Abstract
Background:
Use of smokeless tobacco (ST, moist snuff and chewing tobacco) is elevated among male rural youth, particularly participants in certain sports, including baseball.
Objectives:
This study aimed to assess factors associated with adolescent male athletes’ ST-related behaviors over time, including: baseline use, initiation, and progression in use intensity in a school-based longitudinal cohort.
Methods:
Baseline and one-year follow up questionnaires assessed socio-demographic characteristics, environmental factors, and tobacco-related perceptions and behaviors among 9–12th grade interscholastic baseball players in 36 rural California schools. Population characteristics were compared among ST use categories (never, experimental, and experienced users). Multivariable models using generalized estimating equations were estimated for outcomes among baseline ST never-users (ST susceptibility and future initiation) and experimenters (ST expectations and progression in ST use).
Results:
Of 594 participants, over half (57%) had ever tried a tobacco product and the most common products tried were ST (36%) and electronic cigarettes (36%). Being older, perceiving less ST harm, being Non-Hispanic White, using alcohol or other tobacco products, having family or friends who use ST, and being receptive to advertising were associated with greater baseline ST use. Baseline alcohol consumption, lower perceived ST harm, peer use, and susceptibility and expectations were predictive of ST initiation and/or progression at one-year follow-up.
Conclusion/Importance:
Certain environmental, socio-demographic, cognitive, and behavioral factors predict ST susceptibility and later initiation and progression in use. Interventions addressing these factors have potential to prevent ST uptake and continued use within this high-risk adolescent population.
Keywords: Smokeless tobacco, spit tobacco, snuff, adolescence, athletics, longitudinal studies, rural health
While cigarette use among adolescents in the United States (US) has declined to an all-time low, a similar decline has not been achieved for smokeless tobacco: approximately 8–9% of male high school students nationally currently use smokeless tobacco (ST, moist snuff and chewing tobacco), matching high school male cigarette smoking in prevalence (Kann et al., 2018; Wang et al., 2018). ST use in adolescence is associated with increased risk of future cigarette smoking (Severson, Forrester, & Biglan, 2007), and ST use in general is associated with oral and pancreatic cancer (IARC Working Group on the Evaluation of Carcinogenic Risks to Humans, 2007; Wyss et al., 2016). ST use is notably higher in non-urban areas (Nelson et al., 2006; Pesko & Robarts, 2017): regions that are also frequently underrepresented in research and beyond the reach of tobacco control policies originating in urban centers (Doogan et al., 2017; Pesko & Robarts, 2017). Despite elevated risk of ST use among younger rural adolescents, relatively few longitudinal studies have examined risk factors for ST initiation and progression among rural youth, particularly under the present context of increasingly popular non-cigarette tobacco and nicotine products, such as tobacco waterpipe (hookah) and electronic cigarettes (e-cigarettes). New products may be viewed as superior alternatives to more traditional forms of tobacco, potentially drawing users away from conventional ST; in contrast, emerging product messaging might reinforce positive aspects of non-combustible tobacco relative to cigarettes that could normalize its use (Escobedo et al., 2018).
Adolescents participating in certain sports, including hockey, rodeo, and baseball, are especially vulnerable to ST initiation and continued use (Gansky, Ellison, Kavanagh, Isong, & Walsh, 2009; Severson, Klein, Lichtensein, Kaufman, & Orleans, 2005; Walsh, Hilton, Ernster, Masouredis, & Grady, 1994). Indeed, current ST use among US high school male athletes has remained persistently elevated, staying at approximately 17% from 2001–2013 (Agaku et al., 2015). One study reported that ST use among high school baseball players was nearly 3 times higher than among peers not participating any sport or agriculture club, such as Future Farmers of America (Gansky et al., 2009). Marketing connecting ST to popular sports (Agaku, Odani, Sturgis, Harless, & Glover-Kudon, 2016; Ling, Haber, & Wedl, 2010), masculinity, outdoor activities, and athletic competition (Richardson, Ganz, Stalgaitis, Abrams, & Vallone, 2014), as well as real and perceived ST use among admired professional athletes (Chaffee, Couch, & Gansky, 2018), contributes to social acceptance and normalization of tobacco use, particularly for young rural males.
Adolescent athletes may prefer ST to combustible tobacco because they recognize the adverse effects of cigarette smoking on health and athletic performance (Agaku et al., 2015; Couch, Darius, Walsh, & Chaffee, 2017). Contrasted with cigarette smoking, adolescent athletes may perceive ST as less harmful and more socially acceptable. ST users may overlook potential long-term health consequences, including cancer, gum disease, tooth loss, and nicotine dependence (Boffetta, Hecht, Gray, Gupta, & Straif, 2008; Ebbert, Carr, & Dale, 2004; Warnakulasuriya et al., 2010).
Multiple existing studies have examined correlates and predictors of ST use among youth (Ary, Lichtenstein, & Severson, 1987; Gansky et al., 2009; Goebel, Crespo, Abraham, Masho, & Glover, 2000; Gottlieb, Pope, Rickert, & Hardin, 1993; Riley, Barenie, Mabe, & Myers, 1991; Walsh, Ellison, Hilton, Chesney, & Ernster, 2000). Few such studies were longitudinal (Ary et al., 1987; Hu et al., 1996), and, of these, many either took place in urban areas (Dent, Sussman, Johnson, Hansen, & Flay, 1987; Hu et al., 1996) or followed a national sample (Tomar & Giovino, 1998), rather than focusing on high-risk rural communities. Studies have often considered ST use combined with cigarettes or alcohol (Ary et al., 1987; Dent et al., 1987; Walsh et al., 2000), but not with new and emerging products, such as e-cigarettes. Furthermore, studying youths’ ST susceptibility and future expectations, before unhealthy behaviors begin, may help to identify high-risk individuals for timely preventive interventions.
Existing theoretical models applied to adolescent tobacco use include the tobacco consumer response model (Rees et al., 2009) and theory of planned behavior (Ajzen, 1991). Common across theoretical models, socio-demographic, peer, and environmental variables combine with marketing exposure and past or present substance use to shape individuals’ tobacco-related attitudes and perceptions, which in turn, predict tobacco use intentions and expectations. Intentions regarding whether or not to use ST in the future, one dimension of tobacco susceptibility, predict future tobacco behaviors, including initiation among non-users and progression to established use among tobacco experimenters (Choi, Pierce, Gilpin, Farkas, & Berry, 1997; Pierce, Choi, Gilpin, Farkas, & Merritt, 1996).
Informed by this theoretical framework, the objectives of the present study were to examine smokeless tobacco use behaviors over time and identify risk factors associated with ST use among a relatively under-studied, but high-risk population – rural high school baseball athletes. Specifically, this investigation aimed to identify risk factors associated with ST-related outcomes in three subsets of the study population: 1) baseline ST use in the overall population; 2) ST susceptibility and subsequent ST initiation among baseline ST never users; and 3) ST expectation and progression in ST use among baseline ST experimenters.
Methods
Recruitment and Study Sample
The present study follows a prospective cohort of male baseball players at rural California high schools. Interscholastic teams were enrolled during three spring seasons (2014: 9 schools; 2015: 15 schools; 2016: 12 schools), with each school revisited one year later (i.e., 2015–2017). At each school visit, participants completed in-person confidential surveys on tablet computers to record their tobacco-related beliefs, attitudes, and behaviors. Participants not present the day of one-year follow-up were contacted by email and telephone for an online follow-up survey.
Schools were invited to participate through purposeful sampling. Administrators and athletic coaches were contacted at schools deemed initially eligible, based on having an active baseball program, location in a California county with a population density <1000 persons/mile2 and a municipality <50,000 residents (Hewitt, 1989), and previous participation in a similar research study (Gansky et al., 2009). Schools in the same interscholastic baseball leagues or recommended by coaches or administrators at previously enrolled schools were also contacted. Of 53 schools that met with the study team, 36 (68%) agreed to participate, representing 21 central and northern California counties. At each school, potential participants either returned signed parental consent and granted assent (ages 14–17) or provided self-consent (age 18). Figure 1 depicts participant flow throughout the study. Recruitment targets were designed to estimate past 30-day ST use prevalence (expected: 17%) with a precision of ±2.6% (half-width of 95% confidence interval). The actual baseline sample size (N=594) allowed precision of ±3.0%.
Figure 1.
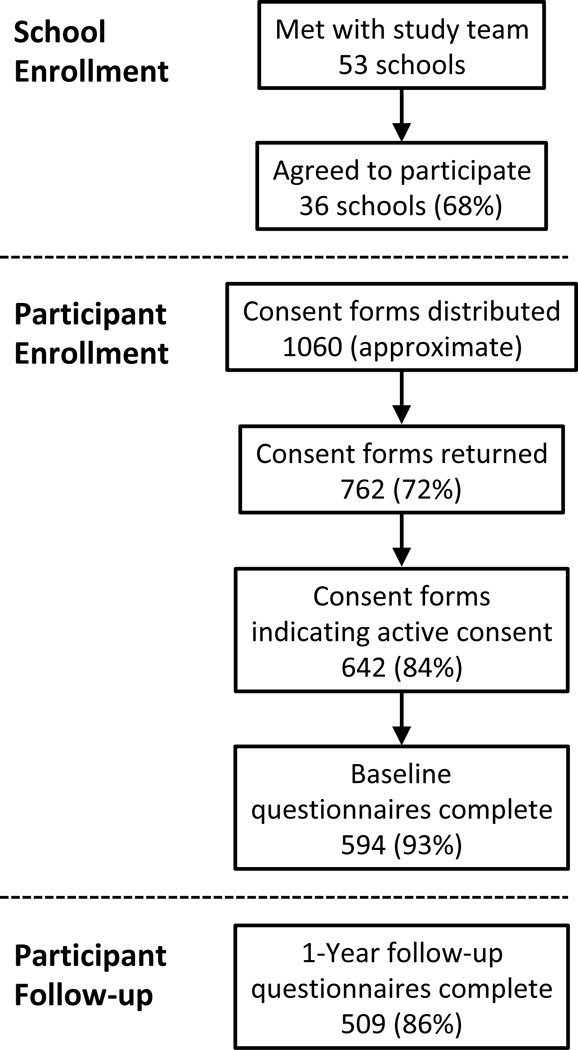
Participant Flow During the Study
An Institutional Review Board of the University of California San Francisco approved all study procedures. Participating schools received $150 to $300, based on the percentage of signed consent forms returned (regardless of affirming or declining participation). Individual respondents received $10 credit to an online retailer at baseline and at follow-up, as well as a letter of commendation from the study.
Survey Instrument
Survey items were reproduced or slightly modified from existing national surveys (Hyland et al., 2017; Wang et al., 2018). Representative images and brief descriptions were shown in separate question blocks for 7 tobacco products: cigarettes, cigars (including premium cigars, little cigars, and cigarillos), e-cigarettes (including cigarette-like disposable, rechargeable, and larger refillable devices), waterpipe, snus, dissolvable tobacco, and conventional smokeless tobacco (oral snuff and chewing tobacco, listed in surveys as dip and chew, respectively). Dissolvable tobacco was excluded from analysis due to leaving the market and low reported baseline prevalence (past-month use: 0.3%).
For each tobacco product, questions related to use included: “Have you ever tried [tobacco product]?”; “During the past 30 days, on how many days did you use [tobacco product]?”; and “About how many times have you used [tobacco product] in your entire life?” (options: 1, 2–10, 11–20, 21–50, 51–99, 100 times or more) (Hyland et al., 2017).
Three baseline ST behavior categories were defined. “Never” users had not used ST, even once. “Experimenters” had tried ST but had not used more than 20 times. “Experienced” users had used ST >20 times, including at least once in the past 30 days. A small number (n=8) of former users who had used ST >20 times, but not within the past 30 days, were not included in these categories. One individual with missing data for lifetime number of times used ST was excluded. Longitudinal outcomes of interest included ST initiation (conversion from ST never use to ST ever use between baseline and follow-up) and progression in ST use (conversion from baseline ST experimenter to current experienced ST user at follow-up). The selection of 20 times as the threshold to define a higher level of accumulated lifetime experience was made a priori based on subjective judgment. This threshold was high enough to require finishing multiple ST containers but low enough that a sufficient number of individuals were expected to reach this threshold within one year of follow-up to allow statistical analysis.
Adolescents who had never tried ST were asked whether they would use ST if “one of your best friends offered” (willingness), and all participants were asked whether they “will be using dip or chew a year from now” (expectation). Each of these items had four Likert-type response options: definitely yes, probably yes, probably not, and definitely not. Failure to strongly reject both of these items with an answer of “definitely not” was considered susceptible to ST use. Questions were based on similarly worded items for cigarettes (Pierce et al., 1996), and this susceptible categorization has been shown to predict future smoking among adolescents (Forrester, Biglan, Severson, & Smolkowski, 2007; Nodora et al., 2014; Pierce et al., 1996). The present measures substitute the words “dip/chew” for “cigarettes.”
Individual and Environmental Covariates
Participants were asked to provide their age, grade in school, self-identified ethnicity and race (later categorized: Non-Hispanic White, Hispanic/Latino, other), the educational attainment of each parent (later dichotomized: ≥1 parent with a college degree vs. less), and whether they had used alcohol (ever and within the past 30 days). Family ST use included use by a father, mother, siblings, or grandparents, adapted for this study based on prior work (Ary et al., 1987; Chassin, Presson, Sherman, McLaughlin, & Gioia, 1985). Advertising receptivity was defined as being able to name the brand of a favorite or attention-grabbing tobacco advertisement (Pierce, Choi, Gilpin, Farkas, & Berry, 1998). Frequency of seeing tobacco warning labels (any tobacco product) was later combined into at least “sometimes” vs. “rarely” or “never.” Perceived ST use by friends (response options: none, few, some, about half, most) was asked regarding friends on or not on the baseball team, adapted from prior work (Ary et al., 1987). A visual analog scale assessed perceived ST harm. Participants were asked, “In your opinion, how harmful is using dip or chew to general health?” and moved a horizontal bar from 0 (not at all harmful) to 100 (extremely harmful) (Chaffee et al., 2015).
Statistical Analysis
To assess whether ST never-users, experimenters, and experienced users were different in individual and environmental characteristics at baseline, and if any of the baseline characteristics were associated with ST use initiation and progression at follow-up among baseline ST never-users and baseline ST experimenters, respectively, parametric (chi-square, ANOVA) and non-parametric (Kruskal-Wallis) tests compared baseline characteristics, as appropriate. The Benjamini-Hochberg procedure for multiple hypothesis testing was used to determine statistical significance while maintaining the overall false discovery rate (alpha) at 0.05 (Benjamini & Hochberg, 1995).
Sensitivity and specificity values were calculated to assess whether baseline ST susceptibility predicted ST initiation and whether baseline ST expectation predicted progression in ST use. Sensitivity was defined as the percentage of all participants with the behavioral outcome at follow-up (i.e., ST use) who were identified as ST susceptible at baseline; whereas specificity was the percentage of all participants without the behavioral outcome (i.e., no ST use at follow-up) who were identified as not ST susceptible at baseline.
To identify additional potentially important factors associated with ST susceptibility, expectation, initiation, and progression, four separate multivariable models were estimated using generalized estimating equations (logit link; exchangeable working correlation structure for clustering within school) for the following outcomes: 1) baseline ST susceptibility among baseline ST never-users; 2) ST initiation at follow-up among baseline ST never-users; 3) baseline ST expectation among baseline ST experimenters; and 4) progression in ST use at follow-up among baseline ST experimenters. Model covariates were based on a priori hypothesized risk factors for ST use, with exclusions for collinear variables (e.g., grade in school included while excluding age). Multiple imputation (chained equations, 25 replicates) was used for missing covariate information (5% of possible values). Covariate specification was identical across models with the exception of other tobacco product and alcohol use, which were categorized as ever use in the ST never-user sample due to relatively low prevalence of past 30-day alcohol use among ST never-users. Model robustness checks included fitting analogous logistic regression models with maximum likelihood, using listwise deletion for missing covariate information, and adding inverse-probability of censoring weights to account for losses-to-follow-up. No substantial differences from the main analysis were observed in robustness checks.
Exploratory Analysis
To capture changes in ST behaviors occurring synchronously with changes in use of other tobacco products, we developed additional behavior categories at baseline and follow-up. These categories defined behaviors according to past 30-day use of smokeless (moist snuff, chewing tobacco, and/or snus), combustible (cigarettes, cigars, and/or hookah) and electronic (e-cigarettes) products, alone or in combination. Given the exploratory nature of this analysis, statistical hypothesis tests were not included (Supplemental Table 1).
Results
Baseline ST Use in the Overall Population
At baseline, the majority of study participants (57%) had ever tried a tobacco product; smokeless tobacco (36%) and electronic cigarettes (36%) were most commonly tried (Table 1). Of those who tried ST, 31% were experienced users, having used ST >20 times, including in the past 30 days. Compared to ST never-users and experimenters, experienced users, on average, were older, perceived ST as less harmful, were more likely to identify as Non-Hispanic White, had used other tobacco products and alcohol, reported family ST use, were receptive to tobacco advertising, saw tobacco warning labels, reported that their friends use ST, and expected to be using ST within one year (Table 1).
Table 1. Sample Characteristics at Baseline.
| Smokeless Tobacco Use Category at Baseline |
|||||
|---|---|---|---|---|---|
| Characteristic | Total (N=585)1 |
Never (N=375) |
Experimenter2 (N=145) |
Experienced3 (N=65) |
p-value4 |
| Age in years, mean (SD) | 15.8 (1.2) | 15.6 (1.1) | 16.1 (1.2) | 16.5 (1.1) | <0.001 |
| Grade in school, n (%) | |||||
| 9th | 172 (29) | 134 (36) | 31 (21) | 7 (11) | <0.001 |
| 10th | 160 (27) | 108 (29) | 39 (27) | 13 (20) | |
| 11th | 139 (24) | 82 (22) | 38 (26) | 19 (29) | |
| 12th | 113 (19) | 50 (13) | 37 (26) | 26 (40) | |
| Race/ethnicity, n (%) | 0.002 | ||||
| Non-Hispanic White | 279 (48) | 164 (44) | 69 (48) | 46 (71) | |
| Hispanic/Latino | 237 (41) | 166 (44) | 57 (39) | 14 (22) | |
| Other | 69 (12) | 45 (12) | 19 (13) | 5 (8) | |
| Parental education, n (%) | |||||
| ≥1 parent with college degree | 321 (59) | 197 (56) | 88 (64) | 36 (63) | 0.22 |
| Ever use, n (%) | |||||
| Smokeless Tobacco | 210 (36) | 0 (0) | 145 (100) | 65 (100) | <0.001 |
| Cigarettes | 126 (22) | 31 (8) | 55 (38) | 31 (48) | <0.001 |
| E-Cigarettes | 208 (36) | 78 (21) | 84 (58) | 46 (71) | <0.001 |
| Cigars | 182 (31) | 44 (12) | 81 (56) | 57 (88) | <0.001 |
| Hookah | 180 (31) | 56 (15) | 74 (51) | 50 (77) | <0.001 |
| Any Tobacco | 332 (57) | 122 (33) | 145 (100) | 65 (100) | <0.001 |
| Alcohol | 359 (64) | 177 (49) | 122 (88) | 60 (94) | <0.001 |
| Any family ST use, n (%) | 182 (35) | 87 (27) | 59 (45) | 36 (62) | <0.001 |
| Advertising receptivity, n (%) | 131 (23) | 54 (15) | 40 (29) | 37 (58) | <0.001 |
| Tobacco warning labels, n (%) | |||||
| See sometimes or more | 346 (62) | 194 (54) | 97 (69) | 55 (86) | <0.001 |
| Perceived ST harm, median (IQR) | 80 (60–98) | 89 (71–100) | 71 (53–89) | 42 (25–60) | 0.001 |
| Friends who use ST, n (%) | <0.001 | ||||
| None | 160 (29) | 143 (41) | 15 (11) | 2 (3) | |
| Few or some | 306 (56) | 175 (51) | 95 (69) | 36 (57) | |
| Half or most | 81 (15) | 28 (8) | 28 (20) | 25 (40) | |
| ST Expectation, n (%) | 264 (46) | 103 (28) | 96 (66) | 65 (100) | <0.001 |
Number of observations for some variables may add to less than the total due to missing data
Had ever tried smokeless tobacco but used less than 20 times
Had used smokeless tobacco ≥20 times, including in the past 30 days
Chi-square test (categorical variables), ANOVA (age), or Kruskal-Wallis test (ST harm score) for difference over the three smokeless tobacco use categories
Abbreviations: IQR = interquartile range; SD = standard deviation; ST = smokeless tobacco
ST Initiation Among Baseline Never Users
Many baseline variables associated with ST use cross-sectionally also predicted ST initiation before follow-up (Table 2). Among baseline ST never-users, 13% tried ST within one year (Figure 2). ST initiation was positively associated with perceiving ST as less harmful and having friends who use ST. Using any other tobacco products was associated with initiation (Table 2). Individually, hookah ever-use predicted ST initiation, while cigarette and e-cigarette ever-use did not. Cigar and alcohol use were not statistically significant predictors under the Benjamini-Hochberg multiple testing procedure. The ST susceptibility measures were predictive of initiation: expectation (sensitivity: 58%; specificity: 75%), willingness (sensitivity: 60%; specificity: 72%), susceptible by either measure (sensitivity: 65%; specificity: 68%).
Table 2. Unadjusted Associations with Smokeless Tobacco Initiation Among Baseline Never Users.
| Smokeless Tobacco Use Between Baseline and Follow-up |
||||
|---|---|---|---|---|
| Consistent Never1 (N=288)5 |
Initiation2 (N=43)5 |
Percent Initiation3 |
p-value4 |
|
| Characteristic | ||||
| Age in years, mean (SD) | 15.5 (1.1) | 15.5 (1.2) | - | 0.83 |
| Baseline perceived ST harm, median (IQR) | 90 (74 – 100) | 77 (61 – 91) | - | 0.004 |
| Follow-up perceived ST harm, median (IQR) | 88 (72 – 100) | 64 (47 – 82) | - | <0.001 |
| Grade in school, n | 0.89 | |||
| 9th | 107 | 17 | 14% | |
| 10th | 89 | 11 | 11% | |
| 11th | 64 | 10 | 14% | |
| 12th | 27 | 5 | 16% | |
| Race/ethnicity, n | 0.37 | |||
| Non-Hispanic White | 126 | 23 | 15% | |
| Hispanic/Latino | 125 | 17 | 12% | |
| Other | 37 | 3 | 8% | |
| Parental education, n | 0.34 | |||
| Neither parent with college degree | 114 | 15 | 12% | |
| ≥1 parent with college degree | 153 | 28 | 15% | |
| Ever use, n | ||||
| Cigarettes | 0.81 | |||
| Never | 264 | 40 | 13% | |
| Ever | 23 | 3 | 12% | |
| E-Cigarettes | 0.78 | |||
| Never | 233 | 34 | 13% | |
| Ever | 55 | 9 | 14% | |
| Cigars | 0.037* | |||
| Never | 259 | 34 | 12% | |
| Ever | 29 | 9 | 24% | |
| Hookah | 0.002 | |||
| Never | 252 | 30 | 11% | |
| Ever | 36 | 13 | 27% | |
| Any non-ST Tobacco | 0.018 | |||
| Never | 205 | 23 | 10% | |
| Ever | 82 | 20 | 20% | |
| Alcohol | 0.024* | |||
| Never | 149 | 15 | 9% | |
| Ever | 125 | 27 | 18% | |
| Any family ST use, n | 0.35 | |||
| No | 184 | 23 | 11% | |
| Yes | 67 | 12 | 15% | |
| Advertising receptivity, n | 0.32 | |||
| No | 231 | 33 | 13% | |
| Yes | 42 | 9 | 18% | |
| Tobacco warning labels, n | 0.15 | |||
| Less than sometimes | 130 | 15 | 10% | |
| See sometimes or more | 143 | 27 | 16% | |
| Friends who use ST, n | 0.002 | |||
| None | 119 | 7 | 6% | |
| Few or some | 126 | 32 | 20% | |
| Half or most | 20 | 3 | 13% | |
| ST Expectation, n | <0.001 | |||
| No | 214 | 18 | 8% | |
| Yes | 70 | 25 | 26% | |
| ST Willingness, n | <0.001 | |||
| No | 204 | 17 | 8% | |
| Yes | 80 | 26 | 25% | |
| ST Susceptibility, n | <0.001 | |||
| No | 193 | 15 | 7% | |
| Yes | 91 | 28 | 24% | |
Reporting ST never use at both baseline and follow-up
Converting from ST never use (baseline) to ST ever use (follow-up)
Incidence of new ST use at follow-up among all baseline never users in the category (only applicable for categorical variables)
Chi-square test (categorical variables), T-test (age), or Mann-Whitney U-test (ST harm score) for difference between smokeless tobacco initiators and non-initiators
Number of observations for some variables may add to less than the total due to missing data
Abbreviations: IQR = interquartile range; SD = standard deviation; ST = smokeless tobacco
No longer statistically significant under the Benjamini-Hochberg procedure for multiple hypothesis tests
Figure 2. Longitudinal Changes in Smokeless Tobacco Use Status.
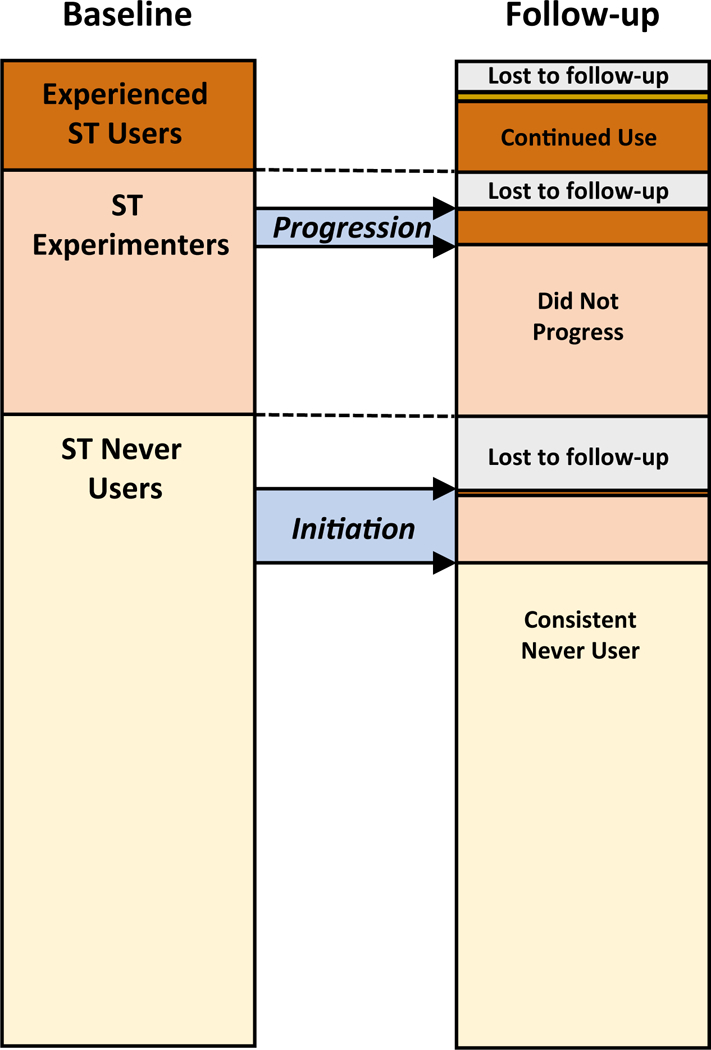
Figure depicts smokeless tobacco (ST) use categories at baseline and follow-up 1 year later, as defined in the analysis; colors represent never user (light yellow; never tried ST, even once or twice), experimental user (beige; ever tried smokeless tobacco but not used >20 times), experienced user (brown; used smokeless tobacco ≥20 times, including ≥1 days in the past 30 days), and former user (gold; baseline experienced user who had not used in the past 30 days at follow-up).
Progression in ST Use Among Baseline Experimenters
Among baseline experimenters (i.e., had tried ST but not >20 times), 17% became current experienced ST users at one-year follow-up (Figure 2). Identifying as Non-Hispanic White and ST use expectation predicted progression at follow-up (Table 3). Perceived ST harm was not statistically significantly lower at baseline among those who progressed, but was lower at follow-up (Table 3). Baseline ST expectation was a sensitive but non-specific predictor of progression (sensitivity: 90%; specificity: 38%). Among baseline experienced ST users, 89% remained current ST users at follow-up.
Table 3.
Unadjusted Associations with Smokeless Tobacco Progression Among Baseline Experimenters
| Characteristic | Smokeless Tobacco Use Between Baseline and Follow-up |
|||
|---|---|---|---|---|
| Did not Progress1 (N=102)5 |
Progressed2 (N=21)5 |
Percent Progressed 3 |
p-value4 | |
| Age in years, mean (SD) | 15.9 (1.1) | 15.6 (0.9) | - | 0.32 |
| Baseline perceived ST harm, median (IQR) | 71 (53 – 86) | 61 (47 – 80) | - | 0.22 |
| Follow-up perceived ST harm, median (IQR) | 69 (52 – 93) | 48 (27 – 70) | - | 0.008* |
| Grade in school, n | 0.66 | |||
| 9th | 24 | 7 | 23% | |
| 10th | 32 | 6 | 16% | |
| 11th | 27 | 6 | 18% | |
| 12th | 19 | 2 | 10% | |
| Race/ethnicity, n | 0.020* | |||
| Non-Hispanic White | 44 | 16 | 27% | |
| Hispanic/Latino | 43 | 3 | 7% | |
| Other | 15 | 2 | 12% | |
| Parental education, n | 0.45 | |||
| Neither parent with college degree | 32 | 8 | 20% | |
| ≥1 parent with college degree | 65 | 11 | 14% | |
| Past month use, n | ||||
| Cigarettes | 0.86 | |||
| No use in past 30-days | 98 | 20 | 17% | |
| Use in past 30-days | 4 | 1 | 20% | |
| E-Cigarettes | 0.20 | |||
| No use in past 30-days | 85 | 15 | 15% | |
| Use in past 30-days | 17 | 6 | 26% | |
| Cigars | 0.53 | |||
| No use in past 30-days | 87 | 19 | 18% | |
| Use in past 30-days | 15 | 2 | 23% | |
| Hookah | 0.53 | |||
| No use in past 30-days | 87 | 19 | 18% | |
| Use in past 30-days | 15 | 2 | 12% | |
| Any non-ST Tobacco | 0.43 | |||
| No use in past 30-days | 72 | 13 | 15% | |
| Use in past 30-days | 30 | 8 | 21% | |
| Alcohol | 0.91 | |||
| No use in past 30-days | 48 | 10 | 17% | |
| Use in past 30-days | 50 | 11 | 18% | |
| Any family ST use, n | 0.90 | |||
| No | 47 | 10 | 18% | |
| Yes | 45 | 9 | 17% | |
| Advertising receptivity, n | 0.46 | |||
| No | 68 | 13 | 16% | |
| Yes | 29 | 8 | 22% | |
| Tobacco warning labels, n | 0.95 | |||
| Less than sometimes | 32 | 7 | 18% | |
| See sometimes or more | 66 | 14 | 18% | |
| Friends who use ST, n | 0.47 | |||
| None | 11 | 1 | 8% | |
| Few or some | 67 | 13 | 16% | |
| Half or most | 19 | 6 | 24% | |
| ST Expectation, n | 0.011* | |||
| No | 39 | 2 | 5% | |
| Yes | 63 | 19 | 23% | |
Reported ST experimenters at baseline and but did not reach threshold for progression at follow-up (past 30-day use and used ≥20 times)
Progressed from ST experimentation (baseline) to experienced ST use (follow-up)
Incidence of progression in ST use at follow-up among all baseline experimenters in the category (only applicable for categorical variables)
Chi-square test (categorical variables), T-test (age), or Mann-Whitney U-test (ST harm score) for difference between those who did and did not progress in ST use
Number of observations for some variables may add to less than the total due to missing data
Abbreviations: IQR = interquartile range; SD = standard deviation; ST = smokeless tobacco
No longer statistically significant under the Benjamini-Hochberg procedure for multiple hypothesis tests
Multivariable Models
Among baseline ST never-users, adjusted for covariates, ever use of other tobacco products was associated with ST susceptibility cross-sectionally and with ST initiation prospectively (Table 4). Perceived ST harm was inversely associated with ST susceptibility and initiation. Alcohol use and grade in school were associated with ST susceptibility, and having friends who use ST was associated with initiation (Table 4).
Table 4.
Correlates of smokeless tobacco susceptibility and initiation among baseline never-users
| Outcome: ST Susceptibility1 Baseline Sample (N = 375) | Outcome: ST Initiation2 Longitudinal Sample (N = 331) | |||||
|---|---|---|---|---|---|---|
| OR | (95% CI) | p-value | OR | (95% CI) | p-value | |
| Grade in school3 | 0.77 | (0.60, 0.99) | 0.04 | 0.94 | (0.65, 1.35) | 0.73 |
| Race/ethnicity | ||||||
| Non-Hispanic White | 1 (reference) | 1 (reference) | ||||
| Hispanic/Latino | 0.94 | (0.52, 1.70) | 0.85 | 1.12 | (0.50, 2.54) | 0.78 |
| Other | 0.82 | (0.37, 1.79) | 0.61 | 0.40 | (0.11, 1.51) | 0.18 |
| Parental education (≥ college) | 0.77 | (0.45, 1.32) | 0.35 | 1.44 | (0.66, 3.13) | 0.36 |
| Ever used non-ST tobacco | 2.13 | (1.24, 3.66) | 0.006 | 2.35 | (1.11, 4.97) | 0.03 |
| Ever used alcohol | 2.48 | (1.44, 4.25) | 0.001 | 1.43 | (0.66, 3.14) | 0.37 |
| Family ST use | 1.67 | (0.92, 3.01) | 0.09 | 1.09 | (0.47, 2.54) | 0.84 |
| Tobacco advertising receptivity | 1.71 | (0.88, 3.31) | 0.11 | 1.56 | (0.64, 3.78) | 0.33 |
| Tobacco warning labels (≥ sometimes) | 0.91 | (0.54, 1.52) | 0.71 | 1.54 | (0.73, 3.27) | 0.26 |
| Perceived ST harm | ||||||
| Least harm | 1 (reference) | 1 (reference) | ||||
| Moderate harm | 0.63 | (0.31, 1.27) | 0.20 | 0.45 | (0.18, 1.14) | 0.09 |
| Greatest harm | 0.17 | (0.08, 0.35) | <0.001 | 0.22 | (0.08, 0.60) | 0.003 |
| Friends who use ST | ||||||
| None | 1 (reference) | 1 (reference) | ||||
| Few or some | 1.12 | (0.64, 1.96) | 0.70 | 2.89 | (1.17, 7.15) | 0.02 |
| Half or most | 1.12 | (0.42, 2.99) | 0.82 | 1.23 | (0.27, 5.54) | 0.79 |
Giving a response other than “definitely not” to ST willingness (try if friend offers) or expectation (using a year from now) among ST never-users at baseline
Converting from ST never use (baseline) to ST ever use (follow-up)
Range: 9–12, specified continuously
Abbreviations: CI = confident interval; OR = odds ratio; ST = smokeless tobacco
Among baseline ST experimenters, in multivariable models, past 30-day alcohol use was associated with baseline expectation about future ST use, whereas Non-Hispanic White identity was associated with progression in ST use (Table 5). Perceiving low ST harm at baseline was associated with baseline ST expectation and future ST use progression (Table 5).
Table 5.
Correlates of smokeless tobacco use expectation and progression in use among baseline experimenters
| Outcome: ST Use Expectation1 Baseline Sample (N = 145) |
Outcome: ST Use Progression2 Longitudinal Sample (N = 123) |
|||||
|---|---|---|---|---|---|---|
| OR | (95% CI) | p-value | OR | (95% CI) | p-value | |
| Grade in school3 | 1.14 | (0.77, 1.67) | 0.51 | 0.74 | (0.41, 1.34) | 0.32 |
| Race/ethnicity | ||||||
| Non-Hispanic White | 1 (reference) | 1 (reference) | ||||
| Hispanic/Latino | 0.63 | (0.23, 1.69) | 0.36 | 0.08 | (0.02, 0.35) | 0.001 |
| Other | 1.64 | (0.43, 6.26) | 0.47 | 0.27 | (0.04, 1.61) | 0.15 |
| Parental education (≥ college) | 0.94 | (0.37, 2.42) | 0.90 | 0.55 | (0.17, 1.76) | 0.31 |
| Past 30-day non-ST tobacco use | 0.73 | (0.28, 1.88) | 0.51 | 2.54 | (0.78, 8.32) | 0.12 |
| Past 30-day alcohol use | 2.52 | (1.06, 6.00) | 0.04 | 0.89 | (0.28, 2.79) | 0.84 |
| Family ST use | 2.20 | (0.79, 6.13) | 0.13 | 0.57 | (0.19, 1.74) | 0.32 |
| Tobacco advertising receptivity | 2.80 | (0.93, 8.42) | 0.07 | 0.89 | (0.26, 3.07) | 0.86 |
| Tobacco warning labels (≥ sometimes) | 0.74 | (0.29, 1.90) | 0.53 | 0.64 | (0.20, 2.07) | 0.46 |
| Perceived ST harm | ||||||
| Least harm | 1 (reference) | 1 (reference) | ||||
| Moderate harm | 0.66 | (0.24, 1.83) | 0.42 | 0.23 | (0.06, 0.87) | 0.03 |
| Greatest harm | 0.10 | (0.03, 0.33) | <0.001 | 0.36 | (0.07, 1.85) | 0.22 |
| Friends who use ST | ||||||
| None | 1 (reference) | 1 (reference) | ||||
| Few or some | 1.21 | (0.29, 4.99) | 0.79 | 1.90 | (0.19, 18.5) | 0.58 |
| Half or most | 1.25 | (0.23, 6.69) | 0.80 | 3.91 | (0.28, 54.7) | 0.31 |
Giving a response other than “definitely not” to expectation (will be using a year from now) among baseline ST experimenters
Converting from ST experimenter (ever used but <20 times) to experienced ST use (used ≥20 times, including in past 30 days) at follow-up
Range: 9–12, specified continuously
Abbreviations: CI = confident interval; OR = odds ratio; ST = smokeless tobacco
Exploratory Analysis
Supplemental Table 1 shows patterns of tobacco use at baseline and follow-up, including use of products other than ST (e.g., e-cigarettes). Among baseline ST-only users, the most common follow-up tobacco behavior was ST dual-use with other products (40%).
Discussion
The present study confirms the persistence of elevated smokeless tobacco use among rural adolescent male athletes. Use was about double the prevalence reported for high school males nationally (Kann et al., 2018; Wang et al., 2018) and in agreement with other studies showing high ST and non-ST tobacco use among high school athletes (Agaku et al., 2015; Davis et al., 1997; Gansky et al., 2009; Walsh et al., 2000). Multiple socio-demographic, family, peer, behavioral (e.g., alcohol and other tobacco use), and psycho-social (e.g., advertising receptivity and tobacco harm perception) measures were associated with baseline ST use; of these, alcohol consumption, perceived ST harm, and peer use predicted ST initiation and/or progression in use within a year. These factors were similarly associated with ST susceptibility and expectations, which in turn, were also good predictors of future ST behaviors. These findings largely conform to a theoretical model, in which personal and environmental influences shape perceived acceptance and intentions related to tobacco and, ultimately, tobacco product use (Rees et al., 2009), as previously applied to ST in other settings (Brubaker & Loftin, 1987). While the present study population may not generalize to all adolescents, it identifies potential targets for ongoing and future interventions tailored to rural male athletes, for whom ST use is a particular public health concern.
In this study, ST susceptibility (willingness to try and expectation to use within one year) was a useful predictor of future ST behavior. In a recent study of high school students in Ontario, similarly constructed susceptibility measures designed for cigarettes were reasonable proxies of susceptibility to other tobacco products (Cole, Kennedy, Chaurasia, & Leatherdale, 2017). A novel finding of the present study is that the ST-specific susceptibility measures demonstrated better sensitivity (at approximately the same specificity) for ST prediction as the cigarette susceptibility measures used in Canada. This suggests added value for product-specific measures. Furthermore, among participants who had already tried ST, most expected to continue using. No baseline experienced ST user expected to stop within a year. Among baseline experimenters, expectation predicted one-year progression in use with high sensitivity, supporting potential use of such a measure to identify at-risk adolescents for more intensive tobacco prevention or cessation interventions.
Having tried non-ST tobacco products was strongly associated with baseline ST use and with ST susceptibility and initiation among baseline never-users. The present data align with existing evidence that dual and poly use of multiple tobacco or nicotine products accounts for an increasing share of youth tobacco users (El-Toukhy, Sabado, & Choi, 2018). Also, it has been demonstrated that use of non-cigarette tobacco products predicts youth cigarette smoking initiation (Watkins, Glantz, & Chaffee, 2018). However, while use of at least one form of non-ST tobacco predicted ST initiation in this study, when products were considered individually, cigar and waterpipe use were associated with ST initiation but cigarette and e-cigarette use were not. This differs from earlier data demonstrating that cigarette smoking predicted future ST uptake (Ary et al., 1987; Dent et al., 1987; Hu et al., 1996; Timberlake, 2016; Tomar & Giovino, 1998). In the present study, conducted two decades later, results differed in that cigarettes were the least often used tobacco product. This may suggest a shift in how different forms of tobacco are used and perceived among rural adolescents: juxtaposed with the widely recognized health risks and decreased social acceptance of smoking, ST may be perceived relatively more favorably (Couch et al., 2017; Persoskie, O’Brien, Nguyen, & Tworek, 2017). As youth cigarette smoking declines, further research is needed to understand why increasingly negative attitudes toward cigarettes may not extend to ST and non-cigarette combustible tobacco products, like waterpipes and cigars.
Alcohol use was higher among more experienced ST users and was positively associated with ST susceptibility and expectation at baseline. Longitudinal associations between alcohol and ST use were not statistically significant. Studies have shown that high school team sport athletes are more likely to consume alcohol and consume in larger quantities than their non-athlete peers (Lisha & Sussman, 2010; Rainey, McKeown, Sargent, & Valois, 1996). We speculate that the high prevalence of alcohol use observed among ST users may reflect simultaneous tobacco and alcohol use in social settings and that substance use prevention strategies may benefit from considering these behaviors together. Alcohol and tobacco in combination deserves particular attention as synergistic risk factors for oral cancer (Franceschi et al., 1990).
Social and cultural factors also play key roles in ST use among interscholastic athletes. Adolescents may see tobacco use as a way to strengthen group bonds with peers (Nemeth et al., 2012), and adolescents with friends, family, or coaches who use ST are more likely to use themselves (Agaku, Ayo-Yusuf, Vardavas, Alpert, & Connolly, 2013; Walsh et al., 2000). In the present study, ST users perceived more ST use among their friends and family than did never-users. Never-users who reported that none of their friends used ST were least likely to initiate use before follow-up. A tobacco cessation program that included peer-led components was effective in promoting ST cessation among high school baseball athletes (Walsh et al., 2003). Further research examining how to incorporate family and peers into ST cessation and prevention may greatly benefit rural youth. In particular, further information on pathways through which culture, environment, and socioeconomic factors interact, potentially in ways specific to certain sports, would inform expanded interventions beyond baseball and into other geographic regions.
Perceiving less harm to health from ST use was strongly associated with experienced ST use at baseline and with ST susceptibility, initiation, and progression in use over time. While perceived harm, generally, serves as a good predictor of behavior, evidence suggests that youth conceptualize potential tobacco harm to include multiple types of health and non-health consequences, including social risks (Halpern-Felsher, Biehl, Kropp, & Rubinstein, 2004; Newman & Shell, 2005; Parsons, Siegel, & Cousins, 1997). Thus, both health and non-health consequences can be important components of youth anti-tobacco communication efforts.
Limitations of the outcome measures and sample size deserve mention. The number of one-year ST progression events in this sample was relatively small, which limited statistical power to identify predictors. It is possible that progression takes place over a longer period. Presumably, additional progression events occurred prior to baseline, as evident by the larger number of ST users already designated as experienced users. Thus, interventions may be more effective if beginning earlier than high school. Additionally, the threshold for defining “experienced” use was based on an arbitrary minimum cut-point of using ST 20 times (approximately 2–5 tins of moist snuff); youth near this minimum may not go on to long-term, regular ST use. Given the lack of previously defined measures of youth smokeless tobacco progress, this threshold was chosen subjectively; its relevance must be tested in independent samples. Notably, however, nearly 90% of baseline experienced ST users continued to use one year later. In future work, data-driven approaches to identify longitudinal behavioral categories, such as group trajectory analysis (Dutra, Glantz, Lisha, & Song, 2017), provide an alternative method to assess ST use patterns over time.
Several other study limitations should be considered. Study participants were exclusively male baseball players from a purposeful sample of rural California schools. Therefore, results do not necessarily generalize to all adolescents, all high school athletes, or other geographic regions. That said, results were congruent with published findings drawn from samples collected elsewhere, suggesting that the present sample was not unusual: behaviors and associations were not greatly divergent from those observed in other populations. Moreover, it is important to examine potential risk factors in high-risk groups facing specific social and environmental contexts, and thus inform potential interventions that may be tailored and targeted to that community. As another possible limitation, tobacco and alcohol use data were based on self-report, and participants may have been hesitant to answer some questions honestly. However, prior research suggests that given assurances of confidentiality, adolescents report their tobacco use accurately (Walsh et al., 2000). Seeing ST warning labels was statistically significantly related to baseline ST use in the positive direction, plausible signifying reverse causation, in which warning labels were seen more often after beginning to engage in ST use. As mentioned, statistical power for some study outcomes, such as ST initiation and progression, was limited, contributing to non-statistically significant findings. Advantageously, the present study provided prospective data from a recent cohort with excellent retention between study waves. The survey instrument assessed multiple conventional and novel tobacco products in addition to ST use, and offered insight into ST susceptibility and future use expectations.
Conclusions
This study demonstrates that rural adolescent male athletes continue to be at elevated risk of smokeless tobacco use, despite living in a state (California) featuring a low prevalence of youth cigarette smoking and known for strong tobacco control policies. During a period of substantial reductions in youth smoking and rising public, academic, and policy interest in new and emerging tobacco and nicotine products, this finding highlights the importance of conventional non-cigarette tobacco products, including ST, as a persistent health risk for adolescents. In the present study population, certain socio-demographic, family, peer, behavioral, and psycho-social factors were readily identified as correlates of ST use and predictive of future ST use over time. Such findings may inform communication, educational, and regulatory strategies aimed at reducing ST use in especially susceptible subpopulations and improving the overall health of rural youth. The finding that much ST initiation had already occurred at baseline suggests a need for such interventions prior to high school.
Supplementary Material
Acknowledgments
Funding details
This work was supported by the US National Institutes of Health National Cancer Institute, National Heart Lung and Blood Institute, and Food and Drug Administration Center for Tobacco Products under grants P50CA180890 and U54HL14712; and the NIH National Center for Advancing Translational Sciences under grant KL2TR001870. The content is solely the responsibility of the authors and does not necessarily represent the views of the NIH or FDA. The authors affirm that there are no conflicts of interest related to the publication of this research.
Footnotes
Disclosure statement
The authors report no conflicts of interest.
References
- Agaku IT, Ayo-Yusuf OA, Vardavas CI, Alpert HR, & Connolly GN (2013). Use of conventional and novel smokeless tobacco products among US adolescents. Pediatrics, 132(3), e578–586. doi: 10.1542/peds.2013-0843 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agaku IT, Odani S, Sturgis S, Harless C, & Glover-Kudon R (2016). Tobacco advertising and promotional expenditures in sports and sporting events - United States, 1992–2013. MMWR Morb Mortal Wkly Rep, 65(32), 821–825. doi: 10.15585/mmwr.mm6532a3 [DOI] [PubMed] [Google Scholar]
- Agaku IT, Singh T, Jones SE, King BA, Jamal A, Neff L, & Caraballo RS (2015). Combustible and smokeless tobacco use among high school athletes - United States, 2001–2013. MMWR Morb Mortal Wkly Rep, 64(34), 935–939. doi: 10.15585/mmwr.mm6434a2 [DOI] [PubMed] [Google Scholar]
- Ajzen I (1991). The theory of planned behavior. Organizational behavior and human decision processes, 50(2), 179–211. [Google Scholar]
- Ary DV, Lichtenstein E, & Severson HH (1987). Smokeless tobacco use among male adolescents: patterns, correlates, predictors, and the use of other drugs. Prev Med, 16(3), 385–401. [DOI] [PubMed] [Google Scholar]
- Benjamini Y, & Hochberg Y (1995). Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc Series B Stat Methodol, 57(1), 289–300. [Google Scholar]
- Boffetta P, Hecht S, Gray N, Gupta P, & Straif K (2008). Smokeless tobacco and cancer. Lancet Oncol, 9(7), 667–675. doi: 10.1016/s1470-2045(08)70173-6 [DOI] [PubMed] [Google Scholar]
- Brubaker RG, & Loftin TL (1987). Smokeless tobacco use by middle school males: a preliminary test of the reasoned action theory. J Sch Health, 57(2), 64–67. [DOI] [PubMed] [Google Scholar]
- Chaffee BW, Couch ET, & Gansky SA (2018). Adolescents’ smokeless tobacco susceptibility by perceived professional baseball players’ use. J Public Health Dent, 78(1), 5–8. doi: 10.1111/jphd.12228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaffee BW, Gansky SA, Halpern-Felsher B, Couch ET, Essex G, & Walsh MM (2015). Conditional risk assessment of adolescents’ electronic cigarette perceptions. Am J Health Behav, 39(3), 421–432. doi: 10.5993/ajhb.39.3.14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chassin L, Presson C, Sherman SJ, McLaughlin L, & Gioia D (1985). Psychosocial correlates of adolescent smokeless tobacco use. Addict Behav, 10(4), 431–435. [DOI] [PubMed] [Google Scholar]
- Choi WS, Pierce JP, Gilpin EA, Farkas AJ, & Berry CC (1997). Which adolescent experimenters progress to established smoking in the United States. Am J Prev Med, 13(5), 385–391. [PubMed] [Google Scholar]
- Cole AG, Kennedy RD, Chaurasia A, & Leatherdale ST (2017). Exploring the predictive validity of the susceptibility to smoking construct for tobacco cigarettes, alternative tobacco products, and e-cigarettes. Nicotine & Tobacco Research. doi: 10.1093/ntr/ntx265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Couch ET, Darius E, Walsh MM, & Chaffee BW (2017). Smokeless tobacco decision-making among rural adolescent males in California. J Community Health, 42(3), 544–550. doi: 10.1007/s10900-016-0286-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis TC, Arnold C, Nandy I, Bocchini JA, Gottlieb A, George RB, & Berkel H (1997). Tobacco use among male high school athletes. J Adolesc Health, 21(2), 97–101. [DOI] [PubMed] [Google Scholar]
- Dent CW, Sussman S, Johnson CA, Hansen WB, & Flay BR (1987). Adolescent smokeless tobacco incidence: Relations with other drugs and psychosocial variables. Prev Med, 16(3), 422–431. [DOI] [PubMed] [Google Scholar]
- Doogan N, Roberts M, Wewers M, Stanton C, Keith D, Gaalema D, … Bunn J (2017). A growing geographic disparity: rural and urban cigarette smoking trends in the United States. Preventive Medicine, 104, 79–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dutra LM, Glantz SA, Lisha NE, & Song AV (2017). Beyond experimentation: Five trajectories of cigarette smoking in a longitudinal sample of youth. PLoS One, 12(2), e0171808. doi: 10.1371/journal.pone.0171808 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ebbert JO, Carr AB, & Dale LC (2004). Smokeless tobacco: an emerging addiction. Med Clin North Am, 88(6), 1593–1605. doi: 10.1016/j.mcna.2004.06.003 [DOI] [PubMed] [Google Scholar]
- El-Toukhy S, Sabado M, & Choi K (2018). Trends in tobacco product use patterns among U.S. youth, 1999–2014. Nicotine Tob Res, 20(6), 690–697. doi: 10.1093/ntr/ntx128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Escobedo P, Cruz TB, Tsai KY, Allem JP, Soto DW, Kirkpatrick MG, … Unger, J. B. (2018). Monitoring tobacco brand websites to understand marketing strategies aimed at tobacco product users and potential users. Nicotine Tob Res, 20(11), 1393–1400. doi: 10.1093/ntr/ntx200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forrester K, Biglan A, Severson HH, & Smolkowski K (2007). Predictors of smoking onset over two years. Nicotine Tob Res, 9(12), 1259–1267. doi: 10.1080/14622200701705357 [DOI] [PubMed] [Google Scholar]
- Franceschi S, Talamini R, Barra S, Baron AE, Negri E, Bidoli E, … La Vecchia, C (1990). Smoking and drinking in relation to cancers of the oral cavity, pharynx, larynx, and esophagus in northern Italy. Cancer Res, 50(20), 6502–6507. [PubMed] [Google Scholar]
- Gansky SA, Ellison JA, Kavanagh C, Isong U, & Walsh MM (2009). Patterns and correlates of spit tobacco use among high school males in rural California. J Public Health Dent, 69(2), 116–124. doi: 10.1111/j.1752-7325.2008.00109.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goebel LJ, Crespo RD, Abraham RT, Masho SW, & Glover ED (2000). Correlates of youth smokeless tobacco use. Nicotine Tob Res, 2(4), 319–325. [DOI] [PubMed] [Google Scholar]
- Gottlieb A, Pope SK, Rickert VI, & Hardin BH (1993). Patterns of smokeless tobacco use by young adolescents. Pediatrics, 91(1), 75–78. [PubMed] [Google Scholar]
- Halpern-Felsher BL, Biehl M, Kropp RY, & Rubinstein ML (2004). Perceived risks and benefits of smoking: differences among adolescents with different smoking experiences and intentions. Prev Med, 39(3), 559–567. doi: 10.1016/j.ypmed.2004.02.017 [DOI] [PubMed] [Google Scholar]
- Hewitt ME (1989). Defining “rural” areas: Impact on health care policy and research. Washington, DC: DIANE Publishing. [Google Scholar]
- Hu FB, Hedeker D, Flay BR, Sussman S, Day LE, & Siddiqui O (1996). The patterns and predictors of smokeless tobacco onset among urban public school teenagers. Am J Prev Med, 12(1), 22–28. [PubMed] [Google Scholar]
- Hyland A, Ambrose BK, Conway KP, Borek N, Lambert E, Carusi C, … Compton WM (2017). Design and methods of the Population Assessment of Tobacco and Health (PATH) Study. Tob Control, 26(4), 371–378. doi: 10.1136/tobaccocontrol-2016-052934 [DOI] [PMC free article] [PubMed] [Google Scholar]
- IARC Working Group on the Evaluation of Carcinogenic Risks to Humans. (2007). Smokeless tobacco and some tobacco-specific N-nitrosamines. IARC Monogr Eval Carcinog Risks Hum, 89, 1–592. [PMC free article] [PubMed] [Google Scholar]
- Kann L, McManus T, Harris WA, Shanklin SL, Flint KH, Queen B, … Ethier KA (2018). Youth risk behavior surveillance - United States, 2017. MMWR Surveill Summ, 67(8), 1–114. doi: 10.15585/mmwr.ss6708a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ling PM, Haber LA, & Wedl S (2010). Branding the rodeo: a case study of tobacco sports sponsorship. Am J Public Health, 100(1), 32–41. doi: 10.2105/ajph.2008.144097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lisha NE, & Sussman S (2010). Relationship of high school and college sports participation with alcohol, tobacco, and illicit drug use: a review. Addict Behav, 35(5), 399–407. doi: 10.1016/j.addbeh.2009.12.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson DE, Mowery P, Tomar S, Marcus S, Giovino G, & Zhao L (2006). Trends in smokeless tobacco use among adults and adolescents in the United States. American Journal of Public Health, 96(5), 897–905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nemeth JM, Liu ST, Klein EG, Ferketich AK, Kwan MP, & Wewers ME (2012). Factors influencing smokeless tobacco use in rural Ohio Appalachia. J Community Health, 37(6), 1208–1217. doi: 10.1007/s10900-012-9556-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newman IM, & Shell DF (2005). Smokeless tobacco expectancies among a sample of rural adolescents. Am J Health Behav, 29(2), 127–136. [DOI] [PubMed] [Google Scholar]
- Nodora J, Hartman SJ, Strong DR, Messer K, Vera LE, White MM, … Pierce, J. P. (2014). Curiosity predicts smoking experimentation independent of susceptibility in a US national sample. Addict Behav, 39(12), 1695–1700. doi: 10.1016/j.addbeh.2014.06.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parsons JT, Siegel AW, & Cousins JH (1997). Late adolescent risk-taking: effects of perceived benefits and perceived risks on behavioral intentions and behavioral change. J Adolesc, 20(4), 381–392. doi: 10.1006/jado.1997.0094 [DOI] [PubMed] [Google Scholar]
- Persoskie A, O’Brien EK, Nguyen AB, & Tworek C (2017). Measuring youth beliefs about the harms of e-cigarettes and smokeless tobacco compared to cigarettes. Addict Behav, 70, 7–13. doi: 10.1016/j.addbeh.2017.01.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pesko MF, & Robarts AM (2017). Adolescent tobacco use in urban versus rural areas of the United States: the influence of tobacco control policy environments. J Adolesc Health, 61(1), 70–76. [DOI] [PubMed] [Google Scholar]
- Pierce JP, Choi WS, Gilpin EA, Farkas AJ, & Berry CC (1998). Tobacco industry promotion of cigarettes and adolescent smoking. JAMA, 279(7), 511–515. [DOI] [PubMed] [Google Scholar]
- Pierce JP, Choi WS, Gilpin EA, Farkas AJ, & Merritt RK (1996). Validation of susceptibility as a predictor of which adolescents take up smoking in the United States. Health Psychol, 15(5), 355–361. [DOI] [PubMed] [Google Scholar]
- Rainey CJ, McKeown RE, Sargent RG, & Valois RF (1996). Patterns of tobacco and alcohol use among sedentary, exercising, nonathletic, and athletic youth. J Sch Health, 66(1), 27–32. [DOI] [PubMed] [Google Scholar]
- Rees VW, Kreslake JM, Cummings KM, O’Connor RJ, Hatsukami DK, Parascandola M, … Connolly, G. N. (2009). Assessing consumer responses to potential reduced-exposure tobacco products: a review of tobacco industry and independent research methods. Cancer Epidemiol Biomarkers Prev, 18(12), 3225–3240. doi: 10.1158/1055-9965.epi-09-0946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richardson A, Ganz O, Stalgaitis C, Abrams D, & Vallone D (2014). Noncombustible tobacco product advertising: how companies are selling the new face of tobacco. Nicotine Tob Res, 16(5), 606–614. doi: 10.1093/ntr/ntt200 [DOI] [PubMed] [Google Scholar]
- Riley WT, Barenie JT, Mabe PA, & Myers DR (1991). The role of race and ethnic status on the psychosocial correlates of smokeless tobacco use in adolescent males. J Adolesc Health, 12(1), 15–21. [DOI] [PubMed] [Google Scholar]
- Severson HH, Forrester KK, & Biglan A (2007). Use of smokeless tobacco is a risk factor for cigarette smoking. Nicotine Tob Res, 9(12), 1331–1337. doi: 10.1080/14622200701705209 [DOI] [PubMed] [Google Scholar]
- Severson HH, Klein K, Lichtensein E, Kaufman N, & Orleans CT (2005). Smokeless tobacco use among professional baseball players: survey results, 1998 to 2003. Tob Control, 14(1), 31–36. doi: 10.1136/tc.2004.007781 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Timberlake DS (2016). Advertising receptivity and youth initiation of smokeless tobacco. Subst Use Misuse, 51(9), 1077–1082. doi: 10.3109/10826084.2016.1160115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomar SL, & Giovino GA (1998). Incidence and predictors of smokeless tobacco use among US youth. Am J Public Health, 88(1), 20–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walsh MM, Ellison J, Hilton JF, Chesney M, & Ernster VL (2000). Spit (smokeless) tobacco use by high school baseball athletes in California. Tob Control, 9 Suppl 2, Ii32–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walsh MM, Hilton JF, Ellison JA, Gee L, Chesney MA, Tomar SL, & Ernster VL (2003). Spit (Smokeless) Tobacco intervention for high school athletes: results after 1 year. Addict Behav, 28(6), 1095–1113. [DOI] [PubMed] [Google Scholar]
- Walsh MM, Hilton JF, Ernster VL, Masouredis CM, & Grady DG (1994). Prevalence, patterns, and correlates of spit tobacco use in a college athlete population. Addict Behav, 19(4), 411–427. [DOI] [PubMed] [Google Scholar]
- Wang TW, Gentzke A, Sharapova S, Cullen KA, Ambrose BK, & Jamal A (2018). Tobacco product use among middle and high school students - United States, 2011–2017. MMWR Morb Mortal Wkly Rep, 67(22), 629–633. doi: 10.15585/mmwr.mm6722a3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warnakulasuriya S, Dietrich T, Bornstein MM, Casals Peidro E, Preshaw PM, Walter C, … Bergstrom J (2010). Oral health risks of tobacco use and effects of cessation. Int Dent J, 60(1), 7–30. [PubMed] [Google Scholar]
- Watkins SL, Glantz SA, & Chaffee BW (2018). Association of noncigarette tobacco product use with future cigarette smoking among youth in the Population Assessment of Tobacco and Health (PATH) Study, 2013–2015. JAMA Pediatr, 172(2), 181–187. doi: 10.1001/jamapediatrics.2017.4173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wyss AB, Hashibe M, Lee YA, Chuang SC, Muscat J, Chen C, … Olshan AF (2016). Smokeless tobacco use and the risk of head and neck cancer: pooled analysis of US studies in the INHANCE Consortium. Am J Epidemiol, 184(10), 703–716. doi: 10.1093/aje/kww075 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


