Abstract
Research suggests that individuals with greater dispositional mindfulness (i.e., non-judgmental, present-focused attention) are more likely to quit smoking, but the underlying mechanisms are unclear. This study investigated mechanisms linking mindfulness and early smoking abstinence using ecological momentary assessment (EMA). Participants were 355 smokers (33% Caucasian, 33% African American, 32% Latino; 55% female) receiving smoking cessation treatment. Mindfulness was assessed at baseline and on the quit date. For 4 days pre-quit and 1 week post-quit, participants completed up to 4 EMAs per day indicating levels of negative affect (NA), positive affect (PA), smoking urges, and affect regulation expectancies. Mean, slope, and volatility were calculated for each pre-quit and post-quit EMA variable. Associations among mindfulness, EMA parameters, and abstinence on the quit day and 7 days post-quit, as well as indirect effects of mindfulness on abstinence through EMA parameters were examined. Mindfulness predicted higher odds of abstinence in unadjusted but not covariate-adjusted models. Mindfulness predicted lower NA, higher PA, and lower affective volatility. Lower stress mediated the association between mindfulness and quit-day abstinence. Higher ratings of happy and relaxed, and lower ratings of bored, sad and angry, mediated the association between mindfulness and post-quit abstinence. Mindfulness appeared to weaken the association between craving and post-quit abstinence. This study elucidates real-time, real-life mechanisms underlying dispositional mindfulness and smoking abstinence. During the early process of quitting smoking, more mindful individuals appear to have more favorable emotional profiles, which predicts higher likelihood of achieving abstinence 1 week after the quit date.
Keywords: mindfulness, smoking cessation, ecological momentary assessment
Although most adult cigarette smokers have tried to quit (Lavinghouze et al., 2015), rates of successful smoking cessation are quite low (Babb, Malarcher, Schauer, Asman, & Jamal, 2017). A significant proportion of smokers attempting to quit lapse within hours or days, and those who lapse early are at high risk for full relapse (Brown, Lejuez, Kahler, Strong, & Zvolensky, 2005; Hughes, Keely, & Naud, 2004). Accordingly, researchers have called for studies to examine not only prolonged abstinence, but milestones throughout the process of quitting (including initial abstinence and early lapses to smoking; Japuntich, Piper, Leventhal, Bolt, & Baker, 2011; Shiffman et al., 2006). A better understanding of factors that promote early abstinence (and how) could inform conceptual models as well as smoking cessation interventions. Dispositional mindfulness (i.e., non-judgmental, present-focused attention in daily life; Brown & Ryan, 2003) is one factor that may not only protect against lapse and relapse, but can be modified via interventions (Davis, Goldberg, et al., 2014; Heppner et al., 2016).
Two recent studies suggest that smokers with greater dispositional mindfulness are more likely to quit smoking. First, among Spanish-speaking smokers of Mexican heritage, those with higher levels of the non-judging aspect of mindfulness (indicating the tendency to accept thoughts and feelings without evaluating them; Baer, Smith, Hopkins, Krietemeyer, & Toney, 2006) exhibited a higher likelihood of achieving long-term abstinence (Spears et al., 2015). Second, among African American smokers, those with greater dispositional mindfulness were more likely to achieve initial abstinence and to recover abstinence after early lapses (Heppner et al., 2016). A growing body of research also supports mindfulness-based interventions (which aim to increase dispositional mindfulness) for promoting smoking cessation (Brewer et al., 2011; Davis, Fleming, Bonus, & Baker, 2007; Davis, Goldberg, et al., 2014; Davis, Manley, Goldberg, Smith, & Jorenby, 2014; Davis et al., 2013; Froeliger et al., 2017; Vidrine et al., 2016).
There is a need for research to elucidate how mindfulness (both mindfulness training and dispositional mindfulness) might target core mechanisms underlying addictive behaviors (Witkiewitz & Black, 2014; Witkiewitz et al., 2014). Psychological models of addiction often highlight that escaping, avoiding, or reducing negative affect is a key driver of substance use (Baker, Piper, McCarthy, Majeskie, & Fiore, 2004). Brewer, Elwafi, and Davis (2013) described the “addictive loop,” through which unpleasant cues elicit negative affect, which triggers craving and smoking behavior. Over time, smoking becomes a habitual reaction to negative affect and craving via negative reinforcement.
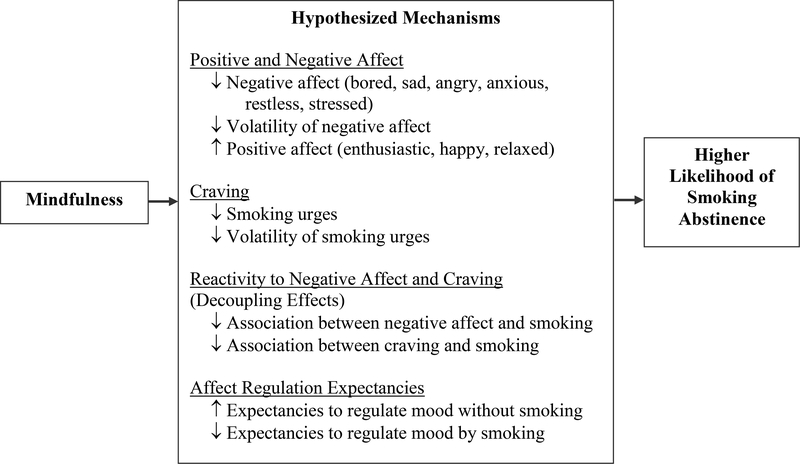
Mindfulness is thought to impact several aspects of the addictive loop (see Figure 1). First, mindfulness might promote more positive and less negative emotions. By promoting nonjudgmental attention to negative emotions, mindfulness might lessen the intensity of negative emotions that are often triggers for smoking. For example, greater dispositional mindfulness has been linked to lower negative affect and perceived stress among smokers (Adams et al., 2015; Paulus, Langdon, Wetter, & Zvolensky, 2017; Waters et al., 2009). Heppner et al. (2016) found that lower negative affect (i.e., depressive symptoms, anger, and sadness) during the early postcessation period mediated the association of dispositional mindfulness with smoking cessation. Similarly, Spears et al. (2017) found that compared to usual care, participants receiving mindfulness-based addiction treatment (MBAT) reported lower anxiety, which predicted a higher likelihood of quitting smoking.
Figure 1.
Hypothesized Mechanisms Underlying Mindfulness and Smoking Abstinence.
Greater volatility (i.e., lability/scatter) of negative affect has been shown to predict lapse and relapse to smoking (Piasecki, Jorenby, Smith, Fiore, & Baker, 2003a, 2003b). Conversely, mindful attention to experiences during the smoking cessation process (e.g., nonjudgmental observation of thoughts, emotions, and physical sensations associated with craving) might promote greater emotional stability. Research suggests that more mindful smokers exhibit less volatility of negative affect during a quit attempt (Adams et al., 2014) and that mindfulness-based smoking cessation treatment reduces volatility of anger (Spears et al., 2017). Among non-smokers, dispositional mindfulness has been linked to lower lability of both positive and negative emotions (Hill & Updegraff, 2012). However, another study found that mindfulness predicted lower volatility of negative, but not positive affect in a sample of Asian undergraduate students (Keng & Tong, 2016). Research is needed to clarify associations among mindfulness, volatility of discrete emotions, and smoking cessation.
Although much less research has explored the role of positive emotions in smoking cessation, mindfulness may also improve cessation outcomes by increasing positive emotions. Low levels of positive affect have been predictive of relapse (Leventhal, Ramsey, Brown, LaChance, & Kahler, 2008) and both higher mean levels and increasing positive emotions predict lower lapse likelihood (Vinci et al., 2017). Through broadening attention and greater cognitive flexibility, mindfulness may promote more positive emotions (Garland et al., 2010). Indeed, dispositional mindfulness has been linked to higher positive affect among smokers (Waters et al., 2009), which could be protective in the smoking cessation process. However, affective scientists have highlighted the need to examine how discrete emotions (e.g., happiness, excitement, sadness, anger) influence decision making and health risk behaviors (Ferrer, Green, & Barrett, 2015). Dispositional mindfulness has been related to lower levels of anger and sadness during the course of smoking cessation (Heppner et al., 2016), but the role of discrete positive emotions in the association between mindfulness and smoking cessation is unclear.
Second, mindfulness might target the addictive loop by reducing craving. That is, non-evaluative attention to the experience of craving could serve to diminish craving intensity. Indeed, greater dispositional mindfulness is related to lower craving among smokers (Vidrine et al., 2009). Mindfulness-Based Relapse Prevention has been shown to reduce craving among individuals with substance use disorders, and these effects were mediated by increases in acceptance, awareness, and nonjudgment (Witkiewitz, Bowen, Douglas, & Hsu, 2013). Furthermore, lower craving has been shown to mediate the effect of mindfulness training vs. usual care on smoking cessation (Spears et al., 2017).
Third, in addition to reducing the intensity of craving and negative emotions, mindfulness might reduce reactivity to these inevitable sensations during the process of quitting smoking (Brewer et al., 2013; Wilson et al., 2017; Witkiewitz et al., 2014). That is, mindfulness may reduce (or “decouple”) the associations of negative emotions and craving with smoking, such that more mindful smokers are able to observe craving and negative affect without automatically reacting by smoking. For example, Elwafi, Witkiewitz, Mallik, Iv, and Brewer (2013) found that while there was a strong correlation between craving and higher smoking frequency at baseline, that association was no longer significant after a mindfulness-based treatment. Neuroimaging research also suggests that mindful attention reduces reactivity to craving among smokers viewing smoking-related images (Westbrook et al., 2013). Regarding dispositional mindfulness, Adams et al. (2015) found that more mindful smokers not only experienced lower levels of perceived stress, but that the associations between stress and alcohol use were weaker for those individuals. Research also supports decoupling as a mechanism of change in studies of mindfulness more broadly (e.g., in the areas of disordered eating, chronic pain, relationships, and self-harm; Levin, Luoma, & Haeger, 2015).
In a similar vein, because evidence suggests that mindfulness is associated with better emotional self-regulation (Guendelman, Medeiros, & Rampes, 2017; Tang, Tang, & Posner, 2016), more mindful smokers might have higher expectancies regarding their ability to regulate emotions without smoking (and lower expectancies of regulating their emotions by smoking). Prior research has suggested that smokers with greater mindfulness have lower expectancies of regulating their emotions by smoking and higher expectancies of regulating emotions by other means (Vidrine et al., 2009), and Heppner et al. (2016) found that lower expectancies regarding the ability of smoking to regulate negative affect mediated the association of dispositional mindfulness with early smoking abstinence.
The vast majority of research on mindfulness and smoking cessation has been limited by reliance on retrospective questionnaire data, which can be hampered by biased or inaccurate reporting. Ecological momentary assessment (EMA) can reduce bias and errors by assessing phenomena at the moment of occurrence in natural settings (Shiffman, 2009; Shiffman, Stone, & Hufford, 2008). Since EMA is often used for multiple assessments throughout the day, trajectories of experiences can be characterized by parameters including the mean level, a linear slope representing direction and rate of change (e.g., worsening levels of negative affect over time), and volatility (i.e., the degree of scatter or instability of affect over time; Cofta-Woerpel et al., 2011; Piasecki et al., 2003a). EMA studies have indicated that higher negative affect and greater volatility of negative affect predict lapse and relapse during a smoking cessation attempt (Cofta-Woerpel et al., 2011; Piasecki et al., 2003a, 2003b; Piasecki et al., 2000; Shiffman et al., 2007; Shiffman, Paty, Gnys, Kassel, & Hickcox, 1996; Shiffman & Waters, 2004). Vinci et al. (2017) recently reported that among smokers making a quit attempt, higher EMA ratings of happiness and relaxation, as well as increasing ratings of happiness, relaxation, and enthusiasm predicted lower likelihood of smoking the next day. However, no known research has examined whether EMA measures of these variables mediate the relationship between mindfulness and smoking cessation. For example, Heppner et al. (2016) found that lower levels of anger and sadness mediated the association between dispositional mindfulness and early abstinence using general questionnaire measures, but these constructs are known to fluctuate on a moment-to-moment basis. In addition, more research has focused on negative (rather than positive) emotions in relation to mindfulness and smoking cessation. EMA data could provide important information about how mindfulness predicts moment-to-moment responding in terms of both discrete positive and discrete negative emotions in smokers’ natural environments.
This study investigated the mechanisms linking dispositional mindfulness with abstinence early in a quit attempt (i.e., on the quit day and during the first week post-quit) using EMA. We expected that mindfulness would target several aspects of the addictive loop (Brewer et al., 2013). As shown in Figure 1, we hypothesized that greater dispositional mindfulness would predict lower levels and lower volatility of negative emotions, higher positive emotions, lower levels and lower volatility of craving, lower expectancies of regulating emotions by smoking, and higher expectancies of regulating emotions by other means, and that each of these parameters would predict greater likelihood of abstinence on the quit day and during the first week post-quit (critical milestones in the smoking cessation process; Shiffman et al., 2006). In addition, mindfulness was hypothesized to moderate (decouple) the associations of negative affect and craving with smoking abstinence, such that those associations would be weaker among participants with higher vs. lower levels of dispositional mindfulness.
Method
Participants
Data were collected as part of a longitudinal cohort study designed to examine the effects of race/ethnicity and social/environmental influences on the process of smoking cessation through 26 weeks post-quit. Participants were recruited from the Houston, TX metropolitan area using media and community outreach. Eligible participants were at least 21 years old, current smokers with a history of smoking at least five cigarettes per day on average over the past year, motivated to quit smoking in the next 30 days, able to provide a home address and functioning telephone number, and able to speak, read, and write in English at or above the sixth grade level. Exclusion criteria were: contraindication for the nicotine patch; active substance use disorder; regular use of tobacco products other than cigarettes; use of bupropion or nicotine replacement products other than the patch provided in the study; another household member enrolled in the study; or participation in a smoking cessation program in the past 90 days. The study was approved by the University of Texas MD Anderson Cancer Center Institutional Review Board.
Procedures
Screening and study orientation.
After telephone screening, eligible participants were scheduled for an in-person orientation session to learn more about the study and provide written informed consent. Then they were scheduled for their baseline session.
In-person visits and treatment.
Participants received six smoking cessation counseling sessions (10–20 minutes each), beginning at the baseline session. In-person counseling sessions were scheduled on the same days as assessment visits, and occurred at baseline (one week before the quit date), on the quit date, and at weeks 1, 2, and 4 post-quit. Participants received an additional counseling session via telephone at week 3 post-quit. Counseling sessions were based on the Treating Tobacco Use and Dependence Clinical Practice Guideline (Fiore et al., 2008), in addition to self-help materials. Counseling sessions and self-help materials did not specifically include mindfulness training. Rather, they provided psychoeducation about nicotine dependence and quitting smoking, encouraged participants to identify and plan for high-risk situations, and taught cognitive and behavioral techniques (e.g., distraction, modifying routines) for avoiding and coping with high-risk situations. Participants were provided with a 6-week course of nicotine patch therapy and instructed to begin using patches on the quit date.
EMA procedures.
At baseline, participants were trained in EMA procedures. EMA assessments occurred for 5 contiguous weeks (1 week pre-cessation through 4 weeks postcessation) using a palmtop personal computer (Etcheverry et al., 2016). Participants completed urge assessments (user-initiated assessments whenever they experienced an urge to smoke), slip assessments (user-initiated assessments whenever they smoked a cigarette), and random assessments (four computer-initiated assessments at random times throughout each day). Because prompts could occur at inconvenient times, random assessments could be delayed for up to 20 minutes total (4 delays of 5 minutes each). Participants were also asked to complete a daily diary assessment as soon as possible each morning. For the present study, potential mediators were assessed in random EMA assessments from the 4 days directly preceding the quit day (pre-quit trajectories), and for the quit day and 6 subsequent days (i.e., 7 days comprising the post-quit trajectories). Post-quit EMA data were drawn from the first week after the quit date because of our interest in predictors of early abstinence (given high lapse rates in the first week; Hughes et al., 2004) and data suggesting that EMA parameters during the first week predict early smoking lapses (Cofta-Woerpel et al., 2011).
Measures
Covariates.
Demographic variables (assessed at baseline) included age, gender, race/ethnicity, partner status, and education. Number of cigarettes per day (which was controlled in analyses predicting day 7 abstinence) was determined for the quit day and each of the 6 days post-quit based on both EMA data (random, slip, and urge assessments) and daily diary data.
Mindfulness.
Dispositional mindfulness was assessed at baseline and on the quit day using the Mindful Attention Awareness Scale (MAAS; Brown & Ryan, 2003), a 15-item self-report measure of the tendency for mindful attention in daily life. Participants rated each item (e.g., “I find myself doing things without paying attention”) using a 6-point Likert scale with reversed endpoints (1 = Almost Always, 6 = Almost Never), and items were summed such that higher scores reflect greater mindfulness. Cronbach’s alpha indicated excellent internal consistency at both baseline and quit day (α = .91 and .92, respectively). Descriptive statistics for the MAAS were as follows: Baseline: M = 4.20, SD = .94; Quit day: M = 4.30, SD = .97. The correlation between the MAAS at the two time points was .74 (p < .001), and a paired-samples t-test indicated no overall changes in MAAS from baseline to quit day, p = .31.
Potential Mediators.
The following potential mediators were assessed in EMA random assessments over the four days directly preceding the quit date (pre-quit trajectories) and on the quit date and subsequent six days (post-quit trajectories). All of the below variables were rated using a 5-point Likert scale (1= Strongly Disagree, 5 = Strongly Agree unless otherwise noted), and participants were asked to “mark the response that most applies to you RIGHT NOW.”
Negative Affect.
Participants rated the extent to which they currently felt each of 6 negative emotions (“I feel... bored, sad, angry, anxious, restless, stressed”). These items were largely drawn from the PANAS-X (Watson & Clark, 1994) and past EMA studies of negative affect and smoking behavior (Shiffman, 2005; Shiffman et al., 2002).
Positive Affect.
Participants rated the extent to which they currently felt each of 3 positive emotions (“I feel. enthusiastic, happy, relaxed”). These items were drawn from the PANAS-X (Watson & Clark, 1994) and have been shown to predict lower likelihood of smoking lapses (Vinci et al., 2017).
Smoking Urges.
Three items were averaged to create an index of smoking urges at each assessment: “I have an urge to smoke,” “I really want to smoke,” and “I need a cigarette.”
Affect Regulation Expectancies.
Expectancies for regulating emotions with and without smoking were assessed with two items: “I am confident that I could do something other than smoke to improve my mood” and “I am confident that smoking would improve my mood.” These items were based on the Affective Information Processing Questionnaire (Wetter, Brandon, & Baker, 1992) and EMA research suggesting that expectancies for smoking to improve mood are associated with greater smoking urges (Cano et al., 2014).
Smoking abstinence.
EMA data were used to determine whether participants smoked on the quit day. If participants indicated smoking a cigarette via a random, slip, or urge assessment on the quit day, they were considered to have lapsed. In addition, if participants indicated in the next-day daily diary that they had smoked on the quit day, they were coded as having lapsed on the quit day. Twenty-four hour abstinence at 7 days after the quit day was assessed via self-report and verified with expired carbon monoxide < 6ppm (Marrone, Paulpillai, Evans, Singleton, & Heishman, 2010; Vidrine et al., 2016). This outcome was chosen rather than 7-day continuous abstinence so that the mediators (assessed over the first week post-quit) and outcome (abstinence) would not overlap in time. Abstinence data at this time point were missing for 17 of the 258 participants included in analyses predicting post-quit abstinence. Thus, analyses were initially conducted with missing data coded as non-abstinent. In addition, sensitivity analyses were conducted with the 241 participants with complete abstinence data.
Statistical Analyses
First, logistic regression analyses were conducted to examine associations between baseline mindfulness and quit-day abstinence, and between quit day mindfulness and day 7 abstinence. Next, a pre-quit trajectory was created for each participant from random assessment data over the four days directly preceding the quit date for each potential mediator (negative affect, positive affect, smoking urges, and affect regulation expectancies), by following the penalized splines methodology in Vinci et al (2017). A post-quit trajectory was created for each participant from random assessment data on the quit day and subsequent 6 days, controlling for self-reported number of cigarettes smoked on each day, by following the orthogonal polynomials regression methodology in Piasecki et al. (2003 a). The mean (indicating the average level over all assessments), slope (indicating increasing or decreasing trends), and volatility (scatter/lability of assessments) were calculated from each participant’s trajectories. Volatility was calculated according to the definition of the mean square successive difference (MSSD; Jahng, Wood, & Trull, 2008), which captures both variability and temporal instability.
Two sets of mediation analyses were conducted to examine: 1) mediators of the association between baseline mindfulness and quit-day abstinence, and 2) mediators of the association between quit-day mindfulness and day 7 abstinence. Analyses determined associations between mindfulness and mediators (path a); associations between mediators and abstinence, controlling for mindfulness (path b); and indirect effects of mindfulness on abstinence through mediators (which would suggest mediation). Each of the aforementioned parameters (mean, slope, and volatility) were tested as mediators in separate analyses. Analyses controlled for age, gender, race/ethnicity, partner status, and education. Mediation analyses were conducted using bootstrapping with Hayes’ (2013) PROCESS macro for SPSS. Bias-corrected 95% confidence intervals were calculated based on 10,000 bootstrap samples for indirect effects.
Finally, moderation analyses were conducted to examine interactions between negative affect/craving and mindfulness in predicting abstinence on the quit day and at 7 days post-quit. As with mediation analyses, moderation was examined using Hayes’ (2013) PROCESS macro for SPSS, controlling for age, gender, race/ethnicity, partner status, and education. Interaction terms were constructed as the product of negative/affect craving variables (in separate models) and dispositional mindfulness (assessed at baseline in predicting quit day abstinence and on the quit day in predicting day 7 abstinence). Negative affect/craving variables included in interaction terms were the mean levels of bored, sad, angry, anxious, restless, stressed, and smoking urges. For significant interactions, associations between negative affect/craving and abstinence were examined at the mean and +/− one standard deviation from the mean of mindfulness.
Results
Participant Characteristics
Of the 434 adult smokers who consented to participate in the parent study, 396 attended the baseline visit. Five participants did not complete any EMAs and were therefore eliminated from EMA analyses, resulting in 391 participants. Of these 391 individuals, 36 had no pre-quit EMA data for the 4 days prior to quit day. Thus, the total number of participants for the current analyses with pre-quit EMA data was 355. As reported by Vinci et al. (2017), this subsample was just over half (55.21%) female and had an average age of 41.76 (SD = 11.23). The sample was 32.68% Caucasian, 33.24% African American, and 32.11% Latino, and 40.34% reported high school or less education. On average, participants smoked 20.79 (SD = 9.68) cigarettes per day and 47.89% reported smoking their first cigarette within 5 minutes of waking at baseline. Overall, participants completed 77.7% of random assessments during the pre-quit period.
Participants were allowed to change their quit date, and pre-quit trajectories for the 355 participants were created based on their individual quit dates. For 258 of these participants, the actual quit date was the same day as the in-person “day 0” assessment. Thus, in order to create post-quit trajectories for the first week of quitting prior to the day 7 in-person assessment, only the 258 participants whose quit date was day 0 were included in post-quit analyses. There were no significant differences between participants who were included in these analyses and those who were excluded because they changed their quit day in terms of demographics or whether they abstained from smoking on their quit day. Among the 258 individuals included in post-quit analyses, participants completed 77.5% of random assessments during the first week post-quit.
Based on EMA data, 62.8% of participants achieved abstinence on the quit day. At 7 days post-quit, 40.7% achieved biochemically-confirmed 24-hour abstinence.
Associations between Mindfulness and Abstinence
Baseline mindfulness predicted higher odds of quit-day abstinence (OR = 1.27 [95% CI: 1.00, 1.60], p = .046) in an unadjusted logistic regression, but did not reach significance once demographic covariates were included (OR = 1.25 [95% CI: 0.98, 1.58], p = .071). Similarly, quit-day mindfulness approached significance in predicting day 7 abstinence in the unadjusted analysis (OR = 1.30 [95% CI: 1.00, 1.69], p = .052) but not in the adjusted analysis (OR = 1.21 [95% CI: 0.92, 1.60], p = .178). We proceeded to examine indirect effects given that statistical power to detect overall effects may have been limited relative to the power to detect other links within the mediation chain (Mackinnon & Fairchild, 2009; O’Rourke & MacKinnon, 2015) and given that current approaches highlight the importance of testing mediation even in the absence of significant total effects (O’Rourke & MacKinnon, 2018).
Mechanisms Underlying Mindfulness and Abstinence
Table 1 shows results for all pathways within the mediational chains predicting quit-day abstinence. The tables present results for mean levels of potential mediators (rather than slope or volatility), and findings regarding slope and volatility are described in the text because there were fewer significant results for those parameters. Mindfulness predicted lower mean ratings for all negative emotions (bored, sad, angry, anxious, restless, stressed) and higher mean ratings for all positive emotions (enthusiastic, happy, relaxed; see Table 1). Mindfulness was also related to lower mean ratings of smoking urges and lower expectancies of smoking in order to improve mood. Furthermore, mindfulness predicted lower volatility for all negative and positive emotions except enthusiastic (happy [b = −.10, p = .005], relaxed [b = −.09, p = .03], bored [b = −.13, p < .001], sad [b = −.10, p = .01], angry [b = −.19, p < .001], anxious [b = −.15, p < .001], restless [b = −.14, p = .002], stressed [b = −.14, p = .01]). Mindfulness did not predict the slope of any variables, and neither volatility nor slope predicted quit-day abstinence. The only significant indirect effect was for stress as a mediator, b = .10 (95% CI: .016, .216). Mindfulness predicted lower stress, which predicted higher likelihood of abstinence on the quit day. There were no significant interactions between mindfulness and negative affect or craving in predicting quit-day abstinence.
Table 1.
Associations among Baseline Mindfulness, Pre-Quit Mean Levels of Potential Mediators, and Quit Day Abstinence. (n = 355)
| Variable | a path (mindfulness associated with mediator) | b path (mediator associated with abstinence) | Indirect Effect (SE) | BC 955% CI | Sobel test p value | |
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Positive Affect | ||||||
| Enthusiastic | .12** | .15 | .02 (.02) | −.018 | .078 | .41 |
| Happy | .18*** | .16 | .03 (.04) | −.036 | .112 | .39 |
| Relaxed | .17*** | .27 | .05 (.04) | −.019 | .132 | .20 |
| Negative Affect | ||||||
| Bored | −.23*** | −.02 | .004 (.04) | −.084 | .091 | .93 |
| Sad | −.24*** | −.29 | .07 (.04) | −.014 | .163 | .12 |
| Angry | −.19*** | −.33 | .06 (.04) | −.003 | .145 | .08 |
| Anxious | −.24*** | −.18 | .04 (.04) | −.039 | .132 | .27 |
| Restless | −.26*** | −.08 | .02 (.05) | −.072 | .115 | .66 |
| Stressed | −.29*** | −.36* | .10 (.05)* | .016 | .206 | .03 |
| Smoking Urges | ||||||
| Smoking Urges | −.12** | −.12 | .02 (.02) | −.025 | .070 | .49 |
| Affect Regulation Expectancies | ||||||
| Improve mood without smoking | .02 | −.10 | −.002 (.01) | −.038 | .008 | .80 |
| Improve mood by smoking | −.09* | −.04 | .003 (.02) | −.024 | .045 | .84 |
Notes. Mindfulness was assessed at baseline. Pre-quit mean levels of potential mediators are based on EMA data from 4 days preceding quit date. “a path” = association between mindfulness and mediator; “b path” = association between mediator and abstinence, controlling for mindfulness; “indirect effect” = indirect effect of mindfulness on abstinence through mediator (abstinence coded as 1, smoking as 0). Models controlled for age, gender, race/ethnicity, partner status, and education. SE = standard error of indirect effect. BC 95% CI = bias-corrected 95% confidence intervals for indirect effects.
Table 2 shows results for all pathways within the mediational chains predicting abstinence at 7 days post-quit. Mindfulness predicted lower mean ratings for all negative emotions and higher mean ratings for all positive emotions during the first week post-quit. Mindfulness was also associated with lower expectancies of smoking to improve mood and higher expectancies of doing something other than smoking to improve mood. Mindfulness predicted lower volatility of several negative emotions (bored [b = −.06, p = .04], sad [b = −.09, p = .001], angry [b = −.11, p < .001], restless [b = −.07, p = .01]) and one positive emotion (relaxed [b = −.06, p = .02]). Indirect effects were significant for mean ratings of the following emotions: happy (b = .14, 95% CI: .040, .290), relaxed (b = .15, 95% CI: .026, .297), bored (b = .16, 95% CI: .050, .318), sad (b = .22, 95% CI: .072, .416), and angry (b = .19, 95% CI: .069, .364). That is, mindfulness predicted higher ratings of feeling happy and relaxed, and lower ratings of feeling bored, sad, and angry during the first week post-quit, each of which predicted higher odds of abstinence at 7 days post-quit.
Table 2.
Associations among Quit Day Mindfulness, Post-Quit Mean Levels of Potential Mediators, and 24-hour Abstinence at 7 Days Post-Quit. (n = 258)
| Variable | a path (mindfulness associated with mediator) | b path (mediator associated with abstinence) | Indirect Effect (SE) | BC 95% CI | Sobel test p value | |
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Positive Affect | ||||||
| Enthusiastic | .19*** | .29 | .06 (.05) | −.028 | .174 | .22 |
| Happy | .21*** | .69** | .14 (.07)* | .040 | .290 | .02 |
| Relaxed | .22*** | .66* | .15 (.07)* | .026 | .297 | .03 |
| Negative Affect | ||||||
| Bored | −.23*** | − 71** | .16 (.07)** | .050 | .318 | .01 |
| Sad | −.29*** | −.77** | .22 (.09)** | .072 | .416 | .01 |
| Angry | −.22*** | − 86*** | .19 (.07)** | .069 | .364 | .01 |
| Anxious | −.23*** | −.10 | .02 (.05) | −.074 | .127 | .64 |
| Restless | −.31*** | −.41 | .13 (.08) | −.017 | .287 | .08 |
| Stressed | −.35*** | −.16 | .06 (.08) | −.084 | .217 | .44 |
| Smoking Urges | ||||||
| Smoking Urges | −.08 | −.15 | .01 (.02) | −.015 | .090 | .56 |
| Affect Regulation Expectancies | ||||||
| Improve mood without smoking | .12** | .45 | .05 (.04) | .001 | .162 | .13 |
| Improve mood by smoking | −.15** | −.23 | .03 (.04) | −.018 | .132 | .28 |
Notes.
p <.05.
p ≤ .01.
p ≤ .001.
Mindfulness was assessed on quit day. Post-quit mean levels of potential mediators are based on EMA data from quit day through 6 days after the quit date and control for cigarettes per day. “a path” = association between mindfulness and mediator; “b path” = association between mediator and abstinence, controlling for mindfulness; “indirect effect” = indirect effect of mindfulness on abstinence through mediator (abstinence coded as 1, smoking as 0). Models controlled for age, gender, race/ethnicity, partner status, and education. SE = standard error of indirect effect. BC 95% CI = bias-corrected 95% confidence intervals for indirect effects.
There was a significant interaction between mindfulness and smoking urges in predicting abstinence at 7 days post-quit, b = .40, SE = .20, p = .04. While higher urges predicted lower likelihood of abstinence at 1 standard deviation below the mean of mindfulness (b = −.59, SE = .30, p = .048), there were not significant associations at the mean (p = .32) or 1 standard deviation above the mean of mindfulness (p = .46).
Sensitivity analyses including only the 241 participants with complete post-quit abstinence data revealed identical patterns for both mediation and moderation.
Discussion
To the best of our knowledge, this is the first study to use EMA to examine the mechanisms linking dispositional mindfulness to smoking abstinence early in a quit attempt. During both the pre- and post-quit periods, mindfulness predicted lower levels of negative emotions, higher levels of positive emotions, and lower affective volatility (i.e., greater emotional stability). In predicting quit-day abstinence, stress was the only significant mediator, such that more mindful smokers reported less pre-quit stress, which predicted higher odds of abstinence on the quit day. In predicting day 7 abstinence, the association between mindfulness and abstinence was mediated by lower levels of sadness, anger, and boredom, and higher levels of happiness and relaxation. In addition, mindfulness appeared to weaken the association between craving and post-quit abstinence. These findings indicate that mindfulness may impact abstinence early in the quit process through enhanced emotional profiles as well as reduced reactivity to craving.
Overall, results are consistent with recent studies suggesting that emotional processes are key mechanisms through which mindfulness promotes smoking cessation (Froeliger et al., 2017; Heppner et al., 2016; Spears et al., 2017). Findings also dovetail with theoretical models suggesting that emotional processes are core mechanisms of addiction (Baker et al., 2004) and that mindfulness targets these emotional processes as key elements in the addictive loop (Brewer et al., 2013). By paying attention to uncomfortable emotions without judging or reacting to them, more mindful smokers may experience less intense negative emotions over time, which appears to enhance their ability to quit. The present study adds to this literature by elucidating how mindfulness predicts discrete emotions, both positive and negative, during both the pre-quit and early post-quit periods. Although mindfulness was related to each of the distinct emotions measured, associations were strongest with lower ratings of stress and restlessness across both the pre-quit and post-quit periods. This is consistent with meta-analyses indicating that some of the more robust effects of mindfulness are on stress (Gotink et al., 2015; Li, Howard, Garland, McGovern, & Lazar, 2017; Spijkerman, Pots, & Bohlmeijer, 2016).
Mindfulness not only predicted higher levels of specific positive and negative emotions but also predicted lower affective volatility. This greater emotional stability is consistent with the concept of “mindful emotion regulation” (Chambers, Gullone, & Allen, 2009; Grecucci, Pappaianni, Siugzdaite, Theuninck, & Job, 2015; Guendelman et al., 2017), through which mindfulness is thought to lessen reactivity to thoughts, feelings, and situations (Brewer et al., 2013; Wilson et al., 2017; Witkiewitz et al., 2014). However, affective volatility did not predict smoking cessation in the current study, which is inconsistent with some previous research (Piasecki et al., 2003a, 2003b). More research is needed to examine associations between affective volatility and various cessation milestones. For example, it is possible that greater affective stability is a stronger predictor of longer-term smoking abstinence.
Interestingly, mechanisms underlying mindfulness and smoking were different for predicting abstinence on the quit day versus one week later. Whereas the indirect effect of mindfulness on quit-day abstinence occurred through lower pre-quit stress, indirect effects of mindfulness on day 7 abstinence occurred through higher post-quit happiness and relaxation and lower sadness, anger, and boredom. In examining each of the mediational pathways, the difference is likely related to differences in the “b path” (associations between mediators and abstinence, controlling for mindfulness as shown in Tables 1 and 2). For example, although mindfulness predicted higher positive emotions and lower negative emotions and urges during the pre-quit period, only pre-quit stress predicted lower likelihood of abstinence on the quit day. However, post-quit happiness, relaxation, boredom, sadness, and anger each predicted abstinence at 7 days post-quit, whereas stress did not. This is consistent with some studies indicating that post-quit variables are more strongly predictive of cessation than pre-quit variables (Gwaltney, Metrik, Kahler, & Shiffman, 2009; Vinci et al., 2017). It may be that certain negative emotions are particularly strong triggers (and positive emotions more salient protective factors) when smokers are experiencing withdrawal symptoms during the post-quit period. Furthermore, mindfulness could be particularly helpful in promoting more adaptive emotion regulation during this challenging time.
Unexpectedly, there were not significant indirect effects of mindfulness on abstinence through either craving or affect regulation expectancies. Although mindfulness did predict lower craving during the pre-quit period, the lack of association between mindfulness and post-quit craving is surprising given findings that mindfulness training reduces post-quit craving (Davis, Manley, et al., 2014; Spears et al., 2017). Our study examined dispositional mindfulness, however, and more research is needed to elucidate associations of both dispositional mindfulness and mindfulness training with craving. Furthermore, craving did not predict abstinence at either time point in this study. Systematic reviews of treatment and laboratory studies have revealed inconsistent associations between craving and smoking (Gass, Motschman, & Tiffany, 2014; Wray, Gass, & Tiffany, 2013), and the cognitive processing model suggests that craving is not a necessary precursor to drug use (Tiffany, 1999). Perhaps more importantly, mindfulness might promote more adaptive responses to craving as described below.
Mindfulness moderated the association between craving and post-quit abstinence, such that higher craving was associated with lower likelihood of abstinence among participants with low (but not high) levels of mindfulness. Although mindfulness did not predict lower levels of craving in this study, findings indicate that mindfulness may change smokers’ responses to the inevitable experience of craving. This is consistent with theoretical and empirical work suggesting that decoupling of associations between craving and substance use is a key mechanism through which mindfulness targets addictive behaviors (Brewer et al., 2013; Wilson et al., 2017; Witkiewitz et al., 2014). For example, Enkema and Bowen (2017) found that greater formal mindfulness practice weakened the association between craving and substance use.
Future research should consider the extent to which the mechanisms examined here are specific to the role of mindfulness in smoking cessation. Other individual differences (e.g., neuroticism; Cosci et al., 2009) and interventions (e.g., cognitive behavioral therapy [CBT]; Spears et al., 2017) may also impact smoking cessation through their effects on negative emotions and stress. It is possible that lower affective volatility and lower reactivity (e.g., decoupling the association between craving and smoking) are more specific to mindfulness. For example, Spears et al. (2017) found that mindfulness training for smoking cessation uniquely reduced volatility of anger compared to CBT. In another recent study, participants receiving mindfulness-based treatment for smoking cessation evidenced less neural stress reactivity compared to those receiving CBT (Kober, Brewer, Height, & Sinha, 2017). Future studies could also use EMA to examine more construct-specific variables (e.g., state mindfulness) as mechanisms underlying both dispositional mindfulness and mindfulness-based treatment for smoking cessation. Preliminary work suggests that brief mindfulness practice (vs. sham meditation) can increase state mindfulness as assessed with EMA among smokers (Ruscio, Muench, Brede, MacIntyre, & Waters, 2016).
The current study is limited by reliance on self-reported EMA data as well as potential concerns about measurement reactivity (i.e., if engaging in self-monitoring via EMA alters participants’ behavior; Rowan et al., 2007). In addition, the large number of statistical tests could inflate familywise error rate, and research is needed to examine whether findings are replicated. This study only predicted abstinence early in the quit process, and it is possible that results would differ for predicting longer-term cessation. Furthermore, this study examined mindfulness as a naturally-occurring individual difference, and it is unclear whether mindfulness-based treatments might produce similar or different outcomes. Future work might also examine whether individual differences (e.g., baseline levels of nicotine dependence) moderate the effects of both dispositional mindfulness and mindfulness-based treatment on smoking cessation. This study is strengthened by measurement of discrete positive and negative emotions in real time in the real world; examination of smoking cessation milestones in a critical timeframe (given high lapse rates early in quit attempts); and investigation of mindfulness in a racially/ethnically and socioeconomically diverse sample.
In conclusion, more mindful individuals appear to have more favorable emotional profiles early in the process of quitting, which predict higher likelihood of achieving early cessation milestones. Mindfulness may target key emotional processes, thus weakening the negative reinforcement patterns hypothesized to underlie addictions (Baker et al., 2004; Brewer et al., 2013). Findings have implications for understanding mindfulness-based interventions, which aim to increase dispositional mindfulness and may promote smoking cessation through fostering more adaptive emotional profiles. During the pre-quit period, lower stress might be a primary mechanism through which mindfulness enhances cessation. During the first week of quitting, a greater tendency for mindful responding might foster certain emotions (e.g., less sadness, anger, and boredom; greater happiness and relaxation) that promote successful cessation, in addition to decoupling the association between craving and smoking. Future research might use EMA to examine effects of mindfulness-based treatment on hypothesized mechanisms over time; directly compare mechanisms underlying mindfulness vs. other active treatments (e.g., cognitive-behavioral therapy); and examine mechanisms underlying mindfulness and longer-term smoking cessation outcomes.
Acknowledgments
This research was supported by the Huntsman Cancer Foundation, the National Institute on Drug Abuse (R01DA014818, K23DA040933), the National Center for Complementary and Integrative Health (K23AT008442), the National Institute on Minority Health and Health Disparities (R00MD010468), the National Cancer Institute (P30CA016672, P30CA042014), and the National Center for Advancing Translational Sciences (UL1TR00106). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The authors have no conflicts of interest to declare.
Results reported here were presented at the 2018 annual meeting of the Society of Behavioral Medicine and 2017 annual meeting of the Society for Research on Nicotine & Tobacco. This manuscript utilizes ecological momentary assessment (EMA) data from a longitudinal cohort study designed to examine the effects of race/ethnicity and social/environmental influences on the process of smoking cessation (R01DA014818). Other publications using these EMA data examined associations among attentional bias, negative affect, and smoking (Etcheverry et al., 2016) and the role of positive emotions in predicting smoking (Vinci et al., 2017), but neither examined mindfulness.
Contributor Information
Claire A. Spears, Department of Health Policy and Behavioral Sciences, School of Public Health, Georgia State University
Liang Li, Department of Biostatistics, The University of Texas MD Anderson Cancer Center.
Cai Wu, Department of Biostatistics, The University of Texas MD Anderson Cancer Center.
Christine Vinci, Health Outcomes and Behavior, Moffitt Cancer Center.
Whitney L. Heppner, Department of Psychological Science, Georgia College & State University
Diana S. Hoover, Department of Health Disparities Research, The University of Texas MD Anderson Cancer Center
Cho Lam, Department of Population Health Sciences, University of Utah and Huntsman Cancer Institute..
David W. Wetter, Department of Population Health Sciences, University of Utah and Huntsman Cancer Institute.
References
- Adams CE, Cano MA, Heppner WL, Stewart DW, Correa-Fernandez V, Vidrine JI, . . . Wetter DW (2015). Testing a Moderated Mediation Model of Mindfulness, Psychosocial Stress, and Alcohol Use among African American Smokers. Mindfulness, 6(2), 315–325. doi: 10.1007/s12671-013-0263-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adams CE, Chen M, Guo L, Lam CY, Stewart DW, Correa-Fernandez V, . . . Wetter DW (2014). Mindfulness predicts lower affective volatility among African Americans during smoking cessation. Psychology of Addictive Behaviors, 28(2), 580–585. doi: 10.1037/a0036512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Babb S, Malarcher A, Schauer G, Asman K, & Jamal A (2017). Quitting Smoking Among Adults - United States, 2000–2015. MMWR Morbidity and Mortality Weekly Report, 65(52), 1457–1464. [DOI] [PubMed] [Google Scholar]
- Baer RA, Smith GT, Hopkins J, Krietemeyer J, & Toney L (2006). Using self-report assessment methods to explore facets of mindfulness. Assessment, 13, 27–45. doi: 10.1177/1073191105283504 [DOI] [PubMed] [Google Scholar]
- Baker TB, Piper ME, McCarthy DE, Majeskie MR, & Fiore MC (2004). Addiction motivation reformulated: an affective processing model of negative reinforcement. Psychological Review, 111(1), 33–51. doi: 10.1037/0033-295X.111.1.33 [DOI] [PubMed] [Google Scholar]
- Brewer JA, Elwafi HM, & Davis JH (2013). Craving to quit: psychological models and neurobiological mechanisms of mindfulness training as treatment for addictions. Psychology of Addictive Behaviors, 27(2), 366–379. doi: 10.1037/a0028490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewer JA, Mallik S, Babuscio TA, Nich C, Johnson HE, Deleone CM, . . . Rounsaville BJ (2011). Mindfulness training for smoking cessation: results from a randomized controlled trial. Drug and Alcohol Dependence, 119, 72–80. doi: 10.1016/j.drugalcdep.2011.05.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown KW, & Ryan RM (2003). The benefits of being present: mindfulness and its role in psychological well-being. Journal of Personality and Social Psychology, 84, 822–848. [DOI] [PubMed] [Google Scholar]
- Brown RA, Lejuez CW, Kahler CW, Strong DR, & Zvolensky MJ (2005). Distress tolerance and early smoking lapse. Clinical Psychology Review, 25(6), 713–733. doi: 10.1016/j.cpr.2005.05.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cano MA, Lam CY, Chen M, Adams CE, Correa-Fernandez V, Stewart DW, . . . Wetter DW (2014). Positive smoking outcome expectancies mediate the association between negative affect and smoking urge among women during a quit attempt. Exp Clin Psychopharmacol, 22(4), 332–340. doi: 10.1037/a0036749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chambers R, Gullone E, & Allen NB (2009). Mindful emotion regulation: An integrative review. Clinical Psychology Review, 29(6), 560–572. doi: 10.1016/j.cpr.2009.06.005 [DOI] [PubMed] [Google Scholar]
- Cofta-Woerpel L, McClure JB, Li Y, Urbauer D, Cinciripini PM, & Wetter DW (2011). Early cessation success or failure among women attempting to quit smoking: trajectories and volatility of urge and negative mood during the first postcessation week. Journal of Abnormal Psychology, 120(3), 596–606. doi: 10.1037/a0023755 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cosci F, Corlando A, Fornai E, Pistelli F, Paoletti P, & Carrozzi L (2009). Nicotine dependence, psychological distress and personality traits as possible predictors of smoking cessation. Results of a double-blind study with nicotine patch. Addict Behav, 34(1), 28–35. doi: 10.1016/j.addbeh.2008.08.003 [DOI] [PubMed] [Google Scholar]
- Davis JM, Fleming MF, Bonus KA, & Baker TB (2007). A pilot study on mindfulness based stress reduction for smokers. BMC Complementary and Alternative Medicine, 7, 2. doi: 10.1186/1472-6882-7-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis JM, Goldberg SB, Anderson MC, Manley AR, Smith SS, & Baker TB (2014). Randomized trial on mindfulness training for smokers targeted to a disadvantaged population. Substance Use and Misuse, 49(5), 571–585. doi: 10.3109/10826084.2013.770025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis JM, Manley AR, Goldberg SB, Smith SS, & Jorenby DE (2014). Randomized trial comparing mindfulness training for smokers to a matched control. Journal of Substance Abuse Treatment, 47(3), 213–221. doi: 10.1016/j.jsat.2014.04.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis JM, Mills DM, Stankevitz KA, Manley AR, Majeskie MR, & Smith SS (2013). Pilot randomized trial on mindfulness training for smokers in young adult binge drinkers. BMC Complementary and Alternative Medicine, 13, 215. doi: 10.1186/1472-6882-13-215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elwafi HM, Witkiewitz K, Mallik S, Iv TA, & Brewer JA (2013). Mindfulness training for smoking cessation: moderation of the relationship between craving and cigarette use. Drug and Alcohol Dependence, 130(1–3), 222–229. doi: 10.1016/j.drugalcdep.2012.11.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enkema MC, & Bowen S (2017). Mindfulness practice moderates the relationship between craving and substance use in a clinical sample. Drug Alcohol Depend, 179, 1–7. doi: 10.1016/j.drugalcdep.2017.05.036 [DOI] [PubMed] [Google Scholar]
- Etcheverry PE, Waters AJ, Lam C, Correa-Fernandez V, Vidrine JI, Cinciripini PM, & Wetter DW (2016). Attentional bias to negative affect moderates negative affect’s relationship with smoking abstinence. Health Psychol, 35(8), 881–890. doi: 10.1037/hea0000338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrer RA, Green PA, & Barrett LF (2015). Affective science perspectives on cancer control: strategically crafting a mutually beneficial research agenda. Perspectives on Psychological Science, 10(3), 328–345. doi: 10.1177/1745691615576755 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiore MC, Jaen CR, Baker TB, Bailey WC, Benowitz NJ, & Curry SJ (2008). Treating Tobacco Use and Dependence: 2008 Update. Rockville, MD: U.S. Department of Health and Human Services (USDHHS), Public Health Service (PHS). [Google Scholar]
- Froeliger B, Mathew AR, McConnell PA, Eichberg C, Saladin ME, Carpenter MJ, & Garland EL (2017). Restructuring Reward Mechanisms in Nicotine Addiction: A Pilot fMRI Study of Mindfulness-Oriented Recovery Enhancement for Cigarette Smokers. Evidence-Based Complementary and Alternative Medicine, 2017, 7018014. doi: 10.1155/2017/7018014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garland EL, Fredrickson B, Kring AM, Johnson DP, Meyer PS, & Penn DL (2010). Upward spirals of positive emotions counter downward spirals of negativity: insights from the broaden-and-build theory and affective neuroscience on the treatment of emotion dysfunctions and deficits in psychopathology. Clinical Psychology Review, 30(7), 849–864. doi: 10.1016/j.cpr.2010.03.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gass JC, Motschman CA, & Tiffany ST (2014). The Relationship Between Craving and Tobacco Use Behavior in Laboratory Studies: A Meta-Analysis. Psychology of Addictive Behaviors, 28(4), 1162–1176. doi: 10.1037/a0036879 [DOI] [PubMed] [Google Scholar]
- Gotink RA, Chu P, Busschbach JJ, Benson H, Fricchione GL, & Hunink MG (2015). Standardised mindfulness-based interventions in healthcare: An overview of systematic reviews and meta-analyses of RCTs. PLoS One, 10(4), e0124344. doi: 10.1371/journal.pone.0124344 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- Grecucci A, Pappaianni E, Siugzdaite R, Theuninck A, & Job R (2015). Mindful Emotion Regulation: Exploring the Neurocognitive Mechanisms behind Mindfulness. BioMed Research International, 2015, 670724. doi: 10.1155/2015/670724 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guendelman S, Medeiros S, & Rampes H (2017). Mindfulness and Emotion Regulation: Insights from Neurobiological, Psychological, and Clinical Studies. Front Psychol, 8, 220. doi: 10.3389/fpsyg.2017.00220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gwaltney CJ, Metrik J, Kahler CW, & Shiffman S (2009). Self-efficacy and smoking cessation: a meta-analysis. Psychology of Addictive Behaviors, 23(1), 56–66. doi: 10.1037/a0013529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes AF (2013). Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. New York, NY: Guilford. [Google Scholar]
- Heppner WL, Spears CA, Correa-Fernandez V, Castro Y, Li Y, Guo B, . . . Wetter DW (2016). Dispositional Mindfulness Predicts Enhanced Smoking Cessation and Smoking Lapse Recovery. Annals of Behavioral Medicine, 50(3), 337–347. doi: 10.1007/s12160-015-9759-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill CL, & Updegraff JA (2012). Mindfulness and its relationship to emotional regulation. Emotion, 12(1), 81–90. doi: 10.1037/a0026355 [DOI] [PubMed] [Google Scholar]
- Hughes JR, Keely J, & Naud S (2004). Shape of the relapse curve and long-term abstinence among untreated smokers. Addiction, 99(1), 29–38. [DOI] [PubMed] [Google Scholar]
- Jahng S, Wood PK, & Trull TJ (2008). Analysis of affective instability in ecological momentary assessment: Indices using successive difference and group comparison via multilevel modeling. Psychological Methods, 13(4), 354–375. doi: 10.1037/a0014173 [DOI] [PubMed] [Google Scholar]
- Japuntich SJ, Piper ME, Leventhal AM, Bolt DM, & Baker TB (2011). The effect of five smoking cessation pharmacotherapies on smoking cessation milestones. Journal of Consulting and Clinical Psychology, 79(1), 34–42. doi: 10.1037/a0022154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keng SL, & Tong EM (2016). Riding the tide of emotions with mindfulness: Mindfulness, affect dynamics, and the mediating role of coping. Emotion, 16(5), 706–718. doi: 10.1037/emo0000165 [DOI] [PubMed] [Google Scholar]
- Kober H, Brewer JA, Height KL, & Sinha R (2017). Neural stress reactivity relates to smoking outcomes and differentiates between mindfulness and cognitive-behavioral treatments. Neuroimage, 151, 4–13. doi: 10.1016/j.neuroimage.2016.09.042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lavinghouze SR, Malarcher A, Jama A, Neff L, Debrot K, & Whalen L (2015). Trends in Quit Attempts Among Adult Cigarette Smokers - United States, 2001–2013. MMWR Morbidity and Mortality Weekly Report, 64(40), 1129–1135. doi: 10.15585/mmwr.mm6440a1 [DOI] [PubMed] [Google Scholar]
- Leventhal AM, Ramsey SE, Brown RA, LaChance HR, & Kahler CW (2008). Dimensions of depressive symptoms and smoking cessation. Nicotine & Tobacco Research, 10(3), 507–517. doi: 10.1080/14622200801901971 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levin ME, Luoma JB, & Haeger JA (2015). Decoupling as a mechanism of change in mindfulness and acceptance: a literature review. BehavModif, 39(6), 870–911. doi: 10.1177/0145445515603707 [DOI] [PubMed] [Google Scholar]
- Li W, Howard MO, Garland EL, McGovern P, & Lazar M (2017). Mindfulness treatment for substance misuse: A systematic review and meta-analysis. Journal of Substance Abuse Treatment, 75, 62–96. doi: 10.1016/jjsat.2017.01.008 [DOI] [PubMed] [Google Scholar]
- Mackinnon DP, & Fairchild AJ (2009). Current Directions in Mediation Analysis. Current Directions in Psychological Science, 18(1), 16. doi: 10.1111/j.1467-8721.2009.01598.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marrone GF, Paulpillai M, Evans RJ, Singleton EG, & Heishman SJ (2010). Breath carbon monoxide and semiquantitative saliva cotinine as biomarkers for smoking. Hum Psychopharmacol, 25(1), 80–83. doi: 10.1002/hup.1078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Rourke HP, & MacKinnon DP (2015). When the test of mediation is more powerful than the test of the total effect. Behav Res Methods, 47(2), 424–442. doi: 10.3758/s13428-014-0481-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Rourke HP, & MacKinnon DP (2018). Reasons for Testing Mediation in the Absence of an Intervention Effect: A Research Imperative in Prevention and Intervention Research. J Stud Alcohol Drugs, 79(2), 171–181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paulus DJ, Langdon KJ, Wetter DW, & Zvolensky MJ (2017). Dispositional Mindful Attention in Relation to Negative Affect, Tobacco Withdrawal, and Expired Carbon Monoxide On and After Quit Day. J Addict Med. doi: 10.1097/ADM.0000000000000361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piasecki TM, Jorenby DE, Smith SS, Fiore MC, & Baker TB (2003a). Smoking withdrawal dynamics: I. Abstinence distress in lapsers and abstainers. Journal of Abnormal Psychology, 112(1), 3–13. [PubMed] [Google Scholar]
- Piasecki TM, Jorenby DE, Smith SS, Fiore MC, & Baker TB (2003b). Smoking withdrawal dynamics: II. Improved tests of withdrawal-relapse relations. Journal of Abnormal Psychology, 112(1), 14–27. [PubMed] [Google Scholar]
- Piasecki TM, Niaura R, Shadel WG, Abrams D, Goldstein M, Fiore MC, & Baker TB (2000). Smoking withdrawal dynamics in unaided quitters. Journal of Abnormal Psychology, 109(1), 74–86. [DOI] [PubMed] [Google Scholar]
- Rowan PJ, Cofta-Woerpel L, Mazas CA, Vidrine JI, Reitzel LR, Cinciripini PM, & Wetter DW (2007). Evaluating reactivity to ecological momentary assessment during smoking cessation. Experimental and Clinical Psychopharmacology, 15(4), 382–389. doi: 10.1037/1064-1297.15.4.382 [DOI] [PubMed] [Google Scholar]
- Ruscio AC, Muench C, Brede E, MacIntyre J, & Waters AJ (2016). Administration and Assessment of Brief Mindfulness Practice in the Field: a Feasibility Study Using Ecological Momentary Assessment. Mindfulness, 7(4), 988–999. doi: 10.1007/s12671-016-0538-4 [DOI] [Google Scholar]
- Shiffman S (2005). Dynamic influences on smoking relapse process. J Pers, 73(6), 1715–1748. doi:JOPY364 [pii] 10.1111/j.0022-3506.2005.00364.x [DOI] [PubMed] [Google Scholar]
- Shiffman S (2009). How many cigarettes did you smoke? Assessing cigarette consumption by global report, Time-Line Follow-Back, and ecological momentary assessment. Health Psychology, 28(5), 519–526. doi: 10.1037/a0015197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiffman S, Balabanis MH, Gwaltney CJ, Paty JA, Gnys M, Kassel JD, . . . Paton SM (2007). Prediction of lapse from associations between smoking and situational antecedents assessed by ecological momentary assessment. Drug and Alcohol Dependence, 91(2–3), 159–168. doi: 10.1016/j.drugalcdep.2007.05.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiffman S, Gwaltney CJ, Balabanis MH, Liu KS, Paty JA, Kassel JD, . . . Gnys M (2002). Immediate antecedents of cigarette smoking: an analysis from ecological momentary assessment. J Abnorm Psychol, 111(4), 531–545. [DOI] [PubMed] [Google Scholar]
- Shiffman S, Paty JA, Gnys M, Kassel JA, & Hickcox M (1996). First lapses to smoking: within-subjects analysis of real-time reports. Journal of Consulting and Clinical Psychology, 64(2), 366–379. [DOI] [PubMed] [Google Scholar]
- Shiffman S, Scharf DM, Shadel WG, Gwaltney CJ, Dang Q, Paton SM, & Clark DB (2006). Analyzing milestones in smoking cessation: illustration in a nicotine patch trial in adult smokers. Journal of Consulting and Clinical Psychology, 74(2), 276–285. doi: 10.1037/0022-006X.74.2.276 [DOI] [PubMed] [Google Scholar]
- Shiffman S, Stone AA, & Hufford MR (2008). Ecological momentary assessment. Annual Review of Clinical Psychology, 4, 1–32. doi: 10.1146/annurev.clinpsy.3.022806.091415 [DOI] [PubMed] [Google Scholar]
- Shiffman S, & Waters AJ (2004). Negative affect and smoking lapses: a prospective analysis. Journal of Consulting and Clinical Psychology, 72(2), 192–201. doi: 10.1037/0022-006X.72.2.192 [DOI] [PubMed] [Google Scholar]
- Spears CA, Hedeker D, Li L, Wu C, Anderson NK, Houchins SC, . . . Wetter DW (2017). Mechanisms Underlying Mindfulness-Based Addiction Treatment Versus Cognitive Behavioral Therapy and Usual Care for Smoking Cessation. Journal of Consulting and Clinical Psychology, 55(11), 1029–1040. doi: 10.1037/ccp0000229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spears CA, Houchins SC, Stewart DW, Chen M, Correa-Fernandez V, Cano MA, . . . Wetter DW (2015). Nonjudging facet of mindfulness predicts enhanced smoking cessation in Hispanics. Psychology of Addictive Behaviors, 29(4), 918–923. doi: 10.1037/adb0000087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spijkerman MP, Pots WT, & Bohlmeijer ET (2016). Effectiveness of online mindfulness-based interventions in improving mental health: A review and meta-analysis of randomised controlled trials. Clinical Psychology Review, 45, 102–114. doi: 10.1016/j.cpr.2016.03.009 [DOI] [PubMed] [Google Scholar]
- Tang YY, Tang R, & Posner MI (2016). Mindfulness meditation improves emotion regulation and reduces drug abuse. Drug and Alcohol Dependence, 163 Suppl 1, S13–18. doi: 10.1016/j.drugalcdep.2015.11.041 [DOI] [PubMed] [Google Scholar]
- Tiffany ST (1999). Cognitive concepts of craving. Alcohol Research & Health, 23(3), 215–224. [PMC free article] [PubMed] [Google Scholar]
- Vidrine JI, Businelle MS, Cinciripini P, Li Y, Marcus MT, Waters AJ, . . . Wetter DW (2009). Associations of mindfulness with nicotine dependence, withdrawal, and agency. Substance Abuse, 30, 318–327. doi: 10.1080/08897070903252973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vidrine JI, Spears CA, Heppner WL, Reitzel LR, Marcus MT, Cinciripini PM, . . . Wetter DW (2016). Efficacy of mindfulness-based addiction treatment (MBAT) for smoking cessation and lapse recovery: A randomized clinical trial. Journal of Consulting and Clinical Psychology, 84(9), 824–838. doi: 10.1037/ccp0000117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vinci C, Li L, Wu C, Lam CY, Guo L, Correa-Fernandez V, . . . Wetter DW (2017). The Association of Positive Emotion and First Smoking Lapse: An Ecological Momentary Assessment Study. Health Psychology. doi: 10.1037/hea0000535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waters AJ, Reitzel LR, Cinciripini P, Li Y, Marcus MT, Vidrine JI, & Wetter DW (2009). Associations between mindfulness and implicit cognition and self-reported affect. Substance Abuse, 30(4), 328–337. doi: 10.1080/08897070903252080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson D , & Clark LA (1994). The PANAS-X: Manual for the Positive and Negative Affect Schedule—Expanded Form. Ames, Iowa: The University of Iowa. [Google Scholar]
- Westbrook C, Creswell JD, Tabibnia G, Julson E, Kober H, & Tindle HA (2013). Mindful attention reduces neural and self-reported cue-induced craving in smokers. Social Cognitive and Affective Neuroscience, 8(1), 73–84. doi:nsr076 [pii] 10.1093/scan/nsr076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wetter DW, Brandon TH, & Baker TB (1992). The relation of affective processing measures and smoking motivation indices among college-age smokers. Advances in Behaviour Research and Therapy, 14(3), 169–193. [Google Scholar]
- Wilson AD, Roos CR, Robinson CS, Stein ER, Manuel JA, Enkema MC, . . . Witkiewitz K (2017). Mindfulness-based interventions for addictive behaviors: Implementation issues on the road ahead. Psychology of Addictive Behaviors, 31(8), 888–896. doi: 10.1037/adb0000319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witkiewitz K, & Black DS (2014). Unresolved issues in the application of mindfulness-based interventions for substance use disorders. Substand Use and Misuse, 49(5), 601–604. doi: 10.3109/10826084.2014.852797 [DOI] [PubMed] [Google Scholar]
- Witkiewitz K, Bowen S, Douglas H, & Hsu SH (2013). Mindfulness-based relapse prevention for substance craving. Addictive Behaviors, 38(2), 1563–1571. doi: 10.1016/j.addbeh.2012.04.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witkiewitz K, Bowen S, Harrop EN, Douglas H, Enkema M, & Sedgwick C (2014). Mindfulness-based treatment to prevent addictive behavior relapse: theoretical models and hypothesized mechanisms of change. Substand Use and Misuse, 49(5), 513–524. doi: 10.3109/10826084.2014.891845 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wray JM, Gass JC, & Tiffany ST (2013). A Systematic Review of the Relationships Between Craving and Smoking Cessation. Nicotine & Tobacco Research, 15(7), 1167–1182. doi: 10.1093/ntr/nts268 [DOI] [PMC free article] [PubMed] [Google Scholar]