Sarcopenia was identified nearly 60 years ago as a common manifestation of advanced cirrhosis. Although risk prediction in advanced liver disease has been focused on laboratory-derived criteria such as the MELD score, sarcopenia has garnered recent attention due to its association with adverse outcomes independent of MELD1.
Bhanji et al reported the findings of a retrospective study of 293 adults who underwent liver transplantation between 2002 and 20062. They characterized body composition using CT scans performed during routine clinical care and reported a progressive decrease in skeletal muscle index (SMI) with a concomitant increase in myosteatosis both leading up to transplantation with continuation post-operatively. After a year post transplant, only five patients resolved their pre-transplant sarcopenia and an additional 25 developed sarcopenia de novo. A limitation (not unique to this study) is the acquisition of sarcopenia measures from non-protocol-driven imaging resulting in high rates of missing follow-up imaging. Data extrapolated in this manner can also be heavily influenced by selection bias as patients who undergo imaging usually have some concern for complication or are being monitored for cancer, both of which are associated with sarcopenia3. While limited by its retrospective nature, this study broadens our understanding of the time course of sarcopenia post-transplant and its recovery—or lack thereof.
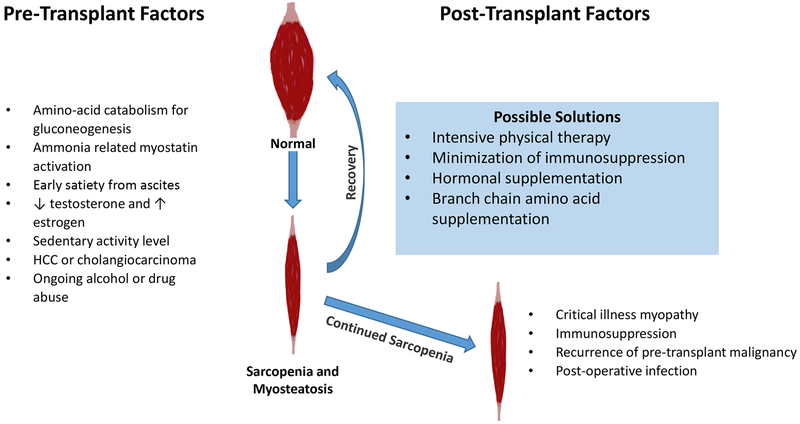
Sarcopenia in cirrhosis is thought to be multifactorial with metabolic, endocrine, and mechanical causes (Figure 1). The primary drivers of sarcopenia may be related to scavenging of skeletal muscle in order to obtain amino acids for gluconeogenesis in the absence of adequate hepatic function, ammonia-related myostatin activity, and low levels of anabolic hormones4. Although early satiety from ascites can be a contributing factor, portosystemic shunting induces skeletal muscle loss even in the absence of cirrhosis or ascites in rat models5. Furthermore, post-transplant recovery may be hampered by immunosuppression with corticosteroids and other anti-rejection therapy. In fact, muscle cell regeneration is thought to be mediated by a calcineurin-driven process6.
Figure 1.
Sarcopenia pathways and possible solutions.
Myosteatosis, denoted by hypoattenuation on CT, is the infiltration of fat into muscle and is associated with poor outcomes. The FrAILT study, among others, found that myosteatosis on CT but not SMI was more tightly correlated with waitlist mortality even after adjustment for grip strength, MELD, and Short Physical Performance Battery1,7.
Despite its rising importance, no treatments definitively improve sarcopenia. Small uncontrolled studies in humans suggest a reversal of sarcopenia with Transjugular Intrahepatic Porosystemic Shunt placement, increased muscle mass with testosterone replacement, and mitigated skeletal muscle loss with branch chain amino acid supplementation.8–10 Despite several studies showing increased muscle mass, quality of life, and exercise capacity after short intensive physical activity programs, there is no existing evidence suggesting that these interventions alter waitlist or post-transplant outcomes11. Given the strong associations found in the literature with poor patient outcomes as well as the concerning signals noted in the study by Bhanji et al, a controlled, prospective study is warranted to track outcomes and body composition changes, and test the efficacy of interventions for this important problem.
Statements of Interests
The writing and preparation of this paper was funded in part by NIH grant T32DK077662 PI MM Abecassis.
References:
- 1.van Vugt JLA, Levolger S, de Bruin RWF, van Rosmalen J, Metselaar HJ, IJzermans JNM. Systematic Review and Meta-Analysis of the Impact of Computed Tomography-Assessed Skeletal Muscle Mass on Outcome in Patients Awaiting or Undergoing Liver Transplantation. Am J Transplant. 2016;16(8):2277–2292. doi: 10.1111/ajt.13732 [DOI] [PubMed] [Google Scholar]
- 2.Bhanji RA, Takahashi N, Moynagh MR, et al. The evolution and impact of sarcopenia pre- and post-liver transplantation. Aliment Pharmacol Ther. 2019;00:1–7. 10.1111/apt.15161 [DOI] [PubMed] [Google Scholar]
- 3.Krell RW, Kaul DR, Martin AR, et al. Association between sarcopenia and the risk of serious infection among adults undergoing liver transplantation. Liver Transpl. 2013;19(12):1396–1402. doi: 10.1002/lt.23752 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Montano-Loza AJ. Clinical relevance of sarcopenia in patients with cirrhosis. World J Gastroenterol. 2014;20(25):8061–8071. doi: 10.3748/wjg.v20.i25.8061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dasarathy S, McCullough AJ, Muc S, et al. Sarcopenia associated with portosystemic shunting is reversed by follistatin. J Hepatol. 2011;54(5):915–921. doi: 10.1016/j.jhep.2010.08.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Semsarian C, Wu M-J, Ju Y-K, et al. Skeletal muscle hypertrophy is mediated by a Ca2+-dependent calcineurin signalling pathway. Nature. 1999;400(6744):576–581. doi: 10.1038/23054 [DOI] [PubMed] [Google Scholar]
- 7.Wang CW, Feng S, Covinsky KE, et al. A Comparison of Muscle Function, Mass, and Quality in Liver Transplant Candidates: Results From the Functional Assessment in Liver Transplantation Study. Transplantation. 2016;100(8):1692–1698. doi: 10.1097/TP.0000000000001232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sinclair M, Grossmann M, Hoermann R, Angus PW, Gow PJ. Testosterone therapy increases muscle mass in men with cirrhosis and low testosterone: A randomised controlled trial. J Hepatol. 2016;65(5):906–913. doi: 10.1016/J.JHEP.2016.06.007 [DOI] [PubMed] [Google Scholar]
- 9.Tsien C, Shah SN, McCullough AJ, Dasarathy S. Reversal of sarcopenia predicts survival after a transjugular intrahepatic portosystemic stent. Eur J Gastroenterol Hepatol. 2013;25(1):85–93. doi: 10.1097/MEG.0b013e328359a759 [DOI] [PubMed] [Google Scholar]
- 10.Kaido T, Ogawa K, Fujimoto Y, et al. Impact of Sarcopenia on Survival in Patients Undergoing Living Donor Liver Transplantation. Am J Transplant. 2013;13(6):1549–1556. doi: 10.1111/ajt.12221 [DOI] [PubMed] [Google Scholar]
- 11.Kruger C, McNeely ML, Bailey RJ, et al. Home Exercise Training Improves Exercise Capacity in Cirrhosis Patients: Role of Exercise Adherence. Sci Rep. 2018;8(1):99. doi: 10.1038/s41598-017-18320-y [DOI] [PMC free article] [PubMed] [Google Scholar]