Abstract
Background
Stress urinary incontinence (SUI) imposes significant health and economic burden on society and the women affected. Laparoscopic colposuspension was one of the first minimal access operations for the treatment of women with SUI, with the presumed advantages of avoiding major incisions, shorter hospital stays and quicker return to normal activities.
Objectives
To determine the effects of laparoscopic colposuspension for urinary incontinence in women.
Search methods
We searched the Cochrane Incontinence Group Trials Register (searched 2 July 2009), and sought additional trials from other sources and by contacting study authors for unpublished data and trials.
Selection criteria
Randomised or quasi‐randomised controlled trials in women with symptomatic or urodynamic diagnosis of stress or mixed incontinence that included laparoscopic surgery as the intervention in at least one arm of the studies.
Data collection and analysis
The review authors evaluated trials for methodological quality and their appropriateness for inclusion in the review. Two review authors extracted data and another cross checked them. Where appropriate, we calculated a summary statistic.
Main results
We identified 22 eligible trials. Ten involved the comparison of laparoscopic with open colposuspension. Whilst the women's subjective impression of cure seemed similar for both procedures, in the short‐ and medium‐term follow‐up, there was some evidence of poorer results of laparoscopic colposuspension on objective outcomes. The results showed trends towards fewer perioperative complications, less postoperative pain and shorter hospital stay for laparoscopic compared with open colposuspension, however, laparoscopic colposuspension was more costly.
Eight studies compared laparoscopic colposuspension with newer 'self‐fixing' vaginal slings. There were no significant differences in the reported short‐ and long‐term subjective cure rates of the two procedures but objective cure rates at 18 months favoured slings. We observed no significant differences for postoperative voiding dysfunction and perioperative complications. Laparoscopic colposuspension had a significantly longer operation time and hospital stay. We found significantly higher subjective and objective one‐year cure rates for women randomised to two paravaginal sutures compared with one suture in a single trial. Three studies compared sutures with mesh and staples for laparoscopic colposuspension and showed a trend towards favouring the use of sutures.
Authors' conclusions
Currently available evidence suggests that laparoscopic colposuspension may be as good as open colposuspension at two years post surgery. However, the newer vaginal sling procedures appear to offer even greater benefits, better objective outcomes in the short term and similar subjective outcomes in the longer term. If laparoscopic colposuspension is performed, the use of two paravaginal sutures appears to be the most effective method. The place of laparoscopic colposuspension in clinical practice should become clearer when there are more data available describing long‐term results. A brief economic commentary (BEC) identified three studies suggesting that tension‐free vaginal tape (TVT) may be more cost‐effective compared with laparoscopic colposuspension but laparoscopic colposuspension may be slightly more cost‐effective when compared with open colposuspension after 24 months follow‐up.
Keywords: Female, Humans, Laparoscopy, Quality of Life, Randomized Controlled Trials as Topic, Urinary Incontinence, Urinary Incontinence/surgery, Urologic Surgical Procedures, Urologic Surgical Procedures/methods
Keyhole (laparoscopic) surgery through the abdomen for treating urinary incontinence in women
Urinary incontinence is a common and often debilitating problem for many women. Around a third of women of child‐bearing age are incontinent during physical exertion or when they cough, laugh or sneeze. When such 'stress' incontinence persists despite non‐surgical treatment, surgery is often recommended. A significant amount of a woman's and their family's income can be spent on management of stress urinary incontinence.
Laparoscopic colposuspension is an operation carried out through a small incision in the abdomen to hold and support the tissues around the neck of the bladder. Women recover more quickly from laparoscopic colposuspension for urinary incontinence than from traditional, open surgery, with similar initial improvement. Longer‐term success rates may be lower but this is uncertain. However, when laparoscopic colposuspension is compared with newer 'self‐fixing' sling procedures, it appears that in the short term the sling procedures offer the greater benefits of minimal access techniques with similar, if not better cure rates. The review of trials found that both traditional colposuspension and newer 'self‐fixing' slings had technically better results in the short term when compared with laparoscopic colposuspension. However, women's experience of improvement, both in the short and long term was similar for each type of operation. Using two stitches in laparoscopic colposuspensions was better than both one suture or the use of mesh. A trend was shown towards better outcomes for the laparoscopic operation when compared to open surgery, such as less postoperative pain, shorter hospital stay, quicker time to return to normal activities and shorter duration of catheterisation. When the laparoscopic technique was compared to the newer vaginal sling procedures, all the aforementioned trends were in favour of the sling procedure.
In terms of costs, a non‐systematic review of economic studies suggested that tension‐free vaginal tape and open colposuspension would be cheaper than laparoscopic colposuspension.
The value of the review is limited by the size and quality of the trials and the few data about long‐term results.
Background
Urinary incontinence is a common and often debilitating problem for many adult women. Some degree of stress incontinence affects around a third of women of child‐bearing age (Wilson 1996). Continence is achieved by a combination of normal anatomical and physiological properties of the bladder, urethra and sphincter, the pelvic floor, and also the nervous system co‐ordinating these organs. Disruption to any of these components may lead to incontinence.
There are different types of urinary incontinence. 'Stress urinary incontinence' (SUI) is defined by the symptom of involuntary loss of urine associated with physical exertion and activities that increase intra‐abdominal pressure. The International Continence Society defines 'urodynamic stress incontinence' (USI) as the involuntary leakage of urine during increased abdominal pressure in the absence of a detrusor contraction, noted during filling cystometry (Abrams 2002). Therefore, diagnosis based on this definition requires urodynamic investigation. 'Urge urinary incontinence' is defined as involuntary loss of urine accompanied by or immediately preceded by urgency. Detrusor overactivity (DO) is a diagnosis of involuntary detrusor muscle contractions that are not due to neurological disorders; and the diagnosis must be made using urodynamic investigations (Abrams 2002). Mixed urinary incontinence is the complaint of involuntary leakage associated with urgency and also with exertion, effort, sneezing or coughing (Abrams 2002). This review includes women with SUI, proven urodynamic stress incontinence, women with symptoms of stress plus urge incontinence or other urinary symptoms diagnosed clinically or urodynamic stress incontinence plus detrusor overactivity diagnosed using urodynamics.
Stress urinary incontinence constitutes a huge financial economic burden to society. In the USA, the annual total direct costs of urinary incontinence in both men and women is over USD 16 billion (1995 USD) (Chong 2011) with societal costs of USD 26.2billion (1995 USD) (Wagner 1998). Approximately, USD 13.12 billion (1995 USD) of the total direct costs of urinary incontinence is spent on SUI (Chong 2011; Kunkle 2015). About 70% of this USD 13.12 billion is borne by people with SUI, mainly through routine care (purchasing pads and disposable underwear (diapers), laundry and dry cleaning). This constitutes a significant individual financial burden. Of the remaining 30% of costs, 14% is spent on nursing home admission, 9% on treatment, 6% on addressing complications and 1% on diagnosis (Chong 2011).
A study in the USA reported that about 1% of the median annual household income (USD 50,000 to USD 59,999 in 2006) was spent by women on incontinence management. This study estimated that women spent an annual mean amount of USD 751 to USD 1277 (2006 USD) on incontinence. This cost increases with the severity of the symptoms (Subak 2008). The indirect cost associated with SUI exerts a social and psychological burden that is unquantifiable (Chong 2011; Kilonzo 2004), nevertheless, Birnbaum 2004 estimated that the annual average direct medical costs of SUI for one year (1998 USD) was USD 5642 and USD 4208 for indirect workplace costs. The cost of management and treatment of SUI appears to have increased over time due to increasing prevalence and increased desire for improved quality of life. This, in turn, has resulted from improved recognition of the condition, as well as increased use of surgical and non‐surgical managements.
Non‐surgical treatments for SUI include conservative (Hay‐Smith 2006; Hay‐Smith 2008; Herbison 2002; Wallace 2004) and pharmacological therapies (Hay‐Smith 2005; Nabi 2006). These interventions are the subject of separate Cochrane Reviews. This review is one of a series of interrelated Cochrane Reviews of surgical approaches to the management of urinary incontinence. We refer the reader to another review in the series (Lapitan 2009) for further background information about the mechanisms of urinary incontinence in women, the principal categories of incontinence and the broad approaches to management. Surgical procedures to remedy SUI generally aim to lift and support the urethro‐vesical junction between the urethra and the bladder and increase bladder outlet resistance. There is disagreement, however, regarding the precise mechanism by which continence is achieved after surgery. The choice of procedures is often influenced by co‐existent problems, a surgeon's specialty or preference and the physical features of the person affected. Numerous surgical methods have been described but essentially they fall into seven categories:
open abdominal retropubic urethropexy (e.g. colposuspension (Burch), Marshall‐Marchetti‐Krantz) (Lapitan 2009);
laparoscopic retropubic colposuspension (this review);
anterior vaginal repair (anterior colporrhaphy) (e.g. Kelly, Pacey) (Glazener 2001);
suburethral slings (traditional and newer 'self‐fixing') (Bezerra 2005; Ogah 2009);
needle suspensions (e.g. Pereyra, Stamey) (Glazener 2004);
periurethral injections (Keegan 2007); and
artificial sphincters.
This review concentrates on laparoscopic retropubic colposuspension; other Cochrane Reviews address six of the other categories.
Laparoscopic incontinence procedures were first introduced in the early 1990s (Vancaillie 1991) with the advantage to women that they avoided the major incisions of conventional open surgery. It was claimed that this would result in shorter lengths of hospital stay and shorten the time to return to normal activities.
The most popular laparoscopic procedure for urinary incontinence is laparoscopic colposuspension. As in open colposuspension, sutures are inserted into the paravaginal tissues on either side of the bladder neck and then attached to the ileopectineal ligaments on the same side. There are, however, technical variations in surgery in respect of the laparoscopic approach (transperitoneal into the abdominal cavity or extraperitoneal) and in the number and types of sutures, the site of anchor and the use of mesh and staples (Jarvis 1999).
Objectives
To determine the effects of laparoscopic colposuspension for urinary incontinence in women.
We tested the following hypotheses.
Laparoscopic colposuspension is better than no treatment or sham operation for the management of urodynamic stress incontinence (urodynamic diagnosis) or for symptoms of stress or mixed incontinence (clinical diagnosis).
Laparoscopic colposuspension is better than conservative interventions (e.g. pelvic floor muscle training, electrical stimulation, cones, biofeedback) for the management of urodynamic stress incontinence (urodynamic diagnosis) or for symptoms of stress or mixed incontinence (clinical diagnosis).
Laparoscopic colposuspension is better than open colposuspension (abdominal surgery) for the management of urodynamic stress incontinence (urodynamic diagnosis) or for symptoms of stress or mixed incontinence (clinical diagnosis).
Laparoscopic colposuspension is better than needle suspension (abdominal and vaginal surgery) for the management of urodynamic stress incontinence (urodynamic diagnosis) or for symptoms of stress or mixed incontinence (clinical diagnosis).
Laparoscopic colposuspension is better than traditional sling procedures (abdominal and vaginal surgery) for the management of urodynamic stress incontinence (urodynamic diagnosis) or for symptoms of stress or mixed incontinence (clinical diagnosis).
Laparoscopic colposuspension is better than newer 'self‐fixing' sling procedures (abdominal and vaginal surgery) for the management of urodynamic stress incontinence (urodynamic diagnosis) or for symptoms of stress or mixed incontinence (clinical diagnosis).
Laparoscopic colposuspension is better than anterior vaginal repair for the management of urodynamic stress incontinence (urodynamic diagnosis) or for symptoms of stress or mixed incontinence (clinical diagnosis).
Laparoscopic colposuspension is better than periurethral injections for the management of urodynamic stress incontinence (urodynamic diagnosis) or for symptoms of stress or mixed incontinence (clinical diagnosis).
Some methods of laparoscopic colposuspension are better than others for the management of urodynamic stress incontinence (urodynamic diagnosis) or for symptoms of stress or mixed incontinence (clinical diagnosis).
Methods
Criteria for considering studies for this review
Types of studies
All randomised or quasi‐randomised controlled trials studying effects of treatment for stress or mixed urinary incontinence in women, where at least one management arm involved laparoscopic colposuspension.
Types of participants
Adult women with urinary incontinence who were diagnosed as having:
urodynamic stress incontinence (urodynamic diagnosis); or
stress incontinence (clinical diagnosis); or
mixed incontinence (stress incontinence plus other urinary symptoms such as urge incontinence).
The definitions for the above diagnoses were those used by the authors of the trial reports.
Types of interventions
At least one arm of a study must have involved laparoscopic colposuspension to treat urinary incontinence.
Comparison interventions were those described in the eight hypotheses above.
Types of outcome measures
We sought data for the following measures of outcome with subjective cure considered as the primary measure.
A. Women's observations
1. Subjective cure within 18 months (women's perception of cure) 2. Subjective cure after 18 months and within five years 3. Subjective cure after five years
B. Quantification of symptoms
4. Incontinent episodes (from self‐completed bladder chart) 5. Pad tests of quantified leakage (mean volume or weight of urine loss)
C. Clinicians' measures
6. Stress testing (alone or at cystometrogram) 7. Urge symptoms or urge incontinence (clinical diagnosis without urodynamics) 8. De novo detrusor instability (urodynamic diagnosis) 9. Voiding dysfunction or difficulty within 18 months, with or without urodynamic confirmation (residual urine estimation, flowmetry) 10. Urodynamically assessed cure (the absence of urinary stress incontinence on filling cystometry)
D. Quality of life
11. General health status measures e.g. Short Form 36 (Ware 1993) or specific instruments designed to assess incontinence
E. Surgical outcome measures
12. Perioperative surgical complications e.g. infection, haemorrhage 13. Pain or analgesia requirements 14. Length of inpatient stay 15. Time to return to normal activity level 16. Repeat incontinence surgery
F. Other outcomes
17. Non‐prespecified outcomes judged important when performing the review
Search methods for identification of studies
We did not impose any language or other limits on the searches.
Electronic searches
This review has drawn on the search strategy developed for Cochrane Incontinence as a whole. We have identified relevant trials primarily from the Cochrane Incontinence Trials Register. The methods used to derive this, including the search strategy, are described under the Group's details in the Cochrane Library. For more details please see the ‘Specialized Register’ section of the Group's module in the Cochrane Library). The register contains trials identified from the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE, CINAHL, and handsearching of journals and conference proceedings.
We searched the Cochrane Incontinence Trials Register using the Group's own keyword system. The search terms used were as follows.
{design.rct* or design.cct*} AND {TOPIC.URINE.INCON*} AND {INTVENT.SURG.LAP*}
All searches were of the keyword field of Reference Manager 2002. The date of the most recent search of the register for this review was 2 July 2009. The trials in the Incontinence Group Specialised Register are also contained in CENTRAL.
We performed additional searches for the brief economic commentary (BEC). These were conducted in MEDLINE (1 January 1946 to March 2017), Embase (1 January 1980 to 2017 Week 12) and NHS EED (1st Quarter 2016). All searches were conducted on 6 April 2017. Details of the searches run and the search terms used can be found in Appendix 1.
Searching other resources
We conducted the following, additional searches for this review: we checked all reference lists of identified trials and other relevant articles; we contacted authors and trialists in the field to identify any additional or unpublished data or studies.
Data collection and analysis
We identified randomised and quasi‐randomised trials using the above search strategy. We excluded studies from the review if they were not randomised or quasi‐randomised controlled trials for incontinent people or if they made comparisons other than those prespecified. Excluded studies are listed with reasons for their exclusion.
The review authors evaluated the reports of all possibly eligible studies for methodological quality and appropriateness for inclusion, without prior consideration of the results. Each review author assessed methodological quality using the Cochrane Incontinence assessment criteria, which include quality of random allocation and concealment, description of dropouts and withdrawals, analysis by intention to treat and blinding during treatment and at outcome assessment. We resolved any differences of opinion by discussion with a third party.
At least two review authors independently undertook data extraction of individual studies. Where data may have been collected but not reported, we sought clarification from the trialists. We planned to group trial data by type of incontinence, either urodynamic stress incontinence, based on a urodynamic diagnosis or stress or mixed incontinence, based upon a symptom classification. In the event, however, all included trials were limited to women with urodynamic stress incontinence.
Included trial data were processed as described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2005). When appropriate, we carried out meta‐analysis. For categorical outcomes, we derived a risk ratio (RR) by relating the number reporting an outcome to the number at risk in each group. For continuous variables we used means and standard deviations to derive a mean difference and combined studies to get a weighted mean difference (WMD). Where appropriate, we used a fixed‐effect model to calculate the combined estimates and their 95% confidence intervals (CI). We examined heterogeneity between trial results using visual inspection of the forest plot and taking into account the results of Chi2 tests for heterogeneity and I2 tests (Higgins 2003). Due to the small number of studies, we could not carry out sensitivity analyses for methodological quality. We subgrouped trial data by type of material used for the laparoscopic colposuspension and the technique used for the self‐fixing sling: either mesh or sutures and tension‐free vaginal tape (TVT) or suprapubic arc (SPARC).
Results
Description of studies
Included and excluded studies
We identified 22 randomised trials of surgery for urinary incontinence, with laparoscopic colposuspension in at least one arm, to be included in this review. There were 14 additional studies to the eight studies identified in 2000 for the original review (Burton 1997; Carey 2000; Fatthy 2001; Persson 2000; Ross 1995; Su 1997; Summitt 2000; Wallwiener 1995). We excluded three studies, two because they were not randomised (Lee 1997; Lernis 1997) and the third study because it compared two‐dimensional view laparoscopy with three‐dimensional view laparoscopy for different gynaecological operations and only three participants had colposuspension, all randomly allocated to the same group (Koster 1996).
Publication type
Two of the 22 included studies had published versions in both English and either German (Wallwiener 1995) or Italian (Adile 2001). Six studies were reported only as abstracts (Adile 2001; Burton 1997; Maher 2004; Mirosh 2005; Morris 2001; Summitt 2000). Where more detailed study information was required we contacted the study authors and used the information gained (some currently unpublished) in the review.
Sample characteristics
Sample sizes ranged from 20 to 300, with the majority of the trials having fewer than 50 women in each arm. Judged on the study reports, all participants had prior urodynamic investigation although this was not always explicitly stated. All studies, therefore, appeared to have been undertaken on women with urodynamic stress incontinence. The inclusion and exclusion criteria varied in other respects. All but two studies (Morris 2001; Ustun 2003) stated their exclusion criteria. Fifteen trials excluded women with previous anti‐incontinence surgery; six did not (Carey 2000; Fatthy 2001; Foote 2004; Kitchener 2006; Maher 2004; Wallwiener 1995) and for one of these studies recurrent urinary stress incontinence was an inclusion criteria (Maher 2004). Twelve trials excluded women who had had previous retropubic surgery (Adile 2001; Ankardal 2004; Ankardal 2005; Burton 1997; Carey 2000; Foote 2004; Kitchener 2006; Mirosh 2005; Persson 2000; Su 1997; Summitt 2000; Zullo 2001). Nine studies excluded women with detrusor overactivity (mixed urinary incontinence) (Fatthy 2001; Foote 2004; Kitchener 2006; Mirosh 2005; Paraiso 2004; Ross 1995; Su 1997; Summitt 2000; Valpas 2004) and one study excluded women with urge incontinence but included women with urgency symptoms (Persson 2000). Ten studies excluded women with varying degrees of pelvic organ prolapse: greater than grade one uterine prolapse or cystocele (Persson 2000; Su 1997; Wallwiener 1995), greater than or equal to stage two (Persson 2002; Zullo 2001), any significant prolapse (Foote 2004; Maher 2004; Paraiso 2004) and grade three prolapse or greater (Fatthy 2001; Mirosh 2005). Eight studies excluded women who required coincident additional gynaecological operations (Adile 2001; Ankardal 2004; Ankardal 2005; Foote 2004; Mirosh 2005; Persson 2002; Summitt 2000; Valpas 2004), making the trial intervention a sole procedure.
Comparison of interventions
Ten studies compared laparoscopic colposuspension with open colposuspension (Ankardal 2004; Ankardal 2005; Burton 1997; Carey 2000; Cheon 2003; Fatthy 2001; Kitchener 2006; Morris 2001; Su 1997; Summitt 2000) but they were not consistent in either the number or type of mesh or sutures used. Burton 1997 used absorbable Dexon sutures, whereas six trials used non‐absorbable sutures, mainly Ethibond (Ankardal 2004; Ankardal 2005; Cheon 2003; Kitchener 2006; Su 1997; Summitt 2000) or polypropylene sutures (Fatthy 2001). All studies with the exception of two (Ankardal 2004; Su 1997) used the same number and type of suspension material for both the laparoscopic and open procedures. In the study by Ankardal and colleagues (Ankardal 2004) a polypropylene mesh and Titan staples were used for the laparoscopic colposuspensions and sutures for the open colposuspensions. Unpublished information by Su and colleagues (Su 1997) revealed that the paravaginal fascia was held by one suture on each side in the laparoscopic procedure and by three sutures each side in the open procedure. The surgeons in three studies (Burton 1997; Cheon 2003; Fatthy 2001) had performed fewer than 20 laparoscopic colposuspensions before starting the trial; other studies either reported surgeons as being senior gynaecologists with extensive experience in both procedures (Ankardal 2004; Ankardal 2005; Carey 2000; Kitchener 2006; Su 1997) or did not report the experience of the surgeons (Morris 2001; Summitt 2000).
Eight studies (Adile 2001; Foote 2004; Maher 2004; Mirosh 2005; Paraiso 2004; Persson 2002; Ustun 2003; Valpas 2004) compared laparoscopic colposuspension with self‐fixing vaginal mesh slings. Seven of these studies used a tension‐free vaginal tape (TVT) for the vaginal sling technique and one study (Foote 2004) used SPARCTM. One study (Valpas 2004) used TackerTM mesh for the laparoscopic colposuspension whereas four studies (Foote 2004; Paraiso 2004; Persson 2002; Ustun 2003) reported using two single‐bite non‐absorbable sutures each side. The main differences between the interventions in this group was the type of anaesthesia used. In all trials the laparoscopic colposuspensions were performed under a general anaesthetic. The self‐fixing sling operations were performed under local anaesthetic with sedation in two studies (Persson 2002; Valpas 2004); under regional anaesthesia (spinal or epidural) in two studies (Adile 2001; Mirosh 2005) and a combination of general, regional and local with sedation in two other studies (Paraiso 2004; Ustun 2003).
Five studies (Ankardal 2005; Persson 2000; Ross 1995; Wallwiener 1995; Zullo 2001) compared different operative techniques or approaches for laparoscopic colposuspension. Of these, Ankardal 2005; Ross 1995 and Zullo 2001 compared polypropylene mesh fixed with staples or tacks with EthibondTM or Gore‐TexTM sutures; Persson 2000 compared two single‐bite Gore‐Tex sutures with one double‐bite suture on each side of the urethra; and Wallwiener 1995 compared extraperitoneal with transperitoneal access using Gore‐Tex sutures or mesh and staples.
Of the included 22 studies just over half stated the method of approach used for the laparoscopic colposuspension. Ten studies used the transperitoneal approach (Ankardal 2004; Burton 1997; Carey 2000; Cheon 2003; Foote 2004; Persson 2000; Ross 1995; Su 1997; Summitt 2000; Zullo 2001), three studies (Fatthy 2001; Paraiso 2004; Valpas 2004) used the extraperitoneal approach and Wallwiener 1995 compared a transperitoneal with an extraperitoneal approach.
Outcome measures
Fifteen studies reported subjective cure measures of operative success (Ankardal 2004; Ankardal 2005; Carey 2000; Cheon 2003; Fatthy 2001; Foote 2004; Maher 2004; Morris 2001; Persson 2000; Persson 2002; Kitchener 2006; Su 1997; Ustun 2003; Valpas 2004; Zullo 2001) although they used different instruments and scales to assess cure.
Thirteen studies performed objective measures in the form of a pad test or reported incontinent episodes (Ankardal 2004; Ankardal 2005; Burton 1997; Cheon 2003; Fatthy 2001; Foote 2004; Kitchener 2006; Morris 2001; Paraiso 2004; Persson 2000; Persson 2002; Su 1997; Valpas 2004). Eleven studies (Burton 1997; Carey 2000; Cheon 2003; Fatthy 2001; Maher 2004; Paraiso 2004; Ross 1995; Summitt 2000; Ustun 2003; Zullo 2001) used urodynamic measurements pre and postoperatively, but put their emphasis on different parameters, not all using the measurements as their definition of cure. All but three studies reported the number of perioperative complications and types of complications (Maher 2004; Morris 2001; Wallwiener 1995). These three studies reported either no major complications or that the number of complications were similar in each arm.
Ten studies (Ankardal 2004; Ankardal 2005; Carey 2000; Cheon 2003; Foote 2004; Kitchener 2006; Maher 2004; Mirosh 2005; Paraiso 2004; Valpas 2004) assessed quality of life as an outcome, however all the studies used various assessment questionnaires (for example (Short Form 36 (SF‐36), King's Health Questionnaire (KHQ), Incontinence Impact Questionnaire (IIQ), Urogenital Distress Inventory (UDI)) and in differing combinations. Two studies (Cheon 2003; Mirosh 2005) that assessed quality of life did not report which validated questionnaire they used and did not report the results.
All studies with the exception of one (Morris 2001) reported follow‐up outcomes within 18 months. Three studies (Burton 1997; Kitchener 2006; Zullo 2001) had a follow‐up time longer than 18 months and within five years and three studies (Burton 1997; Morris 2001; Paraiso 2004) reported on follow up after five years.
Further characteristics of the trials are reported in the tables 'Characteristics of included studies' and 'Characteristics of excluded studies'.
Risk of bias in included studies
Allocation concealment
Ten trials used an adequately concealed group allocation (Ankardal 2004; Ankardal 2005; Burton 1997; Cheon 2003; Fatthy 2001; Kitchener 2006; Summitt 2000; Paraiso 2004; Persson 2002; Persson 2000) while in seven trials no details were given about concealment of group allocation (Carey 2000; Foote 2004; Maher 2004; Ross 1995; Valpas 2004; Wallwiener 1995; Zullo 2001). In one study a random sequence of group allocation had initially been achieved by computer‐generated random numbers in sealed, opaque envelopes; then four participants, who were not willing to undergo laparoscopic colposuspension, were enrolled to the open colposuspension group, the respective next participant was assigned to the laparoscopic procedure and the following participants went back to the sequence of random numbers (Su 1997).
Blinding
Carey 2000 blinded participants and assessors, where the abdominal wounds were dressed in theatre in an identical fashion so that both participants and ward staff were masked to the procedure performed until removal of dressings prior to discharge. In one study participants could refuse one treatment and were allocated to the other group (Su 1997). In four studies assessors were blind to the type of operation performed but the participants were not (Burton 1997; Fatthy 2001; Zullo 2001; Persson 2002). Four study reports mentioned that assessors were not blinded (Persson 2000; Su 1997; Kitchener 2006; Ankardal 2004).
Data‐dependent stopping
Three trials were stopped earlier than intended. Persson 2000 set out to enrol 280 participants but the trialists became convinced during follow‐up that one trial arm had a higher cure rate. For ethical reasons they therefore performed an interim analysis on the objective one‐year cure rate on 108 participants, which confirmed a significantly higher cure rate in one group. Thereafter, further enrolment was stopped and only the 161 participants who had already been recruited were followed up and the analysis was adjusted for the early stopping. Su 1997 employed early stopping rules with evaluation points, which were determined before the beginning of the trial. The trial was stopped at the second evaluation point but no further explanation was given; 92 of 152 intended participants were recruited. In Valpas 2004 the number of women recruited fell short of the target owing to limitations of time and recruiting problems and for these reasons this study was also stopped prematurely. However, in this study the groups were still considered to be comparable and the data were analysed without adjustment after stopping the study.
Dropouts and losses to follow‐up
Eleven studies reported losses to follow‐up and dropouts (Ankardal 2004; Ankardal 2005; Burton 1997; Fatthy 2001; Maher 2004; Paraiso 2004; Persson 2000; Persson 2002; Kitchener 2006; Valpas 2004; Zullo 2001) that ranged from 1 to 22 participants across the studies.
Effects of interventions
Hypothesis 1: laparoscopic colposuspension versus no treatment or sham operation
No eligible studies were found.
Hypothesis 2: laparoscopic colposuspension versus conservative management
No eligible studies were found.
Hypothesis 3: laparoscopic colposuspension versus open colposuspension
Ten trials compared laparoscopic with open colposuspension (Ankardal 2004; Ankardal 2005; Burton 1997; Carey 2000; Cheon 2003; Fatthy 2001; Kitchener 2006; Morris 2001; Su 1997; Summitt 2000). All had different lengths of follow‐up: Carey et al (Carey 2000) for six months; Su et al (Su 1997), Ankardal et al studies (Ankardal 2004; Ankardal 2005), Cheon et al (Cheon 2003) and Summitt et al (Summitt 2000) for one year; Fatthy et al (Fatthy 2001) for six and 18 months; Smith et al (Kitchener 2006) for six, 12 and 24 months; and Burton et al (Burton 1997) for six months, one year, three years and five years. Outcome data for 'six months to 18 months' were therefore available for eight studies. Longer‐term data, over five years, were only available for two studies (Burton 1997; Morris 2001) and the study by Morris et al had only five to seven year follow‐up data with no earlier follow‐up results reported. The ability to synthesise data was also limited by the variable tests and definitions used to measure subjective and objective outcomes across the trials and failure to report standard deviations. For these reasons some data are reported in the 'Additional tables' (Tables 1‐9).
Women's observations
Subjective cure rates ranged from 58% to 96% in the open and 62% to 100% in the laparoscopic group within the 18 months follow‐up, with a non‐significant 5% lower relative subjective cure rate for laparoscopic colposuspension (Comparison 01.01.01; RR 0.95, 95% CI 0.90 to 1.00). Because of concerns about the effects of problems with randomisation and an inconsistent use of sutures for the different operations in the study Su 1997, we re‐ran the analysis after excluding this study and this did not change the results. The statistically significant heterogeneity mostly reflected the results of one Ankardal trial (Ankardal 2004), for which there were concerns that post randomisation withdrawals may have introduced bias. We could not include the results of the Burton 1997 trial in these analyses because of the way they had presented the data. In this trial (Table 4), based on visual analogue scales of 'cure', the open group had better results; increasingly so at three and five years. The Kitchener 2006 trial reported subjective cure rates at two years and there were no differences between the laparoscopic and open groups (Comparison 01.01.02; RR 1.00, 95% CI 0.81 to 1.25). The study Morris 2001 reported data from five to seven years of follow‐up, however, this differed from the results reported in Burton 1997 as they showed that the laparoscopic colposuspension group had a significantly higher subjective cure rate than the open colposuspension group (Comparison 01.01.03; RR 1.53, 95% CI 1.00 to 2.35).
Table 1.
Burton 1997: subjective cure on visual analogue scale 1‐10 (means)
| 6/12 | 1 year | 3 years | 5 years | |
| open | 10.0 | 9.8 | 9.6 | 9.4 |
| laparoscopic | 7.8 | 6.7 | 4.8 | 4.4 |
Quantification of symptoms
Two studies used urinary diaries and pad tests to quantify symptoms at follow‐up (Burton 1997; Fatthy 2001). The results for the Burton 1997 are shown in the Additional tables (Table 5 and Table 6). Although both groups improved significantly after surgery this was less in the laparoscopic group. Furthermore, there was marked deterioration over time in this group such that by five years the mean number of incontinent episodes in the laparoscopic group was approaching the preoperative level. In contrast, there was no apparent difference between the groups in incontinent episodes at 18 months in Fatthy's study (Fatthy 2001) (Comparison 01.02; MD ‐0.12 episodes, 95% CI ‐0.68 to 0.92).
Table 2.
Burton 1997: incontinent episodes / day (mean)
| pre‐op | 6/12 | 1 year | 3 years | 5 years | |
| open | 12 | 0 | 2 | 2 | 3 |
| laparoscopic | 13 | 2 | 6 | 8 | 9 |
Table 3.
Burton 1997: pad test leakage in g (mean)
| pre‐op | 6/12 | 1 year | 3 years | 5 years | |
| open | 22 | 1 | 2 | 3 | 5 |
| laparoscopic | 24 | 5 | 12 | 14 | 15 |
Clinicians' measures
All 10 studies assessed leakage on a clinical stress test and they reported the data as objective cure rates. Six studies used negative urodynamic testing as their definition of cure and four studies (Ankardal 2004; Ankardal 2005; Kitchener 2006; Morris 2001) used a negative pad test as their definition of objective cure. Overall, objective cure rate within 18 months showed a statistically significant reduction of RR in laparoscopic colposuspension, thus favouring open colposuspension (Comparison 01.03.01; RR 0.91, 95% CI 0.86 to 0.96). The analysis for objective cure rates between 18 months and five years showed no significant differences between laparoscopic and open colposuspensions (Comparison 01.03.02; RR 1.01, 95% CI 0.88 to 1.16). There was, however, evidence of heterogeneity with the smaller Burton (Burton 1997) trial greatly favouring open colposuspension. Similar results were seen with the analysis of objective cure rates after five years' follow‐up as Burton 1997 reported objective cure rates favouring the open technique, which was opposite to the findings from Morris 2001 (Comparison 01.03.03; RR 0.94, 95% CI 0.69 to 1.27).
There were no statistically significant differences in de novo detrusor overactivity within 18 months (Comparison 01.04.01; RR 1.29, 95% CI 0.72 to 2.30). Longer‐term follow‐up data (between 18 months and five years and after five years) also showed no statistically significant difference (Comparisons 01.04.02 and 01.04.03; RR 1.00 and 1.22, 95% CI 0.07 to 15.12 and 0.40 to 3.75).
Similarly, there were no statistically significant differences in voiding dysfunction (Comparison 01.05; RR 0.82, 95% CI 0.50 to 1.35). Burton 1997 recorded higher residual urinary volumes at follow up in the laparoscopic group whereas in Fatthy 2001 the residual volumes were similar in the two groups (Table 7).
Table 4.
Residual volumes in ml (mean)
| Study | pre‐op | 6/12 | 1 year | 18/12 | 3 years | 5 years |
| Burton 1997 | ||||||
| open | 24 | 33 | 30 | 26 | 32 | |
| laparoscopic | 21 | 42 | 40 | 42 | 49 | |
| Fatthy 2001 | ||||||
| open | 23.9 | 30.95 | ||||
| laparoscopic | 26.65 | 32.85 |
Six studies used urodynamic investigations to assess cure objectively. Overall, there was a significantly higher success rate following open colposuspension (Comparison 01.06; RR 0.91, 95% CI 0.85 to 0.99). After exclusion of Su 1997 data the results still favoured open colposuspension (RR 0.92, 95% CI 0.84 to 1.00).
Quality of life
Five studies measured quality of life using a variety of questionnaires (Ankardal 2004; Ankardal 2005; Carey 2000; Cheon 2003; Kitchener 2006). Carey 2000 used the SF36 (Short Form 36), SUDI (Short Urogenital Distress Inventory) and IIQ questionnaires; both the SUDI and IIQ scores equally improved postoperatively in the two groups but no further details were available. Cheon 2003 assessed quality of life but details of the instrument used and further results were lacking in the study report. In both their studies, Ankardal and colleagues used a visual analogue score (VAS) to assess the bother symptoms caused and their impact on different quality‐of‐life domains (Ankardal 2004; Ankardal 2005). In Ankardal 2004, the scores had improved in all domains following surgery, in both groups; however, the improvement was greater in the open colposuspension group with regard to physical activity one year following surgery (Table 8). The study by Smith and colleagues (Kitchener 2006) used a number of validated questionnaires; these included SF‐36, the Bristol Female Lower Urinary Tract Symptom Questionnaire (BFLUTS), Symptom Severity and Symptom Impact Index and the EQ‐5D. Results for the SF‐36 and EQ‐5D were reported and showed that both treatment arms had improved scores after two years with no suggestion of any group differences (Table 9).
Table 5.
Ankardal 2004: Improvement on aspects of QoL one year after surgery
| Domain of QoL | laparoscopic colpo | Open colpo | p value |
| Physical activity | 63 (27‐81) | 74 (52‐84) | <0.05 |
| Working ability | 25 (4‐54) | 31 (10‐60) | NS |
| Social life | 37 (15‐66) | 38 (10‐65) | NS |
| Sexual life | 13 (1‐41) | 9 (0‐37) | NS |
| median (range) | median (range) |
Table 6.
Quality of Life at 24 months (EQ‐5D and SF‐36), mean scores (SD)
| Score at 24 months | Laparoscopic colpoe | Open colpo |
| EQ‐5D values | 0.844 (0.259) | 0.825 (0.270) |
| SF‐36 Physical sub‐scale | 79.32 (27.59) | 77.60 (27.74) |
| SF‐36 Mental sub‐scale | 69.51 (21.21) | 69.38 (22.65) |
Surgical outcome measures
There were significantly fewer perioperative complications in the laparoscopic colposuspension group (Comparison 01.07; RR 0.74, 95% CI 0.58 to 0.96). However, 21 bladder injuries were reported amongst 521 laparoscopic procedures compared with 10 amongst 507 open operations (Comparison 01.08; RR 1.88, 95% CI 0.93 to 3.83). Two studies reported cases of laceration to the obturator vein during laparoscopic colposuspension (Carey 2000; Summitt 2000).
Women who underwent a laparoscopic colposuspension appeared to have significantly less pain and needed less postoperative analgesia but data from the studies were not presented in a form suitable for quantitative synthesis (Burton 1997; Carey 2000; Cheon 2003; Fatthy 2001; Kitchener 2006; Su 1997). All studies with the exception of Morris 2001 reported the length of hospital stay to be longer for open colposuspension. Six studies reported data in such a way that could be analysed (Comparison 01.09; WMD 0.86 days, 95% CI 0.65 to 1.06) so favouring laparoscopic colposuspension due to a shorter hospital stay. There was, however, significant heterogeneity between the trials in this respect. The time to return to normal activities, where reported, was longer for open colposuspension (Table 10). Three women (10%) in the laparoscopic group in Burton 1997 had repeat incontinence surgery compared with none in the open group; none of the other studies reported this outcome.
Table 7.
Time to return to normal (days)
| Carey (mean) | Fatthy (mean) | Summitt (mean) | Cheon (mean) | |
| open | 21.8 | 31.5 | 37.3 | 29.3 |
| laparoscopic | 17.3 | 8.5 | 35.5 | 22.2 |
Other outcomes
Laparoscopic surgery took significantly longer than open colposuspension in the majority of the studies (Comparison 01.11; MD 14.06 minutes, 95% CI 11.39 to 16.73). Although there was significant statistical heterogeneity the results of the three largest trials (contributing 85% of the weight) were consistent in suggesting a 14 to 17 minute difference. The estimated blood loss was higher in the open groups in all studies that reported these data (Table 11). The duration of catheterisation was longer after open than after laparoscopic colposuspension in Ankardal 2004; Ankardal 2005; Burton 1997; Carey 2000; Cheon 2003; and Su 1997 but was similar for both procedures in Summitt 2000 (Table 12).
Table 8.
Estimated blood loss (ml)
| Burton(median+range) | Carey (mean) | Fatthy (mean+SD) | Su (mean +SD) | Summitt (mean) | Ankardal (mean) | Cheon (mean) | |
| open | 261 (120 ‐ 410) | 171 | 240.5 (35.5) | 134.3 (102.0) | 131.9 | 105 | 327 |
| laparoscopic | 190 (180 ‐ 290) | 125 | 42.75 (7.2) | 59.3 (42.1) | 112 | 35 | 125 |
Table 9.
Duration of catheterisation (days)
| Burton (mean) | Carey (mean) | Su (mean + SD) | Summitt (mean) | Ankardal (mean + SD) | Cheon (mean +SD) | |
| open | 1.7 | 4.9 | 6.8 (2.3) | 2.7 | 4.9 (8.3) | 3.7 (2.8) |
| laparoscopic | 1.33 | 4.4 | 3.9 (1.9) | 2.7 | 1.9 (2.4) | 3.0 (1.6) |
Hypothesis 4: laparoscopic colposuspension versus needle suspension
No eligible studies were found.
Hypothesis 5: laparoscopic colposuspension versus traditional sling procedures
No eligible studies were found.
Hypothesis 6: laparoscopic colposuspension versus newer 'self‐fixing' sling procedures
Eight studies compared laparoscopic colposuspension with newer 'self‐fixing' sling procedures (Adile 2001; Foote 2004; Mirosh 2005; Maher 2004; Paraiso 2004; Persson 2002; Ustun 2003; Valpas 2004). Within these eight studies there were variations in the techniques (TVT or SPARC slings) and type of material (sutures or mesh) used for both of the procedures; for this reason we have displayed subgroups within the comparison graphs. All studies reported data within 18 months and the majority of the studies had follow‐up at one year postoperatively (Foote 2004; Paraiso 2004; Persson 2002; Mirosh 2005; Valpas 2004). The ability to synthesise data was limited in some areas by the variable tests and definitions used for subjective and objective outcomes and for this reason some data were reported in the Additional tables. A published supplementary version of the study by Paraiso reported long‐term follow‐up (four to eight years) (Paraiso 2004).
Women's observations
Subjective cure rates were near equal in all studies that compared laparoscopy using sutures with vaginal slings, but Valpas 2004 used a mesh for the laparoscopic colposuspension and the subjective cure rate favoured the sling procedure. Overall, there was no statistically significant difference in the reported subjective cure rates between laparoscopic colposuspension and vaginal sling procedures within 18 months (Comparison 02.01; RR 0.91, 95% CI 0.80 to 1.02). This appeared to remain the case in the longer‐term follow‐up (four to eight years), as TVT was reported to have similar subjective cure rates as laparoscopic colposuspension (Paraiso 2004) (Comparison 02.10; RR 1.18, 95% CI 0.36 to 3.81).
Quantification of symptoms
Two studies (Foote 2004; Paraiso 2004) reported the mean number of incontinent episodes per week in each group. Although the reporting was incomplete and not statistically significant, both the means were lower in the laparoscopic groups (Comparison 02.02; WMD ‐1.40, 95% CI ‐3.30 to 0.50). Valpas 2004 reported pad test data but not in a way suitable for analysis.
Clinicians' measures
All but one of the studies (Mirosh 2005) assessed objective cure rates within 18 months . The definitions of objective cure varied across the studies as they used negative pad tests (Persson 2002; Valpas 2004), negative clinical stress tests (Valpas 2004), negative urodynamic tests (Maher 2004; Paraiso 2004; Ustun 2003) or no leaks recorded on urinary diary (Foote 2004). The objective cure rate was higher for TVT when compared with laparoscopy using sutures (Comparison 02.03.01; RR 0.92, 95% CI 0.85 to 0.99) and also in Valpas 2004, when TVT was compared with laparoscopy using mesh (Comparison 02.03.02; RR 0.66, 95% CI 0.51 to 0.86). The report from Adile 2001 was unclear about the exact timing of the follow‐up, which could have been any time from six to 36 months. When we re‐ran the analysis excluding this trial the effect estimate was unchanged but was no longer statistically significant (RR 0.92, 95% CI 0.83 to 1.02). In Foote 2004 there was no statistically significant difference between the groups for the objective cure rates within 18 months when laparoscopy (67% objective cure) was compared with SPARC sling (65% objective cure) (Comparison 02.03.03; RR 1.05, 95% CI 0.72 to 1.52). Overall, laparoscopic colposuspension procedures had statistically significantly lower objective cure rates (RR 0.88, 95% CI 0.81 to 0.95).
Only two studies reported urge symptoms (Foote 2004; Valpas 2004) and showed that urgency was more common in the sling groups (Table 13). There was no difference in de novo detrusor overactivity within 18 months (Comparison 02.04; RR 0.80, 95% CI 0.34 to 1.88); three of the studies reporting this outcome (Adile 2001; Paraiso 2004; Ustun 2003) had higher rates of overactivity in the vaginal sling group but tMaher 2004 reported the opposite, with overactivity being more common in the laparoscopic colposuspension group. Similarly, there was no apparent overall difference in voiding dysfunction (Comparison 02.05; RR 1.06, 95% CI 0.47 to 2.41). However, the numbers in each of the groups with these outcomes were small.
Table 10.
Number reporting Urge symptoms: Lap colpo vs Vaginal sling
| Study | Laparoscopic colpo | Vaginal sling |
| Foote 2004 | 3/40 | 6/40 (SPARC) |
| Valpas 2004 | 0/51 | 2/70 (TVT) |
Urodynamic investigations were used to assess cure objectively in three studies (Maher 2004; Paraiso 2004; Ustun 2003) and showed no difference between the two procedures (Comparison 02.06; RR 0.91, 95% CI 0.80 to 1.03).
Quality of life
Five studies assessed quality of life (QoL) as an outcome (Foote 2004; Maher 2004; Mirosh 2005; Paraiso 2004; Valpas 2004). These studies each used a varying number of validated questionnaires (UDI, IIQ, SF‐36, KHQ and visual analogue scores) and reported the data in different ways so that the results could not be combined. Mirosh 2005 gave no details of the quality‐of‐life instrument used and just reported the QoL scores to be similar in each group at one‐year postsurgery. Foote 2004; Maher 2004; and Paraiso 2004 all reported a significant improvement in QoL measures in both laparoscopic and vaginal sling groups but no differences between the two groups. In one study this improvement was reported to be maintained for the longer‐term follow‐up of four to eight years (Paraiso 2004). Only one study (Valpas 2004) reported a significant difference between the two procedures, in VAS scores and in the majority of the domains in King's Health Questionnaire scores at one year postsurgery; this difference was in favour of the TVT procedure.
Surgical outcome measures
Seven of the studies reported perioperative complications. Only Maher 2004 was lacking this information. However, this study did report that the postoperative complications were similar in each group. There was no difference in the perioperative complication rates between laparoscopic colposuspension and vaginal sling procedures (Comparison 02.07; RR 0.99, 95% CI 0.60 to 1.64).
Only two studies assessed the use of postoperative analgesia and pain relief (Paraiso 2004; Valpas 2004). Valpas 2004 reported that the use and doses of analgesics were lower in the TVT group, whereas Paraiso 2004 reported that the length of time (in hours) that patient‐controlled analgesia was used was equal in both groups.
The length of inpatient stay significantly differed between the two groups although by only one day (Comparison 02.08; MD 1.10, 95% CI 0.79 to 1.41) and favoured the vaginal sling for shortest hospital stay. The time to return to normal activities, where reported, was longer for laparoscopic colposuspension (Table 14).
Table 11.
Mean time to return to normal activities: Lap colpo vs Vaginal sling
| Study | Laparoscopic colpo | Vaginal sling |
| Foote 2004 | 3.8 weeks | 2.8 weeks |
| Maher 2004 | 25 days | 17.9 days |
| Valpas 2004 | 24 days | 15 days |
Persson 2002 reported re‐operation rates at one year, with three out of 38 women in the TVT group and one out of 32 woman in the laparoscopic colposuspension group requiring repeat surgery for non‐cure.
Other outcomes
Laparoscopic surgery took significantly longer than the vaginal sling surgery, by an average of 20 minutes (Comparison 02.09; MD 20.31 minutes, 95% CI 16.75 to 23.86). There was significant statistical heterogeneity reflecting the two trials (Mirosh 2005; Ustun 2003) that contributed least weight to the comparison. The duration of indwelling catheterisation was reported to be longer in the laparoscopic colposuspension group in three trials (Maher 2004; Ustun 2003; Valpas 2004) and longer in the TVT group in one trial Paraiso 2004; we have displayed these results in the Additional tables (Table 15).
Table 12.
Mean duration of catheterisation (days): Lap colpo vs Vaginal sling
| Study | Lap colpo | Vaginal sling (TVT) |
| Maher 2004 | 2.7 | 1.4 |
| Unstan 2003 | 3 (range 1‐5) | 1 (range 0‐7) |
| Valpas 2004 | 24.4 hours | 9.2 hours |
| Paraiso 2004 | 4.9 | 5.2 |
Hypothesis 7: laparoscopic colposuspension versus anterior repair
No eligible studies were found.
Hypothesis 8: laparoscopic colposuspension versus periurethral injections
No eligible studies were found.
Hypothesis 9: one method of laparoscopic colposuspension is better than another method
Five studies looked at different methods of laparoscopic colposuspension. One compared one double‐bite suture with two single‐bite sutures each side of the urethra (Persson 2000), three compared mesh and staples with sutures (Ankardal 2005; Ross 1995; Zullo 2001) and the final study compared two different methods of laparoscopic approach (Wallwiener 1995).
i) One versus two sutures
Women's observations
Persson 2000 reported subjective cure rates using the women's description of: cure, improvement and non‐improvement. A significantly greater number of women felt cured (89%) in the two‐suture compared to the one‐suture group (65%) (Comparison 03.01.01; RR 1.37, 95% CI 1.14 to 1.64).
Quantification of symptoms
Cure was quantified by an 'ultrashort' pad test assessment. The number of cured women was again significantly higher in the two‐suture group compared to one‐suture (Comparison 03.03.01; RR 1.42, 95% CI 1.14 to 1.77) with an 83% cure rate for two sutures compared with a 58% cure rate for one suture.
Clinicians' measures
Four of 83 women in the two‐suture group compared with six of 78 in the one‐suture group had postoperative urge symptoms. The equivalent numbers for voiding dysfunction were 3 and 1 women, respectively (Comparison 03.06.01; RR 2.82, 95% CI 0.30 to 26.54). The mean residual urinary volume at follow up was 25 mL in the one‐suture group and 30 mL in the two‐suture group.
Quality of life
No data reported.
Surgical outcome measures
Fourteen women in the one‐suture group and 15 in the two‐suture group had a perioperative surgical complication (Comparison 03.07.01; RR 0.88, 95% CI 0.45 to 1.70). One woman in the one‐suture group had pubic bone osteitis after the operation. The median length of hospital stay was 1.7 days in both groups. One women in the two‐suture group had repeat incontinence surgery.
Other outcomes
The median operating time was 17 minutes longer among those allocated to two sutures. Among women without additional surgery, mean blood loss was similar in the two groups. The mean time of catheterisation was 2.5 days in both groups. One year after surgery one woman in the one‐suture group and four in the two‐suture group were lost to follow‐ up. Of the remainder, four in the one‐suture group and seven in the two‐suture group did not provide a follow‐up pad test. The cure rates given were for the number of women at follow‐ up.
ii) Sutures versus mesh and staples
Women's observations
Ross 1995 did not report subjective methods of cure or improvement. Ankardal 2005 and Zullo 2001 reported significantly better subjective cure rates with sutures than mesh within 18 months (Comparison 03.01.02 and 02.02; RR 1.28, 95% CI 1.11 to 1.47).
Quantification of symptoms
No data quantifying leakage were reported.
Clinicians' measures
All studies reported failure of objective cure as leakage on the clinical stress test. In Zullo 2001 there were more failures in the mesh and staples group; analysis of the trials showed a significantly better objective cure rate in the suture group within 18 months (Comparison 03.03.02; RR 1.20, 95% CI 1.07 to 1.35 ). Objective cure data were also reported at three years' follow‐up in Zullo 2001 and again, tended to favour the method using sutures, but this was not significant (Comparison 03.04; RR 1.50, 95% CI 0.83 to 2.70). Two studies measured de novo detrusor overactivity and found no difference between the groups (Ross 1995; Zullo 2001) (Comparison 03.05; RR 0.72, 95% CI 0.17 to 3.06).
Quality of life
No data reported.
Surgical outcome measures
There were no statistically significant differences between the number of postoperative complications in two studies (Ross 1995; Zullo 2001) however, the meta‐analysis included the study by Ankardal et al (Ankardal 2005) and resulted in significantly fewer complications in the mesh group (Comparison 03.07.02; RR 1.94, 95% CI 1.09 to 3.48). In both Ankardal 2005 and Ross 1995 there were more (four and two, respectively) bladder perforations in the suture group than in the mesh group (one perforation) and in Zullo 2001 there was one in each of the groups. In two studies (Ross 1995; Zullo 2001), length of hospital stay was the same regardless of whether sutures or mesh were used. In Ankardal 2005, the length of hospital stay was less in the mesh group (Table 16). In Ross 1995 one woman in the mesh group and two women in the suture group had repeat incontinence surgery.
Table 13.
Laparoscopic colposuspension (sutures vs Mesh)
| Mean +/‐ SD | Sutures | Mesh |
| Time of Surgery (min) | 84+/‐30 | 74+/‐25 |
| Time with bladder drainage (days) | 6.2+/‐9.2 | 1.9+/‐2.5 |
| Length of stay in hospital (days) | 3.3+/‐2.5 | 2.1+/‐1.3 |
Other outcomes
Not applicable.
iii) Transperitoneal versus extraperitoneal laparoscopic colposuspension
One study compared a transperitoneal approach with an extraperitoneal approach for laparoscopic colposuspension (Wallwiener 1995), using a mixture of sutures or mesh stapler fixation, but it was not clear which method of fixation was used with which operation. The sample size was small (n = 22).
Women's observations
Subjective assessment by the participants was a criterion for evaluating outcome but no further information was given.
Quantification of symptoms
No data reported.
Clinicians' measures
Urodynamic assessment, clinical findings and perineal sonography to control the anatomic correction of bladder neck descent were performed but no data were given. Overall, 18 out of 22 women were subjectively and objectively cured, one was unchanged and one was worse. One woman had postoperative detrusor overactivity.
Quality of life
No data reported.
Surgical outcome measures
Two perioperative complications were reported of which one was a bladder injury.
Other outcomes
Surgery lasted between 45 to 105 minutes. The length of follow‐up varied between two and 12 months.
Discussion
The 22 eligible trials that were identified addressed only three of the pre‐stated hypotheses. In particular, there were no comparisons with non‐surgical management. Nevertheless, the three hypotheses that were addressed were the most obvious areas of clinical uncertainty. These were whether colposuspension should be performed laparoscopically rather than by open surgery; how laparoscopic colposuspension compares with other, newer minimal access procedures (self‐fixing slings); and what laparoscopic techniques should be used.
To supplement the main systematic review of effects, we sought to identify economic evaluations that have compared laparoscopic colposuspension with any of the other main categories of surgical procedures listed in the background section. A supplementary search in NHS EED, MEDLINE and Embase identified two such economic evaluations.
Hypothesis 3: laparoscopic colposuspension versus open colposuspension
Eight of the 10 trials comparing laparoscopic with open colposuspension were of good quality (Ankardal 2004; Ankardal 2005; Burton 1997; Carey 2000; Cheon 2003; Fatthy 2001; Kitchener 2006; Summitt 2000). Burton 1997 had the potentially confounding factors of using absorbable sutures and the surgeon only having carried out a relatively small number of laparoscopic colposuspensions (fewer than 20) before commencing the trial. Cheon 2003 also involved surgeons with relatively little experience, only 15 previous laparoscopic colposuspensions. These factors may have influenced the results, in particular since there is believed to be a definite, albeit relatively steep, learning curve associated with laparoscopic colposuspension. The first of Ankardal's studies in 2004 (Ankardal 2004) differed from the other studies, as they used a polypropylene mesh and staples for the laparoscopic procedure rather than sutures; this may explain why this study has cure rates in favour of the open technique. However, if this study is removed from the analysis, the overall results do not change. Su 1997 had methodological problems with corrupted randomisation, confounding factors of performance of additional surgery in some participants, and the use of a different number of sutures for laparoscopic colposuspension (one suture) and open colposuspension (three sutures). As shown elsewhere in the review, the number of sutures used appears to have a significant influence on the cure rate, with more sutures resulting in a significantly higher success rate (Persson 2000) (see below). For these reasons, we have repeated some meta‐analyses in this review after excluding data from Su 1997. This, again, did not have an effect on the meta‐analysis results.
Three trials currently have data beyond 18 months' follow‐up (Burton 1997; Morris 2001; Kitchener 2006). Burton 1997 suggested poorer long‐term results after laparoscopic surgery. This finding should be interpreted cautiously, however, as there are concerns that the surgeon's laparoscopic performance may have been suboptimal, as he had performed few laparoscopic colposuspensions when the trial started. The Morris 2001 results disagree and suggest poorer long‐term cure rates for open colposuspension. However this trial has a very limited study report, in abstract form, and only reports five to seven years' follow up, with no earlier data. The data from Kitchener 2006 is more reliable, as it was a larger trial with multiple operators and the follow‐up at two years showed no significant differences between the cure rates of the two procedures.
The data that are available up to a maximum of 18 months showed some inconsistencies. Outcomes assessed by the women participating (arguably the most important outcome) appear equally good in the two groups, whereas objectively and urodynamically‐assessed cure rates were lower in the laparoscopic group.
No significant differences between the two groups were observed for postoperative urgency, voiding dysfunction or de novo detrusor overactivity. Other short‐term outcomes have shown lower perioperative complication rates, longer operation times, less postoperative pain, shorter hospital stay and a quicker overall recovery with laparoscopic colposuspension. All of these are consistent with reviews of other laparoscopic operations (McCormack 2001).
It is noteworthy that this rigorous systematic review has shown significant differences, in comparison with a published conventional review in the British Medical Journal. Thakar and Stanton (Thakar 2000) quoted laparoscopic colposuspension to be 20% less successful than open colposuspension, which is not consistent with our findings. They quoted two references of which one was to a trial of poor methodological quality.
Economic evidence
A cost‐effectiveness analysis by Dumville 2006, alongside a randomised controlled trial, compared open colposuspension with laparoscopic colposuspension in women with SUI in the UK. The cost analysis was conducted from the perspective of the UK NHS and healthcare resource use (2002 to 2003, GBP) relating to the surgery, associated hospital stay and first six months after hospital discharge were collected prospectively for each participant. The data required for the calculation of quality adjusted life years (QALYs) were collected prospectively using the EQ‐5D‐3L questionnaire at baseline, 6, 12 and 24 months.
The economic evaluation was for both a six‐month and up‐to‐24‐month time horizon. Healthcare resource use over six‐month follow‐up resulted in costs of GBP 1805 for the laparoscopic arm and GBP 1433 for the open arm (differential mean cost GBP 372, 95% credibility interval (CrI) 274 to 471). At six months, QALYs were slightly higher on average in the laparoscopic arm relative to the open arm (0.005, 95% CrI –0.012 to 0.023). On average the incremental cost per extra QALY provided by the laparoscopic approach was GBP 74,400 at six months. At 24 months, the laparoscopic arm again had higher mean QALYs compared to the open‐surgery group (0.04, 95% CrI ‐0.009 to 0.086). If the laparoscopic colposuspension did not incur any significant additional costs after six months compared with open colposuspension, then the incremental cost per extra QALY reduced to GBP 9300 at 24 months. The probability that laparoscopic colposuspension is cost effective was 86% when the decision maker was willing to pay up to GBP 30,000 for an additional QALY. Dumville 2006 concluded that laparoscopic colposuspension is not cost effective when compared with open colposuspension during the first six months but the additional QALYs might be judged to be worth the additional cost after 24‐months' follow‐up.
Hypothesis 6: laparoscopic colposuspension versus newer 'self‐fixing' sling procedures
The eight trials that we included in this review comparing laparoscopic colposuspension with sling procedures involved only newer, 'self‐fixing' slings. They were generally of good quality, with the exception of two (Adile 2001; Mirosh 2005). Adile 2001 gave no details of the randomisation process and the exact timing of the follow‐up was unclear, being anywhere between 6 to 36 months. Mirosh 2005 had no description of the randomisation or allocation process and had only a very small number of participants in each group (14 women in the laparoscopic group and 16 women in the TVT group). For these reasons, the data from these two trials must be interpreted with caution. Maher 2004 only recruited women with recurrent urinary stress incontinence and this different inclusion criterion may have influenced the results from this trial.
As the 'self‐fixing' vaginal slings are relatively new procedures, long‐term follow‐up studies are lacking. Only one study reported long‐term follow‐up of four to eight years (Paraiso 2004). Overall, this review has shown that the subjective cure rates are equally good for both of these minimal access techniques, both in the short and long term. However, the objective cure rate within 18 months appears to favour the vaginal sling technique, especially TVT, when compared to laparoscopy using a mesh or sutures. However, three studies assessed the urodynamic cure rate (Maher 2004; Paraiso 2004; Ustun 2003), all comparing laparoscopic sutures with TVT, and there was no significant difference in the outcome rates. There were no significant differences between the two procedures for the rates of postoperative voiding dysfunction, de novo detrusor overactivity and perioperative complications.
Laparoscopy has a longer operation time, longer hospital stay and slower return to normal activities. The re‐operation rates at one year were reported in one trial (Persson 2002) and TVT had a higher re‐operation rate. Longer‐term data are now emerging with regard to laparoscopic colposuspension and there is a need for more long‐term follow‐up of 'self‐fixing' sling procedures. One study in this review (Paraiso 2004) reported long‐term follow‐up and concluded that TVT has similar long‐term satisfaction rates to laparoscopic colposuspension. However, the study also reported that a substantial proportion of subjects had some degree of urinary incontinence at four to eight years following surgery, but the majority was not bothersome. Like laparoscopic surgery, the newer vaginal slings have all the advantages of minimal access techniques, and this review has shown that they are as, if not more, clinically effective than laparoscopic colposuspension. As the skill needed to perform laparoscopic colposuspension is greater than that needed for the 'self‐fixing' slings, many surgeons training in the techniques of surgery for urinary stress incontinence are more likely to become efficient in the sling procedures. While there is still a trend in favour of the sling procedures, more studies reporting longer‐term data are needed as unanticipated and even anticipated complications may arise from these newer procedures.
Economic evidence
Valpas 2006 reported a cost‐effectiveness analysis alongside a randomised controlled trial that compared laparoscopic mesh colposuspension with TVT as a primary surgical treatment in women with SUI over a follow‐up period of one year in Finland. The primary outcome was negative stress test and 48‐hour pad test (<8g/48h) and secondary outcomes were health‐related quality of life. These were collected prospectively during the main period of hospitalisation, six weeks after surgery, and after one year of follow‐up. Cost items included costs of the treatments in each treatment arm, other hospital costs, and productivity costs.
Primary and secondary outcomes in the TVT group were significantly better than laparoscopic mesh colposuspension as measured by the negative stress test (60 versus 29; 95% CI for change between the groups 12.7 to 43.9), visual analogue scale (VAS) (0 = no inconvenience at all; 10 = maximal inconvenience) (0.8 versus 2.4; 95% CI for change between the groups 0.65 to 2.07), and Urinary Incontinence Severity Score (UISS) (1.1 versus 2.8; 95% CI for change between the groups 0.27 to 2.94). The between‐group difference in the 48‐hour pad test did not reach statistical significance (3 versus 12.4; 95% CI for change between the groups ‐2.8 to 30.4; P = 0.105). The total costs per participant at one year of follow‐up for laparoscopic mesh colposuspension was EUR 3262 while TVT cost EUR 2081 (2000 EUR). Valpas 2006 concluded that when the VAS or UISS are used as the outcome measure, TVT is more cost‐effective than laparoscopic mesh colposuspension over a follow‐up period of one year (P < 0.0001).
Another cost‐effectiveness analysis (Cody 2003) compared TVT with Burch colposuspension, laparoscopic colposuspension, traditional suburethral retropubic sling procedure and injectables. The study utilised clinical data from a systematic review of RCTs conducted up to mid‐2002 and the results modelled for a time horizon of up to 10 years. The analysis of costs and resources used was based on the UK payer’s perspective (UK National Health Service). Based on clinical evidence, this study assumed that traditional sling effectiveness was equivalent to open colposuspension, that the effectiveness of laparoscopic colposuspension was equivalent to or possibly worse than open colposuspension, and that use of injectables was the least effective procedure. This study reported the cost (2001 GBP) to be GBP 1058 per woman with an average of 2.9 days hospital stay for TVT, GBP 1317 per woman and average hospital stay of 4.6 days for laparoscopic colposuspension, GBP 1301 per woman and average hospital stay of 7.1 days for open colposuspension, GBP 1340 per woman and average hospital stay of 7.2 days for traditional sling and GBP 1305 per woman with an average hospital stay of 2 days for injectables. The study concluded that TVT was more likely to be considered cost‐effective compared with the other surgical procedures based on the assumptions that traditional slings have the same effectiveness as open colposuspension and are also more costly; that laparoscopic colposuspension has the same or lower effectiveness as open colposuspension and similar costs; and that injectable agents are less effective than TVT but of greater cost.
We did not subject these two identified economic evaluations to critical appraisal and we do not attempt to draw any firm or general conclusions regarding the relative costs or efficiency of laparoscopic colposuspension in treatment of SUI. However, the economic evidence available suggests that laparoscopic colposuspension is not cost‐effective when compared with TVT in the treatment of SUI in women.
Hypothesis 9: different methods of laparoscopic colposuspension
i) One suture versus two sutures
A single study (Persson 2000) comparing different numbers of paravaginal sutures found a significantly higher objective one year cure rate (dry on 'ultrashort' pad test) for women randomised to two sutures compared with one suture, with a 83% cure rate for two sutures and a 58% cure rate for one suture. These findings were supported by a significantly higher subjective impression of cure in the two‐sutures group compared to the one‐suture group, with subjective cure rates of 89% and 65% respectively.
This study was of good quality, with adequate group allocation. However, the trial was stopped early as it became apparent at an interim analysis that two sutures were superior to one suture. Such data‐dependent stopping may lead to an exaggeration of the true effect size. Another concern is the potential confounding from one third of the women having additional surgery.
ii) Sutures versus mesh and staples
Sutures appeared to be more effective than mesh and staples. Two of the studies (Ross 1995; Zullo 2001) were small and the confidence intervals were wide. Cure was not clearly defined and it was unclear how the women were randomised in Ross 1995; we assumed that they used a negative cough stress test as a proof of cure, which was found to be similar for both groups. They did not report subjective measures. The trialists set out to prove equivalence between the two techniques as they found the technique of mesh and staples much easier to apply than sutures. However, the methodological problems mean that this question was not addressed reliably by this study. Zullo 2001 was of a similar size with clearly stated definitions of both objective and subjective cure, and adequate randomisation and concealment of allocation. This study reported outcomes in favour of sutures. The analysis with the addition of Ankardal 2005, which is a larger study and of good quality, showed significant subjective and objective outcomes favouring the use of sutures over mesh. However, Ankardal 2005 had fewer perioperative complications (mainly bladder perforations) with the mesh and staples technique, making the overall analysis results favour the use of mesh for perioperative complications.
iii) Transperitoneal versus extraperitoneal laparoscopic colposuspension
Wallwiener 1995, comparing transperitoneal with extraperitoneal laparoscopic colposuspension, was of poor quality and had very small numbers of participants. It is unclear how randomisation was achieved and it was difficult to interpret which suture material was used for which operation. Their cure rate was expressed as an overall 'subjective and objective' cure. Women's evaluation of cure was part of the outcome measures but it is unclear how it contributed. The cure rate was not given separately for the two groups. All the above make valid conclusions from this study impossible.
Economic evidence
No relevant economic evidence was identified for the brief economic commentary.
Authors' conclusions
Like other laparoscopic operations, laparoscopic colposuspension appears to have short‐term benefits over open surgery, such as quicker recovery, less pain and fewer perioperative complications; but it appears to be more costly and takes longer to perform. A single trial raises concerns about the long‐term performance but this may reflect a learning effect and is not reliable data on its own. The recent addition of medium‐term results from a large, multicentre trial is encouraging for the effectiveness of laparoscopic colposuspension. Newer sling procedures appear to offer even greater benefits of minimal access surgery, have better objective outcomes in the short term, and similar subjective outcomes in the longer term. If laparoscopic colposuspension is performed, two paravaginal sutures appear to be more effective than one suture or the use of mesh and staples. It is unclear whether an extraperitoneal approach has advantages over a transperitoneal method. The place of laparoscopic colposuspension in clinical practice should become clearer when ongoing trials with longer‐term data are reported.
To provide further information there is a need for well‐designed randomised controlled trials with adequate sample sizes to assess the effectiveness of laparoscopic colposuspension in comparison with other surgical and non‐surgical management options. Further recruitment to ongoing trials should be strongly encouraged and good reporting is needed to make these and completed trials worthwhile.
Future research in incontinence treatments should incorporate standardised, validated and simple outcome measures that are relevant to women who have incontinence in order to allow comparison across studies, particularly with regard to quality of life and economic health measures.
Surgical trials related to urinary incontinence should systematically address surgical morbidity outcomes such as adverse perioperative events, pain scores, length of hospital stay, time to return to normal activities, development of urge symptoms or detrusor overactivity and, especially, the need for repeat surgery or alternative interventions.
Long‐term follow‐up is essential for the proper evaluation of incontinence treatments, and this should be included in all trials of laparoscopic colposuspension.
Acknowledgements
For the original review
Jean Hay‐Smith, Peter Herbison and Gaye Ellis were very helpful with discussions on the form of the review, data interpretation and trial selection. Michelle Fynes has critically read and commented on the final draft of the original review.
For this version of the review (May 2006)
We would like to thank the previous authors, Birgit Moehrer and Marcus Carey, for their contributions to the original review.
Appendices
Appendix 1. Search strategies for the brief economic commentary (BEC)
We performed additional searches for the brief economic commentary (BEC). These were conducted in NHS EED (1st Quarter 2016), MEDLINE (1 January 1946 to March 2017) and Embase (1 January 1980 to 2017 Week 12). All searches were conducted on 6 April 2017. We used one search strategy on NHS EED (OVID) and two different search strategies on MEDLINE and Embase (OvidSP). Details of the searches run and the search terms used can be found below.
NHS EED (Ovid) (1st Quarter 2016)
We searched NHS EED using the following search strategy:
1. Urinary incontinence/
2. Urinary incontinence, stress/
3. ((stress$ or mix$ or urg$ or urin$) adj3 incontinen$).tw.
4. Colporrhaphy.tw.
5. Colpoperineoplast$.tw.
6. Sling procedure$.tw.
7. Sling$ procedure$.tw.
8. Bladder neck needle suspension$.tw.
9. Anterior vaginal repair$ .tw.
10. Or/1‐9
MEDLINE (1 January 1946 to March 2017), Embase (1 January 1980 to 2017 Week 12)
We used two different search strategies on MEDLINE and Embase (OvidSP) ‐ these are given below.
Search strategy 1:
1. Economics, Pharmaceutical/ or Economics, Medical/ or Economics/ or Economics, Hospital/ or economics.mp. or Economics, Nursing/
2. exp "costs and cost analysis"/
3. "Value of Life"/
4. exp "fees and charges"/
5. exp budgets/
6. budget*.ti,ab.
7. cost*.ti.
8. (economic* or pharmaco?economic*).ti.
9. (price* or pricing*).ti,ab.
10. (cost* adj2 (effective* or utilit* or benefit* or minimi* or unit* or estimat* or variable*)).ab.
11. (financ* or fee or fees).ti,ab.
12. (value adj2 (money or monetary)).ti,ab.
13. ((energy or oxygen) adj cost).ti,ab.
14. (metabolic adj cost).ti,ab.
15. ((energy or oxygen) adj expenditure).ti,ab.
16. 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15
17. exp Urinary Incontinence/
18. ((stress* or mix* or urg* or urin*) adj3 incontinen*).tw.
19. Urodynamics/ or Urinary Incontinence, Stress/ or Urinary Incontinence/ or Suburethral Slings/ or mixed incontinence.mp. or Urinary Bladder/ or Urinary Incontinence, Urge/
20. 17 or 18 or 19
21. anterior vaginal repair*.tw.
22. 16 and 20 and 21
23. anterior colporrhaphy*.tw.
24. 21 or 23
25. 16 and 20 and 23
26. bladder neck needle suspension$.tw.
27. 16 and 20
28. 26 and 27
29. open abdominal retropubic colposuspension*.tw.
30. retropubic colposuspension*.tw.
31. burch colposuspension*.tw.
32. 29 or 30 or 31
33. 27 and 32
34. laparoscopic retropubic colposuspension*.tw.
35. laparoscopic colposuspension*.tw.
36. 34 or 35
37. 27 and 36
38. traditional suburethral retropubic sling procedure$*.tw.
39. traditional sling procedure$*.tw.
40. suburethral retropubic sling procedure$*.tw.
41. retropubic sling procedure$*.tw.
42. traditional suburethral sling*.tw.
43. Suburethral Slings/ or Urinary Incontinence, Stress/ or Urologic Surgical Procedures/
44. 27 and 43
45. remove duplicates from 44
Search strategy 2:
1. economics.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, fs]
2. value of life.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, fs]
3. exp "costs and cost analysis"/
4. exp economics, hospital/
5. exp economics, medical/
6. economics, nursing.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, fs]
7. economics, pharmaceutical.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, fs]
8. exp "fees and charges"/
9. exp budgets/
10. budget*.ti,ab.
11. cost*.ti.
12. (economic* or pharmaco?economic*).ti.
13. (price* or pricing*).ti,ab.
14. (cost* adj2 (effective* or utilit* or benefit* or minimi* or unit* or estimat* or variable*)).ab.
15. (financ* or fee or fees).ti,ab.
16. (value adj2 (money or monetary)).ti,ab.
17. or/1‐16
18. economics.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, fs]
19. value of life.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, fs]
20. exp "costs and cost analysis"/
21. exp economics, hospital/
22. exp economics, medical/
23. economics, nursing.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, fs]
24. economics, pharmaceutical.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, fs
25. exp "fees and charges"/
26. exp budgets/
27. budget*.ti,ab.
28. cost*.ti.
29. (economic* or pharmaco?economic*).ti.
30. (price* or pricing*).ti,ab.
31. (cost* adj2 (effective* or utilit* or benefit* or minimi* or unit* or estimat* or variable*)).ab.
32. (financ* or fee or fees).ti,ab.
33. (value adj2 (money or monetary)).ti,ab.
34. 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31 or 32 or 33
35. ((energy or oxygen) adj cost).ti,ab.
36. (metabolic adj cost).ti,ab.
37. ((energy or oxygen) adj expenditure).ti,ab.
38. 34 or 35 or 36 or 37
39. urinary incontinence.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
40. ((stress$ or mix$ or urg$ or urin$) adj3 incontinen$).tw.
41. URINARY INCONTINENCE, STRESS.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
42. stress urinary incontinence*.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
43. 39 or 40 or 41 or 42
44. intervention surgery*.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
45. colporrhaphy.tw.
46. Bologna procedure*.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
47. Kelly‐Kennedy.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
48. Marion Kelly.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
49. Diaphragmplasty.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
50. Vaginal urethrocystopexy.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
51. Cystocele repair.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
52. Kelly plication.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
53. anterior vaginal repair$.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
54. anterior colporrhaphy.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
55. 44 or 45 or 46 or 47 or 48 or 49 or 50 or 51 or 52 or 53 or 54
56. 38 and 43 and 55
57. remove duplicates from 56
58. Bladder neck needle suspension$.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
59. 38 and 43 and 58
60. burch colposuspension.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
61. open abdominal retropubic colposuspension.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
62. Paravaginal defect repair.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
63. Marshall‐Marchetti‐Krantz.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
64. abdominal burch.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
65. abdominal colposuspension.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
66. endopelvic Fascia Plication.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
67. 60 or 61 or 62 or 63 or 64 or 65 or 66
68. 38 and 43
69. 67 and 68
70. laparoscopic retropubic colposuspension.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
71. laparoscopic colposuspension.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
72. retropubic colposuspension.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
73. 70 or 71 or 72
74. 68 and 73
75. remove duplicates from 74
76. suburethral sling.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
77. abdominal sling.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
78. traditional sling procedure$*.tw.
79. suburethral sling procedure.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
80. 76 or 77 or 78 or 79
81. 68 and 80
82. remove duplicates from 81
83. mid$urethral sling.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
84. retropubic sling procedure$*.tw.
85. transobturator sling procedure$.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
86. 83 or 84 or 85
87. remove duplicates from 86
88. 68 and 87
89. TVT‐Secur.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
90. mini‐arc.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
91. ajust.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
92. needleless.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
93. solyx.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
94. single$incision sling$.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
95. miniarc.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
96. mini$sling.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
97. Ophira.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
98. Tissue Fixation System.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
99. 89 or 90 or 91 or 92 or 93 or 94 or 95 or 96 or 97 or 98
100. 68 and 99
101. remove duplicates from 100
102. ((urethra$ or periurethra$ or transurethra$) adj3 (agent$ or bulk$ or injection$ or injectable$)).tw.
103. injection therapy.tw.
104. injectable$.tw.
105. (injectable$ adj2 agent$).tw.
106. (bulk$ adj3 agent$).tw.
107. Peri$urethral injection$.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
108. Autologous fat.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
109. Macroplastique.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
110. Calcium hydroxylapatite.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
111. Hyaluronic acid with dextranomer.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
112. Porcine dermal implant.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
113. Ethylene vinyl alcohol copolymer.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
114. Silicon particles.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
115. 102 or 103 or 104 or 105 or 106 or 107 or 108 or 109 or 110 or 111 or 112 or 113 or 114
116. 68 and 115
117. remove duplicates from 116
Data and analyses
Comparison 1.
Laparoscopic urethropexy vs open colposuspension
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Subjective cure | 8 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 Within 18 months | 7 | 1025 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.90, 1.00] |
| 1.2 Between 18 months and 5 years | 1 | 263 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.81, 1.25] |
| 1.3 After 5 years | 1 | 64 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.53 [1.00, 2.35] |
| 2 Incontinent episodes over 24 hours within 18 months | 2 | 133 | Mean Difference (IV, Fixed, 95% CI) | ‐0.12 [‐0.92, 0.68] |
| 3 Objective cure on clinical testing | 10 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.1 Within 18 months | 9 | 1087 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.86, 0.96] |
| 3.2 Between 18 months and 5 years | 2 | 290 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.88, 1.16] |
| 3.3 After 5 years | 2 | 107 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.69, 1.27] |
| 4 De novo detrusor overactivity (urodynamic diagnosis) | 6 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 4.1 Within 18 months | 5 | 512 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.29 [0.72, 2.30] |
| 4.2 Between 18 months and 5 years | 1 | 50 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.07, 15.12] |
| 4.3 After 5 years | 2 | 107 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.22 [0.40, 3.75] |
| 5 Voiding dysfunction within 18 months | 4 | 439 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.82 [0.50, 1.35] |
| 6 Urodynamic cure within 18 months | 6 | 564 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.85, 0.99] |
| 7 Perioperative complications | 9 | 1182 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.74 [0.58, 0.96] |
| 8 Bladder perforations | 7 | 1028 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.88 [0.93, 3.83] |
| 9 Length of inpatient stay (days) | 6 | mean difference (Fixed, 95% CI) | 0.86 [0.65, 1.06] | |
| 10 Operation time (minutes) | 7 | Mean difference (Fixed, 95% CI) | 14.06 [11.39, 16.73] |
Analysis 1.1.
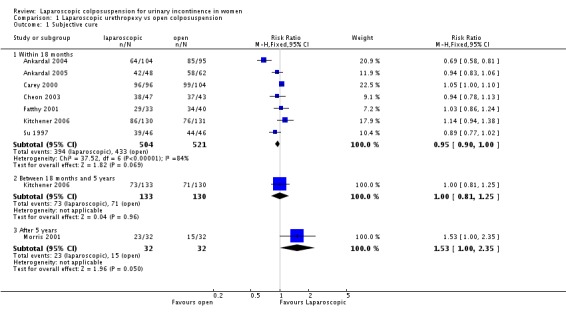
Comparison 1 Laparoscopic urethropexy vs open colposuspension, Outcome 1 Subjective cure.
Analysis 1.2.
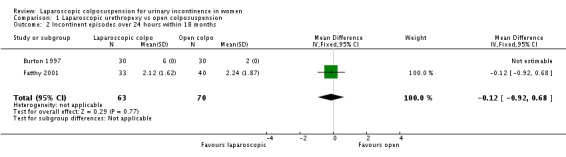
Comparison 1 Laparoscopic urethropexy vs open colposuspension, Outcome 2 Incontinent episodes over 24 hours within 18 months.
Analysis 1.3.
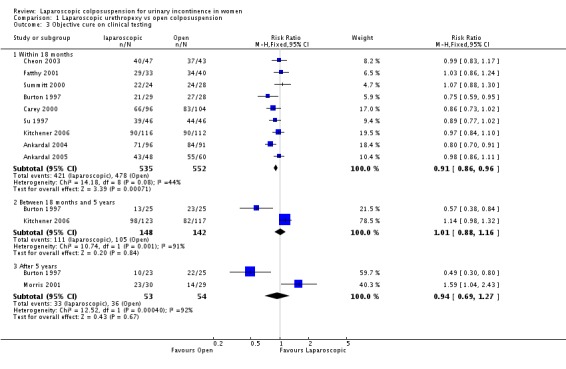
Comparison 1 Laparoscopic urethropexy vs open colposuspension, Outcome 3 Objective cure on clinical testing.
Analysis 1.4.
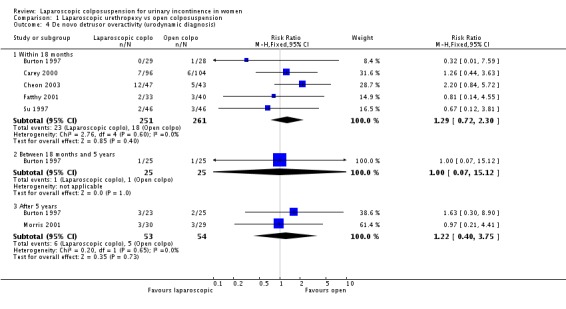
Comparison 1 Laparoscopic urethropexy vs open colposuspension, Outcome 4 De novo detrusor overactivity (urodynamic diagnosis).
Analysis 1.5.
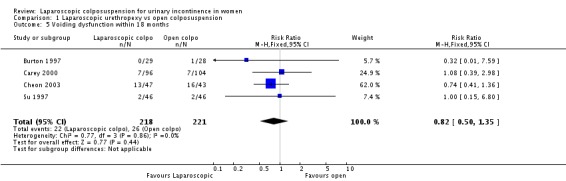
Comparison 1 Laparoscopic urethropexy vs open colposuspension, Outcome 5 Voiding dysfunction within 18 months.
Analysis 1.6.
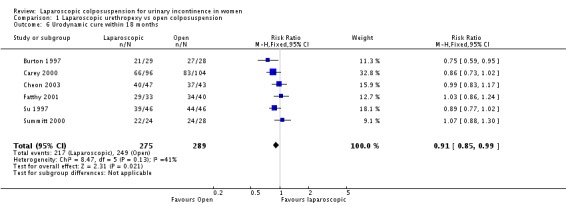
Comparison 1 Laparoscopic urethropexy vs open colposuspension, Outcome 6 Urodynamic cure within 18 months.
Analysis 1.7.
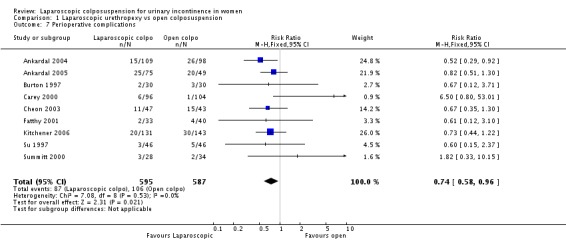
Comparison 1 Laparoscopic urethropexy vs open colposuspension, Outcome 7 Perioperative complications.
Analysis 1.8.
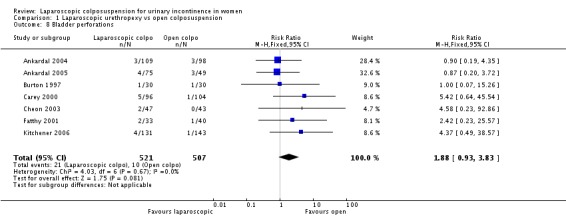
Comparison 1 Laparoscopic urethropexy vs open colposuspension, Outcome 8 Bladder perforations.
Analysis 1.9.
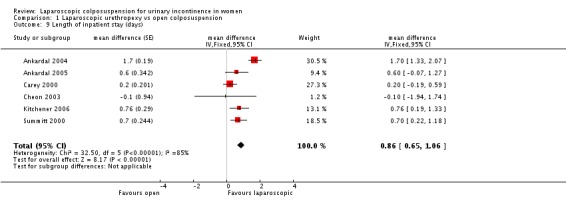
Comparison 1 Laparoscopic urethropexy vs open colposuspension, Outcome 9 Length of inpatient stay (days).
Analysis 1.10.
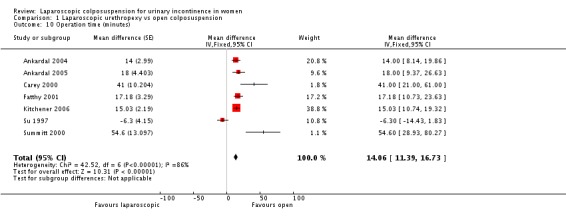
Comparison 1 Laparoscopic urethropexy vs open colposuspension, Outcome 10 Operation time (minutes).
Comparison 2.
Laparoscopc urethropexy vs 'self‐fixing' sling procedures
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Subjective cure within 18 months | 5 | 377 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.80, 1.02] |
| 1.1 Lap (sutures) vs TVT | 3 | 196 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.86, 1.19] |
| 1.2 Lap (mesh) vs TVT | 1 | 121 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.71 [0.55, 0.91] |
| 1.3 Lap vs SPARC sling | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.75, 1.29] |
| 2 Incontinent episodes per week within 18 months | 2 | 143 | Mean Difference (IV, Fixed, 95% CI) | ‐1.4 [‐3.30, 0.50] |
| 2.1 Lap (sutures) vs TVT | 1 | 63 | Mean Difference (IV, Fixed, 95% CI) | ‐1.4 [‐3.30, 0.50] |
| 2.2 Lap vs SPARC sling | 1 | 80 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3 Objective cure on clinical testing within 18 months | 7 | 575 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.81, 0.95] |
| 3.1 Lap (sutures) vs TVT | 5 | 394 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.92 [0.85, 0.99] |
| 3.2 Lap (mesh) vs TVT | 1 | 121 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.66 [0.51, 0.86] |
| 3.3 Lap vs SPARC sling | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.05 [0.72, 1.52] |
| 4 De novo detrusor overactivity within 18 months | 4 | 326 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.80 [0.34, 1.88] |
| 4.1 Lap (sutures) vs TVT | 4 | 326 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.80 [0.34, 1.88] |
| 5 Voiding dysfunction within 18 months | 5 | 412 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.06 [0.47, 2.41] |
| 5.1 Lap (sutures) vs TVT | 3 | 211 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.15 [0.44, 2.99] |
| 5.2 Lap (mesh) vs TVT | 1 | 121 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.37 [0.20, 9.42] |
| 5.3 Lap vs SPARC sling | 1 | 80 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.95] |
| 6 Urodynamic cure within 18 months | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 6.1 Lap (sutures) vs TVT | 3 | 189 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.80, 1.03] |
| 7 Perioperative complications | 7 | 514 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.60, 1.64] |
| 7.1 Lap (sutures) vs TVT | 5 | 350 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.48, 1.60] |
| 7.2 Lap (mesh) vs TVT | 1 | 121 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.92 [0.65, 5.71] |
| 7.3 Lap vs SPARC sling | 1 | 43 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.38 [0.04, 3.40] |
| 8 Length of inpatient stay (days) | 5 | Mean difference (Fixed, 95% CI) | 1.10 [0.79, 1.41] | |
| 8.1 Lap (sutures) vs TVT | 3 | Mean difference (Fixed, 95% CI) | 0.95 [0.57, 1.32] | |
| 8.2 Lap (mesh) vs TVT | 1 | Mean difference (Fixed, 95% CI) | 1.1 [0.46, 1.74] | |
| 8.3 Lap vs SPARC sling | 1 | Mean difference (Fixed, 95% CI) | 2.5 [1.36, 3.64] | |
| 9 Operation time (minutes) | 6 | Mean difference (Fixed, 95% CI) | 20.31 [16.75, 23.86] | |
| 9.1 Lap (sutures) vs TVT | 4 | Mean difference (Fixed, 95% CI) | 21.60 [17.29, 25.92] | |
| 9.2 Lap (mesh) vs TVT | 1 | Mean difference (Fixed, 95% CI) | 18.0 [7.54, 28.46] | |
| 9.3 Lap vs SPARC sling | 1 | Mean difference (Fixed, 95% CI) | 17.3 [9.43, 25.17] | |
| 10 Subjective cure 4‐8 year follow‐up | 1 | 53 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.18 [0.36, 3.81] |
Analysis 2.1.
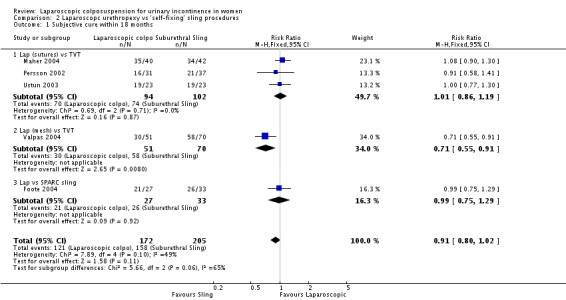
Comparison 2 Laparoscopc urethropexy vs 'self‐fixing' sling procedures, Outcome 1 Subjective cure within 18 months.
Analysis 2.2.
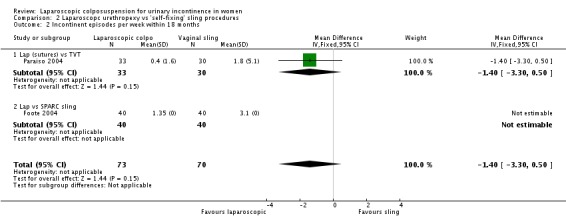
Comparison 2 Laparoscopc urethropexy vs 'self‐fixing' sling procedures, Outcome 2 Incontinent episodes per week within 18 months.
Analysis 2.3.
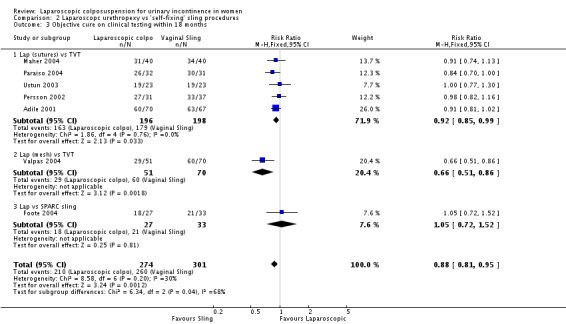
Comparison 2 Laparoscopc urethropexy vs 'self‐fixing' sling procedures, Outcome 3 Objective cure on clinical testing within 18 months.
Analysis 2.4.
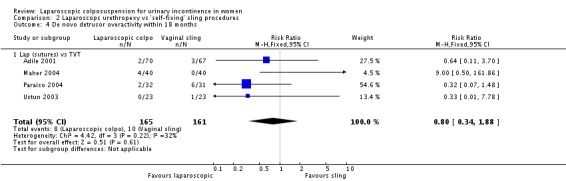
Comparison 2 Laparoscopc urethropexy vs 'self‐fixing' sling procedures, Outcome 4 De novo detrusor overactivity within 18 months.
Analysis 2.5.
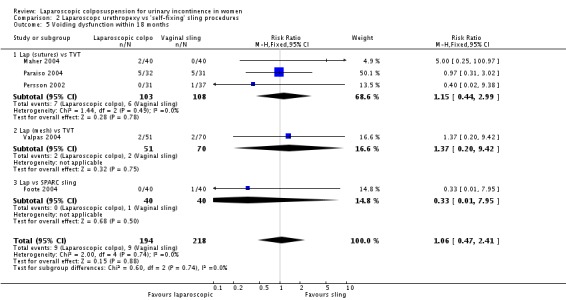
Comparison 2 Laparoscopc urethropexy vs 'self‐fixing' sling procedures, Outcome 5 Voiding dysfunction within 18 months.
Analysis 2.6.
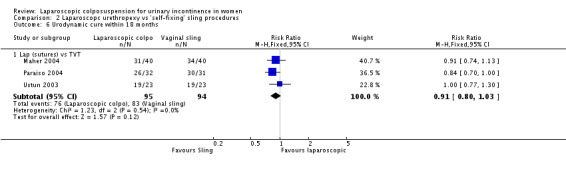
Comparison 2 Laparoscopc urethropexy vs 'self‐fixing' sling procedures, Outcome 6 Urodynamic cure within 18 months.
Analysis 2.7.
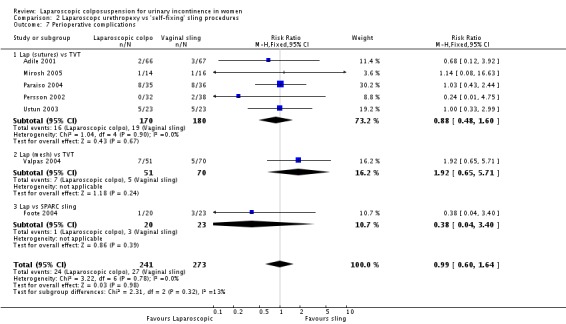
Comparison 2 Laparoscopc urethropexy vs 'self‐fixing' sling procedures, Outcome 7 Perioperative complications.
Analysis 2.8.
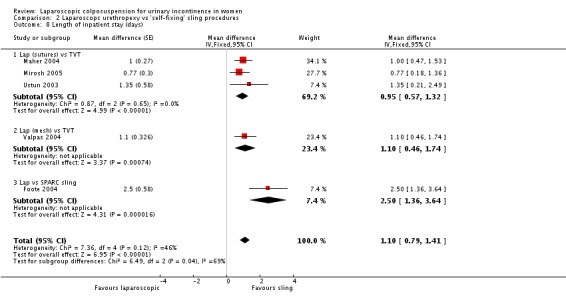
Comparison 2 Laparoscopc urethropexy vs 'self‐fixing' sling procedures, Outcome 8 Length of inpatient stay (days).
Analysis 2.9.
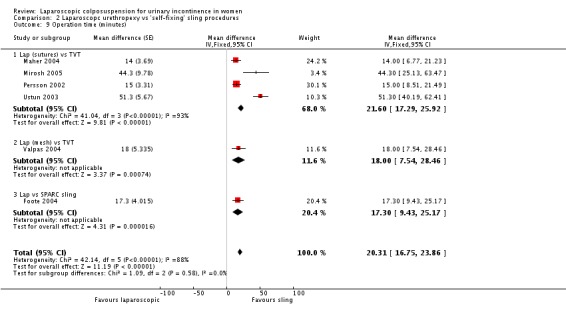
Comparison 2 Laparoscopc urethropexy vs 'self‐fixing' sling procedures, Outcome 9 Operation time (minutes).
Analysis 2.10.
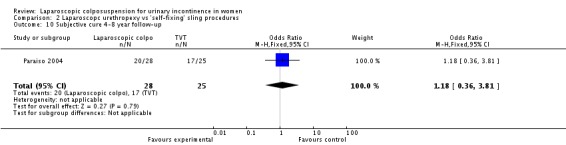
Comparison 2 Laparoscopc urethropexy vs 'self‐fixing' sling procedures, Outcome 10 Subjective cure 4‐8 year follow‐up.
Comparison 3.
Different methods of laparoscopic colposuspension
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Subjective cure within 18 months | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 Two sutures vs one suture | 1 | 158 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.37 [1.14, 1.64] |
| 1.2 Sutures vs mesh | 2 | 180 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.28 [1.11, 1.47] |
| 2 Subjective cure between 18 months and 5 years | 1 | 56 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.16 [0.76, 1.75] |
| 3 Objective cure on clinical testing within 18 months | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.1 Two sutures vs one suture | 1 | 149 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.42 [1.14, 1.77] |
| 3.2 Sutures vs mesh | 3 | 243 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.20 [1.07, 1.35] |
| 4 Objective cure on clinical testing between 18 months and 5 years | 1 | 52 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.5 [0.83, 2.70] |
| 5 De novo detrusor overactivity within 18 months | 2 | 122 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.72 [0.17, 3.06] |
| 6 Voiding dysfunction within 18 months | 1 | 161 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.82 [0.30, 26.53] |
| 6.1 Two sutures vs one suture | 1 | 161 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.82 [0.30, 26.53] |
| 7 Perioperative complications | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 7.1 Two sutures vs one suture | 1 | 161 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.45, 1.70] |
| 7.2 Sutures vs mesh | 3 | 260 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.94 [1.09, 3.48] |
Analysis 3.1.
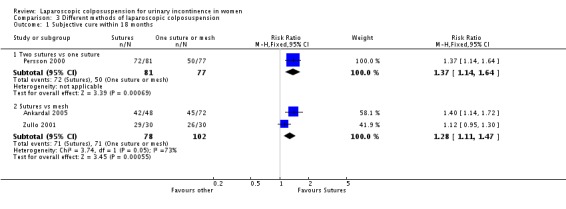
Comparison 3 Different methods of laparoscopic colposuspension, Outcome 1 Subjective cure within 18 months.
Analysis 3.2.
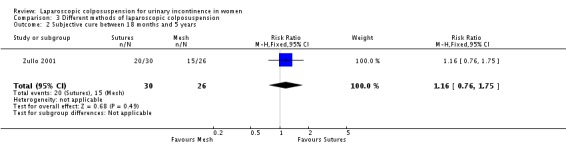
Comparison 3 Different methods of laparoscopic colposuspension, Outcome 2 Subjective cure between 18 months and 5 years.
Analysis 3.3.
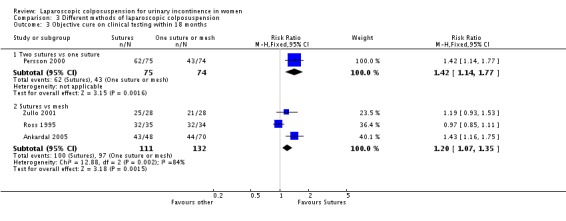
Comparison 3 Different methods of laparoscopic colposuspension, Outcome 3 Objective cure on clinical testing within 18 months.
Analysis 3.4.
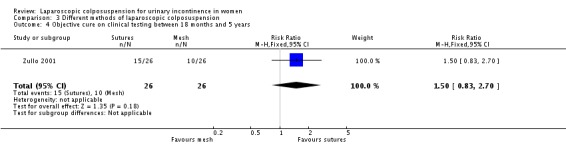
Comparison 3 Different methods of laparoscopic colposuspension, Outcome 4 Objective cure on clinical testing between 18 months and 5 years.
Analysis 3.5.
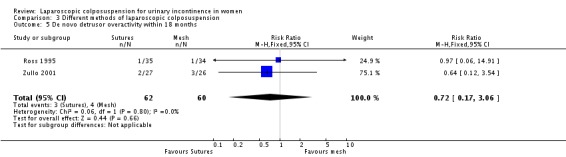
Comparison 3 Different methods of laparoscopic colposuspension, Outcome 5 De novo detrusor overactivity within 18 months.
Analysis 3.6.
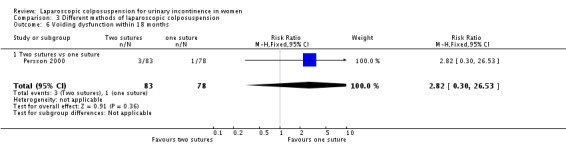
Comparison 3 Different methods of laparoscopic colposuspension, Outcome 6 Voiding dysfunction within 18 months.
Analysis 3.7.
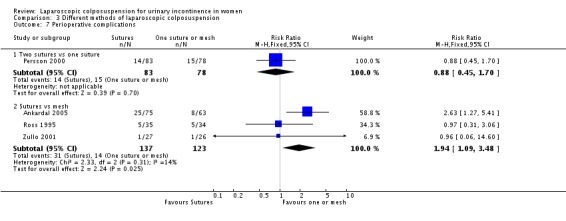
Comparison 3 Different methods of laparoscopic colposuspension, Outcome 7 Perioperative complications.
What's new
Last assessed as up‐to‐date: 16 December 2009.
| Date | Event | Description |
|---|---|---|
| 10 July 2017 | New citation required but conclusions have not changed | Brief economic commentary (BEC) added. Economics‐related sections revised. |
| 10 July 2017 | Amended | Brief economic commentary (BEC) added. Economics‐related sections revised: the Abstract, Plain language summary, Background, Methods (outcomes, search methods), and Discussion were amended. Appendix added with details of search strategies for BECs. |
History
Protocol first published: Issue 3, 2001 Review first published: Issue 1, 2002
| Date | Event | Description |
|---|---|---|
| 16 December 2009 | New search has been performed | Minor update. This updated review includes the long term (4 to 8 years) follow‐up results of a previously included trial, comparing laparoscopic colposuspension and TVT. Overall four studies were identified from the search. Two trials were excluded due to not being randomised and a further study, which was in abstract form, had already been included in the previous updated review in 2007. So only one study has been added in this update. This is the long term (4 to 8 years) follow‐up results of a previously included trial, comparing laparoscopic colposuspension and TVT. Overall the conclusions of the review remain the same, with now emerging evidence that laparoscopic colposuspension has similar long‐term subjective cure rates as TVT. |
| 31 October 2007 | New citation required and conclusions have changed | Substantive amendment This update of the review (Jan 2008) includes additional results from a three‐armed trial comparing two techniques of laparoscopic colposuspension with open colposuspension. Many of the trials in the previously updated review were in abstract form only and now have been published in full and on one occassion the authorship has changed. One trial has also published additional outcomes of cost effectiveness. The overall conclusions of the review remain unchanged for the comparisons of laparoscopic colposuspension with open and newer sling techniques. However, the addition of the three armed trial has lead to both subjective and objective outcomes favouring the use of sutures rather than mesh for the laparoscopic colposuspension procedures. |
| 24 May 2006 | New citation required and conclusions have changed | The last major update of the review (Jan 2006) included the following: The authorship has changed. Nicola Dean and Peter Herbison have been added to the authors, in place of Birgit Moehrer and Marcus Carey. The review includes the results of thirteen extra trials. Four trials compared laparoscopic colposuspension with open colposuspension, involving longer‐term follow‐up data and additional outcomes, such as health economic costs and quality of life scores. Eight trials have been included comparing laparoscopic colposuspension with 'self‐fixing' vaginal sling procedures, reporting short‐term outcomes and allowing for analysis. There is one additional trial comparing techniques of laparoscopic colposupension. The overall conclusion that laparoscopic colposuspension appears, in the short‐term, to have similar subjective and poorer objective cure rates to open colposuspension remains. However, 'self fixing' sling procedures appear to have similar, if not, better cure rates than laparoscopic colposuspension and offer greater benefits of minimal access surgery: shorter operation time, shorter hospital stay, and quicker return to normal activities. |
| 15 January 2002 | New search has been performed | update |
Differences between protocol and review
July 2017 update
Brief economic commentaries (BECs) have been added to all of Cochrane Incontinence's reviews on surgery for urinary incontinence in women. The economic elements throughout the review have been revised – if incorrect they have been stripped out. New economics‐related text has been added. This involved revisions to the Background section, Methods section (e.g. search section referring to an added Appendix), Discussion section, Abstract and Plain Language Summary. An appendix has been added with details of the economics searches. The Conclusions section of the review has not changed. The rest of the review has not changed.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | RCT comparing laparoscopic colposuspension with TVT, F/U 3‐36 months | |
| Participants | 133 women, mean ages 51 years in Laparoscopic colposuspension (LC) and 53 years in TVT; 57.5% postmenopausal in LC group and 28.3% postmenopausal in TVT group. All had urodynamics, Q‐tip test, vaginal profile, pad test. All participants showed USI. Excluded were women who needed additional surgical procedures | |
| Interventions | 66 LC and 67 TVT, surgeons had 6 months training for LC and 15 days for the TVT; GA for LC and regional or local for TVT. Both had Foley catheters and these were removed 3‐4 hours after the procedure. | |
| Outcomes | Duration of surgery, blood loss, haematomas, bladder perforations, duration of hospitalisation, subjective /objective cure rate at 6‐36 months; de novo bladder overactivity | |
| Notes | Unclear regarding method of randomisation, 3 bladder injuries in TVT group and 2 haematomas in laparoscopic colposuspension group | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
| Methods | RCT comparing laparoscopic with open colposuspension. Laparoscopic technique using mesh, power calculation, set in Sweden, 4 hospitals, Follow‐up 1 year | |
| Participants | 240 women randomised (120 in each group), All women referred with USI as their main symptom. Patient characteristics similar in each group | |
| Interventions | Group 1 (n = 109): laparoscopic colposuspension Group 2 (n = 98): open colposuspension; total of 7 surgeons most had performed > 60 laparoscopic colposuspensions before and supervised 2 others starting the technique. The laparoscopic colposuspension was performed by the transperitoneal approach using mesh and staples. 2 non‐absorbable sutures each side were used in the open colposuspension.The laparoscopic group had a urethral catheter inserted at the end of the procedure and the open group had a suprapubic catheter. | |
| Outcomes | Subjective cure and objective cure ( < 8 g/24 h on a 48‐h pad test, and leakage on a frequency/volume chart). VAS used to assess subjective improvement and QoL. Duration of surgery, blood loss, duration of catheter drainage, duration of hospital stay, complications (bladder perforation haematoma leading to re‐operation, UTI within 1 month, wound infection and urinary retention > 5 days) | |
| Notes | Withdrawals before surgery 11 in group 1 (n = 109) and 22 in group 2 (n = 98). Only analysed those that were operated on as they still had enough power, but this may be biased Of the laparoscopic group 5 were converted to open procedures. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
| Methods | 3‐armed RCT comparing laparoscopic colposuspension using sutures, laparoscopic colposuspension using mesh with open colposuspension using sutures. power calculation, set in Sweden, 4 hospitals. Follow‐up 1 year. | |
| Participants | 211 women randomised. All women referred with USI as their main symptom. Patient characteristics similar in each group | |
| Interventions | Group 1 (n = 79): open colposuspension Group 2 (n = 53): laparoscopic colposuspension using sutures Group 3 (n = 79): laparoscopic colposuspension using mesh |
|
| Outcomes | Subjective cure and objective cure ( < 8 g/24 h on a 48‐h pad test, and leakage on a frequency/volume chart). VAS used to assess subjective improvement and QoL. Duration of surgery, blood loss, duration of catheter drainage, duration of hospital stay, complications (bladder perforation haematoma leading to re‐operation, UTI within 1 month, wound infection and urinary retention > 5 days) | |
| Notes | Withdrawls before surgery: group 1 (n = 16); group 2 (n = 4); group 3 (n = 4) due to failure to meet all inclusion criteria or regret decision after randomisation | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
| Methods | RCT comparing laparoscopic with open colposuspension, power calculation, telephone randomisation; F/U: 6/12, 1 year, 3 years, 5 years | |
| Participants | 60 women Inclusion criteria: age ≥ 30 years, moderate‐severe urodynamically proven USI Exclusion criteria: previous bladder neck surgery, previous major abdominal surgery, hysterectomy, > 1st degree prolapse, diabetes, central nervous system condition severe chronic obstructive airways disease, steroid‐dependent asthma, recurrent UTI, MUCP < 25 cm H2O | |
| Interventions | Group 1 (n = 30): laparoscopic colposuspension Group 2 (n = 30): open colposuspension 15 previous laparoscopic colposuspensions to familiarise and standardise technique, transperitoneal approach for laparoscopic colposuspension, same surgeon for all operations, Dexon suture used in both groups, suprapubic catheter | |
| Outcomes | Duration of surgery, blood loss, catheterisation time, duration of hospital stay, analgesia use, adverse events, video cystourethrography, urodynamics, residuals, voiding difficulties, 1‐h pad test, urinary diary, VAS symptoms | |
| Notes | Adverse events: group 1: 1 bladder perforation, 1 UTI; group 2: 1 bladder perforation, 1 voiding difficulties, 1 wound infection 3 participants in group 1 had repeat surgery (3 open colposuspensions) Losses to F/U: none at 6/12, group 1: 7 (3 at 1 year, 5 at 3 years, 7 at 5 years); group 2: 6 (2 at 1 year, 5 at 3 years, 6 at 5 years) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
| Methods | RCT comparing laparoscopic with open colposuspension, power calculation on non patient‐orientated outcomes only F/U: 6/52 and 6/12 | |
| Participants | 200 women with urodynamic evidence of USI and no history of retropubic surgery, participants and ward staff blinded to procedure performed until discharge | |
| Interventions | Group 1 (n = 104): open colposuspension Group 2 (n = 96): laparoscopic colposuspension Different surgical expertise levels, the 2 senior surgeons together performed 70 laparoscopic colposuspensions before starting the trial | |
| Outcomes | Duration of surgery, blood loss, visual assessment scores for post‐op pain, voiding difficulties, duration of hospital stay, urinary continence scores, symptom questionnaire, urodynamics, evaluation of urogenital prolapse, QoL assessment using SF 36, SUDI, SIIQ, return to normal activities, adverse outcomes | |
| Notes | Adverse events: group 1: 1 bladder perforation requiring blood transfusion, group 2: 1 laceration to obturator vein, 5 bladder perforations, 2 of which required conversion to open procedure | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
| Methods | RCT comparing laparoscopic with open colposuspension, computer‐randomised and sealed opaque envelopes, F/U at 1 year | |
| Participants | 90 women with urodynamically proven stress incontinence were randomised. Excluded women who had undergone previous anti‐continence surgery or intrinsic sphincter deficiency. 13 (30.2%) of group 1 and 7 (14.9%) of group 2 had mixed incontinence (stress and urge) | |
| Interventions | Group 1 (n = 43): open colposuspension Group 2 (n = 47): laparoscopic colposuspension 16 (37.2%) of group 1 had concomitant hysterectomy and 7 (14.9%) of group 2 Laparoscopic approaches were both transperitoneal and extraperitoneal, both open and laparoscopic procedures used 2 sutures (Ethibond). 2 surgeons and both had performed more than 15 laparoscopic colposuspensions before starting the study | |
| Outcomes | Subjective cure and improvement, objective urodynamic testing, duration of operation (colposuspension only), estimated blood loss, duration of bladder training, length of in‐patient stay, time to return to normal activities, days leave taken, complications and change in severity of incontinence (1‐h pad test) | |
| Notes | Total perioperative complications group 1 = 15, group 2 = 11. Bladder perforations 2 in laparoscopic group (group 2) and 0 in open colposuspension group 1 1 laparoscopic converted to open procedure | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
| Methods | RCT comparing laparoscopic with open colposuspension. Random number table balanced randomisation with blinding and disguised block length; duration of study: 18/12; F/U: 4/52 post‐op and every 6/12 up to 18/12 | |
| Participants | 74 women Inclusion criteria: urodynamically diagnosed USI Exclusion criteria: detrusor instability, underactive detrusor, intrinsic sphincter deficiency, limited vaginal mobility, stage III and IV vaginal prolapse, contraindications to laparoscopy and surgery in general | |
| Interventions | Group 1 (n = 34): laparoscopic colposuspension Group 2 (n = 40): open colposuspension Extraperitoneal approach, number 1 nonabsorbable polypropylene suture, 1 suture on each side of urethrovesical junction, first surgeon performed 23 and second surgeon 16 laparoscopic procedures before starting the trial, prophylactic cephradine 1 g 3 times/d for 24 h, catheterisation group 1: Foley for 24 h, removed if postvoid volume < 100 mL, group 2: Bonnano suprapubic catheter for 48 h, removed if postvoid volume < 100 mL | |
| Outcomes | 24‐h urinary diary, urodynamics at 6/12 and 18/12 by independent urologist who was blinded to procedure performed, assessment of subjective success by questionnaire about urinary leakage, lack of need to wear pads at rest and at different activity levels, comparison of pre‐and post‐operative symptoms, objective success assessed through cough provocation test, Valsalva leak point pressure, MUCP, max. urethral pressure, operating time, EBL, analgesia use (immediate postoperative pain), voiding difficulties, hospital stay, time to return to light work, pelvic relaxation (post‐op rectocele), dyspareunia Definition of cure: subjective cure: dry ‐ completely continent or only rarely requiring pad with exertion with which the woman was completely satisfied, objective: negative cough stress test and urodynamically absence of leakage during Valsalva manoeuvre and repeated coughing, as well as a significant improvement in MUCP; definition of failure: subjective: change in amount of leakage with which woman was not satisfied, objective: post‐op de novo detrusor instability | |
| Notes | Adverse events: group 1: 1 bladder injury, 1 bladder perforation, 4 dysuria, 2 voiding difficulties; group 2: 1 bladder injury, 2 superficial wound infections, 1 retropubic haematoma, 2 dysuria, 2 voiding difficulties Losses to F/U: 1 in group 2 15 menopausal women were not receiving HRT (8 in group 1, 7 in group 2), they were prescribed HRT for 3/12 before their scheduled surgery, 6 women in group 1 and 9 women in group 2 had additional rectocele repair | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
| Methods | RCT comparing laparoscopic colposuspension with vaginal mesh sling. No details of randomisation, F/U 6 months | |
| Participants | 80 women with urodynamically proven stress incontinence. Women were excluded if they had other diagnosis such as DO or voiding difficulty, previous retropubic surgery, weight > 100 kg, significant prolapse, required other gynae surgery or were unsuitable for laparoscopic surgery | |
| Interventions | Group 1 (n = 40): laparoscopic colposuspension Group 2 (n = 40): vaginal mesh sling 'SPARC'. One surgeon performed all the operations | |
| Outcomes | Urodynamics, bladder diary, VAS score , QoL (York and Urogential distress Inventory) at 6 months. Intraoperative complications | |
| Notes | Adverse events: 1 bladder suturing requiring intraoperative repositioning. 3 needle perforations of the bladder requiring repositioning. 1 mesh erosion. 1 with voiding difficulty in mesh group | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
| Methods | RCT comparing laparoscopic with open colposuspension. Randomisation performed by external centre. ITT and power calculation pro formed. Multi‐centre study involving 6 units in the UK. F/U 6 weeks, 6 , 12 and 24 months | |
| Participants | 291 women with urodynamically proven stress incontinence were recruited between April 1999 and February 2002 | |
| Interventions | Group 1 (n = 144): laparoscopic colposuspension, using 2 Ethibond sutures each side Group 2 (n = 147): open colposuspension. Both groups were treated with the standard surgical procedure of antibiotic prophylaxis, skin preparation, supra‐pubic catheterisation and patient‐controlled analgesia post‐op | |
| Outcomes | Primary outcomes were both subjective: a question of satisfaction with outcome; and objective: a negative 1‐h pad test Secondary outcomes were levels of operative morbidity, time to return to work. | |
| Notes | 88% subjective data available at 2 years and 82.5% objective data available at 2 years | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
| Methods | RCT comparing laparoscopic colposuspension with TVT. Computer‐generated randomisation, power calculation and ITT analysis. Women all had recurrent SUI. F/U 6 weeks and 6 months | |
| Participants | 82 women with recurrent SUI and/or intrinsic sphincter deficiency (MUCP < or = 20 H2O) were randomly allocated. Excluded were women primarily presenting with pelvic organ prolapse, rigid urethra and those unfit for GA | |
| Interventions | Group 1 (n = 40): TVT Group 2 (n = 42): laparoscopic colposuspension 61% of group 1 and 65% of group 2 had had previous continence surgery | |
| Outcomes | Subjective cure, de novo DO, voiding problems, QoL scores (change in SUDI, SIIQ, SF‐36), satisfaction score, length of inpatient stay, time to return to normal activities, operation time, duration of catheter post‐operatively, blood loss, post‐op increase in MUCP | |
| Notes | In the laparoscopic arm 9 underwent open procedures due to BMI > 35. In the TVT group 1 woman had to be converted to open colposuspension and another woman had an incidental finding of grade 1 transitional cell carcinoma | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
| Methods | RCT comparing laparoscopic colposuspension with TVT | |
| Participants | 30 women with urodynamic SUI were randomised ‐ no details of method given. Women were at least 30 years old and had had no previous incontinence surgery, had no need for concurrent surgery. Exclusion criteria included grade 3‐4 pelvic organ prolapse, mixed urinary incontinence | |
| Interventions | Group 1 (n = 16): TVT Group 2 (n = 14): laparoscopic colposuspension TVT operations were performed under spinal anaesthetic and laparoscopic colposuspension performed under GA All performed by a single surgeon | |
| Outcomes | Primary outcomes were anaesthetic, operation, and hospital stay times. Secondary outcomes were patient satisfaction, quality of life scores and complications | |
| Notes | Postoperative complications TVT = 1 urinary retention that needed the tape loosening, Laparoscopic colposuspension = 1 right‐sided ureteric obstruction and needed the right‐sided sutures removing | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
| Methods | RCT comparing laparoscopic with open colposuspension 5‐7 year F/U. | |
| Participants | 73 women with urodynamically (cystometry and pad test) proven stress incontinence. DO was not an exclusion criteria. Figures based on ITT | |
| Interventions | Group 1 (n = 38): laparoscopic colposuspension group 2 (n = 35): open colposuspension | |
| Outcomes | Cystometry repeated at 2 years and pad test at 5‐7 years (median of 6 years). 5 women declined formal review and 9 were lost to F/U. So group 1 (n = 30) and group 2 (n = 29). Objective pad testing, subjective assessment and de novo DO | |
| Notes | Only 5‐7 year F/U data available | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
| Methods | RCT comparing laparoscopic colposuspension with TVT. 1, 2 and 4‐8 (long‐term) year F/U. Computer‐randomised and sealed, opaque envelopes, power calculation. Set in 2 centres Cleveland , Ohio | |
| Participants | 72 women enrolled and randomised. Inclusion criteria: urodynamic stress incontinence, urethral hypermobility (cotton‐tipped swab angle ≥ 30º), ability to undergo a GA and laparoscopy. Exclusion criteria: previous anti‐incontinent surgery, DO on urodynamics, anterior vaginal wall prolapse to or at the hymen |
|
| Interventions | Group 1 (n = 36): laparoscopic colposuspension, combination of extraperitoneal and transperitoneal approaches used, 2 sutures of Ethibond used each side and passed through ipsilateral Cooper's ligament Group 2 (n = 36): TVT, performed under LA with sedation, regional or GA Both procedures had suprapubic catheters post‐operatively. Concurrent surgery: group 1 = 9 (25%) had hysterectomy and 11 (32%) had adhesiolysis group 2 = 8 (22%) had hysterectomy and 4 (11%) had adhesiolysis | |
| Outcomes | Primary outcome of objective cure (no leakage on post‐op urodynamics), de novo DO, voiding difficulty, and post‐void residual. Objective assessment performed at 1 year post‐operatively Subjective assessment, UDI, IIQ, POP‐Q, urinary diaries, VAS, all at 1‐2 and then 4‐8 years post‐operatively Perioperative complications, estimated blood loss, change in haematocrit, analgesia requirement, hospital stay, number of days to normal voiding | |
| Notes | Surgeons each with > 80 laparoscopic colposuspension experience. Many had concurrent surgeries, ranging from bladder biopsy to laparoscopic cholecystectomy 3 participants were lost to F/U from each group. (n = 33 in each group). Further participants lost/withdrew for the longer‐term F/U 1 woman in TVT group required intraoperative blood transfusion 2 bladder perforations in TVT group and 2 participants in laparoscopy group had sutures found in the bladder and were replaced 1 bowel injury in laparoscopic colposuspension, which was repaired at the time of the operation. 3 of laparoscopies were converted to open procedures. Post‐operative complications included 2 in the TVT group requiring tape‐releasing procedures. 74% participants completed long‐term F/U 4‐8 years (25 in the TVT group and 28 in the laparoscopic colposuspension group) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
| Methods | RCT comparing 1 bilateral double‐bite Gore‐Tex suture to 2 bilateral single‐bite Gore‐Tex sutures in laparoscopic colposuspension Randomisation 1:1 F/U: 2/12 telephone interview, 1‐year clinic visit | |
| Participants | 161 women Inclusion criteria: bothersome stress incontinence symptoms, normal urethral closing pressure, hypermobility bladder neck, objective sign of leaking (pad test), stress incontinent with concomitant subdominant urge symptoms without associated urine leakage Exclusion criteria: urge incontinence, stress incontinence due to low urethral closing pressure (< 20 mm H2O), uterovaginal descent more than grade 1 cystocele, incontinence after previous vaginal repair, recurrent incontinence, high risk for GA or surgical complications | |
| Interventions | Group 1 (n = 78): 1 bilateral double‐bite suture group 2 (n = 83): 2 bilateral single‐bite sutures Transperitoneal approach, vaginal fascia fixed against Cooper's ligament with sutures placed approx 2 cm lateral to each side of urethra and 2 cm distal to bladder neck Last 84 women received 2 g intravenous cefoxitin at induction Additional surgery in 63 cases (34 in group 1, 29 in group 2) Indwelling catheter, removed within 24 h post‐op and residuals recorded, if residual < 125 mLs discharge home, remaining women were offered delayed discharge, discharge with indwelling catheter or discharge with intermittent self‐catheterisation | |
| Outcomes | Main objective outcome variables: leakage on ultrashort pad test, operation time Secondary objective outcome variables: post‐op voiding difficulties, complications during and after surgery, EBL Objective cure defined as no leaking at ultrashort pad test, improvement max. 1/3 of pre‐op leaking volume on pad test, unimproved > 1/3 of pre‐op leaking volume on pad test Subjective: women's description of cure, improvement, non‐improvement |
|
| Notes | Study set up to enrol 280 participants, trialists became convinced during F/U that 2 bilateral sutures have higher cure rate and therefore did an interim analysis on objective 1‐year cure rate on 108 participants, which showed a cure rate of 87% in group 2 vs 68% in group 1, therefore further enrolment into the study was stopped and only already enrolled participants were followed up; Losses to F/U: 1 in group 1, 2 in group 2; 9 women refused F/U pad test Minor adverse events only | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
| Methods | RCT comparing laparoscopic colposuspension with TVT. Approached 270 consecutive women presenting for evaluation of stress incontinence at University Hospital, Lund, Sweden. In 156 of the women surgical treatment was indicated | |
| Participants | 79 consenting women were randomised Inclusion criteria: significant stress incontinence proven on urodynamic testing, hypermobility of bladder neck, > 5 mL on ultra‐short pad test, urethral closure > 20 cm H2O, urethral functional length > 25 mm Exclusion criteria: predominant symptom of urge incontinence, previous surgery for prolapse or incontinence, grade 2 or more prolapse, requiring concurrent gynaecological surgery and all with increased risk for GA and laparoscopic surgery | |
| Interventions | Group 1 (n = 32): laparoscopic colposuspension, using 2 sutures (polytetrafluoroethylene) each side, GA Group 2 (n = 38): TVT, LA and sedation | |
| Outcomes | 2‐5 months following surgery, women were telephoned and answered a questionnaire. Any adverse events up to 2 months were noted. Then a 1‐year F/U appointment arranged. Main outcome measures were subjective change in stress‐induced urinary leakage and objective change in pad test results pre and post operatively. | |
| Notes | One surgeon performed all the laparoscopic colposuspensions and 2 surgeons performed the TVT's | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
| Methods | RCT comparing sutures and mesh in laparoscopic colposuspension; same surgeon for all operations F/U at 6/52 and 1 year | |
| Participants | 69 women Inclusion criteria: GSI demonstrated by positive cough stress test with a full bladder, hypermobile urethrovesical junction shown by positive Q‐Tip and US test + negative CMG Exclusion criteria: previous incontinence surgery, detrusor instability, inferred intrinsic sphincter dysfunction | |
| Interventions | Group 1 (n = 35): sutures (either 0 Ethibond or 0 Gortex) Group 2 (n = 34): polypropylene mesh + staples (EMS disposable endostapler) Same transperitoneal approach for both groups, fixation 2 cm lateral to urethrovesical junction and 2 cm lateral to midurethra, paravaginal fascia to Cooper's ligament Simultaneously treated gynaecological problems in both groups: group 1: 9 laparoscopic‐assisted vaginal hysterectomies, 12 modified McCull culdoplasties, 6 sacrocolpopexies, 5 posterior repairs; group 2: 11 laparoscopic‐ assisted vaginal hysterectomies, 17 modified McCull culdoplasties, 4 sacrocolpopexies, 3 posterior repairs | |
| Outcomes | Post‐op: time to void, hospital stay, return to work, complications At 6/52: cough test with full bladder, if leaking CMG At 1 year: Q‐Tip test, perineal US, cough test with full bladder, if leaking CMG to rule out detrusor instability; cure defined as negative Q‐Tip, US, cough stress test and urodynamics; no subjective findings reported | |
| Notes | Adverse events: Group 1: 1 haematuria, 2 UTI's, 2 accidental cystotomies Group 2: 2 UTI's, 1 accidental cystotomy, 1 thrombophlebitis, 1 urinary retention | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
| Methods | RCT comparing laparoscopic with open colposuspension Power calculation, early stopping rules with 3 evaluation points determined before beginning of trial Allocation through computer‐generated random numbers in sealed, opaque envelopes, but 4 participants who were not willing to undergo laparoscopic colposuspension were enrolled to open group, then the next participant was assigned to the laparoscopic procedure and the following participants went back to sequence of random number All operations by senior gynaecologist; F/U at 3/12, and every 6/12 |
|
| Participants | 92 women Exclusion criteria: pathology that limits flexibility of vaginal wall, uterine prolapse, cystocele greater than 1st degree, DO, underactive detrusor, outflow obstruction, previous anti‐incontinent surgery, previous hysterectomy | |
| Interventions | Group 1 (n = 46): laparoscopic colposuspension Group 2 (n = 46): open colposuspension; transperitoneal approach, 1 double‐bite suture at level of urethro‐vesical junction and then to nearest point on ipsilateral Cooper's ligament in laparoscopic procedure, 3 sutures in open procedure, surgeon had done 50 previous laparoscopic colposuspensions; 14 participants in laparoscopic and 19 in open group had hysterectomy at same time Suprapubic catheter, clamped day 2, participants encouraged to void every 2 h, residuals measured with catheter unclamped for 15 min, if 2 successive voids > 200 mLs and residuals < 100 mLs catheter was clamped overnight, if still void > 200 mLs and residuals < 100 mLs catheter was removed | |
| Outcomes | Operation time, blood loss, duration of catheterisation At 1 year F/U: 1‐h pad test, objective stress test, assessment of bladder neck position; if incontinence was found urodynamics were repeated to confirm GSI Cure defined as dry during severe cough and bouncing on urodynamics, otherwise failure In the 14 participants who had total abdominal hysterectomy after laparoscopic colposuspension immediate look at the suture position and tension revealed 5 suboptimal suspension sutures | |
| Notes | Trial was stopped at 2nd evaluation point Adverse effects: group 1: 2 outflow obstruction, 2 DO, 1 UTI; group 2: 2 outflow obstruction, 3 DO, 1 UTI, 2 haematuria | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | High risk | C ‐ Inadequate |
| Methods | Multicentre (5 sites) RCT comparing laparoscopic with open colposuspension; power calculation; computer‐generated randomisation schedule, randomisation numbers in double‐sealed envelopes with project secretary; F/U 2/52, 6/52, 3/12 and 1 year | |
| Participants | 62 women Inclusion criteria: age 21‐75, objective diagnosis of GSI with urine loss with cough and absence of detrusor activity with stress loss of urine, anatomic defect of urethrovesical junction (Q‐tip deviation > 30º from the horizontal) Exclusion criteria: need for concomitant surgical procedures, previous retropubic urethropexy, needle suspension or suburethral sling, neurologic deficit associated with incontinence, type III stress incontinence, detrusor instability that has not been treated and improved, absolute contraindications to laparoscopy (uterine fibroids or pelvic masses > 16 weeks gestational size, conditions in which participant cannot tolerate anaesthesia, severe bleeding disorders, acute peritonitis of upper abdomen with severe distension), pathology present at the time of surgery that requires additional surgery (eg. unsuspected ovarian mass) | |
| Interventions | Group 1 (n = 28): laparoscopic colposuspension Group 2 (n = 34): open colposuspension To ensure similarity of operative technique all co‐investigators met at a common location at beginning of study to observe surgery and participate in animal laboratory Intraperitoneal approach for laparoscopy 0‐Ethibond suture, 2 sutures each side of urethra; suprapubic catheter | |
| Outcomes | Operating time, blood loss, hospital stay, complications, fever, time to resumption of voiding, objective surgical success, urodynamics, time to return to work and normal activity, subjective success | |
| Notes | 3 laparoscopic colposuspensions were converted to open colposuspensions due to severe intraabdominal adhesions | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
| Methods | RCT comparing laparoscopic colposuspension with TVT. Set in a tertiary care university hospital. F/U subjectively at 3, 6, 12 and 18 months and objective cure at 3 months | |
| Participants | 46 consecutive women with proven genuine stress incontinence. All participants were evaluated preoperatively with medical and voiding histories, physical examination, urinalysis, urine culture, multichannel urodynamics with cystometry, uroflowmetry, and measurement of Valsalva leak‐point pressure | |
| Interventions | Group 1 (n = 23): laparoscopic colposuspension, transperitoneal approach, 2 sutures each side under general anaesthetic Group 2 (n = 23): TVT, (5 local and 10 spinal anaesthetic and 8 general anaesthetic) | |
| Outcomes | Operating time, length of catheterisation, hospital stay and surgical complications were recorded. Objective assessment by urodynamics at 3 months. Subjective assessment (with questionnaire and patient history) was also evaluated. Cure was defined as no need for pads and no leakage on urodynamics | |
| Notes | No clear exclusion/inclusion criteria. 4 of TVT women had previous incontinence surgery, otherwise the groups were similar with respect to age, parity and hormonal status. Laparoscopy couldn't be completed in 2 (8.6%) women due to intraoperative complications, so were converted to open procedures. In the TVT group there was 2 (8.6%) bladder lacerations but they did not need treatment | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
| Methods | RCT comparing laparoscopic colposuspension with TVT. Multicentred in Finland. F/U 6 weeks and 1 year. Study ongoing for a 5 year F/U | |
| Participants | 128 women recruited from gynaecology clinic. Inclusion criteria: urodynamically proven stress incontinence with positive stress test Exclusion: previous incontinent surgery, > 3 UTI's with in 2 years, > 70 years old, coincident other gynaecology surgery, unstable bladder in cystometry, urethral pressure < 20, residual volume > 100 mL pre operatively |
|
| Interventions | Group 1 (n = 51): laparoscopic colposuspension, extraperitoneal approach, mesh (2 strips of polypropylene) and tacks used Group 2 (n = 70): TVT, local anaesthetic and sedation | |
| Outcomes | Primary outcomes: negative 48‐h pad test results (< 8 g/48 h) and secondary outcome measures include subjective cure of incontinence (2 symptom scores were assessed the 'urinary Incontinence severity score' and the 'Urge score'. KHQ and VAS were also used to assess the severity of incontinence. Operative complications were also assessed. Length of patient stay, return to normal activities, operation time and post‐operative analgesia requirement | |
| Notes | 7 withdrawals and at 12 months group 1 n = 49 and group 2 (TVT) n = 66 1 bladder perforation in each group. One laparoscopy converted to open procedure. 2 participants in each group with urinary retention (1 TVT had the tape loosened the next day, all others treated with intermittent self‐catheterisation) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
| Methods | RCT comparing laparoscopic transperitoneal with extraperitoneal colposuspension, using Gore‐Tex sutures or Mesh + staples 2‐12/12 F/U | |
| Participants | 22 women with recurrent urinary stress incontinence grade 2‐3, all had prior hysterectomy and at least 1 additional gynae operation Inclusion criteria: flat passive urethral pressure profile (low maximum urethral closure pressure), hypotonic urethra, motoric/sensoric urge component Exclusion criteria: cysto‐ and rectocele or prolapse | |
| Interventions | Group 1 (n = ?): transperitoneal approach Group 2 (n = ?): extraperitoneal approach Using paraurethral Gore‐Tex suture or Mesh stapler fixation All had cystoscopy to exclude bladder lesion and suprapubic catheter for drainage and residuals | |
| Outcomes | Duration of surgery, post‐op bleeding, voiding difficulties, complications Subjective evaluation, urodynamics, post‐op clinical findings, perineal US for control of anatomic correction of bladder neck descent | |
| Notes | Adverse events: 1 bladder lesion, 1 detrusor instability, 1 transient urinary retention 18 participants (92%) subjectively and objectively cured, 1 no improvement, 1 failure Groups too small, F/U too short | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
| Methods | RCT comparing transperitoneal laparoscopic colposuspension using mesh (polypropylene mesh and tacks or staples) with laparoscopic colposuspension using sutures (0‐Ethibond sutures). Power calculation. F/U at 3, 6, 12 months | |
| Participants | 60 women with either mild or moderate stress incontinence were enrolled. Excluded: previous gynae. or incontinent surgery, BMI > 30, prolapse ≥ 2nd degree, previous severe abdopelvic infection, severe stress incontinence (loss of urine on minimal activity) |
|
| Interventions | Group 1 (n = 30): transperitoneal laparoscopic colposuspension with sutures, 1‐2 each side Group 2 (n = 30): transperitoneal laparoscopic colposuspension using mesh and tacks or staples. All similar with regard to baseline characteristics | |
| Outcomes | Intra and postoperative complications were recorded, operating time, blood loss, catheterisation time, resumption to spontaneous voiding, hospital stay. Objective measurement was involuntary loss of urine during cough and Valsalva manoeuvre in standing position with the bladder filled to max. cystometric capacity. VAS used to assess subjective cure | |
| Notes | Researcher assessing objective outcome was blinded to the type of laparoscopy. A total of 7 withdrew from the study (group 1 n = 27 and group 2 n = 26) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
Key for abbreviations: CMG: cystometrogram; DO = detrusor overactivity; EBL: estimated blood loss; F/U = follow‐up; GA = general anaesthetic; GSI: genuine stress incontinence; IIQ: Incontinence Impact Questionnaire; ITT: intention‐to‐treat; KHQ: King's Health Questionnaire; LA = local anaesthetic; LC = laparoscopic colposuspension; MUCP: maximum urethral closure pressure; POP‐Q: Pelvic Organ Prolapse Quantification System; QoL = quality of life; RCT = randomised controlled trial; SIIQ: Short Incontinence Impact Questionnaire; SUDI: Short Urinary Distress Inventory; TVT = tension‐free vaginal tape; UDI: Urogenital Distress Inventory; US: ultrasound; USI = urodynamic stress incontinence; UTI = urinary tract infection; VAS = visual analogue score;
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Foote 2007 | Randomisation broke down when one recruitment source only referred participants for laparoscopic procedure. This led to the study continuing as a cohort study to two surgical techniques, so was excluded from this review |
| Koster 1996 | Comparing two‐dimensional view laparoscopy to three‐dimensional laparoscopy for different gynaecological operations; n = 3 for colposuspension, all randomly allocated to one group |
| Lee 1997 | Comparison of the clinical course and results between laparoscopic and open Burch colposuspension. Not a randomised study |
| Lernis 1997 | Not a randomised study and only reporting experience with laparoscopic colposuspension technique |
| Salam 2004 | Comparison of operative complications and early results between laparoscopic and open colposuspension. Design not stated and not a randomised study |
Contributions of authors
For the original review: Birgit Moehrer wrote the review with advice and editorial help from Don Wilson. Don Wilson and Marcus Carey wrote the original protocol. Gaye Ellis and Birgit Moehrer selected trials, extracted data separately and cross‐checked with Don Wilson. For the first (2005), second (2007) and this update (2009): Nicola Dean wrote the updated review. Gaye Ellis and Nicola Dean assessed the new studies and extracted the data separately. Don Wilson and Peter Herbison checked the new data and commented on the review.
For the July 2017 addition of the brief economic commentary (BEC) to this review ‐ Atefeh Mashayekhi was responsible for the entire BEC‐related work on this review: she ran the search for studies, screened the searches, extracted data from relevant studies, revised any existing economics‐related text, added the BEC‐related text, and responded to any peer referee comments. All review authors had the opportunity to comment on the revised review.
Sources of support
Internal sources
University of Otago, New Zealand.
External sources
-
National Institute for Health Research, UK.
This project, to add brief economic commentaries to Cochrane Incontinence's reviews on surgery for urinary incontinence in women, was supported by the National Institute for Health Research (NIHR), via the Cochrane Review Incentive Scheme 2016, to Cochrane Incontinence. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, NHS or the Department of Health.
-
National Institute for Health Research, UK.
This project was supported by the National Institute for Health Research, via Cochrane Infrastructure funding to Cochrane Incontinence. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, NHS or the Department of Health. The NIHR is the largest single funder of Cochrane Incontinence.
Declarations of interest
Nicola Dean: None known
Gaye Ellis: None known
G Peter Herbison: None known
Don Wilson: None known
Atefeh Mashayekhi: this project, to add brief economic commentaries to Cochrane Incontinence's reviews on surgery for urinary incontinence in women, was supported by the National Institute for Health Research (NIHR), via the Cochrane Review Incentive Scheme 2016, to Cochrane Incontinence. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, NHS or the Department of Health.
Edited (no change to conclusions)
References
References to studies included in this review
- Adile B, Cucinella G, Gugliotta G, Lo BA, Grifo S, Caputo A. A prospective randomised study of Burch laparoscopy versus tension‐free vaginal tape: 2 year follow‐up [Italian]. Urogynaecologia International Journal 2001;15(1 Suppl):121‐2. [13093] [Google Scholar]; Adile B, Granese R, Lo Bue A, Gugliotta G, Cardella AM, Adile C. A prospective randomized study comparing laparoscopic Burch versus TVT. Short and long term follow‐up (Abstract). Proceedings of the International Continence Society, 33rd Annual Meeting; 2003 Oct 5‐9; Florence, Italy. 2003:563. [Google Scholar]; Cucinella G, Adile B, Gugliotta G, Lo Bue A, Grifo S, Caputo A. A prospective randomized study comparing laparoscopic Burch versus TVT. Two years follow‐up (Abstract). International Urogynecology Journal 2001;12(Suppl 3):107. [Google Scholar]
- Ankardal M, Crafoord K, Ekerydh A, Ellstrom M, Franzen K, Olsson J‐H, et al. Burch colposuspension by laparoscopic or abdominal approach: report from a randomised study (Abstract). Proceedings of the International Continence Society (ICS), 31st Annual Meeting; 2001 Sept 18‐21; Seoul, Korea. 2001:Abstract 302. [Google Scholar]; Ankardal M, Ekerydh A, Crafoord K, Milsom I, Stjerndahl JH, Engh ME. A randomised trial comparing open Burch colposuspension using sutures with laparoscopic colposuspension using mesh and staples in women with stress urinary incontinence. BJOG: an International Journal of Obstetrics & Gynaecology 2004;111(9):974‐81. [17915] [DOI] [PubMed] [Google Scholar]
- Ankardal M, Milsom I, Stjerndahl JH, Engh ME. A three‐armed randomized trial comparing open Burch colposuspension using sutures with laparoscopic colposuspension using sutures and laparoscopic colposuspension using mesh and staples in women with stress urinary incontinence. Acta Obstetricia et Gynecologica Scandinavica 2005;84(8):773‐9. [20624] [DOI] [PubMed] [Google Scholar]
- Burton G. A five year prospective randomised urodynamic study comparing open and laparoscopic colposuspension. Neurourology and Urodynamics. 18 1999; Vol. 18, issue 4:295‐6. ; Burton G. A five year prospective randomised urodynamic study comparing open and laparoscopic colposuspension (Abstract). International Urogynecology Journal of Pelvic Floor Dysfunction. 10 1999; Vol. 10, issue Suppl 1:44‐5. ; Burton G. A randomised comparison of laparoscopic and open colposuspension. Neurourology and Urodynamics 1994;13(4):497‐8. [2684] [Google Scholar]; Burton G. A three year prospective randomised urodynamic study comparing open and laparoscopic colposuspension. Neurourology and Urodynamics 1997;16(5):353‐4. [5836] [Google Scholar]
- Carey M, Rosamilia A, Dwyer P, Cornish A, Murray C, Ugoni A, et al. Laparoscopic versus open colposuspension: a prospective multicentre randomised single‐blind comparison. Neurourology and Urodynamics 2000;19(4):389‐91. [Google Scholar]; Carey MP, Goh JT, Rosamilia A, Cornish A, Gordon I, Hawthorne G, et al. Laparoscopic versus open Burch colposuspension: a randomised controlled trial. BJOG: an International Journal of Obstetrics & Gynaecology 2006;113(9):999‐1006. [22334] [DOI] [PubMed] [Google Scholar]; Carey MP, Maher CF, Rosamilla A, Cornish A, Ugoni A. Open or laparoscopic colposuspension ‐ a prospective single blinded randomised control trial. Proceedings of the Annual Meeting of the Royal Australian and New Zealand College of Obstetrics and Gynaecology. 2000. [Google Scholar]; Cornish A, Fynes M, Harmer C, Hawthorne G, Rosamillia A, Carey M, et al. The genitourinary treatment satisfaction score for continence surgery (Abstract). Proceedings of the International Continence Society (ICS), 31st Annual Meeting; 2001 18‐21 Sept; Seoul, Korea. 2001:Abstract 83. [Google Scholar]
- Cheon WC, Mak JH, Liu JY. Prospective randomised controlled trial comparing laparoscopic and open colposuspension. Hong Kong Medical Journal 2003;9(1):10‐4. [PubMed] [Google Scholar]; Mak JHL, Cheon CW, Liu JYS, Lee TK, Tong WM, Wong THK. Prospective randomized controlled trial comparing laparoscopic and open colposuspension (Abstract). Proceedings of the 2nd Scientific Meeting of the Asian Society for Female Urology; 2000 Aug 26‐27; Hong Kong. 2000:59‐61. [Google Scholar]
- Fatthy H, Hao M, Samaha I, Abdallah K. Modified Burch colposuspension: laparoscopy versus laparotomy. The Journal of the American Association of Gynecologic Laparoscopists 2001;8(1):99‐106. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Foote A, Carne C, Lowndes C. Laparoscopic colposuspension vs vaginal mesh sling: a randomised prospective trial (Abstract). Neurourology and Urodynamics 2004;23(5/6):434‐5. [Google Scholar]; Foote AJ, Maughan V, Carne C. Laparoscopic colposuspension versus vaginal suburethral slingplasty: a randomised prospective trial. Australian & New Zealand Journal of Obstetrics & Gynaecology 2006;46(6):517‐20. [22592] [DOI] [PubMed] [Google Scholar]
- Dumville JC, Manca A, Kitchener HC, Smith AR, Nelson L, Torgerson DJ, COLPO Study Group. Cost‐effectiveness analysis of open colposuspension versus laparoscopic colposuspension in the treatment of urodynamic stress incontinence. BJOG: an International Journal of Obstetrics & Gynaecology 2006;113(9):1014‐22. [22332] [DOI] [PubMed] [Google Scholar]; Kitchener HC, Dunn G, Lawton V, Reid F, Nelson L, Smith AR, COLPO Study Group. Laparoscopic versus open colposuspension‐‐results of a prospective randomised controlled trial. BJOG: an International Journal of Obstetrics & Gynaecology 2006;113(9):1007‐13. [22333] [DOI] [PubMed] [Google Scholar]; Reid FM, Smith AR, Dunn G. Which questionnaire? A psychometric evaluation of three patient‐based outcome measures used to assess surgery for stress urinary incontinence. Neurourology and Urodynamics 2007;26(1):123‐8. [22577] [DOI] [PubMed] [Google Scholar]; Smith A, Kitchener H, Dunne G, Torgerson D, Lawton V, Reid F, et al. A prospective randomised controlled trial of open and laparoscopic colposuspension (Abstract). Neurourology and Urodynamics 2005;24(5/6):422‐3. [Google Scholar]
- Maher C, Qatawneh A, Baessler K, Cropper M, Schluter P. Laparoscopic colposuspension or tension‐free vaginal tape for recurrent stress urinary incontinence and/or intrinsic sphincter deficiency ‐ a randomised controlled trial (Abstract). Neurourology and Urodynamics 2004;23(5/6):433‐4. [Google Scholar]
- Mirosh M, Epp A. TVT vs laparoscopic Burch colposuspension for the treatment of stress urinary incontinence (Abstract). Proceedings of the 35th Annual Meeting of the International Incontinence Society (ICS); 2005 28 Aug ‐ 2 Sept; Montreal. 2005:Abstract number 640. [Google Scholar]
- Morris AR, Reilly ETC, Hassan A, Ramsay IN, Hawthorn RJS. 5‐7 year follow‐up of a randomised trial comparing laparoscopic colposuspension (LC) and open colposuspension (OC) in the treatment of genuine stress incontinence (Abstract). International Urogynecology Journal 2001;12(Suppl 3):S6. [Google Scholar]
- Jelovsek JE, Barber MD, Karram MM, Walters MD, Paraiso MF. Randomised trial of laparoscopic Burch colposuspension versus tension‐free vaginal tape: long‐term follow up. BJOG: an International Journal of Obstetrics & Gynaecology 2008;115(2):219‐225, discussion 225. [DOI] [PubMed] [Google Scholar]; Paraiso MF, Walters M, Karram M, Barber M. Laparoscopic Burch colposuspension versus the tension‐free vaginal tape procedure: a randomized clinical trial (Abstract). Neurourology and Urodynamics 2003;22(5):487‐8. [Google Scholar]; Paraiso MF, Walters MD, Karram MM, Barber MD. Laparoscopic Burch colposuspension versus tension‐free vaginal tape: a randomized trial. Obstetrics and Gynecology 2004;104(6):1249‐58. [DOI] [PubMed] [Google Scholar]
- Persson J, Wolner‐Hanssen P. Laparoscopic Burch colposuspension for stress urinary incontinence: a randomized comparison of one or two sutures on each side of the urethra. Obstetrics and Gynaecology 2000;95(1):151‐5. [MEDLINE: ; 9014] [DOI] [PubMed] [Google Scholar]
- Persson J. Stress urinary incontinence among women: aspects of risk factors, evaluation and surgical treatment [PhD thesis]. Lund (Sweden): Department of Obstetrics and Gynecology, Lund University, 2001:1‐61. [Google Scholar]; Persson J, Teleman P, Eten‐Bergquist C, Wolner‐Hanssen P. Cost‐analyses based on a prospective, randomised study comparing laparoscopic colposuspension with tension‐free vaginal tape procedure. Acta Obstetricia et Gynecologica Scandinavica 2002;81(11):1066‐73. [DOI] [PubMed] [Google Scholar]
- Ross J. Two techniques of laparoscopic Burch repair for stress incontinence: a prospective, randomized study. Journal of the American Association of Gynaecologic Laparoscopists 1996;3(3):351‐7. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Su TH, Wang KG, Hsu CY, Wei HJ, Hong BK. Prospective comparison of laparoscopic and traditional colposuspensions in the treatment of genuine stress incontinence. Acta Obstetricia et Gynecologica Scandinavica 1997;6(76):576‐82. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Summitt RL, Lucente VL, Karram MM, Shull BL, Bent AE. Randomised comparison of laparoscopic and transabdominal Burch urethropexy for the treatment of genuine stress incontinence (Abstract). Obstetrics and Gynecology 2000;95(4 Suppl 1):2. [Google Scholar]
- Ustun Y, Engin‐Ustun Y, Gungor M, Tezcan S. Tension‐free vaginal tape compared with laparoscopic Burch urethropexy. Journal of the American Association of Gynecologic Laparoscopists 2003;10(3):386‐9. [DOI] [PubMed] [Google Scholar]
- Valpas A, Kivela A, Penttinen J, Kauko M, Kujansuu E, Tomas E, et al. Comparison of TVT and laparoscopic colposuspension in the treatment of stress urinary incontinence (Abstract). Proceedings of the XXXIII Congress of the Nordic Federation of Societies of Obstetricians and Gynecologists (NFOG); 2002 June 1‐4 ; Umea, Sweden. 2002. [Google Scholar]; Valpas A, Kivela A, Penttinen J, Kauko M, Kujansuu E, Tomas E, et al. Intra‐operative and immediate post‐operative results comparing tensionfree vaginal tape (TVT) and laparoscopic colposuspension (LC) in the treatment of female stress urinary incontinence (SUI) ‐ A randomized clinical trial (Preliminary results). 10th Congress of the European Society for Gynaecological Endoscopy, Proceedings; 2001 Nov 21‐24; Lisbon, Portugal. 2001:355‐8. [Google Scholar]; Valpas A, Kivela A, Penttinen J, Kauko M, Kujansuu E, Tomas E, et al. Tension‐free vaginal tape and laparoscopic mesh colposuspension in the treatment of stress urinary incontinence: immediate outcome and complications‐‐a randomized clinical trial. Acta Obstetricia et Gynecologica Scandinavica 2003;82(7):665‐71. [PubMed] [Google Scholar]; Valpas A, Kivela A, Penttinen J, Kujansuu E, Haarala M, Nilsson CG. Tension‐free vaginal tape and laparoscopic mesh colposuspension for stress urinary incontinence. Obstetrics and Gynecology 2004;104(1):42‐9. [19322] [DOI] [PubMed] [Google Scholar]; Valpas A, Rissanen P, Kujansuu E, Nilsson C. A cost‐effectiveness analysis of tension‐free vaginal tape procedure vs. laparoscopic mesh colposuspension for primary female stress incontinence ‐ a randomised clinical trial (Abstract). Neurourology and Urodynamics 2005;24(5/6):418‐9. [Google Scholar]; Valpas A, Rissanen P, Kujansuu E, Nilsson CG. A cost‐effectiveness analysis of tension‐free vaginal tape versus laparoscopic mesh colposuspension for primary female stress incontinence. Acta Obstetricia et Gynecologica Scandinavica 2006;85(12):1485‐90. [22539] [DOI] [PubMed] [Google Scholar]; Valpas AK, Rissanen P, Kujansuu E, Nilsson CG. In a randomised clinical trial tension‐free vaginal tape is more cost‐effective than laparoscopic colposuspension (Abstract number 111). International Urogynecology Journal 2005;16(Suppl 2):S58‐9. [Google Scholar]
- Wallwiener D, Grischke EM, Rimbach S, Maleika A, Bastert G. Endoscopic retropubic colposuspension: "Retziusscopy" versus laparoscopy‐‐a reasonable enlargement of the operative spectrum in the management of recurrent stress incontinence?. Endoscopic Surgery and Allied Technologies 1995;3(2‐3):115‐8. [MEDLINE: ] [PubMed] [Google Scholar]; Wallwiener D, Grischke EM, Rimbach S, Maleika A, Kaufmann M, Bastert G. Endoscopic retropubic colposuspension: "Retziuscopy" versus laparoscopy ‐ a reasonable enlargement of the operative spectrum in the management of recurrent stress incontinence? [Endoskopische Kolposuspension ("Retziuskopie" versus Laparoskopie). Eine sinnvolle Erweiterung des Operationsspektrum der Stressinkontinenz?]. Geburtshilfe und Frauenheilkunde 1995;5(55):235‐9. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Palomba S, Russo T, Iuzzolino D, Cosco C, Noia R, Arduino B, et al. Comparison between two laparoscopic retropubic urethropexy. Minerva Chirurgica 2002;57(3):323‐9. [PubMed] [Google Scholar]; Zullo F, Morelli M, Russo T, Iuzzolino D, Palomba S. Two techniques of laparoscopic retropubic urethropexy. Journal of the American Association of Gynecologic Laparoscopists 2002;9(2):178‐81. [DOI] [PubMed] [Google Scholar]; Zullo F, Palomba S, Piccione F, Morelli M, Arduino B, Mastrantonio P. Laparoscopic Burch colposuspension: a randomized controlled trial comparing two transperitoneal surgical techniques(1). Obstetrics and Gynecology 2001;98(5 (Pt 1)):783‐8. [DOI] [PubMed] [Google Scholar]; Zullo F, Palomba S, Russo T, Sbano FM, Falbo A, Morelli M, et al. Laparoscopic colposuspension using sutures or prolene meshes: a 3‐year follow‐up. European Journal of Obstetrics, Gynecology, and Reproductive Biology 2004;117(2):201‐3. [19421] [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
- Foote AJ, Moore KH. The cost of urogynaecological treatments: which are more cost‐effective?. Australian & New Zealand Journal of Obstetrics & Gynaecology 2007;47(3):240‐6. [DOI] [PubMed] [Google Scholar]
- Koster S, Volz J, Melchert F. Indications for 3 D laparoscopy in gynecology [Zur Indikation der 3 D‐Laparoskopie in der Gynaekologie]. Geburtshilfe und Frauenheilkunde 1996;56(8):431‐3. [MEDLINE: ; 6892] [DOI] [PubMed] [Google Scholar]
- Lee YS, Kim JH, Seo JT. A comparison of laparoscopic versus open Burch procedure for stress urinary incontinence (Abstract). International Urogynecology Journal of Pelvic Floor Dysfunction. 8 1997; Vol. 8 Suppl, issue 1:37.
- Lernis P, Pantekhis G, Kalakoutis G. Presentation of our experience with laparoscopic colposuspension (Burch) at Makarios Hospital, Nicosia, Cyprus. Acta Obstetricia et Gynecologica Scandinavica 1997;76 Suppl 167(1):14. [Google Scholar]
- Salam TA. Laproscopic versus conventional surgical treatment of genuine urinary stress incontinence (Abstract number 4). Progres en Urologie 2004;14(3 Suppl 3):6. [Google Scholar]
Additional references
- Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, et al. Lower urinary tract function: standardisation of terminology. Neurourology and Urodynamics 2002;21:167‐78. [DOI] [PubMed] [Google Scholar]
- Bezerra CCB, Bruschini H, Cody JD. Traditional suburethral sling operations for urinary incontinence in women. Cochrane Database of Systematic Reviews 2005, Issue 3. [DOI: 10.1002/14651858.CD001754.pub2; CD001754] [DOI] [PubMed] [Google Scholar]
- Birnbaum HG, Leong SA, Oster EF, Kinchen K, Sun P. Cost of stress urinary incontinence: a claims data analysis. Pharmacoeconomics 2004;22(2):95‐105. [DOI] [PubMed] [Google Scholar]
- Chong E, Khan A, Anger J. The financial burden of stress urinary incontinence among women in the United States. Current Urology Reports 2011;12(5):358‐62. [DOI] [PubMed] [Google Scholar]
- Cody J, Wyness L, Wallace S, Glazener C, Kilonzo M, Stearns S, et al. Systematic review of the clinical effectiveness and cost‐effectiveness of tension‐free vaginal tape for treatment of urinary stress incontinence. Health Technology Assessment (Winchester, England) 2003;7(21):iii, 1‐189. [DOI] [PubMed] [Google Scholar]
- Dumville JC, Manca A, Kitchener HC, Smith AR, Nelson L, Torgerson DJ, et al. Cost‐effectiveness analysis of open colposuspension versus laparoscopic colposuspension in the treatment of urodynamic stress incontinence. BJOG: An International Journal of Obstetrics & Gynaecology 2006;113(9):1014‐22. [DOI] [PubMed] [Google Scholar]
- Glazener CMA, Cooper K. Anterior vaginal repair for urinary incontinence in women. Cochrane Database of Systematic Reviews 2001, Issue 1. [DOI: 10.1002/14651858.CD001755] [DOI] [PubMed] [Google Scholar]
- Glazener CMA, Cooper K. Bladder neck needle suspension for urinary incontinence in women. Cochrane Database of Systematic Reviews 2004, Issue 2. [DOI: 10.1002/14651858.CD003636.pub2; CD003636] [DOI] [PubMed] [Google Scholar]
- Hay‐Smith J, Ellis G, Herbison GP. Which anticholinergic drug for overactive bladder symptoms in adults. Cochrane Database of Systematic Reviews 2005, Issue 3. [DOI: 10.1002/14651858.CD005429; CD005429] [DOI] [PubMed] [Google Scholar]
- Hay‐Smith J, Dumoulin C. Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women. Cochrane Database of Systematic Reviews 2006, Issue 1. [DOI: 10.1002/14651858.CD005654; CD005654] [DOI] [PubMed] [Google Scholar]
- Hay‐Smith J, Mørkved S, Fairbrother KA, Herbison GP. Pelvic floor muscle training for prevention and treatment of urinary and faecal incontinence in antenatal and postnatal women. Cochrane Database of Systematic Reviews 2008, Issue 4. [DOI: 10.1002/14651858.CD007471; CD007471] [DOI] [PubMed] [Google Scholar]
- Herbison GP, Dean N. Weighted vaginal cones for urinary incontinence. Cochrane Database of Systematic Reviews 2002, Issue 1. [DOI: 10.1002/14651858.CD002114; CD002114] [DOI] [PubMed] [Google Scholar]
- Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analyses. BMJ 2003;327:557‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions 4.2.5 [updated May 2005]. www.cochrane.org/resources/handbook.htm (accessed 4 January 2006).
- Jarvis GJ, Bent A, Cortesse A, McGuire A, Milani R, Quartey J, et al. Surgical treatment for incontinence in adult women surgery of female lower genito‐urinary fistulae. In: Abrams P, Khoury S, Wein A editor(s). Incontinence: 1st International Consultation on Incontinence. Recommendations of the International Scientific Committee: the evaluation and treatment of urinary incontinence. Vol. 15, Plymouth: Health Publication Limited, 1999:637‐68. [Google Scholar]
- Keegan PE, Atiemo K, Cody JD, McClinton S, Pickard R. Periurethral injection therapy for urinary incontinence in women. Cochrane Database of Systematic Reviews 2007, Issue 3. [DOI: 10.1002/14651858.CD003881.pub2; CD003881] [DOI] [PubMed] [Google Scholar]
- Kilonzo M, Vale L, Stearns SC, Grant A, Cody J, Glazener CMA, et al. Cost effectiveness of tension‐free vaginal tape for the surgical management of female stress incontinence. International Journal of Technology Assessment in Health Care 2004;20(4):455‐63. [DOI] [PubMed] [Google Scholar]
- Kunkle CM, Hallock JL, Hu X, Blomquist J, Thung SF, Werner EF. Cost utility analysis of urethral bulking agents versus midurethral sling in stress urinary incontinence. Female Pelvic Medicine & Reconstructive Surgery 2015;21(3):154‐9. [DOI] [PubMed] [Google Scholar]
- Lapitan MCM, Cody JD, Grant A. Open retropubic colposuspension for urinary incontinence in women. Cochrane Database of Systematic Reviews 2009, Issue 4. [DOI: 10.1002/14651858.CD002912.pub4; CD002912] [DOI] [PubMed] [Google Scholar]
- McCormack K, Scott NW, Go PMNYH, Ross S, Grant AM, the EU Hernia Trialists Collaboration. Laparoscopic techniques versus open techniques for inguinal hernia repair. Cochrane Database of Systematic Reviews 2003, Issue 1. [DOI: 10.1002/14651858.CD001785] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nabi G, Cody JD, Ellis G, Hay‐Smith J, Herbison GP. Anticholinergic drugs versus placebo for overactive bladder syndrome in adults. Cochrane Database of Systematic Reviews 2006, Issue 4. [DOI: 10.1002/14651858.CD003781.pub2; CD003781] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogah J, Cody JD, Rogerson L. Minimally invasive synthetic suburethral sling operations for stress urinary incontinence in women. Cochrane Database of Systematic Reviews 2009, Issue 4. [DOI: 10.1002/14651858.CD006375.pub2; CD006375] [DOI] [PubMed] [Google Scholar]
- ISI ResearchSoft. Reference Manager 9.5 N. Berkeley, CA, USA: ISI ResearchSoft, 2002.
- Subak L, Brubaker L, Chai T, Creasman J, Diokno A, Goode P, et al. High costs of urinary incontinence among women electing surgery to treat stress incontinence. Obstetrics & Gynecology 2008;111(4):899‐907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thakar R, Stanton S. Regular review: management of urinary incontinence in women. BMJ 2000;321(7272):1326‐31. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valpas A, Rissanen P, Kujansuu E, Nilsson CG. A cost‐effectiveness analysis of tension‐free vaginal tape versus laparoscopic mesh colposuspension for primary female stress incontinence. Acta Obstetricia et Gynecologica Scandinavica 2006;85(12):1485‐90. [DOI] [PubMed] [Google Scholar]
- Vancaillie TG, Schuessler W. Laparoscopic bladderneck suspension. Journal of Laparoendoscopic Surgery 1991;1(3):169‐73. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Wagner TH, Hu TW. Economic costs of urinary incontinence in 1995. Urology 1998;51(3):355‐61. [DOI] [PubMed] [Google Scholar]
- Wallace SA, Roe B, Williams K, Palmer M. Bladder training for urinary incontinence in adults. Cochrane Database of Systematic Reviews 2004, Issue 1. [DOI: 10.1002/14651858.CD001308.pub2; CD001308] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ware JE, Snow KK, Kosinski M, Gandek B. SF‐36 Health Survey Manual and Interpretation Guide. Boston, Massachusetts: The Health Institute, New England Medical Centre, 1993. [Google Scholar]
- Wilson PD, Herbison RM, Herbison GP. Obstetric practice and the prevalence of urinary incontinence three months after delivery. British Journal of Obstetrics and Gynaecology 1996;103(2):154‐61. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]


