Abstract
Background
Many people with low back pain (LBP) become frequent users of healthcare services in their attempt to find treatments that minimise the severity of their symptoms. Back School consists of a therapeutic programme given to groups of people that includes both education and exercise. However, the content of Back School has changed over time and appears to vary widely today. This review is an update of a Cochrane review of randomised controlled trials (RCTs) evaluating the effectiveness of Back School. We split the Cochrane review into two reviews, one focusing on acute and subacute LBP, and one on chronic LBP.
Objectives
The objective of this systematic review was to determine the effect of Back School on pain and disability for adults with chronic non‐specific LBP; we included adverse events as a secondary outcome. In trials that solely recruited workers, we also examined the effect on work status.
Search methods
We searched for trials in the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE, Embase, CINAHL, two other databases and two trials registers to 15 November 2016. We also searched the reference lists of eligible papers and consulted experts in the field of LBP management to identify any potentially relevant studies we may have missed. We placed no limitations on language or date of publication.
Selection criteria
We included only RCTs and quasi‐RCTs evaluating pain, disability, and/or work status as outcomes. The primary outcomes for this update were pain and disability, and the secondary outcomes were work status and adverse events.
Data collection and analysis
Two review authors independently performed the 'Risk of bias' assessment of the included studies using the 'Risk of bias' assessment tool recommended by The Cochrane Collaboration. We summarised the results for the short‐, intermediate‐, and long‐term follow‐ups. We evaluated the overall quality of evidence using the GRADE approach.
Main results
For the outcome pain, at short‐term follow‐up, we found very low‐quality evidence that Back School is more effective than no treatment (mean difference (MD) ‐6.10, 95% confidence interval (CI) ‐10.18 to ‐2.01). However, we found very low‐quality evidence that there is no significant difference between Back School and no treatment at intermediate‐term (MD ‐4.34, 95% CI –14.37 to 5.68) or long‐term follow‐up (MD ‐12.16, 95% CI ‐29.14 to 4.83). There was very low‐quality evidence that Back School reduces pain at short‐term follow‐up compared to medical care (MD ‐10.16, 95% CI –19.11 to ‐1.22). Very low‐quality evidence showed there to be no significant difference between Back School and medical care at intermediate‐term (MD ‐9.65, 95% CI ‐22.46 to 3.15) or long‐term follow‐up (MD ‐5.71, 95% CI –20.27 to 8.84). We found very low‐quality evidence that Back School is no more effective than passive physiotherapy at short‐term (MD 1.96, 95% CI –9.51 to 13.43), intermediate‐term (MD ‐16.89, 95% CI ‐66.56 to 32.79), or long‐term follow‐up (MD ‐12.86, 95% CI –61.22 to 35.50). There was very low‐quality evidence that Back School is no better than exercise at short‐ term follow‐up (MD ‐2.06, 95% CI –14.58 to 10.45). There was low‐quality evidence that Back School is no better than exercise at intermediate‐term (MD ‐4.46, 95% CI –19.44 to 10.52) and long‐term follow‐up (MD 4.58, 95% CI –0.20 to 9.36).
For the outcome disability, we found very low‐quality evidence that Back School is no more effective than no treatment at intermediate‐term (MD –5.92, 95% CI –12.08 to 0.23) and long‐term follow‐up (MD ‐7.36, 95% CI ‐22.05 to 7.34); medical care at short‐term (MD –1.19, 95% CI –7.02 to 4.64) and long‐term follow‐up (MD –0.40, 95% CI –7.33 to 6.53); passive physiotherapy at short‐term (MD 2.57, 95% CI –15.88 to 21.01) and intermediate‐term follow‐up (MD 6.88, 95% CI ‐4.86 to 18.63); and exercise at short‐term (MD ‐1.65, 95% CI –8.66 to 5.37), intermediate‐term (MD 1.57, 95% CI –3.86 to 7.00), and long‐term follow‐up (MD 4.54, 95% CI ‐4.44 to 13.52). We found very low‐quality evidence of a small difference between Back School and no treatment at short‐term follow‐up (MD –3.38, 95% CI –6.70 to –0.05) and medical care at intermediate‐term follow‐up (MD –6.34, 95% CI –10.89 to –1.79). Still, at long‐term follow‐up there was very low‐quality evidence that passive physiotherapy is better than Back School (MD 9.60, 95% CI 3.65 to 15.54).
Few studies measured adverse effects. The results were reported as means without standard deviations or group size was not reported. Due to this lack of information, we were unable to statistically pool the adverse events data. Work status was not reported.
Authors' conclusions
Due to the low‐ to very low‐quality of the evidence for all treatment comparisons, outcomes, and follow‐up periods investigated, it is uncertain if Back School is effective for chronic low back pain. Although the quality of the evidence was mostly very low, the results showed no difference or a trivial effect in favour of Back School. There are myriad potential variants on the Back School approach regarding the employment of different exercises and educational methods. While current evidence does not warrant their use, future variants on Back School may have different effects and will need to be studied in future RCTs and reviews.
Plain language summary
Back School for the treatment of chronic low back pain
Background
Many people with low back pain (LBP) seeking treatments that minimise the severity of their symptoms become frequent users of healthcare services. Back School consists of a therapeutic programme given to groups of people that includes both education and exercise. Since its introduction in 1969, the Swedish Back School has frequently been used in the treatment of LBP. However, the content of Back School has changed over time and appears to vary widely today.
Review question
We reviewed the evidence on the effects of Back School on pain and disability in adults with LBP with no specific cause lasting more than 12 weeks compared to no treatment, medical care, physiotherapist‐applied treatment, or exercise. We included adverse events as a secondary outcome. In trials that only recruited workers, we also examined the effect on work status.
Study characteristics
In this update we searched for trials, both published and unpublished, to 15 November 2016. We included 30 trials with 4105 participants comparing Back School to no treatment, medical care, passive physiotherapy (physiotherapist‐applied treatment), or exercise therapy. All studies included a similar population of people with chronic non‐specific LBP.
Key results
Regardless of the comparison used (as well as the outcomes investigated), the results of the meta‐analysis showed no difference or a trivial effect in favour of Back School. Due to a lack of information on adverse effects and work status, we were unable to statistically pool the data.
Quality of evidence
Due to the low‐ to very low‐quality evidence for all treatment comparisons, outcomes, and follow‐up periods investigated, it is uncertain if Back School is effective for chronic low back pain.
Summary of findings
Summary of findings for the main comparison. Back School compared with no treatment for low back pain.
| Back School compared with no treatment for low back pain | |||||
|
Patient or population: people with low back pain Intervention: Back School Comparison: no treatment | |||||
| Outcomes | lIIustrative comparative risks (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | |
| Assumed risk | Corresponding risk* | ||||
| No treatment | Back School | ||||
|
Pain: short‐term follow‐up (< 3 months) Multiple scales: scale from 0 to 100 (worse pain) |
The mean pain at short‐term follow‐up ranged across control groups from 31.8 to 68 points. | The mean pain (short term) in the intervention groups was 6.10 lower (10.18 lower to 2.01 lower). | MD ‐6.10 (‐10.18 to ‐2.01) | 647 participants (6 studies) | ⊕⊝⊝⊝ very low2,3,4 |
|
Pain: intermediate‐term follow‐up (3 to 6 months) Multiple scales: scale from 0 to 100 (worse pain) |
The mean pain at intermediate‐term follow‐up ranged across control groups from 26 to 65 points. | The mean pain (intermediate term) in the intervention groups was 4.34 lower (14.37 lower to 5.68 higher). | MD ‐4.34 (‐14.37 to 5.68) | 257 participants (4 studies) | ⊕⊝⊝⊝ very low1,2,4 |
|
Pain: long‐term follow‐up (> 6 months) Multiple scales: scale from 0 to 100 (worse pain) |
The mean pain at long‐term follow‐up ranged across control groups from 38 to 58 points. | The mean pain (long term) in the intervention groups was 12.16 lower (29.14 lower to 4.83 higher). | MD ‐12.16 (‐29.14 to 4.38) | 244 participants (3 studies) | ⊝⊝⊝⊝ very low1,2,3,4 |
|
Disability: short‐term follow‐up (< 3 months) Multiple scales: scale from 0 to 100 (worse disability) |
The mean disability at short‐term follow‐up ranged across control groups from 29.3 to 60 points. | The mean disability (short term) in the intervention groups was 3.83 lower (6.70 lower to 0.05 lower). | MD ‐3.38 (‐6.70 to ‐0.05) | 426 participants (3 studies) | ⊕⊝⊝⊝ very low2,3,4 |
|
Disability: intermediate‐term follow‐up (3 to 6 months) Multiple scales: scale from 0 to 100 (worse disability) |
The mean disability at intermediate‐term follow‐up ranged across control groups from 39 to 53 points. | The mean disability (intermediate term) in the intervention groups was 5.92 lower (12.80 lower to 0.23 higher). | MD ‐5.92 (‐12.08 to 0.23) | 181 participants (3 studies) | ⊕⊝⊝⊝ very low1,2,4 |
|
Disability: long‐term follow‐up (> 6 months) Multiple scales: scale from 0 to 100 (worse disability) |
The mean disability long‐term follow‐up ranged across control groups from 48 to 51 points. | The mean disability (long term) in the intervention groups was 7.36 lower (22.05 lower to 7.34 higher). | MD ‐7.36 (‐22.05 to 7.34) | 124 participants (2 studies) | ⊕⊝⊝⊝ very low1,2,4 |
| Adverse events Not reported | |||||
| Work status Not reported | |||||
| The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; MD: mean difference | |||||
| GRADE Working Group grades of evidence High‐quality evidence: There are consistent findings among at least 75% of randomised controlled trials with low risk of bias; consistent, direct, and precise data; and no known or suspected publication biases. Further research is unlikely to change either the estimate or our confidence in the results. Moderate‐quality evidence: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low‐quality evidence: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low‐quality evidence: We are very uncertain about the results. No evidence: We identified no randomised controlled trials that addressed this outcome. | |||||
1Downgraded one level due to imprecision (fewer than 400 participants in total). 2Downgraded one level due to risk of bias (> 25% of the participants were from studies with a high risk of bias). 3Downgraded one level due to clear inconsistency of results. 4Downgraded one level due to publication bias.
Summary of findings 2. Back School compared with medical care for low back pain.
| Back School compared with medical care for low back pain | |||||
|
Patient or population: people with low back pain Intervention: Back School Comparison: medical care | |||||
| Outcomes | Illustrative comparative risks (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | |
| Assumed risk | Corresponding risk* | ||||
| Medical care | Back School | ||||
|
Pain: short‐term follow‐up (< 3 months) Multiple scales: scale from 0 to 100 (worse pain) |
The mean pain at short‐term follow‐up ranged across control groups from 17 to 73 points. | The mean pain (short term) in the intervention groups was 10.16 lower (19.11 lower to 1.22 lower). | MD ‐10.16 (‐19.11 to ‐1.22) | 249 participants (3 studies) | ⊕⊝⊝⊝ very low1,2,4 |
|
Pain: intermediate‐term follow‐up (3 to 6 months) Multiple scales: scale from 0 to 100 (worse pain) |
The mean pain at intermediate‐term follow‐up ranged across control groups from 12 to 76 points. | The mean pain (intermediate term) in the intervention groups was 9.65 lower (22.46 lower to 3.15 higher). | MD ‐9.65 (‐22.46 to 3.15) | 545 participants (5 studies) | ⊕⊝⊝⊝ very low2,3,4 |
|
Pain: long‐term follow‐up (> 6 months) Multiple scales: scale from 0 to 100 (worse pain) |
The mean pain at long‐term follow‐up ranged across control groups from 12 to 65 points. | The mean pain (long term) in the intervention groups was 5.71 lower (20.27 lower to 8.84 higher). | MD ‐5.71 (‐20.27 to 8.84) | 406 participants (3 studies) | ⊕⊝⊝⊝ very low2,3,4 |
|
Disability: short‐term follow‐up (< 3 months) Multiple scales: scale from 0 to 100 (worse disability) |
The mean disability at short‐term follow‐up ranged across control groups from 24.8 to 41.2 points. | The mean disability at short‐term follow‐up in the intervention groups was 1.19 lower (7.02 lower to 4.64 higher). | MD ‐1.19 (‐7.02 to 4.64) | 130 participants (2 studies) | ⊕⊝⊝⊝ very low1,2,4 |
|
Disability: intermediate‐term follow‐up (3 to 6 months) Multiple scales: scale from 0 to 100 (worse disability) |
The mean disability at intermediate‐term follow‐up ranged across control groups from 25.8 to 43.3 points. | The mean disability at intermediate‐term follow‐up in the intervention groups was 6.34 lower (10.89 lower to 1.79 lower). | MD ‐6.34 (‐10.89 to ‐1.79) | 331 participants (3 studies) | ⊕⊝⊝⊝ very low1,2,4 |
|
Disability: long‐term follow‐up (> 6 months) Multiple scales: scale from 0 to 100 (worse disability) |
The mean disability at long‐term follow‐up was 32.9 points. | The mean disability at long‐term follow‐up in the intervention groups was 0.40 lower (7.33 lower to 6.53 higher). | MD ‐0.40 (‐7.33 to 6.53) | 201 participants (1 study) | ⊕⊝⊝⊝ very low1,2,4 |
| Adverse events Two workers in the Back School group (n=98) reported a strong increase in low back pain (Heymans 2006). | |||||
| Work status Not reported | |||||
| The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; MD: mean difference | |||||
| GRADE Working Group grades of evidence High‐quality evidence: There are consistent findings among at least 75% of randomised controlled trials with low risk of bias; consistent, direct, and precise data; and no known or suspected publication biases. Further research is unlikely to change either the estimate or our confidence in the results. Moderate‐quality evidence: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low‐quality evidence: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low‐quality evidence: We are very uncertain about the results. No evidence: We identified no randomised controlled trials that addressed this outcome. | |||||
1Downgraded one level due to imprecision (fewer than 400 participants in total). 2Downgraded one level due to risk of bias (> 25% of the participants were from studies with a high risk of bias). 3Downgraded one level due to clear inconsistency of results. 4Downgraded one level due to publication bias.
Summary of findings 3. Back School compared with passive physiotherapy for low back pain.
| Back School compared with passive physiotherapy for low back pain | |||||
|
Patient or population: people with low back pain. Intervention: Back School Comparison: passive physiotherapy | |||||
| Outcomes | Illustrative comparative risks (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | |
| Assumed risk | Corresponding risk* | ||||
| Passive physiotherapy | Back School | ||||
| pain: short‐term follow‐up (< 3 months) Multiple scales: scale from 0 to 100 (worse pain) | The mean pain at short‐term follow‐up ranged across control groups from 7.1 to 88 points. | The mean pain (short‐ term) in the intervention groups was 1.96 higher (9.51 lower to 13.43 higher). | MD 1.96 (‐9.51 to 13.43) | 290 participants (3 studies) | ⊝⊝⊝⊝ very low1,2,3,4 |
|
pain ‐ intermediate‐term follow up (3‐6 months) Multiple scales: scale from 0 to 100 (worse pain) |
The mean pain at intermediate‐term follow‐up ranged across control groups from 13.3 to 65 points. | The mean pain (intermediate‐term) in the intervention groups was 16.89 lower (66.56 lower to 32.79 higher). | MD ‐16.89 (‐66.56 to 32.79) | 290 participants (3 studies) | ⊝⊝⊝⊝ very low1,2,3,4 |
|
pain ‐ long‐term follow‐up (>6 months) Multiple scales: scale from 0 to 100 (worse pain) |
The mean pain at long‐term follow‐up ranged across control groups from 11.6 to 60.5 points. | The mean pain (long‐ term) in the intervention groups was 12.86 lower (61.22 lower to 35.50 higher). | MD ‐12.86 (‐61.22 to 35.50) | 291 participants (3 studies) | ⊝⊝⊝⊝ very low1,2,3,4 |
|
Disability ‐ short‐term follow‐up (<3 months) Multiple scales: scale from 0 to 100 (worse disability) |
The mean disability at short‐term follow‐up ranged across control groups from 9.1 to 60 points. | The mean disability at short‐term follow‐up in the intervention groups was 2.57 higher (15.88 lower to 21.01 higher). | MD 2.57 (‐15.88 to 21.01) | 180 participants (2 studies) | ⊝⊝⊝⊝ very low1,2,3,4 |
|
Disability ‐ intermediate‐term follow up (3‐6 months) Multiple scales: scale from 0 to 100 (worse disability) |
The mean disability at intermediate‐term follow‐up ranged across control groups from 10.4 to 53 points. | The mean disability at short‐term follow‐up in the intervention groups was 6.88 higher (‐4.86 lower to 18.63 higher). | MD 6.88 (‐4.86 to 18.63). | 180 participants (2 studies) | ⊕⊝⊝⊝ very low1,2,4 |
|
Disability ‐ long‐term follow‐up (>6 months) Multiple scales: scale from 0 to 100 (worse disability) |
The mean disability at long‐term follow‐up ranged across control groups from 10.4 to 46 points. | The mean disability at long‐term follow‐up in the intervention groups was 9.60 higher (3.65 higher to 15.54 higher). | MD 9.60 (3.65 to 15.54) | 180 participants (2 studies) | ⊕⊝⊝⊝ very low1,2,4 |
| Adverse events Not reported | |||||
| Work status Not reported | |||||
| The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; MD: mean difference | |||||
| GRADE Working Group grades of evidence High‐quality evidence: There are consistent findings among at least 75% of randomised controlled trials with low risk of bias; consistent, direct, and precise data; and no known or suspected publication biases. Further research is unlikely to change either the estimate or our confidence in the results. Moderate‐quality evidence: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low‐quality evidence: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low‐quality evidence: We are very uncertain about the results. No evidence: We identified no randomised controlled trials that addressed this outcome. | |||||
1 Downgraded one level due to imprecision (fewer than 400 participants, in total). 2 Downgraded one level due to risk of bias (> 25% of the participants were from studies with a high risk of bias). 3 Downgraded one level due to clear inconsistency of results. 4 Downgraded one level due to publication bias.
Summary of findings 4. Back School compared with exercise for low back pain.
| Back School compared with exercise for low back pain | |||||
|
Patient or population: people with low back pain Intervention: Back School Comparison: exercise | |||||
| Outcomes | Illustrative comparative risks (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | |
| Assumed risk | Corresponding risk* | ||||
| Exercise | Back School | ||||
|
Pain: short‐term follow‐up (< 3 months) Multiple scales: scale from 0 to 100 (worse pain) |
The mean pain at short‐term follow‐up ranged across control groups from 25 to 40 points. | The mean pain (short term) in the intervention groups was 2.06 lower (14.58 lower to 10.45 higher). | MD ‐2.06 (‐14.58 to 10.45) | 416 participants (5 studies) | ⊕⊝⊝⊝ very low2,3,4 |
|
Pain: intermediate‐term follow‐up (3 to 6 months) Multiple scales: scale from 0 to 100 (worse pain) |
The mean pain at intermediate‐term follow‐up ranged across control groups from 11.2 to 40 points. | The mean pain (intermediate term) in the intervention groups was 4.46 lower (19.44 lower to 10.52 higher). | MD ‐4.46 (‐19.44 to 10.52) | 619 participants (4 studies) | ⊕⊕⊝⊝ low3,4 |
|
Pain: long‐term follow‐up (> 6 months) Multiple scales: scale from 0 to 100 (worse pain) |
The mean pain at long‐term follow‐up ranged across control groups from 8.6 to 50.9 points. | The mean pain (long term) in the intervention groups was 4.58 higher (0.20 lower to 9.36 higher). | MD 4.58 (‐0.20 to 9.36) | 461 participants (3 studies) | ⊕⊕⊝⊝ low3,4 |
|
Disability: short‐term follow‐up (< 3 months) Multiple scales: scale from 0 to 100 (worse disability) |
The mean disability at short‐term follow‐up ranged across control groups from 4.5 to 29.1 points. | The mean disability at short‐term follow‐up in the intervention groups was 1.65 lower (8.66 lower to 5.37 higher). | MD ‐1.65 (‐8.66 to 5.37) | 471 participants (6 studies) | ⊕⊝⊝⊝ very low2,3,4 |
|
Disability: intermediate‐term follow‐up (3 to 6 months) Multiple scales: scale from 0 to 100 (worse disability) |
The mean disability at intermediate‐term follow‐up ranged across control groups from 2.87 to 29.5 points. | The mean disability at intermediate‐term follow‐up in the intervention groups was 1.57 higher (3.86 lower to 7.00 higher). | MD 1.57 (‐3.86 to 7.00) | 766 participants (6 studies) | ⊕⊝⊝⊝ very low2,3,4 |
|
Disability: long‐term follow‐up (> 6 months) Multiple scales: scale from 0 to 100 (worse disability |
The mean disability at long‐term follow‐up ranged across control groups from 3.3 to 28.3 points. | The mean disability at long‐term follow‐up in the intervention groups was 4.54 higher (4.44 lower to 13.52 higher). | MD 4.54 (‐4.44 to 13.52) | 556 participants (4 studies) | ⊕⊝⊝⊝ very low2,3,4 |
| Adverse events One participant in the Back School group reported a temporary exacerbation of pain (Garcia 2013) and 5 patients in exercise group experienced worsening of leg pain (Dufour 2010) | |||||
| Work status Not reported | |||||
| The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; MD: mean difference | |||||
| GRADE Working Group grades of evidence High‐quality evidence: There are consistent findings among at least 75% of randomised controlled trials with low risk of bias; consistent, direct, and precise data; and no known or suspected publication biases. Further research is unlikely to change either the estimate or our confidence in the results. Moderate‐quality evidence: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low‐quality evidence: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low‐quality evidence: We are very uncertain about the results. No evidence: We identified no randomised controlled trials that addressed this outcome. | |||||
1Downgraded one level due to imprecision (fewer than 400 participants in total). 2Downgraded one level due to risk of bias (> 25% of the participants were from studies with a high risk of bias). 3Downgraded one level due to clear inconsistency of results. 4Downgraded one level due to publication bias.
Background
See glossary of terms in Appendix 1.
Description of the condition
Low back pain (LBP) is a major problem worldwide, and the associated disability is responsible for a significant personal burden (van Tulder 2006). The Global Burden of Disease Study suggests that LBP is one of the 10 leading causes of disease burden globally (Murray 2013; Vos 2010). Many people with LBP become frequent users of healthcare services in their attempt to find treatments that minimise the severity of their symptoms.
Exercise therapy is commonly advised for people with LBP, and it is recommended in clinical practice guidelines as an effective treatment for chronic LBP (European Guidelines 2006). A Cochrane systematic review on this topic also concluded that exercise therapy is effective in decreasing pain and improving function in adults with chronic LBP (Hayden 2005). Education has been recommended in clinical practice guidelines for chronic LBP (European Guidelines 2006). Supervised exercise therapy associated with an educational component has been considered to be one of the most effective interventions in reducing pain and disability in people with chronic LBP (Airaksinen 2006; van Tulder 2006).
Back School is one treatment that provides both exercise and education for the treatment of people with chronic LBP. The original Swedish Back School was introduced by Zachrisson‐Forssell in 1969. It was designed to reduce pain and prevent recurrences of LBP episodes (Forssell 1980; Forssell 1981). Back School was a therapeutic programme including information on the anatomy of the back, biomechanics, optimal posture, ergonomics, and back exercises. Since the introduction of the Swedish Back School, the content and length of the method have changed and appear to vary widely today.
This review is an update of a previously conducted Cochrane review of the effectiveness of Back School for chronic non‐specific LBP. The previous Cochrane review was published in 2004 and concluded that Back School seemed to be more effective than other treatments, placebo, or waiting‐list controls for improving pain, functional status, and return to work (Heymans 2004). Since the completion of this review, new trials about Back School have been published (Andrade 2008; Cecchi 2010a; Costantino 2014; Devasahayam 2014; Donzelli 2006; Dufour 2010; Durmus 2014; Garcia 2013; Heymans 2006; Jaromi 2012; Meng 2009; Morone 2011; Morone 2012; Nentwig 1990; Paolucci 2012a; Paolucci 2012b; Ribeiro 2008; Sahin 2011; Tavafian 2007). Given this substantial amount of new data, and developments in systematic review methods, a revision of the 2004 Cochrane review was needed to provide clinicians and patients up‐to‐date information about the effects of this intervention. Our aim was therefore to perform an update on this topic in order to provide accurate and robust information on the effectiveness of the Back School approach for chronic non‐specific LBP, as compared to no treatment, medical care, passive physiotherapy, or exercise therapy.
Description of the intervention
The original Swedish Back School was introduced by Zachrisson‐Forssell in 1969. It was meant to reduce pain and prevent recurrences of episodes of LBP (Forssell 1980; Forssell 1981). Back School was a therapeutic programme including information on the anatomy of the back, biomechanics, optimal posture, ergonomics, and back exercises and was given to groups of patients. The aim was to reduce back pain and teach people to care for their own backs and back pain in an active way should back pain recur.
How the intervention might work
Back School is a combination of exercises and education, where lessons are given to groups of patients, supervised by a physical therapist or medical specialist. According to the European guidelines (Airaksinen 2006), the combination of exercise programmes and education seems to be the most promising approach for the management of chronic non‐specific LBP. Theoretical information could help patients understand their condition and learn how to modify their behaviour with regard to LBP. People with chronic non‐specific LBP often have maladaptive thoughts, feelings, and beliefs, which have an important role in their experience of LBP (Parsons 2007). Exercise therapy is probably the most commonly used intervention for the treatment of people with chronic non‐specific LBP. It is reported in the literature as effective in decreasing pain and improving function (Hayden 2005). Treatment that combines both interventions has the potential to improve pain and disability in people with chronic non‐specific LBP.
Why it is important to do this review
This review is an update of a previously conducted Cochrane review of randomised controlled trials on the effectiveness of Back School (Heymans 2004). We split this review into two reviews, one focusing on acute and subacute LBP, and one on chronic LBP. This review evaluated the effectiveness of Back School for chronic non‐specific LBP. In previous reviews it was not possible to statistically pool the data because of the heterogeneity of the included studies. Conclusions were generated on the basis of the methodological quality scores of the studies, assessed using a generally accepted criteria list, in combination with a best‐evidence synthesis (van Tulder 2003). Since 2011, a number of new RCTs have been published evaluating the effectiveness of Back School. Method guidelines for Cochrane reviews have also been published by The Cochrane Collaboration (Higgins 2011) and in the field of back pain (Furlan 2015). These were also implemented in the current updated review.
Objectives
The objective of this systematic review was to determine the effect of Back School on pain and disability for adults with chronic non‐specific LBP; we included adverse events as a secondary outcome. In trials that solely recruited workers, we also examined the effect on work status.
Methods
Criteria for considering studies for this review
Types of studies
We included only randomised controlled trials (RCTs) and quasi‐RCTs.
Types of participants
We included studies evaluating people with chronic (more than 12 weeks' duration) non‐specific LBP, aged 18 to 70 years. Low back pain is defined as pain localised below the scapulae and above the cleft of the buttocks; non‐specific indicates that no specific cause was detected, such as infection, neoplasm, metastasis, osteoporosis, fracture, or inflammatory arthritis. We did not include trials enrolling participants with pregnancy‐related LBP.
Types of interventions
We included studies in which one of the treatments consisted of a Back School‐type of intervention. We included trials that used a clear contrast for the Back School intervention, such as usual care, waiting list, or other interventions (e.g. exercise therapy or manipulation). Additional interventions were allowed. However, if the Back School was part of a larger multidisciplinary treatment programme, we only included the study if a contrast existed for the Back School. For example, a study that compared Back School plus a fitness programme against a fitness programme was included, but a study that compared Back School plus fitness programme against a waiting list was not. Trials that studied the effectiveness of Back School in workers or non‐workers without low back pain at study onset were not included because they concerned primary prevention of LBP.
Technique (index dose):
We classified the intensity of the technique as follows.
Intensive: when the length of the session was greater than or equal to 20 hours (intervention time)
Non‐intensive: when the length of the session was less than 20 hours (intervention time)
Not specified
Types of outcome measures
We included trials that reported outcomes for short‐term (less than three months), intermediate‐term (three to six months), and long‐term (more than six months) follow‐up.
Primary outcomes
Pain (e.g. measured by visual analogue scale or numerical rating scale)
Disability (e.g. measured by Oswestry Disability Index (ODI) or Roland‐Morris Disability Questionnaire (RMDQ))
Secondary outcomes
Work status in trials that solely recruited workers (e.g. days of sick leave)
Adverse events (reported by the physiotherapists on standardised forms)
Search methods for identification of studies
Electronic searches
We used the search methods developed by the Cochrane Back and Neck Review Group and Chapter 6 of the Cochrane Handbook for Systematic Reviews of Interventions (Furlan 2015; Higgins 2011). The strategies were developed and updated by the Information Specialist of the Back and Neck Review Group.
We searched for trials in the following databases to 15 November 2016:
Cochrane Central Register of Controlled Trials (CENTRAL, which also includes the Back and Neck Group Trials Register) (the Cochrane Library, Issue 10, 2016);
MEDLINE (OvidSP; Ahead of Print, In‐Process & Other Non‐Indexed Citations, Ovid MEDLINE(R) Daily and Ovid MEDLINE(R); 1946 to 15 November 2016);
Embase (Ovid SP, 1980 to 2016 Week 46);
Cumulative Index to Nursing and Allied Health Literature (CINAHL) (EBSCO, 1981 to 15 November 2016);
PsycINFO (Ovid SP, 2002 to November Week 1 2016);
ClinicalTrials.gov (clinicaltrials.gov/);
World Health Organization International Clinical Trials Registry Platform (WHO ICTRP) (apps.who.int/trialsearch/);
PubMed (www.ncbi.nlm.nih.gov/pubmed).
We added CINAHL and PsycINFO to the search in 2007 and the clinical trials registries in 2011; we searched these from inception to current. We added MEDLINE In‐Process & Other Non‐Indexed Citations in 2015. We searched PubMed in August 2015 to capture any studies published within the previous year using the strategy recommended by Duffy 2014. In 2016, we searched MEDLINE (Ahead of Print, In‐Process & Other Non‐Indexed Citations, Ovid MEDLINE(R) Daily and Ovid MEDLINE(R)), which allows multiple sets of MEDLINE databases to be searched at one time.
The search strategies can be found in Appendix 2.
Searching other resources
We screened reference lists of relevant reviews and included studies, and consulted experts in the field of LBP management to identify any potentially relevant studies we may have missed.
Data collection and analysis
For each of the steps, two review authors (PP and NP) independently selected new studies, assessed risk of bias, and extracted data (using a standardised form). Any disagreements were resolved by consensus or by bringing in a third review author if disagreements persisted (CM).
Selection of studies
For this update, we first reassessed the included studies from the original review to ensure that they met our revised inclusion criteria. Following the same process as in the original review and previous update, two review authors (PP and NP) first screened the titles and abstracts of the new studies. The full texts of all potentially relevant studies were then retrieved for the final selection of eligible studies.
Data extraction and management
Two review authors (PP and NP) independently extracted the data using standardised data extraction forms. We collected the following information:
participant characteristics (patient source or setting, study inclusion criteria, duration of LBP episode);
intervention characteristics (description and types of Back School, duration and number of treatment sessions, intervention delivery type, and co‐interventions); and
outcome data (pain intensity, disability, work status, adverse events);
When several time points fell within the same category, we used the time point closest to six weeks for the short term, four months for the intermediate term, and 12 months for the long term.
Assessment of risk of bias in included studies
Two review authors (PP and NP) independently assessed the risk of bias in included studies. We employed a consensus method to resolve disagreements, consulting a third review author (CM) if disagreement persisted. We used the Cochrane Back and Neck 'risk of bias' criteria (Table 5 and Table 6) (Furlan 2015).
1. Sources of risk of bias.
| Bias domain | Source of bias | Possible answers |
| Selection | (1) Was the method of randomization adequate? | Yes/no/unsure |
| Selection | (2) Was the treatment allocation concealed? | Yes/no/unsure |
| Performance | (3) Was the patient blinded to the intervention? | Yes/no/unsure |
| Performance | (4) Was the care provider blinded to the intervention? | Yes/no/unsure |
| Detection | (5) Was the outcome assessor blinded to the intervention? | Yes/no/unsure |
| Attrition | (6) Was the drop‐out rate described and acceptable? | Yes/no/unsure |
| Attrition | (7) Were all randomized participants analyzed in the group to which they were allocated? | Yes/no/unsure |
| Reporting | (8) Are reports of the study free of suggestion of selective outcome reporting? | Yes/no/unsure |
| Selection | (9) Were the groups similar at baseline regarding the most important prognostic indicators? | Yes/no/unsure |
| Performance | (10) Were co‐interventions avoided or similar? | Yes/no/unsure |
| Performance | (11) Was the compliance acceptable in all groups? | Yes/no/unsure |
| Detection | (12) Was the timing of the outcome assessment similar in all groups? | Yes/no/unsure |
| Other | (13) Are other sources of potential bias unlikely? | Yes/no/unsure |
2. Criteria for a judgment of ‘‘yes’’ for the sources of risk of bias.
| 1 | A random (unpredictable) assignment sequence. Examples of adequate methods are coin toss (for studies with 2 groups), rolling a dice (for studies with 2 or more groups), drawing of balls of different colours, drawing of ballots with the study group labels from a dark bag, computer‐generated random sequence, preordered sealed envelopes, sequentially‐ordered vials, telephone call to a central office, and preordered list of treatment assignments. Examples of inadequate methods are: alternation, birth date, social insurance/security number, date in which they are invited to participate in the study, and hospital registration number. |
| 2 | Assignment generated by an independent person not responsible for determining the eligibility of the patients. This person has no information about the persons included in the trial and has no influence on the assignment sequence or on the decision about eligibility of the patient. |
| 3 | Index and control groups are indistinguishable for the patients or if the success of blinding was tested among the patients and it was successful. |
| 4 | Index and control groups are indistinguishable for the care providers or if the success of blinding was tested among the care providers and it was successful. |
| 5 | Adequacy of blinding should be assessed for each primary outcome separately. This item should be scored ‘‘yes’’ if the success of blinding was tested among the outcome assessors and it was successful or:
|
| 6 | The number of participants who were included in the study but did not complete the observation period or were not included in the analysis must be described and reasons given. If the percentage of withdrawals and drop‐outs does not exceed 20% for short‐term follow‐up and 30% for long‐term follow‐up and does not lead to substantial bias a ‘‘yes’’ is scored. (N.B. these percentages are arbitrary, not supported by literature). |
| 7 | All randomized patients are reported/analyzed in the group they were allocated to by randomization for the most important moments of effect measurement (minus missing values) irrespective of noncompliance and co‐interventions. |
| 8 | All the results from all prespecified outcomes have been adequately reported in the published report of the trial. This information is either obtained by comparing the protocol and the report, or in the absence of the protocol, assessing that the published report includes enough information to make this judgment. |
| 9 | Groups have to be similar at baseline regarding demographic factors, duration and severity of complaints, percentage of patients with neurological symptoms, and value of main outcome measure(s). |
| 10 | If there were no co‐interventions or they were similar between the index and control groups. |
| 11 | The reviewer determines if the compliance with the interventions is acceptable, based on the reported intensity, duration, number and frequency of sessions for both the index intervention and control intervention(s). For example, physiotherapy treatment is usually administered for several sessions; therefore it is necessary to assess how many sessions each patient attended. For single‐session interventions (e.g., surgery), this item is irrelevant. |
| 12 | Timing of outcome assessment should be identical for all intervention groups and for all primary outcome measures. |
| 13 | Other types of biases. For example:
|
Measures of treatment effect
The primary outcome measures were continuous (pain and disability); the secondary outcome measures (work status and adverse events) were mainly dichotomous. For all continuous outcomes, we quantified the treatment effects with the mean difference (MD). To accommodate the different scales used for these outcomes, we converted outcomes to a common 0‐to‐100 scale. We also expected to encounter dichotomous outcomes such as return to work; in such cases we calculated risk ratios (RR) of experiencing the positive outcome. We used effect sizes and 95% confidence intervals (CI) as a measure of treatment effect.
Unit of analysis issues
If trials were sufficiently homogenous, we conducted a meta‐analysis for these follow‐up time points: short (within three months after randomisation), intermediate (at least three months but within 12 months after randomisation), and long term (12 months or longer after randomisation). When multiple time points fell within the same category, we used the one that was closer to the end of treatment, 6 months or 12 months.
Dealing with missing data
We emailed the authors of each study requesting any necessary data that were not comprehensively reported in the manuscript. We also estimated data from graphs in cases where this information was not presented in tables or text. If the standard deviation was not reported, we calculated it from confidence intervals or standard errors (if available). If no measure of variability was presented anywhere in the text, we estimated the standard deviation from the most similar trial in the review, taking the risk of bias of individual studies into consideration.
Assessment of heterogeneity
We based the assessment of heterogeneity on visual inspections of the forest plots (e.g. overlapping confidence intervals) and more formally by the Chi2 test and the I2 statistic, as recommended in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011).
Assessment of reporting biases
To avoid potential language bias, we applied no language restriction to the searches.
Data synthesis
Regardless of whether there were sufficient data available to use quantitative analyses to summarise the data, we assessed the overall quality of the evidence for each outcome. We used the GRADE approach, as recommended in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011), and adapted in the updated Cochrane Back and Neck Review Group method guidelines (Furlan 2015). The GRADE approach to evidence synthesis can be found in Appendix 3.
Subgroup analysis and investigation of heterogeneity
We stratified the analyses based upon the duration of follow‐up reported for each outcome (i.e. short term, intermediate term, and long term).
Sensitivity analysis
We planned sensitivity analyses to see if the overall results on effectiveness between comparison groups changed when in the studies of high risk of bias, defined as fulfilling five or more criteria out of the 13.
Results
Description of studies
Results of the search
The search retrieved 307 trials after duplicates were removed (Figure 1). After the selection and discussion step, based on title, keyword, abstract, and full text screening, both review authors agreed that 19 studies (20 references) met the inclusion criteria (Andrade 2008; Cecchi 2010a; Costantino 2014; Devasahayam 2014; Donzelli 2006; Dufour 2010; Durmus 2014; Garcia 2013; Heymans 2006; Jaromi 2012; Meng 2009; Morone 2011; Morone 2012; Nentwig 1990; Paolucci 2012a; Paolucci 2012b; Ribeiro 2008; Sahin 2011; Tavafian 2007). We found one study that was a protocol for an included study (Garcia 2013). We included 11 studies (15 references) from the previous review (Berwick 1989; Dalichau 1999; Donchin 1990; Hurri 1989; Keijsers 1989; Keijsers 1990; Klaber Moffett 1986; Lankhorst 1983; Lønn 1999; Penttinen 2002; Postacchini 1988). We included a total of 30 studies (35 references) in this update. An additional search for ongoing or registered trials in ClinicalTrials.gov and the WHO ICTRP retrieved one record (IRCT201010184251N2). We consulted experts in the field of LBP research but did not identify any new studies. The most recent search performed on 15 November 2016 retrieved two studies that fulfilled the inclusion criteria (Garcia 2016; Paolucci 2016), and we added them to the 'awaiting classification' section to be incorporated in the next review update.
1.
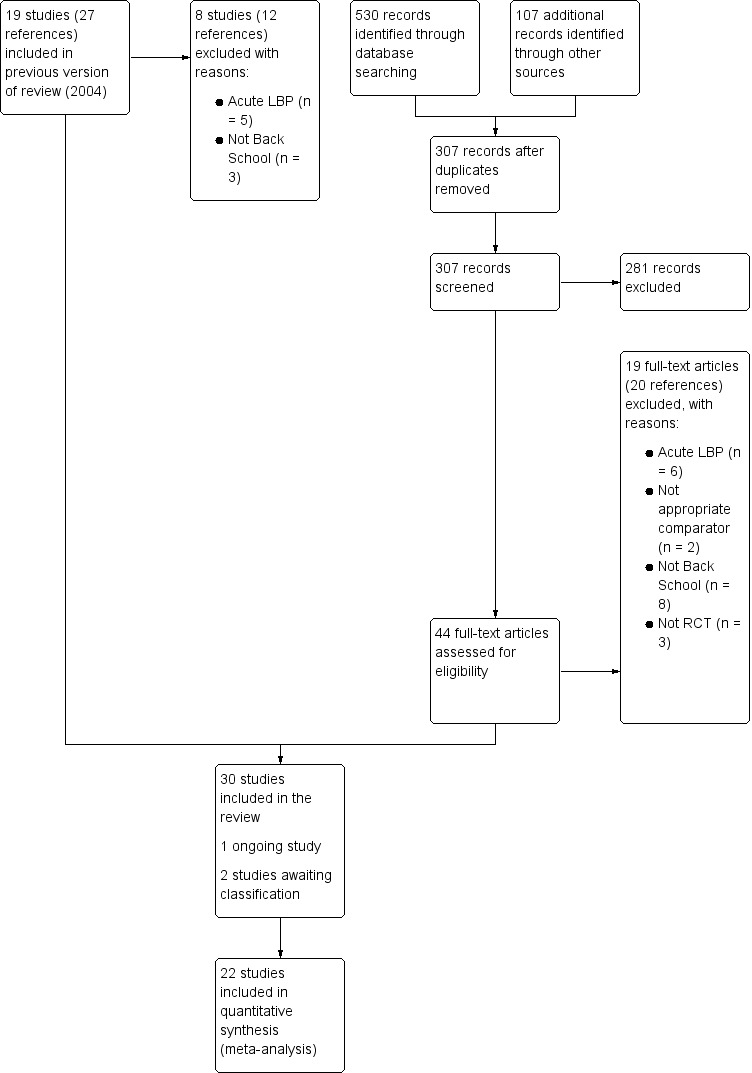
Study flow diagram.
Included studies
We included 30 studies with a total of 4105 participants. The study sample sizes ranged from 37 to 360 participants (mean = 128). Ten studies were not included in the meta‐analysis because they lacked necessary data (Dalichau 1999; Donchin 1990; Dufour 2010; Hurri 1989; Keijsers 1990; Morone 2011; Morone 2012; Nentwig 1990; Paolucci 2012a; Postacchini 1988).
Design
Of the 30 studies included in this review, only one study was a quasi‐RCT (Donzelli 2006).
Types of studies
We identified the following comparisons in this review.
Ten trials compared Back School with no treatment (Andrade 2008; Dalichau 1999; Donchin 1990; Hurri 1989; Keijsers 1989; Keijsers 1990; Lønn 1999; Meng 2009; Nentwig 1990; Postacchini 1988).
Seven trials compared Back School with medical care (Berwick 1989; Morone 2011; Morone 2012; Paolucci 2012a; Paolucci 2012b; Ribeiro 2008; Tavafian 2007).
Four trials compared Back School with passive physiotherapy (Cecchi 2010a; Jaromi 2012; Lankhorst 1983; Postacchini 1988).
Eleven trials compared Back School with exercises (Costantino 2014; Devasahayam 2014; Donchin 1990; Donzelli 2006; Dufour 2010; Durmus 2014; Garcia 2013; Heymans 2006; Klaber Moffett 1986; Penttinen 2002; Sahin 2011).
Two trials had three treatment arms (Donchin 1990; Postacchini 1988), and we included both treatment contrasts.
Study population
Eleven studies included a homogeneous population of LBP patients without radiation (Andrade 2008; Berwick 1989; Cecchi 2010a; Costantino 2014; Devasahayam 2014; Donzelli 2006; Durmus 2014; Garcia 2013; Lankhorst 1983; Meng 2009; Sahin 2011), while 17 studies did not specify if participants had radiating symptoms or not, and five studies included a mixed population of patients with and without radiating symptoms (Dufour 2010; Heymans 2006; Jaromi 2012; Morone 2011; Tavafian 2007). Eight studies reported no data on the sex or age of the groups evaluated (Andrade 2008; Devasahayam 2014; Donzelli 2006; Keijsers 1990; Meng 2009; Nentwig 1990; Paolucci 2012a; Postacchini 1988); three studies included women only (Durmus 2014; Hurri 1989; Linton 1989); and one study included men only (Dalichau 1999). All trials included participants with chronic symptoms (LBP persisting for 12 weeks or more) exclusively.
Primary outcomes
Pain intensity
Seventeen studies measured pain intensity with a visual analogue scale or a numerical rating scale from 0 to 10 (Andrade 2008; Devasahayam 2014; Donzelli 2006; Dufour 2010; Durmus 2014; Garcia 2013; Heymans 2006; Jaromi 2012; Keijsers 1989; Klaber Moffett 1986; Meng 2009; Morone 2011; Morone 2012; Paolucci 2012a; Postacchini 1988; Ribeiro 2008; Sahin 2011). The other instruments were: pain rating (Cecchi 2010a; Dalichau 1999), pain index (Hurri 1989; Keijsers 1990; Morone 2011), McGill Pain Scale, pain severity subscale (Paolucci 2012b), subscale of 36‐Item Short Form Health Survey (SF‐36) (Tavafian 2007), and mean pain (Lankhorst 1983). One study created their own instrument (Nentwig 1990). All scales were converted to a 0‐to‐100 scale.
Disability
Nineteen studies measured disability (Andrade 2008; Cecchi 2010a; Costantino 2014; Devasahayam 2014; Donchin 1990; Donzelli 2006; Dufour 2010; Durmus 2014; Garcia 2013; Heymans 2006; Hurri 1989; Klaber Moffett 1986; Lønn 1999; Meng 2009; Morone 2011; Morone 2012; Penttinen 2002; Ribeiro 2008; Sahin 2011). Seven studies measured disability with the Roland‐Morris Disability Questionnaire (Andrade 2008; Cecchi 2010a; Costantino 2014; Devasahayam 2014; Dufour 2010; Garcia 2013; Heymans 2006). Nine studies measured disability using the Oswestry Disability Index (Donchin 1990; Donzelli 2006; Durmus 2014; Hurri 1989; Klaber Moffett 1986; Morone 2011; Morone 2012; Penttinen 2002; Sahin 2011); one study used the Low Back Disability Scale (Lønn 1999); and one study used the Hannover Functional Ability Questionnaire (Meng 2009). All scales were converted to a 0‐to‐100 scale.
Secondary outcomes
Return to work
Three studies measured return to work (Dalichau 1999; Heymans 2006; Keijsers 1990). Due to insufficient information, we were unable to statistically pool the data.
Adverse events
Three studies measured adverse effects (Dufour 2010; Garcia 2013; Heymans 2006). All studies either reported means without standard deviations or did not report group size; we were therefore unable to statistically pool the data.
Excluded studies
We excluded 19 studies (20 references) in the full –text assessment for eligibility. Of the 19 excluded full‐text articles, six studies did not consider Back School as the intervention (Demoulin 2006; Härkäpää 1989; Härkäpää 1990; Linton 1989; Tavafian 2008; Yang 2010). In one study the results were for a single group (Sadeghi‐Abdollahi 2012). In another study each group was assessed once (the control group at the beginning of the programme, the Back School group at the end) (Morrison 1988). In three studies, the Back School intervention consisted of education only, without exercises (Cecchi 2010b; Indahl 1998; Maul 2005; Mele 2006). In one study the Back School intervention was not a clear contrast for the control group (Meng 2011). In six studies, the average time of symptoms in the inclusion criteria was characterised as acute LBP (Bergquist 1977; Herzog 1991; Hsieh 2002; Indahl 1995; Leclaire 1996; Lindequist 1984).
Risk of bias in included studies
The results from the 'Risk of bias’ assessment for the individual studies are summarised in Figure 2. We considered 10% of the studies to have a low risk of bias. Due to the small number of studies with low risk of bias, it was not possible to run a sensitivity analysis as planned.
2.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
Eleven studies described an appropriate method of randomisation (Andrade 2008; Costantino 2014; Donchin 1990; Dufour 2010; Durmus 2014; Garcia 2013; Heymans 2006; Klaber Moffett 1986; Lønn 1999; Paolucci 2012a; Ribeiro 2008). Only seven studies were at low risk of bias for allocation concealment (Dufour 2010; Durmus 2014; Heymans 2006; Klaber Moffett 1986; Paolucci 2012a; Ribeiro 2008; Sahin 2011).
Blinding
Due to the nature of the intervention, none of the included studies blinded participants or care providers. Nine of the included studies blinded outcome assessment (Andrade 2008; Cecchi 2010a; Devasahayam 2014; Dufour 2010; Garcia 2013; Heymans 2006; Jaromi 2012; Ribeiro 2008; Sahin 2011).
Incomplete outcome data
Most of the included studies (86%) had a good rate of follow‐up, with less than 20% withdrawals and dropouts.
Selective reporting
One of the included studies had a published protocol (Garcia 2013). We scored all studies as at unclear risk of reporting bias, as we could not compare prespecified outcomes with reported ones.
Other potential sources of bias
We considered all studies as having a low risk of other potential sources of bias.
Effects of interventions
See: Table 1; Table 2; Table 3; Table 4
See: Summary of main results, Table 1; Table 2; Table 3; Table 4
Effectiveness of Back School
Comparison 1: Back School versus no treatment
Ten trials compared Back School with no treatment for chronic LBP (Andrade 2008; Dalichau 1999; Donchin 1990; Hurri 1989; Keijsers 1989; Keijsers 1990; Lønn 1999; Meng 2009; Nentwig 1990; Postacchini 1988). Four trials provided insufficient information and were therefore not included in the analysis (Donchin 1990; Hurri 1989; Nentwig 1990; Postacchini 1988).
In the meta‐analysis for the outcome pain, based on six trials (Andrade 2008; Dalichau 1999; Keijsers 1989; Keijsers 1990; Lankhorst 1983; Meng 2009), there was very low‐quality evidence (downgraded due to risk of bias, inconsistency, and publication bias) that Back School reduces pain compared with no treatment at short‐term follow‐up (MD ‐6.10, 95% CI –10.18 to ‐2.01; I2 = 19%). At intermediate‐term follow‐up, four trials provided very low‐quality evidence (downgraded due to imprecision, risk of bias, and publication bias) that there was no substantial difference between Back School and no treatment (MD ‐4.34, 95% CI –14.37 to 5.68; I2 = 71%) (Andrade 2008; Keijsers 1990; Lankhorst 1983; Lønn 1999). Based on three trials (Dalichau 1999; Lankhorst 1983; Lønn 1999), there was very low‐quality evidence (downgraded due to imprecision, risk of bias, inconsistency, and publication bias) that Back School was no better than no treatment at long‐term follow‐up (MD ‐12.16, 95% CI ‐29.14 to 4.83; I2 = 84%) (Analysis 1.1).
1.1. Analysis.

Comparison 1 Back School versus no treatment, Outcome 1 Pain.
In the meta‐analysis for the outcome disability, based on three trials (Andrade 2008; Lankhorst 1983; Meng 2009), there was very low‐quality evidence (downgraded due to risk of bias, inconsistency, and publication bias) at short‐term follow‐up that Back School was slightly better than no treatment (MD –3.38, 95% CI –6.70 to –0.05; I2 = 0%). At intermediate‐term follow‐up, based on three trials (Andrade 2008; Lankhorst 1983; Lønn 1999), there was very low‐quality evidence (downgraded due to imprecision, risk of bias, and publication bias) that Back School was no better than no treatment (MD –5.92, 95% CI –12.08 to 0.23; I2 = 0%). At long‐term follow‐up, based on two trials (Lankhorst 1983; Lønn 1999), there was very low‐quality evidence (downgraded due to imprecision, risk of bias, and publication bias) that there was no important difference between Back School and no treatment (MD ‐7.36, 95% CI ‐22.05 to 7.34; I2 = 76%) (Analysis 1.2).
1.2. Analysis.
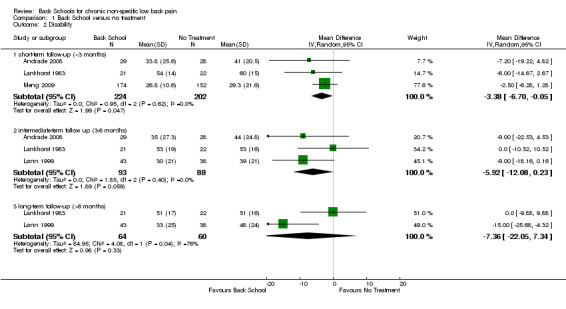
Comparison 1 Back School versus no treatment, Outcome 2 Disability.
None of the included studies reported adverse events or work status.
Comparison 2: Back School versus medical care
Five trials evaluated the effectiveness of Back School compared to medical care for chronic LBP (Berwick 1989; Heymans 2006; Morone 2011; Ribeiro 2008; Tavafian 2007).
In the meta‐analysis for the outcome pain, based on three trials (Berwick 1989; Morone 2011; Ribeiro 2008), there was very low‐quality evidence (downgraded due to imprecision, risk of bias, and publication bias) that Back School reduces pain intensity compared with medical care at short‐term follow‐up (MD ‐10.16, 95% CI –19.11 to ‐1.22; I2 = 62%). At intermediate‐term follow‐up, based on five trials (Berwick 1989; Heymans 2006; Morone 2011; Ribeiro 2008; Tavafian 2007), there was very low‐quality evidence (downgraded due to risk of bias, inconsistency, and publication bias) that there was no important difference between Back School and medical care (MD ‐9.65, 95% CI ‐22.46 to 3.15; I2 = 89%). Based on three trials (Berwick 1989; Heymans 2006; Morone 2011), there was very low‐quality evidence (downgraded due to risk of bias, inconsistency, and publication bias) that Back School was no better than medical care at long‐term follow‐up (MD ‐5.71, 95% CI –20.27 to 8.84; I2 = 87%) (Analysis 2.1).
2.1. Analysis.
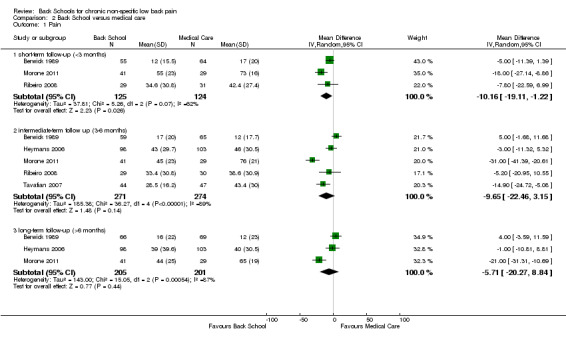
Comparison 2 Back School versus medical care, Outcome 1 Pain.
For the outcome disability, based on two trials (Morone 2011; Ribeiro 2008), there was very low‐quality evidence (downgraded due to imprecision, risk of bias, and publication bias) that Back School was no better than medical care at short‐term follow‐up (MD –1.19, 95% CI –7.02 to 4.64; I2 = 0%). At intermediate‐term follow‐up, three trials provided very low‐quality evidence (downgraded due to imprecision, risk of bias, and publication bias) that Back School was better than medical care (MD –6.34, 95% CI –10.89 to –1.79; I2 = 0%) (Heymans 2006; Morone 2011; Ribeiro 2008). At long‐term follow‐up, one trial, Heymans 2006, provided inconclusive evidence that Back School improves disability compared with medical care (MD –0.40, 95% CI –7.33 to 6.53; I2 = not applicable) (very low quality evidence; downgraded due to imprecision, risk of bias and publication bias) (Analysis 2.2).
2.2. Analysis.
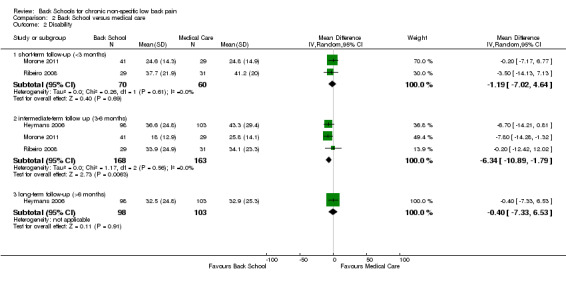
Comparison 2 Back School versus medical care, Outcome 2 Disability.
Only one study (Heymans 2006) measured adverse effects and reported that two workers in the Back School group (n=98), reported a strong increase in low back pain. However, the result reported means without standard deviations or did not report group size; we were therefore unable to statistically pool the data. None of the included studies reported work status.
Comparison 3: Back School versus passive physiotherapy
Four trials evaluated the effectiveness of Back School compared to passive physiotherapy for chronic LBP (Cecchi 2010a; Jaromi 2012; Lankhorst 1983; Postacchini 1988). One trial did not report any usable information (Postacchini 1988).
In the meta‐analysis for the outcome pain, based on three trials (Cecchi 2010a; Jaromi 2012; Lankhorst 1983), there was very low‐quality evidence (downgraded due to imprecision, risk of bias, inconsistency, and publication bias) that Back School is no better than passive physiotherapy at short‐term follow‐up (MD 1.96, 95% CI –9.51 to 13.43; I2 = 94%). Based on three trials (Cecchi 2010a; Jaromi 2012; Lankhorst 1983), it is uncertain that there is any difference between back school and passive physiotherapy at intermediate term (MD ‐16.89, 95% CI ‐66.56 to 32.79; I2 = 100%) and long‐term follow‐up (MD ‐12.86, 95% CI –61.22 to 35.50; I2 = 100%)(very low quality evidence; downgraded due to imprecision, risk of bias, inconsistency, and publication bias) (Analysis 3.1).
3.1. Analysis.
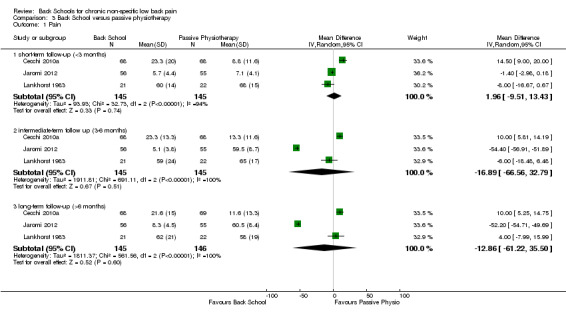
Comparison 3 Back School versus passive physiotherapy, Outcome 1 Pain.
In the meta‐analysis for the outcome disability, based on two trials (Cecchi 2010a; Lankhorst 1983), there was very low‐quality evidence (downgraded due to imprecision, risk of bias, inconsistency, and publication bias) that Back School was no better than passive physiotherapy (MD 2.57, 95% CI –15.88 to 21.01; I2 = 82%) at short‐term follow‐up. At intermediate‐term follow‐up, two trials provided very low‐quality evidence (downgraded due to imprecision, risk of bias, and publication bias) that there was no important difference between Back School and passive physiotherapy (MD 6.88, 95% CI ‐4.86 to 18.63; I2 = 74%) (Cecchi 2010a; Lankhorst 1983). At long‐term follow‐up, two trials, Cecchi 2010a and Lankhorst 1983, provided very low‐quality evidence (downgraded due to imprecision, risk of bias, and publication bias) that passive physiotherapy was better than Back School (MD 9.60, 95% CI 3.65 to 15.54; I2 = 23%) (Analysis 3.2).
3.2. Analysis.
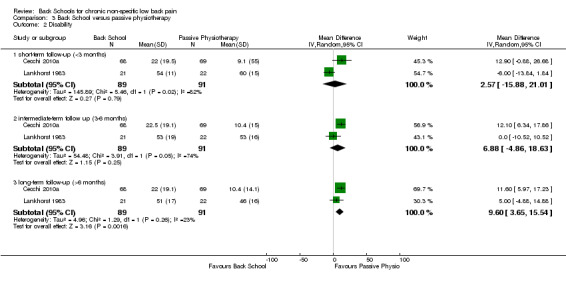
Comparison 3 Back School versus passive physiotherapy, Outcome 2 Disability.
None of the included studies reported adverse events or work status.
Comparison 4: Back School versus exercise
Eight trials evaluated the effectiveness of Back School compared to exercise for chronic LBP (Costantino 2014; Devasahayam 2014; Donzelli 2006; Dufour 2010; Durmus 2014; Garcia 2013; Klaber Moffett 1986; Penttinen 2002).
In the meta‐analysis for the outcome pain, based on five trials (Devasahayam 2014; Donzelli 2006; Durmus 2014; Garcia 2013; Klaber Moffett 1986), there was very low‐quality evidence (downgraded due to risk of bias, inconsistency, and publication bias) that Back School is no better than exercise at short‐term follow‐up (MD ‐2.06, 95% CI –14.58 to 10.45; I2 = 84%). There was low‐quality evidence (downgraded due to inconsistency and publication bias) that there was no important difference between Back School and exercise at intermediate‐term follow‐up (MD ‐4.46, 95% CI –19.44 to 10.52; I2 = 94%) based on four trials (Dufour 2010; Durmus 2014; Garcia 2013; Klaber Moffett 1986). At long‐term follow‐up, three trials provided low‐quality evidence (downgraded due to inconsistency and publication bias) that exercise was no better than Back School in reducing pain (MD 4.58, 95% CI –0.20 to 9.36; I2 = 0%) (Analysis 4.1) (Donzelli 2006; Dufour 2010; Garcia 2013).
4.1. Analysis.

Comparison 4 Back school versus exercise, Outcome 1 Pain.
In the meta‐analysis for the outcome disability, there was very low‐quality evidence (downgraded due to risk of bias, inconsistency, and publication bias) that there was no important difference between Back School and exercise at short‐term follow‐up (MD ‐1.65, 95% CI –8.66 to 5.37; I2 = 85%) based on six trials (Costantino 2014; Devasahayam 2014; Donzelli 2006; Durmus 2014; Garcia 2013; Klaber Moffett 1986). At intermediate‐term follow‐up, six trials provided very low‐quality evidence (downgraded due to risk of bias, inconsistency, and publication bias) that Back School was no better than exercise (MD 1.57, 95% CI –3.86 to 7.00; I2 = 88%) (Costantino 2014; Devasahayam 2014; Dufour 2010; Garcia 2013; Klaber Moffett 1986; Penttinen 2002). Based on four trials (Donzelli 2006; Dufour 2010; Garcia 2013; Penttinen 2002), there was very low‐quality evidence (downgraded due to risk of bias, inconsistency, and publication bias) that there was no significant difference between Back School and exercise at long‐term follow‐up (MD 4.54, 95% CI ‐4.44 to 13.52; I2 = 80%) (Analysis 4.2).
4.2. Analysis.
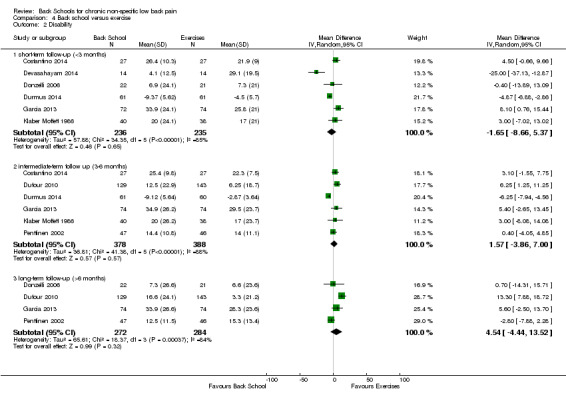
Comparison 4 Back school versus exercise, Outcome 2 Disability.
Two studies (Dufour 2010; Garcia 2013) measured adverse effects. One participant in the Back School group reported a temporary exacerbation of pain (Garcia 2013) and 5 patients in exercise group experienced worsening of leg pain (Dufour 2010). However, the results reported means without standard deviations or did not report group size; we were therefore unable to statistically pool the data. None of the included studies reported work status.
Discussion
Summary of main results
It is uncertain if Back School is effective for chronic non‐specific LBP, as we only located very low‐ to low‐quality evidence. The pooled effect sizes were typically small and/or not statistically significant.
Overall completeness and applicability of evidence
Based on the low number of available studies and limited comparison treatments, the overall evidence is incomplete and the comparative effectiveness of Back School versus other contemporary treatments for chronic LBP is unknown. The Back School interventions varied from intensive (36 sessions during 12 weeks in Dufour 2010) to non‐intensive (4 sessions during 4 weeks in Garcia 2013). This difference in treatment programmes could affect the generalisability of the evidence. Most included trials did not provide information about the care provider, hindering the generalisability of our findings to other settings.
Quality of the evidence
Based on the GRADE approach, the quality of the evidence varied from very low to low, the main problems being inconsistency, risk of bias, and publication bias. The most commonly identified methodological deficiencies were lack of blinding of participants and care providers (scored as high risk of bias in all 30 RCTs); lack of blinding of assessors (scored as high risk of bias or unclear in 18 RCTs); inappropriate method of randomisation (scored as high risk of bias or unclear in 18 RCTs); inadequate concealment of treatment allocation (scored as high risk of bias or unclear in 18 RCTs); and selective reporting (scored as high risk of bias or unclear in 23 RCTs). It is very difficult to blind this type of treatment, and because of the use of self reported outcomes (at least in terms of pain and disability), very difficult to blind the assessor.
Potential biases in the review process
In this systematic review, we aimed to perform a meta‐analysis for some comparisons to provide quantitative estimates of treatment effects. However, some of the trials did not report sufficient information (e.g. means, standard deviations, or group size), which prevented us from providing a quantitative summary of the data from these trials. Furthermore, a limited number of studies reported return‐to‐work outcomes and adverse effects. Due to this lack of information, we were unable to statistically pool the data and consequently performed a best‐evidence synthesis. Of particular note was the heterogeneity among studies for the content of Back School and type of control interventions. Due to a high statistical heterogeneity of some comparisons, we used a random‐effects model to perform the meta‐analysis. An additional limitation was that for most comparisons it was not possible to search for evidence of publication bias using funnel plots as too few studies were included.
Agreements and disagreements with other studies or reviews
In general, the results of this review are reasonably consistent with the previous Cochrane review regarding pain and disability outcomes (Heymans 2004). In the current review, Back School was minimally more effective than no treatment for pain and disability outcomes at short term, but not at intermediate‐ or long‐term follow‐up. This result is consistent with that from the previous review, which found conflicting evidence on the effectiveness of Back School compared to waiting‐list controls or placebo interventions for all outcomes.
The previous review found moderate evidence that Back School is more effective than other treatments for the outcomes pain and functional status at short‐ and intermediate‐term follow‐ups, but not at long‐term follow‐up. In this review, we stratified ‘other treatments’ into medical care, passive physiotherapy, and exercise because we considered these treatments to be sufficiently different that they should be evaluated separately. For all of these control treatments, our results were inconsistent or we did not find any significant differences in effectiveness when compared to Back School for pain and disability outcomes for all time periods.
Authors' conclusions
Implications for practice.
We found only low‐ or very low‐quality evidence for all comparisons, outcomes, and follow‐up periods investigated. Regardless of the comparison treatment used (as well as the outcomes investigated), the results of the meta‐analysis showed no difference or a trivial effect in favour of Back School. There does not seem to be sufficient justification for using Back School in clinical practice.
Implications for research.
Given the scarcity and low quality of evidence in this area, a large, well‐designed randomised controlled trial is very likely to change our conclusions on the effectiveness of Back School for chronic non‐specific low back pain. However, Back School is not endorsed by guidelines. Further research into this area may not be necessary.
What's new
| Date | Event | Description |
|---|---|---|
| 15 November 2016 | New citation required and conclusions have changed | In this update, we identified 19 additional studies for a total of 30 included studies. The conclusions of this review are not in agreement with the previous Cochrane review (Heymans 2004). In the previous Cochrane review, the authors concluded that there was moderate evidence suggesting that Back Schools, in an occupational setting, reduced pain and improved function and return‐to‐work status, in the short and intermediate term, compared to exercises, manipulation, myofascial therapy, advice, placebo, or waiting‐list controls, for people with chronic and recurrent low back pain. In this update, we found low‐ to very low‐quality evidence for all treatment comparisons, outcomes, and follow‐up periods investigated. |
| 10 September 2015 | New search has been performed | Four authors joined the review team (P Parreira, N Poquet, C Maher, and C Lin), and one of the original authors is no longer involved (C Bombardier). We made the following methodological changes: We included quasi‐randomised controlled trials as well as randomised controlled trials. The primary outcomes were pain and disability. The secondary outcomes were work status and adverse events. Finally, we stratified ‘other treatments’ into medical care, passive physiotherapy, and exercise because we considered these treatments to be sufficiently different that they should be evaluated separately. |
Acknowledgements
Patricia Parreira is supported by CAPES (Coordenação de Aperfeiçoamento de Pessoal de Nível Superior), Brazil. Chris Maher is supported by National Health and Medical Research Council of Australia.
Appendices
Appendix 1. Glossary of terms
Bias: a systematic error, or deviation from the truth, in results or inferences. Biases can operate in either direction: different biases can lead to underestimation or overestimation of the true intervention effect. Control of bias in randomised controlled trials is necessary to reduce the risk of making incorrect conclusions about treatment effects.
Biomechanics: the study of muscular activity.
Ergonomics: the arranging of things people use in a way that makes their use safe and less painful.
Medical care: pain medication, physician counselling.
Meta‐analysis: the statistical combination of results from two or more separate studies.
Metastasis: the spreading of cancer.
Neoplasm: tumour.
Osteoporosis: the thinning and weakening of bones which can lead to fractures.
Publication bias: the publication or non‐publication of research findings, depending on the nature and direction of the results.
Scapulae: shoulder blade.
Appendix 2. Search strategies
CENTRAL
Last searched 15 November 2016. The strategy was revised in 2011. Back pain was added to line 3 in 2015.
#1 MeSH descriptor: [Back Pain] explode all trees
#2 dorsalgia
#3 backache or back pain
#4 (lumbar near pain) or (coccyx) or (coccydynia) or (sciatica) or (spondylosis)
#5 MeSH descriptor: [Sciatica] explode all trees
#6 MeSH descriptor: [Spine] explode all trees
#7 MeSH descriptor: [Spinal Diseases] explode all trees
#8 (lumbago) or (discitis) or (disc near herniat*)
#9 spinal fusion
#10 facet near joint*
#11 MeSH descriptor: [Intervertebral Disc] explode all trees
#12 postlaminectomy
#13 arachnoiditis
#14 failed near back
#15 MeSH descriptor: [Cauda Equina] explode all trees
#16 lumbar near vertebra*
#17 spinal near stenosis
#18 slipped near (disc* or disk*)
#19 degenerat* near (disc* or disk*)
#20 stenosis near (spine or root or spinal)
#21 displace* near (disc* or disk*)
#22 prolap* near (disc* or disk*)
#23 (#1 or #2 or #3 or #4 or #5 or #6 or #7 or #8 or #9 or #10 or #11 or #12 or #13 or #14 or #15 or #16 or #17 or #18 or #19 or #20 or #21 or #22)
#24 "back school"
#25 (#23 and #24)
#26 #25 in Trials
#27 #26 Publication Year from 2015 to 2016
January 2009 strategy
#1 MeSH descriptor Back explode all trees
#2 MeSH descriptor Buttocks, this term only
#3 MeSH descriptor Leg, this term only
#4 MeSH descriptor Back Pain explode tree 1
#5 MeSH descriptor Back Injuries explode all trees
#6 MeSH descriptor Low Back Pain, this term only
#7 MeSH descriptor Sciatica, this term only
#8 (low next back next pain)
#9 (lbp)
#10 (#1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8 OR #9)
#11 (back school):ti,ab,kw
#12 (#10 AND #11), from 2007 to 2009
MEDLINE
Last searched 15 November 2016. Back pain was added to line 17 in 2015. Lines 5, 22, 25 and 26 were added in 2014.
1 randomized controlled trial.pt.
2 controlled clinical trial.pt.
3 comparative study.pt.
4 clinical trial.pt.
5 pragmatic clinical trial.pt.
6 randomized.ab.
7 placebo.ab,ti.
8 drug therapy.fs.
9 randomly.ab,ti.
10 trial.ab,ti.
11 groups.ab,ti.
12 or/1‐11
13 (animals not (humans and animals)).sh.
14 12 not 13
15 dorsalgia.ti,ab.
16 exp Back Pain/
17 (backache or back pain).ti,ab.
18 (lumbar adj pain).ti,ab.
19 coccyx.ti,ab.
20 coccydynia.ti,ab.
21 sciatica.ti,ab.
22 exp sciatic neuropathy/
23 spondylosis.ti,ab.
24 lumbago.ti,ab.
25 back disorder$.ti,ab.
26 exp Back Muscles/
27 or/15‐26
28 back school.mp.
29 14 and 27 and 28
30 limit 29 to yr=2015‐2016
31 limit 29 to ed=20150804‐20161115
32 30 or 31
The June 2011 search for MEDLINE used a different entry date filter to current strategy:
randomized controlled trial.pt.
controlled clinical trial.pt.
randomized.ab.
placebo.ab,ti.
drug therapy.fs.
randomly.ab,ti.
trial.ab,ti.
groups.ab,ti.
or/1‐8
(animals not (humans and animals)).sh.
9 not 10
dorsalgia.ti,ab.
exp Back Pain/
backache.ti,ab.
exp Low Back Pain/
(lumbar adj pain).ti,ab.
coccyx.ti,ab.
coccydynia.ti,ab.
sciatica.ti,ab.
sciatica/
spondylosis.ti,ab.
lumbago.ti,ab.
or/12‐22
back school.mp.
11 and 24 and 23
limit 25 to yr="2009 ‐ 2011"
2009$.ed.
2010$.ed.
2011$.ed.
27 or 28 or 29
25 and 30
26 or 31
The April 2007 strategy for MEDLINE used a different study design filter to current strategy
exp "Clinical Trial [Publication Type]"/
randomized.ab,ti.
placebo.ab,ti.
dt.fs.
randomly.ab,ti.
trial.ab,ti.
groups.ab,ti.
or/1‐7
Animals/
Humans/
9 not (9 and 10)
8 not 11
dorsalgia.ti,ab.
exp Back Pain/
backache.ti,ab.
(lumbar adj pain).ti,ab.
coccyx.ti,ab.
coccydynia.ti,ab.
sciatica.ti,ab.
sciatica/
spondylosis.ti,ab.
lumbago.ti,ab.
exp low back pain/
or/13‐23
back school.mp.
12 and 24 and 25
limit 26 to yr="2004 ‐ 2007"
EMBASE
Last searched 15 November 2016. In March 2014, line 31 was changed from 14 and 30 to 14 or 30, line 47 was added, and the animal study filter (lines 32 to 36) was revised from the June 2011 strategy
Clinical Article/
exp Clinical Study/
Clinical Trial/
Controlled Study/
Randomized Controlled Trial/
Major Clinical Study/
Double Blind Procedure/
Multicenter Study/
Single Blind Procedure/
Phase 3 Clinical Trial/
Phase 4 Clinical Trial/
crossover procedure/
placebo/
or/1‐13
allocat$.mp.
assign$.mp.
blind$.mp.
(clinic$ adj25 (study or trial)).mp.
compar$.mp.
control$.mp.
cross?over.mp.
factorial$.mp.
follow?up.mp.
placebo$.mp.
prospectiv$.mp.
random$.mp.
((singl$ or doubl$ or trebl$ or tripl$) adj25 (blind$ or mask$)).mp.
trial.mp.
(versus or vs).mp.
or/15‐29
14 or 30
exp animals/ or exp invertebrate/ or animal experiment/ or animal model/ or animal tissue/ or animal cell/ or nonhuman/
human/ or normal human/ or human cell/
32 and 33
32 not 34
31 not 35
dorsalgia.mp.
back pain.mp.
exp BACKACHE/
(lumbar adj pain).mp.
coccyx.mp.
coccydynia.mp.
sciatica.mp.
ischialgia/
spondylosis.mp.
lumbago.mp.
back disorder$.ti,ab.
or/37‐47
back school.mp.
36 and 48 and 49
limit 50 to yr=2015‐2016
limit 50 to dd=20150804‐20161115
51 or 52
The June 2011 strategy used a different animal study and entry date filter:
Clinical Article/
exp Clinical Study/
Clinical Trial/
Controlled Study/
Randomized Controlled Trial/
Major Clinical Study/
Double Blind Procedure/
Multicenter Study/
Single Blind Procedure/
Phase 3 Clinical Trial/
Phase 4 Clinical Trial/
crossover procedure/
placebo/
or/1‐13
allocat$.mp.
assign$.mp.
blind$.mp.
(clinic$ adj25 (study or trial)).mp.
compar$.mp.
control$.mp.
cross?over.mp.
factorial$.mp.
follow?up.mp.
placebo$.mp.
prospectiv$.mp.
random$.mp.
((singl$ or doubl$ or trebl$ or tripl$) adj25 (blind$ or mask$)).mp.
trial.mp.
(versus or vs).mp.
or/15‐29
14 and 30
human/
Nonhuman/
exp ANIMAL/
Animal Experiment/
33 or 34 or 35
32 not 36
31 not 36
37 and 38
38 or 39
dorsalgia.mp.
back pain.mp.
exp BACKACHE/
(lumbar adj pain).mp.
coccyx.mp.
coccydynia.mp.
sciatica.mp.
exp ISCHIALGIA/
spondylosis.mp.
lumbago.mp.
exp Low back pain/
or/41‐51
back school.mp.
40 and 52 and 53
limit 54 to yr="2009 ‐ 2011"
2009$.em.
2010$.em.
2011$.em.
56 or 57 or 58
54 and 59
55 or 60
CINAHL
Last searched 15 November 2016.
Back pain was added to line 27 in 2015. In 2014 , CINAHL was searched from inception to May 2007 using the current strategy to ensure records were up to date.
S47 S45 OR S46
S46 S44 and EM 20150804‐20161115
S45 S42 AND S43Limiters ‐ Published Date: 20150801‐20161131
S44 S42 AND S43
S43 back school
S42 S24 and S41
S41 S40 or S39 or S38 or S37 or S36 or S35 or S34 or S33 or S32 or S31 or S30 or S29 or S28 or S27 or S26 or S25
S40 lumbago
S39 (MH "Spondylolysis")
S38 (MH "Spondylolisthesis")
S37 lumbar N2 vertebrae
S36 (MH "Lumbar Vertebrae")
S35 back disorder*
S34 coccydynia
S33 coccyx
S32 sciatica
S31 (MH "Sciatica")
S30 (MH "Coccyx")
S29 lumbar N5 pain
S28 lumbar W1 pain
S27 backache or back pain
S26 (MH "Back Pain+")
S25 dorsalgia
S24 S22 not S23
S23 (MH "Animals+")
S22 S21 or S20 or S19 or S18 or S17 or S16 or S15 or S14 or S13 or S12 or S11 or S10 or S9 or S8 or S7 or S6 or S5 or S4 or S3 or S2 or S1
S21 volunteer*
S20 prospectiv*
S19 control*
S18 followup stud*
S17 follow‐up stud*
S16 (MH "Prospective Studies+")
S15 (MH "Evaluation Research+")
S14 (MH "Comparative Studies")
S13 latin square
S12 (MH "Study Design+")
S11 (MH "Random Sample+")
S10 random*
S9 placebo*
S8 (MH "Placebos")
S7 (MH "Placebo Effect")
S6 triple‐blind
S5 single‐blind
S4 double‐blind
S3 clinical W3 trial
S2 randomi?ed controlled trial*
S1 (MH "Clinical Trials+")
June 2011 search. Line S3 was changed from "clinical W8 trial" to "clinical W3 trial" and line S21 and S42 were added:
S51 S49 and S50 Limiters ‐ Published Date from: 20090101‐20111231
S50 "back school"
S49 S28 and S48
S48 S35 or S43 or S47
S47 S44 or S45 or S46
S46 "lumbago"
S45 (MH "Spondylolisthesis") OR (MH "Spondylolysis")
S44 (MH "Thoracic Vertebrae")
S43 S36 or S37 or S38 or S39 or S40 or S41 or S42
S42 lumbar N2 vertebra
S41 (MH "Lumbar Vertebrae")
S40 "coccydynia"
S39 "coccyx"
S38 "sciatica"
S37 (MH "Sciatica")
S36 (MH "Coccyx")
S35 S29 or S30 or S31 or S32 or S33 or S34
S34 lumbar N5 pain
S33 lumbar W1 pain
S32 "backache"
S31 (MH "Low Back Pain")
S30 (MH "Back Pain+")
S29 "dorsalgia"
S28 S26 NOT S27
S27 (MH "Animals")
S26 S7 or S12 or S19 or S25
S25 S20 or S21 or S22 or S23 or S24
S24 volunteer*
S23 prospectiv*
S22 control*
S21 followup stud*
S20 follow‐up stud*
S19 S13 or S14 or S15 or S16 or S17 or S18
S18 (MH "Prospective Studies+")
S17 (MH "Evaluation Research+")
S16 (MH "Comparative Studies")
S15 latin square
S14 (MH "Study Design+")
S13 (MH "Random Sample")
S12 S8 or S9 or S10 or S11
S11 random*
S10 placebo*
S9 (MH "Placebos")
S8 (MH "Placebo Effect")
S7 S1 or S2 or S3 or S4 or S5 or S6
S6 triple‐blind
S5 single‐blind
S4 double‐blind
S3 clinical W3 trial
S2 "randomi?ed controlled trial*"
S1 (MH "Clinical Trials+")
PsycINFO
Last searched 15 November 2016.
1 clinical trials/
2 controlled trial.mp.
3 RCT.mp.
4 Random*.mp. [mp=title, abstract, heading word, table of contents, key concepts, original title, tests & measures]
5 (clin* adj3 trial).mp. [mp=title, abstract, heading word, table of contents, key concepts, original title, tests & measures]
6 (sing* adj2 blind*).mp. [mp=title, abstract, heading word, table of contents, key concepts, original title, tests & measures]
7 (doub* adj2 blind*).mp. [mp=title, abstract, heading word, table of contents, key concepts, original title, tests & measures]
8 placebo.mp. or exp Placebo/
9 latin square.mp.
10 (random* adj2 assign*).mp.
11 prospective studies/
12 (prospective adj stud*).mp.
13 (comparative adj stud*).mp.
14 treatment effectiveness evaluation/
15 (evaluation adj stud*).mp.
16 exp Posttreatment Followup/
17 follow?up stud*.mp.
18 or/1‐17
19 back pain/
20 lumbar spinal cord/
21 (low adj back adj pain).mp. [mp=title, abstract, heading word, table of contents, key concepts, original title, tests & measures]
22 (back adj pain).mp. [mp=title, abstract, heading word, table of contents, key concepts, original title, tests & measures]
23 spinal column/
24 (lumbar adj2 vertebra*).mp. [mp=title, abstract, heading word, table of contents, key concepts, original title, tests & measures]
25 coccyx.mp.
26 sciatica.mp.
27 lumbago.mp.
28 dorsalgia.mp.
29 back disorder*.mp.
30 "back (anatomy)"/
31 ((disc or disk) adj degenerat*).mp. [mp=title, abstract, heading word, table of contents, key concepts, original title, tests & measures]
32 ((disc or disk) adj herniat*).mp.
33 ((disc or disk) adj prolapse*).mp.
34 (failed adj back).mp.
35 or/19‐34
36 back school.mp.
37 18 and 35 and 36
38 limit 37 to yr=2015‐2016
The June 15, 2011 search in Cambridge Scientific Abstracts (CSA)
((KW=(Randomi?ed controlled trial*) OR KW=(clinical trial*) OR KW=(clin* near trail*) OR KW= (sing* near blind*) OR KW=(sing* near mask*) OR (doub* near blind*) OR KW=(doubl* NEAR mask*) OR KW=(trebl* near mask*) OR KW=(trebl* near mask*) OR KW=(tripl* near blind*) OR KW=(tripl* near mask*) OR KW=(placebo*) OR KW=(random*) OR DE=(research design) OR KW=(Latin square) OR KW=(comparative stud*) OR KW=(evaluation stud*) OR KW=(follow up stud*) OR DE=(prospective stud*)OR KW=(control*) OR KW=(prospective*) OR KW=(volunteer*)) AND (DE=(back) OR DE=(back pain) OR DE=(neck))) and(KW=(back school))
ClinicalTrials.gov
Last searched 15 November 2016
Basic search: “back school” and back pain
Received from 08/04/2015 to 11/15/2016
June 2011 search
Condition: back pain
AND
Intervention: back school
WHO ICTRP
Last searched 15 November 2016
Basic search: back school and back pain
June 2011 search
Condition: back pain
AND
Intervention: back school
PubMed
Searched August 4, 2015
((back pain OR backache OR coccydynia OR sciatica OR back disorder OR lumbago OR spondylosis) AND (back school) AND (random OR randomly OR randomized OR randomised OR placebo OR trial) AND (pubstatusaheadofprint OR publisher[sb] OR pubmednotmedline[sb]))
Filters activated: Publication date from 2014/03/04 to 2015/12/31
Appendix 3. The GRADE approach to evidence synthesis
We will categorise the quality of evidence as follows.
High: Further research is very unlikely to change either the estimate or confidence in the results.
Moderate: Further research is likely to have an important impact on confidence in the estimate of effect and may change the estimate.
Low: Further research is very likely to have an important impact on confidence in the estimate of effect and is likely to change the estimate.
Very low: Any estimate of effect is very uncertain.
We will grade the evidence available to answer each subquestion on the domains in the following manner.
Risk of bias
Limitations in the study design and implementation may bias the estimates of the treatment effect. If studies suffer from any major limitation, the accuracy in the estimate of the effect and its recommendation can be affected. We will examine all studies on the following five types of biases.
Selection (random sequence generation, allocation concealment, group similarities at baseline): We will score this item as low risk of bias if two or more of these items are defined as having low risk.
Performance (blinding of participants, blinding of healthcare providers, co‐interventions, and compliance with intervention): We will score this item as low risk of bias if three or more of these items are defined as having low risk.
Attrition (dropouts and intention‐to‐treat analysis): We will score this item as low risk of bias if both of these items are defined as having low risk.
Measurement (blinding of the outcome assessors and timing of outcome assessment): We will score this item as low risk of bias if both of these items are defined as having low risk.
Reporting bias (selective reporting): We will score this item as low risk of bias if it is defined as having low risk.
We will define a study with a low risk of bias as having low risk of bias on four or more of these items.
Inconsistency
Inconsistency refers to an unexplained heterogeneity of results. Widely differing estimates of the treatment effect (i.e. heterogeneity or variability in results) across studies suggest true differences in underlying treatment effect. Inconsistency may arise from differences in populations (e.g. drugs may have larger relative effects in sicker populations), interventions (e.g. larger effects with higher drug doses), or outcomes (e.g. diminishing treatment effect with time). We will downgrade the quality of evidence as follows:
by one level: when the heterogeneity or variability in results is large (e.g. I2 above 80%);
by two levels: when the heterogeneity or variability in results is large AND there was inconsistency arising from populations, interventions, or outcomes.
Indirectness
Indirect population, intervention, comparator, or outcome: the question being addressed in this systematic review differs from the available evidence regarding the population, intervention, comparator, or an outcome in the included randomised trial. We will downgrade the quality of evidence as follows:
by one level: when there is indirectness in only one area;
by two levels: when there is indirectness in two or more areas.
Imprecision
Results are imprecise when studies include relatively few participants and events and thus have wide confidence intervals around the estimate of the effect. In such cases we judge the quality of the evidence as lower than it otherwise would have been because of resulting uncertainty in the results. We consider each outcome separately.
For dichotomous outcomes
We will consider imprecision for either of the following two reasons.
There is only one study. When there is more than one study, the total number of events is less than 300 (a threshold rule‐of‐thumb value) (Mueller 2007).
The 95% confidence interval around the pooled or best estimate of effect includes both a) no effect and b) appreciable benefit or appreciable harm. The threshold for ’appreciable benefit’ or ’appreciable harm’ is a relative risk reduction or relative risk increase greater than 25%.
We will downgrade the quality of the evidence as follows:
by one level: when there is imprecision due to (1) or (2);
by two levels: when there is imprecision due to (1) and (2).
For continuous outcomes
We will consider imprecision for either of the following two reasons.
There is only one study. When there is more than one study, total population size is less than 400 (a threshold rule‐of‐thumb value; using the usual α and β, and an effect size of 0.2 standard deviation, representing a small effect).
The 95% confidence interval includes no effect and the upper or lower confidence limit crosses an effect size (standardised mean difference) of 0.5 in either direction.
We will downgrade the quality of the evidence as follows:
by one level: when there is imprecision due to (1) or (2);
by two levels: when there is imprecision due to (1) and (2).
Publication bias
Publication bias is a systematic underestimate or overestimate of the underlying beneficial or harmful effect due to the selective publication of studies. We will downgrade the quality of evidence by one level when the funnel plot suggests publication bias.
Data and analyses
Comparison 1. Back School versus no treatment.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pain | 7 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 short‐term follow‐up (<3 months) | 6 | 647 | Mean Difference (IV, Random, 95% CI) | ‐6.10 [‐10.18, ‐2.01] |
| 1.2 intermediate‐term follow up (3‐6 months) | 4 | 257 | Mean Difference (IV, Random, 95% CI) | ‐4.34 [‐14.37, 5.68] |
| 1.3 long‐term follow‐up (>6 months) | 3 | 244 | Mean Difference (IV, Random, 95% CI) | ‐12.16 [‐29.14, 4.83] |
| 2 Disability | 4 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 short‐term follow‐up (<3 months) | 3 | 426 | Mean Difference (IV, Random, 95% CI) | ‐3.38 [‐6.70, ‐0.05] |
| 2.2 intermediate‐term follow up (3‐6 months) | 3 | 181 | Mean Difference (IV, Random, 95% CI) | ‐5.92 [‐12.08, 0.23] |
| 2.3 long‐term follow‐up (>6 months) | 2 | 124 | Mean Difference (IV, Random, 95% CI) | ‐7.36 [‐22.05, 7.34] |
Comparison 2. Back School versus medical care.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pain | 5 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 short‐term follow‐up (<3 months) | 3 | 249 | Mean Difference (IV, Random, 95% CI) | ‐10.16 [‐19.11, ‐1.22] |
| 1.2 intermediate‐term follow up (3‐6 months) | 5 | 545 | Mean Difference (IV, Random, 95% CI) | ‐9.65 [‐22.46, 3.15] |
| 1.3 long‐term follow‐up (>6 months) | 3 | 406 | Mean Difference (IV, Random, 95% CI) | ‐5.71 [‐20.27, 8.84] |
| 2 Disability | 3 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 short‐term follow‐up (<3 months) | 2 | 130 | Mean Difference (IV, Random, 95% CI) | ‐1.19 [‐7.02, 4.64] |
| 2.2 intermediate‐term follow up (3‐6 months) | 3 | 331 | Mean Difference (IV, Random, 95% CI) | ‐6.34 [‐10.89, ‐1.79] |
| 2.3 long‐term follow‐up (>6 months) | 1 | 201 | Mean Difference (IV, Random, 95% CI) | ‐0.40 [‐7.33, 6.53] |
Comparison 3. Back School versus passive physiotherapy.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pain | 3 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 short‐term follow‐up (<3 months) | 3 | 290 | Mean Difference (IV, Random, 95% CI) | 1.96 [‐9.51, 13.43] |
| 1.2 intermediate‐term follow up (3‐6 months) | 3 | 290 | Mean Difference (IV, Random, 95% CI) | ‐16.89 [‐66.56, 32.79] |
| 1.3 long‐term follow‐up (>6 months) | 3 | 291 | Mean Difference (IV, Random, 95% CI) | ‐12.86 [‐61.22, 35.50] |
| 2 Disability | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 short‐term follow‐up (<3 months) | 2 | 180 | Mean Difference (IV, Random, 95% CI) | 2.57 [‐15.88, 21.01] |
| 2.2 intermediate‐term follow up (3‐6 months) | 2 | 180 | Mean Difference (IV, Random, 95% CI) | 6.88 [‐4.86, 18.63] |
| 2.3 long‐term follow‐up (>6 months) | 2 | 180 | Mean Difference (IV, Random, 95% CI) | 9.60 [3.65, 15.54] |
Comparison 4. Back school versus exercise.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pain | 6 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 short‐term follow‐up (<3 months) | 5 | 416 | Mean Difference (IV, Random, 95% CI) | ‐2.06 [‐14.58, 10.45] |
| 1.2 intermediate‐term follow up (3‐6 months) | 4 | 619 | Mean Difference (IV, Random, 95% CI) | ‐4.46 [‐19.44, 10.52] |
| 1.3 long‐term follow‐up (>6 months) | 3 | 461 | Mean Difference (IV, Random, 95% CI) | 4.58 [‐0.20, 9.36] |
| 2 Disability | 8 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 short‐term follow‐up (<3 months) | 6 | 471 | Mean Difference (IV, Random, 95% CI) | ‐1.65 [‐8.66, 5.37] |
| 2.2 intermediate‐term follow up (3‐6 months) | 6 | 766 | Mean Difference (IV, Random, 95% CI) | 1.57 [‐3.86, 7.00] |
| 2.3 long‐term follow‐up (>6 months) | 4 | 556 | Mean Difference (IV, Random, 95% CI) | 4.54 [‐4.44, 13.52] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Andrade 2008.
| Methods | RCT | |
| Participants | 57 participants. 1. Back School group n = 29. 2. Waiting‐list group n = 28. Inclusion criteria: non‐specific chronic low back pain for over 3 months, pain present during the study, and cognitive ability to sign the consent form. Exclusion criteria: pregnancy, disc herniation, infectious or inflammatory spondylitis, tumours, fractures, thoracic, shoulder, or neck pain, and fibromyalgia. |
|
| Interventions | 1. Back School group: 4 sessions x 60 minutes in 4 weeks. Information on anatomy, causes of LBP, ergonomics, exercises, and advice on physical activity. 2. Waiting‐list group. |
|
| Outcomes | 1. Pain: visual analogue scale. 2. Disability: Roland‐Morris Disability Questionnaire. |
|
| Notes | Secondary care setting. Funding: N/A. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were randomised using a system developed in Visual Basic into 2 groups: experimental (34 participants) and control (36 participants). |
| Allocation concealment (selection bias) | Unclear risk | The sequence generation procedure or the method of allocation were not mentioned. The title, abstract, and flowchart indicate that it is an RCT. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No mention of any attempts to blind the participants |
| Blinding (performance bias and detection bias) All outcomes | High risk | No mention of any attempts to blind the care providers |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | All participants were evaluated by the same examiner, who was blind to group allocation. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The percentage of withdrawals and dropouts was within the acceptable rate (less than 20%). |
| Intention‐to‐treat Analysis | Unclear risk | No information about intention‐to‐treat analysis |
| Selective reporting (reporting bias) | Unclear risk | It was unclear if the published report included all expected outcomes. |
| Similarity of baseline characteristics? | Low risk | Table I presents the data at baseline of the experimental and control groups, with no statistically significant difference between groups. |
| Co‐interventions avoided or similar? | Unclear risk | Not mentioned |
| Compliance acceptable? | Low risk | Compliance was acceptable based on the reported intensity/dosage, duration, number, and frequency for both the intervention and control groups. |
| Timing outcome assessments similar? | Low risk | All important outcomes assessments for both groups were measured at the same time. |
Berwick 1989.
| Methods | RCT | |
| Participants | 224 participants. 1. Back School group n = 72. 2. Usual care group n = 74. 3. Compliance Package n = 76. Inclusion criteria: low back pain, age 21 to 55 years, no serious comorbidity, no prior surgery, at least 2 weeks pain, maximum 6 months pain, no specific illness causing back pain, no prior episode during the previous year. Exclusion criteria: pain characteristically extended below the level of the knee. |
|
| Interventions | 1. Back School group: a single 4‐hour instruction session on LBP (psycho‐educational). 2. Usual care group: participants were sent a single short pamphlet on LBP. |
|
| Outcomes | Pain: visual analogue scale. | |
| Notes | Primary care setting. Funding: N/A. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The sequence generation procedure or the method of allocation were not mentioned. The title and abstract indicate that it is an RCT. |
| Allocation concealment (selection bias) | Unclear risk | The sequence generation procedure or the method of allocation were not mentioned. The title and abstract indicate that it is an RCT. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No mention of any attempts to blind the participants |
| Blinding (performance bias and detection bias) All outcomes | High risk | No mention of any attempts to blind the care providers |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No mention of any attempts to blind the assessors |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The percentage of withdrawals and dropouts was within the acceptable rate (less than 20%). |
| Intention‐to‐treat Analysis | Unclear risk | Not mentioned |
| Selective reporting (reporting bias) | Unclear risk | It was unclear if the published report included all expected outcomes. |
| Similarity of baseline characteristics? | Low risk | The only significant difference that randomisation failed to prevent was on Sickness Impact Profile |
| Co‐interventions avoided or similar? | Low risk | Balanced for both groups |
| Compliance acceptable? | Unclear risk | Not mentioned |
| Timing outcome assessments similar? | Low risk | All important outcomes assessments for both groups were measured at the same time. |
Cecchi 2010a.
| Methods | RCT | |
| Participants | 210 participants. 1. Back School n = 70. 2. Individual physiotherapy n = 70. 3. Spinal manipulation n = 70. Inclusion criteria: non‐specific low back pain, reported "often" to "always" for at least the past 6 months. Exclusion criteria: neurological signs or symptoms, spondylolisthesis 4 second degree, rheumatoid arthritis or spondylitis, previous vertebral fractures, psychiatric disease, cognitive impairment, or pain‐related litigation. |
|
| Interventions | 1. Back School: 15 sessions x 1 hour for 3 weeks. The first 5 sessions were devoted to information and group discussions on back physiology and pathology, with reassurance on the benign character of common low back pain and education in ergonomics at home and in different occupational settings by slides and demonstrations. The next 10 sessions included relaxation techniques, postural and respiratory group exercises, and individually tailored back exercises. Each Back School group included 8 participants. *All participants received a booklet with evidence‐based, standardised educational information on basic back anatomy and biomechanics, optimal postures, ergonomics, and advice to stay active. 2. Individual physiotherapy: 15 sessions x 60 minutes for 3 weeks. Included passive and assisted mobilisation, active exercise, massage/treatment of the soft tissues, and proprioceptive neuromuscular facilitation, with emphasis on patient education and active treatment. 3. Spinal manipulation: 4 to 6 sessions (as needed) x 20 minutes for 4 to 6 weeks. Spinal manipulation given according to Manual Medicine. |
|
| Outcomes | 1. Pain: Pain Rating Scale. 2. Disability: Roland‐Morris Disability Questionnaire. |
|
| Notes | Setting not specified. Funding: N/A. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Simple (non‐restricted) randomisation led to some imbalances in participants' baseline characteristics. |
| Allocation concealment (selection bias) | Unclear risk | The sequence generation procedure or the method of allocation were not mentioned. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No mention of any attempts to blind the participants |
| Blinding (performance bias and detection bias) All outcomes | High risk | No mention of any attempts to blind the care providers |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | The examiners were blinded to group assignment. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The percentage of withdrawals and dropouts was within the acceptable rate (less than 20%). |
| Intention‐to‐treat Analysis | High risk | Analysis was substantially similar to the intention‐to‐treat analysis commonly adopted in reporting randomised trials due to the minimal dropout (5/210, 2.4%). |
| Selective reporting (reporting bias) | Low risk | It was clear that the published report includes all expected outcomes. |
| Similarity of baseline characteristics? | Low risk | No significant difference across the groups was found. |
| Co‐interventions avoided or similar? | Low risk | Balanced for both groups |
| Compliance acceptable? | Unclear risk | There are not enough data. |
| Timing outcome assessments similar? | Low risk | All important outcomes assessments for both groups were measured at the same time. |
Costantino 2014.
| Methods | RCT | |
| Participants | 54 participants. 1. Back School group n = 27. 2. Hydrotherapy group n = 27. Inclusion criteria: participants aged between 65 and 80 years; diagnosis of chronic non‐specific low back pain. Exclusion criteria: presence of musculoskeletal disorders, severe heart failure, or internal medicine pathologies that could interfere with moderate physical activity; fever or infectious disease; systemic inflammatory or rheumatologic diseases; previous spinal surgery or a history of vertebral traumas/fractures; instrumental physical therapies or physiotherapeutic therapies in the previous 3 months. |
|
| Interventions | 1. Back School group: In the first session, individuals were informed about the anatomy of the spinal column, its functioning and ergonomic position and the basis of the pain‐inducing mechanism, psychological aspects and stress management, whereas in the following sessions they performed stretching and muscular strengthening, associated with proper breathing. 2. Hydrotherapy group: Participants at first performed walking exercises to adapt to the pool conditions, and afterwards performed bilateral stretching and selective muscle strengthening exercises. |
|
| Outcomes | 1. Disability: Roland‐Morris Disability Questionnaire. | |
| Notes | Setting not specified. Funding: N/A. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The participants were randomly allocated using computer randomisation software (RANDI2 software version 0.6.1) to the Back School programme (group A) or to the hydrotherapy programme (group B). |
| Allocation concealment (selection bias) | Unclear risk | The sequence generation procedure or the method of allocation were not mentioned. The title and abstract indicate that it is an RCT. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No mention of any attempts to blind the participants |
| Blinding (performance bias and detection bias) All outcomes | High risk | No mention of any attempts to blind the care providers |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No mention of any attempts to blind the assessors |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The percentage of withdrawals and dropouts was within the acceptable rate (less than 20%). |
| Intention‐to‐treat Analysis | Low risk | All analyses were performed based on the intention‐to‐treat principle. |
| Selective reporting (reporting bias) | Low risk | It was clear that the published report included all expected outcomes. |
| Similarity of baseline characteristics? | Low risk | No significant difference across the groups was found. |
| Co‐interventions avoided or similar? | Low risk | Balanced for both groups |
| Compliance acceptable? | Low risk | Compliance was acceptable based on the reported intensity/dosage, duration, number, and frequency for both the intervention and control groups. |
| Timing outcome assessments similar? | Low risk | All important outcomes assessments for both groups were measured at the same time. |
Dalichau 1999.
| Methods | RCT | |
| Participants | 120 participants. 1. Back School group n = 60. 2. Waiting‐list control group n = 60. Inclusion criteria: chronic, recurrent low back pain, age 20 to 40 years, no use of treatment because of acute back pain, no Back School experience, working full time, no expectation of an occupational disease at the time of enrolment. |
|
| Interventions | 1. Back School group: 6 sessions (6 to 8 different modules) of 90 minutes in 8 weeks including education (anatomy, pathology, ergonomic, optimal posture during work and other activities) and exercises (isometric and dynamic strength, stretching and relaxation exercises, work simulating). 2. Waiting‐list control group. |
|
| Outcomes | Pain: Pain Rating Scale. | |
| Notes | Occupational setting. Funding: N/A. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The sequence generation procedure or the method of allocation were not mentioned. The title and abstract indicate that it is an RCT. |
| Allocation concealment (selection bias) | Unclear risk | The sequence generation procedure or the method of allocation were not mentioned. The title and abstract indicate that it is an RCT. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No mention of any attempts to blind the participants |
| Blinding (performance bias and detection bias) All outcomes | High risk | No mention of any attempts to blind the care providers |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No mention of any attempts to blind the assessors |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The percentage of withdrawals and dropouts was within the acceptable rate (less than 20%). |
| Intention‐to‐treat Analysis | Unclear risk | Not mentioned |
| Selective reporting (reporting bias) | Unclear risk | Not mentioned |
| Similarity of baseline characteristics? | Low risk | Demographic baseline characteristics of the study population are presented in Table 1. |
| Co‐interventions avoided or similar? | Unclear risk | Not mentioned |
| Compliance acceptable? | Unclear risk | Not mentioned |
| Timing outcome assessments similar? | Unclear risk | Not mentioned |
Devasahayam 2014.
| Methods | RCT | |
| Participants | 28 participants. 1. Back School group n = 14. 2. Mat‐based exercises group n = 14. Inclusion criteria: Candidates with non‐specific low back pain with a pain score < 8 on the verbal numerical pain (VNP) scale, and without significantly impaired spinal mobility, were included in this study. Only candidates who could read and speak English were included. Exclusion criteria: Candidates suffering from numbness, paraesthesia, or radicular symptoms were excluded from this study, as were those with any other musculoskeletal disorders of the lower limbs or upper‐ and mid‐back pain. Candidates with red flags such as cancer, fractures, inflammatory or infective diseases, other neurological disorders, and those having spinal surgery less than 6 months prior to the study were also excluded. |
|
| Interventions | 1. Back School group: The participants in the experimental group performed functional back exercises and had back care instruction amounting to 1‐hour duration for each session. The participants received training in specific tasks like lifting, sitting, or mopping in order to correct their body mechanics in their ADL. The first 15 minutes of the session was a PowerPoint presentation on correct postures like upright sitting and standing postures, proper body mechanics of ADL like lifting, mopping and sweeping, walking, going up and down the stairs, information on ergonomic correction and activity pacing. This was followed by a functional task practice of all the above‐mentioned ADL for the next 30 minutes. 2. Mat‐based exercises group: The participants in the control group performed generic mat‐based exercises commonly used to treat people with chronic low back pain. These exercises were not focused on any specific body mechanics or postures. The stretches were performed in reclined position on an exercise mat for the quadriceps, hamstrings, calf, hip external rotators, and spine (such as cat/dog stretches and prayer stretches). Mat exercises (e.g. knee hugs, knee rocking, lumbar rotation, and pelvic tilts in the supine position), mat‐based core stability exercises were also performed. 2 sets of 10 repetitions of each exercise were performed for the 1‐hour duration of each session; this was continued for 4 consecutive sessions once a week. The participants were instructed to follow the exercises as performed by the physiotherapist. The sessions were kept less interactive than they would be in a regular group exercise class. |
|
| Outcomes | 1. Pain: numerical pain scale. 2. Disability: Roland‐Morris Disability Questionnaire. |
|
| Notes | Funding: N/A. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The sequence generation procedure or the method of allocation were not mentioned. The title and abstract indicate that it is an RCT. |
| Allocation concealment (selection bias) | Unclear risk | The sequence generation procedure or the method of allocation were not mentioned. The title and abstract indicate that it is an RCT. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Due to the nature of the interventions, it was not possible to blind the participants. |
| Blinding (performance bias and detection bias) All outcomes | High risk | Due to the nature of the interventions, it was not possible to blind the therapists. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | An independent investigator collected data before and after the exercise classes. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Only 15 participants completed the study; 13 participants dropped out of the study due to non‐compliance or inability to obtain time‐off from work, or both. |
| Intention‐to‐treat Analysis | Unclear risk | Not mentioned |
| Selective reporting (reporting bias) | Unclear risk | Not mentioned |
| Similarity of baseline characteristics? | Low risk | No significant difference across the groups was found. |
| Co‐interventions avoided or similar? | Low risk | Balanced for both groups |
| Compliance acceptable? | High risk | Only 15 participants completed the study; 13 participants dropped out of the study due to non‐compliance or inability to obtain time‐off from work, or both. |
| Timing outcome assessments similar? | Low risk | All important outcomes assessments for both groups were measured at the same time. |
Donchin 1990.
| Methods | RCT | |
| Participants | 138 participants. 1. Back School group n = 46. 2. Calisthenics exercises group n = 46. 3. Waiting‐list control group n = 46. Inclusion criteria: at least 3 annual episodes of low back pain. Exclusion criteria: not described. |
|
| Interventions | 1. Back School group: 4, 90‐minute sessions during a 2‐week period plus a 5th session after 2 months. Each group of 10 to 12 participants was supervised by a physiotherapist (education and exercises for back and abdominal muscles). 2. Calisthenics exercises group: 45‐minute sessions biweekly for 3 months in groups of 10 to 12 participants (flexion and pelvic tilt exercises in order to strengthen the abdominal muscles, expanding spinal forward flexion). 3. Waiting‐list control group. |
|
| Outcomes | Disability: Oswestry Low Back Pain Questionnaire. | |
| Notes | Occupational setting. Funding: N/A. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | After being examined, the participants were allocated to the 3 groups by a systematic random sampling method. |
| Allocation concealment (selection bias) | Unclear risk | The sequence generation procedure or the method of allocation were not mentioned. The title and abstract indicate that it is an RCT. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No mention of any attempts to blind the participants |
| Blinding (performance bias and detection bias) All outcomes | High risk | No mention of any attempts to blind the care providers |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No mention of any attempts to blind the assessors |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The percentage of withdrawals and dropouts was within the acceptable rate (less than 20%). |
| Intention‐to‐treat Analysis | Unclear risk | Not mentioned |
| Selective reporting (reporting bias) | Unclear risk | It was unclear if the published report included all expected outcomes. |
| Similarity of baseline characteristics? | Low risk | Demographic and clinical baseline characteristics of the study population are presented in Table 1. Demographic and clinical baseline characteristics were similar for both groups. |
| Co‐interventions avoided or similar? | Unclear risk | There were few reported co‐interventions in the study. |
| Compliance acceptable? | Low risk | Based on the description of both groups, compliance was acceptable. |
| Timing outcome assessments similar? | Low risk | All important outcomes assessments for both groups were measured at the same time. |
Donzelli 2006.
| Methods | quasi‐RCT | |
| Participants | 43 participants. 1. Back School group n = 22. 2. Pilates group n = 21. Inclusion criteria: chronic LBP without peripheral irradiation for at least 3 months; neurological values within the normal range; negative Lasegue’s test and Wassermann test. Exclusion criteria: clinical history of spinal surgery; neurological values outside the normal range; radicular pain with positive Lasegue’s and Wassermann’s signs and straight leg raise test; structural deformities such as spondylolisthesis; stenosis of the vertebral canal; computed tomography or nuclear magnetic resonance documented disc hernia; rheumatoid arthritis or other rheumatologically related pathologies; conditions unrelated to the spinal column that mimic lumbalgic symptoms. |
|
| Interventions | 1. Back School group: 10 sessions/60 minutes. During each session, participants performed all the exercises listed in the protocol. The protocol included postural education exercises, respiratory education, muscular extension and strengthening exercises of the paravertebral muscles and lower limbs, mobilising exercises for the spinal column and antalgic postures. During each treatment session, the therapist taught the participants some theoretical notions of the anatomy and pathology of the spinal column and in the principles of postural education. 2. Pilates group: 10 sessions/60 minutes. The protocol comprised a programme of exercise modules that made it easier to adapt the exercise to the requirements of each participant in each group. The protocol comprised postural education, stretching exercises, and breathing education. |
|
| Outcomes | 1. Pain: visual analogue scale. 2. Disability: Roland‐Morris Disability Questionnaire. |
|
| Notes | Secondary care setting. Funding: N/A. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Used a quasi‐random procedure |
| Allocation concealment (selection bias) | Unclear risk | The sequence generation procedure or the method of allocation were not mentioned. The title and abstract indicate that it is an RCT. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No mention of any attempts to blind the participants |
| Blinding (performance bias and detection bias) All outcomes | High risk | No mention of any attempts to blind the care providers |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No mention of any attempts to blind the assessors |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The percentage of withdrawals and dropouts was within the acceptable rate (less than 20%). |
| Intention‐to‐treat Analysis | Unclear risk | Not mentioned |
| Selective reporting (reporting bias) | Unclear risk | It was unclear if the published report included all expected outcomes. |
| Similarity of baseline characteristics? | Low risk | Demographic and clinical baseline characteristics were similar for both groups. |
| Co‐interventions avoided or similar? | Unclear risk | There were few reported co‐interventions in the study. |
| Compliance acceptable? | Low risk | Compliance was acceptable based on the descriptions of both groups. |
| Timing outcome assessments similar? | Low risk | All important outcomes assessments for both groups were measured at the same time. |
Dufour 2010.
| Methods | RCT | |
| Participants | 272 participants. 1. Back School group n = 129. 2. Muscle training exercises group n = 143. Inclusion criteria: low back pain lasting more than 12 weeks with or without pain radiating into the leg(s), and aged 18 to 60 years. Exclusion criteria: symptoms of serious spinal pathology such as malignancy, osteoporosis, vertebral fracture, spinal stenosis, clinical symptoms of an acute herniated disc accompanied by nerve root entrapment, unstable spondylolisthesis, spondylitis, health conditions that prevented them from performing strenuous exercise, and language problems. |
|
| Interventions | 1. Back School group: 36 sessions x 2 hours for 12 weeks. Participants received a programme of combined exercise, education, and pain management based on a programme described by Bendix. At the first session, a pre‐programme assessment was performed to familiarise participants with the exercise programme, set treatment goals, and set the initial intensity for each exercise. The bulk of the session consisted of aerobic training and training to strengthen the muscles in the back, gluteus region, and abdominal wall. These exercises were all performed in the supine position using machines and circuit training. A total of 22 hours of exercises was performed. In addition, participants were provided 1.5 hours to play ball games, 1.5 hours of training in hot water, and 2 hours of ball stick training. Bi‐weekly lessons on anatomy, postural techniques, and pain management were provided by a physiotherapist and on back care and lifting techniques by an occupational therapist, for a total of 10 hours. During the second period, 2‐hour exercise sessions were performed twice a week at the study site and once a week at the participant’s home. During the third period, 2‐hour exercise sessions were performed 3 times a week at home. The participants performed a total of 75 hours of moderate muscle training exercise. The treatment‐related cost per participant amounted to 12 hours of therapist assistance. 2. Muscle training exercises group: 24 sessions x 1 hour for 12 weeks. Participants received a programme of specific and intensive muscle training exercises to strengthen and shorten the muscles in the back and gluteus region. The programme did not include stretching or abdominal muscle exercises. |
|
| Outcomes | 1. Pain: visual analogue scale. 2. Disability: Roland‐Morris Disability Questionnaire. 3. Adverse events: reported by the physiotherapists on standardised forms. |
|
| Notes | Secondary care setting. Funding: The Danish National Board of Health. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were allocated by a separate secretary to a group‐based multidisciplinary biopsychosocial rehabilitation programme (group A) or intensive individually therapist‐assisted back muscle strengthening exercises (group B) according to a random number chart made for each subgroup provided by the Copenhagen Trial Unit, Center for Clinical Intervention Research, Rigshospitalet. |
| Allocation concealment (selection bias) | Low risk | Participants were allocated by a separate secretary to a group‐based multidisciplinary biopsychosocial rehabilitation programme (group A) or intensive individually therapist‐assisted back muscle strengthening exercises (group B) according to a random number chart made for each subgroup provided by the Copenhagen Trial Unit, Center for Clinical Intervention Research, Rigshospitalet. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No mention of any attempts to blind the participants |
| Blinding (performance bias and detection bias) All outcomes | High risk | No mention of any attempts to blind the care providers |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | All physical examinations at trial visits were performed by 1 physician who was blinded to the treatment group and had no access to the treatment area. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The percentage of withdrawals and dropouts was within the acceptable rate (less than 20%). |
| Intention‐to‐treat Analysis | Low risk | Data analysis was performed on the actual data on an intention‐to‐treat basis, with the last value carried forward. |
| Selective reporting (reporting bias) | Low risk | It was clear that the published report included all expected outcomes. |
| Similarity of baseline characteristics? | Low risk | Demographic and clinical baseline characteristics of the study population are presented in Table 1. There were no significant differences between the groups. |
| Co‐interventions avoided or similar? | Unclear risk | Not mentioned |
| Compliance acceptable? | Unclear risk | There are insufficient data about the control group. |
| Timing outcome assessments similar? | Low risk | All important outcomes assessments for both groups were measured at the same time. |
Durmus 2014.
| Methods | RCT | |
| Participants | 121 participants. 1. Back School group n = 61. 2. Exercise group n = 60. Inclusion criteria: people with low back pain for at least 3 months. Exclusion criteria: people with acute radicular signs or symptoms, those who had radiographic evidence of inflammatory disease affecting the spine, tumour; serious medical conditions for which exercise is contraindicated; history of spinal surgery; pregnancy. |
|
| Interventions | 1. Back School group: 8 sessions within a 4‐week period. Each session entailed approximately half an hour of didactic training and half an hour of practical training. The program was administered by a physiatrist. 2. Exercise group: The participants in both groups were treated with a group‐exercise programme of 60 minutes of exercise 3 times a week. |
|
| Outcomes | 1. Pain: visual analogue scale. 2. Disability: Oswestry Disability Index. |
|
| Notes | Funding: N/A. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was allocated by numbered‐envelopes method. |
| Allocation concealment (selection bias) | Unclear risk | The sequence generation procedure or the method of allocation were not mentioned. The title and abstract indicate that it is an RCT. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No mention of any attempts to blind the participants |
| Blinding (performance bias and detection bias) All outcomes | High risk | No mention of any attempts to blind the care providers |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No mention of any attempts to blind the assessors |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The percentage of withdrawals and dropouts was within the acceptable rate (less than 20%). |
| Intention‐to‐treat Analysis | Unclear risk | Not mentioned |
| Selective reporting (reporting bias) | Unclear risk | It was unclear if the published report included all expected outcomes. |
| Similarity of baseline characteristics? | Low risk | Demographic and clinical baseline characteristics of the study population are presented in Table 1. There were no significant differences between the groups. |
| Co‐interventions avoided or similar? | Low risk | Balanced for both groups |
| Compliance acceptable? | Unclear risk | Not mentioned |
| Timing outcome assessments similar? | Low risk | All important outcomes assessments for both groups were measured at the same time. |
Garcia 2013.
| Methods | RCT | |
| Participants | 148 participants. 1. Back School group n = 74. 2. McKenzie Method group n = 74. Inclusion criteria: Patients seeking care had to have non‐specific low back pain of at least 3 months’ duration and be between 18 and 80 years of age. Patients with any contraindication to physical exercise based on the recommendations of the guidelines of the American College of Sports Medicine. Exclusion criteria: Serious spinal pathology (e.g. tumours, fractures, inflammatory diseases), previous spinal surgery, nerve root compromise, cardiorespiratory illnesses, or pregnancy. |
|
| Interventions | 1. Back School group: 4 sessions x 60 minutes for 4 weeks. Participants received theoretical and practical information during the treatment sessions. The first session was conducted individually, and the 3 remaining sessions were conducted in groups. 2. McKenzie Method: 4 sessions x 60 minutes for 4 weeks. Participants received theoretical information regarding the care of the spine and performed specific exercises according to the direction of preference of movement according to the McKenzie Method. |
|
| Outcomes | 1. Pain: numerical pain scale. 2. Disability: Roland‐Morris Disability Questionnaire. 3. Adverse events: reported by the physiotherapists on standardised forms. |
|
| Notes | Primary care setting. Funding: Fundação de Amparo a Pesquisa do Estado de São Paulo (FAPESP). |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A simple randomisation sequence was computer generated using Microsoft Excel (Microsoft Corporation, Redmond, Washington) by one of the investigators of the study who was not directly involved with the assessment and treatment of participants. |
| Allocation concealment (selection bias) | Low risk | The allocation was concealed by using consecutively numbered, sealed, opaque envelopes. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Given the nature of the interventions, it was not possible to blind the therapist or participants. |
| Blinding (performance bias and detection bias) All outcomes | High risk | Given the nature of the interventions, it was not possible to blind the therapist or participants. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | This study was a prospectively registered, 2‐arm randomised controlled trial with a blinded assessor. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 146 (98.6%) of participants completed the follow‐up at 1 month for the primary outcome measures of pain and disability and for the secondary outcome measure of quality of life. |
| Intention‐to‐treat Analysis | Low risk | The statistical analysis was conducted on an intention‐to‐treat basis. |
| Selective reporting (reporting bias) | Low risk | It was clear that the published report included all expected outcomes. |
| Similarity of baseline characteristics? | Low risk | Groups did not differ in the baseline characteristics. |
| Co‐interventions avoided or similar? | Low risk | Balanced for both groups |
| Compliance acceptable? | Low risk | Based on the descriptions of both groups, compliance was acceptable. |
| Timing outcome assessments similar? | Low risk | All important outcomes assessments for both groups were measured at the same time. |
Heymans 2006.
| Methods | RCT | |
| Participants | 299 participants. 1. Back School (low‐intensity) group n = 98. 2. Back School (high‐intensity) group n = 98. 3. Usual care group n = 103. Inclusion criteria: workers; non‐specific low back pain; being sick‐listed (completely or partially) between 3 and 6 weeks; age 18 to 65 years; and ability to complete written questionnaires in the Dutch language. Exclusion criteria: sick‐listed due to low back pain less than 1 month before the onset of the current episode of sick‐leave; specific pathology; pregnancy. |
|
| Interventions | 1. Back School (low‐intensity) group: 4 sessions x 120 minutes for 4 weeks. 2. Back School (high‐intensity) group: 16 sessions x 60 minutes for 8 weeks. 3. Usual care group: Participants allocated to this group received usual care provided by the occupational physician according to the Dutch guidelines for the occupational health management of patients with low back pain. After 12 weeks of continued sick‐leave, the occupational physician was advised to refer the worker to more intensive interventions such as Back Schools or a multidisciplinary rehabilitation programme. |
|
| Outcomes | 1. Pain: visual analogue scale. 2. Disability: Roland‐Morris Disability Questionnaire. 3. Return to work: defined as the duration of work absenteeism in calendar days from the first day of sick‐leave until full return to own work or other work with equal earnings for at least 4 weeks without (partial or full) dropout. 4. Adverse events: reported by the physiotherapists on standardised forms. |
|
| Notes | Secondary care setting. Funding: The Netherlands Organisation for Health Research and Development (ZonMw), Dutch Ministries of Health, Welfare and Sports and of Social Affairs and Employment. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Using sealed, opaque envelopes, coded according to a computerised random number generator, participants were randomly allocated to either the low‐intensity Back School, high‐intensity Back School, or usual care group. |
| Allocation concealment (selection bias) | Low risk | Using sealed, opaque envelopes, coded according to a computerised random number generator, participants were randomly allocated to either the low‐intensity Back School, high‐intensity Back School, or usual care group. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Occupational and family physicians and physiotherapists were not blinded for the allocated intervention. |
| Blinding (performance bias and detection bias) All outcomes | High risk | Occupational and family physicians and physiotherapists were not blinded for the allocated intervention. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | An independent research assistant extracted the work absence data. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The percentage of withdrawals and dropouts was within the acceptable rate (less than 20%). |
| Intention‐to‐treat Analysis | Low risk | "Applying the intention‐to‐treat (ITT) principle, we included all patients in the analysis according to the group determined at randomisation." |
| Selective reporting (reporting bias) | Low risk | It was clear that the published report included all expected outcomes. |
| Similarity of baseline characteristics? | Low risk | Participants did not differ in baseline characteristics. |
| Co‐interventions avoided or similar? | Unclear risk | Not mentioned |
| Compliance acceptable? | Low risk | Compliance was acceptable based on the reported intensity/dosage, duration, number, and frequency for both the intervention and control groups. |
| Timing outcome assessments similar? | Low risk | All important outcomes assessments for both groups were measured at the same time. |
Hurri 1989.
| Methods | RCT | |
| Participants | 188 participants. 1. Back School group n = 95. 2. Instruction material of the Back School in written form group n = 93. Inclusion criteria: idiopathic LBP for at least 12 months, LBP present on at least 1 day each week during the preceding month, and/or ADL limitations. Exclusion criteria: rheumatoid arthritis or other connective tissue disease as well as people with a history of back surgery. |
|
| Interventions | 1. Back School group: modified Swedish Back School: 60‐minute education and exercise sessions, 6 times in 3 weeks. Refresher course 2 x 60 minutes after 6 months. Supervised by physiotherapist; 11 participants per group. 2. Instruction material of the Back School in written form group: No actual treatment, but free to use healthcare services. |
|
| Outcomes | 1. Pain: visual analogue scale. 2. Disability: Oswestry Disability Index. |
|
| Notes | Occupational setting. Funding: N/A. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The participants were randomly assigned to one of two groups. |
| Allocation concealment (selection bias) | Unclear risk | The sequence generation procedure or the method of allocation were not mentioned. The title and abstract indicate that it is an RCT. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No mention of any attempts to blind the participants |
| Blinding (performance bias and detection bias) All outcomes | High risk | No mention of any attempts to blind the care providers |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No mention of any attempts to blind the assessors |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The percentage of withdrawals and dropouts was within the acceptable rate (less than 20%). |
| Intention‐to‐treat Analysis | Unclear risk | Not mentioned |
| Selective reporting (reporting bias) | Unclear risk | It was unclear if the published report included all expected outcomes. |
| Similarity of baseline characteristics? | Low risk | The 2 groups were comparable for age and duration of low back pain syndrome. |
| Co‐interventions avoided or similar? | Low risk | Balanced for both groups |
| Compliance acceptable? | Low risk | Compliance was acceptable based on the reported intensity/dosage, duration, number, and frequency for both the intervention and control groups. |
| Timing outcome assessments similar? | Low risk | All important outcomes assessments for both groups were measured at the same time. |
Jaromi 2012.
| Methods | RCT | |
| Participants | 111 participants. 1. Back School group n = 56. 2. Passive physiotherapy group n = 55. Inclusion criteria: nurses working in the inpatient department of the university clinics, having LBP syndrome in their medical history, under 60 years of age; more than 3 months of lower back pain with or without referred pain; and having a current active diagnosis of chronic LBP. Exclusion criteria: pregnancy; previous spinal surgery; current nerve root entrapment accompanied by significant neurological deficit; spinal cord compression; tumours; severe structural deformity; severe instability; severe osteoporosis; inflammatory disease of the spine; spinal infection; severe cardiovascular or metabolic disease; depression; and connective tissue disorder. |
|
| Interventions | 1. Back School group: 6 sessions for 6 weeks. Sessions of ergonomics training and Back School once a week for a duration of 6 weeks. Each therapy session was divided into a 10‐minute ergonomics training exercise, a 20‐minute muscle strengthening and stretching exercise. 2. Passive physiotherapy group: 1 session for 6 weeks of transcutaneous electrical nerve stimulation (TENS) therapy and heat therapy, which participants were advised to practise at home daily. |
|
| Outcomes | 1. Pain: numerical pain scale. | |
| Notes | Occupational setting. Funding: The Netherlands Organisation for Health Research and Development (ZonMw), Dutch Ministries of Health, Welfare and Sports and of Social Affairs and Employment. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Nurses having chronic LBP syndrome were randomised into 2 groups to receive either ergonomics training and Back School (education) or passive therapy. |
| Allocation concealment (selection bias) | Unclear risk | The sequence generation procedure or the method of allocation were not mentioned. The title, abstract, and flowchart indicate that it is an RCT. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No mention of any attempts to blind the participants |
| Blinding (performance bias and detection bias) All outcomes | High risk | No mention of any attempts to blind the care providers |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | The examiner was kept blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The percentage of withdrawals and dropouts was within the acceptable rate (less than 20%). |
| Intention‐to‐treat Analysis | Unclear risk | No information about intention‐to‐treat analysis |
| Selective reporting (reporting bias) | Unclear risk | It was unclear if the published report included all expected outcomes. |
| Similarity of baseline characteristics? | Low risk | Based on Table 1, participants did not differ in baseline characteristics. |
| Co‐interventions avoided or similar? | Low risk | Balanced for both groups |
| Compliance acceptable? | Unclear risk | There are insufficient data about the control group. |
| Timing outcome assessments similar? | Low risk | All important outcomes assessments for both groups were measured at the same time. |
Keijsers 1989.
| Methods | RCT | |
| Participants | 40 participants. 1. Back School treatment group n = 20. 2. Waiting‐list control group n = 20. Inclusion criteria: low back pain for at least 6 months. Exclusion criteria: medical contraindication list which specified medical disorders and diseases. |
|
| Interventions | 1. Back School treatment group: Maastricht Back School: education and skills program in group setting (10 to 12 participants per group), 7 lessons of 2.5 hours and refresher lesson after 8 weeks. Included postural education, exercises, information on psychological factors. 2. Waiting‐list control group. |
|
| Outcomes | 1. Pain: visual analogue scale. | |
| Notes | Setting not specified. Funding: N/A. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The sequence generation procedure or the method of allocation were not mentioned. |
| Allocation concealment (selection bias) | Unclear risk | The sequence generation procedure or the method of allocation were not mentioned. The title and abstract indicate that it is an RCT. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No mention of any attempts to blind the participants |
| Blinding (performance bias and detection bias) All outcomes | High risk | No mention of any attempts to blind the care providers |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No mention of any attempts to blind the assessors |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The percentage of withdrawals and dropouts was within the acceptable rate (less than 20%). |
| Intention‐to‐treat Analysis | Unclear risk | Not mentioned |
| Selective reporting (reporting bias) | Unclear risk | It was unclear if the published report included all expected outcomes. |
| Similarity of baseline characteristics? | Unclear risk | Not mentioned |
| Co‐interventions avoided or similar? | Unclear risk | There were few reported co‐interventions in the study. |
| Compliance acceptable? | Unclear risk | There are insufficient data about the control group. |
| Timing outcome assessments similar? | Unclear risk | Not mentioned |
Keijsers 1990.
| Methods | RCT | |
| Participants | 90 participants. 1. Back School treatment group n = 45. 2. Waiting‐list control group n = 45. Inclusion criteria: LBP for at least 2 months and maximum of 3 years. Exclusion criteria: people eligible for surgical treatment were excluded, as were those who were unable to participate in a physical exercise program and relaxation training. |
|
| Interventions | 1. Back School group: Maastricht Back School, education and skills program in group setting (10 to 12 participants per group), 7 lessons of 2.5 hours and refresher lesson after 6 months. Included postural education, exercises, information on psychological factors. 2. Waiting‐list control group. |
|
| Outcomes | 1. Pain: visual analogue scale. 2. Return to work was expressed in number of days. |
|
| Notes | Primary care setting. Funding: N/A. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The sequence generation procedure or the method of allocation were not mentioned. The title and abstract indicate that it is an RCT. |
| Allocation concealment (selection bias) | Unclear risk | The sequence generation procedure or the method of allocation were not mentioned. The title and abstract indicate that it is an RCT. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No mention of any attempts to blind the participants |
| Blinding (performance bias and detection bias) All outcomes | High risk | No mention of any attempts to blind the care providers |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No mention of any attempts to blind the assessors |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Dropouts exceed 20%. |
| Intention‐to‐treat Analysis | Unclear risk | Not mentioned |
| Selective reporting (reporting bias) | Unclear risk | It was unclear if the published report included all expected outcomes. |
| Similarity of baseline characteristics? | Unclear risk | Not mentioned |
| Co‐interventions avoided or similar? | Unclear risk | Not mentioned |
| Compliance acceptable? | Unclear risk | Not mentioned |
| Timing outcome assessments similar? | Unclear risk | Not mentioned |
Klaber Moffett 1986.
| Methods | RCT | |
| Participants | 78 participants. 1. Back School treatment group n = 40. 2. Exercises group n = 38. Inclusion criteria: chronic (6 months or more) LBP with or without lower limb pain. Exclusion criteria: history of spinal surgery; person concurrently attending physiotherapy treatment; and evidence of underlying disease, such as fracture, ankylosing spondylitis, or multiple myeloma. |
|
| Interventions | 1. Back School treatment group: Swedish Back School, 3 sessions containing education on anatomy and body mechanics, semi‐Fowler position, ergonomic counselling, and exercises aimed at strengthening the abdominal muscles. 2. Exercises group. |
|
| Outcomes | 1. Pain: visual analogue scale. 2. Disability: Oswestry Low Back Pain Questionnaire. |
|
| Notes | Primary care setting. Funding: N/A. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The participants were randomly allocated to 2 groups and were assessed by a rheumatologist who was not aware of treatment allocated. |
| Allocation concealment (selection bias) | Low risk | The participants were randomly allocated to 2 groups and were assessed by a rheumatologist who was not aware of treatment allocated. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No mention of any attempts to blind the participants |
| Blinding (performance bias and detection bias) All outcomes | High risk | No mention of any attempts to blind the care providers |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No mention of any attempts to blind the assessors |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The percentage of withdrawals and dropouts was within the acceptable rate (less than 20%). |
| Intention‐to‐treat Analysis | Unclear risk | Not mentioned |
| Selective reporting (reporting bias) | Unclear risk | It was unclear if the published report included all expected outcomes. |
| Similarity of baseline characteristics? | Low risk | Based on Table 1, participants did not differ in baseline characteristics. |
| Co‐interventions avoided or similar? | Unclear risk | There were few reported co‐interventions in the study. |
| Compliance acceptable? | Low risk | Compliance was acceptable based on the reported intensity/dosage, duration, number, and frequency for both the intervention and control group. |
| Timing outcome assessments similar? | Unclear risk | Not mentioned |
Lankhorst 1983.
| Methods | RCT | |
| Participants | 43 participants. 1. Back School treatment group n = 21. 2. Electrotherapy n = 22. Inclusion criteria: idiopathic LBP of more than 6 months duration, not responding to conventional physiotherapy. Exclusion criteria: inflammatory or other specific disorders of the spine such as ankylosing spondylitis, abnormal reflexes, sensory loss, or muscle weakness. |
|
| Interventions | 1. Back School treatment group: Swedish Back School: 4 sessions of 45 minutes each over the course of 2 weeks (anatomy and causes of LBP, function muscles and posture, ergonomics, advice on physical activity). 2. Electrotherapy: 4 sessions with detuned short‐wave diathermy in a period of 2 weeks. |
|
| Outcomes | 1. Pain: mean pain score (on 10‐point scale). | |
| Notes | Setting not specified. Funding: N/A. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The sequence generation procedure or the method of allocation were not mentioned. The title and abstract indicate that it is an RCT. |
| Allocation concealment (selection bias) | Unclear risk | The sequence generation procedure or the method of allocation were not mentioned. The title and abstract indicate that it is an RCT. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No mention of any attempts to blind the participants |
| Blinding (performance bias and detection bias) All outcomes | High risk | No mention of any attempts to blind the care providers |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No mention of any attempts to blind the assessors |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The percentage of withdrawals and dropouts was within the acceptable rate (less than 20%). |
| Intention‐to‐treat Analysis | Unclear risk | Not mentioned |
| Selective reporting (reporting bias) | Unclear risk | It was unclear if the published report included all expected outcomes. |
| Similarity of baseline characteristics? | Low risk | Based on Table 1, participants did not differ in baseline characteristics. |
| Co‐interventions avoided or similar? | Unclear risk | Not mentioned |
| Compliance acceptable? | Unclear risk | There are insufficient data about the control group. |
| Timing outcome assessments similar? | Unclear risk | Not mentioned |
Lønn 1999.
| Methods | RCT | |
| Participants | 81 participants. 1. Active Back School group n = 43. 2. No‐treatment group n = 38. Inclusion criteria: individuals of both genders, 18 to 50 years of age, at least 1 episode of low back pain in the last year, and finished treatment and sick leave at the time of enrolment. Exclusion criteria: previous surgical procedures for LBP, pregnancy. specific rheumatologic diseases, spondylolisthesis, spinal tumour, spinal fracture, drug or alcohol abuse, and documented mental illness. |
|
| Interventions | 1. Active Back School group: 20 sessions of 1 hour each over 13 weeks, consisting of education (anatomy, biomechanics, pathology, ergonomic principles) and exercise (ergonomic, functional, strength and stretching exercises of upper body, pelvis, and leg muscles and joints, simulation of home and work activities). 2. No‐treatment group. |
|
| Outcomes | 1. Pain: overall experienced pain. | |
| Notes | Mixed study setting. Funding: N/A. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The sequence generation procedure or the method of allocation were not mentioned. The title and abstract indicate that it is an RCT |
| Allocation concealment (selection bias) | Unclear risk | The sequence generation procedure or the method of allocation were not mentioned. The title and abstract indicate that it is an RCT |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No mention of any attempts to blind the participants |
| Blinding (performance bias and detection bias) All outcomes | High risk | No mention of any attempts to blind the care providers |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No mention of any attempts to blind the assessors |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The percentage of withdrawals and dropouts was within the acceptable rate (less than 20%). |
| Intention‐to‐treat Analysis | Unclear risk | Not mentioned |
| Selective reporting (reporting bias) | Unclear risk | It was unclear if the published report included all expected outcomes |
| Similarity of baseline characteristics? | Low risk | Based on Table 1, participants did not differ in baseline characteristics |
| Co‐interventions avoided or similar? | Low risk | Balanced for both groups |
| Compliance acceptable? | Low risk | Compliance was acceptable based on the reported intensity/dosage, duration, number, and frequency for both the intervention and control groups |
| Timing outcome assessments similar? | Low risk | All important outcomes assessments for both groups were measured at the same time |
Meng 2009.
| Methods | RCT | |
| Participants | 360 participants. 1. Back School group n = 187. 2. Usual care group n = 173. Inclusion criteria: people with chronic LBP. |
|
| Interventions | 1. Back School group: 7 sessions x 60 minutes. 2. Usual care group: 7 sessions x 60 minutes. |
|
| Outcomes | 1. Pain: numerical pain scale. | |
| Notes | Secondary care setting. Funding: N/A. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The sequence generation procedure or the method of allocation were not mentioned. The title and abstract indicate that it is an RCT. |
| Allocation concealment (selection bias) | Unclear risk | The sequence generation procedure or the method of allocation were not mentioned. The title and abstract indicate that it is an RCT. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No mention of any attempts to blind the participants |
| Blinding (performance bias and detection bias) All outcomes | High risk | No mention of any attempts to blind the care providers |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No mention of any attempts to blind the assessors |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Dropouts exceeded 20% |
| Intention‐to‐treat Analysis | Unclear risk | Not mentioned |
| Selective reporting (reporting bias) | Unclear risk | It was unclear if the published report included all expected outcomes. |
| Similarity of baseline characteristics? | Unclear risk | Not mentioned |
| Co‐interventions avoided or similar? | Low risk | Balanced for both groups |
| Compliance acceptable? | Unclear risk | There are insufficient data about the control group |
| Timing outcome assessments similar? | Unclear risk | Not mentioned |
Morone 2011.
| Methods | RCT | |
| Participants | 62 participants. 1. Back School group n = 41. 2. Usual care group n = 21. Inclusion criteria: age between 18 and 80 years, chronic non‐specific low back pain persisting for at least 3 months. Exclusion criteria: acute low back pain; pain due to a specific cause (e.g. fracture, spondylolisthesis, disc herniation, and lumbar stenosis); scheduled back surgery; severe cognitive impairments; pregnancy; and the presence of concomitant rheumatological, neurological, psychiatric, cardiological, respiratory, or oncological diseases that could affect spine function or alter the perception of pain. |
|
| Interventions | 1. Back School group: 10 sessions x 60 minutes for 4 weeks. 2. Usual care group: same medical and pharmacological assistance as the other group. |
|
| Outcomes | 1. Pain: visual analogue scale. 2. Disability: Oswestry Disability Index. 3. Disability: Waddell Disability Index. |
|
| Notes | Mixed study setting. Funding: N/A. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The sequence generation procedure or the method of allocation were not mentioned. The title, abstract, and flowchart indicate that it is an RCT |
| Allocation concealment (selection bias) | Unclear risk | The sequence generation procedure or the method of allocation were not mentioned. The title, abstract, and flowchart indicate that it is an RCT |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No mention of any attempts to blind the participants |
| Blinding (performance bias and detection bias) All outcomes | High risk | No mention of any attempts to blind the care providers |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | The study is described as a single‐blind RCT, but there is not enough information to determine who was blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The percentage of withdrawals and dropouts was within the acceptable rate (less than 20%) |
| Intention‐to‐treat Analysis | Unclear risk | No information about intention‐to‐treat analysis |
| Selective reporting (reporting bias) | Unclear risk | It was unclear if the published report included all expected outcomes |
| Similarity of baseline characteristics? | Low risk | Participants did not differ in baseline characteristics |
| Co‐interventions avoided or similar? | Unclear risk | Not mentioned |
| Compliance acceptable? | Low risk | Compliance was acceptable based on the reported intensity/dosage, duration, number, and frequency for both the intervention and control groups |
| Timing outcome assessments similar? | Low risk | All important outcomes assessments for both groups were measured at the same time |
Morone 2012.
| Methods | RCT | |
| Participants | 75 participants. 1. Back School group n = 25. 2. Perceptive rehabilitation group n = 25. 3. Control group n = 25. Inclusion criteria: people aged 18 to 75 years with chronic non‐specific low back pain persisting for at least 3 months. Exclusion criteria: acute pain, LBP due to specific cause (fracture, spondylolisthesis, disc herniation, and lumbar stenosis), presence of rheumatological, neurological or oncological concomitant disease, back surgery before study, cognitive impairment (Mini‐Mental State Examination score < 24), and pregnancy. |
|
| Interventions | 1. Back School group: 10 sessions for 4 weeks. Information on anatomy, causes of LBP, ergonomics, exercises, and advice on physical activity. 2. Perceptive rehabilitation group: 20 sessions x 45 minutes for 4 weeks 3. Control group: same medical and pharmacological assistance as the other groups. |
|
| Outcomes | 1. Pain: visual analogue scale. 2. Pain: McGill Pain Questionnaire. 3. Disability: Oswestry Disability Index. 4. Disability: Waddell Disability index. |
|
| Notes | Secondary care setting. Funding: this research received no specific grant from any commercial or public funding agency. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The sequence generation procedure or the method of allocation were not mentioned. The title, abstract, and flowchart indicate that it is an RCT |
| Allocation concealment (selection bias) | Unclear risk | The sequence generation procedure or the method of allocation were not mentioned. The title, abstract, and flowchart indicate that it is an RCT |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No mention of any attempts to blind the participants |
| Blinding (performance bias and detection bias) All outcomes | High risk | No mention of any attempts to blind the care providers |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | The study is described as a single‐blind RCT, but there is not enough information to determine who was blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The percentage of withdrawals and dropouts was within the acceptable rate (less than 20%) |
| Intention‐to‐treat Analysis | Unclear risk | No information about intention‐to‐treat analysis |
| Selective reporting (reporting bias) | Unclear risk | It was unclear if the published report included all expected outcomes |
| Similarity of baseline characteristics? | Low risk | Based on Table 1, participants did not differ in baseline characteristics |
| Co‐interventions avoided or similar? | Low risk | Balanced for both groups |
| Compliance acceptable? | Low risk | Compliance was acceptable based on the reported intensity/dosage, duration, number, and frequency for both the intervention and control groups |
| Timing outcome assessments similar? | Low risk | All important outcomes assessments for both groups were measured at the same time |
Nentwig 1990.
| Methods | RCT | |
| Participants | 74 participants. 1. Back School group n = 32. 2. Waiting‐list group n = 42. Inclusion criteria: degenerative LBP (on a waiting list for a Back School). Exclusion criteria: acute pain, LBP due to specific cause (fracture, spondylolisthesis, disc herniation, and lumbar stenosis), presence of rheumatological, neurological, or oncological concomitant disease, back surgery before study, cognitive impairment (Mini‐Mental State Examination score < 24), and pregnancy. |
|
| Interventions | 1. Back School group: 4 sessions x 2 hours for 4 weeks. 2. Waiting list. |
|
| Outcomes | 1. Pain (own instrument). | |
| Notes | Setting not specified. Funding: N/A. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The sequence generation procedure or the method of allocation were not mentioned. The title and abstract indicate that it is an RCT. |
| Allocation concealment (selection bias) | Unclear risk | The sequence generation procedure or the method of allocation were not mentioned. The title and abstract indicate that it is an RCT. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No mention of any attempts to blind the participants |
| Blinding (performance bias and detection bias) All outcomes | High risk | No mention of any attempts to blind the care providers |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No mention of any attempts to blind the assessors |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not mentioned |
| Intention‐to‐treat Analysis | Low risk | Not mentioned |
| Selective reporting (reporting bias) | Unclear risk | It was unclear if the published report included all expected outcomes. |
| Similarity of baseline characteristics? | Unclear risk | Not mentioned |
| Co‐interventions avoided or similar? | Unclear risk | Not mentioned |
| Compliance acceptable? | Low risk | Compliance was acceptable based on the reported intensity/dosage, duration, number, and frequency for both the intervention and control groups. |
| Timing outcome assessments similar? | Low risk | All important outcomes assessments for both groups were measured at the same time. |
Paolucci 2012b.
| Methods | RCT | |
| Participants | 50 participants. 1. Back School group n = 29. 2. Medical‐assistance group n = 21. Inclusion criteria: age between 18 and 80 years and a diagnosis of chronic non‐specific low back pain. |
|
| Interventions | 1. Back School group: 10 sessions over 4 weeks. First theoretical lesson and then treated 3 times per week for 3 weeks. All sessions lasted 1 hour. Each group included 4 or 5 participants. First session carried out by physicians: education about general anatomical information related to spine, its functioning, and ergonomic positions in daily living, pain concepts, psychological aspects, stress management, workplace situation, and sport activities. 9 sessions carried out by physiotherapist: exercises based on the re‐education of breathing, self stretching trunk muscles, erector spine reinforcement, abdominal reinforcement, and postural exercises. Ergonomic use of the spine in daily life with self correction and how to cope with spine stressing positions during work were explained. 2. Medical assistance. |
|
| Outcomes | 1. Pain: visual analogue scale. 2. Dsability: Oswestry Disability Index. |
|
| Notes | Secondary care setting. Funding: N/A. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The concealed randomisation was performed by means of sealed envelopes |
| Allocation concealment (selection bias) | Low risk | The concealed randomisation was performed by means of sealed envelopes |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No mention of any attempts to blind the participants |
| Blinding (performance bias and detection bias) All outcomes | High risk | No mention of any attempts to blind the care providers |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No mention of any attempts to blind the assessors |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The percentage of withdrawals and dropouts was within the acceptable rate (less than 20%) |
| Intention‐to‐treat Analysis | Unclear risk | Not mentioned |
| Selective reporting (reporting bias) | Unclear risk | It was unclear if the published report included all expected outcomes |
| Similarity of baseline characteristics? | Low risk | Based on Table 1, participants did not differ in baseline characteristics |
| Co‐interventions avoided or similar? | Unclear risk | Not mentioned |
| Compliance acceptable? | Low risk | Compliance was acceptable based on the descriptions of both groups |
| Timing outcome assessments similar? | Low risk | All important outcomes assessments for both groups were measured at the same time |
Paolucci 2012a.
| Methods | RCT | |
| Participants | 30 participants. 1. Back School group n = 15. 2. Perceptive rehabilitation group n = 15. Inclusion criteria: a diagnosis of chronic non‐specific low back pain and age between 18 and 75 years. |
|
| Interventions | 1. Back School group: 10 sessions x 45 minutes for 4 weeks. Comprised an initial lesson on theory and 3 practical sessions per week for 3 weeks. 2. Perceptive rehabilitation group: Utilised a specific tool called "surface for perceptive rehabilitation" composed of about 100 deformable latex cones with a small top, fixed to a rigid surface. Perceptive rehabilitation is a therapeutic system based on the interaction between the patient’s body trunk and a support surface. |
|
| Outcomes | 1. Pain: McGill Pain Questionnaire. | |
| Notes | Secondary care setting. Funding: N/A. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The sequence generation procedure or the method of allocation were not mentioned. The title, abstract, and flowchart indicate that it is an RCT. |
| Allocation concealment (selection bias) | Unclear risk | The sequence generation procedure or the method of allocation were not mentioned. The title, abstract, and flowchart indicate that it is an RCT. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No mention of any attempts to blind the participants |
| Blinding (performance bias and detection bias) All outcomes | High risk | No mention of any attempts to blind the care providers |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No mention of any attempts to blind the assessors |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not mentioned |
| Intention‐to‐treat Analysis | Unclear risk | No mentioned |
| Selective reporting (reporting bias) | Unclear risk | It was unclear if the published report included all expected outcomes. |
| Similarity of baseline characteristics? | Unclear risk | Not mentioned |
| Co‐interventions avoided or similar? | Unclear risk | Not mentioned |
| Compliance acceptable? | Unclear risk | There are insufficient data about the control group. |
| Timing outcome assessments similar? | Low risk | All important outcomes assessments for both groups were measured at the same time. |
Penttinen 2002.
| Methods | RCT | |
| Participants | 93 participants. 1. Back School group n = 47. 2. Fitness training n = 46. Inclusion criteria: age between 35 and 50 years, non‐specific back pain (excluded if an exact diagnosis was present), gradual development of back pain lasting at least 1 month at the time of selection, no medical problems preventing physical training, and full consent to participate in the Back School. Exclusion criteria: not described. |
|
| Interventions | 1. Back School group: 21 sessions (8 supervised and 13 voluntary group meetings) of 85 minutes each over 10 weeks. Swedish type of Back School including fitness training (muscle force, endurance, and stretching exercises for upper and lower back, trunk flexors, upper arm and leg muscles, and ergonomic work techniques), group discussions (structure, functioning and strain of the back, lifting, principles of physical exercises during leisure time and at work), and extra meetings consisting of physical training and social intercourse. 2. Fitness training: 10 sessions of 1 hour each over 5 weeks. |
|
| Outcomes | 1. Disability: Oswestry Disability Questionnaire. | |
| Notes | Occupational setting. Funding: N/A. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The sequence generation procedure or the method of allocation were not mentioned. The title and abstract indicate that it is an RCT. |
| Allocation concealment (selection bias) | Unclear risk | The sequence generation procedure or the method of allocation were not mentioned. The title and abstract indicate that it is an RCT. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No mention of any attempts to blind the participants |
| Blinding (performance bias and detection bias) All outcomes | High risk | No mention of any attempts to blind the care providers |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No mention of any attempts to blind the assessors |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Dropouts exceeded 20%. |
| Intention‐to‐treat Analysis | Unclear risk | Not mentioned |
| Selective reporting (reporting bias) | Unclear risk | It was unclear if the published report included all expected outcomes. |
| Similarity of baseline characteristics? | Low risk | Based on Table 1, participants did not differ in baseline characteristics. |
| Co‐interventions avoided or similar? | Unclear risk | There were few reported co‐interventions in the study. |
| Compliance acceptable? | Unclear risk | There are insufficient data about the control group. |
| Timing outcome assessments similar? | Low risk | All important outcomes assessments for both groups were measured at the same time. |
Postacchini 1988.
| Methods | RCT | |
| Participants | 240 participants. 1. Back School treatment group n = 50. 2. Spinal manipulation by chiropractor group n = 52. 3. Usual care n = 47. 4. Physiotherapy group n = 91. Inclusion criteria: continuous or almost continuous back pain lasting more than 2 months; episode of acute pain on a chronic history of pain. Exclusion criteria: LBP related to neoplastic diseases of the spine; pregnant or nursing women; people with serious general diseases. |
|
| Interventions | 1. Back School treatment group: based on Canadian Back Education Unit: 4, 1‐hour sessions in a 1‐week period (including muscle exercises). 2. Spinal manipulation by chiropractor: daily for the first week and then twice a week for 6 weeks. 3. Usual care: drug therapy, non‐steroidal anti‐inflammatory drugs (15 to 20 days). 4. Physiotherapy: physiotherapy, light massage, analgesic currents and diathermy daily for 3 weeks. |
|
| Outcomes | 1. Pain: visual analogue scale. | |
| Notes | Secondary care setting. Funding: N/A. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The sequence generation procedure or the method of allocation were not mentioned. The title and abstract indicate that it is an RCT. |
| Allocation concealment (selection bias) | Unclear risk | The sequence generation procedure or the method of allocation were not mentioned. The title and abstract indicate that it is an RCT. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No mention of any attempts to blind the participants |
| Blinding (performance bias and detection bias) All outcomes | High risk | No mention of any attempts to blind the care providers |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No mention of any attempts to blind the assessors |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The percentage of withdrawals and dropouts was within the acceptable rate (less than 20%). |
| Intention‐to‐treat Analysis | Unclear risk | Not mentioned |
| Selective reporting (reporting bias) | Unclear risk | It was unclear if the published report included all expected outcomes. |
| Similarity of baseline characteristics? | Unclear risk | Not mentioned |
| Co‐interventions avoided or similar? | Unclear risk | Not mentioned |
| Compliance acceptable? | Unclear risk | There are insufficient data about the control group. |
| Timing outcome assessments similar? | Unclear risk | Not mentioned |
Ribeiro 2008.
| Methods | RCT | |
| Participants | 55 participants. 1. Back School group n = 26. 2. Medical assistance n = 29. Inclusion criteria: aged 18 to 65 years diagnosed with chronic non‐specific low back pain with mechanical characteristics lasting more than 3 months. Exclusion criteria: previous back surgery, spinal tumour, spinal fracture, pregnancy, fibromyalgia, inflammatory or infectious spinal diseases, and litigant patients. |
|
| Interventions | 1. Back School group: 3 sessions during 2 months. Orientation was given regarding the anatomy and physiology of the spine, causes and treatment of low back pain, and ergonomic guidelines relevant to back problems. Abdominal and back strengthening exercises were also performed. 2. Medical assistance. |
|
| Outcomes | 1. Pain: visual analogue scale. 2. Disability: Roland‐Morris Disability Questionnaire. |
|
| Notes | Secondary care setting. Funding: 2 authors (DCR and DA) received support from the University of Otago (University of Otago Doctoral Scholarship). |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Folded pieces of paper indicating 1 of the groups were placed in sealed envelopes which were placed in a container. Another investigator selected the envelopes to determine to which group individual participants would belong. |
| Allocation concealment (selection bias) | Low risk | Folded pieces of paper indicating 1 of the groups were placed in sealed envelopes which were placed in a container. Another investigator selected the envelopes to determine to which group individual participants would belong. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No mention of any attempts to blind the participants |
| Blinding (performance bias and detection bias) All outcomes | High risk | No mention of any attempts to blind the care providers |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Participants were assessed by an investigator (physiotherapist) blinded to treatment groups. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The percentage of withdrawals and dropouts was within the acceptable rate (less than 20%). |
| Intention‐to‐treat Analysis | High risk | Participants who failed to complete all 4 assessments were also considered dropouts and were excluded from the statistical analysis. |
| Selective reporting (reporting bias) | Unclear risk | It was unclear if the published report included all expected outcomes. |
| Similarity of baseline characteristics? | Low risk | Based on Table 1, participants did not differ in baseline characteristics. |
| Co‐interventions avoided or similar? | Unclear risk | Not mentioned |
| Compliance acceptable? | Low risk | Compliance was acceptable based on the reported intensity/dosage, duration, number, and frequency for both the intervention and control groups. |
| Timing outcome assessments similar? | Low risk | All important outcomes assessments for both groups were measured at the same time. |
Sahin 2011.
| Methods | RCT | |
| Participants | 146 participants. 1. Back School group n = 73. 2. Exercise group n = 73. Inclusion criteria: non‐specific low back pain for longer than 12 weeks without neurological deficits. Exclusion criteria: people who had continuous pain, age ≤ 18 years, those who had already attended the Back School programme, those who had previously undergone surgery, who had structural anomalies, spinal cord compressions, severe instabilities, severe osteoporosis, acute infections, severe cardiovascular or metabolic diseases, who were pregnant, and those with a body mass index above 30 kg/m2. |
|
| Interventions | 1. Back School group: 4 sessions x 60 minutes for 2 weeks, participants received exercise, physical treatment modalities, and a Back School programme. 2. Exercise group: received exercise and physical treatment modalities. |
|
| Outcomes | 1. Pain: visual analogue scale. 2. Disability: Oswestry Disability Index. |
|
| Notes | Funding: N/A. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Concealed randomisation was conducted using sealed, opaque envelopes coded according to a computerised random number generator. |
| Allocation concealment (selection bias) | Low risk | Concealed randomisation was conducted using sealed, opaque envelopes coded according to a computerised random number generator. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No mention of any attempts to blind the participants |
| Blinding (performance bias and detection bias) All outcomes | High risk | No mention of any attempts to blind the care providers |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | All participants were examined by the same physician, who was blind to the type of therapy. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The percentage of withdrawals and dropouts was within the acceptable rate (less than 20%). |
| Intention‐to‐treat Analysis | Unclear risk | Not mentioned |
| Selective reporting (reporting bias) | Unclear risk | It was unclear if the published report included all expected outcomes. |
| Similarity of baseline characteristics? | Low risk | Based on Table 1, participants did not differ in baseline characteristics. |
| Co‐interventions avoided or similar? | Low risk | Balanced for both groups |
| Compliance acceptable? | Low risk | Compliance was acceptable based on the reported intensity/dosage, duration, number, and frequency for both the intervention and control groups. |
| Timing outcome assessments similar? | Low risk | All important outcomes assessments for both groups were measured at the same time. |
Tavafian 2007.
| Methods | RCT | |
| Participants | 102 participants. 1. Back School group n = 50. 2. Medical assistance n = 52. Inclusion criteria: age 18 years and over, suffering from chronic back pain (persisting for 90 days or more), and having a telephone number for regular contact with a responsible caregiver. Exclusion criteria: back surgery within the 2 years prior to the initial observation, or if the complaint was restricted to the sacroiliac joint or the cervical or thoracic regions, or if there was congenital spine disease. People with a low back complaint that had persisted less than 90 days were also excluded. |
|
| Interventions | 1. Back School group: 5 sessions for 4 days. Multidimensional and interdisciplinary educational regimen designed to assess each patient's physical condition, personal characteristics, lifestyle, and subsequent ability to cope. The program utilises an empowerment approach, providing a combination of knowledge, skills, and heightened self awareness regarding values and needs, so that patients can define and achieve their own goals. 2. Medical assistance: only medication. |
|
| Outcomes | 1. Pain: subscale of 36‐Item Short Form Health Survey (SF‐36). | |
| Notes | Secondary care setting. Funding: N/A. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The sequence generation procedure or the method of allocation were not mentioned. The title, abstract, and flowchart indicate that it is an RCT. |
| Allocation concealment (selection bias) | High risk | The treatment allocation was not concealed. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants were not blinded to the intervention. |
| Blinding (performance bias and detection bias) All outcomes | High risk | No mention of any attempts to blind the care providers |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No mention of any attempts to blind the assessors |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The percentage of withdrawals and dropouts was within the acceptable rate (less than 20%). |
| Intention‐to‐treat Analysis | Low risk | The study used an intention‐to‐treat analysis. |
| Selective reporting (reporting bias) | Unclear risk | It was unclear if the published report included all expected outcomes. |
| Similarity of baseline characteristics? | Low risk | Participants did not differ in baseline characteristics. |
| Co‐interventions avoided or similar? | Low risk | Co‐interventions were avoided for both groups. |
| Compliance acceptable? | Low risk | Compliance was acceptable based on the descriptions of both groups. |
| Timing outcome assessments similar? | Low risk | All important outcomes assessments for both groups were measured at the same time. |
ADL: activities of daily living LBP: low back pain N/A: not applicable RCT: randomised controlled trial
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Bergquist 1977 | The average time of symptoms in the inclusion criteria was characterised as acute LBP. |
| Cecchi 2010b | Back School intervention consisted of education only, without exercises. |
| Demoulin 2006 | The intervention was not considered to be Back School. |
| Herzog 1991 | The average time of symptoms in the inclusion criteria was characterised as acute LBP. |
| Hsieh 2002 | The average time of symptoms in the inclusion criteria was characterised as acute LBP. |
| Härkäpää 1989 | Back School intervention consisted of education only, without exercises. |
| Härkäpää 1990 | Back School intervention consisted of education only, without exercises. |
| Indahl 1995 | The average time of symptoms in the inclusion criteria was characterised as acute LBP. |
| Indahl 1998 | Back School intervention consisted of education only, without exercises. |
| Leclaire 1996 | The average time of symptoms in the inclusion criteria was characterised as acute LBP. |
| Lindequist 1984 | The average time of symptoms in the inclusion criteria was characterised as acute LBP. |
| Linton 1989 | The intervention was not considered to be Back School. |
| Maul 2005 | Back School intervention consisted of education only, without exercises. |
| Mele 2006 | Back School intervention consisted of education only, without exercises. |
| Meng 2011 | The Back School intervention was not a clear contrast for the control group. |
| Morrison 1988 | Each group was assessed once, the control group at the beginning of the programme and the Back School group at the end. |
| Sadeghi‐Abdollahi 2012 | The results are for a single group. |
| Tavafian 2008 | The intervention was not considered to be Back School. |
| Yang 2010 | The intervention was not considered to be Back School. |
LBP: low back pain
Characteristics of studies awaiting assessment [ordered by study ID]
Garcia 2016.
| Methods | Randomised controlled trial |
| Participants | 148 people with a diagnosis of chronic low back pain for at least 3 months. |
| Interventions | 1. Back School group: 4 sessions x 60 minutes for 4 weeks. Participants allocated to this group received theoretical and practical information during the treatment sessions. The first session was conducted individually, and the 3 remaining sessions were conducted in groups. 2. McKenzie Method group: 4 sessions x 60 minutes for 4 weeks. Participants allocated to this group received theoretical information regarding the care of the spine and performed specific exercises according to the direction of preference of movement according to the McKenzie Method. |
| Outcomes | 1. Pain: numerical pain scale. 2. Disability: Roland‐Morris Disability Questionnaire. 3. Adverse events: reported by the physiotherapists on standardised forms. |
| Notes |
Paolucci 2016.
| Methods | Randomised controlled trial |
| Participants | 53 people with a diagnosis of chronic low back pain for at least 3 months. |
| Interventions | 1. Experimental group: Participants were treated in outpatient with a Back School programme. Each group consisted of 4 or 5 people who underwent the rehabilitation treatment twice a week for 5 consecutive weeks for a total of 10 sessions, each lasting about 1 hour. 2. Control group: Participants were treated in outpatient with the Feldenkrais Method. Each group consisted of 4 or 5 people who underwent the rehabilitation treatment twice a week for 5 consecutive weeks for a total of 10 sessions, each lasting about 1 hour. |
| Outcomes | 1. Pain: visual analogue scale and McGill Pain Questionnaire. 2. Disability: Waddell Disability Index. 3. Quality of life: 36‐Item Short Form Health Survey. 4. Mind‐body interactions: Multidimensional Assessment of Interoceptive Awareness Questionnaire. |
| Notes | No funding was received in support of this work. Adverse events: not evaluated. |
Characteristics of ongoing studies [ordered by study ID]
IRCT201010184251N2.
| Trial name or title | The effect of lumbar care (based on Back School) on nursing staff’s low back pain and functional disability |
| Methods | Clinical trial, 2 arms, randomised controlled, single‐blind |
| Participants | Individuals diagnosed with chronic low back pain. Inclusion criteria: nursing licence, work at hospital in the morning shift during the study, low back pain (based on self report). Exclusion criteria: does not follow the training, underwent back surgery within previous 2 years, congenital and inflammatory spine disease, pregnancy, severe osteoporosis (based on medical records). |
| Interventions | Intervention: a 3‐hour lumbar care workshop based on Back School method. Control: routine care. |
| Outcomes | 1. Functional disability: Roland‐Morris Disability Questionnaire. 2. Pain: visual analogue scale. |
| Starting date | 06 September 2015 |
| Contact information | Name: Mehdi Pakbaz Address: Kodakyar Ave., Daneshjo Blvd., Evin, Post code: 1985713834, Tehran, Iran Email: ma.pakbaz@uswr.ac.ir; mehdi_pakbaz@live.com Affiliation: University of Social Welfare and Rehabilitation Sciences |
| Notes |
Differences between protocol and review
In 2015 we published a new protocol for this review.
We stratified ‘other treatments’ into medical care, passive physiotherapy, and exercise because we considered these treatments to be sufficiently different that they should be evaluated separately. We classified the intensity of the interventions and clarified how adverse events would be measured. We planned a sensitivity analysis using different cut‐off points, i.e. high quality defined as either five or seven of the 11 items scored positive. However, during the execution of the review, we were guided by the Cochrane group to examine all studies on five types of biases and not the 11 internal validity criteria. Based on that, it was impracticable run the sensitivity analyses. We updated the methods to be in line with the Furlan 2015 method guidelines.
Contributions of authors
Final approval of the protocol: all authors
Collection and assembly of data: Patricia Parreira, Bart W Koes, and Nolwenn Poquet
Analysis and interpretation of the data: Patricia Parreira, Martijn W Heymans, Maurits van Tulder, Rosmin Esmail, Bart W Koes, Chung‐Wei Christine Lin, Nolwenn Poquet, and Chris G Maher
Drafting of the article: Patricia Parreira, Nolwenn Poquet, and Chris G Maher
Final approval of the article: all authors
Sources of support
Internal sources
Christopher Maher has a senior research fellowship by the National Health and Medical Research Council, Australia.
Patricia Parreira is supported by CAPES (Coordenação de Aperfeiçoamento de Pessoal de Nível Superior), Brazil.
Chung‐Wei Christine Lin has a Career Development Fellowship from the National Health and Medical Research Council, Australia.
External sources
VU University Medical Center, Netherlands.
The George Institute for Global Health, Sydney Medical School, The University of Sydney, Australia.
Declarations of interest
PP, MH, RE, BK, NP, CL have no conflicts of interest.
Two review authors (CM and MvT) are on the Editorial Board of the Cochrane Back and Neck Review Group. Editors are required to conduct at least one Cochrane review, which ensures that they are aware of the processes and commitment needed to conduct reviews.
New
References
References to studies included in this review
Andrade 2008 {published data only}
- Andrade SC, Araújo AG, Vilar MJ. Back school for patients with non‐specific chronic low‐back pain: benefits from the association of an exercise program with patient's education. Acta Reumatologica Portuguesa 2008;33:443‐50. [PubMed] [Google Scholar]
Berwick 1989 {published data only}
- Berwick DM, Budman S, Feldstein M. No clinical effect of back schools in an HMO. A randomized prospective trial. Spine 1989;14:339‐44. [DOI] [PubMed] [Google Scholar]
Cecchi 2010a {published data only}
- Cecchi F, Molino‐Lova R, Chiti M, Pasquini G, Paperini A, Conti AA, et al. Spinal manipulation compared with back school and with individually delivered physiotherapy for the treatment of chronic low back pain: a randomized trial with one‐year follow‐up. Clinical Rehabilitation 2010;24:26‐36. [DOI] [PubMed] [Google Scholar]
Costantino 2014 {published data only}
- Costantino C, Romiti D. Effectiveness of Back School program versus hydrotherapy in elderly patients with chronic non‐specific low back pain: a randomized clinical trial. Acta Bio Medica 2014;85(3):52‐61. [PubMed] [Google Scholar]
Dalichau 1999 {published data only}
- Dalichau S, Perrey RM, Solbach T, Elliehausen H‐J. Experience in the implementation of a professional back‐school model in the construction industry [Erfahrungen bei der Durchführung eines berufsbezogenen Rückenschulmodells im Baugewerbe]. Zentralblatt für Arbeitsmedizin 1998;48:72‐80. [Google Scholar]
- Dalichau S, Scheele K, Perrey RM, Elliehausen H‐J, Huebner J. Ultrasonic supported posture and motion analysis of the lumbar spine to demonstrate the effectiveness of a back school [Ultraschallgestützte Haltungs‐ und Bewegungsanalyse der Lendenwirbelsäule zum Nachweis der Wirksamkeit einer Rückenschule]. Zentralblatt für Arbeitsmedizin 1999;49:148‐56. [Google Scholar]
Devasahayam 2014 {published data only}
- Devasahayam A, Lim C, Goh M, Lim You J, Ying Pua P. Delivering a Back School programme with a cognitive behavioural modification: a randomised pilot trial on patients with chronic nonspecific low back pain and functional disability. Proceedings of Singapore Healthcare 2014;23(3):218‐25. [Google Scholar]
Donchin 1990 {published data only}
- Donchin M, Woolf O, Kaplan L, Floman Y. Secondary prevention of low‐back pain. A clinical trial. Spine 1990;15:1317‐20. [DOI] [PubMed] [Google Scholar]
Donzelli 2006 {published data only}
- Donzelli S, Domenica F, Cova AM, Galletti R, Giunta N. Two different techniques in the rehabilitation treatment of low back pain: a randomized controlled trial. Europa Medicophysica 2006;42:205‐10. [PubMed] [Google Scholar]
Dufour 2010 {published data only}
- Dufour N, Thamsborg G, Oefeldt A, Lundsgaard C, Stender S. Treatment of chronic low back pain: a randomized, clinical trial comparing group‐based multidisciplinary biopsychosocial rehabilitation and intensive individual therapist‐assisted back muscle strengthening exercises. Spine 2010;35:469‐76. [DOI] [PubMed] [Google Scholar]
Durmus 2014 {published data only}
- Durmus D, Unal M, Kuru O. How effective is a modified exercise program on its own or with back school in chronic low back pain? A randomized‐controlled clinical trial. Journal of Back and Musculoskeletal Rehabilitation 2014;27(4):553‐61. [DOI] [PubMed] [Google Scholar]
Garcia 2013 {published data only}
- Garcia AN, Costa Lda C, Silva TM, Gondo FL, Cyrillo FN, Costa RA, et al. Effectiveness of back school versus McKenzie exercises in patients with chronic nonspecific low back pain: a randomized controlled trial. Physical Therapy 2013;93:729‐47. [DOI] [PubMed] [Google Scholar]
- Garcia AN, Costa Lda C, Silva TM, Gondo FL, Cyrillo FN, Costa RA, et al. Effects of two physical therapy interventions in patients with chronic non‐specific low back pain: feasibility of a randomized controlled trial. Brazilian Journal of Physical Therapy 2011;15:420‐7. [DOI] [PubMed] [Google Scholar]
Heymans 2006 {published data only}
- Heymans MW, Vet HCW, Bongers PM, Knol DL, Koes BW, Mechelen W. The effectiveness of high‐intensity versus low‐intensity back schools in an occupational setting: a pragmatic randomized controlled trial. Spine 2006;31:1075‐82. [DOI] [PubMed] [Google Scholar]
Hurri 1989 {published data only}
- Hurri H. The Swedish back school in chronic low‐back pain. Part I. Benefits. Scandinavian Journal of Rehabilitation Medicine 1989;21:33‐40. [PubMed] [Google Scholar]
- Hurri H. The Swedish back school in chronic low‐back pain. Part II. Factors predicting the outcome. Scandinavian Journal of Rehabilitation Medicine 1989;21:41‐4. [PubMed] [Google Scholar]
- Julkunen J, Hurri H, Kankainen J. Psychological factors in the treatment of chronic low back pain. Psychotherapy and Psychosomatics 1988;50:173‐81. [DOI] [PubMed] [Google Scholar]
Jaromi 2012 {published data only}
- Jaromi M, Nemeth A, Kranicz J, Laczko T, Betlehem J. Treatment and ergonomics training of work‐related lower back pain and body posture problems for nurses. Journal of Clinical Nursing 2012;21:1776‐84. [DOI] [PubMed] [Google Scholar]
Keijsers 1989 {published data only}
- Keijsers JFEM, Groenman NH, Gerards FM, Oudheusden E, Steenbakkers M. A back school in the Netherlands: Evaluating the results. Patient Education & Counseling 1989;14:31‐44. [DOI] [PubMed] [Google Scholar]
Keijsers 1990 {published data only}
- Keijsers JFME, Steenbakkers WHL, Meertens RM, Bouter LM, Kok GJ. The efficacy of the back school: A randomized trial. Arthritis Care and Research 1990;3:204‐9. [Google Scholar]
Klaber Moffett 1986 {published data only}
- Klaber Moffett JA, Chase SM, Portek I, Ennis JR. A controlled prospective study to evaluate the effectiveness of a back school in the relief of chronic low‐back pain. Spine 1986;11:120‐2. [DOI] [PubMed] [Google Scholar]
Lankhorst 1983 {published data only}
- Lankhorst GJ, Stadt RJ, Vogelaar TW, Korst JK, Prevo AJH. The effect of the Swedish back school in chronic idiopathic low‐back pain. Scandinavian Journal of Rehabilitation Medicine 1983;15:141‐5. [PubMed] [Google Scholar]
Lønn 1999 {published data only}
- Glomsrød B, Lønn JH, Soukup MG, Bø K, Larsen S. Active back school, prophylactic management for low back pain: Three‐year follow‐up of a randomized controlled trial. Journal of Rehabilitation Medicine 2001;33:26‐30. [DOI] [PubMed] [Google Scholar]
- Lønn JH, Glomsrød B, Soukup MG, Bø K, Larsen S. Active back school: Prophylactic management for low back pain. A randomized controlled 1‐year follow‐up study. Spine 1999;24:865‐71. [DOI] [PubMed] [Google Scholar]
Meng 2009 {published data only}
- Meng K, Seekatz B, Rossband H, Worringen U, Faller H, Vogel H. Development of a standardized back school for in‐patient orthopaedic rehabilitation. Rehabilitation 2009;48:335‐44. [DOI] [PubMed] [Google Scholar]
Morone 2011 {published data only}
- Morone G, Paolucci T, Alcuri MR, Vulpiani MC, Matano A, Bureca I, et al. Quality of life improved by multidisciplinary back school program in patients with chronic non‐specific low back pain: a single blind randomized controlled trial. European Journal of Physical & Rehabilitation Medicine 2011;47:533‐41. [PubMed] [Google Scholar]
Morone 2012 {published data only}
- Morone G, Iosa M, Paolucci T, Fusco A, Alcuri R, Spadini E, et al. Efficacy of perceptive rehabilitation in the treatment of chronic nonspecific low back pain through a new tool: a randomized clinical study. Clinical Rehabilitation 2012;26:339‐50. [DOI] [PubMed] [Google Scholar]
Nentwig 1990 {published data only}
- Nentwig CG, Ullrich CH. Effectiveness of a behavioral training for spinal column patients: a prospective controlled study [Wirksamkeit eines Verhaltenstrainings fur Wirbelsaulen patienten: eine prospektive kontrollierte studie]. Orthopädie und orthopädische Chirurgie 1990;3:888‐92. [Google Scholar]
Paolucci 2012a {published data only}
- Paolucci T, Fusco A, Iosa M, Grasso MR, Spadini E, Paolucci S, et al. The efficacy of a perceptive rehabilitation on postural control in patients with chronic nonspecific low back pain. International Journal of Rehabilitation Research 2012;35:360‐6. [DOI] [PubMed] [Google Scholar]
Paolucci 2012b {published data only}
- Paolucci T, Morone G, Iosa M, Fusco A, Alcuri R, Matano A, et al. Psychological features and outcomes of the Back School treatment in patients with chronic non‐specific low back pain. A randomized controlled study. European Journal of Physical & Rehabilitation Medicine 2012;48:245‐53. [PubMed] [Google Scholar]
Penttinen 2002 {published data only}
- Penttinen J, Nevala‐Puranen N, Airaksinen O, Jaaskelainen M, Sintonen H, Takala J. Randomized controlled trial of back school with and without peer support. Journal of Occupational Rehabilitation 2002;12:21‐9. [DOI] [PubMed] [Google Scholar]
Postacchini 1988 {published data only}
- Postacchini F, Facchini M, Palieri P. Efficacy of various forms of conservative treatment in low‐back pain. A comparative study. Neuro‐Orthopedics 1988;6:28‐35. [Google Scholar]
Ribeiro 2008 {published data only}
- Ribeiro LH, Jennings F, Jones A, Furtado R, Natour J. Effectiveness of a back school program in low back pain. Clinical & Experimental Rheumatology 2008;26:81‐8. [PubMed] [Google Scholar]
Sahin 2011 {published data only}
- Sahin N, Albayrak I, Durmus B, Ugurlu H. Effectiveness of back school for treatment of pain and functional disability in patients with chronic low back pain: a randomized controlled trial. Journal of Rehabilitation Medicine 2011;43:224‐9. [DOI] [PubMed] [Google Scholar]
Tavafian 2007 {published data only}
- Tavafian SS, Jamshidi A, Mohammad K, Montazeri A. Low back pain education and short term quality of life: a randomized trial. BMC Musculoskeletal Disorders 2007;8:1‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies excluded from this review
Bergquist 1977 {published data only}
- Bergquist‐Ullman M, Larsson U. Acute low‐back pain in industry. Acta Orthopaedica Scandinavica 1977;170:1‐117. [DOI] [PubMed] [Google Scholar]
Cecchi 2010b {published data only}
- Cecchi F, Molino‐Lova R, Chiti M, Pasquini G, Paperini A, Conti AA, et al. Spinal manipulation provides better short and long‐term reduction in pain and disability for patients with non‐specific chronic low back pain. Clinical Rehabilitation 2010;24:26‐36. [DOI] [PubMed] [Google Scholar]
Demoulin 2006 {published data only}
- Demoulin C, Tomasella M, Croisier J‐L, Crielaard J‐M, Vanderthommen M. Benefits of a physical training program after back school for chronic low back pain patients. Journal of Musculoskeletal Pain 2006;14:21‐31. [Google Scholar]
Härkäpää 1989 {published data only}
- Härkäpää K, Järvikoski A, Mellin G, Hurri H. A controlled study on the outcome of inpatient and outpatient treatment of low back pain. Part I. Pain, disability, compliance, and reported treatment benefits three months after treatment. Scandinavian Journal of Rehabilitation Medicine 1989;21(2):81‐9. [PubMed] [Google Scholar]
Härkäpää 1990 {published data only}
- Härkäpää K, Mellin G, Järvikoski A, Hurri H. A controlled study on the outcome of inpatient and outpatient treatment of low back pain. Part III. Long‐term follow‐up of pain, disability, and compliance. Scandinavian Journal of Rehabilitation Medicine 1990;22(4):181‐8. [PubMed] [Google Scholar]
Herzog 1991 {published data only}
- Herzog W, Conway PJW, Willcox BJ. Effects of different treatment modalities on gait symmetry and clinical measures for sacroiliac joint patients. Journal of Manipulative and Physiological Therapeutics 1991;14:104‐9. [PubMed] [Google Scholar]
Hsieh 2002 {published data only}
- Hsieh CY, Adams AH, Tobis J, Hong CZ, Danielson C, Platt K, et al. Effectiveness of four conservative treatments for subacute low back pain: A randomized clinical trial. Spine 2002;27:1142‐8. [DOI] [PubMed] [Google Scholar]
Indahl 1995 {published data only}
- Indahl A, Haldorsen EH, Holm S, Reikeras O, Ursin H. Five‐year follow‐up study of a controlled clinical trial using light mobilization and an informative approach to low back pain. Spine 1998;23:2625‐30. [DOI] [PubMed] [Google Scholar]
- Indahl A, Velund L, Reikeraas O. Good prognosis for low back pain when left untampered. A randomized clinical trial. Spine 1995;20:473‐7. [DOI] [PubMed] [Google Scholar]
Indahl 1998 {published data only}
- Indahl A, Haldorsen EH, Holm S, Reikeras O, Ursin H. Five‐year follow‐up study of a controlled clinical trial using light mobilization and an informative approach to low back pain. Spine 1998;23(23):2625‐30. [DOI] [PubMed] [Google Scholar]
Leclaire 1996 {published data only}
- Leclaire R, Esdaile JM, Suissa S, Rossignol M, Proulx R, Dupuis M. Back school in a first episode of compensated acute low back pain: a clinical trial to assess efficacy and prevent relapse. Archives of Physical Medicine and Rehabilitation 1996;77:673‐9. [DOI] [PubMed] [Google Scholar]
Lindequist 1984 {published data only}
- Lindequist SL, Lundberg B, Wikmark R, Bergstad B, Loof G, Ottermark AC. Information and regime at low‐back pain. Scandinavian Journal of Rehabilitation Medicine 1984;16:113‐6. [PubMed] [Google Scholar]
Linton 1989 {published data only}
- Linton SJ, Bradley LA, Jensen I, Spangfort E, Sundell L. The secondary prevention of low back pain: a controlled study with follow‐up. Pain 1989;36:197‐207. [DOI] [PubMed] [Google Scholar]
Maul 2005 {published data only}
- Maul I, Oliveri M, Krueger H. Long‐term effects of supervised physical training in secondary prevention of low back pain. European Spine Journal 2005;14:599‐611. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mele 2006 {published data only}
- Mele G, Domenica F, Locati F, Gattoronchieri V, Silingardi M. Rehabilitation, physical therapy or Back School. Reumatismo 2006;28:102‐5. [PubMed] [Google Scholar]
Meng 2011 {published data only}
- Meng K, Seekatz B, Roband H, Worringen U, Vogel H, Faller H. Intermediate and long‐term effects of a standardized back school for inpatient orthopedic rehabilitation on illness knowledge and self‐management behaviours: a randomized controlled trial. Clinical Journal of Pain 2011;27:248‐57. [DOI] [PubMed] [Google Scholar]
Morrison 1988 {published data only}
- Morrison GEC, Chase W, Young V, Roberts WL. Back pain. Treatment and prevention in a community hospital. Archives of Physical Medicine and Rehabilitation 1988;69:605‐9. [PubMed] [Google Scholar]
Sadeghi‐Abdollahi 2012 {published data only}
- Sadeghi‐Abdollahi B, Eshaghi A, Hosseini SN, Ghahremani M, Davatchi F. The efficacy of Back School on chronic low back pain of workers of a pharmaceutical company in a Tehran suburb. International Journal of the Rheumatic Diseases 2012;15:144‐53. [DOI] [PubMed] [Google Scholar]
Tavafian 2008 {published data only}
- Tavafian SS, Jamshidi AR, Montazeri A. A randomized study of back school in women with chronic low back pain: quality of life at three, six, and twelve months follow‐up. Spine 2008;33(15):1617‐21. [DOI] [PubMed] [Google Scholar]
Yang 2010 {published data only}
- Yang EJ, Park WB, Shin HI, Lim JY. The effect of back school integrated with core strengthening in patients with chronic low‐back pain. American Journal of Physical Medicine & Rehabilitation 2010;89:744‐54. [DOI] [PubMed] [Google Scholar]
References to studies awaiting assessment
Garcia 2016 {published data only}
- Garcia A, Costa LCM, Hancock M, Costa L. Identifying patients with chronic low back pain who respond best to mechanical diagnosis and therapy: secondary analysis of a randomized controlled trial. Physical Therapy 2016;96(5):623‐30. [DOI] [PubMed] [Google Scholar]
Paolucci 2016 {published data only}
- NCT02231554. Feldenkrais vs back school for treating chronic low back pain: a randomized controlled trial. clinicaltrials.gov/ct2/show/NCT02231554 (first received 8 August 2014).
- Paolucci T, Zangrando F, Iosa M, Angelis S, Marzoli C, Piccinini G, et al. Improved interoceptive awareness in chronic low back pain: a comparison of Back school versus Feldenkrais method. Disability & Rehabilitation 2016;23(1):8. [DOI] [PubMed] [Google Scholar]
References to ongoing studies
IRCT201010184251N2 {published data only}
- IRCT2015093024277N1. The effect of lumbar care (based on Back School) on nursing staff’s low back pain and functional disability. http://apps.who.int/trialsearch/Trial2.aspx?TrialID=IRCT2015093024277N1 (first received 25 November 2015).
Additional references
Airaksinen 2006
- Airaksinen O, Brox JI, Cedraschi C, Hildebrandt J, Klaber‐Moffett J, Kovacs F. Chapter 4. European guidelines for the management of chronic nonspecific low back pain. European Spine Journal 2006;15(Suppl 2):s169–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
Duffy 2014
- Duffy S, Misso K, Noake C, Ross J, Stirk L. Supplementary searches of PubMed to improve currency of MEDLINE and MEDLINE In‐Process searches via OvidSP. Kleijnen Systematic Reviews Ltd, York. Poster presented at the UK InterTASC Information Specialists' Sub‐Group (ISSG) Workshop; 2014 July 9; Exeter: UK. medicine.exeter.ac.uk/media/universityofexeter/medicalschool/research/pentag/documents/Steven_Duffy_ISSG_Exeter_2014_poster_1.pdf (accessed 6 August 2014).
European Guidelines 2006
- COST Action B13 Working Group. European Guidelines for the Management of Non‐Specific Low Back Pain. European Spine Journal 2006;15(Suppl 2):S1‐S300. [Google Scholar]
Forssell 1980
- Forssell MZ. The Swedish back school. Physiotherapy 1980;66:112‐4. [PubMed] [Google Scholar]
Forssell 1981
- Forssell MZ. The back school. Spine 1981;6:104‐6. [DOI] [PubMed] [Google Scholar]
Furlan 2015
- Furlan AD, Malmivaara A, Chou R, Maher CG, Deyo RA, Schoene M, et al. 2015 Updated Method Guideline for Systematic Reviews in the Cochrane Back and Neck Group. Spine 2015;40(21):1660‐73. [DOI] [PubMed] [Google Scholar]
Hayden 2005
- Hayden JA, Tulder MW, Malmivaara A, Koes BW. Exercise therapy for treatment of non‐specific low back pain. Cochrane Database of Systematic Reviews 2005, Issue 3. [DOI: 10.1002/14651858.CD000335.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Mueller 2007
- Mueller PS, Montori VM, Bassler D, Koenig BA, Guyatt GH. Ethical issues in stopping randomized trials early because of apparent benefit. Ideas and Opinions 2007;146:878‐82. [DOI] [PubMed] [Google Scholar]
Murray 2013
- Murray CJ, Lopez AD. Measuring the global burden of disease. New England Journal of Medicine 2013;369:448‐57. [DOI] [PubMed] [Google Scholar]
Parsons 2007
- Parsons S, Harding G, Breen A, Foster N, Pincus T, Vogel S, Underwood M. The influence of patients' and primary care practitioners' beliefs and expectations about chronicmusculoskeletal pain on the process of care: a systematic review of qualitative studies. [The Clinical Journal of Pain]. Clin J Pain 2007;23(1):91‐8. [DOI] [PubMed] [Google Scholar]
van Tulder 2003
- Tulder M, Furlan A, Bombardier C, Bouter L, Editorial Board of The Cochrane Collaboration Back Review Group. Updated method guidelines for systematic reviews in The Cochrane Collaboration Back Review Group. Spine 2003;28:1290‐9. [DOI] [PubMed] [Google Scholar]
van Tulder 2006
- Tulder M, Becker A, Bekkering T, Breen A, Real MT, Hutchinson A. Chapter 3. European guidelines for the management of acute nonspecific low back pain in primary care. European Spine Journal 2006;15 Suppl 2:S169‐91. [DOI] [PMC free article] [PubMed] [Google Scholar]
Vos 2010
- Vos T, Flaxman AD, Naghavi M. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990‐2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2013;380:2163‐96. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to other published versions of this review
Heymans 2004
- Heymans M, Tulder MW, Esmail R, Bombardier C, Koes BW. Back schools for non‐specific low‐back pain. Cochrane Database of Systematic Reviews 2004, Issue 4. [DOI: 10.1002/14651858.CD000261.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Heymans 2005
- Heymans MW, Tulder MW, Esmail R, Bombardier C, Koes BW. Back schools for nonspecific low back pain: a systematic review within the framework of The Cochrane Collaboration Back Review Group. Spine 2005;30(19):2153‐63. [DOI] [PubMed] [Google Scholar]
van Tulder 1999
- Tulder MW, Esmail R, Bombardier C, Koes BW. Back schools for non‐specific low back pain. Cochrane Database of Systematic Reviews 1999, Issue 3. [DOI: 10.1002/14651858.CD000261.pub2] [DOI] [PubMed] [Google Scholar]


