Abstract
Background
Dental sealants were introduced in the 1960s to help prevent dental caries, mainly in the pits and fissures of occlusal tooth surfaces. Sealants act to prevent bacteria growth that can lead to dental decay. Evidence suggests that fissure sealants are effective in preventing caries in children and adolescents compared to no sealants. Effectiveness may, however, be related to caries incidence level of the population. This is an update of a review published in 2004, 2008 and 2013.
Objectives
To compare the effects of different types of fissure sealants in preventing caries in occlusal surfaces of permanent teeth in children and adolescents.
Search methods
Cochrane Oral Health’s Information Specialist searched: Cochrane Oral Health’s Trials Register (to 3 August 2016), the Cochrane Central Register of Controlled Trials (CENTRAL) (the Cochrane Library, 2016, Issue 7), MEDLINE Ovid (1946 to 3 August 2016), and Embase Ovid (1980 to 3 August 2016). We searched ClinicalTrials.gov and the World Health Organization International Clinical Trials Registry Platform for ongoing trials to 3 August 2016. No restrictions were placed on language or date of publication.
Selection criteria
Randomised controlled trials (RCTs) comparing sealants with no sealant or a different type of sealant material for preventing caries of occlusal surfaces of premolar or molar teeth in children and adolescents aged up to 20 years. Studies required at least 12 months follow‐up. We excluded studies that compared compomers to resins/composites.
Data collection and analysis
Two review authors independently screened search results, extracted data and assessed risk of bias of included studies. We presented outcomes for caries or no caries on occlusal surfaces of permanent molar teeth as odds ratio (OR) or risk ratio (RR). We used mean difference (MD) for mean caries increment. All measures were presented with 95% confidence intervals (CI). We conducted meta‐analyses using a random‐effects model for comparisons where there were more than three trials; otherwise we used the fixed‐effect model. We used GRADE methods to assess evidence quality.
Main results
We included 38 trials that involved a total of 7924 children; seven trials were new for this update (1693 participants). Fifteen trials evaluated the effects of resin‐based sealant versus no sealant (3620 participants in 14 studies plus 575 tooth pairs in one study); three trials with evaluated glass ionomer sealant versus no sealant (905 participants); and 24 trials evaluated one type of sealant versus another (4146 participants). Children were aged from 5 to 16 years. Trials rarely reported background exposure to fluoride of trial participants or baseline caries prevalence.
Resin‐based sealant versus no sealant: second‐, third‐ and fourth‐generation resin‐based sealants prevented caries in first permanent molars in children aged 5 to 10 years (at 24 months follow‐up: OR 0.12, 95% CI 0.08 to 0.19, 7 trials (5 published in the 1970s; 2 in the 2010s), 1548 children randomised, 1322 children evaluated; moderate‐quality evidence). If we were to assume that 16% of the control tooth surfaces were decayed during 24 months of follow‐up (160 carious teeth per 1000), then applying a resin‐based sealant would reduce the proportion of carious surfaces to 5.2% (95% CI 3.13% to 7.37%). Similarly, assuming that 40% of control tooth surfaces were decayed (400 carious teeth per 1000), then applying a resin‐based sealant would reduce the proportion of carious surfaces to 6.25% (95% CI 3.84% to 9.63%). If 70% of control tooth surfaces were decayed, there would be 19% decayed surfaces in the sealant group (95% CI 12.3% to 27.2%). This caries‐preventive effect was maintained at longer follow‐up but evidence quality and quantity was reduced (e.g. at 48 to 54 months of follow‐up: OR 0.21, 95% CI 0.16 to 0.28, 4 trials, 482 children evaluated; RR 0.24, 95% CI 0.12 to 0.45, 203 children evaluated). Although studies were generally well conducted, we assessed blinding of outcome assessment for caries at high risk of bias for all trials (blinding of outcome assessment is not possible in sealant studies because outcome assessors can see and identify sealant).
Glass ionomer sealant versus no sealant: was evaluated by three studies. Results at 24 months were inconclusive (very low‐quality evidence).
One sealant versus another sealant: the relative effectiveness of different types of sealants is unknown (very low‐quality evidence). We included 24 trials that directly compared two different sealant materials. Comparisons varied in terms of types of sealant assessed, outcome measures chosen and duration of follow‐up.
Adverse events: only four trials assessed adverse events. No adverse events were reported.
Authors' conclusions
Resin‐based sealants applied on occlusal surfaces of permanent molars are effective for preventing caries in children and adolescents. Our review found moderate‐quality evidence that resin‐based sealants reduced caries by between 11% and 51% compared to no sealant, when measured at 24 months. Similar benefit was seen at timepoints up to 48 months; after longer follow‐up, the quantity and quality of evidence was reduced. There was insufficient evidence to judge the effectiveness of glass ionomer sealant or the relative effectiveness of different types of sealants. Information on adverse effects was limited but none occurred where this was reported. Further research with long follow‐up is needed.
Plain language summary
Sealants for preventing tooth decay in permanent teeth
Review question
Can sealants prevent tooth decay in permanent teeth and what are the effects of different types of sealants?
Background
Although children and adolescents have healthier teeth than in the past, tooth decay is a problem in some people and places. Most tooth decay in young people occurs on the biting surfaces of back teeth. Tooth decay prevention includes brushing, fluoride supplements (such as tablets), fluoride directly applied to the teeth and dental sealants. Dental sealants aim to prevent bacteria growth that promote tooth decay in grooves of back teeth. Sealants are applied by dentists or dental care team members. The main types used are resin‐based sealants and glass ionomer cements.
Study characteristics
We included 38 studies that involved 7924 young people (aged 5 to 16 years) among whom a variety of dental sealants was used to prevent tooth decay. Young people in the studies represented the general population.
The review includes studies available from a search of the literature up to 3 August 2016. We assessed all studies as being at high risk of bias because the dental professionals who are measuring the outcomes can see whether or not sealant has been used.
Key results
Fifteen studies compared resin‐based sealants to no sealants and found that children who had sealant applied to their back teeth were less likely to have tooth decay in their back teeth than children with no sealant. We were able to combine data from seven of these studies (including two published since 2010), which involved children who were aged from 5 to 10 years when the sealants were applied. This showed that if 40% of back teeth develop decay over 24 months, using sealant reduces this to 6%. Similar benefits for resin‐based sealants were shown up to four years. The effect appeared to persist when measured up to nine years, but there was less evidence.
Results were inconclusive when glass ionomer‐based sealant was compared with no sealant and when one type of sealant material was compared with another.
Four studies assessed possible problems from using sealants; none were reported.
Quality of the evidence
We found moderate‐quality evidence that resin‐based sealant is more effective than no sealant for preventing tooth decay, reducing it by between 11% and 51% more than in children without sealant (measured two years after application). 'Moderate quality' means we are reasonably certain of this finding, although it is possible that future research could change it. Most of the studies included in this analysis were carried out in the 1970s. We are not able to draw conclusions about the other comparisons included in our review as the available evidence is very low quality. More studies with long follow‐up times are needed.
Summary of findings
Summary of findings for the main comparison. Resin‐based sealant versus no sealant for preventing dental caries.
| Resin‐based sealant versus no sealant for preventing dental caries | ||||||
| Patient or population: Children and adolescents Settings: Sealant applications for school children in USA, Canada, China, Colombia Intervention: Resin‐based sealant applications on occlusal tooth surfaces of permanent molars Comparison: No sealant application | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control teeth | Sealed teeth | |||||
|
Dentine caries in permanent molars Follow‐up: 24 months |
Incidence of carious first molars (16%) 160 per 1000a |
Incidence of carious first molars (5.2%) 52 per 1000 (31 to 74) |
OR 0.12 (0.08 to 0.19)c | 1548 children randomised & 1322 evaluated after 24 months (7 studies d, e) | ⊕⊕⊕⊝ moderatef | Benefits of resin‐sealant maintained up to at least 48 months of follow‐upg |
| Incidence of carious first molars (40%) 400 per 1000b |
Incidence of carious first molars (6.3%) 63 per 1000 (38 to 96) |
OR 0.12 (0.08 to 0.19)c | 1548 children randomised & 1322 evaluated after 24 months (7 studiesd, e) | ⊕⊕⊕⊝ moderatef | Benefits of resin‐sealant maintained up to at least 48 months of follow‐upg | |
| Incidence of carious first molars (70%) 700 per 1000b |
Incidence of carious first molars (18.9%) 189 per 1000 (123 to 272) |
OR 0.12 (0.08 to 0.19)c | 1548 children randomised & 1322 evaluated after 24 months (7 studiesd, e) | ⊕⊕⊕⊝ moderatef | Benefits of resin‐based sealant maintained up to at least 48 months of follow‐upg | |
| Adverse effects | Two trials measured adverse effects. None were reported. | |||||
| CI: confidence interval; OR: odds ratio | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
a Two recently conducted Chinese studies reported lower incidence of carious control molars than the five split‐mouth studies published between 1976 and 1979. In Liu 2012, carious first molars were detected in 9/121 children in the sealant group (7.4%) (11 carious teeth of 367 sealed teeth), and in 21/124 children in the placebo group (17%) (28 carious teeth of 379 placebo teeth). Caries prevalence: baseline mean dmft level of 3.4. In Liu 2014b, caries figures were 3% of children in the sealant group and 15% in the control group. (China has been classified as having a very low DMFT‐index in children aged 12 years according to FDI 2015 and WHO 2014 figures (DMFT < 1.2)).
b The incidence of carious control teeth in five split‐mouth trials included in this comparison ranged from 37% to 69% (studies published between 1976 and 1979). We have shown the effect of sealants at each end of this range. These studies did not give information on baseline caries prevalence of the children.
c There was considerable heterogeneity in this estimate (I² = 73%, P = 0.001), but all trials showed a highly statistically significant effect favouring sealants.
d All studies recruited children aged 5 to 10 years. Three studies were conducted in areas with fluoridated water, two studies stated water was not fluoridated and two studies did not report if water supplies were fluoridated.
e Two trials (in addition to the 7 trials included in the analysis) also found significant benefit in favour of resin‐based sealants at two years ‐ one Chinese trial published in 2014 that reported MD of increments of number of decayed, missing and filled surfaces of permanent first molars (DMFS) ‐0.24 (95% CI ‐0.36 to ‐0.12)) (Tang 2014), and one trial from Thailand that reported DFS increment published in 1995 with a mean difference in DFS increment ‐0.65, (95% CI ‐0.83 to ‐0.47), 276 children evaluated (Songpaisan 1995).
f Downgraded by one level due to indirectness of evidence (5 trials were published between 1976 and 1979; it is not unreasonable to anticipate that a new study could change this estimate, even if it found sealants to be effective). In assessing the quality of evidence for this comparison, the main focus was on directness of evidence, consistency of results and precision of estimates. We did not downgrade evidence on the basis of the statistical heterogeneity of results; results from individual trials showed clear significant benefit for the sealant. Nor did we downgrade evidence on the basis of overall risk of bias classification of the studies (all studies were assessed at high risk of bias because blinding of outcome assessment is not possible in sealant studies).The studies were otherwise fairly well conducted.
g The benefit associated with sealant use is maintained at all of the follow‐up estimates (up to 108 months) although numbers of studies and children available for evaluation reduced markedly over this period (e.g. at 48 to 54 months of follow‐up OR 0.21, 95% CI 0.16 to 0.28, 4 studies, 482 children evaluated; RR 0.24, 95% CI 0.12 to 0.45, 1 study, 203 children evaluated).
Summary of findings 2. Glass ionomer‐based sealant versus no sealant for preventing dental caries.
| Glass ionomer‐based sealants versus no sealant for preventing dental caries | ||||
|
Patient or population: Children and adolescents Settings: RCTs conducted in China, Thailand and Brazil Intervention: Low‐viscosity glass ionomer sealant (Fuji III and VII), and resin‐modified glass ionomer (Vitremer) Comparison: No sealant application | ||||
| Outcomes | Impact | Number of participants (studies) | Quality of the evidence (GRADE) | Comments |
|
Dentine caries in permanent molars Follow‐up: 24 months |
Inconclusive results. Two studies slightly favoured glass ionomers compared to no sealant a,b, and one study did not c |
3 trials (The 2 studies favouring glass ionomers, compared to no sealant, evaluated 426 children a,b; the 1 study that did not find a difference between the groups evaluated 404 children c) |
⊕⊝⊝⊝ very lowd | |
| Adverse effects | Not measured | |||
| RCT: randomised controlled trial | ||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||
aLiu 2014b (conducted in China) found slightly significantly (P = 0.03) more caries in control group children than glass ionomer group children (OR 0.46, 95% CI 0.23 to 0.91).
bTagliaferro 2011 (conducted in Brazil) evaluated if additional benefit was derived from using resin‐modified glass ionomer sealants among children receiving a regular oral health education programme. Only the high risk children with sealant application plus oral health education showed statistically lower DMF (decayed, missed and filled) increments on occlusal surfaces of first permanent molars compared with high risk children who received only oral health education.
cSongpaisan 1995 (conducted in Thailand) compared DFS increments for two glass ionomer sealant groups with a control group receiving no treatment for children aged 12 to 13 years. We combined data from the two glass ionomer groups. The difference failed to reach significance (MD in DFS ‐0.18 (95% CI ‐0.39 to 0.03; P = 0.09)
d Downgraded by three levels due to inconsistent effects on caries outcomes, diversity in the interventions, and methodological limitations of the studies (e.g. in Liu 2014b and Songpaisan 1995, description of the randomisation procedure was incomplete, and we assessed the studies at unclear risk of selection bias).
Summary of findings 3. Glass ionomer‐based sealants versus resin sealants.
| Glass ionomer‐based sealants versus resin sealants for preventing caries | ||||
|
Patient or population: Children and adolescents Settings: RCTs conducted in the UK, Scandinavia, USA, Asia, Australia, Brazil and Syrian Arab Republic Intervention: Low‐viscosity glass ionomer sealant (including Fuji III, VII, GC Fuji Triage White, Ketac Silver, Ketac‐fil or Baseline); high‐viscosity glass ionomer (including Fuji IX or Ketac Molar Easymix), and resin‐modified glass ionomer (including Fuji II LC, Vitrebond or Vitremer) Comparison: Resin sealant | ||||
| Outcomes | Impact: Inconsistent effect | Number of participants (studies) | Quality of the evidence (GRADE) | Comments |
|
Dentine caries in permanent molars Follow‐up: 12, 24, 36, 48, 60 and 72 months |
Inconsistent effect. There were differences in: products, comparisons, outcomes, outcome reporting times and background fluoride exposure including water and age groups | 21 trials a (3883 participants randomised) | ⊕⊝⊝⊝ very lowb | |
| Adverse effects | One trial measured adverse effects. None reported. | |||
| RCT: randomised controlled trial | ||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||
a Trials published between 1993 and 2014.
b Downgraded by three levels due to inconsistent effects on caries outcomes, due to the diversity in the interventions, comparisons and time of outcomes reported in the trials, the age groups of children included and variation in reporting of background exposure to fluoride.
Background
Description of the condition
Dental caries (tooth decay) is a multifactorial chronic oral disease that affects most populations throughout the world and has been considered the most important global oral health burden (Petersen 2005). Caries disease is an interplay between specific acidogenic bacteria in the dental plaque biofilm, fermentable carbohydrates and tooth structure. The biofilm bacteria produce organic acids that can cause mineral loss from the tooth surface (demineralisation). In favourable conditions, a reversal, that is, a mineral gain, is possible (remineralisation). If the demineralisation process prevails, visually detectable caries lesions occur. Development of a caries lesion is a dynamic process that may progress, stop or reverse. Assessment of the grade and activity of the lesion is challenging.
Definition of dental caries and a system to measure the caries process is integrated by the International Caries Detection and Assessment System (ICDAS II 2008). In ICDAS II, the codes for coronal caries range from 0 to 6, depending on the severity of the lesion: codes 0 to 3 involve a sound tooth surface to caries in enamel (with or without microcavitation); codes 4 to 6 involve caries in dentine.
Since the 1970s, caries prevalence has declined in most industrialised countries, and has been attributed to general factors, such as improvements in living conditions and oral hygiene, and public health measures, such as widespread use of fluorides and better disease management (Splieth 2016). However, dental caries is still a problem for some people and populations; for example, in many Eastern European and South American countries, the prevalence of caries among 12 year‐olds has been reported to be moderate or high (WHO 2014). Even an increase in caries has been reported in countries where prevalence of caries had previously been quite low (Bagramian 2009).
The period of highest risk for caries lesion development in permanent teeth is the first few years after tooth eruption (Carvalho 2014; Mejàre 2014). Consequently, most efforts to prevent caries have been aimed for children and adolescents. Most of the detected incremental increase in dental caries is confined to pit and fissure surfaces of first molars (Batchelor 2004; Brown 1995; McDonald 1992), where carious lesions often start before teeth fully erupt (Alves 2014; Zenkner 2013), because their anatomy favours biofilm formation and retention. The rate of occlusal caries among young people has not fallen to the same extent as the rate of caries on smooth surfaces (Brown 1995).
The efficacy of any caries‐preventive intervention depends on the actual caries risk of an individual (and population), i.e. if the risk of developing new lesions within a certain follow‐up period is small even without any intervention, then the efficacy of additional preventive method is confined to be small. Current methods for caries risk assessment comprise a range of strategies such as past caries experience, information about sociodemography, oral hygiene and dietary habits, oral bacteria and saliva characteristics (Mejàre 2014). However, the factors are not stable, for example, oral hygiene and dietary habits of an individual can change during follow‐up, decreasing or increasing caries risk.
The evidence on the validity of existing systems to predict future caries risk is limited at present (Tellez 2013). A review by Twetman 2016, summarising the findings of recent systematic reviews, concluded that there is no clearly superior method to predict future caries, whereas a systematic review by Mejàre 2014 found that baseline caries experience of the child was the most accurate single predictor for future caries development (moderate/good accuracy in preschool children and limited accuracy in schoolchildren/adolescents).
Description of the intervention
Dental sealant is applied to a tooth surface to provide a physical barrier that prevents growth of biofilm by blocking nutrition. Although sealants were introduced for preventing caries on occlusal surfaces, they are now considered active agents in controlling and managing initial caries lesions on occlusal surfaces (Splieth 2010) and, recently, on approximal surfaces as well (Dorri 2015; Ekstrand 2012; Splieth 2010).
Sealant materials
Options of occlusal sealant materials are numerous but resins/composites and glass ionomers comprise the main material types. A resin, Bisphenol A glycidyl methacrylate (BIS‐GMA), forms the basis for numerous resin‐based dental sealants and composites that are available. The effectiveness of resin‐based sealants is closely related to the longevity of sealant coverage (i.e. clinical retention) (Ripa 1993). The resin‐based sealants can be divided into generations according to their mechanism for polymerisation or their content. The development of sealants has progressed from first‐generation sealants, which were activated with ultraviolet light, through to second‐ and third‐generation sealants, which are autopolymerised and visible‐light activated, and fourth‐generation sealants which contain fluoride. First‐generation sealants are no longer marketed.
Along with resin‐based sealants, the other main type of sealants consists of glass ionomer cements (combination of silicate and polyacrylate cement system). Glass ionomer cements contain fluoride and are thought to prevent caries through fluoride release over a prolonged period. There is a wide range of glass ionomer materials available in the market. They may be used as the original chemically cured type or as the light cured type, which is modified with resin, for example, for rapid initiation of the curing process (resin‐modified glass ionomers). Chemically cured glass ionomers can further be divided to low‐viscosity and high‐viscosity glass ionomers. Compared to inferior retention of low‐viscosity glass ionomers, there are indications that high‐viscosity glass ionomers may have better retention properties, particularly when placed using the press‐finger atraumatic restorative treatment (ART) (Van 't Hof 2006; Weerheijm 1996). Recently, class carbomers, which are basically glass ionomer‐based materials, have been referred as dental sealants.
Compomers (polyacid‐modified resin composites) were developed to combine the beneficial properties of glass ionomer cements with those of composites (Nicholson 2007; Ruse 1999). Compomers have mostly the same components as conventional dimethacrylate composites (Nicholson 2007). Compomers have been associated with considerably low retention rates (Kühnisch 2012).
In addition to resin/composite‐based and glass ionomer‐based materials, other material types such as ormocers have been tested as dental sealants. Ormocers (an acronym for organically modified ceramics), although composites, have been developed as an alternative to the conventional dimethacrylate‐based composites. Ormocers consist of three components – organic and inorganic portions (glass and ceramic components) and the polysiloxanes (Zimmerli 2010).
Safety of sealant materials
Reports have considered possible adverse oestrogen‐like effects of resin‐based materials including bisphenol A (BPA) (e.g. Azarpazhooh 2008b; Fleisch 2010; Joskow 2006; Kloukos 2013). This synthetic chemical resin is widely used in the production of plastic products intended for every day life. Although it is rarely used as such in dental materials, some dental resins can include low‐levels of BPA, e.g. as trace material from resin production (ADA 2016). Current evidence, however, suggests that people are not at risk of harmful effects when resin‐based sealants are used (ADA 2016; Azarpazhooh 2008b; Fleisch 2010). However, some reports recommend precautionary sealant application techniques to limit possible exposure of BPA (e.g. immediate cleaning and rinsing sealed surfaces after placement of sealants) (Fleisch 2010; Kloukos 2013). Allergic reactions to sealant materials are possible but rare.
Why it is important to do this review
Cochrane Oral Health undertook an extensive prioritisation exercise in 2014 to identify a core portfolio of titles that were the most clinically important to maintain on the Cochrane Library (Worthington 2015). The paediatric expert panel identified this review as a priority title (Cochrane OHG priority review portfolio).
Several systematic reviews have supported the substantial effectiveness of sealants in preventing or controlling occlusal decay compared with no intervention (Ahovuo‐Saloranta 2013; Azarpazhooh 2008a; Griffin 2008; Llodra 1993; Mejàre 2003). However, sealant efficacy may be related to caries incidence levels in the populations. In addition, the relative effectiveness of different sealant materials has not been assessed.
We aimed to (1) compare sealant materials: resin/composite‐based, glass ionomer‐based and new types of fissure sealants (such as ormocer‐based sealants) versus control with no sealant application, and (2) evaluate the relative effectiveness of these material types for preventing dental caries in children and adolescents. These evaluations were carried out for different caries incidence levels in populations during the follow‐up.
This is an update of a review first published in 1999 and last updated in 2013, which found that sealants are effective in children at high risk of caries, but information on the magnitude of the benefit of sealing in other conditions is scarce (Ahovuo‐Saloranta 2013).
Objectives
To compare the effects of different types of fissure sealants in preventing caries in occlusal surfaces of permanent teeth in children and adolescents at different levels of caries incidence.
Specifically:
To evaluate the effectiveness of resin/composite‐based fissure sealants compared with no sealant at different follow‐up times;
To evaluate the effectiveness of glass ionomer‐based fissure sealants compared with no sealant at different follow‐up times;
To evaluate the effectiveness of new types of fissure sealants (such as ormocer‐based sealants) compared with no sealant at different follow‐up times;
To evaluate the relative effectiveness of different sealant material types.
We will also report the safety of sealants and possible harmful effects and the retention of sealants (though retention of sealants is not studied as an objective of the review).
Methods
Criteria for considering studies for this review
Types of studies
We included randomised controlled trials (RCTs) with at least 12 months follow‐up in which fissure sealant was compared with no sealant or with a different type of sealant material for preventing caries in children and adolescents. We included both parallel‐group and split‐mouth study designs. We included quasi‐randomised trials for split‐mouth studies only. The unit of randomisation was the individual, the group (e.g. school, school class), or the tooth or tooth pair.
Types of participants
Children and adolescents from the general population, aged up to 20 years at the start of the study.
Types of interventions
The review was concerned with:
(A) comparing sealant material with no sealant (all sealant materials accepted except the first generation resin‐based sealants) and
(B) comparing one type of fissure sealant with another sealant.
In this update, we considered two main types of sealant materials: resin‐based and glass ionomer‐based sealants with subtypes. We excluded studies comparing compomers to resins/composites because compomers and composites have similar components in common (Nicholson 2007)
The control teeth or control groups were those that did not have a sealant placed (A). When comparing the effectiveness of resin/composite sealants with the effectiveness of other sealant types, the resin sealant group was used as a control group. When comparing new types of sealant materials to conventional materials, the conventional materials were used as a control group (B).
We included studies in which sealants were placed on occlusal surfaces of permanent premolar or molar teeth, not sealed previously, for the purpose of preventing caries. Applications of sealants could be either on sound surfaces or on enamel lesions (if scored using the ICDAS II scale, codes 0, 1, 2 and 3 were accepted). The sealant application method used in the study could either be (a) direct application on the tooth surface or (b) application after mechanically preparing the tooth surface.
We excluded studies where fissure sealants were used concurrently with fillings.
We excluded studies that tested any other caries‐preventive treatments (such as fluoride varnishes) used concurrently with sealants. We did however include studies where fissure sealants were used concurrently both in test and control groups with fluoride toothpaste or with fluoridated water, or the children received oral health instruction or education.
Types of outcome measures
Primary outcomes
Dentine caries in permanent molars
measured dichotomously as incidence of carious lesions on treated occlusal surfaces of molars or premolars (yes or no). Caries was defined as caries in the dentine but if scored using the ICDAS II scale, in addition to codes 4 to 6, code 3 was also accepted as caries (localised enamel breakdown on occlusal surface reflecting established decay).
measured continuously as changes in decayed, missing and filled (DMF) rates at occlusal surface.
Secondary outcomes
Adverse events and safety of sealants
Where studies reported on retention of sealants, we have summarised this information (but retention of sealants is not studied as an objective or outcome of the review).
Search methods for identification of studies
Electronic searches
Cochrane Oral Health’s Information Specialist conducted systematic searches in the following databases for RCTs and controlled clinical trials. There were no language, publication year or publication status restrictions; however, we did not include studies with an abstract only.
Cochrane Oral Health’s Trials Register (searched 3 August 2016) (Appendix 1);
Cochrane Central Register of Controlled Trials (CENTRAL; 2016, Issue 7) in the Cochrane Library (searched 3 August 2016) (Appendix 2);
MEDLINE Ovid (1946 to 3 August 2016) (Appendix 3); and
Embase Ovid (1980 to 3 August 2016) (Appendix 4).
Subject strategies were modelled on the search strategy designed for MEDLINE Ovid. Where appropriate, these were combined with subject strategy adaptations of the highly sensitive search strategy designed by Cochrane for identifying randomised controlled trials and controlled clinical trials as described in the Cochrane Handbook for Systematic Reviews of Interventions Chapter 6 (Lefebvre 2011).
Searching other resources
We searched the following databases for ongoing studies:
US National Institutes of Health Ongoing Trials Register ClinicalTrials.gov (clinicaltrials.gov; searched 6 August 2016) (Appendix 5);
World Health Organization International Clinical Trials Registry Platform (apps.who.int/trialsearch; searched 3 August 2016) (Appendix 6).
We placed no restrictions on language or date of publication.
In the previous versions of this review, we also searched the following electronic databases: SCISEARCH, CAplus, INSPEC, JICST‐EPLUS, NTIS, PASCAL, DARE, NHS EED, HTA, OpenSIGLE and OpenGrey (see Appendix 7). We discontinued these searches for subsequent updates due to poor yields.
We screened the reference lists of already identified trials and review articles for additional relevant studies. For the 2008 review, seven companies known to manufacture sealant materials were contacted and data and references from all published and unpublished trials on sealants were requested.
Results of the search process are presented in Figure 1.
1.
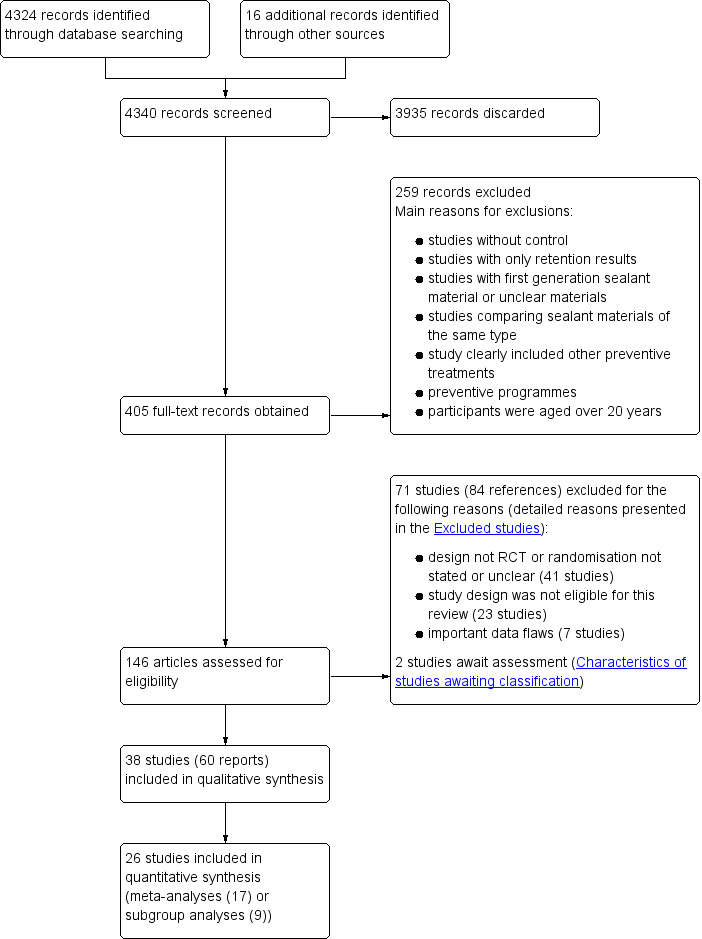
Study flow diagram
Data collection and analysis
Selection of studies
Two review authors (AAS, HF) independently selected papers on the basis of title, keywords and abstract, and decided on eligibility. We obtained the full text reports of all studies considered for inclusion. If information relevant to the inclusion criteria was not available from the abstract, or if the title was relevant but the abstract was not available, we obtained the full text of the report. All information gathering and data recording were done independently, and we resolved disagreements by discussion with a third review author (AN or MM).
We contacted trial authors to request additional information if the study seemed to fulfil review inclusion criteria but information in the report was insufficient to inform final assessment of inclusion or exclusion.
We considered only studies with full‐text reports for inclusion in this review. We excluded studies reported only as abstracts because evidence has suggested discrepancies between data reported in an abstract and those provided in the final published full report, and because information on trial quality indicators is often lacking (Chokkalingam 1998; Hopewell 2006). We felt that the full‐text report was required to ensure reliable data extraction and assessment of risk of bias. To diminish the risk of publication bias, we contacted authors of relevant abstracts to ask if full‐text reports of studies (unpublished or published) were available.
Data extraction and management
Two review authors (AAS, HF) independently extracted data from all included studies in duplicate using a previously prepared data extraction form. The extraction form was pilot‐tested independently by two review authors for the 2004 review (AAS, AH) using a sample of studies to be included.
We attempted to contact study authors to request missing information or seek clarification when necessary.
We extracted the following information on study methods:
trial design;
year the study began; and
length of follow‐up.
We extracted the following participants' characteristics:
location where the study was conducted (country and setting where participants were recruited);
criteria for accepting participants into the study (intact surfaces or surfaces with enamel lesion allowed);
age (range) and mean age at start;
gender;
socioeconomic status;
baseline caries prevalence of participants (caries severity at start (average number of decayed, missing and filled deciduous teeth (dmft); decayed, missing and filled deciduous surfaces (dmfs); decayed, missing and filled permanent surfaces (DMFS); decayed, filled permanent surfaces (DFS); or other measure);
number of randomly assigned participants and number of teeth in treatment and control at study start and after follow‐up; and
number of evaluated participants.
We extracted the following characteristics of interventions:
intervention comparisons (sealant versus control without sealant or sealant versus sealant);
sealant products used in the study;
re‐application of sealants;
isolation method;
information on who applied sealants (dentist with or without assistant or dental hygienist); and
co‐interventions (e.g. background exposure to fluoride sources (toothpaste, water etc)).
We extracted the following outcomes characteristics:
description of outcomes; and
description of outcome measurements.
Outcome information was extracted mainly as the number of dentinal carious lesions or non‐carious lesions on occlusal surfaces of treatment and control teeth at different follow‐up times. If a filling had been put on the occlusal surface or the tooth had been extracted as the result of caries during the study, we coded this as caries. We extracted data that were presented only in graphs and figures when possible. We presented data from the included studies in Table 4 and Table 5.
1. Caries data from studies with binary outcomes.
| Caries data from studies with binary outcomes | ||||||||
| Resin fissure sealant (FS) versus no sealant: 12 months | ||||||||
| Split‐mouth studies with data stated as tooth pair | Study | Both sound | FS sound/ control carious | FS carious/ control sound | Both carious | Proportion of decayed control tooth surfaces to total control surfaces | RR (95% CI) based on paired data | Becker‐Balagtas marginal OR (95% CI) |
| Bojanini 1976 | 188 | 79 | 6 | 2 | 0.29 | RR 0.099 (0.049 to 0.201) | OR 0.07 (0.03 to 0.15) ICC 0.02 |
|
| Charbeneau 1979 | 104 | 82 | 5 | 11 | 0.46 | RR 0.172 (0.107 to 0.276) | OR 0.10 (0.06 to 0.17) ICC 0.13 |
|
| Sheykholeslam 1978 | 132 | 49 | 2 | 3 | 0.28 | RR 0.096 (0.040 to 0.229) | OR 0.07 (0.03 to 0.18) ICC 0.12 |
|
| Split‐mouth studies without summary data of tooth pairs | Study | Desciption of the data | OR (95% CI) | |||||
| Muller‐Bolla 2013 | Adjusted OR based on multivariable conditional tooth‐matched logistic regression analysis | OR 0.26 (0.14 to 0.49) |
||||||
| Split‐mouth studies with data stated only in marginals | Study | FS sound | FS carious | Control sound | Control carious | Proportion of the decayed control tooth surfaces to total control surfaces | Becker‐Balagtas marginal OR (95% CI) | |
| Erdoğan 1987 | 103 | 15 | 96 | 22 | 0.19 | OR 0.64
(0.32 to 1.27) ICC 0.05 |
||
| Richardson 1978 | 375 | 18 | 300 | 93 | 0.24 | OR 0.15
(0.09 to 0.26) ICC 0.05 |
||
| Rock 1978 | 347 | 15 | 316 | 46 | 0.13 | OR 0.30
(0.16 to 0.53) ICC 0.05 |
||
| Pooled | Pooled OR 0.17 (0.10 to 0.30) | |||||||
| Split‐mouth studies without summary data of tooth pairs | Study | Description of the data | Reported result | |||||
| Reisbick 1982 | Paired summary data reported only by tooth sites (3 sites per occlusal surface) but not by tooth surfaces which were the analysis units in this review | Effectiveness based on paired tooth surfaces was reported to be 90% at 14 months | ||||||
| Resin fissure sealant (FS) versus no sealant: 24 months | ||||||||
| Split‐mouth studies with data stated as tooth pair form | Study | Both sound | FS sound/ control carious | FS carious/ control sound | Both carious | Proportion of the decayed control tooth surfaces to total control surfaces | RR (95% CI) based on paired data | Becker‐Balagtas marginal OR (95% CI) |
| Brooks 1979 | 144 | 64 | 3 | 22 | 0.37 | RR 0.29 (0.206 to 0.411) | OR 0.21 (0.14 to 0.31) ICC 0.37 |
|
| Charbeneau 1979 | 53 | 100 | 4 | 29 | 0.69 | RR 0.256 (0.188 to 0.348) | OR 0.10 (0.06 to 0.15) ICC 0.19 |
|
| Sheykholeslam 1978 | 85 | 79 | 1 | 10 | 0.51 | RR 0.124 (0.071 to 0.216) | OR 0.06 (0.03 to 0.12) ICC 0.21 |
|
| Split‐mouth studies with data stated only in marginals | Study | FS sound | FS carious | Control sound | Control carious | Proportion of the decayed control tooth surfaces to total control surfaces | Becker‐Balagtas marginal OR (95% CI) | |
| Bojanini 1976 | 245 | 7 | 159 | 93 | 0.37 | OR 0.05
(0.02 to 0.11) ICC 0.05 |
||
| Richardson 1978 | 326 | 26 | 222 | 130 | 0.37 | OR 0.14
(0.09 to 0.21) ICC 0.05 |
||
| Parallel group studies | Study | Description of the data | OR (95% CI) | |||||
| Liu 2012 | OR based on the model of the multilevel GEE logistic regression | OR 0.32 (0.13 to 0.82) | ||||||
| Liu 2014b | OR based on the analysis by GEE method | OR 0.175 (0.071 to 0.435) | ||||||
| Pooled | Pooled OR 0.12 (0.08 to 0.19) | |||||||
| Parallel‐group study with continuous data | Tang 2014 | The study reported mean increment of DMFS (decayed, missing and filled surfaces of permanent first molars) in sealant group 0.06 (SD 0.26) versus 0.30 (SD 0.79), analysed by ANOVA. In the analysis of this review, the sample sizes of the groups were however reduced to their 'effective sample sizes' because the trial did not report that clustering of data would have been taken into account in the analyses (each child has average 3.8. teeth under evaluation, thus a child is a cluster). This review found significantly (P < 0.0001) more caries in the control group children, with a mean difference (MD) of increments of number of decayed, missing and filled surfaces of permanent first molars (DMFS) = ‐0.24 (95% CI ‐0.36 to ‐0.12) (Analysis 1.7) | ||||||
| Split‐mouth studies without summary data of tooth pairs, and data not included in the meta‐analyses | Study | Description of the data | Reported result | |||||
| Reisbick 1982 | Paired summary data reported only by tooth sites (3 sites per occlusal surface) but not by tooth surfaces which were the analysis units in this review | Effectiveness based on paired tooth surfaces was reported to be 80% at 20 months | ||||||
| Resin fissure sealant (FS) versus no sealant: 32 to 36 months | ||||||||
| Split‐mouth studies with data stated as tooth pair form | Study | Both sound | FS sound/ control carious | FS carious/ control sound | Both carious | Proportion of the decayed control tooth surfaces to total control surfaces | RR (95% CI) based on paired data | Becker‐Balagtas marginal OR (95% CI) |
| Brooks 1979 | 111 | 63 | 4 | 23 | 0.43 | RR 0.314 (0.225 to 0.438) | OR 0.21 (0.14 to 0.31) ICC 0.34 |
|
| Charbeneau 1979 | 45 | 96 | 5 | 47 | 0.74 | RR 0.364 (0.289 to 0.457) | OR 0.13 (0.09 to 0.19) ICC 0.23 |
|
| Hunter 1988 | 302 | 163 | 9 | 35 | 0.39 | RR 0.222 (0.169 to 0.293) | OR 0.15 (0.11 to 0.20) ICC 0.26 |
|
| Split‐mouth studies with data stated only in marginals | Study | FS sound | FS carious | Control sound | Control carious | Proportion of the decayed control tooth surfaces to total control surfaces | Becker‐Balagtas marginal OR (95% CI) | |
| Bojanini 1976 | 250 | 22 | 128 | 144 | 0.53 | OR 0.08 (0.05 to 0.13) ICC 0.05 | ||
| Sheykholeslam 1978 | 142 | 22 | 63 | 101 | 0.62 | OR 0.10 (0.06 to 0.17) ICC 0.05 | ||
| Richardson 1978 | 279 | 58 | 176 | 161 | 0.48 | OR 0.23 (0.16 to 0.32) ICC 0.05 | ||
| Rock 1978 | 253 | 55 | 222 | 86 | 0.28 | OR 0.56
(0.39 to 0.82) ICC 0.05 |
||
| Pooled | Pooled OR 0.17 (0.11 to 0.27) | |||||||
| Split‐mouth studies without summary data of tooth pairs, and data not included in the meta‐analyses | Study | Description of the data | Reported result | |||||
| Reisbick 1982 | Paired summary data reported only by tooth sites (3 sites per occlusal surface) but not by tooth surfaces which were the analysis units in this review | Effectiveness based on paired tooth surfaces was reported to be 70% at 32 months | ||||||
| Resin fissure sealant (FS) versus no sealant: 48 to 54 months | ||||||||
| Split‐mouth studies with data stated as tooth pair form | Study | Both sound | FS sound/ control carious | FS carious/ control sound | Both carious | Proportion of the decayed control tooth surfaces to total control surfaces | RR (95% CI) based on paired data | Becker‐Balagtas marginal OR (95% CI) |
| Brooks 1979 | 61 | 67 | 3 | 37 | 0.62 | RR 0.385 (0.298 to 0.496) | OR 0.19 (0.13 to 0.28) ICC 0.35 |
|
| Charbeneau 1979 | 37 | 81 | 3 | 64 | 0.78 | RR 0.462 (0.385 to 0.554) | OR 0.16 (0.11 to 0.23) ICC 0.31 |
|
| Split‐mouth studies with data stated only in marginals | Study | FS sound | FS carious | Control sound | Control carious | Proportion of the decayed control tooth surfaces to total control surfaces | Becker‐Balagtas marginal OR (95% CI) | |
|
Erdoğan 1987 (54 months) |
82 | 14 | 67 | 29 | 0.30 | OR 0.39 (0.20 to 0.80) ICC 0.05 | ||
|
Richardson 1978 (48 months) |
262 | 68 | 151 | 179 | 0.54 | OR 0.22 (0.15 to 0.31) ICC 0.05 | ||
| Pooled | OR 0.21 (0.16 to 0.28) | |||||||
| Parallel group studies | Study | Description of the data | RR (95% CI) | |||||
| Bravo 2005 | Data are based on requested risk ratio (RR) value with cluster corrected standard error (SE). A school class is a cluster but in addition there were several sealed teeth per child | RR 0.24 (0.12 to 0.45) | ||||||
| Resin fissure sealant (FS) versus no sealant: 60 months | ||||||||
| Split‐mouth studies with data stated only in marginals | Study | FS sound | FS carious | Control sound | Control carious | Proportion of the decayed control tooth surfaces to total control surfaces | Becker‐Balagtas marginal OR (95% CI) | |
| Richardson 1978 | 246 | 85 | 157 | 174 | 0.53 | OR 0.31 (0.23 to 0.43) ICC 0.05 | ||
| Resin fissure sealant (FS) versus no sealant: 72 months | ||||||||
| Split‐mouth studies with data stated as tooth pair form | Study | Both sound | FS sound/ control carious | FS carious/ control sound | Both carious | Proportion of the decayed control tooth surfaces to total control surfaces | RR (95% CI) based on paired data | Becker‐Balagtas marginal OR (95% CI) |
| Brooks 1979 | 50 | 57 | 5 | 38 | 0.63 | RR 0.45 (0.36 to 0.58) | OR 0.23 (0.16 to 0.35) ICC 0.329 |
|
| Resin fissure sealant (FS) versus no sealant: 84 months | ||||||||
| Split‐mouth studies with data stated as tooth pair form | Study | Both sound | FS sound/ control carious | FS carious/ control sound | Both carious | Proportion of the decayed control tooth surfaces to total control surfaces | RR (95% CI) based on paired data | Becker‐Balagtas marginal OR (95% CI) |
| Brooks 1979 | 29 | 41 | 2 | 30 | 0.70 | RR 0.45 (0.34 to 0.59) | OR 0.20 (0.12 to 0.32) ICC 0.355 |
|
| Resin fissure sealant (FS) versus no sealant: 108 months | ||||||||
| Parallel group studies | Study | Description of the data | RR (95% CI) | |||||
| Bravo 2005 | Data are based on requested risk ratio (RR) value with cluster corrected standard error (SE). A school class is a cluster but in addition there were several sealed teeth per child | RR 0.35 (0.22 to 0.55) | ||||||
| Glass ionomer sealant versus no sealant: 24 months | ||||||||
| Parallel group studies | Study | Description of the data | OR (95% CI) | |||||
| Liu 2014b | OR based on the analysis by GEE method | OR 0.459 (0.23 to 0.91) P = 0.03 | ||||||
| Glass ionomer (GI) versus resin sealant: 12 months | ||||||||
| Split‐mouth studies with data stated only in marginals | Study | GI sound | GI carious | Resin sound | Resin carious | Type of glass ionomer sealant material | Becker‐Balagtas marginal OR (95% CI) | |
| Dhar 2012 without surface preparation (no difference) | 23 | 2 | 24 | 1 | Low‐viscosity glass ionomer | OR 2.09
(0.19 to 23.21) P = 0.76 ICC 0.05 |
||
| Dhar 2012 with surface preparation (no difference) | 25 | 0 | 25 | 0 | Low‐viscosity glass ionomer | Not estimable | ||
|
Karlzén‐Reuterving 1995 (no difference) |
72 | 0 | 70 | 2 | Low‐viscosity glass ionomer | OR 0.19
(0.01 to 3.90) P = 0.25 ICC 0.05 |
||
|
Rock 1996 (no difference) |
151 | 7 | 157 | 1 | Low‐viscosity glass ionomer | OR 7.28 (0.91 to 58.12) P = 0.07 ICC 0.05 |
||
|
Sipahier 1995 (no difference) |
80 | 6 | 81 | 5 | Low‐viscosity glass ionomer | OR 1.22
(0.37 to 4.02) P = 0.75 ICC 0.05 |
||
| Resin‐ modified glass ionomer (GI) versus resin sealant: 12 months | ||||||||
| Split‐mouth studies with data stated only in marginals | Study | GI sound | GI carious | Resin sound | Resin carious | Type of glass ionomer sealant material | Becker‐Balagtas marginal OR (95% CI) | |
|
Baseggio 2010 (no difference) |
640 | 0 | 640 | 0 | Resin‐modified glass ionomer | Not estimable | ||
| Parallel group studies | Study | Description of the data | Type of glass ionomer sealant material | OR (95% Cl) | ||||
|
Amin 2008 (no difference) |
Clustered data (2 teeth per child) but not taken into account in the analyses. We decided to analyse the data at child level (whether a child had caries or not) because the numbers of decayed teeth were very small. In analysis, data of resin‐based sealant groups were combined. Numbers of children with caries in glass ionomer sealed teeth 1/13 and in resin sealed teeth 2/28 | Resin‐modified glass ionomer | OR 1.08 (0.09 to 13.15) P = 0.95 | |||||
| Pooled | OR 1.47 (0.64 to 3.37) | |||||||
| Glass ionomer (GI) versus resin sealant: 24 months | ||||||||
| Split‐mouth studies with data stated as tooth pair form | Study | Both sound | GI sound/ resin carious | GI carious/ resin sound | Both carious | Type of glass ionomer sealant material | RR (95% CI) based on paired data | Becker‐Balagtas marginal OR (95% CI) |
|
Chen 2013 (no difference) |
65 | 4 | 4 | 2 | Low‐viscosity glass ionomer | ‐ | OR 1 (0.37 to 2.73) P = 1 ICC 0.275 |
|
|
Poulsen 2001 (resin slightly better) |
191 | 2 | 9 | 1 | Low‐viscosity glass ionomer | RR = 3.33 (1.017 to 10.922) P = 0.065 | OR 3.46 (1.03 to 11.63) P = 0.04 ICC 0.16 |
|
|
Ganesh 2006 (no difference) |
100 | 0 | 0 | 0 | Low‐viscosity glass ionomer | ‐ | OR 1 (0.02 to 46.1) P = 1 |
|
|
Mills 1993 (no difference) |
59 | 0 | 0 | 0 | Low‐viscosity glass ionomer | ‐ | OR 1 (0.02 to 46.4) P = 1 |
|
| Split‐mouth studies with data stated only in marginals | Study | GI sound | GI carious | Resin sound | Resin carious | Type of glass ionomer sealant material | Becker‐Balagtas marginal OR (95% CI) | |
|
Antonson 2012 (no difference) |
27 | 0 | 25 | 2 | Low‐viscosity glass ionomer | OR 0.19
(0.01 to 3.82) P = 0.25 ICC 0.05 |
||
| Dhar 2012 without surface preparation (no difference) | 23 | 2 | 22 | 3 | Low‐viscosity glass ionomer | OR 0.64
(0.10 to 3.99) P = 0.81 ICC 0.05 |
||
| Dhar 2012 with surface preparation (no difference) | 24 | 1 | 21 | 4 | Low‐viscosity glass ionomer | OR 0.22
(0.02 to 2.02) P = 0.38 ICC 0.05 |
||
|
Forss 1998 (no difference) |
144 | 7 | 144 | 7 | Low‐viscosity glass ionomer | OR 1 (0.35 to 2.85) ICC 0.05 |
||
|
Karlzén‐Reuterving 1995 (no difference) |
71 | 1 | 70 | 2 | Low‐viscosity glass ionomer | OR 0.49 (0.05 to 5.25) P = 0.77 ICC 0.05 |
||
|
Rock 1996 (resin better) |
116 | 16 | 130 | 2 | Low‐viscosity glass ionomer | OR 8.96 (2.07 to 38.82) P < 0.001 ICC 0.05 |
||
|
Williams 1996 (resin better) |
274 | 21 | 289 | 6 | Low‐viscosity glass ionomer | OR 3.69 (1.50 to 9.09) P = 0.004 ICC 0.05 |
||
| Parallel group studies | Study | Description of the data | Type of glass ionomer sealant material | OR (95% Cl) | ||||
| Chen 2012 (no difference) | Data of glass ionomer sealant groups were combined (Ketac Molar Easymix with or without LED high energy curing light). Clustered data (mean 3.3 teeth per child). Data were analysed at child level (whether a child had caries or not) because the total number of decayed occlusal surfaces was small and each child who had carious occlusal surface had only 1 carious occlusal surface (9 out of 187 children in combined glass ionomer groups and 3 out of 102 children in resin group had carious occlusal surface). (Information obtained from the author) | High‐viscosity glass ionomer | OR 1.67 (0.44 to 6.30) | |||||
|
Liu 2014a (no difference) |
OR based on the model of GEE logistic regression | High‐viscosity glass ionomer | OR 1.15 (0.35 to 3.82) | |||||
|
Liu 2014b (no difference) |
Caries incidences: in glass ionomer group 6.7% and in resin sealant group 3% after 24 months (P > 0.05) | Low‐viscosity glass ionomer | NR | |||||
| Resin‐ modified glass ionomer (GI) versus resin sealant: 24 months | ||||||||
| Split‐mouth studies with data stated only in marginals | Study | GI sound | GI carious | Resin sound | Resin carious | Type of glass ionomer sealant material | Becker‐Balagtas marginal OR (95% CI) | |
| Baseggio 2010 (resin better) | 583 | 57 | 620 | 20 | Resin‐ modified glass ionomer | OR 3.03 (1.82 to 5.05) P < 0.0001 ICC 0.05 |
||
| Parallel group studies | Study | Description of the data | Type of glass ionomer sealant material | OR (95% Cl) | ||||
|
Amin 2008 (no difference) |
Clustered data (2 teeth per child) but not taken into account in the analyses. We decided to analyse the data at child level (whether a child had caries or not) because the numbers of decayed teeth were very small. In analysis, data of resin‐based sealant groups were combined. Numbers of children with caries in glass ionomer sealed teeth 1/12 and in resin sealed teeth 2/27 | Resin‐ modified glass ionomer | OR 1.14 (0.09 to 13.89) P = 0.92 | |||||
| Pooled | Not pooled | |||||||
| Glass ionomer (GI) sealant versus resin sealant: 36 to 48 months | ||||||||
| Split‐mouth studies with data stated as tooth pair form | Study | Both sound | GI sound/ resin carious | GI carious/ resin sound | Both carious | Type of glass ionomer sealant material | RR (95% CI) based on paired data | Becker‐Balagtas marginal OR (95% CI) |
| Poulsen 2001 (36 months) (resin better) | 156 | 6 | 37 | 7 | Low‐viscosity glass ionomer | RR 3.385 (1.978 to 5.793) P < 0.001 | OR 4.03 (2.23 to 7.29) P < 0.001 ICC 0.21 |
|
| Arrow 1995 (44 months) (ionomer better) | 378 | 28 | 3 | 3 | Low‐viscosity glass ionomer | RR 0.194 (0.087 to 0.431) P < 0.001 | OR 0.18 (0.08 to 0.41) P < 0.001 ICC 0.20 |
|
| Kervanto‐Seppälä 2008 (36 months) (resin better) | 625 | 5 | 25 | 2 | Low‐viscosity glass ionomer | RR 3.857 (1.767 to 8.422) P < 0.001 | OR 3.98 (1.80 to 8.80) P < 0.001 ICC 0.13 |
|
| Split‐mouth studies with data stated only in marginals | Study | GI sound | GI carious | Resin sound | Resin carious | Type of glass ionomer sealant material | Becker‐Balagtas marginal OR (95% CI) | |
|
Karlzén‐Reuterving 1995
(36 months) (no difference) |
71 | 1 | 69 | 3 | Low‐viscosity glass ionomer | OR 0.32 (0.03 to 3.03) P = 0.63 ICC 0.05 |
||
|
Rock 1996
(36 months) (resin better) |
106 | 24 | 126 | 4 | Low‐viscosity glass ionomer | OR 7.13 (2.45 to 20.76) P < 0.001 ICC 0.05 |
||
|
Williams 1996
(48 months) (no difference) |
200 | 22 | 206 | 16 | Low‐viscosity glass ionomer | OR 1.42 (0.73 to 2.73) P = 0.34 ICC 0.05 |
||
| Resin‐modified glass ionomer (GI) versus resin sealant: 36 months | ||||||||
| Study | GI sound | GI carious | Resin sound | Resin carious | Type of glass ionomer sealant material | Becker‐Balagtas marginal OR (95% CI) | ||
| Split‐mouth studies with data stated only in marginals |
Baseggio 2010 (resin better) |
502 | 126 | 572 | 56 | Resin‐ modified glass ionomer | OR 2.56 (1.84 to 3.56) P < 0.001 ICC 0.05 |
|
|
Raadal 1996 (resin better) |
64 | 9 | 73 | 0 | Resin‐ modified glass ionomer | OR 11.38 (1.47 to 88.42) P = 0.012 ICC 0.05 |
||
| Pooled | Not pooled | |||||||
| Glass ionomer (GI) sealant versus resin sealant: 60 months | ||||||||
| Study | Description of the data | Type of glass ionomer sealant material | RR (95% CI) | |||||
| Parallel group studies | Barja‐Fidalgo 2009 (no difference) | Raw data were obtained from the authors because several of a child's teeth had been sealed (a child is a cluster). Raw data were used in calculations | High‐viscosity glass ionomer | RR 0.38 (0.09 to 1.60) | ||||
| Glass ionomer (GI) sealant versus resin sealant: 84 months | ||||||||
| Study | Both sound | GI sound/ resin carious | GI carious/ resin sound | Both carious | Type of glass ionomer sealant material | RR (95% CI) based on paired data | Becker‐Balagtas marginal OR (95% CI) | |
| Split‐mouth studies with data stated as tooth pair form | Forss 1998 (no difference) | 66 | 8 | 15 | 8 | Low‐viscosity glass ionomer | RR 1.44 (0.88 to 2.35) P 0.15 | OR 1.57 (0.86 to 2.89) P = 0.21 ICC 0.275 |
CI = confidence interval; df = degrees of freedom; ICC = intracluster correlation co‐efficient; OR = odds ratio; RR = risk ratio
2. Caries data from parallel‐group study with continuous outcome (Songpaisan 1995).
| Comparison (24 months) | Control number | Control mean | Control SD | Test number | Test mean | Test SD | Mean DFS difference | 95% CI | P value |
| Control versus resin | 143 | 0.70 | 0.96 | 133 | 0.05 | 0.57 | 0.65 | 0.47 to 0.83 | < 0.00001 |
| Control versus GI | 143 | 0.70 | 0.96 | 261 | 0.52 | 1.09 | 0.18 | ‐0.03 to 0.39 | 0.09 |
| Resin versus GI | 133 | 0.05 | 0.57 | 261 | 0.52 | 1.09 | ‐0.47 | ‐0.63 to ‐0.31 | < 0.00001 |
CI = confidence interval; DFS = decayed and filled occlusal surfaces; GI = glass ionomer; SD = standard deviation.
We extracted any information in the trials about retention of sealants (see Table 6).
3. Sealant retention.
| Time | Study | Sealant | Complete (%) | Partial (%) | Lost (%) | Decayed or filled (%) | Total (%) |
| 12 months | Amin 2008 | FUJI II LC (resin‐modified glass ionomer) | 46 | 27 | 27 | ‐ | 100 |
| Amin 2008 | Tetric Flow, Helioseal F (resins, data combined) (mean rates for these two materials) | 82 | 12.5 | 5.5 | ‐ | 100 | |
| Baseggio 2010 | Vitremer (resin‐modified glass ionomer) | 14 | 33 | 54 | ‐ | 101 | |
| Baseggio 2010 | Fluoroshield (resin) | 94 | 6 | 0 | ‐ | 100 | |
| Bojanini 1976 | Delton (resin) | 91 | 6 | 3 | ‐ | 100 | |
| Charbeneau 1979 | Kerr (resin) | 79 | 17 | 4 | ‐ | 100 | |
| De Luca‐Fraga 2001 | Vitremer (resin‐modified glass ionomer) | 86 | 14 | 0 | ‐ | 100 | |
| De Luca‐Fraga 2001 | Dyract (polyacid‐modified composite resin) | 96 | 2 | 2 | ‐ | 100 | |
| Dhar 2012 | GC Fuji Ionomer VII light pink (glass ionomer‐based sealant), without preparation | 0 | 16 | 84 | ‐ | 100 | |
| Dhar 2012 | Clinpro pink (fluoride releasing resin‐based sealant), without preparation | 24 | 28 | 48 | ‐ | 100 | |
| Erdoğan 1987 | Delton (resin) | 77 | 19 | 4 | ‐ | 100 | |
| Karlzén‐Reuterving 1995 | FUJI III (ionomer) | 72 | 17 | 11 | ‐ | 100 | |
| Karlzén‐Reuterving 1995 | Delton (resin) | 97 | 3 | 0 | ‐ | 100 | |
| Muller‐Bolla 2013 | Delton plus (resin) | 53 | 28 | 19 | ‐ | 100 | |
| Pardi 2005 | Vitremer (resin‐modified glass ionomer) | 77 | 17 | 6 | ‐ | 100 | |
| Pardi 2005 | Revolution (flowable resin composite) | 84 | 14 | 2 | ‐ | 100 | |
| Pardi 2005 | Dyract Flow (compomer) | 76 | 22 | 2 | ‐ | 100 | |
|
Reisbick 1982 (14 months) |
Oralin (chemically polymerised resin) | 89 | NR | NR | ‐ | ‐ | |
| Richardson 1978 | resin (the name of the material not stated) | 90 | 6 | 4 | ‐ | 100 | |
| Rock 1978 | Delton (resin) | 53 | 22 | 25 | ‐ | 100 | |
| Rock 1996 | Baseline (ionomer) | 0 | 0 | 96 | 4 | 100 | |
| Rock 1996 | Fluoroshield (resin) | 76.6 | 9.5 | 13.3 | 1.3 | 101 | |
| Sheykholeslam 1978 | Delton (resin) | 92 | 5 | 0 | 3 | 100 | |
| Sipahier 1995 | Ketac‐Silver (glass ionomer‐silver‐cermet cement) | 23 | 34 | 43 | ‐ | 100 | |
| Sipahier 1995 | Delton (resin) | 41 | 48 | 11 | ‐ | 100 | |
| 24 months | Amin 2008 | FUJI II LC (resin‐modified glass ionomer) | 25 | 21 | 54 | ‐ | 100 |
| Amin 2008 | Tetric Flow, Helioseal F (resins, data combined) (mean rates for these two materials) | 83 | 9 | 8 | ‐ | 100 | |
| Antonson 2012 | GC Fuji Triage White (light cured glass ionomer sealant) | 44.4 | 44.4 | 11.1 | ‐ | 99 | |
| Antonson 2012 | Delton Plus+ (light cured resin‐based sealant) | 41 | 52 | 7 | ‐ | 100 | |
| Baseggio 2010 | Vitremer (resin‐modified glass ionomer) | 9 | 12 | 80 | ‐ | 101 | |
| Baseggio 2010 | Fluoroshield (resin) | 94 | 6 | 0 | ‐ | 100 | |
| Bojanini 1976 | Delton (resin) | 89 | 7 | 4 | ‐ | 100 | |
| Brooks 1979 | Delton (resin) | 84 | 10 | 6 | ‐ | 100 | |
| Charbeneau 1979 | Kerr (resin) | 71 | 18 | 11 | ‐ | 100 | |
| Chen 2012 | Ketac Molar Easymix (high‐viscosity glass ionomer) | 78% completely or partially retained | 22 | ‐ | 100 | ||
| Chen 2012 | Ketac Molar Easymix plus LED high energy curing light (high‐viscosity glass ionomer) | 80% completely or partially retained | 20 | ‐ | 100 | ||
| Chen 2012 | Clinpro Sealant (fluoride releasing resin‐based sealant) | 86% completely or partially retained | 14 | ‐ | 100 | ||
| Chen 2013 | Fuji VII (light cured glass ionomer) | 38 | 47 | 15 | ‐ | 100 | |
| Chen 2013 | Concise (resin) | 70 | 30 | 0 | ‐ | 100 | |
| Dhar 2012 | GC Fuji Ionomer VII light pink (glass ionomer‐based sealant), without preparation | 0 | 0 | 100 | ‐ | 100 | |
| Dhar 2012 | Clinpro pink (fluoride releasing resin‐based sealant), without preparation | 0 | 20 | 80 | ‐ | 100 | |
| Forss 1998 | Fuji III (ionomer) | 26 | 26 | 48 | ‐ | 100 | |
| Forss 1998 | Light‐cured Delton (resin) | 82 | 9 | 9 | ‐ | 100 | |
| Ganesh 2006 | Fuji VII (ionomer) | 2 | 68 | 30 | ‐ | 100 | |
| Ganesh 2006 | Concise (resin) | 4 | 66 | 30 | ‐ | 100 | |
| Guler 2013 | Admira Seal (ormocer) | 3 | 83 | 14 | ‐ | 100 | |
| Guler 2013 | Fuji VII (ionomer) | 13 | 80 | 7 | ‐ | 100 | |
| Karlzén‐Reuterving 1995 | FUJI III (ionomer) | 43 | NR | NR | ‐ | ‐ | |
| Karlzén‐Reuterving 1995 | Delton (resin) | 90 | 10 | 0 | ‐ | 100 | |
| Liu 2012 | Clinpro Sealant (fluoride releasing resin) | 46% completely or partially retained | 54 | ‐ | 100 | ||
| Liu 2014a | Ketac‐Molar Easymix (ART sealant; high‐viscosity glass ionomer) | 55% completely or partially retained | 45 | ‐ | 100 | ||
| Liu 2014a | Clinpro (fluoride‐releasing resin) | 79% completely or partially retained | 21 | ‐ | 100 | ||
| Liu 2014b | Helioseal F (light‐cured, fluoride releasing resin‐based sealant) | NR | NR | 6.6 | ‐ | ‐ | |
| Liu 2014b | Fuji VI (Iight cured glass ionomer sealant) | NR | NR | 35.2 | ‐ | ‐ | |
| Mills 1993 | Ketac‐Silver (ionomer) | 83 | 12 | 6 | ‐ | 101 | |
| Mills 1993 | Delton (resin) | 58 | 17 | 25 | ‐ | 100 | |
| Pardi 2005 | Vitremer (resin‐modified glass ionomer) | 47 | 37 | 16 | ‐ | 100 | |
| Pardi 2005 | Revolution (flowable resin composite) | 76 | 17 | 7 | ‐ | 100 | |
| Pardi 2005 | Dyract Flow (compomer) | 58 | 28 | 14 | ‐ | 100 | |
| Poulsen 2001 | Fuji III (ionomer) | 9 | 9 | 82 | ‐ | 100 | |
| Poulsen 2001 | Delton (resin) | 80 | 7 | 13 | ‐ | 100 | |
| Reisbick 1982 (20 months) | Oralin (chemically polymerised resin) | 82 | NR | NR | ‐ | ‐ | |
| Richardson 1978 | resin (the name of the material not stated) | 86 | 9 | 5 | ‐ | 100 | |
| Rock 1996 | Baseline (ionomer) | 0 | 0 | 88 | 12 | 100 | |
| Rock 1996 | Fluoroshield (resin) | 70 | 10 | 19 | 1 | 100 | |
| Sheykholeslam 1978 | Delton (resin) | 85 | 7 | 2 | 6 | 100 | |
| Songpaisan 1995 | Fuji III (ionomer) | < 1 | NR | NR | ‐ | ‐ | |
| Songpaisan 1995 | Delton (resin) | 85 | NR | NR | ‐ | ‐ | |
| Tagliaferro 2011 | (resin‐modified glass ionomer) | NR | NR | 16 | ‐ | ‐ | |
| Tang 2014 | Clinpro TM (light‐cured, fluoride releasing resin‐based sealant) | 90.1 | 6.7 | 3.2 | ‐ | 100 | |
| Williams 1996 | Fuji III (ionomer) | 4 | 3 | 93 | ‐ | 100 | |
| Williams 1996 | Delton (resin) | 80 | 2 | 18 | ‐ | 100 | |
| 36 months | Baseggio 2010 | Vitremer (resin‐modified glass ionomer) | 5 | 6 | 89 | ‐ | 100 |
| Baseggio 2010 | Fluoroshield (resin) | 91 | 8 | 1 | ‐ | 100 | |
| Bojanini 1976 | Delton (resin) | 87 | 9 | 4 | ‐ | 100 | |
| Brooks 1979 | Delton (resin) | 80 | 10 | 10 | ‐ | 100 | |
| Charbeneau 1979 | Kerr (resin) | 61 | 23 | 16 | ‐ | 100 | |
| Hunter 1988 | Delton (resin) | 64 | 19 | 8 | 9 | 100 | |
| Karlzén‐Reuterving 1995 | FUJI III (ionomer) | 28 | 35 | 37 | ‐ | 100 | |
| Karlzén‐Reuterving 1995 | Delton (resin) | 79 | 21 | 0 | ‐ | 100 | |
| Poulsen 2001 | Fuji III (ionomer) | 3 | 7 | 89 | ‐ | 100 | |
| Poulsen 2001 | Delton (resin) | 74 | 16 | 10 | ‐ | 100 | |
| Raadal 1996 | Vitrebond (resin‐reinforced glass ionomer) | 5 | 4 | 91 | ‐ | 100 | |
| Raadal 1996 | Concise White Sealant (resin) | 97 | 1.5 | 1.5 | ‐ | 100 | |
|
Reisbick 1982 (32 months) |
Oralin (chemically polymerised resin) | 78 | NR | NR | ‐ | ‐ | |
| Richardson 1978 | resin (the name of the material not stated) | 75 | 14 | 11 | ‐ | 100 | |
| Rock 1978 | Delton (resin) | 41 | 16 | 43 | ‐ | 100 | |
| Rock 1996 | Baseline (ionomer) | 0 | 0 | 81.5 | 18.4 | 100 | |
| Rock 1996 | Fluoroshield (resin) | 70 | 9.2 | 17.7 | 3.2 | 100 | |
| Sheykholeslam 1978 | Delton (resin) | 77 | 9 | 4 | ‐ | ? | |
| Kervanto‐Seppälä 2008 retention stated by tooth pairs | In total 559 tooth pairs: in 1% ionomer retained, resin lost; in 89% ionomer lost, resin retained; in 6% ionomer retained, resin retained; in 4% ionomer lost, resin lost = 100% | ‐ | ‐ | ‐ | ‐ | ‐ | |
| 44 months | Arrow 1995 retention stated by tooth pairs | In total 465 tooth pairs: in 10% ionomer retained, resin lost; in 18% ionomer lost, resin retained; in 10% ionomer retained, resin retained; in 62% ionomer lost, resin lost = 100% | ‐ | ‐ | ‐ | ‐ | ‐ |
| 48 months | Bravo 2005 | Delton (resin) | 63 | NR | NR | ‐ | ‐ |
| Charbeneau 1979 | Kerr (resin) | 52 | 26 | 22 | ‐ | 100 | |
| Chen 2012 | No information on retention at 48 months | NR | NR | NR | ‐ | ‐ | |
| Richardson 1978 | resin (the name of the material not stated) | 69 | 10 | 21 | ‐ | 100 | |
| Williams 1996 | Fuji III (ionomer) | 4 | 2 | 94 | ‐ | 100 | |
| Williams 1996 | Delton (resin) | 61 | 11 | 28 | ‐ | 100 | |
| 54 months | Brooks 1979 | Delton (resin) | 72 | 14 | 14 | ‐ | 100 |
| Erdoğan 1987 | Delton (resin) | 74 | 22 | 4 | ‐ | 100 | |
| 60 months | Barja‐Fidalgo 2009 | Fuji IX (high‐viscosity glass ionomer) | 29 | 29 | 42 | ‐ | 100 |
| Barja‐Fidalgo 2009 | Delton (resin) | 21 | 21 | 58 | ‐ | 100 | |
| Richardson 1978 | Resin (material name not stated) | 67 | 10 | 23 | ‐ | 100 | |
| 72 months | Brooks 1979 | Delton (resin) | 68 | 16 | 16 | ‐ | 100 |
| 84 months | Brooks 1979 | Delton (resin) | 66 | 14 | 20 | ‐ | 100 |
| Forss 1998 retention stated by tooth pairs | In total 97 tooth pairs: in 6% ionomer retained, resin lost; in 41% ionomer lost, resin retained; in 4% ionomer retained, resin retained; in 49% ionomer lost, resin lost = 100% | ‐ | ‐ | ‐ | ‐ | ‐ | |
| 108 months | Bravo 2005 | Delton (resin) | 39 | NR | NR | ‐ | ‐ |
Results were stated at more than one period of follow‐up period in some studies. All data were extracted at predefined times (annually). We carried out meta‐analyses at predefined times based on available data.
We extracted the following additional information:
factors that might be related to caries incidence (individual behavioural factors e.g. the frequency of eating sugary snacks and oral hygiene habits);
information related to calibration of examiners and kappa statistics; and
funding source.
Assessment of risk of bias in included studies
Two review authors (AAS, HF) independently assessed the risk of bias of included studies. Disagreements were resolved by consensus. We contacted the authors of included studies to request additional information. As recommended in the Cochrane Handbook for Systematic Reviews of Interventions 5.1.0 (Higgins 2011a), we assessed the following six methodological domains: random sequence generation, allocation concealment, blinding of outcome assessment, incomplete outcome data, selective outcome reporting and other sources of bias (baseline comparability of the groups and co‐interventions). Within each domain, we judged each study as low, high or unclear risk of bias. Unclear risk of bias was assigned to indicate lack of information or uncertainty about the potential for bias. See Table 7 for detailed criteria used in our assessments.
4. Criteria for risk of bias assessment.
| Random sequence generation (selection bias) | Was the method used to generate the allocation sequence appropriate to produce comparable groups? | This domain was graded low risk of bias if the authors described a random component in the sequence generation process (e.g. random number table, coin tossing, drawing of lots). In split‐mouth study designs, however, we graded low risk of bias where the method of allocating a tooth to an intervention was not random but quasi‐random (systematic methods that were intended to produce similar groups, e.g. sequence generated by odd or even date of birth or by some rule based on date of admission). Although quasi‐random sequence generation methods include some systematic, non‐random component, we considered that in preventive split‐mouth studies (with mainly sound tooth surfaces), the risk of selection bias is minimal. Our justification is based on the assumption that there is no right‐left asymmetry between contralateral teeth regarding caries risk, as shown by Larmas 1995 when they evaluated timing of the change from a sound erupting tooth to a filled tooth. |
| Allocation concealment (selection bias) | Was the method used to conceal the allocation sequence appropriate to prevent the allocation from being known in advance of, or during, enrolment? | This domain was graded low risk of bias if the authors described adequate concealment (for example, by means of central randomisation, or sequentially numbered, opaque and sealed envelopes), and graded high risk of bias if inadequate concealment was documented (for example, alternation, use of case record numbers, dates of birth or day of the week) or allocation concealment was not used. If there was insufficient or no information on allocation concealment, the judgement was unclear risk. In split‐mouth study designs, however, we considered that the study could be graded low risk of bias if the information about allocation concealment was incomplete or the sequence generation method was quasi‐random. This is because we consider that the risk of selection bias is minimal in preventive split‐mouth designs. |
| Blinding (performance bias) | We did not assess blinding of participants and personnel in this review because we considered that possible knowledge of personnel and participants about which of the 2 intervention groups a child belongs to was unlikely to cause bias (e.g. affect dental behaviour of a child during the trial, especially when follow‐up is long (≥ 1 year in this review)). | |
| Blinding of outcome assessment (detection bias) | Were outcome assessors blinded to the intervention a participant had received? | Trials comparing sealant to no treatment As sealant materials are visible, blinding of the outcome assessor is possible only if a sealant has been lost. Therefore blinding of outcome assessment for caries will be at high risk of bias for all trials. Trials comparing different sealants We decided to assess the blinding of outcome assessment for caries as high risk of bias for all trials because although sealant materials may have a similar appearance when applied, the outcome assessor can discriminate between them at follow‐up (materials change differently by age, e.g. materials including glass‐ionomer lose their glossy appearance more rapidly than resins). |
| Incomplete outcome data (attrition bias) | How complete were the outcome data for caries outcomes? Were drop‐out rates and reasons for withdrawals reported? Were missing data imputed appropriately? | In caries prevention studies, follow‐up times can be several years, and the risk of bias for caries outcome data may differ over time. Studies with long follow‐up may have the problem of high drop‐out rates. We decided to base the judgement of this domain on caries efficacy outcomes at 24 or 36 months (commonly used follow‐up times in sealant studies). When both follow‐up times were reported, we based our judgement on 24 months. If either of these two follow‐up times was not reported, we based our judgement on the first caries efficacy outcome reported in the study (which in this review should be at least 1 year). However, we assessed the risk of bias separately and reported it in the risk of bias table for caries outcomes despite the follow‐up times, and we took the assessments into account in the overall risk of bias assessment for caries outcomes within a study. We decided to grade this domain as having low risk if the proportion of missing outcome data was < 25% at 24 or 36 months (in parallel‐group studies), and the groups were balanced in numbers and reasons for missing data; or if missing data have been imputed using appropriate methods. If no information on reasons for drop‐out across intervention groups was provided, or not reported by group, our judgement was unclear risk. Otherwise the study was judged as high risk of bias. Classifying missing data > 25% as having high risk of bias in all study designs was a pragmatic approach to this domain to make the judgement uniform and transparent. If several teeth were sealed in a child’s mouth (a child is a cluster), missing outcome data had to be stated (or counted) at child level (not at tooth level). |
| Selective reporting (reporting bias) | Were appropriate outcomes reported and were key outcomes missing? | For a trial to be included in this review, caries outcomes had to be reported. However, studies could report the outcome in different ways, for example, incidence of dentinal carious lesion on treated occlusal surfaces of molars or premolars (yes or no); changes in mean figures of decayed, missing and filled occlusal surfaces (DMFS). In this review, selective outcome reporting was graded as ‘low’ risk of bias if the study's prespecified caries outcomes had been reported in the prespecified way. |
| Other sources of bias: comparability of groups at baseline | We decided to base our judgement of comparability of groups on baseline information given to groups available at follow‐up times because if available information is only that provided at the start of the study, it is impossible to assess whether groups are balanced with each other after follow‐up time as well. The comparability of groups after follow‐up is especially problematic when small studies include children with several teeth and the drop‐out rate is high, even if drop‐outs are balanced in numbers and reasons between groups. If no information on the groups was available at follow‐up time, we decided that if the drop‐out rate (regardless of follow‐up time) was < 25% and drop‐outs were balanced in numbers and reasons by group, our judgement would be based on information given for groups at the start of the study. We decided to grade this domain as having ‘low’ risk of bias if: a) groups were balanced in demographic characteristics (such as sex, age and social class), and in baseline caries risk level; b) possible imbalance of groups at baseline and/or after follow‐up had been taken adequately into account in the analyses. If baseline characteristics in parallel‐group studies were not given to groups available at follow‐up and the drop‐out rate was > 25%, we graded the study as having ‘unclear’ risk. | |
| Other sources of bias: co‐interventions | For a trial to be included in this review, only fluoride toothpaste and fluoridated water were accepted as co‐interventions. We decided to grade this domain as having ‘low’ risk of bias if groups were balanced in number and quality of co‐interventions, or if no co‐interventions were included in the protocol, and as having ‘high’ risk of bias if groups received different numbers or quality of co‐interventions during the trial. If no information was provided on co‐interventions, our judgement was unclear risk. | |
Summary assessments of ‘Risk of bias’
To draw conclusions about the overall risk of bias for caries outcomes within a study, we classified studies as low, unclear or high risk of bias. We determined caries outcomes from data of the included studies (all caries data were extracted at pre‐selected times ‐ annually, at 12, 24, 36, 48, 60 months, etc.).
Our classification was based on the following domains: allocation concealment, blinding of outcome assessment, incomplete outcome data, selective outcome reporting and baseline comparability.
We defined overall risk of bias categories as follows.
Low risk of bias (plausible bias unlikely to seriously alter results) if all domains defined above were graded as low risk of bias.
Unclear risk of bias (plausible bias that raises some doubt about results) if one or more of the domains were graded as unclear risk of bias.
High risk of bias (plausible bias that seriously weakens confidence in the results) if one or more domains were graded as high risk of bias.
We completed a 'Risk of bias' assessment for each included study (see Characteristics of included studies). Results are presented graphically by domain (Figure 2) and study (Figure 3).
2.
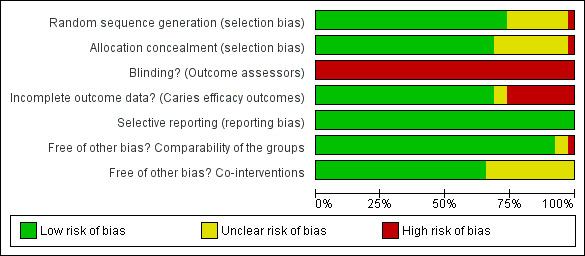
Risk of bias graph: review authors' judgements about each risk of bias domain presented as percentages across all included studies
3.

Risk of bias summary: review authors' judgements about each risk of bias domain for each included study
Measures of treatment effect
We calculated odds ratios (ORs) for differences between sealant and no sealant (or different sealant materials) groups about whether occlusal surfaces were carious, along with appropriate standard errors (SE) and 95% confidence intervals (CI), using RevMan 2014. For split‐mouth studies, we calculated ORs using the Becker‐Balagtas method (BB OR) outlined in Curtin 2002 by R software version 3.3.1 (R for Windows 3.3.1). We chose this method because we intended to pool data from split‐mouth and parallel‐group studies in the same meta‐analyses, and this method facilitated data synthesis (as outlined by Stedman 2011). If an included study presented paired data by tooth pairs, we calculated the intracluster correlation co‐efficient (ICC) (required for BB OR calculations) from paired data. If a split‐mouth study presented data only in marginals (as parallel‐group studies, not as 2 x 2 cross‐classification for paired data), we chose the conservative ICC 0.05.
However, the results of parallel‐group studies with clustered data from Bravo 2005 and Barja‐Fidalgo 2009 were available only as risk ratios (RR) with cluster corrected SEs and we used them as such in the analyses.
For continuous outcomes and data, we used means and standard deviations (SD) to obtain mean differences (MD) and 95% CIs. We chose to use the conservative ICC 0.05 for cluster trials.
Unit of analysis issues
In parallel‐group studies and cluster‐randomised studies, we chose an individual participant to be the unit of analysis. If clustered data were provided (e.g. several measurements per individual (such as more than 1 tooth or surface), clustering of children at school class level), we adjusted the SEs of estimates to take clustering into account (as outlined in Section 16.3.4. of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011b)). However, in the clustered studies by Amin 2008 and Chen 2012, we decided only to dichotomise data (whether a child had caries or not) because the numbers of decayed occlusal surfaces were very small. Results reported by Chen 2012 (although considering for clustering of teeth per child) were not in a form that could be used for this review; the study calculated cumulative survival percentages of dentine carious lesion free pits and fissures of first permanent molars combined.
In split‐mouth studies, we chose a tooth pair of an individual participant to be the unit of analysis. In some studies, more than one pair of tooth surfaces per child could be treated. These pairs are not strictly independent and should be analysed as paired data on a per‐child basis. However, we analysed the pairs independently because otherwise useful information from these studies would have been lost. (We are unaware of any widely used methods to correct and account for dependence of the tooth pairs). This meant that confidence intervals were slightly narrower than they otherwise would have been, and this was taken into consideration when we interpreted the results.
Dealing with missing data
We contacted trial authors to obtain missing data when necessary or feasible.
We performed analyses using an available‐case data analysis approach, as presented in the Cochrane Handbook for Systematic Reviews of Interventions 5.1.0 (Higgins 2011b). This approach for calculating response rates uses the total number of participants for whom data were recorded for the particular outcome in question as a denominator.
In caries‐prevention studies, follow‐up times could include several years. Studies with long follow‐up periods have the challenge of high drop‐out rates, creating uncertainty in the data. A common reason for drop‐out was that children moved away from the study area. We included data from all studies (regardless of drop‐out rates) in the analyses. We assessed studies with high drop‐out rates (over 25% regardless of the follow‐up time) to be at high risk of bias.
Assessment of heterogeneity
We assessed clinical heterogeneity by examining the characteristics of studies and similarities among types of participants, interventions and outcomes (especially caries diagnostic criteria). In studies comparing a sealant with no sealant, we assessed methodological heterogeneity in terms of study design (parallel group, cluster randomised (e.g. school or class), split‐mouth (summary data presented as paired form or only as marginals)). In studies comparing relative effectiveness of glass ionomer‐based sealants with resin‐based sealants, we investigated the effect of the glass ionomer material subtype (low‐viscosity, high‐viscosity and resin‐modified glass ionomers) on effect estimates.
The significance of any discrepancies in the estimates of the treatment effects from the studies was assessed using Cochran's test for heterogeneity and by a measure of I². I² describes the percentage of the variability in effect estimates that is due to heterogeneity rather than sampling error. A value greater than 50% may be considered to represent substantial heterogeneity (Higgins 2003).
If significant heterogeneity was found, we presented only narrative results.
Assessment of reporting biases
We planned that if more than 10 studies were included in any meta‐analysis, we would assess for publication bias according to the recommendations on testing for funnel plot asymmetry described in the Cochrane Handbook for Systematic Reviews of Interventions 5.1.0 (Sterne 2011). If asymmetry was identified, we planned to examine possible causes.
Data synthesis
The included studies presented data comparing sealant versus no sealant, and one sealant material versus another sealant material. We grouped and analysed studies on the basis of sealant material type (resin or composite‐based sealant, glass‐ionomer‐based sealant and ormocer‐based sealant) using different follow‐up periods. We conducted meta‐analyses in RevMan 2014, using the generic inverse variance method and fixed‐effect or random‐effects models. We used the fixed‐effect model in meta‐analyses that included up to three studies and the random‐effects model in meta‐analyses with four or more studies.
We pooled ORs from parallel‐group and split‐mouth studies using the Becker‐Balagtas method when feasible (Stedman 2011).
If we found significant heterogeneity or divergent results between studies, we did not conduct a meta‐analysis, but presented results narratively.
Subgroup analysis and investigation of heterogeneity
In analyses of studies comparing the relative effectiveness of resin sealants and glass ionomer‐based sealants, we created subgroups based on the glass ionomer material subtype (low‐viscosity, high‐viscosity and resin‐modified glass ionomers).
Sensitivity analysis
In analyses of studies comparing resin sealant with no sealant we undertook sensitivity analyses to assess the robustness of results (for caries outcomes) by excluding split‐mouth studies with data presented only in marginals. We used the conservative ICC 0.05 in calculations when data were not available as 2 x 2 cross‐classification for paired data.
‘Summary of findings’ tables and assessing the quality of the evidence
We followed GRADE (Grades of Recommendation, Assessment, Development and Evaluation) methods (GRADE 2004) and used GRADEpro software (GRADEpro GDT 2014) to provide overall grading of the quality of evidence for the main caries outcome for the following comparisons: resin‐based sealant versus no sealant (Table 1); glass ionomer‐based sealant versus no sealant (Table 2); and glass ionomer‐based sealant versus resin‐based sealant (Table 3). We assessed the quality of the body of evidence with reference to overall risk of bias of included studies at each outcome, directness of evidence, inconsistency of results, precision of estimates and risk of publication bias.
Results
Description of studies
Results of the search
Search results (2017 update)
We retrieved a total of 601 records from searches of: Cochrane Oral Health Trials Register (121 records), Cochrane Central Register of Controlled Trials (CENTRAL) (86 records), MEDLINE (202 records), Embase (129 records) and databases for ongoing trials (63 records) for the 2017 update. After removal of duplicates, 353 records remained. We also identified five potentially relevant reports from searching the reference lists of review articles and identified trial articles (n = 358). Following assessment of titles and abstracts, we excluded 336 records (n = 22). We obtained 22 full text study reports for assessment, and following assessment, included seven new studies that involved a total of 1693 children (Antonson 2012; Chen 2013; Guler 2013; Liu 2014a; Liu 2014b; Muller‐Bolla 2013; Tang 2014).
We excluded five studies identified from searches for the 2017 update (Hilgert 2015; Madléna 1993; Marković 2012; Monse 2012; Unal 2015). We also excluded three previously included studies that no longer met inclusion criteria; Beiruti 2006 was quasi‐randomised; Güngör 2004 and Lampa 2004 compared polyacid‐modified resin composite with resin‐based sealant. See Characteristics of included studies and Characteristics of excluded studies.
Two studies await assessment (Gorseta 2014; Ulusu 2012; Characteristics of studies awaiting classification) and there are five potentially eligible ongoing trials (IRCT2013041611960N2; NCT02408601; NCT02443896; NCT02795728; NCT02849925; Characteristics of ongoing studies).
Total search results
We identified a total of 4340 records (3982 from earlier searches and 358 from the 2017 update search). We discarded 3935 records that were not relevant and obtained 405 full‐text reports for assessment. Of these, 259 were excluded for the following reasons: no control; retention results only provided; first‐generation sealant material used or materials used were unclear; comparison of the same type of sealant materials; inclusion of other preventive treatments or programmes; participants were aged over 20 years.
We contacted authors of eight studies to obtain additional information to assess the eligibility of studies for inclusion (Gorseta 2014; Hepp 1990; Hotz 1978; Kervanto‐Seppälä 2008; Li 2008; Marković 2012; Oba 2009; Ulusu 2012); three provided additional information (Hepp 1990; Hotz 1978; Kervanto‐Seppälä 2008).
No language restrictions were applied; all non‐English language reports were translated for assessment. The review authors are fluent in English, German and Scandinavian languages; studies that were potentially eligible for inclusion published in Chinese, French, Hungarian, Italian, Japanese, Polish, Portuguese, Romanian, Russian, Spanish and Thai were translated for assessment.
Included studies
We included 38 (60 reports) studies that involved 7924 children (Amin 2008; Antonson 2012; Arrow 1995; Barja‐Fidalgo 2009; Baseggio 2010; Bojanini 1976; Bravo 2005; Brooks 1979; Charbeneau 1979; Chen 2012; Chen 2013; De Luca‐Fraga 2001; Dhar 2012; Erdoğan 1987; Forss 1998; Ganesh 2006; Guler 2013; Hunter 1988; Karlzén‐Reuterving 1995; Kervanto‐Seppälä 2008; Liu 2012; Liu 2014a; Liu 2014b; Mills 1993; Muller‐Bolla 2013; Pardi 2005; Poulsen 2001; Raadal 1996; Reisbick 1982; Richardson 1978; Rock 1978; Rock 1996; Sheykholeslam 1978; Sipahier 1995; Songpaisan 1995; Tagliaferro 2011; Tang 2014; Williams 1996).
Liu 2014b and Songpaisan 1995 were included in three comparisons (resin‐based sealant versus control without sealant, glass ionomer sealant versus control without sealant, and glass ionomer sealant versus resin‐based sealant).
See Characteristics of included studies and Figure 1.
Comparisons
Resin‐based sealant versus no sealant (n = 15; N = 3620 participants in 14 studies + 575 tooth pairs in 1 study) (Bojanini 1976; Bravo 2005; Brooks 1979; Charbeneau 1979; Erdoğan 1987; Hunter 1988; Liu 2012; Liu 2014b; Muller‐Bolla 2013; Reisbick 1982; Richardson 1978; Rock 1978; Sheykholeslam 1978; Songpaisan 1995; Tang 2014). (Hunter 1988 stated number of tooth pairs only, not children).
-
Glass ionomer‐based fissure sealant versus no sealant (n = 3; N = 905) (Liu 2014b; Songpaisan 1995; Tagliaferro 2011).
Tagliaferro 2011 (N = 218) evaluated if additional benefit was derived by using sealants among children receiving a regular oral health education programme (the evaluation was carried out separately in populations at high‐ and low‐risk of caries).
New types of fissure sealants (such as ormocer‐based sealants) versus no sealant (no studies reported these interventions).
Relative effectiveness of different sealant material types (n = 24; N = 4146) (Amin 2008; Antonson 2012; Arrow 1995; Barja‐Fidalgo 2009; Baseggio 2010; Chen 2012; Chen 2013; De Luca‐Fraga 2001; Dhar 2012; Forss 1998; Ganesh 2006; Guler 2013; Karlzén‐Reuterving 1995; Kervanto‐Seppälä 2008; Liu 2014a; Liu 2014b; Mills 1993; Pardi 2005; Poulsen 2001; Raadal 1996; Rock 1996; Sipahier 1995; Songpaisan 1995; Williams 1996).
23 studies compared glass ionomer‐based sealant versus resin‐based sealant (N = 4096). Guler 2013 with 50 participants compared ormocer‐based sealant versus low‐viscosity glass ionomer.
Study designs
We included 11 parallel‐group design studies (N = 3237) (Amin 2008; Barja‐Fidalgo 2009; Bravo 2005; Chen 2012; Liu 2012; Liu 2014a; Liu 2014b; Pardi 2005; Songpaisan 1995; Tagliaferro 2011; Tang 2014); 27 were split‐mouth studies, in which two interventions (fissure sealant versus no sealant and fissure sealant material versus other fissure sealant material) were randomly or quasi‐randomly allocated to teeth within a tooth pair (N = 4687).
Participants and settings
In the included studies, the children were aged 5 years to 16 years and represented general populations. In most studies, children were recruited from selected schools or dental clinics.
Six of the studies were conducted in China (Chen 2012; Chen 2013; Liu 2012; Liu 2014a; Liu 2014b; Tang 2014), five each in Brazil (Barja‐Fidalgo 2009; Baseggio 2010; De Luca‐Fraga 2001; Pardi 2005; Tagliaferro 2011) and the USA (Antonson 2012; Brooks 1979; Charbeneau 1979; Reisbick 1982; Sheykholeslam 1978), four in the UK (Mills 1993; Rock 1978; Rock 1996; Williams 1996), three in Turkey (Erdoğan 1987; Guler 2013; Sipahier 1995), two each in Finland (Forss 1998; Kervanto‐Seppälä 2008) and India (Dhar 2012; Ganesh 2006), one each in Australia (Arrow 1995), Canada (Richardson 1978), Colombia (Bojanini 1976), Egypt (Amin 2008), France (Muller‐Bolla 2013), New Zealand (Hunter 1988), Norway (Raadal 1996), Spain (Bravo 2005), Sweden (Karlzén‐Reuterving 1995), the Syrian Arab Republic (Poulsen 2001) and Thailand (Songpaisan 1995).
Interventions
Sealants were applied on sound occlusal surfaces or surfaces with enamel lesion of permanent first or second molars. Applications were reported to have been made to sound surfaces (Amin 2008; Arrow 1995; Baseggio 2010; Bojanini 1976; Bravo 2005; Brooks 1979; Charbeneau 1979; Chen 2013; De Luca‐Fraga 2001; Dhar 2012; Erdoğan 1987; Forss 1998; Ganesh 2006; Hunter 1988; Karlzén‐Reuterving 1995; Kervanto‐Seppälä 2008; Mills 1993; Pardi 2005; Raadal 1996; Reisbick 1982; Rock 1978; Rock 1996; Sheykholeslam 1978; Sipahier 1995; Songpaisan 1995; Tagliaferro 2011; Williams 1996), or in the same study on sound surfaces or on surfaces with enamel lesions (Antonson 2012; Barja‐Fidalgo 2009; Chen 2012; Guler 2013; Liu 2012; Liu 2014a; Liu 2014b; Muller‐Bolla 2013; Poulsen 2001; Richardson 1978; Tang 2014). One study reported that sealants were applied on tooth surfaces at caries risk (Kervanto‐Seppälä 2008), and two studies required deep fissures of the surfaces (Amin 2008; Baseggio 2010).
Sealant materials
Studies comparing sealant versus no sealant
The resin‐based sealant materials were autopolymerised resin sealant (bis‐GMA) (n = 10 studies), light‐cured resin sealant (Bravo 2005), and light‐polymerised resin sealant with fluoride (Liu 2012; Liu 2014b; Muller‐Bolla 2013; Tang 2014). Songpaisan 1995 used autopolymerised low‐viscosity glass ionomer sealant, Liu 2014b light‐cured low‐viscosity glass ionomer sealant, and Tagliaferro 2011 used resin‐modified glass ionomer cement.
Studies comparing relative effectiveness of glass ionomer‐based and resin‐based sealants
Low‐viscosity glass ionomer versus resin sealant (n = 15) (Antonson 2012; Arrow 1995; Chen 2013; Dhar 2012; Forss 1998; Ganesh 2006; Karlzén‐Reuterving 1995; Kervanto‐Seppälä 2008; Liu 2014b; Mills 1993; Poulsen 2001; Rock 1996; Sipahier 1995; Songpaisan 1995; Williams 1996).
High‐viscosity glass ionomer versus resin sealant (Barja‐Fidalgo 2009; Chen 2012; Liu 2014a).
Resin‐modified glass ionomer versus resin sealant (Amin 2008; Baseggio 2010; Raadal 1996).
Resin‐modified glass ionomer versus polyacid‐modified composite (compomer) (De Luca‐Fraga 2001).
Pardi 2005 included three sealant arms (resin‐modified glass ionomer, resin sealant, and compomer). Pardi 2005 did not include data in a form suitable for this review. Pardi 2005 defined caries as an active white spot lesion (translucent enamel alteration), presence of a microcavity (diameter < 1.5 mm across the fissure) or large cavity or filling. Results from Pardi 2005 are reported narratively in this review.
Re‐application of sealants
Re‐application of sealants was reported in Bravo 2005 (comparing sealant to control without sealant), Songpaisan 1995 (comparing sealant to no sealant and different sealant materials), and in four studies that compared only relative effectiveness of sealant materials (Arrow 1995; Forss 1998; Kervanto‐Seppälä 2008; Williams 1996). Bravo 2005 re‐applied sealants if there had been partial or total loss since the previous examination after 6, 12, 18, 24 and 36 months. Songpaisan 1995 conducted re‐application for those children whose sealants were either partially or all missing at the six month examination. Arrow 1995 reported that three of 465 teeth (0.6%) were resealed once with glass ionomer and four of 465 teeth (0.9%) with Delton. Forss 1998 reported that 22% of glass ionomer sealants were re‐applied during the first two years. A total of 15% of initially resin sealed teeth were resealed after the sealant was found to be defective in Kervanto‐Seppälä 2008. Williams 1996 reported that 7% of sealants were re‐applied at four years follow‐up (27 teeth with glass ionomer and 6 teeth with resin).
Co‐interventions
Studies comparing sealant versus no sealant
Tap water was fluoridated in areas where three studies took place (Bojanini 1976; Brooks 1979; Sheykholeslam 1978). Half the children in Hunter 1988 used fluoridated water. Water was not fluoridated in seven studies (Liu 2012; Muller‐Bolla 2013; Reisbick 1982; Richardson 1978; Songpaisan 1995; Tagliaferro 2011; Tang 2014). Five studies did not report if water supplies were fluoridated (Bravo 2005; Charbeneau 1979; Erdoğan 1987; Liu 2014b; Rock 1978).
Motivation and instruction, such as achieving good oral hygiene and use of fluoridated toothpaste, were reported in three studies (Muller‐Bolla 2013; Tagliaferro 2011; Tang 2014).
Information on diet (e.g. snacking habits) was provided only by Liu 2012. At study baseline, 13% of children in the sealant group and 29% in the placebo group consumed snacks twice or more daily (no information was provided on snacking habits during the trial) (Liu 2012).
Studies comparing one sealant material versus another sealant material
Tap water was fluoridated in areas where three studies took place (Arrow 1995; Barja‐Fidalgo 2009; Rock 1996). Water was not fluoridated in 11 studies (Amin 2008; Chen 2012; Chen 2013; Dhar 2012; Forss 1998; Ganesh 2006; Guler 2013; Kervanto‐Seppälä 2008; Liu 2014a; Songpaisan 1995; Williams 1996). Ten studies did not report if water supplies were fluoridated. Chen 2013 reported application of topical fluoride foam (6000 ppm) at clinic recalls at 6 and 12 months.
Five studies reported motivation and instruction activities (Amin 2008; Chen 2013; Dhar 2012; Ganesh 2006; Liu 2014a).
Liu 2014a reported information on diet. At study baseline, 26.1% of children in the resin group and 19.4% in the glass ionomer group consumed snacks twice or more daily (Liu 2014a).
Caries prevalence in children at baseline
Studies comparing sealant versus no sealant
The baseline caries prevalence of participants was stated in six studies (Bravo 2005; Liu 2012; Liu 2014b; Muller‐Bolla 2013; Songpaisan 1995; Tagliaferro 2011). Songpaisan 1995 reported the initial mean of decayed, missing, filled permanent teeth (DMFT) of children aged from 12 to 13 years (1.81 ± 1.84); Bravo 2005 (study conducted in the 1990s) reported baseline mean of decayed, filled deciduous teeth (dft) in sealant group (2.24; SD 2.59) and control group (2.98, SD 2.90) children aged 6 to 8 years.
Liu 2012 reported baseline mean decayed, missing, filled deciduous teeth (dmft) (sealant group = 3.19 (2.68); placebo group = 3.55 (2.54)) for children aged 8 years to 10 years. Liu 2014b reported baseline mean dmft‐index (including decayed, missing and filled permanent and deciduous teeth) of children aged 7 years to 9 years (resin‐based sealant group = 5.38 (SD 2.73); glass ionomer sealant group = 5.29 (SD 3.43); control group = 5.18 (SD 3.30)). Muller‐Bolla 2013 reported mean d3‐6mft level of children aged 6 years (2.8 (SD ±3.3)) and mean D3‐6MFT‐M1 (0.2 (SD ± 0.5)). Tagliaferro 2011 reported the baseline mean dmft‐index for high‐caries risk children receiving sealants (4.51 (2.81)) and high‐caries risk children receiving oral health education (4.53 (3.04)). In low‐caries risk groups, dmft + DMFT was zero.
Three studies comparing sealant with no sealant from the 1970s documented that caries‐free children were not included in the studies (Bojanini 1976; Brooks 1979; Sheykholeslam 1978).
Studies comparing one sealant material versus another sealant material
Five studies reported baseline caries prevalence for the study population (Arrow 1995; Chen 2012; Dhar 2012; Kervanto‐Seppälä 2008; Poulsen 2001). Arrow 1995 reported initial dmf (1.64, SD ± 2.45) of children (mean age 7 years); Chen 2012 reported initial dmft (5.0, SD 2.5) in children aged 7 to 9 years. Dhar 2012 reported caries prevalence of children aged 6 to 10 years (63%) and DMFT (2.60). Baseline DMFT was 0.57 in children aged 13 years in Kervanto‐Seppälä 2008. Poulsen 2001 did not report baseline caries information, but referred to general caries levels in Syria. The average DMFT value was 0.6 to 0.7 in children aged 6 to 7 years in Damascus based on data collected by the WHO Regional Demonstration, Training and Research Center for Oral Health (Poulsen 2001).
Seven studies provided some information on caries risk of participants (Antonson 2012; Barja‐Fidalgo 2009; Chen 2013; Forss 1998; Ganesh 2006; Liu 2014a; Rock 1996). Antonson 2012 included children at high risk of developing caries identified according to socio‐economic background; two studies reported that caries‐free children were not included (Barja‐Fidalgo 2009; Rock 1996). Chen 2013 categorised children based on caries risk severity: children with no or one carious tooth (dmft < 2) were included in the low risk group; and children with dmft > 5 were allocated to the high risk caries group. Chen 2013 excluded children with dmft 2 to 5. Liu 2014a did not report baseline caries information for children in the study age (mean age 7.8 years) but referred to caries prevalence of children aged 12 years (29.8%, mean DMFT score 0.54). Forss 1998 assumed the caries risk of participants was low, and in Ganesh 2006, risk was low to high.
Outcome measures
Most included studies (n = 35) reported incidence of dentinal carious lesions on treated occlusal surfaces of first permanent molars dichotomously (yes/no). Three studies reported continuous data as mean decayed, missing and filled (DMF) increments (Songpaisan 1995; Tagliaferro 2011; Tang 2014). As well as visual‐tactile caries diagnostic methods, the studies also used the following methods for caries diagnosis: x‐rays (Barja‐Fidalgo 2009; Raadal 1996) or x‐rays when necessary (Baseggio 2010); fibre‐optic transillumination (Kervanto‐Seppälä 2008); laser fluorescence methods (Baseggio 2010; Liu 2014b); and intra‐oral camera (matching the first and follow‐up images of the sealants) (Guler 2013).
Intra‐examiner agreement for caries diagnosis was stated in eight studies, the kappa co‐efficient was between 0.75 and 0.92 (Chen 2013; Guler 2013; Liu 2012; Muller‐Bolla 2013; Pardi 2005; Poulsen 2001; Songpaisan 1995; Tagliaferro 2011). The inter‐examiner agreement for caries diagnosis was stated in 13 studies (Barja‐Fidalgo 2009; Bravo 2005; Brooks 1979; Charbeneau 1979; Chen 2012; Chen 2013; Dhar 2012; Kervanto‐Seppälä 2008; Liu 2014a; Liu 2014b; Raadal 1996; Tang 2014; Williams 1996). The kappa co‐efficient for inter‐examiner agreement was mainly over 0.8. Two studies reported kappa co‐efficient value of 1.0 (Barja‐Fidalgo 2009: Dhar 2012); the lowest inter‐examiner reliability was reported by Kervanto‐Seppälä 2008 with a value of 0.42 (10 dentists).
Four studies considered adverse events (Bravo 2005; Liu 2012; Liu 2014a; Tagliaferro 2011).
Retention was reported as proportions of completely retained, partially retained and lost sealants.
Detailed outcomes for each study are reported in Characteristics of included studies.
Funding sources
Twelve studies were supported by government or academic sources or independent research foundations (Antonson 2012; Bravo 2005; Chen 2013; Forss 1998; Karlzén‐Reuterving 1995; Kervanto‐Seppälä 2008; Liu 2012; Liu 2014a; Liu 2014b; Pardi 2005; Poulsen 2001; Tagliaferro 2011). Three studies were supported by government or academic sources or independent research foundations, but one or more sealant material was donated by a sealant manufacturer (Chen 2012; De Luca‐Fraga 2001; Songpaisan 1995). Six studies were at least partly supported by a sealant manufacturer (Brooks 1979; Muller‐Bolla 2013; Rock 1978; Rock 1996; Sheykholeslam 1978; Williams 1996). Two authors of the study by Bojanini 1976 were affiliated with a sealant manufacturer. Guler 2013 reported receiving no institutional, private or corporate financial support (the authors were from universities). Fifteen studies did not report on funding sources.
Excluded studies
The Characteristics of excluded studies table presents reasons for exclusion of studies. Only studies that compared sealant with a control without sealant or different sealant material types for prevention of caries were included in the table. We excluded studies without control.
The reasons for exclusion varied, and in many studies, there were several reasons for exclusion. In 41 of 71 excluded studies, randomisation was not stated or unclear; or the study design was clearly other than a randomised clinical trial. Other main reasons for exclusion were that the study design was not eligible for this review or the study included other preventive treatments (23 studies) or the study had significant data flaws (7 studies).
Risk of bias in included studies
We contacted authors of included studies to obtain additional information to assess methodological quality if information in the report was insufficient to make final decisions. We requested additional information from authors of 18 studies (Amin 2008; Barja‐Fidalgo 2009; Bravo 2005; De Luca‐Fraga 2001; Dhar 2012; Forss 1998; Ganesh 2006; Guler 2013; Kervanto‐Seppälä 2008; Liu 2012; Muller‐Bolla 2013; Pardi 2005; Poulsen 2001; Raadal 1996; Sheykholeslam 1978; Sipahier 1995; Songpaisan 1995; Tagliaferro 2011). Additional information for four of those studies was not available for this update (Amin 2008; De Luca‐Fraga 2001; Raadal 1996; Songpaisan 1995).
Overall risk of bias was assessed as high for all studies for the five key domains of allocation concealment, blinding of outcome assessment, incomplete outcome data, selective reporting and baseline comparability of study groups (Figure 3). This was because we assessed that all sealant studies had high detection bias (outcome assessment blinded was not possible).
See detailed criteria for risk of bias assessment for each specific domain in Table 7.
Allocation
Studies comparing sealant versus no sealant
Random sequence generation was adequate indicating low risk of bias in 12 of 16 (75%) studies for this comparison (Bojanini 1976; Brooks 1979; Charbeneau 1979; Hunter 1988; Liu 2012; Muller‐Bolla 2013; Reisbick 1982; Richardson 1978; Rock 1978; Sheykholeslam 1978; Tagliaferro 2011; Tang 2014). Random sequencing methods applied were use of a previously established randomisation table or list of random numbers, using dice or coin tossing. In one split‐mouth study (Hunter 1988), allocation of a tooth to an intervention was quasi‐randomised (the sealed tooth was alternating between the left and right sides of the mouth for tooth pairs) and was graded as low risk of bias (we considered that in preventive split‐mouth studies, the risk of selection bias is minimal, see our justifications in 'Criteria for risk of bias assessment' in Table 7). Bravo 2005 was assessed at high risk of bias, and three studies were at unclear risk of bias (Erdoğan 1987; Liu 2014b; Songpaisan 1995).
We assessed allocation concealment at low risk of bias in 11 studies (69%) (Bojanini 1976; Brooks 1979; Charbeneau 1979; Hunter 1988; Liu 2012; Muller‐Bolla 2013; Reisbick 1982; Richardson 1978; Rock 1978; Sheykholeslam 1978; Tagliaferro 2011). Information on allocation concealment methods and allocation concealment was unclear in four studies (Erdoğan 1987; Liu 2014b; Songpaisan 1995; Tang 2014), and assessed at high risk of bias in Bravo 2005.
Studies comparing one sealant versus another sealant
Random sequence generation was assessed as low risk of bias, in 16 of 24 (67%) studies providing data for comparison of different sealant materials (Antonson 2012; Arrow 1995; Barja‐Fidalgo 2009; Baseggio 2010; Chen 2012; Chen 2013; Dhar 2012; Forss 1998; Ganesh 2006; Guler 2013; Liu 2014a; Mills 1993; Pardi 2005; Poulsen 2001; Rock 1996; Williams 1996). In two split‐mouth studies, allocation of a tooth to an intervention was quasi‐random (Arrow 1995; Baseggio 2010). Eight studies either provided no information, or reporting was unclear, in relation to sequence generation (unclear risk of bias) (Amin 2008; De Luca‐Fraga 2001; Karlzén‐Reuterving 1995; Kervanto‐Seppälä 2008; Liu 2014b; Raadal 1996; Sipahier 1995; Songpaisan 1995).
Allocation concealment was assessed at low risk of bias in 15 (63%) studies (Antonson 2012; Arrow 1995; Barja‐Fidalgo 2009; Baseggio 2010; Chen 2012; Chen 2013; Dhar 2012; Forss 1998; Ganesh 2006; Guler 2013; Liu 2014a; Mills 1993; Poulsen 2001; Rock 1996; Williams 1996). Nine studies either provided no information, or reporting was unclear, in relation to random allocation concealment methods (unclear risk of bias) (Amin 2008; De Luca‐Fraga 2001; Karlzén‐Reuterving 1995; Kervanto‐Seppälä 2008; Liu 2014b; Pardi 2005; Raadal 1996; Sipahier 1995; Songpaisan 1995).
Blinding
Performance bias
Assessment of blinding of participants and personnel was not performed because we thought that possible knowledge of personnel and participants about which intervention group a child belonged was unlikely to cause bias (e.g. affect dental behaviour of a child during the trial, especially when follow‐up was long (≥ 1 year in this review)).
Detection bias
Studies comparing sealant versus no sealant
We assessed blinding of outcome assessment for caries at high risk of bias for all trials because sealant materials are visible and blinding of the outcome assessor was possible only if a sealant had been lost.
Studies comparing one sealant versus another sealant
We assessed blinding of outcome assessment for caries at high risk of bias for all trials because although sealant materials may have similar appearances when applied, the outcome assessor could discriminate between them at follow‐up (materials change over time, e.g. materials including glass‐ionomer lose their glossy appearance more rapidly than resins).
Incomplete outcome data
Studies comparing resin sealant versus no sealant
At 12 months follow‐up, we assessed six of seven studies that compared resin sealant to no sealant at low risk of bias (Bojanini 1976; Charbeneau 1979; Muller‐Bolla 2013; Richardson 1978; Rock 1978; Sheykholeslam 1978). Erdoğan 1987 was assessed at high risk of bias as missing data rate was over 25%.
At 24 months follow‐up, we assessed eight studies at low risk of bias (Bojanini 1976; Brooks 1979; Charbeneau 1979; Liu 2012; Richardson 1978; Sheykholeslam 1978; Songpaisan 1995; Tang 2014). Liu 2014b was assessed at unclear risk of bias.
At 36 months follow‐up, we assessed five studies at low risk of bias (Bojanini 1976; Charbeneau 1979; Hunter 1988; Richardson 1978; Sheykholeslam 1978). Brooks 1979 and Rock 1978 were assessed at high risk of bias.
At 48 to 54 months follow‐up, we assessed two of five studies at low risk of bias (Charbeneau 1979; Richardson 1978), and two studies at high risk of bias (Brooks 1979; Erdoğan 1987). Bravo 2005 provided no information on drop‐outs by group and judged at unclear risk of bias.
Richardson 1978, which reported 60 months follow‐up, was assessed at low risk of bias.
We assessed the only studies that measured outcomes at 72 and 84 months (Brooks 1979) and 108 months (Bravo 2005) to be at high risk of bias for this domain.
Reisbick 1982 was assessed at high risk of bias for all reported follow‐up periods (14, 20 and 32 months).
Studies comparing glass ionomer‐based sealant versus no sealant
Songpaisan 1995 and Tagliaferro 2011 were assessed at low risk of bias at 24 months follow‐up, and Liu 2014b, at unclear risk of bias.
Studies comparing one sealant versus another sealant
Glass ionomer‐based sealant versus resin sealant
All six studies were assessed at low risk of bias at 12 months follow‐up (Amin 2008; Baseggio 2010; Dhar 2012; Karlzén‐Reuterving 1995; Rock 1996; Sipahier 1995).
At 24 months follow‐up, we assessed 11 of 16 studies (69%) at low risk of bias (Amin 2008; Baseggio 2010; Chen 2012; Chen 2013; Dhar 2012; Forss 1998; Ganesh 2006; Karlzén‐Reuterving 1995; Liu 2014a; Rock 1996; Songpaisan 1995). Liu 2014b had unclear risk of bias; and four studies were assessed at high risk of bias (Antonson 2012; Mills 1993; Poulsen 2001; Williams 1996).
At 36 to 48 months follow‐up, we assessed six of nine studies at low risk of bias for this domain (Arrow 1995; Baseggio 2010; Chen 2012; Karlzén‐Reuterving 1995; Raadal 1996; Rock 1996); three studies were at high risk of bias (Kervanto‐Seppälä 2008; Poulsen 2001; Williams 1996).
At 60 months, we assessed the only study in this comparison at high risk of bias (Barja‐Fidalgo 2009). At 84 months, the only study in this comparison was also assessed at high risk of bias (Forss 1998).
Other sealant material comparisons
We assessed De Luca‐Fraga 2001 at one year and Pardi 2005 at 24 months follow‐up at low risk of bias for this domain. Guler 2013 was assessed at high risk of bias after 24 months follow‐up.
Selective reporting
Studies comparing sealant versus no sealant
All 16 studies in this comparison reported all prespecified outcomes adequately and were assessed at low risk of bias.
Studies comparing one sealant versus another sealant
All 24 studies in this comparison reported all prespecified outcomes adequately and were assessed at low risk of bias.
Other potential sources of bias
Studies comparing sealant versus no sealant
Comparability of the groups
Demographic characteristics (such as sex, age, and socio‐economic level) and baseline caries risk were described and assessed to be balanced across groups in all 16 studies providing information for this comparison.
Co‐interventions
In 12 of 16 studies (75%), we assessed this domain at low risk of bias. If co‐interventions were used, they were fluoridated tap water or toothpaste, which were permitted in the protocol for this review. No information was provided in four studies which were assessed at unclear risk of bias (Charbeneau 1979; Erdoğan 1987; Liu 2014b; Rock 1978).
Studies comparing one sealant versus another sealant
Comparability of the groups
Demographic characteristics and baseline caries risk were described and assessed to be balanced across the groups in 21 of 24 (88%) studies comparing different sealant materials. We assessed groups at the analysis point (60 months) to be unbalanced in Barja‐Fidalgo 2009. Information was insufficient in Kervanto‐Seppälä 2008 and Liu 2014a to assess this domain (unclear risk of bias).
Co‐interventions
This domain was assessed at low risk of bias in 14 or 24 studies (58%); 10 studies provided no information and were assessed at unclear risk of bias (Antonson 2012; Baseggio 2010; De Luca‐Fraga 2001; Karlzén‐Reuterving 1995; Liu 2014b; Mills 1993; Pardi 2005; Poulsen 2001; Raadal 1996; Sipahier 1995).
Effects of interventions
See: Table 1; Table 2; Table 3
Effectiveness of sealants: dentine caries in permanent molars
1. Resin/composite‐based fissure sealant versus no sealant
At 12, 24, 36, and 48 to 54 months
Fifteen studies provided data for the comparison of resin sealants to no sealant (10 split‐mouth studies and 5 parallel‐group studies). Eleven studies were pooled for meta‐analysis (2 parallel‐group studies and 9 split‐mouth studies reporting summary data as paired form or as marginals). Seven studies at 12, 24, and 36 months, and four studies at 48 to 54 months were meta‐analysed. Meta‐analyses at 12, 36, and 48 to 54 months included only split‐mouth studies but the meta‐analysis at 24 months also included two parallel‐group studies.
Results of pooled studies in meta‐analyses comparing resin sealant with no sealant were highly significant (P < 0.00001) at 12 months follow‐up (OR 0.17, 95% CI 0.10 to 0.30; Analysis 1.1); 24 months follow‐up (OR 0.12, 95% CI 0.08 to 0.19; Analysis 1.2); 36 months follow‐up (OR 0.17, 95% CI 0.11 to 0.27; Analysis 1.3); and 48 to 54 months follow‐up (OR 0.21, 95% CI 0.16 to 0.28; Analysis 1.4) (Table 4). Becker‐Balagtas ORs were expressed for all split‐mouth studies.
1.1. Analysis.
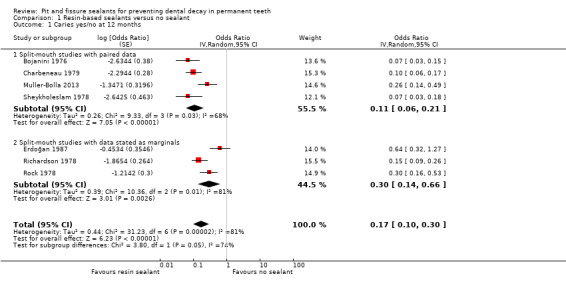
Comparison 1 Resin‐based sealants versus no sealant, Outcome 1 Caries yes/no at 12 months.
1.2. Analysis.
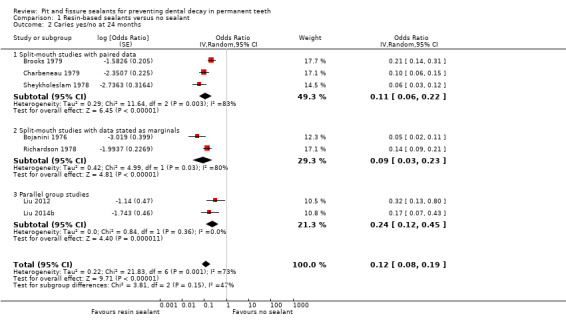
Comparison 1 Resin‐based sealants versus no sealant, Outcome 2 Caries yes/no at 24 months.
1.3. Analysis.
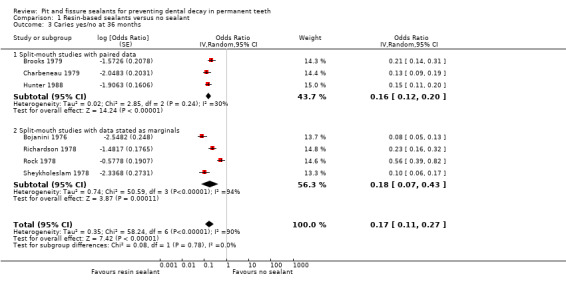
Comparison 1 Resin‐based sealants versus no sealant, Outcome 3 Caries yes/no at 36 months.
1.4. Analysis.
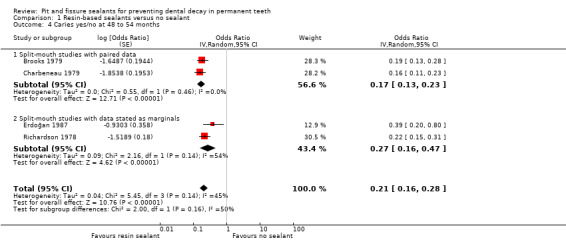
Comparison 1 Resin‐based sealants versus no sealant, Outcome 4 Caries yes/no at 48 to 54 months.
There was significant statistical heterogeneity for these comparisons (Analysis 1.1; Analysis 1.2; Analysis 1.3; Analysis 1.4). However, because all results from individual trials showed significant benefit for the sealant, we felt it was appropriate to pool results in a meta‐analysis using the random‐effects model.
In each meta‐analysis at 12, 24, 36, and 48 to 54 months follow‐up periods, the main findings were based on all studies providing data for those follow‐ups. These results are also presented in Table 1. This was because in sensitivity analyses (excluding split‐mouth studies with data presented only in marginals), the interpretation of results did not alter. Results from split‐mouth studies with data reported in paired form were only slightly more in favour of sealants than from analyses that also included split‐mouth studies with data presented only as marginals at 12 months follow‐up (OR 0.11, 95% CI 0.06 to 0.21); 24 months follow‐up (OR 0.14, 95% CI 0.08 to 0.24); 36 months (OR 0.16, 95% CI 0.12 to 0.20), and 48 to 54 months follow‐up (OR 0.17, 95% CI 0.13 to 0.23). This may be because the conservative intracluster correlation co‐efficient (ICC) 0.05 was used in calculations of studies with data presented only as marginals.
In contrast to other study reports, Liu 2014b recorded enamel lesions with microcavitation as cavitated caries (ICDAS II scale, code 3) (in addition to dentine caries). We saw that this had only a small influence on the pooled effect estimate at 24 months because the outcome in this review was the incidence of caries, and Liu 2014b used the same diagnostic scoring both at the start of the trial and at the follow‐up.
Three parallel‐group studies (Bravo 2005; Songpaisan 1995; Tang 2014) and one split‐mouth study (Reisbick 1982) confirmed the results of the meta‐analyses, from 24 to 48 months. Songpaisan 1995 (a 24 month study) supplied data comparing second generation resin sealant with a control in children aged from 12 to 13 years and found significantly (P < 0.00001) more caries in control group children, with a difference of mean number of decayed, filled permanent surfaces (DFS ‐0.65, 95% CI ‐0.83 to ‐0.47; Analysis 1.6) (Table 5).
1.6. Analysis.
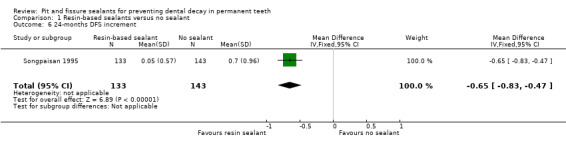
Comparison 1 Resin‐based sealants versus no sealant, Outcome 6 24‐months DFS increment.
Tang 2014 (a 24‐month study) compared light‐cured, fluoride‐releasing resin‐based sealant with control and found significantly (P < 0.0001) more caries in the control group children, with a mean difference (MD) of increments of number of decayed, missing and filled surfaces (DMFS) of permanent first molars (DMFS ‐0.24, 95% CI ‐0.36 to ‐0.12; Analysis 1.7). In the analysis, the sample sizes of the groups were reduced to their effective sample sizes (as recommended in Higgins 2011b; intracluster correlation co‐efficient of 0.05 was used in calculations). The sample sizes were reduced because the trial did not report that clustering of data would have been taken into account in the analyses (each child had an average 3.8. teeth under evaluation, thus a child is a cluster). The study reported mean increment of DMFS in the sealant group of 0.06 (SD 0.26) versus 0.30 (SD 0.79) (ANOVA analysis).
1.7. Analysis.
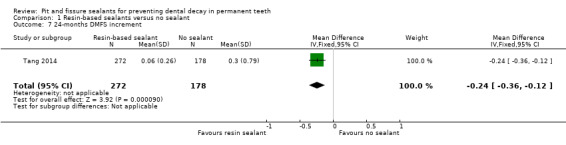
Comparison 1 Resin‐based sealants versus no sealant, Outcome 7 24‐months DMFS increment.
Bravo 2005 found significantly (P < 0.0001) more caries in control group children (RR 0.24, cluster corrected 95% CI 0.12 to 0.45; Analysis 1.5) at 48 months of follow‐up (Table 4).
1.5. Analysis.
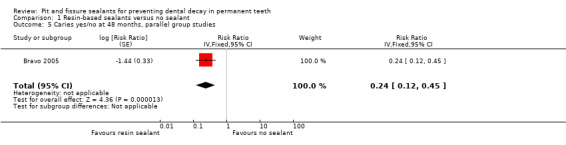
Comparison 1 Resin‐based sealants versus no sealant, Outcome 5 Caries yes/no at 48 months, parallel group studies.
Reisbick 1982, a split‐mouth study, reported effectiveness of 90%, 80%, and 70%, at 14 months, 20 months, and 32 months follow‐up, respectively.
At 60 months
One study provided data at 60 months follow‐up. Richardson 1978 found significantly more caries in control teeth (Becker‐Balagtas OR 0.31, 95% CI 0.23 to 0.43; P < 0.00001; Analysis 1.8).
1.8. Analysis.
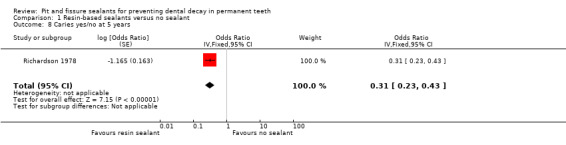
Comparison 1 Resin‐based sealants versus no sealant, Outcome 8 Caries yes/no at 5 years.
At 72 and 84 months
One split‐mouth study provided data for these comparisons. Brooks 1979 found significantly more caries in the control teeth: at 72 months follow‐up (RR 0.45, 95% CI 0.36 to 0.58; Analysis 1.9) and 84 months follow‐up (RR 0.45, 95% CI 0.34 to 0.59; Analysis 1.10). Caries reductions were 55% at 72 and 84 months.
1.9. Analysis.
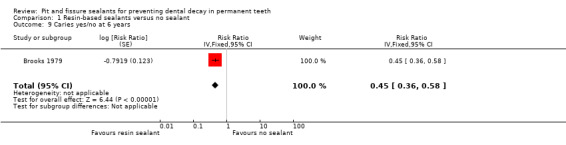
Comparison 1 Resin‐based sealants versus no sealant, Outcome 9 Caries yes/no at 6 years.
1.10. Analysis.
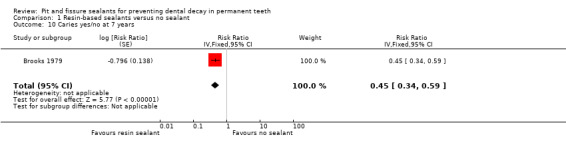
Comparison 1 Resin‐based sealants versus no sealant, Outcome 10 Caries yes/no at 7 years.
At 9 years
One cluster‐randomised study provided data for this comparison. Bravo 2005 found significantly more caries in the control group children (RR 0.35, cluster corrected 95% CI 0.22 to 0.55; P < 0.0001; Analysis 1.11). After nine years, 27% of sealed surfaces were decayed compared to 77% of surfaces without sealant.
1.11. Analysis.
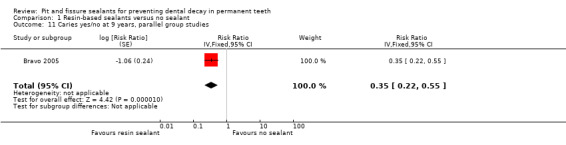
Comparison 1 Resin‐based sealants versus no sealant, Outcome 11 Caries yes/no at 9 years, parallel group studies.
2. Glass ionomer‐based fissure sealant versus no sealant
Glass ionomer sealant versus no sealant at 24 months
Two parallel‐group studies provided data for this comparison comparing low‐viscosity glass ionomers with a control without sealant (Liu 2014b; Songpaisan 1995).
Liu 2014b found slightly more caries in the control group children than the glass ionomer group children (OR 0.46, 95% CI 0.23 to 0.91; P = 0.03; Analysis 2.1). Songpaisan 1995 compared 24‐month DFS increments at age group 12 to 13 years for two glass ionomer sealant groups with one control group of children receiving no treatment. We combined data from the two glass ionomer groups. The difference failed to reach significance (DFS MD ‐0.18, 95% CI ‐0.39 to 0.03; P = 0.09; Analysis 2.2) (Table 5).
2.1. Analysis.
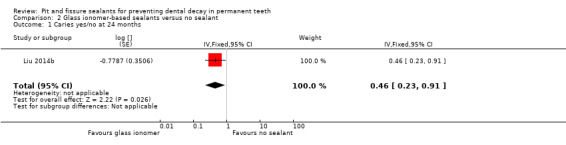
Comparison 2 Glass ionomer‐based sealants versus no sealant, Outcome 1 Caries yes/no at 24 months.
2.2. Analysis.
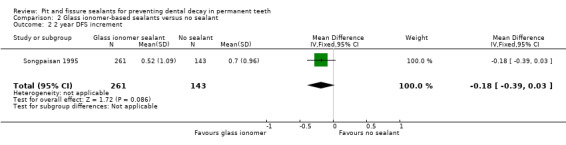
Comparison 2 Glass ionomer‐based sealants versus no sealant, Outcome 2 2 year DFS increment.
Resin‐modified glass ionomer cement plus oral health education programme versus oral health education programme alone at 24 months
Tagliaferro 2011 provided results for comparison resin‐modified glass ionomer cement plus oral health education every three months versus oral health education every three months alone. The comparison was performed separately for high‐risk and low‐risk children. The groups compared were: high‐risk children with sealant application plus oral health education (HRS) versus high‐risk children who received oral health education alone (HRC); and low‐risk children with sealant application plus oral health education (LRS) versus low‐risk children who received oral health education alone (LRC).
After 24 months, only the high‐risk children with sealant and education programme group children showed statistically lower DMF (decayed, missing and filled) increments on occlusal surfaces of first permanent molars compared with the high‐risk children who received oral health education alone. For low‐risk groups, no statistical difference was observed among treatments. Tagliaferro 2011 concluded "that in a 2‐year period, oral health education was sufficient to control occlusal caries in low risk children while for high risk children, sealant application in addition to oral health education was considered the best strategy". The retention rate was reported to be 84% after 24 months (16% of sealed teeth showed total sealant loss).
3. New types of fissure sealants compared with no sealant
No studies comparing new types of fissure sealants with no sealant were included.
4. One sealant material versus another sealant material ‐ glass ionomer‐based sealant versus resin‐based sealant
We included 21 studies (N = 3883) that provided data for comparison of glass ionomer‐based sealant versus resin‐based sealant at 12, 24, 36 to 48, 60 and 84 months follow‐up periods. Six studies found greater caries reductions for resin‐based sealants than glass ionomers (Baseggio 2010; Kervanto‐Seppälä 2008; Poulsen 2001; Raadal 1996; Rock 1996; Songpaisan 1995). Arrow 1995 found that glass ionomers performed better than resin‐based sealants. Twelve studies did not find a difference between these materials (Amin 2008; Antonson 2012; Barja‐Fidalgo 2009; Chen 2013; Dhar 2012; Forss 1998; Ganesh 2006; Karlzén‐Reuterving 1995; Liu 2014a; Liu 2014b; Mills 1993; Sipahier 1995). Williams 1996 found resin‐based sealants performed better than glass ionomers at 24 months but not at 48 months. Chen 2012 found high‐viscosity glass ionomers performed better than resins at 48 months but not at 24 months.
At 12 months
Four studies that compared low‐viscosity glass ionomers versus resin sealants (Dhar 2012; Karlzén‐Reuterving 1995; Rock 1996; Sipahier 1995) and two studies that compared resin‐modified glass ionomers versus resin sealants (Amin 2008; Baseggio 2010) did not find differences between the resin‐based and glass ionomer‐based sealants at 12 months (pooled Becker‐Balagtas (BB) OR 1.47, 95% CI 0.64 to 3.37; P = 0.37; Analysis 4.1) (Table 4). None of the studies favoured either material significantly at 12 months. Dhar 2012 also reported results for teeth where occlusal surfaces were prepared before sealant application (no teeth developed caries during 12 months follow‐up).
4.1. Analysis.
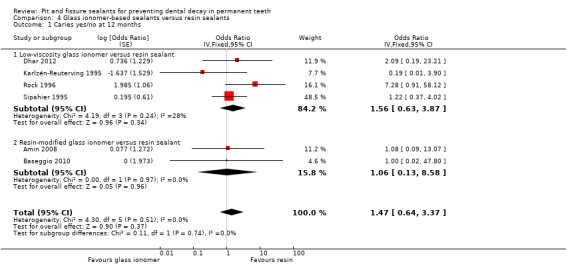
Comparison 4 Glass ionomer‐based sealants versus resin sealants, Outcome 1 Caries yes/no at 12 months.
At 24 months
Sixteen studies provided data for this comparison: 12 compared low‐viscosity glass ionomers with resin‐based sealants (Antonson 2012; Chen 2013; Dhar 2012; Forss 1998; Ganesh 2006; Karlzén‐Reuterving 1995; Liu 2014b; Mills 1993; Poulsen 2001; Rock 1996; Songpaisan 1995; Williams 1996), two compared high‐viscosity glass ionomers with resin‐based sealants (Chen 2012; Liu 2014a) and two compared resin‐modified glass ionomers with resin‐based sealants (Amin 2008; Baseggio 2010).
Eleven studies did not find a difference between materials: eight of 12 studies comparing low‐viscosity glass ionomers with resin‐based sealants (Antonson 2012; Chen 2013; Dhar 2012; Forss 1998; Ganesh 2006; Karlzén‐Reuterving 1995; Liu 2014b; Mills 1993), both studies comparing high‐viscosity glass ionomers with resin‐based sealants (Chen 2012; Liu 2014a), and one out of two studies comparing resin‐modified glass ionomers with resin‐based sealants (Amin 2008) (Table 4; Analysis 4.2).
4.2. Analysis.
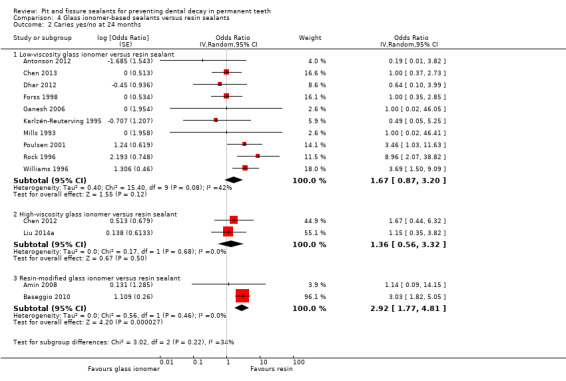
Comparison 4 Glass ionomer‐based sealants versus resin sealants, Outcome 2 Caries yes/no at 24 months.
Five studies favoured resin sealants over glass ionomers. Three studies comparing low‐viscosity glass ionomers with resin‐based sealants found resin‐based sealants significantly superior compared to glass ionomers (Rock 1996; Songpaisan 1995; Williams 1996) (Table 4; Analysis 4.2; Analysis 4.3). Poulsen 2001 found that resin sealants performed slightly better than low‐viscosity glass ionomer. Baseggio 2010, which compared resin‐modified glass ionomer with resin‐based sealant, also found benefits for resins compared to glass ionomer (Analysis 4.2).
4.3. Analysis.
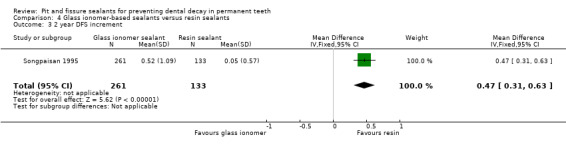
Comparison 4 Glass ionomer‐based sealants versus resin sealants, Outcome 3 2 year DFS increment.
A subgroup analysis comparing low and high viscosity glass ionomers to resins did not find a difference between either form of glass ionomers and resins (OR 1.67, 95% CI 0.87 to 3.20, P = 0.12, and OR 1.36, 95% CI 0.56 to 3.32, P = 0.50, respectively; Analysis 4.2). However, the subgroup analysis comparing resin‐modified glass ionomer with resin‐based sealant (with two studies) favoured resins over glass ionomers (OR 2.92, 95% CI 1.77 to 4.81, P < 0.0001; Analysis 4.2). Only the other study in this analysis favoured resin‐based sealants (Baseggio 2010 with 320 children). The study reported low retention rates for glass ionomers (80% of sealants lost after 24 months) but high retention for resins (0% lost). In contrast to other studies in this comparison, Baseggio 2010 included only adolescents aged from 12 to 16 years and sealed second permanent molars. The study did not report on children's caries risk but the proportion of decayed sealed surfaces was fairly low in both groups (3% of resin sealed teeth and 9% of surfaces sealed with glass ionomer were decayed).
At 36 to 48 months
Nine studies provided data for this comparison: six compared low‐viscosity glass ionomers with resin‐based sealants (Arrow 1995; Karlzén‐Reuterving 1995; Kervanto‐Seppälä 2008; Poulsen 2001; Rock 1996; Williams 1996). Chen 2012 compared high‐viscosity glass ionomer with resin‐based sealant; two studies compared resin‐modified glass ionomers with resin‐based sealants (Baseggio 2010; Raadal 1996).
Because there was significant heterogeneity and divergent results among studies in this comparison, only narrative results are given (Table 4; Analysis 4.4).
4.4. Analysis.
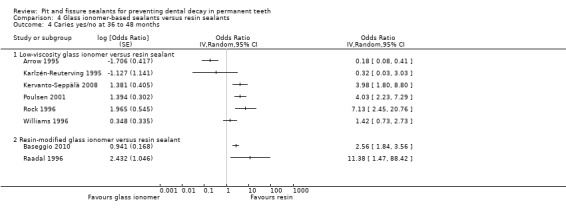
Comparison 4 Glass ionomer‐based sealants versus resin sealants, Outcome 4 Caries yes/no at 36 to 48 months.
Five studies found that resin‐based sealants were significantly superior to glass ionomer‐based sealants. Three studies compared low‐viscosity glass ionomers with resins (Kervanto‐Seppälä 2008; Poulsen 2001; Rock 1996) and two studies compared resin‐modified glass ionomer with resins (Baseggio 2010; Raadal 1996). Poulsen 2001 found a benefit for second‐generation resin sealant (BB OR 4.03, 95% CI 2.23 to 7.29) compared to low‐viscosity glass ionomers, Kervanto‐Seppälä 2008 found benefit for third‐generation sealant (BB OR 3.98, 95% CI 1.80 to 8.80), and Rock 1996 found benefit for fourth‐generation sealant (BB OR 7.13, 95% CI 2.45 to 20.76). Baseggio 2010 found a significant benefit in favour of fluoride‐releasing resin‐based sealant (BB OR 2.56, 95% CI 1.84 to 3.56) compared to resin‐modified glass ionomer, and Raadal 1996 found in favour of second‐generation resin sealant (BB OR 11.38, 95% CI 1.47 to 88.42) (Analysis 4.4).
Two studies did not find differences between low‐viscosity glass ionomers with resins at 36 to 48 months (Karlzén‐Reuterving 1995; Williams 1996) (Analysis 4.4). Two studies found glass ionomer‐based sealants to be superior (Arrow 1995; Chen 2012). The split‐mouth study by Arrow 1995 found a difference in favour of low‐viscosity glass ionomer sealant compared to second‐generation resin sealant at 44 months (BB OR 0.18, 95% CI 0.08 to 0.41; Analysis 4.4). In Chen 2012, the cumulative survival rate of dentin caries lesion‐free pits and fissures in atraumatic restorative treatment (ART) high‐viscosity glass‐ionomer with light‐curing groups (98%) was statistically significantly higher than in the resin‐composite group (96.4%, P = 0.04) after 48 months.
The number of decayed sealed teeth in all studies was rather small regardless of the sealant material used. The proportion of sound surfaces ranged from 86% to 97%.
Over 60 months
One small parallel‐group study with 36 participants provided data for this comparison over 60 months (Barja‐Fidalgo 2009, 36). Barja‐Fidalgo 2009 did not find a difference between high‐viscosity glass ionomer versus resin sealant (RR 0.38, cluster corrected 95% CI 0.09 to 1.6; Analysis 4.5; Table 4).
4.5. Analysis.
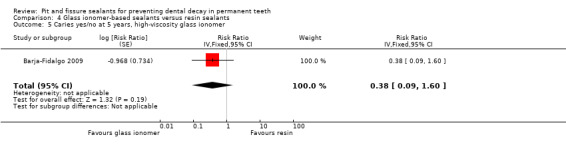
Comparison 4 Glass ionomer‐based sealants versus resin sealants, Outcome 5 Caries yes/no at 5 years, high‐viscosity glass ionomer.
At 84 months follow‐up
One split‐mouth study compared low‐viscosity glass ionomer with resins at 84 months follow‐up (Forss 1998). Forss 1998 did not find a statistically significant difference between materials (RR 1.44, 95% CI 0.88 to 2.35; Analysis 4.6; Table 4). At 84 months follow‐up, 23.5% of the occlusal surfaces sealed with glass ionomer and 16.5% of those sealed with resins were carious or filled.
4.6. Analysis.
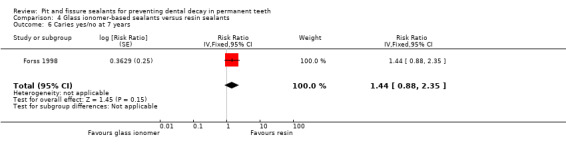
Comparison 4 Glass ionomer‐based sealants versus resin sealants, Outcome 6 Caries yes/no at 7 years.
Results from studies not included in the analyses
De Luca‐Fraga 2001 compared resin‐modified glass ionomer (Vitremer) with polyacid‐modified composite resin sealant (compomer) (Dyract) on the occlusal surfaces of caries‐free mandibular first permanent molars (split‐mouth study design). Because this comparison is not currently relevant, and the chemical compounds of these two materials are similar, we referred only to results from the published report: two restorations were observed in compomer sealed teeth at 12 months follow‐up. Sealants were totally retained on 86% of the tooth surfaces sealed with resin‐modified glass ionomer, and on 96% of teeth sealed with compomer.
Pardi 2005 compared resin‐modified glass ionomer (Vitremer), flowable resin composite (Revolution), and polyacid‐modified composite resin (Dyract Flow). Study data were not presented in a suitable form to include in analyses. (Caries was defined as active white spot lesion (translucent enamel alteration) or presence of a microcavity (diameter under 1.5 mm across fissure) or large cavity or filling). Reported results after 24 months were: 3.1% (3/97) of teeth sealed with resin‐modified glass ionomer, 4.3% (4/93) of teeth sealed with flowable resin composite, and 6.7% (6/89) of teeth sealed with polyacid‐modified composite resin, were carious or filled. After 24 months, sealants were totally retained on: 47% of tooth surfaces sealed with resin‐modified glass ionomer; 76% of teeth sealed with resin composite; and 58% of teeth sealed with polyacid‐modified composite resin.
4b. One sealant material versus another material ‐ Ormocer‐based sealant versus glass ionomer‐based sealant
Guler 2013, comparing ormocer sealant with low‐viscosity glass ionomer sealant, found glass ionomer sealant performed better at 24 months. Because caries data in this study were somewhat unclear, results are provided as they appear in the study report: "...presence of caries was 16% for glass ionomer and 32% for ormocer (P < 0.05)". The dropout rate of the children was high (26%). Only 3% of ormocer sealants and 13% of glass ionomer sealants were completely retained after 24 months.
Effectiveness of sealants related to caries incidence levels
On the whole, there were too few data to enable robust conclusions to be drawn about the effectiveness of sealants in relation to the different caries incidence levels among the populations studied. Only the comparison of resin‐based sealants compared to no sealants provided information on the effectiveness of sealants related to caries incidence levels among the populations; however, our estimations were based only on data from seven studies after 24 months follow‐up.
In studies comparing resin‐based sealants to no sealants, we took the incidence of carious control teeth at 24 months to reflect children's caries risk. If we were to assume that 16% of the control tooth surfaces were decayed during 24 months of follow‐up (160 carious teeth per 1000), then applying a resin‐based sealant would reduce the proportion of carious surfaces to 5.2% (95% CI 3.13% to 7.37%). (This estimate was based on two studies conducted during the 2000s in China; China has been classified as having a very low DMFT‐index among children at 12 years of age according to FDI 2015 and WHO 2014 (DMFT < 1.2). Based on the older five split‐mouth studies in this comparison (studies published between 1976 and 1979): if we were to assume that 40% of the control tooth surfaces were decayed during 24 months of follow‐up (400 carious teeth per 1000), then applying a resin‐based sealant would reduce the proportion of the carious surfaces to 6.25% (95% CI 3.84% to 9.63%). Similarly, if we were to assume that 70% of control tooth surfaces were decayed (700 carious teeth per 1000), then applying a resin‐based sealant would reduce the proportion of the carious surfaces to 18.92% (95% CI 12.28% to 27.18%) (Table 1).
We did not assess caries incidence levels of children in other comparisons (glass ionomer versus control and relative effectiveness of different sealant materials). Only three studies with inconsistent results were available to assess glass ionomer versus control. Results were inconsistent or divergent when the relative effectiveness of sealant materials were compared. Furthermore, the event rate was low in studies comparing relative effectiveness of sealant materials which limited contribution to the results.
Safety of sealants
Only four studies assessed adverse events of the sealants (Bravo 2005; Liu 2012; Liu 2014a; Muller‐Bolla 2013). Bravo 2005, Liu 2012 and Muller‐Bolla 2013 compared resin‐based sealant versus no sealant and Liu 2014a compared glass ionomer versus resin‐based sealant. No adverse events were detected or reported in these four studies.
Retention of sealants
All 38 studies reported data for retention of sealants (see Table 6).
Studies comparing sealant with no sealant
At 12 months follow‐up, four of the eight studies reported about 90% complete retention of resin‐based sealants (Bojanini 1976; Reisbick 1982; Richardson 1978; Sheykholeslam 1978). Muller‐Bolla 2013 and Rock 1978 reported the lowest retention rates (complete retention 53% at 12 months). At 24 months follow‐up, seven of the ten studies reported over 80% complete retention for resin sealants (Bojanini 1976; Brooks 1979; Reisbick 1982; Richardson 1978; Sheykholeslam 1978; Songpaisan 1995; Tang 2014). At 36 months follow‐up, complete retention ranged from 41% (Rock 1978) to 87% (Bojanini 1976). After 48 to 54 months, complete retention of resin‐based sealants was 70% in three of the five studies (Brooks 1979; Erdoğan 1987; Richardson 1978). Bravo 2005 reported 39% complete retention of resins at 108 months follow‐up. In the only study comparing resin‐modified glass ionomer with a control without sealant, Tagliaferro 2011 reported that 16% of resin‐modified glass ionomer sealants were lost after 24 months. Songpaisan 1995 reported 85% complete retention for resin‐based sealants and under 1% for glass ionomer sealants at 24 months follow‐up. Liu 2014b reported 7% loss of sealants among children in the resin group and 35% in the glass ionomer group.
Studies comparing different sealant materials
Glass ionomer‐based versus resin sealant
Low‐viscosity glass ionomer versus resin
Eight studies comparing resin‐based sealants with low‐viscosity glass ionomers reported clearly better retention for resin‐based sealants than glass ionomers (Forss 1998; Karlzén‐Reuterving 1995; Kervanto‐Seppälä 2008; Poulsen 2001; Rock 1996; Sipahier 1995; Songpaisan 1995; Williams 1996). At 36 to 48 months follow‐up, the mean complete retention rate for resin‐based sealants was 76%, and 8% for glass ionomers (based on 5 studies that reported data at these follow‐up points). Forss 1998 reported a significantly higher retention rate for resin‐based sealants than glass ionomers at 84 months follow‐up (10.3% of glass ionomers and 45.4% of resin sealants were fully present).
In four studies, retention was fairly high in both groups after 24 months. Antonson 2012, Chen 2013 and Liu 2014b reported some better retention figures for resins than low‐viscosity glass ionomers (0% to 7% of sealants were lost in resin groups and 11% to 35% lost in glass ionomer groups). Only Mills 1993 reported better retention figures for glass ionomer than resin (6% of sealants in the glass ionomer group and 25% in the resin group were lost).
Retention of both sealant materials was reported to be low in three studies (Arrow 1995; Dhar 2012; Ganesh 2006). Complete retention for both materials was less that 5% at 24 months follow up was less than 5% in Ganesh 2006. In Dhar 2012, 80% of resin sealants (without preparation of the surface before sealant application) and 100% of glass ionomer sealants (without preparation of the surface before sealant application) were lost after 24 months. In Arrow 1995 nearly two‐thirds of participants were found to have lost both sealant materials by 44 months follow‐up.
High‐viscosity glass ionomer versus resin
The three studies that provided data for this comparison reported divergent retention rates. Chen 2012 reported that 20% of sealants were lost from the glass ionomer and 14% from resin groups after 24 months. Liu 2014a reported better retention rates for resins, 55% and 79% of sealants were completely or partially retained in the glass ionomer and resin groups after 24 months, respectively. Barja‐Fidalgo 2009 reported better retention rates for glass ionomers (58%); complete or partial retention rates for resins were 42% after 60 months.
Resin‐modified glass ionomer versus resin
Both studies comparing resin‐modified glass ionomers and resins at 36 months reported clearly better complete retention rates for resins (mean 94% for resins and 5% for resin‐modified glass ionomers) (Baseggio 2010; Raadal 1996).
Discussion
Summary of main results
Effectiveness of pit and fissure sealants
Resin‐based sealants compared with no sealant
We are moderately confident that resin‐based sealants applied on occlusal surfaces of permanent molars of children and adolescents reduce caries up to 48 months when compared to no sealant; after longer follow‐up the quantity and quality of the evidence is reduced (Table 1). Assessment of 10 split‐mouth and five parallel‐group studies that included children aged from 5 to 10 years found a significant difference in favour of second‐, third‐ or fourth‐generation resin‐based sealants on first permanent molars, compared to no sealant. The benefit associated with resin sealant use was maintained up to nine years although both numbers of studies and participants reduced markedly over time.
The effectiveness of resin‐based sealants is related to retention of sealants. Retention of resin sealants was good in studies that compared sealant with a control without sealant. At 12 and 24 months follow‐up, resin sealants were retained completely on average in 80% of cases. After 48 to 54 months, most studies reported 70% retention of sealants. Bravo 2005 reported that sealants were re‐applied up to 36 months; complete retention was 39% at the nine year follow‐up.
Glass ionomer‐based sealants compared with no sealant
Three studies provided data for comparison of glass ionomer sealant with no sealant (low‐viscosity glass ionomer (2 studies) and resin‐modified glass ionomer (1 study)). At 24 months, results were inconsistent for low‐viscosity glass ionomers (Liu 2014b slightly favoured sealants but Songpaisan 1995 did not find a difference between the sealant and control groups). The retention of glass ionomers was better in Liu 2014b than in Songpaisan 1995 with very poor retention of glass ionomers. Tagliaferro 2011, which reported good retention of resin‐modified glass ionomer sealants, concluded that "...in a 2‐year period, oral health education was sufficient to control occlusal caries in low risk children while for high risk children, sealant application in addition to oral health education was considered the best strategy". However, as the quality of the evidence for this comparison was very low, we cannot draw any reliable conclusions.
Sealant versus sealant comparisons
The relative effectiveness of sealant types remained inconclusive. We currently only have very low quality evidence for these comparisons.
Glass ionomer‐based sealant versus resin sealant
Findings of the relative effectiveness of glass ionomers compared to resin sealants remains inconclusive. At 12, sixty and 84 months, there was no difference between materials. At 24 months, most trials favoured neither material, but at 36 to 48 months, results were divergent. Based on three included studies comparing high‐viscosity glass ionomers with resins, caries reduction did not differ significantly between these materials.
Settings and caries risk for children were often unclear, but overall, the proportion of sealed decayed surfaces was small, regardless of material used. For example, in eight studies that provided data at 36 to 48 months, proportions of decayed sealed surfaces ranged from 3% to 14% at 36 to 48 months. In all eight studies, control teeth or control groups without sealants were lacking to further estimate caries risk.
The caries results of the individual trials seemed often to be correlated with retention of sealant materials. For example, in the five studies that found statistically significantly more caries in low‐viscosity glass ionomer and resin‐modified glass ionomer sealed teeth at 36 to 48 months than in resin‐sealed teeth, the complete retention for resin sealants was documented to be good (mean 85%), and for glass ionomers low (mean 4%) (Baseggio 2010; Kervanto‐Seppälä 2008; Poulsen 2001; Raadal 1996; Rock 1996). In the three studies comparing high‐viscosity glass ionomers with resins and with similar caries reductions between these materials, the retention of glass ionomers was fairly good (Barja‐Fidalgo 2009; Chen 2012;Liu 2014a). However, there may be many reasons to account for divergent results (in caries figures) among studies comparing glass ionomers to resin‐based sealants. A straightforward conclusion cannot be drawn based only on retention.
Adverse events and safety of sealants
Only four studies assessed or considered adverse events of sealants, three assessing resin‐based sealant versus no sealant and one comparing glass ionomer and resin‐based sealant. No adverse events (such as allergic reactions) were detected. This is understandable because rare adverse events or long‐term adverse effects are unlikely to be observed in clinical trials.
However, some systematic reviews have considered the possible adverse oestrogen‐like effects of resin‐based materials including Bisphenol A (BPA) (Azarpazhooh 2008b; Fleisch 2010; Kloukos 2013). This synthetic chemical resin is widely used in the production of plastic products used in day‐to‐day living. Dental resins are composed primarily of BPA derivatives rather than pure BPA (Fleisch 2010) but the derivatives (such as bis‐DMA) can hydrolyse to BPA after sealant placement and detected transiently in saliva (Arenholt 1999; Fleisch 2010; Kloukos 2013; Schmalz 1999). BPA has been detected in saliva for up to three hours after application of resin sealants (Fleisch 2010).
The systematic review by Kloukos 2013 found five studies which measured systemic absorption of BPA after application of resin sealants (2 studies measured blood serum samples and 3 studies measured urine samples). Kloukos 2013 concluded that exposure to BPA from dental sealants remains poorly characterised, although the review reported clearly increased levels of BPA in urinary samples after sealant applications. Furthermore, Fleisch 2010 reported the total BPA intake (like contaminated food) can confound making conclusions on exposure of BPA from sealant treatments.
To reduce the possible BPA exposure, some reports recommend precautionary application techniques of resin‐based sealants, meaning e.g. immediate cleaning and rinsing sealed surfaces after placement of sealants (Fleisch 2010; Kloukos 2013).
The current evidence suggests that patients are not at risk of harmful oestrogen‐like effects when sealants are used (ADA 2016; Azarpazhooh 2008b; Fleisch 2010).The American Dental Association concluded that “based on current evidence, the Association agrees with the authoritative government agencies that the low‐level of BPA exposure that may result from dental sealants and composites poses no known health threat” (ADA 2016).
Overall completeness and applicability of evidence
Sealant materials and settings
The studies comparing sealing to control without sealing were mostly conducted as early as in the 1970s and 1980s and it is not straightforward to compare these to recent trials. Nine of 15 studies comparing resin‐based sealant with no sealant were conducted in high‐income countries in the 1970s and 1980s. Two studies were conducted in the 1990s: Bravo 2005 in Spain, and Songpaisan 1995 in Thailand. Four studies were published in the 2010s: three conducted in China (Liu 2012; Liu 2014b; Tang 2014) and one in France (Muller‐Bolla 2013).
Studies comparing different sealant materials were published between 1993 and 2014.
In most of the 38 included studies, children were recruited from schools or community‐oriented dental clinics. In general, these studies were conducted in well‐equipped dental settings.
Variation in caries risk levels
While this review showed that sealants are effective for preventing caries in children and adolescents, the magnitude of effectiveness related to different caries risk levels in the population or children remained unclear. One of our objectives was to evaluate the effectiveness of pit and fissure sealants related to different caries risk levels in the population. The efficacy of any caries‐preventive intervention likely depends on the actual caries risk of an individual (and population), i.e. if the risk of developing new lesions within a certain follow‐up period is small even without any intervention, then the efficacy of additional preventive method is likely to be confined to being small.
We decided to use caries incidence of control teeth (without sealants) as a surrogate factor to estimate caries risk levels of populations, as sealant trials, in general, do not report DMF‐indexes of dentition after follow‐ups. Furthermore, unique definitions of caries risk levels (high, moderate, low, or very low caries risk) with DMF‐classifications are missing. For example, currently the WHO regards 12‐year‐old children as having high caries risk when the DMF‐index is over 4.4 but the FDI (World Dental Federation) when the DMF index is over 3.5 (WHO 2014; FDI 2015). In addition to organisation and time frame, definition of caries risk levels depend, for example, on populations and national trends.
We did not use baseline caries prevalence levels of the populations to estimate the caries risk levels although baseline caries experience of a child has been argued to be the most accurate single predictor for future caries development (e.g. Mejàre 2014). There is, however, a range of various other factors that affect caries risk assessment during the follow‐up, such as sociodemographic factors, oral hygiene and dietary habits, oral bacteria, and saliva characteristics (Carvalho 2014; Mejàre 2014)). Further, these factors are not stable, for example, oral hygiene and dietary habits of an individual can change during the follow‐up, decreasing or increasing caries risk. Moreover, these factors were incompletely reported. Only five out of the 15 studies comparing resin‐based sealant to control without sealant in this review reported information on the baseline caries prevalence of the children. In addition, there was incomplete information on other factors that might be related to caries incidence (factors like individual behavioural factors such as the frequency of eating sugary snacks, the use of fluoridated toothpaste, and other caries‐preventive procedures during the trial (e.g. topical fluoride applications)). Only two studies informed on diet habits, for example.
On the whole, there was incomplete information to draw conclusions about the effectiveness of sealants relative to the caries incidence levels of the children. However, data from studies comparing resin sealants to control without sealants show that resin‐based sealants are effective in children at high caries risk. This information is based on five studies published between 1976 and 1979. The incidence of carious control teeth in these studies ranged from 37% to 69% after 24 months, thus representing populations with high caries risk. Although two sealant studies conducted recently (in 2000s) found statistically significant results favouring sealants after 24 months, the magnitude of effectiveness was clearly lower than that based on the studies conducted in 1970s. After 24 months, the caries incidence of the control teeth was 16% and the caries incidence of the sealed teeth was 5% (the corresponding figures for the studies from 1970s were at lowest 40% and 6.3% and at highest 70% and 19%) (Table 1). Comparison of the results between studies from different decades is, however, not straightforward. For example, it remains unclear whether the populations in the two recent studies represented other caries risk levels (than in those from 1970s) or whether the caries progression rate has been slowing down during the last decades and thus the two‐year follow‐up time was too short to reveal the real caries risk of the populations in recent studies.
Diagnosis
This review was focused on the effect of sealants in preventing or controlling caries, and sealant trials that were mainly intended to manage dental caries were excluded from the review. Studies with sound occlusal surfaces of molars and premolars or with enamel lesions were accepted. Twenty‐seven out of the 38 included studies reported (or implied) that sealants were applied on sound occlusal surfaces, and 11 studies on sound surfaces or on surfaces with enamel lesions. In addition to visual‐tactile caries diagnostic methods, the studies used the following methods in caries diagnostic: two studies reported X‐rays to be used, and one study used X‐rays when necessary; one study used fibre‐optic transillumination; two studies used laser fluorescence methods; and one study used intraoral camera (matching the first and follow‐up images of the sealants).
Caries diagnosis on occlusal surfaces can, however, be challenging. Conventional visual, tactile and radiographic methods in the diagnosis of occlusal caries have not been accurate enough to identify whether a lesion extends into the dentine (McComb 2001). New technologies such as laser fluorescence methods (e.g. DIAGNOdent device) may be sensitive in detecting occlusal dentinal caries (Bader 2004; Twetman 2013), but the likelihood of false‐positive diagnoses may increase when laser fluorescence is used rather than visual methods (Bader 2004). Regardless of the caries diagnostic method used, the condition of an occlusal surface to be sealed remains in any case somewhat unclear.
Quality of the evidence
The body of evidence comparing resin‐based sealants with no sealants comprised 15 randomised trials (3620 participants). We were able to combine seven studies in our main meta‐analysis, which we assessed as moderate quality according to GRADE assessment criteria. Assessment as moderate quality evidence implies that further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. After 24 months of follow‐up in seven studies (1548 participants), the pooled OR for caries was 0.12 (95% CI 0.08 to 0.19). As five of the seven trials were published between 1976 and 1979, it is not unreasonable to anticipate that a new study could change this estimate, even if it found the sealants effective.
We did not further downgrade evidence on the basis of overall risk of bias classifications of the studies (all studies were assessed at high risk of bias because blinding of outcome assessment was not possible in sealant studies). In assessing the quality of evidence for this comparison, the main focus was on directness of evidence, consistency of results, and precision of estimates. Although there was considerable heterogeneity between the results in all comparisons, results from each individual trial showed highly significant benefit for the sealant. The studies were otherwise fairly well conducted: six of nine studies were assessed at low risk of bias regarding allocation concealment, incomplete outcome data, selective outcome reporting and baseline comparability. In three studies (Liu 2014b; Songpaisan 1995; Tang 2014), reporting of randomisation procedures was incomplete, and the studies were assessed at unclear risk of allocation bias. Moreover, it was difficult to assess how likely (or unlikely) it was that the outcome measurement was influenced by lack of blinding of outcome assessors in preventive sealant studies.
Sealing the occlusal surfaces of permanent molars in children and adolescents reduced caries up to 48 months when compared to no sealant. After longer follow‐up the quantity and quality of the evidence was reduced. (Table 1).
The quality of the body of evidence for glass ionomer sealants compared to no sealants (based on 3 studies) was very low, as was evidence comparing one type of sealant with another (24 studies). This was due to inconsistent effects on caries outcomes, due to diversity among interventions, comparisons and outcomes time points reported in the trials, age of included children and variations in reporting background exposure to fluoride. (Table 2; Table 3).
Potential biases in the review process
Study design
Commonly, the efficacy of sealants in preventing caries has been connected with the retention of resin‐based sealants. For example, in the 1980s, most clinical sealant studies were retention studies without caries outcomes. However, the aim of this review was to examine the effectiveness of sealants in caries prevention, measured in caries incidence, rather than retention. This decision was supported by findings from a systematic review by Mickenautsch 2013. Mickenautsch 2013 found that the risk of loss of complete retention of sealant materials was associated with the risk of caries occurrence for resin but not for glass ionomer‐based sealants.
Studies with first‐generation sealants were excluded from this review because retention and caries protection have been shown to be superior for later sealant materials; furthermore, first‐generation sealants are no longer marketed (Ripa 1993). We also excluded studies comparing compomers to resins/composites because compomers have mostly the same components as composites (Nicholson 2007).
We included only randomised studies for this update; quasi‐randomised studies were excluded unless they applied split‐mouth design. Studies with no random sequence generation were excluded to eliminate the possibilities that the person applying sealants intentionally chose teeth or children for sealing, or that certain teeth or children were systematically sealed leaving some teeth or children without sealant.
Analysis issues
We included all studies that fulfilled inclusion criteria whether data were adequately analysed or not. If a split‐mouth study presented data only in marginals (as parallel‐group studies, not as 2 x 2 cross‐classification for paired data), the marginal Becker‐Balagtas method was used for calculating ORs with appropriate standard errors taking the clustering of the teeth within a tooth pair into account. The conservative ICC 0.05 was used in calculations. The Becker‐Balagtas method as proposed by Curtin 2002 and later by Elbourne 2002 was used because Cochrane recommends this approach (Higgins 2011b). (The Becker‐Balagtas method described by Elbourne 2002 was corrected in Stedman 2011). The alternative method introduced by Barker 2011 (based on a hierarchical Bayes structure) is still quite novel but will be considered in future updates.
There was significant heterogeneity for comparisons between resin sealant versus no treatment at several time points. There was, however, incomplete information to investigate the reasons for heterogeneity. Furthermore, in the comparison of resin‐based sealants compared with no sealant, the confidence intervals of ORs and RRs used in the split‐mouth studies are now slightly narrower than they should be because of the dependence of tooth pairs in a child. This is because only one study included only one pair of tooth surfaces per child. In the other studies the average number of tooth pairs per child was 1.6 (children had either one or two tooth pairs under observation). Strictly speaking, the pairs are not independent and should be analysed as 'paired data' on a per child basis. However, we decided to analyse the pairs independently; otherwise, we would need to exclude the trials. (To our knowledge there are no methods to correct and account for dependence of tooth pairs when, for example, only marginals are reported). Due to the substantive evidence for benefit of resin‐based sealants, the interpretation of the results would have been the same.
Reporting bias
We considered only studies published as full‐text reports for inclusion. We excluded studies reported only as abstracts because it has been shown that discrepancies occur between data reported in abstracts and published full reports. It has also been found that information on trial quality indicators is often lacking (Chokkalingam 1998; Hopewell 2006). To diminish risk of publication bias, we contacted authors of potentially eligible abstracts to seek availability of full‐text study reports (unpublished or published).
Authors' conclusions
Implications for practice.
Resin‐based sealants applied to occlusal surfaces of permanent molars reduced caries when compared to no sealant. The incidence of caries at 24 months ranged from 16% to 70% in the control groups of the studies we included, corresponding to absolute reductions in caries risk of between 11% and 51% (moderate‐quality evidence). We found similar results at follow‐up of up to 48 months. Sealants were effective at follow‐up of longer than four years, but this is less certain because of the limited quantity and quality of evidence. Information on adverse effects was limited but none occurred where this was reported. The effectiveness of glass ionomer sealant and the relative effectiveness of different types of sealants has yet to be established.
Implications for research.
Trials with long follow‐up times are needed to research the effectiveness of sealing procedures related to different caries prevalence levels. Long‐term follow‐up studies are needed, especially because caries progression rates in permanent teeth in the future are difficult to predict. Future studies should report characteristics of study populations in terms of risk factors likely to predict caries development. This will help to better determine the applicability of the evidence to different populations and settings, especially where background prevalence is not known. More research is also needed to clarify the relative effectiveness of different sealant material types (representing materials with clearly different chemical compounds). Head‐to‐head comparisons should preferably be studied in controlled settings including a trial arm without sealing. Studies that compare retention of two or more similar types of sealant materials, which report caries rates only on sealed occlusal surfaces, not as increments on the individual level, do not significantly add to the body of evidence and should only be considered as pilot studies preceding more comprehensive trials.
Intervention study designs should be in keeping with the Consolidated Standards of Reporting Trials (CONSORT) statement (www.consort‐statement.org). Information on caries risk in the study population, use of fluoridated water, toothpaste and general preventive methods, as well as other preventive interventions, should be reported to facilitate multivariate analysis of risk factors. Studies should have adequate documentation and follow‐up of drop‐outs, as described by the CONSORT statement.
Currently, sealing procedures are often recommended as a method to control and manage caries, assessed as ICDAS II codes 3 and 4, distinguished such as underlying dentin shadow or localised enamel breakdown on occlusal surfaces. It is therefore advisable that future Cochrane Review updates of sealants also include research conducted on sealants used for controlling and managing occlusal caries.
What's new
| Date | Event | Description |
|---|---|---|
| 24 July 2017 | New citation required but conclusions have not changed | Clinical conclusions are unchanged; but there were several other changes:
|
| 3 August 2016 | New search has been performed | Searches updated. This 2017 update contains 7 new included studies involving 1693 participants (Antonson 2012; Chen 2013; Guler 2013; Liu 2014a; Liu 2014b; Muller‐Bolla 2013; Tang 2014); 8 new excluded studies (3 of which were previously included) (Beiruti 2006; Güngör 2004; Hilgert 2015; Lampa 2004; Madléna 1993; Marković 2012; Monse 2012; Unal 2015); 2 studies awaiting assessment (Gorseta 2014; Ulusu 2012) and 5 ongoing studies. |
History
Protocol first published: Issue 3, 1999 Review first published: Issue 3, 2004
| Date | Event | Description |
|---|---|---|
| 18 February 2009 | Amended | Contact details for lead review author updated. |
| 12 November 2008 | Amended | Format of Additional table 3 slightly changed. |
| 7 August 2008 | Amended | Converted to new review format. |
| 4 August 2008 | New search has been performed | Searches updated. The search strategy for the MEDLINE database was revised to increase its specificity to topic whilst retaining its sensitivity. Further, the search strategy for the SIGLE database was revised. This 2008 update contains 8 new included studies, 19 new excluded studies and 4 studies awaiting assessment. |
| 4 August 2008 | New citation required but conclusions have not changed | This update contains the following changes to the previous version. ‐ Some changes were made to the inclusion criteria. Unlike the previous version, all studies regardless of the drop‐out rate of the participants were included in this update. High drop‐out rates were taken into consideration in handling the data. Further, this version also includes sealant studies with novel materials (the previous version considered only second, third and fourth generation resin‐based sealants and glass ionomer sealants). ‐ In the previous version of this review the study selection was made at two stages using two inclusion criteria: the primary and secondary criteria. To clear up the study selection, the primary and secondary inclusion criteria were combined in this version. ‐ Risk of bias was assessed for each included study as an additional quality assessment tool. Compared to the previous version of the review the overall clinical conclusions were unchanged. |
Acknowledgements
Our gratitude goes to Miss Anne Littlewood at Cochrane Oral Health (COH) in Manchester, UK, for help with searching the literature; Miss Laura CI MacDonald and Mrs Janet Lear, also at COH, for the assistance they provided. We thank Mr Philip Riley and Mr Derek Richards for their comments on the updated draft, and Prof Jan Clarkson, Mr Toby Lasserson, Ms Ruth Floate and Ms Ann Jones, who finalised the review for publication. We also acknowledge Mrs Luisa Fernandez Mauleffinch and Mrs Sue Furness for their help with the previous version of this review. Information specialist Jaana Isojärvi at THL, Finland helped in the literature searches. Trial reports were translated from rare languages by Dr Helena Laasonen, Dr Iris Pasternack, Dr Oleg V Borisenko, Dr Mikako Hayashi, Dr Jordi Pardo, Dr Valeria Marinho, Dr Joanna M Zakrzewska, Dr Giovanni Lodi, Dr Szabolcs Szatmari, Dr Duangjai Lexoboon, Dr May CM Wong, Dr Zongdao Shi, Dr Chunjie Li, Dr Szimonetta Lohner, Dr Chengge Hua and Liyuan Ma. The text was revised by native‐language editor Mark Phillips BA in the previous version.
We would also like to thank the following investigators who provided additional information or translation help in relation to their trials: Dr F Barja‐Fidalgo, Dr M Bravo, Dr V Dhar, Dr W Dukic, Dr C Guler, Dr HC Güngör, Dr M Ganesh, Dr M Houpt, Dr J Frencken, Dr R Holt, Dr P Hotz, Dr GB Gibson, Dr H Forss, Dr S Kervanto‐Seppälä, Dr E Lo, Dr M Muller‐Bolla, Dr BH Oliveira, Dr AC Pereira, Dr S Poulsen, Dr M Raadal, Dr T Ulusu, Dr V Vrbic, Dr EP Tagliaferro. We would also like to thank Dr Manuel Bravo for the manual literature search in the initial review. We are also grateful to Prof Heikki Murtomaa for his expert help and the University of Helsinki, Finland for supporting this study. Dr May CM Wong was very helpful during discussions on statistics in the previous version.
We acknowledge the input of Anne Hiiri to previous versions of this review.
Appendices
Appendix 1. Cochrane Oral Health’s Trials Register search strategy
sealant*
In the 2008 review version, the following search strategy was used: "pit and fissure sealant*" OR pit‐and‐fissure‐sealant* OR (fissure* AND seal*) OR "resin seal*" OR "dental seal*" OR "tooth seal*" OR "enamel seal*" OR (("glass ionomer*" OR glass‐ionomer* OR resin*) AND seal*)
Appendix 2. Cochrane Central Register of Controlled Trials (CENTRAL) search strategy
#1 MeSH descriptor Pit and Fissure Sealants this term only #2 (fissure* in All Text near/6 seal* in All Text) #3 (dental in All Text near/3 sealant* in All Text) #4 (resin* in All Text near/4 sealant* in All Text) #5 (compomer* in All Text near/4 sealant* in All Text) #6 (composite* in All Text near/4 sealant* in All Text) #7 MeSH descriptor Glass Ionomer Cements explode all trees #8 MeSH descriptor Resins, Synthetic explode all trees #9 ("glass ionomer$" in All Text or glassionomer$ in All Text) #10 (#7 or #8 or #9) #11 sealant* in All Text #12 (#10 and #11) #13 (#1 or #2 or #3 or #4 or #5 or #6 or #12)
In the 2008 review version, the following search strategy was used: #1 PIT AND FISSURE SEALANTS #2 (fissure* NEAR/6 seal*) in title, abstract, or keywords #3 (dental* NEAR/3 sealant*) in title, abstract, or keywords #4 (resin NEAR/4 sealant*) in title, abstract, or keywords #5 Exp GLASSIONOMER CEMENTS #6 RESIN CEMENTS #7 ("glass ionomer*" or glassionomer*) in title, abstract, or keywords #8 ((#5 or #6 or #7) AND sealant*) in title, abstract, or keywords #9 #1 or #2 or #3 or #4 or #8
Appendix 3. MEDLINE Ovid search strategy
1. "Pit and Fissure Sealants"/ 2. (fissure$ adj6 seal$).mp. 3. (dental adj3 sealant$).mp. 4. (resin$ adj4 sealant$).mp. 5. (compomer$ adj4 sealant$).mp. 6. (composite$ adj4 sealant$).mp. 7. exp Glass Ionomer Cements/ 8. exp Resins, Synthetic/ 9. ("glass ionomer$" or glassionomer$).mp. 10. 7 or 8 or 9 11. sealant$.mp. 12. 10 and 11 13. 1 or 2 or 3 or 4 or 5 or 6 or 12 The above subject search was linked to the Cochrane Highly Sensitive Search Strategy (CHSSS) for identifying randomised trials in MEDLINE: sensitivity maximising version (2008 revision) as referenced in Chapter 6.4.11.1 and detailed in box 6.4.c of The Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011) (Lefebvre 2011).
1. randomized controlled trial.pt. 2. controlled clinical trial.pt. 3. randomized.ab. 4. placebo.ab. 5. drug therapy.fs. 6. randomly.ab. 7. trial.ab. 8. groups.ab. 9. or/1‐8 10. exp animals/ not humans.sh. 11. 9 not 10
In the 2008 review version, the following search strategy was used: 1. PIT AND FISSURE SEALANTS/ 2. (fissure$ adj6 seal$) 3. dental adj/3 sealant$ 4. resin$ adj/4 sealant$ 5. exp GLASS IONOMER CEMENTS/ 6. RESIN CEMENTS/ 7. "glass ionomer$" or glassionomer$ 8. ((5 or 6 or 7) AND sealant$) 9. 1 or 2 or 3 or 4 or 8
Appendix 4. Embase Ovid search strategy
1. "Pit and Fissure Sealants"/ 2. (fissure$ adj6 seal$).mp. 3. (dental adj3 sealant$).mp. 4. (resin$ adj4 sealant$).mp. 5. (compomer$ adj4 sealant$).mp. 6. (composite$ adj4 sealant$).mp. 7. exp Glass Ionomer Cements/ 8. exp Resins, Synthetic/ 9. ("glass ionomer$" or glassionomer$).mp. 10. 7 or 8 or 9 11. sealant$.mp. 12. 10 and 11 13. 1 or 2 or 3 or 4 or 5 or 6 or 12
This subject search was linked to Cochrane Oral Health’s filter for identifying RCTs in Embase Ovid:
1. random$.ti,ab. 2. factorial$.ti,ab. 3. (crossover$ or cross over$ or cross‐over$).ti,ab. 4. placebo$.ti,ab. 5. (doubl$ adj blind$).ti,ab. 6. (singl$ adj blind$).ti,ab. 7. assign$.ti,ab. 8. allocat$.ti,ab. 9. volunteer$.ti,ab. 10. CROSSOVER PROCEDURE.sh. 11. DOUBLE‐BLIND PROCEDURE.sh. 12. RANDOMIZED CONTROLLED TRIAL.sh. 13. SINGLE BLIND PROCEDURE.sh. 14. or/1‐13 15. (exp animal/ or animal.hw. or nonhuman/) not (exp human/ or human cell/ or (human or humans).ti.) 16. 14 NOT 15
Appendix 5. US National Institutes of Health Ongoing Trials Register (ClinicalTrials.gov) search strategy
Advanced search:
Intervention: sealant Condition: caries
Appendix 6. World Health Organization International Clinical Trials Registry Platform search strategy
Advanced search:
Intervention: sealant* Condition: tooth decay or caries
Appendix 7. Search strategies of the other electronic databases searched in the previous versions of the review
SIGLE and OpenGrey
The System for Information on Grey Literature in Europe (SIGLE) via STN Easy (1976 to December 2004). SIGLE is later known as OpenGrey. The search strategy was adapted to the new system's search language. The search was run on the Exalead search engine at http://www.opengrey.eu/ (from 9 October 2010 to 1 September 2012).
SIGLE search strategy: L1 fissure(4w)seal? L2 glass(w)ionomer(w)cement? L3 glass(w)ionomer? L4 resin(w)cement? L5 (L1 OR L2 OR L3 OR L4) AND ((DENTAL OR FISSURE?(W)SEAL?))
OpenGrey search strategy: ((fissure NEAR/4 seal* OR glass NEAR ionomer NEAR cement* OR glass NEAR ionomer* OR resin NEAR cement*) AND (dental OR fissure* NEAR seal*))
SCISEARCH, CAplus, INSPEC, NTIS, PASCAL searched via STN Easy (to 1 September 2012)
In the 2013 review version, the following search strategy was used: pit and fissure sealant? AND (dental caries or clinical trial) compomer sealant? AND (dental caries or clinical trial) composite sealant? AND (dental caries or clinical trial)
In the previous review versions, the following search strategy was used: pit and fissure sealant? AND dental caries or clinical trial
DARE, NHS EED, HTA
Centre for Reviews and Dissemination databases (CRD): DARE (Database of Abstracts of Reviews of Effectiveness), NHS EED (NHS Economic Evaluation Database), HTA (Health Technology Assessment) via the CAIRS web interface to 29 March 2012 and thereafter via Metaxis interface to September 2012)
In the 2013 review version, the following search strategy was used: ( compomer NEAR sealant OR composite NEAR sealant OR "fissure sealant" OR fissure NEAR sealant OR "glass ionomer cement" OR glass NEAR ionomer ) AND ( "dental caries" OR "dental fissure" OR "tooth deminerali?ation" OR dental NEAR caries OR dental NEAR decay OR tooth NEAR decay OR deminerali?ation NEAR tooth OR deminerali?ation NEAR enamel)
In the previous review versions, the following search strategy was used: ((fissure sealant OR fissure(s)sealant OR glass ionomer cement OR glass(s)ionomer)) AND ((dental caries OR dental fissure or tooth deminerali?ation OR dental(s)caries OR dental(s)decay OR tooth(s)decay or deminerali?ation(s)tooth or deminerali?ation(s)enamel))
JICST‐EPLUS via STN Easy (to February 2002).
The database has no longer been available via STN Easy (closed in 2007).
Data and analyses
Comparison 1. Resin‐based sealants versus no sealant.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Caries yes/no at 12 months | 7 | Odds Ratio (Random, 95% CI) | 0.17 [0.10, 0.30] | |
| 1.1 Split‐mouth studies with paired data | 4 | Odds Ratio (Random, 95% CI) | 0.11 [0.06, 0.21] | |
| 1.2 Split‐mouth studies with data stated as marginals | 3 | Odds Ratio (Random, 95% CI) | 0.30 [0.14, 0.66] | |
| 2 Caries yes/no at 24 months | 7 | Odds Ratio (Random, 95% CI) | 0.12 [0.08, 0.19] | |
| 2.1 Split‐mouth studies with paired data | 3 | Odds Ratio (Random, 95% CI) | 0.11 [0.06, 0.22] | |
| 2.2 Split‐mouth studies with data stated as marginals | 2 | Odds Ratio (Random, 95% CI) | 0.09 [0.03, 0.23] | |
| 2.3 Parallel group studies | 2 | Odds Ratio (Random, 95% CI) | 0.24 [0.12, 0.45] | |
| 3 Caries yes/no at 36 months | 7 | Odds Ratio (Random, 95% CI) | 0.17 [0.11, 0.27] | |
| 3.1 Split‐mouth studies with paired data | 3 | Odds Ratio (Random, 95% CI) | 0.16 [0.12, 0.20] | |
| 3.2 Split‐mouth studies with data stated as marginals | 4 | Odds Ratio (Random, 95% CI) | 0.18 [0.07, 0.43] | |
| 4 Caries yes/no at 48 to 54 months | 4 | Odds Ratio (Random, 95% CI) | 0.21 [0.16, 0.28] | |
| 4.1 Split‐mouth studies with paired data | 2 | Odds Ratio (Random, 95% CI) | 0.17 [0.13, 0.23] | |
| 4.2 Split‐mouth studies with data stated as marginals | 2 | Odds Ratio (Random, 95% CI) | 0.27 [0.16, 0.47] | |
| 5 Caries yes/no at 48 months, parallel group studies | 1 | Risk Ratio (Fixed, 95% CI) | 0.24 [0.12, 0.45] | |
| 6 24‐months DFS increment | 1 | 276 | Mean Difference (IV, Fixed, 95% CI) | ‐0.65 [‐0.83, ‐0.47] |
| 7 24‐months DMFS increment | 1 | 450 | Mean Difference (IV, Fixed, 95% CI) | ‐0.24 [‐0.36, ‐0.12] |
| 8 Caries yes/no at 5 years | 1 | Odds Ratio (Fixed, 95% CI) | 0.31 [0.23, 0.43] | |
| 9 Caries yes/no at 6 years | 1 | Risk Ratio (Fixed, 95% CI) | 0.45 [0.36, 0.58] | |
| 10 Caries yes/no at 7 years | 1 | Risk Ratio (Fixed, 95% CI) | 0.45 [0.34, 0.59] | |
| 11 Caries yes/no at 9 years, parallel group studies | 1 | Risk Ratio (Fixed, 95% CI) | 0.35 [0.22, 0.55] |
Comparison 2. Glass ionomer‐based sealants versus no sealant.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Caries yes/no at 24 months | 1 | (Fixed, 95% CI) | 0.46 [0.23, 0.91] | |
| 2 2 year DFS increment | 1 | 404 | Mean Difference (IV, Fixed, 95% CI) | ‐0.18 [‐0.39, 0.03] |
Comparison 4. Glass ionomer‐based sealants versus resin sealants.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Caries yes/no at 12 months | 6 | Odds Ratio (Fixed, 95% CI) | 1.47 [0.64, 3.37] | |
| 1.1 Low‐viscosity glass ionomer versus resin sealant | 4 | Odds Ratio (Fixed, 95% CI) | 1.56 [0.63, 3.87] | |
| 1.2 Resin‐modified glass ionomer versus resin sealant | 2 | Odds Ratio (Fixed, 95% CI) | 1.06 [0.13, 8.58] | |
| 2 Caries yes/no at 24 months | 14 | Odds Ratio (Random, 95% CI) | Subtotals only | |
| 2.1 Low‐viscosity glass ionomer versus resin sealant | 10 | Odds Ratio (Random, 95% CI) | 1.67 [0.87, 3.20] | |
| 2.2 High‐viscosity glass ionomer versus resin sealant | 2 | Odds Ratio (Random, 95% CI) | 1.36 [0.56, 3.32] | |
| 2.3 Resin‐modified glass ionomer versus resin sealant | 2 | Odds Ratio (Random, 95% CI) | 2.92 [1.77, 4.81] | |
| 3 2 year DFS increment | 1 | 394 | Mean Difference (IV, Fixed, 95% CI) | 0.47 [0.31, 0.63] |
| 4 Caries yes/no at 36 to 48 months | 8 | Odds Ratio (Random, 95% CI) | Totals not selected | |
| 4.1 Low‐viscosity glass ionomer versus resin sealant | 6 | Odds Ratio (Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 Resin‐modified glass ionomer versus resin sealant | 2 | Odds Ratio (Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Caries yes/no at 5 years, high‐viscosity glass ionomer | 1 | Risk Ratio (Fixed, 95% CI) | 0.38 [0.09, 1.60] | |
| 6 Caries yes/no at 7 years | 1 | Risk Ratio (Fixed, 95% CI) | 1.44 [0.88, 2.35] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Amin 2008.
| Methods |
Trial design: parallel group design, 3 randomly assigned treatment arms (resin‐modified glass ionomer, flowable composite, resin‐based sealant). Year the study started: no information on recruitment period Follow‐up: 24 months |
|
| Participants | Location: Egypt Inclusion criteria: children had to have 2 lower first permanent molars with at least two‐thirds of occluso‐cervical length erupted; and deep narrow central fissures and supplemental grooves with no evidence of cavitation, pre‐cavitation, or probe catching with stained fissures. Diagnosis based on clinical examination. Age at baseline: age range 7 to 10 years Gender: not detailed Baseline caries: no information on caries risk levels of the population at baseline Number randomly assigned: 45 children (15 in resin‐modified glass ionomer group; 15 in flowable composite group; 15 in resin‐based sealant group) Number evaluated: 39 children (12 in resin‐modified glass ionomer group; 14 in flowable composite group; 13 in resin‐based sealant group | |
| Interventions | 3 treatment arms:
Sealants were applied on the occlusal surfaces of sound first permanent molars. Isolation method was a rubber dam. No definite information who applied the sealants (likely a dentist). Co‐interventions: oral hygiene instructions; children continued their usual oral hygiene practices including the use of fluoridated toothpaste throughout the study |
|
| Outcomes | Sound or carious occlusal surface of molar, sealant retention status, and long‐term salivary Streptococcus mutans counts. Diagnosis was primarily visual, probing was used only to confirm diagnosis (assessment likely done by a dentist). |
|
| Notes | Inter‐evaluator consistency: no information provided Funding source: no identified funding source |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The children were randomly divided into three equal groups." Comment: No further information on sequence generation (no reply to request for information) |
| Allocation concealment (selection bias) | Unclear risk | No information provided (no reply for request for information) |
| Blinding? (Outcome assessors) | High risk | Comment: this domain was graded as having high risk of bias because we saw that blinding of outcome assessor in clinical trials of this nature cannot be performed, as outcome assessor can discriminate between materials after follow‐up |
| Incomplete outcome data? (Caries efficacy outcomes) | Low risk | Missing data:
2/15 children in glass ionomer group; and 1/15 in conventional resin group and 1/15 in flowable composite group at 12 months. 3/15 children in glass ionomer group; and 2/15 in conventional resin group and 1/15 in flowable composite group at 24 months. In total 4/45 (9%) children and 6/45 (13%) children after 12 and 24 months, respectively. Comment: Missing data were seen to be balanced in numbers across groups. |
| Selective reporting (reporting bias) | Low risk | Outcomes reported: Caries response, sealant retention, and long‐term salivary Streptococcus mutans counts. Comment: Pre‐specified outcomes (in methods) were reported in pre‐specified way. |
| Free of other bias? Comparability of the groups | Low risk | Quote: "The mean number of Streptococcus mutans colony forming units in the three groups were not statistically significant." Comment: Although the information on demographic characteristics is limited, this domain was graded low risk of bias because the information on Streptococcus mutans levels was similar across groups at baseline. |
| Free of other bias? Co‐interventions | Low risk | Quote: "Children received oral hygiene instructions and they continued their usual oral hygiene practices including the use of fluoridated toothpaste throughout the study." Comment: In all groups the same co‐interventions were allowed and of such quality that they were not seen to cause bias. |
Antonson 2012.
| Methods |
Trial design: split‐mouth design, sealant material randomly assigned among tooth pair Year the study started: no information provided Follow‐up: 24 months |
|
| Participants |
Location: USA
Inclusion criteria: Children had to have bilateral partially erupted permanent first molars that were free of restorations, hypoplasia, fracture or cracks; operculum coverage of at least one‐fourth and up to one‐half of the occlusal surface. Teeth with an operculum that covered more than one‐half of the occlusal surface were excluded. One dentist examined the molars with a calibrated laser fluorescence device (DIAGNOdent) for the absence of occlusal caries; teeth for which DIAGNOdent reading was higher than 20 were excluded (thus enamel lesions accepted). Age at baseline: 5 to 9 years Gender: not stated Baseline caries: not stated but children at high risk of developing caries were identified according to socioeconomic background and included in the study. Number randomly assigned: 39 children with 39 tooth pairs Number evaluated: 27 children with 27 tooth pairs |
|
| Interventions |
Comparison: glass ionomer sealant versus resin‐based sealant
Tooth pair: occlusal surface of 1 tooth sealed with glass ionomer sealant (light cured GC Fuji Triage White); occlusal surface of the other tooth of the tooth pair sealed with light cured resin‐based sealant Delton Plus+. Sealants were applied to partially erupted occlusal surfaces of permanent first molars by a dentist. No re‐sealing Co‐interventions: no information provided |
|
| Outcomes | Sound or carious occlusal surface of molar Examinations were performed with the use of a mirror, blunt explorer and air stream | |
| Notes | Calibrated investigators (2 investigators) but there is no information on the kappa‐coefficients. Funding source: Nova Southeastern University President's Faculty Research and Development grant 335381 and GC America, Alsip, Ill |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "We used a coin toss to assign sealants randomly to quadrants" |
| Allocation concealment (selection bias) | Low risk | Comment: Although the information of allocation concealment was incomplete, this domain was graded low risk of bias because we saw that in split‐mouth studies the risk of selection bias is in any case insignificant. |
| Blinding? (Outcome assessors) | High risk | Quote: "Two calibrated investigators who were not involved with the treatment procedures evaluated the sealants". Comment: Although blinding of outcome assessor was indicated, this domain was graded as having high risk of bias because we saw that blinding of outcome assessor in clinical trials of this nature cannot be performed, as outcome assessor can discriminate between materials after follow‐up. |
| Incomplete outcome data? (Caries efficacy outcomes) | High risk | Missing data: 12/39 (31%) children after 24 months. Quote: "At the 24‐month recall visit, 12 participants were absent, mainly because of relocations". Comment: Missing data rate more than 25% |
| Selective reporting (reporting bias) | Low risk | Outcomes reported: incidence of dentinal carious lesion on treated occlusal surfaces of molars, retention Comment: Pre‐specified caries outcomes (in methods) were reported in the pre‐specified way |
| Free of other bias? Comparability of the groups | Low risk | Comment: Split‐mouth design with similar conditions during the follow‐up |
| Free of other bias? Co‐interventions | Unclear risk | No information provided |
Arrow 1995.
| Methods |
Trial design: split‐mouth design, sealant material quasi‐randomly assigned among tooth pair Year the study started: 1989 Follow‐up: on average 44 months |
|
| Participants |
Location: Australia, children were from 7 dental therapy centres. Study conducted among children resident in a fluoridated area.
Inclusion criteria: children had to have recently erupted, sound, unsealed, homologous permanent first molars. Diagnosis based on clinical examination.
Age at baseline: mean age 7 years Gender: 218 girls and 247 boys Baseline caries: mean initial dmf (± SD) 1.64 ± 2.45 Number randomly assigned: 465 children with 465 tooth pairs Number evaluated: 412 children with 412 tooth pairs |
|
| Interventions |
Comparison: glass ionomer sealant versus resin‐based sealant
Tooth pair: occlusal surface of 1 tooth sealed with glass ionomer cement (GIC) (Ketac‐fil); occlusal surface of the other tooth of the tooth pair sealed with second generation resin‐based sealant (autopolymerised Delton) Sealants were applied by dental therapists, and the procedures were carried out in school dental clinics. Isolation method was a saliva ejector and cotton wool rolls. 3 children had their GIC‐sealed tooth resealed once and 4 had their Delton‐sealed tooth resealed once during the trial period. Co‐interventions: study was conducted in a fluoridated area, fluoride toothpaste predominates |
|
| Outcomes | Sound or carious occlusal surface of molar and sealant retention status Outcomes assessed by a dental therapist or a dentist, and examinations were carried out visually or by gentle probing with a sickle probe. Caries was defined as a cavity or a filling on the occlusal surface |
|
| Notes | Inter‐examiner consistency: no information provided Funding source: no identified funding source |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Participants born in an even‐numbered month received a resin sealant on the right permanent first molar and a GIC sealant on the left corresponding tooth. Participants born in an odd‐numbered month received a resin sealant on the left side and GIC on the right." Comment: Although the method of allocation of a tooth to an intervention within a tooth pair is quasi‐random, this domain was graded low risk of bias because we saw that in split‐mouth studies the risk of selection bias is in any case insignificant |
| Allocation concealment (selection bias) | Low risk | Quote: "Participants born in an even‐numbered month received a resin sealant on the right permanent first molar and a GIC sealant on the left corresponding tooth. Participants born in an odd‐numbered month received a resin sealant on the left side and GIC on the right." Comment: Although the method of allocation of a tooth to an intervention within a tooth pair is quasi‐random, this domain was graded low risk of bias because we saw that in split‐mouth studies the risk of selection bias is in any case insignificant. |
| Blinding? (Outcome assessors) | High risk | Comment: this domain was graded as having high risk of bias because we saw that blinding of outcome assessor in clinical trials of this nature cannot be performed, as outcome assessor can discriminate between materials after follow‐up |
| Incomplete outcome data? (Caries efficacy outcomes) | Low risk | Missing data: 53 /465 (11%) children at 44 months. Drop‐outs due to participants leaving Western Australia or moving to very remote areas. Comment: Missing data rate under 25% |
| Selective reporting (reporting bias) | Low risk | Outcomes reported: Caries response and sealant retention Comment: Pre‐specified outcomes (in methods) were reported in pre‐specified way |
| Free of other bias? Comparability of the groups | Low risk | Comment: Split‐mouth design with the same baseline diagnosis of the teeth within a tooth pair (sound surfaces) |
| Free of other bias? Co‐interventions | Low risk | Quote: "The study was conducted among children resident in a fluoridated area, where fluoride toothpaste predominates." Comment: No other co‐interventions included in the protocol |
Barja‐Fidalgo 2009.
| Methods |
Trial design: parallel group study, 2 randomly assigned treatment arms (glass ionomer cement, resin‐based sealant). Several teeth per child (a child is a cluster). Year the study started: 1998 Follow‐up: 60 months |
|
| Participants |
Location: Rio de Janeiro, Brazil, children were from low socio‐economic status families. The setting was a university.
Inclusion criteria: children had to have at least 1 erupted permanent first molar with either occlusal surface sound or with non‐cavitated enamel lesion and 2 or more primary molars decayed, filled, or extracted due to caries. At baseline, clinical examinations and bite wing X‐rays were undertaken. Examinations done by a dentist.
Age at baseline: 6 to 8 years
Gender: 22 girls, 14 boys
Baseline caries: mean initial dmf score for evaluable population at 5 years for resin‐sealed group was 13.9 (95% CI 6.50 to 28.30) and for glass ionomer sealed group 10.9 (95% CI 7.10 to 14.60). Number randomly assigned: 36 children (18 children in both groups) with 92 teeth Number evaluated: 20 children (10 children in glass ionomer group and 10 children in resin group) |
|
| Interventions | 2 treatment arms
Sealants were applied on the occlusal surfaces of sound first permanent molars or surface with non‐cavitated enamel lesion. Sealants were placed by graduate students without the support of a chairside assistant. No re‐sealing Co‐interventions: children supposedly had access to optimally fluoridated tap water because by law the Brazilian population on public water supplies should have access to fluoridated water. Information was obtained from the author |
|
| Outcomes |
Outcomes assessed by a dentist by using dental mirror, and explorer after the teeth had been cleaned with a toothbrush and dried. Bitewing X‐rays were also undertaken |
|
| Notes | Inter‐examiner reliability: Cohen's kappa statistic for caries 1.0. Funding source: no identified funding source |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The children were randomly allocated to the test group or to the control group, using a list of random numbers." Comment: Adequate sequence generation |
| Allocation concealment (selection bias) | Low risk | The sequence of allocation was determined using a list of random numbers generated in MS Excel. Each child was assigned by a member of the research team to the test or control group at the moment of sealant application. The operator was given the material for sealant application according to group assignment. Comment: Information obtained from the author |
| Blinding? (Outcome assessors) | High risk | Quote: "Double‐blind design (outcome assessor and child/caregiver). At the moment of the examination, the outcome assessors did not have access to information about the type of dental sealant that the children had received. Children/caregivers were not informed about the type of material used because keeping them and their children unaware of the specific material used (this was part of the study protocol)." (Detailed information obtained from the author) Comment: Although blinding of outcome assessor was indicated, this domain was graded as having high risk of bias because we saw that blinding of outcome assessor in clinical trials of this nature cannot be performed, as outcome assessor can discriminate between materials after follow‐up |
| Incomplete outcome data? (Caries efficacy outcomes) | High risk | Missing data: 8/18 (44%) children in glass ionomer group and 8/18 (44%) children in resin group after 60 months. Comment: High drop‐out rate and the drop‐out rates regarding the number of sealed teeth per child unevenly distributed across the treatment groups. (At 60 months of follow‐up, there were 7 children who had got glass ionomer sealant at baseline to 1 or 2 teeth and 3 children who had got glass ionomer sealant to 3 or 4 teeth. The corresponding figures to resin sealant children were: 4 children with 1 or 2 resin‐sealed teeth and 6 children with 3 or 4 sealed teeth). Original data obtained from the author |
| Selective reporting (reporting bias) | Low risk | Outcomes reported: Caries response and sealant retention. Comment: Pre‐specified outcomes (in methods) were reported in pre‐specified way |
| Free of other bias? Comparability of the groups | High risk | The study stated the mean initial dmf score for evaluable population at 60 months to be different across the groups: for resin‐sealed group 13.9 (95% CI 6.50 to 28.30) and for glass ionomer sealed group 10.9 (95% CI 7.10 to 14.60). Further, there was significant difference between the original glass ionomer group and evaluable glass ionomer group regarding the mean initial dmfs score (change from 16.5 (95% CI 10.60 to 22.40) to 10.9 (95% CI 7.10 to 14.60)) but the score for the resin group at 60 months was almost the same as at baseline. This indicates that more children with high risk of caries had dropped out in glass ionomer group compared to resin group. Comment: The groups were seen to be imbalanced at 60 months of follow‐up (which was the point of analysis) taking into account that the groups at 60 months were small (10 in each group with different numbers of sealed teeth at baseline) and the notable uncertainty whether the groups were comparable regarding the baseline risk of caries of the children |
| Free of other bias? Co‐interventions | Low risk | The participants lived in Rio de Janeiro, and supposedly had access to optimally fluoridated tap water because by law the Brazilian population on public water supplies should have access to fluoridated water.
The participants may have received bi‐annually fluoride gel applications because they were eligible for comprehensive dental care, and at the time that the study was conducted this was the standard practice. Additional information obtained from the author. Comment: Although some children may have received fluoride gel applications, this domain was graded low risk of bias because fluoride gel applications were not included in the protocol and in both groups the same co‐interventions were allowed |
Baseggio 2010.
| Methods |
Trial design: split‐mouth design, sealant material quasi‐randomly assigned among tooth pair Year the study started: no information provided Follow‐up: 36 months |
|
| Participants |
Location: Brazil; study setting: public health service Inclusion criteria: children had to have at least 1 homologous pair of intact, caries‐free, fully erupted or in‐eruption second permanent molars, with deep and retentive pits and fissures. Diagnosis was based on a visual inspection and laser fluorescence; X‐rays were taken only when necessary. Age at baseline: 12 to 16 years Gender: 152 girls, 168 boys Baseline caries: no information provided. Number randomly assigned: 320 children with 640 tooth pairs Number evaluated: 314 children with 628 tooth pairs |
|
| Interventions |
Comparison: resin‐modified glass ionomer cement versus resin‐based sealant Tooth pair: occlusal surface of 1 tooth sealed with resin‐modified glass ionomer cement (Vitremer, application combined with primer, no etching); occlusal surface of the other tooth of the tooth pair sealed with fluoride‐releasing resin‐based sealant (Fluoroshield) No re‐sealing Sealants were applied by a team of experienced clinicians working with a chairside assistant. Isolation method was a saliva ejector, and a rubber dam in the mandibular arch. Co‐interventions: no information provided |
|
| Outcomes |
Outcomes assessed by 1 dentist. Examination of new caries lesions' was based on visual examination, tactile inspection and laser fluorescence. Conventional radiographs were taken when necessary |
|
| Notes | Funding source: no identified funding source (authors were from universities) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The method to choose which material and which tooth would be sealed first (right or left mandibular molar) was randomly carried out according to the child's birth day." Comment: Although the method of allocation of a tooth to an intervention within a tooth pair is quasi‐random, this domain was graded low risk of bias because we saw that in split‐mouth studies the risk of selection bias is in any case insignificant |
| Allocation concealment (selection bias) | Low risk | Comment: Although the method of allocation of a tooth to an intervention within a tooth pair is quasi‐random, this domain was graded low risk of bias because we saw that in split‐mouth studies the risk of selection bias is in any case insignificant |
| Blinding? (Outcome assessors) | High risk | Comment: this domain was graded as having high risk of bias because we saw that blinding of outcome assessor in clinical trials of this nature cannot be performed, as outcome assessor can discriminate between materials after follow‐up |
| Incomplete outcome data? (Caries efficacy outcomes) | Low risk | Missing data: 6/320 (2%) children at 36 months. Comment: Marginal missing data rate |
| Selective reporting (reporting bias) | Low risk | Outcomes reported: Caries response and sealant retention. Comment: Pre‐specified outcomes (in methods) were reported in pre‐specified way |
| Free of other bias? Comparability of the groups | Low risk | Comment: Split‐mouth design with the same baseline diagnosis of the teeth within a tooth pair (sound surfaces) |
| Free of other bias? Co‐interventions | Unclear risk | No information provided |
Bojanini 1976.
| Methods |
Trial design: split‐mouth design, treatment tooth randomly assigned among tooth pair Year the study started: 1975 Follow‐up: 36‐months |
|
| Participants |
Location: Colombia, children were from the public school system Inclusion criteria: children had to have at least 1 caries‐free homologous pair of first permanent molars. Age at baseline: 6 to 8 years Gender: not stated Baseline caries: no information provided but caries‐free individuals were not included in the study Number randomly assigned: 200 children with 318 tooth pairs Number evaluated: 173 children (275 tooth pairs) at 12 months; 158 children (252 tooth pairs) at 24 months; 170 children (272 tooth pairs) at 36 months |
|
| Interventions |
Comparison: resin‐based sealant versus no sealant Tooth pair: occlusal surface of 1 tooth sealed with resin‐based sealant (second generation resin‐based autopolymerised Delton); occlusal surface of the other tooth of the tooth pair served as a control without sealant. Sealant applications carried out by dental hygienists, with 1 year of formal training, under field equipment. No resealing. Co‐interventions: tap water was fluoridated in the study area |
|
| Outcomes |
Outcomes assessed independently by 2 dentists by visual inspection with use of a mirror and explorer. Any disagreement between the 2 examining dentists was resolved by a combined examination |
|
| Notes | Funding source: no identified funding source but 2 of the authors had affiliation to a sealant manufacturer | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Sealant was applied to the molar of one side while the opposite side homologue(s) served as the untreated control. The treatment was chosen by means of a previously established randomisation table." Comment: Adequate sequence generation |
| Allocation concealment (selection bias) | Low risk | Quote: "The treatment was chosen by means of a previously established randomisation table. To avoid placement errors, an adhesive bandage was placed on the side to be treated." Comment: This domain was graded low risk of bias because the description of the randomisation procedure gives an impression that realization of the random sequence generation was real, and because we saw that in split‐mouth studies the risk of selection bias is in any case insignificant |
| Blinding? (Outcome assessors) | High risk | Comment: this domain was graded as having high risk of bias because we saw that blinding of outcome assessors in clinical trials of this nature cannot be performed, as sealants are visible |
| Incomplete outcome data? (Caries efficacy outcomes) | Low risk | Missing data: 27/200 (13.5%) children at 12 months, 42/200 (21%) children at 24 months, and 30/200 (15%) children at 36 months of follow‐up. Comment: Missing data rate under 25% at all follow‐ups |
| Selective reporting (reporting bias) | Low risk | Outcomes reported: Caries response and sealant retention. Comment: Pre‐specified outcomes (in methods) were reported in pre‐specified way |
| Free of other bias? Comparability of the groups | Low risk | Comment: Split‐mouth design with the same baseline diagnosis of the teeth within a tooth pair (caries‐free surfaces). |
| Free of other bias? Co‐interventions | Low risk | Quote: "Medellin's water has been fluoridated since 1969." Comment: Although there was incomplete information on co‐interventions, this domain was graded low risk of bias because this was a split‐mouth design with equal conditions to teeth within a tooth pair and because it was anticipated that there was no other co‐interventions included in the protocol than fluoridated water and perhaps fluoride toothpaste which were accepted co‐interventions in this review |
Bravo 2005.
| Methods | Trial design: cluster‐randomised design, where 15 school classes were randomly assigned to 3 treatment arms. School classes were conducted at 5 primary schools, which were selected at random from a group of 21 schools. Mean number of teeth per child was 3.5 (a child was an additional cluster) Year the study started: 1990 Follow‐up period: 108 months: 48 month caries preventive programme, plus 60 months after active programme | |
| Participants |
Location: Spain, a non‐fluoridated city (0.07 ppm F ion in tap water)
Children were from middle or lower‐middle socioeconomic status families
Inclusion criteria: children with sound permanent first molars
Age at baseline: 6 to 8 years (average age 7 years)
Gender: girls 68% in sealant group, 51% in control group
Baseline caries: sealant group: mean dft 2.24 (SD 2.59); control group 2.98 (SD 2.90). Number randomly assigned: 362 (112 in sealant group; 115 in fluoride varnish group; 135 in control group) Number evaluated: 75 (37 in sealant group; 38 in fluoride varnish group; 45 in control group). Only children who (1) had at least 1 completely erupted and sound permanent molar at any period during the active programme, and (2) were examined at 48 month follow‐up were included in the analysis at 108 months |
|
| Interventions | Comparison: resin‐based sealant versus control without sealant
(Only sealant and control groups were used in this review) Co‐interventions: none reported |
|
| Outcomes |
|
|
| Notes | Inter‐rater agreement: kappa coefficients for intra‐examiner and inter‐examiner reliability > 0.68 in all measurements Funding source: Spain Ministry of Education and Science. Study authors were from the university |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote from author correspondence: "Each school‐class was numbered. By using a list of random numbers from a statistical book each school‐class was assigned to the 3 groups. When 1 group was full of children (i.e. the sum of the children in the assigned school‐classes was above the sample size needed for a group), then that group was excluded for new random assignations. The school classes allocation was not completely random, since it had some restrictions: For example, the total number of children should be at last more or less equilibrated between the three groups (thus, after the first random assignment, the following were conditional)" Comment: Randomisation procedure was not completely random |
| Allocation concealment (selection bias) | High risk | Comment: The non‐random method used for sequence generation would likely not allow for allocation concealment |
| Blinding? (Outcome assessors) | High risk | Quote: "A different dentist examined the subjects in a blinded fashion" Outcome assessor dentist did not have access to previous records (information was obtained from study authors) Comment: Although blinding of outcome assessor was intended, this domain was graded as having high risk of bias because we saw that blinding of outcome assessors in clinical trials of this nature cannot be performed, as sealants are visible |
| Incomplete outcome data? (Caries efficacy outcomes) | Unclear risk | Missing data: 18% for all 3 groups combined at 48 months (drop‐out rates by group not detailed) Comment: This domain was graded as having unclear risk of bias because no information on drop‐outs was provided by group at 48 month of follow‐up At 108 months of follow‐up, this domain was graded as having high risk of bias because proportion of participants assessed and included in the analysis was 33% (only children who had at least 1 completely erupted and sound permanent molar at any time period during the active programme, and were examined at 48 month follow‐up, were included in the analysis at 108 months) |
| Selective reporting (reporting bias) | Low risk | Outcomes reported: caries response and sealant retention Comment: Pre‐specified outcomes (in methods) were reported in a pre‐specified way |
| Free of other bias? Comparability of the groups | Low risk | Comment: Detailed description of demographic characteristics and caries risk level at baseline was given for groups available at 48 months and 108 months. The groups were assessed to be comparable although baseline mean dft in sealant group was 2.24 (SD 2.59) and in control group 2.98 (SD 2.90), and proportion of girls was 68% in sealant group and 51% in control group |
| Free of other bias? Co‐interventions | Low risk | Quote: "The children received no toothbrushing, fluoride rinse, or fluoride tablet programs" Comment: This domain was graded as having low risk of bias because no co‐interventions were included in the protocol |
Brooks 1979.
| Methods |
Trial design: split‐mouth design, treatment tooth randomly assigned among tooth pair Year the study started: 1974 Follow‐up: 54 months |
|
| Participants |
Location: USA, children were located in 4 elementary schools and represented various socio‐economic backgrounds. Inclusion criteria: a child was eligible for the study if there was at least 1 pair of contralateral, caries‐free first permanent molars. Age at baseline: 5 to 10 years Gender: not detailed Baseline caries: no information provided but included children had to have caries or restorations in at least 1 other tooth. Number randomly assigned: 193 children with 294 tooth pairs Number evaluated: 152 children (233 tooth pairs) at 24 months; 128 children (201 tooth pairs) at 36 months; 110 children (168 tooth pairs) at 54 months; 99 children (150 tooth pairs) at 72 months, 67 children (102 tooth pairs) at 84 months |
|
| Interventions |
Comparison: resin‐based sealant versus no sealant Tooth pair: occlusal surface of 1 tooth sealed with resin‐based sealant (second generation resin‐based autopolymerised sealant (Delton)); occlusal surface of the other tooth of the tooth pair served as a control without sealant. No resealing. Although the study included 2 sealant materials, Delton and Nuva‐Seal, only the Delton group is considered in this review because the first generation resin‐based sealants were not accepted in this review. Sealants were applied by 6 dentists, each with his own assistant in dental clinic consisting of 6 well equipped operatories which were supplied with triplex air‐water syringes and Pelvac or central suction. Isolation method cotton rolls. Co‐interventions: tap water was fluoridated in the study area |
|
| Outcomes |
Outcomes assessed by 2 dentists |
|
| Notes | Inter‐examiner agreement at 3‐year evaluation: the examiners had independent agreement of 92% for tooth status (sound, carious or restored) (2 examiners) Funding source: the study was supported by a university and a sealant manufacturer (authors were from universities) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "A randomised assignment sheet determined which sealant was to be used for each child and on which side of the mouth the teeth were to be treated." Comment: Adequate sequence generation |
| Allocation concealment (selection bias) | Low risk | Quote: "The child received the record form, and had a piece of tape placed on his cheek to indicate the previously assigned treatment side. The final step was an examination by a dentist to check proper sealant placement and accuracy of the record form prior to dismissing the patient." Comment: This domain was graded low risk of bias because the description of the randomisation procedure gives an impression that realisation of the random sequence generation was real, and because we saw that in split‐mouth studies the risk of selection bias is in any case insignificant |
| Blinding? (Outcome assessors) | High risk | Quote: "At the follow‐up examinations, new evaluation forms were used for recording the presence or absence of the sealant and any caries or restorations in the first permanent molars." Comment: Although blinding of outcome assessor was indicated, this domain was graded as having high risk of bias because we saw that blinding of outcome assessors in clinical trials of this nature cannot be performed, as sealants are visible |
| Incomplete outcome data? (Caries efficacy outcomes) | Low risk | Missing data:
Comment: The judgement of this domain is based on 2 years of follow‐up as described in Methods section. At all follow‐ups other than 24 months, this domain was graded high risk of bias because the drop‐out rate was over 25%. These judgements have been taken into account in each follow‐up analysis |
| Selective reporting (reporting bias) | Low risk | Outcomes reported: Caries response and sealant retention. Comment: Pre‐specified outcomes (in methods) were reported in pre‐specified way |
| Free of other bias? Comparability of the groups | Low risk | Comment: Split‐mouth design with the same baseline diagnosis of the teeth within a tooth pair (caries‐free surfaces) |
| Free of other bias? Co‐interventions | Low risk | Quote: "Augusta is a city with fluoridated water." Comment: Although there was incomplete information on co‐interventions, this domain was graded low risk of bias because this was a split‐mouth design with equal conditions to teeth within a tooth pair and because it was anticipated that there was no other co‐interventions included in the protocol than fluoridated water and perhaps fluoride toothpaste which were accepted co‐interventions in this review |
Charbeneau 1979.
| Methods |
Trial design: split‐mouth design, treatment tooth randomly assigned among tooth pair Year the study started: 1973 Follow‐up: 48 months |
|
| Participants |
Location: USA, children were from 2 schools Inclusion criteria: children had to have at least 1 contralateral pair of caries ‐ or restoration‐free permanent first molar. Diagnosis made clinically by mirror and explorer. Age at baseline: 5 to 8 years Gender: no information provided Baseline caries: no information provided Number randomly assigned: 143 children with 229 tooth pairs Number evaluated: 186 tooth pairs at 24 months, 193 tooth pairs at 36 months, 185 tooth pairs at 48 months Drop‐out rate: 26/143 (18%) children at 48 months (information on numbers of children at all follow‐ups not stated). |
|
| Interventions |
Comparison: resin‐based sealant versus no sealant
Tooth pair: occlusal surface of 1 tooth sealed with resin‐based sealant (second generation resin‐based autopolymerised sealant (Kerr Pit and Fissure)); occlusal surface of the other tooth of the tooth pair served as a control without sealant.The occlusal surface was considered acceptable for treatment if the occlusal mesial surface of maxillary molar was sound, even though occlusal distal surface was carious or filled. No resealing. All procedures conducted in a 2‐chair mobile dental van, which provided optimal physical facilities. Co‐interventions: no information provided |
|
| Outcomes | Sound or carious or restored occlusal surface of molar and sealant retention status. Outcomes assessed by 2 dentists |
|
| Notes | Inter‐examiner agreement: 91.2% for tooth status (caries or restoration) at 36 months (2 evaluators) Funding source: no identified funding source (authors were from university) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Sealant was applied to the isolated test tooth that was selected by using a table of random numbers." Comment: Adequate sequence generation |
| Allocation concealment (selection bias) | Low risk | Comment: Although the information of allocation concealment was incomplete, this domain was graded low risk of bias because we saw that in split‐mouth studies the risk of selection bias is in any case insignificant |
| Blinding? (Outcome assessors) | High risk | Comment: this domain was graded as having high risk of bias because we saw that blinding of outcome assessors in clinical trials of this nature cannot be performed, as sealants are visible |
| Incomplete outcome data? (Caries efficacy outcomes) | Low risk | Missing data: 26/143 (18%) children at 48 months. Comment: Drop‐out rate under 25% |
| Selective reporting (reporting bias) | Low risk | Outcomes reported: Caries response and sealant retention. Comment: Pre‐specified outcomes (in methods) were reported in pre‐specified way |
| Free of other bias? Comparability of the groups | Low risk | Comment: Split‐mouth design with the same baseline diagnosis of the teeth within a tooth pair (caries‐free surfaces) |
| Free of other bias? Co‐interventions | Unclear risk | No information provided |
Chen 2012.
| Methods |
Trial design: parallel‐group study, 4 randomly assigned treatment arms (glass‐ionomer, glass‐ionomer plus LED light, glass‐carbomer, composite resin).
Follow‐up: 48 months Year the study started: 2010 |
|
| Participants | Location: China (Wuhan City), high caries‐risk children were chosen from 5 primary schools (grade 2 children). Inclusion criteria: children had to have at least 1 fully erupted first permanent molar, no dentine caries lesion in pits and fissures of these molars, deep and/or intermediate pits and fissures, and a mean dmfs at least 2. Age at baseline: mean age 8.0 years (range 7.0‐9.1) Gender: 215 boys, 190 girls Baseline caries: baseline mean dmft scores with SD: 4.9 (2.6) in combined glass ionomer groups, 5.0 (2.4) in resin‐based sealant group. Baseline mean DMFT scores with SD: 0.15 (0.4) in combined glass ionomer groups, and 0.1 (0.4) in resin sealant group. Number randomly assigned: in total 405 children (with 1304 molars; mean 3.2 teeth per child) in 4 groups: 107 children in composite resin, 97 in glass ionomer, 103 in glass ionomer plus LED, and 98 in glass‐carbomer. Number evaluated: at 24 months: 383 children (102 children in composite resin, 90 in glass ionomer, 99 in glass ionomer plus LED, and 92 in glass‐carbomer groups). At 4 years: 365 children (98 children in composite resin, 84 in glass ionomer, 93 in glass ionomer plus LED, and 90 in glass‐carbomer groups) | |
| Interventions |
Comparison: glass ionomer sealants versus composite resin sealant
Data from glass ionomer sealant groups were combined (group 1 and group 2) at 24 months (because there was no difference in effectiveness of glass ionomer groups at 24 months) but not combined at 4 years (results reported separately for glass ionomer versus resin sealant and glass ionomer with LED light versus resin sealant at 4 years). On the school premises portable equipment (including operating light and adjustable bed) was used for placing the sealants. 3 dentists applied the sealants with a dental ancillary. No resealing. Co‐interventions: tap water was not fluoridated at study area. Fluoridated toothpaste was on the market but there was no information to what extent children had used it. (Additional information obtained from the authors) |
|
| Outcomes | Sound or carious occlusal surface of molar
Molars were assessed at smooth surfaces (pits) and at 3 sections (mesial‐central‐distal) into which the occlusal surface was arbitrarily divided. Outcomes were assessed by 4 evaluators assisted by trained recorders who had also assisted the operators. The examination site was well‐illuminated by an intra‐oral light with attached disposable mirrors |
|
| Notes | Inter‐evaluator consistency: 0.63 at 24 months (2 examiners), 0.86 at 4 years (2 examiners). Funding source: study supported by governmental and academic sources but sealant materials were donated by manufacturers | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "...author randomly allocated each included child to one of the 4 sealant groups, using a list obtained after block randomization (12 children per block for 3 operators) that was prepared by a statistician from the Dental School in Nijmegen (who did not do the analyses)." Comment: Adequate sequence generation |
| Allocation concealment (selection bias) | Low risk | Quote: "...using a list obtained after block randomization that was prepared by a statistician from the Dental School Nijmegen . . . the list was prepared about 7 weeks before the start of the study, placed in a closed envelope and kept concealed until the day before treatment started." Comment: Adequate allocation concealment |
| Blinding? (Outcome assessors) | High risk | Quote: "Blinding of operators in clinical trials of this nature could not be performed. Blinding of the evaluators, by not informing them about the sealant materials used, was only possible at years 0.5, 1 and 2 as the 2 years results had been published. As the three glass‐based sealants did not differ in color and texture, the level of blinding of evaluators is considered to be substantial" |
| Incomplete outcome data? (Caries efficacy outcomes) | Low risk | Missing data: at 24 months: 5/107 (4.7%) in composite resin group, 7/97 (7.2%) in glass ionomer group, 4/103 (3.9%) in glass ionomer plus added energy, and 6/98 (6.1%) in glass‐carbomer group.
At 4 years: 9/107 (8.4%) in composite resin group, 13/97 (13.4%) in glass ionomer group, 10/103 (9.7%) in glass ionomer plus added energy, and 8/98 (8.2%) in glass‐carbomer group. Total drop‐out rate at 4 years: 40/405 (9.9%). Reason of drop‐outs: School transfer; going abroad with parents. Comment: Although there was no information on reasons for drop‐outs by group, the groups were assessed to be balanced with each other. This is because the reasons for drop‐outs were seen not to cause bias |
| Selective reporting (reporting bias) | Low risk | Outcomes reported: Caries response and sealant retention. Comment: Pre‐specified outcomes (in methods) were reported in pre‐specified way |
| Free of other bias? Comparability of the groups | Low risk | Comment: Detailed description on caries risk levels (4 caries indices in permanent and deciduous dentitions) to assess the comparability of the groups at baseline and at 24 months |
| Free of other bias? Co‐interventions | Low risk | Comment: This domain was graded as having low risk of bias because no co‐interventions were included in the protocol |
Chen 2013.
| Methods |
Trial design: split‐mouth design, sealant material randomly assigned among tooth pair Year the study started: no information provided Follow‐up: 24 months |
|
| Participants |
Location: Paediatric department of First Dental Centre, Peking University School and Hospital of Stomatology, China
Inclusion criteria: Children had to have 1 or 2 tooth pairs of totally erupted permanent first molars without caries by visual inspection and probing. Children were divided into two categories based on caries risk severity: a) children with no or one carious tooth (dmft < 2) were included in the low risk group (LR); and b) children with dmft > 5 were placed in the high caries group (HR). Children with dmft 2 to 5 were excluded. Age at baseline: 6 to 9 years (mean 7.2 yr) Gender: not detailed Baseline caries: not reported (see inclusion criteria) Number randomly assigned: 61 children with 79 tooth pairs Number evaluated: 57 children with 75 tooth pairs |
|
| Interventions |
Comparison: glass ionomer sealant versus resin‐based sealant
Tooth pair: occlusal surface of 1 tooth sealed with glass ionomer sealant (light cured Fuji VII); occlusal surface of the other tooth of the tooth pair sealed with resin‐based Concise No re‐sealing Co‐interventions: preventive program that included education in oral hygiene, diet counselling, use of fluoridated toothpaste (600 ppm) and topical fluoridated foam treatment (6000 ppm) at every clinic recall (at 6 and 12 months) |
|
| Outcomes | Sound or carious occlusal surface of molar
Caries status was recorded using visual‐tactile methods Caries data were reported separately for HR (high caries risk) and LR (low caries risk) groups but we decided to combine data of these groups in our analyses (because the groups were small to evaluate separately and the combined design represents more real life) |
|
| Notes | Intra‐evaluator consistency: kappa co‐efficient was 0.91 (2 investigators); and inter‐evaluator consistency for diagnosis of caries (WHO criteria): kappa co‐efficient was 0.75 (2 investigators) Funding source: supported by a grant from the Peking University School and Hospital of Stomatology | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Random numbers determined the material used to seal the teeth" |
| Allocation concealment (selection bias) | Low risk | Comment: Although the information of allocation concealment was incomplete, this domain was graded low risk of bias because we saw that in split‐mouth studies the risk of selection bias is in any case insignificant |
| Blinding? (Outcome assessors) | High risk | Comment: this domain was graded as having high risk of bias because we saw that blinding of outcome assessor in clinical trials of this nature cannot be performed, as outcome assessor can discriminate between materials after follow‐up |
| Incomplete outcome data? (Caries efficacy outcomes) | Low risk | Missing data: 4/61 (6.6%) children after 24 months. Quote: "Reason for dropout: School transfer out of Peking; Immigrant abroad". Comment: Missing data rate under 25% |
| Selective reporting (reporting bias) | Low risk | Outcomes reported: incidence of dentinal carious lesion on treated occlusal surfaces of molars, retention. Comment: Pre‐specified caries outcomes (in methods) were reported in the pre‐specified way |
| Free of other bias? Comparability of the groups | Low risk | Comment: Split‐mouth design with the same baseline diagnosis of the teeth within a tooth pair and with similar conditions during the follow‐up |
| Free of other bias? Co‐interventions | Low risk | Comment: Similar co‐interventions among the sealant teeth during the follow‐up. Although one of the co‐interventions was topical fluoridated foam treatment (6000 ppm) at clinic recalls of 6 and 12 months, we saw that it likely not caused bias because the intervention was marginal and similarly addressed to all sealed teeth |
De Luca‐Fraga 2001.
| Methods |
Trial design: split‐mouth design, sealant material randomly assigned among tooth pair Year the study started: no information provided Follow‐up: 1 year Study evaluated 2 sealant materials (experimental group) to control without sealant (control group). This design is not RCT, and not considered in this review. In the experimental group, sealant material was randomly assigned among each child's tooth pair. The experimental group with randomised split‐mouth design is included in this review, and the description of the study considers only the experimental group |
|
| Participants |
Location: Brazil Inclusion criteria: children had to have caries‐free mandibular first molars Age at baseline: 7 to 8 years Gender: not detailed Baseline caries: no information provided Number randomly assigned: 100 children with 100 tooth pairs Number evaluated: 98 children with 98 tooth pairs |
|
| Interventions |
Comparison: resin‐modified glass ionomer sealant versus polyacid‐modified composite resin Tooth pair: occlusal surface of 1 tooth sealed with resin‐modified glass ionomer (Vitremer)); occlusal surface of the other tooth of the tooth pair sealed with polyacid‐modified composite resin sealant (Dyract) No resealing Sealants were applied by 1 dentist. Isolation method was cotton wool rolls. Co‐interventions: no information provided |
|
| Outcomes | Sound or carious occlusal surface of molar and sealant retention status Because currently the comparison (resin‐modified glass ionomer sealant versus compomer) is not relevant any more and the chemical compounds of these two materials are close to each other, only the results given in the article are referred to in this review (see 'Other comparisons'). Recall examinations were carried out in the children's own school environment and were executed by 2 professionals | |
| Notes | Funding source: study supported by FAPESP‐Sao Paolo Research Support Foundation (independent public foundation) but sealant materials were donated by manufacturers | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "One material was introduced in the right side and the other in the left side, alternately. The first material to be applied in each treated child was also alternated, avoiding results variation. The first choice was random." Comment: No further information on sequence generation |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding? (Outcome assessors) | High risk | Comment: this domain was graded as having high risk of bias because we saw that blinding of outcome assessor in clinical trials of this nature cannot be performed, as outcome assessor can discriminate between materials after follow‐up |
| Incomplete outcome data? (Caries efficacy outcomes) | Low risk | Missing data: 2/100 (2%) children at 12 months. Comment: Marginal missing data rate |
| Selective reporting (reporting bias) | Low risk | Outcomes reported: Caries response and sealant retention. Comment: Pre‐specified outcomes (in methods) were reported in pre‐specified way |
| Free of other bias? Comparability of the groups | Low risk | Comment: Split‐mouth design with the same baseline diagnosis of the teeth within a tooth pair (caries‐free surfaces) |
| Free of other bias? Co‐interventions | Unclear risk | No information provided |
Dhar 2012.
| Methods |
Trial design: split‐mouth design, teeth were randomly selected to be sealed with or without tooth preparation with a glass ionomer or resin‐based sealant Year the study started: no information provided Follow‐up: 24 months |
|
| Participants |
Location: India, children represented low socio‐economic backgrounds Inclusion criteria: children had to have 4 erupted, non‐carious permanent first molars. Clinical examinations carried out by a single examiner with a dental assistant. Age at baseline: 6 to 10 years Gender: not detailed Baseline caries: caries prevalence for the studied age group in the area was 63.2% and DMFT of 2.60 (additional information obtained from the author). Number randomly assigned: 25 children with 50 tooth pairs Number evaluated: 25 children with 50 tooth pairs |
|
| Interventions |
Comparison: glass ionomer sealant versus resin‐based sealant
Tooth pair: occlusal surface of 1 tooth sealed with glass ionomer‐based sealant (GC Fuji Ionomer VII light pink)); occlusal surface of the other tooth of the tooth pair sealed with fluoride releasing resin‐based sealant (Clinpro pink) No resealing Each of the 25 children had their 4 permanent molars subjected randomly to the 4 techniques: a) glass ionomer‐based sealant with tooth preparation, b) glass ionomer‐based sealant without tooth preparation, c) resin‐based sealant with tooth preparation, and d) resin‐based sealant without tooth preparation. The preparation technique involved widening and deepening the fissures with a one quarter round bur, with a slow‐speed handpiece. Sealants were applied by 1 dentist with a dental assistant. Anesthesia and rubber dam application were used to obtain maximum standardisation of sealant placement. Applications and recall examinations were carried out in a dental clinic setting. Co‐interventions: all children were given oral hygiene instructions which was reinforced at each visit, and all children used regularly fluoridated toothpaste. None of the subjects were on fluoride supplements. Tap water was not fluoridated (additional information obtained from the author) |
|
| Outcomes | Sound or carious occlusal surface of molar and sealant retention status
Data concerning teeth without surface preparation were included in review analyses.
Data concerning teeth with surface preparation were reported separately because data were seen not to be comparable with data from the other studies (only this study included teeth with surface preparation). Outcomes were assessed by 1 dentist with the help of a dental assistant. Caries was detected visually for opacity, defects at the margin, or softness by an explorer |
|
| Notes | Inter‐examiner reproducibility: kappa statistic 1.0 Funding source: no identified funding source |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Teeth were randomly selected to be sealed with or without tooth preparation with a glass ionomer or resin‐based sealant." Additional information obtained from the author: Randomisation was performed using the 'chit system'. A 'chit' was a piece of paper on which 1 of the treatment options was written‐ this paper was then carefully folded to conceal the written part. 4 such chits were made with different treatment options. Since the indications for all the 4 treatment options were the same, the provider randomly picked up a chit and provided the sealant type and technique mentioned for the tooth in question. He recorded what treatment was done for each tooth on the record sheet for that patient. |
| Allocation concealment (selection bias) | Low risk | The treatment provider randomly picked up a 'chit' and provided the sealant type and technique mentioned for the tooth in question. Information obtained from the author. Comment: The description gives an impression that the treatment was performed immediately (sealants were applied by 1 dentist with a dental assistant). |
| Blinding? (Outcome assessors) | High risk | Quote: "The examiner was blinded to the technique used, but not to the material used since the materials had different colours." Additional information obtained from the author: All the identifiers were concealed and the record forms of selected children were assigned a code number by a person other than the provider/examiner. The examiner evaluated each patient and filled out a new coded record sheet provided for that patient by the helper. The examiner could not be blinded for the type of sealants since 1 of the sealants used is coloured but did not have any information on whether the tooth was prepared or not. After evaluation was completed all the record sheets were collected by the helper and stapled together with the patient's previous record sheet. A new sheet was filled out by the examiner at each follow‐up visit. |
| Incomplete outcome data? (Caries efficacy outcomes) | Low risk | Missing data rate: 0%. |
| Selective reporting (reporting bias) | Low risk | Outcomes reported: Caries response and sealant retention. Comment: Pre‐specified outcomes (in methods) were reported in pre‐specified way |
| Free of other bias? Comparability of the groups | Low risk | Quote: "Non‐carious molars included." Comment: This domain was graded low risk of bias because we saw that both surfaces within a tooth pair will eventually be in equal risk for caries because of the long follow‐up time (regardless of whether the diagnosis was sound surface or surface with enamel lesion) |
| Free of other bias? Co‐interventions | Low risk | Additional information obtained from the author: All children were given oral hygiene instructions which was reinforced at each visit. All children used regularly fluoridated toothpaste. None of the subjects were on fluoride supplements. Tap water was not fluoridated. Comment: This domain was graded low risk of bias because no other co‐interventions than fluoridated toothpaste were included in the protocol |
Erdoğan 1987.
| Methods |
Trial design: split‐mouth design, sealant tooth randomly assigned among tooth pair Year the study started: no information provided Follow‐up: 54 months |
|
| Participants |
Location: Turkey, children were chosen from primary schools Inclusion criteria: no description of the inclusion criteria of children (however, the way of reporting gives an impression that the children to be included in the study had to have 4 sound first permanent molars) Age at baseline: from 8 to10 years Gender: not detailed Baseline caries: no information provided Number randomly assigned: 85 children with 170 tooth pairs (2 tooth pairs per child) Number evaluated: 236/340 teeth at 12 months, 204 teeth at 18 months, and 192 teeth at 54 months |
|
| Interventions |
Comparison: resin‐based sealant versus no sealant
Tooth pair: occlusal surface of 1 tooth sealed with resin‐based sealant (chemically polymerised Delton); occlusal surface of the other tooth of the tooth pair served as a control without sealant. Bitewing radiographs were taken for more accurate diagnosis before applying sealant Sealants were applied by 1 dentist. Isolation method was a saliva ejector and cotton wool rolls. No resealing. Co‐interventions: no information provided |
|
| Outcomes | Sound or carious or restored occlusal surface of molar and sealant retention status | |
| Notes | Funding source: no identified funding source (authors were from university) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "One maxillary and one mandibular first molar in each child were randomly assigned for treatment, and the other two teeth served as the controls." Comment: No further information on sequence generation |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding? (Outcome assessors) | High risk | Comment: this domain was graded as having high risk of bias because we saw that blinding of outcome assessor in clinical trials of this nature cannot be performed, as sealants are visible |
| Incomplete outcome data? (Caries efficacy outcomes) | High risk | Missing data: 26/88 (31%) children at 12 months, 34/85 (40%) at 18 months, and 37/85 (44%) children at 4.5 years. (Drop‐outs mostly due to children moving schools or areas). Comment: Missing data rate over 25% at all follow‐ups |
| Selective reporting (reporting bias) | Low risk | Outcomes reported: Caries response and sealant retention. Comment: Pre‐specified outcomes (in methods) were reported in pre‐specified way |
| Free of other bias? Comparability of the groups | Low risk | Comment: The way of reporting gives an impression that only molars with sound occlusal surfaces were included. In split‐mouth design we saw that both surfaces within a tooth pair will in any case eventually be in equal risk for caries because of the long follow‐up time (regardless of whether the diagnosis was sound surface or surface with enamel lesion) |
| Free of other bias? Co‐interventions | Unclear risk | No information provided |
Forss 1998.
| Methods |
Trial design: split‐mouth design, sealant material randomly assigned among tooth pair Year the study started: 1988 Follow‐up: on average 7 years (range 6.1 to 7.8 years) |
|
| Participants |
Location: Finland, children were from public health centre system Inclusion criteria: children had to have 1 contralateral pair of newly erupted, sound, unsealed permanent first or second molar teeth. Caries was scored without radiographs at examination. Age at baseline: 5 to14 years (mean age 11 years) Gender: not detailed Baseline caries: not stated (but the authors reported that the overall caries incidence among the same age cohort than the study population was relatively low (DMFT 3.44)). Number randomly assigned: 166 children with 166 tooth pairs Number evaluated: 151 children at 24 months, and 97 children at 7 years |
|
| Interventions |
Comparison: glass ionomer sealant versus resin‐based sealant
Tooth pair: occlusal surface of 1 tooth sealed with glass ionomer sealant (Fuji III); occlusal surface of the other tooth of the tooth pair sealed with third generation resin‐based sealant (light‐cured Delton) Sealants were applied by 3 dentists 22% of glass ionomer sealants were reapplied during the first 24 months of the trial Co‐interventions: no co‐interventions included in the protocol (additional information obtained from the author) |
|
| Outcomes | Sound or carious or restored occlusal surface of molar and sealant retention status Outcomes assessed by 1 dentist. Caries was scored without radiographs at examination | |
| Notes | Inter‐examiner reproducibility: no information provided Funding source: study was supported by a grant from the national dental society |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The side where glass ionomer sealant was applied was chosen randomly and resin‐based sealant was applied to the contralateral tooth." Additional information obtained from the author that the sequence generation was made by a dice, and done just before the sealant application (when the child was already in the dental office). Comment: Adequate sequence generation |
| Allocation concealment (selection bias) | Low risk | Comment: This domain was graded low risk of bias because the description of the randomisation procedure gives an impression that realization of the random sequence generation was real, and because we saw that in split‐mouth studies the risk of selection bias is in any case insignificant. |
| Blinding? (Outcome assessors) | High risk | Comment: this domain was graded as having high risk of bias because we saw that blinding of outcome assessor in clinical trials of this nature cannot be performed, as outcome assessor can discriminate between materials after follow‐up |
| Incomplete outcome data? (Caries efficacy outcomes) | Low risk | Missing data rate: 15/166 (9%) children at 24 months, and 69/166 (42%) children at 7 years.
Comment: Missing data rate under 25% at 24 months. At 7 years the missing data rate was 42%, and judged at high risk of bias |
| Selective reporting (reporting bias) | Low risk | Outcomes reported: Caries response and sealant retention. Comment: Pre‐specified outcomes (in methods) were reported in pre‐specified way |
| Free of other bias? Comparability of the groups | Low risk | Comment: Split‐mouth design with the same baseline diagnosis of the teeth within a tooth pair (sound surfaces) |
| Free of other bias? Co‐interventions | Low risk | No co‐interventions included in the protocol. Additional information obtained from the author |
Ganesh 2006.
| Methods |
Trial design: split‐mouth design, sealant material randomly assigned among tooth pair Year the study started: 2003 Follow‐up: 24 months |
|
| Participants |
Location: India, children were from 7 local government schools, and most of the children hailed from a low socio‐economic population Inclusion criteria: children had to have totally erupted (eruption less than 4 years ago), sound, unsealed, homologous permanent first molars Age at baseline: 6 to 7 years Gender: not detailed Baseline caries: not detailed information but the study population included children with low to high caries risk (additional information obtained from authors) Number randomly assigned: 100 children with 100 tooth pairs Number evaluated: 100 children with 100 tooth pairs |
|
| Interventions |
Comparison: glass ionomer sealant versus resin‐based sealant
Tooth pair: occlusal surface of 1 tooth sealed with glass ionomer sealant (Fuji VII, light‐cured); occlusal surface of the other tooth of the tooth pair sealed with third generation resin‐based sealant (light‐polymerised Concise) (The glass ionomer sealant was protected from moisture with Fuji Varnish after light curing). Isolation method: cotton wool rolls and suction or rubber dam, if needed. No resealing. Co‐interventions: during the study, oral prophylaxis was done for the children. Tap water in the study region was not fluoridated. (Additional information obtained from the author) |
|
| Outcomes | Sound or carious occlusal surface of molar and sealant retention status Evaluation of caries was carried out by visual and tactile method using mirror and explorer probe | |
| Notes | Inter‐ or intra‐examiner reproducibility: no information provided Funding source: no identified funding source |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The children participating in the study were asked to blindly pick up lots (paper chits) for the side of application and the material to be used first followed by the other side and the other material. The randomisation was done just before the sealant application and was done by the operator. Information obtained from the author. Comment: Adequate sequence generation |
| Allocation concealment (selection bias) | Low risk | Comment: This domain was graded low risk of bias because the description of the randomisation procedure gives an impression that realisation of the random sequence generation was real, and because we saw that in split‐mouth studies the risk of selection bias is in any case minimal |
| Blinding? (Outcome assessors) | High risk | The scores were being noted on separate evaluation forms at follow‐ups than at the beginning. (Information obtained from the author) Comment: Although blinding of outcome assessor was indicated, this domain was graded as having high risk of bias because we saw that blinding of outcome assessor in clinical trials of this nature cannot be performed, as outcome assessor can discriminate between materials after follow‐up |
| Incomplete outcome data? (Caries efficacy outcomes) | Low risk | Missing outcome data rate 0% |
| Selective reporting (reporting bias) | Low risk | Outcomes reported: Caries response and sealant retention. Comment: Pre‐specified outcomes (in methods) were reported in pre‐specified way |
| Free of other bias? Comparability of the groups | Low risk | Comment: Split‐mouth design with the same baseline diagnosis of the teeth within a tooth pair (sound surfaces) |
| Free of other bias? Co‐interventions | Low risk | During the study, oral prophylaxis was done for the children. Tap water in the study region was not fluoridated. Information obtained from the author. Comment: This domain was graded low risk of bias because no co‐interventions were included in the study. Oral prophylaxis was not seen to cause bias |
Guler 2013.
| Methods |
Trial design: split‐mouth design, sealant material randomly assigned among tooth pair Year the study started: 2006 (additional information obtained from the author) Follow‐up: 24 months |
|
| Participants |
Location: Ataturk University, Turkey
Inclusion criteria: children had to have fully erupted caries‐free permanent first molars with deep and retentive pit and fissures caries, and children have to live in the same geographical region. Evaluation of caries was performed using an intraoral camera, a DIAGNOdent device and visual examination criteria of Ekstrand. Teeth that showed DIAGNOdent readings of more than 20 as a cut‐off point were not included in the study (outer half enamel caries thus included) Age at baseline: 7 to 13 years (mean age: 8.9 ± 1.3) Gender: girls 29, boys 21 Baseline caries: the study did not evaluate the baseline caries experience of the included children (information obtained from the author) Number randomly assigned: 50 children with 100 tooth pairs Number evaluated: 37 children (74%) |
|
| Interventions |
Comparison: ormocer‐based sealant versus glass ionomer sealant
Tooth pair: occlusal surface of 1 tooth sealed with ormocer‐based sealant (Admira Seal); occlusal surface of the other tooth of the tooth pair sealed with glass ionomer sealant (Fuji VII). Sealants applied by same dentist with assisted by a dental nurse. No re‐sealing Co‐interventions: no fluoride treatments (additional information obtained from the author) |
|
| Outcomes | Sound or carious occlusal surface of molar
Outcomes were assessed by one dentist. Examinations were made with clinical evaluation and matching the first and follow‐up pictures of the sealants (images of the sealants were captured using the intra‐oral camera) Teeth with a lost sealant or a poor marginal integrity (an unacceptable margin with larger crevice present), or a presence of caries were all classified as failures in this study. These tooth surfaces were re‐sealed or otherwise treated and then excluded from the study during the follow‐up. Caries data after 24 months of follow‐up remains unclear although additional information was provided by the author (e.g. caries figures in results and discussion section are not the same). We decided to report the caries results after 24 months as they are stated in the article |
|
| Notes | Intra‐examiner reproducibility: kappa co‐efficient was 0.84 (1 investigator) Funding source: no institutional, private or corporate financial support (additional information obtained from the author). The authors were from universities. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Correspondence from the author: "The method to choose which material (Fuji VII or AS) and which tooth would be sealed first (right or left mandibular molar) was randomly carried out. A randomizing table comprising patient numbers (1‐50) was created for randomized treatment allocation. Type of fissure sealant was randomly allocated to patients from the randomizing table, with odd numbers included in Fuji VII and even numbers included in AS for right maxillary molar. After successfully carrying out the sealing of the affected tooth with the appropriate sealant, the contralateral homologue tooth was sealed with the other material and the opposite quadrants were sealed with the other material to those used first. Both sealants (Fuji VII and AS) were used in the mandibular and maxillary arch." Comment: Adequate random sequence generation, although slightly incompletely reported |
| Allocation concealment (selection bias) | Low risk | Comment: Although the information of allocation concealment was incomplete, this domain was graded low risk of bias because we saw that in split‐mouth studies the risk of selection bias is in any case insignificant |
| Blinding? (Outcome assessors) | High risk | Quote: "This study was designed as a randomised single‐blind clinical trial". Comment: no detailed information on blinding, but although blinding of outcome assessor was perhaps indicated, this domain was graded as having high risk of bias because we saw that blinding of outcome assessor in clinical trials of this nature cannot be performed, as outcome assessor can discriminate between materials after follow‐up |
| Incomplete outcome data? (Caries efficacy outcomes) | High risk | Missing data: 13/50 (26%) children. Comment: missing data over 25% |
| Selective reporting (reporting bias) | Low risk | Outcomes reported: incidence of dentinal carious lesion on treated occlusal surfaces of molars, retention Comment: Pre‐specified caries outcomes (in methods) were reported in the pre‐specified way |
| Free of other bias? Comparability of the groups | Low risk | Comment: Split‐mouth design with the same baseline diagnosis of the teeth within a tooth pair |
| Free of other bias? Co‐interventions | Low risk | Correspondence from the author: "Fluoride treatments, fluoride supplements were not applied at follow‐up examinations". Comment: This domain was graded low risk of bias because no co‐interventions were included in the study |
Hunter 1988.
| Methods |
Trial design: Split‐mouth design, sealant tooth quasi‐randomly assigned among tooth pair
Year the study started: not stated Follow‐up: 36 months |
|
| Participants |
Location: New Zealand; study conducted in 10 school dental clinics (5 in fluoridated towns and 5 in non‐fluoridated towns) to assess the appropriateness of sealants as a preventive procedure in School Dental Service. The main criterion for selection of the clinics was the presence of modern dental equipment with good operating lights, and air and water syringes
Inclusion criteria: children had to have at least 1 contralateral pair of fully erupted first permanent molars with unfilled and caries‐free occlusal surfaces and a retentive fissure pattern
Age at baseline: 5 to 8 years Gender: not detailed Baseline caries: no information provided Number randomly assigned: 575 tooth pairs (the number of the children not stated) Number evaluated: 509 pairs |
|
| Interventions | Comparison: resin‐based sealant versus no sealant Tooth pair: occlusal surface of 1 tooth sealed with second generation resin‐based autopolymerised sealant (Delton); occlusal surface of the other tooth of the tooth pair served as a control without sealant No resealing. Sealants were applied on caries‐free first permanent molars by school dental nurses (nurses had a 1‐hour training session before applications). Co‐interventions: five school dental clinics in fluoridated towns and five in non‐fluoridated towns | |
| Outcomes | Sound or carious or restored occlusal surface of molar and sealant retention status Outcomes assessed by a school dental nurse | |
| Notes | Funding source: no identified funding source | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "One only of each selected pair of teeth was fissure‐sealed alternating between the left and right sides of the mouth for successive tooth pairs." Comment: Although the method of allocation of a tooth to an intervention within a tooth pair is quasi‐random, this domain was graded low risk of bias because we consider that in split‐mouth studies the risk of selection bias is in any case minimal |
| Allocation concealment (selection bias) | Low risk | Quote: "One only of each selected pair of teeth was fissure‐sealed alternating between the left and right sides of the mouth for successive tooth pairs." Comment: Although the method of allocation of a tooth to an intervention within a tooth pair is quasi‐random, this domain was graded low risk of bias because we saw that in split‐mouth studies the risk of selection bias is in any case minimal |
| Blinding? (Outcome assessors) | High risk | Quote: "The records were not checked prior to examination so that the school dental nurse was not aware of the tooth that had been sealed." Comment: Although blinding of outcome assessor was indicated, this domain was graded as having high risk of bias because we saw that blinding of outcome assessor in clinical trials of this nature cannot be performed, as sealants are visible |
| Incomplete outcome data? (Caries efficacy outcomes) | Low risk | Missing data: 66/575 (11.5%) tooth pairs at 36 months. Comment: Information on the number of children at baseline not reported. Although the missing data rate was reported at tooth pair level (not at child level), this domain was graded low risk of bias because the proportion of the children dropped out could not exceed 23% (in calculations assumed the limits: each child would have had 2 tooth pairs at baseline (n = 288 children), but the drop‐out children would have had only 1 tooth pair (n = 66); thus the limit drop‐out would be 66/288) |
| Selective reporting (reporting bias) | Low risk | Outcomes reported: Caries response and sealant retention Comment: Pre‐specified outcomes (in methods) were reported in pre‐specified way |
| Free of other bias? Comparability of the groups | Low risk | Comment: Split‐mouth design with the same baseline diagnosis of the teeth within a tooth pair (caries‐free surfaces) |
| Free of other bias? Co‐interventions | Low risk | Quote: "Ten school dental clinics, five in fluoridated towns and five in non‐fluoridated towns, were selected for the study." Comment: This domain was graded low risk of bias because this was a split‐mouth design with equal conditions to teeth within a tooth pair (despite whether a child lived in fluoridated town or in non‐fluoridated town) |
Karlzén‐Reuterving 1995.
| Methods |
Trial design: split‐mouth design, sealant material randomly assigned among tooth pair Year the study started: 1989 Follow‐up: 36 months |
|
| Participants |
Location: Sweden, children were chosen from community dental clinic Inclusion criteria: children had to have 2 or 4 fully erupted first permanent molars (and their contralaterals), with no previous filling or clinical evidence of caries Age at baseline: mean age 7 years Gender: 26 girls and 21 boys Baseline caries: no information provided Number randomly assigned: 47 children with 74 tooth pairs Number evaluated: 45 children at each all 12, 24, and 36 months of follow‐ups |
|
| Interventions | Comparison: glass ionomer sealant versus resin‐based sealant
Tooth pair: occlusal surface of 1 tooth sealed with glass ionomer cement (GIC) (FUJI III)); occlusal surface of the other tooth of the tooth pair sealed with second generation resin‐based sealant (autopolymerised Delton) Sealants were applied by 1 dentist. No information on resealing but the way of reporting gives an impression that there was no resealing. Co‐interventions: no information provided |
|
| Outcomes | Sound or carious occlusal surface of molar and sealant retention status Sealants were controlled by 1 dentist |
|
| Notes | Funding source: national dental society. Study authors were from university. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The teeth were randomly assigned to treatment with either Delton or Fuji III." Comment: No further information on sequence generation |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding? (Outcome assessors) | High risk | Comment: this domain was graded as having high risk of bias because we saw that blinding of outcome assessor in clinical trials of this nature cannot be performed, as outcome assessor can discriminate between materials after follow‐up |
| Incomplete outcome data? (Caries efficacy outcomes) | Low risk | Missing data: 2/47 (4%) children at 12 months, 2/47 (4%) at 24 months, and 2/47 (4%) children at 36 months of follow‐up. (Due to moving, 2 children could not be evaluated). Comment: Marginal missing data rate |
| Selective reporting (reporting bias) | Low risk | Outcomes reported: Caries response and sealant retention. Comment: Pre‐specified outcomes (in methods) were reported in pre‐specified way. |
| Free of other bias? Comparability of the groups | Low risk | Quote: "Teeth, with no previous filling or clinical evidence of caries, were sealed." Comment: Although the baseline condition of the teeth within a tooth pair was not clearly specified (whether also surfaces with diagnosed enamel lesions included or not), this domain was graded low risk of bias because we saw that both surfaces within a tooth pair will eventually be in equal risk for caries because of the long follow‐up time (regardless of whether the diagnosis was sound surface or surface with enamel lesion) |
| Free of other bias? Co‐interventions | Unclear risk | No information provided |
Kervanto‐Seppälä 2008.
| Methods |
Trial design: split‐mouth design, sealant material quasi‐randomly assigned among tooth pair Year the study started: 1993 Follow‐up: 36 months |
|
| Participants |
Location: Finland, children were from public health centre system Inclusion criteria: children had to have totally erupted, sound, unsealed, homologous permanent second molars at caries risk (the diagnosis and risk assessment of each second molar was based on the case history and on the clinical status of each child) Age at baseline: 12 to 16 years Gender: not detailed Baseline caries: baseline DMFT was 0.57 in the age group of 13 years in 1993 (the largest group of all the age cohorts participating in the study) Number randomly assigned: 599 children with 1 or 2 tooth pairs Number evaluated: 436 children |
|
| Interventions |
Comparison: glass ionomer sealant versus resin‐based sealant
Tooth pair: occlusal surface of 1 tooth sealed with glass ionomer cement (Fuji III, chemically curing); occlusal surface of the other tooth of the tooth pair sealed with third generation resin‐based sealant (light‐polymerised Delton) Sealants were applied by 10 dentists working with a chairside assistant or by 4 dental hygienists operating alone. Teeth with a defective resin‐based sealant or with a re‐exposed fissure were resealed with resin sealant (15.2% were resealed). Defective or lost glass ionomer sealants were not replaced. Co‐interventions: no co‐interventions (the information obtained from the authors) |
|
| Outcomes | Sound or carious occlusal surface of molar and sealant retention status.
Cumulative caries rate of sealed tooth pairs over 36 months. Visual inspection and fibre‐optic transillumination were used routinely at examinations while radiological examination was not routinely used. |
|
| Notes | The dentists participating in the study were earlier calibrated. Mean inter‐examiner reproducibility (using fibre‐optic transillumination as a diagnostic aid): kappa value 0.42 (10 dentists) Funding source: the national dental society |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The sealant material for the first tooth to be sealed per mouth was chosen according to the child's birth date; odd numbers indicating resin sealant, and even numbers indicating glass ionomer. For the following tooth in order of the same child (starting from the upper right quadrant, followed by the upper left, lower left, and finally lower right quadrant), the opposite material was chosen. In case the second upper molar at the right side had not erupted at the time of examination and the others had, the molar from the left side determined the sealant material used. The evaluation was made by combining tooth pairs on contralateral sides in both the upper and lower jaws."
Additional information obtained from the author. Comment: Although a split‐mouth design with quasi‐random allocation method was decided to be graded as low risk of bias in this review, the judgement for this domain for this study was assessed to be unclear risk of bias. This is because the teeth to be sealed within a mouth were allocated systematically (every other tooth was sealed by resin sealant and every other tooth by glass ionomer), and the randomisation (even though by quasi‐random method) was not made within one tooth pair. It is not possible to assess whether or not this systematic procedure causes bias although it was seen unlikely |
| Allocation concealment (selection bias) | Unclear risk | Comment: Although a split‐mouth design with quasi‐random allocation in this review was decided to be graded as low risk of bias, the judgement for this domain for this study was assessed to be unclear risk of bias. This is because teeth to be sealed within a mouth were allocated systematically (every other tooth was sealed by resin sealant and every other tooth by glass ionomer), and the randomisation (even though by quasi‐random method) was not made within one tooth pair. It is not possible to assess whether or not this systematic procedure causes bias although it was seen unlikely |
| Blinding? (Outcome assessors) | High risk | Comment: this domain was graded as having high risk of bias because we saw that blinding of outcome assessor in clinical trials of this nature cannot be performed, as outcome assessor can discriminate between materials after follow‐up |
| Incomplete outcome data? (Caries efficacy outcomes) | High risk | Missing data rate: 163/599 children (27%) at 36 months. Comment: Missing data rate over 25% |
| Selective reporting (reporting bias) | Low risk | Outcomes reported: Caries response and sealant retention. Comment: Pre‐specified outcomes (in methods) were reported in pre‐specified way |
| Free of other bias? Comparability of the groups | Unclear risk | Comment: Both teeth within a tooth pair not necessarily erupted at baseline |
| Free of other bias? Co‐interventions | Low risk | Comment: No co‐interventions were included in the protocol. This information was obtained from the authors. |
Liu 2012.
| Methods |
Trial design: parallel‐group study, 4 randomly assigned treatment arms (sealant, fluoride varnish, silver diamine fluoride solution, and placebo) Year the study started: 2008 Follow‐up: 24 months |
|
| Participants |
Location: China, children were chosen from primary schools Inclusion criteria: children had to have at least 1 sound permanent first molar with deep fissures or fissures with signs of early (enamel) caries viewed as wet, with opacities and discolouration (proportion of early caries 35% of tooth sites). Clinical examinations included DIAGNOdent readings and were done by a dentist. Age at baseline: mean age 9.1 years (range 8 to 10 years) Gender: 248 boys and 253 girls Baseline caries: baseline mean dmft scores with SD for groups: sealant 3.19 (2.68); placebo 3.55 (2.54) (information obtained from the author) Number randomly assigned: 501 children (1539 molars, on average 3 teeth per child) in 4 groups: 124 children in sealant, 124 in fluoride varnish, 125 in silver diamine fluoride solution, and 128 in placebo. 252 children considered in this review (sealant and placebo groups). Number evaluated: 245 (121 children in sealant group, 124 children in placebo group) |
|
| Interventions | 4 treatment arms
Group 1: light‐cured, fluoride releasing resin‐based sealant Clinpro Sealant (applied by a dentist).
Group 2: NaF – semi‐annual application of a 5% NaF varnish (Duraphat) (applied by a dentist).
Group 3: SDF – annual application of a 38% silver diamine fluoride (SDF) solution (applied by a dentist).
Group 4: placebo control – annual application of water (applied by a dentist).
Group 1 and group 4 considered in this review.
Sealants were applied on sound permanent first molars with deep fissures or fissures with signs of early (enamel) caries viewed as wet, with opacities and discolouration.
No resealing. Co‐interventions: no systemic fluoridation in the study area. 90% of the toothpastes on sale contained fluoride. |
|
| Outcomes | Sound or carious occlusal surface of molar and sealant retention status. Each molar was assessed at 2 sites (upper molar – mesial pit/fossa and distal‐palatal groove; lower molar – occlusal fissure and buccal pit/groove). Caries incidence reported as child level, tooth level and fissure site level. Outcomes were assessed by the same blinded examiner using disposable mouth‐mirrors attached to an intra‐oral LED (light‐emitting diode) light and CPI (community periodontal index) probes Adverse events |
|
| Notes | Intra‐examiner reliability: Kappa statistic over 0.9. Funding source: the Hong Kong Research Grants Council (authors were from university) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "An assistant, using computer‐generated random numbers, allocated the children individually among four groups." Comment: Adequate sequence generation |
| Allocation concealment (selection bias) | Low risk | A computer generated random number table (only consisting of numbers 1, 2, 3, and 4) was printed out and kept by a research assistant. The group allocation of the subject, i.e. group 1 to group 4 followed the random numbers in the random number table. The treatment was performed immediately on site by a dentist not involved in the examination of the children according to the group allocation while the research assistant was present. Additional information obtained from the author |
| Blinding? (Outcome assessors) | High risk | Quote: "Status of the molars, including sealant retention and development of caries into dentin (ICDAS codes 4‐6), was assessed every 6 mos by the same blinded examiner." The record forms with group assignment information of the children were kept away from the examiner by the recorder. Additional information obtained from the author. Comment: Although blinding of outcome assessor was indicated, this domain was graded as having high risk of bias because we saw that blinding of outcome assessor in clinical trials of this nature cannot be performed, as sealants are visible |
| Incomplete outcome data? (Caries efficacy outcomes) | Low risk | Missing data: 3/124 (2.4%) in sealant group, and 4/128 (3%) in placebo group. Comment: Marginal drop‐out rate |
| Selective reporting (reporting bias) | Low risk | Outcomes reported: Caries response and sealant retention. Comment: Pre‐specified outcomes (in methods) were reported in pre‐specified way |
| Free of other bias? Comparability of the groups | Low risk | Quote: "Proportionately more children in the sealant group than in other groups had visited a dentist or consumed snacks once a day or less (P < 0.05)." (13% of children in sealant group and 29% in placebo group consumed snacks twice or more often a day) Additional information obtained from the author that there was no statistically significant difference between the groups in the baseline caries risk of the children. The baseline mean dmft scores with SD for groups: sealant 3.19 (2.68); placebo 3.55 (2.54). Comment: We decided to grade this domain as low risk of bias although there was difference in dental visit history and consuming snacks between groups at baseline because baseline caries risk scores of the children were similar. Similar baseline caries risk level was one of the fundamental characteristics in criteria of this domain to be assessed low risk of bias |
| Free of other bias? Co‐interventions | Low risk | Quote: "No systemic fluoridation in the study area. 90% of the toothpastes on sale contained fluoride." Comment: This domain was graded low risk of bias because no other co‐interventions than fluoridated toothpaste were included in the protocol |
Liu 2014a.
| Methods |
Trial design: 4 randomly assigned treatment groups (resin‐based sealant, glass ionomer‐based ART sealant (atraumatic restorative treatment), and 2 topical fluoride groups (SDF‐ silver diamine fluoride solution, NaF ‐ sodium fluoride varnish). There were five possible combinations of two out of the four study groups within a child (resin sealant/ART sealant, resin sealant/SDF, resin sealant/NaF, ART sealant/SDF, ART sealant/NaF).
Year the study started: no information provided Follow‐up: 24 months |
|
| Participants | Location: Southern China Inclusion criteria: Children had to have permanent first molars with occlusal surfaces which were deep or presented with signs of enamel caries lesion (opacity and discolouration seen when viewed wet), similar to ICDAS code 2. The molars were also assessed by DIAGNOdent device; DIAGNOdent readings ≥40 were taken to indicate that the screened molars potentially had dentine caries and these molars were excluded from the trial. Age at baseline: mean age 7.8 years Gender: 56% girls, 44% boys Baseline caries: caries prevalence of the 12‐year‐old children was 29.8% (mean DMFT score 0.54). No information on caries prevalence of the study population. Number randomly assigned: in total 317 children with 383 molars, comprising all groups. (There were only 80 children with resin sealant/ART sealant combination but we decided to include all children in analyses because the effects of fluoride applications to sealed teeth were seen to be minimal and balanced between the sealant material groups.) Number evaluated: 296 children with 357 molars | |
| Interventions |
Comparison: glass ionomer sealant versus resin sealant
Treatment 1: light‐cured, fluoride‐releasing resin‐based sealant Clinpro Sealant
Treatment 2: NaF – semi‐annual application of a 5% sodium fluoride varnish (NaF)
Treatment 3: SDF – annual application of a 38% silver diamine fluoride (SDF) solution
Treatment 4: glass ionomer sealant Ketac‐Molar Easymix (ART sealant; self‐cured high‐viscosity glass ionomer) Only glass ionomer sealant comparison with resin‐based sealant considered in this review. Sealants were provided in the schools by four dentists with help from chair‐side assistants. No re‐sealing. Co‐interventions: Water supply was not fluoridated but fluoride toothpaste was common in the market. Oral hygiene instruction was provided to all children in the study at baseline |
|
| Outcomes | Sound or carious occlusal surface of molar. Adverse events Development of dentine caries (ICDAS codes 4 to 6) was assessed by using intra‐oral LED (light‐emitting diode) light and disposable plane front‐surface mouth mirror (CPI (community periodontal index) probe when necessary) |
|
| Notes | Inter‐evaluator consistency for diagnosis of caries: kappa co‐efficient greater than 0.88 (2 investigators) Funding source: The University of Hong Kong | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Included molars were randomly allocated into one of four parallel study groups (resin sealant, ART sealant, 2 fluoride groups) in units of left/right teeth per subject. At least one and at most two groups would be assigned in the same mouth. Two groups using topical fluorides would not be assigned in the same mouth. There were five possible combinations of two out of the four study groups (resin sealant/ART sealant, resin sealant/SDF, resin sealant/NaF, ART sealant/SDF, ART sealant/NaF) and these were assigned with numbers 1 to 5. Papers with the numbers written on were put into an envelope to be drawn by an assistant to decide the group combination of the included molars of a subject. A coin was then thrown to decide which side of the molars would be assigned the group with smaller group number in the combination. If only molars of one side were included, the other group in the selected combination would be discarded". Comment: Although the description of the randomisation procedure could have been clearer, we decided to grade this domain as having low risk of bias because fundamentally the approach seemed to be sound |
| Allocation concealment (selection bias) | Low risk | Quote: "Papers with the numbers written on were put into an envelope to be drawn by an assistant to decide the group combination of the included molars of a subject. A coin was then thrown to decide which side of the molars would be assigned the group with smaller group number in the combination". Comment: Although the description of the allocation concealment could have been clearer, we decided to grade this domain as having low risk of bias because the description gave the impression that concealment was real |
| Blinding? (Outcome assessors) | High risk | Quote: " Development of dentine caries in the molars was assessed blindly every 6 months by the same two calibrated dentists involved in the baseline examination". Comment: Although blinding of outcome assessor was indicated, this domain was graded as having high risk of bias because we saw that blinding of outcome assessor in clinical trials of this nature cannot be performed, as outcome assessor can discriminate between materials after follow‐up |
| Incomplete outcome data? (Caries efficacy outcomes) | Low risk | Missing data: resin sealant group: 9/157 (5.7 %), glass ionomer group: 12/160 (7.5%) Reasons for lost to follow‐up: children were absent on the day of examination. Comment: No significant difference between the groups in the distribution of children lost to follow‐up |
| Selective reporting (reporting bias) | Low risk | Outcomes reported: caries response, adverse effects Comment: Pre‐specified outcomes (in methods) were reported in a pre‐specified way |
| Free of other bias? Comparability of the groups | Unclear risk | Baseline molar status: higher proportion of molars in the glass ionomer group than in the resin group had signs of enamel caries (19.6% versus 12.2%, P = 0.047). Snacking habits: twice or more a day in 26% of children in resin group and in 19.4% of children in glass ionomer group. Tooth brushing habits: once a day or less in 36% of children in resin group and in 35% of children in glass ionomer group. Comment: this domain was graded as having unclear risk of bias because baseline proportions of molars with enamel lesion was slightly imbalanced between sealant material groups and it is unclear whether this impacted on the results (the study found that presence of incipient caries in the fissures before placement of sealant would increase the risk of dentine caries development, P = 0.008). |
| Free of other bias? Co‐interventions | Low risk | Comment: This domain was graded low risk of bias because no other co‐interventions than fluoridated toothpaste were included in the protocol. |
Liu 2014b.
| Methods |
Trial design: 3 randomly assigned treatment groups (resin‐based sealant, glass ionomer sealant, no‐treatment). The students came from 3 primary schools from Dalian Development District, Dalian, China and the researchers came from Department of Stomatology of Dalian Development District Hospital Year the study started: 2009 Follow‐up: 24 months |
|
| Participants | Location: China Inclusion criteria: children who had at least one sound first permanent molar with deep pit and fissures or pit and fissures with signs of non‐cavitated lesion (ICDAS II scales 1 and 2) were included. Age at baseline: 7 to 9 years (mean age 8.6 years) Gender: 183 (49%) girls, 189 (51%) boys of 372 children at 24 months Baseline caries: baseline mean dmft‐index (including decayed, missing and filled permanent and deciduous teeth): 5.38 (SD 2.73) in resin‐based sealant group, 5.29 (SD 3.43) in glass ionomer sealant group, and 5.18 (SD 3.30) in control group Number randomly assigned: in total 419 children (with 664 molars) in 3 groups (mean teeth number per child 1.6): 136 children (219 teeth) in resin‐based sealant group, 130 children (218 teeth) in glass ionomer group, and 153 children (227 teeth) in no‐treatment group. Number evaluated: in total 372 children (with 587 molars) in 3 groups: 123 children in resin‐based sealant group, 116 in glass ionomer group, and 133 in no‐treatment group | |
| Interventions | Comparisons: resin sealant versus no sealant; glass ionomer sealant versus no sealant; glass ionomer sealant versus resin sealant Treatment 1: light‐cured, fluoride releasing resin‐based sealant Helioseal F (applied by a dentist) Treatment 2: light‐cured Fuji VII glass ionomer sealant (applied by a dentist) Treatment 3: control group without treatments Sealants were applied by two dentists with 5 years experience. No re‐sealing. Co‐interventions: no information provided | |
| Outcomes | Sound or carious occlusal surface of molar Development of caries was recorded using visual methods (by ICDAS II scale: codes 3 to 6 recorded as cavitated caries). The molars were also assessed by DIAGNOdent device; DIAGNOdent readings 16 to 30 indicating that there was no sign of dentin caries. | |
| Notes | Inter‐evaluator consistency for diagnosis of caries: kappa co‐efficient > 0.8 (2 investigators) Funding source: Chinese stomatological association and China Oral Health Foundation | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The subjects were stratified into 4 layers according to the number of first permanent molars included, in each strata the children were allocated into 3 groups by simple randomisation". Comment: no detailed information on randomisation method provided |
| Allocation concealment (selection bias) | Unclear risk | Comment: No information provided |
| Blinding? (Outcome assessors) | High risk | Quote: "singly blinded to the subjects". Comment: "examiners were not blinded" |
| Incomplete outcome data? (Caries efficacy outcomes) | Unclear risk | Missing data: 13/136 (9.6%) children in resin‐based sealant group, 14/130 (10.8%) in the glass ionomer sealant group, and 20/153 (13.1%) in the control group. Reasons for drop‐outs: not stated. Comment: This domain was graded as having unclear risk of bias because no information on reasons for drop‐outs was provided |
| Selective reporting (reporting bias) | Low risk | Outcomes reported: caries response Comment: Pre‐specified outcomes (in methods) were reported in a pre‐specified way |
| Free of other bias? Comparability of the groups | Low risk | Comment: we decided to grade this domain was graded low risk of bias although the proportion of boys was bigger in the glass ionomer group than in the resin‐based sealant and control groups. Further, the proportion of teeth with non‐cavitated caries (compared to deep fissure surface) was significantly bigger in the resin‐based sealant group than in the glass‐ionomer sealant group |
| Free of other bias? Co‐interventions | Unclear risk | No information provided |
Mills 1993.
| Methods |
Trial design: split‐mouth design, sealant material randomly assigned among tooth pair Year the study started: not stated Follow‐up: 24 months |
|
| Participants |
Location: England, children were from a community dental clinic Inclusion criteria: for inclusion in the study group aged 5 to 10 at least 1 pair of caries‐free fissure sites of permanent first molars was required, and in the study group aged 11 to 16 at least 1 pair of caries‐free fissure sites of permanent second molars was required Age at baseline: 5 to 16 years Gender: not detailed Baseline caries: no information provided Number randomly assigned: 53 children with in total 120 pairs of fissure sites Number evaluated: 59 tooth pairs (no information on drop‐out rate of children) |
|
| Interventions |
Comparison: glass ionomer sealant versus resin‐based sealant
Tooth pair: occlusal surface of 1 tooth sealed with silver cermet‐ionomer cement (Ketac Silver); occlusal surface of the other tooth of the tooth pair sealed with second generation resin‐based sealant (autopolymerised Delton) Sealants applied on the occlusal surfaces or buccal grooves of sound first and second permanent molars. Isolation method a saliva ejector and cotton wool rolls. No reporting on resealing. Co‐interventions: no information provided |
|
| Outcomes | Sound or carious or restored occlusal surface of molar and sealant retention status | |
| Notes | Funding source: no identified funding source | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Random allocation of both the sites to be sealed and the choice of material to be used at each site was decided by the dental surgery assistant spinning a coin." Comment: Adequate sequence generation |
| Allocation concealment (selection bias) | Low risk | Comment: this domain was graded low risk of bias because the description of the randomisation procedure gives an impression that realization of the random sequence generation was real, and because we saw that in split‐mouth studies the risk of selection bias is in any case minimal |
| Blinding? (Outcome assessors) | High risk | Comment: this domain was graded as having high risk of bias because we saw that blinding of outcome assessor in clinical trials of this nature cannot be performed, as outcome assessor can discriminate between materials after follow‐up |
| Incomplete outcome data? (Caries efficacy outcomes) | High risk | Missing data rate: 61/120 (51%) tooth pairs at 24 months. Comment: Although the missing data rate was reported at tooth pair level (not at child level), this domain was graded high risk of bias because we saw that the missing data rate stated by tooth pairs was large enough to secure large missing data rate also by children |
| Selective reporting (reporting bias) | Low risk | Outcomes reported: Caries response and sealant retention. Comment: Pre‐specified outcomes (in methods) were reported in pre‐specified way |
| Free of other bias? Comparability of the groups | Low risk | Comment: Split‐mouth design with the same baseline diagnosis of the teeth within a tooth pair (sound surfaces) |
| Free of other bias? Co‐interventions | Unclear risk | No information provided |
Muller‐Bolla 2013.
| Methods |
Trial design: Split‐mouth design, sealant tooth randomly assigned among tooth pair Follow‐up: 12 months |
|
| Participants |
Location: Children were recruited from elementary schools (n = 16) located in the low socio‐economic zones of Nice, France (school‐based dental sealant (SBDS) program)
Inclusion criteria: Children had to have 1 or 2 tooth pairs of totally erupted permanent first molars without caries (ICDAS codes 0 to 2). Age at baseline: mean 6.4 (SD ± 0.4) years Gender: 133 girls, 143 boys Baseline caries: mean d3‐6mft 2.8 (SD ±3.3); mean D3‐6MFT‐M1 0.2 (SD ±0.5). At baseline, 33.1 % of the first graders were totally caries free. However, 90% of children were classified to have high caries risk at baseline, although they regularly used fluoride toothpaste, and none drank soft drinks or ate snacks apart from the three main meals and the classical 4 o'clock snack. Caries risk was considered high when children had one or more carious lesions (ICDAS codes 3‐6) on temporary or permanent teeth, visible dental plaque in large amount without disclosing agent (score 3 of plaque index de Löe and Silness), or a positive salivary test result (caries risk salivary test consisted in the collection of stimulated saliva samples to assess the Streptococcus mutans and Lactobacillus counts). Number randomly assigned: 276 children with 457 tooth pairs Number evaluated: 253 children with 421 tooth pairs |
|
| Interventions |
Comparison: resin‐based sealant versus no sealant
Tooth pair: occlusal surface of 1 tooth sealed with resin‐based sealant (light‐curing Delton plus containing fluoride); occlusal surface of the other tooth of the tooth pair served as a control without sealant. Sealants were applied to completely erupted occlusal surfaces of permanent first molars by 1 dentist assisted by a sixth‐year dental student. Sealing was performed in the first or second grades. No resealing. Co‐interventions: The children were educated on the importance of considering dental caries as a localised disease, toothbrushing with fluoride toothpaste, and adopting healthy dietary habits |
|
| Outcomes | Sound or carious occlusal surface of molar.
Caries status was recorded using visual methods and tactile methods when necessary, after toothbrushing performed by the examiner. Examinations were performed in the school's infirmary using portable equipment that included an air‐water syringe, disposable intraoral mouth mirrors, and a LED headlight for a visual assessment. Adverse events |
|
| Notes | Intra‐evaluator reliability: Kappa co‐efficient 0.75 for diagnosis of caries (1 investigator). Funding source: Dentsply, the city of Nice, the Conseil General des Alpes Maritimes | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The random allocation sequence was generated using block of four by one of the authors". Correspondence from the author: "A block corresponded to 4 children with parental consent and examined in alphabetical order in one class (AABB, ABBA, BAAB, BBAA, ABAB, BABA). In case of one tooth pair, A indicated sealant in cadran 1 or 3 (sealant on 16 for pair 16‐26, and on 36 for pair 36‐46); B indicated sealant in cadran 2 or 4 (26 for pair 16‐26, and 46 for 36‐46). In cases where both pairs were included, the upper pair (16– 26) was used as a reference for randomization. When a maxillary permanent molar was randomly assigned to be sealed, the mandibular permanent molar to be sealed was on the opposite side (16– 36 or 26– 46 were sealed)." Comment: Although the information on sequence generation was incomplete (how the 6 alternatives of blocks and their order were created), this domain was graded as low risk of bias because we saw that in split‐mouth studies the risk of selection bias is in any case minimal |
| Allocation concealment (selection bias) | Low risk | Comment: Although the method of allocation of a tooth to an intervention within a tooth pair was incomplete, this domain was graded low risk of bias because we saw that in split‐mouth studies the risk of selection bias is in any case minimal |
| Blinding? (Outcome assessors) | High risk | Comment: this domain was graded as having high risk of bias because we saw that blinding of outcome assessor in clinical trials of this nature cannot be performed, as sealants are visible |
| Incomplete outcome data? (Caries efficacy outcomes) | Low risk | Missing data: 23 (6.7%) children after 1 year. Quote: "One year later, 23 children (6.7%) had left the school or were absent on the examination day". Comment: Missing data rate under 25% |
| Selective reporting (reporting bias) | Low risk | Outcomes reported: incidence of dentinal carious lesion on treated occlusal surfaces of molars, retention Comment: Pre‐specified caries outcomes (in methods) were reported in the pre‐specified way |
| Free of other bias? Comparability of the groups | Low risk | Comment: Split‐mouth design with similar conditions among the teeth during the follow‐up |
| Free of other bias? Co‐interventions | Low risk | Comment: Similar co‐interventions among the teeth during the follow‐up |
Pardi 2005.
| Methods |
Trial design: parallel‐group study, 3 randomly assigned treatment arms (resin‐modified glass ionomer, flowable resin composite, compomer) Year the study started: no information provided Follow‐up: 24 months |
|
| Participants |
Location: Brazil Inclusion criteria: children had to have at least 1 permanent first molar with no previous filling, sealant or clinical evidence of caries (white spot lesion or cavity). Children were divided into groups of different dmft scores (dmft = 1 e 2, and dmft over 3) before being allocated to groups at random. Age at baseline: 7 to 8 years Gender: not detailed Baseline caries: no information provided Number randomly assigned: 113 children with 356 teeth (117 teeth sealed with Vitremer, 119 teeth sealed with Revolution, 120 teeth sealed with Dyract Flow) Number evaluated: 325 teeth at 12 months (106 teeth sealed with Vitremer, 108 teeth sealed with Revolution, and 111 teeth sealed with Dyract Flow); and 279 teeth at 24 months (97 teeth sealed with Vitremer, 93 teeth sealed with Revolution, 89 teeth sealed with Dyract Flow) |
|
| Interventions | 3 treatments arms Group 1: resin‐modified glass ionomer (Vitremer) (conditioned with 37% phosphoric acid). Group 2: flowable resin composite (Revolution) (conditioned with 37% phosphoric acid). Group 3: compomer (Dyract Flow) (conditioned with 37% phosphoric acid). The clinical procedures were done using portable dentistry equipment. Isolation method cotton rolls. No resealing. Co‐interventions: no information provided |
|
| Outcomes | Sound or carious occlusal surface of molar, and retention status Caries was defined as active white spot lesion (translucent enamel alteration) or presence of a microcavity (diameter under 1.5 mm across fissure) or large cavity or filling. Outcomes assessed by 1 calibrated dentist who used an explorer and a mirror. Data were not used in the analyses in this review because the data reported were not in suitable form for this review (caries was defined as active white spot lesion (translucent enamel alteration) or presence of a microcavity (diameter under 1.5 mm across fissure) or large cavity or filling). Additional information on caries data was inquired from the authors but the information was not available for this update. The results as stated in the original article are reported in this review | |
| Notes | Intra‐examiner reproducibility for caries evaluation: 0.81 Funding source: grant from research support foundation |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Aleatory numbers table. Comment: Information obtained from the authors |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding? (Outcome assessors) | High risk | Comment: this domain was graded as having high risk of bias because we saw that blinding of outcome assessor in clinical trials of this nature cannot be performed, as outcome assessor can discriminate between materials after follow‐up |
| Incomplete outcome data? (Caries efficacy outcomes) | Low risk | Missing data:
11/117 (9.4%) teeth in Vitremer group, 11/119 (9.2%) teeth in Revolution group and 9/120 (7.5%) teeth in Dyract Flow group at 1 year.
20/117 (17%) teeth in Vitremer group, 26/119 (22%) teeth in Revolution group and 31/120 (26%) teeth in Dyract Flow group at 24 months. In total 31/356 (9%) teeth at 1 year, and 77/356 (22%) teeth at 24 months. Comment: Although the missing data rate was reported at tooth level (not at child level) this domain was graded low risk of bias because we saw that the number of the children at start of the study was large enough (37 children per group) to compensate the possible imbalance for missing data in numbers of children across groups, and the drop‐out teeth were evenly distributed between the groups. |
| Selective reporting (reporting bias) | Low risk | Outcomes reported: Caries response and sealant retention Comment: Pre‐specified outcomes (in methods) were reported in pre‐specified way |
| Free of other bias? Comparability of the groups | Low risk | Quote: "The children were divided into groups of different DMFT scores before being allocated to the groups at random." Comment: Although the information on demographic characteristics is limited, this domain was graded low risk of bias because DMFT scores were similar across groups at baseline |
| Free of other bias? Co‐interventions | Unclear risk | No information provided |
Poulsen 2001.
| Methods |
Trial design: split‐mouth design, sealant material randomly assigned among tooth pair Year the study started: 1995 Follow‐up: 36 months |
|
| Participants |
Location: Syrian Arab Republic; in the WHO Regional Demonstration, Training and Research Center for Oral Health in Damascus. Children included in the study were recruited from schools close to the Center Inclusion criteria: children had to have at least 1 pair of permanent first molars sound or with enamel lesion. Diagnosis was based on clinical examination Age at baseline: mean age 7 years Gender: not detailed Baseline caries: average DMFT value 0.6 to 0.7 in children aged 6 to 7 years in Damascus, based on data collected by the WHO Regional Demonstration, Training and Research Center for Oral Health. Number randomly assigned: 170 children with 306 tooth pairs Number evaluated: 115 children at 24 months; 116 children at 36 months |
|
| Interventions | Comparison: glass ionomer sealant versus resin‐based sealant Tooth pair: occlusal surface of 1 tooth sealed with glass ionomer cement (Fuji III); occlusal surface of the other tooth of the tooth pair sealed with second generation resin‐based sealant (autopolymerised Delton) No resealing Co‐interventions: no information provided | |
| Outcomes | Sound or carious occlusal surface of molar and sealant retention status Outcomes were assessed by a dentist. Follow‐up examinations were carried out in a dental chair, with good operating light and using probe and drying with compressed air. |
|
| Notes | Intra‐examiner consistency for caries: kappa value 0.83 at baseline and 0.92 at 36 months Funding source: grant from The Danish Dental Association |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "In each child random numbers were used to decide which tooth should be sealed with the resin material and which tooth should be sealed with glass ionomer." Comment: Adequate sequence generation |
| Allocation concealment (selection bias) | Low risk | Comment: Although the information of allocation concealment was incomplete, this domain was graded low risk of bias because we saw that in split‐mouth studies the risk of selection bias is in any case minimal |
| Blinding? (Outcome assessors) | High risk | Comment: this domain was graded as having high risk of bias because we saw that blinding of outcome assessor in clinical trials of this nature cannot be performed, as outcome assessor can discriminate between materials after follow‐up |
| Incomplete outcome data? (Caries efficacy outcomes) | High risk | Missing data: 55/170 (32%) children, and 54/170 (32%) children at 2 and 36 months, respectively. Missing data: 49/170 (29%) children at 1 year follow‐up. Comment: Missing data rate over 25% |
| Selective reporting (reporting bias) | Low risk | Outcomes reported: Caries response and sealant retention Comment: Pre‐specified outcomes (in methods) were reported in pre‐specified way |
| Free of other bias? Comparability of the groups | Low risk | Comment: Split‐mouth design which included either sound surfaces or surfaces with enamel lesion (but not dentine lesions). In split‐mouth designs we saw that both surfaces within a tooth pair will in any case eventually be in equal risk for caries because of the long follow‐up (regardless of whether the diagnosis was sound surface or surface with enamel lesion) |
| Free of other bias? Co‐interventions | Unclear risk | No information provided |
Raadal 1996.
| Methods |
Trial design: split‐mouth design, sealant material randomly assigned among tooth pair. Sealants were randomly allocated to the 2 sites in each pair of teeth (2 fissure sites were defined in all teeth: the mesial and the distal/lingual in the upper jaw, and the occlusal and buccal in the lower). Year the study started: 1991 Follow‐up: 36 months |
|
| Participants |
Location: Norway, study setting was a public dental clinic Inclusion criteria: children had to have at least 1 pair of newly erupted caries‐free first or second molars with at least 1 fissure site each. Teeth had to be erupted to the extent that the fissures to be sealed were free from gingival tissue. Age at baseline: 5 to 7 years (children with first molars) and 11 and 13 years (children with second molars) Gender: not detailed Baseline caries: no information provided Number randomly assigned: 53 children with 73 tooth pairs (16 children with first molars and 37 with second molars). Number evaluated: 53 at 1, 2, and 36 months |
|
| Interventions |
Comparison: resin‐reinforced glass ionomer cement versus resin‐based sealant
Tooth pair: occlusal surface of 1 tooth sealed with light‐cured resin‐reinforced glass ionomer cement (Vitrebond); occlusal surface of the other tooth of the tooth pair sealed with resin‐based sealant (Concise White Sealant) Sealants were applied by 2 dentists. Isolation method was cotton rolls. No resealing. Co‐interventions: no information provided |
|
| Outcomes | Sound or carious occlusal surface of molar and sealant retention status Outcomes were assessed by 2 dentists. Follow‐up examinations were carried out using a blunt probe. Bitewing radiographs were taken at the 12‐ and 36‐month follow‐ups. Caries was defined as sticking of a blunt probe, or visible cavity, or visible dentine radiolucency on radiograph |
|
| Notes | Inter‐examiner reproducibility: 90% and 100% for caries versus no caries (inter‐examiner reproducibility was assessed twice, before the study started and on commencement of the study). Funding source: no identified funding source |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Two sealants were randomly allocated to the two sites in each pair of teeth." Comment: No further information on sequence generation |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding? (Outcome assessors) | High risk | Quote: "Vitrebond and Concise had a similar opaque‐white appearance on the teeth immediately after application. Although the reviews were intended to be 'blind' this was not possible because Vitrebond lost its glossy appearance more rapidly than Concise and the operators could discriminate between them." |
| Incomplete outcome data? (Caries efficacy outcomes) | Low risk | Quote: "All the children were available for follow‐up." Missing data rate 0% |
| Selective reporting (reporting bias) | Low risk | Outcomes reported: Caries response and sealant retention Comment: Pre‐specified outcomes (in methods) were reported in pre‐specified way |
| Free of other bias? Comparability of the groups | Low risk | Comment: Split‐mouth design with the same baseline diagnosis of the teeth within a tooth pair (caries‐free surfaces) |
| Free of other bias? Co‐interventions | Unclear risk | No information provided |
Reisbick 1982.
| Methods |
Trial design: Split‐mouth design, sealant tooth randomly assigned among tooth pair Year the study started: 1981 (and lasted for 4 days) Follow‐up: 32 months |
|
| Participants |
Location: USA, children were chosen from 7 elementary schools Inclusion criteria: children had to have bilateral non‐carious first permanent molars. Examinations consisted of visual and roentgenographic diagnosis. Teeth allowing tactile enamel penetration by the explorer or displaying interproximal defects were excluded. Students were required to have resided in the study area during the first 5 years of their lives. Age at baseline: 6 to 10 Gender: not detailed Baseline caries: no information provided Number randomly assigned: 437 children with 437 tooth pairs Number evaluated: 317 children at 14 months; 286 children at 20 months; 254 children at 32 months |
|
| Interventions | Comparison: resin‐based sealant versus no sealant Tooth pair: occlusal surface of 1 tooth sealed with resin‐based sealant (chemically polymerised Oralin); occlusal surface of the other tooth of the tooth pair served as a control without sealant. Sealants were applied by 6 pedodontists and their assistants working in USC mobile clinic vans at school site. Isolation method was a rubber dam. No resealing. Co‐interventions: fluoride concentration in the drinking water at the study area was 0.5 ppm | |
| Outcomes | Sound or carious occlusal surface of molar and sealant retention status Sealants were evaluated by 3 evaluators. The study could not be included in the meta‐analyses in this review because it reported paired summary data only by tooth sites (3 sites per occlusal surface) but not by tooth surfaces which were the analysis units in this review. However, the study reported retention and effectiveness figures by treated pair.The results as stated in the original article are reported in this review. | |
| Notes | Funding source: no identified funding source (authors were from university) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The tooth to be sealed was chosen from a random numbers list. Six pedodontists and their assistants applied the sealant." Comment: Adequate sequence generation |
| Allocation concealment (selection bias) | Low risk | Quote: "The tooth to be sealed was chosen from a random numbers list. Six pedodontists and their assistants applied the sealant." Comment: This domain was graded low risk of bias because the description of the randomisation procedure gives an impression that realization of the random sequence generation was real, and because we saw that in split‐mouth studies the risk of selection bias is in any case minimal |
| Blinding? (Outcome assessors) | High risk | Quote: "Evaluation examinations were performed under blind conditions by three evaluators." Comment: Although blinding of outcome assessors was intended, this domain was graded as having high risk of bias because we saw that blinding of outcome assessor in clinical trials of this nature cannot be performed, as sealants are visible |
| Incomplete outcome data? (Caries efficacy outcomes) | High risk | Missing data: 120/437 (27%) children at 14 months, 151/437 (35%) children at 20 months, and 183/437 (42%) children at 32 months of follow‐up. Comment: Missing data rate over 25% |
| Selective reporting (reporting bias) | Low risk | Outcomes reported: Caries response and sealant retention. Comment: Pre‐specified outcomes (in methods) were reported in pre‐specified way |
| Free of other bias? Comparability of the groups | Low risk | Quote: "Teeth allowing tactile enamel penetration by the explorer were excluded." Comment: This domain was graded low risk of bias because we saw that both surfaces within a tooth pair will eventually be in equal risk for caries because of the long follow‐up time (regardless of whether the diagnosis was sound surface or surface with enamel lesion) |
| Free of other bias? Co‐interventions | Low risk | Quote: "The community chosen for the study was Santa Paula, where the fluoride concentration in the drinking water is 0.5." Comment: Although there was incomplete information on co‐interventions, this domain was graded low risk of bias because this was a split‐mouth design with equal conditions across teeth and because it was anticipated that there were no other co‐interventions included in the protocol than perhaps fluoride toothpaste which was an accepted co‐intervention in this review |
Richardson 1978.
| Methods |
Trial design: Split‐mouth design, sealant tooth randomly assigned among tooth pair Year the study started: 1975 Follow‐up: 60 months |
|
| Participants |
Location: Canada, children were chosen from 8 elementary schools (grade 2 children) Inclusion criteria: children had to have sound or sticky occlusal surfaces of erupted first permanent molars (surfaces which offered resistance to explorer removal after moderate pressure, without any visual signs of caries were deemed sticky). Clinical examinations by a dentist, using a portable light, mouth mirrors and explorers. Radiographs were not taken. Age at baseline: grade 2 children Gender: not detailed Baseline caries: no information provided Number randomly assigned: 266 children with 425 tooth pairs Number evaluated: 393 tooth pairs at 12 months; 352 tooth pairs at 24 months; 337 tooth pairs at 36 months; 330 tooth pairs at 48 months; 331 tooth pairs at 60 months |
|
| Interventions |
Comparison: resin‐based sealant versus no sealant
Tooth pair: occlusal surface of 1 tooth sealed with resin‐based sealant (chemically polymerised); occlusal surface of the other tooth of the tooth pair served as a control without sealant. Sealants were applied by a third year dental student assisted by a certified dental assistant in a one‐chair school dental clinic. Isolation method was cotton rolls and a good vacuum system. Co‐interventions: study conducted at a non‐fluoridated middle‐class suburban area of a city |
|
| Outcomes | Sound or carious occlusal surface of molar and sealant retention status The examinations were conducted in school health rooms by same dentist | |
| Notes | Funding source: no identified funding source (authors were from university) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Dice were used to decide which side was to be sealed and which side was to serve as an unsealed control." Comment: Adequate sequence generation |
| Allocation concealment (selection bias) | Low risk | Quote: "Dice were used to decide which side was to be sealed and which side was to serve as an unsealed control. A dental student assisted by a certified dental assistant applied the sealants." Comment: This domain was graded low risk of bias because the description of the randomisation procedure gives an impression that realization of the random sequence generation was real, and because we saw that in split‐mouth studies the risk of selection bias is in any case minimal |
| Blinding? (Outcome assessors) | High risk | Quote: "Predata were not available to the examiner." Comment: Although blinding of outcome assessor was intended, this domain was graded as having high risk of bias because we saw that blinding of outcome assessor in clinical trials of this nature cannot be performed, as sealants are visible |
| Incomplete outcome data? (Caries efficacy outcomes) | Low risk | Missing data: 32/425 (7.5%) tooth pairs at 12 months, 73/425 (17%) tooth pairs at 24 months, 88/425 (20.7%) tooth pairs at 36 months, 95/425 (22%) tooth pairs at 48 months, and 94/425 (22%) tooth pairs at 60 months of follow‐up. Comment: Missing data rate reported by tooth pairs (not by children). This domain was, however, graded low risk of bias because the drop‐out rates by children were also estimated to be under 25% at each follow‐up. (In calculations assumed the same number of tooth pairs per child at follow‐ups than at baseline. The assumption of the 1.6 tooth pairs per child at follow‐ups was based on the large sample size) |
| Selective reporting (reporting bias) | Low risk | Outcomes reported: Caries response and sealant retention. Comment: Pre‐specified outcomes (in methods) were reported in pre‐specified way |
| Free of other bias? Comparability of the groups | Low risk | Quote: "First permanent molars assessed as sound or sticky were included in the study." Comment: This entry was graded as low risk of bias because we saw that both surfaces within a tooth pair will eventually be in equal risk for caries because of the long follow‐up time (regardless of whether the diagnosis was sound surface or surface with enamel lesion) |
| Free of other bias? Co‐interventions | Low risk | Quote: "The study site was a non‐fluoridated middle‐class suburb of Vancouver." Comment: Although there is incomplete information on co‐interventions, this domain was graded low risk of bias because this was a split‐mouth design with equal conditions across teeth and because it was anticipated that there were no other co‐interventions included in the protocol than perhaps fluoride toothpaste which was an accepted co‐intervention in this review |
Rock 1978.
| Methods |
Trial design: Split‐mouth design, sealant tooth randomly assigned among tooth pair Year the study started: no information on recruitment period Follow‐up: 36 months |
|
| Participants |
Location: UK Study included 2 treatment groups: primary school group and secondary school group. Only the primary school group is included in this review because essential information (e.g. the number of the children or tooth pairs at baseline) is not available for the secondary school group. Primary school group was selected from children originally examined at 4 infant schools. Inclusion criteria: children had to have all 4 first molars caries‐free. Diagnosis was made by clinical examination with mirror and probe. Age at baseline: 6 to 7 years Gender: not detailed Baseline caries: no information provided Number randomly assigned: 220 primary school children with 440 tooth pairs Number evaluated: 181 children at 12 months; 154 children at 36 months |
|
| Interventions |
Comparison: resin‐based sealant versus no sealant
Tooth pair: occlusal surface of 1 tooth sealed with resin‐based sealant (chemically polymerised Delton); occlusal surface of the other tooth of the tooth pair served as a control without sealant.
Sealants were applied in a caravan at each school by 2 dentists. Isolation method was cotton rolls and a saliva ejector connected to a high volume aspirator.
No resealing. Co‐interventions: no information provided |
|
| Outcomes | Sound or carious occlusal surface of molar and sealant retention status Both authors were present at recall examinations, small groups of children being seen by 1 or other examiner alternately. If either examiner was in doubt as to how to record the condition of the resin for a particular patient, the opinion of his colleague was sought | |
| Notes | Funding source: grant of a sealant manufacturer (authors were from university) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Resin was applied to one upper and the opposing lower tooth on the same side of the mouth. The side of the test teeth was selected randomly by tossing a coin." Comment: Adequate sequence generation |
| Allocation concealment (selection bias) | Low risk | Quote: "Resin was applied to one upper and the opposing lower tooth on the same side of the mouth. The side of the test teeth was selected randomly by tossing a coin." Comment: This domain was graded low risk of bias because the description of the randomisation procedure gives an impression that realization of the random sequence generation was real, and because we saw that in split‐mouth studies the risk of selection bias is in any case minimal |
| Blinding? (Outcome assessors) | High risk | Quote: "Previous records were not available at recall and the examiner did not know to which teeth resin had been applied and by whom." Comment: Although blinding of outcome assessor was indicated, this domain was graded as having high risk of bias because we saw that blinding of outcome assessor in clinical trials of this nature cannot be performed, as sealants are visible |
| Incomplete outcome data? (Caries efficacy outcomes) | High risk | Missing data: 39/220 (18%) children after 1 year, and 66/220 (30%) children after 36 months. (Drop‐out figures of children not reported but in calculations used the information that each child have 4 teeth at baseline). Comment: The judgement of this domain is based at 36 months of follow‐up as described in Methods section (missing data rate over 25% after 36 months). At 1 year of follow‐up, this domain was graded low risk of bias because the drop‐out rate is 18%. This judgement has been taken into account in the analyses at 1 year |
| Selective reporting (reporting bias) | Low risk | Outcomes reported: Caries response and sealant retention. Comment: Pre‐specified outcomes (in methods) were reported in pre‐specified way |
| Free of other bias? Comparability of the groups | Low risk | Comment: Split‐mouth design with the same baseline diagnosis of the teeth within a tooth pair (caries‐free surfaces) |
| Free of other bias? Co‐interventions | Unclear risk | No information provided |
Rock 1996.
| Methods |
Trial design: split‐mouth design, sealant material randomly assigned among tooth pair Year the study started: 1991 Follow‐up: 36 months |
|
| Participants |
Location: UK, children were selected from 3 junior schools Inclusion criteria: children had to have 4 caries‐free fully erupted first permanent molars but also with there being evidence of caries experience in the primary dentition. Diagnosis based on clinical examination (dental mirror and blunt probe under a dental operating light). Age at baseline: 7 to 8 years Gender: not detailed Baseline caries: no information provided Number randomly assigned: 86 children with 172 tooth pairs Number evaluated: 79 children at 12 months; 66 children at 24 months; 65 children at 36 months |
|
| Interventions | Comparison: glass ionomer sealant versus resin‐based sealant Tooth pair: occlusal surface of 1 tooth sealed with glass ionomer cement (chemically cured Baseline); occlusal surface of the other tooth of the tooth pair sealed with visible light cure composite resin‐based sealant (FluroShield; containing 50% by weight of inorganic filler with releasable fluoride) Sealants were applied by 1 dentist (from academic staff) working in a fully equipped mobile dental surgery at 3 junior schools. Isolation method was a saliva ejector and cotton wool rolls. No resealing. Co‐interventions: tap water was fluoridated in 1987 (before that the water fluoride level was 0.13 ppm) | |
| Outcomes | Sound or carious occlusal surface of molar and sealant retention status Outcomes were assessed by a dentist. Follow‐up examinations were carried out using a mirror and blunt probe |
|
| Notes | Funding source: grant of a dental manufacturer | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Allocation was made before sealant application was begun by using random number tables." Comment: Adequate sequence generation |
| Allocation concealment (selection bias) | Low risk | Quote: "Allocation was made before sealant application was begun by using random number tables." Comment: This domain was graded low risk of bias because the description of the randomisation procedure gives an impression that realization of the random sequence generation was real, and because we saw that in split‐mouth studies the risk of selection bias is in any case minimal |
| Blinding? (Outcome assessors) | High risk | Comment: this domain was graded as having high risk of bias because we saw that blinding of outcome assessor in clinical trials of this nature cannot be performed, as outcome assessor can discriminate between materials after follow‐up. |
| Incomplete outcome data? (Caries efficacy outcomes) | Low risk | Missing data: 20/86 (23%) children after 24 months and 21/86 (24%) children after 36 months. Comment: Missing data rate under 25%. |
| Selective reporting (reporting bias) | Low risk | Outcomes reported: Caries response, sealant retention, and fluoride release from the sealant materials. Comment: Pre‐specified outcomes (in methods) were reported in pre‐specified way |
| Free of other bias? Comparability of the groups | Low risk | Comment: Split‐mouth design with the same baseline diagnosis of the teeth within a tooth pair (caries‐free surfaces) |
| Free of other bias? Co‐interventions | Low risk | Quote: "Tamworth water was fluoridated in 1987." Comment: Although there was incomplete information on co‐interventions, this domain was graded low risk of bias because this was a split‐mouth design with equal conditions across teeth and because it was anticipated that there were no other co‐interventions included in the protocol than perhaps fluoride toothpaste which was an accepted co‐intervention in this review |
Sheykholeslam 1978.
| Methods |
Trial design: split‐mouth design, sealant tooth randomly assigned among tooth pair Year the study started: 1975 Follow‐up: 33 months The results at 6 years were not used in this review because the study reported marginal summary data only by tooth sites (2 sites per maxillary occlusal surfaces) but not by tooth surfaces |
|
| Participants |
Location: USA, children were in grades 1, 2, 3, and 4 of 3 parochial schools in Jersey City Inclusion criteria: a child was selected in the study when there was evidence of caries in the mouth, and a pair of caries‐free, contralateral first permanent molars was present. Age at baseline: 6 to 10 years Gender: not detailed Baseline caries: no information provided Number randomly assigned: 205 children with 205 tooth pairs Number evaluated: 186 children at 11 months; 175 children at 24 months; 164 children at 33 months |
|
| Interventions |
Comparison: resin‐based sealant versus no sealant
Tooth pair: occlusal surface of 1 tooth sealed with second generation resin‐based autopolymerised sealant (Delton); occlusal surface of the other tooth of the tooth pair served as a control without sealant. Sealants applied by dentists. All procedures performed in a mobile van, equipped with 2 operatories. Isolation method cotton rolls. No resealing. Co‐interventions: tap water was fluoridated in the study area |
|
| Outcomes | Sound or carious or restored occlusal surface of molar and sealant retention status | |
| Notes | Funding source: sealant manufacturer (authors were from university) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "We used a table of random numbers to determine which side received the sealant, and which remained as the control." Comment: The information obtained from the authors |
| Allocation concealment (selection bias) | Low risk | Comment: Although the information on allocation concealment was incomplete, this domain was graded low risk of bias because we saw that in split‐mouth studies the risk of selection bias is in any case minimal |
| Blinding? (Outcome assessors) | High risk | Quote: "New examination forms were used at each visit in order to prevent any examiner bias." Comment: Although blinding of outcome assessor was indicated, this domain was graded as having high risk of bias because we saw that blinding of outcome assessor in clinical trials of this nature cannot be performed, as sealants are visible |
| Incomplete outcome data? (Caries efficacy outcomes) | Low risk | Missing data: 19/205 (9%) children after 11 months. 30/205 (15%) children after 24 months. 41/205 (20%) children after 33 months. Comment: Drop‐out rates under 25% at all follow‐ups |
| Selective reporting (reporting bias) | Low risk | Outcomes reported: Caries response and sealant retention. Comment: Pre‐specified outcomes (in methods) were reported in pre‐specified way |
| Free of other bias? Comparability of the groups | Low risk | Comment: Split‐mouth design with the same baseline diagnosis of the teeth within a tooth pair (caries‐free surfaces) |
| Free of other bias? Co‐interventions | Low risk | Quote: "Children were in grades 1, 2, 3, and 4 of three parochial schools in Jersey City (a recently fluoridated community)." Comment: Although there was incomplete information on other co‐interventions, this domain was graded low risk of bias because this was a split‐mouth design with equal conditions to teeth within a tooth pair and because it was anticipated that there were no other co‐interventions included in the protocol than fluoridated water and perhaps fluoride toothpaste which were accepted co‐interventions in this review |
Sipahier 1995.
| Methods |
Trial design: split‐mouth design, sealant material randomly assigned among tooth pair Year the study started: no information provided Follow‐up: 1 year |
|
| Participants |
Location: Turkey Inclusion criteria: children had to have 2 homologous caries‐free permanent first molars with absence of residual gingival tissue on the occlusal surface and no prior therapy. Diagnosis based on visual inspection with the use of a mirror and explorer. Age at baseline: 6 to 15 years Gender: not detailed Baseline caries: no information provided Number randomly assigned: 100 children with 100 tooth pairs Number evaluated: 86 children after 1 year of follow‐up |
|
| Interventions |
Comparison: glass ionomer sealant versus resin‐based sealant
Tooth pair: occlusal surface of 1 tooth sealed with glass ionomer‐silver‐cermet cement (Ketac‐Silver); occlusal surface of the other tooth of the tooth pair sealed with second generation resin‐based sealant (autopolymerised Delton) Sealants were applied by 1 dentist. Isolation method was cotton rolls. Co‐interventions: no information provided |
|
| Outcomes | Sound or carious occlusal surface of molar and sealant retention status | |
| Notes | Funding source: no information on funding. Study authors were from university | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "On a random basis, Delton or Ketac‐Silver was placed by a single operator on the occlusal surfaces of all permanent molars on one side of the side of the mouth; the other sealant was placed on the contralateral side." Comment: No further information on sequence generation |
| Allocation concealment (selection bias) | Unclear risk | No information provided. |
| Blinding? (Outcome assessors) | High risk | Quote: "New record forms were used at each evaluation to prevent examiner bias from occurring through knowledge of previous ratings." Comment: Although blinding of outcome assessor was indicated, this domain was graded as having high risk of bias because we saw that blinding of outcome assessor in clinical trials of this nature cannot be performed, as outcome assessor can discriminate between materials after follow‐up |
| Incomplete outcome data? (Caries efficacy outcomes) | Low risk | Missing data: 14/100 (14%) tooth pairs after 1 year of follow‐up. Comment: Missing data rate under 25% |
| Selective reporting (reporting bias) | Low risk | Outcomes reported: Caries response and sealant retention. Comment: Pre‐specified outcomes (in methods) were reported in pre‐specified way |
| Free of other bias? Comparability of the groups | Low risk | Comment: Split‐mouth design with the same baseline diagnosis of the teeth within a tooth pair (caries‐free surfaces) |
| Free of other bias? Co‐interventions | Unclear risk | No information provided |
Songpaisan 1995.
| Methods |
Trial design: parallel group design, 5 randomly assigned treatment arms (resin‐based sealant, glass ionomer cement Fuji III applied by dentists, glass ionomer cement Fuji III applied by schoolteachers, hydrofluoric acid solution, control) Year the study started: no information provided Follow‐up: 24 months |
|
| Participants |
Location: Thailand, children were selected from 2 secondary schools and they came from very low to medium socio‐economic level families (community‐oriented study). Inclusion criteria: children with at least 3 sound permanent molars (both first and second molars) Age at baseline: 12 to 13 years Gender: not detailed Baseline caries: at study age group of 12 to 13 years, the mean DMFT at baseline was 1.81 ± 1.84 Number randomly assigned: In total 752 children (with on average 7 teeth per child) (numbers of children per group not stated) Number evaluated: 671 children (133 in Delton group; 128 in GIC‐D group; 133 in GIC‐T group; 134 in HF group; and 143 in control group) |
|
| Interventions |
Comparisons: resin‐based sealant versus no sealant; glass ionomer sealant versus no sealant; glass ionomer sealant versus resin‐based sealant
Group 1: autopolymerised resin‐based sealant Delton (applied by a dentist)
Group 2: glass ionomer cement Fuji III applied by dentist (group GIC‐D)
Group 3: glass ionomer cement Fuji III applied by 6 3‐day‐trained schoolteachers (group GIC‐T) Group 4: hydrofluoric acid (HF) solution Group 5: control Group 1, group 2, group 3 and group 5 used in this review (data from groups 2 and 3 were combined). Only children aged 12‐13 years included in this review. The study included also younger age group (7‐8) but that group was excluded in this review because the children in that group rinsed with 0.2% NaF every 2 weeks (co‐intervention was one of the exclusion criteria in this review). With the exception of application of resin sealants, all procedures, including caries registration and retention examinations, were done at the school sites under simple dental mobile settings with the subjects in supine position on a flat table and their heads supported on an attached head rest. Reapplication of sealants was done for those children whose sealants were partially or all missing at the 6‐month examination. Co‐interventions: the central water supply naturally contained 0.1‐0.2 ppm F at the study area |
|
| Outcomes | Sound or carious or filled occlusal surface of molar, DFS increment. Sealant retention status. Outcomes assessed by dentists | |
| Notes | Intra‐examiner consistency: Kappa value for caries and retention at baseline and at 2‐year evaluation was 0.9. Funding sources: Public funding (WHO, Intercountry Centre for Oral Health, and university). 1 sealant material was provided by a sealant manufacturer. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Children were stratified and randomly assigned, based on school and DMFT, into five different groups to be subjected to various preventive programmes." Comment: No further information on sequence generation |
| Allocation concealment (selection bias) | Unclear risk | Comment: No information provided |
| Blinding? (Outcome assessors) | High risk | Comment: this domain was graded as having high risk of bias because we saw that blinding of outcome assessor in clinical trials of this nature cannot be performed, as sealants are visible |
| Incomplete outcome data? (Caries efficacy outcomes) | Low risk | Total amount of the missing data 81/752 (11%) for age group 12‐13 years (not detailed by group). Quote: "The main reason for dropping out was moving out of the area. The other reason was having orthodontic treatment." Comment: This domain was graded low risk of bias although the information on drop‐out rates by group was missing because the numbers of children at 24 months of follow‐up were similar |
| Selective reporting (reporting bias) | Low risk | Outcomes reported: Caries response and sealant retention. Comment: Pre‐specified outcomes (in methods) were reported in pre‐specified way |
| Free of other bias? Comparability of the groups | Low risk | Comment: This domain was graded low risk of bias although the description on demographic characteristics was missing for the groups evaluable at 24 months because the caries risk level at baseline was given to the groups and the groups were assessed to be balanced. |
| Free of other bias? Co‐interventions | Low risk | Quote: "Practically all toothpastes available in Thailand, especially in Bangkok, are fluoridated. The central water supply in Bangkok and adjacent provinces naturally contains 0.1‐0.2 ppm fluoride." Comment: This domain was graded low risk of bias because no other co‐interventions than fluoridated toothpaste were included in the protocol |
Tagliaferro 2011.
| Methods |
Trial design: parallel‐group study, 6 randomly assigned treatment arms Year the study started: no information provided Follow‐up: 24 months |
|
| Participants |
Location: Children were from 2 public schools and lived in a low‐caries‐prevalence city, Brazil
Inclusion criteria: Children had: (1) dmft ≥ 3 and/or ≥ 1 active cavitated lesion, or dmft + DMFT = 0, and (2) ≥ 2 sound permanent first molars
Age at baseline: mean age 7 years
Gender: 52% girls, 48% boys
Baseline caries: Mean (SD) dmft index was 4.51 (2.81) for HRS group and 4.53 (3.04) for HRC group. In low‐caries‐risk groups (LRS, LRV groups), dmft + DMFT was zero
Number randomly assigned: 327 children with mean number (SD) of occlusal surfaces treated 3.47 (0.80) Numbers of children per group: 57 in HRC group; 57 in HRV group; 55 in HRS group; 53 in LRC group; 52 in LRV group; 53 in LRS group Number evaluated: 268 at 24 months (44 children in HRC group; 48 in HRV group; 47 in HRS group; 42 in LRC group; 43 in LRV group; 44 in LRS group) |
|
| Interventions |
Comparison: resin‐modified glass ionomer fissure sealant versus no sealant
6 treatment arms
Groups 1, 2 and 3 included only high‐caries‐risk children
Group 1 (HRC): control group with high‐caries‐risk children receiving oral health education (OHE) program
Group 2 (HRV): OHE and fluoride varnish application biannually
Group 3 (HRS): OHE and single sealant application (resin‐modified glass ionomer cement, Vitremer)
Groups 4, 5 and 6 included only low‐caries‐risk children
Group 4 (LRC): control group receiving oral health education (OHE) program
Group 5 (LRV): OHE and fluoride varnish application biannually
Group 6 (LRS): OHE and single sealant application (resin‐modified glass ionomer cement, Vitremer)
(Only sealant and control groups were considered in this review: groups 1, 3, 4 and 6.)
Sealants were applied by dentist assisted by dental hygienist in dental office (sealants were applied to healthy permanent first molars). Procedure consisted of 4 stages: etching tooth surfaces with 37% phosphoric acid, primer application, ionomer application, finishing gloss application
No resealing
Oral health education was carried out by dentist assisted by dental hygienist. Sessions lasting 1 hour were held every 3 months, with talks covering themes such as dental caries, dental plaque and fluoride. Oral hygiene instructions, supervised tooth brushing and dietary counselling were presented to children by means of lectures, videos, educational games and oral quizzes
Co‐interventions: 93% of children used fluoridated dentifrice. Average fluoride concentration in tap water was 0.7 ppm |
|
| Outcomes | Sound or carious occlusal surface of first permanent molar: Caries increment was stated as mean DMF (decayed, missing and filled) scores One calibrated dentist carried out all examinations. Diagnosis was based on clinical examination, and no radiographs were taken at baseline or at final examinations Adverse events | |
| Notes | Intra‐examiner reliability: Kappa coefficients 0.95 (caries as cavitated lesions) and 0.90 (caries as cavitated and non‐cavitated lesions) Funding source: FAPESP (São Paulo Research Foundation is an independent public foundation) Caries prevalence of population at study area: mean DMFT 1.32 for 12‐years‐olds | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Additional information was obtained from study authors Children were systematically allocated to each treatment group as follows: Approximately 10 children were taken from each classroom at random by a dental hygienist. The hygienist did not know the caries risk of each child. The hygienist organised the 10 children in a queue at random. (In the queue were also those children not included in the study because they did not fulfil the inclusion criteria of the study; those children were excluded after baseline examination by a dentist). The examiner (Pardi V) performed the examination of the first child in the queue, and the main researcher (Tagliaferro EP) recorded data on a specific form and classified the child as having high or low caries risk, according to pre‐established criteria. After each examination day, record forms were organised according to caries risk (low or high) and sequence of examination. After this, for example, the first examined child of that day classified as having high risk of caries was systematically allocated to the control group, the second to the varnish group and the third to the sealant group, and successively. Each child was given an ID code to be used over the whole study period Comment: This domain was graded as having low risk of bias because we saw that the randomisation procedure as a whole was un‐systematic when noting to which treatment group each child was finally allocated |
| Allocation concealment (selection bias) | Low risk | Additional information was obtained from study authors The main researcher (Tagliaferro) called children for treatments as follows: Children allocated to sealant groups were brought to a clinical setting, their names and treatment group were checked and Tagliaferro applied sealants, with the help of a dental hygienist. Then, at another time, Tagliaferro went to the school, called the children allocated to varnish groups and performed varnish applications. The process of calling only children allocated to sealant or varnish groups, when sealant applications or varnish applications were performed, respectively, ensured that each child really received the intended treatment Comment: This domain was graded as having low risk of bias because we saw that despite incomplete allocation concealment (the same main researcher kept the records and made the applications), the large number of children in each allotted group and the fact that implementation of each treatment was centralised gave the impression that concealment was real |
| Blinding? (Outcome assessors) | High risk | Quote: "The study was a systematically randomised, blind, controlled trial. The calibrated dentist was not aware of group assignments during evaluations" The examiner did not see the records used for recording interventions for each child. This information was obtained from study authors Comment: Although blinding of outcome assessor was indicated, this domain was graded as having high risk of bias because we saw that blinding of outcome assessor in clinical trials of this nature cannot be performed, as sealants are visible |
| Incomplete outcome data? (Caries efficacy outcomes) | Low risk | Missing data: 13/57 (22.8%) in HRC group, 8/55 (14.5%) in HRS group,11/53 (20.8%) in LRC group, and 9/53 (17%) in LRS group. Quote: "Many individuals had moved out of the schools where the research was conducted, and some refused to take part in the final examination." Comment: Although there was no information on reasons for drop‐outs by group, the groups (HRC versus HRS; and LRC versus LRS) were assessed to be balanced with each other. This is because the reasons for drop‐outs were seen not to cause bias (many children have moved out of the schools). |
| Selective reporting (reporting bias) | Low risk | Outcomes reported: caries response Comment: Pre‐specified outcomes (in methods) were reported in a pre‐specified way |
| Free of other bias? Comparability of the groups | Low risk | Quote: "At baseline, gender, age, use of fluoridated dentifrice, family income, father's and mother's education were not statistically different among the six groups."
With regard to clinical variables (dmfs, dmft, DMFS, DMFT, number of occlusal surfaces being treated) at baseline, the groups were reported to be balanced. "Baseline caries experience (dmft + DMFT) was not significantly different between full participants and those lost to follow‐up for HRC, HRV, and HRS groups (in the low caries risk groups, dmft + DMFT was 0)." Comment: Detailed description on demographic characteristics (sex, age, and social class), on baseline caries risk level, and on baseline condition of the tooth surfaces to be treated, to assess the comparability of the groups also at 24 months. The groups were assessed to be balanced with each other. |
| Free of other bias? Co‐interventions | Low risk | All children participated in an oral education programme. 93% of children used fluoridated dentifrice. Comment: In all groups the same co‐interventions were allowed |
Tang 2014.
| Methods |
Trial design: 4 randomly assigned treatment groups (resin‐based sealant, fluoride varnish, fluoride foam, and control group). Students were selected from 4 primary schools (representing 33 school classes), and the examiners came from Academic Centres (Shanghai, Jing’an Dental Clinic at regional level and Hospital of Stomatology of 9th People’s Hospital of Shanghai Jiaotong University which is a referral clinic) Year the study started: not stated Follow‐up: 24 months |
|
| Participants |
Location: China
Inclusion criteria: healthy students living in Shanghai Jing’an District for more than 2 and half years with sound occlusal surfaces of first permanent molars or surfaces with enamel lesion. Clinical examinations were done by two dentists with mouth mirror, CPI probe under artificial light. The diagnostic criteria of caries were based on what was recommended by the WHO Oral Health Survey (fifth edition): basic methods.
Age at baseline: 7 to 8 years
Gender: 530 (52%) girls, 486 (48%) boys
Baseline caries: baseline mean DMFT‐index: not stated Number randomly assigned: in total 1016 children in 4 groups: 321 children in resin‐based sealant, 243 in fluoride varnish, 242 in fluoride foam, and 210 in control group. (The number of included teeth not stated.) Number evaluated: in total 977 children in 4 groups: 310 children in resin‐based sealant (1184 teeth; 3.8. teeth per child), 232 in fluoride varnish, 232 in fluoride foam, and 203 in control group. (The number of included teeth in other groups than sealant group not stated) |
|
| Interventions | 4 treatment arms Group 1: fluoride varnish – semi‐annual application of a 0.1% fluoride varnish (Fluor Protector) (applied by a dentist). Group 2: fluoride foam – semi‐annual application of a 0.6% fluoride foam (applied by a dentist). Group 3: light‐cured, fluoride releasing resin‐based sealant Clinpro TM Sealant (applied by a dentist). Group 4: control group with oral hygiene instruction Group 3 and group 4 considered in this review (resin‐based sealant versus control). Four trained dentists applied the sealants. No resealing Co‐interventions: all groups received oral health education. | |
| Outcomes | Sound or carious occlusal surface of molar. Development of dentine caries. Examinations were conducted by 4 dentists |
|
| Notes | Inter‐evaluator consistency for diagnosis of caries: Kappa co‐efficient 0.84 (2 investigators) Funding source: not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Random number table was used to divide subjects into 4 groups" |
| Allocation concealment (selection bias) | Unclear risk | Comment: No information provided |
| Blinding? (Outcome assessors) | High risk | Quote: "examiners were singly blinded". Comment: Although blinding of outcome assessor was indicated, this domain was graded as having high risk of bias because we saw that blinding of outcome assessor in clinical trials of this nature cannot be performed, as sealants are visible |
| Incomplete outcome data? (Caries efficacy outcomes) | Low risk | Missing data: 11/321 (3.4%) in resin‐based sealant group, 11/243 (4.5%) in fluoride varnish group, 10/242 (4.1%) in fluoride foam group, and 7/210 (3.3%) in the control group. Reasons for drop‐outs: "Children transferring to other schools or going abroad with parents." Comment: Marginal drop‐out rates |
| Selective reporting (reporting bias) | Low risk | Outcomes reported: caries incidence, factors effect on caries incidence. Comment: Pre‐specified outcomes (in methods) were reported in a pre‐specified way |
| Free of other bias? Comparability of the groups | Low risk | Comment: This domain was graded low risk of bias although the description on demographic characteristics was missing for the groups evaluable at 24 months because the drop‐out rates in groups were marginal at 24 months. The groups were assessed to be balanced at baseline. |
| Free of other bias? Co‐interventions | Low risk | Comment: This domain was graded low risk of bias because no other co‐interventions than basic oral health education (at baseline of the study) were included in the protocol |
Williams 1996.
| Methods |
Trial design: split‐mouth design, sealant material randomly assigned among tooth pair Year the study started: no information provided Follow‐up: 4 years |
|
| Participants |
Location: UK, selection of the children was carried out through school inspections Inclusion criteria: children had to have recently erupted first permanent molar teeth that were visually free of caries. Diagnosis based on clinical examination, teeth being dried before examination, and probes used only to remove occlusal debris. Age at baseline: mean age 7 years Gender: not detailed Baseline caries: no information provided Number randomly assigned: 228 children with 430 tooth pairs Number evaluated: 157 children at 24 months; 117 children at 4 years |
|
| Interventions |
Comparison: glass ionomer sealant versus resin‐based sealant
Tooth pair: occlusal surface of 1 tooth sealed with glass ionomer cement (Fuji III); occlusal surface of the other tooth of the tooth pair sealed with second generation resin‐based sealant (autopolymerised Delton) Sealants were applied by 2 dentists. Applications and recall examinations were carried out in community dental clinics. Local dental practitioners were asked to continue with routine care as normal. Isolation method was a saliva ejector and cotton rolls. Resealing: 6% of teeth resealed at 24 months of follow‐up (26 teeth with glass ionomer and 8 teeth with resin) and 7% at 4 years of follow‐up (27 teeth with glass ionomer and 6 teeth with resin). Co‐interventions: water fluoride concentration at the study area was from 0.1 to 0.5 mg F/l |
|
| Outcomes | Sound or carious occlusal surface of molar and sealant retention status. Outcomes were assessed by 2 dentists |
|
| Notes | Inter‐examiner reproducibility: Cohen's Kappa statistic 0.75. Funding source: grant from a dental manufacturer. Study authors were from university |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomisation was achieved by using a series of computer generated random numbers to which reference was made before the child entered the surgery." Comment: Adequate sequence generation |
| Allocation concealment (selection bias) | Low risk | Quote: "Randomisation was achieved by using a series of computer generated random numbers to which reference was made before the child entered the surgery." Comment: Adequate allocation concealment |
| Blinding? (Outcome assessors) | High risk | Comment: this domain was graded as having high risk of bias because we saw that blinding of outcome assessor in clinical trials of this nature cannot be performed, as outcome assessor can discriminate between materials after follow‐up |
| Incomplete outcome data? (Caries efficacy outcomes) | High risk | Missing data: 71/228 (31%) children after 24 months and 111/228 (49%) children after 4 years. Comment: Missing data rate over 25% |
| Selective reporting (reporting bias) | Low risk | Outcomes reported: Caries response and sealant retention. Comment: Pre‐specified outcomes (in methods) were reported in pre‐specified way |
| Free of other bias? Comparability of the groups | Low risk | Quote: "First permanent molar teeth that were visually free of caries were noted." Comment: Split‐mouth design with the same baseline diagnosis of the teeth within a tooth pair |
| Free of other bias? Co‐interventions | Low risk | Quote: "Subjects lived in an area receiving a water fluoride concentration between 0.1‐0.5 mgF/l." Comment: Although there was incomplete information on co‐interventions, this domain was graded low risk of bias because this was a split‐mouth design with equal conditions across teeth and because it was anticipated that there were no other co‐interventions included in the protocol than perhaps fluoride toothpaste which was an accepted co‐intervention in this review |
CI = confidence interval; dft = decayed, filled deciduous teeth; dmfs = decayed, missing and filled deciduous surfaces; dmft = decayed, missing and filled deciduous teeth; DMFT = decayed, missing and filled permanent teeth; DFS = decayed and filled occlusal surfaces; F = fluoride; ppm = parts per million; RCT = randomised controlled trial; SD = standard deviation.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Andjelic 1991 | Not RCT. Control group selected from another village |
| Aslanova 2003 | Parallel group study comparing different sealant materials to control without sealant. Not RCT. Random allocation not stated |
| Azul 1990 | Study comparing resin‐based sealant to control without sealant. Not RCT. Random or quasi‐random allocation not stated. |
| Baglioni‐Gouvea 2001 | Conference abstract with split‐mouth study comparing resin sealant to compomer. Comparison excluded in this update. No random or quasi‐random allocation to surfaces within each tooth pair (teeth 26 and 46 were sealed with Fluoroshield, and teeth 16 and 36 with Compoglass). |
| Beiruti 2006 | Quasi‐randomised parallel group study comparing glass ionomer sealant with resin‐based sealant. Quasi‐randomised parallel group designs excluded in this update. (Children were randomly allocated to one of the two sealant treatment groups using the class list. The first child on the list was allocated to the composite resin and the second child to the glass ionomer group and so on. Which treatment group to start with was determined through the flip of a coin.The sequence generation included systematic, non‐random component (class lists)). |
| Boksman 1987 | Split‐mouth study comparing glass ionomer with resin‐based sealant. No random allocation to surfaces within each tooth pair (teeth on the left side of the mouth sealed with a glass ionomer cement, teeth on the right side with resin). |
| Braga 2009 | RCT comparing three treatments: silver diamine fluoride; glass ionomer sealant; and cross toothbrushing technique. Each of these three treatments was used in each child's mouth. Study design neither parallel group nor split‐mouth (however, data analysed as in parallel group designs). |
| Carlsson 1992 | Study mainly intended to estimate the number of Mutans streptococci in saliva after treatment with sealants. Not RCT. Random allocation not stated. Primary teeth included in study. |
| Carlsson 1997 | Parallel group design comparing resin‐based sealant (children at caries risk) with reference group without sealant (children at low caries risk), not randomised. Randomised split‐mouth design within the sealant group comparing two resin‐based sealant materials. |
| Centenaro 2001 | Conference abstract with split‐mouth study comparing resin sealant to glass ionomer. No random or quasi‐random allocation to surfaces within each tooth pair (teeth 16 and 36 were sealed with Fluoroshield, and teeth 26 and 46 with glass ionomer). |
| De Puel 1983 | Split‐mouth design comparing resin‐based sealant to control without sealant. Not RCT. Random or quasi‐random allocation not stated. |
| Dogon 1995 | Conference abstract. Not RCT. Random allocation not stated. Children were divided into five groups by classroom. |
| Duggan 1987 | Test material was a varnish. |
| Flório 2001 | RCT. Three groups: sealant, fluoride varnish and control. Conventional control group was not used; control group children got other preventive treatments than sealants (e.g. fluoride flasks were given to home). |
| Güngör 2004 | RCT study comparing polyacid‐modified resin composite with resin‐based sealant. Comparison excluded in this update. |
| Helle 1975 | Study design comparing resin‐based sealant materials to control without sealant including both permanent and primary teeth (majority of the sealed teeth were sealed by Nuva‐Seal material). Not RCT. Random or quasi‐random allocation not stated. |
| Hepp 1990 | Not RCT. The author was contacted to clarify this. |
| Hickel 1989 | Split‐mouth design comparing glass ionomer to resin‐based sealant. Not RCT. Random or quasi‐random allocation not stated. |
| Hilgert 2015 | Trial comparing three treatments: daily supervised toothbrushing at school, resin‐based sealant and glass ionomer sealant. Not RCT related to comparison of glass ionomer with resin sealant which was the only relevant comparison for this review (randomised only related to comparison of glass ionomer sealant with toothbrushing; schools with equipped with a dental unit were allocated to resin‐based sealant group) |
| Hotz 1978 | Split‐mouth design comparing resin‐based sealant to control without sealant. Study included other preventive treatment (Elmex Fluid around 10,000 ppm F 6 times per year). The author was contacted to clarify this. |
| Irmisch 1992 | Not RCT. Random or quasi‐random allocation not stated. |
| Jodkowska 1984 | Split‐mouth study (resin versus no treatment). Randomisation unclear. |
| Jodkowska 2008 | Resin‐based sealant versus control without sealant comparison.
In total four groups: children were divided into three groups depending on the number and type of teeth to be sealed; the fourth group was a control group.
Group 1: two first molars sealed (one maxillary and one mandibular) with the remaining two left as controls.
Group 2: all four first molars sealed.
Group 3: all molars and premolars sealed as they erupted.
Group 4: control group, no teeth sealed. Three resin‐based sealant materials used (one of those materials was Nuva‐Seal). The quote "Teeth designed for sealing were allotted at random to be sealed with 1 of the materials used" gives an impression that the sealant material for each tooth to be sealed was randomised (but not the tooth or teeth). Allocation of children to groups not randomised. Group 1 could have been handled as split‐mouth design but the selection of teeth to be sealed in each child's mouth remains unclear. Further, Nuva‐Seal was used as sealant material. Study included other preventive treatment (NaF‐rinsing 5 times during the year at 2‐week intervals). |
| Kamala 2008 | Children randomised to two glass ionomer groups, and for each child split‐mouth design was used (the other tooth of the tooth pair was sealed with one of the two glass ionomer materials and the contralateral tooth was left unsealed as control). Randomisation at tooth pair level not stated. It remains unclear how the tooth within a tooth pair to be sealed was selected. |
| Kawakami 1984 | Not RCT. Random or quasi‐random allocation not stated. |
| Komatsu 1994 | Parallel group study comparing glass ionomer to control without sealant. Not RCT (control group was selected using annual school examination records). |
| Lampa 2004 | RCT study comparing polyacid‐modified resin composite with resin‐based sealant. Comparison excluded in this update. |
| Li 2008 | Glass ionomer sealant versus control without sealant. Unclear data: (1) contradictory results in table and text, (2) drop‐out rates not specified by group. Additional information was inquired from the authors to assess the adequacy of the study for this review (no response). |
| Liu 2000 | Conference abstract with split‐mouth study comparing resin‐modified glass ionomer to resin sealant. Not RCT. Random or quasi‐random allocation not stated. |
| Louw 2002 | Conference abstract of RCT comparing glass ionomer to control without sealant on erupting teeth. No full‐text report available (the author was contacted to clarify this). |
| Lovadino 1994 | Split‐mouth design comparing glass ionomer to resin‐based sealant. Not RCT. Random or quasi‐random allocation not stated. |
| Lusanandana 1986 | Not RCT. Random or quasi‐random allocation not stated. |
| Madléna 1993 | Study comparing resin‐based sealant to no treatment. Not RCT. Random allocation not stated (translator‐based information) |
| Manau 1989 | Study comparing resin‐based sealant to no treatment. Children received other preventive treatments (fluoride mouthrinses). |
| Marković 2012 | Glass ionomer sealant versus resin sealant comparison. Unclear data, no information e.g. on: (1) the numbers of teeth under evaluation at baseline in each group, (2) drop‐out rate of children at follow‐up. Additional information was inquired from the authors to assess the adequacy of the study for this review (no response). |
| Mejàre 1990 | Study comparing glass ionomer to resin‐based sealant materials. Not RCT. Random or quasi‐random allocation not stated. Study design neither parallel group nor split‐mouth design with tooth pairs. |
| Mel'nichenko 1994 | Split‐mouth study comparing sealant to control without sealant. No random allocation to surfaces within each tooth pair (right side of each subject control side, and left side sealant side). |
| Monse 2012 | Only the 3 schools without daily toothbrushing program at school could be considered in this review but there were too few clusters for adequate RCT design |
| Morgan 1998 | Study included other preventive treatment (weekly 0.2% NaF‐rinsing). |
| Morrow 1997 | Conference abstract of a randomised study comparing four different sealant materials. No information on numbers of children or numbers of teeth per child in each group at baseline. No information on data at follow‐up in numbers (only in percentages). No contact details of the authors. |
| Noack 1997 | Conference abstract with split‐mouth study comparing compomer to resin sealant. Comparison excluded in this update. Random or quasi‐random allocation to surfaces within each tooth pair not stated. |
| Oba 2009 | RCT comparing glass ionomer to resin‐based sealant. The design stated to be a split‐mouth. However, the number of sealed teeth with each material was different at baseline (91 in glass ionomer cement group and 116 in resin group). The report gives an impression that both materials were used in one child's mouth which has, however, not been taken into account in the analyses. Additional information was inquired from the authors to assess the adequacy of the study for this review (no response). |
| Ohmori 1976 | Not RCT. Split‐mouth study and right side of each subject was the test side. |
| Oliveira 2008 | Study comparing glass ionomer cement with a resin‐based sealant with or without an associated bonding agent (six groups). Not RCT. No random allocation to groups. |
| Pereira 1999 | RCT comparing two glass ionomers to control without sealant. Data remain unclear; some contradictory data in separate reports for the same follow‐ups. |
| Petrovic 1996 | Conference abstract of a study comparing four different sealant materials. Not RCT. Random or quasi‐random allocation not stated. |
| Poulsen 1979 | Study included other preventive treatment (fortnightly fluoride rinses). |
| Poulsen 2006 | Split‐mouth study comparing resin‐based sealant to glass ionomer. Very different follow‐up periods for tooth pairs. |
| Prados‐Atienza 2002 | Assignment to the sealant group was not randomised. |
| Puppin‐Rontani 2006 | Split‐mouth study comparing resin‐based sealant to compomer. Comparison excluded in this update. No random or quasi‐random allocation to surfaces within each tooth pair. |
| Rajić 2000 | Split‐mouth design comparing sealant to control without sealant. Not RCT. Random or quasi‐random allocation not stated. |
| Simonsen 1980 | Not RCT. Study comparing resin‐based sealant to control (sealant group was a random sample; the control group of children was selected). Matched pair analysis was performed. |
| Skrinjaric 2008 | Split‐mouth study (glass ionomer versus resin). Study mainly designed to investigate retention rate of glass ionomer cement heated during setting time. No random allocation to surfaces within each tooth pair (teeth on the left side of the mouth sealed with a glass ionomer cement, teeth on the right side with resin). |
| Smales 1996 | Study comparing resin‐modified glass ionomer to resin sealant. Intra‐individual study design not clearly split‐mouth design with tooth pairs. Patients older than 20 years. Follow‐up time 6 months. |
| Taifour 2003 | Study design comparing glass ionomer to control without sealant. Not RCT. Erupted teeth were sealed and non‐erupted, later erupted teeth were used as controls. |
| Tanguy 1984 | Not RCT. Random or quasi‐random allocation not stated. |
| Tapias Ledesma 2002 | Study comparing sealant with control without sealant. Not RCT (prospective cohort study). Sealant group with other preventive treatments. |
| Thylstrup 1976 | Split‐mouth design comparing resin‐based sealant with control without sealant. Study included other preventive treatments (e.g. fortnightly 0.2% NaF‐rinsing). |
| Tostes 1997 | RCT with three treatments (glass ionomer sealant, resin‐based sealant, and fluoride varnish). Three of each child's teeth were divided to receive one of those treatments; the fourth tooth was left as a control without treatment (in total there were 25 children with 100 teeth). Data reported as summary data for each treatment. Study design not suitable for reliable data analysis (the data could have been treated as a split‐mouth design if they could have been reduced to two treatments which was not the case in this study). |
| Unal 2015 | No data on dentine carious lesions (the trial was designed to evalute the remineralizing capacity of sealants used with or without gaseous ozone; outcome measured by means of changes in the DIAGNOdent values) |
| Valsecki 1992 | Conference abstract. Not RCT. Random or quasi‐random allocation not stated. |
| Vieira 2000 | Conference abstract of a trial comparing glass ionomer to resin‐based sealant. No full‐text report available (the author was contacted to clarify this but the information was not available for this update). |
| Vrbic 1983 | Split‐mouth study, random or quasi‐random allocation to surfaces within each tooth pair not stated. |
| Winkler 1996 | Split‐mouth study comparing resin‐modified glass ionomer to resin‐based sealant. Not RCT. Random or quasi‐random allocation not stated. |
| Wåhlin 1997 | Parallel group design comparing sealing with no sealing, not randomised. The randomised design comparing glass ionomer cement with resin‐based sealant not clear split‐mouth design with tooth pairs. Very different follow‐up periods (in average 4.3 years; range 2 to 5 years). |
| Yakut 2006 | Split‐mouth study comparing resin composite with polyacid‐modified resin composite. Comparison excluded in this update. Not RCT. Random or quasi‐random allocation not stated. |
| Yildiz 2004 | Split‐mouth study comparing resin‐based sealants to control without sealant. Not RCT. Right side in each patient's mouth was the test side, and left side was the control side. |
| Yilmaz 2010 | RCT comparing different sealant materials: two BIS‐GMA resin sealants, ormocer, and compomer. Caries data remain unclear. There are unexplained missing data in all groups at both follow‐ups (e.g. results for 34 teeth are missing at 24 months). |
| Yoshihara 2000 | Study comparing glass ionomer cement to resin‐based sealant. Not RCT. Random or quasi‐random allocation not stated. |
| Zhang 2003 | Split‐mouth study comparing sealant with no treatment. Not RCT. Random or quasi‐random allocation not stated. |
| Zimmer 2009 | Split‐mouth study comparing glass ionomer to resin‐based sealant. Not RCT. Random or quasi‐random allocation not stated. Very different follow‐up periods for tooth pairs (range 1.5 to 4.1 years). |
RCT = randomised controlled trial.
Characteristics of studies awaiting assessment [ordered by study ID]
Gorseta 2014.
| Methods | Trial design: split‐mouth design, sealant material randomly assigned among tooth pair Follow‐up: 12 months |
| Participants | 24 children (mean age at baseline 8 years) with 1 tooth pair of totally erupted caries‐free permanent first or second molars |
| Interventions | Comparison: glass ionomer sealant versus resin‐based sealant Tooth pair: occlusal surface of 1 tooth sealed with glass ionomer sealant (light and heat cured Glass Carbomer); occlusal surface of the other tooth of the tooth pair sealed with resin‐based sealant (Helioseal F) |
| Outcomes | Sound or carious occlusal surface of molar |
| Notes | Much incomplete information e.g. on study setting and participants |
Ulusu 2012.
| Methods | Trial design: split‐mouth design, sealant material randomly assigned among tooth pair Follow‐up: 24 months |
| Participants | 173 children (baseline age range 7‐15 years) with at least 1 tooth pair of caries‐free permanent first molars with deep pits and fissures |
| Interventions | Comparison: glass ionomer sealant versus resin‐based sealant Tooth pair: occlusal surface of 1 tooth sealed with glass ionomer cement; occlusal surface of the other tooth of the tooth pair sealed with resin‐based sealant |
| Outcomes | Sound or carious occlusal surface of molar |
| Notes | Much incomplete information e.g. on data and randomisation (which has been mentioned only in abstract) |
Characteristics of ongoing studies [ordered by study ID]
IRCT2013041611960N2.
| Trial name or title | One year clinical evaluation of glass ionomer and resin based fissure sealants on permanent first molars |
| Methods | RCT, split‐mouth design, follow‐up 12 months |
| Participants | Children aged from 6 to 10 years with dmft index at least 1 and having two first permanent molars in one jaw |
| Interventions | Glass ionomer sealant versus resin‐based sealant |
| Outcomes | Caries development, sealant retention, marginal adaptation, colour adjustment, surface smoothness |
| Starting date | December 2013 |
| Contact information | Dr Nasim Shafiezadeh, Dental branch, Islamic Azad University |
| Notes |
NCT02408601.
| Trial name or title | A Clinical Trial to Assess the Retention and Caries Preventive Effect of Resin Based Sealants Versus ART Sealants |
| Methods | RCT, split‐mouth design, follow‐up 18 months |
| Participants | Children aged from 7 to 10 years with non‐decayed contralateral permanent 1st molars |
| Interventions | Glass ionomer sealant versus resin‐based sealant |
| Outcomes | Caries incidence, sealant retention |
| Starting date | March 2015 |
| Contact information | Dr BH Praveen, Kamineni Institute of Dental Sciences |
| Notes |
NCT02443896.
| Trial name or title | The Use of Pit and Fissure Sealants in Children Requiring Caries Related Dental Extractions |
| Methods | RCT, parallel assignment |
| Participants | Children aged from 5 to 15 years requiring caries related extractions under a chair General Anaesthetic |
| Interventions | Pit and fissure sealant on all 'sealable' permanent molars versus no treatment |
| Outcomes | Caries incidence; time frame 12 months |
| Starting date | April 2014 |
| Contact information | Birmingham Dental Hospital |
| Notes |
NCT02795728.
| Trial name or title | Fuji Type VII Sealant Versus Resin Based Sealant. A Clinical Trial |
| Methods | RCT, split‐mouth design, follow‐up 12 months |
| Participants | Children aged from 7 to 9 years with a fully erupted contralateral permanent mandibular 1st molars with well‐defined deep pits and fissures and molars free of mucosal tissue |
| Interventions | Glass ionomer sealant versus resin‐based sealant |
| Outcomes | Caries incidence, sealant retention |
| Starting date | February 2010 |
| Contact information | Dr BH Praveen, Kamineni Institute of Dental Sciences |
| Notes |
NCT02849925.
| Trial name or title | Randomized Controlled Clinical Trial on the Treatment of Caries Lesions Using Resin or Glass Ionomer Sealants in Permanent Teeth |
| Methods | RCT, parallel assignment, follow‐up 18 months |
| Participants | Children aged from 6 to 12 years with at least one ICDAS 3 lesion in first permanent molars |
| Interventions | Glass ionomer sealant versus resin‐based sealant |
| Outcomes | Number of lesions that evidence progression of caries by a higher ICDAS code, percentage of sealants that were intact |
| Starting date | March 2015 |
| Contact information | Dr RA Giacaman, University of Talca, Chile |
| Notes |
RCT = randomised controlled trial.
Differences between protocol and review
We made the following changes compared to the last updated version from 2013 (Ahovuo‐Saloranta 2013).
We changed the title to "Pit and fissure sealants for preventing dental decay in the permanent teeth". The last version of the review was entitled "Sealants for preventing dental decay in the permanent teeth". (The protocol title was "Pit and fissure sealants for preventing dental decay in the permanent teeth of children and adolescents".)
We included only studies in which sealants were placed on occlusal surfaces of permanent premolar or molar teeth. In the review version from 2013, we considered also studies where sealants were placed on approximal surfaces. The Cochrane review by Dorri 2015 considering approximal surfaces has been published in 2015.
We changed the wording of the objectives and outcomes to clearly specify our comparisons of interest.
We excluded quasi‐randomised trials unless they used a split‐mouth design and studies that compared compomers to resins/composites.
Contributions of authors
Writing of the protocol ‐ Anneli Ahovuo‐Saloranta (AAS), Anne Hiiri (AH), Anne Nordblad (AN) and Marjukka Mäkelä (MM). Study selection ‐ AAS, Helena Forss (HF), and AH in the previous versions. Data extraction ‐ AAS, HF, Helen V Worthington (HW), and AH in the previous versions. Data analysis ‐ AAS, Tanya Walsh (TW), HW. Writing of the review ‐ AAS, HF, AN, MM, TW, HW.
Sources of support
Internal sources
FinOHTA, National Institute for Health and Welfare, Finland.
The University of Manchester; the Manchester Academic Health Sciences Centre (MAHSC); the NIHR Manchester Biomedical Research Centre, UK.
-
Centers for Disease Control and Prevention (CDC), USA.
Contract number 200‐2011‐41717.
External sources
-
Cochrane Oral Health Global Alliance, Other.
The production of Cochrane Oral Health reviews has been supported financially by our Global Alliance since 2011 (oralhealth.cochrane.org/partnerships‐alliances). Contributors over the past year have been the American Association of Public Health Dentistry, USA; the British Association for the Study of Community Dentistry, UK; the British Society of Paediatric Dentistry, UK; the Canadian Dental Hygienists Association, Canada; the Centre for Dental Education and Research at All India Institute of Medical Sciences, India; the National Center for Dental Hygiene Research & Practice, USA; New York University College of Dentistry, USA; NHS Education for Scotland, UK; and Swiss Society for Endodontology, Switzerland.
-
National Institute for Health Research (NIHR), UK.
This project was supported by the NIHR, via Cochrane Infrastructure funding to Cochrane Oral Health. The views and opinions expressed herein are those of the review authors and do not necessarily reflect those of the Systematic Reviews Programme, the NIHR, the NHS or the Department of Health.
Declarations of interest
Anneli Ahovuo‐Saloranta: none known. Helena Forss: none known. Tanya Walsh: none known. I am an Editor with Cochrane Oral Health. Anne Nordblad: none known. Marjukka Mäkelä: none known. Helen V Worthington: none known. I am one of the two Co‐ordinating Editors of Cochrane Oral Health.
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Amin 2008 {published data only}
- Amin HE. Clinical and antibacterial effectiveness of three different sealant materials. Journal of Dental Hygiene 2008;82(5):45. [PubMed] [Google Scholar]
Antonson 2012 {published data only}
- Antonson SA, Antonson DE, Brener S, Crutchfield J, Larumbe J, Michaud C, et al. Twenty‐four month clinical evaluation of fissure sealants on partially erupted permanent first molars: glass ionomer versus resin‐based sealant. Journal of the American Dental Association 2012;143(2):115‐22. [DOI] [PubMed] [Google Scholar]
Arrow 1995 {published data only}
- Arrow P, Riordan PJ. Retention and caries preventive effects of a GIC and a resin‐based fissure sealant. Community Dentistry and Oral Epidemiology 1995;23(5):282‐5. [DOI] [PubMed] [Google Scholar]
Barja‐Fidalgo 2009 {published and unpublished data}
- Barja‐Fidalgo F, Maroun S, Oliveira BH. Effectiveness of a glass ionomer cement used as a pit and fissure sealant in recently erupted permanent first molars. Journal of Dentistry for Children 2009;76(1):34‐40. [PubMed] [Google Scholar]
Baseggio 2010 {published data only}
- Baseggio W, Naufel FS, Davidoff DC, Nahsan FP, Flury S, Rodrigues JA. Caries‐preventive efficacy and retention of a resin‐modified glass ionomer cement and a resin‐based fissure sealant: a 3‐year split‐mouth randomised clinical trial. Oral Health & Preventive Dentistry 2010;8(3):261‐8. [PubMed] [Google Scholar]
Bojanini 1976 {published data only}
- Bojanini J, Garces H, McCune RJ, Pineda A. Effectiveness of pit and fissure sealants in the prevention of caries. Journal of Preventive Dentistry 1976;3(6):31‐4. [PubMed] [Google Scholar]
- McCune RJ, Bojanini J, Abodeely RA. Effectiveness of a pit and fissure sealant in the prevention of caries: three‐year clinical results. Journal of the American Dental Association 1979;99(4):619‐23. [DOI] [PubMed] [Google Scholar]
Bravo 2005 {published and unpublished data}
- Bravo M, Baca P, Llodra JC, Osorio E. A 24‐month study comparing sealant and fluoride varnish in caries reduction on different permanent first molar surfaces. Journal of Public Health Dentistry 1997;57(3):184‐6. [DOI] [PubMed] [Google Scholar]
- Bravo M, Garcia‐Anllo I, Baca P, Llodra JC. A 48‐month survival analysis comparing sealant (Delton) with fluoride varnish (Duraphat) in 6‐ to 8‐year‐old children. Community Dentistry and Oral Epidemiology 1997;25(3):247‐50. [DOI] [PubMed] [Google Scholar]
- Bravo M, Llodra JC, Baca P, Osorio E. Effectiveness of visible light fissure sealant (Delton) versus fluoride varnish (Duraphat): 24‐month clinical trial. Community Dentistry and Oral Epidemiology 1996;24(1):42‐6. [DOI] [PubMed] [Google Scholar]
- Bravo M, Montero J, Bravo JJ, Baca P, Llodra JC. Sealant and fluoride varnish in caries: a randomized trial. Journal of Dental Research 2005;84(12):1138‐43. [DOI] [PubMed] [Google Scholar]
Brooks 1979 {published data only}
- Brooks JD, Mertz‐Fairhurst EJ, Della‐Giustina VE, Fairhurst CW, Williams JE. A comparative study of the retention of two pit and fissure sealants: one‐year results. Journal of Preventive Dentistry 1976;3(5):43‐6. [PubMed] [Google Scholar]
- Brooks JD, Mertz‐Fairhurst EJ, Della‐Giustina VE, Williams JE, Fairhurst CW. A comparative study of two pit and fissure sealants: three‐year results in Augusta, Ga. Journal of the American Dental Association 1979;99(1):42‐6. [DOI] [PubMed] [Google Scholar]
- Brooks JD, Mertz‐Fairhurst EJ, Della‐Giustina VE, Williams JE, Fairhurst CW. A comparative study of two pit and fissure sealants: two‐year results in Augusta, Ga. Journal of the American Dental Association 1979;98(5):722‐5. [DOI] [PubMed] [Google Scholar]
- Mertz‐Fairhurst EJ, Della‐Giustina VE, Brooks JE, Williams JE, Fairhurst CW. A comparative study of two pit and fissure sealants: results after 4 1/2 years in Augusta, Ga. Journal of the American Dental Association 1981;103(2):235‐8. [DOI] [PubMed] [Google Scholar]
- Mertz‐Fairhurst EJ, Fairhurst CW, Williams JE, Della‐Giustina VE, Brooks JD. A comparative clinical study of two pit and fissure sealants: 7‐year results in Augusta, Ga. Journal of the American Dental Association 1984;109(2):252‐5. [DOI] [PubMed] [Google Scholar]
- Mertz‐Fairhurst EJ, Fairhurst CW, Williams JE, Della‐Giustina VE, Brooks JD. A comparative clinical study of two pit and fissure sealants: six‐year results in Augusta, Ga. Journal of the American Dental Association 1982;105(2):237‐9. [DOI] [PubMed] [Google Scholar]
Charbeneau 1979 {published data only}
- Charbeneau GT, Dennison JB. Clinical success and potential failure after single application of a pit and fissure sealant: a four‐year report. Journal of the American Dental Association 1979;98(4):559‐64. [DOI] [PubMed] [Google Scholar]
- Charbeneau GT, Dennison JB, Ryge G. A filled pit and fissure sealant: 18‐month results. Journal of the American Dental Association 1977;95(2):299‐306. [DOI] [PubMed] [Google Scholar]
Chen 2012 {published and unpublished data}
- Chen X, Du M, Fan M, Mulder J, Huysmans MC, Frencken JE. Effectiveness of two new types of sealants: retention after 2 years. Clinical Oral Investigations 2012;16(5):1443‐50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen X, Du MQ, Fan MW, Mulder J, Huysmans MC, Frencken JE. Caries‐preventive effect of sealants produced with altered glass‐ionomer materials, after 2 years. Dental Materials 2012;28(5):554‐60. [DOI] [PubMed] [Google Scholar]
- Zhang W, Chen X, Fan MW, Mulder J, Huysmans MC, Frencken JE. Do light cured ART conventional high‐viscosity glass‐ionomer sealants perform better than resin‐composite sealants: A 4‐year randomized clinical trial. Dental Materials 2014;30(5):487‐92. [DOI] [PubMed] [Google Scholar]
Chen 2013 {published data only}
- Chen XX, Liu XG. Clinical comparison of Fuji VII and a resin sealant in children at high and low risk of caries. Dental Materials Journal 2013;32(3):512‐8. [DOI] [PubMed] [Google Scholar]
De Luca‐Fraga 2001 {published data only}
- Luca‐Fraga LR, Pimenta LA. Clinical evaluation of glass‐ionomer/resin‐based hybrid materials used as pit and fissure sealants. Quintessence International 2001;32(6):463‐8. [PubMed] [Google Scholar]
Dhar 2012 {published and unpublished data}
- Dhar V, Chen H. Evaluation of resin based and glass ionomer based sealants placed with or without tooth preparation ‐ a two year clinical trial. Pediatric Dentistry 2012;34(1):46‐50. [PubMed] [Google Scholar]
Erdoğan 1987 {published data only}
- Erdoğan B, Alaçam T. Evaluation of a chemically polymerized pit and fissure sealant ‐ results after 4, 5 years. Journal of Paediatric Dentistry 1987;3:11‐3. [Google Scholar]
Forss 1998 {published and unpublished data}
- Forss H, Halme E. Retention of a glass ionomer cement and a resin‐based fissure sealant and effect on carious outcome after 7 years. Community Dentistry and Oral Epidemiology 1998;26(1):21‐5. [PubMed] [Google Scholar]
- Forss H, Saarni UM, Seppä L. Comparison of glass‐ionomer and resin‐based fissure sealants: a 2‐year clinical trial. Community Dentistry and Oral Epidemiology 1994;22(1):21‐4. [DOI] [PubMed] [Google Scholar]
Ganesh 2006 {published and unpublished data}
- Ganesh M, Tandon S. Clinical evaluation of FUJI VII sealant material. Journal of Clinical Pediatric Dentistry 2006;31(1):52‐7. [DOI] [PubMed] [Google Scholar]
Guler 2013 {published data only}
- Guler C, Yilmaz Y. A two‐year clinical evaluation of glass ionomer and ormocer based fissure sealants. Journal of Clinical Pediatric Dentistry 2013;37(3):263‐7. [DOI] [PubMed] [Google Scholar]
Hunter 1988 {published data only}
- Hunter PB. A study of pit and fissure sealing in the School Dental Service. New Zealand Dental Journal 1988;84(375):10‐2. [PubMed] [Google Scholar]
Karlzén‐Reuterving 1995 {published data only}
- Karlzén‐Reuterving G, Dijken JW. A three‐year follow‐up of glass ionomer cement and resin fissure sealants. Journal of Dentistry for Children 1995;62(2):108‐10. [PubMed] [Google Scholar]
Kervanto‐Seppälä 2008 {published and unpublished data}
- Kervanto‐Seppälä S, Lavonius E, Pietilä I, Pitkäniemi J, Meurman J, Kerosuo E. Comparing the caries‐preventive effect of two fissure sealing modalities in public health care: a single application of glass ionomer and a routine resin‐based sealant programme. A randomized split‐mouth clinical trial. International Journal of Paediatric Dentistry 2008;18(1):56‐61. [DOI] [PubMed] [Google Scholar]
Liu 2012 {published and unpublished data}
- Liu BY, Lo ECM, Chu CH, Lin HC. Randomized trial on fluorides and sealants for fissure caries prevention. Journal of Dental Research 2012;91(8):753‐8. [DOI] [PubMed] [Google Scholar]
Liu 2014a {published data only}
- Liu BY, Xiao Y, Chu CH, Lo EC. Glass ionomer ART sealant and fluoride‐releasing resin sealant in fissure caries prevention ‐ results from a randomized clinical trial. BMC Oral Health 2014;14(1):54. [DOI] [PMC free article] [PubMed] [Google Scholar]
Liu 2014b {published data only}
- Liu Y, Rong W, Zhao X, Wang M, Jiang Q, Wang W. Caries prevention effect of resin based sealants and glass ionomer sealants. Chinese Journal of Stomatology 2014;49(4):199‐203. [PubMed] [Google Scholar]
Mills 1993 {published data only}
- Mills RW, Ball IA. A clinical trial to evaluate the retention of a silver cermet‐ionomer cement used as a fissure sealant. Operative Dentistry 1993;18(4):148‐54. [PubMed] [Google Scholar]
Muller‐Bolla 2013 {published and unpublished data}
- Muller‐Bolla M, Lupi‐Pégurier L, Bardakjian H, Velly AM. Effectiveness of school‐based dental sealant programs among children from low‐income backgrounds in France: a pragmatic randomized clinical trial. Community Dentistry and Oral Epidemiology 2013;41(3):232‐41. [DOI] [PubMed] [Google Scholar]
Pardi 2005 {published and unpublished data}
- Pardi V, Pereira AC, Ambrosano GMB, Meneghim Mde C. Clinical evaluation of three different materials used as pit and fissure sealant: 24‐months results. Journal of Clinical Pediatric Dentistry 2005;29(2):133‐8. [DOI] [PubMed] [Google Scholar]
Poulsen 2001 {published and unpublished data}
- Poulsen S, Beiruti N, Sadat N. A comparison of retention and the effect on caries of fissure sealing with a glass‐ionomer and a resin‐based sealant. Community Dentistry and Oral Epidemiology 2001;29(4):298‐301. [DOI] [PubMed] [Google Scholar]
Raadal 1996 {published data only}
- Raadal M, Utkilen AB, Nilsen OL. Fissure sealing with a light‐cured resin‐reinforced glass‐ionomer cement (Vitrebond) compared with a resin sealant. International Journal of Paediatric Dentistry 1996;6(4):235‐9. [DOI] [PubMed] [Google Scholar]
Reisbick 1982 {published data only}
- Reisbick MH, Thanos CE, Berson RB, Goldstein CM. Benefit from sealants in a moderately fluoridated community. CDA Journal California Dental Association 1982;10(1):53‐6. [PubMed] [Google Scholar]
Richardson 1978 {published data only}
- Gibson GB, Richardson AS. Sticky fissure management. 30‐month report. Journal of the Canadian Dental Association 1980;46(4):255‐8. [PubMed] [Google Scholar]
- Gibson GB, Richardson AS, Waldman R. The effectiveness of a chemically polymerized sealant in preventing occlusal caries: five‐year results. Pediatric Dentistry 1982;4(4):309‐10. [Google Scholar]
- Richardson AS, Gibson GB, Waldman R. Chemically polymerized sealant in preventing occlusal caries. Journal of the Canadian Dental Association 1980;46(4):259‐60. [PubMed] [Google Scholar]
- Richardson AS, Gibson GB, Waldman R. The effectiveness of a chemically polymerized sealant: Four‐year results. Pediatric Dentistry 1980;2(1):24‐6. [PubMed] [Google Scholar]
- Richardson AS, Waldman R, Gibson GB. The effectiveness of a chemically polymerized sealant in preventing occlusal caries: two year results. Journal of the Canadian Dental Association 1978;44(6):269‐72. [PubMed] [Google Scholar]
Rock 1978 {published data only}
- Rock WP, Bradnock G. Effect of operator variability and patient age on the retention of fissure sealant resin: 3‐year results. Community Dentistry and Oral Epidemiology 1981;9(5):207‐9. [DOI] [PubMed] [Google Scholar]
- Rock WP, Gordon PH, Bradnock G. The effect of operator variability and patient age on the retention of fissure sealant resin. British Dental Journal 1978;145(3):72‐5. [DOI] [PubMed] [Google Scholar]
Rock 1996 {published data only}
- Rock WP, Foulkes EE, Perry H, Smith AJ. A comparative study of fluoride‐releasing composite resin and glass ionomer materials used as fissure sealants. Journal of Dentistry 1996;24(4):275‐80. [DOI] [PubMed] [Google Scholar]
Sheykholeslam 1978 {published and unpublished data}
- Houpt M, Shey Z. Clinical effectiveness of an autopolymerized fissure sealant (Delton) after thirty‐three months. Pediatric Dentistry 1979;1(3):165‐8. [PubMed] [Google Scholar]
- Houpt M, Shey Z. The effectiveness of a fissure sealant after six years. Pediatric Dentistry 1983;5(2):104‐6. [PubMed] [Google Scholar]
- Houpt M, Sheykholeslam Z. The clinical effectiveness of Delton fissure sealant after one year. Journal of Dentistry for Children 1978;45(2):130‐2. [PubMed] [Google Scholar]
- Sheykholeslam Z, Houpt M. Clinical effectiveness of an autopolymerized fissure sealant after 2 years. Community Dentistry and Oral Epidemiology 1978;6(4):181‐4. [DOI] [PubMed] [Google Scholar]
Sipahier 1995 {published and unpublished data}
- Sipahier M, Ulusu T. Glass‐ionomer‐silver‐cermet cements applied as fissure sealants II. Clinical evaluation. Quintessence International 1995;26(1):43‐8. [Google Scholar]
Songpaisan 1995 {published data only}
- Songpaisan Y, Bratthall D, Phantumvanit P, Somridhivej Y. Effects of glass ionomer cement, resin‐based pit and fissure sealant and HF applications on occlusal caries in a developing country field trial. Community Dentistry and Oral Epidemiology 1995;23(1):25‐9. [DOI] [PubMed] [Google Scholar]
- Songpaisan Y, Serinirach R, Kuvatanasuchati J, Bratthall D. Mutans Streptococci in a Thai population: relation to caries and changes in prevalence after application of fissure sealants. Caries Research 1994;28(3):161‐8. [DOI] [PubMed] [Google Scholar]
Tagliaferro 2011 {published and unpublished data}
- Tagliaferro EP, Pardi V, Ambrosano GM, Meneghim Mde C, Silva SR, Pereira AC. Occlusal caries prevention in high and low risk schoolchildren. A clinical trial. American Journal of Dentistry 2011;24(2):109‐14. [PubMed] [Google Scholar]
Tang 2014 {published data only}
- Tang L, Shi L, Yuan S, Lv J, Lu H. Effectiveness of 3 different methods in prevention of dental caries in permanent teeth among children. Shanghai Journal of Stomatology 2014;23(6):736‐9. [PubMed] [Google Scholar]
Williams 1996 {published data only}
- Williams B, Laxton L, Holt RD, Winter GB. Fissure sealants: a 4‐year clinical trial comparing an experimental glass polyalkenoate cement with a bis glycidyl methacrylate resin used as fissure sealants. British Dental Journal 1996;180(3):104‐8. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Andjelic 1991 {published data only}
- Andjelic P, Vojinovic J, Tatic E, Pintaric J. Fissure sealants as primary preventive measures. Four‐year evaluation in Stara Pazova [Fissurenversiegelungen als primäre Vorbeugungsmassnahme. Eine vierjährige Bewertungsstudie in Stara Pazova]. Oralprophylaxe 1991;13(1):3‐10. [PubMed] [Google Scholar]
Aslanova 2003 {published data only}
- Aslanova FK, Seyidbayov OS. Comparative effectiveness assessment of different prophylaxis methods of the second teeth caries. Azerbaijan Medical Journal 2003;4:59‐62. [Google Scholar]
Azul 1990 {published data only}
- Azul AM. Fissure sealants ‐ 5 years of use [Selantes de fissura ‐ 5 anos de utilizacao]. Revista Portuguesa de Estomatologia e Cirurgia Maxilo‐Facial 1990;31(1):27‐33. [PubMed] [Google Scholar]
Baglioni‐Gouvea 2001 {published data only}
- Baglioni‐Gouvea ME, Puppin‐Rontani RM, Komati SM, Centenaro RS. Clinical evaluation of the retention and efficacy of a resin‐based sealant and a compomer in occlusal sealing. Journal of Dental Research 2001;80(4):1036. [Google Scholar]
Beiruti 2006 {published data only}
- Beiruti N, Frencken JE, van't Hof MA, Taifour D, Palenstein Helderman WH. Caries‐preventive effect of a one‐time application of composite resin and glass ionomer sealants after 5 years. Caries Research 2006;40(1):52‐9. [DOI] [PubMed] [Google Scholar]
Boksman 1987 {published data only}
- Boksman L, Gratton DR, McCutcheon E, Plotzke OB. Clinical evaluation of a glass ionomer cement as a fissure sealant. Quintessence International 1987;18(10):707‐9. [PubMed] [Google Scholar]
Braga 2009 {published data only}
- Braga MM, Mendes FM, Benedetto MS, Imparato JC. Effect of silver diammine fluoride on incipient caries lesions in erupting permanent first molars: a pilot study. Journal of Dentistry for Children 2009;76(1):28‐33. [PubMed] [Google Scholar]
Carlsson 1992 {published data only}
- Carlsson Å, Jonsson Y, Svensson K, Stahl B, Twetman S. Pit and fissure sealing and mutans streptococci levels in saliva. American Journal of Dentistry 1992;5(5):280‐2. [PubMed] [Google Scholar]
Carlsson 1997 {published data only}
- Carlsson Å, Petersson M, Twetman S. 2‐year clinical performance of a fluoride‐containing fissure sealant in young schoolchildren at caries risk. American Journal of Dentistry 1997;10(3):115‐9. [PubMed] [Google Scholar]
Centenaro 2001 {published data only}
- Centenaro RS, Puppin‐Rontani RM, Komati SM, Baglioni‐Gouvea ME. Clinical evaluation of the retention of a resin‐based sealant and a glass ionomer for pit and fissure sealing. Journal of Dental Research 2001;80(4):1036. [Google Scholar]
De Puel 1983 {published data only}
- Puel PN, Brassesco MB, Edelberg M. Clinical behavior of pit and fissure sealants. Results after 36 months [Comportamiento clinico de un sellador de fosas y fisuras. Resultados a 36 meses]. Revista de la Asociacion Odontologica Argentina 1983;71(1):4,6. [PubMed] [Google Scholar]
Dogon 1995 {published data only}
- Dogon IL, Ping FI, Liang LG. Three year results of an evaluation of a fluoride sealant. Journal of Dental Reseach 1995;74(Special Issue):404. [Google Scholar]
Duggan 1987 {published data only}
- Duggan G, Midda M. Clinical trial of a new fissure sealant. Journal of the International Association of Dentistry for Children 1987;18(2):17‐20. [PubMed] [Google Scholar]
Flório 2001 {published and unpublished data}
- Flório FM, Pereira AC, Meneghim MC, Ramacciato JC. Evaluation of non‐invasive treatment applied to occlusal surfaces. Journal of Dentistry for Children 2001;68(5‐6):326‐31. [PubMed] [Google Scholar]
Güngör 2004 {published data only}
- Güngör HC, Altay N, Alpar R. Clinical evaluation of a polyacid‐modified resin composite‐based fissure sealant: two‐year results. Operative Dentistry 2004;29(3):254‐60. [PubMed] [Google Scholar]
Helle 1975 {published data only}
- Helle A. Two fissure sealants tested for retention and caries reduction in Finnish children. Proceedings of the Finnish Dental Society 1975;71(3):91‐5. [PubMed] [Google Scholar]
Hepp 1990 {published and unpublished data}
- Hepp K, Tarjan I, Bodoki I. Comparative study of the fissure sealants Concise and Delton [Összehadonlito vizsgalatok Concise es Delton barazdazaro anyaggal]. Fogorvosi Szemle 1990;83(11):337‐9. [PubMed] [Google Scholar]
Hickel 1989 {published data only}
- Hickel R, Voss A. Comparative studies on fissure sealing: composite versus Cermet cement [Vergleichende untersuchung über fissurenversiegelung: komposit versus Cermet‐zement]. Deutsche Zahnärztliche Zeitschrift 1989;44(6):472‐4. [PubMed] [Google Scholar]
Hilgert 2015 {published data only}
- Hilgert LA, Leal SC, Mulder J, Creugers NH, Frencken JE. Caries‐preventive effect of supervised toothbrushing and sealants. Journal of Dental Research 2015;94(9):1218‐24. [DOI] [PubMed] [Google Scholar]
Hotz 1978 {published and unpublished data}
- Hotz P, Hofstetter HW, Rohrbach UJ. Fissure sealing combined with enamel fluoridation. Follow‐up study 2 years after sealing [Fissurenversiegelung in kombination mit schmelzfluorierung. Nachkontrolle von zweijährigen versiegelungen]. Schweizerische Monatsschrift für Zahnheilkunde 1978;88(4):313‐23. [PubMed] [Google Scholar]
Irmisch 1992 {published data only}
- Irmisch B. Caries prophylaxis using fissure sealing [Kariesprophylaxe mittels fissurenversiegelung]. Deutsche Zahnärztliche Zeitschrift 1992;47(11):790‐3. [Google Scholar]
Jodkowska 1984 {published data only}
- Jodkowska E. 2‐year clinical follow‐up after application of Concise Enamel Bond System for sealing defects in the occluding surfaces of teeth [Dwuletnie obserwacje kliniczne po zastosowaniu materialu zlozonego Concise enamel bond system do uszczelnienia powierzchni zujacej zebow]. Czasopismo Stomatologiczne 1984;37(11):839‐46. [PubMed] [Google Scholar]
- Jodkowska E. Effectiveness of sealing measures on the chewing surface of permanent teeth in clinical evaluation. II: Caries reduction [Wirksamkeit von Versiegelungsmassnahmen der Kaufläche bleibender Zähne in klinischer Beurteilung II: Kariesreduction]. Stomatologie der DDR 1985;35(5):275‐9. [PubMed] [Google Scholar]
Jodkowska 2008 {published data only}
- Jodkowska E. Efficacy of pit and fissure sealing ‐ Long‐term clinical observations. Quintessence International 2008;39(7):593‐602. [PubMed] [Google Scholar]
Kamala 2008 {published data only}
- Kamala BK, Hegde AM. Fuji III vs. Fuji VII glass ionomer sealants ‐ A clinical study. Journal of Clinical Pediatric Dentistry 2008;33(1):29‐33. [DOI] [PubMed] [Google Scholar]
Kawakami 1984 {published data only}
- Kawakami S, Komatsu H, Matsuda K, Shimokobe H. Clinical trial of a new glass ionomer cement as a fissure sealant. Shikai Tenbo 1984;64(4):748‐58. [PubMed] [Google Scholar]
Komatsu 1994 {published data only}
- Komatsu H, Shimokobe H, Kawakami S, Yoshimura M. Caries‐preventive effect of glass ionomer sealant reapplication: study presents three‐year results. Journal of the American Dental Association 1994;125(5):543‐9. [DOI] [PubMed] [Google Scholar]
Lampa 2004 {published data only}
- Lampa E, Brechter A, Dijken JW. Effect of a nonrinse conditioner on the durability of a polyacid‐modified resin composite fissure sealant. Journal of Dentistry for Children 2004;71(2):152‐7. [PubMed] [Google Scholar]
Li 2008 {published data only}
- Li SF, Deng M, He GQ, Luo WN. Evaluating the effects of GcFuji II glass ionomer cement in pit and fissure enameloplasty sealant technique. Journal of Clinical Rehabilitative Tissue Engineering Research 2008;12(23):4457‐60. [Google Scholar]
Liu 2000 {published data only}
- Liu JF. Fissure sealing with resin modified glass ionomer: A one‐year clinical study. Pediatric Dentistry 2000;22(3):241. [Google Scholar]
Louw 2002 {published data only}
- Louw AJ. Effect of glass ionomer sealant on caries in erupting molars. Journal of Dental Research 2002;81(Special Issue B, Divisional Abstracts):B‐375. [Google Scholar]
Lovadino 1994 {published data only}
- Lovadino JR, Marcondes Martins LR, Sartini Filho R, Brasil JR, Gardenal Meneguel MA. Evaluation, after one year, of two sealant materials: glass ionomer cement and composite sealant [Avaliacão de dois materiáis utilizados como selante oclusal: ionômero X compósito]. Revista da Associacão Paulista de Cirurgiões Dentistas 1994;48:1243‐6. [Google Scholar]
Lusanandana 1986 {published data only}
- Lusanandana S, Panyangarm R, Charoensupaya O. Retention and effectiveness of sealants on dental caries in a community program. Journal of the Dental Association of Thailand 1986;36(5):145‐52. [PubMed] [Google Scholar]
Madléna 1993 {published data only}
- Madléna M, Kincses S, Alberth M, Keszthelyi G. Short‐term effectiveness of fissure sealants [Barazdazaras hatekonysaganak rövid tavu vizsgalata]. Fogorvosi Szemle 1993;86(1):15‐21. [PubMed] [Google Scholar]
Manau 1989 {published data only}
- Manau C, Cuenca E, Salleras L. [Estudio de la eficiencia de un programa comunitario de sellados de fisuras en un grupo de escolares]. Archivos de Odonto‐Estomatología Preventiva y Comunitaria 1989;1:63‐7. [Google Scholar]
Marković 2012 {published data only}
- Marković D, Petrović B, Perić T, Blagojević D. Microleakage, adaptation ability and clinical efficacy of two fluoride releasing fissure sealants [Ispitivanje mikrocurenja, površinske adaptacije i kliničke efikasnosti dva zalivača fisura sa sposobnošću otpuštanja fluorida]. Vojnosanitetski Pregled 2012;69(4):320‐5. [PubMed] [Google Scholar]
Mejàre 1990 {published data only}
- Mejàre I, Mjör IA. Glass ionomer and resin‐based fissure sealants: a clinical study. Scandinavian Journal of Dental Research 1990;98(4):345‐50. [DOI] [PubMed] [Google Scholar]
Mel'nichenko 1994 {published data only}
- Mel'nichenko EM, Tristen' KS. Experience in preventing dental caries in the children of a city with a low fluorine content in its water. Stomatologiia 1994;73(4):64‐5. [PubMed] [Google Scholar]
Monse 2012 {published data only}
- Monse B, Heinrich‐Weltzien R, Mulder J, Holmgren C, Palenstein Helderman WH. Caries preventive efficacy of silver diammine fluoride (SDF) and ART sealants in a school‐based daily fluoride toothbrushing program in the Philippines. BMC Oral Health 2012;12:52. [DOI: 10.1186/1472-6831-12-52] [DOI] [PMC free article] [PubMed] [Google Scholar]
Morgan 1998 {published data only}
- Morgan MV, Crowley SJ, Wright C. Economic evaluation of a pit and fissure dental sealant and fluoride mouthrinsing program in two nonfluoridated regions of Victoria, Australia. Journal of Public Health Dentistry 1998;58(1):19‐27. [DOI] [PubMed] [Google Scholar]
Morrow 1997 {published data only}
- Morrow TA, Christensen WG, Cordner CI, Hein DK, Smith SL, Christensen RP. 2‐year clinical performance of 4 sealants. Journal of Dental Research 1997;76:191. [Google Scholar]
Noack 1997 {published data only}
- Noack MJ, Noack CB. Early fissure sealing with a compomer in high caries risk children. Journal of Dental Research 1997;5(Divisional Abstracts):1136. [Google Scholar]
Oba 2009 {published data only}
- Oba AA, Dülgergil T, Sönmez IS, Doğan S. Comparison of caries prevention with glass ionomer and composite resin fissure sealants. Journal of the Formosan Medical Association 2009;108(11):844‐8. [DOI] [PubMed] [Google Scholar]
Ohmori 1976 {published data only}
- Ohmori I, Kikuchi K, Masuhara E, Nakabayashi N, Tanaka S. Effect of the methyl methacrylate‐tributylborane sealant in preventing occlusal caries. Bulletin of Tokyo Medical and Dental University 1976;23(3):149‐55. [PubMed] [Google Scholar]
Oliveira 2008 {published data only}
- Oliveira FS, Silva SM, Machado MA, Bijella MF, Lima JE, Abdo RC. Resin‐modified glass ionomer cement and a resin‐based material as occlusal sealants: a longitudinal clinical performance. Journal of Dentistry for Children 2008;75(2):134‐43. [PubMed] [Google Scholar]
Pereira 1999 {published and unpublished data}
- Pardi V, Pereira AC, Mialhe FL, Meneghim Mde C, Ambrosano GM. A 5‐year evaluation of two glass‐ionomer cements used as fissure sealants. Community Dentistry and Oral Epidemiology 2003;31(5):386‐91. [DOI] [PubMed] [Google Scholar]
- Pereira AC, Basting RT, Pinelli C, Castro Meneghim M, Werner CW. Retention and caries prevention of Vitremer and Ketac‐bond used as occlusal sealants. American Journal of Dentistry 1999;12(2):62‐4. [PubMed] [Google Scholar]
- Pereira AC, Pardi V, Basting RT, Menighim Mde C, Pinelli C, Ambrosano GM, et al. Clinical evaluation of glass ionomers used as fissure sealants: twenty‐four‐month results. Journal of Dentistry for Children 2001;68(3):168‐74. [PubMed] [Google Scholar]
- Pereira AC, Pardi V, Mialhe FL, Meneghim Mde C, Ambrosano GM. A 3‐year clinical evaluation of glass‐ionomer cements used as fissure sealants. American Journal of Dentistry 2003;16(1):23‐7. [PubMed] [Google Scholar]
Petrovic 1996 {published data only}
- Petrovic V, Vulovic M, Vulicevic ZR. Clinical evaluation of pit and fissure sealants (IADR Abstract). Journal of Dental Research 1996;75:287. [Google Scholar]
Poulsen 1979 {published data only}
- Poulsen S, Thylstrup A, Christensen PF, Ishöy U. Evaluation of a pit‐ and fissure‐sealing program in a public dental health service after 2 years. Community Dentistry and Oral Epidemiology 1979;7(3):154‐7. [DOI] [PubMed] [Google Scholar]
Poulsen 2006 {published data only}
- Poulsen S, Laurberg L, Vaeth M, Jensen U, Haubek D. A field trial of resin‐based and glass‐ionomer fissure sealants: clinical and radiographic assessment of caries. Community Dentistry and Oral Epidemiology 2006;34(1):36‐40. [DOI] [PubMed] [Google Scholar]
Prados‐Atienza 2002 {published and unpublished data}
- Hita Iglesias C, Prados Atienza MB, Bravo M, Prados Sánchez E, Muñoz Soto E, González Rodríguez MP. Impact of public preventive programmes on oral quality of life of 11 to 12‐yr‐old school students. Medicina Oral, Patología Oral y Cirugía Bucal 2007;12:E408‐11. [PubMed] [Google Scholar]
- Prados‐Atienza MB, Bravo‐Perez M, Muñoz‐Soto E, González‐Rodríguez MP, Prados‐Sánchez E. Effectiveness of fissure sealant and fluoride varnish on different tooth surfaces: A 24‐month field trial [Efectividad de selladores de fisuras más barniz de flúor en distintas superficies dentarias: ensayo de campo a 24 meses]. RCOE 2002;7(2):167‐74. [Google Scholar]
Puppin‐Rontani 2006 {published data only}
- Puppin‐Rontani RM, Baglioni‐Gouvea ME, deGoes MF, Garcia‐Godoy F. Compomer as a pit and fissure sealant: effectiveness and retention after 24 months. Journal of Dentistry for Children 2006;73(1):31‐6. [PubMed] [Google Scholar]
Rajić 2000 {published data only}
- Rajić Z, Gvozdanović Z, Rajić‐Mestrović S, Bagić I. Preventive sealing of dental fissures with Heliosil: a two‐year follow‐up. Collegium Antropologicum 2000;24(1):151‐5. [PubMed] [Google Scholar]
Simonsen 1980 {published data only}
- Simonsen RJ. Retention and effectiveness of a single application of white sealant after 10 years. Journal of the American Dental Association 1987;115(1):31‐6. [DOI] [PubMed] [Google Scholar]
- Simonsen RJ. Retention and effectiveness of dental sealant after 15 years. Journal of the American Dental Association 1991;122(10):34‐42. [DOI] [PubMed] [Google Scholar]
- Simonsen RJ. The clinical effectiveness of a colored pit and fissure sealant at 24 months. Pediatric Dentistry 1980;2(1):10‐6. [PubMed] [Google Scholar]
- Simonsen RJ. The clinical effectiveness of a colored pit and fissure sealant at 36 months. Journal of the American Dental Association 1981;102(3):323‐7. [DOI] [PubMed] [Google Scholar]
Skrinjaric 2008 {published data only}
- Skrinjaric K, Vranic DN, Glavina D, Skrinjaric I. Heat‐treated glass ionomer cement fissure sealants: retention after 1 year follow‐up. International Journal of Paediatric Dentistry 2008;18(5):368‐73. [DOI] [PubMed] [Google Scholar]
Smales 1996 {published data only}
- Smales RJ, Lee YK, Lo FW, Tse CC, Chung MS. Handling and clinical performance of a glass ionomer sealant. American Journal of Dentistry 1996;9(5):203‐5. [PubMed] [Google Scholar]
- Smales RJ, Wong KC. 2‐year clinical performance of a resin‐modified glass ionomer sealant. American Journal of Dentistry 1999;12(2):59‐61. [PubMed] [Google Scholar]
Taifour 2003 {published data only}
- Taifour D, Frencken JE, van't Hof MA, Beiruti N, Truin GJ. Effects of a glass ionomer sealant in newly erupted first molars after 5 years: a pilot study. Community Dentistry and Oral Epidemiology 2003;31(4):314‐9. [DOI] [PubMed] [Google Scholar]
Tanguy 1984 {published data only}
- Tanguy R, Casanova F, Barnaud J. Prevention of tooth fissure caries using a sealing resin in the public health service [Prevention de la carie des sillons dentaires avec une resine de scellement en sante publique]. Revue d' Odonto‐Stomatologie 1984;13(2):125‐30. [PubMed] [Google Scholar]
Tapias Ledesma 2002 {published data only}
- Tapias Ledesma MA, Jiménez‐García R, Lamas F, Gil De Miguel A. Effectiveness of fissure sealants in child population at high risk of caries [Efectividad de los selladores de fisuras en una población infantil con alto riesgo de presentar caries]. Atención Primaria 2002;30(3):150‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Thylstrup 1976 {published data only}
- Thylstrup A, Poulsen S. Retention and effectiveness of a chemically polymerised pit and fissure sealant after 2 years. Scandinavian Journal of Dental Research 1978;86(1):21‐4. [DOI] [PubMed] [Google Scholar]
- Thylstrup A, Poulsen S. Retention and effectiveness of a chemically polymerized pit and fissure sealant after 12 months. Community Dentistry and Oral Epidemiology 1976;4(5):200‐4. [DOI] [PubMed] [Google Scholar]
Tostes 1997 {published data only}
- Tostes M. Prevention of pit and fissure caries in permanent molars using different fluoride materials [Prevenção de cárie de sulcos e fissuras em dentes permanentes com diferentes materiais contendo fluoreto]. Revista Brasileira de Odontologia 1997;54:368‐71. [Google Scholar]
Unal 2015 {published data only}
- Unal M, Oztas N. Remineralization capacity of three fissure sealants with and without caseous ozone on non‐cavitated incipient pit and fissure caries. Journal of Clinical Pediatric Dentistry 2015;39(4):364‐70. [DOI] [PubMed] [Google Scholar]
Valsecki 1992 {published data only}
- Valsecki Jr A, Vertuan V. Retention and efficiency of an occlusal sealant associated with a topical application of fluoride. Journal of Dental Research 1992;71(4):967. [Google Scholar]
Vieira 2000 {published data only}
- Vieira RS, Almeida ICS, Martinhon C, Rodriques CO, Freitas SFT. A 36 months follow‐up of glass ionomer and resin sealants. Journal of Dental Research 2000;79(Special Issue):417. [Google Scholar]
- Vieira RS, Martinhon C, Rodriques C. A 36 month follow‐up of glass ionomer and resin fissure sealant. International Journal of Paediatric Dentistry 1999;9(Suppl 1):45. [Google Scholar]
Vrbic 1983 {published and unpublished data}
- Vrbic V. Five‐year experience with fissure sealing. Quintessence International 1986;17:371‐2. [Google Scholar]
- Vrbic V. Retention of fissure sealant and caries reduction. Quintessence International 1983;14:421‐4. [Google Scholar]
- Vrbic V. Retention of fissure sealant and caries reduction [Obstojnost fisurnega zalitja in zmanjsanje kariesa]. Zobozdravstveni Vestnik 1982;37(3‐4):51‐9. [PubMed] [Google Scholar]
Wåhlin 1997 {published data only}
- Wåhlin G. Fissure sealing with glass ionomer cement and resin‐based material. A comparative clinical study [Fissurförsegling med glasjonomer respektive resinbaserat material. Jämförande klinisk studie]. Tandläkartidningen 1997;89(15):49‐54. [Google Scholar]
Winkler 1996 {published data only}
- Winkler MM, Deschepper EJ, Dean JA, Moore BK, Cochran MA, Ewoldsen N. Using a resin‐modified glass ionomer as an occlusal sealant: a one‐year clinical study. Journal of the American Dental Association 1996;127(10):1508‐14. [DOI] [PubMed] [Google Scholar]
Yakut 2006 {published data only}
- Yakut N, Sönmez H. Resin composite sealant vs. polyacid‐modified resin composite applied to post eruptive mature and immature molars: two year clinical study. Journal of Clinical Pediatric Dentistry 2006;30(3):215‐8. [DOI] [PubMed] [Google Scholar]
Yildiz 2004 {published data only}
- Yildiz E, Dörter C, Efes B, Koray F. A comparative study of two fissure sealants: a 2‐year clinical follow‐up. Journal of Oral Rehabilitation 2004;31(10):979‐84. [DOI] [PubMed] [Google Scholar]
Yilmaz 2010 {published data only}
- Yilmaz Y, Beldüz N, Eyüboğlu O. A two‐year evaluation of four different fissure sealants. European Archives of Paediatric Dentistry 2010;11(2):88‐92. [DOI] [PubMed] [Google Scholar]
Yoshihara 2000 {published data only}
- Yoshihara A, Sakuma S, Miyazaki H. A comparative study of glass ionomer and resin‐based material used as fissure sealants on the first molars with incipient remineralization. Koku Eisei Gakkai Zasshi 2000;50(5):777‐82. [Google Scholar]
Zhang 2003 {published data only}
- Zhang YY, Zhang L, Shan H. Clinical observation of microfilled sealant for first molars in children. Shanghai Kou Qiang Yi Xue/Shanghai Journal of Stomatology 2003;12(4):297‐9. [PubMed] [Google Scholar]
Zimmer 2009 {published data only}
- Zimmer S, Strafela N, Bastendorf KD, Bartsch A, Lang H, Barthel CR. Clinical success rate of a resin modified glass ionomer cement fissure sealant in comparison to a bis‐GMA sealant after three years [Klinische erfolgsraten von fissurenversiegelungen mit kompomer oder bis‐GMA nach drei jahren]. Oralprophylaxe & Kinderzahnheilkunde 2009;31(1):8‐12. [Google Scholar]
References to studies awaiting assessment
Gorseta 2014 {published data only}
- Gorseta K, Glavina D, Borzabadi‐Farahani A, Duinen RN, Skrinjaric I, Hill RG, et al. One‐year clinical evaluation of a glass carbomer fissure sealant, a preliminary study. European Journal of Prosthodontics and Restorative Dentistry 2014;22(2):67‐71. [PubMed] [Google Scholar]
Ulusu 2012 {published data only}
- Ulusu T, Odabaş ME, Tüzüner T, Baygin Ö, Sillelioğlu H, Deveci C, et al. The success rates of a glass ionomer cement and a resin‐based fissure sealant placed by fifth‐year undergraduate dental students. European Archives of Paediatric Dentistry 2012;13(2):94‐7. [DOI] [PubMed] [Google Scholar]
References to ongoing studies
IRCT2013041611960N2 {published data only}
- IRCT2013041611960N2. Clinical evaluation of glass ionomer fissure sealants. en.search.irct.ir/view/13191 (first received 20 December 2013).
NCT02408601 {published data only}
- NCT02408601. A clinical trial to assess the retention and caries preventive effect of resin based sealants versus ART sealants. clinicaltrials.gov/ct2/show/NCT02408601 (first received 24 March 2015).
NCT02443896 {published data only}
- NCT02443896. The use of pit and fissure sealants in children requiring caries related dental extractions. clinicaltrials.gov/ct2/show/NCT02443896 (first received 1 April 2015).
NCT02795728 {published data only}
- NCT02795728. Fuji type VII sealant versus resin based sealant. A clinical trial. clinicaltrials.gov/ct2/show/NCT02795728 (first received 28 May 2016).
NCT02849925 {published data only}
- NCT02849925. Randomized controlled clinical trial on the treatment of caries lesions using resin or glass ionomer sealants in permanent teeth. clinicaltrials.gov/ct2/show/NCT02849925 (first received 21 July 2016).
Additional references
ADA 2016
- ADA American Dental Association. ADA Statement on bisphenol A and dental materials. www.ada.org/en/member‐center/oral‐health‐topics/bisphenol‐a (accessed August 2016).
Alves 2014
- Alves LS, Zenkner JE, Wagner MB, Damé‐Teixeira N, Susin C, Maltz M. Eruption stage of permanent molars and occlusal caries activity/arrest. Journal of Dental Research 2014;93(7 Suppl 1):114‐9S. [DOI] [PMC free article] [PubMed] [Google Scholar]
Arenholt 1999
- Arenholt‐Bindslev D, Breinholt V, Preiss A, Schmalz G. Time‐related bisphenol‐A content and estrogenic activity in saliva samples collected in relation to placement of fissure sealants. Clinical Oral Investigations 1999;3(3):120‐5. [DOI] [PubMed] [Google Scholar]
Azarpazhooh 2008a
- Azarpazhooh A, Main PA. Pit and fissure sealants in the prevention of dental caries in children and adolescents: a systematic review. Journal of the Canadian Dental Association 2008;74(2):171‐7. [PubMed] [Google Scholar]
Azarpazhooh 2008b
- Azarpazhooh A, Main PA. Is there a risk of harm or toxicity in the placement of pit and fissure sealant materials? A systematic review. Journal of the Canadian Dental Association 2008;74(2):179‐83. [PubMed] [Google Scholar]
Bader 2004
- Bader JD, Shugars DA. A systematic review of the performance of a laser fluorescence device for detecting caries. Journal of the American Dental Association 2004;135(10):1413‐26. [DOI] [PubMed] [Google Scholar]
Bagramian 2009
- Bagramian RA, Garcia‐Godoy F, Volpe AR. The global increase in dental caries. A pending public health crisis. American Journal of Dentistry 2009;22:3‐8. [PubMed] [Google Scholar]
Barker 2011
- Barker LK, Griffin SO, Jeon S, Gray SK, Vidakovic B. Ecological‐type inference in matched‐pair studies with fixed marginal totals. Statistics in Medicine 2011;30(5):541‐8. [DOI] [PubMed] [Google Scholar]
Batchelor 2004
- Batchelor PA, Sheiham A. Grouping of tooth surfaces by susceptibility to caries: a study in 5‐16 year‐old children. BMC Oral Health 2004;4(1):2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Brown 1995
- Brown LJ, Selwitz RH. The impact of recent changes in the epidemiology of dental caries on guidelines for the use of dental sealants. Journal of Public Health Dentistry 1995;55(5 Spec No):274‐91. [DOI] [PubMed] [Google Scholar]
Carvalho 2014
- Carvalho JC. Caries process on occlusal surfaces: evolving evidence and understanding. Caries Research 2014;48(4):339‐46. [DOI] [PubMed] [Google Scholar]
Chokkalingam 1998
- Chokkalingam A, Scherer R, Dickersin K. Agreement of data in abstracts compared to full publications. Contemporary Clinical Trials 1998;19(3 (Suppl 1)):S61‐2. [Google Scholar]
Curtin 2002
- Curtin F, Elbourne D, Altman DG. Meta‐analysis combining parallel and cross‐over clinical trials. II: Binary outcomes. Statistics in Medicine 2002;21(15):2145‐59. [DOI] [PubMed] [Google Scholar]
Dorri 2015
- Dorri M, Dunne SM, Walsh T, Schwendicke F. Micro‐invasive interventions for managing proximal dental decay in primary and permanent teeth. Cochrane Database of Systematic Reviews 2015, Issue 11. [DOI: 10.1002/14651858.CD010431.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ekstrand 2012
- Ekstrand K, Martignon S, Bakhshandeh A, Ricketts DNJ. The non‐operative resin treatment of proximal caries lesions. Dental Update 2012;39(9):614‐22. [DOI] [PubMed] [Google Scholar]
Elbourne 2002
- Elbourne DR, Altman DG, Higgins JPT, Curtin F, Worthington HV, Vail A. Meta‐analyses involving cross‐over trials: methodological issues. International Journal of Epidemiology 2002;31(1):140‐9. [DOI] [PubMed] [Google Scholar]
FDI 2015
- FDI World Dental Federation. The challenge of oral disease ‐ A call for global action by FDI World Dental Federation: Tooth decay worldwide. www.fdiworldental.org/media/78201/16_c_map_oh2.pdf (accessed 16 December 2016).
Fleisch 2010
- Fleisch AF, Sheffield PE, Chinn C, Edelstein BL, Landrigan PJ. Bisphenol A and related compounds in dental materials. Pediatrics 2010;126(4):760‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
GRADE 2004
- GRADE Working Group. Grading quality of evidence and strength of recommendations. BMJ 2004;328(7454):1490‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
GRADEpro GDT 2014 [Computer program]
- GRADE Working Group, McMaster University. GRADEpro GDT. Version (accessed prior to 23 May 2017). Hamilton (ON): GRADE Working Group, McMaster University, 2014.
Griffin 2008
- Griffin SO, Oong E, Kohn W, Vidakovic B, Gooch BF, CDC Dental Sealant Systematic Review Work Group, et al. The effectiveness of sealants in managing caries lesions. Journal of Dental Research 2008;87(2):169‐74. [DOI] [PubMed] [Google Scholar]
Higgins 2003
- Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analyses. BMJ 2003;327(7414):557‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011a
- Higgins JPT, Altman DG, Sterne JAC (editors). Chapter 8: Assessing risk of bias in included studies. In: Higgins JPT, Green S editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org. [Google Scholar]
Higgins 2011b
- Higgins JPT, Deeks JJ, Altman DG (editors). Chapter 16: Special topics in statistics. In: Higgins JPT, Green S editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org. [Google Scholar]
Hopewell 2006
- Hopewell S, Clarke M, Askie L. Reporting of trials presented in conference abstracts needs to be improved. Journal of Clinical Epidemiology 2006;59(7):681‐4. [DOI] [PubMed] [Google Scholar]
ICDAS II 2008
- International Caries Detection and Assessment System (ICDAS) Coordinating Committee. ICDAS II International Caries Assessment and Detection System. www.icdas.org/assets/downloads/Appendix.pdf (accessed August 2015).
Joskow 2006
- Joskow R, Boyd Barr D, Barr JR, Calafat AM, Needham LL, Rubin C. Exposure to bisphenol A from bis‐glycidyl dimethacrylate‐based dental sealants. Journal of the American Dental Association 2006;137(3):353‐62. [DOI] [PubMed] [Google Scholar]
Kloukos 2013
- Kloukos D, Pandis N, Eliades T. In vivo bisphenol‐A release from dental pit and fissure sealants: a systematic review. Journal of Dentistry 2013;41(8):659‐67. [DOI] [PubMed] [Google Scholar]
Kühnisch 2012
- Kühnisch J, Mansmann U, Heinrich‐Weltzien R, Hickel R. Longevity of materials for pit and fissure sealing ‐ Results from a meta‐analysis. Dental Materials 2012;28(3):298‐303. [DOI] [PubMed] [Google Scholar]
Larmas 1995
- Larmas MA, Virtanen JI, Bloigu RS. Timing of first restorations in permanent teeth: a new system for oral health determination. Journal of Dentistry 1995;23(6):347‐52. [DOI] [PubMed] [Google Scholar]
Lefebvre 2011
- Lefebvre C, Manheimer E, Glanville J. Searching for studies. Cochrane Handbook for Systematic Reviews of Interventions, Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011, Available from www.cochrane‐handbook.org. [Google Scholar]
Llodra 1993
- Llodra JC, Bravo M, Delgado‐Rodriguez M, Baca P, Galvez R. Factors influencing the effectiveness of sealants ‐ a meta‐analysis. Community Dentistry and Oral Epidemiology 1993;21(5):261‐8. [DOI] [PubMed] [Google Scholar]
McComb 2001
- McComb D, Tam LE. Diagnosis of occlusal caries: Part I. Conventional methods. Journal of the Canadian Dental Association 2001;67(8):454‐7. [PubMed] [Google Scholar]
McDonald 1992
- McDonald SP, Sheiham A. The distribution of caries on different tooth surfaces at varying levels of caries ‐ a compilation of data from 18 previous studies. Community Dental Health 1992;9(1):39‐48. [PubMed] [Google Scholar]
Mejàre 2003
- Mejàre I, Lingström P, Petersson LG, Holm AK, Twetman S, Källestål C, et al. Caries‐preventive effect of fissure sealants: a systematic review. Acta Odontologica Scandinavica 2003;61(6):321‐30. [DOI] [PubMed] [Google Scholar]
Mejàre 2014
- Mejàre I, Axelsson S, Dahlén G, Espelid I, Norlund A, Tranæus S, Twetman S. Caries risk assessment: A systematic review. Acta Odontologica Scandinavica 2014;72(2):81‐91. [DOI] [PubMed] [Google Scholar]
Mickenautsch 2013
- Mickenautsch S, Yengopal V. Validity of sealant retention as surrogate for caries prevention ‐ a systematic review. PLoS ONE 2013;8(10):e77103. [DOI] [PMC free article] [PubMed] [Google Scholar]
Nicholson 2007
- Nicholson JW. Polyacid‐modified composite resins ("compomers") and their use in clinical dentistry. Dental Materials 2007;23(5):615‐22. [DOI] [PubMed] [Google Scholar]
Petersen 2005
- Petersen PE. Sociobehavioural risk factors in dental caries ‐ international perspectives. Community Dentistry and Oral Epidemiology 2005;33(4):274‐9. [DOI] [PubMed] [Google Scholar]
R for Windows 3.3.1 [Computer program]
- R Core Team (2016). R: A language and environment for statistical computing. Version 3.3.1. Vienna, Austria. URL http://www.R‐project.org/.: R Foundation for Statistical Computing, 2016.
RevMan 2014 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Ripa 1993
- Ripa LW. Sealants revisited: an update of the effectiveness of pit‐and‐fissure sealants. Caries Research 1993;27(Suppl 1):77‐82. [DOI] [PubMed] [Google Scholar]
Ruse 1999
- Ruse ND. What is a "compomer"?. Journal of the Canadian Dental Association 1999;65(9):500‐4. [PubMed] [Google Scholar]
Schmalz 1999
- Schmalz G, Preiss A, Arenholt‐Bindslev D. Bisphenol‐A content of resin monomers and related degradation products. Clinical Oral Investigations 1999;3(3):114‐9. [DOI] [PubMed] [Google Scholar]
Splieth 2010
- Splieth CH, Ekstrand KR, Alkilzy M, Clarkson J, Meyer‐Lueckel H, Martignon S, et al. Sealants in dentistry: outcomes of the ORCA Saturday Afternoon Symposium 2007. Caries Research 2010;44(1):3‐13. [DOI] [PubMed] [Google Scholar]
Splieth 2016
- Splieth CH, Christiansen J, Foster Page LA. Caries epidemiology and community dentistry: changes for future improvements in caries risk groups. Outcomes of the ORCA Saturday Afternoon Symposium, Greifswald, 2014. Part 1. Caries Research 2016;50:9‐16. [DOI] [PubMed] [Google Scholar]
Stedman 2011
- Stedman MR, Curtin F, Elbourne DR, Kesselheim AS, Brookhart MA. Meta‐analyses involving cross‐over trials: methodological issues. International Journal of Epidemiology 2011;40(6):1732‐4. [DOI] [PubMed] [Google Scholar]
Sterne 2011
- Sterne JAC, Egger M, Moher D (editors). Chapter 10: Addressing reporting biases. In: Higgins JPT, Green S editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org. [Google Scholar]
Tellez 2013
- Tellez M, Gomez J, Pretty I, Ellwood R, Ismail AI. Evidence on existing caries risk assessment systems: are they predictive of future caries?. Community Dentistry and Oral Epidemiology 2013;41(1):67‐78. [DOI] [PubMed] [Google Scholar]
Twetman 2013
- Twetman S, Axelsson S, Dahlen G, Espelid I, Mejàre I, Norlund A, et al. Adjunct methods for caries detection: a systematic review of literature. Acta Odontologica Scandinavica 2013;71(3‐4):388‐97. [DOI] [PubMed] [Google Scholar]
Twetman 2016
- Twetman S. Caries risk assessment in children: how accurate are we?. European Archives of Paediatric Dentistry 2016;17:27‐32. [DOI] [PubMed] [Google Scholar]
Van 't Hof 2006
- 't Hof MA, Frencken JE, Palenstein Helderman WH, Holmgren CJ. The atraumatic restorative treatment (ART) approach for managing dental caries: a meta‐analysis. International Dental Journal 2006;56(6):345‐51. [DOI] [PubMed] [Google Scholar]
Weerheijm 1996
- Weerheijm KL, Kreulen CM, Gruythuysen RJ. Comparison of retentive qualities of two glass‐ionomer cements used as fissure sealants. ASDC Journal of Dentistry for Children 1996;63(4):265‐7. [PubMed] [Google Scholar]
WHO 2014
- WHO (World Health Organization). Global caries map for 12 year olds (based on the most recent data in CAPP in 2014); Figure: Dental caries levels (DMFT) among 12‐years‐olds, December 2014. www.mah.se/CAPP/Country‐Oral‐Health‐Profiles/According‐to‐WHO‐Regions/Global‐caries‐map‐2013‐‐2014/ (accessed 16 December 2016).
Worthington 2015
- Worthington H, Clarkson J, Weldon J. Priority oral health research identification for clinical decision‐making. Evidence‐based Dentistry 2015;16(3):69‐71. [DOI] [PubMed] [Google Scholar]
Zenkner 2013
- Zenkner JE, Alves LS, Oliveira RS, Bica RH, Wagner MB, Maltz M. Influence of eruption stage and biofilm accumulation on occlusal caries in permanent molars: a generalized estimating equations logistic approach. Caries Research 2013;47(3):177‐82. [DOI] [PubMed] [Google Scholar]
Zimmerli 2010
- Zimmerli B, Strub M, Jeger F, Stadler O, Lussi A. Composite materials: Composition, properties and clinical applications. Schweizer Monatsschrift für Zahnmedizin 2010;120(11):972‐9. [PubMed] [Google Scholar]
References to other published versions of this review
Ahovuo‐Saloranta 1999
- Ahovuo‐Saloranta A, Hiiri A, Nordblad A, Mäkëla M, Murtomaa H. Pit and fissure sealants for preventing dental decay in the permanent teeth of children and adolescents. Cochrane Database of Systematic Reviews 1999, Issue 4. [DOI: 10.1002/14651858.CD001830] [DOI] [PubMed] [Google Scholar]
Ahovuo‐Saloranta 2004
- Ahovuo‐Saloranta A, Hiiri A, Nordblad A, Worthington H, Mäkelä M. Pit and fissure sealants for preventing dental decay in the permanent teeth of children and adolescents. Cochrane Database of Systematic Reviews 2004, Issue 3. [DOI: 10.1002/14651858.CD001830.pub2] [DOI] [PubMed] [Google Scholar]
Ahovuo‐Saloranta 2008
- Ahovuo‐Saloranta A, Hiiri A, Nordblad A, Mäkelä M, Worthington HV. Pit and fissure sealants for preventing dental decay in the permanent teeth of children and adolescents. Cochrane Database of Systematic Reviews 2008, Issue 4. [DOI: 10.1002/14651858.CD001830.pub3] [DOI] [PubMed] [Google Scholar]
Ahovuo‐Saloranta 2013
- Ahovuo‐Saloranta A, Forss H, Walsh T, Hiiri A, Nordblad A, Mäkelä M, Worthington HV. Sealants for preventing dental decay in the permanent teeth. Cochrane Database of Systematic Reviews 2013, Issue 3. [DOI: 10.1002/14651858.CD001830.pub4] [DOI] [PubMed] [Google Scholar]


