Abstract
OBJECTIVES
Despite increasing utilization of reposition devices in the management of benign paroxysmal positional vertigo (BPPV), knowledge on subjective outcomes is insufficient. The objective of the present study was to evaluate subjective vertigo complaints and vertigo-associated emotional distress during reposition chair management for refractory BPPV.
MATERIALS AND METHODS
This was a prospective observational cohort study of subjective and objective data of 31 patients suffering from refractory BPPV representing failed conventional repositioning treatment. At the beginning of each visit, the patients filled out the Dizziness Handicap Inventory (DHI), the Visual Analog Scale (VAS), and the Hospital Anxiety and Depression Scale (HADS). Treatment and re-evaluation were repeated every 2 weeks until the patient was declared disease-free.
RESULTS
Complete remission of BPPV required a mean of two treatments. Mean DHI score decreased from 45 points prior to first treatment to 22 points by finished treatment (p<0.001). Similarly, mean VAS score was reduced from 58 to 25 points (p<0.001), and HADS decreased from 8 to 5 points (p<0.001). Patients with cupulolithiasis reported worse vertigo complaints than those with canalolithiasis. All scores correlated positively.
CONCLUSION
Patients with refractory BPPV improved significantly by reposition chair management according to all subjective outcomes. Thus, the reposition device could significantly reduce disease burden in the group of patients with BPPV who failed to respond to conventional management. The strong correlation between the scores suggests VAS as a useful tool for vertigo-related patient complaints.
Keywords: Vertigo, repositioning maneuvers, canalolithiasis, cupulolithiasis, treatment
INTRODUCTION
Benign paroxysmal positional vertigo (BPPV) is regarded as the most common peripheral vestibular disorder and cause of vertigo [1–3]. BPPV can be a disabling and incapacitating condition [4]. Moreover, BPPV and vestibular disorders can be associated with depression and anxiety and act mutually reinforcing [5, 6]. These issues can be evaluated with self-assessments tools for vestibular, unspecified, or emotional complaints with the Dizziness Handicap Inventory (DHI) [7], the Visual Analog Scale (VAS) [8], and the Hospital Anxiety and Depression Scale (HADS) [9], respectively.
Limitations in conventional repositioning treatment of BPPV have led to the development of reposition devices [10–13]. The TRV chair (TRV Chair®; Interacoustics, Denmark; TRV with respect to the inventor Thomas Richard-Vitton) is a mechanical diagnostic and reposition device created for management of BPPV. The advantages of the TRV chair compared with conventional management include improved analytical feasibility, accurate navigation, and treatment of people unfit for manual treatments [13–16]. A previous review has revealed a shortage of published literature on reposition chairs and the effect on BPPV [13]. To the best of our knowledge, no studies to this day have evaluated subjective outcomes systematically and prospectively in patients receiving reposition treatment in the TRV chair.
In our tertiary university institution, we receive refractory BPPV cases from all parts of the country on a daily basis. The patient group is characterized by intractable BPPV that has failed conventional repositioning treatment. Owing to chronic and disabling vertigo, many patients struggle with emotional distress. Given that the TRV chair offers strict objective control (accurate 3D rotational planes and videonystagmography, VNG), the objective of the study was to evaluate subjective complaints (VAS, DHI, and HADS) during treatment with reposition maneuvers in the TRV chair for this problematic group of patients.
MATERIALS AND METHODS
This was a prospective observational cohort study of both subjective and objective outcomes. Prior to recruitment, inclusion criterion was defined as adult patients with refractory BPPV referred to our tertiary university otorhinolaryngology department. Refractory BPPV was defined as confirmed or suspected BPPV that did not respond to repeated attempts of manual treatment. All patients were referred from other hospitals or private otorhinolaryngology clinics due to failure in management. Exclusion criterion was non-BPPV-related vertigo diagnosed at the first visit. Patients received oral and written information. Informed consent was obtained from all individual participants included in the study. The study was reported to the National Board of Health and Data Protection Agency (journal no. 03305/30-1355). Ethics committee approval was not required. Patient inclusion occurred over a period of 9 months, from September 2014 to May 2015. A total of 31 patients suffering from refractory BPPV were included in the study. Upon diagnosis of BPPV, the type of BPPV was characterized, and subsequent treatment in the TRV chair was selected. Among the 31 patients, five were excluded from the study; two were lost to follow-up (did not attend the following appointments), two did not fill out the questionnaires adequately, and one was under the influence of the anti-anxiety drug pregabalin (that may influence the vestibulo-ocular reflex and the outcome of the questionnaires). Among the 26 included patients, there were 18 (69%) women and 8 (31%) men. The mean age of the patients at first treatment was 57 (standard deviation 14) years.
Patients were re-evaluated two weeks after treatment, and reposition treatment was repeated in case of remaining BPPV. Prior to each individual treatment session and after being declared free of otolith disease, the patient was given the following questionnaires to fill out: DHI, VAS, and HADS. DHI is a 25-item survey created in 1990 for self-perceived handicap owing to vestibular disorder [7]. Items are marked with 0 (no), 2 (sometimes), or 4 (yes) points and are summarized in a total grade ranging from 0 to 100 points. VAS is a measurement tool for intensity of subjective complaints. It is commonly used for pain evaluation. However, it has also been applied to patients with dizziness [8]. The scale we applied was a 100 mm line on which the patient should mark the overall severity of vertigo symptoms. Thus, the grade could be quantified from 0 to 100 points. HADS is a self-assessment survey to detect and manage emotional distress [9]. It is a 14-item survey of which each item is graded from 0 to 3 according to the severity of the symptom, resulting in a total grade ranging from 0 to 42 points.
The TRV device has preset 360° planes for each of the semi-circular canals, allowing diagnosis and treatment of all subtypes of BPPV. VNG goggles eliminate visual fixation and allow for magnification, analysis, and storage of nystagmus patterns during positioning in the TRV chair. The diagnosis for posterior canal BPPV and horizontal (lateral) canal BPPV is performed by Dix-Hallpike and supine roll tests, respectively [17]. The criterion for BPPV is position-dependent positional nystagmus with or without fatigue. TRV chair treatment is based on the Epley and the barbecue (180–270 rotations) maneuvers for posterior BPPV and horizontal BPPV, respectively [12, 17, 18]. Multicanal BPPV is addressed by treating canalolithiasis before cupulolithiasis and repositioning posterior canal otoliths before horizontal canal otoliths. Furthermore, the TRV chair has a potentiated “impact” function, applying decelerating manual forces upon reposition maneuvers. Detailed operational procedures of the TRV chair have previously been published including the clinical distinction between canalolithiasis and cupulolithiasis that relates to the timing and excitation of geotropic or apogeotropic nystagmus, respectively [13, 19]. The TRV setup is displayed in Figure 1.
Figure 1.
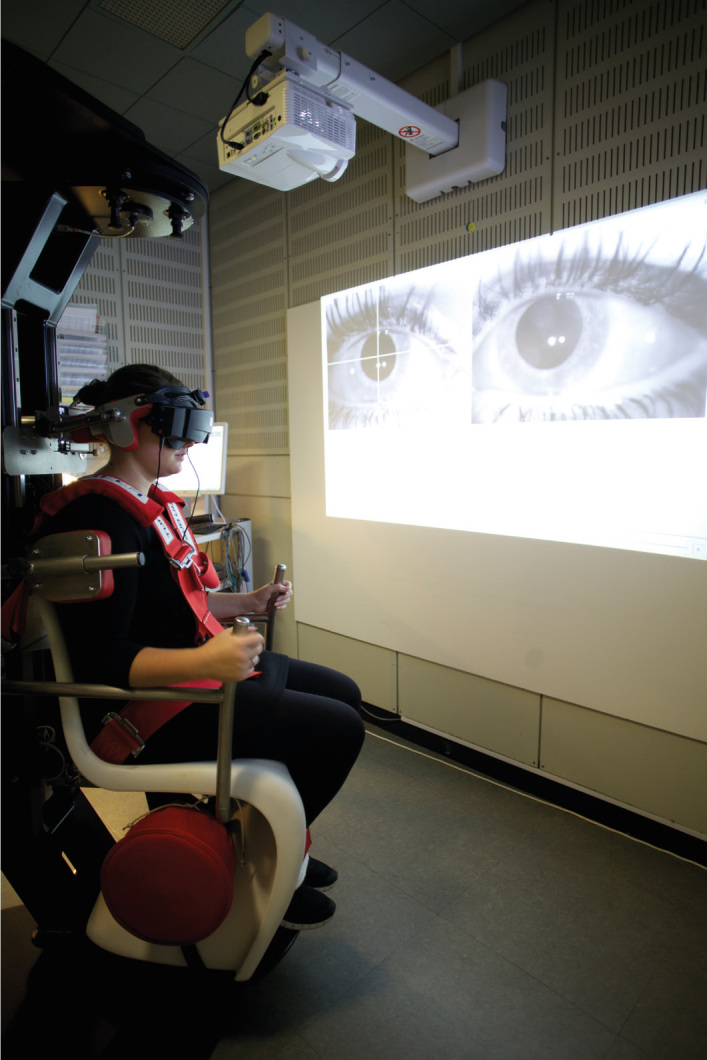
The TRV chair setup. The patient is fixed in the chair and fitted with videonystagmography goggles. Eye movements are presented on the wall monitor.
Statistical Analysis
All subjective data were analyzed as continuous variables. Paired two-tailed Wilcoxon test was used for evaluation of the differences in scores during treatment. Mann–Whitney U test was used for comparison between BPPV subtypes. Spearman’s correlation (rs) was used for correlation analyses of the three scoring systems. Bonferroni correction was performed to address potential type 1 errors. Thus, the significance level of p<0.05 was corrected to p<0.017.
RESULTS
The 26 patients corresponded to a total of 76 treatments. Regarding each individual treatment, patients suffered from posterior canalolithiasis (42 cases of all treatments), posterior cupulolithiasis (30 cases of all treatments), horizontal canalolithiasis (2 cases of all treatments), and horizontal cupulolithiasis (11 cases of all treatments). Of the 76 treatments, multicanal affection accounted for nine cases. All patients had unilateral affection. Seven (27%) patients presented a BPPV subtype conversion during the treatment course, the most predominant being cupulolithiasis switching to canalolithiasis, followed by multicanal affection switching to single canal affection. The mean number of treatments was 2 (range 1–11). The mean number of weeks treated was 6 (range 2–31) weeks. Seven (27%) patients experienced recurrence. The mean time to recurrence after last treatment was 6.5 months. The mean time of observation was 32 months. Table 1 displays the clinical features of the included patients.
Table 1.
Demographic and clinical features of BPPV subjects and TRV treatment
| Clinical features of 26 patients (SD) | |
|---|---|
| Age (mean) | 56.9 (14.6) |
| Sex ratio (female/male) | 18/8 |
| n treatments (mean) | 2 |
| n weeks of treatment (mean) | 6 |
| n recurrence | 7 |
| Time to recurrence in months (mean) | 7 (8) |
| Months of observation (mean) | 33 (3) |
Standard deviation is in parentheses.
DHI: The mean DHI score at first treatment was 45 points. The corresponding end mean end score was 22 points. The difference in DHI scores showed statistical significance (p<0.001).
VAS: The mean VAS score prior to first treatment was 58 points. By the end of treatment, this score had decreased to 25 points (p<0.001).
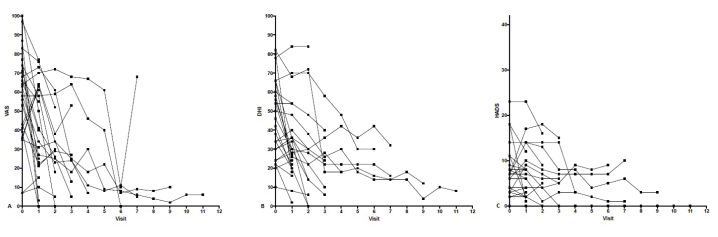
HADS: The first and last mean HADS scores were 8 points and 5 points, respectively. The decrease in HADS score from first to last treatment showed a strong trend (p=0.024). Table 2 and Fig. 2 display the individual scores for each subjective outcome during TRV treatment.
Table 2.
Scores for VAS, DHI, and HADS before the first treatment and after ending treatment
| Mean scores | Before treatment | After treatment | Difference | p |
|---|---|---|---|---|
| DHI | 45.4 (20.4) | 21.7 (17.9) | 23.7 (52%) | <0.001 |
| VAS | 57.7 (23.6) | 25.4 (24.8) | 32.3 (56%) | <0.001 |
| HADS | 8.0 (5.9) | 5.4 (4.6) | 2.6 (33%) | <0.001 |
Parentheses indicate standard deviation and percentage, respectively.
DHI: Dizziness Handicap Inventory; VAS: Visual Analog Scale; HADS: Hospital Anxiety and Depression Scale
Figure 2. a–c.
Vertigo measured with a) VAS and b) DHI and emotional distress measured with c) HADS for each individual patient during TRV treatment. Each line represents a patient and each dot represents an evaluation. The mean number of treatments was two. VAS and DHI are scales ranging from 0 to 100. HADS ranges from 0 to 42.
Correlation analyses between VAS/DHI, VAS/HADS, and DHI/HADS showed positive correlations. VAS and DHI had a strong correlation (rs=0.79, p<0.001). VAS and HADS had a moderately positive correlation (rs=0.43, p<0.001). DHI and HADS similarly showed a moderately positive correlation (rs=0.51, p<0.001).
Grouping according to the canalolithiasis or cupulolithiasis variant of BPPV (the last registered for each patient) enabled subtype comparisons. Any presence of cupulolithiasis (as either single or multicanal affection) was grouped as cupulolithiasis. VAS scores for all canalolithiasis treatments had a mean of 31 points compared with 44 points for cupulolithiasis (p=0.015). DHI scores for all canalolithiasis treatments had a mean of 28 points in contrast to 39 points for cupulolithiasis (p=0.006). The mean HADS score for canalolithiasis treatments was 5 points compared with a mean of cupulolithiasis HADS scores of 6 points (p=0.36). Subgroups regarding semi-circular canal affection were too small to make meaningful statistics since most of the horizontal semi-circular canal affections were multicanal in combination with cupulolithiasis.
DISCUSSION
The present study evaluates the treatment effect of reposition chair treatment on complicated cases of BPPV. Demography for this patient group was in accordance with our expectations and previous studies that had a similar sex ratio and age [10, 13].
VAS, DHI, and HADS outcomes were all substantially responsive to treatment. Since the TRV chair together with VNG has a standardized and accurate ability to identify the presence of otoliths or clear the patient for BPPV, these findings indicate that the subjective burden of symptoms overall matches the objective findings. VAS and DHI were significantly higher for patients who suffered from cupulolithiasis than for those who suffered from canalolithiasis. Previous findings that cupulolithiasis is harder to treat than canalolithiasis could describe this difference [13, 20]. However, there was no difference in scores related to emotional distress as measured by the HADS. These findings are interesting, indicating that fixed otoliths produce more severe subjective vertigo complaints than loose otoliths. However, depression and anxiety issues (as measured by HADS) appear independent of the variant of BPPV (grouped according to cupulolithiasis or canalolithiasis).
The initial (before treatment) mean DHI score of 45 corresponds to a moderate dizziness handicap, whereas a score of 22 corresponds to a mild handicap [7]. The change in scores during treatment represented a 52% decrease. In contrast, VAS showed higher mean scores at both the first (58 points) and the last visits (25 points), signifying a decrease of 56%. Thus, despite showing a strong correlation, VAS scores did not follow DHI scores completely. Though all patients were declared disease-free at the final visit, no mean scores (including HADS scores) were approximating a value of 0. Although a significant improvement occurs, this indicates a discrepancy between objective and subjective parameters. An explanation for this finding could be the post-reposition residual dizziness that subsides after approximately 3 weeks in most cases, but for the minority of patients, it can take 1–3 months [21]. Causes for this phenomenon include remaining otolith debris not generating visible nystagmus and central adaptation. Another reason for scores not declining completely is an inherent bias in the questionnaires being filled out 2 weeks after repositioning. Although the items in the surveys are based on the present situation, some overlap to the recent pathologic situation is likely. The selected group of patients in the study cohort has suffered from long-term refractory BPPV. This could explain why HADS demonstrated a less decrease than the other parameters because HADS focuses on issues that do not respond immediately to successful treatment. Several HADS items include a time aspect (e.g., often, sometimes, not often, and very seldom as answers to the question “I can enjoy a good book or radio or TV program”). It is reasonable to believe that 2 weeks is not sufficient to generate a valid response when taking into account how long the patients have been suffering from BPPV. Future studies should re-evaluate patients with questionnaires at long-term follow-up (e.g., at 6 months after last treatment) to adjust for the new life situation and to counter a potential subjective “backlog.”
VAS was strongly correlated to DHI. This indicates that VAS could be regarded as a validated scoring system of subjective complaints regarding dizziness. VAS is a strong indicator of overall symptomatic burden (physical, emotional, and functional dizziness) and a moderate indicator of anxiety and mood issues. This suggests that VAS could monitor and evaluate subjective treatment effect. However, in addition to providing a greater level of detail, DHI should still be considered a more accurate evaluation tool of subjective BPPV burden. Nevertheless, VAS represents a quick, easy-to-apply evaluation tool for overall subjective complaints associated with BPPV. VAS may be applied for simple evaluation of treatment effect or comparison between individuals or groups.
A limitation of the present study is the lack of a manual control group for comparing reposition chair treatment with conventional reposition treatment. However, in this setting, all patients have failed management with manual procedures prior to consultation in our laboratory. The waiting time from referral to appointment in the clinic was not available for the current period but normally ranges from 6 to 12 months; therefore, patient motivation for voluntary participation in a randomized controlled trial is low. Despite this methodological limitation, to our knowledge, the current study is the only study to prospectively and systematically investigate subjective outcomes for this patient group.
The findings indicate that individuals suffering from refractory and chronic BPPV do not only experience moderate to severe dizziness handicap, but in addition, many patients struggle with secondary emotional issues. This calls for multidisciplinary efforts including physiotherapy and psychological involvement in the vestibular rehabilitation of patients with dizziness that is known to improve patient outcomes in vertigo[22].
CONCLUSION
Patients with refractory BPPV improved significantly by TRV chair management according to subjective outcomes measured by the DHI, the VAS, and the HADS. BPPV was resolved after a mean of two treatments. Thus, the reposition device could significantly reduce disease burden in the group of patients with BPPV who previously failed to respond to conventional treatment. In addition, there was a strong correlation between the scores extracted from DHI and VAS, suggesting VAS as an individual measurement tool for vertigo-related patient complaints.
Acknowledgements
Authors would like to acknowledge vestibular specialist Gerd Hansen for her invaluable work.
Footnotes
This study was presented at the “ONH-dagarna 2018 (Swedish Association for Otorhinolaryngology Head and Neck Surgery)”, April 11, 2018, Linkoping, Sweden.
Ethics Committee Approval: N/A.
Informed Consent: Written informed consent was obtained from the patients who participated in this study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept – N.W, S.B., M.N.M, S.H., M.K.; Design – N.W., S.H., M.N.M., M.K.; Supervision – S.B., M.K.; Resource – S.B., M.N.M., S.H., M.K.; Materials – M.K.; Data Collection and/or Processing – N.W., S.B.; Analysis and/or Interpretation – N.W., S.B.; Literature Search – N.W.; Writing – N.W.; Critical Reviews – S.B., M.N.M., M.K..
Conflict of Interest: NW has been invited by Interacoustics, Denmark, to present the study results at local meetings, however no compensation has been received.
Financial Disclosure: The authors declared that this study has received no financial support.
REFERENCES
- 1.von Brevern M, Lezius F, Tiel-Wilck K, Radtke A, Lempert T. Benign paroxysmal positional vertigo: current status of medical management. Otolaryngol Head Neck Surg. 2004;130:381–2. doi: 10.1016/j.otohns.2003.07.007. [DOI] [PubMed] [Google Scholar]
- 2.Zappia JJ. Benign paroxysmal positional vertigo. Curr Opin Otolaryngol Head Neck Surg. 2013;21:480–6. doi: 10.1097/MOO.0b013e32836463d6. [DOI] [PubMed] [Google Scholar]
- 3.Hansen S, Karlberg M. Benign paroksysmal positionel vertigo - den hyppigste form for otogen vertigo. Ugeskr Laeger. 2007;169:1996–2002. [PubMed] [Google Scholar]
- 4.von Brevern M, Radtke A, Lezius F, Feldmann M, Ziese T, Lempert T, et al. Epidemiology of benign paroxysmal positional vertigo: a population based study. J Neurol Neurosurg Psychiatry. 2006;78:710–5. doi: 10.1136/jnnp.2006.100420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Best C, Tschan R, Eckhardt-Henn A, Dieterich M. Who is at risk for ongoing dizziness and psychological strain after a vestibular disorder? Neuroscience. 2009;164:1579–87. doi: 10.1016/j.neuroscience.2009.09.034. [DOI] [PubMed] [Google Scholar]
- 6.Ferrari S, Monzani D, Baraldi S, Simoni E, Prati G, Forghieri M, et al. Vertigo “in the pink”: The impact of female gender on psychiatric-psychosomatic comorbidity in benign paroxysmal positional vertigo patients. Psychosomatics. 2014;55:280–8. doi: 10.1016/j.psym.2013.02.005. [DOI] [PubMed] [Google Scholar]
- 7.Jacobson GP, Newman CW, Newman CW. The development of the Dizziness Handicap Inventory. Arch Otolaryngol Head Neck Surg. 1990;116:424–7. doi: 10.1001/archotol.1990.01870040046011. [DOI] [PubMed] [Google Scholar]
- 8.Toupet M, Ferrary E, Grayeli AB. Visual analog scale to assess vertigo and dizziness after repositioning maneuvers for benign paroxysmal positional vertigo. J Vestib Res Equilib Orientat. 2011;21:235–41. doi: 10.3233/VES-2011-0420. [DOI] [PubMed] [Google Scholar]
- 9.Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand. 1983;67:361–70. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 10.Hunt WT, Zimmermann EF, Hilton MP. Modifications of the Epley (canalith repositioning) manoeuvre for posterior canal benign paroxysmal positional vertigo (BPPV) Cochrane Database Syst Rev. 2012:CD008675. doi: 10.1002/14651858.CD008675.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nakayama M, Epley JM. BPPV and variants: Improved treatment results with automated, nystagmus-based repositioning. Otolaryngol Head Neck Surg. 2005;133:107–12. doi: 10.1016/j.otohns.2005.03.027. [DOI] [PubMed] [Google Scholar]
- 12.Richard-Vitton BT, Petrak M, Douglas L. The TRV Chair: Introductory Concepts. Hearing Review. 2013;20:52–4. [Google Scholar]
- 13.West N, Hansen S, M⊘ller MN, Bloch SL, Klokker M. Repositioning chairs in benign paroxysmal positional vertigo: implications and clinical outcome. Eur Arch Otorhinolaryngol. 2016;273:573–80. doi: 10.1007/s00405-015-3583-z. [DOI] [PubMed] [Google Scholar]
- 14.Wang J, lu Chi F, hao Jia X, Tian L, Richard-Vitton T. Does benign paroxysmal positional vertigo explain age and gender variation in patients with vertigo by mechanical assistance maneuvers? Neurol Sci. 2014;35:1731–6. doi: 10.1007/s10072-014-1822-5. [DOI] [PubMed] [Google Scholar]
- 15.Richard-vitton T, Viirre E. Unsteadiness and drunkennes sensations as a new sub-type of BPPV. Rev Laryngol Otol Rhinol. 2011;132:75–80. [PubMed] [Google Scholar]
- 16.Tan J, Yu D, Feng Y, Song Q, You J, Shi H, et al. Comparative study of the efficacy of the canalith repositioning procedure versus the vertigo treatment and rehabilitation chair. Acta Otolaryngol. 2014;134:704–8. doi: 10.3109/00016489.2014.899711. [DOI] [PubMed] [Google Scholar]
- 17.Bhattacharyya N, Baugh RF, Orvidas L, Barrs D, Bronston LJ, Cass S, et al. Clinical practice guideline: Benign paroxysmal positional vertigo. Otolaryngol Head Neck Surg. 2008;139(5 Suppl 4):S47–81. doi: 10.1016/j.otohns.2008.08.022. [DOI] [PubMed] [Google Scholar]
- 18.Epley JM. The canalith repositioning procedure: for treatment of benign paroxysmal positional vertigo. Otolaryngol Head Neck Surg. 1992;107:3 99–404. doi: 10.1177/019459989210700310. [DOI] [PubMed] [Google Scholar]
- 19.West N, Hansen S, Bloch SL, M⊘ller MN, Klokker M. Benign paroxysmal positional vertigo treatment. Ugeskr Laeger. 2017;179:2–5. [PubMed] [Google Scholar]
- 20.Pérez P, Franco V, Cuesta P, Aldama P, Alvarez MJ, Méndez JC. Recurrence of Benign Paroxysmal Positional Vertigo. Otol Neurotol. 2012;33:437–43. doi: 10.1097/MAO.0b013e3182487f78. [DOI] [PubMed] [Google Scholar]
- 21.Seok JI, Lee HM, Yoo JH, Lee DK. Residual dizziness after successful repositioning treatment in patients with benign paroxysmal positional vertigo. J Clin Neurol. 2008;4:107–10. doi: 10.3988/jcn.2008.4.3.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Karlberg M, Magnusson M, Malmström EM, Melander A, Moritz U. Postural and symptomatic improvement after physiotherapy in patients with dizziness of suspected cervical origin. Arch Phys Med Rehabil. 1996;77:874–82. doi: 10.1016/S0003-9993(96)90273-7. [DOI] [PubMed] [Google Scholar]