Abstract
Background
Infant acute pain and distress is commonplace. Infancy is a period of exponential development. Unrelieved pain and distress can have implications across the lifespan. This is an update of a previously published review in the Cochrane Database of Systematic Reviews, Issue 10 2011 entitled 'Non‐pharmacological management of infant and young child procedural pain'.
Objectives
To assess the efficacy of non‐pharmacological interventions for infant and child (up to three years) acute pain, excluding kangaroo care, and music. Analyses were run separately for infant age (preterm, neonate, older) and pain response (pain reactivity, immediate pain regulation).
Search methods
For this update, we searched the Cochrane Central Register of Controlled Trials (CENTRAL) in The Cochrane Library (Issue 2 of 12, 2015), MEDLINE‐Ovid platform (March 2015), EMBASE‐OVID platform (April 2011 to March 2015), PsycINFO‐OVID platform (April 2011 to February 2015), and CINAHL‐EBSCO platform (April 2011 to March 2015). We also searched reference lists and contacted researchers via electronic list‐serves. New studies were incorporated into the review. We refined search strategies with a Cochrane‐affiliated librarian. For this update, nine articles from the original 2011 review pertaining to Kangaroo Care were excluded, but 21 additional studies were added.
Selection criteria
Participants included infants from birth to three years. Only randomised controlled trials (RCTs) or RCT cross‐overs that had a no‐treatment control comparison were eligible for inclusion in the analyses. However, when the additive effects of a non‐pharmacological intervention could be assessed, these studies were also included. We examined studies that met all inclusion criteria except for study design (e.g. had an active control) to qualitatively contextualize results. There were 63 included articles in the current update.
Data collection and analysis
Study quality ratings and risk of bias were based on the Cochrane Risk of Bias Tool and GRADE approach. We analysed the standardized mean difference (SMD) using the generic inverse variance method.
Main results
Sixty‐three studies, with 4905 participants, were analysed. The most commonly studied acute procedures were heel‐sticks (32 studies) and needles (17 studies). The largest SMD for treatment improvement over control conditions on pain reactivity were: non‐nutritive sucking‐related interventions (neonate: SMD ‐1.20, 95% CI ‐2.01 to ‐0.38) and swaddling/facilitated tucking (preterm: SMD ‐0.89; 95% CI ‐1.37 to ‐0.40). For immediate pain regulation, the largest SMDs were: non‐nutritive sucking‐related interventions (preterm: SMD ‐0.43; 95% CI ‐0.63 to ‐0.23; neonate: SMD ‐0.90; 95% CI ‐1.54 to ‐0.25; older infant: SMD ‐1.34; 95% CI ‐2.14 to ‐0.54), swaddling/facilitated tucking (preterm: SMD ‐0.71; 95% CI ‐1.00 to ‐0.43), and rocking/holding (neonate: SMD ‐0.75; 95% CI ‐1.20 to ‐0.30). Fifty two of our 63 trials did not report adverse events. The presence of significant heterogeneity limited our confidence in the findings for certain analyses, as did the preponderance of very low quality evidence.
Authors' conclusions
There is evidence that different non‐pharmacological interventions can be used with preterms, neonates, and older infants to significantly manage pain behaviors associated with acutely painful procedures. The most established evidence was for non‐nutritive sucking, swaddling/facilitated tucking, and rocking/holding. All analyses reflected that more research is needed to bolster our confidence in the direction of the findings. There are significant gaps in the existing literature on non‐pharmacological management of acute pain in infancy.
Plain language summary
Drug‐free management of young children's pain during medical procedures
Background: Infant pain has been historically under‐managed.
Review question: This review assessed 24 different ways of reducing young children's pain during medical procedures without using drugs, such as using a pacifier, distracting the child, and rocking a child. We analysed studies separately for babies who were born preterm, full‐term newborns, and older infants from one month to three years. We also looked at if there was a difference on the impact of the interventions depending on whether the infant had just had the painful procedure (pain reactivity), as opposed to calming down from their peak distress (immediate pain regulation).
Study characteristics: This updated review examined 63 randomised controlled trials of 4905 participants.
Key results and Quality of evidence: While there was evidence for non‐nutritive sucking, swaddling and tucking, massage, environment modification, rocking, video distraction, structured non‐parent involvement at different ages, and pain types, none of the analyses were based on sufficient evidence to allow us to draw firm conclusions (i.e. high quality studies from at least two independent laboratories).
Summary of findings
Background
This review is an update of a previously published review in the Cochrane Database of Systematic Reviews, Issue 10 2011 entitled 'Non‐pharmacological management of infant and young child procedural pain'.
Description of the condition
Despite the vigorous responses that result when an infant is subjected to a painful procedure, the premise that infants are insensitive to pain was only recently rejected by the general scientific community (Anand 1987), although exceptions in the literature still remain (e.g. Derbyshire 1999). Early studies suggested that infants did not possess a cortex well developed enough to perceive or localize pain (McGraw 1943). Moreover, initial misinterpretations of common infant pain outcomes, for example, the lack of declarative memory for painful experiences during infancy (Field 1995), the muted responses of premature infants after a barrage of painful procedures (Johnston 1993), and unacceptable rates of cardiac arrest or death due to poor knowledge of infant morphokinetics during the 1950s to 1970s (Berde 2005), all perpetuated widespread neglect of infant pain treatment until the last three decades.
Current research supports the understanding that infants possess the anatomical and functional requirements to perceive pain (Fitzgerald 2005; Slater 2010) and respond during tissue insult in a manner unequivocally interpretable as pain (Grunau 1987). Despite evidence of the long‐term implications of unrelieved pain during infancy (Anand 2000; Grunau 1996; Grunau 2000; Howard 2003; Taddio 1997), evidence that infant pain is still under‐managed and unmanaged is clearly evident (Alexander 2003; Pillai Riddell 2005; Simons 2003; Taddio 2010). A comprehensive and systematic review of pain management strategies is integral to appropriate infant pain management.
Description of the intervention
Generally speaking, pain management can be subdivided into two categories: pharmacological (Barber 2004; treatments that deal with the uses, effects, and modes of action of drugs) and non‐pharmacological (any treatments (environmental, psychological/cognitive, and behavioral strategies) that do not deal with uses, effects, and modes of action of drugs).
In a recent précis of infant non‐pharmacological pain management strategies, pain management was defined as any strategy or technique administered to an infant in pain with the intention of lessening pain experience (Pillai Riddell 2013a). One of the important principles in infant pain management is to recognize that pain is most effectively managed by avoiding, preventing or limiting exposure to pain‐provoking stimuli (Joint Committee 2000). Accordingly, pain management during infancy must be multifaceted and integrated within every step of the decision‐making process; from deciding whether a particular procedure is warranted, to determining the safest and most efficacious pain relieving strategy.
There are comprehensive reviews which summarize assessment and management techniques for painful procedures in neonates or infants, or both, which have recently been published (Anand 2001; Cignacco 2007; Cohen 2008; Johnston 2011; Kleiber 1999; Obeidat 2009; Piira 2005; Prasopkittikun 2003; Schechter 2007; Slifer 2002). To our knowledge, however, aside from our Cochrane Review there are no other comprehensive, systematic meta‐analyses conducted on the efficacy or effectiveness of non‐pharmacological interventions for managing acute pain and distress in infants and young children up to three years of age that:
analyse results according to developmental subcategories within infancy (i.e. infant born preterm, healthy neonate, older infant); and
analyse type of pain response (i.e. responses right after the painful stimulus (pain reactivity) versus those after the initial pain response period (immediate pain regulation). This dichotomy is supported by a program of studies synthesized in a recent review chapter (Pillai Riddell 2013d).
Why it is important to do this review
Both of these above dimensions of analysis are crucial due to the steep trajectory of infant development, both psychologically and physiologically. Moreover, given the different physiological and psychological mechanisms subsuming a person’s immediate reaction to a painful stimulus (automatic or reflexive reactivity, or both) and a person’s reaction during the period of recovering from the painful insult (immediate pain regulation), it was seen as crucial to elucidate this variable to keep moving the literature on infant acute pain management forward. Therefore, this review will take a broader and more in‐depth look at the non‐pharmacological pain‐management literature for infant acute pain.
Objectives
To assess the efficacy of non‐pharmacological interventions for infant and child (up to three years) acute pain, excluding kangaroo care, and music. Analyses were run separately for infant age (preterm, neonate, older infant) and pain response (pain reactivity, immediate pain regulation).
Methods
Criteria for considering studies for this review
Types of studies
We first included randomised controlled trials (RCTs) and randomised cross‐over trials that utilized a no‐treatment control group. This new update also included studies that utilized an active control group if the study design allowed for the determination of an 'additive' effect of a non‐pharmacological intervention. All studies involved the non‐pharmacological management of acute procedural pain in infants and children up to three years of age. We used no language restrictions during the search.
Due to existing work completed by other Cochrane Review authors, this review excluded studies that focused on kangaroo care (Johnston 2013b), sucrose (Stevens 2010), breast milk (Shah 2009), or music (Cepeda 2006) as a pain‐management strategy. In addition, due to other existing Cochrane Reviews on these acute pain stimuli, we also excluded studies that examined pain management for the following types of acute pain stimuli and age group combinations: circumcision procedure for boys aged zero to three years (Brady‐Fryer 2009; Cyna 2010), blood sampling via heel lance or venipuncture in neonates up to 28 days (Shah 2009), and needle‐related or procedural pain in children older than three years (Uman 2006).
Types of participants
Participants included all young children who were undergoing painful acute procedures. Term and preterm infants were also included in the review. Given that research in the area of infant pain management began in the late 1980s, we selected a broad mandate of 'procedural pain' rather than any particular type of procedure. In order to provide general parameters regarding procedures that are covered by the review, sample procedures are provided. Based on two comprehensive references that outline painful procedures in either neonates or older children (Anand 2001; Uman 2006), the following non‐exhaustive list is provided as a sample of procedures that fell under the umbrella of this review (see Table 9). Definitions were derived from two online medical encyclopedic reference sources (i.e. MEDLINE Plus Medical Encyclopedia: www.nlm.nih.gov/medlineplus/mplusdictionary.html; the Merck Manual of Diagnosis and Therapy, 17th Edition, www.merck.com) and by consulting with medical professionals in the area of infant pain.
1. Procedures analyzed under scope of current review.
| Name | Description |
| Heel‐stick | Heel‐stick involves lancing of the lateral aspect of the infant's heel, squeezing the heel, and collecting the pooled blood. |
| Venipuncture (also known as venepuncture) | Surgical puncture of a vein, especially for the withdrawal of blood or for intravenous medication. |
| Needle | The act of forcing a liquid (such as vaccines) into tissue using a sharp needle. |
| Diaper change (preterm only) | Care‐giving intervention in which soiled diapers are changed and causes distress that some suspect to be pain‐related. |
| Endotracheal suctioning | A component of bronchial hygiene for mechanical ventilation and involves the mechanical aspiration of pulmonary secretion from the intubated airway. Its primary purpose is to remove airway secretions in order to prevent obstructions. |
| Weighing procedure (preterm only) | Routine care procedure in which the preterm is weighed on a scale and causes distress that some suspect to be pain‐related. |
| Urinary catheterization | A tube known as a urinary catheter is inserted into a patient's bladder via the urethra. |
Types of interventions
We clustered non‐pharmacological interventions into three different categories based on their hypothesized mechanism of action (Pillai Riddell 2013a):
Environmental strategies
The context in which a painful procedure is conducted modifies behavioral and physiological expressions of infant pain. Interventions that are classified in this category involved modifying the environment to have lower pain reactivity and stress. They tended to involve multiple components that in combination modify the environment in which an infant experiences pain (i.e. low noise and lighting, clustering procedures to avoid over handling, soothing smells).
Cognitive strategies
Any intervention that is suspected to have a mechanism of action that impacts an infant's abilities to perceive the pain experience was classified here. The main intervention falling under this category is distraction. We defined distraction as any procedure aimed at diverting infant attention from the painful stimulus. For the purposes of the review, we defined distraction as either toy‐mediated distraction (use of a children’s toy) versus video‐mediated distraction (use of an audio‐visual screen displaying two‐dimensional moving images with coordinated audio output).
Behavioral strategies
These strategies involve either direct (e.g. rocking) or indirect (e.g. non‐nutritive sucking) manipulation of the infant's body (body part) by a caregiver. Most research on non‐pharmacological pain management strategies has been conducted within this domain. Accordingly, a number of strategies are covered in this review. For ease of use, we grouped strategies that were considered to have a similar (albeit not identical) mechanism of action together into categories. The categories of treatments that were included in the statistical analysis were the following.
Non‐nutritive sucking‐related strategies: an object (e.g. pacifier, non‐lactating nipple) is placed into an infant's mouth to stimulate oro‐tactile or sucking behaviours during a painful event. This may have involved other adjuvant non‐pharmacological interventions that fall under the purvey of the review (e.g. pacifier plus water was included; pacifier plus sucrose was not included unless an 'additive' study; see below).
Swaddling/facilitated tucking: swaddling is when an infant is securely wrapped in a blanket to prevent the child's limbs from moving around excessively. Facilitated tucking involves firmly containing the infant using a caregiver's hands on both head and lower limbs to maintain a 'folded‐in' position. Infant may or may not be wearing clothes.
Touch/massage‐related: an infant’s body is 'stroked' to provide some type of counter‐stimulation to the nociceptive input.
Simulated rocking and water: as opposed to being held by an adult, an infant is placed in a bassinet‐type machine that provides a swaying motion. In addition, water was administered in a manner that did not incite extensive sucking.
Simulated mother's voice: an infant is exposed to a reproduction of his or her mother’s voice within the womb, designed to help simulate the fetal environment.
Swallowing water: water is administered for ingestion without an instrument that would incite extensive sucking (e.g. water administered by a dropper).
Rocking, holding or both: an infant is held or gently moved up and down or side to side (or both) by a caregiver.
Parent presence: simply allowing the parent to be present during a painful procedure but parents are not interacting extensively with their child in a manner thought to be pain‐reducing.
Structured parental involvement: parents are instructed or informed of strategies that are accepted as pain‐reducing but are not given any materials to aid them. A variety of strategies may or may not be enacted such as rocking, holding, shushing, talking, rubbing, tickling, and distracting attention without toy or video.
Structured non‐parental involvement: A non‐parent is instructed about strategies that are accepted as pain reducing.
Therapeutic touch: an alternative approach based on the theory of energy medicine where hands are held over the infant’s body without touching the body.
Familiar odor: familiarizing an infant with the smell of vanilla 24 hours prior to the procedure and subsequently presenting the smell at the time of the procedure.
Unfamiliar odor: exposing the infant to the smell of vanilla only during the procedure.
Co‐bedding: having an infant be with their twin in an incubator.
Heel warming: involved warming the infant's heel prior to a heel‐lance procedure.
A number of strategies were found in the treatment literature which could not be included in the review because they did not have at least one study that met the criteria for the quantitative analysis, most often due to the choice of an active control group. These strategies were olfactory stimulation (providing either a pleasing smell or a familiar smell before, during and after a painful procedure), order of immunizations (providing the most painful immunization last), position during procedure (infant is positioned either prone or supine during procedure), and formula (providing infant formula during the painful procedure). Given the current ethical zeitgeist, the use of no‐treatment controls appears to be on the decline. To address this within the context of the current review, the 'additive' effect of non‐pharmacological strategies was analysed if the study used a design whereby the same intervention was used in both the treatment and control group, but the treatment group had an additional non‐pharmacological intervention. Six analyses of this kind were included in the current review.
Co‐Bedding + Sucrose versus Co‐bedding + Sucrose + Sucking: this allowed for the analysis of the additive effect of sucking on co‐bedding and sucrose.
Sucrose + Holding versus Sucrose+ Holding + Massage: this allowed for the analysis of the additive effect of massage on sucrose + holding.
Sucrose versus Sucrose + Structured non‐parent involvement: this allowed for the analysis of the additive effect of structured non‐parent involvement on sucrose.
Sucrose versus Sucrose + Pacifier: this allowed for the analysis of the additive effect of sucking on sucrose.
Sucking + Sucrose versus Sucking + Sucrose + Facilitated tucking: this allowed for the analysis of the additive effect of facilitated tucking on sucking + sucrose.
Non‐nutritive sucking versus Non‐nutritive sucking + Facilitated tucking: this allowed for the analysis of the additive effect of facilitated tucking on sucking.
Types of outcome measures
Primary outcomes
Due to the limited verbal capacity of the infant, it is important to recognize that pain measures are limited in distinguishing between infant pain and infant distress (Craig 2002). Due to the presence of an objectively painful stimulus in all studies selected for this review, however, we considered all measures of negative reactions, after the administration of a known painful stimulus, to be an indicator of an infant's pain.
Since the purpose of this review was to be able to synthesize intervention‐specific, age‐specific, and pain response‐specific information, outcomes were not subdivided by type of outcome measure. Due to the emerging verbal skills of infants and recommended clinical assessment procedures for infant pain (Franck 2000; Stevens 2007), we made the decision to only analyse objectively measured behavioral responses to pain. When studies had more than one behavioral response to pain, we used the most specific measure available. For example, we used pain facial expression over cry duration. We kept detailed logs about decisions regarding which measure (when multiple were available) was selected from an article and why. The lead authors reviewed all tables to confirm judgments made by other review authors.
Physiological measures are rarely used in clinical practice as the sole indicator of pain and the literature showed considerable inter‐study variance with the measurement of physiological indicators, therefore they were not analysed for the review. No article was completely excluded from the review because it only used physiological indicators. These articles were still qualitatively mentioned in the respective 'Summary of treatment effects' section (at the end of every treatment effect section description, results for each age group and pain response type are summarized briefly). Finally, if well‐established, multi‐dimensional pain measures were utilized, with behavioral and physiological indicators, and it was a reliable and valid measure, we used the total score, for example, the Premature Infant Pain Profile (PIPP) (Stevens 1996).
Secondary outcomes
Adverse events were considered as a secondary outcome. All studies were screened for reporting of adverse events. Three categories were tracked: no mention of adverse effects, explicit statement of no adverse effects, and explicit statement of adverse effects (details tracked regarding group distribution of adverse effects).
Search methods for identification of studies
Electronic searches
In terms of published studies, we designed a unique search strategy for each of five databases in conjunction with librarians affiliated with Cochrane. The search for the original review was on April 30, 2011. For this update, we searched:
The Cochrane Central Register of Controlled Trials (CENTRAL) in The Cochrane Library (Issue 2 of 12, 2015),
MEDLINE (OVID) (April 2011 to 2 March 2015),
EMBASE (OVID) (April 2011 to 3 March 2015),
PsycINFO (OVID) (April 2011 to February 2015),
Cumulative Index to Nursing and Allied Health Literature (CINAHL) (EBSCO) (April 2011 to March 2015).
We also searched reference lists and contacted researchers via electronic list‐serves. See Appendix 1 for the search strategies used.
Searching other resources
We made appeals to paediatric list‐serves (Pain in Child Health [PICH], Pediatric Pain, American Psychological Association’s Division 54 [Pediatric Psychology] list‐serve) for unpublished trials relating to non‐pharmacological pain management in infants. List‐serves are electronic mailing lists that facilitate widespread distribution of information to many Internet users.
Finally, using relevant articles from the pediatric pain literature (i.e., articles cited in the introduction (background) section of this review), we checked their reference lists to check for any potential articles for use in this review.
Data collection and analysis
Selection of studies
Three review authors (RPR, NR, HG) and a research assistant independently screened titles and abstracts of studies from literature searches for inclusion in the review. Review authors were not blinded to authors, institutions, journals, or results. For all abstracts where relevance was questionable, the full article was read by the review authors (RPR, NR) who made the final decision regarding inclusion.
Data extraction and management
Using the full articles, eight review authors (HG, RH, SAK, JHS, KT, LU, DL, BJS) reviewed articles for inclusion. Each article was extracted by at least two authors. For all articles where relevance was questionable, two review authors (RPR, NR) made the final decision at a consensus meeting. We used a data extraction form designed specifically for this review and divided all included articles for extraction between teams. Every included article was extracted independently and both members of the team compared every extracted data point (including risk of bias questions) for every article to ensure accuracy. When the two members of a team disagreed, RPR and NR consulted the original article for pertinent information.
Research assistants compiled data from the studies into an electronic database in SPSS 21.0 (IBM Corp 2012). Data from the studies were entered in RevMan 5.3 (RevMan 2014) and double checked by RPR and NR.
Assessment of risk of bias in included studies
At least two review authors of the extraction team (HG, RH, SAK, JHS, KT, LU, DL, BJS) scored every study included in the review for quality. For articles where there was disagreement, two review authors (RPR, NR) made the final decision. In our initial review, we used the Quality of Study Design and Methods Scale (Yates 2005) as the basis to develop the study quality rating form for this review. In the current review, a two‐pronged strategy was enacted to determine study quality and overall recommendation quality for each treatment (for each possible age‐pain response combination). Upon recommendation from our PaPaS review group, we used a simplified measure of risk of bias based on the Cochrane Handbook for Systematic Reviews of Interventions 5.1.0 (Chapter 8; Table 8.5a) (Higgins 2011a). We rated each included study on randomisation, allocation bias, blinding of participants/personnel, blinding of outcome assessors, attrition, other potential risks of bias, power calculations, and sufficient sample size. Studies were rated as having low, unclear or high risk of bias. Studies were deemed to have high risk of bias if any one of the evaluated domains (e.g. randomization, allocation bias, etc.) indicated high risk of bias. Forty‐seven studies were rated as having a high risk of bias, three studies were rated as having an unclear risk of bias, and 13 studies had a low risk of bias. Further details are provided below. Figures 1 and 2 summarize the ratings for each of the included studies (Figure 1; Figure 2). Our next step was to use these analyses in our grading of the quality of our findings based on the absolute effect of each treatment for each age‐pain response combination. Based on definitions contained within the GRADE learning modules for Cochrane reviewers, which is hosted by McMaster University (http://cebgrade.mcmaster.ca/index.html), the strength of our findings were qualified by the following criteria: design, risk of bias, inconsistency, imprecision, indirectness. They were synthesized using GradeProfiler software (GRADEpro GDT). A 'Summary of findings' table is included for each of the 51 analyses that qualifies the absolute effect of the intervention (for each possible age‐pain response combination) using the GRADE criteria ( Schünemann 2011) (see 'Summary of findings' tables). In addition, one overarching 'Summary of findings' table was created to summarize the entirety of the findings in one place (see Table 10 Summary of overall findings table).
1.
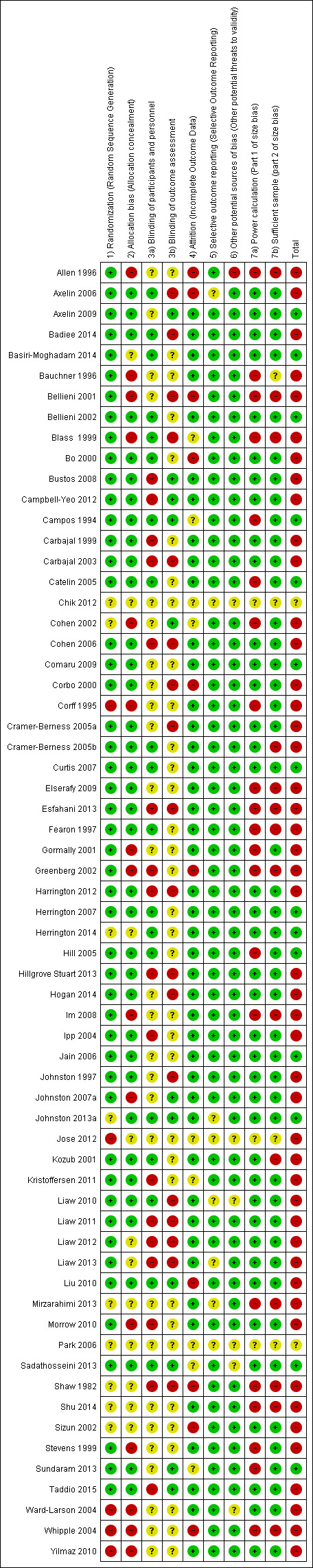
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
2.
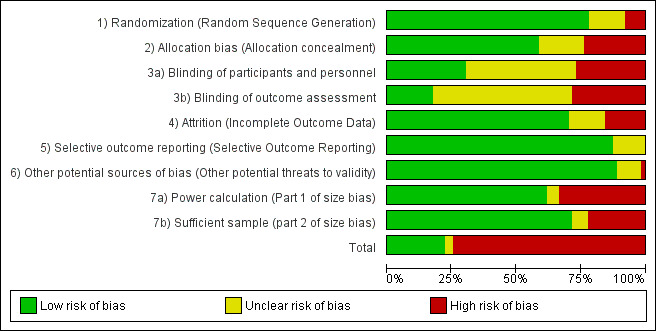
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
2. Summary of overall findings.
|
Non‐pharmacological management of infant and young child procedural pain Patient population: pre‐term born, full‐term born or older Infants Settings: 16 different counties (Australia, Brazil, Canada, China, Finland, France, Hong Kong, India, Iran, Italy, Norway, Saudi Arabia, South Korea, Taiwan, Turkey, and United States). Interventions: 20 separate interventions Comparisons: standard care or additive (as indicated in table) | ||||||
| Preterm Infants | Neonates | Older Infants | ||||
| Reactivity | Immediate regulation | Reactivity | Immediate regulation | Reactivity | Immediate regulation | |
| Non‐nutritive sucking‐related | X + |
✓ ++ |
✓ + |
✓ + |
‐ | ✓ ++ |
| Swaddling/tucking‐related | ✓ + |
✓ + |
✓ + |
‐ | ‐ | ‐ |
| Touch or massage‐related | ✓ ++ |
X + |
X +++ |
X + |
✓ + |
✓ + |
| Environment modification | X + |
✓ +++ |
‐ | ‐ | ‐ | ‐ |
| Simulated rocking and water | X + |
‐ | ‐ | ‐ | ‐ | ‐ |
| Simulated Mother's voice | X + |
‐ | ‐ | ‐ | ‐ | ‐ |
| Swallowing water | X + |
X + |
X + |
X + |
‐ | X + |
| Rocking or holding | ‐ | ‐ | X + |
✓ ++ |
X + |
‐ |
| Toy distraction | ‐ | ‐ | ‐ | ‐ | X ++ |
X + |
| Video distraction | ‐ | ‐ | ‐ | ‐ | ✓ + |
✓ + |
| Parent presence | ‐ | ‐ | ‐ | ‐ | X + |
X + |
| Structured parent involvement | ‐ | ‐ | ‐ | ‐ | X ++ |
X ++ |
| Structured non‐parent involvement | ‐ | ‐ | ‐ | ‐ | ‐ | ✓ + |
| Therapeutic touch | X ++ |
X ++ |
‐ | ‐ | X + |
‐ |
| Familiar odor | ‐ | ‐ | ‐ | ✓ +++ |
‐ | ‐ |
| Unfamiliar odor | ‐ | ‐ | ‐ | X +++ |
‐ | ‐ |
| Co‐bedding | X + |
‐ | ‐ | ‐ | ‐ | ‐ |
| Heel warming | ✓ + |
‐ | ‐ | ‐ | ‐ | ‐ |
| Additive Studies | ||||||
| Co‐bedding + Sucrose Vs. Co‐bedding +Sucrose + Sucking | X + |
X + |
‐ | ‐ | ‐ | ‐ |
| Sucrose + Holding Vs. Sucrose + Holding + Massage | ‐ | ‐ | ‐ | ‐ | X + |
‐ |
| Sucrose Vs. Sucrose + Structured non‐parent involvement | ‐ | ‐ | ‐ | ‐ | ‐ | X + |
| Sucrose Vs. Sucrose + Pacifier | ✓ + |
‐ | ‐ | ‐ | ‐ | ‐ |
| Sucking + Sucrose Vs. Sucking + Sucrose + Facilitated Tucking | X + |
X ++ |
‐ | ‐ | ‐ | ‐ |
| Non‐nutritiev sucking Vs. Non‐nutritive sucking Vs. Facilitated tucking | ✓ ++ |
✓ ++ |
‐ | ‐ | ‐ | ‐ |
Legend:
✓ Evidence supports efficacy for reducing pain behaviours.
X Evidence supports inefficacy for reducing pain behaviours.
+ Very Low quality evidence (GRADE criteria)
++ Low quality evidence (GRADE criteria)
+++ Moderate quality evidence (GRADE criteria)
++++ High quality evidence (GRADE criteria)
Measures of treatment effect
Results were organized according to treatment, then age, then pain response type. For example, an analysis that was conducted to determine if non‐nutritive sucking was effective for preterm infants’ pain reactivity.
We treated all of the outcome data for the included studies as continuous. Due to the decision to include randomised controlled trials (RCTs) and randomised cross‐over trials, we used different procedures, obtained from a Cochrane statistical consultant, to calculate the standardized mean difference (SMD) and the standard error of the mean difference (SE), depending on whether the study was parallel‐group or cross‐over. We calculated the standard error of the SMD as follows for parallel trials: the square root of: (n1 + n2/n1*n2 + [SMD*SMD/2*(n1+n2)]). The standard error of the SMD for cross‐over trials used the square root of: 2*(1‐r)*(1/n+[SMD*SMD/2n]). If a trial provided two arms for one treatment analysis, we divided the control group 'n' such that they were not double‐counted within the same analysis.
Dealing with missing data
For every study that met the inclusion criteria, we contacted study authors when data were missing. Finally, using the recommended formulas from the Cochrane Handbook for Systematic Reviews of Interventions, we attempted to derive the numbers needed from data provided in the article (Higgins 2011b). As an additional level of quality assurance for the review, whenever data was interpolated from a study, a sub‐team of authors (RPR, NR) also conducted a conceptual double‐check ensuring confidence intervals (CIs) from interpolated data were always in line with the findings from the original authors.
Assessment of reporting biases
If more than 20% of the originally randomised participants were not available for the outcome analysis, we did not incorporate the data in the statistical analysis. This event did not occur in any of the studies that were considered for this review. In addition, in order to help overcome publication bias, we imposed no language barriers, contacted known infant pain management researchers through personal emails and list‐serves, and utilized both dissertation and trial registration sites.
Data synthesis
Guiding principles
Two main principles guided the meta‐analysis of the data collected for this review.
-
Under the 24 different categories of treatments, we separated studies into one of three age subcategories.
Preterm ‐ infants born at 36 weeks gestation or less.
Neonate ‐ infants born at 37 weeks until one month of age.
Older infant ‐ infants over one month to 36 months of age.
-
Each study within an age subcategory was further divided into one of two pain response subcategories to reduce heterogeneity among included studies.
Pain reactivity ‐ infant pain response was measured within the first 30 seconds after the acutely painful stimulus was discontinued.
Immediate pain regulation ‐ infant pain response was measured after the first 30 seconds following the acutely painful stimulus. If multiple measurements were taken after the first 30 seconds elapsed, we utilized the measurement closest to the 30 second time point. Our results are best understood as the immediate pain regulation response rather than regulation in a more prolonged sense.
We pooled the results from individual treatment studies using the generic inverse method for a random‐effects model in Review Manager 5.3 (RevMan 2014). Using this statistical methodology, an index of the variability of the sample (standard error) and the number of participants in the sample (sample size) are used to determine how influential each study will be in the final meta‐analytic statistic. The greater the variability (generally associated with small sample sizes), the less a particular study would be weighted in the final analysis. In addition to the SMD and SE, we also reported a 95% confidence interval (CI); which incorporates the standard error of the pooled treatment effect) for the treatment effect.
Subgroup analysis and investigation of heterogeneity
Although we utilized a statistical analysis plan to limit heterogeneity among studies (i.e. treatment x age x pain response analyses), the existence of heterogeneity between studies was inevitable. Given our primary interest in the impact of the heterogeneity (not the presence of heterogeneity), we utilized the I2 statistic (Higgins 2003). In cases where substantial heterogeneity was found, when possible (i.e. more than two studies were analysed), we re‐ran the analyses without the source of heterogeneity (noted using the SMD) and compared to the original findings. These data were incorporated in our GRADE analyses whenever possible and are noted in the footnotes of our individual 'Summary of findings' tables.
Sensitivity analysis
We investigated factors that may have affected our overall results from individual studies using sensitivity analyses. For each pooled result, we conducted the following sensitivity analyses.
We compared each pooled result to the individual studies that contributed to the overall pooled result to determine if any studies were more influential than others and discussed this in the respective summary results narrative section. We re‐ran analyses without significantly influential studies when there were two or more studies left to contribute to an overall pooled result. This was conducted in cases of significant heterogeneity or poor study quality/treatment integrity.
We tracked any experimental study that examined an eligible non‐pharmacological treatment for infant acute pain that was excluded based on our inclusion criteria. There were 22 studies in this category (see Results). Wherever possible these studies were qualitatively described to further contextualize the overall pooled result. Results of these comparisons were included in the 'Summary of treatment effects' section at the end of each analysis but did not impact the interpretation of the quantitative analyses.
For every treatment analysis, we examined the studies that contributed to the overall pooled result in greater detail when they did not agree with the overall pooled result. We examined studies for methodological differences to help offer potential reasons why there was disagreement between the studies. Results of these comparisons were included in the 'Summary of treatment effects' section at the end of each analysis.
Despite our attempt to conduct analyses utilizing homogeneous groups of pain management interventions, age groups, and pain responses, we found substantial heterogeneity among many overall treatment effects. We still presented pooled results and we added attempts to explain heterogeneity among treatment effects to the 'Summary of treatment effects' section at the end of each treatment analysis.
This comprehensive review provides a significant contribution to the infant pain management literature by providing findings specifically tailored to different infant age groups and types of pain responses. Moreover, it elucidates gaps in the current literature and provides direction for future researchers in the field of non‐pharmacological treatments for infant acute pain. We conducted statistical analyses using Review Manager 5.3 software (RevMan 2014).
Results
Description of studies
See the 'Characteristics of included studies' and 'Characteristics of excluded studies' tables.
Results of the search
In the original review, 4772 potential studies were assessed for eligibility resulting in a final selection of 42. For the current updated review, an additional 3355 from 2011 to 2015 (March) were assessed for eligibility to be added to the review. Of these 3355 studies, 21 were selected. This resulted in a total of 63 studies being included in the review. These 63 studies had at least one treatment arm that met all the inclusion criteria of this review. We extracted means and standard deviations from the papers, or when not provided, we calculated them using the procedures outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011c). In addition, we referred to 24 papers on relevant treatments that did not meet our inclusion criteria in a qualitative manor (Aguirre 2008; Bueno 2010; Campos 1989; Cignacco 2008; Cong 2009; Diego 2009; Felt 2000; Huang 2004; Johnston 2008a; Johnston 2009; Lima 2013; Ludington‐Hoe 2005; Morelius 2009; Okan 2010; Vivancos 2010Weissman 2009) or in a separate section at the end of the results section (Goubet 2003; Goubet 2007; Grunau 2004; Ipp 2009; Rattaz 2005; Singh 2012). We were thus able to compare our quantitative results to qualitative literature and there were no notable discrepancies. These 24 studies can be found in the excluded studies section. The following description of included studies refers only to the 63 studies included in the statistical analysis.
Included studies
In the case of studies where only some of the treatment arms were included in the review, only the participants in the treatment arms that met inclusion criteria were counted towards the descriptions below. Figure 3 demonstrates the flow of studies included in the review.
3.
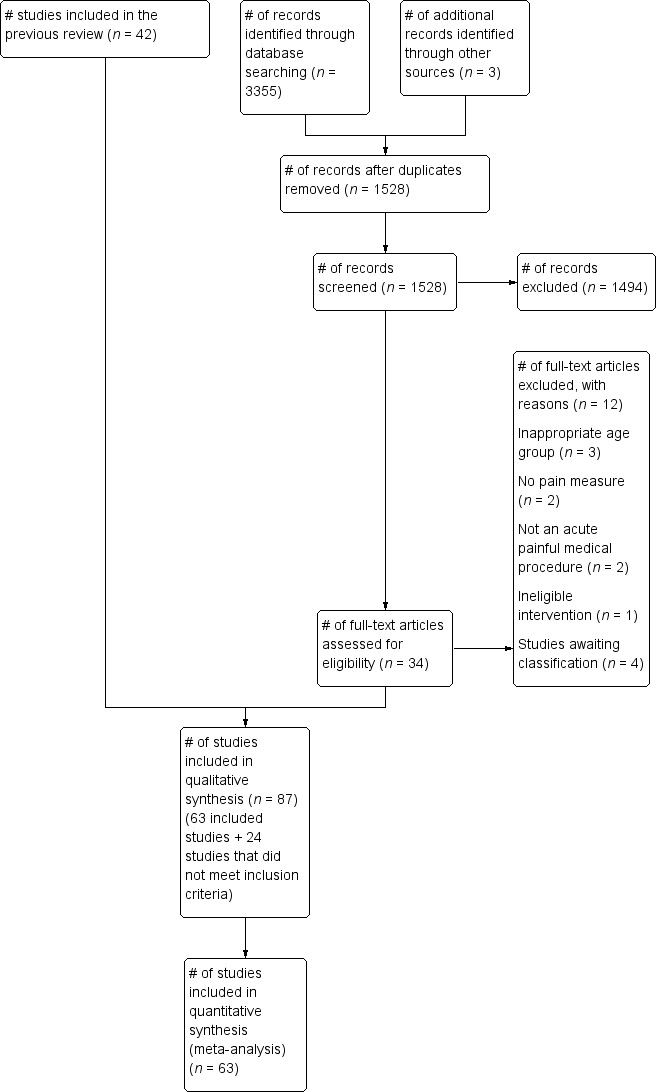
Study flow diagram.
Study design characteristics
Of the total participants that were included in the studies, 3391 were in treatment conditions only, and 1803 were in control conditions. Of these, 1020 participants were in a cross‐over study (i.e. exposure to both the treatment and control conditions).
Twenty‐three of the papers included in the review used cross‐over designs. For cross‐over designs, the participants were only counted once towards the total number of participants. The remaining 40 papers included in the review were between‐groups designs.
Cross‐over designs (23 studies; Axelin 2006; Axelin 2009; Bellieni 2001; Bo 2000; Catelin 2005; Chik 2012; Comaru 2009; Corbo 2000; Corff 1995; Elserafy 2009; Fearon 1997; Herrington 2007; Herrington 2014; Hill 2005; Jain 2006; Johnston 2007a; Kozub 2001; Kristoffersen 2011; Liaw 2012; Sizun 2002; Sundaram 2013; Stevens 1999; Ward‐Larson 2004).
Between‐groups designs (40 studies; Allen 1996; Badiee 2014; Basiri‐Moghadam 2014; Bauchner 1996; Bellieni 2002; Blass 1999; Bustos 2008; Campbell‐Yeo 2012; Campos 1994; Carbajal 1999; Carbajal 2003; Cohen 2002; Cohen 2006; Cramer‐Berness 2005a; Cramer‐Berness 2005b; Curtis 2007; Esfahani 2013; Gormally 2001; Greenberg 2002; Harrington 2012; Hillgrove Stuart 2013; Hogan 2014; Im 2008; Ipp 2004; Johnston 1997; Johnston 2013a; Jose 2012; Liaw 2010; Liaw 2011; Liaw 2013; Liu 2010; Mirzarahimi 2013; Morrow 2010; Park 2006; Sadathosseini 2013; Shaw 1982; Shu 2014; Taddio 2015; Whipple 2004; Yilmaz 2010).
Study nationality characteristics
The 63 included studies were conducted by authors in 16 different counties (Australia, Brazil, Canada, China, Finland, France, Hong Kong, India, Iran, Italy, Norway, Saudi Arabia, South Korea, Taiwan, Turkey, and United States).
Description of study treatment arms
In total, the 63 included studies contributed 104 separate treatment arms (each of which was compared to a control group or control phase). We analysed pain reactivity and immediate pain regulation separately, therefore one treatment arm could be analysed in two separate analyses if data were provided for pain reactivity (right after the pain stimulus) and immediate pain regulation (occurring at least 30 seconds after the pain stimulus) separately.
One treatment arm: 45 studies provided one treatment arm. Of these 45 studies, 11 studies (Axelin 2006; Campbell‐Yeo 2012; Catelin 2005; Corbo 2000; Gormally 2001; Johnston 2013a; Liaw 2010; Liu 2010; Sundaram 2013; Taddio 2015; Yilmaz 2010) provided data for both pain reactivity and immediate pain regulation, providing 22 treatment arms for analysis, and one study provided data for two age groups (Allen 1996 (neonate); Allen 1996 (older infant) for regulation), providing two treatment arms for analysis. Two studies (Chik 2012; Comaru 2009) provided two comparisons as the results were reported separately by order of treatment, providing four treatment arms for analysis. Thirty one provided data on either pain reactivity or immediate pain regulation (Axelin 2009; Badiee 2014; Basiri‐Moghadam 2014; Bellieni 2001; Blass 1999; Bo 2000; Bustos 2008; Carbajal 2003; Cohen 2002; Cohen 2006; Corff 1995; Curtis 2007; Esfahani 2013; Fearon 1997; Greenberg 2002; Herrington 2007; Herrington 2014; Hill 2005; Hogan 2014; Ipp 2004; Jain 2006; Johnston 1997; Johnston 2007a; Jose 2012; Kozub 2001; Liaw 2011; Morrow 2010; Park 2006; Shaw 1982; Sizun 2002; Ward‐Larson 2004), providing 31 treatment arms for analysis.
Two treatment arms: 16 studies provided two treatment arms. Fourteen of these studies provided data on either pain reactivity or immediate pain regulation (Bauchner 1996; Bellieni 2002; Campos 1994; Carbajal 1999; Cramer‐Berness 2005a; Cramer‐Berness 2005b; Harrington 2012; Im 2008; Liaw 2012; Mirzarahimi 2013; Sadathosseini 2013; Shu 2014; Stevens 1999; Whipple 2004), providing 28 treatment arms for analysis. Two of these 16 studies provided two arms for both pain reactivity and immediate pain regulation comparisons (Hillgrove Stuart 2013; Liaw 2013; eight treatment arms total).
Three or more treatment arms: two studies contributed three treatment arms. One study had comparisons of both pain reactivity and immediate pain regulation, each with three treatment arms, resulting in six treatment arms in total (Elserafy 2009). One study provided data on reactivity only, contributing three treatment‐arm comparisons (Kristoffersen 2011).
In analyses where more than one treatment arm was analysed, we split the control group n to avoid the bias associated with 'double‐counting'.
Description of pain responses (pain reactivity versus immediate pain regulation)
A breakdown of which studies contributed to overall findings for pain reactivity (right after the pain stimulus) and immediate pain regulation (occurring at least 30 seconds after the pain stimulus):
Twenty‐eight studies reported pain reactivity outcomes, which was zero to 30 seconds after the painful stimulus (Axelin 2009; Badiee 2014; Basiri‐Moghadam 2014; Bellieni 2001; Bellieni 2002; Bustos 2008; Carbajal 1999; Carbajal 2003; Chik 2012; Cohen 2002; Comaru 2009; Cramer‐Berness 2005a; Cramer‐Berness 2005b; Esfahani 2013; Hill 2005; Hogan 2014; Ipp 2004; Johnston 1997; Johnston 2007a; Kozub 2001; Kristoffersen 2011; Mirzarahimi 2013; Morrow 2010; Shaw 1982; Shu 2014; Sizun 2002; Stevens 1999; Ward‐Larson 2004).
Twenty‐one studies reported immediate pain regulation outcomes, which was the pain measurement closest to 30 seconds after the last painful stimulus (Allen 1996; Bauchner 1996; Blass 1999; Bo 2000; Campos 1994; Cohen 2006; Corff 1995; Curtis 2007; Fearon 1997; Greenberg 2002; Harrington 2012; Herrington 2007; Herrington 2014; Jose 2012; Im 2008; Jain 2006; Liaw 2011; Liaw 2012; Park 2006; Sadathosseini 2013; Whipple 2004).
Fourteen studies reported pain outcomes for both pain reactivity and immediate pain regulation (Axelin 2006; Campbell‐Yeo 2012; Catelin 2005; Corbo 2000; Elserafy 2009; Gormally 2001; Hillgrove Stuart 2013; Johnston 2013a; Liaw 2010; Liaw 2013; Liu 2010; Sundaram 2013; Taddio 2015; Yilmaz 2010).
Participants
Age groupings
Of all the included studies, there were 29 studies that had preterm infants as participants (i.e. born at 36 weeks gestation or less). Fifteen papers had participants in the neonate age category (i.e. infants born at 37 weeks until one month of age). Twenty papers included older infants (i.e. over one month to 36 months of age) as participants. One paper (Allen 1996) was a cross‐sectional study that included a group of neonates and older infants who underwent the same treatment, and the means and standard deviations were reported separately for each age group. For this review, the participants from this study were included separately in the neonate and older infant categories, respectively.
Preterm‐born (29 studies; Axelin 2006; Axelin 2009; Badiee 2014; Bellieni 2001; Campbell‐Yeo 2012; Catelin 2005; Chik 2012; Comaru 2009; Corbo 2000; Corff 1995; Elserafy 2009; Fearon 1997; Herrington 2007; Herrington 2014; Hill 2005; Jain 2006; Johnston 1997; Johnston 2007a; Johnston 2013a; Kristoffersen 2011; Liaw 2010; Liaw 2012; Liaw 2013; Shu 2014; Sizun 2002; Stevens 1999; Sundaram 2013; Ward‐Larson 2004; Whipple 2004).
Neonate (15 studies; Allen 1996; Bellieni 2002; Blass 1999; Bo 2000; Campos 1994; Carbajal 1999; Carbajal 2003; Gormally 2001; Greenberg 2002; Im 2008; Liu 2010; Mirzarahimi 2013; Morrow 2010; Sadathosseini 2013; Yilmaz 2010).
Older infant (20 studies; Allen 1996; Basiri‐Moghadam 2014; Bauchner 1996; Bustos 2008; Cohen 2002; Cohen 2006; Cramer‐Berness 2005a; Cramer‐Berness 2005b; Curtis 2007; Esfahani 2013; Harrington 2012; Hillgrove Stuart 2013; Hogan 2014; Ipp 2004; Jose 2012; Kozub 2001; Liaw 2011; Park 2006; Shaw 1982; Taddio 2015).
It should be noted that one study (Catelin 2005) had 66% preterm participants and 33% full‐term participants. We categorized this study as a preterm study.
Diagnostic status
The diagnostic status of the infants in the 63 included studies:
Healthy infants born full‐term (32 studies; Allen 1996; Basiri‐Moghadam 2014; Bauchner 1996; Bellieni 2002; Blass 1999; Bustos 2008; Campos 1994; Carbajal 1999; Carbajal 2003; Cohen 2002; Cohen 2006; Cramer‐Berness 2005a; Cramer‐Berness 2005b; Curtis 2007; Esfahani 2013; Gormally 2001; Greenberg 2002; Harrington 2012; Hillgrove Stuart 2013; Hogan 2014; Im 2008; Ipp 2004; Jose 2012; Liaw 2011; Liu 2010; Mirzarahimi 2013; Morrow 2010; Park 2006; Sadathosseini 2013; Shaw 1982; Taddio 2015; Yilmaz 2010).
Hospitalized infants born preterm (28 studies; Axelin 2006; Axelin 2009; Badiee 2014; Bellieni 2001; Campbell‐Yeo 2012; Catelin 2005; Comaru 2009; Corbo 2000; Corff 1995; Elserafy 2009; Fearon 1997; Herrington 2007; Herrington 2014; Hill 2005; Jain 2006; Johnston 1997; Johnston 2007a; Johnston 2013a; Kristoffersen 2011; Liaw 2010; Liaw 2012; Liaw 2013; Shu 2014; Sizun 2002; Stevens 1999; Sundaram 2013Ward‐Larson 2004; Whipple 2004).
Infants born full‐term, being monitored or treated for health complications (two studies; Bo 2000; Kozub 2001).
Unknown (one study; Chik 2012)
Types of painful procedures
For a study to be included in the search, the procedure had to be described by the author as painful or causing pain (e.g. diaper change or weighing procedure for preterms). The following painful procedures were used in the included studies:
Heel‐stick (32 studies; Axelin 2009; Badiee 2014; Bellieni 2001; Bellieni 2002; Blass 1999; Bo 2000; Campbell‐Yeo 2012; Campos 1994; Corbo 2000; Corff 1995; Fearon 1997; Gormally 2001; Greenberg 2002; Herrington 2007; Herrington 2014; Im 2008; Jain 2006; Johnston 1997; Johnston 2007a; Johnston 2013a; Kozub 2001; Liaw 2010; Liaw 2012; Liaw 2013; Mirzarahimi 2013; Morrow 2010; Park 2006; Shu 2014; Stevens 1999; Sundaram 2013; Whipple 2004; Yilmaz 2010).
Vaccine/vitamin needle (17 studies; Allen 1996; Basiri‐Moghadam 2014; Bustos 2008; Cohen 2002; Cohen 2006; Cramer‐Berness 2005a; Cramer‐Berness 2005b; Esfahani 2013; Harrington 2012; Hillgrove Stuart 2013; Hogan 2014; Ipp 2004; Jose 2012; Kristoffersen 2011; Liaw 2011; Shaw 1982; Taddio 2015).
Venipuncture (8 studies; Bauchner 1996; Carbajal 1999; Carbajal 2003; Chik 2012; Curtis 2007; Elserafy 2009; Liu 2010; Sadathosseini 2013).
Diaper change (2 studies; Comaru 2009; Sizun 2002).
Endotracheal suctioning technique (2 studies; Axelin 2006; Ward‐Larson 2004).
Weighing procedure (2 studies; Catelin 2005, Hill 2005)
Types of treatment
In total, we analysed 24 different types of treatment for this review. We analysed the efficacy of the 24 different types of treatment separately for preterms, neonates, and older infants. Moreover, within each treatment x age analysis, data were separated into pain types (pain reactivity or immediate pain regulation). None of the 104 treatment arms from the 63 included studies were included twice within any single treatment x age x pain type analyses. Eighteen studies contributed more than one treatment arm. They are distinguished by the suffix "‐1", "‐2" or "‐3" added to the in‐text citation reference. Noteworthy comments regarding the treatment comparisons follow.
We grouped studies that used pacifiers and other methods of non‐nutritive sucking together under 'Non‐nutritive sucking‐related'. Due to a number of studies that included water as a treatment arm (thus enabling a comparison with an actual 'no treatment' arm), this was included as a separate treatment, despite the fact that some studies considered the administration of water (without a sucking tool such as a pacifier) as a control group. We grouped 'swaddling/facilitated tucking' together due to sharing one similar mechanism of comfort (containment), despite having differences in other pain‐reducing qualities beyond that of containment. The intervention of structured parent involvement' were interventions that were grouped together if parents were given some type of instructive suggestion (whether written or oral) on how to reduce pain for their infant with no other tools given. One important distinction to make is that between touch/massage and therapeutic touch. In touch/massage, the infant's body is stroked or rubbed, whereas in therapeutic touch, the hands are held over the infant's body without actually touching the infant.
-
Non‐nutritive sucking‐related (28 treatment arms total)
-
Preterm
Pain reactivity: Bellieni 2001; Corbo 2000; Elserafy 2009‐1; Elserafy 2009‐2; Kristoffersen 2011‐1; Liaw 2010; Stevens 1999‐2
Immediate pain regulation: Corbo 2000; Elserafy 2009‐1; Elserafy 2009‐2; Liaw 2010; Liaw 2012‐2; Whipple 2004‐1; Whipple 2004‐2
-
Neonate
Pain reactivity: Bellieni 2002‐1; Carbajal 1999‐1; Liu 2010; Mirzarahimi 2013‐1; Yilmaz 2010
Immediate pain regulation: Blass 1999; Bo 2000; Campos 1994‐1; Greenberg 2002; Im 2008‐1; Liu 2010; Yilmaz 2010
-
Older infant
Pain reactivity: no studies found.
Immediate pain regulation: Curtis 2007; Liaw 2011
-
-
Swaddling or tucking (15 treatment arms total)
-
Preterm
Pain reactivity: Axelin 2006; Axelin 2009; Comaru 2009‐1; Comaru 2009‐2; Hill 2005; Shu 2014‐1; Stevens 1999‐1; Sundaram 2013; Ward‐Larson 2004
Immediate pain regulation: Axelin 2006; Corff 1995; Fearon 1997; Liaw 2012‐1, Sundaram 2013
-
Neonate
Pain reactivity: Morrow 2010
Immediate pain regulation: no studies found.
Older infant: no studies found.
-
-
Touch or Massage (11 treatment arms)
-
Preterm
Immediate pain regulation: Herrington 2007; Herrington 2014; Jain 2006
-
Neonate
Pain reactivity: Bellieni 2002‐2; Mirzarahimi 2013‐2
-
Older infant
Pain reactivity: Esfahani 2013
Immediate pain regulation: Jose 2012
-
-
Environmental modification (3 treatment arms)
-
Preterm
Pain reactivity: Catelin 2005; Sizun 2002
Immediate pain regulation: Catelin 2005
Neonate: no studies found.
Older infant: no studies found.
-
-
Simulated rocking and water (1 treatment arm)
-
Preterm
Pain reactivity: Johnston 1997
Immediate pain regulation: no studies found.
Neonate: no studies found.
Older infant: no studies found.
-
-
Simulated mother's voice (1 treatment arm)
-
Preterm
Pain reactivity: Johnston 2007a
Immediate pain regulation: no studies found.
Neonate: no studies found.
Older infant: no studies found.
-
-
Swallowing water (6 treatment arms)
-
Preterm
Pain reactivity: Elserafy 2009‐3; Kristoffersen 2011‐2
Immediate pain regulation: Elserafy 2009‐3
-
Neonate
Pain reactivity: Carbajal 1999‐2
Immediate pain regulation: Allen 1996
-
Older infant
Pain reactivity: no studies found.
Immediate pain regulation: Allen 1996
-
-
Rocking, holding or both (5 treatment arms)
Preterm: no studies found.
-
Neonate
Pain reactivity: Carbajal 2003; Gormally 2001
Immediate pain regulation: Campos 1994‐2; Gormally 2001
-
Older infant
Pain reactivity: Ipp 2004
Immediate pain regulation: no studies found.
-
Toy distraction (7 treatment arms
Preterm: no studies found.
Neonate: no studies found.
-
Older infant
Pain reactivity:Basiri‐Moghadam 2014; Cramer‐Berness 2005a‐1; Cramer‐Berness 2005b‐1; Hillgrove Stuart 2013‐1; Hillgrove Stuart 2013‐2
Immediate pain regulation:Hillgrove Stuart 2013‐1; Hillgrove Stuart 2013‐2
-
Video distraction (2 treatment arms)
Preterm: no studies found.
Neonate: no studies found.
-
Older infant
Pain reactivity: Cohen 2002
Immediate pain regulation: Cohen 2006
-
Parent presence (2 treatment arms)
Preterm: no studies found.
Neonate: no studies found.
-
Older infant
Pain reactivity: Shaw 1982I
Immediate pain regulation: Bauchner 1996‐2
-
Structured parent involvement (6 treatment arms)
Preterm: no studies found.
Neonate: no studies found.
-
Older infant
Pain reactivity: Bustos 2008; Cramer‐Berness 2005a‐2; Cramer‐Berness 2005b; Taddio 2015
Immediate pain regulation: Bauchner 1996‐1; Taddio 2015
-
Structured non‐parent involvement (1 treatment arm)
Preterm: no studies found.
Neonate: no studies found.
-
Older infant
Pain reactivity: no studies found.
Immediate pain regulation: Harrington 2012‐1
-
Therapeutic touch (3 treatment arms)
-
Preterm
Pain reactivity: Johnston 2013a
Immediate pain regulation: Johnston 2013a
Neonate: no studies found
-
Older infant
Pain reactivity: Kozub 2001
Immediate pain regulation: no studies found.
-
-
Familiar odor (1 treatment arm)
Preterm: no studies found.
-
Neonate
Pain reactivity: no studies found.
Immediate pain regulation: Sadathosseini 2013‐1
Older infant: no studies found.
-
Unfamiliar odor (1 treatment arm)
Preterm: no studies found.
-
Neonate
Pain reactivity: no studies found.
Immediate pain regulation: Sadathosseini 2013‐2
Older infant: no studies found.
-
Co‐bedding (1 treatment arm)
-
Preterm
Pain reactivity: Badiee 2014
Immediate pain regulation: no studies found.
Neonate: no studies found.
Older infant: no studies found.
-
-
Heel warming (1 treatment arm)
-
Preterm
Pain reactivity: Shu 2014‐2
Immediate pain regulation: no studies found.
Neonate: no studies found.
Older infant: no studies found.
-
-
Co‐bedding + Sucrose vs. Co‐bedding + Sucrose + Sucking (2 treatment arms)
-
Preterm
Pain reactivity: Campbell‐Yeo 2012
Immediate pain regulation: Campbell‐Yeo 2012
Neonate: no studies found.
Older infant: no studies found.
-
-
Sucrose + Holding vs. Sucrose + Holding + Massage (1 treatment arm)
Preterm: no studies found.
Neonate: no studies found.
-
Older infant
Pain reactivity: Hogan 2014
Immediate pain regulation: no studies found.
-
Sucrose vs. Sucrose + Structured non‐parent involvement (1 treatment arm)
Preterm: no studies found.
Neonate: no studies found.
-
Older infant:
Pain reactivity: no studies found.
Immediate pain regulation: Harrington 2012‐2
-
Sucrose vs. Sucrose + Sucking (1 treatment arm)
-
Preterm
Pain reactivity: Kristoffersen 2011‐3
Immediate pain regulation: no studies found.
Neonate: no studies found.
Older infant: no studies found.
-
-
Sucking + Sucrose vs. Sucking + Sucrose + Facilitated tucking (2 treatment arms)
Sucking vs. Sucking +Facilitated tucking (2 treatment arms)
Treatment locations
The treatment interventions described in the studies occurred in the following locations.
Inpatient hospital (50 studies; Allen 1996; Axelin 2006; Axelin 2009; Badiee 2014; Bauchner 1996; Bellieni 2001; Bellieni 2002; Blass 1999; Bo 2000; Campbell‐Yeo 2012; Campos 1994; Carbajal 1999; Carbajal 2003; Catelin 2005; Chik 2012Comaru 2009; Corbo 2000; Corff 1995; Curtis 2007; Elserafy 2009; Fearon 1997; Gormally 2001; Greenberg 2002; Herrington 2007; Herrington 2014; Hill 2005; Im 2008; Jain 2006; Johnston 1997; Johnston 2007a; Johnston 2013a; Kozub 2001; Kristoffersen 2011; Liaw 2010; Liaw 2011; Liaw 2012; Liaw 2013; Liu 2010; Mirzarahimi 2013; Morrow 2010; Park 2006; Sadathosseini 2013; Shu 2014; Sizun 2002; Stevens 1999; Sundaram 2013; Taddio 2015; Ward‐Larson 2004; Whipple 2004; Yilmaz 2010).
Outpatient medical clinic (13 studies; Basiri‐Moghadam 2014; Bustos 2008; Cohen 2002; Cohen 2006; Cramer‐Berness 2005a; Cramer‐Berness 2005b; Esfahani 2013; Harrington 2012; Hogan 2014; Hillgrove Stuart 2013; Ipp 2004; Jose 2012; Shaw 1982).
Pain measurement
The pain measurements used in the included studies were as follows.
Premature Infant Pain Profile (PIPP) (18 studies: Axelin 2009; Badiee 2014; Bellieni 2001; Campbell‐Yeo 2012; Chik 2012; Elserafy 2009; Hill 2005; Johnston 2007a; Johnston 2013a; Kozub 2001; Kristoffersen 2011; Liaw 2010; Liaw 2012; Mirzarahimi 2013; Sizun 2002; Sundaram 2013; Stevens 1999; Ward‐Larson 2004).
Neonatal Infant Pain Scale (NIPS) (11 studies: Axelin 2006; Bo 2000; Catelin 2005; Esfahani 2013; Im 2008; Jain 2006; Liu 2010, Morrow 2010; Park 2006; Shu 2014; Yilmaz 2010).
Duration of cry (8 studies: Allen 1996; Bauchner 1996; Blass 1999; Campos 1994; Corff 1995; Greenberg 2002; Herrington 2007; Herrington 2014; Sadathosseini 2013).
Neonatal Facial Coding System (NFCS) (7 studies: Bustos 2008; Comaru 2009; Fearon 1997; Gormally 2001; Ipp 2004; Johnston 1997; Liaw 2011).
Modified Behavioral Pain Scale (MBPS) (6 studies: Cohen 2002; Cramer‐Berness 2005a; Cramer‐Berness 2005b; Hillgrove Stuart 2013, Hogan 2014; Taddio 2015).
Douleur Aiguë Nouveau‐né (DAN) (3 studies: Bellieni 2002; Carbajal 1999; Carbajal 2003).
Active/Sleep State (1 study: Liaw 2013).
Behavioral Observation Pain Scale (1 study: Jose 2012).
Brazelton Neonatal Behavioral Assessment Scale (BNBAS) (1 study: Corbo 2000).
Face Legs Arms Cry Consolability Scale (FLACC) (1 study: Curtis 2007).
Infant behavioral state (1 study: Whipple 2004).
Infant's Pain Questonnaire (1 study: Basiri‐Moghadam 2014).
Measure of Adult and Infant Soothing and Distress (MAISD) (1 study: Cohen 2006)
Modified Frankl Scale (1 study: Shaw 1982).
Modified Riley Infant Pain Scoring (1 study: Harrington 2012).
Cry Frequency (1 study: Bauchner 1996)
Excluded studies
In the previous version of this review, 4772 abstracts were screened for inclusion. For the update, 3 authors (RPR, NR, HG) and one research assistant screened 3355 abstracts based on the search strategy. From these 3355 abstracts, 34 were selected for further review. Of these 34 studies, we excluded 12 studies, included 20, and one article was already included in the original review. One of the articles selected for further review was extracted twice (Luthy 2013). Sixty‐two articles were excluded in the original review search and 12 were excluded in the current review search. Of the 62 articles that were originally excluded, one was included in the current review because it became available in English (Park 2006) and a translator had not previously been available. In addition, all articles related to kangaroo care (9 articles) were also excluded from the original review. These were the primary reasons for exclusion for 77 studies that were not analysed or discussed qualitatively.
Inappropriate age or infant age group could not be separated from older child group (39 studies: Abedin 2008; Al‐Bekaa 2003; Aslanabadi 2008; Carlson 2000; D'Agostino 2008; Dahlquist 2002; Downey 2012; Drago 2009; Favara‐Scacco 2001; Gedaly‐Duff 1992; Gold 2006; Gonzalez 1989; Gonzalez 1993; Hatem 2006; Heden 2009; Hoffman 2006; Ida 2008; Jackson 2008; Jo 2007; Kivijärvi 2008; Koivusalo 2009; Li 2007; MacLaren 2005; Manne 1990; Marchisotti 2007; Marec‐Berard 2009; McCarthy 2010; Mercer 2013; Michel 2008; Phipps 2005; Reichel 2007; Salmon 2006; Shapiro 2007; Slifer 2009; Sparks 2007; Sundararajan 2007; Tanabe 2002; Zeltzer 1991; Zun 2012).
Ineligible intervention (15 studies: Axelin 2010; Bellieni 2003; Bellieni 2007; Boots 2010; De Jong 2012; Dilen 2010; El‐Naggar 2010; Hanson 2010; He 2010; Holsti 2005; Ipp 2007; Mucignat 2004; Ozdogan 2010; Slater 2010; Wisdorf‐Houtkooper 1997).
No pain or pain not measured on day of procedure (10 studies: Cologna 1999; Duncan 2004; Harrison 2000; Hsu 1995; Huang 1999; Johnston 2007b; Leclair 2007; Luthy 2013 (two extractions); Marin Gabriel 2010; Vignochi 2010).
Student work later published and included in review (one study: Greenberg 1997).
Randomized controlled trial citation originally in progress but now completed (one study: Campbell‐Yeo 2009).
Kangaroo Care (included in original): (9 studies: Akcan 2009; Castral 2008; Chermont 2009; de Sousa 2008; Ferber 2008; Gray 2000; Johnston 2003; Kashaninia 2008; Kostandy 2008).
Not an acute painful medical procedure: (2 studies: Ha 2013; Ucar 2014).
In addition to the above reasons for the exclusion of those 77 articles, 24 studies were in a gray area as they did not meet the full inclusion criteria to be included in the statistical analyses of the review, but it was felt they were relevant to the purpose of the review. These papers were referred to either in the 'Summary of treatment effects' narratives following the relevant quantitative analysis of the included studies OR they were included in a separate section at the end of the results ('Other potentially effective non‐pharmacological interventions') when there was no relevant quantitative intervention analysis for comparison. In this way, qualitative sensitivity analyses could be conducted where the summary outcome of the quantitative analyses could be compared to the results of individual studies that did not meet the inclusion criteria. These studies did not meet complete inclusion criteria for the following reasons.
Control group was an active control/no control group (15 studies: Aguirre 2008; Badiee 2013; Bueno 2010; Campos 1989; Cignacco 2008; Diego 2009; Goubet 2003; Goubet 2007; Grunau 2004; Huang 2004; Ipp 2009; Johnston 2008a; Johnston 2009; Ludington‐Hoe 2005; Rattaz 2005).
No behavioral pain outcome reported or not analysable (two studies: Cong 2009; Okan 2010).
Was not a RCT (seven studies: Abdallah 2013; Felt 2000; Lima 2013; Morelius 2009; Singh 2012; Vivancos 2010; Weissman 2009).
In addition, four studies are still awaiting classification (Ho 2012; Obeidat 2011; Rozenfeld 2012; Taavoni 2013).
Risk of bias in included studies
Eight raters, in four groups of two, participated in study quality rating (NR, HG, LU, DL, RH, JHS, SAK, KT). Each team was assigned a subset of the 63 articles included in the quantitative analysis. Two review authors independently rated each article. Every individual score on the data extraction form (article details, study quality, and treatment integrity) were compared by the two lead authors. Every score that differed between two members of the team was examined by the two lead authors. The data extraction form required raters to put the page and paragraph number (from the original article) that justified their rating. Thus, when scores differed between team members, the original article was consulted and a consensus‐based decision was made. Seven domains of bias were assessed for each study: randomisation, allocation bias, blinding (participants, outcome assessment), data attrition, selective reporting, other potential sources of bias (potential threats to validity) and power (calculation, sample size).
As described earlier, risk of bias was initially calculated using dimensions from Chapter 8 in the 2011 Cochrane Handbook (see Figure 1 and Figure 2) (Higgins 2011a).
High risk of bias (47 studies; Allen 1996; Axelin 2006; Badiee 2014; Bauchner 1996; Bellieni 2001; Blass 1999; Bo 2000; Bustos 2008; Campbell‐Yeo 2012; Carbajal 1999; Carbajal 2003; Cohen 2002; Cohen 2006; Corbo 2000; Corff 1995; Cramer‐Berness 2005a; Cramer‐Berness 2005b; Elserafy 2009; Esfahani 2013; Fearon 1997; Gormally 2001; Greenberg 2002; Harrington 2012; Hillgrove Stuart 2013; Hogan 2014; Im 2008; Ipp 2004; Johnston 1997; Johnston 2007a; Jose 2012; Kozub 2001; Kristoffersen 2011; Liaw 2010; Liaw 2011; Liaw 2012; Liaw 2013; Liu 2010; Mirzarahimi 2013; Morrow 2010; Shaw 1982; Shu 2014; Sizun 2002; Stevens 1999; Taddio 2015; Ward‐Larson 2004; Whipple 2004; Yilmaz 2010).
Unclear risk of bias (2 studies; Chik 2012; Park 2006).
Low risk of bias (14 studies; Axelin 2009; Basiri‐Moghadam 2014; Bellieni 2002; Campos 1994; Catelin 2005; Comaru 2009; Curtis 2007; Herrington 2007; Herrington 2014; Hill 2005; Jain 2006; Johnston 2013a; Sadathosseini 2013; Sundaram 2013).
To further contextualize the overall quality of the studies included in this review, we integrated the risk of bias scores in a synthesis of our results entered into GRADEpro (GRADEpro GDT). We added footnotes to contextualize each of the analyses that were included in this review. For every analysis conducted, we included a 'Summary of findings' table that summarizes the quality of the data pooled for that intervention. In addition, for ease of comprehension, we included one 'Summary of overall findings' table (see Table 10). However, we only provided forest plots for analyses that had more than two studies and total analysis sample size greater than 200.
Effects of interventions
See: Table 1; Table 2; Table 3; Table 4; Table 5; Table 6; Table 7; Table 8
Summary of findings for the main comparison. Non‐nutritive sucking x preterm x pain reactivity.
| Non‐nutritive sucking x preterm x pain reactivity | ||||||
|
Patient or population: Preterm infants
Intervention: Non‐nutritive sucking‐related
Comparison: Standard care Countries: Canada, Italy, Norway, Saudi Arabia, Taiwan Setting: Inpatient Behavioural measurements: PIPP, BNBAS. | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Standard care | Non‐nutritive sucking‐related | |||||
| Pain reactivity behavioural | The mean pain reactivity in the intervention groups was 0.31 standard deviations lower (0.65 lower to 0.04 higher) | 329 (6 studies1) | ⊕⊝⊝⊝ very low2,3,4 | |||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1 One study (Elserafy 2009) contributed two treatment arms. 2 Quality of evidence downgraded by two levels due to serious risk of bias. All six studies were deemed high risk of bias. 3 Quality of evidence downgraded by one level due to serious inconsistency. Heterogeneity and chi2 test analyses suggest that when Kristofferson 2011 (the only study with feeding tube insertion and the strongest study to favour control) is removed, effects remain stable and inconsistency is no longer significant. However, study results are inconsistent regarding its efficacy. 4 Quality of evidence was not downgraded for imprecision as n = 329 for the entire analysis, which exceeds the threshold for imprecision.
Summary of findings 2. Non‐nutritive sucking‐related x preterm x immediate pain regulation.
| Non‐nutritive sucking‐related x preterm x immediate pain regulation | ||||||
|
Patient or population: Preterm infants
Intervention: Non‐nutritive sucking‐related
Comparison: Standard care Countries: Italy, Saudi Arabia, Taiwan, USA Setting: Inpatient Behavioural measurements:PIPP, BNBAS, Infant behavioral state. | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Standard care | Non‐nutritive sucking‐related | |||||
| Immediate pain regulation behaviour | The mean immediate pain regulation in the intervention groups was 0.43 standard deviations lower (0.63 to 0.23 lower) | 260 (5 studies1) | ⊕⊕⊝⊝ low2,3 | |||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1 Two studies (Elserafy 2009, Whipple 2004) contributed two treatment arms. 2 Quality of evidence was downgraded by two levels as all included studies had high risk of bias. 3Quality of evidence was not downgraded (Total sample size for entire analysis was n = 260 in treatment groups. The threshold for imprecision was total treatment number for analyses should exceed n = 30x (where x = number of studies)).
Summary of findings 3. Non‐nutritive sucking‐related x neonate x pain reactivity.
| Non‐nutritive sucking‐related x neonate x pain reactivity | ||||||
|
Patient or population: Neonates
Intervention: Non‐nutritive sucking‐related Comparison: Standard Care Countries: France, Iran, Italy, Taiwan, Turkey Setting: Inpatient Behavioural measurements: PIPP, NIPS, DAN. | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Non‐nutritive sucking‐related | |||||
| Pain reactivity behaviour | The mean pain reactivity in the intervention groups was 1.20 standard deviations lower (2.01 to 0.38 lower) | 270 (5 studies) | ⊕⊝⊝⊝ very low1,2,3 | |||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1 Quality of evidence was downgraded by two levels because four out of the five included studies were observed to have high risk of bias due to methodological issues. 2 Quality was downgraded by one level due to heterogeneity among studies with an I2 statistic = 90%. 3 Quality of evidence was not downgraded for imprecision. Total sample size for entire treatment group was n = 270 patients in the treatment group in the entire analysis. (The threshold for imprecision was total treatment number for analyses should exceed n = 30x).
Summary of findings 4. Non‐nutritive sucking‐related x older infant x immediate pain regulation.
| Non‐nutritive sucking‐related x older infant x immediate pain regulation | ||||||
|
Patient or population: Older infants
Intervention: Non‐nutritive sucking‐related
Comparison: Standard care Countries: Canada, Taiwan Setting: Inpatient and outpatient Behavioural measurements: NFCS, FLACC. | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Standard care | Non‐nutritive sucking‐related | |||||
| immediate pain regulation behaviour | The mean immediate pain regulation in the intervention groups was 1.34 standard deviations lower (2.14 to 0.54 lower) | 151 (2 studies) | ⊕⊕⊝⊝ low1,2,3 | |||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1 Quality of evidence was downgraded by one level because one study had low risk of bias and one study had high risk of bias. 2 Quality of evidence was downgraded by one level due to heterogeneity. Liaw 2011 had a notably stronger effect than Curtis 2007, perhaps due to injection versus venipuncture respectively. 3 There were n = 77 patients in the treatment group in the entire analysis. The quality was not downgraded.
Summary of findings 5. Swaddling/tucking‐related x preterm x pain reactivity.
| Preterm x swaddling/tucking‐related x pain reactivity | ||||||
|
Patient or population: Preterm infants
Intervention: Swaddling/tucking‐related Comparison: Control Countries: Brazil, Canada, Finland, India, Taiwan, , USA, . Setting: Inpatient Behavioural measurements: PIPP, NIPS, NFCS. | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control |
Swaddling/tucking‐ related |
|||||
| Pain reactivity behaviour | The mean pain reactivity in the intervention groups was 0.89 standard deviations lower (1.37 to 0.40 lower) | 331 (8 studies) | ⊕⊝⊝⊝ very low1,2,3 | |||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1 Quality of evidence was downgraded by two levels due to serious risk of bias. Of all the studies, 4/9 treatment arms were high risk of bias and 5/9 had low risk of bias.Therefore, since almost half the treatment arms included were high risk of bias, the overall quality of the studies was downgraded. 2 Quality of evidence was downgraded by one level due to serious inconsistency (8/9 treatment arms found an effect and the overall I2statistic = 85%). 3 There were 331 participants in the treatment conditions, which meets the threshold of n = 30x.
Summary of findings 6. Toy distraction x older infant x pain reactivity.
| Toy distraction x older infant x pain reactivity | ||||||
|
Patient or population: Older infants
Intervention: Toy distraction Comparison: Control Countries: Canada, Iran, USA Setting: Outpatient Behavioural measurements: Infants' Pain Questionnaire, MBPS. | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Toy distraction | |||||
| Pain reactivity behaviour | The mean pain reactivity in the intervention groups was 0.15 standard deviations lower (0.39 lower to 0.08 higher) | 293 (4 studies) | ⊕⊕⊝⊝ low1,2 | |||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1 Quality of evidence was downgraded by two levels due to serious risk of bias. Risk of bias is high in 3 out of 4 studies with 1 low risk of bias because of potential issues with methods i.e. allocation disclosure, blinding of participants and outcome assessors, sample size issues. 2 There was a total of n = 293 participants across 4 treatment arms, which exceeds n = 30x participants per treatment arm.
Summary of findings 7. Structured parent involvement x older infant x pain reactivity.
| Structured parent involvement x older infant x pain reactivity | ||||||
|
Patient or population: Older infants
Intervention: Structured parent involvement Comparison: Control Countries: Australia, Canada, USA Setting: Outpatient Behavioural measurements: NFCS, MBPS | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Structured parent involvement | |||||
| Pain reactivity behaviour | The mean pain reactivity in the intervention groups was 0.24 standard deviations lower (0.51 lower to 0.04 higher) | 369 (4 studies) | ⊕⊕⊝⊝ low1,2 | |||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1 Quality of evidence was downgraded by two levels. Risk of Bias is high for all 4 studies because of potential issues with methods i.e. allocation disclosure, blinding of participants and outcome assessors, sample size issues. 2 The total sample size for 4 studies was n = 369 for treatment which is greater than n = 30x and was thus not downgraded for this.
Summary of findings 8. Structured parent involvement x older infant x immediate pain regulation.
| Structured parent involvement x older infant x immediate pain regulation | ||||||
|
Patient or population: Older infants
Intervention: Structured parent involvement Comparison: Control Countries: Canada, USA Setting: tInpatient Behavioural measurements: MBPS, Duration of cry | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Structured parent involvement | |||||
| Immediate pain regulation behaviour | The mean immediate pain regulation in the intervention groups was 0.04 standard deviations lower (0.23 lower to 0.15 higher) | 444 (2 studies) | ⊕⊕⊝⊝ low1,2 | |||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1 Quality was downgraded by two levels due to both studies having serious risk of bias. 2 Quality of evidence was not downgraded for imprecision as n = 444 exceeded the threshold for imprecision.
To analyse the efficacy of each intervention (see 'Types of treatment' above), we first separated the studies within an intervention category by the age of the sample. Preterm: infants born less than 37 weeks gestation, hospitalised after birth; or neonate: full‐term infants between birth and one month of age; or older infant: full‐term infants, aged from one month to 36 months.
We further subdivided outcomes by the timing of the pain response that was being measured, either pain reactivity (within the first 30 seconds following the painful stimuli) or immediate pain regulation (the next closest time point measured 30 seconds after the painful stimuli). For example, for studies that examined sucking‐related interventions, first we divided into three age groups (preterm, neonate or older infant), then we divided by timing of response measurement (pain reactivity or immediate pain regulation). Thus, findings were age‐specific and pain response‐specific (e.g. sucking‐related treatment recommendation for preterm infants’ pain reactivity), as opposed to a blanket recommendation for sucking‐related interventions.
Due to the emerging verbal skills of infants and recommended assessment procedures for infant pain (Franck 2000; Stevens 2007), we made the decision to only analyse objectively measured behavioral responses to pain (see Types of outcome measures). When studies had more than one behavioral response to pain, we used pain facial expression over any other behavior. Physiological measures were not included due to considerable methodological heterogeneity (including significant missing data for behavioral measures; in these situations it was rare that intention‐to‐treat analyses were done). But, if well‐established, multi‐dimensional pain measures were utilized, with behavioral and physiological indicators, and it was a reliable and valid measure, we used the total score (for example, the Premature Infant Pain Profile (PIPP) (Stevens 1996) to maintain the integrity of scale. Three studies utilized measures of distress that directly followed a painful procedure, therefore, were included as a measure of pain (Corbo 2000; Ferber 2008; Whipple 2004).
We standardized all the scores using the standardized mean difference (SMD) method recommended by Cochrane. Since all the outcomes were behaviorally‐based and standardized but used different types of measurements, we examined them together as either the outcome variable called 'Pain reactivity' or 'Immediate pain regulation'. As such, our outcome measure was treated the same for each intervention and it encapsulated all the above measures of pain‐related distress.
Standardized mean differences (SMDs) using a random‐effects model are displayed in the results below with the 95% confidence intervals included in brackets. Interventions for specific ages and time periods are considered effective when the SMD and the two anchors of the confidence interval fell in the negative range. All participants included in the analyses were randomized and met the inclusion criteria outlined earlier. Studies that examined a relevant non‐pharmacological treatment but did not meet the inclusion criteria were qualitatively compared to the actual quantitative analyses in the individual 'Summary of treatment effects' section.
In terms of interpretation of the effect sizes, 0.2 represents a small effect, 0.5 a moderate effect, and 0.8 a large effect (Cohen 1988). For this review we used the inverse variance method recommended by Cochrane. Using this method, the weight given to each study is the inverse of the variance of the effect estimate. This means that larger studies with smaller standard errors are given more weight than smaller studies with larger standard errors. Thus, since the overall findings are heavily impacted by heterogeneity (i.e. large variance in treatment or control groups), the overall results presented may differ from the results of individual studies. Also, as aforementioned, based on our study quality analyses, studies of lower/unknown quality were examined for their impact on the findings for individual treatments.
The results below examine the effects of 24 separate treatments, analysed by age (preterm or neonate or older infant) x pain response (reactivity or regulation). Fifty‐one separate analyses were conducted. No analyses were based on sufficient evidence. Sufficient evidence for an intervention was based on the following criteria: the analysis must be based on a total treatment number ('n') that exceeds 30x where x is the number of studies; the majority of studies must be of moderate to high quality evidence using GRADE criteria and evidence must come from at least two separate research groups. Criteria were based on recommendations from Cochrane, GRADE criteria and the American Psychological Association (Chambless 2001). Please refer to the Summary of overall findings table (Table 10) for summary.
For our secondary outcome (i.e. adverse events), 52 studies did not mention any adverse events. Eight studies explicitly stated that no adverse events took place. Three studies (Axelin 2009; Campbell‐Yeo 2012; Curtis 2007) reported adverse events (mild acute oxygen desaturation, bradycardia and vomiting). All three studies stated these mild adverse events were equally distributed among treatment groups.
1. Non‐nutritive sucking‐related
Preterm infants
Pain reactivity
Six studies (seven treatment arms) investigated the effects of sucking on preterm pain reactivity (SMD ‐0.31; 95% CI ‐0.65 to 0.04; I2 = 72%). The total number of participants was 329 (control = 52, treatment = 277). The mean sample size across studies was 54.83 (SD = 45.82; range = 17 to 122). Most studies were cross‐over trials (six out of seven treatment arms). One study (Elserafy 2009) contributed two treatment arms to the analysis: a pacifier treatment arm and a pacifier plus water treatment arm. See Analysis 1.1 for the full analysis. Non‐nutritive sucking for preterm pain reactivity was not effective based on very low quality evidence, see Table 1.
1.1. Analysis.
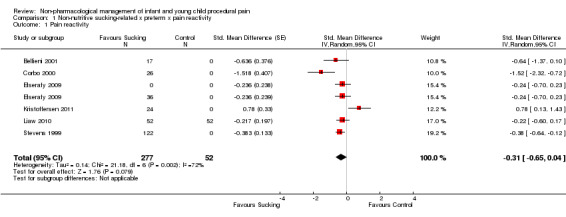
Comparison 1 Non‐nutritive sucking‐related x preterm x pain reactivity, Outcome 1 Pain reactivity.
Immediate pain regulation
Five studies investigated the effects of sucking on preterm immediate pain regulation, with two studies contributing two arms each (Elserafy 2009; Whipple 2004). The total number of participants was 260 (control = 72, treatment = 188). The mean sample size across studies was 52 (SD = 31.72; range = 26 to 104). Most studies were cross‐over trials (four out of seven treatment arms). For the arms included in the analysis, five involved sucking on a pacifier, one involved sucking on a pacifier with water, and one involved sucking on a pacifier with music. There is evidence that sucking is efficacious for improving immediate regulation in preterm infants (SMD ‐0.43; 95% CI ‐0.63 to ‐0.23; I2 = 0%). Of side note, a study not included in the quantitative analyses due to use of an active control group (Campos 1989) also suggests sucking is an effective intervention, when compared to swaddling. See Analysis 2.1 for full analysis. Non‐nutritive sucking for preterm immediate pain regulation was effective based on low quality evidence, see Table 2.
2.1. Analysis.
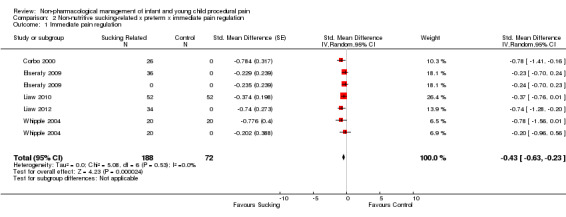
Comparison 2 Non‐nutritive sucking‐related x preterm x immediate pain regulation, Outcome 1 Immediate pain regulation.
Neonates
Pain reactivity
Five studies investigated the effect of sucking on pain reactivity for neonates. The SMD is ‐1.20 (95% CI ‐2.01 to ‐0.38; I2 = 90%) suggesting that for neonates, sucking is efficacious in reducing immediate pain reactivity (Analysis 3.1). The total number of participants was 270 (control = 140, treatment = 130). The mean sample size across studies was 54 (SD = 5.86; range = 40 to 70). All studies were between‐group analyses. One study involved stimulating sucking with water for 30 seconds after the needle, where as the other involved placing a pacifier in the baby’s mouth. Non‐nutritive sucking for neonate pain reactivity was effective based on very low quality evidence, see Table 3.
3.1. Analysis.
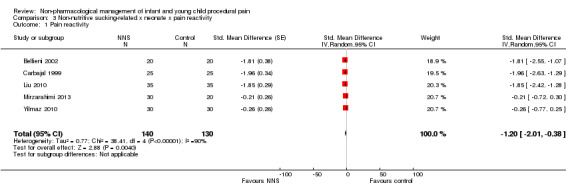
Comparison 3 Non‐nutritive sucking‐related x neonate x pain reactivity, Outcome 1 Pain reactivity.
Immediate pain regulation
Seven studies investigated the effect of sucking on the immediate regulation of pain for neonates. An overall SMD of ‐0.90 (95% CI ‐1.54 to ‐0.25; I2 = 84%) suggests that there is very low quality evidence that sucking is efficacious for improving immediate pain regulation in neonates. The total number of participants was 325 (control = 149, treatment = 176). The mean sample size across studies was 46.43 (SD = 19.41; range = 20 to 70). Most studies were between‐group analyses (six out of seven treatment arms).
Older infants
Immediate pain regulation
Two studies investigated the effect of sucking on the immediate regulation of pain for older infants (see Analysis 4.1). This analysis found that sucking is an efficacious intervention for helping older infants to regulate following a painful procedure (SMD ‐1.34; 95% CI ‐2.14 to ‐0.54;. I2 = 77%) based on very low quality evidence, see Table 4. The total number of participants was 151 (control = 74, treatment = 77). The mean sample size across studies was 75.5 (SD = 48.8; range = 41 to 110). Both studies were between‐group analyses. Sucking‐related interventions are considered a promising intervention with confirmatory evidence needed.
4.1. Analysis.
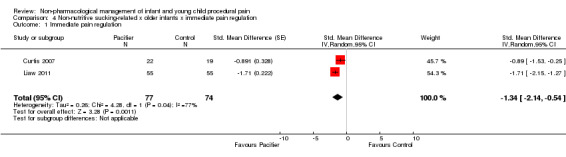
Comparison 4 Non‐nutritive sucking‐related x older infants x immediate pain regulation, Outcome 1 Immediate pain regulation.
Summary of treatment effects: non‐nutritive sucking‐related
Preterm infants. The pooled results from this review suggest that there is evidence that sucking is not efficacious in reducing pain reactivity but is effective for immediate pain regulation in preterm infants. An analysis of significant studies suggests that pain relief will be maximized if sucking begins at least three minutes prior to the painful stimuli. Of peripheral note, two studies that were not included in the analyses due to the use of an active control group (Bueno 2010; Weissman 2009) suggest that sucking helps diminish pain reactivity in preterm infants.
Neonates. The results suggest that sucking is effective for pain reactivity and immediate pain regulation in neonates but this is based on very low quality evidence. Four studies that were not included in the analyses, due to methodological differences with our included studies (Aguirre 2008; Bueno 2010; Campos 1989; Morelius 2009) also lend support to the efficacy of sucking to improve immediate pain regulation for neonates.
Older infants. Evidence suggests that non‐nutritive sucking is effective for the immediate regulation of pain in older infants based on low quality evidence.
2. Swaddling/tucking‐related
Preterm infants
Pain reactivity
Nine treatment arms investigated the effect of swaddling or tucking on pain reactivity in preterm infants. One study reported two groups separately which both received tucking and nesting (Comaru 2009) with separate control groups. These two groups were thus entered into the analysis as separate studies since they used different participants. Swaddling/tucking was found to be effective in reducing pain reactivity in preterm infants (SMD ‐0.89; 95% CI ‐1.37 to ‐0.40). See Analysis 5.1 for the full analysis. The total number of participants was 331 (control = 25 (crossover trial), treatment = 306). The mean sample size across studies was 36.77 (SD = 34.18; range = 12 to 122). Eight treatment arms were cross‐over studies and one was not. This analysis found that swaddling/tucking is an efficacious intervention for pain reactivity based on low quality evidence, see Table 5.
5.1. Analysis.
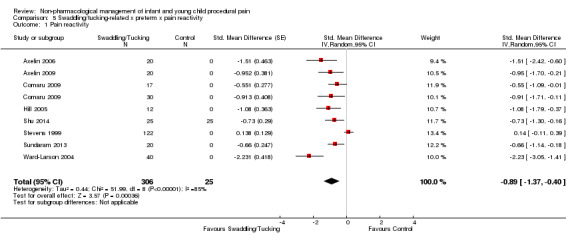
Comparison 5 Swaddling/tucking‐related x preterm x pain reactivity, Outcome 1 Pain reactivity.
Immediate pain regulation
Five studies investigated whether facilitated tucking was effective for immediate pain regulation of preterm infants. The total number of participants was 119 (control = 0 (crossover trial), treatment = 119). The mean sample size across studies was 23.8 (SD = 7.89; range = 15 to 34). All five treatment arms were cross‐over studies. Facilitated tucking was an efficacious intervention for improving the immediate pain regulation of preterm infants (SMD ‐0.71; 95% CI ‐1.00 to ‐0.43) based on very low quality evidence.
Neonates
Pain reactivity
Results from one study (Morrow 2010), with a sample size of 42 (control = 22, treatment = 20), suggest that swaddling/tucking is effective for pain reactivity with a SMD of ‐1.26 (95% CI ‐1.92 to ‐0.60) based on very low quality evidence.
Summary of treatment effects: swaddling/tucking‐related
Preterm infants. There was low to very low quality evidence to support the use of swaddling/tucking as an effective intervention for reducing pain reactivity and immediate pain regulation in preterm infants. Of side note, two studies (Huang 2004; Johnston 2008a) that were not included in the analysis due to use of an active control group, suggested that swaddling was as effective as containment (placing the child in a lateral position for 30 minutes prior to heel‐stick) but not as effective as kangaroo care.
Neonates. Very low quality evidence supports the effectiveness of swaddling/tucking‐related interventions for pain reactivity in the neonates.
3. Touch/massage‐related
Preterm infants
Pain reactivity
Two treatment arms investigated the effect of touch/massage on pain reactivity in preterm infants. The total number of participants was 65 (control = 0, treatment = 65). The mean sample size across treatment arms was 32.5 (SD = 0.71; range = 32 to 33). Both treatment arms were cross‐over. One study reported two groups separately which both received touch/massage (Chik 2012) with separate treatment groups. These two groups were thus entered into the analysis as separate studies since they used different participants. Touch/massage was found to be effective in reducing pain reactivity in preterm infants (SMD ‐1.44; 95% CI ‐2.56 to ‐0.32) based on low quality evidence. One quasi‐experimental study not included in analyses also found massage to be efficacious in reducing acute pain in preterms (Abdallah 2013).
Immediate pain regulation
Three small studies investigated the effect of touch on immediate pain regulation in preterm infants. The total number of participants was 45 (control = 0, treatment = 45). The mean sample size across studies was 15 (SD = 6.93; range = 11 to 23). All treatment arms were cross‐over studies. The results suggest that touch/massage is not efficacious in improving the immediate regulation of preterm infants following a painful procedure (SMD ‐1.11; 95% CI ‐2.33 to 0.11) based on very low quality evidence.
Neonates
Pain reactivity
Two studies with a total sample size of 100, assessed the efficacy of touch/massage on pain reactivity in neonates. Massage was no more efficacious than a no‐treatment control (SMD ‐0.19; 95% CI ‐0.58 to 0.21) based on moderate quality evidence.
Immediate pain regulation
Two studies investigated the effect of touch on the immediate pain regulation of neonates. The total number of participants was 98 (control = 49, treatment = 49). The mean sample size across studies was 49 (SD = 24; range = 32 to 66). All treatment arms were between‐group studies. The two studies did not find it to be efficacious in improving immediate pain regulation in neonates (SMD ‐0.27; 95% CI ‐0.67 to 0.13) based on very low quality evidence.
Older infants
Pain reactivity
One study, with a sample size of 64 (control = 32, treatment = 32), investigated the effect of touch on the immediate pain regulation of older infants. This study found it to be efficacious in improving pain reactivity in older infants (SMD ‐0.86; 95% CI ‐1.37 to ‐0.35) based on very low quality evidence.
Immediate pain regulation
One study, with a sample size of 60 (control = 30, treatment = 30), investigated the effect of touch on the immediate pain regulation of older infants. This study found it to be efficacious in improving immediate pain regulation in older infants (SMD ‐1.91; 95% CI ‐2.52 to ‐1.30) based on very low quality evidence.
Summary of treatment effects: touch or massage‐related
Preterm infants. The findings from this review suggest that touch/massage‐related interventions are efficacious in improving pain reactivity (low quality evidence) but not efficacious for immediate pain regulation (very low quality evidence). Of side note, one study not included in the analysis due to use of a physiological outcome measure (Diego 2009) demonstrated an effect on heart rate.
Neonates. Low to very low quality evidence suggests touch/massage‐related interventions are not an efficacious intervention to reduce pain reactivity or immediate regulation in neonates, based on low quality evidence. Of peripheral note, one study that was not included in the analysis due to methodological choices (Cignacco 2008) provides further support that massage is not an efficacious intervention for reducing acute pain in neonates.
Older infants. Very low quality evidence suggests that touch/massage is efficacious in reducing pain reactivity and immediate pain regulation scores in older infants.
4. Environmental modification
Preterm infants
Pain reactivity
Two studies investigated the effect of environmental modification on pain reactivity in preterm infants. The total number of participants was 64 (control = 0, treatment = 64). The mean sample size across studies was 32 (SD = 18.38; range = 19 to 45). Both treatment arms were cross‐over. Environmental modification was not found to be efficacious in reducing pain reactivity (SMD ‐6.44; 95% CI ‐17.13 to 4.26), based on very low quality evidence.
Immediate pain regulation
The effect of environmental modification on the immediate pain regulation of preterm infants was assessed by one cross‐over study with a sample size of 45 (control = 0, treatment = 45). This intervention was efficacious in improving immediate pain regulation of preterm infants over time following the painful stimuli (SMD ‐4.01; 95% CI ‐5.26 to ‐2.77), based on moderate quality evidence.
Summary of treatment effects: environmental modification
Preterm infants. While the pooled result from two studies suggest that environmental modification was not efficacious for pain reactivity, this was based on very low quality evidence. There is moderate quality evidence to suggest that environmental modification is an efficacious for immediate pain regulation.
5. Simulated rocking and water
Preterm infants
Pain reactivity
One study, with a sample size of 44 (control = 20, treatment = 24), assessed the efficacy of simulated rocking and water on the pain reactivity of preterm infants. This study showed that the intervention was no better than a no‐treatment control in reducing pain reactivity in preterm infants (SMD 0.00; 95% CI ‐0.59 to 0.59) based on very low quality evidence.
Summary of treatment effects: simulated rocking and water
Preterm infants. Very low quality evidence indicates that simulated rocking and water is not an efficacious intervention for reducing pain reactivity for preterm infants.
6. Simulated mother’s voice
Preterm infants
Pain reactivity
Based on one cross‐over study with a sample size of 19 (control = 0, treatment = 19), simulated mother’s voice, which was modified to sound like it would in utero, was not efficacious at reducing pain reactivity for preterm infants (SMD ‐0.29; 95% CI ‐0.94 to 0.35) based on very low quality evidence.
Summary of treatment effect: simulated mother’s voice
Preterm infants. Very low quality evidence indicated that simulated mother’s voice was not more efficacious than a no‐treatment control for reducing pain reactivity for preterm infants.
7. Swallowing water
Preterm infants
Pain reactivity
The effect of swallowing water on pain reactivity in preterm infants was assessed in two studies. The total number of participants was 60 (control = 0, treatment = 60). The mean sample size across studies was 30 (SD = 8.49; range = 24 to 36). Both treatment arms were cross‐over studies. These studies found that water was not more efficacious than a no‐treatment control in reducing preterm pain reactivity (SMD 1.07; 95% CI ‐1.59 to 3.72; I2 = 95%), based on very low quality evidence.
Immediate pain regulation
One cross‐over study, with a sample size of 36 (control = 0, treatment = 36), examined the effect of swallowing water on the immediate pain regulation of preterm infants. Based on this result, water was not an efficacious intervention for improving immediate pain regulation for preterm infants (SMD ‐0.23; 95% CI ‐0.70 to 0.24) based on very low quality evidence.
Neonates
Pain reactivity
The effect of swallowing water on pain reactivity in neonates was assessed in one between‐group study with a sample size of 50 (control = 25, treatment = 25). This study found that water was not efficacious in reducing pain reactivity for neonates (SMD 0.10; 95% CI ‐0.45 to 0.66) based on very low quality evidence.
Immediate pain regulation
One between‐group study, with a sample size of 34 (control = 17, treatment = 17), examined the effect of swallowing water on the immediate pain regulation of neonates. Based on this result, water is not an efficacious intervention for reducing immediate pain regulation for neonates (SMD ‐0.53; 95% CI ‐1.21 to 0.16) based on very low quality evidence.
Older infants
Immediate pain regulation
One between‐group study, with a sample size of 30 (control = 15, treatment = 15), examined the effect of swallowing water on the immediate pain regulation of older infants. Based on the results of one study, water is not more efficacious than a no‐treatment control at improving immediate pain regulation for older infants (SMD 0.00; 95% CI ‐0.72 to 0.72) based on very low quality evidence.
Summary of treatment effects: swallowing water
Preterm infants. There is very low quality evidence showing that water is an ineffective intervention for pain reactivity or immediate pain regulation for preterm infants.
Neonates. There is very low quality evidence showing that water is an ineffective intervention for pain reactivity or immediate pain regulation of neonates.
Older infants. There is very low quality evidence showing that water is an ineffective intervention for immediate pain regulation of older infants.
The above studies used water as a treatment arm (in comparison to a ‘no‐treatment’ control), while most other studies in the literature used water as the ‘no‐treatment’ control group. Given the more common use of water in the literature and the limited evidence at every age group of its inefficacy, it is not recommended that further research explores water as a treatment for young‐child procedural pain.
8. Rocking/holding
Neonates
Pain reactivity
Two studies investigated the effect of holding on the pain reactivity of neonates following a painful procedure. The total number of participants was 131 (control = 66, treatment = 65). The mean sample size across studies was 65.5 (SD = 34.65; range = 41 to 90). Both treatment arms were between groups. The pooled effects found that rocking/holding alone was not more effective than a no‐treatment control group in reducing pain reactivity in neonates (SMD ‐0.33; 95% CI ‐1.05 to 0.39; I2= 73%) based on very low quality evidence.
Immediate pain regulation
The effect of rocking or holding on immediate pain regulation of neonates was examined in two studies. The total number of participants was 81 (control = 41, treatment = 40). The mean sample size across studies was 40.5 (SD = 0.71; range = 40 to 41). Both treatment arms were between groups. The overall pooled effect showed that rocking/holding was more efficacious than a no‐treatment control at improving immediate pain regulation for neonates (SMD ‐0.75; 95% CI ‐1.20 to ‐0.30; I2= 0%) based on low quality evidence.
Older infants
Pain reactivity
The effect of holding an infant during a routine immunization on pain reactivity was examined in one large study with a sample size of 106 (control = 50, treatment = 56). The results from this study indicated that simply holding the infant during the immunization was not more efficacious in reducing pain reactivity than the no‐treatment control (SMD 0.23; 95% CI ‐0.15 to 0.62) based on very low quality evidence.
Summary of treatment effects: holding/rocking
Neonates. The results indicated very low quality evidence to suggest that rocking/holding was not efficacious for pain reactivity in neonates. There is low quality evidence to suggest that rocking/holding is efficacious for immediate pain regulation for neonates.
Older infants. There is very low quality evidence that suggests holding is not an effective intervention for pain reactivity in older infants.
9. Toy distraction
Older infants
Pain reactivity
Four studies with five treatment arms investigated the effects of toy distraction on the pain reactivity of older infants. The total number of participants was 293 (control = 131, treatment = 162). The mean sample size across studies was 58.6 (SD = 23.9; range = 32 to 81). All treatment arms were between groups. One study had two separate treatment arms, both of which involved toy distraction and were included as separate studies (Hillgrove Stuart 2013). Overall, there is evidence that toy distraction is not efficacious in reducing pain reactivity in older infants (SMD ‐0.15; 95% CI ‐0.39 to 0.08; I2= 0) based on low quality evidence. Please see Table 6 and Analysis 6.1.
6.1. Analysis.
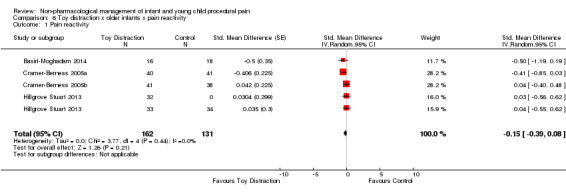
Comparison 6 Toy distraction x older infants x pain reactivity, Outcome 1 Pain reactivity.
Immediate pain regulation
The effect of toy distraction on the immediate pain regulation of older infants was investigated in one study. The total number of participants was 99 (control = 34, treatment = 65) with two treatment arms. Toy distraction was not efficacious in improving immediate pain regulation for older infants (SMD ‐0.08; 95% CI ‐0.50 to 0.33) based on very low quality evidence.
Summary of treatment effects: toy distraction
Older infants. Low to very low quality evidence suggests that toy distraction is not more efficacious than a no‐treatment control for reducing pain reactivity and immediate pain regulation in older infants. Of note, a study not included in the statistical analysis (Singh 2012) showed that distraction was efficacious using a non‐validated behavioral measure of pain.
10. Video distraction
Older infants
Pain reactivity
One study with 90 participants (control = 41, treatment = 49) examined the impact of video on the pain reactivity of older infants. Infants were always distracted with a video during the intervention, and toys may or may not have been used in conjunction. The results indicated that this intervention was efficacious in reducing pain reactivity for older infants (SMD ‐0.70; 95% CI ‐1.13 to ‐0.27) based on very low quality evidence.
Immediate pain regulation
The effects of video distraction on immediate pain regulation for older infants were assessed in one between‐group study with 126 participants (control = 63, treatment = 63). The results indicated that this intervention was more efficacious than a no‐treatment control at improving immediate pain regulation in older infants (SMD ‐0.84; 95% CI ‐1.20 to ‐0.47) based on very low quality evidence.
Summary of treatment effects: video distraction
Older infants. Results from this review indicated that there is very low quality evidence that video distraction is efficacious in reducing pain reactivity and immediate pain regulation.
11. Parent presence
Older infants
Pain reactivity.
One study with 10 participants and very low quality evidence found that parent presence was not effective in reducing pain reactivity.
Immediate pain regulation
Parental presence alone during the painful medical procedure was not found in one trial with 278 participants (control = 131, treatment = 147) to be efficacious in reducing immediate pain regulation for older infants (SMD 0.00; 95% CI ‐0.24 to 0.23) based on very low quality evidence.
Summary of treatment effects: parent presence
Older infants. Very low quality evidence indicated that parent presence was not more efficacious than a no‐treatment control for improving pain reactivity and immediate pain regulation for older infants.
12. Structured parent involvement
Older infants
Pain reactivity
The effect of structured parent involvement was investigated in four studies. Structured parent involvement included studies whereby parents were given specific instructions on what to do with their infant during a painful procedure (either verbally/verbal coaching or via an information sheet). The total number of participants was 369 (control = 184, treatment = 185). The mean sample size across studies was 92.25 (SD = 47.24; range = 50 to 160). All treatment arms were between groups. The overall pooled effect indicates that there is evidence that structured parent involvement was no more efficacious than a no‐treatment control group in reducing pain reactivity in older infants (SMD ‐0.24; 95% CI ‐0.51 to 0.04; I2= 41%) based on very low quality evidence, see Table 7. See Analysis 7.1 for the complete analysis.
7.1. Analysis.
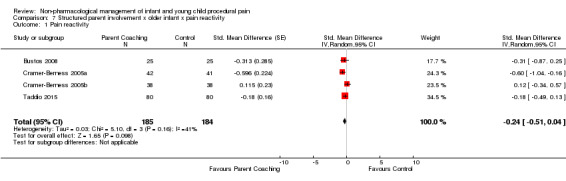
Comparison 7 Structured parent involvement x older infant x pain reactivity, Outcome 1 Pain reactivity.
Immediate pain regulation
The efficacy of structured parent involvement on immediate pain regulation for older infants was assessed in two studies. The total number of participants was 444 (control = 211, treatment = 233). In both studies parents were instructed to stand by their infant's head and talk and touch during the painful procedure. The intervention was not more efficacious than a no‐treatment control in improving pain regulation for older infants (SMD ‐0.04; 95% CI ‐0.23 to 0.15) based on very low quality evidence.
Summary of treatment effects: structured parent involvement
Older infants. Based on very low quality evidence, structured parent involvement is not effective for pain reactivity or pain regulation.
13. Structured non‐parent involvement
Older infants
Immediate pain regulation
The efficacy of structured non‐parent involvement on immediate pain regulation for older infants was assessed in one study. The total number of participants was 114 (control = 56, treatment = 58). In this study, infants were given either water or oral sucrose and using the physical intervention of the 5 S's (shushing, swaddling, sucking, side position, and swinging) during the painful procedure. The intervention was more efficacious than a no‐treatment control in improving immediate pain regulation for older infants (SMD ‐1.09; 95% CI ‐1.48 to ‐0.70), based on very low quality evidence.
Summary of treatment effects: structured non‐parent involvement
Older infants. Based on very low quality evidence, structured parent involvement is not effective for pain regulation.
14. Therapeutic touch
Preterm infants
Pain reactivity
The effect of therapeutic touch was investigated in one study. The total number of participants was 55 (control = 28, treatment = 27). The therapeutic touch intervention was no more efficacious than a no‐treatment control group in reducing pain reactivity in preterm infants (SMD ‐0.09; 95% CI ‐0.44 to 0.62) based on low quality evidence.
Immediate pain regulation
The efficacy of structured therapeutic touch on the regulation of immediate pain regulation for preterm infants was assessed in one study. The total number of participants was 55 (control = 28, treatment = 27). The intervention was not more efficacious than a no‐treatment control in improving immediate pain regulation for preterm infants (SMD 0.22; 95% CI ‐0.31 to 0.75) based on low quality evidence.
Older infants
Pain reactivity
The effect of therapeutic touch was investigated in one cross‐over study. The total number of participants was 20 (control = 0, treatment = 20). The therapeutic touch intervention was no more efficacious than a no‐treatment control group in reducing pain reactivity in older infants (SMD ‐0.21; 95% CI ‐0.84 to 0.41) based on very low quality evidence.
Summary of treatment effects: therapeutic touch
Preterm infants. Low quality evidence for both pain reactivity and immediate pain regulation showed that therapeutic touch is not efficacious.
Older infants. Very low quality evidence for pain reactivity showed that therapeutic touch is not efficacious.
15. Familiar Odor
Neonates
Immediate pain regulation
One study with 90 participants (control = 45, treatment = 45) found that familiar odor was effective in improving immediate pain regulation in neonates (Sadathosseini 2013) based on moderate quality evidence (SMD ‐1.04; 95% CI ‐1.47 to ‐0.61).
16. Unfamiliar Odor
Neonates
Immediate pain regulation:
One study with 90 participants (control = 45, treatment = 45) found that unfamiliar odor was not effective in improving immediate pain regulation in neonates (Sadathosseini 2013) based on moderate quality evidence (SMD ‐0.09; 95% CI ‐0.50 to 0.32).
17. Co‐bedding
Preterm infants
Pain reactivity:
One study with 100 participants (control = 50, treatment = 50) found that co‐bedding was not effective in reducing pain reactivity in preterm neonates (Badiee 2014) based on moderate quality evidence (SMD ‐0.30; 95% CI ‐0.69 to 0.09).
18. Heel Warming
Preterm infants
Pain reactivity
One study with 50 participants (control = 25, treatment = 25) found that heel warming was effective in reducing pain reactivity for neonates based on very low quality evidence (SMD ‐0.58; 95% CI ‐1.15 to ‐0.01).
19. Sucrose + Sucking vs. Co‐bedding + Sucrose + Sucking
Preterm infants
Pain reactivity
The additive effect of co‐bedding on sucrose and sucking was investigated in one study. The total number of participants was 124 (control = 57, treatment = 67). The intervention was no more efficacious than a no‐treatment control group in reducing pain reactivity in preterm infants (SMD ‐0.03; 95% CI ‐0.38 to 0.32) based on very low quality evidence.
Immediate pain regulation
The additive effect of co‐bedding on sucrose and sucking was investigated in one study. The total number of participants was 124 (control = 57, treatment = 67). The intervention was no more efficacious than a no‐treatment control group in improving immediate pain regulation in preterm infants (SMD 0.40; 95% CI 0.04 to 0.75) based on very low quality evidence.
Summary of treatment effects: Co‐bedding + Sucrose + Sucking vs. Sucrose + Sucking
Preterm infants. Very low quality evidence for both pain reactivity and immediate pain regulation showed that co‐bedding did not have an additive effect beyond sucking and sucrose.
20. Sucrose + Holding vs. Massage + Sucrose + Holding
Older infants
Pain reactivity
The additive effect of massage on sucrose and holding was investigated in one study. The total number of participants was 120 (control = 60, treatment = 60). Massage did not have an additive effect for reducing pain reactivity in older infants (SMD ‐0.11; 95% CI ‐0.47 to 0.25), based on very low quality evidence.
Summary of treatment effects: Massage + Sucrose + Holding vs. Sucrose + Holding
Older infants. Very low quality evidence for pain reactivity showed that massage did not have an additive effect in addition to sucrose and holding.
21. Sucrose vs. Structured non‐parent involvement + Sucrose vs.
Older infants
Immediate pain regulation
The additive effect of structured non‐parent involvement on sucrose for the immediate regulation of pain for older infants was assessed in one study. The total number of participants was 116 (control = 58, treatment = 58).The additive effect of structured non‐parent involvement was not more efficacious than sucrose alone in improving immediate pain regulation for older infants (SMD ‐0.27; 95% CI ‐0.64 to 0.09) based on very low quality evidence.
Summary of treatment effects: Structured non‐parent involvement + Sucrose vs. Sucrose
Older infants. Very low quality evidence for immediate pain regulation showed that structured non‐parent involvement did not have an additive effect in addition to sucrose.
22. Sucrose vs. Sucrose + Sucking
Preterm infants
Pain reactivity
The additive effect of a pacifier on sucrose was investigated in one cross‐over study. The total number of participants was 24 (control = 0, treatment = 24). The pacifier in addition to sucrose for preterm infants was more efficacious than sucrose alone in reducing pain reactivity (SMD ‐2.25; 95% CI ‐3.31 to ‐1.19) based on very low quality evidence.
Summary of treatment effects: Pacifier + Sucrose vs. Sucrose
Preterm infants. Very low quality evidence for pain reactivity showed that pacifiers did have an additive effect in addition to sucrose.
23. Sucking + Sucrose vs. Sucking + Sucrose + Facilitated tucking
Preterm infants
Pain reactivity
The additive effect of facilitated tucking on sucking and sucrose was investigated in one study. The total number of participants was 44 (control = 21, treatment = 23). Facilitated tucking did not have an additive effect to sucrose and sucking for reducing pain reactivity in preterm infants (SMD ‐0.44; 95% CI ‐1.05 to 0.17) based on very low quality evidence.
Immediate pain regulation
The additive effect of facilitated tucking on sucking and sucrose was investigated in one study. The total number of participants was 44 (control = 21, treatment = 23). Facilitated tucking did not have an additive effect to sucrose and sucking for improving immediate pain regulation in preterm infants (SMD 0.00; 95% CI ‐0.61 to 0.61) based on very low quality evidence.
Summary of treatment effects: Sucking + Sucrose + Facilitated tucking vs. Sucking + Sucrose
Preterm infants. Very low quality evidence for pain reactivity and immediate pain regulation showed that facilitated tucking did not have an additive effect in addition to sucking and sucrose.
24. Sucking vs. Scking + Facilitated tucking
Preterm infants
Pain reactivity
The additive effect of facilitated tucking on non‐nutritive sucking was investigated in one study. The total number of participants was 45 (control = 23, treatment = 22). Facilitated tucking did have an additive effect to non‐nutritive sucking for reducing pain reactivity in preterm infants (SMD ‐1.37; 95% CI ‐2.02 to ‐0.72) based on very low quality evidence.
Immediate pain regulation
The additive effect of facilitated tucking on non‐nutritive sucking was investigated in one study. The total number of participants was 45 (control = 23, treatment = 22). Facilitated tucking did have an additive effect to non‐nutritive sucking for improving immediate pain regulation in preterm infants (SMD ‐1.60; 95% CI ‐2.27 to ‐0.93) based on very low quality evidence.
Summary of treatment effects: Non‐nutritive sucking + Facilitated tucking vs. Non‐nutritive sucking
Preterm infants. Very low quality evidence for pain reactivity and immediate pain regulation showed that facilitated tucking did have an additive effect on non‐nutritive sucking in preterm infants.
Publication bias
In order to help minimize the influence of publication bias (i.e. the bias resulting from analysing only published studies), we used systematic methods to obtain studies that were not published. This included contacting researchers and clinicians broadly through emails and list‐serves, using dissertation search engines, contacting specific researchers who presented data at relevant paediatric pain or pain conferences we attended, and searching databases that register studies in progress. It is highly unlikely we were able to locate every relevant study but a methodical attempt was made. We also plan to disseminate our findings broadly, by both publishing parts of this review, and presenting it at conferences, with an invitation to researchers and clinicians who have worked on studies currently omitted to contact us, helping to further minimize this bias for future updates.
Discussion
Summary of main results
The overall findings of this review are summarized succinctly in Table 10 with the explanation of the numbers presented in Table 1. These results are based on the 63 studies used for quantitative analyses. In our opinion, this table is the most important page of the review because it summarizes the entirety of the review, including: analysis strategy (treatment x age x pain response), direction of effect (evidence supports efficacy; evidence supports inefficacy) and the quality of the evidence using GRADE criteria. The following summaries are offered, with the caveat that all analyses reflect that more research is needed to bolster our confidence in the direction of the findings.
Across age groups, non‐nutritive sucking‐related (NNS) interventions showed efficacy. It should be noted that this evidence was based on low to very low quality evidence. However, one age difference is that it may not be efficacious for preterm pain reactivity. For preterms, it appears swaddling/tucking type interventions and touch/massage type interventions are promising interventions (although also based on very low to low quality evidence), while therapeutic touch is not currently seen as efficacious (based on low to very low quality evidence). Swaddling/tucking and rocking/holding appear to be promising interventions requiring more research for neonates, while sucking, structured non‐parent involvement and video distraction are promising for older infants (low quality evidence).
Taking a broad view of the results from a pain‐response vantage point, a pattern seems to exist in a number of our non‐pharmacological strategies. Similar to what was seen for NNS interventions, environmental modification also appears to work for preterm pain regulation but not reactivity. Moreover, rocking/holding also seems to have low to very low quality evidence supporting the regulation of pain but not the initial pain reaction in neonates. This suggests an emerging pattern whereby researchers conducting randomised controlled trials with non‐pharmacological strategies should be cautioned to carefully measure separate indicators of the initial response to pain versus the regulation of pain. It seems logical that given some non‐pharmacological strategies do not interfere with primary nociception (i.e. sucking, rocking, environmental modification), they would not impact how an infant initially reacts but rather how quickly an infant soothes or regulates after a painful response.
Our 'additive' trials analyses suggested that for preterm infants, sucking on a pacifier with sucrose was superior to just taking sucrose. Moreover, facilitated tucking also had an additive effect on non‐nutritive sucking.
Overall completeness and applicability of evidence
Our goal was to update our 2011 review and assess the efficacy of all non‐pharmacological interventions, that had not been included in other Cochrane Reviews, for the management of acute pain and distress in infants and children up to three years of age. Given our belief in the steep developmental trajectory that occurs during infancy and that this steep trajectory influences the efficacy of non‐pharmacological treatments, we conducted our analyses for preterms, neonates, and older infants separately. Moreover, due to the fact that different studies may measure acute pain at different time points and are therefore distinct, we analysed pain reactivity (the reaction within 30 seconds after the painful stimulus) and immediate pain regulation (reactions that occur after the initial pain reaction; in our review 30 seconds was chosen as the beginning of the regulation phase) data separately. While there was a considerable body of randomised controlled trials the evidence base is challenged by the lack of sufficient evidence for all of the intervention strategies examined in this review. It should be noted that 52 of our 63 trials did not report adverse events.
The current review included patients from both inpatient and outpatient settings and assessed a broad array of non‐pharmacological interventions, contributing to its overall completeness. Given that healthy and sick infants were included in the review, the findings are generalizable for healthy and typically developing infants as well as those hospitalized for various conditions. The results of the review have been categorized by age and pain response. Results are only applicable and generalizable for the age and pain response for which they were reported. For example, findings with regards to non‐nutritive sucking for preterm infants for pain reactivity would only apply for preterm infants and for the first 30 seconds after the painful procedure.
Quality of the evidence
The quality of the evidence in the review was generally low to very low. Few interventions had moderate quality evidence. This finding behooves researchers and trialists to improve the quality of the randomised controlled trials. Key reasons for the lack of reliable evidence for findings stems from the low quality of randomised controlled trials in the field (such as high risk of bias and imprecision), the small number of studies within the same intervention, and small sample sizes within studies. The best available evidence was used, despite some of the limitations in quality. Criteria were based on recommendations from Cochrane, GRADE criteria and the American Psychological Association (Chambless 2001).
Potential biases in the review process
Four articles were not extracted due to authors not responding to our requests. These articles will be pursued for the next update. Clinical trial registers were not searched for this review, which may have introduced some bias. Additionally, although 24 excluded studies were referenced in the review, they did not impact the interpretation of the included studies as they were not considered in the results synthesis or final conclusions.
Agreements and disagreements with other studies or reviews
Previous systematic reviews assessing pain management in children have focused on very specific forms of pain management strategies, such as music (Cepeda 2006), breast milk (Shah 2009), kangaroo care (Johnston 2013b), and sucrose (Stevens 2010), therefore, none of these pain management strategies were assessed for the purpose of this review. Another major distinction between this review and others in this research area is the division of pain response into pain reactivity and immediate pain regulation. A recent systematic review was done in order to create Clinical Practice Guidelines for Reducing Pain from Vaccine Injections in Children and Adults (Taddio in press), inclusive of included non‐pharmacological interventions, as well as the four above interventions. There were no major disagreements found between these guidelines and our review. Furthermore, the qualitative findings of the 24 relevant studies excluded due to insufficient criteria were all in line with the quantitative results.
Authors' conclusions
Implications for practice.
Preterm infants: The available evidence suggests that for preterm infants, touch/massage is effective in reducing pain immediately after a painful procedure. Non‐nutritive sucking, environmental modification, and swaddling/facilitated tucking can be used to reduce both pain immediately after a procedure and pain 30 seconds after a procedure. Including sucking with sucrose for pain immediately after a needle is effective as is adding facilitated tucking with non‐nutritive sucking for both pain reactivity and immediate pain regulation. All of these findings are based on low to very low quality evidence, which indicates that better quality evidence is needed to further substantiate these results.
Neonates: The available evidence suggests that for neonates, sucking‐related interventions can be used to reduce pain immediately after a painful procedure and 30 seconds after the painful procedure. There is evidence that swaddling and facilitated tucking reduce pain in neonates immediately after a painful procedure. There is evidence that rocking/holding is a useful strategy for helping an infant to regulate from pain, but was not found to be effective in reducing pain immediately after a painful procedure. Finally, familiar odor has also been shown to be promising to reduce pain during the regulatory phase post‐needle. All of these findings are based on low to very low quality evidence, which indicates that better quality evidence is needed to further substantiate these results.
Older infants: The available evidence suggests that for older infants, non‐nutritive sucking, such as a pacifier, is effective to help an infant regulate after a painful procedure. There is also evidence that touch/massage‐related interventions and structured non‐parent involvement are effective in immediate pain regulation. There is evidence for video distraction used to reduce pain throughout the post‐immunization phase. Overall, these findings are also based on low to very low quality evidence, which indicates that better quality evidence is needed to further substantiate these results.
Implications for research.
Based on the results of this review, significant gaps in the existing literature on non‐pharmacological management of acute pain in infancy can be discerned. Among the highest priority gaps are the need for well‐designed trials that study:
Sucking‐related interventions, swaddling/tucking‐related interventions, rocking/holding, touch/massage, familiar odor, video distraction. These have all been shown to be potentially effective but confidence is limited due to poor quality and lack of replication.
Structured‐caregiver interventions (parent and non‐parent) that are informed by established attachment theory. Over the first year of life, it has been argued that the caregiver is the most important context for the infants (Pillai Riddell 2009). Currently, studies that have attempted to formally structure parent behavior have been limited and, thus, shown to be ineffective. It should be stressed that more work on better types of parent/non‐parent interventions, especially ones that capitalize on an infant’s primary developmental need for proximity to the parent (Bowlby 1982), is needed. Teaching caregivers to better meet an infant’s attachment needs during times of pain may lead to more efficacious parent interventions.
In addition, preliminary work from other studies (excluded from our overall quantitative analyses for methodological reasons) suggests that feeding an infant formula, and administering the least painful immunization first are promising non‐pharmacological interventions that may reduce infant pain in the acute setting, but more structured research methodologies need to be applied.
A new aspect of the review, which emerged at the update stage based on changing trends in methodology, is the concept of 'additive' studies. In our analysis, we looked at studies that could offer evidence of the additive effect of a non‐pharmacological treatment on existing treatments. It is important to remember that trials of this nature, only speak to the additive effect of a given intervention on top of another intervention. These trials offer nothing about the original intervention. For example, in a well‐designed trial comparing the additive effect of sucking on co‐bedding + sucrose. There was no additive effect of sucking on co‐bedding + sucrose. But, this does not mean co‐bedding + sucrose does not have merit. Sucrose has been shown to be efficacious in reducing pain‐related behaviour. Whether co‐bedding adds to sucrose as an intervention is undetermined. A major challenge of researchers is to execute 'additive' trials that build on treatments that have demonstrated efficacy, while meeting the ethical guidelines we must uphold. Given the challenge of defining equipoise with a no‐treatment control group (see Harrison 2013, Pillai Riddell 2013c), more work must be done.
Another important point for future trialists is the meaning of heterogeneity estimates. Observational research on a large longitudinal study that used latent class analysis techniques to analyse infant pain responses over time, substantiate the assertion that there are different subgroups of pain responders (Pillai Riddell 2013b) that render average pain estimates (i.e. the key outcome in most non‐pharmacological trials for acute pain) meaningless, particularly in the regulation phase. Using covariates such as temperament estimates or conducting responder analyses may be options to remedy this situation. Additionally, it is not expected that future studies could be done for all interventions at all age groups. For example, non‐nutritive sucking may not be an appropriate intervention for three‐year olds. More research is needed in areas where the intervention would be developmentally appropriate.
Finally, sample size in treatment groups in trials studying non‐pharmacological treatments for infants must increase and investigators should work on replicating trials so that there can be independent corroborating evidence for a particular intervention.
What's new
| Date | Event | Description |
|---|---|---|
| 27 July 2017 | Review declared as stable | See Published notes. |
History
Protocol first published: Issue 4, 2006 Review first published: Issue 10, 2011
| Date | Event | Description |
|---|---|---|
| 4 March 2015 | New search has been performed | This review has been updated to include the results of a new search, new risk of bias tables, application of GRADE criteria and summary of findings tables have been added. |
| 4 March 2015 | New citation required but conclusions have not changed | i. Kangaroo Care section now omitted due to new 2013 Cochrane Review on topic. Eleven new interventions or intervention combinations added to review (structured non‐parent involvement; therapeutic touch; additive effect of sucking to co‐bedding + sucrose; additive effect of massage on sucrose + holding; additive effect of structured parent involvement on sucrose; additive effect of pacifier on sucrose; additive effect of facilitated tucking on sucking + sucrose, familiar odour, unfamiliar odour, co‐bedding, and heel warming) ii. Search updated on March 4, 2015 iii. 21 new studies added (Badiee 2014; Basiri 2014; Campbell‐Yeo 2012; Chik 2012; Esfahani 2013; Harrington 2012; Herrington 2014; Hogan 2014; Johnston 2013; Jose 2012; Kristoffersen 2011; Liaw 2011; Liaw 2012; Liaw 2013; Park 2006; Mirzarahimi 2013; Sadathosseini 2013; Shaw 1982; Shu 2014; Sundaram 2013; Taddio 2015) iv. 1595 new participants in the review. v. GRADE evaluations now embedded in meta‐Summary of Findings (SoF) Table and in individual SoF tables. vi. All conclusions stayed same but confidence of findings is elaborated. The application of GRADE criteria and the new types of interventions are compelling reasons to reread this update and especially SoF tables. |
| 10 November 2008 | Amended | Further RevMan 5 conversion changes. |
| 28 July 2008 | Amended | Converted to new review format. |
Notes
The authors are not aware of any new studies to change the conclusions at present. We are planning to split the review into individual interventions which will serve to update the original. This review has now been stabilised pending further discussion with the authors and editors.
Acknowledgements
We would like to thank the team at Cochrane for their patience (Anna Hobson, Jessica Thomas, Dr. Amanda C de C Williams, and Dr. John Plummer) and support with our complex search strategies (Elizabeth Ulryk, Sylvia Bickley, Caroline Struthers, and Joanne Abbott) over the years. The breadth of the literature reviewed is due to their willingness to listen to our concerns and skilfully adapt the search. We would also like to thank Dr. Ken Craig and Dr. Amanda C de C Williams for their help at the initial protocol stage. Finally, we would like to thank our research assistants at the OUCH lab for extensive help with all the project and data management of this review. We would also like to thank Janet Yamada and Grace Lee for helping with extraction.
In addition, we would like to thank our sources of funding over the creation of this analysis: The Canadian Institutes of Health Research has provided salary support to Dr. Pillai Riddell (Post‐doctoral Fellowship, New Investigator Award); doctoral fellowships to Ms. Nicole Racine, Ms. Jessica Hillgrove Stuart, and Dr. Laila Din Osmun; a Master's level graduate fellowship to Ms. Hannah Gennis; as well as graduate support to Dr. Rachel Horton and Dr. Sara Ahola Kohut. The Ontario Graduate Scholarship Program has provided support to Ms. Racine, Dr. Horton, and Dr. Ahola Kohut. The Social Sciences and Humanities Research Council has provided support to Ms. Racine and Dr. Ahola Kohut. Fonds de Recherche en Santé du Québec provided doctoral funding to Dr. Lindsay Uman. In addition, during this review, The Pain in Child Health (Canadian Institutes for Health Research) strategic training initiative provided support to Ms. Racine, Ms. Gennis, Ms. Hillgrove Stuart, Dr. Uman, Dr. Din Osmun, Dr. Horton, and Dr. Ahola Kohut. Finally, the Lillian Wright Foundation for Maternal‐Child Health has also provided funds to: Ms. Racine, Ms. Gennis, Dr. Din Osmun, and Dr. Horton. In addition, operating funds for this project were provided by funds from York University to Dr. Pillai Riddell.
Cochrane Review Group funding acknowledgement: The National Institute for Health Research (NIHR) is the largest single funder of the Cochrane PaPaS Group. Disclaimer: The views and opinions expressed in this review are those of the authors and do not necessarily reflect those of the NIHR, National Health Service (NHS) or the Department of Health.
Appendices
Appendix 1. MEDLINE (OVID) search strategy 2015 update
1. Needles/
2. needle*.mp.
3. (blood sampl* or immuni* or inoculat* or vaccin* or inject* or "finger prick*" or finger‐prick or "heel prick*" or heel‐prick* or "heel lance*" or heel‐lance* or "heel puncture*" or heel‐puncture* or "heel stick" or suture* or (laceration* adj3 repair*)).mp.
4. ("lumbar puncture" or lumbar‐puncture* or "spinal tap*" or spinal‐tap*).mp.
5. ("bone marrow aspiration" or "bone marrow biops*").mp.
6. (intravenous or intra‐venous or venepuncture* or venipuncture* or venous cannulation* or (arterial blood gas* and cannul*)).mp.
7. ((catheter adj6 insert*) or catheter* or port‐a‐cath* or portacath).mp.
8. ("central line" adj6 (insert* or remov*)).mp.
9. (central venous catheter* adj6 insert*).mp.
10. (local analges* or local anaesthe* or local anesthe*).mp.
11. ((arterial puncture or artery) adj6 puncture*).mp.
12. "arterial line*".mp.
13. (thoracocentesis or paracentesis).mp.
14. or/1‐13
15. exp Pain/
16. Pain Measurement/
17. PAIN THRESHOLD/
18. pain*.mp.
19. or/15‐18
20. 14 and 19
21. ((vaccin* adj6 pain) or (cannul* adj6 pain) or (needle* adj6 pain*) or (needle* adj6 distress*) or (needle* adj6 discomfort) or (needle* adj6 fear*) or (needle* adj6 fright*) or (needle* adj6 anxious) or (needle* adj6 anxiet*) or (procedure* adj6 pain*) or (intervention* adj6 pain*) or (intervention* adj6 distress*) or (procedure adj6 distress*) or (procedure* adj6 discomfort*) or (procedure‐related adj6 pain)).mp.
22. or/20‐21
23. Pain, Postoperative/
24. ((postoperative adj3 pain*) or (post‐operative adj3 pain*) or post‐operative‐pain).mp.
25. ((post‐surgical adj3 pain*) or ("post surgical" adj3 pain*) or (post‐surgery adj3 pain*) or (post adj surg* adj3 pain*)).mp.
26. (post* adj4 pain*).mp.
27. "pain relief after".mp.
28. ("pain following" adj3 surg*).mp.
29. (posttreatment adj3 pain*).mp.
30. ("pain control after" adj4 surg*).mp.
31. ((post surg* or post‐surg*) and (pain* or discomfort)).mp.
32. ((pain* adj3 "after surg*") or (pain* adj3 "after operat*")).mp.
33. ((pain* adj3 "follow* operat*") or (pain* adj3 "follow* surg*")).mp.
34. or/23‐33
35. 22 or 34
36. Child, Preschool/
37. exp Infant/
38. (baby or babies or neonate* or newborn or child* or infant* or paediatric* or pediatric*).mp.
39. or/36‐38
40. 35 and 39
41. randomized controlled trial.pt.
42. controlled clinical trial.pt.
43. randomized.ab.
44. placebo.ab.
45. drug therapy.fs.
46. randomly.ab.
47. trial.ab.
48. or/41‐47
49. exp animals/ not humans.sh.
50. 48 not 49
51. 40 and 50
52 (201104* or 201105* or 201106* or 201107* or 201108* or 201109* or 201110* or 201111* or 201112* or 2012* or 2013*).ed.
53 51 and 52
Appendix 2. PsycINFO (OVID) search strategy 2015 update
1. needle*.mp.
2. (blood sampl* or immuni* or inoculat* or vaccin* or inject* or "finger prick*" or finger‐prick or "heel prick*" or heel‐prick* or "heel lance*" or heel‐lance* or "heel puncture*" or heel‐puncture* or "heel stick" or suture* or (laceration* adj3 repair*)).mp.
3. ("lumbar puncture" or lumbar‐puncture* or "spinal tap*" or spinal‐tap*).mp.
4. ("bone marrow aspiration" or "bone marrow biops*").mp.
5. (intravenous or intra‐venous or venepuncture* or venipuncture* or venous cannulation* or (arterial blood gas* and cannul*)).mp.
6. ((catheter adj6 insert*) or catheter* or port‐a‐cath* or portacath).mp.
7. ("central line" adj6 (insert* or remov*)).mp.
8. (central venous catheter* adj6 insert*).mp.
9. (local analges* or local anaesthe* or local anesthe*).mp.
10. ((arterial puncture or artery) adj6 puncture*).mp.
11. "arterial line*".mp.
12. (thoracocentesis or paracentesis).mp.
13. or/1‐12
14. exp Pain/
15. Pain Measurement/
16. PAIN THRESHOLD/
17. pain*.mp.
18. or/14‐17
19. 13 and 18
20. ((vaccin* adj6 pain) or (cannul* adj6 pain) or (needle* adj6 pain*) or (needle* adj6 distress*) or (needle* adj6 discomfort) or (needle* adj6 fear*) or (needle* adj6 fright*) or (needle* adj6 anxious) or (needle* adj6 anxiet*) or (procedure* adj6 pain*) or (intervention* adj6 pain*) or (intervention* adj6 distress*) or (procedure adj6 distress*) or (procedure* adj6 discomfort*) or (procedure‐related adj6 pain)).mp.
21. or/19‐20
22. ((postoperative adj3 pain*) or (post‐operative adj3 pain*) or post‐operative‐pain).mp.
23. ((post‐surgical adj3 pain*) or ("post surgical" adj3 pain*) or (post‐surgery adj3 pain*) or (post adj surg* adj3 pain*)).mp.
24. (post* adj4 pain*).mp.
25. "pain relief after".mp.
26. ("pain following" adj3 surg*).mp.
27. (posttreatment adj3 pain*).mp.
28. ("pain control after" adj4 surg*).mp.
29. ((post surg* or post‐surg*) and (pain* or discomfort)).mp.
30. ((pain* adj3 "after surg*") or (pain* adj3 "after operat*")).mp.
31. ((pain* adj3 "follow* operat*") or (pain* adj3 "follow* surg*")).mp.
32. or/22‐31
33. 21 or 32
34. (baby or babies or neonate* or newborn or child* or infant* or paediatric* or pediatric*).mp.
35. 33 and 34
36. clinical trials/
37. (randomis* or randomiz*).tw.
38. (random$ adj3 (allocat$ or assign$)).tw.
39. ((clinic$ or control$) adj trial$).tw.
40. ((singl$ or doubl$ or trebl$ or tripl$) adj3 (blind$ or mask$)).tw.
41. (crossover$ or "cross over$").tw.
42. random sampling/
43. Experiment Controls/
44. Placebo/
45. placebo$.tw.
46. exp program evaluation/
47. treatment effectiveness evaluation/
48. ((effectiveness or evaluat$) adj3 (stud$ or research$)).tw.
49. or/36‐48
50. 35 and 49
51 limit 50 to yr="2011 ‐Current"
Appendix 3. EMBASE (OVID) search strategy 2015 update
1. needle*.mp.
2. (blood sampl* or immuni* or inoculat* or vaccin* or inject* or "finger prick*" or finger‐prick or "heel prick*" or heel‐prick* or "heel lance*" or heel‐lance* or "heel puncture*" or heel‐puncture* or "heel stick" or suture* or (laceration* adj3 repair*)).mp.
3. ("lumbar puncture" or lumbar‐puncture* or "spinal tap*" or spinal‐tap*).mp.
4. ("bone marrow aspiration" or "bone marrow biops*").mp.
5. (intravenous or intra‐venous or venepuncture* or venipuncture* or venous cannulation* or (arterial blood gas* and cannul*)).mp.
6. ((catheter adj6 insert*) or catheter* or port‐a‐cath* or portacath).mp.
7. ("central line" adj6 (insert* or remov*)).mp.
8. (central venous catheter* adj6 insert*).mp.
9. (local analges* or local anaesthe* or local anesthe*).mp.
10. ((arterial puncture or artery) adj6 puncture*).mp.
11. "arterial line*".mp.
12. (thoracocentesis or paracentesis).mp.
13. or/1‐12
14. exp Pain/
15. Pain Measurement/
16. PAIN THRESHOLD/
17. pain*.mp.
18. or/14‐17
19. 13 and 18
20. ((vaccin* adj6 pain) or (cannul* adj6 pain) or (needle* adj6 pain*) or (needle* adj6 distress*) or (needle* adj6 discomfort) or (needle* adj6 fear*) or (needle* adj6 fright*) or (needle* adj6 anxious) or (needle* adj6 anxiet*) or (procedure* adj6 pain*) or (intervention* adj6 pain*) or (intervention* adj6 distress*) or (procedure adj6 distress*) or (procedure* adj6 discomfort*) or (procedure‐related adj6 pain)).mp.
21. or/19‐20
22. ((postoperative adj3 pain*) or (post‐operative adj3 pain*) or post‐operative‐pain).mp.
23. ((post‐surgical adj3 pain*) or ("post surgical" adj3 pain*) or (post‐surgery adj3 pain*) or (post adj surg* adj3 pain*)).mp.
24. (post* adj4 pain*).mp.
25. "pain relief after".mp.
26. ("pain following" adj3 surg*).mp.
27. (posttreatment adj3 pain*).mp.
28. ("pain control after" adj4 surg*).mp.
29. ((post surg* or post‐surg*) and (pain* or discomfort)).mp.
30. ((pain* adj3 "after surg*") or (pain* adj3 "after operat*")).mp.
31. ((pain* adj3 "follow* operat*") or (pain* adj3 "follow* surg*")).mp.
32. or/22‐31
33. 21 or 32
34. (baby or babies or neonate* or newborn or child* or infant* or paediatric* or pediatric*).mp.
35. 33 and 34
36. clinical trials/
37. (randomis* or randomiz*).tw.
38. (random$ adj3 (allocat$ or assign$)).tw.
39. ((clinic$ or control$) adj trial$).tw.
40. ((singl$ or doubl$ or trebl$ or tripl$) adj3 (blind$ or mask$)).tw.
41. (crossover$ or "cross over$").tw.
42. random sampling/
43. Experiment Controls/
44. Placebo/
45. placebo$.tw.
46. exp program evaluation/
47. treatment effectiveness evaluation/
48. ((effectiveness or evaluat$) adj3 (stud$ or research$)).tw.
49. or/36‐48
50. 35 and 49
51 limit 50 to yr="2011 ‐Current"
Appendix 4. CINAHL (EBSCO) search strategy 2015 update
S50 S40 AND S49
S49 S41 OR S42 OR S43 OR S44 OR S45 OR S46 OR S47 OR S48
S48 (allocat* random*)
S47 (MH "Quantitative Studies")
S46 (MH "Placebos")
S45 placebo*
S44 (random* allocat*)
S43 (MH "Random Assignment")
S42 (Randomi?ed control* trial*)
S41 (singl* blind* ) or (doubl* blind* ) or (tripl* blind* ) or (trebl* blind* ) or (trebl* mask* ) or (tripl* mask* ) or (doubl* mask* ) or (singl* mask* )
S40 S35 AND S39
S39 S36 OR S37 OR S38
S38 (baby or babies or neonate* or newborn or child* or infant* or paediatric* or pediatric*)
S37 (MH "Infant+")
S36 (MH "Child, Preschool")
S35 S22 OR S34
S34 S23 OR S24 OR S25 OR S26 OR S27 OR S28 OR S29 OR S30 OR S31 OR S32 OR S33
S33 ((pain* N3 "follow* operat*") or (pain* N3 "follow* surg*"))
S32 ((pain* N3 "after surg*") or (pain* N3 "after operat*"))
S31 ((post surg* or post‐surg*) and (pain* or discomfort))
S30 ("pain control after" N4 surg*)
S29 (posttreatment N3 pain*)
S28 ("pain following" N3 surg*)
S27 "pain relief after"
S26 (post* N4 pain*)
S25 ((post‐surgical N3 pain*) or ("post surgical" N3 pain*) or (post‐surgery N3 pain*) or (post adj surg* N3 pain*))
S24 ((postoperative N3 pain*) or (post‐operative N3 pain*) or post‐operative‐pain)
S23 (MH "Postoperative Pain")
S22 S20 OR S21
S21 ((vaccin* N6 pain) or (cannul* N6 pain) or (needle* N6 pain*) or (needle* N6 distress*) or (needle* N6 discomfort) or (needle* N6 fear*) or (needle* N6 fright*) or (needle* N/anxious) or (needle* N6 anxiet*) or (procedure* N6 pain*) or (intervention* N6 pain*) or (intervention* N6 distress*) or (procedure N6 distress*) or (procedure* N6 discomfort*) or (procedure‐related N6 pain))
S20 S14 AND S19
S19 S15 OR S16 OR S17 OR S18
S18 pain*
S17 (MH "Pain Threshold")
S16 (MH "Pain Measurement")
S15 (MH "Pain+")
S14 S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 OR S9 OR S10 OR S11 OR S12 OR S13
S13 (thoracocentesis or paracentesis)
S12 "arterial line*"
S11 ((arterial puncture or artery) N6 puncture*)
S10 (local analges* or local anaesthe* or local anesthe*)
S9 (central venous catheter* N6 insert*)
S8 ("central line" N6 (insert* or remov*))
S7 ((catheter N6 insert*) or catheter* or port‐a‐cath* or portacath)
S6 (intravenous or intra‐venous or venepuncture* or venipuncture* or venous cannulation* or (arterial blood gas* and cannul*))
S5 ("bone marrow aspiration" or "bone marrow biops*")
S4 ("lumbar puncture" or lumbar‐puncture* or "spinal tap*" or spinal‐tap*)
S3 (blood sampl* or immuni* or inoculat* or vaccin* or inject* or "finger prick*" or finger‐prick or "heel prick*" or heel‐prick* or "heel lance*" or heel‐lance* or "heel puncture*" or heel‐puncture* or "heel stick" or suture* or (laceration* N3 repair*))
S2 needle*
S1 (MH "Needles")
Appendix 5. CENTRAL (The Cochrane Library) 2015 update
#1 MeSH descriptor: [Needles] this term only
#2 needle*:ti,ab,kw (Word variations have been searched)
#3 (blood sampl* or immuni* or inoculat* or vaccin* or inject* or "finger prick*" or finger‐prick or "heel prick*" or heel‐prick* or "heel lance*" or heel‐lance* or "heel puncture*" or heel‐puncture* or "heel stick" or suture* or (laceration* near/3 repair*)):ti,ab,kw (Word variations have been searched)
#4 ("lumbar puncture" or lumbar‐puncture* or "spinal tap*" or spinal‐tap*):ti,ab,kw (Word variations have been searched)
#5 ("bone marrow aspiration" or "bone marrow biops*"):ti,ab,kw (Word variations have been searched)
#6 (intravenous or intra‐venous or venepuncture* or venipuncture* or venous cannulation* or (arterial blood gas* and cannul*)):ti,ab,kw (Word variations have been searched)
#7 ((catheter near/6 insert*) or catheter* or port‐a‐cath* or portacath):ti,ab,kw (Word variations have been searched)
#8 ("central line" near/6 (insert* or remov*)):ti,ab,kw (Word variations have been searched)
#9 (central venous catheter* near/6 insert*):ti,ab,kw (Word variations have been searched)
#10 (local analges* or local anaesthe* or local anesthe*):ti,ab,kw (Word variations have been searched)
#11 ((arterial puncture or artery) near/6 puncture*):ti,ab,kw (Word variations have been searched)
#12 "arterial line*":ti,ab,kw (Word variations have been searched)
#13 (thoracocentesis or paracentesis):ti,ab,kw (Word variations have been searched)
#14 #1 or #2 or #3 or #4 or #5 or #6 or #7 or #8 or #9 or #10 or #11 or 12 or #13
#15 MeSH descriptor: [Pain] explode all trees
#16 MeSH descriptor: [Pain Measurement] this term only
#17 MeSH descriptor: [Pain Threshold] this term only
#18 pain*:ti,ab,kw (Word variations have been searched)
#19 #15 or #16 or #17 or #18
#20 #14 and #19
#21 ((vaccin* near/6 pain) or (cannul* near/6 pain) or (needle* near/6 pain*) or (needle* near/6 distress*) or (needle* near/6 discomfort) or (needle* near/6 fear*) or (needle* near/6 fright*) or (needle* near/6 anxious) or (needle* near/6 anxiet*) or (procedure* near/6 pain*) or (intervention* near/6 pain*) or (intervention* near/6 distress*) or (procedure near/6 distress*) or (procedure* near/6 discomfort*) or (procedure‐related near/6 pain)):ti,ab,kw (Word variations have been searched)
#22 #20 or #21
#23 MeSH descriptor: [Pain, Postoperative] this term only
#24 ((postoperative near/3 pain*) or (post‐operative near/3 pain*) or post‐operative‐pain):ti,ab,kw (Word variations have been searched)
#25 ((post‐surgical near/3 pain*) or ("post surgical" near/3 pain*) or (post‐surgery near/3 pain*) or (post adj surg* near/3 pain*)):ti,ab,kw (Word variations have been searched)
#26 (post* near/4 pain*):ti,ab,kw (Word variations have been searched)
#27 "pain relief after":ti,ab,kw (Word variations have been searched)
#28 ("pain following" near/3 surg*):ti,ab,kw (Word variations have been searched)
#29 (posttreatment near/3 pain*):ti,ab,kw (Word variations have been searched)
#30 ("pain control after" near/4 surg*):ti,ab,kw (Word variations have been searched)
#31 ((post surg* or post‐surg*) and (pain* or discomfort)):ti,ab,kw (Word variations have been searched)
#32 ((pain* near/3 "after surg*") or (pain* near/3 "after operat*")):ti,ab,kw (Word variations have been searched)
#33 ((pain* near/3 "follow* operat*") or (pain* near/3 "follow* surg*")):ti,ab,kw (Word variations have been searched)
#34 #23 or #24 or #25 or #26 or #27 or #28 or #29 or #30 or #31 or #32
#35 #22 or #34
#36 MeSH descriptor: [Child, Preschool] this term only
#37 MeSH descriptor: [Infant] explode all trees
#38 (baby or babies or neonate* or newborn or child* or infant* or paediatric* or pediatric*):ti,ab,kw (Word variations have been searched)
#39 #36 or #37 or #38
#40 #35 and #39 from 2011 to 2013
Data and analyses
Comparison 1. Non‐nutritive sucking‐related x preterm x pain reactivity.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pain reactivity | 6 | 329 | Std. Mean Difference (Random, 95% CI) | ‐0.31 [‐0.65, 0.04] |
Comparison 2. Non‐nutritive sucking‐related x preterm x immediate pain regulation.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Immediate pain regulation | 5 | 260 | Std. Mean Difference (Random, 95% CI) | ‐0.43 [‐0.63, ‐0.23] |
Comparison 3. Non‐nutritive sucking‐related x neonate x pain reactivity.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pain reactivity | 5 | 270 | Std. Mean Difference (Random, 95% CI) | ‐1.20 [‐2.01, ‐0.38] |
Comparison 4. Non‐nutritive sucking‐related x older infants x immediate pain regulation.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Immediate pain regulation | 2 | 151 | Std. Mean Difference (Random, 95% CI) | ‐1.34 [‐2.14, ‐0.54] |
Comparison 5. Swaddling/tucking‐related x preterm x pain reactivity.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pain reactivity | 8 | 331 | Std. Mean Difference (Random, 95% CI) | ‐0.89 [‐1.37, ‐0.40] |
Comparison 6. Toy distraction x older infants x pain reactivity.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pain reactivity | 4 | 293 | Std. Mean Difference (Random, 95% CI) | ‐0.15 [‐0.39, 0.08] |
Comparison 7. Structured parent involvement x older infant x pain reactivity.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pain reactivity | 4 | 369 | Std. Mean Difference (Random, 95% CI) | ‐0.24 [‐0.51, 0.04] |
Comparison 8. Structured parent involvement x older infants x immediate pain regulation.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Immediate pain regulation | 2 | 444 | Std. Mean Difference (Random, 95% CI) | ‐0.04 [‐0.23, 0.15] |
8.1. Analysis.
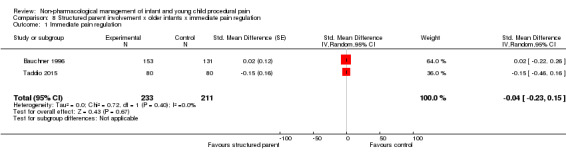
Comparison 8 Structured parent involvement x older infants x immediate pain regulation, Outcome 1 Immediate pain regulation.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Allen 1996.
| Methods |
Study design: randomized between groups Total study duration: unknown |
|
| Participants |
Total number: 285 Setting: hospital ambulatory pediatric clinic Diagnostic criteria: healthy neonates and infants Age: Minimum: 2 weeks Maximum: 18 months Mean: not reported SD: not reported Sex: Males: not mentioned Females: not mentioned Country: USA |
|
| Interventions |
Total number of intervention groups: 1 Control group description: 1 Total number of participants randomized to each of your groups: 2 weeks old = 50 2 months old = 44 4 months old = 50 6 months old = 46 9 months old = 28 15 months old = 30 18 months old = 37 Specific intervention: sterile water Intervention details: the infant orally received 2 mL of sterile water 20 minutes before needle Integrity of intervention: satisfactory |
|
| Outcomes |
Pain outcomes, time points when measured, and scale limits: Pain vocalization (cry) Upper limit: 100% Lower limit: 0% High score = more pain (longer cry) Continuous |
|
| Notes |
Adverse reactions: None reported Key conclusions of study authors: water administered prior to needle lowers pain response only when one needle is given in infants aged two weeks, nine months and 18 months |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 1) Randomization (Random Sequence Generation) | Low risk | 1 ‐ A convincing method of randomization is reported but this did not involve an independent person |
| 2) Allocation bias (Allocation concealment) | High risk | 0 ‐ There is not an adequate description of attempts to deal with potential allocation bias |
| 3a) Blinding of participants and personnel | Unclear risk | 0 ‐ Efforts to reduce measurement bias are not reported or are insufficient, e.g. outcomes collected by therapist |
| 3b) Blinding of outcome assessment | Unclear risk | 0 ‐ Efforts to reduce measurement bias are not reported or are insufficient, e.g. outcomes collected by therapist |
| 4) Attrition (Incomplete Outcome Data) | High risk | 0 ‐ There is no documented evidence or insufficient evidence reported of how attrition was dealt with |
| 5) Selective outcome reporting (Selective Outcome Reporting) | Low risk | There was no selective outcome reporting |
| 6) Other potential sources of bias (Other potential threats to validity) | High risk | 0 ‐ Either equivalence of groups is not reported or there is evidence of non‐equivalence |
| 7a) Power calculation (Part 1 of size bias) | High risk | 0 ‐ Power calculations were not conducted a priori |
| 7b) Sufficient sample (part 2 of size bias) | High risk | 0 ‐ A sufficient sample size based on the power calculation was not obtained |
| Total | High risk | Total score on new Cochrane standard: Low risk (2/9), High risk (5/9), Unclear Risk (2/9) |
Axelin 2006.
| Methods |
Study design: randomized cross‐over trial Total study duration: 10 months (2003 to 2004) |
|
| Participants |
Total number: 20 Setting: Turku University Hospital, NICU Diagnostic criteria: less than and equal to 37 weeks gestation, no major congenital anomalies, a need for regular endotracheal/pharyngeal suctioning, no analgesics for four hours before the procedure. Age: Minimum: 24 weeks gestation, 6 days Maximum: 33 weeks gestation, 37 days Mean: not reported (median: 18 days) SD: not reported Sex: Males: 8 Females: 12 Country: Finland |
|
| Interventions |
Total number of intervention groups: 1 Control group description: 1 Total number of participants randomized to each of your groups: 20 Specific intervention: facilitated tucking Intervention details: facilitated tucking by parents Integrity of intervention: satisfactory |
|
| Outcomes |
Pain outcomes, time points when measured, and scale limits: NIPS Upper limit: 7 Lower limit: 0 High score = more pain Continuous |
|
| Notes |
Adverse reactions: one infant got septicaemia after the experimental care and did not express pain during Funding sources: the South‐Western Finnish Foundation of Neonatal Research Key conclusions of study authors: facilitated tucking by parents is an effective and safe pain management method during suctioning of preterm infants |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 1) Randomization (Random Sequence Generation) | Low risk | 1 ‐ A convincing method of randomization is reported but this did not involve an independent person |
| 2) Allocation bias (Allocation concealment) | Low risk | 1 ‐ An adequate method is reported that removes the potential biases of investigators |
| 3a) Blinding of participants and personnel | Low risk | Personnel could not be blinded but babies were |
| 3b) Blinding of outcome assessment | High risk | Coders could not be blinded to condition |
| 4) Attrition (Incomplete Outcome Data) | High risk | 0 ‐ There is no documented evidence or insufficient evidence reported of how attrition was dealt with |
| 5) Selective outcome reporting (Selective Outcome Reporting) | Unclear risk | Not specified |
| 6) Other potential sources of bias (Other potential threats to validity) | Low risk | There was no baseline inequality |
| 7a) Power calculation (Part 1 of size bias) | Low risk | 1 ‐ Power calculations were conducted a priori |
| 7b) Sufficient sample (part 2 of size bias) | Low risk | 1 ‐ A sufficient sample size based on the power calculation was obtained |
| Total | High risk | Total score on new Cochrane standard: Low risk (6/9), High risk (2/9), Unclear Risk (1/9) |
Axelin 2009.
| Methods |
Study design: randomized cross‐over Study duration: 2 years |
|
| Participants |
Total number: 22 Setting: NICU at university hospital Diagnostic criteria: preterm, but were excluded if they had unstable health conditions Age: Minimum: 23 weeks Maximum: 30 weeks Mean: 28 SD: 2.3 Sex: Males: 12 Females: 8 Country: Finland |
|
| Interventions |
Total number of intervention groups: 1 Control group description: sterile: 2 mL of water on tongue Total number of participants randomized to each of your groups: 22 Specific intervention #1: facilitated tucking Intervention details: parent held infant in a side lying, flexed fetal type position offering support and skin contact (taught parent the procedure in advance) Integrity of intervention: Good |
|
| Outcomes |
Pain outcomes, scale limits, and time points when measured: PIPP Measured for the first 30 seconds Higher scores = more pain Continuous |
|
| Notes |
Adverse reactions: None reported Key conclusions of study authors: facilitated tucking works |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 1) Randomization (Random Sequence Generation) | Low risk | 1 ‐ A convincing method of randomization is reported but this did not involve an independent person |
| 2) Allocation bias (Allocation concealment) | Low risk | 1 ‐ An adequate method is reported that removes the potential biases of investigators |
| 3a) Blinding of participants and personnel | Unclear risk | None specified |
| 3b) Blinding of outcome assessment | Low risk | 1 ‐ A convincing effort to reduce bias in outcomes measurement is reported |
| 4) Attrition (Incomplete Outcome Data) | Low risk | 2 ‐ Documented evidence that the CONSORT guidelines have been followed |
| 5) Selective outcome reporting (Selective Outcome Reporting) | Low risk | There was no selective outcome reporting |
| 6) Other potential sources of bias (Other potential threats to validity) | Low risk | There were no other potential sources of bias reported |
| 7a) Power calculation (Part 1 of size bias) | Low risk | 1 ‐ Power calculations were conducted a priori |
| 7b) Sufficient sample (part 2 of size bias) | Low risk | 1 ‐ A sufficient sample size based on the power calculation was obtained |
| Total | Low risk | Total score on new Cochrane standard: Low risk (8/9), High risk (0/9), Unclear Risk (1/9) |
Badiee 2014.
| Methods |
Study design: between groups Total study duration: May 2012 – December 2012 (7 months) |
|
| Participants |
Total number: 100 Setting: NICU of Shahid Beheshti University Hospital, affiliated to Isfhan University of Medical Sciences Diagnostic criteria: Preterm Age: Minimum: 26 weeks Maximum: 34 weeks Mean: 32.08 weeks (Co‐bedding group), 32.02 weeks (Standard Care group), Overall Mean = 32 SD: 1.8 (Co‐bedding group), 1.7 (Standard Care group), Overall SD = 1.75 Sex: Males: 26 (Co‐bedding), 27 (Standard Care), Total = 53 Females: 24 (Co‐bedding), 23 (Standard Care), Total = 47 Country: Iran |
|
| Interventions |
Total number of intervention groups: 1 Control group description: remained in separate incubators following current NICU standards Total number of participants randomized to each of your groups: intervention #1 = 50; control = 50 Intervention Descriptions: infants in the Co‐bedding group were placed side by side in an incubator without any clothing except for diapers so that they could touch each other freely, with each side of the incubator pertaining to one twin Integrity of intervention: good |
|
| Outcomes |
Pain outcomes, time points when measured, and scale limits: PIPP Time points: 30 seconds after heel lancing Range of possible scores: 0 to 21, higher scores indicating greater pain |
|
| Notes |
Adverse reactions: none reported Key conclusions of study authors: co‐bedding could reduce pain sensation in premature infants as measured by the PIPP, and reduces cry time after heel lance. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 1) Randomization (Random Sequence Generation) | Low risk | “Randomization was performed using a computer generated random number algorithm” (page 263, second paragraph of second column) |
| 2) Allocation bias (Allocation concealment) | Low risk | “Allocation of eligible newborns to intervention and control groups was performed using a sealed opaque envelope” (page 263, second paragraph of second column) |
| 3a) Blinding of participants and personnel | Low risk | “Researchers could not be blinded for the assigned groups” (page 263, paragraph 5 second column) |
| 3b) Blinding of outcome assessment | High risk | “PIPP score was calculated based on the recordings by three researchers.” (page 263, last paragraph second column) – Not sure if these are different researchers than those present for heel stick |
| 4) Attrition (Incomplete Outcome Data) | Low risk | “… 105 of them were included in the study. The main reason that infants could not be included was parental refusal. A few were excluded because there was no need for blood sampling” (page 264, paragraph 3 first column) |
| 5) Selective outcome reporting (Selective Outcome Reporting) | Low risk | There was no selective outcome reporting |
| 6) Other potential sources of bias (Other potential threats to validity) | Low risk | There were no other potential sources of bias reported |
| 7a) Power calculation (Part 1 of size bias) | Low risk | Power calculations were conducted a priori |
| 7b) Sufficient sample (part 2 of size bias) | Low risk | A sufficient sample size based on the power calculation was obtained |
| Total | High risk | Total score on new Cochrane standard: Low risk (8/9), High risk (1/9), Unclear Risk (0/9) |
Basiri‐Moghadam 2014.
| Methods |
Study design: between groups Total study duration: May 2012 – Feb 2013 (9 months) |
|
| Participants |
Total number: 50 Setting: clinic under the Gonabad University of Medical Sciences Diagnostic criteria: healthy Age Minimum: 4 months Maximum: 6 months Mean: 7.39 (including EMLA group) SD: 1.02 Sex Males: N/A Females: N/A Country: Iran |
|
| Interventions |
Total number of intervention groups: 2 Control group description: normal vaccination process Total number of participants randomized to each of your groups: intervention 1= N/A; control= N/A Intervention details: rattles: a rattle was shaken from 30 s before administration to 15 s afterward as a source of distraction. Integrity of intervention: good |
|
| Outcomes |
Pain outcomes, time points when measured, and scale limits: Infants’ Pain Questionnaire Time points: infants were filmed before, during and after injection (15 s). The observer used the films to fill out the questionnaires. Range of possible scores: The questionnaire scores facial expression and body motions in the range of 0 to 3, and at the range of 0 to 4 for crying. All the scores were summed. Maximum and minimum obtained scores of pain behavioural response were 10 and 0 respectively. |
|
| Notes |
Adverse reactions: none reported Key conclusions of study authors: rattles reduced pain more than control, but EMLA was more significant compared to control during needle – NOTE: no significant differences between groups 15 seconds after. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 1) Randomization (Random Sequence Generation) | Low risk | To ensure random selection, the researcher first chose a number out of a random number block and, depending on the right digit of the number, different combinations of words A (EMLA group), B for (rattle group), and C (control group) were adopted (1= ABC, 2 = BAC, 3 = CAB, 4 CBA, 5 = BCA, 6 = ACB; and re‐ selection of number for other digits;(paragraph 5, page 875). |
| 2) Allocation bias (Allocation concealment) | Unclear risk | No allocation concealment reported |
| 3a) Blinding of participants and personnel | Low risk | To determine the severity of pain experienced by the infants and to blind and control the intervention factor, the infants were filmed before, during and after injection (15s). The observer used the films to fill out the questionnaires. Only one individual was in charge of observation, who did not know about the classification of the participants(paragraph 5, page 875). |
| 3b) Blinding of outcome assessment | Unclear risk | There was no report of blinding of outcome assessment. |
| 4) Attrition (Incomplete Outcome Data) | Low risk | Initially, 60 infants were recruited, but 14(23.3%) subsequently had to be excluded; 2(3.33%) did not meet the inclusion criteria, 4(6.66%) were vaccinated by another person, and the questionnaire for 4(6.66%) were not completely filled. The final study size comprised 50(83.33%) infants (paragraph 3, page 876). |
| 5) Selective outcome reporting (Selective Outcome Reporting) | Low risk | There was no selective outcome reporting |
| 6) Other potential sources of bias (Other potential threats to validity) | Low risk | There were no other potential sources of bias reported |
| 7a) Power calculation (Part 1 of size bias) | Low risk | 1 ‐ Power calculations were conducted a priori‐ low |
| 7b) Sufficient sample (part 2 of size bias) | Low risk | 1 ‐ A sufficient sample size based on the power calculation was obtained‐ low |
| Total | Low risk | Total score on new Cochrane standard: Low risk (7/9), High risk (0/9), Unclear Risk (2/9) |
Bauchner 1996.
| Methods |
Study design: between groups Total study duration: unknown |
|
| Participants |
Total number: 431 Setting: pediatric emergency department in a hospital Diagnostic criteria: infants aged 0 to 36 months coming to the pediatric ER, undergoing a venipuncture, intravenous cannulation, or urethral catheterization Age (page 863): Minimum: newborn Maximum: 3 years Mean: unknown SD: unknown Sex: Males: 246 (57%) Females: 185 (43%) Country: USA Socio‐demographics: 87% of the mothers were between the ages 20 and 24 years old; 22% were married; 43% had less than a high school degree Ethnicity: Black: 249 participants Hispanic: , 92 participants White: , 35 participants Other: , 39 participants Note: Although there was a total of 431 participants, ethnicity was only reported for 415 participants. |
|
| Interventions |
Total number of intervention groups: 2 Control group description: 1 (parents not present) Total number of participants randomized to each of your groups: 431 total (present with intervention: 153; present without intervention: 147; control: 131 ) Specific intervention #1: intervention ‐ parent instruction Intervention details: parents asked to sit at the head of the bed and talk to, touch, and maintain eye contact with their child Integrity of intervention: good Specific intervention #2: parent present Intervention details: parent present in the room, with no other instructions given Integrity of intervention: satisfactory |
|
| Outcomes |
Pain outcomes, scale limits, and time points when measured: Cry frequency (analyses) Measured during procedure (unspecified) in Hz. This involved the computerized analysis of cry, whereby each 30‐second cry signal was filtered above 10kHZ and digitized. In general, computerized analysis of cry confirms reports of parents that the cry of children in pain is higher pitched and more turbulent. Higher frequency of cry = more pain Continuous |
|
| Notes |
Adverse reactions: none Funding sources: Maternal and Child Health Bureau Key conclusions of study authors: intervention (parent present, engaging in touch, talking and eye contact) during painful ER procedure are not effective in reducing pain (as measured by cry) in infants aged 0 to 36 months |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 1) Randomization (Random Sequence Generation) | Low risk | 2 ‐ A convincing method for generating a random allocation sequence is reported that used an independent person not involved in enrolment or allocation of participants |
| 2) Allocation bias (Allocation concealment) | High risk | 0 ‐ There is not an adequate description of attempts to deal with potential allocation bias |
| 3a) Blinding of participants and personnel | Unclear risk | None specified |
| 3b) Blinding of outcome assessment | Unclear risk | None specified |
| 4) Attrition (Incomplete Outcome Data) | Low risk | 2 ‐ Documented evidence that the CONSORT guidelines have been followed |
| 5) Selective outcome reporting (Selective Outcome Reporting) | Low risk | There was no selective outcome reporting |
| 6) Other potential sources of bias (Other potential threats to validity) | Low risk | There were no other potential sources of bias reported |
| 7a) Power calculation (Part 1 of size bias) | High risk | 0 ‐ Power calculations were not conducted a priori |
| 7b) Sufficient sample (part 2 of size bias) | Unclear risk | 1 ‐ A sufficient sample size based on the power calculation was obtained |
| Total | High risk | Total score on new Cochrane standard: Low risk (4/9), High risk (2/9), Unclear Risk (3/9) |
Bellieni 2001.
| Methods |
Study design: cross‐over Total study duration: 3 months (December 2000 to February 2001) |
|
| Participants |
Total number: 17 Setting: Siena Hospital NICU Diagnostic criteria: preterm infants Age: all infants were born less than 35 weeks gestation, and the procedure took place within 10 days post natal life Minimum: 28 weeks Maximum: 35 weeks Mean: unknown SD: unknown Sex: Males: 7 Females: 10 Country: Italy |
|
| Interventions |
Total number of intervention groups: 1 Control group description: no intervention whatsoever (just heel lance) Total number of participants randomized to each of your groups: 17 Specific intervention: water was administered orally 30 seconds before and during withdrawal Intervention details: water was instilled on the tip of the tongue with a syringe, introduced in mouth and moved to stimulate sucking. The amount that was administered was that necessary to maintain sucking (0.2 to 0.3 mL) until after the heel prick. Integrity of intervention: satisfactory |
|
| Outcomes |
Pain outcome, scale limits and time points when measured: PIPP Upper limit: 21 Lower limit: 0 High score = more pain Continuous |
|
| Notes |
Adverse reactions: none Key conclusions of study authors: non‐nutritive sucking is effective in reducing pain for preterm infants undergoing heel lance when compared to receiving no treatment at all Miscellaneous comments by review authors: poor description of methods and time in which pain was measured; poor description of sample characteristics |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 1) Randomization (Random Sequence Generation) | Low risk | 1 ‐ A convincing method of randomization is reported but this did not involve an independent person |
| 2) Allocation bias (Allocation concealment) | High risk | 0 ‐ There is not an adequate description of attempts to deal with potential allocation bias |
| 3a) Blinding of participants and personnel | Unclear risk | 1 ‐ A convincing effort to reduce bias |
| 3b) Blinding of outcome assessment | High risk | Coders not blinded to receiving no treatment or water |
| 4) Attrition (Incomplete Outcome Data) | High risk | 0 ‐ There is no documented evidence or insufficient evidence reported of how attrition was dealt with |
| 5) Selective outcome reporting (Selective Outcome Reporting) | Low risk | There was no selective outcome reporting |
| 6) Other potential sources of bias (Other potential threats to validity) | Low risk | There were no other potential sources of bias reported |
| 7a) Power calculation (Part 1 of size bias) | High risk | 0 ‐ Power calculations were not conducted a priori but was significantly powered |
| 7b) Sufficient sample (part 2 of size bias) | High risk | 0 ‐ A sufficient sample size based on the power calculation was not obtained |
| Total | High risk | Low risk (3/9), High risk (5/9), Unclear Risk (1/9) |
Bellieni 2002.
| Methods |
Study design: randomized between groups Total study duration: 5 months (February to June 2001) |
|
| Participants |
Total number: 120 (60 participants meet the requirements of this review) Setting: hospital Diagnostic criteria: healthy newborns Age: Minimum: 38 weeks Maximum: 41 weeks Mean: not reported SD: 2.5 Sex: Males: 31 Females: 29 Country: Italy Ethnicity: Caucasian |
|
| Interventions |
Total number of intervention groups: 2 Control group description: no analgesic procedure Total number of participants randomized to each of your groups: 20 in each group (total of 60) Specific intervention #1: water during heel prick (sucking) Intervention details: the tip of 1 mL syringe without needle was placed in the baby's mouth and 1 mL of distilled water was given with gentle a movement of the syringe to stimulate sucking for 30 s before, during and after heelstick Integrity of intervention: good Specific intervention #2: sensorial saturation without glucose Intervention details: involved laying the infant on its side with legs and arms flexed but free to move; looking at the infant in the face, close up, to attract its attention and simultaneously massaging the infant's face and back; speaking to the infant softly but firmly; letting the infant smell the fragrance of the baby perfume on the physiotherapist's hands Integrity of intervention: good |
|
| Outcomes |
Pain outcomes, scale limits, and time points when measured: Douleur Aiguë Nouveau‐né(DAN) scale 30 seconds pre heelstick 30 seconds post heelstick Upper limit: 10 Lower limit: 0 Higher score = more pain Continuous |
|
| Notes |
Adverse reactions: none Key conclusions of study authors: sensorial stimulation without glucose does not produce an analgesic effect in healthy newborns during the 30‐second post‐heel prick but rather, it increased irritation and awareness Sucking (water oral) does significantly reduce pain scores during 30 seconds post‐heel lance in healthy newborn infants |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 1) Randomization (Random Sequence Generation) | Low risk | 2 ‐ A convincing method for generating a random allocation sequence is reported that used an independent person not involved in enrolment or allocation of participants |
| 2) Allocation bias (Allocation concealment) | Low risk | 1 ‐ An adequate method is reported that removes the potential biases of investigators |
| 3a) Blinding of participants and personnel | Low risk | 1 ‐ A convincing effort to reduce bias in outcomes measurement is reported |
| 3b) Blinding of outcome assessment | Unclear risk | None specified |
| 4) Attrition (Incomplete Outcome Data) | Low risk | 2 ‐ Documented evidence that the CONSORT guidelines have been followed |
| 5) Selective outcome reporting (Selective Outcome Reporting) | Low risk | There was no selective outcome reporting |
| 6) Other potential sources of bias (Other potential threats to validity) | Low risk | There were no other potential sources of bias reported |
| 7a) Power calculation (Part 1 of size bias) | Low risk | 1 ‐ Power calculations were conducted a priori |
| 7b) Sufficient sample (part 2 of size bias) | Low risk | 1 ‐ A sufficient sample size based on the power calculation was obtained |
| Total | Low risk | Total score on new Cochrane standard: Low risk (8/9), High risk (0/9), Unclear Risk (1/9) |
Blass 1999.
| Methods |
Study design: randomized between groups Total study duration: 12 months (June 1997 to June 1998) |
|
| Participants |
Total number: 40 (20 meet the requirements of this review) Setting: hospital (Boston Medical) Diagnostic criteria: healthy newborns Age: Minimum: 34 hours old Maximum: 55 hours old Mean: not reported SD: not reported Sex: Males: 17 Females: 23 Country: USA Ethnicity: 55% African American; 22.5% White; 12.5% Hispanic; 2.5% Asian; 2.5% American Indian; 5% unclassified |
|
| Interventions |
Total number of intervention groups: 1 ‐ pacifier dipped in water Control group description: water only (delivered by syringe) Total number of participants randomized to each of your groups: 20 total (10 in each group) Specific intervention #1: infant was given either water only or a pacifier prior to heel lance Intervention details: 4 minutes pre heel lance, the infant was given a heat pad to warm feet and was wrapped in a blanket and turned supine to his or her bassinet. 60 seconds before the heelstick, the infant was given either water only (delivered by syringe) or pacifier (coated in water). Pacifier was redipped in water every 30 seconds. The heat pad was then removed and the heel lance occurred lasting 1 to 3 minutes. A band‐aid was then placed on the wound. Integrity of intervention: good |
|
| Outcomes |
Pain outcomes, scale limits, and time points when measured: Crying Heel lance (2 minutes post) Recovery (5 minutes post) Upper limit: 100% Lower limit: 0% High score = more pain Continuous Grimacing (furrowing of brow and eye squinting) Heel lance (2 minutes post) Recovery (2 minutes post) Upper limit: 100% Lower limit: 0% Continuous |
|
| Notes |
Adverse reactions: none Funding sources: National Institute of Mental Health Key conclusions of study authors: sucking a water‐dipped pacifier caused modest and variable reductions in grimacing during the 2‐minute post‐heel lance in healthy neonates. Further analyses revealed that this intervention is only effective if the sucking rate is greater than 30 times/minute prior to the heel lance. Miscellaneous comments by review authors: results are not significant and no data are given at the recovery period (2 mins to 5 mins post heel lance) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 1) Randomization (Random Sequence Generation) | Low risk | 1 ‐ A convincing method of randomization is reported but this did not involve an independent person |
| 2) Allocation bias (Allocation concealment) | High risk | 0 ‐ There is not an adequate description of attempts to deal with potential allocation bias |
| 3a) Blinding of participants and personnel | Low risk | 1 ‐ A convincing effort to reduce bias in outcomes measurement is reported |
| 3b) Blinding of outcome assessment | High risk | Not blinded to pacifier versus syringe condition as seeing the face for grimacing would have involved seeing the pacifier in the infant's mouth. |
| 4) Attrition (Incomplete Outcome Data) | Unclear risk | 0 ‐ There is no documented evidence or insufficient evidence reported of how attrition was dealt with |
| 5) Selective outcome reporting (Selective Outcome Reporting) | Low risk | There was no selective outcome reporting |
| 6) Other potential sources of bias (Other potential threats to validity) | Low risk | Some participants had been circumcised the day before the study Some had heel lance before These participants were randomly distributed to both groups |
| 7a) Power calculation (Part 1 of size bias) | High risk | 0 ‐ Power calculations were not conducted a priori |
| 7b) Sufficient sample (part 2 of size bias) | High risk | 0 ‐ A sufficient sample size based on the power calculation was not obtained |
| Total | High risk | Total score on new Cochrane standard: Low risk (4/9), High risk (4/9), Unclear Risk (1/9) |
Bo 2000.
| Methods |
Study design: cross‐over Total study duration: not known |
|
| Participants |
Total number: 27 Setting: special care baby unit, NICU Diagnostic criteria: healthy neonates and premature neonates Age: Minimum: 30 weeks Maximum: 41 weeks Mean: 37 weeks SD: 3.43 weeks Sex: Males: 17 Females: 10 Country: Hong Kong/China Ethnicity: Chinese |
|
| Interventions |
Total number of intervention groups: 1 Control group description: infants were placed in the supine position. Total number of participants randomized to each of your groups: 27 Specific intervention: non‐nutritive sucking Intervention details: infants were given a small, standard, short and hollow soft latex nipple. Gentle pressure was applied to keep it in the infant's mouth. Integrity of intervention: good |
|
| Outcomes |
Pain outcomes, scale limits, and time points when measured: NIPS 1 minute pre heelstick 13 minutes post heelstick Upper limit: 7 Lower limit: 0 Higher score = higher pain Continuous |
|
| Notes |
Adverse reactions: none Key conclusions of study authors: non‐nutritive sucking is an effective intervention for pain regulation after heelstick in neonates |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 1) Randomization (Random Sequence Generation) | Low risk | 1 ‐ A convincing method of randomization is reported but this did not involve an independent person |
| 2) Allocation bias (Allocation concealment) | Low risk | 1 ‐ An adequate method is reported that removes the potential biases of investigators |
| 3a) Blinding of participants and personnel | Low risk | 1 ‐ A convincing effort to reduce bias in outcomes measurement is reported |
| 3b) Blinding of outcome assessment | Unclear risk | None specified |
| 4) Attrition (Incomplete Outcome Data) | High risk | 0 ‐ There is no documented evidence or insufficient evidence reported of how attrition was dealt with. |
| 5) Selective outcome reporting (Selective Outcome Reporting) | Low risk | There was no selective outcome reporting |
| 6) Other potential sources of bias (Other potential threats to validity) | Low risk | There were no other potential sources of bias reported |
| 7a) Power calculation (Part 1 of size bias) | Low risk | 1 ‐ Power calculations were conducted a priori |
| 7b) Sufficient sample (part 2 of size bias) | Low risk | 1 ‐ A sufficient sample size based on the power calculation was obtained |
| Total | High risk | Total score on new Cochrane standard: Low risk (7/9), High risk (1/9), Unclear Risk (1/9) |
Bustos 2008.
| Methods |
Study design: randomized between groups Total study duration: unknown |
|
| Participants |
Total number: 62 Setting: Sydney Children's Hospital Outpatient Immunization Clinic Diagnostic criteria: adequate grasp of English, spoke English to infant Age: Minimum: 5 months Maximum: 7 months Mean: not reported SD: not reported Sex: Males: 24 (in the final sample) Females: 26 (in the final sample) Country: Australia |
|
| Interventions |
Total number of intervention groups: 1 Control group description: standard care Total number of participants randomized to each of your groups: intervention = 30; control group = 32 (total = 62) Specific intervention: coping ‐ promoting verbalizations Intervention details: intervention group received a one‐page information sheet with information about 3 types of parental verbalizations associated with lower pain outcomes for infants. Parents were encouraged to review the sheet before their appointment. All infants were placed in supine position on the treatment table. The injection site was cleaned with an alcohol swab and the injection was then performed. During the injection, parents held infant's leg. Integrity of intervention: good |
|
| Outcomes |
Pain outcomes, scale limits, and time points when measured: NFCS Injection phase: 15 seconds post needle Recovery phase: 15 seconds following injection phase (scored in 5 second blocks) Upper limit: 30 Lower limit: 0 High score = higher expression of pain Continuous |
|
| Notes |
Adverse reactions: none Funding sources: Cavenadian Institutes of Health Research (Pain In Child Health Strategic Training Initiative); Mayday Foundation Key conclusions of study authors: the promotion of parent‐coping verbalizations during an infant's 6 month immunization is able to reduce the duration of infant cry following an injection There was no significant effect of intervention on NFCS outcome measure |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 1) Randomization (Random Sequence Generation) | Low risk | 2 ‐ A convincing method for generating a random allocation sequence is reported that used an independent person not involved in enrolment or allocation of participants |
| 2) Allocation bias (Allocation concealment) | Low risk | 1 ‐ An adequate method is reported that removes the potential biases of investigators |
| 3a) Blinding of participants and personnel | High risk | Efforts to reduce measurement bias are not reported or are insufficient, e.g. outcomes collected by therapist |
| 3b) Blinding of outcome assessment | Low risk | All coders were blinded to group assignment |
| 4) Attrition (Incomplete Outcome Data) | Low risk | 2 ‐ Documented evidence that the CONSORT guidelines have been followed |
| 5) Selective outcome reporting (Selective Outcome Reporting) | Low risk | There was no selective outcome reporting |
| 6) Other potential sources of bias (Other potential threats to validity) | Low risk | Did not examine possible differences between ethnicity or SES |
| 7a) Power calculation (Part 1 of size bias) | Low risk | 1 ‐ Power calculations were conducted a priori |
| 7b) Sufficient sample (part 2 of size bias) | Low risk | 1 ‐ A sufficient sample size based on the power calculation was obtained |
| Total | High risk | Total score on new Cochrane standard: Low risk (8/9), High risk (1/9), Unclear Risk (0/9) |
Campbell‐Yeo 2012.
| Methods |
Study design: between groups Total study duration: 28 months |
|
| Participants |
Total number: 67 sets of twins (134 infants) Setting: NICU Diagnostic criteria: eligibility was based on being preterm (28‐36 weeks gestation), heavier than 1000g, without major anomalies, requiring at least 1 medically indicated heel lance, and medically stable. Age: Mean: 31.85 (getational age) SD: 2.6 Sex: Males: 76 Females: 58 Country: Canada |
|
| Interventions |
Total number of intervention groups: 1 Control group description: standard care: remained in separate incubator. Both the intervention and standard care groups received sucrose 2 min before heel lance as part of hospital policy Total number of participants randomized to each of your groups: intervention = 67; control group = 57 Specific intervention: cobedding Intervention details: placed in diaper clad together in giraffe incubator close to each other, permitting touch. Integrity of intervention: good |
|
| Outcomes |
Pain outcomes, scale limits, and time points when measured: PIPP Time points: 30 secs epochs from the time of the heel lance until the application of the bandage Upper limit: 21 Lower limit: 0 High score = more pain Continuous |
|
| Notes |
Adverse reactions: None Funding sources: Groupe de Recherche Interuniversitaire en Interventions en Sciences Infirmieres du Quebec, the Canadian Nurses Foundation Nursing Care Partnership Program, CIHR, and the IWK Health Centre Key conclusions of study authors: cobedding enhanced the physiologic recovery of preterm twins undergoing heel lance, but did not lead to lower pain scores |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 1) Randomization (Random Sequence Generation) | Low risk | 2 ‐ A convincing method for generating a random allocation sequence is reported that used an independent person not involved in enrolment or allocation of participants |
| 2) Allocation bias (Allocation concealment) | Low risk | 1 ‐ An adequate method is reported that removes the potential biases of investigators |
| 3a) Blinding of participants and personnel | High risk | Participants (i.e., parents) and personnel could not be blinded due to seeing twins in either cobedding arrangement or standard care, “Limitations in our study include the inability to blind care providers to the intervention” (p. 505) |
| 3b) Blinding of outcome assessment | Low risk | Coders were not aware of the purpose of the markers or study objective |
| 4) Attrition (Incomplete Outcome Data) | Low risk | Information included on data in a flow chart. |
| 5) Selective outcome reporting (Selective Outcome Reporting) | Low risk | There was no selective outcome reporting |
| 6) Other potential sources of bias (Other potential threats to validity) | Low risk | No other potential source of bias |
| 7a) Power calculation (Part 1 of size bias) | Low risk | Power calculation was used |
| 7b) Sufficient sample (part 2 of size bias) | Low risk | Adequate sample size based on power calculation was used. |
| Total | High risk | Total score on new Cochrane standard: Low risk (8/9), High risk (1/9), Unclear Risk (0/9) |
Campos 1994.
| Methods |
Study design: between groups Total study duration: unknown |
|
| Participants |
Total number: 60 Setting: mid‐western neo‐natal nursery Diagnostic criteria: full‐term birth; Apgar scores > 7; absence of respiratory or other health problems Age: Minimum: not reported Maximum: not reported Mean: 51.5 hrs SD: 12 hrs Sex: Males: 30 Females: 30 Country: USA |
|
| Interventions |
Total number of intervention groups: 2 Control group description: infants received no comforting care after heelstick; were placed prone in bassinet after heelstick and covered with a blanket Total number of participants randomized to each of your groups: 20 participants in each of the 3 groups, total number of participants is 60 Specific intervention #1: rocking Intervention details: infants were held at the experimenter's shoulder, rocked in a rocking chair at a rate of 30 cycles per minute (auditory signal fed to experimenter) post‐procedure Integrity of intervention: good Specific intervention #2: pacifier Intervention details: infants were held in the experimenter's lap while the pacifier was administered for 8 minutes after heelstick; gentle pressure was applied to keep that pacifier in the infant's mouth Integrity of intervention: good |
|
| Outcomes |
Pain outcomes, scale limits, and time points when measured: Latencies to cry cessation 0 to 2 minutes post heelstick 3 to 4 minutes post heelstick Upper limit: 180 seconds Lower limit: 0 seconds Higher score = longer latency to cry cessation Continuous |
|
| Notes |
Adverse reactions: none Funding sources: National Association of Neonatal Nurses; The University of Illinois Key conclusions of study authors: newborns benefit from both rocking and pacifiers when undergoing heelstick procedures |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 1) Randomization (Random Sequence Generation) | Low risk | 1 ‐ A convincing method of randomization is reported but this did not involve an independent person |
| 2) Allocation bias (Allocation concealment) | Low risk | 1 ‐ An adequate method is reported that removes the potential biases of investigators |
| 3a) Blinding of participants and personnel | Low risk | A convincing effort to reduce bias in outcomes measurement is reported |
| 3b) Blinding of outcome assessment | Low risk | Coders were blinded to group assignment |
| 4) Attrition (Incomplete Outcome Data) | Unclear risk | 0 ‐ There is no documented evidence or insufficient evidence reported of how attrition was dealt with |
| 5) Selective outcome reporting (Selective Outcome Reporting) | Low risk | There was no selective outcome reporting |
| 6) Other potential sources of bias (Other potential threats to validity) | Low risk | There were no other potential sources of bias reported |
| 7a) Power calculation (Part 1 of size bias) | High risk | 0 ‐ Power calculations were not conducted a priori |
| 7b) Sufficient sample (part 2 of size bias) | Low risk | 0 ‐ A sufficient sample size based on the power calculation was not obtained but an effect was found. |
| Total | Low risk | Total score on new Cochrane standard: Low risk (7/9), High risk (1/9), Unclear Risk (1/9) |
Carbajal 1999.
| Methods |
Study design: between groups Total study duration: April 1997 to June 1997 |
|
| Participants |
Total number: 150 Setting: maternity ward of a hospital in France Diagnostic criteria: newborns who had a 5‐minute Apgar score greater than or equal to 7, were medically stable, had not received naloxone during the previous 24 hours, and were not fed in the previous 30 minutes Age: Minimum: 37 weeks Maximum: 42 weeks Mean: 40 weeks SD: not reported Sex: Males: 89 Females: 61 Country: France |
|
| Interventions |
Total number of intervention groups: 5 (but only 1 does not use sucrose) Control group description: placebo, 2 mL of sterile water Total number of participants randomized to each of your groups: 100 (does not indicate how many were in each group) Specific intervention #1: pacifier Specific intervention #2: swallowing water Intervention details: pacifier given to baby Integrity of intervention: unknown |
|
| Outcomes |
Pain outcomes, scale limits, and time points when measured: DAN (Douleur Aiguë Nouveau‐né) Article does not indicate what time points were measured Upper limit: 10 Lower limit: 0 Higher score = more pain Continuous |
|
| Notes |
Adverse reactions: none Funding sources: no external funding Key conclusions of study authors: pacifiers were effective in reducing infant pain |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 1) Randomization (Random Sequence Generation) | Low risk | 2 ‐ A convincing method for generating a random allocation sequence is reported that used an independent person not involved in enrolment or allocation of participants |
| 2) Allocation bias (Allocation concealment) | Low risk | 1 ‐ An adequate method is reported that removes the potential biases of investigators |
| 3a) Blinding of participants and personnel | High risk | 0 ‐ Efforts to reduce measurement bias are not reported or are insufficient e.g. outcomes collected by therapist |
| 3b) Blinding of outcome assessment | Unclear risk | None provided |
| 4) Attrition (Incomplete Outcome Data) | Low risk | 2 ‐ Documented evidence that the CONSORT guidelines have been followed |
| 5) Selective outcome reporting (Selective Outcome Reporting) | Low risk | There was no selective outcome reporting |
| 6) Other potential sources of bias (Other potential threats to validity) | Low risk | Very short article, not a lot of available information |
| 7a) Power calculation (Part 1 of size bias) | Low risk | 1 ‐ Power calculations were conducted a priori |
| 7b) Sufficient sample (part 2 of size bias) | Low risk | 1 ‐ A sufficient sample size based on the power calculation was obtained |
| Total | High risk | Total score on new Cochrane standard: Low risk (7/9), High risk (1/9), Unclear Risk (1/9) |
Carbajal 2003.
| Methods |
Study design: between groups Total study duration: 5 months |
|
| Participants |
Total number: 180 Setting: maternity ward of hospital Diagnostic criteria: equal to or greater than 37 weeks gestation; had APGAR scores of 7 or higher at 5 minutes; were greater than or equal to 24 hours old; undergoing venipuncture; breast‐fed; had not been fed for the previous 30 minutes; no medical instability; no medication in the previous 24 hours Age: Minimum: 39.6 weeks Maximum: 40 weeks Mean: 39.8 SD: 1.23 Sex: Males: 93 Females: 87 Country: France |
|
| Interventions |
Total number of intervention groups: 3 (we will only focus on the first one for this review; other interventions included breast milk and sucrose) Control group description: Infants given sterile water as a placebo Total number of participants randomized to each of your groups: 45 in each group (180 total) Specific intervention: held in mother's arms without breast feeding Intervention details: held in mother's arms, without breast feeding Integrity of intervention: satisfactory |
|
| Outcomes |
Pain outcome, scale limits and time points when measured: Douleur (DAN) scale Time points: unknown Upper limit: 10 Lower limit: 0 High score = more pain Continuous PIPP Time points: unknown Upper limit: 21 Lower limit: 0 Higher score = more pain Continuous |
|
| Notes |
Adverse reactions: none Funding sources: Fondation Pour La Santé, France Key conclusions of study authors: there were no significant differences in pain reactivity between newborns being held in mother's arms or newborns who were given sterile water |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 1) Randomization (Random Sequence Generation) | Low risk | 2 ‐ A convincing method for generating a random allocation sequence is reported that used an independent person not involved in enrolment or allocation of participants |
| 2) Allocation bias (Allocation concealment) | Low risk | 1 ‐ An adequate method is reported that removes the potential biases of investigators |
| 3a) Blinding of participants and personnel | High risk | 0 ‐ Efforts to reduce measurement bias are not reported or are insufficient, e.g. outcomes collected by therapist |
| 3b) Blinding of outcome assessment | High risk | Coders were not blinded |
| 4) Attrition (Incomplete Outcome Data) | Low risk | 2 ‐ Documented evidence that the CONSORT guidelines have been followed |
| 5) Selective outcome reporting (Selective Outcome Reporting) | Low risk | There was no selective outcome reporting |
| 6) Other potential sources of bias (Other potential threats to validity) | Low risk | There were no other potential sources of bias reported |
| 7a) Power calculation (Part 1 of size bias) | Low risk | 1 ‐ Power calculations were conducted a priori |
| 7b) Sufficient sample (part 2 of size bias) | Low risk | 1 ‐ A sufficient sample size based on the power calculation was obtained |
| Total | High risk | Total score on new Cochrane standard: Low risk (7/9), High risk (2/9), Unclear Risk (0/9) |
Catelin 2005.
| Methods |
Study design: cross‐over Total study duration: unknown |
|
| Participants |
Total number: 45 Setting: NIDCAP‐reliable NICU Diagnostic criteria: participants were excluded if they received treatment with a muscle relaxant, sedative, antiepileptic, or analgesic drug (except sucrose) during the last 24 hours; had a congenital defect, a neurological abnormality including convulsion, intraventricular hemorrhage grade higher than II according to the Papile scale, and periventricular leukomalacia Age: Minimum: less than or equal to 32 weeks Maximum: greater than or equal to 37 weeks Mean: 34.47 weeks SD: 1.0 weeks Sex: Males: 27 Females: 18 Country: France |
|
| Interventions |
Total number of intervention groups: 1 Control group description: no EBI, no specific protection from light or noise, in the supine position and without swaddling or any postural support Total number of participants randomized to each of your groups: 45 Specific intervention: Environmental and Behavioral Interventions (EBI) Intervention details: EBI included attenuated noise and light with closed doors and covered incubator, lateral posture with head, back, and feet contacting supportive bedding, and opportunity for grasping or sucking Integrity of intervention: satisfactory |
|
| Outcomes |
Pain outcomes, scale limits, and time points when measured: NIPS 2 minutes before weighing, during weighing and 5 and 30 minutes after weighing Upper limit: 7 Lower limit: 0 High score = more pain Continuous EDIN 2 minutes before and 5 and 30 minutes after weighing Upper limit: 15 Lower limit: 0 High score = more pain Continuous |
|
| Notes |
Adverse reactions: none Funding sources: grants from the French ministry of health, the Foundation de France, SESEP and the Fondation CNP Key conclusions of study authors: EBI procedures were associated with lower heart rates just after weighing procedures |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 1) Randomization (Random Sequence Generation) | Low risk | 2 ‐ A convincing method for generating a random allocation sequence is reported that used an independent person not involved in enrolment or allocation of participants |
| 2) Allocation bias (Allocation concealment) | Low risk | 1 ‐ An adequate method is reported that removes the potential biases of investigators |
| 3a) Blinding of participants and personnel | Low risk | A convincing effort to reduce bias in outcomes measurement is reported |
| 3b) Blinding of outcome assessment | Unclear risk | None specified |
| 4) Attrition (Incomplete Outcome Data) | Low risk | 1 ‐ A reasonable account of how attrition was dealt with is given, but no specific reference to CONSORT |
| 5) Selective outcome reporting (Selective Outcome Reporting) | Low risk | There was no selective outcome reporting |
| 6) Other potential sources of bias (Other potential threats to validity) | Low risk | There were no other potential sources of bias reported |
| 7a) Power calculation (Part 1 of size bias) | High risk | 0 ‐ Power calculations were not conducted a priori. |
| 7b) Sufficient sample (part 2 of size bias) | Low risk | 1 ‐ A sufficient sample size due to significant effect. |
| Total | Low risk | Total score on new Cochrane standard: Low risk (7/9), High risk (1/9), Unclear Risk (1/9) |
Chik 2012.
| Methods |
Study design: crossover study Total study duration: 7 months |
|
| Participants |
Total number: 65 Setting: NICU Diagnostic criteria: infants in NICU Age: Minimum: unknown Maximum: unknown Mean: unknown SD:unknown Sex: Males: unknown Females: uknown Country: Hong Kong |
|
| Interventions |
Total number of intervention groups: 2 Control group description: usual care Total number of participants randomized to each of your groups: intervention = 32; control group = 33 Specific intervention: limb massage Intervention details: 2 min limb massage prior to procedure and vice versa Integrity of intervention: satisfactory |
|
| Outcomes |
Pain outcomes, scale limits, and time points when measured PIPP Time points: right after the intervention and during the first 30 secs of the procedure Upper limit: 21 Lower limit: 0 High score = more pain Continuous |
|
| Notes |
Adverse reactions: none Key conclusions of study authors: upper limb massage may be effective technique for relieving infants' venipuncture pain |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 1) Randomization (Random Sequence Generation) | Unclear risk | Not enough information provided in abstract. |
| 2) Allocation bias (Allocation concealment) | Unclear risk | Not enough information provided in abstract. |
| 3a) Blinding of participants and personnel | Unclear risk | None specified |
| 3b) Blinding of outcome assessment | Unclear risk | None specified |
| 4) Attrition (Incomplete Outcome Data) | Unclear risk | Not enough information provided in abstract. |
| 5) Selective outcome reporting (Selective Outcome Reporting) | Unclear risk | TNot enough information provided in abstract. |
| 6) Other potential sources of bias (Other potential threats to validity) | Unclear risk | Not enough information provided in abstract. |
| 7a) Power calculation (Part 1 of size bias) | Unclear risk | Not enough information provided in abstract. |
| 7b) Sufficient sample (part 2 of size bias) | Unclear risk | Not enough information provided in abstract. |
| Total | Unclear risk | Total score on new Cochrane standard: Low risk (0/9), High risk (0/9), Unclear Risk (9/9) |
Cohen 2002.
| Methods |
Study design: between groups Total study duration: 1 year |
|
| Participants |
Total number: 90 Setting: rural clinic Diagnostic criteria: healthy babies Age: Minimum: 2 months Maximum: 3 years Mean: 12 months SD: 8.6 months Sex: Males: 44 Females: 46 Country: USA Co‐morbidity: none Socio‐demographics: income average was $24,000/year Parents: 2 years of college Ethnicity: 88% were Caucasian |
|
| Interventions |
Total number of intervention groups: 2 Control group description: typical care, interact normally with infant but without movie or toy distraction Total number of participants randomized to each of your groups: Intervention: 49; Control: 41 Specific intervention: video distraction Intervention details: Teletubbies movie or toys, or both Quality of intervention: poor |
|
| Outcomes |
Pain outcomes, scale limits, and time points when measured: MBPS Injection and recovery phase Upper limit: 40 Lower limit: 0 High score = more pain Continuous VAS ‐ Parent During and 3 minutes after immunization Upper limit: 100 Lower limit: 0 High score = more pain Continuous VAS ‐ Nurse During and 3 minutes after immunization Upper limit: 100 Lower limit: 0 Higher score = more pain Continuous |
|
| Notes |
Adverse reactions: none reported Funding sources: none mentioned Key conclusions of study authors: nurse‐directed distraction works but not sure if it is the toy, nurse, parent or combination |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 1) Randomization (Random Sequence Generation) | Unclear risk | 0 ‐ Randomization is mentioned but there is not an adequate description of the methods used |
| 2) Allocation bias (Allocation concealment) | High risk | 0 ‐ There is not an adequate description of attempts to deal with potential allocation bias |
| 3a) Blinding of participants and personnel | Unclear risk | Efforts to reduce measurement bias are not reported or are insufficient, e.g. outcomes collected by therapist |
| 3b) Blinding of outcome assessment | Low risk | Coders were blind to study hypotheses |
| 4) Attrition (Incomplete Outcome Data) | Unclear risk | 0 ‐ There is no documented evidence or insufficient evidence reported of how attrition was dealt with |
| 5) Selective outcome reporting (Selective Outcome Reporting) | Low risk | There was no selective outcome reporting |
| 6) Other potential sources of bias (Other potential threats to validity) | Low risk | None other mentioned. |
| 7a) Power calculation (Part 1 of size bias) | High risk | 0 ‐ Power calculations were not conducted a priori |
| 7b) Sufficient sample (part 2 of size bias) | Low risk | 0 ‐ A sufficient sample size based on the power calculation was not obtained but effect was found |
| Total | High risk | Total score on new Cochrane standard: Low risk (4/9), High risk (2/9), Unclear Risk (3/9) |
Cohen 2006.
| Methods |
Study design: between groups Total study duration: 5 months |
|
| Participants |
Total number: 136 Note: The authors reported that 136 participants were included but only reported on sex for 135 participants. Setting: university‐affiliated medical centre; private practice office Diagnostic criteria: any English‐speaking families with an infant between the ages of 1 and 24 months present for routine checkups and vaccinations Age: Minimum: 1 month Maximum: 21 months Mean: 7.6 months SD: 5 months Sex: Males: 55 Females: 80 Country: USA Socio‐demographics: income ranged from $0 to $170,000, M = $38,740, SD = $29,158 Parent's education ranged from 8th grade‐post baccalaureate, most had completed 1 year of college Ethnicity: 90.4% Caucasian; 2.2% Native American; 1.5% African American; 0.7% Hispanic; 5.2% other |
|
| Interventions |
Total number of intervention groups: 1 Control group description: parent and nurse were encouraged to interact with the infant in their usual manner, no movie or toy distraction provided Total number of participants randomized to each of your groups: approximately 63 per group (total = 136)Specific intervention: distraction ‐ video Intervention details: prior to data collection, nurses engaged in brief intervention training and parents were briefly instructed in distraction techniques. During the immunization, a DVD movie (choice between 2) played on a hand‐held DVD player 6 inches from the child. Parents were instructed that they could redirect attention to DVD. Integrity of intervention: satisfactory |
|
| Outcomes |
Pain outcomes, scale limits, and time points when measured: MAISD (infant distress, crying, screaming or flailing) Coded for 5‐second periods up to 2 minutes post needle Upper limit: 1 Lower limit: 0 High score = higher pain Continuous |
|
| Notes |
Adverse reactions: none Funding sources: Mayday Fund Key conclusions of study authors: video distraction is a simple and practical means of providing distress relief to infants during routine injections |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 1) Randomization (Random Sequence Generation) | Low risk | 2 ‐ A convincing method for generating a random allocation sequence is reported that used an independent person not involved in enrolment or allocation of participants |
| 2) Allocation bias (Allocation concealment) | Low risk | 1 ‐ An adequate method is reported that removes the potential biases of investigators |
| 3a) Blinding of participants and personnel | High risk | Efforts to reduce measurement bias are not reported or are insufficient, e.g. outcomes collected by therapist |
| 3b) Blinding of outcome assessment | High risk | Coders were not blinded |
| 4) Attrition (Incomplete Outcome Data) | Low risk | 1 ‐ A reasonable account of how attrition was dealt with is given, but no specific reference to CONSORT |
| 5) Selective outcome reporting (Selective Outcome Reporting) | Low risk | There was no selective outcome reporting |
| 6) Other potential sources of bias (Other potential threats to validity) | Low risk | There were no other potential sources of bias reported |
| 7a) Power calculation (Part 1 of size bias) | Low risk | 1 ‐ Power calculations were conducted a priori |
| 7b) Sufficient sample (part 2 of size bias) | Low risk | 1 ‐ A sufficient sample size based on the power calculation was obtained |
| Total | High risk | Total score on new Cochrane standard: Low risk (7/9), High risk (2/9), Unclear Risk (0/9) |
Comaru 2009.
| Methods |
Study design: cross‐over Total study duration: April to October 2004 |
|
| Participants |
Total number: 47 Setting: NICU Diagnostic criteria: preterm Age: Minimum: not reported Maximum: 35 weeks Mean: 32 weeks SD: 2 weeks Sex: Males: not reported Females: not reported Country: Brazil Co‐morbidity: respiratory distress syndrome was diagnosed in approximately 35% of the studied babies Socio‐demographics: not reported Ethnicity: not reported |
|
| Interventions |
Total number of intervention groups: 1 Control group description: babies' diaper changed in the incubator Total number of participants randomized to each of your groups: 47 Specific intervention: nesting Intervention details: slightly flexed posture, side lying, limbs directed to midline: head, back, links feet with folded up towel Integrity of intervention: not needed |
|
| Outcomes |
Pain outcomes, scale limits, and time points when measured: NFCS Upper limit: 1 Lower limit: 0 Continuous |
|
| Notes |
Adverse reactions: none Funding sources: Research Support Fund (FIPE) of the Hospital of Clinicas in Porto Alegre and by the CNPq Scholarship Key conclusions of study authors: nesting works in diminishing distress during diaper changes |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 1) Randomization (Random Sequence Generation) | Low risk | 2 ‐ A convincing method for generating a random allocation sequence is reported that used an independent person not involved in enrolment or allocation of participants |
| 2) Allocation bias (Allocation concealment) | Low risk | 1 ‐ An adequate method is reported that removes the potential biases of investigators |
| 3a) Blinding of participants and personnel | Unclear risk | None specified |
| 3b) Blinding of outcome assessment | Unclear risk | None specified |
| 4) Attrition (Incomplete Outcome Data) | Low risk | 1 ‐ A reasonable account of how attrition was dealt with is given, but no specific reference to CONSORT |
| 5) Selective outcome reporting (Selective Outcome Reporting) | Low risk | There was no selective outcome reporting |
| 6) Other potential sources of bias (Other potential threats to validity) | Low risk | There were no other potential sources of bias reported |
| 7a) Power calculation (Part 1 of size bias) | Low risk | 1 ‐ Power calculations were conducted a priori |
| 7b) Sufficient sample (part 2 of size bias) | Low risk | 1 ‐ A sufficient sample size based on the power calculation was obtained |
| Total | Low risk | Total score on new Cochrane standard: Low risk (7/9), High risk (0/9), Unclear Risk (2/9) |
Corbo 2000.
| Methods |
Study design: cross‐over Total study duration: unknown |
|
| Participants |
Total number: 26 Setting: NICU of the Division of Neonatology (University of Naples) Diagnostic criteria: neonates without severe complications Age: Minimum: 2 days Maximum: 15 days Mean: 4.9 days SD: 3.3 days Sex: Males: 16 Females: 10 Country: Italy |
|
| Interventions |
Total number of intervention groups: 1 Control group description: infant in the supine position with their head towards the examiner, in incubator/crib/room, no pacifier Total number of participants randomized to each of your groups: 26 Specific intervention: non‐nutritive sucking (pacifier) Intervention details: the pacifier was placed in the infant's mouth 3 minutes pre‐procedure and for 3 minutes post‐procedure Integrity of intervention: good |
|
| Outcomes |
Pain outcomes, scale limits, and time points when measured: Brazelton Neonatal Behavioral Assessment Scale (BNBAS) State 6 3 minutes post‐procedure Upper limit: 180 seconds Lower limit: 0 seconds Higher score = longer time spent in distressed state Continuous |
|
| Notes |
Adverse reactions: none Funding sources: none reported Key conclusions of study authors: non‐nutritive sucking can reduce the period of behavioral distress in newborn, premature infants following heelstick blood sampling |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 1) Randomization (Random Sequence Generation) | Low risk | 1 ‐ A convincing method of randomization is reported but this did not involve an independent person |
| 2) Allocation bias (Allocation concealment) | Low risk | 1 ‐ An adequate method is reported that removes the potential biases of investigators |
| 3a) Blinding of participants and personnel | Unclear risk | 0 ‐ Efforts to reduce measurement bias are not reported or are insufficient, e.g. outcomes collected by therapist |
| 3b) Blinding of outcome assessment | High risk | Coders were not blind to the condition |
| 4) Attrition (Incomplete Outcome Data) | High risk | 0 ‐ There is no documented evidence or insufficient evidence reported of how attrition was dealt with |
| 5) Selective outcome reporting (Selective Outcome Reporting) | Low risk | There was no selective outcome reporting |
| 6) Other potential sources of bias (Other potential threats to validity) | Low risk | There were no other potential sources of bias reported |
| 7a) Power calculation (Part 1 of size bias) | Low risk | 1 ‐ Power calculations were conducted a priori |
| 7b) Sufficient sample (part 2 of size bias) | Low risk | 1 ‐ A sufficient sample size based on the power calculation was obtained |
| Total | High risk | Total score on new Cochrane standard: Low risk (6/9), High risk (2/9), Unclear Risk (1/9) |
Corff 1995.
| Methods |
Study design: cross‐over Study duration: unknown |
|
| Participants |
Total number: 30 Setting: NICU Diagnostic criteria: less than 22 days old, and no anomalies Age: Minimum: 25 weeks Maximum: 35 weeks Mean: 30 weeks SD: unknown Sex: Males: not reported Females: not reported Country: USA |
|
| Interventions |
Total number of intervention groups: 1 Control group description: normal nursery routine Total number of participants randomized to each of your groups: 30 Specific intervention: facilitated tucking Intervention details: facilitated tucking was supplied during and after the heelstick by one consistent neonatal nurse Integrity of intervention: poor (not reported) |
|
| Outcomes |
Pain outcomes, scale limits, and time points when measured: Total crying time Upper limit: 100% Lower limit: 0 % Longer cry = more distress Continuous |
|
| Notes |
Adverse reactions: none Funding sources: not reported Key conclusions of study authors: facilitated tucking works |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 1) Randomization (Random Sequence Generation) | High risk | 0 ‐ Randomization is mentioned but there is not an adequate description of the methods used |
| 2) Allocation bias (Allocation concealment) | High risk | 0 ‐ There is not an adequate description of attempts to deal with potential allocation bias |
| 3a) Blinding of participants and personnel | Unclear risk | None specified |
| 3b) Blinding of outcome assessment | Unclear risk | None specified |
| 4) Attrition (Incomplete Outcome Data) | Low risk | 1 ‐ A reasonable account of how attrition was dealt with is given, but no specific reference to CONSORT |
| 5) Selective outcome reporting (Selective Outcome Reporting) | Low risk | There was no selective outcome reporting |
| 6) Other potential sources of bias (Other potential threats to validity) | Low risk | There were no other potential sources of bias reported |
| 7a) Power calculation (Part 1 of size bias) | High risk | 0 ‐ Power calculations were not conducted a priori |
| 7b) Sufficient sample (part 2 of size bias) | Low risk | 1 ‐ A sufficient sample size based on the power calculation was obtained, enough power to detect effect |
| Total | High risk | Total score on new Cochrane standard: Low risk (4/9), High risk (3/9), Unclear Risk (2/9) |
Cramer‐Berness 2005a.
| Methods |
Study design: between groups Total study duration: 12 months |
|
| Participants |
Total number: 123 Setting: health care clinic in upstate New York Diagnostic criteria: healthy infants between 2 months and 24 months of age who were receiving routine immunizations Age: Minimum: 2 months Maximum: 24 months Mean: 8.70 months SD: 5.92 months Sex: Males: 60 Females: 63 Country: USA Co‐morbidity: none Socio‐demographics: never married = 59%; married = 28.7%; separated = 9%; divorced = 3.3% Less than $10,000 = 32.5%; $10,000 to $20,000 = 29.8%; $20,001 to $30,000 = 24.6%; greater than $30,001 = 13.2%; did not answer = 7.3% Ethnicity: Caucasian parents = 63.9% Caucasian infants = 51.3%; Hispanic parents = 13.4% Hispanic infants = 7.6%; African American parents = 12.6% African American infants = 15.1%; other parents = 10.1% other infants = 8.4% |
|
| Interventions |
Total number of intervention groups: 2 Control group description: typical care ‐ parents did not receive prompting to engage in usual behaviors or distraction Total number of participants randomized to each of your groups: typical care = 41, supportive care = 42, distraction = 40 (total = 123) Specific intervention #1: supportive care Intervention details: parents were asked what they normally do to reduce infant distress. They were encouraged by the researcher to engage in these techniques. Integrity of intervention: satisfactory Specific intervention #2: distraction Intervention details: parents were encouraged to use a distraction toy and to direct infant's attention towards the toy (e.g. "Look at this!") Integrity of intervention: satisfactory |
|
| Outcomes |
Pain outcomes, scale limits, and time points when measured: MBPS 5 seconds pre‐needle 5 seconds during needle 5 seconds after needle Upper limit: 3 Lower limit: 0 High score = more distress Continuous |
|
| Notes |
Adverse reactions: 3 parents withdrew from the study (no reason given) Funding sources: not reported Key conclusions of study authors: brief prompting for parents to use their normal coping strategies may be more effective than training in helping infants recover more quickly from routine procedure pain. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 1) Randomization (Random Sequence Generation) | Low risk | 1 ‐ A convincing method of randomization is reported but this did not involve an independent person |
| 2) Allocation bias (Allocation concealment) | Low risk | 1 ‐ An adequate method is reported that removes the potential biases of investigators |
| 3a) Blinding of participants and personnel | Unclear risk | 0 ‐ Efforts to reduce measurement bias are not reported or are insufficient, e.g. outcomes collected by therapist |
| 3b) Blinding of outcome assessment | High risk | Coders were not blinded to intervention |
| 4) Attrition (Incomplete Outcome Data) | Low risk | 1 ‐ A reasonable account of how attrition was dealt with is given, but no specific reference to CONSORT |
| 5) Selective outcome reporting (Selective Outcome Reporting) | Low risk | There was no selective outcome reporting |
| 6) Other potential sources of bias (Other potential threats to validity) | Low risk | There were no other potential sources of bias reported |
| 7a) Power calculation (Part 1 of size bias) | Low risk | 1 ‐ Power calculations were conducted a priori |
| 7b) Sufficient sample (part 2 of size bias) | Low risk | 1 ‐ A sufficient sample size based on the power calculation was obtained |
| Total | High risk | Total score on new Cochrane standard: Low risk (7/9), High risk (1/9), Unclear Risk (1/9) |
Cramer‐Berness 2005b.
| Methods |
Study design: randomized between groups Total study duration: 14 months |
|
| Participants |
Total number: 117 Setting: pediatrician's office Diagnostic criteria: healthy infants Age: Minimum: 2 months Maximum: 24 months Mean: 8.61 months SD: 5.78 months Sex: Males: 63 Females: 54 Country: USA Socio‐demographics: Annual household income: Less than $10,000: 29.1% $10,000 to $20,000: 33.3% $20,001 to $30,000: 10.3% $30,001 to $50,000: 10.3% $50,001 and higher: 6.8% Ethnicity: Caucasian parents: 64.1%; Caucasian infants: 55.6% Hispanic parents: 8.5%; Hispanic infants: 6.0% African American parents: 14.5%; African American infants: 12.0% Asian parents: 1.7%; Asian infants: 1.7% Native American parents: 2.6%; Native American infants: 1.7% multiracial parents: 7.7%; multiracial infants: 23.1% |
|
| Interventions |
Total number of intervention groups: 2 Control group description: typical care Total number of participants randomized to each of your groups: Audiovisual distraction: 41; Tactile distraction: 38; Control: 38 Specific intervention #1: audiovisual distraction Intervention details: parents were instructed to encourage infants to focus on toys throughout immunization process by verbal statements such as "look at this!" and engaging behaviors, such as playing music with the toy Integrity of intervention: good Specific intervention #2: tactile distraction Intervention details: parents were instructed to tickle their infants during the immunization and alternate where they tickled with each immunization Integrity of intervention: satisfactory |
|
| Outcomes |
Pain outcomes, scale limits, and time points when measured: MBPS 5 seconds post‐needle Upper limit: 10 Lower limit: 0 High score = more pain Continuous |
|
| Notes |
Adverse reactions: none Funding sources: none reported Key conclusions of study authors: distraction (auditory or tactile) does not reduce pain in healthy infants aged 2 to 24 months during immunization Miscellaneous comments by review authors: if more than 1 needle was given they averaged out the pain score between needles to account for 1 to 4 needles. Therefore, there was a separate score for "during needle" phase. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 1) Randomization (Random Sequence Generation) | Low risk | 2 ‐ A convincing method for generating a random allocation sequence is reported that used an independent person not involved in enrolment or allocation of participants |
| 2) Allocation bias (Allocation concealment) | Low risk | 1 ‐ An adequate method is reported that removes the potential biases of investigators |
| 3a) Blinding of participants and personnel | Low risk | 1 ‐ A convincing effort to reduce bias in outcomes measurement is reported |
| 3b) Blinding of outcome assessment | Unclear risk | none specified |
| 4) Attrition (Incomplete Outcome Data) | Low risk | 2 ‐ Documented evidence that the CONSORT guidelines have been followed |
| 5) Selective outcome reporting (Selective Outcome Reporting) | Low risk | There was no selective outcome reporting |
| 6) Other potential sources of bias (Other potential threats to validity) | Low risk | There were no other potential sources of bias reported |
| 7a) Power calculation (Part 1 of size bias) | Low risk | 1 ‐ Power calculations were conducted a priori |
| 7b) Sufficient sample (part 2 of size bias) | High risk | 0 ‐ A sufficient sample size based on the power calculation was not obtained |
| Total | High risk | Total score on new Cochrane standard: Low risk (7/9), High risk (1/9), Unclear Risk (1/9) |
Curtis 2007.
| Methods |
Study design: between groups; comparison to baseline Total study duration: 6 months |
|
| Participants |
Total number: 41 Setting: pediatric Emergency Department at the Stollery Children's Hospital in Edmonton, Alberta, Canada Diagnostic criteria: all infants up to 6 months corrected age that required venipuncture; participants required to have had nothing by mouth for 5 minutes prior to venipuncture; could not be critically ill; no fructose intolerance; no EMLA at the site of venipuncture Age: Minimum: 0 months Maximum: 6 months Mean: 58.25 days SD: 56.50 days Sex: Males: 44 Females: 40 Socio‐demographics: not reported Country: Canada Ethnicity: not reported |
|
| Interventions |
Total number of intervention groups: 1 (placebo, and placebo and pacifier) Control group description: placebo group received 2 mL of sterile water, administered via syringe over tongue at 2 minutes prior to venipuncture Total number of participants randomized to each of your groups: placebo = 19, pacifier and placebo = 22 Specific intervention: timers used to co‐ordinate events; solution administered by research nurse to anterior aspect of tongue over 30 seconds via syringe and pacifier inserted orally (if deemed necessary) at 2 minutes post intervention. Venipuncture was performed by nurse. Parents interacted with voice and touch as per usual. Integrity of intervention: good |
|
| Outcomes |
Pain outcomes, scale limits, and time points when measured: FLACC Pain Scale Measured before and after procedure (30 to 60 seconds post intervention) Change from baseline = outcome Upper limit: 10 Lower limit: 0 High score = higher pain Continuous |
|
| Notes |
Adverse reactions: There was one episode of vomiting, which occurred in a total of three children. Funding sources: pediatric residents' training committee research award at the Department of Pediatrics, Stollery Children's Hospital Key conclusions of study authors: pacifiers are effective analgesics Miscellaneous comments from the study authors: "Parents interacted with voice or touch as per normal" (page 4). This may have confounded results. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 1) Randomization (Random Sequence Generation) | Low risk | 2 ‐ A convincing method for generating a random allocation sequence is reported that used an independent person not involved in enrolment or allocation of participants |
| 2) Allocation bias (Allocation concealment) | Low risk | 1 ‐ An adequate method is reported that removes the potential biases of investigators |
| 3a) Blinding of participants and personnel | Low risk | 1 ‐ A convincing effort to reduce bias in outcomes measurement is reported |
| 3b) Blinding of outcome assessment | Unclear risk | None specified |
| 4) Attrition (Incomplete Outcome Data) | Low risk | 1 ‐ A reasonable account of how attrition was dealt with is given, but no specific reference to CONSORT |
| 5) Selective outcome reporting (Selective Outcome Reporting) | Low risk | There was no selective outcome reporting |
| 6) Other potential sources of bias (Other potential threats to validity) | Low risk | There were no other potential sources of bias reported |
| 7a) Power calculation (Part 1 of size bias) | Low risk | 1 ‐ Power calculations were conducted a priori |
| 7b) Sufficient sample (part 2 of size bias) | Low risk | 1 ‐ A sufficient sample size based on the power calculation was obtained |
| Total | Low risk | Total score on new Cochrane standard: Low risk (8/9), High risk (0/9), Unclear Risk (1/9) |
Elserafy 2009.
| Methods |
Study design: cross‐over Study duration: January 2005 and May 2007 |
|
| Participants |
Total number: 36 Setting: NICU tertiary care Diagnostic criteria: exclusion criteria were 1) exposure to maternal sedation; 2) occurrence of any procedure performed within 24 hours in preterm infants whose mothers had had general anesthesia during delivery; 3) the presence of major neurologic abnormalities; 4) Apgar scores at 5 minutes of greater than 5; 5) presence of necrotizing intestinal colitis; 6) nothing by mouth status for any reason; 7) being preterm with hyperglycemia Age: Minimum: 27 weeks Maximum: 36 weeks Mean: 32.4 weeks SD: 2.9 Sex: Males: not reported Females: not reported Country: Saudi Arabia |
|
| Interventions |
Total number of intervention groups: 3 Control group description: standardized care Total number of participants randomized to each group: 36 Specific intervention #1: water pacifier Intervention details: infants were given pacifiers coated in 0.5 mL of water 2 minutes prior Integrity of intervention: good Specific intervention #2: pacifier alone Intervention details: standard nipple stuffed with gauze square for resistance, held in infant's mouth for 2 minutes prior Integrity of intervention: good Specific intervention #3: sterile water Intervention details: 0.5 mL of sterile water without pacifier Integrity of intervention: good |
|
| Outcomes |
Pain outcomes, scale limits, and time points when measured: PIPP 15 seconds after the venipuncture Upper limit: 3 Lower limit: 0 Higher score = more pain Continuous |
|
| Notes |
Adverse reactions: none Funding sources: none reported Key conclusions of study authors: water pacifier, pacifier alone, and sterile water were not as effective as sucrose and pacifier. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 1) Randomization (Random Sequence Generation) | Low risk | 2 ‐ A convincing method for generating a random allocation sequence is reported that used an independent person not involved in enrolment or allocation of participants |
| 2) Allocation bias (Allocation concealment) | Low risk | 1 ‐ An adequate method is reported that removes the potential biases of investigators |
| 3a) Blinding of participants and personnel | Unclear risk | 0 ‐ Efforts to reduce measurement bias are not reported or are insufficient, e.g. outcomes collected by therapist |
| 3b) Blinding of outcome assessment | Unclear risk | none specified |
| 4) Attrition (Incomplete Outcome Data) | Low risk | 1 ‐ A reasonable account of how attrition was dealt with is given, but no specific reference to CONSORT |
| 5) Selective outcome reporting (Selective Outcome Reporting) | Low risk | There was no selective outcome reporting |
| 6) Other potential sources of bias (Other potential threats to validity) | Low risk | There were no other potential sources of bias reported |
| 7a) Power calculation (Part 1 of size bias) | High risk | 0 ‐ Power calculations were not conducted a priori |
| 7b) Sufficient sample (part 2 of size bias) | High risk | 0 ‐ A sufficient sample size based on the power calculation was not obtained |
| Total | High risk | Total score on new Cochrane standard: Low risk (5/9), High risk (2/9), Unclear Risk (2/9) |
Esfahani 2013.
| Methods |
Study design: between groups Total study duration: April 2011 – July 2011 (3 months) |
|
| Participants |
Total number: 64 Setting: Navabsafabi Health Care Center Diagnostic criteria: healthy neonates Age Minimum: 6 months Maximum: 12 months Mean: N/A SD: N/A Sex Males: N/A Females: N/A Country: Iran |
|
| Interventions |
Total number of intervention groups: 1 Control group description: vaccination was conducted in the conventional method with no intervention Total number of participants randomized to each of your groups: intervention = 32; control = 32 Intervention descriptions: Massage therapy: researcher massaged the first knuckle of the middle or ring finger of the infants’ palm or sole of the injection side for 60 sec and finally vaccinated the subject. The massage point was corresponding with the injection‐related leg in the body through sujok correspondence system the points are on a miniature map of the body on the palms and soles Integrity of intervention: poor |
|
| Outcomes |
Pain outcomes, time points when measured, and scale limits: NIPS Time points: “During the procedure of vaccination” page 3, paragraph 1 under Materials and Methods – did not specify timing Range of possible scores: 0 (lowest pain score) to 7 (highest pain score); score of 3 shows existence of pain |
|
| Notes |
Adverse reactions: none reported Key conclusions of study authors: massage therapy can be used as a replacement method for breastfeeding (less vaccination pain reported in the massage group compared to the control group); breastfeeding was more effective than massage therapy. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 1) Randomization (Random Sequence Generation) | Low risk | “The type of vaccine to be investigated was randomly selected from 96 envelopes marked as A and B, which the researcher had already made by random number table (zero was ignored; numbers 1, 2, 3 were assigned to the massage group; 4, 5, 6 to the breast feeding group; and 7, 8, 9 to the control group. Envelopes A were assigned to 6‐month‐old infants and envelopes B to 12‐month‐old infants” page 3, paragraph 2 under Materials and Methods |
| 2) Allocation bias (Allocation concealment) | Low risk | Same as above |
| 3a) Blinding of participants and personnel | High risk | Participants and personnel were not blinded because they would see which intervention the child was given |
| 3b) Blinding of outcome assessment | High risk | Coder were not blinded as they evaluated NIPS in the room and would have seen the intervention the infant was assigned to |
| 4) Attrition (Incomplete Outcome Data) | Low risk | A total of 99 infants entered the study, three infants were left out due to restlessness and cry before the injection |
| 5) Selective outcome reporting (Selective Outcome Reporting) | Low risk | All expected and pre‐specified outcomes reported |
| 6) Other potential sources of bias (Other potential threats to validity) | Low risk | No other potential sources of bias reported |
| 7a) Power calculation (Part 1 of size bias) | High risk | No report of power calculation |
| 7b) Sufficient sample (part 2 of size bias) | High risk | No report of having a sufficient sample size due to power calculation |
| Total | High risk | Total score on new Cochrane standard: Low risk (5/9), High risk (4/9), Unclear Risk (0/9) |
Fearon 1997.
| Methods |
Study design: cross‐over Total study duration: not reported |
|
| Participants |
Total number: 15 Setting: NICU Diagnostic criteria: Preterm Age: Minimum: 27 weeks Maximum: 36 weeks Mean: younger group (29.6 weeks) and older group (33.7 weeks) SD: younger group (0.90 weeks) and older group (2.16 weeks) Sex: Males: 9 Females: 6 Country: Canada Socio‐demographics: not collected Ethnicity: not collected |
|
| Interventions |
Total number of intervention groups: 1 Control group description: Typical care Total number of participants randomized to each group: 15 Specific intervention: swaddling Intervention details: placed infant in a supine position on a soft clean cloth. Infant's arms were crossed over in a relaxed position and tucked in on sides. Integrity of intervention: good |
|
| Outcomes |
Pain outcomes, scale limits, and time points when measured: NFCS Pre‐needle, during needle, and post‐needle Upper limit: 10 Lower limit: 0 Higher score = more pain |
|
| Notes |
Adverse reactions: none Funding sources: Ontario Ministry of Health Nursing Innovation Fund grant and the Ontario Ministry of Health Career Scientist Award Key conclusions of study authors: pain behaviors reduced by swaddling |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 1) Randomization (Random Sequence Generation) | Low risk | 1 ‐ A convincing method of randomization is reported but this did not involve an independent person |
| 2) Allocation bias (Allocation concealment) | Low risk | 1 ‐ An adequate method is reported that removes the potential biases of investigators |
| 3a) Blinding of participants and personnel | Low risk | 1 ‐ A convincing effort to reduce bias in outcomes measurement is reported |
| 3b) Blinding of outcome assessment | Unclear risk | None specified |
| 4) Attrition (Incomplete Outcome Data) | Low risk | 1 ‐ A reasonable account of how attrition was dealt with is given, but no specific reference to CONSORT |
| 5) Selective outcome reporting (Selective Outcome Reporting) | Low risk | There was no selective outcome reporting |
| 6) Other potential sources of bias (Other potential threats to validity) | Low risk | There were no other potential sources of bias reported |
| 7a) Power calculation (Part 1 of size bias) | High risk | 0 ‐ Power calculations were not conducted a priori. |
| 7b) Sufficient sample (part 2 of size bias) | High risk | 1 ‐ Small sample size and no effect detected. |
| Total | High risk | Total score on new Cochrane standard: Low risk (7/9), High risk (2/9), Unclear Risk (1/9) |
Gormally 2001.
| Methods |
Study design: randomized between groups Total study duration: unknown |
|
| Participants |
Total number: 41 Setting: community hospital Diagnostic criteria: healthy infants born at term Age: Minimum: 37 weeks Maximum: not reported Mean: 39.3 SD: 1.3 Sex: Males: 22 Females: 19 Country: Canada Socio‐demographics: mothers in control group had a mean age of 29.9 years and 10.7 years of education; mothers in holding group had a mean age of 29.4 years and 11.4 years of education |
|
| Interventions |
Total number of intervention groups: 1 Control group description: no holding and water taste Total number of participants randomized to each of your groups: Intervention: 20, Control: 21 Specific intervention: holding and water taste Intervention details: the infant is held in the arms of a female RA beginning 4 minutes pre heelstick, given sterile water and rested in the morning Integrity of intervention: good |
|
| Outcomes |
Pain outcomes, scale limits, and time points when measured: NFCS (% of the time) 1 minute post‐heel lance, 2 minutes post‐heel lance Upper limit: 100 Lower limit: 0 Higher score = more pain Continuous Cry (% of the time) 1, 2, and 3 minutes post‐heel lance Upper limit: 100 Lower limit: 0 Higher score = more time spent crying/more pain Continuous |
|
| Notes |
Adverse reactions: Non reported Funding sources: Medical Research Council of Canada, Allan Ross Fellowship, Lewis Sessenwein Academic Award Key conclusions of study authors: providing care‐giving context reduces pain in neonates |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 1) Randomization (Random Sequence Generation) | Low risk | 1 ‐ A convincing method of randomization is reported but this did not involve an independent person |
| 2) Allocation bias (Allocation concealment) | High risk | 0 ‐ There is not an adequate description of attempts to deal with potential allocation bias |
| 3a) Blinding of participants and personnel | Unclear risk | none specified |
| 3b) Blinding of outcome assessment | Unclear risk | none specified |
| 4) Attrition (Incomplete Outcome Data) | Low risk | 1 ‐ A reasonable account of how attrition was dealt with is given, but no specific reference to CONSORT |
| 5) Selective outcome reporting (Selective Outcome Reporting) | Low risk | There was no selective outcome reporting |
| 6) Other potential sources of bias (Other potential threats to validity) | Low risk | There were no other potential sources of bias reported |
| 7a) Power calculation (Part 1 of size bias) | High risk | 0 ‐ Power calculations were not conducted a priori |
| 7b) Sufficient sample (part 2 of size bias) | Low risk | 1 ‐ A sufficient sample size based on the power calculation was obtained, an effect was shown |
| Total | High risk | Total score on new Cochrane standard: Low risk (5/9), High risk (2/9), Unclear Risk (2/9) |
Greenberg 2002.
| Methods |
Study design: randomized between groups Total study duration: unknown |
|
| Participants |
Total number: 84 Setting: moderate sized hospital, nursery Diagnostic criteria: birth weight between 2500 and 4000 grams; less than or equal to 72 hours old; no congenital abnormalities; full‐term Age: Minimum: age of birth Maximum: 72 hours Mean: 18.99 hours SD: 5.59 hours Sex: Males: 38 Females: 46 Country: USA Co‐morbidity: none Socio‐demographics: mothers were excluded from the study if there was a history of substance abuse, or chronic or infectious diseases during pregnancy Ethnicity: 73.8% white; 10.7% Hispanic; 4.8% African American; 10.7% other |
|
| Interventions |
Total number of intervention groups: 3 (we will only focus on 1 for review, as the other intervention group included sucrose) Control group description: routine care; no intervention offered during heelstick Total number of participants randomized to each of your groups: 21 in each of the 4 groups (total of 84) Specific intervention: water pacifier Intervention details: a Mini‐Mam 0 to 6‐month orthodontic pacifier moistened with water was gently held in the infant's mouth (without initiating any other contact) during 2 minutes pre‐procedure and 3 minutes post‐procedure Integrity of intervention: satisfactory |
|
| Outcomes |
Pain outcomes, scale limits, and time points when measured: Duration of cry From the start of the procedure to 25 minutes post procedure Upper limit: 1500 seconds (and higher) Lower limit: 0 seconds Higher score = longer cry duration, more pain Continuous |
|
| Notes |
Adverse reactions: none Funding sources: American Cancer Society; California Division Fellowship Key conclusions of the study authors: no significant differences between water pacifier and typical care group were found |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 1) Randomization (Random Sequence Generation) | Low risk | 1 ‐ A convincing method of randomization is reported but this did not involve an independent person |
| 2) Allocation bias (Allocation concealment) | High risk | 0 ‐ There is not an adequate description of attempts to deal with potential allocation bias |
| 3a) Blinding of participants and personnel | High risk | investigator collected all data |
| 3b) Blinding of outcome assessment | Unclear risk | none specified |
| 4) Attrition (Incomplete Outcome Data) | High risk | 0 ‐ There is no documented evidence or insufficient evidence reported of how attrition was dealt with |
| 5) Selective outcome reporting (Selective Outcome Reporting) | Low risk | There was no selective outcome reporting |
| 6) Other potential sources of bias (Other potential threats to validity) | Low risk | There were no other potential sources of bias reported |
| 7a) Power calculation (Part 1 of size bias) | High risk | 0 ‐ Power calculations were not conducted a priori |
| 7b) Sufficient sample (part 2 of size bias) | High risk | 0‐ Small sample size and no effect detected. |
| Total | High risk | Total score on new Cochrane standard: Low risk (3/9), High risk (5/9), Unclear Risk (1/9) |
Harrington 2012.
| Methods |
Study design: between groups Total study duration: 6 months |
|
| Participants |
Total number: 230 Setting: general pediatric outpatient practice located in local hospital Diagnostic criteria: Inclusion criteria: infants with a GA between 32 and 42 weeks at delivery and post natal age of < 20 weeks. Exclusion criteria: acetominophen or ibuprofen administration within 4 hours before immunization, current neurological disorder, known genetic anomaly, moderate to severe illness with or without fever at the time of the immunization, anaphylactic reaction to previous dose of vaccine, or infant was previously enrolled in the study at 2 months. Age: Minimum: 2 months Maximum: 6 months SD: not reported Sex: Males: 124 Females: 106 Country: USA (majority were African American) |
|
| Interventions |
Total number of intervention groups: 3 Control group description: 2 mL of water 2 mins before needle and comfort by parent or guardian after immunization Total number of participants randomized to each of your groups: intervention 1 = 58; intervention 2 = 58; intervention 3 = 58; control group = 56 Specific intervention #1: 2 mL 24% oral sucrose 2 mins before needle and comfort by parent or guardian after immunization Specific intervention #2: 2 mL of water 2 min before needle and physical intervention using the 5 S's by research after immunization Specific intervention #3: 2 mL of 24% oral sucrose 2 min before needle and physical intervention using the 5 S's by researcher after immunization Integrity of intervention: good |
|
| Outcomes |
Pain outcomes, scale limits, and time points when measured: Modified Riley Infant Pain Scoring method Time points: 15 secs intervals for the first 2 min post last needle, then 30 sec intervals to a maximum of 5 mins post last needle, after the infant was calm scoring was continued for an additional 1 minute post cry. Upper limit: 9 Lower limit: 0 High score = more pain Continuous Crying Time points: 15 sec intervals for the first 2 min post last needle, then 30 sec intervals to a maximum of 5 min post last needle Continuous |
|
| Notes |
Adverse reactions: none Key conclusions of study authors: physical intervention of the 5 S's provided decreased pain scores on a validated pain scale and decreased crying time among 2 and 4 month old infants during routine immunizations. The use of the 5 S's did not differ from the 5 S's plus sucrose. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 1) Randomization (Random Sequence Generation) | Low risk | “Infants of parents or guardians who consented were randomly assigned to 1 of 4 study groups by using presealed cards.” (p. 817) |
| 2) Allocation bias (Allocation concealment) | Low risk | “Infants of parents or guardians who consented were randomly assigned to 1 of 4 study groups by using presealed cards. The cards were then selected by the nurses and only reviewed by the nurses to instruct them as to the group assignment” (p. 817) |
| 3a) Blinding of participants and personnel | High risk | Infants and parents not blinded to whether the physical intervention was used. |
| 3b) Blinding of outcome assessment | High risk | Coders not blinded to whether infant received physical intervention |
| 4) Attrition (Incomplete Outcome Data) | Low risk | 0 ‐ There is no documented evidence or insufficient evidence reported of how attrition was dealt with |
| 5) Selective outcome reporting (Selective Outcome Reporting) | Low risk | There was no selective outcome reporting |
| 6) Other potential sources of bias (Other potential threats to validity) | Low risk | There were no other potential sources of bias reported |
| 7a) Power calculation (Part 1 of size bias) | Low risk | 1 ‐ Power calculations were conducted a priori |
| 7b) Sufficient sample (part 2 of size bias) | Low risk | Effect shown and sufficient sample size used |
| Total | High risk | Total score on new Cochrane standard: Low risk (7/9), High risk (2/9), Unclear Risk (0/9) |
Herrington 2007.
| Methods |
Study design: crossover Total study duration: 4 months (October 2006 to January 2007) |
|
| Participants |
Total number: 11 (21 enrolled initially; 1 withdrew, 2 were excluded, 6 discharged, 1 excluded due to video difficulty) Setting: NICU Diagnostic criteria: premature Age: Minimum: 27 weeks Maximum: 33 weeks Mean: 31 weeks SD: not reported Sex: Males: 6 Females: 5 Country: USA Ethnicity: 57.5% of the infants were African American; 40% Caucasian; 2.5% Hispanic origin |
|
| Interventions |
Total number of intervention groups: 1 Control group description: no intervention, PI did not directly touch the infant. Both hands were loosely fisted and placed behind the infant in close approximation to the head and buttocks, but not in contact with the infant. Total number of participants randomized to each of your groups: 11 Specific intervention: gentle human touch Intervention details: gentle positioning support for the infant using warm human hands to contain the infant's body in a flexed position. PI placed both hands in isolette, placing the right hand behind the infant's head and shoulders in a cupped fashion. PI paused for 10 seconds to release tension. The position was held for the entire duration of the heelstick procedure and 2 minutes post heelstick procedure. Integrity of intervention: good |
|
| Outcomes |
Pain outcomes, scale limits, and time points when measured: Cry duration Heelstick and 2 minutes post‐draw recovery Upper limit: (variable) Lower limit: 0 seconds Higher score = more pain Continuous |
|
| Notes |
Adverse reactions: none Funding sources: none reported Key conclusions of the study authors: gentle human touch does not reduce cry duration in moderately premature infants receiving the heelstick procedure Miscellaneous comments by review authors: study was double‐blind; participant information is not known |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 1) Randomization (Random Sequence Generation) | Low risk | 2 ‐ A convincing method for generating a random allocation sequence is reported that used an independent person not involved in enrolment or allocation of participants |
| 2) Allocation bias (Allocation concealment) | Low risk | 1 ‐ An adequate method is reported that removes the potential biases of investigators |
| 3a) Blinding of participants and personnel | Low risk | 1 ‐ A convincing effort to reduce bias in outcomes measurement is reported |
| 3b) Blinding of outcome assessment | Unclear risk | none specified |
| 4) Attrition (Incomplete Outcome Data) | Low risk | 2 ‐ Documented evidence that the CONSORT guidelines have been followed |
| 5) Selective outcome reporting (Selective Outcome Reporting) | Low risk | There was no selective outcome reporting |
| 6) Other potential sources of bias (Other potential threats to validity) | Low risk | There were no other potential sources of bias reported |
| 7a) Power calculation (Part 1 of size bias) | Low risk | 1 ‐ Power calculations were conducted a priori |
| 7b) Sufficient sample (part 2 of size bias) | Low risk | 1 ‐ A sufficient sample size based on the power calculation was obtained |
| Total | Low risk | Total score on new Cochrane standard: Low risk (8/9), High risk (0/9), Unclear Risk (1/9) |
Herrington 2014.
| Methods |
Study design: repeated‐measures crossover design Total study duration: not reported |
|
| Participants |
Total number: 11 Setting: NICU, Sparrow Hospital Diagnostic criteria: premature Age: Minimum: 27 weeks Maximum: 34 weeks Mean: 31 weeks SD: 1.7 weeks Sex Males: 6 Females: 5 Country: USA |
|
| Interventions |
Total number of intervention groups: 1 Control group description: standard care – infants also placed in a side‐lying position and supported with blanket rolls to create a “nest confinement” Total number of participants randomized to each of your groups: intervention = 11; control = 11 Intervention descriptions: Gentle Human Touch was accomplished by placing the infant in a side‐lying position and gently flexing the infant into a tucked position similar to the flexed fetal position infants naturally assume in the womb as they near term gestation. GHT is provided by cupping one hand around the infant’s head while cupping the other hand around the infant’s bottom. This position allowed the infant to move but limited extension and flailing of the extremities Integrity of intervention: good |
|
| Outcomes |
Pain outcomes, time points when measured, and scale limits: Audible Cry Time points: immediately after needle, recovery not specified Range of possible scores: measured in seconds |
|
| Notes |
Adverse reactions: None reported Key conclusions of study authors: Gentle Human Touch reduces pain in premature infants undergoing heel stick |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 1) Randomization (Random Sequence Generation) | Unclear risk | “Infants served as their own controls with random assignment to order of treatment” (p. 109, paragraph 1) ‐ this means that their own scores in the intervention and control group were compared to each other – No mention of how random assignment was generated |
| 2) Allocation bias (Allocation concealment) | Unclear risk | Did not address this outcome |
| 3a) Blinding of participants and personnel | Low risk | “phlebotomist at the bedside so that the phlebotomist was unaware of the experimental assignment of the infant” – p.110 |
| 3b) Blinding of outcome assessment | Unclear risk | Did not address this outcome |
| 4) Attrition (Incomplete Outcome Data) | Low risk | Figure 3 page 111 outlines enrolment and exclusion of participants, repeated‐measures design so same for both conditions |
| 5) Selective outcome reporting (Selective Outcome Reporting) | Low risk | Addressed all expected and pre‐specified outcomes |
| 6) Other potential sources of bias (Other potential threats to validity) | Low risk | Did not report other potential sources of bias. |
| 7a) Power calculation (Part 1 of size bias) | Low risk | The study was powered to detect an effect size of $0.70 using a two‐tailed matched test design with a of .05, considering a ‘‘large effect’’ in Cohen’s classification (paragraph 2, page 109). |
| 7b) Sufficient sample (part 2 of size bias) | Low risk | Power calculatio demonstrates sufficient sample generated. |
| Total | Low risk | Total score on new Cochrane standard: Low risk (6/9), High risk (0/9), Unclear Risk (3/9) |
Hill 2005.
| Methods |
Study design: cross‐over Total study duration: unknown |
|
| Participants |
Total number: 12 Setting: NICU Diagnostic criteria: preterm Age: Minimum: 25 weeks Maximum: 34 weeks Mean: 30.9 weeks SD: 2.5 weeks Sex: Males: 6 Females: 6 Country: USA |
|
| Interventions |
Total number of intervention groups: 1 Control group description: Standard care Total number of participants randomized to each of your groups: 12 Specific intervention: facilitated tucking Intervention details: nurse provided care to the infant while the physical therapist supported the infant in a midline, tucked position Integrity of intervention: good |
|
| Outcomes |
Pain outcomes, scale limits, and time points when measured: PIPP Immediate, during procedure Upper limit: 21 Lower limit: 0 Continuous |
|
| Notes |
Adverse reactions: none Funding sources: none stated. Key conclusions of the study authors: by incorporating facilitated tucking into routine care events, the stress levels of infants born preterm may be reduced |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 1) Randomization (Random Sequence Generation) | Low risk | 1 ‐ A convincing method of randomization is reported but this did not involve an independent person |
| 2) Allocation bias (Allocation concealment) | Low risk | 1 ‐ An adequate method is reported that removes the potential biases of investigators |
| 3a) Blinding of participants and personnel | Low risk | 1 ‐ A convincing effort to reduce bias in outcomes measurement is reported |
| 3b) Blinding of outcome assessment | Unclear risk | none specified |
| 4) Attrition (Incomplete Outcome Data) | Low risk | 2 ‐ Documented evidence that the CONSORT guidelines have been followed |
| 5) Selective outcome reporting (Selective Outcome Reporting) | Low risk | There was no selective outcome reporting |
| 6) Other potential sources of bias (Other potential threats to validity) | Low risk | There were no other potential sources of bias reported |
| 7a) Power calculation (Part 1 of size bias) | High risk | 0 ‐ Power calculations were not conducted a priori |
| 7b) Sufficient sample (part 2 of size bias) | Low risk | 1 ‐ A sufficient sample size was obtained to show an effect |
| Total | Low risk | Total score on new Cochrane standard: Low risk (7/9), High risk (1/9), Unclear Risk (1/9) |
Hillgrove Stuart 2013.
| Methods |
Study design: randomized between groups Total study duration: 11 months |
|
| Participants |
Total number: 99 Setting: pediatrician's clinic Diagnostic criteria: healthy infants Age: Minimum: 12 weeks Maximum: 20 weeks Mean: 14.98 weeks SD: 2.88 weeks Sex: Males: 58 Females: 41 Country: Canada Socio‐demographics: predominantly moderate‐high socioeconomic class Ethnicity: predominantly white |
|
| Interventions |
Total number of intervention groups: 2 Control group description: no intervention Total number of participants randomized to each of your groups: 34 to control, 33 to RA‐led distraction, 32 to parent‐led distraction Specific intervention #1: RA‐led distraction Intervention details: research assistant held toy and distracted infant Integrity of intervention: good Specific intervention #2: parent‐led distraction Intervention details: parent distracted infant throughout procedure Integrity of intervention: good |
|
| Outcomes |
Pain outcomes, scale limits, and time points when measured: MBPS 15 seconds to 1 min after needle Upper limit: (variable): 10 Lower limit: 0 seconds Higher score = more pain Continuous |
|
| Notes |
Adverse reactions: none Funding sources: not stated. Key conclusions of the study authors: toy distraction does not work |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 1) Randomization (Random Sequence Generation) | Low risk | 2 ‐ A convincing method for generating a random allocation sequence is reported that used an independent person not involved in enrolment or allocation of participants |
| 2) Allocation bias (Allocation concealment) | Low risk | 1 ‐ An adequate method is reported that removes the potential biases of investigators |
| 3a) Blinding of participants and personnel | High risk | Personnel and participants were not blind |
| 3b) Blinding of outcome assessment | High risk | Coders were not blinded |
| 4) Attrition (Incomplete Outcome Data) | Low risk | 1 ‐ A reasonable account of how attrition was dealt with is given, but no specific reference to CONSORT |
| 5) Selective outcome reporting (Selective Outcome Reporting) | Low risk | There was no selective outcome reporting |
| 6) Other potential sources of bias (Other potential threats to validity) | Low risk | There were no other potential sources of bias reported |
| 7a) Power calculation (Part 1 of size bias) | Low risk | 1 ‐ Power calculations were conducted a priori |
| 7b) Sufficient sample (part 2 of size bias) | Low risk | 1 ‐ A sufficient sample size based on the power calculation was obtained |
| Total | High risk | Total score on new Cochrane standard: Low risk (7/9), High risk (2/9), Unclear Risk (0/9) |
Hogan 2014.
| Methods |
Study design: between groups Total study duration: 15 months |
|
| Participants |
Total number: 120 Setting: primary care pediatric practice Diagnostic criteria: Inclusion criteria: aged 4‐6 month scheduled to have their DTaP‐IPV‐Hib and PVC vaccines Exclusion criteria:if impaired neurological development, history of seizures, use of local topical analgesics at injection site, use of sedatives or opioids 24 hours prior to procedure, fever or illness that would prevent administration of vaccination, a parent who was unable to use the assessment tool in the study, or a parent who did not speak English. Each infant could only participate once. Age: Minimum: 4 months Maximum: 6 months Mean % of each age group: 4 mos= 71%; 6 mos= 29% SD: unknown Sex: Males: 61 Females: 59 Country: Canada |
|
| Interventions |
Total number of intervention groups: 1 Control group description: no tactile stimulation. Note: all infants received sucrose solution, holding by parent, and injections without aspiration. Total number of participants randomized to each of your groups: intervention = 60; control = 60 Specific intervention: parent‐led tactile stimulation Intervention details: rub ipsilateral thigh distal to injection site for 15 seconds prior, during, and after each needle, using as much pressure as they felt would be suitable without distressing their infant Integrity of intervention: good |
|
| Outcomes |
Pain outcome, scale limits and time points when measured: MBPS Time points: 15 sec intervals before and after each injection Upper limit: 10 Lower limit: 0 High score = more pain Continuous VAS parent rating Time points: during each injection Upper limit: unknown Lower limit: unknown High score = mor epain Duration of crying Time points: first min after each vaccine VAS RA rating During each injection Upper limit: unknown Lower limit: unknown High score = more pain |
|
| Notes |
Adverse reactions: none Key conclusions of study authors: parent‐led tactile stimulation did not reduce pain in infants undergoing immunization when combined with other pain relieving interventions (sucrose & parenting holding). |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 1) Randomization (Random Sequence Generation) | Low risk | “A computer random number generator was used to create the sequence in random blocks of 4 to 8” (page 2) |
| 2) Allocation bias (Allocation concealment) | Low risk | “The randomization code was created by an individual not directly associated with the study. Treatment allocation was concealed in sequentially numbered opaque sealed envelopes that were not opened until after written consent was obtained from a parent” (page 2) |
| 3a) Blinding of participants and personnel | Unclear risk | Participants were blinded but personnel were not |
| 3b) Blinding of outcome assessment | High risk | Coders were blinded to study hypotheses but not blinded to condition |
| 4) Attrition (Incomplete Outcome Data) | Low risk | 1 ‐ A reasonable account of how attrition was dealt with is given, |
| 5) Selective outcome reporting (Selective Outcome Reporting) | Low risk | There was no selective outcome reporting |
| 6) Other potential sources of bias (Other potential threats to validity) | Low risk | There were no other potential sources of bias reported |
| 7a) Power calculation (Part 1 of size bias) | Low risk | 1 ‐ Power calculations were conducted a priori |
| 7b) Sufficient sample (part 2 of size bias) | Low risk | 1 ‐ A sufficient sample size based on the power calculation was obtained |
| Total | High risk | Total score on new Cochrane standard: Low risk (7/9), High risk (1/9), Unclear Risk (1/9) |
Im 2008.
| Methods |
Study design: randomized between groups Total study duration: unknown |
|
| Participants |
Total number: 99 Setting: hospital Diagnostic criteria: healthy neonates Age: Minimum: 38.8 weeks Maximum: 39.1 weeks Mean: approximately 273.4 days gestation SD: approximately 9.31 days gestation Sex: Males: 47 Females: 52 Country: South Korea Socio‐demographics: unknown Ethnicity: Korean |
|
| Interventions |
Total number of intervention groups: 2 Control group description: 1 Total number of participants randomized to each of your groups: touch: 33; non‐nutritive sucking: 33; control: 33 Specific intervention #1: Yakson touch Intervention details: nurse warmed hands to 34 degrees Celsius and approached neonate from behind. Nurse placed left hand under neonate's back. Nurse placed right hand on neonate's abdomen and caressed clockwise (approximately 4 cm in diameter) every 5 seconds. Integrity of intervention: good Specific intervention #2: non‐nutritive sucking Intervention details: neonates were given a small, short and hollow nipple packed with sterile gauze while gentle pressure was applied in the mouth Integrity of intervention: good |
|
| Outcomes |
Pain outcomes, scale limits, and time points when measured: NIPS Taken at one minute post heelstick Upper limit: 7 Lower limit: 0 High score = more pain Continuous |
|
| Notes |
Adverse reactions: none Funding sources: none reported Key conclusions of study authors: touch and non‐nutritive sucking were found not to reduce pain in healthy neonates measured 1 minute after heelstick, as compared to the control group |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 1) Randomization (Random Sequence Generation) | Low risk | 1 ‐ A convincing method of randomization is reported but this did not involve an independent person |
| 2) Allocation bias (Allocation concealment) | High risk | 0 ‐ There is not an adequate description of attempts to deal with potential allocation bias |
| 3a) Blinding of participants and personnel | Unclear risk | 0 ‐ Efforts to reduce measurement bias are not reported or are insufficient, e.g. outcomes collected by therapist |
| 3b) Blinding of outcome assessment | Unclear risk | None specified |
| 4) Attrition (Incomplete Outcome Data) | Low risk | 1 ‐ A reasonable account of how attrition was dealt with is given, but no specific reference to CONSORT |
| 5) Selective outcome reporting (Selective Outcome Reporting) | Low risk | There was no selective outcome reporting |
| 6) Other potential sources of bias (Other potential threats to validity) | Low risk | There were no other potential sources of bias reported |
| 7a) Power calculation (Part 1 of size bias) | High risk | 0 ‐ Power calculations were not conducted a priori |
| 7b) Sufficient sample (part 2 of size bias) | High risk | 0 ‐ A sufficient sample size based on the power calculation was not obtained |
| Total | High risk | Total score on new Cochrane standard: Low risk (4/9), High risk (3/9), Unclear Risk (2/9) |
Ipp 2004.
| Methods |
Study design: randomized between groups Total study duration: unknown |
|
| Participants |
Total number: 106 Setting: community pediatrics office Diagnostic criteria: healthy infants Age: Minimum: 2 months Maximum: 6 months Mean: 123 days SD: 51 days Sex: Males: 47 Females: 59 Country: Canada Co‐morbidity: 60% of the males were circumcised. |
|
| Interventions |
Total number of intervention groups: 1 (held by parent) Control group description: 1 (positioned supine) Total number of participants randomized to each of your groups: 50 in the control group, 56 in the intervention group Specific intervention: holding Intervention details: mothers were instructed to stand and hold the baby in a comfortable way (no specific instructions given) Integrity of intervention: satisfactory |
|
| Outcomes |
Pain outcomes, scale limits, and time when measured: NFCS (brow bulge, nasolabial furrowing, and eyes squeezed shut) Time: not mentioned Upper limit: 300% Lower limit: 0% High score = more pain Continuous Crying 180 seconds Upper limit: 180 seconds Lower limit: 0 More crying = more pain Continuous VAS 15 seconds post needle Upper limit: 100 mm (maximum pain) Lower limit: 0 mm (no pain) High score = more pain Continuous |
|
| Notes |
Adverse reactions: none Funding sources: none reported. Key conclusions of the study authors: holding is not better than the supine positioning in reducing the post needle pain in healthy infants aged 2 to 6 months (based on crying and NFCS and VAS scores) Miscellaneous comments by review authors: it was not mentioned how long NFCS was coded for, though it was stated that the maximum was 180 seconds |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 1) Randomization (Random Sequence Generation) | Low risk | 1 ‐ A convincing method of randomization is reported but this did not involve an independent person |
| 2) Allocation bias (Allocation concealment) | Low risk | 1 ‐ An adequate method is reported that removes the potential biases of investigators |
| 3a) Blinding of participants and personnel | High risk | 0 ‐ Efforts to reduce measurement bias are not reported or are insufficient, e.g. outcomes collected by therapist |
| 3b) Blinding of outcome assessment | Unclear risk | None specified |
| 4) Attrition (Incomplete Outcome Data) | Low risk | 1 ‐ A reasonable account of how attrition was dealt with is given, but no specific reference to CONSORT |
| 5) Selective outcome reporting (Selective Outcome Reporting) | Low risk | There was no selective outcome reporting |
| 6) Other potential sources of bias (Other potential threats to validity) | Low risk | There were no other potential sources of bias reported |
| 7a) Power calculation (Part 1 of size bias) | Low risk | 1 ‐ Power calculations were conducted a priori |
| 7b) Sufficient sample (part 2 of size bias) | Low risk | 1 ‐ A sufficient sample size based on the power calculation was obtained |
| Total | High risk | Total score on new Cochrane standard: Low risk (7/9), High risk (1/9), Unclear Risk (1/9) |
Jain 2006.
| Methods |
Study design: cross‐over Total study duration: unknown |
|
| Participants |
Total number: 23 Setting: hospital NICU Diagnostic criteria: premature infants who were not currently ventilated and not on analgesic for the last 48 hours, and had not undergone surgery in the last 2 weeks Age: Minimum: 28 weeks Maximum: 35 weeks Mean: 31.1 weeks SD: 1.9 weeks Sex: no information stated Country: Canada (Alberta) |
|
| Interventions |
Total number of intervention groups: 1 Control group description: 1 Total number of participants randomized to each of your groups: 23 Specific intervention: massage Intervention details: the infant was wrapped and bundled for 5 minutes prior to heel lance. The heel (from toes to mid thigh) was massaged with gentle pressure using fingers and thumbs. The heel was then covered with a warm cloth for 2 to 3 minutes. Integrity of intervention: good |
|
| Outcomes |
Pain outcomes, scale limits, and time points when measured NIPS 5 minutes post heel lance High score = more pain Continuous |
|
| Notes |
Adverse reactions: data for 3 infants was not included (they were transferred to another hospital) Funding sources: no mentioned. Key conclusions of the study authors: gentle massage prior to heel lance is helpful in reducing pain during heel lance in premature infants |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 1) Randomization (Random Sequence Generation) | Low risk | 1 ‐ A convincing method of randomization is reported but this did not involve an independent person |
| 2) Allocation bias (Allocation concealment) | Low risk | 1 ‐ An adequate method is reported that removes the potential biases of investigators |
| 3a) Blinding of participants and personnel | Unclear risk | 0 ‐ Efforts to reduce measurement bias are noted but not explained. |
| 3b) Blinding of outcome assessment | Unclear risk | None specified |
| 4) Attrition (Incomplete Outcome Data) | Low risk | 2 ‐ Documented evidence that the CONSORT guidelines have been followed |
| 5) Selective outcome reporting (Selective Outcome Reporting) | Low risk | There was no selective outcome reporting |
| 6) Other potential sources of bias (Other potential threats to validity) | Low risk | There were no other potential sources of bias reported |
| 7a) Power calculation (Part 1 of size bias) | Low risk | 1 ‐ Power calculations were conducted a priori |
| 7b) Sufficient sample (part 2 of size bias) | Low risk | 1 ‐ A sufficient sample size based on the power calculation was obtained |
| Total | Low risk | Total score on new cochrane standard: Low risk (7/9), High risk (0/9), Unclear Risk (2/9) |
Johnston 1997.
| Methods |
Study design: between groups Total study duration: unknown |
|
| Participants |
Total number: 44 Setting: NICU Diagnostic criteria: premature sample Age: Minimum: 25 4/7 weeks Maximum: 34 2/7 weeks Mean: 31 weeks SD: not reported Sex: Males: 42 Females: 43 Country: Canada Co‐morbidity: no congenital abnormalities; Apgar scores greater than 3 at 5 minutes Socio‐demographics: not reported Ethnicity: not reported |
|
| Interventions |
Total number of intervention groups: 1 Control group description: baby was handled and repositioned to the side, and 0.05 mL of water was placed on the tongue's surface just prior to starting the heel lance procedure Total number of participants randomized to each group: 24 in rocking condition 20 in control condition Specific intervention: rocking Intervention details: the infant was repositioned to be on the side or in the supine position and was swaddled in a blanket. An air mattress was placed beneath them, that pumped air into the mattress at a rate of 12 cycles per minute. The swaddled baby was left on the oscillating mattress for 15 minutes prior to the heelstick. The infant also received 0.05 ml of water. Integrity of intervention: good |
|
| Outcomes |
Pain outcomes, time points when measured, and scale limits: NFCS Baseline, 30 seconds post needle, 60 seconds post needle, 90 seconds post needle Upper limit: 1 Lower limit: 0 High score = more pain Continuous |
|
| Notes |
Adverse reactions: none Funding sources: FRSQ, NIH Key conclusions: no difference between rocking and control. . |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 1) Randomization (Random Sequence Generation) | Low risk | 2 ‐ A convincing method for generating a random allocation sequence is reported that used an independent person not involved in enrolment or allocation of participants |
| 2) Allocation bias (Allocation concealment) | Low risk | 1 ‐ An adequate method is reported that removes the potential biases of investigators |
| 3a) Blinding of participants and personnel | Unclear risk | 0 ‐ Efforts to reduce measurement bias are not reported or are insufficient, e.g. outcomes collected by therapist |
| 3b) Blinding of outcome assessment | High risk | None specified and suspect coders were not blind due to rocking in an incubator. |
| 4) Attrition (Incomplete Outcome Data) | Low risk | 1 ‐ A reasonable account of how attrition was dealt with is given, but no specific reference to CONSORT |
| 5) Selective outcome reporting (Selective Outcome Reporting) | Low risk | There was no selective outcome reporting |
| 6) Other potential sources of bias (Other potential threats to validity) | Low risk | There were no other potential sources of bias reported |
| 7a) Power calculation (Part 1 of size bias) | Low risk | 1 ‐ Power calculations were conducted a priori |
| 7b) Sufficient sample (part 2 of size bias) | Low risk | 1 ‐ A sufficient sample size based on the power calculation was obtained |
| Total | High risk | Total score on new Cochrane standard: Low risk (7/9), High risk (1/9), Unclear Risk (1/9) |
Johnston 2007a.
| Methods |
Study design: cross‐over Total study duration: not known |
|
| Participants |
Total number: 20 Setting: NICU Diagnostic criteria: preterm infants Age: Minimum: 32 weeks Maximum: 34 5/7 weeks Mean: 33 weeks Std. 0.89 weeks Sex: Males: 57% males Females:43% females Country: Canada |
|
| Interventions |
Total number of intervention groups: 1 Control group description: no intervention Total number of participants randomized to each of your groups: 20 Specific intervention: mother's voice played during heel lance Intervention details: recording of mother's voice either singing, talking, or reading a nursery rhyme was played 1 minute before the procedure began and until heart rate and O2 sat returned to baseline Integrity of intervention: good |
|
| Outcomes |
Pain outcomes, time points when measured, and scale limits: 1) PIPP 30 seconds Upper limit: 21 Lower limit: 0 High score = more pain Continuous |
|
| Notes |
Adverse reactions: none Funding sources: Canadian Institute of Health Research Key conclusions of the authors: playing maternal voice pre and during heel lance has no significant impact on premie pain Miscellaneous comments by review authors: no means, only F provided for PIPP Percentages for NFCS |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 1) Randomization (Random Sequence Generation) | Low risk | 2 ‐ A convincing method for generating a random allocation sequence is reported that used an independent person not involved in enrolment or allocation of participants |
| 2) Allocation bias (Allocation concealment) | High risk | 0 ‐ There is not an adequate description of attempts to deal with potential allocation bias |
| 3a) Blinding of participants and personnel | Unclear risk | 0 ‐ Efforts to reduce measurement bias are not reported or are insufficient, e.g. outcomes collected by therapist |
| 3b) Blinding of outcome assessment | Low risk | Coders blinded to the purpose of the study |
| 4) Attrition (Incomplete Outcome Data) | Low risk | 1 ‐ A reasonable account of how attrition was dealt with is given, but no specific reference to CONSORT |
| 5) Selective outcome reporting (Selective Outcome Reporting) | Low risk | There was no selective outcome reporting |
| 6) Other potential sources of bias (Other potential threats to validity) | Low risk | There were no other potential sources of bias reported |
| 7a) Power calculation (Part 1 of size bias) | Low risk | 1 ‐ Power calculations were conducted a priori |
| 7b) Sufficient sample (part 2 of size bias) | Low risk | 1 ‐ A sufficient sample size based on the power calculation was obtained |
| Total | High risk | Total score on new Cochrane standard: Low risk (7/9), High risk (1/9), Unclear Risk (1/9) |
Johnston 2013a.
| Methods |
Study design: between groups Total study duration: not reported |
|
| Participants |
Total number: 68; only 55 were analyzed Setting: two university‐affiliated level III NICUs in Canada Diagnostic criteria: preterm neonates between 26 0/7 and 28 6/7 weeks’ gestational age. Infants were free of major congenital anomalies, had not experienced severe hypoxia, and were not receiving analgesics or sedatives within 72 hours of the study; however, they could be receiving ventilator support. Age: Minimum: 26 0/7weeks Maximum: 28 0/7weeks Mean: both groups together = 27 2/7 weeks; Therapeutic Touch group only = 27 2/7 weeks; Sham group only = 27 3/7 weeks SD: SD not given for both groups together; Therapeutic Touch group = 1/7 weeks; Sham group = 1.7 weeks Sex: Males: 53% of 27 in Therapeutic Group & 47% of 28 in Sham group Females: 47% of 27 in Therapeutic Group & 53% of 28 in Sham group Country: Canada |
|
| Interventions |
Total number of intervention groups: 1 Control group description: Sham group: the therapist stood beside the incubator with hands at her side and did mental tasks (e.g. mathematical operations) to avoid focusing on the infant. Total number of participants randomized to each of your groups: intervention = 27; control = 28 Specific intervention: Non‐Tactile Therapeutic Touch group Intervention details: The therapist used her hands to assess and rebalance the energy field of the patient using the following steps: (1) centering her state of awareness, (2) assessing the energy field of the patient, and (3) modulating the energy field. The average time for this was 5 minutes. Both therapists and nurses had several years experience in Therapeutic Touch. Integrity of intervention: good |
|
| Outcomes |
Pain outcome, scale limits and time points when measured: PIPP Time points: 30, 60, 90, and 120 seconds post heel lance Upper limit: 21 Lower limit: 3 High score = more pain Continuous |
|
| Notes |
Adverse reactions: none Key conclusions of study authors: Therapeutic Touch given immediately before and after heel lance has no comforting effect in preterm neonates. Other effective strategies involving actual touch should be considered. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 1) Randomization (Random Sequence Generation) | Unclear risk | Unclear whether what was used was a website for random numbers |
| 2) Allocation bias (Allocation concealment) | Low risk | 1 ‐ An adequate method is reported that removes the potential biases of investigators |
| 3a) Blinding of participants and personnel | Low risk | 1 ‐ A convincing effort to reduce bias in outcome measurement is reported |
| 3b) Blinding of outcome assessment | Low risk | Coders were blinded |
| 4) Attrition (Incomplete Outcome Data) | Low risk | For outcome examined there was sufficient outcome data |
| 5) Selective outcome reporting (Selective Outcome Reporting) | Unclear risk | Salivary cortisol results were not fully reported. |
| 6) Other potential sources of bias (Other potential threats to validity) | Low risk | No other source of bias specified |
| 7a) Power calculation (Part 1 of size bias) | Low risk | 1 ‐ Power calculations were conducted a priori |
| 7b) Sufficient sample (part 2 of size bias) | Low risk | 1 ‐ A sufficient sample size based on the power calculation was obtained |
| Total | Low risk | Total score on new cochrane standard: Low risk (7/9), High risk (0/9), Unclear Risk (2/9) |
Jose 2012.
| Methods |
Study design: quasi‐experimental post‐test only design Total study duration: not reported |
|
| Participants |
Total number: 60 Setting: various rural maternal and child welfare centres of Kasturba Medical College, Manipal, India Diagnostic criteria: not reported Age: all infants were 14 weeks old Minimum: 14 weeks Maximum: 14 weeks Mean: 14 weeks SD: 0 weeks Sex: Males: 33 Females: 27 Country: India |
|
| Interventions |
Total number of intervention groups: 1 Control group description: no intervention Total number of participants randomized to each of your groups: intervention = 30; control = 30 Specific intervention: skin‐tap technique Intervention details: tapping the skin with the finger pads of the dominant hand to relax the muscle. The immunization site (i.e. left vastus lateralis) was tapped for a duration of two minutes before immunization, and during and after immunization, the area above the site was tapped for a duration of one minute. To maintain synchrony, the investigator counts one, two and on the count of three, the needle will be inserted. Integrity of intervention satisfactory |
|
| Outcomes |
Pain outcome, scale limits and time points when measured: Behavioral Observation Pain Scale Time points: not specified Upper limit: 20 Lower limit: 0 High score = more pain Continuous |
|
| Notes |
Adverse reactions: none reported Key conclusions of study authors: The study concludes that skin tapping was effective in improving pain during DPT injections among infants. The study recommends application of this technique to nursing practice to minimize the pain experienced by the children they are taking care of. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 1) Randomization (Random Sequence Generation) | High risk | "Quasi experimental post‐test only control group", "the sampling design was purposive sampling with random allocation of treatment using chit method with non replacement technique" |
| 2) Allocation bias (Allocation concealment) | Unclear risk | not specified |
| 3a) Blinding of participants and personnel | Unclear risk | not specified |
| 3b) Blinding of outcome assessment | Unclear risk | not specified |
| 4) Attrition (Incomplete Outcome Data) | Unclear risk | not specified |
| 5) Selective outcome reporting (Selective Outcome Reporting) | Unclear risk | not specified |
| 6) Other potential sources of bias (Other potential threats to validity) | Unclear risk | not specified |
| 7a) Power calculation (Part 1 of size bias) | Unclear risk | not specified |
| 7b) Sufficient sample (part 2 of size bias) | Unclear risk | not specified |
| Total | High risk | Total score on new Cochrane standard: Low risk (0/9), High risk (1/9), Unclear Risk (8/9) |
Kozub 2001.
| Methods |
Study design: cross‐over Total study duration: winter of 2000 |
|
| Participants |
Total number: 20 Setting: pulmonary clinic (hospital) Diagnostic criteria: premature born infants (but older at time of the study), receiving Synagis injections to prevent pulmonary infections Age: Minimum: 1 month Maximum: 15 months Mean: 6.58 months SD: 4.1 months Sex: Males: 12 Females: 8 Country: USA |
|
| Interventions |
Total intervention groups: 1 Control group description: 1 (mimic intervention) Total number of participants randomized to each of your groups: 20 Specific intervention: therapeutic touch Intervention details: Krieger method: centering, assessment, unruffing and direction/modulation of energy Centering: focus attention Assessment: detection of irregular energy areas (chakras) Unruffing: smoothing at energy field Direction/modulation of energy: energy transfer (change flow) and using visualization and intentionality to redistribute energy flow Integrity of intervention: good |
|
| Outcomes |
Pain outcomes, scale limits, and time points when measured: PIPP 30 seconds post injection Upper limit: 21 Lower limit: 0 High score = more distress Continuous |
|
| Notes |
Adverse reactions: none Funding sources: none reported Key conclusions of study authors: therapeutic touch does not reduce immediate (30 seconds) pain during heel‐stick in infants aged 1 to 15 months |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 1) Randomization (Random Sequence Generation) | Low risk | 2 ‐ A convincing method for generating a random allocation sequence is reported that used an independent person not involved in enrolment or allocation of participants |
| 2) Allocation bias (Allocation concealment) | Low risk | 1 ‐ An adequate method is reported that removes the potential biases of investigators |
| 3a) Blinding of participants and personnel | Low risk | 1 ‐ A convincing effort to reduce bias in outcomes measurement is reported |
| 3b) Blinding of outcome assessment | Unclear risk | None specified |
| 4) Attrition (Incomplete Outcome Data) | Low risk | 2 ‐ Documented evidence that the CONSORT guidelines have been followed |
| 5) Selective outcome reporting (Selective Outcome Reporting) | Low risk | There was no selective outcome reporting |
| 6) Other potential sources of bias (Other potential threats to validity) | Low risk | There were no other potential sources of bias reported |
| 7a) Power calculation (Part 1 of size bias) | Low risk | 1 ‐ Power calculations were conducted a priori |
| 7b) Sufficient sample (part 2 of size bias) | High risk | 0 ‐ A sufficient sample size based on the power calculation was not obtained |
| Total | High risk | Total score on new Cochrane standard: Low risk (7/9), High risk (1/9), Unclear Risk (1/9) |
Kristoffersen 2011.
| Methods |
Study design: Cross‐over Total study duration: 42 months; each study participant was examined over a 3‐week study period |
|
| Participants |
Total number: 24 Setting: the NICU at St. Olav’s University Hospital Diagnostic criteria: infants with a gestational age at time for first intervention (i.e. postmenstrual age or PMA) between 28 and 32 weeks, in stable condition, and at low risk for neurologic sequelae. Infants on a ventilator or those receiving continuous positive airway pressure(CPAP) or opioid treatment were excluded, as were infants with ongoing serious infections. Infants who needed to have their tube inserted by mouth were not included. Age: Minimum: PMA of 28 weeks at first intervention Maximum: PMA of 32 weeks at first intervention Mean: not reported SD: not reported Sex: Males: not reported Females: not reported Country: Norway |
|
| Interventions |
Total number of intervention groups: 5 Control group description: no intervention Total number of participants randomized to each of your groups: intervention #1 = 24; intervention #2 = 24; intervention # 3 = 24; intervention #4 = 24; intervention #5 = 24; control = 24 Specific intervention #1: No pacifier + Sterile water Specific intervention #2: No pacifier + Sucrose 30% Specific intervention #3: Pacifier + No fluid Specific intervention #4: Pacifier + Sterile water Specific intervention #5: Pacifier + Sucrose 30% Integrity of intervention: good |
|
| Outcomes |
Pain outcome, scale limits and time points when measured: PIPP Time points: during nasogastric tube insertion. After 1 minute, and after 5 minutes Upper limit: 21 Lower limit: 0 High score = more pain Continuous |
|
| Notes |
Adverse reactions: none reported Key conclusions of study authors: The intervention that best reduced pain reactivity was a pacifier with sucrose |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 1) Randomization (Random Sequence Generation) | Low risk | 2 ‐ A convincing method for generating a random allocation sequence is reported that used an independent person not involved in enrolment or allocation of participants |
| 2) Allocation bias (Allocation concealment) | Low risk | 1 ‐ An adequate method is reported that removes the potential biases of investigators |
| 3a) Blinding of participants and personnel | High risk | Personnel were not blinded |
| 3b) Blinding of outcome assessment | Unclear risk | None specified |
| 4) Attrition (Incomplete Outcome Data) | Unclear risk | 2 ‐ incomplete data accounted for |
| 5) Selective outcome reporting (Selective Outcome Reporting) | Low risk | There was no selective outcome reporting |
| 6) Other potential sources of bias (Other potential threats to validity) | Low risk | There were no other potential sources of bias reported |
| 7a) Power calculation (Part 1 of size bias) | Low risk | 1 ‐ Power calculations were conducted a priori |
| 7b) Sufficient sample (part 2 of size bias) | Low risk | 0 ‐ A sufficient sample size based on the power calculation was obtained |
| Total | High risk | Total score on new Cochrane standard: Low risk (6/9), High risk (1/9), Unclear Risk (2/9) |
Liaw 2010.
| Methods |
Study design: between groups Total study duration: 9 months |
|
| Participants |
Total number: 104 Setting: NICU in Taiwan Diagnostic criteria: healthy, preterm infants, between 3 and 28 days post birth Age: 27 to 37 weeks Minimum: 3 days Maximum: 19 days Mean: 6.48 days SD: 3.11 days Sex: Males: 54 Females: 50 Country: Taiwan |
|
| Interventions |
Total intervention groups: 1 Control group description: routine comfort (gentle touching) without non‐nutritive sucking Total number of participants randomized to each of your groups: 52 Specific intervention: non‐nutritive sucking Intervention details: pacifier was given to infant to suck before touching the foot to initiate the heelstick Integrity of intervention: satisfactory |
|
| Outcomes |
Pain outcomes, scale limits, and time points when measured: PIPP Every minute for before (for 3 minutes), during, and after (for 10 minutes) the procedure Upper limit: 21 Lower limit: 0 High score = more pain Continuous |
|
| Notes |
Adverse reactions: none reported Funding sources: none reported Key conclusions of study authors: non‐nutritive sucking reduces pain, especially mild to moderate pain and behavioral responses |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 1) Randomization (Random Sequence Generation) | Low risk | 2 ‐ A convincing method for generating a random allocation sequence is reported that used an independent person not involved in enrolment or allocation of participants |
| 2) Allocation bias (Allocation concealment) | Low risk | 1 ‐ An adequate method is reported that removes the potential biases of investigators |
| 3a) Blinding of participants and personnel | Low risk | 1 ‐ A convincing effort to reduce bias in outcomes measurement is reported |
| 3b) Blinding of outcome assessment | High risk | None specified but suspect that coders were not blinded due to sucking. |
| 4) Attrition (Incomplete Outcome Data) | Low risk | 1 ‐ A reasonable account of how attrition was dealt with is given, but no specific reference to CONSORT |
| 5) Selective outcome reporting (Selective Outcome Reporting) | Unclear risk | None specified |
| 6) Other potential sources of bias (Other potential threats to validity) | Unclear risk | None specified |
| 7a) Power calculation (Part 1 of size bias) | Low risk | 1 ‐ Power calculations were conducted a priori |
| 7b) Sufficient sample (part 2 of size bias) | Low risk | 1 ‐ A sufficient sample size based on the power calculation was obtained |
| Total | High risk | Total score on new Cochrane standard: Low risk (6/9), High risk (1/9), Unclear Risk (2/9) |
Liaw 2011.
| Methods |
Study design: Between‐subjects Total study duration: 2007‐2008 |
|
| Participants |
Total number: 165 Setting: neonatal nursery at a medical centre in Taipei Diagnostic criteria: inclusion criteria: 1) gestational age (GA) greater than or equal to 36 weeks; 2) birth weight greater than or equal to 2200g; 3) Apgar score greater than or equal to 7 at the first and fifth minute after birth; 4) underwent IM injection for hepatitis B; and 5) mothers healthy without substance abuse. Exclusion criteria: 1) congenital anomalies, 2) neurological impairment, 3) documented congenital or nosocomial sepsis; 4) surgery; 5) substance‐abusing mother; 6) had been administered sedatives, analgesics, or naloxone; and 7) no need for injection against hepatitis B. Age Minimum: 36.43 weeks Maximum: 42.28 weeks Mean: Control: 39.19, Non‐nutritive Sucking: 39.21, Sucrose: 39.22 SD: Control: 1.25, NNS: 1.27, Sucrose: 1.09 Sex Males: 84 Females: 81 Country: Taiwan |
|
| Interventions |
Total number of intervention groups: 2 Control group description: during injection procedures, infants in the routine care group (control group) received gentle touch and verbal comfort. Total number of participants randomized to each of your groups: 55 Specific intervention #1: Non‐nutritive Sucking (NNS). Intervention details: infants in this group were given a standard silicone newborn pacifier manufactured with natural scent to stimulate sucking two minutes before touching the thigh to initiate the injection procedures. Specific intervention #2: sucrose. Intervention details: infants in the sucrose group were fed 2 mL of 20% sucrose through a syringe two minutes before the injection procedures. Integrity of intervention: good |
|
| Outcomes |
Pain outcomes, time points when measured, and scale limits: NFCS Time points: measured every minute during baseline (T1) and injection procedures (T2), and during recovery at the first (T3), second (T4), third (T5), fourth (T6), and fifth (T7) minutes Upper limit: 48 Lower limit: 0 High score = more intense pain Continuous Cry Duration Time points: seconds from the video recording using a stopwatch from the start of the injection procedures to the fifth minute of recovery Greater/longer cry = greater distress |
|
| Notes |
Adverse reactions: none Key conclusions of study authors: pain caused by intra‐muscular injection procedures, as brief as one minute, was lower after administering NNS or 20% oral sucrose than that after routine care. Using NNS and sucrose also enhanced infants’ physiological stability and shortened their cry duration during injections. Furthermore, administering sucrose two minutes before the injection more effectively reduced newborns’ pain during injection than NNS. Clinicians should incorporate NNS and sucrose into caregiving while newborns undergo painful procedures. These study results add to evidence supporting the use of NNS and sucrose for pain relief in newborns during immunization injection. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 1) Randomization (Random Sequence Generation) | Low risk | 2 ‐ A convincing method for generating a random allocation sequence is reported that used an independent person not involved in enrolment or allocation of participants |
| 2) Allocation bias (Allocation concealment) | Low risk | 1 ‐ An adequate method is reported that removes the potential biases of investigators |
| 3a) Blinding of participants and personnel | High risk | Personnel not totally blinded but suspect could be guessed based on sucking |
| 3b) Blinding of outcome assessment | High risk | Coders not completely blind |
| 4) Attrition (Incomplete Outcome Data) | Low risk | 1 ‐ A reasonable account of how attrition was dealt with is given, but no specific reference to CONSORT |
| 5) Selective outcome reporting (Selective Outcome Reporting) | Low risk | None specified |
| 6) Other potential sources of bias (Other potential threats to validity) | Low risk | None specified |
| 7a) Power calculation (Part 1 of size bias) | Low risk | 1 ‐ Power calculations were conducted a priori |
| 7b) Sufficient sample (part 2 of size bias) | Low risk | 1 ‐ A sufficient sample size based on the power calculation was obtained |
| Total | High risk | Total score on new Cochrane standard: Low risk (7/9), High risk (2/9), Unclear Risk (0/9) |
Liaw 2012.
| Methods |
Study design: Cross‐over Total study duration: infants were recruited from January 2006‐October 2008 |
|
| Participants |
Total number: 34 Setting: Level III Neonatal Intensive Care Unit in Taipai Diagnostic criteria: Inclusion criteria: (1) GA 29 ‐ 37 weeks and postmentrual age 30 ‐ 38.5, (2) postbirth age 3 ‐ 28 days, and (3) stable condition (score < 12 on the Neonatal Therapeutic Intervention Scoring System [NTISS] for disease severity). Exclusion criteria: (1) congenital anomalies, (2) neurologic impairment including convulsion, intraventricular haemorrhage > grade II or periventricular leukomalacia, (3) documented congenital or nosocomial sepsis, (4) surgery, (5) severe growth restriction at birth, (6) substance‐abusing mother, and (7) severe medical conditions requiring treatments such as sedatives, muscle relaxants, antiepileptic, or analgesic drugs. Age: Minimum: actual min and max ages not specified, only the ranges that were part of the inclusion criteria were specified (i.e. GA of 28 ‐ 37 weeks, postmentrual age of 30 ‐ 38.5 weeks, and postbirth age of 3 ‐ 28 days) Maximum: see above under 'minimum' Mean: mean GA of 33.06 wks; mean postmenstrual age of 33.98 weeks; mean age of 7.0 days SD: SD for GA was 2.02 weeks; SD for postmenstrual age 2.0 weeks; SD for age of 5.0 days Sex Males: 18 (53 % of 34) Females: 16 (47% of 34) Country: Taiwan |
|
| Interventions |
Total number of intervention groups: 2 Control group description: routine care: infants were given only gentle touch and verbal comfort. Total number of participants randomized to each of your groups: intervention #1 = 34; intervention #2 = 34; control = 34 Specific intervention #1: non‐nutritive sucking Intervention details: infants were given a standard silicone newborn pacifier to stimulate sucking while touching the foot to initiate heel‐stick procedures. Specific intervention #2: facilitated tucking Intervention details: infants were in a flexed posture and gently held by a nurse’s warm hands without strongly restraining the infant’s body and limb movements, one hand on the infant’s head, and the other on the buttocks. Facilitated tucking was also provided while the physician assistant touched the infant for heel stick Integrity of intervention: good |
|
| Outcomes |
Pain outcomes, time points when measured, and scale limits: PIPP Time points: All measures were standardised from baseline to the 10th minute after heel‐stick procedures. Upper limit: 21 Lower limit: 0 High score = more pain Continuous Modified preterm infant behavioural coding scheme Time points: All measures were standardised from baseline to the 10th minute after heel‐stick procedures. The RA coded the behaviours that occurred in every 10 s interval during the five sessions of heel‐stick procedures. Data were transformed to number of 10 s intervals in which the behavior occurred. Higher frequency of behavior = greater distress |
|
| Notes |
Adverse reactions: none Key conclusions of study authors: both non‐nutritive sucking and facilitated tucking effectively reduced pain scores more than routine care during heel‐stick procedures. Non‐nutritive sucking reduced PIPP pain scores more effectively than facilitated tucking. However, facilitated tucking showed broader effects not only on relieving pain, but also on enhancing infants’ physiological and behavioural stability during heel‐stick procedures. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 1) Randomization (Random Sequence Generation) | Low risk | 2 ‐ A convincing method for generating a random allocation sequence is reported that used an independent person not involved in enrolment or allocation of participants |
| 2) Allocation bias (Allocation concealment) | Unclear risk | lack of information |
| 3a) Blinding of participants and personnel | High risk | Personnel not totally blinded |
| 3b) Blinding of outcome assessment | High risk | Coders not blind |
| 4) Attrition (Incomplete Outcome Data) | Low risk | 1 ‐ A reasonable account of how attrition was dealt with is given |
| 5) Selective outcome reporting (Selective Outcome Reporting) | Low risk | None specified |
| 6) Other potential sources of bias (Other potential threats to validity) | Low risk | None specified |
| 7a) Power calculation (Part 1 of size bias) | Low risk | 1 ‐ Power calculations were conducted a priori |
| 7b) Sufficient sample (part 2 of size bias) | Low risk | 1 ‐ A sufficient sample size based on the power calculation was obtained |
| Total | High risk | Total score on new Cochrane standard: Low risk (6/9), High risk (2/9), Unclear Risk (1/9) |
Liaw 2013.
| Methods |
Study design: Between‐subjects Total study duration: infants were screened from August 2010 until December 2011 |
|
| Participants |
Total number: 110 Setting: Level III Neonatal Intensive Care Unit (NICU) and a neonatal special care unit at a medical centre in Taipei Diagnostic criteria: Inclusion criteria: (1) gestational age (GA) 26 ‐ 37 weeks and postmenstrual age (PMA) 26.4 ‐ 38 weeks, (2) postbirth age 2 ‐ 28 days, and (3) disease condition acceptable for observation (illness severity indicated by the Neonatal Therapeutic Intervention Scoring System [NTISS] score ≤ 22) Exclusion criteria: (1) congenital anomalies, (2) neurologic impairment including convulsion, intraventricular haemorrhage > grade II or periventricular leukomalacia, (3) documented congenital or nosocomial sepsis, (4) surgery, (5) severe growth restriction at birth, (6) substance‐abusing mother, and (7) severe medical conditions requiring treatments such as sedatives, muscle relaxants, antiepileptic, or analgesic drugs. Age: Minimum: no min age stated but GA range is 11 Maximum: no max age stated but GA range is 11 Mean: GA = 32.40 weeks, PMA = 33.29 weeks, Age = 6.45 days SD: GA = 3.14 weeks, PMA = 3.05 weeks, Age = 6.62 days Sex: Males: 54 (49.5%) Females: 56 (50.5%) Country: Taiwan |
|
| Interventions |
Total number of intervention groups: 4 Control group description: Routine care: Infants were given only gentle touch and verbal comfort if they were crying Total number of participants randomized to each of your groups: intervention #1 = 22; intervention #2 = 21; intervention #3 = 21; intervention #4 = 23; control = 23 Intervention Descriptions: Non‐nutritive sucking (NNS): infants were given a standard silicone newborn pacifier to stimulate sucking 1 min before touching the foot to initiate heel‐stick procedures. Oral sucrose: Infants were fed 0.2 ‐ 2.0 mL of 20% sucrose through a syringe 2 minutes before the heel‐stick procedures depending on the infants’ GA (GA 26 ‐ 28 weeks: 0.2 mL; GA 28.1 ‐ 30 weeks: 0.5 mL; GA 30.1 ‐ 32 weeks: 1 mL; GA 32.1 ‐ 37 weeks: 1.5 mL; GA > 37 weeks: 2.0 mL). Facilitated tucking (FT): Infants were in a flexed posture and gently held by the intervener’s warm hands without strongly restraining the infant’s head and body, one hand on the infant’s head, and the other on the trunk. FT was provided while the infant was touched by the senior nurse performing heel sticks Specific intervention #1: NNS‐FT group Specific intervention #2: FT‐Sucrose group Specific intervention #3: NNS‐Sucrose group Specific intervention #4: NNS‐Sucrose‐FT group Integrity of intervention: satisfactory |
|
| Outcomes |
Pain outcomes, time points when measured, and scale limits: Active sleep Time points: data was conducted at 1‐min intervals. All data were collected over four phases: (a) baseline (P1, 30 min without stimuli before heel‐stick procedures); (b) intervention (P2, one of five treatment conditions), (c) heel stick procedures (P3), and (d) recovery (P4, 30 min after P3 from when the research nurse finished collecting blood and left the infant to the 30th minute). Range of possible scores: not reported Transition state Time points: data was conducted at 1‐min intervals. All data were collected over four phases: (a) baseline (P1, 30 min without stimuli before heel‐stick procedures); (b) intervention (P2, one of five treatment conditions), (c) heel stick procedures (P3), and (d) recovery (P4, 30 min after P3 from when the research nurse finished collecting blood and left the infant to the 30th minute). Range of possible scores: not reported Active awake and quiet awake Time points: data was conducted at 1‐min intervals. All data were collected over four phases: (a) baseline (P1, 30 min without stimuli before heel‐stick procedures); (b) intervention (P2, one of five treatment conditions), (c) heel stick procedures (P3), and (d) recovery (P4, 30 min after P3 from when the research nurse finished collecting blood and left the infant to the 30th minute). Range of possible scores: not reported Fussing or crying Time points: data was conducted at 1‐min intervals. All data were collected over four phases: (a) baseline (P1, 30 min without stimuli before heel‐stick procedures); (b) intervention (P2, one of five treatment conditions), (c) heel stick procedures (P3), and (d) recovery (P4, 30 min after P3 from when the research nurse finished collecting blood and left the infant to the 30th minute). Range of possible scores: not reported |
|
| Notes |
Adverse reactions: none Key conclusions of study authors: the four treatment combinations differentially reduced infants’ high arousal across heel‐stick procedures. The combined use of oral sucrose‐tucking, sucking‐oral sucrose, and sucking‐oral sucrose‐tucking more effectively reduced occurrences of infant fussing or crying than routine care. Treatment combinations of sucking‐oral sucrose‐tucking and sucking‐oral sucrose also better facilitated infants’ sleep than routine care. To preserve infants’ sleep, clinicians should use combinations of non‐nutritive sucking, oral sucrose, and facilitated tucking to reduce agitation during painful procedures. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 1) Randomization (Random Sequence Generation) | Low risk | 2 ‐ A convincing method for generating a random allocation sequence is reported that used an independent person not involved in enrolment or allocation of participants |
| 2) Allocation bias (Allocation concealment) | Unclear risk | Lack of information |
| 3a) Blinding of participants and personnel | High risk | Personnel not totally blinded |
| 3b) Blinding of outcome assessment | High risk | Coders not blind |
| 4) Attrition (Incomplete Outcome Data) | Low risk | 1 ‐ A reasonable account of how attrition was dealt with is given |
| 5) Selective outcome reporting (Selective Outcome Reporting) | Unclear risk | None specified |
| 6) Other potential sources of bias (Other potential threats to validity) | Low risk | None specified |
| 7a) Power calculation (Part 1 of size bias) | Low risk | 1 ‐ Power calculations were conducted a priori |
| 7b) Sufficient sample (part 2 of size bias) | Low risk | 1 ‐ A sufficient sample size based on the power calculation was obtained |
| Total | High risk | Total score on new Cochrane standard: Low risk (5/9), High risk (2/9), Unclear Risk (2/9) |
Liu 2010.
| Methods |
Study design: randomized control trial, between groups (parallel‐group controlled trial) Total study duration: 5 months (June to October 2006) |
|
| Participants |
Total number: 105 Setting: newborn special care nursery and in a newborn baby room of a teaching hospital in northern Taiwan Diagnostic criteria: neonates were greater than or equal to 32 weeks gestational age, medically stable, scheduled to undergo a newborn screening procedure within 24 hours to 7 days, Apgar scores greater than 7 at 1 and 5 minutes, with no crying in the 5 minutes pre‐venipuncture Age: Minimum: unknown Maximum: unknown Mean: 3.03 days SD: 1.06 days Sex: Males: 48 Females: 57 Country: Taiwan |
|
| Interventions |
Total intervention groups: 1 Control group description: no intervention provided prior to venipuncture. Infants were taken to a quiet, individual room and placed on a heated radial warmer, naked except for their diaper. Infants were observed for 2 minutes to collect baseline data. Total number of participants randomized to each of your groups: 35 in each group (70 in total) Specific intervention: non‐nutritive sucking Intervention details: each neonate was assisted to suck on a pacifier for 2 minutes pre‐sterilization. The pacifier was continuously provided until 2 minutes post needle. Integrity of intervention: good |
|
| Outcomes |
Pain outcomes, scale limits, and time points when measured: NIPS Coded at 1‐minute intervals for 2 minutes in preparation, venipuncture, and recovery phases Upper limit: 7 Lower limit: 0 High score = more pain Continuous |
|
| Notes |
Adverse reactions: none reported Funding sources: no financial sources that might pose a conflict of interest declared Key conclusions of study authors: non‐nutritive sucking can effectively decrease the level of pain |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 1) Randomization (Random Sequence Generation) | Low risk | 2 ‐ A convincing method for generating a random allocation sequence is reported that used an independent person not involved in enrolment or allocation of participants |
| 2) Allocation bias (Allocation concealment) | Low risk | 1 ‐ An adequate method is reported that removes the potential biases of investigators |
| 3a) Blinding of participants and personnel | Low risk | 1 ‐ A convincing effort to reduce bias in outcomes measurement is reported |
| 3b) Blinding of outcome assessment | Low risk | Coders were blind |
| 4) Attrition (Incomplete Outcome Data) | High risk | 0 ‐ There is no documented evidence or insufficient evidence reported of how attrition was dealt with |
| 5) Selective outcome reporting (Selective Outcome Reporting) | Low risk | None specified |
| 6) Other potential sources of bias (Other potential threats to validity) | Low risk | None specified |
| 7a) Power calculation (Part 1 of size bias) | Low risk | 1 ‐ Power calculations were conducted a priori |
| 7b) Sufficient sample (part 2 of size bias) | Low risk | 1 ‐ A sufficient sample size based on the power calculation was obtained |
| Total | High risk | Total score on new Cochrane standard: Low risk (8/9), High risk (1/9), Unclear Risk (0/9) |
Mirzarahimi 2013.
| Methods |
Study design: between‐groups Total study duration: N/A |
|
| Participants |
Total number: 90 Setting: NICU in Alavi hospital at Ardebil Diagnostic criteria: healthy full‐term neonates Age: Minimum: 3 days Maximum: 7 days Mean: N/A SD: N/A Sex: Males: 54 Females: 36 Country: Iran |
|
| Interventions |
Total number of intervention groups: 2 Control group description: "received no intervention" Total number of participants randomized to each of your groups: intervention #1 = 30; intervention # 2 = 30; control = 30 Intervention descriptions: Specific intervention #1: NNS – researcher gave each neonate a standard small, short, hollow soft latex nipple while applying gentle pressure to maintain it in the neonate’s mouth. Specific intervention #2: Massage – two minutes before the heel stick, one of the investigators slowly massaged the outer aspect of the leg chosen for the heel stick from toes to mid thigh by using a firm but gentle pressure by fingers and thumbs. The massage pressure was adjusted to keep the baby comfortable. At the end of the massage intervention (2 min), the heel was wrapped in a warm cloth for 1 min. An assistant nurse performed the heel stick using a lancet. Integrity of intervention: good |
|
| Outcomes |
Pain outcomes, time points when measured, and scale limits: PIPP Time points: did not indicate timing of pain outcome, but seems it was during heel stick Range of possible scores: 0 (no pain) to 21 (maximum pain) – max. value in this study was 18 (still reflecting greater pain) |
|
| Notes |
Adverse reactions: none reported Key conclusions of study authors: single or combined use of massage and a pacifier is effective in reducing pain response in neonates undergoing heel stick. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 1) Randomization (Random Sequence Generation) | Unclear risk | Insufficient information |
| 2) Allocation bias (Allocation concealment) | Unclear risk | Insufficient information |
| 3a) Blinding of participants and personnel | Unclear risk | Insufficient information |
| 3b) Blinding of outcome assessment | Unclear risk | Insufficient information |
| 4) Attrition (Incomplete Outcome Data) | Low risk | No incomplete outcome data, p.77 |
| 5) Selective outcome reporting (Selective Outcome Reporting) | Unclear risk | There was no selective outcome reporting |
| 6) Other potential sources of bias (Other potential threats to validity) | Low risk | Did not report other potential sources of bias |
| 7a) Power calculation (Part 1 of size bias) | High risk | Did not report power calculation |
| 7b) Sufficient sample (part 2 of size bias) | High risk | Did not report sufficient sample size |
| Total | High risk | Total score on new Cochrane standard: Low risk (2/9), High risk (2/9), Unclear Risk (5/9) |
Morrow 2010.
| Methods |
Study design: Between‐groups Total study duration: 3 months (February to April 2008) |
|
| Participants |
Total number: 42 Setting: tertiary hospital serving a major metropolitan area Diagnostic criteria: infants scoring in the high‐intermediate or high‐risk zone by TcB (Transcutaneous Bilirubin) measurement receiving a total serum bilirubin (TSB) evaluation; full‐term neonates Age: greater than or equal to 37 weeks gestation Minimum: not reported Maximum: not reported Mean: 39.13 weeks gestation SD: 1.84 days Sex: Males: 18 Females: 21 Note: Note: The authors reported that 42 participants were included but only reported on sex for 39 participants. Country: USA |
|
| Interventions |
Total intervention groups: 1 Control group description: infants were placed in a standard position (supine while lying in a crib) during a sample collection. The crib was elevated to a 30 degree angle and the leg was elevated during the heel lance. Total number of participants randomized to each of your groups: Intervention:22, Control:20 Specific intervention: swaddling and holding upright Intervention details: infants were swaddled and held upright at a 90 degree angle, with one leg exposed Integrity of intervention: satisfactory |
|
| Outcomes |
Pain outcomes, scale limits, and time points when measured: NIPS Coded immediately after heel lance Upper limit: 7 Lower limit: 0 High score = more pain Continuous |
|
| Notes |
Adverse reactions: none reported Funding sources: no funding sources. Key conclusions of study authors: swaddling infants while holding them in an upright position was superior for pain relief during heel lance procedures when compared with a standard position technique |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 1) Randomization (Random Sequence Generation) | Low risk | 1 ‐ A convincing method of randomization is reported but this did not involve an independent person |
| 2) Allocation bias (Allocation concealment) | High risk | 0 ‐ There is not an adequate description of attempts to deal with potential allocation bias |
| 3a) Blinding of participants and personnel | High risk | Nurses were not blinded |
| 3b) Blinding of outcome assessment | Unclear risk | not specified |
| 4) Attrition (Incomplete Outcome Data) | Low risk | 1 ‐ A reasonable account of how attrition was dealt with is given, but no specific reference to CONSORT |
| 5) Selective outcome reporting (Selective Outcome Reporting) | Low risk | None specified |
| 6) Other potential sources of bias (Other potential threats to validity) | Low risk | None specified |
| 7a) Power calculation (Part 1 of size bias) | Low risk | 1 ‐ Power calculations were conducted a priori |
| 7b) Sufficient sample (part 2 of size bias) | Low risk | 1 ‐ A sufficient sample size based on the power calculation was obtained |
| Total | High risk | Total score on new Cochrane standard: Low risk (6/9), High risk (2/9), Unclear Risk (1/9) |
Park 2006.
| Methods | Study design: Between‐subjects Study duration: Not available |
|
| Participants |
Total number: 32 Setting: In‐hospital setting Diagnostic criteria: Not available Age: Not available Minimum: Not available Maximum: Not available Mean: Not available SD: Not available Sex: Males: Not available Females: Not available Country: Korea |
|
| Interventions |
Total intervention groups: 1 Control group description: Not available Total number of participants randomized to each of your groups: Intervention:16, Control:16 Specific intervention: Touch/massage‐related Intervention details: Not available Integrity of intervention: Not available |
|
| Outcomes |
Pain outcomes, scale limits, and time points when measured: NIPS Coded 5 minutes after heel‐stick Upper limit: 7 Lower limit: 0 High score = more pain Continuous |
|
| Notes |
Adverse reactions: Not availale Funding sources: Not available Key conclusions of study authors: touch/massage‐related intervention reduced pain more than the control condition |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 1) Randomization (Random Sequence Generation) | Unclear risk | Information unknown as only abstract was extracted. |
| 2) Allocation bias (Allocation concealment) | Unclear risk | Information unknown as only abstract was extracted. |
| 3a) Blinding of participants and personnel | Unclear risk | Information unknown as only abstract was extracted. |
| 3b) Blinding of outcome assessment | Unclear risk | Information unknown as only abstract was extracted. |
| 4) Attrition (Incomplete Outcome Data) | Unclear risk | Information unknown as only abstract was extracted. |
| 5) Selective outcome reporting (Selective Outcome Reporting) | Unclear risk | Information unknown as only abstract was extracted. |
| 6) Other potential sources of bias (Other potential threats to validity) | Unclear risk | Information unknown as only abstract was extracted. |
| 7a) Power calculation (Part 1 of size bias) | Unclear risk | Information unknown as only abstract was extracted. |
| 7b) Sufficient sample (part 2 of size bias) | Unclear risk | Information unknown as only abstract was extracted. |
| Total | Unclear risk | Information unknown as only abstract was extracted. |
Sadathosseini 2013.
| Methods |
Study design: between groups Total study duration: 8 weeks to put together sample size |
|
| Participants |
Total number: 135 Setting: Bahrami Children Hospital Diagnostic criteria: healthy Age: Minimum: N/A Maximum: N/A Mean: 5.04 days (familiar scent), 5 days (unfamiliar scent), 5.09 (control), overall mean= 5.05 SD: 1.20 (familiar scent), 1.11 (unfamiliar scent), 5.09 (control), overall SD= 1.18 Sex: Males: 23 (familiar), 21 (unfamiliar), 20 (control), total = 64 Females: 22 (familiar), 24 (unfamiliar), 25 (control), Totalv= 71 Country: Iran |
|
| Interventions |
Total number of intervention groups: 2 Control group description: "No scent was given to the control group" Total number of participants randomized to each of your groups: intervention #1 = 45; intervention #2 = 45; control = 45 Intervention Descriptions: Specific intervention #1: familiar scent: familiarization was performed the night before blood sampling and neonates were exposed to the vanillin scent during the painful procedure. The vanillin solution on the pad was placed near the neonate's head. The next morning, the scented gauze was removed for an average familiarization of 8.65 hours. After 2 minutes, a sterile gauze pad perfumed with ten drops of the vanillin solution was held 1 cm from the neonate's nose without contact. Specific intervention #2: unfamiliar scent: after 2 minutes, a sterile gauze pad perfumed with ten drops of the vanillin solution was held 1 cm from the neonate's nose without contact Integrity of intervention: good |
|
| Outcomes |
Pain outcomes, time points when measured, and scale limits: Cry Duration Time points: Infant cry was recorded from onset after needle insertion until a cessation for 5 seconds, up to a maximum of 1 minute after removing the needle Range of possible scores: 0 to 60 seconds |
|
| Notes |
Adverse reactions: none reported Key conclusions of study authors: stimulating neonates with a familiar scent reduced cry duration compared to other groups. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 1) Randomization (Random Sequence Generation) | Low risk | “Sampling was done only for one group during each week, with groups being randomly selected… On the first day, the name of each group was written on a separate piece of paper, which was enclosed in an envelope, and an independent nurse who worked in the clinical context and was unaware of purpose of the study picked up one envelope randomly as the first group. Then selection was performed the same way for the second group, and the remaining envelope was considered the third group. During each week, eligible cases were recognized and selected by convenience sampling only for one group, and groups were replaced respectively (e.g. first week, unfamiliar scent group; second week, familiar…” Page e197, last paragraph of second column into page e198 |
| 2) Allocation bias (Allocation concealment) | Low risk | See above |
| 3a) Blinding of participants and personnel | Low risk | “… the researcher who performed familiarization and olfactory stimulation was the only person who had knowledge of group assignments” Page e199, 2nd paragraph of 1st column |
| 3b) Blinding of outcome assessment | Low risk | “… the researcher who performed familiarization and olfactory stimulation was the only person who had knowledge of group assignments” Page e199, 2nd paragraph of 1st column |
| 4) Attrition (Incomplete Outcome Data) | Unclear risk | Study did not address this outcome |
| 5) Selective outcome reporting (Selective Outcome Reporting) | Low risk | Reports all expected and pre‐specified outcomes |
| 6) Other potential sources of bias (Other potential threats to validity) | Unclear risk | “Also neonates were excuded if they were not calm before data collection" |
| 7a) Power calculation (Part 1 of size bias) | Low risk | Based on the mean and standard deviation of the neonates’ duration of crying obtained from an earlier study (Goubet et al., 2007) and a = 0.05, b = 0.2, certainty coefficient of 95% and power of 80%, we estimated a sample size of 40 individuals per group" (paragraph 5, page e197). |
| 7b) Sufficient sample (part 2 of size bias) | Low risk | Sufficient sample size addressed by the power calculation |
| Total | Low risk | Total score on new Cochrane standard: Low risk (7/9), High risk (0/9), Unclear Risk (2/9) |
Shaw 1982.
| Methods |
Study design: between groups Total study duration: not reported |
|
| Participants |
Total number: 20 Setting: office of pediatricians in private practice Diagnostic criteria: healthy Age: Minimum: 18 months Maximum: 26 months Mean: 18.7 months SD: N/A Sex: Males: 13 Females: 7 Country: USA |
|
| Interventions |
Total number of intervention groups: 1 Control group description: mother absent: the child was placed in a supine position and, with the parent (in the mother‐present group) or one of the behavior coders (in the mother‐absent group) holding the child's hands, was given the DPT injection in the thigh by the nurse. Children in the mother‐absent group were picked up by the nurse and taken to the waiting room where they were reunited with their mother. Total number of participants randomized to each of your groups: intervention = 10; control = 10 Intervention descriptions: Mother present: the child was placed in a supine position and, with the parent (in the mother‐present group) or one of the behavior coders (in the mother‐absent group) holding the child's hands, was given the DPT injection in the thigh by the nurse. Children in the mother‐present group were immediately picked up by their mothers. Integrity of intervention: good |
|
| Outcomes |
Pain outcomes, time points when measured, and scale limits: Modified Frankl Scale/Crying Duration Time points: the tally sheets used by the behavior coders divided each part of the examination time into 20‐second intervals. The coders recorded, for each interval, the presence of each of the following behaviors Range of possible scores: N/A |
|
| Notes |
Adverse reactions: none reported Key conclusions of study authors: during the immunization, those in the mother‐present condition behaviour was rated as significantly more negative than the mother absent group. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 1) Randomization (Random Sequence Generation) | Unclear risk | No report of randomization |
| 2) Allocation bias (Allocation concealment) | Unclear risk | No report of allocation bias |
| 3a) Blinding of participants and personnel | High risk | No way of blinding this if the mother is absent or present |
| 3b) Blinding of outcome assessment | High risk | No way of blinding this |
| 4) Attrition (Incomplete Outcome Data) | High risk | 10 additional participants were recruited and then never reported on. |
| 5) Selective outcome reporting (Selective Outcome Reporting) | Low risk | There was no selective outcome reporting |
| 6) Other potential sources of bias (Other potential threats to validity) | Low risk | There were no other potential sources of bias reported |
| 7a) Power calculation (Part 1 of size bias) | High risk | Power calculations were not conducted a priori |
| 7b) Sufficient sample (part 2 of size bias) | High risk | A sufficient sample size based on the power calculation was not obtained |
| Total | High risk | Total score on new Cochrane standard: Low risk (2/9), High risk (5/9), Unclear Risk (2/9) |
Shu 2014.
| Methods |
Study design: between subjects Total study duration: July 2009 ‐ December 2010 |
|
| Participants |
Total number: 75 Setting: District hospital in Taiwan Diagnostic criteria: healthy neonates (Apgar scores >7) Age: Minimum: N/A Maximum: N/A Mean: 266.80 days gestation (Control), 269.20 days gestation (Swaddling), 269.60 days gestation (Heel Warming), overall mean = 238.53 SD:15.93 (Contol), 10.86 (Swaddling), 10.43 (Heel Warming), overall SD = 12.41 Sex: Males: 12 (Control), 17 (Swaddling), 11 (Heel Warming), Total = 40 Females: 13 (Control), 8 (Swaddling), 14 (Heel Warming), Total = 35 Country: Taiwan |
|
| Interventions |
Total number of intervention groups: 2 Control group description: Routine care: placed in a supine position while lying inside a crib and left without intervention for 30 minutes before performing heel stick Total number of participants randomized to each of your groups: intervention #1 = 25; intervention #2 = 25; control = 25 Intervention descriptions: Specific intervention #1: Swaddling: neonates were placed face up on a 90 cm blanket. The arms of the neonates were placed close to their torso with both hands clasped. The upper and lower ends of the wrap were kept open, and the upper rim was aligned with the shoulder of the neonate. The horizontal ends of the wrap were folded in opposite directions to cover the torso. An appropriate space was retained at the foot of the wrap before folding it upward to the front, completing the swaddle Specific intervention #2: Heel Warming: superficial heat between 40 ‐ 45 degrees C increases the blood flow. The effects of heat on skin temperature increased rapidly during the first four minutes. We put water at 40 degrees C in a thermal bag and applied the bag against the puncture point for 5 minutes. Integrity of intervention: Good |
|
| Outcomes |
Pain outcomes, time points when measured, and scale limits: NIPS Time points: measured immediately after Range of possible scores: 0‐7, with high scores indicating higher pain reactivity Cry Duration Time points: started measuring from the first cry immediately after heel stick to the moment the crying stopped Range of possible scores: not reported |
|
| Notes |
Adverse reactions: none reported Key conclusions of study authors: swaddling and heel warming reduce the pain response of neonates during the heel stick procedure ‐ heel warming resulted in lower pain response than swaddling during pain recovery |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 1) Randomization (Random Sequence Generation) | Unclear risk | Did not specify |
| 2) Allocation bias (Allocation concealment) | Unclear risk | Did not specify |
| 3a) Blinding of participants and personnel | Unclear risk | Did not specify |
| 3b) Blinding of outcome assessment | Unclear risk | Did not specify |
| 4) Attrition (Incomplete Outcome Data) | Low risk | Depicted in Figure 1 on page 3109 |
| 5) Selective outcome reporting (Selective Outcome Reporting) | Low risk | Report included all expected and pre‐specified outcomes |
| 6) Other potential sources of bias (Other potential threats to validity) | Low risk | No evidence of other sources of bias. |
| 7a) Power calculation (Part 1 of size bias) | High risk | No a‐priori power calculation |
| 7b) Sufficient sample (part 2 of size bias) | High risk | No a‐priori power calculation; therefore not a sufficient sample size |
| Total | High risk | Total score on new Cochrane standard: Low risk (3/9), High risk (2/9), Unclear Risk (4/9) |
Sizun 2002.
| Methods |
Study design: Cross‐over Total study duration: unknown |
|
| Participants |
Total number: 19 Setting: hospital NICU Diagnostic criteria: preterm neonates, younger than 32 weeks Age: Minimum: unknown Maximum: unknown Mean: 29 weeks SD: 1.8 weeks Sex: Males: 10 Females: 9 Country: France |
|
| Interventions |
Total number of intervention groups: 1 Control group description: no protection from light, supine, no supportive bedding, no individualized attention Total number of participants randomized to each of your groups: 19 Specific intervention #1: developmental care Intervention details: decreased light, decreased noise, lateral posture, feet contacting supportive bedding, opportunities for grasping, offered motor support by hard swaddling, grasping, support for state transition Integrity of intervention: satisfactory |
|
| Outcomes |
Pain outcomes, scale limits, and time points when measured: PIPP Immediate Upper limit: 21 Lower limit: 0 Higher score = more pain Continuous |
|
| Notes |
Adverse reactions: none Funding sources: PHRC 1998 grant Key conclusions of study authors: developmental care works on reactivity |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 1) Randomization (Random Sequence Generation) | Unclear risk | 0 ‐ Randomization is mentioned but there is not an adequate description of the methods used |
| 2) Allocation bias (Allocation concealment) | Unclear risk | 0 ‐ There is not an adequate description of attempts to deal with potential allocation bias |
| 3a) Blinding of participants and personnel | Unclear risk | 0 ‐ Efforts to reduce measurement bias are not reported or are insufficient, e.g. outcomes collected by therapist |
| 3b) Blinding of outcome assessment | Unclear risk | none specified |
| 4) Attrition (Incomplete Outcome Data) | High risk | 0 ‐ There is no documented evidence or insufficient evidence reported of how attrition was dealt with |
| 5) Selective outcome reporting (Selective Outcome Reporting) | Low risk | There was no selective outcome reporting |
| 6) Other potential sources of bias (Other potential threats to validity) | Low risk | There were no other potential sources of bias reported |
| 7a) Power calculation (Part 1 of size bias) | Low risk | 1 ‐ Power calculations were conducted a priori |
| 7b) Sufficient sample (part 2 of size bias) | Low risk | 1 ‐ A sufficient sample size based on the power calculation was obtained |
| Total | High risk | Total score on new Cochrane standard: Low risk (4/9), High risk (1/9), Unclear Risk (4/9) |
Stevens 1999.
| Methods |
Study design: Cross‐over Total study duration: 15 months |
|
| Participants |
Total number: 122 Setting: NICU Diagnostic criteria: preterm infants Age: Minimum: 27 weeks Maximum: 31 weeks Mean: 28.6 weeks SD: 0.15 weeks Sex: Males: 70 males Females: 52 females Country: Canada Co‐morbidity: none Socio‐demographics: not reported Ethnicity: 78 white, 12 black, 17 Hispanic, 15 Asian |
|
| Interventions |
Total number of intervention groups: 2 Control group description: in a Snuggle‐Up device for 30 minutes prior to heel lance procedure. Infant was side‐lying or in the supine position in the Snuggle‐Up. Total number of participants randomized to each of your groups: 122 Specific intervention #1: prone positioning Intervention details: infants were positioned prone in Snuggle‐Up, with knees flexed, arms in, arms close to midline and left foot free Integrity of intervention: good Specific Intervention #2: pacifier with water Intervention details: infants were given a pacifier dipped in water and positioned in Snuggle‐Up for 7 minutes pre lance Integrity of intervention: good |
|
| Outcomes |
Pain outcomes, time points when measured, and scale limits: PIPP Immediately (stick 15 seconds) 5 minutes after Upper limit: 21 Lower limit: 0 High score = more pain Continuous |
|
| Notes |
Adverse reactions: none Funding sources: NIH, NINR, NIHPCRC Key conclusions of study authors: pacifier with water was the most effective method in reducing pain |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 1) Randomization (Random Sequence Generation) | Low risk | 2 ‐ A convincing method for generating a random allocation sequence is reported that used an independent person not involved in enrolment or allocation of participants |
| 2) Allocation bias (Allocation concealment) | High risk | 0 ‐ There is not an adequate description of attempts to deal with potential allocation bias |
| 3a) Blinding of participants and personnel | Unclear risk | 0 ‐ Efforts to reduce measurement bias are not reported or are insufficient, e.g. outcomes collected by therapist |
| 3b) Blinding of outcome assessment | Unclear risk | none specified |
| 4) Attrition (Incomplete Outcome Data) | Low risk | 1 ‐ A reasonable account of how attrition was dealt with is given, but no specific reference to CONSORT |
| 5) Selective outcome reporting (Selective Outcome Reporting) | Low risk | There was no selective outcome reporting |
| 6) Other potential sources of bias (Other potential threats to validity) | Low risk | There were no other potential sources of bias reported |
| 7a) Power calculation (Part 1 of size bias) | High risk | 0 ‐ Power calculations were not conducted a priori |
| 7b) Sufficient sample (part 2 of size bias) | Low risk | 1 ‐ A sufficient sample size based on the power calculation was obtained |
| Total | High risk | Total score on new Cochrane standard: Low risk (5/9), High risk (2/9), Unclear Risk (2/9) |
Sundaram 2013.
| Methods |
Study design: Cross‐over Total study duration: less than 1 month |
|
| Participants |
Total number: 20 Setting: NICU Diagnostic criteria: Preterm newborns of both sexes between 28 and 36 weeks of GA who were breathing unassisted, not receiving paralytic, analgesic, or sedative medications within 48 hours, without major congenital anomalies, not suffering from Grade III or IV intraventricular hemorrhage (IVH) or subsequent periventricular leukomalacia (PVH), had not undergone any surgery from a Level – II NICU of a tertiary care hospital through purposive sampling, and from whom parental consent (approved by the institution) was obtained after explaining the purpose and procedure of the study. Age: Minimum: 28 weeks Maximum: > 36 weeks gestation Mean: 34.11 weeks gestation; 7.75 days SD: 2.29 weeks gestation; 7.72 days Sex: Males: 11 Females: 9 Country: India |
|
| Interventions |
Total number of intervention groups: 1 Control group description: Standard care Total number of participants randomized to each of your groups: 20 Specific intervention: facilitated tucking Intervention details: described as holding the infant by placing a hand on his or her hands and feet, positioning them in a flexed midline position while in either a side‐lying, supine, or prone position Integrity of intervention: good |
|
| Outcomes |
Pain outcomes, time points when measured, and scale limits: PIPP Time points: 30, 60, 90 ,120 secs post heel stick Upper limit: 21 Lower limit: 0 High score = more pain Continuous |
|
| Notes |
Adverse reactions: none Key conclusions of study authors: facilitated tucking is an effective non‐pharmacological pain management in preterm newborns during routine neonatal intensive care. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 1) Randomization (Random Sequence Generation) | Low risk | 2 ‐ A convincing method for generating a random allocation sequence is reported that used an independent person not involved in enrolment or allocation of participants |
| 2) Allocation bias (Allocation concealment) | Low risk | There is adequate description of attempts to deal with potential allocation bias |
| 3a) Blinding of participants and personnel | Unclear risk | Not specified |
| 3b) Blinding of outcome assessment | Low risk | Coders were blind |
| 4) Attrition (Incomplete Outcome Data) | Unclear risk | 1 ‐ participants that had missing data were simply eliminated from the analyses |
| 5) Selective outcome reporting (Selective Outcome Reporting) | Low risk | There was no selective outcome reporting |
| 6) Other potential sources of bias (Other potential threats to validity) | Low risk | There were no other potential sources of bias reported |
| 7a) Power calculation (Part 1 of size bias) | High risk | 0 ‐ Power calculations were not conducted a priori |
| 7b) Sufficient sample (part 2 of size bias) | Low risk | 1 ‐ A sufficient sample size was obtained as an effect was detected |
| Total | Low risk | Total score on new Cochrane standard: Low risk (6/9), High risk (2/9), Unclear Risk (1/9) |
Taddio 2015.
| Methods |
Study design: Between‐subjects Total study duration: N/A |
|
| Participants |
Total number: 160 Setting: St. Michael’s Hospital, Toronto, ON Diagnostic criteria: healthy Age: Mean: 75 days (Parent education), 81 days (Control), Overall Mean = 78 SD: 28 (Parent education), 29 (Control), Overall SD = 28.5 Sex: Males: 40 (Parent education), 48 (Control), Total = 88 Females: 40 (Parent education), 32 (Control), Total = 72 Country: Canada |
|
| Interventions |
Total number of intervention groups: 1 Control group description: parents in the control group received general information on the diseases infant immunizations protect against adopted from the Toronto Public Health website. Total number of participants randomized to each of your groups: intervention #1 = 80; control = 80 Intervention Description: Parent Education: parents in the intervention group received information on how they can comfort their infants during immunizations in the form of written and video information. Integrity of intervention: good |
|
| Outcomes |
Pain outcomes, time points when measured, and scale limits: MBPS Time points: 15 seconds post‐needle Range of possible scores: 0 – 10 (Higher numbers, greater pain) Cry Time Time points: 120 seconds post‐needle Range of possible scores: 0 – 120 seconds |
|
| Notes |
Adverse reactions: none reported Key conclusions of study authors: parent education can reduce pain regulation in children during immunizations and parents should be taught about non‐pharm strategies. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 1) Randomization (Random Sequence Generation) | Low risk | Using a computer random number generator, a research assistant (RA) uninvolved with the study retrieved a randomization code for the 4 participating physician practices from the study statistician– 1⁄2 in control and 1⁄2 in intervention group. |
| 2) Allocation bias (Allocation concealment) | Low risk | Didn’t need this as it was a cluster trials |
| 3a) Blinding of participants and personnel | High risk | “The members of the clinical staff and the candidate involved with recruitment, education, and follow‐up could not be blinded to treatment allocation due to the nature of the intervention”; “Parents were blinded to their group allocation” |
| 3b) Blinding of outcome assessment | Low risk | “The trained RAs that scored strategy utilization, pain, and interactions were blinded to the purpose of the study and the treatment allocation. Study personnel collecting data and clinicians were instructed to ensure that any indication of group allocation is not captured during the video recording so as to maintain concealment of treatment allocation.” |
| 4) Attrition (Incomplete Outcome Data) | Low risk | Depicted in Figure 5 |
| 5) Selective outcome reporting (Selective Outcome Reporting) | Low risk | No selective outcome reporting. |
| 6) Other potential sources of bias (Other potential threats to validity) | Low risk | No evidence of other potential sources of bias. |
| 7a) Power calculation (Part 1 of size bias) | Low risk | 1 ‐ Power calculations were conducted a priori |
| 7b) Sufficient sample (part 2 of size bias) | Low risk | 1 ‐ A sufficient sample size based on the power calculation was obtained |
| Total | High risk | Total score on new Cochrane standard: Low risk (8/9), High risk (1/9), Unclear Risk (0/9) |
Ward‐Larson 2004.
| Methods |
Study design: Cross‐over Total study duration: not noted |
|
| Participants |
Total number: 40 Setting: NICU Diagnostic criteria: very preterm infants Age: Minimum: 23 weeks Maximum: 32 weeks Mean: 27.313 weeks SD: 2.430 weeks Sex: Males: 22 Females: 18 Country: USA Co‐morbidity: none Socio‐demographics: none listed Ethnicity: 23 African American, 16 Caucasian, 1 Hispanic |
|
| Interventions |
Total number of intervention groups: 1 Control group description: infants were put in a Snuggle‐Up (provides containment). No hands were on the infants. Total number of participants randomized to each of your groups: 40 Specific intervention: facilitated tucking Intervention details: infants were put in a Snuggle‐Up and turned to their sides. Their backs were curled gently, legs flexed at a 90 degree angle and their shoulders were brought to midline. They remained like this for suctioning and for 30 seconds after. There was a 2‐ to 4‐hour washout period between procedures. Integrity of intervention: good |
|
| Outcomes |
Pain outcomes, time points when measured, and scale limits: PIPP Measured for 30 seconds after suctioning Upper limit: 21 Lower limit: 0 High score = more pain Continuous |
|
| Notes |
Adverse reactions: none Funding sources: not mentioned Key conclusions of study authors: facilitated tucking works |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 1) Randomization (Random Sequence Generation) | High risk | 0 ‐ Randomization is mentioned but there is not an adequate description of the methods used |
| 2) Allocation bias (Allocation concealment) | High risk | 0 ‐ There is not an adequate description of attempts to deal with potential allocation bias |
| 3a) Blinding of participants and personnel | Unclear risk | 0 ‐ Efforts to reduce measurement bias are not reported or are insufficient, e.g. outcomes collected by therapist |
| 3b) Blinding of outcome assessment | Unclear risk | none specified |
| 4) Attrition (Incomplete Outcome Data) | Low risk | 1 ‐ A reasonable account of how attrition was dealt with is given, but no specific reference to CONSORT |
| 5) Selective outcome reporting (Selective Outcome Reporting) | Low risk | There was no selective outcome reporting |
| 6) Other potential sources of bias (Other potential threats to validity) | Unclear risk | Investigator did the coding |
| 7a) Power calculation (Part 1 of size bias) | Low risk | 1 ‐ Power calculations were conducted a priori |
| 7b) Sufficient sample (part 2 of size bias) | Low risk | 1 ‐ A sufficient sample size based on the power calculation was obtained |
| Total | High risk | Total score on new Cochrane standard: Low risk (4/9), High risk (2/9), Unclear Risk (3/9) |
Whipple 2004.
| Methods |
Study design: between groups Total study duration: unknown |
|
| Participants |
Total number: 60 Setting: NICU‐SCN Level III of Hospital in Atlanta, Georgia Diagnostic criteria: low birth weight (< 2500 g), hospitalized in NICU, preterm Age: Minimum: 24.43 weeks Maximum: 35.43 weeks Mean: 31.17 weeks SD: not reported for whole sample Sex: Males: 30 Females: 30 Country: USA |
|
| Interventions |
Total number of intervention groups: 2 Control group description: no contact, infants were not provided with a pacifier or music listening opportunities at any point during heelstick procedure. Standard care and pain management procedures (such as swaddling, cuddling, and sucrose) were not limited to infants of any of the groups. Total number of participants randomized to each of your groups: 20 in each group (total of 60) Specific intervention #1: Sondrez PAL system‐music contingent on sucking Intervention details: intervention began 3 minutes prior to heelstick and continued throughout the procedure until approximately 3 minutes after blood collection. PAL played a lullaby contingent on the sucking of the infant. Integrity of Intervention: satisfactory Specific intervention #2: pacifier provided, no music Intervention details: same procedures as the intervention #1, except that the infants did not receive music reinforcement for sucking Integrity of intervention: satisfactory |
|
| Outcomes |
Pain outcomes, scale limits, and time points when measured: Behavioral state (scored based on the "Assessment of Premature Infant's Behavior") 1 second intervals and 1 minute pre needle, last minute pre needle, 1 minute during needle, 1 minute post needle, last minute post needle Upper limit: 254 Lower limit: 15 High score = high pain Continuous Stress level 1 second intervals and 1 minute pre‐needle, last minute pre‐needle, 1 minute during needle, 1 minute post needle, last minute post needle Upper limit: 837 Lower limit: 54 High score = high pain Continuous |
|
| Notes |
Adverse reactions: none Funding sources: none mentioned Key conclusions of study authors: music reinforced NNS, effectively lowers behavioral states and stress levels in low birthweight, preterm infants undergoing heelstick |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 1) Randomization (Random Sequence Generation) | High risk | 0 ‐ Randomization is mentioned but there is not an adequate description of the methods used |
| 2) Allocation bias (Allocation concealment) | High risk | 0 ‐ There is not an adequate description of attempts to deal with potential allocation bias |
| 3a) Blinding of participants and personnel | Unclear risk | none specified |
| 3b) Blinding of outcome assessment | Unclear risk | none specified |
| 4) Attrition (Incomplete Outcome Data) | High risk | 0 ‐ There is no documented evidence or insufficient evidence reported of how attrition was dealt with |
| 5) Selective outcome reporting (Selective Outcome Reporting) | Low risk | There was no selective outcome reporting |
| 6) Other potential sources of bias (Other potential threats to validity) | Low risk | Were randomized prior to setting the date for the heelstick. Therefore, it was known what condition they were in before the heel procedure was completed. |
| 7a) Power calculation (Part 1 of size bias) | High risk | 0 ‐ Power calculations were not conducted a priori |
| 7b) Sufficient sample (part 2 of size bias) | High risk | 0 ‐ A sufficient sample size based on the power calculation was not obtained |
| Total | High risk | Total score on new Cochrane standard: Low risk (2/9), High risk (5/9), Unclear Risk (2/9) |
Yilmaz 2010.
| Methods |
Study design: Between‐groups Total study duration: 12 months |
|
| Participants |
Total number: 60 Setting: hospital Diagnostic criteria: low birth weight (< 2500 g), Apgar score greater than or equal to 8, fed at least 30 minutes before procedure, no signs of disease or congenital anomalies, C‐Section delivery, blood sampling at the first attempt, mothers holding baby in their arms during the procedure Age: 37 to 42 weeks (gestational age) Minimum: 37 weeks GA Maximum: 42 weeks GA Mean: 3.33 days SD: 1.24 Sex: Males: 61 Females: 59 (49.2%) Country: Turkey |
|
| Interventions |
Total number of intervention groups: 1 Control group description: baby in mother's lap, no interventions Total number of participants randomized to each of your groups: 30 Specific intervention #1: pacifier Intervention details: babies were given a pacifier Integrity of intervention: satisfactory |
|
| Outcomes |
Pain outcomes, scale limits, and time points when measured: NIPS Coded for 2 minutes before, 5 minutes during, and 3 minutes after injections Upper limit: 7 Lower limit: 0 High score = more pain Continuous |
|
| Notes |
Adverse reactions: none mentioned Funding sources: none mentioned Key conclusions of study authors: pacifying shortened the length of crying time and the rate of behavioral responses to pain compared to the control group |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| 1) Randomization (Random Sequence Generation) | High risk | 0 ‐ Randomization is mentioned but there is not an adequate description of the methods used |
| 2) Allocation bias (Allocation concealment) | High risk | 0 ‐ There is not an adequate description of attempts to deal with potential allocation bias |
| 3a) Blinding of participants and personnel | Unclear risk | Efforts to reduce measurement bias are not reported or are insufficient, e.g. outcomes collected by therapist |
| 3b) Blinding of outcome assessment | Unclear risk | none specified |
| 4) Attrition (Incomplete Outcome Data) | Low risk | 1 ‐ A reasonable account of how attrition was dealt with is given, but no specific reference to CONSORT |
| 5) Selective outcome reporting (Selective Outcome Reporting) | Low risk | None specified |
| 6) Other potential sources of bias (Other potential threats to validity) | Low risk | None specified |
| 7a) Power calculation (Part 1 of size bias) | Low risk | 1 ‐ Power calculations were conducted a priori |
| 7b) Sufficient sample (part 2 of size bias) | Low risk | 1 ‐ A sufficient sample size based on the power calculation was obtained |
| Total | High risk | Total score on new Cochrane standard: Low risk (5/9), High risk (2/9), Unclear Risk (2/9) |
CONSORT: Consolidated Standards of Reporting Trials DAN: Douleur Aiguë Nouveau‐né EBI: Environmental and Behavioral Interventions
EDIN: Échelle Douleur Inconfort Nouveau‐Né (neonatal pain and discomfort scale)
EMLA: Eutectic Mixture of Local Anesthetics ER: emergency room FLACC: Face Legs Arms Cry Consolability Scale
FRSQ: Fonds de recherche en santé du Québec GA: gestational age MAISD: Measure of Adult and Infant Soothing and Distress MBPS: Modified Behavioral Pain Scale NFCS: Neonatal Facial Coding System NICU: neonatal intensive care unit NIDCAP: Newborn Individualized Developmental Care and Assessment Program
NIH: National Institute of Health
NIH PCRC: National Institute of Health Pediatric Clinical Research Center
NINR: National Institute of Nursing Research NIPS: Neonatal Infant Pain Scale
NNS: Non‐nutritive sucking
PHRC: French Government Funding Program for Clinical Research
PI: Principal Investigator PIPP: Premature Infant Pain Profile RA: research assistant RCT: randomized controlled trial s: seconds SES: socioeconomic status
SESEP: Société d'Études et de Soins pour les Enfants Paralysés et Malformés
TcB: Transcutaneous Bilirubin VAS: visual analog scale
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Abdallah 2013 | Not a randomized controlled trial |
| Abedin 2008 | Wrong age or age could not be separated |
| Aguirre 2008 | Control group is an active control group Included in 'Summary of treatment effect' section |
| Akcan 2009 | Inappropriate intervention |
| Al‐Bekaa 2003 | Wrong age or age could not be separated |
| Aslanabadi 2008 | Wrong age or age could not be separated |
| Axelin 2010 | Inappropriate intervention |
| Badiee 2013 | No control group |
| Bellieni 2003 | Inappropriate intervention |
| Bellieni 2007 | Inappropriate intervention |
| Boots 2010 | Inappropriate intervention |
| Bueno 2010 | Control group was an active control Included in 'Summary of treatment effect' section |
| Campbell‐Yeo 2009 | Protocol for randomized controlled trial. |
| Campos 1989 | Control group was an active control Included in 'Summary of treatment effect' section |
| Carlson 2000 | Wrong age or age could not be separated |
| Castral 2008 | Inappropriate intervention |
| Chermont 2009 | Inappropriate intervention |
| Cignacco 2008 | Control group was an active control Included in 'Summary of treatment effect' section |
| Cologna 1999 | Not pain or pain is not measured immediately |
| Cong 2009 | No behavioral pain outcome reported Included in 'Summary of treatment effect' section |
| D'Agostino 2008 | Wrong age or age could not be separated |
| Dahlquist 2002 | Wrong age or age could not be separated |
| De Jong 2012 | Post‐op |
| de Sousa 2008 | Inappropriate intervention |
| Diego 2009 | Control group is an active control group Included in 'Summary of treatment effect' section |
| Dilen 2010 | Inappropriate intervention |
| Downey 2012 | Wrong age |
| Drago 2009 | Wrong age or age could not be separated |
| Duncan 2004 | Not pain or pain is not measured immediately. |
| El‐Naggar 2010 | Inappropriate intervention |
| Favara‐Scacco 2001 | Wrong age or age could not be separated |
| Felt 2000 | Not a randomized controlled trial. |
| Ferber 2008 | Inappropriate intervention |
| Gedaly‐Duff 1992 | Wrong age or age could not be separated |
| Gold 2006 | Wrong age or age could not be separated |
| Gonzalez 1989 | Wrong age or age could not be separated |
| Gonzalez 1993 | Wrong age or age could not be separated |
| Goubet 2003 | Control group was an active control Included in 'Summary of treatment effect' section |
| Goubet 2007 | Control group was an active control Included in 'Summary of treatment effect' section |
| Gray 2000 | Inappropriate intervention |
| Greenberg 1997 | Student work later published and included in the review |
| Grunau 2004 | No control group Included in 'Summary of treatment effect' section |
| Ha 2013 | Not an acute painful medical procedure |
| Hanson 2010 | Inappropriate intervention |
| Harrison 2000 | This study did not use a painful stimulus |
| Hatem 2006 | Wrong age or age could not be separated |
| He 2010 | Inappropriate intervention |
| Heden 2009 | Wrong age or age could not be separated |
| Hoffman 2006 | Wrong age or age could not be separated |
| Holsti 2005 | Inappropriate intervention |
| Hsu 1995 | Not pain or pain not measured immediately |
| Huang 1999 | Not pain or pain not measured immediately |
| Huang 2004 | Control group is an active control group Included in 'Summary of treatment effect' section |
| Ida 2008 | Wrong age or age could not be separated |
| Ipp 2007 | Inappropriate intervention |
| Ipp 2009 | No control group Included in 'Summary of treatment effect' section |
| Jackson 2008 | Wrong age or age could not be separated |
| Jo 2007 | Wrong age or age could not be separated |
| Johnston 2003 | Inappropriate intervention |
| Johnston 2007b | Not pain or pain not measured immediately |
| Johnston 2008a | Control group is an active control group Included in 'Summary of treatment effect' section |
| Johnston 2009 | Control group is an active control group Included in 'Summary of treatment effect' section |
| Kashaninia 2008 | Inappropriate intervention |
| Kivijärvi 2008 | Wrong age or age could not be separated |
| Koivusalo 2009 | Wrong age or age could not be separated |
| Kostandy 2008 | Inappropriate intervention |
| Leclair 2007 | Not pain or pain not measured immediately |
| Li 2007 | Wrong age or age could not be separated |
| Lima 2013 | Not a randomized controlled trial |
| Ludington‐Hoe 2005 | Control group was an active control Included in 'Summary of treatment effect' section |
| Luthy 2013 | Not behaviour outcome |
| MacLaren 2005 | Wrong age or age could not be separated |
| Manne 1990 | Wrong age or age could not be separated |
| Marchisotti 2007 | Wrong age or age could not be separated |
| Marec‐Berard 2009 | Wrong age or age could not be separated |
| Marin Gabriel 2010 | Not pain or pain is not measured immediately |
| McCarthy 2010 | Wrong age or age could not be separated |
| Mercer 2013 | Inappropriate age or infant age group could not be separated from older child group |
| Michel 2008 | Wrong age or age could not be separated |
| Morelius 2009 | Not a randomized controlled trial Included in 'Summary of treatment effect' section |
| Mucignat 2004 | Inappropriate intervention |
| Okan 2010 | No means or standard deviations reported Included in 'Summary of treatment effect' section |
| Ozdogan 2010 | Inappropriate intervention |
| Phipps 2005 | Wrong age or age could not be separated |
| Rattaz 2005 | No control group Included in 'Summary of treatment effect' section |
| Reichel 2007 | Wrong age or age could not be separated |
| Salmon 2006 | Wrong age or age could not be separated |
| Shapiro 2007 | Wrong age or age could not be separated |
| Singh 2012 | Not randomized |
| Slater 2010 | Inappropriate intervention |
| Slifer 2009 | Wrong age or age could not be separated |
| Sparks 2007 | Wrong age or age could not be separated |
| Sundararajan 2007 | Wrong age or age could not be separated |
| Tanabe 2002 | Wrong age or age could not be separated |
| Ucar 2014 | Not an acute painful medical procedure |
| Vignochi 2010 | Not pain or pain not measured immediately |
| Vivancos 2010 | Not a randomized controlled trial Included in 'Summary of treatment effect' section |
| Weissman 2009 | Not a randomized controlled trial Included in 'Summary of treatment effect' section |
| Wisdorf‐Houtkooper 1997 | Inappropriate intervention |
| Zeltzer 1991 | Wrong age or age could not be separated |
| Zun 2012 | Could not retrieve data |
Characteristics of studies awaiting assessment [ordered by study ID]
Ho 2012.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Author was contacted to get a copy of the article. There has not been a response to date. |
Obeidat 2011.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Author was contacted to get a copy of the article. There has not been a response to date. |
Rozenfeld 2012.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Author was contacted to get a copy of the article. There has not been a response to date. |
Taavoni 2013.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Author was contacted to get a copy of the article. There has not been a response to date. |
Differences between protocol and review
Only behavioral measures were analysed. Due to significant heterogeneity and missing data, physiological measures were not analysed for our review.
Despite our attempt to find studies examining postoperative pain, none of the studies included in our review were in a postsurgical context.
Due to the complexity involved with a treatment x age x pain response analysis, the decision was made not to analyse studies by the fourth dimension (different types of outcome measures).
Age groups were collapsed into three groups, instead of four, based on the ages found in the located studies.
The standardized mean difference was analysed instead of the mean difference.
Contributions of authors
One review author (RPR) created the search strategy under the guidance of four Cochrane‐affiliated librarians (Elizabeth Ulryk, Sylvia Bickley, Caroline Struthers, and Joanne Abbott). One review author contributed to the modification of the strategies and protocol (RPR). Ten review authors (RPR, NR, HG, KT, LU, RH, LDO, SAK, JHS, AG) independently screened titles and abstracts of studies from literature searches for inclusion in the initial review. For the update, seven authors did the extractions (HG, KT, LU, RH, SAK, JHS, DL). The articles were located and obtained by research assistants. Three review authors reviewed the extractions and came to consensus (RPR, HG, NR). All review authors were involved reviewing the manuscript (RPR, NR, HG, KT, LU, RH, SAK, JHS, BS, DL).
Dr. Rebecca Pillai Riddell is responsible for the update of this review.
Sources of support
Internal sources
-
Lillian Wright Foundation for Maternal‐Child Health, York University, Canada.
Lillian Wright Foundation for Maternal‐Child Health has provided funds to: Ms. Nicole Racine, Ms. Hannah Gennis, Dr. Laila Din Osmun, and Dr. Rachel Horton.
-
York University, Canada.
Operating funds for this project were provided by funds from York University to Dr. Pillai Riddell with salary support through the York Research Chairs Program.
External sources
-
Canadian Institutes for Health Research, Canada.
Provided salary support to Dr. Pillai Riddell (Post‐doctoral Fellowship, New Investigator Award), doctoral fellowships to Ms. Nicole Racine, Ms. Jessica Hillgrove Stuart, and Dr. Laila Din Osmun, a Master's‐level fellowship to Ms. Hannah Gennis, as well as graduate support to Dr. Rachel Horton and Dr. Sara Ahola Kohut.
-
Ontario Graduate Scholarship, Canada.
Provided support to Ms. Nicole Racine, Dr. Rachel Horton, and Dr. Sara Ahola Kohut.
-
Social Sciences and Humanities Research Council, Canada.
Provided support to Ms. Nicole Racine and Dr. Sara Ahola Kohut.
-
Pain In Child Health (Canadian Institutes of Health Research) Strategic Training Initiative, Canada.
Provided support to Ms. Nicole Racine, Ms. Hannah Gennis, Ms. Jessica Hilgrove Stuart, Dr. Laila Din Osmun, Dr. Rachel Horton, and Dr. Sara Ahola Kohut.
Declarations of interest
Dr. Rebecca Pillai Riddell C.Psych.: No conflict to declare.
Nicole Racine, M.A.: No conflict to declare
Hannah Gennis, B.A.: No conflict to declare
Kara Turcotte, M.A.: No conflict to declare.
Dr. Lindsay Uman, R.Psych: No conflict to declare.
Dr. Rachel Horton, C.Psych (supervised practice): No conflict to declare.
Dr. Sara Ahola Kohut, C.Psych: No conflict to declare.
Jessica Hillgrove‐Stuart, M.A.: No conflict to declare.
Dr. Bonnie Stevens, RN, PhD: No conflict to declare.
Diana Lisi, B.A.: No conflict to declare.
Stable (no update expected for reasons given in 'What's new')
References
References to studies included in this review
Allen 1996 {published data only}
- Allen KD, White DD, Walburn JN. Sucrose as an analgesic agent for infants during immunization injections. Archives of Pediatrics & Adolescent Medicine 1996;150(3):270‐4. [DOI] [PubMed] [Google Scholar]
Axelin 2006 {published data only}
- Axelin A, Salantera S, Lehtonen L. Facilitated tucking by parents in pain management of preterm infants ‐ a randomized crossover trial. Early Human Development 2006;82:241‐7. [DOI] [PubMed] [Google Scholar]
Axelin 2009 {published data only}
- Axelin A, Salantera S, Kirjavainen J, Lehtonen L. Oral glucose and parental holding preferable to opioid in pain management in preterm infants. Clinical Journal of Pain 2009;25:138‐45. [DOI] [PubMed] [Google Scholar]
Badiee 2014 {published data only}
- Badiee Z, Nassir Z, Armanian A. Cobedding of twin premature infants: calming effects on pain responses. Pediatrics and Neonatology 2014;55(4):262‐268. [DOI] [PubMed] [Google Scholar]
Basiri‐Moghadam 2014 {published data only}
- Basiri‐Moghadam M, Kianmehr M, Pasban‐Noghabi S, Basiri‐Moghadam K. Comparison of EMLA cream with rattles on reducing immunization pain in four month infants. The Journal of the Pakistan Medical Association 2014;64(8):874‐878. [PubMed] [Google Scholar]
Bauchner 1996 {published data only}
- Bauchner H, Vinci R, Bak S, Pearson C, Corwin MJ. Parents and procedures: a randomized controlled trial. Pediatrics 1996;98(5):861‐7. [PubMed] [Google Scholar]
Bellieni 2001 {published data only}
- Bellieni CV, Buonocore G, Nenci A, Franci N, Cordelli DM, Bagnoli F. Sensorial saturation: an effective analgesic tool for heel‐prick in preterm infants. Biology of the Neonate 2001;80(1):15‐8. [DOI] [PubMed] [Google Scholar]
Bellieni 2002 {published data only}
- Bellieni CV, Bagnoli F, Perrone S, Nenci A, Cordelli DM, Fusi M, et al. Effect of multisensory stimulation on analgesia in term neonates: a randomized controlled trial. Pediatric Research 2002;51(4):460‐3. [DOI] [PubMed] [Google Scholar]
Blass 1999 {published data only}
- Blass EM, Watt LB. Suckling‐ and sucrose‐induced analgesia in human newborns. Pain 1999;83(3):611‐23. [DOI] [PubMed] [Google Scholar]
Bo 2000 {published data only}
- Bo LK, Callaghan P. Soothing pain‐elicited distress in Chinese neonates. Pediatrics 2000;105(4):E49. [DOI: 10.1542/peds.105.4.e49] [DOI] [PubMed] [Google Scholar]
Bustos 2008 {published data only}
- Bustos T, Jaaniste T, Salmon K, Champion GD. Evaluation of a brief parent intervention teaching coping‐promoting behavior for the infant immunization context: a randomized controlled trial. Behavior Modification 2008;32(4):450‐67. [DOI: 10.1177/0145445507309031] [DOI] [PubMed] [Google Scholar]
Campbell‐Yeo 2012 {published data only}
- Campbell‐Yeo ML, Johnston CC, Joseph KS, Feely N, Chambers CT, Barrington KJ. Cobedding and recovery time after heel lance in preterm twins: results of a randomized trial. Pediatrics September 2012;130:500‐6. [DOI] [PubMed] [Google Scholar]
Campos 1994 {published data only}
- Campos RG. Rocking and pacifiers: two comforting interventions for heelstick pain. Research in Nursing & Health 1994;17(5):321‐31. [DOI] [PubMed] [Google Scholar]
Carbajal 1999 {published data only}
- Carbajal R, Chauvet X, Couderc S, Olivier‐Martin M. Randomised trial of analgesic effects of sucrose, glucose, and pacifiers in term neonates. BMJ 1999;319(7222):1393‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Carbajal 2003 {published data only}
- Carbajal R, Veerapen S, Couderc S, Jugie M, Ville Y. Analgesic effect of breast feeding in term neonates: randomised controlled trial. British Medical Journal (Clinical Research Ed.) 2003;326(7379):13. [DOI] [PMC free article] [PubMed] [Google Scholar]
Catelin 2005 {published data only}
- Catelin C, Tordjman S, Morin V, Oger E, Sizun J. Clinical, physiologic, and biologic impact of environmental and behavioral interventions in neonates during a routine nursing procedure. Journal of Pain 2005;6(12):791‐7. [DOI: 10.1016/j.jpain.2005.07.010] [DOI] [PubMed] [Google Scholar]
Chik 2012 {published data only}
- Chik Y, Ip W. The effect of limb massage on infant's venipuncture pain. Journal of Pain 2012;13:S89. [DOI] [PubMed] [Google Scholar]
Cohen 2002 {published data only}
- Cohen LL. Reducing infant immunization distress through distraction. Health Psychology 2002;21(2):207‐11. [PubMed] [Google Scholar]
Cohen 2006 {published data only}
- Cohen LL, MacLaren JE, Fortson BL, Friedman A, DeMore M, Lim CS, et al. Randomized clinical trial of distraction for infant immunization pain. Pain 2006;125(1‐2):165‐71. [DOI] [PubMed] [Google Scholar]
Comaru 2009 {published data only}
- Comaru T, Miura E. Postural support improves distress and pain during diaper change in preterm infants. Journal of Perinatology 2009;29:504‐7. [DOI: 10.1038/jp.2009.13] [DOI] [PubMed] [Google Scholar]
Corbo 2000 {published data only}
- Corbo MG, Mansi G, Stagni A, Romano A, Heuvel J, Capasso L et al. Nonnutritive sucking during heelstick procedures decreases behavioral distress in the newborn infant. Biology of the Neonate 2000;77(3):162‐7. [DOI] [PubMed] [Google Scholar]
Corff 1995 {published data only}
- Corff KE, Seideman R, Venkataraman PS, Lutes L, Yates B. Facilitated tucking: a nonpharmacologic comfort measure for pain in preterm neonates. Journal of Obstetric, Gynecologic, & Neonatal Nursing 1995;24(2):143‐7. [DOI] [PubMed] [Google Scholar]
Cramer‐Berness 2005a {published data only}
- Cramer‐Berness LJ, Friedman AG. Behavioral interventions for infant immunizations. Children's Health Care 2005;34(2):95‐111. [Google Scholar]
Cramer‐Berness 2005b {published data only}
- Cramer‐Berness LJ. A comparison of behavioral interventions for infant immunizations. Dissertation Abstracts International: Section B: The Sciences and Engineering 2005;66(12‐B):6916. [Google Scholar]
Curtis 2007 {published data only}
- Curtis SJ, Jou H, Ali S, Vandermeer B, Klassen T. A randomized controlled trial of sucrose and/or pacifier as analgesia for infants receiving venipuncture in a pediatric emergency department. BMC Pediatrics 2007;7:27. [DOI] [PMC free article] [PubMed] [Google Scholar]
Elserafy 2009 {published data only}
- Elserafy FA, Alsaedi SA, Louwrens J, Bin Sadiq B, Mersal AY. Oral sucrose and a pacifier for pain relief during simple procedures in preterm infants: a randomized controlled trial. Annals of Saudi Medicine 2009;29(3):184‐8. [DOI: 10.4103/0256-4947.52821] [DOI] [PMC free article] [PubMed] [Google Scholar]
Esfahani 2013 {published data only}
- Esfahani MS, Sheykhi S, Abdeyazdan Z, Jodakee M, Boroumandfar K. A comparative study on vaccination pain in the methods of massage therapy and mothers’ breast feeding during injection of infants referring to Navabsafavi Health Care Center in Isfahan. Iranian Journal of Nursing and Midwifery Research 2013;18(6):494‐498. [PMC free article] [PubMed] [Google Scholar]
Fearon 1997 {published data only}
- Fearon I, Kisilevsky BS, Hains SMJ, Muir DW, Tranmer J. Swaddling after heel lance: age‐specific effects on behavioral recovery in preterm infants. Developmental and Behavioral Pediatrics 1997;18(4):222‐32. [PubMed] [Google Scholar]
Gormally 2001 {published data only}
- Gormally S, Barr RG, Wertheim L, Alkawaf R, Calinoiu N, Young SN. Contact and nutrient caregiving effects on newborn infant pain responses. Developmental Medicine & Child Neurology 2001;43(1):28‐38. [DOI] [PubMed] [Google Scholar]
Greenberg 2002 {published data only}
- Greenberg CS. A sugar‐coated pacifier reduces procedural pain in newborns. Pediatric Nursing 2002;28(3):271‐7. [PubMed] [Google Scholar]
Harrington 2012 {published data only}
- Harrington JW, Logan S, Harwell C, Gardner J, Swingle J, McGuire E, et al. Efffective analgesia using physical interventions for infant immunizations. Pediatrics 2012;129(5):815‐22. [DOI] [PubMed] [Google Scholar]
Herrington 2007 {unpublished data only}
- Herrington CJ. Reducing pain of heelstick in premature infants with gentle human touch. Wayne State University Doctoral Dissertation unpublished:1‐229.
Herrington 2014 {published data only}
- Herrington CJ, Chiodo LM. Human touch effectively and safely reduces pain in the newborn intensive care unit. Pain Management Nursing 2014;15(1):107‐115. [DOI] [PubMed] [Google Scholar]
Hill 2005 {published data only}
- Hill S, Engle S, Jorgensen J, Kralik A, Whitman K. Effects of facilitated tucking during routine care of infants born preterm. Pediatric Physical Therapy 2005;17(2):158‐63. [DOI] [PubMed] [Google Scholar]
Hillgrove Stuart 2013 {published data only}
- Hillgrove‐Stuart J, Pillai Riddell R, Horton R, Greenberg S. Toy‐mediated distraction: clarifying the role of the agent of distraction and pre‐needle distress. Pain Research and Management 2013; Vol. 18, issue 4:197‐202. [DOI] [PMC free article] [PubMed]
Hogan 2014 {published data only}
- Hogan ME, Probst J, Wong K, Pillai Riddell R, Katz J, Taddio A. A randomized‐controlled trial of parent‐led tactile stimulation to reduce pain during infant immunization injections. Clinical Journal of Pain 2014;30(3):259‐265. [DOI] [PubMed] [Google Scholar]
Im 2008 {published data only}
- Im H, Kim E, Park E, Sung K, Oh W. Pain reduction of heel stick in neonates: Yakson compared to non‐nutritive sucking. Journal of Tropical Pediatrics 2008;54(1):31‐5. [DOI] [PubMed] [Google Scholar]
Ipp 2004 {published data only}
- Ipp M, Taddio A, Goldbach M, Ben David S, Stevens B, Koren G. Effects of age, gender and holding on pain response during infant immunization. Canadian Journal of Clinical Pharmacology 2004;11(1):e2‐7. [PubMed] [Google Scholar]
Jain 2006 {published data only}
- Jain S, Kumar P, McMillan DD. Prior leg massage decreases pain responses to heel stick in preterm babies. Journal of Paediatrics & Child Health 2006;42(9):505‐8. [DOI: 10.111/j.1440-1754.2006.00912.x] [DOI] [PubMed] [Google Scholar]
Johnston 1997 {published data only}
- Johnston CC, Stremler RL, Stevens BJ, Horton LJ. Effectiveness of oral sucrose and simulated rocking on pain response in preterm neonates. Pain 1997;72(1‐2):193‐9. [DOI] [PubMed] [Google Scholar]
Johnston 2007a {published data only}
- Johnston CC, Filion F, Nuyt AM. Recorded maternal voice for preterm neonates undergoing heel lance. Advances in Neonatal Care 2007;7(5):258‐66. [DOI] [PubMed] [Google Scholar]
Johnston 2013a {published data only}
- Johnston C, Campbell‐Yeo M, Rich B, Whitley J, Filion F, Cogan J, et al. Therapeutic touch is not therapeutic for procedural pain in very preterm neonates. Clinical Journal of Pain 2013;29(9):824‐29. [DOI] [PubMed] [Google Scholar]
Jose 2012 {published data only}
- Jose RM, Soluchana B, Shetty S. Effectiveness of skin tap technique in reducing pain response. International Journal of Nursing Education 2012;4(1):56‐7. [Google Scholar]
Kozub 2001 {unpublished data only}
- Kozub ML. The effect of therapeutic touch on pain response in infants receiving injections. Ohio: Medical College of Ohio, 2001. [Google Scholar]
Kristoffersen 2011 {published data only}
- Kristoffersen L, Skogvoll E, Hafstrom M. Pain reduction in insertion of a feeding tube in preterm infants: a randomized controlled trial. Pediatrics 2011;127(6):1449‐54. [DOI] [PubMed] [Google Scholar]
Liaw 2010 {published data only}
- Liaw J, Yang L, Ti Y, Tucker Blackburn S, Chang Y, Sun L. Non‐nutritive sucking relieves pain for preterm infants during heel stick procedures in Taiwan. Journal of Clinical Nursing 2010;19:2741‐51. [DOI] [PubMed] [Google Scholar]
Liaw 2011 {published data only}
- Liaw JJ, Zeng WP, Yang L, Yuh YS, Yin T, Yang MH. Nonnutritive sucking and oral sucrose relieve neonatal pain during intramuscular injection of hepatitis vaccine. Journal of Pain and Symptom Management 2011;42(6):918‐29. [DOI] [PubMed] [Google Scholar]
Liaw 2012 {published data only}
- Liaw JJ, Yang L, Wang KWK, Chen CM, Chang YC, Yin T. Non‐nutritive sucking and facilitated tucking relieve preterm infant pain during heel‐stick procedures: a prospective, randomised controlled crossover trial. International Journal of Nursing Studies 2012;49:300‐9. [DOI] [PubMed] [Google Scholar]
Liaw 2013 {published data only}
- Liaw JJ, Yang L, Lee CM, Fan HC, Chang YC, Cheng, LP. Effects of combined use of non‐nutritive sucking, oral sucrose, and facilitated tucking on infant behavioural states across heel‐stick procedures: a prospective, randomised controlled trial. International Journal of Nursing Studies 2013;50:883‐94. [DOI] [PubMed] [Google Scholar]
Liu 2010 {published data only}
- Liu M, Lin K, Chou Y, Lee T. Using non‐nutritive sucking and oral glucose solution with neonates to relieve pain: a randomised controlled trial. Journal of Clinical Nursing 2010;19:1604‐11. [DOI] [PubMed] [Google Scholar]
Mirzarahimi 2013 {published data only}
- Mirzarahimi M, Mehrnoush N, Shahizadeh S, Samadi N, Amani F. Effect of non‐nutritive sucking and leg massage on physiological and behavioural indicators of pain following heel blood sampling in term neonates. International Journal of Advanced Nursing Studies 2013;2(2):74‐79. [Google Scholar]
Morrow 2010 {published data only}
- Morrow C, Hidinger A, Wilkinson‐Faulk D. Reducing neonatal pain during routine heel lance procedures. American Journal of Maternal/Child Nursing 2010;35(6):346‐54. [DOI] [PubMed] [Google Scholar]
Park 2006 {published data only}
- Park ES, Sung KS, Oh WO, Im HS, Kim ES, Kim YA, et al. Pain relieving effect of yakson therapy for infants. Taehan Kanho Hakhoe Chi 2006;36(6):10. [DOI] [PubMed] [Google Scholar]
Sadathosseini 2013 {published data only}
- Sadathosseini AS, Negarandeb R, Movahedi Z. The effect of a familiar scent on the behavioural and physiological pain responses in neonates. Pain Management Nursing 2013;14(4):e196‐203. [DOI] [PubMed] [Google Scholar]
Shaw 1982 {published data only}
- Shaw EG, Routh DK. Effect of mother presence on children's reaction to aversive procedures. Journal of Pediatric Psychology 1982;7(1):33‐42. [DOI] [PubMed] [Google Scholar]
Shu 2014 {published data only}
- Shu SH, Lee YL, Hayter M, Wang RH. Efficacy of swaddling and heel warming on pain response to heel stick in neonates: a randomised control trial. Journal of Clinical Nursing 2014;23(21‐22):3107‐3114. [DOI] [PubMed] [Google Scholar]
Sizun 2002 {published data only}
- Sizun J, Ansquer H, Browne J, Tordjman S, Morin JF. Developmental care decreases physiologic and behavioral pain expression in preterm neonates. Journal of Pain 2002;3(6):446‐50. [DOI] [PubMed] [Google Scholar]
Stevens 1999 {published data only}
- Stevens B, Johnston C, Franck L, Petryshen P, Jack A, Foster G. The efficacy of developmentally sensitive interventions and sucrose for relieving procedural pain in very low birth weight neonates. Nursing Research 1999;48(1):35‐43. [DOI] [PubMed] [Google Scholar]
Sundaram 2013 {published data only}
- Sundaram B, Shrivastava S, Pandian JP, Singh VP. Facilitated tucking on pain in pre‐term newborns during neonatal intensive care: a single blinded randomized controlled cross‐over pilot trial. Journal of Pediatric Rehabilitation Medicine 2013;6(1):19‐27. [DOI] [PubMed] [Google Scholar]
Taddio 2015 {published data only}
- Taddio A, Parikh C, Yoon EW, Sgro M, Singh H, Habtom E, et al. Impact of parent‐directed education on parental use of pain treatments during routine infant vaccination: a cluster randomized trial. Pain 2015;156(1):185‐191. [DOI] [PubMed] [Google Scholar]
Ward‐Larson 2004 {published data only}
- Ward‐Larson C, Horn RA, Gosnell F. The efficacy of facilitated tucking for relieving procedural pain of endotracheal suctioning in very low birthweight infants. MCN: The American Journal of Maternal Child Nursing 2004;29(3):151‐6. [DOI] [PubMed] [Google Scholar]
Whipple 2004 {published data only}
- Whipple J. The effect of music‐reinforced nonnutritive sucking on state of preterm, low birthweight infants experiencing heelstick. Florida: The Florida State University, 2004. [DOI] [PubMed] [Google Scholar]
Yilmaz 2010 {published data only}
- Yilmaz F, Arikan D. The effects of various interventions to newborns on pain and duration of crying. Journal of Clinical Nursing 2010;20:1008‐17. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Abdallah 2013 {published data only}
- Abdallah B, Badr LK, Hawwari, M. The efficacy of massage on short and long term outcomes in preterm infants. Infant Behavior and Development 2013;36:662‐669. [DOI] [PubMed] [Google Scholar]
Abedin 2008 {published data only}
- Abedin S, Kapoor G. Peripherally inserted central venous catheters are a good option for prolonged venous access in children with cancer. Pediatric Blood Cancer 2008;51:251‐5. [DOI] [PubMed] [Google Scholar]
Aguirre 2008 {published data only}
- Aguirre Unceta‐Barrenechea A, Saitua Iturriaga G, Sainz de Rozas Aparicio I, Riveira Fernandez D. Analgesia when taking heel‐lance blood in the newborn. Anales de Pediatria 2008;69(6):544‐7. [DOI] [PubMed] [Google Scholar]
Akcan 2009 {published data only}
- Akcan E, Yigit R, Atici A. The effect of kangaroo care on pain in premature infants during invasive procedures. The Turkish Journal of Pediatrics 2009;51:14‐8. [PubMed] [Google Scholar]
Al‐Bekaa 2003 {published data only}
- Al‐Bekaa S. Harmonic scalpel tonsillectomy vs diathermy tonsillectomy: a comparative study. Australian Journal of Otolaryngology 2003;6(2):78‐80. [Google Scholar]
Aslanabadi 2008 {published data only}
- Aslanabadi S, Ghalehgolab‐Behbahan A, Zarrintan S, Jamshidi M, Seyyedhejazi M. Transanal one‐stage endorectal pull‐through for Hirschsprung's disease: a comparison with the staged procedures. Pediatric Surgery International 2008;24:925‐9. [DOI] [PubMed] [Google Scholar]
Axelin 2010 {published data only}
- Axelin A, Lehtonen L, Pelander T, Slantera S. Mothers' different styles of involvement in preterm infant pain care. Journal of Obstetric, Gynecologic and Neonatal Nursing 2010;39:415‐24. [DOI] [PubMed] [Google Scholar]
Badiee 2013 {published data only}
- Badiee Z, Asghari M, Mohammadizadeh M. The calming effect of maternal breast milk odor on premature infants. Pediatrics and Neonatology 2013;54:322‐325. [DOI] [PubMed] [Google Scholar]
Bellieni 2003 {published data only}
- Bellieni CV, Bagnoli F, Cordelli DM, Perrone S, Nenci A, Buonocore G. Analgesia for premature children. Italian Journal of Pediatrics 2003;29(4):286‐90. [Google Scholar]
Bellieni 2007 {published data only}
- Bellieni CV, Cordelli DM, Marchi S, Ceccarelli S, Perrone S, Maffei M, et al. Sensorial saturation for neonatal analgesia. Clinical Journal of Pain 2007;23(3):219‐21. [DOI] [PubMed] [Google Scholar]
Boots 2010 {published data only}
- Boots BK, Edmundson EE. A controlled, randomised trial comparing single to multiple application lidocaine analgesia in paediatric patients undergoing urethral catheterisation procedures. Journal of Clinical Nursing 2010;19:744‐8. [DOI] [PubMed] [Google Scholar]
Bueno 2010 {unpublished data only}
- Bueno M, Bussotti E, DaSilva A, Leao E. Non nutritive sucking and swaddling for pain relief in term neonates. Abstract from the International Symposium on Pediatric Pain 2010:1.
Campbell‐Yeo 2009 {published data only}
- Campbell‐Yeo ML, Johnston C, Joseph KS, Feeley NL, Chambers CT, Barrington KJ. Co‐bedding as a comfort measure for twins undergoing painful procedures (CComForT Trial). BMC Pediatrics 2009;9:76. [10.1 186/1471‐2431‐9‐76] [DOI] [PMC free article] [PubMed] [Google Scholar]
Campos 1989 {published data only}
- Campos RG. Soothing pain‐elicited distress in infants with swaddling and pacifiers. Child Development 1989;60(4):781‐92. [PubMed] [Google Scholar]
Carlson 2000 {published data only}
- Carlson KL, Broome M, Vessey JA. Using distraction to reduce reported pain, fear, and behavioral distress in children and adolescents: a multisite study. Journal of the Society of Pediatric Nurses 2000;5(2):75‐85. [DOI] [PubMed] [Google Scholar]
Castral 2008 {published data only}
- Castral TC, Warnock F, Leite AM, Haas VJ, Scochi, CGS. The effects of skin‐to‐skin contact during acute pain in preterm newborns. European Journal of Pain 2008;12:464‐471. [DOI] [PubMed] [Google Scholar]
Chermont 2009 {published data only}
- Chermont AG, Falcao LFM, Souza Silva EHL, Cassia Xavier Balda R, Guinsburg R. Skin‐to‐skin contact and/or oral 25% dextrose for procedural pain relief for term newborn infants. Pediatrics 2009;124:1101‐7. [DOI: 10.1542/peds.2009-0993] [DOI] [PubMed] [Google Scholar]
Cignacco 2008 {published data only}
- Cignacco E, Hamers JP, Lingen RA, Zimmermann LJI, Muller R, Gessler P, et al. Pain relief in ventilated preterm infants during endotracheal suctioning: a randomized controlled trial. Swiss Medical Weekly 2008;138(43‐44):635‐45. [DOI] [PubMed] [Google Scholar]
Cologna 1999 {published data only}
- Cologna M, Sperandio L. The effect of two different methods of heel lancing on pain reaction in preterm neonates. Assistenza Infermieristica e Ricerca:Air 1999;18(4):185‐92. [PubMed] [Google Scholar]
Cong 2009 {published data only}
- Cong X, Ludington‐Hoe SM, McCain G, Fu P. Kangaroo care modifies preterm infant heart rate variability in response to heel stick pain: pilot study. Early Human Development 2009;85:561‐7. [DOI: 10.1016/j.earlhumdev.2009.05.012] [DOI] [PMC free article] [PubMed] [Google Scholar]
D'Agostino 2008 {published data only}
- D'Agostino R, Tarantino V, Calevo MG. Blunt dissection versus electronic molecular resonance bipolar dissection for tonsillectomy: operative time and intraoperative and postoperative bleeding and pain. International Journal of Pediatric Otorhinolaryngology 2008;72(7):1077‐84. [DOI] [PubMed] [Google Scholar]
Dahlquist 2002 {published data only}
- Dahlquist LM, Pendley JS, Landthrip DS, Jones CL, Steuber CP. Distraction intervention for preschoolers undergoing intramuscular injections and subcutaneous port access. Health Psychology 2002;21(1):94‐9. [PubMed] [Google Scholar]
De Jong 2012 {published data only}
- Jong M, Lucas C, Bredero H, Adrichem L, Ribboel D, Dijk M. Does postoperative 'M' technique massage with or without mandarin oil reduce infants' distress after major craniofacial surgery?. Journal of Advanced Nursing 2012;68(8):1748‐57. [DOI] [PubMed] [Google Scholar]
de Sousa 2008 {published data only}
- Sousa Freire NB, Santos Garcia JB, Carvalho Lamy Z. Evaluation of analgesic effect of skin‐to‐skin contact compared to oral glucose in preterm neonates. Pain 2008;139(1):28‐33. [DOI: 10.1016/j.pain.2008.02.031] [DOI] [PubMed] [Google Scholar]
Diego 2009 {published data only}
- Diego MA, Field T, Hernandez‐Reif M. Procedural pain heart rate responses in massaged preterm infants. Infant Behavior & Development 2009;32:226‐9. [DOI: 10.1016/j.infbeh.2008.12.001] [DOI] [PMC free article] [PubMed] [Google Scholar]
Dilen 2010 {published data only}
- Dilen B, Elseviers M. Oral glucose solution as pain relief in newborns: results of a clinical trial. Birth: Issues in Perinatal Care 2010;37(2):98‐105. [DOI] [PubMed] [Google Scholar]
Downey 2012 {published data only}
- Downey LV, Zun S. The impact of watching cartoons for distraction during painful procedures in the emergency department. Pediatric Emergency Care 2012;28(10):1033‐35. [DOI] [PubMed] [Google Scholar]
Drago 2009 {published data only}
- Drago LA, Singh SB, Douglass‐Bright A, Yaa Yiadom M, Baumann BM. Efficacy of ShotBlocker in reducing pediatric pain associated with intramuscular injections. American Journal of Emergency Medicine 2009;27:536‐43. [DOI: 10.1016/j.ajem.2008.04.011] [DOI] [PubMed] [Google Scholar]
Duncan 2004 {published data only}
- Duncan B, Barton L, Edmonds D, Blashill BM. Parental perceptions of the therapeutic effect from osteopathic manipulation or acupuncture in children with spastic cerebral palsy. Clinical Pediatrics 2004;43(4):349‐53. [DOI] [PubMed] [Google Scholar]
El‐Naggar 2010 {published data only}
- El‐Naggar W, Yiu A, Mohamed A, Shah V, Manley J, McNamara P, et al. Comparison of pain during two methods of urine collection in preterm infants. Pediatrics 2010;125(6):1224‐9. [DOI] [PubMed] [Google Scholar]
Favara‐Scacco 2001 {published data only}
- Favara‐Scacco C, Smirne G, Schiliro G, Cataldo A. Art therapy as support for children with leukemia during painful procedures. Medical & Pediatric Oncology 2001;36(4):474‐80. [DOI] [PubMed] [Google Scholar]
Felt 2000 {published data only}
- Felt BT, Mollen E, Diaz S, Renaud E, Zeglis M, Wheatcroft G, et al. Behavioral interventions reduce infant distress at immunization. Archives of Pediatric and Adolescent Medine 2000;154:719‐724. [DOI] [PubMed] [Google Scholar]
Ferber 2008 {published data only}
- Ferber SG, Makhoul IR. Neurobehavioural assessment of skin‐to‐skin effects on reaction to pain in preterm infants: a randomized, controlled within‐subject trial. Acta Paediatrica 2008;97(2):171‐6. [DOI: 10.1111/j.1651-2227.2007.00607.x] [DOI] [PubMed] [Google Scholar]
Gedaly‐Duff 1992 {published data only}
- Gedaly‐Duff V, Burns C. Reducing children's pain‐distress associated with injections using cold: a pilot study. Journal of the American Academy of Nurse Practitioners 1992;4(3):95‐9. [DOI] [PubMed] [Google Scholar]
Gold 2006 {published data only}
- Gold JI, Kim SH, Kant AJ, Joseph MH, Rizzo AS. Effectiveness of virtual reality for pediatric pain distraction during i.v. placement. Cyberpsychology & Behavior 2006;9(2):207‐12. [DOI] [PubMed] [Google Scholar]
Gonzalez 1989 {published data only}
- Gonzalez JC, Routh DK, Saab PG, Armstrong FD, Shifman L, Guerra E et al. Effects of parent presence on children's reactions to injections: behavioral, physiological, and subjective aspects. Journal of Pediatric Psychology 1989;14(3):449‐62. [DOI] [PubMed] [Google Scholar]
Gonzalez 1993 {published data only}
- Gonzalez JC, Routh DK, Armstrong FD. Effects of maternal distraction versus reassurance on children's reactions to injections. Journal of Pediatric Psychology 1993;18(5):593‐604. [DOI] [PubMed] [Google Scholar]
Goubet 2003 {published data only}
- Goubet N, Rattaz C, Pierrat V, Bullinger A, Lequien P. Olfactory experience mediates response to pain in preterm newborns. Developmental Psychobiology 2003;42(2):171‐80. [DOI] [PubMed] [Google Scholar]
Goubet 2007 {published data only}
- Goubet N, Strasbaugh K, Chesney J. Familiarity breeds content? Soothing effect of a familiar odor on full‐term newborns. Journal of Developmental & Behavioral Pediatrics 2007;28(3):189‐94. [DOI] [PubMed] [Google Scholar]
Gray 2000 {published data only}
- Gray L, Watt L, Blass EM. Skin‐to‐skin contact is analgesic in healthy newborns. Pediatrics 2000;105(1):e14. [DOI] [PubMed] [Google Scholar]
Greenberg 1997 {published data only}
- Greenberg CS. An evaluation of the efficacy of selected nonpharmacologic pain interventions in infants. San Diego: University of San Diego, 1997. [Google Scholar]
Grunau 2004 {published data only}
- Grunau RE, Linhares MB, Holsti L, Oberlander TF, Whitfield MF. Does prone or supine position influence pain responses in preterm infants at 32 weeks gestational age?. Clinical Journal of Pain 2004;20(2):76‐82. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ha 2013 {published data only}
- Ha YO, Kim HS. The effects of audiovisual distraction on children's pain during laceration repair. International Journal of Nursing Practice 2013;19(3):20‐27. [DOI] [PubMed] [Google Scholar]
Hanson 2010 {published data only}
- Hanson D, Hall W, Mills LL, Au S, Bhagat R, Hernandez M, et al. Comparison of distress and pain in infants randomized to groups receiving standard versus multiple immunizations. Infant Behavior and Development 2010;33:289‐96. [DOI] [PubMed] [Google Scholar]
Harrison 2000 {published data only}
- Harrison LL, Williams AK, Berbaum ML, Stem JT, Leeper J. Physiologic and behavioral effects of gentle human touch on preterm infants. Research in Nursing & Health 2000;23(6):435‐46. [DOI] [PubMed] [Google Scholar]
Hatem 2006 {published data only}
- Hatem TP, Lira PI, Mattos SS. The therapeutic effects of music in children following cardiac surgery. Jornal de Pediatria 2006;82(3):186‐92. [DOI] [PubMed] [Google Scholar]
He 2010 {published data only}
- He H, Jahja R, Lee T, Ang E, Sinnappan R, Vehvilainen‐Julkunen K, et al. Nurses' use of non‐pharmacological methods in children's postoperative pain management: educational intervention study. Journal of Advanced Nursing 2010;66(11):2398‐409. [DOI] [PubMed] [Google Scholar]
Heden 2009 {published data only}
- Heden L, Essen L, Ljungman G. Randomized interventions for needle procedures in children with cancer. European Journal of Cancer Care 2009;18:358‐63. [DOI: 10.1111/j.1365-2354.2008.00939.x] [DOI] [PubMed] [Google Scholar]
Hoffman 2006 {published data only}
- Hoffman HG, Richards TL, Bills AR, Oostrom T, Magula J, Seibel EJ, et al. Using fMRI to study the neural correlates of virtual reality analgesia. CNS Spectrums 2006;11(1):45‐51. [DOI] [PubMed] [Google Scholar]
Holsti 2005 {published data only}
- Holsti L, Grunau RE, Oberlander TF, Whitfield MF. Prior pain induces heightened motor responses during clustered care in preterm infants in the NICU. Early Human Development 2005;81(3):293‐302. [DOI] [PubMed] [Google Scholar]
Hsu 1995 {published data only}
- Hsu CY, Huang LM, Lee CY, Lin TY, Lee PI, Chen JM. Local massage after vaccination enhances the immunogenicity of diphtheria‐ tetanus‐pertussis vaccine. Pediatric Infectious Disease Journal 1995;14(7):567‐72. [DOI] [PubMed] [Google Scholar]
Huang 1999 {published data only}
- Huang FY, Huang LM. Effect of local massage on vaccination: DTP and DTPa. Acta Paediatrica Taiwanica 1999;40(3):166‐70. [PubMed] [Google Scholar]
Huang 2004 {published data only}
- Huang CM, Tung WS, Kuo LL, Ying‐Ju C. Comparison of pain responses of premature infants to the heelstick between containment and swaddling. Journal of Nursing Research 2004;12(1):31‐40. [DOI] [PubMed] [Google Scholar]
Ida 2008 {published data only}
- Ida S, Yoshimura N, Nakacho M, Ota M, Mine H, Moriyama H, et al. Evaluation of the use of PenNeedle 32G Taper in children being treated with growth hormone. Clinical Pediatric Endocrinology 2008;17(1):1‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ipp 2007 {published data only}
- Ipp M, Taddio A, Sam J, Goldbach M, Parkin PC. Vaccine‐related pain: randomised controlled trial of two injection techniques. Archives of Disease in Childhood 2007;92(12):1105‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ipp 2009 {published data only}
- Ipp M, Parkin PC, Lear N, Goldbach M, Taddio A. Order of vaccine injection and infant pain response. Archives of Pediatrics & Adolescent Medicine 2009;163(5):469‐72. [DOI] [PubMed] [Google Scholar]
Jackson 2008 {published data only}
- Jackson LA, Starkovich P, Dunstan M, Yu O, Nelson J, Dunn J, et al. Prospective assessment of the effect of needle length and injection site on the risk of local reactions to the fifth diphtheria‐tetanus‐acellular pertussis vaccination. Pediatrics 2008;21(3):e646‐52. [DOI] [PubMed] [Google Scholar]
Jo 2007 {published data only}
- Jo SH, Mathiasen RA, Gurushanthaiah D. Prospective, randomized, controlled trial of a hemostatic sealant in children undergoing adenotonsillectomy. Otolaryngology ‐ Head & Neck Surgery 2007;137(3):154‐8. [DOI] [PubMed] [Google Scholar]
Johnston 2003 {published data only}
- Johnston CC, Stevens B, Pinelli J, Gibbins S, Filion F, Jack A, et al. Kangaroo care is effective in diminishing pain response in preterm neonates. Archives of Pediatrics & Adolescent Medicine 2003;157(11):1084‐8. [DOI] [PubMed] [Google Scholar]
Johnston 2007b {published data only}
- Johnston CC, Gagnon A, Rennick J, Rosmus C, Patenaude H, Ellis J, et al. One‐on‐one coaching to improve pain assessment and management practices of pediatric nurses. Pediatric Nursing 2007;22(6):467‐78. [DOI] [PubMed] [Google Scholar]
Johnston 2008a {published data only}
- Johnston CC, Filion F, Campbell‐Yeo M, Goulet C, Bell L, McNaughton K, et al. Kangaroo mother care diminishes pain from heel lance in very preterm neonates: a crossover trial. BMC Pediatrics 2008;8:13. [DOI: 10.1186/1471-2431-8-13] [DOI] [PMC free article] [PubMed] [Google Scholar]
Johnston 2009 {published data only}
- Johnston CC, Filion F, Campbell‐Yeo M, Goulet C, Bell L, McNaughton K, et al. Enhanced kangaroo mother care for heel lance in preterm neonates: a crossover trial. Journal of Perinatology 2009;29:51‐6. [DOI: 10.1038/jp.2008.113] [DOI] [PubMed] [Google Scholar]
Kashaninia 2008 {published data only}
- Kashaninia Z, Sajedi F, Rahgozar M, Noghabi FA. The effect of kangaroo care on behavioral responses to pain of an intramuscular injection in neonates. Journal for Specialists in Pediatric Nursing 2008;13(4):275‐80. [DOI] [PubMed] [Google Scholar]
Kivijärvi 2008 {published data only}
- Kivijärvi R, Palviainen J. "Just like I had kicked my toe" ‐‐ Children's experiences of postsurgical pain. Sairaanhoitaja 2008;81(1):27‐9. [Google Scholar]
Koivusalo 2009 {published data only}
- Koivusalo AI, Korpela R, Wirtavuori K, Piiparinen S, Rintala RJ, Pakarinen MP. A single‐blinded, randomized comparison of laparoscopic versus open hernia repair in children. Pediatrics 2009;123(1):332‐7. [DOI] [PubMed] [Google Scholar]
Kostandy 2008 {published data only}
- Kostandy RR, Ludington‐Hoe SM, Cong X, Abouelfettoh A, Bronson C, Stankus A, et al. Kangaroo care (skin contact) reduces crying response to pain in preterm neonates: pilot results. Pain Management Nursing 2008;9(2):55‐65. [DOI] [PMC free article] [PubMed] [Google Scholar]
Leclair 2007 {published data only}
- Leclair MD, Plattner V, Mirallie E, Lejus C, Nguyen JM, Podevin G, et al. Laparoscopic pyloromyotomy for hypertrophic pyloric stenosis: a prospective, randomized controlled trial. Journal of Pediatric Surgery 2007;42(4):692‐8. [DOI] [PubMed] [Google Scholar]
Li 2007 {published data only}
- Li HCW, Lopez V, Lee TLI. Effects of preoperative therapeutic play on outcomes of school‐age children undergoing day surgery. Research in Nursing & Health 2007;30(3):320‐32. [DOI] [PubMed] [Google Scholar]
Lima 2013 {published data only}
- Lima AH, Hermont AP, Lima Friche AA. Analgesia in newborns: a case‐control study of the efficacy of nutritive and non‐nutritive sucking stimuli. CoDAS 2013;25(4):365‐368. [DOI] [PubMed] [Google Scholar]
Ludington‐Hoe 2005 {published data only}
- Ludington‐Hoe SM, Hosseini R, Torowicz DL. Skin‐to‐skin contact (kangaroo care) analgesia for preterm infant heel stick. AACN Clinical Issues 2005;16(3):373‐87. [DOI] [PMC free article] [PubMed] [Google Scholar]
Luthy 2013 {published data only}
- Luthy KE, Beckstand RL, Pulsipher A. Evaluation of methods to relieve parental perceptions of vaccine‐associated pain and anxiety in children: a pilot study. Journal of Pediatric Health Care 2013;27(5):351‐58. [DOI] [PubMed] [Google Scholar]
MacLaren 2005 {published data only}
- MacLaren JE, Cohen LL. A comparison of distraction strategies for venipuncture distress in children. Journal of Pediatric Psychology 2005;30(5):387‐96. [DOI] [PubMed] [Google Scholar]
Manne 1990 {published data only}
- Manne SL, Redd WH, Jacobsen PB, Gorfinkle K, Schorr O, Rapkin B. Behavioral intervention to reduce child and parent distress during venipuncture. Journal of Consulting & Clinical Psychology 1990;58(5):565‐72. [DOI] [PubMed] [Google Scholar]
Marchisotti 2007 {published data only}
- Marchisotti FG, Carvalho LR, Berger K, Arnhold IJ, Mendonca BB. Growth hormone (GH) deficiency treatment in children: comparison between uses of pen versus bottles/syringes on GH administration. Arquivos Brasileiros de Endocrinologia e Metabologia 2007;51(7):1093‐6. [DOI] [PubMed] [Google Scholar]
Marec‐Berard 2009 {published data only}
- Marec‐Berard P, Bissery A, Kebaili K, Schell M, Aubert F, Gaillard S, et al. A positioning pillow to improve lumbar puncture success rate in paediatric haematology‐oncology patients: a randomized controlled trial. BMC Cancer 2009;9:21. [DOI: 10.1186/1471-2407-9-21] [DOI] [PMC free article] [PubMed] [Google Scholar]
Marin Gabriel 2010 {published data only}
- Marin Gabriel MA, Llana Martin I, Lopez Escobar A, Fernandez Villalba E, Romero Blanco I, Touza Pol P. Randomized controlled trial of early skin‐to‐skin contact: effects on the mother and the newborn. Acta Paediatrica 2010;99:1630‐4. [DOI] [PubMed] [Google Scholar]
McCarthy 2010 {published data only}
- McCarthy A, Lieiber C, Hanrahan K, Zimmerman B, Westhus N, Allen S. Impact of parent‐provided distraction on child responses to an IV insertion. Children's Health Care 2010;39:125‐41. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mercer 2013 {published data only}
- Mercer M, Whittle E, Nelson L, Ingram C, O'Hare A. Developmental delay confers increased distress prior to first venepuncture: Findings from an RCT of distress‐reducing interventions employing 'Social Stories'. Developmental Medicine & Child Neurology (Poster Session 1) 2013:55. [Google Scholar]
Michel 2008 {published data only}
- Michel RG, Weinstock BI, Tsau K. Safety and efficacy of pressure‐assisted tissue‐welding tonsillectomy: a preliminary evaluation. Ear, Nose & Throat Journal 2008;87(2):100‐12. [PubMed] [Google Scholar]
Morelius 2009 {published data only}
- Morelius E, Theodorsson E, Nelson N. Stress at three‐month immunization: parents' and infants' salivary cortisol response in relation to the use of pacifier and oral glucose. European Journal of Pain 2009;13(2):202‐8. [DOI] [PubMed] [Google Scholar]
Mucignat 2004 {published data only}
- Mucignat V, Ducrocq S, Lebas F, Mochel F, Baudon JJ, Gold F. Analgesic effects of Emla cream and saccharose solution for subcutaneous injections in preterm newborns: a prospective study of 265 injections. Archives de Pediatrie 2004;11(8):921‐5. [DOI] [PubMed] [Google Scholar]
Okan 2010 {published data only}
- Okan F, Ozdil A, Bulbul A, Yapici Z, Nuhoglu A. Analgesic effects of skin‐to‐skin contact and breastfeeding in procedural pain in healthy term neonates. Annals of Tropical Paediatrics 2010;30:119‐28. [DOI] [PubMed] [Google Scholar]
Ozdogan 2010 {published data only}
- Ozdogan T, Akman I, Cebeci D, Bilgen H, Ozek E. Comparison of two doses of breast milk and sucrose during neonatal heel prick. Pediatrics International 2010;52:175‐9. [DOI] [PubMed] [Google Scholar]
Phipps 2005 {published data only}
- Phipps S, Dunavant M, Gray E, Rai SN. Massage therapy in children undergoing hematopoietic stem cell transplantation: results of a pilot trial. Journal of Cancer Integrative Medicine 2005;3(2):62‐70. [Google Scholar]
Rattaz 2005 {published data only}
- Rattaz C, Goubet N, Bullinger A. The calming effect of a familiar odor on full‐term newborns. Journal of Developmental & Behavioral Pediatrics 2005;26(2):86‐92. [DOI] [PubMed] [Google Scholar]
Reichel 2007 {published data only}
- Reichel O, Mayr D, Winterhoff J, Chaux R, Hagedorn H, Berghaus A. Tonsillotomy or tonsillectomy? A prospective study comparing histological and immunological findings in recurrent tonsillitis and tonsillar hyperplasia. European Archives of Oto‐Rhino‐Laryngology 2007;264:277‐84. [DOI] [PubMed] [Google Scholar]
Salmon 2006 {published data only}
- Salmon K, McGuigan F, Pereira JK. Brief report: optimizing children's memory and management of an invasive medical procedure: the influence of procedural narration and distraction. Journal of Pediatric Psychology 2006;31(5):522‐7. [DOI] [PubMed] [Google Scholar]
Shapiro 2007 {published data only}
- Shapiro NL, Bhattacharyya N. Cold dissection versus coblation‐assisted adenotonsillectomy in children. Laryngoscope 2007;117(3):406‐10. [DOI] [PubMed] [Google Scholar]
Singh 2012 {published data only}
- Singh P. Effect of distraction techniques in behaviour responses to pain among toddlers receiving immunisation. Nursing Journal of India 2012;106(4):176‐79. [PubMed] [Google Scholar]
Slater 2010 {published data only}
- Slater R, Cornelissen L, Fabrizi L, Patten D, Yaxen J, Warley A, et al. Oral sucrose as an analgesic drug for procedural pain in newborn infants: a randomised controlled trial. Lancet 2010;376:1225‐32. [DOI] [PMC free article] [PubMed] [Google Scholar]
Slifer 2009 {published data only}
- Slifer KJ, DeMore M, Vona‐Messersmith N, Pulbrook‐Vetter V, Beck M, Dalhquist L, et al. Comparison of two brief parent‐training interventions for child distress during parent‐administered needle procedures. Children's Health Care 2009;38:23‐48. [DOI: 10.1080/02739610802615831] [DOI] [PMC free article] [PubMed] [Google Scholar]
Sparks 2007 {published data only}
- Sparks LA, Setlik J, Luhman J. Parental holding and positioning to decrease IV distress in young children: a randomized controlled trial. Journal of Pediatric Nursing 2007;22(6):440‐7. [DOI] [PubMed] [Google Scholar]
Sundararajan 2007 {published data only}
- Sundararajan L, Parikh DH. Evolving experience with video‐assisted thoracic surgery in congenital cystic lung lesions in a British pediatric center. Journal of Pediatric Surgery 2007;42:1243‐50. [DOI] [PubMed] [Google Scholar]
Tanabe 2002 {published data only}
- Tanabe P, Ferket K, Thomas R, Paice J, Marcantonio R. The effect of standard care, ibuprofen, and distraction on pain relief and patient satisfaction in children with musculoskeletal trauma. Journal of Emergency Nursing 2002;28(2):118‐25. [DOI] [PubMed] [Google Scholar]
Ucar 2014 {published data only}
- Ucar S, Varma M, Altan S. The efficacy of non‐nutritive sucking and sucrose for the relief of pain during eye examinations for retinopathy of prematurity: a randomised controlled trial. Archives of Disease in Childhood 2014;99:A182‐A183. [Google Scholar]
Vignochi 2010 {published data only}
- Vignochi C, Teixeira PP, Nader SS. Effect of aquatic physical therapy on pain and state of sleep and wakefulness among stable preterm newborns in neonatal intensive care units [Efeitos da fisioterapia aquatica na dor e no estado de sono e vigilia de recem‐nascidos pre‐termo estaveis internados em unidade de terapia intensiva neonatal]. Revista Brasileira de Fisioterapia (Brazilian Journal of Physical Therapy) 2010;14(3):214‐20. [PubMed] [Google Scholar]
Vivancos 2010 {published data only}
- Vivancos RBZ, Leite AM, Scochi CGS, dos Santos CB. The skin to skin contact at birth and newborn crying during vaccination against hepatitis B [O contato pele a pele ao nascimento e o choro de recem‐nascidos durante vacinacao contra Hepatite B]. Acta Paul Enferm 2010;23(4):461‐5. [Google Scholar]
Weissman 2009 {published data only}
- Weissman A, Aranovitch M, Blazer S, Zimmer EZ. Heel‐lancing in newborns: behavioral and spectral analysis assessment of pain control methods. Pediatrics 2009;124:921‐6. [DOI: 10.1542/peds.2009-0598] [DOI] [PubMed] [Google Scholar]
Wisdorf‐Houtkooper 1997 {published data only}
- Wisdorf‐Houtkooper KK. The efficacy of pediatric pain management techniques for infants during inoculation procedures. Michigan: Western Michigan University, 1997. [Google Scholar]
Zeltzer 1991 {published data only}
- Zeltzer LK, Dolgin MJ, LeBaron S, LeBaron C. A randomized, controlled study of behavioral intervention for chemotherapy distress in children with cancer. Pediatrics 1991;88(1):34‐42. [PubMed] [Google Scholar]
Zun 2012 {published data only}
- Zun L, Downey L. The use of cartoon distraction in the reduction of pain. Pain Practice 2012;12(s1):1‐199. [Google Scholar]
References to studies awaiting assessment
Ho 2012 {published data only}
- Ho S, Ho L. Effects of facilitated swaddling for controlling procedural pain in premature neonates: a randomized controlled trial. Journal of Pain 2012;1:S59. [Author was contacted to get a copy of the article. There has not been a response to date] [Google Scholar]
Obeidat 2011 {published data only}
- Obeidat HM. The efficacy of containment for relieving painful responses among jordanian preterm infants during heel stick blood drawing. European Journal of Pain Supplements 2011;5(1):59. [Author was contacted to get a copy of the article. There has not been a response to date.] [Google Scholar]
Rozenfeld 2012 {published data only}
- Rozenfeld S, Mantin H, Mussafi H, Taizi T, Landau R, Kadosh D, et al. Effect of Snoezelen on pain perception and anxiety in CF infants during sputum suction. Pediatric Pulmonology 2012;47:41. [Author was contacted to get a copy of the article. There has not been a response to date.] [Google Scholar]
Taavoni 2013 {published data only}
- Taavoni S, Shahali S, Haghani H. Infants' vaccination pain management and effect of breast feeding, sucking the pacifier and mother's hug: A randomized control trial. European Psychiatry, Conference: 21st European Congress of Psychiatry 2013:28. [Author was contacted to get a copy of the article. There has not been a response to date.] [Google Scholar]
Additional references
Alexander 2003
- Alexander J, Manno M. Underuse of analgesia in very young pediatric patients with isolated painful injuries. Annals of Emergency Medicine 2003;41(5):617‐22. [DOI] [PubMed] [Google Scholar]
Anand 1987
- Anand KJS, Hickey PR. Pain and its effects in the human neonate and fetus. New England Journal of Medicine 1987;317(21):1321‐1329. [DOI] [PubMed] [Google Scholar]
Anand 2000
- Anand KJ. Pain, plasticity and premature birth: a prescription for permanent suffering?. Nature and Medicine 2000;6:971‐3. [DOI] [PubMed] [Google Scholar]
Anand 2001
- Anand KJS, International Evidence‐Based Group for Neonatal Pain. Consensus statement for the prevention and management of pain in the newborn. Archives of Pediatrics & Adolescent Medicine 2001;55(2):173‐80. [DOI] [PubMed] [Google Scholar]
Barber 2004
- Barber K. Pharmacology ‐ noun. The Canadian Oxford Dictionary ‐ Oxford Reference Online. University of Toronto Libraries: Oxford University Press, 2004. [Google Scholar]
Berde 2005
- Berde CB, Jaksic T, Lynn AM, Maxwell LG, Soriano SG, Tibboel D. Anesthesia and analgesia during and after surgery in neonates. Clinical Therapeutics 2005;27(6):900‐21. [DOI] [PubMed] [Google Scholar]
Bowlby 1982
- Bowlby J. Attachment. 2nd Edition. USA: Tavistock Institute of Human Relations, 1969/1982. [Google Scholar]
Brady‐Fryer 2009
- Brady‐Fryer B, Wiebe N, Lander JA. Pain relief for neonatal circumcision. Cochrane Database of Systematic Reviews 2009, Issue 1. [DOI: 10.1002/14651858.CD004217.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Cepeda 2006
- Cepeda MS, Carr DB, Lau J, Alvarez H. Music for pain relief. Cochrane Database of Systematic Reviews 2006, Issue 2. [DOI: 10.1002/14651858.CD004843.pub2] [DOI] [PubMed] [Google Scholar]
Chambless 2001
- Chambless DL, Ollendick TH. Empirically supported psychological interventions: controversies and evidence. Annual Review of Psychology 2001;52:685‐716. [DOI] [PubMed] [Google Scholar]
Cignacco 2007
- Cignacco E, Hamers JPH, Stoffel L, Lingen RA, Gessler P, McDougall J, et al. The efficacy of non‐pharmacological interventions in the management of procedural pain in preterm and term neonates. A systematic literature review. European Journal of Pain 2007;11(2):139‐52. [DOI] [PubMed] [Google Scholar]
Cohen 1988
- Cohen J. Statistical power analysis for the behavioral sciences. 2nd Edition. Routledge, 1988. [Google Scholar]
Cohen 2008
- Cohen LL, Lemanek K, Blount RL, Dahlquist LM, Lim CS, Palermo TM, et al. Evidence‐based assessment of pediatric pain. Journal of Pediatric Psychology 2008;33(9):939‐55. [DOI] [PMC free article] [PubMed] [Google Scholar]
Craig 2002
- Craig KD, Korol CT, Pillai RR. Challenges of judging pain in vulnerable infants. Clinics in Perinatology 2002;29:445‐58. [DOI] [PubMed] [Google Scholar]
Cyna 2010
- Cyna AM, Middleton P. Caudal epidural block versus other methods of postoperative pain relief for circumcision in boys. Cochrane Database of Systematic Reviews 2010, Issue 11. [DOI: 10.1002/14651858.CD003005] [DOI] [PMC free article] [PubMed] [Google Scholar]
Derbyshire 1999
- Derbyshire SWG. Locating the beginnings of pain. Bioethics 1999;13(1):1‐31. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Field 1995
- Field T. Infancy is not without pain. Annals of Child Development 1995;10:1‐26. [Google Scholar]
Fitzgerald 2005
- Fitzgerald M. The development of nociceptive circuits. Nature Reviews Neuroscience 2005;6:507‐20. [DOI] [PubMed] [Google Scholar]
Franck 2000
- Franck L, Greenberg C, Stevens B. Pain assessment in infants and children. Pediatric Clinics of North America 2000;47(3):487‐512. [DOI] [PubMed] [Google Scholar]
GRADEpro GDT [Computer program]
- McMaster University (developed by Evidence Prime, Inc) available from www.gradepro.org. GRADEpro Guideline Development Tool. McMaster University (developed by Evidence Prime, Inc) available from www.gradepro.org, 2015.
Grunau 1987
- Grunau R, Craig KD. Pain expression in neonates: facial action and cry. Pain 1987;28(3):395‐410. [DOI] [PubMed] [Google Scholar]
Grunau 1996
- Grunau RVE, Whitfield M, Petrie JH. Children's judgments about pain at age 8‐10 years: do extremely low birthweight children (< 1000g) children differ from full birthweight peers?. Journal of Child Psychology and Psychiatry 1996;39(4):587‐94. [PubMed] [Google Scholar]
Grunau 2000
- Grunau RE. Long‐term consequences of pain in human neonates. In: KJ Anand, BJ Stevens, PJ McGrath editor(s). Pain in Neonates, 2nd Edition. New York: Elsevier, 2000. [Google Scholar]
Harrison 2013
- Harrison D. Naturalistic studies of procedural pain management in infants – is it ethical to not provide pain management?. Pain 2013;154(9):1895‐6. [DOI] [PubMed] [Google Scholar]
Higgins 2003
- Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analyses. BMJ 2003;327(7417):557‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011a
- Higgins JPT, Altman DG, Sterne JAC (editors). Chapter 8: Assessing risk of bias in included studies. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011.. Available from www.cochrane‐handbook.org.
Higgins 2011b
- Higgins JPT, Deeks JJ, Altman DG (editors). Chapter 16: Special topics in statistics. In: Higgins JPT, Green S (editors), Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Higgins 2011c
- Higgins JPT, Deeks JJ (editors). Chapter 7: Selecting studies and collecting data. In: Higgins JPT, Green S (editors), Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Howard 2003
- Howard RF. Current status of pain management in children. JAMA 2003;290(18):2464‐9. [DOI] [PubMed] [Google Scholar]
IBM Corp 2012 [Computer program]
- IBM Corp. IBM SPSS Statistics for Windows, Version 21.0. Armonk, NY: IBM Corp, 2012.
Johnston 1993
- Johnston CC, Stevens B, Craig KD, Grunau RV. Developmental changes in pain expression in premature, full‐term, two‐ and four‐month‐old infants. Pain 1993;52(2):201‐8. [DOI] [PubMed] [Google Scholar]
Johnston 2011
- Johnston CC, Fernandes AM, Campbell‐Yeo M. Pain in neonates is different. Pain 2011;152(3):S65‐S73. [DOI] [PubMed] [Google Scholar]
Johnston 2013b
- Johnston C, Campbell‐Yeo M, Fernandes A, Inglis D, Streiner D, Zee R. Skin‐to‐skin care for procedural pain in neonates. Cochrane Database of Systematic Reviews 2014, Issue 1. [DOI: 10.1002/14651858.CD008435.pub2] [DOI] [PubMed] [Google Scholar]
Joint Committee 2000
- Joint Fetus and Newborn Committee of the Candian Paediatric Society and American Academy of Pediatrics. Prevention and management of pain and stress in the neonate. Pediatrics 2000;105(2):454‐61. [PubMed] [Google Scholar]
Kleiber 1999
- Kleiber C, Harper D. Effects of distraction on children's pain and distress during medical procedures: a meta‐analysis. Nursing Research 1999;48(1):44‐9. [DOI] [PubMed] [Google Scholar]
McGraw 1943
- McGraw MD. The neuromuscular maturation of the human infant. New York: Columbia University Press, 1943. [Google Scholar]
Obeidat 2009
- Obeidat H, Kahalaf I, Callister LC, Froelicher ES. Use of facilitated tucking for nonpharmacological pain management in preterm infants: a systematic review. Journal of Perinatal and Neonatal Nursing 2009;23(4):372. [DOI] [PubMed] [Google Scholar]
Piira 2005
- Piira T, Sugiura T, Champion GD, Donnelly N, Cole ASJ. The role of parental presence in the context of children's medical procedures: a systematic review. Child: Care, Health and Development 2005;31(2):233‐43. [DOI] [PubMed] [Google Scholar]
Pillai Riddell 2005
- Pillai Riddell R, Stevens BJ, Katz J. Expanding the notion of chronic pain to infancy. Presentation at the Canadian Pain Society Annual Meeting. Pain Research & Management. 2005; Vol. 10:85.
Pillai Riddell 2009
- Pillai Riddell R, Racine N. Assessing pain in infancy: the caregiver context. Pain Research and Management 2009;14:27‐32. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pillai Riddell 2013a
- Pillai Riddell RR, Racine N, Stevens BJ. Non‐pharmacological pain management in infancy. The Encyclopedia of Pain. Springer‐Verlag, 2013. [Google Scholar]
Pillai Riddell 2013b
- Pillai Riddell RR, Flora DB, Stevens SA, Stevens BJS, Cohen LL, Greenberg S, et al. Variability in infant acute pain responding meaningfully obscured by averaging pain responses. Pain 2013;154(5):714‐721. [DOI] [PubMed] [Google Scholar]
Pillai Riddell 2013c
- Pillai Riddell, RR. Invited commentary to “Naturalistic studies of procedural pain management in infants – is it ethical to not provide pain management?”. Pain 2013;154(9):1986‐1897. [DOI] [PubMed] [Google Scholar]
Pillai Riddell 2013d
- Pillai Riddell R, Racine N, Craig K, Campbell L. Psychological theories and biopsychosocial models in pediatric pain. In: P.J. McGrath, B. Stevens, S. Walker, W. Zempsky editor(s). Oxford Textbook of Pediatric Pain. London: Oxford, 2013:85‐94. [Google Scholar]
Prasopkittikun 2003
- Prasopkittikun T, Tilokskulchai F. Management of pain from heel stick in neonates ‐ an analysis of research conducted in Thailand. Journal of Perinatal and Neonatal Nursing 2003;17(4):304‐12. [DOI] [PubMed] [Google Scholar]
RevMan 2014 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Schechter 2007
- Schechter NL, Zempsky WT, Cohen LL, McGrath PJ, McMurtry CM, Bright NS. Pain reduction during pediatric immunizations: Evidence‐based review and recommendations. Pediatrics 2007;119(5):184‐98. [DOI] [PubMed] [Google Scholar]
Schünemann 2011
- Schünemann HJ, Oxman AD, Vist GE, Higgins JPT, Deeks JJ, Glasziou P, Guyatt GH. Chapter 12: Interpreting results and drawing conclusions. In: Higgins JPT, Green S (editors), Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Shah 2009
- Shah PS, Aliwalas LL, Shah V. Breastfeeding or breast milk for procedural pain in neonates. Cochrane Database of Systematic Reviews 2009, Issue 1. [DOI: 10.1002/14651858.CD004950.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Simons 2003
- Simons SHP, Dijk M, Anand KS, Roofthooft D, Lingen RA, Tibboel D. Do we still hurt newborn babies?: a prospective study of procedural pain and analgesia in neonates. Archives of Pediatrics & Adolescent Medicine 2003;157(11):1058‐64. [DOI] [PubMed] [Google Scholar]
Slifer 2002
- Slifer KJ, Tucker CL, Dahlquist LM. Helping children and caregivers cope with repeated invasive procedures: how are we doing?. Journal of Clinical Psychology in Medical Settings 2002;9(2):131‐52. [Google Scholar]
Stevens 1996
- Stevens B, Johnston C, Petryshen P, Taddio A. Premature infant pain profile: development and initial validation. Clinical Journal of Pain 1996;12:13‐22. [DOI] [PubMed] [Google Scholar]
Stevens 2007
- Stevens B, Pillai Riddell RR, Oberlander T, Gibbins S. Assessment of pain in neonates and infants. In: Anand KJ, Stevens BJ, McGrath PJ editor(s). Pain in Neonates and Infants. 3rd Edition. New York: Elsevier Limited, 2007. [Google Scholar]
Stevens 2010
- Stevens B, Yamada J, Ohlsson A. Sucrose for analgesia in newborn infants undergoing painful procedures. Cochrane Database of Systematic Reviews 2010, Issue 1. [DOI: 10.1002/14651858.CD001069.pub2] [DOI] [PubMed] [Google Scholar]
Taddio 1997
- Taddio A, Katz J, Ilersich AL, Koren G. Effect of neonatal circumcision on pain response during subsequent routine vaccination. Lancet 1997;349(9052):599‐603. [DOI] [PubMed] [Google Scholar]
Taddio 2010
- Taddio A, Appleton M, Bortolussi R, Chambers C, Dubey V, Halperin S, et al. Reducing the pain of childhood vaccination: an evidence‐based clinical practice guideline (summary). Canadian Medical Association Journal 2010;182(18):1‐7. [DOI: 10.1503/cmaj.092048] [DOI] [PMC free article] [PubMed] [Google Scholar]
Taddio in press
- Taddio A, McMurtry MC, Shah V, Pillai Riddell R, Chambers CT, Noel M, et al. Clinical practice guideline (summary) for reducing pain during vaccination injections. Canadian Medical Association Journal In press. [Google Scholar]
Uman 2006
- Uman LS, Chambers CT, McGrath PJ, Kisely SR. Psychological interventions for needle‐related procedural pain and distress in children and adolescents. Cochrane Database of Systematic Reviews 2013, Issue 10. [DOI: 10.1002/14651858.CD005179.pub3] [DOI] [PubMed] [Google Scholar]
Yates 2005
- Yates SL, Morley S, Eccleston C, Williams AC. A scale for rating the quality of psychological trials for pain. Pain 2005;117:314‐25. [DOI] [PubMed] [Google Scholar]


