ABSTRACT
The 2012 Royal College of Physicians report Hospitals on the edge is clear that ‘decisions about service redesign must be clinically led and clinicians must be prepared to challenge the way services – including their own service – are organised’. This paper describes a service redesign in which we have gained learning and experience in two areas. Firstly, a description of measured improvement by the innovation of redesigning the traditional hospital-based assessment of frail older patients’ home support needs (assess to discharge) into their own home and meeting those needs in real time (discharge to assess). In combination with the formation of a collaborative health and social care community team to deliver this new process, there has been a reduction in the length of stay from completion of acute hospital care to getting home (from 5.5 days to 1.2 days for those patients that require support at home). Secondly, the methodology through which this has been achieved. We describe our translation of a Toyota methodology used for the design of complex cars to use for engaging staff and patients in the design of a healthcare process.
KEYWORDS: Discharge to assess, process design, statistical process control, quality improvement
Introduction
Sheffield is a city in the north of England with a population of approximately 560,000. The health and social care structure is coterminous, consisting of one acute adult NHS foundation trust, one clinical commissioning group and one local authority. In the transforming community services NHS reform of 2011, the acute hospital and community provider underwent vertical integration, thereby removing the organisational divide between hospital- and community-based teams.
At the same time, a framework for system redesign and improvement was established within geriatric medicine and community care with a weekly improvement meeting using Toyota Oobeya (Big Room) design methodology1 with members of front line staff coached by clinicians trained in quality improvement science. The process of redesign of admission to the acute service for older people at the trust had begun, and clinical outcomes had improved.2 The focus of the work was to learn how the discharge process could be improved for older people who were currently undergoing a multidisciplinary assessment in hospital to determine the support required for discharge home.
Methodology
The Big Room meeting staff sought to first understand the current discharge process (Fig 1). This was achieved by a combination of patient stories with process analysis and mapping. This generated a clear picture of the discharge process and allowed the staff to appreciate that patients were often delayed leaving hospital while therapy assessments were carried out in hospital to determine the required support for the person to function safely at home. The team came up with a novel approach that would ‘flip’ the process: rather than ‘assess to discharge’, could a patient that no longer needed acute hospital care be discharged and then assessed in their own home and have the resulting support needs met in real time? The team decided to test this idea.
Fig 1.
The ‘Big Room’ translated from Toyota Oobeya. Reproduced with permission from The Health Foundation.
They started with one discharge from one ward. Once deemed ‘medically fit’ the patient was taken home that day, accompanied by a therapist. At home, assessments were carried out in real time to inform a clinical judgement about the person's need for additional support or equipment to help them function. The results of the test were reported at the next Big Room meeting and studied by the group; the team reflected on what had been learned and what should be done differently next time. This (Plan-Do-Study-Act) cycle of testing was repeated and, as the team's confidence grew, more patients were included.
This methodical, iterative approach, underpinned by improvement science, enabled the team to refine the discharge to assess (D2A) model and implement it in a way that worked for their context. When the first ward piloted the implementation of D2A, within 3 weeks staff on the ward decided the redesigned discharge process should become their standard way of working.
The next step was to scale up the use of D2A as a discharge model, so that more patients in the directorate could benefit. To do this was a significant challenge; the homecare support capacity within the health and social care community systems was insufficient for this new way of working and the skill set to undertake the initial assessment was undergoing development. Serendipitously, the integration that was taking place in the Sheffield health and social care system coincided with a cross-city programme called Right First Time. This enabled an evidence-based discussion, resulting in investment in a new collaborative community service. The Big Room meeting played an important role at this juncture, providing both a time and space for relationships to build, and an established process for improvement that was trusted by the staff attending.
Outcome
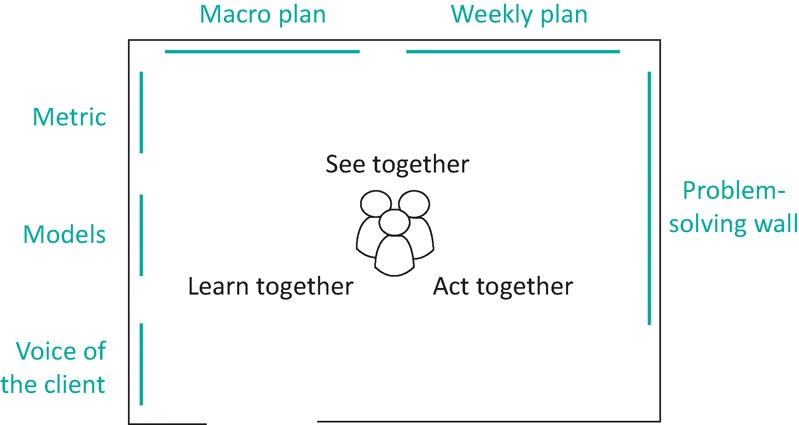
Fig 2, generated with statistical process control software,3 demonstrates two significant reductions in the weekly average wait for patients between hospital referral and being at home with community-based support services. The first reduction corresponds with the establishment of closer collaborative working between the health and social care teams involved in the hospital discharge process: the Community Intermediate Care Service and the local authority's Short Term Intervention Team. It demonstrates a reduction in average wait from 5.5 to 3.6 days. This was a precursor to the more formal reconfiguration into a single service called Active Recovery. This process was informed by the improvement work taking place in the Big Room in 2013 and, our observations suggest, were enabled and accelerated by vertical integration of the hospital and community healthcare systems. By the end of 2013, there was sufficient evidence for a bid to be put to health system leaders requesting increased funding of £1.4 million for the Active Recovery service to allow the predicted required capacity to be established. This bid was successful and by May 2014, the capacity of Active Recovery had increased to match the demand for the service. This resulted in a highly stable system with a mean transfer time from hospital to support at home of 1.2 days. We estimate that approximately 10,400 patients transferred from hospital to Active Recovery in the year 2015. The average reduction in time to transfer from 5.2 to 1.2 days equates to an average of 4 hospital bed days per patient being saved as a result of the redesigned system; using a marginal cost of £300 per hospital bed day, this equates to a highly significant net efficiency improvement.
Fig 2.
Reducing patient wait for active recovery from a hospital bed. AR = Active Recovery; CICS = Community Intermediate Care Service; STIT = Short Term Intervention Team
We assessed balance measures of readmission rate and mortality (Supplementary file S1). There was no observed change in readmissions. There was a short term increase in mortality, which temporally corresponded to the increase in influenza cases resulting from the ineffectiveness of the vaccination that year. There were no other mortality changes.
The reduction in mean times was also associated with a reduction in the absolute range (Supplementary file S1).
Conclusion and next steps
In this case study, we present measured improvements in the discharge process for older people within our organisation, resulting from the application of quality improvement methodology by front line healthcare teams to flip the traditional ‘assess to discharge’ model in to one of ‘discharge to assess’. We have described the leadership and organisational factors that created the conditions for improvement. This is a subset of patients that is exceptionally vulnerable to in-hospital harm, and delayed transfers of care occur almost exclusively in this group. We believe there is potential to develop this model further to improve the quality of care in a way that will significantly affect outcomes for patients.
In parallel to the patient care benefits, this redesign has improved efficiency during a time of increasing austerity in the NHS. It is difficult to apply a precise figure to the cost saving as the hospital bed days saved vary between medical and surgical specialties, which have significant variation in marginal bed day cost. However, our data give us high confidence that the return on investment is several-fold.
Although there are clear efficiency benefits of this work, the initial motivation and aim were to enable staff to achieve an improved patient experience. We believe this is a stronger strategy than initially aiming to save money based on our experience of this work compared with other work we have observed within the NHS in which the initial aim was cost saving.
Key learning points
The model of ‘discharge to assess’ is a patient-centred model of care translatable to other acute trusts. Although common sense, assessments undertaken in the context of the patients’ own homes provide a more accurate measure of support requirement.
In industry, complex products are designed through understanding the current state, prototyping and iterative design. This methodology can be applied to healthcare systems. Prototyping helps overcome the complexity of modern healthcare systems.
Staff provided with the capability and opportunity to redesign care process can achieve transformative improvement in patient experience and efficiency.
The ‘Big Room’ process of improvement is directly transferable to other healthcare settings.
Conflicts of interest
The authors have no conflicts of interest to declare.
Author contributions
TD and PH coached the process design outlined in the case study. NO was an active participant and wrote the first draft of this paper. PH was responsible for data processing and analysis. All authors contributed to the interpretation of the data and critically revising drafts of the paper. All authors read and approved the final version of the manuscript.
Funding
This work was produced by Sheffield Teaching Hospitals NHS Foundation Trust. The initial work to develop the ‘Big Room’ quality improvement methodology was supported by The Health Foundation, an independent charity working to continuously improve the quality of healthcare in the UK.
Supplementary material
Additional supplementary material may be found in the online version of this article at http://futurehospital.rcpjournal.org/:
S1 – Supplementary figures.
References
- 1.Fillingham D, Jones B, Pereira P. The challenge and potential of whole system flow. London: The Health Foundation, 2016. [Google Scholar]
- 2.Silvester KM, Mohammed MA, Harriman P, Girolami A, Downes TW. Timely care for frail older people referred to hospital improves efficiency and reduces mortality without the need for extra resources. Age Ageing 2014;43:472–7. [DOI] [PubMed] [Google Scholar]
- 3.Prism Europe Winchart Professional Edition 4.0. www.prismeurope.co.uk/software/winchart_professional.php [Accessed 13 December 2016].