Abstract
Background.
Although being married with children is associated with a reduced rate of alcohol use disorder (AUD), is this finding independent of a marital effect, different in mothers and fathers and potentially causal in effect.
Methods.
Using Cox proportional hazards, we examined, in 1 252 237 married individuals, the association between a resident younger and older child and risk for AUD registration in national medical, criminal, and pharmacy registers. Using logistic regression, we analyzed, in 600 219 parents, within-person models comparing risk for AUD prior to first pregnancy v. with young children. We examined whether risk for AUD in 1302 parents after a first spousal AUD registration was reduced by having a young resident child.
Results.
Compared with childless married individuals, resident younger children were associated with a reduced risk for AUD in mothers [hazard ratio (HR) 0.36, 95% confidence interval 0.31–0.41] and fathers (HR 0.66, 0.60–0.73). The reduced risk was attenuated but still significant for older children. Within-person models confirmed the protective effect of young children in mothers [odds ratio (OR) 0.49, 0.30–0.80] but yielded inconclusive results in fathers (OR 0.85, 0.58–1.25). After a first spousal registration for AUD, a resident young child was associated with a substantial reduction in risk for mothers and a weaker marginal effect in fathers.
Conclusion.
In married individuals, resident children are associated with a reduction in basal risk for AUD which is stronger in mothers than fathers and with younger v. older children. This effect is also evident during high-risk periods. In mothers, our results are consistent with a largely causal effect.
Keywords: Alcohol use disorder, children, epidemiology, marriage
Risk for alcohol use disorder (AUD) is substantially influenced by genetic factors (Verhulst et al., 2015) and important progress has been made in understanding the neurobiology of the underlying addiction (Koob and Volkow, 2016). However, a wide range of evidence suggests that risk for AUD is also influenced by cultural, social, and interpersonal processes. In particular, changes in social roles in early to mid-adulthood impact on the risk for initiation, regular use, and abuse/dependence of both legal and illegal psychoactive substances (Yamaguchi and Kandel, 1985; Bachman et al., 1997; Leonard and Eiden, 2007).
Two of the most important social roles often adopted in this age period are marriage and parenthood. In nation-wide Swedish data, marriage substantially reduces and divorce substantially increases the risk for a first-time registration for AUD as assessed from legal, medical, and pharmacy registries (Kendler et al., 2016a, 2017). Furthermore, among those who are married with no prior history of AUD, a history of AUD in the spouse is a substantial risk factor for subsequent AUD registration (Kendler et al., 2018). In all three of these analyses, co-relative and/or within-person designs suggested that the observed associations were at least partially causal (Kendler et al., 2016a, 2017, 2018).
In this paper, we turn to an examination of the impact of parenthood on risk for AUD registration. In population surveys, having children is typically associated with lower rates of problematic alcohol consumption (Bachman et al., 1997; Hajema and Knibbe, 1998; Tyssen et al., 1998; Staff et al., 2010; Fergusson et al., 2012; Verges et al., 2012). However, a number of questions remain unanswered in this literature.
First, can we distinguish between the protective effects of parenthood from those of marriage? In a longitudinal study of US HMO cohort, Chilcoat and Breslau found that both marital status and parenthood predicted reduced levels of DSM-III-R alcohol abuse and dependence symptoms (Chilcoat and Breslau, 1996). However, controlling for marital status reduced the parenthood effects to non-significance. In the early midlife assessment from the Monitoring the Future study, Merline et al. found that being a custodial parent was associated with reduced levels of heavy drinking above and beyond the reductions associated with marriage (Merline et al., 2004). There was some evidence that parenthood had a distinctive effect above and beyond marriage in a study of the intergenerational transmission of AUDs; however, these effects differed as a function of the timing of parenthood. Specifically, alcohol consumption declined after the transition to parenthood, except among those who became parents as adolescents (Little et al., 2009)
Second, is the impact of parenthood on problem drinking or risk for AUD similar in men and women? Examination of sex differences has been limited, perhaps due to the focus on women’s drinking during the transition to parenthood given the pathogenic effects of alcohol exposure on fetuses and infants. Moreover, previous analysis of this question has produced inconsistent results. In Monitoring the Future and in the National Epidemiological Survey of Alcohol and Related Conditions, parenthood was associated with reduced drinking and reduced likelihood of AUD onset in both men and women (Staff et al., 2010; Verges et al., 2012). In contrast, in a New Zealand birth cohort and in a population-based Dutch study, parenthood had a stronger protective effect for women compared with men (Neve et al., 2000; Fergusson et al., 2012), and in younger Dutch cohorts having children was associated increased drinking problems in men (Neve et al., 2000). In the US National Longitudinal Survey of Youth, the transition to parenthood was related to less frequent drinking for women but not men (Christie-Mizell and Peralta, 2009).
Third, is the hypothesized protective effect of parenthood on AUD risk similar for the parents of younger and older children? Previous studies have primarily focused on the initial transition to parenthood as part of the process of maturing out from young adult problem drinking (O’Malley, 2004), with relatively fewer studies examining the associations between parenting older children and problem drinking. Caring for younger children requires more time than caring for older children (Craig and Bittman, 2008; Statistics Sweden, 2016); thus, parents may face more constraints on their leisure time when their children are younger compared with when they are older. Consistent with this possibility, the longitudinal British National Child Development Study showed that mothers and fathers were least likely to endorse heavy daily or problem drinking when they had a young child (<5 years) in the home (Staff et al., 2013). Likewise, in the NESARC data, females (but not males) who lived with a child under the age of 1 consumed less alcohol compared with females who did not live with a child under the age of 1 (Levy et al., 2018)
Fourth, is the apparent protective effect of parenthood on AUD risk likely to reflect a causal effect, or a result of confounders – that is, other factors associated both with one’s likelihood of becoming a parent and of developing AUD? With the exception of a study that used fixed-effects regression to control for differences between those who did and did not select into parenthood (Staff et al., 2013), we are unaware of other attempts to use natural experiments or specific statistical tools to gain insight into the degree to which children are affecting their parents’ risk for AUD.
Fifth, would a protective effect of parenthood on AUD risk be observed in the context of a temporally defined risk factor for AUD onset? Previous analyses of the Swedish national data indicate that first AUD registration in one spouse is associated with a pronounced increased risk for an AUD registration in the other spouse (Kendler et al., 2018). Although previous studies have looked at configurations of social roles and their association with alcohol behavior (Kuntsche et al., 2009), to our knowledge, none have examined the protective effect of parenthood in the context of a discrete high-risk environmental exposure.
In these analyses of a general population Swedish sample here reported, we examine the following five questions:
-
(1)
In married couples, is the presence of a resident child associated with a change in the risk for AUD registration?
-
(2)
Does the observed association between resident children and risk for AUD differ in mothers and fathers?
-
(3)
Does the impact on parental risk for AUD differ for resident younger v. older children?
-
(4)
Can we, using a within-person design, provide potential insight into the causal nature of the association between resident children and risk for AUD registration?
-
(5)
Is the impact of having resident children on baseline risk for AUD in a married individual similar to that seen in the high-risk period immediately following the first registration for AUD in the spouse?
Methods
We linked nationwide Swedish registers via the unique 10-digit identification number assigned at birth or immigration to all Swedish residents. The identification number was replaced by a serial number to ensure anonymity. The following sources were used to create our dataset: Total Population Register, containing information about year of birth, sex, family and marital status; Swedish Census, containing household information in 1960, 1965, 1970, 1975, 1980, 1985, and 1990; Multi-Generation Register, linking individuals born after 1932 to their parents; the Hospital Discharge Register, containing hospitalizations for Swedish inhabitants from 1964 to 2012; Prescribed Drug Register, containing all prescriptions in Sweden picked up by patients from 2005 to 2013; Outpatient Care Register, containing information from all outpatient clinics from 2001 to 2012; Crime Register that included national complete data on all convictions in lower court from 1973 to 2012; and Swedish Suspicion Register that included national data on individuals strongly suspected of crime from 1998 to 2012.
Sample
We included men and women born in Sweden between 1960 and 1990 who were married before the end of our follow-up, 31 December 2013, who had no prior AUD registration and were without children before marriage. Our basic design was to follow individuals from age at first marriage, through transitions from marriage with no children, to marriage with children of varying ages with our outcome being either age at AUD registration, or censoring.
Measures
Individuals’ AUD status was identified from Swedish medical registries by the following ICD codes: ICD8: 571.0, 291, 303, 980; ICD9: V79B, 305A, 357F, 571A, 571B, 571C, 571D, 425F, 535D, 291, 303, 980; and ICD 10: E244, G312, G621, G721, I426, K292, K700, K701, K702, K703, K704, K709, K852, K860, O354, T510, T512, T511, T513, T518, T519, F101, F102, F103, F104, F105, F106, F107, F108, F109; and from the Prescribed Drug Register if retrieved disulfiram [Anatomical Therapeutic Chemical (ATC) Classification System N07BB01], acamprosate (N07BB03), or naltrexone (N07BB04). Among females, 3.1% of those assigned an AUD diagnosis (129 women) had a registration of naltrexone use during marriage and were not identified in any other register. For men, the corresponding figure was 1.9% (127 men). In addition, we identified AUD as convicted for or suspected of at least two alcohol-related crimes according to law 1951:649, paragraphs 4 and 4A and law 1994:1009, Chapter 20, paragraphs 4 and 5 from the Swedish Crime Register, and codes 3005 and 3201 in the Suspicion register.
We identified biological children from the Multi-Generation Register and cohabitation status with their parents from the Census (before 1990) and Total Population Register (after 1990). To allow for different effects depending on the child’s age, we created two categories: (i) ‘having young children’ defined as having at least one child below age 7and (ii) ‘having older children’ defined as having at least one child between age 8 and 18 and no child under the age of 7. We chose these ages as children typically begin public schooling in Sweden at the age of 7 and are considering to be ‘of majority’ at age 18. We counted only the children with whom a parent was cohabiting.
Statistical methods
We observed men and women for up to three phases during their first marriage: living without children, living with at least one younger child, and living with older children. We utilized a survival model framework and followed each individual from the age at which they entered a new phase (e.g. starting with first marriage without children, then marriage with at least one younger child, or marriage with older children, etc.) until age at fist AUD registration, or censoring. We censored at a new observational period, death, emigration, divorce, widowhood, or end of follow-up. To account for the non-independence between repeated observations within individuals, we used a frailty model – a survival model that includes a random effect. Each random level thereby represents one individual, or cluster. To explore possible gender differences, we allowed parameters to differ between men and women by including the respective interaction terms in the model. That is, besides the main effects of young and older children, respectively, representing the associations in women, we included two interaction terms, one between male gender and having young children and one between male gender and having older children. The two latter terms represent how the association between young and older children, respectively, is modified if you are a man instead of women. From the full model, we derived the key comparisons, and present the results by gender, namely: younger child v. no child, older child v. no child, and older v. younger child.
Next, we conducted within-person analyses on the subsamples observed as married at least 2 years before childbirth, with observations up to 7 years after childbirth. Subjects with at least one post childbirth observational period are included and to account for the within-individual clustering, we conduct a multilevel logistic regression analysis. As above, such an approach accounts for the repeated observation within individuals. The basal period of risk against which we calculate change is the year prior to pregnancy. As the absolute risk of AUD increases with age in this period in life, we include age as an adjustment factor in the model, assuming that the relative increase in risk is constant by year. The analysis is stratified by gender.
Finally, we estimate the time to first AUD registration from a first AUD registration in spouse. This time to event curve represents the hazard function in a survival model, which can be estimated non-parametrically utilizing the R package bshazard (Rebora et al., 2014). We estimate the hazard functions during the next 3.5 years, separately for wives and husbands, and with and without younger children. If the subject was without children at the time of spousal AUD registration, but later had a child or had a young child who turned 8, we censor at the time of the respective event. To obtain an empirical estimate of the hazard ratio (HR) over follow-up time, we divide the curves with and without young children for wives and husbands, respectively.
The statistical analyses are performed using R version 3.4.1 and the function coxph from the built-in survival package or the function glmer from the built-in lme4 package (R Development Core Team, 2017). Confidence intervals (CIs) were obtained using the built-in multcomp package.
Results
Table 1 presents the sample sizes available for our main analysis, noting that in the course of our study, the same couple may transition across all three categories of having no children, young children, and older children.
Table 1.
Descriptive statistics – children during marriagea
| Males |
Females |
|||
|---|---|---|---|---|
| Total number |
AUD in state (% of number in state) | Total number |
AUD in state (% of number in state) | |
| Married, any time | 299 768 | 3230 (1.1) | 338 193 | 1619 (0.5) |
| Married, no children | 299 465 | 1770 (0.6) | 337 748 | 1045 (0.3) |
| Married, living with child under 7 | 223 294 | 1484 (0.7) | 258 340 | 516 (0.2) |
| Married, living with child aged 8–18 | 92 372 | 801 (0.9) | 115 741 | 407 (0.4) |
The samples are not independent in that over our observation period, a number of individuals move from being married with no children to have a child under 7 and some to having a child between the ages of 8 and 18.
Effects of younger and older children in married couples – frailty models
Table 2 presents results from the frailty analysis and then the estimates of key parameters from that model. Compared with married women without children, the presence of a resident younger child for married women is associated with a large reduction in risk for AUD registration (HR 0.36, 95% CI 0.32–0.40). In married men, having a young child in the home is also associated with a lowered risk (HR 0.66, 0.61–0.71), although the effect is significantly weaker than that observed in women.
Table 2.
Frailty model analyses of the impact of lived-with children in married individuals on the risk for alcohol use disorder registration
| Parameter estimates | |||||
|---|---|---|---|---|---|
| HRs | p value | ||||
| Male v. female | 2.08 (1.90–2.28) | <0.001 | |||
| Child under 7 v. no child | 0.36 (0.32–0.40) | <0.001 | |||
| Child 8–18 v. no child | 0.53 (0.47–0.61) | <0.001 | |||
| Interaction child under 7 and sex | 1.86 (1.63–2.11) | <0.001 | |||
| Interaction child 8–18 and sex | 1.52 (1.31–1.76) | <0.001 | |||
| Key model results | |||||
| Females | Males | p value for sex difference | |||
| HRs | p value | HRs | p value | ||
| Child under 7 v. no child | 0.36 (0.32–0.40) | <0.001 | 0.66 (0.61–0.71) | <0.001 | <0.001 |
| Child 8–18 v. no child | 0.53 (0.47–0.61) | <0.001 | 0.81 (0.73–0.90) | <0.001 | <0.001 |
| Child 8–18 v. child under 7 | 1.50 (1.32–1.71) | <0.001 | 1.23 (1.12–1.35) | <0.001 | <0.001 |
In married women, the presence of a resident older child was also associated with a substantial reduction in risk for AUD registration (HR 0.53, 0.47–0.61), but the effect was significantly weaker than that seen with younger children (HR 1.50, 1.32–1.71). In married men, resident older children were also significantly associated with a modest reduction in AUD risk (HR 0.81, 0.73–0.90). The effect of older children on AUD risk in fathers was significantly weaker than that seen with younger children (HR 1.23, 1.12–1.35) and with older children in women.
Within-person analyses
The frailty model includes the entire population so that the association between having children and reduced risk for AUD could be influenced by systematic differences between the kinds of married individuals who do v. do not have children. To give more insight into potential causal processes, we conducted within-person analyses where we compare risk for AUD registration in the same married individual when they have no children v. a young child using as our baseline the year prior to the beginning of pregnancy. As seen in Table 3, we also controlled for the impact of aging on risk for AUD. The sample size of eligible subjects was 282 420 fathers and 317 799 mothers.
Table 3.
Within-person logistic regression analyses of the impact of lived-with younger children in married individuals on the risk for alcohol use disorder registrationa
| Females |
Males |
|||
|---|---|---|---|---|
| OR | P | OR | P | |
| Change in risk per year | 1.11 (1.04–1.20) | 0.003 | 1.13 (1.07–1.18) | <0.001 |
| Presence of child | 0.49 (0.30–0.80) | 0.005 | 0.85 (0.58–1.25) | 0.417 |
Measured over 7 years after birth against a baseline of the year prior to the beginning of pregnancy.
In our within-person analyses, the presence of a child in the home up until age 7 substantially reduced the risk for AUD registration in the mother compared with seen prior to her pregnancy [odds ratio (OR) 0.49, 0.30–0.80]. Although this effect was in the same direction for the father, the CIs included 1.00 (OR 0.85, 0.58–1.25).
Impact of having children after first AUD registration in spouse
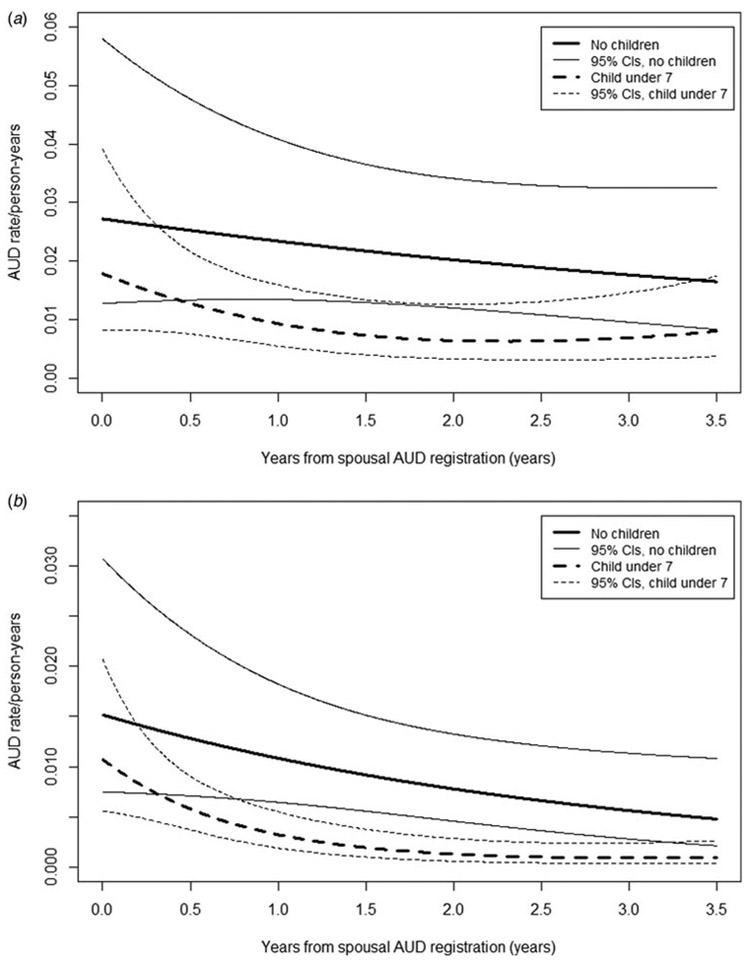
Among husbands whose wife had a first registration for AUD, we identified 1001 and 301 who, respectively, had children under the age of 7 and had no children. The raw risk for first AUD registration for them in the subsequent 3.5 years was 1.9% and 4.0%, respectively. The hazard function, calculated using non-parametric survival methods, representing the absolute risk of a first registration for the husband (± 95% CIs) with young children conditional on his wife’s first registration, is seen as a dotted line in Fig. 1a and can be compared with the corresponding risk for matched fathers with no children depicted by a solid line. The risk is lower in the husbands with young children at home. However, the CIs are broad and overlap over the entire follow-up period.
Fig. 1.
(a) First registration for AUD in husbands when the wives had a first AUD registration – a non-parametric estimate of the hazard function (and 95% CIs) of first AUD registration in husbands as a function of whether there was a resident child in the home (in dotted line) or there were no children (solid line). Estimates are presented in solid lines and 95% Cis in dotted lines. The x-axis is time from registration in the wife in years. The y-axis is rate of AUD registration. (b) First registration for AUD in wives when the husband had a first AUD registration – a non-parametric estimate of the hazard function (and 95% Cis) of first AUD registration in wives as a function of whether there was a resident child in the home (dotted line) or there were no children (solid line). Estimates are presented in solid lines and 95% Cis in dotted lines. The x-axis is time from first registration in the husband in years. The y-axis is rate of AUD registration.
We identified 3089 and 702 wives with and without children under the age of 7 whose husband had a first registration for AUD. The raw risk for first AUD registration for them in the subsequent 3.5 years was 0.7 and 2.1%, respectively. The survival curves are seen for these two groups in Fig. 1b. The risk is considerably lower in the wives with young children at home and the CIs did not overlap with those without children over a considerable portion of the follow-up period.
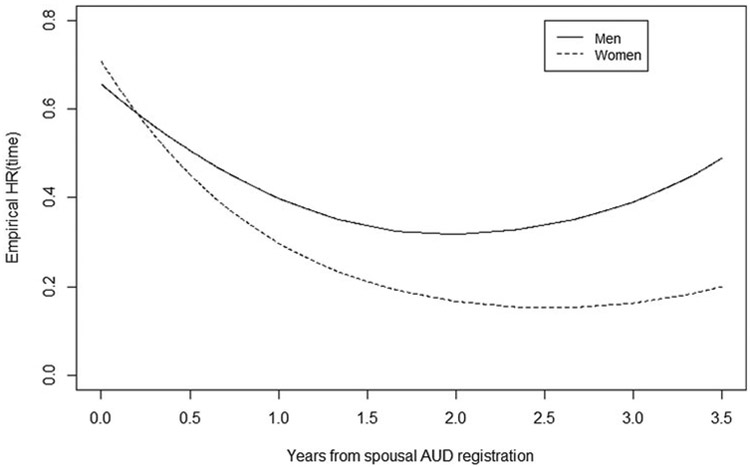
More easily interpretable than the results presented in Figs 1a and b is the ratio of the two hazard functions (the HR in those with young children divided by those without children) which are seen for males and females in Fig. 2. The protective effect of having young children during a period of high risk for AUD onset is both greater in magnitude and more long-lasting in women than in men. Furthermore, the strength of the protective effect (HRs of <0.20 in mothers and <0.40 in fathers) was stronger (although much less precisely known) than those observed in our baseline analyses.
Fig. 2.
Risk ratio for first registration for AUD in men (solid line) and women (dotted line) who had been exposed to a first onset of AUD in their spouse when there was v. was not a resident child in the home. The two curves represent the ratio between the curves seen, respectively, in Figs 1a and b.
Discussion
We attempted, in this paper, to address, in married Swedish couples, five specific questions about the relationship between risk for AUD registration and the presence of children in the home. We review these results in turn.
First, using frailty survival models, we found clear evidence that the presence of children in the home of married couples was strongly associated with a reduced risk for AUD registration. This is consistent with other population-based studies that find that parenthood is associated with reduced drinking and alcohol problems (Bachman et al., 1997; Verges et al., 2012). Importantly, we find that the effect of resident children on likelihood of AUD registration goes above and beyond the protective effect of marriage itself, which is consistent with some (Bachman et al., 1997) but not all (Chilcoat and Breslau, 1996) prior studies comparing the relative impact of these two social roles.
Second, we found consistent and significant evidence that children living in the home were associated with a larger reduction in risk for AUD registration in mothers than in fathers. Previous studies on this point have been mixed, with some suggesting that mothers and fathers benefit equally from the protective effect of parenthood on risk for AUD onset (Verges et al., 2012) while others have found stronger effects for mothers than for fathers (Neve et al., 2000; Fergusson et al., 2012). These gendered effects may reflect time-constraint differences related to child-rearing, as Swedish women spend more time caring for children compared with men (Staff et al., 2013; Statistics Sweden, 2016).
Third, the reduction in risk for AUD in both mothers and fathers was stronger for younger than for older children. This is consistent with an earlier study that looked at whether the protective effect of parenthood changed as a function of children’s age, which found that mothers’ and fathers’ likelihood of heavy drinking and alcohol problems was lowest when their children were younger (<5 years) (Staff et al., 2013). It is also congruent with the hypothesis that constraints on unstructured leisure time, which are more intense for younger than older children (Craig and Bittman, 2008), are one mechanism through which parenthood may have a protective effect on risk for AUD (O’Malley, 2004).
Fourth, we sought to gain insight into the potential causal nature of the association between children and risk for AUD by also conducting within-person analyses which control for possible confounders. The estimates obtained in the frailty analyses are consistent with the interpretation that the effects of young children on maternal risk for AUD are largely causal rather than a result of confounders. For fathers, the results are less clear. They are so imprecisely known that they are consistent both with the hypothesis that the effects are largely causal or entirely the result of confounders. As a set, these findings are at least partially consistent with the protective effects of parenthood on problem drinking seen from an earlier study that used a fixed-effects regression model to control for individual differences associated with selection into parenthood (Staff et al., 2013). More broadly, these parenthood results are congruent with findings from earlier work on family roles in the Swedish population, which show that marriage has a likely causal, protective effect against the onset of AUD registration (Kendler et al., 2016a), while the loss of marriage through divorce or widowhood increases risk for AUD registration (Kendler et al., 2017).
Finally, we examined, for the first time to our knowledge, the impact of young children on parental risk for AUD in a more dynamic manner. In a married couple neither of whom had prior AUD, when one spouse gets a first AUD registration, the other spouse has a very large increased risk for an AUD registration over the next 4 years (Kendler et al., 2018). We showed that in this situation, having young children in the home was associated with a large reduction in risk. Our finding that the protective effect of children is strongest for those who are at greatest risk suggests that parenthood may be particularly potent, positive turning point in an otherwise high-risk trajectory (Rutter, 1996; Schulenberg et al., 2003). These protective effects were more robust than seen in our frailty analyses and, like those analyses, stronger in mothers than fathers. These analyses highlight the importance of considering how acute social risk for AUD interfaces with parenting roles to influence AUD onset.
Limitations
These results should be interpreted in the context of five possible methodological limitations. First, we ascertained subjects with AUD from medical, legal, and pharmacy records. This approach does not rely on respondent cooperation or unbiased recall, but cannot be expected to reproduce precisely results from interview-based epidemiological surveys. The population prevalence of AUD in our sample is lower than that found in an interview survey in nearby Norway (Kringlen et al., 2001) as our methods will miss mildly affected individuals who avoid pharmacological treatment and medical and legal complications of their drinking. However, the validity of our detection method is supported by the high rates of concordance observed across our ascertainment methods shown in our previous work (Kendler et al., 2015) and replicated for the specific samples used in this report examining both the ORs and Yule’s Y (Yule, 1912) (online Supplementary appendix Table S1) and by the pattern of resemblance in relatives (Kendler et al., 2015, 2016b) which is very similar to that found in interview-based studies (Heath et al., 1997; Prescott and Kendler, 1999).
Second, while of obvious interest, we were unable to examine the impact of children on AUD risk in unmarried couples as Swedish registries cannot unambiguously identify romantically involved unmarried individuals. Third, for our within-person analyses, to maximize our sample size and statistical power, we used as a baseline the year prior to pregnancy. We examined whether this baseline might be biased by some women reducing alcohol intake in preparation of a planned pregnancy by comparing rates of AUD 2 v. 1 year prior to pregnancy. We actually saw a slight increase in rates of AUD 1 v. 2 years prior to pregnancy, suggesting that taking the 1-year prior period as a baseline would not bias upward estimates of the effect of resident children.
Fourth, to maximize power, we included, as subjects, men and women born in Sweden between 1960 and 1990. A disadvantage of this approach is the possibility that our approach obscured important cohort effects. We therefore repeated our main analyses on three cohorts (1960–69, 1970–79, and 1980–89) (online Supplementary appendix Table S2). While we had too short a follow-up period in the youngest cohort to obtain stable parameter estimates, results from the first two cohorts were quite similar. It is unlikely that our aggregate results masked large historical differences across our 30-year ascertainment window.
Finally, families with both younger and older children were classified as having younger children raising a possible confound between the presence of a young children in the home and the number of children. We therefore studied families with only one child within our ascertainment window. As seen in online Supplementary appendix Table S3, in both the mothers and fathers in these families, risk for AUD was significantly lower when their child was below v. above the age of 8. These results support our interpretation of our main findings. That is, younger children in the home have a stronger protective effect on parental risk for AUD than older children.
Conclusions
For married individuals, living with a child substantially reduces risk for AUD. This effect is stronger in mothers than fathers, with younger v. older children and is likely largely causal in mothers while the results of causal analysis in men are inconclusive. The protective effect is also clearly seen and particularly strong at times of high risk. While the genetic and neurobiological roots of AUD are firmly established (Verhulst et al., 2015; Koob and Volkow, 2016), these results, along with our prior findings with marriage (Kendler et al., 2016a), demonstrate that intimate interpersonal relationships can also play a strong protective role in the pathways to AUD onset.
Supplementary Material
ACKNOWLEDGMENTS
This project was supported by grants R01AA023534 and K01AA024152 from the National Institutes of Health, the Swedish Research Council (K2012-70X-15428-08-3), the Swedish Research Council for Health, Working Life and Welfare (In Swedish: Forte; Reg.nr: 2013-1836), the Swedish Research Council (2012-2378; 2014-10134) and FORTE (2014-0804) as well as ALF funding from Region Skåne awarded.
Role of the funder/sponsor. The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Footnotes
Supplementary material. The supplementary material for this article can be found at https://doi.org/10.1017/S0033291718002969.
Conflict of interest. None.
Ethical standards. The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
References
- Bachman JG, Wadsworth KN, O’Malley PM, Johnston LD and Schulenberg JE (1997) Smoking, Drinking, and Drug Use in Young Adulthood: The Impacts of New Freedoms and New Responsibilities. Mahwah, NJ: Lawrence Erlbaum Associates. [Google Scholar]
- Chilcoat HD and Breslau N (1996) Alcohol disorders in young adulthood: effects of transitions into adult roles. Journal of Health and Social Behavior 37, 339–349. [PubMed] [Google Scholar]
- Christie-Mizell CA and Peralta RL (2009) The gender gap in alcohol consumption during late adolescence and young adulthood: gendered attitudes and adult roles. Journal of Health and Social Behavior 50, 410–426. [DOI] [PubMed] [Google Scholar]
- Craig L and Bittman M (2008) The incremental time costs of children: an analysis of children’s impact on adult time use in Australia. Feminist Economics 14, 59–88. [Google Scholar]
- Fergusson DM, Boden JM and John HL (2012) Transition to parenthood and substance use disorders: findings from a 30-year longitudinal study. Drug and Alcohol Dependence 125, 295–300. [DOI] [PubMed] [Google Scholar]
- Hajema KJ and Knibbe RA (1998) Changes in social roles as predictors of changes in drinking behaviour. Addiction 93, 1717–1727. [DOI] [PubMed] [Google Scholar]
- Heath AC, Bucholz KK, Madden PA, Dinwiddie SH, Slutske WS, Bierut LJ, Statham DJ, Dunne MP, Whitfield JB and Martin NG (1997) Genetic and environmental contributions to alcohol dependence risk in a national twin sample: consistency of findings in women and men. Psychological Medicine 27, 1381–1396. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Ji J, Edwards AC, Ohlsson H, Sundquist J and Sundquist K (2015) An extended Swedish national adoption study of alcohol use disorder. JAMA Psychiatry 72, 211–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler KS, Lonn SL, Salvatore J, Sundquist J and Sundquist K (2016a) Effect of marriage on risk for onset of alcohol use disorder: a longitudinal and co-relative analysis in a Swedish national sample. American Journal of Psychiatry 173, 911–918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler KS, PirouziFard M, Lonn S, Edwards AC, Maes HH, Lichtenstein P, Sundquist J and Sundquist K (2016b) A national Swedish twin-sibling study of alcohol use disorders. Twin Research and Human Genetics 19, 430–437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler KS, Lonn SL, Salvatore J, Sundquist J and Sundquist K (2017) Divorce and the onset of alcohol use disorder: a Swedish population-based longitudinal cohort and co-relative study. American Journal of Psychiatry 174, 451–458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler KS, Lönn SL, Salvatore J, Sundquist J and Sundquist K (2018) The origin of spousal resemblance for alcohol use disorder. JAMA Psychiatry 75, 280–286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koob GF and Volkow ND (2016) Neurobiology of addiction: a neurocircuitry analysis. The Lancet Psychiatry 3, 760–773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kringlen E, Torgersen S and Cramer V (2001) A Norwegian psychiatric epidemiological study. American Journal of Psychiatry 158, 1091–1098. [DOI] [PubMed] [Google Scholar]
- Kuntsche S, Knibbe RA and Gmel G (2009) Social roles and alcohol consumption: a study of 10 industrialised countries. Social Science and Medicine 68, 1263–1270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leonard KE and Eiden RD (2007) Marital and family processes in the context of alcohol use and alcohol disorders. Annual Review of Clinical Psychology 3, 285–310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levy F, Le Strat Y, Hoertel N, Ancelet C and Dubertret C (2018) Childbirth and alcohol consumption impact of recent childbirth on alcohol consumption. Journal of Child and Family Studies 27, 2245–2253. [Google Scholar]
- Little M, Handley E, Leuthe E and Chassin L (2009) The impact of parenthood on alcohol consumption trajectories: variations as a function of timing of parenthood, familial alcoholism, and gender. Developmental Psychopathology 21, 661–682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merline AC, O’Malley PM, Schulenberg JE, Bachman JG and Johnston LD (2004) Substance use among adults 35 years of age: prevalence, adulthood predictors, and impact of adolescent substance use. American Journal of Public Health 94, 96–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neve RJ, Lemmens PH and Drop MJ (2000) Changes in alcohol use and drinking problems in relation to role transitions in different stages of the life course. Substance Abuse 21, 163–178. [DOI] [PubMed] [Google Scholar]
- O’Malley PM (2004) Maturing out of problematic alcohol use. Alcohol Research &Health 28, 202–204. [Google Scholar]
- Prescott CA and Kendler KS (1999) Genetic and environmental contributions to alcohol abuse and dependence in a population-based sample of male twins. American Journal of Psychiatry 156, 34–40. [DOI] [PubMed] [Google Scholar]
- R Development Core Team (2017) R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing. Online Source. [Google Scholar]
- Rebora P, Salim A and Reilly M (2014) bshazard: Nonparametric Smoothing of the Hazard Function R package version 1.0. Vienna, Austria: The R Foundation for Statistical Computing. Online Source. [Google Scholar]
- Rutter M (1996) Transitions and turning points in developmental psychopathology: as applied to the age span between childhood and midadulthood. International Journal of Behavioral Development 19, 603–626. [Google Scholar]
- Schulenberg J, Maggs JL and O’Malley PM (2003) How and why the understanding of developmental continuity and discontinuity is important: the sample case of long-term consequences of adolescent substance use In Mortimer JT & Shanaham M (eds), Handbook of the Life Course. New York: Kluwer Academic/Plenum Publishers, pp. 413–436. [Google Scholar]
- Staff J, Schulenberg JE, Maslowsky J, Bachman JG, O’Malley PM, Maggs JL and Johnston LD (2010) Substance use changes and social role transitions: proximal developmental effects on ongoing trajectories from late adolescence through early adulthood. Developmental Psychopathology 22, 917–932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Staff J, Greene KM, Maggs JL and Schoon I (2013) Family transitions and changes in drinking from adolescence through mid-life. Addiction 109, 227–236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sweden Statistics (2016) Women and men in Sweden: Facts and Figures 2016. Örebro: Statistics Sweden, Population Statistics Unit. SE-701 89. Online Source. [Google Scholar]
- Tyssen R, Vaglum P, Aasland OG, Gronvold NT and Ekeberg O (1998) Use of alcohol to cope with tension, and its relation to gender, years in medical school and hazardous drinking: a study of two nation-wide Norwegian samples of medical students. Addiction 93, 1341–1349. [DOI] [PubMed] [Google Scholar]
- Verges A, Jackson KM, Bucholz KK, Grant JD, Trull TJ, Wood PK and Sher KJ (2012) Deconstructing the age-prevalence curve of alcohol dependence: why ‘maturing out’ is only a small piece of the puzzle. Journal of Abnormal Psychology 121, 511–523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verhulst B, Neale MC and Kendler KS (2015) The heritability of alcohol use disorders: a meta-analysis of twin and adoption studies. Psychological Medicine 45, 1061–1072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yamaguchi K and Kandel DB (1985) On the resolution of role incompatibility – a life event history analysis of family roles and marijuana use. American Journal of Sociology 90, 1284–1325. [Google Scholar]
- Yule GU (1912) On the methods of measuring association between two attributes. Journal of the Royal Statistical Society 75, 579–652. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.