Abstract
Adolescents who are particularly sensitive to social stress may be vulnerable to earlier alcohol consumption and related problems. While a small literature supports this contention, previous studies mostly rely on retrospective self-report. The current study used discrete-time survival analysis (DTSA) to test whether real-time social stress responding (via laboratory induction) and social anxiety symptoms predicted 12-month alcohol onset in an alcohol-naïve sample of young female adolescents. Anxiety elicited by the task was expected to predict greater and earlier rates of alcohol incidence, particularly among girls with higher levels of self-reported social anxiety symptoms. Participants were 104 community-recruited girls (12–15 years) who completed a modified Trier Social Stress Test and questionnaires; follow-up calls were conducted at 3-, 6-, 9-, and 12-months after the laboratory visit. Self-reported anxiety was assessed in response to the stressor following acclimation (baseline), instruction (anticipation), and speech (post-task). By 12-months, 30.8% of the sample had consumed a full alcoholic beverage. The DTSA revealed that girls with higher levels of social anxiety and greater elevations in anticipatory (but not post-task) anxiety compared to baseline, had earlier alcohol initiation. This is the first study to examine the role of both laboratory-induced anxious responding and retrospective reports of social anxiety as prospective predictors of alcohol incidence. These preliminary findings suggest that adolescent girls who are more sensitive to social stress may be at risk for experimenting with alcohol earlier than their peers.
Keywords: Adolescent, alcohol incidence, social stress responding, anticipatory anxiety, discrete-time survival analysis (DTSA)
Introduction
The majority of individuals in the US will experiment with alcohol use during adolescence (e.g., ~61% by 12th grade; Miech et al., 2017), making early to middle adolescence key for prospectively studying the equifinality of initial alcohol use and subsequent risk. Adolescent alcohol use is linked to extensive societal costs and personal consequences (e.g., poor health outcomes, poorer academic achievement; Boden & Fergusson, 2011). Some estimates place the cost of underage drinking in the U.S. at $61.9 billion annually, including $34.7 billion related to violent crime and $13.7 billion to traffic accidents (Miller, Levy, Spicer, & Taylor, 2006). Although underage alcohol use often reflects experimentation related to normative developmental processes (Jessor, 1991; Johnston et al., 2017), the initiation of alcohol use prior to age 16 years is associated with heightened risk for alcohol-related and other substance use problems (Jenkins et al., 2011; Wittchen et al., 2008). For instance, drawing from data collected in the National Longitudinal Study of Adolescent Health, Moss, Chen, and Yi (2014) found that adolescents who consumed alcohol prior to 16 years of age were significantly more likely to report daily cigarette smoking, recent binge drinking, prescription and illicit drug misuse (e.g., methamphetamine) in young adulthood (ages 24–32 years) as compared to those who had not yet consumed alcohol. Similarly, in a large sample of twin girls, participants who reported initial use prior to age 16 were over 3 times as likely to develop an alcohol use disorder (AUD) by age 30, with 32.9% of early users meeting AUD criteria as compared to 12% of those who reported initiation later in life (Jenkins et al., 2011). These findings suggest that initial alcohol use in adolescence (particularly before age 16) may pose a risk for the development of later alcohol related problems.
Although much of the literature has focused on externalizing pathways to adolescent substance use, a small but growing body of work has begun to highlight the importance of internalizing pathways (Hussong et al., 2011) and maladaptive social stress responding in particular (Battista, Stewart, & Ham, 2010). This literature presents mixed findings, supporting positive, negative, and null associations between internalizing symptoms and stress responses with alcohol use indices (e.g., Battista et al., 2010; Colder et al., 2013; Fröjd, Ranta, Kaltiala-Heino, & Marttunen, 2011). One potential explanation for these inconsistent findings is that heterogeneity in internalizing symptoms, when broadly defined to include all depression and anxiety symptoms, may be masking divergent associations with specific symptom clusters (e.g., social anxiety versus separation anxiety; Buckner et al., 2008; Marmorstein et al., 2010). This suggests there may be utility in focusing on specific symptom clusters, rather than general internalizing symptoms. Social anxiety and related social stress may be particularly important for understanding adolescent alcohol use. Adolescence is a period of increased sensitivity to social rewards and susceptibility to peer influence, and adolescent drinking commonly occurs in the context of peers (e.g., Anderson & Brown, 2011; Steinberg, 2007). Although social anxiety is not consistently associated with use frequency, with some notable exceptions (Tomlinson & Brown, 2012), elevated social fears, including social anxiety disorder, relate to problematic alcohol use among both adolescents and adults (Blumenthal, Leen-Feldner, Badour, & Babson, 2011; Buckner, Heimberg, Ecker, & Vinci, 2013; Buckner & Schmidt, 2009). While these findings suggest that sensitivity to social stressors are associated with greater alcohol use related problems, the inconsistent associations with use frequency (e.g., Keough, Badawi, Nitka, O’Connor, & Stewart, 2016) make it difficult to explain how these patterns emerge. Of note, the majority of this literature relies solely on retrospective report of anxiety symptoms which are subject to several biases (e.g., recall biases, introspective accuracy).
Experimental psychopathology techniques that incorporate real-time assessments can be used to maximize internal validity and minimize common biases of retrospective self-reports (Zvolensky, Lejuez, Stuart, & Curtin, 2001). Indeed, to circumvent potential biases, research conducted with adults has used real-time, laboratory-based tasks and assessments in the examination of acute social stress (e.g., giving an impromptu speech) and alcohol relevant responses (e.g., sensory bias, reported craving, self-administration; Battista et al., 2010). Several studies have found that anxiety elicited by laboratory-induced social stress is positively correlated with alcohol craving and consumption among heavy drinking (Field & Powell, 2007; Nesic & Duka, 2006) and socially drinking adults (de Wit, Sӧderpalm, Nikolayev, & Young, 2003; Magrys & Olmstead, 2015), and that the relation is especially pronounced among adults with relevant internalizing problems (e.g., social anxiety disorder; Abrams, Kushner, Medina, & Voight, 2002). Further, individuals with a current AUD have been found to respond more strongly to an evaluative speech task than those presenting with past AUD or no AUD history (Starcke, Holst, Brink, Veltman, & Goudriaan, 2013). Lastly, in the one laboratory study to date conducted with adolescents (ages 14–17 years; recent alcohol consumption), symptoms of social anxiety were positively correlated with the acute desire to drink following introduction to the novel, socially-relevant laboratory protocol (Blumenthal, Ham, Cloutier, Bacon, & Douglas, 2016). While these findings suggest current drinkers may be prone to consume alcohol in new, potentially stressful social contexts, it is unclear as to whether sensitivity to social stress might also be related to risk of early initial alcohol use among alcohol-naïve youth.
Finally, based on historical data indicating elevated alcohol use and disorder prevalence among men as compared to women, the majority of work has targeted adult men and boys (Nolen-Hoeksema & Hilt, 2006; Schulte, Ramo, & Brown, 2009). However, in the past two decades, the gender gap in alcohol use has begun to close. In fact, recent national data indicate that prior drinking, recent drinking, and past year AUD prevalence are now higher among adolescent girls than boys (CDC, 2016; Forman-Hoffman, Edlund, Glasheen, & Ridenour, 2017; Miech et al., 2017; Perou et al., 2013). Further, young women evidence greater immediate risk of alcohol-related problems and injury (Stockwell et al., 2002), as well as a faster transition from use to disorder as compared to men (Diehl et al., 2007; Johnson, Richter, Kleber, McLellan, & Carise, 2005). A growing body of work details differential structural and functional neuro-correlates of AUD among adult and adolescent women, suggesting not only distinct but elevated risk for the neurotoxic effects of alcohol among women (Caldwell et al., 2005; Medina et al., 2008). Collectively, sex-specific differences in risk and consequences of use, alongside an underrepresentation of women in this literature (Foster et al., 2014) and greater rates of social anxiety disorder diagnoses in girls (Merikangas et al., 2011) emphasize the need for research examining markers, processes, and outcomes among adolescent girls specifically (Brady & Randall, 1999; Medina et al., 2008).
The Current Study
Early alcohol use initiation (before age 16) poses significant risk for experiencing problems in adulthood, particularly among female adolescents; therefore, it is critical to obtain a better understanding of the processes that may underlie early alcohol use. When paired with longitudinal designs, laboratory analogues can be used to establish the temporal ordering of co-occurring phenomenon (e.g., social anxiety and AUD) and provide enhanced sensitivity to prodromal symptoms (e.g., preclinical social anxiety; Zvolensky et al., 2001). To date, several laboratory studies with adults and at least one study with adolescents suggest that elevated social stress responses may lead to increased alcohol use among current drinkers. The present study seeks to build upon this work by examining whether alterations in stress responding might precede initial alcohol use among adolescents.
Specifically, the current study tests whether real-time social stress responding (elicited in the laboratory) would predict 12-month alcohol incidence in an alcohol-naïve sample of young female adolescents using discrete-time survival analysis (DTSA). It was expected that anxiety elicited by the task would positively relate to initiation of alcohol use over the following 12month period. Individuals with higher levels of social anxiety symptoms more generally are known to be particularly sensitive to social stressors and may therefore be more likely to initiate alcohol use as a means of coping with their acute anxiety. Accordingly, we also tested the potential interactions of trait level social anxiety symptoms with anxious reactivity to the task as predictors of alcohol incidence. Given their noted history with alcohol incidence, age, ethnicity, and race were considered as potential covariates (Forman-Hoffman et al., 2017). Though alcohol-naivety was considered ‘never consuming a full alcoholic beverage’, there is recent evidence to suggest that youth often try small amounts of alcohol months or years before consuming a full alcoholic beverage (Colder, Shyhalla, & Frndak, 2018). Therefore, in the current study, baseline alcohol sipping history was included as a statistical control variable.
Method
Participants
Participants were drawn from a larger laboratory-based investigation on pubertal development and emotional vulnerability among community-recruited girls between the ages of 12 and 15 years (N = 138). Recruitment for this project ran concurrently with a second project screening for adolescent boys and girls (ages 14–17 years) who consumed a full alcoholic beverage within the past year (Blumenthal, Cloutier, Douglas, Kearns, & Carey, 2018). Because participants could not participate in both studies, the current sample is comprised of alcohol-naïve girls or girls who have never consumed a full standard alcoholic beverage at screening (n = 119). Following the initial laboratory component, participants completed telephone follow-up interviews for one year at three-month intervals, retention rates (from baseline) were 82.6% (3months), 71.0% (6-months), 62.3% (9-months), and 53.6% (12-months).
The current analyses include only girls who reported no lifetime alcohol use or less than a full standard alcoholic beverage at baseline and had complete data on the primary baseline variables (i.e., scores on all three Subjective Units of Distress Scale anxiety assessments and the Revised Child Anxiety and Depression Scale social anxiety subscale) as well as on at least one follow-up call. Thus, the final sample includes 104 early adolescent girls with a mean age of 13.9 years at baseline. The racial composition of the final sample was comparable to that of the local community (Denton County, TX; U.S. Census Bureau, 2016): 65.7% Caucasian, 11.4% African American, 3.8% Asian, 2.9% Native American, 15.2% multi-racial, and 1.0% “other”. However, the proportion of Hispanics/Latinos was slightly lower (14.0%) than that of the local community (19.2%; Denton County, TX; U.S. Census Bureau, 2016). A series of independent samples t-tests and chi-square tests with baseline data indicated that there were no statistically significant differences in attrition or selection rates by age, SA symptoms, stress responsivity, ethnicity, race, or sipping status.
Measures and Task
Alcohol Use.
Participants were asked about their alcohol use at initial screening, during the laboratory visit, and through telephone interviews 3, 6, 9, and 12 months following the laboratory appointment.
Baseline alcohol use/Sipping at baseline.
At initial screening participants were asked “Have you ever consumed an alcoholic beverage, even just one or two sips?”. If any alcohol use was endorsed, participants were asked to indicate whether they had consumed a full alcoholic beverage. Only participants who reported never consuming more than a few sips at the initial telephone screening were included in the current study. To control for sipping history, all screening responses were treated as a dichotomous variable such that 0 reflects ‘no alcohol use’ and 1 reflects ‘endorsed sipping’.
For 27 of 109 cases telephone screening data was not available (i.e. ages 12–13 years; drinking status not assessed at screening for those under age 14) but otherwise had complete baseline and follow-up data. To retain these cases and maintain statistical power, data from the Adolescent Alcohol and Drug Involvement Scale (AADIS; Moberg, 2000) administered in the laboratory was used to infer use history. Specifically, the alcohol item asks how often participants have used alcohol but does not confirm whether positive endorsements refer to full alcoholic beverages or just a few sips. Most participant responses from the laboratory assessment reflected no lifetime alcohol use (n = 22) which was coded as 0 for ‘no alcohol use’ on the sipping variable. However, the five cases that endorsed trying alcohol ‘once or twice’ were excluded resulting in a final sample of 104.
12-month alcohol use.
During the follow-up calls participants reported on their alcohol use frequency via the Adolescent Alcohol and Drug Involvement Scale (AADIS; Moberg, 2000; Moberg & Hahn, 1991). The AADIS was administered in an interview format with a trained research assistant who would read the instructions, list the substance (i.e., alcohol), and each of the response items. Participants are asked to select a single response that best reflects how often they use alcohol on a scale of 0 (never used) to 7 (several times a day). Each response point is accompanied by a written descriptor, and higher numbers reflect increased frequency of use (e.g., 2 = several times a year; 3 = several times a month). If endorsed, research assistants confirmed that participants had consumed a full alcoholic beverage (i.e., not just sips). For the current analyses, responses were dichotomized such that reporting ‘never used’ or ‘sips only’ by 12 months was coded as a ‘0,’ and any other positive endorsement at any follow-up call was coded as a ‘1’ so long as the endorsement included full alcoholic beverages. The AADIS is a face-valid scale that has been shown to strongly correspond with clinical assessments of use patterns (i.e. non-use, abuse, dependence; Moberg & Hahn, 1991) and has been successfully employed in prior work examining substance use in similar community-based samples of adolescents (e.g., Blumenthal, Leen-Feldner, Frala, Badour, & Ham, 2010).
Social anxiety.
The Revised Child Anxiety and Depression Scale - Social phobia subscale (RCADS-SA; Chorpita, Yim, Moffitt, Umemoto, & Francis, 2000) was used as a continuous measure of typical, or trait-like, SA symptoms. This 9-item self-report subscale includes items such as “I am afraid of looking foolish in front of other people” and “I worry about what others think of me,” which participants rate on a four-point Likert-type scale (0 = never, 1 = sometimes, 2 = often, and 3 = always) as to how often each statement reflects how they typically feel. Responses are summed to create a total SA score. The RCADS evidences sound psychometric properties, demonstrating convergent validity with existing measures of childhood anxiety and anxiety disorders, test-retest reliability (SA test-retest coefficient=.80), as well as internal consistency (e.g., current sample Cronbach’s alpha [α] = .86; Chorpita et al., 2000). The RCADS also has been used in other studies of adolescent social anxiety and substance use (e.g., Cloutier, Mischel, & Blumenthal, 2016).
Social stress induction.
Social stress was elicited through the Modified Trier Social Stress Test (TSST-M; Yim, Quas, Cahill, & Hayakawa, 2010). Participants were informed that they would complete a 5-minute speech task for which they should imagine that they were introducing themselves to a new classroom and convincing the class that they would be a good student. Participants also had to include at least one good thing and one bad thing about themselves. They were given 3 minutes to prepare with paper and pencil but were informed that they would not be allowed to use any notes during the actual speech. Participants also were told that researchers would be viewing and evaluating their speech from the adjoining room via the camera located above them. The participants prepared for their speech in private, then after the 3-minute period, a research assistant re-entered the room, instructed the participant to stand up, look directly into a camera, then begin their speech as soon as the researcher left the room and said ‘Go’. Participants then spoke freely; however, if the participant stopped speaking for more than 10 seconds a researcher in the adjoining room would remind the participant to continue speaking. Because the rooms were separated by a doorway, the researcher could provide prompts to the participant without the participant seeing the researcher. If, after several prompts, the participant continued to stop speaking a researcher would ask open-ended questions relevant to their speech. The TSST has a long history of safely and successfully eliciting socially-relevant psychobiological stress among adults, adolescents, and children (Kudielka, Hellhammer, & Kirschbaum, 2007; Yim et al., 2010).
Real-Time Social Stress Response.
Participants self-reported their acute emotional state immediately before task instructions (i.e., baseline), post-instructions/pre-speech (i.e., in anticipation of task), and post-speech via the well-established Subjective Unites of Distress Scale (SUDS; Gotlib, Traill, Montoya, Joormann, & Chang, 2005; Wolpe, 1958). Specifically, a single item measurement of how ‘anxious’ the participant felt was rated on a scale of 0 (Not at all) to 10 (A lot). To create change scores reflecting increases in anxiety in anticipation and immediately following the task, baseline anxiety values were subtracted from the post-instructions/pre-speech anxiety values and post-speech anxiety values, respectively. This resulted in a possible range of – 10 (high baseline anxiety; low anticipatory/post-task anxiety) to 10 (low baseline anxiety; high anticipatory/post-task anxiety).
Procedures
All study procedures were approved by the University Institutional Review Board. Participants were passively recruited from the local community with flyers and information booths at local events. Interested guardians and youth who contacted the laboratory were informed about study procedures. Eligibility (i.e., ages 12–15 years, female sex) was assessed via a brief telephone screener at which point the initial laboratory visit was scheduled. Upon arrival, written guardian consent (for child) and assent was obtained for the lab visit as well as the follow-up calls. Thereafter, youth completed 45 minutes of questionnaires, followed by the baseline SUDS assessment. Participants then completed the social stress task described above as well as a series of interviews and questionnaires unrelated to the current study. At the end of the 2.5hr protocol, participants were fully debriefed and compensated $30 for their time. Participants then scheduled their first, 3-month follow-up call.
Follow-up calls were always scheduled with respect to the period since the laboratory date (e.g., 90 days from lab appointment). When participants did not complete their scheduled call, research assistants were instructed to attempt contact/call completion up to 30 days after their original call date, at which point their call was ‘skipped’ until the next scheduled call (e.g., 180 days from lab appointment) or the participant asked to withdraw from the study. At the completion of each call, participants scheduled their next follow-up call and were mailed $5 for their time.
Data Structure
The raw data were prepared based on recommendations by Muthen and Masyn (2005) so that the Discrete Time Survival Analyses (DTSA) could be modeled in a latent variable framework. A total of four binary time-specific event indicators were constructed to reflect the three-month intervals between the earliest post-lab visit initiation onset (i.e., within 3-months) and the latest post-lab visit initiation onset (i.e., between 9 and 12-months) that was assessed. For ease, the binary time-specific indicators will be referred to by the month of assessment (i.e., 3-, 6-, 9-, and 12-month interview). The participant was considered to have experienced the event of interest in the interval in which they reported drinking at least one full standard alcoholic beverage for the first time. First time endorsements of alcohol use were coded as “1” on the binary time-specific event indicators, prior event indicators were coded as “0” meaning the event had not occurred, and subsequent event indicators were coded as missing since they already experienced the event.
Analytic Approach
Repeated measures ANOVA was conducted as a manipulation check to confirm that anxiety increased in anticipation of the speech and following the speech as compared to baseline. Descriptive statistics were computed for the entire sample and a series of independent samples t-tests (age) and chi-square tests (ethnicity, race, sipping history) were conducted to identify potential baseline differences among girls who initiated alcohol use and those who did not by the 12-month follow-up.
For the primary analyses, the relations between the selected baseline covariates and the alcohol onset outcomes were examined using a series of DTSA with a latent hazard function representing the event time distribution. The discrete-time hazard is the conditional probability that an adolescent will consume her first alcoholic beverage in a time period, given that she did not report alcohol use in previous time periods (Singer & Willett, 2003). The DTSA model provides information on whether the participant consumes an alcoholic beverage (i.e., event occurrence) as well as when it occurs within the assessment period. The survival function is the sample’s cumulative probability of not reporting any alcohol use across the one-year assessment period; in other words, it is the probability of “surviving” through the 12-month follow-up as a non-user (Muthen & Masyn, 2005). This survival function approximates the Cox regression model used in traditional continuous time survival models and is preferred when the data are categorical with fewer than 20 categories (Asparouhov et al., 2006).
Based on the procedures outlined by Muthen and Masyn (2005), the DTSA was modeled as a special case within the latent variable framework in which a single-class latent class analysis corresponded to binary time-specific indicators. First, the constancy of the hazard rate assumption was tested to determine whether changes in the survival rate were constant across time. An unconditional survival model was fit that allowed the hazard rate to vary across the four, binary time-specific event indicators for alcohol incidence. This model was then compared to one that constrained the hazard rate to equality across intervals using a likelihood-ratio test from the model deviance statistics. The hazard assumption is met if the constrained model fits as well as, or better than, the unconstrained model.
Second, the proportionality assumption for each of the predictors and covariates was tested to evaluate whether the effect of each covariate on the latent hazard function was equivalent across time. For each predictor/covariate, a model constraining their effect to equality was compared to a model allowing the variable to vary across time. The proportionality assumption for each variable is met if the constrained models fit as well as, or better than, the unconstrained models.
Third, a multivariate model with all the predictors was estimated such that the latent hazard function (with its 4 binary time-specific event indicators) was regressed on the set of predictors. This model provided estimates for the individual effects of each variable on alcohol incidence as well as the interactions of theoretical interest after controlling for all the other variables in the model. Two separate models are reported which include the main and interaction effects of anticipatory anxiety change scores with RCADS social anxiety symptoms (Model 1) and post-task anxiety change scores with RCADS social anxiety symptoms (Model 2). To increase confidence in the final maximum likelihood values, automatically generated starting values with random perturbations (100 random sets of starting values with 30 full optimizations) were used for all models.
Results
Manipulation Check of the Stressor Task
First, the Repeated Measures ANOVA indicated statistically significant within-subject differences in anxiety (F [2, 206] = 12.946, p < .001, η2p = .112) across time. Specifically, pairwise comparisons confirmed statistically significant increases in anxiety both in anticipation of the speech (M = 4.16, SD = 3.13, p < .001) and following the speech (M = 4.20, SD = 3.11, p < .001) compared to baseline levels (M = 3.15, SD = 2.74).
Demographics & Covariate Selection
Table 1 presents baseline demographic information of the total sample and by overall initiation status. By 12-months, 30.8% of the sample consumed a full alcoholic beverage. Specifically, 13.5% of the sample newly initiated at 3-months, 8.7% newly initiated at 6-months, 3.9% newly initiated at 9-months, and 4.8% newly initiated at 12-months. Adolescents who initiated alcohol use were slightly older (t [101] = −2.69, p = .008) and were more likely to have sipped alcohol (χ2 [1] = 19.13, p < .001) at baseline compared to non-initiators. There were no differences in terms of SA symptoms (t [101] = −1.32, p = .190), ethnicity (χ2 [1] = 0.41, p = .524), race (χ2 [4] = 1.874, p = .759), or grade in school (χ2 [5] = 6.907, p = .228) across initiation groups. Additional t-tests exploring whether individuals who reported a sipping history (compared to those without a sipping history) differed on any of the acute measures of anxiety during the TSST (i.e., baseline, anticipatory, post-task, anticipatory-baseline change scores, post-task – baseline change scores) or RCADS social anxiety were not statistically significant (p’s > .05; data not shown). Based on these initial analyses, the only covariates included in the final model were age and sipping history.
Table 1.
Baseline Demographics
| Total (N = 104) | Never Initiated (n= 72) | Initiated (n = 32) | |
|---|---|---|---|
| Age | 13.95 (0.97) | 13.78 (0.99) | 14.31 (0.82) |
| Social Anxiety Symptoms | 12.70 (6.73) | 12.20 (6.55) | 14.08 (6.97) |
| Anticipatory Anxiety Change Score | 1.01 (2.27) | 0.78 (2.42) | 1.47 (1.90) |
| Post-Task Anxiety Change Score | 1.05 (2.21) | 0.79 (2.32) | 1.50 (1.81) |
| Ethnicity (Hispanic/Latino) | 12.9% | 14.3% | 9.7% |
| Race: | |||
| Caucasian/White | 68.7% | 68.7% | 68.8% |
| African American/Black | 10.1% | 9.0% | 12.5% |
| Asian American | 4.0% | 4.5% | 3.1% |
| Native American | 3.0% | 4.5% | 0.0% |
| Other/Multiracial | 14.1% | 13.4% | 15.6% |
| Year in School: | |||
| 6th Grade | 5.8% | 5.6% | 6.3% |
| 7th Grade | 10.7% | 12.7% | 6.3% |
| 8th Grade | 16.5% | 21.1% | 6.3% |
| 9th Grade | 42.7% | 40.8% | 46.9% |
| 10th Grade | 23.3% | 18.3% | 34.4% |
| Other (Homeschooled) | 1.0% | 1.4% | 0.0% |
| Sipping | 25.2% | 12.7% | 53.1% |
Note. Bolded category values were statistically different p <.05 for initiators and non-initiators.
Discrete Time Survival Analyses
Unconditional Survival Model.
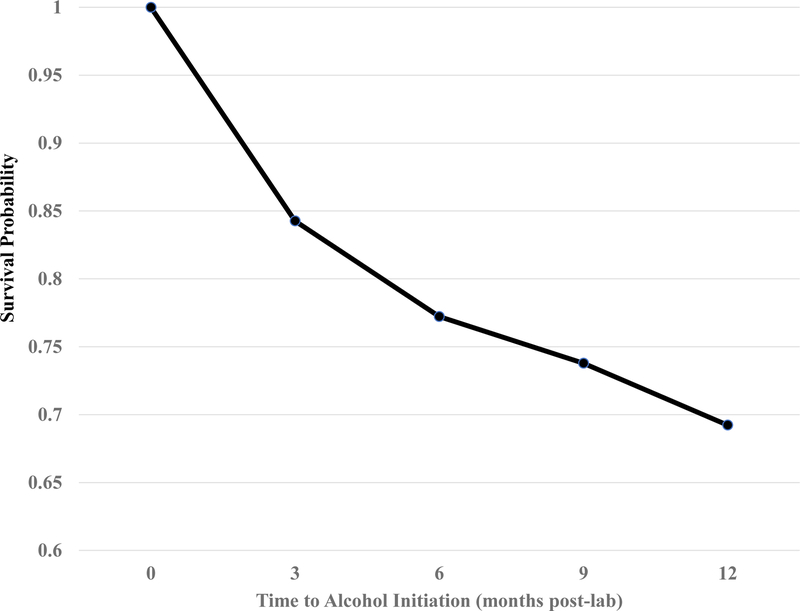
The unconditional hazard function in Figure 1 demonstrates a gradual decrease in rates of “surviving” alcohol onset across the one-year follow-up period. Approximately 69.2% of girls did not report any alcohol use by their final interview. The likelihood ratio test comparing the unconditional hazard model with time-varying hazard rates to one that constrained the hazard rates to equality was not statistically significant, meeting the constancy of the baseline hazard rate assumption. Therefore, the hazard rate function was constrained to equality across all models.
Figure 1-.
Fitted survival probabilities for onset of alcohol use following lab assessment
Univariate Covariate Effects.
None of the likelihood ratio tests comparing the models where the effects of each of the predictor variables on alcohol onset were allowed to vary, against models where the effects were constrained across time, were significant (analyses not shown). Because all the predictor variables met the proportionality assumption, the effect of each predictor was estimated to be proportional across time.
The parameter estimates (i.e., log hazard odds) for the univariate effects of each covariate on the hazard probabilities are listed in Table 2, under the Univariate Effects heading. Three baseline predictors were statistically significant in the expected direction: older age, sipping history, and higher change scores on post-task anxiety from baseline were all associated with increased alcohol onset. Univariate change scores in anticipatory anxiety from baseline were also in the expected direction (p = .06).
Table 2.
Predicting the Hazard Function of Alcohol Onset (n = 104)
| Univariate Effects | Full Model | |||||
|---|---|---|---|---|---|---|
| Est (SE) | t | OR (95%CI) | Est (SE) | t | OR (95%CI) | |
| Model 1- Anticipatory Anxiety | ||||||
| Age | 0.60 (.24) | 2.47 | 1.83 (1.13–2.95) | 0.24 (.27) | 0.88 | 1.26 (0.75–2.14) |
| Any Sipping | 1.87 (.44) | 4.29 | 6.50 (2.77–15.28) | 1.89 (.49) | 3.85 | 6.61 (2.52–17.31) |
| Social Anxiety (SA) | 0.03 (.03) | 0.89 | 1.03 (0.97–1.08) | 0.01 (.03) | 0.21 | 1.01 (0.94–1.08) |
| Antic. Anxiety Δ | 0.14 (.07) | 1.88 | 1.14 (0.99–1.31) | 0.17 (.09) | 1.92 | 1.18 (0.99–1.40) |
| SA x Antic. Anxiety Δ | - | - | - | 0.03 (.01) | 2.17 | 1.03 (1.00–1.05) |
| Model 2- Post-Task Anxiety | ||||||
| Age | 0.60 (.24) | 2.47 | 1.83 (1.13–2.95) | 0.38 (.24) | 1.62 | 1.47 (0.92–2.33) |
| Any Sipping | 1.87 (.44) | 4.29 | 6.50 (2.77–15.28) | 1.77 (.45) | 3.96 | 5.89 (2.45–14.18) |
| Social Anxiety (SA) | 0.03 (.03) | 0.89 | 1.03 (0.97–1.08) | 0.02 (.03) | 0.74 | 1.02 (0.96–1.09) |
| Post-Anxiety Δ | 0.15 (.07) | 2.07 | 1.16 (1.01–1.34) | 0.15 (.09) | 1.72 | 1.17 (0.98–1.39) |
| SA x Post-Anxiety Δ | - | - | - | 0.02 (.01) | 1.83 | 1.02 (0.99–1.05) |
Note. Model 1 tests the interaction of SA and Anticipatory Anxiety as the primary predictor while controlling for main effects and baseline variables; Model 2 tests the interaction of SA and Post-Speech Anxiety as the primary predictor while controlling for main effects and baseline variables. Antic. Anxiety Δ = Anticipatory Anxiety Change Score; calculated by subtracting the baseline report of SUDS Anxiety from Pre-Task SUDS Anxiety. Post-Anxiety Δ = Post-Task Anxiety Change Score; calculated by subtracting the baseline report of SUDS Anxiety from Post-Task SUDS Anxiety.
Multivariate Survival Model.
In Table 2, the log hazard odds for each variable are presented under the Full Model heading. After adjusting for the effects of all other variables, sipping history and the interaction term for change scores in anticipatory anxiety and social anxiety symptoms were statistically significant (p’s < .05). The interaction term between post-task anxiety change scores and social anxiety did not reach the threshold for statistical significance (p = .06).
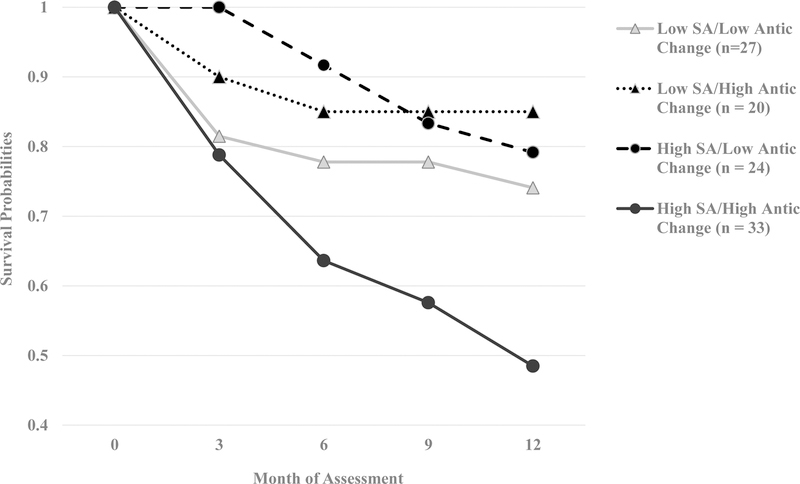
To provide a visual representation of the interaction terms, a series of tables (data not shown) ordering the new alcohol initiations at 3-, 6-, 9-, and 12-months by dichotomized subgroups of the main effect variables were created. Median splits were used to create binary variables for RCADS SA (< 11 vs. 11+), anticipatory anxiety change scores from baseline (< 1 vs. 1+), and post-task anxiety change scores from baseline (< 1 vs. 1+). For both sets of interactions, four subgroups were created, with the survival function calculated for each subgroup individually and graphed across time. Figure 2 shows the rate of alcohol onset (i.e., decreased survival/abstinence rates) across the 4 subgroups formed by crossing high/low categories of SA and anticipatory anxiety change scores from baseline. The only group to not show an immediate decrease in survival at 3-months was the High SA/Low Anticipatory change group (100% survival rate); though they did show a gradual decline at 6-, 9-, and 12-months. Both the Low SA/Low Anticipatory Change and High SA/High Anticipatory Change groups showed immediate sharp declines in survival at 3-month (78 – 82%); however, where the Low SA/Low Anticipatory Change group survival rate appeared to stabilize through the 12-month assessment (74 – 78%), the High SA/High Anticipatory change group continued to decline steadily to ~48% survival rate.
Figure 2-.
Survival probabilities of alcohol onset by social anxiety/anticipatory anxiety change score subgroups.
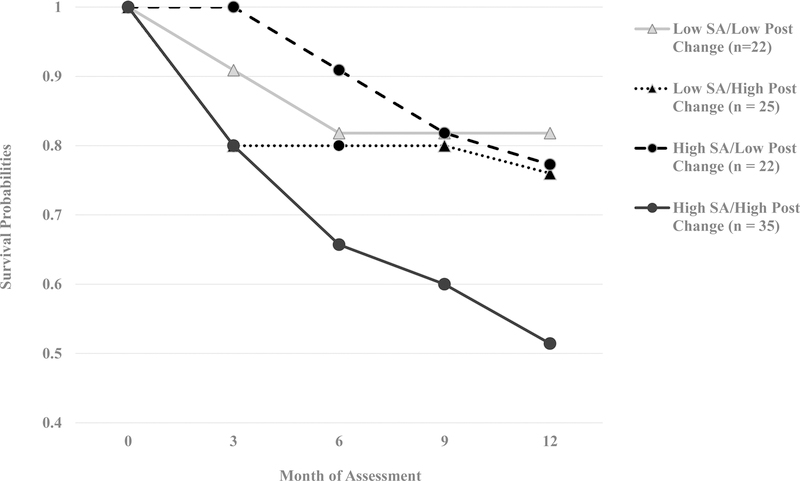
Figure 3 shows the rate of alcohol onset (i.e., decreased survival/abstinence rates) across the 4 subgroups formed by crossing high/low categories of SA and post-task anxiety change scores from baseline. Overall, the findings were similar to the interaction findings between SA and anticipatory anxiety change scores. The only group to not show an immediate decrease in survival at 3-months was the High SA/Low Post-Task Anxiety Change group (100% survival rate); though they did show a gradual decline at 6-, 9-, and 12-months. The Low SA/Low Post-Task Anxiety Change had a decline in survival that was slightly more gradual (e.g., 90% at 3-months) than the corresponding Anticipatory Anxiety change interaction noted above (e.g., 78% at 3-months), though did stabilize again between 6- and 12-months at 82%. The Low SA/High Post-Task Anxiety Change group had a steeper immediate decline in survival (80% at 3-months) than the corresponding anticipatory anxiety interaction noted above (90%), but then stabilized through 12-months. Finally, the High SA/High Post-Task Anxiety Change group evidenced the steepest decline in survival rates starting at 3-months (80%), continuing through 12-months (51%).
Figure 3-.
Survival probabilities of alcohol onset by social anxiety/post-task anxiety change score subgroups.
Discussion
Early alcohol use initiation (before age 16) is often associated with alcohol related problems in adulthood. To date, most studies examining internalizing pathways are limited to retrospective self-report, often of global symptoms. While there is some evidence to suggest sensitivity to social stress is related to acute alcohol desires among current drinkers, whether exaggerated stress responses might precede initial alcohol use and related problems among adolescents is not well understood. The present study sought to build upon the existing literature by testing whether social stress reactivity elicited in the laboratory was related to 12-month incidence of drinking among young female adolescents who never consumed a full alcoholic beverage. Consistent with hypotheses, increased anxiety elicited by the task was associated with greater and earlier rates of alcohol initiation over the following 12-month period. However, this association was only statistically significant in regard to anticipatory anxiety and not post-task anxiety. Girls with elevated anticipatory anxiety and greater levels of retrospectively reported social anxiety symptoms appeared to have the greatest and earliest rates of onset. Findings were robust to the inclusion of age and alcohol sipping history at baseline. Building off a tension-reduction framework, it is possible that the exaggerated responses to a social stressor may be a marker of inadequate coping mechanisms, and therefore risk for alcohol initiation. Indeed, social relationships with peers are a central concern to adolescents (e.g., Steinberg, 2007) – alcohol may be viewed as a means of coping with social stress, which in turn, prompts the initiation of early alcohol use (Kuntsche, Knibbe, Engels, & Gmel, 2007).
Prior research has found that exaggerated stress/anxiety responding is associated with alcohol craving among current drinkers and those with an AUD (e.g., Blumenthal et al., 2016; Starcke et al., 2013). We extend this work by examining the prospective association between laboratory induced social stress/anxiety and alcohol initiation. Theoretical accounts of why internalizing symptoms, such as social stress and anxiety, are associated with alcohol use have been based in large part on self-medication and tension reduction models, proposing that people use alcohol as a means of coping with acute and/or anticipated emotional distress (Khantzian, 1985). Self-medication models have been expanded to include a variety of relevant factors (e.g., genetics, social factors; Buckner et al., 2008; Hussong et al., 2011), and an implicit assumption in this work is that people need to experience the anxiolytic effects of alcohol in order to self-medicate. One interpretation of these models suggests that social stress and anxiety may not be germane to understanding initiation and early experimentation of alcohol use (c.f., heavy use or AUD). In contrast, the present findings suggest that exaggerated anxiety responses to anticipated social stressors may temporally precede alcohol incidence and is involved in the early stages of adolescent drinking.
That this effect was only statistically significant in terms of anticipatory anxiety (c.f., task anxiety) is consistent with several findings in which anticipation of stressors often elicits greater anxiety/stress responses than the experience of the stressor itself (e.g., den Bos, Rooji, Miers, Bokhorst, & Westenberg, 2014; Evans, Greaves-Lord, Euser, Franken, & Huizink, 2012). It may also be important to view anticipatory anxiety through a developmental lens when considering initiation of alcohol use. During adolescence, there is an increase in sensitivity to potentially negative social evaluations (Ollendick & Hirshfeld-Becker, 2002; Westenberg, Drewes, Goedhart, Sieblink, & Treffers, 2004). In a two-year prospective study where children and adolescents (ages 8–17 at baseline) completed two speech tasks, children evidenced the greatest stress responding during the speech whereas adolescents evidenced the greatest response in anticipation of the speech (den Bos et al., 2014). With emerging and shifting expectancies about alcohol in early adolescence (Dunn & Goldman, 2000; Smit et al., 2018), adolescents may initiate alcohol use as a coping strategy (Johnston et al., 2017; Steinberg, 2007) or in an attempt to ‘fit in’ or avoid negative evaluations (Blumenthal et al., 2011; Buckner & Schmidt, 2009).
Of note, the findings somewhat diverge from a significant body of work that argues blunted stress/anxiety reactivity is a precursor to alcohol initiation and problems (e.g., Evans et al., 2012). The underlying argument is that certain individuals are less reactive to their environment, including stressors, therefore, they begin using alcohol as a means of enhancing their internal state (e.g., sensation seeking; Goeders, 2003). Although we found that the Low SA/Low Anticipatory Anxiety Change group evidenced similar drops in survival as the High SA/High Anticipatory Change group at Month 3, their rates of survival plateaued through the 12-month assessment. It is possible that the cross-sectional examinations of blunted stress/anxiety with clinical samples are capturing associations later in the etiological process (i.e., blunted responding develops after alcohol onset). It is also possible that with a longer evaluation period, the Low SA/Low Anticipatory Change group would have caught up with or even surpassed the High SA/High Anticipatory Change group, supporting the equifinality of alcohol-related risk as well as highlighting two distinct high-risk groups for alcohol initiation/later alcohol problems. Nonetheless, as the first study to report these findings, replication is key. In particular, future studies should incorporate specific physiological and subjective measures of stress responding as well as repeated stress task administrations beginning before alcohol initiation (e.g., 12–15 years of age) with sufficient follow-ups to assess changes in both stress responses and various alcohol patterns (e.g., incidence to problematic drinking). While this would require substantially larger samples and more complex analyses to account for normative changes in incidence and progression, such findings would provide clear and comprehensive insight into the underlying physiological and cognitive processes that drive changes in alcohol use.
While measuring internalizing symptomology as anxious reactivity to a social stressor is a novel, methodological strength, we did not include real-time assessments of other internalizing symptoms (e.g., feeling sad). Future researchers should consider the extent to which the findings are specific to anxiety (c.f., internalizing symptoms/negative affect more broadly). The current study also did not include potential covariates from the externalizing domain. Externalizing symptoms and related variables are robust correlates of initiation of adolescent alcohol use, and recent work has highlighted the importance of examining internalizing and externalizing symptoms concurrently (e.g., Colder et al., 2013; Colder et al., 2017; Hussong, Ennett, Cox, & Haroon, 2017). It is possible that the association between anticipatory anxiety and alcohol incidence would be better accounted for by co-occurring externalizing symptoms such as impulsivity or behavioral disruptiveness (Gibbons et al., 2016; Kessler et al., 2006). For example, externalizing behaviors may further moderate the association between acute anxiety symptoms and alcohol incidence (Colder et al., 2017; Keough et al., 2016). Further, recent studies have shown that impulsivity moderates the association between social anxiety symptoms, coping-motivated drinking, and other drinking outcomes which could help explain the lack of main effects for social anxiety in the present study (e.g., Keough et al., 2016). Laboratory tasks that tap into certain aspects of externalizing such as impulsivity (e.g., BART; Lejuez, Aklin, Zvolensky, & Pedulla, 2003; Lejuez et al., 2002) or inattentiveness (e.g., CAARS; Conners, Erhardt, & Sparrow, 1999), may aid in parsing apart these relations. Future researchers should consider additional ways in which externalizing behaviors (e.g., behavioral disruption) might be modeled statistically as well as in laboratory settings. Finally, most of the literature has examined externalizing- and internalizing-type problems as (at least statistically) mutually exclusive; research seeking to understand the additive, interactive, and reinforcing links among behaviors traditionally conceptualized as internalizing or externalizing is needed (e.g., Colder et al., 2013).
In the current study, sipping history was included as a potential covariate based on recent literature indicating that youth begin trying alcohol months, or even years, before consuming their first full alcoholic beverage (Colder et al., 2018). As expected, we found that girls who reported sipping alcohol at baseline were more likely to initiate alcohol use within the following year and at earlier rates than those who did not report any sipping at baseline. While this finding is consistent with the limited work in this area, it is worth noting that the 95% confidence intervals for that variable were fairly large preventing us from drawing any conclusions regarding precisely how strong the effect of sipping behaviors has on alcohol initiation. Notably, wide CI’s generally occur with low-base rate behaviors and small sample sizes. While we are fairly confident that sipping history would lead to earlier rates of alcohol onset, larger epidemiological studies on this new topic area are certainly warranted.
The present study includes several additional limitations that need to be addressed. First, the present study only recruited young adolescent girls as a means of reducing gender biased effects. While these findings contribute to a literature that has historically focused on male-only samples, and there are recent data suggesting minimal gender differences in terms of substance use rates and stress responding (e.g., den Bos et al., 2014; Miech et al., 2017), the lack of male representation in the current study precludes the possibility of directly testing potential gender differences. Males and females may differ in the way they react to stressors, particularly those that are more socially-oriented. Second, a modified version of the Trier Social Stress Task (Yim et al., 2010) was selected as the social stressor, backed by decades of empirical data showing that it effectively elicits both subjective and psychobiological stress responses (Kudielka et al., 2007). However, performance-oriented stressors such as the speech task may not be ideally suited to model real-life stressors that relate to alcohol use, particularly among adolescents. Rejection and peer-evaluation tasks (e.g., Cyberball, Yale Interpersonal Stressor; Stroud, Tanofsky-Kraff, Wilfley, & Salovey, 2000; Williams & Jarvis, 2006) may elicit responses that are more consistent with real-life stressors related to alcohol use. Third, although we statistically controlled for age and early sipping history, there were several additional covariates not assessed and should be considered in future work (e.g., parent/friend substance use; Ennett et al., 2016). Last, although the aim of the current project was focused exclusively on predicting alcohol incidence, there is a wealth of data highlighting adolescence as a period of trying a variety of substances beyond alcohol (e.g., cigarettes, cannabis; Johnston et al., 2017) as well as the role of anxious reactivity in the development of problematic use associated with those substances (Blumenthal et al., 2011). Future work should consider the role of real-time anxious reactivity and social anxiety symptoms as predictors of initiating multiple substances across a longer time frame. Further research is also needed to examine the extent to which real-time anxious reactivity and social anxiety symptoms might predict varying levels of use or use patterns by including continuous measures of alcohol use frequency and additional measures of alcohol-related behaviors/consequences (e.g., Savage et al., 2016).
Together, the current study found that girls who were more sensitive to acute social stress also were more likely to initiate alcohol use in the following year. This is the first study to recruit largely alcohol-naïve youth from the community, collect real-time assessments of reactions to a stressor task, and conduct prospective follow-ups. The current findings support the potential utility of targeting social stress responding and management of such distress in the development of selective intervention efforts. Indeed, despite decades of research, early intervention efforts aimed at reducing adolescent alcohol use incidence and problems evidence mixed findings (e.g., Cuijpers, 2002; Sandler et al., 2014). Some of the most consistent, promising data emerge from selective intervention efforts built upon preclinical work identifying risk markers and factors (e.g., high anxiety sensitivity) and related mechanisms (e.g., coping with acute distress). For example, the PreVenture program tailors intervention modules to match one of four identified risk factors (i.e. anxiety sensitivity, hopelessness, impulsivity, sensation seeking) to reduce rates of alcohol initiation and risky-drinking behavior among adolescents (e.g., binge drinking; Conrod, Stewart, Comeau, & Maclean, 2006; Conrod et al., 2013). Consistent with the development and testing of this program, continued efforts aimed at clarifying the nature and boundaries of the social anxiety-alcohol use risk link will aid in further refining such targeted intervention. It is important to note that no other studies to date have examined the role of acute social stress responses and subsequent alcohol initiation among adolescents, therefore replication of these initial effects as well as work targeting moderators (e.g., use expectancies; coping styles; peer affiliation) and mediators (e.g., use willingness) of this association is needed (Anderson et al., 2014; Fromme & D’Amico, 2000). Additional research pairing a range of real-time assessments (e.g., laboratory stressors, ecological momentary assessment) with prospective follow-ups is needed, particularly with adolescent samples.
Acknowledgments
The first author was partially supported by a National Institute on Drug Abuse National Research Service Award (1F31DA041105) during the writing of this manuscript. The authors have no conflicts of interest to declare. The authors would like to thank Dr. Craig Colder for his thoughtful review of earlier drafts of this manuscript.
Footnotes
This paper has not been, nor will be, published by any other journal and is not under consideration for publication elsewhere. Earlier versions of the ideas and data appearing in this manuscript were presented at poster sessions at the Collaborative Perspectives on Addiction Conference (2016) and Research Society on Alcoholism Meeting (2018).
Contributor Information
Renee M. Cloutier, University of North Texas
Heidemarie Blumenthal, University of North Texas.
Ryan S. Trim, University of California San Diego
Megan E. Douglas, University of North Texas
Kristen G. Anderson, Reed College
References
- Abrams K, Kushner MG, Medina KL, & Voight A (2002). Self-administration of alcohol before and after a public speaking challenge by individuals with social phobia. Psychology of Addictive Behaviors, 16(2), 121. [PubMed] [Google Scholar]
- Anderson KG, Brackenbury L, Quackenbush M, Buras M, Brown SA, & Price J (2014). A-SIDE: Video simulation of teen alcohol and marijuana use contexts. Journal of Studies on Alcohol and Drugs, 75(6), 953–957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson KG & Brown SA (2011). Middle school drinking: Who, where and when. Journal of Child and Adolescent Substance Abuse, 20(1), 48–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asparouhov T, Masyn K, & Muthen B (2006, August). Continuous time survival in latent variable models. In Proceedings of the Joint Statistical Meeting in Seattle (pp. 180–187). [Google Scholar]
- Battista SR, Stewart SH, & Ham LS (2010). A critical review of laboratory-based studies examining the relationships of social anxiety and alcohol intake. Current Drug Abuse Reviews, 3(1), 3–22. [DOI] [PubMed] [Google Scholar]
- Blumenthal H, Cloutier RM, Douglas ME, Kearns NT, & Carey C (2018). The desire to drink as a function of laboratory-induced social stress among adolescents Manuscript under Review. [DOI] [PMC free article] [PubMed]
- Blumenthal H, Ham LS, Cloutier RM, Bacon AK, & Douglas ME (2016). Social anxiety, disengagement coping, and alcohol-use behaviors among adolescents. Anxiety, Stress, & Coping, 29(4), 432–446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blumenthal H, Leen-Feldner EW, Badour CL, & Babson KA (2011). Anxiety psychopathology and alcohol use among adolescents: A critical review of the empirical literature and recommendations for future research. Journal of Experimental Psychopathology, 2(3), 318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blumenthal H, Leen-Feldner EW, Frala JL, Badour CL, & Ham LS (2010). Social anxiety and motives for alcohol use among adolescents. Psychology of Addictive Behaviors, 24(3), 529–534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brady KT, & Randall CL (1999). Gender differences in substance use disorders. Psychiatric Clinics, 22(2), 241–252. [DOI] [PubMed] [Google Scholar]
- Buckner JD, Heimberg RG, Ecker AH, & Vinci C (2013). A biopsychosocial model of social anxiety and substance use. Depression and Anxiety, 30(3), 276–284. [DOI] [PubMed] [Google Scholar]
- Buckner JD, & Schmidt NB (2009). Understanding social anxiety as a risk for alcohol use disorders: Fear of scrutiny, not social interaction fears, prospectively predicts alcohol use disorders. Journal of Psychiatric Research, 43(4), 477–483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boden JM, & Fergusson DM (2011). The short and long term consequences of adolescent alcohol use. Young People and Alcohol: Impact, Policy, Prevention and Treatment, 32–46.
- Buckner JD, Schmidt NB, Lang AR, Small JW, Schlauch RC, & Lewinsohn PM (2008). Specificity of social anxiety disorder as a risk factor for alcohol and cannabis dependence. Journal of Psychiatric Research, 42(3), 230–239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caldwell LC, Schweinsburg AD, Nagel BJ, Barlett VC, Brown SA, & Tapert SF (2005). Gender and adolescent alcohol use disorders on BOLD (blood oxygen level dependent) response to spatial working memory. Alcohol and Alcoholism, 40(3), 194–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control (CDC;2016) Youth Risk Behavior Surveillance — United States, 2015. MMWR Surveillance Summaries 65(6):1–174. 10.15585/mmwr.ss6506a1. [DOI] [PubMed] [Google Scholar]
- Chorpita BF, Yim L, Moffitt C, Umemoto LA, & Francis SE (2000). Assessment of symptoms of DSM-IV anxiety and depression in children: A revised child anxiety and depression scale. Behaviour Research and Therapy, 38(8), 835–855. [DOI] [PubMed] [Google Scholar]
- Cloutier RM, Blumenthal H, & Mischel ER (2016). An examination of social anxiety in marijuana and cigarette use motives among adolescents. Substance Use & Misuse, 51(3), 408–418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colder CR, Scalco M, Trucco EM, Read JP, Lengua LJ, Wieczorek WF, & Hawk LW (2013). Prospective associations of internalizing and externalizing problems and their co-occurrence with early adolescent substance use. Journal of Abnormal Child Psychology, 41(4), 667–677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colder CR, Shyhalla K, & Frndak SE (2018). Early alcohol use with parental permission: psychosocial characteristics and drinking in late adolescence. Addictive Behaviors, 76, 82–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colder CR, Shyhalla K, Frndak S, Read JP, Lengua LJ, Hawk LW, & Wieczorek WF (2017). The prospective association between internalizing symptoms and adolescent alcohol involvement and the moderating role of age and externalizing symptoms. Alcoholism: Clinical and Experimental Research, 41(12), 2185–2196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conners CK, Erhardt D, Sparrow EP Conners’ Adult ADHD Rating Scales (CAARS; 1999) Multi-Health Systems, North Tonawanda; 1999. [Google Scholar]
- Conrod PJ, Stewart SH, Comeau N, & Maclean AM (2006). Efficacy of cognitive–behavioral interventions targeting personality risk factors for youth alcohol misuse. Journal of Clinical Child & Adolescent Psychology, 35, 550–563. 10.1207/s15374424jccp3504_6 [DOI] [PubMed] [Google Scholar]
- Conrod PJ, O’Leary-Barrett M, Newton N, Topper L, Castellanos-Ryan N, Mackie C, & Girard A (2013). Effectiveness of a selective, personality-targeted prevention program for adolescent alcohol use and misuse: a cluster randomized controlled trial. JAMA Psychiatry, 70, 334–342. 10.1001/jamapsychiatry.2013.651 [DOI] [PubMed] [Google Scholar]
- Cuijpers P (2002). Effective ingredients of school-based drug prevention programs: A systematic review. Addictive Behaviors, 27, 1009–1023. 10.1016/S0306-4603(02)00295-2 [DOI] [PubMed] [Google Scholar]
- de Wit H, Söderpalm AH, Nikolayev L, & Young E (2003). Effects of acute social stress on alcohol consumption in healthy subjects. Alcoholism: Clinical and Experimental Research, 27(8), 1270–1277. [DOI] [PubMed] [Google Scholar]
- den Bos E, Rooij M, Miers AC, Bokhorst CL, & Westenberg PM (2014). Adolescents’ increasing stress response to social evaluation: Pubertal effects on cortisol and alpha- amylase during public speaking. Child Development, 85(1), 220–236. [DOI] [PubMed] [Google Scholar]
- Dunn ME, & Goldman MS (2000). Validation of multidimensional scaling-based modeling of alcohol expectancies in memory: Age and drinking-related differences in expectancies of children assessed as first associates. Alcoholism: Clinical and Experimental Research, 24(11), 1639–1646. [PubMed] [Google Scholar]
- Diehl A, Croissant B, Batra A, Mundle G, Nakovics H, & Mann K (2007). Alcoholism in women: is it different in onset and outcome compared to men?. European Archives of Psychiatry and Clinical Neuroscience, 257(6), 344–351. [DOI] [PubMed] [Google Scholar]
- Ennett ST, Jackson C, Cole VT, Haws S, Foshee VA, Reyes HLM, … & Cai L (2016). A multidimensional model of mothers’ perceptions of parent alcohol socialization and adolescent alcohol misuse. Psychology of Addictive Behaviors, 30(1), 18–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans BE, Greaves-Lord K, Euser AS, Franken IH, & Huizink AC (2012). The relation between hypothalamic–pituitary–adrenal (HPA) axis activity and age of onset of alcohol use. Addiction, 107(2), 312–322. [DOI] [PubMed] [Google Scholar]
- Field M, & Powell H (2007). Stress increases attentional bias for alcohol cues in social drinkers who drink to cope. Alcohol and Alcoholism, 42(6), 560–566. [DOI] [PubMed] [Google Scholar]
- Forman-Hoffman VL, Edlund M, Glasheen C, & Ridenour T (2017). Alcohol initiation and progression to use, heavy episodic use, and Alcohol Use Disorder among young adolescents ages 12–14 living in US households. Journal of Studies on Alcohol and Drugs, 78(6), 853–860. [DOI] [PubMed] [Google Scholar]
- Foster KT, Hicks BM, Iacono WG, & McGue M (2014). Alcohol use disorder in women: Risks and consequences of an adolescent onset and persistent course. Psychology of Addictive Behaviors, 28(2), 322–335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fröjd S, Ranta K, Kaltiala-Heino R, & Marttunen M (2011). Associations of social phobia and general anxiety with alcohol and drug use in a community sample of adolescents. Alcohol and Alcoholism, 46(2), 192–199. [DOI] [PubMed] [Google Scholar]
- Fromme K, & D’amico EJ (2000). Measuring adolescent alcohol outcome expectancies. Psychology of Addictive Behaviors, 14(2), 206–212. [DOI] [PubMed] [Google Scholar]
- Gibbons FX, Kingsbury JH, Wills TA, Finneran SD, Dal Cin S, & Gerrard M (2016). Impulsivity moderates the effects of movie alcohol portrayals on adolescents’ willingness to drink. Psychology of Addictive Behaviors, 30(3), 325–334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gotlib IH, Traill SK, Montoya RL, Joormann J, & Chang K (2005). Attention and memory biases in the offspring of parents with bipolar disorder: indications from a pilot study. Journal of Child Psychology and Psychiatry, 46(1), 84–93. [DOI] [PubMed] [Google Scholar]
- Goeders NE (2003). The impact of stress on addiction. European Neuropsychopharmacology, 13(6), 435–441. [DOI] [PubMed] [Google Scholar]
- Hussong AM, Ennett ST, Cox MJ, & Haroon M (2017). A systematic review of the unique prospective association of negative affect symptoms and adolescent substance use controlling for externalizing symptoms. Psychology of Addictive Behaviors, 31(2), 137–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hussong AM, Jones DJ, Stein GL, Baucom DH, & Boeding S (2011). An internalizing pathway to alcohol use and disorder. Psychology of Addictive Behaviors, 25(3), 390–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jenkins MB, Agrawal A, Lynskey MT, Nelson EC, Madden PA, Bucholz KK, & Heath AC (2011). Correlates of alcohol abuse/dependence in early- onset alcohol- using women. The American Journal on Addictions, 20(5), 429–434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jessor R (1991). Risk behavior in adolescence: A psychosocial framework for understanding and action. Journal of Adolescent Health, 12(8), 597–605. [DOI] [PubMed] [Google Scholar]
- Johnson PB, Richter L, Kleber HD, McLellan AT, & Carise D (2005). Telescoping of drinking-related behaviors: Gender, racial/ethnic, and age comparisons. Substance Use & Misuse, 40(8), 1139–1151. 10.1081/JA-200042281 [DOI] [PubMed] [Google Scholar]
- Johnston LD, O’Malley PM, Miech RA, Bachman JG, & Schulenberg JE 2017. Monitoring the Future national survey results on drug use, 1975–2016: Overview, key findings on adolescent drug use Ann Arbor, Michigan: Institute for Social Research, The University of Michigan. [Google Scholar]
- Keough MT, Badawi G, Nitka D, O’Connor RM, & Stewart SH (2016). Impulsivity increases risk for coping-motivated drinking in undergraduates with elevated social anxiety. Personality and Individual Differences, 88, 45–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Adler L, Barkley R, Biederman J, Conners CK, Demler O, … & Spencer T (2006). The prevalence and correlates of adult ADHD in the United States: results from the National Comorbidity Survey Replication. American Journal of Psychiatry, 163(4), 716–723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khantzian EJ (1985). The self-medication hypothesis of addictive disorders: focus on heroin and cocaine dependence. American Journal of Psychiatry, 142(11), 1259–1264. [DOI] [PubMed] [Google Scholar]
- Kudielka BM, Hellhammer DH, & Kirschbaum C (2007). Ten years of research with the Trier Social Stress Test--revisited. In Harmon-Jones E & Winkielman P (Eds.), Social neuroscience: Integrating biological and psychological explanations of social behavior (pp. 56–83). New York, NY, US: Guilford Press. [Google Scholar]
- Kuntsche E, Knibbe R, Engels R, & Gmel G (2007). Drinking motives as mediators of the link between alcohol expectancies and alcohol use among adolescents. Journal of Studies on Alcohol and Drugs, 68(1), 76–85. [DOI] [PubMed] [Google Scholar]
- Lejuez CW, Aklin WM, Zvolensky MJ, & Pedulla CM (2003). Evaluation of the Balloon Analogue Risk Task (BART) as a predictor of adolescent real-world risk-taking behaviours. Journal of Adolescence, 26(4), 475–479. [DOI] [PubMed] [Google Scholar]
- Lejuez CW, Read JP, Kahler CW, Richards JB, Ramsey SE, Stuart GL, … & Brown RA (2002). Evaluation of a behavioral measure of risk taking: the Balloon Analogue Risk Task (BART). Journal of Experimental Psychology: Applied, 8(2), 75. [DOI] [PubMed] [Google Scholar]
- Magrys SA, & Olmstead MC (2015). Acute stress increases voluntary consumption of alcohol in undergraduates. Alcohol and Alcoholism, 50(2), 213–218. [DOI] [PubMed] [Google Scholar]
- Marmorstein NR, White H, Chung T, Hipwell A, Stouthamer-Loeber M, & Loeber R (2010). Associations between first use of substances and change in internalizing symptoms among girls: Differences by symptom trajectory and substance use type. Journal of Clinical Child & Adolescent Psychology, 39(4), 545–558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Medina KL, McQueeny T, Nagel BJ, Hanson KL, Schweinsburg AD, & Tapert SF (2008). Prefrontal cortex volumes in adolescents with alcohol use disorders: Unique gender effects. Alcoholism: Clinical and Experimental Research, 32(3), 386–394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merikangas KR, He JP, Burstein M, Swanson SA, Avenevoli S, Cui L, … & Swendsen J (2010). Lifetime prevalence of mental disorders in US adolescents: results from the National Comorbidity Survey Replication–Adolescent Supplement (NCS-A). Journal of the American Academy of Child & Adolescent Psychiatry, 49(10), 980–989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miech RA, Johnston LD, O’Malley PM, Bachman JG, & Schulenberg JE, & Patrick ME (2017). Monitoring the Future national survey results on drug use, 1975–2016: Volume I, secondary school students Ann Arbor, Michigan: Institute for Social Research, The University of Michigan. [Google Scholar]
- Miller TR, Levy DT, Spicer RS, & Taylor DM (2006). Societal costs of underage drinking. Journal of Studies on Alcohol, 67(4), 519–528. [DOI] [PubMed] [Google Scholar]
- Moberg DP (2000). The Adolescent Alcohol and Drug Involvement Scale Retrieved from https://psycentre.apps01.yorku.ca/wp/adolescent-alcohol-and-drug-involvement-scale-aadis-and-adolescent-drug-involvement-scale-adis/. [DOI] [PubMed]
- Moberg DP, & Hahn L (1991). The Adolescent Drug Involvement Scale. Journal of Adolescent Chemical Dependency, 2, 75–88. [Google Scholar]
- Moss HB, Chen CM, & Yi HY (2014). Early adolescent patterns of alcohol, cigarettes, and marijuana polysubstance use and young adult substance use outcomes in a nationally representative sample. Drug and Alcohol Dependence, 136, 51–62. [DOI] [PubMed] [Google Scholar]
- Muthén B, & Masyn K (2005). Discrete-time survival mixture analysis. Journal of Educational and Behavioral Statistics, 30(1), 27–58. [Google Scholar]
- Nesic J, & Duka T (2006). Gender specific effects of a mild stressor on alcohol cue reactivity in heavy social drinkers. Pharmacology Biochemistry and Behavior, 83(2), 239–248. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S, & Hilt L (2006). Possible contributors to the gender differences in alcohol use and problems. The Journal of General Psychology, 133(4), 357–374. [DOI] [PubMed] [Google Scholar]
- Ollendick TH, & Hirshfeld-Becker DR (2002). The developmental psychopathology of social anxiety disorder. Biological Psychiatry, 51(1), 44–58. [DOI] [PubMed] [Google Scholar]
- Perou R, Bitsko RH, Blumberg SJ, Pastor P, Ghandour RM, Gfroerer JC, … & Parks SE (2013). Mental health surveillance among children—United States, 2005–2011. Morbidity and Mortality Weekly Report Surveillance Summary, 62(Suppl 2), 1–35. [PubMed] [Google Scholar]
- Sandler I, Wolchik SA, Cruden G, Mahrer NE, Ahn S, Brincks A, & Brown CH (2014). Overview of meta-analyses of the prevention of mental health, substance use, and conduct poblems. Annual Review of Clinical Psychology, 10, 243–273. 10.1146/annurev-clinpsy-050212-185524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Savage JE, Kaprio J, Korhonen T, Pulkkinen L, Rose RJ, Verhulst B, & Dick DM (2016). The effects of social anxiety on alcohol and cigarette use across adolescence: Results from a longitudinal twin study in Finland. Psychology of Addictive Behaviors, 30(4), 462–474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulte MT, Ramo D, & Brown SA (2009). Gender differences in factors influencing alcohol use and drinking progression among adolescents. Clinical Psychology Review, 29(6), 535–547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singer JD, Willett JB, & Willett JB (2003). Applied longitudinal data analysis: Modeling change and event occurrence Oxford University Press. [Google Scholar]
- Smit K, Voogt C, Hiemstra M, Kleinjan M, Otten R, & Kuntsche E (2018). Development of alcohol expectancies and early alcohol use in children and adolescents: A systematic review. Clinical Psychology Review 60 136–146. 10.1016/j.cpr.2018.02.002 [DOI] [PubMed] [Google Scholar]
- Staff J, Schulenberg JE, Maslowsky J, Bachman JG, O’Malley PM, Maggs JL, & Johnston LD (2010). Substance use changes and social role transitions: Proximal developmental effects on ongoing trajectories from late adolescence through early adulthood. Development and Psychopathology, 22(4), 917–932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Starcke K, Holst RJ, Brink W, Veltman DJ, & Goudriaan AE (2013). Physiological and endocrine reactions to psychosocial stress in alcohol use disorders: duration of abstinence matters. Alcoholism: Clinical and Experimental Research, 37(8), 1343–1350. [DOI] [PubMed] [Google Scholar]
- Steinberg L (2007). Risk taking in adolescence: New perspectives from brain and behavioral science. Current Directions in Psychological Science, 16(2), 55–59. [Google Scholar]
- Stockwell T, McLeod R, Stevens M, Phillips M, Webb M, & Jelinek G (2002). Alcohol consumption, setting, gender and activity as predictors of injury: A population-based case-control study. Journal of Studies on Alcohol, 63(3), 372–379. [DOI] [PubMed] [Google Scholar]
- Stroud LR, Tanofsky-Kraff M, Wilfley DE, & Salovey P (2000). The Yale Interpersonal Stressor (YIPS): Affective, physiological, and behavioral responses to a novel interpersonal rejection paradigm. Annals of Behavioral Medicine, 22(3), 204–213. [DOI] [PubMed] [Google Scholar]
- Tomlinson KL, & Brown SA (2012). Self-medication or social learning? A comparison of models to predict early adolescent drinking. Addictive Behaviors, 37(2), 179–186. [DOI] [PubMed] [Google Scholar]
- United States Census Bureau (2016). Quick facts Denton County, Texas: All facts Retrieved from https://www.census.gov/quickfacts/fact/table/dentoncountytexas/PST045216
- Westenberg PM, Drewes MJ, Goedhart AW, Siebelink BM, & Treffers PD (2004). A developmental analysis of self-reported fears in late childhood through mid-adolescence: social-evaluative fears on the rise?. Journal of Child Psychology and Psychiatry, 45(3), 481–495. [DOI] [PubMed] [Google Scholar]
- Williams KD, & Jarvis B (2006). Cyberball: A program for use in research on interpersonal ostracism and acceptance. Behavior Research Methods, 38(1), 174–180. [DOI] [PubMed] [Google Scholar]
- Wolpe J (1958). Psychotherapy by reciprocal inhibition Stanford, CA: Stanford University Press. [Google Scholar]
- Wittchen HU, Behrendt S, Höfler M, Perkonigg A, Lieb R, Bühringer GEEA, & Beesdo K (2008). What are the high risk periods for incident substance use and transitions to abuse and dependence? Implications for early intervention and prevention. International Journal of Methods in Psychiatric Research, 17(S1) 16–29. 10.1002/mpr.254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yim IS, Quas JA, Cahill L, & Hayakawa CM (2010). Children’s and adults’ salivary cortisol responses to an identical psychosocial laboratory stressor. Psychoneuroendocrinology, 35(2), 241–248. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Lejuez CW, Stuart GL, & Curtin JJ (2001). Experimental psychopathology in psychological science. Review of General Psychology, 5(4), 371. [Google Scholar]