Abstract
Background
Urinary incontinence is a common and potentially debilitating problem. Stress urinary, incontinence as the most common type of incontinence, imposes significant health and economic burdens on society and the women affected. Open retropubic colposuspension is a surgical treatment which involves lifting the tissues near the bladder neck and proximal urethra in the area behind the anterior pubic bones to correct deficient urethral closure to correct stress urinary incontinence.
Objectives
The review aimed to determine the effects of open retropubic colposuspension for the treatment of urinary incontinence in women. A secondary aim was to assess the safety of open retropubic colposuspension in terms of adverse events caused by the procedure.
Search methods
We searched the Cochrane Incontinence Group Specialised Register, which contains trials identified from the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE, MEDLINE in process, ClinicalTrials.gov, WHO ICTRP and handsearching of journals and conference proceedings (searched 5 May 2015), and the reference lists of relevant articles. We contacted investigators to locate extra studies.
Selection criteria
Randomised or quasi‐randomised controlled trials in women with symptoms or urodynamic diagnoses of stress or mixed urinary incontinence that included open retropubic colposuspension surgery in at least one trial group.
Data collection and analysis
Studies were evaluated for methodological quality or susceptibility to bias and appropriateness for inclusion and data extracted by two of the review authors. Trial data were analysed by intervention. Where appropriate, a summary statistic was calculated.
Main results
This review included 55 trials involving a total of 5417 women.
Overall cure rates were 68.9% to 88.0% for open retropubic colposuspension. Two small studies suggested lower incontinence rates after open retropubic colposuspension compared with conservative treatment. Similarly, one trial suggested lower incontinence rates after open retropubic colposuspension compared to anticholinergic treatment. Evidence from six trials showed a lower incontinence rate after open retropubic colposuspension than after anterior colporrhaphy. Such benefit was maintained over time (risk ratio (RR) for incontinence 0.46; 95% CI 0.30 to 0.72 before the first year, RR 0.37; 95% CI 0.27 to 0.51 at one to five years, RR 0.49; 95% CI 0.32 to 0.75 in periods beyond five years).
Evidence from 22 trials in comparison with suburethral slings (traditional slings or trans‐vaginal tape or transobturator tape) found no overall significant difference in incontinence rates in all time periods evaluated (as assessed subjectively RR 0.90; 95% CI 0.69 to 1.18, within one year of treatment, RR 1.18; 95%CI 1.01 to 1.39 between one and five years, RR 1.11; 95% CI 0.97 to 1.27 at five years and more, and as assessed objectively RR 1.24; 95% CI 0.93 to 1.67 within one year of treatment, RR 1.12; 95% CI 0.82 to 1.54 for one to five years follow up, RR 0.70; 95% CI 0.30 to 1.64 at more than five years). However, subgroup analysis of studies comparing traditional slings and open colposuspension showed better effectiveness with traditional slings in the medium and long term (RR 1.35; 95% CI 1.11 to 1.64 from one to five years follow up, RR 1.19; 95% CI 1.03 to 1.37).
In comparison with needle suspension, there was a lower incontinence rate after colposuspension in the first year after surgery (RR 0.66; 95% CI 0.42 to 1.03), after the first year (RR 0.56; 95% CI 0.39 to 0.81), and beyond five years (RR 0.32; 95% CI 15 to 0.71).
Patient‐reported incontinence rates at short, medium and long‐term follow‐up showed no significant differences between open and laparoscopic retropubic colposuspension, but with wide confidence intervals. In two trials incontinence was less common after the Burch (RR 0.38; 95% CI 0.18 to 0.76) than after the Marshall Marchetti Krantz procedure at one to five year follow‐up. There were few data at any other follow‐up times.
In general, the evidence available does not show a higher morbidity or complication rate with open retropubic colposuspension compared to the other open surgical techniques, although pelvic organ prolapse is more common than after anterior colporrhaphy and sling procedures. Voiding problems are also more common after sling procedures compared to open colposuspension.
Authors' conclusions
Open retropubic colposuspension is an effective treatment modality for stress urinary incontinence especially in the long term. Within the first year of treatment, the overall continence rate is approximately 85% to 90%. After five years, approximately 70% of women can expect to be dry. Newer minimal access sling procedures look promising in comparison with open colposuspension but their long‐term performance is limited and closer monitoring of their adverse event profile must be carried out. Open colposuspension is associated with a higher risk of pelvic organ prolapse compared to sling operations and anterior colporrhaphy, but with a lower risk of voiding dysfunction compared to traditional sling surgery. Laparoscopic colposuspension should allow speedier recovery but its relative safety and long‐term effectiveness is not yet known. A Brief Economic Commentary (BEC) identified five studies suggesting that tension‐free vaginal tape (TVT) and laparoscopic colposuspension may be more cost‐effective compared with open retropubic colposuspension.
Plain language summary
Open retropubic colposuspension for urinary incontinence in women
Importance of the Review / Background
Stress urinary incontinence is losing urine when coughing, laughing, sneezing or exercising. It can be caused by changes to muscles and ligaments holding up the bladder. Mixed urinary incontinence is also losing urine when there is an urge to void as well as when coughing and laughing. Muscle‐strengthening exercises can help, and there are surgical procedures to improve support or correct problems. A significant amount of a woman's and their family's income can be spent on management of stress urinary incontinence. Open retropubic colposuspension is an operation which involves lifting the tissues around the junction between the bladder and the urethra.
Main Findings
The review of trials found that this is an effective surgical technique for stress and mixed urinary incontinence in women, resulting in long‐term cure for most women. It provides better cure rates compared to anterior colporrhaphy a (suturing of the top wall of the vagina) and needle suspension surgery (passing a needle with sutures at the sides of the urethra to lift up the tissues beside it).New techniques, particularly sling operations (including the use of tapes to lift up the urethra)and keyhole (laparoscopic) colposuspension, look promising but need further research particularly on long‐term performance. Procedures involving surgery to insert a tape under the urethra showed better cure rates in the medium and long term, compared to open colposuspension. In terms of costs, a non‐systematic review of economic studies suggested that open retropubic colposuspension would be cheaper than laparoscopic colposuspension, but more expensive than tension‐free vaginal tape (TVT).
Adverse Events
Laparoscopic colposuspension allows for faster recovery compared to open colposuspension. Studies did not reveal a higher complication rate with open colposuspension compared with the other surgical techniques, although pelvic organ prolapse was found to be more common. Abnormal voiding was less common after open colposuspension compared to sling surgery.
Limitations
Limited information was available on the long term adverse events of open colposuspension and its effect on the quality of life.
Background
Description of the condition
Urinary incontinence has been identified by the World Health Organization as an important global health issue. It is a common and potentially debilitating problem. The overall prevalence of incontinence is reported to be between 10% to 40% of adult women, and is considered severe in about 3% to 17% (Hunskaar 2002). The wide range of prevalence estimates is due to variations in the definition of incontinence used, populations sampled, and study methods (Herzog 1990). It is believed that the true magnitude of the problem is still unknown due to under‐reporting.
Continence is achieved through an interplay of the normal anatomical and physiological properties of the bladder, urethra and sphincter, pelvic floor, and the nervous system co‐ordinating these organs. The active relaxation of the bladder, coupled by the ability of the urethra and sphincter to contain urine within the bladder by acting as a closure mechanism during filling, allow storage of urine until an appropriate time and place to void is reached. The role of the pelvic floor in providing support to the bladder and urethra, and allowing normal abdominal pressure transmission to the proximal urethra, is also considered essential in the maintenance of continence. Crucial to the healthy functioning of the bladder, urethra, sphincter and pelvic floor is co‐ordination between them, facilitated by an intact nervous system control.
Incontinence occurs when this normal relationship between the lower urinary tract components is disrupted, resulting from nerve damage or direct mechanical trauma to the pelvic organs. Advancing age, higher parity, vaginal delivery, obesity and menopause are associated with an increase in risk (Wilson 1996).
There are different types of urinary incontinence. Stress incontinence is the symptom of involuntary loss of urine during situations of increased intra‐abdominal pressure, such as coughing or sneezing. The International Continence Society defines 'urodynamic stress incontinence' as the involuntary loss of urine with increased intra‐abdominal pressure during filling cystometry, in the absence of detrusor (bladder wall muscle) contraction (Abrams 2002). Thus, urodynamic evaluation is a prerequisite for the diagnosis of urodynamic stress incontinence. It is not clear, however, especially from the clinical management standpoint, whether urodynamic diagnosis is imperative for successful treatment of stress incontinence. Therefore, this review included women diagnosed with either stress urinary incontinence (symptom alone) or urodynamic stress incontinence.
Stress urinary incontinence (SUI) constitutes a huge financial economic burden to society. In the USA, the annual total direct costs of urinary incontinence in both men and women is over USD 16 billion (1995 USD) (Chong 2011), with societal costs of USD 26.2 billion (Wagner 1998). Approximately, USD 13.12 billion of the total direct costs of urinary incontinence is spent on SUI (Chong 2011; Kunkle 2015).
About 70% of this USD 13.12 billion is borne by the patients, mainly through routine care (purchasing pads and disposable underwear (diapers), laundry and dry cleaning). This constitutes a significant individual financial burden. Of the remaining 30% of costs, 14% is spent on nursing home admission, 9% on treatment, 6% on addressing complications and 1% on diagnosis (Chong 2011).
A study in the USA reported that about 1% of the median annual household income (USD 50,000 to USD 59,999 in 2006) was spent by women on incontinence management. This study estimated that women spent an annual mean cost of USD 751 to USD 1277 (2006 USD) on incontinence. This cost increases with the severity of the symptoms (Subak 2008a). The indirect cost associated exerts a social and psychological burden which is unquantifiable. (Chong 2011; Kilonzo 2004). Nevertheless, Birnbaum 2004 estimated that the annual average direct medical costs of SUI for one year (1998 USD) was USD 5642 and USD 4208 for indirect workplace costs. The cost of management and treatment of SUI appears to have increased over time, due to increasing prevalence and increased desire for improved quality of life (QOL). This in turn has resulted from improved recognition of the condition, as well as increased use of surgical and non‐surgical managements.
Two types of stress incontinence are recognised, one from a hypermobile but otherwise healthy urethra and one from deficiency of the sphincter itself (Blaivas 1988). Urethral hypermobility is a manifestation of weakened support of the proximal urethra while sphincter deficiency is an indication of compromised ability of the urethra to act as a watertight outlet. Both types were considered together for this review for three reasons. Firstly, few studies have distinguished between them; secondly, a standardised test is not available to differentiate between them accurately; and lastly, there is increasing belief that both types are present most of the time although to differing degrees.
Urge incontinence is the symptom of involuntary loss of urine associated with a sudden, strong desire to void (urgency). It is usually a manifestation of uncontrolled bladder wall contraction (detrusor overactivity). Bladder overactivity may be suspected clinically from symptoms of frequency and urgency. When detected urodynamically, bladder overactivity is termed either as 'neurogenic detrusor overactivity' if there is an underlying neurologic pathology associated with it, or 'idiopathic detrusor overactivity' when there is none. Women with urge incontinence alone were not included in this review.
Mixed incontinence is the condition of urine leakage with features of both stress and urgency. Women with mixed incontinence were included in this review. They could either have stress incontinence with symptoms of frequency and urgency, stress and urge incontinence (either diagnosed by symptom alone or by urodynamics), or stress incontinence with detrusor overactivity, or urodynamic stress incontinence with detrusor overactivity.
Description of the intervention
Treatment for urinary incontinence includes 'conservative', pharmacological and surgical interventions. Conservative management includes physical therapies (for example pelvic floor muscle training, electrical stimulation, biofeedback and vaginal weighted cones), lifestyle modification (for example weight loss, regulation of fluid intake), behavioural interventions (for example bladder retraining, timed voiding) and mechanical devices (for example urethral plugs and inserts to prevent or reduce urine leakage). Drug therapies include alpha‐adrenergic agents and duloxetine (mainly for stress urinary incontinence), anticholinergics and antispasmodics (for urge incontinence) and estrogens. Conservative therapy, with or without the use of medications, is generally undertaken before resorting to surgery. These interventions are the subject of separate Cochrane reviews.
Surgical procedures to treat stress urinary incontinence generally aim to improve the support to the urethro‐vesical junction and correct deficient urethral closure. There is disagreement, however, regarding the precise mechanism by which continence is achieved with surgical manipulation. The surgeon's preference, co‐existing pelvic floor problems, and the anatomical features of the patient and her general health condition often influence the choice of procedure. Numerous surgical methods have been described but essentially they fall into seven categories, with one category subdivided into three.
Open retropubic colposuspension.
Vaginal anterior repair (anterior colporrhaphy) (Glazener 2001).
-
Suburethral sling procedures:
traditional suburethral sling procedure (Rehman 2011);
self‐fixing suburethral sling procedure (Ford 2015);
single incision sling procedure (Nambiar 2014).
Bladder neck needle suspension (Glazener 2014).
Laparoscopic retropubic colposuspension (Dean 2006).
Periurethral injections (Kirchin 2012).
Artificial urethral sphincters.
This review focused on the first of these. Other Cochrane reviews have or will focus on the other six categories (Dean 2006; Glazener 2001; Glazener 2014; Nambiar 2014; Kirchin 2012; Ford 2015; Rehman 2011). There is also a Cochrane review which looks at treatment of recurrent stress urinary incontinence after failed minimally invasive synthetic suburethral tape surgery in women (Bakali 2013). There is as yet no Cochrane review of artificial urethral sphincters.
How the intervention might work
Retropubic colposuspension is the surgical approach of lifting the tissues near the bladder neck and proximal urethra in the area of the pelvis behind the anterior pubic bones. When it is an 'open' procedure, the approach is through an incision over the lower abdomen. There are generally three variations of open retropubic colposuspension:
Burch;
Marshall‐Marchetti‐Krantz (MMK);
Paravaginal defect repair or vagina‐obturator shelf repair.
The Burch colposuspension is the elevation of the anterior vaginal wall and paravesical tissues towards the ileopectineal line of the pelvic side wall using two to four sutures on either side (Burch 1961). The Marshall‐Marchetti‐Krantz procedure is the suspension of the vesico‐urethral junction (bladder neck) onto the periosteum of the symphysis pubis (Mainprize 1988). The paravaginal defect repair, or the vagina‐obturator shelf repair, is a modification of the Burch with placement of the sutures extended laterally and anchored at the obturator shelf rather than the ileopectineal line (Richardson 1976). It aims to close the fascial defect rather than elevate the tissues at the paravesical area.
Why it is important to do this review
The wide variety of treatment options for stress incontinence indicates the lack of a clear consensus as to which procedure is the most effective. Several organisations have produced guidelines for provision of good healthcare service (Fantl 1996; Leach 1997). However, these reports were based on studies of mixed quality and consequently some recommendations were based on consensus rather than reliable evidence. The International Consultation on Incontinence (ICI), now in its fourth iteration, is another similar initiative which uses evidence of mixed quality (www.congress‐urology.org). Systematic and methodical analyses of well‐designed randomised controlled trials have also been performed (for example Black 1996; Jarvis 1994; Novara 2008) but each has its own limitations in terms of database, methodology and, more importantly, updating in the event of new evidence.
While stress urinary incontinence is now generally managed surgically with minimally invasive procedures, particularly with the use of mid‐urethral slings, such procedures are not readily available in many countries. This is partly because of the limitations of expertise but also, more importantly, because of the difficulty in acquiring the slings, either because of their unavailability or their prohibitive cost.
Objectives
The review aimed to determine the effects of open retropubic colposuspension for the treatment of urinary incontinence in women. A secondary aim was to assess the safety of open retropubic colposuspension in terms of adverse events caused by the procedure.
Methods
Criteria for considering studies for this review
Types of studies
All randomised or quasi‐randomised (using for example alternation) controlled trials which involved open retropubic colposuspension in at least one arm.
Types of participants
Adult women with urinary incontinence diagnosed as having:
urodynamic stress incontinence; or
stress incontinence (clinical diagnosis); or
mixed incontinence (stress incontinence plus other urinary symptoms, eg urgency, urge incontinence, frequency whether confirmed by urodynamics or based on symptoms alone).
Classification of diagnoses was accepted as defined by the trialists.
Participants with previous incontinence surgery or with other co‐morbid diseases (for example prolapse disease) were included in the review.
Types of interventions
At least one arm of a trial involved open retropubic colposuspension to treat stress or mixed incontinence.
Comparison interventions included conservative therapy, drug therapy and other surgical techniques.
The following comparisons were made:
open retropubic colposuspension versus no treatment or sham operation for the management of urodynamic stress incontinence and for symptoms of stress or mixed incontinence (clinical diagnosis);
open retropubic colposuspension versus conservative interventions (pelvic floor muscle training, electrical stimulation, biofeedback) for the management of urodynamic stress incontinence and for symptoms of stress or mixed incontinence (clinical diagnosis);
open retropubic colposuspension versus drug therapy for the management of urodynamic stress incontinence and for symptoms of stress or mixed incontinence (clinical diagnosis);
open retropubic colposuspension versus vaginal anterior repair (anterior colporrhaphy) for the management of urodynamic stress incontinence and for symptoms of stress or mixed incontinence (clinical diagnosis);
-
open retropubic colposuspension versus sling procedures (abdominal and vaginal approach, including self‐fixing slings) for the management of urodynamic stress incontinence and for symptoms of stress or mixed incontinence (clinical diagnosis);
open retropubic colposuspension versus traditional sling procedures (abdominal and vaginal approach) for the management of urodynamic stress incontinence and for symptoms of stress or mixed incontinence (clinical diagnosis);
open retropubic colposuspension versus self‐fixing sling procedures (tension‐free vaginal tape (TVT), transobturator tape (TOT)) for the management of urodynamic stress incontinence and for symptoms of stress or mixed incontinence (clinical diagnosis);
open retropubic colposuspension versus single‐incision sling procedures for the management of urodynamic stress incontinence and for symptoms of stress or mixed incontinence (clinical diagnosis);
open retropubic colposuspension versus bladder neck needle suspension for the management of urodynamic stress incontinence and for symptoms of stress or mixed incontinence (clinical diagnosis);
open retropubic colposuspension versus laparoscopic retropubic colposuspension for the management of urodynamic stress incontinence and for symptoms of stress or mixed incontinence (clinical diagnosis);
open retropubic colposuspension versus periurethral injection procedures for the management of urodynamic stress incontinence and for symptoms of stress or mixed incontinence (clinical diagnosis);
-
methods of open retropubic colposuspension versus other methods of open retropubic colposuspension for the management of urodynamic stress incontinence and for symptoms of stress or mixed incontinence (clinical diagnosis):
Burch colposuspension versus Marshall‐Marchetti‐Krantz procedure,
Burch colposuspension versus paravaginal defect repair or vaginal obturator shelf repair,
Marshall‐Marchetti‐Krantz procedure versus paravaginal defect repair or vaginal obturator shelf repair.
Types of outcome measures
This review adopted the recommendations by the Standardisation Committee of the International Continence Society on the outcome domains of research investigating the effect of therapeutic interventions for women with urinary incontinence. These outcome domains include: the woman's observation (symptoms), quantification of symptoms, the clinician's observations (anatomical and functional) and quality of life measures (Lose 1998).
A crucial consideration in the choice of surgical intervention for benign disease is the attendant complications and consequences of the different procedures. Thus, this review included adverse events as outcome measures.
Women's observations
1. Number not cured (worse, unchanged or improved versus cured) within first year (self‐reported, subjective) 2. Number not cured (worse, unchanged or improved versus cured) after first year (self‐reported, subjective) 3. Number not cured (worse, unchanged or improved versus cured) after five years (self‐reported, subjective) 4. Number not improved (worse or unchanged versus improved or cured) within first year (self‐reported, subjective) 5. Number not improved (worse or unchanged versus improved or cured) after first year (self‐reported, subjective) 6. Number not improved (worse or unchanged versus improved or cured) after five years (self‐reported, subjective)
Quantification of symptoms
7. Number of pad changes over 24 hours (from self‐reported number of pads used) 8. Number of incontinent episodes over 24 hours (from self‐completed urinary diary) 9. Mean volume or weight of urine loss on pad tests
Clinicians' observations
10. Number not cured (worse, unchanged or improved versus cured) within first year (objective test) 11. Number not cured (worse, unchanged or improved versus cured) after first year (objective test) 12. Number not cured (worse, unchanged or improved versus cured) after five years (objective test)
Quality of life
13. General health status measures e.g. Short Form‐36 (Ware 1993) 14. Condition‐specific health measures (specific instruments designed to assess incontinence)
Surgical outcome measures
15. Length of operating time 16. Length of inpatient hospital stay 17. Time to return to normal activity level 18. Time to catheter removal
Adverse events
19. Number with perioperative surgical complications (e.g. infection, haemorrhage, etc) 20. Number with de novo urge symptoms or urge incontinence (clinical diagnosis without urodynamics) 21. Number with de novo detrusor overactivity (urodynamic diagnosis) 22. Number with voiding dysfunction or voiding difficulty (with or without urodynamic confirmation) 23. Number with recurrent or new prolapse (enterocoele, rectocoele, vaginal prolapse, uterine prolapse) 24. Number undergoing repeat incontinence surgery 25. Number with other complications inherent to the procedure (e.g. osteitis for Marshall‐Marchetti‐Krantz procedure) 26. Number with bladder perforation
Other outcomes
Non pre‐specified outcomes judged important when performing the review
The surgical outcome measures were not considered in the comparisons made between open retropubic colposuspension and conservative management or drug treatment.
For this review, the following were considered to be the primary outcomes.
Numbers not cured at one year (symptomatic)
Number not cured at one year (objective)
Number not improved at one year (symptomatic)
Number not cured at five years (symptomatic)
Condition‐specific health measures
Search methods for identification of studies
We did not impose any language or other restrictions on any of the searches.
Electronic searches
This review has drawn on the search strategy developed for the Incontinence Review Group. Relevant trials were identified from the Group's Specialised Register of controlled trials, which is described under the Incontinence Group's module in the Cochrane Library. The Register contains trials identified from the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE, MEDLINE in process, ClinicalTrials.gov, and WHO ICTRP and handsearching of journals and conference proceedings. The date of the most recent search was: 5 May 2015.
Most of the trials in the Incontinence Group Specialised Register are also contained in CENTRAL.
We searched the Incontinence Group Specialised Register using the Group's own keyword system, the search terms used are given in Appendix 1.
We performed additional searches for the Brief Economic Commentary (BEC). We conducted them in MEDLINE(1 January 1946 to March 2017), Embase (1 January 1980 to 2017 Week 12) and NHS EED (1st Quarter 2016). We ran all searches on 6 April 2017. Details of the searches run and the search terms used can be found in Appendix 2.
Searching other resources
We searched the reference lists of relevant articles for other possible relevant trials.
We contacted investigators to ask for other possible relevant trials, published or unpublished.
For earlier versions of this review we handsearched conference proceedings as described in Appendix 3.
Data collection and analysis
Selection of studies
Two review authors appraised the titles and, where possible, the abstracts of all studies identified by the searches to ascertain those likely to be assessments of the effectiveness of open retropubic colposuspension. We retrieved reports of potentially eligible trials in full. The review authors, without prior consideration of the results, evaluated the full reports of all possibly eligible studies for methodological quality and appropriateness for inclusion.
If studies were not randomised or quasi‐randomised controlled trials for incontinent women, or if they made comparisons other than those pre‐specified, we excluded them from the review. Excluded studies are listed in the 'Characteristics of excluded studies' table with the reasons for their exclusion.
Data extraction and management
Both review authors independently undertook data extraction using a standard form containing pre‐specified outcomes. Where data may have been collected but not reported, we sought clarification from the investigators.
Subjective cure and objective cure were as study authors defined them. However if more than one form of the result was available, we used the women's report of having or not having the symptom of leakage as the measure of subjective cure and the result of the stress test or the pad test, depending on which test was used by the majority of the trials in the comparison, as the measure of objective cure. Number with voiding dysfunction included those having urinary retention and voiding difficulty, those needing a bladder drainage procedure such as intermittent or indwelling catheterisation. Time to catheter removal was considered equivalent to time to normal or spontaneous voiding, as defined by the trialists.
When more than one result for an outcome was reported due to multiple determinations at different time intervals within the trial, the latest available data set was used and entered into the table of comparisons.
We resolved any differences of opinion related to study inclusion, methodological quality or data extraction by discussion amongst the review authors and, when necessary, by referral to a third party for arbitration.
Assessment of risk of bias in included studies
Each review author independently undertook the assessment of risk of bias using the Cochrane Collaboration's risk of bias tool (Higgins 2011). We based the system for classifying risk of bias of controlled trials on an assessment of the three principal potential sources of bias. These are: selection bias from insecure random allocation of treatments; attrition bias from dropouts or losses to follow‐up, particularly if there was a differential dropout rate between groups; and biased ascertainment (detection bias) of outcome where knowledge of the allocation might have influenced the measurement of outcome. In addition, we examined the calculation of sample size and definition of used terms.
Measures of treatment effect
We used the standard Cochrane software Review Manager (RevMan) to conduct this review (RevMan 2014) and processed included trial data as described in the Cochrane Collaboration Handbook (Deeks 2011). When we identified more than one eligible study, we carried out quantitative synthesis. Where appropriate, we calculated a combined estimate of treatment effect across similar studies for each pre‐specified outcome. For categorical (dichotomous) outcomes we related the numbers reporting an outcome to the numbers at risk in each group to derive a risk ratio (RR). For continuous variables, we used means and standard deviations to derive a mean difference (MD), and generated 95% confidence intervals (CI), where possible.
Where statistical synthesis of data from more than one study was not possible or not considered appropriate, we undertook a narrative review of eligible studies. We sought data on the number of women with each outcome event by allocated treatment group, irrespective of compliance and whether or not the participant was later thought to be ineligible or otherwise excluded from treatment or follow‐up, to allow an intention‐to‐treat analysis when possible. For trials with missing data, we based the primary analysis upon the observed data, as reported, without imputation for missing data. We carried out sensitivity analyses using different assumptions about missing data.
When appropriate, we separated trial data into those performed for primary incontinence and those for recurrent incontinence from failed previous surgery; and those performed as a single procedure or in combination with another surgical procedure (for example hysterectomy or repair of prolapse).
Data synthesis
We used a fixed‐effect model approach to the analysis unless there was evidence of heterogeneity across studies.
Subgroup analysis and investigation of heterogeneity
We grouped trial data by type of incontinence, either urodynamic stress incontinence or stress or mixed incontinence, based upon a symptom classification.
When appropriate, we separated trial data into those performed for primary incontinence and those for recurrent incontinence from failed previous surgery; and those performed as a single procedure or in combination with another surgical procedure (for example hysterectomy or repair of prolapse).
We investigated differences between trials when apparent from either visual inspection of the results or when statistically significant heterogeneity was demonstrated by using the Chi2 test at the 10% probability level or assessment of the I2 statistic (Higgins 2003). If there was no obvious reason for the heterogeneity (after consideration of populations, interventions, outcomes and settings of the individual trials) or it persisted despite the removal of outlying trials, we used a random‐effects model.
Results
Description of studies
The reader is directed to the Characteristics of included studies table for a more detailed account.
Search results
We screened 428 records produced by the literature search. Altogether, we have reviewed 231 full‐text articles for eligibility, of which 152 reports of 55 studies were included in the review. One trial report is still awaiting classification (Helmy 2012), pending verification if it is a new trial or a report of an already included study (Albo 2007). Of the trials that were excluded, the majority were either not randomised trials or had participants that were not incontinent at the beginning of the trial. Two references were studies comparing one sling technique with another (Debodinance 1993; Debodinance 1994). One trial (Baessler 1998) was excluded because it compared one technique of open retropubic colposuspension (Burch) with the same technique in combination with another (paravaginal repair) and another trial (Costantini 2007b) because it compared a type of prolapse repair with Burch colposuspension and the same repair without the Burch.
Two new trials (El‐Din Shawki 2012; Trabuco 2014), and a new report from a previously included trial (Albo 2007), were identified for inclusion in this review update (2015). The PRISMA diagram showing the flow of literature through the assessment process is given in Figure 1 (Liberati 2009).
1.
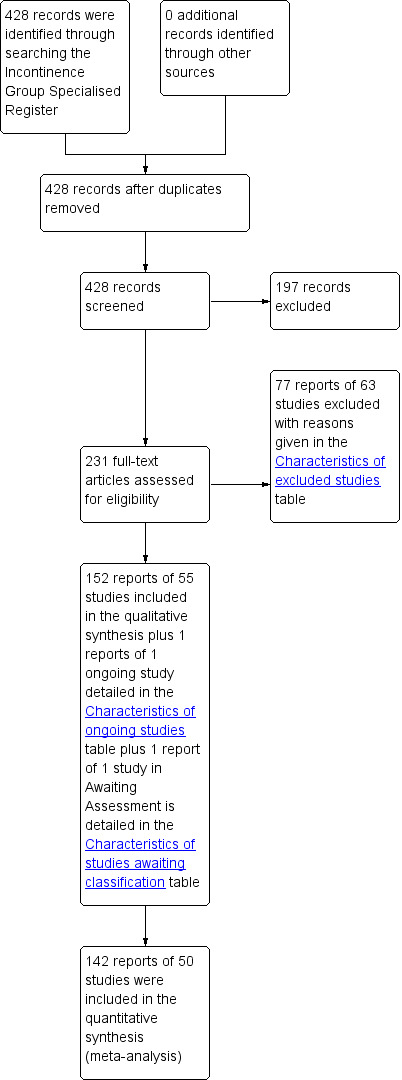
PRISMA study flow diagram.
Publication types
The primary reference for the 55 included trials were: 36 full text, published journal articles; 18 abstracts from conference proceedings; and data from one unpublished full paper (Holmes 1985) published as abstracts in three conference proceedings. We received additional information for five trials (Colombo 2000; Gilja 1998; Palma 1985; Su 1997; Ward 2002) as a result of correspondence with the trialists. One report was published in German (Enzelsberger 1996). Information and data were extracted from an English translation performed by a medical practitioner not involved in the review. One report was published in Turkish (Tuygun 2006). The information used in this review from that report was limited to that contained in the English abstract, pending translation of the full text.
Sample characteristics
The 55 trials included a total of 5417 women randomised into the different treatment groups. Outcomes from 5198 women were available for analysis (at the time of the latest assessment).
Follow up
Two trials reported complete follow‐up while 25 reported dropouts (mostly lost to follow‐up) ranging from 1.3% to 28.4% of the study population. No information regarding completeness of the follow‐up was available in the other trials.
Primary or recurrent incontinence
Twenty‐five trials included women presenting with primary urinary incontinence alone, nine included both primary and recurrent cases and one trial included only recurrent cases. Twenty trials failed to indicate whether the women studied had either primary or recurrent urinary incontinence, or had both.
Diagnosis of incontinence
For the subgroup analysis, we divided the trials into those that studied women diagnosed with urodynamically‐confirmed stress urinary incontinence and those that included women diagnosed by symptoms alone. Most of the trials included women with urodynamically‐confirmed stress urinary incontinence. Four trials (Albo 2007; Enzelsberger 1996; Kitchener 2006, Trabuco 2014) used the symptom diagnosis of stress urinary incontinence. It could not be determined whether urodynamics was used to confirm the diagnosis in five trials (Drahoradova 2004; El‐Din Shawki 2012; Palma 1985; Quadri 1999; Tuygun 2006).
The majority of the trials (36 out of 55) included women with stress urinary incontinence alone; two of these trials limited inclusion to women with low maximum urethral closing pressure (MUCP) or intrinsic sphincter deficiency (Quadri 1999; Sand 2000). Ten trials specifically mentioned exclusion of women with low maximum urethral closing pressure or other evidence of intrinsic sphincter deficiency (Bai 2005; Colombo 1994; Colombo 1996; El Barky 2005; Fatthy 2001; Kammerer‐Doak 1999; Liapis 2002; Mak 2000; McCrery 2005; Stangel‐Wojcikiewicz 2008). Three trials included women with stress urinary incontinence who had symptoms of detrusor overactivity or detrusor instability on urodynamics. Six trials included women with stress incontinence and some with mixed incontinence. One trial only had women with mixed incontinence (Osman 2003). Nine trials failed to indicate whether the population included women with mixed incontinence or mixed symptoms.
Setting
The majority of the trials were conducted in Europe (29 out of 55), of which seven were carried out in the UK. Nine were done in the United States, seven in Asia, two in Australia, one in Canada, one in South America, and five in the Middle East. Nearly all trials were carried out in university‐based hospitals, 27 of which were under the department of obstetrics and gynaecology, five in urology, 11 in centres specialising in incontinence management (urogynaecology, incontinence centres, urodynamic centres), and one in three departments (urology, gynaecology and radiology) (Klarskov 1986). One trial was performed by the minimal access unit of the department of obstetrics and gynaecology (Fatthy 2001). Five were multi‐centre trials (Albo 2007; Corcos 2001; El Barky 2005; Kitchener 2006; Ward 2002). Ward 2002 included district hospitals as trial centres. For three trials it was not clear what type of centre they were conducted in.
Intervention comparisons
The following comparators were included.
No trial was identified comparing open retropubic colposuspension with no treatment or a sham procedure.
Two trials compared open retropubic colposuspension with conservative treatment, both using physical therapy (Klarskov 1986; Tapp 1989).
One trial compared open retropubic colposuspension with anticholinergic therapy as part of a three‐armed study (Osman 2003).
Nine trials compared open retropubic colposuspension with anterior colporrhaphy, including four that included three arms in the trial (Bergman 1989a; Bergman 1989b; El‐Din Shawki 2012; Liapis 1996).
Comparisons between colposuspension and a sling procedure were investigated in 22 trials, 12 of which included the TVT procedure (Bai 2005; Drahoradova 2004; El Barky 2005; Elshawaf 2009; Halaska 2001; Han 2001; Koelbl 2002; Liapis 2002; O'Sullivan 2000; Tellez Martinez‐Fornes 2009; Wang 2003; Ward 2002) and four investigated the TOT procedure (Bandarian 2011; El‐Din Shawki 2012; Elshawaf 2009; Sivaslioglu 2007).
Comparison between open retropubic colposuspension and needle suspension procedures was performed in six trials, including two with three arms (Bergman 1989a; Bergman 1989b).
Open colposuspension was compared with laparoscopic colposuspension in 12 trials (Ankardal 2001; Burton 1994; Carey 2000; Fatthy 2001; Kitchener 2006; Mak 2000; Morris 2001; Stangel‐Wojcikiewicz 2008; Su 1997; Summitt 2000; Tuygun 2006; Ustun 2005).
One trial compared Burch colposuspension and collagen periurethral injection (Corcos 2001).
Four trials compared one technique of colposuspension with another. Four evaluated the Burch against the Marshall‐Marchetti‐Krantz procedure (Colombo 1994; Liapis 1996; McCrery 2005; Quadri 1999), one trial compared Burch colposuspension with two types of sling surgery, TVT and TOT (Elshawaf 2009) and one compared the Burch colposuspension with paravaginal repair (Colombo 1996).
The majority of the full text references either described the details of the technique in each intervention used or provided a citation, allowing verification of type of operation in ambiguous cases. This proved to be important in Gilja 1998, in which we assessed the third arm of the trial (termed as trans‐vaginal Burch or Gilja operation) to actually be a needle bladder neck suspension procedure, and hence analysed it as such. We used the name of the operation reported by the trialists to categorise a technique when a technical description of the intervention was absent, for example in trials where the only published report was an abstract. Ankardal 2001 was a three‐armed trial with two arms using laparoscopic colposuspension; one using mesh and staples and one using sutures. For this review, these two arms were combined as a comparison against open colposuspension
Outcomes
Three trials (Burton 1994; Halaska 2001; O'Sullivan 2000) did not report any outcome data that could be used in the meta‐analysis.
Definition of cure
The most consistently reported outcome among the trials was cure or success rate. In the majority, cure was defined both subjectively and objectively while subjective cure alone was reported for two studies (Demirci 2001; German 1994) and objective cure alone for four trials (Athanassopoulos 1996; Henriksson 1978; Liapis 2002; Trabuco 2014). In one study (Quadri 1985) cure was not defined. Five studies did not report cure rates (Athanasopoulos 1999; Burton 1994; Halaska 2001; Han 2001; O'Sullivan 2000). Objective cure was commonly defined by a negative stress test although others used a pad test and urodynamic parameters, either solely or as additional criteria.
Adverse effects
Twenty‐eight trials reported data on adverse events and 10 on recurrence or occurrence of prolapse, or surgery for prolapse.
Quality of life and impact of incontinence
Six studies (Corcos 2001; Fischer 2001; Kammerer‐Doak 1999; Osman 2003; Trabuco 2014; Ward 2002) included a condition‐specific outcome measure. Fischer 2001 and Kammerer‐Doak 1999 used the Incontinence Impact Questionnaire (IIQ) scoring while Osman 2003 and Ward 2002 utilised the Stress‐related leakage, Emptying ability, Anatomy, Protection, Inhibition (SEAPI) and Bristol‐Female Lower Urinary Tract Symptom (B‐FLUTS) scoring systems, respectively. Fischer 2001 also used the Urinary Distress Index (UDI) scoring.. Trabuco 2014 used the SUI sub‐scale of the Medical, Epidemiological, Social Aging Questionnaire. Corcos 2001 did not specify which scoring system was used. Fifteen trials used several urodynamic parameters as outcomes.
Quality of life measures were reported in five trials (Carey 2000; Corcos 2001; Kitchener 2006; Mak 2000; Ward 2002). Ankardal 2001 used a questionnaire with VAS to assess the impact of incontinence on the quality of life.Patient satisfaction was reported in two trials (Albo 2007; Trabuco 2014).
Length of follow up
Participant follow‐up was less than one year in 13 trials. Long‐term (at least five years) follow‐up was performed in three trials, while the rest had follow‐up between one and five years.
Risk of bias in included studies
Assessment of risk of bias of the included studies was difficult, in general, due to the insufficient detail provided by the authors, particularly on random allocation concealment and blinding. Whilst this might be expected in the abstracts, such was the case even in full reports. The information is summarised in Figure 2 and Figure 3.
2.
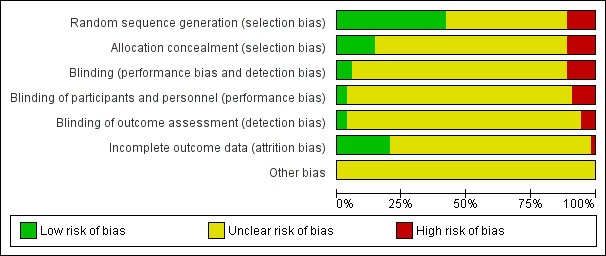
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
3.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
There were five quasi‐randomised trials where allocation was by a method of alternation (Demirci 2001; Henriksson 1978; Liapis 2002; Mundy 1983) or by date of birth (Athanassopoulos 1996).
Three trials had combined allocation methods wherein randomisation was performed in assigning the women to the major intervention arms but assignment to a specific technique depended on particular clinical characteristics (Corcos 2001; Klarskov 1986; Osman 2003):
Corcos 2001 randomly allocated women to either collagen injection therapy or surgery. Those assigned to the surgical arm were given the option of undergoing the Burch colposuspension, bladder neck suspension, or the sling procedure.
Klarskov 1986 randomly allocated women to either the conservative management or the surgical treatment arm. Within the surgical treatment arm, women were assigned to the Burch colposuspension arm or the anterior colporrhaphy arm based on the type of pelvic organ prolapse.
Osman 2003 randomly allocated women to either the drug therapy arm or the surgical arm. Women were assigned to the Burch colposuspension arm or the pubovaginal sling arm based on the Valsalva leak point pressure (VLPP) result.
In 15 trials, random sequence generation was through a random number list or computer‐generated list. One trial used tossing of a coin for randomisation (McCrery 2005). No description of the randomisation method was provided in the other trials.
Two trials (Colombo 2000; Gilja 1998) used an open list, suggesting a lack of allocation concealment. Only five trials (Ankardal 2001; Fatthy 2001; Mak 2000; Summitt 2000; Ustun 2005) specifically mentioned the use of sealed or opaque envelopes to ensure adequate concealment of allocation. One trial specifically mentioned the absence of opaque envelopes in the trial (Colombo 1996). The rest of the trials did not provide information regarding allocation concealment.
Blinding
Blinding was not mentioned in any trial except two (Carey 2000; Palma 1985,) wherein the patient, ward staff and the assessor were all blinded to the intervention, one (McCrery 2005) wherein the women were blinded to the treatment they received, and one (Trabuco 2014) where the stress test on follow up was performed by a masked observer. Liapis 2002 stated that it was a "blind study with respect to the surgeon", although it was not clear how this was implemented in the trial. Four trials (Albo 2007; Ankardal 2001; Drahoradova 2004; Kitchener 2006) stated that no blinding was attempted.
Incomplete outcome data
Thirty‐two trials did not mention if there were any withdrawals; that is, the number of participants stated as those entered into the study matched the number with outcomes at the time of assessment, without explicitly stating that there were no dropouts during the study. Five studies had 'trialist‐determined' dropouts or exclusions (Bergman 1989a; Corcos 2001; Fischer 2001; Gilja 1998; Wang 2003). SIx reported only the number and failed to indicate the reason for the withdrawals (Albo 2007; Burton 1994; Demirci 2001; Fatthy 2001; Trabuco 2014; Ward 2002). The rest cited loss to follow‐up or non‐attendance as the reason for the dropout.
Among those reporting withdrawals, 12 trials had a dropout rate of less than 10% (Bergman 1989a; Bergman 1989b; Carey 2000,Colombo 2000; Fatthy 2001; Holmes 1985; Kitchener 2006; Liapis 1996; Sand 2000; Tellez Martinez‐Fornes 2009; Trabuco 2014; Ward 2002). The rest had a dropout rate ranging from 12.9% (Bergman 1989a) to 28.4% (Gilja 1998). Of those that reported separate dropout rates according to treatment group, five trials (Corcos 2001; Fischer 2001; Morris 2001; Wang 2003; Ward 2002) had significantly different rates between the groups with more dropouts or withdrawals in the colposuspension group. In one trial (McCrery 2005) there were more women lost to follow up in the Marshall‐Marchetti‐Krantz procedure group compared to the Burch colposuspension group.
One trial (Albo 2007) reported its five year follow up data as a long‐term observational study wherein not all women initially enrolled in the trial were included. In this extension study, incontinent participants were more likely to be enrolled (85.5% vs 52.2%, P <0.0001).
Other bias
Intention‐to‐treat analysis
A form of intention‐to‐treat analysis was done in one trial (Ward 2002) wherein different assumptions and scenarios were described and corresponding results calculated. We opted to report the actual data, making no assumptions about these women. One trial (Morris 2001) stated that analysis of data was done on an intention‐to‐treat basis although the particulars were not provided. One trial deliberately did not perform an intention‐to‐treat analysis (Sand 2000). The rest of the trials did not explicitly state if intention‐to‐treat analysis was performed or if an attempt was made to do so. Details on how women crossing over between treatment groups were handled, and if outcomes among the withdrawals and dropouts were sought, were either not provided or were insufficient to allow the review authors to execute an intention‐to‐treat analysis.
Sample size
Sand 2000 and Ward 2002 did not attain the projected sample size judged necessary to detect a pre‐determined difference in the primary outcome. The sample size of Wang 2003 was based on detecting a difference in the obstructive effect of the two interventions studied rather than cure rates. One trial (Liapis 2002) attempted to perform a back calculation of the study sample's power, suggesting a marginally underpowered trial.
In general, the trial sample sizes were small, with each arm usually having a population of less than 40. The largest trial was a two‐armed trial on open colposuspension versus a sling procedure, enrolling more than 200 women per treatment arm (Albo 2007). Five larger studies (sample size more than 100) were three‐armed trials (Ankardal 2001; Bergman 1989a; Bergman 1989b; Gilja 1998; Liapis 1996). However, we had to convert three of these (Ankardal 2001; Gilja 1998; Liapis 1996) into two‐armed trials since the review authors assessed two of the three interventions to be of the same category. In Gilja 1998 the data of the Raz procedure and the trans‐vaginal Burch and Gilja groups were combined, since the latter was assessed to be a needle procedure as well. The Burch and Marshall‐Marchetti groups in Liapis 1996 were combined as the open colposuspension group in comparison with the anterior colporrhaphy group. In Arkandal 2001, the two laparoscopic colposuspension arms were combined as one comparator group against open colposuspension.
There were seven moderately‐sized two‐armed trials Carey 2000; Drahoradova 2004; Kitchener 2006; Koelbl 2002; McCrery 2005; Quadri 1985; Ward 2002).
Effects of interventions
Comparison 1: open retropubic colposuspension versus no treatment
There were no trials identified comparing open retropubic colposuspension with no treatment or sham operation.
Comparison 2: open retropubic colposuspension versus conservative treatment
Two small studies (Klarskov 1986; Tapp 1989) compared open retropubic colposuspension with conservative treatment and involved a total of 97 women, 40 of whom underwent the surgical intervention. Klarskov 1986 compared Burch colposuspension with pelvic floor muscle training (PFMT) in a subset of its study population with defective posterior bladder support. Tapp 1989 compared women undergoing colposuspension with either PFMT alone or PFMT with electrical stimulation. The methodological quality of both studies was poor. There were inconsistencies in the results reported in the two versions of Tapp 1989, primarily in the stated total number of women enrolled in the study.
The studies showed consistency of results favouring surgery for open colposuspension versus PFMT in the short term:
in subjective incontinence (Klarskov 1986), 3/16 versus 10/13 (RR 0.24; 95% CI 0.08 to 0.71, Analysis 2.1); and
objective incontinence (Tapp 1989), 6/24 versus 42/44 (RR 0.26; 95% CI 0.13 to 0.53, Analysis 2.3).
2.1. Analysis.

Comparison 2 Open retropubic colposuspension versus conservative interventions, Outcome 1 Number with incontinence within first year (subjective).
2.3. Analysis.

Comparison 2 Open retropubic colposuspension versus conservative interventions, Outcome 3 Number with incontinence within the first year (objective).
In Klarskov 1986, incontinence did improve in the majority of women, but the numbers were too small to test the difference between surgery and conservative treatment (number of women failing to improve 2/16 versus 2/13 (RR 0.81; 95% CI 0.13 to 5.01, Analysis 2.2)). Long‐term results (up to eight years) were available for Klarskov 1986 but the data could not be used as the results in the surgery group were not reported separately according to type of surgical procedure (Burch or anterior repair or both procedures).
2.2. Analysis.
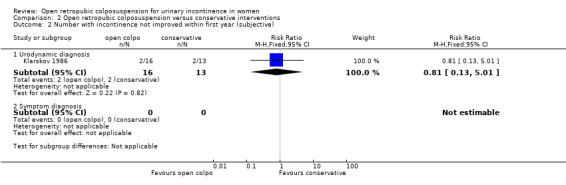
Comparison 2 Open retropubic colposuspension versus conservative interventions, Outcome 2 Number with incontinence not improved within first year (subjective).
Klarskov 1986 noted the occurrence of adverse events in the form of retropubic pain (1/16, 6%) and detrusor overactivity (1/16, 6%), persistent pelvic pain (1/16, 6%), and persistent dyspareunia with loss of libido (1/16, 6%) in the colposuspension group compared to no adverse events in the conservative therapy group. The very small numbers limited the significance of such results.
No formal comparisons were made between the two treatment groups in terms of surgical parameters or quality of life.
Comparison 3: open retropubic colposuspension versus drug therapy
One small trial (Osman 2003) compared open retropubic colposuspension with anticholinergic treatment in a subset of 44 women, of whom 21 received oxybutynin 5 mg twice daily with titration and 23 underwent Burch colposuspension (the remaining 24 women of the total study population underwent a pubovaginal sling procedure). The methodological quality of the trial was poor. A mixed surgical approach was taken and although the two groups were originally randomised, participants were then selected for colposuspension or sling procedure on the basis of the Valsalva leak point pressure. The estimation of effect size for this study may have been biased in favour of the drug therapy because those who failed to complete the anticholinergic treatment were excluded from the analysis.
The only useable outcome measures for this review were the subjective cure rates and a quantitative symptom scoring system as means of assessing improvement. One hundred per cent failed subjectively after drug therapy compared with three out of 23 after colposuspension (Analysis 3.1). The subjective symptom scores showed improvement in both treatment groups, with the colposuspension group having a greater degree of improvement compared to the drug therapy group (P < 0.05). Post‐treatment subjective and objective symptom scores after open retropubic colposuspension showed significantly lower (better) scores compared with oxybutynin treatment. Women undergoing colposuspension scored a mean 3.3 points lower (95% CI ‐3.96 to ‐2.64) and a mean 3.8 points lower (95% CI ‐4.59 to ‐3.01, Analysis 3.2) on subjective and objective scoring, respectively, than those scores of women receiving oxybutynin.
3.1. Analysis.

Comparison 3 Open retropubic colposuspension versus drug therapy, Outcome 1 Number with incontinence within first year (subjective).
3.2. Analysis.

Comparison 3 Open retropubic colposuspension versus drug therapy, Outcome 2 Condition specific health measure.
Objective cure rates were not reported. Quality of life measures and adverse events were not evaluated.
Comparison 4: open retropubic colposuspension versus anterior colporrhaphy (repair)
A total of nine trials (Berglund 1996; Bergman 1989a; Bergman 1989b; Colombo 2000; El‐Din Shawki 2012; Holmes 1985; Kammerer‐Doak 1999; Liapis 1996; Quadri 1985) compared open retropubic colposuspension with anterior colporrhaphy. These trials involved 627 women with 353 randomised to undergo retropubic colposuspension (note: these totals do not include the women from El‐Din Shawki 2012 because the distribution of the study population into the treatment groups was not reported). Two trials (Bergman 1989a; Liapis 1996) had moderate rather than small sample sizes (200 and 155 participants, respectively) although both were three‐armed trials.
The methodological quality of the studies was generally satisfactory. However, there was a lack of detail on blinding and concealment of allocation. Most trials had co‐interventions (mostly addressing prolapse when present) and there was some variation in the study populations across the trials in terms of inclusion of recurrent cases and presence of significant prolapse at study entry. Two out of the nine trials included recurrent incontinence cases (Kammerer‐Doak 1999; Quadri 1985). Six trials included women with prolapse (Bergman 1989a; Colombo 2000; Holmes 1985; Kammerer‐Doak 1999; Liapis 1996; Quadri 1985). Estimates of effect derived from these six were similar to those derived from the two trials that excluded women with prolapse.
For this section, the results for Marshall‐Marchetti‐Krantz (MMK) were considered with those for Burch colposuspension. Berglund 1996 described the technique used for open colposuspension, termed in the report as "retropubic urethropexy" as that of the MMK while Liapis 1996 had three treatment arms, wherein one arm underwent the Burch procedure, another had the MMK procedure, and anterior repair was performed on the third group. When the results of the Burch and the MMK groups were considered together in Liapis 1996, the estimates of effects were consistent with those from the other trials which performed only the Burch procedure, and no statistical heterogeneity was noted during the meta‐analysis.
However, there was evidence of statistical heterogeneity in the results of the studies for the three different outcomes examined, that is, long‐term objective cure rate, length of hospital stay and occurrence of new prolapse, which appeared to reflect Berglund 1996. We performed sensitivity analysis excluding Berglund 1996 from the meta‐analysis, and another excluding the MMK arm in Liapis 1996, to explore any difference in the results for outcomes which included data from these trials. We also carried out a subgroup analysis reporting the results from these two different operations separately (Burch versus anterior repair and MMK versus anterior repair)(Analysis 4.19, Analysis 4.20).
4.19. Analysis.

Comparison 4 Open retropubic colposuspension versus anterior colporrhapy, Outcome 19 Number not cured within first year (subjective) Burch vs MMK.
4.20. Analysis.

Comparison 4 Open retropubic colposuspension versus anterior colporrhapy, Outcome 20 Number not cured after first year but before five years (subjective) Burch vs MMK.
Women's observations (outcomes 4.1 to 4.3)
Evidence from seven trials evaluating a total of 695 women (with assessments available at different time periods) showed a lower incontinence rate for subjective cure after open retropubic colposuspension than after anterior colporrhaphy. Such benefit was maintained over time:
incontinence rates 9% versus 19% (RR 0.46; 95% CI 0.30 to 0.72) before the first year (Analysis 4.1);
14% versus 36% (RR 0.37; 95% CI 0.27 to 0.51) at one to five years (Analysis 4.2); and
28% versus 53% (RR 0.49; 95% CI 0.32 to 0.75) in periods beyond five years (Analysis 4.3).
4.1. Analysis.

Comparison 4 Open retropubic colposuspension versus anterior colporrhapy, Outcome 1 Number with incontinence within first year (subjective).
4.2. Analysis.

Comparison 4 Open retropubic colposuspension versus anterior colporrhapy, Outcome 2 Number with incontinence after first year but before five years (subjective).
4.3. Analysis.

Comparison 4 Open retropubic colposuspension versus anterior colporrhapy, Outcome 3 Number with incontinence after five years (subjective).
A sensitivity analysis excluding Berglund 1996 (because the operation tested was MMK rather than Burch) removed the heterogeneity and strengthened the long‐term result in favour of the Burch procedure (RR 0.29; 95% CI 0.16 to 0.52).
Quantification of symptoms (outcome 4.12)
Data from one small trial (Berglund 1996) showed no difference in the two‐hour pad test results but with a wide confidence interval (MD 1.1 gm; 95% CI ‐4.41 to 6.61, Analysis 4.7).
4.7. Analysis.

Comparison 4 Open retropubic colposuspension versus anterior colporrhapy, Outcome 7 Volume/weight of urine loss in 2 hour pad test.
Clinician's observations (outcomes 4.9 to 4.11)
Consistent with the results for subjective cure, there was also evidence that open retropubic colposuspension was more effective than anterior colporrhaphy for objective cure rates. The benefit was maintained over time:
incontinence rates 9% versus 25% (RR 0.36; 95% CI 95% 0.22 to 0.58) within one year (Analysis 4.4);
16% versus 44% (RR 0.34; 95% CI 0.25 to 0.47) at one year but before five years (Analysis 4.5); and
26% versus 54% (RR 0.48; 95% CI 0.31 to 0.73) after five years (Analysis 4.6).
4.4. Analysis.

Comparison 4 Open retropubic colposuspension versus anterior colporrhapy, Outcome 4 Number with incontinence within the first year (objective).
4.5. Analysis.

Comparison 4 Open retropubic colposuspension versus anterior colporrhapy, Outcome 5 Number with incontinence after first and before five years (objective).
4.6. Analysis.

Comparison 4 Open retropubic colposuspension versus anterior colporrhapy, Outcome 6 Number with incontinence at and after five years (objective).
As would be expected, sensitivity analyses excluding Berglund 1996 removed the heterogeneity. There was some indirect evidence that the Burch procedure was more effective than the MMK procedure (Analysis 4.19).
Overall, the risk of failing to cure urinary incontinence through open retropubic colposuspension was only half that of anterior repair, with an estimated absolute risk difference (ARR) of around 20% (ARR 0.21; 95% CI 0.15 to 0.27). To put this another way, for every five women treated, one extra was cured after open retropubic colposuspension.
Quality of life measures (outcome 4.14)
There was only one small trial (Kammerer‐Doak 1999) that investigated the impact of both types of surgery on the quality of life through an incontinence rating score. Scores improved in both treatment groups. There was a small (less than 1 point) but statistically significantly better improvement in the quality of life scores in the open retropubic colposuspension group compared to the anterior colporrhaphy group (MD ‐0.59; 95% CI ‐1.11 to ‐0.07, Analysis 4.8).
4.8. Analysis.

Comparison 4 Open retropubic colposuspension versus anterior colporrhapy, Outcome 8 Condition specific health measure.
Surgical outcome measures (outcomes 4.16 to 4.19)
Data from one small trial (Holmes 1985) showed a longer operating time for colposuspension (MD 14.40 minutes, 95% CI 5.43 to 23.37, Analysis 4.9).
4.9. Analysis.

Comparison 4 Open retropubic colposuspension versus anterior colporrhapy, Outcome 9 Operative time (minutes).
The pattern of results for length of hospital stay differed between the two trials with data. In one (Berglund 1996), women had an average three fewer days in hospital after open retropubic colposuspension compared with anterior repair, whereas the other trial (Colombo 2000) showed no difference. Because of the heterogeneity no attempt was made to derive an estimate from combined data (Analysis 4.10).
4.10. Analysis.

Comparison 4 Open retropubic colposuspension versus anterior colporrhapy, Outcome 10 Length of hospital stay (days).
The estimates for the time to catheter removal post‐operatively, available from three trials (outcome 4.19) (Bergman 1989a; Bergman 1989b; Holmes 1985) were not statistically significantly different (MD ‐0.28 days, 95% CI ‐0.83 to 0.27, Analysis 4.11).
4.11. Analysis.

Comparison 4 Open retropubic colposuspension versus anterior colporrhapy, Outcome 11 Time to catheter removal (days).
Adverse events (outcomes 4.20 to 4.26)
The included trials reported adverse events in different ways, with only one or two providing data for a particular event. Thus, there were limited data to draw conclusions confidently for each adverse event. Based on two trials with data, the number of perioperative complications was significantly lower with open retropubic colposuspension (outcome 4.20: RR 0.39; 95% CI 0.19 to 0.83, Analysis 4.12). Holmes 1985 and Berglund 1996 reported more wound infections in the retropubic colposuspension group, but more haemorrhage (Holmes 1985) and more positive urine cultures (Berglund 1996) in the anterior repair group. Bergman 1989a reported no difference in post‐operative complications between the treatment groups, although specific data were not provided.
4.12. Analysis.

Comparison 4 Open retropubic colposuspension versus anterior colporrhapy, Outcome 12 Number of perioperative surgical complications.
Estimates of the risk for de novo urge symptoms and urge incontinence, and risk for detrusor were inconclusive as the data were not statistically significant and had wide confidence intervals (Colombo 2000; Holmes 1985; Kammerer‐Doak 1999; Liapis 1996). In three trials with data, there were fewer women with de novo urge symptoms or incontinence after open retropubic colposuspension but the difference was not statistically significant (RR 0.53; 95% CI 0.25 to 1.14, Analysis 4.13). In four small trials with data there was no statistically significant difference in the risk for developing urodynamically demonstrable de novo detrusor overactivity post‐operatively (event rates: 8% versus 6% (RR 1.26; 95% CI 0.54 to 2.94, Analysis 4.14)).
4.13. Analysis.

Comparison 4 Open retropubic colposuspension versus anterior colporrhapy, Outcome 13 Number with de novo urge symptoms and urge incontinence.
4.14. Analysis.

Comparison 4 Open retropubic colposuspension versus anterior colporrhapy, Outcome 14 Number with de novo detrusor instability.
Four trials evaluated the risk for voiding difficulty after open retropubic colposuspension and anterior repair. Across the four trials there were only three events of voiding difficulty, all occurring in the open colposuspension group (Analysis 4.15). For this reason no combined estimate was derived.
4.15. Analysis.

Comparison 4 Open retropubic colposuspension versus anterior colporrhapy, Outcome 15 Number with voiding difficulty.
Data on the risk of recurrent or new prolapse were available from five trials (Bergman 1989b; Colombo 2000; Holmes 1985; Liapis 1996; Quadri 1985). It is of note that all trials had an adequate mean follow up of at least one year at the time of assessment of the prolapse. However, there was significant heterogeneity in the results between the trials and the groups were statistically different in only two trials (Colombo 2000; Quadri 1985). Although there were more women with prolapse in the open colposuspension groups (16% versus 5%), this did not reach statistical significance when a random‐effects model was used (RR 2.51; 95% CI 0.62 to 10.10, Analysis 4.16). Examination of study design and population characteristics across the trials did not reveal any possible source of difference that could explain the heterogeneity. The largest difference in post‐operative prolapse rates was demonstrated in Colombo 2000, which had a very long follow‐up of at least eight years and showed a risk difference of over 50% in favour of anterior repair.
4.16. Analysis.

Comparison 4 Open retropubic colposuspension versus anterior colporrhapy, Outcome 16 Number with new or recurrent prolapse.
Consistent with the findings on cure, fewer women in the colposuspension group had repeat anti‐incontinence surgery (6.3% versus 23.4% (RR 0.11; 95% CI 0.04 to 0.30, Analysis 4.17); estimated absolute difference 21% from the three trials with data).
4.17. Analysis.

Comparison 4 Open retropubic colposuspension versus anterior colporrhapy, Outcome 17 Number with repeat anti‐incontinence surgery.
Comparison 5: open retropubic colposuspension versus sling procedures (traditional and self‐fixing slings)
Twenty‐two trials (Albo 2007; Bai 2005; Bandarian 2011; Demirci 2001; Drahoradova 2004; El Barky 2005; El‐Din Shawki 2012; Elshawaf 2009; Enzelsberger 1996; Fischer 2001; Halaska 2001; Han 2001; Henriksson 1978; Koelbl 2002; Liapis 2002; O'Sullivan 2000; Sand 2000; Sivaslioglu 2007; Tellez Martinez‐Fornes 2009; Trabuco 2014; Wang 2003; Ward 2002) compared open retropubic colposuspension with sling procedures. These involved 2343 randomised women, at least 1089 of whom underwent colposuspension. One trial (El‐Din Shawki 2012) involving 60 participants did not specify the numbers allocated to the three treatment groups.
Traditional slings
Six trials involved traditional suburethral sling procedures. Two trials involved the pubovaginal sling technique using autologous rectus muscle fascia (Albo 2007; Demirci 2001). Enzelsberger 1996 used the lyodura sling, Henriksson 1978 used the Zoedler sling, and Sand 2000 used the Gortex type synthetic material. Fischer 2001 did not specify the sling material.
Midurethral tapes
Twelve trials (Bai 2005; Drahoradova 2004; El Barky 2005; Elshawaf 2009; Halaska 2001; Han 2001; Koelbl 2002; Liapis 2002; O'Sullivan 2000; Tellez Martinez‐Fornes 2009; Wang 2003; Ward 2002) used the tension‐free vaginal tape (TVT) as the sling procedure. One of these trials was a three‐armed study which compared open Burch colposuspension, the transobturator tape procedure (TOT), and the TVT (Elshawaf 2009). Three trial used TOT as the sling procedure (Bandarian 2011; El‐Din Shawki 2012; Sivaslioglu 2007).
One trial did not specify whether TVT or TOT procedure was the approach taken (Trabuco 2014). In one trial (Trabuco 2014), women in both treatment groups underwent abdominal sacrocolpopexy for pelvic organ prolapse, in addition to the incontinence procedure.
Data issues
We distributed data on the subjective cure rates of the Burch colposuspension group from Bai 2005 between the subcategories of open colposuspension versus traditional sling procedures and open colposuspension versus self‐fixing sling procedures to avoid double counting for the meta‐analysis. For Elshawaf 2009, we planned to combine the data for the TOT and TVT groups. However, we could not extract any usable data from the report as the results were limited to a narrative description.
We could not enter data from Halaska 2001 into RevMan (RevMan 2014) as the results of a visual analogue scale were presented in a graph and it was not clear how the figures were derived. A conference abstract on a subset of women from that trial reported that the results in two‐ and six‐month follow‐up revealed no difference in the clinical outcomes between TVT and Burch. It was also reported that TVT was superior to the Burch procedure in terms of restoring normal sexual activity. One study (Henriksson 1978) reported equivalent results in both treatment groups but no data were provided. Outcomes studied in O'Sullivan 2000, which were based on tissue collagen analysis results, were not used in this review. We used data from the longest follow‐up from trials which reported the event rates at different time periods In the analysis of the risk for prolapse.
Albo 2007 used various criteria to define success. We selected symptoms as the criterion to define subjective cure (using self‐reported incontinence using a questionnaire) and the pad test results to define objective cure because the other trials in this comparison used these parameters to define subjective and objective cure.
Only three trials (Albo 2007; Sand 2000; Ward 2002) had long‐term results (at and after five years). However, the extension study of Albo 2007 only included a proportion of the initially enrolled study population (482/665) and incontinent women were more likely to enrol in the follow up study (P <0.0001). The numbers used in the analysis for the number of incontinent women, based on self‐reported incontinence questionnaires, were difficult to determine, as the paper stated the number of women who completed the study at five years but data for more women were available for different outcomes. Hence, the denominators for the continence rates used in this review were only derived values based on reported percentages and counts in the paper. The inclusion of this long‐term outcomes data, being part of an observational study, rather than part of the randomized trial, was subjected to sensitivity analysis.
While El‐Din Shawki 2012 reported outcomes, we were not able to include the data in the review because it did not specify how the participants were allocated across the three treatment groups.
Women's observations (outcomes 5.1 to 5.6)
Short‐term cure
Evidence from eight trials including traditional and self‐fixing slings (Bai 2005; Demirci 2001; Drahoradova 2004; El Barky 2005; Sand 2000; Sivaslioglu 2007; Tellez Martinez‐Fornes 2009; Ward 2002) showed no statistically significant difference between the two treatment groups in the risk for incontinence as assessed subjectively (RR 0.90; 95% CI 0.69 to 1.18, Analysis 5.1) within one year of treatment. The confidence interval was wide, however, and from the data we cannot rule out a difference favouring open colposuspension or slings.
5.1. Analysis.

Comparison 5 Open retropubic colposuspension versus sling procedure, Outcome 1 Number with incontinence within first year (subjective).
Subgroup analysis of those trials including traditional slings only showed no statistical difference between open colposuspension and traditional slings but the confidence interval was wide and again we cannot rule out favouring either open colposuspension or traditional slings (RR 1.92; 95% CI 0.57 to 6.50, Analysis 5.1).
The meta‐analysis of five trials (Bai 2005; El Barky 2005; Sivaslioglu 2007; Tellez Martinez‐Fornes 2009; Ward 2002) using the TVT procedure (RR 0.88; 95% CI 0.67 to 1.16, Analysis 5.1) demonstrated a narrower confidence interval but not narrow enough to say there was no difference between the procedures.
One small trial (El Barky 2005) was too small to provide evidence of any difference in subjective improvement rates within one year between open colposuspension and sling procedures (Analysis 5.4).
5.4. Analysis.
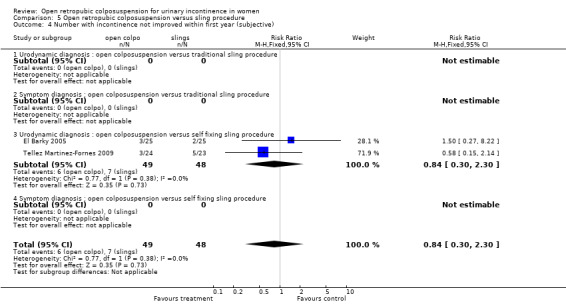
Comparison 5 Open retropubic colposuspension versus sling procedure, Outcome 4 Number with incontinence not improved within first year (subjective).
Medium‐term cure
Data for incontinence rates at one‐ to five‐year follow‐up were available from six trials (Albo 2007; Enzelsberger 1996; Sivaslioglu 2007; Tellez Martinez‐Fornes 2009; Wang 2003; Ward 2002). The summary statistic, combining traditional slings and self‐fixing slings, showed a lower incontinence rate in women who had sling procedures (RR 1.18; 95% CI 1.01 to 1.39, Analysis 5.2), which was primarily due to the results of the Albo 2007 trial which used the traditional sling procedure. Data from studies using traditional slings alone showed lower incontinence rates with traditional slings (RR 1.35; 95% CI 1.03 to 1.37). Data from the TVT trials alone showed no clear difference in medium‐term subjective incontinence rate (Analysis 5.2) or improvement rate (Analysis 5.5) between open colposuspension and the TVT procedure.
5.2. Analysis.

Comparison 5 Open retropubic colposuspension versus sling procedure, Outcome 2 Number with incontinence after first year but before five years (subjective).
5.5. Analysis.

Comparison 5 Open retropubic colposuspension versus sling procedure, Outcome 5 Number with incontinence not improved after first year but before five years (subjective).
Long‐term cure
Data beyond five years was provided by three trials (Albo 2007; Sand 2000; Ward 2002), demonstrating no overall significant difference in effects (RR 1.11; 95% CI 0.97 to 1.27, Analysis 5.3). However, traditional slings continued to be more effective than open colposuspension at long term follow up in one trial (RR1.19; 95% CI 1.03 to 1.37) (Albo 2007).
5.3. Analysis.

Comparison 5 Open retropubic colposuspension versus sling procedure, Outcome 3 Number with incontinence after five years (subjective).
Clinician's observations (outcomes 5.9 to 5.11)
Consistent with the results in the subjective assessment of cure, in objective incontinence rates there were no statistically significant differences within any time periods:
RR 1.21, 95% CI 0.84 to 1.75 within one year of treatment, Analysis 5.6;
RR 1.12; 95% CI 0.82 to 1.54 for one to five years follow up, Analysis 5.7; and
RR 0.70; 95% CI 0.30 to 1.64 at more than five years, Analysis 5.8.
5.6. Analysis.

Comparison 5 Open retropubic colposuspension versus sling procedure, Outcome 6 Number with incontinence within the first year (objective).
5.7. Analysis.

Comparison 5 Open retropubic colposuspension versus sling procedure, Outcome 7 Number with incontinence after first and before five years (objective).
5.8. Analysis.

Comparison 5 Open retropubic colposuspension versus sling procedure, Outcome 8 Number with incontinence at and after five years (objective).
Again the confidence intervals could not rule out a favouring of open colposuspension or slings. This was based on data from eight studies (Fischer 2001; Henriksson 1978; Sand 2000; Sivaslioglu 2007; Tellez Martinez‐Fornes 2009; Trabuco 2014; Wang 2003; Ward 2002) with objective assessment within the first year of treatment, from five studies with data for assessments between one to five years (Albo 2007; Enzelsberger 1996; Liapis 2002; Tellez Martinez‐Fornes 2009; Ward 2002) and from three trials (Albo 2007; Sand 2000; Ward 2002) with long‐term data. Sensitivity analysis of the long‐term data, with inclusion/exclusion of the data from the Albo 2007 extension study, showed a shift from the tendency to favour sling procedures with inclusion of the data to a tendency to favour open colposuspension with the exclusion of the data, but with both results showing no statistically significant difference.
Surgical outcomes (outcomes 5.16 to 5.19)
Data on surgical parameters came from 12 studies (Albo 2007; Bai 2005; Bandarian 2011; Demirci 2001; El Barky 2005; Enzelsberger 1996; Koelbl 2002; Liapis 2002; Sand 2000; Sivaslioglu 2007; Tellez Martinez‐Fornes 2009; Ward 2002; ).
The four trials (; Sivaslioglu 2007; Tellez Martinez‐Fornes 2009; Ward 2002) that compared the operative times between colposuspension and sling procedure showed conflicting results (Analysis 5.10). This discrepancy is likely to be due to the different types of sling operations performed. Demirci 2001, which used a free rectus fascial sling through a combined abdominoperineal approach, showed a longer operative time while the self‐fixing sling trials using TVT had a significantly shorter operative time when compared to open colposuspension.
5.10. Analysis.

Comparison 5 Open retropubic colposuspension versus sling procedure, Outcome 10 Operative time (minutes).
Hospital stay was reported by eight trials. Two trials showed similar lengths of stay for both treatment groups (Demirci 2001; Sand 2000). One trial (Enzelsberger 1996) reported that women stayed in hospital eight fewer days in the colposuspension group compared to the traditional sling group. The six trials that compared open colposuspension with TVT (Bandarian 2011; El Barky 2005; Koelbl 2002; Liapis 2002; Sivaslioglu 2007; Ward 2002) consistently showed shorter hospital stays with the self‐fixing (TVT) group. Summary data of the TVT trials alone showed a shorter hospital stay of four days (MD 3.99; 95% CI 3.71 to 4.28, Analysis 5.11).
5.11. Analysis.
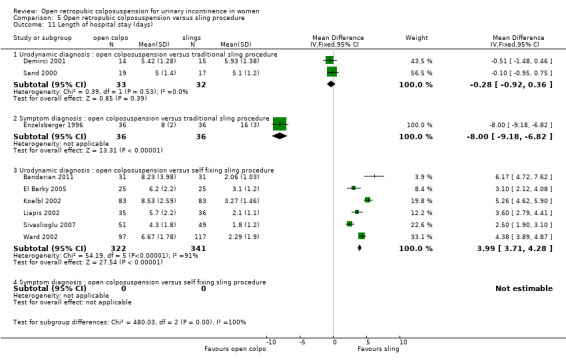
Comparison 5 Open retropubic colposuspension versus sling procedure, Outcome 11 Length of hospital stay (days).
The data on the time to catheter removal from three trials (Enzelsberger 1996; Koelbl 2002; Sand 2000) again showed significant heterogeneity (Analysis 5.12). While the different types of sling procedures used and the different method of diagnosis of incontinence may explain the disparity in the results between Koelbl 2002 and Enzelsberger 1996, they do not explain the difference between the results of Koelbl 2002 and Sand 2000. Different policies in the removal of catheters post‐operation that was adopted in the different trials could explain the diversity of results. However, this could not be verified due to lack of such information in the trial reports. Because of the heterogeneity of results across trials, we did not perform meta‐analysis of data for this outcome.
5.12. Analysis.

Comparison 5 Open retropubic colposuspension versus sling procedure, Outcome 12 Time to catheter removal (days).
Quality of life (outcomes 5.13 to 5.14)
One trial (Ward 2002) compared quality of life using Short Form‐36 (SF‐36) (Ware 1993), EQ‐5D and Bristol Female Lower Urinary Tract Symptoms (B‐FLUTS) scoring systems after open retropubic colposuspension with the TVT procedure. There was no difference in these measures apart from the SF‐36 showing that women in the colposuspension group had significantly less improvement in emotional and social functioning, vitality and mental health dimensions at six months and at two years. There was no difference between the groups in any of the health dimensions measured by the SF‐36 at five years. There was also no significant difference in the quality‐adjusted life years between the two groups.
Another trial (Fischer 2001) reported no significant difference in the Incontinence Impact Questionnaire (IIQ) and Urogenital Distress Inventory (UDI) scores between the colposuspension group and the sling group, although actual numbers were not reported.
Adverse effects (outcomes 5.20 to 5.27)
In eight trials (Albo 2007; Bandarian 2011; Demirci 2001; Enzelsberger 1996; Han 2001; Liapis 2002; Sand 2000; Tellez Martinez‐Fornes 2009), there were statistically significantly fewer perioperative surgical complications in the open colposuspension group. This result reflected the result from the relatively large Albo 2007 trial (complication rates RR 0.76; 95% CI 0.66 to 0.87, Analysis 5.13.2). In the subgroup analysis looking at trials that compared open colposuspension and self‐fixing slings, there was no significant difference in the perioperative complications rates between the two procedures (RR 1.11; 95% CI 0.66 to 1.87, Analysis 5.13.3). In addition, Wang 2003 reported no significant differences in complications although the numbers were not provided.
5.13. Analysis.

Comparison 5 Open retropubic colposuspension versus sling procedure, Outcome 13 Number of perioperative surgical complications.
There was insufficient evidence to assess whether or not there were differences in the risks of de novo urgency symptoms (Analysis 5.14) and de novo detrusor overactivity (Analysis 5.15) between the two treatment procedures. Pooled data from 11 trials (Albo 2007; Bai 2005; Bandarian 2011; Drahoradova 2004; El Barky 2005; Enzelsberger 1996; Liapis 2002; Sand 2000; Sivaslioglu 2007; Tellez Martinez‐Fornes 2009; Ward 2002) showed nearly 40% lesser risk of developing voiding difficulties after open colposuspension compared to sling procedures (RR 0.41; 95% CI 0.26 to 0.67, Analysis 5.16). This result was highly influenced by the large Albo 2007 trial that reported having almost no risk of developing voiding dysfunction after open colposuspension compared to the traditional sling procedure. On the other hand, consistent data from the TVT trials showed no significant difference in the risk of voiding dysfunction between the two groups.
5.14. Analysis.

Comparison 5 Open retropubic colposuspension versus sling procedure, Outcome 14 Number with de novo urge symptoms and urge incontinence.
5.15. Analysis.

Comparison 5 Open retropubic colposuspension versus sling procedure, Outcome 15 Number with de novo detrusor instability.
5.16. Analysis.

Comparison 5 Open retropubic colposuspension versus sling procedure, Outcome 16 Number with voiding difficulty.
Based on evidence from three trials (Demirci 2001; Enzelsberger 1996; Ward 2002) women undergoing open retropubic colposuspension were nearly twice at risk of developing new or recurrent prolapse compared to those undergoing sling procedures (33.9% versus 20.1% (RR 1.85; 95% CI 1.25 to 2.75, Analysis 5.17)). Ward 2002 trial reported a significant reduction in objective cystocoele but more enterocoele and vault or cervical prolapse cases in the colposuspension group compared with the TVT group, both at six months, two years and five years after surgery. However, if only symptomatic prolapse was considered, there were no significant differences between the two groups. This trial also reported on the need for repeat continence surgery, but the numbers were too few for reliable analysis (Analysis 5.18).
5.17. Analysis.

Comparison 5 Open retropubic colposuspension versus sling procedure, Outcome 17 Number with new or recurrent prolapse.
5.18. Analysis.

Comparison 5 Open retropubic colposuspension versus sling procedure, Outcome 18 Number with repeat anti‐incontinence surgery.
Nine trials reported data on bladder perforation (Albo 2007; Bandarian 2011; El Barky 2005; Han 2001; Koelbl 2002; Liapis 2002; Sivaslioglu 2007; Tellez Martinez‐Fornes 2009; Ward 2002). Results from the lone trial using the traditional sling differed from those trials using the TVT (Albo 2007). Data from this trial showed that there was a five‐fold higher risk of having sutures pass through the bladder during open colposuspension compared to during the pubovaginal sling procedure (perforation rates: 3% versus 0.06% (RR 4.95; 95% CI 1.09 to 22.44, Analysis 5.20.)). In contrast, data from the TVT trials consistently showed a trend towards lesser risk for bladder perforation during open colposuspension (perforation rate: 0.9% versus 6.3% (RR 0.20; 95% CI 0.08 to 0.49, Analysis 5.20)).
5.20. Analysis.

Comparison 5 Open retropubic colposuspension versus sling procedure, Outcome 20 Number with bladder perforation.
There was also a significant vascular injury during TVT. None of these complications had serious consequences. Sand 2000 reported that one woman required urethrolysis for persistent urinary retention and two women suffered from partial erosions after the TVT procedure in the long‐term follow‐up.
Ward 2002 reported that the long term outcome involving the TVT procedure showed tape complications in a total of six women out of 170 at five‐year follow‐up.
We performed sensitivity analysis of the data by excluding the three trials which were quasi‐randomised, but this did not materially change the findings (data not shown).
Comparison 6: open retropubic colposuspension versus needle suspension procedure
Seven trials (Athanassopoulos 1996; Bergman 1989a; Bergman 1989b; German 1994; Gilja 1998; Mundy 1983; Palma 1985) compared open retropubic colposuspension with needle suspension procedures, with a total population of 570 women of whom 278 underwent colposuspension. The methodological qualities of the studies were generally satisfactory although the sample sizes of all except one (Bergman 1989a) were small and two trials were quasi‐randomised (Athanassopoulos 1996; Mundy 1983).
The most consistently reported outcomes were short‐ and medium‐term cure rates, for which data were generally available from at least five of the six trials. No trials examined quality of life or symptom quantification outcomes.
Women's observations
Fewer women were incontinent after colposuspension in the first year after surgery:
incontinence rate: 11% versus 15% (RR 0.66; 95% CI 0.42 to 1.03, Analysis 6.1);
after the first year, incontinence rate: 14% versus 23% (RR 0.56; 95% CI 0.39 to 0.81, Analysis 6.2); and
beyond five years, incontinence rate: 18% versus 57% (RR 0.32; 95% CI 0.15 to 0.71, Analysis 6.3).
6.1. Analysis.

Comparison 6 Open retropubic colposuspension versus needle suspension, Outcome 1 Number with incontinence within first year (subjective).
6.2. Analysis.

Comparison 6 Open retropubic colposuspension versus needle suspension, Outcome 2 Number with incontinence after first year but before five years (subjective).
6.3. Analysis.

Comparison 6 Open retropubic colposuspension versus needle suspension, Outcome 3 Number with incontinence after five years (subjective).
This was compared to those undergoing needle suspension, with the difference in incontinence rates increasing over time. There were few data describing subjective improvement (Analysis 6.4; Analysis 6.5; Analysis 6.6).
6.4. Analysis.

Comparison 6 Open retropubic colposuspension versus needle suspension, Outcome 4 Number with incontinence not improved within first year (subjective).
6.5. Analysis.

Comparison 6 Open retropubic colposuspension versus needle suspension, Outcome 5 Number with incontinence not improved after first year but before five years (subjective).
Clinician's observations
Data describing objective incontinence also favoured open colposuspension:
incontinence rate: 9% versus 14.% (RR 0.56; 95% CI 0.32 to 0.97) at less than one year, Analysis 6.6;
13% versus 21% (RR 0.59; 95% CI 0.40 to 0.88) at one year but less than five years, Analysis 6.7;
and from a single trial (Bergman 1989b) 18% versus 57% (RR 0.32; 95% CI 0.15 to 0.71) at more than five years' follow‐up (Analysis 6.8).
6.6. Analysis.

Comparison 6 Open retropubic colposuspension versus needle suspension, Outcome 6 Number with incontinence within the first year (objective).
6.7. Analysis.

Comparison 6 Open retropubic colposuspension versus needle suspension, Outcome 7 Number with incontinence after first and before five years (objective).
6.8. Analysis.
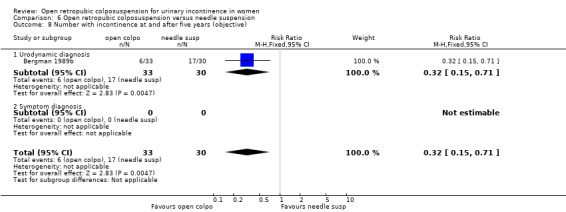
Comparison 6 Open retropubic colposuspension versus needle suspension, Outcome 8 Number with incontinence at and after five years (objective).
Surgical parameters
In the two trials with data the average time to catheter removal was shorter after colposuspension but the difference was not statistically significant (MD ‐0.40; 95% CI ‐0.95 to 0.15, Analysis 6.9). Other surgical parameters (operative time, length of hospitalisation) were not reported for any of the included trials.
6.9. Analysis.

Comparison 6 Open retropubic colposuspension versus needle suspension, Outcome 9 Time to catheter removal (days).
Adverse events
Combining data from the three trials (Athanassopoulos 1996; German 1994; Mundy 1983) reporting perioperative complications suggested that women undergoing open colposuspension had a lower risk of developing such complications (complication rate: 30% versus 48% (RR 0.66; 95% CI 0.46, 0.94, Analysis 6.10)). However, there was heterogeneity in the results between trials.
6.10. Analysis.

Comparison 6 Open retropubic colposuspension versus needle suspension, Outcome 10 Number of perioperative surgical complications.
There was insufficient evidence to judge whether or not the two procedures differed in:
de novo urge symptoms, total events: 19: 4% versus 8% (RR 0.56; 95% CI 0.22 to 1.41, Analysis 6.11);
de novo detrusor instability, event rate: 4% versus 13% (RR 0.34; 95% CI 0.09 to 1.37, Analysis 6.12);
voiding difficulty, total events 18: 12% versus 12% (RR 0.97; 95% CI 0.42 to 2.24, Analysis 6.13); or
new or recurrent prolapse (RR 0.45; 95% CI 0.04 to 4.72, Analysis 6.14).
6.11. Analysis.

Comparison 6 Open retropubic colposuspension versus needle suspension, Outcome 11 Number with de novo urge symptoms and urge incontinence.
6.12. Analysis.

Comparison 6 Open retropubic colposuspension versus needle suspension, Outcome 12 Number with de novo detrusor instability.
6.13. Analysis.

Comparison 6 Open retropubic colposuspension versus needle suspension, Outcome 13 Number with voiding difficulty.
6.14. Analysis.

Comparison 6 Open retropubic colposuspension versus needle suspension, Outcome 14 Number with new or recurrent prolapse.
We performed sensitivity analysis of the data by excluding the two quasi‐randomised trials (Athanassopoulos 1996; Mundy 1983). For one outcome (perioperative complications) the significant advantage of the open colposuspension when the quasi‐randomised trials were included in the meta‐analysis disappeared with the exclusion. Otherwise, the estimates were similar before and after exclusion.
Comparison 7: open retropubic colposuspension versus laparoscopic colposuspension
Twelve trials (Ankardal 2001; Burton 1994; Carey 2000; Fatthy 2001; Kitchener 2006; Mak 2000; Morris 2001; Stangel‐Wojcikiewicz 2008; Su 1997; Summitt 2000; Tuygun 2006; Ustun 2005) compared open with laparoscopic approaches to colposuspension, with a total of 1260 women studied. However, the results as reported by Burton 1994 could not be utilised for this review's statistical analysis since outcomes were reported as visual analogue scores. In Burton 1994, outcomes were better after open retropubic colposuspension in terms of post‐operative scoring for stress incontinence, number of incontinence episodes and pad test results, both in the short‐ and long‐term follow‐up. Data from the other 11 studies (Ankardal 2001; Carey 2000; Fatthy 2001; Kitchener 2006; Mak 2000; Morris 2001; Stangel‐Wojcikiewicz 2008; Su 1997; Summitt 2000; Tuygun 2006; Ustun 2005) are summarised below.
Ankardal 2001 had three citations, two of which referred to a multi‐centre trial on open versus laparoscopic colposuspension using mesh and staples, while the third was on a single institution, three‐armed trial on open versus laparoscopic colposuspension using mesh and staples versus laparoscopic colposuspension using sutures. Women in the open colposuspension and laparoscopic colposuspension using mesh in the three‐armed trial were also enrolled in the multi‐centre trial. Data from the multi‐centre trial were included in the meta‐analysis. Results from the three‐armed trial were presented separately in the text and in the additional tables when indicated.
The data on some of the surgical outcomes from Carey 2000 were not included in the meta‐analysis because no estimates of variance were provided. However, they were considered in the qualitative analysis of the different outcomes.
Kitchener 2006 reported subjective cure in terms of proportions of women who were perfectly happy or pleased, as well as proportions of women who never leaked and those who leaked less than once a month. For this review, the number of women who reported any leakage or leakage more than once a month was used for subjective incontinence.
Women's observations
Although data on patient‐reported incontinence rates were available from all 12 trials, they related to differing lengths of follow‐up. Furthermore, there appeared to be some heterogeneity between studies and the estimates from the meta‐analyses depended on which trials were used to contribute data.
In the short‐term, the combined estimate showed a wide confidence interval, consistent with as much as 20% favouring of either intervention (RR 0.97; 95% CI 0.79 to 1.18, Analysis 7.1). In the medium‐term (between one and five years), the combined estimate favoured open surgery (RR 0.88; 95% CI 0.75 to 1.03, Analysis 7.2) but this was not statistically significant and there was significant heterogeneity. This was due to Ankardal 2001 which used both sutures and mesh and staples (and where mesh and staples were used in the majority of patients) during the laparoscopic colposuspension (rather than sutures as in the other trials) and its removal eliminated the heterogeneity. Without the Ankardal data (which reported highly significantly better results with open colposuspension and was given a considerable weight in the meta‐analysis), no difference in the cure rates between the open and laparoscopic colposuspension could be demonstrated (RR 0.95; 95% CI 0.80 to 1.11). In the long term, the single small trial (Morris 2001) with 64 participants tended to favour laparoscopic repair (RR 1.89; 95% CI 0.99 to 3.59, Analysis 7.3), however the result did not quite reach statistical significance.
7.1. Analysis.

Comparison 7 Open retropubic colposuspension versus laparoscopic retropubic colposuspension, Outcome 1 Number with incontinence within first year (subjective).
7.2. Analysis.

Comparison 7 Open retropubic colposuspension versus laparoscopic retropubic colposuspension, Outcome 2 Number with incontinence after first year but before five years (subjective).
7.3. Analysis.

Comparison 7 Open retropubic colposuspension versus laparoscopic retropubic colposuspension, Outcome 3 Number with incontinence after five years (subjective).
Only one trial (Mak 2000) reported on improvement rates: three women in total failed to improve (out of 90) in the medium term (Analysis 7.4); the confidence interval was very wide.
7.4. Analysis.

Comparison 7 Open retropubic colposuspension versus laparoscopic retropubic colposuspension, Outcome 4 Number with incontinence not improved after first year but before five years (subjective).
Clinician's observations
To a large extent, the same issues applied to objective measures of incontinence. The meta‐analyses of data (six trials) available at less than one year (RR 0.88; 95% CI 0.64 to 1.21, Analysis 7.5) and between one and five years (seven trials) (RR 0.92; 95% CI 0.71 to 1.19, Analysis 7.6) did not show any significant differences in objective incontinence rates between the two treatment groups. Again, there was heterogeneity in the medium‐term results because of Ankardal 2001. However, inclusion or exclusion of the data did not change the results of the meta‐analysis. The single small trial of Morris 2001 showed a statistically significant result favouring laparoscopic repair (Analysis 7.7). However, the incontinence rate after open colposuspension was over 50%, which is much higher than that usually reported in other studies of open colposuspension with long‐term follow‐up.
7.5. Analysis.

Comparison 7 Open retropubic colposuspension versus laparoscopic retropubic colposuspension, Outcome 5 Numbers with incontinence within the first year (objective).
7.6. Analysis.

Comparison 7 Open retropubic colposuspension versus laparoscopic retropubic colposuspension, Outcome 6 Numbers with incontinence after first and before five years (objective).
7.7. Analysis.

Comparison 7 Open retropubic colposuspension versus laparoscopic retropubic colposuspension, Outcome 7 Numbers with incontinence at and after five years (objective).
Quality of life
Two trials (Carey 2000; Kitchener 2006) reported general health measures on quality of life, both using the SF‐36 physical and mental subscales. Both trials demonstrated significant improvement in both sub‐scales after open and laparoscopic colposuspension. The combined result of the two trials showed that laparoscopic colposuspension had lower (worse) post‐operative scores in the mental sub‐scale when compared to the open technique (MD 3.94; 95% CI 1.07 to 6.81, Analysis 7.8.2). The result was driven by the results of Carey 2000, which has the larger weighting.
7.8. Analysis.

Comparison 7 Open retropubic colposuspension versus laparoscopic retropubic colposuspension, Outcome 8 General health status measure.
Surgical parameters
FIve trials (Ankardal 2001; Fatthy 2001; Stangel‐Wojcikiewicz 2008; Su 1997;Tuygun 2006) evaluated the operative time, with conflicting results. Ankardal 2001, Fatthy 2001, , Stangel‐Wojcikiewicz 2008 and Tuygun 2006 reported a shorter operative time with open colposuspension, by 15 to 30 minutes, while Su 1997 reported the opposite (Analysis 7.9). This may be due to the use of only one suture per side in the laparoscopic colposuspension in the Su trial while using three sutures for the open procedure. Because of significant heterogeneity, pooling of the data was not done. Sensitivity analysis excluding the Su trial still showed statistical heterogeneity (p < 0.01, I2 = 72%).
7.9. Analysis.

Comparison 7 Open retropubic colposuspension versus laparoscopic retropubic colposuspension, Outcome 9 Operative time (minutes).
Seven studies (Carey 2000; Fatthy 2001; Kitchener 2006; Mak 2000; Stangel‐Wojcikiewicz 2008; Su 1997; Tuygun 2006) reported length of stay and there were large differences between trials (Analysis 7.10). The Fatthy 2001, Su 1997, Stangel‐Wojcikiewicz 2008 and Tuygun 2006 trials reported a longer hospital stay after open compared to laparoscopic colposuspension. Mak 2000, however, reported no significant difference. Carey 2000 reported similar lengths of hospital stay for both groups (3.9 days versus 3.7 days, no standard deviations provided); these were comparable to those in the Mak 2000 trial. It should be noted that among all the trials only Carey 2000 made special arrangements to ensure blinding of assessors and caregivers, which may have had an impact and resulted in the comparable hospital stays of the women in both groups. Because of the heterogeneity we made no attempt to derive a 'typical' estimate.
7.10. Analysis.

Comparison 7 Open retropubic colposuspension versus laparoscopic retropubic colposuspension, Outcome 10 Length of hospital stay (days).
In the two trials with data (Mak 2000; Tuygun 2006) the time to return to normal activities was longer in the open colposuspension group. There was significant heterogeneity in the results of the two trials so we did not combine the data (Analysis 7.11).
7.11. Analysis.

Comparison 7 Open retropubic colposuspension versus laparoscopic retropubic colposuspension, Outcome 11 Time to return to normal activity (days).
In the three trials providing standard deviations (Mak 2000; Su 1997; Tuygun 2006), time to catheter removal was longer after open colposuspension (MD 2.25; 95% CI 0.95 to 3.55, Analysis 7.12). Similarly, the time to catheter removal was longer after colposuspension in the Carey 2000 trial but this was not significant (4.9 versus 4.4 days, P = 0.8).
7.12. Analysis.

Comparison 7 Open retropubic colposuspension versus laparoscopic retropubic colposuspension, Outcome 12 Time to catheter removal (days).
Adverse events
There were no significant differences in the risk for developing adverse events in terms of:
perioperative complications, total events from four trials 36, complication rate: 14% versus 12% (RR 1.18; 95% CI 0.64 to 2.16, Analysis 7.13);
de novo urge symptoms or urge incontinence, total events from one trial 5: 7% versus 4% (RR 1.50; 95% CI 0.26 to 8.56, Analysis 7.14);
de novo detrusor overactivity, total events from six trials 51: 8% versus 11% (RR 0.82; 95% CI 0.48 to 1.38, Analysis 7.15);
voiding difficulties, total events from six trials 57, 10% versus 9% (RR 1.12; 95% CI 0.70 to 1.79, Analysis 7.16)); or
new or recurrent prolapse, total events from two trials 39, prolapse rate: 9% versus 11% (RR 0.76, 95% CI 0.39 to 1.52, Analysis 7.17).
7.13. Analysis.

Comparison 7 Open retropubic colposuspension versus laparoscopic retropubic colposuspension, Outcome 13 Number of perioperative surgical complications.
7.14. Analysis.

Comparison 7 Open retropubic colposuspension versus laparoscopic retropubic colposuspension, Outcome 14 Number with de novo urge symptoms and urge incontinence.
7.15. Analysis.

Comparison 7 Open retropubic colposuspension versus laparoscopic retropubic colposuspension, Outcome 15 Number with de novo detrusor instability.
7.16. Analysis.

Comparison 7 Open retropubic colposuspension versus laparoscopic retropubic colposuspension, Outcome 16 Number with voiding difficulty.
7.17. Analysis.

Comparison 7 Open retropubic colposuspension versus laparoscopic retropubic colposuspension, Outcome 17 Number with new or recurrent prolapse.
Four trials (Carey 2000; Kitchener 2006; Stangel‐Wojcikiewicz 2008; Tuygun 2006) provided some evidence of a greater tendency for laparoscopic colposuspension to have more complications specifically related to the procedure (bladder perforation: 0.6% versus 3% (RR 0.22; 95% CI 0.06 to 0.87, Analysis 7.18)).
7.18. Analysis.

Comparison 7 Open retropubic colposuspension versus laparoscopic retropubic colposuspension, Outcome 18 Number with bladder perforation.
Comparison 8: open retropubic colposuspension versus periurethral injections
A single trial (Corcos 2001) was identified which compared periurethral injection with surgery. Surgery included Burch colposuspension, needle suspension and slings. The data for all types of surgery were reported together so it was not possible to extract data to compare open retropubic colposuspension alone with periurethral injection. Of 66 women receiving collagen injections and 67 undergoing surgery, the authors reported that 19% of women were more likely to be cured with surgery than injections. There were significantly fewer and less severe complications with collagen injection (36 events for collagen versus 84 events for surgery, P = 0.003) but no statistically significant differences were reported for satisfaction, quality of life, or disease‐specific questions.
Comparison 9, 10 and 11: one type of open retropubic colposuspension versus another
Comparison 09: Burch colposuspension versus Marshall‐Marchetti‐Krantz procedure
Four trials (Colombo 1994; Liapis 1996; McCrery 2005; Quadri 1999) compared Burch colposuspension and the Marshall‐Marchetti‐Krantz (MMK) procedure, randomising a total of 353 women with 175 undergoing the Burch procedure. The methodological quality of the trials was acceptable.
No data were found describing differences in symptom quantification and quality of life measures between the treatment groups.
Women's observations (Comparisons 09.01 to 09.08)
Limited data were available from two trials at up to one year; these were not conclusive ( 9% versus 12% (RR 0.73; 95% CI 0.28 to 1.95, Analysis 9.1)). However, after the first year and before five years women treated with a Burch procedure were less likely to be incontinent (23% versus 34% (RR 0.72; 95% CI 0.52 to 0.99, Analysis 9.2)). No data were available for other outcomes based on women's observations.
9.1. Analysis.

Comparison 9 Burch colposuspension versus MMK, Outcome 1 Number with incontinence within first year (subjective).
9.2. Analysis.

Comparison 9 Burch colposuspension versus MMK, Outcome 2 Number with incontinence after first year but before five years (subjective).
Clinician's observations (Comparisons 09.09 to 09.12)
The result for objective cure also favoured Burch but was not statistically significant. At one to five years after surgery the incontinence rates were 19% versus 30% (RR 0.64; 95% CI 0.39 to 1.05, Analysis 9.5), but very few data were available at other times and none for other outcomes based on clinician observations.
9.5. Analysis.

Comparison 9 Burch colposuspension versus MMK, Outcome 5 Number with incontinence after first and before five years (objective).
Surgical parameters (Comparisons 09.17 to 09.19)
In the single trial with data (Colombo 1994), use of the Burch procedure was associated with a shorter hospital stay by an estimated one day (MD ‐1.10; 95% CI ‐1.74 to ‐0.46, Analysis 9.6). In three trials, women were catheterised for over six days less after the Burch procedure than after MMK (MD ‐6.35; 95% CI ‐9.15 to ‐3.56, Analysis 9.7).
9.6. Analysis.

Comparison 9 Burch colposuspension versus MMK, Outcome 6 Length of hospital stay (days).
9.7. Analysis.
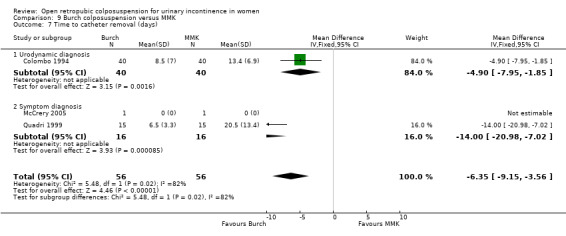
Comparison 9 Burch colposuspension versus MMK, Outcome 7 Time to catheter removal (days).
Adverse effects (Comparisons 09.20 to 09.26)
There was insufficient evidence to determine whether or not there were any differences between the Burch and MMK procedures in the risks of adverse effects in terms of perioperative complications (Analysis 9.8), de novo urge symptoms or urge incontinence (Analysis 9.9), detrusor overactivity (Analysis 9.10), or repeat anti‐incontinence surgery (RR 0.47; 95% CI 0.04 to 5.05, Analysis 9.13). One trial reported a lesser risk for voiding difficulties after Burch colposuspension compared to MMK (3/40 versus 11/40 (RR 0.27; 95% CI 0.08 to 0.90, Analysis 9.11)). Although more women developed a new or recurrent prolapse after Burch (versus none after MMK), this did not reach significance and the confidence interval was implausibly wide (Colombo 1994; Liapis 1996) (6/94 versus 0/91 (RR 6.75; 95% CI 0.84 to 54.31, Analysis 9.12)).
9.8. Analysis.

Comparison 9 Burch colposuspension versus MMK, Outcome 8 Number of perioperative surgical complications.
9.9. Analysis.

Comparison 9 Burch colposuspension versus MMK, Outcome 9 Number with de novo urge symptoms and urge incontinence.
9.10. Analysis.

Comparison 9 Burch colposuspension versus MMK, Outcome 10 Number with de novo detrusor overactivity.
9.13. Analysis.

Comparison 9 Burch colposuspension versus MMK, Outcome 13 Number with repeat anti‐incontinence surgery.
9.11. Analysis.

Comparison 9 Burch colposuspension versus MMK, Outcome 11 Number with voiding difficulty.
9.12. Analysis.

Comparison 9 Burch colposuspension versus MMK, Outcome 12 Number with new or recurrent prolapse.
Comparison 10: Burch colposuspension versus paravaginal defect repair
There was only one small study comparing Burch colposuspension with paravaginal defect repair (Colombo 1996). There were insufficient data to draw any conclusions in relation to any of the outcomes.
Comparison 11: Marshall‐Marchetti‐Krantz versus paravaginal defect repair or vaginal obturator shelf repair
There were no trials comparing Burch colposuspension with paravaginal defect repair or vaginal obturator shelf repair.
Discussion
Numerous surgical methods have been described for managing urinary incontinence, yet the quest for the ideal procedure with the highest effectiveness, least morbidity, and highest cost effectiveness is still ongoing. Large numbers of studies have been conducted and the need to integrate the results from high quality research into a meaningful and clinically useful recommendation has become imperative. This systematic review aimed to address this in respect to open retropubic colposuspension.
Summary of main results
Overall, open retropubic colposuspension has been shown to provide significantly better cure rates, both subjectively and objectively, compared to most of the other management options. Of all the other methods studied, the sling procedures and the laparoscopic technique of performing colposuspension seem to most closely approximate the efficacy of open colposuspension.
Open retropubic colposuspension was regarded as the gold standard treatment for urinary incontinence in women before the advent of new, minimally invasive procedures such as TVT. However, in countries where minimally invasive suburethral tapes are not available or the cost is prohibitive, open colposuspension remains the treatment of choice with its high success rates and acceptable levels of associated morbidity. The results of this systematic review present the evidence supporting such a view. The results of the trials considered in this review have shown overall cure rates of 69% to 88% for open retropubic colposuspension. These figures are consistent with those reported in other reviews, such as those conducted by Black 1996 and Jarvis 1994. Women must be given a balanced view, however, of the likely benefits and possible risks to help them make informed decisions.
Two small trials showed a significant advantage of open retropubic colposuspension over conservative management, with effect differences of 60% to 70%. While it is instinctive among women to favour conservative treatment over surgery, the prospect of achieving dryness offered by open retropubic colposuspension compared to conservative measures may be enough to make a woman seriously consider undergoing the procedure, despite the risks of surgery, especially in cases of severe, incapacitating incontinence.
More important perhaps than its short‐ to medium‐term performance is the durability of effectiveness several years after an open retropubic colposuspension operation. This is its main strength and has been the primary basis for considering it as the gold standard in the surgical treatment of urinary incontinence in women. Based on the results of this review, one can expect a decline in the cure rate of only 15% to 20% even beyond five years after open colposuspension. In contrast, anterior colporrhaphy and needle suspension procedures showed a decline of at least 40% and 30%, respectively, over a similar period of time.
The two interventions that compare most favourably with open colposuspension are the sling procedure and the laparoscopic technique of colposuspension. Long‐term trial results, although small in number, seem to show a similar enduring effect on continence rates from these procedures, comparable with open colposuspension.
To supplement the main systematic review of effects, we sought economic evaluations which have compared open retropubic colposuspension with any of the other main categories of surgical procedures listed in the Background section. A supplementary search in NHS EED, MEDLINE and Embase identified four such economic evaluations.
Colposuspension versus slings
The comparison of open colposuspension with TVT is largely dependent on a single medium‐sized trial (Ward 2002). To an extent, the interpretation of this depends on what assumptions are made about the women who refused their allocated procedure, most of whom were allocated to the colposuspension group. It is plausible that they were women with milder incontinence at trial entry; assuming that they would all have been cured by colposuspension, this tilts the comparison in favour of colposuspension. Nevertheless, this trial does illustrate the substantial short‐term advantages of TVT in terms of less post‐operative morbidity and more rapid return to normal activities. The main perioperative complication of TVT is bladder perforation, although this does not appear to have longer‐term implications.
With the inclusion of more data on traditional slings and TVT, a further examination of the effects of these two types of procedures and their comparison against open colposuspension was possible in this update. The inclusion of extra long‐term data from a large trial of traditional slings (Albo 2007) demonstrated that the traditional slings had better long‐term cure rates but a higher chance of post‐operative voiding dysfunction rates compared to open colposuspension. On the other hand, the TVT trials have only shown non‐inferiority in terms of cure rates when compared with open colposuspension. This possible difference in the effects of the traditional sling and the TVT should be explored and studied, and are the subjects of other Cochrane reviews (Ford 2015; Rehman 2011).
Clinicians must therefore inform women of the differences in adverse event profiles for each technique. Open colposuspension has been shown to be associated with pelvic organ prolapse, particularly in the long term. On the other hand, sling operations put women at a higher risk for postoperative voiding dysfunction.
Economic evidence
Four studies compared the use of tension‐free vaginal tape (TVT) with Burch colposuspension in the treatment of SUI in women (Kilonzo 2004; Laudano 2013; Manca 2003; Wu 2007) using clinical data from our MEDLINE search of RCTs (Kilonzo 2004) or both RCTs and observational studies (Laudano 2013; Wu 2007) and from a prospective multicentre randomised controlled trial (Manca 2003). Two studies (Laudano 2013; Wu 2007) adopted the perspective of the US healthcare system with a time horizon of 10 years, while Kilonzo 2004 and Manca 2003 adopted the UK payer’s perspective (UK National Health Service) with up to 10 years and less than a year time horizon, respectively. The Burch colposuspension procedure was reported to be more expensive than TVT in all studies. Wu 2007 reported an average cost in 2005 US Dollars of USD 9320 for Burch colposuspension and USD 8082 for TVT (P values and Cl not reported). Laudano 2013 reported an average cost of USD 10,545 for Burch colposuspension and USD 8651 for TVT (price year and Cl not reported) While Kilonzo 2004 reported the cost (2001 GBP) of GBP 1345 and GBP 1588 (after 1 year from initial surgery) and GBP 1645 and GBP 1920 (after 10 years from initial surgery) for TVT and open colposuspension, respectively. Manca 2003 reported the cost (1999 ‐ 2000 GBP) of GBP 1058 for TVT and GBP 1301 for open colposuspension (Differential costs: ‐243 (‐341 to ‐201)).
Burch colposuspension was on average slightly more effective, generating 0.01 more quality‐adjusted life years (QALYs) over 10 years compared to TVT (7.26 QALYs versus 7.25 QALYs), resulting in an incremental cost effectiveness ratio (ICER) of USD 98,755 per QALY gained (Wu 2007). Laudano 2013, Kilonzo 2004 and Manca 2003, however, reported that TVT generated on average 0.01 more QALYs at 10 years (Kilonzo 2004) and six months (Manca 2003) than the Burch procedure. The number of QALYs for each procedure and each study were; 5.79 QALYs for TVT versus 5.78 QALYs for Burch, 7.69 QALYs for TVT versus 7.68 QALYs for Burch and 0.397 QALYs for TVT versus 0.387 QALYs for Burch reported in Laudano 2013, Kilonzo 2004 and Manca 2003, respectively.
Wu 2007 concluded that TVT was more cost‐effective compared to Burch colposuspension based on the higher costs and minimal additional QALYs gained from the Burch colposuspension (probability not reported). Laudano 2013 also concluded that TVT was cost‐effective, with 90% probability that it was more cost‐effective than Burch colposuspension in the treatment of SUI in women. Burch colposuspension was estimated to only be more cost‐effective than TVT if the failure rate of TVT increases over time or when the cure rate was less than 42%. Kilonzo 2004 concluded that there was an 86% probability that TVT was cost‐effective compared to open colposuspension with a willingness‐to‐pay of GBP 30,000. TVT was found to be slightly less effective than open colposuspension in terms of QALYs for the first four years; beyond five years TVT became effective. Manca 2003 concluded that for a 12‐month follow‐up the probability that TVT was more cost‐effective than colposuspension was 94.6% when the decision‐maker is willing to pay at least GBP 30,000 per additional QALY.
Open abdominal colposuspension versus laparoscopic colposuspension
Shorter hospital stay was seen in trials that compared laparoscopic colposuspension with the open technique. However, failure to ensure blinding of the participants' care providers in the included trials may have introduced some bias towards earlier discharge from hospital for those undergoing laparoscopy. As noted in the results, for trials wherein blinding was employed, no significant difference in the length of hospitalisation was noted between women undergoing open and laparoscopic colposuspension. Also, hospital stay, particularly in elective surgical cases, is usually subject to institutional policies more than a reflection of actual patient needs. It is unclear from the reports if policies have been properly controlled or standardised in the conduct of the trials. There was not enough evidence in this review to judge whether laparoscopic colposuspension has an advantage or disadvantage compared to the open procedure in terms of subjective and objective cure rates, safety, longer‐term complications and quality of life.
Economic evidence
A cost‐effectiveness analysis by Dumville 2006 alongside a randomised controlled trial comparing open colposuspension with laparoscopic colposuspension in patients with SUI in the UK. The cost analysis was conducted from the perspective of the UK NHS. Healthcare resource use (2002 ‐ 2003 GBP) relating to the surgery, associated hospital stay and first six months after hospital discharge were collected prospectively for each participant. The data required for the calculation of QALYs were collected prospectively using the EQ‐5D‐3L questionnaire at baseline, 6, 12 and 24 months.
The economic evaluation was for both a six‐month and up to 24‐month time horizons. Healthcare resource use over six‐month follow‐up resulted in costs of GBP 1805 for the laparoscopic arm and GBP 1433 for the open arm (differential mean cost GBP 372; 95% credibility interval [CrI]: 274 to 471). At six months, QALYs were slightly higher on average in the laparoscopic arm relative to the open arm (0.005, 95% CrI –0.012 to 0.023). On average the incremental cost per extra QALY provided by the laparoscopic approach was GBP 74,400 at six months. At 24 months, the laparoscopic arm again had a higher mean QALYs compared to the open surgery group (0.04, 95% CrI ‐0.009 to 0.086). If the laparoscopic colposuspension did not incur any significant additional costs after six months compared with open colposuspension, then the incremental cost per extra QALY reduced to GBP 9300 at 24 months. The probability that laparoscopic colposuspension is cost‐effective was 86% when the decision‐maker is willing to pay up to GBP 30,000 for an additional QALY. Dumville 2006 concluded that laparoscopic colposuspension is not cost‐effective when compared with open colposuspension during the first six months, but the additional QALYs might be judged to be worth the additional cost after 24 months follow‐up.
Burch colposuspension versus Marshall‐Marchetti‐Krantz procedure
Despite the relatively small combined sample size of the trials comparing the Burch colposuspension and the Marshall‐Marchetti‐Krantz procedure, the pooled data provide enough evidence that the Burch technique results in higher cure rates. In addition, sensitivity analysis of the data limiting the trials to those which employed the Burch procedure in comparison with the other techniques showed greater benefits for open retropubic colposuspension Thus, it is reasonable to conclude that the Burch technique should be regarded as the standard open retropubic colposuspension procedure.
Economic evidence
We found no relevant economic evidence for the Brief Economic Commentary.
Overall completeness and applicability of evidence
Options for adrenergic drug treatment of stress urinary incontinence are limited (Alhasso 2005). A Cochrane review of the serotonin and noradrenaline reuptake inhibitor duloxetine was published in 2005; it does not include trials comparing duloxetine with surgery (Mariappan 2005).
With respect to alternative approaches to surgery, some of the findings in this review may not be relevant to current practice. This is especially true with regard to the infrequent to almost non‐existent use of anterior colporrhaphy and needle suspension procedures in the treatment of urinary incontinence, particularly in Western countries. However, it is believed that in certain Asian countries, anterior colporrhaphy is still widely offered as a first‐line treatment for urinary incontinence. One of the main arguments for this practice is the perceived lower morbidity rates associated with vaginal surgery compared to the retropubic or abdominal approach. This review has not shown any significantly higher risk for perioperative complications and adverse effects for open colposuspension compared with the other surgical techniques. However, the combined trial populations included in this review may be too small in number, and thus lack the power, to detect such a difference. On the other hand, it is noteworthy that this review indicates higher post‐operative morbidity rates associated with needle suspension procedures and anterior colporrhaphy when directly compared with open colposuspension. Such a finding seems to be in conflict with prevailing views and recommendations, which are mostly based on observational studies.
The evaluation provided by this review was limited by the fact that very few studies focused on the impact of the various treatment modalities on quality of life after treatment, long term outcomes on cosmesis, voiding dysfunction, sexual function and repeat incontinence surgery of alternative procedures. These parameters could be key determinants for decision making.
Estimates of outcomes in surgical trials may not reflect real life settings. The effect of the surgeon's skills on the outcome, when several surgeons are involved in the trial are not taken into account. Also, expertise of surgeons in trials may not necessarily be comparable to those in pure clinical practice.
We did intend to assess the impact of certain participant characteristics on the estimates of treatment effects. Among the factors were method of diagnosis of incontinence (symptom‐based versus urodynamics), previous anti‐incontinence surgery, presence of pre‐operative prolapse, and presence of signs and symptoms of detrusor overactivity or mixed incontinence. As only three trials (Albo 2007; Enzelsberger 1996; Kitchener 2006) relied on symptoms as their main diagnostic criteria for inclusion, the influence of having a urodynamic diagnosis on the outcomes could not be ascertained in this review. It could not be determined whether urodynamics was used to confirm the diagnosis in a further four trials (Drahoradova 2004; Palma 1985; Quadri 1999; Summitt 2000). Most studies did not describe their participants in sufficient detail, according to our pre‐specified factors, and hence it was not possible to assess the influence of these factors on the outcomes.
Also, we did not subject these four identified economic evaluations to critical appraisal and we do not attempt to draw any firm or general conclusions about the relative costs or efficiency of open retropubic colposuspension in treatment of SUI. However, the economic evidence available indicates that open retropubic colposuspension is not cost‐effective when compared with TVT, but is likely be cost‐effective in the short term (i.e. first six months following surgery) when compared with laparoscopic colposuspension in the treatment of SUI.
Authors' conclusions
Implications for practice.
1. The evidence available indicates that open retropubic colposuspension is an effective treatment for stress urinary incontinence, especially in the long term. Within the first year of treatment, the overall continence rate is approximately 85% to 90%. After five years, approximately 80% of women can expect to be dry. The review showed better cure and improvement rates after open retropubic colposuspension compared to conservative management, anterior colporrhaphy, and needle suspension surgery without any significant increase in morbidity. Therefore, retropubic colposuspension could be offered to women seeking open surgical treatment for urinary incontinence.
2. The minimally invasive sling procedures confer similar success rates in comparison to open colposuspension. However, traditional slings provide better cure rates at the expense of more voiding dysfunction in the short term. The long‐term adverse event profile of the sling procedures, in particular with the use of the TVT, is still unclear.
3. Laparoscopic colposuspension should allow speedier recovery, and available evidence shows comparable effectiveness with open surgery.
4. In general, the evidence available does not show a higher morbidity or complication rate with open retropubic colposuspension compared to the other surgical techniques, as has often been claimed. However, we found greater risk for post‐operative pelvic organ prolapse after open colposuspension, when compared with anterior colporrhaphy and sling procedures.
5. The available evidence suggests that the Burch procedure should be the preferred technique for open colposuspension. The Burch colposuspension provides better cure rates compared to the Marshall‐Marchetti‐Krantz procedure. There was no evidence on paravaginal repair.
Implications for research.
1. The methodology of the trials in the review could have been more scientifically valid. Future trials of incontinence surgery should have a well‐described sequence generation and secure concealment of allocation, standardised procedures with minimal co‐interventions and confounders, larger sample sizes to provide sufficiently precise estimates of effects, proper blinding, and longer follow‐up of all women randomised irrespective of the treatment actually received, intention‐to‐treat analyses, and detailed accounts of dropouts and withdrawals with explicit description of handling attrition.
It was not clear whether the methodological limitations in the trials reviewed were actual study design errors or poor reporting. It is highly recommended that clinical trials should be reported following the CONSORT guidelines (Schulz 2010).
2. There is an urgent need for further trials of adequate power to assess the effectiveness, safety and cost‐effectiveness of open retropubic colposuspension in comparison with (a) suburethral slings, using both traditional and minimally invasive approaches, and (b) the laparoscopic technique. In addition, the long‐term outcomes of existing trials could and should be reported: this would be a cost‐effective way of providing the information that is most important to women, i.e. for how long the operations remain effective, and at what cost in terms of adverse effects or the need for further treatment for urinary incontinence, prolapse or adverse effects.
Future trials should be designed in ways that allow exploration of effects in specific subgroups of women characterised by prognostic factors, and potential confounding by these factors. These include previous anti‐incontinence surgery, co‐existing prolapse, mixed incontinence, and low maximal urethral closure pressure (MUCP) or leak point pressures, or suspicion of having a significant component of intrinsic sphincter deficiency.
3. Future research on surgical treatment of urinary incontinence must provide more information on long‐term outcomes, particularly on adverse events and quality of life.
What's new
| Date | Event | Description |
|---|---|---|
| 10 July 2017 | New citation required but conclusions have not changed | Brief economic commentary (BEC) added. Economics‐related sections revised. |
| 10 July 2017 | Amended | Brief economic commentary (BEC) added. Economics related sections revised: the Abstract, Plain language summary, Background, Methods (outcomes, search methods), and Discussion were amended. Appendix added with details of search strategies for BECs. |
History
Protocol first published: Issue 1, 2001 Review first published: Issue 1, 2003
| Date | Event | Description |
|---|---|---|
| 15 February 2016 | New search has been performed | Review updated with two additional studies (El‐Din Shawki 2012, Trabuco 2014), follow up data on one trial (Albo 2007) |
| 15 February 2016 | New citation required but conclusions have not changed | Review updated with two additional studies (El‐Din Shawki 2012, Trabuco 2014), follow up data on one trial (Albo 2007) |
| 16 May 2012 | New citation required but conclusions have not changed | review updated with seven additional studies |
| 16 May 2012 | New search has been performed | review updated with seven additional studies |
| 27 January 2009 | New citation required but conclusions have not changed | new citation |
| 12 November 2008 | New search has been performed | For this update, we identified 39 new reports that appeared to meet the inclusion criteria. Upon further assessment, 10 reports were excluded for one of the following reasons : not randomised to the anti‐incontinence treatment, patients not incontinent at start of study, interventions or outcomes were not among prespecified in the protocol. Of the remaining 29 reports, 23 were citations to 7 new trials (Albo 2007, Bai 2005, Drahoradova 2004, El Barky 2005, Kitchener 2006, McCrery 2005, Quadri 1999) and 6 were citations to 4 trials previous included in the earlier version of the review (Ankardal 2001, Carey 2000, Corcos 2001, Ward 2002). Of these 4 trials, new data were available for 3 (Ankardal 2001, Carey 2000, Ward 2002). |
| 2 April 2008 | Amended | Converted to new review format. |
| 2 March 2005 | New citation required and conclusions have changed | March 2005: First update, we identified 42 (or 48??) new reports that appeared to meet the inclusion criteria of the review. Upon further review, 24 were excluded as patients were either not randomized to treatment or the studies included patients who were not incontinent . Of the remaining 18 reports, 6 were additional publications of already included studies (Milani 85, Demirci 2001, Ward 2002), 6 were follow up reports of previously included studies (Sand 2000, Mak 2000, Corcos 2001, Ward 2002), and 6 were citations of protocols of ongoing randomized trials (Boyd 1996; Brubaker 2003; Bump 2002; MRC Colpo Trial; Tincello 2004). Six new trials were identified for inclusion into this review update (Ankardal 2001, Koelbl 2002, Liapis 2002, O'Sullivan 2000, Osman 2003, Wang 2003). |
| 1 November 2002 | New search has been performed | We identified 123 reports of 69 studies that used open retropubic colposuspension in at least one arm and apparently met the review criteria. Of the 69 studies, 33 were included, 25 were excluded and 11 are awaiting assessment, pending confirmation from the authors on the random allocation of the participants. Of the 25 trials that were excluded, the majority were either not randomised trials or had participants that were not incontinent at the beginning of the trial. Two references were studies done comparing one sling technique with another (Debodinance 1993; Debodinance 1994). One trial (Baessler 1998) was excluded because it compared one technique of open retropubic colposuspension (Burch) with the same technique in combination with another (paravaginal repair). Hence, the review includes 33 trials. |
Acknowledgements
We thank Sheila Wallace for all her help with searching for the studies. We would also like to thank the following Cochrane Incontinence Group editorial base staff members for their help and support with this review: Cathryn Glazener, Muhammad Imran Omar, Suzanne Macdonald and Erika Magnago. We are also thankful to Nicola Dean (Contact Editor) and Peter Herbison (Statistical Editor) of the review.
The following authors and trialists provided additional important information regarding their respective works:
Dr David Holmes;
Dr Ivan Gilja;
Dr Paolo Palma;
Dr Paul Hilton;
Dr TH Su;
Dr Wiggo Fischer‐Rasmussen;
Dr Mario Colombo;
Dr RG Condie;
Dr Maud Arkandal.
We also thank the following who assisted us in the translation of non‐English manuscripts:
Mr Neil Scott;
Dr Donald Jude Meguizo.
Appendices
Appendix 1. Specialised Register ‐ search terms used
The Incontinence Group Specialised Register was searched using the Group's own keyword system, the search terms used were: topic.urine.incon* AND ({design.cct*} OR {design.rct*}) AND ({intvent.surg.abdo.} OR {intvent.surg.abdo.burch.} OR {intvent.surg.abdo.colposusp.} OR {intvent.surg.abdo.mmk.} OR {intvent.surg.burch.} OR {intvent.surg.colpo*} OR {intvent.surg.endopelvicFasciaPlication.}).
(All searches were in the keywords field of Reference Manager 2012)
The date of the most recent search was: 5 May 2015.
Appendix 2. Search strategies for brief economic commentary
We performed additional searches for the Brief Economic Commentary (BECs). We conducted them in MEDLINE(1 January 1946 to March 2017), Embase (1 January 1980 to 2017 Week 12) and NHS EED (1st Quarter 2016). We ran all searches on 6 April 2017. We used two different search strategies on MEDLINE and Embase (OvidSP) and one on NHS EED (OVID). Details of the searches run and the search terms used can be found below.
NHS EED (Ovid) (1st Quarter 2016)
NHS EED was searched using the following search strategy:
1. Urinary incontinence/
2. Urinary incontinence, stress/
3. ((stress$ or mix$ or urg$ or urin$) adj3 incontinen$).tw.
4. Colporrhaphy.tw.
5. Colpoperineoplast$.tw.
6. Sling procedure$.tw.
7. Sling$ procedure$.tw.
8. Bladder neck needle suspension$.tw.
9. Anterior vaginal repair$ .tw.
10. Or/1‐9
MEDLINE (1 January 1946 to March 2017) and Embase (1 January 1980 to 2017 Week 12)
We used two different search strategies on MEDLINE and EMBASE (OvidSP) ‐ these are given below.
Search strategy 1:
1. Economics, Pharmaceutical/ or Economics, Medical/ or Economics/ or Economics, Hospital/ or economics.mp. or Economics, Nursing/
2. exp "costs and cost analysis"/
3. "Value of Life"/
4. exp "fees and charges"/
5. exp budgets/
6. budget*.ti,ab.
7. cost*.ti.
8. (economic* or pharmaco?economic*).ti.
9. (price* or pricing*).ti,ab.
10. (cost* adj2 (effective* or utilit* or benefit* or minimi* or unit* or estimat* or variable*)).ab.
11. (financ* or fee or fees).ti,ab.
12. (value adj2 (money or monetary)).ti,ab.
13. ((energy or oxygen) adj cost).ti,ab.
14. (metabolic adj cost).ti,ab.
15. ((energy or oxygen) adj expenditure).ti,ab.
16. 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15
17. exp Urinary Incontinence/
18. ((stress* or mix* or urg* or urin*) adj3 incontinen*).tw.
19. Urodynamics/ or Urinary Incontinence, Stress/ or Urinary Incontinence/ or Suburethral Slings/ or mixed incontinence.mp. or Urinary Bladder/ or Urinary Incontinence, Urge/
20. 17 or 18 or 19
21. anterior vaginal repair*.tw.
22. 16 and 20 and 21
23. anterior colporrhaphy*.tw.
24. 21 or 23
25. 16 and 20 and 23
26. bladder neck needle suspension$.tw.
27. 16 and 20
28. 26 and 27
29. open abdominal retropubic colposuspension*.tw.
30. retropubic colposuspension*.tw.
31. burch colposuspension*.tw.
32. 29 or 30 or 31
33. 27 and 32
34. laparoscopic retropubic colposuspension*.tw.
35. laparoscopic colposuspension*.tw.
36. 34 or 35
37. 27 and 36
38. traditional suburethral retropubic sling procedure$*.tw.
39. traditional sling procedure$*.tw.
40. suburethral retropubic sling procedure$*.tw.
41. retropubic sling procedure$*.tw.
42. traditional suburethral sling*.tw.
43. Suburethral Slings/ or Urinary Incontinence, Stress/ or Urologic Surgical Procedures/
44. 27 and 43
45. remove duplicates from 44
Search strategy 2:
1. economics.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, fs]
2. value of life.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, fs]
3. exp "costs and cost analysis"/
4. exp economics, hospital/
5. exp economics, medical/
6. economics, nursing.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, fs]
7. economics, pharmaceutical.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, fs]
8. exp "fees and charges"/
9. exp budgets/
10. budget*.ti,ab.
11. cost*.ti.
12. (economic* or pharmaco?economic*).ti.
13. (price* or pricing*).ti,ab.
14. (cost* adj2 (effective* or utilit* or benefit* or minimi* or unit* or estimat* or variable*)).ab.
15. (financ* or fee or fees).ti,ab.
16. (value adj2 (money or monetary)).ti,ab.
17. or/1‐16
18. economics.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, fs]
19. value of life.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, fs]
20. exp "costs and cost analysis"/
21. exp economics, hospital/
22. exp economics, medical/
23. economics, nursing.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, fs]
24. economics, pharmaceutical.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, sy, tn, dm, mf, dv, kw, fs
25. exp "fees and charges"/
26. exp budgets/
27. budget*.ti,ab.
28. cost*.ti.
29. (economic* or pharmaco?economic*).ti.
30. (price* or pricing*).ti,ab.
31. (cost* adj2 (effective* or utilit* or benefit* or minimi* or unit* or estimat* or variable*)).ab.
32. (financ* or fee or fees).ti,ab.
33. (value adj2 (money or monetary)).ti,ab.
34. 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31 or 32 or 33
35. ((energy or oxygen) adj cost).ti,ab.
36. (metabolic adj cost).ti,ab.
37. ((energy or oxygen) adj expenditure).ti,ab.
38. 34 or 35 or 36 or 37
39. urinary incontinence.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
40. ((stress$ or mix$ or urg$ or urin$) adj3 incontinen$).tw.
41. URINARY INCONTINENCE, STRESS.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
42. stress urinary incontinence*.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
43. 39 or 40 or 41 or 42
44. intervention surgery*.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
45. colporrhaphy.tw.
46. Bologna procedure*.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
47. Kelly‐Kennedy.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
48. Marion Kelly.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
49. Diaphragmplasty.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
50. Vaginal urethrocystopexy.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
51. Cystocele repair.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
52. Kelly plication.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
53. anterior vaginal repair$.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
54. anterior colporrhaphy.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
55. 44 or 45 or 46 or 47 or 48 or 49 or 50 or 51 or 52 or 53 or 54
56. 38 and 43 and 55
57. remove duplicates from 56
58. Bladder neck needle suspension$.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
59. 38 and 43 and 58
60. burch colposuspension.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
61. open abdominal retropubic colposuspension.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
62. Paravaginal defect repair.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
63. Marshall‐Marchetti‐Krantz.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
64. abdominal burch.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
65. abdominal colposuspension.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
66. endopelvic Fascia Plication.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
67. 60 or 61 or 62 or 63 or 64 or 65 or 66
68. 38 and 43
69. 67 and 68
70. laparoscopic retropubic colposuspension.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
71. laparoscopic colposuspension.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
72. retropubic colposuspension.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
73. 70 or 71 or 72
74. 68 and 73
75. remove duplicates from 74
76. suburethral sling.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
77. abdominal sling.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
78. traditional sling procedure$*.tw.
79. suburethral sling procedure.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
80. 76 or 77 or 78 or 79
81. 68 and 80
82. remove duplicates from 81
83. mid$urethral sling.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
84. retropubic sling procedure$*.tw.
85. transobturator sling procedure$.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
86. 83 or 84 or 85
87. remove duplicates from 86
88. 68 and 87
89. TVT‐Secur.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
90. mini‐arc.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
91. ajust.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
92. needleless.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
93. solyx.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
94. single$incision sling$.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
95. miniarc.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
96. mini$sling.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
97. Ophira.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
98. Tissue Fixation System.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
99. 89 or 90 or 91 or 92 or 93 or 94 or 95 or 96 or 97 or 98
100. 68 and 99
101. remove duplicates from 100
102. ((urethra$ or periurethra$ or transurethra$) adj3 (agent$ or bulk$ or injection$ or injectable$)).tw.
103. injection therapy.tw.
104. injectable$.tw.
105. (injectable$ adj2 agent$).tw.
106. (bulk$ adj3 agent$).tw.
107. Peri$urethral injection$.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
108. Autologous fat.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
109. Macroplastique.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
110. Calcium hydroxylapatite.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
111. Hyaluronic acid with dextranomer.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
112. Porcine dermal implant.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
113. Ethylene vinyl alcohol copolymer.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
114. Silicon particles.mp. [mp=ti, ab, ot, nm, hw, kf, px, rx, ui, an, eu, pm, sy, tn, dm, mf, dv, kw, fs]
115. 102 or 103 or 104 or 105 or 106 or 107 or 108 or 109 or 110 or 111 or 112 or 113 or 114
116. 68 and 115
117. remove duplicates from 116
Appendix 3. Handsearch conducted for earlier versions of this review
The following conference proceedings were searched:
International Urogynecological Association (IUGA) ‐ 32nd Annual Meeting, Cancun, Mexico, 12‐16 Jun 2007 ‐ the proceedings published in the International Urogynecology Journal (2007) volume 18, Supplement 1 were handsearched.
AUA 2007 ‐ Anaheim, CA ‐ the 2007 poster sessions are available online at http://www.aua2008.org/ and were searched using the terms: Burch; colposuspension; colposuspensions; urethropexy; and urethropexies. The titles of the relevant sessions on incontinence were also scanned.
ICS 2007 ‐ 37th Annual Meeting, Rotterdam, Netherlands, 20‐24 Aug 2007 ‐ the abstracts are available to search online at https://www.icsoffice.org/ASPNET_Membership/Membership/Home.aspx and were searched using the terms: Burch; colposuspension; colposuspensions; urethropexy; and urethropexies.
Data and analyses
Comparison 2. Open retropubic colposuspension versus conservative interventions.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Number with incontinence within first year (subjective) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 Urodynamic diagnosis | 1 | 29 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.24 [0.08, 0.71] |
| 2 Number with incontinence not improved within first year (subjective) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 Urodynamic diagnosis | 1 | 29 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.81 [0.13, 5.01] |
| 2.2 Symptom diagnosis | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3 Number with incontinence within the first year (objective) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.1 Urodynamic diagnosis | 1 | 68 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.26 [0.13, 0.53] |
| 4 Number with de novo detrusor instability | 1 | 29 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.47 [0.11, 56.03] |
| 4.1 Urodynamic diagnosis | 1 | 29 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.47 [0.11, 56.03] |
| 5 Number with other complication inherent to procedure | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 5.1 Urodynamic diagnosis | 1 | 29 | Risk Ratio (M‐H, Fixed, 95% CI) | 5.76 [0.32, 102.44] |
2.4. Analysis.

Comparison 2 Open retropubic colposuspension versus conservative interventions, Outcome 4 Number with de novo detrusor instability.
2.5. Analysis.
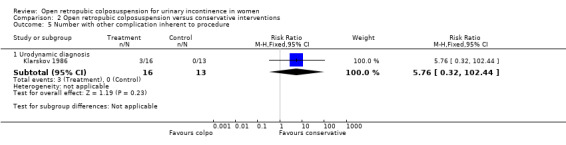
Comparison 2 Open retropubic colposuspension versus conservative interventions, Outcome 5 Number with other complication inherent to procedure.
Comparison 3. Open retropubic colposuspension versus drug therapy.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Number with incontinence within first year (subjective) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 Urodynamic diagnosis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Condition specific health measure | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 2.1 Urodynamic diagnosis | 1 | 44 | Mean Difference (IV, Fixed, 95% CI) | ‐3.80 [‐4.59, ‐3.01] |
| 2.2 Symptom diagnosis | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
Comparison 4. Open retropubic colposuspension versus anterior colporrhapy.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Number with incontinence within first year (subjective) | 6 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 Urodynamic diagnosis | 6 | 576 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.46 [0.30, 0.72] |
| 1.2 Symptom diagnosis | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 2 Number with incontinence after first year but before five years (subjective) | 7 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.1 Urodynamic diagnosis | 7 | 628 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.37 [0.27, 0.51] |
| 2.2 Symptom diagnosis | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3 Number with incontinence after five years (subjective) | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3.1 Urodynamic diagnosis | 3 | 174 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.49 [0.32, 0.75] |
| 3.2 Symptom diagnosis | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Number with incontinence within the first year (objective) | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 4.1 Urodynamic diagnosis | 4 | 428 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.36 [0.22, 0.58] |
| 4.2 Symptom diagnosis | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Number with incontinence after first and before five years (objective) | 6 | 505 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.34 [0.25, 0.47] |
| 5.1 Urodynamic diagnosis | 6 | 505 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.34 [0.25, 0.47] |
| 5.2 Symptom diagnosis | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Number with incontinence at and after five years (objective) | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 6.1 Urodynamic diagnosis | 3 | 174 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.48 [0.31, 0.73] |
| 6.2 Symptom diagnosis | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Volume/weight of urine loss in 2 hour pad test | 1 | 45 | Mean Difference (IV, Fixed, 95% CI) | 1.10 [‐4.41, 6.61] |
| 7.1 Urodynamic diagnosis | 1 | 45 | Mean Difference (IV, Fixed, 95% CI) | 1.10 [‐4.41, 6.61] |
| 7.2 Symptom diagnosis | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 8 Condition specific health measure | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 8.1 Urodynamic diagnosis | 1 | 35 | Mean Difference (IV, Fixed, 95% CI) | ‐0.59 [‐1.11, ‐0.07] |
| 8.2 Symptom diagnosis | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 9 Operative time (minutes) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 9.1 Urodynamic diagnosis | 1 | 51 | Mean Difference (IV, Fixed, 95% CI) | 14.4 [5.43, 23.37] |
| 9.2 Symptom diagnosis | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 10 Length of hospital stay (days) | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 10.1 Urodynamic diagnosis | 2 | 113 | Mean Difference (IV, Random, 95% CI) | ‐1.53 [‐4.45, 1.39] |
| 10.2 Symptom diagnosis | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 11 Time to catheter removal (days) | 3 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 11.1 Urodynamic diagnosis | 3 | 324 | Mean Difference (IV, Fixed, 95% CI) | ‐0.28 [‐0.83, 0.27] |
| 11.2 Symptom diagnosis | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 12 Number of perioperative surgical complications | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 12.1 Urodynamic diagnosis | 2 | 96 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.39 [0.19, 0.83] |
| 12.2 Symptom diagnosis | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 13 Number with de novo urge symptoms and urge incontinence | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 13.1 Urodynamic diagnosis | 3 | 241 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.53 [0.25, 1.14] |
| 13.2 Symptom diagnosis | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 14 Number with de novo detrusor instability | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 14.1 Urodynamic diagnosis | 4 | 306 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.26 [0.54, 2.94] |
| 14.2 Symptom diagnosis | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 15 Number with voiding difficulty | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 15.1 Urodynamic diagnosis | 4 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 15.2 Symptom diagnosis | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 16 Number with new or recurrent prolapse | 5 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 16.1 Urodynamic diagnosis | 5 | 447 | Risk Ratio (M‐H, Random, 95% CI) | 2.51 [0.62, 10.10] |
| 16.2 Symptom diagnosis | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 17 Number with repeat anti‐incontinence surgery | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 17.1 Urodynamic diagnosis | 3 | 271 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.11 [0.04, 0.30] |
| 17.2 Symptom diagnosis | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 18 Number with other complication inherent to procedure | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 18.1 Urodynamic diagnosis | 2 | 119 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.78 [0.58, 39.54] |
| 18.2 Symptom diagnosis | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 19 Number not cured within first year (subjective) Burch vs MMK | 6 | Odds Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 19.1 Burch trials | 4 | 427 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.47 [0.26, 0.85] |
| 19.2 MMK trials | 2 | 146 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.58 [0.25, 1.36] |
| 20 Number not cured after first year but before five years (subjective) Burch vs MMK | 2 | 146 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.77 [0.38, 1.55] |
| 20.1 MMK | 2 | 146 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.77 [0.38, 1.55] |
4.18. Analysis.

Comparison 4 Open retropubic colposuspension versus anterior colporrhapy, Outcome 18 Number with other complication inherent to procedure.
Comparison 5. Open retropubic colposuspension versus sling procedure.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Number with incontinence within first year (subjective) | 8 | 817 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.69, 1.18] |
| 1.1 Urodynamic diagnosis : open colposuspension versus traditional sling procedure | 3 | 131 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.92 [0.57, 6.50] |
| 1.2 Symptom diagnosis : open colposuspension versus traditional sling procedure | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 1.3 Urodynamic diagnosis : open colposuspension versus self fixing sling procedure | 5 | 547 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.67, 1.16] |
| 1.4 Symptom diagnosis : open colposuspension versus self fixing sling procedure | 1 | 139 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.04, 2.87] |
| 2 Number with incontinence after first year but before five years (subjective) | 6 | 1019 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.18 [1.01, 1.39] |
| 2.1 Urodynamic diagnosis : open colposuspension versus traditional sling procedure | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 2.2 Symptom diagnosis : open colposuspension versus traditional sling procedure | 2 | 592 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.35 [1.11, 1.64] |
| 2.3 Urodynamic diagnosis : open colposuspension versus self fixing sling procedure | 4 | 427 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.68, 1.22] |
| 2.4 Symptom diagnosis : open colposuspension versus self fixing sling procedure | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3 Number with incontinence after five years (subjective) | 3 | 658 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.11 [0.97, 1.27] |
| 3.1 Urodynamic diagnosis : open colposuspension versus traditional sling procedure | 1 | 28 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.43 [0.04, 4.25] |
| 3.2 Symptom diagnosis : open colposuspension versus traditional sling procedure | 1 | 453 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.19 [1.03, 1.37] |
| 3.3 Urodynamic diagnosis : open colposuspension versus self fixing sling procedure | 1 | 177 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.83 [0.54, 1.26] |
| 3.4 Symptom diagnosis : open colposuspension versus self fixing sling procedure | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Number with incontinence not improved within first year (subjective) | 2 | 97 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.84 [0.30, 2.30] |
| 4.1 Urodynamic diagnosis : open colposuspension versus traditional sling procedure | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4.2 Symptom diagnosis : open colposuspension versus traditional sling procedure | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4.3 Urodynamic diagnosis : open colposuspension versus self fixing sling procedure | 2 | 97 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.84 [0.30, 2.30] |
| 4.4 Symptom diagnosis : open colposuspension versus self fixing sling procedure | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Number with incontinence not improved after first year but before five years (subjective) | 2 | 277 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.11 [0.64, 1.91] |
| 5.1 Urodynamic diagnosis : open colposuspension versus traditional sling procedure | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5.2 Symptom diagnosis : open colposuspension versus traditional sling procedure | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5.3 Urodynamic diagnosis : open colposuspension versus self fixing sling procedure | 2 | 277 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.11 [0.64, 1.91] |
| 5.4 Symptom diagnosis : open colposuspension versus self fixing sling procedure | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Number with incontinence within the first year (objective) | 7 | 603 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.21 [0.84, 1.75] |
| 6.1 Urodynamic diagnosis : open colposuspension versus traditional sling procedure | 3 | 88 | Risk Ratio (M‐H, Fixed, 95% CI) | 6.69 [0.89, 50.43] |
| 6.2 Symptom diagnosis : open colposuspension versus traditional sling procedure | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6.3 Urodynamic diagnosis : open colposuspension versus self fixing sling procedure | 4 | 515 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.08 [0.74, 1.57] |
| 6.4 Symptom diagnosis : open colposuspension versus self fixing sling procedure | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Number with incontinence after first and before five years (objective) | 5 | 940 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.12 [0.82, 1.54] |
| 7.1 Urodynamic diagnosis : open colposuspension versus traditional sling procedure | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7.2 Symptom diagnosis : open colposuspension versus traditional sling procedure | 2 | 592 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.11 [0.75, 1.66] |
| 7.3 Urodynamic diagnosis : open colposuspension versus self fixing sling procedure | 3 | 348 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.14 [0.69, 1.88] |
| 7.4 Symptom diagnosis : open colposuspension versus self fixing sling procedure | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 8 Number with incontinence at and after five years (objective) | 2 | 149 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.70 [0.30, 1.64] |
| 8.1 Urodynamic diagnosis : open colposuspension versus traditional sling procedure | 1 | 28 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.38 [0.23, 83.62] |
| 8.2 Symptom diagnosis : open colposuspension versus traditional sling procedure | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 8.3 Urodynamic diagnosis : open colposuspension versus self fixing sling procedure | 1 | 121 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.52 [0.20, 1.36] |
| 8.4 Symptom diagnosis : open colposuspension versus self fixing sling procedure | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 9 Mean change in IIQ score from baseline | 1 | 655 | Mean Difference (IV, Fixed, 95% CI) | 5.80 [‐11.03, 22.63] |
| 9.1 Urodynamic diagnosis : open colposuspension versus traditional sling procedure | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 9.2 Symptom diagnosis : open colposuspension versus traditional sling procedure | 1 | 655 | Mean Difference (IV, Fixed, 95% CI) | 5.80 [‐11.03, 22.63] |
| 9.3 Urodynamic diagnosis : open colposuspension versus self fixing sling procedure | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 9.4 Symptom diagnosis : open colposuspension versus self fixing sling procedure | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 10 Operative time (minutes) | 4 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 10.1 Urodynamic diagnosis : open colposuspension versus traditional sling procedure | 1 | 29 | Mean Difference (IV, Fixed, 95% CI) | ‐6.02 [‐12.56, 0.52] |
| 10.2 Symptom diagnosis : open colposuspension versus traditional sling procedure | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 10.3 Urodynamic diagnosis : open colposuspension versus self fixing sling procedure | 3 | 361 | Mean Difference (IV, Fixed, 95% CI) | 18.06 [14.67, 21.46] |
| 10.4 Symptom diagnosis : open colposuspension versus self fixing sling procedure | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 11 Length of hospital stay (days) | 9 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 11.1 Urodynamic diagnosis : open colposuspension versus traditional sling procedure | 2 | 65 | Mean Difference (IV, Fixed, 95% CI) | ‐0.28 [‐0.92, 0.36] |
| 11.2 Symptom diagnosis : open colposuspension versus traditional sling procedure | 1 | 72 | Mean Difference (IV, Fixed, 95% CI) | ‐8.0 [‐9.18, ‐6.82] |
| 11.3 Urodynamic diagnosis : open colposuspension versus self fixing sling procedure | 6 | 663 | Mean Difference (IV, Fixed, 95% CI) | 3.99 [3.71, 4.28] |
| 11.4 Symptom diagnosis : open colposuspension versus self fixing sling procedure | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 12 Time to catheter removal (days) | 3 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 12.1 Urodynamic diagnosis : open colposuspension versus traditional sling procedure | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 12.2 Symptom diagnosis : open colposuspension versus traditional sling procedure | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 12.3 Urodynamic diagnosis : open colposuspension versus self fixing sling procedure | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 12.4 Symptom diagnosis : open colposuspension versus self fixing sling procedure | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 13 Number of perioperative surgical complications | 8 | 1023 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.79 [0.69, 0.91] |
| 13.1 Urodynamic diagnosis : open colposuspension versus traditional sling procedure | 2 | 65 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.18, 5.57] |
| 13.2 Symptom diagnosis : open colposuspension versus traditional sling procedure | 2 | 727 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.76 [0.66, 0.87] |
| 13.3 Urodynamic diagnosis : open colposuspension versus self fixing sling procedure | 4 | 231 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.11 [0.66, 1.87] |
| 13.4 Symptom diagnosis : open colposuspension versus self fixing sling procedure | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 14 Number with de novo urge symptoms and urge incontinence | 6 | 730 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.11 [0.67, 1.83] |
| 14.1 Urodynamic diagnosis : open colposuspension versus traditional sling procedure | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 14.2 Symptom diagnosis : open colposuspension versus traditional sling procedure | 1 | 72 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.4 [0.08, 1.93] |
| 14.3 Urodynamic diagnosis : open colposuspension versus self fixing sling procedure | 4 | 342 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.28 [0.65, 2.50] |
| 14.4 Symptom diagnosis : open colposuspension versus self fixing sling procedure | 2 | 316 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.28 [0.51, 3.16] |
| 15 Number with de novo detrusor instability | 4 | 521 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.43 [0.84, 2.44] |
| 15.1 Urodynamic diagnosis : open colposuspension versus traditional sling procedure | 2 | 70 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.61 [0.75, 9.05] |
| 15.2 Symptom diagnosis : open colposuspension versus traditional sling procedure | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 15.3 Urodynamic diagnosis : open colposuspension versus self fixing sling procedure | 3 | 451 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.28 [0.71, 2.32] |
| 15.4 Symptom diagnosis : open colposuspension versus self fixing sling procedure | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 16 Number with voiding difficulty | 11 | 1668 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.41 [0.26, 0.67] |
| 16.1 Urodynamic diagnosis : open colposuspension versus traditional sling procedure | 2 | 92 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.24 [0.04, 1.43] |
| 16.2 Symptom diagnosis : open colposuspension versus traditional sling procedure | 2 | 727 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.06 [0.01, 0.30] |
| 16.3 Urodynamic diagnosis : open colposuspension versus self fixing sling procedure | 7 | 710 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.85 [0.47, 1.53] |
| 16.4 Symptom diagnosis : open colposuspension versus self fixing sling procedure | 1 | 139 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.66 [0.06, 7.09] |
| 17 Number with new or recurrent prolapse | 3 | 246 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.85 [1.25, 2.75] |
| 17.1 Urodynamic diagnosis : open colposuspension versus traditional sling procedure | 1 | 34 | Risk Ratio (M‐H, Fixed, 95% CI) | 5.0 [0.26, 97.00] |
| 17.2 Symptom diagnosis : open colposuspension versus traditional sling procedure | 1 | 72 | Risk Ratio (M‐H, Fixed, 95% CI) | 5.0 [0.61, 40.70] |
| 17.3 Urodynamic diagnosis : open colposuspension versus self fixing sling procedure | 1 | 140 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.64 [1.10, 2.44] |
| 17.4 Symptom diagnosis : open colposuspension versus self fixing sling procedure | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 18 Number with repeat anti‐incontinence surgery | 1 | 316 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.46 [0.40, 5.32] |
| 18.1 Urodynamic diagnosis : open colposuspension versus traditional sling procedure | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 18.2 Symptom diagnosis : open colposuspension versus traditional sling procedure | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 18.3 Urodynamic diagnosis : open colposuspension versus self fixing sling procedure | 1 | 316 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.46 [0.40, 5.32] |
| 18.4 Symptom diagnosis : open colposuspension versus self fixing sling procedure | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 19 Number with other complication inherent to procedure | 5 | 577 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.23 [0.09, 0.58] |
| 19.1 Urodynamic diagnosis : open colposuspension versus traditional sling procedure | 1 | 28 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.18 [0.01, 3.34] |
| 19.2 Symptom diagnosis : open colposuspension versus traditional sling procedure | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 19.3 Urodynamic diagnosis : open colposuspension versus self fixing sling procedure | 4 | 549 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.24 [0.09, 0.62] |
| 19.4 Symptom diagnosis : open colposuspension versus self fixing sling procedure | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 20 Number with bladder perforation | 9 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 20.1 Urodynamic diagnosis : open colposuspension versus traditional sling procedure | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 20.2 Symptom diagnosis : open colposuspension versus traditional sling procedure | 1 | 655 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.95 [1.09, 22.44] |
| 20.3 Urodynamic diagnosis : open colposuspension versus self fixing sling procedure | 8 | 862 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.20 [0.08, 0.49] |
| 20.4 Symptom diagnosis : open colposuspension versus self fixing sling procedure | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
5.9. Analysis.

Comparison 5 Open retropubic colposuspension versus sling procedure, Outcome 9 Mean change in IIQ score from baseline.
5.19. Analysis.

Comparison 5 Open retropubic colposuspension versus sling procedure, Outcome 19 Number with other complication inherent to procedure.
Comparison 6. Open retropubic colposuspension versus needle suspension.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Number with incontinence within first year (subjective) | 5 | 517 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.66 [0.42, 1.03] |
| 1.1 Urodynamic diagnosis | 5 | 517 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.66 [0.42, 1.03] |
| 1.2 Symptom diagnosis | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 2 Number with incontinence after first year but before five years (subjective) | 6 | 569 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.56 [0.39, 0.81] |
| 2.1 Urodynamic diagnosis | 6 | 569 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.56 [0.39, 0.81] |
| 2.2 Symptom diagnosis | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3 Number with incontinence after five years (subjective) | 1 | 63 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.32 [0.15, 0.71] |
| 3.1 Urodynamic diagnosis | 1 | 63 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.32 [0.15, 0.71] |
| 3.2 Symptom diagnosis | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Number with incontinence not improved within first year (subjective) | 1 | 50 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.33 [0.13, 13.74] |
| 4.1 Urodynamic diagnosis | 1 | 50 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.33 [0.13, 13.74] |
| 4.2 Symptom diagnosis | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Number with incontinence not improved after first year but before five years (subjective) | 1 | 51 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.17, 2.68] |
| 5.1 Urodynamic diagnosis | 1 | 51 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.17, 2.68] |
| 5.2 Symptom diagnosis | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Number with incontinence within the first year (objective) | 3 | 417 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.56 [0.32, 0.97] |
| 6.1 Urodynamic diagnosis | 3 | 417 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.56 [0.32, 0.97] |
| 6.2 Symptom diagnosis | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Number with incontinence after first and before five years (objective) | 5 | 519 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.59 [0.40, 0.88] |
| 7.1 Urodynamic diagnosis | 5 | 519 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.59 [0.40, 0.88] |
| 7.2 Symptom diagnosis | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 8 Number with incontinence at and after five years (objective) | 1 | 63 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.32 [0.15, 0.71] |
| 8.1 Urodynamic diagnosis | 1 | 63 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.32 [0.15, 0.71] |
| 8.2 Symptom diagnosis | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 9 Time to catheter removal (days) | 2 | 271 | Mean Difference (IV, Fixed, 95% CI) | ‐0.40 [‐0.95, 0.15] |
| 9.1 Urodynamic diagnosis | 2 | 271 | Mean Difference (IV, Fixed, 95% CI) | ‐0.40 [‐0.95, 0.15] |
| 9.2 Symptom diagnosis | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 10 Number of perioperative surgical complications | 3 | 152 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.66 [0.46, 0.94] |
| 10.1 Urodynamic diagnosis | 3 | 152 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.66 [0.46, 0.94] |
| 10.2 Symptom diagnosis | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 11 Number with de novo urge symptoms and urge incontinence | 4 | 297 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.56 [0.22, 1.41] |
| 11.1 Urodynamic diagnosis | 4 | 297 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.56 [0.22, 1.41] |
| 11.2 Symptom diagnosis | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 12 Number with de novo detrusor instability | 2 | 101 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.34 [0.09, 1.37] |
| 12.1 Urodynamic diagnosis | 2 | 101 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.34 [0.09, 1.37] |
| 12.2 Symptom diagnosis | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 13 Number with voiding difficulty | 3 | 152 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.97 [0.42, 2.24] |
| 13.1 Urodynamic diagnosis | 3 | 152 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.97 [0.42, 2.24] |
| 13.2 Symptom diagnosis | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 14 Number with new or recurrent prolapse | 1 | 72 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.45 [0.04, 4.72] |
| 14.1 Urodynamic diagnosis | 1 | 72 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.45 [0.04, 4.72] |
| 14.2 Symptom diagnosis | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 15 Number with other complication inherent to procedure | 1 | 51 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.14 [0.01, 2.53] |
| 15.1 Urodynamic diagnosis | 1 | 51 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.14 [0.01, 2.53] |
| 15.2 Symptom diagnosis | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
6.15. Analysis.

Comparison 6 Open retropubic colposuspension versus needle suspension, Outcome 15 Number with other complication inherent to procedure.
Comparison 7. Open retropubic colposuspension versus laparoscopic retropubic colposuspension.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Number with incontinence within first year (subjective) | 6 | 690 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.97 [0.79, 1.18] |
| 1.1 Urodynamic diagnosis | 5 | 630 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.81, 1.20] |
| 1.2 Symptom diagnosis | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.61 [0.15, 2.51] |
| 2 Number with incontinence after first year but before five years (subjective) | 6 | 831 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.75, 1.03] |
| 2.1 Urodynamic diagnosis | 5 | 771 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.77, 1.06] |
| 2.2 Symptom diagnosis | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.57 [0.29, 1.12] |
| 3 Number with incontinence after five years (subjective) | 1 | 64 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.89 [0.99, 3.59] |
| 3.1 Urodynamic diagnosis | 1 | 64 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.89 [0.99, 3.59] |
| 3.2 Symptom diagnosis | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Number with incontinence not improved after first year but before five years (subjective) | 1 | 90 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.19 [0.21, 23.26] |
| 4.1 Urodynamic diagnosis | 1 | 90 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.19 [0.21, 23.26] |
| 4.2 Symptom diagnosis | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Numbers with incontinence within the first year (objective) | 6 | 682 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.64, 1.21] |
| 5.1 Urodynamic diagnosis | 6 | 682 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.64, 1.21] |
| 5.2 Symptom diagnosis | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Numbers with incontinence after first and before five years (objective) | 7 | 928 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.92 [0.71, 1.19] |
| 6.1 Urodynamic diagnosis | 7 | 928 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.92 [0.71, 1.19] |
| 6.2 Symptom diagnosis | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Numbers with incontinence at and after five years (objective) | 1 | 59 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.22 [1.06, 4.64] |
| 7.1 Urodynamic diagnosis | 1 | 59 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.22 [1.06, 4.64] |
| 7.2 Symptom diagnosis | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 8 General health status measure | 2 | 878 | Mean Difference (IV, Fixed, 95% CI) | 1.65 [‐0.38, 3.68] |
| 8.1 Urodynamic diagnosis : SF‐36 physical subscale | 2 | 438 | Mean Difference (IV, Fixed, 95% CI) | ‐0.64 [‐3.51, 2.23] |
| 8.2 Urodynamic diagnosis : SF‐36 mental subscale | 2 | 440 | Mean Difference (IV, Fixed, 95% CI) | 3.94 [1.07, 6.81] |
| 8.3 Symptom diagnosis : SF‐36 physical subscale | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 8.4 Symptom diagnosis : SF‐36 mental subscale | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 9 Operative time (minutes) | 5 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 9.1 Urodynamic diagnosis | 4 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 9.2 Symptom diagnosis | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 10 Length of hospital stay (days) | 6 | 714 | Mean Difference (IV, Random, 95% CI) | 1.53 [1.07, 1.98] |
| 10.1 Urodynamic diagnosis | 5 | 654 | Mean Difference (IV, Random, 95% CI) | 1.44 [0.92, 1.97] |
| 10.2 Symptom diagnosis | 1 | 60 | Mean Difference (IV, Random, 95% CI) | 1.90 [1.42, 2.38] |
| 11 Time to return to normal activity (days) | 2 | 150 | Mean Difference (IV, Random, 95% CI) | 15.10 [0.33, 29.88] |
| 11.1 Urodynamic diagnosis | 1 | 90 | Mean Difference (IV, Random, 95% CI) | 7.10 [‐0.36, 14.56] |
| 11.2 Symptom diagnosis | 1 | 60 | Mean Difference (IV, Random, 95% CI) | 22.2 [20.49, 23.91] |
| 12 Time to catheter removal (days) | 3 | 242 | Mean Difference (IV, Random, 95% CI) | 2.25 [0.95, 3.55] |
| 12.1 Urodynamic diagnosis | 2 | 182 | Mean Difference (IV, Random, 95% CI) | 1.81 [‐0.35, 3.97] |
| 12.2 Symptomatic diagnosis | 1 | 60 | Mean Difference (IV, Random, 95% CI) | 3.0 [2.59, 3.41] |
| 13 Number of perioperative surgical complications | 4 | 279 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.18 [0.64, 2.16] |
| 13.1 Urodynamic diagnosis | 4 | 279 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.18 [0.64, 2.16] |
| 13.2 Symptom diagnosis | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 14 Number with de novo urge symptoms and urge incontinence | 1 | 92 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.5 [0.26, 8.56] |
| 14.1 Urodynamic diagnosis | 1 | 92 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.5 [0.26, 8.56] |
| 14.2 Symptom diagnosis | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 15 Number with de novo detrusor instability | 6 | 566 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.82 [0.48, 1.38] |
| 15.1 Urodynamic diagnosis | 6 | 566 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.82 [0.48, 1.38] |
| 15.2 Symptom diagnosis | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 16 Number with voiding difficulty | 6 | 602 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.12 [0.70, 1.79] |
| 16.1 Urodynamic diagnosis | 5 | 542 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.18 [0.73, 1.91] |
| 16.2 Symptom diagnosis | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.41 [0.04, 4.27] |
| 17 Number with new or recurrent prolapse | 2 | 290 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.76 [0.39, 1.52] |
| 17.1 Urodynamic diagnosis | 2 | 290 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.76 [0.39, 1.52] |
| 17.2 Symptom diagnosis | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 18 Number with bladder perforation | 4 | 659 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.22 [0.06, 0.87] |
| 18.1 Urodynamic diagnosis | 3 | 599 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.21 [0.05, 0.96] |
| 18.2 Symptom diagnosis | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.27 [0.01, 6.48] |
Comparison 9. Burch colposuspension versus MMK.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Number with incontinence within first year (subjective) | 2 | 135 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.73 [0.28, 1.95] |
| 1.1 Urodynamic diagnosis | 1 | 105 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.35 [0.10, 1.26] |
| 1.2 Symptom diagnosis | 1 | 30 | Risk Ratio (M‐H, Fixed, 95% CI) | 7.0 [0.39, 124.83] |
| 2 Number with incontinence after first year but before five years (subjective) | 4 | 353 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.72 [0.52, 0.99] |
| 2.1 Urodynamic diagnosis | 2 | 185 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.38 [0.18, 0.76] |
| 2.2 Symptom diagnosis | 2 | 168 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.66, 1.34] |
| 3 Number with incontinence not improved after first year but before five years (subjective) | 2 | 218 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.42 [0.22, 0.80] |
| 3.1 Urodynamic diagnosis | 1 | 80 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3.2 Symptom diagnosis | 1 | 138 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.42 [0.22, 0.80] |
| 4 Number with incontinence within the first year (objective) | 2 | 135 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.58 [0.22, 1.50] |
| 4.1 Urodynamic diagnosis | 1 | 105 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.35 [0.10, 1.26] |
| 4.2 Symptom diagnosis | 1 | 30 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.5 [0.29, 7.73] |
| 5 Number with incontinence after first and before five years (objective) | 3 | 215 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.64 [0.39, 1.05] |
| 5.1 Urodynamic diagnosis | 2 | 185 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.44 [0.25, 0.77] |
| 5.2 Symptom diagnosis | 1 | 30 | Risk Ratio (M‐H, Fixed, 95% CI) | 7.0 [0.98, 50.16] |
| 6 Length of hospital stay (days) | 1 | 80 | Mean Difference (IV, Fixed, 95% CI) | ‐1.10 [‐1.74, ‐0.46] |
| 6.1 Urodynamic diagnosis | 1 | 80 | Mean Difference (IV, Fixed, 95% CI) | ‐1.10 [‐1.74, ‐0.46] |
| 6.2 Symptom diagnosis | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Time to catheter removal (days) | 3 | 112 | Mean Difference (IV, Fixed, 95% CI) | ‐6.35 [‐9.15, ‐3.56] |
| 7.1 Urodynamic diagnosis | 1 | 80 | Mean Difference (IV, Fixed, 95% CI) | ‐4.9 [‐7.95, ‐1.85] |
| 7.2 Symptom diagnosis | 2 | 32 | Mean Difference (IV, Fixed, 95% CI) | ‐14.0 [‐20.98, ‐7.02] |
| 8 Number of perioperative surgical complications | 1 | 80 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.01, 4.04] |
| 8.1 Urodynamic diagnosis | 1 | 80 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.01, 4.04] |
| 8.2 Symptom diagnosis | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 9 Number with de novo urge symptoms and urge incontinence | 1 | 105 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.63 [0.11, 3.62] |
| 9.1 Urodynamic diagnosis | 1 | 105 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.63 [0.11, 3.62] |
| 9.2 Symptom diagnosis | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 10 Number with de novo detrusor overactivity | 2 | 185 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.53 [0.20, 1.36] |
| 10.1 Urodynamic diagnosis | 2 | 185 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.53 [0.20, 1.36] |
| 10.2 Symptom diagnosis | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 11 Number with voiding difficulty | 1 | 80 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.27 [0.08, 0.90] |
| 11.1 Urodynamic diagnosis | 1 | 80 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.27 [0.08, 0.90] |
| 11.2 Symptom diagnosis | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 12 Number with new or recurrent prolapse | 2 | 185 | Risk Ratio (M‐H, Fixed, 95% CI) | 6.75 [0.84, 54.31] |
| 12.1 Urodynamic diagnosis | 2 | 185 | Risk Ratio (M‐H, Fixed, 95% CI) | 6.75 [0.84, 54.31] |
| 12.2 Symptom diagnosis | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 13 Number with repeat anti‐incontinence surgery | 1 | 105 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.47 [0.04, 5.05] |
| 13.1 Urodynamic diagnosis | 1 | 105 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.47 [0.04, 5.05] |
| 13.2 Symptom diagnosis | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
9.3. Analysis.

Comparison 9 Burch colposuspension versus MMK, Outcome 3 Number with incontinence not improved after first year but before five years (subjective).
9.4. Analysis.

Comparison 9 Burch colposuspension versus MMK, Outcome 4 Number with incontinence within the first year (objective).
Comparison 10. Burch colposuspension versus paravaginal defect repair.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Number with incontinence after first year but before five years (subjective) | 1 | 36 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.09 [0.01, 1.53] |
| 1.1 Urodynamic diagnosis | 1 | 36 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.09 [0.01, 1.53] |
| 1.2 Symptom diagnosis | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 2 Number with incontinence not improved within first year (subjective) | 1 | 36 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.09 [0.01, 1.53] |
| 2.1 Urodynamic diagnosis | 1 | 36 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.09 [0.01, 1.53] |
| 2.2 Symptom diagnosis | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3 Number with incontinence after first and before five years (objective) | 1 | 36 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.07 [0.00, 1.09] |
| 3.1 Urodynamic diagnosis | 1 | 36 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.07 [0.00, 1.09] |
| 3.2 Symptom diagnosis | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Length of hospital stay (days) | 1 | 36 | Mean Difference (IV, Fixed, 95% CI) | 0.20 [‐0.36, 0.76] |
| 4.1 Urodynamic diagnosis | 1 | 36 | Mean Difference (IV, Fixed, 95% CI) | 0.20 [‐0.36, 0.76] |
| 4.2 Symptom diagnosis | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Number with de novo urge symptoms and urge incontinence | 1 | 36 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.0 [0.13, 69.09] |
| 5.1 Urodynamic diagnosis | 1 | 36 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.0 [0.13, 69.09] |
| 5.2 Symptom diagnosis | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Number with de novo detrusor instability | 1 | 36 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.0 [0.13, 69.09] |
| 6.1 Urodynamic diagnosis | 1 | 36 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.0 [0.13, 69.09] |
| 6.2 Symptom diagnosis | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Number with voiding difficulty | 1 | 36 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.5 [0.28, 7.93] |
| 7.1 Urodynamic diagnosis | 1 | 36 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.5 [0.28, 7.93] |
| 7.2 Symptom diagnosis | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
10.1. Analysis.

Comparison 10 Burch colposuspension versus paravaginal defect repair, Outcome 1 Number with incontinence after first year but before five years (subjective).
10.2. Analysis.

Comparison 10 Burch colposuspension versus paravaginal defect repair, Outcome 2 Number with incontinence not improved within first year (subjective).
10.3. Analysis.

Comparison 10 Burch colposuspension versus paravaginal defect repair, Outcome 3 Number with incontinence after first and before five years (objective).
10.4. Analysis.

Comparison 10 Burch colposuspension versus paravaginal defect repair, Outcome 4 Length of hospital stay (days).
10.5. Analysis.

Comparison 10 Burch colposuspension versus paravaginal defect repair, Outcome 5 Number with de novo urge symptoms and urge incontinence.
10.6. Analysis.

Comparison 10 Burch colposuspension versus paravaginal defect repair, Outcome 6 Number with de novo detrusor instability.
10.7. Analysis.

Comparison 10 Burch colposuspension versus paravaginal defect repair, Outcome 7 Number with voiding difficulty.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Albo 2007.
| Methods | RCT by electronic treatment assignment Two arms Not blinded Follow up at 24 months and at 5 years (but this was an extension study where not all patients were enrolled) Analysis with intention to treat |
|
| Participants | N = 655
14 ineligible after randomisation (11‐sling, 3‐Burch), 1 did not undergo allocated treatment. Only 520 assessed at end of trial (265‐sling, 255‐Burch) but all included in analysis In the 5‐year follow up, only 482 patients were enrolled in the extension study, and only 357 completed the 5‐year follow up Symptom‐based diagnosis, confirmed by standard stress test Incl: documented pure or predominant symptom of SUI for at least 3 months, positive standardised urinary stress test Excl: age < 21 years, nonambulatory, pregnancy, current cancer chemo‐ or radiotherapy, systemic disease affecting bladder function, urethral diverticulum, prior augmentation cystoplasty or artificial urethral sphincter, recent pelvic surgery, < 12 months postpartum Groups similar in age, ethnic group, marital status, BMI, vaginal deliveries, hormone treatment, smoking, mixed UI, POP, UDS, concomitant surgery Multi‐centre. Tertiary referral centres. USA. |
|
| Interventions | I: Burch (329)
II: Sling (326) Burch as modified by Tanagho Sling procedure using autologous rectus fascia at level of the bladder neck and proximal urethra Interventions standardised across the centres |
|
| Outcomes | Number with overall success, number with SUI‐specific success, pad test, number of incontinence episodes in a three‐day voiding diary, POP, adverse event, voiding dysfunction (use of a catheter), post‐operative UUI. Overall success defined as no self‐reported symptoms of UI, no incontinence on three‐day diary, negative stress test, no retreatment. SUI‐specific success defined as no symptoms, negative stress test and no retreatment for SUI. All outcomes reported at two years' follow‐up New reports reporting the following outcomes: patient satisfaction |
|
| Notes | Full text with several other reports in full text and abstract form | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "randomized"; "use of permuted‐block randomisation schedule with stratification according to clinic site, by electronic treatment assignment |
| Allocation concealment (selection bias) | Unclear risk | no further description of allocation concealment in any of the reports |
| Blinding (performance bias and detection bias) All outcomes | High risk | "unmasked" |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | "unmasked" |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | "unmasked" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Analysis done by intention to treat. Not all patients were examined at the end of the trial (Burch = 74, Sling = 61, did not complete the follow up) |
| Other bias | Unclear risk | no other bias identified |
Ankardal 2001.
| Methods | RCT. Method not described. Three arms. Blinding not mentioned. No power calculation. Not stated if ITT analysis. Follow up at 1 year | |
| Participants | N = 187. Recruited 211 but only 198 with one year follow up at time of report Groups comparable at baseline Only primary incontinence. Some patients with mixed incontinence Excl: recurrent UI, other major surgery |
|
| Interventions | I: Burch (79)
II: Lap with mesh and staplers (72)
III: Lap with sutures (49) Techniques for open and lap described Participating surgeons with pre‐specified skill level |
|
| Outcomes | Number with objective and subjective continence Subjective cure : report as “dry” Objective cure : <8g leakage/24 hours Stress objective cure : <5g leakage / 24 hours Operative time Hospital stay (number of postoperative nights in hospital) QoL using a VAS Complications (Bladder perforation, hematoma, UTI, wound infection, urinary retention >5 days) |
|
| Notes | Full text | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | method of randomization not mentioned |
| Allocation concealment (selection bias) | Low risk | used opaque dealed envelopes |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | not mentioned |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | not mentioned |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | not mentioned |
| Other bias | Unclear risk | no other source of bias identified |
Athanassopoulos 1996.
| Methods | Quasi‐RCT (by date of birth). Two arms Blinding not mentioned No power calculation Not stated if ITT analysis Follow up 8 months to 27 months | |
| Participants | N = 51. No withdrawals mentioned UDS‐confirmed SUI Combined primary and recurrent. Includes those with previous surgery and with prolapse Mean age: 50 years (range 20‐78), 50.9% menopausal, 14% with previous pelvic operations Inclusion/exclusion criteria not listed No baseline comparison of treatment groups Single‐centre, university‐based hospital Greece |
|
| Interventions | I: Burch (27)
II: Stamey needle suspension surgery (24) Description of both procedures referenced All done by one surgeon |
|
| Outcomes | Number cured
Number improved
UDS parameters (Qmax, RU, MCC, Pvesmax, Pdet/Qmax, FUL, Pclosmax)
Length of stay
Complications, Urinary retention
Urgency Cure = complete freedom from SUI Failure = persistent or recurrent UI Urinary retention not defined. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | "randomly (by date of birth)" |
| Allocation concealment (selection bias) | High risk | "randomly (by date of birth)" |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | not mentioned |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | not mentioned |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | no withdrawals mentioned |
| Other bias | Unclear risk | no other bias identified |
Bai 2005.
| Methods | RCT. Method not described. Three arms. Blinding not mentioned. Unclear if ITT Follow‐up at one year with assessments at 3 months, 6 months and 9 months. | |
| Participants | N = 92. No withdrawals mentioned UDS confirmed. No mixed incontinence Groups comparable as to age, parity, BMI, menopausal status, MUCP, VLPP, functional urethral length and peak flow rates at baseline Incl: USI grade I and II Excl: grade III incontinence, detrusor overactivity, UTI, ISD, POP > grade II Ob & Gyne. South Korea |
|
| Interventions | I: Burch (33)
II: Sling (28)
III: TVT (31) Sling procedure was a pubovaginal sling using autologous rectus muscle fascia TVT technique according to Ulmsten All procedures performed by one surgeon |
|
| Outcomes | Number cured (3 months, 6 months,12 months); complication rate (number with idiopathic detrusor overactivity, hesitancy, urinary retention) Cure defined as absence of subjective complaints of leakage and absence of urinary leakage on stress test |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | randomization method not described |
| Allocation concealment (selection bias) | Unclear risk | not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | not mentioned |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | not mentioned |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | all patients with complete follow‐up; no mention of dropouts |
| Other bias | Unclear risk | no other bias identified |
Bandarian 2011.
| Methods | RCT; simple randomisation method | |
| Participants | N = 62 (Burch = 31, TOT = 31) Incl: proven SUI who were candidates for surgery for the first time, did not respond to treatment Excl: chronic disease such as collagen vascular disease, neuropathy, coagulopathy, history of urogenital cancer, pregnancy, history of pelvic radiation, previous surgery for incontinence, urge incontinence, urodynamic detrusor overactivity or genital prolapse of POP‐Q stage II or more Department of Obstetrics and Gynecology Tehran University of Medical Sciences Tehran, Iran |
|
| Interventions | Burch colposuspension (N = 31) TOT (N = 31) All procedures done by one surgeon No description of the interventions |
|
| Outcomes | Cure: absence of urinary incontinence Improvement: urinary incontinence less than once in two weeks Failure: urinary incontinence more than once a week (note: paper states "long term outcome" but did not specify any particular time of assessment) Surgical complications such as bleeding, urethral and bladder damage, urinary retention, urinary infection, wound infection, vaginal erosion, pelvic hematoma Hospital stay Operation time Patient satisfaction (asked to express using rate of very satisfied, moderately satisfied, less satisfied and unsatisfied) Mean duration of follow‐up: Burch: 28 months (12‐38) TOT: 22 months (8‐26) (note: no specific time of follow up specified in the methods) Post‐operative follow‐up done by a senior surgeon who did not take part in the operation |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "simple randomisation" |
| Allocation concealment (selection bias) | Unclear risk | not mentioned in the paper |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | not mentioned in the paper |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | "all procedures performed by one surgeon" but no mention specifically regarding blinding |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | "follow up was done by a senior surgeon who did not take part in the operation" but no mention specifically regarding blinding |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | timing of follow‐up was not clearly defined and there is a difference in the mean between the two groups |
| Other bias | Unclear risk | no other bias identified |
Berglund 1996.
| Methods | RCT. Method not described. Two arms Blinding not mentioned Not mentioned if ITT analysis No power calculation Follow‐up 1 year | |
| Participants | N = 45. No withdrawals mentioned Diagnosis by symptoms alone All primary UI. Unclear if mixed UI included Mean age: 50 years (SD6.6); parity: 2.6; 44% menopausal No baseline comparison of groups Incl: not listed Excl: age > 65, previous anti‐incontinence surgery, other gynaecological disease needing surgery, severe medical disease Single centre, university‐based, Dept of Gyne Sweden |
|
| Interventions | I: Retropubic urethropexy (30)
II: Pubococcygeal repair (15) Description of techniques referenced : Based on these, the reviewers assessed “Retropubic urethropexy” is also the Marshall‐Marchetti‐Krantz. And “Pubococcygeal repair” is also anterior colporrhaphy Both groups had instructions for pelvic floor exercise from physiotherapist Surgeon not specified |
|
| Outcomes | Number cured at one year, subjective and objective
Time to catheter removal
Number with severe post‐op pain
Urine loss by 2‐hour pad test
Length of stay
Number of post‐op complications
Number with voiding difficulty Obj Cure = no leak by pad test Subj Cure = no leak by history Catheter removed if residual urine < 100 ml |
|
| Notes | Berglund paper (primary reference) includes patients excluded in the Lalos 1993 paper | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | method of randomization not described |
| Allocation concealment (selection bias) | Unclear risk | not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | not mentioned |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | not mentioned |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | no dropouts/withdrawals reported |
| Other bias | Unclear risk | no other bias identified |
Bergman 1989a.
| Methods | RCT. Randomisation table (to intervention and surgeon). Three arms Blinding not mentioned No power calculation Not ITT analysis Follow‐up one year | |
| Participants | N = 342 enrolled, 298 analysed. Three technically difficult hysterectomy excluded, 41 lost to follow‐up UDS‐confirmed SUI. Only primary incontinence All had pelvic relaxation Mean age: 57 years (range 31‐80), mean parity: 3 (1‐13), 191 were menopausal (received Premarin), 19 had previous vaginal hysterectomy Treatment groups comparable as to age, parity, menopausal status Incl: primary GSI with prolapse requiring vaginal correction Excl: previous anti‐incontinence surgery, DI, other gynae condition needing surgery Single centre, university‐based hospital, urogynaecology unit. USA |
|
| Interventions | I : Burch (101)
II: Pereyra needle suspension surgery (98)
III: Anterior colporrhaphy (99) All procedures described, standard. Prolapse surgery ± vaginal hysterectomy performed together with anti‐incontinence surgery. |
|
| Outcomes | Number cured at 3 months and 12 months
UDS parameters (MUCP, functional length, abd pressure transmission)
Days on catheter Cure = no history of UI, no UI on evaluation, negative cough profile on UDS Catheter removed when RU < 50 ml with spontaneous void |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "randomization table" |
| Allocation concealment (selection bias) | Unclear risk | not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | not mentioned |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | not mentioned |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | no withdrawals mentioned |
| Other bias | Unclear risk | no other bias identified |
Bergman 1989b.
| Methods | RCT. Randomisation table (to intervention and surgeon). Three arms. Blinding not mentioned. No power calculation. Not ITT analysis | |
| Participants | N = 127. 107 at one year, 93 at five years Fourteen lost to follow up at one year. No baseline comparison of treatment groups Mean age: 55 years (range 29‐77), mean parity: 3 (1‐12), 74 menopausal UDS‐confirmed SUI. Only primary incontinence Excl: other gynaecological disease needing surgery, previous anti‐incontinence surgery Single centre, university based, Urogyne. USA | |
| Interventions | I: Burch (38) II: modified Pereyra needle suspension surgery (34) III: Anterior colporrhaphy (35) All procedures described and referenced. Done by house staff and one senior surgeon, randomised | |
| Outcomes | Number cured UDS parameters (functional length, urethral closure pressure, abdominal pressure transmission) Prolapse Days on catheter | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | randomisation table |
| Allocation concealment (selection bias) | Unclear risk | not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | not mentioned |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | not mentioned |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | "14 lost to follow up" |
| Other bias | Unclear risk | no other bias identified |
Burton 1994.
| Methods | RCT. Method not described. Two arms Blinding not mentioned No power calculation Not ITT analysis Follow‐up 5 years | |
| Participants | N = 60. No detail on how the 60 was distributed to the groups. Thirteen withdrawals, no reason given (lap = 7, open = 6) UDS‐confirmed SUI No Incl/ Excl criteria given Unclear if included recurrent or mixed UI Baseline comparison of treatment group similar for age, degree of GSI, parity but details not given Single centre. Australia | |
| Interventions | I: open colposuspension II: lap colposuspension Not described, specific technique of open procedure not mentioned Number of surgeons not mentioned | |
| Outcomes | VAS for frequency, urge incontinence, stress incontinence, urgency Pad test Number of incontinence episodes UDS parameters | |
| Notes | Written to authors regarding population per treatment group All abstracts |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | method not described |
| Allocation concealment (selection bias) | Unclear risk | not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | not mentioned |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | not mentioned |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | equivalent dropout rates between groups; no reason given to the withdrawals |
| Other bias | Unclear risk | no other bias identified |
Carey 2000.
| Methods | RCT. Computer‐generated randomisation list held by the non‐surgical investigator. Two arms Patient, ward staff and assessor blinded to intervention Not ITT analysis No power calculation Follow‐up = 6 months Later report with 24 month and 3 year to 5 year follow‐up | |
| Participants | N = 200
Lost to follow‐up at 6 months: open colpo = 12, lap colpo = 13; at 24 months: open colpo = 2, lap colpo = 6; at 3 years to 5 years: open colpo = 2, lap colpo = 1 UDS‐confirmed SUI. All primary SUI. No mixed UI Mean age: 52.3/50.7 years; Mean parity: 2.6/2.8; Mean BMI: 29.7/29.6. Baseline characteristics comparable Incl: GSI Excl: previous surgery Multicentre (9 urogynae departments), Australia |
|
| Interventions | I: open colposuspension (N = 104)
II: laparoscopic colposuspension (N = 96) Techniques described Six surgeons of different expertise |
|
| Outcomes | Number cured (objective and subjective) Patient satisfaction Operative time Blood loss VAS for pain Number with voiding difficulty Length of stay Time to return to normal activity Cost, number of days of catheterisation, SUDI, SIIQ, GUTSS Cure not defined QoL SF36 |
|
| Notes | N = 201 in 1999 paper 2000 reports showed percentage of subjective cure at six months but did not indicate actual number of patients assessed. 2006 report now indicates actual numbers assessed at six months but outcome of "subjective cure" no longer reported. Pending clarification from the authors, only data from the 2005 report was used in the 2007 version of the review and the data from 2000 reports previously included were withdrawn Senior author performed 70 laparoscopies prior to study |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | computer‐generated randomisation list |
| Allocation concealment (selection bias) | Unclear risk | list held by non surgical investigator |
| Blinding (performance bias and detection bias) All outcomes | Low risk | patient and ward staff blinded to intervention |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | patient and ward staff blinded to intervention |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | assessor blinded to intervention |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | not mentioned |
| Other bias | Unclear risk | no other bias identified |
Colombo 1994.
| Methods | RCT. computer‐generated random assignment. Two arms Blinding not mentioned No power calculation Not mentioned if ITT analysis Follow‐up two to seven years, mean 3.1‐3.5 years | |
| Participants | N = 80. No withdrawals UDS‐confirmed diagnosis. All primary UI, No mixed UI Mean age: 49.8/51.4 years, parity: 2.6/2.3; with menopause: 40%/47.5% Baseline comparison of groups similar in age, parity, number post‐menopausal, BMI, clinical score Incl: minimum incontinence score of 4; pure GSI Excl: ISD with MUCP < 30 cm H2O, DI, prolapse ≥ 2nd degree, urethral diverticulum, fistula, previous anti‐incontinence surg Single centre, university‐based, Dept of Ob&Gyn Italy |
|
| Interventions | I: Burch (40)
II: modified MMK (40) MMK done with bladder dome opened Additional culdoplasty done in some patients (Burch = 14; MMK = 8) No mention of surgeon |
|
| Outcomes | Number cured (subjective and objective)
Number Improved (subjective)
Number of incontinence episodes/day
Number with post‐op complications
Length of stay
Number with voiding difficulty
Number with DI
Number with prolapse
UDS parameters (functional length, MUCP)
Time to normal void Subj Cure = No incontinence by history Obj Cure = no urine loss by stress test Improved = score decreased from 8 to ≤ 4 or from 4 to ≤ 2 |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | computer‐generated random assignment |
| Allocation concealment (selection bias) | Unclear risk | not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | not mentioned |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | not mentioned |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | no withdrawals |
| Other bias | Unclear risk | no other bias identified |
Colombo 1996.
| Methods | RCT. Computer‐generated random table. No opaque envelope available. Two arms Blinding not mentioned No power calculation Not ITT Follow‐up 3 years | |
| Participants | N = 36. No withdrawals UDS‐confirmed SUI. Only primary UI. No mixed UI Mean age: 47.8/49.2 years; parity 2.1/1.9; menopausal: 22%/39% Baseline comparison of groups similar in age, parity, number of vaginal deliveries, % menopausal, BMI, incontinence score Incl: GSI, grade I urethrocoele, incontinence score of 4 or 8 Excl: MUCP < 20 cm H2O, DI, previous anti‐incontinence surgery Single centre, university‐based, Dept Ob&Gyn Italy |
|
| Interventions | I: Burch (18)
II: Paravaginal defect repair (18) Both techniques described Culdoplasty done if with deep cul de sac of Douglas in both groups Additional abdominal hysterectomy: Burch = 14, Paravag = 16 Surgeon not mentioned |
|
| Outcomes | Number cured (objective and subjective)
Number improved (subjective)
Length of stay
Time to spontaneous void
Number with urge symptoms
Number with voiding difficulty
Number with prolapse
UDS parameters Subj Cure = no incontinence by history Obj Cure = no urine loss by stress test Normal void = RU ≤ 50ml Improved = clinical score dropped from 8 to ≤ 4 or from 4 to ≤ 2 |
|
| Notes | Study discontinued due to ethical issues | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | computer‐generated random table |
| Allocation concealment (selection bias) | High risk | "no opaque envelopes available" |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | not mentioned |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | not mentioned |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | not mentioned |
| Other bias | Unclear risk | study was discontinued due to ethical reasons |
Colombo 2000.
| Methods | RCT. Open list of computer‐generated random nos. Two arms Blinding not mentioned No power calculation Not ITT but possible Follow‐up 8 years to 17 years | |
| Participants | N = 71. Dropouts from loss to follow‐up: 2 = Burch; 1 = anterior colporrhaphy UDS‐confirmed diagnosis. All primary UI. No mixed UI. All had MUCP > 30 cm H20 Mean age: 54.9/55.7 years, parity: 3/3, % menopausal: 66%/67%. Baseline comparison of groups similar Incl: GSI, grade 2 or 3 cystocoele; (+) Qtip test Excl: DI, prev anti‐incontinence or prolapse surgery; pelvic disease requiring laparotomy, high surgical risk Single centre, university‐based, Dept Ob&Gyn Italy |
|
| Interventions | I: Burch (35)
II: Anterior colporrhaphy (33) Both techniques described Group I had total abdominal hysterectomy ± Moschowitz; Group II had vaginal hysterectomy with Douglas obliteration Surgeon not mentioned |
|
| Outcomes | Number cured (subjective and objective)
Number with recurrent prolapse of grade 2 or 3
Number with dyspareunia for sexually active
Length of hospital stay
Number with post‐op DI
Vaginal length post‐op Subjective cure = no incontinence by history; Objective cure = negative stress test |
|
| Notes | Different anti‐prolapse surgery done in each group Additional information on methods and outcome results provided by author on further communication |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | computer‐generated random number |
| Allocation concealment (selection bias) | High risk | "randomization list was open" |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | not mentioned |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | not mentioned |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | equivalent proportion of lost to follow‐up between groups |
| Other bias | Unclear risk | no other bias identified |
Corcos 2001.
| Methods | RCT. method not described Blinding not mentioned Not ITT analysis No power calculation Follow‐up 12 months | |
| Participants | N = 133 women
15 refused intervention; Injection = 2
Surgery = 13 SUI Age not mentioned Inclusion/exclusion not listed No baseline comparisons of treatment group Multi‐centre, Canada |
|
| Interventions | I: Collagen (66) II: surgery (67) I:2/66 II: 13/67 refused intervention. Results reported for I:64 II:54
I: (64) submucosal urethral injection, one to four injections in six months, follow‐up started after last injection. II: (54) option of BNS (6), sling (24) or Burch (24). Four centres, does not mention number of surgeons |
|
| Outcomes | Numbers not cured or improved at 12 months, urodynamics, QOL questionnaire score, numbers not satisfied, complications | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | method not described; randomisation done for collagen versus surgery but specific surgical procedure was according to the surgeon's assessment/selection |
| Allocation concealment (selection bias) | Unclear risk | not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | not mentioned |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | not mentioned |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | more patients refused the surgical intervention after randomisation |
| Other bias | Unclear risk | no other bias identified |
Demirci 2001.
| Methods | Quasi RCT. Procedures were "performed successively" Blinding not mentioned No power calculation Not ITT Follow‐up 1 year |
|
| Participants | N = 46
Six dropouts from each group UDS confirmed GSI ALl primary UI. No mixed UI Mean age: sling group 48.86 years (± 6.31) Burch group 48.13 years (± 6.73) Inclusion: type I and II incontinence, no preoperative detrusor instability, no recurrent GSI, no severe pelvic prolapse, Valsalva leak point pressure > 90 cm water Exclusion: patients with additional abdominal hysterectomy Baseline comparisons comparable Single centre, university‐based hospital Istanbul, Turkey |
|
| Interventions | I : Burch colposuspension II : Pubovaginal sling : free rectus fascial sling |
|
| Outcomes | Subjective cure, Operating time, hospital stay, urinary tract infection | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | "procedures were performed successively" |
| Allocation concealment (selection bias) | High risk | "procedures were performed successively" |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | not mentioned |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | not mentioned |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | equal dropouts in both groups, reason for dropout not mentioned |
| Other bias | Unclear risk | no other bias identified |
Drahoradova 2004.
| Methods | RCT. Method not described. Two arms Unblinded. Unclear if ITT. Follow‐up at 3 months, 6 months and 12 months | |
| Participants | N = 139. No withdrawals mentioned No mention if diagnosis of SUI was by symptom alone or by urodynamics No inclusion or exclusion criteria mentioned Baseline comparison of groups by age, BMI, parity Single centre. Ob&Gyne. Czech Republic |
|
| Interventions | I: Burch (60)
II:TVT (79) No description of technique |
|
| Outcomes | Recurrence of SUI (3 mo, 1 year); IQOL; de novo urge incontinence; de novo urge symptoms; voiding difficulties; TVT erosions | |
| Notes | Abstract | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | method not described |
| Allocation concealment (selection bias) | Unclear risk | not mentioned |
| Blinding (performance bias and detection bias) All outcomes | High risk | unblinded |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | unblinded |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | unblinded |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | no withdrawals mentioned; complete follow‐up |
| Other bias | Unclear risk | no other bias identified |
El Barky 2005.
| Methods | RCT. Method not described. Two arms Blinding not mentioned. Follow‐up every 3 months to 6 months for a minimum of two years (but outcomes reported at first 3 months to 6 months after surgery) | |
| Participants | N = 50. No withdrawals mentioned UDS‐confirmed SUI. Only primary incontinence. No mixed incontinence Excl: uninhibited detrusor contraction > 15 cm H20, incompetent urethral sphincter, more than grade I cystocoele, previous failed surgical repair Groups comparable by age, parity, duration of symptoms at baseline Multi‐centre. Kuwait and Egypt |
|
| Interventions | I: Burch (25)
II: TVT (25) Both techniques described. Cystocath bladder drainage for Burch. Foley urethral catheter drainage for TVT. Cystoscopy performed after TVT but not after Burch. |
|
| Outcomes | Number cured (at 3 months to 6 months after surgery); number improved; operative time; post‐operative analgesia; hospital stay; return to normal activity; intra‐ and perioperative complications (bladder perforation, urine retention, de novo urgency, wound infection, UTI) Cure defined as "no SUI 3‐6 months after the surgical procedure" Improved defined as "experienced occasional SUI at 3‐6 months after surgery but not as severe as prior to surgery" |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | method not described |
| Allocation concealment (selection bias) | Unclear risk | not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | not mentioned |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | not mentioned |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | no withdrawals mentioned |
| Other bias | Unclear risk | no other bias identified |
El‐Din Shawki 2012.
| Methods | RCT. method not described. Three arms. Blinding not mentioned. Follow up at three months | |
| Participants | N = 60, no distribution mentioned across the groups no inclusion / exclusion criteria details no mention of baseline group comparison single‐centre, department of obstetrics and gynaecology. Egypt |
|
| Interventions | I: Burch II: transobturator vaginal tape (TOT) III: anterior repair + Kelly's plication No description / details of intervention. No mention of co‐interventions |
|
| Outcomes | Subjective and objective cure rate (no definition stated) Operative time (mins) Intraoperative blood loss (ml) cCmplications |
|
| Notes | Abstract only Investigator emailed for further information No response yet |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | method not mentioned |
| Allocation concealment (selection bias) | Unclear risk | not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | not mentioned |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | not mentioned |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | not mentioned |
| Other bias | Unclear risk | no other bias identified |
Elshawaf 2009.
| Methods | RCT Three arms |
|
| Participants | N = 75 Incl: diagnosis of urodynamic GSUI (genuine stress urinary incontinence) Exclusion criteria not mentioned in the publication Urology and Obstetric and Gynaecology Departments university hospital Kingdom of Saudi Arabia |
|
| Interventions | Three arms Group I: Burch colposuspension (N = 25) Group II: TVT procedure (N = 25) Group III: TOT procedure (N = 25) |
|
| Outcomes | ‐ operative details: type of anaesthesia, duration of the procedure ‐ hospital stay ‐ return to normal activity ‐ perioperative complications, including symptoms of voiding dysfunction ‐ objective cure rate ‐ patient satisfaction follow‐up at 2 weeks and 6 months following the primary surgical procedure |
|
| Notes | No data reported in a usable format for the review as results were narrative. Reported no difference between the groups as regard objective cure rates at 6 months TOT was regarded the "simplest operation as regards type of anaesthesia, duration of the procedure, hospital stay and return to normal activity" Perioperative complications associated with TOT procedure were potentially less serious than those associated with either TVT or Burch |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "randomized" |
| Allocation concealment (selection bias) | Unclear risk | not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | not mentioned |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | not mentioned |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | no mention of lost to follow up patients |
| Other bias | Unclear risk | no other bias identified |
Enzelsberger 1996.
| Methods | RCT by randomisation chart: odd/even. Two arms Blinding not mentioned No power calculation Not mentioned if ITT analysis Follow‐up 32 months to 48 months | |
| Participants | N = 72. No withdrawals Diagnosis by symptom. All recurrent UI. No mixed UI Mean age: 58 years (45‐72), 57 were menopausal Baseline comparison of treatment groups similar Incl: history of recurrent SUI post‐surgery for incontinence Excl: UTI, unstable bladder, voiding difficulty (Qmax <15ml/s), grade 3 cysto‐ or rectocoele SIngle centre, university‐based, Dept of Ob&Gyn. Austria |
|
| Interventions | I: modified Burch (36)
II: Lyodura sling (36) Both techniques described. Mod Burch = 2 sutures per side. Sling = vaginal placement One surgeon for all procedures No other procedures done in both groups |
|
| Outcomes | Number cured
UDS parameters
Sonographic variables
Number with post‐op complications
Number with new prolapse
Number with urge
Number with voiding difficulty
Length of stay
Time to normal void
Time to catheter removal Cure = dry, symptom‐free, no leak on cough or jump when bladder filled to 300 ml or positive UCP on stress Normal void = RU < 100 ml |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | by randomisation chart |
| Allocation concealment (selection bias) | Unclear risk | not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | not mentioned |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | not mentioned |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | no withdrawals |
| Other bias | Unclear risk | no other bias identified |
Fatthy 2001.
| Methods | RCT. Random number tables. Statistician did not allow surgeon or patients to know the next allocation Blinding not mentioned No power calculation Not ITT analysis Follow‐up 4 months to 18 months | |
| Participants | N = 74
One patient lost to follow‐up UDS ‐ confirmed SUI Combined primary and recurrent Includes women with prolapse Mean age in lap group 40.29 years (range 30‐55) Open group 42.9 years (range 30‐65) 74% menopausal, 35% previous pelvic operations Inclusion: not mentioned Exclusion: detrusor instability, underactive detrusor, intrinsic sphincter deficiency, limited vaginal mobility, stages III and IV vaginal prolapse, or contradictions to laparoscopy and surgery in general Baseline comparison of groups similar in age, weight, parity, menopausal status, pelvic relaxation, previous surgery, pre‐operative urodynamics Single centre, university‐based, department of Ob & Gyn. Cairo, Egypt |
|
| Interventions | I: Burch (40) II: Laparascopic Burch colposuspension (34) Similar technique used for both groups; one anchoring suture per side. | |
| Outcomes | Number cured UDS parameters Length of stay; complications; operating time; wound infection; blood loss; haematoma; spontaneous voiding; analgesia frequency; detrusor instability; post op pain; pelvic relaxation, dyspareunia | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | random numbers table |
| Allocation concealment (selection bias) | Low risk | "statistician did not allow patients and surgeon to know the next allocation" |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | not mentioned |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | not mentioned |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | one patient lost to follow up |
| Other bias | Unclear risk | no other bias identified |
Fischer 2001.
| Methods | RCT. Randomisation not described Blinding not mentioned No power calculation Not mentioned if ITT analysis Follow‐up: 6 months | |
| Participants | N = 22
No withdrawals UDS‐confirmed SUI Unclear if only primary UI Inclusion: intrinsic sphincter deficiency by low urethral closure pressure and/or positive Valsalva leak point pressure and urethrovesical junction hypermobility and/or urethral displacement Exclusion: end‐stage urethral neuropathy Single centre, university based. Indianapolis, USA |
|
| Interventions | I: Burch (11)
II: Suburethral sling (11) Procedures not described Correction of other pelvic floor support defects as indicated Surgeon not mentioned |
|
| Outcomes | Number cured Objective success = negative standing stress test at cystometric capacity Subjective success = comparison of preoperative and 6 month postoperative IIQ and UDI No of days with post‐operative voiding, dysfunction, Incontinence questionnaires, surgical failure |
|
| Notes | Patients with recurrence of UVJ hypermobility or displacement were considered failures and excluded from final analysis for the neurophysiologic testing of the pelvic floor but outcomes for incontinence reported | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "randomized"; method not described |
| Allocation concealment (selection bias) | Unclear risk | not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | not mentioned |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | not mentioned |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | no dropouts mentioned |
| Other bias | Unclear risk | no other bias identified |
German 1994.
| Methods | RCT. Method not described. Two arms Blinding not mentioned Not mentioned if ITT analysis Follow‐up mean 2 years (range 12 months to 44 months). | |
| Participants | N = 50. No withdrawals UDS‐confirmed SUI. Both primary and recurrent UI. No mixed UI Mean age: 50/53 years, Mean weight: 68.4/70.9 Baseline comparison of groups matched to age and weight Incl: GSI Excl: not listed Number with previous surgery: Needle group = 10 VOS group = 11 Single centre, Urology UK |
|
| Interventions | I: Vagina/obturator shelf repair (24)
II: modified needle suspension (26): modified Stamey operation involving helical full thickness suture through the vagina and a silastic buttress inferiorly Both techniques described Surgeon not mentioned |
|
| Outcomes | Number of success
Length of stay
Number with infection
Number with voiding problems
Number with post‐op pain
Time to normal activity
Number with urge Success = complete dryness or occasional incontinence Failures = slight improvement or no improvement |
|
| Notes | Separate analysis of primary and recurrent cases possible | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "randomized", method not described |
| Allocation concealment (selection bias) | Unclear risk | not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | not mentioned |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | not mentioned |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | no withdrawals/dropouts mentioned |
| Other bias | Unclear risk | no other bias identified |
Gilja 1998.
| Methods | RCT by open randomisation list. Three arms Blinding not mentioned Not ITT analysis Follow‐up 3 years | |
| Participants | N = 204, 58 lost to follow‐up due to war UDS‐confirmed diagnosis. Unclear if only primary UI Mean age 36 years (range 28‐48); mean parity 3.1 (1‐8) Baseline comparison of groups similar in age & parity No incl/excl criteria listed Single centre, general hospital. Dept of Urology Croatia |
|
| Interventions | I: Burch
II: Raz
III: Transvaginal Burch/Gilja Burch and Raz described and referenced Gilja = combination of open & needle but basically a needle suspension Single surgeon for all |
|
| Outcomes | Number cured (subjective and objective)
Number with de novo urge incontinence
Number with de novo DI Cure not defined |
|
| Notes | With additional info from author Author emphasised strict evaluation of results for cure |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "with use of a randomization list" |
| Allocation concealment (selection bias) | Unclear risk | not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | not mentioned |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | not mentioned |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | High risk | "58 patients were lost to follow‐up"; 204 women randomized, no description of the distribution of lost patients across the treatment groups, analysis limited to those available for follow‐up |
| Other bias | Unclear risk | no other bias identified |
Halaska 2001.
| Methods | RCT 6 month follow up | |
| Participants | Women with genuine stress incontinence | |
| Interventions | Burch 11 participants versus TVT 15 participants | |
| Outcomes | Cure rates (visual analogue score) sexual life | |
| Notes | Abstract | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "randomized", method not described |
| Allocation concealment (selection bias) | Unclear risk | not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | not mentioned |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | not mentioned |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | no withdrawals mentioned |
| Other bias | Unclear risk | report available only in abstract form; no full text publication |
Han 2001.
| Methods | RCT. Randomisation and allocation concealment not described Blinding not mentioned No power calculation ITT unclear Follow‐up 6 months | |
| Participants | N = 50 No withdrawals UDS confirmed SUI Mean age: not reported Parity: not reported Baseline comparison not mentioned Inclusion: SUI Exclusion: not mentioned Single centre Singapore | |
| Interventions | I: Burch (25) II: TVT (25) Procedure not described Surgeons not mentioned | |
| Outcomes | Operation time, blood loss, time in hospital, complications, pain | |
| Notes | No cure rates reported Abstract | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "randomised", method not described |
| Allocation concealment (selection bias) | Unclear risk | not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | not mentioned |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | not mentioned |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | no description of withdrawals |
| Other bias | Unclear risk | no other bias identified |
Henriksson 1978.
| Methods | Quasi‐RCT. Alternate allocation. Two arms Blinding not mentioned No power calculation Not mentioned if ITT analysis Follow‐up 3 months | |
| Participants | N = 30. No withdrawals mentioned UDS‐confirmed diagnosis. Not clear if recurrent UI included. No mixed UI Mean age 50 years (sling) / 56 years (MMK) Baseline comparison of groups similar as to age and parity Incl: not listed Excl: prolapse, urge incontinence, neurogenic bladder, UTI, tumour, other urogenital tract disorder Single centre, university‐based, Dept of Ob&Gyn Sweden |
|
| Interventions | I: Abdominal urethrocystopexy / MMK (15)
II: Zoedler suburethral/vaginal sling (15) Abdominal urethrocystopexy reference made to MMK procedure. Sling technique described Surgeon not mentioned |
|
| Outcomes | Number cured (objective)
UDS parameters (intraurethral pressure, MUCP, intravesical pressure, functional urethral length) Cure = no urine leak during coughing in the standing position |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | "... were used in alternate patients" |
| Allocation concealment (selection bias) | High risk | alternate allocation |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | not mentioned |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | not mentioned |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | no description of withdrawals |
| Other bias | Unclear risk | no other bias identified |
Holmes 1985.
| Methods | RCT. Computer‐randomisation code to intervention and surgeon. Two arms Blinding not mentioned Not ITT analysis Follow‐up 2 years | |
| Participants | N = 51. Three withdrawals (Colpo = 2, Ant rep = 1), lost to follow‐up UDS‐confirmed stable bladder but some had symptoms of urge incontinence. Primary UI only Mean age 44‐47; parity 3.2‐2.9. Baseline comparison of groups similar as to age, parity weight, previous hysterectomy Incl: not listed (additional information sent by the author indicate that some women with the following characteristics were included in the study : with previous hysterectomy, with urgency incontinence, with detrusor instability, with significant anterior wall prolapse) Excl: previous anti‐inc. surgery, previous surgery for prolapse Two‐centres, Dept of Ob&Gyn UK |
|
| Interventions | I: Colposuspension (26)
II: Anterior repair (25) Techniques not described Additional hysterectomy done (I = 1, II = 4) Randomisation to surgeon done |
|
| Outcomes | Number cured (subjective and objective) Symptom severity Number with voiding difficulty Number with prolapse Pad test Number with DI Number with post‐op complications UDS parameters (Qmax, Pdetmax, RU) | |
| Notes | Full text, unpublished paper supplied by author | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | computer randomisation code |
| Allocation concealment (selection bias) | Unclear risk | not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | not mentioned |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | not mentioned |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | no description of withdrawals |
| Other bias | Unclear risk | no other bias identified |
Kammerer‐Doak 1999.
| Methods | RCT. Computer‐generated random list. Two arms All blinded prior to day of surgery No power calculation Not mentioned if ITT analysis Follow‐up 1 year | |
| Participants | N = 35. No withdrawals, one woman in each group refused one year urodynamic testing UDS‐confirmed diagnosis. Included recurrent UI. No mixed UI Burch group younger and more were pre‐menopausal Incl: GSI (allowed inclusion of women with prolapse) Excl: neuro cause for incontinence, DI, previous radical pelvic surgery, pelvic radiation, ISD, interstitial cystitis Single‐centre, university‐based, Dept of Ob&Gyn USA |
|
| Interventions | I: Burch (19)
II: Modified anterior colporrhaphy (16) Techniques not described Other surgical procedures done to both groups, significantly more paravaginal repairs to Burch group Surgery by senior residents with supervision |
|
| Outcomes | Number cured (subjective and objective)
Incontinence rating (IIQ)
Pad test
Number with morbidity Length on suprapubic catheter Subjective cure = not defined; objective cure = negative cough and Valsalva test at supine and standing with bladder filled to MCC |
|
| Notes | No values given to length of stay, post‐op complication rate and length on catheter but noted no difference in both groups | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | computer‐generated randomisation table |
| Allocation concealment (selection bias) | Unclear risk | not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | "everyone was blinded prior to day of surgery" |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | "everyone was blinded prior to day of surgery" |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | "everyone was blinded prior to day of surgery" |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | not mentioned |
| Other bias | Unclear risk | Burch group was significantly younger and more were pre‐menopausal; anterior colporrhaphy was more frequent in the modified anterior colporrhaphy group and paravaginal defect repair was more common in the Burch group |
Kitchener 2006.
| Methods | RCT. Randomisation performed by telephone using random permuted blocks, stratified by centre, age > 50 years and previous bladder neck surgery. Two arms Unblinded. ITT analysis. Follow‐up at 6 months, 12 months, 24 months | |
| Participants | N = 291. Withdrawals: Burch = 14, Lap = 9 Reasons: unfit for anaesthesia, COLPO surgeon not available, operation cancelled, moved, husband died, psychiatric problems, withdrawn, data destroyed by flood, unknown UDS‐confirmed. Allowed for previous anti‐incontinence surgery but not previous retropubic surgery. No mixed incontinence Excl: detrusor overactivity, previous retropubic surgery, grossly obese women Groups comparable to age, parity, previous bladder neck surgery, pad test, at baseline Multi‐centre. UK |
|
| Interventions | I: Burch (147)
II: Lap (144) Minimum of 2 sutures required for both procedures. No other surgery allowed Different surgeons |
|
| Outcomes | Objective cure (24 months); subjective cure; morbidity, time to return to work, QOL: SF‐36 physical and mental Objective cure defined as negative 1‐hour pad test. Subjective cure defined as response of "perfectly happy" to question 33 of Bristol questionnaire |
|
| Notes | MRC COLPO trial | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "using random permuted block sizes 2 and 4 with a dispersed block throughout the string, stratified by centre, age > 50 years and previous bladder neck surgery" |
| Allocation concealment (selection bias) | Low risk | "performed by telephone at University of York" (not a participating centre) |
| Blinding (performance bias and detection bias) All outcomes | High risk | "no attempt to blind the surgical procedure" |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | "no attempt to blind the surgical procedure" |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | "no attempt to blind the surgical procedure" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | withdrawal numbers equivalent across groups, reasons for withdrawals stated; some cross‐overs but ITT analysis done |
| Other bias | Unclear risk | no other bias identified |
Klarskov 1986.
| Methods | RCT. Method not described Two arms but surgical group stratified to three techniques. Choice of type of surgery based on VCUG result/ anatomy. Blinding not mentioned No power calculation Not mentioned if ITT analysis Follow‐up 12 months | |
| Participants | N = 52. Withdrawals not mentioned UDS‐confirmed diagnosis. Only primary GSI Median age = 48 years (range 31‐66) Baseline comparison of groups not mentioned Incl: GSI Excl: previous surgery, previous PFMT, other indication for surgery, inability to follow instruction Single‐centre, university hospital, Depts of Uro, Gyne & Radiol Denmark |
|
| Interventions | I: PFMT (24) by physiotherapist, at least 5 lessons, outpatient
II: Surgery
IIa: Burch (16) for ant. suspension defect
IIb: Anterior colpo (7) for post. suspension defect
IIc: Burch and Ant colpo, (3) for both defects Choice of surgery based on VCUG results If patient unhappy w/ tx, allowed to shift to other tx after 3 mos Surgeon not mentioned |
|
| Outcomes | Number cured (subjective and objective)
Urine loss
Number of incontinence episodes
UDS parameters Subjective cure based on patient satisfaction Graded into worse, unchanged, improved, cured |
|
| Notes | Some results given in surgical groups cannot be broken down to the 3 subgroups Burch versus anterior colporrhaphy data not used in this review because treatment allocation was not randomised |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "randomized", method not described |
| Allocation concealment (selection bias) | Unclear risk | not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | not mentioned |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | not mentioned |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | withdrawals not described |
| Other bias | Unclear risk | no other bias identified |
Koelbl 2002.
| Methods | RCT. Method not described but mentioned stratified random treatment assignment and block randomisation. Two arms. Blinding not mentioned. No power calculation. ITT analysis not mentioned. Follow‐up not specified but may have been limited to the in hospital stay of patients | |
| Participants | N = 166. No mention of dropouts UDS‐confirmed SUI Groups comparable in age, BMI Excl: PVR > 50 ml, UTI, mixed UI, DI, urgency, pelvic floor disorders |
|
| Interventions | I: Burch (83)
II: TVT (83) Techniques referenced Procedures done by three urogynaecologists per centre |
|
| Outcomes | Number cured, operation time, post‐operative complications, hospital stay, normal voids | |
| Notes | Abstract | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "stratified random treatment assignment and block randomization" |
| Allocation concealment (selection bias) | Unclear risk | not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | not mentioned |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | not mentioned |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | no description of withdrawals |
| Other bias | Unclear risk | no other bias identified |
Liapis 1996.
| Methods | RCT. Assigned according to a randomisation list. Three arms Blinding not mentioned No power calculation Not ITT analysis Follow‐up 5 years |
|
| Participants | N = 170. 15 dropouts (10 not yet due for 5 year follow up, 5 lost to follow up). UDS‐confirmed diagnosis. All primary UI. No mixed UI Mean age 50.6 years, parity 3, 97 menopausal No baseline comparison of groups Incl: GSI Excl: DI, gyne disease needing hysterectomy, other gyne disease needing surgery, previous anti‐incontinence surgery Single centre, university‐based, Dept of Ob&Gyn Greece |
|
| Interventions | I: Burch (54)
II: MMK (51)
III: Anterior colporrhaphy (50) All techniques described Additional posterior colporrhaphy done in all patients in groups I and III. Post colporrhaphy done in group II only if with rectocoele Surgeon not mentioned |
|
| Outcomes | Number cured (subjective and objective)
Number with post‐op urge incontinence
Number with DI
Number with repeat incontinence surgery
Number with prolapse
Days on catheter
UDS parameters Subjective cure = based on history Objective cure = based on UDS Catheter removal = if RU ≤ 150 ml and voided vol ≥ 200 ml |
|
| Notes | With additional information from author | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "assigned according to a randomization list" |
| Allocation concealment (selection bias) | Unclear risk | not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | not mentioned |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | not mentioned |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 15 patients were not included in the final analysis because 5‐year period was not completed (10 patients) or because they neglected their follow up (5 patients); no description of the distribution of these withdrawals |
| Other bias | Unclear risk | no other bias identified |
Liapis 2002.
| Methods | Quasi‐RCT by alternate method. Two arms. Blinding not mentioned. Back calculation of sample size showed only 76.9% power to detect difference in efficacy. ITT analysis not mentioned Follow‐up 24 months |
|
| Participants | N = 71. Withdrawals not mentioned Primary incontinence only. No mixed UI Incl: not mentioned Excl: previous operations, urge incontinence, ISD Groups comparable at baseline in age, parity, BMI |
|
| Interventions | I: Burch (35)
II: TVT (36) Techniques described. Surgeon not mentioned |
|
| Outcomes | Number cured (objective), number improved, analgesia needs, operative time, hospital stay, return to normal activity, uroflowmetric parameters | |
| Notes | None | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | "on an alternate fashion" |
| Allocation concealment (selection bias) | Unclear risk | not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | not mentioned |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | not mentioned |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | not mentioned |
| Other bias | Unclear risk | no other bias identified |
Mak 2000.
| Methods | RCT. Randomisation using computer‐generated random schedule. Used sealed opaque envelopes Blinding not mentioned No power calculation Not mentioned if ITT analysis Follow‐up 1 year | |
| Participants | N = 90 No withdrawals UDS confirmed SUI Mean age: Laparoscopic 51.1 years, open 50.4 years Parity Lap 2.7, open 2.9 Baseline characteristics comparable for age, parity, duration of incontinence, pre‐op pad test, of vaginal deliveries, no. with pre‐existing DI Inclusion: UDS‐confirmed SUI Excl: ISD, previous anti incontinence surgery, MUCP < 20 cm H20, VLPP < 60 Ccm H20, fibrotic vagina. | |
| Interventions | I. Laparoscopic (47) II. Open colposuspension (43) Co‐intervention: All received bladder training once patient was mobile, some had concomitant hysterectomy Procedures described Two senior surgeons performed the procedures | |
| Outcomes | Number cured (objective cure = dry during urodynamics, subjective cure = cure or improvement according to patient's report) using urinary symptom questionnaire, urodynamics, pad test and quality of life Length of stay, time to return to normal activities Complications |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "randomised according to a computer‐generated random table" |
| Allocation concealment (selection bias) | Low risk | "sequentially numbered sealed, opaque envelope" |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | not mentioned |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | not mentioned |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | no withdrawals mentioned |
| Other bias | Unclear risk | no other bias identified |
McCrery 2005.
| Methods | RCT. By coin toss. Two arms. Patients blinded. No mention on blinding of care giver. Independent assessor. Follow‐up mean of 28.8 months in Burch and 24.2 months in MMK | |
| Participants | N = 138
Lost to follow‐up: 6 in Burch, 11 in MMK Symptom‐based diagnosis (not all had UDS). Only primary incontinence. With mixed incontinence Incl: with anterior wall prolapse and SUI, urethral mobility of > 30 degrees from horizontal or USI, at least 6 months follow‐up. Excl: prior incontinence surgery; with diabetes, neuro disorders, spinal injuries; known CLPP < 60 cm H20 or MUCP < 20 cm H20. Similar in age, number of vaginal deliveries, weight and urodynamic parameters at baseline Women's hospital university‐affiliated, single centre |
|
| Interventions | I: Burch (66)
II: MMK (72) Both treatment groups underwent paravaginal defect repair. Both techniques described Single surgeon with with variable resident/fellow participation |
|
| Outcomes | Number cured subjectively, success rate, postop voiding problems, time to resumption of spontaneous voiding Subjective cure defined as no SUI and bladder problems assessed to be better Success is the combined number of cured and improved |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "randomized by a coin toss" |
| Allocation concealment (selection bias) | Unclear risk | not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | not mentioned |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | not mentioned |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | "losing 11 patients from MMK and 6 from Burch", but analysis was by intention to treat |
| Other bias | Unclear risk | mean length of follow‐up was significantly longer in the MMK group (28.8 mos versus 24.2) and reported results were "after controlling for the difference in months of follow up" |
Morris 2001.
| Methods | RCT. Randomisation not described Blinding not mentioned No power calculation ITT analysis as stated, details not described Follow‐up median of 72 months (interquartile range 67 months to 82 months). | |
| Participants | N = 73
Five declined formal review with UDS (Burch = 3, Lap = 2), 9 lost to follow‐up (Burch = 3, Lap = 6) UDS confirmed diagnosis Baseline comparison statistically similar Inclusion/Exclusion: not mentioned Single centre, Dept of Ob & Gyne, Glasgow, UK |
|
| Interventions | I: Open colposuspension (35)
II: Laparascopic colposuspension (38)
No description of techniques Surgeon not mentioned |
|
| Outcomes | Number cured subjectively and objectively Detrusor instability, de novo detrusor instability | |
| Notes | Abstract | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "randomised", method not described |
| Allocation concealment (selection bias) | Unclear risk | not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | not mentioned |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | not mentioned |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Five declined formal review with UDS (Burch = 3, Lap = 2), 9 lost to follow‐up with no reasons given (Burch = 3, Lap = 6) |
| Other bias | Unclear risk | no other bias identified |
Mundy 1983.
| Methods | Quasi‐randomised RCT (alternate allocation) Stratification between primary and recurrent GSI. Two arms Blinding not mentioned No power calculation ITT analysis Follow up minimum 1 year | |
| Participants | N = 51. No withdrawals Inclusion criteria: GSI (urodynamic diagnosis), combined primary and recurrent UI. No mixed UI Mean age 48 years (29 to 70). No baseline comparison of groups Single‐centre, Department of Urology, UK | |
| Interventions | (I) Colposuspension (Burch) (26)
(II) Needle (modified Stamey) (25) Colposuspension referenced; modified Stamey described Single surgeon for all cases |
|
| Outcomes | Number cured (subjective and objective)
Number with DI
Number with voiding difficulty Subjective cure = not defined Objective cure = negative nappy test and video UDS Subjective cure = not defined Objective cure = negative nappy test and video UDS Failure rate (subjective) at 12 months: (I) 3/26; (II) 6/25 Failure rate (objective) at 12 months: (I) 6/26; (II) 15/25 DI: (I) 2/26; (II) 5/25 Voiding difficulty: (I) 3/26; (II) 6/25 Peri‐operative complications (UTI, stitch removal, Dacron sheath removal): (I) 0/26; (II) 10/25 (II) 3 of the 10 needed removal of suprapubic Dacron buffer |
|
| Notes | Colposuspension described as Burch Cannot do separate analysis for recurrent GSI alone | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | "alternately allocated" |
| Allocation concealment (selection bias) | High risk | "alternately allocated" |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | not mentioned |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | not mentioned |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | no description of withdrawals |
| Other bias | Unclear risk | no other bias identified |
O'Sullivan 2000.
| Methods | RCT. Method not described. Two arms. Blinding not mentioned. ITT analysis not mentioned Follow‐up 6 months |
|
| Participants | N = 20. No withdrawals mentioned Groups comparable as to age, parity, menopausal status, use of HRT Excl: prior surgery for prolapse, radiotherapy, clinically significant prolapse |
|
| Interventions | I: colposuspension (9)
II: TVT (11) Techniques and surgeon not mentioned |
|
| Outcomes | Total collagen content, proteoglycan, protein content, mature cross links, immature cross links, elastin | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "randomised", method not described |
| Allocation concealment (selection bias) | Unclear risk | not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | not mentioned |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | not mentioned |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | not mentioned |
| Other bias | Unclear risk | data presented only in abstract form, no full text publication available |
Osman 2003.
| Methods | RCT (block randomisation technique). Four arm. Randomisation to surgery vs. drugs but type of surgery dictated by VLPP. Blinding not mentioned. Power calculation not done. ITT analysis not mentioned Follow‐up 6 months to 12 months, mean 9.3, SD =1.7 |
|
| Participants | N = 75. Seven patients lost to follow‐up Incl: combination of SUI and UUI > 6 months, no treatment for UI > for ≥ 3 months, sterile urine culture, negative cystometrogram for motor detrusor overactivity, unobstructed uroflow, no previous surgery for incontinence, no suspicion of other pathology Mean age 49.8 years, range 35‐61 |
|
| Interventions | I: anticholinergics (21)
IIa: Burch (23)
IIb: Pubovaginal sling (24)
III: Burch or Pubovaginal sling (20) Anticholinergic treatment used oxybutynin HCl 5 mg 3 x per day with titration Surgical techniques all described All procedures done by single surgeon |
|
| Outcomes | Number cured objectively and subjectively; SEAPI score, number with SUI and UUI | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "random selection, using the block‐randomization technique" |
| Allocation concealment (selection bias) | Unclear risk | not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | not mentioned |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | not mentioned |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Four patients lost to follow‐up in anticholinergics group, one patient lost in Burch group, no reasons given |
| Other bias | Unclear risk | no other bias identified |
Palma 1985.
| Methods | RCT, method not described Author replied patients, care givers and assessors were blinded Not mentioned if ITT analysis Follow up: (I) mean 34 months, (range 19 to 56); (II) 21 (2 to 44) | |
| Participants | N = 70. No withdrawals mentioned Previous surgery (Kelly or MMK): (I) 3/30, (II) 10/40 Urodynamics used to confirm SUI if in doubt Age: (I) mean 46 years (range 28 to 69); (II) 44 (26 to 67) Inclusion/exclusion not mentioned No statistical baseline comparisons of groups Single‐centre. Department of Obstetrics and Gynaecology, university‐based hospital, Campinas, Brazil | |
| Interventions | (I) MMK (30) (II) Needle suspension (Stamey) (40) Procedures described Surgeon not mentioned | |
| Outcomes | Not cured in first year: (I) 4/30, (II) 1/20 Not cured after first year: (I) 7/30, (II) 10/20 Not improved in first year: (I) 2/30, (II) 1/20 New urge or urge incontinence: (I) 0/30, (II) 2/20 New detrusor overactivity: (I) 0/30, (II) 1/20 Operating time: (I) 30 minutes, (II) 35 minutes Length of stay: (I) 3 days, (II) 2 days Voiding dysfunction: (I) 0/30, (II) 1/20 | |
| Notes | Abstract Correspondence from author to clarify if randomised. Extra data also obtained | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "randomised"; method not described |
| Allocation concealment (selection bias) | Unclear risk | not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Low risk | patients, caregivers and outcome assessors blinded (as per correspondence with author) |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | patients, caregivers and outcome assessors blinded (as per correspondence with author) |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | patients, caregivers and outcome assessors blinded (as per correspondence with author) |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | no withdrawals described |
| Other bias | Unclear risk | no other bias identified |
Quadri 1985.
| Methods | RCT, method unspecified | |
| Participants | 103 women with mixed incontinence (urethral sphincter incompetence in all, detrusor instability in I,12/55 ; II,7/48), moderate (I,25; II, 34) to severe (I, 30; II, 14) prolapse. Age: I, 58 yr (range 38‐76); II, 54 (36‐75) Previous incontinence surgery (anterior vaginal repair): I, 7/55; II, 2/48 Additional operations during trial: I, 55 had vaginal hysterectomy, 52 had posterior repair; II, 43 had abdominal hysterectomy, 2 had vaginal hysterectomy, 10 had Douglas obliteration, 15 had posterior repair | |
| Interventions | I: Retropubic colposuspension (48)
II: Anterior colporrhaphy (55) Techniques not described Surgeon not mentioned Other co‐interventions allowed |
|
| Outcomes | Number cured
Number with prolapse Cure not defined Incontinence at 3 m: I, 17/55; II, 16/48 Incontinence persisted at 12 m (failed): I, 11/55; II, 8/48. Further 5/55 and 4/48 later 'cured' using drugs Incontinence at 5 years (subjective): I: 8/50, II: 4/49 Incontinence at 5 years (objective): I: 6/50, II: 4/49 Prolapse recurred: I, 3/55; II, 13/48 [Type of prolapse: I, moderate cystocele 2, vaginal cuff 1; II, moderate to severe urethrocystocele 7, vaginal cuff 6] Later prolapse recurrence: I: 1/50, II: 16/49 Dyspareunia amongst sexually active: I: 30%, II: 13% P < 0.05 (number not given) Vaginal length: I: 4.9 cm (SD 1.7), II: 7.3 (1) |
|
| Notes | Reported in 3 conference abstracts only, further data not available. Recruitment period, data and numbers slightly different in each abstract Follow up 3 months, 3 years and 5 years. For recurrent prolapse, data from 1993 abstract used (at 5 year follow up) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "randomly selected to a surgical schedule" |
| Allocation concealment (selection bias) | Unclear risk | not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | not mentioned |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | not mentioned |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | no withdrawals described |
| Other bias | Unclear risk | information available in abstract only; no full text publication available |
Quadri 1999.
| Methods | RCT. By computer‐generated random assignment. Two arms. Blinding not mentioned. Unclear if ITT. Follow‐up at 2 months and 1 year | |
| Participants | N = 30. No withdrawals mentioned No mention if diagnosis based on symptom alone or by urodynamics. Allowed recurrent incontinence. No mention if included mixed incontinence Incl: only patients with MUCP < = 20 cm H20. Groups similar in age, parity, post‐menopausal status, BMI, subjective SUI score, previous vaginal delivery, presence of cystocoele < gr. 2 at baseline. Single centre. Urogyne unit. Italy |
|
| Interventions | I: Burch (15)
II: MMK (15) Both techniques described. MMK utilised video urethroscopy but not the Burch Foley catheter used for bladder drainage in Burch. Cystofix used for MMK 3 surgeons |
|
| Outcomes | Post‐operative complications Subjective cure |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "computer‐generated randomization" |
| Allocation concealment (selection bias) | Unclear risk | not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | not mentioned |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | not mentioned |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | no withdrawals described |
| Other bias | Unclear risk | MMK utilised video urethroscopy but not the Burch. Foley catheter used for bladder drainage in Burch. Cystofix used for MMK |
Sand 2000.
| Methods | RCT. Randomisation by random number table. Two arms Blinding not mentioned, 80% power to detect lower success for Burch if n > = 30 (based on a cure rate for Burch = 46% and for sling = 92%) Not ITT analysis Follow‐up 3 months and 72 months | |
| Participants | N = 36 (37 were randomised, only 36 operated on), 8 dropouts at 72 month follow‐up, 4 from each group. UDS‐confirmed diagnosis. Both primary and recurrent UI. With mixed UI Baseline comparison of groups similar to age, parity, UDS parameters but Burch group had higher rate of pre‐op DI and RU. Incl: GSI with urethral hypermobility, MUCP ≤ 20 cm H2O Excl: significant pelvic support defects Single centre, continence centre USA |
|
| Interventions | I: Modified Burch (19)
II: Suburethral transabdominal sling (17) Both techniques described Additional procedures done: group I (1); group II (2) Surgeon not mentioned |
|
| Outcomes | Number cured (subjective and objective), immediate complication, bladder training days, hospital stay, leave days, return to normal activities, operating time Subj Cure = no history of UI Obj Cure = no leak at MCC while coughing or doing Valsalva when sitting or standing |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "randomization was performed...using a random number table" |
| Allocation concealment (selection bias) | Unclear risk | not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Low risk | "only study participants were blinded as to group assignment" |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | "only study participants were blinded as to group assignment" |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | equal numbers of withdrawals across groups, noted two deaths but did not specify to which group these patients belong to |
| Other bias | Unclear risk | none |
Sivaslioglu 2007.
| Methods | RCT Computer‐based stratified randomisation using menopausal status as a block |
|
| Participants | N = 100 Incl: urodynamically proven SUI Excl: previous incontinence surgery, urge incontinence, urodynamic detrusor overactivity, genital prolapse of POP‐Q stage II or more both groups similar as regards age, BMI, parity, % post‐menopausal, % hormone replacement therapy, duration of stress urinary incontinence All participants available for evaluation at 1‐year follow‐up (Burch = 51, TOT = 49) Only 63 patients available for evaluation at 2 years (Burch = 31, TOT = 32) Urogynecology department Maternity and Women's Teaching Hospital Ankara, Turkey |
|
| Interventions | Burch (N = 51) ‐ as described by Walters TOT (N = 49) ‐ performed under spinal anaesthesia ‐ described in the paper Cystoscopy routinely performed after both procedures, Foley catheter was removed from the bladder 24 h after the operations; patients discharged when post‐void residual volume was < 100 ml (by ultrasonography) |
|
| Outcomes | Objective Cure = supine cough test negative and patient reported the restoration of urinary incontinence Subjective Cure = if the patient reported the restoration of urinary incontinence bu the supine cough test was positive Duration of procedure Hospital stay Operative complications (bleeding, bladder injury) Post‐operative complications (urinary retention, urinary tract infection) De novo urge incontinence Evaluation done at 6 weeks, 6 months, 1 year and 2 years |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | computer‐based stratified randomisation using menopausal status as a block |
| Allocation concealment (selection bias) | Unclear risk | not mentioned |
| Blinding (performance bias and detection bias) All outcomes | High risk | "patients were not blinded, all procedures performed by first author, postoperative assessment done by a senior surgeon who did not take part in the operation" |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | "patients were not blinded to the operative procedure", all procedures performed by first author |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | "single blind", "postoperative assessment done by a senior surgeon who did not take part in the operation", but no specific mention if this assessor was blinded to the intervention received by participant |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | complete follow up at 1 year assessment; equivalent losses for both groups at 2 year assessment; no reasons given |
| Other bias | Unclear risk | no other bias identified |
Stangel‐Wojcikiewicz 2008.
| Methods | RCT | |
| Participants | N = 108 Urodynamically diagnosed genuine stress urinary incontinence Excl: OAB, hyperactive detrusor, ISD (VLPP < 65 cm H20), MUCP < 20 cm H20), POP‐Q grade III and IV, with diabetes mellitus, neurological disorders, with contraindications for open procedure and for laparoscopy Poland |
|
| Interventions | Laparotomy for Burch/open Burch (N = 57) Laparoscopic Burch colposuspension (N = 51) |
|
| Outcomes | ||
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "randomized"; method not described |
| Allocation concealment (selection bias) | Unclear risk | not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | not mentioned |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | not mentioned |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | no withdrawals mentioned |
| Other bias | Unclear risk | none |
Su 1997.
| Methods | RCT comparing laparoscopic with open colposuspension Power calculation, early stopping rules with three evaluation points determined before beginning of trial; allocation through computer‐generated random numbers in sealed opaque envelopes, but four patients who were not willing to undergo laparoscopic colposuspension were enrolled to open group, then the next patient was assigned to the laparoscopic procedure and the following patients went back to sequence of random number All operations by senior gynaecologist F/U at 3/12, and every 6/12 | |
| Participants | 92 women Exclusion criteria: pathology that limits flexibility of vaginal wall, uterine prolapse, cystocele greater than 1st degree, DO, underactive detrusor, outflow obstruction, previous anti‐incontinent surgery, previous hysterectomy | |
| Interventions | Group 1 (N = 46): laparoscopic colposuspension Group 2 (N = 46): open colposuspension; transperitoneal approach, 1 double bite suture at level of urethro‐vesical junction and then to nearest point on ipsilateral Cooper's ligament in laparoscopic procedure, 3 sutures in open procedure, surgeon had done 50 previous laparoscopic colposuspensions Fourteen patients in laparoscopic and 19 in open group had hysterectomy at same time Suprapubic catheter, clamped day 2, patients encouraged to void every 2 hours, residuals measured with catheter unclamped for 15 min, if 2 successive voids > 200 mls and residuals < 100 mls catheter was clamped overnight, if still void > 200 mls and residuals < 100 mls catheter was removed | |
| Outcomes | Cure defined as dry during severe cough and bouncing on urodynamics, otherwise failure Numbers cured, pad test, operative time, length of stay, complications, de novo urge symptoms, de novo detrusor, voiding dysfunction, prolapse Adverse effects: Group 1: 2 outflow obstruction, 2 DI, 1 UTI; Group 2: 2 outflow obstruction, 3 DI, 1 UTI, 2 haematuria Operation time, blood loss, duration of catheterisation At 1 year F/U: 1‐hour pad test, objective stress test, assessment of bladder neck position; if incontinence was found urodynamics were repeated to confirm GSI Cure defined as dry during severe cough and bouncing on urodynamics, otherwise failure In the 14 patients who had TAH after laparoscopic colposuspension immediate look at the suture position and tension revealed 5 suboptimal suspension sutures |
|
| Notes | Trial was stopped at 2nd evaluation point
Adverse effects:
Group 1: 2 outflow obstruction, 2 DO, 1 UTI; Group 2: 2 outflow obstruction, 3 DO, 1 UTI, 2 haematuria Additional information supplied by the authors |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "according to a computer‐generated random number table" |
| Allocation concealment (selection bias) | Low risk | "assigned by opening the next sequentially numbered, sealed, opaque envelope" |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | not mentioned |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | not mentioned |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | no withdrawals described |
| Other bias | Unclear risk | A few patients were not willing to undergo laparoscopic colposuspension. They were thus enrolled to the traditional groups. Then, the next patient was assigned to the laparoscopic procedure and the following patients went back to the sequence of the random number table. Early stopping rules employed. Trial was stopped on the second evaluation point (after 90th patient recruited) |
Summitt 2000.
| Methods | RCT. Randomisation: computer‐generated randomisation schedule, numbers in double sealed envelope with project secretary Blinding not mentioned No power calculation Not mentioned if ITT analysis Follow‐up: 2 and 6 weeks, 3 and 12 months | |
| Participants | N = 62
No withdrawals or dropouts
UDS confirmed SUI
Exclusion criteria: need for concomitant surgical procedures, previous retropubic urethropexy, needle suspension or suburethral sling, neurologic deficit associated with incontinence, type III stress incontinence, detrusor instability that has not been treated and improved, absolute contraindications to laparoscopy (uterine fibroids or pelvic mass > 16 weeks gestational size, conditions in which patient cannot tolerate anaesthesia, severe bleeding disorders, acute peritonitis of upper abdomen with severe distension), pathology present at the time of surgery that requires additional surgery (eg. unsuspected ovarian mass) Multi‐centre trial 5 sites, Memphis, USA |
|
| Interventions | I: Laparoscopic colposuspension (N = 28) II: Open colposuspension (N = 34) To ensure similarity of operative technique all co‐investigators met at a common location at beginning of study to observe surgery and participate in animal laboratory Intraperitoneal approach for laparoscopy 0‐Ethibond suture, 2 sutures each side of urethra; suprapubic catheter | |
| Outcomes | Operating time, blood loss, hospital stay, complications, fever, time to resumption of voiding, objective surgical success, urodynamics, time to return to work and normal activity, subjective success | |
| Notes | Abstract Personal communication with reviewers on Lap review Three laparoscopic colposuspensions were converted to open due to severe intra‐abdominal adhesions | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "randomly assigned" |
| Allocation concealment (selection bias) | Low risk | not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | not mentioned |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | not mentioned |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | no withdrawals described |
| Other bias | Unclear risk | abstract |
Tapp 1989.
| Methods | RCT. Method not described. Three‐arm Blinding not mentioned No power calculation Not mentioned if ITT analysis Follow‐up 6 months | |
| Participants | N = 68 (81 entered but 13 withdrew) UDS‐confirmed diagnosis. All primary UI. No mixed UI Population characteristic not given. No baseline comparison of groups mentioned Incl: GSI Excl: history of urologic or vaginal surgery, other UDS abnormality Single centre, urodynamic unit UK |
|
| Interventions | I: Burch ( 24)
II: Pelvic floor exercise (21)
III: Pelvic floor exercise with faradic stimulation (23) PFE = 14 sessions over 3 months Patients not satisfied with PFE results allowed to have surgery at 3 months |
|
| Outcomes | Number cured (objective)
Number improved (subjective) Cure not defined |
|
| Notes | Abstract only Unclear if withdrawals were before or after randomisation |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | method not described |
| Allocation concealment (selection bias) | Unclear risk | not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | not mentioned |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | not mentioned |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | no withdrawals described |
| Other bias | Unclear risk | abstract |
Tellez Martinez‐Fornes 2009.
| Methods | RCT Randomisation using an automatic computerised system on being added to the surgical waiting list |
|
| Participants | N = 49 Women aged 35 years to 70 years Incl: completed their families; indicated for surgical treatment of SUI; clinically demonstrated SUI by positive Bonney test and by urodynamic study Excl: prior incontinence, vesicular or pelvic surgery due to any cause, urodynamic study with results for overactive bladder or urinary obstruction (maximum flow <15 ml/s, detrusor expulsion pressure > 50 cm H20, or post void volume > 100 ml, grade I or above cystocele, prior hysterectomy, major obesity with BMI > = 40, poorly controlled diabetes, neurological disorders, repetitive urinary infections, genital atrophy which inhibits vaginal surgery, non‐bleeding diathesis or anticoagulant treatment and, no informed consent TVT: 24 randomised, 23 received treatment, 1 excluded due to adnexal mass and no SUI operation; 2 follow up losses (no reason given), 23 with complete data available Burch: 25 randomised, 23 received treatment, 2 excluded (1 had Burch with hysterectomy, 1 not operated), 24 with complete data, 1 follow‐up loss (no reason given) Treatment groups similar as regard parity, proportion at menopause, age, duration of incontinence, ISI and IIQ score, BMI, baseline one hour pad test weight, leak point pressure, maximal urethral closure pressure and functional urethral length More patients had cystocele in the Burch colposuspension group Urology department general hospital Madrid, Spain |
|
| Interventions | TVT procedure (N = 24, only 23 analysed) ‐ as described by Ulmsten ‐ vesicular probe was maintained for 24 hours ‐ vaginal plug maintained for 12 hours to 24 hours ‐ discharged 24 hours after the procedure Burch colposuspension (N = 25, only 23 analysed) ‐ performed according to the usual technique followed in the centre with 2 Ethi bond No. 1 sutures on each side of the urethra and vesicular cervix on the paravaginal fascia and anchored to the Cowper ligament ‐ vaginal plug maintained for 12 hours to 24 hours ‐ vesicular probe maintained for 72 hours ‐ discharged after post void residual control Two urologists performed the procedure |
|
| Outcomes | Subjective cure of SUI, evaluated with IIQ and ISI questionnaires Cure = meets all the following criteria: IIQ score < 2, ISI score < 1; negative one‐hour pad test, normal uroflowmetry (Qmax < 12ml/s, post‐void residue <100ml), absence of obstructive symptoms and/or urinary urgency Improvement = IIQ score between 3 and 6 (and lower than before surgery); ISI score between 1 and 3 (and lower than before surgery); negative one‐hour pad test, flowmetry with post void residue < 100 ml, and the presence of obstructive symptoms and/or urinary urgency acceptable to patient Failure: all of the remaining cases that did not meet the cure or improvement criteria Intraoperative complications (vesicular lesion, urethral lesion, transfusion, etc) Post‐operative complications (urinary tract infection, acute urinary retention, surgical wound infection) Readmissions Surgical time Post‐operative stay Adequacy of the clinical route designed for the procedure Amount of analgesics consumed in the postoperative period Total cost of the procedure Patients assessed at 7 days for postoperative complication assessment; follow up schedules at 6 months, 1 year, 3 years follow‐up variable at different assessment points |
|
| Notes | Need to clarify with author re numbers in the treatment group for the results tables and the actual SDs for the IIQ and ISI scores. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | automatic computerised system |
| Allocation concealment (selection bias) | Unclear risk | not mentioned |
| Blinding (performance bias and detection bias) All outcomes | High risk | difference in surgical technique prevent masking to the surgeons |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | open clinical trial; all patients were informed of the type of surgery they would undergo |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | follow‐up losses noted in both groups; TVT = 2, Burch = 1 |
| Other bias | Unclear risk | none |
Trabuco 2014.
| Methods | RCT. "dynamic allocation process". Two arms, single‐assessor blinded. Follow up at 6 months | |
| Participants | N = 113 Included women with symptomatic SUI and pelvic organ prolapse undergoing abdominal sacrocolpopexy. Included both SUI and stress predominant mixed incontinence women. Groups comparable at baseline in age, BMI, history of prior incontinence surgery, pre‐operative diagnosis, prolapse stage, or baseline incontinence severity Single‐centre. University‐based/academic hospital, USA |
|
| Interventions | I: Burch colposuspension (N = 56) II : retropubic mid urethral sling (N = 57) No description of the interventions Both groups underwent abdominal sacrocolpopexy |
|
| Outcomes | Objective continence, defined as 1) negative standardised stress test, 2) no interim re‐treatment for stress urinary incontinence, and 2) no self‐reported urinary incontinence = ICIQ‐SF score = 0 Stress‐specific continence = fulfilled criteria 1 and 2 above and had "never" or "rarely" response to all 6 questions from the SUI subscale of the MESA questionnaire Improvement of the urgency urinary incontinence satisfaction rate perception of improvement measured as VAS Global impression of severity Complications |
|
| Notes | Abstract only | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "randomized dynamic allocation approach" |
| Allocation concealment (selection bias) | Unclear risk | "dynamic allocation approach" |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | not mentioned |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | not mentioned |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | "blinded standardized cough test" / "stress test performed by a masked observer" |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | loss to follow up, small and equivalent in both groups : 5/56 (Burch), 4/57 (Sling) |
| Other bias | Unclear risk | none |
Tuygun 2006.
| Methods | RCT | |
| Participants | Women with primary stress incontinence | |
| Interventions | Open Burch 27 (participants) versus laparoscopic Burch (33 participants) follow up 38.7 +/‐ 10.2 months open Burch, laparoscopic Burch 42.12 +/‐ 13.8 months | |
| Outcomes | Objective cure, complications including bladder perforation | |
| Notes | Data derived only from the English abstract. Turkish study | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "randomized" |
| Allocation concealment (selection bias) | Unclear risk | not mentioned in abstract |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | not mentioned in abstract |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | not mentioned in abstract |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | not mentioned in abstract |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | complete follow‐up at 3 years |
| Other bias | Unclear risk | none |
Ustun 2005.
| Methods | RCT Computer‐generated randomisation list, in sealed envelopes |
|
| Participants | N = 52 with symptoms of genuine stress incontinence and with GSI on urodynamic investigation and also requiring additional gynaecologic operations Excl: detrusor instability on tests Groups similar as regard to age, parity, menopausal status, concomitant gynaecologic procedures performed Department of Obstetrics and Gynecology university hospital Ankara, Turkey |
|
| Interventions | Laparotomic Burch procedure (N = 26) ‐ two suspending sutures in the paravaginal fascia and tied to Cooper's ligament Laparoscopic Burch procedure (N = 26) ‐ under general anaesthesia ‐ as described by Tanagho ‐ two sutures ‐ indwelling catheter removed within 24 hours of surgery |
|
| Outcomes | Cure = no need for the use of pads and the urodynamic evaluation was dry Subjective cure = by history and questionnaire Objective cure = by multichannel urodynamic evaluation and Qtip Intraoperative and postoperative complications De novo detrusor instability Urinary retention Follow‐up done at 4 weeks, 3 months, and every 6 months (mean follow‐up at 14.19 months, ranging from 3 months to 24 months) |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | computer‐generated randomisation list |
| Allocation concealment (selection bias) | Low risk | "in sealed envelopes" |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | not mentioned |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | not mentioned |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | complete follow up; no reported patients lost to follow up at 12 months |
| Other bias | Unclear risk | none |
Wang 2003.
| Methods | RCT using computer‐generated randomisation schedule. Blinding not mentioned Power calculation based on probability of voiding difficulty Follow‐up 12 months to 36 months, median = 22 months. |
|
| Participants | N = 98 (108 randomised but some excluded because of bladder outlet obstruction). Eight patients, all in the Burch group, lost to follow‐up, went overseas UDS‐confirmed SUI. Only primary UI Groups comparable by age, parity, body weight, number of menopausal women, number with additional procedures, urodynamic parameters Excl: pre‐operative bladder outlet obstruction (by pre‐specified urodynamic parameters), previous anti‐incontinence surgery |
|
| Interventions | I: Burch (41)
II: TVT (49) Techniques described and referenced |
|
| Outcomes | Number with objective cure (1 hour pad wt < 2 g); number with objective improvement (less than half of pre‐operative pad weight); number with subjective cure (no loss of urine during physical exercise as reported), number with subjective improvement (less than half of amount lost pre‐operatively) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "predetermined computer‐generated randomization code" |
| Allocation concealment (selection bias) | Unclear risk | not mentioned |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | not mentioned |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | not mentioned |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Eight patients, all from the Burch group, were lost to follow‐up because they went overseas |
| Other bias | Unclear risk | no other bias identified |
Ward 2002.
| Methods | RCT of TVT versus Burch colposuspension ITT analysis (non‐attenders as failures) | |
| Participants | Women who had completed their family who presented with USI unresponsive to pelvic floor muscle training were included. Excluded were those with detrusor overactivity, vaginal prolapse requiring treatment, previous surgery for prolapse or incontinence, a major degree of voiding dysfunction (defined at cystometry as a voiding pressure > 50 cm H20, maximum flow < 15 ml/s, and residual urine volume > 100 ml), neurological disease, and allergy to local anaesthetic. Urodynamic evaluation was performed. Patients were asked to complete a urinary diary for one week, and a 1‐hour perineal pad test was performed according to the recommendations of the International Continence Society. Patients' perceptions of changes in their symptoms and treatment outcome were measured with the generic SF36 and the disease‐specific Bristol Female Lower Urinary Tract Symptoms (B‐FLUTS) questionnaire. Six weeks after surgery a postal questionnaire was sent out comprising the SF36 and questions about recovery. Six months after surgery reassessment was undertaken with symptom review, clinical examination, the one‐hour pad test, and urodynamic studies. Other assessments were performed at 1 year, 2 years and 5 years after surgery. |
|
| Interventions | Group 1: TVT (N = 170) Group 2: Colposuspension (N = 146) |
|
| Outcomes | The primary outcome measure was objective cure of stress incontinence defined as a negative stress test on urodynamic testing and a negative one‐hour pad test (< 1 g change in weight). Secondary outcome measures included subjective cure of incontinence and the development of voiding problems, urge symptoms, and vaginal prolapse. These were measured with the B‐FLUTS questionnaire and by interview with patients | |
| Notes | 344 women were randomised. Five from TVT and 23 from colposuspension did not receive allocated treatment because of withdrawn consent, declined surgery, ineligibility for trial. At 6 months 2 women withdrew and 1 was lost to follow up from the TVT group and 1 withdrew and 8 lost to follow up from the colposuspension group. (The baseline characteristics of the patients who withdrew before surgery were similar to the participants, with the exception of a lower change in pad weight in the colposuspension group) Complete data was available in 152 and 127 women from TVT and colposuspension groups respectively at 6‐months' follow‐up Complete data was available in 125 and 101 respectively at 2‐years' follow‐up Complete data was available in 72 and 49 respectively at 5‐years' follow‐up |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "randomization was computer‐generated using randomly varying block sizes of 4 and 6" |
| Allocation concealment (selection bias) | Low risk | "via a telephone system which allocated trial identification number and treatment group" |
| Blinding (performance bias and detection bias) All outcomes | High risk | "not possible to blind patients or investigators" |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | "not possible to blind patients or investigators" |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | not mentioned |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | more patients in the colposuspension group did not receive treatment as allocated (23 versus 5), more patients lost to follow‐up in colposuspension group; however results reported and analysed by intention to treat |
| Other bias | Unclear risk | no other bias identified |
BMI = body mass index; CLPP + cough leak point pressure; DI = detrusor instability; Excl = exclusion criteria; FUL = functional urethral length; GSI = genuine stress incontinence; GUTSS = Genito‐urinary Treatment Satisfaction Scale; Gyne = gynaecology; Incl = inclusion criteria; ISD = intrinsic sphincter deficiency; ITT = intention to treat; MCC = maximum cystometric capacity; MMK = Marshall‐Marchetti‐Krantz; MUCP = maximum urethral closing pressure; Ob&Gyne = obstetrics and gynaecology; PFMT = pelvic floor muscle training; POP = pelvic organ prolapse; PTR = pressure transmission ratio; PVR = post‐void residual volume;Qmax = maximum urine flow, SIIQ = Short Incontinence Impact Questionnaire; SUDI = Short Urinary Distress Inventory; RCT = randomised controlled trial; RU = residual urine; TOT = transobturator tape procedure; TVT = tension‐free vaginal tape; UDS = urodynamic; SUI = stress urinary incontinence; UI = urinary incontinence; UTI = urinary tract infection; VAS = visual analogue score; lap = laparoscopic; VLPP = Valsalva leak point pressure
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Adile 2001 | Not RCT |
| Adile 2001b | Not RCT |
| Ankardal 2007 | Not a trial |
| Baessler 1998 | Comparison was between one technique of open retropubic colposuspension (Burch) with the same technique in combination with another (paravaginal repair) |
| Barber 2002 | Patients entered to the surgical arm by choice. Randomisation done for the other arms of the trial |
| Benson 1993 | Participants not incontinent |
| Benson 1996a | Participants not incontinent |
| Benson 1996b | Participants not incontinent |
| Bhatia 1985a | Not randomised, surgeon chose the intervention |
| Bhatia 1985b | All participants had Burch, randomisation was on the use of antibiotics |
| Brubaker 2002 | Participants not incontinent at study entry |
| Brubaker 2009 | Analysis of the data was not by treatment group; focus of the analysis was on the change in sexual function after surgery in general |
| Bump 1988 | Participants not incontinent |
| Bump 1995 | Participants not incontinent |
| Bump 1996 | Participants not incontinent |
| Byrne 1989 | Study "not properly controlled" upon correspondence with co‐author (Condie) |
| Colombo 1997 | Not all participants are incontinent; comparison interventions are anterior colporrhaphy and variations of needle suspension procedures |
| Cornish 2001 | Study was on the relevance of questionnaires |
| Costantini 2007a | Participants were not incontinent at the start of the trial |
| Costantini 2007b | Treatment groups not among the pre‐specified comparison groups (compared colposacropexy with Burch versus colposacropexy without Burch). |
| Costantini 2008 | Treatment groups not among the pre‐specified comparison groups (compared colposacropexy with versus without Burch) |
| Costantini 2010 | Treatment groups not among the pre‐specified comparison groups (compared colposacropexy with versus without Burch) |
| Costantini 2011 | Participants were not incontinent at the start of the trial |
| Debodinance 1993 | Both treatment arms are sling procedures |
| Debodinance 1994 | Both treatment arms are sling procedures |
| Di Palumbo 2003 | Review of the technique of 4 corner bladder suspension assessed to be a variant of a needle suspension surgery |
| el‐Toukhy 2001 | Not RCT, patients chose operation |
| Fischer‐Rasmussen 87 | Not RCT |
| Foote 2007 | Trial was planned and initially conducted as an RCT but was converted to a cohort study after a failure in the randomisation process as reported |
| Goldberg 2001a | Participants were cadavers; not incontinent; outcomes not relevant for the review |
| Goldberg 2001b | Participants were randomised to the type of prolapse repair and not to the different anti‐incontinence surgical procedures that were done concomitantly |
| Jongen 1999 | Not an RCT |
| Lee 1997 | Randomisation could not be confirmed. Written to author regarding clarification but no reply received |
| Lemack 2008 | Analysis of the data was according to the presence of voiding dysfunction preoperatively rather than the treatment group allocation |
| Lemieux 1991 | Interventions were on clamping versus non‐clamping of catheters post anti‐incontinence surgery |
| Martan 2000 | No comparison group |
| Martan 2001 | Not RCT ‐ the abstract in the study report uses the term 'randomised' but all patients received Burch colposuspension |
| McClure 2006 | Study did not involve a comparison of the efficacy of surgical techniques but rather on the methodology of assessing outcomes |
| Meschia 2001 | Surgery for prolapse rather than incontinence |
| Morley 1995 | Intervention not abdominal open colposuspension |
| Mundy 1982 | Unclear regarding treatment assignment. Written to author for clarification but no reply received |
| Obrink 1978 | Not clear how patients were allocated. Author written to in Oct 2001, no reply received to date |
| Ostrzenski 1996 | Study on prolapse surgery rather than incontinence surgery |
| Palomba 2001 | All participants had Burch; trial was on effect of pre‐operative oestrogen |
| Pifarotti 2001 | Not RCT |
| Quadri 2000 | The study groups were on prostaglandin injection and control, not the types of surgery for incontinence |
| Reid 2007 | The study did not deal with the efficacy of the surgical techniques but rather on the validity of the patient‐based outcome measures used to assess the outcomes of surgery |
| Richter 2007 | Analysis of the data not according to treatment groups but according to treatment outcome |
| Richter 2008a | Analysis of the data not according to treatment groups but according to age group |
| Richter 2008b | Analysis of the data not according to treatment groups but according to age group |
| Roca 1994 | Not RCT |
| Rogers 2006 | Not a trial of incontinence surgery |
| Salam 2004 | Study design not mentioned; contact information of author not available |
| Salinas 1994 | Not RCT |
| Salinas 1995 | Not RCT |
| Schostak 2001 | Interventions were sling and needle suspension |
| Stanton 1979 | Unclear regarding treatment assignment. Written to author regarding clarification but no reply received |
| Subak 2008b | Not RCT |
| Surkont 2007 | Not randomised |
| Tincello 2009 | Not RCT. Patient preference study |
| Virseda Chamorro 1995 | Not RCT |
| Walter 1982 | Not RCT. Surgeon chose intervention |
| Zhu 1998 | After translation from Chinese established not an RCT. Allocated to treatment according to preference of surgeon |
Characteristics of studies awaiting assessment [ordered by study ID]
Helmy 2012.
| Methods | Long‐term observational study of women who participated in a randomized surgical trial |
| Participants | N = 482 (73.6%) of women who participated in a surgical trial |
| Interventions | I: Burch urethropexy II: fascial sling |
| Outcomes | Continence rate at 5 years Satisfaction at 5 years Adverse event rate |
| Notes | Abstract. Contacted authors to verify if this report is from the SISTEr trial (Albo 2007) |
Characteristics of ongoing studies [ordered by study ID]
Boyd 1996.
| Trial name or title | Laparoscopic treatment for female urinary incontinence |
| Methods | |
| Participants | |
| Interventions | Laparoscopic colposuspension versus traditional open colposuspension |
| Outcomes | Surgical success rates, infection rates, intraoperative blood loss, post‐operative pyrexia, length of stay, urinary infection rates, rates of catheter problems, patient satisfaction |
| Starting date | 01/03/94 |
| Contact information | Dr Karen Boyd Yorkshire Health Department of Obstetrics and Gynaecology Belmont Grove Leeds LS2 9NS UK 0113432799 |
| Notes | Trial should have been completed by 1996; however no other publication of this trial could be located, other than its registration with the metaregister of controlled trials |
Differences between protocol and review
The comparison between open colposuspension and sling procedures was subdivided into three subcategories: (1) open colposuspension versus traditional slings, (2) open colposuspension versus self‐fixing slings, and (3) open colposuspension versus single‐incision slings because of the increase in the number of trials using minimally invasive sling procedures with its variations. This is also in keeping with the Cochrane Incontinence Review Group's move to have separate reviews for these different types of sling procedures.
July 2017 update: We have added Brief Economic Commentaries (BECs) to all of our 'Surgery for UI in women' Cochrane Reviews. The economic elements throughout the review have been revised; if incorrect, we have stripped them out. We have added new economics‐related text. This involved revisions to the Background section, Methods section, e.g. search section referring to added Appendix, Discussion section, Abstract and Plain Language Summary. We have added an appendix with details of the economics searches. The Conclusions section of the review has not changed. The rest of the review has not changed.
Contributions of authors
Marie Carmela Lapitan wrote the protocol and the text of the main review. She performed the initial screening of studies for inclusion into the review, assessment of methodological quality, data extraction, and analysis of results. She was also responsible for the clinical input for the review.
June Cody performed the second and confirmatory screening of studies for inclusion, assessment of methodological quality, and data extraction. Adrian Grant and June Cody assisted in the analysis and interpretation of the results. Adrian Grant made a significant input to the writing of the review.
For the July 2017 addition of the BECs to this review: Atefeh Mashayekhi was responsible for the entire BECs‐related work on this review, i.e. she ran the search for studies, screened the search results, extracted data from relevant studies, revised any existing economics‐related text, added the BECs‐related text, and responded to any peer referee comments. All authors had the opportunity to comment on the revised review.
Sources of support
Internal sources
National Institutes of Health, University of Philippines ‐ Manila, Philippines.
Chief Scientist Office, Scottish Executive Health Department, UK.
External sources
-
National Institute for Health Research, UK.
This project was supported by the National Institute for Health Research, via Cochrane Infrastructure, Cochrane Programme Grant or Cochrane Incentive funding to the Incontinence Group. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, NHS or the Department of Health. The NIHR is the largest single funder of the Cochrane Incontinence Group.
-
National Institute for Health Research, UK.
This project, to add Brief Economic Commentaries to our 'Surgery for UI in women' reviews, was supported by the National Institute for Health Research (NIHR), via the Cochrane Review Incentive Scheme 2016, to the Cochrane Incontinence Group. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, NHS or the Department of Health.
Declarations of interest
Marie Carmela Lapitan: none known June Cody: none known Atefeh Mashayekhi: This project, to add Brief Economic Commentaries to our 'Surgery for UI in women' reviews, was supported by the National Institute for Health Research (NIHR), via the Cochrane Review Incentive Scheme 2016, to the Cochrane Incontinence Group. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, NHS or the Department of Health.
Edited (no change to conclusions)
References
References to studies included in this review
Albo 2007 {published data only}
- Albo M, Wruck L, Baker J, Brubaker L, Chai T, Dandreo KJ, et al. for the Urinary Incontinence Treatment Network (UITN). The relationships among measures of incontinence severity in women undergoing surgery for stress urinary incontinence. Journal of Urology 2007;177(5):1810‐4. [sr‐incont23120] [DOI] [PubMed] [Google Scholar]
- Albo ME, Richter HE, Brubaker L, Norton P, Kraus SR, Zimmern PE, et al. for the Urinary Incontinence Treatment Network (UITN). Burch colposuspension versus fascial sling to reduce urinary stress incontinence. New England Journal of Medicine 24‐5‐2007;356(21):2143‐55. [sr‐incont23077] [DOI] [PubMed] [Google Scholar]
- Brubaker L. Five year continence rates, satisfaction and adverse events of Burch urethropexy and fascial sling surgery for urinary incontinence (Abstract). European Urology Supplements 2012;11(1):e172. [NCT00064662; TrialID.SISTEr.; sr‐incont62253] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brubaker L, Barber MD, Nygaard I, Nager CW, Varner E, Schaffer J, et al. Quantification of vaginal support: are continuous summary scores better than POPQ stage?. American Journal of Obstetrics & Gynecology 2010;203(5):512‐6. [NCT00065845; sr‐incont40592] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brubaker L, Richter HE, Norton PA, Albo M, Zyczynski HM, Chai TC, et al. 5‐year continence rates, satisfaction and adverse events of Burch urethropexy and fascial sling surgery for urinary incontinence. Journal of Urology 2012;187(4):1324‐30. [NCT00064662; TrialID.SISTEr.; sr‐incont44723] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bump RC, Brubaker LT, Fine PL, Norton PA, Chancellor MB, Zyczynski H, et al. Randomised clinical trial of Burch vs sling procedure for stress urinary incontinence (known as SISTEr trial). CRISP database 2002. [sr‐incont17205]
- Burgio KL, Brubaker L, Richter HE, Wai CY, Litman HJ, France DB, et al. Patient satisfaction with stress incontinence surgery. Neurourology & Urodynamics 2010;29(8):1403‐9. [sr‐incont40322] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chai T, Albo M, Richter H, Norton P, Dandreo K, Kenton K, et al. Adverse events from a randomized trial for the surgical treatment of stress urinary incontinence (Abstract number 512). 37th Annual Meeting of the International Continence Soceity (ICS), 20‐24 Aug 2007, Rotterdam, Netherlands. 2007. [sr‐incont23535]
- Chai TC, Albo ME, Richter HE, Norton PA, Dandreo KJ, Kenton K, et al. Complications in women undergoing Burch colposuspension versus autologous rectus fascial sling for stress urinary incontinence. Journal of Urology 2009;181(5):2192‐7. [sr‐incont31150] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diokno AC, Richter HE, Kenton K, Norton P, Albo M, Kraus S, et al. Risk factors associated with failure of surgical treatment for stress urinary incontinence at 24 months follow‐up (Abstract number 115). Neurourology and Urodynamics 2007;26(5):745. [sr‐incont23533] [Google Scholar]
- FitzGerald MP, Burgio KL, Borello‐France DF, Menefee SA, Schaffer J, Kraus S, et al. Pelvic‐floor strength in women with incontinence as assessed by the Brink scale. Physical Therapy 2007;87(10):1316‐24. [sr‐incont23825] [DOI] [PubMed] [Google Scholar]
- Kenton K, Tennstedt S, Litman H, Zimmern P, Getti C, Kusek JW, et al. Improvement in quality of life in women at two years after undergoing the Burch colposuspension or fascial sling procedure (Abstract number 206). Proceedings of the 38th Annual Meeting of the International Continence Society (ICS), 2008 Oct 20‐24, Cairo, Egypt. 2008. [sr‐incont31863]
- Kraus SR, Lemack GE, Sirls LT, Chai TC, Brubaker L, Albo M, et al. Urodynamic changes associated with successful stress urinary incontinence surgery: is a little tension a good thing?. Urology 2011;78(6):1257‐62. [sr‐incont42989] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kraus SR, Markland A, Chai TC, Stoddard A, FitzGerald MP, Leng W, et al. Race and ethnicity do not contribute to differences in preoperative urinary incontinence severity or symptom bother in women who undergo stress incontinence surgery. American Journal of Obstetrics and Gynecology. 2007;197(1):92‐6. [sr‐incont23802] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lemack G, Krauss S, Litman H, FitzGerald M, Chai T, Nager C, et al. Preoperative urodynamic testing does not predict postoperative voiding dysfunction among women undergoing surgery for SUI: Results from a prospective randomized trial comparing Burch versus pubovaginal sling (Abstract number 7, poster). Neurourology and Urodynamics 2008;27(2):123. [sr‐incont26919] [Google Scholar]
- Lemack GE, Xu Y, Brubaker L, Nager C, Chai T, Moalli P, et al. for the Urinary Incontinence Treatment Network (UITN). Clinical and demographic factors associated with valsalva leak point pressure among women undergoing Burch bladder neck suspension or autologous rectus fascial sling procedures. Neurourology and Urodynamics 2007;26(3):392‐6. [sr‐incont23233] [DOI] [PubMed] [Google Scholar]
- Markland AD, Kraus SR, Richter HE, Nager CW, Kenton K, Kerr L, et al. Prevalence and risk factors of fecal incontinence in women undergoing stress incontinence surgery. American Journal of Obstetrics and Gynecology. 2007;197(6):662‐7. [sr‐incont26334] [DOI] [PubMed] [Google Scholar]
- Nager C, Chai T, FitzGerald M, Lemack G, Kraus S, Sirls L, et al. for the Urinary Incontinence Treatment Network (UITN). Valsalva leak point pressure and detrusor overactivity do not predict, but urodynamic stress incontinence does predict continence outcomes after Burch or pubovaginal sling procedures (Abstract number 85). Neurourology and Urodynamics 2007;26(5):709‐11. [sr‐incont23532] [Google Scholar]
- Nager CW, Albo ME, FitzGerald MP, McDermott S, Wruck L, Kraus S, et al. for the Urinary Incontinence Treatment Network (UITN). Reference urodynamic values for stress incontinent women. Neurourology and Urodynamics 2007;26(3):333‐40. [sr‐incont23232] [DOI] [PubMed] [Google Scholar]
- Nygaard I, Brubaker L, Chai TC, Markland AD, Menefee SA, Sirls L, et al. Risk factors for urinary tract infection following incontinence surgery. International Urogynecology Journal 2011;22(10):1255‐65. [sr‐incont42698] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richter HE, Brubaker L, Stoddard AM, Xu Y, Zyczynski HM, Norton P, et al. Patient related factors associated with long‐term urinary continence after Burch colposuspension and pubovaginal fascial sling surgeries. Journal of Urology 2012;188(2):485‐9. [NCT00064662; sr‐incont45162] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richter HE, Burgio KL, Brubaker L, Moalli PA, Markland AD, Mallet V, et al. Urinary Inc. Factors associated with incontinence frequency in a surgical cohort of stress incontinent women. American Journal of Obstetrics and Gynecology 2005;193(6):2088‐93. [sr‐incont21231] [DOI] [PubMed] [Google Scholar]
- Richter HE, Diokno A, Kenton K, Norton P, Albo M, Kraus S, et al. Predictors of treatment failure 24 months after surgery for stress urinary incontinence. Journal of Urology 2008;179(3):1024‐30. [sr‐incont27213] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richter HE, Kenton K, Huang L, Nygaard I, Kraus S, Whitcomb E, et al. The impact of obesity on urinary incontinence symptoms, severity, urodynamic characteristics and quality of life. Journal of Urology 2010;183(2):622‐8. [NCT00064662; NCT00325039; sr‐incont49290] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steers WD. Randomized clinical trial of the Burch modified Tanagho and autologous fascia sling procedures for women with predominantly stress urinary incontinence (Trial registration number: NCT00064662). http://clinicaltrials.gov/show/NCT00064662 2002. [NCT00064662; sr‐incont49815]
- Subak LL, Brubaker L, Chai TC, Creasman JM, Diokno AC, Goode PS, et al. High costs of urinary incontinence among women electing surgery to treat stress incontinence. Obstetrics and Gynecology 2008;111(4):899‐907. [sr‐incont27122] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subak LL, Goode PS, Brubaker L, Kusek JW, Schembri M, Lukacz ES, et al. Urinary incontinence management costs are reduced following Burch or sling surgery for stress incontinence. American Journal of Obstetrics & Gynecology 2014;211(2):171‐7. [NCT00064662; sr‐incont62600] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tennstedt S, Borello‐France D, FitzGerlad MP, Goode P, Kraus S, Kusek J, et al. Identification of factors related to health‐related quality of life in women with stress urinary incontinence that may improve with surgical treatment (Abstract number 321). Proceedings of the 35th Annual International Continence Society (ICS), Montreal, 28 Aug ‐ 2 Sept. 2005. [sr‐incont21098]
- Tennstedt S, for the Urinary Incontinence Treatment Network (UITN). Design of the Stress Incontinence Surgical Treatment Efficacy Trial (SISTEr). Urology 2005;66(6):1213‐7. [sr‐incont21530] [DOI] [PubMed] [Google Scholar]
- Walsh LP, Zimmern PE, Pope N, Shariat SF, Urinary Inc. Comparison of the Q‐tip test and voiding cystourethrogram to assess urethral hypermobility among women enrolled in a randomized clinical trial of surgery for stress urinary incontinence. Journal of Urology 2006;176(2):646‐9, discussion 650. [sr‐incont22387] [DOI] [PubMed] [Google Scholar]
- Zimmern P, Nager CW, Albo M, FitzGerald MP, McDermott S, for the Urinary Incontinence Treatment Network (UITN). Interrater reliability of filling cystometrogram interpretation in a multicenter study. Journal of Urology 2006;175(6):2174‐7. [sr‐incont22424] [DOI] [PubMed] [Google Scholar]
- Zimmern P, for the Urinary Incontinence Treatment Network (UITN). Design of the SISTEr (Stress Incontinence Surgical Treatment Efficacy Trial) Study: A randomized surgical trial comparing Burch colposuspension and the autologous rectus fascia sling. A clinical trial of the NIH/NIDDK Urinary Incontinence Treatment Network (UITN). Progres en Urologie 2004;14(3 Suppl 3):26. [sr‐incont19780] [Google Scholar]
Ankardal 2001 {published data only}
- Ankardal M, Crafoord K, Ekerydh A, Ellstrom M, Franzen K, Olsson J‐H, et al. Burch colposuspension by laparoscopic or abdominal approach: report from a randomised study (Abstract number 302). Proceedings of the International Continence Society (ICS), 31st Annual Meeting, 18‐21 Sept, Seoul, Korea. 2001. [sr‐incont14383]
- Ankardal M, Ekerydh A, Crafoord K, Milsom I, Stjerndahl JH, Engh ME. A randomised trial comparing open Burch colposuspension using sutures with laparoscopic colposuspension using mesh and staples in women with stress urinary incontinence. BJOG: an International Journal of Obstetrics and Gynaecology 2004;111(9):974‐81. [sr‐incont17915] [DOI] [PubMed] [Google Scholar]
- Ankardal M, Jarbrink K, Milsom I, Heiwall B, Lausten‐Thomsen N, Ellstrom‐Engh M. Comparison of health care costs for open Burch colposuspension, laparoscopic colposuspension and tension‐free vaginal tape in the treatment of female urinary incontinence. Neurourology & Urodynamics 2007;26(6):761‐6. [sr‐incont23845] [DOI] [PubMed] [Google Scholar]
- Ankardal M, Milsom I, Stjerndahl JH, Engh ME. A three‐armed randomized trial comparing open Burch colposuspension using sutures with laparoscopic colposuspension using sutures and laparoscopic colposuspension using mesh and staples in women with stress urinary incontinence. Acta Obstetricia et Gynecologica Scandinavica 2005;84(8):773‐9. [sr‐incont20624] [DOI] [PubMed] [Google Scholar]
Athanassopoulos 1996 {published data only}
- Athanasopoulos A, Liatsikos EN, Perimenis P, Barbalias GA. Female stress urinary incontinence: predictive factors for the operative correction (Abstract). International Urogynecology Journal and Pelvic Floor Dysfunction. 10 1999; Vol. 10, issue Suppl 1:S140. [sr‐incont9840]
- Athanassopoulos A, Barbalias G. Burch colposuspension versus Stamey endoscopic bladder neck suspension: a urodynamic appraisal. Urologia Internationalis 1996;56(1):23‐7. [sr‐incont4816] [DOI] [PubMed] [Google Scholar]
Bai 2005 {published data only}
- Bai SW, Sohn WH, Chung DJ, Park JH, Kim SK. Comparison of the efficacy of Burch colposuspension, pubovaginal sling, and tension‐free vaginal tape for stress urinary incontinence. International Journal of Gynaecology and Obstetrics 2005;91(3):246‐51. [sr‐incont21260] [DOI] [PubMed] [Google Scholar]
Bandarian 2011 {published data only}
- Bandarian M, Ghanbari Z, Asgari A. Comparison of transobturator tape (TOT) vs Burch method in treatment of stress urinary incontinence. Journal of Obstetrics and Gynaecology 2011;31(6):518‐20. [sr‐incont41697] [DOI] [PubMed] [Google Scholar]
Berglund 1996 {published data only}
- Berglund AL, Eisemann M, Lalos A, Lalos O. Predictive factors of the outcome of primary surgical treatment of stress incontinence in women. Scandinavian Journal of Urology and Nephrology 1997;31(1):49‐55. [sr‐incont5650] [DOI] [PubMed] [Google Scholar]
- Berglund AL, Lalos O. The pre‐ and postsurgical nursing of women with stress incontinence. Journal of Advanced Nursing 1996;23(3):502‐11. [sr‐incont2794] [DOI] [PubMed] [Google Scholar]
- Lalos O, Berglund AL, Bjerle P. The long‐term outcome of retropubic urethrocystopexy (sutures and fibrin sealant) and pubococcygeal repair. Acta Obstetricia et Gynecologica Scandinavica 2000;79(2):135‐9. [sr‐incont12900] [DOI] [PubMed] [Google Scholar]
- Lalos O, Bergmund AL, Bjerle P. Urodynamics in women with stress incontinence before and after surgery. European Journal of Obstetrics, Gynecology, and Reproductive Biology 1993;48:197‐205. [sr‐incont4948] [DOI] [PubMed] [Google Scholar]
Bergman 1989a {published data only}
- Bergman A, Ballard CA, Koonings PP. Primary stress urinary incontinence and pelvic relaxation: prospective randomized comparison of 3 different operations (Abstract). Neurourology and Urodynamics 1989; Vol. 8, issue 4:334‐5. [sr‐incont4512] [DOI] [PubMed]
- Bergman A, Koonings PP, Ballard CA. Primary stress urinary incontinence and pelvic relaxation: prospective randomized comparison of three different operations. American Journal of Obstetrics and Gynecology 1989;161(1):97‐101. [sr‐incont444] [DOI] [PubMed] [Google Scholar]
- Klutke JJ, Klutke CG, Bergman J, Elia G. Urodynamic changes in voiding after anti‐incontinence surgery: an insight into the mechanism of cure. Urology 1999;54(6):1003‐7. [sr‐incont9121] [DOI] [PubMed] [Google Scholar]
Bergman 1989b {published data only}
- Bergman A, Ballard CA, Koonings PP. Comparison of three different surgical procedures for genuine stress incontinence: prospective randomized study. American Journal of Obstetrics and Gynecology 1989;160(5 Pt 1):1102‐6. [sr‐incont450] [DOI] [PubMed] [Google Scholar]
- Bergman A, Elia G. Three surgical procedures for genuine stress incontinence: five‐year follow‐up of a prospective randomized study. American Journal of Obstetrics and Gynecology 1995;173(1):66‐71. [sr‐incont2962] [DOI] [PubMed] [Google Scholar]
- Elia G, Bergman A. Prospective randomized comparison of 3 surgical procedures for stress urinary incontinence: five‐year follow‐up (Abstract). Neurourology and Urodynamics 1994; Vol. 13, issue 4:498‐500. [sr‐incont2685]
Burton 1994 {published data only}
- Burton G. A five year prospective randomised urodynamic study comparing open and laparoscopic colposuspension (Abstract). International Urogynecology Journal and Pelvic Floor Dysfunction 1999; Vol. 10, issue Suppl 1:S44‐5. [sr‐incont9841]
- Burton G. A five year prospective randomised urodynamic study comparing open and laparoscopic colposuspension (Abstract). Neurourology and Urodynamics 1999;18(4):295‐6. [sr‐incont9875] [Google Scholar]
- Burton G. A randomised comparison of laparoscopic and open colposuspension (Abstract). Neurourology and Urodynamics. 13 1994; Vol. 13, issue 4:497‐8. [sr‐incont2684]
- Burton G. A three year prospective randomised urodynamic study comparing open and laparoscopic colposuspension (Abstract). Neurourology and Urodynamics 1997; Vol. 16, issue 5:353‐4. [sr‐incont5836]
Carey 2000 {published data only}
- Carey M, Maher C, Rosamilia A, Cornish A, Ugoni A. Open or laparoscopic colposuspension ‐ a prospective single blinded randomised control trial (Abstract). Proceedings of the Annual Meeting of the Royal Australian and New Zealand College of Obstetrics and Gynaecology (RANZCOG), July, Cairns. 2000. [sr‐incont12089]
- Carey M, Rosamilia A, Maher C, Cornish A, Murray C, Ugoni A, et al. Laparoscopic versus open colposuspension: A prospective multi‐centre randomised single‐blind comparison (Abstract). Neurourology and Urodynamics 2000; Vol. 19, issue 4:389‐91. [sr‐incont9868]
- Carey MP, Goh JT, Rosamilia A, Cornish A, Gordon I, Hawthorne G, et al. Laparoscopic versus open Burch colposuspension: a randomised controlled trial. BJOG: an International Journal of Obstetrics & Gynaecology 2006;113(9):999‐1006. [sr‐incont22334] [DOI] [PubMed] [Google Scholar]
- Carey MP, Maher CF, Rosamilia A, Cornish A, Murray C, Moran P, et al. Laparoscopic versus open colposuspension: early results of a single blind prospective randomized control trial (Abstract number 532). Proceedings of the International Continence Society (ICS), 29th Annual Meeting, 23‐29 Aug, Denver, Colorado. 1999:224‐5. [sr‐incont8023]
- Carey MP, Rosamilia A, Maher C, Tsaltas J. Laparoscopic versus open colposuspension ‐ results of a single blind prospective randomized control trial. IX Annual Scientific Meeting of the Australian Gynaecological Endoscopic Society 99, Adelaide, Australia. 1999:51. [sr‐incont18194]
- Cornish A, Carey M. Laparoscopic versus open colposuspension for women with stress urinary incontinence: A prospective multicentre randomised single blind comparison of urodynamic cure of stress urinary incontinence at 6 months following surgery. http://www.anzctr.org.au/ACTRN12605000439640.aspx (accessed 5 May 2015) 2005. [ACTRN12605000439640; sr‐incont64630]
Colombo 1994 {published data only}
- Colombo M, Scalambrino S, Maggioni A, Milani R. Burch colposuspension versus modified Marshall‐Marchetti‐Krantz urethropexy for primary genuine stress urinary incontinence: a prospective, randomized clinical trial. American Journal of Obstetrics and Gynecology 1994;171(6):1573‐9. [sr‐incont3125] [DOI] [PubMed] [Google Scholar]
- Milani R, Maggioni A, Colombo M, Pisani G, Quinto M. Burch colposuspension versus modified Marshall‐Marchetti‐Krantz for stress urinary incontinence: A controlled clinical study (Abstract). Neurology and Urodynamics 1991;10(4):454‐5. [sr‐incont4661] [Google Scholar]
Colombo 1996 {published data only}
- Colombo M, Milani R, Vitobello D, Maggioni A. A randomized comparison of Burch colposuspension and abdominal paravaginal defect repair for female stress urinary incontinence. American Journal of Obstetrics and Gynecology 1996;175(1):78‐84. [sr‐incont2756] [DOI] [PubMed] [Google Scholar]
- Milani R, Vitobello D, Teruzzi M, Colombo M. Comparison of Burch colposuspension and paravaginal defect repair for patients with genuine stress urinary incontinence (Abstract). Proceedings of the International Continence Society (ICS), 25th Annual Meeting, 17‐20 Oct, Sydney, Australia. 1995:475. [sr‐incont9866]
Colombo 2000 {published data only}
- Colombo M, Vitobello D, Proietti F, Milani R. Randomised comparison of Burch colposuspension versus anterior colporrhaphy in women with stress urinary incontinence and anterior vaginal wall prolapse. British Journal of Obstetrics and Gynaecology 2000;107(4):544‐51. [sr‐incont8978] [DOI] [PubMed] [Google Scholar]
Corcos 2001 {published data only}
- Corcos J, Collet JP, Shapiro S, Herschorn S, Radomski SB, Schick E, et al. Multicenter randomized clinical trial comparing surgery and collagen injections for treatment of female stress urinary incontinence. Urology 2005;65(5):898‐904. [sr‐incont20346] [DOI] [PubMed] [Google Scholar]
- Corcos J, Collet JP, Shapiro S, Schick E, Macramallah E, Tessier J, et al. Surgery vs collagen for the treatment of female stress urinary incontinence (SUI): results of a multicentric randomized trial (Abstract). Journal of Urology 2001;165(5 Suppl):198. [sr‐incont12912] [Google Scholar]
- Oremus M, Tarride JE. An economic evaluation of surgery versus collagen injection for the treatment of female stress urinary incontinence. Canadian Journal of Urology 2010;17(2):5087‐93. [sr‐incont39605] [PubMed] [Google Scholar]
Demirci 2001 {published data only}
- Demirci F, Yucel O. Comparison of free rectus fascial sling and Burch colposuspension procedures in type I and type II genuine stress incontinence (Abstract). International Urogynecology Journal and Pelvic Floor Dysfunction 2000;11(Suppl 1):S48. [sr‐incont13419] [Google Scholar]
- Demirci F, Yucel O. Comparison of pubovaginal sling and Burch colposuspension procedures in type I/II genuine stress incontinence. Archives of Gynecology and Obstetrics 2001;265(4):190‐4. [sr‐incont13079] [DOI] [PubMed] [Google Scholar]
Drahoradova 2004 {published data only}
- Drahoradova P, Masata J, Martan A, Svabik K. Comparative development of quality of life between TVT and Burch colposuspension (Abstract). Proceedings of the International Continence Society (34th Annual Meeting) and the International UroGynecological Association, 23‐27 August, 2004, Paris. 2004:Abstract number 278. [sr‐incont19049]
El Barky 2005 {published data only}
- Barky E, Shazly A, Wahab OA, Kehinde EO, Al Hunayan A, Al Awadi KA. Tension free vaginal tape versus Burch colposuspension for treatment of female stress urinary incontinence. International Urology and Nephrology 2005;37(2):277‐81. [sr‐incont20774] [DOI] [PubMed] [Google Scholar]
El‐Din Shawki 2012 {published data only}
- El‐Din Shawki H, Kamel HH, El‐Moghazy DA, El‐Adawy AR, Mohammed HF. The role of transobturator vaginal tape (TVT‐O) and some traditional surgical interventions in the management of female genuine stress urinary incontinence ‐ randomized controlled trial (Abstract number 0217). International Journal of Gynaecology and Obstetrics 2012;119(Suppl 3):S337. [sr‐incont62241] [Google Scholar]
Elshawaf 2009 {published data only}
- Elshawaf H, Al bahaie Y. Randomized prospective trial comparing Burch colposuspension to tension free vaginal tape and transobturator suburethral tape procedures in treating female genuine stress urinary incontinence (Abstract number 857). Proceedings of the 39th Annual Meeting of the International Continence Society (ICS), 2009 Sep 29 ‐ Oct 3, San Francisco, CA 2009. [sr‐incont35631]
Enzelsberger 1996 {published data only}
- Enzelsberger H, Helmer H, Schatten C. Comparison of Burch and lyodura sling procedures for repair of unsuccessful incontinence surgery. Obstetrics and Gynecology 1996;88(2):251‐6. [sr‐incont2759] [DOI] [PubMed] [Google Scholar]
- Enzelsberger H, Kurz C, Seifert M, Raimann H, Schatten C. Surgical treatment of recurrent stress incontinence: Burch versus lyodura sling operation ‐ a prospective study [Zur operativen Behandlung der RezidivstreBinkontinenz: Burch versus Lyoduraschlingeoperation ‐ eine prospektive studie]. Geburtshilfe und Frauenheilkunde 1993;53(7):467‐71. [sr‐incont100] [DOI] [PubMed] [Google Scholar]
Fatthy 2001 {published data only}
- Fatthy H, Hao M, Samaha I, Abdallah K. Modified Burch colposuspension: laparoscopy versus laparotomy. Journal of the American Association of Gynecologic Laparoscopists 2001;8(1):99‐106. [sr‐incont11967] [DOI] [PubMed] [Google Scholar]
Fischer 2001 {published data only}
- Fischer JR, Hale DS, McClellan E, Benson JT. The use of urethral electrodiagnosis to select the method of surgery in women with intrinsic sphincter deficiency (Abstract). International Urogynecology Journal and Pelvic Floor Dysfunction 2001;12(Suppl 1):S33. [sr‐incont12008] [Google Scholar]
German 1994 {published data only}
- German K, Goodman C, Haynes R, Stephenson TP. A randomised trial comparing a modified needle suspension procedure with the vagina/obturator shelf procedure for genuine stress incontinence (Abstract 256). Proceedings of the International Continence Society (ICS), 22nd Annual Meeting, 1‐4 Sept, Halifax, UK. 1992. [sr‐incont12071]
- German KA, Kynaston H, Weight S, Stephenson TP. A prospective randomized trial comparing a modified needle suspension procedure with the vagina/obturator shelf procedure for genuine stress incontinence. British Journal of Urology 1994;74(2):188‐90. [sr‐incont2104] [DOI] [PubMed] [Google Scholar]
Gilja 1998 {published data only}
- Gilja I, Puskar D, Mazuran B, Radej M. Comparative analysis of bladder neck suspension using Raz, Burch and transvaginal Burch procedures. A 3‐year randomized prospective study. European Urology 1998;33:298‐302. [sr‐incont5872] [DOI] [PubMed] [Google Scholar]
Halaska 2001 {published data only}
- Halaska M, Kolbl H, Petri E, Danes L, Voigt R, Otcenasek M, et al. Preliminary results of a prospective randomized study comparing Burch colposuspension and tension‐free vaginal tape ‐ urodynamic and sexuological aspects (Abstract). Neurourology and Urodynamics 2001;20(4):421‐2. [sr‐incont12128] [Google Scholar]
Han 2001 {published data only}
- Han WHC. Burch colposuspension or tension‐free vaginal tape for female stress urinary incontinence? (Abstract). International Urogynecology Journal and Pelvic Floor Dysfunction 2001;12(Suppl 3):S23. [sr‐incont12580] [Google Scholar]
Henriksson 1978 {published data only}
- Henriksson L, Asmussen M, Löfgren O, Ulmsten U. A urodynamic comparison between abdominal urethrocystopexy and vaginal sling plasty in female stress incontinence. Urologia Internationalis 1978;33:111‐6. [sr‐incont5152] [Google Scholar]
- Henriksson L, Ulmsten U. A urodynamic evaluation of the effects of abdominal urethrocystopexy and vaginal sling urethroplasty in women with stress incontinence. American Journal of Obstetrics and Gynecology 1978;131(1):77‐82. [sr‐incont2670] [DOI] [PubMed] [Google Scholar]
Holmes 1985 {published and unpublished data}
- Holmes D, Stanton S, Chamberlain GVP. Randomised trial to compare the colposuspension with the anterior repair in the management of genuine stress incontinence. Personal communication 1985. [sr‐incont9859]
- Stanton SL, Chamberlain G, Holmes DM. The anterior repair or colposuspension for the cure of stress incontinence due to urethral sphincter incompetence. A randomised study (Abstract). Proceedings of the 24th British Congress of Obstetrics and Gynaecology. 1986:156. [sr‐incont8016]
- Stanton SL, Chamberlain GVP, Holmes DM. Randomised study of the anterior repair and colposuspension operation in the control of genuine stress incontinence (Abstract). Proceedings of the International Continence Society (ICS),15th Annual Meeting, 1985 Sep 3‐6, London, UK. 1985:236‐7. [sr‐incont5145]
- Stanton SL, Chamberlain GVP, Holmes DM. The control of stress incontinence: comparison of anterior colporrhaphy and colposuspension (Abstract). Archives of Gynecology 1985;237 Suppl:401‐2. [sr‐incont9858] [Google Scholar]
Kammerer‐Doak 1999 {published data only}
- Kammerer‐Doak DN, Dorin MH, Rogers RG, Cousin MO. A randomized trial of Burch retropubic urethropexy and anterior colporrhaphy for stress urinary incontinence. Obstetrics and Gynecology 1999;93(1):75‐8. [sr‐incont8256] [DOI] [PubMed] [Google Scholar]
Kitchener 2006 {published data only}
- Dumville JC, Manca A, Kitchener HC, Smith AR, Nelson L, Torgerson DJ, COLPO Study Group. Cost‐effectiveness analysis of open colposuspension versus laparoscopic colposuspension in the treatment of urodynamic stress incontinence. BJOG: an International Journal of Obstetrics and Gynaecology 2006;113(9):1014‐22. [sr‐incont22332] [DOI] [PubMed] [Google Scholar]
- Kitchener HC. A randomised trial of open versus laparoscopic colposuspension for genuine stress incontinence (MRC COLPO Trial). http://isrctn.org/ISRCTN14969683 (accessed 5 May 2015) 2000. [sr‐incont16345]
- Kitchener HC, Dunn G, Lawton V, Reid F, Nelson L, Smith AR, COLPO Study Group. Laparoscopic versus open colposuspension‐‐results of a prospective randomised controlled trial. BJOG: an International Journal of Obstetrics and Gynaecology 2006;113(9):1007‐13. [sr‐incont22333] [DOI] [PubMed] [Google Scholar]
- Smith A, Kitchener H, Dunne G, Torgerson D, Lawton V, Reid F, Ali N. A prospective randomised controlled trial of open and laparoscopic colposuspension (Abstract). Neurourology and Urodynamics 2005;24(5/6):422‐3. [sr‐incont20986] [Google Scholar]
Klarskov 1986 {published data only}
- Klarskov P, Belving D, Bischoff N, Dorph S, Gerstenberg T, Hald T, et al. Pelvic floor exercise versus surgery for female urinary stress incontinence: preliminary results (Abstract). Proceedings of the International Continence Society (ICS), 14th Annual Meeting, Sept, Innsbruck, Austria. 1984:159. [sr‐incont9874]
- Klarskov P, Belving D, Bischoff N, Dorph S, Gerstenberg T, Okholm B, et al. Pelvic floor exercise versus surgery for female urinary stress incontinence. Urologia Internationalis 1986;41(2):129‐32. [sr‐incont592] [DOI] [PubMed] [Google Scholar]
- Klarskov P, Kroyer K, Kromann B, Maegaard E. Long term results of pelvic floor training and surgery for female genuine stress incontinence (Abstract). Neurourology and Urodynamics. 8 1989; Vol. 8, issue 4:357‐9. [sr‐incont4516]
- Klarskov P, Nielson KK, Kromann‐Andersen B, Maegaard E. Long term results of pelvic floor training and surgery to female genuine stress incontinence. International Urogynaecology Journal 1991;2:132‐5. [sr‐incont6655] [Google Scholar]
- Klarskov P, Vedel Jepsen P, Dorph S. Reliability of voiding colpocystourethrography in female urinary stress incontinence before and after treatment. Acta Radiologica 1988;29:685‐8. [sr‐incont469] [PubMed] [Google Scholar]
Koelbl 2002 {published data only}
- Koelbl H, Halaska M, Ostermann S, Lautenschlaeger C. Burch colposuspension and TVT ‐ perioperative results of a prospective randomized trial in patients with genuine stress incontinence (Abstract). Neurourology and Urodynamics 2002;21(4):327. [sr‐incont14541] [Google Scholar]
Liapis 1996 {published data only}
- Liapis A, Pyrgiotis E, Kontoravdis A, Louridas C, Zourlas PA. Genuine stress incontinence: prospective randomized comparison of two operative methods. European Journal of Obstetrics, Gynecology, and Reproductive Biology 1996;64(1):69‐72. [sr‐incont2723] [DOI] [PubMed] [Google Scholar]
- Liapis AE, Asimiadis V, Loghis CD, Pyrgiotis E, Zourlas PA. A randomized prospective study of three operative methods for genuine stress incontinence. Journal of Gynecologic Surgery 1996;12(1):7‐14. [sr‐incont4537] [Google Scholar]
Liapis 2002 {published data only}
- Liapis A, Bakas P, Creatsas G. Burch colposuspension and tension‐free vaginal tape in the management of stress urinary incontinence in women. European Urology 2002;41(4):469‐73. [sr‐incont14229] [DOI] [PubMed] [Google Scholar]
- Liapis A, Bakas P, Creatsas G. Comparison of open retropubic colposuspension with tension‐free vaginal tape for the treatment of genuine stress incontinence in women (Abstract). Neurourology and Urodynamics 2000;19(4):385‐6. [sr‐incont9872] [Google Scholar]
Mak 2000 {published data only}
- Cheon WC, Mak JH, Liu JY. Prospective randomised controlled trial comparing laparoscopic and open colposuspension. Hong Kong Medical Journal 2003;9(1):10‐4. [sr‐incont15758] [PubMed] [Google Scholar]
- Mak JHL, Cheon CW, Liu JYS, Lee TK, Tong WM, Wong THK. Prospective randomized controlled trial comparing laparoscopic and open colposuspension (Abstract). Proceedings of the Asian Society for Female Urology, 2nd Scientific Meeting, 26‐27 Aug, Hong Kong. 2000:59‐61. [sr‐incont12120]
McCrery 2005 {published data only}
- McCrery RJ, Thompson PK. Outcomes of urethropexy added to paravaginal defect repair: a randomized trial of Burch versus Marshall‐Marchetti‐Krantz. Journal of Pelvic Medicine & Surgery 2005;11(3):137‐43. [sr‐incont22982] [Google Scholar]
Morris 2001 {published data only}
- Morris AR, Reilly ETC, Hassan A, Ramsay IN, Hawthorn RJS. 5‐7 year follow‐up of a randomised trial comparing laparoscopic colposuspension (LC) and open colposuspension (OC) in the treatment of genuine stress incontinence (Abstract). International Urogynecology Journal and Pelvic Floor Dysfunction 2001;12(Suppl 3):S6. [sr‐incont12582] [Google Scholar]
Mundy 1983 {published data only}
- Mundy AR. A trial comparing the Stamey bladder neck suspension procedure with colposuspension for the treatment of stress incontinence. British Journal of Urology 1983;55(6):687‐90. [sr‐incont672] [DOI] [PubMed] [Google Scholar]
O'Sullivan 2000 {published data only}
- O'Sullivan S, Avery N, Balley A, Keane D. The effect of surgery on the collagen metabolism of paraurethral tissue in women with genuine stress incontinence (Abstract O10). International Urogynaecology Journal 2000;11 Suppl 1:S5. [sr‐incont11903] [Google Scholar]
Osman 2003 {published data only}
- Osman T. Stress incontinence surgery for patients presenting with mixed incontinence and a normal cystometrogram. BJU International 2003;92(9):964‐8. [sr‐incont16660] [DOI] [PubMed] [Google Scholar]
Palma 1985 {published data only}
- Palma P, David S, Pinotti JA. Comparative study between the Marshall‐Marchetti‐Krantz operation and the endoscopic suspension of the bladder neck for surgical correction of stress urinary incontinence (Abstract). Archives of Gynecology 1985;237 Suppl:402. [sr‐incont9864] [Google Scholar]
- Palma PC, Soffiatti SA, Almeida SC, Pinotti JA. Stress urinary incontinence: a comparative study of surgical treatment by the Marshall‐Marchetti‐Krantz technique with endoscopic suspension of the bladder neck. Second report. Asia Oceania Journal of Obstetrics and Gynaecology 1988;14(1):31‐6. [sr‐incont15461] [DOI] [PubMed] [Google Scholar]
- Palma PCR, Suely A, Soffiatti D, Pinotti JA. Stress urinary incontinence: a comparative study of the surgical treatment by the Marshall‐Marchetti‐Krantz technique with endoscopic suspension of the bladder neck. Second report. Ginecologia and Obstetricia (Sociedad Peruana de Obstetricia y Ginecologia) 1986;30(2):15‐9. [sr‐incont15464] [Google Scholar]
Quadri 1985 {published data only}
- Colombo M, Scalambrino S, Gallazzi S, Milani R. Burch colposuspension versus anterior repair in severe genital prolapse with stress incontinence: long term follow‐up (Abstract number 174). Proceedings of the International Continence Society, 23rd Annual Meeting, 1993 Sep 8‐11, Rome, Italy. 1993:440‐2. [sr‐incont12045]
- Milani R, Scalambrino S, Vicandone G, Sirtori P, Spazzini D. Complementary drug therapy improving results of surgery for incontinence and prolapse into two randomized procedures: vaginal versus suprapubic operation (Abstract). Proceedings of the International Continence Society (ICS), 14th Annual Meeting, Sept, Innsbruck, Austria. 1984:440‐1. [sr‐incont9867]
- Quadri G, Scalambrino S, Boisio N, Marchesin R, Milani R. Randomized surgery for incontinence and prolapse: Retropubic colposuspension vs anterior repair (Abstract). Archives of Gynecology 1985;237 Suppl:402. [sr‐incont8019] [Google Scholar]
- Scalambrino S, Biosio N, Marchesin R, Quadri G, Alegri M, Milani R. Clinical and urodynamic results in a surgical trial for incontinence and prolapse (Abstract). Proceedings of the International Continence Society (ICS), 15th Annual Meeting, 3‐6 Sept, London, UK. 1985:484‐5. [sr‐incont9865]
Quadri 1999 {published data only}
- Quadri G, Magatti F, Belloni C, Barisani D, Natale N. Marshall‐Marchetti‐Krantz urethropexy and Burch colposuspension for stress urinary incontinence in women with low pressure and hypermobility of the urethra: early results of a prospective randomized clinical trial. American Journal of Obstetrics and Gynecology 1999;181(1):12‐8. [sr‐incont8864] [DOI] [PubMed] [Google Scholar]
Sand 2000 {published data only}
- Culligan PJ, Goldberg RP, Sand PK. A randomized controlled trial comparing a modified Burch procedure and a suburethral sling: long‐term follow‐up. International Urogynecology Journal 2003;14(4):229‐33. [sr‐incont16706] [DOI] [PubMed] [Google Scholar]
- Culligan PJ, Winkler HA, Blackhurst DW, Sand PK. A prospective randomized study of modified Burch retropubic urethropexy and suburethral sling for genuine stress incontinence and low pressure urethra. Proceedings of the International Continence Society (ICS), 28th Annual Meeting, 1998 Sep 14‐17, Jerusalem, Israel. 1998:133. [sr‐incont5689]
- Goldberg RP, Culligan PJ, Koduri S, Sand PK. A prospective randomized study comparing modified Burch retropubic urethropexy and suburethral sling: long term follow‐up (Abstract). International Urogynaecology Journal 2000;11(Suppl 1):S8. [sr‐incont11904] [Google Scholar]
- Goldberg RP, Sand PK, Koduri S, Culligan PJ. A prospective randomized study comparing modified Burch retropubic urethropexy and suburethral sling: long term follow‐up (Abstract). International Urogynecology Journal and Pelvic Floor Dysfunction 2001;12(Suppl 1):S6. [sr‐incont12004] [Google Scholar]
- Sand PK, Winkler H, Blackhurst DW, Culligan PJ. A prospective randomized study comparing modified Burch retropubic urethropexy and suburethral sling for treatment of genuine stress incontinence with low‐pressure urethra. American Journal of Obstetrics and Gynecology 2000;182(1 Pt 1):30‐4. [sr‐incont9013] [DOI] [PubMed] [Google Scholar]
Sivaslioglu 2007 {published data only}
- Sivaslioglu AA, Caliskan E, Dolen I, Haberal A. A randomized comparison of transobturator tape and Burch colposuspension in the treatment of female stress urinary incontinence. International Urogynecology Journal 2007;18(9):1015‐9. [sr‐incont23854] [DOI] [PubMed] [Google Scholar]
Stangel‐Wojcikiewicz 2008 {published data only}
- Stangel‐Wojcikiewicz K. Laparoscopic Burch colposuspension compared to laparotomy for treatment urinary stress incontinence (Abstract number 121). Neurourology and Urodynamics 2008;27(7):714. [sr‐incont31857] [Google Scholar]
Su 1997 {published data only}
- Su TH, Wang KG, Hsu CY, Wei HJ, Hong BK. Prospective comparison of laparoscopic and traditional colposuspensions in the treatment of genuine stress incontinence. Acta Obstetricia et Gynecologica Scandinavica 1997;76:576‐82. [sr‐incont5558] [DOI] [PubMed] [Google Scholar]
Summitt 2000 {published data only}
- Summitt RL, Lucente V, Karram MM, Shull BL, Bent AE. Randomized comparison of laparoscopic and transabdominal Burch urethropexy for the treatment of genuine stress incontinence (Abstract). Obstetrics and Gynecology 2000;95(4):S2. [sr‐incont11862] [Google Scholar]
Tapp 1989 {published data only}
- Tapp AJS, Hills B, Cardozo L. Pelvic floor physiotherapy compared with the Burch colposuspension in the treatment of genuine stress incontinence. Proceedings of the Silver Jubilee British Congress of Obstetrics and Gynaecology. 1989:65. [sr‐incont8015]
- Tapp AJS, Hills B, Cardozo L, Tapp AJ. Randomised study comparing pelvic floor physiotherapy with the Burch colposuspension. Neurourology and Urodynamics 1989;8:356‐7. [sr‐incont4515] [Google Scholar]
Tellez Martinez‐Fornes 2009 {published data only}
- Tellez Martinez‐Fornes M. A Three Year Follow‐up Prospective Open Randomized Trial of Tension‐Free Vaginal Tape and Colposuspension for Primary Urodynamic Stress Incontinence. http://clinicaltrials.gov/show/NCT00782990 (accessed 5 May 2015) 2001. [sr‐incont62910]
- Tellez Martinez‐Fornes M, Fernandez Perez C, Fouz Lopez C, Fernandez Lucas C, Borrego Hernando J. A three year follow‐up of a prospective open randomized trial to compare tension‐free vaginal tape with Burch colposuspension for treatment of female stress urinary incontinence. Actas Urologicas Espanolas 2009;33(10):1088‐96. [sr‐incont39608] [PubMed] [Google Scholar]
Trabuco 2014 {published data only}
- Trabuco E, Klingele C, Blandon R, Occhino J, McGree M, Weaver A, et al. A randomized comparison of incontinence procedures performed concomitantly with abdominal sacrocolpopexy: the Burch versus mid‐urethral sling trial (Abstract number 689). Neurourology and Urodynamics 2014;33(6):1005. [NCT00934999; sr‐incont64705] [Google Scholar]
Tuygun 2006 {published data only}
- Tuygun C, Bakirtas H, Eroglu M, Alisir I, Zengin K, Imamoglu A. Comparison of two different surgical approaches in the treatment of stress urinary incontinence: Open and laparoscopic Burch colposuspension. Turk Uroloji Dergisi 2006;32(2):248‐53. [sr‐incont26724] [Google Scholar]
Ustun 2005 {published data only}
- Ustun Y, Engin‐Ustun Y, Gungor M, Tezcan S. Randomized comparison of Burch urethropexy procedures concomitant with gynecologic operations. Gynecologic and Obstetric Investigation 2005;59(1):19‐23. [sr‐incont20187] [DOI] [PubMed] [Google Scholar]
Wang 2003 {published data only}
- Wang AC, Chen MC. Comparison of tension‐free vaginal taping versus modified Burch colposuspension on urethral obstruction: a randomized controlled trial. Neurourology and Urodynamics 2003;22(3):185‐90. [sr‐incont16021] [DOI] [PubMed] [Google Scholar]
- Wang AC, Liang CC, Lo TS, Tseng LH. Does tension‐free vaginal tape procedure really exert no tension on the urethra? ‐ A randomized controlled study using the voiding mechanism (Abstract). International Urogynecology Journal 2001;12(Suppl 3):S111. [sr‐incont15459] [Google Scholar]
Ward 2002 {published and unpublished data}
- Abrams P, Martin K, Bulmer P, Donovan J, Hilton P. Responsiveness of the Bristol female lower urinary tract symptoms questionnaire (BFLUTS‐Q) to surgical intervention in a randomised controlled trial (Abstract). Proceedings of the International Continence Society (ICS), 30th Annual Meeting, 28‐31 Aug, Tampere, Finland. 2000:A173. [sr‐incont9954]
- Brookes ST, Donovan JL, Wright M, Jackson S, Abrams P. A scored form of the Bristol Female Lower Urinary Tract Symptoms questionnaire: data from a randomized controlled trial of surgery for women with stress incontinence. American Journal of Obstetrics and Gynecology 2004;191(1):73‐82. [sr‐incont19277] [DOI] [PubMed] [Google Scholar]
- Manca A, Sculpher MJ, Ward K, Hilton P. A cost‐utility analysis of tension‐free vaginal tape (TVT) versus colposuspension for primary genuine stress incontinence (unpublished material). Personal communication 2002. [sr‐incont12892]
- Manca A, Sculpher MJ, Ward K, Hilton P. A cost‐utility analysis of tension‐free vaginal tape versus colposuspension for primary urodynamic stress incontinence. BJOG: an International Journal of Obstetrics and Gynaecology 2003;110:255‐62. [sr‐incont14361] [PubMed] [Google Scholar]
- Sculpher MJ, Ward KL, Hilton P. A comparison of the hospital cost of tension‐free vaginal tape and colposuspension (Abstract). Proceedings of the International Continence Society (ICS), 30th Annual Meeting, 28‐31 Aug, Tampere, Finland. 2000:333‐4. [sr‐incont9871]
- Ward K, Hilton P. Multicentre randomised trial of tension‐free vaginal tape and colposuspension for primary urodynamic stress incontinence: five year follow up (Abstract number 50). Neurourology and Urodynamics 2006;25(6):568‐9. [23328] [Google Scholar]
- Ward K, Hilton P on behalf of the United Kingdom and Ireland Tension‐Free Vaginal Tape Trial Group. Prospective multicentre randomised trial of tension‐free vaginal tape and colposuspension as primary treatment for stress incontinence. BMJ 2002;325(7355):67‐73. [sr‐incont14365] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ward K, Hilton P, on behalf of the UK & Ireland TVT trial group. A randomised trial of colposuspension and 'TVT' TM for primary Genuine Stress Incontinence ‐ 2 year follow‐up (Revised Abstract). Personal communication only 2001. [sr‐incont12573]
- Ward K, Hilton P, on behalf of the UK & Ireland TVT trial group. A randomised trial of colposuspension and tension‐free vaginal tape (TVT) for primary genuine stress incontinence ‐ 2 yr follow‐up (Abstract). International Urogynecology Journal and Pelvic Floor Dysfunction. 12 2001; Vol. 12, issue Suppl 3:S7. [sr‐incont12574]
- Ward K, Hilton P, on behalf of the UK & Ireland TVT trial group. A randomised trial of tension‐free vaginal tape (TVT) and colposuspension for primary genuine stress incontinence (unpublished material). Personal communication 2002. [sr‐incont12891]
- Ward KL, Hilton P, Browning J. Urodynamic variables in a randomized comparison of colposuspension and tension‐free vaginal tape for primary genuine stress incontinence (Abstract). Neurourology and Urodynamics 2000;19(4):388‐9. [sr‐incont9870] [Google Scholar]
- Ward KL, Hilton P, Browning J on behalf of the UK and Ireland TVT Trial group. A randomized trial of colposuspension and tension‐free vaginal tape for primary genuine stress incontinence (Abstract). Neurourology and Urodynamics 2000;19(4):386‐8. [sr‐incont9869] [Google Scholar]
- Ward KL, Hilton P, Browning J, (on behalf of the UK and Ireland TVT Trial Group). Changes in quality of life following surgery with tension free vaginal tape (TVT) or colposuspension for primary genuine stress incontinence (Abstract). Proceedings of the International Continence Society (ICS), 30th Annual Meeting, 28‐31 Aug, Tampere, Finland. 2000:314. [sr‐incont14348]
- Ward KL, Hilton P, UK and Ireland TVT Trial Group. A prospective multicenter randomized trial of tension‐free vaginal tape and colposuspension for primary urodynamic stress incontinence: two‐year follow‐up. American Journal of Obstetrics and Gynecology 2004;190(2):324‐31. [sr‐incont17301] [DOI] [PubMed] [Google Scholar]
- Ward KL, Hilton P, UK and Ireland TVT Trial Group. Tension‐free vaginal tape versus colposuspension for primary urodynamic stress incontinence: 5‐year follow up. BJOG: an International Journal of Obstetrics and Gynaecology 2008;115(2):226‐33. [sr‐incont26268] [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Adile 2001 {published data only}
- Adile B, Liguori P, Pisapia G, Alvino G, Bova C. Tension‐free vaginal tape for surgical treatment of stress urinary incontinence. An Italian multicenter study and two year follow‐up. [Italian]. Urogynaecologia International Journal 2001;15(Suppl 1):68. [Google Scholar]
Adile 2001b {published data only}
- Adile B, Cucinella G, Gugliotta G, Lo BA, Grifo S, Caputo A. A prospective randomized study on Burch laparoscopy versus tension‐free vaginal tape: 2 year follow‐up. [Italian]. Urogynaecologia International Journal 2001;15(Suppl 1):121‐2. [Google Scholar]
Ankardal 2007 {published data only}
- Ankardal M, Jarbrink K, Milsom I, Heiwall B, Lausten‐Thomsen N, Ellstrom‐Engh M. Comparison of health care costs for open Burch colposuspension, laparoscopic colposuspension and tension‐free vaginal tape in the treatment of female urinary incontinence. Neurourology and Urodynamics 2007;26(6):761‐6. [DOI] [PubMed] [Google Scholar]
Baessler 1998 {published data only}
- Baessler K, Keller M, Draths R, Hohl MK, Schuessler B. Are there less voiding difficulties if a paravaginal repair is performed in addition to an abdominal colposuspension? ‐ Preliminary results of a randomised controlled trial (Abstract). Proceedings of the International Continence Society (ICS), 28th Annual Meeting, 14‐17 Sept, Jerusalem, Israel. 1998.
Barber 2002 {published data only}
- Barber MD, Visco AG, Wyman JF, Fantl JA, Bump RC, Continence Program for Women Research Group. Sexual function in women with urinary incontinence and pelvic organ prolapse. Obstetrics and Gynecology 2002;99(2):281‐9. [sr‐incont12932] [DOI] [PubMed] [Google Scholar]
Benson 1993 {published data only}
- Benson JT, McClellan E. The effect of vaginal dissection on the pudendal nerve. Obstetrics and Gynecology 1993;82(3):387‐9. [PubMed] [Google Scholar]
Benson 1996a {published data only}
- Benson JT, Lucente V, McClellan E. VAG vs ABD reconstructive pelvic surgery: a prospective randomised study with long term outcome evaluation (Abstract). Proceedings of the International Continence Society (ICS), 26th Annual Meeting, 27‐30 Aug, Athens,Greece. 1996:132.
Benson 1996b {published data only}
- Benson JT, Lucente V, McClellan E. Vaginal versus abdominal reconstructive surgery for the treatment of pelvic support defects: a prospective randomized study with long‐term outcome evaluation. American Journal of Obstetrics and Gynecology 1996;175(6):1418‐22. [DOI] [PubMed] [Google Scholar]
Bhatia 1985a {published data only}
- Bhatia NN, Bergman A. Modified Burch versus Pereyra retropubic urethropexy for stress urinary incontinence. Obstetrics and Gynecology 1985;66(2):255‐61. [PubMed] [Google Scholar]
Bhatia 1985b {published data only}
- Bhatia NN, Bergman A. Role of antibiotic prophylaxis in surgery for stress urinary incontinence (Abstract). Proceedings of the American Urogynecology Society, 6th Annual Meeting, Nov 6‐9, 1985, San Diego, California. 1985. [sr‐incont14559]
Brubaker 2002 {published data only}
- Bradley CS, Nygaard IE, Brown MB, Gutman RE, Kenton KS, Whitehead WE, et al. Bowel symptoms in women 1 year after sacrocolpopexy. American Journal of Obstetrics and Gynecology. 2007;197(6):642‐8. [DOI] [PubMed] [Google Scholar]
- Brubaker L. Colpopexy and urinary reduction efforts (CARE) protocol: a protocol of the pelvic floor disorders network. ClinicalTrials.gov (http://clinicaltrials.gov/show/NCT00065845) (accessed 5 May 2015) 2002. [sr‐incont15048; sr‐incont49823]
- Brubaker L, Cundiff G, Fine P, Nygaard I, Richter H, Visco A, et al. A randomized trial of colpopexy and urinary reduction efforts (CARE): design and methods. Controlled Clinical Trials 2003;24(5):629‐42. [sr‐incont16703] [DOI] [PubMed] [Google Scholar]
- Brubaker L, Cundiff GW, Fine P, Nygaard I, Richter HE, Visco AG, et al. Abdominal sacrocolpopexy with Burch colposuspension to reduce urinary stress incontinence. New England Journal of Medicine 13‐4‐2006;354(15):1557‐66. [sr‐incont21842] [DOI] [PubMed] [Google Scholar]
- Brubaker L, Pelvic Floor Disorders Network. The Colpopexy And urinary Reduction Efforts (CARE) trial: two year outcomes (Abstract number 5). Neurourology and Urodynamics 2007;26(5):608. [sr‐incont23531] [Google Scholar]
- Burgio KL, Nygaard IE, Richter HE, Brubaker L, Gutman RE, Leng W, et al. Bladder symptoms 1 year after abdominal sacrocolpopexy with and without Burch colposuspension in women without preoperative stress incontinence symptoms. American Journal of Obstetrics and Gynecology. 2007;197(6):647.e1‐6. [DOI] [PubMed] [Google Scholar]
- Nygaard I, Brubaker L, Zyczynski HM, Cundiff G, Richter H, Gantz M, et al. Long‐term outcomes following abdominal sacrocolpopexy for pelvic organ prolapse [Erratum appears in JAMA. 2013 Sep 11;310(10):1076]. JAMA : the journal of the American Medical Association 2013;309(19):2016‐24. [NCT00099372; TrialID.CARE.; sr‐incont47934] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nygaard I, Handa VL, Brubaker L, Borello‐France D, Wei J, Wells E, et al. Changes in physical activity after abdominal sacrocolpopexy for advanced pelvic organ prolapse. American Journal of Obstetrics and Gynecology. 2008;198(5):570‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Brubaker 2009 {published data only}
- Brubaker L, Chiang S, Zyczynski H, Norton P, Kalinoski DL, Stoddard A, et al. The impact of stress incontinence surgery on female sexual function. American Journal of Obstetrics & Gynecology. 2009;200(5):562.e1‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bump 1988 {published data only}
- Bump RC, Copeland WE, Hurt WG, Fantl JA. Dynamic urethral pressure/profilometry pressure transmission ratio determinations in stress‐incontinent and stress‐continent subjects. American Journal of Obstetrics and Gynecology 1988;159(3):749‐55. [DOI] [PubMed] [Google Scholar]
Bump 1995 {published data only}
- Bump RC, Hurt WG, Elser DM, Theofrastous JP, Fantl JA, McClish DK. Reliability of intra‐operative anatomic, endoscopic and urodynamic measurements and their correlation with post‐operative pressure transmission in women undergoing bladder neck suspension surgery. Neurourology and Urodynamics. 14 1995; Vol. 14, issue 5:490‐1.
Bump 1996 {published data only}
- Bump RC, Hurt WG, Theofrastous JP, Addison WA, Fantl JA, Wyman JF, et al. Randomized prospective comparison of needle colposuspension versus endopelvic fascia plication for potential stress incontinence prophylaxis in women undergoing vaginal reconstruction for stage III or IV pelvic organ prolapse. The Continence Program for Women Research Group. American Journal of Obstetrics and Gynecology 1996;175(2):326‐35. [DOI] [PubMed] [Google Scholar]
Byrne 1989 {published data only}
- Byrne P, Condie R, Shafi M. A comparison of the Burch colposuspension and Aldridge sling operation for the treatment of stress incontinence (Abstract). Proceedings of the International Continence Society (ICS), Louvain, Belgium. 1989.
Colombo 1997 {published data only}
- Colombo M, Maggioni A, Scalambrino S, Vitobello D, Milani R. Surgery for genitourinary prolapse and stress incontinence: a randomized trial of posterior pubourethral ligament plication and Pereyra suspension. American Journal of Obstetrics and Gynecology 1997;176(2):337‐43. [DOI] [PubMed] [Google Scholar]
Cornish 2001 {published data only}
- Cornish A, Fynes M, Harmer C, Hawthorne G, Rosamillia A, Carey M, et al. The genitourinary treatment satisfaction score for continence surgery (Abstract). Proceedings of the International Continence Society (ICS), 31st Annual Meeting, Seoul, Korea, 18‐21 Sept 2001. 2001:Abstract 83. [sr‐incont14493]
Costantini 2007a {published data only}
- Costantini E, Zucchi A, Giannantoni A, Mearini L, Bini V, Porena M. Must colposuspension be associated with sacropexy to prevent postoperative urinary incontinence?. European Urology 2007;51(3):788‐94. [sr‐incont22549] [DOI] [PubMed] [Google Scholar]
Costantini 2007b {published data only}
- Costantini E, Lazzeri M, Bini V, Zingaro M, Frumenzio E, Porena M. Pelvic organ prolapse repair with and without concomitant Burch colposuspension in incontinent women: a randomised controlled trial with at least 5‐year followup. Obstetrics and Gynecology International 2012;2012:Article ID 967923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costantini E, Lazzeri M, Giannantoni A, Zingaro M, Fioretti F, Zucchi A, et al. Abdominal integral pelvic reconstruction plus or minus Burch colposuspension in the treatment of severe uro‐genital prolapse associated to urinary incontinence. A RCT with a mid‐term follow‐up (Abstract number 476). 37th Annual Meeting of the International Continence Soceity (ICS), 20‐24 Aug 2007, Rotterdam, Netherlands. 2007. [sr‐incont23534]
- Costantini E, Lazzeri M, Giannantoni A, Zingaro M, Fioretti F, Zucchi A, et al. Abdominal integral pelvic reconstruction plus or minus Burch colposuspension in the treatment of severe uro‐genital prolapse associated to urinary incontinence. A RCT with a mid‐term follow‐up (Abstract number 476). Proceedings of the 37th Annual Meeting of the International Continence Soceity (ICS), 20‐24 Aug 2007, Rotterdam, Netherlands. 2007.
Costantini 2008 {published data only}
- Costantini E, Lazzeri M, Bini V, Zingaro M, Zucchi A, Porena M. Burch colposuspension does not provide any additional benefit to pelvic organ prolapse repair in patients with urinary incontinence: a randomized surgical trial. Journal of Urology 2008;180(3):1007‐12. [DOI] [PubMed] [Google Scholar]
Costantini 2010 {published data only}
- Costantini E, Lazzeri M, Frumenzio E, Zingaro M, Bruno R, Salvini E, et al. Burch colposuspension and pelvic organ prolapse repair in patients with or without urinary incontinence. Results: from two randomised surgical trials (Abstract). Neurourology and Urodynamics 2010;29(2S):111‐2. [Google Scholar]
Costantini 2011 {published data only}
- Costantini E, Lazzeri M, Bini V, Zingaro M, Zucchi A, Porena M. Pelvic organ prolapse repair with and without prophylactic concomitant Burch colposuspension in continent women: a randomized, controlled trial with 8‐year followup. Journal of Urology 2011;185(6):2236‐40. [DOI] [PubMed] [Google Scholar]
Debodinance 1993 {published data only}
- Debodinance P, Querleu D. Comparison of the Bologna and Ingelman‐Sundberg procedures for stress incontinence associated with genital prolapse: prospective randomized study. European Journal of Obstetrics, Gynecology, and Reproductive Biology 1993;52(1):35‐40. [DOI] [PubMed] [Google Scholar]
Debodinance 1994 {published data only}
- Debodinance P, Bievre P, Parmentier D, Dubrulle R, Querleu D, Crepin G. [The "hazards" of using a Gore‐Tex sling in the treatment of stress urinary incontinence]. [French]. Journal de Gynecologie, Obstetrique et Biologie de la Reproduction 1994;23(6):665‐70. [PubMed] [Google Scholar]
Di Palumbo 2003 {published data only}
- Palumbo VS. Four‐corner bladder and urethral retropubic suspension versus anterior colporrhaphy in the correction of stress urinary incontinence with urethrocystocele 3‐4. Randomized clinical trial. Urogynaecologia International Journal 2003;17(2):57‐68. [Google Scholar]
el‐Toukhy 2001 {published data only}
- Toukhy TA, Davies AE. The efficacy of laparoscopic mesh colposuspension: results of a prospective controlled study. BJU International 2001;88(4):361‐6. [DOI] [PubMed] [Google Scholar]
Fischer‐Rasmussen 87 {published data only}
- Fischer‐Rasmussen W, Thunedborg P, Bjerregaard S. Colposuspension versus anterior colporraphy in the treatment of stress incontinence in patients with posterior bladder suspension defect (Abstract). Proceedings of the International Continence Society (ICS), 17th Annual Meeting, 2‐5 Sept, Bristol, UK. 1987:48‐9.
- Thunedborg P, Fischer‐Rasmussen W, Jensen SB. Stress urinary incontinence and posterior bladder suspension defects. Results of vaginal repair versus Burch colposuspension. Acta Obstetricia at Gynecologica Scandinavia 1990;69 (1):55‐9. [DOI] [PubMed] [Google Scholar]
Foote 2007 {published data only}
- Foote AJ, Moore KH. The cost of urogynaecological treatments: Which are more cost‐effective. Australian & New Zealand Journal of Obstetrics & Gynaecology 2007;47(3):240‐6. [DOI] [PubMed] [Google Scholar]
Goldberg 2001a {published data only}
- Goldberg RP, Culligan P, Koduri PK, Sand PK. The tensile strength of Cooper's ligament suturing: comparison of the transvaginal versus abdominal techniques (Abstract). Proceedings of the International Continence Society (ICS), 31st Annual Meeting, 18‐21 Sept, Seoul, Korea. 2001:Abstract 244. [sr‐incont14470]
Goldberg 2001b {published data only}
- Goldberg RP, Koduri S, Lobel RW, Culligan PJ, Tomezsko JE, Winkler HA, et al. Long‐term effects of three different anti‐incontinence procedures on the posterior compartment (Abstract). Proceedings of the International Continence Society (ICS), 31st Annual Meeting, Seoul, Korea, 18‐21 Sept 2001. 2001:Abstract 243. [sr‐incont14471]
Jongen 1999 {published data only}
- Jongen VHWM, Brouwer WK. Comparison of the modified Pereyra procedure and Burch urethropexy. Subjective results of a one to six years follow‐up survey. International Urogynaecology Journal 1997;8(1):S3. [sr‐incont9817] [Google Scholar]
- Jongen VHWM, Brouwer WK. Comparison of the modified Pereyra procedure using permanent suture material and Burch urthropexy. European Journal of Obstetrics, Gynecology, and Reproductive Biology 1999;84:7‐11. [DOI] [PubMed] [Google Scholar]
Lee 1997 {published data only}
- Lee YS, Kim JH, Seo JT. A comparison of laparoscopic versus open Burch procedure for stress urinary incontinence. International Urogynecology Journal and Pelvic Floor Dysfunction. 8 1997; Vol. 8, issue 1:S37.
Lemack 2008 {published data only}
- Lemack GE, Krauss S, Litman H, FitzGerald MP, Chai T, Nager C, et al. Normal preoperative urodynamic testing does not predict voiding dysfunction after Burch colposuspension versus pubovaginal sling. Journal of Urology 2008;180(5):2076‐80. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lemieux 1991 {published data only}
- Lemieux MC, Kung R, Drutz HP. Suprapubic clamping routine after anti‐incontinence surgery: a randomized prospective study comparing continuous vs intermittent clamping (Abstract). Proceedings of the American Urogynecology Society, 12th Annual Meeting, Oct 23‐26, Newport Beach, California, USA. 1991. [sr‐incont14575]
Martan 2000 {published data only}
- Martan A, Masata J, Halaska M, Otcenasek M. Ultrasonic assessment of a paravaginal defect before and after surgical treatment in women with the stress type incontinence. Ceska Gynekologie 2000;65(3):152‐5. [sr‐incont11017] [PubMed] [Google Scholar]
Martan 2001 {published data only}
- Martan A, Masata J, Halaska M, Voigt R. Ultrasound imaging of the lower urinary system in women after Burch colposuspension. Ultrasound in Obstetrics & Gynecology 2001;17(1):58‐64. [DOI] [PubMed] [Google Scholar]
McClure 2006 {published data only}
- McClure LA, Brown MB. A likelihood approach to analyzing clinical trial data when treatments favor different outcomes. Contemporary Clinical Trials 2006;27(4):340‐52. [sr‐incont22391] [DOI] [PubMed] [Google Scholar]
Meschia 2001 {published data only}
- Meschia M, Spennacchio M, Amicarelli F, Pifarotti P, Cavoretto P, Stoppelli S. A randomized prospective comparison of TVT and endopelvic fascia plication in the treatment of occult stress urinary incontinence in patients with genital prolapse: preliminary data (Abstract). Neurourology and Urodynamics 2001;20(4):423‐4. [Google Scholar]
Morley 1995 {published data only}
- Morley R, Cumming J, Birch BRP. Staple colpofixation: a new minimally invasive treatment for stress incontinence (Abstract). Proceedings of the International Continence Society (ICS), 25th Annual Meeting, 17‐20 Oct, Sydney, Australia. 1995:471.
Mundy 1982 {published data only}
- Mundy AR. The role of the Stamey bladder neck suspension procedure in the treatment of stress incontinence of urine (Abstract). Proceedings of the International Continence Society (ICS), 12th Annual Meeting, Leiden, Germany. 1982:137.
Obrink 1978 {published data only}
- Obrink A, Bunne G. The margin to incontinence after three types of operation for stress incontinence. Scandinavian Journal of Urological Nephrology 1978;12:209‐14. [DOI] [PubMed] [Google Scholar]
Ostrzenski 1996 {published data only}
- Ostrzenski A. Laparoscopic colposuspension for total vaginal prolapse. International Journal of Gynaecology and Obstetrics 1996;55(2):147‐52. [sr‐incont4775] [DOI] [PubMed] [Google Scholar]
Palomba 2001 {published data only}
- Palomba S, Napolitano V, Sammartino A, Spiezio SA, Vassallo M, Mandato V, et al. [Effect of estriol treatment per vaginam before Burch culposuspension]. [Italian]. Minerva Ginecologica 2001;53(2):141‐5. [sr‐incont12281] [PubMed] [Google Scholar]
Pifarotti 2001 {published data only}
- Pifarotti P, Frigerio A, Gattei U, Ronchetti A, Stoppelli S, Meschia M. Results and urodynamic effects of Tension‐Free Vaginal Tape. [Italian]. Urogynaecologia International Journal 2001;15(Suppl 1):58‐60. [Google Scholar]
- Pifarotti P, Spennacchio M, Gattei U, Ronchetti A, Stoppelli S, Meschia M. A randomized prospective comparison of TVT and endopelvic fascia plication in the treatment of occult stress urinary incontinence in patients with genital prolapse: Preliminary data. Urogynaecologia International Journal 2001;15(Suppl 1):55‐7. [Google Scholar]
Quadri 2000 {published data only}
- Quadri G, Natale N, Spreafico C, Belloni C, Barisani D, Lahodny J. Intravesical prostaglandin E2 effectiveness in the prevention of urinary retention after transvaginal reconstruction of the pubo‐cervical fascia and short arm sling according to lahodny: A prospective randomized clinical trial. Urogynaecologia International Journal 2000;14(1):15‐24. [sr‐incont18130] [Google Scholar]
Reid 2007 {published data only}
- Reid FM, Smith AR, Dunn G. Which questionnaire? A psychometric evaluation of three patient‐based outcome measures used to assess surgery for stress urinary incontinence. Neurourology and Urodynamics 2007;26(1):123‐8. [sr‐incont22577] [DOI] [PubMed] [Google Scholar]
Richter 2007 {published data only}
- Richter HE, Diokno AC, Kenton K, Norton P, Albo M, Kraus S, et al. Predictors of treatment failure 24 months after surgery for stress urinary incontinence (Abstract number 5 Oral). Journal of Pelvic Medicine & Surgery 2007;13(5):227‐8. [Google Scholar]
Richter 2008a {published data only}
- Richter H, Goode P, Brubaker L, Zyczynski H, Stoddard A, Dandreo K, et al. Two‐year outcomes after surgery for stress urinary incontinence in older versus younger women (Abstract number 95). Neurourology and Urodynamics 2008;27(7):682‐3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Richter 2008b {published data only}
- Richter HE, Goode PS, Brubaker L, Zyczynski H, Stoddard AM, Dandreo KJ, et al. Two‐year outcomes after surgery for stress urinary incontinence in older compared with younger women. Obstetrics and Gynecology 2008;112(3):621‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Roca 1994 {published data only}
- Roca Edreira A, Gutierrez Banos JL, Martin Garcia B, Hernandez Rodriguez R, Portillo Martin JA, Correas Gomez MA, et al. [Stress urinary incontinence. Comparative study of suprapubic and vaginal surgical techniques]. [Spanish]. Archivos Espanoles de Urologia 1994;47(7):711‐4. [PubMed] [Google Scholar]
Rogers 2006 {published data only}
- Rogers RG, Kammerer‐Doak D, Darrow A, Murray K, Qualls C, Olsen A, et al. Does sexual function change after surgery for stress urinary incontinence and/or pelvic organ prolapse? A multicenter prospective study. American Journal of Obstetrics and Gynecology. 2006;195(5):e1‐4. [DOI] [PubMed] [Google Scholar]
Salam 2004 {published data only}
- Salam TA. Laproscopic versus conventional surgical treatment of genuine urinary stress incontinence (Abstract number 4). Progres en Urologie 2004;14(3 Suppl 3):6. [Google Scholar]
Salinas 1994 {published data only}
- Salinas Casado J, Virseda Chamorro M, Ramirez Fernandez JC, Rapariz Gonzalez M, Esteban Fuertes M, Resel Estevez L. [Comparative results of different types of urethropexy in the treatment of stress urinary incontinence in women]. [Spanish]. Archivos Espanoles de Urologia 1994;47(8):761‐8. [PubMed] [Google Scholar]
Salinas 1995 {published data only}
- Salinas Casado J, Virseda Chamorro M, Ramirez Fernandez JC, Rapariz Gonzalez M, Esteban Fuertes M, Samblas Garcia R, et al. [Effects of urethropexy on urination. A price to pay?]. [Spanish]. Archivos Espanoles de Urologia 1995;48(7):709‐16. [PubMed] [Google Scholar]
Schostak 2001 {published data only}
- Schostak M, Gottfried HW, Heicappell R, Muller M, Sauter T, Steiner U, et al. Minimally invasive bone anchoring for female stress incontinence: a treatment with moderate results (Abstract). European Urology 2001;39(Suppl 5):3. [16374] [Google Scholar]
Stanton 1979 {published data only}
- Stanton SL, Cardozo LD. A comparison of vaginal and suprapubic surgery in the correction of incontinence due to urethral sphincter incompetence. British Journal of Urology 1979;51:497‐9. [DOI] [PubMed] [Google Scholar]
Subak 2008b {published data only}
- Subak LL, Brubaker L, Chai TC, Creasman JM, Diokno AC, Goode PS, et al. High costs of urinary incontinence among women electing surgery to treat stress incontinence. Obstetrics and Gynecology 2008;111(4):899‐907. [DOI] [PMC free article] [PubMed] [Google Scholar]
Surkont 2007 {published data only}
- Surkont G, Wlazlak E, Dunicz‐Sokolowska A, Suzin J. [The efficacy of SUI treatment with Burch colposuspension evaluated with use of ITT analysis] [Polish]. Ginekologia Polska 2007;78(5):378‐80. [PubMed] [Google Scholar]
Tincello 2009 {published data only}
- Tincello D. Colposuspension or tension free vaginal tape with anterior repair for urinary incontinence and prolapse: a pilot study CARPET 1. ISRCTN (http://isrctn.org/ISRCTN34759911) 2006. [sr‐incont62311] [DOI] [PubMed]
- Tincello DG, Kenyon S, Slack M, Toozs‐Hobson P, Mayne C, Jones D, et al. Colposuspension or TVT with anterior repair for urinary incontinence and prolapse: results of and lessons from a pilot randomised patient‐preference study (CARPET 1). BJOG: an International Journal of Obstetrics and Gynaecology 2009;116(13):1809‐14. [sr‐incont34323] [DOI] [PubMed] [Google Scholar]
- Tincello DG, Mayne CJ, Toozs‐Hobson P, Slack M. Randomised controlled trial of colposuspension versus anterior repair plus TVT for urodynamic stress incontinence with anterior vaginal prolapse: proposal (Abstract). Proceedings of the International Continence Society, 11th Annual Scientific Meeting (ICS), 18‐19 Mar, Bournemouth, United Kingdom. 2004:46. [sr‐incont17170]
Virseda Chamorro 1995 {published data only}
- Virseda Chamorro M, Salinas Casado J, Ramirez Fernandez JC, Rapariz Gonzalez M, Esteban Fuertes M, Nacarino Corbacho L, et al. [Impact of bladder irritative symptoms and detrusor instability on the outcome of urethropexy]. [Spanish]. Archivos Espanoles de Urologia 1995;48(6):595‐601. [PubMed] [Google Scholar]
Walter 1982 {published data only}
- Walter S, Olesen KP, Hald T, Jensen HK, Pedersen PH. Urodynamic evaluation after vaginal repair and colposuspension. British Journal of Urology 1982;54(4):377‐80. [DOI] [PubMed] [Google Scholar]
Zhu 1998 {published data only}
- Zhu L, Lang J, Liu Z. Comparison of different surgical procedures for urinary stress incontinence. Chung‐Hua i Hsueh Tsa Chih [Chinese Medical Journal] 1998;78(8):601‐3. [PubMed] [Google Scholar]
References to studies awaiting assessment
Helmy 2012 {published data only}
- Helmy H, El‐Gamal S. Three‐year continence rates, satisfaction and adverse events of Burch urethropexy and fascial sling surgery for urinary incontinence (Abstract number 589). Proceedings of the 42nd Annual Meeting of the International Continence (ICS), 2012 Oct 15 to 19, Beijing, China. 2012. [sr‐incont45471]
References to ongoing studies
Boyd 1996 {published data only}
- Boyd K. Laparoscopic treatment for female urinary incontinence. http://isrctn.org/ISRCTN44339585 (accessed 9 June 2004) 2004. [sr‐incont17206]
Additional references
Abrams 2002
- Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, et al. The standardization of terminology of lower urinary tract function: Report from the standardisation sub‐committee of the International Continence Society. Neurourology and Urodynamics 2002;21:167‐78. [sr‐incont12909] [DOI] [PubMed] [Google Scholar]
Alhasso 2005
- Alhasso A, Glazener CMA, Pickard R, N'Dow JMO. Adrenergic drugs for urinary incontinence in adults. Cochrane Database of Systematic Reviews 2005, Issue 3. [DOI: 10.1002/14651858.CD001842.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Athanasopoulos 1999
- Athanasopoulos A, Liatsikos EN, Perimenis P, Barbalias GA. Female stress urinary incontinence: predictive factors for the operative correction (Abstract). International Urogynecology Journal and Pelvic Floor Dysfunction. 10 1999; Vol. 10, issue Suppl 1:S140.
Bakali 2013
- Bakali E, Buckley BS, Hilton P, Tincello DG. Treatment of recurrent stress urinary incontinence after failed minimally invasive synthetic suburethral tape surgery in women. Cochrane Database of Systematic Reviews 2013, Issue 2. [DOI: 10.1002/14651858.CD009407.pub2] [DOI] [PubMed] [Google Scholar]
Birnbaum 2004
- Birnbaum HG, Leong SA, Oster EF, Kinchen K, Sun P. Cost of stress urinary incontinence: a claims data analysis. Pharmacoeconomics 2004;22(2):95‐105. [DOI] [PubMed] [Google Scholar]
Black 1996
- Black NA, Downs SH. The effectiveness of surgery for stress incontinence in women: a systematic review. British Journal of Urology 1996;78(4):497‐510. [DOI] [PubMed] [Google Scholar]
Blaivas 1988
- Blaivas JG, Olsson CA. Stress incontinence: classification and surgical approach. Journal of Urology 1988;139(4):727‐31. [DOI] [PubMed] [Google Scholar]
Burch 1961
- Burch JC. Urethrovaginal fixation to Cooper's ligament for correction of stress incontinence, cystocoele and prolapse. American Journal of Obstetrics and Gynecology 1961;81(2):281‐90. [DOI] [PubMed] [Google Scholar]
Chong 2011
- Chong E, Khan A, Anger J. The financial burden of stress urinary incontinence among women in the United States. Current Urology Reports 2011;12(5):358‐62. [DOI] [PubMed] [Google Scholar]
Dean 2006
- Dean N, Ellis G, Herbison GP, Wilson D. Laparoscopic colposuspension for urinary incontinence in women. Cochrane Database of Systematic Reviews 2006, Issue 3. [DOI: 10.1002/14651858.CD002239.pub2] [DOI] [PubMed] [Google Scholar]
Deeks 2011
- Deeks JJ, Higgins JPT, Altman DG (editors). Chapter 9: Analysing data and undertaking meta‐analyses. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Dumville 2006
- Dumville JC, Manca A, Kitchener HC, Smith AR, Nelson L, Torgerson DJ, et al. Cost‐effectiveness analysis of open colposuspension versus laparoscopic colposuspension in the treatment of urodynamic stress incontinence. BJOG: An International Journal of Obstetrics & Gynaecology 2006;113(9):1014‐22. [DOI] [PubMed] [Google Scholar]
Fantl 1996
- Fantl JA, Newman DK, Colling J, DeLancey JOL, Keeys C, Loughery R, et al. Urinary incontinence in adults: acute and chronic management. Clinical practice guideline. No. 2, 1996 update. Rockville (MD): US Department of Health and Human Services. Public Health Service, Agency for Health Care Policy and Research, 1996 Mar. AHCPR Publication No.: 96‐0682:1‐154. [AHCPR Publication No. 96‐0682] [Google Scholar]
Ford 2015
- Ford AA, Rogerson L, Cody JD, Ogah J. Mid‐urethral sling operations for stress urinary incontinence in women. Cochrane Database of Systematic Reviews 2015, Issue 7. [DOI: 10.1002/14651858.CD006375.pub3] [DOI] [PubMed] [Google Scholar]
Glazener 2001
- Glazener CMA, Cooper K. Anterior vaginal repair for urinary incontinence in women. Cochrane Database of Systematic Reviews 2001, Issue 1. [DOI: 10.1002/14651858.CD001755] [DOI] [PubMed] [Google Scholar]
Glazener 2014
- Glazener CMA, Cooper K. Bladder neck needle suspension for urinary incontinence in women. Cochrane Database of Systematic Reviews 2014, Issue 12. [DOI: 10.1002/14651858.CD003636.pub3] [DOI] [PubMed] [Google Scholar]
Herzog 1990
- Herzog AR, Flutz NH. Prevalence and incidence of urinary incontinence in community‐dwelling populations. Journal of American Geriatric Society 1990;38:273‐81. [DOI] [PubMed] [Google Scholar]
Higgins 2003
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analyses. BMJ 2003;327(7414):557‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Altman DG, Sterne JAC (editors). Chapter 8: Assessing risk of bias in included studies. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Hunskaar 2002
- Hunskaar S, Burgio K, Diokno AC, Herzog AR, Hjalmas K, Lapitan MC. Epidemiology and natural history of urinary incontinence (UI). In: Abrams P, Cardozo L, Khoury S, Wein A editor(s). Incontinence: second international consultation on incontinence. Recommendations of the International Scientific Committee: the evaluation and treatment of urinary incontinence. Paris, 1‐3 July 2001. Plymouth, UK: Health Publication Ltd, 2002:165‐201. [Google Scholar]
Jarvis 1994
- Jarvis GJ. Surgery for genuine stress incontinence. British Journal of Obstetrics and Gynaecology 1994;101(5):371‐4. [DOI] [PubMed] [Google Scholar]
Kilonzo 2004
- Kilonzo M, Vale L, Stearns SC, Grant A, Cody J, Glazener CM, et al. Cost effectiveness of tension‐free vaginal tape for thesurgical management of female stress incontinence. International Journal of Technology Assessment in Health Care 2004;20(4):455‐63. [DOI] [PubMed] [Google Scholar]
Kirchin 2012
- Kirchin V, Page T, Keegan PE, Atiemo K, Cody JD, McClinton S. Urethral injection therapy for urinary incontinence in women. Cochrane Database of Systematic Reviews 2012, Issue 2. [DOI: 10.1002/14651858.CD003881.pub3] [DOI] [PubMed] [Google Scholar]
Kunkle 2015
- Kunkle CM, Hallock JL, Hu X, Blomquist J, Thung SF, Werner EF. Cost utility analysis of urethral bulking agents versusmidurethral sling in stress urinary incontinence. Female Pelvic Medicine & Reconstructive Surgery 2015;21(3):154‐9. [DOI] [PubMed] [Google Scholar]
Laudano 2013
- Laudano MA, Seklehner S, Chughtai B, Lee U, Tyagi R, Kavaler E, et al. Cost‐effectiveness analysis of tension‐free vaginal tape vs burch colposuspension for female stress urinary incontinence in the USA. BJU International 2013;112(2):E151‐8. [DOI] [PubMed] [Google Scholar]
Leach 1997
- Leach GE, Dmochowski RR, Appell RA, Blaivas JG, Hadley HR, Luber KM, et al. Female Stress Urinary Incontinence Clinical Guidelines Panel summary report on surgical management of female stress urinary incontinence. The American Urological Association. Journal of Urology 1997;158(3 Pt 1):875‐80. [DOI] [PubMed] [Google Scholar]
Liberati 2009
- Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta‐analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Medicine 2009;6:e1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lose 1998
- Lose G, Fantl JA, Victor A, Walter S, Wells TL. Outcome measures for research in adult women with symptoms of lower urinary tract dysfunction. Neurourology and Urodynamics 1998;17(3):255‐62. [DOI] [PubMed] [Google Scholar]
Mainprize 1988
- Mainprize TC, Drutz HP. The Marshall‐Merchetti‐Krantz procedure: a critical review. Obstetrics and Gynecology Survey 1988;43(12):724‐9. [DOI] [PubMed] [Google Scholar]
Manca 2003
- Manca A, Sculpher MJ, Ward K, Hilton P. A cost‐utility analysis of tension‐free vaginal tape versus colposuspension for primary urodynamic stress incontinence. BJOG: An International Journal of Obstetrics & Gynaecology 2003;110(3):255‐62. [PubMed] [Google Scholar]
Mariappan 2005
- Mariappan P, Alhasso AA, Grant A, N'Dow JMO. Serotonin and noradrenaline reuptake inhibitors (SNRI) for stress urinary incontinence in adults. Cochrane Database of Systematic Reviews 2005, Issue 3. [DOI: 10.1002/14651858.CD004742.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Nambiar 2014
- Nambiar A, Cody JD, Jeffery ST. Single‐incision sling operations for urinary incontinence in women. Cochrane Database of Systematic Reviews 2014, Issue 6. [DOI: 10.1002/14651858.CD008709.pub2] [DOI] [PubMed] [Google Scholar]
Novara 2008
- Novara G, Galfano A, Boscolo‐Berto R, Secco S, Cavalleri S, Ficarra V, et al. Complication rates of tension‐free midurethral slings in the treatment of female stress urinary incontinence: a systematic review and meta‐analysis of randomized controlled trials comparing tension‐free midurethral tapes to other surgical procedures and different devices. European Urology 2008;53(2):288‐309. [DOI] [PubMed] [Google Scholar]
Reference Manager 2012 [Computer program]
- Thomson Reuters. Reference Manager Professional Edition Version 12. New York: Thomson Reuters, 2012.
Rehman 2011
- Rehman H, Bezerra CCB, Bruschini H, Cody JD. Traditional suburethral sling operations for urinary incontinence in women. Cochrane Database of Systematic Reviews 2011, Issue 1. [DOI: 10.1002/14651858.CD001754.pub3] [DOI] [PubMed] [Google Scholar]
RevMan 2014 [Computer program]
- The Nordic Cochrane Centre, Cochrane. Review Manager (RevMan). Version 5.3. Copenhagen: The Nordic Cochrane Centre, Cochrane, 2014.
Richardson 1976
- Richardson AC, Lyon FB, Williams NL. A new look at pelvic relaxation. American Journal of Obstetrics and Gynecology 1976;126:568‐73. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Schulz 2010
- Schulz KF, Altman DG, Moher D, for the CONSORT Group. CONSORT 2010 Statement: updated guidelines for reporting parallel group randomised trials. BMJ 2010;340:c332. [PUBMED: 20332509] [DOI] [PMC free article] [PubMed] [Google Scholar]
Subak 2008a
- Subak LL, Brubaker L, Chai TC, Creasman JM, Diokno AC, Goode PS, et al. High costs of urinary incontinence among women electing surgery to treat stress incontinence. Obstetrics & Gynecology 2008;111(4):899‐907. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wagner 1998
- Wagner T, Hu T. Economic costs of urinary incontinence in 1995. Urology 1998;51(3):355‐361. [DOI] [PubMed] [Google Scholar]
Ware 1993
- Ware JE, Snow KK, Kosinski M, Gandek B. SF‐36 Health survey manual and interpretation guide. Boston, MA: The Health Institute, New England Medical Centre, 1993. [Google Scholar]
Wilson 1996
- Wilson PD, Herbison RM, Herbison GP. Obstetric practice and the prevalence of urinary incontinence three months after delivery. British Journal of Obstetrics and Gynaecology 1996;103(2):154‐61. [DOI] [PubMed] [Google Scholar]
Wu 2007
- Wu JM, Visco AG, Weidner AC, Myers ER. Is Burch colposuspension ever cost‐effective compared with tension‐free vaginal tape for stress incontinence?. American Journal of Obstetrics & Gynecology 2007;197(1):62.e1‐5. [DOI] [PubMed] [Google Scholar]


