Abstract
Objective:
Demographic differences (race/ethnicity/sex) in 9–1–1 emergency medical services (EMS) access and utilization have been reported for various time-dependent critical illnesses along with associated outcome disparities. However, data are lacking with respect to measuring the various components of time taken to reach definitive care facilities following the onset of acute stroke symptoms (i.e., stroke onset to 9–1–1 call, EMS response, time on-scene, transport interval) and particularly with respect to any differences across ethnicities and sex. Therefore, the specific aim of this study was to measure the various time intervals elapsing following the first symptom onset (FSO) from an acute stroke until stroke hospital arrival (SHA) and to delineate any race/ethnic/sex-related differences among any of those measurements.
Methods:
The Florida-Puerto Rico Stroke Registry (FLPRSR) is an on-going, voluntary stroke registry of hospitals participating in the Get with the Guidelines-Stroke initiative. The study population included patients treated at Florida hospitals participating in the FLPRSR between 2010 and 2014 who had called 9–1–1 and were managed and transported by EMS. In total, 10,481 patients (16% black, 8% Hispanic, 74% white) had complete data-sets that included birthdate/year, sex, ethnic background, date/hour/minute of FSO and date/hour/minute of EMS response, scene arrival and SHA.
Results:
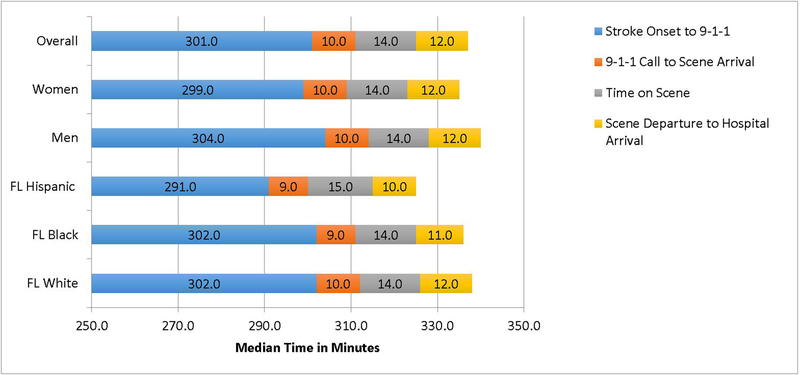
Median time from FSO to SHA was 339 minutes (interquartile range [IQR] of 284–442), 301 of which constituted the time elapsed from FSO to the 9–1–1 call (IQR=249–392) versus only 10 from 9–1–1 call to EMS arrival (IQR=7–14), 14 on-scene (IQR=11–18) and 12 for transport to SHA (IQR=8–19). The FSO to 9–1–1 call interval, being by far the longest interval, was longest among whites and blacks (302 minutes for both) versus 291 for Hispanics (p=0.01). However, this 11-minute difference was not deemed clinically-significant. There were no significant sex-related differences nor any racial/ethnic/sex differences in the relatively short EMS-related intervals.
Conclusions:
Following acute stroke onset, time elapsed for EMS response and transport is relatively short compared to the lengthy intervals elapsing between symptom onset and 9–1–1 system activation, regardless of demographics. Exploration of innovative strategies to improve public education regarding stroke symptoms and immediate 9–1–1 system activation are strongly recommended.
Keywords: Stroke, Race/Ethnicity, EMS, stroke center, 9–1–1 dispatcher, Response Intervals
INTRODUCTION
The 2001 Know Stroke campaign and the 2003 national stroke plan, Ensuring the Chain of Recovery for Stroke, both developed by the National Institute of Neurological Disorders and Stroke, were promulgated in large part to: 1) facilitate public awareness of the time-dependent, critical need to recognize stroke signs/symptoms; and 2) emphasize the importance of calling 9–1–1 immediately to ensure rapid stroke treatment/interventions.1–3
Since that time, efforts to improve the public health system of stroke recognition, response and care have increased significantly, particularly with the formal development and designations of comprehensive stroke centers along with applicable triage protocols to enhance EMS recognition of stroke.4–7 Nonetheless, there remain concerns that many stroke patients still do not arrive at stroke care facilities until many hours after stroke symptom onset, diminishing the chances of successful treatment.
In that regard, data are still lacking with respect to measuring the various components of time taken to reach definitive care facilities following the onset of acute stroke symptoms, including the time elapsed before calling 9–1–1, the time it takes for EMS to respond, time EMS spends on-scene and the time taken to transport to a stroke care hospital.
In addition, previous studies concerning certain time-dependent medical conditions, including stroke, have indicated outcome disparities that might be related to demographics (race/ethnicity/sex).8,9 Therefore, further identification of any differences with respect to ethnicity and sex might be extremely important information to guide either the need for EMS quality assurance improvements (e.g., training, protocol revisions) or the need for other public health interventions (e.g., faster activation of 9–1–1 by the public).
Conceivably, demographics (e.g. language barriers, cultural perspectives, economic concerns) could play a possible role in affecting the time it takes to initiate an 9–1–1 activation. In addition, such factors may even influence EMS management (beginning with dispatch call-intake interactions to on-scene interface with patients and families, and even transport decision-making).
Therefore, as a basic starting point, the specific aim of this study was to delineate any race/ethnic/sex differences in terms of the time elapsed from first symptom onset (FSO) from an acute stroke until eventual stroke hospital arrival (SHA). In doing so, the investigators sought to better elucidate the specific opportunities for improvements based on identifying any respective time-component delays in getting to definitive care facilities.
METHODS
Institutional Review Board Approval:
The study was part of an on-going series of research projects approved by the Institutional Review Board (IRB) of the University of Miami (Miami, FL) and the conduct of the current study is compliant with relevant federal and state guidelines for ethical conduct of studies.10 No additional informed consent was required by the IRB for this de-identified data-set analysis.
Setting:
The Florida-Puerto Rico Stroke Registry (FLPRSR) is an on-going, previously-described, voluntary and IRB-approved/monitored registry.10 The study includes stroke patients who arrived by EMS and who were treated at Florida hospitals participating in the registry. This constitutes 67 stroke receiving facilities and 161 EMS agencies across Florida. The registry data were matched with the respective records from EMSTARS (the EMS Tracking and Reporting System in Florida). These two databases were matched using probabilistic linkage by date of birth, age, sex, year and admission date +/− one day, and hospital identification number.
Subjects:
Although many patients may seek medical care for stroke symptoms by way of public and private transportation or they first seek care at clinics or facilities that are not stroke centers, for the purposes of this study, investigators purposely limited the study sample to those stroke patients for whom 9–1–1 was called between 2010 and 2014 and who were subsequently transported directly to a participating stroke center. Only patients with complete and accurate data-sets (as previously described) were included. The final merged data-set (from EMSTARS and FLPRFR) that was to be evaluated involved 10,481 patients for whom: 1) 9–1–1 was called; 2) subsequent transport was made directly to a stroke facility; and 3) valid data were recorded for all variables of interest.
Definitions of Variables and End-Points:
Measured time segments extending from stroke symptom onset to stroke hospital arrival were categorized into the following interval components: 1) FSO (stroke onset) to 9–1–1 call; 2) 9–1–1 call answer to EMS (ambulance) on-scene arrival; 3) EMS time on scene; 4) scene departure to SHA; and 5) the total sum of these component intervals (FSO-SHA). Stroke symptom onset date and time were variables recorded in the American Heart Association Get with the Guidelines for Stroke (GWTG-S) database utilized by the Florida registry.9,10 Other time points were derived from the in-field data recorded by the EMS providers. Scene arrival was defined as arriving/stopping at the street address (not arrival at the patient’s side). On-scene time includes time taken to retrieve carry-in equipment/stretchers and then traverse a building or residence (frequently with small elevators, stairwells, small back bedroom or other logistical barriers). It also includes the time taken to exit across those same logistical challenges, but now with a monitored patient and inserted catheters to secure.
For the purpose of this study, extreme outliers for each timespan were excluded using the following restrictions: FSO to 9–1–1 call (two days), 9–1–1 call to EMS arrival on-scene (>100 minutes), EMS time on scene with patient (>60 minutes) and scene departure to hospital arrival (>140 minutes). As a result, less than 0.5% of records were excluded. We also conducted a sensitivity analysis restricting FSO to 9–1–1 call within 24 hours, resulting in 10 additional records removed.
Due to skewed distributions of the timespan endpoints, we examined the relationships between sex and race/ethnicity with the four time segments from FSO to hospital arrival by quantile regression using the median of the timespans. The quantile regression models were mutually adjusted for sex and race/ethnicity (with whites as the reference category), and also adjusted for age and the National Institutes of Health (NIH) stroke score (NIHSS). These analyses were conducted using SAS version 9.4 (Cary, NC). We also examined the distribution of time for FSO to 9–1–1 activation, stratified by hour-of-the-day, as one methodology to attempt to identify any potential influence of “wake-up strokes” in terms of lengthening 9–1–1 activation intervals.
As all of the hospitals participating in the registry were stroke receiving facilities, the EMS time stamp for hospital arrival defined the SHA time-point. As noted above, only cases with direct transport from EMS to the stroke care facility were purposely part of the analysis. Due to the prehospital focus of this study, in-hospital time intervals to various interventions were not targeted or reported here.
RESULTS
Among the 10,481 stroke cases analyzed, 16% were black, 8% Hispanic, 74% white, and 51% were women (Table 1). The overall median time (in minutes) from symptom onset to hospital arrival (FSO-SHA) was 339 (5 hours, 39 minutes) with an interquartile range (IQR) of 284 to 442. While there were no significant differences identified with respect to sex in any category (Table 1), the FSO-SHA interval was longest among whites (340), followed by blacks (337), and shortest (327 min.) for Hispanics (Figure 1; Table 1). The 13-minute interval difference (i.e., Hispanics vs. whites) was statistically significant (p=0.003), but not deemed clinically significant given the long overall time span from FSO to SHA. Those differences were largely driven by the time interval elapsing from FSO to 9–1–1 call, for which Hispanics had the shortest median timespan at 291 versus 302 for whites (p=0.01 vs. Hispanics) and blacks alike (also 302 min.). These comparisons were all adjusted for age and NIHSS.
Table 1.
Race/ethnic and sex-related differences with respect to time from stroke symptom onset to hospital arrival.
| Symptom Onset until Stroke Hospital Arrival (Minutes) | Symptom Onset to 9–1–1 Call (Minutes) | 9–1–1 Call to Scene Arrival (Minutes) | On-Scene (Minutes) | Scene Departure to Hospital Arrival (Minutes) | |
|---|---|---|---|---|---|
| Overall (n=10,481) Median (IQR) |
339 (284–442) | 301 (249–392) | 10 (7–14) | 14 (11–18) | 12 (8–19) |
| Black (n=1,691) Median (IQR) Effect (P value) a |
337 (283–456) −5.20 (0.10) |
302 (249–416) −1.68 (0.67) |
9 (7–13) −1.38 (<0.0001) |
14 (10–18) −0.46 (0.06) |
11 (7–17) −1.82 (<0.0001) |
| White (n=7,746) Median (IQR) (reference group) |
340 (286–348) | 302 (250–388) | 10 (7–14) | 14 (11–18) | 12 (8–20) |
| Hispanic (n=834) Median (IQR) Effect (P value) a |
327 (272–423) −13.28 (0.003) |
291 (239–380) −11.62 (0.01) |
9 (7–13) −0.94 (<0.0001) |
15 (11–20) 1.07 (<0.0001) |
10 (6–16) −2.28 (<0.0001) |
| Men (n=5,173) Median (IQR) Effect (P value) a |
342 (286–449) 3.67 (0.08) |
304 (251–399) 2.60 (0.16) |
10 (7–14) 0.06 (0.59) |
14 (10–18) −0.07 (0.53) |
12 (8–18) −0.28 (0.12) |
| Women(n=5,308) Median (IQR) (reference group) |
336 (282–431) | 299 (247–385) | 10 (7–14) | 14 (11–18) | 12 (8–18) |
Adjusted for race/ethnicity, sex, age, National Institutes of Health Stroke Score (NIHSS)
Figure 1.
Race/ethnic and sex differences with respect to time from stroke symptom onset to hospital arrival. Comparison of race/ethnicity- and sex-related differences among stroke patients with respect to the overall time elapsed (in minutes) from stroke symptom onset to stroke hospital arrival, and then respectively compared in terms of: the time elapsed prior to 9–1–1 system activation; the ambulance response interval; time spent on-scene; and the time elapsing from scene departure until arrival at the receiving stroke hospital.
Though the analysis did project statistically significant race/ethnic differences comparing the various EMS time intervals (time elapsing from the 9–1–1 call to EMS arrival on-scene, time on-scene and time of scene departure to SHA), these differences (Fig. 1) were quite small (1 minute apart) and the total time elapsed for EMS response, scene and transport were identical (median 34 min. each) for blacks and Hispanics and similar to whites (median 36 min.).
Moreover, despite the scene logistics, barriers to access (and egress) and despite the required key assessments and procedures to be accomplished on-scene for stroke patients, the total time elapsed from EMS first arriving at the street address until hospital arrival (average transport time of about 11–12 minutes) was less than a half-hour in over half of the cases (median 26 minutes). While the time elapsed from stroke symptom onset to hospital arrival was similar among men and women, each of the three EMS-related intervals were also identical for men and women (Table 1; Figure 1).
When the analyses were restricted to those who called 9–1–1 within a day of FSO, most of the results remained consistent. However, the decreased time from FSO to hospital arrival for blacks was shorter than that for whites (effect estimate=−7.42, P=0.03), but again not deemed clinically significant given the long overall time span from FSO to SHA.
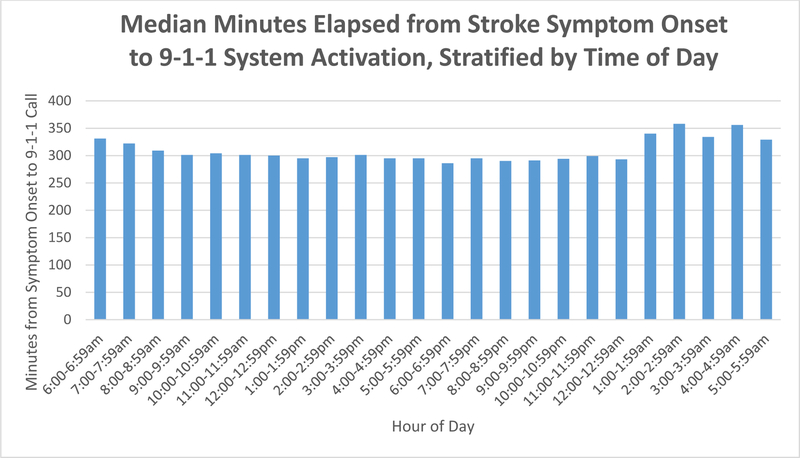
The time elapsed from FSO to the 9–1–1 call was slightly longer between 1:00 am to 7:00 am (Figure 2), with median timespans approximately 5.5 to 6 hours during those hours compared to ~5 hours for all other hours of the day. However, total EMS time intervals (9–1–1 response to SHA) remained relatively consistent throughout the daily cycle.
Figure 2.
Median time from stroke symptom onset to 9–1–1 activation, by hour of day.
DISCUSSION
In addition to other emergency conditions for which time-dependent treatment is critical, race/ethnic/sex differences have been documented previously with respect to the overall time taken for a patient with acute stroke to reach definitive hospital-based treatment.8 Often these, delays and disparities are attributed to socio-economic concerns, transportation limitations or initially utilizing alternative facilities for medical care that later require subsequent transfer to a stroke care hospital. However, the current study revealed that in the relatively optimal subset of patients directly utilizing the 9–1–1 system and who were directly transported to a participating stroke center, the main delay occurs prior to 9–1–1 activation, regardless of demographics or sex.
This study design, as an initial exploratory venture, did not drill down on the factors causing that delay within each of the individual demographics (or overall). Intuitively, there are several reasons that demographics could possibly play a role in affecting the time it takes to initiate an 9–1–1 system activation including lack of medically-related public education, language barriers, communication sources, cultural perspectives, domestic circumstances, socio-economic barriers or even prior experiences with the healthcare system. Financial issues are another subtle concern as are cultural stoicism versus cultural proclivity to call for help.
The other considerations for delayed time to hospital arrival after stroke onset have traditionally included activities involved after 9–1–1 (EMS) activation.2 These elements can range from time spent during the 9–1–1 center call-intake (including verifying correct location) as well as dispatcher assessments and instructions to those on-scene. It also involves the time taken for EMS to find patients at the location (e.g. large apartment complex, shopping mall, country road or high-rise) and then deliver required on-scene assessment and procedures. Transport decision-making can involve by-pass of a closer hospital or patient reluctance to go to a hospital amplified by possible cultural and socio-economic factors. Therefore, as a starting point, the specific objective of this study was to begin to identify which of these time-consuming elements might indicate areas of significant delay especially in terms of any ethnic and sex-related disparities.
Accordingly, the current study clearly demonstrates that, regardless of racial/ethnic/sex disparities in other situations, the time interval from stroke symptom onset until calling 9–1–1 for help is, universally, the major cause for delay in getting to a stroke care hospital. It is recognized that even more significant (avoidable) delays can occur within the hospital, but the specific aim here was to examine the prehospital components. The crude overall results indicate that rapid stroke recognition by the patient, family, friends and the public at-large with immediate EMS activation (or some other reluctance factors) appear to be the main barriers causing delays in stroke care, regardless of racial/ethnic background, sex or EMS system interface. This point is underscored even further given the consideration that the current study sample represents the presumptive “best-case scenario”. Specifically, the target stroke patient group studied was the subset of stroke patients for whom EMS services were activated (at some point after stroke symptoms) and who were then transported and treated at a GWTG-participating stroke center. In other words, even among the subset of patients who called 9–1–1 directly and arrived directly by EMS at a stroke center, the delay to call 9–1–1 was extremely long in the great majority of cases.
The study did identify (statistically-speaking) significant race/ethnic differences, but, contrary to previous experience, among those arriving by ambulance, Hispanic and black patients arrived at stroke hospitals somewhat sooner than whites. However, from a clinical (and intuitive) point of view, differences in median FSO-SHA intervals were negligible when one compares a median time of 5 hours 40 minutes for whites versus 5 hours 37 minutes for blacks and 5 hours 27 minutes for Hispanics. Most importantly, for all groups, the pre-9–1–1 activation phase approximated 5 hours with only an 11-minute difference for Hispanics versus whites and blacks (291 vs. 302 minutes) and there were no sex-related disparities nor any racial/ethnic/sex differences in terms of any of the EMS-related time phases (once 9–1–1 was called).
Possible reasons for a slightly longer delay to 9–1–1 calls among whites, or any of the groups, are not clear. Overall, FLPRSR data indicate that whites are the most likely to travel to hospital via EMS and also more likely to activate 9–1–1 for transport, even after lengthy delays following symptom onset.10 While this may explain why they are represented more in this current EMS-oriented study, it does not yet explain any (relative) delay. One conjecture might be that whites have higher NIH stroke scores (representing more severe strokes) and therefore more aphasia/neglect and inability to call 9–1–1 themselves, but that is purely speculative.10
With the caveat that this study purposely was focused on patients directly transported to stroke care facilities in EMS-activated responses, the findings may likely be different if studying patients who arrive by private vehicle, bus or if they first went to a non-stroke care facility or clinic. However, presumptively, all of those factors would have lengthened the time taken to reach definitive care facilities and it is not intuitive that patients with more worrisome or overt symptoms would have bypassed the 9–1–1 system. Nevertheless, those cases not involving direct EMS activation also deserve further attention (beyond this study) to confirm or refute those presumptions.
Still, the observations of this targeted study all strengthen the argument that, in this circumstance (EMS-managed prehospital stroke care), many of the ethnic, cultural and socio-economic barriers within the populations studied were less of a concern. Instead, there is an overall common indication for bettering our public education and public health interventions regarding stroke identification and rapid action by patients, families, friends and bystanders.
Public education campaigns have already improved knowledge about stroke signs/symptoms and swift 9–1–1 activation.11–13 In the more recent 2014 National Health Interview Survey, 66% of respondents had some knowledge of stroke symptoms and they further acknowledged the importance of calling 9–1–1. This result far exceeded previous estimates, ranging from 17% to 51% between 2004 and 2009.14 In the 2014 survey, women were more knowledgeable than men and whites more so than blacks and Hispanics, theoretically indicating the need for culturally-tailored strategies.14
Other studies are in concurrence with that recommendation.8,9,15 For example, socio-cultural factors, including living arrangements among older populations, can have a specific impact among women and black stroke patients in particular and these factors are further influenced by cultural and gender-related societal roles.15 Also, subtle differences in stroke symptoms and presentation can vary by sex and race/ethnicity.9 Likewise, socio-economic factors and social discomfort may influence the utilization of either EMS transportation or an emergency department visit. Both may be perceived as incurring substantial and non-reimbursable charges as well, thus an important issue requiring further attention. Therefore, all of these factors need to be considered when developing outreach education and any other related public health interventions.
In terms of some study limitations, not all stroke patients were analyzed including a subset of those calling 9–1–1. Patients without complete merged datasets were not included nor were patients not transported to a stroke center. In some cases, relevant data were missing from some EMS agencies (including those in some high-volume 9–1–1 systems), but, more importantly, only a third of presumed stroke patients transported by EMS had been linked prospectively in terms of conjoint EMSTARS and GWTG-S datasets.
At first glance, purposely excluding so many patients could be considered a type of selection bias, but the strict criteria for inclusion were decided upon a priori in terms of achieving the study purpose. The specific study design was to ensure that only patients with a complete and valid data-set would be included so that investigators could specifically determine which time-phase(s) resulted in the greatest delays to stroke care and to see if ethnic/racial/sex-related differences existed with respect to those various phases.
Interestingly, in reviewing many of the excluded patients, many of the likely-eligible (but unlinked) patients took even longer to arrive at the hospital after stroke onset and they were more likely to be Hispanic and less likely to be white. Therefore, the investigators could not rule out the potential for some type of selection bias in this study, but the residual study population consisting of patients with complete datasets was still quite large (over 10,000 subjects across a large state with a robust dataset). More importantly, the study sample likely represented more of an ideal situation (EMS activation, rapid management and transport directly to a stroke center). Therefore, had additional patients been included, even worse outcomes might be expected. Regardless, the findings remain clear, time to 9–1–1 activation for stroke patients is far too long.
Also, looking back, a large percentage of unmatched patients (those without conjoint EMSTARS and GWTG-S datasets) were likely due to the patients being initially identified in good faith by EMS as possible stroke patients, but who later did not receive a confirmed stroke diagnosis at the hospital. Such “over-triage” should actually be expected, however, particularly with the current emphasis on increasing sensitivity and not missing a treatable stroke.
While comparative work for stroke cases not directly involving EMS care/transport is also equally needed, the consistency of the findings here, especially in terms of the EMS interface components, is compelling. Patients arriving by EMS generally achieve SHA faster and they receive CT imaging, intravenous tissue plasminogen activator (tPA) therapy and endovascular rescue treatment sooner.16,17 Stroke mortality and disability outcomes are highly-influenced by the timespan from stroke symptom onset to treatment.15,18 Therefore, even in this presumably best-case scenario of EMS-managed response, the delays identified should be considered even more concerning. There is always the caveat that these data may not be applicable elsewhere, but the face-value results indicate that delays in calling 9–1–1 occurred across the board, regardless of sex or ethnicity, across a large state involving all types of urban and non-urban locales. These findings emphasize that we need to become more creative to further improve public education interventions regarding stroke. Accordingly, work in this public health arena needs to be prioritized. The sophisticated interventions we now possess will be of lesser effectiveness, or not effective at all, without eliminating these delays in access. Also, it is the authors’ opinion that these interventional programs should be tailored as indicated in culturally-specific ways. This recommendation is not only intuitive recognizing language, educational and socio-economic disparities, but it is also supported by previous work which, in contrast to this study sample, identified race/ethnic differences in accessing early stroke care when 9–1–1 services are not utilized.9
Prior studies have evaluated the overall time from FSO to SHA, but this study is the first to link a state-wide EMS database with the GWTG-S registry data-set using electronic EMS time stamps. In turn, it was able to reliably delineate and compare the various component time segments for the various demographic groups studied. Although this very large merged data-set requires further refinements and development, it still resulted in an exceptionally robust analysis for our purposes here, allowing investigators to reliably examine the various segments of that timespan. With such a large sample size and completeness of the data sets, this analysis should have allowed us to easily document the race/ethnic and sex disparities that we had suspected prior to study. Instead, the dataset revealed a common problem independent of demographics that needs to be more creatively addressed and embraced a clear priority to better ensure the effectiveness of contemporary stroke interventions now at our disposal.
CONCLUSIONS:
Following acute stroke onset, the time consumed for EMS response and transport is exceptionally brief whereas the time intervals elapsing between symptom onset and 9–1–1 system activation is quite lengthy (over 5 hours for half of the patients). This finding is consistent across all categories of basic demographics such as sex and racial/ethnic differences. This observation calls for an urgent reappraisal and likely re-invention of public education and interventions regarding identification of acute stroke symptoms as well as stressing the importance of making 9–1–1 calls immediately following onset of those symptoms.
Acknowledgments:
The authors extend their deepest appreciation to the men and women of the involved EMS agencies who respond daily in 9–1–1 systems to rescue and attend to the needs of stroke patients and many others with critical illness and injury. Their actions and documentation made this study possible as did the leadership and staff members from the numerous participating hospitals in the Florida-Puerto Rico Stroke Registry.
Sources of Funding: This work was supported by the National Institutes of Health (NIH)/National Institute of Neurological Disorders and Stroke (NINDS) under grant # U54-NS081763
Footnotes
Disclosures of Conflict of Interest:
None of the authors have any conflicts of interest to disclose relevant to this research, its findings or manuscript development.
REFERENCES
- 1.https://stroke.nih.gov/index.htm (Date accessed: January 3, 2018)
- 2.Pepe PE, Zachariah BS, Sayre MR, Floccare D. Ensuring the chain of recovery for stroke in your community. Acad Emerg Med. 1998;5:352–358. [DOI] [PubMed] [Google Scholar]
- 3.National Institute of Neurological Disorders and Stroke Symposium: Improving the Chain of Recovery for Acute Stroke in Your Community. Publication of the National Institutes of Health (NIH) National Institute for Neurological Disorders and Stroke (NINDS); September 2003; https://azslide.com/a-national-institute-of-neurological-disorders-and-stroke-symposium-improving-th_59b048c01723ddd637f5ace5.html (Date accessed: December 23, 2017). [Google Scholar]
- 4.Fassbender K, Balucani C, Walter S, Levine SR, Haass A, Grotta J. Streamlining of prehospital stroke management: the golden hour. Lancet Neurol. 2013;12:585–596. [DOI] [PubMed] [Google Scholar]
- 5.Alberts MJ, Latchaw RE, Selman WR, Hadley HM, Brass LM, Koroshetz W, Marler JR, Booss J Zorowtiz RD, Croft JB, Magnis E, Mulligan D, Jagoda A, O’Connor R, Cawley CM, Connors JJ, Rose-DeRenzy JA, Emr M, Warren M, Walker MD; Brain Attack Coalition. Recommendations for comprehensive stroke centers: a consensus statement from the brain attack coalition. Stroke. 2005;36:1597–1616. [DOI] [PubMed] [Google Scholar]
- 6.McKinney JS, Deng Y, Kasner SE, Kostis JB. Comprehensive stroke centers overcome the weekend versus weekday gap in stroke treatment and mortality. Stroke. 2011;42:2403–2409. [DOI] [PubMed] [Google Scholar]
- 7.Iihara K, Nishimura K, Kada A, Iihara K, Nishimura K, Kado A, Nakagawara J, Ogasawara K, Ono J, Shiokawa Y, Aruga T, Miyachi S, Nagata I, Toyoda K, Matsuda S, Miyamoto Y, Suzuki A, Ishikawa KB, Matsuda S, Kataoka H, Nakamura F, Kamitani S. Effects of comprehensive stroke care capabilities on in-hospital mortality of patients with ischemic and hemorrhagic stroke: J-aspect study. PLoS One. 2014;9:e96819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cruz-Flores S, Rabinstein A, Biller J, Elkind MS, Griffith P, Gorelick PB, Howard G, Leira EC, Morgenstern LB, Ovbiagele B, Peterson E, Rosamond W, Trimble B, Valderrama AL; American Heart Association Stroke Council; Council on Cardiovascular Nursing; Council on Epidemiology and Prevention; Council on Quality of Care and Outcomes Research. Racial-ethnic disparities in stroke care -- the American experience: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2011;42:2091–2116. [DOI] [PubMed] [Google Scholar]
- 9.Mochari-Greenberger H, Xian Y, Hellkamp AS, Schulte PJ, Bhatt DL, Fonarow GC, Reeves MJ, Schwamm LH, Smith EE. Racial/ethnic and sex differences in emergency medical services transport among hospitalized U.S. stroke patients: analysis of the national Get with The Guidelines-Stroke Registry. J Am Heart Assoc. 2015;4:e002099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sacco RL, Gardener H, Wang K, Dong C, Ciliberti-Vargas MA, Gutierrez CM2, Asdaghi N, Burgin WS, Carrasquillo O, Garcia-Rivera EJ, Nobo U, Oluwole S, Rose DZ, Waters MF, Zevallos JC, Robichaux M, Waddy SP, Romano JG, Rundek T; FL‐PR CReSD Investigators and Collaborators. Racial-ethnic disparities in acute stroke care in the Florida-Puerto Rico Collaboration to Reduce Stroke Disparities study. J Am Heart Assoc. 2017;6:pii:e004073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Becker K, Fruin M, Gooding T, Tirschwell D, Love P, Mankowski T. Community-based education improves stroke knowledge. Cerebrovasc Dis. 2001;11:34–43. [DOI] [PubMed] [Google Scholar]
- 12.Fogle CC, Oser CS, McNamara MJ, Helgerson SD, Gohdes D, Harwell TS. Impact of media on community awareness of stroke warning signs: a comparison study. J Stroke Cerebrovasc Dis. 2010;19:370–375. [DOI] [PubMed] [Google Scholar]
- 13.Payne GH, Fang J, Fogle CC, Oser CC, Wigand DA, Theisen V, Farris RP. Stroke awareness: surveillance, educational campaigns, and public health practice. J Public Health Manag Pract. 2010;16:345–358. [DOI] [PubMed] [Google Scholar]
- 14.Ojike N, Ravenell J, Seixas A, Masters-Israilov A, Rogers A, Jean-Louis G, Ogedegbe G, McFarlane SI. Racial disparity in stroke awareness in the US: an analysis of the 2014 National Health Interview Survey. J Neurol Neurophysiol. 2016;7:pii:365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Moser DK, Kimble LP, Alberts MJ, et al. Moser DK, Kimble LP, Alberts MJ, Alonzo A, Croft JB, Dracup K, Evenson KR, Go AS, Hand MM, Kothari RU, Mensah GA, Morris DL, Panciolo AM, Riegel B, Zerwic JJ. Reducing delay in seeking treatment by patients with acute coronary syndrome and stroke: a scientific statement from the American Heart Association Council on Cardiovascular Nursing and Stroke Council. Circulation. 2006;114:168–182. [DOI] [PubMed] [Google Scholar]
- 16.Ekundayo OJ, Saver JL, Fonarow GC, Schwamm LH, Xian Y, Zhao X, Hernandez AF, Peterson ED, Cheng EM. Patterns of emergency medical services use and its association with timely stroke treatment: findings from Get with the Guidelines-Stroke. Circ Cardiovasc Qual Outcomes. 2013;6:262–269. [DOI] [PubMed] [Google Scholar]
- 17.Sozener CB, Barsan WG. Impact of regional pre-hospital emergency medical services in treatment of patients with acute ischemic stroke. Ann NY Acad Sci. 2012;1268:51–56. [DOI] [PubMed] [Google Scholar]
- 18.Emberson J, Lees KR, Lyden P, Blackwell L, Albers G, Bluhmki E, Brott T, Cohen G, Davis S, Donnan G, Grotta J, Howard G, Kaste M, Koga M, von Kummer R, Lansberg M, Lindley RI, Murray G, Olivot JM, Parsons M, Tilley B, Toni D, Toyoda K, Wahlgren N, Wardlaw J, Whiteley W, del Zoppo GJ, Baigent C, Sandercock P, Hacke W; Stroke Thrombolysis Trialists’ Collaborative Group. Effect of treatment delay, age, and stroke severity on the effects of intravenous thrombolysis with alteplase for acute ischaemic stroke: a meta-analysis of individual patient data from randomised trials. Lancet. 2014;384(9958):1929–1935. [DOI] [PMC free article] [PubMed] [Google Scholar]