Abstract
Background
This review is the first update of a previously published review in The Cochrane Library (Issue 7, 2015). Interleukin‐5 (IL‐5) is the main cytokine involved in the activation of eosinophils, which cause airway inflammation and are a classic feature of asthma. Monoclonal antibodies targeting IL‐5 or its receptor (IL‐5R) have been developed, with recent studies suggesting that they reduce asthma exacerbations, improve health‐related quality of life (HRQoL) and lung function. These are being incorporated into asthma guidelines.
Objectives
To compare the effects of therapies targeting IL‐5 signalling (anti‐IL‐5 or anti‐IL‐5Rα) with placebo on exacerbations, health‐related qualify of life (HRQoL) measures, and lung function in adults and children with chronic asthma, and specifically in those with eosinophilic asthma refractory to existing treatments.
Search methods
We searched the Cochrane Airways Trials Register, clinical trials registries, manufacturers' websites, and reference lists of included studies. The most recent search was March 2017.
Selection criteria
We included randomised controlled trials comparing mepolizumab, reslizumab and benralizumab versus placebo in adults and children with asthma.
Data collection and analysis
Two authors independently extracted data and analysed outcomes using a random‐effects model. We used standard methods expected by Cochrane.
Main results
Thirteen studies on 6000 participants met the inclusion criteria. Four used mepolizumab, four used reslizumab, and five used benralizumab. One study in benralizumab was terminated early due to sponsor decision and contributed no data. The studies were predominantly on people with severe eosinophilic asthma, which was similarly but variably defined. Eight included children over 12 years but these results were not reported separately. We deemed the risk of bias to be low, with all studies contributing data being of robust methodology. We considered the quality of the evidence for all comparisons to be high overall using the GRADE scheme, with the exception of intravenous mepolizumab because this is not currently a licensed delivery route.
All of the anti‐IL‐5 treatments assessed reduced rates of 'clinically significant' asthma exacerbation (defined by treatment with systemic corticosteroids for three days or more) by approximately half in participants with severe eosinophilic asthma on standard of care (at least medium‐dose inhaled corticosteroids (ICS)) with poorly controlled disease (either two or more exacerbations in the preceding year or Asthma Control Questionnaire (ACQ) 1.5 or more). Non‐eosinophilic participants treated with benralizumab also showed a significant reduction in exacerbation rates, but no data were available for non‐eosinophilic participants, and mepolizumab or reslizumab.
We saw modest improvements in validated HRQoL scores with all anti‐IL‐5 agents in severe eosinophilic asthma. However these did not exceed the minimum clinically important difference for ACQ and Asthma Quality of Life Questionnaire (AQLQ), with St. George's Respiratory Questionnaire (SGRQ) only assessed in two studies. The improvement in HRQoL scores in non‐eosinophilic participants treated with benralizumab, the only intervention for which data were available in this subset, was not statistically significant, but the test for subgroup difference was negative.
All anti‐IL‐5 treatments produced a small but statistically significant improvement in mean pre‐bronchodilator forced expiratory flow in one second (FEV1) of between 0.08 L and 0.11 L.
There were no excess serious adverse events with any anti‐IL‐5 treatment, and indeed a reduction in favour of mepolizumab that could be due to a beneficial effect on asthma‐related serious adverse events. There was no difference compared to placebo in adverse events leading to discontinuation with mepolizumab or reslizumab, but significantly more discontinued benralizumab than placebo, although the absolute numbers were small (36/1599 benralizumab versus 9/998 placebo).
Mepolizumab, reslizumab and benralizumab all markedly reduced blood eosinophils, but benralizumab resulted in almost complete depletion, whereas a small number remained with mepolizumab and reslizumab. The implications for efficacy and/or adverse events are unclear.
Authors' conclusions
Overall our study supports the use of anti‐IL‐5 treatments as an adjunct to standard of care in people with severe eosinophilic asthma and poor control. These treatments roughly halve the rate of asthma exacerbations in this population. There is limited evidence for improved HRQoL scores and lung function, which may not meet clinically detectable levels. There were no safety concerns regarding mepolizumab or reslizumab, and no excess serious adverse events with benralizumab, although there remains a question over adverse events significant enough to prompt discontinuation.
Further research is needed on biomarkers for assessing treatment response, optimal duration and long‐term effects of treatment, risk of relapse on withdrawal, non‐eosinophilic patients, children (particularly under 12 years), and comparing anti‐IL‐5 treatments to each other and, in people eligible for both, to anti‐immunoglobulin E. For benralizumab, future studies should closely monitor rates of adverse events prompting discontinuation.
Keywords: Adolescent; Adult; Child; Humans; Adrenal Cortex Hormones; Adrenal Cortex Hormones/administration & dosage; Anti‐Asthmatic Agents; Anti‐Asthmatic Agents/administration & dosage; Anti‐Asthmatic Agents/adverse effects; Antibodies, Monoclonal, Humanized; Antibodies, Monoclonal, Humanized/administration & dosage; Antibodies, Monoclonal, Humanized/adverse effects; Asthma; Asthma/etiology; Asthma/therapy; Disease Progression; Injections, Intravenous; Injections, Subcutaneous; Interleukin‐5; Interleukin‐5/antagonists & inhibitors; Quality of Life; Randomized Controlled Trials as Topic; Receptors, Interleukin‐5; Receptors, Interleukin‐5/antagonists & inhibitors
Mepolizumab, reslizumab or benralizumab for people already taking inhaled steroids and long‐acting beta2‐agonists for their asthma
Review question
We considered in this review whether taking the new drugs mepolizumab, reslizumab or benralizumab in addition to standard treatment (e.g. inhaled steroids and combination inhalers) are better than a placebo for people with asthma.
Background
Asthma is an inflammatory lung condition characterised by the narrowing of the airways, breathlessness, a tight chest and reduced quality of life. By the year 2025, there may be up to 400 million people with asthma worldwide. Mepolizumab, reslizumab and benralizumab are new 'anti‐IL‐5' treatments that may help to reduce asthma symptoms.
Study characteristics
Thirteen studies compared mepolizumab, reslizumab or benralizumab to a placebo in 6000 people with asthma, most with severe disease. We summarised the results as they related to the occurrence of asthma attacks requiring additional treatment, quality of life, breathing tests, effects on a blood biomarker, and side effects.
Key results
We found that participants with severe asthma, who had high numbers of a certain type of inflammatory cell (eosinophils) in the blood, benefited from taking mepolizumab, reslizumab or benralizumab through reduced asthma attacks. There were small improvements in quality of life and breathing tests, but these may be too small to be detected by patients. We agree with international guidelines that say that these treatments can be added to standard treatment for people with severe asthma. However, we think that further research is needed to clarify some aspects, such as how to assess treatment response and how long to give treatment for.
Quality of the evidence
The evidence included in this review is provided by very well‐designed studies. We consider these studies to be at low risk of bias in the following important respects: the procedure that determined who received which treatment, the blinding processes and the clarity of detail concerning participants who did not complete the study. Overall the evidence was high to moderate quality.
Summary of findings
Summary of findings for the main comparison.
Mepolizumab subcutaneous (SC) compared to placebo for asthma
| Mepolizumab (SC) compared to placebo for asthma | ||||||
| Patient or population: people with asthma Setting: community Intervention: mepolizumab (SC) Comparison: placebo | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Risk with placebo | Risk with mepolizumab (SC) | |||||
| Rate of exacerbations requiring systemic corticosteroids Follow‐up: range 24 to 32 weeks | The mean rate in the placebo group was 1.48 events per participant per yeara | The mean rate in the intervention group was 0.81 fewer events per participant per year (95% CI 0.66 fewer to 0.94 fewer) | Rate ratio 0.45 (0.36 to 0.55) | 936 (2 RCTs) | ⊕⊕⊕⊕ High | |
| Rate of exacerbations requiring emergency department treatment or admission Follow‐up: range 24 to 32 weeks | The mean rate in the placebo group was 0.15 events per patient per yearb | The mean rate in the intervention group was 0.10 fewer events per participant per year (95% CI 0.05 fewer to 0.12 fewer) | Rate ratio 0.36 (0.20 to 0.66) | 936 (2 RCTs) | ⊕⊕⊕⊕ High | |
| Health‐related quality of life (ACQ) Scale from: 0 to 6 (lower is better) Follow‐up: range 24 to 32 weeks | The mean change in the placebo group ranged from −0.4 to −0.5 units | The mean in the intervention group was ‐0.42 units fewer (‐0.56 fewer to ‐0.28 fewer) | ‐ | 936 (2 RCTs) | ⊕⊕⊕⊝ Moderatec | A change of ≥ 0.5 is considered the minimum clinically significant difference |
| Health‐related quality of life (SGRQ) Scale from: 0 to 100 (lower is better) Follow‐up: range 24 to 32 weeks | The mean change in the placebo group ranged from −7.9 to −9.0 units | The mean change in the intervention group was ‐7.4 units fewer (‐9.5 fewer to ‐5.29 fewer) | ‐ | 936 (2 RCTs) | ⊕⊕⊕⊕ High | A change of ≥ 4 is considered the minimum clinically significant difference |
| Pre‐bronchodilator FEV1 (L) Follow‐up: range 24 to 32 weeks | The mean change in the placebo group ranged from 0.086 L (± 0.031 L) to 0.120 L (0.047 to 0.192 L) | The mean difference from placebo was a further 0.11 L (0.06 L to 0.17 L) | ‐ | 936 (2 RCTs) | ⊕⊕⊕⊕ High | |
| Adverse events leading to discontinuation Follow‐up: range 24 to 32 weeks | 15 per 1000 | 7 per 1000 (2 to 27) | Risk ratio 0.45 (0.11 to 1.80) | 936 (2 RCTs) | ⊕⊕⊕⊝ Moderated | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). ACQ: Asthma Control Questionnaire; CI: confidence interval; FEV1 : forced expiratory volume in 1 second; RR: risk ratio; SC: subcutaneous; SGRQ: St. George's Respiratory Questionnaire | ||||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low quality: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect Very low quality: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect | ||||||
aRounded mean of the rate in the placebo group of the two studies: 1.21 and 1.74. bRounded mean of the rate in the placebo group of the two studies: 0.10 and 0.20. cThe mean difference (‐0.42) is smaller than the minimum clinically significant difference (a reduction of 0.5 points). dThe 95% CI crosses the line of no effect, thus we downgraded the quality of evidence to moderate because of imprecision.
Summary of findings 2.
Mepolizumab intravenous (IV) compared to placebo for asthma
| Mepolizumab (IV) compared to placebo for asthma | ||||||
| Patient or population: people with asthma Setting: community Intervention: mepolizumab (IV) Comparison: placebo | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Risk with placebo | Risk with mepolizumab (IV) | |||||
| Rate of clinically significant exacerbations Follow‐up: range 32 weeks to 52 weeks | The mean rate in the placebo group was 2.51 events per participant per yeara | The mean rate in the intervention groups was 1.18 fewer events per participant per year (1.41 fewer to 0.90 fewer) | Rate ratio 0.53 (0.44 to 0.64) | 751 (3 RCTs) | ⊕⊕⊕⊝ Moderatec | |
| Rate of exacerbations requiring emergency department treatment or admission Follow‐up: range 32 weeks to 52 weeks | The mean rate in the placebo group was 0.32 events per participant per yearb | The mean rate in the intervention groups was 0.15 fewer events per participant per year (0.22 fewer to 0.04 fewer) | Rate ratio 0.52 (0.31 to 0.87) | 690 (2 RCTs) | ⊕⊕⊕⊝ Moderatec | |
| Health‐related quality of life (AQLQ) Scale from: 1 to 7 (higher is better) Follow‐up: range 32 weeks to 52 weeks | The mean change in the placebo group ranged from 0.18 to 0.71 units | MD 0.21 higher (‐0.06 lower to 0.47 higher) | ‐ | 677 (2 RCTs) | ⊕⊕⊕⊝ Moderatec | A change of ≥ 0.5 is considered the minimum clinically significant difference |
| Health‐related quality of life (ACQ) Scale from: 0 to 6 (lower is better) Follow‐up: range 32 weeks to 52 weeks | The mean change in the placebo group ranged from −0.59 to −0.50 units | MD ‐0.11 lower (‐0.32 lower to 0.09 higher) | ‐ | 369 (2 RCTs) | ⊕⊕⊕⊝ Moderatec | A change of ≥ 0.5 is considered the minimum clinically significant difference |
| Pre‐bronchodilator FEV1 (L) Follow‐up: range 32 weeks to 52 weeks | The mean change in the placebo group ranged from 0.060 L (± 0.038 L) to 0.086 L (± 0.031 L) | MD 0.08 L (0.02 L higher to 0.15 L higher) |
‐ | 690 (2 RCTs) | ⊕⊕⊕⊝ Moderatec | |
| Adverse events leading to discontinuation Follow‐up: range 32 weeks to 52 weeks | 26 per 1000 | 19 per 1000 (5 to 77) | RR 0.72 (0.18 to 2.92) | 751 (3 RCTs) | ⊕⊕⊕⊝ Moderatec | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). ACQ: Asthma Control Questionnaire; AQLQ: Asthma Quality of Life Questionnaire; CI: confidence interval; FEV1 : forced expiratory volume in 1 second; MD: mean difference; IV: intravenous; RR: risk ratio | ||||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low quality: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect Very low quality: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect | ||||||
aRounded mean of the rate in the placebo group of the three studies: 1.74, 2.40 and 3.4. bRounded mean of the rate in the placebo group of the two studies: 0.20 and 0.43. cThe intravenous route is not currently licenced for mepolizumab; one point deducted for indirectness.
Summary of findings 3.
Reslizumab intravenous (IV) compared to placebo for asthma
| Reslizumab (IV) compared to placebo for asthma | ||||||
| Patient or population: people with asthma Setting: community Intervention: reslizumab (IV) Comparison: placebo | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Risk with placebo | Risk with reslizumab (IV) | |||||
| Rate of exacerbations requiring systemic corticosteroids Follow‐up: 52 weeks | The mean rate in the placebo group was 1.54 events per participant per year | The mean rate in the intervention groups was 0.93 fewer events per participant per year (1.09 fewer to 0.73 fewer) | Rate ratio 0.43 (0.33 to 0.55) | 953 (2 RCTs) | ⊕⊕⊕⊕ High | |
| Rate of exacerbations requiring emergency department treatment or admission Follow‐up: 52 weeks | The mean rate in the placebo group was 0.12 events per participant per year | The mean rate in the intervention groups was 0.04 fewer events per participant per year (0.07 fewer to 0.02 more) | Rate ratio 0.67 (0.39 to 1.17) | 953 (2 RCTs) | ⊕⊕⊕⊕ High | |
| Health‐related quality of life (AQLQ) Scale from: 1 to 7 (higher is better) Follow ‐p: range 16 weeks to 52 weeks | The mean change in the placebo group ranged from 0.779 to 0.89 units | MD 0.28 higher (0.17 higher to 0.39 higher)a | ‐ | 1164 (3 RCTs) | ⊕⊕⊕⊕ High | A change of ≥ 0.5 is considered the minimum clinically significant difference |
| Health‐related quality of life (ACQ) Scale from: 0 to 6 (lower is better) Follow‐up: range 16 weeks to 52 weeks | The mean change in the placebo group ranged from −0.368 to −0.80 units | MD ‐0.25 lower (‐0.33 lower to ‐0.17 lower)b | ‐ | 1652 (4 RCTs) | ⊕⊕⊕⊕ High | A change of ≥ 0.5 is considered the minimum clinically significant difference |
| Pre‐bronchodilator FEV1 (L) Follow‐up: range 16 weeks to 52 weeks | The mean change in the placebo group ranged from 0.002 L (± 0.1216 L) to 0.215 (± 0.0484 L) | MD 0.11 L higher (0.07 L higher to 0.15 L higher) | ‐ | 1652 (4 RCTs) | ⊕⊕⊕⊕ High | |
| Serious adverse events Follow‐up: range 16 weeks to 52 weeks | 91 per 1000 | 72 per 1000 (51 to 102) | RR 0.79 (0.56 to 1.12) | 1656 (4 RCTs) | ⊕⊕⊕⊕ High | |
| Adverse events leading to discontinuation Follow‐up: range 16 weeks to 52 weeks | 58 per 1000 | 38 per 1000 (25 to 59) | RR 0.66 (0.43 to 1.02) | 1659 (4 RCTs) | ⊕⊕⊕⊕ High | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). ACQ: Asthma Control Questionnaire; AQLQ: Asthma Quality of Life Questionnaire; CI: confidence interval; FEV1 : forced expiratory volume in 1 second; MD: mean difference; IV: intravenous; RR: risk ratio | ||||||
| GRADE Working Group grades of evidence High quality: We are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low quality: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low quality: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | ||||||
a The mean difference (0.28) is smaller than the minimum clinically significant difference (a reduction of 0.5 points). b The mean difference (‐0.25) is smaller than the minimum clinically significant difference (a reduction of 0.5 points)
Summary of findings 4.
Benralizumab subcutaneous (SC) compared to placebo for asthma
| Benralizumab (SC) compared to placebo for asthma | ||||||
| Patient or population: people with asthma Setting: community Intervention: benralizumab (SC) Comparison: placebo | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Risk with placebo | Risk with benralizumab (SC) | |||||
| Rate of exacerbations requiring systemic corticosteroids Follow‐up: range 48 weeks to 56 weeks | The mean rate in the placebo group was 0.98 events per participant per yeara | The mean rate in the intervention groups was 0.37 fewer events per participant per year (0.44 fewer to 0.29 fewer) | Rate ratio 0.62 (0.55 to 0.70) | 2456 (3 RCTs) | ⊕⊕⊕⊕ High | |
| Rate of exacerbations requiring emergency department treatment or admission Follow‐up: range 48 weeks to 56 weeks | The mean rate in the placebo group was 0.11 events per participant per yearb | The mean rate in the intervention groups was 0.04 fewer events per participant per year (0.06 fewer to 0.002 fewer) | Rate ratio 0.68 (0.47 to 0.98) | 1537 (2 RCTs) | ⊕⊕⊕⊝ Moderatee | There is greater heterogeneity (I² = 43%) owing to inclusion of less severe participants in FitzGerald 2016 (a larger proportion who had only suffered one exacerbation the previous year, with correspondingly less potential for exacerbation) |
| Health‐related quality of life (AQLQ) Scale from: 1 to 7 (higher is better) Follow‐up: range 48 weeks to 56 weeks | The mean change in the placebo group ranged from 0.98 to 1.31 units | MD 0.23 higher (0.11 higher to 0.35 higher)c | ‐ | 1541 (3 RCTs) | ⊕⊕⊕⊕ High | A change of ≥ 0.5 is considered the minimum clinically significant difference |
| Health‐related quality of life (ACQ) Scale from: 0 to 6 (lower is better) Follow up: range 48 weeks to 56 weeks | The mean change in the placebo group ranged from −1.19 to −0.76 units | MD ‐0.20 lower (‐0.29 lower to ‐0.11 lower)d | ‐ | 2359 (3 RCTs) | ⊕⊕⊕⊕ High | A change of ≥ 0.5 is considered the minimum clinically significant difference |
| Pre‐bronchodilator FEV1 (L) Follow‐up: range 48 weeks to 56 weeks | The mean change in the placebo group ranged from ‐0.01 L to 0.239 L | MD 0.10 L higher (0.05 L higher to 0.14 L higher) | ‐ | 2355 (3 RCTs) | ⊕⊕⊕⊕ High | |
| Serious adverse events Follow‐up: range 48 weeks to 56 weeks | 135 per 1000 | 109 per 1000 (89 to 136) | RR 0.81 (0.66 to 1.01) | 2648 (4 RCTs) | ⊕⊕⊕⊕ High | |
| Adverse events leading to discontinuation Follow‐up: range 48 weeks to 56 weeks | 9 per 1000 | 19 per 1000 (9 to 41) | RR 2.15 (1.02 to 4.57) | 2597 (3 RCTs) | ⊕⊕⊕⊕ High | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). ACQ: Asthma Control Questionnaire; AQLQ: Asthma Quality of Life Questionnaire; CI: confidence interval; FEV1 : forced expiratory volume in 1 second; MD: mean difference; IV: intravenous; RR: risk ratio | ||||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low quality: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect Very low quality: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect | ||||||
a Rounded mean of the rate in the placebo group of the eosinophilic and non‐eosinophilic arms (as applicable) or the three studies: 1.33, 1.21, 0.68, 0.49, 0.93, 1.21. b Rounded mean of the rate in the placebo group of the two studies: 0.18 and 0.04. c The mean difference (0.23) is less than the minimum clinically significant difference (≥ 0.5). d The mean difference (‐0.2) is less than the minimum clinically significant difference (≥ ‐0.5) e One point deducted to reflect the level of heterogeneity on this outcome.
Background
This review is the first update of a previously published review in The Cochrane Library (Issue 7, 2015), evaluating the effects of therapies targeting IL‐5 signalling (anti‐IL‐5 or anti‐IL‐5Rα) with placebo on asthma.
Description of the condition
Asthma is a chronic inflammatory condition affecting the airways in the lungs. It is defined by symptoms of breathlessness, chest tightness, wheeze, and cough. These symptoms are a consequence of variable airway hyperresponsiveness, with subsequent bronchoconstriction and airflow obstruction. These symptoms are variably and intermittently present in the natural course of the disease, with periods of acutely increased symptomatology called exacerbations.
A recent global estimate suggested 300 million people currently live with asthma, and predicted this to increase to 400 million by 2025 (WHO 2007). Asthma causes a significant degree of morbidity and mortality: every year in the UK alone there are an estimated 2.7 million GP consultations, 121,000 hospital attendances, 93,900 admissions, and over 1000 deaths (Mukherjee 2016). The annual cost in the UK has been estimated at GBP 1.1 billion. Current treatments, such as inhaled corticosteroids (ICS) and bronchodilators are well established, yet despite these almost half of people living with asthma experience an exacerbation each year (Price 2014).
Asthma is increasingly recognised as a heterogenous disease comprised of a number of different clinical phenotypes and molecular endotypes, although the precise definition of these remains a work in progress (Wenzel 2012). 'Atopic asthma' is generally considered the most common phenotype, representing roughly half of all asthmatics (Woodruff 2009). Atopic asthma is thought to be driven by an excess of 'type 2 inflammation': an elevated number of type 2 helper T (Th2) cells and the cytokines they secrete, interleukin 4 (IL‐4), IL‐5 and IL‐13. A separate pathophysiological mechanism, in which type 2 innate lymphoid cells (ILC2s) produce large amounts of IL‐5 and IL‐13 (and to a lesser degree, IL‐4), is hypothesised to be important in a subgroup of asthma sufferers with eosinophilia but no allergies (Brusselle 2013). This group are particularly important because they have severe disease that is largely resistant to ICS, and so have a high burden of disease.
The cytokines IL‐4, IL‐5 and IL‐13 produce many of the classic features of atopic asthma, for example, eosinophilia (IL‐5 controls the proliferation, survival and recruitment of eosinophils), raised immunoglobulin E (IgE) levels (the result of B cell class switching in response to IL‐4 and IL‐13), mucus hypersecretion and airway hyperresponsiveness (both a potential consequence of IL‐13) (Chung 2015). Treatments targeting so called 'type 2 cytokines' have subsequently been developed and investigated for their potential in asthma.
Description of the intervention
One of the core pathological features of asthma is eosinophilic infiltration of the bronchial mucosa and airways (Kay 2015). Pro‐inflammatory mediators secreted by eosinophils cause damage to the epithelium, initiating vasodilatation, smooth muscle contraction and increased mucous secretion, which in turn is associated with increased airway hyperresponsiveness, asthma symptoms and airway narrowing (Liu 2013). Thus increased eosinophil counts, for example following reduction in the dose of maintenance ICS, are associated with increased symptoms and asthma exacerbations (Jatakanon 2000).
The proliferation, maturation, activation, recruitment and survival of eosinophils is under the control of IL‐5 (Lopez 1986), with the IL‐5 receptor being selectively expressed on eosinophils and basophils. Elevated levels of IL‐5 mRNA are seen in the bronchial biopsies of people with asthma and correlate with disease severity (Humbert 1997). IL‐5 signalling is therefore an attractive target in asthma, and has yielded three monoclonal antibodies: mepolizumab (trade name Nucala; GlaxoSmithKline), reslizumab (trade names Cinqair or Cinqaero; Teva) and benralizumab (MedImmune/AstraZeneca). Mepolizumab and reslizumab both target IL‐5, whereas benralizumab binds the alpha chain of the IL‐5 receptor (IL‐5Rα), found on eosinophils and basophils.
How the intervention might work
Mepolizumab and reslizumab bind IL‐5 and interfere with its ligation to the IL‐5 receptor on eosinophils and basophils. Both have been shown to reduce serum eosinophils (Wang 2009).
Benralizumab binds IL‐5Rα to inhibit its activation. In addition it appears to induce eosinophil and basophil apoptosis (Kolbeck 2010). Benralizumab has also been shown to be effective in reducing serum eosinophil counts (Busse 2010).
Mepolizumab and reslizumab have marketing licenses for use in people with 'eosinophilic' asthma (variably defined) and it is logical that these drugs would be most effective in this subgroup of patients. Anti‐IL‐5 therapies might also theoretically be effective in patients with more relaxed definitions of eosinophilia, or in those defined as 'non‐eosinophilic' based on their serum eosinophil count but who may have an isolated elevation of eosinophils in the airways (i.e. sputum eosinophilia), or whose eosinophils may be suppressed due to ICS treatment, or both.
Why it is important to do this review
As anti‐IL‐5 therapies become incorporated into national and international guidelines (e.g. the Global Initiatve for Asthma (GINA)'s 2017 guidelines, GINA 2017) and clinical practice, it is important that the evidence is reviewed and made available in the Cochrane Library. The first Cochrane Review focused on mepolizumab, at the time the only anti‐IL‐5 agent licensed (Powell 2015).
Since then reslizumab has been approved by the US Food & Drug Administration and European Medicines Agency. With phase 3 clinical trials of benralizumab recently being reported as having met their primary endpoints, it seems likely that benralizumab will also be approved soon. These anti‐IL‐5 agents are likely to compete directly with each other and so the scope of this review has been broadened to consider all anti‐IL‐5 therapies. They are compared to each other rather than pooled as there are potentially important differences in dose, route of administration (subcutaneous versus intravenous), and in the case of benralizumab, a significant difference in the mechanism of action that uniquely induces eosinophil and basophil apoptosis ‐ which could improve efficacy, but equally increase the incidence of adverse events.
Objectives
To compare the effects of therapies targeting IL‐5 signalling (anti IL‐5 or anti‐IL‐5Rα) with placebo on exacerbations, health‐related quality of life (HRQoL) measures, and lung function in adults and children with chronic asthma, and specifically in those with eosinophilic asthma refractory to existing treatments.
Methods
Criteria for considering studies for this review
Types of studies
We included randomised controlled trials (RCTs). We included studies reported as full text, those published as abstracts only and unpublished data.
Types of participants
We included both adults and children with a diagnosis of asthma. We focused on collating data from people who had been reported as having eosinophilic asthma to analyse these individuals as a subgroup. We examined individual articles in order to determine how this group should be defined.
Individuals with respiratory comorbidities such as cystic fibrosis were excluded, as were current smokers.
Types of interventions
We included trials comparing anti‐IL‐5 therapy with placebo, in addition to current standard of care for asthma (ICS, with or without a second controller such as a long‐acting beta2 agonist (LABA), provided the treatment period was 16 weeks or longer.
In the case of dose‐ranging studies, we included data only for participants on doses likely to be used clinically, that is, 75 mg intravenous (IV) or 100 mg subcutaneous (SC) injections of mepolizumab, 3 mg/kg IV reslizumab, 20 to 30 mg SC benralizumab. For mepolizumab SC and reslizumab IV, these are the licensed doses. For benralizumab, we took the 30 mg dose used in the two phase 3 studies (Bleecker 2016; FitzGerald 2016), which is likely to be the licensed dose, and included the 20 mg dose in the three previous phase 2a dose‐ranging studies (Castro 2015a; Castro 2015b; Park 2016).
Studies that initiated a reduction in standard asthma management (e.g. corticosteroids) as part of the protocol were excluded, as this is unlikely to reflect clinical practice in the majority of cases.
We planned to include the following co‐interventions provided they were not part of the randomised treatment: leukotriene antagonists (LTRA), inhaled bronchodilators (including LABA), inhaled (ICS) and oral corticosteroids (OCS), oral aminophylline and macrolide antibiotics.
Types of outcome measures
We referred to the joint American Thoracic Society (ATS) and European Respiratory Society (ERS) statement on standardising endpoints for asthma clinical trials to identify appropriate outcome measures (Reddel 2009). These recommend that clinical trials should assess outcomes relevant to both goals of asthma management: current control of asthma symptoms, and reduced risk of exacerbations and other adverse outcomes (e.g. accelerated lung function decline, treatment side effects). Moreover the authors note that these aspects are often discordant, thus endpoints assessing each need to be considered.
Exacerbations are responsible for most of the morbidity, mortality and healthcare costs related to asthma, and therefore considered the primary outcome measure. The ATS/ERS statement defines severe exacerbations as including either use of systemic corticosteroids for at least three days, or emergency department treatment or admission requiring systemic corticosteroids (definitions in terms of changes from baseline in lung function, symptoms, or short‐acting β2 agonist use are not validated).
Lung function, specifically low pre‐bronchodilator forced expiratory flow in one second (FEV1) (the most commonly reported lung function measure in clinical trials), is a strong independent predictor of asthma exacerbations (Osborne 2007), and is objective and reproducible. However lung function and symptoms correlate poorly over time in individual patients, so it is recommended that both are monitored. There is no gold standard score for assessing asthma symptoms, with several validated and regularly used including the Asthma Control Questionnaire (ACQ) (Juniper 1999), Asthma Control Test (ACT) (Nathan 2004), Asthma Quality of Life Questionnaire (AQLQ) (Juniper 1992), and the St George's Respiratory Questionnaire (SGRQ) (Jones 1991). We considered any one of these an adequate measure of symptoms and health‐related quality of life (HRQoL).
Identifying potential patient safety issues are a priority in the evaluation of new drugs. We consider the decision to discontinue study medication because of an adverse event to be a useful clinical marker of severity with real‐world applicability, and have included this alongside serious adverse events, which would likely outweigh any potential benefits of the intervention.
Anti‐IL‐5 treatments should result in a reduction in eosinophils. Moreover as discussed earlier, increased eosinophil counts are associated with symptoms and exacerbations (Jatakanon 2000). We have therefore included eosinophil counts in the peripheral blood, a measure that is readily available in hospitals and clinics, as a secondary outcome.
Primary outcomes
'Clinically significant' asthma exacerbation, as defined by treatment with a course (three days or more) of systemic corticosteroids (with or without hospital admission)
Secondary outcomes
Asthma exacerbation requiring hospital admission
HRQoL (as measured by a validated questionnaire e.g. ACQ, AQLQ, SGRQ)
Measures of lung function (e.g. FEV1)
Serious adverse events
'Clinically significant' adverse events, as defined by those that prompted discontinuation of the intervention and withdrawal from the study
Eosinophil counts in peripheral blood
Reporting one or more of the outcomes listed here in the trial was not an inclusion criterion for the review.
Search methods for identification of studies
Electronic searches
We identified trials from the Cochrane Airways Trials Register, which is maintained by the Information Specialist for the Group. The Cochrane Airways Trials Register contains studies identified from several sources:
monthly searches of the Cochrane Central Register of Controlled Trials (CENTRAL), through the Cochrane Register of Studies Online (crso.cochrane.org);
weekly searches of MEDLINE Ovid SP 1946 to date;
weekly searches of Embase Ovid SP 1974 to date;
Monthly searches of PsycINFO Ovid SP;
Monthly searches of CINAHL EBSCO (Cumulative Index to Nursing and Allied Health Literature);
Monthly searches of AMED EBSCO (Allied and Complementary Medicine);
handsearches of the proceedings of major respiratory conferences.
Studies contained in the Trials Register are identified through search strategies based on the scope of Cochrane Airways. Details of these strategies, as well as a list of handsearched conference proceedings are in Appendix 1. See Appendix 2 for search terms used to identify studies for this review.
We also conducted a search of ClinicalTrials.gov (www.clinicaltrials.gov) and the World Health Organization (WHO) trials portal (www.who.int/ictrp/en).
We searched all databases from their inception to the present and imposed no restriction on language of publication. The search was first conducted in November 2013 and was updated in November 2014 and March 2017.
Searching other resources
We checked the bibliographies of all primary studies and review articles for additional references. We searched relevant manufacturers' websites for trial information (clinical trials registers on the GlaxoSmithKline (manufacturer of mepolizumab) and AstraZeneca (benralizumab) websites; the Teva (reslizumab) website does not have a clinical trials register).
We searched for errata and retractions relevant to the included studies published in full text on PubMed (www.ncbi.nlm.nih.gov/pubmed) and planned to report the date this was done within the review if this was an issue.
Data collection and analysis
Selection of studies
Two review authors (HF, CP) independently screened titles and abstracts of all the potential studies identified in the search and coded them as 'retrieve' (eligible or potentially eligible/unclear) or 'do not retrieve'. We retrieved the full‐text study reports/publications, and two review authors (HF, CP) independently screened the full text and identified studies for inclusion, identifying and recording reasons for excluding the ineligible studies. We planned to resolve any disagreement through discussion or, if required, by consulting a third review author (SJM); however, this was not necessary. We identified and excluded duplicates and collated multiple reports of the same study so that each study rather than each report was the unit of interest in the review. We recorded the selection process in sufficient detail to complete a PRISMA flow diagram (Moher 2009) (Figure 1) and a 'Characteristics of excluded studies' table.
Figure 1.
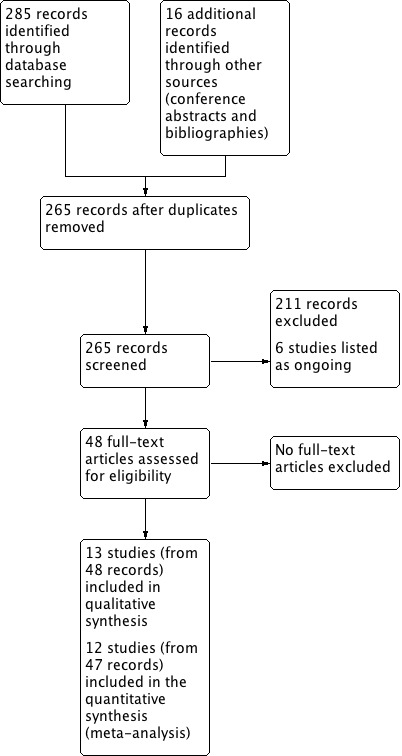
Study flow diagram
Data extraction and management
We used a data collection form to record study characteristics and outcome data that had been piloted on at least one study in the review. Two review authors (HF, AW) extracted the following study characteristics from included studies.
Methods: study design, total duration of study, details of any run‐in period, number of study centres and location, study setting, withdrawals and date of study
Participants: number, mean age, age range, gender, severity of condition, diagnostic criteria, baseline lung function, smoking history, inclusion criteria and exclusion criteria
Interventions: intervention, comparator, concomitant medications and excluded medications
Outcomes: primary and secondary outcomes specified and collected, and time points reported
Notes: funding for trial and notable conflicts of interest of trial authors
Two review authors (HF, AW) independently extracted outcome data from included studies. We noted in the 'Characteristics of included studies' table if outcome data were not reported in a usable way. We planned to resolve disagreements by consensus or by involving a third author (CP), but this was not necessary. One review author (HF) transferred data into Review Manager 5 (RevMan 5) (RevMan 2014). We double‐checked that data were entered correctly by comparing the data presented in the systematic review with the study reports. The data extracted were additionally checked by the Cochrane Airways' statistician. A second review author (SJM) spot‐checked study characteristics for accuracy against the trial report.
Assessment of risk of bias in included studies
Two review authors (HF, AW) independently assessed risk of bias for each study using the criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We planned to resolve any disagreements by discussion or by involving another review author (SJM), but this was not necessary. We assessed the risk of bias according to the domains:
random sequence generation;
allocation concealment;
blinding of participants and personnel;
blinding of outcome assessment;
incomplete outcome data;
selective outcome reporting;
other bias.
We graded each potential source of bias as high, low or unclear, and provided a quotation from the study report together with a justification for this judgement in the 'Risk of bias' table. We summarised the risk of bias judgements across different studies for each of the domains listed. We considered blinding separately for different key outcomes where necessary (e.g. for an unblinded outcome assessment, risk of bias for all‐cause mortality may be very different than that for a patient‐reported pain scale). Where information on risk of bias related to unpublished data or correspondence with a trialist, we noted this in the 'Risk of bias' table.
When considering treatment effects, we took into account the risk of bias for the studies that contributed to that outcome.
We conducted the review according to this published protocol and have reported any deviations from it in the 'Differences between protocol and review' section of the systematic review.
Measures of treatment effect
We analysed dichotomous data as rate ratios and risk ratios, and continuous data as mean differences or standardised mean differences, which are presented with 95% confidence intervals. We entered data presented on a scale with a consistent direction of effect.
We have undertaken meta‐analyses only where this was meaningful (i.e. if the treatments, participants and underlying clinical question were sufficiently similar for pooling to make sense).
Where multiple trial arms were reported in a single trial (Bjermer 2016; Castro 2014a; Park 2016; Pavord 2012a), we only included the arms with doses likely to be used clinically, that is, 75 mg intravenous (IV) or 100 mg subcutaneous (SC) injections of mepolizumab, 3 mg/kg IV reslizumab, 20 to 30 mg SC benralizumab. We considered four‐weekly and eight‐weekly dosing schedules to be equally clinically valid and therefore pooled these data (Bleecker 2016; FitzGerald 2016). Mepolizumab can be administered by different routes (IV or SC); for the purpose of this review we considered these separately.
In future updates of this review, we will narratively describe skewed data reported as medians and interquartile ranges. Where multiple trial arms are reported in a single trial, we will include only the relevant arms. If two comparisons (e.g. drug A versus placebo and drug B versus placebo) are combined in the same meta‐analysis, we will halve the control group to avoid double‐counting.
Unit of analysis issues
We did not identify any cross‐over studies or cluster‐randomised trials for inclusion in this version of the review. If cross‐over trials are identified in the future, we will seek data from a paired analysis from the trial report or authors in order to appropriately include data in the review using the inverse variance method. If we identify cluster‐randomised trials in the future, then analyses will be at the level of the individual while allowing for the clustering in the data by using the intracluster correlation coefficient. If this is not reported in the trial, then we will impute it from similar studies.
Dealing with missing data
We contacted investigators in order to verify key study characteristics and obtain missing numerical outcome data where possible (e.g. when a study was identified as an abstract only). If this was not possible and the missing data were thought to introduce serious bias, we planned to explore the impact of including such studies in the overall assessment of results by a sensitivity analysis.
Assessment of heterogeneity
Statistical heterogeneity between studies was assessed visually by inspection of the forest plots and using the Chi2 test (a P value less than 0.10 was considered significant due to the low power of the test). We also calculated the I² statistic (Higgins 2003); this describes the percentage of the variability in effect estimates that is due to heterogeneity rather than sampling error (chance). Values of I² range from 0% to 100%, with 0% representing no heterogeneity and 100% representing considerable heterogeneity.
For this review, we defined heterogeneity as reported using the I² statistic as follows.
0% to 40%: heterogeneity might not be important.
30% to 60%: may represent moderate heterogeneity.
50% to 90%: may represent substantial heterogeneity.
75% to 100%: considerable heterogeneity.
Assessment of reporting biases
If we are able to pool more than 10 trials for future versions, we will create and examine a funnel plot to explore possible small study biases and publication bias.
Data synthesis
In view of the considerable clinical heterogeneity between the included studies, we used a random‐effects model.
Data on outcomes were combined at 6 months and 12 months. Where data for other time points were reported, these were also described.
Subgroup analysis and investigation of heterogeneity
Provided sufficient studies were included, we planned to carry out subgroup analyses according to:
eosinophilic individuals versus non‐eosinophilic individuals (as eosinophilia may be a prescribing requirement e.g. NICE 2017); and
age (0 to 5 years, 6 to 16 years, 17 years and older).
Using the outcomes:
'clinically significant' asthma exacerbations;
HRQoL (as measured by a validated questionnaire); and
measures of lung function (e.g. FEV1).
We used the formal test for subgroup interactions in RevMan 2014.
Sensitivity analysis
We planned to carry out the following sensitivity analyses if sufficient studies were included:
excluding studies with an overall high risk of bias;
excluding cross‐over trials and cluster‐randomised trials.
'Summary of findings' table
We created 'Summary of findings' tables using the following outcomes.
Asthma exacerbations
HRQoL (as measured by a validated questionnaire)
Measures of lung function (e.g. FEV1)
Adverse events
We used the five GRADE considerations (study limitations, consistency of effect, imprecision, indirectness and publication bias) to assess the quality of the body of evidence as it related to the studies that contributed data to the meta‐analyses for the prespecified outcomes. We used methods and recommendations described in Section 8.5 (Higgins 2011) and Chapter 12 (Schünemann 2011) of the Cochrane Handbook for Systematic Reviews of Interventions using GRADEpro GDT software (GRADEpro GDT 2015). We have justified all decisions to downgrade or upgrade the quality of studies using footnotes, and we have made comments to aid the reader's understanding of the review where necessary.
Results
Description of studies
Results of the search
We identified 301 records in our literature searches (Figure 1):
159 in database searches for the original mepolizumab review (last search April 2015)
126 in updated database searches for this review (in August 2016 and March 2017)
13 relevant studies reported in conference abstracts and two in study bibliographies in September 2016, and
A further study in April 2017 (identified on reviewing the ongoing studies and finding one had completed and published).
After removing duplicates, 265 records remained.
Thirteen (13) studies met our inclusion criteria ('Characteristics of included studies' table), and six others were included in the ongoing studies category ('Characteristics of ongoing studies' table). The thirteen studies included had 48 records:
The four included studies comparing mepolizumab versus placebo had 16 records: two for Chupp 2017, four for Haldar 2009, eleven for Ortega 2014 and six for Pavord 2012a.
The four included studies comparing reslizumab versus placebo had 16 records: five for Castro 2015a; three for Castro 2015b; four for Bjermer 2016, and three for Corren 2016.
The five included studies for benralizumab versus placebo had 16 records: three for Bleecker 2016; six for Castro 2014a; three for FitzGerald 2016; three for Park 2016, and one for NCT01947946 2013.
The remaining 211 records were excluded for various reasons ('Characteristics of excluded studies' table). In particular, Nair 2009 and Bel 2014 were excluded as the dose of prednisolone was reduced four weeks after the first dose of mepolizumab.
Included studies
Table 9 compares the design, numbers, interventions and participant groups in the included trials.
Table 1.
Comparisons of study characteristics
| Study (Number of Participants) | Design, follow‐up (weeks) | Baseline asthma severity | Baseline treatment | Intervention (route) | Primary and secondary outcomes |
| Chupp 2017 (551) | RCT, double‐blind, placebo‐controlled (24) | Blood eosinophils ≥ 150 cells/μL at screening or ≥ 300 cells/μL in previous 12 months; and ≥ 2 exacerbations in previous 12 months; and FEV1 < 80% | High‐dose ICS for ≥ 12 months; + additional controller for ≥ 3 months; ± maintenance OCS | Mepolizumab 100 mg (SC) or placebo every 4 weeks for 24 weeks (last dose at 20 weeks) | ‐ SGRQ ‐ Mean change from baseline pre‐bronchodilator FEV1 ‐ Proportion of SGRQ total score responders at week 24 ‐ Mean change from baseline in ACQ‐5 |
| Haldar 2009 (61) | RCT, double‐blind, placebo‐controlled, parallel‐group (50) | ≥ 3% sputum eosinophils; and ≥ 2 exacerbations in previous 12 months | High‐dose ICS | Mepolizumab 75 (IV) or matched placebo (150 mL of 0.9% saline) at monthly intervals for 1 y | ‐ Severe exacerbations per person ‐ Change in AQLQ ‐ post‐bronchodilator FEV1 ‐ Airway hyperresponsiveness ‐ Blood/sputum eosinophil counts |
| Ortega 2014 (576) | RCT, double‐blind, double‐dummy, phase 3 (32) | Blood eosinophils ≥ 150 cells/μL at screening or ≥ 300 cells/μL in previous 12 months; and ≥ 2 exacerbations in previous 12 months; and FEV1 < 80% | High‐dose ICS for ≥ 12 months; + additional controller for ≥ 3 months; ± maintenance OCS | Mepolizumab 75 mg (IV) or 100 mg (SC) or placebo every 4 weeks for 32 weeks | ‐ Exacerbations per y ‐ Mean change from baseline pre‐bronchodilator FEV1 ‐ Mean change from baseline SGRQ total score |
| Pavord 2012a (621) | Multicentre, double‐blind, placebo‐controlled (52) | ≥ 3% sputum eosinophils or blood eosinophil ≥ 300 cells/μL; and ≥ 2 exacerbations in previous 12 months | High‐dose ICS (i.e. ≥ 880 μg/d FP or equivalent daily); + additional controller; ± maintenance OCS | Mepolizumab 75 mg, 250 mg or 750 mg (IV) or placebo every 4 weeks for 13 doses | ‐ Time to first clinically significant exacerbation ‐ Frequency of exacerbations requiring hospitalisation ‐ Time to first exacerbation requiring hospitalisation or ED visit ‐ Mean change from baseline pre‐bronchodilator FEV1 ‐ Mean change from baseline post‐bronchodilator FEV1 ‐ Mean change from baseline ACQ |
| Bjermer 2016 (315) | RCT, double‐blind, placebo‐controlled, parallel‐group, fixed‐dosage, multicentre phase 3 (16) | Blood eosinophils ≥ 400 cells/μL during 2‐4 weeks screening period; and ACQ‐7 score ≥ 1.5 | Medium‐dose ICS; maintenance OCS not allowed | Reslizumab 0.3 mg/kg or 3 mg/kg (IV) or placebo every 4 weeks for 4 doses | ‐ Pre‐bronchodilator FEV1, FVC, FEF25‐75 ‐ ACQ, ACQ‐6, ACQ‐5 ‐ ASUI ‐ AQLQ ‐ Rescue inhaler use ‐ Blood eosinophil levels |
|
Castro 2015a (489) and Castro 2015b (464) |
2 x duplicate RCT double‐blind, placebo‐controlled, parallel‐group, multicentre, phase 3 (52) | Blood eosinophils ≥ 400 cells/μL during 2‐4 week screening period; and ACQ‐7 score ≥ 1.5 | Medium‐dose ICS (i.e. ≥ 440 μg/day FP or equivalent daily); ± additional controller or maintenance OCS | Reslizumab 3 mg/kg (IV) or matching placebo every 4 weeks for 13 doses (last dose week 48) | ‐ Annual frequency of exacerbations ‐ Change in FEV1 from baseline over 16 weeks ‐ ACQ‐7 score ‐ ASUI score ‐ Rescue use of SABA ‐ Blood eosinophil count ‐ AQLQ total score at weeks 16, 32 and 52 |
| Corren 2016 (496) | RCT double‐blind, placebo‐controlled, multicentre phase 3 (16) | ACQ‐7 score ≥ 1.5 (no selection based on blood eosinophils) | Medium‐dose ICS; maintenance OCS not allowed | Reslizumab 3 mg/kg (IV) or matching placebo every 4 weeks for 4 doses | ‐ Change in FEV1 from baseline ‐ ACQ‐7 score ‐ Rescue (SABA) use within previous 3 days ‐ FVC ‐ Blood eosinophils |
| Bleecker 2016 (1204) | RCT double‐blind, parallel‐group, placebo‐controlled multicentre (52) | ≥ 2 exacerbations in the previous 12 months; and ACQ‐6 score ≥ 1.5 at enrolment; and FEV1 < 80% (if 12‐17 years old, < 90%) | Adults (> 18 y) high‐dose (≥ 500 μg/d FP or equivalent) ICS/LABA for ≥ 12 months Children (12‐17 y) at least medium‐dose (≥ 250 μg/day FP or equivalent) ICS/LABA |
Benralizumab 30 mg (SC) or placebo either every 4 weeks or every 4 weeks for the first 3 doses then every 8 weeks or placebo for 48 weeks | ‐ Annual exacerbation rate ‐ Pre‐bronchodilator FEV1 ‐ Total asthma symptom score ‐ Time to first exacerbation ‐ Annual rate of exacerbations requiring ED visit or hospital admission ‐ Post‐bronchodilator FEV1 ‐ ACQ‐6 ‐ AQLQ(S)+12 score |
| Castro 2014a (606) | RCT double‐blind, placebo‐controlled, multicentre dose‐ranging (52) | 2‐6 exacerbations in the previous 12 months; and ACQ‐6 score ≥ 1.5 at least twice during screening; and morning pre‐bronchodilator FEV1 40%‐90% | Medium‐ to high‐dose ICS in combination with LABA for ≥ 12 months | Benralizumab 2 mg, 20 mg or 100 mg (SC) or placebo every 4 weeks for the first 3 doses, then every 8 weeks (total 7 doses) | ‐ Annual exacerbation rate ‐ Change from baseline in FEV1 ‐ Mean ACQ‐6 score ‐ Overall symptom score ‐ Mean AQLQ score |
| FitzGerald 2016 (1306) | RCT, double‐blind, parallel‐group, placebo‐controlled multicentre (56) | ≥ 2 exacerbations in the previous 12 months; and ACQ‐6 score ≥ 1.5 at enrolment; and FEV1 < 80% | Medium‐ (≥ 250 μg/d FP or equivalent) to high‐dose (≥ 500 μg/d FP or equivalent) ICS/LABA for ≥ 12 months; high‐dose ICS/LABA for ≥ 3 months | Benralizumab 30 mg (SC) or placebo either every 4 weeks or every 4 weeks for the first 3 doses then every 8 weeks or placebo | ‐ Annual exacerbation rate for participants with blood eosinophils ≥ 300 cells/μL ‐ Pre‐bronchodilator FEV1 ‐ Total asthma symptom score ‐ Time to first exacerbation ‐ Annual rate of exacerbations requiring ED visit or hospital admission ‐ Post‐bronchodilator FEV1 ‐ ACQ‐6 ‐ AQLQ(S)+12 score |
|
NCT01947946 2013 (13) |
RCT double‐blind, parallel‐group, placebo‐controlled multicentre (48) | Uncontrolled asthma taking medium‐dose ICS plus LABA | Medium‐dose ICS (>250ug and ≤500ug fluticasone dry powder formulation equivalents total daily dose) and LABA for at least 3 month prior to first visit | Benralizumab 30 mg (SC) or placebo either every 4 weeks or every 4 weeks for the first 3 doses then every 8 weeks or placebo | Asthma exacerbations over 48‐week treatment period |
| Park 2016 (103) | RCT double‐blind, placebo‐controlled, dose‐ranging multicentre (52) | 2‐6 exacerbations in the previous 12 months; and ACQ‐6 score ≥ 1.5 at least twice during screening; and morning pre‐bronchodilator FEV1 40%‐90% | Medium‐ to high‐dose ICS in combination with LABA for ≥ 12 months | Benralizumab 2 mg, 20 mg or 100 mg (SC) or placebo every 4 weeks for the first 3 doses, then every 8 weeks (total 7 doses) | ‐ Annual exacerbation rate ‐ Lung function ‐ ACQ‐6 ‐ FeNO ‐ Blood eosinophil counts |
ACQ: Asthma Control Questionnaire; AQLQ: Asthma Quality of Life Questionnaire; ASUI: Asthma Symptom Utility Index; BDP: beclomethasone dipropionate; b: day; ECP: eosinophil cationic protein; ED: emergency department; FEF25‐75 : forced expiratory flow at 25% to 75% of FVC; FeNO: exhaled fraction of nitric oxide; FEV1 : Forced expiratory volume in 1 second; FVC: forced vital capacity; FP; fluticasone propionate; ICS; inhaled corticosteroid; IV: intravenous; LABA: long‐acting beta2 agonistOCS; oral corticosteroid; PC20 : histamine provocative concentration causing a 20% drop in FEV1; PEFR: peak expiratory flow rate; RCT: randomised controlled trial; SABA: short‐acting beta2‐agonists; SC: subcutaneous; SGRQ: St George's Respiratory Questionnaire; y: year
Mepolizumab
We included four studies comparing mepolizumab versus placebo ('Characteristics of included studies' table), involving 1809 total participants distributed as follows: Chupp 2017 n = 551; Haldar 2009 n = 61; Ortega 2014 n = 576, and Pavord 2012a n = 621. Mepolizumab was administered intravenously (IV) in Haldar 2009 (at a dose of 750 mg) and Pavord 2012a (at doses of 75 mg, 250 mg and 750 mg), subcutaneously (SC) in Chupp 2017, and via both routes (75 mg IV or 100 mg SC) in Ortega 2014 over a range of treatment periods. For Pavord 2012a, we only included the arm dosed at 75 mg, as this is considered comparable to the 100 mg SC dose that is licensed (according to manufacturer's evidence submission to the UK's National Institute for Health and Care Excellence in November 2015).
The studies only included participants with severe eosinophilic asthma. In all four studies severe disease was defined as requiring high‐dose ICS and a second controller medication plus a history of at least two exacerbations in the preceding 12 months. In addition Chupp 2017 and Ortega 2014 required that participants had impaired lung function despite treatment with an FEV1 of less than 80%. Eosinophilia was defined as a serum eosinophil count of 150 cells or more per μL at screening or 300 cells or more per μL at some time during the previous year (Chupp 2017; Ortega 2014), or either a sputum eosinophil count of 3% or more (Haldar 2009) and/or a blood eosinophil count of 300 cells or more per μL (Pavord 2012a). The blood eosinophil thresholds used in Chupp 2017 and Ortega 2014 were identified as those that best predicted response to mepolizumab in a secondary analysis of previous studies (Ortega 2014; Pavord 2012a).
Reslizumab
Four studies comparing reslizumab versus placebo were included ('Characteristics of included studies' table), involving 1764 total participants distributed as follows: Bjermer 2016 n = 315, Castro 2015a n = 489; Castro 2015b n = 464; and Corren 2016 n = 496. Reslizumab was administered intravenously in all four studies over a range of treatment periods at a dose of 3.0 mg/kg, with an additional arm at a dose of 0.3 mg/kg in Bjermer 2016, which was not included as it is 10 times lower than the licensed dose of 3.0 mg/kg.
All the participants had moderate to severe asthma, defined as requiring medium‐dose ICS. In addition they had inadequate symptom control, with an ACQ of 1.5 or more. In addition Castro 2015a and Castro 2015b required a history of at least one exacerbation in the preceding 12 months. Three studies of reslizumab (Bjermer 2016; Castro 2015a; Castro 2015b) required that participants had a blood eosinophil count of 400 cells or more per μL, which has been shown to be predictive of a sputum eosinophil count of 3% or more in studies of participants with paired blood and sputum samples (Farooqui 2009; Van Veen 2009). Corren 2016 included participants with a range of eosinophil counts.
Benralizumab
We included five studies comparing benralizumab versus placebo ('Characteristics of included studies' table), involving 3232 total participants distributed as follows: Bleecker 2016 n = 1204; Castro 2014a n = 606; FitzGerald 2016 n = 1306, NCT01947946 2013 n = 13 and Park 2016 n = 103. The benralizumab was administered subcutaneously in all studies, with dosage varying from 2 mg to 100 mg every four or eight weeks over a range of treatment periods. We only included participants dosed with 20 mg or 30 mg benralizumab in the analysis, as the other doses are unlikely to be licensed and therefore used clinically. NCT01947946 2013 was terminated due to sponsor decision after randomising 13 participants and contributes no data to the review.
The severity of asthma among participants varied from moderate to severe, defined as a requirement for maintenance therapy with medium‐ or high‐dose ICS plus LABA. Participants also had poor asthma control, determined by a history of at least two exacerbations in the previous 12 months and an ACQ of 1.5 or above in the studies contributing data. All five benralizumab trials included participants regardless of eosinophilia, but results were stratified by blood eosinophil count using a threshold of 300 cells or more per μL.
Excluded studies
We excluded 187 studies from the review (from 211 references). Of these: 117 (61%) because anti‐IL‐5 therapy had not been included in the study; 32 (17%) were not randomised placebo‐controlled studies; 14 (8%) had a treatment period of less than 16 weeks; 11 (6%) were conducted on participants without a diagnosis of asthma; 9 (5%) were an aggregation of trials, and 4 (2%) because the focus was on steroid reduction. (See 'Characteristics of excluded studies' table).
Risk of bias in included studies
Details of our 'Risk of bias' assessments are available in the 'Characteristics of included studies' table, and a summary of our assessment can be seen in Figure 2 and Figure 3.
Figure 2.
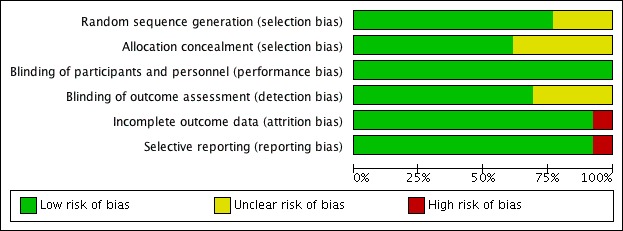
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies
Figure 3.
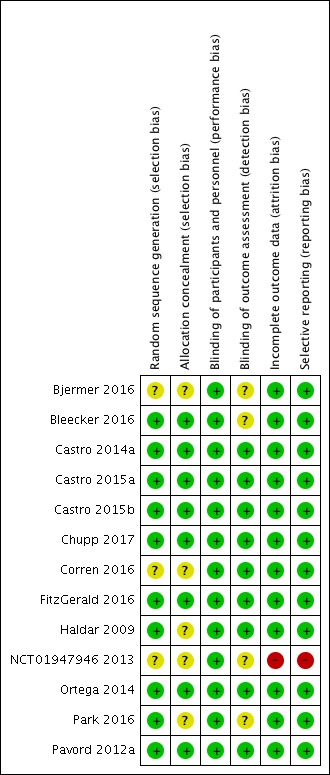
Risk of bias summary: review authors' judgements about each risk of bias item for each included study
Allocation
We deemed the majority of studies to be at low risk of bias for both random sequence generation and allocation concealment. Three studies (Bjermer 2016; Corren 2016; NCT01947946 2013) presented no details on either random sequence generation or allocation concealment, whereas a further two (Haldar 2009; Park 2016) presented no details on allocation concealment only (Figure 3).
Blinding
We determined that all 13 studies were at low risk of performance bias, and nine were at low risk of detection bias; the risk of detection bias was unclear for four studies (Bjermer 2016; Bleecker 2016; NCT01947946 2013; Park 2016) (Figure 3).
Incomplete outcome data
We considered all 12 studies contributing data to be at low risk of attrition bias (Figure 3). One study, in which no participant completed the trial, was deemed to be at high risk (NCT01947946 2013).
Selective reporting
We considered the risk of reporting bias to be low in 12 studies (Figure 3) and high in the terminated study (NCT01947946 2013).
Other potential sources of bias
We did not note any other potential sources of bias.
Effects of interventions
See: Table 1; Table 2; Table 3; Table 4
Mepolizumab (SC) versus placebo
The data for this comparison come from two studies, Chupp 2017 and Ortega 2014, with a combined 936 participants with severe eosinophilic asthma. In both studies this was defined as a serum eosinophil count of 300 cells or more per μL in the preceding 12 months or 150 cells or more per μL at screening. Our confidence in the results below is high, as both studies were large with a robust methodology.
Primary Outcomes
'Clinically significant' asthma exacerbation (as defined by treatment with a course of systemic corticosteroids, with or without hospital attendance or admission)
The meta‐analysis produced a statistically significant effect favouring mepolizumab, versus placebo, from the two studies contributing data to this outcome Chupp 2017; Ortega 2014 (rate ratio 0.45, 95% confidence interval (CI) 0.36 to 0.55; participants = 936; studies = 2) (Analysis 1.1).
Analysis 1.1.
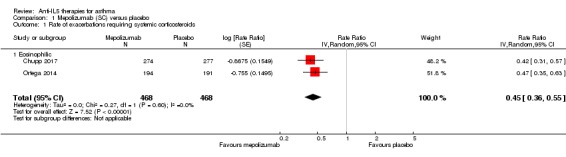
Comparison 1 Mepolizumab (SC) versus placebo, Outcome 1 Rate of exacerbations requiring systemic corticosteroids.
Secondary outcomes
Exacerbations requiring emergency department treatment or admission
The rate of exacerbations requiring emergency department treatment or admission from the two studies (Chupp 2017; Ortega 2014) contributing to this outcome was significantly lower in the mepolizumab condition (rate ratio 0.36, 95% CI 0.20 to 0.66; participants = 936; studies = 2) (Analysis 1.2); and the rate of exacerbations requiring admission in the same two studies similarly favoured mepolizumab versus placebo (rate ratio 0.31, 95% CI 0.13 to 0.73; participants = 936; studies = 2) (Analysis 1.3).
Analysis 1.2.
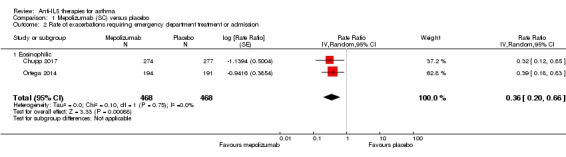
Comparison 1 Mepolizumab (SC) versus placebo, Outcome 2 Rate of exacerbations requiring emergency department treatment or admission.
Analysis 1.3.
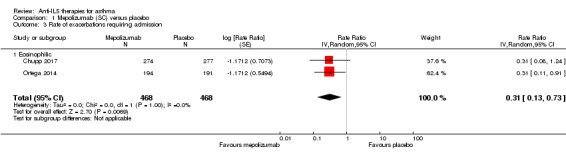
Comparison 1 Mepolizumab (SC) versus placebo, Outcome 3 Rate of exacerbations requiring admission.
HRQoL (as measured by a validated questionnaire e.g. ACQ, AQLQ, SGRQ)
Two studies (Chupp 2017; Ortega 2014) contributed HRQoL data measured by the ACQ instrument, indicating a statistically significant effect in favour of mepolizumab versus placebo (mean difference (MD) ‐0.42, 95% CI ‐0.56 to ‐0.28; participants = 936; studies = 2) (Analysis 1.4), but this did not meet the minimum clinically important difference (MCID) of 0.5 points in the ACQ. However there was a statistically and clinically significant improvement in the SGRQ in these studies (MD ‐7.40, 95% CI ‐9.50 to ‐5.29; participants = 936; studies = 2) (Analysis 1.5); the MCID is ‐4 points for the SGRQ). The SGRQ is a 50‐item questionnaire with questions covering three domains: symptoms, activity, and impacts (psycho‐social). The ACQ has between five and seven items (there are three variations) focused on asthma symptoms and airflow limitation (the seven‐item ACQ includes short‐acting bronchodilator use for symptom relief and FEV1). Thus the intervention may have had broader effects on activity and psycho‐social aspects that were not captured by the ACQ.
Analysis 1.4.
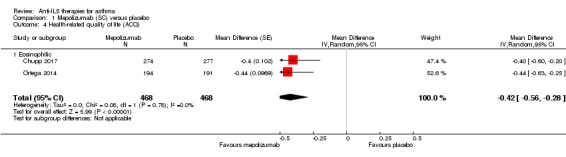
Comparison 1 Mepolizumab (SC) versus placebo, Outcome 4 Health‐related quality of life (ACQ).
Analysis 1.5.
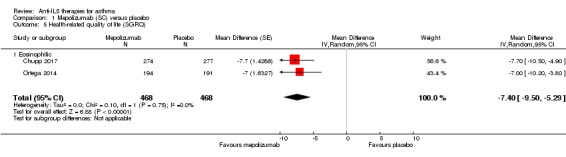
Comparison 1 Mepolizumab (SC) versus placebo, Outcome 5 Health‐related quality of life (SGRQ).
In a responder analysis, Chupp 2017 found 59% of participants experienced an improvement greater than the MCID of 0.5 points in the ACQ, versus 42% of participants on placebo (P = 0.0014), and 73% had an improvement of greater than the MCID of 4 points in the SGRQ, versus 55% in the placebo arm (P < 0.0001).
Measures of lung function (e.g. FEV1)
We observed a statistically significant increase of 110 mL in pre‐bronchodilator FEV1 in the mepolizumab condition of the aggregated studies (Chupp 2017; Ortega 2014) (MD 0.11 L, 95% CI 0.06 to 0.17; participants = 936; studies = 2) (Analysis 1.6). This is a relatively modest increase; although there is no universally accepted MCID for FEV1 in asthma, variability within a single testing session can be up to 0.12 L (data from a mixed pool of respiratory patients, Enright 2004).
Analysis 1.6.
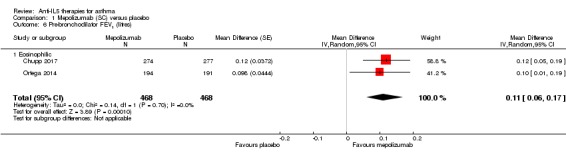
Comparison 1 Mepolizumab (SC) versus placebo, Outcome 6 Pre‐bronchodilator FEV1 (litres).
Serious adverse events
Overall there were statistically fewer serious adverse events in the mepolizumab condition when we combined data from Chupp 2017 and Ortega 2014 (risk ratio 0.63, 95% CI 0.41 to 0.97; participants = 936; studies = 2) (Analysis 1.7). This may be due to a reduction in asthma‐related serious adverse events (e.g. exacerbations requiring hospitalisation, which were significantly reduced), although neither study achieved statistical significance alone and therefore this was not commented on by the investigators. It is also possible that the inclusion of asthma‐related serious adverse effects, which were reduced, could mask a relatively smaller increase in non‐asthma‐related serious adverse effects; in future it would be useful for this to be separated.
Analysis 1.7.
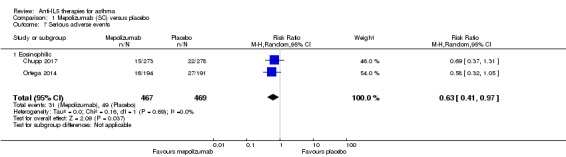
Comparison 1 Mepolizumab (SC) versus placebo, Outcome 7 Serious adverse events.
'Clinically significant' adverse events (defined as those prompting participants to stop the intervention)
There was no significant statistical difference between the two conditions with respect to this outcome (risk ratio 0.45, 95% CI 0.11 to 1.80; participants = 936; studies = 2; I² = 0%) (Analysis 1.8).
Analysis 1.8.
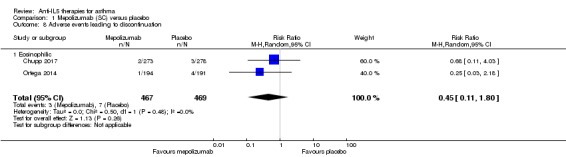
Comparison 1 Mepolizumab (SC) versus placebo, Outcome 8 Adverse events leading to discontinuation.
Serum eosinophil counts
Insufficient data were available to analyse this outcome. However Ortega 2014 reported a decrease in serum eosinophil counts by week 4, with a maximal drop of 86% by week 12 that was maintained during the study.
Mepolizumab (IV) versus placebo
The data for this comparison come from three studies (Haldar 2009; Ortega 2014; Pavord 2012a) with a combined 751 participants, all with severe eosinophilic asthma; there were no subgroups with non‐eosinophilic participants. Our confidence in the results is moderate, as IV delivery is not currently a licenced delivery route for mepolizumab, and although the results for exacerbations mirror those with mepolizumab SC, those for HRQoL measures do not.
Primary Outcomes
'Clinically significant' asthma exacerbation (as defined by treatment with a course of systemic corticosteroids, with or without hospital attendance or admission)
The rate of 'clinically significant' exacerbations was significantly lower in the mepolizumab condition (rate ratio 0.53, 95% CI 0.44 to 0.64; participants = 751; studies = 3 (Haldar 2009; Ortega 2014; Pavord 2012a)) (Analysis 2.1).
Analysis 2.1.
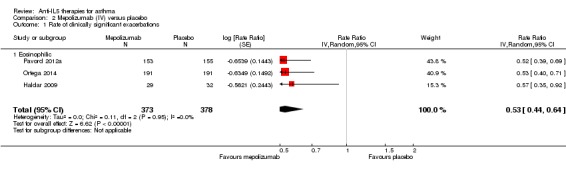
Comparison 2 Mepolizumab (IV) versus placebo, Outcome 1 Rate of clinically significant exacerbations.
Secondary outcomes
Exacerbations requiring emergency department treatment or admission
The rate of exacerbations requiring emergency department treatment or admission was significantly lower in the mepolizumab condition (rate ratio 0.52, 95% CI 0.31 to 0.87; participants = 690; studies = 2 (Ortega 2014; Pavord 2012a)) (Analysis 2.2). The rate of exacerbations requiring admission favoured the intervention group but this did not reach statistical significance (rate ratio 0.61, 95% CI 0.33 to 1.13; participants = 690; studies = 2 (Ortega 2014; Pavord 2012a)) (Analysis 2.3).
Analysis 2.2.
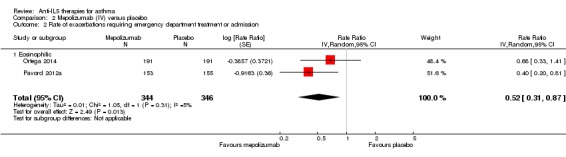
Comparison 2 Mepolizumab (IV) versus placebo, Outcome 2 Rate of exacerbations requiring emergency department treatment or admission.
Analysis 2.3.
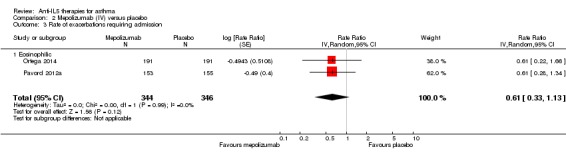
Comparison 2 Mepolizumab (IV) versus placebo, Outcome 3 Rate of exacerbations requiring admission.
These findings are consistent with results from a smaller trial (participants = 61; Haldar 2009), which reported three admissions for asthma exacerbations in the mepolizumab group (n = 29) compared to 11 in the placebo group (n = 32; P = 0.07). However there was no significant difference between mepolizumab versus placebo in terms of people experiencing one or more exacerbations in this smaller trial (Haldar 2009; risk ratio 0.82, 95% CI 0.61 to 1.09; participants = 61; studies = 1) (Analysis 2.4).
Analysis 2.4.
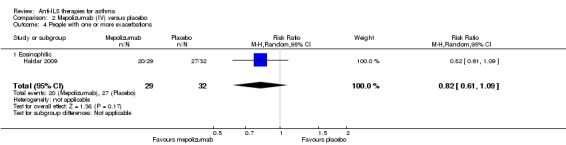
Comparison 2 Mepolizumab (IV) versus placebo, Outcome 4 People with one or more exacerbations.
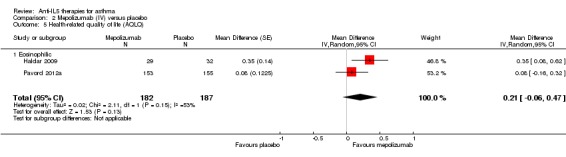
HRQoL (as measured by a validated questionnaire e.g. ACQ, AQLQ, SGRQ)
There was no significant difference between mepolizumab and placebo for HRQoL when measured using the AQLQ instrument (MD 0.21, 95% CI ‐0.06 to 0.47; participants = 369; studies = 2 (Haldar 2009; Pavord 2012a)) (Analysis 2.5). Similarly there was no statistically reliable difference between the two conditions when measuring HRQoL using the ACQ in these studies (MD ‐0.11, 95% CI ‐0.32 to 0.09; participants = 369; studies = 2) (Analysis 2.6). However, we observed a statistically significant benefit favouring mepolizumab in HRQoL using the SGRQ in a single study (MD ‐6.40, 95% CI ‐9.65 to ‐3.15; participants = 382; studies = 1 (Ortega 2014)) (Analysis 2.7). These results conflict with those with mepolizumab SC, but in those cases where statistical significance was not reached, the trend was in favour of mepolizumab and so it may be that the effect is relatively small and this outcome is therefore underpowered.
Analysis 2.5.
Comparison 2 Mepolizumab (IV) versus placebo, Outcome 5 Health‐related quality of life (AQLQ).
Analysis 2.6.
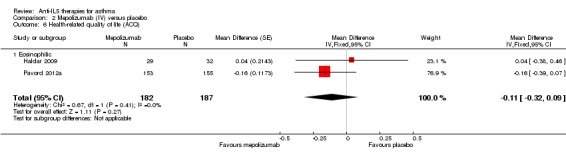
Comparison 2 Mepolizumab (IV) versus placebo, Outcome 6 Health‐related quality of life (ACQ).
Analysis 2.7.
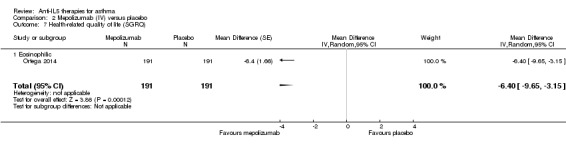
Comparison 2 Mepolizumab (IV) versus placebo, Outcome 7 Health‐related quality of life (SGRQ).
Measures of lung function (e.g. FEV1)
We observed a statistically significant benefit favouring mepolizumab in pre‐bronchodilator FEV1 (litres) (MD 0.08, 95% CI 0.02 to 0.15; participants = 690; studies = 2 (Ortega 2014; Pavord 2012a)) (Analysis 2.8). This increase is comparable, but slightly smaller, than that for mepolizumab SC and, at an individual participant level, would be considered within the normal range of variability at a single session (Enright 2004).
Analysis 2.8.
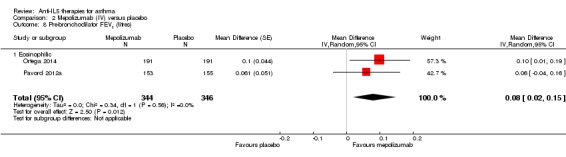
Comparison 2 Mepolizumab (IV) versus placebo, Outcome 8 Pre‐bronchodilator FEV1 (litres).
Serious adverse events
Significantly fewer serious adverse events occurred in the mepolizumab condition (risk ratio 0.59, 95% CI 0.37 to 0.94; participants = 751; studies = 3 (Haldar 2009; Ortega 2014; Pavord 2012a); I² = 27%) (Analysis 2.9). As with mepolizumab SC, this may be due to a reduction in asthma‐related serious adverse events but as the individual studies did not report a clear effect, there is no comment by the investigators.
Analysis 2.9.
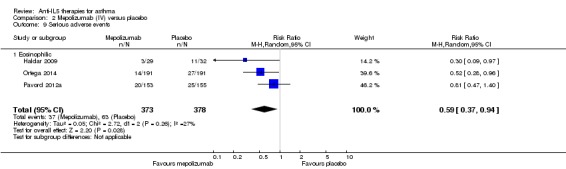
Comparison 2 Mepolizumab (IV) versus placebo, Outcome 9 Serious adverse events.
'Clinically significant' adverse events (defined as those prompting discontinuation)
For this outcome there was no significant difference between mepolizumab versus placebo (risk ratio 0.72, 95% CI 0.18 to 2.92; participants = 751; studies = 3 (Haldar 2009; Ortega 2014; Pavord 2012a); I² = 24%) (Analysis 2.10).
Analysis 2.10.
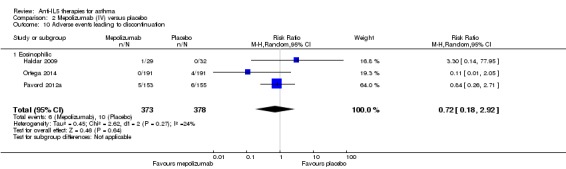
Comparison 2 Mepolizumab (IV) versus placebo, Outcome 10 Adverse events leading to discontinuation.
Serum eosinophil counts
We included a single small study (Haldar 2009) in the analysis as it was the only one to report serum eosinophil counts. This reported a significant benefit favouring mepolizumab (MD ‐170.00, 95% CI ‐230.00 to ‐110.00; participants = 61; studies = 1 (Haldar 2009)) (Analysis 2.11).
Analysis 2.11.
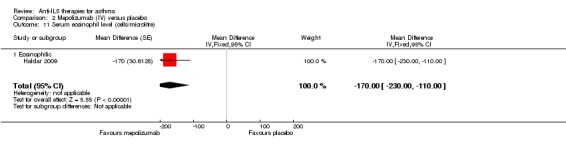
Comparison 2 Mepolizumab (IV) versus placebo, Outcome 11 Serum eosinophil level (cells/microlitre).
Ortega 2014 also reported a decrease in serum eosinophil counts by week 4, with a maximal drop of 83% by week 12 that was maintained during the study, but did not provide absolute counts that could be included.
Reslizumab (IV) versus placebo
The data for this comparison come from four studies (Bjermer 2016; Castro 2015a; Castro 2015b; Corren 2016) with a combined 1652 participants. One of these studies included participants with non‐eosinophilic asthma (Corren 2016). Our confidence in the results as applied to eosinophilic participants is high, as the studies were large and had a robust methodology. Where data were available for non‐eosinophilic participants we have compared the effect estimate with that for eosinophilic participants using the test for subgroup difference.
Primary Outcomes
'Clinically significant' asthma exacerbation (as defined by treatment with a course of systemic corticosteroids, with or without hospital attendance or admission)
There were significantly fewer 'clinically significant' asthma exacerbations in the reslizumab condition (rate ratio 0.43, 95% CI 0.33 to 0.55; participants = 953; studies = 2 (Castro 2015a; Castro 2015b)) (Analysis 3.1). This only included eosinophilic participants; there were no data for non‐eosinophilic participants.
Analysis 3.1.
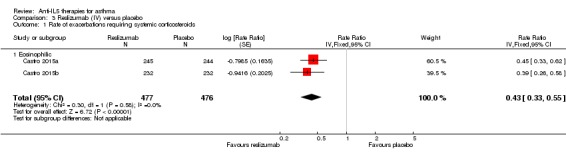
Comparison 3 Reslizumab (IV) versus placebo, Outcome 1 Rate of exacerbations requiring systemic corticosteroids.
Secondary outcomes
Exacerbations requiring emergency department treatment or admission
There was no significant difference between reslizumab versus placebo on this outcome (rate ratio 0.67, 95% CI 0.39 to 1.17; participants = 953; studies = 2 (Castro 2015a; Castro 2015b)) (Analysis 3.2). This only included eosinophilic participants; there were no data for non‐eosinophilic participants.
Analysis 3.2.
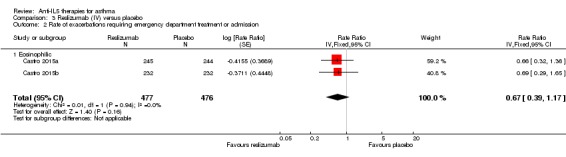
Comparison 3 Reslizumab (IV) versus placebo, Outcome 2 Rate of exacerbations requiring emergency department treatment or admission.
HRQoL (as measured by a validated questionnaire e.g. ACQ, AQLQ, SGRQ)
Participants in the reslizumab condition experienced a significantly better HRQoL measured by the AQLQ instrument (MD 0.28, 95% CI 0.17 to 0.39; participants = 1164; studies = 3 (Bjermer 2016; Castro 2015a; Castro 2015b)) (Analysis 3.3), although this failed to meet the MCID of 0.5 points or more. This only included eosinophilic participants; there were no data for non‐eosinophilic participants.
Analysis 3.3.
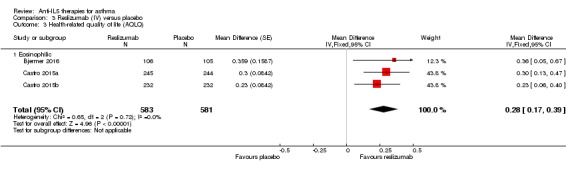
Comparison 3 Reslizumab (IV) versus placebo, Outcome 3 Health‐related quality of life (AQLQ).
We found the same effect when using the ACQ (MD ‐0.25, 95% CI ‐0.33 to ‐0.17; participants = 1652; studies = 4 (Bjermer 2016; Castro 2015a; Castro 2015b; Corren 2016)) (Analysis 3.4), again, lower than the MCID of ‐0.5 points or more. In this analysis data were available (in only one study, Corren 2016) from non‐eosinophilic participants and for that particular group there was no significant difference between reslizumab versus placebo on this outcome. However, the formal test for subgroup difference was not significant (P = 0.19, I² = 41.1%).
Analysis 3.4.
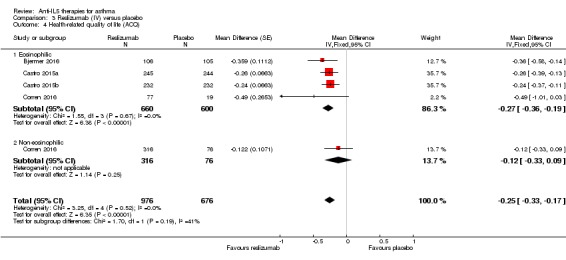
Comparison 3 Reslizumab (IV) versus placebo, Outcome 4 Health‐related quality of life (ACQ).
Measures of lung function (e.g. FEV1)
We noted a clear, statistically significant increase in pre‐bronchodilator FEV1 with reslizumab treatment (MD 0.11 L, 95% CI 0.07 to 0.15; participants = 1652; studies = 4 (Bjermer 2016; Castro 2015a; Castro 2015b; Corren 2016)) (Analysis 3.5). For this outcome data from non‐eosinophilic participants were available (again in only one study, Corren 2016) and for that subgroup we observed no significant difference between reslizumab versus placebo. As in the ACQ data, there was a significant benefit only in eosinophilic participants. However, as before, the formal test for subgroup differences was not significant (P = 0.13, I² = 56.3%). Again it is worth noting that the absolute difference of 0.11 L is relatively modest, although there is no consensus around a MCID in FEV1 in asthma.
Analysis 3.5.
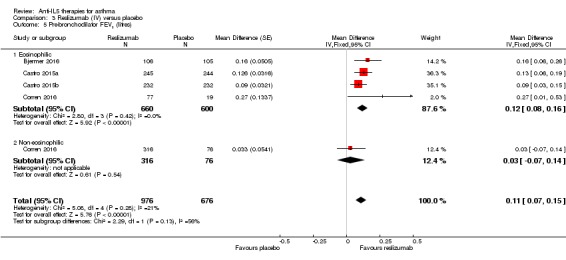
Comparison 3 Reslizumab (IV) versus placebo, Outcome 5 Pre‐bronchodilator FEV1 (litres).
Serious adverse events
There was no significant difference in the number of serious adverse events occurring in the two conditions (risk ratio 0.79, 95% CI 0.56 to 1.12; participants = 1656; studies = 4 (Bjermer 2016; Castro 2015a; Castro 2015b; Corren 2016); I² = 0%) (Analysis 3.6).
Analysis 3.6.
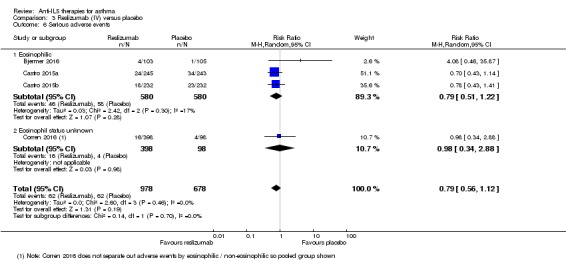
Comparison 3 Reslizumab (IV) versus placebo, Outcome 6 Serious adverse events.
There was a reduction favouring the treatment group with the pooled mepolizumab trials, which may have been due to a reduction in asthma‐related serious adverse events (the pooled studies showed significantly fewer asthma exacerbations requiring hospital admission, which would qualify as a serious adverse event). However there was no significant difference in the rate of hospitalisations due to asthma exacerbations in studies of reslizumab, which may explain the discrepancy in serious adverse events compared to mepolizumab.
'Clinically significant' adverse events (defined as those prompting discontinuation)
There was no significant difference between reslizumab versus placebo on this outcome (risk ratio 0.66, 95% CI 0.43 to 1.02; participants = 1659; studies = 4 (Bjermer 2016; Castro 2015a; Castro 2015b; Corren 2016); I² = 0%) (Analysis 3.7).
Analysis 3.7.
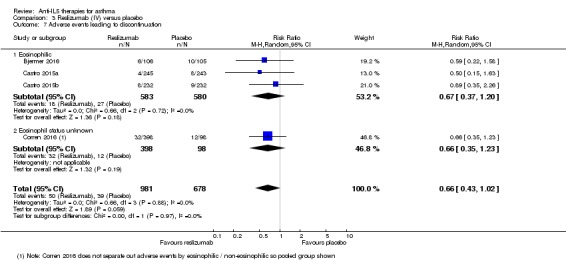
Comparison 3 Reslizumab (IV) versus placebo, Outcome 7 Adverse events leading to discontinuation.
Serum eosinophil counts
The serum eosinophil counts were significantly reduced in the reslizumab condition (MD ‐476.83, 95% CI ‐499.32 to ‐454.34; participants = 1656; studies = 4 (Bjermer 2016; Castro 2015a; Castro 2015b; Corren 2016)) (Analysis 3.8). This only included eosinophilic participants; note that a reduction in eosinophils amongst participants whose eosinophil counts are within the normal range to start with is not necessarily desirable or achievable.
Analysis 3.8.
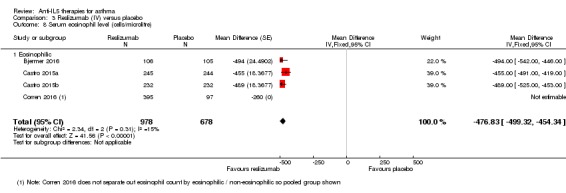
Comparison 3 Reslizumab (IV) versus placebo, Outcome 8 Serum eosinophil level (cells/microlitre).
Benralizumab (SC) versus placebo
The data for this comparison come from four studies (Bleecker 2016; Castro 2014a; FitzGerald 2016; Park 2016) with a combined 2648 participants. All four studies included participants with an eosinophilic and non‐eosinophilic phenotype, with more complete data presented for eosinophilic participants. In addition two studies had additional treatment arms for four‐weekly and eight‐weekly dosing regimens (Bleecker 2016; FitzGerald 2016), which we have shown separately in the meta‐analyses with the placebo group split across them (and adjusted accordingly). Our confidence in the results is high, as the studies were large and had a robust methodology. However limited data were available on non‐eosinophilic subgroups, and these were variably consistent with the findings in eosinophilic subgroups.
Primary Outcomes
'Clinically significant' asthma exacerbation (as defined by treatment with a course of systemic corticosteroids, with or without hospital attendance or admission)
Significantly fewer 'clinically significant' asthma exacerbations occurred in the benralizumab condition (rate ratio 0.62, 95% CI 0.55 to 0.70; participants = 2456; studies = 3 (Bleecker 2016; Castro 2014a; FitzGerald 2016)) (Analysis 4.1). We observed this effect in both eosinophilic and non‐eosinophilic participants, with a slightly larger effect for the eosinophilic subgroup (eosinophilic: rate ratio 0.59, 95% CI 0.51 to 0.68 versus non‐eosinophilic: rate ratio 0.69, 95% CI 0.56 to 0.85) but the test for subgroup difference was non‐significant (P = 0.22, I² = 33.9%).
Analysis 4.1.
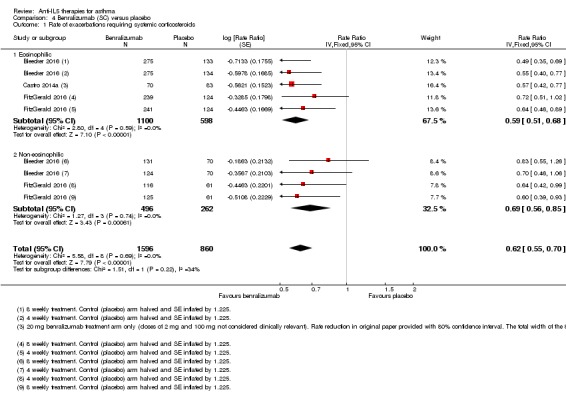
Comparison 4 Benralizumab (SC) versus placebo, Outcome 1 Rate of exacerbations requiring systemic corticosteroids.
Secondary outcomes
Exacerbations requiring emergency department treatment or admission
There were significantly fewer exacerbations requiring emergency department treatment or admission for participants in the benralizumab condition (rate ratio 0.68, 95% CI 0.47 to 0.98; participants = 1537; studies = 2 (Bleecker 2016; FitzGerald 2016)) (Analysis 4.2). This only included eosinophilic participants; there were no data for non‐eosinophilic participants. However there was a considerable degree of heterogeneity (I² = 43%), despite the Bleecker 2016 and FitzGerald 2016 studies having the same design. Both studies noted heterogeneity in the exacerbation history of their participants, FitzGerald 2016 specifically commenting that participants recruited in Eastern Europe and South America had fewer exacerbations in the year before study entry than those recruited elsewhere. These would therefore have less scope for a reduction in exacerbation. FitzGerald 2016 noted that participants who had had three or more exacerbations in the previous year had the greatest effects of benralizumab treatment, at rates comparable to the Bleecker 2016 study.
Analysis 4.2.
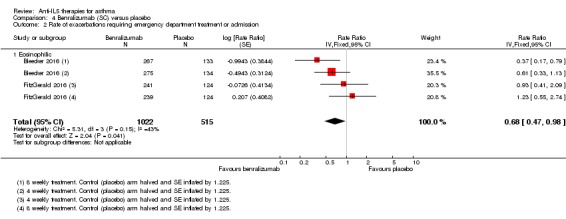
Comparison 4 Benralizumab (SC) versus placebo, Outcome 2 Rate of exacerbations requiring emergency department treatment or admission.
HRQoL (as measured by a validated questionnaire e.g. ACQ, AQLQ, SGRQ)
HRQoL (AQLQ mean difference) was significantly better in the benralizumab condition (MD 0.23, 95% CI 0.11 to 0.35; participants = 1541; studies = 3 (Bleecker 2016; Castro 2014a; FitzGerald 2016)) (Analysis 4.3); on this particular outcome data were available only from eosinophilic participants. However a similar significant advantage in favour of benralizumab was also observed with both eosinophilic and non‐eosinophilic participants when measuring HRQoL with the ACQ instrument (MD ‐0.20, 95% CI ‐0.29 to ‐0.11; participants = 2359; studies = 3 (Bleecker 2016; Castro 2014a; FitzGerald 2016)) (Analysis 4.4). When taking the non‐eosinophilic subgroup only this fell short of statistical significance (MD ‐0.14, 95% CI ‐0.30 to 0.02), although the test for subgroup difference was non‐significant (P = 0.36, I² = 0%). Neither difference reached the MCID of 0.5 points or more on either the AQLQ or ACQ scale.
Analysis 4.3.
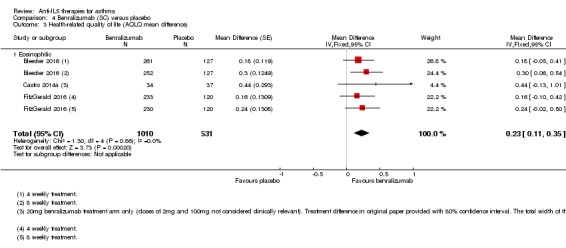
Comparison 4 Benralizumab (SC) versus placebo, Outcome 3 Health‐related quality of life (AQLQ mean difference).
Analysis 4.4.
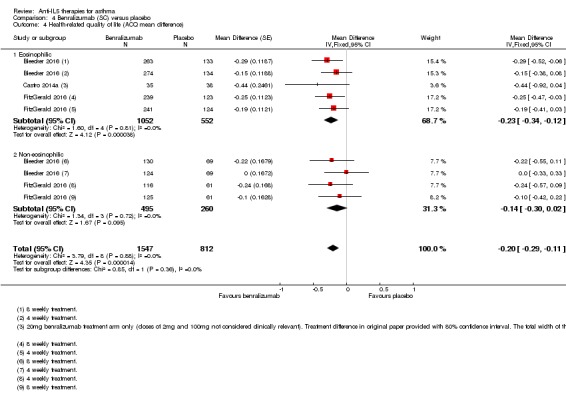
Comparison 4 Benralizumab (SC) versus placebo, Outcome 4 Health‐related quality of life (ACQ mean difference).
Measures of lung function (e.g. FEV1)
Pre‐bronchodilator FEV1 was significantly superior in the benralizumab condition (MD 0.10, 95% CI 0.05 to 0.14; participants = 2355; studies = 3 (Bleecker 2016; Castro 2014a; FitzGerald 2016)) (Analysis 4.5). However on closer inspection it was apparent that only eosinophilic participants had experienced this benefit, with a significant test for subgroup difference between eosinophilic and non‐eosinophilic participants (P = 0.02, I² = 82.0%). This improvement of 0.10 L is of a similar magnitude to that seen with mepolizumab and reslizumab, and is relatively modest.
Analysis 4.5.
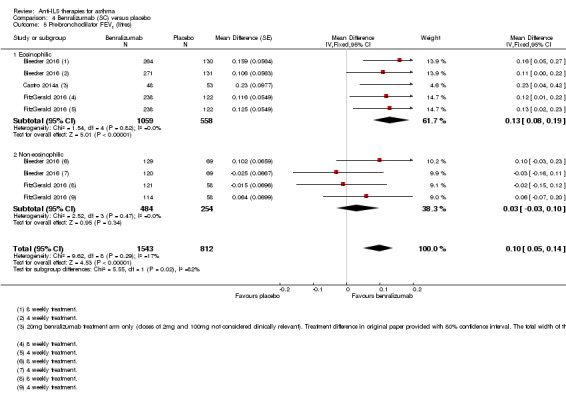
Comparison 4 Benralizumab (SC) versus placebo, Outcome 5 Pre‐bronchodilator FEV1 (litres).
Serious adverse events
There was no significant difference in the number of serious adverse events occurring in the two conditions (risk ratio 0.81, 95% CI 0.66 to 1.01; participants = 2648; studies = 4 (Bleecker 2016; Castro 2014a; FitzGerald 2016; Park 2016); I² = 0%)( Analysis 4.6), based on eosinophilic and non‐eosinophilic participants (including a subgroup of participants whose eosinophil status was not defined).
Analysis 4.6.
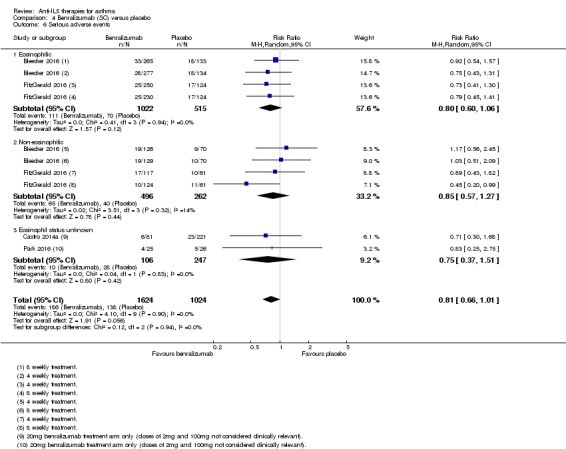
Comparison 4 Benralizumab (SC) versus placebo, Outcome 6 Serious adverse events.
This is slightly surprising given that the pooled analysis for mepolizumab showed a reduction in serious adverse events compared to placebo, which may have been due to a reduction in asthma‐related serious adverse events such as exacerbations requiring admission, which was also seen with benralizumab (significantly fewer exacerbations requiring admission or emergency department treatment). However the size of the effect on asthma exacerbations requiring admission or emergency department treatment was smaller with benralizumab (rate ratio 0.68, 95% CI 0.47 to 0.98) than mepolizumab (rate ratio 0.36, 95% CI 0.20 to 0.66 for mepolizumab SC; rate ratio 0.52, 95% CI 0.31 to 0.87 for mepolizumab IV). The dilution of this by including other adverse events may have been sufficient to make it non‐significant. Indeed examining the rate ratios suggests that this is the case both for mepolizumab, where the 95% CIs are nearer to 1 than it is for the asthma exacerbation outcomes, and benralizumab, where the upper CI is 1.01. Equally it is possible that benralizumab results in relatively greater numbers of non‐asthma‐related serious adverse events than mepolizumab (or reslizumab), given its different mechanism of action. It will be important in future to distinguish asthma‐related from non‐asthma‐related serious adverse events and, if licensed, to monitor real‐world data.
'Clinically significant' adverse events (defined as those prompting discontinuation)
There were significantly fewer 'clinically significant' adverse events in the placebo condition (risk ratio 2.15, 95% CI 1.02 to 4.57; participants = 2597; studies = 3 (Bleecker 2016; Castro 2014a; FitzGerald 2016); I² = 0%) (Analysis 4.7), based on eosinophilic and non‐eosinophilic participants (including a subgroup of participants whose eosinophil status was not defined). The individual studies did not find a statistically significant effect and thus there was no comment by the investigators. However benralizumab has a different mechanism of action resulting in a much larger reduction in eosinophils, which could result in an increase in adverse events. This is an area for further research.
Analysis 4.7.
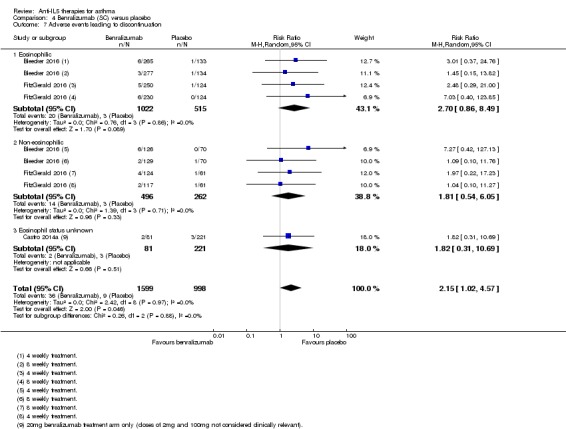
Comparison 4 Benralizumab (SC) versus placebo, Outcome 7 Adverse events leading to discontinuation.
Serum eosinophil levels (% change from baseline)
The serum eosinophil levels were significantly reduced in the benralizumab condition (MD ‐104.74, 95% CI ‐116.12 to ‐93.35; participants = 2295; studies = 2 (Bleecker 2016; FitzGerald 2016)) (Analysis 4.8). This included both eosinophilic and non‐eosinophilic participants. This is shown as a percentage change rather than absolute number, which was not available. There was also a marked reduction in serum eosinophils in Castro 2014a, with mean values of 46 to 56 cells per μL in participants with 300 or more cells per μL at baseline, and in Park 2016, to around 0 cells per μL from a mean of 564 to 824 cells per μL (these data were shown graphically and could not be extracted for inclusion in the meta‐analysis).
Analysis 4.8.
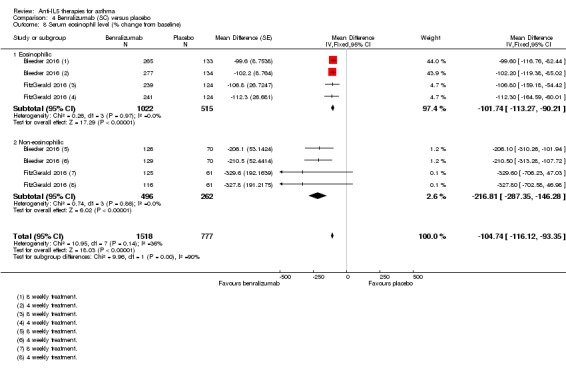
Comparison 4 Benralizumab (SC) versus placebo, Outcome 8 Serum eosinophil level (% change from baseline).
Discussion
Summary of main results
Thirteen studies met the inclusion criteria for this systematic review (Bjermer 2016; Bleecker 2016; Castro 2014a; Castro 2015a; Castro 2015b; Chupp 2017; Corren 2016; FitzGerald 2016; Haldar 2009; NCT01947946 2013; Ortega 2014; Park 2016; Pavord 2012a). Five studies included adult participants only (Castro 2014a; Corren 2016; Haldar 2009; NCT01947946 2013; Park 2016) while the remaining eight (Bjermer 2016; Bleecker 2016; Castro 2015a; Castro 2015b; Chupp 2017; FitzGerald 2016; Pavord 2012a; Ortega 2014) included participants aged 12 years and over. Results in adolescents were not reported separately and thus we could not perform a subgroup analysis on this population.
The results suggest that treatments targeting IL‐5 or the IL‐5 receptor reduce 'clinically significant' asthma exacerbation rates by approximately half in participants with severe eosinophilic asthma already on standard of care therapy with a history of poor control ('clinically significant' exacerbations defined as episodes requiring at least three days' treatment with systemic corticosteroids; standard of care defined as at least medium‐dose ICS; poor control defined as either two or more exacerbations in the preceding 12 months or an ACQ score of 1.5 or more). The effect size was largest with reslizumab and mepolizumab SC, although the study design and populations studied differed across trials and no head‐to‐head trials were performed. In addition, treatment with mepolizumab SC and benralizumab significantly reduced rates of exacerbations requiring emergency department attendance or hospital admission, with mepolizumab IV and reslizumab also showing a non‐significant trend towards this. Non‐eosinophilic participants experienced a significant, albeit smaller, reduction in asthma exacerbation rates when treated with benralizumab (with the test for subgroup difference non‐significant); no data were available for mepolizumab or reslizumab treatment in participants with non‐eosinophilic asthma. Whether this finding will be replicated with mepolizumab and reslizumab is uncertain.
Mepolizumab SC, reslizumab and benralizumab all produced modest improvements in validated HRQoL scores (e.g. ACQ, AQLQ) in severe eosinophilic asthma. However these did not exceed the MCID for ACQ and AQLQ. Improvements in the SGRQ did reach the MCID but came from only two studies (Chupp 2017; Ortega 2014). This may be due to differences between the different tools used. The SGRQ is a longer (50‐item) questionnaire with three domains (symptoms, activity, and psychosocial impact); the ACQ is much shorter (five to seven items) and focuses on asthma symptoms and airflow limitation; however the AQLQ is more like the SGRQ, with 32 items in four domains (symptoms, activity, emotional function, environmental stimuli). It is therefore not entirely clear why there were differences between the SGRQ and the AQLQ in particular, although an analysis of the results by question domain might be illuminating in that regard.
We saw no improvement in HRQoL scores in those treated with mepolizumab IV or non‐eosinophilic participants treated with benralizumab (data not available for mepolizumab or reslizumab), although in both cases there was a non‐significant trend in this direction. The effect size was largest with mepolizumab, although again the study designs and populations enrolled differed with no head‐to‐head studies to assess this.
All anti‐IL‐5 interventions produced a small but statistically significant improvement in mean pre‐bronchodilator FEV1 of between 0.08 L and 0.11 L. There is no agreed definition of a MCID in FEV1 in asthma, but the reproducibility of FEV1 values in a single session in participants with a range of respiratory conditions is up to 0.12 L (Enright 2004) suggesting that the increase with anti‐IL‐5 is modest.
Treatment with mepolizumab (SC and IV) and reslizumab appeared to be safe, although there remain safety concerns over benralizumab. Pooling the results of the clinical trials of mepolizumab (SC and IV), but not benralizumab or reslizumab, showed a small but statistically significant reduction in severe adverse events in favour of the active treatment group. This may well be attributable to the impact of the study drug on asthma‐related adverse events, particularly those leading to hospital admission that would be classed as serious adverse events (although the split of asthma‐ and non‐asthma‐related adverse events was not provided). When considering adverse events prompting participants to discontinue the study drug, there was a small but significant increase with benralizumab compared to placebo, which was not the case for mepolizumab (SC or IV) or reslizumab. This may be due to the different mechanism of action of benralizumab; further research is needed.
There were marked reductions in blood eosinophil levels with all anti‐IL‐5 treatments. Benralizumab resulted in almost complete depletion of eosinophils from the peripheral circulation, in both eosinophilic and non‐eosinophilic participants, unlike mepolizumab and reslizumab where a small number of residual eosinophils remained. This is attributed to a difference in its mechanism of action (anti‐IL‐5 receptor rather than anti‐IL‐5). It is unclear whether this translates into greater clinical efficacy or greater risk of adverse events (e.g. parasitic or helminth infections) or both.
Overall our study supports the use of anti‐IL‐5 treatments as an adjunct to standard of care (at least medium‐dose ICS) in people with severe eosinophilic asthma and a history of poor control (either two or more exacerbations in the preceding 12 months or an ACQ score of 1.5 or more).
Overall completeness and applicability of evidence
A reduction in asthma exacerbations is considered to be one of the key goals of asthma management (GINA 2017). Asthma exacerbations are of major clinical significance as they are the primary cause of morbidity and mortality in asthma, and drive increased healthcare utilisation and cost (Zeiger 2016). This is particularly the case for those with severe asthma, who continue to suffer from frequent exacerbations despite existing treatment options and therefore have a high unmet need (Custovic 2013).
We found evidence of a reduction in the rate of clinically significant exacerbations in adults with severe eosinophilic asthma with poor control given anti‐IL‐5 treatment, with low heterogeneity between studies. Secondary outcomes included safety data showing that anti‐IL‐5 treatments are well tolerated.
Whilst statistically significant improvements in symptoms (as assessed by validated HRQoL scores) and lung function (FEV1) were evident with anti‐IL‐5 interventions, these changes were modest and likely to be below levels that would be clinically detected by patients. There were also large reductions in blood eosinophil levels, but a relationship between these and symptoms is not established and thus this may also be of limited direct relevance to patients.
The included studies did not directly compare the different anti‐IL‐5 treatments, however, the effect sizes versus placebo were similar. Pragmatically, mepolizumab is given subcutaneously every four weeks, reslizumab is given by intravenous infusion necessitating a healthcare setting, whereas benralizumab can be given subcutaneously every eight weeks. Thus there are practical advantages to benralizumab treatment.
Given the mechanism of action of anti‐IL‐5 agents, the studies were predominantly conducted in participants with severe eosinophilic asthma and poor control. None extended beyond a year. It is therefore not possible to draw any conclusions about those with milder or better‐controlled (e.g. ACQ less than 1.5 with no exacerbations) disease, non‐eosinophilic asthma, nor about the long‐term effects of treatment. Eosinophilic and severe asthma were variably defined. Most studies considered blood eosinophil counts, although others used sputum eosinophil counts which are not readily available in most hospitals or clinics (Haldar 2009; Pavord 2012a). The thresholds used to determine eosinophilia in blood counts varied, with the mepolizumab studies considering 150 cells or more per μL at screening or 300 cells or more per μL in the previous year, benralizumab studies using a cut‐off of 300 or more cells per μL and reslizumab 400 cells or more per μL. All the included studies defined severe asthma as a requirement to be on stable treatment with at least medium‐dose ICS, but most specified high‐dose ICS, often with additional controller medication(s). In addition all studies restricted participants to those with uncontrolled asthma. This was either defined in terms of exacerbation history (usually at least two in the previous 12 months; e.g. the studies of mepolizumab), ACQ score (1.5 or more; e.g. the studies of reslizumab), or both (e.g. the studies of benralizumab). Given this heterogeneity, it is unclear exactly how best to select patients for anti‐IL‐5 treatment, although current evidence suggests that a measure of eosinophilia, treatment with at least medium‐dose ICS, and a history of poor control, defined as either two or more exacerbations in the last 12 months or an ACQ score of 1.5 or more, are necessary.
The evidence on mepolizumab IV is of limited applicability as it is currently only available subcutaneously.
In summary, anti‐IL‐5 agents represent a new treatment option for severe eosinophilic asthma with poor control, a patient population with a high, unmet need.
Quality of the evidence
Using the GRADE system, we considered the quality of the evidence for all comparisons to be high overall, with the exception of mepolizumab IV, which is not currently a licensed delivery route (so we would regard this as indirect evidence). We are aware of the limitations in some of the studies and have detailed them in the Results section, Figure 2 and Figure 3. We did not formally assess publication bias through the construction of a funnel plot due to the small number of included studies. However, our search strategy was thorough, including searching conference abstracts and ongoing studies, in order to identify unpublished studies.
Potential biases in the review process
This review and update was based on a published protocol (Powell 2013). We acknowledge the potential for publication bias in this review, as it is possible that we failed to identify unpublished trials that may have provided positive or negative outcomes, which in turn could have altered the treatment benefits. However, to the best of our knowledge, we identified a significant number of trials meeting our inclusion criteria through comprehensive and systematic database searches. We tried to address any study selection bias by having two review authors who independently evaluated all the identified studies. We also ensured that the assessment of each trial was consistently in line with the inclusion criteria.
Agreements and disagreements with other studies or reviews
This review is an update on a previous Cochrane Review of mepolizumab in asthma (Powell 2015), which noted one previous review with similar findings (Liu 2013). Since then, several reviews have been published on the topic:
Wang 2016, which considered all anti‐IL‐5 treatments, but also included studies with a treatment duration of less than 16 weeks and those with concomitant oral steroid reduction, and which did not include Chupp 2017;
Cabon 2017, which also assessed all anti‐IL‐5 treatments and included studies with a treatment duration of less than 16 weeks or concomitant oral steroid reduction. However fewer studies were included as the search was up to September 2015;
Yancey 2017, which only included studies of mepolizumab in asthma;
Li 2017, which only included studies of reslizumab in asthma;
Our findings are consistent with these reviews, despite the application of more rigorous inclusion criteria (in terms of treatment duration and allowed concomitant treatments, that is, standard of care rather than oral steroid reduction) and inclusion of an additional recent trial (Chupp 2017). All the reviews highlight the need for further research in this area.
Authors' conclusions
The currently available studies provide evidence to support the use of anti‐IL‐5 treatments in adults with severe eosinophilic asthma, which is now being incorporated into national and international guidelines (e.g. GINA 2017). These treatments appear to roughly halve the rate of asthma exacerbations in this patient population, for whom exacerbations are particularly troublesome (Custovic 2013). Importantly there were no safety concerns regarding mepolizumab or reslizumab, and no excess serious adverse events with benralizumab, although a question over adverse events significant enough to prompt discontinuing this treatment. There is limited evidence for improvement in health‐related quality‐of‐life scores and lung function, which may not meet clinically detectable levels.
Whilst the majority of studies included children over the age of 12, these did not provide sufficient evidence to reach a conclusion about efficacy and safety in this population.
Further research is needed to identify biomarkers for assessing treatment response, what the optimal duration of treatment is, the long‐term effects of treatment and risk of relapse on withdrawal, the impact of eosinophil‐depleting treatment on parasitic or helminth infections, and to clarify how best to define the people who will benefit from this treatment, considering the availability of tests (e.g. sputum cell differentials) and thresholds (for blood eosinophil counts). Research is also needed in people with non‐eosinophilic asthma and younger age groups, both under 12 years old, in whom there have been no trials, and 12 years to 18 years old, for whom data has not been reported separately.
With regards to benralizumab in particular, future trials and observational studies should closely monitor the incidence of adverse events leading to discontinuation.
There will be some people who are eligible for more than one anti‐IL‐5 agent and potentially also treatment with anti‐immunoglobulin E. At present there are no direct comparisons from head‐to‐head trials, leaving the clinician faced with such patients in an evidence‐free quandary. A network meta‐analysis could provide much needed guidance, but ultimately high‐quality head‐to‐head trials are required.
Acknowledgements
We would particularly like to acknowledge the excellent support and assistance from Emma Dennett, Liz Stovold and Emma Jackson of the Cochrane Airways Review Group, together with the greatly appreciated guidance from Chris Cates (Cochrane Airways Review Group Co‐ordinating Editor). The support provided by librarians Judith Scammel, Jane Appleton and Hilary Garrett at St George's University of London is also greatly appreciated. We thank Dr Anette Blümle and Dr Birgit Smith for their excellent support with translation.
Chris Cates was the Editor for this review and commented critically on the review.
The information provided by Prof. Peter Barnes regarding a study included in the previous version of this review (Leckie 2000) and the support provided by Birgit Smith, Jane Dennis, Laura Sansum and Anette Blümle with translation on non‐English trial reports is also very much appreciated.
The Background and Methods section of this review are based on a standard template used by Cochrane Airways.
We gratefully acknowledge the significant contribution on the previous version of this review Powell 2015 by Kerry Dwan (KD) and Nicola Walters (NW).
This project was supported by the National Institute for Health Research (NIHR), via Cochrane Infrastructure funding to the Cochrane Airways Group. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, NHS, or the Department of Health.
Appendices
Appendix 1. Sources and search methods for the Cochrane Airways Trials Register
Electronic searches: core databases
| Database | Frequency of search |
| CENTRAL (the Cochrane Library) | Monthly |
| MEDLINE (Ovid) | Weekly |
| Embase (Ovid) | Weekly |
| PsycINFO (Ovid) | Monthly |
| CINAHL (EBSCO) | Monthly |
| AMED (EBSCO) | Monthly |
Handsearches: core respiratory conference abstracts
| Conference | Years searched |
| American Academy of Allergy, Asthma and Immunology (AAAAI) | 2001 onwards |
| American Thoracic Society (ATS) | 2001 onwards |
| Asia Pacific Society of Respirology (APSR) | 2004 onwards |
| British Thoracic Society Winter Meeting (BTS) | 2000 onwards |
| Chest Meeting | 2003 onwards |
| European Respiratory Society (ERS) | 1992, 1994, 2000 onwards |
| International Primary Care Respiratory Group Congress (IPCRG) | 2002 onwards |
| Thoracic Society of Australia and New Zealand (TSANZ) | 1999 onwards |
MEDLINE search strategy used to identify trials for the Register
Asthma search
1. exp Asthma/
2. asthma$.mp.
3. (antiasthma$ or anti‐asthma$).mp.
4. Respiratory Sounds/
5. wheez$.mp.
6. Bronchial Spasm/
7. bronchospas$.mp.
8. (bronch$ adj3 spasm$).mp.
9. bronchoconstrict$.mp.
10. exp Bronchoconstriction/
11. (bronch$ adj3 constrict$).mp.
12. Bronchial Hyperreactivity/
13. Respiratory Hypersensitivity/
14. ((bronchial$ or respiratory or airway$ or lung$) adj3 (hypersensitiv$ or hyperreactiv$ or allerg$ or insufficiency)).mp.
15. ((dust or mite$) adj3 (allerg$ or hypersensitiv$)).mp.
16. or/1‐15
Filter to identify RCTs
1. exp "clinical trial [publication type]"/
2. (randomised or randomised).ab,ti.
3. placebo.ab,ti.
4. dt.fs.
5. randomly.ab,ti.
6. trial.ab,ti.
7. groups.ab,ti.
8. or/1‐7
9. Animals/
10. Humans/
11. 9 not (9 and 10)
12. 8 not 11
The MEDLINE strategy and RCT filter are adapted to identify trials in other electronic databases.
Appendix 2. Search strategy for Cochrane Airways Trials Register
#1 AST:MISC1
#2 MeSH DESCRIPTOR Asthma Explode All
#3 asthma*:ti,ab
#4 #1 or #2 or #3
#5 MeSH DESCRIPTOR Antibodies, Monoclonal
#6 MeSH DESCRIPTOR Antibodies, Monoclonal, Humanized
#7 mepolizumab*
#8 SB24056 or SB‐24056
#9 human* NEAR2 monoclonal* NEAR2 antibod*
#10 Bosatria or Nucala #11 benralizumab* #12 MEDI‐563 #13 reslizumab* #14 Cinquil or Cinqair #15 CEP‐38072 #16 "anti‐interleukin 5" #17 "anti‐IL5" #18 "anti‐IL‐ 5" #19 #5 or #6 or #7 or #8 or #9 or #10 or #11 or #12 or #13 or #14 or #15 or #16 or #17 or #18 #20 #4 AND #19
[In search line #1, MISC1 denotes the field where the reference has been coded for condition, in this case, asthma]
Data and analyses
Comparison 1.
Mepolizumab (SC) versus placebo
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Rate of exacerbations requiring systemic corticosteroids | 2 | 936 | Rate Ratio (Random, 95% CI) | 0.45 [0.36, 0.55] |
| 1.1 Eosinophilic | 2 | 936 | Rate Ratio (Random, 95% CI) | 0.45 [0.36, 0.55] |
| 2 Rate of exacerbations requiring emergency department treatment or admission | 2 | 936 | Rate Ratio (Random, 95% CI) | 0.36 [0.20, 0.66] |
| 2.1 Eosinophilic | 2 | 936 | Rate Ratio (Random, 95% CI) | 0.36 [0.20, 0.66] |
| 3 Rate of exacerbations requiring admission | 2 | 936 | Rate Ratio (Random, 95% CI) | 0.31 [0.13, 0.73] |
| 3.1 Eosinophilic | 2 | 936 | Rate Ratio (Random, 95% CI) | 0.31 [0.13, 0.73] |
| 4 Health‐related quality of life (ACQ) | 2 | 936 | Mean Difference (Random, 95% CI) | ‐0.42 [‐0.56, ‐0.28] |
| 4.1 Eosinophilic | 2 | 936 | Mean Difference (Random, 95% CI) | ‐0.42 [‐0.56, ‐0.28] |
| 5 Health‐related quality of life (SGRQ) | 2 | 936 | Mean Difference (Random, 95% CI) | ‐7.40 [‐9.50, ‐5.29] |
| 5.1 Eosinophilic | 2 | 936 | Mean Difference (Random, 95% CI) | ‐7.40 [‐9.50, ‐5.29] |
| 6 Pre‐bronchodilator FEV1 (litres) | 2 | 936 | Mean Difference (Random, 95% CI) | 0.11 [0.06, 0.17] |
| 6.1 Eosinophilic | 2 | 936 | Mean Difference (Random, 95% CI) | 0.11 [0.06, 0.17] |
| 7 Serious adverse events | 2 | 936 | Risk Ratio (M‐H, Random, 95% CI) | 0.63 [0.41, 0.97] |
| 7.1 Eosinophilic | 2 | 936 | Risk Ratio (M‐H, Random, 95% CI) | 0.63 [0.41, 0.97] |
| 8 Adverse events leading to discontinuation | 2 | 936 | Risk Ratio (M‐H, Random, 95% CI) | 0.45 [0.11, 1.80] |
| 8.1 Eosinophilic | 2 | 936 | Risk Ratio (M‐H, Random, 95% CI) | 0.45 [0.11, 1.80] |
Comparison 2.
Mepolizumab (IV) versus placebo
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Rate of clinically significant exacerbations | 3 | 751 | Rate Ratio (Random, 95% CI) | 0.53 [0.44, 0.64] |
| 1.1 Eosinophilic | 3 | 751 | Rate Ratio (Random, 95% CI) | 0.53 [0.44, 0.64] |
| 2 Rate of exacerbations requiring emergency department treatment or admission | 2 | 690 | Rate Ratio (Random, 95% CI) | 0.52 [0.31, 0.87] |
| 2.1 Eosinophilic | 2 | 690 | Rate Ratio (Random, 95% CI) | 0.52 [0.31, 0.87] |
| 3 Rate of exacerbations requiring admission | 2 | 690 | Rate Ratio (Random, 95% CI) | 0.61 [0.33, 1.13] |
| 3.1 Eosinophilic | 2 | 690 | Rate Ratio (Random, 95% CI) | 0.61 [0.33, 1.13] |
| 4 People with one or more exacerbations | 1 | 61 | Risk Ratio (M‐H, Random, 95% CI) | 0.82 [0.61, 1.09] |
| 4.1 Eosinophilic | 1 | 61 | Risk Ratio (M‐H, Random, 95% CI) | 0.82 [0.61, 1.09] |
| 5 Health‐related quality of life (AQLQ) | 2 | 369 | Mean Difference (Random, 95% CI) | 0.21 [‐0.06, 0.47] |
| 5.1 Eosinophilic | 2 | 369 | Mean Difference (Random, 95% CI) | 0.21 [‐0.06, 0.47] |
| 6 Health‐related quality of life (ACQ) | 2 | 369 | Mean Difference (Fixed, 95% CI) | ‐0.11 [‐0.32, 0.09] |
| 6.1 Eosinophilic | 2 | 369 | Mean Difference (Fixed, 95% CI) | ‐0.11 [‐0.32, 0.09] |
| 7 Health‐related quality of life (SGRQ) | 1 | 382 | Mean Difference (Random, 95% CI) | ‐6.4 [‐9.65, ‐3.15] |
| 7.1 Eosinophilic | 1 | 382 | Mean Difference (Random, 95% CI) | ‐6.4 [‐9.65, ‐3.15] |
| 8 Pre‐bronchodilator FEV1 (litres) | 2 | 690 | Mean Difference (Random, 95% CI) | 0.08 [0.02, 0.15] |
| 8.1 Eosinophilic | 2 | 690 | Mean Difference (Random, 95% CI) | 0.08 [0.02, 0.15] |
| 9 Serious adverse events | 3 | 751 | Risk Ratio (M‐H, Random, 95% CI) | 0.59 [0.37, 0.94] |
| 9.1 Eosinophilic | 3 | 751 | Risk Ratio (M‐H, Random, 95% CI) | 0.59 [0.37, 0.94] |
| 10 Adverse events leading to discontinuation | 3 | 751 | Risk Ratio (M‐H, Random, 95% CI) | 0.72 [0.18, 2.92] |
| 10.1 Eosinophilic | 3 | 751 | Risk Ratio (M‐H, Random, 95% CI) | 0.72 [0.18, 2.92] |
| 11 Serum eosinophil level (cells/microlitre) | 1 | Mean Difference (Fixed, 95% CI) | ‐170.0 [‐228.00, ‐110.00] | |
| 11.1 Eosinophilic | 1 | Mean Difference (Fixed, 95% CI) | ‐170.0 [‐228.00, ‐110.00] |
Comparison 3.
Reslizumab (IV) versus placebo
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Rate of exacerbations requiring systemic corticosteroids | 2 | 953 | Rate Ratio (Fixed, 95% CI) | 0.43 [0.33, 0.55] |
| 1.1 Eosinophilic | 2 | 953 | Rate Ratio (Fixed, 95% CI) | 0.43 [0.33, 0.55] |
| 2 Rate of exacerbations requiring emergency department treatment or admission | 2 | 953 | Rate Ratio (Fixed, 95% CI) | 0.67 [0.39, 1.17] |
| 2.1 Eosinophilic | 2 | 953 | Rate Ratio (Fixed, 95% CI) | 0.67 [0.39, 1.17] |
| 3 Health‐related quality of life (AQLQ) | 3 | 1164 | Mean Difference (Fixed, 95% CI) | 0.28 [0.17, 0.39] |
| 3.1 Eosinophilic | 3 | 1164 | Mean Difference (Fixed, 95% CI) | 0.28 [0.17, 0.39] |
| 4 Health‐related quality of life (ACQ) | 4 | 1652 | Mean Difference (Fixed, 95% CI) | ‐0.25 [‐0.33, ‐0.17] |
| 4.1 Eosinophilic | 4 | 1260 | Mean Difference (Fixed, 95% CI) | ‐0.27 [‐0.36, ‐0.19] |
| 4.2 Non‐eosinophilic | 1 | 392 | Mean Difference (Fixed, 95% CI) | ‐0.12 [‐0.33, 0.09] |
| 5 Pre‐bronchodilator FEV1 (litres) | 4 | 1652 | Mean Difference (Fixed, 95% CI) | 0.11 [0.07, 0.15] |
| 5.1 Eosinophilic | 4 | 1260 | Mean Difference (Fixed, 95% CI) | 0.12 [0.08, 0.16] |
| 5.2 Non‐eosinophilic | 1 | 392 | Mean Difference (Fixed, 95% CI) | 0.03 [‐0.07, 0.14] |
| 6 Serious adverse events | 4 | 1656 | Risk Ratio (M‐H, Random, 95% CI) | 0.79 [0.56, 1.12] |
| 6.1 Eosinophilic | 3 | 1160 | Risk Ratio (M‐H, Random, 95% CI) | 0.79 [0.51, 1.22] |
| 6.2 Eosinophil status unknown | 1 | 496 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.34, 2.88] |
| 7 Adverse events leading to discontinuation | 4 | 1659 | Risk Ratio (M‐H, Random, 95% CI) | 0.66 [0.43, 1.02] |
| 7.1 Eosinophilic | 3 | 1163 | Risk Ratio (M‐H, Random, 95% CI) | 0.67 [0.37, 1.20] |
| 7.2 Eosinophil status unknown | 1 | 496 | Risk Ratio (M‐H, Random, 95% CI) | 0.66 [0.35, 1.23] |
| 8 Serum eosinophil level (cells/microlitre) | 4 | 1656 | Mean Difference (Fixed, 95% CI) | ‐476.83 [‐499.32, ‐454.34] |
| 8.1 Eosinophilic | 4 | 1656 | Mean Difference (Fixed, 95% CI) | ‐476.83 [‐499.32, ‐454.34] |
Comparison 4.
Benralizumab (SC) versus placebo
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Rate of exacerbations requiring systemic corticosteroids | 3 | 2456 | Rate Ratio (Fixed, 95% CI) | 0.62 [0.55, 0.70] |
| 1.1 Eosinophilic | 3 | 1698 | Rate Ratio (Fixed, 95% CI) | 0.59 [0.51, 0.68] |
| 1.2 Non‐eosinophilic | 2 | 758 | Rate Ratio (Fixed, 95% CI) | 0.69 [0.56, 0.85] |
| 2 Rate of exacerbations requiring emergency department treatment or admission | 2 | 1537 | Rate Ratio (Fixed, 95% CI) | 0.68 [0.47, 0.98] |
| 2.1 Eosinophilic | 2 | 1537 | Rate Ratio (Fixed, 95% CI) | 0.68 [0.47, 0.98] |
| 3 Health‐related quality of life (AQLQ mean difference) | 3 | 1541 | Mean Difference (Fixed, 95% CI) | 0.23 [0.11, 0.35] |
| 3.1 Eosinophilic | 3 | 1541 | Mean Difference (Fixed, 95% CI) | 0.23 [0.11, 0.35] |
| 4 Health‐related quality of life (ACQ mean difference) | 3 | 2359 | Mean Difference (Fixed, 95% CI) | ‐0.20 [‐0.29, ‐0.11] |
| 4.1 Eosinophilic | 3 | 1604 | Mean Difference (Fixed, 95% CI) | ‐0.23 [‐0.34, ‐0.12] |
| 4.2 Non‐eosinophilic | 2 | 755 | Mean Difference (Fixed, 95% CI) | ‐0.14 [‐0.30, 0.02] |
| 5 Pre‐bronchodilator FEV1 (litres) | 3 | 2355 | Mean Difference (Fixed, 95% CI) | 0.10 [0.05, 0.14] |
| 5.1 Eosinophilic | 3 | 1617 | Mean Difference (Fixed, 95% CI) | 0.13 [0.08, 0.19] |
| 5.2 Non‐eosinophilic | 2 | 738 | Mean Difference (Fixed, 95% CI) | 0.03 [‐0.03, 0.10] |
| 6 Serious adverse events | 4 | 2648 | Risk Ratio (M‐H, Random, 95% CI) | 0.81 [0.66, 1.01] |
| 6.1 Eosinophilic | 2 | 1537 | Risk Ratio (M‐H, Random, 95% CI) | 0.80 [0.60, 1.06] |
| 6.2 Non‐eosinophilic | 2 | 758 | Risk Ratio (M‐H, Random, 95% CI) | 0.85 [0.57, 1.27] |
| 6.3 Eosinophil status unknown | 2 | 353 | Risk Ratio (M‐H, Random, 95% CI) | 0.75 [0.37, 1.51] |
| 7 Adverse events leading to discontinuation | 3 | 2597 | Risk Ratio (M‐H, Random, 95% CI) | 2.15 [1.02, 4.57] |
| 7.1 Eosinophilic | 2 | 1537 | Risk Ratio (M‐H, Random, 95% CI) | 2.70 [0.86, 8.49] |
| 7.2 Non‐eosinophilic | 2 | 758 | Risk Ratio (M‐H, Random, 95% CI) | 1.81 [0.54, 6.05] |
| 7.3 Eosinophil status unknown | 1 | 302 | Risk Ratio (M‐H, Random, 95% CI) | 1.82 [0.31, 10.69] |
| 8 Serum eosinophil level (% change from baseline) | 2 | 2295 | Mean Difference (Fixed, 95% CI) | ‐104.74 [‐116.12, ‐93.35] |
| 8.1 Eosinophilic | 2 | 1537 | Mean Difference (Fixed, 95% CI) | ‐101.74 [‐113.27, ‐90.21] |
| 8.2 Non‐eosinophilic | 2 | 758 | Mean Difference (Fixed, 95% CI) | ‐216.81 [‐287.35, ‐146.28] |
What's new
| Date | Event | Description |
|---|---|---|
| 29 March 2017 | New search has been performed | New literature search run |
| 29 March 2017 | New citation required and conclusions have changed | Scope broadened to encompass all Anti IL 5 therapies (reslizumab and benralizumab), rather than mepolizumab alone Review substantively redrafted Inclusion criteria applied more strictly resulting in exclusion of five (out of eight) mepolizumab studies Search updated leading to the inclusion of 10 new studies (one mepolizumab, four reslizumab and five benralizumab) Groups on doses of the trial medications that are not clinically relevant (e.g. 10 times higher or lower) have been excluded from the analysis Outcomes revised to focus on validated symptom scores, only a pre‐bronchodilator measure of lung function, subgroups for eosinophilia or otherwise New author team |
Differences between protocol and review
We initially planned to use a fixed‐effect model for meta‐analysis, but we agreed with a peer reviewer who suggested that a random‐effects model was more appropriate in view of the substantial clinical heterogeneity between the trials.
The scope was broadened to encompass all anti‐IL‐5 therapies, that is, including reslizumab and benralizumab in addition to mepolizumab. Since the previous review, reslizumab has been licensed and benralizumab has entered phase 3 clinical trials with a licensing decision due from the US Food & Drug Administration and European Medicines Agency in 2017. These agents are all designed for the same patients and are therefore comparable.
Data from study arms on doses not deemed clinically relevant (e.g. 10 times more or less than the dose that has marketing approval) was excluded. Similarly studies where an additional intervention was the withdrawal of systemic corticosteroid were also excluded.
Outcomes were revised to focus on validated symptom scores (i.e. excluding non‐validated scores, as these cannot be readily compared across studies) and only a pre‐bronchodilator measure of lung function (as per American Thoracic Society/European Respiratory Society guidelines on standardising endpoints for clinical asthma trials). Subgroups were set as eosinophilic or otherwise, as these agents are primarily designed for eosinophilic asthma.
The original protocol stated that included trials should be a minimum of 16 weeks in duration; we have clarified that there should be a minimum of 16 weeks treatment.
Congenital heart disease had been listed as an exclusion criteria previously but this was removed as there was no reason why these conditions in particular should be excluded.
The number of studies identified was insufficient to conduct subgroup analyses or formally assess for reporting bias.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | Parallel, double‐blind RCT with a 16‐week treatment phase | |
| Participants | 315 participants (42 male) with moderate‐severe asthma, with airway reversibility, blood eosinophilia, ACQ score of at least 1.5, and taking ICS
|
|
| Interventions | IV infusion of reslizumab 0.3 mg/kg, reslizumab 3.0 mg/kg, or placebo once every 4 weeks (total of 4 doses) | |
| Outcomes | Primary outcome
Secondary outcomes
|
|
| Notes | 68 locations across 13 countries Funded by Teva Branded Pharmaceutical Products R&D, Inc |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated, no clarification available from study authors |
| Allocation concealment (selection bias) | Unclear risk | Not stated, no clarification available from study authors |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double blind |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated, no clarification available from study authors |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Slightly more withdrawals in placebo group (20/105, 19%) than treatment arms (12‐17%) |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Methods | Randomised, double‐blind, parallel‐group, placebo‐controlled trial run over 48 weeks | |
| Participants | 1204 participants with symptomatic asthma were randomised to 1 of 3 groups (benralizumab 30 mg 4 weeks, benralizumab 30 mg 8 weeks, or placebo)
|
|
| Interventions | SC benralizumab 30 mg/mL every 4 weeks or every 8 weeks versus placebo | |
| Outcomes | Primary outcomes
Secondary outcomes
|
|
| Notes | Multi‐centre trial in 374 centres from 17 countries Funded by AstraZeneca and Kyowa Hakko Kirin |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Each participant was assigned a unique enrolment number and randomisation code by an interactive web‐based voice response system |
| Allocation concealment (selection bias) | Low risk | The identity of the treatment allocation was not made available to the participants, investigators involved in participant treatment or clinical assessment, or study funder |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double blind (participant, caregiver and investigator) |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated, no clarification available from study authors |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Withdrawal rates were relatively low (10.1%‐12.8%) |
| Selective reporting (reporting bias) | Low risk | Unless otherwise specified, all results were presented for participants with baseline blood eosinophilia |
| Methods | Randomised, controlled, double‐blind, dose‐ranging trial | |
| Participants | 606 participants with uncontrolled asthma randomised and 535 completed
|
|
| Interventions | 6 arms: benralizumab 2 mg or benralizumab 20 mg or benralizumab 100 mg or placebo delivered by 2 SC injections every 4 weeks for the first 3 doses (weeks 1, 4, and 8), then every 8 weeks (weeks 16, 24, 32, and 40) | |
| Outcomes | Primary outcomes
Secondary outcomes in eosinophilic individuals
|
|
| Notes | 52‐year multi‐national study with sites in 10 countries. The study protocol was developed by MedImmune and the corresponding author. The investigators collected and had full access to all study data, which were analysed by the funding source. The analysis was done solely by MedImmune; however, study authors helped determine which analyses were done and could request further ad‐hoc analyses. The report was written by the study authors with a medical writer funded by the funding source. The corresponding author had final responsibility for decision to submit for publication. Funding: MedImmune |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Interactive web/voice‐response system for random assignment |
| Allocation concealment (selection bias) | Low risk | Allocation concealment was ensured by the vendor systems and no study personnel or site had access to the system. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Participants, treating physicians, study investigators, and study statisticians were masked to treatment allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | As above |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The withdrawal rates were even across groups |
| Selective reporting (reporting bias) | Low risk | Results for most but not all listed primary and secondary outcomes were reported (e.g. symptoms score, AQLQ – shown in supplementary material in graphs only) |
| Methods | Double‐blind, placebo‐controlled, parallel‐group study | |
| Participants | 489 participants with moderate‐severe asthma (medium dose of ICS, inadequate control ACQ ≥ 1.5, and at least 1 exacerbation in the past 12 months)
|
|
| Interventions | IV infusion of reslizumab 3 mg/kg or matching placebo every 4 weeks (13 doses with last dose in week 48) | |
| Outcomes | Primary outcomes (per protocol)
Secondary outcomes (per protocol):
|
|
| Notes | 128 clinical research centres. The research was funded by Teva Branded Pharmaceutical Products R&D. Teva employees were involved in the study design, data collection and analysis, and in the writing of this manuscript. All study authors had full access to all study data and had final responsibility for the decision to submit for publication. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was done with use of interactive response technology with computerised central randomisation. |
| Allocation concealment (selection bias) | Low risk | The funder’s clinical personnel involved in the study were also masked to the study drug identity until the database was locked for analysis and the treatment assignment |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Participants and investigators remained masked to treatment assignment during the study |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Participants and investigators remained masked to treatment assignment during the study |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The withdrawal rates were relatively low and even across the groups (11%‐14%) |
| Selective reporting (reporting bias) | Low risk | All primary and secondary outcome measures were reported. |
| Methods | Double‐blind, placebo‐controlled, parallel‐group study | |
| Participants | 464 participants with moderate‐severe asthma (medium does of ICS, inadequate control ACQ ≥1.5 and at least 1 exacerbation in the past 12 months).
|
|
| Interventions | IV infusion of reslizumab 3 mg/kg or matching placebo every 4 weeks (13 doses with last dose in week 48) | |
| Outcomes | Primary outcomes (per protocol):
Secondary outcomes (per protocol):
|
|
| Notes | Funding: Teva Branded Pharmaceutical Products R&D. Teva employees were involved in the study design, data collection and analysis, and in the writing of this manuscript. All study authors had full access to all the data in the study and had final responsibility for the decision to submit for publication. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was done with use of interactive response technology with computerised central randomisation. |
| Allocation concealment (selection bias) | Low risk | The funder’s clinical personnel involved in the study were also masked to the study drug identity until the database was locked for analysis and the treatment assignment |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Participants and investigators remained masked to treatment assignment during the study. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Participants and investigators remained masked to treatment assignment during the study. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The withdrawal rates were relatively low and even across the groups (11%‐14%) |
| Selective reporting (reporting bias) | Low risk | All primary and secondary outcome measures were reported |
| Methods | Multicentre, placebo‐controlled, double‐blind, parallel‐group study | |
| Participants | 551 participants with severe eosinophilic asthma Males (%): mepolizumab 125 (46); placebo, 101 (36)
|
|
| Interventions | Mepolizumab 100 mg SC every 4 weeks for a period of 24 weeks (total of 6 doses) along with their respective standard care of treatment, versus placebo (0.9% sodium chloride) SC every 4 weeks for a period of 24 weeks (total of 6 doses) along with their respective standard care of treatment | |
| Outcomes | Primary outcomes
Secondary outcomes
|
|
| Notes | Funding: GlaxoSmithKline | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomised using an interactive voice‐response system and a centralised, computer‐generated, permuted‐block design of block size six |
| Allocation concealment (selection bias) | Low risk | Participants, investigators, other site staff, and the entire study team including those assessing outcomes data were masked to treatment assignment. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Participants and investigators remained masked to treatment assignment during the study. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Participants and investigators remained masked to treatment assignment during the study. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | In the treatment arm 5 participants were withdrawn from the study: 2 withdrew consent, 2 experienced an adverse event and 1 was lost to follow‐up. In the placebo arm 14 participants were withdrawn from study: 6 withdrew consent, 2 experienced an adverse event, 2 withdrew due to poor efficacy, 2 were lost to follow‐up and 2 were withdrawn on a physician's decision. |
| Selective reporting (reporting bias) | Low risk | No indication of reporting bias |
| Methods | Parallel, double‐blind | |
| Participants | 496 participants with moderate‐severe asthma (based on at least medium‐dose ICS, inadequate control ACQ ≥ 1.5)
|
|
| Interventions | IV reslizumab 3.0 mg/kg or placebo once every 4 weeks (total of 4 doses) | |
| Outcomes | Primary outcomes
Secondary outcomes
|
|
| Notes | 66 study locations across the USA Funding: Teva Branded Pharmaceutical Products R&D, Inc |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated, no clarification available from study authors |
| Allocation concealment (selection bias) | Unclear risk | Not stated, no clarification available from study authors |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double blind |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Double blind |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropouts comparable in each group (16/98, 16%, placebo vs 58/398, 15%, reslizumab) |
| Selective reporting (reporting bias) | Low risk | All primary and secondary outcomes reported with numbers, except blood eosinophil counts only shown as a chart |
| Methods | Multicentre, randomised, double‐blind, parallel‐group, placebo‐controlled trial | |
| Participants | 1306 participants with moderate‐severe (medium‐high‐dose ICS + LABA, ≥ 2 asthma exacerbations last 12 months, FEV1 < 80% predicted), ACQ‐6 ≥ 1.5 at enrolment
|
|
| Interventions | 56 weeks (final follow‐up at 60 weeks). SC benralizumab 30 mg every 4 weeks for 56 weeks or every 4 weeks for 3 doses then 8 weeks thereafter for 56 weeks | |
| Outcomes | Primary outcomes
Secondary outcomes
|
|
| Notes | Funding: AstraZeneca and Kyowa Hakko Kirin. 303 clinical research centres in 11 countries | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were assigned to treatment groups using an interactive web‐based voice‐response system. Randomisation was stratified by ICS dosage at enrolment (high or medium), geographic region, age group (adult or adolescent), and peripheral blood eosinophil count at enrolment (< 300 cells per μL or ≥ 300 cells per μL) |
| Allocation concealment (selection bias) | Low risk | The study investigator assigned randomisation codes sequentially in each stratum as participants became eligible for randomisation, until each stratum was full |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | To preserve blinding, participants and study centre staff were masked to treatment allocation, placebo solution was visually matched with benralizumab solution, and both placebo and benralizumab were provided in accessorised (needle guards and finger phalanges), prefilled syringes. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | As above |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | The withdrawal rates were relatively low: placebo 11.1% (49/440); benralizumab 30 mg every four weeks 9.6% (41/425); benralizumab 30 mg every eight weeks 13.4% (59/441) |
| Selective reporting (reporting bias) | Low risk | Results for all listed primary and secondary outcomes were reported |
| Methods | Randomised, double‐blind, placebo‐controlled, parallel‐group trial | |
| Participants | 61 participants had refractory eosinophilic asthma and a history of recurrent severe exacerbations.
|
|
| Interventions | Intravenous mepolizumab (750 mg) versus matched placebo (150 mL of 0.9% saline) at monthly intervals for 1 year | |
| Outcomes | Reported as: "[P]rimary outcome measure was the number of severe exacerbations per participant during the 50‐week treatment phase. Secondary outcomes included a change in asthma symptoms, scores on the Asthma Quality of Life Questionnaire (AQLQ, in which scores range from 1 to 7, with lower values indicating more severe impairment and a change of 0.5 unit considered to be clinically important), forced expiratory volume in 1 second (FEV1) after use of a bronchodilator, airway hyperresponsiveness, and eosinophil counts in the blood and sputum." | |
| Notes | Single centre trial conducted at Institute for Lung Health, Leicester, UK Supported by GlaxoSmithKline |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Reported as: "Stratified randomisation with use of the minimisation method, which was performed by an independent clinician. Participants were randomly assigned with the use of the minimisation method to receive 12 infusions of either 750 mg of mepolizumab delivered intravenously or matched placebo (150 mL of 0.9% saline) at monthly intervals between visits 3 and 14. The criteria used for minimisation were the frequency of exacerbations in the previous 12 months, the baseline eosinophil count in the sputum and the number of participants taking oral corticosteroids." |
| Allocation concealment (selection bias) | Unclear risk | Details not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Reported as double blind |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Reported as double blind |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Reported as: "A total of 61 of the 63 participants ( one required and operation and one withdrew consent) who were screened started treatment and constituted the modified intention‐to‐treat population. Thirty‐two participants were randomly assigned to receive placebo. Overall, 94.9% of treatment visits were completed. Participants who withdrew completed a mean of 4.6 treatment visits (38.3%)." |
| Selective reporting (reporting bias) | Low risk | No apparent indication of reporting bias |
| Methods | Multicentre, randomised, double‐blind, parallel‐group, placebo‐controlled, phase 3 efficacy and safety study | |
| Participants | 13 participants with uncontrolled asthma taking medium‐dose ICS plus long‐acting beta2 agonist (LABA)
|
|
| Interventions | Fixed 30 mg dose of benralizumab every 4 weeks or fixed 30 mg dose of benralizumab, every 4 weeks for the first 3 doses and then every 8 weeks thereafter versus placebo | |
| Outcomes | Primary outcomes
Secondary outcomes
|
|
| Notes | Study terminated due to sponsor decision after recruitment of 13 participants. No participant completed the study | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Described as randomised but no further details |
| Allocation concealment (selection bias) | Unclear risk | No details given |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Reported as double blind |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Reported as double blind, but blinding of outcome assessment not specifically described |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Study terminated due to decision of sponsor after recruitment of 13 participants. No reason given for decision to terminate |
| Selective reporting (reporting bias) | High risk | Study terminated due to decision of sponsor after recruitment of 13 participants. No reason given for decision to terminate. Original secondary outcomes listed removed from trial registration. Outcomes could not be incorporated into meta‐analysis |
| Methods | Randomised, double‐blind, double‐dummy, phase 3 study | |
| Participants | 576 participants with recurrent asthma exacerbations and evidence of eosinophilic inflammation despite high doses of inhaled glucocorticoids to 1 of 3 study groups
|
|
| Interventions | Mepolizumab in a 75 mg intravenous dose versus mepolizumab in a 100 mg subcutaneous dose versus placebo every 4 weeks for 32 weeks | |
| Outcomes | Primary outcomes
Secondary outcomes:
|
|
| Notes | 32‐week treatment intervention, with 1‐6 weeks run‐in and 8‐week follow‐up. Conducted in Baltimore, Middlesex, Ghent, Vancouver, Parma, Marseille and Paris Funding: GlaxoSmithKline |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Centralised computer‐generated permuted block schedule |
| Allocation concealment (selection bias) | Low risk | Treatment allocations will be concealed via the RandAll system |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Mepolizumab and placebo were identical in appearance and were administered by a staff member who was unaware of the study group assignments. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | The study drugs were prepared by staff members who were aware of the study group assignments but were not involved in study assessments. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 6% (placebo), 8% (IV), 5% ( SC) did not complete the study |
| Selective reporting (reporting bias) | Low risk | All outcome measures reported |
| Methods | Parallel | |
| Participants | 103. 38 males. (age 53.2, 55.6, 51.4, 50.8 Moderate/severe (based on ICS dose (medium/high), exacerbation history, and ACQ ≥ 1.5 on at least 2 occasions) participants also had to demonstrate post‐bronchodilator FEV1 reversibility ≥ 12% and ≥ 200 mL, or a positive response to methacholine challenge (PC20 ≤ 8 mg/mL)
|
|
| Interventions | Subcutaneous doses given at weeks 1, 4, 8, 16, 24, 32, 40. Benralizumab 2 mg, 20 mg or 100 mg subcutaneously | |
| Outcomes | Primary outcomes
Secondary outcomes
Exploratory endpoints included blood eosinophil counts. |
|
| Notes | 32 sites in South Korea and Japan | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Eosinophilic participants were randomised using a central, interactive web‐response system |
| Allocation concealment (selection bias) | Unclear risk | Not stated, no clarification available from study authors |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | The study medication was administered … in a blinded fashion |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated, no clarification available from study authors |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition rates relatively high but even across groups (19.2% for placebo vs 16.0%‐23.1% for treatment groups) |
| Selective reporting (reporting bias) | Low risk | All outcomes reported |
| Methods | Multicentre, double‐blind, placebo‐controlled trial | |
| Participants | 621 participants with severe asthma despite receiving high doses of standard asthma medications
|
|
| Interventions | 13 total intravenous infusions of mepolizumab (750 mg), mepolizumab (250 mg), mepolizumab (75 mg) or placebo given every 4 weeks | |
| Outcomes | Primary outcomes
Secondary outcomes
|
|
| Notes | 52‐week study conducted at 81 centres in 13 countries (Argentina, Australia, Canada, Chile, France, Germany, South Korea, Poland, Romania, Russia, Ukraine, the UK and the USA) Supported by GlaxoSmithKline |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Central telephone‐based system and computer‐generated randomly permuted block schedule stratified by whether treatment with OCS was required |
| Allocation concealment (selection bias) | Low risk | Mepolizumab and placebo were prepared by unmasked site staff who were not involved in study assessments |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Mepolizumab and placebo were prepared by unmasked site staff who were not involved in study assessments. Both treatments were identical in appearance and were given to participants by a masked member of the site staff |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Data analysts were masked to treatment allocation |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants accounted for with information on reasons for having withdrawn. Some participants not included in results due to ‘poor efficacy’ |
| Selective reporting (reporting bias) | Low risk | No apparent indication of reporting bias |
ACQ: Asthma Control Questionnaire; ALT: alanine aminotransferase; Alk Phos: alkaline phosphatase; AQLQ: Asthma Quality of Life Questionnaire; AST: aspartate aminotransferase; ECP: eosinophil cationic protein; ED: emergency department; FeNO: exhaled fraction of nitric oxide; FEV1 : Forced expiratory volume in 1 second; FP: fluticasone propionate; FVC: forced vital capacity; HRQoL: health‐related quality of life; ICS: inhaled corticosteroid; ICU: intensive care unit; IL: interleukin; IQR: interquartile range; IV: intravenous; JACQ: Juniper Asthma Control Questionnaire; OCS: oral corticosteroids; PC20 : histamine provocative concentration causing a 20% drop in FEV1;PEFR: peak expiratory flow rate; SC: subcutaneous; SD: standard deviation; SGRQ: St. George's Respiratory Questionnaire; ULN: Upper Limit of Normal; VC: vital capacity. aQTc(F): a measure of the time between the start of the Q wave and the end of the T wave in the heart's electrical cycle, corrected for the heart rate using Fredericia's formula.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Albers 2016 | Post‐hoc analysis of observational study |
| Alvarez‐Cuesta 1994 | Intervention used in study (cat extract immunotherapy) is not anti‐IL‐5 therapy |
| Armentia 1992 | Intervention used in study (immunotherapy) is not anti‐IL‐5 therapy |
| Austin 2016 | Aggregation of two clinical trials |
| Ayres 2004 | Intervention used in study (omalizumab) is not anti‐IL‐5 therapy |
| Bel 2014 | Focus of trial is on steroid reduction and therefore does not meet our predefined inclusion criteria |
| Berger 2003 | Intervention used in study (omalizumab) is not anti‐IL‐5 therapy |
| Blanken 2012 | Intervention used in study (omalizumab) is not anti‐IL‐5 therapy |
| Blanken 2013 | Intervention used in study (pavilizumab) is not anti‐IL‐5 therapy |
| Boulet 1997 | Intervention used in study (anti‐IgE antibody e25) is not anti‐IL‐5 therapy |
| Bousquet 2004 | Intervention used in study (omalizumab) is not anti‐IL‐5 therapy |
| Bousquet 2011 | Intervention used in study (omalizumab) is not anti‐IL‐5 therapy |
| Brightling 2014 | Intervention used in study (tralokinumab) is not anti‐IL‐5 therapy |
| Brown 2007 | Intervention used in study (omalizumab) is not anti‐IL‐5 therapy |
| Brusselle 2016 | Aggregation of two clinical trials |
| Bryant 1975a | Not a RCT |
| Bryant 1975b | Not a RCT |
| Buhl 2000a | Intervention used in study (rhumab‐25) is not anti‐IL‐5 therapy |
| Buhl 2000b | Intervention used in study (rhumab‐25) is not anti‐IL‐5 therapy |
| Buhl 2002 | Intervention used in study (omalizumab) is not anti‐IL‐5 therapy |
| Bush 1985 | Intervention used in study (soybean oil) is not anti‐IL‐5 therapy |
| Busse 2001 | Intervention used in study (omalizumab) is not anti‐IL‐5 therapy |
| Busse 2008 | Intervention used in study (omalizumab) is not anti‐IL‐5 therapy |
| Busse 2015 | Intervention used in study (tralokinumab) is not anti‐IL‐5 therapy |
| Buttner 2003 | Treatment < 16 weeks |
| Caffarelli 2000 | Intervention used in study (immunotherapy) is not anti‐IL‐5 therapy |
| Canvin 2016 | Aggregation of two clinical trials |
| Castro 2011 | < 16 weeks in length |
| Castro 2014b | Intervention used in study (dupilumab) is not anti‐IL‐5 therapy |
| Chandra 1989 | Intervention used in study (various foods) is not anti‐IL‐5 therapy |
| Chervinsky 2003 | Intervention used in study (omalizumab) is not anti‐IL‐5 therapy |
| Clavel 1998 | Intervention used in study (immunotherapy) is not anti‐IL‐5 therapy |
| Corren 2003 | Intervention used in study (omalizumab) is not anti‐IL‐5 therapy |
| Corren 2010 | Intervention used in study (il‐4ralpha antagonist) is not anti‐IL‐5 therapy |
| Cullell‐Young 2002 | Not a RCT |
| Dasgupta 2016 | Participants did not have a diagnosis of asthma (COPD patients) |
| De Boever 2014 | Intervention used in study (anti‐IL‐13 mab) is not anti‐IL‐5 therapy |
| Djukanovic 2004 | Intervention used in study (omalizumab) is not anti‐IL‐5 therapy |
| Ebner 1989 | Intervention used in study (immunotherapy) is not anti‐IL‐5 therapy |
| Eckman 2010 | Intervention used in study (immunotherapy) is not anti‐IL‐5 therapy |
| El‐Nawawy 2000 | Not a RCT |
| EUCTR2012‐004385‐17‐BE | The study participants did not have asthma |
| EUCTR2014‐002666‐76‐GB | Treatment period < 16 weeks |
| EUCTR2014‐003162‐25‐DE | The study participants did not have asthma |
| EUCTR2015‐001152‐29‐BE | Not an RCT and endpoints are not applicable as this is a long‐term access programme |
| EUCTR2015‐003697‐32‐NL | Not placebo‐controlled. Single treatment arm only |
| EUCTR2016‐001831‐10‐NL | No placebo arm/single treatment arm and treatment duration < 16 weeks |
| EUCTR2016‐002405‐19‐DE | Participants do not have a diagnosis of asthma, no placebo arm, treatment duration < 16 weeks |
| Fahy 1997 | Intervention used in study (anti‐IgE) is not anti‐IL‐5 therapy |
| Fahy 1999 | Intervention used in study (anti‐IgE) is not anti‐IL‐5 therapy |
| Ferrguson 2016 | Treatment duration < 16 weeks in length |
| Finn 2003 | Intervention used in study (omalizumab) is not anti‐IL‐5 therapy |
| Flood‐Page 2003 | Treatment < 16 weeks |
| Flood‐Page 2007 | Treatment < 16 weeks |
| Frew 1998 | Intervention used in study (anti‐IgE) is not anti‐IL‐5 therapy |
| Garcia 2013 | Intervention used in study (omalizumab) is not anti‐IL‐5 therapy |
| Gauvreau 2011 | Intervention used in study ( anti‐IL‐13) is not anti‐IL‐5 therapy |
| Gauvreau 2014a | Intervention used in study ( anti‐tslp) is not anti‐IL‐5 therapy |
| Gauvreau 2014b | Intervention used in study (ox40l antagonism) is not anti‐IL‐5 therapy |
| Gauvreau 2014c | Intervention used in study (quilizumab) is not anti‐IL‐5 therapy |
| Gauvreau 2015a | Intervention used in study (ligelizumab) is not anti‐IL‐5 therapy |
| Gauvreau 2015b | Intervention used in study (ligelizumab) is not anti‐IL‐5 therapy |
| Gevaert 2013 | Intervention used in study (omalizumab) is not anti‐IL‐5 therapy |
| Gordon 1972 | Intervention used in study is not anti‐IL‐5 therapy |
| Greenberg 1991 | Participants do not have a diagnosis of asthma |
| Gunsoy 2016 | Not a randomised, placebo‐controlled trial |
| Han 2009 | Intervention used in study ( jade screen powder) is not anti‐IL‐5 therapy |
| Hanania 2011 | Intervention used in study (omalizumab) is not anti‐IL‐5 therapy |
| Hanania 2013 | Intervention used in study (omalizumab) is not anti‐IL‐5 therapy |
| Hanania 2014 | Intervention used in study (lebrikizumab) is not anti‐IL‐5 therapy |
| Hanania 2015 | Intervention used in study (lebrikizumab) is not anti‐IL‐5 therapy |
| Harris 2016 | Intervention used in study (quilizumab) is not anti‐IL‐5 therapy |
| Hendeles 2015 | Intervention used in study (omalizumab) is not anti‐IL‐5 therapy |
| Hill 1982 | Intervention used in study (immunotherapy) is not anti‐IL‐5 therapy |
| Hodsman 2013 | Intervention used in study ( anti‐IL‐13) is not anti‐IL‐5 therapy |
| Holgate 2004 | Intervention used in study (omalizumab) is not anti‐IL‐5 therapy |
| Hoshino 2012 | Intervention used in study (omalizumab) is not anti‐IL‐5 therapy |
| Humbert 2005 | Intervention used in study (omalizumab) is not anti‐IL‐5 therapy |
| Humbert 2008 | Intervention used in study (omalizumab) is not anti‐IL‐5 therapy |
| Humbert 2009 | Intervention used in study (omalizumab) is not anti‐IL‐5 therapy |
| Jacquemin 1995 | Intervention used in study (immunotherapy) is not anti‐IL‐5 therapy |
| Jutel 2005 | Intervention used in study (immunotherapy) is not anti‐IL‐5 therapy |
| Kang 1988 | Intervention used in study (immunotherapy) is not anti‐IL‐5 therapy |
| Kips 2003 | Treatment < 16 weeks |
| Kon 2001 | Intervention used in study (anti‐cd4) is not anti‐IL‐5 therapy |
| Kopp 2009 | Intervention used in study (omalizumab) is not anti‐IL‐5 therapy |
| Kopp 2013 | Intervention used in study (omalizumab) is not anti‐IL‐5 therapy |
| Kulus 2010 | Intervention used in study (omalizumab) is not anti‐IL‐5 therapy |
| Lanier 2003 | Intervention used in study (omalizumab) is not anti‐IL‐5 therapy |
| Lanier 2009 | Intervention used in study (omalizumab) is not anti‐IL‐5 therapy |
| Laviolette 2013 | Treatment < 16 weeks |
| Leckie 2000 | Treatment < 16 weeks |
| Leynadier 2004 | Intervention used in study (omalizumab) is not anti‐IL‐5 therapy |
| Li 2016 | Review article, not a RCT |
| Lizaso 2008 | Intervention used in study (immunotherapy) is not anti‐IL‐5 therapy |
| Lugogo 2016 | Not a randomised, placebo‐controlled trial |
| Maspero 2016 | Combined secondary analysis of two trials: NCT01287039 and NCT01285323 |
| Massanari 2009 | Intervention used in study (omalizumab) is not anti‐IL‐5 therapy |
| Massanari 2010 | Intervention used in study (omalizumab) is not anti‐IL‐5 therapy |
| Metzger 1998 | Intervention used in study (omalizumab) is not anti‐IL‐5 therapy |
| Milgrom 1999 | Intervention used in study (anti‐IgE) is not anti‐IL‐5 therapy |
| Milgrom 2001 | Intervention used in study (omalizumab) is not anti‐IL‐5 therapy |
| Modlin 1977 | Participants do not have diagnosis of asthma |
| Moss 1987 | Intervention used in study (immunotherapy) is not anti‐IL‐5 therapy |
| Nair 2009 | Focus of trial is on steroid reduction and therefore does not meet our predefined inclusion criteria |
| Nair 2016 | All participants do not have a diagnosis of asthma |
| NCT00783289 2008 | Treatment duration < 16 weeks |
| NCT00802438 | Non randomised study |
| NCT01290887 2011 | Study does not include a placebo arm |
| NCT01366521 | Phase 2 study comparing three doses of mepolizumab. This trial does not have a placebo arm |
| NCT01471327 | Focus of study was on tolerability, pharmacokinetics and pharmacodynamics of single dose SB‐240563 administered intravenously to Japanese healthy male participants. People with asthma were not included in the study. |
| NCT01691859 | This study does not include a placebo group. Multi‐centre, open‐label, long‐term safety study with total sample receiving 100 mg mepolizumab administered subcutaneously (no control group) |
| NCT01842607 | This study does not include a placebo group. Multi‐centre, open‐label, long‐term safety study with total sample receiving 100 mg mepolizumab administered subcutaneously (no control group) |
| NCT02075255 2014 | Focus of trial is on oral steroid reduction |
| NCT02135692 | This study does not include a placebo group. Multi‐center, open‐label, long‐term study of subcutaneously (SC) administered mepolizumab 100 mg in addition to standard of care (SOC), in participants with severe eosinophilic asthma |
| NCT02258542 2014 | Not a RCT (an extension study with no placebo arm) |
| NCT02293265 | Aim of study is to provide a 'reliable description of the severe asthma patient landscape with respect to the potential eligibility for treatment with mepolizumab, omalizumab, and reslizumab'. No pharmaceutical intervention in study |
| NCT02417961 2015 | Not a RCT |
| NCT02501629 2015 | Focus of trial is on oral steroid reduction |
| NCT02559791 | Not placebo‐controlled ‐ single treatment arm only |
| NCT02808819 2016 | Not a RCT |
| NCT02814643 2016 | Treatment duration < 16 weeks |
| NCT02869438 | Treatment duration < 16 weeks |
| NCT02937168 | Treatment duration < 16 weeks |
| NCT02968914 | Not a placebo‐controlled trial |
| NCT03014674 | Not a placebo‐controlled trial and treatment duration < 16 weeks |
| NCT03021304 | No placebo arm/single treatment arm, treatment duration < 16 weeks |
| Newbold 2016 | Not a RCT |
| Niven 2008 | Intervention used in study (omalizumab) is not anti‐IL‐5 therapy |
| Noga 2003 | Intervention used in study (omalizumab) is not anti‐IL‐5 therapy |
| Noga 2008 | Intervention used in study (omalizumab) is not anti‐IL‐5 therapy |
| Noonan 2013 | Intervention used in study (lebrikizumab) is not anti‐IL‐5 therapy |
| Nowak 2015 | Treatment < 16 weeks |
| Oba 2004 | Intervention used in study (omalizumab) is not anti‐IL‐5 therapy |
| Oh 2013 | Intervention used in study (anti‐IL‐9) is not anti‐IL‐5 therapy |
| Ohashi 1997 | Participants do not have a diagnosis of asthma |
| Ohman 1984 | Intervention used in study (immunotherapy) is not anti‐IL‐5 therapy |
| Ohta 2009 | Intervention used in study (omalizumab) is not anti‐IL‐5 therapy |
| Ong 2005 | Intervention used in study (omalizumab) is not anti‐IL‐5 therapy |
| Park 1998 | Not a RCT |
| Parker 2010 | Intervention used in study (anti‐IL‐9) is not anti‐IL‐5 therapy |
| Pauli 1984 | Intervention used in study (immunotherapy) is not anti‐IL‐5 therapy |
| Pavord 2012b | Posthoc analysis of Pavord 2012a and Ortega 2014 stratified by prior use of anti‐IgE therapy |
| Pelaia 2016 | Study is not a RCT |
| Pham 2016 | An analysis of sera collected from asthma patients enrolled in two clinical studies: NCT00659659 and NCT00783289 |
| Piper 2012 | Intervention used in study (tralokinumab) is not anti‐IL‐5 therapy |
| Piper 2013 | Intervention used in study (tralokinumab) is not anti‐IL‐5 therapy |
| Pouliquen 2015 | Study has no placebo arm or clinical endpoints |
| Pouliquen 2016 | Aggregation of two clinical trials |
| Prazma 2016 | Study is not a randomised, placebo controlled trial |
| Prieto 2006 | Intervention used in study (omalizumab) is not anti‐IL‐5 therapy |
| Pui 2010 | Intervention used in study (air/diesel exhaust +/‐ antioxidant) is not anti‐IL‐5 therapy |
| Ranade 2015 | Intervention used in study (tralokinumab) is not anti‐IL‐5 therapy |
| Rose 2009 | Intervention used in study (pneumococcal vaccine) is not anti‐IL‐5 therapy |
| Sakamoto 1984 | Not a RCT |
| Scheerens 2011 | Intervention used in study (lebrikizumab) is not anti‐IL‐5 therapy |
| Scheerens 2012 | Intervention used in study (lebrikizumab) is not anti‐IL‐5 therapy |
| Scheerens 2014 | Intervention used in study (lebrikizumab) is not anti‐IL‐5 therapy |
| Siergiejko 2011 | Intervention used in study (omalizumab) is not anti‐IL‐5 therapy |
| Silk 1998 | Intervention used in study (pneumococcal vaccine) is not anti‐IL‐5 therapy |
| Silkoff 2004 | Intervention used in study (omalizumab) is not anti‐IL‐5 therapy |
| Simoes 2007 | Intervention used in study (pavilizumab) is not anti‐IL‐5 therapy |
| Singh 2010 | Intervention used in study (anti‐IL‐13) is not anti‐IL‐5 therapy |
| Slavin 2009 | Intervention used in study (omalizumab) is not anti‐IL‐5 therapy |
| Soler 2001 | Intervention used in study (omalizumab) is not anti‐IL‐5 therapy |
| Sorkness 2013 | Intervention used in study (omalizumab) is not anti‐IL‐5 therapy |
| Sthoeger 2007 | Intervention used in study (omalizumab) is not anti‐IL‐5 therapy |
| Sugaya 1994 | Intervention used in study (influenza vaccine) is not anti‐IL‐5 therapy |
| Swanson 2014 | Intervention used in study (dupilumab) is not anti‐IL‐5 therapy |
| Szymaniak 1998 | Not a RCT |
| Tanaka 1993 | Intervention used in study (influenza vaccine) is not anti‐IL‐5 therapy |
| Terr 1969 | Study predates monoclonal treatments |
| Van Rensen 2009 | Intervention used in study (omalizumab) is not anti‐IL‐5 therapy |
| Vignola 2004 | Intervention used in study (omalizumab) is not anti‐IL‐5 therapy |
| Virchow 2016 | Aggregation of two clinical trials |
| Wang 2015 | Pharmacometrics assessment of phase IIb data to characterize the exposure‐response relationship with Benralizumab in adults with asthma. |
| Wark 2003 | Intervention used in study (itraconazole) is not anti‐IL‐5 therapy |
| Weinstein 2016 | Combined secondary analysis of two trials: NCT01287039 and NCT01285323 |
| Wenzel 2009 | Intervention used in study (golimumab) is not anti‐IL‐5 therapy |
| Wenzel 2013a | Intervention used in study (dupilumab) is not anti‐IL‐5 therapy |
| Wenzel 2013b | Interventionused in study (dupilumab) is not anti‐IL‐5 therapy |
| Wenzel 2014 | Intervention used in study (dupilumab) is not anti‐IL‐5 therapy |
| Yan 2015 | Participants do not have a diagnosis of asthma |
| Zetterstrom 1972 | Participants do not all have diagnosis of asthma |
| Zhu 2013 | Intervention used in study (omalizumab) is not anti‐IL‐5 therapy |
| Zielen 2013 | Intervention used in study (omalizumab) is not anti‐IL‐5 therapy |
RCT: randomised controlled trial
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | Mepolizumab and exacerbation frequency in refractory eosinophilic asthma. A randomised, double blind, placebo controlled, parallel group trial |
| Methods | Randomised, double‐blind, placebo‐controlled, parallel‐group trial |
| Participants | Target recruitment = 60 participants with refractory eosinophilic asthma Principal inclusion criteria
|
| Interventions | Mepolizumab IV Placebo |
| Outcomes | Main objective To investigate whether mepolizumab effectively suppresses the presence of eosinophils in sputum and whether this translates into a fall in the frequency of asthma exacerbations in a cohort of refractory asthmatics who otherwise require a high dose of inhaled corticosteroids and, in some cases, regular oral corticosteroids to control their asthma. Secondary objectives To assess the effects of mepolizumab on:
|
| Starting date | Date of competent authority/ethics committee decision 2005‐11‐16 |
| Contact information | (No contact details listed) Sponsored by University Hospitals of Leicester www.clinicaltrialsregister.eu/ctr‐search/trial/2005‐001932‐61/GB |
| Notes | Non‐commercial |
| Trial name or title | Mepolizumab treatment for rhinovirus‐induced asthma exacerbations (MATERIAL) |
| Methods | Randomised, double‐blind trial |
| Participants | People with mild allergic asthma with viral airway infections Target recruitment = 48 participants Inclusion criteria
Exclusion criteria:
|
| Interventions | 3 monthly intravenous infusions of 750 mg versus 3 monthly intravenous infusions with saline |
| Outcomes | Primary outcome measures
Secondary outcome measures:
|
| Starting date | January 2012 |
| Contact information | Suzanne Bal +31 205668043 s.m.bal@amc.uva.nl Koenraad van der Sluijs +31 205668224 kvandersluijs@amc.uva.nl Principal Investigator: René Lutter, Academisch Medisch Centrum ‐ Universiteit van Amsterdam (AMC‐UvA) |
| Notes | Also known as "MATERIAL" study. Clinicaltrials.gov website notes "The recruitment status of this study is unknown. The completion date has passed and the status has not been verified in more than two years." Estimated study completion date March 2014 |
| Trial name or title | A 52‐week double‐blind, placebo‐controlled, parallel‐group efficacy and safety study of reslizumab 110 mg fixed, subcutaneous dosing in patients with uncontrolled asthma and elevated blood eosinophils |
| Methods | Double‐blind, placebo‐controlled, parallel‐group study |
| Participants | 469 participants with unstable asthma Inclusion criteria
|
| Interventions | Reslizumab will be administered subcutaneously in a dose of 110 mg every 4 weeks versus placebo |
| Outcomes | The primary objective of this study is to determine the effect of reslizumab (110 mg) administered subcutaneously every 4 weeks on clinical asthma exacerbations in adults and adolescents with asthma and elevated blood eosinophils who are inadequately controlled on standard‐of‐care asthma therapy. Primary outcome measures
Secondary outcome measures
|
| Starting date | September 2015 |
| Contact information | Study Director: Teva Medical Expert, MD |
| Notes | Estimated study completion date: January 2018 Responsible party: Teva Branded Pharmaceutical Products, R&D Inc. International multicentre study with 200 centres |
| Trial name or title | Cessation versus continuation of long‐term mepolizumab in severe eosinophilic asthma patients |
| Methods | Multi‐center, randomised, double‐blind, placebo‐controlled, parallel‐group study |
| Participants | 300 participants
|
| Interventions | Mepolizumab 100 mg versus placebo |
| Outcomes | Primary outcome measures
Secondary outcome measures
|
| Starting date | January 2016 |
| Contact information | US GSK Clinical Trials Call Center GSKClinicalSupportHD@gsk.com |
| Notes | Estimated study completion date: January 2019 |
| Trial name or title | A randomised, double‐blind, placebo‐controlled, mono‐center study to evaluate the effects of mepolizumab on airway physiology in patients with eosinophilic asthma: the MEMORY Study |
| Methods | Randomised, double‐blind, placebo‐controlled, mono‐centre study |
| Participants | 29 participants with severe eosinophilic asthma Inclusion criteria
|
| Interventions | Mepolizumab 100 mg SC every 4 weeks for 13 injections and placebo |
| Outcomes | Primary outcome measures
Secondary outcome measures
|
| Starting date | November 2015 |
| Contact information | PI Dr. Stephanie Korn, Johannes Gutenberg University Mainz |
| Notes | GlaxoSmithKline collaborator Estimated study completion date August 2018 |
| Trial name or title | A double‐bind, randomised, parallel group, placebo‐controlled multi‐centre study to evaluate the effect of benralizumab on allergen‐induced inflammation in mild, atopic asthmatics |
| Methods | Randomised, double‐blind, parallel‐group, placebo‐controlled study |
| Participants | Estimated enrolment 42 participants with mild atopic asthma Inclusion criteria
|
| Interventions | Benralizumab administered subcutaneously compared with placebo administered subcutaneously Allergen challenge (all participants) |
| Outcomes | Primary outcome measures
Secondary outcome measures
Other outcome measures:
|
| Starting date | October 2016 |
| Contact information | AstraZeneca Clinical Study Information Center 1‐877‐240‐9479 information.center@astrazeneca.com |
| Notes | Still recruiting April 2017 Estimated completion date February 2019 |
BDP: beclomethasone dipropionate; CO: carbon monoxide; ECG: electrocardiogram; ED: emergency department; eNO: exhaled nitric oxide; FEV1 : Forced expiratory volume in 1 second; FVC: forced vital capacity; GETE: global evaluation of treatment effectiveness; IC: inspiratory capacity; ICU: intensive care unit; NO: nitric oxide; PC20 : histamine provocative concentration causing a 20% drop in FEV1: RV: residual volume; TLC: total lung capacity;
Contributions of authors
On the current version of this review, SM, HF and CP contributed to the rewriting of the Background and Methods sections. HF and CP independently selected trials for the review, HF and AW extracted the data, and HF entered the data into the RevMan 2014 file with cross‐checking by Christopher Cates, the Cochrane Airways Group statistician. HF, SM and AW wrote the Results section, and HF, CP and SM co‐authored the Discussion and Conclusions.
On the previous version (Powell 2015), SM, KD, NW and CP contributed to the writing of the protocol. NW and CP independently selected trials for the review, NW and LB extracted the data, and KD entered the data into the RevMan 2014 file with cross‐checking by SM. KD and SM wrote the Results section, and NW, LB, CP, KD and SM coauthored the Discussion and Conclusions.
Sources of support
Internal sources
The authors declare that no such funding was received for this systematic review, Other.
External sources
The authors declare that no such funding was received for this systematic review, Other.
Declarations of interest
HF: none known.
AW: none known.
CP: none known.
LB: none known.US Food & Drug Administration
SM: none known.
New search for studies and content updated (conclusions changed)
References
References to studies included in this review
- Bjermer L, Lemiere C, Maspero J, Ciesielska M, O'Brien C, Zangrilli J. A randomized phase 3 study of the efficacy and safety of reslizumab in subjects with asthma with elevated eosinophils. European Respiratory Journal 2014;44(Suppl 58):P299. [CENTRAL: 1053372; CRS: 4900126000028560; EMBASE: 71849984] [Google Scholar]; Bjermer L, Lemiere C, Maspero J, Weiss S, Zangrilli J, Germinaro M. Reslizumab for inadequately controlled asthma with elevated blood eosinophil levels: a randomized phase 3 study. Chest 2016;150(4):789‐98. [CENTRAL: 1139859 ; CRS: 4900132000017682; PUBMED: 27056586] [DOI] [PubMed] [Google Scholar]; Maspero J, Bjermer L, Lemiere C, Ciesielska M, O'Brien C, Zangrilli J. A randomized phase 3 study assessing patient reported outcomes and safety of reslizumab in patients with asthma with elevated eosinophils. Annals of Allergy, Asthma and Immunology 2014;113(5 SUPPL. 1):A21. [CENTRAL: 1020022; CRS: 4900126000021720; EMBASE: 71679175] [Google Scholar]; NCT01270464. A study to evaluate the efficacy and safety of reslizumab (0.3 or 3.0 mg/kg) as treatment for patients (12‐75 years of age) with eosinophilic asthma. clinicaltrials.gov/ct2/show/NCT01270464 (first received 29 December 2010).
- Bleecker E, FitzGerald JM, Chanez P, Papi A, Weinstein SF, Barker P, et al. Benralizumab provides significant improvements for patients with severe, uncontrolled asthma: SIROCCO Phase III results. European Respiratory Journal 2016;48:OA4832. [Google Scholar]; Bleecker ER, FitzGerald JM, Chanez P, Papi A, Weinstein SF, Barker P, et al. Efficacy and safety of benralizumab for patients with severe asthma uncontrolled with high‐dosage inhaled corticosteroids and long‐acting beta2‐agonists (SIROCCO): a randomised, multicentre, placebo‐controlled phase 3 trial. Lancet 2016;388(10056):2115–27. [DOI] [PubMed] [Google Scholar]; NCT01928771. Efficacy and safety study of benralizumab added to high‐dose inhaled corticosteroid plus LABA in patients with uncontrolled asthma. clinicaltrials.gov/show/NCT01928771 (first received 16 August 2013). [CRS: 4900132000027654]
- Castro M, Gossage DL, Ward CK, Wu Y, Khatri DB, Molfino NA, et al. Benralizumab reduces exacerbations and improves lung function in adults with uncontrolled eosinophilic asthma. American Journal of Respiratory and Critical Care Medicine 2014;189:B101. [CENTRAL: 1131488; CRS: 4900132000009717; EMBASE: 72043211] [Google Scholar]; Castro M, Wenzel S, Kolbeck R, Khatry D, Christine W, Wu Y, et al. A phase 2 study of benralizumab on exacerbations, lung function, and asthma control in adults with uncontrolled eosinophilic asthma. European Respiratory Journal 2014;44(Suppl 58):2909. [CENTRAL: 1053384; CRS: 4900126000028573] [Google Scholar]; Castro M, Wenzel SE, Bleecker ER, Pizzichini E, Kuna P, Busse WW, et al. Benralizumab, an anti‐interleukin 5 receptor alpha monoclonal antibody, versus placebo for uncontrolled eosinophilic asthma: a phase 2b randomised dose‐ranging study. Lancet Respiratory Medicine 2014;2(11):879‐9. [PUBMED: 25306557] [DOI] [PubMed] [Google Scholar]; Eck S, Castro M, Sinibaldi D, White W, Folliot K, Gossage D, et al. Benralizumab effect on blood basophil counts in adults with uncontrolled asthma. European Respiratory Journal 2014;44(Suppl 58):297. [CENTRAL: 1053403; CRS: 4900126000028594; EMBASE: 71849982]25082908 [Google Scholar]; NCT01238861. Study to evaluate the efficacy and safety of MEDI‐563 in adults with uncontrolled asthma. clinicaltrials.gov/ct2/show/NCT01238861 (first received 9 November 2010). ; Wang B, Yan L, Hutmacher M, White WI, Ward CK, Nielsen J, et al. Exposure‐response analysis for determination of benralizumab optimal dosing regimen in adults with asthma. American Journal of Respiratory and Critical Care Medicine 2014;189:A1324. [CENTRAL: 1035648; CRS: 4900126000023160; EMBASE: 72043774] [Google Scholar]
- Brusselle G, Germinaro M, Weiss S, Zangrilli J. Reslizumab in patients with inadequately controlled late‐onset asthma and elevated blood eosinophils. Pulmonary Pharmacology and Therapeutics 2017;43:39‐45. [DOI] [PubMed] [Google Scholar]; Castro M, Zangrilli J, Wechsler ME. Corrections. Reslizumab for inadequately controlled asthma with elevated blood eosinophil counts: results from two multicentre, parallel, double‐blind, randomised, placebo‐controlled, phase 3 trials. Lancet Respiratory Medicine 2015;3(4):e15. [CRS: 4900126000028793; DOI: 10.1016/S2213-2600(15)00042-9; EMBASE: 2015833476] [DOI] [PubMed] [Google Scholar]; Castro M, Zangrilli J, Wechsler ME, Bateman ED, Brusselle GG, Bardin P, et al. Reslizumab for inadequately controlled asthma with elevated blood eosinophil counts: results from two multicentre, parallel, double‐blind, randomised, placebo‐controlled, phase 3 trials. Lancet Respiratory Medicine 2015;3(5):355‐66. [DOI] [PubMed] [Google Scholar]; NCT01287039. A study to evaluate the efficacy and safety of reslizumab (3.0 mg/kg) in the reduction of clinical asthma exacerbations in patients (12‐75 years of age) with eosinophilic asthma. clinicaltrials.gov/ct2/show/NCT01287039 (first received 28 January 2011).
- Castro M, Zangrilli J, Wechsler ME. Corrections to Reslizumab for inadequately controlled asthma with elevated blood eosinophil counts: results from two multicentre, parallel, double‐blind, randomised, placebo‐controlled, phase 3 trials. Lancet Respiratory Medicine 2015;3(4):e15. [CRS: 4900126000028793; EMBASE: 2015833476] [DOI] [PubMed] [Google Scholar]; Castro M, Zangrilli J, Wechsler ME, Bateman ED, Brusselle GG, et al. Reslizumab for inadequately controlled asthma with elevated blood eosinophil counts: results from two multicentre, parallel, double‐blind, randomised, placebo‐controlled, phase 3 trials. Lancet Respiratory Medicine 2015;3(5):355‐66. [DOI] [PubMed] [Google Scholar]; NCT01285323. A study to evaluate the efficacy and safety of reslizumab in patients with eosinophilic asthma. clinicaltrials.gov/ct2/show/NCT01285323 (first received 25 January 2011).
- Chupp GL, Bradford ES, Albers FC, Bratton DJ, Wang‐Jairaj J, Nelsen LM, et al. Efficacy of mepolizumab add‐on therapy on health‐related quality of life and markers of asthma control in severe eosinophilic asthma (MUSCA): a randomised, double‐blind, placebo‐controlled, parallel‐group, multicentre, phase 3b trial. Lancet Respiratory Medicine 2017;5(5):390‐400. [DOI] [PubMed] [Google Scholar]; NCT02281318. A randomised, double‐blind, placebo‐controlled, parallel‐group, multi‐centre 24‐week study to evaluate the efficacy and safety of mepolizumab adjunctive therapy in subjects with severe eosinophilic asthma on markers of asthma control. clinicaltrials.gov/show/NCT02281318 (first received 30 October 2014). [CRS: 4900126000021132]
- Corren J, Weinstein S, Janka L, O'Brien C, Zangrilli J. A randomized phase 3 study of reslizumab efficacy in relation to blood eosinophil levels in patients with moderate to severe asthma. European Respiratory Journal 2014;44(Suppl 58):4673. [CENTRAL: 1053393; CRS: 4900126000028582; EMBASE: 71849958] [Google Scholar]; Corren J, Weinstein S, Janka L, Zangrilli J, Garin M. Phase 3 study of reslizumab in patients with poorly controlled asthma: effects across a broad range of eosinophil counts. Chest 2016;150(4):799‐810. [CENTRAL: 1139856; CRS: 4900132000017663; PUBMED: 27018175] [DOI] [PubMed] [Google Scholar]; NCT01508936. A 16‐week, randomized, double‐blind, placebo‐controlled study to evaluate the efficacy and safety of reslizumab (3.0 mg/kg) treatment in patients with moderate to severe asthma. clinicaltrials.gov/show/NCT01508936 (first received 3 January 2012). [CRS: 4900132000027649]
- FitzGerald JM, Bleecker E, Nair P, Korn S, Ohta K, Lommatzsch M, et al. Benralizumab reduces exacerbations in severe, uncontrolled asthma: results of the phase III CALIMA trial [OA1969]. European Respiratory Society 26th Annual Congress; 2016 Sep 3‐7; London. 2016. [Google Scholar]; FitzGerald JM, Bleecker ER, Nair P, Korn S, Ohta K, Lommatzsch M, et al. Benralizumab, an anti‐interleukin‐5 receptor α monoclonal antibody, as add‐on treatment for patients with severe, uncontrolled, eosinophilic asthma (CALIMA): a randomised, double‐blind, placebo‐controlled phase 3 trial. Lancet 2016;388(10056):2128‐41. [DOI] [PubMed] [Google Scholar]; NCT01914757. A multicentre, randomized, double‐blind, parallel group, placebo controlled, phase 3 study to evaluate the efficacy and safety of benralizumab in asthmatic adults and adolescents inadequately controlled on inhaled corticosteroid plus long‐acting beta2 agonist (CALIMA). clinicaltrials.gov/show/NCT01914757 (first received 31 July 2013). [CRS: 4900132000027659]
- Gupta S, Halder P, Hargadon B, Sousa A, Marshall RP, Wardlaw AJ, et al. Assessment of changes in airways dimensions with mepolizumab treatment in refractory eosinophilic asthma. American Thoracic Society International Conference; 2009 May 15‐20 San Diego. 2009:A3641. [] [Google Scholar]; Haldar P, Brightling C, Hargadon B, Gupta S, Monteiro W, Sousa A, et al. Mepolizumab (Anti‐IL5) and exacerbation frequency in refractory eosinophilic asthma. American Journal of Critical Care and Respiratory Medicine 2009;179:A3638. [] [Google Scholar]; Haldar P, Brightling CE, Hargadon B, Gupta S, Monteiro W, Sousa A, et al. Mepolizumab and exacerbations of refractory eosinophilic asthma. New England Journal of Medicine 2009;360(10):973‐84. [] [DOI] [PMC free article] [PubMed] [Google Scholar]; Haldar P, Brightling CE, Singapuri A, Hargadon B, Gupta S, Monteiro W, et al. Outcomes after cessation of mepolizumab therapy in severe eosinophilic asthma: a 12‐month follow‐up analysis. The Journal of Allergy and Clinical Immunology 2014;133(3):921‐3. [CRS: 4900126000009453; EMBASE: 2014156329; PUBMED: 24418480] [DOI] [PubMed] [Google Scholar]
- NCT01947946. Efficacy and safety study of benralizumab added to medium‐dose inhaled corticosteroid plus LABA in patients with uncontrolled asthma. clinicaltrials.gov/show/NCT01947946 (first received 11 September 2013). [CRS: 4900132000027663]
- Albers FC, Lugogo N, Gilson MJ, Price R, Yancey SW. Long‐term safety and efficacy of mepolizumab in patients with severe eosinophilic asthma. Journal of Allergy and Clinical Immunology 2016;137(2 SUPPL 1):AB14. [CENTRAL: 1135293; CRS: 4900132000016843; EMBASE: 72196801] [Google Scholar]; Albers FC, Price R, Ortega H, Yancey SW, Nelsen LM. Effect of mepolizumab in severe eosinophilic asthma patients in relation to their baseline ACQ‐5 and SGRQ scores. European Journal of Allergy and Clinical Immunology 2016;71:257‐8. [Google Scholar]; Basu A, Dalal A, Canonica GW, Forshag M, Yancey SW, Nagar S, et al. Economic analysis of the phase III MENSA study evaluating mepolizumab for severe asthma with eosinophilic phenotype. Expert Review of Pharmacoeconomics and Outcomes Research 2017;17(2):121‐31. [DOI] [PubMed] [Google Scholar]; Forshag M, Dalal AA, Ortega H, Yancey S, Gunsoy NB, Canonica G. Healthcare resource use associated with exacerbations in patients with severe eosinophilic asthma. American Journal of Respiratory and Critical Care Medicine 2015;191:A4174. [CENTRAL: 1107017; CRS: 4900132000010497; EMBASE: 72052049] [Google Scholar]; Magnan AA, Bourdin A, Prazma CM, Albers FC, Price RG, Yancey SW, et al. Treatment response with mepolizumab in severe eosinophilic asthma patients with previous omalizumab treatment. European Journal of Allergy and Clinical Immunology 2016;71(9):1335‐44. [DOI] [PMC free article] [PubMed] [Google Scholar]; NCT01691521. MEA115588 A randomised, double‐blind, double‐dummy, placebo‐controlled, parallel‐group, multi‐centre study of the efficacy and safety of mepolizumab adjunctive therapy in subjects with severe uncontrolled refractory asthma. clinicaltrials.gov/ct2/show/NCT01691521 (first received 20 September 2012). []; Ortega H, Liu M, Pavord I, Brusselle G, FitzGerald JM, Chetta A, et al. Reduction in exacerbations with mepolizumab in severe eosinophilic asthma: MENSA study. European Respiratory Journal 2014;44(Suppl 58):2906. [CENTRAL: 1053453; CRS: 4900126000028649] [Google Scholar]; Ortega H, Mayer B, Yancey S, Katial R. Response to treatment with mepolizumab in elderly patients. American Journal of Respiratory and Critical Care Medicine 2015;191:A4177. [CENTRAL: 1107016; CRS: 4900132000010495; EMBASE: 72052052] [Google Scholar]; Ortega HG, Liu MC, Pavord ID, Brusselle GG, FitzGerald JM, Chetta A, et al. Mepolizumab treatment in patients with severe eosinophilic asthma. New England Journal of Medicine 2014;371(13):1198‐207. [CRS: 4900126000019751; EMBASE: 25199059; PUBMED: 25199059] [DOI] [PubMed] [Google Scholar]; Ortega HG, Yancey SW, Mayer B, Gunsoy NB, Keene ON, Bleecker ER, et al. Severe eosinophilic asthma treated with mepolizumab stratified by baseline eosinophil thresholds: a secondary analysis of the DREAM and MENSA studies. Lancet Respiratory Medicine 2016;4(7):549–56. [CENTRAL: 1161094; CRS: 4900132000021649; PUBMED: 27177493] [DOI] [PubMed] [Google Scholar]; Shimoda T, Odajima H, Okamasa A, Kawase M, Komatsubara M, Mayer B, et al. Efficacy and safety of mepolizumab in Japanese patients with severe eosinophilic asthma. Allergology International 2017;66(3):445‐51. [DOI] [PubMed] [Google Scholar]
- Adachi M, Kim M‐K, Imai N, Nakanishi T, Ohta K, Tohda Y, et al. A phase 2a study of benralizumab for patients with eosinophilic asthma in South Korea and Japan. American Journal of Respiratory and Critical Care Medicine 2015;191(Meeting Abstracts):A2495. [CENTRAL: 1101040; CRS: 4900132000009869; EMBASE: 72050330] [Google Scholar]; NCT01412736. A phase IIa study of KHK4563 (4563‐003). clinicaltrials.gov/show/NCT01412736 (first received 7 August 2011). [CRS: 4900132000027662]; Park HS, Kim MK, Imai N, Nakanishi T, Adachi M, Ohta K, et al. A phase 2a study of benralizumab for patients with eosinophilic asthma in South Korea and Japan. International Archives of Allergy and Immunology 2016;169(3):135‐45. [CENTRAL: 1152856; CRS: 4900132000019460; EMBASE: 20160326586; PUBMED: 27097165] [DOI] [PubMed] [Google Scholar]
- NCT01000506. Dose ranging efficacy and safety with mepolizumab in severe asthma (DREAM). clinicaltrials.gov/ct2/show/NCT01000506 (accessed 16 January 2015). []; Ortega H, Chupp G, Bardin P, Bourdin A, Garcia G, Hartley B, et al. The role of mepolizumab in atopic and nonatopic severe asthma with persistent eosinophilia. European Respiratory Journal 2014;44(1):239‐41. [DOI] [PubMed] [Google Scholar]; Ortega H, Li H, Suruki R, Albers F, Gordon D, Yancey S. Cluster analysis and characterization of response to mepolizumab: a step closer to personalized medicine for patients with severe asthma. Annals of the American Thoracic Society 2014;11(7):1011‐7. [CRS: 4900126000015693; PUBMED: 24983709] [DOI] [PubMed] [Google Scholar]; Ortega HG, Chupp G, Bardin P, Bourdin A, Hartley B, Humbert M. The role of mepolizumab in atopic and non‐atopic patients with refractory eosinophilic asthma. American Journal of Respiratory and Critical Care Medicine 2013;187:A3861. [CENTRAL: 1129378; CRS: 4900132000007150; EMBASE: 71983360] [Google Scholar]; Pavord I, Korn S, Howarth P, Bleecker E, Buhl R, Keene O, et al. Mepolizumab (anti‐IL‐5) reduces exacerbations in patients with refractory eosinophilic asthma. Proceedings of the European Respiratory Society 22nd Annual Congress; 2012 Sep 1‐5; Vienna. European Respiratory Journal 2012;40(Suppl 56):36s [349]. [] [Google Scholar]; Pavord ID, Korn S, Howarth P, Bleecker ER, Buhl R, Keene ON, et al. Mepolizumab for severe eosinophilic asthma (DREAM): a multicentre, double‐blind, placebo‐controlled trial. The Lancet 2012;380(9842):651‐9. [] [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
- Albers F, Cockle S, Gunsoy N, Shin JY, Nelsen L, Muellerova H. Eligibility for mepolizumab, omalizumab and reslizumab in the EU population: The IDEAL study [PA4216]. European Respiratory Society 26thAnnual Congress; 2016 Sep 3‐7; London. 2016. [Google Scholar]
- Alvarez‐Cuesta E, Cuesta‐Herranz J, Puyana‐Ruiz J, Cuesta‐Herranz C, Blanco‐Quiros A. Monoclonal antibody‐standardized cat extract immunotherapy: risk‐benefit effects from a double‐blind placebo study. Journal of Allergy and Clinical Immunology 1994;93(3):556‐66. [] [DOI] [PubMed] [Google Scholar]
- Armentia A, Arranz M, Martin JM, Fuente R, Sanchez P, Barber D, et al. Evaluation of immune complexes after immunotherapy with wheat flour in bakers' asthma. Annals of Allergy 1992;69(5):441‐4. [] [PubMed] [Google Scholar]
- Austin D, Pouliquen I, Keene O, Yancey S. Blood eosinophil dose response to oral corticosteroids in a population of patients with severe asthma [PA1110]. European Respiratory Society 26th Annual Congress; 2016 Sep 3‐7; London. 2016. [Google Scholar]
- Ayres JG, Higgins B, Chilvers ER, Ayre G, Blogg M, Fox H. Efficacy and tolerability of anti‐immunoglobulin E therapy with omalizumab in patients with poorly controlled (moderate‐to‐severe) allergic asthma. Allergy 2004;59(7):701‐8. [] [DOI] [PubMed] [Google Scholar]
- Bel EH, Wenzel SE, Thompson PJ, Prazma CM, Keene O, Yancey SW, et al. Oral corticosteroid‐sparing effect of mepolizumab in severe eosinophilic asthma: The SIRIUS study. European Respiratory Journal 2014;44(Suppl 58):2907. [CENTRAL: 1053369; CRS: 4900126000028557] [Google Scholar]; Bel EH, Wenzel SE, Thompson PJ, Prazma CM, Keene ON, Yancey SW, et al. Oral glucocorticoid‐sparing effect of mepolizumab in eosinophilic asthma. New England Journal of Medicine 2014;371(13):1189‐97. [CENTRAL: 1013105; CRS: 4900126000019750; EMBASE: 25199060; PUBMED: 25199060] [DOI] [PubMed] [Google Scholar]; NCT01691508. Mepolizumab steroid‐sparing study in subjects with severe refractory asthma. clinicaltrials.gov/ct2/show/NCT01691508 (first received 20 September 2012). []; Sehmi R, Smith SG, Kjarsgaard M, Radford K, Boulet LP, Lemiere C, et al. Role of local eosinophilopoietic processes in the development of airway eosinophilia in prednisone‐dependent severe asthma. Clinical and Experimental Allergy 2015;46(6):793‐802. [CENTRAL: 1129187; CRS: 4900132000012252; PUBMED: 26685004] [DOI] [PubMed] [Google Scholar]
- Berger W, Gupta N, McAlary M, Fowler‐Taylor A, McAlary M, Fowler‐Taylor A. Evaluation of long‐term safety of the anti‐IgE antibody, omalizumab, in children with allergic asthma. Annals of Allergy, Asthma and Immunology 2003;91(2):182‐8. [; 4900102000000524] [DOI] [PubMed] [Google Scholar]
- Blanken M, Rovers M, Sanders E, Bont L. Ethical considerations and rationale of the MAKI trial: a multicenter double‐blind randomized placebo‐controlled trial into the preventive effect of palivizumab on recurrent wheezing associated with respiratory syncytial virus infection in children with a gestational age of 33‐35 weeks. Contemporary Clinical Trials 2012;33(6):1287‐92. [] [DOI] [PubMed] [Google Scholar]
- Blanken MO, Rovers MM, Molenaar JM, Winkler‐Seinstra PL, Meijer A, Kimpen JL, et al. Respiratory syncytial virus and recurrent wheeze in healthy preterm infants. New England Journal of Medicine 2013;368(19):1791‐9. [; 4900100000077900] [DOI] [PubMed] [Google Scholar]
- Boulet LP, Chapman KR, Cote J, Kalra S, Bhagat R, Swystun VA, et al. Inhibitory effects of an anti‐IgE antibody E25 on allergen‐induced early asthmatic response. American Journal of Respiratory and Critical Care Medicine 1997;155(6):1835‐40. [] [DOI] [PubMed] [Google Scholar]
- Bousquet J, Wenzel S, Holgate S, Lumry W, Freeman P, Fox H. Predicting response to omalizumab, an anti‐IgE antibody, in patients with allergic asthma. Chest 2004;125(4):1378‐86. [] [DOI] [PubMed] [Google Scholar]
- Bousquet J, Siergiejko Z, Swiebocka E, Humbert M, Rabe KF, Smith N, et al. Persistency of response to omalizumab therapy in severe allergic (IgE‐mediated) asthma. Allergy 2011;66(5):671‐8. [] [DOI] [PubMed] [Google Scholar]
- Brightling CE, She D, Ranade K, Piper E. Efficacy and safety of tralokinumab, an anti‐il‐13 monoclonal antibody, in a phase 2b study of uncontrolled severe asthma. American Journal of Respiratory and Critical Care Medicine 2014;189:A6670. [CENTRAL: 1035526; CRS: 4900126000023037; EMBASE: 72047302] [Google Scholar]
- Brown R, Turk F, Dale P, Bousquet J. Cost‐effectiveness of omalizumab in patients with severe persistent allergic asthma. Allergy 2007;62(2):149‐53. [; 4900100000019948] [DOI] [PubMed] [Google Scholar]
- Brusselle G, McElhattan J, Canvin J, Buhl R. Reslizumab (RES) in asthma patients (pts) with severe eosinophilic asthma stratified by GINA asthma steps 4 and 5: Analysis of two phase 3, placebo (PBO)‐controlled trials [PA4107]. European Respiratory Society 26thAnnual Congress; 2016 Sep 3‐7; London. 2016. [Google Scholar]
- Bryant DH, Burns MW, Lazarus L. Identification of IgG antibody as a carrier of reaginic activity in asthmatic patients. The Journal of Allergy and Clinical Immunology 1975;56(6):417‐28. [] [DOI] [PubMed] [Google Scholar]
- Bryant DH, Burns MW, Lazarus L. The correlation between skin tests, bronchial provocation tests and the serum level of IgE specific for common allergens in patients with asthma. Clinical Allergy 1975;5(2):145‐57. [] [DOI] [PubMed] [Google Scholar]
- Buhl R, Kunkel G, Soler M, Bensch G, Wolfe J, Noga O, et al. RhuMAb‐25 improves asthma‐specific quality of life in patients with allergic asthma. European Respiratory Journal 2000;16(Suppl 31):465s. [] [DOI] [PubMed] [Google Scholar]
- Buhl R, Soler M, Fox H, Ashby M, McAlary M, Cooper J, et al. Recombinant humanized monoclonal antibody (rhuMAb) E25 in the prevention of serious asthma exacerbations. European Respiratory Journal 2000;16(Suppl 31):277s. [] [Google Scholar]
- Buhl R, Soler M, Matz J, Townley R, O'Brien J, Noga O, et al. Omalizumab provides long‐term control in patients with moderate‐to‐ severe allergic asthma. European Respiratory Journal 2002;20(1):73‐8. [] [DOI] [PubMed] [Google Scholar]
- Bush RK, Taylor SL, Nordlee JA, Busse WW. Soybean oil is not allergenic to soybean‐sensitive individuals. The Journal of Allergy and Clinical Immunology 1985;76(2 Pt 1):242‐5. [] [DOI] [PubMed] [Google Scholar]
- Busse WW, Corren J, Lanier BQ, McAlary M, Fowler‐Taylor A, Della Cioppa G, et al. Omalizumab, anti‐IgE recombinant humanized monoclonal antibody, for the treatment of severe allergic asthma. Journal of Allergy and Clinical Immunology 2001;108(2):184‐90. [; 4900100000010636] [DOI] [PubMed] [Google Scholar]
- Busse WW, Israel E, Nelson HS, Baker JW, Charous BL, Young DY, et al. Daclizumab improves asthma control in patients with moderate to severe persistent asthma: a randomized, controlled trial. American Journal of Respiratory and Critical Care Medicine 2008;178(10):1002‐8. [] [DOI] [PubMed] [Google Scholar]
- Busse WW, Wang M, Gibson J, Gottlow M, Braddock M, Colice G. TROPOS: designing a clinical trial to evaluate the oral corticosteroid‐sparing effect of a biologic in severe asthma. Clinical Investigation 2015;5(8):723‐30. [CENTRAL: 1096145; CRS: 4900132000008837; EMBASE: 2015401568] [Google Scholar]
- Buttner C, Lun A, Splettstoesser T, Kunkel G, Renz H. Monoclonal anti‐interleukin‐5 treatment suppresses eosinophil but not T‐cell functions. European Respiratory Journal 2003;21(5):799‐803. [] [DOI] [PubMed] [Google Scholar]; Buttner C, Splettstosser T, Lun A, Renz H, Kunkel G. The influence of anti‐IL‐5 anti‐bodies on leucocyte differentiation and function in patients with asthmatic. Pneumologie (Stuttgart, Germany) 2001;55(SH1):S69. [CRS: 4900100000048746; 4900100000048746] [Google Scholar]
- Caffarelli C, Sensi LG, Marcucci F, Cavagni G. Preseasonal local allergoid immunotherapy to grass pollen in children: a double‐blind, placebo‐controlled, randomized trial. Allergy 2000;55(12):1142‐7. [] [DOI] [PubMed] [Google Scholar]
- Canvin J, Noble R, Djukanovic R, Curran M, Weiss S, et al. Early identification of responders to reslizumab at 16 weeks using an algorithm derived from the pivotal clinical studies of severe eosinophilic asthma (SEA) patients [OA2998]. European Respiratory Society 26th Annual Congress; 2016 Sep 3‐7; London. 2016. [Google Scholar]
- Castro M, Mathur S, Hargreave F, Boulet LP, Xie F, Young J, et al. Reslizumab for poorly controlled, eosinophilic asthma: a randomized, placebo‐controlled study. American Journal of Respiratory and Critical Care Medicine 2011;184(10):1125‐32. [] [DOI] [PubMed] [Google Scholar]; Castro M, Mathur S, Hargreave F, Xie F, Young J, Wilkins HJ, et al. Reslizumab in the treatment of poorly controlled asthma in patients with eosinophilic airway inflammation. Annals of Allergy, Asthma and Immunology 2010;105(5 Suppl):A43. [] [Google Scholar]; Mathur S, Castro M, Hargreave F, Xie F, Wilkins HJ, Henkel T, et al. Efficacy of reslizumab in patients with poorly controlled eosinophilic asthma: subgroup analysis of patients with nasal polyps. Journal of Allergy and Clinical Immunology 2011;127(2 Suppl 1):AB84. [] [Google Scholar]; NCT00587288. Efficacy and safety study of reslizumab to treat poorly controlled asthma. clinicaltrials.gov/show/NCT005872882008. [CRS: 4900132000027648]
- Castro M, Teper A, Wang L, Pirozzi G, Radin A, Graham N, et al. Responder analysis for FEV1 improvement with dupilumab in patients with persistent asthma and elevated eosinophil levels. American Journal of Respiratory and Critical Care Medicine 2014;189:A1321. [CENTRAL: 1131453; CRS: 4900132000009662; EMBASE: 72043771] [Google Scholar]
- Chandra RK, Singh G, Shridhara B. Effect of feeding whey hydrolysate, soy and conventional cow milk formulas on incidence of atopic disease in high risk infants. Annals of Allergy 1989;63(2):102‐6. [] [PubMed] [Google Scholar]
- Chervinsky P, Casale T, Townley R, Tripathy I, Hedgecock S, Fowler‐Taylor A, et al. Omalizumab, an anti‐IgE antibody, in the treatment of adults and adolescents with perennial allergic rhinitis. Annals of Allergy, Asthma and Immunology 2003;91(2):160‐7. [; 4900100000015346] [DOI] [PubMed] [Google Scholar]
- Clavel R, Bousquet J, Andre C. Clinical efficacy of sublingual‐swallow immunotherapy: a double‐blind, placebo‐controlled trial of a standardized five‐grass‐pollen extract in rhinitis. Allergy 1998;53(5):493‐8. [] [DOI] [PubMed] [Google Scholar]
- Corren J, Casale T, Deniz Y, Ashby M. Omalizumab, a recombinant humanized anti‐IgE antibody, reduces asthma‐related emergency room visits and hospitalizations in patients with allergic asthma. The Journal of Allergy and Clinical Immunology 2003;111(1):87‐90. [] [DOI] [PubMed] [Google Scholar]
- Corren J, Busse W, Meltzer EO, Mansfield L, Bensch G, Fahrenholz J, et al. A randomized, controlled, phase 2 study of AMG 317, an IL‐4Ralpha antagonist, in patients with asthma. American Journal of Respiratory and Critical Care Medicine 2010;181(8):788‐96. [] [DOI] [PubMed] [Google Scholar]
- Cullell‐Young M, Bayes M, Leeson PA. Omalizumab: treatment of allergic rhinitis, treatment of asthma. Drugs of the Future 2002;27(6):537‐45. [] [Google Scholar]
- Dasgupta A, Kjarsgaard M, Capaldi D, Radford K, Aleman F, Parraga G, et al. Mepolizumab in COPD with eosinophilic bronchitis: a randomized clinical trial [PA305]. European Respiratory Society 26th Annual Congress; 2016 Sep 3‐7; London. 2016. [Google Scholar]
- Boever EH, Ashman C, Cahn AP, Locantore NW, Overend P, Pouliquen IJ, et al. Efficacy and safety of an anti‐IL‐13 mAb in patients with severe asthma: a randomized trial. The Journal of Allergy and Clinical Immunology 2014;133(4):989‐96. [CENTRAL: 984687; CRS: 4900126000011203; EMBASE: 2014224342; PUBMED: 24582316] [DOI] [PubMed] [Google Scholar]
- Djukanovic R, Wilson SJ, Kraft M, Jarjour NN, Steel M, Chung KF, et al. Effects of treatment with anti‐immunoglobulin E antibody omalizumab on airway inflammation in allergic asthma. American Journal of Respiratory and Critical Care Medicine 2004;170(6):583‐93. [] [DOI] [PubMed] [Google Scholar]
- Ebner H, Neuchrist C, Havelec L, Kraft D. Comparative studies of the effectiveness of specific immunotherapy in house dust mite allergy [Vergleichende untersuchungen zur wirksamkeit einer spezifischen immuntherapie bei hausstaubmilben‐allergie]. Wiener Klinische Wochenschrift 1989;101(15):504‐11. [] [PubMed] [Google Scholar]
- Eckman JA, Sterba PM, Kelly D, Alexander V, Liu MC, Bochner BS, et al. Effects of omalizumab on basophil and mast cell responses using an intranasal cat allergen challenge. The Journal of Allergy and Clinical Immunology 2010;125(4):889‐95.e7. [] [DOI] [PMC free article] [PubMed] [Google Scholar]
- El‐Nawawy AA, Massoud MN, El‐Nazzar SY, Ramy BB. Pulmonary tuberculosis as a cause of recurrent wheezy chest: the value of serological diagnosis using IgG antibodies to mycobacterium 38 kDa antigen. Journal of Tropical Pediatrics 2000;46(1):53‐4. [] [DOI] [PubMed] [Google Scholar]
- 2012‐004385‐17. Study of mepolizumab versus placebo in addition to standard of care for the treatment of eosinophilic granulomatosis with polyangiitis [A double‐blind, randomised, placebo‐controlled study to investigate the efficacy and safety of mepolizumab in the treatment of eosinophilic granulomatosis with polyangiitis in subjects receiving standard of care therapy]. www.clinicaltrialsregister.eu/ctr‐search/ (first received 2 November 2013).
- NCT02377427. Pharmacokinetics and pharmacodynamics of mepolizumab administered subcutaneously in children. clinicaltrials.gov/ct2/show/NCT02377427 (first received 26 February 2015).
- NCT02020889. A study to investigate mepolizumab in the treatment of eosinophilic granulomatosis with polyangiitis. clinicaltrials.gov/ct2/show/NCT02020889 (first received 19 December 2013).
- 2015‐001152‐29. A long‐term access programme for asthmatic subjects who participated in a GSK‐sponsored clinical study with mepolizumab. www.clinicaltrialsregister.eu/ctr‐search/search?query=A+long‐term+access+programme+for+asthmatic+subjects+who+participated+in+a+GSK‐sponsored+clinical+study+with+mepolizumab (first received 10 July 2015).
- NCT02654145. Omalizumab to mepolizumab switch study in severe eosinophilic asthma patients. clinicaltrials.gov/ct2/show/NCT02654145 (first received 11 January 2016).
- 2016‐001831‐10. A real‐world use study of safety syringe for the administration of mepolizumab in severe asthma. clinicaltrialsregister.eu/ctr‐search/search?query=A+Real‐World+Use+Study+of+Safety+Syringe+for+the+Administration+of+Mepolizumab+in+Severe+Asthma (first received 14 February 2017).
- 2016‐002405‐19. A phase 3 pharmacokinetic study in healthy volunteers of mepolizumab as liquid formulation versus powder for solution formulation. clinicaltrialsregister.eu/ctr‐search/ (first received 5 December 2017).
- Fahy JV, Fleming HE, Wong HH, Liu JT, Su JQ, Reimann J, et al. The effect of an anti‐IgE monoclonal antibody on the early‐ and late‐phase responses to allergen inhalation in asthmatic subjects. American Journal of Respiratory and Critical Care Medicine 1997;155(6):1828‐34. [] [DOI] [PubMed] [Google Scholar]
- Fahy JV, Cockcroft DW, Boulet LP, Wong HH, Deschesnes F, Davis EE, et al. Effect of aerosolized anti‐IgE (E25) on airways responses to inhaled allergen in asthmatic subjects. American Journal of Respiratory and Critical Care Medicine 1999;160(3):1023‐7. [; 4900100000006519] [DOI] [PubMed] [Google Scholar]
- Ferguson G, FitzGerald JM, Bleecker E, Laviolette M, Bernstein D, LaForce C, et al. Benralizumab for mild to moderate, persistent asthma: The BISE phase III study. European Respiratory Society 26th Annual Congress; 2016 Sep 3‐7; London. 2016; Vol. 48:Suppl 60. [Google Scholar]
- Finn A, Gross G, Bavel J, Lee T, Windom H, Everhard F, et al. Omalizumab improves asthma‐related quality of life in patients with severe allergic asthma. Journal of Allergy and Clinical Immunology 2003;111(2):278‐84. [] [DOI] [PubMed] [Google Scholar]
- Flood‐Page P, Menzies‐Gow A, Wangoo A, Barnes NC, Barkans J, Phipps S, et al. Intravenous administration of an anti‐IL‐5 monoclonal antibody to mild atopic asthmatics reduces the expression of tenascin, procollagen 111 and lumican in the bronchial mucosal reticular basement membrane: evidence for a role for eosinophils in airways remodelling. QJM : Monthly Journal of the Association of Physicians 2003;96(11):860. [CENTRAL: 493553; CRS: 4900100000017354; 4900100000017354] [Google Scholar]; Flood‐Page PT, Menzies‐Gow AN, Kay AB, Robinson DS. Eosinophil's role remains uncertain as anti‐interleukin‐5 only partially depletes numbers in asthmatic airway. American Journal of Respiratory and Critical Care Medicine 2003;167(2):199‐204. [; 4900100000013790] [DOI] [PubMed] [Google Scholar]; Flood‐Page PT, Menzies‐Gow AN, Phipps S, Compton C, Walls C, Barnes NC, et al. Reduction of tissue eosinophils in mild atopic asthmatics by an anti‐IL‐5 monoclonal antibody (Mepolizumab) is associated with inhibition of tenascin deposition with the bronchial epithelial basement. American Journal of Respiratory and Critical Care Medicine 2002;165(Suppl 8):B42. [] [Google Scholar]; Flood‐Page PT, Menzies‐Gow AN, Phipps S, Ying S, Wangoo A, Ludwig MS, et al. Anti‐IL‐5 treatment reduces deposition of ECM proteins in the bronchial subepithelial basement membrane of mild atopic asthmatics. Journal of Clinical Investigation 2003;112(7):1029‐36. [] [DOI] [PMC free article] [PubMed] [Google Scholar]; Kay AB, Flood‐Page PT, Menzies‐Gow AN, Robinson DS. Effect of anti‐Il‐5 (mezolizumab) on airway eosinophils in asthmatics. Allergy and Clinical Immunology International 2004;Suppl 1:298‐301. [; 4900100000051661] [Google Scholar]; Menzies‐Gow AN, Flood‐Page PT, Compton C, Walls C, Sehmi R, Robinson DS, et al. A double‐blind placebo‐controlled, parallel group study to assess the effect of mepolizumab (humanised monoclonal anti‐il‐5‐antibody) on bone marrow and peripheral blood eosinophils and eosinophil progenitors in atopic asthmatics. American Journal of Respiratory and Critical Care Medicine 2002;165(Suppl 8):B50. [] [Google Scholar]; Menzies‐Gow AN, Flood‐Page PT, Sehmi R, Burman J, Hamid Q, Robinson DS, et al. Anti‐IL‐5 (mepolizumab) therapy induces bone marrow eosinophil maturational arrest and decreases eosinophil progenitors in the bronchial mucosa of atopic asthmatics. Journal of Allergy and Clinical Immunology 2003;111(4):714‐9. [; 4900100000015225] [DOI] [PubMed] [Google Scholar]; Phipps S, Flood‐Page PT, Menzies‐Gow AN, Wangoo A, Barnes N, Barkans J, et al. Anti‐IL‐5 (mepolizumab) reduces the expression of tenascin procollagen III and lumican in the reticular basement membrane of human atopic asthmatics. Journal of Allergy and Clinical Immunology 2003;111(2 Suppl):S278. [] [Google Scholar]
- Flood‐Page PT, Swenson C, Faiferman I, Matthews J, Williams M, Brannick L, et al. A study to evaluate safety and efficacy of mepolizumab in patients with moderate persistent asthma. American Journal of Respiratory and Critical Care Medicine 2007;176(11):1062‐71. [] [DOI] [PubMed] [Google Scholar]
- Frew AJ. Effects of anti‐IgE in asthmatic subjects. Thorax 1998;53(Suppl 2):S52‐7. [; 4900100000010183] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia G, Magnan A, Chiron R, Contin‐Bordes C, Berger P, Taillé C, et al. A proof‐of‐concept, randomized, controlled trial of omalizumab in patients with severe, difficult‐to‐control, nonatopic asthma. Chest 2013;144(2):411‐9. [CENTRAL: 872766; CRS: 4900100000089187; EMBASE: 2013508319; PUBMED: 23579324] [DOI] [PubMed] [Google Scholar]
- Gauvreau GM, Boulet LP, Cockcroft DW, Fitzgerald JM, Carlsten C, Davis BE, et al. Effects of interleukin‐13 blockade on allergen‐induced airway responses in mild atopic asthma. American Journal of Respiratory and Critical Care Medicine 2011;183(8):1007‐14. [] [DOI] [PubMed] [Google Scholar]
- Gauvreau GM, O'Byrne PM, Boulet LP, Wang Y, Cockcroft D, Bigler J, et al. Effects of an anti‐TSLP antibody on allergen‐induced asthmatic responses. New England Journal of Medicine 2014;370(22):2102‐10. [CENTRAL: 991614; CRS: 4900126000014666; 4900126000014666; PUBMED: 24846652] [DOI] [PubMed] [Google Scholar]
- Gauvreau GM, Boulet LP, Cockcroft DW, Fitzgerald JM, Mayers I, Carlsten C, et al. OX40L blockade and allergen‐induced airway responses in subjects with mild asthma. Clinical and Experimental Allergy 2014;44(1):29‐37. [CENTRAL: 961627; CRS: 4900126000003111; EMBASE: 2013812052; PUBMED: 24224471] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gauvreau GM, Harris JM, Boulet LP, Scheerens H, Fitzgerald JM, Putnam WS, et al. Targeting membrane‐expressed IgE B cell receptor with an antibody to the M1 prime epitope reduces IgE production. Science Translational Medicine 2014;6(243):243ra85. [CENTRAL: 994063; CRS: 4900126000015683; PUBMED: 24990880] [DOI] [PubMed] [Google Scholar]
- Gauvreau GM, Boulet LP, Leigh R, Cockcroft DW, Davis BE, Mayers I, et al. QGE031 (ligelizumab) is more effective than omalizumab and placebo in inhibiting allergen‐induced early asthmatic response: Results from a predictive modeling study. European Respiratory Journal 2015;46(Suppl 59):PA5091. [CENTRAL: 1135083; CRS: 4900132000012742; EMBASE: 72107321] [Google Scholar]
- Gauvreau G, Boulet L‐P, Leigh R, Cockcroft DW, Davis BE, Mayers I, et al. A predictive model for determining the efficacy of multiple doses of QGE031 (ligelizumab) versus omalizumab and placebo in inhibiting the allergen‐induced early asthmatic response. American Journal of Respiratory and Critical Care Medicine 2015;191(Meeting Abstracts):A2488. [CENTRAL: 1101075; CRS: 4900132000009906; EMBASE: 72050323] [Google Scholar]
- Gevaert P, Calus L, Zele T, Blomme K, Ruyck N, Bauters W, et al. Omalizumab is effective in allergic and nonallergic patients with nasal polyps and asthma. Journal of Allergy and Clinical Immunology 2013;131(1):110‐6.e1. [] [DOI] [PubMed] [Google Scholar]
- Gordon VH, Caplinger KJ, Meade JHJ, Thompson C. Correlation of type specific fluorescent antibodies to ragweed with symptomatology: double‐blind study. Annals of Allergy 1972;30(9):507‐17. [] [PubMed] [Google Scholar]
- Greenberg RN, Wilson KM, Kunz AY, Wedel NI, Gorelick KJ. Randomized, double‐blind phase II study of anti‐endotoxin antibody (E5) as adjuvant therapy in humans with serious gram‐negative infections. Progress in Clinical and Biological Research 1991;367:179‐86. [] [PubMed] [Google Scholar]
- Gunsoy N, Cockle S, Nelsen L, Albers F, Doyle S. Association between EQ‐5D and changes in asthma symptoms, severity, and Qol in patients with severe eosinophilic asthma. Value in Health 2016;19(7):A558. [Google Scholar]
- Han JQ, Zhu YX. Efficacy and regulation of humoral immunity of jade screen powder as an adjunct therapy in children with asthma [搜索关键词]. Zhongguo Dang Dai Er Ke Za Zhi [Chinese Journal of Contemporary Pediatrics] 2009;11(7):587‐8. [] [PubMed] [Google Scholar]
- Hanania NA, Alpan O, Hamilos DL, Condemi JJ, Reyes‐Rivera I, Zhu J, et al. Omalizumab in severe allergic asthma inadequately controlled with standard therapy: a randomized trial. Annals of Internal Medicine 2011;154(9):573‐82. [] [DOI] [PubMed] [Google Scholar]
- Hanania NA, Wenzel S, Rosen K, Hsieh HJ, Mosesova S, Choy DF, et al. Exploring the effects of omalizumab in allergic asthma: an analysis of biomarkers in the EXTRA study. American Journal of Respiratory and Critical Care Medicine 2013;187(8):804‐11. [; 4900100000077549] [DOI] [PubMed] [Google Scholar]
- Hanania NA, Noonan MJ, Corren J, Korenblat P, Zheng Y, Putnam W, et al. Efficacy and safety of lebrikizumab in severe uncontrolled asthma: results from the LUTE and VERSE phase II randomized, double‐blind, placebo‐controlled trials. Journal of Allergy and Clinical Immunology 2014;133(2 Suppl):AB402. [CENTRAL: 985853; CRS: 4900126000010490; EMBASE: 71351759] [Google Scholar]
- Hanania NA, Noonan M, Corren J, Korenblat P, Zheng Y, Fischer SK, et al. Lebrikizumab in moderate‐to‐severe asthma: pooled data from two randomised placebo‐controlled studies. Thorax 2015;70(8):748‐56. [CENTRAL: 1072983; CRS: 4900132000002592; EMBASE: 2015350098; PUBMED: 26001563] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris JM, Maciuca R, Bradley MS, Cabanski CR, Scheerens H, Lim J, et al. A randomized trial of the efficacy and safety of quilizumab in adults with inadequately controlled allergic asthma. Respiratory Research 2016;17(1):29. [CENTRAL: 1139820; CRS: 4900132000016979; EMBASE: 20160229671; PUBMED: 26993628] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hendeles L, Khan YR, Shuster JJ, Chesrown SE, Abu‐Hasan M. Omalizumab therapy for asthma patients with poor adherence to inhaled corticosteroid therapy. Annals of Allergy, Asthma and Immunology 2015;114(1):58‐62.e2. [CENTRAL: 1038271; CRS: 4900126000023439; EMBASE: 2014983010; PUBMED: 25528738] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill DJ, Smart IJ, Hosking CS. Specific cellular and humoral immunity in children with grass pollen asthma. Clinical Allergy 1982;12(1):83‐9. [] [DOI] [PubMed] [Google Scholar]
- Hodsman P, Ashman C, Cahn A, Boever E, Locantore N, Serone A, et al. A phase 1, randomized, placebo‐controlled, dose‐escalation study of an anti‐IL‐13 monoclonal antibody in healthy subjects and mild asthmatics. British Journal of Clinical Pharmacology 2013;75(1):118‐28. [] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holgate ST, Chuchalin AG, Hebert J, Lotvall J, Persson GB, Chung KF, et al. Efficacy and safety of a recombinant anti‐immunoglobulin E antibody (omalizumab) in severe allergic asthma. Clinical and Experimental Allergy 2004;34(4):632‐8. [] [DOI] [PubMed] [Google Scholar]
- Hoshino M, Ohtawa J. Effects of adding omalizumab, an anti‐immunoglobulin E antibody, on airway wall thickening in asthma. Respiration; International Review of Thoracic Diseases 2012;83(6):520‐8. [] [DOI] [PubMed] [Google Scholar]
- Humbert M, Beasley R, Ayres J, Slavin R, Hebert J, Bousquet J, et al. Benefits of omalizumab as add‐on therapy in patients with severe persistent asthma who are inadequately controlled despite best available therapy (GINA 2002 step 4 treatment): INNOVATE. Allergy 2005;60(3):309‐16. [] [DOI] [PubMed] [Google Scholar]
- Humbert M, Berger W, Rapatz G, Turk F. Add‐on omalizumab improves day‐to‐day symptoms in inadequately controlled severe persistent allergic asthma. Allergy 2008;63(5):592‐6. [; 4900100000021856] [DOI] [PubMed] [Google Scholar]
- Humbert M, Boulet LP, Niven RM, Panahloo Z, Blogg M, Ayre G. Omalizumab therapy: patients who achieve greatest benefit for their asthma experience greatest benefit for rhinitis. Allergy 2009;64(1):81‐4. [] [DOI] [PubMed] [Google Scholar]
- Jacquemin MG, Saint‐Remy JM. Specific down‐regulation of anti‐allergen IgE and IgG antibodies in humans associated with injections of allergen‐specific antibody complexes. Therapeutic Immunology 1995;2(1):41‐52. [] [PubMed] [Google Scholar]
- Jutel M, Jaeger L, Suck R, Meyer H, Fiebig H, Cromwell O. Allergen‐specific immunotherapy with recombinant grass pollen allergens. Journal of Allergy and Clinical Immunology 2005;116(3):608‐13. [] [DOI] [PubMed] [Google Scholar]
- Kang BC, Johnson J, Morgan C, Chang JL. The role of immunotherapy in cockroach asthma. Journal of Asthma 1988;25(4):205‐18. [] [DOI] [PubMed] [Google Scholar]
- Kips JC, O'Connor BJ, Langley SJ, Woodcock A, Kerstiens HAM, Postma DS, et al. Results of a phase I trial with SCH55700, a humanized anti‐IL‐5 antibody, in severe persistent asthma. American Journal of Respiratory and Critical Care Medicine 2000;161(3 Suppl):A505. [CENTRAL: 429039; CRS: 4900100000014606] [DOI] [PubMed] [Google Scholar]; Kips JC, O'Connor BJ, Langley SJ, Woodcock A, Kerstjens HA, Postma DS, et al. Effect of SCH55700, a humanized anti‐human interleukin‐5 antibody, in severe persistent asthma: a pilot study. American Journal of Respiratory and Critical Care Medicine 2003;167(12):1655‐9. [] [DOI] [PubMed] [Google Scholar]
- Kon OM, Sihra BS, Loh LC, Barkans J, Compton CH, Barnes NC, et al. The effects of an anti‐CD4 monoclonal antibody, keliximab, on peripheral blood CD4+ T‐cells in asthma. European Respiratory Journal 2001;18(1):45‐52. [; 4900100000011111] [DOI] [PubMed] [Google Scholar]
- Kopp MV, Hamelmann E, Zielen S, Kamin W, Bergmann KC, Sieder C, et al. Combination of omalizumab and specific immunotherapy is superior to immunotherapy in patients with seasonal allergic rhinoconjunctivitis and co‐morbid seasonal allergic asthma. Clinical and Experimental Allergy 2009;39(2):271‐9. [] [DOI] [PubMed] [Google Scholar]
- Kopp MV, Hamelmann E, Bendiks M, Zielen S, Kamin W, Bergmann KC, et al. Transient impact of omalizumab in pollen allergic patients undergoing specific immunotherapy. Pediatric Allergy and Immunology 2013;24(5):427‐33. [CENTRAL: 870929; CRS: 4900100000087210; EMBASE: 2013483684; PUBMED: 23799935] [DOI] [PubMed] [Google Scholar]
- Kulus M, Hebert J, Garcia E, Fowler Taylor A, Fernandez Vidaurre C, Blogg M. Omalizumab in children with inadequately controlled severe allergic (IgE‐mediated) asthma. Current Medical Research and Opinion 2010;26(6):1285‐93. [] [DOI] [PubMed] [Google Scholar]
- Lanier BQ, Corren J, Lumry W, Liu J, Fowler‐Taylor A, Gupta N. Omalizumab is effective in the long‐term control of severe allergic asthma. Annals of Allergy, Asthma and Immunology 2003;91(2):154‐9. [CENTRAL: 440250; CRS: 4900100000015345; PUBMED: 12952109] [DOI] [PubMed] [Google Scholar]
- Lanier B, Bridges T, Kulus M, Taylor AF, Berhane I, Vidaurre CF. Omalizumab for the treatment of exacerbations in children with inadequately controlled allergic (IgE‐mediated) asthma. Journal of Allergy and Clinical Immunology 2009;124(6):1210‐6. [CENTRAL: 731495; CRS: 4900100000024431; EMBASE: 2009623072; PUBMED: 19910033] [DOI] [PubMed] [Google Scholar]
- Gossage DL, Laviolette M, Gauvreau GM, Leigh R, Kolbeck R, Wu Y. Depletion of airway eosinophils by benralizumab an anti‐IL5 receptor alpha monoclonal antibody. American Journal of Respiratory and Critical Care Medicine 2012;185(Meeting Abstracts):A3961. [CENTRAL: 834337; CRS: 4900100000060605; EMBASE: 71988597] [Google Scholar]; Laviolette M, Gossage DL, Gauvreau G, Leigh R, Olivenstein R, Katial R, et al. Effects of benralizumab on airway eosinophils in asthmatic patients with sputum eosinophilia. Journal of Allergy and Clinical Immunology 2013;132(5):1086‐96.e5. [CENTRAL: 874819; CRS: 4900126000001561; EMBASE: 2013693094; PUBMED: 23866823] [DOI] [PMC free article] [PubMed] [Google Scholar]; NCT00659659. A study to evaluate the safety, tolerability and effects of MEDI‐563 in adults with asthma. clinicaltrials.gov/ct2/show/NCT00659659 (first received 11 April 2008).
- Leckie MJ, Brinke A, Khan J, Diamant Z, O'Connor BJ, Walls CM, et al. Effects of an interleukin‐5 blocking monoclonal antibody on eosinophils, airway hyper‐responsiveness, and the late asthmatic response. Lancet 2000;356(9248):2144‐8. [] [DOI] [PubMed] [Google Scholar]
- Leynadier F, Doudou O, Gaouar H, Gros V, Bourdeix I, Guyomarch‐Cocco L, et al. Effect of omalizumab in health care workers with occupational latex allergy. Journal of Allergy and Clinical Immunology 2004;113(2):360‐1. [] [DOI] [PubMed] [Google Scholar]
- Li J, Lin C, Du J, Xiao B, Du C, Sun J, et al. The efficacy and safety of reslizumab for inadequately controlled asthma with elevated blood eosinophil counts: a systematic review and meta‐analysis. Journal of Asthma 2016;54(3):300‐7. [CRS: 4900132000026751; PUBMED: 27435534] [DOI] [PubMed] [Google Scholar]
- Lizaso MT, Tabar AI, Garcia BE, Gomez B, Algorta J, Asturias JA, et al. Double‐blind, placebo‐controlled alternaria alternata immunotherapy: in vivo and in vitro parameters. Pediatric Allergy and Immunology 2008;19(1):76‐81. [] [DOI] [PubMed] [Google Scholar]
- Lugogo N, Domingo C, Chanez P, Leigh R, Gilson MJ, Price RG, et al. Long‐term efficacy and safety of mepolizumab in patients with severe eosinophilic asthma: a multi‐center, open‐label, phase IIIb study. Clinical Therapeutics 2016;0149‐2918 (Linking):1879‐114X (Electronic). [DOI] [PubMed] [Google Scholar]
- Maspero J, Jacobs J, Garin M. Improvements in asthma quality of life questionnaire (AQLQ) domains with reslizumab in patients with inadequately controlled asthma and elevated blood eosinophils. Journal of Allergy and Clinical Immunology 2016;137(2 SUPPL. 1):AB15. [CENTRAL: 1135292; CRS: 4900132000016842; EMBASE: 72196802] [Google Scholar]
- Massanari M, Kianifard F, Zeldin RK, Geba GP. Efficacy of omalizumab in cat‐allergic patients with moderate‐to‐severe persistent asthma. Allergy and Asthma Proceedings 2009;30(5):534‐9. [CENTRAL: 728392; CRS: 4900100000024363; PUBMED: 19467177] [DOI] [PubMed] [Google Scholar]
- Massanari M, Nelson H, Casale T, Busse W, Kianifard F, Geba GP, et al. Effect of pretreatment with omalizumab on the tolerability of specific immunotherapy in allergic asthma. Journal of Allergy and Clinical Immunology 2010;125(2):383‐9. [] [DOI] [PubMed] [Google Scholar]
- Metzger WJ, Fick RB, Bush RK, Busse W, Casale T, Chodosh S. Corticosteroid (CS) withdrawal in a study of recombinant humanized monoclonal antibody to IgE (rhu MAbE25) [Abstract]. Journal of Allergy and Clinical Immunology 1998;101(1 Suppl):S231. [] [Google Scholar]
- Milgrom H, Fick RB, Su JQ, Reimann JD, Bush RK, Watrous ML, et al. Treatment of allergic asthma with monoclonal anti‐IgE antibody. RhuMAb‐E25 Study Group. New England Journal of Medicine 1999;341(26):1966‐73. [] [DOI] [PubMed] [Google Scholar]
- Milgrom H, Berger W, Nayak A, Gupta N, Pollard S, McAlary M, et al. Treatment of childhood asthma with anti‐immunoglobulin E antibody (omalizumab). Pediatrics 2001;108(2):E36. [] [DOI] [PubMed] [Google Scholar]
- Modlin JF, Smith DH, Harding L. Clinical trials of bivalent A/New Jersey/76‐A/Victoria/75 influenza vaccines in high‐risk children. Journal of Infectious Diseases 1977;136(Suppl):S626‐31. [] [DOI] [PubMed] [Google Scholar]
- Moss RB, Hsu YP, Kwasnicki JM, Sullivan MM, Reid MJ. Isotypic and antigenic restriction of the blocking antibody response to ryegrass pollen: correlation of rye group I antigen‐specific IgG1 with clinical response. Journal of Allergy and Clinical Immunology 1987;79(2):387‐98. [] [DOI] [PubMed] [Google Scholar]
- Ayars AG, Altman LC, Potter‐Perigo S, Radford K, Wight TN, Nair P. Sputum hyaluronan and versican in severe eosinophilic asthma. International Archives of Allergy and Immunology 2013;161(1):65‐73. [] [DOI] [PMC free article] [PubMed] [Google Scholar]; Ayars AG, Altman LC, Potter‐Perigo S, Wight TN, Nair P. Sputum hyaluronan as a biomarker of airway remodeling in severe asthma. Journal of Allergy and Clinical Immunology 2011;127(2 Suppl 1):AB8. [] [Google Scholar]; NCT00292877. The prednisone‐sparing effect of anti‐IL‐5 antibody (SB‐240563). clinicaltrials.gov/ct2/show/NCT00292877 (first received 15 February 2006). []; Nair P, Kjarsgaard M, Armstrong S, Efthimiadis A, O'Byrne PM, Hargreave FE. Nitric oxide in exhaled breath is poorly correlated to sputum eosinophils in patients with prednisone‐dependent asthma. Journal of Allergy and Clinical Immunology 2010;126(2):404‐6. [CENTRAL: 759797; CRS: 4900100000025377; PUBMED: 20621343] [DOI] [PubMed] [Google Scholar]; Nair P, Pizzichini M, Kjarsgaard M, Inman M, Efthimiadis A, Pizzichini E, et al. Prednisone sparing effect of mepolizumab on eosinophilic bronchitis with or without asthma a randomized placebo controlled trial. American Thoracic Society International Conference; 2008 May 16‐21; Toronto. 2008:A568[#509]. [] [Google Scholar]; Nair P, Pizzichini MM, Kjarsgaard M, Inman MD, Efthimiadis A, Pizzichini E, et al. Mepolizumab for prednisone‐dependent asthma with sputum eosinophilia. New England Journal of Medicine 2009;360(10):985‐93. [] [DOI] [PubMed] [Google Scholar]
- Nair PK, Dasgupta A, Kjarsgaard M, Capaldi D, Radford K, Aleman FP, et al. Mepolizumab in COPD with eosinophilic bronchitis: a randomized clinical trial. Journal of Allergy and Clinical Immunology 2016;137(2 SUPPL. 1):AB392. [CENTRAL: 1135274; CRS: 4900132000016691; EMBASE: 72197694] [Google Scholar]
- NCT00783289. A phase 2a study to evaluate the safety and tolerability of MEDI‐563 in adults with asthma (MEDI‐563). clinicaltrials.gov/show/NCT00783289 (first received 30 October 2008). [CRS: 4900132000027655]
- NCT00802438. Eosinophilic airway inflammation and mepolizumab. clinicaltrials.gov/ct2/show/NCT00802438 (first received 4 December 2008). []
- NCT01290887. Open‐label extension study to evaluate the long‐term safety and efficacy of reslizumab (3.0 mg/kg) as treatment for patients (12 through 75 years of age) with eosinophilic asthma. clinicaltrials.gov/show/NCT01290887 (first received 4 February 2011). [CRS: 4900132000027651]
- NCT01366521. Dose ranging pharmacokinetics and pharmacodynamics study with mepolizumab in asthma patients with elevated eosinophils. clinicaltrials.gov/ct2/show/NCT01366521 (first received 12 May 2011). []
- NCT01471327. Japanese phase 1 study of mepolizumab. clinicaltrials.gov/ct2/show/NCT01471327 (first received 10 November 2011). []
- NCT01691859. MEA112997 open‐label long term extension safety study of mepolizumab in asthmatic subjects. clinicaltrials.gov/ct2/show/NCT01691859 (first received 13 September 2012). []
- NCT01842607. A study to determine long‐term safety of mepolizumab in asthmatic subjects. clinicaltrials.gov/ct2/show/NCT01842607 (first received 25 April 25 2013). []
- NCT02075255. Efficacy and safety study of benralizumab to reduce OCS use in patients with uncontrolled asthma on high dose inhaled corticosteroid plus LABA and chronic OCS therapy. clinicaltrials.gov/show/NCT02075255 (first received 14 February 2014). [CRS: 4900132000027653]
- NCT02135692. A Phase 3a, repeat dose, open‐label, long‐term safety study of mepolizumab in asthmatic subjects. clinicaltrials.gov/show/NCT02135692 (first received 8 May 2014). [CRS: 4900126000021136]
- NCT02258542. A safety extension study to evaluate the safety and tolerability of benralizumab (MEDI‐563) in asthmatic adults and adolescents on inhaled corticosteroid plus LABA (BORA). clinicaltrials.gov/show/NCT02258542 (first received 14 September 2014). [CRS: 4900132000027660]
- NCT02293265. Cross‐sectional study for identification and description of severe asthma patients. clinicaltrials.gov/show/NCT02293265 (first received 27 October 2014). [CRS: 4900126000021134]
- NCT02417961. Study to assess functionality, reliability, and performance of a pre‐filled syringe with benralizumab administered at home. clinicaltrials.gov/show/NCT02417961 (first received 12 March 2015). [CRS: 4900132000027656]
- NCT02501629. An efficacy and safety study of reslizumab subcutaneous in patients with oral corticosteroid dependent asthma and elevated blood eosinophils. clinicaltrials.gov/show/NCT02501629 (first received 14 July 2015). [CRS: 4900132000027650]
- NCT02559791. Anti‐interleukin‐5 (IL5) monoclonal antibody (MAb) in prednisone‐dependent eosinophilic asthma. clinicaltrials.gov/ct2/show/NCT02559791 (first received 22 September 2015).
- NCT02808819. A safety extension study with benralizumab for asthmatic adults on inhaled corticosteroid plus long‐acting beta2 agonist (MELTEMI). clinicaltrials.gov/show/NCT02808819 (first received 7 June 2016). [CRS: 4900132000027657]
- NCT02814643. Study to evaluate the potential effect of benralizumab on the humoral immune response to the seasonal influenza vaccination in adolescent and young adult patients with severe asthma (ALIZE). clinicaltrials.gov/show/NCT02814643 (first received 15 June 2016). [CRS: 4900132000027661]
- NCT02869438. A study to evaluate the onset of effect and time course of change in lung function with benralizumab in severe, uncontrolled asthma patients with eosinophilic inflammation. clinicaltrials.gov/ct2/show/NCT02869438 (first received 16 August 2016).
- NCT02937168. An imaging study using PET/CT to characterize the effect of intravenous reslizumab on airway inflammation. clinicaltrials.gov/show/NCT02937168 (first received 14 October 2016).
- NCT02968914. Pharmacokinetic comparability of benralizumab using accessorized pre‐filled syringe or autoinjector in healthy volunteers. clinicaltrials.gov/show/NCT02968914 (first received 28 October 2016).
- NCT03014674. A study to compare the pharmacokinetics of mepolizumab as a liquid drug in a safety syringe or an autoinjector versus lyophilised drug. clinicaltrials.gov/show/NCT03014674 (first received 15 December 2016).
- NCT03021304. Study of mepolizumab safety syringe in asthmatics. clinicaltrials.gov/ct2/show/NCT03021304 (first received 12 January 2017).
- Newbold P, Liu H, Pham T‐H, Damera G, Sridhar S. Modulation of inflammation by benralizumab in eosinophilic airway disease. European Respiratory Society 26th Annual Congress; 2016 Sep 3‐7; London. 2016:[PA4902]. [Google Scholar]
- Niven R, Chung KF, Panahloo Z, Blogg M, Ayre G. Effectiveness of omalizumab in patients with inadequately controlled severe persistent allergic asthma: an open‐label study. Respiratory Medicine 2008;102(10):1371‐8. [] [DOI] [PubMed] [Google Scholar]
- Noga O, Hanf G, Kunkel G. Immunological and clinical changes in allergic asthmatics following treatment with omalizumab. International Archives of Allergy and Immunology 2003;131(1):46‐52. [; 4900100000015254] [DOI] [PubMed] [Google Scholar]
- Noga O, Hanf G, Kunkel G, Kleine‐Tebbe J. Basophil histamine release decreases during omalizumab therapy in allergic asthmatics. International Archives of Allergy and Immunology 2008;146(1):66‐70. [CENTRAL: 628876; CRS: 4900100000021809; PUBMED: 18087163] [DOI] [PubMed] [Google Scholar]
- Noonan M, Korenblat P, Mosesova S, Scheerens H, Arron JR, Zheng Y, et al. Dose‐ranging study of lebrikizumab in asthmatic patients not receiving inhaled steroids. Journal of Allergy and Clinical Immunology 2013;132(3):567‐74.e12. [CENTRAL: 872124; CRS: 4900100000088876; EMBASE: 2013545353; PUBMED: 23726041] [DOI] [PubMed] [Google Scholar]
- Molfino NA, Nowak R, Silverman RA, Rowe BH, Smithline H, Khan F. Reduction in the number and severity of exacerbations following acute severe asthma: results of a placebo‐controlled, Randomized clinical trial with benralizumab. American Journal of Respiratory and Critical Care Medicine 2012;185(Meeting Abstracts):A2753. [CENTRAL: 834405; CRS: 4900100000060673; EMBASE: 71987342] [Google Scholar]; NCT00768079. A phase 2 study to evaluate the safety and efficacy of intravenously administered MEDI‐563 (MEDI‐563). clinicaltrials.gov/ct2/show/NCT00768079 (first received 3 October 2008). ; Nowak RM, Parker JM, Silverman RA, Rowe BH, Smithline H, Khan F, et al. A randomized trial of benralizumab, an antiinterleukin 5 receptor alpha monoclonal antibody, after acute asthma. American Journal of Emergency Medicine 2015;33(1):14‐20. [CENTRAL: 1038284; CRS: 4900126000023932; EMBASE: 2014976517; PUBMED: 25445859] [DOI] [PubMed] [Google Scholar]
- Oba Y, Salzman GA. Cost‐effectiveness analysis of omalizumab in adults and adolescents with moderate‐to‐severe allergic asthma. Journal of Allergy and Clinical Immunology 2004;114(2):265‐9. [] [DOI] [PubMed] [Google Scholar]
- Oh CK, Leigh R, McLaurin KK, Kim K, Hultquist M, Molfino NA. A randomized, controlled trial to evaluate the effect of an anti‐interleukin‐9 monoclonal antibody in adults with uncontrolled asthma. Respiratory Research 2013;14:93. [CENTRAL: 871533; CRS: 4900100000090024; EMBASE: 2013599844; 4900100000090024; PUBMED: 24050312] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ohashi Y, Nakai Y, Tanaka A, Kakinoki Y, Ohno Y, Masamoto T, et al. Serum levels of specific IgE, soluble interleukin‐2 receptor, and soluble intercellular adhesion molecule‐1 in seasonal allergic rhinitis. Annals of Allergy, Asthma and Immunology 1997;79(3):213‐20. [] [DOI] [PubMed] [Google Scholar]
- Ohman JLJ, Findlay SR, Leitermann KM. Immunotherapy in cat‐induced asthma. Double‐blind trial with evaluation of in vivo and in vitro responses. Journal of Allergy and Clinical Immunology 1984;74(3 Pt 1):230‐9. [] [DOI] [PubMed] [Google Scholar]
- Ohta K, Miyamoto T, Amagasaki T, Yamamoto M, 1304 Study Group. Efficacy and safety of omalizumab in an Asian population with moderate‐to‐severe persistent asthma. Respirology 2009;14(8):1156‐65. [] [DOI] [PubMed] [Google Scholar]
- Ong YE, Menzies‐Gow A, Barkans J, Benyahia F, Ou TT, Ying S, et al. Anti‐IgE (omalizumab) inhibits late‐phase reactions and inflammatory cells after repeat skin allergen challenge. Journal of Allergy and Clinical Immunology 2005;116(3):558‐64. [] [DOI] [PubMed] [Google Scholar]
- Park CS, Choi YS, Ki SY, Moon SH, Jeong SW, Uh ST, et al. Granulocyte macrophage colony‐stimulating factor is the main cytokine enhancing survival of eosinophils in asthmatic airways. European Respiratory Journal 1998;12(4):872‐8. [CENTRAL: 156846; CRS: 4900100000006169; PUBMED: 9817161] [DOI] [PubMed] [Google Scholar]
- Parker J, Brazinsky S, Miller DS, Nayak A, Korenblat PE, Sari S, et al. Randomized, double‐blind, placebo‐controlled, multicenter phase 2A study to evaluate the effect of a humanized interleukin‐9 monoclonal antibody (MEDI‐528) on exercise‐induced bronchospasm. American Journal of Respiratory and Critical Care Medicine 2010;181:A5394. [] [Google Scholar]
- Pauli G, Bessot JC, Bigot H, Delaume G, Hordle DA, Hirth C, et al. Clinical and immunologic evaluation of tyrosine‐adsorbed Dermatophagoides pteronyssinus extract: a double‐blind placebo‐controlled trial. The Journal of Allergy and Clinical Immunology 1984;74(4 Pt 1):524‐35. [] [DOI] [PubMed] [Google Scholar]
- Albers FC, Price RG, Yancey SW, Bradford E. Efficacy of mepolizumab in reducing exacerbations in patients with severe eosinophilic asthma who would be eligible for omalizumab treatment. 35th Annual Congress of the European Academy of Allergy and Clinical Immunology; 2016 11‐15 June; Vienna 2016;71:66‐67. [Google Scholar]
- Pelaia G, Vatrella A, Busceti MT, Gallelli L, Preiano M, Lombardo N, et al. Role of biologics in severe eosinophilic asthma ‐ focus on reslizumab. Therapeutics and Clinical Risk Management 2016;12:1075‐82. [CRS: 4900132000026857; EMBASE: 20160514755] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pham T‐H, Damera G, Newbold P, Ranade K. Reductions in eosinophil biomarkers by benralizumab in patients with asthma. Respiratory Medicine 2016;111:21‐9. [CENTRAL: 1139843; CRS: 4900132000017428; EMBASE: 20160044298] [DOI] [PubMed] [Google Scholar]
- Piper E, She D, Molfino NA. Subgroup analysis of a phase 2A randomized, double‐blind, placebo‐controlled study of tralokinumab, an anti‐IL‐13 monoclonal antibody, in moderate to severe asthma. American Journal of Respiratory and Critical Care Medicine 2012;185:A2759. [CENTRAL: 1107530; CRS: 4900132000006867; EMBASE: 71987348] [Google Scholar]
- Piper E, Brightling C, Niven R, Oh C, Faggioni R, Poon K, et al. A phase II placebo‐controlled study of tralokinumab in moderate‐to‐severe asthma. European Respiratory Journal 2013;41(2):330‐8. [] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pouliquen IJ, Kornmann O, Barton SV, Price JA, Ortega HG. Characterization of the relationship between dose and blood eosinophil response following subcutaneous administration of mepolizumab. International Journal of Clinical Pharmacology and Therapeutics 2015;53(12):1015‐27. [CENTRAL: 1096155; CRS: 4900132000008918; EMBASE: 20160138058; PUBMED: 26445140] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pouliquen I, Austin D, Gunsoy N, Yancey S. A weight‐based exacerbation dose‐response analysis of mepolizumab in severe asthma with eosinophilic phenotype [PA4106]. European Respiratory Society 26th Annual Congress; 2016 Sep 3‐7; London. 2016. [Google Scholar]
- Prazma CM, Bel EH, Barnes NC, Price R, Albers FC, Yancey SW. Steroid sparing response with mepolizumab: durability of steroid reduction in severe asthma. Journal of Allergy and Clinical Immunology 2016;137(2 SUPPL. 1):AB16. [CENTRAL: 1135291; CRS: 4900132000016838; EMBASE: 72196807] [Google Scholar]
- Prieto L, Gutierrez V, Colas C, Tabar A, Perez‐Frances C, Bruno L, et al. Effect of omalizumab on adenosine 5'‐monophosphate responsiveness in subjects with allergic asthma. International Archives of Allergy and Immunology 2006;139(2):122‐31. [] [DOI] [PubMed] [Google Scholar]
- Pui M, Lay JC, Alexis NE, Carlsten C. Flow cytometry to identify leukocyte sub‐populations in blood and induced sputum in asthmatic and healthy volunteers exposed to diesel exhaust. Allergy, Asthma, and Clinical Immunology 2010;6(Suppl 3):P7. [] [Google Scholar]
- Ranade K, Manetz S, Liang M, Lee R, Kuziora M, She D, et al. Effect of tralokinumab on serum periostin and IgE levels in uncontrolled severe asthma. European Respiratory Journal 2015;46(Suppl 59):OA1770. [CENTRAL: 1135122; CRS: 4900132000012861; EMBASE: 72106787] [Google Scholar]
- Rose MA, Gruendler M, Schubert R, Kitz R, Schulze J, Zielen S. Safety and immunogenicity of sequential pneumococcal immunization in preschool asthmatics. Vaccine 2009;27(38):5259‐64. [] [DOI] [PubMed] [Google Scholar]
- Sakamoto Y, Nakagawa T, Ito K, Miyamoto T. Solid‐phase radioimmunoassay for the measurement of IgG antibodies specific for the house dust mite, Dermatophagoides farinae. Annals of Allergy 1984;52(4):303‐8. [] [PubMed] [Google Scholar]
- Scheerens H, Arron J R, Su Z, Zheng Y, Putnam W, Erickson RW, et al. Predictive and pharmacodynamic biomarkers of interleukin‐13 blockade: effect of lebrikizumab on late phase asthmatic response to allergen challenge. Journal of Allergy and Clinical Immunology 2011;127(2 Suppl 1):AB164. [] [Google Scholar]
- Scheerens H, Arron J, Choy D, Mosesova S, Lal P, Matthews J. Lebrikizumab reduces serum periostin in asthma patients with elevated baseline periostin. European Respiratory Journal 2012;40(Suppl 56):387s [P2167]. [CENTRAL: 839426; CRS: 4900100000068033; EMBASE: 71926597] [Google Scholar]
- Scheerens H, Arron JR, Zheng Y, Putnam WS, Erickson RW, Choy DF, et al. The effects of lebrikizumab in patients with mild asthma following whole lung allergen challenge. Clinical and Experimental Allergy 2014;44(1):38‐46. [CENTRAL: 961626; CRS: 4900126000003110; EMBASE: 2013812053; PUBMED: 24131304] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siergiejko Z, Swiebocka E, Smith N, Peckitt C, Leo J, Peachey G, et al. Oral corticosteroid sparing with omalizumab in severe allergic (IgE‐mediated) asthma patients. Current Medical Research and Opinion 2011;27(11):2223‐8. [] [DOI] [PubMed] [Google Scholar]
- Silk H, Zora J, Goldstein J, Tinkelman D, Schiffman G. Response to pneumococcal immunization in children with and without recurrent infections. Journal of Asthma 1998;35(1):101‐12. [] [DOI] [PubMed] [Google Scholar]
- Silkoff PE, Romero FA, Gupta N, Townley RG, Milgrom H. Exhaled nitric oxide in children with asthma receiving Xolair (omalizumab), a monoclonal anti‐immunoglobulin E antibody. Pediatrics 2004;113(4):e308‐12. [] [DOI] [PubMed] [Google Scholar]
- Simoes EA, Groothuis JR, Carbonell‐Estrany X, Rieger CH, Mitchell I, Fredrick LM, et al. Palivizumab prophylaxis, respiratory syncytial virus, and subsequent recurrent wheezing. Journal of Pediatrics 2007;151(1):34‐42, 42.e1. [] [DOI] [PubMed] [Google Scholar]
- Singh D, Kane B, Molfino NA, Faggioni R, Roskos L, Woodcock A. A phase 1 study evaluating the pharmacokinetics, safety and tolerability of repeat dosing with a human IL‐13 antibody (CAT‐354) in subjects with asthma. BMC Pulmonary Medicine 2010;10:3. [] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slavin RG, Ferioli C, Tannenbaum SJ, Martin C, Blogg M, Lowe PJ. Asthma symptom re‐emergence after omalizumab withdrawal correlates well with increasing IgE and decreasing pharmacokinetic concentrations. Journal of Allergy and Clinical Immunology 2009;123(1):107‐113.e3. [; 4900100000022846] [DOI] [PubMed] [Google Scholar]
- Soler M, Matz J, Townley R, Buhl R, O'Brien J, Fox H, et al. The anti‐IgE antibody omalizumab reduces exacerbations and steroid requirement in allergic asthmatics. European Respiratory Journal 2001;18(2):254‐61. [] [DOI] [PubMed] [Google Scholar]
- Sorkness CA, Wildfire JJ, Calatroni A, Mitchell HE, Busse WW, O'Connor GT, et al. Reassessment of omalizumab‐dosing strategies and pharmacodynamics in inner‐city children and adolescents. Journal of Allergy and Clinical Immunology in Practice 2013;1(2):163‐71. [CENTRAL: 991371; CRS: 4900126000012068; PUBMED: 24565455] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sthoeger ZM, Eliraz A, Asher I, Berkman N, Elbirt D. The beneficial effects of Xolair (Omalizumab) as add‐on therapy in patients with severe persistent asthma who are inadequately controlled despite best available treatment (GINA 2002 step IV ‐ the Israeli arm of the INNOVATE study). Israel Medical Association Journal 2007;9(6):472‐5. [] [PubMed] [Google Scholar]
- Sugaya N, Nerome K, Ishida M, Matsumoto M, Mitamura K, Nirasawa M. Efficacy of inactivated vaccine in preventing antigenically drifted influenza type A and well‐matched type B. JAMA 1994;272(14):1122‐6. [] [PubMed] [Google Scholar]
- Swanson BN, Wang L, Ming J, Hamilton JD, Teper A, Dicioccio T, et al. Exhaled nitric oxide (FENO) and t‐helper 2 cell biomarkers: can they predict treatment response to dupilumab, an il‐4ra antibody, in an eosinophilic asthma population?. Journal of Allergy and Clinical Immunology 2014;133(2 Suppl):AB85. [CENTRAL: 985863; CRS: 4900126000010595; EMBASE: 71351035] [Google Scholar]
- Szymaniak L. An attempt to block histamine release from basophils granulocytes with antibodies obtained as a result of long‐term immunization [Proba blokowania uwalniania histaminy z granulocytow zasadochlonnych przeciwcialami uzyskanymi w wyniku dlugotrwalej immunizacji bakteriami]. Annales Academiae Medicae Stetinensis 1998;44:45‐64. [] [PubMed] [Google Scholar]
- Tanaka Y, Ueda K, Miyazaki C, Nakayama M, Kusuhara K, Okada K, et al. Trivalent cold recombinant influenza live vaccine in institutionalized children with bronchial asthma and patients with psychomotor retardation. Pediatric Infectious Disease Journal 1993;12(7):600‐5. [] [DOI] [PubMed] [Google Scholar]
- Terr AI. Immunologic bases for injection therapy of allergic diseases. Medical Clinics of North America 1969;53(6):1257‐64. [] [PubMed] [Google Scholar]
- Rensen EL, Evertse CE, Schadewijk WA, Wijngaarden S, Ayre G, Mauad T, et al. Eosinophils in bronchial mucosa of asthmatics after allergen challenge: effect of anti‐IgE treatment. Allergy 2009;64(1):72‐80. [] [DOI] [PubMed] [Google Scholar]
- Vignola AM, Humbert M, Bousquet J, Boulet LP, Hedgecock S, Blogg M, et al. Efficacy and tolerability of anti‐immunoglobulin E therapy with omalizumab in patients with concomitant allergic asthma and persistent allergic rhinitis: SOLAR. Allergy 2004;59(7):709‐17. [] [DOI] [PubMed] [Google Scholar]
- Virchow JC, Zangrilli J, Weiss S, Korn S. Reslizumab (RES) in patients (pts) with inadequately controlled asthma and elevated blood eosinophils (EOS): analysis of two phase 3, placebo‐controlled trials [OA1797]. European Respiratory Society 26thAnnual Congress; 2016 Sep 3‐7; London. 2016. [Google Scholar]
- Wang B, Yan L, Hutmacher M, Roskos L. Pharmacometrics enabled rational determination of optimal dosing regimen for benralizumab pivotal studies in adults and adolescents with asthma. Clinical Pharmacology and Therapeutics 2015;97:S78. [CENTRAL: 1066945; CRS: 4900126000025854; EMBASE: 71771470] [Google Scholar]
- Wark PA, Hensley MJ, Saltos N, Boyle MJ, Toneguzzi RC, Epid GD, et al. Anti‐inflammatory effect of itraconazole in stable allergic bronchopulmonary aspergillosis: a randomized controlled trial. Journal of Allergy and Clinical Immunology 2003;111(5):952‐7. [] [DOI] [PubMed] [Google Scholar]
- Weinstein SF, Germinaro M, Bardin P, Korn S, Bateman ED. Efficacy of reslizumab with asthma, chronic sinusitis with nasal polyps and elevated blood eosinophils. Journal of Allergy and Clinical Immunology 2016;137(2 SUPPL. 1):AB86. [CENTRAL: 1135290; CRS: 4900132000016805; EMBASE: 72197039] [Google Scholar]
- Wenzel SE, Barnes PJ, Bleecker ER, Bousquet J, Busse W, Dahlén SE, et al. A randomized, double‐blind, placebo‐controlled study of tumor necrosis factor‐alpha blockade in severe persistent asthma. American Journal of Respiratory and Critical Care Medicine 2009;179(7):549‐58. [; 4900100000023441] [DOI] [PubMed] [Google Scholar]
- Wenzel S, Ford L, Pearlman D, Spector S, Sher L, Skobieranda F, et al. Dupilumab in persistent asthma with elevated eosinophil levels. New England Journal of Medicine 2013;368(26):2455‐66. [] [DOI] [PubMed] [Google Scholar]
- Wenzel SE, Pirozzi G, Wang L, Kirkesseli S, Rocklin R, Radin A, et al. Efficacy and safety of SAR231893/REGN668 in patients with moderate‐to‐severe, persistent asthma and elevated eosinophil levels. American Journal of Respiratory and Critical Care Medicine 2013;187(Meeting Abstracts):A6068. [CENTRAL: 870803; CRS: 4900100000087948; EMBASE: 71984701] [Google Scholar]
- Wenzel SE, Teper A, Wang L, Pirozzi G, Radin A, Graham N, et al. ACQ5 improvement with dupilumab in patients with persistent asthma and elevated eosinophil levels: responder analysis from a 12‐week proof‐of‐concept placebo‐controlled trial. American Journal of Respiratory and Critical Care Medicine 2014;189:A1323. [CENTRAL: 1131452; CRS: 4900132000009661; EMBASE: 72043773] [Google Scholar]
- Yan L, Roskos L, Ward CK, She D, Merwe R, Wang B. Pharmacokinetics and pharmacodynamics of benralizumab in subjects with moderate‐to‐severe chronic obstructive pulmonary disease. Clinical Pharmacology and Therapeutics 2015;97:S95. [CENTRAL: 1066944; CRS: 4900126000025853; EMBASE: 71771521] [Google Scholar]
- Zetterstrom O, Fagerberg E, Wide L. An investigation of pollen extracts from different deciduous trees in patients with springtime allergy in Sweden. Acta Allergologica 1972;27(1):15‐21. [] [DOI] [PubMed] [Google Scholar]
- Zhu R, Zheng Y, Putnam WS, Visich J, Eisner MD, Matthews JG, et al. Population‐based efficacy modelling of omalizumab in patients with severe allergic asthma inadequately controlled with standard therapy. AAPS Journal 2013;15(2):559‐70. [] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zielen S, Lieb A, Motte S, Wagner F, Monchy J, Fuhr R, et al. Omalizumab protects against allergen‐induced bronchoconstriction in allergic (immunoglobulin E‐mediated) asthma. International Archives of Allergy and Immunology 2013;160(1):102‐10. [] [DOI] [PubMed] [Google Scholar]
References to ongoing studies
- EUCTR2005‐001932‐61‐GB. Mepolizumab and exacerbation frequency in refractory eosinophilic asthma. A randomised, double blind, placebo controlled, parallel group trial. clinicaltrialsregister.eu/ctr‐search/search?query=EUCTR2005‐001932‐61‐GB (first received 16 November 2005).
- NCT01520051. Mepolizumab treatment for rhinovirus‐induced asthma exacerbations (MATERIAL) [The efficacy of mepolizumab treatment on rhinovirus induced asthma exacerbations]. clinicaltrials.gov/show/NCT01520051 (first received 25 January 2012). []
- NCT02452190. Study of reslizumab in patients with uncontrolled asthma and elevated blood eosinophils. clinicaltrials.gov/show/NCT02452190 (first received 13 May 2015). [CRS: 4900132000027647]
- NCT02555371. Cessation versus continuation of long‐term mepolizumab in severe eosinophilic asthma patients. clinicaltrials.gov/show/NCT02555371 (first received 17 September 2015). [CRS: 4900132000027646]
- NCT02594332. Effects of mepolizumab compared to placebo on airway physiology in patients with eosinophilic asthma: MEMORY study (MEMORY). clinicaltrials.gov/show/NCT02594332 (first received 31 August 2015). [CRS: 4900132000027645]
- NCT02821416. Study to evaluate the effect of benralizumab on allergen‐induced inflammation in mild, atopic asthmatics (ARIA). clinicaltrials.gov/show/NCT02821416 (first received 17 June 2016). [CRS: 4900132000027652]
Additional references
- Brusselle GG, Maes T, Bracke KR. Eosinophils in the spotlight: eosinophilic airway inflammation in nonallergic asthma. Nature Medicine 2013;19(8):977‐9. [PUBMED: 23921745] [DOI] [PubMed] [Google Scholar]
- Busse WW, Katial R, Gossage D, Sari S, Wang B, Kolbeck R, et al. Safety profile, pharmacokinetics, and biologic activity of MEDI‐563, an anti‐IL‐5 receptor alpha antibody, in a phase I study of subjects with mild asthma. Journal of Allergy and Clinical Immunology 2010;125(6):1237‐1244.e2. [PUBMED: 20513521] [DOI] [PubMed] [Google Scholar]
- Cabon Y, Molinari N, Marin G, Vachier I, Gamez AS, Chanez P, et al. Comparison of anti‐interleukin‐5 therapies in patients with severe asthma: global and indirect meta‐analyses of randomized placebo‐controlled trials. Clinical and Experimental Allergy 2017;47(1):129‐38. [PUBMED: 27859832] [DOI] [PubMed] [Google Scholar]
- Chung KF. Targeting the interleukin pathway in the treatment of asthma. Lancet 2015;386(9998):1086‐96. [PUBMED: 26383000] [DOI] [PubMed] [Google Scholar]
- Custovic A, Johnston SL, Pavord I, Gaga M, Fabbri L, Bel EH, et al. EAACI position statement on asthma exacerbations and severe asthma. Allergy 2013;68(12):1520‐31. [PUBMED: 24410781] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enright PL, Beck KC, Sherrill DL. Repeatability of spirometry in 18,000 adult patients. American Journal of Respiratory and Critical Care Medicine 2004;169(2):235‐8. [PUBMED: 14604836] [DOI] [PubMed] [Google Scholar]
- Farooqui N, Khan BQ, Wan JY, Lieberman P. Blood eosinophils as markers of inflammation in asthma. Annals of Allergy, Asthma, and Immunology 2009;103(5):A56. [Google Scholar]
- Global Initiative for Asthma (GINA). Global Initiative for Asthma. Global Strategy for Asthma Management and Prevention, 2017. www.ginasthma.org2017.
- McMaster university (developed by Evidence Prime). GRADEpro GDT. Version accessed March 2017. Hamilton (ON): McMaster university (developed by Evidence Prime), 2015.
- Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analyses. BMJ 2003;327:557‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins JPT, Altman DG, Sterne JAC (editors). Chapter 8: Assessing risk of bias in included studies. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
- Humbert M, Corrigan CJ, Kimmitt P, Till SJ, Kay AB, Durham SR. Relationship between IL‐4 and IL‐5 mRNA expression and disease severity in atopic asthma. American Journal of Respiratory and Critical Care Medicine 1997;156(3 Pt 1):704‐8. [PUBMED: 9309982] [DOI] [PubMed] [Google Scholar]
- Jatakanon A, Lim S, Barnes PJ. Changes in sputum eosinophils predict loss of asthma control. American Journal of Respiratory and Critical Care Medicine 2000;161(1):64‐72. [PUBMED: 10619799] [DOI] [PubMed] [Google Scholar]
- Jones PW, Quirk FH, Baveystock CM. The St George's Respiratory Questionnaire. Respiratory Medicine 1991;85:25‐31. [DOI] [PubMed] [Google Scholar]
- Juniper EF, Guyatt GH, Epstein RS, Ferrie PJ, Jaeschke R, Hiller TK. Evaluation of impairment of health related quality of life in asthma: development of a questionnaire for use in clinical trials. Thorax 1992;47(2):76‐83. [PUBMED: 1549827] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Juniper EF, O'Byrne PM, Guyatt GH, Ferrie PJ, King DR. Development and validation of a questionnaire to measure asthma control. The European Respiratory Journal 1999;14(4):902‐7. [PUBMED: 10573240] [DOI] [PubMed] [Google Scholar]
- Kay AB. The early history of the eosinophil. Clinical and Experimental Allergy 2015;45(3):575‐82. [PUBMED: 25544991] [DOI] [PubMed] [Google Scholar]
- Kolbeck R, Kozhich A, Koike M, Peng L, Andersson CK, Damschroder MM, et al. MEDI‐563, a humanized anti‐IL‐5 receptor alpha mAb with enhanced antibody‐dependent cell‐mediated cytotoxicity function. Journal of Allergy and Clinical Immunology 2010;125(6):1344‐1353.e2. [PUBMED: 20513525] [DOI] [PubMed] [Google Scholar]
- Li J, Wang F, Lin C, Du J, Xiao B, Du C, et al. The efficacy and safety of reslizumab for inadequately controlled asthma with elevated blood eosinophil counts: a systematic review and meta‐analysis. Journal of Asthma 2017;54(3):300‐7. [PUBMED: 27435534] [DOI] [PubMed] [Google Scholar]
- Liu Y, Zhang S, Li DW, Jiang S‐J. Efficacy of anti‐interleukin‐5 therapy with mepolizumab in patients with asthma: a meta‐analysis of randomized placebo‐controlled trials. PLoS One 2013;8(3):e59872. [DOI: 10.1371/journal.pone.0059872] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez AF, Begley CG, Williamson DJ, Warren DJ, Vadas MA, Sanderson CJ. Murine eosinophil differentiation factor. An eosinophil‐specific colony‐stimulating factor with activity for human cells. Journal of Experimental Medicine 1986;163(5):1085‐99. [PUBMED: 3486243] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group (2009). Preferred Reporting Items for Systematic Reviews and Meta‐Analyses: The PRISMA Statement. PLoS Medicine 6;7:e1000097. [DOI: 10.1371/journal.pmed1000097] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mukherjee M, Stoddart A, Gupta RP, Nwaru BI, Farr A, Heaven M, et al. The epidemiology, healthcare and societal burden and costs of asthma in the UK and its member nations: analyses of standalone and linked national databases. BMC Medicine 2016;14(1):113. [PUBMED: 27568881] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nathan RA, Sorkness CA, Kosinski M, Schatz M, Li JT, Marcus P, et al. Development of the asthma control test: a survey for assessing asthma control. The Journal of Allergy and Clinical Immunology 2004;113(1):59‐65. [PUBMED: 14713908] [DOI] [PubMed] [Google Scholar]
- National Institute for Health and Care Excellence (NICE). Mepolizumab for treating severe refractory eosinophilic asthma. www.nice.org.uk/guidance/ta431 (accessed prior to 20 July 2017).
- Osborne ML, Pedula KL, O'Hollaren M, Ettinger KM, Stibolt T, Buist AS, et al. Assessing future need for acute care in adult asthmatics: the Profile of Asthma Risk Study: a prospective health maintenance organization‐based study. Chest 2007;132(4):1151‐61. [PUBMED: 17573515] [DOI] [PubMed] [Google Scholar]
- Price D, Fletcher M, Molen T. Asthma control and management in 8,000 European patients: the REcognise Asthma and LInk to Symptoms and Experience (REALISE) survey. NPJ Primary Care Respiratory Medicine 2014;24:14009. [PUBMED: 24921985] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reddel HK, Taylor DR, Bateman ED, Boulet LP, Boushey HA, Busse WW, et al. AmericanThoracic Society/European Respiratory Society Task Force on Asthma Control and Exacerbations. An official American Thoracic Society/European Respiratory Society statement: asthma control and exacerbations: standardizing endpoints for clinical asthma trials and clinical practice. American Journal of Respiratory and Critical Care Medicine 2009;180(1):59‐99. [DOI: 10.1164/rccm.200801-060ST; PUBMED: 19535666] [DOI] [PubMed] [Google Scholar]
- Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager 5 (RevMan 5). Version 5.3. Copenhagen: Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
- Schünemann HJ, Oxman AD, Vist GE, Higgins JPT, Deeks JJ, Glasziou P, et al. Chapter 12: Interpreting results and drawing conclusions. In: Higgins JPT, Green S (editors), Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
- Veen IH, Brinke A, Gauw SA, Sterk PJ, Rabe KF, Bel EH. Consistency of sputum eosinophilia in difficult‐to‐treat asthma: a 5‐year follow‐up study. Journal of Allergy and Clinical Immunology 2009;124(3):615‐7, 617.e1‐2. [PUBMED: 19733302] [DOI] [PubMed] [Google Scholar]
- Wang YH, Liu YJ. Thymic stromal lymphopoietin, OX40‐ligand, and interleukin‐25 in allergic responses. Clinical and Experimental Allergy 2009;39(6):798‐806. [PUBMED: 19400908] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang FP, Liu T, Lan Z, Li SY, Mao H. Efficacy and safety of anti‐interleukin‐5 therapy in patients with asthma: a systematic review and meta‐analysis. PloS One 2016;11(11):e0166833. [PUBMED: 27875559] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wenzel SE. Asthma phenotypes: the evolution from clinical to molecular approaches. Nature Medicine 2012;18(5):716‐25. [PUBMED: 22561835] [DOI] [PubMed] [Google Scholar]
- Cruz AA, Mantzouranis E, Matricardi PM, Minelli E, Aït‐Khaled N, Bateman ED, et al. In: Bousquet N, Khaltaev N editor(s). Global Surveillance, Prevention and Control of Chronic Respiratory Diseases. A Comprehensive Approach. Geneva: World Health Organization, 2007. [Google Scholar]
- Woodruff PG, Modrek B, Choy DF, Jia G, Abbas AR, Ellwanger A, et al. T‐helper type 2‐driven inflammation defines major sub phenotypes of asthma. American Journal of Respiratory and Critical Care Medicine 2009;180(5):388‐95. [PUBMED: 19483109] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yancey SW, Ortega HG, Keene ON, Mayer B, Gunsoy NB, Brightling CE, et al. Meta‐analysis of asthma‐related hospitalization in mepolizumab studies of severe eosinophilic asthma. Journal of Allergy and Clinical Immunology 2017;139(4):1167‐1175.e2. [PUBMED: 27726946] [DOI] [PubMed] [Google Scholar]
- Zeiger RS, Schatz M, Dalal AA, Qian L, Chen W, Ngor EW, et al. Utilization and costs of severe uncontrolled asthma in a managed‐care setting. Journal of Allergy and Clinical Immunology 2016;4(1):120‐9.e3. [PUBMED: 26439182] [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
- Powell C, Milan SJ, Dwan K, Walters N. Mepolizumab versus placebo for asthma. Cochrane Database of Systematic Reviews 2013, Issue 11. [DOI: 10.1002/14651858.CD010834] [DOI] [PubMed] [Google Scholar]
- Powell C, Milan SJ, Dwan K, Bax L, Walters N. Mepolizumab versus placebo for asthma. Cochrane Database of Systematic Reviews 2015, Issue 7. [DOI: 10.1002/14651858.CD010834.pub2] [DOI] [PubMed] [Google Scholar]


