Abstract
Background
Urinary incontinence is a very common and debilitating problem affecting about 50% of women at some point in their lives. Stress urinary incontinence (SUI) is a predominant cause in 30% to 80% of these women imposing significant health and economic burden on society and the women affected. Mid‐urethral sling (MUS) operations are a recognised minimally invasive surgical treatment for SUI. MUS involves the passage of a small strip of tape through either the retropubic or obturator space, with entry or exit points at the lower abdomen or groin, respectively. This review does not include single‐incision slings.
Objectives
To assess the clinical effects of mid‐urethral sling (MUS) operations for the treatment of SUI, urodynamic stress incontinence (USI) or mixed urinary incontinence (MUI) in women.
Search methods
We searched: Cochrane Incontinence Specialised Register (including: CENTRAL, MEDLINE, MEDLINE In‐Process, ClinicalTrials.gov) (searched 26 June 2014); Embase Classic (January 1947 to Week 25 2014); WHO ICTRP (searched 30 June 2014); reference lists.
Selection criteria
Randomised or quasi‐randomised controlled trials amongst women with SUI, USI or MUI, in which both trial arms involve a MUS operation.
Data collection and analysis
Two review authors independently assessed the methodological quality of potentially eligible studies and extracted data from included trials.
Main results
We included 81 trials that evaluated 12,113 women. We assessed the quality of evidence for outcomes using the GRADE assessment tool; the quality of most outcomes was moderate, mainly due to risk of bias or imprecision.
Fifty‐five trials with data contributed by 8652 women compared the use of the transobturator route (TOR) and retropubic route (RPR). There is moderate quality evidence that in the short term (up to one year) the rate of subjective cure of TOR and RPR are similar (RR 0.98, 95% CI 0.96 to 1.00; 36 trials, 5514 women; moderate quality evidence) ranging from 62% to 98% in the TOR group, and from 71% to 97% in the RPR group. Short‐term objective cure was similar in the TOR and RPR groups (RR 0.98, 95% CI 0.96 to 1.00; 40 trials, 6145 women). Fewer trials reported medium‐term (one to five years) and longer‐term (over five years) data, but subjective cure was similar between the groups (RR 0.97, 95% CI 0.87 to 1.09; 5 trials, 683 women; low quality evidence; and RR 0.95, 95% CI 0.80 to 1.12; 4 trials, 714 women; moderate quality evidence, respectively). In the long term, subjective cure rates ranged from 43% to 92% in the TOR group, and from 51% to 88% in the RPR group.
MUS procedures performed using the RPR had higher morbidity when compared to TOR, though the overall rate of adverse events remained low. The rate of bladder perforation was lower after TOR (0.6% versus 4.5%; RR 0.13, 95% CI 0.08 to 0.20; 40 trials, 6372 women; moderate quality evidence). Major vascular/visceral injury, mean operating time, operative blood loss and length of hospital stay were lower with TOR.
Postoperative voiding dysfunction was less frequent following TOR (RR 0.53, 95% CI 0.43 to 0.65; 37 trials, 6200 women; moderate quality evidence). Overall rates of groin pain were higher in the TOR group (6.4% versus 1.3%; RR 4.12, 95% CI 2.71 to 6.27; 18 trials, 3221 women; moderate quality evidence) whereas suprapubic pain was lower in the TOR group (0.8% versus 2.9%; RR 0.29, 95% CI 0.11 to 0.78); both being of short duration. The overall rate of vaginal tape erosion/exposure/extrusion was low in both groups: 24/1000 instances with TOR compared with 21/1000 for RPR (RR 1.13, 95% CI 0.78 to 1.65; 31 trials, 4743 women; moderate quality evidence). There were only limited data to inform the need for repeat incontinence surgery in the long term, but it was more likely in the TOR group than in the RPR group (RR 8.79, 95% CI 3.36 to 23.00; 4 trials, 695 women; low quality evidence).
A retropubic bottom‐to‐top route was more effective than top‐to‐bottom route for subjective cure (RR 1.10, 95% CI 1.01 to 1.19; 3 trials, 477 women; moderate quality evidence). It incurred significantly less voiding dysfunction, and led to fewer bladder perforations and vaginal tape erosions.
Short‐and medium‐term subjective cure rates between transobturator tapes passed using a medial‐to‐lateral as opposed to a lateral‐to‐medial approach were similar (RR 1.00, 95% CI 0.96 to 1.06; 6 trials, 759 women; moderate quality evidence, and RR 1.06, 95% CI 0.91 to 1.23; 2 trials, 235 women; moderate quality evidence). There was moderate quality evidence that voiding dysfunction was more frequent in the medial‐to‐lateral group (RR 1.74, 95% CI 1.06 to 2.88; 8 trials, 1121 women; moderate quality evidence), but vaginal perforation was less frequent in the medial‐to‐lateral route (RR 0.25, 95% CI 0.12 to 0.53; 3 trials, 541 women). Due to the very low quality of the evidence, it is unclear whether the lower rates of vaginal epithelial perforation affected vaginal tape erosion (RR 0.42, 95% CI 0.16 to 1.09; 7 trials, 1087 women; very low quality evidence).
Authors' conclusions
Mid‐urethral sling operations have been the most extensively researched surgical treatment for stress urinary incontinence (SUI) in women and have a good safety profile. Irrespective of the routes traversed, they are highly effective in the short and medium term, and accruing evidence demonstrates their effectiveness in the long term. This review illustrates their positive impact on improving the quality of life of women with SUI. However, a brief economic commentary (BEC) identified three studies suggesting that transobturator may be more cost‐effective compared with retropubic. Fewer adverse events occur with employment of a transobturator approach with the exception of groin pain. When comparing transobturator techniques of a medial‐to‐lateral versus a lateral‐to‐medial insertion, there is no evidence to support the use of one approach over the other. However, a bottom‐to‐top route was more effective than top‐to‐bottom route for retropubic tapes.
A salient point illustrated throughout this review is the need for reporting of longer‐term outcome data from the numerous existing trials. This would substantially increase the evidence base and provide clarification regarding uncertainties about long‐term effectiveness and adverse event profile.
Plain language summary
Mid‐urethral sling operations for stress urinary incontinence in women
Background information
Stress urinary incontinence (involuntary leakage of urine on effort or exertion; or on sneezing, coughing or laughing) is the commonest form of incontinence in women and leads to a reduction in their quality of life. Women with stress urinary incontinence can also have problems with sexual intercourse, as leakage of urine can occur. A significant amount of the woman's and her family's income can be spent on managing the symptoms. One in three women over the age of 18 years will be affected by stress urinary incontinence at some point in her lifetime.
Over the years, surgery to stop this problem has become less invasive. Mid‐urethral sling operations are one of the various types of surgeries available. These operations are suitable for women who are having their first operation and those who had previous unsuccessful surgery. In a mid‐urethral sling operation a tape is placed underneath the urethra, which is the tube that carries urine out of the bladder. When the woman coughs, the tape compresses the tube, thus providing the support necessary to prevent urine leakage.
There are two main ways of carrying out these operations, either by inserting a tape behind the pubic bone through the abdomen ('retropubic'), or through the groin ('transobturator').
What this review tried to find out
We looked at the effects and costs of mid‐urethral sling operations using the two different methods. We also compared different ways of inserting the tape, and using tapes made from different materials. The purpose of this review was to find out how effective these operations are in the treatment of stress urinary incontinence and help determine potential complications rate.
Main findings of this review
We performed a thorough literature search up to June 2014. We identified 81 trials that had a total of 12,113 women. These trials showed that over 80% of women with stress urinary incontinence are cured, or have significant improvement in their symptoms, with either operation, for up to five years after surgery, irrespective of the tapes used and the route of tape insertion. The studies used different questionnaires to assess quality of life, which meant that we could not combine their results . However, the information available for quality of life shows that it improves as a result of these operations, though there is no clear difference between the two procedures. In terms of costs, a non‐systematic review of economic studies suggested that transobturator had lower costs than retropubic methods. Only a few trials provided information about the effectiveness of these tapes more than five years after surgery. The evidence that we have been able to assess indicates that the positive effects persist.
Adverse effects
Tapes passing behind the pubic bone (retropubic) seem to carry a greater risk of injuring the bladder during the operation and of women experiencing problems emptying their bladder completely after surgery. However, this operation leads to less groin pain in the short term. There is some limited evidence that this way of inserting the tape has a lower risk of requiring a repeat operation in the long term compared to tapes passing through the groin (transobturator). There is moderate quality evidence that overall reported rates of tape‐related complications are low, such as erosion of the tape into the vagina at about 2% for both routes of tape insertion. The reported occurrence of problems with sexual intercourse including pain was low, and leakage of urine during intercourse are improved following insertion of these tapes.
Limitations of the review
Most of our results are based on moderate quality evidence. Most trials did not describe their methods clearly, thus leading to some degree of uncertainty in the findings. At present there are only a limited number of randomised controlled trials (these produce the most reliable results) that have published data beyond five years after surgery. This means that evidence about how effective and safe these procedures are in the longer term lags behind the evidence for them in the short and medium term (up to five years). Longer‐term data are required to help increase the reliability of longer‐term results.
Summary of findings
Summary of findings for the main comparison. Transobturator (TOR) compared to retropubic (RPR) route for stress urinary incontinence in women.
| Transobturator (TOR) compared to retropubic (RPR) route for stress urinary incontinence in women | ||||||
| Patient or population: women with stress urinary incontinence Settings: Secondary care Intervention: transobturator (TOR) Comparison: retropubic (RPR) route | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Retropubic (RPR) route | Transobturator (TOR) | |||||
| Subjective cure (Short term < 1 year) | Study population | RR 0.98 (0.96 to 1.00) | 5514 (36 RCTs) | ⊕⊕⊕⊝ MODERATE 1 | ||
| 844 per 1000 | 827 per 1000 (810 to 844) | |||||
| Mean control group risk across studies | ||||||
| 833 per 1000 | 816 per 1000 (800 to 833) | |||||
| Subjective cure (medium term, 1 to 5 years) | Study population | RR 0.97 (0.92 to 1.03) | 683 (5 RCTs) | ⊕⊕⊝⊝ LOW 2,3 | ||
| 881 per 1000 | 854 per 1000 (810 to 907) | |||||
| Mean control group risk across studies | ||||||
| 869 per 1000 | 843 per 1000 (799 to 895) | |||||
| Subjective cure (long term, > 5 years) | Study population | RR 0.95 (0.87 to 1.04) | 714 (4 RCTs) | ⊕⊕⊕⊝ MODERATE 4 | ||
| 707 per 1000 | 671 per 1000 (615 to 735) | |||||
| Mean control group risk across studies | ||||||
| 843 per 1000 | 801 per 1000 (733 to 877) | |||||
| Bladder or urethral perforation | Study population | RR 0.13 (0.08 to 0.20) | 6372 (40 RCTs) | ⊕⊕⊕⊝ MODERATE 5 | ||
| 49 per 1000 | 6 per 1000 (4 to 10) | |||||
| Mean control group risk across studies | ||||||
| 25 per 1000 | 3 per 1000 (2 to 5) | |||||
| Voiding dysfunction (short and medium term, up to 5 years) | Study population | RR 0.53 (0.43 to 0.65) | 6217 (37 RCTs) | ⊕⊕⊕⊝ MODERATE 6 | ||
| 72 per 1000 | 38 per 1000 (31 to 47) | |||||
| Mean control group risk across studies | ||||||
| 55 per 1000 | 29 per 1000 (24 to 36) | |||||
| De novo urgency or urgency incontinence (short term, up to 12 months) | Study population | RR 0.98 (0.82 to 1.17) | 4923 (31 RCTs) | ⊕⊕⊕⊝ MODERATE 7 | ||
| 82 per 1000 | 80 per 1000 (67 to 96) | |||||
| Mean control group risk across studies | ||||||
| 83 per 1000 | 81 per 1000 (68 to 97) | |||||
| Groin pain | Study population | RR 4.62 (3.09 to 6.92) | 3226 (18 RCTs) | ⊕⊕⊕⊝ MODERATE 8 | ||
| 14 per 1000 | 66 per 1000 (44 to 99) | |||||
| Mean control group risk across studies | ||||||
| 45 per 1000 | 208 per 1000 (139 to 311) | |||||
| Suprapubic pain | Study population | RR 0.29 (0.11 to 0.78) | 1105 (4 RCTs) | ⊕⊕⊕⊝ MODERATE 9 | ||
| 29 per 1000 | 8 per 1000 (3 to 23) | |||||
| Mean control group risk across studies | ||||||
| 18 per 1000 | 5 per 1000 (2 to 14) | |||||
| Vaginal tape erosion (short and medium term, up to 5 years) | Study population | RR 1.13 (0.78 to 1.65) | 4743 (31 RCTs) | ⊕⊕⊕⊝ MODERATE 10 | ||
| 20 per 1000 | 22 per 1000 (15 to 32) | |||||
| Mean control group risk across studies | ||||||
| 21 per 1000 | 24 per 1000 (16 to 34) | |||||
| Repeat incontinence surgery (short term, within 12 months) | Study population | RR 1.64 (0.85 to 3.16) | 1402 (9 RCTs) | ⊕⊕⊕⊝ MODERATE 11 | ||
| 19 per 1000 | 31 per 1000 (16 to 60) | |||||
| mean control group across studies | ||||||
| 24 per 1000 | 39 per 1000 (20 to 76) | |||||
| Repeat incontinence surgery (long term, > 5 years) | Study population | RR 8.79 (3.36 to 23.00) | 695 (4 RCTs) | ⊕⊕⊝⊝ LOW 12,13 | ||
| 11 per 1000 | 100 per 1000 (38 to 262) | |||||
| Mean control group across studies | ||||||
| 67 per 1000 | 589 per 1000 (225 to 1000) | |||||
| Quality of life | 16 different validated questionnaires were used by different studies to assess QoL. This outcome was reported in 11 RCTs, but reported in different ways which precluded meta‐analysis. In all but one of the RCTs where QoL was assessed there was improvement in the QoL in women after the intervention, irrespective of which route was used, with no significant difference in scores between groups. Where assessment of sexual function was performed, there was an equal amount of improvement in sexual function following surgical treatment, irrespective of the route employed | ‐ | (11 RCTs) | |||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI).
CAD: Canadian dollars CI: confidence interval RCT: randomised controlled trial RPR: retropubic route RR: risk ratio QoL: quality of life TOR: transobturator route | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate Very low quality: We are very uncertain about the estimate | ||||||
1Random sequence generation was unclear in 13 studies and at high risk of bias in 2 studies, and allocation concealment was unclear in 20 studies and at high risk in 2/37 studies
2Allocation concealment was unclear in 2/5 trials and sequence generation was unclear in 1/5 trials, so we decided to downgrade by 1 level
3There was potential substantial heterogeneity with an I² value of 67%, so we downgraded the quality rating by 1 level
4There was potential substantial heterogeneity among studies with an I² value of 65%, which lead us to downgrade by 1 level
5As allocation concealment was unclear in 18/40 trials and at high risk in 3/40, and sequence generation was unclear in 14/40 trials and at high risk in 3/40, we decided to downgrade by 1 level
6As allocation concealment was unclear in 16/37 trials and at high risk in 2/37, and sequence generation was unclear in 11/37 trials and at high risk in 2/37, we decided to downgrade by 1 level
7Random sequence generation was unclear in 10/31 studies and at high risk of bias in 2/31, and allocation concealment was unclear in 15/31 studies and at high risk in 2/31, so we downgraded by 1 level
8Random sequence generation was unclear in 4/18 studies and at high risk in 2/18, and allocation concealment was unclear in 9/18 studies and at high risk in 2/18, so we downgraded the quality of the evidence by 1 level
9Random sequence generation was at high risk in 1/4 studies, while allocation concealment was unclear in 2/4 and at high risk in 1/4, so we downgraded by 1 level
10Allocation concealment was unclear in 12/31 trials and at high risk in 1/31, while sequence generation was unclear in 6/31 trials and at high risk in 1/31, so we decided to downgrade by 1 level
11The wide confidence interval was judged to include a threshold for appreciable harm considered to be > 25% increase in RR, in this case there was much more than a 25% increase in RR for harm, so we downgraded the level by 1
12There was potential substantial heterogeneity with an I² value of 46%, so we downgraded the quality rating by 1 level
13Due to the low number of studies reporting data for this outcome, and the low number of events and wide CI around the estimate of the effect, we downgraded the quality of evidence by 1 level due to imprecision
Summary of findings 2. Retropubic bottom‐to‐top approach compared to retropubic top‐to‐bottom approach for stress urinary incontinence in women.
| Retropubic bottom‐to‐top approach compared to retropubic top‐to‐bottom approach for stress urinary incontinence in women | ||||||
| Patient or population: women with stress urinary incontinence Settings: Secondary care Intervention: retropubic bottom‐to‐top approach Comparison: retropubic top‐to‐bottom approach | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| retropubic top‐to‐bottom approach | Retropubic bottom‐to‐top approach | |||||
| Subjective cure (short term, ≤ 1 year) | Study population | RR 1.10 (1.01 to 1.20) | 492 (3 RCTs) | ⊕⊕⊕⊝ MODERATE 1 | ||
| 770 per 1000 | 847 per 1000 (778 to 924) | |||||
| Mean control group across studies | ||||||
| 890 per 1000 | 979 per 1000 (899 to 1000) | |||||
| Subjective cure (medium term, 1 to 5 years) | No studies reported this outcome | ‐ | (0 studies) | |||
| Subjective cure long term: > 5 years | No studies reported this outcome | ‐ | (0 studies) | |||
| Bladder or urethral perforation | Study population | RR 0.55 (0.31 to 0.98) | 631 (5 RCTs) | ⊕⊕⊕⊝ MODERATE 2 | ||
| 85 per 1000 | 47 per 1000 (26 to 83) | |||||
| Mean control group across studies | ||||||
| 115 per 1000 | 63 per 1000 (36 to 113) | |||||
| Voiding dysfunction | Study population | RR 0.40 (0.18 to 0.90) | 631 (5 RCTs) | ⊕⊕⊕⊝ MODERATE 2 | ||
| 60 per 1000 | 24 per 1000 (11 to 54) | |||||
| Mean control group across studies | ||||||
| 49 per 1000 | 20 per 1000 (9 to 44) | |||||
| De novo urgency or urgency incontinence | Study population | RR 0.84 (0.52 to 1.34) | 547 (4 RCTs) | ⊕⊕⊝⊝ LOW 3,4 | ||
| 123 per 1000 | 103 per 1000 (64 to 165) | |||||
| Mean control group across studies | ||||||
| 187 per 1000 | 157 per 1000 (97 to 250) | |||||
| Vaginal tape erosion | Study population | RR 0.27 (0.08 to 0.95) | 569 (4 RCTs) | ⊕⊕⊕⊝ MODERATE 5 | ||
| 35 per 1000 | 9 per 1000 (3 to 33) | |||||
| Mean control group across studies | ||||||
| 69 per 1000 | 19 per 1000 (6 to 65) | |||||
| Repeat incontinence surgery short term | No studies reported this outcome | ‐ | (0 studies) | |||
| Repeat incontinence surgery long term | No studies reported this outcome | ‐ | (0 studies) | |||
| Quality of life (IIQ scores) | The mean quality of life (IIQ scores) in the control group was 49.9 | The mean quality of life (IIQ scores) in the intervention group was 4.6 lower (14.17 lower to 4.97 higher) | ‐ | 84 (1 RCT) | ||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI).
CI: confidence interval IIQ: Incontinence Impact questionnaire RCT: randomised controlled trial RR risk ratio; | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate Very low quality: We are very uncertain about the estimate. | ||||||
1Sequence generation and allocation concealment was unclear in 2/3 trials, so we downgraded by 1 level
2Sequence generation and allocation concealment was unclear in 3/5 trials, so we downgraded by 1 level
3Sequence generation was unclear in 2/4 studies and allocation concealment unclear in 3/4 studies, so we downgraded by 1 level
4The wide confidence interval was judged to include a threshold for appreciable harm considered to be > 25% increase in RR, in this case there was much more than a 25% increase in RR for harm, so we downgraded the level by 1
5Sequence generation unclear in 3/4 studies and allocation concealment unclear in 2/4 studies, so we downgraded by 1 level
Summary of findings 3. Obturator medial‐to‐lateral approach compared to obturator lateral‐to‐medial approach for stress urinary incontinence in women.
| Obturator medial‐to‐lateral approach compared to obturator lateral‐to‐medial approach for stress urinary incontinence in women | ||||||
| Patient or population: women with stress urinary incontinence Settings: Secondary care Intervention: obturator medial‐to‐lateral approach Comparison: obturator lateral‐to‐medial approach | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Obturator lateral‐to‐medial approach | Obturator medial‐to‐lateral approach | |||||
| Subjective cure (short term ≤ 1 year) | Study population | RR 1.00 (0.96 to 1.06) | 759 (6 RCTs) | ⊕⊕⊝⊝ LOW 1 | ||
| 877 per 1000 | 877 per 1000 (842 to 930) | |||||
| Mean control group risk across studies | ||||||
| 880 per 1000 | 880 per 1000 (845 to 933) | |||||
| Subjective cure (medium term, 1 to 5 years) | Study population | RR 1.06 (0.91 to 1.23) | 235 (2 RCTs) | ⊕⊕⊝⊝ LOW 2 | ||
| 711 per 1000 | 753 per 1000 (647 to 874) | |||||
| Mean control group risk across studies | ||||||
| 736 per 1000 | 780 per 1000 (670 to 905) | |||||
| Subjective cure | No studies reported this outcome | ‐ | (0 studies) | |||
| Bladder or urethral perforation | Study population | RR 0.38 (0.07 to 1.92) | 794 (6 RCTs) | ⊕⊕⊕⊝ MODERATE 3 | ||
| 11 per 1000 | 4 per 1000 (1 to 20) | |||||
| Mean control group risk across studies | ||||||
| 6 per 1000 | 2 per 1000 (0 to 12) | |||||
| Voiding dysfunction (short and medium term, up to 5 years) | Study population | RR 1.74 (1.06 to 2.88) | 1121 (8 RCTs) | ⊕⊕⊕⊝ MODERATE 4 | ||
| 40 per 1000 | 70 per 1000 (43 to 116) | |||||
| Mean control group risk across studies | ||||||
| 55 per 1000 | 96 per 1000 (58 to 158) | |||||
| De novo urgency or urgency incontinence (short term, up to 12 months) | Study population | RR 1.01 (0.46 to 2.20) | 357 (3 RCTs) | ⊕⊕⊝⊝ LOW 5 | ||
| 63 per 1000 | 63 per 1000 (29 to 138) | |||||
| Mean control group risk across studies | ||||||
| 64 per 1000 | 65 per 1000 (29 to 141) | |||||
| Groin pain | Study population | RR 1.15 (0.75 to 1.76) | 837 (6 RCTs) | ⊕⊝⊝⊝ VERY LOW 6,7 | ||
| 80 per 1000 | 92 per 1000 (60 to 140) | |||||
| Mean control group risk across studies | ||||||
| 74 per 1000 | 85 per 1000 (56 to 130) | |||||
| Vaginal tape erosion (short and medium term, up to 5 years) | Study population | RR 0.42 (0.16 to 1.09) | 1087 (7 RCTs) | ⊕⊝⊝⊝ VERY LOW 7,8 | ||
| 24 per 1000 | 10 per 1000 (4 to 26) | |||||
| Mean control group risk across studies | ||||||
| 17 per 1000 | 7 per 1000 (3 to 19) | |||||
| Repeat incontinence surgery (short term, up to 12 months) | Study population | RR 0.64 (0.32 to 1.30) | 532 (2 RCTs) | ⊕⊕⊝⊝ LOW 7,9 | ||
| 71 per 1000 | 45 per 1000 (23 to 92) | |||||
| Mean control group risk across studies | ||||||
| 58 per 1000 | 37 per 1000 (19 to 75) | |||||
| Repeat incontinence surgery | No studies reported this outcome | ‐ | (0 studies) | |||
| Quality of life | The mean quality of life in the control group was 0 | The mean quality of life in the intervention group was 16.54 higher (4.84 higher to 28.24 higher) | ‐ | 46 (1 RCT) | ⊕⊝⊝⊝ VERY LOW 10,11 | |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI).
CI: confidence interval RCT: randomised controlled trial RR: risk ratio; | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate Very low quality: We are very uncertain about the estimate | ||||||
1Random sequence generation was unclear in 4/6 studies, allocation concealment was unclear in5/6 and at high risk in 1/6 studies, so we downgraded the quality of evidence due to risk of bias by 2 levels
2Random sequence generation was unclear in all both studies, allocation concealment was unclear in 1 and high risk of bias in the other study, so we downgraded by 2 levels
3Sequence generation was unclear in 2 studies and allocation concealment was unclear in 3 studies, so we downgraded the quality rating by 1 level
4Sequence generation was unclear in 3 studies and at high risk in 1 study, while allocation concealment was unclear in 4 studies and at high risk in 1 study, so we downgraded by 1 level
5Sequence generation was unclear in 2/3 studies and at high risk in 1/3, allocation concealment was unclear in 2/3 studies and high in 1/3, so we downgraded by 2 levels
6Random sequence generation was unclear in 2/5 and high in 1/5 studies, while allocation concealment was unclear in 2/5 and high in 2/5 studies, so we downgraded the quality of evidence due to high risk of bias by 2 levels
7The wide confidence interval was judged to include a threshold for appreciable harm considered to be > 25% increase in RR, in this case there was > 65% increase in RR for harm, so we downgraded by 1 level
8Sequence generation was unclear in 3/7 studies and at high risk in 1/7. Allocation concealment was unclear in 5/7 studies and at high risk in 1/7. We downgraded the quality rating by 2 levels
9Sequence generation and allocation concealment were unclear in 1/2 studies, so we downgraded by 1 level
10Sequence generation and allocation concealment were unclear, so we downgraded by 1 level
11As there was only 1 study with very few events and CIs around estimates of effect included appreciable benefit and appreciable harm, we downgraded by 2 levels
Summary of findings 4. Monofilament compared to multifilament tapes for stress urinary incontinence in women.
| Monofilament compared to multifilament tapes for stress urinary incontinence in women | ||||||
| Patient or population: women with stress urinary incontinence Settings: Secondary care Intervention: monofilament Comparison: multifilament tapes | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| multifilament tapes | Monofilament | |||||
| Subjective cure (short term ≤ 1 year) | Study population | RR 1.07 (0.98 to 1.16) | 505 (4 RCTs) | ⊕⊕⊕⊝ MODERATE 1 | ||
| 784 per 1000 | 839 per 1000 (768 to 909) | |||||
| Mean control group risk across studies | ||||||
| 810 per 1000 | 867 per 1000 (794 to 939) | |||||
| Subjective cure (medium term: 1 to 5 years) | No studies reported this outcome | ‐ | (0 studies) | |||
| Subjective cure (long term: > 5 years) | No studies reported this outcome | ‐ | (0 studies) | |||
| Bladder or urethral perforation | Study population | RR 0.76 (0.29 to 1.99) | 496 (4 RCTs) | ⊕⊕⊕⊝ MODERATE 1 | ||
| 37 per 1000 | 28 per 1000 (11 to 73) | |||||
| Mean control group risk across studies | ||||||
| 32 per 1000 | 25 per 1000 (9 to 64) | |||||
| Voiding dysfunction | Study population | RR 2.20 (0.98 to 4.92) | 400 (3 RCTs) | ⊕⊕⊝⊝ LOW 2,3 | ||
| 41 per 1000 | 89 per 1000 (40 to 200) | |||||
| Mean control group risk across studies | ||||||
| 65 per 1000 | 143 per 1000 (64 to 320) | |||||
| De novo urgency or urgency incontinence | Study population | RR 1.09 (0.66 to 1.82) | 496 (4 RCTs) | ⊕⊕⊝⊝ LOW 4,5 | ||
| 102 per 1000 | 111 per 1000 (67 to 186) | |||||
| Mean control group risk across studies | ||||||
| 107 per 1000 | 117 per 1000 (71 to 195) | |||||
| Vaginal tape erosion | Study population | RR 0.43 (0.16 to 1.14) | 396 (3 RCTs) | ⊕⊕⊕⊕ HIGH | ||
| 62 per 1000 | 26 per 1000 (10 to 70) | |||||
| Mean control group risk across studies | ||||||
| 43 per 1000 | 18 per 1000 (7 to 49) | |||||
| Repeat incontinence surgery (short term ≤ 1 year) | No studies reported this outcome | ‐ | (0 studies) | |||
| Repeat incontinence surgery (long term > 5 years) | No studies reported this outcome | ‐ | (0 studies) | |||
| Quality of life scores ICIQ | The mean quality of life scores ICIQ in the control group was 2.1 | The mean quality of life scores ICIQ in the intervention group was 0.6 lower (0.76 lower to 0.44 lower) | ‐ | 96 (1 RCT) | ⊕⊕⊕⊕ HIGH | |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI).
CI: confidence interval ICIQ: International Consultation on Incontinence questionnaire RCT: randomised controlled trial RR: risk ratio | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate Very low quality: We are very uncertain about the estimate | ||||||
1Random sequence generation and allocation concealment unclear in 2/4 studies, so we downgraded by 1 level
2Random sequence generation and allocation concealment unclear in 2/3 studies, so downgraded by 1 level
3The wide confidence interval was judged to include a threshold for appreciable harm considered to be > 25% increase in RR, in this case there was much more than a 25% increase in RR for harm, so we downgraded by 1 level
4Sequence generation and allocation concealment were unclear in 2/4 studies, so we downgraded the quality rating by 1 level
5The wide confidence interval was judged to include a threshold for appreciable harm considered to be > 25% increase in RR, in this case there was > 65% increase in RR for harm, so we downgraded by 1 level
Background
Urinary incontinence is a very common condition in women. It is associated with significant physical morbidity, sexual dysfunction, loss of independence and a reduction in psychological well being, with consequent decreased participation in social and domestic activities (Wetle 1995; Thom 1998; Van Oyen 2002; Salonia 2004; Botlero 2010). Overall the prevalence of urinary incontinence in adult women has been estimated to be between 10% and 40%, and is considered severe in about 3% to 17%, with annual incidence ranging from 2% to 11% (Hunskaar 2002; Milsom 2009). The prevalence of stress urinary incontinence (SUI) in women is between 12% to 46% (Botlero 2008; Coyne 2009; Irwin 2006). This is a potentially debilitating social problem, with significant cost implications to the individuals and the healthcare service. The estimated annual cost to the healthcare system in the UK exceeds GBP 700 million (1999/2000 GBP) (Turner 2004) while in the USA, the annual total direct costs in both men and women is over USD 16 billion (1995 USD) (Chong 2011) with societal costs of USD 26.2 billion (1995 USD) (Wagner 1998). Approximately, USD 13.12 billion (1995 USD) of the total direct costs of urinary incontinence is spent on SUI (Chong 2011; Kunkle 2015). In the USA,about 70% of this USD 13.12 billion is borne by the patients mainly through routine care (purchasing pads and disposable underwear (diapers), laundry and dry cleaning). Of the remaining 30%, 14% is spent on nursing home admission, 9% on treatment, 6% on addressing complications and 1% on diagnosis (Chong 2011). In the UK an estimated more than GBP 178 million (1999/2000 GBP) is borne by women on an individual basis annually (Turner 2004; Papanicolaou 2005).This constitutes a significant individual financial burden.
A study reported that about 1% of the median annual household income (USD 50,000 to USD 59,999) was spent by women on incontinence management. This study estimated that women spent an annual mean cost of USD 751 to USD 1277 (2006 USD) on incontinence. This cost increases based on the severity of the symptoms (Subak 2008).The indirect cost associated exerts social and psychological burdens which are unquantifiable. (Chong 2011; Kilonzo 2004). Nevertheless, Birnbaum 2004 estimated that the annual average direct medical costs of SUI for one year (1998 USD) was USD 5642 and USD 4208 for indirect workplace costs.The cost of management and treatment of SUI appears to have increased over time due to increasing prevalence and an increased desire for improved quality of life (QOL). This in turn has resulted from improved recognition of the condition, as well as increased use of surgical and non‐surgical managements.
Continence is achieved through interplay of the normal anatomical and physiological properties of the bladder, urethra, urethral sphincter and pelvic floor, with the nervous system co‐ordinating these organs. The urethra and its sphincter act as a closure mechanism during bladder filling to contain urine within the bladder, thereby allowing storage of urine until a convenient time and place to void is reached. The pelvic floor provides support to the bladder and urethra, and allows normal abdominal pressure transmission to the proximal urethra, which is essential in the maintenance of continence. Crucial to the healthy functioning of the bladder, urethra, sphincter and pelvic floor is co‐ordination between them, which is facilitated by an intact nervous system.
There are many theories hypothesizing the pathophysiology of stress urinary incontinence. Historically Goran Enhorning was first to measure simultaneous bladder and urethral pressures. He suggested that during the cough impulse, pressure is transmission from the abdomen to the urethra with a concurrent reduction in urethral closure pressure that results in SUI (Enhorning 1961). McGuire’s modified classification of SUI emphasizes the principle of intrinsic sphincter deficiency (ISD) as a cause of SUI. This is said to occur due to poor urethral closure function resulting from defective urethral mucosal coaptation. These two theories informed procedures such as the Burch Colposuspension and Marshall Marchetti Krantz operations. De Lancey’s 'hammock' theory suggested that abdominal pressure transmission to the bladder neck and urethra leads to the proximal urethra being compressed against the pubo‐vesical fascia and anterior vaginal wall, thus maintaining continence (DeLancey 1994).
Recent findings on the pathophysiology of urinary incontinence have demonstrated that mid‐urethral support, provided by the pubo‐urethral ligaments, also plays an important role in maintaining continence when the intra‐abdominal pressure rises. This has led to the 'integrated theory' for the maintenance of continence in female SUI (Petros 1990; Petros 1993). This theory, in turn, is the basis for the current use of minimally invasive mid‐urethral tapes in the treatment of SUI.
When performing mid‐urethral tape surgery there are different types of synthetic materials used. Synthetic meshes are divided into four groups:
type 1 are macroporous, monofilament;
type 2 are microporous;
type 3 are macroporous, multifilament;
type 4 are submicronic, coated biomaterials with pore sizes of less than 1 μm.
Type 1 mesh has the highest biocompatibility with the least propensity for infection. Differences in their efficacy and complications are likely to be due to several factors including the different knits and weaves of the various tape materials, their biomechanical properties and histological biocompatibility. Pore size affects the inflammatory response and resultant connective tissue formation within and into the mesh, and the rearrangement of materials such as collagen within the mesh structure. Macroporous meshes (pore size in excess of 75 μm) easily allow macrophages, leukocytes, fibroblasts, blood vessels and collagen to transverse the pores: thus macroporous meshes promote tissue host ingrowth with resultant biocompatibility and low risk of infection (Amid 1997). Monofilament tapes are widely available and now predominate in current clinical practice.
In contrast, microporous meshes (pore size greater than 10 μm) allow bacteria to pass through and replicate, but exclude macrophages. Multifilament tapes have smaller pore sizes, and are thus microporous. This perhaps explains why tape erosion was more common in the multifilament tapes, though statistical significance was not reached.
Description of the condition
Incontinence occurs when this normal relationship between the lower urinary tract components is disrupted, as a result of nerve damage or direct mechanical disruption to the pelvic organs. Advancing age, higher parity, vaginal delivery, obesity and post menopausal status are all associated with an increased risk of urinary incontinence (Wilson 1996).
There are different forms of urinary incontinence of which SUI is the most common type, accounting for at least 50% of cases of urinary incontinence in women (Hannestad 2000). SUI is the involuntary loss of urine that occurs with physical exertion (e.g. sporting activities), or on sneezing or coughing (Haylen 2010). Urodynamic stress incontinence (USI) is the involuntary leakage of urine observed during filling cystometry, it is associated with increased intra‐abdominal pressure, in the absence of a detrusor contraction (Haylen 2010). Two mechanisms for stress incontinence are recognized: hyper‐mobility or significant displacement of the urethra and bladder neck during exertion, and intrinsic urethral sphincter deficiency (Blaivas 1988). These mechanisms may co‐exist in women (O'Donnell 1994). Few clinical trials have distinguished between the two conditions, probably because there is currently no standardised and validated test available for this (Blaivas 1988; McGuire 1993). We considered women whose incontinence could be due to either mechanism together in this review.
The diagnosis of urodynamic stress incontinence implies that urodynamic investigation has been done to confirm stress incontinence; it may also identify the presence of detrusor overactivity, in mixed urinary incontinence. Standard clinical assessment includes history taking, physical examination, frequency/volume charts and urine analysis. Some authors described women with the symptom of stress urinary incontinence only (diagnosis made on clinical evaluation without urodynamics). Women with stress urinary incontinence and those with urodynamic stress incontinence have been included in this review.
Urgency urinary incontinence (UUI) is a sudden, compelling desire to pass urine, which is difficult to defer (urgency), accompanied by the involuntary loss of urine. Detrusor overactivity (DO) is a diagnosis that denotes involuntary detrusor contractions observed during the filling phase of a urodynamic assessment. It may be spontaneous or provoked and can be qualified according to cause ‐ neurogenic or idiopathic (Haylen 2010). We included women with UUI and the formal urodynamic diagnosis of DO in the review only if they had co‐existing stress incontinence (so called mixed urinary incontinence (MUI)).
Women with MUI who were included in this review had symptoms of SUI plus either urgency or UUI, or urodynamic stress incontinence (USI) plus DO (urodynamic diagnosis).
Description of the intervention
Management of SUI includes conservative, mechanical, pharmacological and surgical interventions.
Conservative management centres on lifestyle modifications, physical methods including pelvic floor muscle training, electrical stimulation, biofeedback and the use of weighted cones.
Mechanical devices that prevent or reduce urinary leakage are available, and include metal plugs or patches and urethral or vaginal inserts.
Drug therapies, such as oestrogens and alpha adrenergic agents, have been used in the past. Recently, inhibitors of serotonin and norepinephrine reuptake have been proposed as new drug therapy for SUI, used alone or in combination with other conservative management (Ghoniem 2005).
A trial of such conservative treatments should be undertaken before resorting to surgery. The following interventions are the subject of separate Cochrane reviews.
Lifestyle interventions for the treatment of urinary incontinence in adults (Imamura 2010).
Bladder training for urinary incontinence in adults (Wallace 2004).
Comparisons of approaches to pelvic floor muscle training for urinary incontinence in women (Hay‐Smith 2011).
Feedback or biofeedback to augment pelvic floor muscle training for urinary incontinence in women (Herderschee 2011).
Pelvic floor muscle training added to another active treatment versus the same active treatment alone for urinary incontinence in women (Ayeleke 2013).
Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women (Dumoulin 2014).
Combined conservative interventions for urge, stress or mixed incontinence in adults (French 2010).
Weighted vaginal cones for urinary incontinence (Herbison 2013).
Mechanical devices for urinary incontinence in women (Lipp 2011).
Oestrogen therapy for urinary incontinence in post‐menopausal women (Cody 2012).
Adrenergic drugs for urinary incontinence in adults (Alhasso 2005).
Serotonin and noradrenaline reuptake inhibitors (SNRI) for stress urinary incontinence in adults (Mariappan 2005).
Acupuncture for stress urinary incontinence in adults (Wang 2013).
Surgical procedures to remedy SUI generally aim to lift and support the urethro‐vesical junction, but in the last decade the emphasis has been on suburethral support at the mid‐urethral level. Owing to disagreement on the precise mechanism by which continence is achieved, the choice of surgical procedure is influenced by co‐existent problems, surgeon's preference and the physical features of the person affected.
Numerous surgical methods for SUI have been described and evaluated in Cochrane reviews. Traditionally, they fall into seven categories:
suburethral slings (including traditional suburethral slings and minimally invasive sling operations; Rehman 2011);
open abdominal retropubic suspension (e.g. colposuspension (Burch/modified Burch), Marshall‐Marchetti‐Krantz (MMK); Lapitan 2012);
laparoscopic retropubic suspension (Dean 2006);
anterior vaginal repair (anterior colporrhaphy; Glazener 2001);
needle suspensions (Glazener 2004);
urethral injections (Kirchin 2012); and
artificial sphincters.
Suburethral slings have become the favourite primary continence surgery in current clinical practice. Several developments in type and technique have resulted in the separation of the original sling review, Bezerra 2005, into three different reviews focusing on:
traditional suburethral slings (Rehman 2011)
minimally invasive slings such as TVT and TOT (Ogah 2009), and
single incision slings, also known as mini‐slings (Nambiar 2014).
The materials that have been used for slings may be biological or synthetic. The first of these reviews concentrates on traditional (biological) suburethral sling operations (Rehman 2011). A traditional suburethral sling operation requires a combined abdominal and vaginal approach. Strips of material are tunnelled under the proximal urethra. They are attached either to the rectus muscle or the iliopectineal ligaments, resulting in a tightening of the sling and increased bladder support every time the woman strains to prevent leaking. They are applied under open surgery and are fixed with sutures.
This current review is an update of the second of these reviews, focusing on minimally invasive suburethral sling operations using artifical (synthetic) non‐absorbable sling materials (Ogah 2009). The techniques of these procedures are described below. This review does not include single incision slings.
The third of these reviews is a new, recently published review that compares a new type of sling, the single incision sling, which is also known as the mini‐sling (Nambiar 2014). The technique differs from that of the original synthetic slings in that a single incision is made within the vagina using a significantly shorter tape and there are no tape exit incisions.
How the intervention might work
The current review focuses on mid‐urethral sling operations. These involve the insertion of a tape covered by a plastic sheath around the mid‐urethra without suture fixation, performed in some centres under local anaesthesia (Ulmsten 1995a; Ulmsten 1996; Smith 2002). The aim is to restore or enhance the patient's urethral support during a sudden movement, such as a cough or sneeze, which would prevent the involuntary loss of urine. Ultrasound studies suggest that the mechanism of action is the intermittent or dynamic obstruction of the urethra by the tape when increased abdominal pressure occurs (such as when coughing or sneezing; Dietz 2004).
There are two main types of surgical approaches.
Retropubic: This procedure involves the insertion of two needles passed through the retropubic space blindly from the vagina to abdomen or from the abdomen to the vagina. Cystoscopy is recommended to detect any perforation of the bladder or urethra (Ulmsten 1995a; Ulmsten 1995b).
Transobturator; This is another type of minimally invasive synthetic suburethral sling operation in which the tape is inserted in a horizontal plane underneath the middle of the urethra between the two obturator foramina. The ends of the tape are tunnelled percutaneously with a tunneller (curved needle), again without suture fixation. As the retropubic space is not breached, it is argued that cystoscopy is not required (Delorme 2001; Delorme 2003; Delorme 2004). Shortly after the development of this technique a similar operation was described in which a tape is passed percutaneously through the obturator foramina, using an inside‐to‐outside technique, i.e. medio‐lateral (de Leval 2003; de Leval 2005).
We included only mid‐urethral sling operations, with synthetic tape materials applied through minimally invasive surgeries, either through the retropubic space or the transobturator route in this review. However, a number of modifications of transobturator surgery using the same route have been described and we have included these too.
In this update, in contrast to the original review in which trials of minimally invasive slings were compared to traditional slings, open colposuspension, or laparoscopic colposuspension, these comparator techniques have not been included, as these are now covered by other Cochrane reviews (Dean 2006; Rehman 2011; Lapitan 2012).
A concern of using synthetic material is the potential risk of complications caused by infection and tissue reaction to the tapes. Some aspects of the material that may vary include pore size, mono‐ or multifilament design, and biocompatibility. We included all types of mesh used in different minimally invasive slings in this review, and assessed possible differences between the risk of complications.
Why it is important to do this review
There is a plethora of minimally invasive synthetic tapes available and used worldwide for treatment of SUI. The reported effectiveness and safety of these procedures have made them very popular, but in the past there has been controversy about which of these procedures is best, as the introduction of many of these procedures and tapes was market driven and was not accompanied by rigorous prospective randomised controlled trials of effectiveness. Now more randomised controlled trials that assess their effectiveness have been published, but many trials are too small to draw definitive conclusions, hence the need for the first review.
Our initial review, Ogah 2009, showed evidence of efficacy in the short‐term, as many trials only reported a 12‐month follow‐up. A significant advantage of a Cochrane review is not only the rigorous database search and methodology, but most importantly the ability to update the review and meta‐analysis as new evidence becomes available. This meta‐analysis of the trials available is necessary to help make judgements on medium‐ and longer‐term efficacy, since we now have 18 years‐worth of data since the initial report of the retropubic mid‐urethral tape, and it is over 11 years since the first randomised trials of the tension‐free vaginal tape and transobturator tapes were published. It is also necessary to provide evidence on medium‐ and longer‐term safety of the devices both suspected and expected, and the unexpected adverse events in the long‐term. This review update aims to clarify the uncertainty surrounding the use mid‐urethral slings in terms of surgical approach, route of insertion and the type of tape used.
This current update analyses only the effects of mid‐urethral slings, and excludes both single incision slings and other surgical procedures e.g. traditional slings and colposuspension. The options of no treatment, conservative treatment and pharmacological treatment are also excluded, as this will be addressed in a future Cochrane review.
Objectives
To assess the clinical effects of mid‐urethral sling (MUS) operations for the treatment of stress urinary incontinence (SUI), urodynamic stress incontinence (USI) or mixed urinary incontinence (MUI) in women.
Methods
Criteria for considering studies for this review
Types of studies
Randomised or quasi‐randomised controlled trials amongst women with USI (urodynamic diagnosis), or symptoms of SUI or MUI (clinical diagnosis), in which both trial arms involve a mid‐urethral sling operation.
Types of participants
Adult women with SUI due to hyper‐mobility and intrinsic sphincter deficiency, or both, diagnosed clinically or with urodynamics, and women with MUI in which stress incontinence was the predominant symptom. Classification of diagnoses were accepted as defined by the trialists.
Types of interventions
Both trial arms of a study must involve mid‐urethral sling operations to treat SUI or MUI.
We made the following comparisons.
Transobturator route (TOR) versus retropubic route (RPR).
Retropubic bottom‐to‐top approach versus retropubic top‐to‐bottom approach.
Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach.
One method of mid‐urethral tape insertion versus another method, same route.
One type of tape material versus another
Comparisons with other types of surgery (i.e. traditional slings, single incision slings and colposuspension) for urinary incontinence are covered in other recent Cochrane reviews. The options of no treatment, conservative treatment and pharmacological treatment have also been removed as these will be addressed in a future Cochrane review.
Types of outcome measures
Primary outcomes
We selected the outcome measures used in this review on the basis of their relevance to the clinical cure or improvement of incontinence. We regarded the principal measures of effectiveness as being:
1. Women's observations
the proportion of women cured (continent or dry) following surgery;
the proportion of women whose incontinence is improved;
cure and improvement measured in the short term (less than one year); medium term (one to five years); and long term (more than five years).
Secondary outcomes
2. Women's observations
Urgency symptoms or urgency incontinence.
3. Quantification of symptoms
Pad changes (from self‐reported number of pads used).
Incontinence episodes (from self‐completed bladder chart).
Pad tests of quantified leakage (mean volume or weight of urine loss).
4. Clinician's observations
Objective cure rates in the short term (less than one year); medium term (one to five years); and long term (more than five years).
De novo detrusor overactivity (urodynamic diagnosis).
5. Surgical outcome measures
Duration of operation.
Length of inpatient stay.
Time to return to normal activity level.
Operative blood loss.
6. Adverse events
Major vascular or visceral injury.
Bladder, urethral or bowel perforation.
Nerve damage.
Perioperative surgical complications (e.g. infection, bacteriuria, haemorrhage with or without major vessel lesion).
Voiding dysfunction or difficulty after three months (with or without urodynamic confirmation) or need for long‐term catheterisation.
Infection related to use of synthetic mesh.
Tape erosion or extrusion or exposure into the vagina.
Tape erosion or extrusion or exposure into the bladder or urethra.
7. Need for further treatment
Physiotherapy treatment.
Drug treatment for urinary incontinence or symptoms.
Pelvic organ prolapse (e.g. cystocoele, rectocoele, enterocoele).
Repeat incontinence surgery.
Later prolapse surgery.
8. Quality of life
Quality of life assessed by means of:
general health status measures (e.g. Short Form 36 (Ware 1993));
condition‐specific instruments designed to assess incontinence, e.g. the Bristol Female Lower Urinary Tract Symptoms questionnaire (BFLUTS; Jackson 1996);
condition‐specific sexual function assessment e.g. via Pelvic Organ Prolapse/Urinary Incontinence Sexual Function Questionnaire (PISQ‐12;Rogers 2003);
psychological measures.
9. Other outcomes
Non‐prespecified outcomes judged to be important when performing the review.
Search methods for identification of studies
Unless otherwise stated we did not impose language or other restrictions on any of the searches which are described below.
Electronic searches
This review drew on the search strategy developed for the Cochrane Incontinence Group. We identified relevant trials from the Cochrane Incontinence Group Specialised Trials Register. For more details of the search methods used to build the Specialised Register please see the Group's module in The Cochrane Library. The Register contains trials identified from the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE, and MEDLINE in process, ClinicalTrials.gov and handsearching of journals and conference proceedings. Most of the trials in the Cochrane Incontinence Group Specialised Register are also contained in CENTRAL. The date of the last search was 26 June 2014.
The terms used to search the Incontinence Group Specialised Register are given in Appendix 1.
Additionally the following electronic databases were searched, details of the searches and the terms used are given in Appendix 1.
Embase and Embase Classic (January 1947 to Week 25 2014; searched on 26 June 2014; limited to those years not searched via the CENTRAL search of Embase, i.e. 1 January 2010 to Week 25 2014 inclusive).
WHO ICTRP (searched on 30 June 2014)
Details of the searches performed for the previous version of this review can be found in Appendix 2.
We performed additional searches for the Brief Economic Commentaries (BECs). We conducted them in MEDLINE(1 January 1946 to March 2017), Embase (1 January 1980 to 2017 Week 12) and NHS EED (1st Quarter 2016). We ran all searches on 6 April 2017. Details of the searches run and the search terms used can be found in Appendix 3.
Searching other resources
We searched the reference lists of relevant articles.
Data collection and analysis
Selection of studies
Randomised and quasi‐randomised trials were identified using the above search strategy. We excluded studies from the review if they were not randomised or quasi‐randomised controlled trials for incontinent women, or if they made comparisons other than those pre‐specified. Excluded studies are listed in the Characteristics of excluded studies table along with reasons for their exclusion. We evaluated all potentially eligible studies for appropriateness for inclusion without prior consideration of the results. We retrieved reports of potentially eligible trials in full.
Data extraction and management
We extracted data independently using a standard form containing pre‐specified outcomes. Where data may have been collected but not reported, we sought clarification from the trialists. We processed included trial data as described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We resolved differences of opinion relating to study inclusion, methodological quality or data extraction by discussion among the reviewers, and when necessary, referred them to a third party for arbitration.
Assessment of risk of bias in included studies
Miss Abigail Ford and Mr Joseph Ogah (review authors) extracted data and independently assessed the included trials for methodological quality and validity using the 'Risk of bias' assessment tool (Higgins 2011). We assessed the risk of bias in the results of the included trials by examining the following features: selection bias, which results from insecure random allocation of treatments; performance bias that occurs when knowledge of the procedure actually performed might have affected the participant or care provider; attrition bias caused by incomplete reporting of outcome data, or from dropouts or losses to follow‐up, particularly if there is a differential dropout rate between groups; and biased ascertainment (detection bias) of outcome where knowledge of the allocation might have influenced the measurement of outcome. These were assessed under the headings below:
sequence generation;
allocation sequence concealment;
blinding of participants and personnel;
blinding of outcome assessment;
incomplete outcome data.
These were presented in the 'Risk of bias' tables, graphs and summary figures.
The GRADE (Grades of Recommendation, Assessment, Development and Evaluation) system was used to assess and grade the quality of evidence for each individual outcome (Guyatt 2011a; Guyatt 2011b; Guyatt 2013a; Guyatt 2013b).
Measures of treatment effect
The review was conducted using the standard Cochrane software Review Manager 'Revman' version 5.2 (Reference Manager 2012). For categorical outcomes we related the numbers reporting an outcome to the numbers at risk in each group to derive a summary risk ratio (RR). For continuous variables we used means and standard deviations to derive a mean difference (MD) if the outcomes were measured in the same way between trials. Any continuous data that were the product of a number of different scales (for example, scales used to assess symptoms such as pain or quality of life) we summarised as the standardised mean difference (SMD) using a fixed‐effect model. A fixed‐effect model was used for calculation of all summary estimates and 95% confidence intervals (CIs) except when there was significant heterogeneity. When appropriate, we undertook meta‐analysis.
We undertook a narrative review of eligible trials where statistical synthesis of data from more than one study was not possible, or considered inappropriate.
Unit of analysis issues
We did not perform analysis of trials with non‐standard designs, such as cross‐over trials and cluster‐randomised trials, as there were no such trials. We analysed trials with multiple treatment groups by treating each pair of arms as a separate comparison, as appropriate.
Dealing with missing data
We defined 'intention‐to‐treat analysis' as meaning that all participants were analysed in their randomised groups whether or not they received the allocated intervention. We included data as they were reported for each outcome and did not impute missing values, but used the data as presented by the trialists. Where intraoperative outcomes were reported, we used the number of patients undergoing the described procedure as the denominator. Follow‐up outcomes were reported with the exclusion of patients lost to follow‐up. We would have performed sensitivity analyses had there been differential dropout from the randomised groups, or another reason to suspect systematic bias from missing data.
Assessment of heterogeneity
We used a fixed‐effect approach for the analysis unless there was evidence of heterogeneity across trials. Differences between trials were investigated when apparent either through visual inspection of the results, or when statistically significant heterogeneity was demonstrated by using the Chi² test at the 10% probability level or assessment of the I² statistic (Higgins 2003).
Assessment of reporting biases
We examined publication bias by means of a funnel plot where there were 10 or more trials contributing to a meta‐analysis.
Data synthesis
We used fixed‐effect model analysis for the meta‐analyses, except when significant heterogeneity was suspected, when we used a random‐effects model.
Subgroup analysis and investigation of heterogeneity
Heterogeneity
Where there was no obvious reason for heterogeneity to exist (after consideration of populations, interventions, outcomes and settings of the individual trials), or it persisted despite the removal of trials that were clearly different from the others, we used a random‐effects model.
Subgroup analysis
Clinical factors such as symptoms of SUI, USI, MUI, diagnosis of intrinsic urethral sphincter deficiency or urethral hypermobility, obesity, previous incontinence surgery, presence or absence of prolapse, anaesthesia used, or experience of the surgeon and other concomitant surgical intervention, might all influence the outcomes of surgery and consideration of subgroup analysis was taken into account.
Sensitivity analysis
We performed sensitivity analysis to explore the robustness of the results in some outcomes. We planned to carry out sensitivity analysis for the primary outcomes by restricting our analysis to trials assessed as having a low risk of bias for the of domain attrition bias; if more than 30% of participants had been lost to follow‐up, these trials would have been excluded from sensitivity analyses. This was not necessary.
Summary of findings
We employed the GRADE approach to interpret findings (Guyatt 2011a; Guyatt 2011b; Guyatt 2013a; Guyatt 2013b; Langendam 2013), and the GRADE profiler (GRADEpro) was used to import data from RevMan 5.2 to create 'Summary of findings’ tables. These tables provide outcome‐specific information concerning the overall quality of evidence from trials included in a comparison, the magnitude of effect of the interventions examined, and the sum of the available data on the outcomes we considered.
We included the following outcomes in the 'Summary of findings’ tables.
Subjective cure: medium term (one to five years).
Subjective cure: long term (more than 5 years).
Bladder or urethral perforation.
Voiding dysfunction: short term and medium term (up to five years).
De novo urgency or urgency incontinence: short term (less than one year).
Vaginal tape erosion: short term and medium term (up to five years).
Repeat continence surgery: short term (less than one year).
Repeat continence surgery: long term (more than five years).
Groin pain: short term (less than one year).
Quality of life.
We assessed the overall quality of evidence for these outcomes and downgraded the evidence level from high quality by one level for serious, or by two levels for very serious study limitations (risk of bias), indirectness of evidence, serious inconsistency, imprecision of effect estimates or potential publication bias.
Results
Description of studies
Results of the search
We screened the 841 records identified by the literature searches and obtained a total of 290 full‐text articles for further assessment. Altogether 217 reports concerning 81 randomised trials met the inclusion criteria. A further two trials were ongoing.
We excluded 551 records on the basis of either the title or abstract alone, and 71 reports relating to 62 studies after retrieval of the full text publication. Exclusion was either because they were not randomised trials, they did not include a mid‐urethral sling operation, or because the women included in the trial were not urinary incontinent. A full description of these trials can be found in the Characteristics of excluded studies section of this review. The flow of literature through the assessment process is shown in Figure 1.
1.
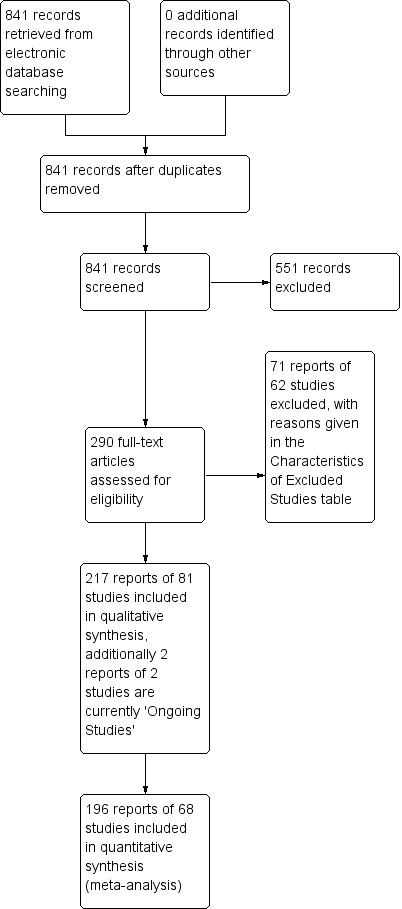
PRISMA study flow diagram
We analysed trials with multiple treatment groups by treating each pair of arms as a separate comparison, as appropriate. There were six trials in this review that supplied data and for which this method was employed, thus leading to 87 comparisons. There were no trials with non‐standard designs, such as cross‐over trials and cluster‐randomised trials.
Included studies
Further characteristics of the trials are reported in the Characteristics of included studies table.
Comparisons and interventions
1. Transobturator (TOR) versus retropubic route (RPR)
This comparison of mid‐urethral sling operations was based on the routes that the tapes traverse, i.e. transobturator route (TOR) versus retropubic route (RPR). There were 55 trials that investigated this (Aigmuller 2014; Alkady 2009; Andonian 2007; Aniuliene 2009; Araco 2008; Barber 2008; Barry 2008; Cervigni 2006; Chen 2010; Chen 2012; Choe 2013; Darabi Mahboub 2012; David‐Montefiore 2006; Deffieux 2010; de Tayrac 2004; Diab 2012; El‐Hefnawy 2010; Enzelsberger 2005; Freeman 2011; Hammoud 2011; Jakimiuk 2012; Kamel 2009; Karateke 2009; Kilic 2007; Kim 2005; Krofta 2010; Laurikainen 2007; Leanza 2009; Lee 2007; Liapis 2006; Mansoor 2003; Mehdiyev 2010; Meschia 2007; Nerli 2009; Nyyssonen 2014; Oliveira 2006; Palomba 2008; Porena 2007; Rechberger 2009; Richter 2010; Riva 2006; Ross 2009; Salem 2014; Scheiner 2012; Schierlitz 2008; Tanuri 2010; Tarcan 2011; Teo 2011; van Leijsen 2013; Wang 2006; Wang 2008; Wang 2009; Wang 2010; Wang 2011; Zullo 2007).
2. Retropubic bottom‐to‐top approach versus retropubic top‐to‐bottom approach
Trials in this group compared the retropubic bottom‐to‐top approach (e.g. tension‐free vaginal tape (TVTTM); tape inserted from the vagina through the retropubic space and exiting onto the abdominal skin in the suprapubic region) with a retropubic top‐to‐bottom approach (e.g. suprapubic urethral support sling (SPARCTM); tape inserted from the abdomen in the suprapubic region through the retropubic space and exiting in the vagina). There were five such trials (Andonian 2005; Kim 2004; Lim 2005; Lord 2006; Tseng 2005).
3. Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach
Ten trials reported on this comparison which compared tapes traversing the obturator route: obturator lateral‐to‐medial approach, (e.g. TOTTM tape inserted in the thigh crease and through the obturator route exiting in the vagina) with obturator medial‐to‐lateral approach (e.g. TVT‐OTM tape inserted in the vagina and through the obturator route exiting in the thigh crease; Abdel‐Fattah 2010; But 2008; Chen 2010; Hassan 2013; Houwert 2009; Lee 2008; Liapis 2008; Park 2012; Peattie 2006; Scheiner 2012).
4. One method of mid‐urethral tape insertion versus another method, same route
Ten trials compared different methods of carrying out operations using the same route (Cho 2010; de Leval 2011; Elbadry 2014; Juang 2007; Naumann 2006; Paparella 2010; Rechberger 2011; Tommaselli 2012; Ugurlucan 2013; Zhang 2011).
The trials compared the following operations.
Transobturator lateral to medial
Monarc® TOT versus TOT® (Cho 2010).
TOT versus adjustable TOT (Elbadry 2014).
TOT versus TOT with two‐point fixation sutures (Rechberger 2011).
Synthetic TOT versus biological TOT (Paparella 2010; Ugurlucan 2013).
Transobturator medial to lateral
TVT‐O versus modified TVT‐O (shorter tape and less lateral dissection; de Leval 2011).
TVT‐O versus TVT‐O plus Ingleman‐Sundberg bladder denervation procedure (Juang 2007).
TVT‐O versus modified TVT‐O (reduced dissection; Tommaselli 2012).
TVT‐O versus modified TVT‐O (self‐tailored mesh; Zhang 2011).
Retropubic
TVT versus modified TVT, bottom‐to‐top (suburethral pad; Naumann 2006).
5. One type of tape material versus another
A final group compared different mid‐urethral sling operations based on the properties of the tape material. All used synthetic non‐absorbable mesh for the tape material, but differed in the structure of the material, i.e. monofilament tapes versus multifilament tapes. There were four such trials (Lim 2005; Meschia 2006; Okulu 2013; Rechberger 2003), which made the following comparisons.
Monofilament (TVT SPARC) verus multifilament (IVS; Lim 2005).
Monofilament (TVT) versus multifilament (IVS; Meschia 2006).
Synthetic monofilament (prolene light mesh) versus a combined synthetic mesh coated with a biological film (Ultrapro mesh) versus a multifilament mesh (Vypro; Okulu 2013).
Monofilament (TVT) versus multifilament (IVS; Rechberger 2003).
Publication type and sample characteristics
1. Retropubic route versus transobturator route
The sample sizes ranged from 20 to 597; with a median of 131.
Twelve of the 55 trials were reported only as abstracts (Cervigni 2006; Choe 2013; Darabi Mahboub 2012; Diab 2012; Hammoud 2011; Kamel 2009; Leanza 2009; Mansoor 2003; Oliveira 2006; Riva 2006; Salem 2014; Tarcan 2011).
Inclusion and exclusion criteria were not clearly stated in eight trials (Cervigni 2006; Chen 2010; Darabi Mahboub 2012; Kamel 2009; Mansoor 2003; Mehdiyev 2010; Oliveira 2006; Tarcan 2011).
All trials had women either presenting with SUI or had USI confirmed. In addition other characteristics included:
23 trials included women with MUI (Alkady 2009; Aigmuller 2014; Andonian 2007; Barber 2008; Barry 2008; Cervigni 2006; David‐Montefiore 2006; Deffieux 2010; El‐Hefnawy 2010; Freeman 2011; Kim 2005; Krofta 2010; Laurikainen 2007; Lee 2007; Nerli 2009; Nyyssonen 2014; Porena 2007; Richter 2010; Riva 2006; Scheiner 2012; Tarcan 2011; van Leijsen 2013; Wang 2011).
ten trials included women with previous incontinence surgery (Andonian 2007; Aniuliene 2009; Barber 2008; Barry 2008; David‐Montefiore 2006; de Tayrac 2004; Kim 2005; Lee 2007; Richter 2010; Wang 2010).
28 trials included women with pelvic organ prolapse (POP; Alkady 2009; Andonian 2007; Aniuliene 2009; Barber 2008; Barry 2008; Cervigni 2006; Chen 2012; David‐Montefiore 2006; El‐Hefnawy 2010; Freeman 2011; Krofta 2010; Laurikainen 2007; Mansoor 2003; Meschia 2007; Nerli 2009; Porena 2007; Rechberger 2009; Richter 2010; Riva 2006; Scheiner 2012; Schierlitz 2008; Tanuri 2010; Tarcan 2011; van Leijsen 2013; Wang 2006; Wang 2008; Wang 2009; Wang 2010).
in 13 trials women had concomitant pelvic or prolapse surgery (Andonian 2007; Barber 2008; Barry 2008; Cervigni 2006; David‐Montefiore 2006; Richter 2010; Riva 2006; Scheiner 2012; Schierlitz 2008; Tarcan 2011; Wang 2008; Wang 2009; Wang 2010).
Follow‐up for women ranged from one month to five years with a median follow‐up of 12 months.
2. Retropubic bottom‐to‐top approach versus retropubic top‐to‐bottom approach
Five trials investigated a retropubic bottom‐to‐top approach versus a retropubic top‐to‐bottom approach (Andonian 2005; Kim 2004; Lim 2005; Lord 2006; Tseng 2005). One of the five trials was reported only as an abstract (Kim 2004), and this was the only study without clear inclusion and exclusion criteria.
The sample sizes ranged from 62 to 304; the average sample size, 'n' (standard deviation), for retropubic in‐out was 62 (49) and for retropubic out‐in was 64 (53).
All trials had women either presenting with SUI or had USI confirmed. All trials except Tseng 2005 included women with MUI. Andonian 2005 and Lord 2006 included women with previous incontinence surgery.
All the trials included women with POP and had concomitant pelvic or POP surgery performed.
Follow‐up for women ranged from 1.5 months to 2 years with a median of 12 months.
3. Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach
Nine trials compared the obturator medial‐to‐lateral approach with the obturator lateral‐to‐medial approach (Abdel‐Fattah 2010; But 2008; Chen 2010; Hassan 2013; Houwert 2009; Lee 2008; Liapis 2008; Park 2012; Scheiner 2012). With the exception of Hassan 2013, which was reported only as an abstract, the other eight trials were reported as full articles. Peattie 2006 appears in a trials registry but its status is unclear; we have contacted the authors and are awaiting a response.
The sample sizes ranged from 74 to 341 with a median size of 110.
Inclusion and exclusion criteria were not clearly stated in two trials (But 2008; Hassan 2013).
All trials had women either presenting with SUI or had USI confirmed.
Five trials included women with MUI (Abdel‐Fattah 2010; But 2008; Lee 2008; Park 2012; Scheiner 2012), and two trials included women who had undergone previous incontinence surgery (Abdel‐Fattah 2010; Scheiner 2012). Scheiner 2012 included women with POP and women with concomitant pelvic or POP surgery.
Follow‐up ranged from three months to three years with a median follow up of 12 months.
4. One method of mid‐urethral tape insertion versus another method, same route
Ten trials investigated one method of mid‐urethral tape versus another method, using the same route (Cho 2010; de Leval 2011; Elbadry 2014; Juang 2007; Naumann 2006; Paparella 2010; Rechberger 2011; Tommaselli 2012; Ugurlucan 2013; Zhang 2011). Three of these trials were reported only as abstract publications (Cho 2010; Elbadry 2014; Naumann 2006). The sample sizes ranged from 72 to 463 with a median of 156.
All the trials included women with SUI or USI. Rechberger 2011 reported women with ISD. Inclusion and exclusion criteria were not clearly defined in four of the ten trials (Cho 2010; Elbadry 2014; Juang 2007; Naumann 2006). Juang 2007, Tommaselli 2012 and Ugurlucan 2013 included women with MUI, whilst de Leval 2011 and Ugurlucan 2013 included women who had undergone previous incontinence surgery. Women with prolapse were included in de Leval 2011 and Ugurlucan 2013, but concomitant POP surgery was performed only in Ugurlucan 2013.
Follow‐up ranged from three months to three years.
5. One type of tape material versus another
Four trials investigated the use of monofilament tape versus multifilament tape (Lim 2005; Meschia 2006; Okulu 2013; Rechberger 2003). All four trials were reported as full article publications.
The sample sizes ranged from 70 to 182 with a median value of 144.
The trials had women either presenting with SUI or had USI confirmed: all had clear inclusion and exclusion criteria. Three trials included women with POP (Lim 2005; Meschia 2006; Rechberger 2003). Two trials included women with MUI (Lim 2005; Meschia 2006). Three trials included women with previous incontinence surgery (Lim 2005; Okulu 2013; Rechberger 2003), whereas only Lim 2005 included women who had concomitant pelvic or POP surgery.
Follow‐up for women ranged from three months to three years.
Outcomes
The trials reported their outcomes in a variety of different ways. The primary outcome, subjective cure of urinary incontinence (UI), was defined as follows:
no subjective report of UI (Aniuliene 2009; Barber 2008; But 2008; Cho 2010; Darabi Mahboub 2012; de Leval 2011; de Tayrac 2004; Deffieux 2010; El‐Hefnawy 2010; Freeman 2011; Hassan 2013; Houwert 2009; Jakimiuk 2012; Kim 2004; Laurikainen 2007; Leanza 2009; Liapis 2006; Lim 2005; Lord 2006; Mansoor 2003; Naumann 2006; Nerli 2009; Okulu 2013; Paparella 2010; Porena 2007; Richter 2010; Riva 2006; Scheiner 2012; Schierlitz 2008; Tanuri 2010; Tarcan 2011; Ugurlucan 2013; van Leijsen 2013; Wang 2010; Wang 2011; Zhang 2011);
no subjective report of UI and negative stress test (Lee 2007; Meschia 2006; Meschia 2007; Park 2012; Rechberger 2003; Rechberger 2009; Wang 2008);
no or improved subjective report of UI (Abdel‐Fattah 2010; Aigmuller 2014; Barry 2008; Karateke 2009; Ross 2009; Teo 2011; Zullo 2007).
Secondary outcome objective cure was defined by the trialists as follows:
absence of USI on urodynamics (UDS) (Abdel‐Fattah 2010; Araco 2008; Barry 2008; Cervigni 2006; Enzelsberger 2005; Kamel 2009; Karateke 2009; Kilic 2007; Kim 2005; Krofta 2010; Lim 2005; Riva 2006; Schierlitz 2008; Zullo 2007);
absence of SUI and negative stress test (Alkady 2009; Paparella 2010; Porena 2007);
one‐hour pad test less than 2 g (Andonian 2005; Andonian 2007; But 2008; Ross 2009; Tseng 2005);
24‐hour pad test less than 5 g (Darabi Mahboub 2012; Okulu 2013; Teo 2011);
negative stress test (Aigmuller 2014; Aniuliene 2009; Barber 2008; Chen 2010; David‐Montefiore 2006; de Leval 2011; de Tayrac 2004; Deffieux 2010; El‐Hefnawy 2010; Juang 2007; Kim 2004; Kim 2005; Laurikainen 2007; Lord 2006; Meschia 2007; Nerli 2009; Tarcan 2011; van Leijsen 2013; Wang 2009; Wang 2011);
multiple objective measures used (El‐Hefnawy 2010; Juang 2007; Kamel 2009; Kim 2005; Krofta 2010; Liapis 2006; Liapis 2008; Mansoor 2003; Meschia 2006; Naumann 2006; Nyyssonen 2014; Oliveira 2006; Rechberger 2011; Richter 2010; Scheiner 2012; Tanuri 2010; Tommaselli 2012; Wang 2006; Wang 2008; Wang 2010).
Excluded studies
We excluded 62 studies after retrieval of the full text publication because they were not randomised trials, did not include a mid‐urethral sling operation, the participants did not have urinary incontinence, or the participants were randomised to an intervention other than a mid‐urethral sling (such as no treatment, pelvic floor muscle training, drugs, or a different class of surgery). The details of the reasons for exclusion are given in the Characteristics of excluded studies table.
Ongoing trials
There are two ongoing trials: Cavkaytar 2013 and Sung 2013.
Cavkaytar 2013 is a randomised controlled trial (RCT) comparing RPR and TOR for the treatment of SUI in women with no intrinsic sphincter deficiency. This study is currently recruiting and includes women with SUI and excludes women with MUI or detrusor overactivity (DO), previous incontinence surgery, and women with a body mass index greater than 35. Fifty women have been randomly assigned into each arm for evaluation.
Sung 2013 is an RCT comparing mid‐urethral sling operations and behavioural or pelvic floor therapy in combination versus suburethral sling operations alone for women with MUI. The ESTEEM trial includes women over 18 years of age who have had urodynamic investigation within the last 18 months, and excludes women with prolapse, previous incontinence surgery, and women currently on antimuscarinic medication. This trial is currently recruiting participants.
Studies awaiting classification
There are no studies awaiting classification.
New trials included in this update
We have included 48 new trials in this update (Abdel‐Fattah 2010; Aigmuller 2014; Alkady 2009; Andonian 2007; Aniuliene 2009; Chen 2010; Chen 2012; Cho 2010; Choe 2013; Darabi Mahboub 2012; de Leval 2011; Diab 2012; Elbadry 2014; El‐Hefnawy 2010; Freeman 2011; Hassan 2013; Hammoud 2011; Jakimiuk 2012; Juang 2007; Kamel 2009; Karateke 2009; Kilic 2007; Krofta 2010; Leanza 2009; Mehdiyev 2010; Naumann 2006; Nerli 2009; Nyyssonen 2014; Okulu 2013; Palomba 2008; Paparella 2010; Park 2012; Peattie 2006; Rechberger 2011; Richter 2010; Ross 2009; Salem 2014; Scheiner 2012; Tanuri 2010; Tarcan 2011; Teo 2011; Tommaselli 2012; Ugurlucan 2013; van Leijsen 2013; Wang 2008; Wang 2010; Wang 2011; Zhang 2011).
Previously included trials with new outcome data
We have included new data from 11 trials previously included in this review, including the report of medium‐ or long‐term outcomes (Barber 2008; But 2008; David‐Montefiore 2006; Deffieux 2010; Houwert 2009; Laurikainen 2007; Porena 2007; Rechberger 2009; Schierlitz 2008; Wang 2009; Zullo 2007).
Previously included trials with no new outcome data
Twenty‐two trials included in the earlier version of this review have not published new outcome data (Andonian 2005; Araco 2008; Barry 2008; Cervigni 2006; de Tayrac 2004; Enzelsberger 2005; Kim 2004; Kim 2005; Lee 2007; Lee 2008; Liapis 2006; Liapis 2008; Lim 2005; Lord 2006; Mansoor 2003; Meschia 2006; Meschia 2007; Oliveira 2006; Rechberger 2003; Riva 2006; Tseng 2005; Wang 2006).
Risk of bias in included studies
Details of the criteria used to assess the risk of bias and the ratings for each study are reported in the 'Risk of bias' tables that accompany the Characteristics of included studies. Further information on the risk of bias in included trials is shown in Figure 2 the 'Risk of bias' graph and Figure 3 the ‘Risk of bias' summary.
2.
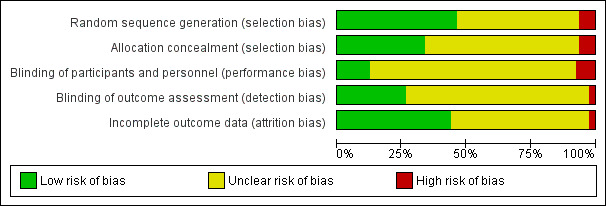
Risk of bias graph: review authors' judgments about each risk of bias item presented as percentages across all included studies.
3.
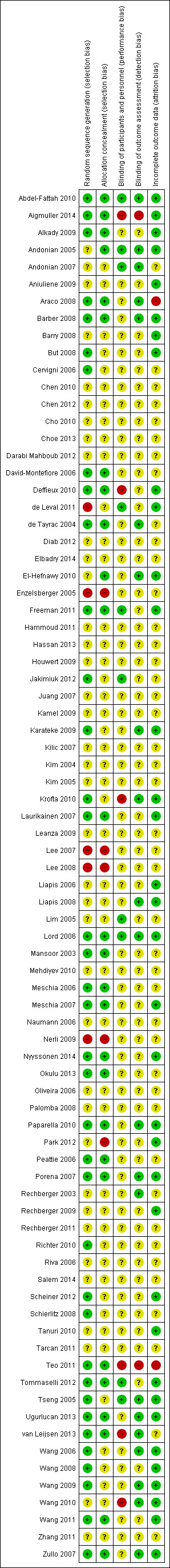
Risk of bias summary: review authors' judgments about each risk of bias item for each included study.
The risk of bias in the trials included was variable, though overall only few trials were judged to be at high risk of bias. In over 50% of trials the random sequence generation was judged to be adequate, for example with the use of a computer‐generated list or a table of random numbers. Approximately 30% of trials confirmed that secure concealment of the randomisation process was used, for example allocation by a remote person or the use of sealed envelopes.
Blinding of participants was unclear in the majority of trials. This is an obvious limitation with trials comparing surgical interventions, though one trial described the use of a 'sham' procedure (Jakimiuk 2012). Blinding of patients and the post‐operative reviewer was not reported in most trials. Loss to follow‐up in most trials was minimal, and in approximately 50% of included trials the risk of attrition bias was judged to be low.
We judged that 39 trials had adequate random sequence generation (Abdel‐Fattah 2010; Aigmuller 2014; Alkady 2009; Andonian 2005; Araco 2008; Barber 2008; But 2008; Cervigni 2006; Chen 2012; David‐Montefiore 2006; Deffieux 2010; de Tayrac 2004; Freeman 2011; Jakimiuk 2012; Karateke 2009; Krofta 2010; Laurikainen 2007; Lord 2006; Mansoor 2003; Meschia 2006; Meschia 2007; Nyyssonen 2014; Okulu 2013; Paparella 2010; Porena 2007; Richter 2010; Ross 2009; Scheiner 2012; Schierlitz 2008; Teo 2011; Tommaselli 2012; Tseng 2005; Ugurlucan 2013; van Leijsen 2013; Wang 2006; Wang 2008; Wang 2009; Wang 2011; Zullo 2007).
We judged that adequate allocation concealment occurred in 26 trials (Abdel‐Fattah 2010; Aigmuller 2014; Alkady 2009; Andonian 2005; Araco 2008; Barber 2008; David‐Montefiore 2006; Deffieux 2010; de Tayrac 2004; El‐Hefnawy 2010; Freeman 2011; Laurikainen 2007; Lord 2006; Mansoor 2003; Meschia 2006; Meschia 2007; Nyyssonen 2014; Okulu 2013; Paparella 2010; Porena 2007; Ross 2009; Teo 2011; Tommaselli 2012; van Leijsen 2013; Wang 2011; Zullo 2007).
We judged that 24 trials had an adequate randomisation process and secure concealment of the randomisation process (Aigmuller 2014; Alkady 2009; Andonian 2005; Araco 2008; Barber 2008; David‐Montefiore 2006; Deffieux 2010; de Tayrac 2004; Freeman 2011; Laurikainen 2007; Lord 2006; Mansoor 2003; Meschia 2006; Meschia 2007; Nyyssonen 2014; Okulu 2013; Paparella 2010; Porena 2007; Ross 2009; Teo 2011; Tommaselli 2012; van Leijsen 2013; Wang 2011; Zullo 2007).
We judged that 22 trials adequately blinded outcome assessors (Abdel‐Fattah 2010; Andonian 2005; Andonian 2007; Araco 2008; Barber 2008; de Tayrac 2004; El‐Hefnawy 2010; Karateke 2009; Krofta 2010; Liapis 2006; Liapis 2008; Lord 2006; Paparella 2010; Porena 2007; Rechberger 2003; Tseng 2005; Ugurlucan 2013; van Leijsen 2013; Wang 2006; Wang 2009; Wang 2010; Zullo 2007).
We judged 36 trials to be at a low risk of attrition bias (Abdel‐Fattah 2010; Aigmuller 2014; Alkady 2009; Andonian 2005; Aniuliene 2009; Barber 2008; Barry 2008; But 2008; Deffieux 2010; de Leval 2011; El‐Hefnawy 2010; Freeman 2011; Karateke 2009; Krofta 2010; Laurikainen 2007; Liapis 2006; Liapis 2008; Lord 2006; Meschia 2007; Nyyssonen 2014; Paparella 2010; Park 2012; Porena 2007; Rechberger 2009; Ross 2009; Scheiner 2012; Tanuri 2010; Tommaselli 2012; Tseng 2005; Ugurlucan 2013; Wang 2006; Wang 2008; Wang 2009; Wang 2010; Wang 2011; Zullo 2007).
Effects of interventions
See: Table 1; Table 2; Table 3; Table 4
The results of all the included studies can be found in Table 5.
1. Tabulated Results of Included Studies.
| Study | Outcome data |
| Abdel‐Fattah 2010 | Group A: TVT‐O (n = 170) Group B: TOT (n = 171) Loss to follow up at 1yr: A: 18/170, B: 24/171 Loss to follow up at 3yrs: A: 44/170, B: 59/171 Objective cure: A: 114/121, B: 96/109 Subjective success: A: 121/149, B: 111/143 Bladder/urethral perforation: A: 1/170, B: 2/171 Voiding dysfunction: A: 12/170, B: 9/171 Tape erosion: A: 3/153, B: 5/149 Groin pain: A: 27/150, B: 19/147 Repeat continence surgery: A: 7/170, B: 15/171 QoL assessed via: King’s Health Questionnaire (KHQ) [10], Birmingham Bowel Urinary Symptom (BBUSQ‐22) [11] and Pelvic Organ Prolapse/Incontinence Sexual Function Questionnaire (PISQ‐12). In addition Patient Global Impression of Improvement (PGI‐I) [13] and International Consultation on Incontinence Questionnaire‐ Short form (ICIQ‐SF) [14] questionnaires. QOL scores were much improve following surgery with no significant inter group (A vs B) differences. Sexual dysfunction: PISQ‐12 employed. 199 patients completed this assessment and in most domains a significant improvement in postoperative PISQ‐12 scores was found with no significant difference demonstrated between the two groups. Intermediate (3 yr) Subjective success (very much & much improved) on PGI‐I: A: 93/126, B: 81/112 |
| Aigmuller 2014 | Group A: TVT: (n = 285; 38 of whom were lost to follow‐up) Group B: TVT‐O: (n = 269; 36 of whom were lost to follow‐up) Participants were evaluated at 3 months, with a further evaluation scheduled at 5 years
At 5‐year review:
|
| Alkady 2009 | Group A: TVT (n = 15) Group B: TVT‐O (n = 15)
|
| Andonian 2005 | Group A: SPARC Group B: TVT
|
| Andonian 2007 | Group A: Obtape (n = 78) Group B: DUPS (n = 32) ‐ suspended Group C: TVT (n = 80)
|
| Aniuliene 2009 | Group A: TVT‐O (n = 150) Group B: TVT (n = 114)
|
| Araco 2008 | Group A: TVT‐O (n = 120)
Group B: TVT (n = 120)
|
| Barber 2008 | Group A: TVT (n = 88) Group B: TOT (n = 82)
|
| Barry 2008 | Group A: TOT (n = 58)
Group B: TVT (n = 82)
|
| But 2008 | Group A: TVT‐O (n = 60) Group B: TOT (n = 60)
|
| Cervigni 2006 | Numbers in each group unreported. It was, thus, impossible to abstract results |
| Chen 2010 | Group A: TVT (n = 77) Group B: TOT (n = 45) Group C: TVT‐O (n = 65)
|
| Chen 2012 | A: TVT (n = 102) B: TVT‐O (n = 103)
|
| Cho 2010 | Group A: Monarc TOT (n = 48) Group B: TOT (n = 45)
|
| Choe 2013 | We were not able to use the data provided, as the number in each group was not specified |
| Darabi Mahboub 2012 | Group A: TOT (n = 40) Group B: TVT (n = 40) Operative time (minutes (SD): A: 64.50 (9.04), B: 64.00 (9.48) Mean hospital stay (days): A: 2.56 (0.51), B: 2.52 (0.47) |
| David‐Montefiore 2006 | Group A: RPR (n = 42) Group B: TOR (n = 46)
|
| de Leval 2011 | Group A: TVT‐O (n = 87) Group B: modified TVT‐O (n = 88)
At 3‐year follow‐up:
|
| de Tayrac 2004 | Group: A: TOT (n = 30) Group: B: TVT (n = 31)
|
| Deffieux 2010 | Group A: TVT (n = 75) Group B: TVT‐O (n = 74)
|
| Diab 2012 | Group A: TOT (n = 31) Group B: TVT (n = 32)
All the preoperative parameters were comparable in both groups. The mean operative time was significantly longer and bladder injury was significantly higher in the TVT group. There were no significant difference in cure rates, voiding dysfunction, de novo urgency and reoperation rate. The postoperative groin/thigh pain was higher in the TOT group. |
| El‐Hefnway 2010 | Preliminary results: Group A: TVT: (n = 19) Group B: TOT: (n = 21) At 24 months: Group A: TVT: (n = 45) Group B: TOT: (n = 42)
|
| Elbadry 2014 | Group A: adjustable TOT (n = 48) Group B: TOT: (n = 48)
|
| Enzelsberger 2005 | Group A: TOT (n = 56) Group B: TVT (n = 54)
|
| Freeman 2011 | Group A: Monarc TOT (n = 100) Group B: Gynaecare TVT (n = 92)
|
| Hammoud 2011 | Group A: TVT (n = 60) Group B: TVT‐O (n = 50) Subjective cure: A: 56/60, B: 48/50 |
| Hassan 2013 | Group A: inside‐out TOT (n = 125) Group B: outside‐in TOT (n = 125)
|
| Houwert 2009 | Group A: TVT‐O (n = 93) Group B: Monarc TOT (n = 98)
|
| Jakimiuk 2012 | Group A: TVT (n = 19) Group B: TVT‐O (n = 16)
|
| Juang 2007 | Group A: TVT‐O (n = 47) Group B: TVT‐O plus IS: (n = 49)
|
| Kamel 2009 | A: TVT (n = 60) B: TVT‐O (n = 60)
|
| Karateke 2009 | Group A: TVT (n = 83) Group B: TVT‐O (n = 84)
|
| Kilic 2007 | Group A: TVT (n = 10) Group B: TOT (n = 10)
|
| Kim 2004 | Group A: TVT (n = 32) Group B: SPARC (n = 30) Group C: IRIS (n = 34).
|
| Kim 2005 | Group A: Monarc (n = 65) Group B: SPARC (n = 65)
|
| Krofta 2010 | Group A: TVTTM (n = 149) Group B: TVT –OTM (n = 151)
|
| Laurikainen 2007 | Group A: TVT‐O (n = 131)
Group B: TVT (n = 136)
QoL: The scores of the condition specific quality of life questionnaires were significantly lower at the 3 and 5 year follow up compared with pre‐operative scores. This improvements were statistically significant, but with no difference between the groups. 84% of women with pre‐operative moderate and severe frequency and urgency symptoms were cured of these symptoms at the 5 year follow up. |
| Leanza 2009 | Group A: r‐TICT (n = 229; retropubic) Group B: t‐TICT (n = 220; transobturator) Subjective cure: A: 190/215, B: 178/208 |
| Lee 2007 | Group A: TVT (n = 60) Group B: TVT‐O (n = 60)
|
| Lee 2008 | Group A: TVT‐O (n = 50) Group B: TOT (n = 50)
|
| Liapis 2006 | Group A: TVT (n = 46) Group B: TVT‐O (n = 43)
|
| Liapis 2008 | Group A: TVT‐O (n = 61) Group B: Monarc TOT (n = 53)
|
| Lim 2005 | Group A: TVT (n = 61) Group B: IVS (n = 60) Group C: SPARC (n = 61)
|
| Lord 2006 | Group A: TVT (n = 147)
Group B: SPARC (n = 154)
|
| Mansoor 2003 | Group A: TVT‐O (n = 48)
Group B: TVT (n = 54)
|
| Mehdiyev 2010 | A: TOT (n = 17) B: TVT (n = 15)
|
| Meschia 2006 | Group A: TVT (n = 92)
Group B: IVS (n = 87)
|
| Meschia 2007 | Group A: TVT‐O (n = 117) Group B: TVT (n = 114)
|
| Naumann 2006 | Group A: TVT (n = 123) Group B: LIFT (n = 125)
|
| Nerli 2009 | Group A: TVT (n = 18) Group B: TOT (n = 18)
|
| Nyyssonen 2014 | Group A: TOT (n = 50) Group B: TVT (n = 50)
|
| Okulu 2013 | Group A: Vypro mesh: (n = 48; multifilament) Group B: Ultrapro mesh: (n = 48; monofilament + biological combined mesh) Group C: Prolene light mesh: (n = 48; monofilament)
|
| Oliveira 2006 | Group A: TVT (n = 17)
Group B: TVT‐O (n = 28)
|
| Palomba 2008 | Trial terminated. |
| Paparella 2010 | Group A: synthetic UretexTO® (n = 34) Group B: biological PelviLaceTO® (n‐36)
|
| Park 2012 | Group A: TVT‐O (n = 39) Group B: TOT Monarc (n = 35)
|
| Peattie 2006 | No published data. |
| Porena 2007 | Group A: TVT (n = 70) Group B: TOT (n = 75)
|
| Rechberger 2003 | Group A: TVT (n = 50) Group B: IVS (n = 50)
|
| Rechberger 2009 | Group A: retropubic (IVS‐02; n = 269) Group B: transobturator (IVS‐04; n = 268)
|
| Rechberger 2011 | Group A: TOT (n = 232) Group B: TOT with fixation (n = 231)
|
| Richter 2010 | Group A: retropubic sling (TVT; n = 298) Group B: transobturator tapes (TVT‐O, and TOT Monarc; n = 299) (Group C (?): TVT‐O (inside‐out) ‐ separate data not provided) (Group D (?): TOT (Monarch, outside‐in) ‐ separate data not provided) Objective cure at 1 year: A: 232/280 (80.8%), B: 233/285 (77.7%) Subjective cure at 1 year: A: 181/280 (62.2%), B: 163/285 (55.8%) Secondary outcomes:
PISQ‐12 (Prolapse / urinary incontinence sexual questionnaire): Analysis of results for group A and group B combined showed significant improvement in sexual function in both groups with a mean PISQ‐12 score increase from 32.8+/‐7.1 at baseline to 37.3+/‐ 6 at 24 months. These changes are >0.6 SD units, which reflects “medium” improvement in the PISQ‐12 score after surgery. Compared with women with successful surgery, women who experienced surgical failure, regardless of assigned type of surgery, reported worse adjusted sexual function scores at all postoperative time points. Improvement in PISQ‐12 scores was consistent with change in the 3 specific items from the sexual function measure of interest: (1) the experience of pain during sexual activity, (2) UI during sexual activity, and (3) fear of incontinence during sexual activities. Pain with intercourse was reported by 153 of 406 of sexually active women (38%) at baseline and decreased to 27% at 12 months after surgery (P.003). Self‐reported UI and the fear of incontinence occurring during sexual activity also significantly improved by 12 months after surgery, regardless of sling route. To specifically investigate the association of synthetic mesh slings on dyspareunia, we repeated the analysis on the 247 women who underwent MUS only (no concurrent procedures) and who completed baseline and 12‐month assessments. In this subset of women, dyspareunia decreased from 57% at baseline to 43% at 12 months after surgery (P .03). 5‐year data provided, but without numbers in each group, so could not be used for meta‐analysis |
| Riva 2006 | Group A: TOT (n = 65) Group B: TVT (n = 66) |
| Salem 2014 | Group A: TOT (n = 37) Group B: TVT (n = 39) No significant difference was noticed between the two groups as regard the mean operative time, perioperative complications, intraoperative blood loss, hospital stay, and time to return to normal activities. The mean of abdominal leak point pressure and urethral closure pressure showed marked and maintained improvement for 5 years later in group I whereas in group II, they showed marked and maintained improvement for only one year then shows significant decline in comparison with group I. As regard the mean of objective SEAPI score shows marked decrease (improvement) in both groups and this was maintained for the five years in group I but in group II, it increased after one year later. No usable data provided. |
| Scheiner 2012 | Group A: TVT (n = 80) Group B: TOT outside‐in approach (Monarc; n = 40) Group C: TVT‐O inside‐out approach (Gynecare; n = 40)
|
| Schierlitz 2008 | Group A: TVT (n = 81) Group B: Monarc sling (n = 82)
|
| Tanuri 2010 | Group A: Safyre VS retropubic tape (n = 10) Group B: Safyre T transobturator tape (n = 20)
|
| Tarcan 2011 | Group A: TVT (n = 27) Group B: TOT (n = 27) 12‐month follow‐up assessed:
2 year follow‐up assessed:
|
| Teo 2011 | Group A: TVT (n = 66) Group B: TVT‐O (n = 61)
|
| Tommaselli 2012 | Group A: TVT‐O (n = 48) Group B: modified TVT‐O (n = 24)
|
| Tseng 2005 | Group A: SPARC (n = 31)
Group B: TVT (n = 31)
|
| Ugurlucan 2013 | Group A: biological PELVILACE TO (n = 50) Group B: synthetic TOT ALIGN ®TO (n = 50)
|
| van Leijsen 2013 | Group A: RPR (n = 33) Group B: TOT (n = 90)
|
| Wang 2006 | Group A: Monarc (n = 31) Group B: SPARC (n = 29)
|
| Wang 2008 | Group A: TVT (n = 35) Group B: TVT‐O (n = 34)
|
| Wang 2009 | Group A: TVT (n = 154) Group B: TVT‐O (n = 146)
|
| Wang 2010 | Group A: TVT (n = 70) Group B: TOT (n = 70)
|
| Wang 2011 | Group A: TVT (n = 32) Group B: TVT‐O (n = 36)
|
| Zhang 2011 | Group A: TVT‐O (n = 76) Group B: modified TVT‐O (n = 80)
|
| Zullo 2007 | Group A: TVT (n = 35) Group B: TVT‐O (n = 37)
|
Abbreviations
BFLUTS: Bristol lower urinary tract symptoms questionnaires
BMI: body‐mass index
DO: detrusor overactivity
DUP: distal urethral polypropylene sling
EQOL‐5D: Euro Quality of life ‐5 Dimension
hr: hour/s
HRT: hormone replacement therapy
ICIQ: International Consultation on Incontinence questionnaire
ICIQ‐FLUTS: International Consultation on Incontinence questionnaire ‐ female lower urinary tract symptoms
ICIQ‐ LUTSquol: International Consultation on Incontinence questionnaire ‐ lower urinary tract quality of life questionnaire
ICIQ‐SF: International Consultation on Incontinence questionnaire short form
ICIQ‐SF15: International Consultation on Incontinence questionnaire short form 15
IIQ: Incontinence Impact questionnaire
ICS: International Continence Society
I‐QoL: Incontinence Quality of Life questionnaire
ISD: intrinsic sphincter deficiency
IVS: intravaginal slingoplasty
KHQ: King's Health questionnaireMUI: mixed urinary incontinence
MUCP: Maximum urethral closure pressure
MUI: mixed urinary incontinence
OAB: overactive bladder
PGI‐I: Patient Global Impression of Improvment
PGI‐S: Patient Global Impression of Severity
PISQ‐12: pelvic organ prolapse/urinary incontinence sexual questionnaire
POP: pelvic organ prolapse
POP‐Q: pelvic organ prolapse quantification
POP‐Q ICS: pelvic organ prolapse quantification International Continence Society
PVR: post void residual
RCT: randomized controlled trial
RPR: retropubic route
QoL: quality of life
QRCT: quasi‐randomised trial
SEAPI‐QMM: Stress related leak, Empyting ability, Anatomy, Protection, Inhibition‐Quality of life, Mobility and Mental status incontinence classification system
SD: standard deviation
SIS: Single incision sling
SPARC: suprapubic arc (procedure)
SUI: stress urinary incontinence
TOR: transobturator
TOT: transobturator tape
TOT‐ARIS: transobturator tape‐ARIS
TVT: tension‐free vaginal tape
TVT‐O: transobturator tension‐free vaginal tape
UDI: Urinary Distress Impact questionnaire
UDI‐6: Urinary Distress Impact questionnaire short form
UDS: urodynamics study
UI: urinary incontinence
UISS: urinary incontinence severity score
USI: urodynamic stress incontinence
USS: ultrasound
UTI: urinary tract infection
UUI: urgency urinary incontinence
VAS: visual analogue scale
VLPP: Valsalval leak point pressure
Comparison 1. Transobturator versus retropubic route
Fifty‐five trials addressed this comparison (Aigmuller 2014; Alkady 2009; Andonian 2007; Aniuliene 2009; Araco 2008; Barber 2008; Barry 2008; Cervigni 2006; Chen 2010; Chen 2012; Choe 2013; Darabi Mahboub 2012; David‐Montefiore 2006; de Tayrac 2004; Deffieux 2010; Diab 2012; El‐Hefnawy 2010; Enzelsberger 2005; Freeman 2011; Hammoud 2011; Jakimiuk 2012; Kamel 2009; Karateke 2009; Kilic 2007; Kim 2005; Krofta 2010; Laurikainen 2007; Leanza 2009; Lee 2007; Liapis 2006; Mansoor 2003; Mehdiyev 2010; Meschia 2007; Nerli 2009; Nyyssonen 2014; Oliveira 2006; Palomba 2008; Porena 2007; Rechberger 2009; Richter 2010; Riva 2006; Ross 2009; Salem 2014; Scheiner 2012; Schierlitz 2008; Tanuri 2010; Tarcan 2011; Teo 2011; van Leijsen 2013; Wang 2006; Wang 2008; Wang 2009; Wang 2010; Wang 2011; Zullo 2007).
1.1 Women's observations
Subjective cure within 12 months was reported in 36 trials with a total of 5514 participants. Assessment of cure was self‐reported by participants and by responses to symptom‐based questionnaires. The combined results from the 36 trials showed no statistically significant difference in the subjective cure rates between the two routes (RR 0.98, 95% CI 0.96 to 1.00; Analysis 1.1). The short‐term subjective cure ranged from 62% to 98% for TOR and from 71% to 97% for RPR.
1.1. Analysis.
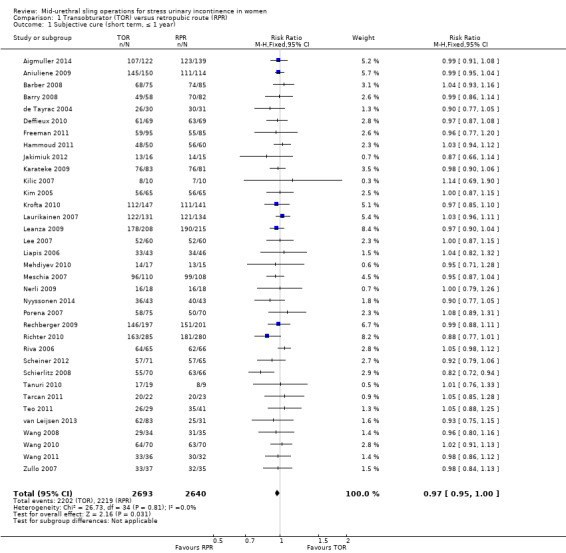
Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 1 Subjective cure (short term, ≤ 1 year).
The mean subjective cure rate across both groups was 83.3% and, using this as the assumed control subjective cure rate in the RPR group, for every 1000 women there were 17 fewer cured in the TOR group (95% CI from 0 fewer to 33 fewer per 1000). This was not statistically significant and is also unlikely to be considered to be a clinically significant difference. The funnel plot inspection shows no strong evidence of publication bias Figure 4.
4.
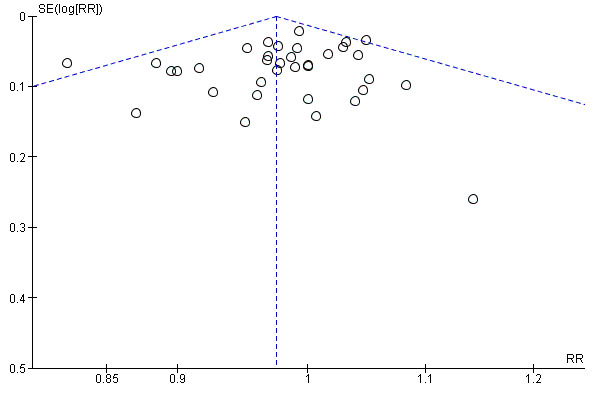
Funnel plot of comparison: 1 Transobturator (TOR) versus retropubic (RPR) route, outcome: 1.1 Subjective cure (short term, ≤ 1 year)
There was also no statistically significant difference between the two groups in terms of symptomatic improvement and cure rate (RR 0.98, 95% CI 0.96 to 1.00; Analysis 1.2).
1.2. Analysis.
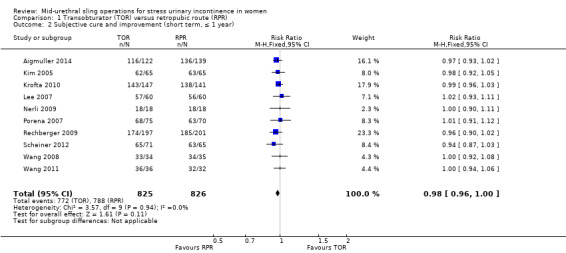
Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 2 Subjective cure and improvement (short term, ≤ 1 year).
Medium‐term outcomes
Only seven trials provided information after the first year (Deffieux 2010; Laurikainen 2007; Nyyssonen 2014; Porena 2007; Schierlitz 2008; Tarcan 2011; Zullo 2007). Five trials (683 participants) contributed medium‐term data between one and five years after surgery, which showed no significant difference in subjective cure between the two groups (RR 0.97, 95% CI 0.87 to 1.09; Analysis 1.3). Subjective cure rates ranged from 82% to 91% in the TOR group and from 77% to 98% in the RPR group.
1.3. Analysis.
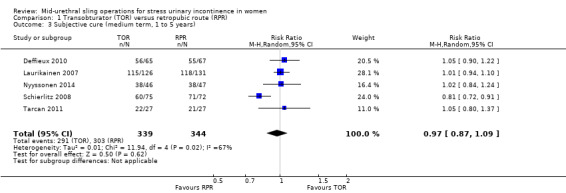
Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 3 Subjective cure (medium term, 1 to 5 years).
The average medium‐term subjective cure rate across both groups was 86.9% and, using this as the assumed control cure rate in the RPR group, for every 1000 women there were 26 fewer women cured in the TOR group (95% CI from 26 per 1000 more to 70 per 1000 fewer).
Long‐term outcomes
Four trials (714 women) reported long‐term results for subjective cure after five years (Laurikainen 2007; Porena 2007; Richter 2010; Zullo 2007); the difference between the groups was not statistically significant (RR 0.95, 95% CI 0.80 to 1.12; Analysis 1.4). Subjective cure rates range from 43% to 92% in the TOR group and from 51% to 88% in the RPR group.
1.4. Analysis.
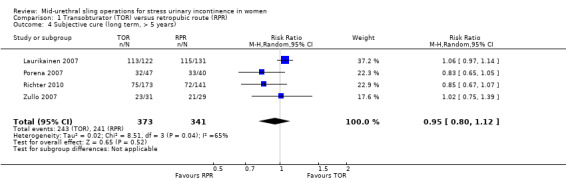
Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 4 Subjective cure (long term, > 5 years).
The average long‐term subjective cure rate across both groups was 84.3% and, using this as the assumed control cure rate in the RPR group, for every 1000 women there were 42 fewer women cured in the TOR group (95% CI from 110 per 1000 less to 34 per 1000 more).
Two trials with 340 women reported long‐term data for subjective cure and improvement and the difference between the groups was not statistically significant (RR 0.92, 95% CI 0.67 to 1.28; Analysis 1.5); due to significant heterogeneity we also performed a random‐effects analysis that produced similar results and, as there were only two trials, the fixed‐effect analysis was maintained.
1.5. Analysis.
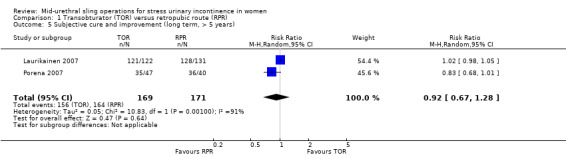
Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 5 Subjective cure and improvement (long term, > 5 years).
1.2 Quantification of symptoms
Only two trials provided data about pad test weights (Tanuri 2010 used a non standardised modified/simplified pad test and Wang 2006 used the standard one‐hour pad test). The information provided was not suitable for meta‐analysis, but each reported a significant reduction in pad weight postoperatively in each group without a significant difference between the groups.
1.3 Clinician's observations
Objective cure was assessed by 40 trials with 6145 participants in the short term using a variety of measures such as urodynamic assessment, negative cough‐stress test, one‐hour pad test of 2 g or less, one‐hour pad test of 1 g or less, and 24‐hour pad test of 5g or less. The cure rate with the obturator route was 85.7% versus 87.2% for the RPR (RR 0.98, 95% CI 0.96 to 1.00, Analysis 1.6). The confidence interval was narrow and this statistically non significant difference between the groups (2%) is unlikely to represent a clinically significant difference in outcome between the two methods in the short term.
1.6. Analysis.
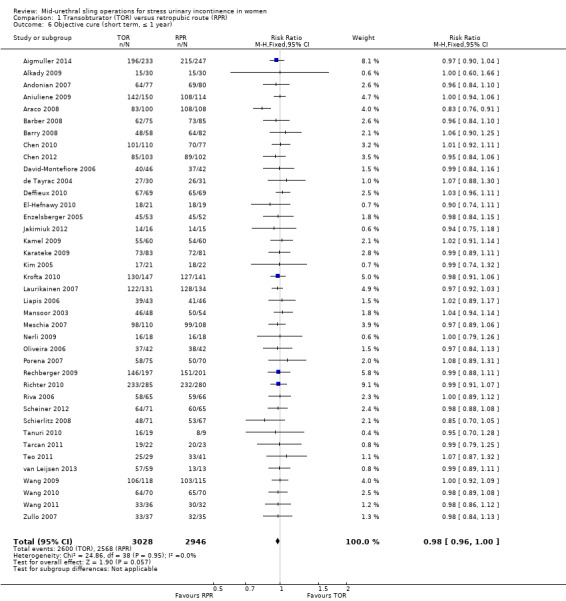
Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 6 Objective cure (short term, ≤ 1 year).
The small difference in the objective cure and improvement rate in the short term was not statistically ‐ nor was it likely to be clinically ‐ significant (RR 0.98, 95% CI 0.96 to 1.01; 10 studies, 1478 women; Analysis 1.7). The same holds true for the medium‐term objective cure rates (RR 1.00, 95% CI 0.95 to 1.06; 5 studies, 596 women; Analysis 1.8), and long‐term cure rates (RR 0.97, 95% CI 0.90 to 1.06; 3 studies, 400 women; Analysis 1.9).
1.7. Analysis.
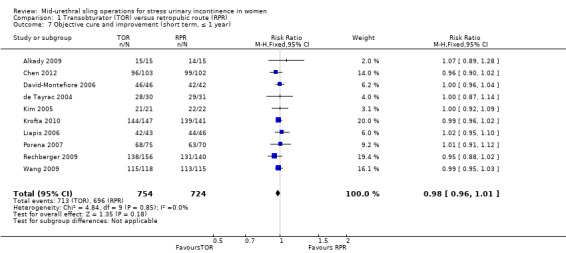
Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 7 Objective cure and improvement (short term, ≤ 1 year).
1.8. Analysis.
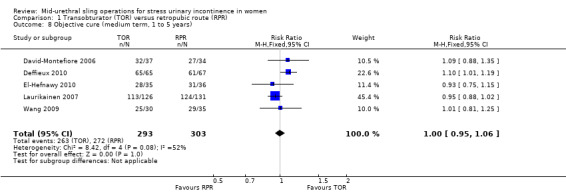
Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 8 Objective cure (medium term, 1 to 5 years).
1.9. Analysis.
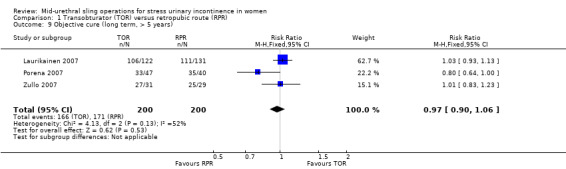
Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 9 Objective cure (long term, > 5 years).
1.4 Surgical outcome measures
Duration of operation was significantly shorter, by an average of approximately seven minutes, with the TOR compared with the RPR (MD ‐7.54 minutes, 95% CI ‐9.31 to ‐5.77). There was statistically significant heterogeneity, but all the trials reported a shorter operating time with the TOR. This may be attributable to most surgeons routinely performing a cystoscopy following a RPR procedure, but not necessarily doing this after a TOR procedure.
To investigate this theory, we performed a sensitivity analysis to assess the difference in operative time between the RPR and TOR approach in trials where cystoscopy was performed in both comparison groups as defined by the trialists. In eight trials where cystoscopy was performed in both TOR and RPR groups we still found a shorter operating time with the TOR in comparison to the RPR (MD ‐6.50 95% CI ‐7.57 to ‐5.44) although high heterogeneity persisted. Using a random‐effects method on the full analysis of 31 trials still showed the duration of operation to be statistically significantly shorter with TOR approach (MD ‐7.54 minutes, 95% CI ‐9.31 to ‐5.77; Analysis 1.10).
1.10. Analysis.
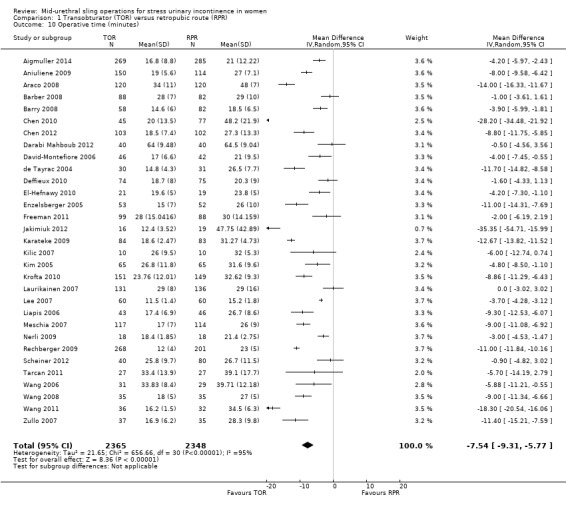
Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 10 Operative time (minutes).
Intraoperative blood loss was small (mean loss ranged from 15 ml to 125 ml), but was significantly less with the TOR approach (MD ‐6.49 ml, 95% CI ‐12.33 to ‐0.65; Analysis 1.11). There was significant heterogeneity that was accounted for by three small trials (Nerli 2009; Wang 2008; Zullo 2007). In view of the small blood volumes involved, this is unlikely to be a clinically significant finding.
1.11. Analysis.
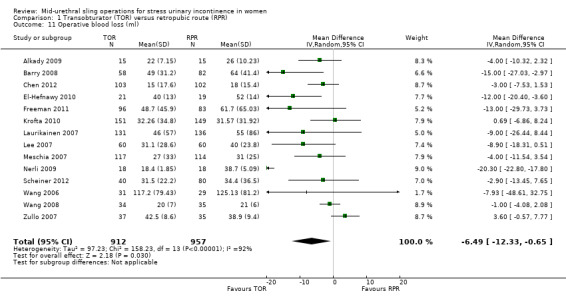
Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 11 Operative blood loss (ml).
Length of stay was also significantly shorter by an average of 0.17 days with the TOR compared with the retropubic route (MD ‐0.17, 95% CI ‐0.25 to ‐0.10; Analysis 1.12). A high level of between‐study heterogeneity (I² 94%) was present with the length of stay, thus a random‐effects model was used, which then showed no significant difference (MD ‐0.25, 95% CI ‐0.59 to 0.09; Analysis 1.12).
1.12. Analysis.
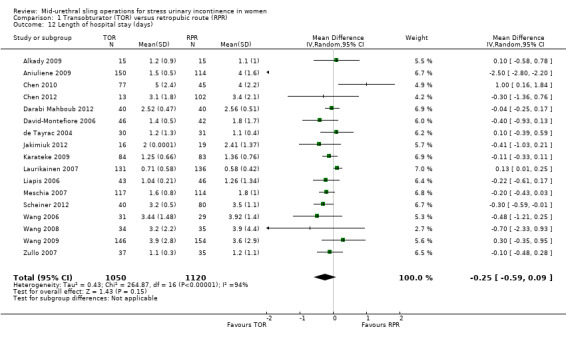
Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 12 Length of hospital stay (days).
The mean time the women took to return to normal activity ranged from under two weeks to just over five weeks, with no statistically significant difference between the two surgical approaches (MD ‐0.05, 95% CI ‐0.15 to 0.06; Analysis 1.13). This confirms the minimally invasive nature of both operations, compared with a more normal recovery period of three months after major abdominal surgery.
1.13. Analysis.
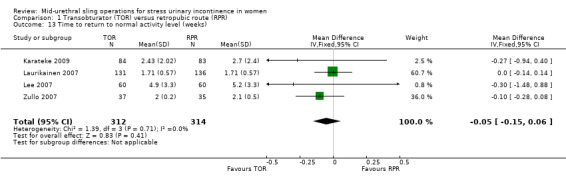
Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 13 Time to return to normal activity level (weeks).
1.5 Adverse events
In trials where overall perioperative complication rates were reported there were no statistically significant differences in the rate of perioperative complications between the TOR and RPR groups (RR 0.91, 95% CI 0.73 to 1.14; Analysis 1.14).
1.14. Analysis.
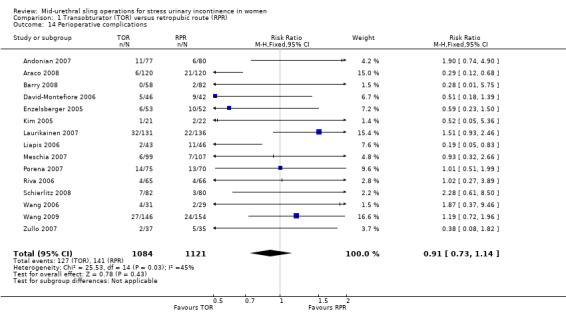
Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 14 Perioperative complications.
In trials where specific complications were recorded there were significant differences in the rate of each individual complication sustained.
Major vascular/visceral injury
Major vascular injury such as retropubic haematoma or major visceral injury, for example bowel perforation, was reported by 28 trials with 4676 women. This occurred significantly less often with TOR than with RPR (RR 0.33, 95% CI 0.19 to 0.55; Analysis 1.15).
1.15. Analysis.
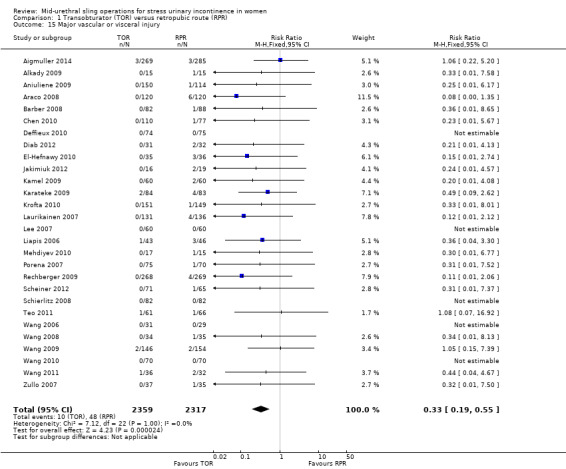
Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 15 Major vascular or visceral injury.
Bladder/urethral perforation
Forty trials assessed rate of bladder perforation. The rate was significantly lower in the TOR group than the RPR group (RR 0.13, 95% CI 0.08 to 0.20; Analysis 1.16). The average bladder perforation rate across both groups was 2.54% and, using this as the assumed control bladder perforation rate in the RPR group, there were 22 fewer perforations per 1000 in the TOR group (95% CI from 20 to 23 per 1000 fewer). There was some degree of asymmetry in the funnel plot, which raised the possibility of some publication bias Figure 5.
1.16. Analysis.
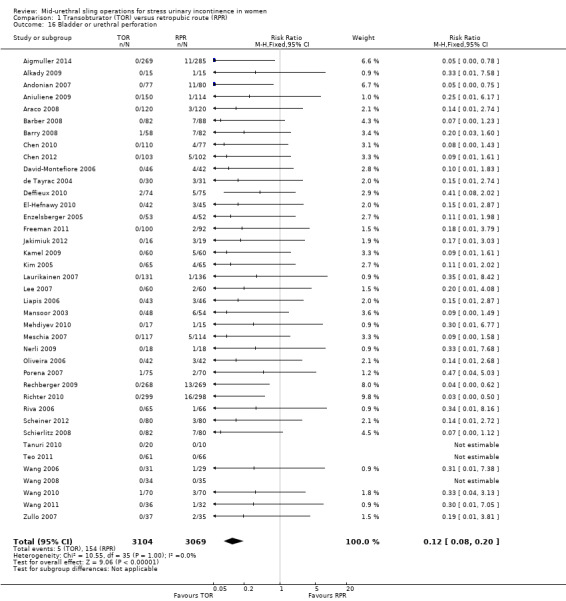
Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 16 Bladder or urethral perforation.
5.
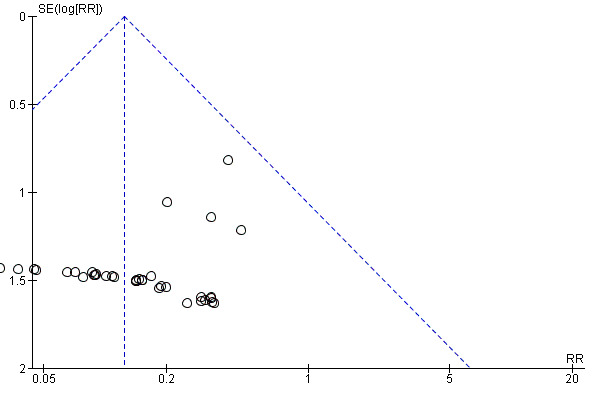
Funnel plot of comparison: 1 Transobturator (TOR) versus retropubic (RPR) route, outcome: 1.16 Bladder or urethral perforation
Postoperative voiding dysfunction (POVD)
Rates of postoperative voiding dysfunction (POVD) was assessed in 37 trials with 6200 participants. This showed significantly lower rates in the TOR group than in the RPR group (RR 0.53 95% CI 0.43 to 0.65; Analysis 1.17). The average POVD rate across both groups was 5.53% and, using this as the assumed control rate in the RPR group, there were 26 fewer POVD per 1000 in the TOR group (95% CI from 19 to 32 per 1000 fewer). The funnel plot showed symmetry on visual inspection, which suggests a low likelihood of publication bias Figure 6.
1.17. Analysis.
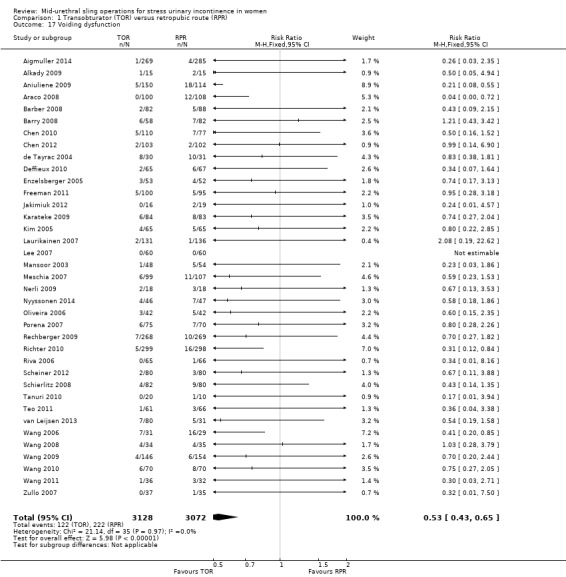
Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 17 Voiding dysfunction.
6.
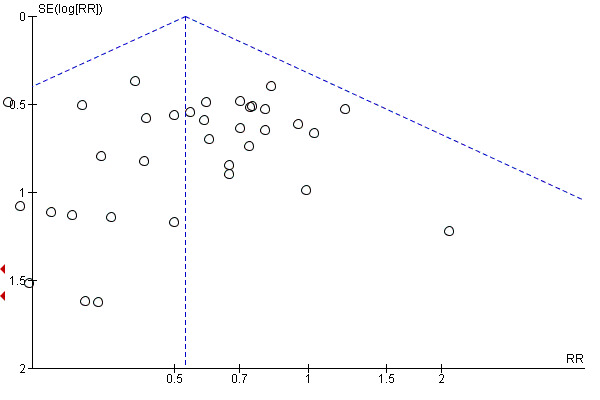
Funnel plot of comparison: 1 Transobturator (TOR) versus retropubic (RPR) route, outcome: 1.17 Voiding dysfunction
Urgency and urgency urinary incontinence (UUI)
The 31 trials (4923 women) that reported de novo urgency and urgency urinary incontinence (UUI) showed no statistically significant difference between the two groups (RR 0.98, 95% CI 0.82 to 1.17; Analysis 1.18). In the short term the average rate of de novo urgency/UUI across both groups was 8.35% and, using this as the assumed control rate in the RPR group, there were two fewer cases per 1000 in the TOR group (95% CI from 15 per 1000 fewer to 14 per 1000 more).
1.18. Analysis.
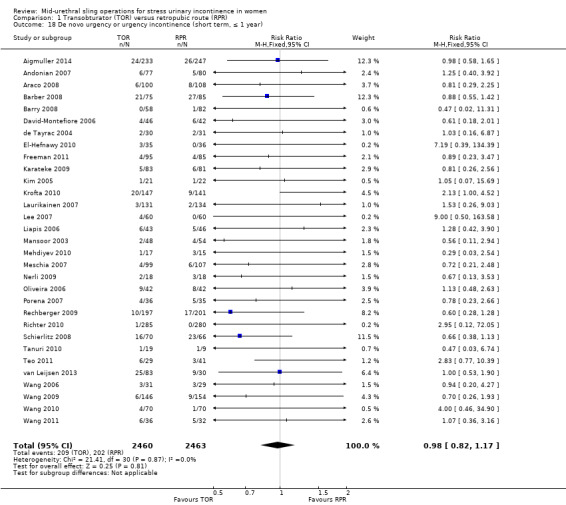
Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 18 De novo urgency or urgency incontinence (short term, ≤ 1 year).
Equally, in the medium term the rate of de novo urgency and UUI was not significantly different (RR 0.98, 95% CI 0.55 to 1.73, Analysis 1.19). Laurikainen 2007 reported long‐term data for de novo urgency and UUI for 253 women; this showed no difference between the groups (RR 0.81, 95% CI 0.18 to 3.53; 253 women; Analysis 1.20).
1.19. Analysis.
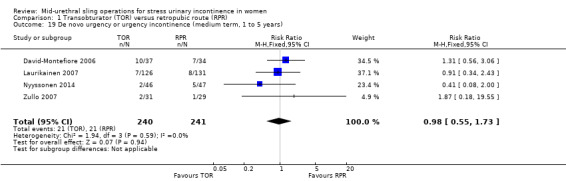
Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 19 De novo urgency or urgency incontinence (medium term, 1 to 5 years).
1.20. Analysis.
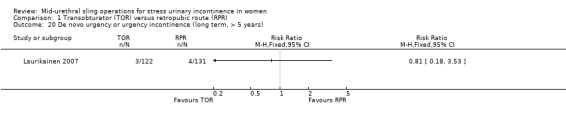
Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 20 De novo urgency or urgency incontinence (long term, > 5 years).
Four trials with 853 women with DO showed a rate of 8% in both groups (RR 1.00, 95% CI 0.58 to 1.73; Analysis 1.21).
1.21. Analysis.
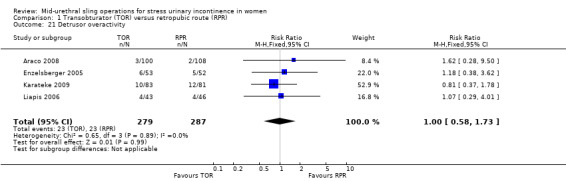
Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 21 Detrusor overactivity.
In one trial of women with MUI (Laurikainen 2007), 84% who had pre‐existing moderate or severe urinary frequency and urgency symptoms were cured of these symptoms post operatively at the five‐year follow‐up.
Vaginal tape erosion
Vaginal tape erosion was assessed in 31 trials with 4743 participants. No significant difference was demonstrated between the groups (RR 1.13, 95% CI 0.78 to 1.65; Analysis 1.22). The average rate of vaginal tape erosion across both groups was 2.09%, and, using this as the assumed control rate in the RPR group, there were three more cases per 1000 in the TOR group (95% CI from 5 per 1000 fewer to 14 per 1000 more). The funnel plot showed symmetry on visual inspection suggesting low likelihood of publication bias Figure 7. In the one trial that reported long‐term tape erosion (Laurikainen 2007), no tape erosion was reported in either group. Bladder or urethral tape erosion was assessed in four trials with 374 participants. No significant difference was demonstrated between the groups (RR 0.34, 95% CI 0.01 to 8.13; Analysis 1.23).
1.22. Analysis.
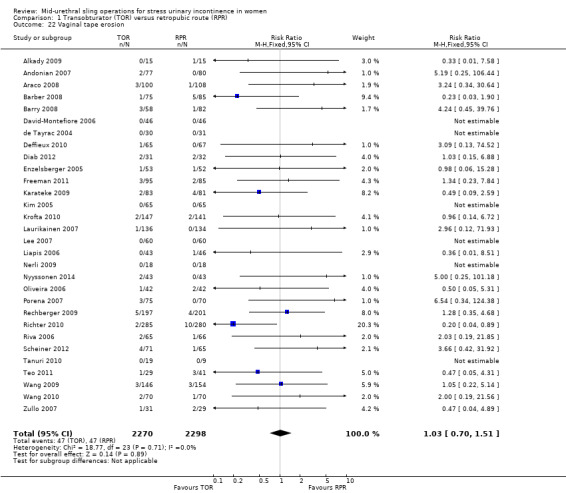
Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 22 Vaginal tape erosion.
7.
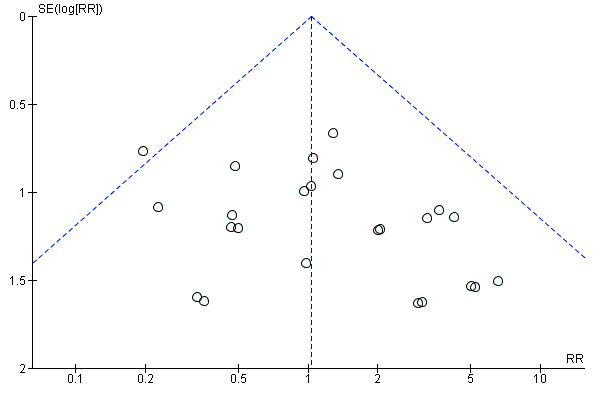
Funnel plot of comparison: 1 Transobturator (TOR) versus retropubic (RPR) route, outcome: 1.22 Vaginal tape erosion
1.23. Analysis.
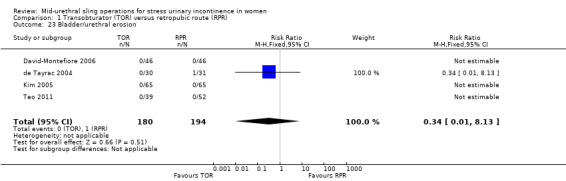
Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 23 Bladder/urethral erosion.
Pain
There was a significantly higher occurrence of groin pain in women who underwent a TOR procedure than in women who underwent a RPR procedure (RR 4.12, 95% CI 2.71 to 6.27; Analysis 1.24). The average rate of groin pain across both groups was 4.51% and, using this as the assumed control rate in the RPR group, there were 163 more cases per 1000 in the TOR group (95% CI from 94 to 266 per 1000 more). Conversely, suprapubic pain was found to be significantly lower in women who underwent a TOR procedure than a RPR procedure (RR 0.29, 95% CI 0.11 to 0.78; Analysis 1.25). Both groin and suprapubic pain occurrence were short‐lasting, with most resolving within the first six months. The duration of pain ranged from two to 52 weeks, with a median duration of eight weeks. The funnel plot for groin pain showed symmetry on visual inspection, suggesting low likelihood of publication bias Figure 8.
1.24. Analysis.
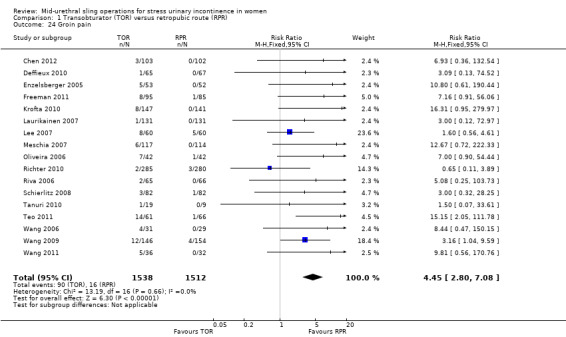
Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 24 Groin pain.
1.25. Analysis.
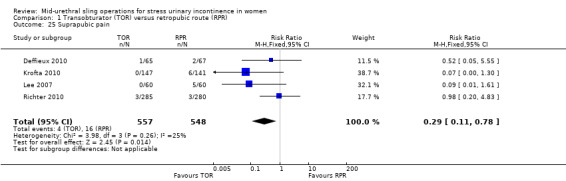
Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 25 Suprapubic pain.
8.
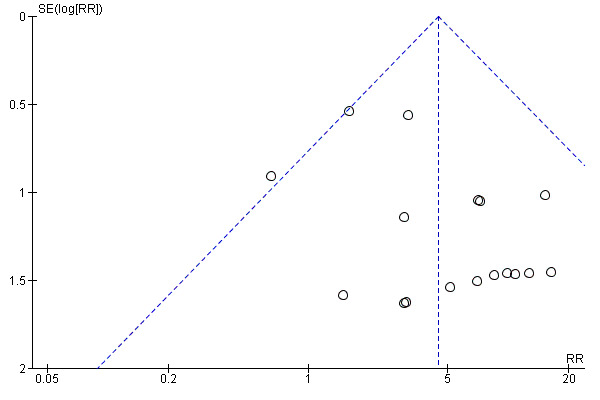
Funnel plot of comparison: 1 Transobturator (TOR) versus retropubic (RPR) route, outcome: 1.24 Groin pain
1.6 Need for further treatment
Nine trials (1402 women) reported the number of women who required repeat incontinence surgery in the short term (up to one year). The difference between the TOR and RPR groups was not statistically significant (RR 1.64, 95% CI 0.85 to 3.16; Analysis 1.26). The average rate of repeat incontinence surgery in the short term across both groups was 2.43% and, using this as the assumed control rate in the RPR group, there were 12 more cases per 1000 in the TOR group (95% CI from 3 per 1000 fewer to 41 per 1000 more).
1.26. Analysis.
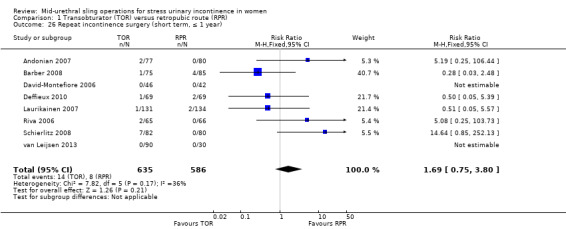
Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 26 Repeat incontinence surgery (short term, ≤ 1 year).
More women required repeat incontinence surgeries in the TOR group in the medium term (RR 21.89, 95% CI 4.36 to 109.77; two studies, 355 women; Analysis 1.27).
1.27. Analysis.
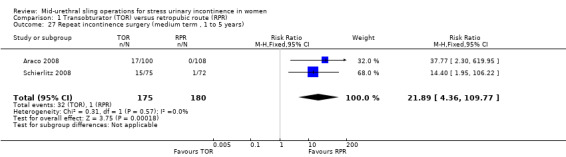
Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 27 Repeat incontinence surgery (medium term , 1 to 5 years).
In the long term, three trials with data from 487 women, found that more women required repeat incontinence surgery in the TOR group (RR 8.79, 95% CI 3.36 to 23.00; Analysis 1.28). The average rate of repeat incontinence surgery in the long term across both groups was 5.34% and, using this as the assumed control rate in the RPR group, there were 231 more cases per 1000 in the TOR group (95% CI from 45 to 767/1000 more).
1.28. Analysis.
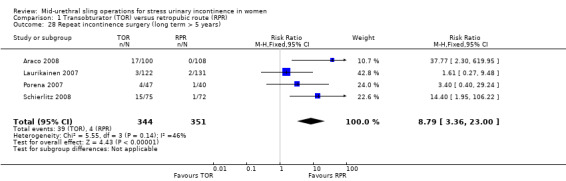
Comparison 1 Transobturator (TOR) versus retropubic route (RPR), Outcome 28 Repeat incontinence surgery (long term > 5 years).
1.7 Quality of life
Thirty‐three of the 55 trials in this comparison assessed quality of life (QoL; Aigmuller 2014; Andonian 2007; Barber 2008; Barry 2008; Chen 2012; Darabi Mahboub 2012; David‐Montefiore 2006; Deffieux 2010; de Tayrac 2004; El‐Hefnawy 2010; Freeman 2011; Jakimiuk 2012; Karateke 2009; Kim 2005; Krofta 2010; Laurikainen 2007; Leanza 2009; Mansoor 2003; Meschia 2007; Nerli 2009; Porena 2007; Richter 2010; Riva 2006; Ross 2009; Scheiner 2012; Schierlitz 2008; Tanuri 2010; Tarcan 2011; Teo 2011; Wang 2008; Wang 2010; Wang 2011; Zullo 2007); however only 11 of these trials reported QoL scores (Andonian 2007; Barber 2008; Barry 2008; David‐Montefiore 2006; de Tayrac 2004; Laurikainen 2007; Meschia 2007; Porena 2007; Riva 2006; Schierlitz 2008; Wang 2008).
A wide variety of measures were used by different trials to assess this outcome, including:
Condition‐specific measures
Incontinence Impact Questionnaire (IIQ‐7).
Urogenital Distress Inventory (UDI‐6).
International Consultation on Incontinence Questionnaire (ICIQ).
Urinary Incontinence Quality of Life Scale (I‐QOL).
Kings Health Questionnaire (KHQ).
Bristol Female Lower Urinary Tract Symptoms questionnaire (BFLUTS).
Women Irritative Prostate Symptoms Score (W‐IPSS).
Urinary Incontinence Severity Score (UISS).
Detrusor Instability Score (DIS).
A Visual Analogue Scale (VAS).
CONTILIFE.
Generic measures
EuroQoL 5‐Dimensional Classification Component Scores (EuroQoL‐5D).
Short‐Form Health‐Related QoL (SF‐36).
Patient Global Impression of Severity (PGI‐S).
Patient Global Impression of Improvement (PGI‐I).
The data on quality of life outcomes were reported in different ways, which precluded meta‐analysis. In general, with the exception of Araco 2008, all trials found that women's QoL improved significantly post‐operatively within each group, but no statistically significant differences were found between the randomised groups. Only the Araco 2008 trial found the I‐QOL scores to be statistically significantly higher postoperatively after the retropubic approach.
Sexual function quality of life measures
Sexual function was addressed in 10 trials (Barber 2008; Barry 2008; Deffieux 2010; de Tayrac 2004; Freeman 2011; Krofta 2010; Richter 2010; Ross 2009; Scheiner 2012; Schierlitz 2008), which used a variety of measures including validated questionnaires and direct questioning. Questionnaires employed were:
Prolapse/Incontinence Symptoms Questionairre (PISQ‐12);
Bristol Female Lower Urinary Tract Symptoms questionnaire (BFLUTS);
International Consultation on Incontinence Questionnaire Lower Urinary Tract Symptoms quality of life questionnaire (ICIQ‐LUTSqol); and
Visual Analogue Scale (VAS).
In all the trials there was significant improvement in sexual function from baseline scores during the follow‐up period that spanned six to 24 months. There were no significant differences between the two groups. At 24‐month follow‐up, rates of superficial and deep dyspareunia were low, with no difference between the groups.
Comparison 2. Retropubic bottom‐to‐top approach versus retropubic top‐to‐bottom approach
Five small trials, with 636 women in total, addressed this comparison (Andonian 2005; Kim 2004; Lim 2005; Lord 2006; Tseng 2005).
2.1 Women's observations
Three trials (477 women) investigated subjective cure defined as self‐reported absence of urinary leakage on stress (Kim 2004; Lim 2005; Lord 2006). In the 12 months following surgery, women were significantly more often dry with the bottom‐to‐top approach (TVTTM) compared to the top‐to‐bottom approach (SPARCTM; 87.34% versus 79.58%; RR 1.10, 95% CI 1.01 to 1.19; Analysis 2.1).
2.1. Analysis.
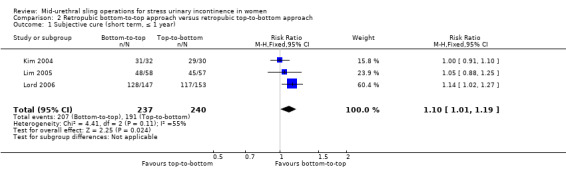
Comparison 2 Retropubic bottom‐to‐top approach versus retropubic top‐to‐bottom approach, Outcome 1 Subjective cure (short term, ≤ 1 year).
2.2 Quantification of symptoms
No data were reported for this outcome.
2.3 Clinician's observation
Five trials assessed objective cure using a variety of measures (Andonian 2005; Kim 2004; Lim 2005; Lord 2006; Tseng 2005): one‐hour pad test of 2g or less, negative stress test on urodynamics (UDS), the observed absence of urinary leakage when the patient coughed while supine and with a comfortably full bladder, and one‐hour pad test of 1g or less, respectively. In a total of 622 participants, the objective cure rate was similar between the two groups (94.19% versus 89.10%; RR 1.06, 95% CI 0.97 to 1.17; Analysis 2.2).
2.2. Analysis.
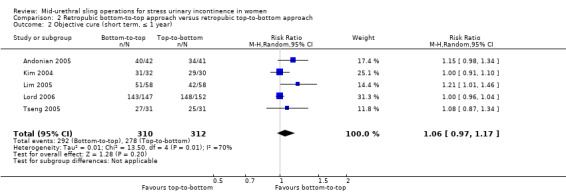
Comparison 2 Retropubic bottom‐to‐top approach versus retropubic top‐to‐bottom approach, Outcome 2 Objective cure (short term, ≤ 1 year).
2.4 Surgical outcome measures
Two small trials, Kim 2004 and Tseng 2005, reported that there were no statistically significant differences in duration of operation (Analysis 2.3) or length of hospital stay (Analysis 2.4).
2.3. Analysis.

Comparison 2 Retropubic bottom‐to‐top approach versus retropubic top‐to‐bottom approach, Outcome 3 Operative time (minutes).
2.4. Analysis.
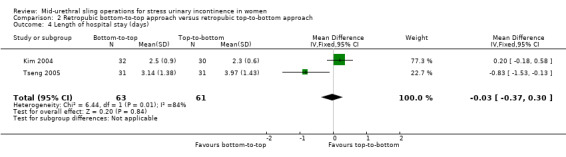
Comparison 2 Retropubic bottom‐to‐top approach versus retropubic top‐to‐bottom approach, Outcome 4 Length of hospital stay (days).
2.5 Adverse events
No statistically significant difference was seen in overall perioperative complications, but the confidence interval was wide (RR 0.98, 95% CI 0.53 to 1.84; Analysis 2.5).
2.5. Analysis.
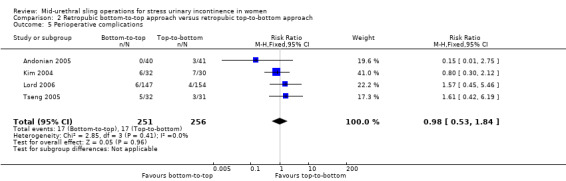
Comparison 2 Retropubic bottom‐to‐top approach versus retropubic top‐to‐bottom approach, Outcome 5 Perioperative complications.
Significantly fewer women experienced certain complications with the bottom‐to‐top approach (TVTTM), which included:
bladder perforation (RR 0.55, 95% CI 0.31 to 0.98; 5 trials; Analysis 2.6);
voiding dysfunction after the bottom‐to‐top approach (TVTTM; RR 0.40, 95% CI 0.18 to 0.90; 5 trials; Analysis 2.7);
vaginal tape erosions (RR 0.27, 95% CI 0.08 to 0.95; 4 trials; Analysis 2.10).
2.6. Analysis.
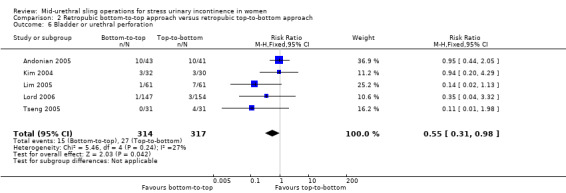
Comparison 2 Retropubic bottom‐to‐top approach versus retropubic top‐to‐bottom approach, Outcome 6 Bladder or urethral perforation.
2.7. Analysis.
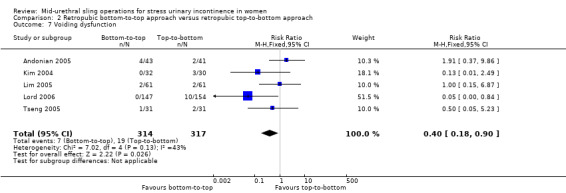
Comparison 2 Retropubic bottom‐to‐top approach versus retropubic top‐to‐bottom approach, Outcome 7 Voiding dysfunction.
2.10. Analysis.
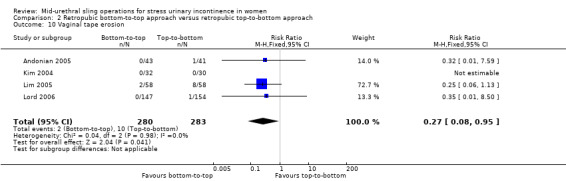
Comparison 2 Retropubic bottom‐to‐top approach versus retropubic top‐to‐bottom approach, Outcome 10 Vaginal tape erosion.
There were no statistically significant differences between the two groups with respect to:
postoperative de novo urgency symptoms and UUI (RR 0.84, 95% CI 0.52 to 1.34; 4 trials; Analysis 2.8); or
DO (1 trial; Analysis 2.9).
2.8. Analysis.

Comparison 2 Retropubic bottom‐to‐top approach versus retropubic top‐to‐bottom approach, Outcome 8 De novo urgency or urgency incontinence.
2.9. Analysis.
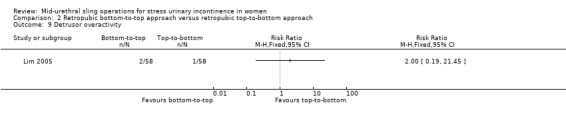
Comparison 2 Retropubic bottom‐to‐top approach versus retropubic top‐to‐bottom approach, Outcome 9 Detrusor overactivity.
However, the confidence intervals were wide for each of these five outcomes, which reflects the small number of trials.
2.6 Need for further treatment
No data were reported on the need for further treatment.
2.7 Quality of life
Only one of the five trials, Andonian 2005, assessed the QoL of women using the Incontinence Impact Questionnaire (IIQ; Shumaker 1994), where a score of less than 50 represents a good QoL, 50 to 70 represents moderate QoL, and over 70 indicates a poor QoL. In this study the mean IIQ scores were similar in the groups preoperatively and improved postoperatively, but there was no significant difference between the groups after operation. At one year follow‐up, there was no statistically significant difference in the mean IIQ scores (mean difference of ‐4.6; 95% CI: ‐7.5 to 16.7).
Comparison 3. Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach
Ten trials reported this comparison (Abdel‐Fattah 2010; But 2008; Chen 2010; Hassan 2013; Houwert 2009; Lee 2008; Liapis 2008; Park 2012; Peattie 2006; Scheiner 2012).
3.1 Women's observations
Six trials investigated short‐term subjective cure rate and five of these assessed subjective cure and improvement in the short term (within 12 months of surgery). There were no statistically significant differences in either subjective cure rates (RR 1.0, 95% CI 0.96 to 1.06; Analysis 3.1) or subjective cure and improvement rates (RR 1.02, 95% CI 0.97 to 1.08 Analysis 3.2), and the confidence intervals for each were quite narrow. Two trials reported no statistically significant difference in subjective cure in the medium term (RR 1.06, 95% CI 0.91 to 1.23; Analysis 3.3) and a further two trials reported no significant difference in subjective cure and improvement in the medium term (RR 1.00, 95% CI 0.90 to 1.11; Analysis 3.4). There are no published trials with long‐term data.
3.1. Analysis.

Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 1 Subjective cure (short term, ≤ 1 year).
3.2. Analysis.
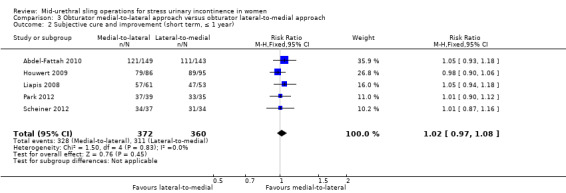
Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 2 Subjective cure and improvement (short term, ≤ 1 year).
3.3. Analysis.
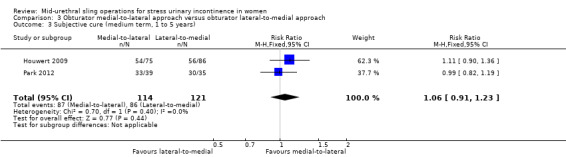
Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 3 Subjective cure (medium term, 1 to 5 years).
3.4. Analysis.
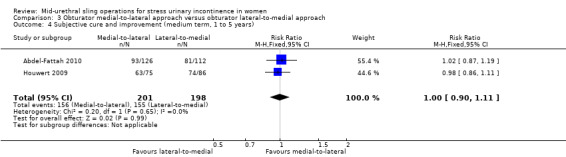
Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 4 Subjective cure and improvement (medium term, 1 to 5 years).
3.2 Quantification of symptoms
No data were reported for this comparison.
3.3 Clinician's observation
Six trials assessed objective cure (short term, ≤ 1 year); there was no statistically significant difference between the two groups (RR 0.99, 95% CI 0.95 to 1.04; Analysis 3.5), and the confidence interval was narrow. There was also no statistically significant difference in the objective cure or improvement rate between the two groups (RR 1.00, 95% CI 0.95 to 1.07; Analysis 3.6).
3.5. Analysis.
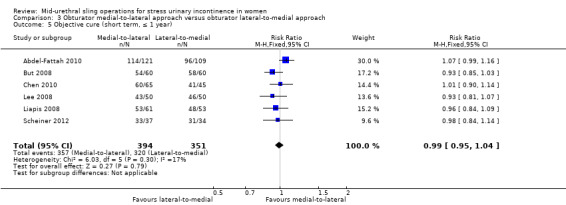
Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 5 Objective cure (short term, ≤ 1 year).
3.6. Analysis.

Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 6 Objective cure and improvement (short term, ≤ 1 year).
3.4 Surgical outcome measures
There were no statistically significant differences between the two groups in terms of:
duration of operation, (in minutes, MD 0.52, 95% CI ‐1.09 to 2.13; 4 studies, 481 women; Analysis 3.7);
operative blood loss (in ml, MD 1.11, 95% CI ‐6.01 to 8.22; 3 studies, 255 women; Analysis 3.8);
length of hospital stay (in days, MD ‐0.77, 95% CI ‐2.54 to 0.99; 2 studies, 190 women; Analysis 3.9);
time to return to normal activity (in weeks, MD ‐0.60, 95% CI ‐1.80 to 0.60; 1 study, 100 women; Analysis 3.10).
3.7. Analysis.
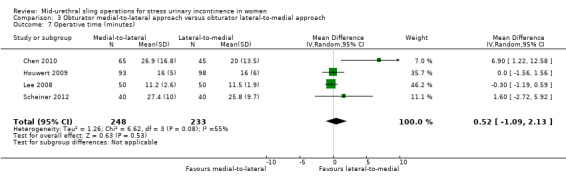
Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 7 Operative time (minutes).
3.8. Analysis.
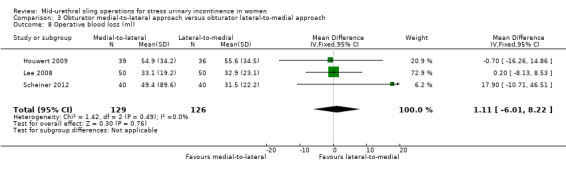
Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 8 Operative blood loss (ml).
3.9. Analysis.
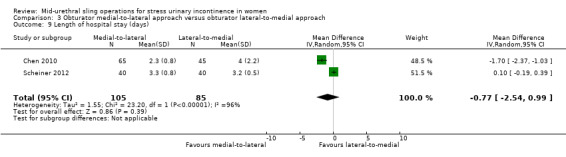
Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 9 Length of hospital stay (days).
3.10. Analysis.
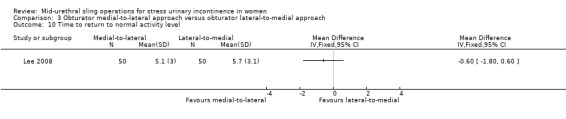
Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 10 Time to return to normal activity level.
3.5 Adverse events
Vaginal perforation was significantly less likely to occur with the medial‐to‐lateral approach (RR 0.25, 95% CI 0.12 to 0.53; I² of 43%; Analysis 3.13). The average rate of vaginal wall perforation across both groups was 7.39% and, using this as the assumed control rate in the lateral‐to‐medial group, there were 55 fewer cases per 1000 in the medial‐to‐lateral group (95% CI from 35 per 1000 fewer to 65 per 1000 more).
3.13. Analysis.
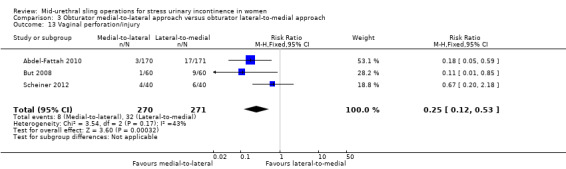
Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 13 Vaginal perforation/injury.
Voiding dysfunction occurred significantly more in the medial‐to‐lateral compared to the lateral‐to‐medial group (RR 1.74, 95% CI 1.06 to 2.88; I² of 0%; 8 studies, 1121 women; Analysis 3.15). The average rate of POVD across both groups was 5.53% and, using this as the assumed control rate in the lateral‐to‐medial group, there were 41 more cases per 1000 in the medial‐to‐lateral group (95% CI from 3 to 104 per 1000 more).
3.15. Analysis.
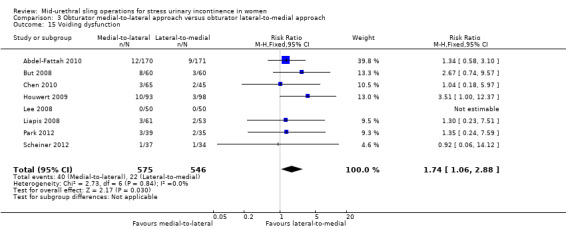
Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 15 Voiding dysfunction.
There were no statistically significant differences between the two groups in terms of:
overall perioperative complication rate (RR 1.30, 95% CI 0.23 to 7.51; 2 studies, 214 women; Analysis 3.11);
major vascular/visceral injury (RR 0.71, 95% CI 0.23 to 2.19; 4 studies, 622 women; Analysis 3.12);
bladder perforation (RR 0.38, 95% CI 0.07 to 1.92; 6 studies, 794 women; Analysis 3.14);
de novo urgency symptoms and UUI rates (RR 1.01, 95% CI 0.46 to 2.20; 3 studies, 357 women; Analysis 3.16);
detrusor overactivity (RR 0.87, 95% CI 0.27 to 2.84; 1 study, 114 women; Analysis 3.17);
vaginal tape erosions (RR 0.42, 95% CI 0.16 to 1.09; 7 studies, 1087 women; Analysis 3.18);
groin/thigh pain (9.2% versus 8%; RR 1.15, 95% CI 0.75 to 1.76; 6 studies, 837 women; Analysis 3.19).
3.11. Analysis.
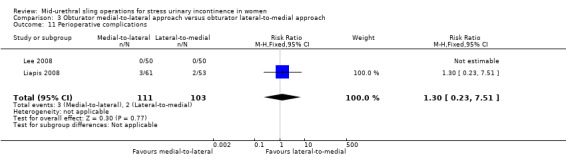
Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 11 Perioperative complications.
3.12. Analysis.
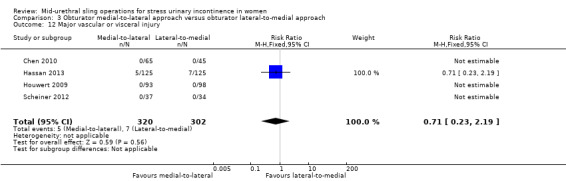
Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 12 Major vascular or visceral injury.
3.14. Analysis.
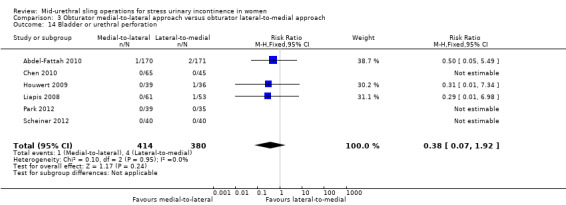
Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 14 Bladder or urethral perforation.
3.16. Analysis.
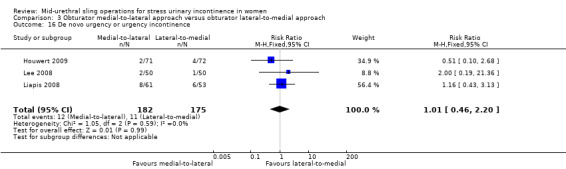
Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 16 De novo urgency or urgency incontinence.
3.17. Analysis.
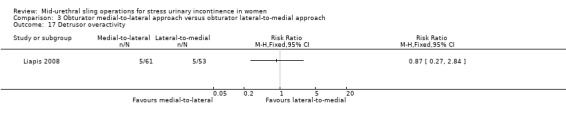
Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 17 Detrusor overactivity.
3.18. Analysis.
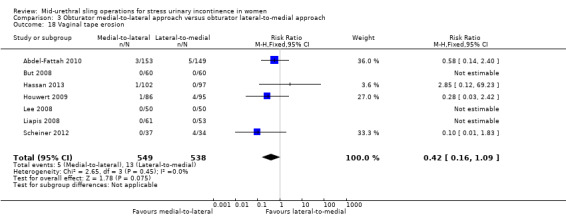
Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 18 Vaginal tape erosion.
3.19. Analysis.
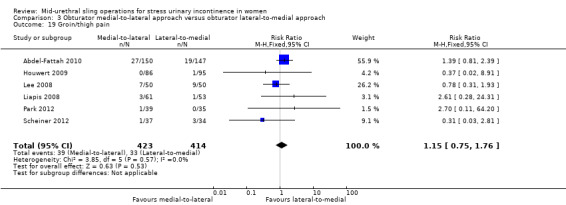
Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 19 Groin/thigh pain.
3.6 Need for further treatment
Two large trials showed no significant difference in the rates of repeat incontinence surgery in the medium term (4.6% versus 7.1%; RR 0.64, 95% CI 0.32 to 1.30; Analysis 3.20).
3.20. Analysis.
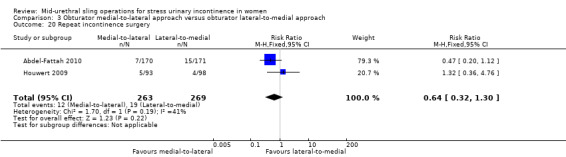
Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 20 Repeat incontinence surgery.
3.7 Quality of life
Quality of life was assessed in five of the ten trials using validated QoL questionnaires. All of these trials reported QoL scores.
Condition‐specific QoL scores
Houwert 2009 used the short forms of the IIQ‐7 and UDI‐6. Within each group there was significant improvement postoperatively compared to scores obtained preoperatively, but no significant postoperative differences between the two groups (MD 16.54, 95% CI 4.84 to 28.24; 1 study, 42 women).
But 2008 assessed QoL with IIQ and UDI questionnaires and VAS scores, but reported no results.
Lee 2008 used a validated Korean version of the Incontinence QoL questionnaire (I‐QoL) and showed improvements within the groups, but with no significant differences between the groups after surgery.
Scheiner 2012 used the KHQ and found no significantly difference between the groups at baseline and postoperatively, but with improvement following surgery compared to baseline scores in all domains.
Abdel‐Fattah 2010 used the KHQ, Birmingham Bowel and Urinary Symptoms Questionnaire (BBUSQ‐22), PISQ‐12, PGI‐I and the short form of the ICIQ (ICIQ‐SF) to assess QoL. Overall there was statistically significant improvement in total scores, as well as in each of the nine domains of the KHQ. This remained the case when comparing baseline score in each group postoperatively; there was no significant difference in the QoL scores between the two routes.
Sexual function
Sexual function was addressed in three trials that used a variety of measures including validated questionnaires and direct questioning (Abdel‐Fattah 2010; Houwert 2009; Park 2012). Questionnaires included: the PISQ‐12, and BFLUTS (Abdel‐Fattah 2010). There was significant improvement in PISQ‐12 scores following surgery (improved sexual function compared to baseline), but no significant difference between the two groups at follow‐up. Rates of dyspareunia following surgery were extremely low, with evidence of resolution by 24 months.
Comparison 4. One method of mid‐urethral tape insertion versus another method, same route
Ten trials compared different methods of carrying out TOR and RPR operations using the same route (Cho 2010; de Leval 2011; Elbadry 2014; Juang 2007; Naumann 2006; Paparella 2010; Rechberger 2011; Tommaselli 2012; Ugurlucan 2013; Zhang 2011). The following operations were compared.
Transobturator lateral‐to‐medial
Monarc® TOT versus TOT® (Cho 2010).
TOT versus adjustable TOT (Elbadry 2014).
TOT versus TOT with two‐point fixation sutures (Rechberger 2011).
Synthetic TOT versus biological TOT (Paparella 2010; Ugurlucan 2013).
Transobturator medial‐to‐lateral
TVT‐O versus modified TVT‐O (shorter tape and less lateral dissection; de Leval 2011).
TVT‐O versus TVT‐O plus Ingleman‐Sundberg bladder denervation procedure (Juang 2007).
TVT‐O versus modified TVT‐O (reduced dissection; Tommaselli 2012).
TVT‐O versus modified TVT‐O (self‐tailored mesh; Zhang 2011).
Retropubic
TVT versus modified TVT, bottom‐to‐top (suburethral pad; Naumann 2006).
Each comparison group included only a small single trial, which precluded any meaningful statistical analysis of the outcomes measured, except for the synthetic versus biological TOT comparison, for which there were two small trials (Analysis 4.1; Analysis 4.2; Analysis 4.3; Analysis 4.5; Analysis 4.4; Analysis 4.6; Analysis 4.7; Analysis 4.8; Analysis 4.10; Analysis 4.11; Analysis 4.12; Analysis 4.13; Analysis 4.14; Analysis 4.15; Analysis 4.16). Naumann 2006 reported no usable data.
4.1. Analysis.
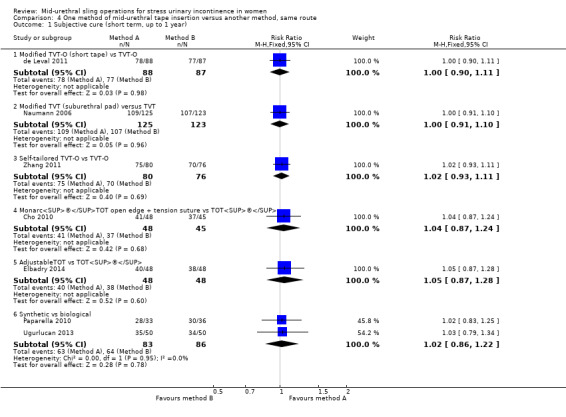
Comparison 4 One method of mid‐urethral tape insertion versus another method, same route, Outcome 1 Subjective cure (short term, up to 1 year).
4.2. Analysis.
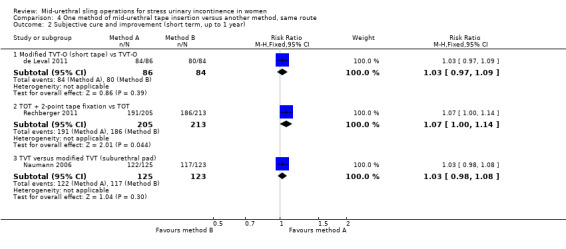
Comparison 4 One method of mid‐urethral tape insertion versus another method, same route, Outcome 2 Subjective cure and improvement (short term, up to 1 year).
4.3. Analysis.
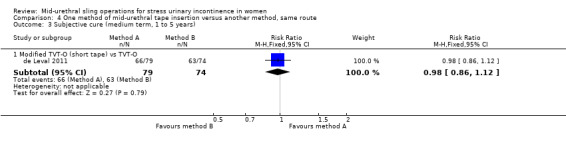
Comparison 4 One method of mid‐urethral tape insertion versus another method, same route, Outcome 3 Subjective cure (medium term, 1 to 5 years).
4.5. Analysis.
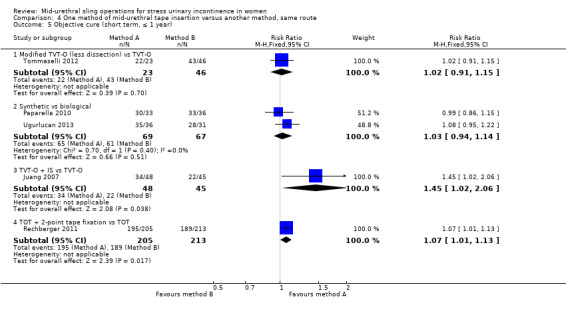
Comparison 4 One method of mid‐urethral tape insertion versus another method, same route, Outcome 5 Objective cure (short term, ≤ 1 year).
4.4. Analysis.
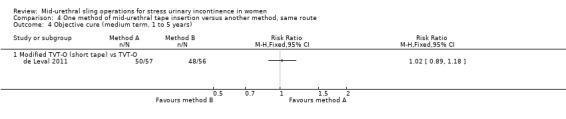
Comparison 4 One method of mid‐urethral tape insertion versus another method, same route, Outcome 4 Objective cure (medium term, 1 to 5 years).
4.6. Analysis.
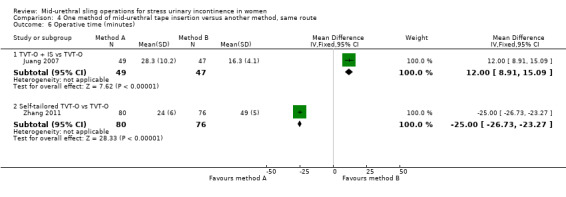
Comparison 4 One method of mid‐urethral tape insertion versus another method, same route, Outcome 6 Operative time (minutes).
4.7. Analysis.
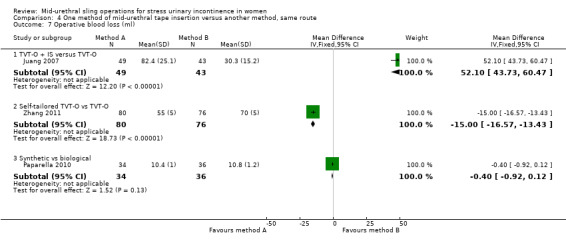
Comparison 4 One method of mid‐urethral tape insertion versus another method, same route, Outcome 7 Operative blood loss (ml).
4.8. Analysis.
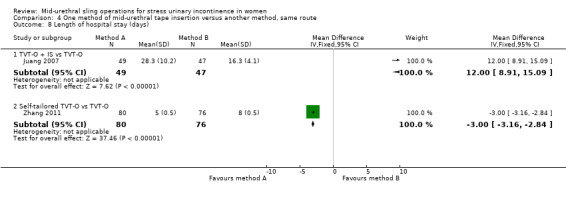
Comparison 4 One method of mid‐urethral tape insertion versus another method, same route, Outcome 8 Length of hospital stay (days).
4.10. Analysis.
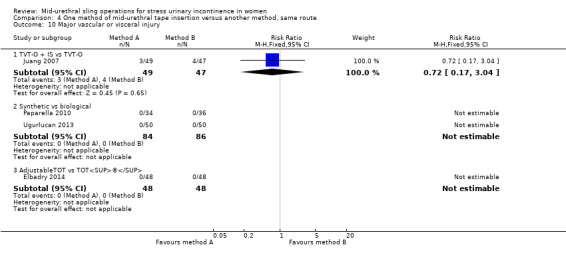
Comparison 4 One method of mid‐urethral tape insertion versus another method, same route, Outcome 10 Major vascular or visceral injury.
4.11. Analysis.
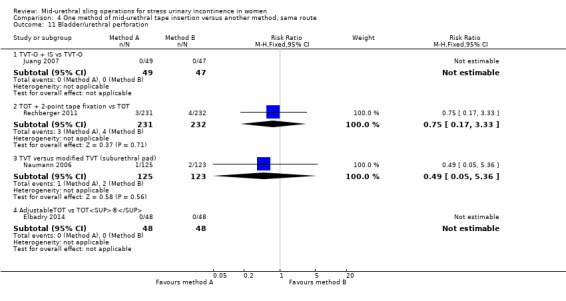
Comparison 4 One method of mid‐urethral tape insertion versus another method, same route, Outcome 11 Bladder/urethral perforation.
4.12. Analysis.
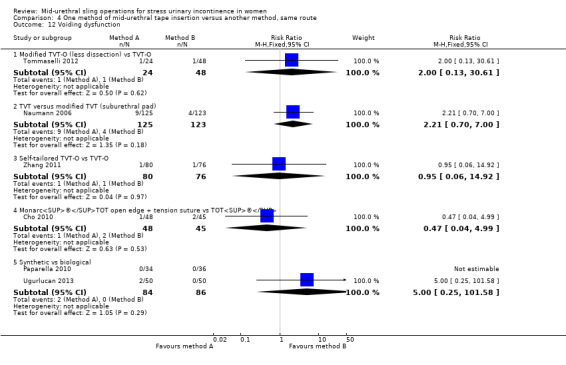
Comparison 4 One method of mid‐urethral tape insertion versus another method, same route, Outcome 12 Voiding dysfunction.
4.13. Analysis.
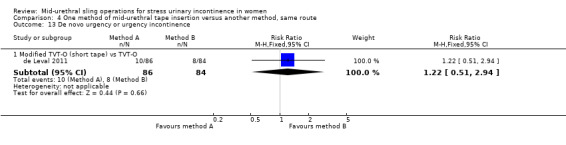
Comparison 4 One method of mid‐urethral tape insertion versus another method, same route, Outcome 13 De novo urgency or urgency incontinence.
4.14. Analysis.
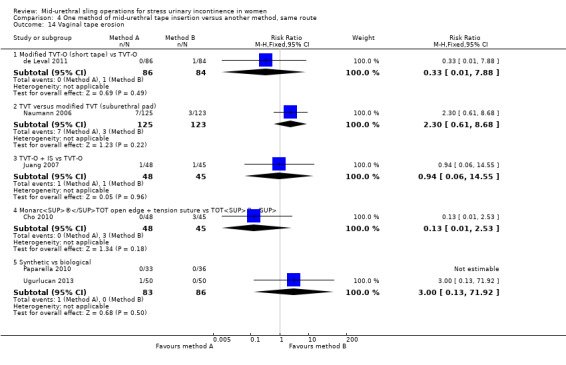
Comparison 4 One method of mid‐urethral tape insertion versus another method, same route, Outcome 14 Vaginal tape erosion.
4.15. Analysis.
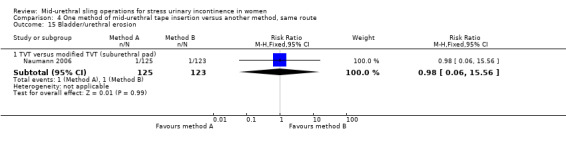
Comparison 4 One method of mid‐urethral tape insertion versus another method, same route, Outcome 15 Bladder/urethral erosion.
4.16. Analysis.
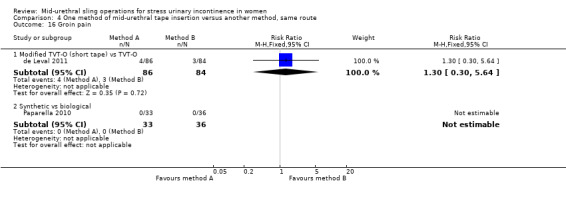
Comparison 4 One method of mid‐urethral tape insertion versus another method, same route, Outcome 16 Groin pain.
For all outcomes measured in each trial, there were no statistically significant differences reported, with the exception of Juang 2007, where significant differences were found in favour of TVT‐O plus Ingleman‐Sundberg bladder denervation procedure for objective cure, operative time and intraoperative blood loss. Objecture cure in the short term for synthetic versus biological TOT showed no significant difference (RR 1.03, 95% CI 0.94 to 1.14; 2 trials; Analysis 4.5.2)
Sexual function was assessed by Paparella 2010 and Tommaselli 2012 using the PISQ‐12. The PISQ‐12 scores decreased after the procedure in both groups, indicating improved sexual function after surgery. No significant differences were observed between groups after the procedures.
Comparison 5. One type of tape material versus another
Four trials compared different mid‐urethral sling operations based on their tape properties, e.g. monofilament tapes versus multifilament tapes (Lim 2005; Meschia 2006; Okulu 2013; Rechberger 2003). The interventions compared were:
monofilament (TVT SPARC) verus multifilament (IVS; Lim 2005);
monofilament (TVT) versus multifilament (IVS; Meschia 2006);
synthetic monofilament (prolene light mesh) versus combined synthetic and biological (Ultrapro mesh) versus multifilament mesh (Vypro; Okulu 2013);
monofilament (TVT) versus multifilament (IVS; Rechberger 2003).
5.1 Women's observations
In the short and medium term there was no statistically significant difference between monofilament and multifilament tapes in terms of their subjective cure rates; neither was there a significant difference found where the combined synthetic and biological tapes were compared to monofilament tapes (RR 1.03, 95% CI 0.95 to 1.10; RR 0.91, 95% CI 0.79 to 1.05; RR 1.10, 95% CI 0.96 to 1.26; Analysis 5.1: RR 1.03, 95% CI 0.85 to 1.23; RR 0.91, 95% CI 0.78 to 1.06; RR 1.13, 95% CI 0.96 to 1.32; Analysis 5.2).
5.1. Analysis.
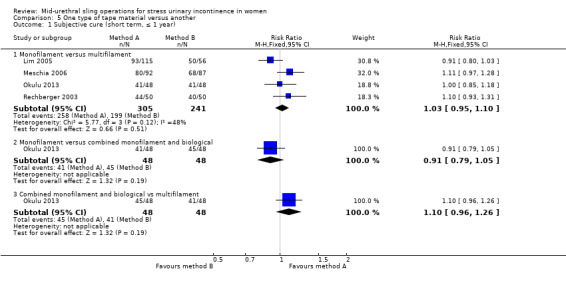
Comparison 5 One type of tape material versus another, Outcome 1 Subjective cure (short term, ≤ 1 year).
5.2. Analysis.
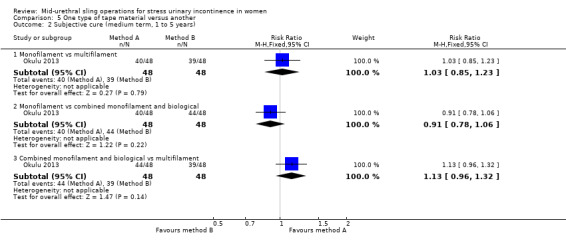
Comparison 5 One type of tape material versus another, Outcome 2 Subjective cure (medium term, 1 to 5 years).
5.2 Quantification of symptoms
No data were reported for this comparison.
5.3 Clinician's observation
The objective cure rate for monofilament tape and multifilament tapes show no significant difference between the groups (RR 1.07, 95% CI 0.96 to 1.19; Analysis 5.3).
5.3. Analysis.
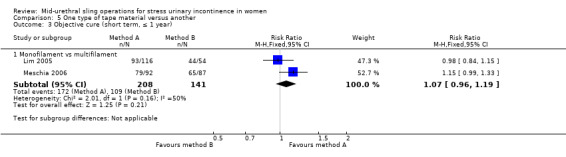
Comparison 5 One type of tape material versus another, Outcome 3 Objective cure (short term, ≤ 1 year).
5.4 Surgical outcome measures
There were no statistically significant differences in the duration of operation or length of hospital stay reported (RR 0.00, 95% CI ‐1.49 to 1.49; Analysis 5.4: RR 0.20, 95% CI ‐0.09 to 0.49; Analysis 5.5).
5.4. Analysis.
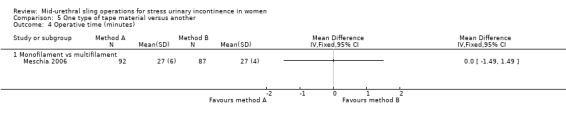
Comparison 5 One type of tape material versus another, Outcome 4 Operative time (minutes).
5.5. Analysis.
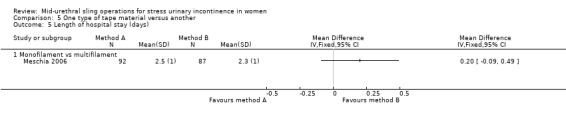
Comparison 5 One type of tape material versus another, Outcome 5 Length of hospital stay (days).
5.5 Adverse events
There were few perioperative complications with no statistically significant difference between the groups (RR 1.16, 95% CI 0.36 to 3.69; Analysis 5.6). No major vascular/visceral injury was reported in any of the trials (Analysis 5.7). Bladder perforation occurred in 4.49% of monofilament and 3.67% of multifilament tape procedures (RR 1.15, 95% CI 0.49 to 2.70; Analysis 5.8).
5.6. Analysis.
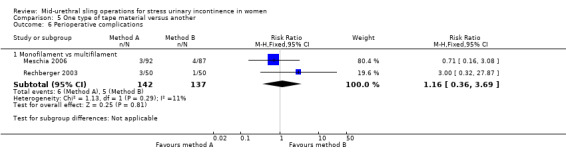
Comparison 5 One type of tape material versus another, Outcome 6 Perioperative complications.
5.7. Analysis.
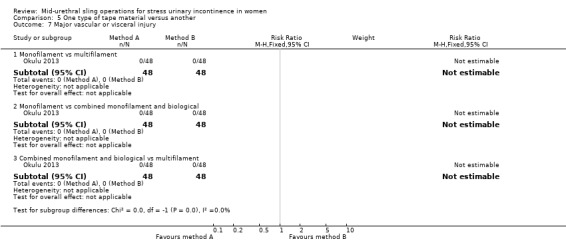
Comparison 5 One type of tape material versus another, Outcome 7 Major vascular or visceral injury.
5.8. Analysis.
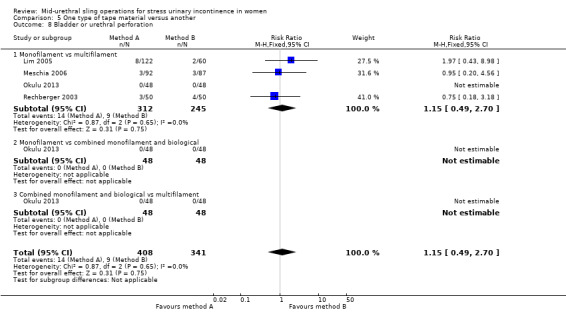
Comparison 5 One type of tape material versus another, Outcome 8 Bladder or urethral perforation.
There were no statistically significant differences between the groups for:
POVD (RR 2.10, 95% CI 0.96 to 4.59; Analysis 5.9);
de novo urgency symptoms and UUI (RR 1.11, 95% CI 0.68 to 1.82; Analysis 5.10);
DO (RR 0.70, 95% CI 0.12 to 4.06; Analysis 5.11).
5.9. Analysis.
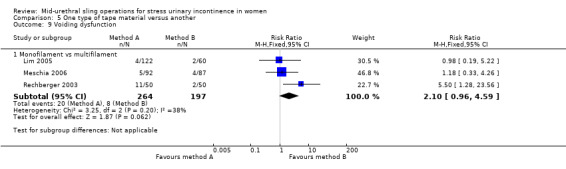
Comparison 5 One type of tape material versus another, Outcome 9 Voiding dysfunction.
5.10. Analysis.
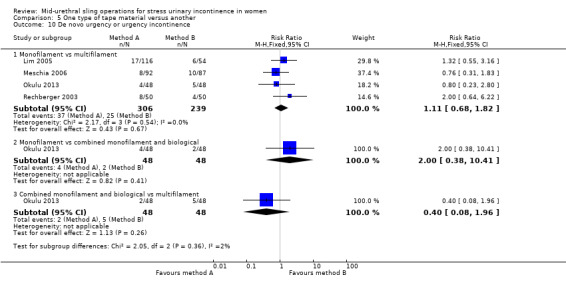
Comparison 5 One type of tape material versus another, Outcome 10 De novo urgency or urgency incontinence.
5.11. Analysis.
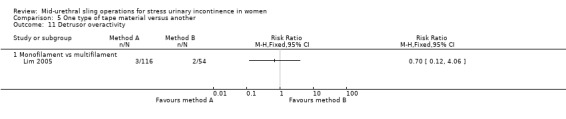
Comparison 5 One type of tape material versus another, Outcome 11 Detrusor overactivity.
In three trials, vaginal tape erosions were more common in the multifilament group, but this did not reach statistical significance (RR 0.79, 95% CI 0.09 to 6.84; Analysis 5.12).
5.12. Analysis.
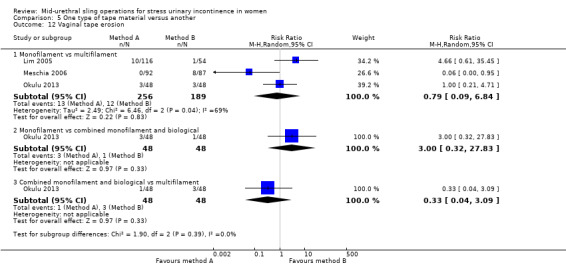
Comparison 5 One type of tape material versus another, Outcome 12 Vaginal tape erosion.
5.6 Need for further treatment
No data were reported regarding the need for further treatment in this comparison.
5.7 Quality of life
Only the Okulu 2013 study assessed QoL and showed improvement from baseline scores, with no significant difference between the comparison groups. At 48 months mean postoperative ICI‐Q QoL scores were significantly better in the monofilament group than in the multifilament group (MD ‐0.06, 95% CI ‐0.76 to ‐0.44; 1 study, 96 women; Analysis 5.13).
5.13. Analysis.

Comparison 5 One type of tape material versus another, Outcome 13 QoL specific (ICIQ).
Discussion
Summary of main results
1. Transobturator (TOR) versus retropubic route (RPR)
Comparison of the transobturator (TOR) versus retropubic route (RPR) was addressed by 55 trials that included 8652 women. Thirty‐six of these trials (5514 women) contributed data to the primary outcome of subjective cure, which showed that in the short term there was no difference between TOR and RPR. Only six of these 53 trials reported medium‐ or long‐term data, again with relatively small numbers of women showing no significant difference in symptomatic cure. These small numbers limit the judgements that can be made about cure rates in the longer term for both the efficacy of individual tapes, or for comparison of the route of tape insertion. There was potential for at least 22 of these trials to have published either medium‐ or longer‐term outcomes, given their dates of publication. Similarly, objective cure rates showed no significant difference between the two routes.
Evidence from 40 trials (6372 women) showed a 30 fold percentage increase in the rate of bladder perforation with the RPR approach compared to the TOR approach. In practice, for this reason, some clinicians favour the TOR for patients at higher risk of bladder/urethral perforation, for example, those who have had previous pelvic or incontinence surgery. Similarly, 37 trials (6217 women) that assessed postoperative voiding dysfunction (POVD) showed this adverse outcome to be significantly less frequent when the TOR was employed. However, the reported sequale for both of these outcomes is usually of short duration.
Thirty‐one trials (4743 women) that assessed vaginal tape erosion showed no significant difference when either route was used. More women experienced groin pain in the TOR group than in the RPR group. This groin pain was usually of short duration and resolved within eight weeks in most cases. The occurrence of suprapubic pain following an RPR procedure was poorly reported. This was more common in the RPR group; however, when data was provided, only a minority of women suffered this symptom and for a short period of time.
Overall mid‐urethral slings are a highly effective treatment for stress urinary incontinence (SUI). In the short term there is equivalence in the efficacy between the two routes, and this persists into the medium and longer term, though the data for this is somewhat limited by small numbers. There is some evidence that suggests women are more likely to require repeat incontinence surgery in the longer term with the TOR, but this requires cautious interpretation, as there are extremely small numbers. There is an equal improvement in the overall quality of life of women for both routes. Sexual function improved in both groups as a result of the surgery, most probably from reduction in coital incontinence, with no significant difference in sexual function between the two groups.
To supplement the main systematic review of effects, we sought to identify economic evaluations which have compared TOR with RPR in the treatment of SUI in women. A supplementary search in Ovid MEDLINE, Embase and NHS EED, identified three economic evaluations (Lier 2011; Lier 2016; Seklehner 2014). The search strategies used are given in Appendix 3. Lier 2016 reported both a cost‐utility and cost‐effectiveness analysis while Lier 2011 was a cost‐effectiveness analysis. Both studies analysed costs and resources used from public payer perspective (Alberta, Canada) and used clinical data from the same RCT (Ross 2009) with results presented at one year (Lier 2011) and five years (Lier 2016) post‐surgery. Seklehner 2014 reported a decision model based cost‐effectiveness analysis with clinical evidence collected from MEDLINE search of RCTs on TOR and RPR. This study adopted a US healthcare system perspective with a 10‐year time horizon. Lier 2016, which was a further follow‐up of Lier 2011, reported that TOR was slightly more effective than RPR with a mean QALY gain of 0.04 over five years (95% Cl ‐0.06 to 0.14). Seklehner 2014 reported that on average TOR was slightly more effective, with a QALY gain of 0.03 over 10 years. Both Lier 2016 and Lier 2011 reported no statistically significant difference in the cure rate (81% for TOR versus 77% for RPR, P value not stated) but there was a significant difference in the number of patients in the TOR arm with groin pain and palpation of the surgical tape on vaginal examination (26% difference, P = 0.001) even after five years (Lier 2016). In all three studies TOR was less costly in when compared with RPR (Lier 2011; Lier 2016; Seklehner 2014). In Lier 2016, TOR was on average less costly, with an average total cost difference which rose from CAD ‐414 (95% Cl ‐1415 to 587) (Lier 2011) to CAD ‐2368 (95% Cl ‐7166 to 2548) at five years (2011 Canadian dollars). In Seklehner 2014 the average cost difference was CAD ‐562 (Cl not stated).The three studies each suggested that TOR may be cost‐effective.
2. Retropubic bottom‐to‐top approach versus retropubic top‐to‐bottom approach
Five trials with 636 women compared the retropubic bottom‐to‐top with the retropubic top‐to‐bottom approach. These showed that passage of the tape through the retropubic route in a bottom‐to‐top path (e.g. TVTTM) was more effective than passage in a top‐to‐bottom path (e.g. SPARCTM), and resulted in fewer intra and postoperative adverse events.We took the same approach for TOR versus RPR to identify economic evaluations, but found no results.
3. Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach
Ten trials with 1199 women compared the obturator medial‐to‐lateral approach with the obturator lateral‐to‐medial approach. Evidence from the ten trials, two of which reported medium‐term data, showed no difference between the two approaches with respect to most outcomes measured. The only exceptions were voiding dysfunction, where higher rates were reported in the medial‐to‐lateral group, and vaginal perforation, which had higher rates in the lateral‐to‐medial group. Despite this, there was no resultant increase in the rate of tape erosion. It is, therefore, not unreasonable to exercise operator preference when deciding which of these two approaches to adopt. Notably, each route improved quality of life and sexual function postoperatively. We took the same approach for TOR versus RPR to identify economic evaluations, but found no results.
4. One method of mid‐urethral tape insertion versus another method, same route
Ten trials with 1569 women compared one method of mid‐urethral tape insertion with another using the same route. Despite several design or procedural modifications to tapes traversing the same route, there was no difference in the efficacy, surgical outcomes or occurrence of adverse events.The same approach done for TOR versus RPR was carried out to identify economic evaluations but yielded no result.
5. One type of tape material versus another
Four trials with 505 women compared monofilament tapes with multifilament tapes. There was no statistical difference in physician‐observed cure rates or patient‐reported cure between the groups. There was no significant difference in the rate of vaginal tape erosion. We took the same approach for TOR versus RPR to identify economic evaluations, but found no results.
Overall completeness and applicability of evidence
Many of the trials contributing to this review did provide evidence regarding the primary outcome, which was to determine the effectiveness of mid‐urethral sling operations in the treatment of urinary incontinence. They confirm that mid‐urethral sling operations for SUI are an effective surgical treatment available in current practice. A major limitation was the variable quality of many of the trials.
We did not attempt to analyse the data by subgroups according to the clinical characteristics of the women, such as symptoms of SUI, urodynamic stress incontinence, diagnosis of intrinsic urethral sphincter deficiency or urethral hypermobility, obesity, previous incontinence surgery, presence or absence of prolapse, anaesthesia used, or experience of the surgeon. In fact the majority of trials did not describe these characteristics of the women.
We did not subject the three identified economic evaluations to critical appraisal and we do not attempt to draw any firm or general conclusions about the relative costs or efficiency of TOR for treatment of SUI. However, the economic evidence available suggests that TOR is cost‐effective when compared with RPR in the treatment of SUI in women.
Complications
Major complications such as nerve, bowel or major vascular injuries, pelvic haematoma, necrotizing fasciitis, ischiorectal abscess and death are uncommon and unlikely to be picked up by small randomised controlled trials (RCTs). There is potential to determine a more accurate incidence from large national registries and voluntary reporting registries or databases for reporting complications, such as the United States Food and Drug Administration's (FDA) manufacturer and user facility device experience (MAUDE). One must bear in mind, though, the limitations of this method. Several of these registries have reported their findings (Collinet 2008; Dyrkorn 2010; Kuuva 2002; Koops 2005; Tamussino 2001; Tamussino 2007; Tincello 2011).
Retropubic tapes
From the above list of registries, for tension‐free vaginal tape the number of procedures reported ranged from 809 to 4281, and there were found to be low rates of major complications.
Bladder perforation occurred in 2.7% to 3.9% of cases.
Reoperation rates relating to tape insertion or postoperative voiding dysfunction (POVD) ranged from 1.6% to 2.4%.
Urinary retention rate was 1.6%.
Pelvic haematoma occurred in 0.7% to 1.9% of women.
Infection rate was 0.7%.
Vaginal tape erosion/extrusion rate was 1.5%.
Groin pain occurred in 0.4% of women.
These rates are largely of the same order as those reported in the trials included in this review. There were also a few cases of major visceral injuries such as bowel and urethral injuries.
Transobturator tapes
Registries of transobturator tapes reported much lower rates of complications.
Bladder perforation occurred in 0.4% of cases.
Reoperation rates relating to tape insertion ranged from 0.8% to 2.2%.
Urinary retention rate was 0.5%.
Pelvic haematoma occurred in 0.5% of women.
Infection rate was 0.6%.
Vaginal tape erosion/extrusion rate was 0.4%.
Groin pain occurred in 1.6% of women.
The FDA received 1876 reports of complications associated with the use of slings for SUI in the period between 1 January 2008 to 30 September 2011. The most common complications reported were pain, vaginal tape erosion (exposure, extrusion or protrusion), infection, urinary problems, recurrent incontinence, pain during sexual intercourse (dyspareunia), bleeding, organ perforation, neuro‐muscular problems and vaginal scarring. Many of these complications required further medical intervention, and sometimes required surgical treatment or hospitalisation, or both. With the exception of tape erosion, the above complications were also found to occur following non‐mesh surgical repairs for SUI. It should be borne in mind that this sort of reporting system is a passive surveillance system limited by the inclusion of the potential submission of incomplete or inaccurate data, under‐reporting of events, lack of denominator data (number of tapes), and the lack of report timeliness.
It should be noted that the latest FDA white paper and safety communications on meshes released in 2011 ‐ unlike the previous 2008 release (FDA 2008) ‐ relates to ongoing concern with mesh used to treat pelvic organ prolapse (POP) and not the small strip of mesh/tape/sling used to treat SUI (FDA 2011a; FDA 2011b). In fact the FDA states that the safety and effectiveness of mid‐urethral slings is well established in clinical trials with 1‐year follow‐up (FDA 2013).
Equally, because of the increasing numbers of adverse events and patient concerns reported, in 2012 the Medicines and Healthcare Products and Regulatory Agency (MHRA) in Europe published a commissioned report on the most frequently reported adverse events associated with different meshes/tapes/slings (MHRA 2012). The report showed that for the treatment of SUI the rate of vaginal tape erosion was low, at between 1.1% to 2.5%. Even in a selected cohort of women presenting primarily with adverse events of mesh, those with mid‐urethral sling were significantly less likely to present with mesh erosions than those who had mesh for POP repair. Presentation of mesh erosion following SUI treatment is less severe, and less likely to require surgical treatment under general anaesthesia than erosion following mesh insertion for POP repair. This relates to complication classification severity grade 4 (Abbott 2014; Strasberg 2009).
In their 2014 report, the MHRA concluded that from the review of the information available, there appeared to be no evidence that vaginal mesh implants for SUI are unsafe, nor was there evidence to justify MHRA taking enforcement action to take them off the market, or remove them from use. The report concluded that the overall benefit outweighed the relatively low rate of complications (MHRA 2014).
Although the number of adverse events was generally low and they were rarely serious, it is recognised that the ability of RCTs to identify rarer adverse effects is poor. With the increasing popularity of MUS procedures the occurrence of complications in the short term is well established, but in general these are easily treated or resolve spontaneously. However, because few trialists have carried out long‐term follow‐up, there is very little information about whether there is a hidden cache of serious adverse effects that might be set against the benefits of curing incontinence.
Longer‐term outcomes after MUS
Observational studies of MUS show data confirming effectiveness in the long term with some data that cover 15 to 17 years (Aigmueller 2011; Athanasiou 2014; Heinonen 2013; Nilsson 2013; Serati 2012; Serati 2013; Svenningsen 2013a; Svenningsen 2013b). These trials of MUS, like similar observational studies for open colposuspension, show a decline in effectiveness that is time‐dependent, and also reveal high rates of de novo urgency symptoms (15%) and voiding difficulties (23%). It is difficult to elucidate the reasons for these long‐term symptoms, but they could be age related, or due to new pathology, or a true consequence of the surgery. Nevertheless, they emphasise the need for longer‐term data from RCTs to help counsel women appropriately.
With regard to long‐term data from RCTs, there is a paucity of trials that reported longer‐term outcomes and most long‐term data reported for both open colposuspension and MUS are for five to six years. If evidence from RCTs mirrors that from observational studies, we will not only require the many RCTs that have been published for MUS to report their longer‐term data, but will in fact need to follow these women up for at least 10 to 15 years. This would allow us to discover whether there is a time‐dependent decline in effectiveness, and enable us to elucidate the development in the long term of new adverse effects.
Comparisons with other methods of continence surgery
'Gold standard' surgical treatment for stress urinary incontinence (SUI)
Open abdominal retropubic colposuspension used to be considered the gold standard treatment for SUI. It is noteworthy that there are no randomised controlled trials of open colposuspension versus no treatment. Two small trials that compared open colposuspension with conservative treatment were unreliable because of very small numbers of participant and a high risk of bias (Lapitan 2012). Equaliy the evidence for MUS versus no treatment or conservative treatment is limited and we will be addressing this in a future Cochrane review.
Our initial review showed the effectiveness of MUS in the short term and, as time has moved on, it was hoped that with reports of long‐term data it would become clear whether long‐term efficacy of MUS could be compared with that of open retropubic colposuspension. A Cochrane review of open retropubic colposuspension identified 15 RCTs that compared the mid‐urethral sling operations (12 RPR and three TOR) with colposuspension (Lapitan 2012). This review concluded that there was no significant difference in incontinence rates between the two procedures for all time periods assessed. Both procedures led to improvement in the quality of life of women. While some complications, such as bladder perforation, were reported more with MUS, the numbers were small. Other complications such as POVD, which were reported to be higher with MUS, were influenced by a large trial that reported no risk of voiding difficulties at all after colposuspension, but consistent data from TVT trials showed no significant difference in the risk of voiding dysfunction between MUS and colposuspension. MUS had a shorter operating time, length of hospital stay and cost. Only one RCT that compared MUS with open colposuspension has reported results for a five‐year follow‐up, and it failed to detect significant difference between the success rates of MUS and colposuspension. It also showed that the effect on cure of incontinence and improvement in quality of life was maintained for both procedures at five years (Ward 2008).
Observational data for open colposuspension with follow‐up of 10 to 20 years show high rates of effectiveness in the long term (Alcalay 1995; Kjolhede 2005; Brubaker 2012). This long‐term cure is shown to be time‐dependent with cure rates plateauing at about 69% at 10 to 12 years. In addition some reports show continence rates of only 44% at 14 years, with high rates of voiding difficulties (of 36%) at 14‐year follow‐up.
Mid‐urethral sling operations versus traditional slings
Historically, traditional suburethral sling procedures were used for women who had recurrent stress incontinence (after a previous failed continence operation). However, the review did not report the results separately for women with new or recurrent incontinence (Rehman 2011). These procedures were designed to restore normal urethrovesical junction support by mechanical compression or kinking of the proximal urethra.
Minimally invasive synthetic suburethral slings appeared to be as effective as traditional suburethral slings in short‐term incontinence rates (RR 0.97; 95% CI 0.78 to 1.20), although the confidence interval is compatible with minimally invasive slings being 20% better or 12% worse. The operating time and length of stay were also significantly shorter with minimally invasive synthetic suburethral sling operations, and women had fewer perioperative complications and less detrusor overactivity.
Mid‐urethral sling operations versus open retropubic colposuspension
Although 14 RCTs were found that compared TVT operations with colposuspension (Lapitan 2012), data from five of them showed no clear differences in the short‐ or medium‐term chance of incontinence compared with open colposuspension. While there were more complications after the sling operations, the numbers were small.
Mid‐urethral sling operations versus laparoscopic colposuspension
Another Cochrane review identified eight trials that compared mid‐urethral sling operations to laparoscopic colposuspension (Dean 2006). Overall, the review showed that the subjective cure rates were similar for both of these minimal access techniques in the short term, while operation times were shorter for the slings. Long‐term data are lacking, however.
Mid‐urethral sling operations versus single incision slings
Single‐incision slings compared with retropubic mid‐urethral slings
Women were twice as likely to be incontinent after a single‐incision sling as after a retropubic TVT (RR 2.08, 95% CI 1.04 to 4.14; Nambiar 2014), although the surgery took less time to perform. However, this finding mostly related to one type of single‐incision sling (TVT‐Secur), which has now been withdrawn from the market due to this lack of efficacy.
Single‐incision slings compared with transobturator mid‐urethral slings
Women were twice as likely to be incontinent after a single‐incision sling procedure as after a transobturator sling procedure (RR 1.91, 95% CI 1.53 to 2.39; Nambiar 2014). In addition, they were more likely to need a further operation for complications or repeat surgery for their incontinence. However, the risks of postoperative pain and long‐term pain were slightly higher with transobturator slings.
For the economic evidence, two cost‐effectiveness analyses also compared single‐incision mini‐slings with transobturator mid‐urethral slings. These adopted the perspective of the Spanish (Castañeda 2014) and UK healthcare systems (Boyers 2013) respectively. Boyers 2013 used clinical evidence from a prospective RCT (Mostafa 2012), while Castañeda 2014 used evidence from a retrospective observational study, using a one‐year follow‐up in both cases. Both studies reported no statistically significant differences in the clinical outcomes: 6.7% difference, 95% Cl ‐6.6 to 20.0, P = 0.527 (Castañeda 2014); 5% difference, 95% Cl 0.38 to 2.26, P = 1.000 (Boyers 2013), and also no statistically significant differences in intraoperative complications: P = 0.023 (Boyers 2013); P = 0.553 (Castañeda 2014). Boyers 2013 also reported the impact on health‐related quality of life reported as quality adjusted life years (QALYs). There was no significant difference in QALYs (mean difference ‐0.003, 95% Cl ‐0.008 to 0.002) (Boyers 2013).However, in the single‐incision sling arm, there were statistically significant improved postoperative pain scores up to four weeks with a pain score of zero compared with mid‐urethral slings with a total pain score of two (P < 0.001, 95% Cl 1.245 to 1.853). There was also a statistically significant one day earlier return to normal activities with single‐incision slings (P = 0.025, 95% Cl 6.1 to 9.4 days) (Boyers 2013) and less repeated urinary tract infections (Castañeda 2014). Single‐incision mini‐slings were less costly in both studies. The mean total direct cost of single‐incision mini‐sling in Boyers 2013 was GBP 1277 (2011 GBP) while that of transobturator sling procedure was GBP 1462 (2011 GBP), with a 94% probability (95% Cl GBP ‐316.99 to GBP 32.17) of being cost‐saving compared to the transobturator sling procedure, irrespective of whether single‐incision mini‐slings were performed under local or general anaesthesia. In Castañeda 2014, the average cost of single‐incision mini‐slings (2013 euro) was EUR 2059 (95% Cl 1914 to 2285), while the cost of the transobturator sling procedure was EUR 2821 (95% Cl 2661 to 2997). There was a 100% probability of single‐incision mini‐slings being cost‐saving. Both studies (Boyers 2013; Castañeda 2014) suggested that the transobturator sling procedure is less cost‐effective when compared with mini‐sling based on comparative effectiveness of both interventions and lower costs associated with single‐incision mini‐slings.
Mid‐urethral sling operations versus anterior repair
To date, no trials have been identified that compared the original operation for SUI, anterior repair (with urethral buttressing sutures, or Kelly sutures) directly to mid‐urethral slings (Glazener 2001). However, in the current climate of concern about adverse effects from the use of synthetic mesh or tape materials, perhaps it is time to reassess the value of this operation, not least because of its additional role in the management of prolapse.
Quality of the evidence
We judged the quality of evidence using the GRADE classification as moderate for the majority of outcomes. The remaining outcomes assessed were low level evidence. The main reason for the decrease in the quality of evidence for many outcomes was a high risk of bias where allocation concealment or random sequence generation were deemed uncertain. Imprecision of effects estimates also contributed to the variable quality of evidence in some outcomes.
In the main comparison between TOR and RPR, the quality of evidence for most outcomes was moderate. The downgrade from high quality to moderate quality evidence was mainly because of a small proportion of trials in which there was a high risk of bias from either study design or implementation, which then reduced our confidence in the estimates of effects.
Potential biases in the review process
GRADE‐specific outcomes were selected at the time of the original review. These have been modified for this update. There is potential for introduction of bias, as ideally these GRADE‐specific outcomes should have been selected at the time of the protocol, and there would have been consistency between the outcomes selected in the original review and in the update.
Authors' conclusions
Implications for practice.
Mid‐urethral sling operations are now widely accepted as a routine surgical treatment for stress urinary incontinence (SUI). This review has identified evidence that addresses the comparative effects of different ways of inserting tapes, including different insertion routes, surgical approaches and tapes.
Irrespective of the routes traversed, these procedures are highly effective in the short and medium term and mounting evidence demonstrates their effectiveness in the long term.
There is low to moderate quality evidence that retropubic tapes and transobturator tapes have comparable effects on cure of incontinence between one and five years, and limited evidence for the same in the long term. With the exception of a two‐fold increase in the incidence of groin pain, transobturator tapes have fewer adverse events. Retropubic tapes have an eight‐fold increase in the incidence of bladder perforation and a two‐fold increase in the incidence of post operative voiding difficulties. Although women's outcomes for quality of life and sexual function improved significantly after all surgical approaches, our analyses could not establish whether there was any difference between retropubic and transobturator tapes. Evidence for longer‐term effects is required to evaluate the need for further surgery following either approach.
There was moderate quality evidence that when a retropubic route (RTR) is employed a bottom‐to‐top approach is more effective in terms of subjective cure than a top‐to‐bottom approach. When traversing the transobturator route (TOR), there was moderate quality evidence showing that medial‐to‐lateral ('inside‐out') and lateral‐to‐medial ('outside‐in') approaches have similar effects.
Implications for research.
Many trials have evaluated the use of mid‐urethral tapes in the short term. However, the long‐term effects of surgery, and how the different insertion routes affect long‐term outcome, have not been established. It is unfortunate that although 35 of the 81 trials included should be in a position to report their long‐term data (i.e. over five years), only three have done so. More of the trials included in this review should publish the results of their longer‐term follow‐up to increase the robustness of evidence supporting the use of mid‐urethral sling (MUS) in the long term, to provide answers about the long‐term adverse events of these operations, including whether there is a significant decline in the effectiveness of these procedures over time, and to identify the point at which decline becomes significant enough to require women to need repeat procedures.
More research is required into trials assessing the clinical effectiveness of different routes (RPR or TOR) in women with urodynamic stress incontinence where hypermobility is differentiated from intrinsic urethral sphincter deficiency, as data for most of the outcomes are sparse. Equally, trials assessing the effectiveness of RPR or TOR in a cohort of women presenting with recurrent SUI after a failed MUS procedure are needed. More adequately powered trials are needed to address the issue of MUS in women who also have symptomatic or asymptomatic pelvic organ prolapse, as presently it is unclear whether concomitant pelvic organ prolapse surgery is necessary, and, if performed, whether it enhances or detracts from the effectiveness of the MUS. Conversely, there is only indirect evidence to suggest that MUS are more effective than anterior repair, as no RCTs have compared them directly.
Future randomised controlled trials should be robustly designed to be of good quality and adequately powered with standardised woman‐reported (subjective) outcome measures and objective outcomes. When reporting, these trials should follow the CONSORT guidelines (Moher 2001; Schulz 2010). There needs to be long‐term follow‐up and adequate reporting of adverse effects. It is essential that outcomes relevant to both women and policy makers who commission treatments are incorporated into these trials. In particular, quality of life, sexual function and economic implications should be assessed.
What's new
| Date | Event | Description |
|---|---|---|
| 10 July 2017 | Amended | Brief economic commentary (BEC) added. Economics related sections revised: the Abstract, Plain language summary, Background, Methods (outcomes, search methods), and Discussion were amended. Appendix added with details of search strategies for BECs. |
| 10 July 2017 | New citation required but conclusions have not changed | Brief economic commentary (BEC) added. Economics‐related sections revised. |
History
Protocol first published: Issue 1, 2007 Review first published: Issue 4, 2009
Acknowledgements
We thank Sheila Wallace for all her help and also for conducting the literature search.
We thank Dr Muhammad Imran Omar and Professor Cathryn Glazener for their input and help with arbitration of disagreements.
We also thank Dr Michaela Weingarten who assisted us in the translation of non‐English manuscripts.
We would like to thank Dr Carlos Bezerra and Dr Mauricio S Plata for their contribution to the original protocol.
Appendices
Appendix 1. Searches performed for the 2014 version of this review
Cochrane Incontinence Group Specialised Register
The terms used to search the Incontinence Group Specialised Register 26 June 2014 are given below:
(TOPIC.URINE.INCON*) AND ({DESIGN.CCT*} OR {DESIGN.RCT*}) AND {INTVENT.SURG.SLIN*} OR {INTVENT.SURG.SUBURETHRAL SLING.} OR {INTVENT.SURG.ABDO.SLING.} (All searches were of the keyword field of Reference Manager 2012.)
Embase and Embase Classic (on OVID SP) was searched from 1947 to Week 25 20014 on 26 June 2014 and was limited to those years not fully covered by the Embase search for CENTRAL carried out by the Cochrane Collaboration. Limited to: (2010* to 2014*).em. The following search strategy was used:
1. Randomized Controlled Trial/
2. crossover procedure/ or double blind procedure/ or parallel design/ or single blind procedure/
3. Placebo/
4. placebo$.tw,ot.
5. random$.tw,ot.
6. ((singl$ or doubl$ or trebl$ or tripl$) adj25 (blind$ or mask$)).tw,ot.
7. crossover.tw,ot.
8. cross over$.tw,ot.
9. allocat$.tw,ot.
10. trial.ti.
11. parallel design/
12. triple blind procedure/
13. or/1‐12
14. exp animals/ or exp invertebrate/ or animal experiment/ or animal model/ or animal tissue/ or animal cell/
15. exp human/ or exp "human tissue, cells or cell components"/
16. 14 and 15
17. 14 not 16
18. 13 not 17
19. incontinence/ or mixed incontinence/ or stress incontinence/ or urge incontinence/ or urine incontinence/
20. continence/
21. overactive bladder/
22. micturition disorder/ or lower urinary tract symptom/ or pollakisuria/
23. urinary dysfunction/ or bladder instability/ or detrusor dyssynergia/ or neurogenic bladder/ or urinary urgency/ or urine extravasation/
24. (incontinen$ or continen$).tw.
25. ((bladder or detrusor or vesic$) adj5 (instab$ or stab$ or unstab* or irritab$ or hyperreflexi$ or dys?ynerg$ or dyskinesi$ or irritat$)).tw.
26. (urin$ adj2 leak$).tw.
27. ((bladder or detrusor or vesic$) adj2 (hyper$ or overactiv$)).tw.
28. (bladder$ adj2 (neuropath$ or neurogen* or neurolog$)).tw.
29. (nervous adj pollakisur$).tw.
30. or/19‐29
31. (tape* or sling*).tw.
32. 18 and 30 and 31
33. (2010* or 2011* or 2012* or 2013* or 2014*).em.
34. 32 and 33
WHO ICTRP (on http://www.who.int/ictrp/en/) was searched on 30 June 2014 using the following search string: Continent OR continence OR incontinent OR incontinence AND tape* OR sling* AND random*
Appendix 2. Search terms for the first version of this review published in 2009
The terms that we used to search the Incontinence Group Specialised Register are given below: (TOPIC.URINE.INCON*) AND ({DESIGN.CCT*} OR {DESIGN.RCT*}) AND {INTVENT.SURG.SLIN*} OR {INTVENT.SURG.SUBURETHRAL SLING.} OR {INTVENT.SURG.ABDO.SLING.} (All searches were of the keyword field of Reference Manager 9.5 N, ISI ResearchSoft). Date of last search: 20 March 2008.
The review authors also searched MEDLINE (January 1950 to April 2008), EMBASE (January 1988 to April 2008), CINAHL (January 1982 to April 2008), and AMED (January 1985 to April 2008) on 28 April 2008.
The following terms were used to search these electronic databases:
(Urinary incontinence OR urodynamic stress incontinence OR urgency urinary incontinence OR urge incontinence urinary)
AND
(suburethral slings OR tension free vaginal tape OR tvt OR transvaginal tape OR transobturator tape OR tot OR tvt‐o OR ivs OR uretrex OR safyre OR I‐stop OR sparc OR lynx OR monarc OR obtryx OR obtape OR aris)
The review authors also searched the UK National Research Register and ClinicalTrials.gov on 28 April 2008 using the term: urinary incontinence.
Appendix 3. Search strategies for brief economic commentary
We performed additional searches for the Brief Economic Commentary (BECs). These were conducted in MEDLINE(1 January 1946 to March 2017), Embase (1 January 1980 to 2017 Week 12) and NHS EED (1st Quarter 2016). All searches were conducted on 6 April 2017. We used two different search strategies on MEDLINE and EMBASE (OvidSP) and one on NHS EED (OVID). Details of the searches run and the search terms used can be found below. There were no year, publication type or language restrictions applied.
NHS EED (Ovid) (1st Quarter 2016)
NHS EED was searched using the following search strategy:
1. Urinary incontinence/
2. Urinary incontinence, stress/
3. ((stress$ or mix$ or urg$ or urin$) adj3 incontinen$).tw.
4. Colporrhaphy.tw.
5. Colpoperineoplast$.tw.
6. Sling procedure$.tw.
7. Sling$ procedure$.tw.
8. Bladder neck needle suspension$.tw.
9. Anterior vaginal repair$ .tw.
10. Or/1‐9
MEDLINE (1 January 1946 to March 2017) and Embase (1 January 1980 to 2017 Week 12)
We used two different search strategies on MEDLINE and Embase (OvidSP) ‐ these are given below.
Search strategy 1:
1. Economics, Pharmaceutical/ or Economics, Medical/ or Economics/ or Economics, Hospital/ or economics.mp. or Economics, Nursing/
2. exp "costs and cost analysis"/
3. "Value of Life"/
4. exp "fees and charges"/
5. exp budgets/
6. budget*.ti,ab.
7. cost*.ti.
8. (economic* or pharmaco?economic*).ti.
9. (price* or pricing*).ti,ab.
10. (cost* adj2 (effective* or utilit* or benefit* or minimi* or unit* or estimat* or variable*)).ab.
11. (financ* or fee or fees).ti,ab.
12. (value adj2 (money or monetary)).ti,ab.
13. ((energy or oxygen) adj cost).ti,ab.
14. (metabolic adj cost).ti,ab.
15. ((energy or oxygen) adj expenditure).ti,ab.
16. 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15
17. exp Urinary Incontinence/
18. ((stress* or mix* or urg* or urin*) adj3 incontinen*).tw.
19. Urodynamics/ or Urinary Incontinence, Stress/ or Urinary Incontinence/ or Suburethral Slings/ or mixed incontinence.mp. or Urinary Bladder/ or Urinary Incontinence, Urge/
20. 17 or 18 or 19
21. anterior vaginal repair*.tw.
22. 16 and 20 and 21
23. anterior colporrhaphy*.tw.
24. 21 or 23
25. 16 and 20 and 23
26. bladder neck needle suspension$.tw.
27. 16 and 20
28. 26 and 27
29. open abdominal retropubic colposuspension*.tw.
30. retropubic colposuspension*.tw.
31. burch colposuspension*.tw.
32. 29 or 30 or 31
33. 27 and 32
34. laparoscopic retropubic colposuspension*.tw.
35. laparoscopic colposuspension*.tw.
36. 34 or 35
37. 27 and 36
38. traditional suburethral retropubic sling procedure$*.tw.
39. traditional sling procedure$*.tw.
40. suburethral retropubic sling procedure$*.tw.
41. retropubic sling procedure$*.tw.
42. traditional suburethral sling*.tw.
43. Suburethral Slings/ or Urinary Incontinence, Stress/ or Urologic Surgical Procedures/
44. 27 and 43
45. remove duplicates from 44
Search strategy 2:
1. economics.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, fs]
2. value of life.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, fs]
3. exp "costs and cost analysis"/
4. exp economics, hospital/
5. exp economics, medical/
6. economics, nursing.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, fs]
7. economics, pharmaceutical.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, fs]
8. exp "fees and charges"/
9. exp budgets/
10. budget*.ti,ab.
11. cost*.ti.
12. (economic* or pharmaco?economic*).ti.
13. (price* or pricing*).ti,ab.
14. (cost* adj2 (effective* or utilit* or benefit* or minimi* or unit* or estimat* or variable*)).ab.
15. (financ* or fee or fees).ti,ab.
16. (value adj2 (money or monetary)).ti,ab.
17. or/1‐16
18. economics.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, fs]
19. value of life.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, fs]
20. exp "costs and cost analysis"/
21. exp economics, hospital/
22. exp economics, medical/
23. economics, nursing.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, fs]
24. economics, pharmaceutical.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, fs
25. exp "fees and charges"/
26. exp budgets/
27. budget*.ti,ab.
28. cost*.ti.
29. (economic* or pharmaco?economic*).ti.
30. (price* or pricing*).ti,ab.
31. (cost* adj2 (effective* or utilit* or benefit* or minimi* or unit* or estimat* or variable*)).ab.
32. (financ* or fee or fees).ti,ab.
33. (value adj2 (money or monetary)).ti,ab.
34. 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31 or 32 or 33
35. ((energy or oxygen) adj cost).ti,ab.
36. (metabolic adj cost).ti,ab.
37. ((energy or oxygen) adj expenditure).ti,ab.
38. 34 or 35 or 36 or 37
39. urinary incontinence.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
40. ((stress$ or mix$ or urg$ or urin$) adj3 incontinen$).tw.
41. URINARY INCONTINENCE, STRESS.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
42. stress urinary incontinence*.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
43. 39 or 40 or 41 or 42
44. intervention surgery*.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
45. colporrhaphy.tw.
46. Bologna procedure*.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
47. Kelly‐Kennedy.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
48. Marion Kelly.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
49. Diaphragmplasty.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
50. Vaginal urethrocystopexy.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
51. Cystocele repair.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
52. Kelly plication.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
53. anterior vaginal repair$.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
54. anterior colporrhaphy.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
55. 45 or 46 or 47 or 48 or 49 or 50 or 51 or 52 or 53 or 54
56. 38 and 43 and 55
57. remove duplicates from 56
58. Bladder neck needle suspension$.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
59. 38 and 43 and 58
60. burch colposuspension.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
61. open abdominal retropubic colposuspension.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
62. Paravaginal defect repair.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
63. Marshall‐Marchetti‐Krantz.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
64. abdominal burch.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
65. abdominal colposuspension.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
66. endopelvic Fascia Plication.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
67. 60 or 61 or 62 or 63 or 64 or 65 or 66
68. 38 and 43
69. 67 and 68
70. laparoscopic retropubic colposuspension.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
71. laparoscopic colposuspension.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
72. retropubic colposuspension.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
73. 70 or 71 or 72
74. 68 and 73
75. remove duplicates from 74
76. suburethral sling.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
77. abdominal sling.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
78. traditional sling procedure$*.tw.
79. suburethral sling procedure.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
80. 76 or 77 or 78 or 79
81. 68 and 80
82. remove duplicates from 81
83. mid$urethral sling.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
84. retropubic sling procedure$*.tw.
85. transobturator sling procedure$.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
86. 83 or 84 or 85
87. remove duplicates from 86
88. 68 and 87
89. TVT‐Secur.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
90. mini‐arc.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
91. ajust.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
92. needleless.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
93. solyx.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
94. single$incision sling$.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
95. miniarc.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
96. mini$sling.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
97. Ophira.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
98. Tissue Fixation System.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
99. 89 or 90 or 91 or 92 or 93 or 94 or 95 or 96 or 97 or 98
100. 68 and 99
101. remove duplicates from 100
102. ((urethra$ or periurethra$ or transurethra$) adj3 (agent$ or bulk$ or injection$ or injectable$)).tw.
103. injection therapy.tw.
104. injectable$.tw.
105. (injectable$ adj2 agent$).tw.
106. (bulk$ adj3 agent$).tw.
107. Peri$urethral injection$.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
108. Autologous fat.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
109. Macroplastique.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
110. Calcium hydroxylapatite.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
111. Hyaluronic acid with dextranomer.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
112. Porcine dermal implant.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
113. Ethylene vinyl alcohol copolymer.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
114. Silicon particles.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
115. 102 or 103 or 104 or 105 or 106 or 107 or 108 or 109 or 110 or 111 or 112 or 113 or 114
116. 68 and 115
117. remove duplicates from 116
Data and analyses
Comparison 1. Transobturator (TOR) versus retropubic route (RPR).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Subjective cure (short term, ≤ 1 year) | 35 | 5333 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.97 [0.95, 1.00] |
| 2 Subjective cure and improvement (short term, ≤ 1 year) | 10 | 1651 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.96, 1.00] |
| 3 Subjective cure (medium term, 1 to 5 years) | 5 | 683 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.87, 1.09] |
| 4 Subjective cure (long term, > 5 years) | 4 | 714 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.80, 1.12] |
| 5 Subjective cure and improvement (long term, > 5 years) | 2 | 340 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.67, 1.28] |
| 6 Objective cure (short term, ≤ 1 year) | 39 | 5974 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.96, 1.00] |
| 7 Objective cure and improvement (short term, ≤ 1 year) | 10 | 1478 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.96, 1.01] |
| 8 Objective cure (medium term, 1 to 5 years) | 5 | 596 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.95, 1.06] |
| 9 Objective cure (long term, > 5 years) | 3 | 400 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.97 [0.90, 1.06] |
| 10 Operative time (minutes) | 31 | 4713 | Mean Difference (IV, Random, 95% CI) | ‐7.54 [‐9.31, ‐5.77] |
| 11 Operative blood loss (ml) | 14 | 1869 | Mean Difference (IV, Random, 95% CI) | ‐6.49 [‐12.33, ‐0.65] |
| 12 Length of hospital stay (days) | 17 | 2170 | Mean Difference (IV, Random, 95% CI) | ‐0.25 [‐0.59, 0.09] |
| 13 Time to return to normal activity level (weeks) | 4 | 626 | Mean Difference (IV, Fixed, 95% CI) | ‐0.05 [‐0.15, 0.06] |
| 14 Perioperative complications | 15 | 2205 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.73, 1.14] |
| 15 Major vascular or visceral injury | 28 | 4676 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.19, 0.55] |
| 16 Bladder or urethral perforation | 39 | 6173 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.12 [0.08, 0.20] |
| 17 Voiding dysfunction | 37 | 6200 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.53 [0.43, 0.65] |
| 18 De novo urgency or urgency incontinence (short term, ≤ 1 year) | 31 | 4923 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.82, 1.17] |
| 19 De novo urgency or urgency incontinence (medium term, 1 to 5 years) | 4 | 481 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.55, 1.73] |
| 20 De novo urgency or urgency incontinence (long term, > 5 years) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 21 Detrusor overactivity | 4 | 566 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.58, 1.73] |
| 22 Vaginal tape erosion | 30 | 4568 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.70, 1.51] |
| 23 Bladder/urethral erosion | 4 | 374 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.34 [0.01, 8.13] |
| 24 Groin pain | 17 | 3050 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.45 [2.80, 7.08] |
| 25 Suprapubic pain | 4 | 1105 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.29 [0.11, 0.78] |
| 26 Repeat incontinence surgery (short term, ≤ 1 year) | 8 | 1221 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.69 [0.75, 3.80] |
| 27 Repeat incontinence surgery (medium term , 1 to 5 years) | 2 | 355 | Risk Ratio (M‐H, Fixed, 95% CI) | 21.89 [4.36, 109.77] |
| 28 Repeat incontinence surgery (long term > 5 years) | 4 | 695 | Risk Ratio (M‐H, Fixed, 95% CI) | 8.79 [3.36, 23.00] |
Comparison 2. Retropubic bottom‐to‐top approach versus retropubic top‐to‐bottom approach.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Subjective cure (short term, ≤ 1 year) | 3 | 477 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.10 [1.01, 1.19] |
| 2 Objective cure (short term, ≤ 1 year) | 5 | 622 | Risk Ratio (M‐H, Random, 95% CI) | 1.06 [0.97, 1.17] |
| 3 Operative time (minutes) | 2 | 124 | Mean Difference (IV, Fixed, 95% CI) | ‐2.15 [‐4.68, 0.38] |
| 4 Length of hospital stay (days) | 2 | 124 | Mean Difference (IV, Fixed, 95% CI) | ‐0.03 [‐0.37, 0.30] |
| 5 Perioperative complications | 4 | 507 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.53, 1.84] |
| 6 Bladder or urethral perforation | 5 | 631 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.55 [0.31, 0.98] |
| 7 Voiding dysfunction | 5 | 631 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.40 [0.18, 0.90] |
| 8 De novo urgency or urgency incontinence | 4 | 541 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.84 [0.52, 1.34] |
| 9 Detrusor overactivity | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 10 Vaginal tape erosion | 4 | 563 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.27 [0.08, 0.95] |
| 11 QoL specific | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected |
2.11. Analysis.
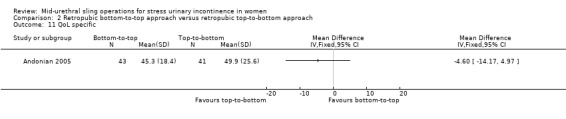
Comparison 2 Retropubic bottom‐to‐top approach versus retropubic top‐to‐bottom approach, Outcome 11 QoL specific.
Comparison 3. Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Subjective cure (short term, ≤ 1 year) | 6 | 759 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.96, 1.06] |
| 2 Subjective cure and improvement (short term, ≤ 1 year) | 5 | 732 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.97, 1.08] |
| 3 Subjective cure (medium term, 1 to 5 years) | 2 | 235 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.06 [0.91, 1.23] |
| 4 Subjective cure and improvement (medium term, 1 to 5 years) | 2 | 399 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.90, 1.11] |
| 5 Objective cure (short term, ≤ 1 year) | 6 | 745 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.95, 1.04] |
| 6 Objective cure and improvement (short term, ≤ 1 year) | 2 | 214 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.95, 1.07] |
| 7 Operative time (minutes) | 4 | 481 | Mean Difference (IV, Random, 95% CI) | 0.52 [‐1.09, 2.13] |
| 8 Operative blood loss (ml) | 3 | 255 | Mean Difference (IV, Fixed, 95% CI) | 1.11 [‐6.01, 8.22] |
| 9 Length of hospital stay (days) | 2 | 190 | Mean Difference (IV, Random, 95% CI) | ‐0.77 [‐2.54, 0.99] |
| 10 Time to return to normal activity level | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 11 Perioperative complications | 2 | 214 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.30 [0.23, 7.51] |
| 12 Major vascular or visceral injury | 4 | 622 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.71 [0.23, 2.19] |
| 13 Vaginal perforation/injury | 3 | 541 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.25 [0.12, 0.53] |
| 14 Bladder or urethral perforation | 6 | 794 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.38 [0.07, 1.92] |
| 15 Voiding dysfunction | 8 | 1121 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.74 [1.06, 2.88] |
| 16 De novo urgency or urgency incontinence | 3 | 357 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.46, 2.20] |
| 17 Detrusor overactivity | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 18 Vaginal tape erosion | 7 | 1087 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.42 [0.16, 1.09] |
| 19 Groin/thigh pain | 6 | 837 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.15 [0.75, 1.76] |
| 20 Repeat incontinence surgery | 2 | 532 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.64 [0.32, 1.30] |
| 21 QoL specific | 1 | 46 | Mean Difference (IV, Fixed, 95% CI) | 16.54 [4.84, 28.24] |
3.21. Analysis.
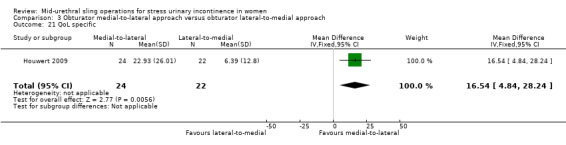
Comparison 3 Obturator medial‐to‐lateral approach versus obturator lateral‐to‐medial approach, Outcome 21 QoL specific.
Comparison 4. One method of mid‐urethral tape insertion versus another method, same route.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Subjective cure (short term, up to 1 year) | 7 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 Modified TVT‐O (short tape) vs TVT‐O | 1 | 175 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.90, 1.11] |
| 1.2 Modified TVT (suburethral pad) versus TVT | 1 | 248 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.91, 1.10] |
| 1.3 Self‐tailored TVT‐O vs TVT‐O | 1 | 156 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.93, 1.11] |
| 1.4 Monarc®TOT open edge + tension suture vs TOT® | 1 | 93 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.04 [0.87, 1.24] |
| 1.5 AdjustableTOT vs TOT® | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.05 [0.87, 1.28] |
| 1.6 Synthetic vs biological | 2 | 169 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.86, 1.22] |
| 2 Subjective cure and improvement (short term, up to 1 year) | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 Modified TVT‐O (short tape) vs TVT‐O | 1 | 170 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.97, 1.09] |
| 2.2 TOT + 2‐point tape fixation vs TOT | 1 | 418 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.07 [1.00, 1.14] |
| 2.3 TVT versus modified TVT (suburethral pad) | 1 | 248 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.98, 1.08] |
| 3 Subjective cure (medium term, 1 to 5 years) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.1 Modified TVT‐O (short tape) vs TVT‐O | 1 | 153 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.86, 1.12] |
| 4 Objective cure (medium term, 1 to 5 years) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4.1 Modified TVT‐O (short tape) vs TVT‐O | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Objective cure (short term, ≤ 1 year) | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 5.1 Modified TVT‐O (less dissection) vs TVT‐O | 1 | 69 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.91, 1.15] |
| 5.2 Synthetic vs biological | 2 | 136 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.94, 1.14] |
| 5.3 TVT‐O + IS vs TVT‐O | 1 | 93 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.45 [1.02, 2.06] |
| 5.4 TOT + 2‐point tape fixation vs TOT | 1 | 418 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.07 [1.01, 1.13] |
| 6 Operative time (minutes) | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 6.1 TVT‐O + IS vs TVT‐O | 1 | 96 | Mean Difference (IV, Fixed, 95% CI) | 12.0 [8.91, 15.09] |
| 6.2 Self‐tailored TVT‐O vs TVT‐O | 1 | 156 | Mean Difference (IV, Fixed, 95% CI) | ‐25.0 [‐26.73, ‐23.27] |
| 7 Operative blood loss (ml) | 3 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 7.1 TVT‐O + IS versus TVT‐O | 1 | 92 | Mean Difference (IV, Fixed, 95% CI) | 52.10 [43.73, 60.47] |
| 7.2 Self‐tailored TVT‐O vs TVT‐O | 1 | 156 | Mean Difference (IV, Fixed, 95% CI) | ‐13.00 [‐16.57, ‐13.43] |
| 7.3 Synthetic vs biological | 1 | 70 | Mean Difference (IV, Fixed, 95% CI) | ‐0.40 [‐0.92, 0.12] |
| 8 Length of hospital stay (days) | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 8.1 TVT‐O + IS vs TVT‐O | 1 | 96 | Mean Difference (IV, Fixed, 95% CI) | 12.0 [8.91, 15.09] |
| 8.2 Self‐tailored TVT‐O vs TVT‐O | 1 | 156 | Mean Difference (IV, Fixed, 95% CI) | ‐3.0 [‐3.16, ‐2.84] |
| 9 Perioperative complications | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 9.1 Synthetic vs biological | 2 | 170 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 10 Major vascular or visceral injury | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 10.1 TVT‐O + IS vs TVT‐O | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.72 [0.17, 3.04] |
| 10.2 Synthetic vs biological | 2 | 170 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 10.3 AdjustableTOT vs TOT® | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 11 Bladder/urethral perforation | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 11.1 TVT‐O + IS vs TVT‐O | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 11.2 TOT + 2‐point tape fixation vs TOT | 1 | 463 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.75 [0.17, 3.33] |
| 11.3 TVT versus modified TVT (suburethral pad) | 1 | 248 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.49 [0.05, 5.36] |
| 11.4 AdjustableTOT vs TOT® | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 12 Voiding dysfunction | 6 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 12.1 Modified TVT‐O (less dissection) vs TVT‐O | 1 | 72 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.0 [0.13, 30.61] |
| 12.2 TVT versus modified TVT (suburethral pad) | 1 | 248 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.21 [0.70, 7.00] |
| 12.3 Self‐tailored TVT‐O vs TVT‐O | 1 | 156 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.06, 14.92] |
| 12.4 Monarc®TOT open edge + tension suture vs TOT® | 1 | 93 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.47 [0.04, 4.99] |
| 12.5 Synthetic vs biological | 2 | 170 | Risk Ratio (M‐H, Fixed, 95% CI) | 5.0 [0.25, 101.58] |
| 13 De novo urgency or urgency incontinence | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 13.1 Modified TVT‐O (short tape) vs TVT‐O | 1 | 170 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.22 [0.51, 2.94] |
| 14 Vaginal tape erosion | 6 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 14.1 Modified TVT‐O (short tape) vs TVT‐O | 1 | 170 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.88] |
| 14.2 TVT versus modified TVT (suburethral pad) | 1 | 248 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.30 [0.61, 8.68] |
| 14.3 TVT‐O + IS vs TVT‐O | 1 | 93 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.06, 14.55] |
| 14.4 Monarc®TOT open edge + tension suture vs TOT® | 1 | 93 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.13 [0.01, 2.53] |
| 14.5 Synthetic vs biological | 2 | 169 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.0 [0.13, 71.92] |
| 15 Bladder/urethral erosion | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 15.1 TVT versus modified TVT (suburethral pad) | 1 | 248 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.06, 15.56] |
| 16 Groin pain | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 16.1 Modified TVT‐O (short tape) vs TVT‐O | 1 | 170 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.30 [0.30, 5.64] |
| 16.2 Synthetic vs biological | 1 | 69 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
4.9. Analysis.
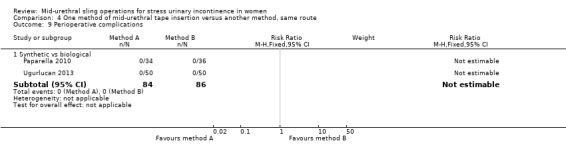
Comparison 4 One method of mid‐urethral tape insertion versus another method, same route, Outcome 9 Perioperative complications.
Comparison 5. One type of tape material versus another.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Subjective cure (short term, ≤ 1 year) | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 Monofilament versus multifilament | 4 | 546 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.95, 1.10] |
| 1.2 Monofilament versus combined monofilament and biological | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.79, 1.05] |
| 1.3 Combined monofilament and biological vs multifilament | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.10 [0.96, 1.26] |
| 2 Subjective cure (medium term, 1 to 5 years) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 Monofilament vs multifilament | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.85, 1.23] |
| 2.2 Monofilament vs combined monofilament and biological | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.78, 1.06] |
| 2.3 Combined monofilament and biological vs multifilament | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.13 [0.96, 1.32] |
| 3 Objective cure (short term, ≤ 1 year) | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.1 Monofilament vs multifilament | 2 | 349 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.07 [0.96, 1.19] |
| 4 Operative time (minutes) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4.1 Monofilament vs multifilament | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Length of hospital stay (days) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 5.1 Monofilament vs multifilament | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Perioperative complications | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 6.1 Monofilament vs multifilament | 2 | 279 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.16 [0.36, 3.69] |
| 7 Major vascular or visceral injury | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 7.1 Monofilament vs multifilament | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7.2 Monofilament vs combined monofilament and biological | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7.3 Combined monofilament and biological vs multifilament | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 8 Bladder or urethral perforation | 4 | 749 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.15 [0.49, 2.70] |
| 8.1 Monofilament vs multifilament | 4 | 557 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.15 [0.49, 2.70] |
| 8.2 Monofilament vs combined monofilament and biological | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 8.3 Combined monofilament and biological vs multifilament | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 9 Voiding dysfunction | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 9.1 Monofilament vs multifilament | 3 | 461 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.10 [0.96, 4.59] |
| 10 De novo urgency or urgency incontinence | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 10.1 Monofilament vs multifilament | 4 | 545 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.11 [0.68, 1.82] |
| 10.2 Monofilament vs combined monofilament and biological | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.0 [0.38, 10.41] |
| 10.3 Combined monofilament and biological vs multifilament | 1 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.4 [0.08, 1.96] |
| 11 Detrusor overactivity | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 11.1 Monofilament vs multifilament | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 12 Vaginal tape erosion | 3 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 12.1 Monofilament vs multifilament | 3 | 445 | Risk Ratio (M‐H, Random, 95% CI) | 0.79 [0.09, 6.84] |
| 12.2 Monofilament vs combined monofilament and biological | 1 | 96 | Risk Ratio (M‐H, Random, 95% CI) | 3.0 [0.32, 27.83] |
| 12.3 Combined monofilament and biological vs multifilament | 1 | 96 | Risk Ratio (M‐H, Random, 95% CI) | 0.33 [0.04, 3.09] |
| 13 QoL specific (ICIQ) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 13.1 Monofilament vs multifilament | 1 | 96 | Mean Difference (IV, Fixed, 95% CI) | ‐0.60 [‐0.76, ‐0.44] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Abdel‐Fattah 2010.
| Methods | RCT of TVT‐O vs TOT–ARIS | |
| Participants | 341 women from the west of Scotland, UK, Urogynaecology tertiary referral centre Inclusion criteria: women with USI or MUI (but with SUI as the predominant troublesome symptom). Women with previous incontinence surgery were included. All women had failed or declined pelvic floor muscle training Exclusion criteria: predominant OAB symptoms; or had specific co‐morbidities such as known neurological conditions (e.g. multiple sclerosis); diabetes; ≥ stage 2 POP‐Q or concomitant surgery, or both There were no significant differences in participant characteristics between the 2 groups Mean age (years): Group A: 51.5; Group B: 52.1 Mean BMI kg/m²: Group A: 28.1; Group B: 28.9 MUI: Group A: 40/170; Group B: 43/171 Previous incontinence surgery: Group A: 28/170; Group B: 18/171 |
|
| Interventions | Group A: TVT‐O (n = 170) Group B: TOT (n = 171) |
|
| Outcomes | Primary outcome: absence of USI on UDS Secondary outcome measures:
|
|
| Notes | Loss to follow up at 1 year: Group A: 18/170, Group B: 24/171 Loss to follow up at 3 years: Group A: 44/170, Group B: 59/171 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "A single‐blinded, prospective, randomized study … Women were assigned to either procedure by random allocation (computer generated)" |
| Allocation concealment (selection bias) | Low risk | Quote: "Allocation was concealed using opaque sealed envelopes, which were opened by the nursing staff on the morning of the operation" |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: “a single‐blinded, prospective, randomized study… Women were informed about the type of operation if they wished, for ethical considerations, but they were instructed not to disclose this information to the clinician at follow‐up” |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: “Post‐operative assessment at 6 months was performed by an independent clinician who was blinded to the type of surgery … “ |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: “No woman assigned to an arm asked to change her operation or to withdraw from the study prior to the operation. Withdrawals, unattendants and untraceables were accounted for without significant inter group differences” |
Aigmuller 2014.
| Methods | RCT of Gynecare TVT vs Gynecare TVT‐O; Gynecare, Ethicon | |
| Participants | Trial conducted by Austrian Urogynecology Working Group in 25 gynaecology units in Austria and Germany 554 women Inclusion criteria: women with USI (positive cough stress test at bladder filling of 300 ml); no concomitant prolapse surgery or hysterectomy Exclusion criteria: DO or a predominant complaint of OAB; concomitant prolapse surgery; other major concomitant surgery (e.g. hysterectomy); previous incontinence surgery other than colporrhaphy; residual urine ≥100 ml; neurologic disease; allergy to local anaesthetic agents; and coagulation disorders or other contraindications for surgery Age (years): Group A: 59.7 ± 11.3; Group B: 58.6 ± 10.7 BMI kg/m²: Group A: 27.7 ± 5.3; Group B: 28.5 ± 4.9 Parity: Group A: 2.2 ± 1.2; Group B: 2.2 ± 1.3 |
|
| Interventions | Group A: TVT: (n = 285; 38 of whom were lost to follow‐up) Group B: TVT‐O: (n = 269; 36 of whom were lost to follow‐up) |
|
| Outcomes | Participants were evaluated at 3 months, with a further evaluation scheduled at 5 years
|
|
| Notes | QoL: Short‐Form Health Survey (SF‐12), EuroQol‐5D (EQ‐5D) condition‐specific QoL was assessed with the German language version of the KHQ, the Incontinence Outcome Questionnaire (IOQ), and PGI‐S and PGI‐I Cystoscopy was performed with all retropubic placements but not routinely with transobturator insertions The number of women in each group seen at 5‐year follow‐up was not available, so the data reported could not be used for meta‐analysis |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "randomized according to a computer generated random list allocating trial identification number and treatment group. Randomization was by fax through the central office" |
| Allocation concealment (selection bias) | Low risk | Quote: "computer generated random list allocating trial identification number and treatment group" |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Patients, surgeons, and physicians performing follow‐up exams were not blinded to the type of surgery |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Patients, surgeons, and physicians performing follow‐up exams were not blinded to the type of surgery |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Accounted for and no differentials in the groups in terms of loss to follow‐up |
Alkady 2009.
| Methods | RCT of TVT vs TVT‐O | |
| Participants | 30 women with SUI in Kuwait Maternity Hospital Inclusion criteria: SUI with or without a prolapse; USI with or without urethral hypermobility; MUI without urodynamic DO; absence of a contractile urinary bladder or obstruction Exclusion criteria: acute cystitis; predominant urge incontinence; urodynamic DO; maximum flow (Qmax) less than 15 ml/s and/or PVR urine of more than 20% of the volume voided; genital prolapse of stage 4 or 5 Menopausal: Group A: 3/15; Group B: 4/15 |
|
| Interventions | Group A: TVT (n = 15) Group B: TVT‐O (n = 15) |
|
| Outcomes |
|
|
| Notes | No participants lost to follow‐up at 6 and 12 months | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Women were randomised using numbered, opaque, sealed envelopes containing computer‐generated random allocations in a ratio of 1:1 in balanced blocks of 10. |
| Allocation concealment (selection bias) | Low risk | Women were randomised using numbered, opaque, sealed envelopes containing computer‐generated random allocations in a ratio of 1:1 in balanced blocks of 10. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: “All accounted for” |
Andonian 2005.
| Methods | RCT comparing TVT with SPARC | |
| Participants | 84 women presenting with SUI, or SUI with MUI if cystometrogram showed normal capacity, compliance and no uninhibited contractions. Women with previous failed anti‐incontinence surgeries or bulking agents treatments were also eligible for the study. Both groups were similar in terms of age, severity of symptoms, 1‐h pad test and preoperative IIQ (of Shumaker) | |
| Interventions | Group A: SPARC (n = 41) Group B: TVT (n = 43) |
|
| Outcomes | Primary endpoint: objective cure defined as 1‐h pad test of 2g Secondary endpoint: QoL assessed through Shumaker's IIQ, a score of <50 represented good QoL, 50‐70 moderate QoL, and >70 poor QoL | |
| Notes | Follow‐up assessment of cure at 1 year was unavailable in 1 woman (Group B) who died from a myocardial infarct | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Patients were blinded to the procedure and had envelope randomization immediately prior to the start of the surgery" |
| Allocation concealment (selection bias) | Low risk | Adequate |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Both groups and outcome assessors were said to have been blinded but how this was achieved was not clear. Quote: "Patients were blinded to the procedure and had envelope randomization immediately prior to the start of the surgery" |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Outcome assessors blinded, quote: "dedicated UDS nurse (BS), who was blinded to the procedure" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Addressed |
Andonian 2007.
| Methods | RCT of TOT (Obtape) versus distal urethral polypropylene sling (DUPS) versus TVT | |
| Participants | 190 women Inclusion criteria: women with SUI with or without POP or pelvic surgery; previous failed anti‐incontinence surgeries or bulking agent treatments permitted; women with MUI were not excluded as long as their cystometrogram showed normal capacity; compliance and no uninhibited contractions Exclusion criteria: obstruction; unstable bladder function, or neurogenic bladder; UTI |
|
| Interventions | Group A: Obtape (n = 78) Group B: DUPS (n = 32) Group C: TVT (n = 80) 1 participant in the Obtape group had a urethral diverticulum, which was repaired, but the Obtape procedure was cancelled, leaving 77 patients in the Obtape group for the final analysis |
|
| Outcomes | Primary outcome: objective cure defined by 1‐h pad test of ≤ 2 g Secondary outcome: subjective cure rates determined by the ICIQ‐SF Postoperatively, all women were re‐evaluated by history and physical examination at 1, 6, and 12 months. At the 12‐month visit, participants completed the ICIQ‐SF, and underwent the 1‐h pad test conducted by the dedicated UDS nurse who was blinded to the procedure |
|
| Notes | Mentor's Obtape is a non woven monofilament thermally bonded micropore (50 µm) polypropylene mesh which was withdrawn by its manufacturers in 2006. There have been many reports of tape erosions and some cases of ischiorectal abscess and necrotizing fasciitis DUPS is not a minimally invasive sling, but a woven polypropylene mesh (by Ethicon, New Jersey). Absorbable sutures are used to fix the sling into position until adhesions form and adhere it naturally to the retropubic space. As it was not a minimally invasive sling there was no need to compare DUPS in the review The DUPS procedure was discontinued because of a higher postoperative retention rate combined with several complaints of suprapubic abdominal discomfort on straining |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Randomization was performed by an envelope method immediately before the start of surgery." |
| Allocation concealment (selection bias) | Unclear risk | Not mentioned |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | The patients were blinded to the procedure |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Outcome assessors blinded, but how this was achieved was not explained |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Unclear |
Aniuliene 2009.
| Methods | A prospective RCT of TVT‐O vs TVT | |
| Participants | 264 women with SUI in Lithuania hospital setting. The degree of incontinence was 2–3 according to the Ingelman‐Sundberg scale Inclusion criteria: women with SUI Exclusion criteria: urogenitale prolapse greater than stage 2; urinary retention; OAB and psychiatric problems Post menopausal: Group A: 47/150; Group B: 48/114 Mean BMI kg/m² (SD): Group A: 28.2 (3.8); Group B: 27.9 (4.0) Previous incontinence surgery: Group A: 18/150; Group B: 16/114 POP‐Q stage 2: Group A: 29/150; Group B: 22/114 |
|
| Interventions | Group A: TVT‐O (n = 150) Group B: TVT (n = 114) |
|
| Outcomes |
|
|
| Notes | Urodynamics assessment was not performed in all participants Cystoscopy and cough test were routinely performed only in the TVT group No patients were lost to follow‐up |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No participants lost to follow‐up |
Araco 2008.
| Methods | RCT of TVT‐O versus TVT | |
| Participants | 240 women with different degrees of SUI Inclusion criteria: symptomatic SUI grades 1 and 2a (McGuire classification) Exclusion criteria: women with ISD; OAB; associated prolapses; neurovegetative disorders and recurrent SUI or under rehabilitative/medical therapies Diagnosis based on ambulatory UDS Average age of 54 years |
|
| Interventions | Group A: TVT‐O (n = 120) Group B: TVT (n = 120) | |
| Outcomes | Primary outcome: cure rate of SUI evaluated with the postoperative ambulatory urodynamic tests 1 year after surgery
Secondary outcomes:
A positive pad weight result was defined as > 2g of leakage |
|
| Notes | The participants were classified according to the SUI system on the basis of urodynamics studies (McGuire classification), performed at 250 ml bladder volume. SUI was classified into 3 grades considering the severity of symptoms referred (SUI1 = loss of urine during excessive strains, SUI2 = during minor strains, SUI3 = at rest) and the urodynamic evaluation (McGuire classification: SUI1 = abdominal leak‐point pressure (ALPP) > 90 cm water, SUI2 = ALPP of 60‐90 cm water, SUI 3 = intrinsic sphincter deficiency and ALPP < 60 cm water)
Cystoscopy was performed in all cases Loss to follow‐up: 32 women were lost to follow‐up due to work commitments, Group A:12/120 TVT, Group B: 20/120 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "A stratified randomisation was carried out. Presented two identical closed envelopes to patients, one containing the paper “TVT” and the other “TVT‐O”. After choosing and opening of the envelope, further stratification was performed with a sampling chart. Four groups were formed on the basis of which operation they were going to receive." |
| Allocation concealment (selection bias) | Low risk | Quote: "Presented two identical closed envelopes to patients, one containing the paper “TVT” and the other “TVT‐O” |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "Data was analysed by a surgeon who was not involved in the surgical intervention" |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Disproportionately higher numbers lost to follow‐up in TVT‐O group |
Barber 2008.
| Methods | RCT of TVT vs Monarc TOT | |
| Participants | Setting: 3 USA tertiary academic medical centres Inclusion criteria: 170 women aged over 21 years with USI with or without concurrent POP Exlusion criteria: DO; previous incontinence surgery; PVR > 100 ml; desiring future childbearing; history of hidradenitis suppurativa, inguinal lymphadenopathy, or an inguinal or vulvar mass; history of a bleeding diathesis or ongoing anticoagulation therapy; current genitourinary fistula or urethral diverticulum Mean age in years (SD): Group A: 52 (11); Group B: 53 (12) Mean BMI kg/m² (SD): Group A: 30 (7); Group B: 29 (6) Postmenopausal: Group A: 53/88; Group B: 58/82 Previous continence surgery: Group A: 5/88; Group B: 10/82 MUI: Group A: 76/88; Group B: 66/82 VLPP: < 60 cm/H2O: Group A: 14/88; Group B: 16/82 |
|
| Interventions | Group A: TVT (n = 88) Group B: TOT (n = 82) |
|
| Outcomes | Primary outcome: presence or absence of 'abnormal bladder function', a composite outcome defined as the presence of any the following: incontinence symptoms ‐ any type (ISI > 0), a positive cough‐stress test, re‐treatment for SUI or postoperative urinary retention assessed 1‐year after surgery Secondary outcomes: assessed by use of SF12, PISQ‐12, bladder diary at 12 and 24 months:
|
|
| Notes | Intraoperative cystoscopy performed in both groups Concomitant surgery performed in Group A: 48/88; Group B: 45/82 Loss to follow‐up: Group A: 3/88; Group B: 7/82 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "were randomised using computer generated random allocation" |
| Allocation concealment (selection bias) | Low risk | Quote: "group assignment were concealed in consecutively numbered sealed opaque envelopes" |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Quote: "blinding of surgeon and participants was not possible ..." |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "all post op assessments were performed by research nurses who were blinded to treatment given" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All accounted for |
Barry 2008.
| Methods | RCT of TOT (Monarc) versus TVT Random allocation of participants but method of sequence generation and allocation concealment not described |
|
| Participants | 140 women diagnosed with USI Participants in both groups had similar background characteristics including age, BMI, parity, HRT use, menopausal status, previous incontinence surgery, prolapse etc Inclusion criteria: participants had either failed conservative management for symptomatic stress incontinence or required prophylactic incontinence surgery during prolapse repair for occult stress incontinence (no preoperative subjective complaint of urinary stress leakage but found to have USI) Exclusion criteria: significant voiding dysfunction (maximum urine flow rate < 10th percentile according to Liverpool nomogram and PVR volume > 50 ml); known allergy to polypropylene; immunosuppressant therapy and a past history of neurological disease; urogenital malignancy; fistula or pelvic radiotherapy |
|
| Interventions | Group A: TOT (n = 58) Group B: TVT (n = 82) | |
| Outcomes | Outcomes included Immediate‐ and short‐term complications, cure rates and patient satisfaction Primary outcome: reduction in incidence of bladder injury Secondary outcomes:
Improvement of a particular symptom denoted at least 50% reduction in frequency of occurrence in 3‐day bladder diary when compared to preoperative state Measures used for assessment included:
|
|
| Notes | 23 women from the TVT group and 21 from TOT group were lost to follow‐up. Thus, at follow‐up complete data set available for 82 women in TVT group and 58 in the TOT group. There were no differences between the group unavailable for analysis when compared to those finally analysed No mention of intraoperative cystoscopy in either group |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Participants were blinded and randomly allocated in a balanced way (blocks of 20) Randomisation was stratified according to a history of previous incontinence surgery |
| Allocation concealment (selection bias) | Unclear risk | Unclear |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Participants were blinded. How this was achieved was not explained |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No differential loss to follow‐up or differential attrition |
But 2008.
| Methods | RCT of TVT‐O versus TOT (Monarc) | |
| Participants | 120 women with SUI (31) and MUI (89) Inclusion criteria: women with SUI, or MUI, with SUI as the predominant symptom Exclusion criteria: MUI with predominant UUI Performed under local anaesthesia Mean age years (SD): 52.6 (6.8) |
|
| Interventions | Group A: TVT‐O (n = 60) Group B: TOT (n = 60) |
|
| Outcomes |
|
|
| Notes | Follow‐up 3 months All women attended for follow‐up |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Before the beginning of the study, the computer‐generated list of 120 random numbers (from one to 120) was made for two groups (60 random numbers for each group, optimum allocation ratio 1)" |
| Allocation concealment (selection bias) | Unclear risk | Quote: "the consecutive study numbers were given after admission, and based on this admission number, either inside‐out or outside‐in procedure was selected later in the OR according to a computer‐ generated list of random number" |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All data/information accounted for at follow‐up |
Cervigni 2006.
| Methods | RCT of TVT versus Monarc TOT | |
| Participants | 118 women Inclusion criteria: women with SUI and POP‐Q ≥ stage 2 Mean age 57.43 years All women had cystocoele repair and levator myorraphy 73 women were post menopausal |
|
| Interventions | Group A: TVT Group B: TOT (exact numbers in each group not reported) |
|
| Outcomes | Cure rates: TVT (98.3%), TOT (97.1%) as exact number of women in each group was not given there were no data that could be extracted Intraoperative and postoperative complications |
|
| Notes | Numbers in each group unreported. It was, thus, impossible to abstract results | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Women randomised into 2 groups (computer generated randomisation list) |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No information |
Chen 2010.
| Methods | RCT comparing TVT, TOT and TVT‐O | |
| Participants | 187 women Inclusion criteria: women with urodynamically proven SUI in the urology department of a Chinese hospital |
|
| Interventions | Group A: TVT (n = 77) Group B: TOT (n = 45) Group C: TVT‐O (n = 65) |
|
| Outcomes |
|
|
| Notes | No quality of life measures undertaken Cystoscopy performed in TVT group |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No information |
Chen 2012.
| Methods | RCT of TVT vs TVT‐O Recruitment Feb 2009‐Feb 2010 |
|
| Participants | 205 women with SUI Inclusion criteria: women with urodynamically proven SUI with or without prolapse Exclusion criteria: DO; MUI All women had similar background characteristics |
|
| Interventions | A: TVT (n = 102) B: TVT‐O (n = 103) |
|
| Outcomes | Follow‐up 12‐24 months
|
|
| Notes | Needs translation for further information Article written in Chinese and translated to English for interpretation and extraction |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Stated: ‘randomly allocated ’ |
| Allocation concealment (selection bias) | Unclear risk | Stated: ‘randomized’ |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No information |
Cho 2010.
| Methods | RCT of Monarc system and TOT system | |
| Participants | 93 women having urodynamic evaluation | |
| Interventions | Group A: Monarc TOT (n = 48) Group B: TOT (n = 45) |
|
| Outcomes | Outcomes assessed 12 months postoperatively
|
|
| Notes | Monarc is outside‐to‐in TOT with open edge polypropylene mesh that contains an absorbable tensioning suture threaded into the length of the mesh. The tension free obturator tape (TOT) system used here is the same outside‐in type, but has a closed edge polypropylene mesh without absorbable tensioning suture | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "93 female patients were prospectively, randomly assigned to the study" |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No information |
Choe 2013.
| Methods | RCT OF TVT vs TOT | |
| Participants | 41 women Inclusion criteria: women with SUI; able to complete a questionnaire Exclusion criteria: prior spine surgery; back pain; scoliosis; traumatic spine injury; neurological disease; or hip or knee surgery |
|
| Interventions | 41 women, number in each group was not given | |
| Outcomes | Postoperative pain was assessed using a 10‐point visual analogue scale (VAS) at fixed time‐points: 30 minutes, 3hr and 24hr after surgery Length of procedure (minutes) |
|
| Notes | We were not able to use the data provided, as the number in each group was not specified | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "were randomized to receive" |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No information |
Darabi Mahboub 2012.
| Methods | RCT of TOT versus TVT | |
| Participants | Women with SUI Age in years (SD): Group A: 52.02 (0.88); Group B: 52.27 (7.34) |
|
| Interventions | Group A: TOT (n = 40) Group B: TVT (n = 40) |
|
| Outcomes | A validated stress and urge incontinence questionnaire 24‐h pad test 6‐month follow‐up of ICIQ Operative time Mean hospital stay |
|
| Notes | Intraoperative cystoscopy not mentioned in either group | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: “In this randomised clinical trial, eighty female patients with SUI were randomly allocated to “ |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No information |
David‐Montefiore 2006.
| Methods | RCT comparing TOR and RTR of sling procedures for SUI using the I‐STOP device | |
| Participants | Multicentre (3 gynaecology and 2 urology departments in France) 88 women Inclusion criteria: women > 18 years with SUI, proven by clinical and urodynamic examinations, or MUI Exclusion criteria: women with previous history of radio‐ or chemotherapy; on anticoagulant or antipsychotic treatment; or pregnant Mean age: Group A: 58.8 years; Group B: 53.4 years |
|
| Interventions | Group A: RPR (n = 42) Group B: TOR (n = 46) The I‐STOP device (CL Medical, Lyon, France) was used for both the RPR and the TOR procedures |
|
| Outcomes |
|
|
| Notes | Loss to follow‐up at 4 years: Group A: 8/42; Group B: 9/46 Length of follow‐up ranged from 48 months to 61 months (RPR) and 48 months to 63 months (TOR) The mean follow‐up was 10 months, with 37 women having 6 months of follow‐up and 51 women having at least 12 months of follow‐up Cystoscopy was performed for both procedures |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | " ... Prospective randomised Multicentre study .... using a predetermined computer generated randomisation code ..." |
| Allocation concealment (selection bias) | Low risk | Surgeon informed of allocated procedures by an uninvolved third‐party immediately before the operation |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Unclear |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Unclear |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Unclear |
de Leval 2011.
| Methods | QRCT of TVT‐O vs modified TVT‐O | |
| Participants | 175 women Inclusion criteria: women aged 25‐85 years with USI; positive stress test with at least a maximum cystometric capacity of 300 ml Exclusion criteria: DO or detrusor acontractility; neurogenic bladder; or POP stage 3 or above Mean age years (SD): Group A: 60.0 (11.7); Group B: 57.2 (2.7) BMI kg/m² (SD): Group A: 26.4 (4.8) Group B: 26.8 (5.3) Previous surgery for SUI: Group A: 4/87; B Group: 4/88 Previous surgery for POP: Group A: 4/87; Group B: 2/88 |
|
| Interventions | Group A: TVT‐O (n = 87) Group B: modified TVT‐O (n = 88) |
|
| Outcomes | At 1 ‐year follow‐up:
At 3‐year follow‐up:
|
|
| Notes | The modified TVT‐O was shortened to a total tape length of 12 cm and had a reduction in the depth of lateral dissection, the obturator membrane was not perforated with the scissors or the guide Follow‐up assessments carried out at 1, 6, 12 months, and 3 years Lost to follow‐up:
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote: "The randomisation process was performed with five sequential patients undergoing one approach before alternating surgical modality" |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Patients were blinded to the type of surgery they underwent |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "no patients withdrew from the study prior to their operation". 2 participants were completely lost to follow‐up after the 1‐month visit and 2 more after the 6‐month visit. One patient died before the 6‐month visit; the cause of death was unrelated to the surgery |
de Tayrac 2004.
| Methods | RCT comparing TVT with TOT | |
| Participants | 61 women Inclusion criteria: USI Exclusion criteria: predominant urge incontinence; urodynamic detrusor instability; or prolapse Mean age (years; SD): Group A: 54.7 (11.9); Group B: 53.6 (12.5) Mean BMI kg/m² (SD): Group A: 24 (3.2); Group B: 25.2 (4.3) Postmenopausal status: Group A: 18/30; Group B: 16/31 Previous continence surgery: Group A: 4/30; Group B: 1/31 Previous prolapse surgery: Group A: 4/30; Group B: 1/31 ISD: Group A: 4/30; Group B: 3/31 |
|
| Interventions | Group: A: TOT (n = 30) Group: B: TVT (n = 31) |
|
| Outcomes |
|
|
| Notes | The full article was retracted at the request of authors because appropriate ethics committee approval was not received prior to starting study. Nevertheless, participants did give written consent to be included in the trial and consented for the procedures. No methodological flaws were identified: the review authors therefore decided to include the data TOT: Uratape mentor‐porges Cystoscopy performed following TVT procedure |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Women were randomised using numbered, opaque sealed envelopes containing computer‐generated random allocations in a ratio of 1:1 in balanced blocks of 10. Envelopes were opened in the operating room by a nurse just before starting the procedure |
| Allocation concealment (selection bias) | Low risk | Adequate |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Outcome assessors were blinded |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No information |
Deffieux 2010.
| Methods | RCT of TVT and TVT‐O | |
| Participants | Multicentred RCT, 14 centres in France (university hospitals and 3 general hospitals) 149 women with SUI Inclusion criteria: age >18 years; isolated or mixed USI; indication for surgical treatment of USI; positive cough stress test Exclusion criteria: concomitant POP surgery; concomitant hysterectomy; previous incontinence surgery; pregnancy; anticoagulant therapy; higher than stage 1 urogenital prolapse (POP‐Q ICS) All women had similar background characteristics Mean age (years; SD): Group A: 54.6 (10.9); Group B: 52.8 (9.8) Mean BMI kg/m² (SD): Group A: 26.3 (4.5); Group B: 26.3 (5.7) Postmenopausal: Group A: 43/75; Group B: 40/74 POP‐Q stage 1: Group A: 245/75; Group B: 24/74 |
|
| Interventions | Group A: TVT (n = 75) Group B: TVT‐O (n = 74) |
|
| Outcomes | Outcomes assessed at 2, 6, 12 and 24 months
|
|
| Notes | Cystoscopy performed in both groups Loss to follow‐up: at 12 months: Group A: 6/75; Group B: 5/74 Loss to follow‐up at 24 months: Group A: 8/75; Group B: 9/74 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The patients were randomized using sealed opaque envelopes, following computer‐generated random allocations" |
| Allocation concealment (selection bias) | Low risk | Quote: "The patients were randomized using sealed opaque envelopes, following computer‐generated random allocations, with a ratio of 1:1 in balanced blocks of four. The envelopes were opened just before each participant's surgical procedure" |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: "blinding of surgeons and participants not possible" |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data complete |
Diab 2012.
| Methods | RCT of TOT vs TVT | |
| Participants | 70 women with SUI | |
| Interventions | Group A: TOT (n = 31) Group B: TVT (n = 32) |
|
| Outcomes |
|
|
| Notes | Mean follow up in months (SD): A: 28 (12.3) and B: 26 (13.6) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "were randomly distributed to two groups" |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No information |
El‐Hefnawy 2010.
| Methods | RCT comparing Gynecare TVT R and Aris TOTR outside‐in | |
| Participants | 40 women Inclusion criteria: women with urodynamically proven SUI Exclusion criteria: women who reported urgency incontinence as predominant complaint; had pelvic or vaginal surgery within the preceding 6 months; had associated urethral and/or bladder pathology or active UTI; neuropathic bladder; POP > stage 2 (Baden Walker classification) Mean age (years; SD): Group A:47 (5); Group B: 45 (7) Concomitant POP stage 1‐2: Group A: 10; Group B: 13 Mean BMI kg/m² (SD): Group A: 34 (5); Group B: 32(5) |
|
| Interventions | Preliminary results: Group A: TVT: (n = 19) Group B: TOT: (n = 21) At 24 months: Group A: TVT: (n = 45) Group B: TOT: (n = 42) |
|
| Outcomes | Follow‐up at 3, 6, 12 and 24 months
|
|
| Notes | Intraoperative cystoscopy carried out only in the TVT group to exclude bladder or urethral injury Concomittant surgery was performed in 9 participants; 5 participants underwent abdominal hysterectomy, 4 participants underwent anterior colporrhaphy Lost to follow‐up at 12 months: Group A: 0/19; Group B: 0/21 Lost to follow‐up at 24 months: Group A: 9/45; Group B: 7/42 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Patient’s randomisation is accomplished through closed envelopes. A randomly selected envelope is dispatched to a running nurse with the patient’s name and ID hand typed on the envelope" |
| Allocation concealment (selection bias) | Low risk | Quote: “randomisation is accomplished through closed envelopes. A randomly selected envelope is dispatched to a running nurse with the patient’s name and ID hand typed on the envelope” |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: “Follow up was carried out by a nurse blinded to the procedure” |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All outcomes included |
Elbadry 2014.
| Methods | RCT of adjustable TOT vs TOT | |
| Participants | 96 women with SUI, with a mean age of 53 + 9.9 years | |
| Interventions | Group A: adjustable TOT (n = 48) Group B: TOT: (n = 48) |
|
| Outcomes |
|
|
| Notes | The advantage of the adjustable tape is that it can be adjusted postoperatively to address over‐ or under‐correction | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Patients were randomized into 2 equal groups" |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No information |
Enzelsberger 2005.
| Methods | QRCT comparing TVT and TOT | |
| Participants | 110 women Inclusion criteria: women with SUI, all had preoperative stress test Exclusion criteria: previous surgery for SUI; mixed incontinence; renal disease; metabolic disorders; or POP Mean age was 51 years |
|
| Interventions | Group A: TOT (n = 56) Group B: TVT (n = 54) |
|
| Outcomes |
|
|
| Notes | No mention of intraoperative cystoscopy Followed‐up at 15 months |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quasi‐RCT |
| Allocation concealment (selection bias) | High risk | Inadequate |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No information |
Freeman 2011.
| Methods | RCT comparing TOT and TVT | |
| Participants | Multicentre RCT – 21 centres across the UK 192 women Inclusion criteria: women >21 years of age; USI or MUI for which SUI was the predominant symptom; must have failed with conservative measures Exclusion criteria: women with neurological disease; previous surgery for USI (those with previous prolapse surgery were not excluded); urodynamic DO or low compliance; POP extending beyond the hymen |
|
| Interventions | Group A: Monarc TOT (n = 100) Group B: Gynaecare TVT (n = 92) |
|
| Outcomes | Follow‐up at 4 weeks, 6 months and 12 months
|
|
| Notes | The trial was a non‐inferiority design. Outcome measures calculated by intention‐to‐treat Assessed via ICIQ‐FLUTS long form, ICIQ LUTSqol; KHQ questionnaires and 4‐day urinary diary Sexual function assessed by ICIQ‐LUTSqol question, ‘does your urinary problem affect your sex life?’ Cystoscopy: not mentioned whether routinely performed in either group Lost to follow‐up: Group A: 5/100; Group B: 7/92 (and 1 excluded as she did not have the operation) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "randomisation list was stratified by study sites, using randomly permuted blocks of varying sizes of 4, 6 and 8" |
| Allocation concealment (selection bias) | Low risk | Quote: "The study co‐ordinator placed a treatment into consecutively numbered opaque envelopes which were opened immediately before surgery by someone other than the surgeon. Allocation concealment was therefore ensured" |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "Patients and ward staff were blinded to the intervention group by ensuring that dressings were applied both suprapubically and to the obturator areas" |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Patients and their data accounted for |
Hammoud 2011.
| Methods | RCT of TVT vs TVT‐O | |
| Participants | 110 women with SUI | |
| Interventions | Group A: TVT (n = 60) Group B: TVT‐O (n = 50) |
|
| Outcomes | Subjective cure: | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "in a prospective randomized trial ... women were randomized between TVT and TVT‐O for treatment" |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No information |
Hassan 2013.
| Methods | RCT of inside‐out TOT vs outside‐in TOT | |
| Participants | 250 women Inclusion criteria: women with SUI in a university teaching hospital in Cairo, Egypt |
|
| Interventions | Group A: inside‐out TOT (n = 125) Group B: outside‐in TOT (n = 125) |
|
| Outcomes | Primary outcomes:
Secondary outcomes:
|
|
| Notes | Lost to follow‐up: Group A: 23/125; Group B: 28/125 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "A prospective single‐blinded randomised trial" |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No information |
Houwert 2009.
| Methods | RCT of TVT‐O and TOT (Monarc) | |
| Participants | 191 women Inclusion criteria: women with SUI, USI and MUI. Those with MUI failed anti‐cholinergic medical treatment before surgical treatment Exclusion criteria: women with recurrent UTIs; those with predominantly symptoms of UUI; post voiding residuals of > 150 ml and bladder capacity < 100ml There was no concomitant POP surgery Preoperative multichannel urodynamic investigation was carried in all women Mean age (years; SD): Group A: 49.2 (8.9); Group B: 49.5 (10.3) SUI: Group A: 74/93 (80%); Group B: 74 /98 (76%) MUI: Group A: 19/93 (20%); Group B: 23/98 (24%) Postmenopausal: Group A: 33/93; Group B: 34/98 Previous incontinence surgery: Group A: 8/93; Group B: 9/98 Previous POP surgery: Group A: 19/93; Group B: 15/98 Urethral hypermobility: Group A: 80/93; Group B: 90/98 POP ≥ grade 1: Group A: 25/93; Group B: 24/98 ISD: Group A: 5/93; Group B: 1/98 DO: Group A: 5/93; Group B: 7/98 |
|
| Interventions | Group A: TVT‐O (n = 93) Group B: Monarc TOT (n = 98) |
|
| Outcomes |
|
|
| Notes | No concomitant urogynaecological surgery performed Follow‐up occurred at 12 months and at 2 ‐4 years Loss to follow‐up at 12 months: Group A: 15/39; Group B: 14/36. Loss to follow‐up at 4 years: Group A: 18/93; Group B: 12/98 Cystoscopy was performed only when bloody urine was encountered Analysis of cure used the numbers that completed follow‐up as denominator |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Women with an indication for surgical treatment of SUI were at random assigned to either TVT‐O or Monarc..."(from abstract Vervest HAM 2005) |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No information |
Jakimiuk 2012.
| Methods | RCT comparing TVT and TVT‐O: POLTOS study | |
| Participants | Multicentre RCT in Poland 35 women Inclusion criteria: women with urodynamically proven (bladder filled to a minimum of 300 ml) SUI; no prior incontinence surgery Exclusion criteria: women with UTI; BMI > 33 kg/m²; previous hysterectomy; neurological incontinence; POP; PVR > 150 ml; OAB and MUI Age: 40‐80 years |
|
| Interventions | Group A: TVT (n = 19) Group B: TVT‐O (n = 16) |
|
| Outcomes |
|
|
| Notes | Follow‐up at 6 months Cystoscopy was performed in both groups Lost to follow‐up: Group A: 4/19; Group B: 0/16 (3 participants with bladder perforation had the tape removed and were excluded) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: “The randomisation was done through a web page secured with a 128‐bit code” |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: “every patient had extra skin incisions for masking the type of procedure (“sham operation”). Each patient had 4 skin incisions in localization typical for needle introduced in TVT and TVT‐O procedure” |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Information not clear |
Juang 2007.
| Methods | RCT of trans‐obturator tension‐free vaginal tape (TVT‐O) versus TVT‐O with modified Ingelman‐Sundberg (IS) procedure | |
| Participants | 96 women Inclusion criteria: women with MUI after poor response to medical treatment DO at baseline: Group A: 19/43; Group B: 15/49 Post menopausal: Group A: 32/43; Group B: 27/49 |
|
| Interventions | Group A: TVT‐O (n = 47) Group B: TVT‐O plus IS: (n = 49) |
|
| Outcomes |
Follow‐up QOL scores: Both IIQ‐7 and UDI‐6 demonstrated a significant decrease at the 3‐months follow‐up in the TVT‐O plus IS group. Scores remained relatively stable after 3 months of follow‐up and until the end of the study. |
|
| Notes | The IS bladder denervation procedure is designed to disrupt most of the innervations from the inferior hypogastric plexus to the bladder to treat refractory urgency or urge incontinence (the vaginal epithelium and perivesical fascia were dissected off the trigone. The plane of dissection was just within the serosal layer of the bladder. Lateral and posterior sharp dissection was performed to obtain more extensive division in the area of the terminal branches of the pelvic nerve). Follow‐up was at 12‐months, but urodynamic profile was repeated at the 3‐month follow‐up Loss to follow‐up: Group A: 2/47; Group B: 1/49 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: “After an objective evaluation, 96 eligible patients were randomised” |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No information |
Kamel 2009.
| Methods | RCT of TVT vs TVT‐O | |
| Participants | 120 women Inclusion criteria: women with urodynamically proven SUI and urethral hypermobility Exclusion criteria: not defined |
|
| Interventions | A: TVT (n = 60) B: TVT‐O (n = 60) |
|
| Outcomes |
|
|
| Notes | TVT group underwent cystoscopy | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Stated: "randomised" |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No information |
Karateke 2009.
| Methods | RCT comparing TVT and TVT‐O | |
| Participants | 167 women Inclusion criteria: women with urodynamically proven SUI Exclusion criteria: urogenital prolapse > stage 1 (POP‐Q); DO; symptoms of OAB; urinary retention; previous anti‐incontinence surgery including anterior colporrhaphy and neurological bladder Mean age (years; SD): Group A: 49.31 (5.00); Group B: 49.08 (4.93) Postmenopausal: Group A: 16/83; Group B: 14/84 Mean BMI kg/m² (SD): Group A: 25.99 (1.27); Group B: 26.18 (1.88) |
|
| Interventions | Group A: TVT (n = 83) Group B: TVT‐O (n = 84) |
|
| Outcomes |
|
|
| Notes | Cystoscopy only performed in TVT group Lost to follow‐up: Group A: 2/83; Group B: 1/84 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "predetermined computer‐generated randomisation code" |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "two independent physicians blinded to the different procedures" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All data included |
Kilic 2007.
| Methods | RCT of TVT vs TOT | |
| Participants | 20 women Inclusion criteria: women with SUI confirmed on urodynamics Mean age (years; SD): Group A: 55.8 (13.7); Group B: 60.2 (12.2) |
|
| Interventions | Group A: TVT (n = 10) Group B: TOT (n = 10) |
|
| Outcomes |
|
|
| Notes | None lost to follow‐up Follow‐up assessment at 12 months |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No information |
Kim 2004.
| Methods | RCT comparing the IRIS (Innovative Replacement of Incontinence Surgery) tape with TVT and SPARC procedure | |
| Participants | 96 women with SUI were randomised | |
| Interventions | Group A: TVT (n = 32) Group B: SPARC (n = 30) Group C: IRIS (n = 34). All 3 groups had comparable background characteristics |
|
| Outcomes |
|
|
| Notes | Follow‐up was for 1 year | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "In this controlled, prospective, randomised study ...." |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No information |
Kim 2005.
| Methods | RCT comparing Monarc TOT with SPARC retropubic tape | |
| Participants | 130 women Inclusion criteria: women with SUI with similar background characteristics Preoperative assessment included the use of voiding diaries, stress and pad tests, and urodynamics Mean age (years; SD): Group A: 45.7 (9.8); Group B: 45.4 (12.4) |
|
| Interventions | Group A: Monarc (TOR; n = 65) Group B: SPARC (RPR; n = 65) |
|
| Outcomes |
|
|
| Notes | Follow‐up at 3 months. Cystoscopy only in the TVT group | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "43 women withUI were randomly assigned..." |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No information |
Krofta 2010.
| Methods | RCT of TVT vs TVT‐O | |
| Participants | 300 women Inclusion criteria: women with SUI after failed conservative treatment. All confirmed on a positive stress test (cough provocation). Women with symptoms of MUI were included if SUI was the predominant symptom Exclusion criteria: DO; previous incontinence, POP surgery, or pelvic radiotherapy; POP‐Q ≥ stage 2; PVR > 100 ml; preoperative use of anticholinergics; need for concomitant surgery Cough provocation test, multichannel UDS, urethral pressure profilometry and uroflometry were done preoperatively and at 12‐month follow‐up |
|
| Interventions | Group A: TVTTM (n = 149) Group B: TVT –OTM (n = 151) |
|
| Outcomes |
|
|
| Notes | All women with TVT had intraoperative cystoscopy but this was not performed in those with TVT‐O Loss to follow‐up: Group A: 8/141; Group B: 4/147 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "women were prospectively, randomly assigned to the study. We used the method of block randomisation with a random‐number generator" |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: "The current randomised, non‐blinded study" |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | All participants were evaluated at follow‐up by 3 urogynaecologists, blinded to the different procedures |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "In the TVT group, 141/149 patients returned for a 1‐year follow‐up (dropout rate of 5.3%), and in the TVT‐O group, 147/151 patients were present for the 1‐year follow‐up (dropout rate of 2.6%)" |
Laurikainen 2007.
| Methods | RCT comparing TVT and TVT‐O | |
| Participants | Multicenter study from 7 Finnish hospitals (4 university hospitals and 3 central hospitals)
267 of the 273 patients originally randomized underwent the allocated operation. After randomisation 6 patients dropped out Inclusion criteria: history of SUI; indication for surgical treatment of stress incontinence; positive cough‐stress test; detrusor instability score (DIS) ≤ 7 Exclusion criteria: previous incontinence surgery; PVR volume > 100 ml; lower urinary tract anomaly; current (UTI or > 3 UTI episodes within the past year; urogenital prolapse of more than second degree (Baden‐Walker); BMI > 35 kg/m²; previous radiation therapy of the pelvis; active malignancy; anticoagulant therapy; haemophilia; neurogenic disease that can be associated with bladder disorders; anticholinergic medication; duloxetine medication; patient unable to understand the purpose of the trial; patient immobile |
|
| Interventions | Group A: TVT‐O (n = 131) Group B: TVT (n = 136) | |
| Outcomes |
|
|
| Notes | Cystoscopy with 70° optic was performed twice during the TVT and once during the TVT‐O to detect possible bladder injury Follow‐up was for 5 years:
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The investigator called an independent randomisation centre to enter the patient participant in the allocated group. Participant were randomized using computer‐generated random allocations in a ratio of 1:1 in balanced blocks of 4. |
| Allocation concealment (selection bias) | Low risk | The investigator called an independent randomisation centre to enter the patient participant in the allocated group. Participant were randomized using computer‐generated random allocations in a ratio of 1:1 in balanced blocks of 4. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | The 3‐year postoperative evaluation was performed by an independent physician or by the operating surgeon together with a study nurse |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All data accounted for |
Leanza 2009.
| Methods | RCT of retropubic versus transobturator tension‐free incontinence cystocoele treatment (TICT) procedures | |
| Participants | 449 women with USI | |
| Interventions | Group A: r‐TICT (n = 229; retropubic) Group B: t‐TICT (n = 220; transobturator) |
|
| Outcomes |
|
|
| Notes | TICT, a retropubic technique developed using a polypropylene T‐shaped mesh made up by a central body (positioned under both urethra and bladder) and 2 wings that cross the Retzius (retropubic TICT or r‐TICT) and the transobturator foramen (transobturator TICT or t‐TICT). The advantage of T‐shaped mesh is to give a good support both on the mid‐urethral complex (with tapes) and on the whole anterior compartment (with body of mesh). The target consists of treating the functional (incontinence) and the anatomical defect (cystocoele) Average follow‐up was 45 months. Loss to follow‐up: Group A: 14/229; Group B: 12/220 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: “women with urodynamic stress incontinence were randomly allocated to 2 treatment groups” |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No information |
Lee 2007.
| Methods | RCT of TVT versus TVT‐O | |
| Participants | 120 women Inclusion criteria: women with USI Exclusion criteria: predominant urge incontinence or POP Women had similar characteristics with regard to age, parity, incontinence symptoms and menopausal status |
|
| Interventions | Group A: TVT (n = 60) Group B: TVT‐O (n = 60) |
|
| Outcomes |
Follow‐up was for 12 months |
|
| Notes | Cystoscopy was performed only in the TVT group Mean follow‐up 13 months |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote: "Patients were alternately assigned to the TVT or TVT‐O group" (Randomisation was by alternation method) |
| Allocation concealment (selection bias) | High risk | Not concealed |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No information |
Lee 2008.
| Methods | QRCT comparing the efficacy and safety of TVT‐O and TOT (TOT, Dow Medics, Korea) | |
| Participants | 100 women Inclusion criteria: women with USI Exclusion criteria: predominant urge incontinence or POP Preoperative work‐up included a medical history, physical examination, urinalysis, urodynamic evaluation, and I‐QOL questionnaire |
|
| Interventions | Group A: TVT‐O (n = 50) Group B: TOT (n = 50) |
|
| Outcomes | Surgical outcomes were evaluated by the cough‐stress test and symptom questionnaire and scored as cured, improved, or failed. Participants were considered ‘cured’ of SUI if they had a negative cough‐stress test result and there were no reports of urine leakage during stress. Participants were considered ‘improved’ if they did not leak on the cough‐stress test but may have had occasional urine leakage during stress; this occasional leakage did not influence their daily activities or require further treatment. Participants who did not meet these criteria were considered to have ‘failed’ treatment | |
| Notes | Surgical outcomes in the 2 groups were compared about 1 year after surgery. TOT, Dow Medics, Korea = woven monofilament polypropylene mesh |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | 100 women with SUI were alternately assigned |
| Allocation concealment (selection bias) | High risk | Quasi‐randomised study with no mention of allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No information |
Liapis 2006.
| Methods | RCT comparing TVT and TVT‐O | |
| Participants | 89 women Inclusion criteria: women with confirmed SUI without DO Exclusion criteria: DO; other gynaecological disease requiring hysterectomy; other gynaecologic operation; failed surgical treatment for incontinence Mean age (years): Group A: 53; Group B 52 Post menopausal: Group A: 22/46; Group B: 26/43 |
|
| Interventions | Group A: TVT (n = 46) Group B: TVT‐O (n = 43) |
|
| Outcomes | Participants assessed by means of voiding diaries, pad test, negative cough‐stress test at UDS, unvalidated symptom questionnaire
Subjective cure and failure determined by direct questions using an unvalidated questionnaire Follow‐up 12 months |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "... All patients were randomly assigned to an operation from the outpatient department ..." |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No differential loss to follow‐up or differential attrition |
Liapis 2008.
| Methods | RCT comparing Monarc TOT and TVT‐O | |
| Participants | 120 women were randomised
Inclusion criteria: women with USI without DO Exclusion criteria: preoperative maximum urethral closure pressure < 20 cm water; urodynamic findings of DO; previous operation of the anterior vaginal wall or prolapse > stage 1 according to the ICS classification |
|
| Interventions | Group A: TVT‐O (n = 61) Group B: Monarc TOT (n = 53) |
|
| Outcomes |
|
|
| Notes | Both groups had perioperative cystoscopy.
Groin or thigh pain was resolved with simple analgesics within 1 week to 4 months Follow‐up was 12 months. 6 lost to follow‐up leaving a total of 114 women |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The patients were randomly allocated on an alternative fashion to one or another operation." |
| Allocation concealment (selection bias) | Unclear risk | Unclear |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No differential loss to follow‐up or differential attrition |
Lim 2005.
| Methods | RCT comparing TVT with IVS and SPARC | |
| Participants | 195 women Inclusion criteria: women with USI were randomly allocated to suburethral slingoplasty with either TVT, IVS or SPARC. Exclusion criteria: women with a past history of urogenital malignancy, fistula or pelvic radiotherapy At 6‐12 weeks follow‐up, 4, 5 and 4 women from the TVT, IVS and SPARC groups, respectively, were excluded from statistical analysis because of incomplete or missing hospital charts |
|
| Interventions | Group A: TVT (n = 61) Group B: IVS (n = 60) Group C: SPARC (n = 61) |
|
| Outcomes |
|
|
| Notes | Group A: 4 patients; Group B: 5 patients; and Group C: 4 patients were excluded from the analysis due to incomplete or missing data. Those with missing records, those lost to follow‐up and those who failed to have postoperative UDS were assumed to be failures in the assessment of objective cure. Occult cases were excluded from subjective cure rates Follow‐up initially for 12 weeks and results reported, a follow‐on study reviewed the incidence of erosion and tape infections |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "...195 consenting patients with urodynamic stress incontinence (USI) were randomly allocated in a balanced way (three groups of 65 patients each)..." |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: " ... and the patients were blinded to the type of slings being implanted ..." No description of how this was achieved. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Unclear |
Lord 2006.
| Methods | RCT comparing TVT with SPARC sling | |
| Participants | 301 women Inclusion criteria: women presenting with SUI whether or not they had had previous incontinence or other pelvic surgery, or both Exclusion criteria: < 18 years old; pregnant; had a major voiding dysfunction specified as an abnormal flow (i.e. maximum urinary flow rate < 10 ml/s) or residual urinary volume of > 150 ml 254 women had UDS and USI diagnosed MUI: 47 women |
|
| Interventions | Group A: TVT (n = 147) Group B: SPARC (n = 154) | |
| Outcomes | Primary outcome: bladder perforation Secondary outcomes:
The subjective assessments of cure were the participants' reported use of protection, their perceptions of the severity of their SUI symptoms and a scale of improvement (1 to 100). The objective definition of cure was the observed absence of urinary leakage when the participant coughed while supine and with a comfortably full bladder Follow‐up was 6 weeks |
|
| Notes | The women and the outcome assessors were blinded, but no clear description was provided for how this was achieved | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were stratified based on previous UI surgery (yes, no) and the experience of the surgeon (consultant, registrar) and allocated to either TVT or SPARC using computer‐generated random numbers. The biostatistician generated the random allocations, which were sealed in opaque, sequentially numbered envelopes. The surgeons recruited participants and accessed the allocations by a telephone call to a third party. Varying block sizes of 4, 6 and 8 were used within each stratum to preclude prediction of allocation by the surgeons |
| Allocation concealment (selection bias) | Low risk | Concealed |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "The analyst was unaware of the treatment allocation, but it was obviously not possible to ensure that the surgeons were unaware of treatment, although the patients were unable to detect, from their incisions, which sling they had received" |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "The analyst was unaware of the treatment allocation, but it was obviously not possible to ensure that the surgeons were unaware of treatment, although the patients were unable to detect, from their incisions, which sling they had received" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No differential loss to follow‐up or differential attrition |
Mansoor 2003.
| Methods | RCT comparing TVT‐O and TVT | |
| Participants | 102 women with SUI with or without POP Preoperative urodynamics carried out |
|
| Interventions | Group A: TVT‐O (n = 48) Group B: TVT (n = 54) | |
| Outcomes |
|
|
| Notes | Follow‐up 6 months | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "A prospectively randomised and comparative study....." |
| Allocation concealment (selection bias) | Low risk | Quote:"...technique was randomly drawn using blinded envelopes containing the same no of ..." |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No information |
Mehdiyev 2010.
| Methods | RCT of TVT vs TOT | |
| Participants | 32 women with SUI | |
| Interventions | A: TOT (n = 17) B: TVT (n = 15) |
|
| Outcomes | Subjective cure Bladder Injury Major vascular injury: De novo UUI Mean operative time |
|
| Notes | I‐QoL questionnaire was used | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The patients were randomised for TOT and TVT operations" |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No information |
Meschia 2006.
| Methods | RCT of TVT compared with IVS | |
| Participants | 190 women randomised with 11 lost to follow‐up, thus 179 available for analysis at 2‐year follow‐up. The 2 groups were no different in terms of age, parity, BMI, previous hysterectomy, or presence of OAB symptoms
Inclusion criteria: women with urodynamically proven SUI and urethral hypermobility Exclusion criteria: previous anti‐incontinence surgery; vaginal prolapse requiring treatment; coexisting pelvic pathology; known bleeding diathesis or current anticoagulant therapy; DO; and urethral hypomobility (Q‐tip <20° from the horizontal with straining) |
|
| Interventions | Group A: TVT (n = 92) Group B: IVS (n = 87) | |
| Outcomes | Primary outcome: success rate Secondary outcome measure: complication rate The outcome of surgical treatment was estimated both subjectively and objectively. Objective cure was defined as no leakage of urine while performing the cough provocation test, with at least 300 ml of saline in the bladder and as a pad weight gain < 1g during the 1‐h test. Test‐retest reliability of the cough test and 1‐hr pad test have been previously demonstrated. Subjective cure was defined as no urine loss during 'stress' and failure as any reported leakage of urine during exertion |
|
| Notes | IVS = multifilament threads with smaller pores with insertion similar to TVT | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "...a prospective randomised multicenter trial ... were randomly assigned to treatments according to a centralized computer‐generated random list.... Researchers randomly assigned participants by a telephone system to 1 of the treatment groups" |
| Allocation concealment (selection bias) | Low risk | Concealed |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No information |
Meschia 2007.
| Methods | RCT of TVT versus TVT‐O | |
| Participants | Inclusion criteria: women with urodynamic SUI and urethral hypermobility Exclusion criteria: previous anti‐incontinence surgery; vaginal prolapse requiring treatment; coexisting pelvic pathology; known bleeding diathesis or current anticoagulant therapy; DO and urethral hypomobility (Q‐tip <20° from the horizontal with straining) |
|
| Interventions | 206 women randomised, but 25 lost to follow‐up
Group A: TVT (n = 114) Group B: TVT‐O (n = 117) |
|
| Outcomes | Primary outcome: success rate Secondary outcome: complication rate Outcome of surgical treatment was estimated both subjectively and objectively. Objective cure was defined as no leakage of urine whilst performing the cough provocation test. Subjective cure was defined as no urine loss during ‘stress’, and failure as any reported leakage of urine during exertion ICIQ‐SF, Women Irritative Prostate Symptoms Score (W‐IPSS), PGI‐S and PGI‐I questionnaires were used to evaluate the impact of incontinence and voiding dysfunction on QoL, and to measure the participant’s perception of incontinence severity and improvement |
|
| Notes | Median follow‐up time was 6 months 6 women from Group A and 7 from Group B were lost to follow‐up without outcome data; reasons for loss to follow‐up not explored Cystoscopy was performed in all cases of TVT and 50% of cases of TVT‐O |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Women with SUI and urethral hypermobility were randomised to treatments according to a centralised computer‐generated random list. Researchers randomised participants by a telephone system to one of the treatment groups |
| Allocation concealment (selection bias) | Low risk | Concealed |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No differential loss to follow‐up or differential attrition |
Naumann 2006.
| Methods | RCT of classic TVT tape by Gynecare compared with LIFT by Cousin Biotech, with the distinctive feature of a suburethral pad (assumed to be inserted as classic TVT) | |
| Participants | 254 women with SUI | |
| Interventions | Group A: TVT (n = 123) Group B: LIFT (n = 125) |
|
| Outcomes |
|
|
| Notes | Follow‐up 12 months LIFT is a woven monofilament polypropylene tape that can be passed through the transobturator and also the retropubic routes The study seemed to compare the 2 tapes (TVT and LIFT), which have similar characteristics and were both passed through the retropubic routes |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "..an open, prospective, randomised, multicentric study". How sequence generation was achieved not mentioned |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No information |
Nerli 2009.
| Methods | QRCT of TVT vs TOT | |
| Participants | Inclusion criteria: women > 18 years; with SUI or MUI if SUI is the predominant symptom; women with ISD Exclusion criteria: predominant urge incontinence; UTI; malignancy; pregnancy; POP stage 3 or 4 Mean age (years; SD): Group A: 39.5 (1.95); Group B: 50.2 (1.89) Post menopausal status: Group A 8/18; Group B: 6/18 |
|
| Interventions | Group A: TVT (n = 18) Group B: TOT (n = 18) |
|
| Outcomes |
|
|
| Notes | Cystoscopy performed only in the TVT group I‐QOL questionnaire assessed at 12 month F/U: significant improvement in I‐QOL total scores in both groups from the pre‐operative baseline scores. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Allocation of participants by alternation (quasi randomised) |
| Allocation concealment (selection bias) | High risk | Allocation not concealed |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No information |
Nyyssonen 2014.
| Methods | RCT of TVT (Gynecare) vs TOT ('outside‐in' Monarc) | |
| Participants | 100 women Inclusion criteria: women with SUI or MUI with a predominant stress component, after failed conservative treatment Exclusion criteria: urge incontinence; previous mini invasive operation for SUI and the need for another concomitant surgical procedure SUI diagnosed with a positive cough test Urodynamic testing was only done in 5 patients (10%) Pure SUI: Group A: 38/50; Group B: 30/50 Preoperative characteristics similar between groups |
|
| Interventions | Group A: TOT (n = 50) Group B: TVT (n = 50) |
|
| Outcomes |
Follow‐up at 3, 14 and 46 months Cough stress test was performed. Subjective cure and patient satisfaction recorded with aid of UISS and Detrusor Instability Score questionnaires with a specific question about satisfaction |
|
| Notes | Cystoscopy only performed in the TVT group Number available for follow‐up assessments: 14 months: Group A: 43/50; Group B: 43/50 At 46 months: Group A: 46/50; Group B: 47/50 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "This prospective randomized study included ... 100 patients were randomized either to the TVT or to the TOT" |
| Allocation concealment (selection bias) | Low risk | Quote: "randomization was performed with sealed and numbered envelopes" |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No evidence suggestive of attrition bias |
Okulu 2013.
| Methods | RCT of Vypro mesh (Ethicon, USA) vs Ultrapro mesh (Ethicon) vs Prolene light mesh (condensed monofilament non‐absorbable polypropylene) | |
| Participants | 144 women with SUI in Turkey Inclusion criteria: previous incontinence surgery or hysterectomy; SUI or USI; positive stress test Exclusion criteria: urodynamically MUI and DO; ≥ 100 ml PVR; contraindication to anaesthesia; POP; pregnancy; neurogenic bladder; bladder outlet obstructions; urinary fistula; or active urinary or vaginal infection Mean age (years; SD): Group A: 50.06 (9.2); Group B: 50.9 (8.8); Group C: 48.1 (7.9) Mean BMI kg/m² (SD): Group A: 27.8 (3.4); Group B: 27.9 (4.1); Group C: 27.7 (2.9) Post menopausal: Group A: 10/48; Group B: 11/48; Group C: 8/48 Previous incontinence surgery: Group A: 4/48; Group B: 5/48; Group C:4/48 |
|
| Interventions | Group A: Vypro mesh: (n = 48; multifilament) Group B: Ultrapro mesh: (n = 48; monofilament + biological combined mesh) Group C: Prolene light mesh: (n = 48; monofilament) |
|
| Outcomes | Primary outcome: urinary continence rates at 4‐year follow‐up Secondary outcomes assessed at 4‐year follow‐up:
|
|
| Notes | Follow‐up at 6, 12, 24 and 48 months Loss to follow‐up Group A: 2/48; Group B: 0/48; Group C: 1/48 QoL and incontinence was evaluated with the ICIQ‐SF |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: “The patients and the mesh materials were randomised 1:1:1 to each group in blocks of three via a centralized computerized system to ensure a good balance of participant characteristics in each group." |
| Allocation concealment (selection bias) | Low risk | Quote: “via a centralized computerized system to ensure a good balance of participant characteristics in each group” |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No information |
Oliveira 2006.
| Methods | RCT of TVT‐O and TVT | |
| Participants | 45 women Inclusion criteria: women with SUI with and without ISD Exclusion criteria: women with stage 2 or more POP, women with ISD Mean age of 53.9 years Participants had preoperative UDS diagnosis |
|
| Interventions | Group A: TVT (n = 17) Group B: TVT‐O (n = 28) | |
| Outcomes |
|
|
| Notes | Follow‐up 12 months | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "...women with SUI were randomly assigned ..." |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No information |
Palomba 2008.
| Methods | RCT of TOT + mesh repair of POP vs TVT + mesh repair of POP | |
| Participants | Inclusion criteria: 15 women with cystocoele and SUI with urethral hypermobility Exclusion criteria: BMI > 30 kg/m²; previous incontinence surgery and detrusor instability and/or intrinsic sphincter dysfunction |
|
| Interventions | Group A: TOT + mesh repair of POP Group B: TVT + mesh repair of POP |
|
| Outcomes | Trial terminated due to poor recruitment, no results published | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Stated: "randomised" |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No information |
Paparella 2010.
| Methods | RCT of synthetic UretexTO® vs biological PelviLaceTO® outside‐inside TOT | |
| Participants | Inclusion criteria: women with SUI and USI; SUI with urethro‐vesical junction hypermobility without ISD Exclusion criteria: POP > stage 1; previous urogynaecological or anti‐incontinence surgery; concurrent diseases such as psychiatric disease, diabetes, peripheral vascular disease; history of pelvic radiation; urge and mixed incontinence; DO; urgency or neurologic bladder; maximum urethral closure pressure < 20 cm H2O and VLPP < 60 cm H2O (indicators of intrinsic sphincter deficiency); maximum flow ≤ 12 ml/s; and PVR volume ≥ 100 ml Mean age (years; SD): Group A: 60.7 (7.1); Group B: 59.4 (8.4) Mean BMI kg/m² (SD): Group A: 25.4 (1.8); Group B: 24.9 (1.8) Menopausal: Group A: 26/34; Group B: 30/36 (participants in menopause were subjected to at least 1 month of local hormone replacement therapy both before and after the surgery) QoL and sexual impact measured via: KHQ and PISQ‐12 |
|
| Interventions | Group A: synthetic UretexTO® (n = 34) Group B: biological PelviLaceTO® (n‐36) |
|
| Outcomes |
|
|
| Notes | Group A: synthetic (UretexTO®; Bard, Covington, GA) is self‐anchoring transobturator suburethral sling (1.2 cm wide and 45 cm long) made of the same monofilament polypropylene fibres used in many modern tension‐free sling devices (for example TVT, TVT‐O, TOT Monarc, TOT ARIS etc). Polypropylene is a very biocompatible material that has been used for many years in the construction of medical‐grade synthetic meshes. The important difference is how the polypropylene fibres are knitted to form a cohesive macroporous mesh Group B: biological material (PelviLaceTO®; Bard, Covington, GA) is a tension‐free and self‐anchoring transobturator suburethral sling (1.5 cm wide and 40 cm long). It consists of a porcine dermal collagen implant that is intended to provide a matrix for the incorporation of new tissue, cells and blood vessels, thanks to a natural porosity and artificial V‐shaped holes along the arms. Its collagen matrix consists of 3 amino acid chains arranged in a triple helix that has been cross‐linked with hexamethylenediisocyanate to improve durability making the collagen non‐resorbable by the collagenase (enzymes produced by inflammatory cells and fibroblasts that increase during surgery). It is also described as an acellular and deproteinised material so it should not cause an immune response Follow‐up evaluation was carried out after 6 weeks, 6 months, 1, and 2 years 2‐year follow‐up: Group A: 16.6 (3.0); Group B: 17.2 (3.0) Loss to follow‐up: Group A: 1/34; Group B: 0/36 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: “Randomization was done using sealed opaque envelopes containing computer‐generated random allocations in a ratio of 2:2 in balanced blocks of 4” |
| Allocation concealment (selection bias) | Low risk | Quote: “Randomization was done using sealed opaque envelopes containing computer‐generated random allocations in a ratio of 2:2 in balanced blocks of 4” |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: “Follow‐up evaluation was carried out after 6 weeks, 6 months, 1, and 2 years (and/or earlier if problems were experienced) for all patients by two independent physicians” |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: “All patients in both arms completed the follow‐up (2 years)” |
Park 2012.
| Methods | Pseudo RCT of TVT‐O vs TOT (Monarc) | |
| Participants | 74 women Inclusion criteria: women with SUI including those with MUI Exclusion criteria: neurogenic bladder; POP; suspected ISD; or a past history of radical pelvic surgery Mean age (years): Group A: 54.4 (10.13); Group B: 55.1 (10.63) Mean BMI kg/m²: Group A: 28.9 (0.53); Group B: 25.9 (0.48) Urgency/UUI: Group A: 25/39; Group B: 22/35 |
|
| Interventions | Group A: TVT‐O (n = 39) Group B: TOT Monarc (n = 35) |
|
| Outcomes | Cure was defined as the absence of any episodes of involuntary urine leakage during stressful activities and a stress test. Improvement was defined as a significant reduction in urine leakage, such that it did not require further treatment
|
|
| Notes | Cystoscopy was performed in all women | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: “were included in this randomised, prospective, observational study” |
| Allocation concealment (selection bias) | High risk | Quote: "The procedure was performed by a single surgeon, and patients underwent one of the two techniques in accordance with the scheduling order (MONARC and TVT‐O), in alternation" |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All accounted for |
Peattie 2006.
| Methods | RCT TVT‐O vs Monarc TOT | |
| Participants | Inclusion criteria: women having a primary continence procedure without other surgery; diagnosis of USI; completed course of physiotherapy; completed family Exclusion criteria: previous continence or prolapse surgery; neurological disease; pregnancy; UTI or vaginal infection; DO; voiding problem; anticoagulant use |
|
| Interventions | Group A: TVT‐O Group B: TOT |
|
| Outcomes | Primary outcomes: objective and subjective cure of USI Secondary outcomes:
|
|
| Notes | Note: trial started recruitment 2006 but no evidence of current status i.e. completed or recruitment stopped or abandoned. No data published | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "patient allocation by random numbers with blocking" |
| Allocation concealment (selection bias) | Low risk | Quote: "patient allocation by random numbers with blocking" |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No information. |
Porena 2007.
| Methods | RCT of TVT versus TOT | |
| Participants | 145 women Inclusion criteria: women with stress or MUI (stress component clinically predominant) associated with urethral hypermobility (ICS definitions) Exclusion criteria: previous anti‐incontinence surgery and POP > stage 1, according to the Half‐Way system and POP‐Q system classification, in any vaginal compartment With the exception of DO, which was significantly more common in the TOT group, no significant intergroup differences emerged with regard to surgical histories, SUI grade, frequency of mixed incontinence, preoperative voiding or storage symptoms and preoperative urodynamic parameters VLPP determined at a bladder volume of 200 mL and participants performed several Valsalva manoeuvers with a gradual increase in abdominal pressure. Participants stratified by VLPP > 60 cm H2O or VLPP ≤ 60 cm H2O VLPP ≤ 60 cm H2O (ISD): Group A: 25/70; Group B: 25/75 Mean age (years; SD): Group A: 61.8 (10.7); Group B: 60.6 (10) Postmenopausal: Group A: 61/70; Group B: 64/75 SUI: Group A: 42/70; Group B: 41/75 MUI: Group A: 28/70; Group B: 34/75 DO: Group A: 4/70; Group B: 14/75 |
|
| Interventions | Group A: TVT (n = 70) Group B: TOT (n = 75) |
|
| Outcomes | Primary outcomes:
Secondary outcomes:
All participants completed 2 validated questionnaires on QoL, the UDI‐6 and the IIQ‐7 before surgery, at 3, 6, 12 months postoperatively and then annually Patient satisfaction outcome was measured via a VAS scale Objective cure (dry) Objective cure and improved (dry + wet but improved) Subjective cure (dry) Subjective cure and improved(dry + wet but improved) Bladder injury Vaginal perforation Major vascular injury Voiding Dysfunction Tape erosion Long‐term follow‐up (> 6 years, mean 99 ± 19 months): 83 participants (45 TOT; 38 TVT) underwent a telephone interview in October 2012. |
|
| Notes | TVTTM (Gynecare; Ethicon, Somerville, NJ, USA) TOTTM was a fusion‐welded, non woven, non knitted polypropylene tape (Obtapej; Mentor‐Porges, Le Plessis‐Robinson, France) All participants underwent a preoperative urodynamic assessment and intraoperative cystoscopy Follow‐up was at 3, 6, and 12 months postoperatively, and then annually Lower urinary tract dysfunctions and continence status were measured at each follow‐up visit by a blinded assessor The overall median follow‐up was 35 months |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "prospectively randomized by a predetermined computer‐generated randomization code, to the retropubic approach (TVT) or the transobturator route (TOT)" |
| Allocation concealment (selection bias) | Low risk | Quote: " Randomization was done using sealed, opaque, numbered envelopes, which contained the randomized allocation" |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Outcome assessors were blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "No patient was lost during follow‐up" |
Rechberger 2003.
| Methods | RCT comparing TVT and IVS | |
| Participants | 100 women Inclusion criteria: women with USI without concomitant pelvic pathology requiring surgery, some had had anti‐incontinence surgery previously Exclusion criteria: ISD |
|
| Interventions | Group A: TVT (n = 50) Group B: IVS (n = 50) |
|
| Outcomes |
Participants were considered totally cured when free of all SUI symptoms, and cough tests in supine and standing positions were negative. The operation was noted as a failure if the participant still reported urine leakage during increases in intra‐abdominal pressure, the cough test with a comfortably full bladder was positive, and the woman had to change her pads because of being wet during the day In the improvement group the cough test was negative but participants still experienced stress urinary leakage (much less frequent than previously) and the pads were occasionally wet Postoperative UDS was not performed |
|
| Notes | Median follow‐up of 13.5 months (range 4 to 18 months) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Unclear |
| Allocation concealment (selection bias) | Unclear risk | Simple randomisation was used from pseudo‐random numbers (pseudo‐random number means that the participants were operated on by the TVT or the IVS method in a ratio of 1:1). Generated by computer in order to allocate participant to the monofilament or the multifilament group. Investigator KR was not involved in surgical procedure but was responsible for proper randomisation. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Blinded |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Unclear |
Rechberger 2009.
| Methods | RCT of retropubic IVS‐02 vs transobturator IVS‐04, multifilament type 3 tape | |
| Participants | Inclusion criteria: women with SUI with a positive cough provocation test Exclusion criteria: presence of uterine myoma; ovarian cyst; or advanced uterine or vaginal prolapse (POP‐Q scale > grade 1) Mean age (years; SD): Group A: 55.56 (10.19); Group B: 55.75 (11.29) Postmenopausal: Group A: 119/269; Group B: 125/268 VLPP: leak pressure during Valsalva manoeuvre was measured. VLPP was determined at 180 ml of bladder filling. ISD was defined as VLPP of ≤ 60 cm H2O ISD: Group A: 45/269; Group B: 40/268 |
|
| Interventions | Group A: retropubic (IVS‐02; n = 269) Group B: transobturator (IVS‐04; n = 268) |
|
| Outcomes |
|
|
| Notes | The follow‐up visits were at 1, 4, 6, 12, and 18 months Cystoscopy only performed in the retropubic group Loss to follow‐up: Group A: 68/269; Group B: 71/268 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: “Simple randomisation was used from pseudorandom numbers generated by a computer to allocate patients into the IVS‐02 group or the IVS‐04 group” |
| Allocation concealment (selection bias) | Unclear risk | Investigators Jankiewicz and Futyma were not involved in the surgical procedures, but they were responsible for the randomisation process |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Quote: "the surgeon was aware of the procedure being used” |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Quote:"Only investigators Jankiewicz and Futyma were involved in the follow‐up process, and they were blinded with regard to the treatment procedure used" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All outcome data accounted for and the equivalent no of women were lost to follow‐up in the 2 groups |
Rechberger 2011.
| Methods | RCT of standard TOT vs TOT with 2‐point tape fixation sutures to prevent tape displacement | |
| Participants | 463 women Inclusion criteria: women with urodynamically proven SUI, Including women with ISD Exclusion criteria: OAB, MUI Mean age (years; SD): Group A: 55.8 (11.3); Group B: 54.8 (9.8) Mean BMI kg/m² (SD): Group A: 28.9 (6.7); Group B: 28.2 (3.8) ISD: Group A: 41/232; Group B: 42/231 |
|
| Interventions | Group A: TOT (n = 232) Group B: TOT with fixation (n = 231) |
|
| Outcomes |
|
|
| Notes | Both tapes were monofilament Lost to follow‐up: Group A: 19/232; Group B: 26/231 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Patients were randomly allocated to 2 groups" |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No information |
Richter 2010.
| Methods | RCT: multi‐centre randomised equivalence trial conducted in the USA | |
| Participants | 597 women Inclusion criteria: age >21 years; predominant SUI for >3 months (urgency UI allowed); positive urinary stress test; bladder volume >300 ml Exclusion criteria: not defined Baseline characteristics similar between groups Mean age (years; SD): Group A: 52.7 (10.5); Group B: 53.1 (11.5) Previous incontinence surgery: Group A: 38/297; Group B: 41/298 Previous prolapse surgery: Group A: 13/297; Group B: 10/298 Postmenopausal: Group A: 209/297; Group B: 206/298 BMI kg/m²: Group A: 30.6; Group B: 30 HRT: Group A: 81/297; Group B: 90/298 Concomitant pelvic surgery: Group A: 73/298; Group B: 78/299 |
|
| Interventions | Group A: retropubic sling (TVT; n = 298) Group B: transobturator tapes (TVT‐O, and TOT Monarc; n = 299) (Group C (?): TVT‐O (inside‐out) ‐ separate data not provided) (Group D (?): TOT (Monarch, outside‐in) ‐ separate data not provided) |
|
| Outcomes | Composite primary outcomes:
Secondary outcomes:
|
|
| Notes | TOMUS trial NCT00325039 Per protocol Lost to follow‐up: Group A: 18/298; Group B: 14/299 PISQ measures dyspareunia, coital incontinence and fear of coital incontinence |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Permuted block randomisation schedule with stratification by centre |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Quote: "patients who were lost to follow‐up were considered to have had treatment failure and when patients who were lost to follow‐up were excluded” |
Riva 2006.
| Methods | RCT TVT versus TOT | |
| Participants | Inclusion criteria: SUI with urethral hypermobility; age 40‐85 years; urethro‐cystocoele of grade 0‐2 Exclusion criteria: previous prolapse or IU surgery; anterior or posterior vaginal wall repair with mesh No difference recorded between the 2 groups for age, parity, or incontinence severity |
|
| Interventions | Group A: TOT (n = 65) Group B: TVT (n = 66) |
|
| Outcomes | Gynaecological examination, full urodynamic evaluation, voiding diary and KHQ were performed pre‐ and postoperatively | |
| Notes | 12‐month follow‐up | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "A randomised study". No description of how randomisation was achieved or if allocation was concealed |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No information |
Salem 2014.
| Methods | RCT of TOT vs TVT | |
| Participants | 76 women with SUI, all had urodynamics | |
| Interventions | Group A: TOT (n = 37) Group B: TVT (n = 39) |
|
| Outcomes |
|
|
| Notes | No usable data provided | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "were included in this randomized controlled study .... Patients were randomly grouped" |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No information |
Scheiner 2012.
| Methods | RCT of TVT vs TOT (Monarc) vs TVT‐O | |
| Participants | 2 public teaching hospitals in Switzerland Inclusion criteria: women with urodynamically confirmed SUI, or MUI with predominant SUI Exclusion criteria: missing urodynamic assessment; previous sling procedure; predominant OAB; a PVR > 100 ml Mean age (years; SD): Group A: 57.8 (13.0); Group B: 56.6 (10.3); Group C: 59.3 (12.1) Mean BMI kg/m² (SD): Group A: 26.4 (3.7) Group B: 27.8 (4.6); Group C: 27.6 (4.8) |
|
| Interventions | Group A: TVT (n = 80) Group B: TOT outside‐in approach (Monarc; n = 40) Group C: TVT‐O inside‐out approach (Gynecare; n = 40) |
|
| Outcomes |
|
|
| Notes | Preoperatively, conservative measures for SUI were recommended, such as use of local estrogens, pelvic floor re‐education, or incontinence pessaries. A symptomatic cystocele stage 2 or higher according to the POP‐Q system was corrected first. Participants with concomitant sling insertion to repair prolapse were included Cystoscopy was mandatory for every procedure Lost to follow‐up: Group A: 15; Group B: 6; Group C: 3 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Predetermined computer generated block randomisation in blocks of 8 to promote group balance |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants accounted for |
Schierlitz 2008.
| Methods | RCT of retropubic (TVT™ ) versus transobturator (Monarc™)) sling in the treatment of women with USI and ISD | |
| Participants | 163 women Inclusion criteria: women with SUI who had unsuccessful conservative therapy and, on UDS, had a diagnosis of USI and ISD ISD was defined as either a maximum urethral closure pressure (measured both with the bladder empty and at capacity) of <20 cm H2O and/or a pressure rise from baseline required to cause incontinence (Valsalva or cough leak point pressure) of ≤60 cm H2O Exclusion criteria: presence of pelvic infection; a persistent PVR volume > 100 ml; malignancy; fistula; or congenital or neurogenic bladder disorder Mean age (years; SD): Group A: 60 (11.5); Group B: 60 (10.9) Post menopausal: Group A: 66/82; Group B: 68/82 Previous incontinence surgery: Group A: 6/82; Group B: 11/82 Concomitant surgery: Group A: 29/82; Group B: 26/82 |
|
| Interventions | Group A: TVT (n = 81) Group B: Monarc sling (n = 82) |
|
| Outcomes |
|
|
| Notes | Follow‐up was at 6 weeks and 6 months, then yearly for 3 years Loss to follow‐up: Group A: 5/82; Group B: 4/82 At 3‐year follow‐up: Group A: 72 followed‐up with 70 completing questionnaires, and 48 completing examination Group B: 75 followed‐up with 60 completing questionnaires, and 40 completing examination The number available for follow up or number lost to follow up at 5yrs was not made clear (authors have been contacted and response is awaited) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "... A prospective, randomised controlled trial was conducted using computer generated random allocation." |
| Allocation concealment (selection bias) | Unclear risk | No description of how allocation was concealed |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | The number of participants who withdrew or were lost to follow‐up (dropouts) was higher in the TVT group |
Tanuri 2010.
| Methods | RCT of retropubic Safyre VS adjustable sling system and Safyre T adjustable transobturator sling system | |
| Participants | 30 women Inclusion criteria: women with SUI Exclusion criteria: use of drugs (adrenergic, anticholinergic or serotonergic); hormone therapy within the previous 6 months; prior pelvic radiotherapy or current chemotherapy or hormone therapy; POP > stage 2; MUI |
|
| Interventions | Group A: Safyre VS retropubic tape (n = 10) Group B: Safyre T transobturator tape (n = 20) |
|
| Outcomes |
|
|
| Notes | Follow‐up was at 1, 6 and 12 months | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Participants were randomised into 2 groups |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data for all participants accounted for |
Tarcan 2011.
| Methods | RCT: TVT (AdvantageR) vs TOT (ObtryxR) | |
| Participants | 54 women with urodynamic SUI SUI: n = 10; MUI: n = 35 Median age in years (range): 54 (31‐76) BMI kg/m²: Group A: 27.8 (4.6); Group B: 27.4 (4.04) Concomittant POP surgery: Group A: 5/27; Group B: 2/27 |
|
| Interventions | Group A: TVT (n = 27) Group B: TOT (n = 27) |
|
| Outcomes | 12‐month follow‐up assessed:
2 year follow‐up assessed:
|
|
| Notes | Concomitant POP surgery was performed in 7 women (6 cystocele, 1 rectocoele) No mention of intraoperative cystoscopy |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No information |
Teo 2011.
| Methods | RCT of TVT vs TVT‐O | |
| Participants | 127 women recruited from 2 hospitals in the UK Inclusion criteria: women with USI Exclusion criteria: previous continence surgery; OAB symptoms; DO; POP‐Q > stage 1; presence of voiding dysfunction (defined as maximum flow rate < 15 ml/s or PVR volume ≥ 100 ml) Women in both groups had similar background characteristics, degree of severity of symptoms and QoL scores Mean age (years; SD): Group A: 52.4 (11.8); Group B: 50.9 (11.4) Median BMI kg/m² (range): Group A: 27 (21‐37); Group B: 29 (21‐50) Postmenopausal: Group A: 24/66; Group B: 19/61 |
|
| Interventions | Group A: TVT (n = 66) Group B: TVT‐O (n = 61) |
|
| Outcomes |
|
|
| Notes | Intraoperative cystoscopy with a 70° cystoscope performed in all cases Loss to follow‐up at 12 months: Group A: 25/66; Group B: 32/61 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was done by a computer generated list randomised in blocks to ensure balanced allocation |
| Allocation concealment (selection bias) | Low risk | Randomization was done by a computer generated list randomised in blocks to ensure balanced allocation. Block size was randomised between 4 and 10. Numbered opaque envelopes were opened immediately before surgery |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and assessors were not blinded to the treatment received |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participants and assessors were not blinded to the treatment received |
| Incomplete outcome data (attrition bias) All outcomes | High risk | High numbers lost to follow‐up; disproportionately higher in TVT‐O group |
Tommaselli 2012.
| Methods | RCT comparing TVT‐O and a modified version of TVT‐O | |
| Participants | 72 women Inclusion criteria: urodynamically proved SUI; age > 30 years; and previously failed pelvic floor muscle training Exclusion criteria: previous surgery for SUI; isolated OAB; POP ≥ stage 2; neurological disease Mean age (years; SD): Group A: 51 (9.5); Group B: 55 (6.8) Mean BMI kg/m² (SD): Group A: 27.5 (4.9); Group B: 28.9 (3.7) |
|
| Interventions | Group A: TVT‐O (n = 48) Group B: modified TVT‐O (n = 24) |
|
| Outcomes |
|
|
| Notes | For the modified TVT‐O: “Briefly, in contrast with the traditional technique, the paraurethral dissection was minimal and carried only up to the pubic ramus, without perforating the obturator membrane with the scissors The aim of this reduced dissection was to create a passage of very limited size to introduce the guide only up to the bone, without perforating the membrane. Thus, as opposed to the original procedure, the obturator membrane was perforated only by the helical passer” Lost to follow‐up: Group A: 2/48; Group B: 1/24 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: “Patients were randomised using a randomisation list generated by computer” |
| Allocation concealment (selection bias) | Low risk | Quote: "The allocation sequence was concealed from the researchers (CF and AF) who enrolled, assessed, and assigned the participants to the interventions in sequentially numbered, opaque, sealed, and stapled envelopes. The envelopes were opened on the morning of the procedure for the surgeon to perform the allocated procedure" |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: “Patients were blinded to the procedure until the end of the study” |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All data accounted for |
Tseng 2005.
| Methods | RCT comparing TVT with SPARC | |
| Participants | 62 women Inclusion criteria: women with USI with or without POP Exclusion criteria: those with POP > ICS stage 2 and those with previous anti‐incontinence surgery Mean age was 51 years and median parity of 3. The 2 groups were similar in terms of age, parity and menopausal status |
|
| Interventions | Group A: SPARC (n = 31) Group B: TVT (n = 31) | |
| Outcomes | Objective cure: defined as pad weight ≤1g Improved: participants whose loss decreased to < half of the preoperative value were considered to have improved |
|
| Notes | All women had routine suprapubic ultrasonography for detecting unrecognised subcutaneous or retropubic haematoma on the day immediately after the operation, and 7/8 of those with retropubic haematoma of >5 cm diameter were discharged uneventfully from the hospital within 7 days of the operation. Ultrasonography performed at the 1 month follow‐up visit revealed complete resolution of the haematoma for every participant Follow‐up at 2 years Women and their outcome assessors were blinded, but the exact method used to achieve this was unclear |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | By using a predetermined computer‐generated randomisation code, those subjects who acquiesced and satisfied the inclusion criteria were assigned randomly by the authors (except LHT) to the SPARC or TVT procedure at the outpatient clinic |
| Allocation concealment (selection bias) | Unclear risk | Unclear |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "The patients were blinded to the procedure, but the principle based on the integral theory was briefly explained to them" |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No differential loss to follow‐up or differential attrition |
Ugurlucan 2013.
| Methods | RCT of PELVILACE TO (biological TOT material) vs synthetic TOT material (ALIGN TO urethral support system) | |
| Participants | 100 women Inclusion criteria: women >18 years with SUI, MUI or USI in whom conservative treatment had failed. Women with or without POP were included Exclusion criteria: women with ISD Pre‐ and postoperative assessments included evaluation of urinalysis and urine culture POP evaluation using POP‐Q system, 1‐hr pad test, 4‐day bladder diary, stress test, Q‐tip test, and QoL assessment using the KHQ, UDI‐6, and the IIQ‐7. This was repeated at the 12‐month follow‐up. Postoperative urodynamics was performed in all patients accepting the procedure Mean age (years; SD): Group A: 55.0 (12.3); Group B: 52.9 (10.6) Mean BMI kg/m² (SD): Group A: 31.8 (6.6); Group B: 31.3 (4.8) Postmenopausal: Group A: 29 (56.9%); Group B: 30 (58.8%) Previous incontinence surgery: Group A: 2 (4%); Group B: 2 (4%) Concomitant POP surgery: Group A: 28/50; Group B: 28/50 |
|
| Interventions | Group A: biological PELVILACE TO (n = 50) Group B: synthetic TOT ALIGN ®TO (n = 50) |
|
| Outcomes | Primary outcome: patient‐reported improvement in urinary incontinence (either completely dry or improvement in symptoms of SUI; reported as 'cure,' 'better than before,' 'no change at all,' and 'worse than before.')
Secondary outcomes:
|
|
| Notes | Biological tape was PELVILACE® TO system; Bard, Covington, GA, USA and the synthetic tape was ALIGN ®TO urethral support system; Bard TOT operation. The PELVILACE® TO system consists of a PELVICOL® self‐anchoring, natural tissue sling implant and an introducer system. This system contains a self‐anchoring, 1.5 cm wide, and 40 cm long suburethral sling of porcine dermal collagen. The ALIGN® TO urethral support system is a suburethral sling device made of type 1 monofilament polypropylene mesh designed for the treatment of SUI through the TOR Postmenopausal patients received local estrogen treatment for 1 month before and after the operation Concomitant POP was performed in a cohort of women |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: " In this prospective randomized study ... Randomization was carried out using computer‐generated random allocations prepared by an investigator with no clinical involvement in the trial" |
| Allocation concealment (selection bias) | Low risk | Quote: "computer‐generated random allocations prepared by an investigator with no clinical involvement in the trial" |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Quote: "The patients were blinded to the sling material used." |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "Follow‐up was performed ... by the same physician who was blinded to the type of sling used" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All accounted for |
van Leijsen 2013.
| Methods | RCT comparing RPR and TOT | |
| Participants | Dutch multicentre diagnostic cohort study with an embedded RCT 587 women with SUI; 123 randomised to surgery Inclusion criteria: women with urodynamically‐proven SUI, or MUI with SUI as predominant symptom following failed conservative treatment Exclusion criteria: prior incontinence surgery; POP > stage 2 POP‐Q; post PVR of >150 ml (by USS or characterisation) MUI: Group A: 18/33; Group B: 61/90 |
|
| Interventions | Group A: RPR (n = 33) Group B: TOT (n = 90) |
|
| Outcomes | Outcome results for TOT and RPR not reported as separate figures; we contacted the authors who supplied separate figures
|
|
| Notes | QoL questionnaires: UDI | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "A web‐based application was used for block randomisation and computer‐generated random number list prepared by a database designer" |
| Allocation concealment (selection bias) | Low risk | Quote: "Patient data were entered into a password‐protected web‐ based database" |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: "Participants and health professionals were not blinded to the allocated arm and the urodynamic results" |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "Data input of subjective outcome measurements was per‐formed by researchers who were blinded to the treat‐ment allocation" |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No information |
Wang 2006.
| Methods | RCT of TOT (Monarc) and SPARC suburethral sling procedures | |
| Participants | 60 women with an average age of 50 years (SD 10.71 )
Inclusion criteria: women with USI Exclusion criteria: women suffering from preoperative voiding dysfunction, which was defined as either: free Q max of ≤ 12ml/s in repeated free uroflow studies combined with Pdet Q max of ≥20cm H2O, PVR urine ≥ 100 ml, and participants with a pad increase of at least 10cm H2O, compared to the baseline abdominal pressure in a pressure‐flow study. Women who had previous anti‐incontinence surgery and/or with pelvic prolapse > stage 2 of the ICS grading system were also excluded. |
|
| Interventions | Group A: Monarc (n = 31) Group B: SPARC (n = 29) |
|
| Outcomes | Assessed via 1‐hr pad test, multichannel urodynamic assessment, complications and postoperative voiding function. Transabdominal USS to detect subcutaneous, retropubic or obturator haematoma | |
| Notes | The women were blinded to the procedure performed Intraoperative cystoscopy was performed in both groups |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "By using a predetermined computer‐generated randomisation code ... were assigned randomly by the senior author ..." |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Quote: " ... The patients were blinded to the procedure ..." How this was achieved was not explained |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "an independent continence advisor and one of the authors both of whom were blinded to the procedures performed carried out the follow‐up examinations and post operative outcome assessments" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No differential loss to follow‐up or differential attrition |
Wang 2008.
| Methods | RCT of TVT vs TVT‐O Single‐blinded |
|
| Participants | 69 women Inclusion criteria: severe female SUI with or without prolapse (< POP‐Q stage 3) Exclusion criteria: pregnancy; previous surgery for urinary incontinence Mean BMI kg/m² (SD): Group A: 25 (3); Group B: 25 (3) Mean age (years; SD): Group A: 52 (11); Group B: 52 (11) |
|
| Interventions | Group A: TVT (n = 35) Group B: TVT‐O (n = 34) |
|
| Outcomes |
|
|
| Notes | Concomittant surgery: some women also had transvaginal hysterectomy and prolapse repair Follow‐up: mean 14.5 months Cystoscopy performed in TVT group only Article written in Chinese and translated to English for interpretation and data extraction |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomisation schedule |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Single‐blinded (no information about who was blinded) |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Single‐blinded (no information about who was blinded) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "All patients were evaluable" |
Wang 2009.
| Methods | RCT of TVT vs inside‐out TVT‐O 55 were participants in a previous study (ref 8, Zhu 2007: 23870; 27325) – already included |
|
| Participants | 300 women Inclusion criteria: demonstrable severe SUI, or mild to moderate SUI that failed to respond to conservative treatment. All women had urodynamically confirmed USI (no detrusor contraction on leakage) Exclusion criteria: ;ISD MUI; pregnancy; UTI; UUI; PVR volume > 100 ml; neurological disease; urogenital malignancy, fistula, or pelvic radiotherapy Menopausal: Group A: 87/154; Group B: 88/146 Previous prolapse surgery: Previous incontinence surgery: Group A: 5; Group B: 5 |
|
| Interventions | Group A: TVT (n = 154) Group B: TVT‐O (n = 146) |
|
| Outcomes |
|
|
| Notes | Signed informed consent, approved by Ethics committee Mean follow‐up: (months; SD): Group A: 19.6 (11.9); Group B: 20.5 (10.7; twice in first year, then yearly) Loss to follow‐up: Group A: 6; Group B: 8, + 1 withdrawn (operation postponed) Cystoscopy only performed in the TVT group Concomitant prolapse and other surgery |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The 315 women were allocated to the TVT or the TVT‐O group by an SAS randomisation schedule (SAS Institute Inc, Cary, NC, USA) |
| Allocation concealment (selection bias) | Unclear risk | Stated: ‘randomly allocated’, no further information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Outcome assessors blind: ‘independent gynaecologist’ |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No differential dropout (Group A: 6; Group B: 9) |
Wang 2010.
| Methods | RCT comparing TVT and TOT‐outside/in | |
| Participants | 140 women Inclusion criteria: women with urodynamically proven SUI Exclusion criteria: OAB syndrome dry or wet Age (years; SD): Group A: 60 (10.8); Group B: 58 (11.6) Previous incontinence surgery: Group A: 5; Group B: 3 BMI kg/m² (SD): Group A: 24 (2.4); Group B: 24.6 (2.6) Concomitant POP: Group A: 30/70; Group B: 22/70 |
|
| Interventions | Group A: TVT (n = 70) Group B: TOT (n = 70) |
|
| Outcomes |
|
|
| Notes | Cystoscopy only performed when bladder perforation suspected in TOT group. All TVT participants cystoscoped post procedure Concomitant surgery: All participants with POP had this repaired at the time of tape insertion Lost to follow‐up: Group A: 0 women; Group B: 0 women |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: “Our study was a single blind randomised trial and the patients were randomly allocated to ...” |
| Allocation concealment (selection bias) | Unclear risk | Quote: “Our study was a single blind randomised trial and the patients were randomly allocated to ...” |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: “The patients were not blinded to the operative procedure” |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: “post op assessment was performed by FMW who did not take part in the operation , YFS who performed the surgery was not involved in follow up” |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No participants withdrew. None were lost to follow‐up |
Wang 2011.
| Methods | RCT comparing TVT, TVT‐O and TVT‐Secur | |
| Participants | Total of 102 women included in this Chinese trial Inclusion criteria: women with urodynamically proven SUI. If MUI, then SUI was the predominant symptom Exclusion criteria: women with previous surgical procedures for SUI Mean age (years; SD): Group A: 56.6 (9.6); Group B: 56.0 (9.1) Mean BMI kg/m² (SD): Group A: 25.3 (2.0); Group B: 27.3 (1.9) |
|
| Interventions | Group A: TVT (n = 32) Group B: TVT‐O (n = 36) Group C: TVT‐ Secur (data not included in this review) |
|
| Outcomes |
|
|
| Notes | Power test calculation performed Women with SUI were put on anticholinergic treatment prior to surgery QoL assessment was performed using the ICI‐Q‐SF pre‐operatively; no data for post‐operative scores Cystoscopy routinely performed in TVT. Cystoscopy only performed if bladder injury was suspected in the TVT‐O group Follow‐up 1, 3, 6 and 12 months All women completed the trial (no loss to follow‐up) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "computer generated randomisation" |
| Allocation concealment (selection bias) | Low risk | Quote: “allocation was concealed using opaque sealed envelopes” |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants completed follow‐up. All outcomes reported |
Zhang 2011.
| Methods | RCT comparing TVT‐O with a modified version of TVT‐O using a self‐tailored mesh | |
| Participants | 156 women in a Chinese hospital Inclusion criteria: women with SUI aged > 18 years Exclusion criteria: women with urgency; persistent urinary retention (PVR > 50 ml); dysuria; other urologic diseases and psychiatric disorders Mean age (years; SD): Group A: 61.4 (5.4); Group B: 62.6 (3.2) |
|
| Interventions | Group A: TVT‐O (n = 76) Group B: modified TVT‐O (n = 80) |
|
| Outcomes |
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: “stratified randomisation” |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No information |
Zullo 2007.
| Methods | RCT comparing TVT and TVT‐O | |
| Participants | 72 women Inclusion criteria: women affected by SUI with no contraindications to vaginal surgery Excluded criteria: women with urogenital prolapse > stage 1; DO; symptoms of OAB; intrinsic urethral sphincter deficiency; urinary retention; previous anti‐incontinence surgery; neurologic bladder; and psychiatric disease Age (years; SD): Group A: 52.8 (11.8); Group B: 53.4 (10.7) BMI kg/m²: Group A: 25.7 (2.9); Group B: 26.5 (2.7) Menopausal: Group A: 6/35; Group B: 8/37 POP stage 1 and 2: Group A: 34/35; Group B: 35/37 |
|
| Interventions | Group A: TVT (n = 35) Group B: TVT‐O (n = 37) |
|
| Outcomes |
|
|
| Notes | Intraoperative cystoscopy only performed in the TVT group 12 participants did not return for 5‐year follow‐up: 3 participants were lost (2 in the TVT group and 1 in the TVT‐O group), and 9 withdrew (4 in the TVT group and 5 in the TVT‐O group) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: " .. were randomly allocated to undergo a TVT or TVTO procedure by using a predetermined computer‐generated randomisation code" |
| Allocation concealment (selection bias) | Low risk | Allocation concealed |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | " ... outcome assessors at 5 years follow up blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No differential loss to follow‐up or differential attrition |
Abbreviations
BFLUTS: Bristol lower urinary tract symptoms questionnaires
BMI: body‐mass index
DO: detrusor overactivity
DUP: distal urethral polypropylene sling
EQOL‐5D: Euro Quality of life ‐5 Dimension
g: gram
hr: hour
HRT: hormone replacement therapy
ICIQ: International Consultation on Incontinence questionnaire
ICIQ‐FLUTS: International Consultation on Incontinence questionnaire ‐ female lower urinary tract symptoms
ICIQ‐ LUTSquol: International Consultation on Incontinence questionnaire ‐ lower urinary tract quality of life questionnaire
ICIQ‐SF: International Consultation on Incontinence questionnaire short form
ICIQ‐SF15: International Consultation on Incontinence questionnaire short form 15
IIQ: Incontinence Impact questionnaire
ICS: International Continence Society
I‐QoL: Incontinence Quality of Life questionnaire
ISD: intrinsic sphincter deficiency
IVS: intravaginal slingoplasty
KHQ: King's Health questionnaireMUI: mixed urinary incontinence
MUCP: Maximum urethral closure pressure
MUI: mixed urinary incontinence
OAB: overactive bladder
PGI‐I: Patient Global Impression of Improvment
PGI‐S: Patient Global Impression of Severity
PISQ‐12: pelvic organ prolapse/urinary incontinence sexual questionnaire
POP: pelvic organ prolapse
POP‐Q: pelvic organ prolapse quantification
POP‐Q ICS: pelvic organ prolapse quantification International Continence Society
PVR: post void residual
RCT: randomized controlled trial
RPR: retropubic route
QoL: quality of life
QRCT: quasi‐randomised trial
SEAPI‐QMM: Stress related leak, Empyting ability, Anatomy, Protection, Inhibition‐Quality of life, Mobility and Mental status incontinence classification system
SD: standard deviation
SIS: Single incision sling
SPARC: suprapubic arc (procedure)
SUI: stress urinary incontinence
TOR: transobturator
TOT: transobturator tape
TOT‐ARIS: transobturator tape‐ARIS
TVT: tension‐free vaginal tape
TVT‐O: transobturator tension‐free vaginal tape
UDI: Urinary Distress Impact questionnaire
UDI‐6: Urinary Distress Impact questionnaire short form
UDS: urodynamics study
UI: urinary incontinence
UISS: urinary incontinence severity score
USI: urodynamic stress incontinence
USS: ultrasound
UTI: urinary tract infection
UUI: urgency urinary incontinence
VAS: visual analogue scale
VLPP: Valsalval leak point pressure
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Al‐Tayyem 2007 | Not an RCT |
| Amat 2007 | Sling apparently equivalent to TVT, but too little information provided to determine equivalence |
| Ballert 2010 | Not an RCT |
| Bekker 2009 | Sexual function analysis of 2 retrospective studies (not RCTs) |
| Borrell 2005 | Retrospective study, not an RCT |
| Bracken 2012 | RCT of bupivacaine and saline versus saline only for hydrodissection during TVT |
| Bruschini 2005 | Not an RCT |
| Chen 2008 | Not randomized |
| Chen 2011 | Prospective comparative study with participants assigned not randomized. |
| Chene 2009 | Was prospective, but not stated that randomized |
| Chong 2003 | All women had TVT. Intervention groups were division vs no division of tape |
| Corcos 2001 | Traditional slings. No minimally invasive sling |
| Corcos 2005 | No minimally invasive sling |
| Cotte 2006 | An ultrasound study comparing tape position between RPR and TOR |
| Courtney‐Watson 2002 | Trial stopped due to difficulty recruiting. Planned to recruit 30 participants to each arm but actually randomized less than 15 participants in total |
| Debodinance 2006 | Non randomized prospective study |
| Dietz 2005 | Imaging study: aim of the study was to determine the mobility of the slings from ultrasound imaging of slings inserted in the parent trial (SUSPEND trial, Lim 2005) |
| Du 2008 | Not an RCT |
| Falconer 2001 | All had TVT |
| Fischer 2005 | Not an RCT |
| Foote 2012 | Monarc vs mini single incision sling |
| Goldberg 2001 | No minimally invasive sling |
| Gopinath 2013 | Qualitative analysis on nonresponders of single incision sling RCT |
| Harmanli 2011 | RCT of antibiotic use preoperatively for TVT and TOT (surgeons discretion for what tape was used) |
| Jackson 2013 | RCT of antibiotic vs. placebo for MUS surgery |
| Jeon 2008 | Not an RCT |
| Jones 2010 | Not an RCT |
| Karagkounis 2007 | A prospective cohort study not an RCT |
| Kim 2005a | Retrospective review of medical records |
| Kim 2006 | Not an RCT |
| Kulseng‐Hanssen 2004 | RCT ‐ does not meet the inclusion criteria. Not MUS vs MUS. Tradition Sling vs TVT. This trial compares three techniques for performing sling surgery: TVT, porcine xenograft (Pelvicol) sling and the short autologous fascial sling technique 'Sling on a string'. |
| Kulseng‐Hanssen 2007 | A prospective cohort study not an RCT |
| Kwon 2002 | Prolapse trial not urinary incontinence |
| Liapis 2007 | RCT with randomisation based on the type of anaesthesia used for one minimally invasive sling procedure (TVT) |
| Liapis 2010 | RCT of TVT‐O vs TVT‐O plus 6 months postoperative estrodiol therapy. Both groups had TVT‐O performed |
| Markland 2007 | RCT of Burch colposuspension versus traditional sling ‐ SISTEr Trial. Not MUS vs MUS |
| McClure 2006 | Statistical modelling and not a trial in itself. No minimally invasive sling |
| Meschia 2002 | 1 tape used (TVT) and only occult urinary incontinence investigated |
| Osman 2003 | No minimally invasive sling arm in the trial |
| Pace 2008 | Prospective study of SPARC vs Monarc TOT but no evidence of randomisation |
| Padilla‐Fernández 2013 | Randomisation based on immediate or deferred cutting and readjustment of tape |
| Park 2008 | Same tape TOT randomized to either high‐tension or tension‐free |
| Sabadell 2008 | Cohort study, not an RCT |
| Schierlitz 2007 | Investigated occult incontinence |
| Schostak 2001 | Not an RCT and no minimally invasive sling |
| Seo 2007 | Not an RCT, retrospective study |
| Shin 2010 | Non randomized longitudinal study |
| Sivaslioglu 2007 | No minimally invasive sling |
| Surkont 2007 | Not an RCT and only 1 arm, IVS |
| Takeyama 2006 | Improvised instrument used |
| Tantanasis 2013 | A review article, not an RCT |
| Tincello 2009 | RCT of colposuspension or TVT with concomitant anterior repair (1 tape) |
| Tinelli 2007 | Same tape TVT: randomized to either immediate TVT or TVT after 21 days of preoperative estrogen treatment |
| Trezza 2001 | Investigated occult urinary incontinence |
| Wang 2001 | All women received TVT. Compared types of anaesthesia |
| Wei 2012 | RCT of women with occult stress urinary incontinence undergoing POP surgery with and without concomitant MUS insertion |
| Williams 2003 | Statistical modelling and not a trial in itself |
| Yang 2012 | Non randomised inferiority study |
| Yoo 2007 | A comparative study but not an RCT |
| Yoon 2011 | RCT of single incision sling and TOT |
| Zaccardi 2010 | RCT of pelvic floor muscle training on comfort. |
| Zullo 2005 | All had TVT. Women were randomly allocated to receive TVT plus postoperative vaginal oestrogen therapy (ET group) or TVT without adjunctive medical treatment (no ET group) |
Abbreviations
IVS: intravaginal slingoplasty
MUS: mid‐urethral sling
POP: pelvic organ prolapse
RCT: randomized controlled trial
RPR: retropubic route
SIS: Single incision sling
TOR: transobturator route
TOT: transobturator tape
TVT: tension‐free vaginal tape
TVT‐O: tension‐free vaginal tape ‐ Obturator
Characteristics of ongoing studies [ordered by study ID]
Cavkaytar 2013.
| Trial name or title | Prospective randomised study comparing TVT and TOT in female SUI with no ISD |
| Methods | RCT |
| Participants | Inclusion criteria: women aged 18‐70 years; with USI; with or without POP Exclusion criteria: previous incontinence surgery; UI or OAB; mixed incontinence; ISD; BMI > 35 |
| Interventions | Participants underwent either TVT or TOT procedures |
| Outcomes | Primary outcome: postoperative UDI‐6 and IIQ‐7 score <10 and negative cough test will be defined as 'cured' Secondary outcomes:
|
| Starting date | June 2013 |
| Contact information | |
| Notes | NCT01903590, expected completion date June 2014 |
Sung 2013.
| Trial name or title | Effects of surgical treatment enhanced with exercise for mixed urinary incontinence (ESTEEM) |
| Methods | |
| Participants | Women > 21 years Inclusion criteria:
Exclusion criteria:
|
| Interventions | Group A: mid‐urethral sling combined with peri‐ and postoperative behavioral/pelvic floor therapy Group B: mid‐urethral sling |
| Outcomes | |
| Starting date | October 2013, expected completion date October 2016 |
| Contact information | |
| Notes | NCT01959347 |
Abbreviations
BMI: body‐mass index BPTx: behavioural/pelvic floor therapy ESTEEM: Effects of surgical treatment enhanced with exercise for mixed urinary incontinence trial IE; incontinence event IIQ‐7: Incontinence Impact questionnaire ISD: intrinsic sphincter deficiency MUI: mixed urinary incontinence OAB: overactive bladder POP: pelvic organ prolapse POP‐Q: pelvic organ prolapse quantification PVF: post void residual SUI: stress urinary incontinence TOT: transobturator tape TVT: tension‐free vaginal tape UDI: Urinary Distress Impact questionnaire UDI‐6: Urinary Distress Impact questionnaire short form UI: urinary incontinence USI: urodynamic stress incontinence UUI: urgency urinary incontinence
Differences between protocol and review
The review authors decided to focus this update on the use of minimally invasive mid‐urethral slings in women with urinary incontinence, as this has become the gold standard for surgery for stress urinary incontinence (SUI). The alternative surgical treatments, including single incision slings, have been addressed in linked Cochrane reviews and are therefore not included, but are summarised and referenced in the Discussion. Conservative and pharmacological treatments will be addressed in a future Cochrane review. This review therefore now addresses the effectiveness of mid‐urethral slings in the treatment of SUI in women compared to another mid‐urethral sling.
The primary outcome remains the same, but has been measured in time scales that differ from those previously set out; short term (less than 12 months), medium term (one to five years) and long term (over five years). This was done after the first review showed evidence of tape efficacy to establish whether this procedure continued to be effective in the longer term. The primary outcome was repeated as a secondary outcome and this repetition has been amended.
A Dealing with missing data section has been added into the review. Very few trials reported outcome data for clinically relevant subgroups, therefore no subgroup analyses were performed.
July 2017 update: we have added Brief Economic Commentaries (BECs) to all of our 'Surgery for UI in women' Cochrane Reviews. We have revised the economic elements throughout the review; if incorrect, we have stripped them out. We have added new economics‐related text. This involved revisions to the Background section, Methods section, e.g. search section referring to added Appendix, Discussion section, Abstract and Plain Language Summary. We have added an appendix with details of the economics searches. The Conclusions section of the review has not changed. The rest of the review has not changed.
Contributions of authors
Abigail Ford and Joseph Ogah wrote the text of the main review.
Abigail Ford performed the initial screening of studies for inclusion into the review, assessment of methodological quality, data extraction, and analysis of results.
Joseph Ogah performed the second and confirmatory screening of studies for inclusion, assessment of methodological quality, and data extraction.
Abigail Ford, Joseph Ogah, June Cody and Lynne Rogerson assisted in the analysis and interpretation of the results.
Abigail Ford, Joseph Ogah and Lynne Rogerson were also responsible for the clinical input for the review and made a significant input to the writing of the final review.
For the July 2017 addition of the BECs to this review: Patricia Aluko was responsible for the entire BECs‐related work on this review, i.e. she ran the search for studies, screened the search results, extracted data from relevant studies, revised any existing economics‐related text, added the BECs‐related text, and responded to any peer referee comments. All authors had the opportunity to comment on the revised review.
Sources of support
Internal sources
No sources of support supplied
External sources
-
The National Institute for Health Research (NIHR), UK.
This project was supported by the National Institute for Health Research, via Cochrane Infrastructure funding to the Cochrane Incontinence Group. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, NHS or the Department of Health. The NIHR is the largest single funder of the Cochrane Incontinence Group.
-
National Institute for Health Research, UK.
This project, to add Brief Economic Commentaries to our surgery for UI in women reviews, was supported by the National Institute for Health Research (NIHR), via the Cochrane Review Incentive Scheme 2016, to the Cochrane Incontinence Group. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, NHS or the Department of Health.
Declarations of interest
Abigail A Ford: For the 2015 review: Johnson and Johnson for part sponsorship to attend International Urogynaecology Association conference (IUGA), Washington, 2014. For the 2017 BECs review update: Astellas: money given towards travel costs to IUGA meeting 2016, no other financial benefit. This had no impact on this current work.
Lynne Rogerson: For the 2015 review: Astellas: Paid in full for attendance at European Urogynaecological Association meeting in Berlin. For the 2017 BECs review update: registration fee for ICS Rio 2014 paid by Boston Scientific for October 2014 ‐ paid directly to the conference but nothing to do with Cochrane.
June D Cody: For the 2015 review: nothing to declare. For the 2017 BECs review update: None known.
Joseph Ogah: For the 2015 review: part sponsorship for conference registration fees and speaker honoraria by Astellas UK; sponsored to attend workshops by Johnson and Johnson and Speciality European Pharma. All these sponsorships are unrelated to this review. For the 2017 BECs review update: None known.
Patricia Aluko: For the 2017 BECs review: This project, to add Brief Economic Commentaries to our 'Surgery for UI in women' reviews, was supported by the National Institute for Health Research (NIHR), via the Cochrane Review Incentive Scheme 2016, to the Cochrane Incontinence Group. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, NHS or the Department of Health.
Edited (no change to conclusions)
References
References to studies included in this review
Abdel‐Fattah 2010 {published data only}
- Abdel‐Fattah M, Familusi A, Ramsay I, Ayansina D, Mostafa A. Preoperative determinants for failure of transobturator tapes in the management of female urodynamic stress incontinence. International Journal of Gynaecology and Obstetrics 2010;110(1):18‐22. [ETOT; NCT00136071; srincont40971] [DOI] [PubMed] [Google Scholar]
- Abdel‐Fattah M, Familusi A, Ramsay I, N'Dow J. A randomised prospective single‐blinded study comparing "inside‐out" versus "outside‐in" transobturator tapes in the management of female stress urinary incontinence (E‐TOT study); 3 years follow‐up (Abstract number 18). Neurourology and Urodynamics 2011;30(6):825‐6. [ETOT; NCT00136071; srincont42168] [Google Scholar]
- Abdel‐Fattah M, Hasafa Z, Mostafa A. Correlation of three validated questionnaires for assessment of outcomes following surgical treatment of stress urinary incontinence in women. European Journal of Obstetrics, Gynecology, and Reproductive Biology 2011;157(2):226‐9. [ETOT; NCT00136071; srincont41753] [DOI] [PubMed] [Google Scholar]
- Abdel‐Fattah M, Mostafa A, Familusi A, Ramsay I, N'Dow J. Prospective randomised controlled trial of transobturator tapes in management of urodynamic stress incontinence in women: 3‐year outcomes from the evaluation of transobturator tapes study. European Urology 2012;62(5):843‐51. [ETOT; NCT00136071; srincont45947] [DOI] [PubMed] [Google Scholar]
- Abdel‐Fattah M, Mostafa A, Young D, Ramsay I. Evaluation of transobturator tension free vaginal tapes in management of women with stress urinary incontinence and previous failed incontinence surgery (Abstract number 156). Neurourology and Urodynamics 2010;29(6):1027‐9. [ETOT; NCT00136071; srincont40148] [Google Scholar]
- Abdel‐Fattah M, Mostafa A, Young D, Ramsay I. Evaluation of transobturator tension‐free vaginal tapes in the management of women with mixed urinary incontinence: one‐year outcomes. American Journal of Obstetrics and Gynecology 2011;205(2):150‐6. [ETOT; NCT00136071; srincont42990] [DOI] [PubMed] [Google Scholar]
- Abdel‐Fattah M, Mostafa A, Young D, Ramsay I. Impact of transobturator tension free vaginal tapes on quality of life and sexual function in women with mixed urinary incontinence (Abstract number 28). Neurourology and Urodynamics 2010;29(6):844‐5. [ETOT; NCT00136071; srincont40119] [Google Scholar]
- Abdel‐Fattah M, Ramsay I. Transvaginal tension free vaginal tape‐obturator (TVT‐O) versus transobturator tape‐mentor (TOT) in the management of urodynamic stress urinary incontinence. ClinicalTrials.gov (http://ClinicalTrials.gov/show/NCT00136071) (accessed 20 September 2010) 2005. [ETOT; NCT00136071; srincont40211]
- Abdel‐Fattah M, Ramsay I, Pringle S, Hardwick C, Ali H. Evaluation of transobturator tapes (E‐TOT) study: randomised prospective single‐blinded study comparing inside‐out vs. outside‐in transobturator tapes in management of urodynamic stress incontinence: short term outcomes. European Journal of Obstetrics, Gynecology, & Reproductive Biology 2010;149(1):106‐11. [39661; ETOT; NCT00136071; srincont39661] [DOI] [PubMed] [Google Scholar]
- Abdel‐Fattah M, Ramsay I, Pringle S, Hardwick C, Ali H, Young D, et al. Evaluation of transobturator tension‐free vaginal tapes in management of women with recurrent stress urinary incontinence. Urology 2011;77(5):1070‐5. [ETOT; NCT00136071; srincont41485] [DOI] [PubMed] [Google Scholar]
- Abdel‐Fattah M, Ramsay I, Pringle S, Hardwick C, Ali H, Young D, et al. Randomised prospective single‐blinded study comparing 'inside‐out' versus 'outside‐in' transobturator tapes in the management of urodynamic stress incontinence: 1‐year outcomes from the E‐TOT study. BJOG: an International Journal of Obstetrics & Gynaecology 2010;117(7):870‐8. [ETOT; NCT00136071; srincont39920] [DOI] [PubMed] [Google Scholar]
- Abdel‐Fattah M, Ramsay I, Pringle S, Hardwick C, Tierney J, Ali H. (E‐TOT) Study: a randomised prospective single‐blinded study of two transobturator tapes in management of urodynamic stress incontinence: objective & patient reported outcomes (Abstract number 2). International Urogynecology Journal 2008;19(Suppl 2):S2‐3. [ETOT; NCT00136071; srincont31053] [Google Scholar]
- Abdel‐Fattah M, Ramsay I, Pringle S, Hardwick C, Tierney J, Young D. (E‐TOT) Study: a randomised prospective single blinded study of two transobturator tapes in management of urodynamic stress incontinence: quality of life; sexual function at 1‐year (Abstract number 200). International Urogynecology Journal 2008; Vol. 19, issue Suppl 2:S168‐9. [ETOT; NCT00136071; srincont31050]
- Hopper LR, Mostafa A, Abdel‐Fattah M. The effectiveness of transobturator tapes in the surgical management of women with mixed urinary incontinence: 3 year outcomes (Abstract number 612). Proceedings of the 43rd Annual Meeting of the International Continence Society (ICS), 2013 Aug 26‐30, Barcelona, Spain. 2013. [NCT00136071; srincont60036]
- Mostafa A, Madhuvrata P, Abdel‐Fattah M. Preoperative urodynamic predictors of short‐term voiding dysfunction following a transobturator tension‐free vaginal tape procedure. International Journal of Gynaecology and Obstetrics 2011;115(1):49‐52. [NCT00136071; srincont42671] [DOI] [PubMed] [Google Scholar]
Aigmuller 2014 {published data only}
- Aigmuller T, Tammaa A, Tamussino K, Hanzal E, Umek W, Kolle D, et al. Retropubic vs. transobturator tension‐free vaginal tape for female stress urinary incontinence: 3‐month results of a randomized controlled trial. International Urogynecology Journal 2014;25(8):1023‐30. [DOI: 10.1007/s00192-014-2384-z; NCT00441454; sr‐incont62534; PUBMED: 24819327] [DOI] [PubMed] [Google Scholar]
- Bjelic Radisic V, Trutnovsky G, Tammaa A, Hanzal E, Umek W, Koelle D, et al. Quality of life in patients with stress incontinence: results of a randomized trial comparing retropubic and transobturator tension‐free vaginal tape (Abstract number 042). International Urogynecology Journal 2013;24(Suppl 1):S36‐7. [sr‐incont62184] [Google Scholar]
- Tammaa A, Aigmueller T, Umek W, Hanzal E, Kropshofer S, Lang P, et al. Retropubic versus transobturator TVT: five‐year results of the Austrian trial (Abstract number: Oral Poster 18). Journal of Minimally Invasive Gynecology 2014;21(2 Suppl 1):S21. [sr‐incont62148] [Google Scholar]
- Tamussino K, Tammaa A, Hanzal E, Umek W, Bjelic V, Koelle D. TVT vs. TVT‐O for primary stress incontinence: a randomized clinical trial (Abstract number 112). International Urogynecology Journal 2008;19(Suppl 1):S20‐1. [sr‐incont26969] [Google Scholar]
Alkady 2009 {published data only}
- Alkady HM, Eid A. Tension‐free vaginal tape versus transobturator vaginal tape inside‐out for the treatment of female stress urinary incontinence. Medical Journal of Cairo University 2009;77(4):317‐26. [sr‐incont50307] [Google Scholar]
Andonian 2005 {published data only}
- Andonian S, Chen T, Denis B, Corcos J. Randomized clinical trial comparing suprapubic arch sling (SPARC) and tension‐free vaginal tape (TVT): one‐year results. European Urology 2005;47(4):537‐41. [sr‐incont20378] [DOI] [PubMed] [Google Scholar]
- Andonian S, Chen TY, Corcos J. Randomized clinical trial comparing SPARC and TVT procedure for the treatment of SUI: preliminary report on peri‐operative and short term complications (Abstract). Proceedings of the 33rd Annual Meeting of the International Continence Society (ICS), 203 Oct 5‐9, Florence, Italy. 2003:547‐8. [sr‐incont17163]
Andonian 2007 {published data only}
- Andonian S, St‐Denis B, Lemieux MC, Corcos J. Prospective clinical trial comparing Obtape and DUPS to TVT: one‐year safety and efficacy results. European Urology 2007;52(1):245–2. [sr‐incont23793] [DOI] [PubMed] [Google Scholar]
Aniuliene 2009 {published data only}
- Aniuliene R. Tension‐free vaginal tape versus tension‐free vaginal tape obturator (inside‐outside) in the surgical treatment of female stress urinary incontinence. Medicina (Kaunas, Lithuania) 2009;45(8):639‐43. [sr‐incont34372] [PubMed] [Google Scholar]
Araco 2008 {published data only}
- Araco F, Gravante G, Sorge R, Overton J, Vita D, Sesti F, et al. TVT‐O vs TVT: a randomized trial in patients with different degrees of urinary stress incontinence. International Urogynecology Journal 2008;19(7):917‐26. [DOI: 10.1007/s00192-007-0554-y; sr‐incont27794] [DOI] [PubMed] [Google Scholar]
- Araco F, Gravante G, Sorge R, Piccione E. TVT‐O vs. TVT: reply to comments by Burton et al [letter]. International Urogynecology Journal 2009;20:371‐2. [DOI 10.1007/s00192‐008‐0795‐4; sr‐incont27794] [Google Scholar]
- Burton C, Latthe P, Toozs‐Hobson P. Comments on Araco et al: TVT‐O vs TVT: a randomized trial in patients with different degrees of urinary stress incontinence [comment] [letter]. International Urogynecology Journal. 1920;20(3):369. [sr‐incont27794; srincont31410] [DOI] [PubMed] [Google Scholar]
Barber 2008 {published data only}
- Barber M, Kleeman S, Karram M, Paraiso MF, Walters M, Vasavada S, et al. A multi‐center randomized trial comparing the transobturator tape with tension‐free vaginal tape for the surgical treatment of stress urinary incontinence (Abstract number 113). Neurourology and Urodynamics 2007;26(5):742‐3. [sr‐incont23758] [Google Scholar]
- Barber MD, Kleeman S, Karram MM, Paraiso MF, Ellerkmann M, Vasavada S, et al. Risk factors associated with failure 1 year after retropubic or transobturator midurethral slings. American Journal of Obstetrics and Gynecology 2008;199(6):666.e1‐7. [NCT00475839; srincont29239] [DOI] [PubMed] [Google Scholar]
- Barber MD, Kleeman S, Karram MM, Paraiso MF, Walters MD, Vasavada S, et al. Transobturator tape compared with tension‐free vaginal tape for the treatment of stress urinary incontinence: a randomized controlled trial. Obstetrics and Gynecology 2008;111(3):611‐21. [NCT00475839; srincont26837] [DOI] [PubMed] [Google Scholar]
- Barber MD, Kleeman SD, Karram MM, Paraiso MF, Walters MD, Vasavada S, et al. A multi‐center randomized trial comparing the transobturator tape with tension‐free vaginal tape for the surgical treatment of stress urinary incontinence (Abstract number 9 Oral). Journal of Pelvic Medicine & Surgery 2007;13(5):234‐5. [srincont34199] [Google Scholar]
- Chen CC, Rooney CM, Paraiso MF, Kleeman SD, Walters MD, Karram MM, et al. Leak point pressure does not correlate with incontinence severity or bother in women undergoing surgery for urodynamic stress incontinence. International Urogynecology Journal 2008;19(9):1193‐8. [srincont27712] [DOI] [PubMed] [Google Scholar]
- Frick AC, Ridgeway B, Ellerkmann M, Karram MM, Paraiso MF, Walters MD, et al. Comparison of responsiveness of validated outcome measures after surgery for stress urinary incontinence. Journal of Urology 2010;184(5):2013‐7. [srincont40342] [DOI] [PubMed] [Google Scholar]
Barry 2008 {published data only}
- Barry C, Lim YN, Muller R, Hitchins S, Corstiaans A, Foote A, et al. A multi‐centre, randomised clinical control trial comparing the retropubic (RP) approach versus the transobturator approach (TO) for tension‐free, suburethral sling treatment of urodynamic stress incontinence: the TORP study. International Urogynecology Journal 2008;19(2):171–8. [sr‐incont26462] [DOI] [PubMed] [Google Scholar]
- Barry CL, Lim Y, Muller R, Greenland H, Hitchens S, Corstiaans A, et al. A multi‐centre, prospective, randomised trial comparing the retropubic (RP‐SUS) approach versus the transobturator approach (TO‐SUS) for tension free, suburethral sling treatment of urodynamic stress incontinence ‐ the TORP study (Abstract number 53). Neurourology and Urodynamics 2006;25(6):572‐3. [sr‐incont23754] [DOI] [PubMed] [Google Scholar]
But 2008 {published data only}
- But I, Faganelj M. Complications and short‐term results of two different transobturator techniques for surgical treatment of women with urinary incontinence: a randomized study. International Urogynecology Journal 2008;19(6):857‐61. [srincont27423] [DOI] [PubMed] [Google Scholar]
- But I, Zegura B, Pakiz M, Rakic S. Outside‐in vs inside‐out transobturator approach in women with stress and mixed urinary incontinence: a prospective, randomized, head‐to‐head comparison study (Abstract number 18). International Urogynecology Journal and Pelvic Floor Dysfunction 2007;18(Suppl 1):S11‐2. [srincont27320] [Google Scholar]
Cervigni 2006 {published data only}
- Cervigni M, Natale F, Penna C, Agostini M, Antomarchi F, Lo Voi R, et al. Surgical correction of stress urinary incontinence associated with pelvic organ prolapse: trans‐obturator approach (MONARC) versus retropubic approach (TVT) (Abstract number 280). International Urogynecology Journal 2006;17(Suppl 2):S215. [srincont29660] [Google Scholar]
- Cervigni M, Natale F, Penna C, Agostini M, Antomarchi F, Lo Voi R, et al. Surgical correction of stress urinary incontinence associated with pelvic organ prolapse: trans‐obturator approach (MONARC) versus retropubic approach (TVT) (Abstract number 36). Neurourology and Urodynamics 2006;25(6):552. [sr‐incont23756] [Google Scholar]
Chen 2010 {published data only}
- Chen Z, Chen Y, Du GH, Yuan XY, Wu J, Zeng XY, et al. Comparison of three kinds of mid‐urethral slings for surgical treatment of female stress urinary incontinence. Urologia (Treviso) 2010;77(1):37‐42. [srincont40354] [PubMed] [Google Scholar]
Chen 2012 {published data only}
- Chen H‐X, Lv J‐W, Leng J, Li J‐Y, Bo J‐J, Huang Y‐R. Efficacy and complications of TVT procedure and TVT‐O procedure in treatment of female stress urinary incontinence [Chinese]. Journal of Shanghai Jiaotong University (Medical Science) 2012;32(4):412‐5. [srincont59712] [Google Scholar]
Cho 2010 {published data only}
- Cho ST, Lee ST, Kim K, Lee YG, Kim KK, Choi NG. A sequential comparison of postoperative voiding pattern and uroflowmetry between two transobturator midurethral tape procedures (Monarc (trademark) and TOT (trademark)) (Abstract number 750). Proceedings of the Joint Meeting of the International Continence Society (ICS) and the International Urogynecological Association, 2010 Aug 23‐27, Toronto, Canada 2010. [srincont40199]
Choe 2013 {published data only}
- Choe JH, Lee HD, Park SH, Jo DG, Lee HS, Lee JS, et al. Comparison of postoperative pain after transobturator or retropubic suburethral sling for female stress urinary incontinence: a prospective randomized study (Abstract number MP17‐08). Journal of Endourology 2013;27(S1):A263. [srincont62161] [Google Scholar]
Darabi Mahboub 2012 {published data only}
- Darabi MR, Keshvari M, Sheikhi Z. Evaluation study between tension‐free vaginal tape (TVT) and transobturator tape (TOT) in treatment stress incontinence in female (Abstract number S88). European Urology Supplements 2013;12(4):e1196. [sr‐incont62158] [Google Scholar]
- Darabi Mahboub MR, Keshvari M, Sheikhi Z. Evaluation study between tension ‐ free vaginal tape (TVT) and transobturator tape (TOT) in treatment stress incontinence in female (Abstract number 788). Proceedings of the 42nd Annual Meeting of the International Continence (ICS), 2012 Oct 15‐19, Beijing, China 2012. [srincont48402]
- Mahbob MRD. Evaluation study between Tension‐Free Vaginal Tape and Transobturator Tape in treatment stress incontinence in women. Iranian Registry of Clinical Trials (IRCT) (available at: http://www.irct.ir/searchresult.php?id=8228&number=4 ) 2009. [sr‐incont 62304]
- Mahboub MRD, Keshvari M, Sheikhi Z. Evaluation study between tension free vaginal tape and transobturator tape in treatment stress incontinence in female (Abstract number BR03‐09). Journal of Endourology 2011;25(Suppl 1):A12. [srincont62292] [Google Scholar]
David‐Montefiore 2006 {published data only}
- Ballester M, Bui C, Frobert JL, Grisard‐Anaf M, Lienhart J, Fernandez H, et al. Four‐year functional results of the suburethral sling procedure for stress urinary incontinence: a French prospective randomized multicentre study comparing the retropubic and transobturator routes. World Journal of Urology 2012;30(1):117‐22. [srincont44520] [DOI] [PubMed] [Google Scholar]
- Darai E, Frobert JL, Grisard‐Anaf M, Lienhart J, Fernandez H, Dubernard G, et al. Functional results after the suburethral sling procedure for urinary stress incontinence: a prospective randomized multicentre study comparing the retropubic and transobturator routes. European Urology 2007;51(3):795‐802. [srincont22550] [DOI] [PubMed] [Google Scholar]
- David‐Montefiore E, Frobert JL, Grisard‐Anaf M, Liehart J, Fernandez H, Dubernard G, et al. Functional results after suburethral sling procedure for urinary stress incontinence at 1 year: a French prospective randomised multicentre study comparing the retropubic and transobturator routes (Abstract number 063). International Urogynecology Journal 2006;17(Suppl 2):S95. [sr‐incont49146] [Google Scholar]
- David‐Montefiore E, Frobert JL, Grisard‐Anaf M, Lienhart J, Bonnet K, Poncelet C, et al. Peri‐operative complications and pain after the suburethral sling procedure for urinary stress incontinence: a French prospective randomised multicentre study comparing the retropubic and transobturator routes. European Urology 2006;49(1):133‐8. [srincont21623] [DOI] [PubMed] [Google Scholar]
Deffieux 2010 {published data only}
- Deffieux X, Daher N, Mansoor A, Debodinance P, Deval B, Salet‐Lizee D, et al. Tension‐free vaginal tape (TVT) and trans‐obturator suburethral tape from inside to outside (TVT‐O) for surgical treatment of female stress urinary incontinence: a multicenter randomised controlled trial (Abstract number 33). International Urogynecology Journal and Pelvic Floor Dysfunction 2007;18(Suppl 1):S19‐20. [NCT00135616; srincont27322] [Google Scholar]
- Deffieux X, Daher N, Mansoor A, Debodinance P, Muhlstein J, Fernandez H. Transobturator TVT‐O versus retropubic TVT: results of a multicenter randomized controlled trial at 24 months follow‐up. International Urogynecology Journal 2010;21(11):1337‐45. [NCT00135616; srincont40895; PUBMED: 20552165] [DOI] [PubMed] [Google Scholar]
- Deffieux X, Fernandez H. Female sexual function following trans‐obturator suburethral tape from inside to outside (TVT‐O) and tension‐free vaginal tape (TVT): a randomized controlled trial (Abstract number 70). Journal of Minimally Invasive Gynecology 2009;16(6):S22. [NCT00135616; srincont40862] [Google Scholar]
- Trichot C, Salet‐Lizee D, Descamps P, Deval B, Hocke C, Fatton B, et al. [Functional results following transobturator and retropubic mid‐urethral sling] [French]. Journal de Gynecologie, Obstetrique et Biologie de la Reproduction 2010;39(8):614‐23. [NCT00135616; srincont41067] [DOI] [PubMed] [Google Scholar]
de Leval 2011 {published data only}
- Thomas A, Waltregny D, Leval J. One year results of a prospective randomized trial comparing the original inside‐out transobturator (TVT‐O) procedure and a modified version using a shortened tape and reduced dissection for the treatment of female stress urinary incontinence (Abstract number 153). Neurourology and Urodynamics 2010;29(6):1023‐5. [ISRCTN65635093; srincont40146] [Google Scholar]
- Waltregny D. Clincial comparison between the original TVT‐O and a modified procedure (mini TVT‐O) for the surgical treatment of female stress urinary incontinence: a randomised clinical trial with 1‐year follow‐up. http://isrctn.org/ISRCTN65635093 2007. [sr‐incont62307]
- Waltregny D, Thomas A, Blockx C, Leval J. Three year results of a prospective randomized trial comparing the original inside‐out transobturator (TVT‐OTM) procedure with a modified version using a shortened tape and reduced dissection for the treatment of female stress urinary incontinence (Abstract number 254). Neurourology and Urodynamics 2012;31(6):1056‐7. [ISRCTN65635093; srincont46716] [Google Scholar]
- Waltregny D, Leval J. New surgical technique for treatment of stress urinary incontinence TVT‐ABBREVO from development to clinical experience. Surgical Technology International 2012;22:149‐57. [srincont49404] [PubMed] [Google Scholar]
- Leval J, Thomas A, Waltregny D. The original versus a modified inside‐out transobturator procedure: 1‐year results of a prospective randomized trial. International Urogynecology Journal 2011;22(2):145‐56. [ISRCTN65635093; srincont40993] [DOI] [PubMed] [Google Scholar]
de Tayrac 2004 {published data only}
- Tayrac R, Deffieux X, Droupy S, Chauveaud‐Lambling A, Calvanese‐Benamour L, Fernandez H. A prospective randomized trial comparing tension‐free vaginal tape and transobturator suburethral tape for surgical treatment of stress urinary incontinence. American Journal of Obstetrics and Gynecology 2004;190(3):602‐8. [sr‐incont17259] [DOI] [PubMed] [Google Scholar]
- Tayrac R, Droupy S, Calvanese L, Fernandez H. A prospective randomized study comparing TVT and transobturator suburethral tape (T.O.T.) for the surgical treatment of stress incontinence (Abstract). Proceedings of the 33rd Annual Meeting of the International Continence Society (ICS), 203 Oct 5‐9, Florence, Italy. 2003:266‐7. [sr‐incont17153]
Diab 2012 {published data only}
- Diab DE, Zayed AM, Allam MN, Maroof AM, Ibraheem E, El‐Sayed DE. A prospective randomized study comparing the safety and efficacy of transobturator tape (TOT) versus tension free vaginal tape (TVT) in treatment of female stress urinary incontinence (Abstract number 177). European Urology Supplements 2012;11(1):e177. [srincont62249] [Google Scholar]
Elbadry 2014 {published data only}
- Elbadry M, Shaaban A, Gabre A. Adjustable versus ordinary trans‐obturator tape for female stress incontinence...is there a difference? A randomized trial (Abstract number MP75‐09). Journal of Urology 2014;191(4 Suppl 1):e876. [srincont62136] [Google Scholar]
El‐Hefnawy 2010 {published data only}
- El‐Hefnawy AS, Wadie BS, Mekresh M, Nabeeh A, Bazeed MA. TOT for treatment of stress urinary incontinence: how should we assess its equivalence with TVT?. International Urogynecology Journal 2010;21(8):947‐53. [srincont40077] [DOI] [PubMed] [Google Scholar]
- Wadie BS, Elhefnawy AS. TVT versus TOT, 2‐year prospective randomized study. World Journal of Urology 2013;31(3):645‐9. [srincont48133] [DOI] [PubMed] [Google Scholar]
Enzelsberger 2005 {published data only}
- Enzelsberger H, Schalupny J, Heider R, Mayer G. TVT versus TOT ‐ a prospective randomized study for the treatment of female stress urinary incontinence at a follow‐up of 1 year [German]. Geburtshilfe und Frauenheilkunde 2005;65(5):506‐11. [srincont21007] [Google Scholar]
Freeman 2011 {published data only}
- Freeman R, Holmes D, Hillard T, Smith P, James M, Sultan A, et al. What patients think: patient‐reported outcomes of retropubic versus trans‐obturator mid‐urethral slings for urodynamic stress incontinence‐a multi‐centre randomised controlled trial. International Urogynecology Journal 2011;22(3):279‐86. [srincont41009] [DOI] [PubMed] [Google Scholar]
- Freeman R, Holmes D, Smith P, Hillard T, Yang Q, Agur W, et al. Is trans‐obturator tape (TOT) as effective as tension‐free vaginal tape (TVT) in the treatment of women with urodynamic stress incontinence? Results of a multicentre RCT (Abstract number 3). Neurourology and Urodynamics 2008;27(7):573‐4. [srincont31849] [Google Scholar]
Hammoud 2011 {published data only}
- Hammoud K, Elsheikh M, Haitham M, Fayad A, Ghamrawy H, Aboumohamed A. Tension‐free vaginal tape versus transobturator vaginal tape in management of female stress urinary incontinence. Long‐term follow‐up: which to choose (Abstract number UP‐01.075). Urology 2011;78(3 Suppl 1):S209‐10. [srincont62233] [Google Scholar]
- Hammoud KM, Sheikh MG, Haitham M, Fayad AS, Ghamrawy HK, Mohamed AARA. Tension‐free vaginal tape versus trans‐obturator vaginal tape in the management of female stress urinary incontinence long term follow‐up: which to choose (Abstract number MP07‐01). Journal of Endourology 2012;26(Suppl 1):A59. [srincont62245] [Google Scholar]
Hassan 2013 {published data only}
- Hassan S, Aly H. Randomised Comparative study between inside‐out transobturator tape and outside‐in transobturator tape for urodynamic stress incontinence. Neurourology and Urodynamics 2013;32(6):777. [srincont49205] [Google Scholar]
Houwert 2009 {published data only}
- Houwert M, Vos MC, Vervest HAM. Transobturator tape (TOT), inside‐out versus outside‐in approaches: outcome after 1 year (Abstract number 56). International Urogynecology Journal and Pelvic Floor Dysfunction 2007;18(Suppl 1):S33. [srincont27326] [Google Scholar]
- Houwert RM, Renes‐Zijl C, Vos MC, Vervest HA. TVT‐O versus Monarc after a 2‐4‐year follow‐up: a prospective comparative study. International Urogynecology Journal and Pelvic Floor Dysfunction 2009;20(11):1327‐33. [sr‐incont50308; PUBMED: 19597718] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vervest H, Bruin JP, Renes‐Zeijl CC. Transobturator tape (TOT), inside‐out or outside‐in approaches: does it matter? (Abstract number 167). International Urogynecology Journal 2005;16(2 Suppl):S69‐70. [sr‐incont27406] [Google Scholar]
Jakimiuk 2012 {published data only}
- Jakimiuk AJ, Issat T, Fritz‐Rdzanek A, Maciejewski T, Rogowski A, Baranowski W. Is there any difference? A prospective, multicenter, randomized,single blinded clinical trial, comparing TVT with TVT‐O (POLTOS study) in management of stress urinary incontinence. Short‐term outcomes. Pelviperineology 2012;31:5‐9. [sr‐incont50305] [Google Scholar]
- Jakimiuk AJJ, Maciejewski TM, Fritz AF, Baranowski WB, Wladysiuk‐Blicharz MWB. Single‐blind randomized clinical trial comparing efficacy and safety of TVT (tension free vaginal tape) vs TVT‐O (tension free vaginal tape obturator system) in treatment of stress urinary incontinence (POLTOS) preliminary report (Abstract number 348). International Urogynecology Journal and Pelvic Floor Dysfunction 2007;18(Suppl 1):S189. [srincont27324] [Google Scholar]
Juang 2007 {published data only}
- Juang CM, Yu KJ, Chou P, Yen MS, Twu NF, Horng HC, et al. Efficacy analysis of trans‐obturator tension‐free vaginal tape (TVT‐O) plus modified Ingelman‐Sundberg procedure versus TVT‐O alone in the treatment of mixed urinary incontinence: a randomized study. European Urology 2007;51(6):1671‐9. [srincont23260] [DOI] [PubMed] [Google Scholar]
Kamel 2009 {published data only}
- Kamel A. A comparison between TVT & TVTO as regards safety. An African experience (Abstract number 830). Proceedings of the 39th Annual Meeting of the International Continence Society (ICS), 2009 Sep 29 ‐ Oct 3, San Francisco, CA 2009. [srincont35630]
Karateke 2009 {published data only}
- Karateke A, Haliloglu B, Cam C, Sakalli M. Comparison of TVT and TVT‐O in patients with stress urinary incontinence: short‐term cure rates and factors influencing the outcome. A prospective randomised study. Australian & New Zealand Journal of Obstetrics & Gynaecology 2009;49(1):99‐105. [srincont31429] [DOI] [PubMed] [Google Scholar]
Kilic 2007 {published data only}
- Kilic G, Olgun G, Bilen MA, Orhan A, Dunn B. [The comparison of TVT (tension free vaginal tape) and TOT (trans‐obturator vaginal tape) in the treatment of the urinary incontinence and literature search]. Jinekoloji Ve Obstetrik Dergisi 2007;21(1):26‐31. [srincont28036] [Google Scholar]
Kim 2004 {published data only}
- Kim J, Baek U, Kwon S, Jung H, Moon K, Park T, et al. The efficacy of Iris procedure in stress urinary incontinence: comparison with TVT and SPARC (Abstract). Proceedings of the International Continence Society (34th Annual Meeting) and the International Urogynecological Association, Joint Meeting, 23‐27 Aug, 2004, Paris. 2004:Abstract number 313. [srincont19058]
Kim 2005 {published data only}
- Kim Y‐W, Na Y‐G, Sul C‐K. [Randomized prospective study between pubovaginal sling using SPARC sling system and MONARC sling system for the treatment of female stress urinary incontinence: short term results]. Korean Journal of Urology 2005;46(10):1078‐82. [srincont22116] [Google Scholar]
- Na YG, Rob AS, Youk SM, Kim YW, Kim HS, Sul CK, et al. A prospective multicentre randomized study comparing transvaginal tapes (SPARC sling system) and transobturator suburethral tapes (Monarc sling system) for the surgical treatment of stress urinary incontinence (Abstract number 49). European Urology Supplements 2005;4(3):15. [srincont26609] [Google Scholar]
Krofta 2010 {published data only}
- Krofta L, Feyereisl J, Otcenasek M, Kasikova E, Pan M. [Tension free vaginal tape and transobturator suburethral tape for surgical treatment of stress urinary incontinence] [Czech]. Ceska Gynekologie 2008;73(4):231‐9. [sr‐incont27504] [PubMed] [Google Scholar]
- Krofta L, Feyereisl J, Otcenasek M, Velebil P, Kasikova E, Krcmar M. TVT and TVT‐O for surgical treatment of primary stress urinary incontinence: prospective randomized trial. International Urogynecology Journal 2010;21(2):141‐8. [sr‐incont39511] [DOI] [PubMed] [Google Scholar]
Laurikainen 2007 {published data only}
- Brubaker L, Brincat C, Mueller E. Are we satisfied? Perspective on five‐year outcomes of midurethral slings [editorial]. European Urology 2014;65(6):1115‐6. [sr‐incont67651; PUBMED: 24568893] [DOI] [PubMed] [Google Scholar]
- Laurikainen E, Takala T, Aukee P, Kivela A, Rinne K, Valpas A, et al. Retropubic TVT compared with transobturator TVT (TVT‐O) in treatment of stress urinary incontinence: five‐year results of a randomized trial (Abstract number 2). Neurourology and Urodynamics 2011;30(6):803‐5. [NCT00379314; srincont42162] [Google Scholar]
- Laurikainen E, Valpas A, Aukee P, Kivela A, Rinne K, Takala T, et al. Five‐year results of a randomized trial comparing retropubic and transobturator midurethral slings for stress incontinence. European Urology 2014;65(6):1109‐14. [sr‐incont60594; PUBMED: 24508070] [DOI] [PubMed] [Google Scholar]
- Laurikainen E, Valpas A, Kiilholma P, Takala T, Kivela A, Aukee P, et al. A prospective randomised trial comparing TVT and TVT‐O procedures for the treatment of SUI: immediate outcome and complications (Abstract no 077). International Urogynecology Journal 2006;17(Suppl 2):S104‐5. [sr‐incont49149] [Google Scholar]
- Laurikainen E, Valpas A, Kivela A, Kalliola T, Rinne K, Takala T, et al. Retropubic compared with transobturator tape placement in treatment of urinary incontinence: a randomized controlled trial. Obstetrics and Gynecology 2007;109(1):4‐11. [sr‐incont22553] [DOI] [PubMed] [Google Scholar]
- Nilsson CG. A randomized, prospective, multicenter trial comparing TVT with TVT‐O procedures in treatment of female primary urinary stress incontinence (Trial registry number: NCT00379314). http://clinicaltrials.gov/show/NCT00379314 2004. [NCT00379314; srincont49342]
- Palva K, Nilsson CG. Prevalence of urinary urgency symptoms decreases by mid‐urethral sling procedures for treatment of stress incontinence. International Urogynecology Journal 2011;22(10):1241‐7. [NCT00379314; srincont42695] [DOI] [PubMed] [Google Scholar]
- Palva K, Rinne K, Aukee P, Kivela A, Laurikainen E, Takala T, et al. A randomized trial comparing tension‐free vaginal tape with tension‐free vaginal tape‐obturator: 36‐month results. International Urogynecology Journal 2010;21(9):1049‐55. [NCT00379314; srincont40052] [DOI] [PubMed] [Google Scholar]
- Rinne K. Comparison of two mid‐urethral sling operations and their effect on urethral mobility assessed by dynamic magnetic resonance imaging [dissertation]. Dissertations in Health Sciences (Publications of the University of Eastern Finland) 2010; Vol. 33:1‐77. [ISBN: 978‐952‐61‐0236‐8 (pdf); ISSN:1798‐5714 (pdf); NCT00379314; srincont 60054]
- Rinne K, Aukee P, Heikkinen AM, Kalliola T, Kiilholma P, Kivela A, et al. A randomized clinical trial comparing TVT with TVT‐O for treatment of stress urinary incontinence: 12 months results (Abstract number 48). International Urogynecology Journal and Pelvic Floor Dysfunction 2007;18(Suppl 1):S28‐9. [srincont27323] [Google Scholar]
- Rinne K, Laurikainen E, Kivela A, Aukee P, Takala T, Valpas A, et al. A randomized trial comparing TVT with TVT‐O: 12‐month results. International Urogynecology Journal 2008;19(8):1049‐54. [NCT000379314; srincont31311] [DOI] [PubMed] [Google Scholar]
Leanza 2009 {published data only}
- Leanza V, Dati S, Gasbarro N. A multicenter randomized trial of prepubic and retropubic Leanza‐Gasbarro‐Caschetto tension‐free procedures (Abstract number 001). International Urogynaecology Journal 2009;20(Suppl 2):S73. [srincont39881] [Google Scholar]
- Leanza V, Dati S, Gasbarro N, Leanza G. Retropubic versus transobturator tension free procedures: a comparative study (Abstract number 7). Neurourology and Urodynamics 2011;30(S1):6‐7. [DOI: 10.1002/nau.21134; sr‐incont50306] [DOI] [Google Scholar]
Lee 2007 {published data only}
- Lee KS, Han DH, Choi YS, Yum SH, Song SH, Doo CK, et al. A prospective trial comparing tension‐free vaginal tape and transobturator vaginal tape inside‐out for the surgical treatment of female stress urinary incontinence: 1‐year follow up. Journal of Urology 2007;177(1):214‐8. [sr‐incont28039] [DOI] [PubMed] [Google Scholar]
- Ryu KH, Shin JS, Du JK, Choo MS, Lee KS. Randomized trial of tension‐free vaginal tape (TVT) vs. tension‐free vaginal tape obturator (TVT‐O) in the surgical treatment of stress urinary incontinence: comparison of operation related morbidity (Abstract number 50). European Urology Supplements 2005;4(3):15. [srincont26610] [Google Scholar]
Lee 2008 {published data only}
- Lee K‐S, Choo M‐S, Lee YS, Han J‐Y, Kim J‐Y, Jung BJ, et al. Prospective comparison of the ‘inside–out’ and ‘outside–in’ transobturator tape procedures for the treatment of female stress urinary incontinence. International Urogynecology Journal Including Pelvic Floor Dysfunction 2008;19(4):577‐82. [sr‐incont34482] [DOI] [PubMed] [Google Scholar]
Liapis 2006 {published data only}
- Liapis A, Bakas P, Giner M, Creatsas G. Tension‐free vaginal tape versus tension‐free vaginal tape obturator in women with stress urinary incontinence. Gynecologic and Obstetric Investigation 2006;62(3):160‐4. [srincont22245] [DOI] [PubMed] [Google Scholar]
Liapis 2008 {published data only}
- Liapis A, Bakas P, Creatsas G. Monarc vs TVT‐O for the treatment of primary stress incontinence: a randomised study. International Urogynecology Journal 2008;19:185‐90. [sr‐incont26461] [DOI] [PubMed] [Google Scholar]
Lim 2005 {published data only}
- Balakrishnan S, Lim YK, Barry C, Corstiaans A, Kannan K, Rane A. Sling distress: a subanalysis of the IVS tapes from the SUSPEND trial. Australian & New Zealand Journal of Obstetrics & Gynaecology 2007;47(6):496‐8. [sr‐incont26475] [DOI] [PubMed] [Google Scholar]
- Lim YN, Muller R, Corstiaans A, Dietz HP, Barry C, Rane A. Suburethral slingplasty evaluation study in North Queensland, Australia: the SUSPEND trial. Australian & New Zealand Journal of Obstetrics & Gynaecology 2005;45(1):52‐9. [srincont20403] [DOI] [PubMed] [Google Scholar]
- Lim YN, Rane A, Barry C, Corstiaans A, Dietz HP, Muller R. The suburethral slingplasty evaluation study in North Queensland (SUSPEND): a randomized controlled trial (Abstract). Neurourology and Urodynamics 2004;23(5/6):495‐6. [srincont19012] [Google Scholar]
Lord 2006 {published data only}
- Lord HE, Taylor JD, Finn JC, Tsokos N, Jeffery JT, Atherton MJ, et al. A randomized controlled equivalence trial of short‐term complications and efficacy of tension‐free vaginal tape and suprapubic urethral support sling for treating stress incontinence. BJU International 2006;98(2):367‐76. [srincont22369] [DOI] [PubMed] [Google Scholar]
Mansoor 2003 {published data only}
- Mansoor A, Vedrine N, Darcq C. Surgery of female urinary incontinence using transobturator tape (TOT): a prospective randomised comparative study with TVT (Abstract). Neurourology and Urodynamics 2003;22(5):488‐9. [sr‐incont17107] [Google Scholar]
Mehdiyev 2010 {published data only}
- Mehdiyev M, Itil IM, Sendag F, Akdemir A, Askar N. Comparing the transvaginal tape (TVT) and transobturator tape (TOT) in stress urinary incontinance for their efficiency and their effects on quality of life. Turk Jinekoloji ve Obstetrik Dernegi Dergisi 2010;7(2):117‐24. [srincont62297] [Google Scholar]
Meschia 2006 {published data only}
- Meschia M, Pifarotti P, Bernasconi F, Magatti F, Vigano R. Multicenter randomized trial of TVT and IVS for the treatment of stress urinary incontinence in women (Abstract). Proceedings of the 33rd Annual Meeting International Continence Society (ICS), 2003 Oct 5‐9, Florence. 2003:318‐9. [sr‐incont16339]
- Meschia M, Pifarotti P, Bernasconi F, Magatti F, Vigano R, Bertozzi R, et al. Tension‐free vaginal tape (TVT) and intravaginal slingplasty (IVS) for stress urinary incontinence: a multicenter randomized trial. American Journal of Obstetrics and Gynecology 2006;195(5):1338‐42. [sr‐incont22268] [DOI] [PubMed] [Google Scholar]
- Pifarotti P, Meschia M, Gattei U, Bernasconi F, Magatti F, Vigano R. Multicenter randomized trial of tension‐free vaginal tape (TVT) and intravaginal slingplasty (IVS) for the treatment of stress urinary incontinence in women (Abstract). Neurourology and Urodynamics 2004;23(5/6):494‐5. [sr‐incont19011] [Google Scholar]
Meschia 2007 {published data only}
- Meschia M, Bertozzi R, Pifarotti P, Baccichet R, Bernasconi F, Guercio E, et al. Peri‐operative morbidity and early results of a randomised trial comparing TVT and TVT‐O. International Urogynecology Journal 2007;18(11):1257‐61. [srincont23958] [DOI] [PubMed] [Google Scholar]
- Meschia M, Pifarotti P, Baccichet R, Bernasconi F, Cortese P, Magatti F, et al. A multicenter randomized comparison of tension‐free vaginal tape (TVT) and trans‐obturator in‐out technique (TVT‐O) for the treatment of stress urinary incontinence: one year results (Abstract number 3). International Urogynecology Journal and Pelvic Floor Dysfunction 2007;18(Suppl 1):S2. [srincont27318] [Google Scholar]
- Meschia M, Pifarotti P, Bernasconi F, Baccichet R, Magatti F, Cortese P, et al. A multicentre randomised comparison of tension free vaginal tape (TVT) and transobturator in‐out technique (TVT‐O) for the treatment of stress urinary incontinence (Abstract number 059). International Urogynecology Journal 2006;17(Suppl 2):S92‐S93. [sr‐incont49147] [Google Scholar]
- Minassian VA, Parekh M, Langroudi MH. Comment on Meschia et al: peri‐operative morbidity and early results of a randomised trial comparing TVT and TVT‐O [comment]. International Urogynecology Journal 2008;19(12):1725. [srincont31222] [DOI] [PubMed] [Google Scholar]
Naumann 2006 {published data only}
- Naumann G, Lobodasch K, Bettin S, Meyer P, Koelbl H. Tension free vaginal tape (TVT) vs less invasive free tape (LIFT) ‐ a randomized multicentric study of suburethral sling surgery (Abstract number 062). International Urogynecology Journal 2006;17(Suppl 2):S94‐5. [sr‐incont49145] [Google Scholar]
- Naumann G, Lobodasch K, Bettin S, Meyer P, Koelbl H. Tension free vaginal tape (TVTTM) vs less invasive free tape (LIFTTM) ‐ a randomized multicentre study of suburethral sling surgery (Abstract number 481). Proceedings of the 36th Annual Meeting of the International Continence Society (ICS), 2006 Nov 27‐Dec 1, Christchurch, New Zealand. 2006. [sr‐incont23752]
Nerli 2009 {published data only}
- Nerli RB, Kumar AG, Koura A, Prabha V, Alur SB. Transobturator vaginal tape in comparison to tension‐free vaginal tape: a prospective trial with a minimum 12 months follow‐up. Indian Journal of Urology 2009;25(3):321‐5. [srincont40242] [DOI] [PMC free article] [PubMed] [Google Scholar]
Nyyssonen 2014 {published data only}
- Nyyssonen V, Talvensaari‐Mattila A, Santala M. A prospective randomized trial comparing tension‐free vaginal tape versus transobturator tape in patients with stress or mixed urinary incontinence: subjective cure rate and satisfaction in median follow‐up of 46 months. Scandinavian Journal of Urology 2014;48(3):309‐15. [sr‐incont62072; PUBMED: 24286482] [DOI] [PubMed] [Google Scholar]
Okulu 2013 {published data only}
- Okulu E. Synthetic mesh materials in sling surgery. www.ClinicalTrials.gov (accessed 19 December 2011) 2011. [NCT01348334; srincont42756]
- Okulu E, Kayigil O, Aldemir M, Onen E. Use of three types of synthetic mesh material in sling surgery: a prospective randomized clinical trial evaluating effectiveness and complications. Scandinavian Journal of Urology 2013;47(3):217‐24. [sr‐incont48505; PUBMED: 23095128] [DOI] [PubMed] [Google Scholar]
Oliveira 2006 {published data only}
- Oliveira L, Sartori M, Castro R, Fonseca E, Rodrigues A, Girao M. A prospective randomized study to compare TVT, TVT‐O and pre‐pubic TVT for the treatment of women with stress urinary incontinence, with or without intrinsic sphincter deficiency (Abstract number 208). International Urogynecology Journal 2008; Vol. 19, issue Suppl 2:S173‐4. [srincont31051]
- Oliveira LM, Girao MJBC, Sartori MGF, Castro RA, Fonseca ESM. Comparison of retro‐pubic TVT, pre‐pubic TVT and TVT transobturator in surgical treatment of women with stress urinary incontinence (Abstract number 203). International Urogynecology Journal 2005;16(Suppl 2):S80. [srincont27307] [Google Scholar]
- Oliveira LM, Girao MJBC, Sartori MGF, Castro RA, Fonseca ESM, Prior EL. Comparison of retro pubic TVT, pre pubic TVT and TVT transobturator in surgical treatment of women with stress urinary incontinence (Abstract number 354). International Urogynecology Journal 2006;17(Suppl 2):S253. [srincont27309] [Google Scholar]
- Oliveira LM, Girao MJBC, Sartori MGF, Castro RA, Fonseca ESM. Comparison of retro‐pubic TVT, pre‐pubic TVT and TVT transobturator in surgical treatment of women with stress urinary incontinence (Abstract number 328). International Urogynecology Journal 2007;18(Suppl 1):S180. [srincont27310] [Google Scholar]
Palomba 2008 {published data only}
- Palomba S, Zullo F. A Comparison in Terms of Efficacy and Safety Between Transobturator and Transvaginal Tape Performed at the Same Time of Anterior Defect Correction With Mesh. http://clinicaltrials.gov/show/NCT00743535 2008. [NCT00743535; srincont49348]
Paparella 2010 {published data only}
- Paparella R, Marturano M, Pelino L, Scarpa A, Scambia G, Torre G, et al. Prospective randomized trial comparing synthetic vs biological out‐in transobturator tape: a mean 3‐year follow‐up study. International Urogynecology Journal 2010;21(11):1327‐36. [srincont40360] [DOI] [PubMed] [Google Scholar]
- Riva D, Baccichet R, Paparella L, Cianci A, Simonazzi M, Pisapia Cioffi G. Synthetic versus biological trans‐obturator sling for stress urinary incontinence: a randomized study (Abstract number 1). International Urogynecology Journal 2008; Vol. 19, issue Suppl 2:S1. [srincont31054]
Park 2012 {published data only}
- Kim D, Jang HC. Randomized control study of Monarc (trademark) vs. tension‐free vaginal tape obturator (TVT‐O) (trademark) in the treatment of female urinary incontinence in: comparison of medium term cure rate (Abstract number: 219). Neurourology and Urodynamics 2010;29(6):1123‐4. [srincont40160] [Google Scholar]
- Park YJ, Kim DY. Randomized controlled study of MONARC [Registered trademark] vs. tension‐free vaginal tape obturator (TVT‐O [Registered trademark]) in the treatment of female urinary incontinence: comparison of 3‐year cure rates. Korean Journal of Urology 2012;53(4):258‐62. [srincont44720] [DOI] [PMC free article] [PubMed] [Google Scholar]
Peattie 2006 {published data only}
- Peattie A. Randomised controlled trial of transvaginal tension‐free vaginal tape‐obturator (TVT‐O) versus Monarc in treatment of urodynamic stress incontinence. ISRCTN (http://isrctn.org/ISRCTN71562338) 2006. [ISRCTN71562338; sr‐incont62312]
Porena 2007 {published data only}
- Costantini E, Kocjancic E, Saccomanni M, Giannantoni A, Porena M, Frea B. Tension free vaginal tape vs trans obturator tape as surgery for stress urinary incontinence: results of a multicenter randomised trial (Abstract number 54). Neurourology and Urodynamics 2006;25(6):573‐5. [sr‐incont23753] [Google Scholar]
- Costantini E, Lazzeri M, Giannantoni A, Bini V, Kocjancic E, Porena M, et al. Retropubic versus transobturator mid‐urethral slings: in a randomised controlled trial preoperative VLPP may not predict mid‐term outcome (Abstract number 112). Neurourology and Urodynamics 2007;26(5):741‐2. [sr‐incont23757] [Google Scholar]
- Costantini E, Lazzeri M, Giannantoni A, Bini V, Vianello A, Kocjancic E, et al. Preoperative Valsava leak point pressure may not predict outcome of mid‐urethral slings. Analysis from a randomized controlled trial of retropubic versus transobturator mid‐urethral slings. International Braz J Urol 2008;34(1):73‐81; discussion 81‐3. [srincont27817] [DOI] [PubMed] [Google Scholar]
- Costantini E, Lazzeri M, Kocjancic E, Biase M, Salvini E, Porena M. Prolonged follow‐up shows continence deterioration after trans‐obturator tape: results from a randomised controlled study. Neurourology and Urodynamics 2013;32(6):525‐6. [sr‐incont49187] [Google Scholar]
- Costantini E, Lazzeri M, Zucchi A, Bruno R, Salvini E, Pietropaolo A, et al. Deterioration of continence after TOT when the follow‐up is extended: results from a randomised controlled study (Abstract number 729). European Urology Supplements 2013;12(1):e729. [sr‐incont62144] [Google Scholar]
- Costantini E, Lazzeri M, Zucchi A, Biase M, Porena M. Long‐term efficacy of the transobturator and retropubic midurethral slings for stress urinary incontinence: single‐center update from a randomized controlled trial. European Urology 2014;66(3):599‐603. [sr‐incont64001; PUBMED: 24768493] [DOI] [PubMed] [Google Scholar]
- Kocjancic E, Constantini E, Crivellaro S, Tosco L, Grossetti B, Frea B, et al. Mixed incontinence: the best solution for a difficult task (Abstract number 485). Proceedings of the 38th Annual Meeting of the International Continence Society (ICS), 2008 Oct 20‐24, Cairo, Egypt 2008. [srincont31875]
- Kocjancic E, Costantini E, Giannantoni A, Crivellaro S, Mearini L, Frea B, et al. Tension free vaginal tape (TVT) and trans obturator suburethral tape (TOT) a prospective randomized study (Poster abstract number 1462). Proceedings of the American Urological Association (AUA) Annual Meeting, 2007 May 19‐24, Anaheim, CA. 2007. [sr‐incont23765]
- Porena M, Costantini E, Frea B, Giannantoni A, Ranzoni S, Mearini L, et al. Tension‐free vaginal tape versus transobturator tape as surgery for stress urinary incontinence: results of a multicentre randomised trial. European Urology 2007;52(5):1481‐91. [srincont23832] [DOI] [PubMed] [Google Scholar]
- Porena M, Kocjancic E, Costantini E, Cecchetti G, Bini V, Crivellaro S, et al. Tension free vaginal tape vs trans obturator tape as surgery for stress urinary incontinence: results of a multicenter randomised trial (Abstract). Neurourology and Urodynamics 2005;24(5/6):416‐8. [sr‐incont20982] [Google Scholar]
Rechberger 2003 {published data only}
- Rechberger T, Rzezniczuk K, Skorupski P, Adamiak A, Tomaszewski J, Baranowski W, et al. A randomized comparison between monofilament and multifilament tapes for stress incontinence surgery. International Urogynecology Journal 2003;14(6):432‐6. [sr‐incont16673] [DOI] [PubMed] [Google Scholar]
Rechberger 2009 {published data only}
- Rechberger T, Adamiak A, Jankiewicz K, Futyma K, Skorupski P. The comparison of clinical effectiveness of retropubic (IVS 02) and transobturator (IVS04) midurethral slings (Abstract number 076). International Urogynecology Journal 2006;17(Suppl 2):S104. [sr‐incont49148] [Google Scholar]
- Rechberger T, Futyma K, Jankiewicz K, Adamiak A, Bogusiewicz M, Skorupski P. Body mass index does not influence the outcome of anti‐incontinence surgery among women whereas menopausal status and ageing do: a randomised trial. International Urogynecology Journal 2010;21(7):801‐6. [srincont40095] [DOI] [PubMed] [Google Scholar]
- Rechberger T, Futyma K, Jankiewicz K, Adamiak A, Skorupski P. The clinical effectiveness of retropubic (IVS‐02) and transobturator (IVS‐04) midurethral slings: randomized trial. European Urology 2009; Vol. 56, issue 1:24‐30. [srincont35437] [DOI] [PubMed]
- Rechberger T, Jankiewicz K, Futyma K, Adamiak A, Skorupski P. Clinical effectiveness of retropubic (IVS‐02) and transobturator (IVS‐04) slings in the treatment of female stress urinary incontinence ‐ a semi‐randomized trial on 398 patients (Abstract number 515). Proceedings of the 38th Annual Meeting of the International Continence Society (ICS), 2008 Oct 20‐24, Cairo, Egypt 2008. [srincont31877]
- Rechberger T, Jankiewicz K, Skorupski P, Adamiak A, Futyma K, Gogacz M, et al. Transobturator vs retropubic vaginal tape for female stress urinary incontinence: one year follow‐up in 296 patients (Abstract number 288). Proceedings of the 37th Annual Meeting of the International Continence Society (ICS), 2007 Aug 20‐24, Rotterdam, The Netherlands. 2007. [sr‐incont23763]
Rechberger 2011 {published data only}
- Rechberger T, Futyma K, Jankiewicz K, Adamiak A, Bogusiewicz M, Bartuzi A, et al. Tape fixation: an important surgical step to improve success rate of anti‐incontinence surgery. Journal of Urology 2011;186(1):180‐4. [srincont41735] [DOI] [PubMed] [Google Scholar]
Richter 2010 {published data only}
- Brubaker L, Norton PA, Albo ME, Chai TC, Dandreo KJ, Lloyd KL, et al. Adverse events over two years after retropubic or transobturator midurethral sling surgery: findings from the Trial of Midurethral Slings (TOMUS) study. American Journal of Obstetrics and Gynecology 2011;205(5):498.e1‐6. [NCT00325039; TOMUS; srincont43397] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brubaker L, Rickey L, Stoddard A, Lemack G, Xu Y, Ghetti C, et al. Symptoms of combined prolapse and urinary incontinence in large surgical cohorts (Abstract 020). International Urogynaecology Journal 2009;20(Suppl 2):S96‐7. [NCT00064662; srincont39882] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chai TC, Huang L, Kenton K, Richter HE, Baker J, Kraus S, et al. Association of baseline urodynamic measures of urethral function with clinical, demographic, and other urodynamic variables in women prior to undergoing midurethral sling surgery. Neurourology and Urodynamics 2012;31(4):496‐501. [NCT00325039; TOMUS; srincont49292] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chai TC, Kenton K, Xu Y, Sirls L, Zyczynski H, Wilson TS, et al. Effects of concomitant surgeries during midurethral slings (MUS) on postoperative complications, voiding dysfunction, continence outcomes, and urodynamic variables. Urology 2012;79(6):1256‐61. [NCT00325039; srincont44637] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gormley A. TOMUS‐Trial Of Mid‐Urethral Slings [results posted online] (Trials registry number: NCT00325039). ClinicalTrials.gov (http://clinicaltrials.gov/show/NCT00325039) 2006. [NCT00325039; TOMUS; srincont49293]
- Kenton K, Stoddard A, Zyczynski H, Rickey L, Wai C, Albo M, et al. 5‐year outcomes after retropubic and transobturator midurethral sling (Abstract number PII‐03). Journal of Urology 2014;191(4 Suppl 1):e493. [sr‐incont62138] [Google Scholar]
- Kenton K, Stoddard AM, Zyczynski H, Albo M, Rickey L, Norton P, et al. 5‐year longitudinal followup after retropubic and transobturator mid urethral slings. The Journal of Urology 2014;193:203‐10. [sr‐incont64661; PUBMED: 25158274] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kraus S, Lemack G, Chai T, Leng W, Albo M, Mueller E, et al. Urodynamic changes 12 months after retropubic and transobturator midurethral slings (Abstract number 13). Neurourology and Urodynamics 2011;30(6):819‐20. [NCT00325039; TOMUS; sr‐incont42167] [Google Scholar]
- Kraus S, Lemack G, Chai T, Leng W, Albo M, Mueller E, et al. Urodynamic changes 12 months after retropubic and transobturator midurethral slings (Abstract: Podium number 14). Neurourology and Urodynamics 2011;30(2):210. [NCT00325039; TOMUS; srincont41349] [Google Scholar]
- Lemack GE, Litman HJ, Nager C, Brubaker L, Lowder J, Norton P, et al. Preoperative clinical, demographic, and urodynamic measures associated with failure to demonstrate urodynamic stress incontinence in women enrolled in two randomized clinical trials of surgery for stress urinary incontinence. International Urogynecology Journal 2013;24(2):269‐74. [NCT00064662; NCT00325039; SISTEr; TOMUS; srincont47045] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norton PA, Nager CW, Chai TC, Mueller E, Stoddard A, Lowder J, et al. Risk factors for incomplete bladder emptying after midurethral sling. Urology 2013;82(5):1038‐41. [NCT00325039; srincont50470] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nygaard I, Brubaker L, Chai TC, Markland AD, Menefee SA, Sirls L, et al. Risk factors for urinary tract infection following incontinence surgery. International Urogynecology Journal 2011;22(10):1255‐65. [NCT00064662; NCT00325039; SISTEr; TOMUS; srincont42698] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richter HE, Albo ME, Zyczynski HM, Kenton K, Norton PA, Sirls LT, et al. Retropubic versus transobturator midurethral slings for stress incontinence. New England Journal of Medicine 2010;362(22):2066‐76. [NCT00325039; TOMUS; srincont39867] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richter HE, Litman HJ, Lukacz ES, Sirls LT, Rickey L, Norton P, et al. Demographic and clinical predictors of treatment failure one year after midurethral sling surgery. Obstetrics and Gynecology 2011;117(4):913‐21. [NCT00325039; TOMUS; srincont41490] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rickey LM, Huang L, Rahn DD, Hsu Y, Litman HJ, Mueller ER. Risk factors for urgency incontinence in women undergoing stress urinary incontinence surgery. Advances in Urology 2013;2013:567375. [NCT00064662; NCT00325039; srincont50474] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sirls LT, Tennstedt S, Albo M, Chai T, Kenton K, Huang L, et al. Factors associated with quality of life in women undergoing surgery for stress urinary incontinence. Journal of Urology 2010;184(6):2411‐5. [NCT00325039; srincont49291] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sirls LT, Tennstedt S, Lukacz E, Rickey L, Kraus SR, Markland AD, et al. Condition‐specific quality of life 24 months after retropubic and transobturator sling surgery for stress urinary incontinence. Female Pelvic Medicine & Reconstructive Surgery 2012;18(5):291‐5. [NCT00325039; srincont45799] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Urinary Incontinence Treatment Network (UITN). The trial of mid‐urethral slings (TOMUS): design and methodology. Journal of Applied Research 2008;8(1):1‐13. [NCT00325039; srincont27938] [PMC free article] [PubMed] [Google Scholar]
- Wai CY, Curto TM, Zyczynski HM, Stoddard AM, Burgio KL, Brubaker L, et al. Patient satisfaction after midurethral sling surgery for stress urinary incontinence. Obstetrics and Gynecology 2013;121(5):1009‐16. [NCT00325039; srincont49289] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zyczynski HM, Brubaker L. Sexual activity and function in women for two years after midurethral slings (Abstract number 176). European Urology Supplements 2012;11(1):e176. [sr‐incont62250] [Google Scholar]
- Zyczynski HM, Rickey L, Dyer KY, Wilson T, Stoddard AM, Gormley EA, et al. Sexual activity and function in women more than 2 years after midurethral sling placement. American Journal of Obstetrics and Gynecology 2012;207(5):421‐6. [NCT00325039; TOMUS; srincont45909] [DOI] [PMC free article] [PubMed] [Google Scholar]
Riva 2006 {published data only}
- Riva D, Sacca V, Tonta A, Casolati E, Luerti M, Banfi G, et al. TVT versus TOT a randomised study at 1 year follow up (Abstract number 060). International Urogynecology Journal 2006;17(Suppl 2):S93. [sr‐incont49150] [Google Scholar]
Salem 2014 {published data only}
- Salem H, Mostafa M, Diab DE, Abdulla A, Nageeb M, Hashem SA. A prospective randomized study comparing the safety and efficacy of transobturator tape (TOT) versus tension free vaginal tape (TVT) in treatment of female stress urinary incontinence (Abstract number MP33‐13). Journal of Urology 2014;191(4 Suppl 1):e342‐3. [srincont62143] [Google Scholar]
Scheiner 2012 {published data only}
- Scheiner D, Betschart C, Kollbrunner S, Werder H, Fink D, Perucchini D. Retropubic or transobturator out‐in or in‐out sling? A prospective randomized study! (Abstract number 484). Proceedings of the 38th Annual Meeting of the International Continence Society (ICS), 2008 Oct 20‐24, Cairo, Egypt 2008. [NCT00642109; srincont31874]
- Scheiner D, Betschart C, Werder H, Fink D, Perucchini D. Retropubic TVT vs transobturator outside‐in TOT and inside‐out TVT‐O one‐year results from our prospective randomized study (Abstract number 4). Neurourology and Urodynamics 2009;28(7):585‐6. [NCT00642109; srincont34588] [Google Scholar]
- Scheiner DA, Betschart C, Wiederkehr S, Seifert B, Fink D, Perucchini D. Twelve months effect on voiding function of retropubic compared with outside‐in and inside‐out transobturator midurethral slings. International Urogynecology Journal 2012;23(2):197‐206. [srincont44532] [DOI] [PubMed] [Google Scholar]
Schierlitz 2008 {published data only}
- Souza A, Dwyer PL, Rosamilia A, Hiscock R, Lim YN, Murray C, et al. Sexual function following retropubic TVT and transobturator Monarc sling in women with intrinsic sphincter deficiency: a multicentre prospective study. International Urogynecology Journal 2012;23(2):153‐8. [srincont44534] [DOI] [PubMed] [Google Scholar]
- Souza A, Schierlitz L, Rosamilia A, Dwyer P, Murray C, Thomas E, et al. Sexual function following retropubic TVT and transobturator Monarc sling in women with intrinsic sphincter deficiency (Abstract). Australian and New Zealand Continence Journal 2008;14(4):104. [srincont29144] [DOI] [PubMed] [Google Scholar]
- Murray C, Schierlitz L, Dwyer PL, Rosamilia A, Hiscock R, Souza A, et al. Overactive bladder (OAB) symptoms following retropubic TVT and Monarc TOT in women with intrinsic sphincter deficiency (ISD) and stress incontinence (Abstract). Australian and New Zealand Continence Journal 2008;14(4):102. [srincont29145] [Google Scholar]
- Plotti F, Calcagno M, Sansone M, Panici PB. Effectiveness of tension‐free vaginal tape compared with transobturator tape in women with stress urinary incontinence and intrinsic sphincter deficiency: a randomized controlled trial [comment] [letter]. Obstetrics and Gynecology 2009;113(6):1368; author reply 1368‐9. [srincont31355] [DOI] [PubMed] [Google Scholar]
- Schierlitz L, Dwyer P, Rosamilia A, Murray C, Thomas E, Fitzgerald E, et al. A randomized controlled study to compare tension free vaginal tape (TVT) and Monarc trans‐obturator tape in the treatment of women with urodynamic stress incontinence (USI) and intrinsic sphincter deficiency (ISD): the three year follow up (Abstract number 1). Neurourology and Urodynamics 2010;29(6):805‐6. [srincont40112] [Google Scholar]
- Schierlitz L, Dwyer PL, Rosamilia A, Hiscock R, Souza A, Lim YN, et al. A randomised controlled study to compare tension‐free vaginal tape (TVT) and Monarc (trademark) transobturator tape in the treatment of women with urodynamic stress incontinence (USI) and intrinsic sphincter deficiency (ISD): the three‐year follow‐up (Abstract). Australian and New Zealand Continence Journal 2010;16(4):120‐2. [srincont40800] [Google Scholar]
- Schierlitz L, Dwyer PL, Rosamilia A, Murray C, Thomas E, Souza A, et al. Effectiveness of tension‐free vaginal tape compared with transobturator tape in women with stress urinary incontinence and intrinsic sphincter deficiency: a randomized controlled trial. Obstetrics and Gynecology 2008;112(6):1253‐61. [ACTRN12608000093381; srincont28699] [DOI] [PubMed] [Google Scholar]
- Schierlitz L, Dwyer PL, Rosamilia A, Murray C, Thomas E, Souza A, et al. Three‐year follow‐up of tension‐free vaginal tape compared with transobturator tape in women with stress urinary incontinence and intrinsic sphincter deficiency. Obstetrics and Gynecology 2012;119(2 Pt 1):321‐7. [ ACTRN12608000093381; srincont43343] [DOI] [PubMed] [Google Scholar]
- Schierlitz LHE, Dwyer PL, Rosamilia A, Murray C, Thomas E, Taylor N, et al. A randomized controlled study to compare tension free vaginal tape (TVT) and Monarc trans‐obturator tape in the treatment of women with urodynamic stress incontinence (USI) and intrinsic sphincter deficiency (ISD) (Abstract number 32). International Urogynecology Journal and Pelvic Floor Dysfunction 2007;18(Suppl 1):S19. [srincont27321] [Google Scholar]
Tanuri 2010 {published data only}
- Tanuri AL, Feldner PC Jr, Bella ZI, Castro RA, Sartori MG, Girao MJ. [Retropubic and transobturator sling in treatment of stress urinary incontinence.] [Portuguese]. Revista Da Associacao Medica Brasileira 2010;56(3):348‐54. [srincont40054] [DOI] [PubMed] [Google Scholar]
Tarcan 2011 {published data only}
- Tarcan T, Mangir N, Tanidir Y, Top T, IIker Y. A randomised study comparing transvaginal and transobturator mid‐urethral sling surgeries in women with stress urinary incontinence (Abstract number 845). Proceedings of the 41st Annual Meeting of the International Continence Society (ICS), 2011 Aug 29‐Sept 2, Glasgow, Scotland 2011. [srincont42237]
- Tarcan T, Sahan A, Sulukaya M, Mangir N, Ilker Y. 2‐year results of a randomized study comparing retropubic and transobturator mid‐urethral slings in the treatment of urodynamic female stress urinary incontinence (Abstract number 448). Proceedings of the 43rd Annual Meeting of the International Continence Society (ICS), 2013 Aug 26‐30, Barcelona, Spain. 2013. [srincont60034]
Teo 2011 {published data only}
- Mayne C. Randomised trial of tension‐free vaginal tape and transobturator tape as treatment for urinary stress incontinence in women. ISRCTN (http://isrctn.org/ISRCTN34377436) 2004. [sr‐incont62313]
- Teo R, Moran P, Mayne C, Tincello D. Randomised trial of TVT and TVT‐O for the treatment of urodynamic stress incontinence in women (Abstract number 2). Neurourology and Urodynamics 2008;27(7):572‐3. [srincont31848] [Google Scholar]
- Teo R, Moran P, Mayne C, Tincello D. Randomised trial of tension‐free vaginal tape and transobturator tape for the treatment of urodynamic stress incontinence in women (Abstract number 283). Proceedings of the 37th Annual Meeting of the International Continence Society (ICS), 2007 Aug 20‐24, Rotterdam, The Netherlands. 2007. [srincont23761]
- Teo R, Moran P, Mayne C, Tincello D. Randomized trial of tension‐free vaginal tape and tension‐free vaginal tape‐obturator for urodynamic stress incontinence in women. Journal of Urology 2011;185(4):1350‐5. [srincont41497] [DOI] [PubMed] [Google Scholar]
Tommaselli 2012 {published data only}
- Tommaselli GA, D'Afiero A, Di CC, Formisano C, Fabozzi A, Nappi C. Efficacy of a modified technique for TVT‐O positioning: a 12 month, randomized, single‐blind, multicentre, non inferiority study. European Journal of Obstetrics, Gynecology, and Reproductive Biology 2013;167(2):225‐9. [sr‐incont47602] [DOI] [PubMed] [Google Scholar]
- Tommaselli GA, D'Afiero A, Carlo C, Formisano C, Fabozzi A, Nappi C. Effect of a modified surgical technique for the positioning of TVT‐O on post‐operative pain (Abstract number 110). International Urogynecology Journal and Pelvic Floor Dysfunction 2011;22(Suppl 1):S110. [sr‐incont62263] [Google Scholar]
- Tommaselli GA, Formisano C, Carlo C, Fabozzi A, Nappi C. Effects of a modified technique for TVT‐O positioning on postoperative pain: single‐blind randomized study. International Urogynecology Journal 2012;23(9):1293‐9. [srincont45107] [DOI] [PubMed] [Google Scholar]
Tseng 2005 {published data only}
- Tseng LH, Wang AC, Lin YH, Li SJ, Ko YJ. Randomized comparison of the suprapubic arc sling procedure vs tension‐free vaginal taping for stress incontinent women. International Urogynecology Journal 2005;16(3):230‐5. [srincont20354] [DOI] [PubMed] [Google Scholar]
Ugurlucan 2013 {published data only}
- Ugurlucan FG, Erkan HA, Onal M, Yalcin O. Randomized trial of graft materials in transobturator tape operation: biological versus synthetic. International Urogynecology Journal 2013;24(8):1315‐23. [sr‐incont48489; PUBMED: 23184140] [DOI] [PubMed] [Google Scholar]
van Leijsen 2013 {published data only}
- Mengerink BB. The impact of midurethral sling operation on sexual function in women with stress urinary incontinence, a multicenter prospective study (Abstract number 193). International Urogynecology Journal and Pelvic Floor Dysfunction 2013;24(1 Suppl):S147. [sr‐incont62175] [Google Scholar]
- Leijsen SA, Kluivers KB, Mol BW, Hout Ji, Milani AL, Roovers JP, et al. Value of urodynamics before stress urinary incontinence surgery: a randomized controlled trial. Obstetrics and Gynecology 2013;121(5):999‐1008. [sr‐incont47434; PUBMED: 23635736] [DOI] [PubMed] [Google Scholar]
- Leijsen SA, Kluivers KB, Mol BWJ, Broekhuis SR, Milani FL, Vaart CHvan D, et al. Protocol for the value of urodynamics prior to stress incontinence surgery (VUSIS) study: a multicenter randomized controlled trial to assess the cost effectiveness of urodynamics in women with symptoms of stress urinary incontinence in whom surgical treatment is considered. BMC Women's Health 2009;9:22. [sr‐incont32078; PUBMED: 19622153] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wang 2006 {published data only}
- Wang AC, Lin YH, Tseng LH, Chih SY, Lee CJ. Prospective randomized comparison of transobturator suburethral sling (Monarc) vs suprapubic arc (Sparc) sling procedures for female urodynamic stress incontinence. International Urogynecology Journal 2006;17(5):439‐43. [srincont22217] [DOI] [PubMed] [Google Scholar]
Wang 2008 {published data only}
- Wang WY, Zhu L, Lang JH, Sun ZJ, Hai N. [Clinical study on tension‐free vaginal tape and tension‐free vaginal tape obturator for surgical treatment of severe stress urinary incontinence] [Chinese]. Chung‐Hua Fu Chan Ko Tsa Chih [Chinese Journal of Obstetrics & Gynecology] 2008;43(3):180‐4. [srincont27746] [PubMed] [Google Scholar]
Wang 2009 {published data only}
- Wang W, Zhu L, Lang J. Transobturator tape procedure versus tension‐free vaginal tape for treatment of stress urinary incontinence. International Journal of Gynaecology and Obstetrics 2009;104(2):113‐6. [srincont29200] [DOI] [PubMed] [Google Scholar]
- Wang WY, Zhu L, Lang JH, Li B. [A prospective randomized trial of comparing the clinical outcome of tension‐free vaginal tape and transobturator tape for stress urinary incontinence] [Chinese]. Chung‐Hua i Hsueh Tsa Chih [Chinese Medical Journal] 2011;91(13):898‐901. [srincont41799] [PubMed] [Google Scholar]
- Zhu I, Lang J. A prospective randomised trial comparing tension free vaginal tape and transobturator suburethral tape for surgical treatment of slight and moderate stress urinary incontinence (Abstract number 461). International Urogynecology Journal 2006;17(Suppl 2):S307. [sr‐incont49151] [Google Scholar]
- Zhu I, Lang J, Chen R, Hai N, Wong F. Comparing TVT and TVT‐O sub urethral tape for treatment patients with mild and moderate stress urinary incontinence (Abstract number 364). International Urogynecology Journal and Pelvic Floor Dysfunction 2007;18(Suppl 1):S198. [srincont27325] [Google Scholar]
- Zhu L, Lang J, Hai N, Wong F. Comparing vaginal tape and transobturator tape for the treatment of mild and moderate stress incontinence. International Journal of Gynaecology and Obstetrics 2007;99(1):14‐7. [srincont23870] [DOI] [PubMed] [Google Scholar]
Wang 2010 {published data only}
Wang 2011 {published data only}
- Wang YJ, Li FP, Wang Q, Yang S, Cai XG, Chen YH. Comparison of three mid‐urethral tension‐free tapes (TVT, TVT‐O, and TVT‐Secur) in the treatment of female stress urinary incontinence: 1‐year follow‐up. International Urogynecology Journal 2011;22(11):1369‐74. [srincont42639] [DOI] [PubMed] [Google Scholar]
Zhang 2011 {published data only}
- Zhang Y, Jiang M, Tong XW, Fan BZ, Li HF, Chen XL. The comparison of an inexpensive‐modified transobturator vaginal tape versus TVT‐O procedure for the surgical treatment of female stress urinary incontinence. Taiwanese Journal of Obstetrics & Gynecology 2011;50(3):318‐21. [srincont42665] [DOI] [PubMed] [Google Scholar]
Zullo 2007 {published data only}
- Angioli R, Plotti F, Muzii L, Montera R, Panici PB, Zullo MA. Tension‐free vaginal tape versus transobturator suburethral tape: five‐year follow‐up results of a prospective, randomised trial. European Urology 2010;58(5):671‐7. [srincont41500] [DOI] [PubMed] [Google Scholar]
- Zullo MA, Plotti F, Calcagno M, Marullo E, Palaia I, Bellati F, et al. One‐year follow‐up of tension‐free vaginal tape (TVT) and trans‐obturator suburethral tape from inside to outside (TVT‐O) for surgical treatment of female stress urinary incontinence: a prospective randomised trial. European Urology 2007;51(5):1376‐82; discussion 1383‐4. [srincont23246] [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Al‐Tayyem 2007 {published data only}
- Al‐Tayyem A, Benness C, Korda A, Farnsworth B, Burton G. TVT vs TVT‐O: a study comparing early complications (Abstract number 062). International Urogynecology Journal 2007;18(Suppl 1):S37. [27330] [Google Scholar]
Amat 2007 {published data only}
- Amat LL, Martinez F, Hernandez S, Vela M. Needleless: a new technique for the correction of urinary incontinence. Randomised controlled trial compared with TVT‐O. Preliminary results (Abstract number 225). International Urogynecology Journal 2007;18(Suppl 1):S128. [Google Scholar]
Ballert 2010 {published data only}
- Ballert KN, Rose AE, Biggs GY, Rosenblum N, Nitti VW. Outcomes of patients lost to followup after mid urethral synthetic slings‐‐successes or failures?. The Journal of Urology 2010;183(4):1455‐8. [PUBMED: 20171698] [DOI] [PubMed] [Google Scholar]
Bekker 2009 {published data only}
- Bekker M, Beck J, Putter H, Venema P, Nijeholt A, Pelger R, et al. Sexual function improvement following surgery for stress incontinence: the relevance of coital incontinence. Journal of Sexual Medicine 2009;6(11):3208‐13. [DOI] [PubMed] [Google Scholar]
Borrell 2005 {published data only}
- Borrell PA, Chicote FP, Beltran MJF, Queipo ZJA, Esteve Claramunt J, Pastor Sempere F. Comparison of different suburethral slings for the treatment of stress urinary incontinence. Actas Urologicas Espaňolas 2005;29:757‐63. [DOI] [PubMed] [Google Scholar]
Bracken 2012 {published data only}
- Bracken JN, Huffaker RK, Yandell PM, Handcock T, Higgins EW, Kuehl TJ, et al. A randomized comparison of bupivacaine versus saline during placement of tension‐free vaginal tape. Female Pelvic Medicine & Reconstructive Surgery 2012;18(2):93‐6. [PUBMED: 22453319] [DOI] [PubMed] [Google Scholar]
- Huffaker RK, Bracken JN, Yandell PM, Handcock T, Higgins EW, Kuehl TJ, et al. A randomised, double‐blind comparison of bupivacaine containing saline with saline only hydrodissection on voiding function and pain control in the postoperative interval following placement of tension‐free vaginal tape (Abstract number 854). Proceedings of the 41st Annual Meeting of the International Continence Society (ICS), 2011 Aug 29‐Sept 2, Glasgow, Scotland. 2011. [Sricont42239]
Bruschini 2005 {published data only}
- Bruschini H, Nunes R, Truzzi JC, Simonetti R, Cury J, Otiz V, et al. Low cost polypropylene sling procedure for correction of stress urinary incontinence: a possible solution for developing countries? (Abstract number 360). Proceedings of the International Continence Society (ICS), 35th Annual Meeting, 2005 Aug 28‐Sep 2, Montreal, Canada. 2005. [Srincont21055]
Chen 2008 {published data only}
- Chen HY, Ho M, Hung YC, Huang LC. Analysis of risk factors associated with vaginal erosion after synthetic sling procedures for stress urinary incontinence. International Urogynecology Journal 2008;19(1):117‐21. [srincont27217] [DOI] [PubMed] [Google Scholar]
Chen 2011 {published data only}
- Chen X, Jiang M, Tong X, Li H, Qiu J, Shao L, et al. A modified inexpensive transobturator vaginal tape inside‐out procedure versus tension‐free vaginal tape for the treatment of SUI: a prospective comparative study. Archives of Gynecology and Obstetrics 2011;284(6):1461‐6. [srincont59743] [DOI] [PubMed] [Google Scholar]
Chene 2009 {published data only}
- Chene G, Tardieu A‐S, Cotte B, Chauleur C, Savary D, Krief M, et al. [Health‐related quality of life in women operated on by surgical anti‐incontinence procedures: comparison of three techniques]. Gynecologie Obstetrique Fertilite 2009;36(1):3‐10. [srincont40235] [DOI] [PubMed] [Google Scholar]
Chong 2003 {published data only}
- Chong C, Bane A, Corstiaans A. Intraoperative division of tensionless vaginal tape (TVT) ‐ prospective randomized trial (Abstract). Singapore Journal of Obstetrics & Gynaecology 2003;34(Suppl 1):55. [17187] [Google Scholar]
Corcos 2001 {published data only}
- Corcos J, Collet JP, Shapiro S, Schick E, Macramallah E, Tessier J, et al. Surgery vs collagen for the treatment of female stress urinary incontinence (SUI): results of a multicentric randomized trial (Abstract). Journal of Urology 2001;165(5 Suppl):198. [12912] [Google Scholar]
Corcos 2005 {published data only}
- Corcos J, Collet JP, Shapiro S, Herschorn S, Radomski SB, Schick E, et al. Multicenter randomized clinical trial comparing surgery and collagen injections for treatment of female stress urinary incontinence. Urology 2005;65(5):898‐904. [20346] [DOI] [PubMed] [Google Scholar]
Cotte 2006 {published data only}
- Cotte B, Dumousset E, Boda C, Mansoor A. Comparison of transobturator tape (TO) and tension free vaginal tape (TVT) using perineal ultrasound. Gynecologie, Obstetrique & Fertilite 2006;34:298‐303. [DOI] [PubMed] [Google Scholar]
Courtney‐Watson 2002 {published data only}
- Courtney‐Watson C. Comparison of two surgical methods for curing stress incontinence (recurrent). Data on file 2002. [16382]
Debodinance 2006 {published data only}
- Debodinance P. Transobturator urethral sling for surgical correction of female urinary incontinence: outside‐in (Monarc) versus inside‐out (TVT‐O). Are both ways safe?. Journal de Gynecologie Obstetrique et Biologie de la Reproduction 2006;35(6):571‐7. [DOI] [PubMed] [Google Scholar]
Dietz 2005 {published data only}
- Dietz HP, Barry C, Lim Y, Rane A. 2D and 3D ultrasound imaging of suburethral slings: data from the 'suspend' randomized controlled trial (Abstract number 674). Proceedings of the International Continence Society (34th Annual Meeting) and the International Urogynecological Association, 2004 Aug 25‐27, Paris. 2004. [19084]
- Dietz HP, Barry C, Lim YN, Rane A. Two‐dimensional and three‐dimensional ultrasound imaging of suburethral slings. Ultrasound in Obstetrics & Gynecology 2005;26(2):175‐9. [20763] [DOI] [PubMed] [Google Scholar]
Du 2008 {published data only}
- Du G‐H, Chen Z, HU WF, Zhang C‐H, Zhang J‐Y, Zhu Z‐Q, et al. [A multicenter study of mid urethral sling procedures in treatment of female stress urinary incontinence] [Chinese]. Chung‐Hua Wai Ko Tsa Chih [Chinese Journal of Surgery] 2008;46(20):1529‐32. [srincont29216] [PubMed] [Google Scholar]
Falconer 2001 {published data only}
- Falconer C, Rosblad P‐G. A randomized comparative study between local and low spinal anesthesia for tension‐free vaginal tape operation. International Urogynecology Journal 2001;12(Suppl 3):S21. [15455] [Google Scholar]
Fischer 2005 {published data only}
- Fischer A, Fink T, Zachmann S, Eickenbusch U. Comparison of retropubic and outside‐in transoburator sling systems for the cure of female genuine stress urinary incontinence. European Urology 2005;48(5):799‐804. [DOI] [PubMed] [Google Scholar]
Foote 2012 {published data only}
- Foote A. A randomised trial comparing two vaginal prolene sling surgeries for female urinary incontinence. www.anzctr.org (accessed 19 Sep 2012) 2012. [ACTRN12612000314820 ; srincont45458]
Goldberg 2001 {published data only}
- Goldberg RP, Koduri S, Lobel RW, Culligan PJ, Tomezsko JE, Winkler HA, et al. Long‐term effects of three different anti‐incontinence procedures on the posterior compartment (Abstract number 243). Proceedings of the 31st Annual Meeting of the International Continence Society (ICS), 2001 Sept 18‐21, Seoul, Korea. 2001. [14471]
Gopinath 2013 {published data only}
- Gopinath D, Smith AR, Holland C, Reid FM. Why don't women participate? A qualitative study on non‐participation in a surgical randomised controlled trial. International Urogynecology Journal 2013;24(6):969‐75. [srincont48114] [DOI] [PubMed] [Google Scholar]
Harmanli 2011 {published data only}
- Harmanli O, Boyer R, Metz S, Jones K, Tunitsky E. Double‐blinded randomized trial of preoperative antibiotics in midurethral sling procedures (Abstract number 1184). Proceedings of the Joint Meeting of the International Continence Society (ICS) and the International Urogynecological Association, 2010 Aug 23‐27, Toronto, Canada. 2010. [Srincont 40210]
- Harmanli O, Boyer RL, Metz S, Tunitsky E, Jones KA. Double‐blinded randomized trial of preoperative antibiotics in midurethral sling procedures and review of the literature. International Urogynecology Journal 2011;22(10):1249‐53. [PUBMED: 21789661] [DOI] [PubMed] [Google Scholar]
Jackson 2013 {published data only}
- Jackson D, Higgins E, Bracken J, Yandell PM, Shull B, Foster RT Sr. Antibiotic prophylaxis for urinary tract infection after midurethral sling: a randomized controlled trial. Female Pelvic Medicine & Reconstructive Surgery 2013;19(3):137‐41. [CARPET; NCT00734968; srincont48136] [DOI] [PubMed] [Google Scholar]
Jeon 2008 {published data only}
- Jeon MJ, Chung da J, Park JH, Kim SK, Kim JW, Bai SW. Surgical therapeutic index of tension‐free vaginal tape and transobturator tape for stress urinary incontinence. Gynecologic and Obstetric Investigation 2008;65(1):41‐6. [srincont26783] [DOI] [PubMed] [Google Scholar]
Jones 2010 {published data only}
- Jones R, Abrams P, Hilton P, Ward K, Drake M. Risk of tape‐related complications after TVT is at least 4%. Neurourology and Urodynamics 2010;29(1):40‐1. [srincont39866; PUBMED: 20025030] [DOI] [PubMed] [Google Scholar]
Karagkounis 2007 {published data only}
- Karagkounis SC, Pantelis A, Parashou GC, Paplomata E, Madenis N, Chrisanthoupoulos C, et al. Stress urinary incontinence: TVT OB system versus Duloxetine‐HCL and the winner is? (Abstract number 005). International Urogynecology Journal 2007;18(Suppl 1):S3‐4. [Google Scholar]
Kim 2005a {published data only}
- Kim YB, Jeon YT, Jee BC, Park KH, Suh CS. The efficacy and safety of tension‐free vaginal tape and transobturator suburethral tape in the surgical treatment of stress urinary incontinence (Abstract number 237). International Urogynecology Journal 2005;16(Suppl 2):S87. [srincont27308] [Google Scholar]
Kim 2006 {published data only}
- Kim WT, Kim KT, Kim JW, Choe JH, Lee JS, Seo JT. [Comparative study of the tension‐free vaginal tape (TVT) procedure and the suprapubic arc sling (SPARC) procedure for treating female stress urinary incontinence: A 1‐year follow‐up]. Korean Journal of Urology 2006;47(4):397‐401. [srincont27044] [Google Scholar]
Kulseng‐Hanssen 2004 {published data only}
- Kulseng‐Hanssen S. Do preoperative objective and subjective findings predict the outcome of TVT operations in females complaining of mixed urinary incontinence? (Abstract number 310). Proceedings of the International Continence Society (34th Annual Meeting) and the International Urogynecological Association, 2004, Aug 23‐27, Paris. 2004. [19057]
Kulseng‐Hanssen 2007 {published data only}
- Kulseng‐Hanssen S, Husby H, Schiotz HA. The tension free vaginal tape operation for women with mixed incontinence: do preoperative variables predict the outcome?. Neurourology and Urodynamics 2007;26:115‐21. [DOI] [PubMed] [Google Scholar]
Kwon 2002 {published data only}
- Kwon C, Goldberg R, Sanjay G, Sumana K, Krotz S, Sand P. Protective effect of transvaginal slings on recurrent anterior vaginal wall prolapse after pelvic reconstructive surgery (Abstract). Neurourology and Urodynamics 2002;21(4):321‐2. [14540] [Google Scholar]
Liapis 2007 {published data only}
- Liapis A, Bakas P, Creatsas G. Assessment of TVT efficacy in the management of patients with genuine stress incontinence with the use of epidural vs intravenous anesthesia. International Urogynecology Journal 2007;18:1197–200. [DOI] [PubMed] [Google Scholar]
Liapis 2010 {published data only}
- Liapis A, Bakas P, Georgantopoulou C, Creatsas G. The use of oestradiol therapy in postmenopausal women after TVT‐O anti‐incontinence surgery. Maturitas 2010;66(1):101‐6. [srincont39604] [DOI] [PubMed] [Google Scholar]
Markland 2007 {published data only}
- Kirby AC, Nager CW, Litman HJ, FitzGerald MP, Kraus S, Norton P, et al. Preoperative voiding detrusor pressures and stress incontinence surgery outcomes (Abstract number 38). Neurourology and Urodynamics 2010;29(6):860‐1. [Srincont 40122] [Google Scholar]
- Kirby AC, Nager CW, Litman HJ, FitzGerald MP, Kraus S, Norton P, et al. Preoperative voiding detrusor pressures do not predict stress incontinence surgery outcomes. International urogynecology journal 2011;22(6):657‐63. [PUBMED: 21153471] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markland AD, Kraus SR, Richter HE, Nager CW, Kenton K, Kerr L, et al. Prevalence and risk factors of fecal incontinence in women undergoing stress incontinence surgery. American Journal of Obstetrics and Gynecology 2007;197(6):662.e1‐7. [PUBMED: 18060972] [DOI] [PubMed] [Google Scholar]
McClure 2006 {published data only}
- McClure LA, Brown MB. A likelihood approach to analyzing clinical trial data when treatments favour different outcomes. Contemporary Clinical Trials 2006;27(4):340‐52. [22391] [DOI] [PubMed] [Google Scholar]
Meschia 2002 {published data only}
- Meschia M, Pifarotti P, Gattei U, Ronchetti A, Stoppelli S, Lampugnani F. TVT and prolapse repair for treatment of occult stress urinary incontinence: a randomized study (Abstract). Proceedings of the 32nd Annual Meeting of the International Continence Society (ICS), 2002 Aug 28‐30, Heidelberg, Germany. 2002:198‐9. [14518]
Osman 2003 {published data only}
- Osman T. Stress incontinence surgery for patients presenting with mixed incontinence and a normal cystometrogram. BJU International 2003;92(9):964‐8. [16660] [DOI] [PubMed] [Google Scholar]
Pace 2008 {published data only}
- Pace G, Vicentini C. Female sexual function evaluation of the tension‐free vaginal tape (TVT) and transobturator suburethral tape (TOT) incontinence surgery: results of a prospective study. Journal of Sexual Medicine 2008;5(2):387‐93. [srincont27116] [DOI] [PubMed] [Google Scholar]
Padilla‐Fernández 2013 {published data only}
- Padilla‐Fernandez B, Garcia‐Cenador MB, Collazos‐Robles RE, Garcia‐Sanchez MH, Garcia‐Sanchez A, Lorenzo‐Gomez MF. Transobturator tape with whipstitch edges for urinary incontinence allows postoperative adjustment and improves outcomes (Abstract number 606). Proceedings of the 43rd Annual Meeting of the International Continence Society (ICS), 2013 Aug 26‐30, Barcelona, Spain. 2013. [srincont60035]
Park 2008 {published data only}
- Park HK, Lee HW, Kim HG, Lee KS. Does tape tension have an effect on the success rate of transobturator tape surgery? (Abstract number 122). Neurourology and Urodynamics 2008;27(7):714‐5. [srincont31858] [Google Scholar]
Sabadell 2008 {published data only}
- Sabadell J, Luis Poza J, Sanchez‐Iglesias JL, Martinez‐Gomez X, Pla F, Xercavins J. [Comparison of the outside‐in and inside‐out routes in the use of transobturator tapes for the treatment of stress urinary incontinence]. Progresos en Obstetricia y Ginecologia 2008;51(8):464‐70. [srincont40241] [Google Scholar]
Schierlitz 2007 {published data only}
- Schierlitz L, Dwyer P, Rosamilia A, Murray C, Thomas E, Taylor N, et al. A prospective randomised controlled study comparing vaginal prolapse repair with and without tension free vaginal tape (TVT) in women with severe pelvic organ prolapse and occult stress incontinence (Abstract number 114). Neurourology and Urodynamics 2007;26(5):743‐4. [23759] [Google Scholar]
Schostak 2001 {published data only}
- Schostak M, Gottfried HW, Heicappell R, Muller M, Sauter T, Steiner U, et al. Minimally invasive bone anchoring for female stress incontinence: a treatment with moderate results (Abstract). European Urology 2001;39(Suppl 5):3. [16374] [Google Scholar]
Seo 2007 {published data only}
- Seo JH, Lee JW, Kim DY, Lee YG, Seo YJ, Kwon TG, et al. Treatment of obstructive voiding dysfunction after transobturator sling surgery: results of multicenter study (Abstract number 287). Proceedings of the 37th Annual Meeting of the International Continence Society (ICS), 2007 Aug 20‐24, Rotterdam, The Netherlands. 2007. [23762]
Shin 2010 {published data only}
- Shin JH, Lim JS, Song KH, Sul CK, Na YG. Prospective study comparing the suprapubic arc (Sparc) procedure and the transobturator (Monarc) procedure for treating female stress urinary incontinence. LUTS: Lower Urinary Tract Symptoms 2010;2(1):37‐42. [srincont59687] [DOI] [PubMed] [Google Scholar]
Sivaslioglu 2007 {published data only}
- Sivaslioglu AA, Unlubilgin E, Dolen I, Kaplan M. The comparison of tissue fixation system (TFS) with transobturator tape (TOT) in the treatment of stress urinary incontinence (Abstract no. 061). International Urogynecology Journal 2007;18(Suppl 1):S36. [Google Scholar]
Surkont 2007 {published data only}
- Surkont G, Wlazlak E, Kazimierak W, Dunicz‐Sokolowska A, Suzin J. The influence of SUI operative treatment with use of IVS tape on quality of life. Ginekologia Polska 2007;78(5):381‐3. [PubMed] [Google Scholar]
Takeyama 2006 {published data only}
- Takeyama M, Fukumoto Y, Noma M, Yamamoto K, Yamanaka M, Uesaka Y. A prospective study about trans‐obturator‐tape (TOT) procedures with the tape from the Gynecare TVT device and a C‐shape tunneller ‐ comparison between outside‐in and inside‐out procedures (Abstract number 489). Proceedings of the 36th Annual Meeting of the International Continence Society (ICS), 2006 Nov 27‐Dec 1, Christchurch, New Zealand. 2006. [23751]
Tantanasis 2013 {published data only}
- Tantanasis T, Daniilidis A, Pantelis A, Chatzis P, Vrachnis N. Minimally invasive techniques for female stress urinary incontinence, how, why, when. Archives of Gynecology and Obstetrics 2013;288(5):995‐1001. [srincont49470] [DOI] [PubMed] [Google Scholar]
Tincello 2009 {published data only}
- Bakali E, Pitchforth E, Tincello DG, Kenyon S, Slack M, Toozs‐Hobson P, et al. Clinicians' views on the feasibility of surgical randomized trials in urogynecology: results of a questionnaire survey. Neurourology and Urodynamics 2011;30(1):69‐74. [PUBMED: 20658541] [DOI] [PubMed] [Google Scholar]
- Jackson CJ, Dixon‐Woods M, Eborall H, Kenyon S, Toozs‐Hobson P, Tincello DG. Women's views and experiences of a patient preference trial in surgery: a qualitative study of the CARPET1 trial. Clinical Trials 2010;7(6):696‐704. [CARPET1; ISRCTN34759911; srincont40885] [DOI] [PubMed] [Google Scholar]
- Tincello DG, Kenyon S, Slack M, Toozs‐Hobson P, Mayne C, Jones D, et al. Colposuspension or TVT with anterior repair for urinary incontinence and prolapse: results of and lessons from a pilot randomised patient‐preference study (CARPET 1). BJOG : an international journal of obstetrics and gynaecology 2009;116(13):1809‐14. [PUBMED: 19781044] [DOI] [PubMed] [Google Scholar]
Tinelli 2007 {published data only}
- Tinelli A, Malvasi A, D'Anna L, Tinelli R, Perrone A, Tinelli FG. Presurgical promestriene therapy in postmenopausal women with stress urinary incontinence. Gynecological Endocrinology 2007;23(8):445‐50. [srincont23949] [DOI] [PubMed] [Google Scholar]
Trezza 2001 {published data only}
- Trezza G, Rotondi M, Palmisano B, Iervolino P. Uterovaginal prolapse and occult urinary incontinence: a prospective randomized study on the necessity to associate reconstructive surgery and antiincontinence procedure. [Italian]. Urogynaecologia International Journal 2001;15(1 Suppl):152‐4. [13713] [Google Scholar]
Wang 2001 {published data only}
- Wang AC, Chen MC. Randomized comparison of local versus epidural anesthesia for tension‐free vaginal tape operation. Journal of Urology 2001;165(4):1177‐80. [12424] [PubMed] [Google Scholar]
Wei 2012 {published data only}
- Wei J. A midurethral sling prevents incontinence among women undergoing vaginal prolapse repair ‐ the OPUS trial. Neurourology and Urodynamics 2011;30(6):809‐10. [SRINCONT 42165] [Google Scholar]
- Wei J, Nygaard I, Richter H, Brown M, Barber M, Xiao Xu, et al. Outcomes following vaginal prolapse repair and mid urethral sling (OPUS) trial‐‐design and methods. Clinical Trials 2009;6(2):162‐71. [srincont31120] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wei JT, Nygaard I, Richter HE, Nager CW, Barber MD, Kenton K, et al. A midurethral sling to reduce incontinence after vaginal prolapse repair. The New England Journal of Medicine 2012;366(25):2358‐67. [PUBMED: 22716974] [DOI] [PMC free article] [PubMed] [Google Scholar]
Williams 2003 {published data only}
- Williams JG, Cheung WY, Cohen DR, Hutchings HA, Longo MF, Russell IT. Can randomised trials rely on existing electronic data? A feasibility study to explore the value of routine data in health technology assessment. Health Technology Assessment (Winchester, England) 2003;7(26):1‐117. [16488] [DOI] [PubMed] [Google Scholar]
Yang 2012 {published data only}
- Yang X, Jiang M, Chen X, Tong X, Li H, Qiu J, et al. TVT‐O vs. TVT for the treatment of SUI: a non‐inferiority study. International Urogynecology Journal 2012;23(1):99‐104. [srincont44553] [DOI] [PubMed] [Google Scholar]
Yoo 2007 {published data only}
- Yoo ES, Jung HC, Shin HS, Seo JH, Seo YJ. Comparison of the two different approaches for the treatment of female stress urinary incontinence (Abstract number 282). Proceedings of the 37th Annual Meeting of the International Continence Society (ICS), 2007 Aug 20‐24, Rotterdam, The Netherlands. 2007. [23760]
Yoon 2011 {published data only}
- Yoon H, Lee DH, Kim YJ. Early results of comparison of Contasure‐needleless (trademark) and TOT outside‐in midurethral slings (Abstract number 852). Proceedings of the 41st Annual Meeting of the International Continence Society (ICS), 2011 Aug 29‐Sept 2, Glasgow, Scotland. 2011.
Zaccardi 2010 {published data only}
- Zaccardi JE, Wilson L, Mokrzycki ML. The effect of pelvic floor re‐education on comfort in women having surgery for stress urinary incontinence. Urologic Nursing 2010;30(2):137‐46, 148. [PUBMED: 20469573] [PubMed] [Google Scholar]
Zullo 2005 {published data only}
- Zullo MA, Plotti F, Calcagno M, Palaia I, Muzii L, Manci N, et al. Vaginal estrogen therapy and overactive bladder symptoms in postmenopausal patients after a tension‐free vaginal tape procedure: a randomized clinical trial. Menopause 2005;12(4):421‐7. [20805] [DOI] [PubMed] [Google Scholar]
References to ongoing studies
Cavkaytar 2013 {published data only}
- Cavkaytar S, Aksakal SO, Kokanali MK, Topcu HO, Doganay M. Prospective randomized study comparing TVT and TOT in female stress urinary incontinence with no intrinsic sphincter deficiency. http://clinicaltrials.gov/show/NCT01903590 2013. [NCT01903590; srincont49363]
Sung 2013 {published data only}
- Sung VW, Wallace D. Effects of Surgical Treatment Enhanced with Exercise for Mixed Urinary Incontinence (ESTEEM). http://clinicaltrials.gov/show/NCT01959347 2013. [ESTEEM; NCT01959347; srincont49234]
Additional references
Abbott 2014
- Abbott S, Unger CA, Evans JM, Jallad K, Mishra K, Karram MM, et al. Evaluation and management of complications from synthetic mesh after pelvic reconstructive surgery: a multicenter study. American Hournal of Obstetrics and Gynecology 2014;210(2):163.e1‐8. [PUBMED: 24126300] [DOI] [PubMed] [Google Scholar]
Aigmueller 2011
- Aigmueller T, Trutnovsky G, Tamussino K, Kargl J, Wittmann A, Surtov M, et al. Ten‐year follow‐up after the tension‐free vaginal tape procedure. American Journal of Obstetrics and Gynecology 2011;205(5):496.e1‐5. [PUBMED: 21944223] [DOI] [PubMed] [Google Scholar]
Alcalay 1995
- Alcalay M, Monga A, Stanton SL. Burch colposuspension: a 10‐20 year follow up. British Journal of Obstetrics and Gynaecology 1995;102(9):740‐5. [PUBMED: 7547767] [DOI] [PubMed] [Google Scholar]
Alhasso 2005
- Alhasso A, Glazener CMA, Pickard R, N'dow J. Adrenergic drugs for urinary incontinence in adults. Cochrane Database of Systematic Reviews 2005, Issue 3. [DOI: 10.1002/14651858.CD001842.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Amid 1997
- Amid P. Classification of biomaterials and their related complications in abdominal wall hernia surgery. Hernia 1997;1(1):15‐21. [Google Scholar]
Athanasiou 2014
- Athanasiou S, Grigoriadis T, Zacharakis D, Skampardonis N, Lourantou D, Antsaklis A. Seven years of objective and subjective outcomes of transobturator (TVT‐O) vaginal tape: why do tapes fail?. International Urogynecology Journal 2014;25(2):219‐25. [PUBMED: 23892532] [DOI] [PubMed] [Google Scholar]
Ayeleke 2013
- Ayeleke RO, Hay‐Smith EJ, Omar MI. Pelvic floor muscle training added to another active treatment versus the same active treatment alone for urinary incontinence in women. Cochrane Database of Systematic Reviews 2013, Issue 11. [DOI: 10.1002/14651858.CD010551.pub2; PUBMED: 24259154] [DOI] [PubMed] [Google Scholar]
Bezerra 2005
- Bezerra CCB, Bruschini H, Cody JD. Traditional suburethral sling operations for urinary incontinence in women. Cochrane Database of Systematic Reviews 2005, Issue 3. [DOI: 10.1002/14651858.CD001754.pub2] [DOI] [PubMed] [Google Scholar]
Birnbaum 2004
- Birnbaum HG, Leong SA, Oster EF, Kinchen K, Sun P. Cost of stress urinary incontinence: a claims data analysis.. Pharmacoeconomics 2004;22(2):95‐105. [PUBMED: 14731051] [DOI] [PubMed] [Google Scholar]
Blaivas 1988
- Blaivas JG, Olsson CA. Stress‐incontinence ‐ classification and surgical approach. Journal of Urology 1988;139(4):727‐31. [DOI] [PubMed] [Google Scholar]
Botlero 2008
- Botlero R, Urquhart DM, Davis SR, Bell RJ. Prevalence and incidence of urinary incontinence in women: review of the literature and investigation of methodological issues. International Journal of Urology : official journal of the Japanese Urological Association 2008;15(3):230‐4. [PUBMED: 18304218] [DOI] [PubMed] [Google Scholar]
Botlero 2010
- Botlero R, Bell RJ, Urquhart DM, Davis SR. Urinary incontinence is associated with lower psychological general well‐being in community‐dwelling women. Menopause (New York, N.Y.) 2010;17(2):332‐7. [PUBMED: 20216275] [DOI] [PubMed] [Google Scholar]
Boyers 2013
- Boyers D, Kilonzo M, Mostafa A, Abdel‐Fattah M. Comparison of an adjustable anchored single‐incision mini‐sling, Ajust((R)) , with a standard mid‐urethral sling, TVT‐O(TM) : a health economic evaluation. BJU international 2013;112(8):1169‐77. [DOI] [PubMed] [Google Scholar]
Brubaker 2012
- Brubaker L, Richter HE, Norton PA, Albo M, Zyczynski HM, Chai TC, et al. 5‐year continence rates, satisfaction and adverse events of burch urethropexy and fascial sling surgery for urinary incontinence. The Journal of Urology 2012;187(4):1324‐30. [PUBMED: 22341290] [DOI] [PMC free article] [PubMed] [Google Scholar]
Castañeda 2014
- Castañeda E, Sanz‐Granda Á, HidalgoÁ, Meza D, Carreras M, MarquetaJ. Cost Effectiveness analysis of surgical treatment of stress urinary incontinence using single‐incision mini‐slings vs. tension‐free vaginal obturator in Spain. Surgical Research ‐ Open Journal 2014;1(1):17‐24. [DOI: 10.17140/SROJ-1-103; PUBMED: 27201564] [DOI] [PubMed] [Google Scholar]
Chong 2011
- Chong E, Khan A, Anger J. The financial burden of stress urinary incontinence among women in the United States. Current Urology Reports 2011;12(5):358‐62. [DOI: 10.1007/s11934-011-0209-x.] [DOI] [PubMed] [Google Scholar]
Cody 2012
- Cody JD, Jacobs ML, Richardson K, Moehrer B, Hextall A. Oestrogen therapy for urinary incontinence in post‐menopausal women. Cochrane Database of Systematic Reviews 2012, Issue 10. [DOI: 10.1002/14651858.CD001405.pub3; PUBMED: 23076892] [DOI] [PMC free article] [PubMed] [Google Scholar]
Collinet 2008
- Collinet P, Ciofu C, Costa P, Cosson M, Deval B, Grise P, et al. The safety of the inside‐out transobturator approach for transvaginal tape (TVT‐O) treatment in stress urinary incontinence: French registry data on 984 women. International Urogynecology Journal 2008;19(5):711‐5. [DOI] [PubMed] [Google Scholar]
Coyne 2009
- Coyne KS, Sexton CC, Thompson CL, Milsom I, Irwin D, Kopp ZS, et al. The prevalence of lower urinary tract symptoms (LUTS) in the USA, the UK and Sweden: results from the Epidemiology of LUTS (EpiLUTS) study. BJU international 2009;104(3):352‐60. [PUBMED: 19281467] [DOI] [PubMed] [Google Scholar]
de Leval 2003
- Leval J. Novel surgical technique for the treatment of female stress urinary incontinence: transobturator vaginal tape inside‐out. European Urology 2003;44(6):724‐30. [DOI] [PubMed] [Google Scholar]
de Leval 2005
- Leval J, Waltregny D. New surgical technique for treatment of stress urinary incontinence TVT‐Obturator: new developments and results. Surgical Technology International 2005;14:212‐21. [PubMed] [Google Scholar]
Dean 2006
- Dean NM, Ellis G, Wilson PD, Herbison PH. Laparoscopic colposuspension for urinary incontinence in women. Cochrane Database of Systematic Reviews 2006, Issue 3. [DOI: 10.1002/14651858.CD002239.pub2] [DOI] [PubMed] [Google Scholar]
DeLancey 1994
- DeLancey JO. Structural support of the urethra as it relates to stress urinary incontinence: the hammock hypothesis. American Journal of Obstetrics and Gynecology 1994;170(6):1713‐20; discussion 1720‐3. [PUBMED: 8203431] [DOI] [PubMed] [Google Scholar]
Delorme 2001
- Delorme E. [Transobturator urethral suspension: mini‐invasive procedure in the treatment of stress urinary incontinence in women]. Progres en Urologie 2001;11(6):1306‐13. [PubMed] [Google Scholar]
Delorme 2003
- Delorme E, Droupy S, Tayrac R, Delmas V. [Transobturator tape (Uratape). A new minimally invasive method in the treatment of urinary incontinence in women]. Progres en Urologie 2003;13(4):656‐9. [PubMed] [Google Scholar]
Delorme 2004
- Delorme E, Droupy S, Tayrac R, Delmar V. Transobturator tape (Uratape): a new minimally invasive procedure to treat female urinary incontinence. European Urology 2004;45(2):203‐7. [DOI] [PubMed] [Google Scholar]
Dietz 2004
- Dietz HP, Wilson PD. The 'iris effect': how two‐dimensional and three‐dimensional ultrasound can help us understand anti‐incontinence procedures. Ultrasound in Obstetrics & Gynecology 2004;23(3):267‐71. [DOI] [PubMed] [Google Scholar]
Dumoulin 2014
- Dumoulin C, Hay‐Smith EJ, Mac Habee‐Seguin G. Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women. Cochrane Database of Systematic Reviews 2014, Issue 5. [DOI: 10.1002/14651858.CD005654.pub3; PUBMED: 24823491] [DOI] [PubMed] [Google Scholar]
Dyrkorn 2010
- Dyrkorn OA, Kulseng‐Hanssen S, Sandvik L. TVT compared with TVT‐O and TOT: results from the Norwegian National Incontinence Registry. International Urogynecology Journal 2010;21(11):1321‐6. [PUBMED: 20559618] [DOI] [PubMed] [Google Scholar]
Enhorning 1961
- Enhorning G. Simultaneous recording of intravesical and intra‐urethral pressure. A study on urethral closure in normal and stress incontinent women. Acta Chirurgica Scandinavica. Supplementum 1961;Suppl 276:1‐68. [PUBMED: 13696922] [PubMed] [Google Scholar]
FDA 2008
- US Food, Drug Administration (FDA). FDA Public Health Notification: serious complications associated with transvaginal placement of surgical mesh in repair of pelvic organ prolapse and stress urinary incontinence. FDA Public Health Notification (www.fda.gov/MedicalDevices/Safety/AlertsandNotices/ucm262435.htm) 2008. [srincont47910] [DOI] [PubMed]
FDA 2011a
- US Food, Drug Administration (FDA). FDA Safety Communication: UPDATE on serious complications associated with transvaginal placement of surgical mesh for pelvic organ prolapse. FDA Public Health Notification (www.fda.gov/MedicalDevices/Safety/AlertsandNotices/ucm262435.htm) 2011. [srincont47910]
FDA 2011b
- FDA. Urogynecologic Surgical Mesh; Update on the Safety and Effectiveness of Vaginal Placement for Pelvic Organ Prolapse. www.fda.gov/downloads/medicaldevices/safety/alertsandnotices/UCM262760.pdf 2011.
FDA 2013
- FDA. Considerations about surgical mesh for SUI. www.fda.gov/MedicalDevices/ProductsandMedicalProcedures/ImplantsandProsthetics/UroGynSurgicalMesh/ucm345219.htm 2013.
French 2010
- French B, Thomas LH, Leathley MJ, Sutton CJ, Booth J, Brittain K, et al. Combined conservative interventions for urge, stress or mixed incontinence in adults. Cochrane Database of Systematic Reviews 2010, Issue 12. [DOI: 10.1002/14651858.CD008910; CD008910] [DOI] [Google Scholar]
Ghoniem 2005
- Ghoniem GM, Leeuwen JS, Elser DM, Freeman RM, Zhao YD, Yalcin I, et al (Duloxetine/Pelvic Floor Muscle Training Clinical Trial Group). A randomized controlled trial of duloxetine alone, pelvic floor muscle training alone, combined treatment and no active treatment in women with stress urinary incontinence. Journal of Urology 2005;173(5):1453‐4. [DOI] [PubMed] [Google Scholar]
Glazener 2001
- Glazener CMA, Cooper K. Anterior vaginal repair for urinary incontinence in women. Cochrane Database of Systematic Reviews 2001, Issue 1. [DOI: 10.1002/14651858.CD001755] [DOI] [PubMed] [Google Scholar]
Glazener 2004
- Glazener CMA, Cooper K. Bladder neck needle suspension for urinary incontinence in women. Cochrane Database of Systematic Reviews 2004, Issue 2. [DOI: 10.1002/14651858.CD003636.pub2] [DOI] [PubMed] [Google Scholar]
Guyatt 2011a
- Guyatt GH, Oxman AD, Schunemann HJ, Tugwell P, Knottnerus A. GRADE guidelines: a new series of articles in the Journal of Clinical Epidemiology. Journal of Clinical Epidemiology 2011;64(4):380‐2. [DOI] [PubMed] [Google Scholar]
Guyatt 2011b
- Guyatt GH, Oxman AD, Sultan S, Glasziou P, Akl EA, Alonso‐Coello P, et al. GRADE guidelines: 9. Rating up the quality of evidence. Journal of Clinical Epidemiology 2011;64(12):1311‐6. [DOI] [PubMed] [Google Scholar]
Guyatt 2013a
- Guyatt GH, Thorlund K, Oxman AD, Walter SD, Patrick D, Furukawa TA, et al. GRADE guidelines: 13. Preparing summary of findings tables and evidence profiles‐continuous outcomes. Journal of Clinical Epidemiology 2013;66(2):173‐83. [DOI] [PubMed] [Google Scholar]
Guyatt 2013b
- Guyatt GH, Oxman AD, Santesso N, Helfand M, Vist G, Kunz R, et al. GRADE guidelines: 12. Preparing Summary of Findings tables‐binary outcomes. Journal of Clinical Epidemiology 2013;66(2):158‐72. [DOI] [PubMed] [Google Scholar]
Hannestad 2000
- Hannestad YS, Rortveit G, Sandvik H, Hunskaar S. A community‐based epidemiological survey of female urinary incontinence: the Norwegian EPINCONT study. Epidemiology of Incontinence in the County of Nord‐Trondelag. Journal of Clinical Epidemiology 2000;53(11):1150‐7. [PUBMED: 11106889] [DOI] [PubMed] [Google Scholar]
Hay‐Smith 2011
- Hay‐Smith EJ, Herderschee R, Dumoulin C, Herbison GP. Comparisons of approaches to pelvic floor muscle training for urinary incontinence in women. Cochrane Database of Systematic Reviews 2011, Issue 12. [DOI: 10.1002/14651858.CD009508; PUBMED: 22161451] [DOI] [PubMed] [Google Scholar]
Haylen 2010
- Haylen BT, Ridder D, Freeman RM, Swift SE, Berghmans B, Lee J, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourology and Urodynamics 2010;29(1):4‐20. [PUBMED: 19941278] [DOI] [PubMed] [Google Scholar]
Heinonen 2013
- Heinonen P, Ala‐Nissila S, Raty R, Laurikainen E, Kiilholma P. Objective cure rates and patient satisfaction after the transobturator tape procedure during 6.5‐year follow‐up. Journal of Minimally Invasive Gynecology 2013;20(1):73‐8. [PUBMED: 23312245] [DOI] [PubMed] [Google Scholar]
Herbison 2013
- Herbison GP, Dean N. Weighted vaginal cones for urinary incontinence. Cochrane Database of Systematic Reviews 2013, Issue 7. [DOI: 10.1002/14651858.CD002114.pub2; PUBMED: 23836411] [DOI] [PMC free article] [PubMed] [Google Scholar]
Herderschee 2011
- Herderschee R, Hay‐Smith EJ, Herbison GP, Roovers JP, Heineman MJ. Feedback or biofeedback to augment pelvic floor muscle training for urinary incontinence in women. Cochrane Database of Systematic Reviews 2011, Issue 7. [DOI: 10.1002/14651858.CD009252; PUBMED: 21735442] [DOI] [PubMed] [Google Scholar]
Higgins 2003
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analyses. BMJ 2003;327(7414):557‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Hunskaar 2002
- Hunskaar S, Burgio K, Diokno AC, Herzog AR, Hjalmas K, Lapitan MC. Epidemiology and natural history of urinary incontinence (UI). Incontinence: 2nd International Consultation on Incontinence. Recommendations of the International Scientific Committee: the evaluation and treatment of urinary incontinence. 2001 Jul 1‐3, Paris. Plymouth, UK, 2002.
Imamura 2010
- Imamura M, Williams K, Wells M, McGrother C. Lifestyle interventions for the treatment of urinary incontinence in adults. Cochrane Database of Systematic Reviews 2010, Issue 9. [DOI: 10.1002/14651858.CD003505.pub4; CD003505] [DOI] [PMC free article] [PubMed] [Google Scholar]
Irwin 2006
- Irwin DE, Milsom I, Hunskaar S, Reilly K, Kopp Z, Herschorn S, et al. Population‐based survey of urinary incontinence, overactive bladder, and other lower urinary tract symptoms in five countries: results of the EPIC study. European Urology 2006;50(6):1306‐14; discussion 1314‐5. [PUBMED: 17049716] [DOI] [PubMed] [Google Scholar]
Jackson 1996
- Jackson S, Donovan J, Brookes S, Eckford S, Swithinbank L, Abrams P. The Bristol Female Lower Urinary Tract Symptoms questionnaire: development and psychometric testing. British Journal of Urology 1996;77(6):805‐12. [DOI] [PubMed] [Google Scholar]
Kilonzo 2004
- Kilonzo M, Vale L, Stearns S, Grant A, Cody J, Glazener C, et al. Cost effectiveness of tension‐free vaginal tape for the surgical management of female stress incontinence. International Journal of Technology Assessment in Health Care 2004;20(4):455‐63. [DOI] [PubMed] [Google Scholar]
Kirchin 2012
- Kirchin V, Page T, Keegan PE, Atiemo K, Cody JD, McClinton S. Urethral injection therapy for urinary incontinence in women. Cochrane Database of Systematic Reviews 2012, Issue 2. [DOI: 10.1002/14651858.CD003881.pub3; PUBMED: 22336797] [DOI] [PubMed] [Google Scholar]
Kjolhede 2005
- Kjolhede P. Long‐term efficacy of Burch colposuspension: a 14‐year follow‐up study. Acta Obstetricia et Gynecologica Scandinavica 2005;84(8):767‐72. [PUBMED: 16026403] [DOI] [PubMed] [Google Scholar]
Koops 2005
- Schraffordt Koops SE, Bisseling TM, Heintz AP, Vervest HAM. Prospective analysis of complications of tension‐free vaginal tape from the Netherlands Tension‐free Vaginal Tape study. American Journal of Obstetrics and Gynecology 2005;193(1):45‐52. [DOI] [PubMed] [Google Scholar]
Kunkle 2015
- Kunkle C, Hallock J, Hu X, Blomquist J, Thung S, Werner E. Cost utility analysis of urethral bulking agents versus midurethral sling in stress urinary incontinence. Female Pelvic Medicine & Reconstructive Surgery 2015;21(3):154‐9. [DOI] [PubMed] [Google Scholar]
Kuuva 2002
- Kuuva N, Nilsson CG. A nationwide analysis of complications associated with the tension‐free vaginal tape (TVT) procedure. Acta Obstetricia et Gynecologica Scandinavica 2002;81(1):72‐7. [DOI: 10.1034/j.1600-0412.2002.810113.x] [DOI] [PubMed] [Google Scholar]
Langendam 2013
- Langendam MW, Akl EA, Dahm P, Glasziou P, Guyatt G, Schunemann HJ. Assessing and presenting summaries of evidence in Cochrane Reviews. Systematic Reviews 2013;2:81. [PUBMED: 24059250] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lapitan 2012
- Lapitan MCM, Cody JD. Open retropubic colposuspension for urinary incontinence in women. Cochrane Database of Systematic Reviews 2012, Issue 6. [DOI: 10.1002/14651858.CD002912.pub5; PUBMED: 22696331] [DOI] [PubMed] [Google Scholar]
Lier 2011
- Lier D, Ross S, Tang S, Robert M, Jacobs P, Calgary Women's Pelvic Health Research Group. Trans‐obturator tape compared with tension‐free vaginal tape in the surgical treatment of stress urinary incontinence: a cost utility analysis. BJOG 2011;118(5):550‐6. [sr‐incont41520] [DOI] [PubMed] [Google Scholar]
Lier 2016
- Lier D, Robert M, Tang S, Ross S. Surgical treatment of stress urinary incontinence–trans‐obturator tape compared with tension‐free vaginal tape–5‐year follow up: an economic evaluation. BJOG: An International Journal of Obstetrics & Gynaecology 2016 Aug 10 [Epub ahead of print]. [DOI: 10.1111/1471-0528.14227] [DOI] [PubMed]
Lipp 2011
- Lipp A, Shaw C, Glavind K. Mechanical devices for urinary incontinence in women. Cochrane Database of Systematic Reviews 2011, Issue 7. [DOI: 10.1002/14651858.CD001756.pub5; PUBMED: 21735385] [DOI] [PubMed] [Google Scholar]
Mariappan 2005
- Mariappan P, Ballantyne Z, N'Dow JMO, Alhasso AA. Serotonin and noradrenaline reuptake inhibitors (SNRI) for stress urinary incontinence in adults. Cochrane Database of Systematic Reviews 2005, Issue 3. [DOI: 10.1002/14651858.CD004742.pub2] [DOI] [PubMed] [Google Scholar]
McGuire 1993
- McGuire EJ, Fitzpatrick CC, Wan J, Bloom D, Sanvordenker J, Ritchey M, et al. Clinical assessment of urethral sphincter function. Journal of Urology 1993;150(5 Pt 1):1452‐4. [PUBMED: 8411422] [DOI] [PubMed] [Google Scholar]
MHRA 2012
- Mahon J, Cikalo M, Varley D, Glanville J, York Health Economics Consortium. Summaries of the safety/adverse effects of vaginal tapes/slings/meshes for stress urinary incontinence and prolapse. Final report. November 2012 [report]. London: MHRA, Medicines and Healthcare Products Regulatory Agency, Department of Health, 2012. Available at: https://www.mhra.gov.uk/home/groups/comms‐ic/documents/websiteresources/con205383.pdf (accessed 21 May 2015). [Google Scholar]
MHRA 2014
- Medicines and Healthcare Products Regulatory Agency (MHRA). A summary of the evidence on the benefits and risks of vaginal mesh implants [report]. London: Medicines and Healthcare Products Regulatory Agency (MHRA), 28 October 2014. Document available at: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/402162/Summary_of_the_evidence_on_the_benefits_and_risks_of_vaginal_mesh_implants.pdf. Relevant MHRA webpage: https://www.gov.uk/government/publications/vaginal‐mesh‐implants‐summary‐of‐benefits‐and‐risks. [Google Scholar]
Milsom 2009
- Milsom I, Altman D, Lapitan MC, Nelson R, Sillen U, Thom D. Epidemiology of urinary incontinence (UI) anal incontinence (AI) and pelvic organ prolapse (POP). Incontinence: 4th International Consultation on Incontinence (ICI). Recommendations of the International Scientific Committee: evaluation and treatment of urinary incontinence, pelvic organ prolapse and faecal incontinence, 2008 Jul 5‐8, Paris, France. Plymouth, UK: Health Publication Ltd, 2008.
Moher 2001
- Moher D, Schulz KF, Altman DG. The CONSORT statement: revised recommendations for improving the quality of reports of parallel group randomized trials. BMC Medical Research Methodology 2001;1:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mostafa 2012
- Mostafa A, Agur W, Abdel‐All M, Guerrero K, Lim C, Allam M, et al. A multicentre prospective randomised study of single‐incision mini‐sling (Ajust) versus tension‐free vaginal tape‐obturator (TVT‐O) in the management of female stress urinary incontinence: pain profile and short‐term outcomes. European Journal of Obstetrics & Gynecology and Reproductive Biology 2012;165(1):115‐21. [DOI] [PubMed] [Google Scholar]
Nambiar 2014
Nilsson 2013
- Nilsson CG, Palva K, Aarnio R, Morcos E, Falconer C. Seventeen years' follow‐up of the tension‐free vaginal tape procedure for female stress urinary incontinence. International Urogynecology Journal 2013;24(8):1265‐9. [PUBMED: 23563892] [DOI] [PubMed] [Google Scholar]
O'Donnell 1994
- O'Donnell P. Goals of therapy and mechanisms of urethral incontinence. In: McGuire EJ, Kursh ED editor(s). Female Urology. 1st Edition. Philadelphia, Pensylvania, USA: J B Lippincott Company, 1994:175‐201. [Google Scholar]
Papanicolaou 2005
- Papanicolaou S, Pons ME, Hampel C, Monz B, Quail D, Schulenburg MG, et al. Medical resource utilisation and cost of care for women seeking treatment for urinary incontinence in an outpatient setting: examples from three countries participating in the PURE study. Maturitas 2005;52(Supplement 2):35‐47. [DOI] [PubMed] [Google Scholar]
Petros 1990
- Petros PE, Ulmsten UI. An integral theory of female urinary incontinence. Experimental and clinical considerations. Acta Obstetricia et Gynecologica Scandinavica. Supplement 1990;153:7‐31. [PUBMED: 2093278] [DOI] [PubMed] [Google Scholar]
Petros 1993
- Petros PE, Ulmsten UI. An integral theory and its method for the diagnosis and management of female urinary incontinence. Scandinavian Journal of Urology and Nephrology. Supplementum 1993;153:1‐93. [PUBMED: 8108659] [PubMed] [Google Scholar]
Reference Manager 2012 [Computer program]
- Thomson Reuters. Reference Manager Professional Edition Version 12. New York: Thomson Reuters, 2012.
Rehman 2011
- Rehman H, Bezerra CC, Bruschini H, Cody JD. Traditional suburethral sling operations for urinary incontinence in women. Cochrane Database of Systematic Reviews 2011, Issue 1. [DOI: 10.1002/14651858.CD001754.pub3; PUBMED: 21249648] [DOI] [PubMed] [Google Scholar]
Rogers 2003
- Rogers RG, Coates KW, Kammerer‐Doak D, Khalsa S, Qualls C. A short form of the Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire (PISQ‐12). International Urogynecology Journal and Pelvic Floor Dysfunction 2003;14(3):164‐8; discussion 168. [PUBMED: 12955337] [DOI] [PubMed] [Google Scholar]
Ross 2009
- Ross S, Robert M, Swaby C, Dederer L, Lier D, Tang S, et al. Randomized trial of trans‐obturator tape versus tension‐free vaginal tape for stress incontinence. Obstetrics and Gynecology 2009;114(6):1287‐94. [DOI: 10.1097/AOG.0b013e3181c2a151; PUBMED: 19935032] [DOI] [PubMed] [Google Scholar]
Salonia 2004
- Salonia A, Zanni G, Nappi RE, Briganti A, Deho F, Fabbri F, et al. Sexual dysfunction is common in women with lower urinary tract symptoms and urinary incontinence: results of a cross‐sectional study. European Urology 2004;45(5):642‐8; discussion 648. [PUBMED: 15082208] [DOI] [PubMed] [Google Scholar]
Schulz 2010
- Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. PLoS medicine 2010;7(3):e1000251. [PUBMED: 20352064] [DOI] [PMC free article] [PubMed] [Google Scholar]
Seklehner 2014
- Seklehner S, Laudano MA, Te AE, Kaplan SA, Chughtai B, Lee RK. A cost‐effectiveness analysis of retropubic midurethral sling versus transobturator midurethral sling for female stress urinary incontinence. Neurourology and Urodynamics 2014;33(8):1186‐92. [DOI: 10.1002/nau.22483] [DOI] [PubMed] [Google Scholar]
Serati 2012
- Serati M, Ghezzi F, Cattoni E, Braga A, Siesto G, Torella M, et al. Tension‐free vaginal tape for the treatment of urodynamic stress incontinence: efficacy and adverse effects at 10‐year follow‐up. European Urology 2012;61(5):939‐46. [PUBMED: 22305110] [DOI] [PubMed] [Google Scholar]
Serati 2013
- Serati M, Bauer R, Cornu JN, Cattoni E, Braga A, Siesto G, et al. TVT‐O for the treatment of pure urodynamic stress incontinence: efficacy, adverse effects, and prognostic factors at 5‐year follow‐up. European Urology 2013;63(5):872‐8. [PUBMED: 23274106] [DOI] [PubMed] [Google Scholar]
Shumaker 1994
- Shumaker SA, Wyman JF, Uebersax JS, McClish D, Fantl JA. Health‐related quality of life measures for women with urinary incontinence: the Incontinence Impact Questionnaire and the Urogenital Distress Inventory. Continence Program in Women (CPW) Research Group. Quality of Life Research 1994;3(5):291‐306. [DOI] [PubMed] [Google Scholar]
Smith 2002
- Smith ARB, Daneshgari F, Dmochowski R, Ghoniem G, Jarvis GJ, Nitti V, et al. Surgical treatment of incontinence in women. In: Abrams P, Cardozo L, Khoury S, Wein A editor(s). Incontinence. 2nd International Consultation on Incontinence, 2001 Jul 1‐3, Paris, France. Plymouth, UK: Health Publication Ltd, 2002:823‐63. [Google Scholar]
Strasberg 2009
- Strasberg SM, Linehan DC, Hawkins WG. The accordion severity grading system of surgical complications. Annals of Surgery 2009;250(2):177‐86. [PUBMED: 19638919] [DOI] [PubMed] [Google Scholar]
Subak 2008
- Subak L, Brubaker, L, Chai T, Creasman J, Diokno A, Goode P, et al. High costs of urinary incontinence among women electing surgery to treat stress incontinence. Obstetrics & Gynecology 2008;111(4):899‐907. [DOI: 10.1097/AOG.0b013e31816a1e12] [DOI] [PMC free article] [PubMed] [Google Scholar]
Svenningsen 2013a
Svenningsen 2013b
- Svenningsen R, Staff AC, Schiotz HA, Western K, Kulseng‐Hanssen S. Long‐term follow‐up of the retropubic tension‐free vaginal tape procedure. International Urogynecology Journal 2013;24(8):1271‐8. [PUBMED: 23417313] [DOI] [PubMed] [Google Scholar]
Tamussino 2001
- Tamussino KF, Engelbert H, Kolle D, Ralph G, Riss PA. Tension‐free vaginal tape operation: results of the Austrian registry. Obstetrics and Gynecology 2001;98(5 (Pt 1)):732‐6. [DOI] [PubMed] [Google Scholar]
Tamussino 2007
- Tamussino K, Hanzal E, Koelle D, Tammaa A, Preyer O, Umek W, et al. Transobturator tapes for stress urinary incontinence: results of the Austrian registry. American Journal of Obstetrics and Gynecology 2007;197(6):634‐5. [DOI] [PubMed] [Google Scholar]
Thom 1998
- Thom DH, Brown JS. Reproductive and hormonal risk factors for urinary incontinence in later life: a review of the clinical and epidemiologic literature. Journal of the American Geriatrics Society 1998;46(11):1411‐7. [PUBMED: 9809764] [DOI] [PubMed] [Google Scholar]
Tincello 2011
- Tincello DG, Botha T, Grier D, Jones P, Subramanian D, Urquhart C, et al. The TVT Worldwide Observational Registry for Long‐Term Data: safety and efficacy of suburethral sling insertion approaches for stress urinary incontinence in women. The Journal of Urology 2011;186(6):2310‐5. [PUBMED: 22014817] [DOI] [PubMed] [Google Scholar]
Turner 2004
- Turner DA, Shaw C, McGrother CW, Dallosso HM, Cooper NJ. The cost of clinically significant urinary storage symptoms for community dwelling adults in the UK. BJU International 2004;93(9):1246‐52. [DOI] [PubMed] [Google Scholar]
Ulmsten 1995a
- Ulmsten U. Intravaginal slingplasty (IVS): an ambulatory surgical procedure for treatment of female urinary incontinence. Scandinavian Journal of Urology and Nephrology 1995;29(1):75‐82. [DOI] [PubMed] [Google Scholar]
Ulmsten 1995b
- Ulmsten U, Petros P. Intravaginal slingplasty (IVS): an ambulatory surgical procedure for treatment of female urinary incontinence. Scandinavian Journal of Urology and Nephrology 1995;29(1):75‐82. [PUBMED: 7618052] [DOI] [PubMed] [Google Scholar]
Ulmsten 1996
- Ulmsten U, Henriksson L, Johnson P, Varhos G. An ambulatory surgical procedure under local anesthesia for treatment of female urinary incontinence. International Urogynecology Journal including Pelvic Floor Dysfunction 1996;7(2):81‐5. [DOI] [PubMed] [Google Scholar]
Van Oyen 2002
- Oyen H, Oyen P. Urinary incontinence in Belgium; prevalence, correlates and psychosocial consequences. Acta Clinica Belgica 2002;57(4):207‐18. [PUBMED: 12462797] [DOI] [PubMed] [Google Scholar]
Wagner 1998
- Wagner T, Hu T. Economic costs of urinary incontinence in 1995. Urology 1998;51(3):355‐61. [DOI] [PubMed] [Google Scholar]
Wallace 2004
- Wallace SA, Roe B, Williams K, Palmer M. Bladder training for urinary incontinence in adults. Cochrane Database of Systematic Reviews 2004, Issue 1. [DOI: 10.1002/14651858.CD001308.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wang 2013
- Wang Y, Zhishun L, Peng W, Zhao J, Liu B. Acupuncture for stress urinary incontinence in adults. Cochrane Database of Systematic Reviews 2013, Issue 7. [DOI: 10.1002/14651858.CD009408.pub2; PUBMED: 23818069] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ward 2008
- Ward KL, Hilton P. Tension‐free vaginal tape versus colposuspension for primary urodynamic stress incontinence: 5‐year follow up. BJOG : an international journal of obstetrics and gynaecology 2008;115(2):226‐33. [PUBMED: 17970791] [DOI] [PubMed] [Google Scholar]
Ware 1993
- Ware JE, Snow KK, Kosinski M, Gandek B. SF‐36 Health survey manual and interpretation guide. Boston (MA): The Health Institute, New England Medical Centre, 1993. [Google Scholar]
Wetle 1995
- Wetle T, Scherr P, Branch LG, Resnick NM, Harris T, Evans D, et al. Difficulty with holding urine among older persons in a geographically defined community: prevalence and correlates. Journal of the American Geriatrics Society 1995;43(4):349‐55. [PUBMED: 7706622] [DOI] [PubMed] [Google Scholar]
Wilson 1996
- Wilson PD, Herbison RM, Herbison GP. Obstetric practice and the prevalence of urinary incontinence three months after delivery. British Journal of Obstetrics and Gynaecology 1996;103(2):154‐61. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Ogah 2009
- Ogah J, Cody JD, Rogerson L. Minimally invasive synthetic suburethral sling operations for stress urinary incontinence in women. Cochrane Database of Systematic Reviews 2009, Issue 4. [DOI: 10.1002/14651858.CD006375.pub2; PUBMED: 19821363] [DOI] [PubMed] [Google Scholar]


