Abstract
Background
People with asthma who come from minority groups often have poorer asthma outcomes, including more acute asthma‐related doctor visits for flare‐ups. Various programmes used to educate and empower people with asthma have previously been shown to improve certain asthma outcomes (e.g. adherence outcomes, asthma knowledge scores in children and parents, and cost‐effectiveness). Models of care for chronic diseases in minority groups usually include a focus of the cultural context of the individual, and not just the symptoms of the disease. Therefore, questions about whether tailoring asthma education programmes that are culturally specific for people from minority groups are effective at improving asthma‐related outcomes, that are feasible and cost‐effective need to be answered.
Objectives
To determine whether culture‐specific asthma education programmes, in comparison to generic asthma education programmes or usual care, improve asthma‐related outcomes in children and adults with asthma who belong to minority groups.
Search methods
We searched the Cochrane Register of Controlled Trials (CENTRAL), the Cochrane Airways Group Specialised Register, MEDLINE, Embase, review articles and reference lists of relevant articles. The latest search fully incorporated into the review was performed in June 2016.
Selection criteria
Randomised controlled trials (RCTs) comparing the use of culture‐specific asthma education programmes with generic asthma education programmes, or usual care, in adults or children from minority groups with asthma.
Data collection and analysis
Two review authors independently selected, extracted and assessed the data for inclusion. We contacted study authors for further information if required.
Main results
In this review update, an additional three studies and 220 participants were added. A total of seven RCTs (two in adults, four in children, one in both children and adults) with 837 participants (aged from one to 63 years) with asthma from ethnic minority groups were eligible for inclusion in this review. The methodological quality of studies ranged from very low to low. For our primary outcome (asthma exacerbations during follow‐up), the quality of evidence was low for all outcomes. In adults, use of a culture‐specific programme, compared to generic programmes or usual care did not significantly reduce the number of participants from two studies with 294 participants for: exacerbations with one or more exacerbations during follow‐up (odds ratio (OR) 0.80, 95% confidence interval (CI) 0.50 to 1.26), hospitalisations over 12 months (OR 0.83, 95% CI 0.31 to 2.22) and exacerbations requiring oral corticosteroids (OR 0.97, 95% CI 0.55 to 1.73). However, use of a culture‐specific programme, improved asthma quality of life scores in 280 adults from two studies (mean difference (MD) 0.26, 95% CI 0.17 to 0.36) (although the MD was less then the minimal important difference for the score). In children, use of a culture‐specific programme was superior to generic programmes or usual care in reducing severe asthma exacerbations requiring hospitalisation in two studies with 305 children (rate ratio 0.48, 95% CI 0.24 to 0.95), asthma control in one study with 62 children and QoL in three studies with 213 children, but not for the number of exacerbations during follow‐up (OR 1.55, 95% CI 0.66 to 3.66) or the number of exacerbations (MD 0.18, 95% CI ‐0.25 to 0.62) among 100 children from two studies.
Authors' conclusions
The available evidence showed that culture‐specific education programmes for adults and children from minority groups are likely effective in improving asthma‐related outcomes. This review was limited by few studies and evidence of very low to low quality. Not all asthma‐related outcomes improved with culture‐specific programs for both adults and children. Nevertheless, while modified culture‐specific education programs are usually more time intensive, the findings of this review suggest using culture‐specific asthma education programmes for children and adults from minority groups. However, more robust RCTs are needed to further strengthen the quality of evidence and determine the cost‐effectiveness of culture‐specific programs.
Plain language summary
Culture‐specific programs for children and adults from minority groups who have asthma
Background
People with asthma who come from minority groups have poorer asthma outcomes. Asthma education that is culturally specific may improve asthma‐related outcomes.
Review question
Do culture‐specific asthma education programmes (compared to generic asthma education programmes or usual care) improve asthma‐related outcomes in children and adults with asthma who belong to minority groups?
What evidence did we find?
Seven studies with 837 participants, aged from one to 63 years old were included in this review update. This review was limited by few studies and the quality of evidence was very low to low. In adults, we found that culture‐specific programmes did not improve any of our primary outcomes, but were better in improving quality of life (although the mean difference was less that the minimum important difference for the score) (secondary outcome). In children however, when data were combined from studies, culture‐specific programmes reduced severe exacerbations requiring hospitalisation (primary outcome), while single studies showed improved asthma control, asthma knowledge and adherence outcomes for our secondary outcomes.
Conclusion
The available evidence showed that culture‐specific education programmes for adults and children from minority groups are likely effective in improving asthma‐related outcomes. Although more robust evidence is required, asthma education programmes should be as culturally specific as possible in the context of chronic disease management and the complexity of health outcomes and culture, In the absence of any economic data, cost‐effectiveness studies are also required
Quality of the evidence
The quality of the evidence was very low to low for all outcomes.
Summary of findings
Background
Description of the condition
Asthma education is regarded as an important management step in national asthma guidelines (National Asthma Council Australia 2015; BTS 2016). Asthma education, defined as provision of information on asthma, encompasses various formats which include face‐to‐face encounters, group sessions, outreach, home visits, provision of asthma action plans, recognition of loss of asthma control and self‐management skills (BTS 2016). The effects on asthma‐related outcomes of many of these various forms of education have been addressed in other Cochrane reviews (Powell 2002; Wolf 2002; Gibson 2002a; Gibson 2002b; Tapp 2007; Toelle 2011).
Racial and socio‐economic factors can influence both asthma severity and rates of recurrent acute presentations to emergency health facilities (Coultas 1994; de Oliveira 1999; Sin 2002; Haselkorn 2008). The reasons for this are unclear, however contributing factors are arguably likely to include broad service delivery issues rather than a reflection of intrinsic asthma severity (Enarson 1999; Chang 2002). Other cultural influences and barriers on the management of asthma include symptom perception, low literacy levels, and understanding of disease and self‐management (Enarson 1999; Poureslami 2012; Stewart 2013; Harrington 2015).
Description of the intervention
An appropriate model of care is important to successfully deliver services to improve outcomes for people with asthma (Partridge 2000; Chang 2002; Mitchell 2016). The model of care should arguably be culturally appropriate (Enarson 1999; Poureslami 2012; Press 2012) and modified to fit within the local context. As outlined by the World Health Organization's model of health care for chronic diseases in low‐income settings, "health care should facilitate an ongoing relationship between provider and patient and help patients to make full use of their own and their community's resources for health" (Swartz 2002). This is further supported by the implementation of chronic care models in low‐ to middle‐income countries to facilitate chronic disease care (Beaglehole 2008) and asthma guidelines (National Asthma Council Australia 2015; BTS 2016). Not surprisingly, in the health literature, the model of care for chronic diseases in Indigenous people includes the involvement of Indigenous healthcare workers (IHWs) (Hamdorf 1996; Chino 2006; Abbott 2007). Amongst other factors, involvement of IHWs in a supportive service delivery system would theoretically facilitate provider‐patient relationships and could potentially reduce prejudices and inequities that exist in some areas of healthcare systems (Eades 2000; Schmidt 2016). The involvement of IHWs specifically as an inclusion factor has been addressed in another Cochrane review (Chang 2010).
How the intervention might work
For a variety of reasons (e.g. availability) not all culture‐specific asthma programmes involve intervention by IHWs (Anderson 2004). Also, many minority groups are non‐Indigenous to their country of residence (e.g. Latino groups in the United States of America). People from these groups have also been shown to have poorer asthma outcomes (Anderson 2004; La Roche 2006; Alicea‐Alvarez 2014). Furthermore, there is a growing body of literature highlighting the need to tailor asthma education programs specifically for ethnic and cultural groups to improve asthma outcomes (Poureslami 2012; Press 2012; Douglas 2013; Stewart 2013; Alicea‐Alvarez 2014; Speck 2014; National Asthma Council Australia 2015; BTS 2016). It is therefore not surprising that publications such as the Australian National Strategic Improvement Framework for Asthma makes special reference to disadvantaged/minority groups (NHPAC 2006). However, culture‐specific programmes are likely more expensive than generic programmes as they involve specifically designed programmes to fit within the local context. It is therefore important that the efficacy of culture‐specific education programmes for asthma is systematically examined.
There is no universally accepted definition of a culture appropriate program; however it usually refers to adapting the program to the culture‐values, language, and/or using educators that come from the same culture, inclusion of beliefs and practices, culturally appropriate role models, involvement of local community health workers to support clinical teams, to that of the recipients (BTS 2016). Such adaptation impacts on the understanding and/or how well it is received and thus more likely to be effective (compared to non adapted programs).
Why it is important to do this review
Arguably, the most important asthma education outcome is to improve self‐management, so as to prevent morbidity and death from acute exacerbations. Other outcomes include reduction of day to day morbidity from asthma symptoms (e.g. improved asthma control scores and quality of life measures) and objective measurements of asthma severity (e.g. lung function data) (National Asthma Council Australia 2015; BTS 2016).
This systematic review update examines whether culture‐specific asthma education programmes improve asthma‐related outcomes in children and adults from minority groups who have asthma. This review update will provide much needed evidence to guide asthma specific clinical practice guidelines and health policy.
Objectives
To determine whether culture‐specific asthma education programmes in comparison to generic asthma education programmes or usual care, improve asthma‐related outcomes in children and adults diagnosed with asthma who belong to minority groups.
Methods
Criteria for considering studies for this review
Types of studies
We included randomised controlled trials (RCTs) with parallel group design, comparing specifically developed culture‐orientated asthma education programmes in comparison to generic asthma education programmes or usual care for children and adults who belong to minority groups.
Types of participants
Inclusion criteria: Children (≤ 18 years) and adults from minority groups with physician diagnosed asthma. Minority was defined by study authors according to their respective country's definition.
Exclusion criteria: Eosinophilic bronchitis, asthma related to an underlying lung disease such as bronchiectasis and chronic obstructive airway disease, or diagnostic categories such as 'cough variant asthma' and 'wheezy bronchitis' where controversy exists.
Types of interventions
We included RCTs involving comparisons of specifically developed culture‐orientated asthma programmes with their local generic asthma education programmes or usual care. We considered studies that involved the use of other education and other interventions for inclusion if all participants had equal access to such interventions. An education programme is defined as a programme which transfers information about asthma in any form, including but not limited to, adapting the program to the culture‐values, language, and/or using educators who come from the same culture, inclusion of beliefs and practices, culturally appropriate role models, involvement of local community health workers to support clinical teams etc,
Types of outcome measures
Attempts were made to obtain data on at least one of the following outcome measures. All analyses were planned separately for adults and children.
Primary outcomes
Asthma exacerbations during follow‐up defined as:
Number of participants who had one or more exacerbation over the study period
Number of exacerbations over 52 weeks (exacerbation rate)
Severe exacerbations requiring oral corticosteroids over the study period
Severe exacerbations requiring hospitalisation over the study period
Secondary outcomes
Objective measurements of asthma control (FEV1, peak flow, airway hyper‐responsiveness)
Asthma Control Score (score ≤ 19 = uncontrolled asthma)
Asthma quality of life (QoL) score
Other asthma symptom scores (e.g. diary cards)
Adherence outcomes
Asthma knowledge factors
Economic data
Search methods for identification of studies
Electronic searches
Studies were identified from the following sources.
The Cochrane Airways Group Specialised Trials Register (1950 to June 2016).
The Cochrane Central Register of Controlled Trials (CENTRAL), the Cochrane Library, 2016, Issue 6.
MEDLINE (1950 to June 2016). Topic search strategy combined with the RCT search filter as outlined in the Airways Group module.
Embase (1980 to June 2016).Topic search strategy combined with the RCT search filter as outlined in the Airways Group module.
Clinical trials registries: ClinicalTrials.gov and the WHO trials portal (all years to June 2016).
Conference abstracts and grey literature were searched for through the CENTRAL database. We did not impose any restrictions on language of publication. Full search strategies are listed in Appendix 1.
Searching other resources
In addition to the electronic search, we checked reference lists of relevant publications for additional studies.
Data collection and analysis
Selection of studies
Retrieval of studies: Using article titles abstracts, or descriptors, two review authors (EJB and ABC in original and 2009 reviews; GBM and ABC in search from 2009 to 2016) independently reviewed literature searches to identify potentially relevant studies for full review. They conducted searches of bibliographies and texts to identify additional studies. From the full‐text articles, the two review authors independently assessed studies for inclusion on the basis of specific criteria.
Data extraction and management
We had no disagreements but had planned to resolve disagreements through discussion with another review author (PSM). We extracted data using a standardised data collection form and entered the data in Review Manager 5.3 (Review Manager (RevMan)), in accordance with recommendations provided in the Cochrane Handbook for Systematic Review of Interventions (Higgins 2011). When required, we sought further information from study authors. We recorded the selection process in the PRISMA flow diagram (Figure 1).
1.
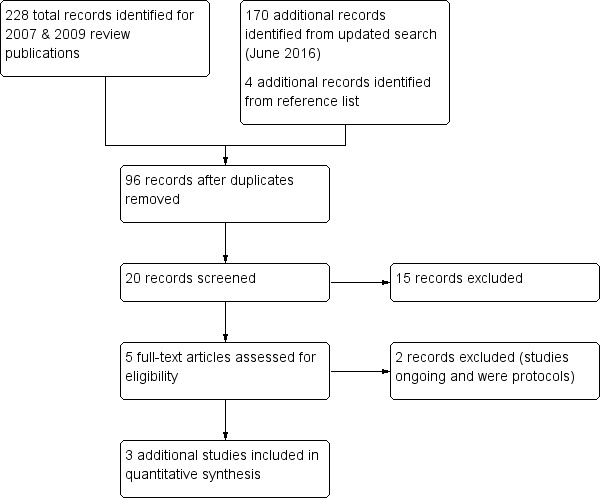
Study flow diagram.
Assessment of risk of bias in included studies
Two review authors (GBM and ABC) independently assessed risk of bias for each study using the criteria outlined in the Cochrane Handbook for Systematic Review of Interventions (Higgins 2011). It was planned that disagreements would be resolved by discussion or by third party adjudication. We assessed risk of bias according to the following domains.
Allocation sequence generation (selection bias)
Concealment of allocation (selection bias)
Blinding of participants (performance bias)
Outcome assessment (detection bias)
Incomplete outcome data (attrition bias)
Selective outcome reporting (reporting bias)
We graded each potential source of bias as low, unclear or high and provided a justification for our judgement in the "Risk of bias" tables (Figure 2).
2.
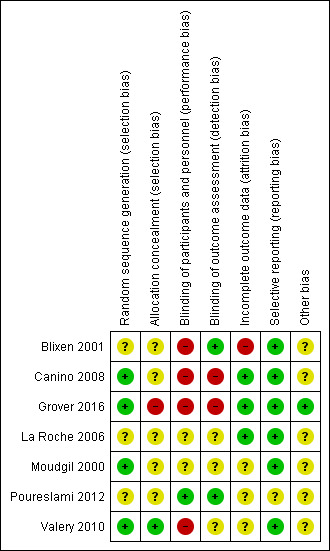
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Measures of treatment effect
We analysed dichotomous data as odds ratios (OR) and continuous data as mean difference (MD) and planned to use standardised mean difference (SMD) if necessary. We then entered data presented as a scale with a consistent direction of effect. We undertook meta‐analyses only where it was meaningful. This took into account differences in study populations, inclusion/exclusion criteria, interventions, outcome assessment, and estimated effect size. We described skewed data which was reported as medians and interquartile ranges (IQR) in the text.
Unit of analysis issues
For dichotomous data, we reported the proportion of participants contributing to each outcome in comparison with the total number randomised. For rate ratios of common events whereby one participant may have more than one event, generic inverse variance (GIV) was used. The rate ratios were taken from the published papers and the standard errors calculated from confidence intervals or P values published in the papers. Cross‐over trials are not appropriate for this intervention and therefore were not planned for inclusion in any meta‐analysis performed.
Dealing with missing data
We planned to contact investigators or study sponsors to verify key study characteristics and to provide missing numerical outcome data when necessary. Three study authors (Canino 2008; Poureslami 2012; Valery 2010) were contacted for further information, with responses from all three (Canino 2008; Poureslami 2012; Valery 2010).
Assessment of heterogeneity
It was proposed that any heterogeneity between the study results would be described and tested to see if it reached statistical significance using a Chi2. The 95% confidence interval (CI), estimated using a random‐effects model, would be included whenever there are concerns about statistical heterogeneity. Heterogeneity is considered significant when the P value is less than 0.10 (Higgins 2011).
Assessment of reporting biases
If reporting bias was suspected (see 'Selective reporting (reporting bias)' in the 'Risk of bias in included studies' table), we planned to contact the study authors to ask them to provide missing outcome data. We planned that if missing data were not provided, and if this was thought to introduce serious bias, the impact of including such studies in the overall assessment would be explored through a sensitivity analysis.
Data synthesis
The results from studies that met the inclusion criteria and which reported any of the outcomes of interest (as defined above) were included in the subsequent meta‐analyses. The summary weighted rate ratio and 95% CI (fixed‐effect model) was calculated (Review Manager (RevMan) using generic inverse ratio (GIV), whereby one participant may have more than one event. The risk ratios were taken from the published papers and the standard errors were calculated from CIs or P values in the published papers. The outcome indices would be assumed to be normally distributed continuous variables so theMD in outcomes could be estimated. If studies had reported outcomes using different measurement scales, we planned to estimate the SMD.
'Summary of findings' (SoF) tables
We created 'Summary of findings' tables, using the primary outcomes (where able) (Table 1; Table 2)
Summary of findings for the main comparison. Summary of findings (paediatric studies).
| Culture‐specific asthma education program compared to Generic asthma education (or usual care) for asthma in children | ||||||
|
Patient or population: Children from minority groups with doctor diagnosed asthma Settings: Any Intervention: Culture‐specific asthma education program Comparison: Generic asthma education program (or usual care) | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Risk with generic asthma education or usual care | Risk with Culture‐specific asthma education program | |||||
| Severe exacerbations requiring hospitalisation over the study period follow‐up: 6‐12 months | 434 per 1,000 |
545 per 1000 (336 to 737) |
OR 1.55 (0.6 to 3.66) | 88 (1 RCT) | ⊕⊕⊝⊝ LOW* | |
| Number of exacerbations over 52 weeks follow‐up: 12 months | ‐ | Mean number of exacerbations over 52 weeks (exacerbation rate) in the intervention group was 0.18 MD higher (0.25 lower to 0.62 higher) | ‐ | 110 (2 RCTs) | ⊕⊕⊕⊝ LOW# | |
| Severe exacerbations requiring hospitalisation over the study period follow‐up: 6‐12 months | RR 0.48 (0.24 to 0.95) | ‐ | 305 (2 RCTs) | ⊕⊕⊕⊝ LOW^ | ||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: rate ratio; OR: Odds ratio | ||||||
| This table was created using the GRADE Pro software (GRADEpro GDT 2015) GRADE Working Group grades of evidence High quality: We are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low quality: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low quality: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | ||||||
* Only one study with small number of participants was included in this analysis. This RCT was unblinded (downgrades for risk of bias and imprecision) (Valery 2010)
# One study by Valery 2010 carried 85.4% of the weight of the results, which may have introduced bias. This RCT was also unblinded (downgrades for risk of bias and imprecision).
^ One study carried 75.1% of the analysis weight (Canino 2008). Both studies (Canino 2008; Valery 2010) were unblinded which may have introduced bias (downgrades for risk of bias and inconsistency).
Summary of findings 2. Summary of Findings (adult studies).
| Culture‐specific asthma education program compared to generic asthma education (or usual care) for asthma in adults | ||||||
| Participant or population: Adults from minority groups with doctor diagnosed asthma Setting: Any Intervention: Culture‐specific asthma education program Comparison: Generic asthma education program (or usual care) | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Risk with generic asthma education or usual care | Risk with Culture‐specific asthma education program | |||||
| Number of participants who had one or more exacerbation of the study period follow‐up: 12 months | 559 per 1,000 | 504 per 1000 (388 to 615) | OR 0.80 (0.50 to 1.26) | 294 (1 RCT) | ⊕⊝⊝⊝ VERY LOW* | |
| Number of participants requiring oral corticosteroids over the study period follow‐up: 12 months | 203 per 1,000 | 198 per 1000 (123 to 306) | OR 0.97 (0.55 to 1.73) | 294 (1 RCT) | ⊕⊝⊝⊝ VERY LOW* | |
| Severe exacerbations requiring hospitalisation over the study period follow‐up: 12 months | 63 per 1,000 | 53 per 1000 (20 to 130) | OR 0.83 (0.31 to 2.22) | 294 (1 RCT) | ⊕⊝⊝⊝ VERY LOW* | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; OR: Odds ratio | ||||||
| This table was created using the GRADE Pro software (GRADEpro GDT 2015) GRADE Working Group grades of evidence High quality: We are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low quality: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low quality: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | ||||||
* The sole study (Moudgil 2000) was of very low quality. There were many uncertainties in this study particularly with regard to outcomes reported (e.g. participants from the age of 11 were included, however the data presented combine adult data, thus outcomes are not shown separately for the paediatric population), allocation concealment, performance/detection bias, reporting bias and imprecision (3 downgrades for these items).
Subgroup analysis and investigation of heterogeneity
We planned to carry out the following a priori subgroup analysis.
Different settings (rural versus non‐rural: as defined by study authors)
Sensitivity analysis
Sensitivity analyses were planned to assess the impact of the potentially important factors on the overall outcomes.
Study quality (adequate allocation concealment and blinding)
Study size
Variation in the inclusion criteria
Differences in outcome measures
Analysis using random‐effects model
Analysis by "treatment received"
Results
Description of studies
See Characteristics of included studies, Characteristics of excluded studies and Characteristics of ongoing studies.
Results of the search
From the previous versions of this review (2007 and 2009), the Cochrane Airways Group Specialised Register (CAGR) identified 228 potentially relevant titles (29 abstracts with four studies satisfying the inclusion criteria for the reviews) (Figure 1). An additional 170 articles were identified from the updated search (up to June 2016), with a further four titles identified from reference lists. After duplicates were removed, 96 titles were considered for the review. After assessing abstracts, 20 studies were retrieved for full review, 15 studies were excluded, with three additional studies (Valery 2010; Poureslami 2012; Grover 2016) fulfilling the eligibility criteria for this update (Figure 1). Two other studies remain ongoing at the time of the review (Janevic 2012; Patel 2014) (see'Characteristics of ongoing studies'). Another two studies are awaiting classification (Buist 2001; Butz 2004) (see 'Characteristics of studies awaiting classification'). An update search run in June 2017 returned three potentially relevant trials which have been added to Studies awaiting classification (Feldman 2016; Griffiths 2016; Patel 2016) and have not been fully incorporated into the review.
Included studies
For this review update seven studies were included (see 'Characteristics of included studies'). A total of 837 participants with asthma from an ethnic minority group were included in this review. Two studies were multi‐centre (Moudgil 2000; Valery 2010) and five were single‐centre studies (Blixen 2001; La Roche 2006; Canino 2008; Poureslami 2012; Grover 2016). Two studies (Blixen 2001; Poureslami 2012) examined adults and four studies examined children (La Roche 2006; Canino 2008; Valery 2010; Grover 2016). The study by (Moudgil 2000) included both adults and children, however specific results for adults and children were not presented in the published paper. The study by (Poureslami 2012), reported outcomes from four treatment groups. For our analysis, we chose to report data from group three (intervention) and group four (control) as we believe group three was the true intervention (participants viewed both the community and knowledge video). The study duration varied ranging from six to 12 months. Exacerbations were defined differently in each study. Culture‐specific programs and controls were defined differently for each study and are further described in (Table 3).
1. Summary description of culture‐specific programs vs control programs Study ID.
| Study ID | Setting | Definition of minority | Participants | Description of Culture‐specific intervention | Description of control |
| Paediatric studies | |||||
| La Roche 2006 | Community Health Centre | African‐American and Hispanic people living in the USA | African‐American or Hispanic descent, children aged 7‐13 years (n = 22) | Multi‐family asthma group treatment (MFAGT) was based on allocentric self‐orientation and socio‐economic context of ethnic minorities. Program delivery included a Hispanic and African‐American educator/psychologist emphasising relational and collaborative asthma management among children, families, primary physician, and mental health specialist (as opposed to learning in isolation from others). Families received three one‐hour education sessions (separate days) covering three modules 1. Identify and monitor asthma symptoms; effectively use medications/resources (e.g. peak flow, medications) to control symptoms. 2. Identifying and preventing asthma triggers 3. Preventing and coping with an asthma attack (e.g. asthma action plans) |
Standard Psycho‐educational Asthma Intervention (SPAI). SPAI has the same 3 education modules as intervention group but followed a structured teaching approach without locating asthma symptoms within the socioeconomic or cultural context. |
| Canino 2008 | Home visits | Socially disadvantaged (low‐income and poor) Puerto Rican families living in the USA. They were identified from the national health plan insurance claims database | Poor Puerto Rican children aged 5 to 12 years (n = 221) | Eight asthma education modules, delivered at 2 home visits with telephone contact for follow‐up and reinforcement of recommended plans and assignments. Modules were culturally adapted with inclusions such as common practices and myths that Puerto Rican parents have about asthma, home remedies, culturally congruent pictures, and common asthma triggers in the island, such as Sahara dust and eruptions from Caribbean volcanoes. | Participants given 5 flyers that contained information on asthma (e.g. what is asthma, control and rescue medications, common allergens (including food) and triggers, how to take care of asthma equipment. |
| Valery 2010 | Community Health Centre | First nations people of Australia who make up a minority of the whole Australian population. They are generally a socially disadvantaged group in a high‐income country | Aboriginal or Torres Strait Islander children aged < 18 years (n = 113) | Three additional education sessions delivered by trained Indigenous Health Care Workers, using existing paediatric asthma and respiratory education resources which were adapted to support Torres Strait culture at baseline, 1, 3 and 6 months | Education session (identical to intervention group) delivered at baseline |
| Grover 2016 | Hospital (chest clinic) | Indian residents whose first language was not English living in India | Indian children aged between 7 and 12 years (n = 40) | Culturally adapted asthma education program to Indian parents and children with asthma (underpinned by GINA guidelines) using age appropriate, graphically appealing and culturally relevant educational materials. The education program was designed based on key principles of health education and pedagogy and intervention delivered by 2 pharmacists. Asthma education was delivered over 1 hr with child/family, workbooks, goal setting and setting asthma action plan with physician. | Parents and children were given a standard information pack for asthma in line with GINA guidelines. |
| Adult studies | |||||
| Moudgil 2000 | General practitioners | A sub group of Indian sub‐continent people living in the UK whose first language was not English | White European (WE) or Indian sub‐continent (ISC) participants aged between 11 to 59 years (n = 689) | Individual asthma education session of 40 minutes duration with an asthma educator fluent in each participants own dialect (e.g. English, Punjabi, Hindi or Urdu). Education sessions included; advising GP changes to treatment; optimising treatment, drug delivery, technique, improved knowledge of asthma, disease severity and medication. | Usual care and follow‐up; 'generic' asthma programme. |
| Blixen 2001 | Hospital | African‐American people living in the USA. They are generally a socially disadvantaged group in a high‐income country | African‐American adults aged between 18 to 50 years (n = 28) | Three one‐hour individual asthma self‐management educational sessions; workbook modified to be culturally appropriate to African Americans; MDI technique and peak flow monitoring video featuring a well‐known African‐American asthma researcher. | Usual care and follow‐up; 'generic' asthma programme. |
| Poureslami 2012 | Usually home or pulmonary clinic | Immigrants to Canada whose first language was not English (e.g. non‐Indigenous to Canada) | Migrants in greater Vancouver Area, who spoke Mandarin, Cantonese or Punjabi with asthma aged > 21 years (n = 92) | Effectiveness of different formats of culturally and linguistically modified asthma education and their impact on self‐management.Participants were allocated to one of three groups below. 1. Physician‐led knowledge video 2. Patient‐generated community video 3. Knowledge and community video |
Received a pictorial pamphlet on asthma. |
Participants
The seven studies used different inclusion and exclusion criteria for participation. All participants had 'doctor diagnosed asthma', but the definition varied across the studies.
Paediatric studies
La Roche 2006 enrolled families (of African‐American or Hispanic descent) with children aged one to 13 years with physician diagnosed asthma. Canino 2008 enrolled poor (defined by utilisation of the Peurto Rico Health Insurance Administration Agency Plan which required that the family be close to the poverty level) Peurto Rican families, with a child aged five to 12 years who had utilised health services for asthma within the previous 12 months. Valery 2010 enrolled Australian Indigenous children (Aboriginal or Torres Strait Islander) aged one to 17 years from Thursday Island and Horn Island with doctor diagnosed asthma. The study by Grover 2016 enrolled Indian children aged seven to 12 years with asthma, who had at least two asthma‐related visits to hospital in the previous 12 months.
Adult studies
Moudgil 2000 enrolled participants (adults and children) with asthma aged 11 to 59 years from participating General Practices (GP) in the United Kingdom (UK). Specific data for children could not be obtained. Of the 689 participants, only 344 were from of an ethnic minority (i.e. Indian Sub‐Continent (ISC)). The remainder (n = 345) were of White European descent. We included this study in the review but only examined data relevant to the ISC participants as published outcomes were stratified by ethnic descent as well as intervention group allocation. Blixen 2001 enrolled African‐American adults, aged 18 to 50 years who had been hospitalised for at least one night with a primary diagnosis of asthma. Poureslami 2012 enrolled adults aged > 21 years with physician diagnosed asthma who had immigrated to Canada within the last 20 years, lived in the Greater Vancouver Area, and spoke Mandarin, Cantonese or Punjabi.
Outcomes
Paediatric studies
Three studies (La Roche 2006; Canino 2008; Valery 2010) used asthma exacerbations as their primary outcome. The study by Grover 2016 used paediatric asthma caregiver quality of life (QoL) as their primary outcome. For other primary outcomes, Canino 2008 was the only study to report the use of oral corticosteroids over the study period. Two studies (Canino 2008; Valery 2010) reported on severe asthma exacerbations requiring hospitalisation.
Secondary outcomes varied between studies. Two studies (Canino 2008; Valery 2010) used the change in Juniper Asthma QoL (Juniper 1992; Juniper 1993). Valery 2010 also reported on adherence outcomes using parents' descriptions of asthma action plan (AAP). Asthma knowledge factors were assessed differently between studies. La Roche 2006 used the individualism‐collectivism scale to measure asthma behavioural assessment for both career/parent and children; where Canino 2008 used change in carers knowledge on triggers and treatment. Grover 2016 used modified scores for asthma knowledge, asthma control and medication adherence.
Adult studies
Two studies (Moudgil 2000; Blixen 2001) used asthma exacerbations as their primary outcome. Moudgil 2000 also reported other primary outcomes such as the use of oral corticosteroids over the study period and severe exacerbations requiring hospitalisation.
Secondary outcomes varied between studies. Objective measurements (FEV1) were used in the Moudgil 2000 study. Symptoms of asthma (QoL) were used in the Moudgil 2000 and Blixen 2001 studies. Asthma knowledge factors were reported by a single study (Poureslami 2012). Poureslami 2012 reported on the proper use of inhaler technique and knowledge of asthma symptoms.
All study characteristics are described in the Characteristics of included studies table.
Excluded studies
The main reason that studies were excluded from the review related to non culture‐specific interventions in minority groups, or non‐randomised controlled studies (see 'Characteristics of excluded studies' table).
Risk of bias in included studies
Risk of bias for included studies are summarised in Figure 2.
Allocation
Valery 2010 was the sole study assessed at low risk for both selection bias domains, as the authors adequately described the method of randomisation using computer‐generated block randomisation sequencing with concealed allocation. Moudgil 2000 and Canino 2008 reported that randomisation was computer generated and randomly allocated, however did not describe the method of concealment allocation (unclear risk). The three remaining studies (Blixen 2001; La Roche 2006; Poureslami 2012) were assessed as an unclear risk; Blixen 2001 and Poureslami 2012 did not describe the method of randomisation or method of concealment allocation. La Roche 2006 reported that randomisation was computer generated, yet did not describe method or how the allocation method was maintained. The study by Grover 2016 reported that randomisation was generated randomly, however it was considered high risk, as the authors reported that allocation concealment was not implemented. There was an imbalance of allocation of treatment groups at baseline.
Blinding
One study (Poureslami 2012) was assessed as low risk for both blinding domains. The authors adequately described how outcome measures were assessed where blinding was not feasible. Two studies (Canino 2008; Grover 2016) were assessed as a high risk for both domains, as they did not describe how blinding was maintained for participants, study personal and did not describe if outcome assessors were blinded. The study by Valery 2010 was assessed as high risk for performance bias as participants and study personal were unblinded and unclear risk for detection bias,as it was not clear whether outcome assessors were blinded. The study by Blixen 2001 was assessed as high risk for performance bias, as participants were unblinded, but low risk for detection bias as outcome assessors were blinded to groups. The remaining two studies (Moudgil 2000; La Roche 2006;) were assessed as an unclear risk as study authors did not describe how blinding was maintained or if outcome assessors were blinded to treatment allocation.
Incomplete outcome data
Three studies (La Roche 2006; Canino 2008; Grover 2016) were assessed as low risk, as > 90% of participants were followed up. Three studies (Moudgil 2000; Poureslami 2012; Valery 2010) were assessed as an unclear risk. In the Moudgil 2000 study, clinical data were only available in 86% of participants and 76% for asthma QoL at the 12‐month follow‐up. Poureslami 2012 did not describe if any participants withdrew or were lost to follow‐up. The Valery 2010 study described that authors did not follow‐up five children due to costs of travel. The study by Blixen 2001 was assessed as high risk as only 46% of participants were able to be contacted for the six‐month follow‐up.
Selective reporting
Six studies (Moudgil 2000; Blixen 2001; La Roche 2006; Canino 2008; Valery 2010; Grover 2016) were assessed as low risk. They adequately described method of analysis (e.g. intention‐to‐treat or by per protocol analysis). Poureslami 2012 was assessed as an unclear risk, as they did not report complete baseline data (some variables presented as grouped data), thus it was difficult to determine differences between the four groups.
Other potential sources of bias
Sources of bias were determined by the review authors and reported in each 'Risk of bias' table.
Effects of interventions
See 'Summary of findings' tables for the main comparisons (Table 1; Table 2).
Three paediatric (La Roche 2006; Canino 2008; Valery 2010) and two adult (Moudgil 2000; Blixen 2001) studies used asthma exacerbations as their primary outcome. The study by Grover 2016 did not report any primary outcome data. Primary and secondary outcome data are reported below in accordance to the adult or paediatric studies.
Paediatric studies (Comparison 1)
Primary outcome
Asthma exacerbations during follow‐up defined as:
Number of participants who had one or more exacerbations over the study period
Three studies (La Roche 2006; Canino 2008; Valery 2010) reported exacerbation data, however we were only able to obtain data for one study (Valery 2010), thus meta‐analysis was not possible. The study by Valery 2010 reported exacerbation data over a 12‐month period in 88 children. There was no significant difference between groups for this outcome (odds ratio (OR) 1.55, 95% confidence interval (CI) 0.66 to 3.66) (Analysis 1.1; Figure 3).
1.1. Analysis.
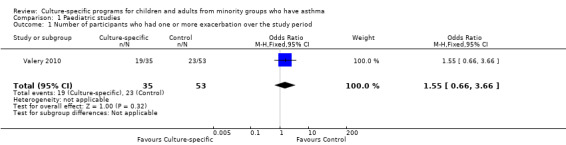
Comparison 1 Paediatric studies, Outcome 1 Number of participants who had one or more exacerbation over the study period.
3.
Forest plot of comparison: 1 Paediatric studies, outcome: 1.1 Number of participants who had one or more exacerbation over the study period.
Number of exacerbations over 52 weeks (exacerbation rate)
Combined data from two studies in 110 children (La Roche 2006; Valery 2010) did not show significant differences of the number of exacerbations over 52 weeks between groups (mean difference (MD 0).18, 95% CI ‐0.25 to 0.62) (Analysis 1.2; Figure 4). Canino 2008 presented data on emergency department (ED) presentations post intervention (in the following six‐month period), but these data could not be combined in the meta‐analysis.
1.2. Analysis.
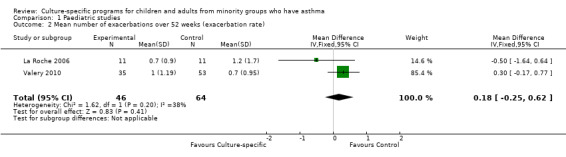
Comparison 1 Paediatric studies, Outcome 2 Mean number of exacerbations over 52 weeks (exacerbation rate).
4.
Forest plot of comparison: 1 Paediatric studies, outcome: 1.2 Mean number of exacerbations over 52 weeks (exacerbation rate).
Severe exacerbations requiring oral corticosteroids over the study period
Canino 2008 reported this outcome over the 12‐month study period. The number of events per group include 33 in the culture‐specific group compared to 30 in the controls. We were, however unable to obtain further data from the study authors.
Severe exacerbations requiring hospitalisations
Combined data from two studies in 305 children (Canino 2008; Valery 2010) showed significantly improved outcomes in the culture‐specific group compared to the control group (Rate Ratio 0.48, 95% CI 0.24 to 0.95) (Analysis 1.3; Figure 5). It is important to note that Canino 2008 reported on hospitalisations for asthma in the six‐month period, whilst Valery 2010 study reported on hospitalisations for asthma in the 12‐month period.
1.3. Analysis.
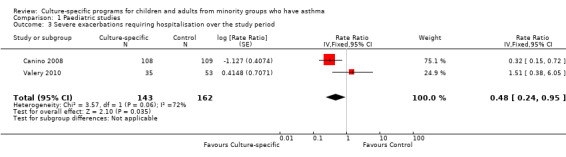
Comparison 1 Paediatric studies, Outcome 3 Severe exacerbations requiring hospitalisation over the study period.
5.
Forest plot of comparison: 1 Paediatric studies, outcome: 1.3 Severe exacerbations requiring hospitalisation over the study period.
Secondary outcomes
Objective measurements of asthma control (FEV1, peak flow, airway hyper‐responsiveness)
No studies reported this outcome.
Asthma Control Score
Asthma Control Score
One study (Canino 2008) reported this outcome over the 12‐month study period, with the outcome being the proportion of children (n=62) with good asthma control based on the score. They reported an OR 3.35, (95% CI 1.45 to 7.73), significantly favouring the group receiving the culture‐specific intervention compared to the control group (Analysis 1.4; Figure 6).
1.4. Analysis.
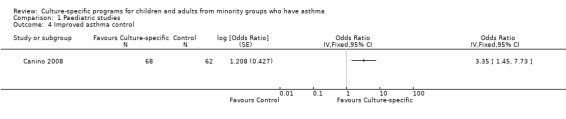
Comparison 1 Paediatric studies, Outcome 4 Improved asthma control.
6.
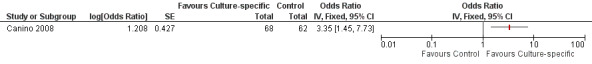
Forest plot of comparison: 1 Paediatric studies, outcome: 1.4 Improved asthma control.
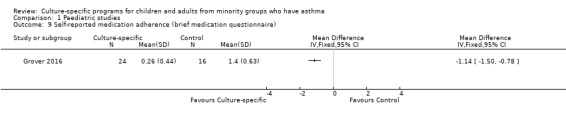
Asthma Control Questionnaire
One study (Grover 2016) reported this outcome in 40 children over the six‐month study period. They used a validated modified Hindi/English version of the asthma control questionnaire and reported a significant improvement in the intervention group compared to controls (Analysis 1.5).
1.5. Analysis.
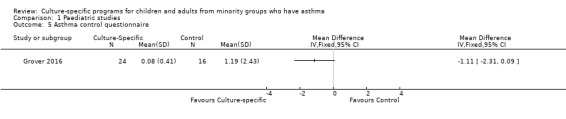
Comparison 1 Paediatric studies, Outcome 5 Asthma control questionnaire.
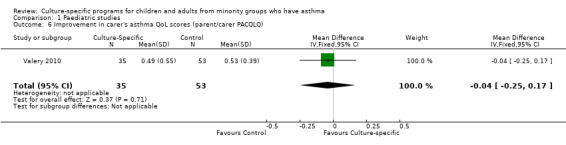
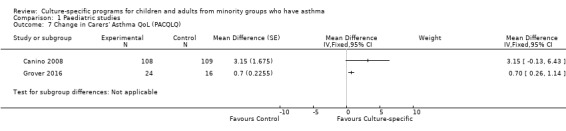
Change in parent proxy asthma QoL score
Three studies (Canino 2008; Valery 2010; Grover 2016) reported this outcome. Data from Valery 2010 could not be combined.The follow‐up period varied for each study; six months in Grover 2016 and 12 months in Canino 2008 and Valery 2010. Additional data were obtained directly from the study authors (Valery 2010; Grover 2016). The study by Valery 2010 measured the change in parent QoL at 12 months (88 parents), but there was no significant difference between the groups (MD ‐0.04; 95% CI ‐0.25 to 0.17). The studies by Canino 2008 and Grover 2016 reported an improvement favouring the culturally‐specific group, but these were not significant. Canino 2008 in 109 parents (MD 3.15; 95% CI ‐0.13 to 6.43) and Grover 2016 in 16 parents (MD 0.70; 95% CI 0.26 to 1.14). The study by Grover 2016 was a feasibility study and of low quality and thus the certainty of this outcome is poor. The clinically minimum important difference (MID) in the QOL scores differ in accordance to the type of QoLs. The most common asthma QoL used in studies is that of Junper where the MID is 0.5 points (Juniper 1996).
Other asthma symptoms scores (e.g. diary cards)
No studies reported this outcome.
Adherence outcomes
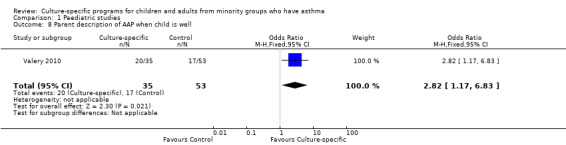
Parent description of Asthma Action Plan (AAP)
Two studies reported on use of AAP (Valery 2010; Grover 2016) but data were only available in the Valery 2010 study. Valery 2010 measured the change in 88 parents' description of AAP when the child was well. The outcome significantly favoured the group who received the culture‐specific program (OR 2.82, 95% CI 1.17 to 6.83) (Figure 7). The study by Grover 2016 reported that none of the participants in either treatment group had a written AAP at baseline. All children in the intervention group were subsequently provided an AAP after baseline and education session. By six months, all participants in the intervention group reported they were confident in using their AAP. Children in the control group were provided a blank template in their information pack at baseline, however no additional data were provided if they were completed or used.
7.
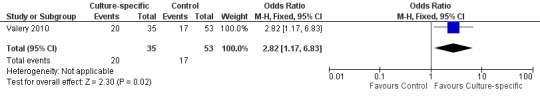
Forest plot of comparison: 1 Paediatric studies, outcome: 1.8 Parent description of AAP when child is well.
Self‐reported medication adherence (using brief medication questionnaire)
A single study (Grover 2016), measured adherence to medications in 40 participants using a validated medication adherence questionnaire (see Characteristics of included studies tables). Study authors reported an improvement in score from baseline in the culture‐specific group compared to the controls.
Asthma knowledge factors
Parent asthma knowledge scores
One study La Roche 2006 reported this outcome in 22 parents. They used a behavioural assessment score. There was an improvement in mean asthma knowledge scores favouring the culture‐specific intervention, but the confidence interval includes no between‐group difference (MD 1.90, 95% CI ‐0.04 to 3.84) (Analysis 1.10).
1.10. Analysis.
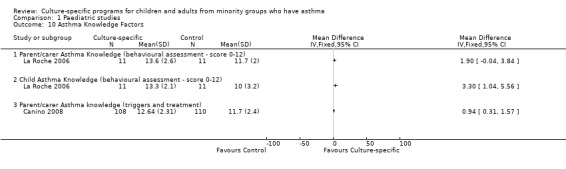
Comparison 1 Paediatric studies, Outcome 10 Asthma Knowledge Factors.
Child asthma knowledge scores
Only one study La Roche 2006 reported this outcome in 22 parents. The outcome significantly favoured the group who received the culture‐specific programme; MD 3.30, (95% CI 1.04 to 5.56) (Analysis 1.10).
Asthma knowledge (change in parent knowledge on triggers and treatment)
The Canino 2008 study presented change from baseline for 218 parents asthma knowledge on asthma triggers and treatment. This outcome favoured the group receiving the culture‐specific program (MD 0.94, 95% CI 0.31 to 1.57) (Analysis 1.10).
Change in asthma knowledge
The study by Grover 2016, used a customised knowledge questionnaire and reported that participants in the intervention group had significantly higher knowledge at the six‐month follow‐up compared to those in the control group.
Economic data
The La Roche 2006 study estimated that the economic savings made by using the culturally specific education programme, based on the reduction of ED presentations was $4675. The estimated total cost of the culturally specific programme for asthma education was $2295.
Adult studies (Comparison 2)
Primary outcome
Asthma exacerbations during follow‐up defined as:
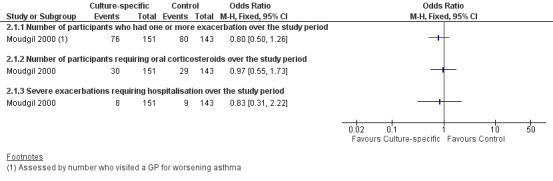
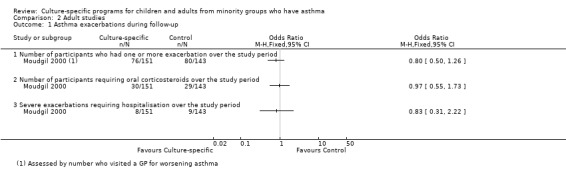
Number of participants who had one or more exacerbations over the study period
Two studies (Moudgil 2000; Blixen 2001) reported exacerbations but numerical data were only provided by one paper (Moudgil 2000), therefore meta‐analysis was not possible. Blixen 2001 stated that there was no statistically significant differences between groups in asthma‐related healthcare resource (defined as hospitalisations, ED visits and physician visits) but no figures were given. In the Moudgil 2000 study, we used the outcome of GP consultations for asthma exacerbations in 294 participants. There was no significant differences between groups (OR 0.80; 95% CI 0.50 to 1.26) (Figure 8).
8.
Forest plot of comparison: 2 Adult studies, outcome: 2.1 Asthma exacerbations during follow‐up.
Number of exacerbations over 52 weeks (exacerbation rate)
Two studies reported exacerbations over 52 weeks. Moudgil 2000 reported the number of events in each group (e.g. culture‐specific n = 218 compared to controls n = 212), however we were unable to obtain or calculate the standard error. Blixen 2001 stated that there was no statistically significant differences between groups but no figures were given. Thus meta‐analysis was not possible for this outcome.
Severe exacerbations requiring oral corticosteroids over the study period
One study (Moudgil 2000) reported data for this outcome. There was no significant difference between groups for those participants (n=294) who required additional corticosteroids (OR 0.97; 95% CI 0.55 to 1.73) (Figure 8).
Severe exacerbations requiring hospitalisations
Two studies (Moudgil 2000; Blixen 2001) reported this outcome, but numerical data could only be obtained from one study (Moudgil 2000). Blixen 2001 stated that there was no statistically significant differences between groups. There was no significant difference between the groups for number of participants (n=294) who were hospitalised for asthma (OR 0.83; 95% CI 0.31 to 2.22) (Figure 8).
Secondary outcomes
Objective measurements of asthma control (FEV1, peak flow, airway hyper‐responsiveness)
One study (Moudgil 2000) reported there was no statistically significant differences between groups for lung function, however numerical data were not provided, therefore meta‐analysis was not possible. We were unable to obtain any further details from study authors.
Asthma Control Score
No studies reported this outcome.
Change in asthma QoL score
Two studies reported this outcome (Moudgil 2000; Blixen 2001). An improved asthma QoL score (the change in score Analysis 2.2) was seen in those who received the culture‐specific education programme when compared to controls (MD 0.26, 95% CI 0.17 to 0.36) (Figure 9). For this outcome, the study authors (Moudgil 2000) report that 280 participants completed the end of study QoL, but the specific numbers for each group was not reported and we assumed that n = 140 was for each group. We could not obtain any further data from the primary author.
2.2. Analysis.
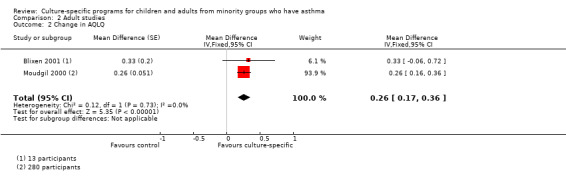
Comparison 2 Adult studies, Outcome 2 Change in AQLQ.
9.
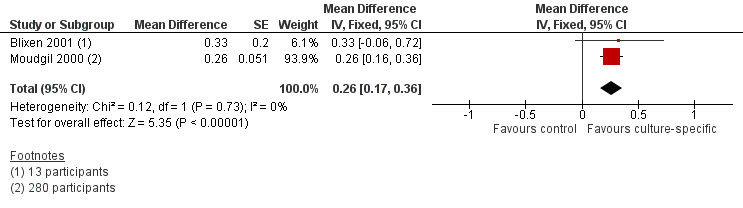
Forest plot of comparison: 2 Adult studies, outcome: 2.2 Change in AQLQ.
Other asthma symptoms scores (e.g. diary cards)
No studies reported this outcome.
Adherence outcomes
No studies reported this outcome.
Asthma knowledge factors
Proper use of inhaler
One study (Poureslami 2012) reported outcome data on improvement of the proper use of inhaler technique in 42 participants. There was no significant differences between groups (Analysis 2.3).
2.3. Analysis.
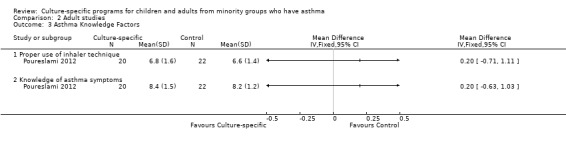
Comparison 2 Adult studies, Outcome 3 Asthma Knowledge Factors.
Knowledge of asthma symptoms
One study (Poureslami 2012) reported improvement in knowledge of asthma symptoms in 42 participants. There was no significant difference between groups (Analysis 2.3).
Economic data
No studies reported this outcome.
Subgroup analysis
Different settings (rural versus non‐rural)
We did not perform a separate subgroup analysis, as there was only one study in each subgroup (Analysis 1.2). The study by La Roche 2006 was conducted in an urban setting in Boston, USA, whereas the study by Valery 2010 was conducted in two Indigenous communities in remote Australia.
Sensitivity analysis
There were insufficient data to undertake any sensitivity analysis.
Discussion
Summary of main results
In this updated review, an additional three studies and 220 participants were added, with a total of seven randomised controlled trials (RCTs) with 837 participants with asthma from ethnic minority groups. Two were multi‐centre and five single‐centre with study durations ranging from six to 12 months. There were two adult‐based studies and four paediatric‐based studies, while one study included both adult and children. This updated review improves the evidence from the previous review supporting the use of culture‐specific asthma education programmes for adults and children from minority groups with asthma. The benefit of culture‐specific asthma education programmes (compared to generic or usual education programme) was stronger in children than in adults. In children, significant differences between groups were found for reducing hospitalisations and improving the outcomes of asthma control, asthma knowledge and adherence. In adults, asthma‐related QoL was the only outcome where there was statistical significance between groups (although clinically the evidence was weak). In both children and adults, there was no difference between groups for the outcome of all exacerbations. A single study examined economic cost and described a significant benefit in cost saving when culture‐specific asthma education programmes were used.
Overall completeness and applicability of evidence
This systematic review is substantially limited by few studies and by a lack of available data preventing combining outcomes for meta‐analysis. Statistical difference between the groups were not found in all outcomes, although this may be related to insufficient sample size (discussed below). While the studies shared some common themes, there were also differences among the studies; notably, the type of interventions used, ethnic groups being investigated and outcomes measured. Furthermore, several studies did not report follow‐up data for clinical outcomes; Blixen 2001 did not report hospitalisations, emergency department (ED) visits etc, and Moudgil 2000 did not report objective measurements e.g. peak flow. Also, La Roche 2006 and colleagues' study was small, leading to baseline imbalances in the asthma knowledge scores. It was also unclear whether there were any participants lost to follow‐up in the Poureslami 2012 study. The study by Grover 2016 was a small feasibility RCT which had some baseline imbalances at randomisation.
The absence of a significant difference between groups for all‐types of asthma exacerbations may be related to a type 1 error (inadequate sample size). Therefore, while both this review and the review from Tapp 2007 found no improvement in adult ED presentations or exacerbations over the study period, the type of educational intervention used can affect self‐reported asthma‐related QoL of participants. In this instance, we could theorise that the use of a culture‐specific programme enables participants (adults) to more fully engage in the education being provided and in turn have a positive effect on QoL scores. These results however should be interpreted with caution due to the small number of included studies that measured asthma QoL (two studies) and the relatively small sample size (n = 308) in those studies (Moudgil 2000; Blixen 2001). Similar to previous updates, we were unable to include results from Canino 2008, which also included an asthma QoL outcome. In children however, a reduction with severe asthma exacerbations requiring hospitalisations was seen (Figure 5).
For the purpose of this review, it was assumed that 'usual care' for asthma presentations would include the provision of generic asthma education, in accordance with recommendations such as the 1997 National Asthma Education and Prevention Program Guidelines (Edmond 1998). Therefore, while the studies by Blixen 2001 and Moudgil 2000 do not specify the nature of the education that control group participants received, it has been assumed that through the provision of 'usual care', participants would have received some form of education during the clinical encounter.
Ideally, this review would have included RCTs in both adults and children with larger sample sizes and have presented more data regarding asthma exacerbation outcomes (e.g. hospitalisations, ED visits, use of rescue oral corticosteroids). This review is limited by the relatively small number of studies and sample sizes, and by the high rate of attrition of participants (clinical outcomes were measured for 329 participants from an original total sample size of 396). It should be noted that three of the studies (Blixen 2001; La Roche 2006; Grover 2016) were pilot/feasibility studies. There were significant differences in several outcomes, however where outcomes did not reach statistical significance, the direction of results tended to favour the culture‐specific programmes.
It has been recognized by Swartz and Dick that in models of care for chronic diseases, the focus must be on the person in his or her own context (Swartz 2002). Certainly this ideal has been met with the intervention in the study by La Roche and colleagues, with one focus of the intervention being to locate the signs and symptoms of asthma within the cultural context of the participant and family (La Roche 2006). La Roche and colleagues also trialled their culturally specific intervention against a generic education programme (La Roche 2006), whereas the control groups in the two other included studies (Moudgil 2000; Blixen 2001) received 'usual care' (standard asthma education) and participants were asked to continue with their usual follow‐up routine. The interventions used by Blixen 2001 and Moudgil 2000 could be argued to be culturally modified, rather than culturally specific, with both studies using interventions that have been used in populations understood to be white participants, and modified through the use of language, images and other additions. However, the decision was made to include these two studies as it was felt that the modifications and delivery of the intervention were specific to the ethnic groups to which the participants belonged. It should also be noted that while all the studies trialled interventions in minority groups, only two studies (Valery 2010; Grover 2016) involved a population who were Indigenous to the study setting.
Quality of the evidence
The 'Summary of findings' tables report the available evidence for our primary outcomes related to asthma exacerbations and our justification for the quality of evidence (Table 1; Table 2). Overall, the quality of evidence of the studies was very low to low, due to methodological differences, lack of objective measurements, reporting and imprecision of data.
Potential biases in the review process
One of the authors of this review is the senior author on the Valery 2010 paper. Additional data were obtained by direct contact with A/Prof Valery and data extraction was performed by another review author using data from another Cochrane review (Chang 2010).
Agreements and disagreements with other studies or reviews
This review's findings are in agreement with the review examining the efficacy of involvement of an Indigenous healthcare worker (IHW) in comparison to absence of an IHW in asthma education programs in improving asthma‐related outcomes in Indigenous children and adults with asthma (Chang 2010). Other systematic reviews on culture‐specific interventions have like‐wise found that culture‐adapted programs were more efficacious than generic programs such as interventions that target smoking cessation, diet, and/or physical activity (Nierkens 2013). However, for health promotion interventions, other systematic reviews have also called for more evidence as there is yet insufficient evidence on the clinical effectiveness or cost‐effectiveness of these adapted approaches although it has been shown that culturally adapting interventions increases salience, acceptability and uptake (Liu 2012; Davidson 2014).
The results of another Cochrane review in adults found that asthma education interventions in the ED, while effective at reducing hospital admission, did not significantly reduce subsequent ED visits (Tapp 2007). The review by Tapp and colleagues also found no significant difference in QoL scores between treatment and control groups (Tapp 2007), whereas the review presented here found a significant improvement in asthma QoL scores for adult participants, although the difference between groups was lower then the minimum important difference for the QoL tool.
Authors' conclusions
Implications for practice.
The evidence presented in this review suggests that culture‐specific education programmes for adults and children from minority groups may be effective in improving asthma‐related outcomes, but our confidence is limited by the small number of randomised controlled trials (RCTs) identified and difficulties encountered in performing meta‐analysis. However, the benefits seen are in keeping with the wider body of evidence and current guidance and it is therefore justified that asthma education programmes for children and adults from minority groups should be culture‐specific and considered for health service and policy (where able) to reduce ongoing disparities and poorer health outcomes faced by disadvantaged and minority groups.
Implications for research.
Given the diversity of settings and complexities of health outcomes of people with asthma from minority groups, evidence from seven RCTs suggests that culture‐specific education programmes are effective in improving some but not all asthma‐related health outcomes.
Further high‐quality parallel RCTs are needed to further assess the role of culturally specific education programmes for people with asthma from minority groups. Trials should include both adults and children (including families), and should compare the culture‐specific programmes with generic education programmes (as opposed to usual care). Collection of clinical outcomes of asthma exacerbations and severity, as well as other asthma‐related outcomes including QoL, knowledge, self‐management behaviours, adherence outcomes and economic impact should be included in future trials to gain a better perspective on the efficacy of culture‐specific programmes for people with asthma from minority groups. Trials involving minority groups indigenous to their country of residence should also be conducted. The type and extend of 'culture‐specific' approaches should also be explicit. Given that there was only one study that reported economic data, economic data for the intervention are also required.
What's new
| Date | Event | Description |
|---|---|---|
| 10 June 2016 | New citation required but conclusions have not changed | Author group changed and review updated to current Cochrane format. Primary and secondary outcomes modified for clarification, and to reflect current asthma‐related outcomes. Subgroup analysis ‐ adults versus children and types of education have been removed. Adults and children are now analysed separately. New studies included (Valery 2010; Poureslami 2012; Grover 2016) including an additional 220 participants. New 'Risk of bias' tool used. SoF table included. |
| 10 June 2016 | New search has been performed | Literature search updated to June 2016. An update literature search in July 2017 was not fully incorporated and three studies were added to studies awaiting classification. |
History
Protocol first published: Issue 3, 2007 Review first published: Issue 2, 2008
| Date | Event | Description |
|---|---|---|
| 1 December 2008 | New citation required but conclusions have not changed | Author list changed |
| 17 October 2008 | New citation required but conclusions have not changed | One new author added to the byline of the review. The conclusions of the review have not been substantively amended by the addition of the study by Canino et al |
| 30 August 2008 | New search has been performed | Literature searches re‐run; One new study added (Canino 2008). |
| 17 June 2008 | Amended | Converted to new review format. |
| 11 December 2007 | New citation required and conclusions have changed | Substantive amendment |
Acknowledgements
We also thank Elizabeth Stovold for performing the original and updated searchers and for obtaining the relevant papers. We further thank Dr Martin La Roche, Dr Fitzgerald, Dr Poureslami, Dr Canino, Dr Grover and A/Prof Patricia Valery for responding to our queries about their study. We are grateful to the Airways Group for their on‐going support.
Christian Osadnik was the Editor for this review.
The Background and Methods sections of this review are based on a standard template used by Cochrane Airways.
This project was supported by the National Institute for Health Research (NIHR), via Cochrane Infrastructure funding to the Cochrane Airways Group. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, NHS, or the Department of Health.
We are very grateful to Dr Chris Cates for advice and help with extracting data and analysis.
Appendices
Appendix 1. Search strategies
Cochrane Airways Register of trials
#1 AST:MISC1 #2 MeSH DESCRIPTOR Asthma Explode All #3 asthma*:ti,ab #4 #1 or #2 or #3 #5 MeSH DESCRIPTOR Oceanic Ancestry Group #6 aboriginal* or aborigine* #7 indigenous* #8 MeSH DESCRIPTOR Minority Groups #9 MeSH DESCRIPTOR Culture Explode All #10 MeSH DESCRIPTOR Ethnology #11 culture* NEAR3 (specific* OR appropriate* or tailored*) #12 cultural* #13 MeSH DESCRIPTOR Cultural Diversity #14 MeSH DESCRIPTOR Cultural Deprivation #15 MeSH DESCRIPTOR Cultural Characteristics #16 MeSH DESCRIPTOR Anthropology, Cultural Explode All #17 #5 or #6 or #7 or #8 or #9 or #10 or #11 or #12 or #13 or #14 or #15 or #16 #18 MeSH DESCRIPTOR Self Care #19 MeSH DESCRIPTOR Self Administration #20 MeSH DESCRIPTOR Self Medication #21 MeSH DESCRIPTOR Self Efficacy #22 self* NEXT manage* #23 MeSH DESCRIPTOR Patient Acceptance of Health Care Explode All #24 MeSH DESCRIPTOR Patient Education as Topic #25 MeSH DESCRIPTOR Patient Care Planning Explode All #26 MeSH DESCRIPTOR Patient‐Centered Care #27 MeSH DESCRIPTOR Health Services, Indigenous #28 indigenous* NEAR3 health* #29 aboriginal* NEAR3 health* #30 (educat*) or (program*) or (learn*) or (specific*) #31 #18 or #19 or #20 or #21 or #22 or #23 or #24 or #25 or #26 or #27 or #28 or #29 or #30 #32 #4 AND #17 AND #31
CENTRAL (Cochrane Library)
#1 MeSH descriptor Asthma explode all trees
#2 MeSH descriptor Bronchial Spasm explode all trees
#3 asthma*
#4 wheez*
#5 bronchospas*
#6 bronch* near spas*
#7 bronchoconstrict*
#8 bronch* near constrict*
#9 (#1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8)
#10 MeSH descriptor Oceanic Ancestry Group, this term only
#11 (aboriginal* or aborigine*)
#12 indigenous
#13 MeSH descriptor Minority Groups, this term only
#14MeSH descriptor Culture, this term only
#15 MeSH descriptor Ethnology, this term only
#16 culture‐specific
#17 cultural
#18 MeSH descriptor Cultural Diversity, this term only
#19MeSH descriptor Cultural Deprivation, this term only
#20 MeSH descriptor Cultural Characteristics, this term only
#21 MeSH descriptor Anthropology, Cultural, this term only
#22 (#10 OR #11 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18 OR #19 OR #20 OR #21)
#23 MeSH descriptor Self Care, this term only
#24 MeSH descriptor Self Administration, this term only
#25 MeSH descriptor Self Medication, this term only
#26 MeSH descriptor Self Efficacy, this term only
#27 self manage*
#28 MeSH descriptor Patient Acceptance of Health Care explode all trees
#29 MeSH descriptor Patient Education explode all trees
#30 MeSH descriptor Patient Care Planning explode all trees
#31 MeSH descriptor Patient‐Centered Care explode all trees
#32 MeSH descriptor Health Services, Indigenous, this term only
#33 indigenous health*
#34 aboriginal* health*
#35 (educat*) or (program*) or (learn*) or (specific)
#36 (#23 OR #24 OR #25 OR #26 OR #27 OR #28 OR #29 OR #30 OR #31 OR #32 OR #33 OR #34 OR #35
#37 (#9 AND #22 AND #36)
MEDLINE (Ovid)
1. exp asthma/ 2. exp Bronchial Spasm/ 3. asthma$.tw. 4. wheez$.tw. 5. bronchospas$.tw. 6. (bronch$ adj3 spas$).tw. 7. bronchoconstrict$.tw. 8. (bronch$ adj3 constrict$).tw. 9. or/1‐8 10. oceanic ancestry group/ or (aboriginal$ or aborigine$).tw. 11. minority groups/ or indigenous.tw. 12. culture/ or ethnology/ or culture specific.tw. or cultural.tw. 13. or/10‐12 14. self care/ or self administration/ or self medication/ or self efficacy/ or self manage$.tw. 15. "patient acceptance of health care"/ or patient compliance/ or patient participation/ or patient satisfaction/ or treatment refusal/ 16. patient education/ or patient care planning/ or patient‐centered care/ 17. health services indigenous/ or indigenous health$.tw. 18. (educat$ or program$ or learn$ or specific).tw. 19. or/14‐18 20. 9 and 13 and 19 21. (controlled clinical trial or randomized controlled trial).pt. 22. (randomized or randomised).ab,ti. 23. placebo.ab,ti. 24. dt.fs. 25. randomly.ab,ti. 26. trial.ab,ti. 27. groups.ab,ti. 28. or/21‐27 29. Animals/ 30. Humans/ 31. 29 not (29 and 30) 32. 28 not 31
Embase (Ovid)
1. exp asthma/ 2. Bronchospasm/ 3. asthma$.tw. 4. wheez$.tw. 5. bronchospas$.tw. 6. (bronch$ adj3 spas$).tw. 7. bronchoconstrict$.tw. 8. (bronch$ adj3 constrict$).tw. 9. or/1‐8 10. (aboriginal$ or aborigine$ or indigenous).tw. or exp minority group/ 11. culture/ or ethnology/ or culture specific.tw. or cultural.tw. 12. 10 or 11 13. self care/ or self administration/ or self medication/ or self efficacy/ or self manage$.tw. 14. patient attitude/ or patient compliance/ or patient participation/ or patient satisfaction/ or refusal to participate/ or treatment refusal/ 15. health education/ or health promotion/ or nutrition education/ or patient education/ 16. exp patient care/ or health care planning/ or patient care planning/ 17. health services indigenous/ or indigenous health$.tw. or aboriginal$ health$.tw. or aborigine$ health$.tw. 18. (educat$ or program$ or learn$ or specific).tw. 19. or/13‐18 20. 9 and 12 and 19 21. Randomized Controlled Trial/ 22. randomization/ 23. controlled clinical trial/ 24. Double Blind Procedure/ 25. Single Blind Procedure/ 26. Crossover Procedure/ 27. (clinica$ adj3 trial$).tw. 28. ((singl$ or doubl$ or trebl$ or tripl$) adj3 (mask$ or blind$ or method$)).tw. 29. exp Placebo/ 30. placebo$.ti,ab. 31. random$.ti,ab. 32. ((control$ or prospectiv$) adj3 (trial$ or method$ or stud$)).tw. 33. (crossover$ or cross‐over$).ti,ab. 34. or/21‐33 35. exp animals/ or exp invertebrate/ or animal experiment/ or animal model/ or animal tissue/ or animal cell/ or nonhuman/ 36. human/ or normal human/ or human cell/ 37. 35 and 36 38. 35 not 37 39. 34 not 38
Data and analyses
Comparison 1. Paediatric studies.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Number of participants who had one or more exacerbation over the study period | 1 | 88 | Odds Ratio (M‐H, Fixed, 95% CI) | 1.55 [0.66, 3.66] |
| 2 Mean number of exacerbations over 52 weeks (exacerbation rate) | 2 | 110 | Mean Difference (IV, Fixed, 95% CI) | 0.18 [‐0.25, 0.62] |
| 3 Severe exacerbations requiring hospitalisation over the study period | 2 | 305 | Rate Ratio (Fixed, 95% CI) | 0.48 [0.24, 0.95] |
| 4 Improved asthma control | 1 | Odds Ratio (Fixed, 95% CI) | Totals not selected | |
| 5 Asthma control questionnaire | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 6 Improvement in carer's asthma QoL scores (parent/carer PACQLQ) | 1 | 88 | Mean Difference (IV, Fixed, 95% CI) | ‐0.04 [‐0.25, 0.17] |
| 7 Change in Carers' Asthma QoL (PACQLQ) | 2 | Mean Difference (Fixed, 95% CI) | Subtotals only | |
| 8 Parent description of AAP when child is well | 1 | 88 | Odds Ratio (M‐H, Fixed, 95% CI) | 2.82 [1.17, 6.83] |
| 9 Self‐reported medication adherence (brief medication questionnaire) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 10 Asthma Knowledge Factors | 2 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 10.1 Parent/carer Asthma Knowledge (behavioural assessment ‐ score 0‐12) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 10.2 Child Asthma Knowledge (behavioural assessment ‐ score 0‐12) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 10.3 Parent/carer Asthma knowledge (triggers and treatment) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
1.6. Analysis.
Comparison 1 Paediatric studies, Outcome 6 Improvement in carer's asthma QoL scores (parent/carer PACQLQ).
1.7. Analysis.
Comparison 1 Paediatric studies, Outcome 7 Change in Carers' Asthma QoL (PACQLQ).
1.8. Analysis.
Comparison 1 Paediatric studies, Outcome 8 Parent description of AAP when child is well.
1.9. Analysis.
Comparison 1 Paediatric studies, Outcome 9 Self‐reported medication adherence (brief medication questionnaire).
Comparison 2. Adult studies.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Asthma exacerbations during follow‐up | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 Number of participants who had one or more exacerbation over the study period | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Number of participants requiring oral corticosteroids over the study period | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 Severe exacerbations requiring hospitalisation over the study period | 1 | Odds Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Change in AQLQ | 2 | Mean Difference (Fixed, 95% CI) | 0.26 [0.17, 0.36] | |
| 3 Asthma Knowledge Factors | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3.1 Proper use of inhaler technique | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Knowledge of asthma symptoms | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
2.1. Analysis.
Comparison 2 Adult studies, Outcome 1 Asthma exacerbations during follow‐up.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Blixen 2001.
| Methods | An open, prospective, randomised controlled study evaluating the use of an asthma education program specifically targeted for African Americans compared with no education (control group). | |
| Participants |
Inclusion criteria: African‐American adults aged between 18 to 50 years hospitalised overnight at a single hospital with a primary diagnosis of asthma Exclusion criteria: No information described Participants were identified and approached whilst hospitalised with an asthma episode. Verbal consent was obtained from those who wished to participate. A face‐to‐face baseline interview was arranged (whilst still hospitalised). Following baseline interview, participants were randomly assigned to either the intervention or control group. Telephone interviews were conducted at 3 and 6 months consisting of the same questions asked at baseline plus additional information about any asthma events since the last interview. Number approached: n = 40 Number declined: n = 12 Number consented and randomised: n = 28 (n = 14 intervention group and n = 14 control group) Baseline: Intervention group n = 14, Control group n = 14 3 month follow‐up: Intervention group n = 10, Control group n = 11 6 month follow‐up: Intervention group n = 7, Control group n = 6 |
|
| Interventions |
Recruitment dates: July to November 1997 Sample size: n = 30 (15 per arm) Intervention group: received three one‐hour individual asthma self‐management educational sessions with a nurse educator while hospitalised with a primary diagnosis of asthma. The aim of the sessions was to teach patients the rationale and skills required to manage asthma as a chronic inflammatory process rather than an episodic crisis‐driven process. During these educational sessions, participants received a number of resources as outlined. 1. Workbook (Learn Asthma Control in Seven Days) which was modified to be culturally appropriate to African Americans. This included a discussion on handling the stressors common to many African Americans. The goals of the educational intervention were to;
To achieve these goals a video on MDI technique and peak flow monitoring was shown during the educational sessions. The video featured a well‐known African‐American asthma researcher (Dr Marvella Ford). Participants rehearsed the demonstration until appropriate technique was mastered, and which included:
2. Participants were shown a video on MDI‐technique and peak flow monitoring. The video, "Managing Your Asthma: Understanding Proper Inhaler and Peak Flow Technique" was produced by Glaxo‐Wellcome and featured an African‐American asthma specialist showing African‐American patients how to use MDIs and Peak flow meters. Participants then rehearsed the demonstration until the technique was mastered. Participants were given the video, a peak flowmeter and a spacer for an MDI to take home. Written materials to reinforce the concepts and self‐management techniques introduced in the educational sessions were mailed to the intervention group participants at 3 and 6 months. Control group: were asked to continue with their usual care and follow‐up, which represented the 'generic' asthma programme. |
|
| Outcomes |
Outcome measures
Outcome assessments were performed by telephone interview at three and six months post intervention. |
|
| Notes |
Lost to follow‐up at final assessment: n = 15 Funding: The Nursing Research Program‐Clinical Applications Research‐GlaxoWellcome and The Agency for Health Care Policy and Research |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of randomisation was not described by authors |
| Allocation concealment (selection bias) | Unclear risk | Study authors did not describe method of allocation concealment and how this was maintained |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding of participants was not possible after randomisation, given the nature of the intervention compared to the control group |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | The randomisation status of participants at 3 and 6 months interviews were concealed by using a different trained interviewer who did not participate in the education program and was not aware of randomisation status |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Attrition was high, with only 13/28 (46%) participants able to be contacted for the 6‐month post discharge follow‐up interview due to disconnected phone or moving without a forwarding address |
| Selective reporting (reporting bias) | Low risk | Descriptive data reported. Intention‐to‐treat analysis not used |
| Other bias | Unclear risk | Education intervention aimed to optimise anti‐inflammatory therapy by improving metered dose inhalation and peak flow ‐ data not reported in paper |
Canino 2008.
| Methods | Single‐blinded randomised controlled trial comparing intervention "Take Control, Empower Yourself and Achieve Management of Asthma" (CALMA) program with control (usual care group). All study participants completed a one hour in‐home baseline interview and similar post‐interview 4 months after randomisation. Randomisation by computer algorithm based on mixed block design. |
|
| Participants | Participants were identified and screened for eligibility before invitation to participate. Inclusion criteria:
Exclusion criteria:
All study participants completed a one‐hour in‐home baseline interview and similar post‐interview 4 months after randomisation. Randomisation by computer algorithm based on mixed block design. Number screened: n = 332 Number eligible: n = 256 Number randomised: n = 221 (Intervention group n = 110 and Control group n = 111) 1 participant from control group and 2 participants from CALMA (intervention) group were lost to follow‐up. All analyses were based on intention‐to‐treat. |
|
| Interventions |
Recruitment dates: April 2006 to October 2006 Sample size: Not stated Intervention group: CALMA is the abbreviation of the Spanish for "Take Control, Empower Yourself and Achieve Asthma Managment". The intervention was developed for reducing asthma morbidity in poor Puerto Rican children (aged 5 to 12 years) with asthma. Children and families enrolled in the intervention group received 8 asthma education modules, delivered over the course of 2 home visits with telephone contact for follow‐up and reinforcement of recommended plans and assignments. The modules aimed to help the patient/family with the following goals.
The modules were culturally adapted with inclusions such as common practices and myths that Puerto Rican parents have about asthma, proper use of home remedies, culturally congruent pictures, and common asthma triggers in the island, such as Sahara dust and eruptions from Caribbean volcanoes. Educational material was developed relating to coping with marital and family stress resulting from the consequences of the child's asthma, increasing parental empowerment to deal with the Puerto Rican health system and educating parents how to teach their child and others how to manage asthma. Control group: received five flyers of educational materials that contained information about:
|
|
| Outcomes |
Primary outcome
Secondary outcome
Assessments were performed at baseline and 4 months post randomisation |
|
| Notes |
Lost to follow‐up at final assessment: n = 3 Funding: National Centre for Minority Health and Health Disparities and the National Institutes of Health |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Study authors state randomisation was done based on a mixed block randomisation scheme |
| Allocation concealment (selection bias) | Unclear risk | Randomisation by computerised algorithm based on mixed block randomisation scheme. No information provided on how allocation concealment was maintained |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Complete blinding was not possible after randomisation, given the nature of the intervention compared to the control group |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Study authors do not describe if outcome assessment was completed by study personnel who were blinded to treatment allocation, yet describe the strict training and certification of asthma counsellors |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Complete outcome data were measured in > 95% of participants |
| Selective reporting (reporting bias) | Low risk | Intention to treat analysis used |
| Other bias | Unclear risk | Nil |
Grover 2016.
| Methods | A single‐centre randomised controlled trial aiming to develop, implement and evaluate the efficacy of a culturally contextualised asthma education program for Indian parents and children with asthma | |
| Participants |
Inclusion criteria: Indian children aged between 7 and 12 years; family spoke either English/Hindi; child diagnosed with asthma and child had at least 2 asthma‐related visits to the hospital in the 12 months prior to study Exclusion criteria: Not stated Clinical asthma: Child needed to be diagnosed with asthma, however not defined as to who made diagnosis Recruitment strategy: Eligible participants were recruited and invited by their physician or by medical record review when attending asthma outpatient clinic in a Chest Diseases Hospital in New Dehli Number approached: Not stated Number refused: Not stated Number randomised (parent‐child pairs): n = 24 (intervention group; n = 16 control group (usual care) |
|
| Interventions |
Education program development: The overarching aim was to develop, implement and evaluate the efficacy of a culturally adapted asthma education program to parents and children with asthma. The asthma education program was designed based on key principles of health education and pedagogy and was split into three key components:
The asthma education content was underpinned by international asthma guidelines (Global initiative for Asthma ‐ GINA). Participant recruitment dates: July to December 2012 Sample size: n = 20 per arm (total n = 40) Parents and children were invited to participate in the RCT when attending asthma outpatient visit. It was not clear if the intervention was done at the time of the outpatient visit or arranged for another time convenient to families. While not reported, it was assumed that the intervention was individualised with parent‐carer pairs. Both the intervention and control group completed data collection at the baseline visit. This included asthma caregiver quality of life questionnaire, paediatric asthma control, asthma knowledge, asthma control, medication adherence, inhaler use competence and asthma action plan ownership. Intervention group: This was delivered by two allied health professionals (pharmacists) and asthma educators (researchers x 2) and included:
Further data collection was done at 3 months (phone call) and at 6 months (face to face follow‐up) to collect primary and secondary outcome data. Control group: After baseline data were collected (identical to intervention group), parents and children were given a standard information pack for asthma in line with GINA guidelines. They were assessed at 6 months (face‐to‐face follow‐up) to collect primary and secondary outcome data. |
|
| Outcomes |
Primary outcome
Secondary outcomes
Outcomes were assessed at baseline, 3 and 6 months |
|
| Notes | It was not clear how many people were screened or if written informed consent was provided. Study reached sample size, however baseline imbalance between groups (n = 24 intervention group and n = 16 control group). Analysis of baseline characteristics was not clinically significant. Funding: Nil |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Authors describe participants were recruited from asthma outpatient clinic and through note reviews. Generated using Microsoft Excel, using number sequence generation |
| Allocation concealment (selection bias) | High risk | Authors acknowledge in discussions that allocation concealment was not implemented |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | It was not clear when the intervention took place with the parent‐child at the time of outpatient visit, or arranged for another time convenient for the family. It was not possible to keep participants blinded after randomisation |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Outcome assessors were not blinded to treatment groups |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Authors report all participants remained in study until end of study at 6 months |
| Selective reporting (reporting bias) | Low risk | Authors report primary and secondary outcomes |
| Other bias | Low risk | Nil |
La Roche 2006.
| Methods | Randomised single‐blind, parallel comparison of 2 types of interventions: Multifamily asthma group treatment (MFAGT) vs. Standard Psycho‐educational Asthma Intervention (SPAI) in children with asthma. These two interventions were also compared to controls (no additional education program provided) that were randomly selected from a pool of patients with asthma. |
|
| Participants | Families with children with asthma were enrolled from Martha Eliot Health Centre, an inner‐city community health centre which is part of the Boston's children Hospital. Inclusion criteria: African‐American or Hispanic descent, aged 7‐13 years with physician diagnosed asthma Exclusion criteria: Nil described Number families screened: n = 46 Number families randomised: n = 24 Number families completed study: n = 22 16 (73%) were Hispanic and 6 (27%) were African American. Mean age of children randomised was 10.2 years. 13 (59%) were male and 9 (41%) were female. The control group had 11 families and were matched to the intervention group by ethnicity, age and sex. All children were from low socio‐economic background. Participants competed 2 assessments (see outcome measures); one at enrolment and the second at one year following enrolment. Lost to follow‐up: n = 2 participants at final assessment |
|
| Interventions |
Recruitment dates: Not stated Sample size: Not stated Intervention group: MFAGT is based on allocentric self‐orientation and socio‐economic context of ethnic minorities. Program delivery included a Hispanic and African‐American educator/psychologist. MFAGT also emphasised relational and collaborative asthma management among children, families, primary physician, and mental health specialist (as opposed to learning in isolation from others). Families in the intervention group received three one‐hour education sessions (on separate days) each covering one module of the education programme. The content of each module consisted of:
Control group: SPAI has the same 3 education modules above but followed a structured teaching approach without locating asthma symptoms within the socio‐economic or cultural context. This asthma education/management strategy did not include contingency plans that emphasised cultural resources and reflected a generic approach to asthma education. Therefore, participants in the MFAGT arm of the study received the 'culturally specific' programme, whereas the SPAI participants served as a control group receiving the generic asthma education programme. |
|
| Outcomes |
Primary outcome 1. Number of asthma‐related Emergency Department visits Secondary outcome
Outcomes were assessed 12 months post intervention |
|
| Notes | The paper provided data that compared MFAGT to SPAI and to controls. However, as the control group was not randomised, control group data were not included in the analysis. Funding: Office of Sponsored Projects of the Childrens Hospital Boston and Harvard Medical School, Center of Excellence in Minority Health and Health Disparities. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomisation by computer, allocation method not described |
| Allocation concealment (selection bias) | Unclear risk | Study authors do not provide information on how allocation concealment was maintained |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Study authors do not describe how blinding was maintained throughout study |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Study authors do not describe if outcome assessment was completed by study personnel who were blinded to treatment allocation. While treatment (exacerbations outcome) was given by health professionals unrelated to trial, for the outcome of asthma knowledge, risk is high as this was a single blind study |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All completed the trial, however two families did not complete 2nd evaluation (these families were omitted from analysis) |
| Selective reporting (reporting bias) | Low risk | Paper provided data that compared MFAGT to SPAI and to controls. However, as the control group was not randomised, control group data was not included in analysis. Intention‐to‐treat analysis not used |
| Other bias | Unclear risk | Authors do not provide data for control children ‐ not included in analysis |
Moudgil 2000.
| Methods | Open, prospective, randomised, controlled, parallel group study examining individually‐based asthma education and structured follow‐up for people with asthma. | |
| Participants | Potential participants were identified through registration and diagnostic records inner city general practices in the Birmingham area. All eligible patients were requested to attend their general practice for review by the researcher. Participants were randomised to either the intervention or control group prior to initial appointments being sent. Inclusion criteria: All white European (WE) or Indian sub‐continent (ISC) participants with asthma, from 12 participating general practices in the Birmingham area, aged 11 to 59 years Exclusion criteria: Minority groups (e.g. Afro‐Caribbean and some mixed race) and a small number of Bangladeshi and/or only Bengali speaking patients who did not speak English, Punjabi, Urdu or Hindu Number identified: n = 1217 Number randomised: n = 689 (Intervention group: n = 343 and Control group: n = 346) |
|
| Interventions |
Study dates: August 1995 to 1996 Sample size: n = 331 in each arm Intervention group participants: received individual asthma education session of 40 minutes duration with an asthma educator fluent in each participants own dialect (e.g. English, Punjabi, Hindi or Urdu). Emphasis during the session was on:
Participants were given peak flow meters free of charge and a booklet to record measurements during the 12‐month intervention period, along with an individually‐tailored asthma management plan and educational literature (in the appropriate dialect) describing aspects of asthma and asthma management. Plans were based on existing BTS guidelines. Educational literature in the relevant ethnic dialect, describing aspects of asthma and its management, including triggers, medication, delivery devices etc were distributed to all participants in the intervention group (literature provided by Allen & Hanburys). Educational intervention was reinforced at 4 and 8 months, although it is not stated how this was done. Control group participants: attended their GP at the start and end of the study for outcome assessment and were asked to continue their usual asthma follow‐up and care for asthma (e.g. generic asthma programme). |
|
| Outcomes |
Outcome measures 1. Number of asthma‐related hospital admissions 2. Number of asthma‐related presentations to the ED 3. Number of asthma‐related home visits from GP 4. Number of asthma‐related visits (during regular hours) to GP 5. Prescriptions of oral steroids 6. Prescriptions of antibiotic 7. Asthma QoL (Juniper ‐ 32 questions about asthma events in the last 2 weeks and scores responses on 7‐point scale (1 = severe limitation or most of the time; 7 = no limitation or none of the time)) Outcomes were performed 12 months post intervention |
|
| Notes | Although the study included participants from the age of 11, data presented combines adult data, thus outcomes are not shown separately for the paediatric population. Study measured clinical outcomes for 294 (of 344) participants, and Asthma QoL outcomes for 280 (of 344) participants. Domains for activity limitation, symptoms, emotional function and exposure to environmental stimuli. Some terms did not translate directly into the different dialects used and the terms used were agreed by two bilingual persons after a translation‐back translation process. Funding: West Midlands Regional Health Authority and North Birmingham Health Authority |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was computer‐generated and randomly allocated |
| Allocation concealment (selection bias) | Unclear risk | Participants were reviewed at local GP clinics by researcher. Study authors did not describe how allocation was concealed |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Unclear if outcome assessor was blinded to intervention groups |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Study authors did not describe if outcomes assessor was blinded to intervention groups |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Clinical data was available for (86%) and 76% for Asthma QoL |
| Selective reporting (reporting bias) | Low risk | Intention‐to‐treat analysis not used. Per protocol analysis |
| Other bias | Unclear risk | Objective measurement of airflow obstruction (e.g. peak flow) recorded for 12 months ‐ nil data reported in paper |
Poureslami 2012.
| Methods | A randomised controlled trial to determine the effectiveness of different formats of culturally relevant asthma education on self‐management in Punjabi and Chinese asthma patients in Canada. | |
| Participants |
Inclusion criteria: Adults with a physician diagnosis of asthma, used asthma medications daily, > 21 years, immigrated to Canada within the last 20 years, lives in the Greater Vancouver Area, and spoke Mandarin, Cantonese or Punjabi. Exclusion criteria: Not stated Number physician confirmed asthmatics: n = 167 Number participated in development of educational intervention: n = 35 Number participated in focus group session: n = 40 Number randomised in the educational intervention: n = 92 (n = 4 groups)
|
|
| Interventions | The overarching purpose of this study was to conduct a community‐based research project to develop culturally and linguistically appropriate educational intervention to improve self‐management of asthma among immigrants to Canada. 167 asthmatic adults were recruited at a University Pulmonary medical clinic in Vancouver using a convenience sampling method. This study was subsequently split into three parts. Part 1 ‐ Development of educational resources (two educational videos on knowledge and community views and educational pamphlet) (n = 35 participants) Part 2 ‐ Randomised controlled trial (n = 92 participants) Part 3 ‐ Focus group session (n = 40 participants) Participants recruitment dates for RCT: Not stated Sample size: n = 92 Intervention group: Education interventions took place in a convenient place for participants (usually in their home or clinic). Participants were interviewed using bilingual and bicultural experienced moderators who were blinded to study groups and study hypothesis. Participants in the intervention group consisted of three groups.
Participants undertook a pre‐test assessment, followed by a 1‐month education intervention based on their group allocation. This was followed by a 3‐month follow‐up post‐test assessment. Immediately after receiving the education intervention, participants were asked a series of standardised qualitative questions. 6 months after the post‐test assessment, participants were called to assess their self‐management using a shorter version of the study questionnaire. Control group: Education interventions took place in a convenient place for participants (usually in their home or clinic). Participants were interviewed using bilingual and bicultural experienced moderators who were blinded to study groups and study hypothesis. Control participants (group) four received a pictorial pamphlet for asthma. They followed the same process as the intervention group with respect to pre and post assessments. |
|
| Outcomes |
Outcomes were assessed at baseline, 3 and 6 months |
|
| Notes | It was not clear if any participants were lost to follow‐up. We assumed all participants were included in the final analysis (n = 92). Funding: Canadian Institutes of Health Research and The Centre for Lung Health at the University of British Columbia, Vancouver. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Authors describe participants were recruited from a convenience sample, however randomisation process not described |
| Allocation concealment (selection bias) | Unclear risk | Study authors did not describe how allocation was concealed |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Education intervention and assessments were done individually at participants home or in clinic. Personnel conducting assessments were blinded to study groups |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Personnel conducting assessments were blinded to study groups |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Authors do not describe if any participants withdrew or were lost to follow‐up. Baseline characteristics were reported as one group |
| Selective reporting (reporting bias) | Unclear risk | Authors do not report descriptive data. Intention‐to‐treat analysis not used |
| Other bias | Unclear risk | Unclear whether the original 167 asthmatics participated in more than one step of the development phase (e.g. development of asthma education or focus group) |
Valery 2010.
| Methods | A multi‐centre randomised controlled trial to assess the outcomes of an education intervention for childhood asthma conducted by Australian Indigenous Health Care Workers (ICHWs). | |
| Participants |
Inclusion criteria: Indigenous children (Aboriginal or Torres Strait Islander) aged < 18 years from Thursday Island and Horn Island with a provisional diagnosis of asthma or had been referred by Indigenous healthcare workers for assessment with respiratory specialist were eligible. Exclusion criteria: Not stated Clinical asthma was defined as repeated episodes of wheeze with dyspnoea that responded to bronchodilators (in children aged 3‐6 years, 2 or more episodes of wheezy illness associated with cough and shortness of breath and documented amelioration of symptoms and clinical signs after administration of a bronchodilator). Severity of asthma was classified as persistent, frequent episodic, or infrequent episodic, based on the clinical pattern in the last 12 months. Number screened for asthma: n = 484 Number with physician confirmed asthma: n = 117 Number refused: n = 4 Number randomised: Total n = 113 (Intervention group: n = 42 and Control group: n = 71) |
|
| Interventions | Prior to the RCT, 67 ICHWs were trained in 7 separate 3‐day asthma education workshops on Thursday Island during 2005 and 2008. ICHWs also attended respiratory specialist clinics where asthma management knowledge and skills were reinforced. Existing paediatric asthma and respiratory education resources were adapted to support Torres Strait culture, including child‐friendly and age‐specific asthma booklets. Participant recruitment dates: April 2005 to March 2007 Sample Size: n = 54 children per arm After children (n = 484) were screened by the respiratory physician, those with a confirmed diagnosis of asthma (n = 117) received an education session delivered by trained ICHWs, using existing paediatric asthma and respiratory education resources which were adapted to support Torres Strait culture. Training included using a child‐friendly age‐specific asthma booklet at enrolment (prior to randomisation). Eligibility for the RCT was subsequently confirmed and consented children (n = 113) were then randomised to the intervention or control group. Intervention group: Children received additional education sessions delivered by ICHWs at 1, 3 and 6 months after the baseline visit (randomisation). Children were also clinically assessed by the ICHWs at baseline, 1,3, 6 and 12 months to collect primary and secondary outcome data. Control group: Control group children did not receive any further education sessions. Children were clinically assessed by ICHWs at the baseline visit (randomisation) and again 12 months later. |
|
| Outcomes |
Primary outcome:
Secondary outcomes:
Data for primary outcome were collected 12 months prior and 12 months post intervention. Data for secondary outcomes were collected as baseline (randomisation) 1, 3, 6 and 12 months |
|
| Notes |
Lost to follow‐up at final assessment: n = 19. A further five children who were infrequent episodic asthmatics were excluded as study investigators could not justify the cost of transport from a remote island for the clinical assessment at 12 months. Funding: National Health and Medical Research Council, Rural Health Suport, Education and Training grant, Telstra Foundation and Royal Children's Hospital Foundation |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A randomly generated list (using a computer‐generated permuted block design) stratified by age |
| Allocation concealment (selection bias) | Low risk | Allocation to intervention groups was revealed after enrolment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Study was unblinded |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Unblinded study, but staff collecting data from medical records were blinded to intervention study allocation |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Five participants who had infrequent data were excluded from the 12 month follow‐up, as investigators decided it was not cost‐effective to fly participants in for this review |
| Selective reporting (reporting bias) | Low risk | Progress of all randomly assignment participants was clearly described. Participants analysed using a per protocol analysis (n = 88) |
| Other bias | Unclear risk | Nil |
AAP: asthma action plan RCT: randomised controlled trial: QoL; quality of life
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Alicea‐Alvarez 2014 | Excluded as study was not an RCT. |
| Anderson 2004 | Excluded as study was not an RCT. |
| Apter 2003 | Excluded as study was not an RCT. |
| Baren 2001 | Excluded as the intervention was not culture‐specific. |
| Bruzzese 2011 | Excluded as study was not an RCT. |
| Butz 2006 | Excluded as the intervention was not culture‐specific. |
| Choy 1999 | Excluded as study was not an RCT. |
| Clark 2004 | Excluded as the intervention was not culture‐specific. |
| Crowder 2012 | Excluded as study was not an RCT. |
| DePue 2007 | Non RCT and intervention was not culture‐specific. |
| Evans 1997 | Non RCT and participants were staff of the clinics rather than asthma patients. Intervention was not culture‐specific. |
| Evans 1999 | Excluded as intervention was not culture‐specific. |
| Fisher 2009 | Excluded as intervention was not culture‐specific. |
| Ford 1997 | Excluded as this re‐analysis was not an RCT. |
| Griffiths 2005 | Excluded as asthma management was nested within an RCT for chronic diseases. |
| Gundelman 2004 | Excluded as intervention was not culture‐specific. |
| Kay 2006 | Excluded as intervention was not culture‐specific. |
| Kelso 1995 | Excluded as study was not an RCT. |
| Mc Manus 2010 | Excluded as study was not an RCT. |
| Mitchell 1986 | Excluded as intervention was not culture‐specific. |
| Mosnaim 2013 | Excluded as intervention was not culture‐specific. |
| Nelson 2011 | Excluded as intervention was not culture‐specific. |
| Partridge 2000 | Excluded as study was not an RCT. |
| Perez 1999 | Excluded as intervention was not culture‐specific. |
| Persky 2007 | Excluded as study was not an RCT. |
| Pilcher 2014 | Excluded as intervention was not culture‐specific. |
| Poureslami 2011 | Excluded as study was not an RCT. |
| Press 2012 | Excluded as study was not an RCT. |
| Sperber 1995 | Excluded as study was not an RCT. |
| Sullivan 2002 | Excluded as study was not an RCT. |
| Tatis 2005 | Excluded as study was not an RCT. |
| Velsor‐Freidrich 2004 | Excluded as study was not an RCT. |
| Velsor‐Friedrich 2005 | Excluded as intervention was not culture‐specific. |
| Wise 2010 | Excluded as intervention was not culture‐specific and was not an RCT. |
| Zar 2012 | Excluded as study was not an RCT. |
| Zorc 2009 | Excluded as intervention was not culture‐specific. |
RCT: randomised controlled trial
Characteristics of studies awaiting assessment [ordered by study ID]
Buist 2001.
| Methods | Not available |
| Participants | White, Asian (Hawaii), Hispanic and African‐American persons with asthma |
| Interventions | Does not use a culturally specific education intervention |
| Outcomes | No data available |
| Notes | Start date in January 2001. Unable to establish if study is ongoing. Information from author in 2007 (Buist AS ‐ Principal Investigator; buists@ohsu.edu). |
Butz 2004.
| Methods | Unknown |
| Participants | African American (93%) |
| Interventions | Includes teaching children communication skills in order to communicate asthma health issues to their primary care provider. Parents completed a one‐page cue card when talking with the child's physician, which included child's symptom frequency, number of emergency department visits or hospitalisations in the last 12 months, current medications and worries, health beliefs or expectations about their child's asthma. |
| Outcomes | No data available |
| Notes | Study completed in July 2008, however no further data available on Clinical.Trials.Gov (last checked 25th January 2017) |
Feldman 2016.
| Methods | Randomised controlled trial |
| Participants | Latino persons 18 years or older with asthma and panic disorder (PD) |
| Interventions | Cognitivie behavior psychophysiological therapy (CBPT) culturally adapted for Latino people compared with music and relaxation therapy (MRT) for 8 weekly sessions to reduce PD severity, improve asthma control and inhaled corticosteroid adherence by 3 months |
| Outcomes |
Primary outcome:
Secondary outcomes:
Data for primary and secondary outcomes were collected at baseline and again at 3 months. Attrition was high (40%). Both groups showed improvements in PD severity, asthma control and several other anxiety and asthma outcome measures from baseline to 3 months. CBPT was more effective over MRT for improved adherence to inhaled corticosteroids. |
| Notes | Trial registered with ClinicalTrials.gov (NCT01583296) |
Griffiths 2016.
| Methods | Cluster randomised controlled trial |
| Participants | South Asians with asthma aged 3 year or older |
| Interventions | Culturally adapted Physician Asthma Care Education (PACE) programme and the Chronic Disease Self Management Programme (CDSMP), compared to usual practice. Participants in the intervention group received education on key messages about asthma with asthma specialist nurses using the PACE and CDSMP program, including self management plans and a follow up appointment either their general practitioner or practice nurses. Participants in the control group received standardised structured education from an asthma specialist. Participants were interviewed in both groups by researchers (blinded to randomisation status) at baseline, 3 and 12 months. Medical records were reviewed at baseline and then again at 12 months. |
| Outcomes |
Primary outcomes: 1. Time to first unscheduled contact with an asthma exacerbation. 2. Proportion of participants without unscheduled care Secondary outcomes 1. Time to first asthma review in primary care 2. Asthma‐specific and generic health related quality of life, using AQ20, North of England and EQ5D scales 3. Prescribing assessed from patient records and interviews Data for primary and secondary outcomes were collected at baseline, 3 and 12 months. The intervention group did not have any effect on time to first unscheduled attendance for asthma, yet did improve follow‐up in primary care, self‐efficacy and quality of life. |
| Notes | Unclear if trial was registered |
Patel 2016.
| Methods | Randomised controlled trial |
| Participants | African American women with persistent asthma |
| Interventions | To evaluate a telephone‐based self‐regulation intervention that emphasised African women's management of asthma compared to usual care in a series of six sessions. |
| Outcomes | Behavioral factors, symptoms and asthma control, asthma‐related quality of life, and health care use were collected at baseline and 2 years later. |
| Notes | Trial registered with ClinicalTrials.gov (NCT01117805) |
Characteristics of ongoing studies [ordered by study ID]
Janevic 2012.
| Trial name or title | Study protocol for women of color and asthma control: A randomised controlled trial of an asthma‐managment intervention for African‐American women |
| Methods | Randomised controlled trial |
| Participants | Inclusion Criteria: African‐American women > 18 years with asthma who have access to a telephone or cell phone, not pregnant and willing to be involved in the study. Exclusion Criteria: Patients with chronic respiratory conditions, including cystic fibrosis and chronic obstructive pulmonary disease (COPD) |
| Interventions | African‐American women comparing a five‐session asthma‐management intervention (over telephone by trained health care educator) compared with usual care. |
| Outcomes | No data available |
| Starting date | May 2010 |
| Contact information | Mary R Janevic ‐ Investigator mjanevic@umich.edu |
| Notes | Last clinical trials registry update ‐ June 2016 (recruitment completed) |
Patel 2014.
| Trial name or title | Study protocol for improving asthma outcomes through cross‐cultural communication training for physicians: a randomised trial of physician training |
| Methods | Parallel randomised controlled trial |
| Participants | Inclusion criteria: Primary healthcare physicians who treat African‐American and Latino/Hisapanic children with asthma |
| Interventions | Three‐arm randomised controlled trial to compare effectiveness of Physician Asthma Care Education (PACE) with cross‐cultural communication training on health outcomes of African‐American and Latino/Hisapanic children with asthma |
| Outcomes | No data available |
| Starting date | December 2010 |
| Contact information | Minal R Patel ‐ Principal Investigator minalrp@umich.edu |
| Notes | Last clinical trials registry update ‐ May 2016 (recruitment completed) |
Differences between protocol and review
The primary and secondary outcomes in this version were altered for clarity (compared to the previous version of the review) and to reflect current asthma‐related outcomes. In the previous review (Bailey 2009b), we used a hierarchy of assessment which made it confusing. In this version, our primary and secondary outcomes are in line with other Cochrane reviews on asthma with exacerbation being the primary outcome and secondary outcomes reflecting other components of asthma morbidity (lung function, QoL, etc).
Contributions of authors
Previous version: ABC and EJB wrote protocol, selected studies, extracted data and drafted the review (2009). Other previous authors (NB, PM, SK) reviewed the manuscript. Current review: GBM and ABC selected relevant papers from searches, extracted and analysed data and updated the review. PSM and NB contributed to writing the review.
Sources of support
Internal sources
-
Australian Cochrane Airways Scholarship, Other.
Gabrielle McCallum received a scholarship to complete review
External sources
National Health and Medical Research Council, Australia.
Australian Cochrane Airways Group Network Scholarship, Australia.
Declarations of interest
GBM: none known.
PSM: none known.
NB: none known.
ABC: was an author in one of the included studies.
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Blixen 2001 {published data only}
- Blixen CE, Hammel JP, Murphy D, Ault V. Feasibility of a nurse‐run asthma education program for urban African‐Americans: a pilot study. Journal of Asthma 2001;38(1):23‐8. [PubMed] [Google Scholar]
Canino 2008 {published data only}
- Canino G, Vila D, Norman S, Acosta‐Perez E, Ramirez R, Garcia P, et al. Reducing asthma health disparities in poor Puerto Rican children: The effectiveness of a culturally tailored family intervention. Journal of Allergy and Clinical Immunology 2008;121(3):665‐70. [DOI] [PMC free article] [PubMed] [Google Scholar]
Grover 2016 {published data only}
- Grover C, Goel N, Armour C, Asperen PP, Gaur SN, Moles RJ, et al. Medication education program for Indian children with asthma: A feasibility study. Nigerian Journal of Clinical Practice 2016;19(1):76‐84. [DOI] [PubMed] [Google Scholar]
La Roche 2006 {published and unpublished data}
- Roche M, Koinis‐Mitchell D, Gualdron M. A culturally competent asthma management intervention: a randomized controlled pilot study. Annals of Allergy, Asthma and Immunology 2006;96:80‐5. [DOI] [PubMed] [Google Scholar]
Moudgil 2000 {published data only}
- Moudgil H, Marshall T, Honeybourne D. Asthma education and quality of life in the community: a randomised controlled study to evaluate the impact on white European and India subcontinent ethnic groups from socio‐economically deprived areas in Birmingham, UK. Thorax 2000;55(3):177‐83. [DOI] [PMC free article] [PubMed] [Google Scholar]
Poureslami 2012 {published data only}
- Poureslami, I. Nimmon L, Doyle‐Waters M, Rootman I, Schulzer M, Kuramoto L, et al. Effectiveness of educational interventions on asthma self‐management in Punjabi and Chinese asthma patients: a randomized controlled trial. Journal of Asthma 2012;49(5):542‐51. [DOI] [PubMed] [Google Scholar]
Valery 2010 {published data only}
- Valery PC, Masters IB, Taylor B, Laifoo Y, Chang AB. An education intervention for childhood asthma by Aboriginal and Torres Strait Islander health workers: a randomised controlled trial. Medical Journal of Australia 2010;192(10):574‐9. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Alicea‐Alvarez 2014 {published data only}
- Alicea‐Alvarez N, Swanson‐Biearman B, Kelsen SG. A review of barriers to effective asthma management in Puerto Ricans: cultural, healthcare system and pharmacogenomic issues. [Review]. Journal of Asthma 2014;51(1):97‐105. [DOI] [PubMed] [Google Scholar]
Anderson 2004 {published data only}
- Anderson ME, Freas MR, Wallace AS, Kempre A, Glefand EW, Liu AH. Successful school based intervention for inner‐city children with persistent asthma. Journal of Asthma 2004;41(4):445‐53. [DOI] [PubMed] [Google Scholar]
Apter 2003 {published data only}
- Apter A, Boston R, George M, Norfleet A, Tenhave T, Coyne J, et al. Modifiable barriers to adherence to inhaled steroids among adults with asthma: It's not just black and white. Journal of Allergy and Clinical Immunology 2003;111:1219‐26. [DOI] [PubMed] [Google Scholar]
Baren 2001 {published data only}
- Baren JM, Shofer FS, Ivey B, Reinhard S, Degeus J, Stahmer SA, et al. A randomized, controlled trial of a simple emergency department intervention to improve the rate of primary care follow‐up for patients with acute asthma exacerbations. Annals of Emergency Medicine 2001;38(2):115‐22. [DOI] [PubMed] [Google Scholar]
Bruzzese 2011 {published data only}
- Bruzzese JM, Kingston S, Sheares BJ, Cespedes A, Sadeghi H, Evans D. Feasibility and preliminary outcomes of a school‐based intervention for inner‐city, ethnic minority adolescents with undiagnosed asthma. Patient Education and Counseling 2011;85(2):290‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Butz 2006 {published data only}
- Butz AM, Tsoukleris M, Donithan M, Doren H, Zuckerman I, Mudd K, at al. Effectiveness of nebulizer use‐targeted asthma education on undeserved children with asthma. Archives of Pediatric and Adolescent Medicine 2006;160(6):622‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Choy 1999 {published data only}
- Choy DK, Tong M, Ko F, Li ST, Ho A, Chan J, et al. Evaluation of the efficacy of a hospital‐based asthma education programme in patients of low socio‐economic status in Hong Kong. Clinical and Experimental Allergy 1999;29(1):84‐90. [DOI] [PubMed] [Google Scholar]
Clark 2004 {published data only}
- Clark NM, Brown R, Joseph CL, Anderson EW, Liu M, Valerio MA. Effects of a comprehensive school‐based asthma program on symptoms, parent management, grades and absenteeism. Chest 2004;125:1674‐9. [DOI] [PubMed] [Google Scholar]
Crowder 2012 {published data only}
- Crowder S, Johnson B, Marion E. A framework to evaluate the cultural appropriateness of intervention research. Western Journal of Nursing Research 2012;34(8):1002‐22. [DOI] [PubMed] [Google Scholar]
DePue 2007 {published data only}
- DePue J, McQuaid E, Koinis‐Mitchell D, Camillo C, Alario A, Klein R. Providence School Asthma Partnership: school‐based asthma program for inner‐city families. Journal of Asthma 2007;44(6):449‐53. [DOI] [PubMed] [Google Scholar]
Evans 1997 {published data only}
- Evans D, Mellins R, Lobach K, Ramos‐Bonoan C, Pinkett‐Heller M, Weisemann S, et al. Improving care for minority children with asthma: professional education in public health clinics. Pediatrics 1997;99:157‐64. [DOI] [PubMed] [Google Scholar]
Evans 1999 {published data only}
- Evans R, Gergen P, Mitchell H, Kattan M, Kercsmar C, Crain E, et al. A randomized clinical trial to reduce asthma morbidity among inner‐city children: results of the National Cooperative Inner‐city Asthma Study. Journal of Paediatrics 1999;135:332‐8. [DOI] [PubMed] [Google Scholar]
Fisher 2009 {published data only}
- Fisher EB, Strunk RC, Highstein GR, Kelley‐Sykes R, Tarr KL, Trinkaus K, et al. A randomized controlled evaluation of the effect of community health workers on hospitalization for asthma: The Asthma Coach. Archives of Pediatrics and Adolescent Medicine 2009;163(3):225‐32. [DOI] [PubMed] [Google Scholar]
Ford 1997 {published data only}
- Ford ME, Havstad SL, Tilley BC, Boulton MB. Health outcomes among African American and Caucasian adults following a randomized trial of an asthma education program. Ethnicity and Health 1997;2(4):329‐39. [DOI] [PubMed] [Google Scholar]
Griffiths 2005 {published data only}
- Griffiths C, Motlib J, Azad A, Ramsay J, Eldridge S, Feder G, et al. Randomised controlled trial of a lay‐led self‐management programme for Bangladeshi patients with chronic disease. British Journal of General Practice 2005;55(520):831‐7. [PMC free article] [PubMed] [Google Scholar]
Gundelman 2004 {published data only}
- Gundelman S, Meade K, Chen YQ, Benson M. Asthma control and hospitalizations among inner‐city children: Results of a randomized trial. Telemedicine Journal and E‐Health 2004;10(Suppl 2):S6‐14. [PubMed] [Google Scholar]
Kay 2006 {published data only}
- Kay Bartholemew L, Sockrider M, Abramson SL, Swank PR, Czyzewski DI, Tortolero SR, et al. Partners in school asthma management: evaluation of a self management program for children with asthma. Journal of School Health 2006;76(6):283‐90. [DOI] [PubMed] [Google Scholar]
Kelso 1995 {published data only}
- Kelso TM, Self TH, Rumbak MJ, Stephens MA, Garret W, Arheart KL. Educational and long‐term therapeutic intervention in the ED: Effect on outcomes in adult indigent minority asthmatics. American Journal of Emergency Medicine 1995;13(6):632‐7. [DOI] [PubMed] [Google Scholar]
Mc Manus 2010 {published data only}
- Manus V, Savage E. Cultural perspectives of interventions for managing diabetes and asthma in children and adolescents from ethnic minority groups. [Review]. Child 2010;36(5):612‐22. [DOI] [PubMed] [Google Scholar]
Mitchell 1986 {published data only}
- Mitchell EA, Ferguson V, Norwood M. Asthma education by community child health nurses. Archives of Disease in Childhood 1986;61(12):1184‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mosnaim 2013 {published data only}
- Mosnaim G, Li H, Martin M, Richardson D, Belice PJ, Avery E, et al. The Iimpact of peer support and mp3 messaging on adherence to inhaled corticosteroids in minority adolescents with asthma: a randomized, controlled trial. Journal of Allergy and Clinical Immunology: In practice 2013;1(5):485‐93. [DOI] [PMC free article] [PubMed] [Google Scholar]
Nelson 2011 {published data only}
- Nelson KA, Highstein GR, Garbutt J, Trinkaus K, Fisher EB, Smith SR, et al. A randomized controlled trial of parental asthma coaching to improve outcomes among urban minority children. Archives of Pediatrics and Adolescent Medicine 2011;165(6):520‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Partridge 2000 {published data only}
- Partridge M. In what way may race, ethnicity or culture influence asthma outcomes?. Thorax 2000;55:175‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Perez 1999 {published data only}
- Perez MG, Feldman L, Caballera F. Effects of a self‐management educational program for the control of childhood asthma. Patient Education and Counselling 1999;36(1):47‐55. [DOI] [PubMed] [Google Scholar]
Persky 2007 {published data only}
- Persky V, Turyk M, Piorkowski J, Coover L, Knight J, Wagner C, et al. Inner‐city asthma: the role of the community. Chest 2007;132:831‐9. [DOI] [PubMed] [Google Scholar]
Pilcher 2014 {published data only}
- Pilcher J, Patel M, Smith A, Davies C, Travers J, Weatherall M, et al. The budesonide/formoterol inhaler as maintenance and reliever therapy in Maori asthmatics [Conference abstract]. Respirology 2014;19:842‐51. [DOI] [PubMed] [Google Scholar]
Poureslami 2011 {published data only}
- Poureslami I, Rootman I, Doyle‐Waters MM, Nimmon L, FitzGerald JM. Health literacy, language, and ethnicity‐related factors in immigrant asthma patients to Canada: a qualitative study. Journal of Immigrant and Minority Health 2011;13(2):315‐22. [DOI] [PubMed] [Google Scholar]
Press 2012 {published data only}
- Press VG, Pappalardo AA, Conwell WD, Pincavage AT, Prochaska MH, Arora VM. Interventions to improve outcomes for minority adults with asthma: a systematic review. [Review]. Journal of General Internal Medicine 2012;27(8):1001‐15. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sperber 1995 {published data only}
- Sperber K, Ibrahin H, Hoffman B, Eisenmesser B, Hsu H, Corn B. Effectiveness of a specialized asthma clinic in reducing asthma morbidity in an inner‐city minority population. Journal of Asthma 1995;32(5):335‐43. [DOI] [PubMed] [Google Scholar]
Sullivan 2002 {published data only}
- Sullivan SD, Weiss KB, Lynn H, Mitchell H, Kattan M, Gergen PJ, et al. The cost‐effectiveness of an inner‐city asthma intervention for children. Journal of Allergy and Clinical Immunology 2002;110(4):576‐81. [DOI] [PubMed] [Google Scholar]
Tatis 2005 {published data only}
- Tatis V, Remache D, DiMango E. Results of a culturally directed asthma intervention program in an inner‐city latino community. Chest 2005;128:1163‐7. [DOI] [PubMed] [Google Scholar]
Velsor‐Freidrich 2004 {published data only}
- Velsor‐Freidrich B, Pigott TD, Louloudes A. The effects of a school based intervention on the self‐care and health of African‐American inner‐city children with asthma. Journal of Pediatric Nursing 2004;19(4):247‐56. [DOI] [PubMed] [Google Scholar]
Velsor‐Friedrich 2005 {published data only}
- Velsor‐Friedrich B, Pigott T, Srof A. A practitioner‐based asthma intervention program with African American inner‐city school children. Journal of Pediatric Health Care 2005;19(3):163‐71. [DOI] [PubMed] [Google Scholar]
Wise 2010 {published data only}
- Wise M, Pulvermacher A, Shanovich KK, Gustafson DH, Sorkness C, Bhattacharya A. Using action research to implement an integrated pediatric asthma case management and eHealth intervention for low‐income families. Health Promotion Practice 2010;11(6):798‐806. [DOI] [PMC free article] [PubMed] [Google Scholar]
Zar 2012 {published data only}
- Zar H, Levin M. Challenges in treating pediatric asthma in developing countries. Paediatric Drugs 2012;14(6):353‐9. [DOI] [PubMed] [Google Scholar]
Zorc 2009 {published data only}
- Zorc J, Chew A, Allen J, Shaw K. Beliefs and barriers to follow‐up after an emergency department asthma visit: A randomized trial. Pediatrics 2009;124(4):1135‐42. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies awaiting assessment
Buist 2001 {unpublished data only}
Butz 2004 {unpublished data only}
Feldman 2016 {published data only}
- Feldman JM, Matte L, Interian A, Lehrer PM, Lu SE, Scheckner B, et al. Psychological treatment of comorbid asthma and panic disorder in Latino adults: Results from a randomized controlled trial. Behaviour Research and Therapy 2016;87:142‐54. [DOI: 10.1016/j.brat.2016.09.007] [DOI] [PMC free article] [PubMed] [Google Scholar]
Griffiths 2016 {published data only}
- Griffiths C, Bremner S, Islam K, Sohanpal R, Vidal DL, Dawson C, et al. Effect of an Education Programme for South Asians with Asthma and Their Clinicians: A Cluster Randomised Controlled Trial (OEDIPUS). PloS One 2016;11(12):e0158783. [DOI: 10.1371/journal.pone.0158783] [DOI] [PMC free article] [PubMed] [Google Scholar]
Patel 2016 {published data only}
- Patel MR, Song PX, Sanders G, Nelson B, Kaltsas E, Thomas LJ, et al. A randomized clinical trial of a culturally responsive intervention for African American women with asthma. Annals of Allergy, Asthma & Immunology 2016;118(2):212‐9. [DOI: 10.1016/j.anai.2016.11.016] [DOI] [PMC free article] [PubMed] [Google Scholar]
References to ongoing studies
Janevic 2012 {unpublished data only}
- Study protocol for women of color and asthma control: A randomised controlled trial of an asthma‐managment intervention for African‐American women. Ongoing study May 2010. [DOI] [PMC free article] [PubMed]
Patel 2014 {unpublished data only}
- Study protocol for improving asthma outcomes through cross‐cultural communication training for physicians: a randomised trial of physician training. Ongoing study December 2010. [DOI] [PMC free article] [PubMed]
Additional references
Abbott 2007
- Abbott P, Gordon E, Davison J. Expanding roles of Aboriginal health workers in the primary care setting: seeking recognition. Contemporary Nurse 2007;26(1):66‐73. [DOI] [PubMed] [Google Scholar]
Beaglehole 2008
- Beaglehole R, Epping‐Jordan J, Patel V, Chopra M, Shah E, Kidd M, et al. Improving the prevention and management of chronic disease in low‐income and middle‐income countries: a priority for primary health care. Lancet 2008;372:940‐9. [DOI] [PubMed] [Google Scholar]
BTS 2016
- SIGN 153. British guideline on the management of asthma. https://www.brit‐thoracic.org.uk/document‐library/clinical‐information/asthma/btssign‐asthma‐guideline‐2016/ (accessed 25 January 2017).
Chang 2002
- Chang AB, Grimwood K, Mulholland EK, Torzillo PJ. Bronchiectasis in Indigenous children in remote Australian communities. Medical Journal of Australia 2002;177(4):200‐4. [DOI] [PubMed] [Google Scholar]
Chang 2010
- Chang AB, Taylor B, Masters IB, Laifoo Y, Brown ADH. Indigenous health worker involvement for Indigenous adults and children with asthma. Cochrane Database of Systematic Reviews 2010, Issue 5. [DOI: 10.1002/14651858.CD006344.pub2] [DOI] [PubMed] [Google Scholar]
Chino 2006
- Chino M, DeBruyn L. Building true capacity: indigenous models for indigenous communities. American Journal of Public Health 2006;96(4):596‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Coultas 1994
- Coultas DB, Gong H, Grad R, Handler A, McCurdy SA, Player R, et al. Respiratory diseases in minorities of the United States. American Journal of Respiratory and Critical Care Medicine 1994;149(3 Pt 2):S93‐131. [DOI] [PubMed] [Google Scholar]
Davidson 2014
- Davidson EM, Liu JJ, Bhopal RS, White M, Johnson MR, Netto G, et al. Consideration of ethnicity in guidelines and systematic reviews promoting lifestyle interventions: a thematic analysis. European Journal of Public Health 2014;24(3):508‐13. [DOI] [PubMed] [Google Scholar]
de Oliveira 1999
- Oliveira MA, Faresin SM, Bruno VF, Bittencourt AR, Fernandes AL. Evaluation of an educational programme for socially deprived asthma patients. European Respiratory Journal 1999;14(4):908‐14. [DOI] [PubMed] [Google Scholar]
Douglas 2013
- Douglas ML, McGhan SL, Tougas D, Fenton N, Sarin C, Latycheva O, et al. Asthma education program for First Nations children: an exemplar of the knowledge‐to‐action framework. Canadian Respiratory Journal 2013;20(4):295‐300. [DOI] [PMC free article] [PubMed] [Google Scholar]
Eades 2000
- Eades SJ. Reconciliation, social equity and Indigenous health. Medical Journal of Australia 2000;172(10):468‐9. [DOI] [PubMed] [Google Scholar]
Edmond 1998
- Edmond SD, Camargo CA, Nowak RM. 1997 National Asthma Education and Prevention Program Guidelines: A practical summary for emergency physicians. Annals of Emergency Medicine 1998;31(5):579‐89. [DOI] [PubMed] [Google Scholar]
Enarson 1999
- Enarson DA, Ait Khaled N. Cultural barriers to asthma management. Pediatric Pulmonology 1999;28(4):297‐300. [DOI] [PubMed] [Google Scholar]
Gibson 2002a
- Gibson PG, Powell H, Coughlan J, Wilson AJ, Hensley MJ, Abramson M, et al. Limited (information only) patient education programs for adults with asthma. Cochrane Database of Systematic Reviews 2002, Issue 1. [DOI: 10.1002/14651858.CD001005] [DOI] [PubMed] [Google Scholar]
Gibson 2002b
- Gibson PG, Powell H, Coughlan J, Wilson AJ, Abramson M, Haywood P, et al. Self‐management education and regular practitioner review for adults with asthma. Cochrane Database of Systematic Reviews 2002, Issue 3. [DOI: 10.1002/14651858.CD001117] [DOI] [PubMed] [Google Scholar]
GRADEpro GDT 2015
- GRADEpro GDT. GRADEpro Guideline Development Tool [Software]. McMaster University, 2015 (developed by Evidence Prime, Inc.) Available from gradepro.org. 2015.
Hamdorf 1996
- Hamdorf M, Wallace P, Gillam C, Stevenson M. Aboriginal health in the peel region of Western Australia. Australian Family Physician 1996;25(9 Suppl 2):S81‐S85. [PubMed] [Google Scholar]
Harrington 2015
- Harrington KF, Zhang B, Magruder T, Bailey WC, Gerald LB. The impact of parents' health literacy on pediatric asthma outcomes. Pediatric Allergy, Immunology and Pulmonology 2015;28(128):20‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Haselkorn 2008
- Haselkorn T, Lee JH, Mink DR, Weiss ST, TENOR Study Group. Racial disparities in asthma‐related health outcomes in severe or difficult‐to‐treat asthma. Annals of Allergy, Asthma & Immunolgy 2008;101(3):256‐63. [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 1.0. Available from www.cochrane‐handbook.org: The Cochrane Collaboration, Updated March 2011. [Google Scholar]
Juniper 1992
- Juniper EF, Guyatt GH, Epstein RS, Ferrie PJ, Jaeschke R, Hiller TK. Evaluation of impairment of health‐related quality of life in asthma: development of a questionnaire for use in clinical trials. Thorax 1992;47(2):76‐83. [DOI] [PMC free article] [PubMed] [Google Scholar]
Juniper 1993
- Juniper EF, Guyatt GH, Ferrie PJ, Griffith LE. Measuring quality of life in asthma. American Review of Respiratory Disease 1993;147(4):832‐8. [DOI] [PubMed] [Google Scholar]
Juniper 1996
- Juniper EF, Guyatt GH, Feeny DH, Ferrie PJ, Griffith LE, Townsend M. Measuring quality of life in the parents of children with asthma.. Quality of Life Research 1996;5(1):27‐34. [DOI] [PubMed] [Google Scholar]
Liu 2012
- Liu J, Davidson E, Bhopal R, White M, Johnson M, Netto G, et al. Adapting health promotion interventions to meet the needs of ethnic minority groups: mixed‐methods evidence synthesis. Health Technology Assessment 2012;16(44):1‐469. [DOI: 10.3310/hta16440] [DOI] [PMC free article] [PubMed] [Google Scholar]
Mitchell 2016
- Mitchell SJ, Bilderback AL, Okelo SO. Racial disparities in asthma morbidity among pediatric patients seeking asthma specialist care. Academic Pediatrics 2016;16(1):64‐7. [DOI] [PubMed] [Google Scholar]
National Asthma Council Australia 2015
- National Asthma Council Australia. Australian Asthma Handbook, Version 1.1. http://www.asthmahandbook.org.au/download‐order/complete‐handbook (accessed 18 August 2016).
NHPAC 2006
- National Health Priority Action Council (NHPAC). National Service Improvement Framework for Asthma. http://www.healthinfonet.ecu.edu.au/key‐resources/promotion‐resources?lid=13452 (accessed 18 August 2016).
Nierkens 2013
- Nierkens V, Hartman MA, Nicolaou M, Vissenberg C, Beune EJAJ, Hosper K, et al. Effectiveness of cultural adaptations of interventions aimed at smoking cessation, diet, and/or physical activity in ethnic minorities. a systematic review. PLOS One 2013;8(10):e73373. [DOI] [PMC free article] [PubMed] [Google Scholar]
Powell 2002
- Powell H, Gibson PG. Options for self‐management education for adults with asthma. Cochrane Database of Systematic Reviews 2002, Issue 3. [DOI: 10.1002/14651858.CD004107] [DOI] [PMC free article] [PubMed] [Google Scholar]
Review Manager (RevMan) [Computer program]
- Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Schmidt 2016
- Schmidt B, Campbell S, McDermott R. Community health workers as chronic care coordinators: evaluation of an Australian Indigenous primary healthcare program. Australian and New Zealand Journal of Public Health 2016;40(Suppl 1):S107‐14. [DOI] [PubMed] [Google Scholar]
Sin 2002
- Sin DD, Wells H, Svenson LW, Man SF. Asthma and COPD among aboriginals in Alberta, Canada. Chest 2002;121(6):1841‐6. [DOI] [PubMed] [Google Scholar]
Speck 2014
- Speck AL, Nelson B, Jefferson SO, Baptist AP. Young, African American adults with asthma: what matters to them?. Annals of Allergy, Asthma and Immunology 2014;112(1):35‐9. [DOI] [PubMed] [Google Scholar]
Stewart 2013
- Stewart M, King M, Blood R, Letourneau N, Masuda JR, Anderson S, Bearskin LB. Health inequities experienced by Aboriginal children with respiratory conditions and their parents. Canadian Journal of Nursing Research 2013;45(3):6‐27. [DOI] [PubMed] [Google Scholar]
Swartz 2002
- Swartz L, Dick J. Managing chronic diseases in less developed countries. BMJ 2002;325(7370):914‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tapp 2007
- Tapp S, Lasserson TJ, Rowe BH. Education interventions for adults who attend the emergency room for acute asthma. Cochrane Database of Systematic Reviews 2007, Issue 3. [DOI: 10.1002/14651858.CD003000.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Toelle 2011
- Toelle BG, Ram FSF. Written individualised management plans for asthma in children and adults. Cochrane Database of Systematic Reviews 2011, Issue 7. [DOI: 10.1002/14651858.CD002171.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wolf 2002
- Wolf FM, Guevara JP, Grum CM, Clark NM, Cates CJ. Educational interventions for asthma in children. Cochrane Database of Systematic Reviews 2002, Issue 4. [DOI: 10.1002/14651858.CD000326] [DOI] [PMC free article] [PubMed] [Google Scholar]
References to other published versions of this review
Bailey 2007
- Bailey EJ, Chang AB. Culture‐specific programs for children and adults from minority groups who have asthma. Cochrane Database of Systematic Reviews 2007, Issue 3. [DOI: 10.1002/14651858.CD006580] [DOI] [PubMed] [Google Scholar]
Bailey 2008
- Bailey EJ, Kruske SG, Morris PS, Cates CJ, Chang AB. Culture‐specific programs for children and adults from minority groups who have asthma. Cochrane Database of Systematic Reviews 2008, Issue 2. [DOI: 10.1002/14651858.CD006580.pub2] [DOI] [PubMed] [Google Scholar]
Bailey 2009a
- Bailey EJ, Cates CJ, Kruske SG, Morris PS, Chang AB, Brown N. Culture‐specific programs for children and adults from minority groups who have asthma. Cochrane Database of Systematic Reviews 2009, Issue 1. [DOI: 10.1002/14651858.CD006580.pub3] [DOI] [PubMed] [Google Scholar]
Bailey 2009b
- Bailey EJ, Cates CJ, Kruske SG, Morris PS, Brown N, Chang AB. Culture‐specific programs for children and adults from minority groups who have asthma. Cochrane Database of Systematic Reviews 2009, Issue 2. [DOI: 10.1002/14651858.CD006580.pub4] [DOI] [PubMed] [Google Scholar]


