Abstract
Background
Cancer patients are 1.4 times more likely to be unemployed than healthy people. Therefore it is important to provide cancer patients with programmes to support the return‐to‐work (RTW) process. This is an update of a Cochrane review first published in 2011.
Objectives
To evaluate the effectiveness of interventions aimed at enhancing RTW in cancer patients compared to alternative programmes including usual care or no intervention.
Search methods
We searched the Cochrane Central Register of Controlled Trials (CENTRAL, in the Cochrane Library Issue 3, 2014), MEDLINE (January 1966 to March 2014), EMBASE (January 1947 to March 2014), CINAHL (January 1983 to March, 2014), OSH‐ROM and OSH Update (January 1960 to March, 2014), PsycINFO (January 1806 to 25 March 2014), DARE (January 1995 to March, 2014), ClinicalTrials.gov, Trialregister.nl and Controlled‐trials.com up to 25 March 2014. We also examined the reference lists of included studies and selected reviews, and contacted authors of relevant studies.
Selection criteria
We included randomised controlled trials (RCTs) of the effectiveness of psycho‐educational, vocational, physical, medical or multidisciplinary interventions enhancing RTW in cancer patients. The primary outcome was RTW measured as either RTW rate or sick leave duration measured at 12 months' follow‐up. The secondary outcome was quality of life.
Data collection and analysis
Two review authors independently assessed trials for inclusion, assessed the risk of bias and extracted data. We pooled study results we judged to be clinically homogeneous in different comparisons reporting risk ratios (RRs) with 95% confidence intervals (CIs). We assessed the overall quality of the evidence for each comparison using the GRADE approach.
Main results
Fifteen RCTs including 1835 cancer patients met the inclusion criteria and because of multiple arms studies we included 19 evaluations. We judged six studies to have a high risk of bias and nine to have a low risk of bias. All included studies were conducted in high income countries and most studies were aimed at breast cancer patients (seven trials) or prostate cancer patients (two trials).
Two studies involved psycho‐educational interventions including patient education and teaching self‐care behaviours. Results indicated low quality evidence of similar RTW rates for psycho‐educational interventions compared to care as usual (RR 1.09, 95% CI 0.88 to 1.35, n = 260 patients) and low quality evidence that there is no difference in the effect of psycho‐educational interventions compared to care as usual on quality of life (standardised mean difference (SMD) 0.05, 95% CI ‐0.2 to 0.3, n = 260 patients). We did not find any studies on vocational interventions. In one study breast cancer patients were offered a physical training programme. Low quality evidence suggested that physical training was not more effective than care as usual in improving RTW (RR 1.20, 95% CI 0.32 to 4.54, n = 28 patients) or quality of life (SMD ‐0.37, 95% CI ‐0.99 to 0.25, n = 41 patients).
Seven RCTs assessed the effects of a medical intervention on RTW. In all studies a less radical or functioning conserving medical intervention was compared with a more radical treatment. We found low quality evidence that less radical, functioning conserving approaches had similar RTW rates as more radical treatments (RR 1.04, 95% CI 0.96 to 1.09, n = 1097 patients) and moderate quality evidence of no differences in quality of life outcomes (SMD 0.10, 95% CI ‐0.04 to 0.23, n = 1028 patients).
Five RCTs involved multidisciplinary interventions in which vocational counselling, patient education, patient counselling, biofeedback‐assisted behavioral training and/or physical exercises were combined. Moderate quality evidence showed that multidisciplinary interventions involving physical, psycho‐educational and/or vocational components led to higher RTW rates than care as usual (RR 1.11, 95% CI 1.03 to 1.16, n = 450 patients). We found no differences in the effect of multidisciplinary interventions compared to care as usual on quality of life outcomes (SMD 0.03, 95% CI ‐0.20 to 0.25, n = 316 patients).
Authors' conclusions
We found moderate quality evidence that multidisciplinary interventions enhance the RTW of patients with cancer.
Plain language summary
Interventions to enhance return‐to‐work for cancer patients
Research question
What is the best way to help cancer patients get back to work when compared to care as usual?
Background
Each year more and more people who get cancer manage to get through treatment alive. Many cancer survivors live well, although they can continue to experience long‐lasting problems such as fatigue, pain and depression. These long‐term effects can cause problems with cancer survivors' participation in working life. Therefore, cancer is a significant cause of absence from work, unemployment and early retirement. Cancer patients, their families and society at large all carry part of the burden. In this Cochrane review we evaluated how well cancer patients can be helped to return to work.
Study characteristics
The search date was 25 March 2014. Fifteen randomised controlled trials including 1835 cancer patients met the inclusion criteria. We found four types of interventions. In the first, psycho‐educational interventions, participants learned about physical side effects, stress and coping and they took part in group discussions. In the second type of physical intervention participants took part in exercises such as walking. In the third type of intervention, participants received medical interventions ranging from cancer drugs to surgery. The fourth kind concerned multidisciplinary interventions in which vocational counselling, patient education, patient counselling, biofeedback‐assisted behavioral training and/or physical exercises were combined.We did not find any studies on vocational interventions aimed at work‐related issues.
Key results
Results suggest that multidisciplinary interventions involving physical, psycho‐educational and/or vocational components led to more cancer patients returning to work than when they received care as usual. Quality of life was similar. When studies compared psycho‐educational, physical and medical interventions with care as usual they found that similar numbers of people returned to work in all groups.
Quality of the evidence
We found low quality evidence of similar return‐to‐work rates for psycho‐educational interventions compared to care as usual. We also found low quality evidence showing that physical training was not more effective than care as usual in improving return‐to‐work. We also found low quality evidence that less radical cancer treatments had similar return‐to‐work rates as more radical treatments. Moderate quality evidence showed multidisciplinary interventions involving physical, psycho‐educational and/or vocational components led to higher return‐to‐work rates than care as usual.
Summary of findings
Background
The number of people who survive cancer is increasing (American Cancer Society 2015; de Boer 2014; Hoffman 2005) due to the sustained improvements in strategies to detect cancer early and treat it effectively. Since the population is ageing in most countries and cancer survival is prolonged, the prevalence of cancer survivors is expected to rise further in the future (Aziz 2007). In the absence of other competing causes of death, 68% of adults now diagnosed with cancer can expect to be alive five years post‐diagnosis (American Cancer Society 2015).
Cancer diagnoses in working age people are becoming more common, with almost half of the adult cancer survivors aged less than 65 years (Short 2005; Verdecchia 2009). Each year an estimated 14.1 million new cases of cancer are diagnosed worldwide (American Cancer Society 2015) and thus approximately seven million working‐age people are diagnosed with cancer each year.
Many survivors do well in general terms, although a significant proportion of survivors continue to experience physical, emotional and social problems such as fatigue, pain, cognitive deficits, anxiety and depression, which may become chronic or persistent (Cooper 2013; Smith 2007). These long‐term medical and psychological effects of cancer or its treatment may cause impairments that diminish social functioning, including obtaining or retaining employment (Cooper 2013; Mehnert 2013; Taskila 2007a). Fortunately, many cancer patients are both willing and able to return‐to‐work (RTW) following treatment (Taskila 2007a) without residual disabilities (Steiner 2010).
Returning to work is important for both cancer patients themselves and society. From the viewpoint of society, it is economically imperative to encourage patients to RTW whenever possible (Verbeek 2007). From the individual point of view, employment is an important component of quality of life (QoL) (de Boer 2014). Work is invaluable as it can provide a sense of purpose, dignity and an income thus enabling people to support themselves and their families. There is strong evidence that good work is beneficial for physical and mental health, whereas unemployment and long‐term sickness absence have a harmful impact (Marmot 2012). This also applies to cancer patients who consider returning to work very important (Mehnert 2013; Verbeek 2007) because it is regarded as a marker of complete recovery (Spelten 2002) and regaining normality (Kennedy 2007). Moreover, returning to work can improve cancer patients' QoL and it can have a positive effect on self‐esteem and social or family roles (Verbeek 2007).
Since 1980, several studies have documented the impact of cancer on employment and they have reported approximately 60% (ranging from 30% to 93%) of the cancer patients returning to work after one to two years (Mehnert 2011; Spelten 2002; Taskila 2007a). However, cancer patients can experience problems getting back to work (Feuerstein 2007). Overall, cancer survivors are 1.4 times more likely to be unemployed than healthy controls although the rate differs depending on the diagnosis (de Boer 2009). Some studies have stated that cancer patients may experience impairments in mental and physical health as a result of their illness, and that these impairments sometimes lead to a decrease in their ability to work (Short 2005). More specifically, work ability of cancer patients who work at the time of their diagnosis is severely impaired in the first months of treatment but does improve in the months afterwards (de Boer 2008). Beyond the first months, a Finnish study found that 26% of the cancer patients reported deteriorated physical work ability and 19% deteriorated mental work ability, two to six years after diagnosis (Taskila 2007b).
Therefore, it is important to provide employed cancer patients with programmes to support their RTW process. A recent Macmillan report has proposed that successful vocational rehabilitation can have a major impact on cancer patients' capability to RTW and remain in work life (Macmillan 2013). There has been increasing interest in improving RTW outcomes for people with cancer. Thus it is reasonable to expect that more studies of interventions with vocational aspects for cancer patients have been conducted since the publication of the first version of this review in 2011 (De Boer 2011).
Objectives
To evaluate the effectiveness of interventions aimed at enhancing RTW in cancer patients compared to alternative programmes including usual care or no intervention.
Methods
Criteria for considering studies for this review
Types of studies
We included all eligible randomised controlled trials (RCTs) and cluster‐RCTs.
Types of participants
We limited the population to adults (≧ 18 years old) who had been diagnosed with cancer and were in paid employment (employee or self‐employed) at the time of diagnosis. We included studies conducted with people who had any type of cancer diagnosis.
Types of interventions
We included any type of intervention aiming to enhance RTW. Interventions may have been carried out either with an individual or in a group and in a clinical setting or in the community. Interventions could primarily focus on different factors which influence RTW, such as coping (in psycho‐educational interventions), workplace adjustments (in vocational interventions), physical exercises (in physical interventions), minimal surgery (in medical interventions) or on a combination of those factors (in multidisciplinary interventions). Thereby we divided interventions into:
Psycho‐educational: interventions that included any type of psycho‐educational intervention such as counselling, education, training in coping skills, and problem solving therapy (PST), undertaken by any qualified professional (e.g. psychologist, social worker or oncology nurse).
Vocational: interventions that included any type of intervention focused on employment. Vocational interventions might be person‐directed or work‐directed. Person‐directed vocational interventions are aimed at the patient and incorporate programmes which aim to encourage RTW, vocational rehabilitation, or occupational rehabilitation. Work‐directed vocational interventions are aimed at the workplace and include workplace adjustments such as modified work hours, modified work tasks, or modified workplace and improved communication with or between managers, colleagues and health professionals.
Physical: interventions that included any type of physical training (such as walking), physical exercises (such as arm lifting) or training of bodily functions (such as vocal training).
Medical or pharmacological: interventions that incorporated any type of medical intervention (e.g. surgical) or medication (such as hormone treatment).
Multidisciplinary: any combination of psycho‐educational, vocational, physical and medical interventions.
Types of outcome measures
Primary outcomes
Our primary outcome was RTW. RTW included return to either full‐ or part‐time employment, to the same or a reduced role and to either the previous job or any new employment. We extracted two types of RTW data:
RTW measured as event data such as RTW rates or (change in) disability pension rates.
RTW measured as time‐to‐event data, such as number of days between reporting sick and any work resumption or the number of days on sick leave during the follow‐up period.
We extracted outcome data from the follow‐up measurement. When study authors reported multiple follow‐up measurements, we extracted the 12‐month follow‐up data.
Secondary outcomes
QoL which included overall QoL, physical QoL and emotional QoL measured with validated and unvalidated questionnaires.
We extracted outcome data from the follow‐up measurement. When study authors reported multiple follow‐up measurements, we extracted the 12‐month follow‐up data.
Search methods for identification of studies
This is an update of the Cochrane review: Interventions to enhance return‐to‐work for cancer patients (De Boer 2011). We considered studies published in any language.
Electronic searches
First, we identified relevant trials from the following sources:
Cochrane Central Register of Controlled Trials (CENTRAL, in the Cochrane Library Issue 3, 2014).
MEDLINE (1966 to 25 March 2014).
EMBASE (1947 to 25 March 2014).
CINAHL (1983 to 25 March 2014).
OSH‐ROM and OSH Update (Occupational Safety and Health, 1960 to 25 March 2014).
PsycINFO (1806 to 25 March 2014).
Abstracts of Reviews of Effectiveness (DARE, 1995 to 25 March 2014).
ClinicalTrials.gov, accessed 25 March 2014.
Trialregister.nl, accessed 25 March 2014.
Controlled‐trials.com, accessed 25 March 2014.
We selected cancer‐related and work–related search terms from an earlier meta‐analysis on cancer and employment (de Boer 2006). We based all systematic searches in electronic databases on the MEDLINE search strategy (Appendix 1) using the revised Cochrane RCT filter (Robinson 2002) and the sensitive search of the Cochrane Occupational Safety and Health Group for retrieving studies of occupational health interventions. For future review updates we will only use the RCT filter. We adapted the search to fit the specifications for CENTRAL, EMBASE, CINAHL, OSH‐ROM, PsycINFO (Appendix 2) and DARE(Appendix 3) . Searches on cancer and employment tended to result in many studies on occupational exposure, occupational diseases and biological research. Therefore, we used a set of search terms to exclude those studies.
Searching other resources
We checked the reference lists of all studies that we retrieved as full papers and the reference lists of all retrieved systematic and narrative reviews in order to identify other potentially eligible studies. We wrote to the corresponding authors of all identified studies that fulfilled our inclusion criteria but provided insufficient data to request any additional published or unpublished study that may be relevant to this Cochrane review.
Data collection and analysis
Selection of studies
Two review authors (AdB, TT) independently screened all titles and abstracts of studies that we identified from the search strategy for inclusion and appropriateness based on the selection criteria. Review authors were not blinded to the name(s) of the author(s), institution(s) or publication source at any level. If the title and abstract provided sufficient information to decide that it did not satisfy the inclusion criteria, we excluded the study. When there was a difference of opinion, a third review author (JV) arbitrated. We documented the reasons for exclusion at this stage. Two review authors (AdB, TT) independently examined the full‐text articles of the included studies to determine which studies fulfilled all inclusion criteria. Where necessary, we contacted study authors for further information. Again, a third review author (JV) arbitrated in case of a difference of opinion. We documented the reasons for exclusion at this stage as well. We discussed reasons for inclusion and exclusion of studies of the two review authors and listed these reasons in the Characteristics of included studies and Characteristics of excluded studies tables.
Data extraction and management
We constructed a data extraction form that enabled two review authors (AdB, TT) to independently extract the following data from the studies: study type, setting, country, recruitment, randomisation, blinding, funding, inclusion and exclusion criteria, number of patients, patient characteristics including diagnosis, medical treatment, sociodemographic data, and employment situation at baseline, intervention (content, duration, provider, discipline, context), co‐interventions, follow‐up time and follow‐up measurements, number of patients lost to follow‐up, RTW outcome measures used, statistical methods, and results for each RTW outcome measure at each follow‐up measurement point for each group. We summarised the diagnoses in diagnostic groups such that if at least 50% of the patients had a specific diagnosis then we included the study in that specific cancer diagnostic group; otherwise we designated it as mixed diagnoses. We discussed all the results of data extraction by the two independent review authors and we entered study data relevant to this review into RevMan 2014.
We entered the details of the interventions into an additional, Table 5, in RevMan 2014.
1. Characteristics of included studies.
| Study | Country | Diagnosis | Design | Number | Intervention(s) | Control | Type |
| Ackerstaff 2009 | Netherlands | Head, neck | RCT | 34 versus 28 | Intra‐arterial chemoradiation | Intravenous chemoradiation | Medical |
| Berglund 1994 | Sweden | Breast | RCT | 81 versus 73 | Physical training, patient education and training of coping skills re RTW | Care as usual | Multidisciplinary |
| Burgio 2006 | USA | Prostate | RCT | 28 versus 29 | Biofeedback behavioral training | Care as usual | Multidisciplinary |
| Emmanouilidis 2009 | Germany | Thyroid | RCT | 7 versus 6 | L‐thyroxine after surgery | Later provision of L‐thyroxine | Medical |
| Friedrichs 2010 | Germany | Leukemia | RCT | 163 versus 166 | Peripheral blood progenitor cell transplantation | Bone marrow transplantation | Medical |
| Hillman 1998 | USA | Laryngeal | RCT | 80 versus 63 | Chemotherapy | Laryngectomy | Medical |
| Hubbard 2013 | UK | Breast | RCT | 7 versus 11 | Physical, occupational, psycho‐educational support services, multi‐disciplinary | Booklet work and cancer | Multidisciplinary |
| Johnsson 2007 | Sweden | Breast | RCT | 53 versus 17 55 versus 17 64 versus 17 |
|
No endocrine therapy | Medical |
| Kornblith 2009 | USA | Endometrial | RCT | 164 versus 73 | Laparoscopy | Laparotomy | Medical |
| Lee 1992 | UK | Breast | RCT | 44 versus 47 | Breast conservation | Mastectomy | Medical |
| Lepore 2003 | USA | Prostate | RCT | 41 versus 20 43 versus 20 |
|
Care as usual | Psycho‐educational |
| Maguire 1983 | UK | Breast | RCT | 42 versus 46 | Physical training, individual counselling and encouragement of RTW. | Care as usual | Multidisciplinary |
| Purcell 2011 | Australia | Radiotherapy patients | RCT | 43 versus 48 21 versus 24 |
|
Flyer with generic information about fatigue. | Psycho‐educational |
| Rogers 2009 | USA | Breast | RCT | 14 versus 14 | Physical activity training | Care as usual | Physical |
| Tamminga 2013 | Netherlands | Breast | RCT | 65 versus 68 | Vocational support, counselling, education, multi‐disciplinary, RTW advice. | Care as usual | Multidisciplinary |
When an article reported more than one intervention and compared each intervention against a control group, we entered each intervention as a separate evaluation.
Assessment of risk of bias in included studies
Two review authors (AdB, TT) assessed the included studies' risk of bias independently according to the procedures described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We assessed each included study within ten domains of risk of bias: adequacy of sequence generation, allocation concealment and blinding, how incomplete outcome data (drop‐outs) were addressed, use of intention‐to‐treat (ITT) analysis, similarity of baseline characteristics, similarity or avoidance of co‐interventions, acceptability of compliance, similarity of the timing of outcome assessments, and evidence of selective outcome reporting.
We judged studies to have a low overall risk of bias when we judged five or more of the domains to have a low risk of bias.
We used a sample of three included studies to test whether the two review authors (AdB, TT) applied the assessment criteria consistently. We followed any disagreement about the criteria by a discussion until we reached consensus. If we could not resolve the difference of opinion, we consulted a third review author (JV). We discussed all the results of the two independent review authors and reported one final assessment of risk of bias for each study.
Measures of treatment effect
For dichotomous data, such as RTW rates, we used risk ratios (RRs) as the measure of treatment effect. For continuous variables, such as the number of days on sick leave during the follow‐up period, we used the mean difference (MD). For QoL outcomes, we calculated standardised mean difference (SMD) values. All estimates included a 95% confidence interval (CI).
Unit of analysis issues
For trials with multiple arms and if two or more interventions were compared with the same control group in one meta‐analysis, we divided the number of patients in the control group equally over the intervention studies, i.e. we halved the number of control patients if there were two intervention groups.
Dealing with missing data
We contacted the authors of the following studies to obtain data that were missing in their report that we needed to assess eligibility of the studies or as input for meta‐analysis, or both: Ackerstaff 2009; Emmanouilidis 2013; Jones 2005; Rogers 2009; Tamminga 2013; and Wiggins 2009 . All of these study authors kindly provided the information we requested. If statistics were missing, such as standard deviations (SDs) we calculated them from other available statistics such as P values according to the methods described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011).
Assessment of heterogeneity
We first decided whether or not studies were sufficiently homogeneous to be able to synthesize the results into one summary‐measure. We defined studies to be sufficiently homogeneous when they had similar designs, similar interventions and similar outcomes measured at the same follow‐up point.
We considered the following categories of interventions as sufficiently similar to be combined: psycho‐educational, vocational, physical, medical and multidisciplinary interventions.
We considered both RTW outcomes and sick leave duration outcomes as similar enough to be combined. We considered general QoL outcomes measured with different instruments similar enough to be merged. We combined different diagnoses within one analysis because we hypothesized that the mechanism of RTW interventions is similar over the different cancer diagnoses.
We also tested for statistical heterogeneity with the I² statistic. We considered studies to be statistically heterogeneous if the I² statistic was greater than 50%.
Assessment of reporting biases
We assessed publication bias with a funnel plot when more than five studies were available for a particular comparison.
Data synthesis
We pooled studies with sufficient data that we judged to be clinically homogeneous with RevMan 2014. We combined studies that were statistically heterogeneous with a random‐effects model; otherwise we used a fixed‐effect model.
For RTW outcomes, we aimed at combining rate of RTW, which is a dichotomous measure, and the number of days on sick leave, which is a continuous measure. Therefore, we calculated effect sizes in order to enter them in the same comparison. For studies with continuous outcomes, we calculated the SMD using RevMan 2014. We subsequently expressed SMDs as log odds ratios by multiplying them by 1.814 (Chinn 2000) as is the recommended method in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). For studies with dichotomous RTW rates, we recalculated the risk ratios (RRs) into odds ratios (ORs) and then into log odds ratios. Next, we calculated for both types of studies the standard errors (SE) of the log odds ratios from the 95% CI of the log odds ratios. We used the formula: SE = (upper limit log odds ratio ‐ lower limit log odds ratio)/3.92, as is the recommended method in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We then used these log odds ratios and their SEs as input into the meta‐analysis using the generic inverse variance method as implemented in RevMan 2014.
Since RTW rates in cancer patients are much higher than 10%, the ORs overestimate the treatment effect considerably. Therefore we recalculated the ORs back into risk ratios using the formula: RR = OR/((1‐P0)+(P0*OR)) as recommended by Zhang 1998. In this formula, OR refers to the pooled OR produced by RevMan 2014 and P0 to the incidence in the non‐exposed group. P0 was estimated from the studies reporting dichotomous RTW rates by selecting the median P0 of the non‐exposed group from these studies.
GRADE assessment
Finally, we used the GRADE approach to assess the quality of the evidence per comparison and per outcome, as described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). Starting from an assumed level of high quality, we reduced the quality of the evidence by one or more levels if there were one or more limitations in the following domains: risk of bias, consistency, directness of the evidence, precision of the pooled estimate and the possibility of publication bias. Thus, we rated the level of evidence as either high, moderate, low or very low depending on the number of limitations. For the most important comparisons and outcomes, we used the programme GRADEpro GDT 2015 to generate 'Summary of findings' tables. We present the results of our GRADE assessment in Table 6.
2. Quality of the evidence (GRADE).
| Comparison/outcome | Number of studies | Study limitations | Inconsistency | Indirectness | Imprecision | Publication bias | Overall quality of evidence |
| Psycho‐educational versus Care as usual/ RTW |
2 RCTs | Yes: 1 high 1 low risk 1 level down |
No inconsistency | No | Wide CI 1 level down |
Only two studies | Low |
| Physical versus Care as usual/ RTW |
1 RCT | No: Low risk | No | No | Wide CI 2 levels down |
Only one study | Low |
| Medical function conserving versus Medical more radical/ RTW |
7 RCTs | No: 2/7 high risk studies contribute 25% | High: I² statistic = 51% | No | Wide CI 1 level down |
Not observed | Low |
| Multidisciplinary physical, psycho‐educational and/or vocational interventions versus Care as usual/ RTW |
5 RCTs | Yes: 3/5 high risk 1 level down |
No: I² statistic = 0% | No | Narrow CIs | Not observed | Moderate |
| Psycho‐educational versus Care as usual/QoL | 2 RCTs | Yes: 1 high, 1 low risk 1 level down |
No: I² statistic = 0% | No | Wide CI 1 level down |
Only two studies | Low |
| Physical versus Care as usual/ QoL |
1 RCT | No: Low risk | Not applicable | No | Wide CI 1 level down |
Only one study | Low |
| Medical function conserving versus Medical more radical/QoL | 2 RCTs | No: Low risk studies | No: I² statistic = 0% | No | Wide CI 1 level down |
Only two studies | Moderate |
| Multidisciplinary physical, psycho‐educational and/or vocational interventions versus Care as usual/QoL | 2 RCTs | Yes: 1 low, 1 high risk studies 1 level down |
No: I² statistic = 17% | No | Wide CI 1 level down |
Only two studies | Low |
Column headings (with explanations in parentheses): Study design (RCT = randomised controlled trial); study limitations (likelihood of reported results not being an accurate estimate of the truth); inconsistency (lack of similarity of estimates of treatment effects); indirectness (not representing PICO well); imprecision (insufficient number of patients or wide CIs) of results; and publication bias (probability of selective publication of trials and outcomes) across all studies that measured that particular outcome.
Subgroup analysis and investigation of heterogeneity
We intended to perform further subgroup analyses according to diagnosis. However, the number of studies in the subgroups was too low to perform such subgroup analyses.
Sensitivity analysis
We intended to analyse how sensitive our results were to the risk of bias in the included studies. However, there was an insufficient number of studies available per comparison to do such an analysis.
Results
Description of studies
Results of the search
Figure 1 shows the PRISMA study flow diagram of included and excluded studies. Through a comprehensive literature search of electronic databases, we identified a total of 5088 potentially relevant records with most (61%) retrieved by MEDLINE. After removing duplicates, we screened a total of 4742 potentially relevant references for eligibility. We excluded a total of 4664 references based on the title and abstract, with the most frequent reasons for exclusion being: 1) study not aimed at cancer patients (39%); 2) study does not assess the effectiveness of an intervention (22%); and 3) no RTW outcomes reported (19%). Other reasons were: no control group (11%); study involved survivors of childhood cancer (5%); study was aimed at cancer as an occupational disease (3%); or study is a review (0.5%).
1.
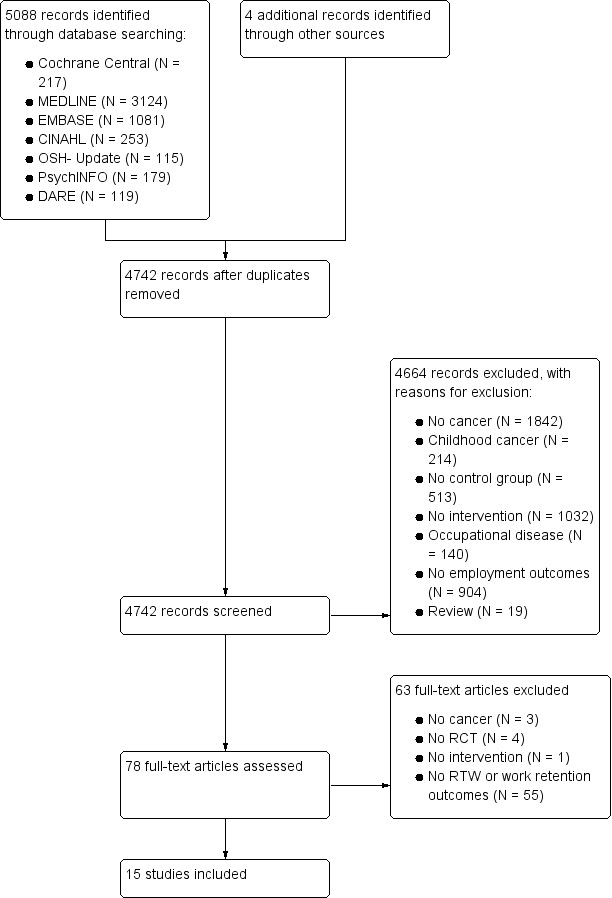
PRISMA flow diagram of reference selection and study inclusion.
From our search of the websites ClinicalTrials.gov, Trialregister.nl and Controlled‐trials.com we identified three ongoing RCT studies (NCT00639210; NCT01799031; NTR2138) which are listed in the Characteristics of ongoing studies table.
We also checked the reference lists of 19 retrieved systematic and narrative reviews (Beck 2003; De Backer 2009; Egan 2013; Fors 2011; Haaf 2005; Harvey 1982; Hersch 2009; Hoving 2009; Irwin 2004; Kirshblum 2001; Kirshbaum 2007; Liu 2009; McNeely 2006; Oldervoll 2004; Scott 2013; Silver 2013; Stanton 2006; Steiner 2010; van der Molen 2009) to identify additional potentially eligible studies. We found four additional titles of potentially eligible studies.
We contacted the corresponding authors of six studies that fulfilled our inclusion criteria but did not provide sufficient data to request any additional relevant published or unpublished study data. Based on the information kindly provided by the trial authors, we included three studies (Ackerstaff 2009; Rogers 2009; Tamminga 2013) and excluded three studies (Emmanouilidis 2013; Gordon 2005; Wiggins 2009). We also checked the reference lists of all studies that we retrieved as full papers in order to identify further potentially eligible studies but did not identify any additional studies.
Included studies
Characteristics of studies and participants
We included 15 studies describing RCTs. Of these, three had multiple study arms and thus we included 19 evaluations of interventions, which we entered as separate evaluations in RevMan 2014. These studies included a total of 1835 participants. Table 5 gives an overview of the main characteristics of the 15 studies and 19 evaluations. All included studies were conducted in high income countries, with most describing research from the United States of America (USA) (N = 5) while another nine studies were conducted in Europe (UK (N = 3); Sweden (N = 2); the Netherlands (N = 2); Germany (N = 2)) and Australia (N = 1). Seven studies aimed interventions at breast cancer patients (Berglund 1994; Hubbard 2013; Johnsson 2007; Lee 1992; Maguire 1983; Rogers 2009; Tamminga 2013). Two studies involved prostate cancer patients (Burgio 2006; Lepore 2003) and one study each showed results for thyroid cancer patients (Emmanouilidis 2009), gynaecological patients (Kornblith 2009), head and neck cancer patients (Ackerstaff 2009), laryngeal cancer patients (Hillman 1998), leukaemia patients (Friedrichs 2010) and mixed cancer diagnoses patients (Purcell 2011).
Funding sources were charities (Berglund 1994; Hubbard 2013; Johnsson 2007; Lee 1992; Maguire 1983; Rogers 2009), national institutes (Burgio 2006; Hillman 1998; Kornblith 2009; Lepore 2003; Purcell 2011; Tamminga 2013), were not received (Emmanouilidis 2009; Friedrichs 2010) or not reported (Ackerstaff 2009). For further details regarding the study populations and settings see the Characteristics of included studies table.
Type of RTW interventions
This Cochrane Review reports on the results of two psycho‐educational interventions, one physical intervention, seven medical interventions and five multidisciplinary interventions which were a combination of psycho‐educational, vocational and/or physical interventions. We did not find any vocational interventions nor multidisciplinary interventions that included a medical intervention.
Psycho‐educational interventions
The psycho‐educational intervention study by Lepore 2003 included one study arm on patient education alone and one on combination of patient education and group discussion. The intervention that only included patient education involved lectures delivered by an expert on things such as physical side effects, stress and coping which was compared with care as usual. In a second intervention group, group discussions to improve coping were added to the patient education and also compared to care as usual. The article by Purcell 2011 describes education aimed at teaching patients self‐care behaviours to reduce cancer‐related fatigue. Pre‐radiotherapy programme was delivered one week prior to radiotherapy planning and the post‐radiotherapy programme was delivered one to two weeks after radiotherapy completion.
Physical interventions
The physical intervention in Rogers 2009 included a moderate walking programme. This training programme included an individually supervised exercise session, face‐to‐face counselling sessions with an exercise specialist, and home‐based exercises.
Medical interventions
The seven medical interventions were diverse and were aimed at intra‐arterial chemoradiation (Ackerstaff 2009), thyroid stimulating hormones after surgery (Emmanouilidis 2009), chemotherapy (Hillman 1998), adjuvant endocrine therapy (Johnsson 2007), laparoscopy (Kornblith 2009), breast conservation (Lee 1992), and peripheral blood progenitor cell transplantation (Friedrichs 2010). Ackerstaff 2009 compared a group of head and neck patients receiving intra‐arterial cisplatin infusion versus a group receiving the standard intravenous chemoradiation. Another RCT evaluated the effect of the use of recombinant human TSH directly after thyroidectomy, hence avoiding hypothyroidism compared to the use of recombinant human TSH after a period of withholding thyroid hormones (Emmanouilidis 2009). Three RCTs studied the effect of an intervention using minimal surgery compared to more radical surgery with RTW as one of the outcomes. Hillman 1998 compared chemotherapy and surgery and Kornblith 2009 compared laparoscopy and laparotomy whereas Lee 1992 compared conservation surgery to mastectomy in breast cancer patients. Johnsson 2007 compared minimal adjuvant treatment (no medication) with the administration of three different types of adjuvant endocrine therapy on RTW in breast cancer patients. Friedrichs 2010 compared the effects of peripheral blood progenitor cell transplantation with bone‐marrow transplantation in leukaemia patients.
Multidisciplinary interventions
The five included multidisciplinary interventions involved vocational counselling, patient education, patient counselling, biofeedback‐assisted behavioral training and/or physical exercises. In Maguire 1983 a nurse advised breast cancer patients on exercise, examined arm movements, checked exercises, and encouraged RTW and becoming socially active. The Berglund 1994 study combined training of coping skills regarding RTW with psychical activity exercises while the Burgio 2006 study combined physical exercise with behavioural biofeedback. In the Hubbard 2013 study a case manager working in a multidisciplinary team referred cancer patients to physical, occupational or psychological support services. Patients in the Tamminga 2013 study were supported by an oncology nurse or medical social worker working in a multidisciplinary team who provided them with vocational support, counselling, education and RTW advice.
Setting, design and outcomes
Thirteen studies were conducted in a hospital, one study was set in the community (Rogers 2009) and in one study the setting was not reported (Berglund 1994). All fifteen studies employed a RCT design.
RTW was measured as event rates, such as RTW rates in 11 studies (Ackerstaff 2009; Berglund 1994; Burgio 2006; Friedrichs 2010; Hillman 1998; Johnsson 2007; Lee 1992; Lepore 2003; Maguire 1983; Purcell 2011; Tamminga 2013). Four studies reported time‐to‐event data, such as number of days between reporting sick and any work resumption or the number of days on sick leave during the follow‐up period (Emmanouilidis 2009; Hubbard 2013; Kornblith 2009; Rogers 2009). QoL was measured as a secondary outcome in eight RCTs (Ackerstaff 2009; Berglund 1994; Burgio 2006; Kornblith 2009; Lepore 2003; Purcell 2011; Rogers 2009; Tamminga 2013). Seven of these measured QoL with validated questionnaires: EORTC (Ackerstaff 2009), SF‐36 (Burgio 2006, Kornblith 2009; Lepore 2003; Tamminga 2013), EQ‐5D (Purcell 2011), and FACT‐B (Rogers 2009) and one used an unvalidated questionnaire (Berglund 1994).
Excluded studies
Of the 4742 potentially relevant records, we retrieved 78 studies for more detailed evaluation. Of these 78 full‐text studies, we excluded 63 because the intervention was not aimed at cancer patients (N = 3), the study design was not RCT (N = 4) or the article did not describe an intervention (N = 1). We excluded 55 studies because they did not report any RTW outcomes. Of these 55 studies, six trials used the vocational environment scale instead of RTW and three studies used the outcome return to normal activity including household tasks, social and family roles. We excluded one study of a contacted author (Emmanouilidis 2013) because it was based on the same data as an earlier, included study (Emmanouilidis 2009). For a detailed description of the reasons for exclusion see the Characteristics of excluded studies table.
Risk of bias in included studies
For results of 'Risk of bias' assessment of RCTs, see the Characteristics of included studies table. The results are summarised in the 'Risk of bias' graph (Figure 2) which is an overview of the review authors' judgements about each risk of bias item presented as percentages across all included studies. Figure 3 shows the 'Risk of bias' summary of each 'Risk of bias' item for each included study.
2.
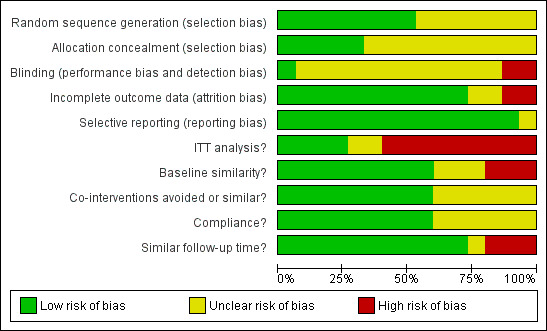
'Risk of bias' graph: review authors' judgements about each 'Risk of bias' item presented as percentages across all included studies.
3.
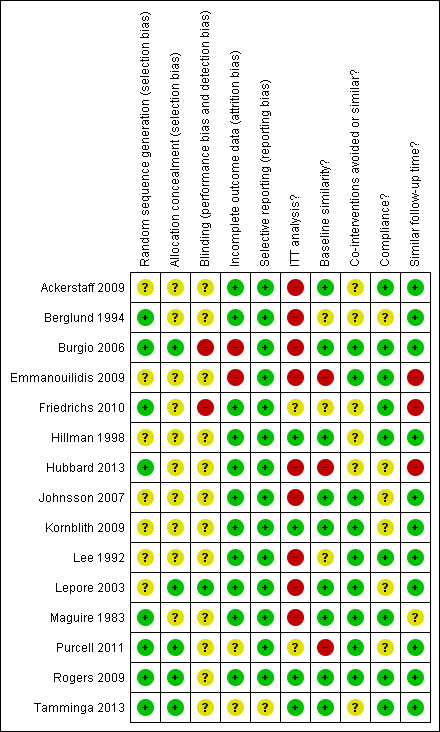
'Risk of bias' summary: review authors' judgements about each 'Risk of bias' item for each included study.
Allocation
Of the 15 included studies describing a RCT, eight studies reported adequate random sequence generation or adequate allocation concealment, or both (Berglund 1994; Burgio 2006; Friedrichs 2010; Hubbard 2013; Maguire 1983; Purcell 2011; Rogers 2009; Tamminga 2013). The trial authors reported having used random numbers generated by a computer or random number tables. According to our judgment, allocation was adequately concealed in all of these studies because a research nurse or an independent interviewer performed the randomisation.
Blinding
Twelve of the 15 RCTs did not report any information on blinding of either the patients, the people performing the intervention or the assessors of the outcomes. Lepore 2003 reported blinding the interviewer assessing the outcomes and blinding the patients for the hypothesis. Two studies explicitly reported that patients and intervention providers were not blinded (Burgio 2006; Friedrichs 2010).
Incomplete outcome data
Thirteen studies reported reasons for drop‐out of the patients and thus addressed the issue of incomplete outcome data. Burgio 2006 did not provide any information about patients with missing data whereas Emmanouilidis 2009 reported not having any drop‐outs. There was no adequate adjustment for confounding in the analyses because 11 studies did not perform ITT analyses. Three studies performed ITT analyses between the two randomised groups even if the patients changed over to the other group (Hillman 1998; Rogers 2009; Tamminga 2013), and in one study 21% of the patients changed over to the control group but the trial authors still performed ITT analyses (Kornblith 2009).
Selective reporting
We judged all included RCT studies to be free of selective reporting of the outcomes because the trial authors reported all outcomes described in the methods.
Other potential sources of bias
Baseline characteristics of the patients were similar in 12 studies, except for Emmanouilidis 2009, Hubbard 2013 and Purcell 2011. However, five studies included a heterogeneous group of patients but obviously could only perform the analyses on employment outcomes in patients employed at baseline. Separate data on the similarity of baseline characteristics on these groups of employed patients were not given (Burgio 2006; Hillman 1998; Kornblith 2009; Lepore 2003; Rogers 2009). Two studies stated that baseline characteristics were similar but did not report the actual data (Lee 1992; Maguire 1983). One study provided no baseline characteristics (Berglund 1994) and in one study the baseline characteristics were significantly different (Emmanouilidis 2009).
Co‐interventions were avoided or similar in both groups in all included studies. Compliance with the intervention was not always reported but was satisfactory in those studies that did report it (Ackerstaff 2009; Burgio 2006; Emmanouilidis 2009; Friedrichs 2010; Hillman 1998; Lee 1992; Rogers 2009; Tamminga 2013). Follow‐up time was similar in all studies except for Emmanouilidis 2009, Friedrichs 2010 and Hubbard 2013 and unclear in Maguire 1983.
Overall risk of bias in studies
We rated nine studies as having a low overall risk of bias (Ackerstaff 2009; Hillman 1998; Johnsson 2007; Kornblith 2009; Lee 1992; Lepore 2003; Maguire 1983; Rogers 2009; Tamminga 2013). We rated six studies (Berglund 1994; Burgio 2006; Emmanouilidis 2009; Friedrichs 2010; Hubbard 2013; Purcell 2011) as having a high overall risk of bias because they had less than five domains at low risk of bias (Table 6; Figure 3).
Effects of interventions
See: Table 1; Table 2; Table 3; Table 4
Summary of findings for the main comparison. Multidisciplinary physical, psycho‐educational and/or vocational interventions versus Care as usual for cancer.
| Multidisciplinary physical, psycho‐educational and/or vocational interventions versus Care as usual for cancer | |||||
| Patient or population: Patients with cancer Settings: Hospital Intervention: Multidisciplinary physical, psycho‐educational and/or vocational interventions versus Care as usual | |||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | |
| Assumed risk | Corresponding risk | ||||
| Control | Multidisciplinary physical, psycho‐educationaland/or vocational interventions versus Care as usual | ||||
| RTW Follow‐up: median 12 months | 786 per 10001 | 872 per 1000 (810 to 912) | RR 1.11 (1.03 to 1.16) | 450 (5 studies) | ⊕⊕⊕⊝ moderate2 |
| QoL Follow‐up: mean 12 months | ‐ | The mean QoL in the intervention groups was 0.03 standard deviations higher (0.20 lower to 0.25 higher) | ‐ | 316 (2 studies) | ⊕⊕⊝⊝ low3,4 |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RR: risk ratio;RTW: return‐to‐work; QoL: quality of life. | |||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | |||||
1Median RTW rate in control groups. 2Three out of five trials with high risk of bias, downgraded one level. 3Wide CIs, downgraded one level. 4One study with high and one with low risk of bias, downgraded one level.
Summary of findings 2. Psycho‐educational care versus Care as usual for return to work in cancer patients.
| Psycho‐educational care versus Care as usual for return to work in cancer patients | |||||
| Patient or population: Patients with cancer Settings: Hospital Intervention: Psycho‐educational care Comparison: Care as usual | |||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | |
| Assumed risk | Corresponding risk | ||||
| Care as usual | Psycho‐educationalcare | ||||
| Return to work (RTW) Follow‐up: 1.5 to 12 months | 491 per 10001 | 535 per 1000 (432 to 663) | RR 1.09 (0.88 to 1.35) | 260 (2 studies) | ⊕⊕⊝⊝ low2,3 |
| Quality of life (QoL) Various scales Follow‐up: 1.5 to 12 months | ‐ | The mean QoL in the intervention groups was 0.05 standard deviations higher (0.2 lower to 0.3 higher) | ‐ | 260 (2 studies) | ⊕⊕⊝⊝ low2,4 |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RR: risk ratio; RTW: return‐to‐work; QoL: quality of life. | |||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | |||||
1Average of control groups' RTW rates. 2One study with high and one with low risk of bias, downgraded one level. 3Wide CIs overlapping with 1, downgraded one level. 4Wide CI including 0 and small effect size, downgraded one level.
Summary of findings 3. Physical exercise versus Care as usual for RTW in cancer.
| Physical exercise versus Care as usual for return to work in cancer | |||||
| Patient or population: Patients with cancer Settings: Community Intervention: Physical exercise Comparison: Care as usual | |||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | |
| Assumed risk | Corresponding risk | ||||
| Care as usual | Physical exercise | ||||
| RTW | 357 per 10001 | 429 per 1000 (114 to 1000) | RR 1.2 (0.32 to 4.54) | 28 (1 study) | ⊕⊕⊝⊝ low2 |
| QoL Various scales Follow‐up: 12 months | ‐ | The mean QoL in the intervention groups was 0.37 standard deviations lower (0.99 lower to 0.25 higher) | ‐ | 41 (1 study) | ⊕⊕⊝⊝ low2 |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RR: risk ratio; RTW: return‐to‐work; QoL: quality of life. | |||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | |||||
1RTW rate in the control group. 2Wide CIs, only one included study, downgraded with two levels.
Summary of findings 4. Medical function conserving treatment versus Medical more radical treatment for cancer.
| Medical function conserving treatment versus Medical more radical treatment for cancer | |||||
| Patient or population: Patients with cancer Settings: Hospital Intervention: Medical function conserving treatment Comparison: Medical more radical treatment | |||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | |
| Assumed risk | Corresponding risk | ||||
| Medical more radical treatment | Medical function conserving treatment | ||||
| RTW Follow‐up: median 18 months | 850 per 10001 | 884 per 1000 (816 to 926) | RR 1.04 (0.96 to 1.09) | 1097 (7 studies) | ⊕⊕⊝⊝ low2,3 |
| QoL Various instruments Follow‐up: mean 9 months | ‐ | The mean QoL in the intervention groups was 0.10 standard deviations higher (0.04 lower to 0.23 higher) | ‐ | 1028 (2 studies) | ⊕⊕⊕⊝ moderate3 |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RR: risk ratio; RTW: return‐to‐work; QoL: quality of life. | |||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | |||||
1 Median RTW rate in control groups of this comparison. 2 I² statistic = 51%, downgraded one level. 3 CIs overlap with one, downgraded one level.
The 15 included studies evaluated the effects of four types of interventions in cancer patients: psycho‐educational interventions, physical interventions, medical interventions and combinations of psycho‐educational, vocational and/or physical interventions.
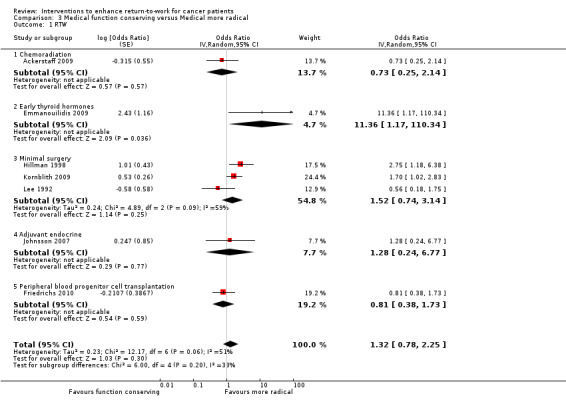
Psycho‐educational interventions
The studies assessing psycho‐educational interventions included a total of 260 patients with 148 patients in intervention groups and 112 in control groups. Two arms of one RCT reported in the same article (Lepore 2003) compared the effect of a psycho‐educational intervention or a psycho‐educational intervention combined with group discussion to care as usual. Similarly, two arms of another RCT compared the effects of either post‐ or pre‐and post radiotherapy fatigue education to care as usual (Purcell 2011). The combined results of these four evaluations from two RCTs indicated that there is low quality evidence of no considerable difference in the effect of psycho‐educational interventions compared to care as usual on RTW (RR 1.09, 95% CI 0.88 to 1.35, n=260 patients; Table 2; Analysis 1.1.
1.1. Analysis.
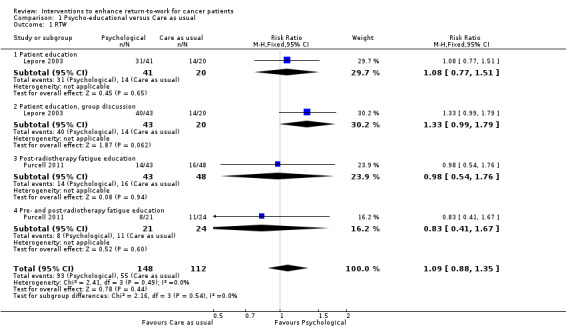
Comparison 1 Psycho‐educational versus Care as usual, Outcome 1 RTW.
The results for the secondary outcome QoL of both studies (Lepore 2003; Purcell 2011) showed that there is low quality evidence of no difference in the effect of psycho‐educational interventions compared to care as usual (SMD 0.05, 95% CI ‐0.2 to 0.3, n=260 patients; Table 2; Analysis 1.2).
1.2. Analysis.
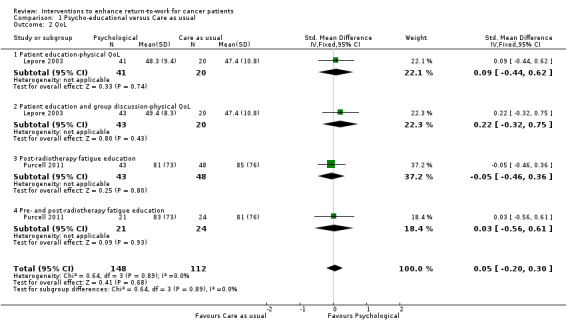
Comparison 1 Psycho‐educational versus Care as usual, Outcome 2 QoL.
Vocational interventions
We did not find any studies that assessed the effectiveness of vocational interventions.
Physical interventions
Rogers 2009 reported an RCT in which breast cancer patients were offered a physical training programme. Results showed that there is low quality evidence that the physical training programme (N = 14) was not more effective than care as usual (N = 14) in improving RTW (RR = 1.20, 95% CI 0.32 to 4.54, n = 28 patients) or QoL (SMD = ‐0.37, 95% CI ‐0.99 to 0.25; n = 28 patients Table 3; Analysis 2.1; Analysis 2.2).
2.1. Analysis.
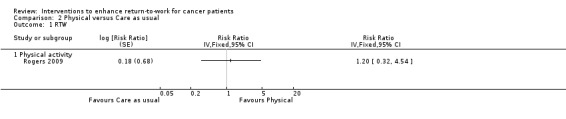
Comparison 2 Physical versus Care as usual, Outcome 1 RTW.
2.2. Analysis.
Comparison 2 Physical versus Care as usual, Outcome 2 QoL.
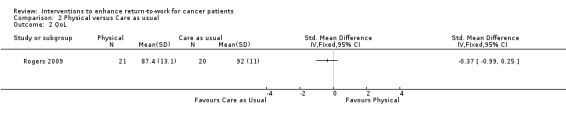
Medical interventions
Seven RCTs conducted with 1097 patients assessed the effects of a medical intervention on RTW (Ackerstaff 2009; Emmanouilidis 2009; Friedrichs 2010; Hillman 1998; Johnsson 2007; Kornblith 2009; Lee 1992). In all studies a less radical or function‐conserving medical intervention was compared with a more radical treatment, with the hypothesis that a function‐conserving medical treatment would improve RTW in cancer patients.
When we pooled the results of the seven individual studies in meta‐analysis we found low quality evidence that function conserving approaches yielded similar RTW rates as more radical treatments (calculated RR = 1.04, 95% CI 0.96 to 1.09 (median P0 of six dichotomous studies was 0.85), n = 1097 patients; Table 4; Analysis 3.1).
3.1. Analysis.
Comparison 3 Medical function conserving versus Medical more radical, Outcome 1 RTW.
We assessed possible publication bias associated with the eight included RCT studies assessing the effect of a less radical medical treatment on RTW. The funnel plot (Figure 4) shows that there might be publication bias and that small studies reported non‐significant results.
4.
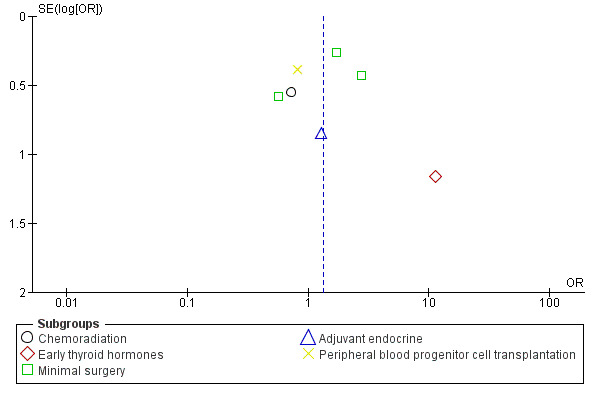
Funnel plot of comparison: 4 Medical function conserving versus Medical more radical‐RCTs, outcome: 4.1 RTW.
We also found two studies showing moderate quality evidence of no differences in the effect of function conserving medical interventions compared to more radical treatment on QoL outcomes (SMD = 0.10, 95% CI ‐0.04 to 0.23, n = 1028 patients; Table 4; Analysis 3.2).
3.2. Analysis.
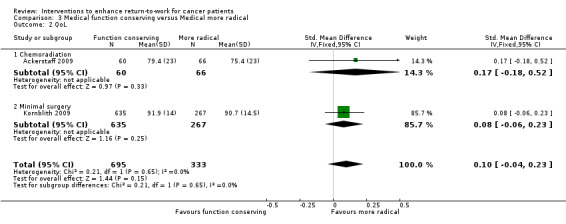
Comparison 3 Medical function conserving versus Medical more radical, Outcome 2 QoL.
Multidisciplinary interventions
Five RCTs conducted with 450 patients assessed the effect of multidisciplinary interventions on RTW (Berglund 1994; Burgio 2006; Hubbard 2013; Maguire 1983; Tamminga 2013). Meta‐analysis produced moderate quality evidence that multidisciplinary interventions in which vocational counselling, patient education, patient counselling, biofeedback‐assisted behavioral training and/or physical exercises were combined led to higher RTW rates than care as usual (calculated RR = 1.11, 95% CI 1.03 to 1.16 (median P0 of four dichotomous studies was 0.79), n = 450 patients; Table 1; Analysis 4.1).
4.1. Analysis.
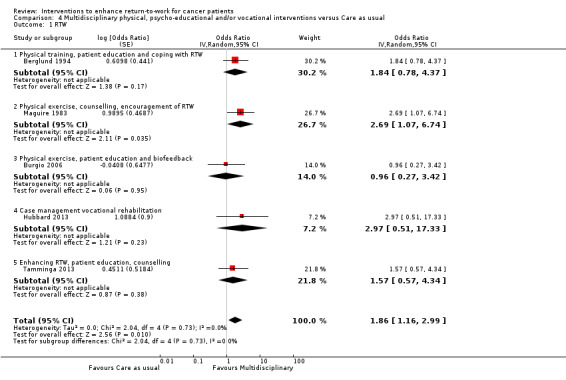
Comparison 4 Multidisciplinary physical, psycho‐educational and/or vocational interventions versus Care as usual, Outcome 1 RTW.
We also found two studies yielding low quality evidence of no differences in the effect of multidisciplinary interventions compared to care as usual on QoL outcomes (SMD = 0.03, 95% CI ‐0.20 to 0.25;, n = 316 patients Table 1; Analysis 4.2).
4.2. Analysis.
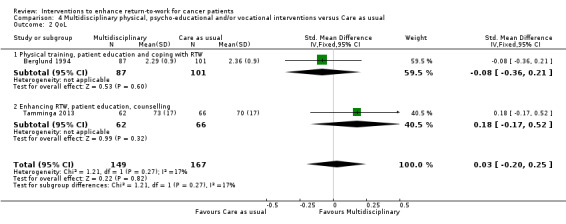
Comparison 4 Multidisciplinary physical, psycho‐educational and/or vocational interventions versus Care as usual, Outcome 2 QoL.
Discussion
Summary of main results
Fifteen studies met the inclusion criteria of this Cochrane Review with a total of 1835 included participants. There was moderate quality evidence from two RCTs with multiple study arms that psycho‐educational interventions do not improve RTW (Lepore 2003; Purcell 2011). We did not find any studies that had assessed the effectiveness of vocational interventions. One trial compared physical training with care as usual and produced low quality evidence of no significant differences on RTW (Rogers 2009).
Seven RCTs yielded low quality evidence of no differences between function conserving versus more radical medical interventions on RTW outcomes (Ackerstaff 2009; Emmanouilidis 2009; Friedrichs 2010; Hillman 1998; Kornblith 2009; Lee 1992; Johnsson 2007). There was moderate quality evidence from five RCTs that multidisciplinary interventions that combine vocational counselling, patient education, patient counselling, biofeedback‐assisted behavioral training and/or physical exercises, produced a higher RTW rate than care as usual (Berglund 1994; Burgio 2006; Hubbard 2013; Maguire 1983; Tamminga 2013).
Overall completeness and applicability of evidence
The included studies were conducted over a 40‐year time span. While one study was conducted in the 1970s and reported in the 1980s (Maguire 1983), we could not find any studies that were performed in the 1980s and only three studies that were conducted in the 1990s (Berglund 1994; Hillman 1998; Lee 1992). Thereby 11 included studies were performed after the year 2000 (Ackerstaff 2009; Burgio 2006; Emmanouilidis 2009; Friedrichs 2010; Hubbard 2013; Johnsson 2007; Kornblith 2009; Lepore 2003; Purcell 2011; Rogers 2009; Tamminga 2013). In these 40 years, medical treatment for cancer has changed enormously. For this reason, older medical studies (Hillman 1998; Lee 1992) may describe medical treatments that are not used anymore. Also the way in which psycho‐educational and multidisciplinary interventions are performed today differs considerably from what is described in the older included studies. Nowadays, interventions are more evidence‐based, more cognitive behavioural therapy‐oriented, briefer, more targeted and more effective than 20 to 30 years ago.
This Cochrane review considers patients from the USA and Europe. Social security systems and labour markets differ widely between countries and thus the effects of cancer survivorship on employment vary. However, in all included studies the effect of the interventions were compared in the same country and with an RCT study design and therefore the influence of a social security system was equal within studies. However, when generalising the results from one country to another, the potential effect of a particular country's social security system should still be considered. For the generalisation of the results of this review to countries outside Europe or the USA, cultural differences regarding employment and cancer disclosure should be taken into account.
Patients with breast cancer were the most studied diagnosis group (Berglund 1994; Hubbard 2013; Johnsson 2007; Lee 1992; Maguire 1983; Rogers 2009; Tamminga 2013) while other studies were aimed at patients with prostate cancer (Burgio 2006; Lepore 2003), thyroid cancer (Emmanouilidis 2009), gynaecological cancer (Kornblith 2009), head and neck cancer (Ackerstaff 2009), laryngeal cancer (Hillman 1998), mixed cancer diagnosis patients (Purcell 2011) and leukaemia patients (Friedrichs 2010). Breast cancer is the most prevalent cancer diagnosis within the working population followed by blood and lymph cancers, prostate cancer, thyroid cancer and colorectal cancer (Short 2005). We did not find any studies that were aimed at patients with colorectal cancer (despite being common in cancer survivors of working age) nor aimed at less prevalent cancer diagnoses including brain cancer, bone cancer and other gastro‐intestinal cancers. We think that the mechanisms of the psycho‐educational, physical training and multidisciplinary RTW interventions are similar regardless of cancer diagnosis and thus patients with colorectal or other types of cancer will experience the same benefits from any of these interventions aimed at improving RTW. However, long‐term and late effects of specific treatments for specific cancers, such as solid versus non‐solid tumours, may differ and play a role in the RTW process. Ultimately, we do not know this because of the lack of evidence. The mechanism behind the effect on RTW of medical interventions should be interpreted with caution, because many of the interventions of the included studies were specific for certain types of cancer and there were inconsistent results. With regard to multidisciplinary interventions we found that multidisciplinary interventions in which vocational counselling, patient education, patient counselling, biofeedback‐assisted behavioral training and/or physical exercises were combined, were effective in improving RTW. These studies were conducted in patients with breast cancer (Berglund 1994; Hubbard 2013; Maguire 1983; Tamminga 2013) or prostate cancer (Burgio 2006) so it is not proven that patients with any other diagnoses will benefit from multidisciplinary interventions.
Although most multidisciplinary interventions did have a vocational component, we did not find any studies assessing vocational interventions focusing on employment issues. This is remarkable because one would expect interventions aimed at RTW to consist of work‐related components, such as work adjustments or involvement of the supervisor. Earlier research in young cancer survivors concluded that vocational rehabilitation interventions, such as vocational training, job search assistance, job placement services, on‐the job support and maintenance services, were all associated with increased odds for employment (Strauser 2010). This latter study was, however, aimed at unemployed cancer patients and the results might therefore not be easily generalised to employed cancer patients. Since our findings showed multidisciplinary interventions containing vocational counselling or coping with employment issues to be effective, more specific or more targeted vocational interventions should be developed and evaluated.
Quality of the evidence
Eleven of the 15 included studies did not report having performed ITT analyses. Moreover, the included studies did not, in most cases, implement blinding of providers, patients or outcome assessors or the blinding was unclear. It can be argued that blinding is not feasible in this type of study and that lack of blinding should not be considered a weakness, but the absence of blinding can be associated with bias even though blinding is not feasible. However, blinding of the outcome assessors and blinding of the patients to the hypothesis of the study are possible. The possibility for bias should therefore be taken into account. Unfortunately it was not discussed in most of the reports. We judged most included studies to have an unclear risk of bias due to sequence generation and allocation concealment, which may indicate further selection bias.
In this Cochrane review we analysed a total of 15 RCTs involving a considerable number of cancer patients (1835 participants). However, the number of patients analysed in the individual studies was generally low, with nine studies providing less than 50 patients in each group thus limiting the power of the studies. In addition, we assessed altogether four different types of interventions, each of which contained several subtypes of interventions. As a result the subtypes of interventions only described one to seven studies. Therefore, it was not possible to perform subgroup analyses according to diagnosis or study risk of bias.
For multidisciplinary interventions compared to care as usual, we included five studies with 450 patients, and concluded that there is moderate quality evidence that multidisciplinary interventions improve RTW more than care as usual RTW. However, for most other comparisons and outcomes, we downgraded the quality of the evidence due to few available studies, risk of bias, indirect results and imprecise effect estimates. GRADE assessments are partly based on subjective judgements and are not definite. Nevertheless GRADE does provide a transparent and consistent classification of the quality of evidence for relevant comparisons and outcomes.
One methodological consideration is the lack of information on baseline characteristics for the patients analysed in this review. In ten of 15 included studies the trial authors analysed data on RTW only for the patients who provided these data, i.e. the employed cancer patients in the study (Ackerstaff 2009; Burgio 2006; Emmanouilidis 2009; Friedrichs 2010; Hillman 1998; Kornblith 2009; Lee 1992; Lepore 2003; Maguire 1983; Rogers 2009). However, the authors reported baseline characteristics only for the total group of cancer patients in these studies including the retired patients and homemakers. Therefore we could not extract and report the baseline characteristics of the employed cancer patients that we included in our analyses. As these baseline characteristics have not been reported we could not check if both groups within the studies had equal distributions of age, sex, and education which could have influenced the effects of the intervention on RTW. However, because allstudies were randomised we assume that the distributions of age, sex and education in both groups of employed patients in each study were similar.
Potential biases in the review process
We sought to conduct a comprehensive and transparent review. We performed the entire process of study search, study selection, data extraction and management, and two review authors independently assessed risk of bias of included studies and we discussed all results until we reached consensus.
The reader can see from the 'Risk of bias' tables attached to the Characteristics of included studies tables that we scored some domains as 'unclear'. This implies that the primary publications did not supply enough details to assess this point. Ideally the number of domains assessed as 'unclear' should be reduced by obtaining supplementary information from the trial authors. For the sake of simplicity we chose to complete our 'Risk of bias' assessment based solely on the information printed in the primary papers.
We searched for eligible studies in ten electronic databases using 130 keywords or combinations of keywords whilst imposing no restrictions on language or publication date. We supplemented our systematic search process with checking the reference lists of included studies and selected reviews. We documented in duplicate and discussed all reasons for exclusion and inclusion of all 4742 potentially relevant studies. Two review authors independently extracted data and performed 'Risk of bias' assessment using an eight‐page form with each included study. We combined the contents of these forms in one consensus form, and a third review author gave advice in case of uncertainties. In case of any missing data or doubt on the correctness of data, we contacted the original trial authors. All six contacted trial authors replied and provided the requested data. Therefore, we think we have done our best to minimise the risk of bias due to the review process. Even though our search strategy was comprehensive and not restricted by language, there is always the risk that relevant citations may have been lost in the review process.
Agreements and disagreements with other studies or reviews
In this Cochrane review we conclude that multidisciplinary physical, psycho‐educational and/or vocational interventions enhance RTW for cancer patients. Another Cochrane review has assessed the effectiveness of vocational rehabilitation programmes compared to care as usual on RTW of people with multiple sclerosis (MS) (Khan 2009). Results of the studies included in Khan 2009 showed that there was inconclusive evidence to support vocational rehabilitation for people with MS because one study aimed at job retention did not find any positive effect while the other study geared towards RTW reported a significant positive effect. This is in line with this review, because the effective studies in this review, two of which contain a vocational rehabilitation component, were also aimed at RTW and not at work retention. Another recent Cochrane review on patients with depression also found that multidisciplinary interventions combing a work‐directed intervention to a clinical intervention reduced the number of days on sick leave compared to a clinical intervention alone (Nieuwenhuijsen 2014). This is similar to the results of our review in which the multidisciplinary interventions were conducted within a hospital setting.
A systematic review including meta‐analysis on the efficacy of multidisciplinary interventions on RTW for people on sick leave due to low‐back pain indicated that multidisciplinary interventions, including behaviour‐oriented physiotherapy, cognitive behavioural therapy, behavioural medicine, light mobilisation, rehabilitation problem‐solving therapy, and behavioural graded activity or personal information, more effectively improve RTW than the alternatives (Norlund 2009). This result is also in agreement with our meta‐analysis which showed that multidisciplinary interventions are more effective than alternative programmes in improving RTW in cancer patients.
The studies we found in our literature search were all person‐directed interventions aimed at the patients. We did not find any work‐directed vocational interventions that were aimed at the workplace and included workplace adjustments, such as modified work hours, modified work tasks, or modified workplaces or improved communication with or between managers, colleagues and health professionals. An earlier systematic review on workplace‐based RTW interventions found strong evidence that work disability duration is significantly reduced by work accommodation offers and contact between healthcare provider and workplace (Franche 2005). The same review also found moderate evidence that work disability duration is reduced by interventions that include early contact with affected workers by their workplaces, ergonomic work site visits and presence of a RTW coordinator (Franche 2005). Although we found that multidisciplinary interventions enhance RTW for cancer patients, this effect might be increased by adding work‐directed vocational components to the interventions.
In this Cochrane review we found low quality evidence that psychosocial interventions are as effective as care as usual in enhancing RTW in cancer patients. The evidence being of low quality is caused by heterogeneity in the RCTs from which the effect was assessed. An earlier meta‐analysis found that cognitive behaviour training (CBT) has a positive effect on QoL, depression and anxiety in adult cancer survivors but that patient education (PE) does not (Osborn 2006). Results from our review show that interventions with patient education do have a positive effect in RTW of cancer patients, especially when they are part of a multidisciplinary intervention.
This review is an update of De Boer 2011. Compared to the earlier version of the review, we have now included four new studies (Friedrichs 2010; Hubbard 2013; Purcell 2011; Tamminga 2013). Furthermore, we have excluded non‐randomised studies in this update because it became clear that randomised studies are feasible and have been conducted. This resulted in the exclusion of three non‐randomised studies (Borget 2007; Capone 1980; Gordon 1980). In this update we have entered each intervention as a separate evaluation when an article reported more than one intervention (multiple study arms) and compared each intervention against a control group. In the earlier version of this review, we entered these evaluations (study arms) as different studies (De Boer 2011). The inclusion of the four new studies, exclusion of the three non‐randomised studies and reorganisation of the study arms into different evaluations rather than different studies did not change the conclusions of this review update compared to the first version of this review (De Boer 2011).
Authors' conclusions
Implications for practice.
There is moderate quality evidence that multidisciplinary interventions combining physical training, psycho‐educational and/or vocational elements improve the RTW of cancer patients. The most apparent setting for this intervention would be the hospital because all multidisciplinary providers are located there and it is the main focal point for the patients. Interventions conducted in a hospital setting are feasible for recently diagnosed cancer patients who are engaged in curative treatment and who are expected to have sufficient recovery to RTW. Other possible settings for RTW interventions for cancer patients would be multidisciplinary rehabilitation outpatient services in community or reintegration teams at large workplaces or multinational corporations. Furthermore, we need to provide effective guidelines to employers needing to deal with a cancer patient returning to work. Thus, it is possible to find ways to improve RTW for people who survive cancer.
There is low quality evidence that psycho‐educational, physical interventions and function‐conserving medical interventions yield similar RTW rates compared to care as usual.
Implications for research.
Multidisciplinary interventions enhance RTW for cancer patients. Most research so far has been conducted in breast cancer patients and prostate cancer patients. Research should additionally focus on patients with other prevalent diagnoses of cancer in the working population, such as colorectal cancer and blood or lymph cancers. Other important patient characteristics, such as age, education and ethnicity, should also be measured. Future research on enhancing RTW in cancer patients should involve multidisciplinary interventions with a physical, psycho‐educational and vocational component. The vocational component should not be just patient‐oriented but should also be directed at the work environment (including work adjustments and supervisors). With regard to psycho‐educational interventions it is unclear whether patient education or patient counselling is most effective. Both interventions should be compared against each other and care as usual.
We did not find any studies assessing vocational interventions aimed at enhancing RTW in cancer patients for this review although one would expect the largest impact on RTW from this kind of intervention. Future research should focus on vocational interventions that include any type of intervention focused on employment. Vocational interventions might be person‐directed, that is, aimed at the patient to encourage RTW, meaning vocational rehabilitation or occupational rehabilitation, or they might be work‐directed, that is, aimed at the workplace by means of workplace adjustments such as modified work hours, modified work tasks, or modified workplaces and improved communication with or between managers, colleagues and health professionals.
So far, not all studies comparing the effect of an intervention on RTW with care as usual or an alternative intervention have been conducted using a RCT design. Consequently there is uncertainty about effectiveness and we need more high‐quality RCTs. Therefore, all studies evaluating the effect of an intervention on RTW should employ a RCT design although this might be sometimes difficult in daily practice. These RCTs should perform ITT analysis. In some cases, a cluster‐RCT design might have to be chosen in which the providers of the intervention or the settings are randomised and not the patients. In addition, the studies described in this review were all relatively small and thus we need RCTs with a much greater number of recruited patients.
With regard to outcome measures, many more clinical trials should incorporate RTW measures. For instance, currently many trials are being conducted evaluating the effect of physical exercise on physical fitness, fatigue or QoL, but almost none of these studies will evaluate effects on sick leave duration or RTW although it is reasonable to expect these interventions to be beneficial for employment. With regard to medical interventions, the search is always on for less radical or less invasive treatments that give comparable medical outcomes. When evaluating the effectiveness of these interventions studies should not only measure medical outcomes or QoL but also work‐related outcome measures. In future research, work‐related outcome measures should not only include the rate of patients returning to work because this measure is a valid, but broad and general indication of RTW. Other work‐related outcome measures that are more precise measures of RTW and should be measured include: total number of days of sick leave from first day of sick leave until first day of return, measures of work retention once back at work, and work productivity. Studies also need to define what RTW is: return to full‐time or part‐time work or return to the same job or a lesser job.
RTW is an important outcome measure for cancer patients indicating recovery and return to normalcy. In this Cochrane Review, we found no difference in QoL in the included studies while people had returned to work. This would imply that probably most cancer patients return to work only when it is feasible. After patients have returned to work, it is important that cancer patients are able to remain working. Research beyond RTW, focusing on work retention and factors associated with it, is needed (Moskowitz 2014). Based on these factors associated with remaining at work, researchers should develop new interventions for work retention of cancer patients.
Finally, many treatments for cancer take several months and result in long‐lasting side effects. This might influence the effectiveness of interventions aimed at RTW of cancer patients. Furthermore, work disability can be episodic. Given these fluctuations in work absence we need studies with long term follow‐up.
Feedback
Wrong classification of intervention in Burgio 2006 study, 15 December 2015
Summary
Thank you for a very interesting and important review. While I think your work is of the utmost high quality, I was nonetheless rather surprised when reading through it carefully I noticed a possible error regarding the categorisation of one included study. You state in the Abstract: “Five RCTs involved multidisciplinary interventions in which vocational counselling was combined with patient education, patient counselling, and biofeedback‐assisted behavioral training or physical exercises.” This implies that the study by Burgio 2006 would have vocational counselling AND biofeedback‐assisted behavioral training, i.e. a combination of the two. This seems not to be the case. I have read through the Burgio 2006 paper and their intervention clearly does not have a vocational counselling component. Could it be that you have made a mistake in categorising this study and that you should in fact remove this study from the comparison Multidisciplinary physical, psycho‐educational and vocational interventions versus Care as usual? This might affect the results of your meta‐analyses also? Heidi Miettinen
Reply
Thank you very much for pointing this out. We realise that the statement in the abstract is misleading because it was meant to refer to any combination of the interventions and not to the combination of vocational rehabilitation with the other interventions. We have now changed this sentence into: "Five RCTs involved multidisciplinary interventions in which vocational counselling, patient education, patient counselling, biofeedback‐assisted behavioral training and/or physical exercises were combined." We hope that this resolves the confusion.
Angela de Boer
Contributors
Heidi Mietttinen (provided feedback), Riitta Sauni (feedback editor), Angela de Boer (review author)
What's new
| Date | Event | Description |
|---|---|---|
| 4 July 2017 | Feedback has been incorporated | Confusion about classification of the intervention in one study. No change in conclusions |
History
Protocol first published: Issue 1, 2009 Review first published: Issue 2, 2011
| Date | Event | Description |
|---|---|---|
| 14 July 2015 | New citation required but conclusions have not changed | We excluded non‐randomised studies. We reorganised comparisons in such a way that we included studies with multiple arms as different evaluations rather than different studies. Four new studies met the inclusion criteria. |
| 15 June 2015 | New search has been performed | We updated our literature search to 25 March 2014. |
| 18 December 2012 | Amended | We recalculated odd ratios (ORs) into risk ratios (RRs) for medical interventions. |
| 4 July 2012 | Amended | We recalculated ORs into RRs. |
| 15 February 2012 | Amended | We amended errors in references. |
| 8 February 2011 | Amended | A minor edit was made for Issue 3, 2011. |
| 14 April 2008 | Amended | We converted to a new review format. |
Acknowledgements
We thank Emma Sydenham and the Cochrane Injuries Group peer referees for their valuable comments. We also thank the Cochrane Work Group Trials Search Coordinator Leena Isotalo and Consumer Editor Wim van Veelen for their feedback on the systematic searches and the trade unions' point of views respectively. We are grateful to Charlotte Archibald from Wiley Blackwell and Jani Ruotsalainen from Cochrane Work for their copy edit support. We thank Christina Mischke from Cochrane Work for her help on recalculating all ORs into RRs.
Appendices
Appendix 1. MEDLINE search strategy
1. neoplasms (MeSH Terms) 2. cancer* (Text Word) 3. neoplasm* (Text Word) 4.carcinoma* (Text Word) 5. oncolog* (Text Word) 6. malignan* (Text Word) 7. tumor (Text Word) 8. tumour (Text Word) 9. tumors (Text Word) 10. tumours (Text Word) 11. leukemia* (Text Word) 12. sarcoma* (Text Word) 13. lymphoma* (Text Word) 14. melanoma* (Text Word) 15. blastoma* (Text Word) 16. radiotherapy (Text Word) 17. chemotherapy (Text Word) 18. 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 19. “return‐to‐work” (Text word) 20. employment (MeSH Terms) 21. employment (Text Word) 22. unemployment (MeSH Terms) 23. unemployment (Text Word) 24. unemployed (Text Word) 25. retirement (Text Word) 26. “sick leave” (MeSH Terms) 27. sick leave (Text Word) 28. Sickness absence (Text Word) 29. absenteeism (MeSH Terms) 30. absenteeism (Text word) 31. “work” (MeSH Terms) 32. occupations (MeSH Terms) 33. “occupational medicine” (MeSH Terms) 34. “occupational health” (MeSH Terms) 35. “occupational health services” (MeSH Terms) 36. “disability management” (Text word) 37. “rehabilitation, vocational” (MeSH Terms) 38. occupation* (Text Word) 39. rehabilitation (MeSH Terms:NoExp) 40. “neoplasms/rehabilitation” (MeSH Terms) 41. vocational* (Text Word) 42. “work ability” (Text Word) 43. “work capacity” (Text Word) 44. “work activity” (Text Word) 45. “work disability” (Text Word) 46. “work rehabilitation” (Text Word) 47. “work status” (Text Word) 48. “work retention” (Text Word) 49. workability (Text Word) 50. employability (Text Word) 51. employable (Text Word) 52. employee* (Text Word) 53. 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31 or 32 or 33 or 34 or 35 or 36 or 37 or 38 or 39 or 40 or 41 or 42 or 43 or 44 or 45 or 46 or 47 or 48 or 49 or 50 or 51 or 52 54. randomized‐controlled‐trial (pt) 55. controlled clinical trial (pt) 56. randomized controlled trials (mh) 57. random allocation (mh) 58. double blind method (mh) 59. single blind method (mh) 60. clinical trial (pt) 61. clinical trials (mh) 62. (clin* adj25 trial*) (ti,ab) 63. ((singl*(tw) OR doubl*(tw) OR trebl*(tw) OR tripl*(tw)) AND (mask*(tw) OR blind*(tw))) 64. placebos (mh) 65. placebo*(tw) 66. random*(tw) 67. research design(mh:noexp) 68. comparative study(pt) 69. evaluation studies(pt) 70. follow‐up studies(mh) 71. prospective studies(mh) 72. cross‐over studies(mh) 73. control*(tw) 74. prospectiv*(tw) 75. volunteer*(tw)) 76. Evaluate* (tw) 77. Compare* (tw) 78. Program* (tw) 79. 54 or 55 or 56 or 57 or 58 or 59 or 60 or 61 or 62 or 63 or 64 or 65 or 66 or 67 or 68 or 69 or 70 or 71 or 72 or 73 or 74 or 75 or 76 or 77 or 78 80. “primary prevention” (MeSH Terms) 81. "Neoplasms/prevention and control"(MeSH Terms) 82. "Smoking/prevention and control"(MeSH) 83. “smoking cessation” (MeSH Terms) 84. Smoking/adverse effects"(MeSH Terms) 85. “occupational exposure” (MeSH Terms) 86. occupational exposure (Text Word) 87. “occupational diseases” (MeSH Terms) 88. occupational risk factor (Text Word) 89. “protective clothing” (MeSH Terms) 90. “inhalation exposure” (MeSH Terms ) 91. exposure (Text Word) 92. exposed (Text Word) 93. body mass (tw) 94. tobacco (tw) 95. occupational vitiligo (Text Word) 96. "Antineoplastic Agents"(Mesh) 97. "Molecular Structure"(Mesh) 98. "Immunoconjugates"(Mesh) 99. "Mutagenesis"(Mesh) 100. "Apoptosis"(Mesh) 101. apoptosis (Text Word) 102. "Tumor Markers, Biological"(Mesh) 103. marker* (tw) 104. genet* (tw) 105. "Signal Transduction"(Mesh) 106. toxin (Text Word) 107. toxin* (Text Word) 108. toxic* (Text Word) 109. toxic (Text Word) 110. "Toxicology"(Mesh) 111. “case control” (tw) 112. epidemiol* (tw) 113. "Carcinogens, Environmental/adverse effects"(MeSH) 114. “Mass Screening” (MeSH Terms) 115. screening (tw) 116. “Palliative Care” (MeSH Terms) 117. “end of life” (tw) 118. palliative (tw) 119. “Neoplasm Metastasis” (MeSH Terms) 120. “Mortality” (MeSH Terms) 121. “aged, 80 and over” (MeSH Terms) 122. “terminal care” (MeSH Terms) 123. “geriatric assessment” (MeSH Terms) 124. “non‐cancer” (tw) 125. “non‐malignant” (tw) 126. “gene expression profiling” (MeSH Terms) 127. "Radiology/education"(MeSH Terms) 128. 80 or 81 or 82 or 83 or 84 or 85 or 86 or 87 or 88 or 89 or 90 or 91 or 92 or 93 or 94 or 95 or 96 or 97 or 98 or 99 or 100 or 101 or 102 or 103 or 104 or 105 or 106 or 107 or 108 or 109 or 110 or 111 or 112 or 113 or 114 or 115 or 116 or 117 or 118 or 119 or 120 or 121 or 122 or 123 or 124 or 125 or 126 or 127 129. (18 and 53 and 79) not 128 130. (animal(mh) NOT human(mh)) 131. 129 not 130
Appendix 2. EMBASE, CINAHL, OSH‐ROM & PsycINFO: identical search strategy via Ovid
1. cancer.mp. (*)
2. *Neoplasm/ or neoplasm*.mp.
3. carcinoma*.mp.
4. oncolog*.mp.
5. malignan*.mp.
6. tumor*.mp.
7. tumour*.mp.
8. leukemi*.mp.
9. sarcom*.mp.
10. lymphom*.mp.
11. melanom*.mp.
12. blastom*.mp.
13. radiotherapy.mp.
14. chemotherapy.mp.
15. 6 or 11 or 3 or 7 or 9 or 12 or 2 or 14 or 8 or 1 or 4 or 13 or 10 or 5
16. exp Work Resumption/ or return to work.mp.
17. exp Employment/ or exp Employment Status/ or employment.mp.
18. exp Unemployment/ or unemployment.mp.
19. unemployed.mp.
20. retirement.mp.
21. (sick leave or Sickness absence or absenteeism).mp.
22. (vocational* or work ability or work capacity or work activity or work disability or work rehabilitation or work status or work retention or workability or employability or employable or employee*).mp.
23. randomized controlled trial.mp.
24. controlled clinical trial.mp.
25. (random allocation or double blind method or single blind method or clinical trial or placebo* or random* or comparative study or follow‐up study or cross‐over study or control* or prospectiv* or volunteer* or Evaluate* or Compare* or Program*).mp.
26. (primary prevention or smoking cessation or occupational disease* or occupational risk factor or protective clothing or exposure or exposed or body mass or tobacco or occupational vitiligo or Antineoplastic Agents or Molecular Structure or Immunoconjugates or Mutagenesis or Apoptosis or genet* or Signal Transduction or toxin or toxin* or toxic* or toxic or case control or epidemiol* or screening or end of life or palliative or Metastas* or terminal care or geriatric assessment or non‐malignant or gene expression).mp.
27. animal.mp. or exp Animal/
28. 24 or 25 or 23
29. occupation.mp.
30. exp Vocational Rehabilitation/ or exp Work Disability/
31. disability management.mp.
32. exp Vocational Rehabilitation/ or work rehabilitation.mp.
33. 21 or 30 or 17 or 20 or 32 or 18 or 22 or 31 or 16 or 19
34. 33 and 28 and 15
35. 34 not 26
36. 35 not 27
* ([mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer name])
Appendix 3. DARE search strategy
DARE: (more terms not possible)
(cancer OR neoplasm* OR carcinoma* OR oncolog* OR malignan* OR tumor* OR tumour* OR leukemi* OR sarcom* OR lymphom* OR melanom* OR blastom* OR radiotherapy OR chemotherapy) AND (return to work OR employment OR unemployment OR unemployed OR retirement OR sick leave OR Sickness absence OR absenteeism OR occupation* OR vocational* OR work ability OR work capacity OR work activity OR work disability OR work rehabilitation OR work status OR work retention OR workability OR employability OR employable OR employee*) NOT (primary prevention OR smoking cessation OR palliative OR Metastasis OR terminal)
Data and analyses
Comparison 1. Psycho‐educational versus Care as usual.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 RTW | 2 | 260 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.09 [0.88, 1.35] |
| 1.1 Patient education | 1 | 61 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.08 [0.77, 1.51] |
| 1.2 Patient education, group discussion | 1 | 63 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.33 [0.99, 1.79] |
| 1.3 Post‐radiotherapy fatigue education | 1 | 91 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.54, 1.76] |
| 1.4 Pre‐ and post‐radiotherapy fatigue education | 1 | 45 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.83 [0.41, 1.67] |
| 2 QoL | 2 | 260 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.05 [‐0.20, 0.30] |
| 2.1 Patient education‐physical QoL | 1 | 61 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.09 [‐0.44, 0.62] |
| 2.2 Patient education and group discussion‐physical QoL | 1 | 63 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.22 [‐0.32, 0.75] |
| 2.3 Post‐radiotherapy fatigue education | 1 | 91 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.05 [‐0.46, 0.36] |
| 2.4 Pre‐ and post‐radiotherapy fatigue education | 1 | 45 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.03 [‐0.56, 0.61] |
Comparison 2. Physical versus Care as usual.
Comparison 3. Medical function conserving versus Medical more radical.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 RTW | 7 | Odds Ratio (Random, 95% CI) | 1.32 [0.78, 2.25] | |
| 1.1 Chemoradiation | 1 | Odds Ratio (Random, 95% CI) | 0.73 [0.25, 2.14] | |
| 1.2 Early thyroid hormones | 1 | Odds Ratio (Random, 95% CI) | 11.36 [1.17, 110.34] | |
| 1.3 Minimal surgery | 3 | Odds Ratio (Random, 95% CI) | 1.52 [0.74, 3.14] | |
| 1.4 Adjuvant endocrine | 1 | Odds Ratio (Random, 95% CI) | 1.28 [0.24, 6.77] | |
| 1.5 Peripheral blood progenitor cell transplantation | 1 | Odds Ratio (Random, 95% CI) | 0.81 [0.38, 1.73] | |
| 2 QoL | 2 | 1028 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.10 [‐0.04, 0.23] |
| 2.1 Chemoradiation | 1 | 126 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.17 [‐0.18, 0.52] |
| 2.2 Minimal surgery | 1 | 902 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.08 [‐0.06, 0.23] |
Comparison 4. Multidisciplinary physical, psycho‐educational and/or vocational interventions versus Care as usual.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 RTW | 5 | Odds Ratio (Random, 95% CI) | 1.86 [1.16, 2.99] | |
| 1.1 Physical training, patient education and coping with RTW | 1 | Odds Ratio (Random, 95% CI) | 1.84 [0.78, 4.37] | |
| 1.2 Physical exercise, counselling, encouragement of RTW | 1 | Odds Ratio (Random, 95% CI) | 2.69 [1.07, 6.74] | |
| 1.3 Physical exercise, patient education and biofeedback | 1 | Odds Ratio (Random, 95% CI) | 0.96 [0.27, 3.42] | |
| 1.4 Case management vocational rehabilitation | 1 | Odds Ratio (Random, 95% CI) | 2.97 [0.51, 17.33] | |
| 1.5 Enhancing RTW, patient education, counselling | 1 | Odds Ratio (Random, 95% CI) | 1.57 [0.57, 4.34] | |
| 2 QoL | 2 | 316 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.03 [‐0.20, 0.25] |
| 2.1 Physical training, patient education and coping with RTW | 1 | 188 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.08 [‐0.36, 0.21] |
| 2.2 Enhancing RTW, patient education, counselling | 1 | 128 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.18 [‐0.17, 0.52] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Ackerstaff 2009.
| Methods | RCT, hospital setting | |
| Participants | Head and neck cancer patients Inclusion criteria: Inoperable stage IV head and neck cancer Exclusion criteria: Not reported |
|
| Interventions | Intervention group (N = 34): Intra‐arterial cisplatin infusion Provider: Oncologist Setting: Hospital Control group (N = 28): Standard intravenous chemoradiation |
|
| Outcomes | Primary outcome measure (RTW outcomes): RTW rate: Number of patients returned to work Registered by: Patient at baseline and 12 months after intervention Secondary outcome measure (QoL outcomes): Eortc‐qlq c30 plus head and neck Registered by: Patient at baseline, 7 weeks, 3 and 12 months |
|
| Funding | Not reported | |
| Objectives of the study | Assessing QoL in advanced neck/head cancer: Intra‐arterial vs standard intravenous chemoradiation | |
| Country | Netherlands | |
| Notes | Results for working patients only in trial of 126 patients | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported. |
| Allocation concealment (selection bias) | Unclear risk | Not reported. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All reasons for drop out described. |
| Selective reporting (reporting bias) | Low risk | All outcomes from methods are reported. |
| ITT analysis? | High risk | Protocol violations were excluded. |
| Baseline similarity? | Low risk | Demographics and disease characteristics similar. |
| Co‐interventions avoided or similar? | Unclear risk | Overall 25% patients had radiotherapy but unclear how many in each group. |
| Compliance? | Low risk | After omission of 3 protocol violations. |
| Similar follow‐up time? | Low risk | All after 12 months. |
Berglund 1994.
| Methods | RCT, setting not reported. Efron's method for randomisation of small groups: Group sizes were forced towards equality by proportionately increasing the probability of assignment to the smaller group. | |
| Participants | Cancer patients (80% breast cancer, 8% ovarian cancer). Inclusion criteria: Age below 75 years, curative treatment for a primary tumour, inclusion within 2 months after post‐operative treatment with radio‐ or chemotherapy. Exclusion criteria: Not reported |
|
| Interventions | Intervention group (N = 87): During the first 4 weeks, patients met twice a week, once for information and once for physical training. The last 3 weeks were devoted to one session of coping skills training each week. An oncology nurse specialised in psychosocial issues conducted the groups during all sessions. She was accompanied by a specialist of the theme dealt with at each session. Physical training: Exercises to increase mobility, muscle strength, fitness, relaxation. Instruction for relaxation at home. Information: Effects of treatment, diet, development trough crises, alternative treatment. Coping: Role plays, how to handle attitudes towards cancer, meeting people asking too much, problem situations at hospital, anxiety and how to handle it. Intervention lasted 7 weeks Sessions: 11 sessions of 2 hours Provider: Oncology nurse and specialist Setting: Not reported Control group (N = 89) N = 36 received single information session (oncologist and dietician information included in the intervention session); N = 53: care as usual. |
|
| Outcomes | Primary outcome measure (RTW outcomes): Work status: Number not working Registered by: Patient at baseline, 3, 6, 12 months Secondary outcome measure (QoL outcomes): Problems with QoL ‐ 2 items Registered by: Patient at baseline, 8 to 12 weeks, 3, 6, 12 months |
|
| Funding | Swedish Cancer Foundation | |
| Objectives of the study | To investigate the short‐term gains of the starting again programme over a follow‐up period of 1 year | |
| Country | Sweden | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Efron's method for randomisation of small samples. |
| Allocation concealment (selection bias) | Unclear risk | Not reported. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Reasons for non‐response for all assessments are reported. |
| Selective reporting (reporting bias) | Low risk | All outcomes from methods are reported. |
| ITT analysis? | High risk | Not performed. |
| Baseline similarity? | Unclear risk | No baseline characteristics reported. |
| Co‐interventions avoided or similar? | Unclear risk | Not reported. |
| Compliance? | Unclear risk | Not reported. |
| Similar follow‐up time? | Low risk | All outcomes were measured 8 to 12 weeks post‐intervention. |
Burgio 2006.
| Methods | RCT, hospital setting | |
| Participants | Prostate cancer patients Inclusion criteria: Be ambulatory, be continent, be identified for the study at least 1 week prior to surgery, elected for radical prostectomy, prostate cancer. Exclusion criteria: > 2 episodes urinary incontinence in previous 6 months, incontinence, prior prostectomy, impaired mental status, less 1 week prior to surgery. |
|
| Interventions | Intervention group (N = 28): Single session of biofeedback assisted behavioral training, including pelvic floor muscle control and exercise. Use of rectal probe to provide information on rectal pressure. Feedback and verbal instructions and reinforcement. Daily home practice. Intervention lasted 6 months Sessions: 1 session + daily at home Provider: Not reported Setting: Hospital and at home Control group (N = 29): Brief verbal instructions to interrupt the urinary stream during voiding |
|
| Outcomes | Primary outcome measure (RTW outcomes): RTW rate at 6 months (Results for patients with paid employment at baseline): Number returned to work Registered by: Patient at baseline and 6 months Secondary outcome measure (QoL outcomes): Medical Outcomes Studies‐Short Form (MOS‐SF) Registered by: Patient at baseline and 6 months |
|
| Funding | National Institute for Diabetes and Digestive and Kidney Diseases, National Institutes of Health. | |
| Objectives of the study | To test effectiveness of preoperative biofeedback assisted behavioral training for hastening the recovery of urinary control, decreasing the severity of post‐operative incontinence and improving QoL in the 6 months following radical prostatectomy | |
| Country | USA | |
| Notes | Results for patients with paid employment at baseline of a total of 102 patients | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer generated numbers. |
| Allocation concealment (selection bias) | Low risk | Randomised schedule was implemented by research nurse, so the interventionists would be blinded to next group assignment. |
| Blinding (performance bias and detection bias) All outcomes | High risk | No blinding to patients or interventionists. Blinding of data handling people or researchers or outcome assessors (patients) unknown. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Work‐related outcomes: No information was provided for patients with missing data and no non‐response analysis. For the work‐related data for people working at baseline no attrition/exclusion statistics were given. |
| Selective reporting (reporting bias) | Low risk | All outcomes from methods are reported. |
| ITT analysis? | High risk | Work‐related outcomes: No information was provided for patients with incomplete data and no ITT analysis. For the work‐related data for people working at baseline no attrition/exclusion statistics were given. |
| Baseline similarity? | Low risk | Similarity for age, sex; unknown for education. |
| Co‐interventions avoided or similar? | Low risk | No co‐interventions. |
| Compliance? | Low risk | 70% were still doing exercises at home after 6 months. |
| Similar follow‐up time? | Low risk | The same time points. |
Emmanouilidis 2009.
| Methods | RCT, hospital setting | |
| Participants | Thyroid cancer patients, thyroidectomised Inclusion criteria: Differentiated thyroid cancer, thyroidectomised, received K1 a/b central lymphadenectomy Exclusion criteria: Not reported |
|
| Interventions | Intervention group (N = 7): L‐Thyroxine (T4) medication initiated a day after thyroidectomy, followed by the use of recombinant human TSH stimulation and subsequent radioablation therapy (RAT) at first hospitalisation immediately after surgery Provider: Endocrinologist Setting: Hospital Control group (N = 6): L‐l‐thyroxine medication abstinence for 4 weeks, then radioablative therapy (RAT) |
|
| Outcomes | Primary outcome measure (RTW outcomes): Sick leave time from day of discharge of department of surgery until completion of first RAT Registered by: Not reported Follow‐up time: Not reported |
|
| Funding | Reported none received | |
| Objectives of the study | To determine whether the use of recombinant human TSH to stimulate radioiodine uptake after thyroidectomy is as efficacious as a period of withholding thyroid hormones, while at the same time avoiding hypothyroidism, reducing sick leave time and shortening the hospital stay | |
| Country | Germany | |
| Notes | Results for working patients only in trial of 25 patients | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported. |
| Allocation concealment (selection bias) | Unclear risk | Not reported. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not reported. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | No drop outs reported. |
| Selective reporting (reporting bias) | Low risk | All outcomes from methods are reported. |
| ITT analysis? | High risk | Not reported. |
| Baseline similarity? | High risk | They are different. |
| Co‐interventions avoided or similar? | Low risk | Scintigrapy and ultrasound identical in both groups. |
| Compliance? | Low risk | No conversion reported. |
| Similar follow‐up time? | High risk | Length of follow‐up seems to be not the same, but not reported. |
Friedrichs 2010.
| Methods | RCT, hospital | |
| Participants | Leukemia patients. Inclusion criteria: 1) aged 18 to 55 years; 2) diagnosed with de‐novo acute myeloid leukaemia (AML) or acute lymphoblastic leukaemia in first or second remission (AAL), chronic myeloid leukaemia (CML) in first chronic or accelerated phase, or myelodysplastic syndrome (MDS) |
|
| Interventions | Intervention (N = 163): Peripheral blood progenitor cell transplantation (PBPCT) Provider: Oncologist Setting: Hospital Control (N = 166): Bone marrow transplant (BMT) |
|
| Outcomes | Number of patients RTW Registered by: patients' physician. Follow‐up time: > 5 years. |
|
| Funding | No funding received | |
| Objectives of the study | To compare long‐term outcomes of patients treated with peripheral blood compared to bone marrow grafts | |
| Country | 13 European countries, Israel, Australia | |
| Notes | Questionnaires were sent to the centres for all patients who were know to be alive > 5 years after transplantation. Questionnaires were answered by the patient's physicians. The physicians filled in if the patient had returned to work at the last follow‐up. This might be highly biased because the physician might have forgotten to ask the patient. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation centre. |
| Allocation concealment (selection bias) | Unclear risk | Not possible. |
| Blinding (performance bias and detection bias) All outcomes | High risk | Assessors were not blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Yes, reasons for drop out addressed. |
| Selective reporting (reporting bias) | Low risk | All outcomes from methods are reported. |
| ITT analysis? | Unclear risk | ITT not reported. |
| Baseline similarity? | Unclear risk | No tests performed. At randomisation stage, stratification criteria was set up to ensure similarity between groups but whether there was actual differences were not reported. |
| Co‐interventions avoided or similar? | Unclear risk | Not described. |
| Compliance? | Low risk | Only a few people did not receive the intervention. |
| Similar follow‐up time? | High risk | Range 3 to 12 years. |
Hillman 1998.
| Methods | RCT, hospital setting | |
| Participants | Laryngeal cancer patients Inclusion criteria: Biopsy proven, previously untreated, stage 3 or 4 squamous cell carcinoma of the larynx Exclusion: T1N1 carcinoma, pyriform sinus lesions, unresectable cancers, distant metastases, prior head and neck radiotherapy, or prior malignancy with the exception of non‐melanoma skin cancer |
|
| Interventions | Intervention (N = 80): Laryngectomy plus radiotherapy Provider: Specialist Setting: Hospital Control (N = 63): Induction chemotherapy plus radiotherapy Provider: Specialist Setting: Hospital |
|
| Outcomes | Primary outcome measure (RTW outcomes): Number of patients: Disabled due to cancer, on sick leave, cannot find work, not seeking work, lesser job, same job Registered by: Patient at baseline (hospital admission) and 1, 6, 12, 18, 24 months after baseline Secondary outcome measure (QoL outcomes) |
|
| Funding | Department of Veterans Affairs Co‐operative Studies | |
| Objectives of the study | To assess employment status for patients who received one of the two treatment modalities for advanced laryngeal cancer | |
| Country | USA | |
| Notes | Results for working patients only in trial of 325 patients | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information about randomisation procedure. |
| Allocation concealment (selection bias) | Unclear risk | Not reported. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Only seven drop‐outs. Data of drop‐outs was censored. |
| Selective reporting (reporting bias) | Low risk | All outcomes from methods are reported. |
| ITT analysis? | Low risk | ITT‐analyses compared the voice assessment and employment between the two randomised groups even if the procedure was converted to the other randomisation group. |
| Baseline similarity? | Low risk | Groups were similar in terms of age, gender, tumour size and site of lesion. |
| Co‐interventions avoided or similar? | Unclear risk | People with different voice preservation were compared. |
| Compliance? | Low risk | Final procedure reported. |
| Similar follow‐up time? | Low risk | Same timing for each group. |
Hubbard 2013.
| Methods | RCT, hospital and community | |
| Participants | Breast cancer patients Inclusion criteria: 1) Aged 18 to 65 years; 2) in paid employment or self‐employed; 3) living or working in Lothian or Tayside, Scotland; 4) diagnosed with an invasive breast cancer tumour or ductal carcinoma in situ; 5) treated first with surgery Exclusion criteria: First, women who worked in large companies were excluded but later included when the recruitment criteria was changed |
|
| Interventions | Intervention (N = 7): Working Health Services established by the Scottish centre with an multi‐disciplinary approach whereby case‐management is used to assess individuals needs to enable work retention or return through signposting or direct referral for a range supportive services according to need, such as physiotherapy, occupational therapy, occupational health nurse, occupation health doctor, counsellor or psychological therapy and complementary therapy. Participants were allocated a case manager who conducted a telephone assessment. Setting: Hospital and phone interview Provider: Case manager and referral to physiotherapy, occupational therapy, occupational health nurse, occupation health doctor, counsellor or psychological therapy and complementary therapy. Control (N = 11): No formal employment support. Participants received a copy of the booklet work and cancer published by Macmillan. |
|
| Outcomes | Number of days off work due to ill health within the first 6 months after surgery. Duration of sick leave in the 4 weeks before the date of 6 and 12‐month follow‐up. Left or remained in employment, job role and hours worked. Secondary outcome measure (QoL outcomes): FACT‐B Registered by: Patient Follow‐up time: 6 and 12 months |
|
| Funding | MacMillan cancer support and Scottish centre for healthy working lives | |
| Objectives of the study | To assess the feasibility and acceptability of an existing case management VR service fro women with breast cancer. It was anticipated that participants referred to the VR service would experience fewer days off work due to sickness in the first 6 months post‐surgery, lower levels of fatigue and increased QoL. | |
| Country | Scotland, UK | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Statistician‐computer. |
| Allocation concealment (selection bias) | Unclear risk | Not reported. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Assessors were blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Incomplete data addressed. |
| Selective reporting (reporting bias) | Low risk | All outcomes from methods are reported. |
| ITT analysis? | High risk | No per protocol although all randomised followed their intervention. |
| Baseline similarity? | High risk | No tests performed. They seem very different. |
| Co‐interventions avoided or similar? | Unclear risk | Not described |
| Compliance? | Unclear risk | Only a few people (2 out of 7) did actually receive interventions and referrals. |
| Similar follow‐up time? | High risk | Timeframe differed in each of the three hospitals. |
Johnsson 2007.
| Methods | RCT, hospital setting | |
| Participants | Breast cancer patients Inclusion criteria: Invasive breast cancer, pre‐menopausal status, primary surgery radical mastectomy plus axillary dissection, node‐positive axillary nodes or tumour > 10 mm, no distant metastases Exclusion criteria: Inoperable cancer, prior radiotherapy, prior neoadjuvant chemotherapy, prior or current endocrine therapy |
|
| Interventions | Intervention groups of adjuvant endocrine therapy: 1. Tamifen only (N = 53) Durtation of treatment: 2 years Setting: Hospital Provider: Treating specialist 2. Goserelin only (N = 55) Duration of treatments: 2 years Setting: Hospital Provider: Treating specialist 3. Tamoxifen + Goserelin (N = 64) Duration of treatments: 2 years Setting: Hospital Provider: Treating specialist Control group (N = 50): No adjuvant endocrine therapy |
|
| Outcomes | Primary outcome measure (RTW outcomes): RTW rate at 24 months Registered by: Patient at baseline (hospital admission) and 12, 18, 24, 36 months after baseline |
|
| Funding | Stockholm Cancer Society and King Gustav V Jubilee Fund | |
| Objectives of the study | To investigate whether socio‐economic and treatment‐related factors were associated with problems of returning to work among pre‐menopausal women included in a randomised trial of adjuvant endocrine therapy | |
| Country | Sweden | |
| Notes | All patients in paid employment at baseline | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported. |
| Allocation concealment (selection bias) | Unclear risk | Not reported. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Blinding of data handling people or researchers or outcome assessors (patients) unknown. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Reasons for drop out were given. |
| Selective reporting (reporting bias) | Low risk | All outcomes from methods are reported. |
| ITT analysis? | High risk | No ITT analysis. |
| Baseline similarity? | Low risk | Similarity for age, sex, education, marital status. |
| Co‐interventions avoided or similar? | Low risk | Surgery, radiotherapy and chemotherapy similar. |
| Compliance? | Unclear risk | No information about the intervention compliance. |
| Similar follow‐up time? | Low risk | The same time points. |
Kornblith 2009.
| Methods | RCT, hospital setting | |
| Participants | Endometrial cancer patients Inclusion criteria: Endometrial cancer, no metastatic cancer, adequate bone marrow, renal, and hepatic function, performance status 0 to 3, speaking English, French or Spanish Exclusion criteria: Not reported |
|
| Interventions | Intervention group (N = 164): Laparoscopy Provider: Surgeon Setting: Hospital Control group (N = 73): Laparotomy Provider: Surgeon Setting: Hospital |
|
| Outcomes | Primary outcome measure (RTW outcomes): RTW in days Registered by: Patient at baseline (hospital admission) and 6 months* post‐surgery Secondary outcome measure (QoL outcomes): FACT‐G and SF‐36, 1, 3, 6 weeks and 6 months post‐surgery |
|
| Funding | National Cancer Institute | |
| Objectives of the study | To compare QoL of patients with endometrial cancer undergoing surgical staging via laparoscopy vs laparotomy | |
| Country | USA | |
| Notes | *6 weeks in article but authors emailed it is 6 months. Results for working patients only in trial of 653 patients | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported. |
| Allocation concealment (selection bias) | Unclear risk | Not reported. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Every loss to follow‐up reason is described. |
| Selective reporting (reporting bias) | Low risk | All outcomes from methods are reported. |
| ITT analysis? | Low risk | 21% converted to control group but ITT performed. |
| Baseline similarity? | Low risk | Age, race. |
| Co‐interventions avoided or similar? | Low risk | None. |
| Compliance? | Unclear risk | 21% converted is acceptable? |
| Similar follow‐up time? | Low risk | 6 months post‐surgery. |
Lee 1992.
| Methods | RCT, hospital setting | |
| Participants | Breast cancer patients Inclusion criteria: Single invasive breast carcinoma 4 cm diameter or less in patients less than 70 years Exclusion criteria: Not reported |
|
| Interventions | Intervention group (N = 44): Breast conservation comprising tumourectomy, axillary clearance, iridium implant and subsequent external beam radiotherapy. Provider: Surgeon Setting: Hospital Control group (N = 47): Modified radical mastectomy |
|
| Outcomes | Primary outcome measure (RTW outcomes): Number returned to original employment (of those employed at baseline) Registered by: Patient at baseline (hospital admission) and 12 months post‐operatively |
|
| Funding | Imperial Cancer Research Fund | |
| Objectives of the study | To test the hypothesis that conservation of the breast with good cosmetic result leads to less psychosocial morbidity | |
| Country | UK | |
| Notes | Results for working patients only in trial of 197 patients | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomisation process not reported. |
| Allocation concealment (selection bias) | Unclear risk | Not clear who and how the randomisation was carried out. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All drop‐outs and reasons for refusal reported. |
| Selective reporting (reporting bias) | Low risk | All outcomes from methods are reported. |
| ITT analysis? | High risk | Analyses done in anxiety and depression between participants and refusals, but not in RTW. |
| Baseline similarity? | Unclear risk | No data given, but groups were similar in terms of sociodemographic factors except social class. |
| Co‐interventions avoided or similar? | Low risk | All patients aged less than 65 years who had axillary nodal metastases were further randomised to receive 12 cycles of adjuvant therapy or no further treatment. |
| Compliance? | Low risk | Attitudes toward treatment procedures measured. |
| Similar follow‐up time? | Low risk | Same timing in both groups. |
Lepore 2003.
| Methods | RCT, hospital setting | |
| Participants | Prostate cancer patients Inclusion criteria: Localised prostate cancer, no history of other cancer, primary residence within 1 hour driving, nonmetastatic disease Exclusion criteria: Not reported |
|
| Interventions | Intervention groups: 1. Education only (N = 41): Six weekly 1 hour lectures delivered by an expert: Prostate cancer biology (oncologist), control physical side effects (urologist), nutrition (dietician), stress and coping (oncology nurse), relationships and sexuality (clinical psychologist), follow‐up care and future health concerns (urologist). Printed material. Intervention lasted 6 weeks Sessions: 6 sessions of 1 hour Providers: Oncologist, urologist, dietician, oncology nurse, clinical psychologist. Setting: Not reported 2. Education plus discussion (N = 43): Lecture series and 45 additional minutes of group discussion (male clinical psychologist), discussion on how lecture topic was relevant to t group. Female family members's own discussion with female oncology nurse. Intervention lasted 6 weeks Sessions: 6 sessions of 1 hour 45 minutes Providers: Oncologist, urologist, dietician, oncology nurse, clinical psychologist. Setting: Not reported Control group (N = 40): Nothing beyond standard medical care. |
|
| Outcomes | Primary outcome measure (RTW outcomes): Employment status only for those working at baseline: Number returned to work and in steady employment Registered by: Patient at baseline (2 months post‐treatment), 2 weeks, 6 months, 12 months Secondary outcome measure (QoL outcomes): SF‐36 Registered by: Patient at baseline (2 months post‐treatment), 2 weeks, 6 months, 12 months |
|
| Funding | National Institute of Health | |
| Objectives of the study | To compare QoL outcomes in patients receiving standard medical care (control) or one of two types of group education interventions | |
| Country | USA | |
| Notes | Results for working patients only in trial of 250 patients | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Sealed envelope. |
| Allocation concealment (selection bias) | Low risk | Randomisation was carried out by an interviewer who was blinded to experimental condition and did not participate in the interventions. |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Interviewer blinded at baseline; patients were not informed about the hypothesis. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition was unrelated to experimental condition. Reasons for drop out given. |
| Selective reporting (reporting bias) | Low risk | All outcomes from methods are reported. |
| ITT analysis? | High risk | No ITT‐analyses conducted in work‐related outcomes. |
| Baseline similarity? | Low risk | Groups were similar in all important background variables. |
| Co‐interventions avoided or similar? | Low risk | No reported co‐intervention. |
| Compliance? | Unclear risk | No report of patients' compliance about the intervention. |
| Similar follow‐up time? | Low risk | Timing of outcomes same in each group. |
Maguire 1983.
| Methods | RCT, hospital setting | |
| Participants | 42 vs 46 breast cancer patients Inclusion criteria: Breast cancer, mastectomy Exclusion criteria: Not reported |
|
| Interventions | Intervention group (N = 42): Within a few days of surgery the nurse advised on exercise, looked at her scar, discussed how she felt about losing a breast, demonstrated breast prothesis. After discharge at home, the nurse examined arm movements, checked exercises, clarified how patient felt about scar, encouraged being open with her partner. Nurse encouraged RTW and becoming socially active. She followed the patient up every two months to monitor the progress until patient adapted well. Intervention lasted several months Sessions: 2 or more sessions Provider: Oncology nurse Setting: Hospital, home Control group (N = 46): Care normally given by the surgical unit |
|
| Outcomes | Primary outcome measure (RTW outcomes): Employment status rate: Number returned to work Registered by: Patient at 12 to 18 months post‐surgery |
|
| Funding | Cancer Research Campaign and the North West Regional Health Authority | |
| Objectives of the study | To assess if a specialist nurse improved the physical and social recovery of patients after mastectomy | |
| Country | UK | |
| Notes | Results for working patients only in trial of 152 patients | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Half of the weeks were designed as counselling weeks and the other half as control weeks using a random number table". |
| Allocation concealment (selection bias) | Unclear risk | Not reported. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Reasons for drop out reported. |
| Selective reporting (reporting bias) | Low risk | All outcomes from methods are reported. |
| ITT analysis? | High risk | No ITT analysis. |
| Baseline similarity? | Low risk | Stated in the article that baseline characteristics were similar. |
| Co‐interventions avoided or similar? | Low risk | No co‐interventions or similar visits to social worker. |
| Compliance? | Low risk | Stated in the article that each patient in the counsel group was advised and counselled by the nurse. |
| Similar follow‐up time? | Unclear risk | Broad follow‐up measurement point: 12 to 18 months. |
Purcell 2011.
| Methods | RCT, hospital | |
| Participants | Radiotherapy patients Inclusion criteria: Patients undergoing outpatient radiotherapy treatment, aged 18 years and over, booked for 20 or more days of radiotherapy for cancer treatment Exclusion criteria: Patients were excluded if the following criteria were present: (1) low performance status (Karnofsky level of < 60/100 requiring at least considerable assistance and frequent medical care); (2) undergoing treatment with palliative intent; (3) undergoing other concurrent cancer treatments (e.g. chemotherapy); (4) involvement in other programmes or research specifically targeting fatigue; (5) inability to complete questionnaires due to cognitive or literacy levels |
|
| Interventions | Intervention groups: Fatigue education: The education programme aimed to reduce participant's level of fatigue by employing self‐care behaviours designed to minimise fatigue. Programme components included a Powerpoint presentation, and a participant handbook, a goal setting sheet and progress diary. Session content addressed radiotherapy and its processes, potential treatment side effects including fatigue, and behavioral strategies to reduce fatigue including activity modification, participation in exercise/activity, maintaining weight/nutrition, sleep hygiene tips and relaxation techniques. Two follow‐up phone calls using a structured script were provided 2 and 4 weeks after each education session to reinforce information. Session duration: 60 minutes Provider: Multidisciplinary team Setting: Via hospital 1) Post‐radiotherapy fatigue education (N = 43): Post‐radiotherapy programme was delivered 1 to 2 weeks after the completion of radiotherapy. 2) Pre‐ and post‐radiotherapy fatigue education (N = 23): Pre‐radiotherapy programme was delivered 1 week prior to radiotherapy planning and post‐radiotherapy programme was delivered 1 to 2 weeks after the completion of radiotherapy. Control (N = 48 and 24): A one‐page flyer was provided with generic information about fatigue. |
|
| Outcomes | Employment status: Full time, part time, casual, not working (baseline). Outcome measure: Health and labour questionnaire: participation in paid work (yes/no) Registered by: Patient at 6 weeks follow‐up Secondary outcome measure (QoL outcomes): EQ‐5D |
|
| Funding | Queensland Healh Cancer Control Team, Queensland Health, Health Practitioner Research Scheme, Princess Alexandria Hospital Cancer Collaborative Group: indirect funding and no direct involvement | |
| Objectives of the study | To assess if providing pre‐radiotherapy fatigue education, post‐radiotherapy education or pre‐ and post‐radiotherapy education reduces the severity of fatigue of cancer patients experienced 6 weeks after radiotherapy | |
| Country | Australia | |
| Notes | Results for the pre‐radiotherapy fatigue education (N = 27) alone were not reported for work outcomes | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer generated. |
| Allocation concealment (selection bias) | Low risk | Sealed opaque envelope. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Blinded from assessor. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not reported. |
| Selective reporting (reporting bias) | Low risk | All outcomes from methods are reported. |
| ITT analysis? | Unclear risk | Not reported. |
| Baseline similarity? | High risk | Not on education. |
| Co‐interventions avoided or similar? | Low risk | Similar. |
| Compliance? | Unclear risk | Mainly self‐management intervention, not clear whether participants completed or not. |
| Similar follow‐up time? | Low risk | 6 weeks follow‐up. |
Rogers 2009.
| Methods | RCT, community setting | |
| Participants | Breast cancer patients Inclusion criteria: English speaking, female, breast cancer survivor, 18 to 70 years, stage I, II or IIIA, expected on hormonal therapy of the duration of the study (8 months), medical clearance by physician, at least 8 weeks after surgery Exclusion criteria: Dementia, organic brain syndrome, medical/psychological/social problems, contradiction for physical activity (angina etc), breast cancer recurrence or metastatic, inability to ambulate, planning to relocate, or engaged in > 60 min of vigorous physical activity or > 150 min of moderate vigorous activity per week |
|
| Interventions | Intervention group (N = 14): 12‐week physical activity behaviour change intervention. Goal: 150 min of moderate walking per week. Six discussion group sessions with clinical psychologist. 12 individual supervised exercise sessions + 3 face to face counselling sessions with exercise specialist. Home‐based exercises.(40). Intervention lasted 12 weeks Sessions: 21 sessions Provider: Clinical psychologist, exercise specialist Setting: Not reported and home Control group (N = 14): Provision of written materials from the Internet |
|
| Outcomes | Primary outcome measure (RTW outcomes): Sick leave days missed from work in past month. Registered by: Patient at baseline and 3 months after the intervention Secondary outcome measure (QoL outcomes): FACT‐General + breast Registered by: Patient at baseline and 3 months after the intervention |
|
| Funding | Southern Illinois University, Brooks Medical Research Fund, Memorial Medical Center Foundation. | |
| Objectives of the study | To determine feasibility and preliminary effectiveness of a physical activity behavior change intervention | |
| Country | USA | |
| Notes | Results for working patients only in trial of 39 patients | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer generated. |
| Allocation concealment (selection bias) | Low risk | Sealed envelope. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Reasons for drop‐out are given. |
| Selective reporting (reporting bias) | Low risk | All outcomes from methods are reported. |
| ITT analysis? | Low risk | ITT analysis performed. |
| Baseline similarity? | Low risk | Groups were compared on demographic, medical, diet, physical activity, other health‐related outcomes. |
| Co‐interventions avoided or similar? | Low risk | Vigorous exercise excluded. |
| Compliance? | Low risk | Intervention adherence monitored. |
| Similar follow‐up time? | Low risk | 3 months after baseline. |
Tamminga 2013.
| Methods | RCT, hospital | |
| Participants | Female cancer patients, 64% breast cancer, 23% cervix Inclusion criteria: 1) Cancer patients; 2) 18 to 60 years; 3) treated with curative intent, i.e. and expected 1‐year survival rate of approximately 80%; 4) had paid work; 5) were on sick leave. Exclusion criteria: 1) Not sufficiently able to speak, read or write Dutch; 2) severe mental illness; 3) other severe comorbidity; 4) primary diagnosis of cancer more that 2 months previously. |
|
| Interventions | Intervention (N = 65): Delivering patient education and support at the hospital, as part of usual psycho‐oncological care; improving communication between the treating physician and the occupational physician, and drawing up a concrete and gradual RTW plain in collaboration with the cancer patient, the occupational physician and the employer. Session duration: 4 meetings lasting 15 minutes; spread across a maximum of 14 months Provider: Oncology nurse or medical social worker Setting: Hospital Control (N = 68): Care as usual. |
|
| Outcomes | RTW rate at 12‐months follow‐up of patients alive and with a life expectancy of more than a few months at 12 months. Ibid for those who died within the follow‐up period or those with a life expectancy of only a few months. Number of calendar days between the first day of sickness and the first day at work (either full‐time or part‐time) that was sustained for at least 4 weeks. Registered by: Patient at baseline and 6 and 12 months of follow‐up Secondary outcome measure (QoL outcomes): SF‐36 |
|
| Funding | Stichting Instituut GAK and part of the research programme Pathways to work. | |
| Objectives of the study | To determine the effect of a hospital‐based work support intervention for cancer patients on RTW and QoL | |
| Country | Netherlands | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Stratified, computer generated. |
| Allocation concealment (selection bias) | Low risk | Computer generated for each patient after inclusion. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Assessors were not blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Numbers on drop out are unable to determine. |
| Selective reporting (reporting bias) | Unclear risk | All outcomes from methods are reported. |
| ITT analysis? | Low risk | Yes, ITT. |
| Baseline similarity? | Low risk | Tested, no differences found. |
| Co‐interventions avoided or similar? | Unclear risk | Not described. |
| Compliance? | Low risk | 8/68 people did not receive the intervention. |
| Similar follow‐up time? | Low risk | 12 months in both groups. |
Abbreviations: vs: versus; RCT: randomised controlled trial; RTW: return‐to‐work; QoL: quality of life; MOS‐SF: Medical Outcomes Studies‐Short Form.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Adamsen 2009 | No RTW outcomes reported. |
| Berglund 1993 | Not a RCT or CBA. |
| Berglund 2003 | No RTW outcomes reported. |
| Bertheussen 2012 | No control group. |
| Bird 2010 | No RTW outcomes reported. |
| Bloom 2008 | No RTW outcomes reported. |
| Borget 2007 | Not a randomised study |
| Budin 2008 | Outcome is not sick leave or RTW but vocational environment scale. |
| Burak 2002 | Outcome is not sick leave or RTW but return to normal activity. |
| Böttcher 2013 | Not a RCT. |
| Bürger 2011 | No RTW outcomes reported. |
| Cadmus‐Bertram 2013 | No RTW outcomes reported. |
| Cain 1986 | Outcome is not sick leave or RTW but vocational environment scale. |
| Capone 1980 | Not a randomised study. |
| Chan 2005 | No RTW outcomes reported. |
| Cherrier 2013 | No RTW outcomes reported. |
| Cho 2006 | No RTW outcomes reported. |
| Egan 2013 | Review. |
| Emmanouilidis 2013 | Same data as in Emmanouilidis 2009. |
| Eyigor 2010 | No RTW outcomes reported. |
| Fassoulaki 2000 | No RTW outcomes reported. |
| Fors 2011 | Review. |
| Gordon 1980 | Not a randomised study. |
| Gordon 2005 | No RTW outcomes reported. |
| Greer 1992 | Outcome is not sick leave or RTW but vocational environment scale. |
| Griffith 2009 | No RTW outcomes reported. |
| Harrison‐Paul 2006 | No RTW outcomes reported. |
| Hartmann 2007 | No RTW outcomes reported. |
| Hegel 2011 | No RTW outcomes reported. |
| Heim 2007 | No RTW outcomes reported. |
| Høybye 2010 | No RTW outcomes reported. |
| Janson 2005 | No RTW outcomes reported for intervention. |
| Jiang 2009 | Outcome is not sick leave or RTW but includes normal routine activity. |
| Jones 2005 | No RTW outcomes reported. |
| Jørgensen 2009 | No RTW outcomes reported. |
| Korstjens 2008 | No RTW outcomes reported. |
| Lauchlan 2011 | No RTW outcomes reported. |
| Lee 2009 | No cancer. |
| Madore 2014 | No RTW outcomes reported. |
| May 2009 | No RTW outcomes reported. |
| McNeely 2008 | No RTW outcomes reported. |
| Meneses 2007 | No RTW outcomes reported. |
| Meraviglia 2013 | No RTW outcomes reported. |
| Mock 1994 | No RTW outcomes reported. |
| Norager 2006 | No RTW outcomes reported. |
| Nowrouzi 2009 | No intervention. |
| O'Brien 2014 | No RTW outcomes reported. |
| Persson 2010 | No cancer. |
| Poppelreuter 2009 | No RTW outcomes reported. |
| Rotstein 1989 | Only half of the patients were employed at baseline. |
| Salonen 2010 | No RTW outcomes reported. |
| Scott 2013 | No patients. |
| Seibaek 2009 | No RTW outcomes reported. |
| Seiler 2005 | Outcome is not sick leave or RTW but return to normal daily activity. |
| Semple 2009 | No RTW outcomes reported. |
| Shelton 2009 | No RTW outcomes reported. |
| Sherer 1997 | Not a RCT or CBA study. |
| Sherman 2010 | No RTW outcomes reported. |
| Sherman 2012 | No RTW outcomes reported. |
| Shimada 2007 | No RTW outcomes reported. |
| Silver 2013 | Review. |
| Vos 2006 | No RTW outcomes reported. |
| Wenzel 1995 | Outcome is not sick leave or RTW but vocational environment scale. |
| Wiggins 2009 | No RTW outcomes reported. |
Characteristics of ongoing studies [ordered by study ID]
NCT01799031.
| Trial name or title | Educational Intervention for Reducing Work Disability in Breast Cancer Survivors. |
| Methods | Allocation: Randomized Endpoint Classification: Efficacy Study Intervention Model: Parallel Assignment Masking: Open Label Primary Purpose: Supportive Care |
| Participants |
|
| Interventions | Patients receive access to the WISE web‐based educational intervention to help BCS manage their symptoms, identify ergonomic workplace problems and risks, and implement ergonomic modifications. Patients also receive standard of care comprising symptom management therapies and a pamphlet on employment rights. Patients receive standard of care comprising symptom management therapies and a pamphlet on employment rights. |
| Outcomes | Employment status |
| Starting date | February 21, 2013 |
| Contact information | https://clinicaltrials.gov/ct2/show/NCT01799031 |
| Notes |
NTR2138.
| Trial name or title | Physical Activity during Cancer Treatment study |
| Methods | Randomized, 2 arms |
| Participants | Patients diagnosed with breast or colon cancer (M0) who will be treated with chemotherapy. Inclusion criteria are: 1. Histological diagnosis of cancer < 6 weeks ago; 2. Adjuvant treatment including chemotherapy; 3. Age 25‐75 years; 4. Able to read and understand the Dutch language; 5. Karnofsky Performance Status ¡Ý 60; 6. Able to walk ¡Ý 100 meter. |
| Interventions | The intervention group will receive an 18 week supervised group exercise program based on Bandura’s social cognitive theory (SCT) during cancer treatment. The exercise program will start earliest one week after surgery and at least within six weeks (breast cancer) or ten weeks (colon cancer) after definitive cancer diagnosis. The control group will receive care as usual (no exercise program). |
| Outcomes | 1. Fatigue; 2. Health service utilization; 3. Sick leave. |
| Starting date | 1‐jan‐2010 |
| Contact information | http://www.trialregister.nl/trialreg/admin/rctview.asp?TC=2138 |
| Notes |
Differences between protocol and review
For this 2015 Cochrane review update we excluded non‐randomised studies because it was clear that randomised studies are feasible and have been conducted. This proved that our earlier understanding was mistaken in that it would be difficult to randomise in this context. This had been the main reason for including non‐randomised studies.
Contributions of authors
AdB is the main review author and has been involved with all aspects of the protocol. She wrote the protocol and the review. She designed and conducted the search strategy. TT, ST, MF‐D, MF and JV contributed to the draft version of the protocol and review and will contribute to subsequent versions and revisions of the review. AdB and TT screened eligible studies, conducted the quality assessment of eligible studies and extracted data from the included studies. JV and AdB conducted the data synthesis. JV performed GRADE data synthesis.
Sources of support
Internal sources
Coronel Institute of Occupational Health, Netherlands.
Cochrane Occupational Safety and Health Review Group, Finland.
University of Birmingham, UK.
Uniformed Services University of the Health Sciences, USA.
Centre for Workforce Effectiveness, The Work Foundation, London, UK.
External sources
SIG Pathways to Work. University Research Programme, Netherlands.
Finnish Work Environment Fund, Finland.
COST Action CANWON IS1211, Not specified.
Declarations of interest
Angela de Boer: I am an author of Tamminga 2013.
Tyna Taskila: None known.
Sietske Tamminga: I am an author of Tamminga 2013.
Michael Feuerstein: I have received consultancy fees from Paradigm Health Corp and travel support and royalties from Springer but these are not related to the topic of this Cochrane review. Neither the grant I currently have nor the retirement investments I have (managed by TIAA‐CREF) are also not related to the topic of this Cochrane review.
Monique Frings‐Dresen: I am an author of Tamminga 2013.
Jos Verbeek: I am an author of Tamminga 2013 and I am employed by the Finnish Institute of Occupational Health to coordinate the Cochrane Work Review Group.
Edited (no change to conclusions), comment added to review
References
References to studies included in this review
Ackerstaff 2009 {published and unpublished data}
- Ackerstaff AH, Balm AJM, Rasch CRN, Boer JP, Wiggenraad R, Rietveld DHF, et al. First‐year quality of life assessment of an intra‐arterial (radplat) versus intravenous chemoradiation phase III trial. Head & Neck 2009;31(1):77‐84. [DOI] [PubMed] [Google Scholar]
Berglund 1994 {published data only}
- Berglund G, Bolund C, Gustafsson UL, Sjödén P‐O. One‐year follow‐up of the 'Starting Again' group rehabilitation programme for cancer patients. European Journal of Cancer 1994;30A(12):1744‐51. [DOI] [PubMed] [Google Scholar]
Burgio 2006 {published data only}
- Burgio KL, Goode PS, Urban DA, Umlauf MG, Locher JL, Bueschen A, et al. Preoperative biofeedback assisted behavioral training to decrease post‐prostatectomy incontinence: a randomized, controlled study. Journal of Urology 2006;175(1):196‐201. [DOI] [PubMed] [Google Scholar]
Emmanouilidis 2009 {published data only}
- Emmanouilidis N, Müller JA, Jäger MD, Kaaden S, Helfritz FA, Güner Z, et al. Surgery and radioablation therapy combined: introducing a 1‐week‐condensed procedure bonding total thyroidectomy and radioablation therapy with recombinant human TSH. European Journal of Endocrinology 2009;161(5):763‐9. [DOI] [PubMed] [Google Scholar]
Friedrichs 2010 {published data only}
- Friedrichs B, Tichelli A, Bacigalupo A, Russell NH, Ruutu T, Shapira MY, et al. Long‐term outcome and late effects in patients transplanted with mobilised blood or bone marrow: a randomised trial. The Lancet Oncology 2010;11(4):331‐8. [DOI] [PubMed] [Google Scholar]
Hillman 1998 {published data only}
- Hillman RE, Walsh MJ, Wolf GT, Fisher SG, Hong WK. Functional outcomes following treatment for advanced laryngeal cancer. Part I‐‐Voice preservation in advancedlaryngeal cancer. Part II‐‐Laryngectomy rehabilitation: the state of the art in the VA System. Research Speech‐Language Pathologists. Department of Veterans Affairs Laryngeal Cancer Study Group. Annals of Otology, Rhinology and Laryngology 1998;172:1‐27. [PubMed] [Google Scholar]
Hubbard 2013 {published data only}
- Hubbard G, Gray NM, Ayansina D, Evans JM, Kyle RG. Case management vocational rehabilitation for women with breast cancer after surgery: a feasibility study incorporating a pilot randomised controlled trial. Trials 2013;14:175. [DOI] [PMC free article] [PubMed] [Google Scholar]
Johnsson 2007 {published data only}
- Johnsson A, Fornander T, Olsson M, Nystedt M, Johansson H, Rutqvist LE. Factors associated with return to work after breast cancer treatment. Acta Oncologica 2007;46(1):90‐6. [DOI] [PubMed] [Google Scholar]
Kornblith 2009 {published data only}
- Kornblith AB, Huang HQ, Walker JL, Spirtos NM, Rotmensch J, Cella D. Quality of life patients with endometrial cancer undergoing laparoscopic international federation of gynecology and obstetrics staging compared with laparotomy: a Gynecologic Oncology Group study. Journal of Clinical Oncology 2009;27(32):5337‐42. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lee 1992 {published data only}
- Lee MS, Love SB, Mitchell JB, Parker EM, Rubens RD, Watson JP, et al. Mastectomy or conservation for early breast cancer: psychological morbidity. European Journal of Cancer 1992;28A(8‐9):1340‐4. [DOI] [PubMed] [Google Scholar]
Lepore 2003 {published data only}
- Lepore SJ, Helgeson VS, Eton DT, Schulz R. Improving quality of life in men with prostate cancer: a randomized controlled trial of group education interventions. Health Psychology 2003;22(5):443‐52. [DOI] [PMC free article] [PubMed] [Google Scholar]
Maguire 1983 {published data only}
- Maguire P, Brooke M, Tait A, Thomas C, Sellwood R. The effect of counselling on physical disability and social recovery after mastectomy. Clinical Oncology 1983;9(4):319‐24. [PubMed] [Google Scholar]
Purcell 2011 {published data only}
- Purcell A, Fleming J, Burmeister B, Bennett S, Haines T. Is education an effective management strategy for reducing cancer‐related fatigue?. Supportive Care in Cancer 2011;19(9):1429‐39. [DOI] [PubMed] [Google Scholar]
Rogers 2009 {published and unpublished data}
- Rogers LQ, Hopkins‐Pryce P, Vicari S, Pamenter R, Courneya KS, Markwell S, et al. A randomized trial to increase physical activity in breast cancer survivors. Medical Science Sports Exercises 2009;41(4):935‐46. [DOI] [PubMed] [Google Scholar]
Tamminga 2013 {published and unpublished data}
- Tamminga SJ, Verbeek JH, Bos MM, Fons G, Kitzen JJ, Plaisier PW, et al. Effectiveness of a hospital‐based work support intervention for female cancer patients ‐ a multi‐centre randomised controlled trial. PLoS One 2013;8(5):e63271. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies excluded from this review
Adamsen 2009 {published data only}
- Adamsen L, Quist M, Andersen C, Møller T, Herrstedt J, Kronborg D, et al. Effect of a multimodal high intensity exercise intervention in cancer patients undergoing chemotherapy: randomised controlled trial. BMJ 2009;339:b3410. [DOI] [PMC free article] [PubMed] [Google Scholar]
Berglund 1993 {published data only}
- Berglund G, Bolund C, Gustavsson UL, Sjödén PO. Starting again‐‐a comparison study of a group rehabilitation program for cancer patients. Acta Oncologica 1993;32(1):15‐21. [DOI] [PubMed] [Google Scholar]
Berglund 2003 {published data only}
- Berglund G, Petersson LM, Eriksson KR, Häggman M. "Between men": patient perceptions and priorities in a rehabilitation program for men with prostate cancer. Patient Education and Counselling 2003;49(3):285‐92. [DOI] [PubMed] [Google Scholar]
Bertheussen 2012 {published data only}
- Bertheussen GF, Kaasa S, Hokstad A, Sandmæl JA, Helbostad JL, Salvesen Ø, et al. Feasibility and changes in symptoms and functioning following inpatient cancer rehabilitation. Acta Oncologica 2012;51(8):1070‐80. [DOI] [PubMed] [Google Scholar]
Bird 2010 {published data only}
- Bird L, Arthur A, Niblock T, Stone R, Watson L, Cox K. Rehabilitation programme after stem cell transplantation: randomized controlled trial. Journal of Advanced Nursing 2010;66(3):607‐15. [DOI] [PubMed] [Google Scholar]
Bloom 2008 {published data only}
- Bloom JR, Stewart SL, D'Onofrio CN, Luce J, Banks PJ. Addressing the needs of young breast cancer survivors at the 5 year milestone: can a short‐term, low intensity intervention produce change?. Journal of Cancer Survivorship 2008;2(3):190‐204. [DOI] [PubMed] [Google Scholar]
Borget 2007 {published data only}
- Borget I, Corone C, Nocaudie M, Allyn M, Iacobelli S, Schlumberger M, et al. Sick leave for follow‐up control in thyroid cancer patients: comparison between stimulation with Thyrogen and thyroid hormone withdrawal. European Journal of Endocrinology 2007;156(5):531‐8. [DOI] [PubMed] [Google Scholar]
Böttcher 2013 {published data only}
- Böttcher HM, Steimann M, Ullrich A, Rotsch M, Zurborn KH, Koch U, et al. Evaluation of a vocationally oriented concept within inpatient oncological rehabilitation [Evaluation eines berufsbezogenen Konzepts im Rahmen der stationären onkologischen Rehabilitation]. Die Rehabilitation 2013;52(5):329‐36. [DOI] [PubMed] [Google Scholar]
Budin 2008 {published data only}
- Budin WC, Hoskins CN, Haber J, Sherman DW, Maislin G, Cater JR, et al. Breast cancer: education, counseling, and adjustment among patients and partners: a randomized clinical trial. Nursing Research 2008;57(3):199‐213. [DOI] [PubMed] [Google Scholar]
Burak 2002 {published data only}
- Burak J, Hollenbeck ST, Zervos EE, Hock KL, Kemp LC, Young DC. Sentinel lymph node biopsy results in less postoperative morbidity compared with axillary lymph node dissection for breast cancer. American Journal of Surgery 2002;183(1):23‐7. [DOI] [PubMed] [Google Scholar]
Bürger 2011 {published data only}
- Bürger W, Streibelt M. Who benefits from stepwise occupational reintegration provided under the statutory pension insurance scheme? [Wer profitiert von Stufenweiser Wiedereingliederung in Trägerschaft der gesetzlichen Rentenversicherung?]. Die Rehabilitation 2011;50(3):178‐85. [DOI] [PubMed] [Google Scholar]
Cadmus‐Bertram 2013 {published data only}
- Cadmus‐Bertram L, Littman AJ, Ulrich CM, Stovall R, Ceballos RM, McGregor BA, et al. Predictors of adherence to a 26‐week viniyoga intervention among post‐treatment breast cancer survivors. Journal of Alternative and Complementary Medicine 2013;19(9):751‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cain 1986 {published data only}
- Cain EN, Kohorn EI, Quinlan DM, Latimer K, Schwartz PE. Psychological benefits of a cancer support group. Cancer 1986;57(1):183‐9. [DOI] [PubMed] [Google Scholar]
Capone 1980 {published data only}
- Capone MA, Good RS, Westie KS, Jacobson AF. Psychosocial rehabilitation of gynecologic oncology patients. Archives of Physical Medical and Rehabilitation 1980;61(3):128‐32. [PubMed] [Google Scholar]
Chan 2005 {published data only}
- Chan YM, Lee PW, Fong DY, Fung AS, Wu LY, Choi AY, et al. Effect of individual psychological intervention in Chinese women with gynecologic malignancy: a randomized controlled trial. Journal of Clinical Oncology 2005;23(22):4913‐24. [DOI] [PubMed] [Google Scholar]
Cherrier 2013 {published data only}
- Cherrier MM, Anderson K, David D, Higano CS, Gray H, Church A, et al. A randomized trial of cognitive rehabilitation in cancer survivors. Life Sciences 2013;93(17):617‐22. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cho 2006 {published data only}
- Cho OH, Yoo YS, Kim NC. Efficacy of comprehensive group rehabilitation for women with early breast cancer in South Korea. Nursing Health Science 2006;8(3):140‐6. [DOI] [PubMed] [Google Scholar]
Egan 2013 {published data only}
- Egan MY, McEwen S, Sikora L, Chasen M, Fitch M, Eldred S. Rehabilitation following cancer treatment. Disability and Rehabilitation 2013;35(26):2245‐58. [DOI] [PubMed] [Google Scholar]
Emmanouilidis 2013 {published data only}
- Emmanouilidis N, Schrem H, Winkler M, Klempnauer J, Scheumann GF. Long‐term results after treatment of very low‐, low‐, and high‐risk thyroid cancers in a combined setting of thyroidectomy and radio ablation therapy in euthyroidism. International Journal of Endocrinology 2013;2013:769473. [DOI] [PMC free article] [PubMed] [Google Scholar]
Eyigor 2010 {published data only}
- Eyigor S, Karapolat H, Yesil H, Uslu R, Durmaz B. Effects of pilates exercises on functional capacity, flexibility, fatigue, depression and quality of life in female breast cancer patients: a randomized controlled study. European Journal of Physical and Rehabilitation Medicine 2010;46(4):481‐7. [PubMed] [Google Scholar]
Fassoulaki 2000 {published data only}
- Fassoulaki A, Sarantopoulos C, Melemeni A, Hogan Q. EMLA reduces acute and chronic pain after breast surgery for cancer. Regional Anesthesia and Pain Medicine 2000;25(4):350‐5. [DOI] [PubMed] [Google Scholar]
Fors 2011 {published data only}
- Fors EA, Bertheussen GF, Thune I, Juvet LK, Elvsaas IK, Oldervoll L, et al. Psychosocial interventions as part of breast cancer rehabilitation programs? Results from a systematic review. Psychooncology 2011;20(9):909‐18. [DOI] [PubMed] [Google Scholar]
Gordon 1980 {published data only}
- Gordon WA, Freidenbergs I, Diller L, Hibbard M, Wolf C, Levine L, et al. Efficacy of psychosocial intervention with cancer patients. Journal of Consulting and Clinical Psychology 1980;48(6):743‐59. [DOI] [PubMed] [Google Scholar]
Gordon 2005 {published and unpublished data}
- Gordon LG, Scuffham P, Battistutta D, Graves N, Tweeddale M, Newman B. A cost‐effectiveness analysis of two rehabilitation support services for women with breast cancer. Breast Cancer Research and Treatment 2005;94(2):123‐33. [DOI] [PubMed] [Google Scholar]
Greer 1992 {published data only}
- Greer S, Moorey S, Baruch JD, Watson M, Robertson BM, Mason A, et al. Adjuvant psychological therapy for patients with cancer: a prospective randomised trial. BMJ 1992;304(6828):675‐80. [DOI] [PMC free article] [PubMed] [Google Scholar]
Griffith 2009 {published data only}
- Griffith K, Wenzel J, Shang J, Thompson C, Stewart K, Mock V. Impact of a walking intervention on cardiorespiratory fitness, self‐reported physical function, and pain in patients undergoing treatment for solid tumors. Cancer 2009;115(20):4874‐84. [DOI] [PMC free article] [PubMed] [Google Scholar]
Harrison‐Paul 2006 {published data only}
- Harrison‐Paul J, Drummond AER. A randomised controlled trial of occupational therapy in oncology: challenges in conducting a pilot study. British Journal of Occupational Therapy 2006;69(3):130‐3. [Google Scholar]
Hartmann 2007 {published data only}
- Hartmann U, Muche R, Reuss‐Borst M. Effects of a step‐by‐step inpatient rehabilitation programme on quality of life in breast cancer patients. A prospective randomised study. Onkologie 2007;30(4):177‐82. [DOI] [PubMed] [Google Scholar]
Hegel 2011 {published data only}
- Hegel MT, Lyons KD, Hull JG, Kaufman P, Urquhart L, Li Z, et al. Feasibility study of a randomized controlled trial of a telephone‐delivered problem‐solving‐occupational therapy intervention to reduce participation restrictions in rural breast cancer survivors undergoing chemotherapy. Psychooncology 2011;20(10):1092‐101. [DOI] [PMC free article] [PubMed] [Google Scholar]
Heim 2007 {published data only}
- Heim ME, Malsburg ML, Niklas A. Randomized controlled trial of a structured training program in breast cancer patients with tumor‐related chronic fatigue. Onkologie 2007;30(8‐9):429‐34. [DOI] [PubMed] [Google Scholar]
Høybye 2010 {published data only}
- Høybye MT, Dalton SO, Deltour I, Bidstrup PE, Frederiksen K, Johansen C. Effect of Internet peer‐support groups on psychosocial adjustment to cancer: a randomised study. British Journal of Cancer 2010;102(9):1348‐54. [DOI] [PMC free article] [PubMed] [Google Scholar]
Janson 2005 {published data only}
- Janson M, Carlsson P, Haglind E, Anderberg B. Data validation in an economic evaluation of surgery for colon cancer. International Journal of Technology Assessment in Health Care 2005;21(2):246‐52. [PubMed] [Google Scholar]
Jiang 2009 {published data only}
- Jiang J, Zheng X, Qin J, Zheng M, Mao Q, Zhang Z, et al. Health‐related quality of life after hand‐assisted laparoscopic and open radical nephrectomies of renal cell carcinoma. International Urolology and Nephrology 2009;41(1):23‐7. [DOI] [PubMed] [Google Scholar]
Jones 2005 {published and unpublished data}
- Jones WG, Fossa SD, Mead GM, Roberts JT, Sokal M, Horwich A, et al. Randomized trial of 30 versus 20 Gy in the adjuvant treatment of stage I Testicular Seminoma: a report on Medical Research Council Trial TE18, European Organisation for the Research and Treatment of Cancer Trial 30942 (ISRCTN18525328). Journal of Clinical Oncology 2005;23(6):1200‐8. [DOI] [PubMed] [Google Scholar]
Jørgensen 2009 {published data only}
- Jørgensen IL, Frederiksen K, Boesen E, Elsass P, Johansen C. An exploratory study of associations between illness perceptions and adjustment and changes after psychosocial rehabilitation in survivors of breast cancer. Acta Oncologica 2009;48(8):1119‐27. [DOI] [PubMed] [Google Scholar]
Korstjens 2008 {published data only}
- Korstjens I, May AM, Weert E, Mesters I, Tan F, Ros WJ, et al. Quality of life after self‐management cancer rehabilitation: a randomized controlled trial comparing physical and cognitive‐behavioral training versus physical training. Psychosomatic Medicine 2008;70(4):422‐9. [DOI] [PubMed] [Google Scholar]
Lauchlan 2011 {published data only}
- Lauchlan DT, McCaul JA, McCarron T, Patil S, McManners J, McGarva J. An exploratory trial of preventative rehabilitation on shoulder disability and quality of life in patients following neck dissection surgery. European Journal of Cancer Care 2011;20(1):113‐22. [DOI] [PubMed] [Google Scholar]
Lee 2009 {published data only}
- Lee WL, Liu WM, Cheng MH, Chao HT, Fuh JL, Wang PH. Uterine vascular occlusion in management of leiomyomas: laparoscopy vs laparotomy. Journal of Minimal Invasive Gynecology 2009;16(5):562‐8. [DOI] [PubMed] [Google Scholar]
Madore 2014 {published data only}
- Madore S, Kilbourn K, Valverde P, Borrayo E, Raich P. Feasibility of a psychosocial and patient navigation intervention to improve access to treatment among underserved breast cancer patients. Supportive Care in Cancer 2014;22(8):2085‐93. [DOI] [PubMed] [Google Scholar]
May 2009 {published data only}
- May A, Korstjens I, Weert E, Borne B, Hoekstra‐Weebers J, Schans CP, et al. Long‐term effects on cancer survivors' quality of life of physical training versus physical training combined with cognitive‐behavioral therapy: results from a randomized trial. Supportive Care in Cancer 2009;17(6):653‐63. [DOI] [PubMed] [Google Scholar]
McNeely 2008 {published data only}
- McNeely ML, Parliament MB, Seikaly H, Jha N, Magee DJ, Haykowsky MJ, et al. Effect of exercise on upper extremity pain and dysfunction in head and neck cancer survivors: a randomized controlled trial. Cancer 2008;113(1):214‐22. [DOI] [PubMed] [Google Scholar]
Meneses 2007 {published data only}
- Meneses KD, McNees P, Loerzel VW, Su X, Zhang Y, Hassey LA. Transition from treatment to survivorship: effects of a psychoeducational intervention on quality of life in breast cancer survivors. Oncology Nursing Forum 2007;34(5):1007‐16. [DOI] [PubMed] [Google Scholar]
Meraviglia 2013 {published data only}
- Meraviglia M, Stuifbergen A, Parsons D, Morgan S. Health promotion for cancer survivors: adaptation and implementation of an intervention. Holistic Nursing Practice 2013;27(3):140‐7. [DOI] [PubMed] [Google Scholar]
Mock 1994 {published data only}
- Mock V, Burke MB, Sheehan P, Creaton EM, Winningham ML, McKenney‐Tedder S, et al. A nursing rehabilitation program for women with breast cancer receiving adjuvant chemotherapy. Oncology Nursing Forum 1994;21(5):899‐907. [PubMed] [Google Scholar]
Norager 2006 {published data only}
- Norager CB, Jensen MB, Madsen MR, Qvist N, Laurberg S. Effect of darbepoetin alfa on physical function in patients undergoing surgery for colorectal cancer. A randomized, double‐blind, placebo‐controlled study. Oncology 2006;71(3‐4):212‐20. [DOI] [PubMed] [Google Scholar]
Nowrouzi 2009 {published data only}
- Nowrouzi B, Lightfoot N, Cote K, Watson R. Workplace support for employees with cancer. Current Oncology 2009;16(5):15‐22. [DOI] [PMC free article] [PubMed] [Google Scholar]
O'Brien 2014 {published data only}
- O'Brien L, Loughnan A, Purcell A, Haines T. Education for cancer‐related fatigue: could talking about it make people more likely to report it?. Supportive Care in Cancer 2014;22(1):209‐15. [DOI] [PubMed] [Google Scholar]
Persson 2010 {published data only}
- Persson P, Brynhildsen J, Kjølhede P, Hysterectomy Multicentre Study Group in South‐East Sweden. Short‐term recovery after subtotal and total abdominal hysterectomy‐‐a randomised clinical trial. BJOG 2010;117(4):469‐78. [DOI] [PubMed] [Google Scholar]
Poppelreuter 2009 {published data only}
- Poppelreuter M, Weis J, Bartsch HH. Effects of specific neuropsychological training programs for breast cancer patients after adjuvant chemotherapy. Journal of Psychosocial Oncology 2009;27(2):274‐96. [DOI] [PubMed] [Google Scholar]
Rotstein 1989 {published data only}
- Rotstein S, Nilsson B, Gustavson‐Kadaka E, Andersson S. Long‐term follow‐up of sickness periods in breast cancer patients primarily treated with surgery and radiotherapy or surgery only. Acta Oncologica 1989;28(6):817‐22. [DOI] [PubMed] [Google Scholar]
Salonen 2010 {published data only}
- Salonen P, Kellokumpu‐Lehtinen PL, Tarkka MT, Koivisto AM, Kaunonen M. Changes in quality of life in patients with breast cancer. Journal of Clinical Nursing 2011;20(1‐2):255‐66. [DOI] [PubMed] [Google Scholar]
Scott 2013 {published data only}
- Scott DA, Mills M, Black A, Cantwell M, Campbell A, Cardwell CR, et al. Multidimensional rehabilitation programmes for adult cancer survivors. Cochrane Database of Systematic Reviews 2013, Issue 3. [DOI: 10.1002/14651858.CD007730.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Seibaek 2009 {published data only}
- Seibaek L, Petersen L. Nurse‐led rehabilitation after gynaecological cancer surgery: preliminary results from a clinically controlled, prospective questionnaire study. Supportive Care in Cancer 2009;17(5):601‐5. [DOI] [PubMed] [Google Scholar]
Seiler 2005 {published data only}
- Seiler CA, Wagner M, Bachmann T, Redaelli CA, Schmied B, Uhl W, et al. Randomized clinical trial of pylorus‐preserving duodenopancreatectomy versus classical Whipple resection ‐ long term results. British Journal of Surgery 2005;92(5):547‐56. [DOI] [PubMed] [Google Scholar]
Semple 2009 {published data only}
- Semple C, Dunwoody L, Kernohan W, McCaughan E. Development and evaluation of a problem‐focused psychosocial intervention for patients with head and neck cancer. Supportive Care in Cancer 2009;17(4):379‐88. [DOI] [PubMed] [Google Scholar]
Shelton 2009 {published data only}
- Shelton ML, Lee JQ, Morris GS, Massey PR, Kendall DG, Munsell MF, et al. A randomized control trial of a supervised versus a self‐directed exercise program for allogeneic stem cell transplant patients. Psycho‐Oncology 2009;18(4):353‐9. [DOI] [PubMed] [Google Scholar]
Sherer 1997 {published data only}
- Shere M, Meyers CA, Bergloff P. Efficacy of post‐acute brain injury rehabilitation for patients with primary malignant brain tumors. Cancer 1997;80(2):250‐7. [PubMed] [Google Scholar]
Sherman 2010 {published data only}
- Sherman KA, Heard G, Cavanagh KL. Psychological effects and mediators of a group multi‐component program for breast cancer survivors. Journal of Behavioral Medicine 2010;33(5):378‐91. [DOI] [PubMed] [Google Scholar]
Sherman 2012 {published data only}
- Sherman DW, Haber J, Hoskins CN, Budin WC, Maislin G, Shukla S, et al. The effects of psychoeducation and telephone counseling on the adjustment of women with early‐stage breast cancer. Applied Nursing Research 2012;25(1):3‐16. [DOI] [PubMed] [Google Scholar]
Shimada 2007 {published data only}
- Shimada Y, Chida S, Matsunaga T, Sato M, Hatakeyama K, Itoi E. Clinical results of rehabilitation for accessory nerve palsy after radical neck dissection. Acta Otolaryngology 2007;127(5):491‐7. [DOI] [PubMed] [Google Scholar]
Silver 2013 {published data only}
- Silver JK, Baima J, Newman R, Galantino ML, Shockney LD. Cancer rehabilitation may improve function in survivors and decrease the economic burden of cancer to individuals and society. Work 2013;46(4):455‐72. [DOI] [PubMed] [Google Scholar]
Vos 2006 {published data only}
- Vos PJ, Visser AP, Garssen B, Duivenvoorden HJ, Haes HC. Effects of delayed psychosocial interventions versus early psychosocial interventions for women with early stage breast cancer. Patient Education and Counselling 2006;60(2):212‐9. [DOI] [PubMed] [Google Scholar]
Wenzel 1995 {published data only}
- Wenzel LB, Robinson SE, Blake DD. The effects of problem‐focused group counselling for earl‐stage gynecologic cancer patients. Journal of Mental Health Counselling 1995;17(1):81‐93. [Google Scholar]
Wiggins 2009 {published and unpublished data}
- Wiggins MS, Simonavice EM. Quality of life benefits in cancer survivorship with supervised exercise. Psychological Reports 2009;104(2):421‐4. [DOI] [PubMed] [Google Scholar]
References to ongoing studies
NCT01799031 {published data only}
- NCT01799031. Educational Intervention for Reducing Work Disability in Breast Cancer Survivors. https://clinicaltrials.gov/ct2/show/NCT01799031 (accessed 27 August 2015).
NTR2138 {published data only}
- NTR2138. Physical Activity during Cancer Treatment study. http://www.trialregister.nl/trialreg/admin/rctview.asp?TC=2138 (accessed 27 August 2015).
Additional references
American Cancer Society 2015
- American Cancer Society. Cancer facts & figures 2015. http://www.cancer.org/acs/groups/content/@editorial/documents/document/acspc‐044552.pdf (accessed 27 August 2015).
Aziz 2007
- Aziz NM. Cancer survivorship research: state of knowledge, challenges and opportunities. Acta Oncologica 2007;46(4):417‐32. [DOI] [PubMed] [Google Scholar]
Beck 2003
- Beck LA. Cancer rehabilitation: does it make a difference?. Rehabilitation Nursing 2003;28(2):42‐7. [DOI] [PubMed] [Google Scholar]
Chinn 2000
- Chinn S. A simple method for converting an odds ratio to effect size for use in meta‐analysis. Statistics in Medicine 2000;19(22):3127‐31. [DOI] [PubMed] [Google Scholar]
Cooper 2013
- Cooper AF, Hankins M, Rixon L, Eaton E, Grunfeld EA. Distinct work‐related, clinical and psychological factors predict return to work following treatment in four different cancer types. Psychooncology 2013;22(3):659‐67. [DOI] [PubMed] [Google Scholar]
De Backer 2009
- Backer IC, Schep G, Backx FJ, Vreugdenhil G, Kuipers H. Resistance training in cancer survivors: a systematic review. International Journal of Sports Medicine 2009;30(10):703‐12. [DOI] [PubMed] [Google Scholar]
de Boer 2006
- Boer AG, Verbeek JH, Dijk FJ. Adult survivors of childhood cancer and unemployment: A metaanalysis. Cancer 2006;107(1):1‐11. [DOI] [PubMed] [Google Scholar]
de Boer 2008
- Boer AG, Verbeek JH, Spelten ER, Uitterhoeve AL, Ansink AC, Reijke TM, et al. Work ability and return‐to‐work in cancer patients. British Journal of Cancer 2008;98(8):1342‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
de Boer 2009
- Boer AG, Taskila T, Ojajärvi A, Dijk FJ, Verbeek JH. Cancer survivors and unemployment: a meta‐analysis and meta‐regression. JAMA 2009;301(7):753‐62. [DOI] [PubMed] [Google Scholar]
de Boer 2014
- Boer AG. The European Cancer and Work Network: CANWON. Journal of Occupational Rehabilitation 2014;24(3):393‐8. [DOI] [PubMed] [Google Scholar]
Feuerstein 2007
- Feuerstein M, Hansen JA, Calvio LC, Johnson L, Ronquillo JG. Work productivity in brain tumor survivors. Journal of Occupational and Environmental Medicine 2007;49(7):803‐11. [DOI] [PubMed] [Google Scholar]
Franche 2005
- Franche RL, Cullen K, Clarke J, Irvin E, Sinclair S, Frank J. Workplace‐based return‐to‐work interventions: a systematic review of the quantitative literature. Journal of Occupational Rehabilitation 2005;15(4):607‐31. [DOI] [PubMed] [Google Scholar]
GRADEpro GDT 2015 [Computer program]
- McMaster University (developed by Evidence Prime, Inc.). GRADEpro GDT: GRADEpro Guideline Development Tool. Available from www.gradepro.org. McMaster University (developed by Evidence Prime, Inc.), 2015.
Haaf 2005
- Haaf HG. Findings on the effectiveness of rehabilitation [Ergebnisse zur Wirksamkeit der Rehabilitation]. Die Rehabilitation 2005;44(5):259‐76. [DOI] [PubMed] [Google Scholar]
Harvey 1982
- Harvey RF, Jellinek HM, Habeck RV. Cancer rehabilitation. An analysis of 36 program approaches. JAMA 1982;247(15):2127‐31. [DOI] [PubMed] [Google Scholar]
Hersch 2009
- Hersch J, Juraskova I, Price M, Mullan B. Psychosocial interventions and quality of life in gynaecological cancer patients: a systematic review. Psycho‐oncology 2009;18(8):795‐810. [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Hoffman 2005
- Hoffman B. Cancer survivors at work: a generation of progress. CA: A Cancer Journal for Clinicians 2005;55(5):271‐80. [DOI] [PubMed] [Google Scholar]
Hoving 2009
- Hoving JL, Broekhuizen MLA, Frings‐Dresen MHW. Return to work of breast cancer survivors: a systematic review of intervention studies. BMC Cancer 2009;9:117. [DOI] [PMC free article] [PubMed] [Google Scholar]
Irwin 2004
- Irwin ML, Ainsworth BE. Physical activity interventions following cancer diagnosis: methodologic challenges to delivery and assessment. Cancer Investigation 2004;22(1):30‐50. [DOI] [PubMed] [Google Scholar]
Kennedy 2007
- Kennedy F, Haslam C, Munir F, Pryce J. Returning to work following cancer: a qualitative exploratory study into the experience of returning to work following cancer. European Journal of Cancer Care 2007;16(1):17‐25. [DOI] [PubMed] [Google Scholar]
Khan 2009
- Khan F, Ng L, Turner‐Stokes L. Effectiveness of vocational rehabilitation intervention on the return to work and employment of persons with multiple sclerosis. Cochrane Database of Systematic Reviews 2009, Issue 1. [DOI: 10.1002/14651858.CD007256.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kirshbaum 2007
- Kirshbaum MN. A review of the benefits of whole body exercise during and after treatment for breast cancer. Journal of Clinical Nursing 2007;16(1):104‐21. [DOI] [PubMed] [Google Scholar]
Kirshblum 2001
- Kirshblum S, O'Dell MW, Ho C, Barr K. Rehabilitation of persons with central nervous system tumors. Cancer 2001;92(4 Suppl):1029‐38. [DOI] [PubMed] [Google Scholar]
Liu 2009
- Liu RD, Chinapaw MJ, Huijgens PC, Mechelen W. Physical exercise interventions in haematological cancer patients, feasible to conduct but effectiveness to be established: a systematic literature review. Cancer Treatment Reviews 2009;35(2):185‐92. [DOI] [PubMed] [Google Scholar]
Macmillan 2013
- Macmillan Cancer Support. Making the Shift – Providing specialist work support to people with cancer. http://www.macmillan.org.uk/Documents/GetInvolved/Campaigns/WorkingThroughCancer/Making‐the‐shift‐specialist‐work‐support‐for‐people‐with‐cancer.pdf (accessed 27 August 2015).
Marmot 2012
- Marmot M, Allen J, Bell R, Bloomer E, Goldblatt P, Consortium for the European Review of Social Determinants of Health and the Health Divide. WHO European review of social determinants of health and the health divide. Lancet 2012;380(9846):1011‐29. [DOI] [PubMed] [Google Scholar]
McNeely 2006
- McNeely ML, Campbell KL, Rowe BH, Klassen TP, Mackey JR, Courneya KS. Effects of exercise on breast cancer patients and survivors: a systematic review and meta‐analysis. Canadian Medical Association Journal 2006;175(1):34‐41. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mehnert 2011
- Mehnert A. Employment and work‐related issues in cancer survivors. Critical Reviews in Oncology/Hematology 2011;77(2):109‐30. [DOI] [PubMed] [Google Scholar]
Mehnert 2013
- Mehnert A, Boer A, Feuerstein M. Employment challenges for cancer survivors. Cancer 2013;119(Suppl 11):2151‐9. [DOI] [PubMed] [Google Scholar]
Moskowitz 2014
- Moskowitz MC, Todd BL, Chen R, Feuerstein M. Function and friction at work: a multidimensional analysis of work outcomes in cancer survivors. Journal of Cancer Survivorship: Research and Practice 2014;8(2):173‐82. [DOI] [PubMed] [Google Scholar]
Nieuwenhuijsen 2014
- Nieuwenhuijsen K, Faber B, Verbeek JH, Neumeyer‐Gromen A, Hees HL, Verhoeven AC, et al. Interventions to improve return to work in depressed people. Cochrane Database of Systematic Reviews 2014, Issue 12. [DOI: 10.1002/14651858.CD006237.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Norlund 2009
- Norlund A, Ropponen A, Alexanderson K. Multidisciplinary interventions: review of studies of return to work after rehabilitation for low back pain. Journal of Rehabilitation Medicine 2009;41(3):115‐21. [DOI] [PubMed] [Google Scholar]
Oldervoll 2004
- Oldervoll LM, Kaasa S, Hjermstad MJ, Lund JA, Loge JH. Physical exercise results in the improved subjective well‐being of a few or is effective rehabilitation for all cancer patients?. European Journal of Cancer 2004;40(7):951‐62. [DOI] [PubMed] [Google Scholar]
Osborn 2006
- Osborn RL, Demoncada AC, Feuerstein M. Psychosocial interventions for depression, anxiety, and quality of life in cancer survivors: meta‐analyses. International Journal of Psychiatry in Medicine 2006;36(1):13‐34. [DOI] [PubMed] [Google Scholar]
RevMan 2014 [Computer program]
- The Nordic Cochrane Centre. The Cochrane Collaboration. Review Manager (RevMan). Version 5.3. Copenhagen: The Nordic Cochrane Centre. The Cochrane Collaboration, 2014.
Robinson 2002
- Robinson KA, Dickersin K. Development of a highly sensitive search strategy for the retrieval of reports of controlled trials using PubMed. International Journal of Epidemiology 2002;31(1):150‐3. [DOI] [PubMed] [Google Scholar]
Short 2005
- Short P, Vasey JJ, Tuncelli K. Employment pathways in a large cohort of adult cancer survivors. Cancer 2005;103(6):1292‐301. [DOI] [PubMed] [Google Scholar]
Smith 2007
- Smith T, Stein KD, Mehta CC, Kaw C, Kepner JL, Buskirk T, et al. The rationale, design, and implementation of the American Cancer Society's studies of cancer survivors. Cancer 2007;109(1):1‐12. [DOI] [PubMed] [Google Scholar]
Spelten 2002
- Spelten ER, Sprangers MA, Verbeek JH. Factors reported to influence the return to work of cancer survivors: a literature review. Psycho‐oncology 2002;11(2):124‐31. [DOI] [PubMed] [Google Scholar]
Stanton 2006
- Stanton AL. Psychosocial concerns and interventions for cancer survivors. Journal of Clinical Oncology 2006;24(32):5132‐7. [DOI] [PubMed] [Google Scholar]
Steiner 2010
- Steiner JF, Nowels CT, Main DS. Returning to work after cancer: quantitative studies and prototypical narratives. Psycho‐oncology 2010;19(2):115‐24. [DOI] [PMC free article] [PubMed] [Google Scholar]
Strauser 2010
- Strauser D, Feuerstein M, Chan F, Arango J, Silva Cardoso E, Chiu CY. Vocational services associated with competitive employment in 18‐25 year old cancer survivors. Journal of Cancer Survivorship: Research and Practice 2010;4(2):179‐86. [DOI] [PubMed] [Google Scholar]
Taskila 2007a
- Taskila T, Lindbohm ML. Factors affecting cancer survivors' employment and work ability. Acta Oncologica 2007;46(4):446‐51. [DOI] [PubMed] [Google Scholar]
Taskila 2007b
- Taskila T, Martikainen R, Hietanen P, Lindbohm ML. Comparative study of work ability between cancer survivors and their referents. European Journal of Cancer 2007;43(5):914‐20. [DOI] [PubMed] [Google Scholar]
van der Molen 2009
- Molen LA, Rossum MAA, Burkhead LM, Smeele LE, Hilgers FJ. Functional outcomes and rehabilitation strategies in patients treated with chemoradiotherapy for advanced head and neck cancer: a systematic review. European Archives of Oto‐rhino‐laryngology 2009;266(6):889‐900. [DOI] [PubMed] [Google Scholar]
Verbeek 2007
- Verbeek J, Spelten E. Work. In: Feuerstein M editor(s). Handbook of Cancer Survivorship. Berkeley: Springer, 2007. [Google Scholar]
Verdecchia 2009
- Verdecchia A, Guzzinati S, Francisci S, Angelis R, Bray F, Allemani C, et al. Survival trends in European cancer patients diagnosed from 1988 to 1999. European Journal of Cancer 2009;45(6):1042‐66. [DOI] [PubMed] [Google Scholar]
Zhang 1998
- Zhang J, Yu KF. What's the relative risk? A method of correcting the odds ratio in cohort studies of common outcomes. JAMA 1998;280(19):1690‐1. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
De Boer 2011
- Boer AG, Taskila T, Tamminga SJ, Frings‐Dresen MH, Feuerstein M, Verbeek JH. Interventions to enhance return‐to‐work for cancer patients. Cochrane Database of Systematic Reviews 2011, Issue 2. [DOI: 10.1002/14651858.CD007569.pub2] [DOI] [PubMed] [Google Scholar]


