Abstract
Background
Cystic fibrosis is a genetic disorder which can lead to multiorgan dysfunction. Malabsorption of fat and fat‐soluble vitamins (A, D, E, K) may occur and can cause subclinical deficiencies of some of these vitamins. Vitamin K is known to play an important role in both blood coagulation and bone formation. Supplementation with vitamin K appears to be one way of addressing the deficiency, but there is very limited agreement on the appropriate dose and frequency of use of these supplements. This is an updated version of the review.
Objectives
To assess the effects of vitamin K supplementation in people with cystic fibrosis and to determine the optimal dose and route of administration of vitamin K for both routine and therapeutic use.
Search methods
We searched the Cochrane Cystic Fibrosis and Genetic Disorders Group's Trials Register comprising references identified from comprehensive electronic database searches and handsearches of relevant journals and abstract books of conference proceedings.
Most recent search: 30 January 2017.
Selection criteria
Randomised and quasi‐randomised controlled trials of all preparations of vitamin K used as a supplement compared to either no supplementation (or placebo) at any dose or route and for any duration, in children or adults diagnosed with cystic fibrosis (by sweat test or genetic testing).
Data collection and analysis
Two authors independently screened papers, extracted trial details and assessed their risk of bias.
Main results
Two trials (total of 32 participants) each lasting one month were included in the review and were assessed as having a moderate risk of bias. One was a dose‐ranging parallel group trial in children (aged 8 to 18 years); and the other (with an older cohort) had a cross‐over design comparing supplements to no treatment, but no separate data were reported for the first intervention period. Neither of the trials addressed any of the primary outcomes (coagulation, bone formation and quality of life). Both trials reported the restoration of serum vitamin K and undercarboxylated osteocalcin levels to the normal range after one month of daily supplementation with 1 mg of vitamin K.
Authors' conclusions
Evidence from randomised controlled trials on the benefits of routine vitamin K supplementation for people with CF is currently weak and limited to two small trials of short duration. However, no harm was found and until further evidence is available, the present recommendations should be adhered to.
Plain language summary
Vitamin K supplementation for cystic fibrosis
Review question
We reviewed the evidence to see whether supplementing vitamin K in people with cystic fibrosis counteracts the effects of deficiency on blood clotting, bone strength and quality of life in people with cystic fibrosis. We tried to determine the best dose needed to prevent this deficiency. This is an update of an earlier review.
Background
Cystic fibrosis is an inherited condition which causes disease, most noticeably in the lungs, digestive system and pancreas. In people with cystic fibrosis, the pancreas often does not produce enough enzymes to allow the body to absorb digested food properly and this may also be linked to deficiencies of fat‐soluble vitamins like vitamin K. Vitamin K is needed for adequate blood clotting, bone formation and some metabolic functions.
Search date
The evidence is current to: 30 January 2017.
Study characteristics
We included two trials (total of 32 participants) in the review. In one trial (14 children aged 8 to 18 years old) for one month half of the participants were given oral vitamin K supplements at a dose of 1 mg/day and the other half were given 5 mg/day. In the second trial all the 18 volunteers (aged 13 to 35 years) were given 5 mg oral vitamin K supplement or nothing for one month and then they swapped to the other group for another month. Unfortunately, we could not analyse the data from this second trial because the investigators did not report data just from the first part of the trial (only from the end of the trial when all volunteers had been in both groups), so we could not tell if the effects were due to supplements or no supplements.
Key results
Neither trial addressed any of the review's primary outcomes (blood clotting, bone formation and quality of life). Both trials reported that in patients who had low levels of vitamin K measured in the blood and also another laboratory marker of vitamin K (undercarboxylated osteocalcin), these levels returned to the normal range after one month of daily supplementation with 1 mg of vitamin K.
Quality of the evidence
We were satisfied that both trials reported all the outcomes they planned to and that the results were not at risk of being biased due to volunteers dropping out of the trials. We did not have enough details to decide whether results would be affected by the way the trials were set up or in case volunteers could tell which treatment they were receiving (it would be obvious in the trial comparing supplements to no treatment),
Background
Description of the condition
Cystic fibrosis (CF) is a multisystem disorder that primarily affects the respiratory and gastrointestinal (GI) systems (Morgan 1999). It is caused by homozygous presence of a mutation in the gene encoding the cystic fibrosis transmembrane conductance regulator (CFTR) protein.
In the UK there are over 8000 people affected by CF and in the United States of America this figure is approximately 30,000; most are diagnosed by six months of age and the median survival has reached the fifth decade of life (Davis 2006; Goss 2004; Staab 2004). It is the most common, life‐threatening, autosomal‐recessively inherited disease in the white population, with a carrier rate of 1 in 25 and an incidence of 1 in 2500 live births (Ratjen 2003); CF is less common in other ethnic groups, approximately 1 in 46 Hispanics, 1 in 65 Africans and 1 in 90 Asians carry at least one abnormal CFTR gene (Bobadilla 2002).
The CFTR protein is a chloride ion channel, important in tissues that produce sweat, digestive juices and mucus. The dominant symptoms of CF relate to the respiratory and GI systems (Wagener 2003). In the GI system, liver dysfunction, intestinal obstruction and exocrine pancreatic insufficiency are the most common morbidities. Pancreatic insufficiency (PI) affects up to 90% of people with CF and causes fat malabsorption (Dodge 2006). Fat‐soluble vitamins (A, D, E and K) are co‐absorbed with fat and thus deficiency of these vitamins may occur (Dodge 2006). Hence ,vitamin K deficiency is well recognised in patients with CF and PI. While deficiencies may occur from the disease process of CF and from insufficient supplementation, another additional co‐factor is the long‐term use of certain types of antibiotics. These can put some individuals at additional risk of vitamin K deficiency by altering intestinal flora which produce vitamin K (Conway 2005). Long‐term effects of bowel resection, an intervention required for intestinal obstruction in some newborns with CF and varying degrees of liver dysfunction can pose a further additional risk for vitamin K deficiency (Fuchs 1998).
The manifestations of vitamin K deficiency can range from a mild subclinical identification (e.g. low levels of vitamin K in the blood) to widespread coagulopathy (defect in the body's mechanism for blood clotting). Such manifestations may include mucosal bleeding (e.g. in the nose, gastro‐intestinal system, and in the urine) and subcutaneous bleeding (e.g. oozing from venipuncture sites and susceptibility to bruising). Vitamin K is also involved in the calcium binding proteins in the bone and its deficiency is implicated in defective bone remineralization and thus osteoporosis (Conway 2005).
The majority of CF centres routinely administer vitamins A, D, and E as supplements from the neonatal period. Vitamin K administration is usually prescribed when clinical deficiencies are detected or following routine investigations. The limited storage capacity and rapid metabolic turnover of vitamin K (Olsen 1994) supports the recommendations for daily rather than weekly supplementation of vitamin K (Beker 1997).
Description of the intervention
Two forms of vitamin K (K1 and K2) occur naturally and synthetic forms of the vitamin (K3, K4, and K5) are also available. Naturally occurring vitamin K is found in green vegetables i.e. kale, collards, spinach and salads (K1 ‐phytonadione) and a small amount is made in human gut by bacteria (K2‐menaquinones). Therapeutic vitamin K is available in both water soluble and insoluble forms (Durie 1994). The enteral forms of vitamin K supplementation are commonly prescribed. These can be in tablet, ampoule (Borowitz 2002; Cystic Fibrosis Trust 2007) or multivitamin preparations (Durie 1994). Vitamin K can also be administered by intramuscular (Shearer 1995) or intravenous injections (Verghese 2003).
How the intervention might work
Vitamin K functions as the cofactor of the enzyme vitamin K‐dependent carboxylase. This enzyme catalyses the post‐translation formation of gamma‐carboxyglutamyl (Gla) residues in specific proteins. Vitamin K‐dependent proteins are: blood coagulation factors (prothrombin and Factors VII, IX and X); other plasma proteins (protein C, protein S and protein Z); two proteins from bone (osteocalcin and matrix Gla‐protein); and proteins from lung, kidney, spleen, testis, placenta and other tissues (Uotila 1990).
Blood coagulation requires activation of inactive proenzymes, hence vitamin K is a vital factor in synthesis of clotting factors and causes haemostasis in vitamin K‐dependant bleeding manifestations.
Vitamin K‐related carboxylation allows the activation of the bone matrix protein, osteocalcin, resulting in osteoblast function and bone formation; vitamin‐K deficiency impairs this process and thus impairs bone formation (Okano 2005).
Why it is important to do this review
Vitamin K deficiency is common in people with CF with pancreatic insufficiency. In a recent study of people with CF, the pathological PIVKA‐II concentration (≥ 2 ng/ml) was found in 42.8% of the population studied and an abnormal percentage of osteocalcin (≥ 20%) in 35.7% of people studied (Krzyzanowska 2015). Supplementation (often oral and occasionally parenteral) appears to the most immediate measure to address the deficiency, although there is limited consensus on the dose and frequency of supplements for routine or therapeutic use (Rashid 1999). In 1992 the Consensus Committee of the Cystic Fibrosis Foundation (CFF) suggested a particular dosage (Ramsey 1992); but the recommendations were later proved ineffectual by another study (Beker 1997). The 2002 American Consensus Committee recommended a low‐dose supplementation of vitamin K for all ages (0.3 to 0.5 mg/day), but emphasized that no adverse effects had been reported at any dosage level of vitamin K (Borowitz 2002). Recent recommendations from Europe and the UK have suggested varying dose regimens ranging from 0.3 to 1 mg/day to 10 mg/week (Cystic Fibrosis Trust 2002; Sinaasappel 2002). There is a suggestion from one study that only a higher level of supplementation can normalise vitamin K levels in people with CF (Dougherty 2010). Another study found that vitamin K deficiency occurs in people with CF despite applied supplementation (Krzyzanowska 2010). The study authors suggested that an accurate supplementation dose should be estimated individually and the assessment of its effectiveness requires studies allowing investigators to determine the real body resources of vitamin K.
There is no uniform consensus on routine or at‐risk vitamin K supplementation in individuals with CF. There is increasing evidence that the prevalence of vitamin K deficiency in CF is associated with an increased morbidity (Rashid 1999). Thus, a systematic review on vitamin K supplementation in people with CF could provide evidence to guide clinical practice.
This is an update of previous review versions (Jagannath 2010; Jagannath 2011; Jagannath 2013; Jagannath 2015).
Objectives
To determine the effects of vitamin K supplementation on the morbidities in people with CF.
To investigate the hypotheses that vitamin K will decrease deficiency‐related coagulopathy, increase bone mineral density, decrease risk of fractures and improve quality of life in people with CF.
To determine the optimal dose and route of administration of vitamin K for people with CF (for both routine and therapeutic use).
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials and quasi‐randomised controlled trials.
Types of participants
Children and adults with a diagnosis of CF (defined by sweat test or genetic testing or both).
Exclusion criteria: Any intervention which may affect the interpretation of the effects of vitamin K or any allergy to vitamin K:
any anticoagulation in the past three months (will make interpretation of vitamin K effects on blood coagulation difficult);
bisphosphonates in the past six months (will make interpretation of vitamin K effects on bone metabolism difficult);
allergy to vitamin K.
Types of interventions
All preparations of vitamin K used as a supplement compared to placebo or no supplementation at any dose and for any duration. Studies comparing different doses and regimens of vitamin K were considered.
Types of outcome measures
Primary outcomes
-
Clinical outcomes related to coagulopathy (Sutor 1995)
time to cessation of bleeding manifestations (symptomatic coagulopathy)
time to normalisation of sub‐therapeutic international normalized ratio (INR) (asymptomatic or sub‐clinical coagulopathy)
-
Bone formation outcome measures
bone mineral density at the spine (L1‐L4) and the total hip (measured by dual energy X‐ray absorptiometry (DEXA) scans with z score compared to reference population) (Borowitz 2002)
reduction in risk of bone fractures
Quality of life (e.g. the CFQ‐R (Quittner 2000) and the CFQoL (Gee 2000))
Secondary outcomes
-
Nutritional parameters (including z scores or centiles)
weight
height
body mass index (BMI)
-
Adverse events
mild (not requiring intervention)
moderate (requiring treatment)
severe (life threatening or requiring hospitalisation)
-
Serum levels
serum undercarboxylated osteocalcin (ucOC)
ucOC/cOC (carboxylated osteocalcin) ratio (UCR)
-
Vitamin K‐specific laboratory outcomes
plasma level of vitamin K1 (measured by high performance liquid chromatography (HPLC) and fluorescence detection (Wang 2004)
proteins induced by vitamin K absence or antagonism factor II (PIVKA II) levels (measured by enzyme‐linked immunosorbent assay (ELISA)) (Belle 1991; Belle 1995)
Search methods for identification of studies
There are no restrictions regarding language or publication status.
Electronic searches
We identified relevant trials from the Group's Cystic Fibrosis Trials Register using the term: 'vitamin K'.
A systematic search without language restrictions was conducted using the optimally sensitive strategy developed for the Cochrane Collaboration to identify all relevant published and unpublished randomised controlled trials (Lefebvre 2009) in the Cystic Fibrosis Trials Register which is compiled from electronic searches of the Cochrane Central Register of Controlled Trials (CENTRAL) (updated each new issue of the Cochrane Library), weekly searches of MEDLINE, a search of Embase to 1995 and the prospective handsearching of two journals ‐ Pediatric Pulmonology and the Journal of Cystic Fibrosis. Unpublished work is identified by searching the abstract books of three major cystic fibrosis conferences: the International Cystic Fibrosis Conference; the European Cystic Fibrosis Conference and the North American Cystic Fibrosis Conference. For full details of all searching activities for the register, please see the relevant sections of the Cystic Fibrosis and Genetic Disorders Group website.
Date of the latest search: 30 January 2017.
We also searched the clinical trials registries: clinicaltrials.gov; International Standard Randomised Controlled Trials Number (ISRCTN) Registry and WHO ICTRP using the search terms "vitamin K" and "cystic fibrosis".
Date of the latest search: 01 April 2017.
Searching other resources
The following additional resources were used:
the bibliographical references of identified studies were searched for citations to additional studies;
personal contact with corresponding authors of relevant trials or reviewers and other experts.
Data collection and analysis
Selection of studies
Up to the 2017 update, two review authors (Vanitha Jagannath (VJ) and Zbys Fedorowicz (ZF)) independently assessed the abstracts of trials resulting from the searches. We obtained full text copies of all relevant and potentially relevant trials, those appearing to meet the inclusion criteria, and those for which there was insufficient detail in the title and abstract to make a clear decision. The two authors then independently assessed the full text papers. There were no disagreements; however, if there are any disagreements on the eligibility of trials in the future, we will resolve these through discussion and consensus, or through a third party (Vidhu Thaker (VT)). All irrelevant records were excluded and details of the trials and the reasons for their exclusion were noted in the tables (Characteristics of excluded studies) in RevMan (RevMan 2014).
Data extraction and management
We entered details for the included trials into the tables (Characteristics of included studies) in RevMan (RevMan 2014) and collected outcome data using a pre‐determined form designed for this purpose. For the original review, two review authors (VJ, ZF) extracted data independently and in duplicate and only included these if there was a consensus; there were no disagreements; if these occur in the future, we will resolve them by consulting with a third review author (VT).
The authors extracted the following details.
-
Trial methods
method of allocation
masking of participants, trialists and outcome assessors
exclusion of participants after randomisation and proportion and reasons for losses at follow‐up
-
Participants
country of origin and study setting
sample size
age
gender
inclusion and exclusion criteria
-
Intervention
type
dose and frequency
duration of intervention in follow‐up
-
Control
type
dose and frequency
duration of intervention in follow‐up
Outcomes: primary and secondary outcomes mentioned in the Types of outcome measures section of this review and categorised and grouped accordingly: short term (less than 12 months) data at 3, 6 and 12 months and medium to long term (over 12 months)
If stated in the trial reports, we recorded the sources of funding of any of the included trials.
The review authors used this information to help them assess clinical heterogeneity and the external validity of any included trials.
Assessment of risk of bias in included studies
For the original review, two authors (VJ, ZF) independently graded the selected trials using a simple contingency form and followed the domain‐based evaluation described in chapter 8 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011a). The authors compared evaluations and discussed and resolved any inconsistencies in these evaluations.
The authors assessed the following domains as 'Yes' (i.e. low risk of bias), 'Unclear' (uncertain risk of bias) or 'No' (i.e. high risk of bias):
sequence generation;
allocation concealment;
blinding (of participants, personnel and outcome assessors);
incomplete outcome data addressed;
free of selective outcome reporting;
free of other bias.
The authors categorised the risk of bias in any included studies according to the following:
low risk of bias (plausible bias unlikely to seriously alter the results) if all criteria met;
unclear risk of bias (plausible bias that raises some doubt about the results) if one or more criteria assessed as unclear; or
high risk of bias (plausible bias that seriously weakens confidence in the results) if one or more criteria not met.
We report these assessments for each trial in the tables (Risk of bias in included studies) in the review.
Measures of treatment effect
For dichotomous outcomes, we planned to express results as odds ratios (OR) with 95% confidence intervals (CI). For continuous outcomes, we calculated the mean difference (MD); we would have calculated the standardized mean difference (SMD) if different measurement scales had been used. We planned to express any time‐to‐event outcomes data as ORs or hazards ratios.
Unit of analysis issues
We included trials with a parallel group design, such that participants were randomised to either intervention or control with subsequent analysis at individual allocation level. Unit of analysis issues can arise with cross‐over trials and therefore we decided not to include end‐of‐trial data from these trials because the effects of vitamin K on bone metabolism are likely to be long‐term and an appropriate wash‐out period cannot be defined. However, we planned to include any data reported from the first intervention period.
Dealing with missing data
We attempted to contact the authors of any trials where we needed clarification of trial design or results (at all stages of the review and updates). We have only received a response the investigators from one of the trials (Drury 2008). We obtained individual patient data which we have included in the analysis.
Assessment of heterogeneity
As we were only able to include two trials in this review, we did not assess heterogeneity; but in future updates of this review, if we are able to include further trials, we will apply the following methods of assessment.
We will assess clinical diversity between the trials by examining the trial characteristics, the similarity between the types of participants, the interventions and the outcomes as specified in the inclusion criteria.
We will assess statistical heterogeneity using a Chi² test and the I² statistic, where I² values of 30% to 60% indicate moderate to high, 50% to 90% substantial and 75% to 100% considerable heterogeneity. We will consider heterogeneity to be significant when the P value is less than 0.10 (Higgins 2003).
Assessment of reporting biases
The paucity of trials included in this review did not permit an assessment of publication bias. If we had identified a sufficient number of trials for inclusion in this review (at least 10), we would have assessed publication bias according to the recommendations on testing for funnel plot asymmetry as described in chapter 10 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011b). If we had then identified asymmetry, we would have tried to assess other possible causes and explored these further in the Discussion section of the review, if appropriate.
Data synthesis
For the original review, two review authors (VJ and ZF) analysed the data in Review Manager (RevMan 2014) and reported them as specified in chapter 9 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011c).
Although we included two trials in this review, we were only able to report reliable data from one of them (Drury 2008) and therefore did not carry out a meta‐analysis. If at a later date we include further trials in this review, we will apply the following methods of data synthesis. When we include sufficient numbers of trials investigating similar interventions, we will conduct the analysis in RevMan (RevMan 2014). In general, we will use the fixed‐effect model; but if there is substantial clinical diversity, we will use the random‐effects model with trials grouped by action.
Subgroup analysis and investigation of heterogeneity
Lack of data did not permit a subgroup analysis, but in future updates and if further data become available we plan to carry out the following subgroup analyses:
cumulative dose (as per kg body weight per day) of vitamin K2;
route of administration (oral or parenteral);
baseline plasma level of vitamin K1 (subnormal versus normal);
presence or absence of any of the following: pancreatic insufficiency, liver dysfunction, bowel resection or prolonged usage of antibiotics and chronic steroid administration;
mean 25OH vitamin D level.
Sensitivity analysis
In view of the low number of trials included in this review, a sensitivity analysis was not possible. For future updates and if we are able to include sufficient trials, we will undertake sensitivity analyses to assess the robustness of our review results by repeating the analysis with the following adjustments:
exclusion of trials with unclear or inadequate allocation concealment;
exclusion of trials with unclear or inadequate blinding of outcomes assessment;
exclusion of trials with unclear or inadequate completeness of follow‐up;
exclusion of quasi‐randomised trials.
Results
Description of studies
Results of the search
The electronic searches retrieved references to nine trials. After examination of the titles and abstracts of these references, all of those which did not match our inclusion criteria and were clearly ineligible were eliminated from the review. Full text copies of the remaining potentially eligible trials were obtained and subjected to further evaluation. The review authors discussed the eligibility of these trials, resolved any remaining uncertainties by consensus. Two trials were included (Beker 1997; Drury 2008), five trials were excluded (Cornelissen 1992; Grey 2008; Mosler 2003; Nicolaidou 2006; Wilson 2001), and two trials are awaiting classification until we obtain further information from the trialists (van Hoorn 2003; van Hoorn 2008).
The search of the Cystic Fibrosis Trials Register in 2012 retrieved one reference, which is an abstract of the ongoing trial in the review which will be assessed for inclusion as soon as it has been published (Kuitert 2010).
Included studies
Two trials, neither of which addressed any of our primary outcomes and only reported on two of the secondary outcomes were included in this review. Albeit these two trials were assessed as having a moderate risk of bias, and provided limited data, it was considered that their inclusion and the reporting of their results would provide at least some evidence towards answering this research question.
One of the trials was cross‐over in design, but did not include a wash‐out period and thus the potential risk of bias as a consequence of the carry‐over of treatment effect could not be ruled out (Beker 1997). Although trials with a cross‐over design were eligible for inclusion in this review, we had specified that only data from the first intervention period would be used. Unfortunately, the trial investigators only provided an analysis across both treatment periods and, even though we were unable to contact the authors to obtain the first period data, this trial has been included in the review but it has not been possible to enter the data into a meta‐analysis.
The second trial included in this review was a dose‐ranging randomised controlled trial which reported some data for two of our secondary outcomes, but these were presented as graph‐plots from which we were unable to obtain precise data (Drury 2008). After successful contact with the principal investigator via electronic mail we received the relevant individual patient data for these two outcomes and have presented them in this review.
Characteristics of the trial setting and investigators
Both were single centre trials, one was conducted at the Montreal Children's Hospital CF Clinic in Canada (Drury 2008), and the other was carried out at the CF Clinic of the Children's National Medical Center (CNMC), Washington DC, USA (Beker 1997).
Although the overall duration of the two trials differed, the active treatment period was the same (i.e. one month). Thus, in the cross‐over trial, the participants were allocated to either active intervention or no‐treatment control for a four‐week period and then crossed over for a further four weeks but without undergoing a wash‐out period (Beker 1997).
The providers of care in both trials were hospital staff and the assessors of outcomes were the investigators and other healthcare providers (Beker 1997; Drury 2008).
Characteristics of the participants
The total sample size comprised of 32 participants between the ages of 8 and 35 years. In the Beker study, the diagnosis of CF was confirmed by duplicate sweat test (Beker 1997). Although Drury did not report the method used to confirm the diagnosis of CF, it is most probable that participants with CF were enrolled in this trial (Drury 2008).
All of the participants in the Beker trial were pancreatic insufficient, as documented by previous fecal fat measurement, and they received replacement therapy of 750 to 200 units of lipase/kg of body weight at meal times during the course of the trial (Beker 1997). The investigators in the Drury trial reported that only pancreatic insufficient participants were included, but provided no further details (Drury 2008). Participants with liver disease (diagnosed by ultrasound, liver function tests or hepatomegaly or both) and those who were taking supplemental therapeutic vitamin K to treat coagulopathies at enrolment were excluded from both trials (Beker 1997; Drury 2008).
Characteristics of the interventions
The active intervention in the Beker trial consisted of 5 mg oral vitamin K1 supplementation per week and the control was no supplementation for four weeks; participants then crossed over for a second four‐week period (Beker 1997). Compliance with the intervention by participants was verified by the trial coordinator at each visit. Oral antibiotic medications of cephalosporin; sulfamethoxazole; erythromycin as well as concomitant usage of bronchodilators and standard multivitamins and 200 to 400 IU vitamin E were allowed during the course of the trial.
The participants in the Drury trial were randomised to either the orally administered injectable formulation of vitamin K1 phytonadione of 1 mg/day (diluted to 1 mg/ml) or the 5 mg/day dose (Drury 2008).
Characteristics of the outcome measures
None of the primary outcomes specified in the protocol for the review were considered in either of the included trials (Beker 1997; Drury 2008). Both trials carried out assessments of plasma Vitamin K1 levels and serum undercarboxylated osteocalcin levels; these were measured at entry and at the completion of the trial by Drury (Drury 2008), and at the end of each period by Beker (Beker 1997). Dietary intake records to estimate the extent of dietary contribution of Vitamin K1 were maintained by the participants in one trial (Beker 1997). The vitamin K1 data of foods were analysed using Nutritionist III software, the database, however, did not have complete vitamin K1 data for many foods.
Excluded studies
Five trials were excluded from the review since these were not randomised controlled trials. Further information about the reasons for exclusion of trials is available in the Excluded studies table.
Risk of bias in included studies
The risks of bias for the two included trials in this review were classified as previously described (Assessment of risk of bias in included studies).
Both included trials were judged as having an 'unclear' risk of bias overall (Beker 1997; Drury 2008). These assessments were to a certain extent based on the inadequate reporting of several of the criteria that are considered to be important in the evaluation of methodological rigour in terms of trial design and conduct.
For further details see the risk of bias tables in Characteristics of included studies, the risk of bias graph (Figure 1) and the risk of bias summary (Figure 2).
1.
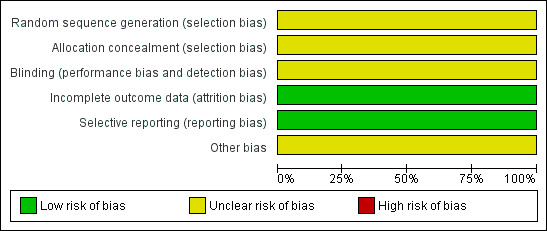
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
2.
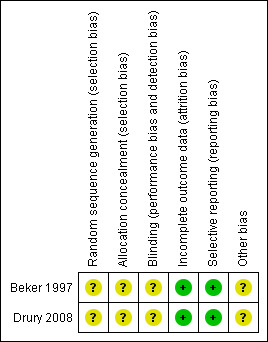
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
The methods used to generate the allocation sequence were not reported in either trial. Moreover, neither of the trials described how the allocation sequence was concealed, which did not allow us to determine whether intervention allocations could have been foreseen in advance of, or during, enrolment. Inadequate reporting quality did not permit a clear judgement to be made for both domains in either of the included trials (Beker 1997; Drury 2008).
Blinding
The measures used to blind trial participants and personnel from knowledge of which intervention a participant received or any information relating to whether the intended blinding was effective were not reported in either trial (Beker 1997; Drury 2008). However, whilst it may be accepted that blinding of participants and investigators in the Beker trial may not have been feasible, it was unclear if the assessors of the outcomes were adequately blinded (Beker 1997). Therefore the judgement given for this domain in both trials was 'unclear'.
Incomplete outcome data
There were no withdrawals and no missing or incomplete data in the Beker trial (Beker 1997); and the only missing data in the Drury trial was as a result of the inability of the investigators to make the final outcome assessment for one participant (Drury 2008). Therefore, we judge there to be a low risk of bias from incomplete outcome data in both trials.
Selective reporting
Although neither trial protocols were available, based on information presented in the methods sections of each of the reports, the investigators appear to have reported on all of their stated objectives and expected outcomes, a number of which were pre‐specified inclusion criteria for this systematic review (Beker 1997; Drury 2008). We therefore judge there to be a low risk of bias from selective reporting for these trials.
Other potential sources of bias
Insufficient information was provided in the reports to assess whether any other important risk of bias exists, and therefore the judgement for this domain in both trials was 'unclear' (Beker 1997; Drury 2008).
Effects of interventions
Primary outcomes
None of the primary outcomes specified in the protocol for this review were considered in either of the included trials (Beker 1997; Drury 2008).
Secondary outcomes
1. Nutritional parameters
These were not considered in either of the included trials (Beker 1997; Drury 2008).
2. Adverse events
No adverse events were reported in either of the trials (Beker 1997; Drury 2008).
3. Serum levels
The Drury trial was under‐powered (Drury 2008). Even though we managed to obtain individual patient data, the small number of participants and the degree of baseline imbalance in vitamin K and undercarboxylated osteocalcin levels (both within and between the groups) did not support analysis of the magnitude of individual response to treatment or control, i.e. the measure of change from baseline. Although it is likely that baseline imbalance may reflect the clinical variability of CF, neither report provided sufficient clinical detail of the participants to enable any assessment of the degree of variability in presentation of CF (Beker 1997; Drury 2008). Therefore, the data for both of these outcomes have been presented in the analysis as the end of trial mean response for the total number of participants in each of the treatment and control groups. We also report the baseline means and SDs alongside the end of trial values in the additional tables (Table 2; Table 3).
1. Serum undercarboxylated osteocalcin (ucOC) percentage (Drury 2008).
| Dose | n | UcOC % Baseline mean (SD) | UcOC % End of study mean (SD) |
| 1 mg/day | 7 | 46 (14.4) | 28 (8.26) |
| 5 mg/day | 6 | 47.6 (9.45) | 30.2 (13.09) |
SD: standard deviation ucOC: undercarboxylated osteocalcin
2. Serum vitamin K levels (Drury 2008).
| Dose | n | Serum vitamin K levels (nmol/L) Baseline mean (SD) | Serum vitamin K levels (nmol/L) End of study mean (SD) |
| 1 mg/day | 7 | 0.28 (0.25) | 2.52 (2.61) |
| 5 mg/day | 6 | 0.15 (0.19) | 6.98 (9.95) |
SD: standard deviation
In the Beker trial, the data for this outcome were analysed across both treatment periods and therefore we only report the end of trial data narratively (Beker 1997). We advise caution in its interpretation and in any comparison with data from the other trial included in this review.
a. Serum undercarboxylated osteocalcin (ucOC)
In the Drury trial, all of the participants had elevated (in excess of 21%) concentrations of ucOC before supplementation, but these levels were reduced after one month of vitamin K1 supplementation (Drury 2008). The overall level of ucOC decreased from a median of 46.8% to 29.1%, and the undercarboxylated osteocalcin levels decreased and returned to levels within the normal range in three (one in the 5 mg/day group, two in the 1 mg/day group) out of the 13 participants by the end of the trial. The mean end of trial difference in ucOC between the two intervention groups was ‐2.20 (95% CI ‐14.33 to 9.93) (Analysis 1.1).
1.1. Analysis.
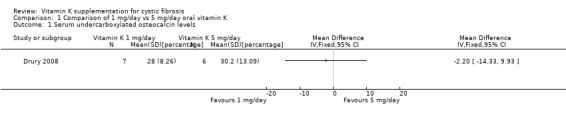
Comparison 1 Comparison of 1 mg/day vs 5 mg/day oral vitamin K, Outcome 1 Serum undercarboxylated osteocalcin levels.
There was no evidence of any difference between the 5 mg/day and the 1 mg/day vitamin K dosage in terms of statistically significant effect on ucOC levels at the end of the one‐month trial period (Drury 2008).
In the Beker trial, all of the participants had increased serum undercarboxylated osteocalcin concentrations (ucOC) at enrolment and prior to supplementation (Beker 1997). It was reported that following supplementation and by the end of the trial the majority had successfully achieved the normal reference mean levels (21%) of ucOC (Beker 1997).
b. ucOC/cOC (carboxylated osteocalcin) ratio (UCR)
This was not evaluated in either of the trials (Beker 1997; Drury 2008).
4. Vitamin K‐specific laboratory outcomes
a. Plasma level of vitamin K1
In the Drury trial, the baseline vitamin K levels in seven out of the 14 participants were sub‐optimal (defined as less than 0.3 nmol/L) (Drury 2008). The paper reported that serum vitamin K levels appeared to improve significantly (P < 0.001) with supplementation, rising into the normal range in all of the participants who were below the optimum level. There was no statistically significant difference in effect between the 5 mg/day and the 1 mg/day vitamin K dose; MD ‐4.46 (95% CI ‐12.65 to 3.73) (Analysis 1.2).
1.2. Analysis.
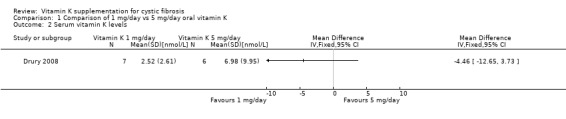
Comparison 1 Comparison of 1 mg/day vs 5 mg/day oral vitamin K, Outcome 2 Serum vitamin K levels.
In the Beker trial, a substantial number of the participants had below normal serum vitamin K levels at trial entry (Beker 1997). Although the mean concentration of plasma vitamin K was higher in the supplemented group, in only less than half of the total number of participants were these levels reportedly brought into the normal range after supplementation with the 5 mg dose (Beker 1997).
b. Proteins induced by vitamin K absence or antagonism factor II (PIVKA II) levels
Drury did not consider or report on this outcome (Drury 2008). In the Beker trial PIVKA‐II concentrations were elevated prior to supplementation and almost one third of the participants had PIVKA‐II levels within the normal range (≤ 2 ng/ml) following supplementation (Beker 1997).
Discussion
Summary of main results
The results from both of the included trials could not be pooled and entered into a meta‐analysis; however, both trials reported an increase in serum vitamin K levels, and a decrease in the undercarboxylated osteocalcin levels which returned to normal following supplementation with oral vitamin K 1 mg/day for one month. There did not appear to be any significant difference in these outcomes when a dose of 1 mg/day was compared with 5 mg/day in the Drury trial (Drury 2008). The PIVKA levels also showed a decrease and a return to normal in the Beker trial following supplementation (Beker 1997).
Overall completeness and applicability of evidence
The noticeable absence in the included trials of any assessments of important clinical outcomes related to coagulopathy or growth and improvement in quality of life as a result of vitamin K supplementation does somewhat limit the overall completeness and ultimately the generalisability of the evidence to the wider CF population. Equally, the short duration and follow‐up of the included trials does not permit any conclusions to be made about the longer‐term benefits and any potential harms of vitamin K supplementation.
Future research should aim to close this gap in the evidence by focusing more closely on some of the patient‐relevant and preferred outcomes rather than solely on biochemical laboratory analyses.
Quality of the evidence
The two trials included in this review were underpowered and of short duration which was illustrated by the wide confidence intervals in the comparisons of treatment effect and reflected the degree of imprecision in these results (Beker 1997; Drury 2008). Some of the practical and methodological difficulties faced by investigators of this research question were highlighted in these trials. The key factors which are likely to have had a degree of impact on the quality level of the evidence for the outcomes sought in this review can be linked to the design and implementation of the included trials, and in particular to the effective concealment of the allocation sequence and adequate blinding of investigators and outcome assessors.
Potential biases in the review process
Although it would be not unreasonable to assume that the comprehensive electronic searches employed in this review will have identified all existing randomised controlled trials and thereby helped to limit bias in the conduct of this review, the absence of any other published randomised trials over the intervening ten years between the two included trials and their scant contribution to the outcomes specified for this review, might presuppose an indication of publication bias.
Agreements and disagreements with other studies or reviews
Several trials have indicated a degree of support for the requirement of supplementation in addition to emphasising the comparative safety of oral supplementation with vitamin K in people with CF (Beker 1997; Borowitz 2002; Ramsey 1992; Sinaasappel 2002); but there is no agreement amongst the trials about the dosage of supplementation. However, there is some concern that the adequacy of dosing based on measurement of vitamin K levels may be inaccurate and that PIVKA levels and ucOC levels may be better indicators of effectiveness of supplementation. Some trials suggest a complimentary role for quantified dietary intake of vitamin K in people with CF (Dougherty 2010). This review did not show anything conclusively to agree or disagree with these trials.
Authors' conclusions
Implications for practice.
People with CF are at risk of vitamin K deficiency. Routine supplementation along with the other fat soluble vitamins is common clinical practice; however, there appears to be very little consensus about the exact dosage that should be prescribed. Until further evidence is available supplementation should continue to follow published ECFS and CFF guidelines (Borowitz 2002; Cystic Fibrosis Trust 2002; Sinaasappel 2002) and be guided by monitoring of the PIVKA or ucOC levels at annual clinical reviews.
Implications for research.
There is now a better understanding of the important effect of vitamin K on gamma‐carboxylation of osteocalcin synthesized in the bones over and above its well‐acknowledged requirement for synthesis of coagulation proteins in the liver. Well‐designed randomised controlled trials are still needed to determine the impact of vitamin K on the outcomes relevant to bone health in addition to routine supplementation and its benefits in people with CF. Research in this area is currently limited and long‐term and large‐scale trials are needed to provide clear answers to these issues. Additional issues that need to be considered are the sensitivity and reliability of markers for vitamin K deficiency, as well as the diagnostic accuracy and associated costs of laboratory equipment and tests.
Thus randomised controlled trials of vitamin K supplementation should be placebo‐controlled trials of parallel‐design involving both children and adults (considered separately). Outcomes should include clinical measures (e.g. coagulation effects), bone measures (density scans) and biochemical markers. In addition patient‐orientated measures such as quality of life and patient satisfaction should also be evaluated. Possible adverse events should also be specifically recorded and reported.
Further research recommendations based on the EPICOT format (Brown 2006) are presented in the additional tables (Table 4).
3. Research recommendations based on a gap in the evidence on Vitamin K supplementation for cystic fibrosis.
| Core elements | Issues to consider | Status of research for this review |
| Evidence (E) | What is the current state of evidence? | A systematic review found only limited high quality evidence in relation to the effectiveness or otherwise of vitamin K supplementation for people with CF. |
| Population (P) | Diagnosis, disease stage, comorbidity, risk factor, sex, age, ethnic group, specific inclusion or exclusion criteria, clinical setting | Any age group with a diagnosis of CF (defined by sweat test or genetic testing or both). Pancreatic insufficient. |
| Intervention (I) | Type, prognostic factor | All preparations of vitamin K used as a supplement at any dose and for any duration. |
| Comparison (C) | Type, prognostic factor | Placebo with a dose, frequency, duration comparable to the intervention, or no supplementation. Trials comparing different doses and dose regimens of vitamin K will also be considered. Compliance to be recorded via pill counts and any concomitant medications. |
| Outcome (O) | Which clinical or patient related outcomes will the researcher need to measure, improve, influence or accomplish? Which methods of measurement should be used? | Clinical outcomes related to:
Biochemical analysis:
Quality of life:
Adverse events Data type: continuous and dichotomous |
| Time stamp (T) | Date of literature search or recommendation | 15 April 2010. |
| Study type | What is the most appropriate study design to address the proposed question? | RCT (adequately powered/large sample size, sufficient duration) Methods: concealment of allocation sequence Blinding: participants and investigators, but if not feasible then outcomes assessors and data analysts should be blinded. Setting: CF Clinic |
BMI: body mass index CF: cystic fibrosis cOC: carboxylated osteocalcin DEXA: dual energy X‐ray absorptiometry ELISA: enzyme‐linked immunosorbent assay HPLC: high performance liquid chromatography PIVKA‐II: proteins induced by vitamin K absence or antagonism factor II RCT: randomised controlled trial ucOC: undercarboxylated osteocalcin
What's new
| Date | Event | Description |
|---|---|---|
| 20 June 2017 | New search has been performed | A search of the Cochrane Cystic Fibrosis and Genetic Disorders Review Group's Cystic Fibrosis Trials Register did not identify any new references potentially eligible for inclusion in this review. |
| 20 June 2017 | New citation required but conclusions have not changed | A former co‐author, Prof Zbys Fedorowicz, has stepped down from the review and been replaced by Dr Amy Price. No new studies have been included in this updated review, therefore our conclusions remain the same. |
History
Protocol first published: Issue 4, 2010 Review first published: Issue 1, 2011
| Date | Event | Description |
|---|---|---|
| 13 April 2015 | Amended | Contact details updated. |
| 4 February 2015 | Amended | Source of support for author VT clarified and added. |
| 18 December 2014 | New search has been performed | A search of the Cystic Fibrosis and Genetic Disorders Group's Cystic Fibrosis Trials Register did not identify any potentially eligible references for this review. |
| 18 December 2014 | New citation required but conclusions have not changed | We have not been able to include any new information, hence our conclusions remain the same. |
| 21 January 2013 | New search has been performed | A search of the Group's Cystic Fibrosis Register identified a single new reference to an ongoing study already listed in the review (Kuitert 2010). |
| 21 January 2013 | New citation required but conclusions have not changed | No new information has been added to the review, therefore the conclusions have not changed. |
| 22 May 2012 | Amended | Contact details updated. |
Acknowledgements
The authors would like to thank Nikki Jahnke of the Cochrane Cystic Fibrosis and Genetic Disorders Group for her support throughout this review.
We would also like to thank Professor Zbys Fedorowicz for his contributions to the review from its inception up to the update in 2017.
This project was supported by the National Institute for Health Research, via Cochrane Infrastructure funding to the Cochrane Cystic Fibrosis and Genetic Disorders Group. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, NHS or the Department of Health.
Appendices
Appendix 1. Glossary
| Term | Meaning |
| bisphosphonate | a class of drugs that prevent the loss of bone mass, used to treat osteoporosis and similar diseases |
| carboxylation | a chemical reaction in which a carboxylic acid group is introduced in a substrate |
| coagulopathy | a defect in the body's mechanism for blood clotting |
| cofactor | a non‐protein chemical compound that is bound to a protein and is required for the protein's biological activity |
| gamma‐glutamyl carboxylase | an enzyme that catalyses the gamma‐carboxylation of glutamic acid residues in bone matrix proteins such as osteocalcin |
| haemostasis | a complex process which causes the bleeding process to stop |
| homozygous | in genetics having identical alleles for a single characteristic |
| mucosal bleeding | bleeding in mucus membranes |
| osteoblast | mononucleate cells that are responsible for bone formation |
| post‐translational modification | the chemical modification of a protein after its translation (the production of proteins by decoding messenger RNA); the post‐translational modification extends the range of functions of the protein. |
| subclinical | describes an early stage or mild form of a medical condition, where no symptoms are detectable. |
| subcutaneous bleeding | bleeding under the skin |
Data and analyses
Comparison 1. Comparison of 1 mg/day vs 5 mg/day oral vitamin K.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Serum undercarboxylated osteocalcin levels | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2 Serum vitamin K levels | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Beker 1997.
| Methods | Randomised cross‐over trial (2 periods of 4 weeks). CF Clinic Children's National Medical Center (CNMC), Washington DC. No date specified. | |
| Participants | Randomised: N = 18 (8 male, 10 female); mean age 20 years (range 13 ‐ 35 years). Inclusion criteria
Exclusion criteria
Withdrawal or loss to follow‐up: none reported. |
|
| Interventions | Intervention: 5 mg oral vitamin K1 supplementation per week. Control: no supplementation. 4 weeks of first treatment then crossed over to the other treatment for a second 4‐week period. Concomitant medications permitted: cephalosporin (13); sulfamethoxazole (3); erythromycin (1); bronchodilators; standard multivitamins and 200 ‐ 400 IU vitamin E. |
|
| Outcomes | Primary outcomes: none reported Secondary outcomes (assessments at entry and end of each trial period)
3‐day dietary intake records were completed during each treatment period, but these did not correspond with the nutritional parameters sought as secondary outcomes for this review. Patient compliance was verified by the trial coordinator at each visit. |
|
| Notes | Randomised cross‐over trial, vitamin K supplementation compared with no treatment. No wash‐out period with a potential carry‐over of treatment effect. No first‐period data available. "Supported in part by grants from the Board of Lady Visitors, Children's National Medical Center, Washington, DC, and the University of Maryland, College Park, Maryland." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "randomly assigned" Page 512 Comment: insufficient information to make a clear judgement of 'Yes' or 'No'. |
| Allocation concealment (selection bias) | Unclear risk | Not reported. Probably not done. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Participants: not possible; control was 'no treatment'. Healthcare providers: not possible; control was 'no treatment'. Outcomes assessors and data analysts: unclear. Comment: overall judgement unclear. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | There were no withdrawals and no missing or incomplete data. |
| Selective reporting (reporting bias) | Low risk | Although the protocol was not available all relevant outcomes appear to have been addressed. |
| Other bias | Unclear risk | Quote: "Supported in part by grants from the Board of Lady Visitors, Children's National Medical Center, Washington, DC, and the University of Maryland, College Park, Maryland." Comment: it is unclear to what extent the support provided may have had on the results of this study. Insufficient information to assess whether an important risk of bias exists. |
Drury 2008.
| Methods | Randomised control trial over 1‐month period. Montreal Children's Hospital Cystic Fibrosis Clinic, Canada. Date not specified. | |
| Participants | Randomised: N = 14; 8 to 18 years, gender unspecified. Inclusion criteria
Exclusion criteria:
Withdrawal or loss to follow‐up: missing data (1) from 5 mg group at final assessment. |
|
| Interventions | Intervention: oral administration of injectable formulation of vitamin K1 phytonadione (Sandoz Canada, Boucherville, Qc) diluted 1 mg/1 ml. Dose 1 mg/day for 1 month. Control: identical but dose 5 mg/day for 1 month. | |
| Outcomes | Primary outcomes: none reported Secondary outcomes
Measured at the beginning of the trial and at the end of 1 month. |
|
| Notes | This project was funded by the Canadian CF Foundation. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "were randomised to receive either 1 mg/day, or 5 mg/day" Page 458. Comment: insufficient information to make a clear judgement of 'Yes' or 'No'. |
| Allocation concealment (selection bias) | Unclear risk | Not reported. Probably not done. |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Participants: not reported. Healthcare providers: unclear. Outcomes assessors and data analysts: unclear. Comment: overall judgement unclear. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote "One subject in the 5 mg group lost consciousness at the time of the second blood procurement". Page 458 Comment: incomplete data for one participant. |
| Selective reporting (reporting bias) | Low risk | The stated objectives of the trial appear to match the listed outcomes. There was no evidence of selective reporting of outcomes. |
| Other bias | Unclear risk | Quote: "This project was funded by the Canadian CF Foundation". Comment: it is unclear to what extent the support provided may have had on the results of this trial. Insufficient information to assess whether an important risk of bias exists. |
ALT: alanine aminotransferase AST: aspartate aminotransferase BMI: body mass index CF: cystic fibrosis IU: international units NCHS: National Center for Health Statistics PIVKA‐II: proteins induced by vitamin K absence or antagonism factor II RCT: randomised controlled trial
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Cornelissen 1992 | Non‐RCT. |
| Grey 2008 | Non‐RCT. |
| Mosler 2003 | Non‐RCT. |
| Nicolaidou 2006 | Non‐RCT, non‐CF control group. |
| Wilson 2001 | Uncontrolled study, non‐RCT. |
CF: cystic fibrosis RCT: randomised controlled trial
Characteristics of studies awaiting assessment [ordered by study ID]
van Hoorn 2003.
| Methods | Case controlled study |
| Participants | People with CF |
| Interventions | Vitamin K in 3 different groups ‐ no supplements, low supplements or high supplements |
| Outcomes | serum ucOC level |
| Notes | Awaiting inclusion until the response form the authors about randomisation in the study |
van Hoorn 2008.
| Methods | Randomised controlled study |
| Participants | 26 participants not receiving vitamin K supplementation before |
| Interventions | 0.1 mg and 1 mg vitamin K supplementation for 2 years |
| Outcomes | ucOC levels and BMD |
| Notes | Only abstract is available now, likely to be included, but we will consider after we get further information from the investigators |
BMD: bone mineral density CF: cystic fibrosis ucOC: undercarboxylated osteocalcin
Characteristics of ongoing studies [ordered by study ID]
Kuitert 2010.
| Trial name or title | Investigating the effect of vitamin K supplementation on markers of bone turnover and bone density in adolescents and adults with CF |
| Methods | RCT |
| Participants | Patients with a diagnosis of CF (positive sweat test or genotype testing) aged over 16 years (post pubertal‐stage IV Tanner), either sex, pancreatic insufficient (i.e. with a positive faecal elastase test, and requiring pancreatic enzyme supplementation) and no overt liver disease. |
| Interventions | 10 mg of menadiol phosphate (water soluble form of vitamin K) once daily orally for 12 months versus placebo. |
| Outcomes |
|
| Starting date | 09/05/2008 |
| Contact information | Lieske Kuitert, Department of Respiratory Medicine, London Chest Hospital, Bonner Road, E2 9JX, London, United Kingdom |
| Notes | Stated on www.controlled‐trials.com that trial completed, await publication of results. |
CF: cystic fibrosis DEXA: dual energy x‐ray absorptiometry RCT: randomised controlled trial
Contributions of authors
VJ, ZF and VT were responsible for:
organising the retrieval of papers;
writing to authors of papers for additional information;
screening search results;
screening retrieved papers against inclusion criteria;
appraising the quality of papers;
data collection for the review;
extracting data from papers; and
obtaining and screening data on unpublished trials;
the analysis and interpretation of data.
VJ and VT were responsible for :
designing the review;
co‐ordinating the review;and
data extraction and management for the review.
All review authors contributed to writing the review. VJ conceived the idea for the review and is the guarantor of the review.
Sources of support
Internal sources
No sources of support supplied
External sources
-
National Health and Medical Research Council, Australia.
Support for AC (Practitioner Fellowship grant number 545216)
-
NIH training grant, USA.
Training grant T32DK007699/DK/NIDDK awarded to Vidhu Thaker.
Declarations of interest
Anne Chang declares she has received a grant provided by GSK which is unrelated to this topic. She is also the principal investigator on a study examining azithromycin for bronchiolitis in Indigenous children.
The remaining authors declare no financial conflicts of interest and that they do not have any associations with any parties who may have vested interests in the results of this review.
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Beker 1997 {published data only}
- Beker LT, Ahrens RA, Fink RJ, O'Brien ME, Davidson KW, Sokoll LJ, et al. Effect of vitamin K1 supplementation on vitamin K status in cystic fibrosis patients. Journal of Pediatric Gastroenterology and Nutrition 1997;24(5):512‐7. [PUBMED: 9161943] [DOI] [PubMed] [Google Scholar]
- Beker LT, Ahrens RA, Fink RJ, Sadowski JA, Davidson KW, Sokoll LJ, et al. Abnormal Vitamin K status in cystic fibrosis patients [abstract]. Pediatric Pulmonology 1994;18 Suppl 10:358. [DOI] [PubMed] [Google Scholar]
Drury 2008 {published and unpublished data}
- Drury D, Grey VL, Ferland G, Gundberg C, Lands LC. Efficacy of high dose phylloquinone in correcting vitamin K deficiency in cystic fibrosis. Journal of Cystic Fibrosis 2008;7(5):457‐9. [PUBMED: 18511355] [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Cornelissen 1992 {published data only}
- Cornelissen EA, Lieburg AF, Motohara K, Oostrom CG. Vitamin K status in cystic fibrosis. Acta Paediatrica 1992;81(9):658‐61. [PUBMED: 1421902] [DOI] [PubMed] [Google Scholar]
Grey 2008 {published data only}
- Grey V, Atkinson S, Drury D, Casey L, Ferland G, Gundberg C, et al. Prevalence of low bone mass and deficiencies of vitamins D and K in pediatric patients with cystic fibrosis from 3 Canadian centers. Pediatrics 2008;122(5):1014‐20. [PUBMED: 18977981] [DOI] [PubMed] [Google Scholar]
Mosler 2003 {published data only}
- Mosler K, Kries R, Vermeer C, Saupe J, Schmitz T, Schuster A. Assessment of vitamin K deficiency in CF‐‐how much sophistication is useful?. Journal of Cystic Fibrosis 2003;2(2):91‐6. [PUBMED: 15463856] [DOI] [PubMed] [Google Scholar]
Nicolaidou 2006 {published data only}
- Nicolaidou P, Stavrinadis I, Loukou I, Papadopoulou A, Georgouli H, Douros K, et al. The effect of vitamin K supplementation on biochemical markers of bone formation in children and adolescents with cystic fibrosis. European Journal of Pediatrics 2006;165(8):540‐5. [PUBMED: 16622660] [DOI] [PubMed] [Google Scholar]
Wilson 2001 {published data only}
- Wilson DC, Rashid M, Durie PR, Tsang A, Kalnins D, Andrew M, et al. Treatment of vitamin K deficiency in cystic fibrosis: Effectiveness of a daily fat‐soluble vitamin combination. Journal of Pediatrics 2001;138(6):851‐5. [PUBMED: 11391328] [DOI] [PubMed] [Google Scholar]
References to studies awaiting assessment
van Hoorn 2003 {published data only}
- Hoorn JH, Hendriks JJ, Vermeer C, Forget PP. Vitamin K supplementation in cystic fibrosis. Archives of Disease in Childhood 2003;88(11):974‐5. [PUBMED: 14612359] [DOI] [PMC free article] [PubMed] [Google Scholar]
van Hoorn 2008 {published data only}
- Hoorn JH, Schurgers JJ, Vermeer C, Escher HC, Hendriks HJ. The effect of vitamin K supplementation on bone status in children with cystic fibrosis [abstract]. Pediatric Pulmonology 2008;43(S31):421. [Google Scholar]
References to ongoing studies
Kuitert 2010 {published and unpublished data}
- Powell M, Kuitert L. Effect of vitamin K supplementation over one year on bone health in adolescents and adults with cystic fibrosis. Pediatric Pulmonology 2010;45(S33):421. [Abstract no: 421; CFGD Register: CO47] [Google Scholar]
Additional references
Belle 1991
- Belle M, Hanss M, Guillaumont M, Leclercq M, Guinet R. Des‐gamma‐carboxyprothrombin detection by immunoblotting after polyacrylamide gelaffinoelectrophoresis in human plasmas. Electrophoresis 1991;12(4):294‐7. [PUBMED: 2070784] [DOI] [PubMed] [Google Scholar]
Belle 1995
- Belle M, Brebant R, Guinet R, Leclercq M. Production of a new monoclonal antibody specific to human des‐gamma‐carboxyprothrombin in the presence of calcium ions. Application to the development of a sensitive ELISA‐test. Journal of Immunoassay 1995;16(2):213‐29. [PUBMED: 7629279] [DOI] [PubMed] [Google Scholar]
Bobadilla 2002
- Bobadilla JL, Macek M Jr, Fine JP, Farrell PM. Cystic fibrosis: a worldwide analysis of CFTR mutations‐correlation with incidence data and application to screening. Human Mutation 2002;19(6):575‐606. [DOI] [PubMed] [Google Scholar]
Borowitz 2002
- Borowitz D, Baker RD, Stallings V. Consensus report on nutrition for paediatric patients with cystic fibrosis. Journal of Pediatric Gastroenterology & Nutrition 2002;35:246‐59. [DOI] [PubMed] [Google Scholar]
Brown 2006
- Brown P, Brunnhuber K, Chalkidou K, Chalmers I, Clarke M, Fenton M, et al. How to formulate research questions. BMJ 2006;333(7572):804‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Conway 2005
- Conway SP, Wolfe SP, Brownlee KG, White H, Oldroyd B, Truscott JG, et al. Vitamin K status among children with cystic fibrosis and its relationship to bone mineral density and bone turnover. Pediatrics 2005;115(5):1325‐31. [DOI] [PubMed] [Google Scholar]
Cystic Fibrosis Trust 2002
- Cystic Fibrosis Trust Nutrition Working Group. Nutritional management of cystic fibrosis. London: Cystic Fibrosis Trust 2002.
Cystic Fibrosis Trust 2007
- UK CF Trust. Bone Mineralisation in Cystic Fibrosis.Report of the UK Cystic Fibrosis Trust Bone Mineralisation Working Group. www.cftrust.org.uk/aboutcf/publications/consensusdoc/Bone‐Mineral‐Booklet.pdf February 2007.
Davis 2006
- Davis PB. Cystic fibrosis since 1938. American Journal of Respiratory and Critical Care Medicine 2006;173(5):475‐82. [PUBMED: 16126935] [DOI] [PubMed] [Google Scholar]
Dodge 2006
- Dodge JA, Turck D. Cystic fibrosis: nutritional consequences and management. Best Practice & Research. Clinical Gastroenterology 2006;20(3):531‐46. [DOI] [PubMed] [Google Scholar]
Dougherty 2010
- Dougherty KA, Schall JI, Stallings VA. Suboptimal vitamin K status despite supplementation in children and young adults with cystic fibrosis. American Journal of Clinical Nutrition 2010;92(3):660‐7. [PUBMED: 20554788] [DOI] [PMC free article] [PubMed] [Google Scholar]
Durie 1994
- Durie PR. Vitamin K and the management of patients with cystic fibrosis. CMAJ 1994;151(7):933‐6. [PUBMED: 7922929] [PMC free article] [PubMed] [Google Scholar]
Fuchs 1998
- Fuchs JR, Langer JC. Long‐term outcome after neonatal meconium obstruction. Pediatrics 1998;101(4):E7. [PUBMED: 9521973] [DOI] [PubMed] [Google Scholar]
Gee 2000
- Gee L, Abbott J, Conway SP, Etherington C, Webb AK. Development of a disease specific health related quality of life measure for adults and adolescents with cystic fibrosis. Thorax 2000;55(11):946‐54. [PUBMED: 11050265] [DOI] [PMC free article] [PubMed] [Google Scholar]
Goss 2004
- Goss CH, Rosenfeld M. Update on Cystic Fibrosis Epidemiology. Current Opinion in Pulmonary Medicine 2004;10(6):510‐4. [PUBMED: 15510059] [DOI] [PubMed] [Google Scholar]
Higgins 2003
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analyses. BMJ 2003;327(7414):557‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011a
- Higgins JPT, Altman DG. Chapter 8: Assessing risk of bias in included studies. In: Higgins JPT, Green S (editors). Cochrane Handbook of Systematic Reviews of Interventions. Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Higgins 2011b
- Sterne JAC, Egger M, Moher D, on behalf of the Cochrane Bias Methods Group. Chapter 10: Addressing reporting biases. In: Higgins JPT, Green S (editors). Cochrane Handbook of Systematic Reviews of Interventions. Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Higgins 2011c
- Deeks JJ, Higgins JPT, Altman DG. Chapter 9: Analysing data and undertaking meta‐analyses. In: Higgins JPT, Green S (editors). Cochrane Handbook of Systematic Reviews of Interventions. Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org 2011. [REFWORKS: ID: 1335]
Krzyzanowska 2010
- Krzyzanowska P, Lisowska A, Skorupa W, Pogorzelski A, Kaminska B, Cichy W, et al. Vitamin K deficiency in patients with CF despite supplementation [Niedobor witaminy K u chorych na mukowiscydoze pomimo stosowanej suplementacji]. Medycyna Wieku Rozwojowego 2010;14(1):68‐72. [PUBMED: 20608431] [PubMed] [Google Scholar]
Krzyzanowska 2015
- Krzyzanowska P, Pogorzelski A, Skorupa W, Moczko J, Grebowiec P, Walkowiak J. Exogenous and endogenous determinants of vitamin K status in cystic fibrosis. Scientific Reports 2015;5:12000. [DOI: 10.1038/srep12000; PUBMED: 26160248] [DOI] [PMC free article] [PubMed] [Google Scholar]
Morgan 1999
- Morgan WJ, Butler SM, Johnson CA, Colin AA, FitzSimmons SC, Geller DE, et al. Epidemiologic study of cystic fibrosis: design and implementation of a prospective, multicenter, observational study of patients with cystic fibrosis in the U.S. and Canada. Pediatric Pulmonology 1999;28(4):231‐41. [DOI] [PubMed] [Google Scholar]
Okano 2005
- Okano T. Vitamin D, K and bone mineral density. Clinical Calcium 2005;15(9):1489‐94. [PUBMED: 16137948] [PubMed] [Google Scholar]
Olsen 1994
- Olson RE. Vitamin K. In: Shils ME, Olson JA, Shike M editor(s). Modern Nutrition in Health and Disease. 8th Edition. Baltimore: Williams and Wilkins, 1994:343‐58. [Google Scholar]
Quittner 2000
- Quittner AL, Sweeny S, Watrous M, Munzenberger P, Bearss K, Gibson NA, et al. Translation and Linguistic Validation of a Disease‐Specific Quality of Life Measure for Cystic Fibrosis. Journal of Pediatric Psychology 2000;25(6):403‐14. [DOI] [PubMed] [Google Scholar]
Ramsey 1992
- Ramsey BW, Farrell PM, Pencharz P, and the Consensus Committee. Nutritional assessment and management in cystic fibrosis: a consensus report. American Journal of Clinical Nutrition 1992;55(1):108‐16. [DOI] [PubMed] [Google Scholar]
Rashid 1999
- Rashid M, Durie P, Andrew M, Kalnins D, Shin J, Corey M, et al. Prevalence of vitamin K deficiency in cystic fibrosis. American Journal of Clinical Nutrition 1999;70(3):378–82. [DOI] [PubMed] [Google Scholar]
Ratjen 2003
- Ratjen F, Döring G. Cystic fibrosis. Lancet 2003;361(9358):681‐9. [DOI] [PubMed] [Google Scholar]
RevMan 2014 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Shearer 1995
- Shearer MJ. Vitamin K. Lancet 1995;345(8944):229‐34. [PUBMED: 7823718] [DOI] [PubMed] [Google Scholar]
Sinaasappel 2002
- Sinaasappel M, Stern M, Littlewood J, Wolfe S, Steinkamp G, Heijerman HG, et al. Nutrition in patients with cystic fibrosis: a European Consensus. Journal of Cystic Fibrosis 2002;1(2):51‐75. [PUBMED: 15463811] [DOI] [PubMed] [Google Scholar]
Staab 2004
- Staab D. Cystic fibrosis ‐ therapeutic challenge in cystic fibrosis children. European Journal of Endocrinology / European Federation of Endocrine Societies 2004;151 Suppl 1:S77‐80. [PUBMED: 15339249] [DOI] [PubMed] [Google Scholar]
Uotila 1990
- Uotila L. The metabolic functions and mechanism of action of vitamin K. Scandinavian Journal of Clinical and Laboratory Investigation 1990;201 Suppl:109‐17. [PUBMED: 2244179] [PubMed] [Google Scholar]
Verghese 2003
- Verghese T, Beverley D. Vitamin K deficient bleeding in cystic fibrosis. Archives of Disease in Childhood 2003;88(6):553. [PUBMED: 12765934] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wagener 2003
- Wagener JS, Headley AA. Cystic fibrosis: current trends in respiratory care. Respiratory Care 2003;48(3):234‐45. [PubMed] [Google Scholar]
Wang 2004
- Wang LY, Bates CJ, Yan L, Harrington DJ, Shearer MJ, Prentice A. Determination of phylloquinone (vitamin K1) in plasma and serum by HPLC with fluorescence detection. Clinica Chimica Acta 2004;347(1‐2):199‐207. [PUBMED: 15313159] [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Jagannath 2010
- Jagannath VA, Fedorowicz Z, Thaker V, Chang AB, Al‐Harthy N. Vitamin K supplementation for cystic fibrosis. Cochrane Database of Systematic Reviews 2010, Issue 4. [DOI: 10.1002/14651858.CD008482] [DOI] [Google Scholar]
Jagannath 2011
- Jagannath VA, Fedorowicz Z, Thaker V, Chang AB. Vitamin K supplementation for cystic fibrosis. Cochrane Database of Systematic Reviews 2011, Issue 1. [DOI: 10.1002/14651858.CD008482.pub2] [DOI] [PubMed] [Google Scholar]
Jagannath 2013
- Jagannath VA, Fedorowicz Z, Thaker V, Chang AB. Vitamin K supplementation for cystic fibrosis. Cochrane Database of Systematic Reviews 2013, Issue 4. [DOI: 10.1002/14651858.CD008482.pub3] [DOI] [PubMed] [Google Scholar]
Jagannath 2015
- Jagannath VA, Fedorowicz Z, Thaker V, Chang AB. Vitamin K supplementation for cystic fibrosis. Cochrane Database of Systematic Reviews 2015, Issue 1. [DOI: 10.1002/14651858.CD008482.pub4] [DOI] [PMC free article] [PubMed] [Google Scholar]


