Abstract
Objective:
To test the short-term efficacy of a brief, fully manualized marital communication and interpersonal support intervention for couples facing recently diagnosed breast cancer.
Methods:
A total of 322 women diagnosed within 6 months with Stage 0-III breast cancer and their 322 spouse caregivers were enrolled. Spouses in the experimental group received five, 30 to 60-minute intervention sessions at 2-week intervals by Masters prepared patient educators; controls received the booklet, “What’s Happening to the Woman I Love?” Outcomes were assessed at 3, 6 and 9 months using Linear Mixed Models within an intent to treat analysis.
Results:
Compared to controls, at 3 months spouse caregivers significantly improved on standardized measures of depressed mood, anxiety, cancer-related marital communication, interpersonal support, and self-care. All differences except depressed mood and anxiety were sustained at 9 months. Wives significantly improved at 3 months on marital communication and positive appraisal of spouses’ interpersonal support; gains remained significant at 9 months. Compared to controls on chemotherapy, wives in the experimental group additionally improved on depressed mood and tended to improve on anxiety.
Conclusions:
A brief, fully manualized intervention delivered directly to spouse caregivers early in the course of their wives’ medical treatment improves caregivers’ self-care and behavioral-emotional adjustment and wives’ positive view of their spouses’ support and communication. The brevity and manualized structure of the intervention argue strongly for its scalability, use in cost-sensitive settings, and its potential dissemination through e-health channels.
Keywords: Cancer, oncology, caregiver, marital communication, skill training, support, randomized clinical trial, self-care, self-efficacy, spouse
Background
Spouse caregivers of women with breast cancer suffer substantial distress during initial treatment of their wives’ breast cancer that goes well beyond simple “caregiving burden” [1, 2]. An estimated 22–32% of them reach or exceed clinical levels of anxiety or depressed mood or both [3] and there is early evidence that caregiving can put spouses at risk for dysregulation of their pro- and anti-inflammatory pathways [4, 5].
Breast cancer also takes a toll on the couples’ relationship, including the quality of marital communication and interpersonal support and marital tension or discord [2, 6–16]. Both the quality and type of marital communication about the cancer, including partner supportive responses, significantly affect the diagnosed woman’s psychological distress [7, 8] and relationship satisfaction [7].
Spouse caregivers self-describe as being unprepared for all aspects of their role [17]; struggle with what to say and do to support their ill partner [10, 18]; commonly misjudge how to help her, emphasizing instrumental, not interpersonal support [19]; struggle with her emotional lability from the cancer and its treatment [10]; and carry serious fears that, despite the best medical treatment, they may lose her to the disease [20].
Despite the magnitude of distress and the large numbers affected, there has never been a randomized control clinical trial of a fully manualized in-person intervention that is delivered directly to spouse caregivers with hypothesized benefits to both members of the dyad. What we do know is that lengthy, multiple, face-to-face, in-home, or group-delivered interventions conjointly delivered to the dyad have significantly improved patients’ and caregivers’ anxiety, depressive symptoms, cancer-specific distress, and positive well-being [14–16, 21]. However, these interventions are not scalable or sustainable and none have attempted to benefit the dyad by intervening solely with the spouse caregiver.
Specific Aims
The purpose of the current study was to test the short-term efficacy of a 5-session skill and efficacy-building communication and interpersonal support intervention delivered to spouses with hypothesized benefits to recently diagnosed wives with Stage 0-III breast cancer. Goals were to improve spouse caregivers’ and wives’ depressed mood, anxiety, and cancer-related marital communication; spouses’ behavioral skills and confidence in interpersonally supporting their wife and managing their own cancer-related distress; and increase wives’ positive appraisal of spouses’ interpersonal support and cancer-related marital communication.
Methods
The study was a 2-group randomized control trial with block randomization that was centrally managed by the study’s biostatistician using a computer random allocation program. Assessments were carried out at baseline and 3, 6 and 9 months. Women and their caregivers were eligible if women were diagnosed within 6 months with in situ or invasive breast cancer (Stage 0, I, IIA, IIB, or III); were married or in an intimate relationship with her spouse (either gender) caregiver; read and wrote English among their languages of choice; and lived within 100 miles of the study center.
After Human Subjects approval at the study center and each recruitment site, the data collection team obtained signed informed consent from caregivers and patients and baseline measures in couples’ homes. Data collectors, study participants, site intermediaries and referring medical providers were masked on randomization status for the duration of the study. Dosage and fidelity were monitored by comparing each digitally recorded intervention session against standardized session-specific performance criteria.
Experimental Intervention
The Helping Her Heal Program consisted of 5 fully scripted, in-person psychoeducational sessions delivered in person to the spouse caregiver every 2 weeks by a Masters prepared patient educator (nurse, certified health educator, or social worker). The theoretical basis of the intervention derived from the Relational Model of Adjustment to Cancer, an extension of family systems theory for dyads and families affected by cancer [2, 7, 8, 11–13, 22–26] and Bandura’s Social Cognitive Theory [27–29]. Each session began with a brief didactic text to frame the session and all sessions incorporated written and interactional assignments between the caregiver and patient educator. Content was unique to each session, complemented by at-home exercises the caregiver practiced with the patient educator, and sessions lasted 30–60 minutes each. See details in Lewis [30].
Control Group
Participants randomized to the control group were mailed a 16-page booklet available in the public domain, “What’s Happening to the Woman I Love?” which described what the spouse caregiver could do to emotionally and physically support his wife; identified strategies for strengthening their relationship; and suggested methods the caregiver could use to decrease distress in their caregiver role.
Study Measures
Diagnosis, demographic and treatment-related data were obtained from the medical record and self-report.
Depressed mood.
Depressed mood was measured by the Center for Epidemiologic Studies-Depression Scale (CES-D), a 20-item scale that measures the recent occurrence of symptoms of depression [31, 32]. Internal consistency reliability and validity are well established, ranging between .84 and .85 [31–33]. Internal consistency reliability for the study sample for caregivers was 0.892 and 0.894 for patients.
Anxiety.
Spouse caregivers’ and patients’ anxiety were measured by the state component of the Spielberger State-Trait Anxiety Inventory (STAI), a 20-item self-report questionnaire which evaluates feelings of apprehension, tension, nervousness, and worry “right now, at this moment” [34, 35]. Reliability and validity are well established [36]. Internal consistency reliability for the study sample was 0.935 for caregivers and 0.945 for patients.
Marital Communication.
Marital communication was measured by the Mutuality & Interpersonal Sensitivity Scale (MIS), a self-report questionnaire that measures both the content and ways in which couples communicate with each other about the breast cancer [20, 24]. The measure has two subscales: Open Communication, e.g., “We spend a lot of time talking about how things are going with the breast cancer” and Expressing Sad Feelings, e.g., “We don’t talk together about the sadness I feel about the breast cancer.” Higher scores denote a higher quality of marital communication about the cancer. The internal consistency reliabilities for wives’ and spouses’ Open Communication subscale for the study sample was 0.92 and 0.86, respectively, and 0.88 and 0.82 for the Expressing Sad Feelings subscale for wives and spouses, respectively.
Spouse’s Skills.
Spouse’s skills were measured by the What I Do for Her Checklist, a spouse-reported measure developed by the study team that describes the specific communication and interpersonal support skills the spouse carries out with the wife related to the breast cancer. The wife support subscale (6 items) measures spouses’ ways of behaviorally interacting with her about the cancer, e.g., “I ask my wife/partner about specific ways I can be supportive to her about her breast cancer.” The self-care subscale (6 items) measures spouses’ ways of managing their own cancer-related stress, e.g., “I take regular time out for myself.” The scale was assessed for content validity by 3 expert clinicians. Construct validity was evaluated by examining its correlation with spouses’ depressed mood, anxiety, self-efficacy and wife-reported perceived support. The internal consistency reliability for the study sample was 0.64 (wife support) and 0.51 (self-care) subscales.
Self-efficacy Scale.
Spouses’ self-efficacy was measured by the Cancer Self-Efficacy Scale (CASE), a 19-item self-report measure of the spouse’s degree of self-confidence to support his wife and carry out his own self-care [20, 24]. The questionnaire consists of two subscales: a Wife-focused subscale and a Self-care focused subscale [30, 37]. The Wife-focused subscale (14 items) measures spouses’ confidence in talking with the patient about her cancer-related concerns and be supportive, e.g., “I know what to do to be supportive to my wife/partner about the breast cancer.” The Self-care subscale (5 items) measures caregivers’ confidence in helping themselves deal with the demands and challenges of the cancer, e.g., “I know what resources to use to help me personally cope with my wife’s breast cancer.” The internal consistency reliability for the Total scale was 0.952 for the study sample and 0.949 for the Wife-focused and 0.810 for the Self-care subscales.
Wife’s Appraisal of Spouse’s Support.
The What He Does for Me Questionnaire is an 18-item measure of support that describes the wife’s perception of specific, observable behaviors of support she receives from her spouse related to her breast cancer. Example items read, “My husband/partner listens to me when I tell him/her sad or negative things about my breast cancer;” “My husband/partner starts up conversations with me when I’m sad or worried about my breast cancer.” The scale’s internal consistency reliability for the study sample was 0.88.
Data Analytic Strategy
Prior to evaluating efficacy, data were inspected for sampling distributions, outliers, covariates, and floor and ceiling effects. All measures were approximately normally distributed. Primary tests of efficacy examined differences between groups at 3 months. Changes between baseline and 6 and 9 months evaluated the stability of changes. Linear Mixed Models, based on Maximum Likelihood Estimation, were used to evaluate efficacy [38, 39]. Pre-treatment equivalence between experimental and control groups was examined at baseline; groups were comparable on all demographic, treatment, and outcome measures.
Target Sample Size & Power Calculations
Prior to conducting the study, a sample size of 220 (110 in each group) was calculated a priori to detect an Effect size of 0.25–0.5 on all spouse caregivers’ and patients’ outcomes assessed at 3 months-post baseline. Power calculations were based on two-tailed t-tests, p=0.05.
Sample
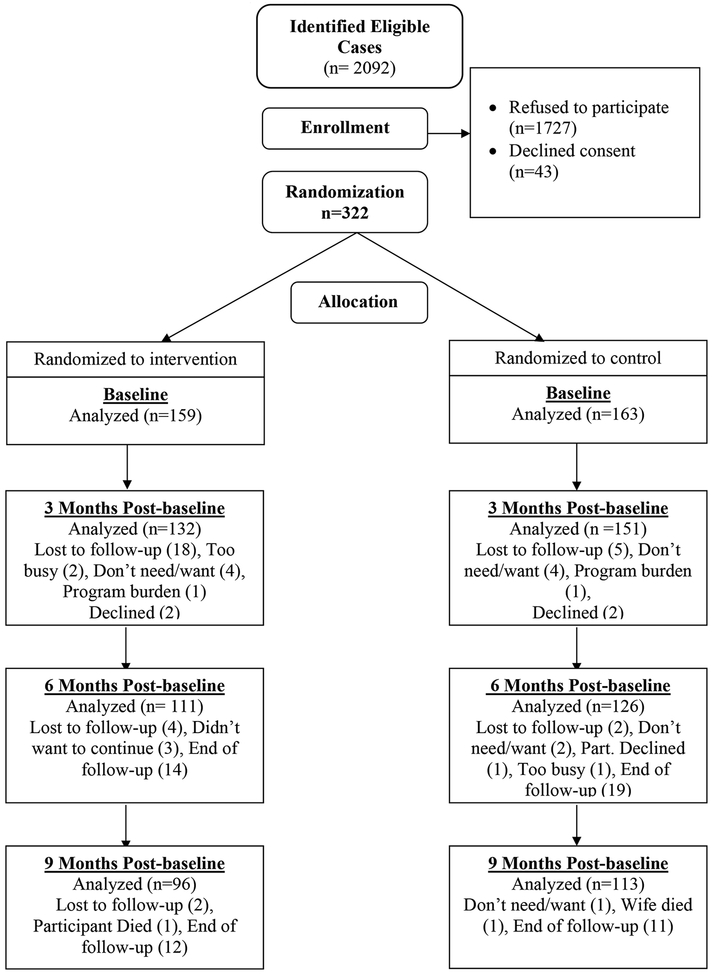
A total of 2,092 eligible spouse caregivers were identified of which 322 enrolled, 159 were randomized to experimental and 163 to control. See Figure 1. Patients were diagnosed an average of 3.3 months (SD 1.2) at baseline and 123 (45.1%) were treated with non-breast conserving surgery (partial, total or bilateral mastectomy). Patients had primarily Stage I breast cancer 126 (39.4%); 114 (35.6%) had Stage II disease; 30 (9.4%) had Stage III disease; and 52 (15.6%) had in situ (Stage 0) disease. More than half (59%) of the women received adjuvant chemo- or radiation therapy or a combination during the study. Patients were primarily Caucasian 285 (88.5%); 7 (2.2%) were Hispanic; 13 (4.0%) Asian; 2 (0.6%) African American; and 15 (4.7%) were other ethnicities, including Native American and Pacific Islander. Patients were primarily college educated (72%), averaged 53.1 years of age (SD 11.4) and married an average of 23.1 (SD 12.9) years. At baseline, 44.4% scored at or above 16 on the CES-D and 36.3% scored at or above 40 on the STAI, scores indicative of distress.
Figure 1:
Study Participant Flow Sheet
Spouse caregivers were primarily Caucasian 286 (88.8%); 7 (2.2 %) Hispanic; 14 (4.3%) Asian; 5 (1.6%) African American; and 10 (3.1%) were other ethnicities, including Native American and Pacific Islander. Caregivers averaged 54.8 years of age (SD 12.2), were primarily college educated 228 (70.8%), and 234 (72.7%) were working full or part time at time of study participation. At baseline, 32.3% of the spouse caregivers scored at or above 16 on the CES-D and 29.8% scored at or above 40 on the STAI.
Results
Tables 1 and 2 contain study results for spouse caregivers and diagnosed wives at baseline, 3, 6 and 9 months. Prior to analysis, comparisons were made between study completers and those who withdrew. There was one significant difference between these two groups on demographic, treatment, and outcome measures. Patients who withdrew had significantly higher anxiety scores on the STAI (Mean: 41.6/SD 14.4) than patients who completed 3-month assessments (Mean: 35.8/SD 11.8). Comparisons were also made between participants who dropped from the study and study completers and between study participants randomized to the experimental group who withdrew after 1 or more intervention sessions compared to those who completed all 5 intervention sessions. There were no significant differences between drops between baseline and 3 months on demographic, treatment, or outcome variables or between those who dropped from the intervention after 1 or more sessions and those who completed all 5 intervention sessions.
Table 1:
Spouses’ Measures over Time by Randomization Group
| Baseline | 3 Months Post-baseline | 6 Months Post-baseline | 9 Months Post-baseline | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Control | Experimental | Control | Experimental | Control | Experimental | Control | Experimental | ||||||||||||
| Mean | (SE) | Mean | (SE) | Mean | (SE) | Mean | (SE) | Cohen’s d p-valuea | Mean | (SE) | Mean | (SE) | Cohen’s d p-valueb | Mean | (SE) | Mean | (SE) | Cohen’s d p-valuec | |
| Depressed Mood | 12.10 | (0.6) | 12.48 | (0.6) | 10.68 | (0.7) | 8.83 | (0.7) | 0.29/0.006 | 10.51 | (0.7) | 9.61 | (0.8) | 0.11/0.162 | 9.36 | (0.8) | 8.40 | (0.9) | 0.17/0.199 |
| Anxiety | 33.46 | (0.8) | 34.82 | (0.8) | 32.64 | (0.8) | 30.88 | (0.9) | 0.36/<.001 | 32.56 | (0.9) | 31.87 | (0.9) | 0.23/0.033 | 30.91 | (0.9) | 30.50 | (1.0) | 0.18/0.096 |
| Marital Communication | |||||||||||||||||||
| Total Scale | 86.68 | (0.9) | 85.40 | (0.9) | 86.45 | (0.9) | 89.40 | (1.0) | 0.41/<.001 | 85.18 | (1.0) | 87.04 | (1.1) | 0.24/0.022 | 83.50 | (1.2) | 86.61 | (1.2) | 0.40/0.004 |
| Open Communication | 30.34 | (0.4) | 30.09 | (0.4) | 30.68 | (0.4) | 31.84 | (0.4) | 0.32/0.003 | 30.07 | (0.4) | 30.84 | (0.5) | 0.22/0.080 | 29.89 | (0.5) | 31.41 | (0.5) | 0.38/0.006 |
| Expressing Sad Feelings | 31.49 | (0.4) | 30.57 | (0.4) | 31.44 | (0.4) | 32.63 | (0.5) | 0.36/<.001 | 30.90 | (0.5) | 31.79 | (0.5) | 0.29/0.004 | 30.28 | (0.5) | 31.56 | (0.6) | 0.39/0.002 |
| Skills | |||||||||||||||||||
| Wife support | 47.24 | (0.4) | 47.23 | (0.4) | 48.41 | (0.4) | 52.10 | (0.4) | 0.74/<.001 | 48.33 | (0.4) | 50.67 | (0.4) | 0.48/<.001 | 48.20 | (0.4) | 50.67 | (0.5) | 0.48/<.001 |
| Self-care | 16.43 | (0.3) | 16.73 | (0.3) | 17.20 | (0.3) | 19.45 | (0.3) | 0.54/<.001 | 17.15 | (0.3) | 19.48 | (0.3) | 0.54/<.001 | 17.41 | (0.3) | 19.58 | (0.3) | 0.52/<.001 |
| Self-efficacy | |||||||||||||||||||
| Total Scale | 118.31 | (1.6) | 119.29 | (1.6) | 143.92 | (1.7) | 154.88 | (1.7) | 0.39/<.001 | 145.78 | (1.8) | 152.06 | (1.9) | 0.19/0.045 | 146.28 | (2.0) | 154.05 | (2.2) | 0.25/0.018 |
| Self-care | 31.81 | (0.5) | 31.71 | (0.5) | 38.05 | (0.5) | 40.38 | (0.5) | 0.34/<.001 | 38.23 | (0.6) | 40.39 | (0.6) | 0.30/0.006 | 38.75 | (0.6) | 40.99 | (0.6) | 0.29/0.017 |
| Wife-focused | 86.50 | (13) | 87.58 | (13) | 105.85 | (1.3) | 114.47 | (14) | 0.39/<.001 | 107.55 | (14) | 111.61 | (15) | 0.13/0.138 | 107.51 | (16) | 113.02 | (17) | 0.21/0.046 |
Cohen’s d/p-value = Effect size and p value for the change from baseline to 3 months by randomization group
Cohen’s d/p-value = Effect size and p value for the change from baseline to 6 months by randomization group
Cohen’s d/p-value = Effect size and p value for the change from baseline to 9 months by randomization group
Table 2:
Wives’ Measures over Time by Randomization Group
| Baseline | 3 Months Post-baseline | 6 Months Post-baseline | 9 Months Post-baseline | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Control | Experimental | Control | Experimental | Control | Experimental | Control | Experimental | ||||||||||||
| Mean | (SE) | Mean | (SE) | Mean | (SE) | Mean | (SE) | Cohen’s d p-valuea | Mean | (SE) | Mean | (SE) | Cohen’s d p-valueb | Mean | (SE) | Mean | (SE) | Cohen’s d p-valuec | |
| Depressed Mood | 14.62 | (0.7) | 15.83 | (0.7) | 13.92 | (0.7) | 13.12 | (0.8) | 0.13/0.181 | 11.04 | (0.8) | 13.00 | (0.8) | 0.15/0.510 | 10.60 | (0.8) | 11.02 | (0.9) | 0.06/0.510 |
| Anxiety Marital Communication | 35.44 | (0.9) | 37.72 | (0.9) | 32.53 | (0.9) | 34.07 | (0.9) | 0.03/0.554 | 31.29 | (1.0) | 35.04 | (1.0) | 0.17/0.287 | 31.39 | (1.0) | 32.86 | (1.0) | 0.02/0.593 |
| Marital Communication | |||||||||||||||||||
| Total Scale | 87.22 | (1.1) | 85.44 | (1.2) | 86.03 | (1.2) | 87.07 | (1.2) | 0.24/0.017 | 84.08 | (1.3) | 83.69 | (1.4) | 0.16/0.369 | 81.31 | (1.5) | 82.72 | (1.5) | 0.31/0.074 |
| Open Communication | 36.93 | (0.5) | 36.45 | (0.5) | 37.21 | (0.5) | 37.51 | (0.5) | 0.16/0.144 | 36.67 | (0.5) | 36.34 | (0.5) | 0.05/0.838 | 36.11 | (0.6) | 36.48 | (0.6) | 0.18/0.269 |
| Expressing Sad Feelings | 32.90 | (0.5) | 32.12 | (0.5) | 33.19 | (0.5) | 33.44 | (0.5) | 0.19/0.084 | 32.53 | (0.6) | 32.60 | (0.6) | 0.18/0.264 | 31.17 | (0.6) | 32.24 | (0.7) | 0.36/0.032 |
| Appraised Spouse Support | 65.08 | (0.8) | 63.40 | (0.9) | 64.34 | (0.9) | 66.24 | (0.9) | 0.39/<.001 | 64.57 | (1.0) | 64.26 | (1.0) | 0.15/0.267 | 62.62 | (1.1) | 64.55 | (1.2) | 0.37/0.009 |
Cohen’s d/p-value = Effect size and p value for change from baseline to 3 months by randomization group
Cohen’s d/p-value = Effect size and p value for change from baseline to 6 months by randomization group
Cohen’s d/p-value = Effect size and p value for change from baseline to 9 months by randomization group
Spouse Caregivers’ Outcomes
Depressed Mood:
Compared to controls, depressed mood in spouses in the experimental group significantly declined at 3 months [Mean 8.83 vs Mean 10.68; p<.006; Cohen’s d =0.29]. By 6 and 9 months, there was no significant difference between experimental and control groups.
Anxiety:
Compared to controls, anxiety significantly decreased in the experimental group at 3 months [Mean 30.88 vs Mean 32.64; p<.001; Cohen’s d =0.36] and at 6 months [Mean 31.87 vs Mean 32.56; p=.033; Cohen’s d =0.23]. By 9 months, experimental group spouses’ anxiety tended to be lower than controls but was no longer significantly different [Mean 30.50 vs Mean 30.91, p=0.096; Cohen’s d =0.18].
Marital Communication:
Spouses in the experimental group significantly improved on both dimensions of cancer-related marital communication compared to controls. Open Communication [Mean 31.84 vs Mean 30.68, p=.003; Cohen’s d =0.32] and Expressing Sad Feelings [Mean 32.63 vs Mean 31.44, p<.001; Cohen’s d =0.36] significantly improved at 3 months. Differences were sustained at 6 months [Mean 31.79 vs Mean 30.90, p=0.004; Cohen’s d =0.29] and 9 months [Mean 31.56 vs Mean 30.28, p=0.002; Cohen’s d =0.39].
Skills:
Compared to controls, spouses in the experimental group significantly improved on both dimensions of spouses’ skills, What I Do for Her Checklist. The Wife support subscale significantly increased at 3 months [Mean 52.10 vs Mean 48.41; p <.001, d =0.74] and remained significantly greater than controls at both 6 months [Mean 50.67 vs Mean 48.33; p< .001, Cohen’s d =0.48] and 9 months [Mean 50.67 vs Mean 48.20; p <.001, Cohen’s d =0.48].
Spouses’ self-care skills were significantly greater in the experimental group at 3 months [Mean 19.45 vs Mean 17.20; p <.001, Cohen’s d =0.54]. Changes were sustained at 6 months [Mean 19.48 vs Mean 17.15; p< .001, Cohen’s d =0.54] and 9 months [Mean 19.58 vs Mean 17.41; p <.001, Cohen’s d= 0.52].
Cancer Self-efficacy:
Compared to controls, spouses in the experimental group significantly improved at 3 months on both dimensions of self-efficacy: wife-focused [Mean 114.47 vs Mean 105.85; p<.001; Cohen’s d =0.39] and self-care focused [Mean 40.38 vs Mean 38.05; p<.001; Cohen’s d =0.34]. Gains in spouses’ self-care were sustained at 6 [Mean 40.39 vs Mean 38.23; p=.006; Cohen’s d =0.30] and 9 months [Mean 40.99 vs Mean 38.75; p=0.17; Cohen’s d=0.29]. Initial gains at 3 months in the spouse’s confidence in helping his wife manage were not sustained at 6 months but were significantly improved at 9 months compared to baseline [Mean 113.02 vs 107.51; p=.046; Cohen’s d= 0.21].
Wives’ Outcomes
Depressed Mood:
There were no significant differences in depressed mood between wives in the experimental and control groups at 3, 6 or 9 months.
Anxiety:
There were no significant differences on anxiety between wives in the experimental and control groups at 3, 6 or 9 months.
Marital Communication:
Compared to controls, wives in the experimental group significantly improved on the Total scale score of marital communication at 3 months [Mean 87.07 vs Mean 86.03, p=.017, Cohen’s d= 0.24] and tended to increase on the Expressing Sad Feelings subscale [Mean 33.44 vs Mean 33.19, p= .084, Cohen’s d =0.19]. Although subscale scores on Expressing Sad Feelings were not significantly different for wives in the experimental compared to the control group [Mean 32.60 vs Mean 32.53, p=.26, Cohen’s d=0.18] at the initial post-intervention assessment or at 6 months, by 9 months, wives’ expression of sad feelings was significantly improved compared to controls [Mean 32.24 vs Mean 31.17, p=.032, Cohen’s d =0.36]. The pattern was for wives in the control group to decrease in their expression of sad feelings while wives in the experimental group increased. Subscale analyses showed no significant changes on the Open communication subscale at 3, 6, or 9 months.
Appraised Spouse Support:
Compared to controls, wives in the experimental group increased in their positive appraisal of spouses’ interpersonal support. Improvements were significant at 3 months [Mean 66.24 vs 64.34, p<.001; Cohen’s d= 0.39] and at 9 months [Mean 64.55 vs Mean 62.62, p=.009, Cohen’s d =0.37].
Discussion and Conclusions
The Helping Her Heal Program (HHH) is the first randomized trial of a skill-building cancer-related marital communication and interpersonal support intervention delivered directly to spouse caregivers with significant benefits to both caregivers and wives. At 3 months, the primary assessment period, the program significantly improved spouses’ depressed mood, anxiety, marital communication, interpersonal support to his wife, his self-care, and his self-confidence compared to controls. Effect sizes ranged from small to moderate: 0.29–0.74. Most significant improvements at 3 months were sustained at 6 and 9 months.
Improvements were more limited for wives than spouses. Compared to controls, wives in the experimental group had significantly improved marital communication about the cancer and significantly higher positive appraisal of spouses’ interpersonal support. However, the intervention did not significantly affect wives’ depressed mood or anxiety. Three plausible causes were considered: program failure, measurement failure, and design failure, none of which explained the differential impact of the intervention on some but not all wives’ outcomes. We speculated that analyses on the total sample was potentially insensitive to changes in a subgroup of women at potentially high risk for anxiety and depressed mood: women on chemotherapy. A single post-hoc analysis was computed comparing women on chemotherapy in the experimental with those in the control group. Prior to analysis, pre-treatment equivalence on background, treatment, and baseline measures was confirmed. Compared to controls, women in the experimental group had significantly decreased depressed mood (11.71 vs 14.24, p=.05, Effect size d=0.34) and significantly improved scores on the total scale score on marital communication (Mean 88.77 vs 87.16, p=.04, Cohen’s d=0.46), on the openness of their communication with their spouse about the cancer (Mean 37.97 vs 37.07, p=.05, Cohen’s d=0.39), and on the degree to which they were able to express sad or negative thoughts and feelings about the cancer (34.15 vs 32.92, p=.008, Cohen’s d=0.56). There was also a tendency for wives’ anxiety to be reduced but that change was not statistically significant. These differences between experimental and control women on chemotherapy are clinically significant given both the effect sizes and that the improvements were achieved by only intervening with the spouse.
Contrary to Scott’s study that required the concurrent presence of patient and caregiver [25], current study results show that directly intervening with the spouse can improve adjustment of both members of the dyad. Contrary to a study by Manne’s team [21], the current intervention did not require conjoint therapy, mutual disclosure, nor group delivery.
Study Limitations
Caution is needed in interpreting results. The sample was biased toward well-educated, middle class couples in long-term heterosexual marriages; results may not generalize to other populations. The measure of spouses’ skills had low internal consistency reliability. Future studies need to test efficacy on a more diverse population, use a more reliable measure of spouses’ skills, and use less costly methods of delivery.
Clinical Implications
Results suggest the potential benefits of directly intervening with spouse caregivers early during treatment for breast cancer. Spouses’ sustained positive outcomes on marital adjustment and communication and wives’ sustained positive appraisal of spouses’ interpersonal support and marital communication are clinically significant results given that all were achieved in approximately 3.3 hours of contact time between the spouse and patient educator. The significant improvements in marital communication and depressed mood for wives on adjuvant chemotherapy reinforce the importance of enrolling caregivers early during treatment.
Acknowledgements
Research reported was supported by the National Cancer Institute of the National Institutes of Health, R01-CA-114–561 (Lewis, PI). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The authors acknowledge the spouse caregivers and patients who participated in the study, physicians whose patients were recruited, and the multiple site intermediaries. Special thanks to Julie R. Gralow, M.D., Sandi Johnson, LMSW, John Wynn, M.D., DFAPA, Natasha Grossman, Taryn Ostereich, Alicia Korkowski and Tessa Floyd.
Clinical trials registration number: NCT01723943, NCI-2013–01838
Footnotes
Conflict of Interest Statement
The authors have no conflicts of interest to report.
References
- 1.Feldman B and Broussard CA, The Influence of relational factors on men’s adjustment to their partners’ newly-diagnosed breast cancer. J Psychosoc Oncol, 2005. 23(2–3): p. 23–43. [DOI] [PubMed] [Google Scholar]
- 2.Wimberly SR, et al. , Perceived partner reactions to diagnosis and treatment of breast cancer: Impact on psychosocial and psychosexual adjustment. J Consult Clin Psychol, 2005. 73(2): p. 300–11. [DOI] [PubMed] [Google Scholar]
- 3.Northouse LL and Swain MA, Adjustment of patients and husbands to the initial impact of breast cancer. Nurs Res, 1987. 36(4): p. 221–5. [PubMed] [Google Scholar]
- 4.Lutgendorf SK and Laudenslager ML, Care of the caregiver: Stress and dysregulation of inflammatory control in cancer caregivers. J Clin Oncol, 2009. 27(18): p. 2894–5. [DOI] [PubMed] [Google Scholar]
- 5.Rohleder N, et al. , Biologic cost of caring for a cancer patient: Dysregulation of pro- and anti-inflammatory signaling pathways. J Clin Oncol, 2009. 27(18): p. 2909–15. [DOI] [PubMed] [Google Scholar]
- 6.DeLongis A, et al. , Social support and social strain among husbands and wives: a multilevel analysis. J Fam Psychol, 2004. 18(3): p. 470–9. [DOI] [PubMed] [Google Scholar]
- 7.Manne SL, et al. , Couples’ support-related communication, psychological distress, and relationship satisfaction among women with early stage breast cancer. J Consult Clin Psychol, 2004. 72(4): p. 660–70. [DOI] [PubMed] [Google Scholar]
- 8.Manne SL, et al. , Partner unsupportive responses, avoidant coping, and distress among women with early stage breast cancer: Patient and partner perspectives. Health Psychol, 2005. 24(6): p. 635–41. [DOI] [PubMed] [Google Scholar]
- 9.Shands ME, et al. , Core concerns of couples living with early stage breast cancer. Psychooncology, 2006. 15(12): p. 1055–64. [DOI] [PubMed] [Google Scholar]
- 10.Zahlis EH and Lewis FM, Coming to grips with breast cancer: The spouse’s experience with his wife’s first six months. J Psychosoc Oncol, 2010. 28(1): p. 79–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Manne SL, et al. , Cancer-related relationship communication in couples coping with early stage breast cancer. Psychooncology, 2006. 15(3): p. 234–47. [DOI] [PubMed] [Google Scholar]
- 12.Manne SL, et al. , Cancer-specific relationship awareness, relationship communication, and intimacy among couples coping with early stage breast cancer. J Soc Pers Relat, 2014. 31(3): p. 314–334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Segrin C, et al. , Dyadic interdependence on affect and quality-of-life trajectories among women with breast cancer and their partners. Journal of Social and Personal Relationships, 2005. 22(5): p. 673–689. [Google Scholar]
- 14.Heinrichs N, et al. , Cancer distress reduction with a couple-based skills training: A randomized controlled trial. Ann Behav Med, 2012. 43(2): p. 239–52. [DOI] [PubMed] [Google Scholar]
- 15.Hopkinson JB, et al. , The effectiveness of patient-family carer (couple) intervention for the management of symptoms and other health-related problems in people affected by cancer: A systematic literature search and narrative review. J Pain Symptom Manage, 2012. 43(1): p. 111–42. [DOI] [PubMed] [Google Scholar]
- 16.Kuijer RG, et al. , Effects of a brief intervention program for patients with cancer and their partners on feelings of inequity, relationship quality and psychological distress. Psychooncology, 2004. 13(5): p. 321–34. [DOI] [PubMed] [Google Scholar]
- 17.Lethborg CE, Kissane D, and Burns WI, ‘It’s not the easy part’: The experience of significant others of women with early stage breast cancer, at treatment completion. Social Work in Health Care, 2003. 37(1): p. 63–85. [DOI] [PubMed] [Google Scholar]
- 18.Zahlis EH and Shands ME, Breast cancer: Demands of the illness on the patient’s partner. Journal of Psychosocial Oncology, 1991. 9(1): p. 75–93. [Google Scholar]
- 19.Reynolds JS and Perrin NA, Mismatches in social support and psychosocial adjustment to breast cancer. Health Psychol, 2004. 23(4): p. 425–30. [DOI] [PubMed] [Google Scholar]
- 20.Lewis FM, et al. , Predictors of depressed mood in spouses of women with breast cancer. J Clin Oncol, 2008. 26(8): p. 1289–95. [DOI] [PubMed] [Google Scholar]
- 21.Manne SL, et al. , A randomized clinical trial of a supportive versus a skill-based couple-focused group intervention for breast cancer patients. J Consult Clin Psychol, 2016. 84(8): p. 668–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lewis FM, et al. , The family’s functioning with chronic illness in the mother: The spouse’s perspective. Soc Sci Med, 1989. 29(11): p. 1261–9. [DOI] [PubMed] [Google Scholar]
- 23.Lewis FM, Advancing family-focused oncology nursing research, in Advancing oncology nursing science, Phillips JM and King CR, Editors. 2009, Oncology Nursing Society: Pittsburgh, PA. [Google Scholar]
- 24.Northouse LL, et al. , Randomized clinical trial of a brief and extensive dyadic intervention for advanced cancer patients and their family caregivers. Psychooncology, 2013. 22(3): p. 555–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Scott JL, Halford WK, and Ward BG, United we stand? The effects of a couple-coping intervention on adjustment to early stage breast or gynecological cancer. J Consult Clin Psychol, 2004. 72(6): p. 1122–35. [DOI] [PubMed] [Google Scholar]
- 26.Lewis FM, Family issues in cancer care, in Oncology nursing : Assessment and clinical care, Miaskowski C and Buchsel PC, Editors. 1999, Mosby: St. Louis. [Google Scholar]
- 27.Bandura A, Self-efficacy: The exercise of control. 1997, NY: W.H. Freeman and Company. [Google Scholar]
- 28.Bandura A, Social cognitive theory: An agentic perspective. Annu Rev Psychol, 2001. 52: p. 1–26. [DOI] [PubMed] [Google Scholar]
- 29.Bandura A, Health promotion by social cognitive means. Health Educ Behav, 2004. 31(2): p. 143–64. [DOI] [PubMed] [Google Scholar]
- 30.Lewis FM, et al. , Helping Her Heal: A pilot study of an educational counseling intervention for spouses of women with breast cancer. Psychooncology, 2008. 17(2): p. 131–7. [DOI] [PubMed] [Google Scholar]
- 31.Conerly RC, et al. , Measuring depression in African American cancer survivors: The reliability and validity of the Center for Epidemiologic Study--Depression (CES-D) Scale. J Health Psychol, 2002. 7(1): p. 107–14. [DOI] [PubMed] [Google Scholar]
- 32.Radloff LS, The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1977. 1(3): p. 385–401. [Google Scholar]
- 33.Given C, et al. , Does a symptom management intervention affect depression among cancer patients: Results from a clinical trial. Psychooncology, 2004. 13(11): p. 818–30. [DOI] [PubMed] [Google Scholar]
- 34.Spielberger CD, Manual for the State-Trait Anxiety Inventory (Form Y). 2nd ed 1983, Palo Alto, CA: Consulting Psychologists Press. [Google Scholar]
- 35.Spielberger CD, et al. , Measuring anxiety and anger with the State-Trait Anxiety Inventory (STAI) and the State-Trait Anger Expression Inventory (STAXI), in The Use of Psychological Testing for Treatment Planning and Outcomes Assessment: Instruments for Adults, Maruish ME, Editor. 1999, Lawrence Erlbaum Associates: Mahwah, N. p. 993–1021. [Google Scholar]
- 36.Edwards B and Clarke V, The psychological impact of a cancer diagnosis on families: the influence of family functioning and patients’ illness characteristics on depression and anxiety. Psychooncology, 2004. 13(8): p. 562–76. [DOI] [PubMed] [Google Scholar]
- 37.Lewis FM, Therapy for parental cancer and dependent children, in Handbook of psychotherapy in cancer care, Watson M and Kissane D, Editors. 2011, Wiley: NY: p. 225–234. [Google Scholar]
- 38.Twisk JW, Longitudinal data analysis. A comparison between generalized estimating equations and random coefficient analysis. Eur J Epidemiol, 2004. 19(8): p. 769–76. [DOI] [PubMed] [Google Scholar]
- 39.West BT, Welch KB, and Galecki AT, Linear mixed models: A practical guide using statistical software. 2007, Boca Raton, FL: Chapman & Hall/CRC. [Google Scholar]