Abstract
Background
Urinary incontinence has been shown to affect up to 50% of women. Studies in the USA have shown that up to 80% of these women have an element of stress urinary incontinence. This imposes significant health and economic burden on society and the women affected. Colposuspension and now mid‐urethral slings have been shown to be effective in treating patients with stress incontinence. However, associated adverse events include bladder and bowel injury, groin pain and haematoma formation. This has led to the development of third‐generation single‐incision slings, also referred to as mini‐slings.
It should be noted that TVT‐Secur (Gynecare, Bridgewater, NJ, USA) is one type of single‐incision sling; it has been withdrawn from the market because of poor results. However, it is one of the most widely studied single‐incision slings and was used in several of the trials included in this review. Despite its withdrawal from clinical use, it was decided that data pertaining to this sling should be included in the first iteration of this review, so that level 1a data are available in the literature to confirm its lack of efficacy.
Objectives
To assess the effectiveness of mini‐sling procedures in women with urodynamic clinical stress or mixed urinary incontinence in terms of improved continence status, quality of life or adverse events.
Search methods
We searched: Cochrane Incontinence Specialised Register (includes: CENTRAL, MEDLINE, MEDLINE In‐Process) (searched 6 February 2013); ClinicalTrials.gov, WHO ICTRP (searched 20 September 2012); reference lists.
Selection criteria
Randomised or quasi‐randomised controlled trials in women with urodynamic stress incontinence, symptoms of stress incontinence or stress‐predominant mixed urinary incontinence, in which at least one trial arm involves one of the new single‐incision slings. The definition of a single‐incision sling is “a sling that does not involve either a retropubic or transobturator passage of the tape or trocar and involves only a single vaginal incision (i.e. no exit wounds in the groin or lower abdomen).”
Data collection and analysis
Three review authors assessed the methodological quality of potentially eligible trials and independently extracted data from individual trials.
Main results
We identified 31 trials involving 3290 women. Some methodological flaws were observed in some trials; a summary of these is given in the 'Risk of bias in included studies' section.
No studies compared single‐incision slings versus no treatment, conservative treatment, colposuspension, laparoscopic procedures or traditional sub‐urethral slings. No data on the comparison of single‐incision slings versus retropubic mid‐urethral slings (top‐down approach) were available, but the review authors believe this did not affect the overall comparison versus retropubic mid‐urethral slings.
Types of single‐incision slings included in this review: TVT‐Secur (Gynecare); MiniArc (American Medical Systems, Minnetonka, USA); Ajust (CR Bard Inc., Covington, USA); Needleless (Mayumana Healthcare, Lisse, The Netherlands); Ophira (Promedon, Cordoba, Argentina); Tissue Fixation System (TFS PTY Ltd, Sydney, Australia) and CureMesh (DMed Co. Inc., Seoul, Korea).
Women were more likely to remain incontinent after surgery with single‐incision slings than with retropubic slings such as tension‐free vaginal tape (TVTTM) (121/292, 41% vs 72/281, 26%; risk ratio (RR) 2.08, 95% confidence interval (CI) 1.04 to 4.14). Duration of the operation was slightly shorter for single‐incision slings but with higher risk of de novo urgency (RR 2.39, 95% CI 1.25 to 4.56). Four of five studies in the comparison included TVT‐Secur as the single‐incision sling.
Single‐incision slings resulted in higher incontinence rates compared with inside‐out transobturator slings (30% vs 11%; RR 2.55, 95% CI 1.93 to 3.36). The adverse event profile was significantly worse, specifically consisting of higher risks of vaginal mesh exposure (RR 3.75, 95% CI 1.42 to 9.86), bladder/urethral erosion (RR 17.79, 95% CI 1.06 to 298.88) and operative blood loss (mean difference 18.79, 95% CI 3.70 to 33.88). Postoperative pain was less common with single‐incision slings (RR 0.29, 95% CI 0.20 to 0.43), and rates of long‐term pain or discomfort were marginally lower, but the clinical significance of these differences is questionable. Most of these findings were derived from the trials involving TVT‐Secur: Excluding the other trials showed that high risk of incontinence was principally associated with use of this device (RR 2.65, 95% CI 1.98 to 3.54). It has been withdrawn from clinical use.
Evidence was insufficient to reveal a difference in incontinence rates with other single‐incision slings compared with inside‐out or outside‐in transobturator slings. Duration of the operation was marginally shorter for single‐incision slings compared with transobturator slings, but only by approximately two minutes and with significant heterogeneity in the comparison. Risks of postoperative and long‐term groin/thigh pain were slightly lower with single‐incision slings, but overall evidence was insufficient to suggest a significant difference in the adverse event profile for single‐incision slings compared with transobturator slings. Evidence was also insufficient to permit a meaningful sensitivity analysis of the other single‐incision slings compared with transobturator slings, as all confidence intervals were wide. The only significant differences were observed in rates of postoperative and long‐term pain, and in duration of the operation, which marginally favoured single‐incision slings.
Overall results show that TVT‐Secur is considerably inferior to retropubic and inside‐out transobturator slings, but additional evidence is required to allow any reasonable comparison of other single‐incision slings versus transobturator slings.
When one single‐incision sling was compared with another, evidence was insufficient to suggest a significant difference between any of the slings in any of the comparisons made.
Authors' conclusions
TVT‐Secur is inferior to standard mid‐urethral slings for the treatment of women with stress incontinence and has already been withdrawn from clinical use. Not enough evidence has been found on other single‐incision slings compared with retropubic or transobturator slings to allow reliable comparisons. A brief economic commentary (BEC) identified two studies which reported no difference in clinical outcomes between single‐incision slings and transobturator mid‐urethral slings, but single‐incision slings may be more cost‐effective than transobturator mid‐urethral slings based on one‐year follow‐up. Additional adequately powered and high‐quality trials with longer‐term follow‐up are required. Trials should clearly describe the fixation mechanism of these single‐incisions slings: It is apparent that, although clubbed together as a single group, a significant difference in fixation mechanisms may influence outcomes.
Plain language summary
Single‐incision sling operations for urinary incontinence in women
Stress urinary incontinence (leakage of urine on effort or exertion, or on coughing, sneezing or laughing) is a common condition that affects up to one in three women worldwide. It is usually the result of weakening of the muscular support of the pipe that conducts urine (urethra), or weakening of the sphincter (circular) muscle at the base of the bladder, which maintains continence. It is more common in women who have had children by vaginal delivery and in those who have weakness in the pelvic floor muscles for other reasons. A significant amount of the woman's and her family's income can be spent on managing the symptoms.
Historically many types of surgery have been performed to treat women with stress urinary incontinence. Over the past 10 years, the accepted standard technique has been the mid‐urethral sling operation, whereby an artificial tape or mesh is placed directly beneath the urethra and is anchored to the tissues in adjacent parts of the groin or just above the pubic bone. Examples of such slings that are commonly used are tension‐free vaginal tape (TVTTM) and transobturator tape (TOT). These operations are usually quite successful, with success rates approaching 80% or 90%. However, they have been shown to result in significant side effects, which can be bothersome and sometimes even dangerous, such as damage to the bladder caused by tape insertion, erosion of the tape into the urethra during the healing period or chronic thigh/groin pain.
In an effort to maintain efficacy while eliminating some of the side effects, a new generation of slings has been developed, called 'single‐incision slings' or 'mini‐slings'; these slings are the subject of this review. They are designed to be shorter (in length) than standard mid‐urethral slings and do not penetrate the tissues as deeply as standard slings. It was therefore thought that they would cause fewer side effects while being no less effective. Examples of single‐incision slings include TVT‐Secur, MiniArc, Ajust and Needleless slings, among others.
We looked for all trials that allocated participants at random to single‐incision slings versus any other treatment for stress incontinence in women, especially comparisons with mid‐urethral slings. We identified a total of 31 trials, involving 3290 women, all of which compared a type of single‐incision sling versus a type of mid‐urethral sling, or different types of single‐incision slings against each other. Overall the quality of the trials was moderate.
We found that subtle differences in the way individual mini‐slings work have sometimes made comparisons difficult. TVT‐Secur is a specific type of mini‐sling that has consistently been shown to provide poorer control of incontinence, along with higher rates of side effects, compared with standard mid‐urethral slings. It has already been withdrawn from clinical use.
In terms of costs, a non‐systematic review of economic studies suggested that single‐incision slings are cheaper than mid‐urethral slings. However, no clear evidence was presented on the differences in costs and effects.
As most trials currently available for inclusion in this review assess TVT‐Secur, trials comparing other single‐incision slings versus standard mid‐urethral slings were too few to allow meaningful comparisons. Some evidence suggests that single‐incision slings were quicker to perform and may cause less postoperative pain, but more trials are needed to adequately assess whether the other types of mini‐slings are in fact as good as or safer than standard mid‐urethral slings.
Background
Urinary incontinence (UI) is an extremely common yet under‐reported, under‐diagnosed, under‐treated and potentially manageable condition that is prevalent throughout the world. It can cause a great deal of distress and embarrassment to individuals, as well as significant financial costs to those individuals and to societies. Estimates of prevalence vary from 10% to 40% depending on the definition and type of incontinence studied, with annual incidence ranging from 2% to 11% (Hunskaar 2002; Milsom 2009). Studies in the USA have shown that up to 80% of women with incontinence have an element of stress urinary incontinence (Hampel 1997). At the turn of the century, Turner estimated that the total annual cost to the United Kingdom National Health Service of treating clinically significant urinary incontinence was GBP 233 million (1999/2000 GDP), with the cost to individuals estimated at an additional GBP 178 million (Turner 2004). In the USA the annual direct costs of urinary incontinence in both men and women is over USD 16 billion (1995 USD) (Chong 2011), with a societal cost of USD 26.2 billion (1995 USD) (Wagner 1998). Approximately USD 13.12 billion (1995 USD) of the total direct costs of urinary incontinence are spent on SUI (Chong 2011; Kunkle 2015). About 70% of this USD 13.12 billion is borne by the patients, mainly through routine care (purchasing pads and disposable underwear (diapers), laundry and dry cleaning). This constitute a significant individual financial burden. Of the remaining 30%, 14% is spent on nursing home admissions, 9% on treatment, 6% on addressing complications and 1% on diagnosis (Chong 2011). Subak 2008 reported that about 1% of the median annual household income (USD 50,000 to USD 59,999) was spent by women on incontinence management. This study estimated that women spent an annual mean cost of USD 751 to USD 1277(2006 USD) on incontinence. This cost increases based on the severity of the symptoms (Subak 2008).The indirect cost associated exerts social and psychological burdens which are unquantifiable. (Chong 2011; Kilonzo 2004). Nevertheless, Birnbaum 2004 estimated that the annual average direct medical costs of SUI for one year (1998 USD) was USD 5642, and USD 4208 for indirect workplace costs.The cost of management and treatment of SUI appears to have increased over time, due to increasing prevalence and increased desire for improved quality of life. This in turn has resulted from improved recognition of the condition, as well as increased use of surgical and non‐surgical managements.
The surgical approach to stress urinary incontinence has progressed rapidly over the past one and a half decades. In the mid‐1990s, a prospective randomised study confirmed the superiority of the colposuspension over the Kelly plication and modified Pereyra needle suspension techniques, with five‐year cure rates in excess of 80% (Bergman 1995). This established the colposuspension as the standard approach to stress incontinence surgery. A colposuspension, however, entails major surgery with substantial operating time and lengthy hospital stay, as well as significant potential for morbidity (Lapitan 2012). The pubovaginal sling, which employs a fascial strip for support, is an effective alternative to the colposuspension, with similar efficacy (Rehman 2011). The incidence of severe adverse events following these procedures is high, for example, 10% after colposuspension (Lapitan 2012) and 13% after pubovaginal slings (Bezerra 2005).
Description of the condition
Classically, UI is subdivided into three main types.
Stress urinary incontinence (SUI) is characterised by leakage that occurs mainly during 'stress,' which can be brought about by coughing, sneezing, exercise or any manoeuvre that increases intra‐abdominal pressure. SUI is generally due to an anatomical/mechanical abnormality or weakness in the urethra/sphincter/pelvic floor support, and it is commonly treated with an anatomical/mechanical solution (i.e. surgery).
Urgency urinary incontinence (UUI) is characterised by leakage associated with a sense of urgency (defined as a sudden compelling desire to pass urine that cannot be postponed for fear of leakage). UUI is thought to be caused by involuntary detrusor contractions, which may be neurogenic or idiopathic, and it is treated with medication (most commonly anti‐muscarinic drugs), intra‐vesical botulinum toxin injections or, in extreme cases, surgery.
Mixed urinary incontinence (MUI) is a combination of stress and urgency incontinence.
Surgical management of SUI or stress‐predominant MUI is most commonly achieved these days by using a mid‐urethral support in the form of a tape or mesh. A great deal of research continues to be conducted to find the best balance of efficacy and minimal adverse events in choosing the right kind of tape.
Women with SUI or stress‐predominant MUI, diagnosed clinically or on urodynamics, have been included in this review.
Description of the intervention
In 1993 Ulmsten and Petros proposed the integral theory, a new concept in the maintenance of female urinary continence (Petros 1993). This is considered to be one of the drivers for the development of “tension‐free vaginal tape” (TVT), which was the first effective minimally invasive procedure for stress incontinence in women (Ulmsten 1998). The five‐year efficacy of TVT has been shown to be comparable with that of the Burch colposuspension, with the added benefits of shorter operating time and decreased hospital stay (Ward 2008).
The major disadvantage of the TVT procedure is that it involves the “blind” passage of a retropubic needle, which poses a significant risk for bladder, bowel and major vessel damage. The incidence of bladder injury is approximately 6% (Ogah 2009). This led to the development of the next generation of sub‐urethral sling procedures with the launch of transobturator tape (TOT) (Delorme 2001). Objective and subjective cure rates for both types of mid‐urethral tape have been shown to be equivalent (Nambiar 2012), but the transobturator passage resulted in fewer injuries to the bladder and other organs. A recent Cochrane review (Ogah 2009) describes lower complication rates with TOT, including less bladder perforation and shorter operating time. The transobturator approach is not without complications, and it has been shown to be associated with significant risk of groin and hip pain following surgery. A meta‐analysis (Latthe 2007) reported an incidence of 12% for groin and hip pain following an obturator‐type sling compared with only 1% for the retropubic approach.
The significant risk of visceral injury associated with the retropubic tape and the high incidence of groin pain following the transobturator route have led to the development of a new generation of stress incontinence devices. Popularly known as the “mini‐slings” (Moore 2009), these third‐generation devices differ from previous sling procedures in that a single incision is made within the vagina with no tape exit incisions. They have also been called single‐incision slings (Molden 2008). The tape used in these devices is significantly shorter (eight to 14 cm) in length than first‐ and second‐generation slings. The insertion pass stops short of the obturator membrane or pelvic floor. This less invasive approach is thought to reduce complications, including bladder/bowel and vascular injury and groin and thigh pain, with a shorter hospital stay and less postoperative pain. Interest is gradually increasing regarding the efficacy and safety of the mini‐slings, but at present, clinical data on these procedures are lacking.
How the intervention might work
Single‐incision slings have been developed that are based on the same mechanistic principles as minimally invasive slings, that is, to restore or enhance the woman's urethral support during a sudden rise in intra‐abdominal pressure, such as during a cough or sneeze, thus preventing involuntary loss of urine. At the same time, they aim to minimise the risk of major side effects associated with minimally invasive slings, such as bladder/vaginal/urethral/vascular perforations or erosions and chronic pain. To try to achieve this, these slings have shorter tape lengths and different fixation systems compared with minimally invasive slings. The main difference in these fixation systems is that they do not penetrate the obturator fossa (hence potentially minimising the risk of groin pain) or the retropubic space (minimising the risk of major vessel or visceral injury).
Currently six minimally invasive sling devices are available, including TVT Secur, MiniArc, Ajust, Needleless, Tissue Fixation System and Ophira. Differences between the various devices include the following.
The TVT‐Secur is inserted with a metal introducer that anchors the device in the obturator membrane. It is placed snugly against the urethra.
The MiniArc has a curved introducer that clips into two plastic anchoring hooks on the ends of the sling; this is used to insert the sling and secure it into the obturator membrane.
The Ajust also has a curved introducer with plastic anchoring hooks, but it differs from the other devices in that it has a pulley‐like system that allows adjustment following insertion.
The Needleless device is 60% longer than the other mini‐slings. It has a pocket‐like fold on each end, and an artery forceps is placed onto the end of the sling in this pouch. The sling is pushed laterally and through the obturator membrane at insertion.
The Ophira mini‐sling is a type 1 polypropylene monofilament mesh with two fixation arms that penetrate the obturator internus muscle on either side with the help of a retractile insertion guide.
The TFS consists of non‐stretch multi‐filament polypropylene tape with two polypropylene soft tissue anchors at either end. The tape is passed in the same direction as standard TVT, but the anchors are embedded into the pubourethral ligament inferior to the pubic symphysis.
CureMesh is a 14‐cm polypropylene mesh similar to the MiniArc sling but manufactured domestically in South Korea.
Why it is important to do this review
Various observational trials have reported cure rates of 77% (Debodinance 2008) and 81% (Meschia 2009) for the TVT‐Secur and 77% for the MiniArc (Gauruder‐Burmester 2009). Preliminary data also suggest lower rates of bladder injury and groin or hip pain following insertion of these devices.
With the introduction of new devices, clinicians have to decide whether they are going to adopt the new technique. Studies of surgical devices can be notoriously difficult to conduct and to report and interpret. It is therefore imperative that a high‐quality review is conducted to pool relevant data from randomised controlled trials to try to answer the question of whether these new single‐incision slings are capable of providing adequate treatment for stress incontinence with a lower rate of side effects compared with currently available standard methods of treatment. This is even more important in the current clinical climate in 2014, when implantable meshes and tapes are under intense scrutiny, both in the media and in clinical circles.
Objectives
To assess the effectiveness of mini‐sling procedures in women with urodynamic clinical stress or mixed urinary incontinence in terms of improved continence status, quality of life or adverse events.
Methods
Criteria for considering studies for this review
Types of studies
Randomised or quasi‐randomised controlled trials in which at least one trial arm involves one of the new single‐incision slings.
Types of participants
Adult women with stress urinary incontinence due to urethral hypermobility or intrinsic sphincter deficiency diagnosed urodynamically (urodynamic stress incontinence (USI)) or clinically (stress urinary incontinence (SUI)). Trials involving women with mixed urinary incontinence (MUI) were also included, if these women were shown to have stress‐predominant symptoms.
Types of interventions
At least one arm of the trial included a single‐incision sling (as defined above) to treat stress or mixed urinary incontinence. The comparison intervention included other surgical techniques and non‐surgical interventions. The definition of a single‐incision sling was “a sling that does not involve either a retropubic or transobturator passage of the tape or trocar and involves only a single vaginal incision (i.e. no exit wounds in the groin or lower abdomen).”
The following comparisons were made.
Single‐incision slings versus no treatment.
Single‐incision slings versus conservative treatment.
Single‐incision slings versus colposuspension.
Single‐incision slings versus laparoscopic procedures.
Single‐incision slings versus traditional sub‐urethral slings.
Single‐incision slings versus retropubic minimally invasive slings (subgrouped: 'bottom‐up' and 'top‐down' approach).
Single‐incision slings versus obturator minimally invasive slings (subgrouped: medial‐to‐lateral 'inside out' approach and lateral‐to‐medial 'outside‐in' approach).
One single‐incision sling versus another.
Comparisons were made on the basis of brand of sling, as significant differences between these products have been noted.
Types of outcome measures
The primary outcome measure was the proportion of women who still had urinary incontinence following surgery.
Primary outcomes
Primary effectiveness outcome: number of women with urinary incontinence.
Secondary outcomes
Women’s observations
Number of women with no improvement in urinary incontinence.
Quantification of symptoms
Number of pad changes.
Incontinence episodes.
Pad tests (weights).
Clinicians’ observations
Objective measurement of incontinence (such as observation, leakage observed at urodynamics).
Quality of life
General health status measures (e.g. Short Form 36).
Condition‐specific health measures (specific instruments designed to assess incontinence).
Surgical outcome measures
Duration of the operation.
Operative blood loss.
Duration of inpatient stay.
Time to return to normal activity level.
Adverse events
Major vascular or visceral injury.
Bladder or urethral perforation.
Inadvertent vaginal wall perforation (“button‐holing”).
Urinary retention and need for catheterisation in the short or long term.
Nerve damage.
Other perioperative surgical complications.
Wound dehiscence.
Infection related to use of synthetic mesh.
Erosion to vagina.
Erosion to bladder or urethra.
Long‐term pain/discomfort including pain/discomfort when sitting.
Dyspareunia.
De novo urgency symptoms or urgency incontinence.
(New) detrusor overactivity (urodynamic diagnosis).
Repeat incontinence surgery.
New prolapse surgery.
Need for additional or repeat treatment for incontinence.
Other outcomes
Non‐prespecified outcomes judged important when the review was performed.
Search methods for identification of studies
We imposed no language or other limits on the searches.
Electronic searches
This review drew on the search strategy developed for the Cochrane Incontinence Group. We identified relevant trials from the Cochrane Incontinence Group Specialised Trials Register. For more details on the search methods used to build the Specialised Register, please see the Group's module in The Cochrane Library. This register contains trials identified from the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE and MEDLINE in process, and by handsearching of journals and conference proceedings. Most of the trials in the Cochrane Incontinence Group Specialised Register are also contained in CENTRAL. The date of the last search was 6 February 2013.
The terms used to search the Incontinence Group Specialised Register are given below.
(({DESIGN.CCT*} OR {DESIGN.RCT*}) AND {INTVENT.SURG.SLINGS.MINISLING*} AND {TOPIC.URINE.INCON*})
(All searches were of the keyword field of Reference Manager 2012.)
Other specific searches in a trials register and a trial portal were performed for this review.
ClinicalTrials.gov (searched 20 September 2012).
World Health Organization (WHO) Internatonal Clinical Trials Registry Platform (ICTRP) (searched 20 September 2012).
The search terms used are given in Appendix 1.
We performed additional searches for the Brief Economic Commentary (BECs). We conducted them in MEDLINE(1 January 1946 to March 2017), Embase (1 January 1980 to 2017 Week 12) and NHS EED (1st Quarter 2016). We ran all searches on 6 April 2017. Details of the searches run and the search terms used can be found in Appendix 2.
Searching other resources
Reference lists of all relevant reviews and trial reports were searched to identify further relevant studies.
Data collection and analysis
All data abstraction, synthesis and analysis for this review were conducted in accordance with standard guidelines and criteria of The Cochrane Collaboration. Data abstraction was carried out independently by two review authors and was checked by a third. All three review authors contributed towards the analysis.
Selection of studies
Randomised and quasi‐randomised trials were identified using the above search strategy. Studies were excluded if they were not randomised or quasi‐randomised controlled trials for women with stress incontinence or stress‐predominant mixed incontinence. All eligible trials were evaluated for appropriateness for inclusion before the results were considered by the three review authors. Excluded studies are listed in the Characteristics of excluded studies table, along with the reasons for their exclusion.
Data extraction and management
Trials were assessed independently by two review authors starting with the titles and gaining further clarity from the abstracts when necessary. Reports of potentially eligible trials were retrieved in full, assessed independently by two review authors and checked by a third. When data may have been collected but not reported, clarification was sought from the trialists when possible. Disagreements were resolved by discussion. Data extraction was performed independently by all three review authors; this approach served as a robust cross‐check for errors.
We extracted data independently using a standard form containing prespecified outcomes. Included trial data were processed as described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). Differences of opinion related to study inclusion, methodological quality or data extraction were resolved by discussion among review authors and, when necessary, were referred to a third party for arbitration.
Assessment of risk of bias in included studies
The Cochrane Collaboration risk of bias tool was used to examine the following features: sequence generation, allocation sequence concealment, blinding and incomplete outcome data. Two review authors assessed risk of bias independently. These assessments are presented in the risk of bias tables, graphs and summary figures.
Measures of treatment effect
We used RevMan software version 5.2.3 to conduct a meta‐analysis when two or more eligible trials were identified. A combined estimate of treatment effect across trials was calculated for each specified outcome. For categorical outcomes, the numbers reporting an outcome were related to the numbers at risk in each group to derive a risk ratio (RR). For continuous variables, means and standard deviations were used to derive a mean difference (MD). When feasible, intention‐to‐treat data were used. If similar outcomes were reported on different scales, we calculated the standard mean difference (SMD). We reversed the direction of effect, if necessary, to ensure consistency across trials.
Data synthesis
We used a fixed‐effect approach to the analysis unless evidence of heterogeneity was noted across trials, in which case a random‐effects model was used.
Subgroup analysis and investigation of heterogeneity
Differences between trials were investigated when apparent from visual inspection of the results, or when statistically significant heterogeneity was demonstrated by using the Chi2 test at the 10% probability level or assessment of the I2 statistic (Higgins 2003). When no obvious reason was noted for heterogeneity to exist (after consideration of populations, interventions, outcomes and settings of the individual trials), or when it persisted despite the removal of trials that were clearly different from the others, we used a random‐effects model.
No subgroup analyses were preplanned, but clinical factors such as symptoms of stress urinary incontinence, urodynamic stress incontinence, mixed urinary incontinence, diagnosis of intrinsic urethral sphincter deficiency or urethral hypermobility, obesity, previous incontinence surgery, presence or absence of prolapse, anaesthesia used or experience of the surgeon might all influence the outcomes of surgery and may be taken into account in future reviews.
Sensitivity analysis
Concomitant stress incontinence with prolapse is a common problem that is frequently corrected simultaneously at surgery; therefore we believed it was important to assess single‐incision slings in this clinically relevant scenario. When appropriate, sensitivity analyses have been conducted, with exclusion of trials in which concomitant surgery was performed.
Timing of outcome measures can vary between trials, and this can serve as a potential source of bias. When comparisons have been made between trials with significantly different mean duration of follow‐up, sensitivity analyses have been performed to assess whether this could be a source of bias.
Results
Description of studies
Trials included in this review have been named in such a way as to make identification and comparisons in tables more intuitive. Trials have been named in the format of <First author surname><Year of publication><Abbreviation of single‐incision sling(s) included in the study>. Abbreviations of single‐incision slings used in this review are as follows.
TVT‐Secur (SEC).
MiniArc (ARC).
Ajust (AJS).
Contasure Needleless (NDL).
Tissue Fixation System (TFS).
Ophira (OPH).
CureMesh (CUR).
For example, Abdelwahab 2010 SEC is a trial report published by Abdelwahab in 2010 including TVT‐Secur as the single‐incision sling intervention; Pardo 2010 SEC ARC included both TVT‐Secur and MiniArc as interventions. This naming system allows easy identification of the types of single‐incision slings used in each study for evaluation of the figures and tables in this review.
Characteristics of the different single‐incision slings
One of the important differences between the different types of single‐incision slings is whether a fixation system, or hook, holds them in place.
Slings that include a fixation system or hook are MiniArc (ARC), CureMesh (CUR), Ajust (AJS), Contasure Needleless (NDL) and Tissue Fixation System (TFS).
Slings that do not include a fixation system or hook are TVT‐Secur (SEC) and Ophira (OPH).
These divisions, however, are subject to further scrutiny because it is difficult to define what is meant by a good 'fixation system.' For example, the Contasure Needleless (NDL) system uses fascial pockets at both ends, in which normal artery forceps are placed to guide the ends of the sling to the obturator tunnel. Technically these pockets act as anchors once the forceps have been removed, but the strength and pull‐out forces could be quite different from those of the tissue fixation system (TFS), which anchors into the pubourethral ligament/muscle complex. Nevertheless, they are regarded as third‐generation sub‐urethral slings, as they do share several common characteristics. The review authors decided that for this iteration of the review, they would be assessed as one group, in line with the protocol.
Results of the search
We identified 81 reports of studies from the literature search (Figure 1). We excluded 13, and ongoing studies will be taken into account for future updates (Characteristics of ongoing studies). As the result of overlap between abstracts and published papers, and through separation of single‐centre reports from multi‐centre trials, we finally identified 31 trials that met the inclusion criteria.
1.
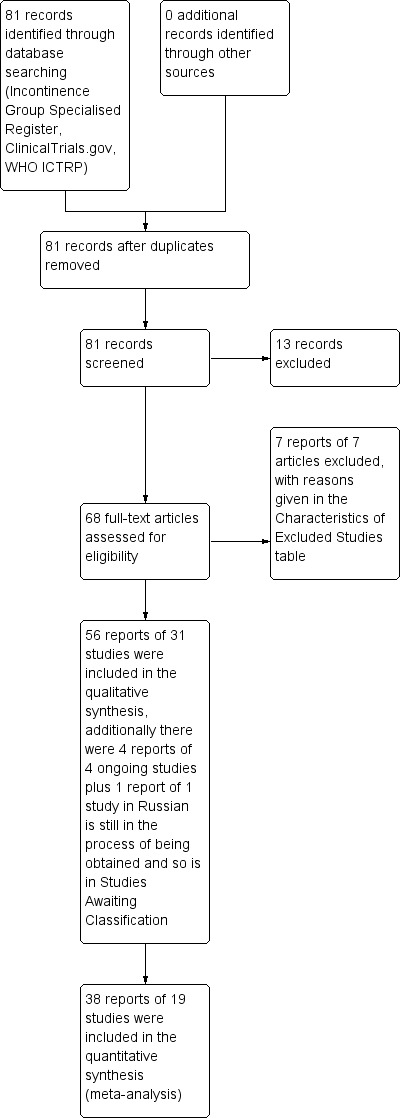
PRISMA study flow diagram.
19 full published papers (Abdelwahab 2010 SEC; Amat 2011 NDL; Andrada Hamer 2012 SEC; Barber 2012 SEC; Basu 2010 ARC; Enzelsberger 2010 ARC; Hinoul 2011 SEC; Hota 2012 SEC; Lee 2010 SEC; Liapis 2010 SEC; Martan 2012 ARC AJS; Masata 2012 SEC; Mostafa 2012 AJS; Oliveira 2011 ARC SEC; Palomba 2012 AJS ARC SEC; Sivaslioglu 2012 TFS; Sottner 2012 ARC AJS; Tommaselli 2010 SEC; Wang 2011 SEC).
One thesis (Mackintosh 2010 AJS).
11 abstracts (Bianchi 2012 SEC; Djehdian 2010 OPH; Friedman 2009 SEC; Kim 2010 SEC; Lee 2010 CUR/SEC; Lee 2012 ARC; Pardo 2010 SEC ARC; Schweitzer 2012 AJS; Seo 2011 SEC; Smith 2011 ARC; Yoon 2011 NDL).
Four ongoing trials were identified (Foote 2012; Maslow 2011; Robert 2012; Rosamilia 2012; Characteristics of ongoing studies). One paper, in Russian, that we are still trying to obtain is listed in Studies awaiting classification (Pushkar 2011).
Included studies
In all, 31 trials met the inclusion criteria. These include 19 fully published papers, one thesis and 11 abstracts. The characteristics of included trials varied considerably and have been described in detail in Characteristics of included studies. A brief descriptive summary follows.
No trials were identified that compared single‐incision slings versus no treatment, conservative treatment, colposuspension, laparoscopic procedures or traditional sub‐urethral slings.
Single‐incision slings versus retropubic mid‐urethral slings
Five trials were identified. These were further sub‐divided on the basis of comparisons with top‐to‐bottom or bottom‐to‐top approaches of retropubic slings; however no trials compared single‐incision slings versus top‐to‐bottom retropubic slings. All five trials were fully published papers and compared single‐incision slings versus bottom‐to‐top retropubic slings (Abdelwahab 2010 SEC; Andrada Hamer 2012 SEC; Barber 2012 SEC; Basu 2010 ARC; Wang 2011 SEC).
Women with prolapse
One study included women with concomitant prolapse (Barber 2012 SEC) but did not present separate data for participants who underwent sling surgery alone. Two trials were unclear about inclusion of women with associated prolapse (Andrada Hamer 2012 SEC; Wang 2011 SEC). No other significant difference was noted between participant groups. Methodology was not well described in Abdelwahab 2010 SEC but was adequate in the four other trials.
Single‐incision slings versus transobturator mid‐urethral slings
These trials were further sub‐divided by type of trans‐obturator sling into inside‐out (TVT‐O) and outside‐in (TOT).
Inside‐out slings
Thirteen trials compared single‐incision slings versus inside‐out transobturator slings. Eight were fully published papers (Amat 2011 NDL; Hinoul 2011 SEC; Hota 2012 SEC; Masata 2012 SEC; Mostafa 2012 AJS; Oliveira 2011 ARC SEC; Tommaselli 2010 SEC; Wang 2011 SEC), four were abstracts (Bianchi 2012 SEC; Friedman 2009 SEC; Schweitzer 2012 AJS; Seo 2011 SEC) and one was a thesis (Mackintosh 2010 AJS). Reporting and adequacy of methodology were variable—methodological information in all abstracts was minimal, as it was in Oliveira 2011 ARC SEC, but in Amat 2011 NDL, the randomisation method used was considered inadequate. The other full papers described methodology well.
Women with prolapse
Amat 2011 NDL; Friedman 2009 SEC; and Hota 2012 SEC included participants with associated prolapse who may have had concomitant prolapse surgery. Bianchi 2012 SEC; Hinoul 2011 SEC; Masata 2012 SEC; Mostafa 2012 AJS; Oliveira 2011 ARC SEC; and Tommaselli 2010 SEC excluded patients with associated prolapse. Mackintosh 2010 AJS; Schweitzer 2012 AJS; and Seo 2011 SEC did not specify this in their exclusion criteria.
Outside‐in slings
Seven trials compared single‐incision slings versus outside‐in transobturator slings (TOTs). Only one is a fully published paper (Sivaslioglu 2012 TFS); the others were abstracts (Djehdian 2010 OPH; Enzelsberger 2010 ARC; Kim 2010 SEC; Lee 2012 ARC; Smith 2011 ARC; Yoon 2011 NDL). Enzelsberger 2010 ARC is a German paper that contains an English language abstract with minimal information. A full translation was not obtained, but we will try to request this for future updates. Methodological quality of these trials was variable. In Lee 2012 ARC; Sivaslioglu 2012 TFS; and Smith 2011 ARC,randomisation methods were adequately described, but allocation and blinding were not described. Randomisation was unequal, and the method was not described in Djehdian 2010 OPH, was inadequately performed in Yoon 2011 NDL, and was not clearly described in Kim 2010 SEC.
Prolapse and overactive bladder symptoms
Djehdian 2010 OPH excluded patients with significant genitourinary prolapse, and Sivaslioglu 2012 TFS excluded patients with predominant overactive bladder symptoms, but Enzelsberger 2010 ARC; Kim 2010 SEC; Lee 2012 ARC; Smith 2011 ARC; and Yoon 2011 NDL were unclear about inclusion/exclusion of these patient groups.
One type of single‐incision sling versus another
Nine trials were identified: five full papers (Lee 2010 SEC; Liapis 2010 SEC; Masata 2012 SEC; Oliveira 2011 ARC SEC; Palomba 2012 AJS ARC SEC) and four abstracts (Lee 2010 CUR/SEC; Martan 2012 ARC AJS; Pardo 2010 SEC ARC; Sottner 2012 ARC AJS). Methodological quality was variable even among fully published papers, ranging from inadequate randomisation methods used in Liapis 2010 SEC to overall very robust and well‐reported methodology used in Palomba 2012 AJS ARC SEC. Methodology as reported in the abstracts was generally unclear. Comparisons varied in these trials and have been grouped into three owing to the difference in fixation systems of the different types of single‐incision slings: TVT‐SECUR versus MiniArc, U‐type versus H‐type of TVT‐Secur and MiniArc versus Ajust. The Sottner 2012 ARC AJS paper was published in Czech with an English abstract, but no useful data were available, and no translation was obtained; however, this will be requested for future updates.
Excluded studies
Seven studies were excluded because they were not randomised control trials or because they did not include single‐incision slings as one of the comparators. Four trials were ongoing at the time of writing of this review and therefore were not included in the analysis but may be considered in future updates. One trial is awaiting classification because currently available information is lacking; however, it will be considered in future updates. The details of these studies are given under Characteristics of excluded studies.
Five other studies are awaiting assessment or are ongoing trials; details are given in the Characteristics of studies awaiting classification and Characteristics of ongoing studies sections.
Risk of bias in included studies
The risk of bias in included trials was variable, with about half of the trials using adequate methods of randomisation and allocation concealment, while in the other half, methods used were inadequate or were not described. Attempts to double‐blind were even less rigorous, with only five trials carrying out some kind of blinding of participants. Although blinding can be notoriously difficult to achieve in surgical trials, it is nonetheless possible to a reasonable degree; therefore the review authors believed it was warranted to utilise this as a criterion in the risk of bias section. The findings of the risk of bias assessment are summarised in Figure 2 and Figure 3.
2.
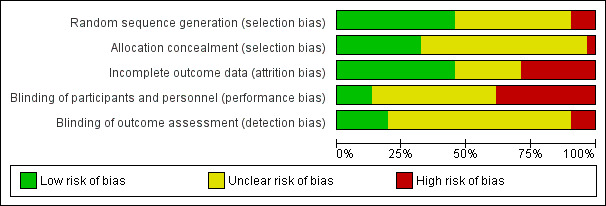
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
3.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
Random sequence generation
The risk of bias was considered to be low for random sequence generation for 14 trials, in which the sequence was generated most often by using a computer (Barber 2012 SEC; Basu 2010 ARC; Hinoul 2011 SEC; Lee 2010 SEC; Lee 2012 ARC; Mackintosh 2010 AJS; Martan 2012 ARC AJS; Masata 2012 SEC; Mostafa 2012 AJS; Palomba 2012 AJS ARC SEC; Sivaslioglu 2012 TFS; Smith 2011 ARC; Tommaselli 2010 SEC; Wang 2011 SEC).
The risk of bias was considered high for three trials, in which allocation was based on medical record number (Amat 2011 NDL), participants were allocated alternately (Liapis 2010 SEC) or the method of randomisation was inadequately described (Pardo 2010 SEC ARC).
The risk of bias was considered unclear in the remaining 14 trials, in which no description was given in the report (Abdelwahab 2010 SEC; Andrada Hamer 2012 SEC; Bianchi 2012 SEC; Djehdian 2010 OPH; Enzelsberger 2010 ARC; Friedman 2009 SEC; Hota 2012 SEC; Kim 2010 SEC; Kim 2010 SEC; Lee 2010 CUR/SEC; Oliveira 2011 ARC SEC; Schweitzer 2012 AJS; Seo 2011 SEC; Sottner 2012 ARC AJS; Yoon 2011 NDL).
Allocation concealment
Eleven trials used an adequate allocation concealment method (most often opaque envelopes) (Andrada Hamer 2012 SEC; Barber 2012 SEC; Basu 2010 ARC; Hota 2012 SEC; Lee 2012 ARC; Mackintosh 2010 AJS; Martan 2012 ARC AJS; Masata 2012 SEC; Mostafa 2012 AJS; Palomba 2012 AJS ARC SEC; Wang 2011 SEC).
The other 20 trials failed to describe any method of allocation concealment.
Blinding
Blinding of participants or personnel
Only five trials carried out some kind of blinding of participants. The Barber trial (Barber 2012 SEC) used sham incisions in the mini‐sling arm to facilitate blinding. In the Basu trial (Basu 2010 ARC), participants were blinded but researchers could not be blinded because of differences in devices. The Palomba trial (Palomba 2012 AJS ARC SEC) stated that participants and data assessors were masked to the procedure. The Schweitzer trial (Schweitzer 2012 AJS) reported that women were blinded to the type of procedure by use of a sham incision in the Ajust group. Tommaselli et al (Tommaselli 2010 SEC) reported that participants "were left blinded to the devices used until the end of the procedure." The other trials made no mention of blinding or stated that it was not possible.
Blinding of outcome assessors
Six trials mentioned methods of reducing risk of bias through blinded outcome assessment (Andrada Hamer 2012 SEC; Barber 2012 SEC; Mackintosh 2010 AJS; Mostafa 2012 AJS; Palomba 2012 AJS ARC SEC; Sivaslioglu 2012 TFS). Three were considered to be at high risk of bias owing to unblinded outcome assessment or inadequate information for assessment (Pardo 2010 SEC ARC; Schweitzer 2012 AJS; Smith 2011 ARC).
Incomplete outcome data
The risk of bias was considered high for eight trials (Amat 2011 NDL; Andrada Hamer 2012 SEC; Hinoul 2011 SEC; Hota 2012 SEC; Liapis 2010 SEC; Schweitzer 2012 AJS; Smith 2011 ARC; Tommaselli 2010 SEC) as the result of high dropout rates. Of these, differential dropout rates were observed in Andrada Hamer 2012 SEC and Hinoul 2011 SEC. Hota 2012 SEC failed to recruit the required number of participants and was stopped at interim analysis.
Effects of interventions
Single‐incision slings versus no treatment
No trials that compared single‐incision slings versus no treatment were found.
Single‐incision slings versus conservative treatment
No trials that compared single‐incision slings versus conservative treatment were found.
Single‐incision slings versus colposuspension
No trials that compared single‐incision slings versus colposuspension were found.
Single‐incision slings versus laparoscopic procedures
No trials that compared single‐incision slings versus laparoscopic procedures were found.
Single‐incision slings versus traditional sub‐urethral slings
No trials that compared single‐incision slings versus traditional sub‐urethral slings were found.
Single‐incision slings versus retropubic minimally invasive slings (subgrouped: 'bottom‐up' and 'top‐down' approach)
Five trials met the inclusion criteria (Abdelwahab 2010 SEC; Andrada Hamer 2012 SEC; Barber 2012 SEC; Basu 2010 ARC; Wang 2011 SEC). All single‐incision slings were compared with 'bottom‐up' retropubic minimally invasive slings. All but one trial (Basu 2010 ARC) involved one type of mini‐sling: TVT‐Secur. The study authors note that the Andrada Hamer 2012 SEC study was stopped at interim analysis (two months) because of poor efficacy and complication rates with the TVT‐Secur.
No trials that compared a single‐incision sling versus a 'top‐down' retropubic sling were identified. These types of slings are no longer used in clinical practice, but if we had identified such trials, they would have been included for completeness.
Number of women with urinary incontinence (primary outcome)
All five trials were included in this meta‐analysis. The overall result showed that more women had persistent urinary incontinence after the single‐incision surgery (121/292, 41% vs 72/281, 26%; RR 2.08, 95% CI 1.04 to 4.14; Analysis 6.1), and this was statistically significant in favour of retropubic slings. One trial (Basu 2010 ARC) compared the MiniArc sling against TVT; the other four compared TVT‐Secur against TVT.
6.1. Analysis.
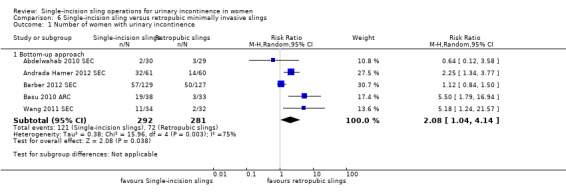
Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 1 Number of women with urinary incontinence.
Statistical heterogeneity is apparent in this meta‐analysis, possibly as a result of the inconclusive results of the small Abdelwahab trial and the larger Barber trial. Clinical heterogeneity may also be a factor: One trial (Barber 2012 SEC) did include women with concomitant prolapse, and almost half of the study population underwent some form of concomitant surgery. Two of the other trials (Andrada Hamer 2012 SEC; Wang 2011 SEC) were not clear about whether women with concomitant prolapse were included. However, the result remained statistically significant in favour of retropubic tape when a more conservative random‐effects model was used.
Follow‐up ranged from nine months (Abdelwahab 2010 SEC) to three years (Basu 2010 ARC) but was one year for the other three trials (Andrada Hamer 2012 SEC; Barber 2012 SEC; Wang 2011 SEC). Most trials used a composite measure of cure consisting of subjective and objective measures of incontinence. Although one‐year follow‐up data are reported for the Andrada Hamer 2012 SEC study, it must be noted that only half of the planned number of subjects were recruited because the trial was stopped at interim analysis. Nevertheless, the review authors believed that the reported data should be included in the meta‐analysis.
Number of women with no improvement
Three trials were included in the meta‐analysis (Abdelwahab 2010 SEC; Andrada Hamer 2012 SEC; Wang 2011 SEC). The overall result showed that almost all women had improved, but no statistically significant difference was observed between the two treatments, and the confidence interval was wide (Analysis 6.2).
6.2. Analysis.
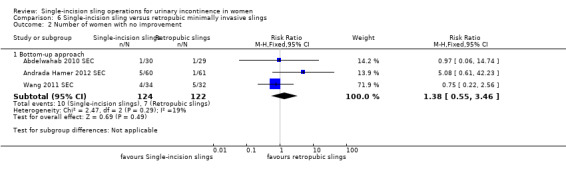
Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 2 Number of women with no improvement.
Objective measurement of incontinence
Two trials were included in the meta‐analysis (Andrada Hamer 2012 SEC; Basu 2010 ARC). The Andrada Hamer trial compared TVT‐Secur against TVT with follow‐up at one year. Investigators performed both cough test and pad test for objective measurement of SUI; we have used the results of the cough test in this analysis. The Basu trial compared the MiniArc against TVT with follow‐up of three years; however urodynamic evaluation of incontinence (the objective measurement criterion used in the trial) was done at six‐month follow‐up, and these data were used in this comparison. The overall result reflected the individual results of the separate trials and was statistically significant favouring retropubic slings (RR 4.44, 95% CI 2.06 to 9.56) (Analysis 6.3).
6.3. Analysis.
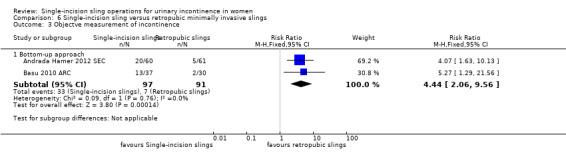
Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 3 Objectve measurement of incontinence.
Quality of life
The Barber trial (Barber 2012 SEC) measured condition‐specific quality of life at one year using the Incontinence Severity Index score. Quality of life was statistically significantly better in the retropubic group (Analysis 6.4).
6.4. Analysis.
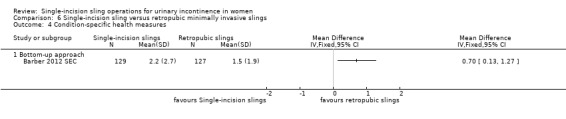
Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 4 Condition‐specific health measures.
Surgical outcome measures
Duration of operation
Three trials were included in the meta‐analysis (Abdelwahab 2010 SEC; Barber 2012 SEC; Wang 2011 SEC). Andrada Hamer 2012 SEC also provided data for mean duration of operation, but the standard deviation was not given; therefore it could not be included in the meta‐analysis. The duration of the operation was significantly shorter for the single‐incision sling (17 minutes, 95% CI 3 to 32 minutes) (Analysis 6.5). However, statistical heterogeneity may be explained clinically by differences in the definition of what constitutes "duration of operation." Statistical significance persisted when the more conservative random‐effects model was used, and all three trials favoured the single‐incision arm.
6.5. Analysis.
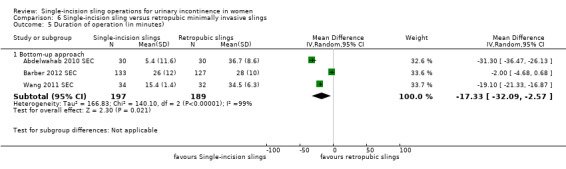
Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 5 Duration of operation (in minutes).
Operative blood loss
Only one study was included in this analysis (Abdelwahab 2010 SEC), but lower blood loss with a single‐incision sling was not statistically significant (Analysis 6.6).
6.6. Analysis.
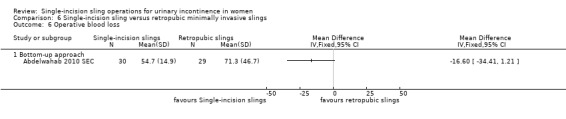
Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 6 Operative blood loss.
Length of in‐patient stay
One study was included in the analysis (Abdelwahab 2010 SEC), but the results were not statistically significant and the confidence interval was wide (Analysis 6.7).
6.7. Analysis.
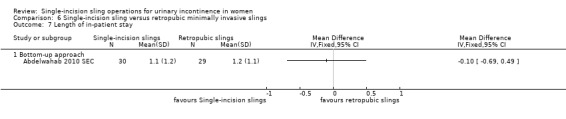
Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 7 Length of in‐patient stay.
Adverse events
Major vascular or visceral injury; vaginal wall perforation
The small Andrada Hamer trial (Andrada Hamer 2012 SEC) reported that one woman had major vascular or visceral injury (Analysis 6.8), and one in each group had vaginal wall perforation (Analysis 6.9); however, the results were not statistically significant because wide confidence intervals implied lack of evidence in favour of either procedure.
6.8. Analysis.
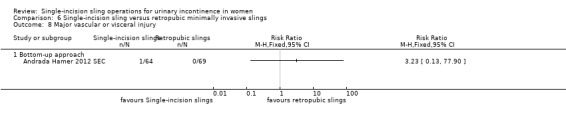
Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 8 Major vascular or visceral injury.
6.9. Analysis.
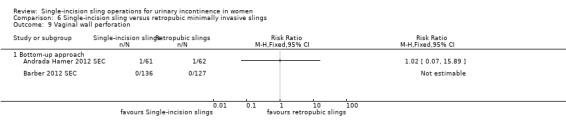
Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 9 Vaginal wall perforation.
Bladder or urethral perforation
Bladder or urethral perforation was reported in four trials (Andrada Hamer 2012 SEC; Barber 2012 SEC; Basu 2010 ARC; Wang 2011 SEC) and was not common (<4%). The overall result was not statistically significant and the confidence interval was wide (Analysis 6.10). Apart from the Basu trial (Basu 2010 ARC), which compared the MiniArc with TVT, all other trials used TVT‐Secur as the experimental intervention, but no statistical heterogeneity was evident.
6.10. Analysis.
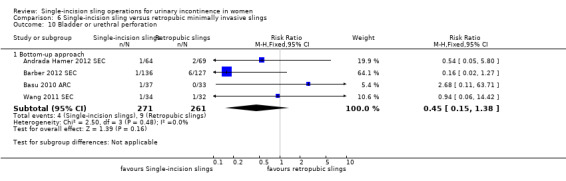
Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 10 Bladder or urethral perforation.
Urinary retention and the need for catheterisation
Five trials reported on this outcome (Abdelwahab 2010 SEC; Andrada Hamer 2012 SEC; Barber 2012 SEC; Basu 2010 ARC; Wang 2011 SEC). Less than 4% of women experienced difficulty voiding; the difference between groups was not statistically significant and the confidence interval was wide (Analysis 6.11).
6.11. Analysis.
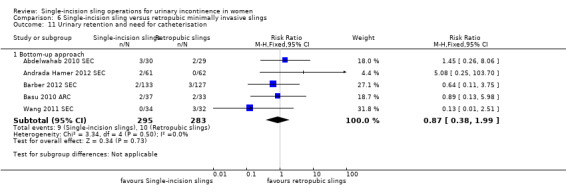
Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 11 Urinary retention and need for catheterisation.
Infection due to synthetic mesh; dyspareunia
Infection related to the use of synthetic mesh and dyspareunia were reported in one small study (Abdelwahab 2010 SEC), but no evidence showed a difference between the procedures (Analysis 6.12; Analysis 6.16).
6.12. Analysis.
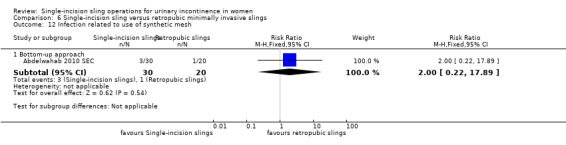
Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 12 Infection related to use of synthetic mesh.
6.16. Analysis.
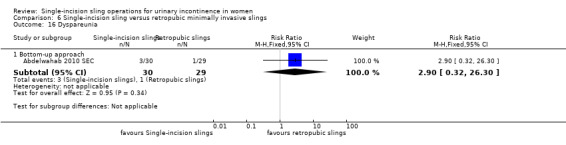
Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 16 Dyspareunia.
Vaginal mesh exposure
Vaginal exposure (erosion) of mesh was reported in three women in two trials (Barber 2012 SEC; Basu 2010 ARC); this result was not statistically significant and the confidence interval was wide (Analysis 6.13).
6.13. Analysis.
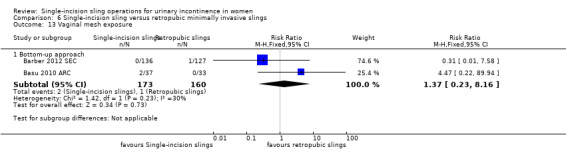
Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 13 Vaginal mesh exposure.
Mesh extrusion into bladder or urethra
Mesh extrusion into the bladder or urethra was reported in five women in three trials (Abdelwahab 2010 SEC; Andrada Hamer 2012 SEC; Barber 2012 SEC); the combined result showed no evidence of a difference between the two procedures and the confidence interval was wide (Analysis 6.14).
6.14. Analysis.
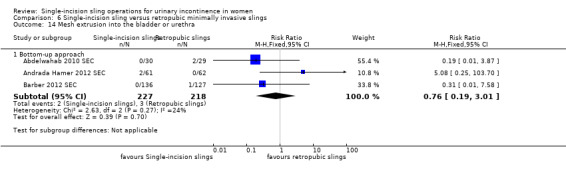
Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 14 Mesh extrusion into the bladder or urethra.
Long‐term pain or discomfort
Two trials reported this outcome (Barber 2012 SEC; Wang 2011 SEC). None of the 329 women reported this adverse effect.
De novo urgency; new‐onset detrusor overactivity
De novo urgency was reported in three trials (Abdelwahab 2010 SEC; Andrada Hamer 2012 SEC; Wang 2011 SEC), all of which compared TVT‐Secur versus TVT. It was more common in the single‐incision group, and the meta analysis showed a statistically significant difference favouring the retropubic TVT procedure (27/125, 22% vs 11/123, 9% after TVT; RR 2.39, 95% CI 1.25 to 4.56) (Analysis 6.17).
6.17. Analysis.
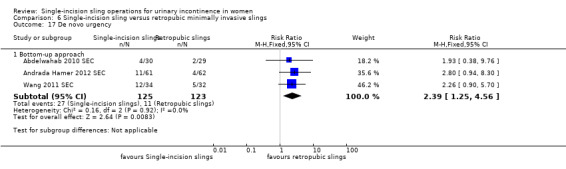
Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 17 De novo urgency.
One small trial (Basu 2010 ARC) reported that two women in each group developed new‐onset detrusor overactivity (Analysis 6.18).
6.18. Analysis.
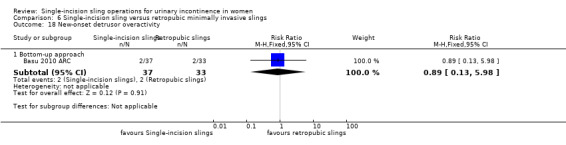
Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 18 New‐onset detrusor overactivity.
Repeat stress incontinence surgery
Repeat stress incontinence surgery was reported in only two trials (Barber 2012 SEC; Basu 2010 ARC), which used different single‐incision slings. In the Basu trial (Basu 2010 ARC), nine women required further incontinence surgery after a single‐incision sling compared with none in the retropubic sling group—a result that was statistically significant in favour of retropubic slings versus the MiniArc. Although the Barber trial (Barber 2012 SEC) showed no statistically significant difference in the comparison between retropubic slings versus TVT‐Secur, only six women required further surgery and the confidence interval was wide (Analysis 6.19).
6.19. Analysis.
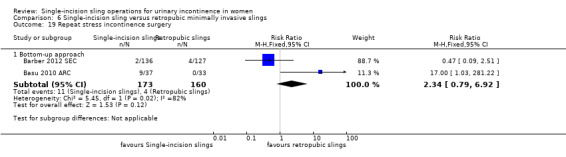
Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 19 Repeat stress incontinence surgery.
Need for any other additional or new surgical procedure to treat complications
This outcome was reported in Barber 2012 SEC and Basu 2010 ARC. No significant difference was noted in the number of women who required additional procedures to treat complications of the index surgery (Analysis 6.20).
6.20. Analysis.
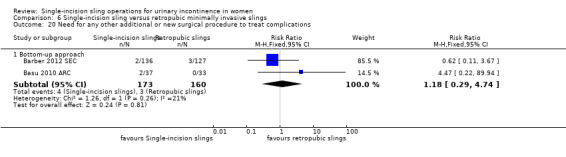
Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 20 Need for any other additional or new surgical procedure to treat complications.
Single‐incision slings versus obturator minimally invasive slings (subgrouped: medial‐to‐lateral 'inside out' approach and lateral‐to‐medial 'outside‐in' approach)
Twenty trials met the inclusion criteria.
Thirteen trials compared single‐incision slings versus inside‐out transobturator slings (Amat 2011 NDL; Bianchi 2012 SEC; Friedman 2009 SEC; Hinoul 2011 SEC; Hota 2012 SEC; Mackintosh 2010 AJS; Masata 2012 SEC; Mostafa 2012 AJS; Oliveira 2011 ARC SEC; Schweitzer 2012 AJS; Seo 2011 SEC; Tommaselli 2010 SEC; Wang 2011 SEC).
Seven trials compared single‐incision slings versus outside‐in transobturator slings (Djehdian 2010 OPH; Enzelsberger 2010 ARC; Kim 2010 SEC; Lee 2012 ARC; Sivaslioglu 2012 TFS; Smith 2011 ARC; Yoon 2011 NDL).
The combined overall results for single‐incision slings versus any types of transobturator slings are stated when available.
Number of women with urinary incontinence (primary outcome)
Ten trials that compared a single‐incision sling (eight TVT‐Secur, two AJS and one ARC) against inside‐out transobturator slings were included in the meta‐analysis (Bianchi 2012 SEC; Friedman 2009 SEC; Hinoul 2011 SEC; Hota 2012 SEC; Mackintosh 2010 AJS; Masata 2012 SEC; Mostafa 2012 AJS; Oliveira 2011 ARC SEC; Seo 2011 SEC; Wang 2011 SEC). Both Masata 2012 SEC and Oliveira 2011 ARC SEC were three‐arm trials with two types of single‐incision devices. For purposes of this analysis, the data from the single‐incision arms have been combined for each trial. More women had urinary incontinence in the single‐incision sling arms (172/572, 30%), and the overall result was statistically significant in favour of inside‐out transobturator slings (incontinence in 55/481, 11% of women; RR 2.55, 95% CI 1.94 to 3.36) (Analysis 7.1.1). A sensitivity analysis excluding the two trials that did not use TVT‐Secur (Mackintosh 2010 AJS; Mostafa 2012 AJS) made no difference in the results (RR 2.65, 95% CI 1.98 to 3.54) (Analysis 7.1.1). This device has been withdrawn from clinical use.
7.1. Analysis.
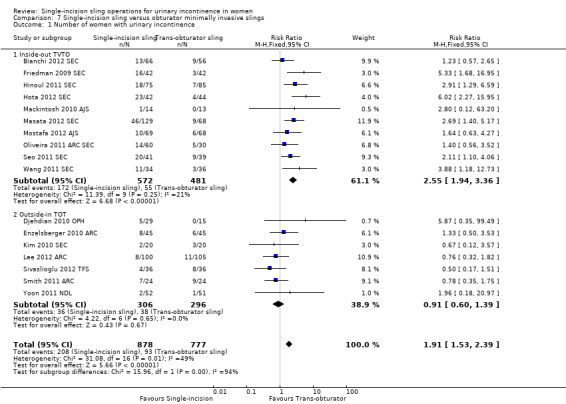
Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 1 Number of women with urinary incontinence.
Follow‐up for all trials was 12 months, apart from Bianchi 2012 SEC; Friedman 2009 SEC; and Masata 2012 SEC, which reported two‐year follow‐up, and Mackintosh 2010 AJS, which reported three‐month follow‐up. Exclusion of the Mackintosh 2010 AJS study made no difference in the results.
Seven trials compared five different types of single‐incision slings against outside‐in transobturator slings (Djehdian 2010 OPH; Enzelsberger 2010 ARC; Kim 2010 SEC; Lee 2012 ARC; Sivaslioglu 2012 TFS; Smith 2011 ARC; Yoon 2011 NDL). The overall result was not statistically significant (36/306, 12% vs 38/296, 13%; RR 0.91, 95% CI 0.60 to 1.39; Analysis 7.1), nor was individual comparison by subtype of single‐incision sling. Considerable variation in the range of follow‐up was seen, from four weeks (Yoon 2011 NDL) to five years (Sivaslioglu 2012 TFS). Djehdian 2010 OPH is an ongoing trial with unequal randomisation reported at six‐month follow‐up.
When results for transobturator slings were combined as a single group, the result was still statistically significant in favour of transobturator slings (RR 1.91, 95% CI 1.53 to 2.39) (Analysis 7.1), but this introduces a degree of heterogeneity, with an I2 statistic of 49%.
Number of women with no improvement
Four trials that compared TVT‐Secur against inside‐out transobturator slings were included in the meta‐analysis (Masata 2012 SEC; Oliveira 2011 ARC SEC; Seo 2011 SEC; Wang 2011 SEC). Oliveira 2011 ARC SEC was a three‐arm trial; for purposes of analysis, the two single‐incision arms were combined, but a sensitivity analysis showed that this had little impact on the combined result. Masata 2012 SEC had the longest follow‐up, at two years. Similar to the analysis of participant‐reported incontinence rates, the overall result was statistically significant in favour of inside‐out transobturator slings (RR 4.80, 95% CI 2.00 to 11.55; Analysis 7.2).
7.2. Analysis.
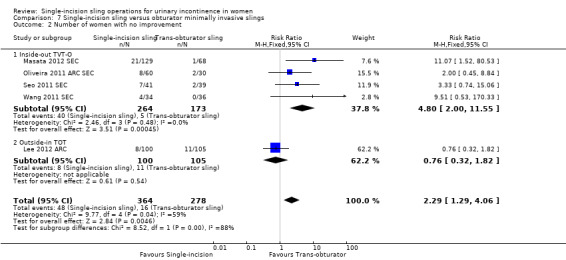
Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 2 Number of women with no improvement.
One small trial (Lee 2012 ARC) compared MiniArc against an outside‐in transobturator tape, but the result was not statistically significant.
The combined result was still statistically significant in favour of transobturator slings (RR 2.29, 95% CI 1.29 to 4.06) but with a degree of heterogeneity (I2 = 59%).
Objective measurement of incontinence
Seven trials that compared TVT‐Secur against inside‐out transobturator slings were included in the meta‐analysis (Bianchi 2012 SEC; Hinoul 2011 SEC; Hota 2012 SEC; Mackintosh 2010 AJS; Masata 2012 SEC; Mostafa 2012 AJS; Tommaselli 2010 SEC). Women were nearly three times more likely to be incontinent with a single‐incision sling, and the overall result was statistically significant in favour of inside‐out transobturator slings (RR 2.91, 95% CI 2.00 to 4.25) (Analysis 7.3.1). Evidence of some statistical heterogeneity was seen in this result, but the direction of effect was the same in all trials.
7.3. Analysis.
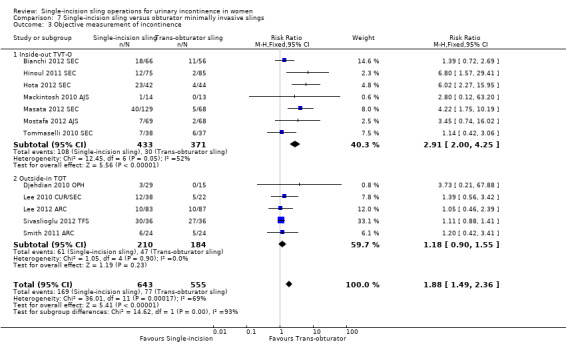
Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 3 Objective measurement of incontinence.
Five trials that compared different types of single‐incision slings against outside‐in transobturator slings were included in the meta‐analysis (Djehdian 2010 OPH; Lee 2010 CUR/SEC; Lee 2012 ARC; Sivaslioglu 2012 TFS; Smith 2011 ARC). The result was not statistically significant, but confidence intervals were too wide to ensure no differences between the groups.
Overall, the results obtained when both types of transobturator tapes were combined still favoured the latter (RR 1.88, 95% CI 1.49 to 2.36) (Analysis 7.3).
Incontinence episodes
One study (Smith 2011 ARC) compared MiniArc against outside‐in transobturator slings but was too small to show a difference in the number of incontinence episodes at a mean follow up of 33 months (Analysis 7.4).
7.4. Analysis.
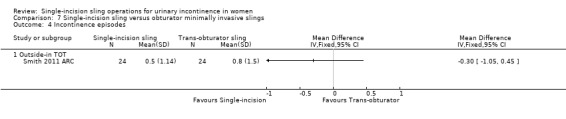
Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 4 Incontinence episodes.
Pad test (weight of urine lost)
Two trials (Djehdian 2010 OPH; Lee 2012 ARC) performed pad tests at six months. However, it must be noted that Djehdian 2010 OPH reported one‐hour pad weights and Lee reported 24‐hour pad weights. Although no statistically significant difference was observed between the groups, the confidence interval was wide (Analysis 7.5).
7.5. Analysis.
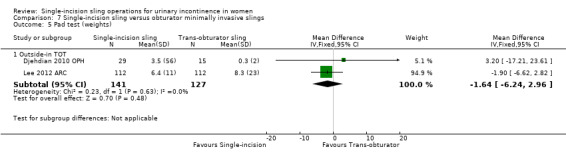
Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 5 Pad test (weights).
Quality of life
Two trials (Hinoul 2011 SEC; Mostafa 2012 AJS) of single‐incision versus inside‐out transobturator slings are included in this meta‐analysis. Different condition‐specific health questionnaires were used (Urinary Distress Inventory (UDI)‐6 and International Consultation on Incontinence Modular Questionnaire, Short Form (ICIQ‐SF)); therefore results were combined by using standardised mean differences. The result was not statistically significant (Analysis 7.6.1) and the confidence interval was wide.
7.6. Analysis.
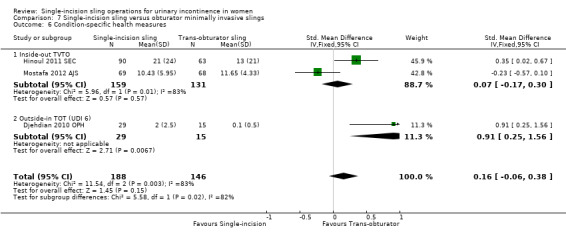
Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 6 Condition‐specific health measures.
One small trial compared a single‐incision sling versus an outside‐in transobturator sling (Djehdian 2010 OPH) and favoured the TOT, but a large discrepancy was noted in recruitment for this study, with the single‐incision group almost double the TOT group; therefore the results must be interpreted with caution (Analysis 7.6.2).
Surgical outcome measures
Duration of operation
Six trials (Hinoul 2011 SEC; Masata 2012 SEC; Mostafa 2012 AJS; Schweitzer 2012 AJS; Tommaselli 2010 SEC; Wang 2011 SEC) compared single‐incision slings versus inside‐out transobturator slings, and three trials (Enzelsberger 2010 ARC; Lee 2012 ARC; Yoon 2011 NDL) compared single‐incision slings versus outside‐in transobturator slings.
The overall duration of the operation was one minute less for single‐incision slings (MD ‐1.17 minutes, 95% CI ‐1.60 to ‐0.75) (Analysis 7.7), but the clinical and economic advantages of a one‐minute reduction in theatre time are likely to be negligible. Significant statistical heterogeneity may be explained by differences in the definition of what constitutes "duration of operation."
7.7. Analysis.
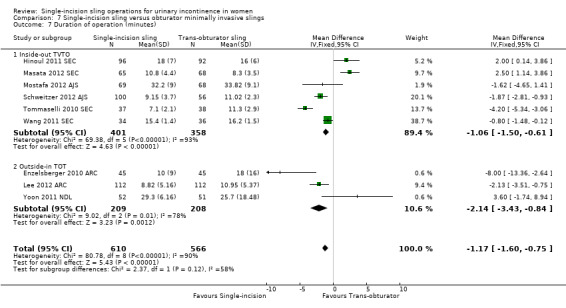
Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 7 Duration of operation (minutes).
Operative blood loss
Two trials (Hinoul 2011 SEC; Masata 2012 SEC) comparing TVT‐Secur against inside‐out TVT‐O showed that women lost 19 mL less blood with the TVT‐O; this is a statistically significant result favouring TVT‐O (MD 19, 95% CI 4 to 34 mL; Analysis 7.8.1).
7.8. Analysis.
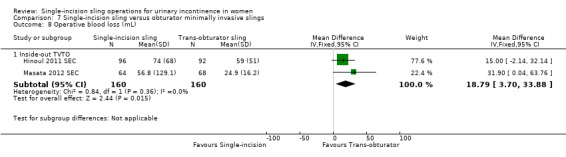
Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 8 Operative blood loss (mL).
Length of in‐patient stay
One study (Hinoul 2011 SEC) reported this outcome, but the result was not statistically significant.
Adverse events
Major vascular or visceral injury
This outcome was reported in three trials (Hinoul 2011 SEC; Masata 2012 SEC; Tommaselli 2010 SEC), all of which compared TVT‐Secur against inside‐out transobturator slings. Very few events were reported, and no evidence suggested superiority of either procedure (Analysis 7.10.1)
7.10. Analysis.
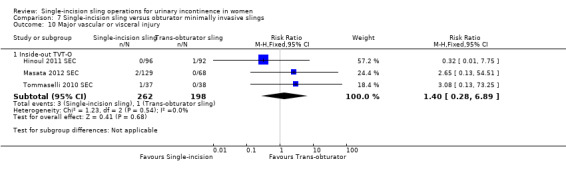
Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 10 Major vascular or visceral injury.
Bladder or urethral perforation
This rare outcome (four women in all) was reported in five trials (Amat 2011 NDL; Hinoul 2011 SEC; Masata 2012 SEC; Schweitzer 2012 AJS; Wang 2011 SEC) that compared single‐incision slings versus inside‐out transobturator slings, and in four versus outside‐in TOT (Djehdian 2010 OPH; Enzelsberger 2010 ARC; Lee 2010 CUR/SEC; Sivaslioglu 2012 TFS). The overall results were not statistically significant (Analysis 7.11), but the confidence intervals were wide.
7.11. Analysis.
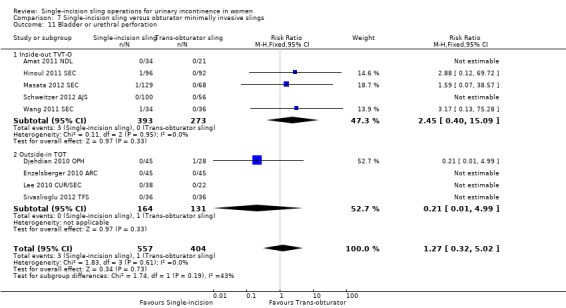
Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 11 Bladder or urethral perforation.
Vaginal wall perforation
Six women had vaginal wall perforation, as reported in five trials (Friedman 2009 SEC; Hinoul 2011 SEC; Masata 2012 SEC; Oliveira 2011 ARC SEC; Schweitzer 2012 AJS) that compared single‐incision slings against inside‐out transobturator slings, and in one trial versus an outside‐in transobturator sling (Djehdian 2010 OPH). The overall result was not statistically significant, and the confidence interval was wide (Analysis 7.12).
7.12. Analysis.
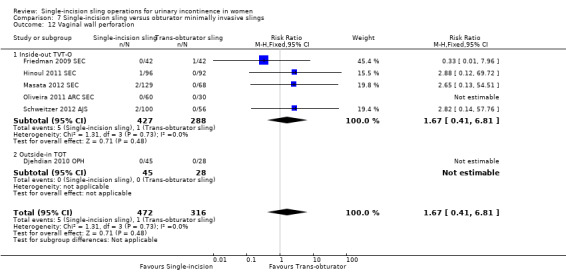
Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 12 Vaginal wall perforation.
Urinary retention and the need for catheterisation
Ten trials reported this outcome by comparing single‐incision slings against inside‐out transobturator slings (Amat 2011 NDL; Bianchi 2012 SEC; Friedman 2009 SEC; Hinoul 2011 SEC; Hota 2012 SEC; Mackintosh 2010 AJS; Masata 2012 SEC; Oliveira 2011 ARC SEC; Tommaselli 2010 SEC; Wang 2011 SEC). Few women had this complication (2% to 3%), and the overall result was not statistically significant, with a wide confidence interval (RR 0.72, 95% CI 0.34 to 1.52) (Analysis 7.13.1).
7.13. Analysis.
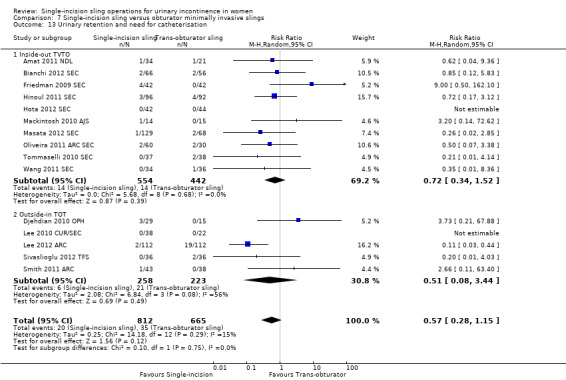
Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 13 Urinary retention and need for catheterisation.
Five trials compared single‐incision slings against outside‐in transobturator slings (Djehdian 2010 OPH; Lee 2010 CUR/SEC; Lee 2012 ARC; Sivaslioglu 2012 TFS; Smith 2011 ARC). Three times as many women required catheterisation after an outside‐in transobturator sling as after a single‐incision sling (2.5%) or an inside‐out transobturator sling (3.2%); this is difficult to explain. The overall result was statistically significant in favour of single‐incision slings, but the trials were not consistent in this respect. This result was driven mainly by the larger Lee 2012 ARC study, which was given the highest weight in the meta‐analysis. Statistical heterogeneity was apparent, and when a random‐effects model was used, the overall result was no longer statistically significant (Analysis 7.13.2).
The combined result was not statistically significant either and had a wide confidence interval, implying that evidence was insufficient to suggest any difference (RR 0.57, 95% CI 0.28 to 1.15) (Analysis 7.13).
Infection related to the use of synthetic mesh
One study reported this outcome in comparing single‐incision slings against inside‐out transobturator slings (Hinoul 2011 SEC), but the overall result was not statistically significant and the confidence interval was wide (Analysis 7.14.1).
7.14. Analysis.
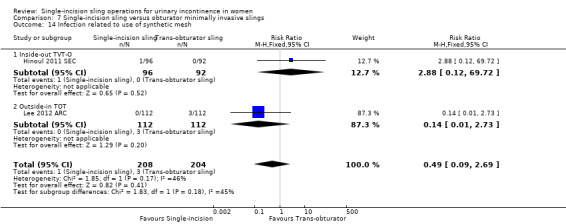
Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 14 Infection related to use of synthetic mesh.
Another study also reported this outcome in comparing single‐incision slings against outside‐in transobturator slings (Lee 2012 ARC), but again the overall result was not statistically significant and the confidence interval was wide (Analysis 7.14.2).
Vaginal exposure of mesh
Vaginal exposure (erosion) of mesh was reported in five trials (Bianchi 2012 SEC; Hinoul 2011 SEC; Hota 2012 SEC; Mostafa 2012 AJS; Tommaselli 2010 SEC) that compared single‐incision slings (all TVT‐Secur) against inside‐out transobturator slings. More women in the single‐incision groups had exposure (18/284, 6% vs 4/278, 1%), and the overall result was statistically significant, favouring inside‐out transobturator slings (RR 3.75, 95% CI 1.42 to 9.86) (Analysis 7.15.1). Four trials (Djehdian 2010 OPH; Lee 2010 CUR/SEC; Sivaslioglu 2012 TFS; Smith 2011 ARC) compared single‐incision slings against outside‐in transobturator slings. The number of cases was fewer, and the overall result was not statistically significant, with a wide confidence interval (Analysis 7.15.1).
7.15. Analysis.
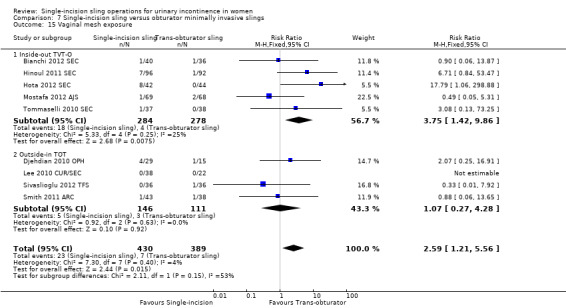
Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 15 Vaginal mesh exposure.
The combined overall result was still significant in favour of transobturator slings (RR 2.59, 95% CI 1.21 to 5.56) (Analysis 7.15).
Mesh extrusion into bladder or urethra
Only two small trials reported on this outcome (Hota 2012 SEC; Lee 2010 CUR/SEC). Only eight women were reported to have this complication, all in the single‐incision sling group in one of the trials: A statistically significant result favouring transobturator slings was of dubious reliability because of the small numbers (Analysis 7.16).
7.16. Analysis.
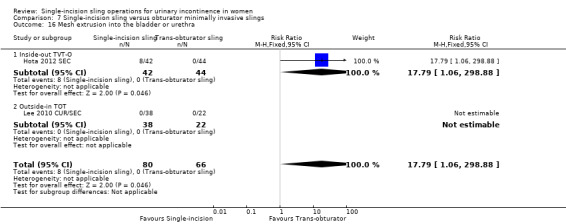
Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 16 Mesh extrusion into the bladder or urethra.
Post‐operative pain or discomfort
Pain was reported in eight trials (Amat 2011 NDL; Bianchi 2012 SEC; Friedman 2009 SEC; Lee 2012 ARC; Mackintosh 2010 AJS; Mostafa 2012 AJS; Seo 2011 SEC; Tommaselli 2010 SEC). The overall result was statistically significant favouring single‐incision slings: Fewer women (27/415, 7%) had pain versus 90/391 (23%) after an inside‐out transobturator sling (RR 0.29, 95% 0.20 to 0.43) (Analysis 7.17.1). Most of the trials used TVT‐Secur as the experimental intervention, apart from Amat 2011 NDL; Lee 2012 ARC; and Mackintosh 2010 AJS, but a sensitivity analysis excluding these trials made little difference in the results for individual single‐incision sling subtypes. Two trials (Lee 2012 ARC; Sivaslioglu 2012 TFS) compared single‐incision slings against outside‐in transobturator slings, and the result was similar, with statistical significance in favour of single‐incision slings (Analysis 7.17.2).
7.17. Analysis.
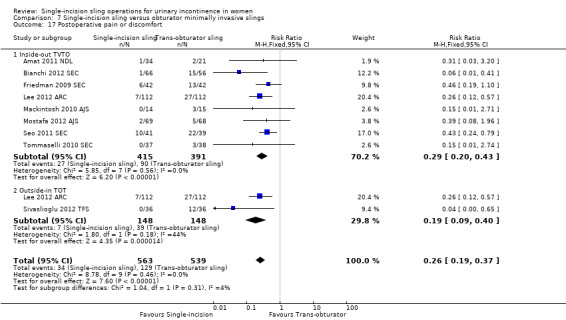
Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 17 Postoperative pain or discomfort.
The combined overall result showed that women had less short‐term pain or discomfort after a single‐incision sling (34/563, 6% vs 129/539, 23.9% after a TOT; RR 0.26, 95% CI 0.19 to 0.37) (Analysis 7.17), but the relevance of this difference may not be clinically important to women.
Long‐term pain or discomfort
This was rare and was reported in only three trials comparing TVT‐Secur against inside‐out transobturator slings (Oliveira 2011 ARC SEC; Tommaselli 2010 SEC; Wang 2011 SEC) and in two trials comparing single‐incision slings against outside‐in transobturator slings (Djehdian 2010 OPH; Sivaslioglu 2012 TFS). A statistically significant difference favoured single‐incision slings in the latter case only (RR 0.12, 95% CI 0.02 to 0.82) (Analysis 7.18.2).
7.18. Analysis.
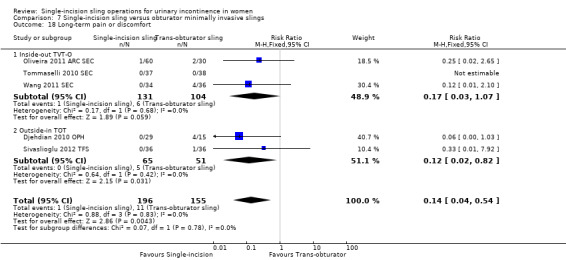
Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 18 Long‐term pain or discomfort.
Although uncommon, women were significantly less likely to have long‐term pain after a single‐incision sling than after a transobturator sling, and the overall result favoured single‐incision slings (1/196, 0.5% vs 11/155, 7.1%; RR 0.14, 95% CI 0.04 to 0.54) (Analysis 7.18).
De novo urgency
Eight trials were included in the meta‐analysis comparing TVT‐Secur versus inside‐out transobturator tapes (Abdelwahab 2010 SEC; Bianchi 2012 SEC; Friedman 2009 SEC; Masata 2012 SEC; Mostafa 2012 AJS; Oliveira 2011 ARC SEC; Tommaselli 2010 SEC; Wang 2011 SEC). Overall no statistically significant difference between the groups was observed (Analysis 7.19.1). Two trials compared single‐incision slings versus outside‐in transobturator tapes (Djehdian 2010 OPH; Smith 2011 ARC) and again found no statistically significant difference between the groups (Analysis 7.19.2).
7.19. Analysis.
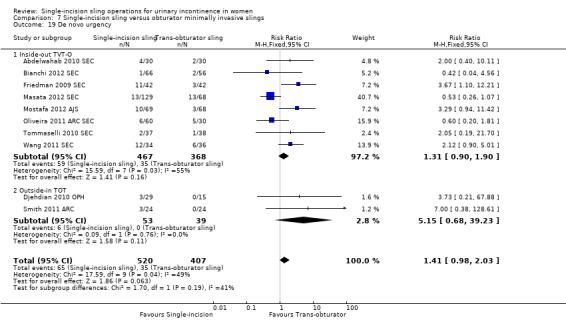
Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 19 De novo urgency.
Around 10% of women reported this symptom. The overall result was not quite statistically significant in favour of transobturator slings but the confidence intervals were wide (RR 1.41, 95% CI 0.98 to 2.03) (Analysis 7.19).
Repeat stress incontinence surgery
Three trials compared TVT‐Secur against inside‐out transobturator slings (Hota 2012 SEC; Masata 2012 SEC; Mostafa 2012 AJS); the pooled analysis showed that women were nearly six times more likely to need further stress incontinence surgery after a single‐incision sling—a significant difference in favour of transobturator slings (28/240, 12% vs 3/180, 2%; RR 5.86, 95% CI 2.0 to 17.21) (Analysis 7.20.1). Two trials compared MiniArc versus outside‐in transobturator tapes (Lee 2012 ARC; Smith 2011 ARC) but found no difference between the groups, as did one study (Sivaslioglu 2012 TFS) that compared the tissue fixation system single‐incision sling (TFS) versus outside‐in transobturator tapes (Analysis 7.20.2).
7.20. Analysis.
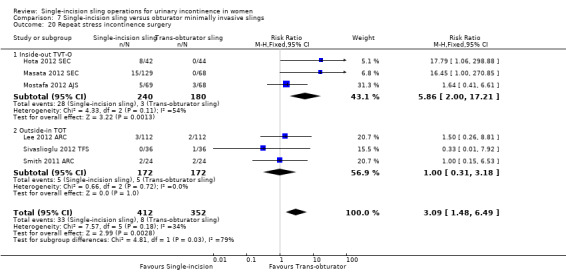
Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 20 Repeat stress incontinence surgery.
The overall result was still statistically significant in favour of transobturator slings: Women are three times more likely to need repeat incontinence surgery after a single‐incision sling (33/412, 8.0% vs 8/352, 2.3%; RR 3.09, 95% CI 1.48 to 6.49) (Analysis 7.20). However, this result was driven by the two trials that used TVT‐Secur (Hota 2012 SEC; Masata 2012 SEC). Without these two trials, no significant difference in repeat surgery rates would be reported.
Need for any other additional or new surgical procedure to treat complications
For this outcome, we assessed any subsequent procedures required to treat complications of the index surgery (e.g. cutting for voiding difficulty, removing tape for mesh exposure or extrusion).
Five trials were included in the meta‐analysis comparing TVT‐Secur against inside‐out transobturator slings (Friedman 2009 SEC; Hinoul 2011 SEC; Hota 2012 SEC; Masata 2012 SEC; Oliveira 2011 ARC SEC). The results were statistically significant in favour of transobturator slings (Analysis 7.21.1). Three trials compared single‐incision slings against outside‐in transobturator slings but found no difference between the groups (Analysis 7.21.2).
7.21. Analysis.
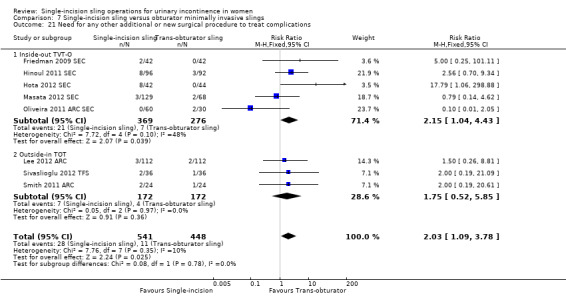
Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 21 Need for any other additional or new surgical procedure to treat complications.
The overall result was still statistically significant in favour of transobturator slings: Twice as many women required surgery for complications after a single‐incision sling (28/541, 5.2% vs 11/448, 2.5%; RR 2.03, 95% CI 1.09 to 3.78) (Analysis 7.21).
One single‐incision sling versus another
Comparisons were made on the basis of brand of sling because significant differences between various products were possible.
Nine trials met the inclusion criteria (Lee 2010 SEC; Lee 2010 CUR/SEC; Liapis 2010 SEC; Martan 2012 ARC AJS; Masata 2012 SEC; Oliveira 2011 ARC SEC; Palomba 2012 AJS ARC SEC; Pardo 2010 SEC ARC; Sottner 2012 ARC AJS). The only one of these trials that was methodologically robust on every dimension of risk of bias was Palomba 2012 AJS ARC SEC. Follow‐up varied among trials, ranging from 30 days (Palomba 2012 AJS ARC SEC) to two years (Martan 2012 ARC AJS; Masata 2012 SEC).
Because of the numerous types of slings compared, very few data could be combined in meta‐analysis and evidence was insufficient to allow the review authors to confidently identify any differences between any of the different types of single‐incision sling.
Number of women with urinary incontinence (primary outcome)
TVT‐Secur versus MiniArc
Two trials were included in this analysis (Oliveira 2011 ARC SEC; Pardo 2010 SEC ARC) and data were too few to allow inferences of any difference between the groups (Analysis 8.1.1).
8.1. Analysis.
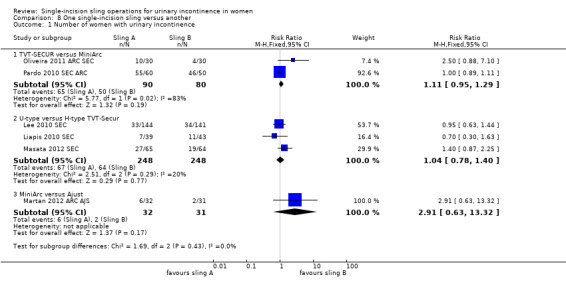
Comparison 8 One single‐incision sling versus another, Outcome 1 Number of women with urinary incontinence.
U‐type versus H‐type TVT‐Secur
Three trials were included in this analysis (Kim 2010 SEC; Liapis 2010 SEC; Masata 2012 SEC) and showed no significant differences between groups, but the confidence interval was wide (Analysis 8.1.2).
MiniArc versus Ajust
Only one study was included in this analysis (Martan 2012 ARC AJS); it showed no significant differences between groups and the confidence interval was wide (Analysis 8.1.3).
Number of women with no improvement
TVT‐Secur versus MiniArc
Two trials were included in this analysis (Oliveira 2011 ARC SEC; Pardo 2010 SEC ARC); although the trials seem to favour the MiniArc procedure, no statistically significant differences between groups were reported (Analysis 8.2.1).
8.2. Analysis.
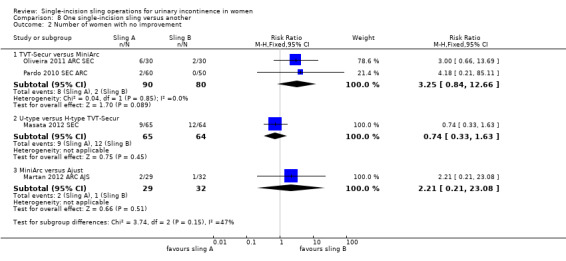
Comparison 8 One single‐incision sling versus another, Outcome 2 Number of women with no improvement.
U‐type versus H‐type TVT‐Secur
Only one study was included in this analysis (Masata 2012 SEC) and data were too few to allow inferences about any differences between groups (Analysis 8.2.2).
MiniArc versus Ajust
Only one study was included in this analysis (Martan 2012 ARC AJS) and the data were too few to allow inferences about any differences between groups (Analysis 8.2.3).
Objective measurement of incontinence
MiniArc versus Ajust
Only one study was included in this analysis (Martan 2012 ARC AJS) and data were too few to allow inferences about any differences between groups (Analysis 8.3.1).
8.3. Analysis.
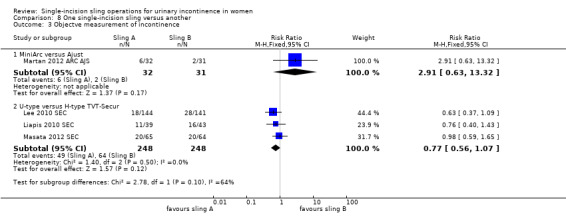
Comparison 8 One single‐incision sling versus another, Outcome 3 Objectve measurement of incontinence.
U‐type versus H‐type TVT‐Secur
Three trials were included in this analysis (Lee 2010 SEC; Liapis 2010 SEC; Masata 2012 SEC); although the results favoured the U‐type procedure, the result was not statistically significant. (Analysis 8.3.2).
Quality of life
MiniArc versus Ajust
Only one study was included in this analysis, which measured condition‐specific health (Martan 2012 ARC AJS). No significant differences between groups were reported and the confidence interval was wide (Analysis 8.4.1).
8.4. Analysis.
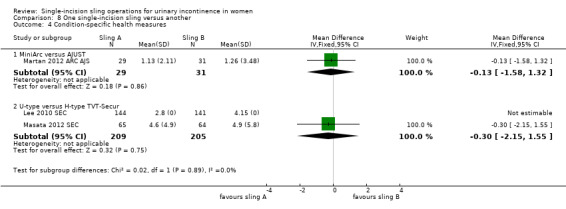
Comparison 8 One single‐incision sling versus another, Outcome 4 Condition‐specific health measures.
U‐type versus H‐type TVT‐Secur
Two trials were included in this analysis and measured condition‐specific health (Lee 2010 SEC; Masata 2012 SEC). No significant differences between groups were reported and the confidence interval was wide (Analysis 8.4.2).
Surgical outcome measures
Duration of operation
TVT‐Secur versus MiniArc
Two trials were included in this analysis (Palomba 2012 AJS ARC SEC; Pardo 2010 SEC ARC). No significant differences between groups were reported (Analysis 8.5.1).
8.5. Analysis.
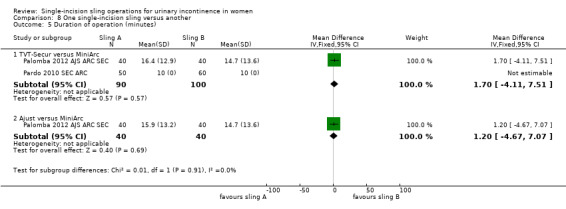
Comparison 8 One single‐incision sling versus another, Outcome 5 Duration of operation (minutes).
Ajust versus MiniArc
Only one study, which was methodologically robust, was included in this analysis (Palomba 2012 AJS ARC SEC); it showed no significant differences between groups (Analysis 8.5.2).
Operative blood loss
U‐type versus H‐type TVT‐Secur
Two trials (Lee 2010 SEC; Masata 2012 SEC) compared U‐ versus H‐type TVT‐Secur. The trialists did not provide standard deviations (SDs), so the data could not be analysed (Analysis 8.6.1).
8.6. Analysis.
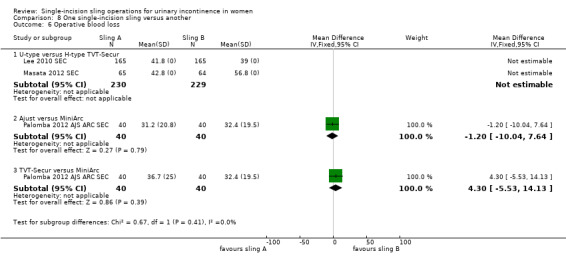
Comparison 8 One single‐incision sling versus another, Outcome 6 Operative blood loss.
Ajust versus MiniArc
One trial compared Ajust versus MiniArc (Palomba 2012 AJS ARC SEC); the data were too few to allow inferences of any differences between groups (Analysis 8.6.2).
TVT‐Secur versus MiniArc
One trial compared TVT‐Secur versus MiniArc (Palomba 2012 AJS ARC SEC); no significant differences between groups were noted in any of these comparisons (Analysis 8.6.3).
Adverse events
U‐type versus H‐type TVT‐Secur
Major vascular or visceral injury was reported in two trials (Lee 2010 SEC; Masata 2012 SEC), but no significant differences between groups were noted and the confidence interval was wide (Analysis 8.7.1).
8.7. Analysis.
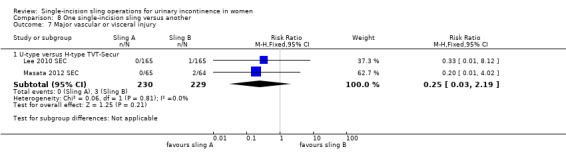
Comparison 8 One single‐incision sling versus another, Outcome 7 Major vascular or visceral injury.
Bladder or urethral perforation was reported in two trials (Lee 2010 SEC; Masata 2012 SEC); no differences between groups were noted and the confidence interval was very wide (Analysis 8.8.1).
8.8. Analysis.
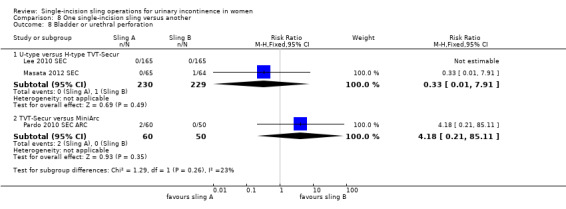
Comparison 8 One single‐incision sling versus another, Outcome 8 Bladder or urethral perforation.
Vaginal erosion was reported in two trials (Lee 2010 SEC; Masata 2012 SEC), which showed no significant differences between groups (Analysis 8.11.1).
8.11. Analysis.
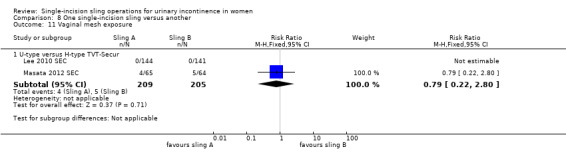
Comparison 8 One single‐incision sling versus another, Outcome 11 Vaginal mesh exposure.
Vaginal wall perforation was reported in one study that compared U‐ and H‐type TVT‐Secur (Lee 2010 SEC). No significant difference between either of the groups was noted, and the confidence interval was wide (Analysis 8.9.2).
8.9. Analysis.
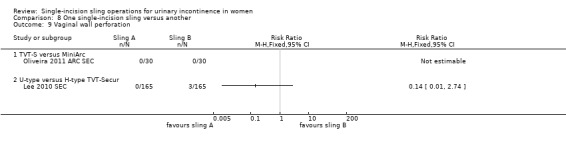
Comparison 8 One single‐incision sling versus another, Outcome 9 Vaginal wall perforation.
Urinary retention and need for catheterisation were reported in one trial comparing U‐ and H‐type TVT‐Secur (Lee 2010 SEC). No significant differences between groups were observed in any of these comparisons (Analysis 8.10.2).
8.10. Analysis.
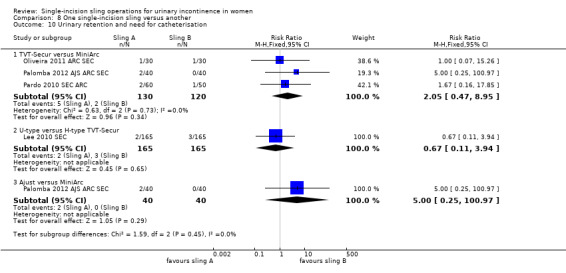
Comparison 8 One single‐incision sling versus another, Outcome 10 Urinary retention and need for catheterisation.
TVT‐Secur versus MiniArc
Bladder or urethral perforation was recorded in one study (Pardo 2010 SEC ARC). No significant differences were noted in either of the groups and the confidence interval was very wide (Analysis 8.8.2).
Vaginal wall perforation was reported in one study comparing TVT‐Secur and MiniArc (Oliveira 2011 ARC SEC). No significant differences were noted between either of the groups (Analysis 8.9.1).
Urinary retention and need for catheterisation were reported in three trials comparing TVT‐Secur versus MiniArc (Oliveira 2011 ARC SEC; Palomba 2012 AJS ARC SEC; Pardo 2010 SEC ARC), No significant differences between groups were reported in any of these comparisons (Analysis 8.10.1).
Postoperative pain or discomfort was reported in one three‐arm study that compared TVT‐Secur versus MiniArc (Palomba 2012 AJS ARC SEC). No significant differences between groups were reported (Analysis 8.12.2).
8.12. Analysis.
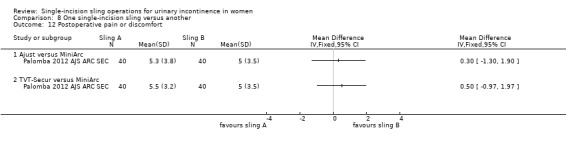
Comparison 8 One single‐incision sling versus another, Outcome 12 Postoperative pain or discomfort.
Ajust versus MiniArc
Urinary retention and need for catheterisation were reported in one study (Palomba 2012 AJS ARC SEC). No significant differences between groups were reported (Analysis 8.10.3).
Postoperative pain or discomfort was reported in one three‐arm study (Palomba 2012 AJS ARC SEC); no significant differences between groups were reported in either comparison (Analysis 8.12.1).
De novo urgency
TVT‐Secur versus MiniArc
Three trials were included in the comparison (Oliveira 2011 ARC SEC; Palomba 2012 AJS ARC SEC; Pardo 2010 SEC ARC) and showed no significant differences between groups (Analysis 8.13.1).
8.13. Analysis.
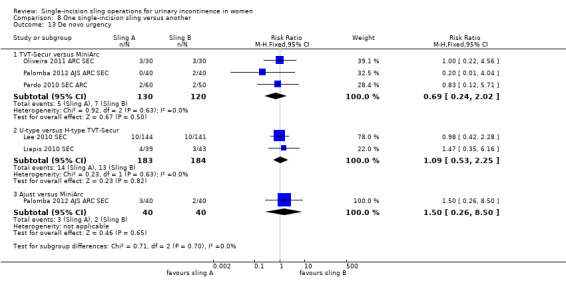
Comparison 8 One single‐incision sling versus another, Outcome 13 De novo urgency.
U‐type versus H‐type TVT‐Secur
Two trials were included in the comparison (Lee 2010 SEC; Liapis 2010 SEC) and showed no significant differences between groups (Analysis 8.13.2).
Ajust versus MiniArc
One study was included in this comparison (Palomba 2012 AJS ARC SEC) and showed no significant differences between groups (Analysis 8.13.3).
Repeat stress incontinence surgery
Two trials were included in this analysis, which compared U‐ and H‐type TVT‐Secur (Lee 2010 SEC; Masata 2012 SEC). About 5% of women required repeat incontinence surgery. The data were too few to allow inferences about any differences between groups (Analysis 8.14.1).
8.14. Analysis.
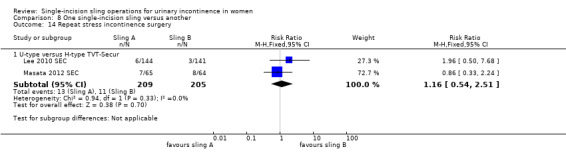
Comparison 8 One single‐incision sling versus another, Outcome 14 Repeat stress incontinence surgery.
Need for any other additional or new surgical procedure to treat complications
Two trials were included in the analysis, which compared U‐ and H‐type TVT‐Secur (Lee 2010 SEC; Masata 2012 SEC). No differences between groups were reported and confidence intervals were wide (Analysis 8.15.1). One study compared TVT‐Secur versus Mini‐Arc (Pardo 2010 SEC ARC) but again showed no differences between groups (Analysis 8.15.2).
8.15. Analysis.
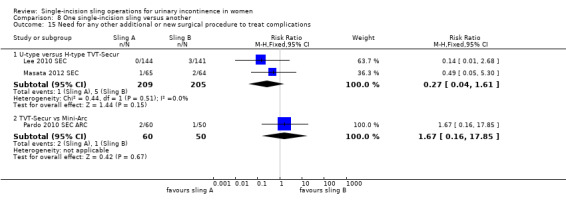
Comparison 8 One single‐incision sling versus another, Outcome 15 Need for any other additional or new surgical procedure to treat complications.
Subgroup analyses
No subgroup analyses were preplanned, but clinical factors such as symptoms of urinary stress incontinence, urodynamic stress incontinence, mixed urinary incontinence, diagnosis of intrinsic urethral sphincter deficiency or urethral hypermobility, obesity, previous incontinence surgery, presence or absence of prolapse, anaesthesia used or experience of the surgeon have been noted and might influence the outcome of surgery. This may be taken into account in future reviews.
Discussion
Summary of main results
We found no trials that compared single‐incision slings versus conservative treatment, colposuspension, laparoscopic surgery or traditional sub‐urethral slings. To supplement the main systematic review of effects, we sought economic evaluations which have compared single‐incision slings with any of the other main categories of surgical procedures listed under the 'Types of interventions' in the Methods section. A supplementary search in MEDLINE and Embase identified two economic evaluations which compared single‐incision slings with transobturator slings. We found no economic evaluation for the other types of interventions.The search strategies used are given in Appendix 2.
Single‐incision slings versus retropubic minimally invasive slings
Four of the five trials in this comparison compared TVT‐Secur against bottom‐up retropubic slings. The overall rate of cure of incontinence for single‐incision slings was worse (RR 2.08, 95% CI 1.04 to 4.14) (Analysis 6.1), as was the objective rate of cure of incontinence (RR 4.44, 95% CI 2.06 to 9.56). Women were more likely to have de novo urgency after single‐incision slings (RR 2.39, 95% CI 1.25 to 4.56) (Analysis 6.17) but evidence was insufficient to confirm a difference between the slings in terms of rates of other adverse events or need for repeat incontinence surgery. Single‐incision slings require less time to perform (mean difference ‐17.33 minutes, 95% CI ‐32.09 to ‐2.57) (Analysis 6.5), but the confidence interval for this comparison is quite wide and may not be clinically important.
No comparisons of singe‐incisions slings versus top‐down retropubic slings were performed, but the review authors believe this did not have an impact on the overall comparison.
A supplementary search carried out to identify economic evaluations for the brief economic commentary yielded no result.
Single‐incision slings versus obturator minimally invasive slings (subgrouped: medial‐to‐lateral 'inside out' approach and lateral‐to‐medial 'outside‐in' approach)
These results were subgrouped on the basis of whether the comparator was an inside‐out transobturator sling or an outside‐in transobturator sling.
Comparison with inside‐out transobturator slings
Generally TVT‐Secur was compared with inside‐out slings, and other types of mini‐slings were compared with outside‐in slings. Single‐incision slings resulted in higher incontinence rates compared with inside‐out transobturator slings (30% vs 11%, RR 2.55, 95% CI 1.93 to 3.36) (Analysis 7.1.1). Participants were also more likely to require repeat procedures to cure their persistent incontinence (RR 5.86, 95% CI 2.00 to 17.21) (Analysis 7.20.1). The adverse event profile was significantly worse, specifically, higher risk of vaginal mesh exposure, bladder/urethral erosion and operative blood loss. Participants were also more likely to require additional procedures to treat complications of the index surgery (RR 2.15, 95% CI 1.04 to 4.43) (Analysis 7.21.1). Postoperative pain was less common with single‐incision slings, and rates of long‐term pain or discomfort were marginally lower, but few trials reported these outcomes and the clinical significance of these differences is questionable. On the other hand, duration of the operation was marginally shorter for single‐incision slings.
However, most of these findings were due to the trials involving TVT‐Secur: Excluding the other trials showed that the high risk of incontinence was principally due to this device (RR 2.65, 95% CI 1.98 to 3.54). This sling has now been withdrawn from clinical use.
Overall these results show that TVT‐Secur is considerably inferior to inside‐out transobturator slings. Evidence of a difference in adverse event profiles for other single‐incision slings compared with inside‐out transobturator slings was insufficient to allow any further conclusions.
Economic evidence
The two cost‐effectiveness analyses compared single‐incision slings with inside‐out transobturator mid‐urethral slings.These adopted the perspective of the Spanish (Castañeda 2014) and UK (Boyers 2013) healthcare systems respectively. Boyers 2013 used clinical evidence from a prospective RCT (Mostafa 2012), while Castañeda 2014 used evidence from a retrospective observational study, to one‐year follow‐up in both cases. Both studies reported no statistically significant differences in the clinical outcomes: 6.7% difference, 95% Cl ‐6.6 to 20.0, P = 0.527 (Castañeda 2014); 5% difference, 95% Cl 0.38 to 2.26, P = 1.00 (Boyers 2013). Boyers 2013 reported no significant difference in peri‐operative complications (data and P value not reported). Castañeda 2014 also reported no statistically significant differences in intraoperative complication (P = 0.55). Boyers 2013 also reported the impact on health‐related quality of life, expressed as quality‐adjusted life years (QALYs). There was no significant difference in QALYs (mean difference ‐0.003, 95% Cl ‐0.008 to 0.002) (Boyers 2013). However, in the single‐incision sling arm, there were statistically significant improved postoperative pain scores up to four weeks with a pain score of zero compared with mid‐urethral slings with a total pain score of two (P < 0.001, 95% Cl 1.245 to 1.853). There was also a statistically significant one day earlier return to normal activities with single‐incision slings (P = 0.025, 95% Cl 6.1 to 9.4 days) (Boyers 2013), and fewer repeated urinary tract infections (Castañeda 2014). Single‐incision sling was less costly in both studies. The mean total direct cost of single‐incision sling in Boyers 2013 was GBP 1277 (2011 GBP), while that of transobturator slings was GBP 1462 (2011 GBP), with a 94% probability (95% Cl GBP ‐316.99 to GBP 32.17) of being cost‐saving compared to transobturator slings, irrespective of whether single‐incision sling was performed under local or general anaesthesia. In Castañeda 2014, the average cost of single‐incision sling (2013 euros) was EUR 2059 (95% Cl EUR 1914 to 2285) while transobturator slings were EUR 2821(95% Cl EUR 2661 to 2997), with a 100% probability of single‐incision sling being cost‐saving. Castañeda 2014 suggested that the mini‐sling might be more cost‐effective compared with transobturator slings, based on the relative effectiveness of both intervention and the lower cost associated with a single‐incision sling. Boyers 2013 also concluded that the single‐incision sling procedure, especially when performed under local anaesthesia, was likely to be more cost‐effective than transobturator slings over a one‐year follow‐up, but said that a longer follow‐up was required.
Comparison with outside‐in transobturator slings
Too little information was provided on other single‐incision slings for a reliable comparison of efficacy and adverse event profiles versus outside‐in transobturator slings. However, the duration of surgery and risks of postoperative and chronic pain were less with single‐incision slings. Comparisons between other single‐incision slings and inside‐out transobturator slings were too few to allow further conclusions.
Comparison with any transobturator sling
The combined results show that transobturator slings have lower incontinence rates than single‐incision slings overall but with significant heterogeneity in the comparisons due to differences in the trials. Women who have transobturator slings have a lower risk of vaginal erosion (RR 2.59, 95% CI 1.21 to 5.56) (Analysis 7.15) and a lesser chance of requiring repeat incontinence surgery (RR 3.09, 95% CI 1.48 to 6.49) (Analysis 7.20) or repeat surgery to treat complications (RR 2.03, 95% CI 1.09 to 3.78) (Analysis 7.21). Risks of postoperative pain and long‐term pain are slightly higher with transobturator slings. Evidence was insufficient to reveal any differences in the rates of other adverse events.
Sensitivity analysis excluding TVT‐Secur trials
Not enough evidence was obtained in a sensitivity analyses comparing all other single‐incision slings (excluding TVT‐Secur) versus transobturator slings to allow any conclusions regarding continence rates or most adverse events. Differences in the rates of postoperative pain (favouring single‐incisions slings; RR 0.23, 95% CI 0.14 to 0.38) (Analysis 7.17) and long‐term pain (favouring single incision slings; RR 0.15, 95% CI 0.03 to 0.67) (Analysis 7.18) were noted, but the magnitude of these differences was small. Single‐incision slings remained quicker to perform in this analysis (RR ‐1.98, 95% CI ‐2.68 to ‐1.2), but again the margin of difference (less than two minutes) is too small to be clinically important.
One single‐incision sling versus another
Seven trials compared one type of single‐incision sling versus another, but too few data were obtained for the review authors to infer any significant differences between the slings in any of the comparisons made. It is interesting that direct comparison of TVT‐Secur versus other single‐incision slings showed no significant difference, but it must be noted that very few trials made this comparison.
A supplementary search carried out to identify economic evaluations for the brief economic commentary yielded no result.
Overall completeness and applicability of evidence
We identified no studies that compared single‐incision slings versus conservative management, laparoscopic surgery or open colposuspension. For economic evidence, we did not subject the two economic evaluations to critical appraisal, and we do not attempt to draw any firm or general conclusions about the relative costs or efficiency of single‐incision slings in treatment of SUI. Taking into account the limitation of the need for a longer time horizon to explore the downstream costs associated with these interventions, the economic evidence from both studies were consistent, and suggested that single‐incision slings were likely to be cost‐effective up to one‐year follow‐up when compared with transobturator mid‐urethral slings.. Also,given that retropubic and transobturator mid‐urethral slings have become the gold standard treatment for stress urinary incontinence in women, it is reasonable for single‐incision slings to be routinely compared with these mid‐urethral slings in clinical trials.
Differences in fixation systems
The review authors believe it is important to note that although single‐incision slings have been clubbed together as a single group, a significant difference in the fixation systems between some of these slings has been noted. Whereas some simply rely on tissue in‐growth into the porous mesh to hold them in place, others use anchors or other fixation mechanisms to anchor them to tissue. These differences make comparisons difficult. TVT‐Secur is the single‐incision sling that has been studied most widely, and the evidence clearly shows it to be inferior to both retropubic slings and inside‐out transobturator slings in achieving cure of stress incontinence while leading to higher risk of adverse events. It does not have a fixation system, and this may have contributed to its poor performance. Undoubtedly the results of these trials have contributed to withdrawal of this particular sling from the market.
The data are less consistent for other single‐incision slings. Fewer trials of variable quality make interpretation difficult, and again, grouping these slings together is not always intuitive because of the different fixation mechanisms involved. At present evidence is insufficient to suggest that these slings are inferior to outside‐in transobturator slings, and comparisons versus inside‐out transobturator slings are too few to allow any meaningful conclusions. However in the current clinical climate, where implantable meshes and tapes are under intense scrutiny, evidence suggests that these slings must be used with caution.
Trials including TVT‐Secur
The inclusion of such a large number of trials including TVT‐Secur as a comparator inevitably has had a major influence on the overall results. Given that this sling has subsequently been removed from the market, it could be questioned why it was included in this review at all. The review authors came to the unanimous conclusion that it should be included in the first iteration of this review, so that level 1 evidence is available to demonstrate its lack of efficacy. Currently lack of available evidence on other single‐incision slings prevents any meaningful conclusions. However, we are aware of a number of ongoing trials and therefore plan to update the review towards the end of 2014, at which stage all TVT‐Secur data will be excluded.
Choice of outcomes
Objective cure is relatively easily assessed, and various methods, such as cough stress tests, pad tests and urodynamic assessment, are used to measure it. But subjective cure can be more difficult to assess and is greatly dependant on the patient's perceptions of success. We have defined subjective cure or patient‐reported success as the most important outcome for this type of surgery, and indeed many trials use subjective success or cure rate as the primary outcome measure. It is therefore critical to establish before surgery what a patient's expectations of success are, so that postoperative evaluations can be based on these definitions. Without this, there is a real danger of introducing significant clinical heterogeneity into a meta‐analysis of these outcomes. However, the included trials differed markedly in their definitions of incontinence and cure, and we have used an inclusive approach to interpretation to maximise the available data.
Quality of the evidence
As stated in the Risk of bias in included studies section, the quality of included trials varied widely. Thirty‐two trials (19 fully published papers, one thesis and 12 abstracts) were included in this review, including overall 3427 women.
The trials included in the comparison of single‐incision slings versus retropubic mid‐urethral slings were of moderate and consistent quality, with no major differences apart from inclusion of some women with concomitant prolapse in up to three of the trials. Results are also consistent across the trials, and hence the results of the meta‐analysis can be considered robust.
Trials comparing single‐incision slings versus inside‐out transobturator slings were more heterogenous in terms of methodology and consistency of results. Fourteen trials (eight fully published papers, five abstracts and one thesis) comprising a total of 1542 women were included. Despite these general inconsistencies, efficacy outcomes were consistently better for inside‐out transobturator slings across the trials, and results of the pooled meta‐analysis give a statistically significant result, even though results in some individual trials may not have reached significance.
Seven trials comprising a total of 658 women compared single‐incision slings versus outside‐in transobturator slings; only one was a fully published paper, and the rest were abstracts. This made evaluation of methodology difficult because of the limited information provided in some of the abstracts. Efficacy outcomes were not statistically significant, but it must be noted that this comparison is a composite of different types of single‐incision slings (MiniArc, CureMesh, Ajust, TFS and Contasure Needleless). The difference in fixation systems between these slings makes the value of a pooled analysis debatable. However none of the individual trials reported a statistically significant difference in efficacy. Duration of the operation was found to be significantly shorter for single‐incision slings, but for the same reasons as were stated for the previous comparison, a high degree of statistical and clinical heterogeneity is present here.
Nine trials comprising a total of 1007 women (five fully published papers and four abstracts) compared one type of single‐incision sling versus another. Methdological quality was variable, and comparisons were made mainly between three different types of single‐incision slings (MiniArc vs TVT‐Secur, U‐ vs H‐type TVT‐Secur and MiniArc vs Ajust). None of the overall comparisons reached statistical significance; neither did any of the individual comparisons in individual trials. Therefore the only possible conclusion is that currently not enough evidence is available to suggest whether any differences between single‐incision slings can be found based on direct comparisons.
Potential biases in the review process
Data were independently checked by three review authors. No restrictions were placed on language of included papers, and two full papers are included that were written in languages other than English (one German, one Czech). These papers included English abstracts in the text and data were extracted from these as far as possible. However, translations could not be obtained; therefore some data may not have been identified.
Ranges of follow‐up varied considerably between trials, and sometimes trials with significantly different mean durations of follow‐up were included in the same comparison. However, when this was the case, sensitivity analyses could be performed to assess whether this could represent a source of bias.
The review authors decided not to include selective outcome reporting for assessment of risk of bias, as considerable variation was found in the availability of this information. This might introduce a potential source of bias.
Agreements and disagreements with other studies or reviews
Other relevant systematic reviews include Abdel‐Fattah 2011; Jeffery 2010; Tommaselli 2011; and Walsh 2011.
Abdel‐Fattah 2011 (literature search up to January 2011) included nine studies of 758 women (six studies of TVT‐Secur) and concluded that single‐incision slings were associated with inferior patient‐reported and objective cure rates on short‐term follow‐up, as well as higher reoperation rates for SUI, while having a significantly shorter operative time, lower day one pain scores and less postoperative groin pain.
Jeffery 2010 included 57 studies, of which only 32 provided information about the type of study conducted (three RCTs, nine retrospective studies and 20 prospective studies). Overall cure rates were reported to range between 70% and 81%, with less than 1% risk of bladder injury and groin or hip pain.
Tommaselli 2011 was a systematic review similar in design to Jeffery 2010 but limited to studies involving TVT‐Secur. It included 54 studies (35 prospective studies, seven RCTs and 12 retrospective studies) and concluded that the objective cure rate for TVT‐Secur did not reach 80% (significantly lower than that of standard mid‐urethral slings), while subjective cure rates were somewhat higher. Complication rates were lower than 10%, and complications were limited to vaginal erosion, bladder injury, de novo urgency and reoperation for SUI.
Walsh 2011 reported 12‐month outcomes after TVT‐Secur in 10 studies including 1178 women and reported objective and subjective cure rates of 76%, a 10% incidence of de novo urgency and 2.4% of mesh exposure. Rates of other complications were low.
Overall the results of these reviews are in keeping with ours, bearing in mind the lower number of randomised studies included in the above reviews. The conclusion of poor performance of TVT‐Secur has been reiterated in this review, which only strengthens this conclusion.
It is generally thought that there is no difference in efficacy between retropubic and transobturator slings for cure of stress incontinence (Nambiar 2012; Ogah 2009), but a difference in the adverse event profile has been reported (Nambiar 2012). It is therefore still relevant to compare single‐incision slings versus both types of synthetic mid‐urethral slings. However descriptions of the types of slings being studied, along with descriptions of the fixation systems and clear documentation of the common adverse events, are important.
An adverse event that is commonly used to define differences between all types of slings is the occurrence of groin/thigh pain. It should be clearly documented in trial reports whether this is postoperative pain (short‐term) or long‐term chronic pain. By convention, short‐term pain is generally taken to be any pain lasting up to six to eight weeks postoperatively, and long‐term or chronic pain lasts beyond six months. Some effort should also be made to document the nature of the pain to try to identify those patients whose pain could reasonably have been caused by sling insertion.
Authors' conclusions
Implications for practice.
TVT‐Secur is inferior to TVT and has already been withdrawn from clinical use.
Women were more likely to remain incontinent after surgery with single‐incision slings than after use of inside‐out transobturator tapes, although operating times were shorter and less short‐term postoperative pain was reported. They were more likely to need further continence surgery and had mesh exposure more often.
Not enough evidence was found for the review authors to conclude whether single‐incision slings were different from outside‐in transobturator tapes in terms of efficacy, but some evidence suggests that they required a shorter operating time and had a slightly lower risk of postoperative pain.
Evidence was insufficient to suggest that one type of single‐incision sling is superior to another in direct comparisons, in terms of efficacy or a more favourable adverse event profile.
Implications for research.
Additional high‐quality trials are required to definitively answer the question whether single‐incision slings are equivalent to standard mid‐urethral slings for the treatment of stress urinary incontinence in women. Specifically these trials need to be adequately powered with appropriate outcome measures, so that conclusions may be drawn regarding individual single‐incision slings as a meta‐analysis of a combination of these slings introduces significant heterogeneity. Future trials of single‐incision slings should compare them against standard retropubic and transobturator slings with meticulous descriptions of the fixation system and defined primary and secondary outcomes. Long‐term follow‐up of at least five years is required for assessment of long‐term benefits and, particularly, risks.
Participant‐reported outcomes are becoming increasingly important and relevant in clinical trials. The woman's report of cure of stress incontinence is generally the desired outcome of sling surgery and should be the primary outcome of any efficacy trial. The method of assessing cure should therefore be clearly documented by trialists.
Another consideration is to identify whether niche group of patients may benefit from this particular type of sling surgery, who may not be suitable for other forms of open or minimally invasive surgery.
What's new
| Date | Event | Description |
|---|---|---|
| 11 July 2017 | New citation required but conclusions have not changed | Brief economic commentary (BEC) added. Economics‐related sections revised. |
| 11 July 2017 | Amended | Brief economic commentary (BEC) added. Economics related sections revised: the Abstract, Plain language summary, Background, Methods (outcomes, search methods), and Discussion were amended. Appendix added with details of search strategies for BEC. |
Acknowledgements
We thank Sheila Wallace for her efficiency and professionalism in conducting the literature search.
We thank Cathryn Glazener for her input and help with arbitration of disagreements.
We would like to acknowledge Peter de Jong, Zeelha Abdool, Frans van Wijk, Vincent Lucente and Miles Murphy for their contributions to the original protocol.
Appendices
Appendix 1. Searches of trials registers and portals
Both of the searches described below were last run on 20 September 2012.
ClinicalTrials.gov Used Advanced search with Search terms = tvt‐s OR tvt‐secur OR mini‐arc OR ajust OR needleless OR solyx OR single‐incision sling OR single incision slings OR altis OR miniarc OR TFS OR minisling OR mini‐sling OR minitape OR mini‐tape OR Ophira OR Zippere OR EPILOG OR arc‐to‐arc.
WHO ICTRP the same terms were used as were used in ClinicalTrials.gov (listed above). The search string was copied and pasted straight into the search line.
Appendix 2. Search strategies for economic evaluations for the brief economic commentary
We performed additional searches for the Brief Economic Commentary (BECs). These were conducted in MEDLINE(1 January 1946 to March 2017), Embase (1 January 1980 to 2017 Week 12) and NHS EED (1st Quarter 2016). All searches were conducted on 6 April 2017. We used two different search strategies on MEDLINE and EMBASE (OvidSP) and one on NHS EED (OVID). Details of the searches run and the search terms used can be found below. There were no year, publication type or language restrictions applied to the searches.
NHS EED (Ovid) (1st Quarter 2016)
NHS EED was searched using the following search strategy:
1. Urinary incontinence/
2. Urinary incontinence, stress/
3. ((stress$ or mix$ or urg$ or urin$) adj3 incontinen$).tw.
4. Colporrhaphy.tw.
5. Colpoperineoplast$.tw.
6. Sling procedure$.tw.
7. Sling$ procedure$.tw.
8. Bladder neck needle suspension$.tw.
9. Anterior vaginal repair$ .tw.
10. Or/1‐9
MEDLINE (1 January 1946 to March 2017) and Embase (1 January 1980 to 2017 Week 12)
We used two different search strategies on MEDLINE and EMBASE (OvidSP) ‐ these are given below.
Search strategy 1:
1. Economics, Pharmaceutical/ or Economics, Medical/ or Economics/ or Economics, Hospital/ or economics.mp. or Economics, Nursing/
2. exp "costs and cost analysis"/
3. "Value of Life"/
4. exp "fees and charges"/
5. exp budgets/
6. budget*.ti,ab.
7. cost*.ti.
8. (economic* or pharmaco?economic*).ti.
9. (price* or pricing*).ti,ab.
10. (cost* adj2 (effective* or utilit* or benefit* or minimi* or unit* or estimat* or variable*)).ab.
11. (financ* or fee or fees).ti,ab.
12. (value adj2 (money or monetary)).ti,ab.
13. ((energy or oxygen) adj cost).ti,ab.
14. (metabolic adj cost).ti,ab.
15. ((energy or oxygen) adj expenditure).ti,ab.
16. 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15
17. exp Urinary Incontinence/
18. ((stress* or mix* or urg* or urin*) adj3 incontinen*).tw.
19. Urodynamics/ or Urinary Incontinence, Stress/ or Urinary Incontinence/ or Suburethral Slings/ or mixed incontinence.mp. or Urinary Bladder/ or Urinary Incontinence, Urge/
20. 17 or 18 or 19
21. anterior vaginal repair*.tw.
22. 16 and 20 and 21
23. anterior colporrhaphy*.tw.
24. 21 or 23
25. 16 and 20 and 23
26. bladder neck needle suspension$.tw.
27. 16 and 20
28. 26 and 27
29. open abdominal retropubic colposuspension*.tw.
30. retropubic colposuspension*.tw.
31. burch colposuspension*.tw.
32. 29 or 30 or 31
33. 27 and 32
34. laparoscopic retropubic colposuspension*.tw.
35. laparoscopic colposuspension*.tw.
36. 34 or 35
37. 27 and 36
38. traditional suburethral retropubic sling procedure$*.tw.
39. traditional sling procedure$*.tw.
40. suburethral retropubic sling procedure$*.tw.
41. retropubic sling procedure$*.tw.
42. traditional suburethral sling*.tw.
43. Suburethral Slings/ or Urinary Incontinence, Stress/ or Urologic Surgical Procedures/
44. 27 and 43
45. remove duplicates from 44
Search strategy 2:
1. economics.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, fs]
2. value of life.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, fs]
3. exp "costs and cost analysis"/
4. exp economics, hospital/
5. exp economics, medical/
6. economics, nursing.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, fs]
7. economics, pharmaceutical.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, fs]
8. exp "fees and charges"/
9. exp budgets/
10. budget*.ti,ab.
11. cost*.ti.
12. (economic* or pharmaco?economic*).ti.
13. (price* or pricing*).ti,ab.
14. (cost* adj2 (effective* or utilit* or benefit* or minimi* or unit* or estimat* or variable*)).ab.
15. (financ* or fee or fees).ti,ab.
16. (value adj2 (money or monetary)).ti,ab.
17. or/1‐16
18. economics.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, fs]
19. value of life.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, fs]
20. exp "costs and cost analysis"/
21. exp economics, hospital/
22. exp economics, medical/
23. economics, nursing.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, fs]
24. economics, pharmaceutical.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, fs
25. exp "fees and charges"/
26. exp budgets/
27. budget*.ti,ab.
28. cost*.ti.
29. (economic* or pharmaco?economic*).ti.
30. (price* or pricing*).ti,ab.
31. (cost* adj2 (effective* or utilit* or benefit* or minimi* or unit* or estimat* or variable*)).ab.
32. (financ* or fee or fees).ti,ab.
33. (value adj2 (money or monetary)).ti,ab.
34. 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31 or 32 or 33
35. ((energy or oxygen) adj cost).ti,ab.
36. (metabolic adj cost).ti,ab.
37. ((energy or oxygen) adj expenditure).ti,ab.
38. 34 or 35 or 36 or 37
39. urinary incontinence.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
40. ((stress$ or mix$ or urg$ or urin$) adj3 incontinen$).tw.
41. URINARY INCONTINENCE, STRESS.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
42. stress urinary incontinence*.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
43. 39 or 40 or 41 or 42
44. intervention surgery*.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
45. colporrhaphy.tw.
46. Bologna procedure*.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
47. Kelly‐Kennedy.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
48. Marion Kelly.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
49. Diaphragmplasty.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
50. Vaginal urethrocystopexy.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
51. Cystocele repair.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
52. Kelly plication.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
53. anterior vaginal repair$.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
54. anterior colporrhaphy.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
55. 44 or 45 or 46 or 47 or 48 or 49 or 50 or 51 or 52 or 53 or 54
56. 38 and 43 and 55
57. remove duplicates from 56
58. Bladder neck needle suspension$.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
59. 38 and 43 and 58
60. burch colposuspension.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
61. open abdominal retropubic colposuspension.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
62. Paravaginal defect repair.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
63. Marshall‐Marchetti‐Krantz.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
64. abdominal burch.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
65. abdominal colposuspension.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
66. endopelvic Fascia Plication.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
67. 60 or 61 or 62 or 63 or 64 or 65 or 66
68. 38 and 43
69. 67 and 68
70. laparoscopic retropubic colposuspension.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
71. laparoscopic colposuspension.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
72. retropubic colposuspension.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
73. 70 or 71 or 72
74. 68 and 73
75. remove duplicates from 74
76. suburethral sling.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
77. abdominal sling.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
78. traditional sling procedure$*.tw.
79. suburethral sling procedure.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
80. 76 or 77 or 78 or 79
81. 68 and 80
82. remove duplicates from 81
83. mid$urethral sling.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
84. retropubic sling procedure$*.tw.
85. transobturator sling procedure$.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
86. 83 or 84 or 85
87. remove duplicates from 86
88. 68 and 87
89. TVT‐Secur.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
90. mini‐arc.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
91. ajust.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
92. needleless.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
93. solyx.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
94. single$incision sling$.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
95. miniarc.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
96. mini$sling.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
97. Ophira.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
98. Tissue Fixation System.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
99. 89 or 90 or 91 or 92 or 93 or 94 or 95 or 96 or 97 or 98
100. 68 and 99
101. remove duplicates from 100
102. ((urethra$ or periurethra$ or transurethra$) adj3 (agent$ or bulk$ or injection$ or injectable$)).tw.
103. injection therapy.tw.
104. injectable$.tw.
105. (injectable$ adj2 agent$).tw.
106. (bulk$ adj3 agent$).tw.
107. Peri$urethral injection$.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
108. Autologous fat.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
109. Macroplastique.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
110. Calcium hydroxylapatite.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
111. Hyaluronic acid with dextranomer.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
112. Porcine dermal implant.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
113. Ethylene vinyl alcohol copolymer.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
114. Silicon particles.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
115. 102 or 103 or 104 or 105 or 106 or 107 or 108 or 109 or 110 or 111 or 112 or 113 or 114
116. 68 and 115
117. remove duplicates from 116
Data and analyses
Comparison 6. Single‐incision sling versus retropubic minimally invasive slings.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Number of women with urinary incontinence | 5 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.1 Bottom‐up approach | 5 | 573 | Risk Ratio (M‐H, Random, 95% CI) | 2.08 [1.04, 4.14] |
| 2 Number of women with no improvement | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 Bottom‐up approach | 3 | 246 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.38 [0.55, 3.46] |
| 3 Objectve measurement of incontinence | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.1 Bottom‐up approach | 2 | 188 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.44 [2.06, 9.56] |
| 4 Condition‐specific health measures | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4.1 Bottom‐up approach | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Duration of operation (in minutes) | 3 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 5.1 Bottom‐up approach | 3 | 386 | Mean Difference (IV, Random, 95% CI) | ‐17.33 [‐32.09, ‐2.57] |
| 6 Operative blood loss | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 6.1 Bottom‐up approach | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Length of in‐patient stay | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 7.1 Bottom‐up approach | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8 Major vascular or visceral injury | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 8.1 Bottom‐up approach | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 9 Vaginal wall perforation | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 9.1 Bottom‐up approach | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 10 Bladder or urethral perforation | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 10.1 Bottom‐up approach | 4 | 532 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.45 [0.15, 1.38] |
| 11 Urinary retention and need for catheterisation | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 11.1 Bottom‐up approach | 5 | 578 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.87 [0.38, 1.99] |
| 12 Infection related to use of synthetic mesh | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 12.1 Bottom‐up approach | 1 | 50 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.0 [0.22, 17.89] |
| 13 Vaginal mesh exposure | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 13.1 Bottom‐up approach | 2 | 333 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.37 [0.23, 8.16] |
| 14 Mesh extrusion into the bladder or urethra | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 14.1 Bottom‐up approach | 3 | 445 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.76 [0.19, 3.01] |
| 15 Long‐term pain or discomfort | 2 | 329 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 15.1 Bottom‐up approach | 2 | 329 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 16 Dyspareunia | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 16.1 Bottom‐up approach | 1 | 59 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.9 [0.32, 26.30] |
| 17 De novo urgency | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 17.1 Bottom‐up approach | 3 | 248 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.39 [1.25, 4.56] |
| 18 New‐onset detrusor overactivity | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 18.1 Bottom‐up approach | 1 | 70 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.13, 5.98] |
| 19 Repeat stress incontinence surgery | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 19.1 Bottom‐up approach | 2 | 333 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.34 [0.79, 6.92] |
| 20 Need for any other additional or new surgical procedure to treat complications | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 20.1 Bottom‐up approach | 2 | 333 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.18 [0.29, 4.74] |
6.15. Analysis.
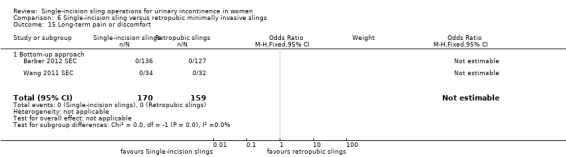
Comparison 6 Single‐incision sling versus retropubic minimally invasive slings, Outcome 15 Long‐term pain or discomfort.
Comparison 7. Single‐incision sling versus obturator minimally invasive slings.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Number of women with urinary incontinence | 17 | 1655 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.91 [1.53, 2.39] |
| 1.1 Inside‐out TVTO | 10 | 1053 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.55 [1.94, 3.36] |
| 1.2 Outside‐in TOT | 7 | 602 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.60, 1.39] |
| 2 Number of women with no improvement | 5 | 642 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.29 [1.29, 4.06] |
| 2.1 Inside‐out TVT‐O | 4 | 437 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.80 [2.00, 11.55] |
| 2.2 Outside‐in TOT | 1 | 205 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.76 [0.32, 1.82] |
| 3 Objective measurement of incontinence | 12 | 1198 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.88 [1.49, 2.36] |
| 3.1 Inside‐out TVT‐O | 7 | 804 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.91 [2.00, 4.25] |
| 3.2 Outside‐in TOT | 5 | 394 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.18 [0.90, 1.55] |
| 4 Incontinence episodes | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4.1 Outside‐in TOT | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Pad test (weights) | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 5.1 Outside‐in TOT | 2 | 268 | Mean Difference (IV, Fixed, 95% CI) | ‐1.64 [‐6.24, 2.96] |
| 6 Condition‐specific health measures | 3 | 334 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.16 [‐0.06, 0.38] |
| 6.1 Inside‐out TVTO | 2 | 290 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.07 [‐0.17, 0.30] |
| 6.2 Outside‐in TOT (UDI 6) | 1 | 44 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.91 [0.25, 1.56] |
| 7 Duration of operation (minutes) | 9 | 1176 | Mean Difference (IV, Fixed, 95% CI) | ‐1.17 [‐1.60, ‐0.75] |
| 7.1 Inside‐out TVTO | 6 | 759 | Mean Difference (IV, Fixed, 95% CI) | ‐1.06 [‐1.50, ‐0.61] |
| 7.2 Outside‐in TOT | 3 | 417 | Mean Difference (IV, Fixed, 95% CI) | ‐2.14 [‐3.43, ‐0.84] |
| 8 Operative blood loss (mL) | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 8.1 Inside‐out TVTO | 2 | 320 | Mean Difference (IV, Fixed, 95% CI) | 18.79 [3.70, 33.88] |
| 9 Length of in‐patient stay | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 9.1 Inside‐out TVTO | 1 | 188 | Mean Difference (IV, Fixed, 95% CI) | ‐0.08 [‐0.33, 0.17] |
| 10 Major vascular or visceral injury | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 10.1 Inside‐out TVT‐O | 3 | 460 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.40 [0.28, 6.89] |
| 11 Bladder or urethral perforation | 9 | 961 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.27 [0.32, 5.02] |
| 11.1 Inside‐out TVT‐O | 5 | 666 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.45 [0.40, 15.09] |
| 11.2 Outside‐in TOT | 4 | 295 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.21 [0.01, 4.99] |
| 12 Vaginal wall perforation | 6 | 788 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.67 [0.41, 6.81] |
| 12.1 Inside‐out TVT‐O | 5 | 715 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.67 [0.41, 6.81] |
| 12.2 Outside‐in TOT | 1 | 73 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 13 Urinary retention and need for catheterisation | 15 | 1477 | Risk Ratio (M‐H, Random, 95% CI) | 0.57 [0.28, 1.15] |
| 13.1 Inside‐out TVTO | 10 | 996 | Risk Ratio (M‐H, Random, 95% CI) | 0.72 [0.34, 1.52] |
| 13.2 Outside‐in TOT | 5 | 481 | Risk Ratio (M‐H, Random, 95% CI) | 0.51 [0.08, 3.44] |
| 14 Infection related to use of synthetic mesh | 2 | 412 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.49 [0.09, 2.69] |
| 14.1 Inside‐out TVT‐O | 1 | 188 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.88 [0.12, 69.72] |
| 14.2 Outside‐in TOT | 1 | 224 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.14 [0.01, 2.73] |
| 15 Vaginal mesh exposure | 9 | 819 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.59 [1.21, 5.56] |
| 15.1 Inside‐out TVT‐O | 5 | 562 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.75 [1.42, 9.86] |
| 15.2 Outside‐in TOT | 4 | 257 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.07 [0.27, 4.28] |
| 16 Mesh extrusion into the bladder or urethra | 2 | 146 | Risk Ratio (M‐H, Fixed, 95% CI) | 17.79 [1.06, 298.88] |
| 16.1 Inside‐out TVT‐O | 1 | 86 | Risk Ratio (M‐H, Fixed, 95% CI) | 17.79 [1.06, 298.88] |
| 16.2 Outside‐in TOT | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 17 Postoperative pain or discomfort | 9 | 1102 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.26 [0.19, 0.37] |
| 17.1 Inside‐out TVTO | 8 | 806 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.29 [0.20, 0.43] |
| 17.2 Outside‐in TOT | 2 | 296 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.19 [0.09, 0.40] |
| 18 Long‐term pain or discomfort | 5 | 351 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.14 [0.04, 0.54] |
| 18.1 Inside‐out TVT‐O | 3 | 235 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.17 [0.03, 1.07] |
| 18.2 Outside‐in TOT | 2 | 116 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.12 [0.02, 0.82] |
| 19 De novo urgency | 10 | 927 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.41 [0.98, 2.03] |
| 19.1 Inside‐out TVT‐O | 8 | 835 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.31 [0.90, 1.90] |
| 19.2 Outside‐in TOT | 2 | 92 | Risk Ratio (M‐H, Fixed, 95% CI) | 5.15 [0.68, 39.23] |
| 20 Repeat stress incontinence surgery | 6 | 764 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.09 [1.48, 6.49] |
| 20.1 Inside‐out TVT‐O | 3 | 420 | Risk Ratio (M‐H, Fixed, 95% CI) | 5.86 [2.00, 17.21] |
| 20.2 Outside‐in TOT | 3 | 344 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.31, 3.18] |
| 21 Need for any other additional or new surgical procedure to treat complications | 8 | 989 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.03 [1.09, 3.78] |
| 21.1 Inside‐out TVT‐O | 5 | 645 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.15 [1.04, 4.43] |
| 21.2 Outside‐in TOT | 3 | 344 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.75 [0.52, 5.85] |
7.9. Analysis.
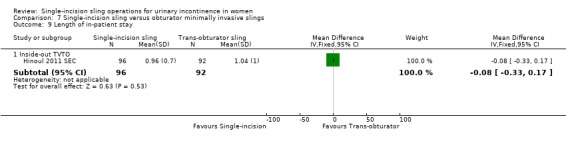
Comparison 7 Single‐incision sling versus obturator minimally invasive slings, Outcome 9 Length of in‐patient stay.
Comparison 8. One single‐incision sling versus another.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Number of women with urinary incontinence | 6 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 TVT‐SECUR versus MiniArc | 2 | 170 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.11 [0.95, 1.29] |
| 1.2 U‐type versus H‐type TVT‐Secur | 3 | 496 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.04 [0.78, 1.40] |
| 1.3 MiniArc versus Ajust | 1 | 63 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.91 [0.63, 13.32] |
| 2 Number of women with no improvement | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 TVT‐Secur versus MiniArc | 2 | 170 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.25 [0.84, 12.66] |
| 2.2 U‐type versus H‐type TVT‐Secur | 1 | 129 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.74 [0.33, 1.63] |
| 2.3 MiniArc versus Ajust | 1 | 61 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.21 [0.21, 23.08] |
| 3 Objectve measurement of incontinence | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.1 MiniArc versus Ajust | 1 | 63 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.91 [0.63, 13.32] |
| 3.2 U‐type versus H‐type TVT‐Secur | 3 | 496 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.77 [0.56, 1.07] |
| 4 Condition‐specific health measures | 3 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 4.1 MiniArc versus AJUST | 1 | 60 | Mean Difference (IV, Fixed, 95% CI) | ‐0.13 [‐1.58, 1.32] |
| 4.2 U‐type versus H‐type TVT‐Secur | 2 | 414 | Mean Difference (IV, Fixed, 95% CI) | ‐0.30 [‐2.15, 1.55] |
| 5 Duration of operation (minutes) | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 5.1 TVT‐Secur versus MiniArc | 2 | 190 | Mean Difference (IV, Fixed, 95% CI) | 1.70 [‐4.11, 7.51] |
| 5.2 Ajust versus MiniArc | 1 | 80 | Mean Difference (IV, Fixed, 95% CI) | 1.20 [‐4.67, 7.07] |
| 6 Operative blood loss | 3 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 6.1 U‐type versus H‐type TVT‐Secur | 2 | 459 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6.2 Ajust versus MiniArc | 1 | 80 | Mean Difference (IV, Fixed, 95% CI) | ‐1.20 [‐10.04, 7.64] |
| 6.3 TVT‐Secur versus MiniArc | 1 | 80 | Mean Difference (IV, Fixed, 95% CI) | 4.30 [‐5.53, 14.13] |
| 7 Major vascular or visceral injury | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 7.1 U‐type versus H‐type TVT‐Secur | 2 | 459 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.25 [0.03, 2.19] |
| 8 Bladder or urethral perforation | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 8.1 U‐type versus H‐type TVT‐Secur | 2 | 459 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.91] |
| 8.2 TVT‐Secur versus MiniArc | 1 | 110 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.18 [0.21, 85.11] |
| 9 Vaginal wall perforation | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 9.1 TVT‐S versus MiniArc | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 9.2 U‐type versus H‐type TVT‐Secur | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 10 Urinary retention and need for catheterisation | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 10.1 TVT‐Secur versus MiniArc | 3 | 250 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.05 [0.47, 8.95] |
| 10.2 U‐type versus H‐type TVT‐Secur | 1 | 330 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.11, 3.94] |
| 10.3 Ajust versus MiniArc | 1 | 80 | Risk Ratio (M‐H, Fixed, 95% CI) | 5.0 [0.25, 100.97] |
| 11 Vaginal mesh exposure | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 11.1 U‐type versus H‐type TVT‐Secur | 2 | 414 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.79 [0.22, 2.80] |
| 12 Postoperative pain or discomfort | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 12.1 Ajust versus MiniArc | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 12.2 TVT‐Secur versus MiniArc | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 13 De novo urgency | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 13.1 TVT‐Secur versus MiniArc | 3 | 250 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.69 [0.24, 2.02] |
| 13.2 U‐type versus H‐type TVT‐Secur | 2 | 367 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.09 [0.53, 2.25] |
| 13.3 Ajust versus MiniArc | 1 | 80 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.5 [0.26, 8.50] |
| 14 Repeat stress incontinence surgery | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 14.1 U‐type versus H‐type TVT‐Secur | 2 | 414 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.16 [0.54, 2.51] |
| 15 Need for any other additional or new surgical procedure to treat complications | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 15.1 U‐type versus H‐type TVT‐Secur | 2 | 414 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.27 [0.04, 1.61] |
| 15.2 TVT‐Secur vs Mini‐Arc | 1 | 110 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.67 [0.16, 17.85] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Abdelwahab 2010 SEC.
| Methods | Prospective RCT of TVT versus TVT‐Secur in the treatment of female SUI | |
| Participants | 60 female patients with SUI Exclusion criteria: detrusor overactivity, bladder capacity < 200 mL, grade III or IV cystocoele, type 0 SUI (Blaivas and Olsson classification 1988), recurrent SUI |
|
| Interventions | TVT (bottom‐to‐top) (30) TVT‐Secur (U‐type) (30) |
|
| Outcomes | Main outcome measures: operative time, bleeding, duration of catheterisation, intraoperative and postoperative complications, Impact of incontinence on quality‐of‐life questionnaire (IQoL), length of hospital stay, urodynamic assessment 9 months' follow‐up Well matched for baseline characteristics |
|
| Notes | Quote: "cure means completely dry, while improvement means wetting but less than before surgery. Success rate includes cure and improvement" | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "patients were randomly divided into two equal groups" |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All enrolled participants were included in the analysis |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not described |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described |
Amat 2011 NDL.
| Methods | Quasi‐randomised prospective study comparing Contasure Needleless (C‐NDL) versus TVT‐O in a non‐inferiority design | |
| Participants | 158 women with SUI with or without associated prolapse | |
| Interventions | TVT‐O (60) (21 had SUI surgery alone) Contasure Needleless (C‐NDL) (72) (34 had SUI surgery alone) |
|
| Outcomes | Objective cure (stress test); subjective cure (Sandvik severity test, clinical history); Q‐tip test, ICIQ‐SF, urodynamics, complications, blood loss, postoperative pain | |
| Notes | Cure defined as negative stress test postoperatively, or score 0 on Sandvik questionnaire. Surgical procedure for stress incontinence only (with no prolapse surgery) done on 55 participants (34 in C‐NDL and 21 in TVT‐O) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote: "patients were assigned to one or other group of treatment depending on the last figure of their medical history number; last even figure was allocated for technical TVT‐O and last odd figure for C‐NDL" Comment: inadequate randomisation method |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 26 participants did not complete follow‐up schedule but were excluded from analysis. Statistical analysis performed on 60 participants in the TVT‐O group and on 72 in the C‐NDL group; these numbers are reported as adequate for analysis as per power calculation |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding of surgeon not possible because of difference in technique. Blinding of participants not described |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described |
Andrada Hamer 2012 SEC.
| Methods | Prospective randomised multi‐centre study comparing TVT versus TVT‐Secur | |
| Participants | 123 women with primary SUI or MUI with predominant SUI Inclusion criteria: age > 18 years; desires surgical treatment; does not desire future pregnancy; >= 3 mL leakage on standardised pad test; cough‐synchronous leakage on cough stress test Exclusion criteria: need for concomitant surgery for pelvic organ prolapse; regular PFMT for less than 3 months; planned or current pregnancy; previous surgery for urinary incontinence, bladder capacity < 300 mL; residual urinary volume > 100 mL; known detrusor instability; cystitis more than 4 times in the past 12 months |
|
| Interventions | TVT (62) TVT‐Secur (61) |
|
| Outcomes | Pad test, stress test, KHQ, voiding diary, visual analogue scale | |
| Notes | 2011 paper follow‐up at 2 months, but this is a full article. The 2012 paper is an abstract but reports 1‐year outcomes Subjective cure rate assessed but method of interpretation not defined. Study stopped at interim analysis because of poor outcomes and high rate of serious complications with TVT‐S 133 participants randomly assigned. Loss to follow‐up in 2 patients. 4 women were excluded because of protocol violations, and 4 declined surgery for personal reasons after they had been randomly assigned. Intention‐to‐treat analysis not done or reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Consenting women who fulfilled all inclusion criteria were randomised in a proportion of 1:1" |
| Allocation concealment (selection bias) | Low risk | Quote: "an equal proportion of assignments were mixed and placed in opaque envelopes which were then sealed, mixed again and numbered and kept at a central study secretariat" |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 133 participants randomly assigned. Loss to follow‐up in 2 patients. 4 women were excluded because of protocol violations, and 4 declined the surgery for personal reasons after they had been randomly assigned. Intention‐to‐treat analysis not done or reported |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Surgeon and participant blinding not possible because of the nature of the procedure |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "the follow up was performed by an independent evaluator, usually a urotherapist" |
Barber 2012 SEC.
| Methods | Multi‐centre RCT of TVT‐Secur versus retropubic TVT for treatment of SUI. Non‐inferiority design. 24‐month follow‐up | |
| Participants | 263 women with urodynamic SUI, with or without genital prolapse Eligibility criteria: at least 21 years of age, demonstrated urodynamic SUI, desiring surgical treatment for incontinence Exclusion criteria: DO on urodynamics; PVR greater than 100 mL; history of previous synthetic, biological or fascial sub‐urethral sling; desire for future pregnancy; currently using anticoagulation or known bleeding diathesis; urethral diverticulum or fistula Patients who received TVT were more likely to undergo concurrent hysterectomy (26% vs 9% in TVT‐Secur arm) |
|
| Interventions | TVT‐Secur (U‐type) (127) TVT (bottom‐up approach) (129) |
|
| Outcomes | Primary outcome: subjective cure (absence of any urinary incontinence or retreatment) at 1 year Secondary outcome measures: bladder diary, postoperative pain, short‐ and long‐term complications, quality of life scores (Incontinence Severity Index, Pelvic Floor Distress Inventory‐20, Pelvic Floor Impact Questionnaire‐7, Patient Global Index of Improvement), change in sexual function |
|
| Notes | Surgeons instructed to set tension of TVT so as to be 'tension‐free' (a spacer can be introduced between urethra and sling), whereas with TVT‐Secur, tension was set tightly, so that sling was directly opposed to the urethra and spacer could not be introduced | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random allocation with randomly permuted blocks used; stratified by site and presence or absence of prolapse beyond the hymen |
| Allocation concealment (selection bias) | Low risk | Consecutively numbered, sealed, opaque envelopes used |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 12 individuals randomly assigned to the mini‐sling arm had technical difficulties during insertion; 7 ended up receiving a TVT (6) or other retropubic sling (1) |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Sham incisions used in mini‐sling arm to facilitate blinding |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Research staff not involved in operation performed postoperative assessments |
Basu 2010 ARC.
| Methods | Prospective, single‐centre RCT | |
| Participants | 71 women with SUI Inclusion criteria: SUI symptoms together with objective evidence of USI, which had failed to resolve with conservative measures Exclusion criteria: previous continence surgery, evidence of voiding dysfunction, known bladder pathology, pelvic organ prolapse (POP‐Q stage 2 or above), recurrent UTI, plan to conceive in the future |
|
| Interventions | Retropubic TVT (Advantage TVT) (33) Mini‐sling (MiniArc) (38) |
|
| Outcomes | Primary outcome was presence of SUI at 6 weeks and 6 months postoperatively (KHQ and PGI‐I). Secondary outcomes were SUI and urodynamics at 6 months and complications | |
| Notes | 6‐Month follow‐up data from 2010 paper used for cure and operative outcomes In 2012 paper of MiniArc, 35/38 returned 3‐year questionnaires; Retropubic TVT, 26/33 returned 3‐year questionnaires. Data were used for redo surgery outcome |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Subjects were randomised using computer‐generated block randomisation sequence" |
| Allocation concealment (selection bias) | Low risk | Quote: "allocation to each group being performed via a series of opaque envelopes, by a member of the research team" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Subjective data available on all participants. Three participants declined urodynamics at 6 months (all in TVT arm) |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Participants blinded but researchers could not be blinded because of differences in devices |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not mentioned |
Bianchi 2012 SEC.
| Methods | Prospective single‐centre RCT comparing TVT‐O versus TVT‐Secur | |
| Participants | 122 women with SUI Exclusion criteria: DO, concomitant prolapse > stage 2 |
|
| Interventions | TVT‐0 (56) TVT‐Secur (66) |
|
| Outcomes | Clinical evaluation, pad test, KHQ, urodynamics. Mean follow‐up 24 months | |
| Notes | Abstract only. Ongoing study with additional data from Bianchi 2010; therefore 2012 abstract used | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data available on all randomly assigned participants |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not described |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described |
Djehdian 2010 OPH.
| Methods | Prospective RCT comparing Ophira mini‐sling versus transobturator tape (Unitape, outside‐in) | |
| Participants | 73 women with SUI and no prolapse > stage 1 Exclusion criteria: PVR > 100 mL; coagulation disorders; current UTI; sequelae of previous radiation therapy of pelvis; anticoagulant therapy; vulvovaginitis; anaesthesia contraindication |
|
| Interventions | Ophira mini‐sling performed under LA (45) Unitape TOT performed under regional anaesthesia (28) |
|
| Outcomes | Primary outcome was objective cure at 6 months (defined as a 1‐hour pad weighing < 2 g and a negative stress test) Secondary outcome measures included quality of life and symptom severity scores ( I‐QOL, UDI‐6, respectively) and rate of complications |
|
| Notes | Conference abstract only. 6‐Month follow‐up data available for only 29 Ophira and 15 Unitape participants reported here. Operative complications are reported for the full cohort | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomisation method not described. Unequal ratio of randomisation with no reason stated |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All outcome data described for all participants |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not described |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described |
Enzelsberger 2010 ARC.
| Methods | Prospective RCT of MinArc versus Monarc | |
| Participants | 90 women with SUI undergoing primary anti‐incontinence surgery | |
| Interventions | Mini‐Arc (45) Monarc (TVTO) (45) |
|
| Outcomes | Clinical and urodynamic evaluation at 24 months | |
| Notes | German paper, only abstract in English | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "women were randomly allocated" |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All outcome data reported |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not described |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described |
Friedman 2009 SEC.
| Methods | Prospective, single‐centre RCT of TVT‐Secur versus TVT‐O | |
| Participants | 84 women with SUI Patients may have undergone concomitant prolapse surgery Groups well matched for baseline characteristics. |
|
| Interventions | TVT‐Secur (Hammock type) (42) TVT‐O (42) |
|
| Outcomes | Primary outcomes were intra‐operative complications, peri‐operative morbidity and post‐operative efficacy (at 1 year) | |
| Notes | Abstract only | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No description |
| Allocation concealment (selection bias) | Unclear risk | No description |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participant data included in analysis |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No description |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No description |
Hinoul 2011 SEC.
| Methods | Prospective, multi‐centre, unblinded RCT comparing TVT‐Secur versus TVT‐O | |
| Participants | 194 women with SUI, demonstrable during clinical and/or urodynamic evaluation. Exclusion criteria: recurrent SUI; concomitant surgery; stage 2 or greater genital prolapse |
|
| Interventions | TVT SECUR (97) TVT‐O (98) |
|
| Outcomes | Primary outcome was objective cure of SUI at 1 year, measured by standing cough stress test measured at 300 mL bladder volume or 70% of maximum bladder capacity, according to the participant voiding diary. Secondary outcome measures were perioperative morbidity, general quality of life scores using SF‐36 and disease‐specific QoL using UDI (Dutch version), pain VAS scores, subjective SUI reporting, urgency and or urgency urinary incontinence | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Patients were assigned to surgical treatment by balanced non‐restricted randomisation. Block randomisation was done at each participating centre using a computerised random number generator" |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Relatively high dropout rate, but statistical analysis revealed no significant or clinically relevant difference between respondents and non‐respondents |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: "Blinding of investigators and patients to group allocation was not possible since one procedure resulted in skin wound whilst the other was exit free" |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described |
Hota 2012 SEC.
| Methods | Single‐centre non‐blinded RCT of TVT‐Secur versus TVTO | |
| Participants | 43 women with SUI Inclusion criteria: SUI with demonstrable impact of SUI on quality‐of‐life questionnaires and positive cough stress test in urodynamics Exclusion criteria: intrinsic sphincter deficiency (MUCP < 20 cm H2O), previous sub‐urethral sling, predominant OAB symptoms, women planning future pregnancy, bleeding diathesis or anticoagulant therapy, immunosuppression, progressive neurological disease, evidence of systemic infection Patients with concomitant prolapse were also included, and some underwent concomitant repair Participants well matched for baseline characteristics |
|
| Interventions | TVT‐Secur (42) TVTO (44) |
|
| Outcomes | Reported at 12 weeks and 1 year Primary outcomes: objective failure (SUI demonstrated on cough test) Secondary outcomes: quality of life symptom questionnaires (PFDI‐20, PFIQ‐7), postoperative pain, mesh erosion or exposure, intraoperative estimated blood loss, length of procedure, postoperative pain (verbal analogue scale), need for sling revision, length of catheterisation postoperatively, need for second anti‐incontinence procedure |
|
| Notes | Power analysis recommended 67 participants in each arm, but study was stopped early because of "several investigators voicing concerns about an increasing number of positive post‐operative CST in women undergoing TVT‐S." The study is therefore underpowered, and this unplanned interim analysis represents a high risk of bias | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Women were randomized in a 1:1 allocation" |
| Allocation concealment (selection bias) | Low risk | Sequentially numbered, opaque, sealed envelopes used |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Study terminated early, therefore underrecruited |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Neither surgeon nor participants blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described |
Kim 2010 SEC.
| Methods | Prospective RCT of TVT‐Secur versus TOT | |
| Participants | 40 women with SUI | |
| Interventions | TVT‐Secur (20) TOT (20) |
|
| Outcomes | Urodynamics, KHQ, subjective cure, operative complications | |
| Notes | Abstract only. Minimal details on randomisation and methodology to allow judgement of the reliability of outcomes | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not described |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described |
Lee 2010 CUR/SEC.
| Methods | Prospective single‐centre RCT | |
| Participants | 60 women with SUI | |
| Interventions | TVT‐Secur (38) CureMesh (22) |
|
| Outcomes | Primary outcome: objective cure (no leakage on cough test with full bladder at 1 year) Secondary outcomes: participant perception of urgency severity, IQoL, BFLUTS, VAS |
|
| Notes | Conference abstract only | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "women with SUI were randomly assigned" |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not described. Given the unequal allocation, this could be a significant risk |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not described |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described |
Lee 2010 SEC.
| Methods | Prospective, multi‐centre RCT of U‐ and H‐type methods of TVT‐Secur | |
| Participants | 285 women with urodynamic SUI, or MUI with predominant SUI Exclusion criteria: pelvic organ prolapse > stage 2; intention to have more children; neurological disease Age, menopausal status percentage of women with DO and number of urgency episodes were not balanced between groups |
|
| Interventions | U‐type TVT Secur (165) H‐type TVT Secur (165) |
|
| Outcomes | Primary outcome: objective cure (no leakage on stress test), subjective cure (response to Sandvik questionnaire) Secondary outcomes: Sandvik questionnaire, I‐QOL, ICIQ‐FLUTS, I‐VAS, 3‐day voiding diary |
|
| Notes | 330 women recruited, 45 not in final analysis (including 28 lost to follow‐up at 1 year) from 41375 ICS abstract with 2‐year data on the same participants in Kim 2010. Five papers refer to the same study; Kim 2010 is a single‐centre report from the multi‐centre study, whereas Lee 2010 and 2011 are reports of the multi‐centre study. Data from the mutli‐centre study have been used |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "the centre applied a stratified and permuted block randomisation method" |
| Allocation concealment (selection bias) | High risk | Quote: "consenting patients were randomly allocated in the operating room" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Outcome data adequately analysed |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Unclear whether participants were blinded; surgeons could not be blinded because of a difference in technique |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described |
Lee 2012 ARC.
| Methods | Prospective, single‐centre RCT of MiniArc versus Monarc | |
| Participants | 224 women with SUI or urodynamic stress incontinence Exclusion criteria: intrinsic sphincter deficiency; previous MUS; untreated DO; significant voiding dysfunction Patients who had previous SUI surgery were included Groups well matched at baseline |
|
| Interventions | MiniArc (112) Monarc (112) |
|
| Outcomes | Primary outcomes: objective cure (negative urodynamic stress or cough stress test), subjective cure (absence of participant‐reported SUI) Secondary outcomes: ICIQ‐SF, ICIQ OAB, PISQ12, IIQ‐7, PGII questionnaires, 24‐hr pad weight gain |
|
| Notes | Abstract only | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Computer‐generated random allocation was concealed and stratified to centre" |
| Allocation concealment (selection bias) | Unclear risk | As above, method not described |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All randomly assigned participants completed follow‐up |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: "Surgeons or patients were not blinded once allocation was revealed" |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described |
Liapis 2010 SEC.
| Methods | Quasi‐randomised, single‐centre RCT of H‐type versus U‐type TVT‐Secur | |
| Participants | 87 women with SUI Exclusion criteria: MUCP < 20 cm H2O, detrusor overactivity, history of anterior vaginal wall surgery or prolapse > stage 1 | |
| Interventions | H‐type TVT‐Secur (45) U‐type TVT‐Secur (42) |
|
| Outcomes | Objective cure (absence of urine leakage on cough test), subjective cure (simple questionnaire), urodynamics. | |
| Notes | Prospective study but not adequately randomly assigned | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | "Patients were allocated alternatively" |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 5 participants did not attend follow‐up and were excluded |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not described |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described |
Mackintosh 2010 AJS.
| Methods | Prospective, pilot RCT comparing Ajust and TVT‐O | |
| Participants | 29 women with SUI Inclusion criteria: SUI or MUI with predominant SUI; women undergoing primary incontinence surgery; BMI < 35; previously failed or declined PFMT Exclusion criteria: predominant OAB; unwilling for randomisation; inability to understand English; concomitant surgery; patients requiring postoperative hospital stay for medical/social reasons Well matched for baseline characteristics |
|
| Interventions | TVT‐O (15) Ajust (14) |
|
| Outcomes | Primary outcomes: feasibility of recruitment and randomisation, acceptability and feasibility of the use of local anaesthetic in the mini‐sling arm Secondary outcomes: complications and short‐term success rate |
|
| Notes | This report was submitted as a thesis for fulfilment of a bachelor of medicine degree and was primarily a feasibility study, but it reported on efficacy and complication rates as secondary outcome measures and is therefore included | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated sequence used |
| Allocation concealment (selection bias) | Low risk | Allocation sequence kept electronically and concealed in opaque envelopes |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data available for all participants at 4‐week follow‐up. 2 participants unavailable for 3‐month follow‐up in TVT‐O arm |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Neither participants nor surgeons blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Reported as beyond available resources for this small study, but assessments done by individuals not involved directly with index procedure |
Martan 2012 ARC AJS.
| Methods | Prospective multi‐centre RCT comparing MiniArc versus Ajust system | |
| Participants | 66 women with previously untreated SUI | |
| Interventions | MiniArc (33) Ajust (33) |
|
| Outcomes | Subjective cure assessed by 5‐point Likert scale, objective cure assessed by cough test | |
| Notes | Abstract only. English summary of results from Martan 2011 study. 43009 Non‐English abstract. Study results presented in Martan 2012 abstract (English), which has been included |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Women were randomly allocated by the envelope method" |
| Allocation concealment (selection bias) | Low risk | "Women were randomly allocated by the envelope method" |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 3 participants did not complete 24‐month follow‐up. ITT analysis not done |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not described |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described |
Masata 2012 SEC.
| Methods | Prospective, single‐centre RCT comparing TVT‐S U and H‐types versus TVT‐O | |
| Participants | 197 women with proven urodynamic stress incontinence who had failed conservative therapy Exclusion criteria: predominant UUI, urodynamic detrusor instability, previous failed anti‐incontinence surgery, previous radiotherapy, PVR > 100 mL, bladder capacity < 300 mL, >= stage 2 pelvic organ prolapse, planned concomitant surgery, immobile urethra Well‐matched groups at baseline |
|
| Interventions | TVT‐O (68) TVT‐S (H‐type) (64) TVT‐S (U‐type) (65) |
|
| Outcomes | Primary outcomes: objective cure (stress test), subjective cure (ICIQ‐SF) Secondary outcomes: IQoL questionnaires, ultrasound examination, intraoperative and postoperative complications |
|
| Notes | Unplanned interim analysis performed at two years; high failure rate in TVT‐S group, which calls into question the risk of bias due to unblinding of outcome assessors. After this interim analysis at two years, the study was only stopped at 3 years once "the minimum number of patients needed for final statistical analysis was achieved" Multiple papers included under this study heading, all referring to the same trial |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: “We implemented randomization by placing pieces of paper containing the randomization allocation in sealed envelopes which were arranged for sequential opening” |
| Allocation concealment (selection bias) | Low risk | “We implemented randomization by placing pieces of paper containing the randomization allocation in sealed envelopes which were arranged for sequential opening” |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Unplanned interim analysis, but adequate numbers recruited as per power calculation |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: "The patients were not blinded" |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described |
Mostafa 2012 AJS.
| Methods | Multi‐centre prospective randomised study comparing Ajust versus TVT‐O | |
| Participants | 137 women with SUI who have failed or declined PFMT, undergoing primary anti‐incontinence procedure with the ability to understand the information leaflet Exclusion criteria: mixed incontinence with uncontrolled OAB symptoms or neurological symptoms such as MS |
|
| Interventions | SIMS‐Ajust (69) performed under LA as an opt‐out policy TVT‐O (68) under GA |
|
| Outcomes | Primary outcome: postoperative pain profile up to 4 weeks postoperatively Secondary outcomes: participant‐reported and objective success rates (cough stress test), reoperation rates, ICIQ‐FLUTS, KHQ, PISQ‐12, UPS, PGI‐I questionnaires |
|
| Notes | Multiple reports of same trial. Full report from European Journal of Obstetrics & Gynaecology 2012 used as primary source of data | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Block randomisation was done for each centre using number allocation software" |
| Allocation concealment (selection bias) | Low risk | Quote: "allocation to each group was performed via a telephone randomisation" |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 8 lost to follow‐up in TVT‐O arm; sensitivity analysis performed but not reported in abstract |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants could not be blinded, as only Ajust was done under LA |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Follow‐up conducted by an independent researcher who was blinded to type of procedure |
Oliveira 2011 ARC SEC.
| Methods | Exploratory randomised phase 2 trial | |
| Participants | 90 women with clinically and urodynamically proven SUI and urethral hypermobility Exclusion criteria: previous surgery for SUI; genital prolapse >= stage 2 (by POP‐Q score); complaints of urgency, frequency, nocturia or demonstrable detrusor overactivity |
|
| Interventions | TVT‐O (30), TVT‐SECUR (30) or MiniArc (30) | |
| Outcomes | Primary outcome: cure rate (considered cured if participants did not report any episodes of urine leakage, ceased to wear incontinence protection and had a negative cough test) Secondary outcomes: KHQ |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participant outcome data assessed adequately |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not described |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described |
Palomba 2012 AJS ARC SEC.
| Methods | Multi‐centre, prospective RCT comparing three vaginal kits of single‐incision mini‐slings (Ajust, MiniArc and TVT‐Secur) | |
| Participants | 120 women with SUI who remained incontinent after at least three months of PFMT, or patients with MUI who had clinically demonstrable SUI while on oral antimuscarinic therapy Participants well matched for baseline characteristics. None had significant pelvic organ prolapse |
|
| Interventions | Ajust (40), MiniArc (40) and TVT‐Secur (40) | |
| Outcomes | Operative time, blood loss, intraoperative and postoperative complications, feasibility (number of surgeries completed under local anaesthesia/total number of surgeries), degree of surgical difficulty, number of analgesic vials, participant satisfaction (using a visual analogue scale (VAS) ranging from 0 (absolutely unsatisfied) to 10 (completely satisfied) administered at hospital discharge) and postoperative pain | |
| Notes | Only surgical data reported in this paper. Data analysed by ITT | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The random allocation sequence was made in single blocks, using a single sequence of random assignment, obtained with the use of a computer‐generated randomization list" |
| Allocation concealment (selection bias) | Low risk | Quote: "The sequence was concealed from all investigators until the interventions were assigned using sequentially numbered opaque sealed envelopes, prepared distant from the study site, until surgeries were assigned (before entering the operating room)" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Outcome data given for all enrolled participants |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "The study protocol was double‐blind, i.e. patients and data assessors were masked to the SIMS assigned" |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "The study protocol was double blind, i.e., patients and data assessors were masked to the SIMS assigned" |
Pardo 2010 SEC ARC.
| Methods | Prospective RCT of TVT‐Secur versus MiniArc | |
| Participants | 110 women with at least one‐year symptomatic SUI | |
| Interventions | TVT‐SECUR (60) versus Mini‐Arc (50) | |
| Outcomes | Primary outcome: cure rate (absence of incontinence) | |
| Notes | Abstract only | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote: "The randomisation was: each physician explained the pathology and the technique to use, offering only one" Comment: inadequate randomisation methods |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Outcome data available for all participants |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unblinded (from the description of randomisation) |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | As above |
Schweitzer 2012 AJS.
| Methods | Single‐blind RCT comparing TVT‐O with Ajust in 2:1 design | |
| Participants | 156 women with clinically proven SUI (stress test) | |
| Interventions | Ajust (92) versus TVT‐O (51) | |
| Outcomes | Main outcomes were surgery‐related pain, efficacy and complications. Physical exam including cough stress test, UDI, IIQ, PGIS, PGII questionnaires. | |
| Notes | Abstract only. Reported before end of recruitment and some outcome measures reported at 6 weeks, others at 6 months | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 7 women withdrew after randomisation, 3 received the wrong type of sling after allocation and were excluded, and 3 were yet to receive intervention at the time of writing. No ITT analysis |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "Women were blinded to the type of procedure by using a sham skin incision in the Ajust group" |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Surgeon not blinded. Single‐blind trial |
Seo 2011 SEC.
| Methods | Prospective, single‐centre RCT comparing TVT‐O versus TVT‐Secur | |
| Participants | 80 women with SUI, reportedly well matched for baseline characteristics | |
| Interventions | TVT‐O (39) vs TVT‐S (41) | |
| Outcomes | Outcomes assessed at 3 and 12 months: physical exam, voiding diary, urodynamics, Stamey symptom severity scale, VAS (pain). Sandvik questionnaire for surgical outcomes assessed at 6 hours postoperatively. Unclear which was the primary outcome | |
| Notes | Abstract only | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Patients were randomly assigned" Comment: limited information from abstract |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Limited information available from abstract |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not described |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described |
Sivaslioglu 2012 TFS.
| Methods | 5‐Year results of prospective RCT of TOT versus TFS (tissue fixation system) | |
| Participants | 80 female patients with only urodynamically proven SUI. Exclusions: patients with overflow incontinence, those with OAB and those who underwent previous anti‐incontinence surgery Groups well matched for baseline characteristics |
|
| Interventions | Group 1: TOT (40) Group 2: TFS (40) |
|
| Outcomes | Simplified QoL score (grade 1‐5 to describe the limitation of normal activities by incontinence), CSPT (preweighed pad placed on vulva and participant with full bladder, asked to cough ten times. Pad weight increase greater than 1 gm assessed as positive, less than 1 gm assessed as negative) At 5 years: If supine, CSPT negative after the operation and participant reported restoration of continence, it was regarded as an objective cure. If participant reported restoration of continence but the supine CSPT was positive, it was regarded as subjective cure. If there was no change in incontinence after the operation, it was regarded as failure. Primary outcome measures: objective cure, subjective cure and failure at 5 years Secondary outcome measures: procedure duration, postoperative groin pain, postoperative urinary retention and mesh extrusion |
|
| Notes | 4 participants from each group lost to follow‐up at 5 years. Not powered, as there were no published long‐term data on TOT/TFS at the time of starting the trial to perform a power analysis. Sample size chosen based on "expectations and practical considerations" | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "participants were randomly allocated according to a computer program" |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 4 patients in each group lost to follow‐up because of moving away from the area |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not described |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "Post‐operative assessment conducted by a senior surgeon at the urogynaecology clinic who did not participate in the operations" |
Smith 2011 ARC.
| Methods | Interim analysis of a prospective, randomised, non‐blinded study at a single institution | |
| Participants | Patients with urodynamically proven SUI, excluding those who had previous anti‐incontinence surgery, urodynamically diagnosed ISD (VLPP < 60 and/or MUCP < 40) or mixed incontinence with predominant detrusor overactivity. Groups well matched for baseline characteristics | |
| Interventions | Transobturator (Monarc) (38) or single incision (MiniArc) (43) | |
| Outcomes | Primary outcome: presence or absence of urine leakage on standard cough stress test Secondary outcomes: intraoperative data, UDI‐6, IIQ‐7, ICIQ and 3‐day voiding diary |
|
| Notes | Abstract only | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Allocation to treatment group was performed by a computer generated randomsation scheme and both surgeon and patient were blinded to allocation until onset of anaesthesia" |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Interim analysis. Aim to randomly assign 80 participants, 40 in each group. Only follow‐up of 24 in each arm included |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Surgeons not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Described as a non‐blinded study but no further details given |
Sottner 2012 ARC AJS.
| Methods | Prospective randomised study of TVT‐O versus MiniArc versus Ajust | |
| Participants | 43 institutionalised elderly patients (nursing home residents) with predominant SUI | |
| Interventions | TVT‐O versus MiniArc versus Ajust | |
| Outcomes | ICIQ, intraoperative complications, de novo urgency, success rate | |
| Notes | Czech article with abstract in English but no usable data in abstract | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not described |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not described |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described |
Tommaselli 2010 SEC.
| Methods | Prospective, single‐centre RCT of TVT‐O versus TVT‐Secur | |
| Participants | 84 women with urodynamically proven SUI and symptomatic for at least 2 years Exclusion criteria: previous surgical/pharmacological treatment of SUI, predominant urge incontinence, genital prolapse >= stage 2, serious contraindication to surgery Groups were well matched for baseline characteristics |
|
| Interventions | TVT‐Secur (37) versus TVT‐O (38) | |
| Outcomes | Primary outcome: objective sure of SUI (during cough test and exertion required in urodynamic evaluation) Secondary outcomes: duration of procedure, complications, PVR, ICIQ‐SF, KHQ, urinary diary |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "randomization list generated by a computer" |
| Allocation concealment (selection bias) | Unclear risk | No description |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Outcome data provided for only 75 participants, others excluded as they did not complete follow‐up |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: "patients were left blinded to the devices used until the end of the procedure" Comment: unclear as to whether this means participant blind was broken after the procedure Quote: "surgeon was obviously not blinded to the technique being used" |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described |
Wang 2011 SEC.
| Methods | Prospective RCT comparing TVT, TVT‐O and TVT‐Secur | |
| Participants | 102 women with SUI Exclusion criteria: previous surgery for SUI |
|
| Interventions | TVT (32), TVT‐O (36) and TVT‐Secur (34) | |
| Outcomes | Primary outcome: cure (defined as negative cough stress test and absence of urine leak by subjective sense) Secondary outcomes: surgical time, blood loss, complications |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "patients were assigned by random allocation (computer generated)" Comment: probably done |
| Allocation concealment (selection bias) | Low risk | Quote: "allocation was concealed using opaque sealed envelopes" Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Outcome data available for all 102 participants |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Surgeon blinding not possible because of the nature of the techniques |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described |
Yoon 2011 NDL.
| Methods | Prospective RCT of Contasure Needleless versus TOT | |
| Participants | 103 women with SUI | |
| Interventions | Contasure Needleless (52) versus TOT (51) | |
| Outcomes | 3‐Day frequency‐volume chart, PVR, symptom questionnaire, complications, operative time, symptoms | |
| Notes | Abstract only; 4‐week follow‐up period | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "(patients) were randomly divided into two groups according to their procedure" Comment: methods unclear |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Limited information available from abstract |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not described |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not described |
Abbreviations:
BMI: Body Mass Index
CST: Cough Stress Test
GA: General Anaesthetic
ICIQ‐SF: International Consultation on Incontinence Questionnaire – Short Form
ITT: Intention To Treat
KHQ: Kings Health Questionnaire
LA: Local Anaesthetic
MUCP: Mean Urethral Closure pressure
MUI: Mixed Urinary Incontinence
PFMT: Pelvic Floor Muscle Training
POP‐Q: Pelvic Organ Prolapse Quotient
PVR: Post‐Void Residual
QoL: Quality of Life
RCT: Randomised Controlled Trial
SUI: Stress Urinary Incontinence
TVT: Tension‐free Vaginal Tape
UDI: Urogenital Distress Inventory
USI: Urodynamic Stress Incontinence
UTI: Urinary Tract Infection
VAS: Visual Analogue Scale
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Araco 2011 | Randomised trial of local versus general anaesthesia, all had TVT procedure |
| Choo 2011 | This is an ongoing prospective, multi‐centre registry. Not an RCT |
| de Leval 2011 | Comparator is not a single‐incision sling |
| Diallo 2012 | No mini‐sling comparator arm (TVT‐O vs another) |
| Martan 2008 | Non‐randomised study correlating ultrasound findings with clinical signs of cure or failure in a subset of participants who had undergone TVT‐Secur (mini‐sling) from an RCT |
| Okulu 2011 | Experimental interventions do not conform to the definition of single‐incision slings |
| Porena 2012 | This study compares pelvic organ prolapse (POP) repair plus mini‐sling versus POP repair alone |
Abbreviations:
TVT: Tension‐free Vaginal Tape
RCT: Randomised Controlled Trial
POP: Pelvic Organ Prolapse
Characteristics of studies awaiting assessment [ordered by study ID]
Pushkar 2011.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | This paper is in Russian; we were unable to obtain a copy and an English translation. We hope to include this in future updates |
Characteristics of ongoing studies [ordered by study ID]
Foote 2012.
| Trial name or title | A randomised trial comparing two vaginal prolene sling surgeries for female urinary incontinence |
| Methods | RCT |
| Participants | Women with USI and no need for concomitant surgery |
| Interventions | Monarc versus MiniArc |
| Outcomes | Postoperative pain score assessed by visual analogue scale, continence rates (2‐day bladder diary), blood loss |
| Starting date | January 2012, target enrolment 50 |
| Contact information | Dr Andrew Foote |
| Notes | Identified from ANZCTR |
Maslow 2011.
| Trial name or title | Trial comparing TVT‐Secur system and transvaginal obturator tape for surgical management of stress urinary incontinence |
| Methods | RCT |
| Participants | Women with clinically demonstrable SUI (cough test) but no POP > stage 1, predominant UUI or DO |
| Interventions | TVT‐Secur versus TVT‐O |
| Outcomes | Objective cure (cough test) |
| Starting date | May 2008, target enrolment 106 |
| Contact information | Ken D Maslow, St Boniface Hospital, Canada |
| Notes | Identified from clinicaltrials.gov |
Robert 2012.
| Trial name or title | Transvaginal tape (TVT)‐Secur versus TVT: a randomised controlled trial |
| Methods | RCT |
| Participants | Women with SUI not requiring prolapse surgery |
| Interventions | TVT‐Secur versus TVT |
| Outcomes | Objective cure (pad test, < 1 g increase in pad weight), subjective cure, UDI‐6, IIQ‐7, voiding dysfunction, sexual function, surgical complications, |
| Starting date | May 2008, target enrolment 74 |
| Contact information | Magaly Robert, University of Calgary |
| Notes | Identified from clinicaltrials.gov |
Rosamilia 2012.
| Trial name or title | Tension‐free vaginal tape (TVT) Abbrevo and MiniArc sub‐urethral sling in women with stress urinary incontinence—a randomised controlled trial |
| Methods | RCT |
| Participants | Women 18 to 80 years of age with USI but not ISD enrolled from the urodynamic clinic |
| Interventions | TVT Abbrevo and MiniArc |
| Outcomes | Objective cure (cough test), subjective cure (ICIQ‐SF), IIQ‐7, PGI‐I, sexual function (PISQ‐12) |
| Starting date | December 2011, target sample 230 |
| Contact information | |
| Notes | Identified from ANZCTR |
Differences between protocol and review
The original protocol stated that trials in which concomitant surgery was performed (e.g. genitourinary prolapse repair) would be excluded. However it was found that a number of trials included, or were unclear about the inclusion of, women undergoing concomitant prolapse surgery, and on further discussion the review authors believed that not including these trials could represent a source of bias. Concomitant stress incontinence and prolapse are common problems that are frequently corrected simultaneously at surgery; therefore we believed it was important to assess single‐incision slings in this clinically relevant scenario. When appropriate, sensitivity analyses were conducted, excluding those trials in which concomitant surgery was performed.
The review authors decided not to carry out assessment of bias due to selective outcome reporting.
We did not include qualitative studies in this review.
Sensitivity analyses were performed when it was thought that differences in duration of follow‐up may represent a source of bias.
Although subgroup analysis was planned in the Protocol, not enough information was available to allow this to be carried out in the review: this may be incorporated in future versions.
July 2017 update: We have added Brief Economic Commentaries (BECs) to all of our 'Surgery for UI in women' Cochrane Reviews. We have revised the economic elements throughout the review; if incorrect, we have stripped them out. We have added new economics‐related text. This involved revisions to the Background section, Methods section, e.g. search section referring to added Appendix, Discussion section, Abstract and Plain Language Summary. We have added an appendix with details of the economics searches. The Conclusions section of the review has not changed. The rest of the review has not changed.
Contributions of authors
Arjun Nambiar wrote the text of the main review. He performed the initial screening of studies for inclusion, assessment of methodological quality of included trials, data extraction and analysis of results.
June D Cody made significant input to writing of the final review, including writing the risk of bias section. She performed confirmatory screening of studies for inclusion, assessment of methodological quality, data extraction and analysis of the results.
Stephen T Jeffery wrote the original protocol and incorporated comments from co‐authors. He performed screening of studies for inclusion, assessment of methodological quality and data extraction. He also performed confirmatory analysis of the results.
Stephen T Jeffery and Arjun Nambiar were responsible for clinical input for the review. June D Cody provided methodological input.
For the July 2017 addition of the BECs to this review: Patricia Aluko was responsible for the entire BECs‐related work on this review, i.e. she ran the search for studies, screened the search results, extracted data from relevant studies, revised any existing economics‐related text, added the BECs‐related text, and responded to any peer referee comments. All authors had the opportunity to comment on the revised review.
Sources of support
Internal sources
No sources of support supplied
External sources
-
National Institute for Health Research (NIHR), UK.
This project was supported by the National Institute for Health Research, via Cochrane Infrastructure funding to the Cochrane Incontinence Group. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, NHS or the Department of Health. The National Institute for Health Research (NIHR) is the largest single funder of the Cochrane Incontinence Group.
-
National Institute for Health Research, UK.
This project, to add Brief Economic Commentaries to our surgery for UI in women reviews, was supported by the National Institute for Health Research (NIHR), via the Cochrane Review Incentive Scheme 2016, to the Cochrane Incontinence Group. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, NHS or the Department of Health.
Declarations of interest
Arjun Nambiar: June 2014: has received travel and educational grants from Pfizer, Astellas and GSK. July 2017: has received educational grants towards travel and accommodation for attending conferences and meetings from the following pharmaceutical companies: Ferring and Takeda; he is also a member of the EAU guideline panel on Urinary Incontinence.
June D Cody: June 2014 and July 2017: has no conflicts of interest to declare.
Stephen T Jeffery: June 2014: is a speaker for Johnson and Johnson (Women’s Health and Urology) and Bard Medical and is part of a randomised trial on Contasure Needleless. He has received honoraria and travel and educational grants from Bard, Johnson and Johnson and Boston Scientific. July 2017: Has received support from Boston Scientific for support for travel to meetings for the study or other purposes and outside the submitted work has received travel support and honoraria from Boston Scientific and received payment for lectures from Pfizer (on complications of sling surgery) and from Boston Scientific for a lecture at a symposium at an IUGA annual meeting. He has received speaker's fees for Aspen.
Patricia Aluko: July 2017: This project, to add Brief Economic Commentaries to our 'Surgery for UI in women' reviews, was supported by the National Institute for Health Research (NIHR), via the Cochrane Review Incentive Scheme 2016, to the Cochrane Incontinence Group. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, NHS or the Department of Health.
Edited (no change to conclusions)
References
References to studies included in this review
Abdelwahab 2010 SEC {published data only}
- Abdelwahab O, Shedid I, Al‐Adl AM. Tension‐free vaginal tape versus secure tension‐free vaginal tape in treatment of female stress urinary incontinence. Current Urology 2010;4:93‐8. [42740] [Google Scholar]
Amat 2011 NDL {published data only}
- Amat L, Franco E, Vicens JM. Contasure‐Needleless compared with transobturator‐TVT for the treatment of stress urinary incontinence. International Urogynecology Journal 2011;22(7):827‐33. [42952] [DOI] [PubMed] [Google Scholar]
- Amat LL, Franco EM, Saavedra AH, Martinez AV. Needleless (R): a new technique for correction of urinary incontinence. Randomized controlled trial compared with TVT‐O (R). Preliminary results (Abstract number 225). International Urogynecology Journal and Pelvic Floor Dysfunction 2007;18(Suppl 1):S128. [27329] [Google Scholar]
Andrada Hamer 2012 SEC {published data only}
- Andrada Hamer M, Larsson PG, Teleman P, Eten‐Bergquist C, Persson J. One year results of a prospective randomized evaluator blinded multicenter study comparing TVT and TVT‐Secur (Abstract number 3). Neurourology & Urodynamics 2012;31(6):728‐9. [45455] [Google Scholar]
- Andrada Hamer M, Larsson PG, Teleman P, Eten‐Bergqvist C, Persson J. Short‐term results of a prospective randomized evaluator blinded multicenter study comparing TVT and TVT‐Secur. International Urogynecology Journal 2011;22(7):781‐7. [41716] [DOI] [PubMed] [Google Scholar]
Barber 2012 SEC {published data only}
- Barber MD, Weidner AC, Sokol AI, Amundsen CL, Jelovsek JE, Karram MM, et al. Single‐incision mini‐sling compared with tension‐free vaginal tape for the treatment of stress urinary incontinence: a randomized controlled trial. Obstetrics and Gynecology 2012;119(2 Pt 1):328‐37. [43342] [DOI] [PubMed] [Google Scholar]
Basu 2010 ARC {published data only}
- Basu M, Duckett J. A randomised trial of a retropubic tension‐free vaginal tape versus a mini‐sling for stress incontinence. BJOG: an International Journal of Obstetrics & Gynaecology 2010;117(6):730‐5. [39624] [DOI] [PubMed] [Google Scholar]
- Basu M, Duckett J. A randomised trial of the Miniarc single incision sling versus a retropubic TVT in the management of women with stress urinary incontinence—three year follow up (Abstract number 92). International Urogynecology Journal 2012;23(Suppl 2):S141‐2. [45466] [Google Scholar]
Bianchi 2012 SEC {published data only}
- Bianchi AH, Jarmy‐Di‐Bella ZI, Castro RA, Sartori MG, Girao MJ. Randomised trial of TVT‐O (trademark) and TVT‐S (trademark) for the treatment of stress urinary incontinence (Abstract number 164). International Urogynecology Journal 2012;23(Suppl 2):S216‐7. [45465] [Google Scholar]
- Bianchi AM, Jarmy‐Di Bella Z, Castro R, Sartori M, Girao M. Randomised trial of TVTO (trademark) and TVTS (trademark) for the treatment of stress urinary incontinence. Preliminary study (Abstract number 154). Neurourology and Urodynamics 2010;29(6):1025‐6. [40147] [Google Scholar]
Djehdian 2010 OPH {published data only}
- Djehdian L, Araujo M, Takano C, Roy C, Castro R, Sartori MGF, et al. Randomised trial of Ophira mini‐sling system and unitape for the treatment of stress incontinence in women. First experiences after a follow‐up of 6 months. (Abstract number 768). Proceedings of the Joint Meeting of the International Continence Society (ICS) and the International Urogynecological Association, 2010 Aug 23‐27, Toronto, Canada. 2010. [40201]
Enzelsberger 2010 ARC {published data only}
- Enzelsberger H, Cemer I, Enzelsberger S, Schalupny J. [MiniArc versus Monarc a prospective randomized study of the treatment of female stress urinary incontinence with a follow‐up of 2 years]. Geburtshilfe und Frauenheilkunde 2010;70(6):499‐502. [42521] [Google Scholar]
Friedman 2009 SEC {published data only}
- Friedman M. TVT‐O vs TVT‐S: first randomized, prospective, comparative study of intraoperative complications, perioperative morbidity and one year postoperative results (Abstract: oral presentation 12). Journal of Pelvic Medicine & Surgery 2009;15(2):48. [SR‐INCONT42743] [Google Scholar]
- Friedman M. TVT‐S vs TVT‐O: randomized, prospective comparative study of intraoperative complications, perioperative morbidity and short‐term postoperative results (Abstract number 377). International Urogynecology Journal and Pelvic Floor Dysfunction 2007;18(Suppl 1):S204. [27328] [Google Scholar]
Hinoul 2011 SEC {published data only}
- Hinoul P. A multi‐centre randomised comparison of the effectiveness and safety of TVT‐O and TVT‐S, 2008. www.trialregister.nl (accessed 20 September 2012). [45470; NTR1141]
- Hinoul P, Vervest HA, Boon J, Venema PL, Lakeman MM, Milani AL, et al. A randomized, controlled trial comparing an innovative single incision sling with an established transobturator sling to treat female stress urinary incontinence. Journal of Urology 2011;185(4):1356‐62. [41495] [DOI] [PubMed] [Google Scholar]
- Page AS, Page GH. Re: A Randomized, Controlled Trial Comparing an Innovative Single Incision Sling With an Established Transobturator Sling to Treat Female Stress Urinary Incontinence P. Hinoul, H. A. Vervest, J. den Boon, P. L. Venema, M. M. Lakeman, A. L. Milani and J. P. Roovers Journal of Urology 2011;185:1356‐62. Journal of Urology 2012;187(1):357‐8. [43003] [DOI] [PubMed] [Google Scholar]
Hota 2012 SEC {published data only}
- Hota LS, Hanaway K, Hacker MR, Disciullo A, Elkadry E, Dramitinos P, et al. TVT‐Secur (Hammock) versus TVT‐obturator: a randomized trial of suburethral sling operative procedures. Female Pelvic Medicine & Reconstructive Surgery 2012;18(1):41‐5. [44507] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kim 2010 SEC {published data only}
- Kim Y, Jung W, Jo SW, Kim WT, Yun SJ, Lee S, et al. Prospective comparative study between the TVT‐Secur and TOT procedures for treatment of stress urinary incontinence patients (Abstract number 1182). Proceedings of the Joint Meeting of the International Continence Society (ICS) and the International Urogynecological Association, 2010 Aug 23‐27, Toronto, Canada. 2010. [40209]
Lee 2010 CUR/SEC {published data only}
- Lee JS, Kim JH, Kim JH, Seo JT. One‐year surgical outcomes and quality of life in minimally invasive slings for the treatment of female stress urinary incontinence: TVT SECUR (trademark) vs. CureMesh (trademark) (Abstract number 806). Proceedings of the Joint Meeting of the International Continence Society (ICS) and the International Urogynecological Association, 2010 Aug 23‐27, Toronto, Canada. 2010. [40203]
Lee 2010 SEC {published data only}
- Kim JJ, Lee YS, Lee KS. Randomized comparative study of the U‐ and H‐type approaches of the TVT‐Secur procedure for the treatment of female stress urinary incontinence: one‐year follow‐up. Korean Journal of Urology 2010;51(4):250‐6. [39595] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee HN, Cho WJ, Han J‐Y, Choo M‐S, Lee K‐S. Randomized comparative study of the U‐ and H‐type approaches of the TVT‐Secur (trademark) procedure for the treatment of female stress urinary incontinence: two‐year follow‐up (Abstract) (Poster number NM7). Neurourology & Urodynamics 2011;30(2):259. [41375] [Google Scholar]
- Lee HN, Lee Y, Cho WJ, Lee HS, Lee K. Randomized, comparative study of the U‐ and H‐type approaches of the TVT‐Secur (trademark) procedure for the treatment of female stress urinary incontinence: two‐year follow‐up (Abstract number 849). Proceedings of the 41st Annual Meeting of the International Continence Society (ICS), 2011 Aug 29 to Sept 2, Glasgow, Scotland 2011. [42733]
- Lee K, Lee Y, Seo JT, Na YG, Seo JH, Lee JG, et al. A prospective multicenter randomized study of 'U' and 'H' approach of TVT‐SECUR procedure for the treatment of female stress urinary incontinence: one‐year follow‐up (Abstract number 5). Neurourology & Urodynamics 2009;28(7):587‐8. [35633] [Google Scholar]
- Lee KS, Lee YS, Seo JT, Na YG, Choo MS, Kim JC, et al. A prospective multicenter randomized comparative study between the U‐ and H‐type methods of the TVT SECUR procedure for the treatment of female stress urinary incontinence: 1‐year follow‐up. European Urology 2010;57(6):973‐9. [40317] [DOI] [PubMed] [Google Scholar]
Lee 2012 ARC {published data only}
- Dwyer PL, Rosamilia A, Lim YN, Lee J, Thomas E. MiniArc and Monarc suburethral sling in women with stress urinary incontinencea randomised controlled trial, 2012. www.anzctr.org (accessed 17 January 2012). [ACTRN12608000624381; SR‐INCONT43056]
- Lee J, Rosamilia A, Dwyer P, Lim YN, Thomas E, Murray C, et al. MiniArc and Monarc suburethral sling in women with stress urinary incontinencea randomised controlled trial (Abstract number 93). International Urogynecology Journal 2012;23(Suppl 2):S142‐4. [45459] [Google Scholar]
Liapis 2010 SEC {published data only}
- Liapis A, Bakas P, Creatsas G. Comparison of the TVT SECUR System "Hammock" and "U" tape positions for management of stress urinary incontinence. International Journal of Gynecology and Obstetrics 2010;111(3):233‐6. [42524] [DOI] [PubMed] [Google Scholar]
Mackintosh 2010 AJS {published data only}
- Mackintosh A. A pilot, randomised, prospective study of transobturator tape versus single incision sub‐urethral tape in the management of female, urodynamic stress incontinence [thesis]. Aberdeen, UK: University of Aberdeen, 2010. [41122] [Google Scholar]
Martan 2012 ARC AJS {published data only}
- Martan A, Masata J, Svabik K, Halaska M, Zachoval R, Horcicka L, et al. Evaluation of experience with MiniArc and Ajust system mini‐sling anti‐incontinence procedures, considering changes in the cure rate over time (Abstract number 165). International Urogynecology Journal 2012; Vol. 23, issue Suppl 2:S217‐8. [45464]
- Martan A, Masata J, Svabik K, Halaska M, Zachoval R, Horcicka L, et al. Evaluation of experience with Miniarc and Ajust system mini‐sling anti‐incontinence procedures (Abstract number 4). Neurourology & Urodynamics 2012;31(6):729‐30. [45304] [Google Scholar]
- Martan A, Svabik K, Halaska M, Zachoval R, Horcicka L, Krhut J. [Evaluation of initial experience with safety and short efficacy of mini‐sling antiincontinence procedures MiniArc and AJUST system]. [Czech]. Ceska Gynekologie 2011;76(5):349‐55. [43009] [PubMed] [Google Scholar]
Masata 2012 SEC {published data only}
- Masata J, Svabik K, Drahoradova P, Hubka P, Zvara K, El‐Haddad R, et al. Randomized prospective trial of a comparison of the efficacy of TVT‐O and TVT Secur system in the treatment of stress urinary incontinent women comparison of the long‐ and short‐term results (Abstract number 3). Neurourology and Urodynamics 2011;30(6):805‐6. [42163] [Google Scholar]
- Masata J, Svabik K, Hubka P, Elhaddad R, Drahoradova P, Martan A. What happens with single incision tape (TVT‐S) after surgery, in comparison with TVT‐O? an ultrasound study results from a randomized trial (Abstract number 23). International Urogynecology Journal 2012;23(Suppl 2):S69‐71. [45468] [Google Scholar]
- Masata J, Svabik K, Hubka P, Zvara K, Haddad R, Drahoradova P, et al. Is the fixation of single incision tape (TVT‐S) as good as a transobturator tape (TVT‐O)? An ultrasound study, results from randomized trial (Abstract number 6). Neurourology & Urodynamics 2012;31(6):731‐3. [45456] [Google Scholar]
- Masata J, Svabik K, Zvara K, Drahodradova P, Hubka P, Elhaddad R, et al. [Comparison of short term results of TVT‐O and TVT‐S in the surgical treatment of stress urinary incontinence]. [Czech]. Ceska Gynekologie 2012;77(4):350‐7. [45851] [PubMed] [Google Scholar]
- Masata J, Svabik K, Zvara K, Drahoradova P, Haddad R, Hubka P, et al. Randomized trial of a comparison of the efficacy of TVT‐O and single‐incision tape TVT SECUR systems in the treatment of stress urinary incontinent women‐2‐year follow‐up. International Urogynecology Journal 2012;23(10):1403‐12. [45853] [DOI] [PubMed] [Google Scholar]
Mostafa 2012 AJS {published data only}
- Boyers D, Kilonzo M, Mostafa A, Abdel‐Fattah M. Single incision mini‐slings versus standard mid‐urethral slings in surgical management of female stress urinary incontinence: a cost‐effectiveness analysis alongside a randomised controlled trial (Abstract number 2). Neurourology & Urodynamics 2012;31(6):726‐7. [45457] [Google Scholar]
- Mostafa A, Agur W, Abdel‐All M, Guerrero K, Allam M, Lim C, et al. A multicentre randomised trial of single‐incision mini‐sling (AJUSTc) and tension‐free vaginal tape‐obturator (TVT‐O trademark) in management of female stress urinary incontinence (Abstract number 4). Neurourology and Urodynamics 2011;30(6):806‐8. [42164] [Google Scholar]
- Mostafa A, Agur W, Abdel‐All M, Guerrero K, Lim C, Allam M, et al. A multicentre prospective randomised study of single‐incision mini‐sling (Ajust([REGISTERED])) versus tension‐free vaginal tape‐obturator (TVT‐OTM) in the management of female stress urinary incontinence: pain profile and short‐term outcomes. European Journal of Obstetrics, Gynecology, & Reproductive Biology 2012;165(1):115‐21. [45867] [DOI] [PubMed] [Google Scholar]
- Mostafa A, Agur W, Abdel‐All M, Guerrero K, Lim C, Allam M, et al. Multicentre prospective randomised study of single‐incision midurethral sling (SIMS‐ Ajust∏) versus tension‐free vaginal tape‐obturator (TVT‐OTM) in management of female stress urinary Incontinence (SUI): a minimum of one year follow‐up (Abstract number 1). Neurourology & Urodynamics 2012;31(6):724‐5. [45454] [Google Scholar]
- Mostafa A, Swami S, Fielding S, N'Dow J, Abdel‐Fattah M. Exploring factors affecting women's decision to participate in randomised controlled trials assessing surgical treatment for stress urinary incontinence (Abstract number 359). Proceedings of the 41st Annual Meeting of the International Continence Society (ICS), 2011 Aug 29 to Sept 2, Glasgow, Scotland. 2011. [42217; NCT01230450]
Oliveira 2011 ARC SEC {published data only}
- Oliveira R, Botelho F, Silva P, Resende A, Silva C, Dinis P, et al. Exploratory study assessing efficacy and complications of TVT‐O, TVT‐Secur, and Mini‐Arc: results at 12‐month follow‐up. European Urology 2011;59(6):940‐4. [41493] [DOI] [PubMed] [Google Scholar]
- Santos Oliveira R, Botelho F, Silva P, Silva CMPM, Dinis P, Cruz FJMR. Randomized clinical trial comparing TVT‐O (trademark), TVT‐Secur (trademark) and Mini‐Arc (trademark). Outcome at 12 months follow‐up (Abstract 391). European Urology Supplements 2010;9(2):145. [41579] [Google Scholar]
Palomba 2012 AJS ARC SEC {published data only}
- Palomba S, Oppedisano R, Torella M, Falbo A, Maiorana A, Materazzo C, et al. A randomized controlled trial comparing three vaginal kits of single‐incision mini‐slings for stress urinary incontinence: surgical data. European Journal of Obstetrics Gynecology and Reproductive Biology 2012;163(1):108‐12. [44508] [DOI] [PubMed] [Google Scholar]
Pardo 2010 SEC ARC {published data only}
- Pardo J, Sola V, Ricci P. Effectiveness of TVT‐Secur compared with MiniArc for stress urinary incontinence: a randomized controlled trial with mini‐sling (Abstract number 221). Neurourology and Urodynamics 2010;29(6):1126‐7. [40161] [Google Scholar]
Schweitzer 2012 AJS {published data only}
- Schweitzer KJ, Cromheecke GJ, Milani AL, Eijndhoven HW, Gietelink D, Hallenleben E, et al. A randomised controlled trial comparing the TVT‐O® with the Ajust® as primary surgical treatment of female stress urinary incontinence. (Abstract number 32). International Urogynecology Journal 2012;23(Suppl 2):S77‐8. [45467] [Google Scholar]
Seo 2011 SEC {published data only}
- Seo JH, Kim GN, Kim JY, Seo HJ, Lee JW, Lee WG, et al. Comparison between transobturator vaginal tape inside out and single incision sling system in the treatment of female stress urinary incontinence: prospective randomized study (Abstract number 23). Neurourology and Urodynamics 2011;30(6):832. [42169] [Google Scholar]
Sivaslioglu 2012 TFS {published data only}
- Sivaslioglu AA, Unlubilgin E, Aydogmus S, Celen E, Dolen I. A prospective randomized comparison of transobturator tape and tissue fixation system minisling in 80 patient with stress urinary incontinence 5 year results. Journal of Urology 2012;188(1):194‐9. [43318] [DOI] [PubMed] [Google Scholar]
- Sivaslioglu AA, Unlubilgin E, Aydogmus S, Celen E, Dolen I. A prospective randomized comparison of transobturator tape and tissue fixation system minisling in 80 patient with stress urinary incontinence—3 year results. Pelviperineology 2010;29(2):56‐9. [43317] [Google Scholar]
- Sivaslioglu AA, Unlubilgin E, Dolen I, Kaplan M. The comparison of tissue fixation (TFS) system with transobturator tape (TOT) in the treatment of stress urinary incontinence (Abstract number 61). International Urogynecology Journal and Pelvic Floor Dysfunction 2007;18(Suppl 1):S36‐7. [27327] [Google Scholar]
Smith 2011 ARC {published data only}
- Smith AL, Castillo P, Karp D, Gross C, Davila G, Aguilar VC. Transobturator versus single incision slings in women with stress urinary incontinence: a prospective randomised controlled trial (Abstract presentation number 52). International Urogynecology Journal 2011;22 Suppl 1:S54‐5. [45303] [Google Scholar]
Sottner 2012 ARC AJS {published data only}
- Sottner O, Halaska M, Vlacil J, Maxova K, Mala I, Krombholz R, et al. [A comparison of different types of suburethral slings in the treatment of urinary incontinence in geriatric patients]. [Czech]. Ceska Gynekologie 2012;77(5):403‐7. [45893] [PubMed] [Google Scholar]
Tommaselli 2010 SEC {published data only}
- Tommaselli GA, Carlo C, Gargano V, Formisano C, Scala M, Nappi C. Efficacy and safety of TVT‐O and TVT‐Secur in the treatment of female stress urinary incontinence: 1‐year follow‐up. International Urogynecology Journal 2010;21(10):1211‐7. [40921] [DOI] [PubMed] [Google Scholar]
Wang 2011 SEC {published data only}
- Wang YJ, Li FP, Wang Q, Yang S, Cai XG, Chen YH. Comparison of three mid‐urethral tension‐free tapes (TVT, TVT‐O, and TVT‐Secur) in the treatment of female stress urinary incontinence: 1‐year follow‐up. International Urogynecology Journal 2011;22(11):1369‐74. [42639] [DOI] [PubMed] [Google Scholar]
Yoon 2011 NDL {published data only}
- Yoon H, Lee DH, Kim YJ. Early results of comparison of Contasure‐needleless (trademark) and TOT outside‐in midurethral slings (Abstract number 852). Proceedings of the 41st Annual Meeting of the International Continence Society (ICS), 2011 Aug 29 to Sept 2, Glasgow, Scotland. 2011. [42238]
References to studies excluded from this review
Araco 2011 {published data only}
- Araco F, Gravante G, Sorge R, Overton J, Castri F, Primicerio M, et al. Sedation with local versus general anesthesia for the tension‐free vaginal tape Secur hammock procedure. International Journal of Gynaecology & Obstetrics 2011;113(2):108‐11. [DOI] [PubMed] [Google Scholar]
Choo 2011 {published data only}
- Choo M‐S, Lee K‐S, Lee HN, Lee YS, Seo JT. Clinical evaluation of the Needleless® Sling, 2011. www.ClinicalTrials.gov (accessed 1 March 2013). [42755]
de Leval 2011 {published data only}
- Leval J, Thomas A, Waltregny D. The original versus a modified inside‐out transobturator procedure: 1‐year results of a prospective randomized trial. International Urogynecology Journal 2011;22(2):145‐56. [40993] [DOI] [PubMed] [Google Scholar]
Diallo 2012 {published data only}
- Diallo S, Cour F, Josephson A, Vidart A, Botto H, Lebret T, et al. Evaluating single‐incision slings in female stress urinary incontinence: the usefulness of the CONSORT statement criteria. Urology 2012;80(3):535‐41. [DOI] [PubMed] [Google Scholar]
Martan 2008 {published data only}
- Martan A, Svabik K, Masata J, Koleska T, Haddad R, Pavlikova M. [The solution of stress urinary incontinence in women by the TVT‐S surgical method—correlation between the curative effect of this method and changes in ultrasound findings]. [Czech]. Ceska Gynekologie 2008;73(5):271‐7. [29223] [PubMed] [Google Scholar]
Okulu 2011 {published data only}
- Okulu E. Synthetic mesh materials in sling surgery, 2011. www.ClinicalTrials.gov (accessed 1 March 2013). [SR‐INCONT42756]
Porena 2012 {published data only}
- Porena M. Urinary incontinence and uro‐genital prolapse: a randomized trial of pelvic organ prolapse repair plus mini‐sling versus pelvic organ prolapse repair alone, 2012. www.ClinicalTrials.gov (accessed 1 March 2013). [SR‐INCONT45469]
References to studies awaiting assessment
Pushkar 2011 {published data only}
- Pushkar' DI, Kasian GR, Gvozdev MI, Lynova IL, Kupriianov IA. [Mini‐invasive operations for correction of urinary incontinence in females] [Russian]. Urologiia (Moscow, Russia) 2011, issue 4:16‐20. [SR‐INCONT43390] [PubMed]
References to ongoing studies
Foote 2012 {published data only}
- Foote A. A randomised trial comparing two vaginal prolene sling surgeries for female urinary incontinence, 2012. www.anzctr.org (accessed 1 March 2013). [45458]
Maslow 2011 {published data only}
- Maslow KD. Trial comparing TVT SECUR system and transvaginal obturator tape for surgical management of stress urinary incontinence, 2011. www.ClinicalTrials.gov (accessed 1 March 2013). [SR‐INCONT42750]
Robert 2012 {published data only}
- Robert M, Ross S, Schulz J. Transvaginal tape (TVT) Secur versus TVT randomised controlled trial (RCT), 2012. www.ClinicalTrials.gov (accessed 1 March 2013). [SR‐INCONT43064]
Rosamilia 2012 {published data only}
Additional references
Abdel‐Fattah 2011
- Abdel‐Fattah M, Ford JA, Lim CP, Madhuvrata P. Single‐incision mini‐slings versus standard midurethral slings in surgical management of female stress urinary incontinence: a meta‐analysis of effectiveness and complications. European Urology 2011;60(3):468‐80. [DOI] [PubMed] [Google Scholar]
Bergman 1995
- Bergman A, Elia G. Three surgical procedures for genuine stress incontinence: five‐year follow‐up of a prospective randomized study. American Journal of Obstetrics & Gynecology 1995;173(1):66‐71. [DOI] [PubMed] [Google Scholar]
Bezerra 2005
- Bezerra CCB, Bruschini H, Cody JD. Traditional suburethral sling operations for urinary incontinence in women. Cochrane Database of Systematic Reviews 2005, Issue 3. [DOI: 10.1002/14651858.CD001754.pub2] [DOI] [PubMed] [Google Scholar]
Birnbaum 2004
- Birnbaum HG, Leong SA, Oster EF, Kinchen K, Sun P. Cost of stress urinary incontinence: a claims data analysis. Pharmacoeconomics 2004;22(2):95‐105. [PUBMED: 14731051] [DOI] [PubMed] [Google Scholar]
Boyers 2013
- Boyers D, Kilonzo M, Mostafa A, Abdel‐Fattah M. Comparison of an adjustable anchored single‐incision mini‐sling, Ajust , with a standard mid‐urethral sling, TVT‐O : a health economic evaluation. BJU international 2013;112(8):1169‐77. [DOI] [PubMed] [Google Scholar]
Castañeda 2014
- Castañeda E, Sanz‐Granda Á, Hidalgo A, Meza D, Carreras M, Marqueta J. Cost effectiveness analysis of surgical treatment of stress urinary incontinence using single‐incision mini‐slings vs. tension‐free vaginal obturator in Spain. Surgical Research ‐ Open Journal 2014;1(1):17‐24. [DOI: 10.17140/SROJ-1-103] [DOI] [PubMed] [Google Scholar]
Chong 2011
- Chong E, Khan A, Anger J. The financial burden of stress urinary incontinence among women in the United States. Current Urology Reports 2011;12(5):358‐62. [DOI: 10.1007/s11934-011-0209-x.] [DOI] [PubMed] [Google Scholar]
Debodinance 2008
- Debodinance P, Lagrange E, Amblard J, Lenoble C, Lucot J.‐P, Villet R, et al. TVT SecurTM: more and more minimally invasive. Preliminary prospective study on 110 cases. Journal de Gynécologie Obstétrique et Biologie de la Reproduction 2008;37:229‐36. [DOI] [PubMed] [Google Scholar]
Delorme 2001
- Delorme E. Transobturator urethral suspension: mini‐invasive procedure in the treatment of stress urinary incontinence in women. Progres en Urologie 2001;11(6):1306‐13. [PubMed] [Google Scholar]
Gauruder‐Burmester 2009
- Gauruder‐Burmester A, Popken G. The MiniArc® sling system in the treatment of female stress urinary incontinence. International Brazilian Journal of Urology 2009;35(3):334‐43. [DOI] [PubMed] [Google Scholar]
Hampel 1997
- Hampel C, Wienhold D, Benken N, Eggersmann C, Thuroff JW. Definition of overactive bladder and epidemiology of urinary incontinence. Urology 1997;50(Suppl):4‐14. [DOI] [PubMed] [Google Scholar]
Higgins 2003
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analyses. BMJ 2003;327(7414):557‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. www.cochrane‐handbook.org.
Hunskaar 2002
- Hunskaar S, Burgio K, Diokno AC, Herzog AR, Hjalmas K, Lapitan MC. Epidemiology and natural history of urinary incontinence (UI). In: Abrams P, Cardozo L, Khoury S editor(s). Incontinence. 2nd Edition. Plymouth, UK: Health Publication Ltd, 2002. [Google Scholar]
Jeffery 2010
- Jeffery S, Acharyya R, Algar M, Makhene M, Makhene M. Mini‐sling procedures in stress urinary incontinence: a systematic review of efficacy and complications (Abstract number 5). Neurourology and Urodynamics 2010;29(6):811‐2. [Google Scholar]
Kilonzo 2004
- Kilonzo M, Vale L, Stearns S, Grant A, Cody J, Glazener C, et al. Cost effectiveness of tension‐free vaginal tape for the surgical management of female stress incontinence. International Journal of Technology Assessment in Health Care 2004;20(4):455‐63. [DOI] [PubMed] [Google Scholar]
Kunkle 2015
- Kunkle C, Hallock J, Hu X, Blomquist J, Thung S, Werner E. Cost Utility Analysis of Urethral Bulking Agents Versus Midurethral Sling in Stress Urinary Incontinence. Female Pelvic Medicine & Reconstructive Surgery. Female Pelvic Medicine & Reconstructive Surgery 2015;21(3):154‐9. [DOI] [PubMed] [Google Scholar]
Lapitan 2012
- Lapitan MCM, Cody JD. Open retropubic colposuspension for urinary incontinence in women. Cochrane Database of Systematic Reviews 2012, Issue 6. [DOI: 10.1002/14651858.CD002912.pub5] [DOI] [PMC free article] [PubMed] [Google Scholar]
Latthe 2007
- Latthe P, Foon R, Toozs‐Hobson P. Transobturator and retropubic tape procedures in stress urinary incontinence: a systematic review and meta‐analysis of effectiveness and complications. BJOG: an international journal of obstetrics and gynaecology 2007;114:522‐31. [DOI] [PubMed] [Google Scholar]
Meschia 2009
- Meschia M, Barbacini P, Ambrogi V, Pifarotti P, Ricci L, Spreafico L. TVT‐secur: a minimally invasive procedure for the treatment of primary stress urinary incontinence. One year data from a multi‐centre prospective trial. International Urogynecology Journal 2009;20:313‐7. [DOI] [PubMed] [Google Scholar]
Milsom 2009
- Milsom I, Altman D, Lapitan MC, Nelson R, Sillén U, Thom D. Epidemiology of urinary (UI) and faecal (FI) incontinence, pelvic organ prolapse (POP). In: Abrams P. Cardozo L, Khoury S, Wein A editor(s). Incontinence: 4th International Consultation on Incontinence, July 5‐8 2008. 4th Edition. Plymouth, UK: Health Publication Ltd, 2009. [Google Scholar]
Molden 2008
- Molden SM, Lucente VR. New minimally invasive slings: TVT secur. Current Urology Reports 2008;9(5):358‐61. [DOI] [PubMed] [Google Scholar]
Moore 2009
- Moore RD, Serels SR, Davila GW, Settle P. Minimally invasive treatment for female stress urinary incontinence (SUI): a review including TVT, TOT, and mini‐sling. Surgery Technology International 2009;18:157‐73. [PubMed] [Google Scholar]
Mostafa 2012
- Mostafa A, Agur W, Abdel‐All M, Guerrero K, Lim C, Allam M, et al. A multicentre prospective randomised study of single‐incision mini‐sling (Ajust) versus tension‐free vaginal tape‐obturator (TVT‐O) in the management of female stress urinary incontinence: pain profile and short‐term outcomes. European Journal of Obstetrics & Gynecology and Reproductive Biology 2012;165(1):115‐21. [DOI] [PubMed] [Google Scholar]
Nambiar 2012
- Nambiar A, Madden T, Lucas M. Retropubic vs transobturator slings for stress incontinence: a comprehensive systematic review and meta‐analysis of efficacy and adverse events. (Abstract number 255). Neurourology and Urodynamics 2012;31(6):1058‐9. [Google Scholar]
Ogah 2009
- Ogah J, Cody JD, Rogerson L. Minimally invasive synthetic suburethral sling operations for stress urinary incontinence in women. Cochrane Database of Systematic Reviews 2009, Issue 4. [DOI: 10.1002/14651858.CD006375.pub2] [DOI] [PubMed] [Google Scholar]
Petros 1993
- Petros PE, Ulmsten UI. An integral theory and its method for the diagnosis and management of female urinary incontinence. Scandinavian Journal of Urology & Nephrology 1993;153(Suppl):1‐93. [PubMed] [Google Scholar]
Reference Manager 2012
- Reference Manager Professional Edition Version 12. New York: Thomson Reuters, 2012.
Rehman 2011
- Rehman H, Bezerra CCB, Bruschini H, Cody JD. Traditional suburethral sling operations for urinary incontinence in women. Cochrane Database of Systematic Reviews 2011, Issue 1. [DOI: 10.1002/14651858.CD001754.pub3] [DOI] [PubMed] [Google Scholar]
Subak 2008
- Subak L, Brubaker, L, Chai T, Creasman J, Diokno A, et al. High Costs of Urinary Incontinence Among Women Electing Surgery to Treat Stress Incontinence. Obstetrics & Gynecology 2008;111(4):899‐907. [DOI: 10.1097/AOG.0b013e31816a1e12] [DOI] [PMC free article] [PubMed] [Google Scholar]
Tommaselli 2011
- Tommaselli GA, Carlo C, D'Afiero A, Formisano C, Fabozzi A, Nappi C. Efficacy and safety of TVT‐secure (trademark) in the treatment of female stress urinary incontinence: a systematic review (Abstract number 867). Proceedings of the 41st Annual Meeting of the International Continence Society (ICS), 2011 Aug 29 to Sept 2, Glasgow, Scotland. 2011.
Turner 2004
- Turner DA, Shaw C, McGrother CW, Dallosso HM, Cooper NJ, MRC Incontinence Team. The cost of clinically significant urinary storage symptoms for community dwelling adults in the UK. BJU International 2004;93(9):1246‐52. [DOI] [PubMed] [Google Scholar]
Ulmsten 1998
- Ulmsten U, Falconer C, Johnson P, Jomaa M, Lannér L, Nilsson CG, et al. A multicenter study of tension‐free vaginal tape (TVT) for surgical treatment of stress urinary incontinence. International Urogynecology Journal and Pelvic Floor Dysfunction 1998;9(4):210‐3. [DOI] [PubMed] [Google Scholar]
Wagner 1998
- Wagner T, Hu T. Economic costs of urinary incontinence in 1995. Urology 1998;51(3):355‐61. [DOI] [PubMed] [Google Scholar]
Walsh 2011
- Walsh CA. TVT‐Secur mini‐sling for stress urinary incontinence: a review of outcomes at 12 months. [Review]. BJU International 2011;108(5):652‐7. [DOI] [PubMed] [Google Scholar]
Ward 2008
- Ward KL, Hilton P, UK and Ireland TVT Trial Group. Tension‐free vaginal tape versus colposuspension for primary urodynamic stress incontinence: 5‐year follow up. BJOG: an international journal of obstetrics and gynaecology 2008;115(2):226‐33. [DOI] [PubMed] [Google Scholar]


