Abstract
Alcohol consumption and interpersonal trauma (IPT) co-occur at high rates, particularly in college populations. Two non-mutually exclusive theories of this comorbidity are the risky behavior model, suggesting that substance use increases likelihood of IPT, and the self-medication model, suggesting that individuals use substances to cope with trauma-related symptoms. Few have simultaneously tested these theories in a sample of college students. Thus, the overarching aim of this longitudinal study (n=1320) was to identify whether alcohol consumption and IPT are associated with one another, and if IPT and/or posttraumatic stress disorder (PTSD) impacts use of alcohol to cope with trauma-related distress. Data were collected from a longitudinal study of college students attending a large public university. Participants in the current study were on average 18.46 years old at study entry, primarily female (70%), and of diverse racial/ethnic backgrounds (e.g., 49.4% White, 19.7% Black, 17.2% Asian). Results from auto-regressive, cross-lagged models indicated that alcohol consumption preceded IPT exposure. In contrast, IPT was not prospectively associated with alcohol consumption. Those reporting probable PTSD, but not IPT, reported more use of alcohol to cope with trauma-related distress. These findings provide support for the risky behavior model, indicating that those with higher levels of alcohol consumption may be a vulnerable group in terms of likelihood of IPT. Findings also suggest that those reporting probable PTSD may be at risk for use of alcohol to cope with trauma-related distress. Implications of these findings, in light of study limitations, are discussed.
Keywords: College students, alcohol use, interpersonal trauma, drinking to cope, autoregressive, cross-lagged model
Since the mid-1990’s, alcohol use in college students has been considered an important public health issue (Read, Wardell, & Colder, 2013; Sher, Wood, Wood, & Raskin, 1996; Wechsler, Lee, Kuo, & Lee, 2000), and remains a pressing issue on campuses. Indeed, college is a time of increased vulnerability for alcohol use and risk for alcohol use disorder (AUD, e.g., Dawson, Grant, Stinson, & Chou, 2004; Wechsler et al., 2000) with evidence that college students drink more alcohol (Slutske et al., 2004) and are at higher risk for alcohol-related problems (Slutske, 2005), compared to their non-college peers. Alcohol consumption is associated with a myriad of adverse consequences, including mood and anxiety disorders (Grant et al., 2004), increased impulsivity (Squeglia & Gray, 2016), cognitive deficits (H. R. White et al., 2011), and death (White & Hingson, 2013). Thus, identifying those most at risk for alcohol misuse among college student populations is warranted.
Similar to alcohol misuse, traumatic events, and in particular interpersonal trauma (IPT; i.e., physical or sexual abuse or assault), a more potent form of trauma in terms of its consistent effects on post-trauma distress (Cottler et al., 1992; R.C. Kessler, A. Sonnega, E. Bromet, M. Hughes, & C.B. Nelson, 1995), is another prevalent public health concern (Krebs, Lindquist, Warner, Fisher, & Martin, 2007; Krug, Mercy, Dahlberg, & Zwi, 2002) ocurring at particularly high rates (estimates as high as 68–90%, Breslau, 2002) during college (Read et al., 2012). As IPT is linked to posttraumatic stress disorder (PTSD), generalized anxiety disorder, panic disorder, depression, and alcohol and drug misuse (Kilpatrick et al., 2003), as well as increasing risk for re-exposure to further IPT (Widom, Czaja, & Dutton, 2008), there is a great need to better understand risk for IPT over the college years.
“Risky Behavior” Model of Alcohol Use and Trauma
Research suggests that IPT and alcohol use commonly co-occur in college students (e.g., Abbey, 2002; Goldstein, Flett, & Wekerle, 2010). There are a number of potential explanations for this co-occurrence, and notably, these models are not mutually exclusive (Khantzian, 1985; Stewart, 1996). One proposed explanation is the “risky behavior hypothesis.” This theory posits that substance use/misuse increases vulnerability to trauma exposure, such that those who use substances are more likely to experience high-risk situations, including interpersonal traumas (e.g., victimization; Windle, 1994), and in turn potentially increased PTSD symptoms (Read, Bachrach, Wright, & Colder, 2016). Indeed, substance use has been linked to revictimization (Messman-Moore, Coates, Gaffey, & Johnson, 2008; Messman-Moore, Ward, & Zerubavel, 2013), potentially in part because it impairs one’s ability to detect danger cues in the environment (Davis, Stoner, Norris, George, & Masters, 2009). Although much of this work has been cross-sectional in nature and/or focused on the role of substance use in predicting revictimization specifically, in one prospective study, Kilpatrick, Acierno, Resnick, Saunders, and Best (1997) found that substance use significantly predicted risk for IPT exposure two years later in a sample of adult women. Thus, the current study tests if alcohol consumption prospectively predicts IPT exposure in a sample of male and female college students.
“Self-Medication” Model of Alcohol Use and Trauma
Another hypothesis proposed to explain the co-occurrence of alcohol use and trauma exposure is the “self-medication hypothesis”, suggesting that individuals may use alcohol or other substances in order to reduce their experience of aversive anxiety- or trauma-related symptoms (Chilcoat & Breslau, 1998; Kushner, Abrams, & Borchardt, 2000). In this model, the aversive symptoms precede substance use or dependence (e.g., Brady, Killeen, Brewerton, & Lucerini, 2000). Prior research indicates that following IPT, individuals may increase in their alcohol use to avoid an aversive emotional reaction (Waldrop, Back, Verduin, & Brady, 2007) or trauma-related sequaelae (e.g., disruption of social connections, Shin, Miller, & Teicher, 2013; Walsh et al., 2012) including PTSD symptoms (Cross, Crow, Powers, & Bradley, 2015). Thus, in order to add to this work, we aimed to examine whether IPT and/or probable PTSD are prospectively associated with alcohol consumption in college.
Further, prior research indicates that negative affect following trauma exposure been found to be associated with coping-oriented drinking (Veilleux, 2014) and recriprocal associations between PTSD symptoms and negative coping among college students with prior trauma exposure have been found (Read, Griffin, Wardell, & Ouimette, 2014). However, much of this work has focused on drinking to cope more generally, using measures such as the Drinking Motives Questionnaire (M. L. Cooper, Russell, Skinner, & Windle, 1992) which focuses on broad affect-related drinking (e.g., “I drink to forget my worries”) while there is a lack of research examining drinking to cope in the context of trauma exposure and trauma- specific distress (i.e., PTSD symptoms). Thus, the current study is novel in that it seeks to expand the existing literature by examining whether IPT is associated with trauma-related drinking (i.e, TRD).
Following trauma, research has also demonstrated that individuals who experience more PTSD symptoms are more likely to endorse use of substances to cope (Ullman, Relyea, Peter- Hagene, & Vasquez, 2013), defined as more broad drinking to cope motives (Dixon, Leen- Feldner, Ham, Feldner, & Lewis, 2009; Waldrop, Back, Verduin, & Brady, 2007). It remains unclear, however, whether those who experience IPT may be at risk for more specific trauma- related drinking to cope because of increased PTSD symptoms. Thus, in continuing to examine facets of the “self-medication” hypothesis, we tested whether probable PTSD was associated with increased risk for use of alcohol to cope specifically with trauma-related distress.
Risky Behavior and Self-Medication Models are Not Mutually Exclusive
The risky behavior and self-medication models are not mutually exclusive. For instance, it may be that one model explains the process of initiating alcohol use, while the other is more salient once use has been initiated. There is also research suggesting that there may be shared risk factors that increase risk for both alcohol consumption and trauma/IPT (Haller & Chassin, 2014; McLeod et al., 2001). Thus, it is possible that we may find support for both the risky behavior and self-medication models.
Present Study
In order to build on the existing research, the current study tested the following hypotheses over the course of college. The first hypothesis, which tested the risky behavior model, purported that alcohol use would prospectively predict exposure to IPT events. The second hypothesis investigated the self-medication model, specifically that the presence of a prior IPT and probable PTSD would prospectively predict alcohol consumption, over the course of college, and that both would predict use of alcohol to cope with trauma-related distress. As the self-medication and risky behavior models of substance use are not mutually exlcusive, it was hypothesized that support for both would be found.
We also controlled for relevant covariates in the proposed analyses. Specifically, given the work suggesting that sex (e.g., women are at higher risk for PTSD, Breslau, 2002), age (e.g., linear relation between age and alcohol use in college, Johnson L.D., 2007) and race/ethnicity (e.g., PTSD is highest among Blacks, compared to Whites; Roberts, Gilman, Breslau, Breslau, & Koenen, 2011) impact associations among study variables, these were included as covariates. Additionally, general anxiety (e.g., Kaplow, Curran, Angold, & Costello, 2001) and depressive symptoms (e.g., Hankin, Fraley, Lahey, & Waldman, 2005) may impact relations between IPT and alcohol use and were also included as covariates. Finally, as broad drinking behaviors are associated with drinking motives (Ham, Bonin, & Hope, 2007; Holahan, Moos, Holahan, Cronkite, & Randall, 2001), alcohol consumption was also included as a covariate in predicting TRD.
Method
Larger, Parent Study Sample
Participants for the current project came from a large, on-going longitudinal study of behavioral and emotional well-being of college students at a mid-Atlantic public university (author et al., 2014). The parent study was approved by the university review board. Participants read through an online consent document, indicated that they understood the potential risks and benefits of participating, and were paid $10 for each survey. For the baseline assessment, incoming first-year students 18 years of age or older were invited via email to complete the survey starting one week before their arrival on-campus up until the tenth week of the fall semester. Baseline and follow-up data were collected on four consecutive cohorts during the fall and the spring, respectively, of participants’ first year of college via online surveys administered using Research Electronic Data Capture (REDCap, Harris et al., 2009) electronic data capture tools hosted at Virginia Commonwealth University. REDCap is a secure, web-based application designed to support data capture for research studies, providing an intuitive interface for validated data entry.
Within the parent study, of the 14,959 individuals who were eligible to complete the baseline fall assessment, 9,889 participated (cohort 1 entering college in 2011 [n = 2,707], cohort 2 entering college in 2012 [n = 2,481], cohort 3 entering college in 2013 [n = 2,391], cohort 4 entering college in 2014 [n=2,310]). Of these, 38.2% were male, 61.1% were female, 0.7% declined to identify sex. The sample reflected the population from which it was drawn: 49.4% White, 18.9% Black, 16.3% Asian, 6% Hispanic/Latino, 9.4% other/multirace/unknown/declined to respond. The average age at baseline assessment was 18.5 years. Those who completed the baseline survey were subsequently invited via email to complete a follow-up assessment between weeks 7 and 14 of the spring semester of their freshman year. Of those who completed the baseline assessment and who were still enrolled at the University, 4,820 also completed the follow-up assessment (59% retention). Individuals were invited to complete a survey during the spring of each of their subsequent years (e.g., spring sophomore year, spring junior year). In comparing those who completed at least one follow-up to those who did not complete any, those who participated were more likely to be female (63.8% versus 55.00%; χ2: 63.769, p<.001; Cramer’s V: .08), younger (18.49 versus 18.55, t=5.26, p<.001; Cohen’s d: .13), Caucasian versus another race (52% versus 43.8%, χ251.01, p<.001; Cramer’s V:.07), and were less likely to have experienced at IPT at baseline (38.5% versus 49%, χ2: 69.66 p<.001; Cramer’s V:.09). However, these differences were all small effects. There were no differences in terms of probable PTSD or log transformed alcohol consumed at baseline.
Current, Spinoff Study Sample
A spinoff-study was conducted to assess in detail trauma history and TRD. Individuals from the parent study who reported at least one traumatic event and who used alcohol at least once were invited to participate in the study (n=7,423) in the Fall of 2016 or the Spring of 2017. Of those invited, 2,175 (29%) expressed an interest in participating in this spin-off study and were emailed a survey link. Of these students, 1896 (87%) provided data for the spin-off study.Of individuals who were eligible but did not participate compared to those who were eligible and who did participate in this spinoff study, those who participated were more likely to be Caucasian compared to another race (50.7% versus 46.9% χ2: 7.936, p<.01; Cramer’s V: .03), younger (18.46 versus 18.52, t=4.60, p<.001; Cohen’s d: .14), female (70.2% versus 61.8%, χ2: 42.65, p<.001; Cramer’s V: .08), and reported less log transformed mean alcohol consumption across fall year 1 (0.96 versus 1.12, t=3.15, p<.01; Cohen’s d:. 11). All effects were small. There were no differences on whether the two groups endorsed an IPT or met criteria for probable PTSD at any time point, or on alcohol consumption at any time after year 1 fall.
As the goal of this study was to understand these inter-relations over the course of college, and not just at the beginning of college, the analytic sample for the present study included those in cohorts 1–3 who could have had four (i.e., could have missing data on) assessments of IPT, probable PTSD, and alcohol consumption preceeding assessment of TRD in the spinoff study. Additionally, in order for the path model to be conducted in Mplus Version 8 (B. Muthen, 2009; L. K. Muthen & Muthen, 2017), only those with non-missing data on the distal outcome, trauma-related drinking, were included (n=1,320); see Figure 1.
Figure 1.
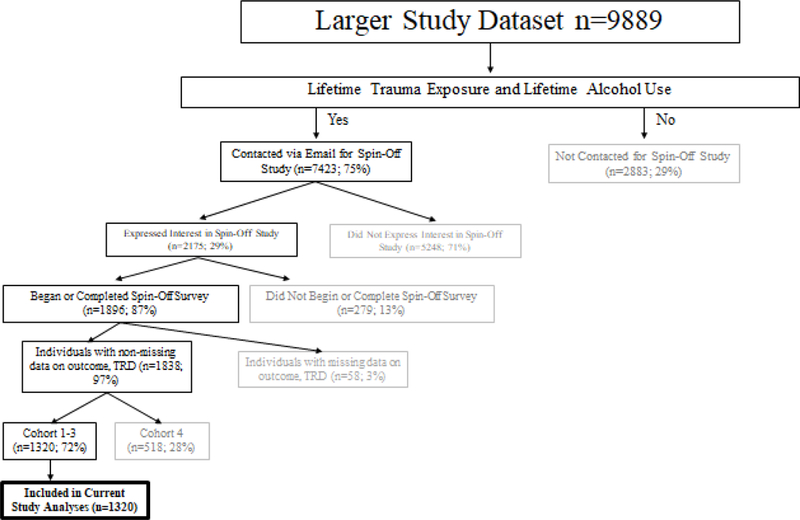
Depiction of How Individuals were Included in the Current Study.
Those 1,320 included in current study analyses were also compared to those included in the spin-off study who were not included in current study analyses (n=576). Those who were included in the spin-off study reported less log transformed alcohol consumption at year 1 fall (.88 versus 1.13, t=3.14, p<.01, Cohen’s d: .19), year 1 spring (1.21 versus 1.57, t=5.20, p<.001; Cohen’s d:.27), year 2 spring (1.45 versus 1.67, t=2.94, p<.01; Cohen’s d: .17), and year 3 spring (1.69 versus 2.02; t=5.41, p<.001; Cohen’s d: .35). Additionally, those included were less likely to report probable PTSD at year 1 spring (26.6% versus 37.8%, χ2: 11.92, p<.001; Cramer’s V: .108), and less likely to report an IPT at year 1 spring (21.1% versus 25.9%, χ2: 4.79, p<.001; Cramer’s V: .053) and year 2 spring (22% versus 27.7%, χ2: 5.57, p<.05; Cramer’s V: .061). Of note, all of these effects were small or small-medium. There were no differences on age, trauma-related drinking, ethnicity, gender, or IPT or probable PTSD at any of the other time points.
Individuals in present study analyses were on average 18.46 years old at the Freshman fall assessment (baseline) (SD: .42). Most participants self-reported as female (70%). Individuals reported on their race/ethnicity at baseline. Whites comprised the largest group (49.4%), followed by Blacks (19.7%), Asians (17.2%), 6.8% more than one race, 5.7% Hispanic/Latino, .6% unknown, .4% Native Hawaiian/Other Pacific Islander, .2% American Indian. In order to reduce the number of parameters, one dummy coded variable was used to compare the largest group (Whites) to others. Finally, individuals for these analyses came from cohort 1 (entering college in Fall 2011; 29.5%), cohort 2 (entering in Fall 2012; 28.9%), or cohort 3 (entering in Fall 2013; 41.6%).
Measures
Main Variables of Interest among Those in Current Study Sub-sample
Alcohol Consumption (measured in Fall Freshman Year and each Spring after).
Participants reported on their recent alcohol use with ordinal frequency and quantity items from the Alcohol Use Disorders Identification Test (AUDIT, Bush, Kivlahan, McDonell, Fihn, & Bradley, 1998). Within the larger study, the full AUDIT was given at some of the time points and only the consumption items were given at the others. In order to harmonize data across multiple time points and cohorts, the consumption items were utilized. These ordinal frequency and quantity items were combined to create a single “grams of ethanol consumed per month” alcohol use variable using a method previously reported in (Dawson, 2000), and utilized by (Salvatore et al., 2016). Because this variable was highly skewed (range: 4.13–5.52) and kurtotic (range: 26.21–44.04), it was log transformed, with the resulting skew (range: −1.19- −.16) and kurtosis (range: −1.46– 2.31) much improved. Over the four time points, the means were .86,1.15, 1.29, and 1.64, and the SDs were 1.48, 1.47, 1.38, and 1.18.
IPTExposure (measured in Fall Freshman Year and each Spring after).
Individuals reported on recent interpersonal traumatic events using a shortened version of the Life Events Checklist (Weathers et al., 2013). Specifically, they indicated whether they had experienced a physical assault, sexual assault, or any other unwanted touching or sexual activity (yes or no for each item). Participants indicated at their freshman fall interview whether they had experienced these events in their lifetimes, and at the freshman spring interview, if they had experienced these events since beginning college. They also indicated whether they had experienced these events in the past year during their sophomore spring and junior spring interviews. This measure was dichotomized to indicate whether or not individuals had experienced an IPT ever (during the Fall Freshman interview, reported by 41% of those in the current study sub-sample), or since the last assessment (i.e., a new IPT; reported by 18.7%, 20.5%, and 17.5% of participants for new onset events occurring during freshman, sophomore, and junior years, respectively).
Probable PTSD (measured in Fall Freshman Year and each Spring after).
A modified version of the Primary Care-PTSD screener (Prins et al., 2016) was used, asking individuals to indicate whether any of their traumas had resulted in them experiencing nightmares, avoiding situations or thoughts of the event, feeling constantly on guard or easily startled, or feeling numb or detached from others/surroundings. The percent endorsing this item fluctuated somewhat over the four time points (37.3%, 26.6%, 37.3%, 34.5%).
Covariates
Demographic Variables.
Participants age, ethnicity, sex, and cohort were included as covariates. Given the preliminary analyses suggesting that cohort 1 consumed less alcohol than cohorts 2 and/or 3 during the Freshman year spring through Junior year spring assessments (F’s: 4.03–14.77,p’s<.01), two dummy coded variables were used to compare those in cohort 1 to those in cohort 2, and as well as cohort 1 to cohort 3.
Depressive and Anxiety Symptoms (measured in Fall Freshman Year and each Spring after).
Participants reported on their depressive and anxiety symptoms in the past week using items from the Symptom Checklist-90 Revised (SCL-90, Todd, 1997). The SCL-90 asks participants about their symptoms using a 5-point scale (1=not at all, 5=extremely). A sum of the five depression items (e.g., feeling blue, blaming yourself for things) and five anxiety items (e.g., nervousness or shakiness, worrying too much) was created at each of the four study time points. Sum scores for depression and anxiety at all time points were within the acceptable range of skew and kurtosis (i.e., +/− 2 and 7, respectively). The means for depression were 8.79 (SD=3.60) for Freshman fall, 9.72 (SD=3.78) for Freshman spring, 9.70 (SD=4.04) for Sophomore spring, and 9.53 (SD=3.97) for Junior spring. The means for the anxiety sum scales were 6.82 (SD=3.04) for Freshman fall, 6.97 (SD=3.22) for Freshman spring, 6.57 (SD=3.11) for Sophomore spring, and 6.79 (SD=3.14) for Junior spring. These values are comparable to or a bit lower than other college samples (Chang & Bridewell, 1998) and are lower than those found in clinical samples (Schmitz et al., 2000).
Outcome
Spinoff Study: Trauma-related Drinking to Cope (TRD).
A study specific measure of trauma-related drinking to cope (TRD) was created for and administered as part of the the spin-off study battery, given that one did not exist in the literature. Therefore, participants in the parent study who endorsed ever having experienced a trauma and having ever consumed alcohol who enrolled in the spin-off study were administered this measure. This measure was completed between six months and two years and six months after the year 3 spring interview. Specifically, cohort 1 completed the assessment 2.5 years after the year 3 spring asessment, cohort 2, 1.5 years after the year 3 spring asessment, and cohort 3, six months after the year 3 spring asessment.
Using the same response options from the Drinking Motives Questionnaire-Revised (DMQ-R, M Lynne Cooper, 1994), which query frequency of use of drinking motives on a 1 to 5 likert scale (1=Almost Never/Never to 5=Almost Always/Always), frequency of alcohol to cope with symptoms specific to each of the four PTSD clusters (i.e., re-experiencing, avoidance, negative cognitions and mood, and arousal) were assessed. Specifically, individuals indicated the extent to which they drank alcohol to cope with repeated feelings or memories of the event, drank to avoid reminders of the event, drank to cope with negative cognitions related to the event, or drank to avoid aversive emotional and physiological aspects of the event. Answer choices ranged from 1 (almost never/never) to 5 (almost always/always) (Cronbach’s Alpha: .876). The sum (M: 5.22, SD: 2.43) of these four items was highly skewed (2.83) and kurtotic (9.33). Therefore, this variable was log transformed. This score (M=.69, SD: 0.15) showed improvement in skew (1.82) and kurtosis (2.77), and thus was used as the measure of TRD for these analyses.
Data Analytic Plan
All continuous predictors and covariates were grand mean centered prior to conducting analyses. The longitudinal auto-regressive, cross-lagged model was conducted using MPlus Version 8 (L. K. Muthen & Muthen, 2017). Missing data was estimated using Full Information Maximum Likelihood under the missingness at random assumption (Schafer & Graham, 2002). Analyses were assessed for goodness of fit using the chi-square goodness of fit test statistic, Comparative Fit Index (CFI) and Tucker Lewis Index (TLI): ≥ .95 and Root Mean Square Error of Approximation (RMSEA) ≤ .08 (Hu, 1999).
Within the auto-regressive cross-lagged model, four time points for study constructs was included (i.e., year 1 fall, year 1 spring, year 2 spring, and year 3 spring). The spin-off study variable (i.e., TRD) was used as the distal outcome, as these data were collected after these first four time points. For the auto-regressive, cross-lagged portion of the model, the stability paths among alcohol consumption at each time point to the next, as well as stability paths among new onset IPT at each time point to the next, were estimated. The effects of alcohol consumption and IPT at the last time they were assessed (i.e., year 3 spring) in predicting drinking to cope, were tested. Additionally, the effect of probable PTSD was included in predicting IPT and alcohol consumption at each time point, as well as TRD. The covariates age, sex, cohort, anxiety symptoms, and depressive symptoms were included in predicting IPT and alcohol consumption at each time point, as well as TRD.
The rationale for including the effects of year 3 IPT, PTSD, and alcohol consumption as predictors of TRD was that if an individual met criteria for probable PTSD at some earlier time point (e.g., year 1 fall, spring, or year 2 spring) but did not meet criteria for probable PTSD at year 3 spring, it would not be expected that individuals would drink to cope with their trauma-related distress—that is, if probable PTSD had remitted. Additionally, there was concern about potential issues with multicollinearity, as correlations within construct across any two time points were as high as r=.67.
In order to test for evidence of the risky behavior model, paths from alcohol consumption at each time point to IPT at the next, were included (e.g., year 1 fall alcohol consumption to year 1 spring IPT). In order to test for evidence of the self-medication model, paths from IPT at each time point to alcohol consumption at the next, were included (e.g., year 1 fall IPT to year 1 spring alcohol consumption). Additionally, the effects of IPT and probable PTSD at year 3 spring on TRD, were tested.
Results
Zero-Order Correlations
In terms of associations among key study variables, alcohol consumption was associated with IPT exposure at all subsequent time points (e.g., alcohol consumption at year 1 fall and IPT at year 1 spring; r’s=.064-.203, p<.05). IPT exposure was also associated with alcohol consumption at all subsequent time points (e.g., IPT at year 1 fall and alcohol consumption at year 1 spring; r’s=.099-.125, p<.05). Probable PTSD during year 3 spring was associated with more TRD (r=.142 p<.05), as was IPT exposure (r: .172, p<.05) at this same time.
Auto-regressive, Cross-lagged Model
The final study model showed good fit to the data. Specifically, fit indices were as follows: CFI: .991, TLI: .967, and RMSEA: .027. See Table and Figure 2 for full model results.
Table.
Auto-Regressive, Cross-Lagged Model Results(n=1,320).
| Predictor | Alcohol Consumption Year 1 Spring |
IPT Year 1 Spring | Alcohol Consumption Year 2 Spring |
IPT Year 2 Spring | Alcohol Consumption Year 3 Spring |
IPT Year 3 Spring | Trauma-related Drinking to Cope |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B | SE | B | SE | B | SE | B | SE | B | SE | B | SE | B | SE | |
| Sex | −.002 | .095 | .131** | .036 | −.087* | .080 | −.075 | .044 | .003 | .069 | .138** | .045 | −.012 | .013 |
| Age | .012 | .077 | .038 | .069 | −.001 | .069 | .075 | .036 | .082* | .065 | −.069 | .039 | .014 | .011 |
| Race | −.021 | .088 | −.111** | .069 | −.021 | .069 | .057 | 039 | −.087* | .063 | −.015 | .040 | .021 | .012 |
| Cohort:1–2 | −.030 | .102 | .115* | .038 | .019 | .090 | −.180** | .055 | .079* | .082 | .111* | .050 | −.040 | .014 |
| Cohort:1–3 | .101** | .108 | .088 | .036 | .089* | .094 | −.127* | .050 | −.001 | .063 | .060 | .045 | .017 | .018 |
| Alcohol Consumption-Y ear 1 Fall | 732*** | .045 | .188*** | .013 | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| IPT- Year 1 Fall | .037 | .099 | .248*** | .032 | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Depression- Year 1 Fall | .104* | .084 | .250*** | .030 | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Anxiety- Year 1 Fall | −.087 | .088 | −.090 | .031 | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Probable PTSD- Year 1 Fall | .047 | .112 | .103* | .038 | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Alcohol Consumption- Year 1 Spring | -- | -- | -- | -- | .703*** | .032 | .012 | .015 | -- | -- | -- | -- | -- | -- |
| IPT- Year 1 Spring | -- | -- | -- | -- | .074 | .130 | .482*** | .079 | -- | -- | -- | -- | -- | -- |
| Depression- Year 1 Spring | -- | -- | -- | -- | .028 | .037 | .092 | .029 | -- | -- | -- | -- | -- | -- |
| Anxiety- Year 1 Spring | -- | -- | -- | -- | .002 | .058 | .100 | .030 | -- | -- | -- | -- | -- | -- |
| Probable PTSD- Year 1 Spring | -- | -- | -- | -- | -.005 | .102 | 257*** | .050 | -- | -- | -- | -- | -- | -- |
| Alcohol Consumption- Year 2 Spring | -- | -- | -- | -- | -- | -- | -- | -- | 679*** | .029 | .202*** | .017 | -- | -- |
| IPT- Year 2 Spring | -- | -- | -- | -- | -- | -- | -- | -- | .001 | .101 | 464*** | .069 | -- | -- |
| Depression- Year 2 Spring | -- | -- | -- | -- | -- | -- | -- | -- | −.017 | .043 | .144* | .028 | -- | -- |
| Anxiety- Year 2 Spring | -- | -- | -- | -- | -- | -- | -- | -- | .025 | .061 | −.002 | .036 | -- | -- |
| Probable PTSD-Year 2 Spring | -- | -- | -- | -- | -- | -- | -- | -- | −.029 | .119 | .028 | .057 | -- | -- |
| Alcohol Consumption-Year 3 Spring | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | .225*** | .005 |
| IPT- Year 3 Spring | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | .055 | .017 |
| Depression- Year 3 Spring | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | .222*** | 007 |
| Anxiety- Year 3 Spring | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | .007 | .011 |
| Probable PTSD- Year 3 Spring | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | 247*** | .037 |
Notes:
p<.05
p<.01
p<.001.
Standardized coefficients are reported. Sex is coded 0 for males and 1 for females; Race: White=0, Other=1; Cohort: Cohort 1=0, Cohort 2 or 3=1. IPT=Interpersonal Trauma; Probable PTSD=Probable Posttraumatic Stress Disorder
Figure 2.
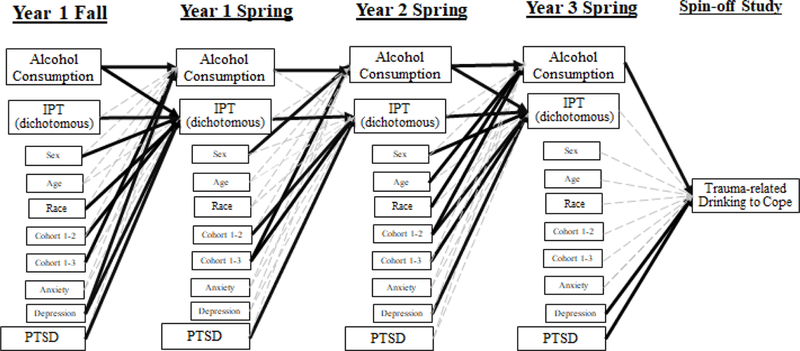
Depiction of auto-regressive, cross-lagged model with drinking to cope as the distal outcome (n=1,320).Notes. Bolded black lines indicate significant effects (p<.05). Dashed gray lines indicate non-significant effects. For increased clarity, correlations between constructs within time are not shown but were estimated as part of the full model. IPT=Interpersonal Trauma; Probable PTSD=Probable Posttraumatic Stress Disorder.
Testing the Risky Behavior Model
Over and above covariates and stability paths for alcohol consumption and IPT (which were significant at all time points), more alcohol consumption at year 1 fall was associated with greater risk for reporting an IPT at year 1 spring. Additionally, more year 2 spring alcohol consumption was associated with higher risk for IPT at year 3 spring. There was a non-significant association between year 1 spring alcohol consumption and year 2 spring IPT. Thus, at two of three time points, alcohol consumption prospectively predicted exposure to IPT.
Testing the Self-Medication Model
Over and above study covariates and stability paths, at no time point was IPT associated with alcohol consumption, nor IPT at year 3 spring with TRD. Additionally, probable PTSD was not prospectively related to alcohol consumption at any time point. However, probable PTSD at the year 3 spring assessment was associated with more TRD1,2.
Covariate Effects
In predicting alcohol consumption, males reported higher levels than females at year 2 spring, Whites reported more than Others at year 3 spring, and those in cohort 3 reported higher levels than those in cohort 1 at year 1 and 2 spring, and those in cohort 2 reported higher levels than those in cohort 1 at year 3 spring. Those with more depressive symptoms at year 1 fall reported more alcohol consumption at year 1 spring. Older individuals consumed more alcohol than younger individuals at year 3 spring. No other covariate effects were significant in predicting alcohol consumption.
In predicting IPT, those with more depressive symptoms at year 1 fall and year 2 spring were more likely to report IPT at year 1 spring and 3 spring, respectively. The presence of probable PTSD was prospectively associated with risk for IPT between year 1 fall-year 1 spring and year 1 spring-year 2 spring. Additionally, females were more likely to report IPT at year 1 spring and year 3 spring. Those in cohort 1 were at lower risk than cohort 2 for IPT at year 1 spring and year 3 spring, but higher risk than cohort at year 2 spring. At year 2 spring, those in cohort 1 were at higher risk for IPT, compared to those in cohort 3.
In predicting TRD, those with more depressive symptoms during year 3 spring and those who consumed more alcohol during year 3 spring reported more use of alcohol to cope with trauma-related distress. No other covariates predicted TRD.
Discussion
“Risky Behavior” Model
We did find evidence for the “risky behavior” model, in that between year 1 fall and year 1 spring, and year 2 spring and year 3 spring, alcohol consumption was prospectively associated with new onset IPT exposure. Notably, analyses take into account the association between IPT and alcohol consumption (as well as covariates) at each time point and suggest that above and beyond these associations, alcohol consumption is associated with an increased likelihood of new IPT exposure. Present findings add to a body of literature suggesting that substance use/misuse may indeed increase vulnerability to subsequent IPT exposure. Recent work examining intimate partner violence in college students has shown that alcohol misuse was associated with victimization in men and that drug misuse was associated with victimization in both males and females (Sabina, Schally, & Marciniec, 2017). Further examination of factors associated with increased alcohol use, potentially relevant for IPT exposure as well, include factors such as impulsivity (i.e., sensation seeking and lack of premeditation) which have been shown to be relevant for problem drinking in a college student sample with sex-related alcohol expectancies shown to mediate the relation between impulsivity traits and both problem drinking and drinking in the context of sexual encounters (Banks & Zapolski, 2017).
“Self-Medication” Model
Contrary to our hypothesis, we found only weak evidence for the self-medication model. Specifically, we did not find evidence for new onset IPT or probable PTSD on alcohol consumption over the course of college. Although prior research has found a link between sexual harassment and alcohol problems (e.g., neglecting responsibilities, Wolff, Rospenda, & Colaneri, 2017), other work in trauma-exposed college students using daily online assessments (over 30 days) did not find support for a trauma-alcohol use/misuse link (Bachrach & Read, 2017). Our study findings suggest that IPT was not associated with alcohol consumption or TRD. The fact that new onset IPT was not associated with TRD signifies, perhaps, that trauma-related distress (i.e., PTSD symptoms) rather than simply trauma exposure(s) per say, is related to TRD. Indeed, individuals reporting probable PTSD were more likely to endorse more TRD, over and above IPT. This is consistent with prior work finding that PTSD is uniquely associated with substance use outcomes (Jakupcak et al., 2010; McDevitt-Murphy et al., 2010) and strengthens such findings by also including examination of trauma exposure to determine that PTSD is related to substance use above and beyond exposure.
There are other possible explanations for the lack of support for the self-medication model in the current dataset. For instance, the time lag between assessments may be too far apart to detect associations between IPT and alcohol consumption, or it may be that the link between IPT and TRD was non-significant because individuals are drinking to cope with some event not assessed (e.g., traumatic/unexpected death of a loved one). It may also be that the self-medication model is more salient for individuals at other developmental periods. For example, early IPTs in childhood or adolescence may increase the likelihood of earlier and more problematic alcohol use, such that individuals then begin college consuming more alcohol than their peer group. It may be that this increased alcohol use at the beginning and during college then increases those individuals’ risk for future interpersonal trauma events. In addition to these pathways not being mutually exclusive with one another, they are also not mutually exclusive with a third variable model in which shared risk factors may increase propensity for both alcohol use/misuse and trauma exposure (e.g., Haller & Chassin, 2014). For istance, there is work suggesting shared genetic risk for this comorbidity (McLeod et al., 2001). Future, longitudinal work extracting sub-groups of individuals with co-occurring trauma/IPT and alcohol use/misuse based on whether they show evidence of risky-behavior, self-medication, or the shared risk model, or potentially more than one at different developmental stages, is warranted, and would have potentially important clinical implications for prevention/treatment.
Notably, probable PTSD showed an association with trauma-related drinking after controlling for alcohol use and interpersonal trauma, suggesting that while individuals may not drink to cope with IPT directly, they appear to be drinking to cope with symptoms subsequent to exposure, above and beyond their alcohol use frequency in and of itself. The small body of work focusing on associations between PTSD and coping motives has found support for this link in a sample of sexual assault survivors (Ullman, Filipas, Townsend, & Starzynski, 2005). However, ours is the first study to find that PTSD is associated with drinking to cope with trauma-related distress, and not simply broad negative affect.
Non-hypothesized Effects
All models tested also included relevant covariates, some of which are worth noting. First, individuals reporting greater alcohol consumption were more likely to endorse TRD, in line with existing work documenting the association of drinking to cope motives broadly and alcohol consumption (Beseler, Aharonovich, & Hasin, 2011). Coping motives are clearly relevant at multiple points in the relation between trauma exposure, distress, alcohol use and misuse, and further longitudinal work examining such motives will be fruitful and likely inform upon important treatment and prevention targets. Present study findings also suggest that TRD is a useful measure and is operating as would be expected. Second, study findings aligned with the broader existing literature, with Whites and males endorsing the highest rates of alcohol consumption (Delker, Brown, & Hasin, 2016). Those with more depression symptoms were more likely to experience new onset IPT at the first and last time points. In addition to PTSD’s effect on TRD, depressive symptoms also exerted a significant effect. Notably, anxiety symptoms were not associated with alcohol consumption, new IPT or TRD at any of the time points.
Implications, Limitations, and Conclusions
Present study findings are associated with a number of clinical implications. First, the association of alcohol use with subsequent IPT exposure suggests the importance of targeting alcohol use, particularly in the early stages of college, in prevention efforts aimed at reducing sexual assault and other IPT exposures on college campuses. Existing work has shown the efficacy of brief interventions aimed at reducing heavy drinking (see systematic review by (Sundstrom, Blankers, & Khadjesari, 2017); future work should examine whether such interventions lead to decreased IPT. Attempts to further examine, and in turn, address the alcohol use and IPT relation should also include factors such as context and peer influence that appear to be important, as existing work has shown that peer/acquaintance and friend alcohol behavior moderated the relation between PTSD symptoms and drinking in varying ways (i.e., was both a protective and a risk factor depending on context and level of symptomatology, Bachrach & Read, 2017). Finally, study findings suggest that trauma-related distress, but not trauma exposure itself, appears to be associated with trauma-related drinking. Thus, more focused examination of the function of drinking, above and beyond alcohol consumption itself, in relation to distress remains an important area of focus.
Results should also be considered in the context of a number of limitations. First, there are limitations with regard to the phenotypes examined. Specifically, the trauma assessment questions do not provide detail into the nature of the endorsed trauma (e.g., the frequency or recency of each type of endorsed interpersonal trauma), and is limited in the breadth of types of events queried (e.g., only three interpersonal traumas). Thus, a more nuanced assessment of trauma frequency is recommended for future research. Additionally, the trauma-related drinking measure is preliminary, was only administered at one time point (precluding examination of change in this pattern over time), and did not ask participants to think about a specific time frame. Additional work attempting to replicate/extend these findings in a longitudinal framework, while asking participants to think about their current PTSD symptoms, is needed. In addition, the measure of probable PTSD also only involved one item, and thus study findings may differ if we had used a more refined measure. However, in order to attempt to test this question empirically, total PTSD symptoms as assessed using a well-validated measure (PTSD Checklist, PCL; Weathers et al., 2013) measured during the spin-off study was substituted for this one item screener as a predictor of trauma-related drinking, and the findings did not change. Thus, this potential explanation is less likely.
Another limitation is that across the many time points of the larger study, varying alcohol use questions were asked. Our alcohol measure, while noted to be strongly associated with outcomes, consists of a quantity and frequency measure only. We did not have information on alcohol misuse outcomes (e.g., binge drinking), associated negative consequences of drinking (e.g., missing class due to hangovers), or alcohol use disorder at all time points. In order to harmonize data across multiple time points and cohorts, the consumption items were utilized in these analyses.Thus, findings can inform upon alcohol use overall, which is broadly developmentally normative (“Alcohol Facts and Statistics,” 2017), but it is unknown at present whether findings would generalize to populations endorsing clinical levels of alcohol use problems.
A final limitation is that although the larger parent study is representative of the university, those eligible for the spin-off study are necessarily different from those not in the spin-off study in the larger study, and those who completed the spin-off study survey did differ in some ways from those eligible but who did not complete the survey. Although most of the differences were small effects, those who completed the spin-off study consumed significantly less alcohol than those who were eligible but did not complete it, and this difference was a small- medium effect. Thus, these study findings may not generalize to the larger population from which this sub-sample was pulled.
Using a college student sample, given emerging alcohol problems and rates of IPT at this age and in this environment, longitudinal data allowed for the examination of the inter-relations of IPT and alcohol consumption over the college years. Present results found support for the risky behavior hypothesis, suggesting that greater alcohol consumption is associated with increased likelihood of IPT. These patterns are informative with regard to identifying those at risk for later IPT exposure. Additionally, the association of probable PTSD with trauma related drinking adds to the literature on coping motives for drinking, and suggests the relevance of more specific, trauma-related coping motives; additional work examining trauma-related coping motives over time, as well as more alcohol misuse, will be particularly useful in understanding this pattern of risk.
Acknowledgements:
Spit for Science has been supported by Virginia Commonwealth University, P20 AA017828, R37AA011408, K02AA018755, and P50 AA022537 from the National Institute on Alcohol Abuse and Alcoholism, and UL1RR031990 from the National Center for Research Resources and National Institutes of Health Roadmap for Medical Research. We would like to thank the Spit for Science participants for making this study a success, as well as the many University faculty, students, and staff who contributed to the design and implementation of the project. Additional funding for this project has come from F31AA025820 (PI: Hawn), and T32 MH020030 andAA025692 (Sheerin).
Footnotes
These data have not been presented at a conference or meeting, posted on a listserv, shared on a website, etc.
. As 17.7% of participants in this subscample reported zero PTSD symptoms but were still administered the trauma-related drinking questionnaire, this final model was estimated when these individuals were omitted. The main study findings remained the same when these individuals were no longer included in analyses.
. We were also curious if/how findings might change in alcohol consumption, IPT, and PTSD measures at all four time points were used to predict TRD. Year 3 fall alcohol consumption remained a positive, significant predictor (B: .110, p<.05), and Year 3 IPT remained a non-significant predictor. Year 2 spring probable PTSD was positively associated with TRD (B: .289, p<.05) and Year 3 spring probable PTSD became a marginally significant negative predictor (B: −.472, p=.08). The fact that this effect of Year 3 PTSD had previously been positive and became negative with the inclusion of Year 2 PTSD may indicate the presence of a suppressor effect, in which one predictor hides or suppresses the effect of another on the outcome (Cohen, 2003). No other effects of alcohol consumption, IPT, or probable PTSD were significantly associated with TRD.
References
- Abbey A (2002). Alcohol-related sexual assault: A common problem among college students. Journal of Studies on Alcohol, Supplement, 14, 118–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alcohol Facts and Statistics. (2017). Retrieved from https://www.niaaa.nih.gov/alcohol-health/overview-alcohol-consumption/alcohol-facts-and-statistics
- Bachrach RL, & Read JP (2017). Peer alcohol behavior moderates within-level associations between posttraumatic stress disorder symptoms and alcohol use in college students. Psychol Addict Behav, 31(5), 576–588. doi: 10.1037/adb0000285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banks DE, & Zapolski TCB (2017). Impulsivity and Problem Drinking in College: Examining the Mediating Role of Sex-Related Alcohol Expectancies and Alcohol Use at Sex. Subst Use Misuse, 52(8), 992–1002. doi: 10.1080/10826084.2016.1268629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beseler CL, Aharonovich E, & Hasin DS (2011). The enduring influence of drinking motives on alcohol consumption after fateful trauma. Alcohol Clin Exp Res, 35(5), 1004–1010. doi: 10.1111/j.1530-0277.2010.01431.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brady KT, Killeen TK, Brewerton T, & Lucerini S (2000). Comorbidity of psychiatric disorders and posttraumatic stress disorder. Journal of Clinical Psychiatry, 61, 22–32. [PubMed] [Google Scholar]
- Breslau N (2002). Epidemiologic studies of trauma, posttraumatic stress disorder, and other psychiatric disorders. Can J Psychiatry, 47(10), 923–929. doi: 10.1177/070674370204701003 [DOI] [PubMed] [Google Scholar]
- Bush K, Kivlahan DR, McDonell MB, Fihn SD, & Bradley KA (1998). The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Ambulatory Care Quality Improvement Project (ACQUIP). Alcohol Use Disorders Identification Test. Arch Intern Med, 158(16), 1789–1795. [DOI] [PubMed] [Google Scholar]
- Chang EC, & Bridewell WB (1998). Irrational beliefs, optimism, pessimism, and psychological distress: a preliminary examination of differential effects in a college population. J Clin Psychol, 54(2), 137–142. [DOI] [PubMed] [Google Scholar]
- Chilcoat HD, & Breslau N (1998). Posttraumatic stress disorder and drug disorders: Testing Causal Pathways. Arch Gen Psychiatry, 55, 913–917. [DOI] [PubMed] [Google Scholar]
- Cohen J, Cohen P, West S, & Aiken L (2003). Applied multiple regression/correlation analysis for the behavioral sciences. Mahwah, NJ: Erlbaum. [Google Scholar]
- Cooper ML (1994). Motivations for alcohol use among adolescents: Development and validation of a four-factor model. Psychol Assess, 6(2), 117. [Google Scholar]
- Cooper ML, Russell M, Skinner JB, & Windle M (1992). Development and validation of a three-dimensional measure of drinking motives. Psychol Assess, 4, 123–132. [Google Scholar]
- Cross D, Crow T, Powers A, & Bradley B (2015). Childhood trauma, PTSD, and problematic alcohol and substance use in low-income, African-American men and women. Child Abuse Negl, 44, 26–35. doi: 10.1016/j.chiabu.2015.01.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis KC, Stoner SA, Norris J, George WH, & Masters NT (2009). Women’s awareness of and discomfort with sexual assault cues: effects of alcohol consumption and relationship type. Violence Against Women, 15(9), 1106–1125. doi: 10.1177/1077801209340759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson DA (2000). US low-risk drinking guidelines: an examination of four alternatives.Alcohol Clin Exp Res, 24(12), 1820–1829. [PubMed] [Google Scholar]
- Dawson DA, Grant BF, Stinson FS, & Chou PS (2004). Another look at heavy episodic drinking and alcohol use disorders among college and noncollege youth. J Stud Alcohol, 65(4), 477–488. [DOI] [PubMed] [Google Scholar]
- Delker E, Brown Q, & Hasin DS (2016). Alcohol Consumption in Demographic Subpopulations: An Epidemiologic Overview. Alcohol Res, 35(1), 7–15. [PMC free article] [PubMed] [Google Scholar]
- Dixon LJ, Leen-Feldner EW, Ham LS, Feldner MT, & Lewis SF (2009). Alcohol use motives among traumatic event-exposed, treatment-seeking adolescents: associations with posttraumatic stress. Addict Behav, 34(12), 1065–1068. doi: 10.1016/j.addbeh.2009.06.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein AL, Flett GL, & Wekerle C (2010). Child maltreatment, alcohol use and drinking consequences among male and female college students: An examination of drinking motives as mediators. Addict Behav, 35(6), 636–639. doi: 10.1016/j.addbeh.2010.02.002 [DOI] [PubMed] [Google Scholar]
- Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, . . . Kaplan K (2004). Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry, 61(8), 807–816. doi: 10.1001/archpsyc.61.8.807 [DOI] [PubMed] [Google Scholar]
- Haller M, & Chassin L (2014). Risk pathways among traumatic stress, posttraumatic stress disorder symptoms, and alcohol and drug problems: a test of four hypotheses. Psychol Addict Behav, 25(3), 841–851. doi: 10.1037/a0035878 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ham LS, Bonin M, & Hope DA (2007). The role of drinking motives in social anxiety and alcohol use. J Anxiety Disord, 21(8), 991–1003. doi: 10.1016/j.janxdis.2006.10.014 [DOI] [PubMed] [Google Scholar]
- Hankin BL, Fraley RC, Lahey BB, & Waldman ID (2005). Is depression best viewed as a continuum or discrete category? A taxometric analysis of childhood and adolescent depression in a population-based sample. JAbnorm Psychol, 114(1), 96–110. doi: 10.1037/0021-843x.114.1.96 [DOI] [PubMed] [Google Scholar]
- Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, & Conde JG (2009). Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. Journal of biomedical informatics, 42(2), 377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holahan CJ, Moos RH, Holahan CK, Cronkite RC, & Randall PK (2001). Drinking to cope, emotional distress and alcohol use and abuse: a ten-year model. J Stud Alcohol, 62(2), 190–198. [DOI] [PubMed] [Google Scholar]
- Hu LB, P M (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives Structural Equation Modeling: A Multidisciplinary Journal, 6(1), 1–55. [Google Scholar]
- Jakupcak M, Tull MT, McDermott MJ, Kaysen D, Hunt S, & Simpson T (2010). PTSD symptom clusters in relationship to alcohol misuse among Iraq and Afghanistan war veterans seeking post-deployment VA health care. Addict Behav, 35(9), 840–843. doi: 10.1016/j.addbeh.2010.03.023 [DOI] [PubMed] [Google Scholar]
- Johnson LD, O M, P M,Bachman JG, & Schulenberg JE (2007). Monitoring the Future: National Survey Results on Drug Use, 1975–2006. I. [Google Scholar]
- Kaplow JB, Curran PJ, Angold A, & Costello EJ (2001). The prospective relation between dimensions of anxiety and the initiation of adolescent alcohol use. J Clin Child Psychol, 30(3), 316–326. doi: 10.1207/s15374424jccp3003_4 [DOI] [PubMed] [Google Scholar]
- Khantzian EJ (1985). The self-medication hypothesis of addictive disorders: focus on heroin and cocaine dependence. American Journal of Psychiatry, 142(11), 1259–1264. [DOI] [PubMed] [Google Scholar]
- Kilpatrick DG, Acierno R, Resnick HS, Saunders BE, & Best CL (1997). A 2-year longitudinal analysis of the relationship between violent assault and substance abuse in women. J Consult Clin Psychol, 65, 834–847. [DOI] [PubMed] [Google Scholar]
- Kilpatrick DG, Ruggiero KJ, Acierno R, Saunders BE, Resnick HS, & Best CL (2003). Violence and risk of PTSD, major depression, substance abuse/dependence, and comorbidity: results from the National Survey of Adolescents. J Consult Clin Psychol, 71(4), 692–700. [DOI] [PubMed] [Google Scholar]
- Kushner MG, Abrams K, & Borchardt C (2000). The relationship between anxiety disorders and alcohol use disorders: A review of major perspectives and findings. Clin Psychol Rev, 20, 149–171. [DOI] [PubMed] [Google Scholar]
- McDevitt-Murphy ME, Williams JL, Bracken KL, Fields JA, Monahan CJ, & Murphy JG (2010). PTSD symptoms, hazardous drinking, and health functioning among U.S.OEF and OIF veterans presenting to primary care. J Trauma Stress, 23(1), 108–111. doi: 10.1002/jts.20482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLeod S, Koenen KC, Meyer J, Lyons MJ, Eisen S, True W, & Goldberg D (2001). Genetic and environmental influences on the relationship among combat exposure, posttraumatic stress disorder symptoms, and alcohol use. J Trauma Stress, 14(4), 259–275. [DOI] [PubMed] [Google Scholar]
- Messman-Moore TL, Coates AA, Gaffey KJ, & Johnson CF (2008). Sexuality, substance use, and susceptibility to victimization: risk for rape and sexual coercion in a prospective study of college women. JInterpers Violence, 23(12), 1730–1746. doi: 10.1177/0886260508314336 [DOI] [PubMed] [Google Scholar]
- Messman-Moore TL, Ward RM, & Zerubavel N (2013). The role of substance use and emotion dysregulation in predicting risk for incapacitated sexual revictimization in women: results of a prospective investigation. Psychol Addict Behav, 27(1), 125–132. doi: 10.1037/a0031073 [DOI] [PubMed] [Google Scholar]
- Muthen B (2009). Missing on x-variables. Retrieved fromhttp://www.statmodel.com/discussion/messages/22/4448.html
- Muthen LK, & Muthen BO (2017). Mplus Version 8 User’s Guide: Muthen & Muthen. [Google Scholar]
- Prins A, Bovin MJ, Smolenski DJ, Marx BP, Kimerling R, Jenkins-Guarnieri MA, . . Tiet QQ (2016). The Primary Care PTSD Screen for DSM-5 (PC-PTSD-5): Development and Evaluation Within a Veteran Primary Care Sample. J Gen Intern Med, 31(10), 1206–1211. doi: 10.1007/s11606-016-3703-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Read JP, Bachrach RL, Wright AG, & Colder CR (2016). PTSD symptom course during the first year of college. Psychol Trauma, 8(3), 393–403. doi: 10.1037/tra0000087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Read JP, Colder CR, Merrill JE, Ouimette P, White J, & Swartout A (2012). Trauma and posttraumatic stress symptoms predict alcohol and other drug consequence trajectories in the first year of college. J Consult Clin Psychol, 80(3), 426–439. doi: 10.1037/a0028210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Read JP, Griffin MJ, Wardell JD, & Ouimette P (2014). Coping, PTSD symptoms, and alcohol involvement in trauma-exposed college students in the first three years of college. Psychol Addict Behav, 28(4), 1052–1064. doi: 10.1037/a0038348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Read JP, Wardell JD, & Colder CR (2013). Reciprocal associations between PTSD symptoms and alcohol involvement in college: a three-year trait-state-error analysis. J Abnorm Psychol, 122(4), 984–997. doi: 10.1037/a0034918 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts AL, Gilman SE, Breslau J, Breslau N, & Koenen KC (2011). Race/ethnic differences in exposure to traumatic events, development of post-traumatic stress disorder, and treatment-seeking for post-traumatic stress disorder in the United States. Psychol Med, 41(1), 71–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sabina C, Schally JL, & Marciniec L (2017). Problematic alcohol and drug use and the risk of partner violence victimization among male and female college students. Journal of Family Violence, 32(3), 305–316. [Google Scholar]
- Salvatore JE, Thomas NS, Cho SB, Adkins A, Kendler KS, & Dick DM (2016). The role of romantic relationship status in pathways of risk for emerging adult alcohol use. Psychol Addict Behav, 30(3), 335–344. doi: 10.1037/adb0000145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schafer JL, & Graham JW (2002). Missing data: our view of the state of the art. Psychol Methods, 7(2), 147–177. [PubMed] [Google Scholar]
- Schmitz N, Hartkamp N, Kiuse J, Franke GH, Reister G, & Tress W (2000). The Symptom Check-List-90-R (SCL-90-R): a German validation study. QualLife Res, 9(2), 185–193. [DOI] [PubMed] [Google Scholar]
- Sher KJ, Wood MD, Wood PK, & Raskin G (1996). Alcohol outcome expectancies and alcohol use: a latent variable cross-lagged panel study. JAbnorm Psychol, 105(4), 561–574. doi: 10.1037/0021-843x.105.4.561 [DOI] [PubMed] [Google Scholar]
- Shin SH, Miller DP, & Teicher MH (2013). Exposure to childhood neglect and physical abuse and developmental trajectories of heavy episodic drinking from early adolescence into young adulthood. Drug Alcohol Depend, 127(1–3), 31–38. doi: 10.1016/j.drugalcdep.2012.06.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slutske WS (2005). Alcohol use disorders among US college students and their non-college- attending peers. Arch Gen Psychiatry, 62(3), 321–327. doi: 10.1001/archpsyc.62.3.321 [DOI] [PubMed] [Google Scholar]
- Slutske WS, Hunt-Carter EE, Nabors-Oberg RE, Sher KJ, Bucholz KK, Madden PA, . . . Heath, A. C. (2004). Do college students drink more than their non-college- attending peers? Evidence from a population-based longitudinal female twin study. J Abnorm Psychol, 113(4), 530–540. doi: 10.1037/0021-843x.113.4.530 [DOI] [PubMed] [Google Scholar]
- Squeglia LM, & Gray KM (2016). Alcohol and Drug Use and the Developing Brain. Curr Psychiatry Rep, 18(5), 46. doi: 10.1007/s11920-016-0689-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart SH (1996). Alcohol abuse in individuals exposed to trauma: a critical review. Psychol Bull, 120(1), 83–112. [DOI] [PubMed] [Google Scholar]
- Sundstrom C, Blankers M, & Khadjesari Z (2017). Computer-Based Interventions for Problematic Alcohol Use: a Review of Systematic Reviews. Int JBehavMed, 24(5), 646–658. doi: 10.1007/s12529-016-9601-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Todd DM, Deane FP, & McKenna PA (1997). Appropriateness of SCL-90-R Adolescent and Adult Norms for Outpatient and Nonoutpatient College Students. Journal of Counseling Psychology, 44(3), 294–301. [Google Scholar]
- Ullman SE, Filipas HH, Townsend SM, & Starzynski LL (2005). Trauma exposure, posttraumatic stress disorder and problem drinking in sexual assault survivors. J Stud Alcohol, 66(5), 610–619. [DOI] [PubMed] [Google Scholar]
- Ullman SE, Relyea M, Peter-Hagene L, & Vasquez AL (2013). Trauma histories, substance use coping, PTSD, and problem substance use among sexual assault victims. Addict Behav, 38(6), 2219–2223. doi: 10.1016/j.addbeh.2013.01.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Veilleux J, Skinner K, Reese ED, & Shaver JA,. (2014). Negative affect intensely influences drinking to cope through facets of emotion dysregulation. Personality and Individual Differences, 59, 96–101. [Google Scholar]
- Waldrop AE, Back SE, Verduin ML, & Brady KT (2007). Triggers for cocaine and alcohol use in the presence and absence of posttraumatic stress disorder. Addict Behav, 32(3), 634–639. [DOI] [PubMed] [Google Scholar]
- Walsh K, Danielson CK, McCauley J, Hanson RF, Smith DW, Resnick HS, . . . Kilpatrick DG (2012). Longitudinal trajectories of posttraumatic stress disorder symptoms and binge drinking among adolescent girls: the role of sexual victimization. J Adolesc Health, 50(1), 54–59. doi: 10.1016/j.jadohealth.2011.05.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weathers F, Litz B, Keane T, Palmieri P, Marx B, & Schnurr P (2013). The PTSD Checklist for DSM-5 (PCL-5). Scale available from the National Center for PTSD at www.ptsd.va.gov. [Google Scholar]
- Wechsler H, Lee JE, Kuo M, & Lee H (2000). College binge drinking in the 1990s: a continuing problem. Results of the Harvard School of Public Health 1999 College Alcohol Study. J Am Coll Health, 48(5), 199–210. doi: 10.1080/07448480009599305 [DOI] [PubMed] [Google Scholar]
- White A, & Hingson R (2013). The burden of alcohol use: excessive alcohol consumption and related consequences among college students. Alcohol Res, 35(2), 201–218. [PMC free article] [PubMed] [Google Scholar]
- Windle M (1994). Substance use, risky behaviors, and victimization among a US national adolescent sample. Addiction, 89(2), 175–182. [DOI] [PubMed] [Google Scholar]
- Wolff JM, Rospenda KM, & Colaneri AS (2017). Sexual Harassment, Psychological Distress, and Problematic Drinking Behavior Among College Students: An Examination of Reciprocal Causal Relations. J Sex Res, 54(3), 362–373. doi: 10.1080/00224499.2016.1143439 [DOI] [PMC free article] [PubMed] [Google Scholar]


