Abstract
Background
Anterior vaginal repair (anterior colporrhaphy) is an operation traditionally used for moderate or severe stress urinary incontinence (SUI) in women. About a third of adult women experience urinary incontinence. SUI imposes significant health and economic burden to the society and the women affected.
Objectives
To determine the effects of anterior vaginal repair (anterior colporrhaphy) on urinary incontinence in comparison with other management options.
Search methods
We searched the Cochrane Incontinence Group Specialised Trials Register (searched 1 September 2009) and the reference lists of relevant articles.
Selection criteria
Randomised or quasi‐randomised trials that included anterior vaginal repair for the treatment of urinary incontinence.
Data collection and analysis
Two review authors independently extracted data and assessed trial quality. Three trial investigators were contacted for additional information.
Main results
Ten trials were identified which included 385 women having an anterior vaginal repair and 627 who received comparison interventions.
A single small trial provided insufficient evidence to assess anterior vaginal repair in comparison with physical therapy. The performance of anterior repair in comparison with bladder neck needle suspension appeared similar (risk ratio (RR) for failure after one year 1.16, 95% confidence interval (CI) 0.86 to 1.56), but clinically important differences could not be confidently ruled out. No trials compared anterior repair with suburethral sling operations or laparoscopic colposuspensions, or compared alternative vaginal operations.
Anterior vaginal repair was less effective than open abdominal retropubic suspension based on patient‐reported cure rates in eight trials both in the medium term (failure rate within one to five years after anterior repair 97/259 (38%) versus 57/327 (17%); RR 2.29, 95% confidence Interval (CI) 1.70 to 3.08) and in the long term (after five years, (49/128 (38%) versus 31/145 (21%); RR 2.02, 95% CI 1.36 to 3.01). There was evidence from three of these trials that this was reflected in a need for more repeat operations for incontinence (25/107 (23%) versus 4/164 (2%); RR 8.87, 95% CI 3.28 to 23.94). These findings held, irrespective of the co‐existence of prolapse (pelvic relaxation). Although fewer women had a prolapse after anterior repair (RR 0.24, 95% CI 0.12 to 0.47), later prolapse operation appeared to be equally common after vaginal (3%) or abdominal (4%) operation.
In respect of the type of open abdominal retropubic suspension, most data related to comparisons of anterior vaginal repair with Burch colposuspension. The few data describing comparison of anterior repair with the Marshall‐Marchetti‐Krantz procedure were consistent with those for Burch colposuspension.
Authors' conclusions
There were not enough data to allow comparison of anterior vaginal repair with physical therapy or needle suspension for primary urinary stress incontinence in women. Open abdominal retropubic suspension appeared to be better than anterior vaginal repair judged on subjective cure rates in eight trials, even in women who had prolapse in addition to stress incontinence (six trials). The need for repeat incontinence surgery was also less after the abdominal operation. However, there was not enough information about postoperative complications and morbidity.A Brief Economic Commentary (BEC) identified one study suggesting that vaginoplasty may be more cost‐effective compared with tension‐free vaginal tape (TVT‐O).
Plain language summary
Anterior vaginal repair for urinary incontinence in women
Urinary incontinence is the inability to prevent urine leakage. Stress urinary incontinence is loss of urine when a person coughs or exercises. A significant amount of a woman's or her families income can be spent on management of stress urinary incontinence. Damage to the muscles that hold up the bladder, and injuries to the nerves during childbirth, may be causes. When non‐surgical methods, such as exercising the muscles in the pelvic floor (the base of the abdomen), have not worked, surgery is sometimes used to lift and support the bladder. Anterior vaginal repair aims to achieve this, operating through the vaginal wall. The review of 10 trials in 1012 women found some evidence that surgery through the abdomen may be better than vaginal repair. However, there was not enough information about side‐effects, or in comparison with other physical or surgical methods of treating urine leakage.
Background
Incontinence of urine is a common and potentially debilitating problem. A degree of incontinence is reported by between 17% and 45% of adult women (Jolleys 1988; Thomas 1980). Some degree of stress incontinence affects around a third of women of childbearing age (MacArthur 1991; Wilson 1996). The outcome of care is often unsatisfactory. This reflects uncertainty about which of the available treatment options are the most appropriate and effective, which may in part be due to lack of standardisation of diagnostic criteria and outcomes in studies investigating this issue (Blaivas 1997a; Blaivas 1997b).
Stress Urinary Incontinence (SUI) constitutes a huge financial economic burden to society. In the USA, the annual total direct costs of urinary incontinence in both men and women is over USD 16 billion (1995 USD) (Chong 2011) with a societal cost of USD 26.2 billion (1995 USD) (Wagner 1998). Approximately, USD 13.12 billion (1995 USD) of the total direct costs of urinary incontinence is spent on SUI (Chong 2011; Kunkle 2015). About 70% of this USD 13.12 billion is borne by the patients, mainly through routine care (purchasing pads, diapers, laundry and dry cleaning). This constitutes a significant individual financial burden. Of the remaining 30% of costs, 14% is spent on nursing home admission, 9% on treatment, 6% on addressing complications and 1% on diagnosis (Chong 2011).
A study in the USA reported that about 1% of the median annual household income (USD 50,000 to USD 59,999 in 2006) was spent by women on incontinence management. This study estimated that women spent an annual mean cost of USD 751 to USD 1277 (2006 USD) on incontinence. This cost increases with the severity of the symptoms (Subak 2008). The indirect cost associated exerts a social and psychological burden which is unquantifiable. (Chong 2011; Kilonzo 2004). Nevertheless, Birnbaum 2004 estimated that the annual average direct medical costs of SUI for one year (1998 USD) was USD 5642 and USD 4208 for indirect workplace costs. The cost of management and treatment of SUI appears to have increased over time due to increasing prevalence and increased desire for improved QOL. This in turn has resulted from improved recognition of the condition, as well as increased use of surgical and non‐surgical management procedures.
Description of the condition
Continence is maintained by a combination of an intact sphincter urethrae (the muscle around the junction between the bladder and the urethra, which encircles the top half of the urethra), normal abdominal pressure transmission to the proximal urethra (the part of the urethra where it enters the bladder), and structural and functional integrity of the neuro‐musculature and fascia (nerves, muscles and connective tissue) of the pelvic floor. This requires a 'compliant' enlargement of the bladder, achieved by active relaxation of the bladder muscle during filling. Normal voiding occurs when the muscles of the sphincter and pelvic floor relax under voluntary control, and the detrusor muscle (in the bladder wall) contracts.
Incontinence can result from damage to the nerve supply to the bladder or the pelvic floor muscles, or from direct mechanical trauma to the pelvic floor. The risk is increased by vaginal (particularly assisted) delivery, increasing age and parity, obesity and the menopause (MacArthur 1993; Thom 1997; Wilson 1996).
There are different types of urinary incontinence.
'Stress urinary incontinence' (SUI) is defined as the symptom of involuntary loss of urine associated with physical exertion (such as coughing, exercise, and changes of position) (Abrams 2002). It is a symptom, not a condition, which may be caused by pathological, anatomical or physiological factors (Blaivas 1997a).
The International Continence Society defines 'urodynamic stress incontinence' (USI) as the involuntary loss of urine occurring when, in the absence of a detrusor (bladder wall muscle) contraction, the intravesical (bladder) pressure exceeds the urethral pressure (Abrams 1988; Blaivas 1997a). Diagnosis based on this definition therefore requires urodynamic investigation in addition to history taking, physical examination, frequency/volume charts and urine analysis.
Both patients with the symptoms of 'stress urinary incontinence' (based on clinical evaluation without urodynamics) and those diagnosed by urodynamics as having 'urodynamic stress incontinence' (USI) were included in this review.
Two types of stress incontinence are recognised: one resulting from a hypermobile but otherwise normal urethra, and one from deficiency of the sphincter itself (Blaivas 1988). Available investigations, such as urethral pressure profilometry and leak point pressures, have been proposed to distinguish between these two types (Bump 1997), but await validation, and at present have no accepted normal values or reliable cut‐off points (Blaivas 1998; McGuire 1993). The two types are considered together for the purpose of this review for three reasons: first, to date, few studies have distinguished between them; second, a standardised test is not available to differentiate between them accurately; and third, it is likely that some patients have a combination of these two conditions. In addition, the International Continence Society has recently suggested that this division may be simplistic and arbitrary, and that further research is required before these are accepted as distinct categories (Abrams 2002).
Further types of urinary incontinence are also recognised.
'Urge urinary incontinence' (UUI) is the symptom of involuntary loss of urine associated with a sudden, strong desire to void (urgency).
'Detrusor overactivity' (DO) is a diagnosis that denotes involuntary detrusor muscle contractions that are not due to neurological disorders, and the diagnosis must be made using urodynamic techniques (Abrams 2002; Blaivas 1997a). Urge incontinence is usually associated with involuntary contractions of the bladder wall muscle.
When urge incontinence co‐exists with stress incontinence, the person affected is said to have 'mixed urinary incontinence' (MUI). Patients with MUI were included in this review. They could have symptoms of stress plus urge incontinence or other urinary symptoms (diagnosed clinically); or urodynamic stress incontinence (USI) plus detrusor overactivity (diagnosed using urodynamics); or stress plus other types of incontinence or other urinary symptoms.
Description of the intervention
Treatments for urinary incontinence include conservative, pharmacological and surgical interventions. Conservative treatments centre on physical methods, including pelvic floor muscle training, electrical stimulation, biofeedback and weighted cones. Mechanical devices that prevent or reduce urinary leakage are available, such as meatal plugs/patches and urethral and vaginal inserts. Drug therapies, principally oestrogens (Cody 2009), and less often adrenergic agents (Alhasso 2005), can be used. Conservative therapy such as pelvic floor muscle training is generally undertaken before resorting to surgery (Hay‐Smith 2006). These interventions are the subjects of separate Cochrane reviews.
This review focuses on anterior vaginal repair (anterior colporrhaphy).
Anterior vaginal repair (anterior colporrhaphy) is a surgical approach through the vagina. The vaginal mucosa below the urethra is dissected, ending just in front of the cervix. One to three sutures (often referred to as Kelly sutures) are placed in the peri‐urethral tissue and the pubocervical fascia to support and elevate the bladder neck. Excess vaginal tissue is removed and then the dissected area is closed. A wide variety of techniques and modifications have been described, including Bologna procedure, Kelly‐Kennedy, Marion Kelly, diaphragmplasty, vaginal urethrocystopexy, cystocele repair and Kelly plication (Downs 1996).
Some women with urinary incontinence have a co‐existent vaginal prolapse (pelvic relaxation). There is debate about whether the prolapse needs to be repaired at the same time as the continence procedure, and if so, how it should be done. In this review, trials of continence procedures which report separately on women with co‐existent prolapse are also included.
How the intervention might work
Surgical procedures to remedy urinary incontinence generally aim to lift and support the urethro‐vesical junction. There is disagreement, however, regarding the precise mechanism by which continence is achieved. The choice of procedures is often influenced by co‐existent problems, surgeon's preference and the physical features of the person affected. Numerous surgical methods have been described, but essentially they fall into seven categories.
Open abdominal retropubic suspension (e.g. Burch colposuspension, Marshall‐Marchetti‐Krantz) (Lapitan 2009).
Laparoscopic colposuspension (Dean 2006).
Anterior vaginal repair (anterior colporrhaphy) (e.g. Pacey, Kelly) (current review).
Suburethral sling procedures (Bezerra 2005); and minimally invasive synthetic suburethral sling operations (Ogah 2009).
Bladder neck needle suspensions (e.g. Pereyra, Stamey) (Glazener 2004).
Peri‐urethral injections (Keegan 2007).
Artificial sphincters.
Why it is important to do this review
The wide variety of surgical treatments for urinary incontinence indicates the lack of consensus as to which procedure is the best. Guidelines using the available literature have been published, but were based on studies of mixed quality (Fantl 1996; Leach 1997). Provided that a sufficient number of trials of adequate quality have been conducted, the most reliable evidence is likely to come from consideration of all well‐designed randomised controlled trials.
Hence, there is a need for an easily accessible, periodically updated, comprehensive systematic review of such trials, which will not only help to identify optimal practice, but also highlight gaps in the evidence base.
Objectives
To determine the effects of anterior vaginal repair (anterior colporrhaphy) on stress or mixed urinary incontinence in women
The following comparisons were made:
anterior vaginal repair versus no treatment or sham operation;
anterior vaginal repair versus conservative interventions (physical therapies such as pelvic floor muscle training, electrical stimulation, cones, biofeedback; lifestyle interventions such as weight loss, fluid changes, modification of activities; behavioural therapies such as bladder training; and devices such as urethral plugs, pessaries);
anterior vaginal repair versus open abdominal retropubic suspensions (abdominal surgery, e.g. Burch colposuspension, Marshall‐Marchetti‐Krantz) for all women;
anterior vaginal repair (vaginal surgery) versus abdominal surgery (open abdominal retropubic suspension) for women with co‐existent prolapse;
anterior vaginal repair versus bladder neck needle suspensions (abdominal and vaginal surgery);
anterior vaginal repair versus suburethral sling procedures (abdominal and vaginal surgery);
anterior vaginal repair versus laparoscopic colposuspensions;
different methods of anterior vaginal repair compared with others.
Methods
Criteria for considering studies for this review
Types of studies
All randomised or quasi‐randomised trials studying the effectiveness of treatment for stress or mixed urinary incontinence in women, in which at least one management arm involved anterior vaginal repair.
Types of participants
Adult women with urinary incontinence diagnosed as having:
urodynamic stress incontinence (urodynamic diagnosis); or
stress urinary incontinence (clinical diagnosis); or
mixed urinary incontinence (any stress incontinence plus other urinary symptoms, e.g. detrusor overactivity (urodynamic diagnosis), or urge urinary incontinence (clinical diagnosis), frequency or other urinary problems).
Classification of diagnoses was accepted as defined by the trialists.
Types of interventions
At least one arm of a trial must have involved anterior vaginal repair (anterior colporrhaphy) to treat stress or mixed urinary incontinence. Comparison interventions included other surgical techniques, drugs or conservative therapies. Surgery classed as open abdominal retropubic suspension included Burch colposuspension and Marshall‐Marchetti‐Krantz. Non‐prespecified comparison interventions were to be included if found.
Types of outcome measures
We selected the outcome measures used in this review on the basis of their relevance to the clinical cure or improvement of incontinence. We regard the principal measures of effectiveness as the proportion of patients cured (continent or dry) following surgery, and the proportion of women whose condition is improved.
We adopted the recommendations made by the Standardisation Committee of the International Continence Society for outcomes of research investigating the effect of therapeutic interventions for women with urinary incontinence. These outcome categories include: women's observation (symptoms), quantification of symptoms, the clinician's measures (anatomical and functional), and quality of life (Lose 1998).
Trialists obtained data from history and questionnaire assessment, supplemented by the use of urinary diaries (including time and type of incontinence, frequency of micturition and voided volumes) and pad tests (quantitative estimate of weight of urine lost under standard conditions). This review also included other surgical measures and adverse events as outcome measures.
A. Women's observations
Perception of cure and improvement in the short term (less than one year), medium term (one to five years) and longer term (greater than five years)
B. Quantification of symptoms (objective measures)
Pad changes over 24 hours (from self‐reported number of pads used)
Incontinent episodes over 24 hours (from self‐completed bladder chart)
Urge symptoms or urge incontinence (clinical diagnosis without urodynamics, new or persistent)
Pad tests of quantified leakage (mean volume or weight of urine loss)
C. Clinician's observations
Objective assessment of incontinence at urodynamics
Detrusor overactivity (urodynamic diagnosis, new or persistent)
New or recurrent/persistent prolapse
D. Quality of life
General health status measures (physical, psychological, other)
Condition‐specific health measures (specific instruments designed to assess incontinence)
E. Surgical outcome measures
Voiding dysfunction /difficulty after three months (with or without urodynamic confirmation)
Perioperative surgical complications (e.g. infection, bacteriuria, haemorrhage, blood loss)
Length of inpatient stay
Time to return to normal activity level
Repeat incontinence surgery
Later prolapse surgery
Death
Dyspareunia (pain with intercourse)
F. Other outcomes
Non‐prespecified outcomes judged important when performing the review
Search methods for identification of studies
We did not impose any language or other restrictions on any of these searches, details are given below.
Electronic searches
This review has drawn on the search strategy developed for the Incontinence Review Group. We identified relevant trials from the Incontinence Group Specialised Register of controlled trials which is described under the Incontinence Group's details in the Cochrane Library (For more details please see the ‘Specialized Register’ section of the Group’s module in The Cochrane Library). The register contains trials identified from the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE, CINAHL, and handsearching of journals and conference proceedings. The trials in the Incontinence Group Specialised Register are also contained in CENTRAL.
The terms used to search the Incontinence Group Specialised Register are given in Appendix 1. Date of the most recent search of the register for this review is 1 September 2009.
We performed additional searches for the Brief Economic Commentary (BECs). These were conducted in MEDLINE(1 January 1946 to March 2017), Embase (1 January 1980 to 2017 Week 12) and NHS EED (1st Quarter 2016). All searches were conducted on 6 April 2017. Details of the searches run and the search terms used can be found in Appendix 2.
Searching other resources
The review authors also searched the reference lists of relevant articles.
Data collection and analysis
Selection of trials
We identified randomised and quasi‐randomised trials using the above search strategy. Studies were excluded if they were not randomised or quasi‐randomised trials for incontinent women. Excluded studies are listed with reasons for their exclusion. We resolved any differences of opinion related to study inclusion, methodological quality or data extraction by discussion with a third party.
Quality of trials
The review authors evaluated reports of all possibly eligible trials for methodological quality and appropriateness for inclusion without prior consideration of the results. Each review author independently assessed methodological quality using the Incontinence Group's assessment criteria which include quality of random allocation and concealment, description of dropouts and withdrawals, analysis by intention‐to‐treat, and 'blinding' during treatment and at outcome assessment. We resolved any differences of opinion by discussion with a third party.
Data extraction and processing
Two review authors independently extracted data on included trials and these were cross‐checked. We sought clarification from the trialists for data that may have been collected but not reported. Trial data were subgrouped by type of incontinence ‐ either urodynamic stress incontinence (USI) based on a urodynamic diagnosis, or stress urinary incontinence (SUI) based upon a symptom classification. Mixed incontinence was defined when either type of stress incontinence co‐existed with detrusor overactivity, urge urinary incontinence or other urinary symptoms.
Statistical analysis
Included trial data were processed as described in the Cochrane Handbook for Systematic Reviews of Interventions (Deeks 2006). When appropriate, meta‐analysis was undertaken. For categorical outcomes we related the numbers reporting an outcome to the numbers at risk in each group to derive a risk ratio (RR). For continuous variables we used means and standard deviations to derive a mean difference (MD). We used a fixed‐effect model to calculate pooled estimates and their 95% confidence intervals (CIs).
We only combined trials if the interventions were similar enough on clinical criteria. When important heterogeneity was then suspected from visual inspection of the results, we used the Chi2 test for heterogeneity (at 10%) or the I2 statistic (Higgins 2003). When concern about heterogeneity persisted, we could have used a random‐effects model.
Subgroup analyses included different diagnostic groups (i.e. USI, SUI or MUI), types of operations and groups with and without co‐existing prolapse. We would have carried out sensitivity analysis for individual methodological criteria if the data allowed (e.g. quality of concealment of randomisation) but the data were insufficient.
For the purpose of the analysis, we considered the Burch colposuspension and Marshall‐Marchetti‐Krantz operations together. However, we considered the results of each operation separately in an additional statistical analysis (not shown on Comparison graphs). Trials which included women with prolapse were also considered separately from those which excluded women with prolapse in an additional analysis.
Results
Description of studies
Results of the search
We identified 10 randomised trials of surgery for urinary incontinence which included anterior vaginal repair in one arm, from six countries (UK, USA, Greece, Denmark, Sweden and Italy). They included a total of 1012 women, of whom 385 had an anterior repair. Sample sizes ranged from 16 to 289. Twelve further studies were excluded because they were not randomised controlled trials, the women were not all incontinent or none of the surgical arms included anterior repair alone. One ongoing trial was also identified (Tincello 2004).
Included studies
All 10 trials were restricted to primary procedures. All gave specific inclusion criteria, and seven included only patients with urodynamic stress incontinence, diagnosed using urodynamics or cystometry, while three included women with mixed incontinence (Di Palumbo 2003; Holmes 1985; Quadri 1985). Some or all women in seven trials also had prolapse (pelvic relaxation) (Bergman 1989b; Colombo 2000; Di Palumbo 2003; Holmes 1985; Kammerer‐Doak 1999; Liapis 1996a; Quadri 1985). In another trial, the type of operation was dictated by the anatomical findings (Klarskov 1986). In that trial, only 16 women with anterior bladder descent were considered for anterior vaginal repair and the analysis in this review was confined to these 16 women.
Long‐term follow‐up at four years was given in only one trial (Liapis 1996a) and at five to 15 years in three trials (Bergman 1989a; Colombo 2000; Lalos 1993).
All trials but one (Quadri 1985), excluded women with other gynaecological disease or previous operations for incontinence: one other trial did not specify past gynaecological procedures but all women had a Grade 3 or 4 anterior prolapse (Di Palumbo 2003). Both pre‐ and post‐menopausal women were included in all trials: one study excluded women aged over 65 years (Lalos 1993). Some studies used adjuvant oestrogen treatment for postmenopausal women either during initial treatment (Bergman 1989a; Bergman 1989b), or at follow‐up if urge incontinence developed (Liapis 1996a). In one trial, all women had a hysterectomy at the time of the primary operation (Colombo 2000); in three trials, some women had a hysterectomy or prolapse repair as well as the anti‐incontinence procedure (Di Palumbo 2003; Kammerer‐Doak 1999; Quadri 1985).
Further characteristics of the trials are reported in the Characteristics of included studies and Characteristics of excluded studies tables.
Risk of bias in included studies
Three trials failed to provide any information about the randomisation process (Klarskov 1986; Lalos 1993; Quadri 1985); one used sealed envelopes (Di Palumbo 2003); and the remainder used 'randomisation lists or tables' without explaining how they were actually used. Patients could not be blinded to comparisons of surgery with physical interventions, nor between abdominal compared with vaginal operations. Blinding of outcome assessors was not reported. The type of surgical intervention in one trial was determined by anatomical findings (Klarskov 1986): results are presented only for women who had a posterior suspension defect (16 women, of whom seven had an anterior repair).
Baseline comparability of the groups was not mentioned in two trials (Lalos 1993; Liapis 1996a). Another trial reported 'comparable' numbers of incontinent episodes at baseline without giving details (Klarskov 1986). One trial provided data which showed that the groups were not comparable in the baseline characteristics of age and menopausal status (Kammerer‐Doak 1999). The others stated that the groups were 'comparable' in terms of age, parity and menopausal status, although only three provided specific data (Colombo 2000; Di Palumbo 2003; Holmes 1985; Quadri 1985). Six trials reported dropouts or loss to follow‐up, ranging from 4% to 16% of eligible patients.
Effects of interventions
01. Anterior vaginal repair versus no treatment or sham operation (Comparison 01)
No trials were identified in which anterior vaginal repair was compared with a sham or mock procedure, or no treatment.
02. Anterior vaginal repair versus conservative interventions (Comparison 02)
Anterior repair was compared with pelvic floor muscle training in one small trial (Klarskov 1986). The trial included only 16 participants who were suitable for anterior repair. The relevant part of this study was therefore too small to provide useful data.
03. Anterior vaginal repair versus open abdominal retropubic suspension in all women(Comparison 03)
Anterior repair was compared with open abdominal retropubic suspension in eight trials (Bergman 1989a; Bergman 1989b; Colombo 2000; Holmes 1985; Kammerer‐Doak 1999; Lalos 1993; Liapis 1996a; Quadri 1985). All trials used Burch colposuspension except one, which in addition allocated one group of women to Marshall‐Marchetti‐Krantz (Liapis 1996a). In the main analysis, the results from the women who had a Burch colposuspension were combined with those who had a Marshall‐Marchetti‐Krantz (Liapis 1996a).
Effectiveness (cure/failure)
Anterior repair was less effective than abdominal suspension, based on subjective outcomes within the first year after surgery (82 of 279 (29%) versus 50 of 346 (14%) still incontinent; risk ratio (RR) for failure 1.89, 95% confidence interval (CI) 1.39 to 2.59, Analysis 3.1) (Bergman 1989a; Bergman 1989b; Holmes 1985; Lalos 1993; Liapis 1996a; Quadri 1985), medium‐term follow‐up in six trials between one and five years 97 of 259 (38%) versus 57 of 327 (17%); RR 2.29, 1.70 to 3.08, Analysis 3.2) (Bergman 1989b; Holmes 1985; Kammerer‐Doak 1999; Lalos 1993; Liapis 1996a; Quadri 1985), and long‐term follow‐up in four trials after five years (49 of 128 (38%) versus 31 of 145 (21%); RR 2.02, 95% CI 1.36 to 3.01, Analysis 3.3) (Bergman 1989a; Colombo 2000; Lalos 1993; Quadri 1985). There was significant heterogeneity, which was reduced or removed after removal of the Lalos trial, which appeared to report lower failure rates in the anterior repair group compared with after colposuspension (Lalos 1993), in contrast to the results of the other trials. However, there was no obvious explanation as to why this trial differed from the others.
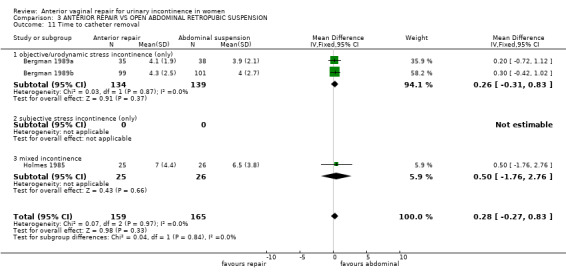
3.1. Analysis.
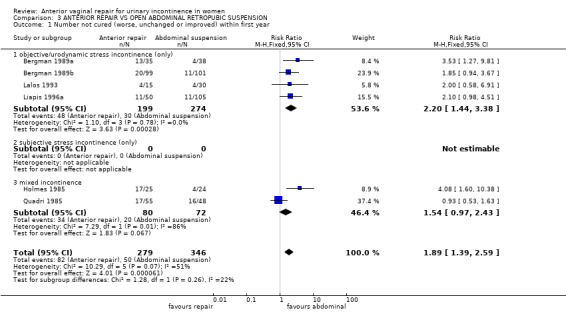
Comparison 3 ANTERIOR REPAIR VS OPEN ABDOMINAL RETROPUBIC SUSPENSION, Outcome 1 Number not cured (worse, unchanged or improved) within first year.
3.2. Analysis.
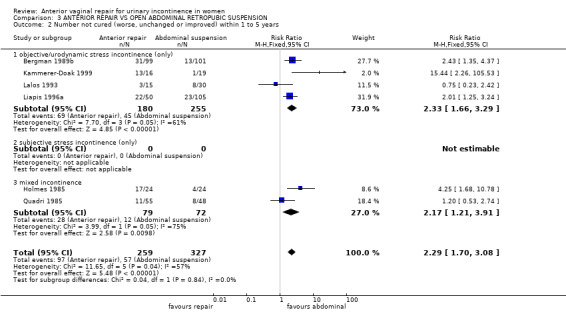
Comparison 3 ANTERIOR REPAIR VS OPEN ABDOMINAL RETROPUBIC SUSPENSION, Outcome 2 Number not cured (worse, unchanged or improved) within 1 to 5 years.
3.3. Analysis.
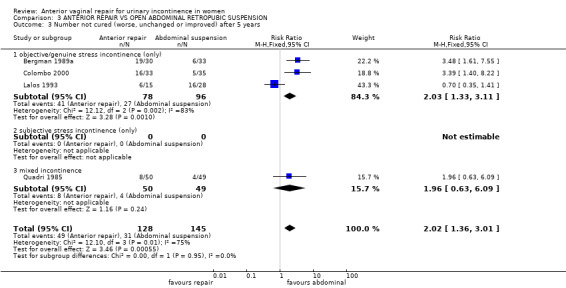
Comparison 3 ANTERIOR REPAIR VS OPEN ABDOMINAL RETROPUBIC SUSPENSION, Outcome 3 Number not cured (worse, unchanged or improved) after 5 years.
Complications
One trial reported more positive urine cultures after anterior repair (Lalos 1993), another found one bladder perforation, during Burch colposuspension (Colombo 1997), and a third reported more intra‐operative complications during colposuspension but more postoperative pyrexia and bleeding after anterior repair (Holmes 1985), giving a RR for perioperative complications of 1.57 (95% CI 0.84 to 2.95, Analysis 3.9) (Colombo 2000; Holmes 1985; Lalos 1993). No difference in complications was reported in another trial, although specific data were not provided (Bergman 1989a).
3.9. Analysis.
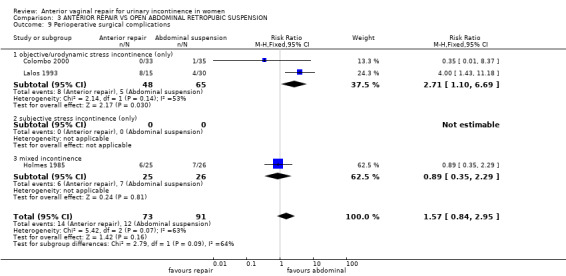
Comparison 3 ANTERIOR REPAIR VS OPEN ABDOMINAL RETROPUBIC SUSPENSION, Outcome 9 Perioperative surgical complications.
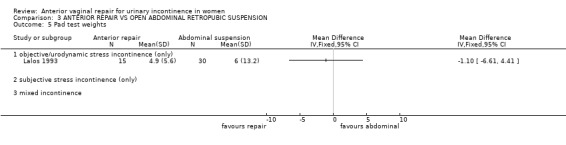
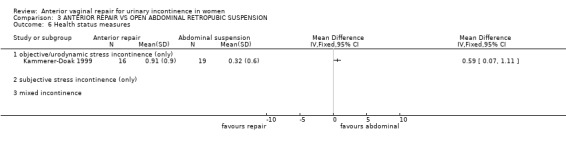
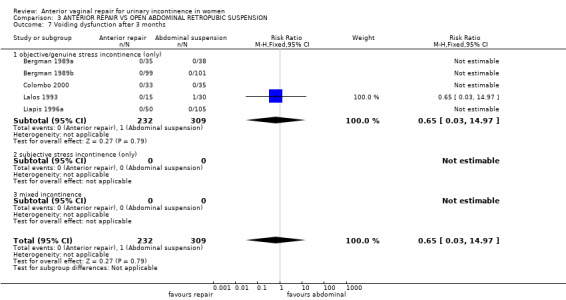
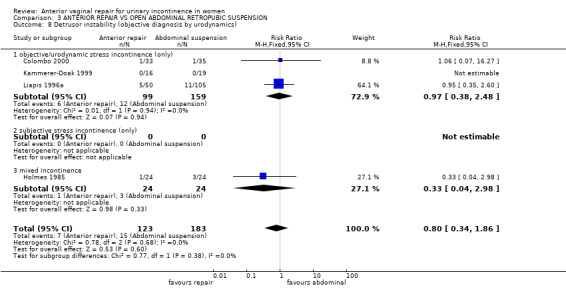
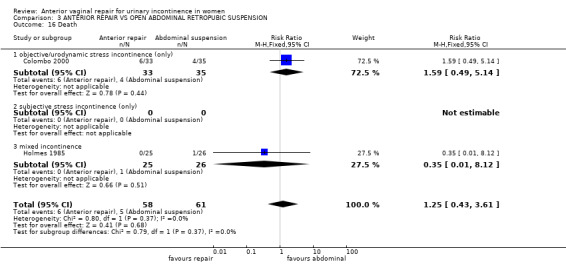
Other outcomes
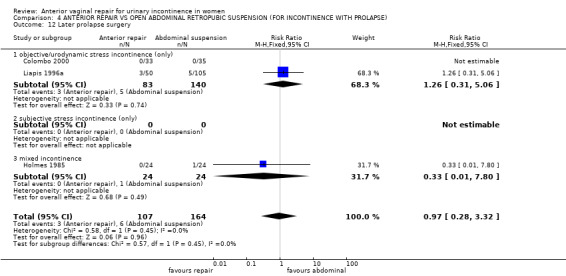
Data describing subsequent urge incontinence or detrusor overactivity (Colombo 2000; Holmes 1985; Liapis 1996a; Kammerer‐Doak 1999), pad test weights (Lalos 1993) and deaths (Colombo 2000; Holmes 1985) were too few to show a difference. Neither was there a significant difference in the chance of voiding difficulty or dysfunction after three months (one woman after abdominal surgery in one of the five trials which reported it). Although women were less likely to have a new or recurrent prolapse after anterior repair in five trials (eight of 192 (4%), versus 43 of 251 (17%); RR 0.24, 95% CI 0.12 to 0.47, Analysis 3.13) (Bergman 1989a; Colombo 2000; Holmes 1985; Liapis 1996a; Quadri 1985), there was no difference in subsequent prolapse repair rates in three trials (three of 107 (3%) versus six of 164 (4%); RR 0.97, 95% CI 0.28 to 3.32, Analysis 3.15) (Colombo 2000; Holmes 1985; Liapis 1996a). On the other hand, more women required repeat surgery for recurrent incontinence after anterior repair (25 of 107 (23%) versus four of 164 (2%); RR 8.87, 95% CI 3.28 to 23.94, Analysis 3.14) (Colombo 2000; Holmes 1985; Liapis 1996a).
3.13. Analysis.
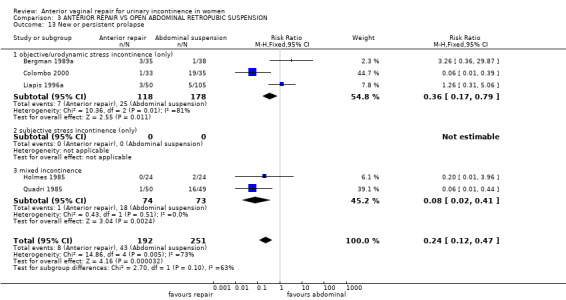
Comparison 3 ANTERIOR REPAIR VS OPEN ABDOMINAL RETROPUBIC SUSPENSION, Outcome 13 New or persistent prolapse.
3.15. Analysis.
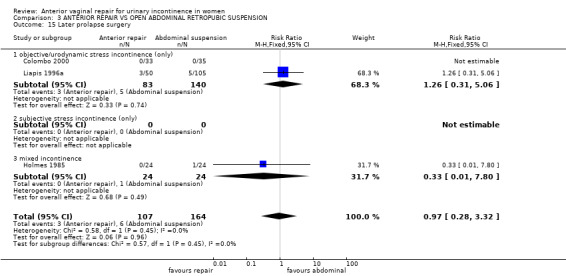
Comparison 3 ANTERIOR REPAIR VS OPEN ABDOMINAL RETROPUBIC SUSPENSION, Outcome 15 Later prolapse surgery.
3.14. Analysis.
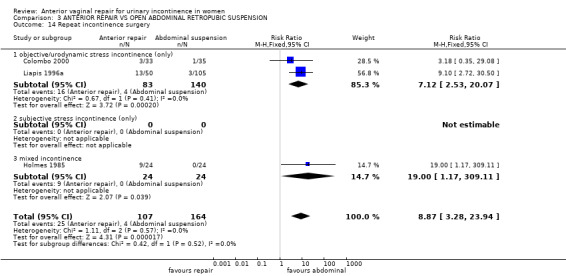
Comparison 3 ANTERIOR REPAIR VS OPEN ABDOMINAL RETROPUBIC SUSPENSION, Outcome 14 Repeat incontinence surgery.
Dyspareunia (pain with intercourse) was reported in one trial (Colombo 2000). All women in the anterior vaginal repair group (of whom only 23 were sexually active) also had a vaginal posterior repair (colporrhapy with perineorrhaphy), whereas only 10 (of 24) sexually active women in the Burch group were thought to need this procedure. Dyspareunia was more common after anterior vaginal repair (57%) amongst sexually active women compared with 20% amongst women who had a posterior repair in the Burch group (RR 2.83, 95% CI 0.78 to 10.27Analysis 3.17.1) (Colombo 2000), but these data did not reach statistical significance and were derived from non‐comparable groups.
3.17. Analysis.
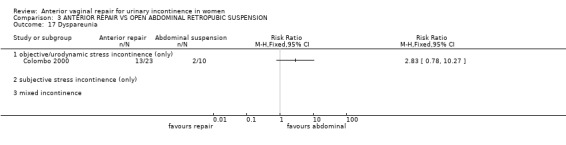
Comparison 3 ANTERIOR REPAIR VS OPEN ABDOMINAL RETROPUBIC SUSPENSION, Outcome 17 Dyspareunia.
Quality of life
Quality of life, measured using an 'incontinence impact questionnaire' was marginally better in the abdominal group in one small trial (mean difference (MD) 0.59, 95% CI 0.07 to 1.11) (Kammerer‐Doak 1999).
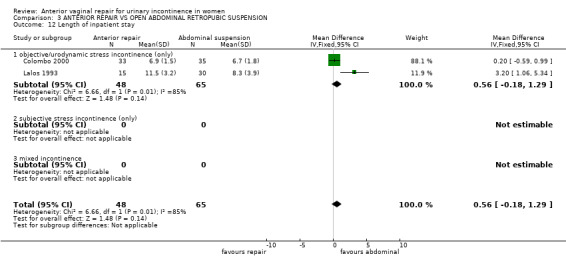
Surgical outcomes
Some trials reported outcomes could be used as the basis for comparisons, such as operative time in theatre, length of stay and duration of use before removal of an indwelling catheter. Anterior repair took about 15 minutes less time in theatre in one trial (MD ‐14.50 minutes, 95% CI ‐23.47 to ‐5.53, Analysis 3.10.3) (Holmes 1985) but the data for time before catheter removal (three trials) and length of stay (two trials) did not show significant differences.
3.10. Analysis.
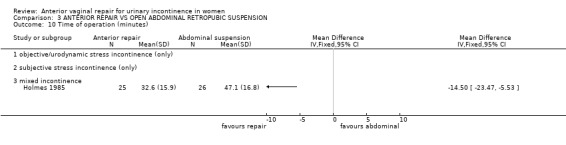
Comparison 3 ANTERIOR REPAIR VS OPEN ABDOMINAL RETROPUBIC SUSPENSION, Outcome 10 Time of operation (minutes).
Anterior vaginal repair versus different types of open abdominal retropubic suspension operations The ability to assess within this review whether one type of open abdominal retropubic suspension performed better than another when compared with anterior repair was limited. Burch colposuspension was evaluated in all eight trials but the Marshall‐Marchetti‐Krantz procedure was only evaluated in one arm of one of these trials (Liapis 1996a). The results of Burch colposuspension alone compared with anterior repair favoured the Burch approach (failure with anterior repair after the first year, RR 2.83, 95% CI 2.12 to 3.79; analysis not shown on Comparison graphs), reflecting the overall results of this comparison. In one trial (Liapis 1996a), a comparison of anterior repair with Marshall‐Marchetti‐Krantz suspension tended to favour the abdominal approach but did not reach significance (RR 1.32, 95% CI 0.80 to 2.17) (not shown on Comparison graphs) and the numbers were small.
04. Anterior vaginal repair versus open abdominal retropubic suspension in trials including women with co‐existing prolapse (Comparison 04)
The only trials that compared anterior repair with abdominal surgery for women with prolapse in addition to their urinary incontinence used open abdominal retropubic suspension as the comparison operation: there were six trials (Bergman 1989b; Colombo 2000; Holmes 1985; Kammerer‐Doak 1999; Liapis 1996a; Quadri 1985). When these six trials were considered alone, open abdominal retropubic suspension was better than anterior vaginal repair in terms of subjective failure rates in both:
* the medium term (RR 2.49, 95% CI 1.83 to 3.39, Analysis 4.2) (Bergman 1989b; Holmes 1985; Kammerer‐Doak 1999; Liapis 1996a; Quadri 1985) and * the long term (RR 3.39, 95% CI 1.4 to 8.22, Analysis 4.3.1) (Colombo 2000).
4.2. Analysis.
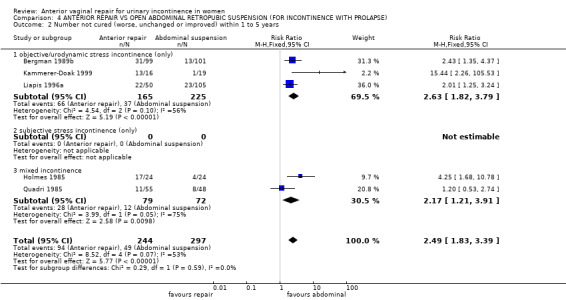
Comparison 4 ANTERIOR REPAIR VS OPEN ABDOMINAL RETROPUBIC SUSPENSION (FOR INCONTINENCE WITH PROLAPSE), Outcome 2 Number not cured (worse, unchanged or improved) within 1 to 5 years.
4.3. Analysis.
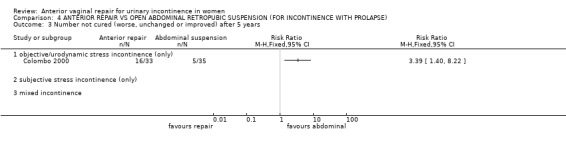
Comparison 4 ANTERIOR REPAIR VS OPEN ABDOMINAL RETROPUBIC SUSPENSION (FOR INCONTINENCE WITH PROLAPSE), Outcome 3 Number not cured (worse, unchanged or improved) after 5 years.
This was reflected in a greater need for repeat continence surgery (25 of 107 (23%) versus four of 164 (2%); RR 8.87, 95% CI 3.28 to 23.94, Analysis 4.11) (Colombo 2000; Holmes 1985; Liapis 1996a). There were no significant differences in voiding dysfunction, perioperative surgical complications, length of hospital stay, subsequent urge incontinence, detrusor overactivity or deaths but the confidence intervals were wide.
4.11. Analysis.
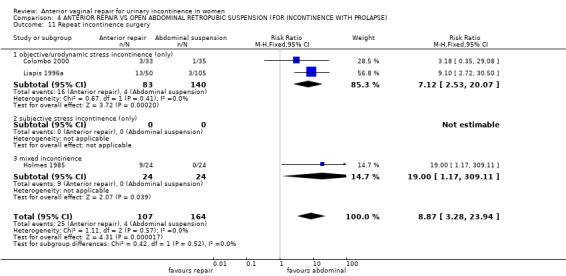
Comparison 4 ANTERIOR REPAIR VS OPEN ABDOMINAL RETROPUBIC SUSPENSION (FOR INCONTINENCE WITH PROLAPSE), Outcome 11 Repeat incontinence surgery.
Although there was an excess of continuing or recurrent prolapse/enterocele amongst the Burch group (RR in favour of anterior vaginal repair 0.12, 95% CI 0.05 to 0.32, Analysis 4.8) (Colombo 2000; Holmes 1985; Quadri 1985), the aggregated chance of actually having further prolapse surgery was similar (three of 107 (3%) and six of 164 (4%), RR 0.97, 95% CI 0.28 to 3.32, Analysis 4.12) (Colombo 2000; Holmes 1985; Liapis 1996a). Of the 19 in the Burch group who had recurrent prolapse in one trial (Colombo 2000), six were recommended to have further surgery but they refused: even if these are counted as if they actually had surgery, the risk of later prolapse surgery still would not differ between the groups (anterior vaginal repair three of 107 (3%) versus 12 of 164 (7%), RR 0.46, 95% CI 0.16 to 1.28, data not shown in Comparison).
4.8. Analysis.
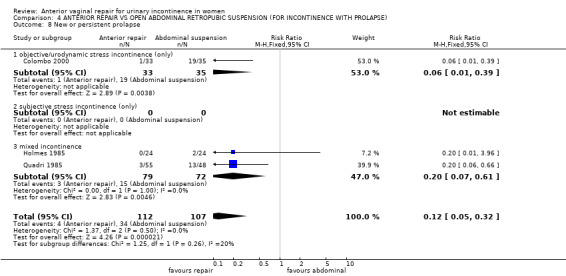
Comparison 4 ANTERIOR REPAIR VS OPEN ABDOMINAL RETROPUBIC SUSPENSION (FOR INCONTINENCE WITH PROLAPSE), Outcome 8 New or persistent prolapse.
4.12. Analysis.
Comparison 4 ANTERIOR REPAIR VS OPEN ABDOMINAL RETROPUBIC SUSPENSION (FOR INCONTINENCE WITH PROLAPSE), Outcome 12 Later prolapse surgery.
05. Anterior vaginal repair versus bladder neck needle suspensions (Comparison 05)
Anterior repair was compared with needle suspension in three trials (Bergman 1989a; Bergman 1989b; Di Palumbo 2003). The performance of the two operations appeared similar in terms of subjective incontinence rates after one year (e.g. 64 of 181, 35% versus 50 of 156, 32%; RR for failure 1.16, 95% CI 0.86 to 1.56, Analysis 5.2) (Bergman 1989a; Bergman 1989b; Di Palumbo 2003) and voiding dysfunction (no women reported this complication, Analysis 5.6) whether the women had prolapse in addition to stress incontinence (Bergman 1989b; Di Palumbo 2003) or not (Bergman 1989a). The numbers were not large, however, and clinically important differences could not be ruled out.
5.2. Analysis.
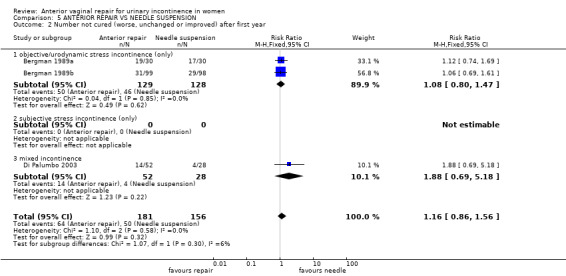
Comparison 5 ANTERIOR REPAIR VS NEEDLE SUSPENSION, Outcome 2 Number not cured (worse, unchanged or improved) after first year.
5.6. Analysis.
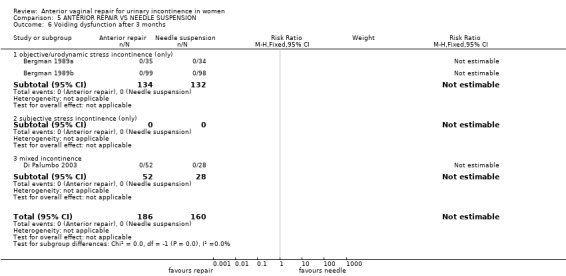
Comparison 5 ANTERIOR REPAIR VS NEEDLE SUSPENSION, Outcome 6 Voiding dysfunction after 3 months.
06. Anterior vaginal repair versus suburethral sling operations (Comparison 06)
No trials were identified which compared anterior vaginal repair with suburethral sling procedures.
07. Anterior vaginal repair versus laparoscopic colposuspensions (Comparison 07)
No trials were identified which compared anterior vaginal repair with laparoscopic colposuspension.
08. One type of anterior vaginal repair versus another (Comparison 08)
No trials were identified which compared different methods or techniques of performing anterior vaginal repair with each other.
Discussion
This review is one of a series of reviews of surgical operations for urinary incontinence and it should be viewed in that context.
This review was confined to the effects of anterior repair in women who had urinary incontinence. The role of anterior vaginal repair in the management of women with cystocele (anterior prolapse) but who do not have urinary incontinence, has been assessed separately in a review of surgery for prolapse (Maher 2007).
Summary of main results
There was evidence that open abdominal retropubic suspension was better than anterior vaginal repair in terms of cure rates (83% dry at one to five years after operation versus 63%, respectively) and, in three trials, avoiding the need for repeat operation. This applied to women with and without associated prolapse. All trials included Burch colposuspension, but one also included Marshall‐Marchetti‐Krantz: the data available for the latter were consistent with the results for the Burch procedure but were too few to draw reliable conclusions.
In the one trial in which it was reported (Colombo 2000), dyspareunia was attributed to posterior repair resulting in over‐narrowing of the vaginal introitus. Amongst sexually active women, there was a trend for more dyspareunia after anterior vaginal repair, but the data were derived from non‐comparable groups, as only some of the comparison group were given a posterior repair. The authors recommend that routine posterior repair should be avoided, particularly amongst sexually active women.
Bladder neck needle suspension appeared to give results similar to those after anterior vaginal repair in women with and without prolapse, both in the short term and long term, but the numbers were small and a clinically important difference could not be ruled out. However, indirect evidence from a review of abdominal retropubic suspension suggests that anterior repair and needle suspension were of broadly similar (lower) effectiveness when each was compared separately with abdominal retropubic suspension (Lapitan 2009).
Although there were no direct comparisons between anterior vaginal repair and suburethral slings, evidence from a Cochrane review comparing abdominal retropubic suspension with slings in six trials suggested that they were broadly equally effective (RR 0.89; 95% CI 0.66 to 1.19 at one year follow‐up, Lapitan 2009), suggesting indirectly that slings would be more effective than anterior repair in a direct comparison. There were no comparisons between anterior repair and laparoscopic procedures, nor different techniques of anterior vaginal repair with each other, and so there was no rigorous evidence to suggest which might be better.
To supplement the main systematic review of effects, we sought to identify economic evaluations which have compared anterior vaginal repair with any of the other main categories of surgical procedures listed in the background section. A supplementary search in NHS EED, MEDLINE and Embase identified one such economic evaluation.
A cost‐benefit analysis (Hana 2012), compared vaginoplasty by Kelly with obturator tension‐free vaginal tape (TVT‐O) in 60 patients with stress urinary Incontinence (SUI) in the period from January 2007 to August 2010 in Bosnia and Herzegovina. The study was a retrospective‐prospective cohort study and calculated by the total cost of treatment of SUI, including the costs associated with the surgery itself and costs related to the disease based on data from the medical records including duration of surgery, length of hospital stay, intra‐operative and early postoperative complications (30 days after surgery) and late postoperative complications (three to six months after surgery). Benefits were based upon impact on society’s productivity based on the valuation of days off work over the follow‐up period; this was valued using the gross national income (GNI ‐ a measure of the wealth of a country) per person per day. The value used for GNI per capita per day was EUR 3.95 (Newsletter of the European Union 2003), this value appears too low for the vast majority of upper‐income countries. The average cost‐benefit ratio for each intervention was calculated as C/B ratio = number of patients x cost of treatment/GNI per day for the total number of absences from work for x number of patients (Bidmead 2002).
The total cost of vaginoplasty was estimated to be EUR 483, while TVT‐O was EUR 817 (no price year stated), but the average number of days off work was higher in the vaginoplasty (10 days) compared to TVT‐O (four days). The C/B ratio was 12.2 and 51.7 for vaginoplasty and TVT‐O, respectively. The study concluded that the benefit of TVT‐O method is up to 4.2 times greater than the benefit of conventional vaginoplasty over a postoperative period of six months. However, the correct interpretation of this result is that the extra costs of TVT‐0 are not worth additional time at usual activities based on the data used.
Overall completeness and applicability of evidence
All but one of the trials excluded women who had undergone previous surgery for incontinence, and that trial included only nine of 103 such women (Quadri 1985); therefore none of the trials addressed the question of the choice of repeat procedure after failed primary surgery. Only one trial compared conservative physical therapies such as pelvic floor muscle training with anterior vaginal repair and was so small that it did not contribute usefully (Klarskov 1986).
Outcome measures were generally limited, with little evidence of reliability and validity. Only one small trial included measurement of quality of life (Kammerer‐Doak 1999). Patient satisfaction with, and acceptability of, the treatment were not addressed but are important factors in choice of management. No mental health outcomes were reported (Black 1997; Kelleher 1997).
Objective urodynamic outcome measures, for example change in functional urethral length or maximal urethral pressure (Bump 1988; Hilton 1983) were reported in four of the trials (Bergman 1989a; Bergman 1989b; Lalos 1993; Liapis 1996a). These are measurable continuous variables, which allow trials with smaller numbers of participants to obtain relatively precise statistical estimates of any differences. However, urodynamic outcome measures are of limited help in determining optimal treatment because they have no proven correlation with clinical outcomes (Meyer 1994; Swift 1995). Until accepted normal values, which correlate with clinical signs and symptoms, are available for these tests, they will not be included in this review.
On the other hand, morbidity outcomes relevant to surgical complications (such as pain, voiding dysfunction, detrusor overactivity, prolapse, dyspareunia, wound and urinary infections) were not consistently reported. Such morbidity is of particular importance in decision making when treating benign disease. Treatment failure reported in terms of the need for repeat surgery both for incontinence and prolapse, or the need for additional interventions, would be particularly useful.
We did not subject this one identified economic evaluation to critical appraisal and we do not attempt to draw any firm or general conclusions regarding the relative costs or efficiency of anterior vaginal repair in the treatment of SUI. However, whilst the limited economic evidence suggests anterior repair looks promising the scarcity of relevant economic evaluations indicates that robust economic evidence is currently lacking.
Quality of the evidence
The number of participants and the quality of the trials that addressed the effects of anterior vaginal repair surgery for stress incontinence was poor. Only 333 women received anterior repair and were compared, in nine trials, with 599 comparable women randomised to another intervention. Although six of the trials stated they used 'randomisation lists', no further details were available about the process of allocation. Long‐term follow‐up beyond the first year was only available in six trials (Bergman 1989a; Colombo 2000; Holmes 1985; Kammerer‐Doak 1999; Lalos 1993; Liapis 1996a). Most trials reported dropouts, but this did not affect reported group size. One study was only reported in three abstracts from oral presentations (Quadri 1985).
Authors' conclusions
Implications for practice.
The limited evidence indicates that the open abdominal approach (retropubic suspension) is better than anterior vaginal repair for the treatment of primary urodynamic stress incontinence (USI). The effect was longer lasting, whether or not the women had associated prolapse. Three trials also reported less need for repeat surgery for incontinence than after vaginal repair. Although there was a higher incidence of prolapse after abdominal operations, this did not require surgical correction more often. Dyspareunia could be minimised by avoiding routine use of posterior repair. There was inadequate data on which to compare anterior vaginal repair with physical therapy or needle suspension, and no data for comparison with suburethral slings or laparoscopic retropubic suspensions.
Since postoperative surgical morbidity was poorly reported, and quality of life measures hardly at all, the alternative treatments could not be compared in other ways. In treating benign disease, long‐term morbidity must be balanced against the chance of cure or improvement.
Although the methodological quality of the evidence was not high, anterior vaginal repair did not seem to be better than any of the comparison interventions, and seemed worse than open abdominal retropubic suspension. This suggests that its use in the treatment of urinary incontinence should be restricted to women deemed unsuitable for alternative treatment.
Implications for research.
Future research in incontinence should incorporate standardised, validated, preferably objective and simple outcome measures that are relevant to women who have incontinence in order to allow comparison between trials. In particular, long‐term morbidity, quality of life, psychological and economic outcomes should be incorporated.
Surgical trials related to stress incontinence should systematically address surgical morbidity outcomes such as adverse perioperative events, length of hospital stay, time to return to normal activities, development of urge symptoms or detrusor overactivity and especially the need for repeat surgery or alternative interventions. Long‐term follow‐up (at least one year, preferably five years or more) is essential for the proper evaluation of incontinence treatments.
What's new
| Date | Event | Description |
|---|---|---|
| 10 July 2017 | Amended | BECs added. Economics‐related sections revised: Abstract, Plain Language Summary, Background, Methods (outcomes, search methods), and Discussion were amended. Appendix added with details of search strategies for BECs. |
| 10 July 2017 | New citation required but conclusions have not changed | Brief economic commentary (BECs) added. Economics‐related sections revised. |
History
Protocol first published: Issue 3, 1999 Review first published: Issue 1, 2000
| Date | Event | Description |
|---|---|---|
| 7 September 2009 | Review declared as stable | Procedure no longer carried out as first‐choice procedure in routine practice so no further RCTs expected |
| 12 September 2008 | Amended | Converted to new review format. |
| 28 February 2007 | New search has been performed | Issue 3 2007 (minor update) One trial added (di Palumbo 2003), results amended, conclusions unaltered. |
| 15 February 2005 | New search has been performed | Issue 2 2005 (minor update) One further trial excluded (Meschia 2004) and one ongoing trial added (Tincello 2004) |
| 15 February 2003 | New search has been performed | Issue 2 2003 (minor update) Long‐term data for two trials (Lalos 1993, Quadri 1985) added. Results amended, conclusions unaltered. |
| 29 November 2000 | New citation required and conclusions have changed | Substantive amendment. Issue 1 2001. Two new trials added (Holmes 1985 and Quadri 1985). One new trial excluded (Gilja 1998). Extra/replacement data added to Lalos 1993 (data from Berglund 1996). |
| 3 May 2000 | New citation required and conclusions have changed | Substantive Update. Issue 3 2000 Two new trials (Kammerer‐Doak 1999 and Colombo 2000) added to review, data incorporated, abstract, results, discussion and conclusions revised. |
Notes
Anterior repair is an old procedure, no new trials
Acknowledgements
Professor A. Liapis provided extra data for an included trial, and information which enabled another to be excluded. Dr Mario Colombo gave extra information about randomisation process and data on dyspareunia. Dr David Holmes provided extra data from a trial published only in conference abstracts. We also thank the external peer reviewers.
We would like to express our thanks to Kirsty Louden for copy‐editing the review.
Appendices
Appendix 1. Search terms used to search the Cochrane Incontinence Group Specialised Register
(TOPIC.URINE.INCON*) AND ({DESIGN.CCT*} OR {DESIGN.RCT*}) AND ({INTVENT.SURG.} OR {INTVENT.SURG.ABDO.*} OR {INTVENT.SURG.ASSESS.} OR {INTVENT.SURG.colpofixation.staple.} OR {INTVENT.SURG.COLPORRHAPHY.ANTERIOR.} OR {INTVENT.SURG.CYSTOPLASTY.} OR {INTVENT.SURG.DIATHERMY.} OR {intvent.surg.endopelvicFasciaPlication.} OR {INTVENT.SURG.KELLY.} OR {INTVENT.SURG.PARVAGINALdefectrepair.} OR {INTVENT.SURG.PELVICFLOORREPAIR.} OR {INTVENT.SURG.PEREYRA*} OR {INTVENT.SURG.PERINEAL*} OR {INTVENT.SURG.RAMIREZ.} OR {INTVENT.SURG.RAZ.} OR {INTVENT.SURG.STAPLING.} OR {INTVENT.SURG.SUSPENSION.URETHRAL.} OR {INTVENT.SURG.URETHROCYSTOPEXY.ABDO.} OR {INTVENT.SURG.URETHROPEXY.MODPEREYRA.} OR {INTVENT.SURG.VAGINAL/PERINEAL.} OR {INTVENT.SURG.VAGINAL/PERINEAL.ANTERIOR REPAIR} OR {INTVENT.SURG.VAGINAL/PERINEAL.COLPORRHAPHY} OR {INTVENT.SURG.VAGINAL/PERINEAL.MICROWAVE}) (All searches were of the keyword field of Reference Manager 9.5 N, ISI ResearchSoft).
We did not impose any language or other restrictions on any of these searches.
Appendix 2. Search strategies for brief economic commentary
We performed additional searches for the Brief Economic Commentary (BECs). These were conducted in MEDLINE(1 January 1946 to March 2017), Embase (1 January 1980 to 2017 Week 12) and NHS EED (1st Quarter 2016). All searches were conducted on 6 April 2017. We used two different search strategies on MEDLINE and Embase (OvidSP) and one on NHS EED (OVID). Details of the searches run and the search terms used can be found below. There were no year, publication type or language restrictions applied to the searches.
NHS EED (Ovid) (1st Quarter 2016)
NHS EED was searched using the following search strategy:
1. Urinary incontinence/
2. Urinary incontinence, stress/
3. ((stress$ or mix$ or urg$ or urin$) adj3 incontinen$).tw.
4. Colporrhaphy.tw.
5. Colpoperineoplast$.tw.
6. Sling procedure$.tw.
7. Sling$ procedure$.tw.
8. Bladder neck needle suspension$.tw.
9. Anterior vaginal repair$ .tw.
10. Or/1‐9
MEDLINE (1 January 1946 to March 2017) and Embase (1 January 1980 to 2017 Week 12)
We used two different search strategies on MEDLINE and Embase (OvidSP) ‐ these are given below.
Search strategy 1:
1. Economics, Pharmaceutical/ or Economics, Medical/ or Economics/ or Economics, Hospital/ or economics.mp. or Economics, Nursing/
2. exp "costs and cost analysis"/
3. "Value of Life"/
4. exp "fees and charges"/
5. exp budgets/
6. budget*.ti,ab.
7. cost*.ti.
8. (economic* or pharmaco?economic*).ti.
9. (price* or pricing*).ti,ab.
10. (cost* adj2 (effective* or utilit* or benefit* or minimi* or unit* or estimat* or variable*)).ab.
11. (financ* or fee or fees).ti,ab.
12. (value adj2 (money or monetary)).ti,ab.
13. ((energy or oxygen) adj cost).ti,ab.
14. (metabolic adj cost).ti,ab.
15. ((energy or oxygen) adj expenditure).ti,ab.
16. 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15
17. exp Urinary Incontinence/
18. ((stress* or mix* or urg* or urin*) adj3 incontinen*).tw.
19. Urodynamics/ or Urinary Incontinence, Stress/ or Urinary Incontinence/ or Suburethral Slings/ or mixed incontinence.mp. or Urinary Bladder/ or Urinary Incontinence, Urge/
20. 17 or 18 or 19
21. anterior vaginal repair*.tw.
22. 16 and 20 and 21
23. anterior colporrhaphy*.tw.
24. 21 or 23
25. 16 and 20 and 23
26. bladder neck needle suspension$.tw.
27. 16 and 20
28. 26 and 27
29. open abdominal retropubic colposuspension*.tw.
30. retropubic colposuspension*.tw.
31. burch colposuspension*.tw.
32. 29 or 30 or 31
33. 27 and 32
34. laparoscopic retropubic colposuspension*.tw.
35. laparoscopic colposuspension*.tw.
36. 34 or 35
37. 27 and 36
38. traditional suburethral retropubic sling procedure$*.tw.
39. traditional sling procedure$*.tw.
40. suburethral retropubic sling procedure$*.tw.
41. retropubic sling procedure$*.tw.
42. traditional suburethral sling*.tw.
43. Suburethral Slings/ or Urinary Incontinence, Stress/ or Urologic Surgical Procedures/
44. 27 and 43
45. remove duplicates from 44
Search strategy 2:
1. economics.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, fs]
2. value of life.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, fs]
3. exp "costs and cost analysis"/
4. exp economics, hospital/
5. exp economics, medical/
6. economics, nursing.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, fs]
7. economics, pharmaceutical.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, fs]
8. exp "fees and charges"/
9. exp budgets/
10. budget*.ti,ab.
11. cost*.ti.
12. (economic* or pharmaco?economic*).ti.
13. (price* or pricing*).ti,ab.
14. (cost* adj2 (effective* or utilit* or benefit* or minimi* or unit* or estimat* or variable*)).ab.
15. (financ* or fee or fees).ti,ab.
16. (value adj2 (money or monetary)).ti,ab.
17. or/1‐16
18. economics.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, fs]
19. value of life.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, fs]
20. exp "costs and cost analysis"/
21. exp economics, hospital/
22. exp economics, medical/
23. economics, nursing.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, fs]
24. economics, pharmaceutical.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, fs
25. exp "fees and charges"/
26. exp budgets/
27. budget*.ti,ab.
28. cost*.ti.
29. (economic* or pharmaco?economic*).ti.
30. (price* or pricing*).ti,ab.
31. (cost* adj2 (effective* or utilit* or benefit* or minimi* or unit* or estimat* or variable*)).ab.
32. (financ* or fee or fees).ti,ab.
33. (value adj2 (money or monetary)).ti,ab.
34. 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31 or 32 or 33
35. ((energy or oxygen) adj cost).ti,ab.
36. (metabolic adj cost).ti,ab.
37. ((energy or oxygen) adj expenditure).ti,ab.
38. 34 or 35 or 36 or 37
39. urinary incontinence.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
40. ((stress$ or mix$ or urg$ or urin$) adj3 incontinen$).tw.
41. URINARY INCONTINENCE, STRESS.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
42. stress urinary incontinence*.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
43. 39 or 40 or 41 or 42
44. intervention surgery*.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
45. colporrhaphy.tw.
46. Bologna procedure*.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
47. Kelly‐Kennedy.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
48. Marion Kelly.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
49. Diaphragmplasty.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
50. Vaginal urethrocystopexy.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
51. Cystocele repair.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
52. Kelly plication.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
53. anterior vaginal repair$.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
54. anterior colporrhaphy.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
55. 44 or 45 or 46 or 47 or 48 or 49 or 50 or 51 or 52 or 53 or 54
56. 38 and 43 and 55
57. remove duplicates from 56
58. Bladder neck needle suspension$.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
59. 38 and 43 and 58
60. burch colposuspension.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
61. open abdominal retropubic colposuspension.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
62. Paravaginal defect repair.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
63. Marshall‐Marchetti‐Krantz.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
64. abdominal burch.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
65. abdominal colposuspension.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
66. endopelvic Fascia Plication.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
67. 60 or 61 or 62 or 63 or 64 or 65 or 66
68. 38 and 43
69. 67 and 68
70. laparoscopic retropubic colposuspension.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
71. laparoscopic colposuspension.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
72. retropubic colposuspension.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
73. 70 or 71 or 72
74. 68 and 73
75. remove duplicates from 74
76. suburethral sling.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
77. abdominal sling.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
78. traditional sling procedure$*.tw.
79. suburethral sling procedure.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
80. 76 or 77 or 78 or 79
81. 68 and 80
82. remove duplicates from 81
83. mid$urethral sling.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
84. retropubic sling procedure$*.tw.
85. transobturator sling procedure$.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
86. 83 or 84 or 85
87. remove duplicates from 86
88. 68 and 87
89. TVT‐Secur.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
90. mini‐arc.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
91. ajust.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
92. needleless.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
93. solyx.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
94. single$incision sling$.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
95. miniarc.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
96. mini$sling.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
97. Ophira.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
98. Tissue Fixation System.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
99. 89 or 90 or 91 or 92 or 93 or 94 or 95 or 96 or 97 or 98
100. 68 and 99
101. remove duplicates from 100
102. ((urethra$ or periurethra$ or transurethra$) adj3 (agent$ or bulk$ or injection$ or injectable$)).tw.
103. injection therapy.tw.
104. injectable$.tw.
105. (injectable$ adj2 agent$).tw.
106. (bulk$ adj3 agent$).tw.
107. Peri$urethral injection$.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
108. Autologous fat.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
109. Macroplastique.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
110. Calcium hydroxylapatite.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
111. Hyaluronic acid with dextranomer.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
112. Porcine dermal implant.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
113. Ethylene vinyl alcohol copolymer.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
114. Silicon particles.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
115. 102 or 103 or 104 or 105 or 106 or 107 or 108 or 109 or 110 or 111 or 112 or 113 or 114
116. 68 and 115
117. remove duplicates from 116
Data and analyses
Comparison 2. ANTERIOR REPAIR VS PELVIC FLOOR MUSCLE TRAINING.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Number not cured (worse, unchanged or improved) within first year | 1 | 16 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.25 [0.84, 1.86] |
| 1.1 objective/urodynamic stress incontinence (only) | 1 | 16 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.25 [0.84, 1.86] |
| 1.2 subjective stress incontinence (only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 1.3 mixed incontinence | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 2 Number not improved (worse or unchanged) within first year | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.1 objective/urodynamic stress incontinence (only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 subjective stress incontinence (only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 mixed incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Number not improved (worse or unchanged) after first year | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.1 objective/urodynamic stress incontinence (only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 subjective stress incontinence (only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.3 mixed incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
2.1. Analysis.
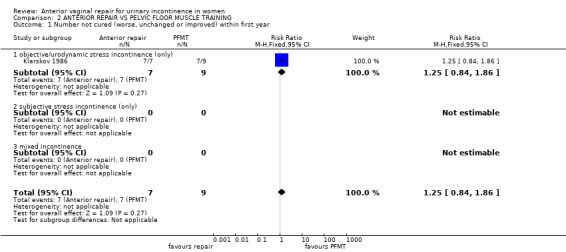
Comparison 2 ANTERIOR REPAIR VS PELVIC FLOOR MUSCLE TRAINING, Outcome 1 Number not cured (worse, unchanged or improved) within first year.
2.2. Analysis.
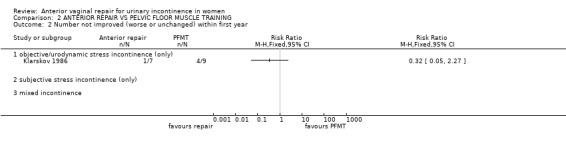
Comparison 2 ANTERIOR REPAIR VS PELVIC FLOOR MUSCLE TRAINING, Outcome 2 Number not improved (worse or unchanged) within first year.
2.3. Analysis.
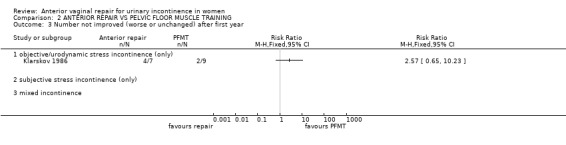
Comparison 2 ANTERIOR REPAIR VS PELVIC FLOOR MUSCLE TRAINING, Outcome 3 Number not improved (worse or unchanged) after first year.
Comparison 3. ANTERIOR REPAIR VS OPEN ABDOMINAL RETROPUBIC SUSPENSION.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Number not cured (worse, unchanged or improved) within first year | 6 | 625 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.89 [1.39, 2.59] |
| 1.1 objective/urodynamic stress incontinence (only) | 4 | 473 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.20 [1.44, 3.38] |
| 1.2 subjective stress incontinence (only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 1.3 mixed incontinence | 2 | 152 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.54 [0.97, 2.43] |
| 2 Number not cured (worse, unchanged or improved) within 1 to 5 years | 6 | 586 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.29 [1.70, 3.08] |
| 2.1 objective/urodynamic stress incontinence (only) | 4 | 435 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.33 [1.66, 3.29] |
| 2.2 subjective stress incontinence (only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 2.3 mixed incontinence | 2 | 151 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.17 [1.21, 3.91] |
| 3 Number not cured (worse, unchanged or improved) after 5 years | 4 | 273 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.02 [1.36, 3.01] |
| 3.1 objective/genuine stress incontinence (only) | 3 | 174 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.03 [1.33, 3.11] |
| 3.2 subjective stress incontinence (only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3.3 mixed incontinence | 1 | 99 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.96 [0.63, 6.09] |
| 4 Urge symptoms or urge incontinence | 3 | 239 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.36 [0.89, 2.08] |
| 4.1 objective/urodynamic stress incontinence (only) | 2 | 190 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.85 [0.83, 4.15] |
| 4.2 subjective stress incontinence (only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4.3 mixed incontinence | 1 | 49 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.12 [0.70, 1.78] |
| 5 Pad test weights | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 5.1 objective/urodynamic stress incontinence (only) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.2 subjective stress incontinence (only) | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.3 mixed incontinence | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Health status measures | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 6.1 objective/urodynamic stress incontinence (only) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.2 subjective stress incontinence (only) | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.3 mixed incontinence | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Voiding dysfunction after 3 months | 5 | 541 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.65 [0.03, 14.97] |
| 7.1 objective/genuine stress incontinence (only) | 5 | 541 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.65 [0.03, 14.97] |
| 7.2 subjective stress incontinence (only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7.3 mixed incontinence | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 8 Detrusor instability (objective diagnosis by urodynamics) | 4 | 306 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.80 [0.34, 1.86] |
| 8.1 objective/urodynamic stress incontinence (only) | 3 | 258 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.97 [0.38, 2.48] |
| 8.2 subjective stress incontinence (only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 8.3 mixed incontinence | 1 | 48 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.04, 2.98] |
| 9 Perioperative surgical complications | 3 | 164 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.57 [0.84, 2.95] |
| 9.1 objective/urodynamic stress incontinence (only) | 2 | 113 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.71 [1.10, 6.69] |
| 9.2 subjective stress incontinence (only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 9.3 mixed incontinence | 1 | 51 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.35, 2.29] |
| 10 Time of operation (minutes) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 10.1 objective/urodynamic stress incontinence (only) | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 10.2 subjective stress incontinence (only) | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 10.3 mixed incontinence | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 11 Time to catheter removal | 3 | 324 | Mean Difference (IV, Fixed, 95% CI) | 0.28 [‐0.27, 0.83] |
| 11.1 objective/urodynamic stress incontinence (only) | 2 | 273 | Mean Difference (IV, Fixed, 95% CI) | 0.26 [‐0.31, 0.83] |
| 11.2 subjective stress incontinence (only) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 11.3 mixed incontinence | 1 | 51 | Mean Difference (IV, Fixed, 95% CI) | 0.5 [‐1.76, 2.76] |
| 12 Length of inpatient stay | 2 | 113 | Mean Difference (IV, Fixed, 95% CI) | 0.56 [‐0.18, 1.29] |
| 12.1 objective/urodynamic stress incontinence (only) | 2 | 113 | Mean Difference (IV, Fixed, 95% CI) | 0.56 [‐0.18, 1.29] |
| 12.2 subjective stress incontinence (only) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 12.3 mixed incontinence | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 13 New or persistent prolapse | 5 | 443 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.24 [0.12, 0.47] |
| 13.1 objective/urodynamic stress incontinence (only) | 3 | 296 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.36 [0.17, 0.79] |
| 13.2 subjective stress incontinence (only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 13.3 mixed incontinence | 2 | 147 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.08 [0.02, 0.41] |
| 14 Repeat incontinence surgery | 3 | 271 | Risk Ratio (M‐H, Fixed, 95% CI) | 8.87 [3.28, 23.94] |
| 14.1 objective/urodynamic stress incontinence (only) | 2 | 223 | Risk Ratio (M‐H, Fixed, 95% CI) | 7.12 [2.53, 20.07] |
| 14.2 subjective stress incontinence (only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 14.3 mixed incontinence | 1 | 48 | Risk Ratio (M‐H, Fixed, 95% CI) | 19.0 [1.17, 309.11] |
| 15 Later prolapse surgery | 3 | 271 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.97 [0.28, 3.32] |
| 15.1 objective/urodynamic stress incontinence (only) | 2 | 223 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.26 [0.31, 5.06] |
| 15.2 subjective stress incontinence (only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 15.3 mixed incontinence | 1 | 48 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.80] |
| 16 Death | 2 | 119 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.25 [0.43, 3.61] |
| 16.1 objective/urodynamic stress incontinence (only) | 1 | 68 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.59 [0.49, 5.14] |
| 16.2 subjective stress incontinence (only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 16.3 mixed incontinence | 1 | 51 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.35 [0.01, 8.12] |
| 17 Dyspareunia | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 17.1 objective/urodynamic stress incontinence (only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 17.2 subjective stress incontinence (only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 17.3 mixed incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
3.4. Analysis.
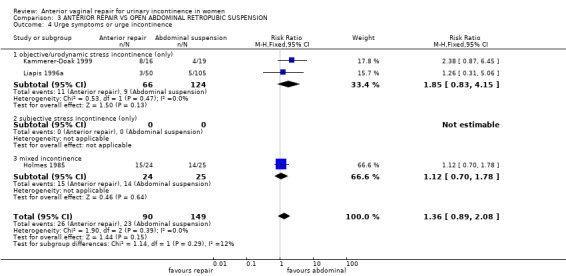
Comparison 3 ANTERIOR REPAIR VS OPEN ABDOMINAL RETROPUBIC SUSPENSION, Outcome 4 Urge symptoms or urge incontinence.
3.5. Analysis.
Comparison 3 ANTERIOR REPAIR VS OPEN ABDOMINAL RETROPUBIC SUSPENSION, Outcome 5 Pad test weights.
3.6. Analysis.
Comparison 3 ANTERIOR REPAIR VS OPEN ABDOMINAL RETROPUBIC SUSPENSION, Outcome 6 Health status measures.
3.7. Analysis.
Comparison 3 ANTERIOR REPAIR VS OPEN ABDOMINAL RETROPUBIC SUSPENSION, Outcome 7 Voiding dysfunction after 3 months.
3.8. Analysis.
Comparison 3 ANTERIOR REPAIR VS OPEN ABDOMINAL RETROPUBIC SUSPENSION, Outcome 8 Detrusor instability (objective diagnosis by urodynamics).
3.11. Analysis.
Comparison 3 ANTERIOR REPAIR VS OPEN ABDOMINAL RETROPUBIC SUSPENSION, Outcome 11 Time to catheter removal.
3.12. Analysis.
Comparison 3 ANTERIOR REPAIR VS OPEN ABDOMINAL RETROPUBIC SUSPENSION, Outcome 12 Length of inpatient stay.
3.16. Analysis.
Comparison 3 ANTERIOR REPAIR VS OPEN ABDOMINAL RETROPUBIC SUSPENSION, Outcome 16 Death.
Comparison 4. ANTERIOR REPAIR VS OPEN ABDOMINAL RETROPUBIC SUSPENSION (FOR INCONTINENCE WITH PROLAPSE).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Number not cured (worse, unchanged or improved) within first year | 4 | 507 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.73 [1.23, 2.43] |
| 1.1 objective/urodynamic stress incontinence (only) | 2 | 355 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.95 [1.17, 3.25] |
| 1.2 subjective stress incontinence (only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 1.3 mixed incontinence | 2 | 152 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.54 [0.97, 2.43] |
| 2 Number not cured (worse, unchanged or improved) within 1 to 5 years | 5 | 541 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.49 [1.83, 3.39] |
| 2.1 objective/urodynamic stress incontinence (only) | 3 | 390 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.63 [1.82, 3.79] |
| 2.2 subjective stress incontinence (only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 2.3 mixed incontinence | 2 | 151 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.17 [1.21, 3.91] |
| 3 Number not cured (worse, unchanged or improved) after 5 years | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.1 objective/urodynamic stress incontinence (only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 subjective stress incontinence (only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.3 mixed incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Urge symptoms or urge incontinence | 3 | 239 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.36 [0.89, 2.08] |
| 4.1 objective/urodynamic stress incontinence (only) | 2 | 190 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.85 [0.83, 4.15] |
| 4.2 subjective stress incontinence (only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4.3 mixed incontinence | 1 | 49 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.12 [0.70, 1.78] |
| 5 Health status measures | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 5.1 objective/urodynamic stress incontinence (only) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.2 subjective stress incontinence (only) | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.3 mixed incontinence | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Voiding dysfunction after 3 months | 3 | 423 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6.1 objective/urodynamic stress incontinence (only) | 3 | 423 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6.2 subjective stress incontinence (only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6.3 mixed incontinence | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Detrusor instability (objective diagnosis by urodynamics) | 4 | 306 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.80 [0.34, 1.86] |
| 7.1 objective/urodynamic stress incontinence (only) | 3 | 258 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.97 [0.38, 2.48] |
| 7.2 subjective stress incontinence (only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7.3 mixed incontinence | 1 | 48 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.04, 2.98] |
| 8 New or persistent prolapse | 3 | 219 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.12 [0.05, 0.32] |
| 8.1 objective/urodynamic stress incontinence (only) | 1 | 68 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.06 [0.01, 0.39] |
| 8.2 subjective stress incontinence (only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 8.3 mixed incontinence | 2 | 151 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.20 [0.07, 0.61] |
| 9 Perioperative surgical complications | 2 | 119 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.23 [0.44, 3.49] |
| 9.1 objective/urodynamic stress incontinence (only) | 1 | 68 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.35 [0.01, 8.37] |
| 9.2 subjective stress incontinence (only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 9.3 mixed incontinence | 1 | 51 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.56 [0.50, 4.88] |
| 10 Length of inpatient stay | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 10.1 objective/urodynamic stress incontinence (only) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 10.2 subjective stress incontinence (only) | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 10.3 mixed incontinence | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 11 Repeat incontinence surgery | 3 | 271 | Risk Ratio (M‐H, Fixed, 95% CI) | 8.87 [3.28, 23.94] |
| 11.1 objective/urodynamic stress incontinence (only) | 2 | 223 | Risk Ratio (M‐H, Fixed, 95% CI) | 7.12 [2.53, 20.07] |
| 11.2 subjective stress incontinence (only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 11.3 mixed incontinence | 1 | 48 | Risk Ratio (M‐H, Fixed, 95% CI) | 19.0 [1.17, 309.11] |
| 12 Later prolapse surgery | 3 | 271 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.97 [0.28, 3.32] |
| 12.1 objective/urodynamic stress incontinence (only) | 2 | 223 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.26 [0.31, 5.06] |
| 12.2 subjective stress incontinence (only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 12.3 mixed incontinence | 1 | 48 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.80] |
| 13 Death | 2 | 119 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.25 [0.43, 3.61] |
| 13.1 objective/urodynamic stress incontinence (only) | 1 | 68 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.59 [0.49, 5.14] |
| 13.2 subjective stress incontinence (only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 13.3 mixed incontinence | 1 | 51 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.35 [0.01, 8.12] |
| 14 Dyspareunia | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 14.1 objective/urodynamic stress incontinence (only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 14.2 subjective stress incontinence (only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 14.3 mixed incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
4.1. Analysis.
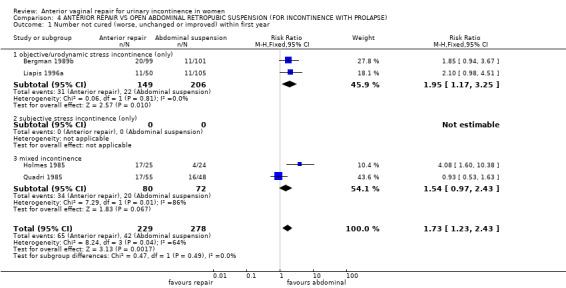
Comparison 4 ANTERIOR REPAIR VS OPEN ABDOMINAL RETROPUBIC SUSPENSION (FOR INCONTINENCE WITH PROLAPSE), Outcome 1 Number not cured (worse, unchanged or improved) within first year.
4.4. Analysis.
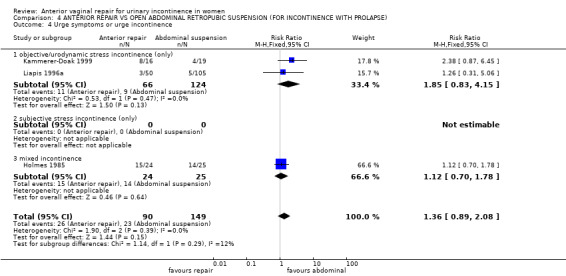
Comparison 4 ANTERIOR REPAIR VS OPEN ABDOMINAL RETROPUBIC SUSPENSION (FOR INCONTINENCE WITH PROLAPSE), Outcome 4 Urge symptoms or urge incontinence.
4.5. Analysis.
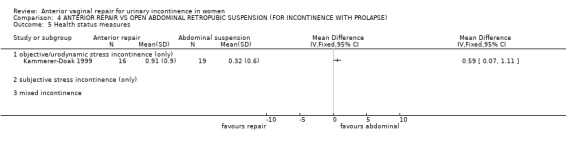
Comparison 4 ANTERIOR REPAIR VS OPEN ABDOMINAL RETROPUBIC SUSPENSION (FOR INCONTINENCE WITH PROLAPSE), Outcome 5 Health status measures.
4.6. Analysis.
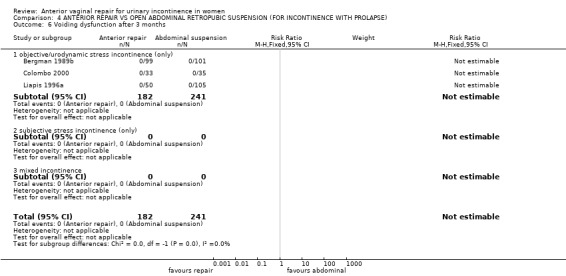
Comparison 4 ANTERIOR REPAIR VS OPEN ABDOMINAL RETROPUBIC SUSPENSION (FOR INCONTINENCE WITH PROLAPSE), Outcome 6 Voiding dysfunction after 3 months.
4.7. Analysis.
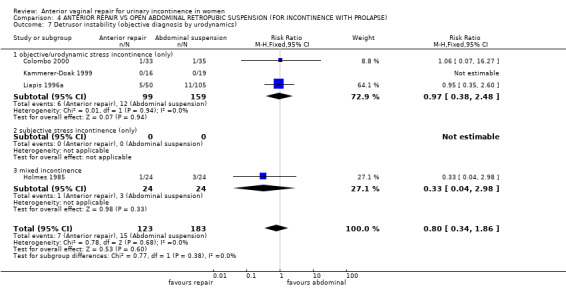
Comparison 4 ANTERIOR REPAIR VS OPEN ABDOMINAL RETROPUBIC SUSPENSION (FOR INCONTINENCE WITH PROLAPSE), Outcome 7 Detrusor instability (objective diagnosis by urodynamics).
4.9. Analysis.
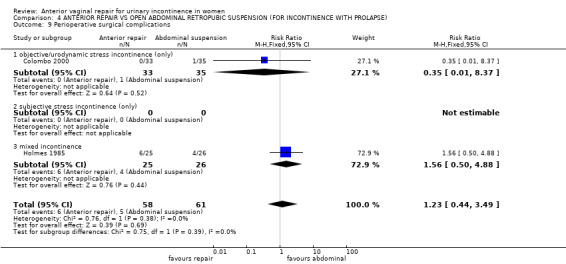
Comparison 4 ANTERIOR REPAIR VS OPEN ABDOMINAL RETROPUBIC SUSPENSION (FOR INCONTINENCE WITH PROLAPSE), Outcome 9 Perioperative surgical complications.
4.10. Analysis.
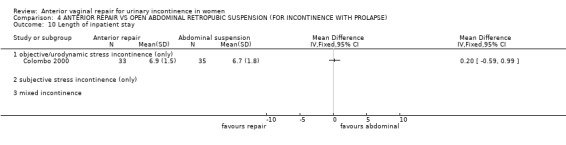
Comparison 4 ANTERIOR REPAIR VS OPEN ABDOMINAL RETROPUBIC SUSPENSION (FOR INCONTINENCE WITH PROLAPSE), Outcome 10 Length of inpatient stay.
4.13. Analysis.
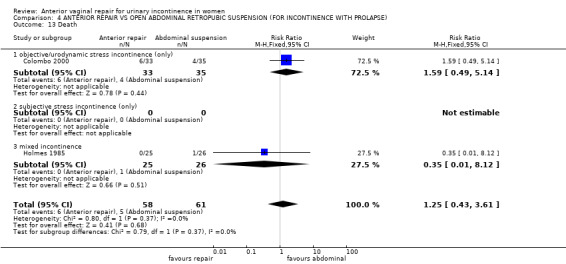
Comparison 4 ANTERIOR REPAIR VS OPEN ABDOMINAL RETROPUBIC SUSPENSION (FOR INCONTINENCE WITH PROLAPSE), Outcome 13 Death.
4.14. Analysis.
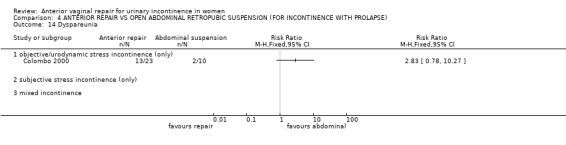
Comparison 4 ANTERIOR REPAIR VS OPEN ABDOMINAL RETROPUBIC SUSPENSION (FOR INCONTINENCE WITH PROLAPSE), Outcome 14 Dyspareunia.
Comparison 5. ANTERIOR REPAIR VS NEEDLE SUSPENSION.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Number not cured (worse, unchanged or improved) within first year | 2 | 266 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.05 [0.69, 1.59] |
| 1.1 objective/urodynamic stress incontinence (only) | 2 | 266 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.05 [0.69, 1.59] |
| 1.2 subjective stress incontinence (only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 1.3 mixed incontinence | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 2 Number not cured (worse, unchanged or improved) after first year | 3 | 337 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.16 [0.86, 1.56] |
| 2.1 objective/urodynamic stress incontinence (only) | 2 | 257 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.08 [0.80, 1.47] |
| 2.2 subjective stress incontinence (only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 2.3 mixed incontinence | 1 | 80 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.88 [0.69, 5.18] |
| 3 Urge symptoms or urge incontinence | 1 | 80 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.29 [0.51, 3.30] |
| 3.1 objective/urodynamic stress incontinence (only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3.2 subjective stress incontinence (only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3.3 mixed incontinence | 1 | 80 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.29 [0.51, 3.30] |
| 4 Perioperative surgical complications | 1 | 80 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.18 [0.01, 4.34] |
| 4.1 objective/urodynamic stress incontinence (only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4.2 subjective stress incontinence (only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4.3 mixed incontinence | 1 | 80 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.18 [0.01, 4.34] |
| 5 New or persistent prolapse | 1 | 80 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.32 [0.08, 1.25] |
| 5.1 objective/urodynamic stress incontinence (only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5.2 subjective stress incontinence (only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5.3 mixed incontinence | 1 | 80 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.32 [0.08, 1.25] |
| 6 Voiding dysfunction after 3 months | 3 | 346 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6.1 objective/urodynamic stress incontinence (only) | 2 | 266 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6.2 subjective stress incontinence (only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6.3 mixed incontinence | 1 | 80 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
5.1. Analysis.
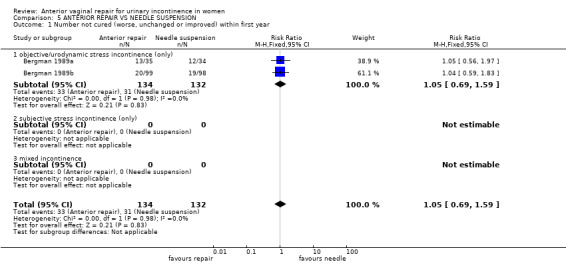
Comparison 5 ANTERIOR REPAIR VS NEEDLE SUSPENSION, Outcome 1 Number not cured (worse, unchanged or improved) within first year.
5.3. Analysis.
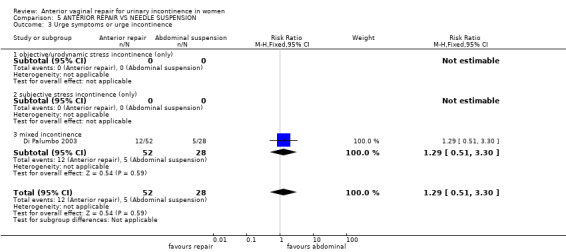
Comparison 5 ANTERIOR REPAIR VS NEEDLE SUSPENSION, Outcome 3 Urge symptoms or urge incontinence.
5.4. Analysis.
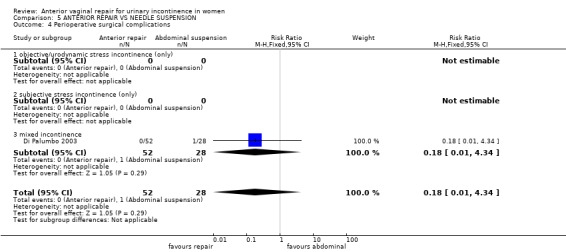
Comparison 5 ANTERIOR REPAIR VS NEEDLE SUSPENSION, Outcome 4 Perioperative surgical complications.
5.5. Analysis.
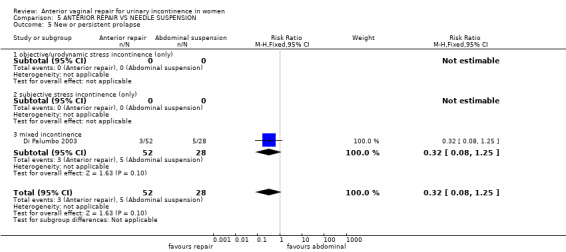
Comparison 5 ANTERIOR REPAIR VS NEEDLE SUSPENSION, Outcome 5 New or persistent prolapse.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Bergman 1989a.
| Methods | RCT. Follow‐up at 3 m, 12 m and 5 yr Patients and surgeons randomly allocated (using randomisation tables) to one of three operations. 20 women lost to follow‐up at 12 m were not reported. | |
| Participants | 127 women recruited, results reported for 107 at 12 m. Results for 64 at 5 yr out of 78 cured at 1 yr. Groups stated to be comparable in mean age, parity and menopausal status but data not given. 53 pre‐menopausal, 74 post‐menopausal. Inclusion criteria: genuine stress incontinence (urodynamic diagnosis); minor cystocele only; post‐menopausal women given oestrogens before and after surgery. Exclusion criteria: other gynaecological disease or operations; previously failed incontinence surgery. | |
| Interventions | Group I anterior vaginal repair (colporrhaphy) (n = 35) (n = 30 at 5 yr) Group II modified Pereyra procedure (needle suspension) (n = 34) (n = 30 at 5 yr) Group III Burch urethropexy (colposuspension) (n = 38) (n = 33 at 5 yr) | |
| Outcomes | Cure defined as no loss of urine in history or on urodynamic investigation Failure rate at 3 m: I: 7/35, at 12 m, 13/35, at 5 yr: 19/30. II: at 3 m: 6/34, at 12 m: 12/34, at 5 yr: 17/30. III: at 3 m: 3/38, at 12 m: 4/38, at 5 yr: 6/33. Failure rate (sensitivity analysis): I: 24/35; II: 21/34; III: 11/38 No subsequent voiding problems in any patient. Postoperative bacteriuria equally frequent in all groups. 3 developed detrusor instability (groups not specified); 6 developed prolapse (I:3; II: 2; III: 1) Urodynamic measurements reported before and 12 m and 5 yr after operation | |
| Notes | Sensitivity analysis at 5 yr for 107 assuming missing 14 were failures and including 29 already failed at 1 yr | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
Bergman 1989b.
| Methods | RCT. Follow‐up at 3 m and 12 m. Patients and surgeons randomly allocated (using randomisation tables) to one of three operations. 3 women excluded for technical reasons, 41 lost to follow‐up: 289 women reported in the study. | |
| Participants | 342 women (289 reported) Mean age 57 yr (range 31‐80); parity 3 (1‐13); 191 post‐menopausal, 151 pre‐menopausal. Groups comparable at baseline but data not given. Post‐menopausal women given oestrogens before and after surgery. Inclusion criteria: urodynamic diagnosis of primary stress incontinence, stable bladder and pelvic relaxation (prolapse). Exclusion criteria: previous incontinence surgery, detrusor instability, gynaecological complications other than prolapse. | |
| Interventions | Group I anterior vaginal repair (n = 99) Group II revised Pereyra procedure (needle suspension) (n = 98) Group III Burch retropubic urethropexy (colposuspension) (n = 101) | |
| Outcomes | Failure rate at 3 m: I: 20/99, at 12 m: 31/99. II: at 3 m: 19/98, at 12 m: 29/98. III: at 3 m: 11/101, at 12 m: 13/101. No postoperative voiding problems Urodynamic measurements reported before and 12 m after operation | |
| Notes | Tertiary referral centre. No power calculation. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
Colombo 2000.
| Methods | RCT. Follow‐up at 3 m and 1‐8 yrs. Used open list of computer‐generated random numbers, allocation known at the time of randomisation. 18/89 women excluded on preset criteria, further 3 lost to follow‐up and excluded from analysis | |
| Participants | 71 women (68 reported), comparable at baseline for age, parity, deliveries, body mass index, menopausal state, severity of incontinence and prolapse. Inclusion criteria: genuine stress incontinence (urodynamic diagnosis); cystocele grade1/2; urethrovesical junction hypermobility (cotton swab test). Exclusion criteria: detrusor instability, previous incontinence or prolapse surgery, laparotomy for other pelvic disease, medical risk factors. | |
| Interventions | Group I anterior vaginal repair (colporrhaphy) (n = 33) Group II Burch colposuspension (n = 35) | |
| Outcomes | Objective cure (+ve stress test) at 3 m: I, 19/33; II, 9/35.
Subjective failure at 1‐12 yr: I, 16/33; II, 5/35.
Death 8‐16 yr later: I,6; II,4.
Perforated bladder: I, 0; II, 1.
Postoperative stay: I, 6.9(1.5); II, 6.7(1.8).
Voiding problems after discharge: I, 13; II, 10.
Repeat incontinence operation: I, 3; II, 1.
Recurrent prolapse: I, 1; II, 19 (none operated).
New detrusor instability: I, 1; II, 1. For sexually active women who also had a posterior repair only: Dyspareunia: I, 13/23; II, 2/10 Vaginal length: I, mean = 4.7 cm (SD 1.2) n = 23; II, mean = 7 cm (1.3) n = 10. |
|
| Notes | All women who had anterior repair also had a vaginal hysterectomy, anchoring of uterosacral ligaments, Douglas obliteration, and posterior repair (posterior colporrhaphy and perineorrhaphy). All women who had Burch colposuspension also had an abdominal hysterectomy and anchoring of uterosacral ligaments, with some having: Pouch of Douglas obliteration (17), and posterior repair (posterior colporrhaphy and perineorrhaphy). (12). Absorbable sutures used for Group I, non‐absorbable for Group II. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | High risk | C ‐ Inadequate |
Di Palumbo 2003.
| Methods | RCT 2:1 randomisation using sealed envelopes Follow‐up: 280 to 1670 days (at 1, 3, 6, 12, 18 and 24 months, then yearly) | |
| Participants | 80 women with SUI + urethrocystocele (anterior prolapse) grade 3 or 4 Age: I: mean 59.8 years (range 41‐79), II: 60.6 (39‐78) Concomitant vaginal hysterectomy: I: 47/52, II: 26/28 Inclusion criteria: Prolapse defect assessed (apical, central, lateral), SUI, UUI, mixed incontinence and overactive bladder diagnosed with Q tip test, stress test, 1‐hour pad test and urodynamics. If urgency, bladder training and anticholinergic treatment before surgery. | |
| Interventions | I: Anterior repair (Nicholls) (52) II: Four‐corner bladder and urethral retropubic suspension (Raz) with thin polypropylene mesh in the spiral suture (28) | |
| Outcomes | SUI (failed): I: 14/52, II: 4/28 (assumed to be after first year) New rectocele at 6 months: I: 3/52, II: 5/28 Urge incontinence: I: 12/52, II: 5/28 Frequency of urination: I: 10/52, II: 2/28 Urinary retention in first 10 days: I: 1/52, II: 1/28 Long‐term retention: I: 0/52, II: 0/28 Time to spontaneous voiding: I: 3.62 days (range 2‐9), II: 4.78 (3‐9) Postoperative hospital stay: I: mean 6 days (range 4‐20), II: 5 (4‐34) (NS) Adverse effects: I: 0/52, II: 1/28 (sepsis, removal of stitches and prolonged hospital stay) | |
| Notes | Women comparable at baseline on age, diabetes, respiratory problems, obstetric history, concomitant vaginal hysterectomy | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
Holmes 1985.
| Methods | RCT. Women randomised by surgeon and by operation. Used open list of computer‐generated random numbers, allocation known at the time of randomisation. | |
| Participants | 51 women, comparable at baseline for age, parity, weight, prolapse (I:6/25, II:8/26), previous hysterectomy, frequency, nocturia, sensation of prolapse, grade of stress incontinence, urgency (I:17/25, II:18/26), urge incontinence (I:13/25, II:14/26) and detrusor instability (I:0/25, II:2/26). Inclusion criteria: genuine stress incontinence, stable bladders at cystometry (but 2 had detrusor instability in Group II), urine sterile. Exclusion criteria: Previous bladder neck surgery for prolapse or incontinence. | |
| Interventions | Group I anterior vaginal repair (n = 25) Group II Burch colposuspension (n = 26) | |
| Outcomes | Blood loss: I,102 mL (SD 86); II, 295 mL (280) Postoperative suprapubic catheter: I, 6.5 days (3.8); II, 7.0 (4.4) Operating time: I, 32.6 min (15.9); II, 47.1 (16.8) Intra‐operative complications: I, 0/25; II, 3/26 Postoperative pyrexia: I, 3; II 2 Postoperative bleeding: I, 3; II, 0 Postoperative wound infection: I, 0; II, 2 Subjective cure 2 m: I, cured 14, improved 7, unchanged 4; II, 26, 0, 0 Objective failure (leak on pad test) at 12 m: I, 17/25; II, 4/24 Objective failure (leak on pad test) at 2 yr: I, 17/24; II, 4/24 Urge incontinence: I, 9/24; II, 7/25. Urge symptoms: I, 15/24; II, 14/25 New detrusor instability: I, 1/24; II, 3/24 Repeat incontinence surgery by 2 yr: I, 9/24; II, 0/24 Recurrent or new prolapse: I, 0/24; II, 2/24 Prolapse surgery: I, 0/24; II, 1/24 | |
| Notes | Unabsorbable sutures (Vicryl or Dexon 1) used for all operations 3 women lost to follow‐up: I, one, continent at 1 yr; II, 1 continent at 2 m, 1 died in first year of carcinoma | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | High risk | C ‐ Inadequate |
Kammerer‐Doak 1999.
| Methods | RCT. Used computer‐generated randomisation table. | |
| Participants | 35 women, 21 with grade 1 or 2 cystocele and 14 with grade 3‐4. Not comparable at baseline for age or menopausal status (Group I older and more often post‐menopausal). Inclusion: genuine stress incontinence (urodynamic diagnosis); cystocele grades 1 to 4. Exclusion: previous radical pelvic surgery or irradiation; intrinsic sphincter deficiency; interstitial cystitis or urethral syndrome. | |
| Interventions | Group I anterior vaginal repair (colporrhaphy) (n = 16) Group II Burch urethropexy (colposuspension) (n = 19) | |
| Outcomes | Cure at 1 yr: Subjective I, 3/16; II, 18/19. Objective I, 5/16; II, 16/18. By pad test I, 6/15; II 15/18. Urge symptoms: I, 8/16; II, 4/19. Detrusor instability: I, 0/16; II, 0/19. Incontinence impact questionnaire (IIQ, mean (SD)): I, 0.91 (0.9); II, 0.32 (0.6). Length of postoperative catheterisation, length of postoperative stay, and postoperative complications (e.g. change in haemoglobin) stated to be the same in both groups. | |
| Notes | Some women had hysterectomy +/‐ prolapse repair as well as incontinence surgery. Randomisation procedure suspect due to differences in baseline characteristics. Trial stopped prematurely after an interim analysis suggested that the Burch group were more likely to be cured than the anterior colporrhaphy group. Non‐absorbable sutures used for Burch, absorbable for vaginal repair. No mention of total number of eligible women or dropouts. No power study. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | High risk | C ‐ Inadequate |
Klarskov 1986.
| Methods | RCT, details not given | |
| Participants | 50 women Median age 48 yrs (range 31‐66) Anatomical defects diagnosed on basis of voiding cystourethrogram, and operations selected accordingly Inclusion criteria: genuine stress incontinence diagnosed by cystometry, with and without prolapse Exclusion criteria: previous surgery, previous systematic PFMT, urge incontinence, other gynaecological surgery needed (e.g. prolapse, hysterectomy) or inability to understand instructions | |
| Interventions | Group I surgery (n = 26) [Burch colposuspension (n = 16) for anterior suspension defect; vaginal repair (n = 7) for posterior bladder descent; both operations (n = 3) for combined defects] Group II Pelvic floor muscle training (PFMT, n = 24) [n = 13 for anterior suspension defect, n = 9 for posterior bladder descent, n = 2 for combined defects] PFMT given by physiotherapists in 5 weekly sessions including pelvic floor anatomy, muscle consciousness training and a home exercise programme. | |
| Outcomes | Subjective cure rates at 4 m: I: 1 worse, 2 unchanged, 7 improved, 16 cured; II: 0 worse, 7 unchanged, 14 improved, 3 cured. I: 5 wanted PFMT at 4 m, 7 wanted PFMT at 12 m (or 19/26 cured at 12 m, 95% CI 52% to 88%)
II: 12 wanted surgery at 4 m, 14 wanted PFMT at 12 m (or 10/24 cured at 12 m, 95% CI 22% to 63%)
Number of incontinent episodes: I: median = 6 (0‐39) at baseline, to 0 (0‐14) at 4m; II: median = 6 (0‐31) at baseline, to 2 (0‐20) at 4 m.
Frequency of micturition: I: 23 (10‐31) at baseline, to 19 (12‐29) at 4 m; II: 26.5 (15‐60) at baseline, to 20 (11‐40) at 4 m.
Side‐effects: I: none; II: 3/26 had long‐term pain after surgery, and 1 developed urge incontinence. Outcomes confined to patients with posterior bladder descent (surgery = anterior repair alone): I: 0 worse, 1 unchanged, 4 improved, 2 cured (of 7) at 4 m II: 0 worse, 4 unchanged, 5 improved, 0 cured (of 9) at 4 m I: 4/7 not improved at 12 m II: 2/9 not improved at 12 m No urodynamic measurements reported |
|
| Notes | Analysis as presented is confined to the 16 women who had posterior bladder descent (cystocele). No comparison of groups at baseline except for number of incontinence episodes. Posterior bladder descent group possibly worse. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
Lalos 1993.
| Methods | RCT of 45/162 eligible patients recruited. Originally 7 excluded because of lack of preoperative cystometry (2) or wrong surgeon (5), later reported in Berglund 1996. Follow‐up at 3 m and 12 m. No details of randomisation. | |
| Participants | RCT of 45/162 eligible patients recruited. Originally 7 excluded because of lack of preoperative cystometry (2) or wrong surgeon (5), later reported in Berglund 1996. Follow‐up at 3 m and 12 m. No details of randomisation. | |
| Interventions | Group I pubococcygeal repair (= anterior repair) (n = 15) Group II retropubic urethrocystopexy (= colposuspension) (n = 30) | |
| Outcomes | Cure rates: I: 11 cured, 4 improved at 3 m; 12 cured, 3 improved at 12 m (subjective, used in analysis) 11/15 failed at 12 m (objective, leaked urine on pad test) II: 26 cured, 4 improved at 3 m; 22 cured, 8 improved at 12 m (subjective, used in analysis) 15/30 failed at 12 m (objective, leaked urine on pad test) Mean urine loss on pad test: I, 4.9 mL (SD 5.6); II, 6 (13.2) Length of stay: I, median 11 days (range 7‐18); II, 6.5 (5‐21) Duration catheterisation: I, mean 8.7 days (range 6‐13); II, 5.9 (3‐18) Positive urine culture: I, 7/15; II, 2/30 Sepsis: I, 1/15; II, 0/30 Wound infection: I, 0/15; II, 2/30 Voiding dysfunction: I: 0/15; II: 1/30 Long‐term follow‐up: Subjective failure rate: I: 6/15; II 16/28 Objective failure rate: I: 4/15; II 10/28 Urinary frequency: I: mean per day 6.2 (range 5‐7); II: 5.6 (5‐7) Urodynamic measurements reported before and after operation | |
| Notes | No power calculation. Reason for selection of 45 from total population of 162 not specified. No baseline comparisons of groups. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
Liapis 1996a.
| Methods | RCT using randomisation list, including type of operation. Pretrial assessment by 7‐day diary and urodynamics 170 patients recruited, 155 followed up at 5 yr (10 dropouts due to lack of elapsed time since operation, 5 lost) | |
| Participants | 155 adult women Age mean 50.6 yr (+/‐ 8.1, range 36‐75); parity mean 3; duration incontinence 7.2 yr (+/‐ 3.9); 97 post‐menopausal, 58 premenopausal. Inclusion criteria: urodynamic diagnosis of genuine stress incontinence, plus pelvic relaxation (prolapse) Exclusion criteria: bladder instability, previous failed incontinence surgery, other gynaecological operations needed | |
| Interventions | Group I anterior repair (plus posterior repair if rectocele present) (n = 50) Group II Marshall‐Marchetti‐Krantz (MMK) (plus posterior repair if rectocele present) (n = 51) Group III Burch colposuspension (plus posterior repair in all cases) (n = 54) | |
| Outcomes | Cure strictly defined (improvement disregarded) I: 11/50 failed at 2 m, 22/50 failed at 4 yr; II: 8/51 failed at 2 m, 17/51 failed at 4 yr; III: 3/54 failed at 2 m, 6/54 failed at 4 yr. Urge incontinence: I: 3/50; II: 3/51; III: 2/54. Detrusor instability: I: 5/50; II: 7/51; III: 4/54 had detrusor instability. 16/155 had subsequent repeat surgery for stress incontinence (I: 13; II: 2; III: 1) 8/155 had subsequent surgery for genital prolapse (I: 3; I: 0; III: 5) Urodynamic measurements reported before and 4 yrs after operation | |
| Notes | Clinical and urodynamic follow‐up at 2 m and 4‐5 yr. No power calculation, no baseline comparison of groups New urge incontinence treated with imipramine (plus conjugated oestrogen vaginal cream if menopausal); detrusor instability treated with oxybutynin | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
Quadri 1985.
| Methods | RCT, method unspecified. | |
| Participants | 103 women with mixed incontinence (urethral sphincter incompetence in all, detrusor instability in I,12/55 ; II,7/48), moderate (I,25; II, 34) to severe (I, 30; II, 14) prolapse. Age: I, 58 yr (range 38‐76); II, 54 (36‐75). Previous incontinence surgery (anterior vaginal repair): I, 7/55; II, 2/48 Additional operations during trial: I, 55 had vaginal hysterectomy, 52 had posterior repair; II, 43 had abdominal hysterectomy , 2 had vaginal hysterectomy, 10 had Douglas obliteration, 15 had posterior repair | |
| Interventions | Group I anterior repair (n = 55) Group II retropubic colposuspension (n = 48) | |
| Outcomes | Incontinence at 3 m: I, 17/55; II, 16/48 Incontinence persisted at 12 m (failed): I, 11/55; II, 8/48. Further 5/55 and 4/48 later 'cured' using drugs Incontinence at 5 years (subjective): I: 8/50, II: 4/49 Incontinence at 5 years (objective): I: 6/50, II: 4/49 Prolapse recurred: I, 3/55; II, 13/48 [Type of prolapse: I, moderate cystocele 2, vaginal cuff 1; II, moderate to severe urethrocystocele 7, vaginal cuff 6] Later prolapse recurrence: I: 1/50, II: 16/49 Dyspareunia amongst sexually active: I: 30%, II: 13% P < 0.05 (number not given) Vaginal length: I: 4.9 cm (SD 1.7), II: 7.3 (1) | |
| Notes | Reported in 3 conference abstracts only, further data not available. Recruitment period, data and numbers slightly different in each abstract Follow‐up 3 months, 3 years and 5 years. For recurrent prolapse, data from 1993 abstract used (at 5‐year follow‐up) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
DO: detrusor overactivity, diagnosed by urodynamics (formerly detrusor instability); n: number; m: month(s); PFMT: pelvic floor muscle training; RCT: randomised controlled trial; SD: standard deviation; SUI: stress urinary incontinence (symptom or sign); UUI: urge urinary incontinence yr: year(s).
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Bump 1996 | Participants were not incontinent. |
| Colombo 1997 | Participants did not all have incontinence. |
| Debodinance 1993 | Participants did not all have incontinence, and results not available separately for incontinent women. |
| Gilja 1998 | RCT but none of the 3 arms included anterior vaginal repair (Burch colposuspension vs Raz needle suspension vs transvaginal Burch, Gilja (needle suspension) |
| Harris 1995 | Not RCT. Interventions: anterior colporrhaphy and retropubic urethropexy performed for genuine stress urinary incontinence, n = 76. Follow‐up for 48‐96 months |
| Liapis 1996b | Patients (96) are a subset of those reported in (Liapis 1996a) (155). |
| Meschia 2004 | Women were not incontinent RCT of TVT and endofascial plication in women with prolapse and occult stress urinary incontinence |
| Park 1988 | Not RCT. Interventions: Marshall‐Marchetti‐Krantz , Kelly plications and Pereyra procedures, n = 680. Long‐term follow‐up, to 10 years. |
| Thunedborg 1990 | Not RCT. Interventions: colposuspension and anterior colporrhaphy |
| van Geelen 1988 | Not RCT. Interventions: anterior vaginal repair and Burch colposuspension, n = 90. Follow‐up for 5‐7 years. |
| Zhu 1998 | After translation from Chinese established not an RCT. Allocated to treatment according to preference of surgeon. |
| Zivkovic 1994 | Not RCT. Interventions: anterior vaginal repair with and without needle suspension. |
RCT = randomised controlled trial TVT: Tension‐free Vaginal Tape
Characteristics of ongoing studies [ordered by study ID]
Tincello 2004.
| Trial name or title | Colposuspension versus TVT with anterior repair |
| Methods | |
| Participants | Women with urodynamic stress urinary incontinence and anterior wall vaginal prolapse Grade II or more |
| Interventions | Colposuspension TVT with anterior repair |
| Outcomes | 3 day urinary diary, 24‐hour pad test, King's Health Questionnaire, POPQ assessment Follow‐up at 3 and 12 months |
| Starting date | |
| Contact information | Dr D Tincello Leicester General Hospital University of Leicester, UK |
| Notes |
POPQ: Pelvic Organ Prolapse Quantification TVT: Tension‐free Vaginal Tape
Differences between protocol and review
July 2017 update – Brief Economic Commentaries (BECs) have been added to all of our surgery for UI in women Cochrane reviews. The economic elements throughout the review have been revised – if incorrect they have been stripped out. The previously used surrogate economic outcomes such as operation time and length of stay have been redefined as ‘Surgical outcomes’. New economics‐related text has been added. This involved revisions to the Background section, Methods section e.g. search section referring to added Appendix, Discussion section, Abstract and Plain language summary. An appendix has been added with details of the economics searches. The Conclusions section of the review has not changed. The rest of the review has not changed.
Contributions of authors
Review authors CG and KC wrote the protocol, selected trials, independently extracted data, interpreted the results and wrote the review.
For the July 2017 addition of the BECs to this review ‐ Atefeh Mashayekhi was responsible for the entire BECs‐related work on this review i.e. she ran the search for studies, screened the searches, extracted data from relevant studies, revised any existing economics‐related text, added the BECs‐related text, and responded to any peer referee comments. All authors had the opportunity to comment on the revised review.
Sources of support
Internal sources
Chief Scientist Office, Scottish Executive Health Department, UK.
External sources
National Health Service Research and Development Programme, UK.
-
National Institute for Health Research, UK.
This project, to add Brief Economic Commentaries to our surgery for UI in women reviews, was supported by the National Institute for Health Research (NIHR), via the Cochrane Review Incentive Scheme 2016, to the Cochrane Incontinence Group. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, NHS or the Department of Health.
-
National Institute for Health Research, UK.
This project was supported by the National Institute for Health Research, via Cochrane Infrastructure funding to the Cochrane Incontinence Group. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, NHS or the Department of Health. The NIHR is the largest single funder of the Cochrane Incontinence Group.
Declarations of interest
Cathryn MA Glazener: None known.
Kevin Cooper: No grants held which are connected with the subject of the Cochrane review. All grants peer reviewed and independently funded.
Atefeh Mashayekhi: This project, to add Brief Economic Commentaries to our surgery for UI in women reviews, was supported by the National Institute for Health Research (NIHR), via the Cochrane Review Incentive Scheme 2016, to the Cochrane Incontinence Group. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, NHS or the Department of Health.
Edited (no change to conclusions)
References
References to studies included in this review
Bergman 1989a {published data only}
- Bergman A, Ballard CA, Koonings PP. Comparison of three different surgical procedures for genuine stress incontinence: prospective randomized study. American Journal of Obstetrics and Gynecology 1989;160(5 Pt 1):1102‐6. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Bergman A, Elia G. Three surgical procedures for genuine stress incontinence: five‐year follow‐up of a prospective randomized study. American Journal of Obstetrics and Gynecology 1995;173(1):66‐71. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Elia G, Bergman A. Prospective randomized comparison of three surgical procedures for stress urinary incontinence: five year follow‐up [Abstract]. Neurourology & Urodynamics 1994;13(4):498‐500. [Google Scholar]
- Elia G, Bergman J, Klutke JJ, Klutke CG. Urethral resistance after surgery for stress urinary incontinence: Do we obstruct to have a successful outcome?. Urodinamica 2000;10(1):32‐7. [18155] [Google Scholar]
Bergman 1989b {published data only}
- Bergman A, Ballard CA, Koonings PP. Primary stress urinary incontinence and pelvic relaxation: prospective randomised comparison of 3 different operations [Abstract]. Neurourology & Urodynamics 1989;8(4):334‐5. [DOI] [PubMed] [Google Scholar]
- Bergman A, Koonings PP, Ballard CA. Primary stress urinary incontinence and pelvic relaxation: prospective randomized comparison of three different operations. American Journal of Obstetrics and Gynecology 1989;161(1):97‐101. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Klutke JJ, Klutke CG, Bergman J, Elia G. Urodynamics changes in voiding after anti‐incontinence surgery: an insight into the mechanism of cure. Urology 1999;54(6):1003‐7. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Colombo 2000 {published and unpublished data}
- Colombo M, Vitobello D, Proietti F, Milani R. Randomised comparison of Burch colposuspension versus anterior colporrhaphy in women with stress urinary incontinence and anterior vaginal wall prolapse. British Journal of Obstetrics & Gynaecology 2000;107(4):544‐51. [DOI] [PubMed] [Google Scholar]
- Glazener CMA, Cooper K. Randomised comparison of Burch colposuspension versus anterior colporrhaphy in women with stress urinary incontinence and anterior vaginal wall prolapse [Letter]. British Journal of Obstetrics & Gynaecology 2000;107(10):1324‐5. [DOI] [PubMed] [Google Scholar]
Di Palumbo 2003 {published data only}
- Palumbo VS. Four‐corner bladder and urethral retropubic suspension versus anterior colporrhaphy in the correction of stress urinary incontinence with urethrocystocele 3‐4. Randomized clinical trial. Urogynaecologia International Journal 2003;17(2):57‐68. [Google Scholar]
Holmes 1985 {published and unpublished data}
- Holmes DM, Stanton SL, Chamberlain GVP. Randomised trial to compare the colposuspension with the anterior repair in the management of genuine stress incontinence (Unpublished Data). personal communication 1985.
- Stanton SL, Chamberlain G, Holmes DM. The anterior repair or colposuspension for the cure of stress incontinence due to urethral sphincter incompetence. A randomised study [Abstract]. Proceedings of the 24th British Congress of Obstetrics and Gynaecology. 1986:156.
- Stanton SL, Chamberlain GVP, Holmes DM. Randomised study of the anterior repair and colposuspension operation in the control of genuine stress incontinence [Abstract]. Proceedings of the International Continence Society, 15th Annual Meeting; 1985 Sept 3‐6. 1985:236‐7.
- Stanton SL, Chamberlain GVP, Holmes DM. The control of stress incontinence: comparison of anterior colporrhaphy and colposuspension [Abstract]. Archives of Gynecology 1985;237 (Suppl):401‐2. [Google Scholar]
Kammerer‐Doak 1999 {published data only}
- Kammerer‐Doak DN, Dorin MH, Rogers RG, Cousin MO. A randomized trial of Burch retropubic urethropexy and anterior colporrhaphy for stress urinary incontinence. Obstetrics and Gynaecology 1999;93(1):75‐8. [DOI] [PubMed] [Google Scholar]
Klarskov 1986 {published data only}
- Klarskov P, Belving D, Bischoff N, Dorph S, Gerstenberg T, Hald T, et al. Pelvic floor exercise versus surgery for female urinary stress incontinence: preliminary results [Abstract]. Proceedings of the International Continence Society (ICS), 14th Annual Meeting; 1984 Sept; Innsbruck, Austria. 1984:159‐61.
- Klarskov P, Belving D, Bischoff N, Dorph S, Gerstenberg T, Okholm B, et al. Pelvic floor exercise versus surgery for female urinary stress incontinence. Urologia Internationalis 1986;41(2):129‐32. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Klarskov P, Kroyer K, Kromann B, Maegaard E. Long term results of pelvic floor training and surgery for female genuine stress incontinence [Abstract]. Neurourology & Urodynamics. 1989; Vol. 8, issue 4:357‐9.
- Klarskov P, Nielson KK, Kromann‐Andersen B, Maegaard E. Long‐term results of pelvic floor training and surgery to female genuine stress incontinence. International Urogynaecology Journal 1991;2:132‐5. [Google Scholar]
- Klarskov P, Vedel Jepsen P, Dorph S. Reliability of voiding colpo‐cysto‐urethrography in female urinary stress incontinence before and after treatment. Acta Radiologica 1988;29(6):685‐8. [MEDLINE: ] [PubMed] [Google Scholar]
Lalos 1993 {published data only}
- Berglund AL, Eisemann M, Lalos A, Lalos O. Predictive factors of the outcome of primary surgical treatment of stress incontinence in women. Scandinavian Journal of Urology & Nephrology 1997;31(1):49‐55. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Berglund AL, Lalos O. The pre‐ and postsurgical nursing of women with stress incontinence. Journal of Advanced Nursing 1996;23(3):502‐11. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Lalos O, Berglund AL, Bjerle P. The long‐term outcome of retropubic urethrocystopexy (sutures and fibrin sealant) and pubococcygeal repair. Acta Obstetricia et Gynecologica Scandinavica 2000;79(2):135‐9. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Lalos O, Berglund AL, Bjerle P. Urodynamics in women with stress incontinence before and after surgery. European Journal of Obstetrics, Gynecology, & Reproductive Biology 1993;48(3):197‐205. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Liapis 1996a {published and unpublished data}
- Liapis AE, Asimiadis V, Loghis CD, Pyrgiotis E, Zourlas PA. A randomized prospective study of three operative methods for genuine stress incontinence. Journal of Gynecologic Surgery 1996;12(1):7‐14. [Google Scholar]
Quadri 1985 {published data only}
- Colombo M, Scalambrino S, Gallazzi S, Milani R. Burch colposuspension versus anterior repair in severe genital prolapse with stress incontinence: long term follow‐up. Proceedings of the 23rd Annual Meeting of the International Continence Society; 1993 Sept 8‐11; Rome, Italy. 1993.
- Milani R, Scalambrino S, Sirtori P, Spazzini D. Complimentary drug therapy improving results of surgery for incontinence and prolapse into two randomized procedures: vaginal versus suprapubic operation [Abstract]. Proceedings of the International Continence Society (ICS), 14th Annual Meeting; 1984 Sept; Innsbruck, Austria. 1984:440‐2.
- Quadri G, Scalambrino S, Boisio N, Marchesin R, Milani R. Randomized surgery for incontinence and prolapse: Retropubic colposuspension vs anterior repair [Abstract]. Archives of Gynecology 1985;237 (Suppl):402. [Google Scholar]
- Scalambrino S, Boisio N, Marchesin R, Quadri G, Algeri M, Milani R. Clinical and urodynamic results in a surgical trial for incontinence and prolapse [Abstract]. Proceedings of the International Continence Society (ICS), 15th Annual Meeting; 1985 Sept 3‐6; London, UK 1985:484‐5.
References to studies excluded from this review
Bump 1996 {published data only}
- Bump RC, Hurt WG, Theofrastous JP, Addison WA, Fantl JA, Wyman JF, et al. Randomized prospective comparison of needle colposuspension versus endopelvic fascia plication for potential stress incontinence prophylaxis in women undergoing vaginal reconstruction for stage III or IV pelvic organ prolapse. The Continence Program for Women Research Group. American Journal of Obstetrics & Gynecology 1996;175(2):326‐35. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Colombo 1997 {published data only}
- Colombo M, Maggioni A, Scalambrino S, Vitobello D, Milani R. Surgery for genitourinary prolapse and stress incontinence: a randomized trial of posterior pubourethral ligament plication and Pereyra suspension. American Journal of Obstetrics & Gynecology 1997;176(2):337‐43. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Colombo M, Milani R, Vitobello D, Maggioni A. A randomized comparison of Burch colposuspension and abdominal paravaginal defect repair for female stress urinary incontinence. American Journal of Obstetrics & Gynecology 1996;175(1):78‐84. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Milani R, Vitobello D, Teruzzi M, Colombo M. Comparison of Burch colposuspension and paravaginal defects repair for patients with genuine stress urinary incontinence. Proceedings of the International Continence Society (ICS), 25th Annual Meeting; 1995 Oct 17‐20; Sydney, Australia 1995:475.
Debodinance 1993 {published data only}
- Debodinance P, Querleu D. Comparison of the Bologna and Ingelman‐Sundberg procedures for stress incontinence associated with genital prolapse: prospective randomized study. European Journal of Obstetrics Gynecology and Reproductive Biology 1993;52(1):35‐40. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Gilja 1998 {published data only}
- Gilja I, Puskar D, Mazuran B, Radej M. Comparative analysis of bladder neck suspension using Raz, Burch and transvaginal Burch procedures. A 3‐year randomized prospective study. European Urology 1998;33:298‐302. [DOI] [PubMed] [Google Scholar]
Harris 1995 {published data only}
- Harris RL, Yancey CA, Wiser WL, Morrison JC, Meeks GR. Comparison of anterior colporrhaphy and retropubic urethropexy for patients with genuine stress urinary incontinence [see comments]. American Journal of Obstetrics & Gynecology 1995;173(6):1671‐4. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Liapis 1996b {published data only}
- Liapis A, Pyrgiotis E, Kontoravdis A, Louridas C, Zourlas PA. Genuine stress incontinence: prospective randomized comparison of two operative methods. European Journal of Obstetrics Gynecology and Reproductive Biology 1996;64(1):69‐72. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Meschia 2004 {published data only}
- Meschia M, Buonaguidi A, Amicarelli F, Pifarotti P, Gattei U, Stoppelli S. A randomized prospective comparison of TVT and endopelvic fascia plication in the treatment of occult stress urinary incontinence in patients with severe genital prolapse (Abstract). International Urogynecology Journal 2001;12(Suppl 3):S10. [Google Scholar]
- Meschia M, Pifarotti P, Gattei U, Ronchetti A, Stoppelli S, Lampugnani F. TVT and prolapse repair for treatment of occult stress urinary incontinence: a randomized study (Abstract). Proceedings of the International Continence Society (ICS), 32nd Annual Meeting; 2002 Aug 28‐30; Heidelberg, Germany. 2002:198‐9.
- Meschia M, Pifarotti P, Spennacchio M, Buonaguidi A, Gattei U, Somigliana E. A randomized comparison of tension‐free vaginal tape and endopelvic fascia plication in women with genital prolapse and occult stress urinary incontinence. American Journal of Obstetrics & Gynecology 2004;190(3):609‐13. [DOI] [PubMed] [Google Scholar]
- Meschia M, Spennacchio M, Amicarelli F, Pifarotti P, Cavoretto P, Stoppelli S. A randomized prospective comparison of TVT and endopelvic fascia plication in the treatment of occult stress urinary incontinence in patients with genital prolapse: preliminary data (Abstract). Neurourology and Urodynamics 2001;20(4):423‐4. [Google Scholar]
Park 1988 {published data only}
- Park GS, Miller EJ, Jr. Surgical treatment of stress urinary incontinence: a comparison of the Kelly plication, Marshall‐Marchetti‐Krantz, and Pereyra procedures. Obstetrics & Gynecology 1988;71(4):575‐9. [MEDLINE: ] [PubMed] [Google Scholar]
Thunedborg 1990 {published data only}
- Fischer‐Rasmussen W, Thunedborg P, Bjerregaard S. Colposuspension versus anterior colporraphy in the treatment of stress incontinence in patients with posterior bladder suspension defect. Proceedings of the International Continence Society (ICS); 17th Annual Meeting; 1987 Sept 2‐5; Bristol, UK. 1987:48‐9.
- Thunedborg P, Fischer‐Rasmussen W, Jensen SB. Stress urinary incontinence and posterior bladder suspension defects. Results of vaginal repair versus Burch colposuspension. Acta Obstetricia et Gynecologica Scandinavica 1990;69(1):55‐9. [DOI] [PubMed] [Google Scholar]
van Geelen 1988 {published data only}
- Geelen JM, Theeuwes AG, Eskes TK, Martin CB, Jr. The clinical and urodynamic effects of anterior vaginal repair and Burch colposuspension. American Journal of Obstetrics & Gynecology 1988;159(1):137‐44. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Zhu 1998 {published data only}
- Zhu L, Lang J, Liu Z. Comparison of different surgical procedures for urinary stress incontinence. Chung‐Hua i Hsueh Tsa Chih [Chinese Medical Journal] 1998;78(8):601‐3. [MEDLINE: ] [PubMed] [Google Scholar]
Zivkovic 1994 {published data only}
- Zivkovic F, Tamussino K, Ralph G, Schied G, Auer‐Grumbach M. Neurourodynamic effects of anterior vaginal repair with or without needle suspension at 1 year [Abstract]. Proceedings of the International Continence Society (ICS), 24th Annual Meeting; 1994 Aug 30 ‐ Sept 2; Prague, Czech Republic. 1994:332.
References to ongoing studies
Tincello 2004 {published data only}
- Tincello DG, Mayne CJ, Toozs‐Hobson P, Slack M. Randomised controlled trial of colposuspension versus anterior repair plus TVT for urodynamic stress incontinence with anterior vaginal prolapse: proposal (Abstract). Proceedings of the International Continence Society United Kingdom 11th Annual Scientific Meeting; 2004 Mar 18‐19; Bournemouth, United Kingdom. 2004:46.
Additional references
Abrams 1988
- Abrams P, Blaivas JG, Stanton SL, Andersen JT. The standardisation of terminology of lower urinary tract function. The International Continence Society Committee on Standardisation of Terminology. Scandinavian Journal of Urologic Nephrology 1988;Suppl 114:5‐19. [PubMed] [Google Scholar]
Abrams 2002
- Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, et al. The standardisation of terminology of lower urinary tract function: Report from the standardisation sub‐committee of the International Continence Society. Neurourology & Urodynamics 2002;21(2):167‐78. [MEDLINE: ; 12909] [DOI] [PubMed] [Google Scholar]
Alhasso 2005
- Alhasso A, Glazener CMA, Pickard R, N'Dow J. Adrenergics for urinary incontinence in adults. Cochrane Database of Systematic Reviews 2005, Issue 3. [DOI: 10.1002/14651858.CD001842.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bezerra 2005
- Bezerra CA, Bruschini H, Cody DJ. Traditional suburethral sling operations for urinary incontinence in women. Cochrane Database of Systematic Reviews 2005, Issue 3. [DOI: 10.1002/14651858.CD001754.pub2] [DOI] [PubMed] [Google Scholar]
Bidmead 2002
- Bidmead J. Urinary incontinence: a gynecologist's experience. European Urology Supplements 2002;1:21‐4. [Google Scholar]
Birnbaum 2004
- Birnbaum HG, Leong SA, Oster EF, Kinchen K, Sun P. Cost of stress urinary incontinence: a claims data analysis. Pharmacoeconomics 2004;22(2):95‐105. [DOI] [PubMed] [Google Scholar]
Black 1997
- Black N, Griffiths J, Pope C, Bowling A, Abel P. Impact of surgery for stress incontinence on morbidity: cohort study. BMJ 1997;315(7121):1493‐8. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Blaivas 1988
- Blaivas JG, Olsson CA. Stress incontinence: classification and surgical approach. Journal of Urology 1988;139(4):727‐31. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Blaivas 1997a
- Blaivas JG, Appell RA, Fantl JA, Leach G, McGuire EJ, Resnick NM, et al. Definition and classification of urinary incontinence: recommendations of the Urodynamic Society. Neurourology & Urodynamics 1997;16(3):149‐51. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Blaivas 1997b
- Blaivas JG, Appell RA, Fantl JA, Leach G, McGuire EJ, Resnick NM, et al. Standards of efficacy for evaluation of treatment outcomes in urinary incontinence: recommendations of the Urodynamic Society. Neurourology & Urodynamics 1997;16(3):145‐7. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Blaivas 1998
- Blaivas JG. Outcome measures for urinary incontinence. Urology 1998;51(2A Suppl):11‐9. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Bump 1988
- Bump RC, Copeland WE Jr, Hurt WG, Fantl JA. Dynamic urethral pressure/profilometry pressure transmission ratio determinations in stress‐incontinent and stress‐continent subjects. American Journal of Obstetrics & Gynecology 1988;159(3):749‐55. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Bump 1997
- Bump RC, Coates KW, Cundiff GW, Harris RL, Weidner AC. Diagnosing intrinsic sphincteric deficiency: comparing urethral closure pressure, urethral axis, and Valsalva leak point pressures. American Journal of Obstetrics & Gynecology 1997;177(2):303‐10. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Chong 2011
- Chong EC, Khan AA, Anger JT. The financial burden of stress urinary incontinence among women in the United States. Current Urology Reports 2011;12(5):358‐62. [DOI] [PubMed] [Google Scholar]
Cody 2009
- Cody JD, Richardson K, Moehrer B, Hextall A, Glazener CMA. Oestrogen therapy for urinary incontinence in post‐menopausal women. Cochrane Database of Systematic Reviews 2009, Issue 4. [DOI: 10.1002/14651858.CD001405.pub2] [DOI] [PubMed] [Google Scholar]
Dean 2006
- Dean NM, Ellis G, Wilson PD, Herbison GP. Laparoscopic colposuspension for urinary incontinence in women. Cochrane Database of Systematic Reviews 2006, Issue 3. [DOI: 10.1002/14651858.CD002239.pub2] [DOI] [PubMed] [Google Scholar]
Deeks 2006
- Deeks JJ, Higgins JPT, Altman DG, editors. Analysing and Presenting Results. Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions 4.2.6 [updated September 2006]; Section 8 http://www.cochrane.org/resources/handbook/hbook.htm (accessed 6th October 2006).
Downs 1996
- Downs S, Black N. Systematic review of the literature on the effectiveness of surgery for stress incontinence in women. Report 21. London: Department of Public Health & Policy Publications, London School of Hygiene & Tropical Medicine, 1996:1‐93. [ISSN 0962‐6115] [Google Scholar]
Fantl 1996
- Fantl JA, Newman DK. Urinary Incontinence in Adults: Acute and Chronic Management. 2. Washington: Agency for Health Care Policy and Research, US Government Printing Office, 1996. [Google Scholar]
Glazener 2004
- Glazener CMA, Cooper K. Bladder neck needle suspension for urinary incontinence in women. Cochrane Database of Systematic Reviews 2004, Issue 2. [DOI: 10.1002/14651858.CD003636.pub2] [DOI] [PubMed] [Google Scholar]
Hana 2012
- Hana D, Amir I, Amel K. Assessment of clinical effectiveness and economic viability of the obturator tension free vaginal tape method for the treatment of stress Urinary Incontinence by Cost Benefit Analysis. European Journal of General Medicine 2012;9(3):178‐82. [Google Scholar]
Hay‐Smith 2006
- Hay‐Smith EJC, Dumoulin C. Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women. Cochrane Database of Systematic Reviews 2006, Issue 1. [DOI: 10.1002/14651858.CD005654] [DOI] [PubMed] [Google Scholar]
Higgins 2003
- Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analyses. BMJ 2003;327(7414):557‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hilton 1983
- Hilton P, Stanton SL. Urethral pressure measurement by microtransducer: the results in symptom‐free women and in those with genuine stress incontinence. British Journal of Obstetrics & Gynaecology 1983;90(10):919‐33. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Jolleys 1988
- Jolleys JV. Reported prevalence of urinary incontinence in women in a general practice. BMJ 1988;296(6632):1300‐2. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Keegan 2007
- Keegan PE, Atiemo K, Cody JD, McClinton S, Pickard R. Periurethral injection therapy for urinary incontinence in women. Cochrane Database of Systematic Reviews 2007, Issue 3. [DOI: 10.1002/14651858.CD003881.pub2] [DOI] [PubMed] [Google Scholar]
Kelleher 1997
- Kelleher CJ, Cardozo LD, Khullar V, Salvatore S. A new questionnaire to assess the quality of life of urinary incontinent women. British Journal of Obstetrics & Gynaecology 1997;104(12):1374‐9. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Kilonzo 2004
- Kilonzo M, Vale L, Stearns SC, Grant A, Cody J, Glazener CM, et al. Cost effectiveness of tension‐free vaginal tape for the surgical management of female stress incontinence. International Journal of Technology Assessment in Health Care 2004;20(4):455‐63. [DOI] [PubMed] [Google Scholar]
Kunkle 2015
- Kunkle CM, Hallock JL, Hu X, Blomquist J, Thung SF, Werner EF. Cost utility analysis of urethral bulking agents versus midurethral sling in stress urinary incontinence. Female Pelvic Medicine & Reconstructive Surgery 2015;21(3):154‐9. [DOI] [PubMed] [Google Scholar]
Lapitan 2009
- Lapitan M, Cody DJ, Grant AM. Open retropubic colposuspension for urinary incontinence in women. Cochrane Database of Systematic Reviews 2009, Issue 4. [DOI: 10.1002/14651858.CD002912.pub4] [DOI] [Google Scholar]
Leach 1997
- Leach GE, Dmochowski RR, Appell RA, Blaivas JG, Hadley HR, Luber KM, et al. Female Stress Urinary Incontinence Clinical Guidelines Panel summary report on surgical management of female stress urinary incontinence. The American Urological Association. Journal of Urology 1997;158(3 Pt 1):875‐80. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Lose 1998
- Lose G, Fantl JA, Victor A, Walter S, Wells TL. Outcome measures for research in adult women with symptoms of lower urinary tract dysfunction. Neurourology and Urodynamics 1998;17(3):255‐62. [DOI] [PubMed] [Google Scholar]
MacArthur 1991
- MacArthur C, Lewis M, Knox EG. Health after Childbirth. London: HMSO, 1991. [DOI] [PubMed] [Google Scholar]
MacArthur 1993
- MacArthur C, Lewis M, Bick D. Stress incontinence after childbirth. British Journal of Midwifery 1993;1(5):207‐15. [Google Scholar]
Maher 2007
- Maher C, Baessler K, Glazener CMA, Adams EJ, Hagen S. Surgical management of pelvic organ prolapse in women. Cochrane Database of Systematic Reviews 2007, Issue 3. [DOI: 10.1002/14651858.CD004014.pub3] [DOI] [PubMed] [Google Scholar]
McGuire 1993
- McGuire EJ, Fitzpatrick CC, Wan J, Bloom D, Sanvordenker J, Ritchey M, et al. Clinical assessment of urethral sphincter function. Journal of Urology 1993;150(5 Pt 1):1452‐4. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Meyer 1994
- Meyer S, Grandi P, Schmidt N, Sanzeni W, Spinosa JP. Urodynamic parameters in patients with slight and severe genuine stress incontinence: is the stress profile useful?. Neurourology & Urodynamics 1994;13(1):21‐8. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Newsletter of the European Union 2003
- Delegation of The European Commission to Bosnia and Herzegovina. EU Newsletter: Delegation of The European Commission to Bosnia and Herzegovina. Sarajevo: Delegation of The European Commission to Bosnia and Herzegovina, April 2003. [Google Scholar]
Ogah 2009
- Ogah J, Cody JD, Rogerson L. Minimally invasive synthetic suburethral sling operations for stress urinary incontinence in women. Cochrane Database of Systematic Reviews 2009, Issue 4. [DOI: 10.1002/14651858.CD006375.pub2] [DOI] [PubMed] [Google Scholar]
Subak 2008
- Subak LL, Brubaker L, Chai TC, Creasman JM, Diokno AC, Goode PS, et al. High costs of urinary incontinence among women electing surgery to treat stress incontinence. Obstetrics & Gynecology 2008;111(4):899‐907. [DOI] [PMC free article] [PubMed] [Google Scholar]
Swift 1995
- Swift SE, Ostergard DR. Evaluation of current urodynamic testing methods in the diagnosis of genuine stress incontinence. Obstetrics & Gynecology 1995;86(1):85‐91. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Thom 1997
- Thom DH, Eeden SK, Brown JS. Evaluation of parturition and other reproductive variables as risk factors for urinary incontinence in later life. Obstetrics & Gynecology 1997;90(6):983‐9. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Thomas 1980
- Thomas TM, Plymat KR, Blannin J, Meade TW. Prevalence of urinary incontinence. British Medical Journal 1980;281(6250):1243‐5. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wagner 1998
- Wagner TH, Hu TW. Economic costs of urinary incontinence in 1995. Urology 1998;51(3):355‐61. [DOI] [PubMed] [Google Scholar]
Wilson 1996
- Wilson PD, Herbison RM, Herbison GP. Obstetric practice and the prevalence of urinary incontinence three months after delivery. British Journal of Obstetrics & Gynaecology 1996;103(2):154‐61. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Glazener 2001
- Glazener CMA, Cooper K. Anterior vaginal repair for urinary incontinence in women. Cochrane Database of Systematic Reviews 2001, Issue 1. [DOI: 10.1002/14651858.CD001755] [DOI] [PubMed] [Google Scholar]


