Abstract
Background
Stress urinary incontinence constitutes a significant health and economic burden to society. Traditional suburethral slings are one of the surgical operations used to treat women with symptoms of stress urinary incontinence.
Objectives
To determine the effects of traditional suburethral slings on stress or mixed incontinence in comparison with other management options.
Search methods
We searched the Cochrane Incontinence Group Specialised Register (searched 3 June 2010) and the reference lists of relevant articles.
Selection criteria
Randomised or quasi‐randomised trials that included traditional suburethral slings for the treatment of stress or mixed urinary incontinence.
Data collection and analysis
At least three reviewers independently extracted data from included trials onto a standard form and assessed trial methodological quality. The data abstracted were relevant to predetermined outcome measures. Where appropriate, we calculated a summary statistic: a relative risk for dichotomous data and a weighted mean difference for continuous data.
Main results
We included 26 trials involving 2284 women. The quality of evidence was moderate for most trials and there was generally short follow‐up ranging from 6 to 24 months.
One medium‐sized trial compared traditional suburethral sling operations with oxybutynin in the treatment of women with mixed urinary incontinence. Surgery appeared to be more effective than drugs in treating participant‐reported incontinence (n = 75, risk ratio (RR) 0.18, 95% confidence interval (CI) 0.08 to 0.43).
One trial found that traditional slings were more effective than transurethral injectable treatment (RR for clinician‐assessed incontinence within a year 0.21, 95% CI 0.09 to 0.21)
Seven trials compared slings with open abdominal retropubic colposuspension. Participant‐reported incontinence was lower with the slings after one year (RR 0.75, 95% CI 0.62 to 0.90), but not when assessed by clinicians. Colposuspension, however, was associated with fewer peri‐operative complications, shorter duration of use of indwelling catheter and less long‐term voiding dysfunction. One study showed there was a 20% lower risk of bladder perforation with the sling procedure but a 50% increase in urinary tract infection with the sling procedure compared with colposuspension. Fewer women developed prolapse after slings (compared with after colposuspension) in two small trials but this did not reach statistical significance.
Twelve trials addressed the comparison between traditional sling operations and minimally invasive sling operations. These seemed to be equally effective in the short term (RR for incontinence within first year 0.97, 95% CI 0.78 to 1.20) but minimally invasive slings had a shorter operating time, fewer peri‐operative complications (other than bladder perforation) and some evidence of less post‐operative voiding dysfunction and detrusor symptoms.
Six trials compared one type of traditional sling with another. Materials included porcine dermis, lyophilised dura mater, fascia lata, vaginal wall, autologous dermis and rectus fascia. Participant‐reported improvement rates within the first year favoured the traditional autologous material rectus fascia over other biological materials (RR 0.45, 95% CI 0.21 to 0.98). There were more complications with the use of non‐absorbable Gore‐Tex in one trial.
Data for comparison of bladder neck needle suspension with suburethral slings were inconclusive because they came from a single trial with a small specialised population.
No trials compared traditional suburethral slings with anterior repair, laparoscopic retropubic colposuspension or artificial sphincters. Most trials did not distinguish between women having surgery for primary or recurrent incontinence when reporting participant characteristics.
For most of the comparisons, clinically important differences could not be ruled out.
Authors' conclusions
Traditional slings seem to be as effective as minimally invasive slings, but had higher rates of adverse effects. This should be interpreted with some caution however, as the quality of evidence for the studies was variable, follow‐up short and populations small, particularly for identifying complication rates. Tradional sling procedures appeared to confer a similar cure rate in comparison to open retropubic colposuspension, but the long‐term adverse event profile is still unclear. A brief economic commentary (BEC) identified two studies suggesting that traditional slings may be more cost‐effective compared with collagen injection but not cost‐effective when compared with minimally invasive sling operations. Reliable evidence to clarify whether or not traditional suburethral slings may be better or worse than other surgical or conservative management options is lacking.
Keywords: Adult; Female; Humans; Suburethral Slings; Suburethral Slings/adverse effects; Suburethral Slings/economics; Polytetrafluoroethylene; Polytetrafluoroethylene/therapeutic use; Randomized Controlled Trials as Topic; Treatment Outcome; Urinary Incontinence; Urinary Incontinence/drug therapy; Urinary Incontinence/surgery; Urinary Incontinence, Stress; Urinary Incontinence, Stress/drug therapy; Urinary Incontinence, Stress/surgery
Traditional sling operations for urinary incontinence in women
Traditional sling operations are used to treat women with stress urinary incontinence. This is loss of urine when coughing, laughing, sneezing or exercising due to damage to the muscles that hold up the bladder, and injuries to the nerves that may occur during childbirth. A significant amount of the woman's and her family's income can be spent on managing the symptoms. Sometimes stress incontinence occurs together with 'urge incontinence' ‐ known as 'mixed incontinence'. The sling operation aims to hold up the bladder with a strip of material which may be biological or synthetic. The results showed that there is not enough information on which to judge whether traditional sling operations are better or worse than any other treatments. Long‐term results are awaited. In terms of costs, a brief review of economic studies, which considered the overall costs and effects, suggested that traditional slings are less costly when compared with collagen injection but expensive when compared with minimally invasive slings. In this review there were few trials, of high quality, comparing slings with other forms of surgery and only one study comparing sling operations with non‐surgical treatment.
Summary of findings
Summary of findings for the main comparison.
Traditional suburethral slings compared to injectable treatment for stress urinary incontinence
| Traditional suburethral slings compared to injectable treatment for stress urinary incontinence | ||||||
| Patient or population: women with stress urinary incontinence Settings: secondary care Intervention: traditional suburethral slings Comparison: injectable treatment | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Injectable treatment | Traditional suburethral slings | |||||
| 4.1 Number with incontinence (worse, unchanged or improved) within the first year (women's observations) | 227 per 10001 | 95 per 1000 (20 to 438) | RR 0.42 (0.09 to 1.93) | 43 (1 study) | ⊕⊝⊝⊝ very low2,3,4,5 | Single trial with few participants |
| 4.2 Number with incontinence (worse, unchanged or improved) after first year (women's observations) | 286 per 10001 | 34 per 1000 (3 to 578) | RR 0.12 (0.01 to 2.02) | 27 (1 study) | ⊕⊕⊝⊝ low2,3,4,5 | Single trial with few participants |
| 4.4 Voiding dysfunction | 45 per 10001 | 189 per 1000 (23 to 1000) | RR 4.19 (0.51 to 34.5) | 43 (1 study) | ⊕⊕⊝⊝ low2,3,4,5 | Single trial with few participants |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1Illustrative comparative risks were based upon the mean risk on control intervention in the studies included in the meta‐analysis. 2Single trial with few participants. 3Uncertainty about method of sequence generation and allocation concealment. 4Single trial thus unable to determine inconsistency. 5Single small trial with large confidence intervals.
Summary of findings 2.
Traditional suburethral sling operation compared to open abdominal retropubic suspension for stress urinary incontinence
| Traditional suburethral sling operation compared to open abdominal retropubic suspension for stress urinary incontinence | ||||||
| Patient or population: women with stress urinary incontinence Settings: secondary care Intervention: traditional suburethral sling operation Comparison: open abdominal retropubic suspension | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Open abdominal retropubic suspension | Traditional suburethral sling operation | |||||
| 5.1 Number with incontinence (worse, unchanged or improved) within the first year (women's observations) | 92 per 10001 | 37 per 1000 (10 to 130) | RR 0.4 (0.11 to 1.41) | 147 (4 studies) | ⊕⊕⊝⊝ low2,3 | Fischer trial did not account for incomplete outcome data |
| 5.3 Number with incontinence (worse, unchanged or improved) after first year (women's observations) | 399 per 10001 | 299 per 1000 (247 to 359) | RR 0.75 (0.62 to 0.9) | 715 (5 studies) | ⊕⊕⊕⊝ moderate2 | Demirci did not account for incomplete outcome data |
| 5.14 Peri‐operative surgical complications | 407 per 10001 | 533 per 1000 (464 to 615) | RR 1.31 (1.14 to 1.51) | 792 (4 studies) | ⊕⊕⊕⊝ moderate2 | |
| 5.15 Bladder perforation | 30 per 10001 | 0 per 1000 (0 to 0) | RR 0 (0 to 0) | 655 (1 study) | ⊕⊕⊕⊝ moderate2 | Single study thus no pooled data available |
| 5.18 Voiding dysfunction after three months | 21 per 10001 | 128 per 1000 (65 to 251) | RR 6.08 (3.1 to 11.95) | 853 (5 studies) | ⊕⊕⊕⊝ moderate2 | |
| 5.21 Repeat incontinence surgery ‐ not reported | See comment | See comment | Not estimable | ‐ | See comment | No data |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1Illustrative comparative risks were based upon the mean risk on control intervention in the studies included in the meta‐analysis. 2Uncertainty in most studies about method of sequence generation and allocation concealment. 395% confidence interval around the pooled data includes both 1) no effect and 2) appreciable benefit or appreciable harm, thus imprecise.
Summary of findings 3.
Traditional suburethral sling operation compared to bladder neck (needle) suspension for stress urinary incontinence
| Traditional suburethral sling operation compared to bladder neck (needle) suspension for stress urinary incontinence | ||||||
| Patient or population: women with stress urinary incontinence Settings: secondary care Intervention: traditional suburethral sling operation Comparison: bladder neck (needle) suspension | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Bladder neck (needle) suspension | Traditional suburethral sling operation | |||||
| 6.1 Number with incontinence (worse, unchanged or improved) within the first year (women's observations) | 200 per 10001 | 100 per 1000 (10 to 934) | RR 0.5 (0.05 to 4.67) | 20 (1 study) | ⊕⊝⊝⊝ very low2,3,4 | |
| 6.2 Number with incontinence (worse, unchanged or improved) after the first year (women's observations) | 300 per 10001 | 99 per 1000 (12 to 807) | RR 0.33 (0.04 to 2.69) | 20 (1 study) | ⊕⊝⊝⊝ very low2,3,4 | |
| 6.4 Peri‐operative surgical complications | 200 per 10001 | 900 per 1000 (256 to 1000) | RR 4.5 (1.28 to 15.81) | 20 (1 study) | ⊕⊕⊝⊝ low2,3,4 | |
| 6.6 Voiding dysfunction after three months ‐ urodynamic stress incontinence (only) | 200 per 10001 | 400 per 1000 (94 to 1000) | RR 2 (0.47 to 8.56) | 20 (1 study) | ⊕⊝⊝⊝ very low2,3,4 | |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1Illustrative comparative risks were based upon the mean risk on control intervention in the studies included in the meta‐analysis. 2Uncertainty about method of sequence generation and allocation concealment. 3Single trial with few participants. 4Single trial thus unable to determine inconsistency.
Summary of findings 4.
Traditional suburethral sling operation compared to minimally invasive synthetic slings for stress urinary incontinence
| Traditional suburethral sling operation compared to minimally invasive synthetic slings for stress urinary incontinence | ||||||
| Patient or population: women with stress urinary incontinence Settings: secondary care Intervention: traditional suburethral sling operation Comparison: minimally invasive slings | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Minimally invasive slings | Traditional suburethral sling operation | |||||
| 9.1 Number with incontinence (worse, unchanged or improved) within the first year (women's observations) | 275 per 10001 | 267 per 1000 (214 to 330) | RR 0.97 (0.78 to 1.2) | 693 (8 studies) | ⊕⊕⊕⊕ high2 | |
| 9.3 Number with incontinence (worse, unchanged or improved) after first year (women's observations) | 253 per 10001 | 311 per 1000 (230 to 420) | RR 1.23 (0.91 to 1.66) | 382 (4 studies) | ⊕⊕⊝⊝ low2,3 | |
| 9.11 Peri‐operative surgical complications | 208 per 10001 | 331 per 1000 (214 to 508) | RR 1.59 (1.03 to 2.44) | 243 (3 studies) | ⊕⊕⊝⊝ low2 | |
| 9.12 Bladder perforations | 82 per 10001 | 51 per 1000 (28 to 91) | RR 0.62 (0.34 to 1.11) | 563 (7 studies) | ⊕⊕⊕⊝ moderate2,4 | |
| 9.16 Voiding dysfunction | 98 per 10001 | 157 per 1000 (92 to 266) | RR 1.6 (0.94 to 2.71) | 375 (5 studies) | ⊕⊕⊕⊝ moderate2,4 | |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1Illustrative comparative risks were based upon the mean risk on control intervention in the studies included in the meta‐analysis. 2Uncertainty in most studies about method of sequence generation and allocation concealment. 3Event rates very low resulting in wide confidence interval. 4Wide confidence interval include possible benefit from both surgical procedures.
Summary of findings 5.
Traditional suburethral sling operation compared to another traditional suburethral sling for stress urinary incontinence
| Traditional suburethral sling operation compared to another traditional suburethral sling for stress urinary incontinence | ||||||
| Patient or population: women with stress urinary incontinence Settings: secondary care Intervention: traditional suburethral sling operation Comparison: another traditional suburethral sling | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Another traditional suburethral sling | Traditional suburethral sling operation | |||||
| 10.1 Number with incontinence (worse, unchanged or improved) within the first year (women's observations) | 336 per 10001 | 299 per 1000 (222 to 400) | RR 0.89 (0.66 to 1.19) | 307 (3 studies) | ⊕⊕⊕⊝ moderate2,3 | |
| 10.3 Number with incontinence (worse, unchanged or improved) after first year (women's observations) | 467 per 10001 | 416 per 1000 (336 to 514) | RR 0.89 (0.72 to 1.1) | 379 (4 studies) | ⊕⊕⊕⊝ moderate2,4 | |
| 10.8 Peri‐operative surgical complications | 360 per 10001 | 335 per 1000 (234 to 479) | RR 0.93 (0.65 to 1.33) | 213 (2 studies) | ⊕⊕⊝⊝ low3,4 | |
| 10.12 Voiding dysfunction | 202 per 10001 | 234 per 1000 (131 to 418) | RR 1.16 (0.65 to 2.07) | 165 (1 study) | ⊕⊕⊕⊝ moderate2,3,5 | |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio; | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1Illustrative comparative risks were based upon the mean risk on control intervention in the studies included in the meta‐analysis. 2Uncertainty in most studies about method of sequence generation and allocation concealment. 395% confidence interval around the pooled data includes both 1) no effect and 2) appreciable benefit or appreciable harm, thus imprecise. 4Widely differing estimates of the treatment effect between trials. 5Single trial thus unable to determine inconsistency.
Background
The prevalence of urinary incontinence in adult women has been estimated to be between 10% to 40%, and is considered severe in about 3% to 17% (Hunskaar 2002). This is a potentially debilitating social problem which leads to high health care costs (Fantl 1996). In the USA, the annual total direct costs of urinary incontinence in both men and women is over USD 16 billion (1995 USD) (Chong 2011) with societal costs of USD 26.2 billion (1995 USD) (Wagner 1998). Approximately, USD 13.12 billion (1995 USD) of the total direct costs of urinary incontinence is spent on stress urinary incontinence (SUI) (Kunkle 2015; Chong 2011). About 70% of this USD 13.12 billion (1995 USD) is borne by people with SUI, mainly through routine care (purchasing pads and disposable underwear (diapers), laundry and dry cleaning). This constitutes a significant individual financial burden. Of the remaining 30%, 14% is spent on nursing home admission, 9% on treatment, 6% on addressing complications and 1% on diagnosis (Chong 2011). A study reported that about 1% of median annual household income (USD 50,000 to USD 59,999 in 2006) was spent by women on incontinence management. This study estimated that women spent an annual mean amount of USD 751 to USD 1277 (2006 USD) on incontinence. This increases based on the severity of the symptoms (Subak 2008). The indirect cost associated exerts social and psychological burden which is unquantifiable. (Chong 2011; Kilonzo 2004). Nevertheless, Birnbaum 2004 estimated that the annual average direct medical costs of SUI for one year (1998) was USD 5642 and USD 4208 for indirect workplace costs. The cost of management and treatment of SUI appears to have increased over time due to increasing prevalence and increased desire for improved quality of life. This in turn has resulted from improved recognition of the condition, as well as increased use of surgical and non‐surgical managements.
Description of the condition
Continence is achieved through an interplay of the normal anatomical and physiological properties of the bladder, urethra and sphincter, pelvic floor and the nervous system co‐ordinating these organs. The active relaxation of the bladder, coupled with the ability of the urethra and sphincter to contain urine within the bladder by acting as a closure mechanism during filling, allow storage of urine until an appropriate time and place to void is reached. The role of the pelvic floor in providing support to the bladder and urethra, and allowing normal abdominal pressure transmission to the proximal urethra is also considered essential in the maintenance of continence. Crucial to the healthy functioning of the bladder, urethra, sphincter and pelvic floor is co‐ordination between them, facilitated by an intact nervous system control.
Incontinence occurs when this normal relationship between the lower urinary tract components is disrupted, resulting from nerve damage or direct mechanical trauma to the pelvic organs. Advancing age, higher parity, vaginal delivery, obesity and menopause are associated with an increase in risk (Wilson 1996). There are different types of urinary incontinence. Stress urinary incontinence is the most common type (Wilson 1996). The symptom of 'stress incontinence' is the involuntary loss of urine from the urethra during physical activities that increase abdominal pressure, in the absence of a detrusor (bladder wall muscle) contraction or an over‐distended bladder (Blaivas 1997a). Two mechanisms for stress incontinence are recognised: hyper‐mobility or significant displacement of the urethra and bladder neck during exertion, and intrinsic urethral sphincter deficiency (Blaivas 1988). In women, these mechanisms may co‐exist (O'Donnell 1994). Few clinical trials have distinguished between the two conditions, probably because there is no standardised and validated test available to date (Blaivas 1988; McGuire 1993). Women whose incontinence may be due to either of these two mechanisms were considered together in this review.
The diagnosis of 'urodynamic stress incontinence' requires urodynamic investigation to exclude detrusor overactivity, in addition to history‐taking, physical examination, frequency/volume charts and urine analysis. Some authors have described women with only the symptom of stress incontinence (diagnosis made on clinical evaluation without urodynamics). Women with stress incontinence, both with and without urodynamic investigation,were eligible for inclusion in this review.
'Urge incontinence' is the symptom of involuntary loss of urine associated with a sudden, strong desire (urgency) to void. 'Detrusor overactivity' is a diagnosis that denotes involuntary detrusor contractions which are not due to neurological disorders, and diagnosis must be made using urodynamic techniques (Blaivas 1997a). Women with both the symptom and the urodynamic diagnosis of detrusor overactivity were eligible for inclusion in the review only if they had co‐existing stress incontinence ('mixed' incontinence).
Women with mixed incontinence included in this review either had symptoms of stress plus urge incontinence or other urinary symptoms (diagnosed clinically), or urodynamic stress incontinence plus detrusor overactivity (diagnosed using urodynamics).
Description of the intervention
Treatments for stress urinary incontinence include conservative, mechanical, pharmacological and surgical interventions.
Conservative treatment centres on physical methods, including pelvic floor muscle training, electrical stimulation, biofeedback and weighted cones.
Mechanical devices, which prevent or reduce urinary leakage are available, such as meatal plugs/patches and urethral and vaginal inserts.
Drug therapies, principally oestrogens and, less often, alpha adrenergic agents, can be used. A trial of conservative therapy is generally undertaken before resorting to surgery.
These interventions are the subject of separate Cochrane Reviews.
Surgical procedures to remedy stress incontinence generally aim to lift and support the urethro‐vesical junction. There is disagreement, however, regarding the precise mechanism by which continence is achieved. Choice of procedures is often influenced by coexistent problems, surgeon's preference and the physical features of the person affected.
Numerous surgical methods have been described, but essentially they fall into eight categories.
Open abdominal retropubic suspension (e.g. colposuspension (Burch), Marshall‐Marchetti‐Krantz (MMK), (Lapitan 2009)
Laparoscopic retropubic suspension (Dean 2006)
Vaginal anterior repair (anterior colporrhaphy) (Glazener 2001)
Traditional suburethral slings
Minimally invasive suburethral slings (Ogah 2010)
Bladder neck needle suspensions (Glazener 2004)
Peri‐urethral injections (Keegan 2007)
Artificial sphincters
In this review we concentrated on traditional suburethral sling operations.
How the intervention might work
The aim is to restore or enhance the woman’s urethral support during a sudden movement, such as a cough or sneeze. This is achieved by lifting and supporting the urethro‐vesical junction with autologous or synthetic material.
A traditional suburethral sling operation requires a combined abdominal and vaginal approach. Strips of material are tunnelled under the urethra and are attached either to the rectus muscle or the ileopectineal ligaments. The materials that have been used for slings may be biological or synthetic. Autologous biological materials include: rectus fascia, fascia lata, pubococcygeal muscle, vaginal wall, aponeurosis and pyramidalis fascia. Exogenous biological materials include: ox fascia and porcine dermis (Pelvicol). Synthetic materials include: Teflon, Mersilene tape in a silicon tube, Lyodura, polytetrafluoroethylene (Gore‐Tex), Marlex mesh and silastic.
A modification of the suburethral sling procedure is the 'minimally invasive' polypropylene mesh applied through a minimally invasive technique (e.g. tension‐free vaginal tape (TVT), suprapubic arc (SPARC)) in which a prolene tape covered by a plastic sheath is inserted around the mid‐urethra without fixation and in some centres under local anaesthesia (Smith 2002). These have been considered in a separate Cochrane Review (Ogah 2010).
We included only traditional sling operations, using an open abdominal approach and fixed with sutures, in this review.
Why it is important to do this review
The wide variety of surgical treatments for urinary incontinence indicates the lack of consensus as to which procedure is the best. Provided that a sufficient number of trials of adequate quality have been conducted, the most reliable evidence is likely to come from consideration of all well‐designed randomised controlled trials. Hence, there is a need for an easily accessible, periodically updated, comprehensive systematic review of such trials, which will not only help to identify optimal practice, but also highlight gaps in the evidence base.
Objectives
To assess the effects of traditional suburethral sling procedures for treatment of urodynamic stress urinary incontinence (urodynamic diagnosis), or for symptoms of stress or mixed incontinence (clinical diagnosis) in women.
We made the following comparisons for traditional suburethral sling procedures (abdominal and vaginal).
Traditional suburethral sling operation versus no treatment or sham operation
Traditional suburethral sling operation versus conservative management (e.g. pelvic floor muscle training, electrical stimulation, cones, biofeedback)
Traditional suburethral sling operation versus drugs
Traditional suburethral sling operation versus injectables
Traditional suburethral sling operation versus colposuspension
Traditional suburethral sling operation versus bladder neck needle suspension (abdominal and vaginal)
Traditional suburethral sling operation versus anterior repair
Traditional suburethral sling operation versus laparoscopic procedures
Traditional suburethral sling operation versus a minimally invasive sling
One type of traditional sling operations versus another traditional sling operation
Methods
Criteria for considering studies for this review
Types of studies
Randomised or quasi‐randomised controlled trials of women with urodynamic stress incontinence (urodynamic diagnosis), or symptoms of stress or mixed urinary incontinence (clinical diagnosis), in which at least one trial arm involved traditional suburethral sling procedures.
Types of participants
Adult women with stress urinary incontinence due to hyper‐mobility or intrinsic sphincter deficiency, or both, diagnosed clinically or with urodynamics, or with mixed incontinence. We accepted classification of diagnoses as defined by the trial authors.
Types of interventions
At least one arm of a study had to involve traditional suburethral sling procedures to treat stress or mixed incontinence. Comparison interventions could include other surgical techniques and non‐surgical interventions.
Types of outcome measures
We selected outcome measures used in this review on the basis of their relevance to the clinical cure or improvement of incontinence. We regarded the principal measures of effectiveness as the proportion of women cured (continent or dry) following surgery, and the proportion of women whose incontinence was improved.
1. Women's observations
Perception of cure and improvement in the short term (less than 12 months) and longer term (more than 12 months)
Urgency symptoms or urgency incontinence
2. Quantification of symptoms
Pad changes over 24 hours (from self‐reported number of pads used)
Incontinent episodes over 24 hours (from self completed bladder chart)
Pad tests of quantified leakage (mean volume or weight of urine loss)
3. Clinician's observations
Cure and improvement in the short term (less than 12 months) and longer term (more than 12 months)
4. Surgical outcome measures
Duration of operation
Length of inpatient stay
Time to return to normal activity level
5. Adverse events
Peri‐operative surgical complications (e.g. infection, bacteriuria, haemorrhage, bladder perforation)
De novo urge symptoms or urge incontinence (clinical diagnosis without urodynamics)
Voiding dysfunction/difficulty after three months (with or without urodynamic confirmation)
Detrusor overactivity (urodynamic diagnosis)
Entero‐rectocele
Repeat incontinence surgery
Later prolapse surgery
Surgical complications and other types of adverse event
6. Quality of life
General health status measures (e.g. Short Form 36 (Ware 1993)), or specific instruments designed to assess incontinence e.g. the Bristol Female Lower Urinary Tract Symptoms questionnaire (BFLUTS) (Jackson 1996)
7. Other outcomes
Non‐prespecified outcomes judged important when performing the review
Search methods for identification of studies
We did not impose language or other restrictions on any of these searches.
Electronic searches
This review has drawn on the search strategy developed for the Cochrane Incontinence Group. We identified relevant trials from the Cochrane Incontinence Group Specialised Register of controlled trials, which is described under Group's details in the Cochrane Library (for more details please see the Specialized Register section of the Group's module in the Cochrane Library). The Register contains trials identified from the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE, CINAHL, and handsearching of journals and conference proceedings. The date of the most recent search of the Register for this review was 3 June 2010.
The trials in the Cochrane Incontinence Specialised Register are also contained in CENTRAL. The terms used to search the Cochrane Incontinence Specialised Register are given below: (TOPIC.URINE.INCON*) AND ({DESIGN.CCT*} OR {DESIGN.RCT*}) AND ({INTVENT.SURG.SLIN*} OR {INTVENT.SURG.SUBURETHRAL SLING.} OR {INTVENT.SURG.ABDO.SLING.}) (All searches were of the keyword field of Reference Manager 2012).
For previous versions of this review one of the review authors performed extra literature searches ‐ these are described in Appendix 1.
On 6 April 2017 we performed additional searches for the brief economic commentary (BEC), conducted in MEDLINE (1 January 1946 to March 2017), Embase (1 January 1980 to 2017 Week 12) and NHS EED (1st Quarter 2016). Details of the searches run and the search terms used can be found in Appendix 2.
Searching other resources
We searched the reference lists of relevant articles for other possibly relevant trials.
Data collection and analysis
We excluded studies from the review if they were not randomised or quasi‐randomised controlled trials for incontinent women or if they made comparisons other than those pre‐specified. Excluded studies are listed in the Characteristics of excluded studies tables, with the reasons for their exclusion.
We processed included trial data as described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2008).
Selection of studies
The review authors evaluated the reports of all possibly eligible studies for appropriateness for inclusion without prior consideration of the results and we retrieved in full any reports of potentially eligible trials.
We resolved any differences of opinion related to study inclusion, methodological quality or data extraction by discussion.
Data extraction and management
At least three review authors independently undertook data extraction using a standard form containing pre‐specified outcomes. Where data may have been collected but not reported, we sought clarification from the trial authors. The review authors resolved any differences of opinion related to study inclusion, methodological quality or data extraction by discussion, and when necessary, we referred to a fourth reviewer for arbitration.
We conducted the review using the standard Cochrane software, Review Manager 5 (RevMan 5) (RevMan 2014) and processed included trial data as described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2008).
Assessment of risk of bias in included studies
Each review author independently undertook 'Risk of bias' assessment. The system for classifying methodological quality of controlled trials was based on an assessment of the three principal potential sources of bias. These are:
selection bias from insecure random allocation of treatments;
attrition bias from dropouts or losses to follow‐up, particularly if there is a differential dropout rate between groups;
biased ascertainment (detection bias) of outcome where knowledge of the allocation might have influenced the measurement of outcome.
Measures of treatment effect
Where appropriate, we calculated a combined estimate of treatment effect across similar studies for each pre‐specified outcome, using risk ratios (RR) for dichotomous outcomes or mean differences for continuous outcomes, with 95% confidence intervals where possible. For categorical (dichotomous) outcomes the numbers reporting an outcome were related to the numbers at risk in each group to derive a RR. For continuous variables we used means and standard deviations to derive a mean difference (MD). We used a fixed‐effect approach to the analysis unless there was evidence of heterogeneity across studies.
Dealing with missing data
Where statistical synthesis of data from more than one study was not possible or considered not appropriate, we undertook a narrative review of eligible studies. We sought data on the number of participants with each outcome event, by allocated treated group, irrespective of compliance and whether or not the participant was later thought to be ineligible or otherwise excluded from treatment or follow‐up to allow an intention‐to‐treat analysis when possible.
We defined an intention‐to‐treat analysis to mean that all participants were analysed in their randomised groups whether or not they received the allocated intervention. We included data as they were reported and did not impute missing values.
Assessment of heterogeneity
We investigated differences between trials when apparent from either visual inspection of the results or when statistically significant heterogeneity was demonstrated by using the Chi2 test at the 10% probability level or assessment of the I2 statistic (Higgins 2003). If there was no obvious reason for the heterogeneity (after consideration of populations, interventions, outcomes and settings of the individual trials) or it persisted despite the removal of outlying trials, we used a random‐effects model.
Data synthesis
We used the Mantel‐Haenszel statistical method for meta‐analysis. We used a fixed‐effect approach to the analysis unless there was evidence of heterogeneity across studies.
Subgroup analysis and investigation of heterogeneity
We grouped trial data by type of incontinence ‐ either urodynamic stress incontinence, based on a urodynamic diagnosis, or stress or mixed incontinence, based on a symptom classification. We carried out quantitative synthesis when we identified more than one eligible study.
Results
Description of studies
This is the second update of the review of traditional suburethral sling operations for urinary incontinence in women. We have added data from 16 RCTs, of which 13 are new RCTs (Albo 2007; Amaro 2007; Bai 2005; Basok 2008; Guerrero 2008; Maher 2005; Pacetta 2005; Sharifiaghdas 2008; Silva Filho 2006; Song 2004; Tcherniakovsky 2009; Teixeira 2008; Wadie 2005) and three are updates of previously included trials (Arunkalaivanan 2003; Kondo 2006; Lucas 2000).
Results of the search
Altogether we reviewed 128 reports of 61 studies, of which we included 26 and excluded 35.
Included studies
We identified 26 randomised or quasi randomised trials that met the inclusion criteria. These trials included 2284 women (1287 with traditional slings), and sample sizes ranging from 20 to 655 participants.
With the exception of the Albo 2007 and Sand 2000 trials, in general, included trials were small with short follow‐up.
One trial (Osman 2003) compared traditional suburethral sling operations with oxybutynin in the treatment of women with mixed urinary incontinence, another (Maher 2005) with suburethral injectable treatment and another (Hilton 1989) with bladder neck needle suspension.
Seven trials compared slings with open abdominal retropubic colposuspension (Albo 2007; Bai 2005; Demirci 2001; Enzelsberger 1996; Fischer 2001; Henriksson 1978; Sand 2000).
Twelve trials addressed the comparison between traditional sling operations and minimally invasive sling operations (Amaro 2007; Arunkalaivanan 2003; Bai 2005; Basok 2008; Kondo 2006; Guerrero 2008; Sharifiaghdas 2008; Silva Filho 2006; Song 2004; Tcherniakovsky 2009; Teixeira 2008; Wadie 2005).
Six trials compared one type of traditional sling with another (Barbalias 1997; Guerrero 2008; Lucas 2000; Pacetta 2005; Shin 2001; Viseshsindh 2003).
There were no trials comparing suburethral slings with anterior repair, laparoscopic retropubic colposuspension or artificial sphincters.
Interventions
The 26 studies used 10 materials for the sling procedure.
Autologous biological materials
Autologous dermal graft patch (Shin 2001)
Autologous fascia lata (Song 2004)
Autologous rectus fascia (Albo 2007; Amaro 2007; Bai 2005; Barbalias 1997; Demirci 2001; Guerrero 2008; Kondo 2006; Lucas 2000; Maher 2005; Osman 2003; Pacetta 2005; Sharifiaghdas 2008; Silva Filho 2006; Tcherniakovsky 2009; Viseshsindh 2003; Wadie 2005)
Autologous rectus fascia of smaller length (Lucas 2000)
Other biological materials
Cadaveric fascia lata (Basok 2008, Shin 2001)
FortaPerm (Pacetta 2005)
Lyphohilised dura matter (Enzelsberger 1996)
Porcine dermis also known as Pelvicol (Arunkalaivanan 2003; Guerrero 2008; Hilton 1989, Teixeira 2008)
Vaginal wall sling ‐ slings made of tissue harvested from the woman's own vaginal wall (Viseshsindh 2003)
Synthetic non‐absorbable materials
Gore‐Tex sling (Barbalias 1997)
Polytetrafluoroethylene ‐ PTFE (Sand 2000)
Teflon Sling (Henriksson 1978)
One trial (Fischer 2001), reported in abstract form, did not mention the type of material used for the suburethral sling.
Comparators
There were seven comparators across 23 studies.
Anticholinergic (Osman 2003)
Intravaginal slingplasty (Basok 2008)
Minimally invasive sling (Amaro 2007; Arunkalaivanan 2003; Bai 2005, Guerrero 2008; Kondo 2006; Sharifiaghdas 2008; Silva Filho 2006; Song 2004; Tcherniakovsky 2009; Teixeira 2008; Wadie 2005)
Retropubic colposuspension: Burch colposuspension (Albo 2007; Bai 2005; Demirci 2001; Enzelsberger 1996; Fischer 2001; Osman 2003; Sand 2000); Marshall‐Marchetti‐Krantz (Henriksson 1978)
Stamey bladder neck (needle) suspension (Hilton 1989)
Transurethral Macroplastique (injectable material, Maher 2005)
One trial was designed to study an anticholinergic agent (oxybutynin) in comparison with surgery (Burch or sling) for women with mixed urinary incontinence (Osman 2003). It was possible to abstract only the data from sling surgery in comparison with medical treatment to include in the analysis.
Participants
Inclusion criteria were not always clearly defined. Seven trials included women with mixed urinary incontinence (MUI, both stress and urgency) (Barbalias 1997; Basok 2008; Kondo 2006; Osman 2003; Sand 2000; Song 2004; Wadie 2005). One large trial involved women with self‐reported stress urinary incontinence (SUI), (Albo 2007). All others were restricted to women with a urodynamic diagnosis of stress incontinence (USI, previously known as genuine stress incontinence). All trials included both pre‐ and post‐menopausal women, but none were treated with hormone replacement therapy. One study was restricted to women with vaginal narrowing due to atrophic vaginitis or previous surgical scars (Hilton 1989).
Previous continence surgery status
Two trials (Henriksson 1978; Silva Filho 2006) only included women without previous interventions for incontinence and another (Enzelsberger 1996) only included women who had had recurrent incontinence after a previous vaginal hysterectomy and at least one anterior repair. The others included women with both primary and recurrent stress incontinence but did not report outcome data separately according to previous continence surgery.
Outcome measures
The included studies did not report outcome measures in a standardised fashion.
Seventeen trials used women's observations to report urinary incontinence outcomes with clinical history or questionnaire about urinary incontinence on effort (SUI) or use of pads (Albo 2007; Amaro 2007; Arunkalaivanan 2003; Bai 2005; Fischer 2001; Kondo 2006; Lucas 2000; Maher 2005; Osman 2003; Pacetta 2005; Sand 2000; Sharifiaghdas 2008; Shin 2001; Song 2004; Tcherniakovsky 2009; Wadie 2005).
Nine trials used clinician's observations of SUI using stress testing or urodynamics (Albo 2007; Barbalias 1997; Demirci 2001; Enzelsberger 1996; Hilton 1989; Kondo 2006; Maher 2005; Osman 2003; Pacetta 2005; Sand 2000; Sharifiaghdas 2008)
Two trials did not adequately describe the parameters on which they based their outcomes (Guerrero 2008; Henriksson 1978). We therefore assumed that data from Guerrero 2008 were patient‐reported.
Three trials (Arunkalaivanan 2003; Basok 2008; Guerrero 2008) assessed woman‐reported improvement of incontinence within 12 months. Arunkalaivanan 2003 assessed improvement using a urinary symptom questionnaire; Basok 2008 considered the use of one or fewer than one incontinence pad per day as subjective improvement; and one trial reported as an abstract did not specify outcome measures (Guerrero 2008).
Follow‐up
Not all studies reported initial and long‐term follow‐up. Seven authors (Bai 2005; Fischer 2001; Henriksson 1978; Silva Filho 2006; Sand 2000; Osman 2003; Viseshsindh 2003; Wadie 2005) presented their results at three‐ and/or six‐ and/or nine‐month assessment. Ten of the studies presented an intermediate follow‐up at around one year (Arunkalaivanan 2003; Basok 2008; Demirci 2001; Guerrero 2008; Lucas 2000; Maher 2005; Pacetta 2005; Sharifiaghdas 2008; Shin 2001; Tcherniakovsky 2009). Seven studies described longer but not ideal, follow‐up of one to five years (Albo 2007; Amaro 2007,Barbalias 1997; Enzelsberger 1996; Hilton 1989; Kondo 2006; Teixeira 2008). One trial provided full information in two reports of short‐ and long‐term (more than five years) follow‐up (Sand 2000). Further characteristics of the trials are reported in the Characteristics of included studies table.
Excluded studies
We excluded 35 studies. Fifteen trials compared minimally invasive or variant sling procedures with each other, or other operations: (Amat 2007; Choe 2000; Chong 2003; Darai 2007; Debodinance 1993; Halaska 2001; Han 2001; Kocjancic 2008; Liapis 2002; Lim 2005; Naumann 2006; O'Sullivan 2000; Seo 2007; Ward 2002a; Yoo 2007). Minimally invasive sling and open colposuspension procedures are considered in other Cochrane Reviews (Ogah 2010; Lapitan 2009). Lemieux 1991 compared clamping and non‐clamping of catheters after incontinence surgery.
Twelve studies were not randomised (Atherton 2000; Bruschini 2005; Corcos 2001; Debodinance 1994; Giri 2004; Giri 2006; Hung 2001; Ishenko 1999; Kuo 2001; Obrink 1978; Schostak 2001; Wang 1999). Choe 2001 did not adequately perform a final analysis.
There was uncertainty regarding the population used in two trials (Aurunkalaivanan 2001; Barrington 2003). Four trials (Goldberg 2001; Kwon 2002; Meschia 2001; Trezza 2001) dealt with a diagnosis other than SUI.
Further details are provided in the Characteristics of excluded studies table.
Risk of bias in included studies
We have summarised our 'Risk of bias' findings in the included trials in Figure 1 and Figure 2.
Figure 1.
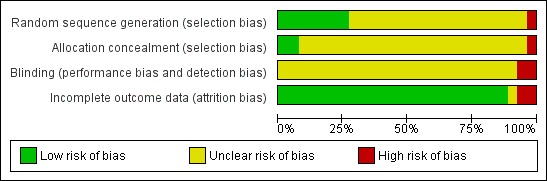
Figure 2.
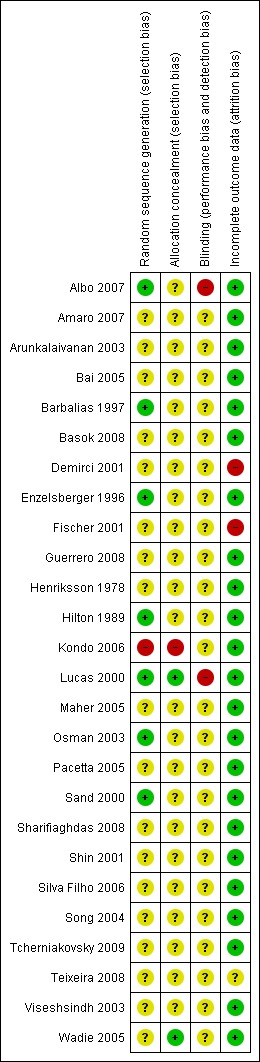
Allocation
Adequate sequence generation
Three trials used an adequate method of sequence generation (Albo 2007; Osman 2003; Sand 2000). Three trials used randomisation charts to generate the randomisation sequence, without providing further information about the process (Barbalias 1997; Enzelsberger 1996; Hilton 1989): nevertheless these were judged to be adequate. Nineteen trials just stated that women were randomised, without any other detail of the process (Amaro 2007; Arunkalaivanan 2003; Bai 2005; Basok 2008; Demirci 2001; Fischer 2001; Guerrero 2008; Henriksson 1978; Maher 2005; Pacetta 2005; Osman 2003; Sharifiaghdas 2008; Shin 2001; Silva Filho 2006; Song 2004; Tcherniakovsky 2009; Teixeira 2008; Viseshsindh 2003; Wadie 2005). There was inadequate sequence generation in one trial (Kondo 2006), which used the date‐of‐birth method, where even dates were assigned to one group and odd to the other. In one trial, one woman was randomised to one arm of the study in comparison with two randomised to the other intervention (Barbalias 1997).
Allocation concealment
The reported method of concealment of randomisation was secure in two trials (Lucas 2000; Wadie 2005). Allocation concealment was unknown for most of the remaining trials as the trial authors did not record it. Inadequate allocation concealment was present in one trial (Kondo 2006) where the date‐of‐birth method was used to randomise participants. Another trial (Sharifiaghdas 2008) mentioned sealed, opaque envelopes, but no mention of numbering, and thus we judged it unclear for allocation concealment.
Blinding
Masking of women or surgeons was not reported in most trials, but is difficult to achieve in surgical trials.
Incomplete outcome data
Most trials had complete outcome data at follow‐up, or losses were evenly distributed between the randomised groups, and thus were unlikely to have had a significant effect on the final analysis. Two trials (Demirci 2001; Fischer 2001) did not account for losses at follow‐up, which might potentially have been a source of bias.
Other potential sources of bias
Comparability of groups at baseline
Baseline comparisons were given in ten trials (Albo 2007; Arunkalaivanan 2003; Bai 2005; Basok 2008; Demirci 2001; Enzelsberger 1996; Hilton 1989; Kondo 2006; Lucas 2000; Maher 2005; Sand 2000; Sharifiaghdas 2008; Song 2004; Tcherniakovsky 2009; Wadie 2005). One author stated that the two groups were comparable without supplying data (Henriksson 1978), and the others did not mention baseline comparisons between the groups (Barbalias 1997; Fischer 2001; Osman 2003; Shin 2001; Viseshsindh 2003). Third party outcome assessment was not performed in any of the trials.
Definition of cure
We calculated the number of incontinent women from the cure rate provided in the reports of trials. The definition of cure was not uniform in the identified studies. For example, although Barbalias 1997 considered only the 'dry' participants as cured, he included the improved ones in the success rates, without reporting what 'improvement' meant. Others only considered 'dry' participants to be cured (Enzelsberger 1996). The most detailed description of results were reported by Albo 2007; Sand 2000 and Lucas 2000, with data describing both objective (pad tests and urodynamics) and subjective (self‐reported, voiding diaries) cure rates. Reporting of other outcomes was variable and incomplete.
Effects of interventions
See: Table 1; Table 2; Table 3; Table 4; Table 5
Outcome measures used in this review were not consistently reported in the trials.
Comparison 1. Traditional suburethral sling operation versus no treatment or sham operation
No trials identified.
Comparison 2. Traditional suburethral sling operation versus conservative management (e.g. pelvic floor muscle training, electrical stimulation, cones, biofeedback)
No trials identified.
Comparison 3. Traditional suburethral sling operation versus drugs
One trial studied women with mixed urinary incontinence treated with oxybutynin or surgery (Osman 2003). Oxybutinin is a drug treatment for urgency urinary incontinence, overactive bladder and detrusor overactivity, not for stress incontinence. The type of surgery was selected according to Valsalva leak point pressure (VLPP) (those with VLPP less than 90 cm of water had rectus fascia sling and those with VLPP more than 90 cm of water had Burch colposuspension). The results for the total surgically managed group were similar to those for the subgroup having slings. We therefore included in tables only data from women with oxybutynin and sling.
The study suggested that slings are significantly better for treating mixed urinary incontinence than oxybutynin. Results were analysed in terms of participant‐reported incontinence within one year (RR 0.18, 95% CI 0.08 to 0.43) (Analysis 3.1). Fewer women had persistent urgency urinary incontinence after the sling surgery (RR 0.29, 95% CI 0.09 to 0.94) (Analysis 3.2).
Analysis 3.1.
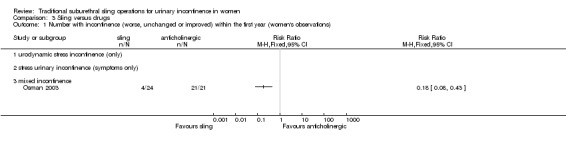
Comparison 3 Sling versus drugs, Outcome 1 Number with incontinence (worse, unchanged or improved) within the first year (women's observations).
Analysis 3.2.
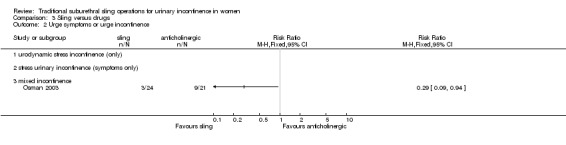
Comparison 3 Sling versus drugs, Outcome 2 Urge symptoms or urge incontinence.
Comparison 4. Traditional suburethral sling versus injectables
We identified one small trial that compared slings (21) with injectable Macroplastique (22) in 45 women (Maher 2005).
The only statistically significant outcome was number with incontinence (clinician‐observed) within the first year, essentially the number not cured, which favours the traditional sling: 4/21 versus 20/22, (RR 0.21, 95% 0.09 to 0.21) (Analysis 4.3).
Analysis 4.3.
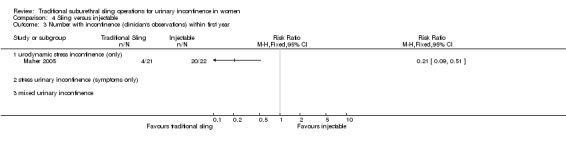
Comparison 4 Sling versus injectable, Outcome 3 Number with incontinence (clinician's observations) within first year.
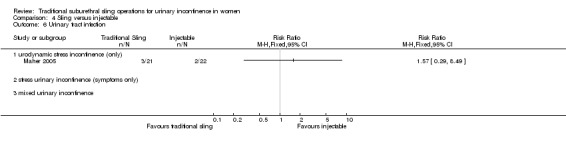
There were no statistically significant differences between groups but we found wide confidence intervals for the following outcomes.
Number of women with incontinence (participant‐reported) within the first year (RR 0.42, 95% CI 0.09 to 1.93) (Analysis 4.1)
Number of women with incontinence (participant‐reported) after the first year (RR 0.12, 95% CI 0.01 to 2.02) (Analysis 4.2)
Voiding dysfunction (RR 4.19, 95% CI 0.51 to 34.50) (Analysis 4.4)
De novo detrusor overactivity (urodynamic diagnosis) (RR 3.14, 95% CI 0.13 to 72.96) (Analysis 4.5)
Urinary tract infection (RR 1.57, 95% CI 0.29 to 8.49) (Analysis 4.6)
Analysis 4.1.
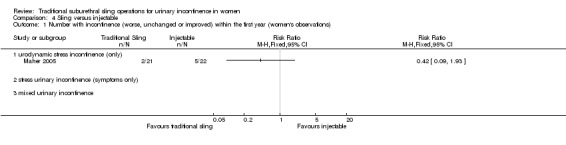
Comparison 4 Sling versus injectable, Outcome 1 Number with incontinence (worse, unchanged or improved) within the first year (women's observations).
Analysis 4.2.
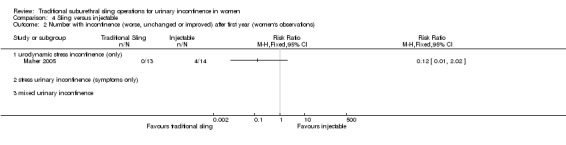
Comparison 4 Sling versus injectable, Outcome 2 Number with incontinence (worse, unchanged or improved) after first year (women's observations).
Analysis 4.4.
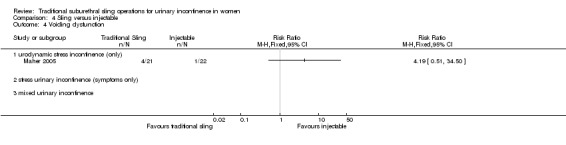
Comparison 4 Sling versus injectable, Outcome 4 Voiding dysfunction.
Analysis 4.5.
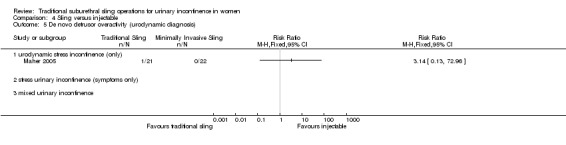
Comparison 4 Sling versus injectable, Outcome 5 De novo detrusor overactivity (urodynamic diagnosis).
Analysis 4.6.
Comparison 4 Sling versus injectable, Outcome 6 Urinary tract infection.
Maher 2005 reported a significant reduction in incontinence impact questionnaire scores compared with baseline (P less than 0.01) in both groups, though he provided no data.
Comparison 5. Traditional suburethral sling versus open abdominal retropubic colposuspension
Seven trials compared slings with open abdominal retropubic colposuspension (Albo 2007; Bai 2005; Demirci 2001; Enzelsberger 1996; Fischer 2001; Henriksson 1978; Sand 2000). The extent to which we could consider the trials together was limited because of differences in the procedures compared, the populations studied, the outcomes assessed, and the length of follow‐up. Two trials involved the pubovaginal sling technique using autologous rectus fascia (Albo 2007; Demirci 2001). Enzelsberger 1996 used a Lyodura sling, Henriksson 1978 used the Zoedler sling, and Sand 2000 used the Gore‐Tex‐type. Fischer (Fischer 2001) did not specify the sling material.
Only one of these trials (Sand 2000) reported follow‐up for more than five years and presented both short‐ and long‐term data in two full reports.
5.1 Women's observations (outcomes 5.1 to 5.4)
Short‐term incontinence or improvement
Evidence from four trials (Bai 2005; Fischer 2001; Henriksson 1978; Sand 2000) showed no statistically significant difference in the number of women reporting incontinence within one year of treatment between the two treatment groups (RR 0.40, 95% CI 0.11 to 1.41) (Analysis 5.1) but the confidence interval was wide and from the data we could not rule out a difference favouring either group.
Analysis 5.1.
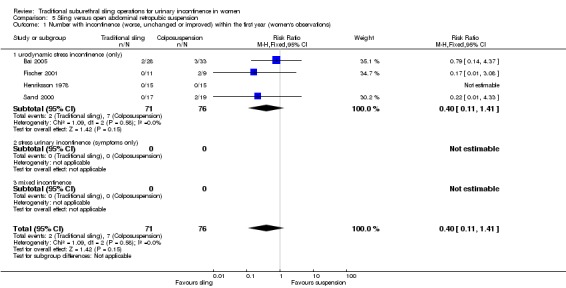
Comparison 5 Sling versus open abdominal retropubic suspension, Outcome 1 Number with incontinence (worse, unchanged or improved) within the first year (women's observations).
Medium‐/long‐term incontinence or improvement
Data for failure rates at one to five year follow‐up were available from five trials (Albo 2007; Bai 2005; Demirci 2001; Enzelsberger 1996; Sand 2000). The summary statistic, combining urodynamic and symptom‐only diagnosis, showed a lower incontinence rate with sling procedures (RR 0.75, 95% CI 0.62 to 0.90) (Analysis 5.3). This reflects the results of the Albo 2007 trial, which had the largest population sample. The data from the trials in which women all had urodynamic stress incontinence showed no significant difference in urinary incontinence after one year (RR 0.72, 95% CI 0.31 to 1.67) (Analysis 5.3.1).
Analysis 5.3.
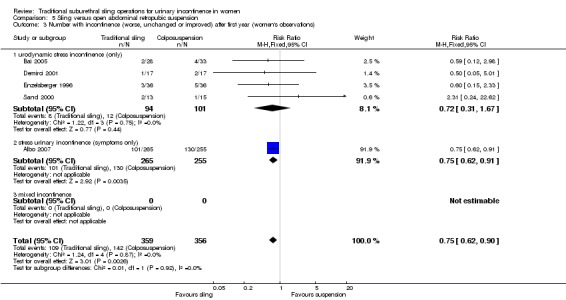
Comparison 5 Sling versus open abdominal retropubic suspension, Outcome 3 Number with incontinence (worse, unchanged or improved) after first year (women's observations).
Long‐term cure
Only one trial provided data beyond five years (Sand 2000, included in the outcome woman‐reported incontinence after one year): there was no statistically significant difference between the groups, but with very wide confidence intervals (RR 2.31, 95% CI 0.24 to 22.62) (Analysis 5.3).
5.2 Quantification of symptoms (outcomes 5.5 to 5.7)
There were no data from any of the trials for these outcomes and thus we could not perform meta‐analysis.
5.3 Clinician's observations (outcomes 5.8 to 5.9)
No data were available for objective cure within one year of treatment.
Consistent with the results in the woman‐reported assessment of incontinence, there were no statistically significant differences in clinically‐assessed incontinence rates at one year (RR 0.95, 95% CI 0.64 to 1.41) (Analysis 5.9). Again, wide confidence intervals mean that we cannot rule out a difference between slings or open colposuspension in either direction. This was based on data from three studies with data on assessment after one year (Albo 2007; Enzelsberger 1996; Sand 2000).
Analysis 5.9.
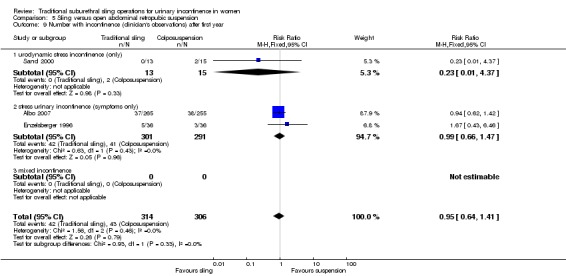
Comparison 5 Sling versus open abdominal retropubic suspension, Outcome 9 Number with incontinence (clinician's observations) after first year.
5.4 Surgical outcome measures (outcomes 5.10 to 5.12)
Data on surgical parameters came from four trials (Albo 2007; Demirci 2001; Enzelsberger 1996; Sand 2000).
One trial (Demirci 2001) compared operative times between groups. There was no statistically significant difference between the groups but the confidence interval was wide (MD 6 minutes, 95% CI ‐0.5 to 13) (Analysis 5.10).
Analysis 5.10.
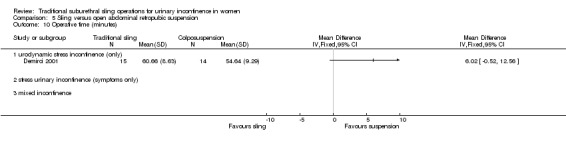
Comparison 5 Sling versus open abdominal retropubic suspension, Outcome 10 Operative time (minutes).
Meta‐analysis of data from two trials (Enzelsberger 1996; Sand 2000) showed that women in the colposuspension group had their catheters removed earlier (MD 8 days, 95% CI 6.8 to 9.2) (Analysis 5.11). However, it is unclear if this was due to the procedures themselves or differences in hospital policies.
Analysis 5.11.
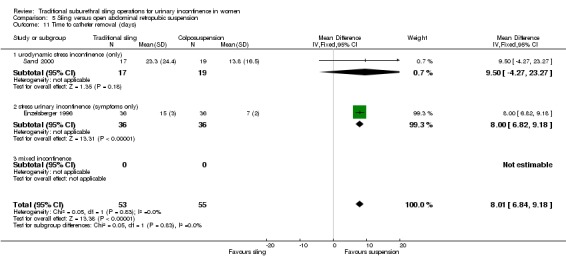
Comparison 5 Sling versus open abdominal retropubic suspension, Outcome 11 Time to catheter removal (days).
Three trials reported length of inpatient stay. Two trials showed similar lengths of stay for both treatment groups (Demirci 2001; Sand 2000). One trial (Enzelsberger 1996) reported that women stayed eight days less after colposuspension compared to after a traditional sling procedure, which is reflected in the statistically significant summary total, (MD 2 days, 95% CI 1.5 to 2.6) (Analysis 5.12). There was statistically significant heterogeneity, which was removed when Enzelsberger 1996 was excluded from the analysis, but it was unclear why this trial reported such a large difference in hospital stay: this may also have been due to differences in hospital policies.
Analysis 5.12.
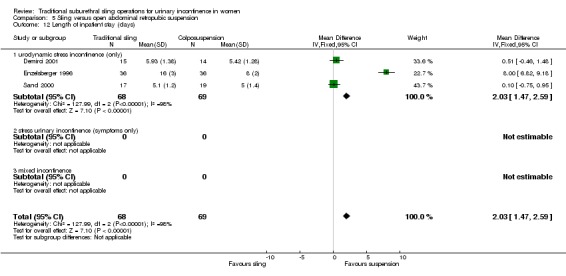
Comparison 5 Sling versus open abdominal retropubic suspension, Outcome 12 Length of inpatient stay (days).
5.5 Adverse events (outcomes 5.14 to 5.21)
In four trials (Albo 2007; Demirci 2001; Enzelsberger 1996; Sand 2000) there were statistically significantly fewer perioperative complications in the open colposuspension group (RR 1.31, 95% CI 1.14 to 1.51) (Analysis 5.14). This finding was mostly due to data from only one, large, trial (Albo 2007), which included data on bladder perforation and urinary tract infection (there was a 20% lower risk of bladder perforation with the sling procedure (RR 0.20, 95% CI 0.04 to 0.91) (Analysis 5.15), and a 50% increase in urinary tract infection with the sling procedure (RR 1.50, 95% CI 1.33 to 1.70) (Analysis 5.16) as compared with colposuspension).
Analysis 5.14.
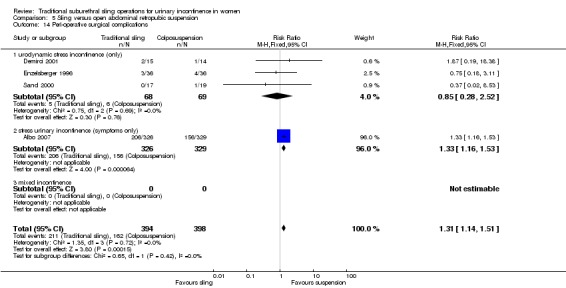
Comparison 5 Sling versus open abdominal retropubic suspension, Outcome 14 Peri‐operative surgical complications.
Analysis 5.15.
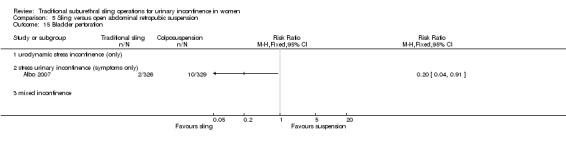
Comparison 5 Sling versus open abdominal retropubic suspension, Outcome 15 Bladder perforation.
Analysis 5.16.
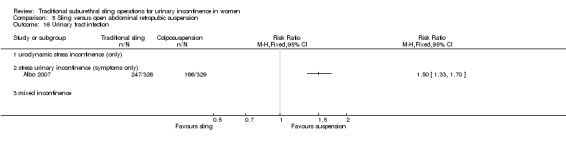
Comparison 5 Sling versus open abdominal retropubic suspension, Outcome 16 Urinary tract infection.
One small trial (Enzelsberger 1996) reported data on de novo urge symptoms or incontinence: there were no statistically significant differences between the groups but the confidence interval was wide (RR 2.00, 95% CI 0.54 to 7.39) (Analysis 5.17). Evidence from four small trials (Bai 2005; Demirci 2001; Enzelsberger 1996; Sand 2000) demonstrated no statistically significant difference in detrusor overactivity between the groups (RR 1.42, 95% CI 0.52 to 3.87) (Analysis 5.18).
Analysis 5.17.
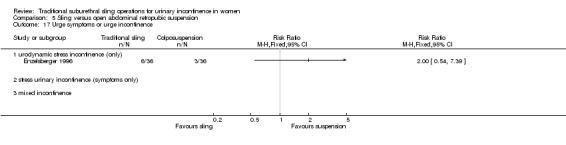
Comparison 5 Sling versus open abdominal retropubic suspension, Outcome 17 Urge symptoms or urge incontinence.
Analysis 5.18.
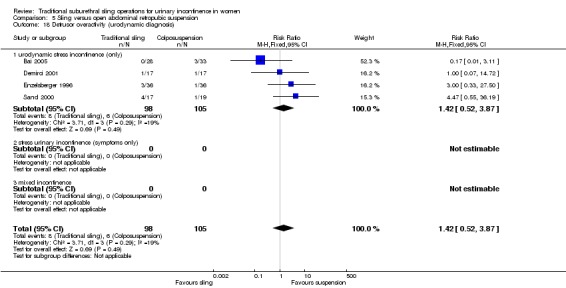
Comparison 5 Sling versus open abdominal retropubic suspension, Outcome 18 Detrusor overactivity (urodynamic diagnosis).
Pooled data from five trials (Albo 2007; Bai 2005; Demirci 2001; Enzelsberger 1996; Sand 2000) showed that significantly more women had voiding dysfunction after sling (13% versus 2% after open colposuspension, RR 6.08, 95% CI 3.10 to 11.95) (Analysis 5.19).
Analysis 5.19.
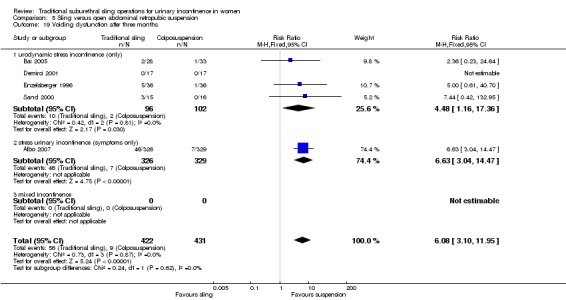
Comparison 5 Sling versus open abdominal retropubic suspension, Outcome 19 Voiding dysfunction after three months.
Two trials (Demirci 2001; Enzelsberger 1996) reported that more women had new or recurrent prolapse after open colposuspension (7/53) compared to after a sling procedure (1/53, RR 0.20, 95% CI 0.04 to 1.11) (Analysis 5.20), but this did not reach statistical significance. However there was no information about subsequent surgery for either urinary incontinence or prolapse in any trial.
Analysis 5.20.
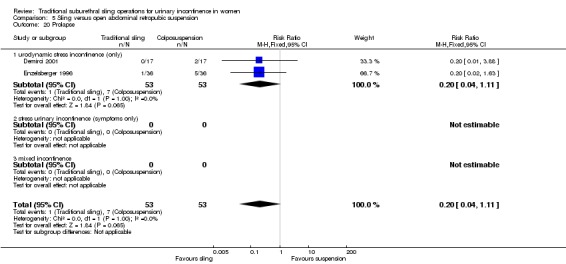
Comparison 5 Sling versus open abdominal retropubic suspension, Outcome 20 Prolapse.
5.6 Quality of life (outcomes 5.22)
Data were reported in different formats, thus meta‐analysis was not possible.
Albo 2007 reported a significantly greater improvement in quality of life for those receiving the Burch procedure compared to the sling procedure, stating their P value was 0.033. Fischer 2001 reported no significant difference in the Incontinence Impact Questionnaire and Urogenital Distress Inventory scores between the colposuspension group and the sling group, although actual numbers were not reported.
Comparison 6. Traditional suburethral sling versus bladder neck needle suspension (abdominal and vaginal)
Only one small trial compared porcine dermis sling with Stamey needle suspension (Hilton 1989). This was a small trial with only 10 women in each arm. The women were unsuitable for abdominal colposuspension (the trial author's preferred procedure) because they had vaginal narrowing secondary to either previous interventions or atrophic vaginitis. All women had urodynamic stress incontinence. Groups were comparable for age, parity, previous interventions and hormonal status. Follow‐up was reported at three and 24 months.
6.1 Women's observations (outcomes 6.1 and 6.2)
Although there were no significant differences in participant‐reported incontinence rates between the groups in the short or longer term, numbers were too small to address such differences (Analysis 6.1; Analysis 6.2).
Analysis 6.1.
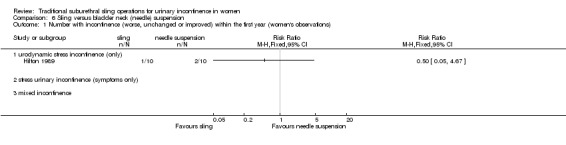
Comparison 6 Sling versus bladder neck (needle) suspension, Outcome 1 Number with incontinence (worse, unchanged or improved) within the first year (women's observations).
Analysis 6.2.
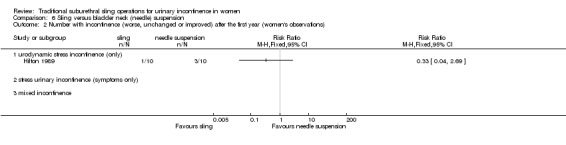
Comparison 6 Sling versus bladder neck (needle) suspension, Outcome 2 Number with incontinence (worse, unchanged or improved) after the first year (women's observations).
6.4 Surgical outcome measures (outcomes 6.3)
The sling group needed an indwelling catheter for longer, and more adjuvant therapy, resulting in a longer stay in hospital (MD 13 days longer, 95% CI 5 to 21) (Analysis 6.3).
Analysis 6.3.
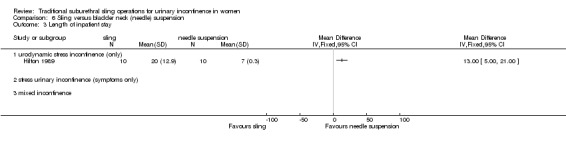
Comparison 6 Sling versus bladder neck (needle) suspension, Outcome 3 Length of inpatient stay.
6.5 Adverse events (outcomes 6.4 to 6.7)
Nine of the 10 women who had sling operations had complications, compared with two of the 10 who had needle suspension. These included: pyrexia, blood loss, wound infection and pulmonary embolus (RR 4.50, 95% CI 1.28 to 15.81) (Analysis 6.4). Data reported for urge incontinence, late voiding dysfunction and detrusor overactivity showed no statistically significant differences, and confidence intervals were wide.
Analysis 6.4.
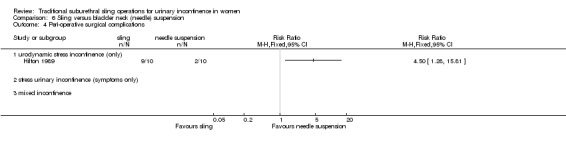
Comparison 6 Sling versus bladder neck (needle) suspension, Outcome 4 Peri‐operative surgical complications.
Comparison 7. Traditional suburethral sling operation versus anterior repair
No trials identified.
Comparison 8. Traditional suburethral sling operation versus laparoscopic procedures
No trials identified.
Comparison 9. Traditional suburethral sling operation versus a minimally invasive sling
Twelve trials addressed this comparison (Amaro 2007; Arunkalaivanan 2003; Bai 2005; Basok 2008; Kondo 2006; Guerrero 2008; Sharifiaghdas 2008; Silva Filho 2006; Song 2004; Tcherniakovsky 2009; Teixeira 2008; Wadie 2005).
9.1 Women's observations (outcomes 9.1 to 9.4)
Short‐term incontinence
Incontinence within 12 months of operation was investigated by eight RCTs with a total of 693 participants. Assessment of failure was self‐reported by participants and by responses to symptom‐based questionnaires. There was no significant difference between participant‐reported incontinence rate (RR 0.97, 95% CI 0.78 to 1.20) (Analysis 9.1). This translates to 267 per 1000 women being incontinent after a traditional sling compared with 275 per 1000 after a minimally invasive sling (Table 4, 9.1).
Analysis 9.1.
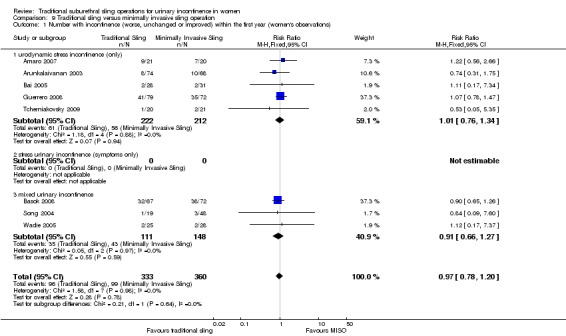
Comparison 9 Traditional sling versus minimally invasive sling operation, Outcome 1 Number with incontinence (worse, unchanged or improved) within the first year (women's observations).
Out of a total of 432 women, 11% of women who had traditional sling operations and 15% of those with minimally invasive sling operations reported no improvement. This was not a statistically significant difference and the confidence intervals were wide (RR 0.78, 95% CI 0.48 to 1.27) (Analysis 9.2).
Analysis 9.2.
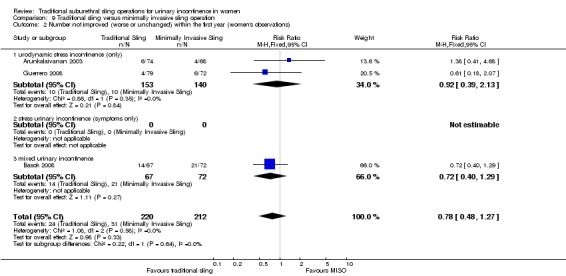
Comparison 9 Traditional sling versus minimally invasive sling operation, Outcome 2 Number not improved (worse or unchanged) within the first year (women's observations).
Medium‐/long‐term incontinence
Data on incontinence after the first year was available from four RCTs (Arunkalaivanan 2003; Bai 2005; Guerrero 2008; Kondo 2006). Incontinence was reported by 31.6% of those women in the traditional sling and 25.3% of those in the minimally invasive slings groups. This was not statistically significant (RR 1.23, 95% CI 0.91 to 1.66) (Analysis 9.3). This translates to 311 per 1000 women being incontinent after a traditional sling compared with 253 per 1000 after a minimally invasive sling (Table 4, 9.3).
Analysis 9.3.
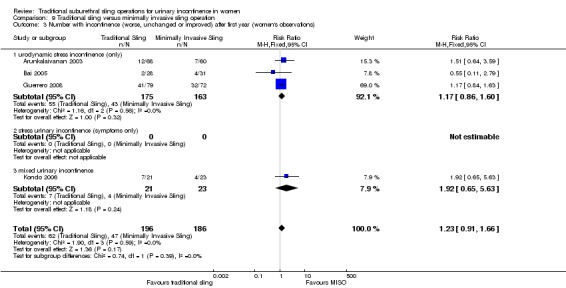
Comparison 9 Traditional sling versus minimally invasive sling operation, Outcome 3 Number with incontinence (worse, unchanged or improved) after first year (women's observations).
Improvement after a year was addressed by two trials (Arunkalaivanan 2003; Guerrero 2008) and there was no statistically significant difference between the two types of sling (RR 1.30, 95% CI 0.57 to 2.94) (Analysis 9.4).
Analysis 9.4.
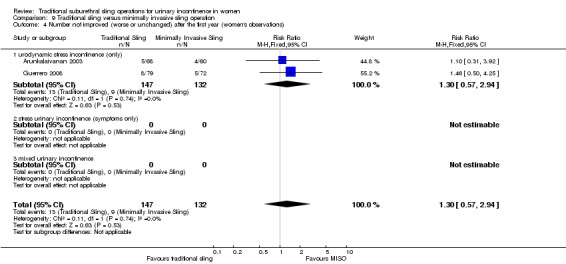
Comparison 9 Traditional sling versus minimally invasive sling operation, Outcome 4 Number not improved (worse or unchanged) after the first year (women's observations).
9.2 Quantification of symptoms (outcome 9.5)
One small trial reported the mean weight of urine on pad test (Silva Filho 2006). The pooled data showed no statistically significant difference in groups (MD 31.00 g, 95% CI ‐57.53 to ‐4.47) (Analysis 9.5).
Analysis 9.5.
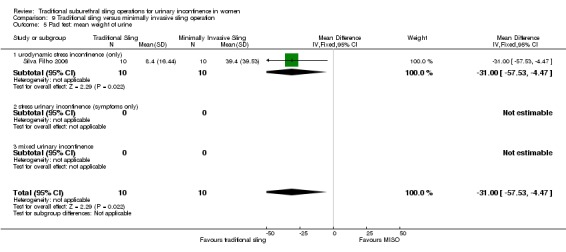
Comparison 9 Traditional sling versus minimally invasive sling operation, Outcome 5 Pad test: mean weight of urine.
9.3 Clinician's observations (outcomes 9.6 and 9.7)
Clinician‐reported incontinence within one year, defined as complete absence of urinary leakage during cough stress test, was assessed in two small trials (Kondo 2006; Sharifiaghdas 2008). There was no statistically significant difference between the two groups (RR 1.29, 95% CI 0.45 to 3.71) (Analysis 9.6). Kondo 2006 further addressed objective cure after the first year but again the findings were not statistically significant and the confidence interval was wide (RR 1.72, 95% CI 0.82 to 3.61) (Analysis 9.7).
Analysis 9.6.
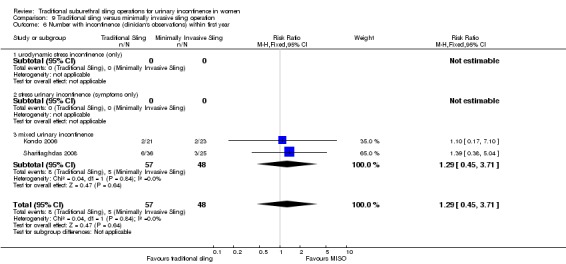
Comparison 9 Traditional sling versus minimally invasive sling operation, Outcome 6 Number with incontinence (clinician's observations) within first year.
Analysis 9.7.
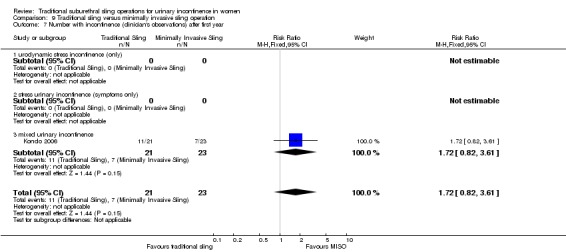
Comparison 9 Traditional sling versus minimally invasive sling operation, Outcome 7 Number with incontinence (clinician's observations) after first year.
9.4 Surgical outcome measures (outcomes 9.8 to 9.10)
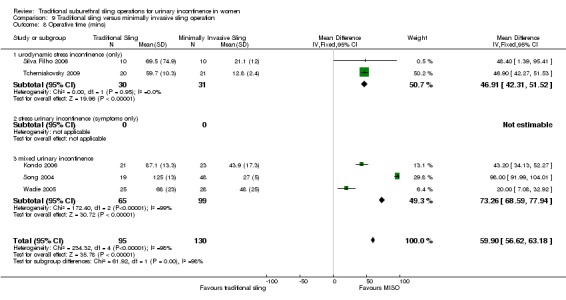
Traditional suburethral sling operations took significantly longer to complete with a mean operating time of 102 minutes compared to 42 minutes for minimally invasive synthetic suburethral sling operations (MD 60 minutes, 95% CI 57 to 63) (Analysis 9.8). There was statistically significant heterogeneity that could not be explained by differences in either the populations, interventions or settings of the individual trials. This heterogeneity persisted even after we performed sensitivity analysis excluding Song 2004, the largest trial, which showed a much longer operating time for the traditional sling operation than the other trials. However, a random‐effects model still showed that traditional suburethral slings took significantly longer to perform (MD 52 minutes, 95% CI 23 to 81) (analysis not shown).
Analysis 9.8.
Comparison 9 Traditional sling versus minimally invasive sling operation, Outcome 8 Operative time (mins).
In two small studies (Kondo 2006; Silva Filho 2006), length of hospital stay was also shorter after minimally invasive synthetic suburethral sling operations (RR 0.49 days, 95% CI 0.26 to 0.72) (Analysis 9.9). Kondo 2006 and Wadie 2005 reported that the time to catheter removal was longer after a traditional sling procedure, but this was not statistically significant (MD 0.11 days, 95% ‐0.07 to 0.30) (Analysis 9.10).
Analysis 9.9.
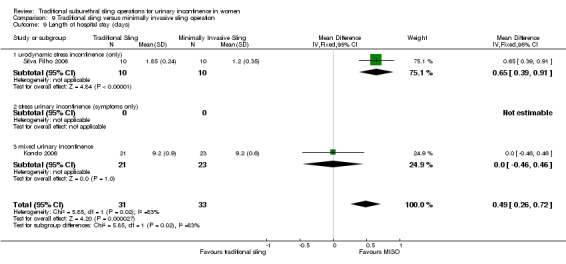
Comparison 9 Traditional sling versus minimally invasive sling operation, Outcome 9 Length of hospital stay (days).
Analysis 9.10.
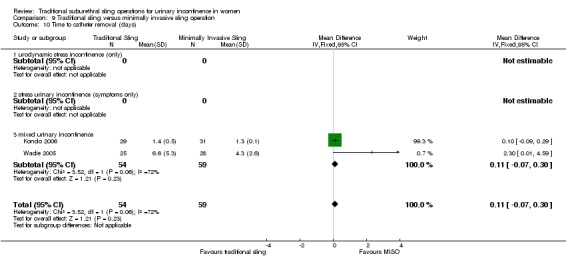
Comparison 9 Traditional sling versus minimally invasive sling operation, Outcome 10 Time to catheter removal (days).
9.5 Adverse events (outcomes 9.11 to 9.20)
Pooled data from three trials (Arunkalaivanan 2003; Kondo 2006; Tcherniakovsky 2009) showed a statistically significant higher risk of perioperative complications after traditional sling operations (RR 1.59, 95% CI 1.03 to 2.44) (Analysis 9.11).
Analysis 9.11.
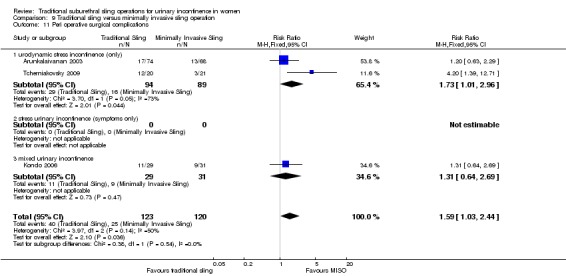
Comparison 9 Traditional sling versus minimally invasive sling operation, Outcome 11 Peri operative surgical complications.
Seven RCTs (Arunkalaivanan 2003; Bai 2005; Kondo 2006; Sharifiaghdas 2008; Song 2004; Tcherniakovsky 2009; Wadie 2005) reported bladder perforation: there were more perforations after minimally invasive slings but this did not reach statistical significance (RR 0.62, 95% CI 0.34 to 1.11) (Analysis 9.12), and the confidence interval was wide. Kondo 2006 further reported urethral injury alone (RR 0.36, 95% CI 0.02 to 8.39) (Analysis 9.13), which again was not statistically significant.
Analysis 9.12.
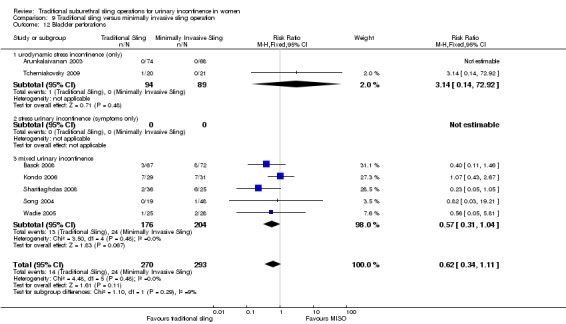
Comparison 9 Traditional sling versus minimally invasive sling operation, Outcome 12 Bladder perforations.
Analysis 9.13.
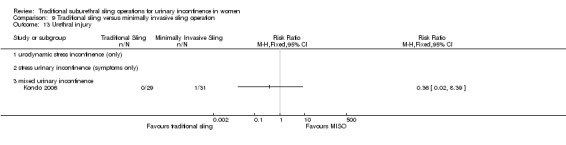
Comparison 9 Traditional sling versus minimally invasive sling operation, Outcome 13 Urethral injury.
The combined results from three trials showed less de novo urgency symptoms or urgency after minimally invasive synthetic suburethral sling operations (RR 3.13, 95% CI 0.96 to 10.24) (Analysis 9.14) but this did not reach statistical significance and the confidence interval was wide. However, three trials showed that de novo detrusor overactivity was significantly less after minimally invasive synthetic suburethral sling operations (RR 3.21, 95% CI 1.29 to 8.03) (Analysis 9.15). This was principally due to the higher weighting given to the largest trial (Basok 2008).
Analysis 9.14.
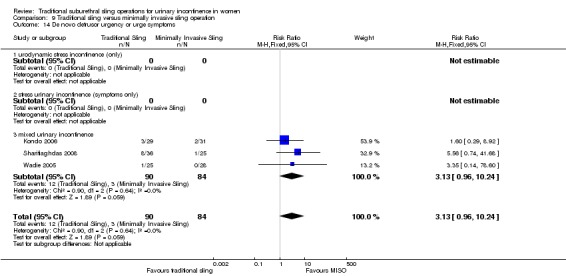
Comparison 9 Traditional sling versus minimally invasive sling operation, Outcome 14 De novo detrusor urgency or urge symptoms.
Analysis 9.15.
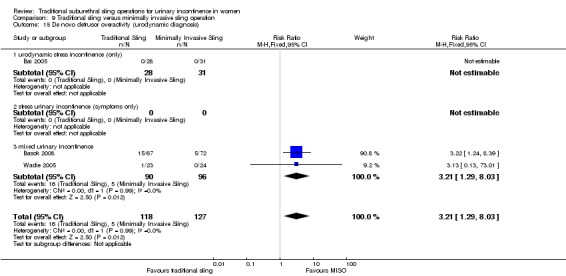
Comparison 9 Traditional sling versus minimally invasive sling operation, Outcome 15 De novo detrusor overactivity (urodynamic diagnosis).
The combined results from five trials showed that more women had postoperative voiding dysfunction after traditional slings than after minimally invasive sling operations (RR 1.60, 95% CI 0.94 to 2.71) (Analysis 9.16) but this did not quite reach statistical significance and the confidence interval was wide.
Analysis 9.16.
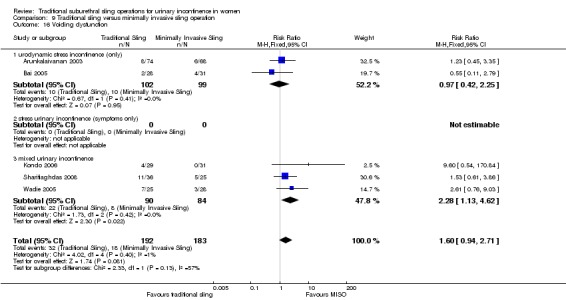
Comparison 9 Traditional sling versus minimally invasive sling operation, Outcome 16 Voiding dysfunction.
More women in the traditional sling group required release of sling (9% versus 2%), reported in two trials (RR 3.67, 95% CI 0.95 to 14.22) (Analysis 9.17) but again this was not statistically significant.
Analysis 9.17.
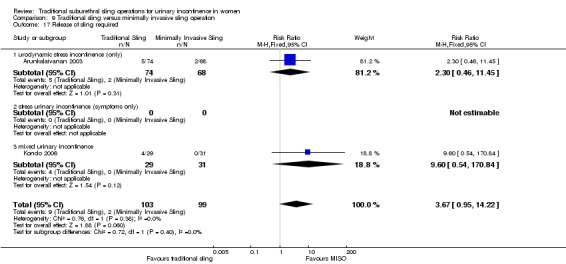
Comparison 9 Traditional sling versus minimally invasive sling operation, Outcome 17 Release of sling required.
There was no statistically significant difference in:
urinary retention up to 6 weeks (RR 5.51, 95% CI 0.68 to 44.63) (Analysis 9.18) reported in one trial;
vaginal erosion (RR 0.35, 95% CI 0.02 to 8.10) (Analysis 9.19) based on one trial.
Analysis 9.18.
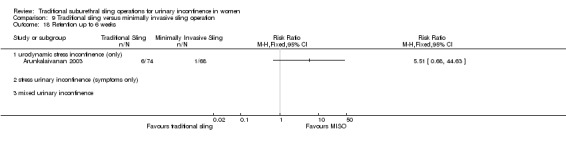
Comparison 9 Traditional sling versus minimally invasive sling operation, Outcome 18 Retention up to 6 weeks.
Analysis 9.19.
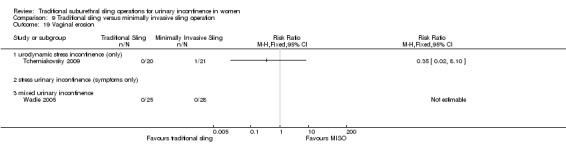
Comparison 9 Traditional sling versus minimally invasive sling operation, Outcome 19 Vaginal erosion.
9.6 Quality of life
Seven studies assessed quality of life. Four of these studies used a number of validated questionnaires, and two studies (Arunkalaivanan 2003; Basok 2008) used invalidated questionnaires. The data were reported in different ways, thus meta‐analysis was not possible and the individual results are reported below .
Amaro 2007 used the Portuguese version of King's Health Questionnaire (KHQ). There were no statistically significant differences between groups in: general health condition; impact of incontinence; role, physical and social limitations; personal relationships; emotions; sleep and severity perception of urinary incontinence at 36 months.
Silva Filho 2006 also used the KHQ, showing a significantly greater improvement in those who underwent the traditional suburethral sling operation in the following domains: general health perception, physical, social and role limitations; and in emotions and severity measures. There were no significant differences in the incontinence impact, personal relationships, sleep or energy domains.
There was statistically significant improvement postoperatively in the Incontinence Impact Questionnaires (IIQ‐7) and Urogenital Distress Inventories (UDI‐6) within both groups but there was no significant difference in the degree of improvement between the groups (Kondo 2006).
IIQ score was also used by Sharifiaghdas 2008 to determine subjective cure. The means were reported 44.3 (range 35.2 to 61.5) in the minimally invasive procedure and 48.5 (range 38.5 to 69.7) in the sling group (P = 0.46). A score less than 50 represents a good quality of life, between 50 and 70 moderate quality of life, and greater than 70 poor quality of life. There was no significant difference in quality of life between groups. Fifteen (72%) of the minimally invasive group and 20 (55%) of the sling group were satisfied with the operation (P value reported by trial authors = 0.3)
There was no significant difference in any of the domains of the Bristol female lower urinary tract symptom score (BFLUTS) assessed in Guerrero 2008.
A subjective 10‐point patient satisfaction questionnaire was used by Basok 2008: there was no evidence of difference between the groups with satisfaction rates of 82% and 87.5% in the traditional sling and minimally invasive sling respectively.
A 10‐point questionnaire‐based assessment was used by Arunkalaivanan 2003: the mean score was 8.03 for minimally invasive synthetic suburethral slings and 8.05 for traditional sling, with a median of nine for both groups.
Comparison 10. One type of traditional sling operations versus another traditional sling operation
Six trials addressed this comparison (Barbalias 1997; Guerrero 2008; Lucas 2000; Pacetta 2005; Shin 2001; Viseshsindh 2003). Traditional sling in this comparison refers to autologous rectus fascial slings, except for one trial, which used autologous dermal graft patch (Shin 2001). New sling refers to Pelvicol (Guerrero 2008), FortaPerm (Pacetta 2005), Gore‐Tex (Barbalias 1997), cadaveric fascia lata (Shin 2001) and a sling made out of vaginal wall (Viseshsindh 2003). The majority of the trials compared different biological materials with each other, except for Barbalias 1997, in which rectus fascia was compared with Gore‐Tex.
10.1 Women's observations (outcomes 10.1 to 10.5)
Three trials (Guerrero 2008; Lucas 2000; Pacetta 2005) reported this outcome.
Short‐term incontinence
A total of 307 women studied within the first 12 months after surgery showed similar incontinence rates between traditional sling operations using autologous materials (35%, 56/161), and traditional sling operations using Pelvicol, FortaPerm and autologous material of shorter length (34%, 49/146). However, the confidence intervals were wide (RR 0.89, 95% CI 0.66 to 1.19) (Analysis 10.1). Two trials using a biological sling (Pelvicol, Guerrero 2008 and FortaPerm, Pacetta 2005) also reported improvement rates that significantly favoured the traditional autologous sling material rectus fascia (RR 0.22, 95% CI 0.08 to 0.59) (Analysis 10.2.1). However, when the comparator was the synthetic non‐absorbable material Gore‐Tex, the trial was too small to be conclusive (Barbalias 1997).
Analysis 10.1.
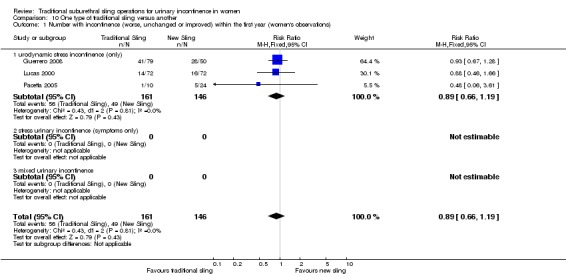
Comparison 10 One type of traditional sling versus another, Outcome 1 Number with incontinence (worse, unchanged or improved) within the first year (women's observations).
Analysis 10.2.
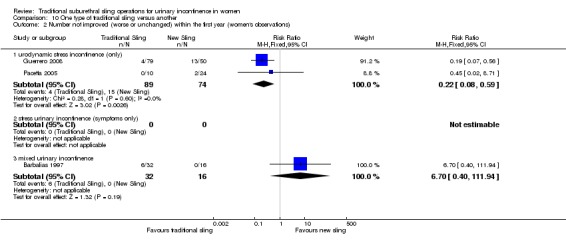
Comparison 10 One type of traditional sling versus another, Outcome 2 Number not improved (worse or unchanged) within the first year (women's observations).
Medium‐/long‐term incontinence rate
A total of 379 women studied after 12 months also showed no statistically significant difference in incontinence rates (RR 0.89, 95% CI 0.72 to 1.10) (Analysis 10.3). However, results once more reported improvement after one year in favour of the traditional autologous sling material rectus fascia (RR 0.33, 95% CI 0.17 to 0.64) (Analysis 10.4).
Analysis 10.3.
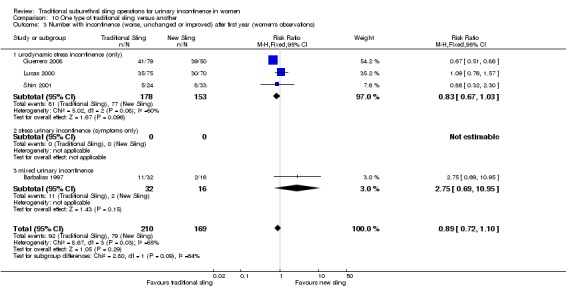
Comparison 10 One type of traditional sling versus another, Outcome 3 Number with incontinence (worse, unchanged or improved) after first year (women's observations).
Analysis 10.4.
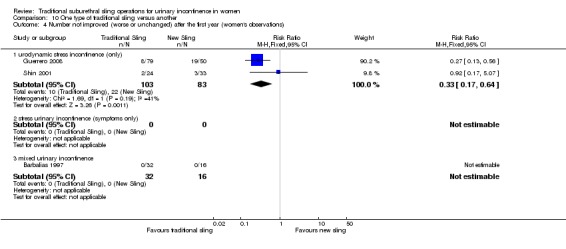
Comparison 10 One type of traditional sling versus another, Outcome 4 Number not improved (worse or unchanged) after the first year (women's observations).
Long‐term incontinence rate
Only one trial reported the incontinence rate after five years (Lucas 2000), and showed no statistically significant difference between different lengths of the autologous material used (RR 1.17, 95% CI 0.86 to 1.59) (Analysis 10.5).
Analysis 10.5.
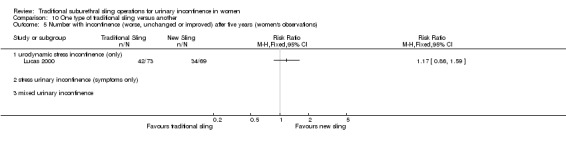
Comparison 10 One type of traditional sling versus another, Outcome 5 Number with incontinence (worse, unchanged or improved) after five years (women's observations).
10.2 Quantification of symptoms (outcome 10.6)
Only one trial (Lucas 2000) reported data on mean weight of urine on a pad test (RR 3.10, 95% CI ‐7.30 to 13.50) (Analysis 10.6): this result was not statistically significant.
Analysis 10.6.
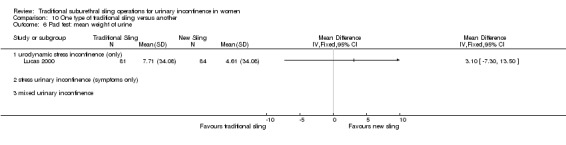
Comparison 10 One type of traditional sling versus another, Outcome 6 Pad test: mean weight of urine.
10.3 Clinician's observations
Number of women with incontinence, as assessed by the clinician, was not reported in any of the trials.
10.4 Surgical outcome measures (outcome 10.7)
The duration of operation for the traditional, long length sling procedure was significantly longer (MD 8.00, 95% CI 3.32 to 12.68) (Analysis 10.7), in one trial (Lucas 2000), which compared long and short lengths of autologous fascia. Length of hospital stay was not reported in any trial.
Analysis 10.7.
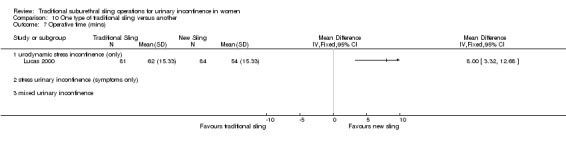
Comparison 10 One type of traditional sling versus another, Outcome 7 Operative time (mins).
10.5 Adverse events (outcomes 10.8 to 10.13)
There was significant heterogeneity in the incidence of adverse effects (perioperative complications) between groups in two trials, which was attributed to more complications with the use of synthetic non‐absorbable Gore‐Tex in one trial (RR 0.05, 95% CI 0.00 to 0.80) (Analysis 10.8.3; Barbalias 1997); in the other trial there was no statistically significant difference between two biological slings (RR 1.14, 95% CI 0.78 to 1.66) (Analysis 10.8.1; Lucas 2000).
Analysis 10.8.
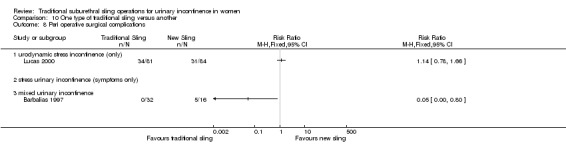
Comparison 10 One type of traditional sling versus another, Outcome 8 Peri operative surgical complications.
No statistically significant difference was found in assessment of the following adverse events, reported in only one trial (Lucas 2000):
bladder perforation (RR 0.69, 95% CI 0.12 to 4.03) (Analysis 10.9);
urinary tract infection (RR 1.73, 95% CI 0.66 to 4.54) (Analysis 10.10);
de novo detrusor urgency or urge symptoms (RR 3.11, 95% CI 0.65 to 14.97) (Analysis 10.11);
voiding dysfunction (RR 1.16, 95% CI 0.65 to 2.07) (Analysis 10.12).
Analysis 10.9.
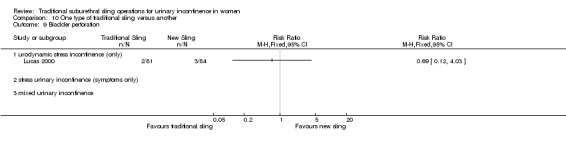
Comparison 10 One type of traditional sling versus another, Outcome 9 Bladder perforation.
Analysis 10.10.
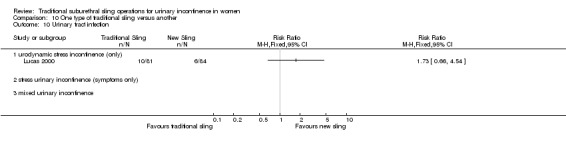
Comparison 10 One type of traditional sling versus another, Outcome 10 Urinary tract infection.
Analysis 10.11.
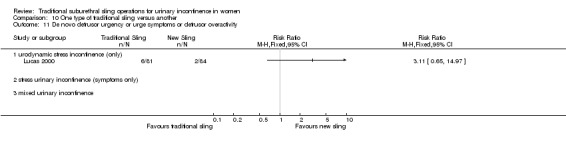
Comparison 10 One type of traditional sling versus another, Outcome 11 De novo detrusor urgency or urge symptoms or detrusor overactivity.
Analysis 10.12.
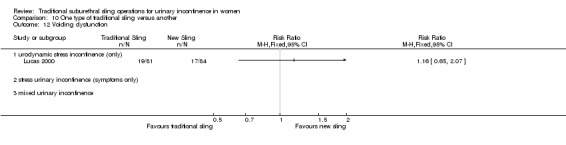
Comparison 10 One type of traditional sling versus another, Outcome 12 Voiding dysfunction.
Two trials reported de novo detrusor overactivity (Barbalias 1997; Shin 2001), once more showing no statistically significant difference between the groups (Analysis 10.13).
Analysis 10.13.
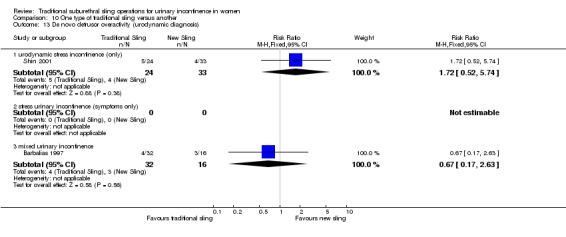
Comparison 10 One type of traditional sling versus another, Outcome 13 De novo detrusor overactivity (urodynamic diagnosis).
10.6 Quality of life
Data were reported in different ways, thus meta‐analysis was not possible.
Lucas 2000 showed significant improvement in the average scores for both the UDI‐6, reported P value = 0.007, and the IIQ‐7, P = 0.002 when compared with baseline. The scores between groups were similar.
Pacetta 2005 evaluated participants using Incontinence Quality of Life (I‐QOL), reporting an improvement from 45 at baseline to 97 at one year in the autologous fascia group and from 39 to 92 for the FortaPerm group.
Discussion
To supplement the main systematic review of effects, we sought to identify economic evaluations that have compared traditional suburethral sling operations with any of the other main categories of surgical methods listed in the background section. A supplementary search in Ovid NHS EED, MEDLINE and Embase identified two such economic evaluations. Details of the search strategies are given in Appendix 2.
Summary of main results
Traditional suburethral sling operation versus no treatment or sham operation
To date, there still remains no RCT comparing traditional sling procedures with laparoscopic procedures for stress urinary incontinence. No related economic evidence was identified for the brief economic commentary.
Traditional suburethral sling operation versus conservative management (e.g. pelvic floor muscle training, electrical stimulation, cones, biofeedback)
We did not find trials comparing suburethral slings with conservative management such as pelvic exercises or vaginal cones, or with some other surgical operations (anterior repair, laparoscopic retropubic suspension, injections or artificial sphincters). No related economic evidence was identified for the brief economic commentary.
Traditional suburethral sling operation versus drugs
One trial compared surgery (Burch or traditional sling procedure) with oxybutynin drug therapy for women with mixed incontinence symptoms (Osman 2003). Oxybutinin is an anticholinergic drug which is usually used to treat urgency urinary incontinence and not stress urinary incontinence. The trial showed significantly better results in the group managed surgically with a traditional sling procedure to treat mixed urinary incontinence than oxybutynin, with a cure rate of 83% for stress urinary incontinence and 88% for urgency incontinence in comparison to 0% and 57%, respectively (Analysis 3.1; Analysis 3.2).
However, post‐operative morbidity was not reported well and the results of a single, medium‐sized trial in determining the effects in either group should be considered cautiously and requires replication.
No related economic evidence was identified for the brief economic commentary.
Traditional suburethral sling versus injectable
Only one small trial assessed this comparison (Maher 2005), showing a clear difference in clinician‐assessed incontinence rate at six months favouring pubovaginal sling (19%; 4/21) versus transurethral Macroplastique (91%; 20/22). Incontinence rate was taken as those women not 'cured'. Cure was defined as no urinary leakage due to stress urinary incontinence on repeat urodynamics.
Advantages to injection therapy were lower morbidity rates: there were equivalent incontinence and participant‐satisfaction rates at six months' follow‐up between groups. At five years 69% (9/13) of women were satisfied with sling surgery versus 29% (4/14) of those who received Macroplastique. There was, however, only a 60% long‐term follow‐up rate in this study, therefore this result must be interpreted with caution.
In a comparative cost analysis of a retrospective observational study conducted by Berman 1997 in the USA, traditional suburethral retropubic sling procedures were compared with transurethral collagen injections in women with SUI. Women were followed up for 15 months post surgery and 71% of the traditional sling arm were symptom free compared with 27% in the collagen injection arm (P = 0.05). The average cost per woman treated with the traditional sling procedure was USD 10,382 (1995 USD), while the collagen injection was USD 4996 (1995 USD) (P < 0.001). Although the cost of the traditional sling is double that of the collagen injection, the study authors argued that traditional suburethral retropubic sling procedure is more cost‐effective than collagen injection due to its higher effectiveness.
Traditional suburethral sling versus open abdominal retropubic colposuspension
The inclusion of the large trial on traditional slings (Albo 2007) strengthened the trend towards a better performance of the traditional slings in terms of participant‐reported incontinence rates, but higher post‐operative voiding dysfunction rates compared to open colposuspension.
The limited data available suggest that the overall rates of peri‐operative and late surgical complications are similar after sling and colposuspension operations. However, the pattern of complications varies.
A cost‐effectiveness analysis (Kilonzo 2004) compared minimally invasive slings with open abdominal retropubic colposuspension, laparoscopic colposuspension, traditional suburethral retropubic sling procedure, and injectables. The data utilised in this study were based on a Technology Assessment Review conducted for the National Institute for Clinical Excellence (NICE), UK (Cody 2003). The study utilised clinical data from a systematic review of RCTs conducted up to mid‐2003 (Lapitan 2003; Moehrer 2002; Ward 2002b) and results based upon economic modelling for a time horizon of up to 10 years. The analysis of costs and resources used was based on the UK payer’s perspective (UK National Health Service). Based on clinical evidence, this study assumed that traditional sling effectiveness was equivalent to open abdominal retropubic colposuspension. The cost of open colposuspension was reported as GBP 1301 per woman (2001) with an operation time of 52.4 minutes and average hospital stay of 7.1 days, while traditional slings cost GBP 1340 per woman (2001 GBP) with an operation time of 45.6 minutes and average hospital stay of 7.2 days.
Traditional suburethral sling versus bladder neck needle suspension (abdominal and vaginal)
The one small trial that compared needle operations with slings included an atypical population who were unsuitable for colposuspension (Hilton 1989). The procedures were restricted to women with vaginal narrowing deemed unsuitable for open abdominal retropubic colposuspension. There were too few women to provide reliable data about cure rates. Although the sling operations were associated with more post‐operative morbidity, the results could not be generalised to the whole population having surgery because of the atypical nature of the women involved in the trial, such that complications may have been caused by surgical difficulties due to vaginal narrowing. However, the group managed by needle suspensions did not seem to have the same complications.
No related economic evidence was identified for the brief economic commentary.
Traditional suburethral sling operation versus anterior repair.
To date, there still remains no RCTs comparing traditional sling procedures with anterior repair for stress urinary incontinence.
No related economic evidence was identified for the brief economic commentary.
Traditional suburethral sling operation versus laparoscopic procedures
To date, there still remains no RCT comparing traditional sling procedures with laparoscopic procedures for stress urinary incontinence.
For the economic evidence, Kilonzo 2004 also assumed that the effectiveness of laparoscopic colposuspension was equivalent or possibly worse than open colposuspension, while the effectiveness of open colposuspension was equivalent to traditional sling. The study reported the cost of laparoscopic colposuspension to be GBP 1317 (2001 GBP) with an operation time of 60 minutes and an average hospital stay of 4.6 days, compared with traditional sling, which costs GBP 1340 (2001 GBP) with an operation time of 45.6 minutes and average hospital stay of 7.2 days.
Traditional suburethral sling operation versus a minimally invasive sling
Historically, traditional suburethral sling procedures were used for women who had recurrent stress incontinence (after a previous failed continence operation). However, the current review includes women with new or recurrent incontinence, without reporting the results separately. They were designed to restore normal urethrovesical junction support by mechanically compressing or kinking the proximal urethra.
Minimally invasive synthetic suburethral sling operations appeared to be as effective as traditional suburethral slings in the short term (RR 0.97, 95% CI 0.78 to 1.20), although the confidence interval was compatible with minimally invasive slings, being 20% better or 12% worse. The operating time and length of stay were also significantly shorter with minimally invasive synthetic suburethral sling operations, and women had fewer perioperative complications and less detrusor overactivity. The main perioperative complication of minimally invasive sling procedures was bladder perforation, although this did not appear to have longer‐term implications. However, because the information was not available, it was not possible to determine if either type of sling was more effective in women who had had previous failed continence surgery.
. More data on the advantages and disadvantages of the different types of biological and synthetic sling materials would be useful to aid decision making. Materials may vary in the degree of discomfort or erosion they cause.
Kilonzo 2004 also reported on this comparison. The study reported the cost in 2001 in GBP to be GBP 1058 (2001 GBP) per woman with an average of 2.9 days hospital stay and 30 minutes operation time for minimally invasive slings, compared with traditional slings, which cost GBP 1340 (2001 GBP) per woman, with an average hospital stay of 7.2 days and operation of time of 45.6 minutes. There was an 86% probability that minimally invasive sling was cost‐effective compared to open colposuspension, with a willingness‐to‐pay of GBP 30,000 (2001 GBP). Minimally invasive sling was found to be slightly less effective than open colposuspension in terms of Quality Adjusted Life Years (QALYs) for the first four years. Beyond five years, minimally invasive sling was more effective. The study concluded that minimally invasive slings were likely to be more cost‐effective than open colposuspensions. Based on the assumption in Kilonzo 2004 that the effectiveness of traditional sling was taken to be equivalent to open colposuspension, therefore the cost‐effectiveness results for the comparison of minimally invasive slings with traditional slings would be similar to the cost‐effectiveness of minimally invasive slings versus open colposuspension.
One type of traditional sling operation versus another traditional sling operation
Some synthetic slings may have a higher incidence of erosion, infections and urge symptoms. There was some evidence that these were more common after Gore‐Tex.
Meta‐analysis showed a significantly greater improvement of symptoms (participant‐reported) both within and after one year, using autologous materials. There was no evidence of a difference in peri‐operative complications or post‐operative morbidity between autologous and other materials. Trials, however, were few in number, with short follow‐up and small populations.
More evidence is needed to compare slings made of autologous materials (e.g. rectus fascia, vaginal wall) with synthetic or exogenous biological materials (e.g. Teflon, polytetrafluoroethylene, porcine dermis, dura mater). Some materials may be inappropriate in particular groups of women, such as those with religious beliefs which preclude the use of animal tissues.
No related economic evidence was identified for the brief economic commentary.
Overall completeness and applicability of evidence
Evidence relating to primary outcome was available, but limited in determining the effectiveness of traditional suburethral sling operations in the treatment of urinary incontinence. The limited evidence suggests that traditional slings may be equally as effective as other surgical treatments currently available, but variability in the quality of trials is a major limiting factor.
None of the trials reviewed contained all relevant participant‐reported outcomes. More data on pain after different procedures (both post‐operative and long term) and time to return to 'normal' daily living following surgery would have been useful.
The review may not be applicable to clinicians everywhere. High‐income countries are increasingly using minimally invasive procedures and synthetic materials as the first‐line treatment for stress urinary incontinence. The use of traditional suburethral operations, which appear to be just as effective, might be reserved for countries where new technology is not available or too expensive.
Where possible, we analysed data in subgroups according to clinical characteristics of the type of incontinence (urodynamic stress incontinence, stress incontinence symptoms or mixed urinary incontinence). Further analysis according to clinical characteristics of women such as: primary versus recurrent SUI, intrinsic urethral sphincter deficiency versus urethral hypermobility, obesity, ethnicity, vaginal delivery versus caesarean‐section, presence or absence of prolapse, anaesthesia used, or experience of the surgeon might make the findings of the review more generalisable. The majority of trials, however, did not report these characteristics.
.Quality of life, emotional well‐being, and social implications were poorly reported, or reported using a variety of instruments, thus precluding meta‐analysis. These outcomes are of great importance to women and decision makers.
For the economic evidence, we did not subject the two identified economic evaluations to critical appraisal and we do not attempt to draw any firm or general conclusions regarding the relative costs or efficiency of traditional suburethral retropubic slings in treatment of stress urinary incontinence. However, based on the economic evidence available, it can be suggested that traditional suburethral retropubic sling procedure is cost‐effective compared to collagen injection but not cost‐effective when compared with minimally invasive slings.
Quality of the evidence
In general, the scientific quality of the trials was low or moderate. Although the trial authors stated that their trials were randomised, most of the reports did not give sufficient detail about the method of sequence generation or concealment of allocation. Only two trials used an adequate randomisation method. Blinding surgeons or women was generally not possible, but none reported external, third‐party, blinded assessment at follow‐up. The total number of women enrolled was 2284, but some trials only recruited 10 women per arm. In addition, several types of slings were compared with different interventions, meaning that different materials had to be grouped together for comparisons. This meant that the numbers in each comparison were small and the confidence intervals wide.
The populations varied, including women with and without previous surgery, and one study included only women who were deemed not suitable for another procedure (Hilton 1989). Although the majority had urodynamic stress incontinence, some trials included women with mixed urinary incontinence. Baseline comparability of the groups was not reported in all trials. Several trials assessed different types of sling in comparison with autologous rectus fascia, suggesting that the latter was considered as the 'standard' comparator. Although seven trials used open abdominal retropubic colposuspension as the comparator, each used a different type of sling, and three followed up the women for only six months. Rather more trials used a minimally invasive sling as the comparator, as this has arguably become the gold standard procedure for continence surgery, at least in high‐income countries.
In general, most trials reported different outcome measures, often poorly. The principal measure of effectiveness used in most studies was the proportion of women with incontinence following surgery. Few researchers have considered other outcomes, such as activities of daily living and quality of life. Few addressed general health status, repeat incontinence surgery, later prolapse surgery and time to return to normal activity level. Satisfaction with, and acceptability of, the treatment were also seldom addressed but are also important factors in choice of management.
Authors' conclusions
Traditional slings seemed to be as effective as minimally invasive slings, but had higher rates of adverse effects. This should be interpreted with some caution however, as the quality of evidence in the studies was variable, follow‐up short, and randomised trials do have inherent limitations in identifying complication rates. Traditional sling procedures appeared to confer a similar cure rate in comparison to open retropubic colposuspension, but the long‐term adverse event profile is still unclear.
The data were too few to address whether the types of suburethral slings tested were as effective as other sling materials, injectables, drugs, or needle suspension. There was limited evidence from one small trial that slings made of non‐absorbable synthetic Gore‐Tex had more complications than slings made of biological rectus fascia.
The broader effects of suburethral slings could not be established since trials did not include appropriate outcome measures, such as general health status, pad testing, third‐party analysis and time to return to normal activity level, and follow‐up was limited.
Evidence to clarify whether or not traditional suburethral slings may be better or worse than surgical or conservative management options, other than those reported in this review, is lacking.
The methodology of trials and their appropriate reporting must be addressed in future research. Some of the evidence was limited by the poor quality and small numbers of the included randomised trials. The CONSORT guidelines should be used to ensure adequate reporting (Schultz 2010).
There is a need for further trials of adequate power, better quality and reporting standard to assess the effectiveness of suburethral slings in comparison with other surgical techniques and different types of slings, and in specific situations such as in women who have already had previous continence surgery, or with anatomical restrictions.
Future research in incontinence treatments should incorporate standardised, validated and simple outcome measures, both participant‐reported and clinician‐observed. Outcomes should be relevant to women who have incontinence and are seeking treatment, and policymakers commissioning treatment, in order to allow comparison between treatments. In particular, quality of life, psychological and economic outcomes should be incorporated. Surgical trials related to urinary incontinence should systematically address surgical morbidity outcomes such as adverse peri‐ and post‐operative events, length of hospital stay, time to return to normal activities, development of urge symptoms or detrusor overactivity and especially the need for repeat surgery or alternative interventions. Long‐term follow‐up (at least one year, preferably five years or more) is essential for the proper evaluation of incontinence treatments.
Acknowledgements
We would like to express our thanks to Sheila Wallace who helped us by providing information not found in Brazil. We are also very grateful to Professor Aldemar Araujo Castro from the Brazilian Cochrane Centre who provided a prompt and valuable contribution to the review. Professor Adrian Grant provided advice with interpretation of data and the final form of the first version of the review. Dr Jonathan Cook provided expert statistical advice.
Appendices
Appendix 1. Details of extra literature searching performed for older versions of this review
For previous versions of this review (which covered all sling types) one of the review authors (Carlos Bezerra) performed extra, specific searches. These are detailed below.
Systematic searches of electronic bibliographic databases:
PubMed ‐ years searched: January 1966 to January 2000, date searched: 30 January 2000;
UK National Research Register ‐ Issue 1, 2001, date searched: May 2001.
Search term used: TVT
Handsearching of conference proceedings: Brazilian Congress of Urology Annual Meeting: 1991 to 2003 inclusive
Appendix 2. Search strategies for brief economic commentary
On 6 April 2017 we performed additional searches for the brief economic commentary. These were conducted in NHS EED (1st Quarter 2016), MEDLINE (1 January 1946 to March 2017), and Embase (1 January 1980 to 2017 Week 12). We used one search strategy on NHS EED (OVID) and two different search strategies on MEDLINE and Embase (OvidSP). Details of the searches run and the search terms used can be found below. We did not apply any year, publication type or language restrictions to the searches.
NHS EED (Ovid) (1st Quarter 2016)
NHS EED was searched using the following search strategy:
1. Urinary incontinence/
2. Urinary incontinence, stress/
3. ((stress$ or mix$ or urg$ or urin$) adj3 incontinen$).tw.
4. Colporrhaphy.tw.
Single‐incision sling operations for urinary incontinence in women
63 / 85
5. Colpoperineoplast$.tw.
6. Sling procedure$.tw.
7. Sling$ procedure$.tw.
8. Bladder neck needle suspension$.tw.
9. Anterior vaginal repair$ .tw.
10. Or/1‐9
MEDLINE (1 January 1946 to March 2017) and Embase (1 January 1980 to 2017 Week 12)
We used two different search strategies on MEDLINE and EMBASE (OvidSP) ‐ these are given below.
Search strategy 1:
1. Economics, Pharmaceutical/ or Economics, Medical/ or Economics/ or Economics, Hospital/ or economics.mp. or
Economics, Nursing/
2. exp "costs and cost analysis"/
3. "Value of Life"/
4. exp "fees and charges"/
5. exp budgets/
6. budget*.ti,ab.
7. cost*.ti.
8. (economic* or pharmaco?economic*).ti.
9. (price* or pricing*).ti,ab.
10. (cost* adj2 (effective* or utilit* or benefit* or minimi* or unit* or estimat* or variable*)).ab.
11. (financ* or fee or fees).ti,ab.
12. (value adj2 (money or monetary)).ti,ab.
13. ((energy or oxygen) adj cost).ti,ab.
14. (metabolic adj cost).ti,ab.
15. ((energy or oxygen) adj expenditure).ti,ab.
16. 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15
17. exp Urinary Incontinence/
18. ((stress* or mix* or urg* or urin*) adj3 incontinen*).tw.
19. Urodynamics/ or Urinary Incontinence, Stress/ or Urinary Incontinence/ or Suburethral Slings/ or mixed incontinence.mp. or Urinary Bladder/ or Urinary Incontinence, Urge/
20. 17 or 18 or 19
21. anterior vaginal repair*.tw.
22. 16 and 20 and 21
23. anterior colporrhaphy*.tw.
24. 21 or 23
25. 16 and 20 and 23
26. bladder neck needle suspension$.tw.
27. 16 and 20
28. 26 and 27
29. open abdominal retropubic colposuspension*.tw.
30. retropubic colposuspension*.tw.
31. burch colposuspension*.tw.
32. 29 or 30 or 31
33. 27 and 32
34. laparoscopic retropubic colposuspension*.tw.
35. laparoscopic colposuspension*.tw.
36. 34 or 35
37. 27 and 36
38. traditional suburethral retropubic sling procedure$*.tw.
39. traditional sling procedure$*.tw.
40. suburethral retropubic sling procedure$*.tw.
41. retropubic sling procedure$*.tw.
42. traditional suburethral sling*.tw.
43. Suburethral Slings/ or Urinary Incontinence, Stress/ or Urologic Surgical Procedures/
44. 27 and 43
45. remove duplicates from 44
Search strategy 2:
1. economics.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, fs]
2. value of life.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, fs]
3. exp "costs and cost analysis"/
4. exp economics, hospital/
5. exp economics, medical/
6. economics, nursing.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, fs]
7. economics, pharmaceutical.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, fs]
8. exp "fees and charges"/
9. exp budgets/
10. budget*.ti,ab.
11. cost*.ti.
12. (economic* or pharmaco?economic*).ti.
13. (price* or pricing*).ti,ab.
14. (cost* adj2 (effective* or utilit* or benefit* or minimi* or unit* or estimat* or variable*)).ab.
15. (financ* or fee or fees).ti,ab.
16. (value adj2 (money or monetary)).ti,ab.
17. or/1‐16
18. economics.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, fs]
19. value of life.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, fs]
20. exp "costs and cost analysis"/
21. exp economics, hospital/
22. exp economics, medical/
23. economics, nursing.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, fs]
24. economics, pharmaceutical.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, fs
25. exp "fees and charges"/
26. exp budgets/
27. budget*.ti,ab.
28. cost*.ti.
29. (economic* or pharmaco?economic*).ti.
30. (price* or pricing*).ti,ab.
31. (cost* adj2 (effective* or utilit* or benefit* or minimi* or unit* or estimat* or variable*)).ab.
32. (financ* or fee or fees).ti,ab.
33. (value adj2 (money or monetary)).ti,ab.
34. 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31 or 32 or 33
Single‐incision sling operations for urinary incontinence in women
65 / 85
35. ((energy or oxygen) adj cost).ti,ab.
36. (metabolic adj cost).ti,ab.
37. ((energy or oxygen) adj expenditure).ti,ab.
38. 34 or 35 or 36 or 37
39. urinary incontinence.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
40. ((stress$ or mix$ or urg$ or urin$) adj3 incontinen$).tw.
41. URINARY INCONTINENCE, STRESS.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
42. stress urinary incontinence*.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
43. 39 or 40 or 41 or 42
44. intervention surgery*.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
45. colporrhaphy.tw.
46. Bologna procedure*.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
47. Kelly‐Kennedy.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
48. Marion Kelly.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
49. Diaphragmplasty.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
50. Vaginal urethrocystopexy.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
51. Cystocele repair.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
52. Kelly plication.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
53. anterior vaginal repair$.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
54. anterior colporrhaphy.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
55. 44 or 45 or 46 or 47 or 48 or 49 or 50 or 51 or 52 or 53 or 54
56. 38 and 43 and 55
57. remove duplicates from 56
58. Bladder neck needle suspension$.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
59. 38 and 43 and 58
60. burch colposuspension.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
61. open abdominal retropubic colposuspension.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw,
fs]
62. Paravaginal defect repair.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
63. Marshall‐Marchetti‐Krantz.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
64. abdominal burch.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
65. abdominal colposuspension.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
66. endopelvic Fascia Plication.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
67. 60 or 61 or 62 or 63 or 64 or 65 or 66
68. 38 and 43
69. 67 and 68
70. laparoscopic retropubic colposuspension.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
71. laparoscopic colposuspension.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
72. retropubic colposuspension.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
73. 70 or 71 or 72
74. 68 and 73
75. remove duplicates from 74
76. suburethral sling.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
77. abdominal sling.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
78. traditional sling procedure$*.tw.
Single‐incision sling operations for urinary incontinence in women
66 / 85
79. suburethral sling procedure.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
80. 76 or 77 or 78 or 79
81. 68 and 80
82. remove duplicates from 81
83. mid$urethral sling.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
84. retropubic sling procedure$*.tw.
85. transobturator sling procedure$.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
86. 83 or 84 or 85
87. remove duplicates from 86
88. 68 and 87
89. TVT‐Secur.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
90. mini‐arc.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
91. ajust.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
92. needleless.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
93. solyx.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
94. single$incision sling$.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
95. miniarc.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
96. mini$sling.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
97. Ophira.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
98. Tissue Fixation System.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
99. 89 or 90 or 91 or 92 or 93 or 94 or 95 or 96 or 97 or 98
100. 68 and 99
101. remove duplicates from 100
102. ((urethra$ or periurethra$ or transurethra$) adj3 (agent$ or bulk$ or injection$ or injectable$)).tw.
103. injection therapy.tw.
104. injectable$.tw.
105. (injectable$ adj2 agent$).tw.
106. (bulk$ adj3 agent$).tw.
107. Peri$urethral injection$.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
108. Autologous fat.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
109. Macroplastique.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
110. Calcium hydroxylapatite.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
111. Hyaluronic acid with dextranomer.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
112. Porcine dermal implant.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
113. Ethylene vinyl alcohol copolymer.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
114. Silicon particles.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
115. 102 or 103 or 104 or 105 or 106 or 107 or 108 or 109 or 110 or 111 or 112 or 113 or 114
116. 68 and 115
117. remove duplicates from 116
Data and analyses
Comparison 3.
Sling versus drugs
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Number with incontinence (worse, unchanged or improved) within the first year (women's observations) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 urodynamic stress incontinence (only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 stress urinary incontinence (symptoms only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 mixed incontinence | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Urge symptoms or urge incontinence | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.1 urodynamic stress incontinence (only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 stress urinary incontinence (symptoms only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 mixed incontinence | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
Comparison 4.
Sling versus injectable
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Number with incontinence (worse, unchanged or improved) within the first year (women's observations) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 urodynamic stress incontinence (only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 stress urinary incontinence (symptoms only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 mixed urinary incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Number with incontinence (worse, unchanged or improved) after first year (women's observations) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.1 urodynamic stress incontinence (only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 stress urinary incontinence (symptoms only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 mixed urinary incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Number with incontinence (clinician's observations) within first year | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.1 urodynamic stress incontinence (only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 stress urinary incontinence (symptoms only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.3 mixed urinary incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Voiding dysfunction | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4.1 urodynamic stress incontinence (only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 stress urinary incontinence (symptoms only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.3 mixed urinary incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 De novo detrusor overactivity (urodynamic diagnosis) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 5.1 urodynamic stress incontinence (only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.2 stress urinary incontinence (symptoms only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.3 mixed urinary incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Urinary tract infection | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 6.1 urodynamic stress incontinence (only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.2 stress urinary incontinence (symptoms only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.3 mixed urinary incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
Comparison 5.
Sling versus open abdominal retropubic suspension
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Number with incontinence (worse, unchanged or improved) within the first year (women's observations) | 4 | 147 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.40 [0.11, 1.41] |
| 1.1 urodynamic stress incontinence (only) | 4 | 147 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.40 [0.11, 1.41] |
| 1.2 stress urinary incontinence (symptoms only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 1.3 mixed incontinence | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 2 Number not improved (worse or unchanged) within the first year (women's observations) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 2.1 urodynamic stress incontinence (only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 2.2 stress urinary incontinence (symptoms only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 2.3 mixed incontinence | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3 Number with incontinence (worse, unchanged or improved) after first year (women's observations) | 5 | 715 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.75 [0.62, 0.90] |
| 3.1 urodynamic stress incontinence (only) | 4 | 195 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.72 [0.31, 1.67] |
| 3.2 stress urinary incontinence (symptoms only) | 1 | 520 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.75 [0.62, 0.91] |
| 3.3 mixed incontinence | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Number not improved (worse or unchanged) after first year (women's observations) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4.1 urodynamic stress incontinence (only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4.2 stress urinary incontinence (symptoms only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4.3 mixed incontinence | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Pad changes over 24 hours | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5.1 urodynamic stress incontinence (only) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5.2 stress urinary incontinence (symptoms only) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5.3 mixed incontinence | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Incontinent episodes over 24 hours | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6.1 urodynamic stress incontinence (only) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6.2 stress urinary incontinence (symptoms only) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6.3 mixed incontinence | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Pad test weights | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7.1 urodynamic stress incontinence (only) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7.2 stress urinary incontinence (symptoms only) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7.3 mixed incontinence | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 8 Number with incontinence (clinician's observations) within the first year | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 8.1 urodynamic stress incontinence (only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 8.2 stress urinary incontinence (symptoms only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 8.3 mixed incontinence | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 9 Number with incontinence (clinician's observations) after first year | 3 | 620 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.64, 1.41] |
| 9.1 urodynamic stress incontinence (only) | 1 | 28 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.23 [0.01, 4.37] |
| 9.2 stress urinary incontinence (symptoms only) | 2 | 592 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.66, 1.47] |
| 9.3 mixed incontinence | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 10 Operative time (minutes) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 10.1 urodynamic stress incontinence (only) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 10.2 stress urinary incontinence (symptoms only) | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 10.3 mixed incontinence | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 11 Time to catheter removal (days) | 2 | 108 | Mean Difference (IV, Fixed, 95% CI) | 8.01 [6.84, 9.18] |
| 11.1 urodynamic stress incontinence (only) | 1 | 36 | Mean Difference (IV, Fixed, 95% CI) | 9.5 [‐4.27, 23.27] |
| 11.2 stress urinary incontinence (symptoms only) | 1 | 72 | Mean Difference (IV, Fixed, 95% CI) | 8.0 [6.82, 9.18] |
| 11.3 mixed incontinence | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 12 Length of inpatient stay (days) | 3 | 137 | Mean Difference (IV, Fixed, 95% CI) | 2.03 [1.47, 2.59] |
| 12.1 urodynamic stress incontinence (only) | 3 | 137 | Mean Difference (IV, Fixed, 95% CI) | 2.03 [1.47, 2.59] |
| 12.2 stress urinary incontinence (symptoms only) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 12.3 mixed incontinence | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 13 Time to return to normal activity level | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 13.1 urodynamic stress incontinence (only) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 13.2 stress urinary incontinence (symptoms only) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 13.3 mixed incontinence | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 14 Peri‐operative surgical complications | 4 | 792 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.31 [1.14, 1.51] |
| 14.1 urodynamic stress incontinence (only) | 3 | 137 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.85 [0.28, 2.52] |
| 14.2 stress urinary incontinence (symptoms only) | 1 | 655 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.33 [1.16, 1.53] |
| 14.3 mixed incontinence | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 15 Bladder perforation | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 15.1 urodynamic stress incontinence (only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 15.2 stress urinary incontinence (symptoms only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 15.3 mixed incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 16 Urinary tract infection | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 16.1 urodynamic stress incontinence (only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 16.2 stress urinary incontinence (symptoms only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 16.3 mixed incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 17 Urge symptoms or urge incontinence | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 17.1 urodynamic stress incontinence (only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 17.2 stress urinary incontinence (symptoms only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 17.3 mixed incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 18 Detrusor overactivity (urodynamic diagnosis) | 4 | 203 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.42 [0.52, 3.87] |
| 18.1 urodynamic stress incontinence (only) | 4 | 203 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.42 [0.52, 3.87] |
| 18.2 stress urinary incontinence (symptoms only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 18.3 mixed incontinence | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 19 Voiding dysfunction after three months | 5 | 853 | Risk Ratio (M‐H, Fixed, 95% CI) | 6.08 [3.10, 11.95] |
| 19.1 urodynamic stress incontinence (only) | 4 | 198 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.48 [1.16, 17.36] |
| 19.2 stress urinary incontinence (symptoms only) | 1 | 655 | Risk Ratio (M‐H, Fixed, 95% CI) | 6.63 [3.04, 14.47] |
| 19.3 mixed incontinence | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 20 Prolapse | 2 | 106 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.04, 1.11] |
| 20.1 urodynamic stress incontinence (only) | 2 | 106 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.04, 1.11] |
| 20.2 stress urinary incontinence (symptoms only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 20.3 mixed incontinence | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 21 Repeat incontinence surgery | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 21.1 urodynamic stress incontinence (only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 21.2 stress urinary incontinence (symptoms only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 21.3 mixed incontinence | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 22 Health status measures | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 22.1 urodynamic stress incontinence (only) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 22.2 stress urinary incontinence (symptoms only) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 22.3 mixed incontinence | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
Comparison 6.
Sling versus bladder neck (needle) suspension
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Number with incontinence (worse, unchanged or improved) within the first year (women's observations) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 urodynamic stress incontinence (only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 stress urinary incontinence (symptoms only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 mixed incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Number with incontinence (worse, unchanged or improved) after the first year (women's observations) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.1 urodynamic stress incontinence (only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 stress urinary incontinence (symptoms only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 mixed incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Length of inpatient stay | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3.1 urodynamic stress incontinence (only) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 stress urinary incontinence (symptoms only) | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.3 mixed incontinence | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Peri‐operative surgical complications | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4.1 urodynamic stress incontinence (only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 stress urinary incontinence (symptoms only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.3 mixed incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Urge symptoms or urge incontinence | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 5.1 urodynamic stress incontinence (only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.2 stress urinary incontinence (symptoms only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.3 mixed incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Voiding dysfunction after three months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 6.1 urodynamic stress incontinence (only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.2 stress urinary incontinence (symptoms only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.3 mixed incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Detrusor overactivity (urodynamic diagnosis) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 7.1 urodynamic stress incontinence (only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.2 stress urinary incontinence (symptoms only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.3 mixed incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
Analysis 6.5.
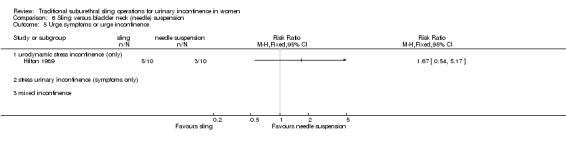
Comparison 6 Sling versus bladder neck (needle) suspension, Outcome 5 Urge symptoms or urge incontinence.
Analysis 6.6.
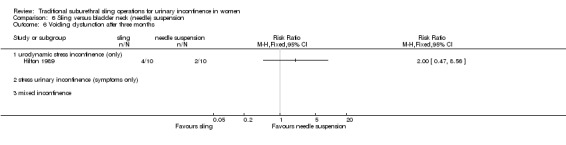
Comparison 6 Sling versus bladder neck (needle) suspension, Outcome 6 Voiding dysfunction after three months.
Analysis 6.7.
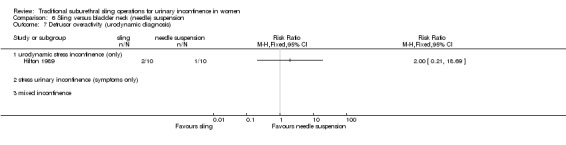
Comparison 6 Sling versus bladder neck (needle) suspension, Outcome 7 Detrusor overactivity (urodynamic diagnosis).
Comparison 9.
Traditional sling versus minimally invasive sling operation
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Number with incontinence (worse, unchanged or improved) within the first year (women's observations) | 8 | 693 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.97 [0.78, 1.20] |
| 1.1 urodynamic stress incontinence (only) | 5 | 434 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.76, 1.34] |
| 1.2 stress urinary incontinence (symptoms only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 1.3 mixed urinary incontinence | 3 | 259 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.66, 1.27] |
| 2 Number not improved (worse or unchanged) within the first year (women's observations) | 3 | 432 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.78 [0.48, 1.27] |
| 2.1 urodynamic stress incontinence (only) | 2 | 293 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.92 [0.39, 2.13] |
| 2.2 stress urinary incontinence (symptoms only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 2.3 mixed urinary incontinence | 1 | 139 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.72 [0.40, 1.29] |
| 3 Number with incontinence (worse, unchanged or improved) after first year (women's observations) | 4 | 382 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.23 [0.91, 1.66] |
| 3.1 urodynamic stress incontinence (only) | 3 | 338 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.17 [0.86, 1.60] |
| 3.2 stress urinary incontinence (symptoms only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3.3 mixed urinary incontinence | 1 | 44 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.92 [0.65, 5.63] |
| 4 Number not improved (worse or unchanged) after the first year (women's observations) | 2 | 279 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.30 [0.57, 2.94] |
| 4.1 urodynamic stress incontinence (only) | 2 | 279 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.30 [0.57, 2.94] |
| 4.2 stress urinary incontinence (symptoms only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4.3 mixed urinary incontinence | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Pad test: mean weight of urine | 1 | 20 | Mean Difference (IV, Fixed, 95% CI) | ‐29.00 [‐57.53, ‐4.47] |
| 5.1 urodynamic stress incontinence (only) | 1 | 20 | Mean Difference (IV, Fixed, 95% CI) | ‐29.00 [‐57.53, ‐4.47] |
| 5.2 stress urinary incontinence (symptoms only) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5.3 mixed urinary incontinence | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Number with incontinence (clinician's observations) within first year | 2 | 105 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.29 [0.45, 3.71] |
| 6.1 urodynamic stress incontinence (only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6.2 stress urinary incontinence (symptoms only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6.3 mixed urinary incontinence | 2 | 105 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.29 [0.45, 3.71] |
| 7 Number with incontinence (clinician's observations) after first year | 1 | 44 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.72 [0.82, 3.61] |
| 7.1 urodynamic stress incontinence (only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7.2 stress urinary incontinence (symptoms only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7.3 mixed urinary incontinence | 1 | 44 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.72 [0.82, 3.61] |
| 8 Operative time (mins) | 5 | 225 | Mean Difference (IV, Fixed, 95% CI) | 59.90 [56.62, 63.18] |
| 8.1 urodynamic stress incontinence (only) | 2 | 61 | Mean Difference (IV, Fixed, 95% CI) | 46.91 [42.31, 51.52] |
| 8.2 stress urinary incontinence (symptoms only) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 8.3 mixed urinary incontinence | 3 | 164 | Mean Difference (IV, Fixed, 95% CI) | 73.26 [68.59, 77.94] |
| 9 Length of hospital stay (days) | 2 | 64 | Mean Difference (IV, Fixed, 95% CI) | 0.49 [0.26, 0.72] |
| 9.1 urodynamic stress incontinence (only) | 1 | 20 | Mean Difference (IV, Fixed, 95% CI) | 0.65 [0.39, 0.91] |
| 9.2 stress urinary incontinence (symptoms only) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 9.3 mixed urinary incontinence | 1 | 44 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [‐0.46, 0.46] |
| 10 Time to catheter removal (days) | 2 | 113 | Mean Difference (IV, Fixed, 95% CI) | 0.11 [‐0.07, 0.30] |
| 10.1 urodynamic stress incontinence (only) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 10.2 stress urinary incontinence (symptoms only) | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 10.3 mixed urinary incontinence | 2 | 113 | Mean Difference (IV, Fixed, 95% CI) | 0.11 [‐0.07, 0.30] |
| 11 Peri operative surgical complications | 3 | 243 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.59 [1.03, 2.44] |
| 11.1 urodynamic stress incontinence (only) | 2 | 183 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.73 [1.01, 2.96] |
| 11.2 stress urinary incontinence (symptoms only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 11.3 mixed urinary incontinence | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.31 [0.64, 2.69] |
| 12 Bladder perforations | 7 | 563 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.62 [0.34, 1.11] |
| 12.1 urodynamic stress incontinence (only) | 2 | 183 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.14 [0.14, 72.92] |
| 12.2 stress urinary incontinence (symptoms only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 12.3 mixed urinary incontinence | 5 | 380 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.57 [0.31, 1.04] |
| 13 Urethral injury | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 13.1 urodynamic stress incontinence (only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 13.2 stress urinary incontinence (symptoms only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 13.3 mixed urinary incontinence | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 14 De novo detrusor urgency or urge symptoms | 3 | 174 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.13 [0.96, 10.24] |
| 14.1 urodynamic stress incontinence (only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 14.2 stress urinary incontinence (symptoms only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 14.3 mixed urinary incontinence | 3 | 174 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.13 [0.96, 10.24] |
| 15 De novo detrusor overactivity (urodynamic diagnosis) | 3 | 245 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.21 [1.29, 8.03] |
| 15.1 urodynamic stress incontinence (only) | 1 | 59 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 15.2 stress urinary incontinence (symptoms only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 15.3 mixed urinary incontinence | 2 | 186 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.21 [1.29, 8.03] |
| 16 Voiding dysfunction | 5 | 375 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.60 [0.94, 2.71] |
| 16.1 urodynamic stress incontinence (only) | 2 | 201 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.97 [0.42, 2.25] |
| 16.2 stress urinary incontinence (symptoms only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 16.3 mixed urinary incontinence | 3 | 174 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.28 [1.13, 4.62] |
| 17 Release of sling required | 2 | 202 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.67 [0.95, 14.22] |
| 17.1 urodynamic stress incontinence (only) | 1 | 142 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.30 [0.46, 11.45] |
| 17.2 stress urinary incontinence (symptoms only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 17.3 mixed urinary incontinence | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 9.6 [0.54, 170.84] |
| 18 Retention up to 6 weeks | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 18.1 urodynamic stress incontinence (only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 18.2 stress urinary incontinence (symptoms only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 18.3 mixed urinary incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 19 Vaginal erosion | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 19.1 urodynamic stress incontinence (only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 19.2 stress urinary incontinence (symptoms only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 19.3 mixed urinary incontinence | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 20 Wound pain (6 months) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 20.1 urodynamic stress incontinence (only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 20.2 stress urinary incontinence (symptoms only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 20.3 mixed urinary incontinence | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
Analysis 9.20.
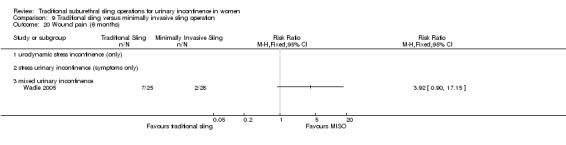
Comparison 9 Traditional sling versus minimally invasive sling operation, Outcome 20 Wound pain (6 months).
Comparison 10.
One type of traditional sling versus another
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Number with incontinence (worse, unchanged or improved) within the first year (women's observations) | 3 | 307 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.66, 1.19] |
| 1.1 urodynamic stress incontinence (only) | 3 | 307 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.66, 1.19] |
| 1.2 stress urinary incontinence (symptoms only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 1.3 mixed urinary incontinence | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 2 Number not improved (worse or unchanged) within the first year (women's observations) | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 urodynamic stress incontinence (only) | 2 | 163 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.22 [0.08, 0.59] |
| 2.2 stress urinary incontinence (symptoms only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 2.3 mixed urinary incontinence | 1 | 48 | Risk Ratio (M‐H, Fixed, 95% CI) | 6.70 [0.40, 111.94] |
| 3 Number with incontinence (worse, unchanged or improved) after first year (women's observations) | 4 | 379 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.72, 1.10] |
| 3.1 urodynamic stress incontinence (only) | 3 | 331 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.83 [0.67, 1.03] |
| 3.2 stress urinary incontinence (symptoms only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3.3 mixed urinary incontinence | 1 | 48 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.75 [0.69, 10.95] |
| 4 Number not improved (worse or unchanged) after the first year (women's observations) | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 4.1 urodynamic stress incontinence (only) | 2 | 186 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.17, 0.64] |
| 4.2 stress urinary incontinence (symptoms only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4.3 mixed urinary incontinence | 1 | 48 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Number with incontinence (worse, unchanged or improved) after five years (women's observations) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 5.1 urodynamic stress incontinence (only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.2 stress urinary incontinence (symptoms only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.3 mixed urinary incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Pad test: mean weight of urine | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 6.1 urodynamic stress incontinence (only) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.2 stress urinary incontinence (symptoms only) | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6.3 mixed urinary incontinence | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Operative time (mins) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 7.1 urodynamic stress incontinence (only) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.2 stress urinary incontinence (symptoms only) | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7.3 mixed urinary incontinence | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8 Peri operative surgical complications | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 8.1 urodynamic stress incontinence (only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.2 stress urinary incontinence (symptoms only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 8.3 mixed urinary incontinence | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 9 Bladder perforation | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 9.1 urodynamic stress incontinence (only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 9.2 stress urinary incontinence (symptoms only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 9.3 mixed urinary incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 10 Urinary tract infection | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 10.1 urodynamic stress incontinence (only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 10.2 stress urinary incontinence (symptoms only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 10.3 mixed urinary incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 11 De novo detrusor urgency or urge symptoms or detrusor overactivity | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 11.1 urodynamic stress incontinence (only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 11.2 stress urinary incontinence (symptoms only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 11.3 mixed urinary incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 12 Voiding dysfunction | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 12.1 urodynamic stress incontinence (only) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 12.2 stress urinary incontinence (symptoms only) | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 12.3 mixed urinary incontinence | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 13 De novo detrusor overactivity (urodynamic diagnosis) | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 13.1 urodynamic stress incontinence (only) | 1 | 57 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.72 [0.52, 5.74] |
| 13.2 stress urinary incontinence (symptoms only) | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 13.3 mixed urinary incontinence | 1 | 48 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.17, 2.63] |
What's new
Last assessed as up‐to‐date: 3 June 2010.
| Date | Event | Description |
|---|---|---|
| 13 July 2017 | New citation required but conclusions have not changed | Brief economic commentary (BEC) added. Economics‐related sections revised. |
| 13 July 2017 | Amended | Brief economic commentary (BEC) added. Economics‐related sections revised: the Abstract, Plain language summary, Background, Methods (outcomes, search methods), and Discussion were amended. Appendix added with details of search strategies for BECs. |
History
Protocol first published: Issue 3, 1999 Review first published: Issue 3, 2000
| Date | Event | Description |
|---|---|---|
| 8 December 2010 | New citation required but conclusions have not changed | 13 new studies added |
| 30 July 2010 | New search has been performed | This is the second update of the review of traditional slings. 13 new RCTs have been added (Albo 2007; Amaro 2007; Bai 2005; Basok 2008; Guerrero 2008; Maher 2005; Pacetta 2005; Sharifiaghdas 2008; Silva Filho 2006; Song 2004; Tcherniakovsky 2009; Teixeira 2008; Wadie 2005 and two have been updated (Arunkalaivanan 2003; Lucas 2000; Kondo 2006) |
| 13 October 2008 | Amended | Converted to new review format. |
| 25 May 2005 | New citation required and conclusions have changed | Substantive amendment. The review was divided into two separate reviews: one on traditional sub‐urethral sling operations (current review, updated) and another on sub‐urethral self fixing sling operations (to include the new TVT and SPARC procedure) to be prepared. The trials on TVT versus other procedures other than traditional suburethral sling operations (four) were moved to the excluded trials list and will be included in the new review. Five new trials were included. |
| 13 February 2003 | New search has been performed | minor update, five studies added |
| 17 May 2001 | New citation required and conclusions have changed | first update |
Differences between protocol and review
July 2017 update – Brief economic commentaries (BECs) have been added to all of Cochrane Incontinence's reviews on surgery for urinary incontinence in women. The economic elements throughout the review have been revised – if incorrect they have been stripped out. New economics‐related text has been added. This involved revisions to the Background section, Methods section (e.g. search section referring to added Appendix), Discussion section, Abstract and Plain language summary. An appendix has been added with details of the economics searches. The conclusions of the review have not changed. The rest of the review has not changed.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | RCT by electronic treatment assignment. 2 arms. Unblinded Follow up at 24 months. Analysis with ITT | |
| Participants | N = 655 4 ineligible after randomisation (3‐Burch, 1‐Sling), 1 did not undergo allocated treatment. Only 520 assessed at end of trial (255‐Burch, 265‐sling) Symptom‐based diagnosis, confirmed by standard stress test Inclusion criteria: documented pure or predominant symptom of SUI for at least 3 months, positive standardised urinary stress test Exclusion criteria: age < 21 years, nonambulatory, pregnancy, current cancer chemo‐ or radiotherapy, systemic disease affecting bladder function, urethral diverticulum, prior augmentation cystoplasty or artificial urethral sphincter, recent pelvic surgery Groups similar in age, ethnic group, marital status, BMI, vaginal deliveries, hormone treatment, smoking, mixed UI, POP, UDS, concomitant surgery Multicentre. Tertiary referral centres. USA |
|
| Interventions | A (326): Sling B (329): Burch Burch as modified by Tanagho Sling procedure using autologous rectus fascia at level of the bladder neck and proximal urethra Interventions standardised across the centres |
|
| Outcomes | Number with overall success, number with SUI‐specific success, pad test, number of incontinence episodes in a 3‐d voiding diary, POP, adverse events, voiding dysfunction (use of a catheter), postoperative UUI Overall success defined as no self‐reported symptoms of UI, no incontinence on 3‐d diary, negative stress test, no re treatment SUI‐specific success defined as no symptoms, negative stress test and no re treatment for SUI All outcomes reported at 2‐year follow‐up Failure (symptoms) at 24 months: A: 101/265, B: 130/255 Failure (pad test) at 24 months: A: 37/265, B: 38/255 Complications: any complications: A: 206/326, B: 156/329; any voiding dysfunction: A: 46/326, B: 7/329; post‐operative cystitis: A: 247/326, B: 166/329; bladder perforation: A: 2/326, B: 10/329 |
|
| Notes | Full text with several other reports in full‐text and abstract form | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Use of permuted‐block randomisation schedule with stratification according to clinical site |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to permit judgement |
| Blinding (performance bias and detection bias) All outcomes | High risk | Participants were aware of study‐group assignments postoperatively. Independent data and safety monitoring board oversaw the progress, interim results, and safety of the study |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 135 women were lost to follow‐up at 2 years. 61 from the sling group and 74 from Burch failed to attend clinic To allow for attrition and missed visits, 655 women had been recruited following power calculation |
| Methods | RCT of autologous fascial sling with TVT. Single blind. Follow‐up assessment carried out at 1, 6, 12 and 36 months | |
| Participants | Women with involuntary detrusor contractions or pre‐existing bladder outlet obstruction during urodynamic study were excluded | |
| Interventions | A (21): autologous fascial sling B (20): TVT |
|
| Outcomes | Cure rates (defined as complete dryness with no usage of pads, operative‐room time, postoperative analgesia, complications, time of hospital stay, postoperative catheterisation, time to return to normal activities. 60‐min pad test used and QoL evaluated using a validated Portuguese version of King's Health Questionnaire Incontinent at 12 months: A: 9/21, B: 7/20 |
|
| Notes | Abstract and poster | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not mentioned |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | "Single blinded" mentioned in abstract, but no description given |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All outcome data assessed. No women lost to follow‐up |
| Methods | RCT, randomisation method unclear. Participants' demographics were well reported. Procedures were standardised. Follow‐up was 2‐6 months, 12 and 24 months (median 12 months) | |
| Participants | 142 women with urodynamic‐proven SUI were recruited. Women with detrusor instability excluded. Groups comparable | |
| Interventions | A (74): Pelvicol B (68): TVT |
|
| Outcomes | Outcome measures: cure rates (subjective, questionnaire‐based; pad used ‐ not weighed), levels of morbidity and impact on QoLand symptom severity Failure at 12 months (incontinence): A: 8/74, B: 10/68 Not Improved at 12 months: A:6/74, B: 4/68 Failure at 36 months (incontinence): A: 12/68, B: 7/60 Not improved at 36 months: A: 5/68, B: 4/60 Complications: any complications: A: 17/74, B: 13/68; any voiding dysfunction: A: 8/74, B: 6/68; Retention up to 6 weeks A: 6/74, B: 1/68; Release of sling required A: 5/74, B: 2/68; Bladder perforations: A: 0/74, B: 0/68 |
|
| Notes | Surgery was only offered after conservative therapy had proved unsuccessful | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not mentioned |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No participants lost to follow‐up at 12 months. All outcome data assessed. At 36 months, in the Pelvicol arm 2 participants died and 4 lost to follow‐up; in the TVT arm 1 died, and 7 lost to follow‐up. Statistical analysis failed to detect significant differences |
| Methods | RCT. Method not described. 3 arms. Blinding not mentioned. Unclear if ITT. Follow‐up at 1 year with assessments at 3, 6, 9 months | |
| Participants | UDS confirmed. No mixed incontinence Groups comparable as to age, parity, BMI, menopausal status, MUCP, VLPP, functional urethral length and peak flow rates at baseline Inclusion criteria : USI grade 1 and 2 Exclusion criteria: grade III incontinence, detrusor overactivity, UTI, ISD, POP > grade II Ob&Gyne. South Korea |
|
| Interventions | A (28): Sling B (33): Burch C (31): TVT Sling procedure was a pubovaginal sling using autologous rectus muscle fascia |
|
| Outcomes | Number cured (3, 6, 12 months); complication rate (number with idiopathic detrusor overactivity, hesitancy, urinary retention) Cure defined as absence of subjective complaints of leakage and absence of urinary leakage on stress test Not cured (6 months): A: 2/28, B: 3/33, C: 2/31 Not cured (12 months): A: 2/28, B: 4/33, C: 4/31 De novo detrusor overactivity: A: 0/28, B: 3/33, C: 0/31 Voiding dysfunction: A: 2/28, B: 1/33, C: 4/31 |
|
| Notes | TVT technique according to Ulmsten All procedures performed by one surgeon |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not mentioned |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No missing outcome data |
| Methods | RCT. Follow‐up at 6 and 30 months. Women allocated to 1/2 interventions by a computer‐generated random table in a 2:1 ratio. All women available at follow‐up | |
| Participants | 48 consecutive women. Inclusion and exclusion criteria not clearly stated, but some participants with mixed incontinence | |
| Interventions | A (32): rectus fascia sling B (16): Gore‐Tex sling operation |
|
| Outcomes | Cure defined as complete freedom from SUI (clinically accessed) or improved (persistence or recurrence of SUI, but in lesser intensity) Failure rates at 6 months: A: 6/32, B: 2/16 Failure rates at 30 months: A:11/32, B: 2/16 Complications: B: 2 cases of erosion of sling and 3 other cases of recurrent UTI |
|
| Notes | Pre‐operative characteristics reported but no comparisons between groups made; statistical analysis reported for urodynamic parameters pre and post operation. No other statistical comparison between groups reported. Some participants with mixed incontinence, but results not stratified by groups or type of incontinence | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer randomised numbers, assigning 2 successive numbers to the fascial group and following number to Gore‐Tex group |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No missing outcome data |
| Methods | RCT. Details of randomisation not given. Two arms. Follow‐up 12 months | |
| Participants | 139 women randomised. Baseline comparison made: number of participants, mean age (years), mean daily pad usage, mean parturition, mean BMI, mixed urinary incontinence. No statistical difference Inclusion criteria: stress urinary incontinence due to urethral hypermobility Exclusion criteria: participants with ISD, uterine prolapse, rectocele, enterocele, grade III or IV cystocele Concomitant urinary urge incontinence was present in some women with mixed urinary incontinence present in 49 participants (73%) in the fascia lata sling group and in 44 participants (61%) in the intravaginal slingplasty group |
|
| Interventions | A (67) Cadaveric fascia lata B (72) Intravaginal slingplasty |
|
| Outcomes | Objective cure rate was evaluated by the pad test, and participant‐satisfaction rate was assessed by a subjective questionnaire. A cure and an improvement were defined as a totally dry participant and 1 pad/d, respectively. Usage of more than 1 pad/d was accepted as surgical failure. The sum of cure and improvement rates was conceded as a total success rate. Other outcomes measured were: mean operating time, bladder perforation, urinary retention, erosion, sling revision, haematoma, persistent urge urinary incontinence, defective vaginal wall, de novo detrusor overactivity. Total success: A: 79.0%, B: 70.8 Satisfaction at 12 months: A: 82.0%, B: 87.5% Incontinent at 12 months: A: 32/67, B: 38/72 Not improved at 12 months: A: 14/67, B: 21/72 Daily mean pad usage (SD): A: 4.1 (3.5), B: 2.9 (1.7) Operative time: A: 50, B: 25 min Adverse events: de novo detrusor overactivity: A: 15/67, B: 5/72; bladder perforation: A: 3/67, B: 8/72; urinary retention: A: 8/67, B: 8/72; vaginal erosion: A: 0/67, B: 0/72; sling revision: A: 2/67, B: 0/72 |
|
| Notes | Preoperative evaluation of all participants included: urogynaecological history, previous pelvic surgery, voiding diary, parturition and daily pad usage The abstract indicated that the QOL was significantly improved in the study, the full article showed that measurement was carried out by participant‐satisfaction questionnaire. No comment was made on the validity and reliability of this questionnaire |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not mentioned |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No missing outcome data |
| Methods | RCT. Follow‐up 12 months. No details of allocation method given. Not all women available in follow‐up | |
| Participants | 46 women recruited, 23 in each arm of the study. 34 women available for follow‐up, reasons for loss to follow‐up not reported. Inclusion and exclusion criteria were well defined | |
| Interventions | A (23): rectus fascia sling B (23): Burch colposuspension |
|
| Outcomes | Cure defined as dry, symptom‐free (subjective based on history and objective on ultrasonography) Failure rate: A:0/17, B: 1/17 Late complications (1‐year follow‐up): A: 1 instability; 3 suprapubic pain and 1 dyspareunia; B: 1 instability, 2 dyspareunia and 2 genital prolapse (enterocele) |
|
| Notes | Ultrasonography for measurement of bladder neck mobility was tested in both groups pre and post operatory and showed significant improvement but no significant differences between the groups | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not mentioned |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 12 women missing lost to follow‐up, reason not reported. No mention of whether loss had impact on final analysis |
| Methods | RCT. Follow‐up at 32‐48 months. Women allocated to 1/2 interventions by open random‐number chart. All women available to follow up | |
| Participants | 72 women recruited, 36 in each arm of the study. Inclusion criteria: all participants with GSI (urodynamic and sonographic diagnosis) had a vaginal hysterectomy and, at least, one previous anterior repair; 57 were postmenopausal without hormone replacement therapy. Exclusion criteria: urinary tract infection, unstable bladder, voiding difficulty and severe cystocele and/or rectocele. Groups were comparable for age, weight, parity, menopausal status, previous surgery and time of follow‐up |
|
| Interventions | A (36) Group II: lyophilised dura mater sling operation B (36) Group I: modified Burch colposuspension (two pairs of sutures instead of three) |
|
| Outcomes | Cure defined as dry, symptom‐free without objective urine loss during stress with bladder filled to 300 mL or positive urethral‐closure pressure during stress provocation. Failure rate at follow‐up at 32‐48 months: A: 3/36, B: 5/36 Urodynamic results reported before and at follow‐up. Reported longer hospital stay and suprapubic catheter permanence for A. Equal frequency pyrexia and bladder laceration Late complications: enterocele or rectocele: A: 1/36, B: 5/36; voiding difficulty A: 5/36, B: 1/36. Both differences statistically significant. Other problems not statistically significant: urgency/urge incontinence (A: 6/36, B: 3/36). 4 participants reported in control because of residual urine for B. Equal good results in sonographic investigation at follow‐up. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number chart, even numbers underwent colposuspension; odd numbers underwent sling procedure |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No missing outcome data |
| Methods | RCT. Details not given. Follow‐up at 6 months | |
| Participants | 22 women with intrinsic sphincter deficiency, 11 in each arm | |
| Interventions | A (11): suburethral sling B (11): Burch retropubic urethropexy |
|
| Outcomes | Cure assessed using IIQ, UDI, stress test, voiding dysfunction Success rate reported as: A: 100% (11/11), B: 77.8% (7/9) P = 0.1 |
|
| Notes | Abstract only Aim to evaluate the prognostic value of urethral electrodiagnosis Two participants in the Burch group were found to have recurrent urethrovisical junction hypermobility or displacement and not included in the final analysis. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not mentioned |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Two participants in the Burch group were found to have recurrent urethrovesical junction hypermobility considered surgical failures and excluded from final analysis. Insufficient information to judge whether appropriately addressed |
| Methods | RCT. Details not given in abstract of trial. 3 treatment arms. 4 centres. Follow‐up 6 months and 1 year | |
| Participants | 201 women randomised (mean age 52 years) to Pelvicol‐50, TVT‐72, autologous sling‐79. 85% were available for follow‐up at 1 year Inclusion criteria: women requiring primary surgical treatment for urodynamic SUI |
|
| Interventions | A (79) autologous sling B (50) Pelvicol C (72) TVT |
|
| Outcomes | Success and improvement rates were described Other outcome measures included: operative details, complications, dry/ improved rates, QoL assessment, catheterisation and re‐operation rates Median theatre time (min): A: 50, B: 35, C: 30 Median length post‐op stay (days): A: 4, B: 4, C: 2 Incontinent at 6 months: A: 41/79, B: 28/50, C: 35/72 Incontinent at 12 months : A: 41/79, B: 39/50, C: 32/72 Not improved at 6 months: A: 4/79, B: 13/50, C: 6/72 Not improved at 12 months: A: 8/79, B: 19/50, C: 5/72 Re‐operation rate: A: 0%, B: 0%, C: 0% Self‐catherterisation at 12 months: A: 1/79, B: 0/50, C: 0/72 |
|
| Notes | High re‐operation rates (1 in 5) in Pelvicol group so arm closed. Study closed at 6 years before target number reached. Interim analysis after the first 50 participants in each group No mention of how success rate was assessed in the abstract, on contacting a listed author, we were informed that the figures were patient‐reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information to make judgement |
| Allocation concealment (selection bias) | Unclear risk | Insufficient information to make judgement |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Insufficient information to make judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No missing outcome data at 12 months. Study closed after 6 years due to failure to recruit target numbers and high reoperation rate |
| Methods | RCT. Details not given. Follow‐up at 4‐6 months | |
| Participants | 30 women randomised, 15 in each arm of the study, all with genuine stress incontinence. All age groups of participants but menopausal status not reported. Exclusion criteria: cystocele, uterine prolapse, urge incontinence, neurogenic bladder, UTIs | |
| Interventions | A (15): Teflon sling (Zoedler urethroplasty) B (15): MMK urethrocystopexy |
|
| Outcomes | Cure defined as complete freedom from SUI (subjective and objective demonstration). All participants cured in both groups. Complications not reported. Main differences observed in stress closing pressure of urethra, which became positive after surgery in both groups | |
| Notes | Groups stated similar but no comparisons made at baseline. Short follow‐up | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not mentioned |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No missing outcome data |
| Methods | RCT. Follow‐up at 2, 3, 12 and 24 months. Women allocated to 1/2 interventions by random tables. All women available at follow‐up | |
| Participants | 20 women recruited, 10 in each arm of the study. Inclusion criteria: GSI (urodynamic diagnosis), vaginal narrowing, post surgical scar, unsuitable for colposuspension. Exclusion criteria: not stated. Groups comparable for age, parity and number of previous surgical incontinence procedures. Menopausal status not reported |
|
| Interventions | A (10): porcine dermis sling operation B (10): Stamey bladder‐neck (needle) suspension |
|
| Outcomes | Cure stated as objective (urodynamic diagnosis, pad test) at 3 months and subjective at 24 months of follow‐up. Failure rates at 3 months: A: 1/10, B: 2/10 Failure rates at 24 months: A: 1/10, B: 3/10 Differences not statistically significant at 3 and 24 months Post op. complications: A: 9/10, B: 2/10 (operative blood loss, pyrexia, infective complications, supra pubic catheter permanence). Hospital stay: A: 20 (12.9), B: 7 (0.3). Late complications not reported. Voiding problems at 3 months: A: 4/10, B:2/10. Detrusor instability: A: 2/10, B: 1/10. Urge incontinence: A: 5/10, B: 3/10. No difference in frequency of uninhibited detrusor contractions, residual volume and maximum voiding pressure. Peak flow significantly reduced for A, although > 15 mL/s |
|
| Notes | Pad test at 12 and 24 months stated but not reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number chart |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No missing outcome data |
| Methods | RCT randomisation by date of birth method. 2 arms. Odd days assigned to TVT arm, even days PVS. Follow‐up 3, 12 and 24 months | |
| Participants | 63 women who complained of SUI were recruited, 3 eventually declined to undergo surgery, therefore a total of 60 women (29‐PVS, 31‐TVT) with urodynamic stress or mixed incontinence were included. Diagnosis made by a cough‐stress test, a 60 min pad‐weighing test, and urodynamic studies | |
| Interventions | A (29): PVS B (31): TVT |
|
| Outcomes | The primary outcome measure was cure of SUI. Objective cure was defined as the complete absence of leakage during the cough‐stress test with 250 or 300 mL of water in the bladder. Subjective cure was consistent with complete dryness or a few drops of water with strong exercises. Other outcome measures (6‐parameter analysis): operation time, numbers of analgesics required in a perioperative period, , changes in haematocrit, length of a Foley catheter, and length of stay Not cured at 24 months (subjective): A: 7/21, B: 4/23 Not cured at 24 months (objective): A: 11/21, B: 7/23 Operative time (mean (SD)): A: 87.1 (13.3), B: 43.9 (17.3) min Length of hospital stay (mean (SD)): A: 9.2 (0.9), B: 9.2 (0.6) days Time to catheter removal (mean (SD)): A: 1.4 (0.5), B: 1.3 (0.1) days Complications: all complications: A: 11/29, B: 9/31; bladder perforation: A: 7/29, B: 7/31; urethral injury: A:0/29, B: 1/31; subcutaneous haematoma: A: 0/29, B: 1/31; voiding dysfunction: A: 4/29, B: 0/31; release of sling surgery: A: 4/29, B: 0/31; de novo detrusor urgency: A: 3/29, B: 2/31 |
|
| Notes | Follow‐up 24 months. Women who underwent concomitant surgery (5‐PVS, 8‐TVT) and/or had revision surgery were excluded from the 6‐parameter analysis because extra interventions made a comparison difficult. Participants for the assessment reduced to 23 women in the TVT and 21 in the PVS group Data updated from new publication |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Date‐of‐birth method |
| Allocation concealment (selection bias) | High risk | Date of birth |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | No mention |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Similar loss across groups at follow‐up, 72% remained in sling arm and 74% in Burch |
| Methods | RCT. Follow‐up at 3, 6 and 12 months. Women allocated to each arm by a central telephone randomisation system. Not blinded ? operation obvious to all medical and nursing personnel. 3 hospitals | |
| Participants | 165 women randomly assigned to 2 groups. Baseline demographics and symptomology were similar: age, height, weight, symptom years, previous surgery, number and type of concurrent problems between both groups Inclusion criteria: participants > 18 years and urodynamically proven SUI exclusion criteria: evidence of neurological disease; urodynamic evidence of detrusor instability and hypocompliance |
|
| Interventions | A (81): standard sling insertion (long) B (84): sling on a string (short) |
|
| Outcomes | Primary outcome was to compare QoL scores in both groups over time. Success rate was measured by recurrence of stress leakage as reported in participant questionnaire Secondary outcomes were measured by participant's QoL, clinical indicators (such as immediate post‐operative complications, time to first void, pad tests); administrative indicators, pain scores and participant satisfaction Participant satisfaction at 12 months: A: 57/73, B: 62/82 Stress leakage at 12 months: A: 14/72, B: 16/72 Stress leakage at 3 years: A: 35/75, B: 30/70 Stress leakage at 6 years: A: 42/73, B: 34/69 De novo urgency: A: 6/81,B: 2/84 Pad test volumes (mL): A: 7.71, B: 4.61; P = 0.56 Mean operative time (min): A: 62 (range 38‐135), B: 54 (25 to 140) P = 0.001, (P used to calculate SD: 15.33 in each group) Mean blood loss (mL): A: 274 (50‐800), B: 230 (50‐700) P = 0.07 Length of stay (ds): A: 6.48, B: 6.73 Voiding dysfunction 12 months: A: 19/81, B: 17/84 Readmission within 3 months: A: 19/79, B: 9/83 Surgery to release sling: A: 1/81, B: 4/84 Further continence surgery: A: 2/56, B: 5/69 Pain at 3 months: A: 52/78, B: 42/82 Adverse effects: perioperative surgical complications: A: 34/81, B: 31/84; bladder perforation A 2/81, B 3/84; UTI A 10/81, B 6/84 |
|
| Notes | Detailed outcome measures at 3, 6 and 12 months were provided. Both groups showed improvement in their QoL with no significant statistical difference between allocated operation. 46 participants had previously undergone one or more forms of incontinence surgery. Data updated from new publication |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomisation schedule |
| Allocation concealment (selection bias) | Low risk | Remote telephone randomisation |
| Blinding (performance bias and detection bias) All outcomes | High risk | Not blinded. Operation performed obvious to all medical and nursing personnel involved in the assessment |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Ouctome data were analysed according to the randomised group, per protocol and best possible. 21 women lost to follow‐up by 12 months, 23 lost by 3 years. The similar losses from each arm were unlikely to affect the final analysis. Actual numbers with outcome reported |
| Methods | RCT of pubovaginal sling vs Macroplastique. Follow‐up 6 months and 1 year. ITT analysis performed | |
| Participants | 45 women randomised. 1 from each arm lost to follow‐up by 1 year Inclusion criteria: women with USI and ISD diagnosed by a MUCP less than or equal to 20 cm H2O, who failed to respond to conservative treatment Exclusion criteria: required prolapse surgery, had undergone a sling procedure or were unsuitable for general anaesthesia Baseline comparison included: age (years), BMI (kg/m2), menopause status, parity, previous surgery (abdominal hysterectomy, vaginal hysterectomy/repair, retropubic continence surgery, needle suspension) |
|
| Interventions | A (22) pubovaginal Sling B (23) transurethral Macroplastique |
|
| Outcomes | Objective success: no leakage due to SUI on repeat urodynamic study Subjective success: no or occasional (less than once a week) stress incontinence Other outcome measures included: voiding dysfunction, participant satisfaction, operating time, blood loss, inpatient days, duration of catheterisation, time to resume normal activities Incontinent within 1st year: A: 2/21, B: 5/22 P = 0.41 Incontinent after 1st year: A: 0/13, B: 4/14 P = 0.1 Incontinent within 1st year (obj): A: 4/21, B: 20/22 P = < 0.0001 Patient satisfaction (self‐reported at 6 months): A: 7/21, B: 13/22 P = 0.41 Patient satisfaction (self‐reported at 5 years): A: 9/13, B: 4/14 P = 0.057 Operative time (mins): A: 60 (25‐105), B: 22 (10‐41) P = < 0.0001 Length of hospital stay (days): A: 4 (3‐81), B: 1 (1‐2) P = < 0.0001 Time to normal activity (weeks): A: 4 (0‐42), B: 28 (0‐35) P = < 0.0001 Time to catheter removal (days): A: 5 (2‐42), B: 1 (0‐7) P = < 0.0001 Further continence surgery: A: 1/21, B: 2/22 Complications: UTI: A: 3/21, B: 2/22; De novo detrusor overactivity: A: 1/21, B: 0/22; voiding dysfunction: A: 4/21, B: 1/22 |
|
| Notes | Tertiary referral centres Macroplastique (uroplasty, Minneapolis, Minnesota, USA) is a vulcanised silicone microimplant (polydiamethylsiloxone) suspended in a povidine gel designed to provided urethral bulking for the treatment of SUI |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Computer randomisation software, no description given |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Ouctome data were analysed according to the randomised group. One woman in each group failed to return or complete any review. Actual numbers with outcome reported |
| Methods | RCT (block‐randomisation technique). Follow‐up reported at 6 months. Selection criteria were well reported | |
| Participants | 75 women with mixed incontinence symptoms and a negative cystometrogram for motor detrusor overactivity. All had proven stress urinary incontinence. No details on demographic data were reported 21 participants (anticholinergic) and 24 (sling) were available to follow up |
|
| Interventions | A (50): surgery (Ai (24) Burch colposuspension, Aii (26) rectus fascia sling) B (25): anticholinergic treatment |
|
| Outcomes | Participants were evaluated by SEAPI score (subjective and objective) and underwent urodynamic examination pre and post treatment Cure for urge symptoms: Aii: 88%; B:57% Cure for SUI: Aii: 83%; B: 0 |
|
| Notes | The study was designed to investigate anticholinergic therapy in comparison with surgery. Participants allocated to surgery had a sling procedure if the Valsalva leak point pressure was < 90 cm H2O. We extracted only data on sling in comparison with anticholinergics | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Block randomisation |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Of 75 women randomised, 68 evaluated at 6 months. Four lost in anticholinergic arm and 3 in surgical arm. Insufficient information to determine whether appropriately addressed or not |
| Methods | RCT. Abstract. Randomisation 2:1. 2 arms. Follow‐up 1 year | |
| Participants | 34 women randomised. No mention of baseline comparison Inclusion criteria: women 30‐77 years old with SUI due to hypermobility or ISD underwent surgical correction |
|
| Interventions | A (10): autologous fascia B (24): FortaPerm |
|
| Outcomes | Objective outcome assessment was urine loss using a provocative pad test Subjective participant evaluations included QoL questionnaire, incontinence diary, pain and global outcome assessments Biopsies were taken at 1 year from FortaPerm implant sites adjacent to urethra for histology Incontinent within 1st year: A: 1/10, B: 5/24 Not improved within 1st year (subjective): A: 0/10, B: 2/24 |
|
| Notes | FortaPerm is absorbable biomaterial composed of laminated sheets of purified porcine collagen matrix | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not mentioned |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No missing outcome data |
| Methods | RCT by random number table. Follow‐up at 3 months and at 72.6 months (mean) | |
| Participants | 36 women with genuine stress incontinence and a maximum urethral closure pressure ≤ 20 cm H2O. Groups comparable in terms of age, parity, and urodynamic variables, except for detrusor instability (> Burch vs sling) and residual volume (> Burch vs sling) | |
| Interventions | A (17): Polytetrafluoroethylene sling operation B (19): modified (overcorrection) Burch colposuspension |
|
| Outcomes | Cure defined as objective (urodynamic) and subjective (history) Objective cure (long‐term): A: 100% 13/13, B: 86% 13/15 Subjective cure (long‐term): A: 84% 11/13, B: 93% 14/15 There were no statistically significant differences in outcome measures |
|
| Notes | The first publication (2000) reported the short‐term follow‐up and was considered the primary reference. The last publication (2003) reported the long‐term results | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number table |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Similar losses in both groups at long‐term assessment |
| Methods | RCT of TVT with autologous rectus fascia sling. Randomisation by sealed, opaque envelopes. Follow‐up 1, 3, 6 and 12 months | |
| Participants | 100 women randomised into 2 groups. However only 61 followed up to 1 year. 16 were lost due to distance and expense of travel, 12 were age‐related and 11 because of dissatisfaction with surgical result (6‐Sling, 5‐TVT) Inclusion criteria: history of USI, 1‐h pad‐test (> 2 g of leakage), objective positive cough (effort or exertion) ? induced stress test, normal cystourethroscopy and urodynamic confirmation of SI, urethral hypermobility and competent bladder neck Exclusion criteria: history of > 3 episodes of UTI in past 2 years, other gynaecological problems such as high grade uterine prolapse, high grade rectocele and enterocele, cystocele ≥ grade 2, abnormal filling phase of urodynamic study, low flow rates (< 15 mL/s), residual urine of more than 100 mL, trabeculated bladder mucosa on cystourethroscopy, a history of major pelvic trauma, and fractures that might negatively affect urethral function Mixed incontinence was included provided urodynamics showed normal capacity, normal compliance and stable bladder The 2 groups had similar characteristics with respect to age, parity, hysterectomy, previous incontinence surgery, sensory urge incontinence, preoperative IIQ score |
|
| Interventions | A (52) pubovaginal sling B (48) TVT |
|
| Outcomes | Objective cure defined as negative cough‐induced stress test with full bladder (at least 250 mL filled) in the lithotomy and standing position and a 1‐h pad‐test ≤ 2 g Subjective cure defined by mean IIQ score in each group Also assessed were: type of anaesthesia, operative time, estimated blood loss, bladder penetration and satisfaction with procedure Incontinent within 1 year (stress test): A: 6/36, B: 3/25 P = 0.9 Incontinent within 1 year (1‐h pad test): A: 10/36, B: 6/25 P = 0.83 Participantsatisfaction at 12 months: A: 20/36, B: 15/25 Operative time (min): A: 80 (50‐180), B: 45 (30‐70) P = 0.01 Length of hospital stay (days): A: 5 (3‐7), B: 2 (1‐5) P = 0.001 Time to catheter removal (days): A: 4.6 (3‐6), B: 1.3 (1‐5) P = 0.001 Complications: de novo urge symptoms: A: 8/36, B: 1/25; voiding dysfunction: A: 11/36, B: 5/25; bladder perforation: A: 2/36, B: 6/25 P = 0.05; bleeding (> 250mL): A: 1/36, B: 1/25 P = 1.00; suprapubic incisional hernia after 8 months: A: 1/36, B: 1/25 |
|
| Notes | Procedures performed by single surgeon All participants were preoperatively evaluated by, physical examination, plain abdominal X‐ray, urinary tract ultrasound, cystourethroscopy and urodynamic study Physical examination assessed degree of prolapsed, basal lab tests (FBC, renal and liver function tests, serum electrolytes, urine analysis, culture) Assumption was made that t‐test was used for operative time, catheterisation and hospital stay |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not mentioned |
| Allocation concealment (selection bias) | Unclear risk | Sealed, opaque envelopes, no mention of numbering |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All outcomes assessed in randomised groups. 39 participants lost to follow‐up. Similar losses in each group |
| Methods | RCT stated. Details not given in the abstract of trial. Follow‐up after first year reported | |
| Participants | 57 women with various types of SUI. Participants' characteristics were not reported | |
| Interventions | A (33): autologous dermal graft patch B (24): cadaveric fascia lata |
|
| Outcomes | Outcome measures reported were success rate (dry/improved), de novo detrusor instability Success rate: A: 91, 6%, B: 93, 2% |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No missing outcome data. (based on abstract) |
| Methods | RCT of SAFYRE TOT with autologous pubovaginal sling. Randomisation method unclear. Follow‐up 6 months | |
| Participants | 20 women (average age of 52.5 years ± 11.8 years) with both USI and SUI but without detrusor overactivity The 2 groups had similar characteristics with respect to age, parity, BMI, menopausal status, presence of pelvic floor defects, and mean Valsalva leak point pressure in the preoperative UDS |
|
| Interventions | A (10): pubovaginal sling B (10): SAFYRE TOT |
|
| Outcomes | Cure rates and intraoperative and postoperative morbidity. Women were declared objectively cured when they had a postoperative pad test of ≤ 8 g All participants were preoperatively evaluated by history, physical examination, QoL questionnaire (King's Health Questionnaire), a 24‐h pad weight test, a 2‐d voiding diary, and a multichannel urodynamic study that included uroflowmetry, post‐void residual volume measurement by urethral catheter, and a cystometrogram. The objective quantification of the severity of incontinence was done by the mean stress leaking point pressure in the urodynamic study. Preoperative measurements included the type of anaesthesia, duration of surgery, intraoperative complications, occurrence of combined procedures, and hospital stay. At 6‐month follow‐up the aforementioned measurements were carried out excluding UDS. Post operative pad test (mean (SD)): A: 8.4 (16.44), B: 39.4 (39.53) g; P = 0.01 Operative time (mean (SD)): A: 69.5 (23.7), B: 21.1 (3.8) min; P < 0.001 Length of hospital stay (mean (SD)): A: 44.4 (5.8), B: 28.8 (8.4) h; P < 0.001 |
|
| Notes | SAFYRE consists of a monofilament polypropylene mesh between two silicone columns that are made of multiple cone‐shaped soft tissue anchors. The two columns are fixed to the obturator muscle. The pubovaginal sling uses rectus fascia | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not mentioned |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No missing outcome data |
| Methods | RCT of TVT compared with autologous fascia lata pubovaginal sling. Single centre | |
| Participants | 67 women with SUI were randomised. Basline comparison of age, menopause status, parity, SUI, mixed incontinence and intrinsic sphincter dysfunction were made Inclusion criteria: type II‐IV SUI, mixed SUI, intrinsic sphincter dysfunction, or failed previous operations Mixed incontinence was included in this study |
|
| Interventions | A (19): autologous fascia lata pubovaginal sling B (48): TVT |
|
| Outcomes | Cure rates and operative morbidity Damage to bladder, urinary retention, difficulty voiding Incontinent at 3 months: A: 1/19, B: 3/48 Not improved at 3 months A: 0/19, B: 0/48 Operative time (SD): A: 125 (13), B: 27 (5) min Mean length of hospital stay: A: 7.2, B: 1.8 ds Mean time to catheter removal: A: 5.3, B: 1 ds Complications: voiding dysfunction: A: 3/19, B: 3/48; urinary retention: A: 2/19, B: 0/48; bladder injury: A: 0/19, B: 2/48; detrusor overactivity: A: 1/19, B: 3/48 |
|
| Notes | Follow‐up on average was between 20‐37 months. Cure rates assessed at 3 months Full text was translated from Chinese |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not mentioned |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No missing outcome data |
| Methods | RCT. Follow‐up 12 months | |
| Participants | 41 women randomly distributed into two groups. Participants had similar baseline characteristics (age, BMI, parity, vaginal births, postmenopausal conditions, hormone replacement therapy, previous SUI surgery, genital prolapse, previous surgery/previous hysterectomy, disease duration) Inclusion criteria: USI, confirmed through medical history, physical exam, and urodynamic investigation |
|
| Interventions | A (20): retropubic sling B (21): SAFYRE TOT |
|
| Outcomes | Cure was reported absence of SUI and no urinary loss during effort manoeuvres at 12‐month follow‐up re‐evaluation. Failure at 12 months: A: 1/20, B: 2/21 Operative time (mean (SD)): A: 59.7 (10.3), B: 12.8 (2.4) mins Time to catheter removal: A: 2, B: 1 ds Complications: all complications: A: 12/20, B: 3/21; UTI: A: 2/20 B: 0/21; bladder perforation: A: 1/20, B: 0/21; urinary retention: B: 3/20, A: 2/21; vaginal mesh erosion (isolated): A: 0/20, B: 1/21 |
|
| Notes | Physical exam specifically evaluated urinary loss through Valsalva manoeuvre and presence of other concurrent dystopias of pelvic floor (anterior, posterior, and apical), using POP‐Q classification. VLPP standardised in this study at 200 mL of vesical repletion Urodynamic study performed on every participant included |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Participants "randomly distributed". No detail provided |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No missing outcome data |
| Methods | RCT. Details not given in abstract. Follow‐up 24 h and 90 ds | |
| Participants | 42 participants were randomised (porcine collagen‐21, polypropylene tapes‐21) Inclusion criteria: stress urinary incontinence |
|
| Interventions | A (21) porcine collagen B (21) polypropylene tapes |
|
| Outcomes | No outcome measure relevant to this review C reactive protein and white blood count measured previous day and at 24 h after surgery Biopsy at 90ds post operation for local inflammatory markers (polymorphonuclear cells, mononuclear cells, giant cells and neovascularisation) and collagen reaction (collagen amount, composition and organisation) |
|
| Notes | Trial assessing systemic and local inflammatory response in different sling materials | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details provided |
| Allocation concealment (selection bias) | Unclear risk | "blindly randomised" no details provided |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 2 participants with missing outcome data. No detail provided on whether losses were similar in both groups, or from a single arm of the trial |
| Methods | RCT. Method not clarified. Only the short‐term follow‐up reported | |
| Participants | 26 women with stress urinary incontinence | |
| Interventions | A (15): fascial sling B (11): vaginal wall sling |
|
| Outcomes | Measures of outcome included SEAPI‐QMN questionnaire, presence of SUI at postoperative period, urinary symptoms and hospital stay. Cure rates: SEAPI scores decreased from 6.1 to 0.9 for B and from 6.3 to 0.8 for A |
|
| Notes | All procedures performed by same surgeon No useable data |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Insufficient information |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No missing outcome data |
| Methods | RCT randomised by closed envelope delivered to surgeon by a third party. Procedures by one surgeon. Follow‐up 6 months | |
| Participants | 53 women (mean age 45.12 years) with SUI were randomised, all had similar background characteristics (age, BMI, parity, grade of associated cystocoele) Inclusion criteria were age > 21 years, Predominant symptom of SUI, willing to give informed consent, life expectancy > 1 year, normal upper urinary tract and normal manual dexterity Exclusion: pelvic or vaginal surgery within 6 months, urge incontinence as predominant symptom, > grade 2 cystocele, associated urethral pathology e.g. diverticulum, associated bladder pathology e.g. fistula, culture proven, active urinary tract infection |
|
| Interventions | A (25): autologous fascial sling B (28): TVT |
|
| Outcomes | Cure, i.e. complete dryness with no usage of pad and negative cough‐stress test Not cured at 6 months: A: 2/25, B: 2/28 Operative time (mean (SD)): A: 68 (23), B: 48 (25) min Time to catheter removal (mean (SD)): A: 6.6 (5.3), B: 4.3 (2.6) d Complications: bladder perforation: A: 1/25, B: 2/28; de novo detrusor overactivity at 6 months: A: 1/23, B: 0/24; stitch sinus at 1 week: A: 0/25, B 1/28; vaginal erosion: A: 0/25, B: 0/28; wound pain at 6 months: A: 7/25, B: 2/28; voiding dysfunction: A: 7/25, B: 3/28 |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not mentioned |
| Allocation concealment (selection bias) | Low risk | Closed, opaque envelopes held by a non‐involved 3rd party who revealed the allocation after participant had been anaesthetised, just before start of surgery |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | No details provided |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No missing data |
BMI = body mass index IIQ = Incontinence Impact Questionnaire ISD = Intrinsic sphincter dysfunction ITT = intention to treat MMK = Marshall‐Marchetti‐Krantz MUCP = maximum urethral closure pressure POP = pelvic organ prolapse QoL = quality of life RCT = randomised controlled trial SEAPI = SEAPI QMM incontinence classification system SUI = stress urinary incontinence TVT = tension‐free vaginal tape UDI = Urinary Distress Inventory UDS = urodynamics UI = urinary incontinence USI = urodynamic stress incontinence UTI = urinary tract infection UUI = urge urinary incontinence VLPP = Valsava leak point pressure
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Amat 2007 | RCT. One minimally invasive sling versus another |
| Atherton 2000 | Non‐randomised |
| Aurunkalaivanan 2001 | We are not sure about the population studied and it could be the same population as Barrington 2003 and Arunkalaivanan 2003 (included in the review); we have written to the trial authors to clarify this point. |
| Barrington 2003 | We are not sure about the population studied and it could be the same population as Aurunkalaivanan 2001 and Arunkalaivanan 2003 (included in the review); we have written to the trial authors to clarify this point. |
| Bruschini 2005 | Not RCT, no comparator group |
| Choe 2000 | Allocation score C (participants randomised by alternating fashion). Trial comparing slings made of vaginal wall and of polytetrafluorethylene mesh impregnated with chorhexidine |
| Choe 2001 | All participants were randomised to undergo preoperative urodynamic evaluation or not. They then had implantation of suburethral mycromesh sling. Therefore the study analyses the impact on effectiveness of sling if the diagnosis of SUI is made with or without urodynamic evaluation |
| Chong 2003 | Participants all had TVT operation, were randomised to division/no division of tape |
| Corcos 2001 | Participants were randomised to surgery or collagen injection but those in the surgery arm were selected to sling by participant's option. Three types of operation could be chosen in the surgery group: Burch, sling or bladder neck suspension. Results were reported in terms of collagen versus surgery |
| Darai 2007 | RCT 1 minimally invasive sling versus another Inlcuded in Minimally Invasive Sling Cochrane Review |
| Debodinance 1993 | Not all participants had stress incontinence (and allocation score C ‐ participants randomised by birth date). Debodinance 2000 is a 10‐year follow‐up of the first published study. The trial is a comparative study between Bologna (a sling made of strips of vaginal wall) and Ingelman‐Sundberg procedure (anterior colporrhaphy with pubococcygeus muscle) |
| Debodinance 1994 | Not clear how participants allocated. Paper in French, need translation |
| Giri 2004 | We are not sure about the population studied and it could be the same population as Giri 2006, which has been excluded as it was a non‐randomised study. We have made attempts to contact the study authors. |
| Giri 2006 | Non‐randomised |
| Goldberg 2001 | Prolapse surgery rather than incontinence surgery |
| Halaska 2001 | Study comparing transvaginal tape with colposuspension; will be included in a separate review on self‐fixing slings |
| Han 2001 | Study comparing transvaginal tape with colposuspension; will be included in a separate review on self‐fixing slings. |
| Hung 2001 | Not clear how participants were allocated, we have written to the study authors |
| Ishenko 1999 | Randomisation and groups unclear ('randomised by age'). Excluded as attempts to contact study authors unsuccessful and insufficient information given in abstract. Interventions: vaginal hysterectomy, modified Pereyra procedure, anterior and posterior repair vs vaginal hysterectomy, sling procedure with Mersilene mesh, anterior and posterior repair |
| Kocjancic 2008 | Study comparing transvaginal tape procedures; will be included in a separate review on self‐fixing slings. |
| Kuo 2001 | Allocation score C (participants randomised by consecutive study entry). Comparison between rectus fascia and polypropylene mesh |
| Kwon 2002 | Not all participants had stress incontinence; all participants were treated for prolapse but one group received concomitant transvaginal sling (processed fascia lata), one group received an alternate surgery for SUI and the last group, didn't have SUI and were submitted only to treatment of prolapse |
| Lemieux 1991 | Interventions were on clamping versus non‐clamping of catheters post‐anti‐incontinence surgery |
| Liapis 2002 | Study comparing transvaginal tape with colposuspension; will be included in a separate review on self‐fixing slings |
| Lim 2005 | This study is comparing minimally invasive sling procedures and will be included in that Cochrane Review. |
| Meschia 2001 | Surgery for prolapse rather than incontinence |
| Naumann 2006 | This study is comparing tape procedures and will be included in the minimally invasive slings Cochrane Review. |
| O'Sullivan 2000 | RCT. Participants randomised to colposuspension or transvaginal tape. Outcome measures (collagen metabolism) reported not included in this review |
| Obrink 1978 | Not clear how participants were allocated. Study author written to in October 2001, no reply received |
| Schostak 2001 | Unclear how participants were allocated. Bone anchoring used |
| Seo 2007 | RCT. One minimally invasive sling versus another |
| Trezza 2001 | Occult incontinence treated at same time as prolapse repair |
| Wang 1999 | Randomised to different types of anaesthetic |
| Ward 2002a | Study comparing transvaginal tape with colposuspension; will be included in a separate review on self‐fixing slings |
| Yoo 2007 | This study is comparing tape procedures and will be added to the minimally invasive slings Cochrane Review. |
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | A prospective randomised comparative trial of a tension free vaginal tape (TVT) and fascial sling procedure for 'secondary' genuine stress incontinence |
| Methods | |
| Participants | 146 planned recruitment |
| Interventions | TVT versus fascial sling |
| Outcomes | No information |
| Starting date | |
| Contact information | |
| Notes |
| Trial name or title | Sling operation for stress urinary incontinence: randomised trial of three operative procedures |
| Methods | |
| Participants | |
| Interventions | TVT versus Pelvicol versus sling on a string |
| Outcomes | |
| Starting date | |
| Contact information | |
| Notes | Possibly same as Lucas 2004 |
Contributions of authors
The review was conceived by CB and HB, and updated by HR and DJC. CB co‐ordinated the steps of the review process with the help of DJC. Screening papers, appraising their quality and abstracting data were done by CB, HB and HR separately (published data only). The review was written by CB who extracted, analysed and interpreted data with the help of HB, and updated by HR. DJC assisted in the update for Feb 2003 by appraising, quality assessing, extracting data and assisting with interpretation.
For the July 2017 addition of the brief economic commentaries (BECs) to this review, Patricia Aluko was responsible for the entire BEC‐related work on this review she ran the search for studies, screened the searches, extracted data from relevant studies, revised any existing economics‐related text, added the BEC‐related text, and responded to any peer referee comments. All review authors had the opportunity to comment on the revised review.
Sources of support
Internal sources
Federal University of Sao Paulo ‐ Sao Paulo, Brazil.
Faculty of Medicine of Foudation of ABC, Brazil.
External sources
-
National Institute for Health Research, UK.
This project was supported by the National Institute for Health Research, via Cochrane Infrastructure funding to Cochrane Incontinence. The views and opinions expressed therein are those of the review authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, NHS or the Department of Health. The NIHR is the largest single funder of Cochrane Incontinence.
-
National Institute for Health Research, UK.
This project, to add brief economic commentaries to Cochrane Incontinence's reviews on surgery for urinary incontinence in women, was supported by the National Institute for Health Research (NIHR), via the Cochrane Review Incentive Scheme 2016, to Cochrane Incontinence. The views and opinions expressed therein are those of the review authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, NHS or the Department of Health.
Declarations of interest
Haroon Rehman: no interests to declare Carlos CB Bezerra: no interests to declare Homero Bruschini: no interests to declare June D Cody: no interests to declare
Patricia Aluko: July 2017 ‐ this project, to add brief economic commentaries to Cochrane Incontinence's reviews on surgery for urinary incontinence in women was supported by the National Institute for Health Research (NIHR), via the Cochrane Review Incentive Scheme 2016, to Cochrane Incontinence. The views and opinions expressed herein are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, NHS or the Department of Health.
Edited (no change to conclusions)
References
References to studies included in this review
- Albo M, Wruck L, Baker J, Brubaker L, Chai T, Dandreo KJ, et al. The relationships among measures of incontinence severity in women undergoing surgery for stress urinary incontinence. Journal of Urology 2007;177(5):1810‐4. [DOI] [PubMed] [Google Scholar]; Albo ME, Richter HE, Brubaker L, Norton P, Kraus SR, Zimmern PE, et al. Burch colposuspension versus fascial sling to reduce urinary stress incontinence. New England Journal of Medicine 2007;356(21):2143‐55. [DOI] [PubMed] [Google Scholar]; Brubaker L, Chiang S, Zyczynski H, Norton P, Kalinoski DL, Stoddard A, et al. The impact of stress incontinence surgery on female sexual function. American Journal of Obstetrics & Gynecology 2009;200(5):562.e1‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]; Brubaker L, Stoddard A, Richter H, Zimmern P, Moalli P, Kraus SR, et al. Mixed incontinence: comparing definitions in women having stress incontinence surgery. Neurourology & Urodynamics 2009;28(4):268‐73. [DOI] [PMC free article] [PubMed] [Google Scholar]; Chai T, Albo M, Richter H, Norton P, Dandreo K, Kenton K, et al. Adverse events from a randomized trial for the surgical treatment of stress urinary incontinence (Abstract number 512). Proceedings of the 37th Annual Meeting of the International Continence Soceity (ICS), 20‐24 Aug 2007, Rotterdam, Netherlands. 2007. [23535] [Google Scholar]; Chai TC, Albo ME, Richter HE, Norton PA, Dandreo KJ, Kenton K, et al. Complications in women undergoing Burch colposuspension versus autologous rectus fascial sling for stress urinary incontinence. Journal of Urology 2009;181(5):2192‐7. [31150] [DOI] [PMC free article] [PubMed] [Google Scholar]; Daneshgari F. Words of wisdom. Re: Burch colposuspension versus fascial sling to reduce urinary stress incontinence. European Urology 2007;52(6):1794‐5. [26271] [DOI] [PubMed] [Google Scholar]; Daneshgari F, Kong W, Swartz M. Complications of mid urethral slings: important outcomes for future clinical trials. Journal of Urology 2008;180(5):1890‐7. [27706] [DOI] [PubMed] [Google Scholar]; Diokno AC, Richter HE, Kenton K, Norton P, Albo M, Kraus S, et al. Risk factors associated with failure of surgical treatment for stress urinary incontinence at 24 months follow‐up (Abstract number 115). Neurourology & Urodynamics 2007;26(5):745. [23533] [Google Scholar]; FitzGerald MP, Burgio KL, Borello‐France DF, Menefee SA, Schaffer J, Kraus S, et al. Pelvic‐floor strength in women with incontinence as assessed by the brink scale. Physical Therapy 2007;87(10):1316‐24. [23825] [DOI] [PubMed] [Google Scholar]; Kenton K, Tennstedt S, Litman H, Zimmern P, Getti C, Kusek JW, et al. Improvement in quality of life in women at two years after undergoing the Burch colposuspension or fascial sling procedure (Abstract number 206). Proceedings of the 38th Annual Meeting of the International Continence Society (ICS), 2008 Oct 20‐24, Cairo, Egypt. 2008. [31863] [Google Scholar]; Kraus SR, Markland A, Chai TC, Stoddard A, FitzGerald MP, Leng W, et al. Race and ethnicity do not contribute to differences in preoperative urinary incontinence severity or symptom bother in women who undergo stress incontinence surgery. American Journal of Obstetrics & Gynecology. 2007;197(1):92‐6. [23802] [DOI] [PMC free article] [PubMed] [Google Scholar]; Lemack G, Krauss S, Litman H, FitzGerald M, Chai T, Nager C, et al. Preoperative urodynamic testing does not predict postoperative voiding dysfunction among women undergoing surgery for SUI: results from a prospective randomized trial comparing Burch versus pubovaginal sling (Abstract number 7, poster). Neurourology & Urodynamics 2008;27(2):123. [26919] [Google Scholar]; Lemack GE, Krauss S, Litman H, FitzGerald MP, Chai T, Nager C, et al. Normal preoperative urodynamic testing does not predict voiding dysfunction after Burch colposuspension versus pubovaginal sling. Journal of Urology 2008;180(5):2076‐80. [27705] [DOI] [PMC free article] [PubMed] [Google Scholar]; Lemack GE, Xu Y, Brubaker L, Nager C, Chai T, Moalli P, et al. Clinical and demographic factors associated with Valsalva leak point pressure among women undergoing Burch bladder neck suspension or autologous rectus fascial sling procedures. Neurourology & Urodynamics 2007;26(3):392‐6. [23233] [DOI] [PubMed] [Google Scholar]; Mallett VT, Brubaker L, Stoddard AM, Borello‐France D, Tennstedt S, Hall L, et al. The expectations of patients who undergo surgery for stress incontinence. American Journal of Obstetrics & Gynecology. 2008;198(3):308.e1‐6. [27182] [DOI] [PubMed] [Google Scholar]; Markland AD, Kraus SR, Richter HE, Nager CW, Kenton K, Kerr L, et al. Prevalence and risk factors of fecal incontinence in women undergoing stress incontinence surgery. American Journal of Obstetrics & Gynecology. 2007;197(6):662‐7. [26334] [DOI] [PubMed] [Google Scholar]; Nager C, Chai T, FitzGerald M, Lemack G, Kraus S, Sirls L, et al. Valsalva leak point pressure and detrusor overactivity do not predict, but urodynamic stress incontinence does predict continence outcomes after Burch or pubovaginal sling procedures (Abstract number 85). Neurourology & Urodynamics 2007;26(5):709‐11. [23532] [Google Scholar]; Nager CW, Albo ME, FitzGerald MP, McDermott S, Wruck L, Kraus S, et al. Reference urodynamic values for stress incontinent women. Neurourology & Urodynamics 2007;26(3):333‐40. [23232] [DOI] [PubMed] [Google Scholar]; Nager CW, Albo ME, FitzGerald MP, McDermott SM, Kraus S, Richter HE, et al. Process for development of multicenter urodynamic studies. Urology 2007;69(1):63‐67; discussion 67‐8. [23195] [DOI] [PMC free article] [PubMed] [Google Scholar]; Nager CW, FitzGerald M, Kraus SR, Chai TC, Zyczynski H, Sirls L, et al. Urodynamic measures do not predict stress continence outcomes after surgery for stress urinary incontinence in selected women. Journal of Urology 2008;179(4):1470‐4. [27210] [DOI] [PubMed] [Google Scholar]; Richter H, Goode P, Brubaker L, Zyczynski H, Stoddard A, Dandreo K, et al. Two‐year outcomes after surgery for stress urinary incontinence in older versus younger women (Abstract number 95). Neurourology and Urodynamics 2008;27(7):682‐3. [31854] [DOI] [PMC free article] [PubMed] [Google Scholar]; Richter HE, Burgio KL, Brubaker L, Moalli PA, Markland AD, Mallet V, et al. Factors associated with incontinence frequency in a surgical cohort of stress incontinent women. American Journal of Obstetrics & Gynecology 2005;193(6):2088‐93. [21231] [DOI] [PubMed] [Google Scholar]; Richter HE, Diokno A, Kenton K, Norton P, Albo M, Kraus S, et al. Predictors of treatment failure 24 months after surgery for stress urinary incontinence. Journal of Urology 2008;179(3):1024‐30. [27213] [DOI] [PMC free article] [PubMed] [Google Scholar]; Richter HE, Diokno AC, Kenton K, Norton P, Albo M, Kraus S, et al. Predictors of treatment failure 24 months after surgery for stress urinary incontinence (Abstract number 5 Oral). Journal of Pelvic Medicine & Surgery 2007;13(5):227‐8. [34197] [DOI] [PMC free article] [PubMed] [Google Scholar]; Richter HE, Goode PS, Brubaker L, Zyczynski H, Stoddard AM, Dandreo KJ, et al. Two‐year outcomes after surgery for stress urinary incontinence in older compared with younger women. Obstetrics & Gynecology 2008;112(3):621‐9. [29193] [DOI] [PMC free article] [PubMed] [Google Scholar]; Strohbehn K. Shades of dry ‐ curing urinary stress incontinence. [comment]. New England Journal of Medicine 2007;356(21):2198‐200. [DOI] [PubMed] [Google Scholar]; Subak LL, Brubaker L, Chai TC, Creasman JM, Diokno AC, Goode PS, et al. High costs of urinary incontinence among women electing surgery to treat stress incontinence. Obstetrics & Gynecology 2008;111(4):899‐907. [27122] [DOI] [PMC free article] [PubMed] [Google Scholar]; Tennstedt S, Borello‐France D, FitzGerlad MP, Goode P, Kraus S, Kusek J, et al. Identification of factors related to health‐related quality of life in women with stress urinary incontinence that may improve with surgical treatment (Abstract number 321). Proceedings of the International Continence Society (ICS), 35th Annual Meeting, 2005 Aug 28‐Sep 2, Montreal, Canada. 2005. [21098] [Google Scholar]; Tennstedt S, Urinary Incontinence Treatment Network. Design of the Stress Incontinence Surgical Treatment Efficacy Trial (SISTEr). Urology 2005;66(6):1213‐7. [21530] [DOI] [PubMed] [Google Scholar]; Tennstedt SL, FitzGerald MP, Nager CW, Xu Y, Zimmern P, Kraus S, et al. Quality of life in women with stress urinary incontinence. International Urogynecology Journal & Pelvic Floor Dysfunction 2007;18(5):543‐9. [30914] [DOI] [PubMed] [Google Scholar]; Tennstedt SL, Litman HJ, Zimmern P, Ghetti C, Kusek JW, Nager CW, et al. Quality of life after surgery for stress incontinence. International Urogynecology Journal 2008;19(12):1631‐8. [31221] [DOI] [PMC free article] [PubMed] [Google Scholar]; Walsh LP, Zimmern PE, Pope N, Shariat SF, Urinary Incontinence Treatment Network. Comparison of the Q‐tip test and voiding cystourethrogram to assess urethral hypermobility among women enrolled in a randomized clinical trial of surgery for stress urinary incontinence. Journal of Urology 2006;176(2):646‐649, discussion 650. [DOI] [PubMed] [Google Scholar]; Zimmern P, Nager CW, Albo M, FitzGerald MP, McDermott S, Urinary Incontinence Treatment Network. Interrater reliability of filling cystometrogram interpretation in a multicenter study. Journal of Urology 2006;175(6):2174‐7. [22424] [DOI] [PubMed] [Google Scholar]; Zimmern P, Tennstedt S, Dickinson T, Dandreo K. Lessons learned from a patient burden survey following a large randomized controlled trial for the surgical management of stress urinary incontinence in women (Abstract number 152). Neurourology & Urodynamics 2009;28(7):770‐1. [20805] [Google Scholar]; Zimmern P, Urinary Incontinence Treatment Network (UITN). Design of the SISTEr (Stress Incontinence Surgical Treatment Efficacy Trial) Study: a randomized surgical trial comparing Burch colposuspension and the autologous rectus fascia sling. A clinical trial of the NIH/NIDDK urinary incontinence treatment network (UITN) (Abstract number 81). Progres en Urologie 2004;14(3 Suppl 3):26. [19780]15217101 [Google Scholar]
- Amaro JL, Yamamoto HA, Kawano PR, Fugita O, Gameiro MOO, Barros G, et al. A prospective randomized trial of autologous fascial sling (AFS) versus tension‐free vaginal tape (TVT) for treatment of stress urinary incontinence (SUI) (Poster abstract number 1460). Journal of Urology 2007;177(4 Suppl 4):482. [Google Scholar]
- Abdel‐Fattah M, Arunkalaivanan AS, Barrington JW. Pelvicol (trademark) implant v TVT (trademark): an update (Abstract). Proceedings of the 27th Annual Meeting of the International Urogynecological Association, 21‐24 Aug 2002, Prague, Czech Republic. 2002. [Google Scholar]; Abdel‐Fattah M, Barrington JW, Arunkalaivanan AS. Pelvicol pubovaginal sling versus tension‐free vaginal tape for treatment of urodynamic stress incontinence: a prospective randomized three‐year follow‐up study. European Urology 2004;46(5):629‐35. [DOI] [PubMed] [Google Scholar]; Arunkalaivan AS, Barrington JW. Randomized trial of porcine dermal sling (Pelvicol TM implant) vs. tension‐free vaginal tape (TVT) in the surgical treatment of stress incontinence: a questionnaire‐based study. International Urogynecology Journal 2003;14:17‐23. [DOI] [PubMed] [Google Scholar]; Arunkalaivanan AS, Barrington JW. Comparison of porcine pubo vaginal sling (Pelvicol) vs tension free vaginal tape (TVT) in the surgical management of stress incontinence (Abstract). International Urogynecology Journal 2001;12(Suppl 3):S21. [DOI] [PubMed] [Google Scholar]
- Bai SW, Sohn WH, Chung DJ, Park JH, Kim SK. Comparison of the efficacy of Burch colposuspension, pubovaginal sling, and tension‐free vaginal tape for stress urinary incontinence. International Journal of Gynaecology & Obstetrics 2005;91(3):246‐51. [21260] [DOI] [PubMed] [Google Scholar]
- Barbalias G, Liatsikos E, Barbalias D. Use of slings made of indigenous and allogenic material (Goretex) in type III urinary incontinence and comparison between them. European Urology 1997;31(4):394‐400. [MEDLINE: ; 5560] [DOI] [PubMed] [Google Scholar]
- Basok EK, Yildirim A, Atsu N, Basaran A, Tokuc R. Cadaveric fascia lata versus intravaginal slingplasty for the pubovaginal sling: surgical outcome, overall success and patient satisfaction rates. Urologia Internationalis 2008;80(1):46‐51. [DOI] [PubMed] [Google Scholar]
- Demirci F, Yucel O. Comparison of free rectus fascial sling and Burch colposuspension procedures in type I and type II genuine stress incontinence (Abstract). International Urogynecology Journal and Pelvic Floor Dysfunction 2000;11(Suppl 1):S48. [13419] [Google Scholar]; Demirci F, Yucel O. Comparison of pubovaginal sling and Burch colposuspension procedures in type I/II genuine stress incontinence. Archives of Gynecology & Obstetrics 2001;265(4):190‐4. [13079] [DOI] [PubMed] [Google Scholar]
- Enzelsberger H, Helmer H, Schatten C. Comparison of Burch and Lyodura sling procedures for repair of unsuccessful incontinence surgery. Obstetrics & Gynecology 1996;88(2):251‐6. [MEDLINE: ; 2759] [DOI] [PubMed] [Google Scholar]; Enzelsberger H, Kurz C, Seifert M, Raimann H, Schatten C. Surgical treatment of recurrent stress incontinence: Burch versus Lyodura sling operation‐‐a prospective study [Zur operativen behandlung der rezidivstre binkontinenz: Burch versus Lyoduraschlingeoperation ‐ eine prospektive studie]. Geburtshilfe und Frauenheilkunde 1993;53(7):467‐71. [MEDLINE: ; 6197] [DOI] [PubMed] [Google Scholar]
- Fischer JR, Hale DS, McClellan E, Benson JT. The use of urethral electrodiagnosis to select the method of surgery in women with intrinsic sphincter deficiency (Abstract). International Urogynecology Journal and Pelvic Floor Dysfunction 2001;12(Suppl 1):S33. [12008] [Google Scholar]
- Guerrero K, Whareham K, Watkins A, Ismail S, Lucas M, Emery S. A randomised control trial comparing TVT, Pelvicol and autologous fascial slings for the management of stress urinary incontinence in women (Abstract number 1). Neurourology and Urodynamics 2008;27(7):571. [31847] [Google Scholar]; Lucas M, Emery S, Alan W, Kathy W. Failure of porcine xenograft sling in a randomised controlled trial of three sling materials in surgery for stress incontinence (Abstract). Proceedings of the International Continence Society (34th Annual Meeting) and the International UroGynecological Association, 23‐27 August, 2004, Paris. 2004:Abstract number 309. [19056] [Google Scholar]
- Henriksson L, Asmussen M, Löfgren O, Ulmsten U. A urodynamic comparison between abdominal urethrocystopexy and vaginal sling plasty in female stress incontinence. Urologia Internationalis 1978;33:111‐6. [5152] [Google Scholar]; Henriksson L, Ulmsten U. A urodynamic evaluation of the effects of abdominal urethrocystopexy and vaginal sling urethroplasty in women with stress incontinence. American Journal of Obstetrics & Gynecology 1978;131(1):77‐82. [MEDLINE: ; 2670] [DOI] [PubMed] [Google Scholar]
- Hilton P. A clinical and urodynamic study comparing the Stamey bladder neck suspension and suburethral sling procedures in the treatment of genuine stress incontinence. British Journal of Obstetrics & Gynaecology 1989;96(2):213‐20. [MEDLINE: ; 453] [DOI] [PubMed] [Google Scholar]
- Kondo A, Isobe Y, Kimura K, Kamihira O, Matsuura O. A randomized control trial of tension‐free vaginal tape vs pubovaginal sling: cure rates and QOL improvement (Abstract number 629). Proceedings of the International Continence Society (ICS), 35th Annual Meeting, 2005 Aug 28‐Sep 2, Montreal, Canada. 2005. [21077] [Google Scholar]; Kondo A, Isobe Y, Kimura K, Kamihira O, Matsuura O, Gotoh M, et al. Efficacy, safety and hospital costs of tension‐free vaginal tape and pubovaginal sling in the surgical treatment of stress incontinence. Journal of Obstetrics & Gynaecology Research 2006;32(6):539‐44. [22233] [DOI] [PubMed] [Google Scholar]; Kondo A, Kimura K, Isobe Y, Kamihira O, Matsuura O. A randomised control trial of tension‐free vaginal tape in comparison with pubovaginal sling in the treatment of stress incontinence (Abstract). Neurourology Urodynamics 2003;22(5):485‐7. [17109] [Google Scholar]
- Guerrero K, Watkins A, Emery S, Wareham K, Stephenson T, Logan V, et al. A randomised controlled trial comparing two autologous fascial sling techniques for the treatment of stress urinary incontinence in women: short, medium and long‐term follow‐up. International Urogynecology Journal 2007;18(11):1263‐70. [23957] [DOI] [PubMed] [Google Scholar]; Lucas M, Emery S, Stephenson T, Wareham K, Cheung I. A randomised study to assess and compare the clinical effectiveness of two surgical techniques for the treatment of stress urinary incontinence in women. Spotlight (Newsletter of The Wales Office of Research)2000. [12901]; Lucas M, Emery S, Stephenson T, Wareham K, Cheung I, Russell I, et al. A randomised study to assess and compare the clinical effectiveness of two surgical techniques for the treatment of stress urinary incontinence in women. Report No. RC080. Cardiff, Wales, UK: The Wales Office of Research & Development for Health & Social Care, 2000. [8995] [Google Scholar]
- Maher CF, Dwyer PL, Carey MP, Cornish A, Schluter PJ. Pubovaginal sling or transurethral Macroplastique for genuine stress incontinence and intrinsic sphincter deficiency: a prospective randomised trial (Abstract). International Urogynecology Journal 2001;12(Suppl 3):S9. [DOI] [PubMed] [Google Scholar]; Maher CF, O'Reilly BA, Dwyer PL, Carey MP, Cornish A, Schluter P. Pubovaginal sling versus transurethral Macroplastique for stress urinary incontinence and intrinsic sphincter deficiency: a prospective randomised controlled trial. BJOG: an International Journal of Obstetrics & Gynaecology 2005;112(6):797‐801. [20579] [DOI] [PubMed] [Google Scholar]
- Osman T. Stress incontinence surgery for patients presenting with mixed incontinence and a normal cystometrogram. BJU International 2003;92:964‐8. [16660] [DOI] [PubMed] [Google Scholar]
- Pacetta AM, Carramao SS, Limoge DC, Mendes V, Date A, Sousa E, et al. Stress urinary incontinence: a prospective randomized study comparing FortaPerm to autologous fascia (Abstract number 109). International Urogynecology Journal 2005;16(Suppl 2):S58. [Google Scholar]
- Culligan PJ, Goldberg RP, Sand PK. A randomized controlled trial comparing a modified Burch procedure and a suburethral sling: long‐term follow‐up. International Urogynecology Journal 2003;14:229‐33. [16706] [DOI] [PubMed] [Google Scholar]; Culligan PJ, Winkler HA, Blackhurst DW, Sand PK. A prospective randomized study of modified Burch retro pubic urethropexy and suburethral sling for genuine stress incontinence and low pressure urethra (Abstract). Proceedings of the International Continence Society (ICS), 28th Annual Meeting, 14‐17 Sept, Jerusalem, Israel. 1998:133. [5689] [Google Scholar]; Goldberg RP, Sand PK, Koduri S, Culligan PJ. A prospective randomized study comparing modified Burch retropubic urethropexy and suburethral sling: long term follow‐up (abstract). International Urogynaecology Journal 2001;12(Suppl 1):S6. [12004] [Google Scholar]; Sand PK, Winkler H, Blackhurst DW, Culligan PJ. A prospective randomized study comparing modified Burch retropubic urethropexy and suburethral sling for treatment of genuine stress incontinence with low‐pressure urethra. American Journal of Obstetrics & Gynecology 2000;182(1 Pt 1):30‐4. [MEDLINE: ; 11781] [DOI] [PubMed] [Google Scholar]
- Sharifiaghdas F, Mortazavi N. Tension‐free vaginal tape and autologous rectus fascia pubovaginal sling for the treatment of urinary stress incontinence: a medium‐term follow‐up. Medical Principles & Practice 2008;17(3):209‐14. [31878] [DOI] [PubMed] [Google Scholar]
- Shin MS, Kim JH, Koh JS, Jung JH. Comparison of the results of sling procedure using autologous dermal graft patch and cadaveric fascia lata as a sling material for stress urinary incontinence (Abstract). Proceedings of the International Continence Society (ICS), 31st Annual Meeting, 18‐21 Sept, Seoul, Korea. 2001:Abstract number 313. [14477] [Google Scholar]
- Silva‐Filho AL, Candido EB, Noronha A, Triginelli SA. Comparative study of autologous pubovaginal sling and synthetic transobturator (TOT) SAFYRE sling in the treatment of stress urinary incontinence. Archives of Gynecology & Obstetrics 2006;273(5):288‐92. [21600] [DOI] [PubMed] [Google Scholar]
- Song YF, Huang HJ, Xu B, Hao L. [Comparative study of tension‐free vaginal tape and fascia lata for stress urinary incontinence]. [Chinese]. Chung‐Hua Fu Chan Ko Tsa Chih [Chinese Journal of Obstetrics & Gynecology] 2004;39(10):658‐61. [PubMed] [Google Scholar]
- Tcherniakovsky M, Fernandes CE, Bezerra CA, Roy CA, Wroclawski ER. Comparative results of two techniques to treat stress urinary incontinence: synthetic transobturator and aponeurotic slings. International Urogynecology Journal 2009;20(8):961‐6. [32120] [DOI] [PubMed] [Google Scholar]
- Teixeira M, Pinto AR, Montalvao M, Candoso B. Systemic and local inflammatory response in collagen vs. polypropylene tapes for stress urinary incontinence: is there any difference? (Abstract number 527). Proceedings of the 38th Annual Meeting of the International Continence Society (ICS), 2008 Oct 20‐24, Cairo, Egypt. 2008. [31878] [Google Scholar]
- Viseshsindh W, Kochakarn W, Waikakul W, Roongruangsilp U. A randomized controlled trial of pubovaginal sling versus vaginal wall sling for stress urinary incontinence. Journal of the Medical Association of Thailand 2003;86(4):308‐15. [15733] [PubMed] [Google Scholar]
- Wadie B, Henawy A. Does urethral pressure measurement correlate to the outcome of incontinence surgery? (Abstract number 546). Proceedings of the 37th Annual Meeting of the ICS, 20‐24 Aug 2007, Rotterdam, The Netherlands. 2007. [26689] [Google Scholar]; Wadie BS, Edwan A, Nabeeh A. Autologous fascial sling verus polypropylene tape at short term follow up, a prospective randomized study (Abstract number 636). Proceedings of the International Continence Society (ICS), 35th Annual Meeting, 2005 Aug 28‐Sep 2, Montreal, Canada. 2005. [21100] [Google Scholar]; Wadie BS, Edwan A, Nabeeh AM. Autologous fascial sling vs polypropylene tape at short‐term follow up: a prospective randomized study. Journal of Urology 2005;174(3):990‐3. [20796] [DOI] [PubMed] [Google Scholar]; Wadie BS, Hefnawy AS. Urethral pressure measurement in stress incontinence: does it help?. International Urology & Nephrology 2009;41(3):491‐5. [32131] [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
- Amat LL, Franco EM, Saavedra AH, Martinez AV. Needleless (R): a new technique for correction of urinary incontinence. Randomized controlled trial compared with TVT‐O (R). Preliminary results (Abstract number 225). International Urogynecology Journal and Pelvic Floor Dysfunction 2007;18(Suppl 1):S128. [27329] [Google Scholar]
- Atherton MJ, Stanton SL. TVT and colposuspension: comparisons and contrasts of possible mechanisms (Abstract). Neurourology and Urodynamics 2000;19(4):396‐8. [Google Scholar]
- Arunkalaivanan AS, Barrington JW. Comparison of porcine pubo vaginal sling (Pelvicol) vs tension free vaginal tape (TVT) in the surgical management of stress incontinence (Abstract). International Urogynecology Journal 2001;12 (Suppl 3):S21. [DOI] [PubMed] [Google Scholar]
- Barrington JW. Pelvicol implant vs TVT ‐ a randomised prospective study. Proceedings of the BARD Satellite Symposium to the International Continence Society Annual Meeting, 7 Oct. 2003; Vol. 8. [Google Scholar]
- Bruschini H, Nunes R, Truzzi JC, Simonetti R, Cury J, Ortiz V, et al. Low cost polypropylene sling procedure for correction of stress urinary incontinence: a possible solution for developing countries? (Abstract number 360). Proceedings of the International Continence Society (ICS), 35th Annual Meeting, 2005 Aug 28‐Sep 2, Montreal, Canada. 2005. [21055] [Google Scholar]
- Choe JM. The use of synthetic materials in pubovaginal sling. Advances in Experimental Medicine & Biology 2003;539(Pt A):481‐92. [DOI] [PubMed] [Google Scholar]; Choe JM, Ogan K, Battino BS. Antimicrobial mesh versus vaginal wall sling: a comparative outcomes analysis. Journal of Urology 2000;163(6):1829‐34. [MEDLINE: ] [PubMed] [Google Scholar]
- Choe JM. Sling surgery performed with and without preoperative urodynamics: a comparative outcomes analysis. Proceedings of the International Continence Society (ICS), 31st Annual Meeting, 18‐21 Sept, Seoul, Korea. 2001:Abstract number 175. [Google Scholar]
- Chong C, Bane A, Corstiaans A. Intraoperative division of tensionless vaginal tape (TVT) ‐ prospective randomized trial (Abstract). Singapore Journal of Obstetrics & Gynaecology 2003;34 (Suppl 1):55. [Google Scholar]
- Corcos J, Collet JP, Shapiro S, Herschorn S, Radomski SB, Schick E, et al. Multicenter randomized clinical trial comparing surgery and collagen injections for treatment of female stress urinary incontinence. Urology 2005;65(5):898‐904. [20346] [DOI] [PubMed] [Google Scholar]; Corcos J, Collet JP, Shappiro S, Schick E, Macramallah E, Tessier J, et al. Surgery vs collagen for the treatment of female stress urinary incontinence (SUI): results of a multicentric randomized trial (Abstract). Journal of Urology 2001;165(5 Suppl):198. [Google Scholar]
- Darai E, Frobert JL, Grisard‐Anaf M, Lienhart J, Fernandez H, Dubernard G, et al. Functional results after the suburethral sling procedure for urinary stress incontinence: a prospective randomized multicentre study comparing the retropubic and transobturator routes. European Urology 2007;51(3):795‐802. [22550] [DOI] [PubMed] [Google Scholar]; David‐Montefiore E, Frobert JL, Grisard‐Anaf M, Liehart J, Fernandez H, Dubernard G, et al. Functional results after suburethral sling procedure for urinary stress incontinence at 1 year: a French prospective randomised multicentre study comparing the retropubic and transobturator routes (Abstract number 063). International Urogynecology Journal 2006;17(Suppl 2):S95. [Google Scholar]; David‐Montefiore E, Frobert JL, Grisard‐Anaf M, Lienhart J, Bonnet K, Poncelet C, et al. Peri‐operative complications and pain after the suburethral sling procedure for urinary stress incontinence: a French prospective randomised multicentre study comparing the retropubic and transobturator routes. European Urology 2006;49(1):133‐8. [21623] [DOI] [PubMed] [Google Scholar]
- Debodinance P. [Comparison of the Bologna and Ingelman‐Sundberg procedures for stress incontinence associated with genital prolapse: ten‐year follow‐up of a prospective randomized study]. [French]. Journal de Gynecologie , Obstetrique et Biologie de la Reproduction 2000;29(2):148‐53. [PubMed] [Google Scholar]; Debodinance P, Querleu D. Comparison of the Bologna and Ingelman‐Sundber procedures for stress incontinence associated with genital prolapse: prospective randomized study . European Journal of Obstetrics, Gynecology, & Reproductive Biology 1993;52(1):35‐40. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Debodinance P, Bievre P, Parmentier D, Dubrulle R, Querleu D, Crepin G. [The "hazards" of using a Gore‐Tex sling in the treatment of stress urinary incontinence]. [French]. Journal de Gynecologie, Obstetrique et Biologie de la Reproduction 1994;23(6):665‐70. [MEDLINE: ] [PubMed] [Google Scholar]
- Giri SK, Hickey JP, Macdonald J, Narasimahulu G, Cashman E, Drumm J, et al. Prospective, randomised trial of xenograft versus rectus fascia pubovaginal sling in the treatment of stress urinary incontinence (abstract number 13). Irish Journal of Medical Science 2004;173(1 Suppl 1):18. [29716]15732230 [Google Scholar]
- Giri SK, Hickey JP, Sil D, Mabadeje O, Shaikh FM, Narasimhulu G, et al. The long‐term results of pubovaginal sling surgery using acellular cross‐linked porcine dermis in the treatment of urodynamic stress incontinence. Journal of Urology 2006;175(5):1788‐92; discussion 1793. [22459] [DOI] [PubMed] [Google Scholar]; Giri SK, Sil D, Drumm J, Mabadeje O, Narasimahulu G, Flood HD. Is acellular porcine dermis material durable for pubovaginal sling surgery? (Abstract number 349). Proceedings of the International Continence Society (ICS), 35th Annual Meeting, 2005 Aug 28‐Sep 2, Montreal, Canada. 2005. [21068] [Google Scholar]
- Goldberg RP, Koduri S, Lobel RW, Culligan PJ, Tomezsko JE, Winkler HA, et al. Long‐term effects of three different anti‐incontinence procedures on the posterior compartment (Abstract). Proceedings of the International Continence Society (ICS), 31st Annual Meeting, 18‐21 Sept, Seoul, Korea. 2001:Abstract number 243. [Google Scholar]
- Halaska M, Kolbl H, Petri E, Danes L, Voigt R, Otcenasek M, et al. Preliminary results of a prospective randomized study comparing Burch colposuspension and tension‐free vaginal tape ‐ urodynamic and sexuological aspects. Neurourology and Urodynamics 2001;20(4):421‐2. [Google Scholar]
- Han WHC. Burch colposuspension or tension‐free vaginal tape for female stress urinary incontinence?. International Urogynecology Journal and Pelvic Floor Dysfunction 2001;12(Suppl 3):S23. [DOI] [PubMed] [Google Scholar]
- Hung MJ. Tension free vaginal tape versus traditional polypropylene pubovaginal sling for the treatment of stress urinary incontinence (Abstract). International Urogynecology Journal and Pelvic Floor Dysfunction 2001;12 (Suppl 3):253. [Google Scholar]
- Ishenko AI, Slobodenyuk AI, Chushkov YV. Modified pereyra and sling procedures in combined surgical treatment in patients with uterine prolapse and stress urinary incontinence ‐ randomized study. European Journal of Obstetrics, Gynecology, & Reproductive Biology 1999;86(Suppl):S15. [Google Scholar]
- Kocjancic E, Constantini E, Crivellaro S, Tosco L, Grossetti B, Frea B, et al. Mixed incontinence: the best solution for a difficult task (Abstract number 485). Proceedings of the 38th Annual Meeting of the International Continence Society (ICS), 2008 Oct 20‐24, Cairo, Egypt. 2008. [Google Scholar]; Kocjancic E, Constantini E, Giannantoni A, Crivellaro S, Mearini L, Frea B, et al. Tension free vaginal tape (TVT) and trans obturator suburethral tape (TOT) a prospective randomized study (Poster abstract number 1462). Proceedings of the American Urological Association (AUA), Annual Meeting, 19‐24 May, Anaheim, CA. 2007. [23765] [Google Scholar]
- Kuo HC. Comparison of video urodynamic results after the pubovaginal sling procedure using rectus fascia and polypropylene mesh for stress urinary incontinence. Journal of Urology 2001;165(1):163‐8. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Kwon C, Goldberg R, Sanjay G, Sumana K, Krotz S, Sand P. Protective effect of transvaginal slings on recurrent anterior vaginal wall prolapse after pelvic reconstructive surgery (abstract). Neurourology and Urodynamics 2002;21(4):321‐2. [Google Scholar]
- Lemieux MC, Kung R, Drutz HP. Suprapubic clamping routine after anti‐incontinence surgery: a randomized prospective study comparing continuous vs intermittent clamping (Abstract). Proceedings of the American Urogynecology Society, 12th Annual Meeting, 23‐26 Oct, California, USA. 1991. [Google Scholar]
- Liapis A, Bakas P, Creatsas G. Burch colposuspension and tension‐free vaginal tape in the management of stress urinary incontinence in women. European Urology 2002;41(4):469‐73. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]; Liapis A, Bakas P, Creatsas G. Comparison of open retropubic colposuspension with tension‐free vaginal tape for the treatment of genuine stress incontinence in women (abstract). Neurourology and Urodynamics 2000;19(4):385‐6. [Google Scholar]
- Lim YN, Muller R, Corstiaans A, Dietz HP, Barry C, Rane A. Suburethral slingplasty evaluation study in North Queensland, Australia: The SUSPEND trial. Australian & New Zealand Journal of Obstetrics & Gynaecology 2005;45(1):52‐9. [DOI] [PubMed] [Google Scholar]
- Meschia M, Spennacchio M, Amicarelli F, Pifarotti P, Cavoretto P, Stoppelli S. A randomized prospective comparison of TVT and endopelvic fascia plication in the treatment of occult stress urinary incontinence in patients with genital prolapse: preliminary data (Abstract). Neurourology and Urodynamics 2001;20(4):423‐4. [Google Scholar]
- Naumann G, Lobodasch K, Bettin S, Meyer P, Koelbl H. Tension free vaginal tape (TVTtm) vs less invasive free tape (LIFTtm) ‐ A randomized multicentric study of suburethral sling surgery (Abstract number 481). Proceedings of the International Continence Society (ICS), 36th Annual Meeting, 2006 Nov 27‐Dec 1, Christchurch, New Zealand. 2006. [Google Scholar]
- O'Sullivan S, Avery N, Bailey A, Keane D. The effect of surgery on the collagen metabollism of paraurethral tissue in women with genuine stress incontinence. International Urogynaecology Journal. 11 2000; Vol. 11, issue Suppl 1:S5. [MEDLINE: ]
- Obrink A, Bunne G. The margin to incontinence after three types of operation for stress incontinence. Scandinavian Journal of Urology and Nephrology 1978;12(3):209‐14. [DOI] [PubMed] [Google Scholar]
- Schostak M, Gottfried HW, Heicappell R, Muller M, Sauter T, Steiner U, et al. Minimally invasive bone anchoring for female stress incontinence: a treatment with moderate results (Abstract). European Urology 2001;39(Suppl 5):3. 11114594 [Google Scholar]
- Seo JH, Lee JW, Kim DY, Lee YG, Seo YJ, Kwon TG, et al. Treatment of obstructive voiding dysfunction after transobturator sling surgery: results of multicenter study (Abstract number 287). Proceedings of the 37th Annual Meeting of the International Continence Society (ICS), 20‐24 Aug, Rotterdam, the Netherlands. 2007. [23762] [Google Scholar]
- Trezza G, Rotondi M, Palmisano B, Iervolino P. Uterovaginal prolapse and occult urinary incontinence: a prospective randomized study on the necessity to associate reconstructive surgery and antiincontinence procedure. Urogynaecologia International Journal 2001;15(1 Suppl):152‐4. [Google Scholar]
- Wang AC. Local anesthesia is superior to epidural blockade in tension‐free vaginal tape installation. International Urogynecology Journal and Pelvic Floor Dysfunction. 10 1999; Vol. 10, issue Suppl 1:S13.
- Abrams P, Martin K, Bulmer P, Donovan J, Hilton P. Responsiveness of the Bristol female lower urinary tract symptoms questionnaire (BFLUTS‐Q) to surgical intervention in a randomised controlled trial. Proceedings of the International Continence Society (ICS), 30th Annual Meeting, 28‐31 Aug, Tampere, Finland. 2000:A173. [Google Scholar]; Sculpher MJ, Ward KL, Hilton P, on behalf of the UK & Ireland TVT trial group. A comparison of the hospital costs of tension free vaginal tape (TVT) and colposuspension. Neurourology and Urodynamics. 19 2000; Vol. 19, issue 4:333‐4. ; Ward K, Hilton P, on behalf of the UK & Ireland TVT trial group. A randomised trial of colposuspension and tension‐free vaginal tape (TVT) for primary genuine stress incontinence ‐ 2 yr follow‐up (Abstract). International Urogynaecological Association, Pelvic Floor Dysfunction. 12 2001; Vol. 12, issue Suppl 3:S7. ; Ward K, Hilton P, on behalf of the United Kingdom and Ireland Tension‐free Vaginal Tape Trial Group. Prospective multicentre randomised trial of tension‐free vaginal tape and colposuspension as primary treatment for stress incontinence. BMJ 2002;325(7355):67‐73. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]; Ward KL, Hilton P, Browning J. A randomized trial of colposuspension and tension‐free vaginal tape (TVT) for primary genuine stress incontinence. Neurourology & Urodynamics 2000;19:386‐8. [Google Scholar]; Ward KL, Hilton P, Browning J. Urodynamic variables in a randomised comparison of colposuspension and tension‐free vaginal tape (TVT) for primary GSI. Neurourology & Urodynamics 2000;19:388‐9. [Google Scholar]
- Yoo ES, Jung HC, Shin HS, Seo JH, Seo YJ. Comparison of the two different approaches for the treatment of female stress urinary incontinence (Abstract number 282). Proceedings of the 37th Annual Meeting of the International Continence Society (ICS), 20‐24 Aug, Rotterdam, the Netherlands. 2007. [Google Scholar]
References to ongoing studies
- Hilton P. A prospective randomised comparative trial of a tension‐free vaginal tape (TVT) and fascial sling procedure for "secondary" genuine stress incontinence. UK National Research Register2002.
- Lucas M. Sling operation for stress urinary incontinence: randomized trial of three operative procedures. UK National Research Register2001.
Additional references
- Berman CJ, Kreder KJ. Comparative cost analysis of collagen injection and fascia lata sling cystourethropexy for the treatment of type III incontinence in women. The Journal of Urology 1997;157(1):122‐4. [PubMed] [Google Scholar]
- Birnbaum HG, Leong SA, Oster EF, Kinchen K, Sun P. Cost of stress urinary incontinence: a claims data analysis. Pharmacoeconomics 2004;22(2):95‐105. [PUBMED: 14731051] [DOI] [PubMed] [Google Scholar]
- Blaivas JG, Olsson CA. Stress incontinence: classification and surgical approach. Journal of Urology 1988;139(4):727‐31. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Blaivas JG, Appell RA, Fantl JA, Leach G, McGuire EJ, Resnick NM, et al. Definition and classification of urinary incontinence: recommendations of the Urodynamic Society. Neurourology & Urodynamics 1997;16(3):149‐51. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Chong E, Khan A, Anger J. The financial burden of stress urinary incontinence among women in the United States. Current Urology Reports 2011;12(5):358‐62. [DOI: 10.1007/s11934-011-0209-x.] [DOI] [PubMed] [Google Scholar]
- Cody J, Wyness L, Wallace S, Glazener C, Kilonzo M, Stearns S, et al. Systematic review of the clinical effectiveness and cost‐effectiveness of tension‐free vaginal tape for treatment of urinary stress incontinence. Health Technology Assessment 2003;7(21):iii, 1‐189. [PUBMED: 13678548] [DOI] [PubMed] [Google Scholar]
- Dean N, Ellis G, Herbison GP, Wilson D. Laparoscopic colposuspension for urinary incontinence in women. Cochrane Database of Systematic Reviews 2006, Issue 3. [DOI: 10.1002/14651858.CD002239.pub2] [DOI] [PubMed] [Google Scholar]
- Debodinance P. [Comparison of the Bologna and Ingelman‐Sundberg procedures for stress incontinence associated with genital prolapse: ten‐year follow‐up of a prospective randomized study]. [French]. Journal de Gynecologie , Obstetrique et Biologie de la Reproduction 2000;29(2):148‐53. [PubMed] [Google Scholar]
- Fantl JA, Newman DK, Colling J, DeLancey JOL, Keeys C, Loughery R, et al. Urinary incontinence in adults: acute and chronic management. Clinical practice guideline. No. 2, 1996 update. Rockville (MD): US Department of Health and Human Services. Public Health Service, Agency for Health Care Policy and Research, 1996 Mar. AHCPR Publication No.: 96‐0682:1‐154. [AHCPR Publication No. 96‐0682] [Google Scholar]
- Glazener CMA, Cooper K. Anterior vaginal repair for urinary incontinence in women. Cochrane Database of Systematic Reviews 2001, Issue 1. [DOI: 10.1002/14651858.CD001755] [DOI] [PubMed] [Google Scholar]
- Glazener CMA, Cooper K. Bladder neck needle suspension for urinary incontinence in women. Cochrane Database of Systematic Reviews 2004, Issue 2. [DOI: 10.1002/14651858.CD003636.pub2] [DOI] [PubMed] [Google Scholar]
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analyses. BMJ 2003;327(7414):557‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.1 [updated Sep 2008). Available from: www.cochrane‐handbook.org: The Cochrane Collaboration, 2008. [Google Scholar]
- Hunskaar S, Burgio K, Diokno AC, Herzog AR, Hjalmas K, Lapitan MC. Epidemiology and natural history of urinary incontinence (UI). In: Abrams P, Cardozo L, Khoury S, Wein A editor(s). Incontinence: 2nd International Consultation on Incontinence. Recommendations of the International Scientific Committee: the evaluation and treatment of urinary incontinence. Paris, 1‐3 July 2001. Plymouth, UK: Health Publication Ltd, 2002. [MEDLINE: ] [Google Scholar]
- Jackson S, Donovan J, Brookes S, Eckford S, Swithinbank L, Abrams P. The Bristol Female Lower Urinary Tract Symptoms questionnaire: development and psychometric testing. British Journal of Urology 1996;77(6):805‐12. [DOI] [PubMed] [Google Scholar]
- Keegan PE, Atiemo K, Cody JD, McClinton S, Pickard R. Periurethral injection therapy for urinary incontinence in women. Cochrane Database of Systematic Reviews 2007, Issue 3. [DOI: 10.1002/14651858.CD003881.pub2] [DOI] [PubMed] [Google Scholar]
- Kilonzo M, Vale L, Stearns S, Grant A, Cody J, Glazener C, et al. Cost effectiveness of tension‐free vaginal tape for the surgical management of female stress incontinence. International Journal of Technology Assessment in Health Care 2004;20(4):455‐63. [DOI] [PubMed] [Google Scholar]
- Kunkle C, Hallock J, Hu X, Blomquist J, Thung S, Werner E. Cost utility analysis of urethral bulking agents versus midurethral sling in stress urinary incontinence. Female Pelvic Medicine & Reconstructive Surgery 2015;21(3):154‐9. [DOI] [PubMed] [Google Scholar]
- Lapitan MC, Cody DJ. Open retropubic colposuspension for urinary stress incontinence in women. Cochrane Database of Systematic Reviews 2003, Issue 1. [DOI: 10.1002/14651858.CD002912] [DOI] [PubMed] [Google Scholar]
- Lapitan MCM, Cody JD, Grant A. Open retropubic colposuspension for urinary incontinence in women. Cochrane Database of Systematic Reviews 2009, Issue 1. [DOI: 10.1002/14651858.CD002912.pub4] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lucas M, Emery S, Alan W, Kathy W. Failure of porcine xenograft sling in a randomised controlled trial of three sling materials in surgery for stress incontinence (Abstract). Proceedings of the International Continence Society (34th Annual Meeting) and the International UroGynecological Association, 23‐27 August, 2004, Paris. 2004:Abstract number 309. [19056] [Google Scholar]
- McGuire EJ, Fitzpatrick CC, Wan J, Bloom D, Sanvordenker J, Ritchey M, et al. Clinical assessment of urethral sphincter function. Journal of Urology 1993;150(5 Pt 1):1452‐4. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Moehrer B, Ellis G, Carey M, Wilson PD. Laparoscopic colposuspension for urinary incontinence in women. Cochrane Database of Systematic Reviews 2002, Issue 2. [DOI: 10.1002/14651858.CD002239] [DOI] [PubMed] [Google Scholar]
- O'Donnell P. Goals of Therapy and Mechanisms of Urethral Incontinence. In: McGuire EJ, Kursh ED editor(s). Female Urology. 1st Edition. Philadelphia, Pensylvania, USA: J. B. Lippincott Company, 1994:175‐201. [Google Scholar]
- Ogah J, Cody JD, Rogerson L. Minimally invasive synthetic suburethral sling operations for stress urinary incontinence in women. Cochrane Database of Systematic Reviews 2009, Issue 4. [DOI: 10.1002/14651858.CD006375.pub2] [DOI] [PubMed] [Google Scholar]
- Thomson Reuters. Reference Manager Professional Edition Version 12. New York: Thomson Reuters, 2012.
- Nordic Cochrane Centre, The Cochrane Collaboration. Review manager 5 (RevMan 5). Copenhagen: Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
- Schulz KF, Altman DG, Moher D, for the CONSORT Group. CONSORT 2010 Statement: updated guidelines for reporting parallel group randomised trials. PLoS Medicine 2010;7(3):e1000251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith ARB, Daneshgari F, Dmochowski R, Ghoniem G, Jarvis GJ, Nitti V, et al. Surgical treatment of incontinence in women. Incontinence. 2nd International Consultation on Incontinence. Plymouth, UK: Health Publication Ltd, 2002. [Google Scholar]
- Subak L, Brubaker, L, Chai T, Creasman J, Diokno A, et al. High costs of urinary incontinence among women electing surgery to treat stress incontinence. Obstetrics & Gynecology 2008;111(4):899‐907. [DOI: 10.1097/AOG.0b013e31816a1e12] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagner T, Hu T. Economic costs of urinary incontinence in 1995. Urology 1998;51(3):355‐61. [DOI] [PubMed] [Google Scholar]
- Ward K, Hilton P, on behalf of the UK & Ireland TVT trial group. Prospective multicentre randomised trial of tension‐free vaginal tape and open colposuspension as primary treatment for stress incontinence. BMJ 2002;325:67‐69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ware JE, Snow KK, Kosinski M, Gandek B. SF‐36 Health survey manual and interpretation guide. Boston (MA): The Health Institute, New England Medical Centre, 1993. [Google Scholar]
- Wilson PD, Herbison RM, Herbison GP. Obstetric practice and the prevalence of urinary incontinence three months after delivery. British Journal of Obstetrics & Gynaecology 1996;103(2):154‐61. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]


