Abstract
Aims: Neck circumference (NC) was found to be related to the risk factors for coronary heart disease (CHD). However, the effects of NC on CHD are still controversial. To evaluate the relationship between NC and CHD, a meta-analysis of observational studies was performed.
Method: Eligible studies on the association between NC and CHD were searched in Medline, Embase, Ovid, and Web of Science databases published in English from January 1980 to December 2016. Moreover, studies published in Chinese in Wanfang and China Hospital Knowledge databases were also searched. Random effects models in the metafor package in statistical analysis software R 3.3.3 were used for the meta-analysis. Heterogeneity was analyzed with Q statistics.
Results: Eight studies were selected for the meta-analysis. A larger NC was associated with a higher prevalence of CHD (OR = 1.18, 95% CI 1.04–1.34, p = 0.0108). The eight studies were further divided into three subgroups according to the criteria for diagnosing CHD. In the subgroup of coronary angiography, NC was also found to be associated with the prevalence of CHD with low heterogeneity (OR = 1.17, 95% CI 1.07–1.28, p = 0.0007, I2 = 17.02%). However, in the subgroup of computed tomography or past history, no association between NC and CHD was found. In addition, subgroup analyses were also conducted according to the regions of the study. No association between NC and CHD was identified in either Chinese studies or Brazil studies (OR = 1.20, 95% CI 0.96–1.49; OR = 1.31, 95% CI 0.82–2.09, respectively).
Conclusion: Larger NC is associated with increased risk of CHD, especially when coronary angiography was taken to diagnose CHD.
Keywords: neck circumference, coronary heart disease, cardiovascular disease
Introduction
Coronary heart disease (CHD) is one of the most common chronic non-communicable diseases in the world. CHD is also the leading reason of all-cause deaths in adults in many countries, accounting for 30.8%–40% of all deaths worldwide (Mozaffarian et al., 2016; National Center for Cardiovascular Disease, 2012). Identifying more risk factors associated with CHD is important for CHD prevention and management.
In recent decades, the prevalence of CHD increased dramatically, and the onset age of CHD significantly decreased with more CHD patients younger than 40 years old. Obesity has been shown to be an important risk factor for CHD, and always accompanied by multiple metabolic abnormalities, such as insulin resistance, diabetes, hypertension, dyslipidemia, and gout. Obesity now is a global health problem, not only in the general population (Finucane et al., 2011), but also in islanders (Finucane et al., 2011; Okihiro & Harrigan, 2005). Several anthropometric indexes, such as body mass index (BMI), waist circumference, waist-to-hip ratio, and neck circumference (NC), are used to evaluate obesity. Several studies have found that upper-body obesity had a stronger association with insulin resistance, diabetes, dyslipidemia, and gout than lower-body obesity (Kissebah et al., 1982; Laakso, Matilainen, & Keinanen-Kiukaanniemi, 2002). NC, as an index for upper-body subcutaneous adipose tissue distribution, has been evaluated in relation to cardiovascular risk factors (Sjostrom, Hakangard, Lissner, & Sjostrom, 1995). The association between NC and insulin resistance (Laakso et al., 2002; Liang et al., 2013; Yang, Samarasinghe, Kane, Amiel, & Aylwin, 2010) and biochemical components of metabolic syndrome (MS) has also been studied (Ben-Noun & Laor, 2006; Kumar, Ismail, Mahesha, Girish, & Tripathy, 2014; Onat et al., 2009). NC has been found to be an independent predictive contributor to cardio-metabolic syndrome (Zhou et al., 2013) and early stage atherosclerosis (Liang et al., 2014).
However, the effects of NC on predicting CHD and CHD events are still controversial (Arjmand, Shidfar, Nojoomi, & Amirfarhangi, 2015; Dai, Wan, Li, & Jin, 2016; Preis et al., 2010). Preis et al. (2010) reported that in the Framingham Heart Study, NC was associated with CHD risk factors even after adjustment for visceral adipose tissue and BMI. However, in a secondary analysis using incident of cardiovascular disease as an outcome, there was no statistically significant association observed between NC and cardiovascular disease in multivariable-adjusted models. In a prospective cohort study performed in China on 12,151 high-risk cardiology outpatients from 2004 until 2014, it was found that a higher NC indicated a higher incidence of future fatal and non-fatal CHD events and all-cause mortality in both male and female high-risk population (Dai et al., 2016). A cross-sectional study performed on people who underwent coronary angiography showed that NC was a better predictor of the risk of coronary artery disease compared to other anthropometric indices (Arjmand et al., 2015).
The controversial results from different studies on association between NC and CHD make it necessary to perform a meta-analysis to evaluate the relationship between NC and CHD by combining the data of all relevant studies. The meta-analysis follows the guideline provided in the Meta-analysis Of Observational Studies in Epidemiology (MOOSE) (Stroup et al., 2000).
Methods
Eligibility Criteria
Eligible studies on the association between NC and CHD were searched in Medline, Embase, Ovid, and Web of Science databases published in English from January 1980 to December 2016. Moreover, studies published in Chinese from January 1980 to December 2016 in Wanfang and China Hospital Knowledge Database (CHKD) databases were also searched. The key words “neck circumference,” “cardiovascular disease,” “coronary heart disease,” and combinations of these were used. References cited in the retrieved articles were also examined to find relevant studies that had not been identified by database searches. The articles were first selected through title and abstract screening. The secondary abstract review was performed on the first screened articles with review of the full text. The final inclusion of articles was determined by consensus between two co-authors. Figure 1 shows the search strategy in the meta-analysis.
Figure 1.
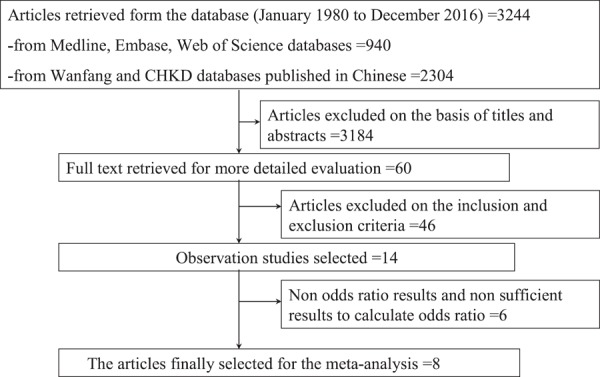
Flow diagram of article selection. Abbreviations: CHKD: China Hospital Knowledge Database.
Selection Criteria
Inclusion criteria included: (i) observation or cohort studies; (ii) adult patients aged 18 years or older; (iii) articles that reported the association between NC and CHD in terms of odds ratios (ORs) or correlation coefficients (r) or other forms of effect sizes. We excluded: (i) abstracts, letters, editorials, expert opinions, case reports, and reviews; (ii) studies that included people aged less than 18 years. Disagreement was solved by the discussion within the team authors.
Data Extraction
Data were extracted using standardized forms. Data recorded included the first authors’ names, years of publication, the locations of studies, study design, numbers of total patients, and adjusted ORs with corresponding 95% confidence intervals (CIs).
Statistical Analysis
Random effects models were utilized to obtain the summary ORs and their 95% CIs for the association between NC and CHD in all eligible studies and subgroup analysis. Statistical heterogeneity among studies was evaluated using the Cochran Q statistics. The heterogeneity was further quantified by inconsistency index (I2) with 25%, 50%, and 75% representing the evidence of low, moderate, and high heterogeneity, respectively (Higgins & Thompson, 2002; Higgins, Thompson, Deeks, & Altman, 2003). According to the p values <0.10 of the heterogeneity test, random effects model were used to estimate OR and corresponding 95% CI. Studies using correlation coefficient (r) as effect sizes were converted to log odds ratios for the meta-analysis.
The funnel plot and radial plot were generated to assess the publication bias. Egger regression asymmetry test for funnel plot asymmetry was also performed to detect publication bias. The metafor package in statistical analysis software R was used for the meta-analysis (Viechtbauer, 2010), and p-values less than 0.05 were considered statistically significant for testing association between NC and CHD.
Sensitivity and Subgroup Analyses
Sensitivity analyses were conducted to measure the robustness of the result. The study with the biggest contribution was removed from the meta-analysis. Then, the two studies using correlation coefficients as effect sizes were removed. Subgroup analysis was based on different nations and different diagnosis criteria for CHD were performed.
Results
Search Results
The screening process for articles used for the meta-analysis is shown in Figure 1. A search of PubMed, Web of Science, and Embase identified a total of 940 articles, and a search of Wanfang and CHKD database identified 2,304 articles. After title and abstract review, 60 studies were selected for a more detailed assessment. We filtered out a total of 46 studies that did not meet the criteria. Finally, eight studies were selected for meta-analysis.
A total of eight articles were included for the meta-analysis. Of them, three were conducted in China (Dai et al., 2016; Liao, Liu, Wang, & Zhang, 2015; G. Yang et al., 2016), three in Brazil (Baena et al., 2016; Chagas et al., 2011; Zen et al., 2012), one in the United States (Pokharel et al., 2014), and one in Iran (Arjmand et al., 2015). In terms of study design, there were seven cross-sectional studies and one cohort study. The sample size varied from 300 (Arjmand et al., 2015) to 12,515 (Dai et al., 2016) (Table 1).
Table 1.
Characteristics of Studies Included in the Meta-analysis
| First author (Publication year) | Location | Study design | Total number (n) | Control number (n) | CHD number (n) | Odds ratio | 95% confidence intervals |
|---|---|---|---|---|---|---|---|
| Zen et al. (2012) | Brazil | Case-control study | 376 | 221 | 155 | 2.40 | 1.10–5.30 |
| G. Yang et al. (2016) | China | Cross-sectional study | 3,176 | 2,560 | 616 | 1.022 | 0.996–1.048 |
| Liao et al. (2015) | China | Case-control study | 677 | 310 | 367 | 1.128 | 1.075–1.185 |
| Arjmand et al. (2015) | Iran | Cross-sectional study | 300 | 68 | 231 | 1.207 | 1.004–1.451 |
| Pokharel et al. (2014) | United States | Cross-sectional study | 845 | 323 | 522 | 1.11 | 0.94–1.31 |
| Baena et al. (2016) | Brazil | Cross-sectional study | 3,929 | 3,004 | 1,148 | 0.94 | 0.78–1.13 |
| Dai et al. (2016) | China | Cohort study | 12,515 | 7,871 | 2,304 | 1.49a | 1.40–1.59a |
| Chagas et al. (2011) | Brazil | Cross-sectional study | 337 | 1.39a | 0.96–2.01a |
CHD: coronary heart disease.
a Calculated according to the data information in the original studies.
Meta-analysis
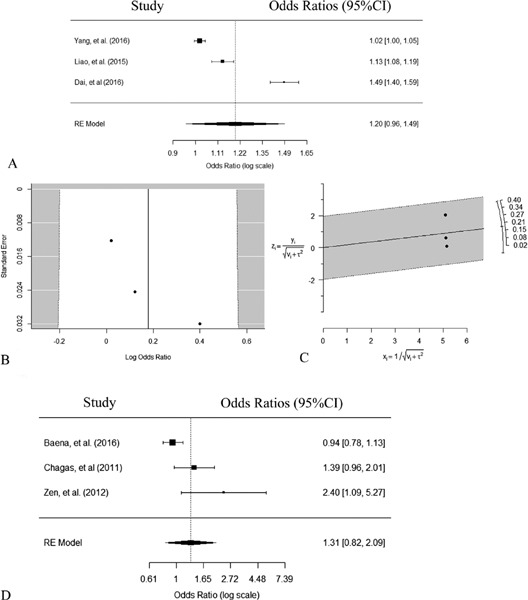
The random-effects model was selected for data analysis, as the test for heterogeneity showed a statistically significant result (I2 = 93.06%, p < 0.05). The weighted odds ratio estimated from the random-effects model indicated that a higher NC was associated with a higher prevalence of CHD (OR = 1.18, 95% CI 1.04–1.34, p = 0.0108), as shown in Figure 2.
Figure 2.
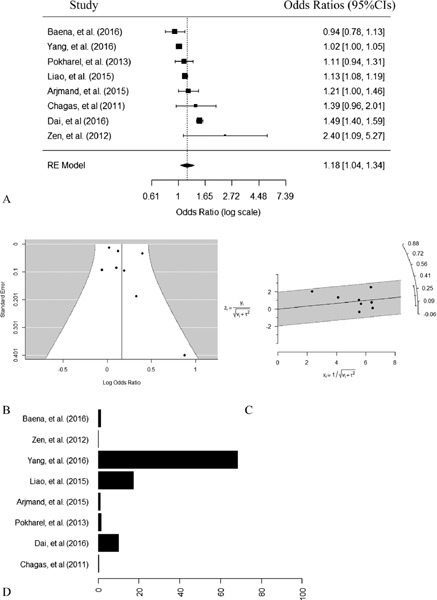
Meta-analysis of neck circumference associated with coronary heart disease (random effects model). (A) Forest plot. (B) Funnel plot. The X-axis was log odds ratio, and the Y-axis represents the standard error. No publication bias was found using regression test for funnel plot asymmetry (p = 0.1574). (C) Radial plot. x stands for the inverse of the standard errors, y stands for the outcome, z stands for standardized outcome, both v and τ stand for standard errors with v denoting the standard errors from the fixed effects part and τ denoting the standard errors from the random effects part. (D) Contribution plot.
Publication Bias
The homogeneity was analyzed with Q statistics and I2. Heterogeneity was found to be statistically significant (Q = 132.2043, I2 = 94.05%, p < 0.05). The publication bias was assessed using funnel plot and radial plot because the heterogeneity existed. The funnel plot showed relative symmetry (Figure 2). Egger regression test for funnel plot asymmetry was performed, indicating no significant bias among these studies (z = 1.4140, p = 0.1574).
Sensitivity Analysis
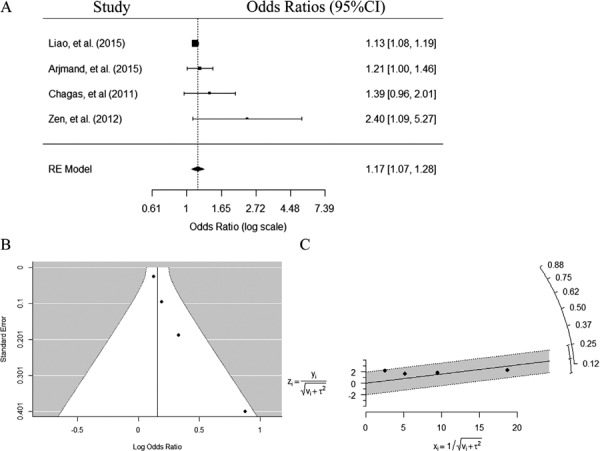
To measure the robustness of the result, sensitivity analyses were conducted. According to the contribution plots of each study, the study with the largest contribution was done by G. Yang et al. (2016), as shown in Figure 2. First, we removed the study with the largest contribution and analysed the remaining results. NC remained to be associated with CHD in a random-effects model (OR = 1.22, 95% CI 1.06–1.40, p = 0.0063, Figure 3). The I2 for heterogeneity was 87.78% (p < 0.05). The funnel plot showed relative symmetry (Figure 3). Egger regression test for funnel plot asymmetry model indicated no significant bias among these studies (z = 1.1586, p = 0.2466).
Figure 3.
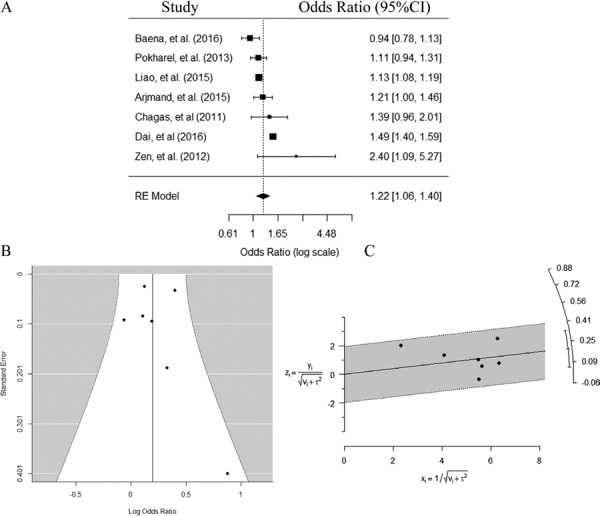
Meta-analysis of neck circumference associated with coronary heart disease after removing the study with the biggest contribution (random effects model). (A) Forest plot. (B) Funnel plot. The X-axis was log odds ratio, and the Y-axis represents the standard error. No publication bias was found using regression test for funnel plot asymmetry (p = 0.2466). (C) Radial plot. x stands for the inverse of the standard errors, y stands for the outcome, z stands for standardized outcome, both v and τ stand for standard errors with v denoting the standard errors from the fixed effects part and τ denoting the standard errors from the random effects part.
Next, we removed the two studies using correlation coefficients as effect sizes (Chagas et al., 2011; Dai et al., 2016). After removing, NC was associated with CHD in a random-effects model (OR = 1.08, 95% CI 1.01–1.16, p = 0.0345, Figure 4). The I2 for heterogeneity was 71.09% (p < 0.05). The funnel plot remained relative symmetry (Figure 4). Egger regression test for funnel plot asymmetry model show no significant bias among these studies (z = 1.5618, p = 0.1183).
Figure 4.
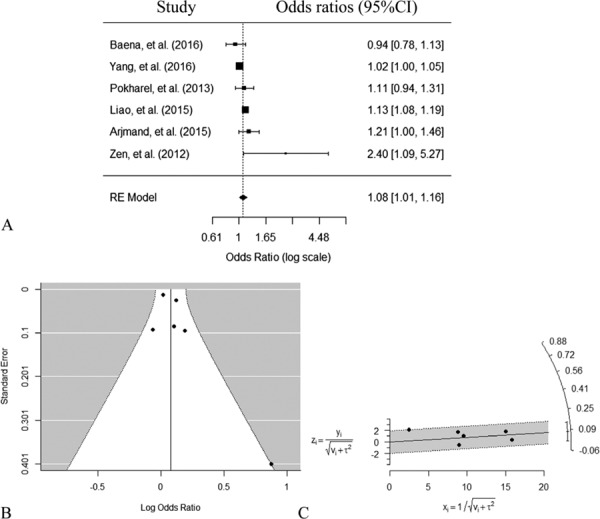
Meta-analysis of neck circumference associated with coronary heart disease after removing two studies using correlation coefficients as effect sizes (random effects model). (A) Forest plot. (B) Funnel plot. The X-axis was log odds ratio, and the Y-axis represents the standard error. No publication bias was found using regression test for funnel plot asymmetry (p = 0.7811). (C) Radial plot. x stands for the inverse of the standard errors, y stands for the outcome, z stands for standardized outcome, both v and τ stand for standard errors with v denoting the standard errors from the fixed effects part and τ denoting the standard errors from the random effects part.
Subgroup Analysis
Subgroup based on Different Nations
Subgroup analysis was conducted stratified by nations. Among the eight studies in the meta-analysis, three studies were conducted in China (Dai et al., 2016; Liao et al., 2015; G. Yang et al., 2016). A random-effects model on the three studies showed no significant association between NC and CHD (OR = 1.20, 95% CI 0.96–1.49, p = 0.113, Figure 5). The I2 for heterogeneity was 98.7% (p = 0.001). The funnel plot remained relative symmetry (Figure 5). Egger regression test for funnel plot asymmetry model showed no significant bias among these studies (z = 2.4227, p = 0.0154).
Figure 5.
Meta-analysis of neck circumference associated with coronary heart disease in subgroups based on different nations (random effects model). (A) Forest plot for the studies conducted in China. (B) Funnel plot for the studies conducted in China. The X-axis was log odds ratio, and the Y-axis represents the standard error. No publication bias was found using regression test for funnel plot asymmetry (p = 0.0154). (C) Radial plot for the studies conducted in China. x stands for the inverse of the standard errors, y stands for the outcome, z stands for standardized outcome, both v and τ stand for standard errors with v denoting the standard errors from the fixed effects part and τ denoting the standard errors from the random effects part. (D) Forest plot for the studies conducted in Brazil.
There were three studies conducted in Brazil (Baena et al., 2016; Chagas et al., 2011; Zen et al., 2012). NC was not associated with CHD in a random-effects model including the three Brazil studies (OR = 1.31, 95% CI 0.82–2.09, p = 0.2604, Figure 5). The I2 for heterogeneity was 77.11% (p = 0.0193). Egger regression test for funnel plot asymmetry model show that there were no significant bias among these studies (z = 2.7787, p = 0.0055).
Subgroup based on Different Diagnosis Criteria for CHD
There were four studies in which coronary angiography was performed to diagnose CHD (Arjmand et al., 2015; Chagas et al., 2011; Liao et al., 2015; Zen et al., 2012). NC was found to be associated with CHD in a random-effects model (OR = 1.17, 95% CI 1.07–1.28, p = 0.0007, Figure 6). The I2 for heterogeneity was 17.02% (p = 0.1668). The funnel plot remained relative symmetry (Figure 6). Egger regression test for funnel plot asymmetry model did not indicate significant bias among these studies (z = 2.1600, p = 0.0308).
Figure 6.
Meta-analysis of neck circumference associated with coronary heart disease in subgroup using coronary angiography to diagnose coronary heart disease (random effects model). (A) Forest plot. (B) Funnel plot. The X-axis was log odds ratio, and the Y-axis represents the standard error. No publication bias was found using regression test for funnel plot asymmetry (p = 0.0308). (C) Radial plot. x stands for the inverse of the standard errors, y stands for the outcome, z stands for standardized outcome, both v and τ stand for standard errors with v denoting the standard errors from the fixed effects part and τ denoting the standard errors from the random effects part.
There were two studies in which computed tomography was performed to evaluate the conditions of the coronary arteries (Baena et al., 2016; Pokharel et al., 2014). NC was not associated with CHD in a random-effects model (OR = 1.03, 95% CI 0.87–1.21, p = 0.7606, Figure 7). The I2 for heterogeneity was 43.23% (p = 0.1844).
Figure 7.
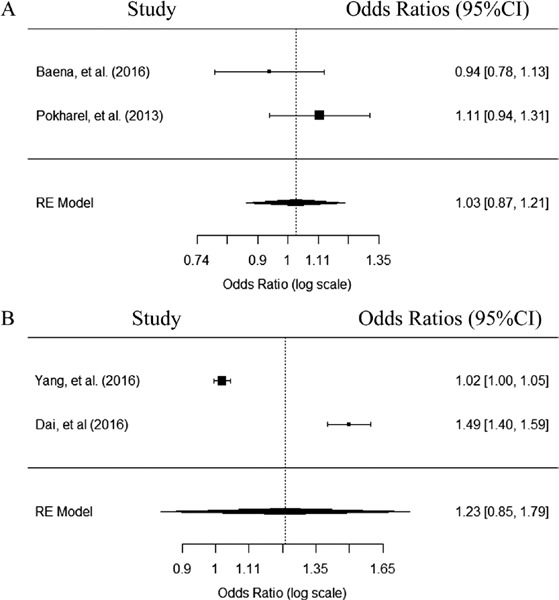
Forest plot of neck circumference associated with coronary heart disease in subgroups using computed tomography and the past history to diagnose coronary heart disease (random effects model). (A) Forest plot for studies using computed tomography to diagnose heart disease. (B) Forest plot for studies using the past history to diagnose coronary heart disease.
In the two studies, CHD was diagnosed by the history of past myocardial infarction, acute coronary syndrome, and cardiac death (Dai et al., 2016; G. Yang et al., 2016). NC was not associated with CHD (OR = 1.23, 95% CI 0.85–1.79, p = 0.2721, Figure 7). The I2 for heterogeneity was 99.16% (p < 0.001).
Discussion
Overweight/obesity is recognized as one of the most common risk factors for CHD (Mongraw-Chaffin, Peters, Huxley, & Woodward, 2015; Wormser et al., 2011). NC was shown in many studies to be an indicator for evaluating overweight/obesity. In this meta-analysis with eight studies, NC was associated with CHD. In the subgroup analysis, when coronary angiography was performed to diagnose CHD, NC was also found to be associated with CHD with low heterogeneity. However, the association between NC and CHD was not found in the other subgroup analysis.
There are several anthropometric indicators to evaluate overweight/obesity, such as BMI, waist circumference, waist hip ratio, and NC. Several meta-analysis studies on the association between anthropometric indicators with CHD showed that BMI, measured continuously or categorically, had deleterious effects on the risk of incident CHD in people across diverse populations (Mongraw-Chaffin et al., 2015). In a meta-analysis study of 82,864 individuals from nine nationwide British cohorts, greater waist circumference and waist hip ratio were found to be associated with an increased cardiovascular mortality (Czernichow, Kengne, Stamatakis, Hamer, & Batty, 2011). However, there was a lack of meta-analysis about the association between NC and CHD.
Since NC was first evaluated in relation to cardiovascular risk factors by Sjöström et al. in 1995 (Sjostrom et al., 1995), many studies were performed to assess the effects of NC in clinical practice. First, NC was used to evaluate overweight and obesity (Ben-Noun & Laor, 2003; Onat et al., 2009; L. Yang et al., 2010). Then it was used to assess obesity related disease, such as insulin resistance, obstructive sleep apnea syndrome, and metabolic syndrome (Ben-Noun & Laor, 2006; Liang et al., 2013). The prevalence of obesity increases in most countries in recent decades. In 2009–2010, the prevalence of obesity was about 35% in U.S. adults (Flegal, Carroll, Kit, & Ogden, 2012). The increase in obesity was seen not only in North America, but also in the Asian/Pacific islanders. An analysis in Australian adults aged over 45 years found that the prevalence of obesity was nearly 30% (Buchmueller & Johar, 2015). It was reported that the mean BMI increased by above 2.0 kg/m2 per decade from 1980 to 2008 in the Cook and Nauru Islanders (Finucane et al., 2011). The Pacific Islander Health Study had shown that the majority of the male Pacific Islander adult was already overweight by aged 18 years (84% of Samoan and 65% of Tongan males being obese) (Panapasa, McNally, Heeringa, & Williams, 2015). The association of NC with cardiovascular disease risks was also studied in Asian/Pacific Islanders (Aoi et al., 2016; Dixon & O’Brien, 2002; Lindarto, Shierly, & Syafril, 2016). A study conducted in obese premenopausal Australian women found that NC was a significant predictive factor of hyperinsulinemia (Dixon & O’Brien, 2002). An observation study conducted in Indonesia reported that NC was related to BMI and may be useful in evaluating overweight/obesity (Lindarto et al., 2016). Another prospective cohort study conducted in a Japan community found that change in NC was related to atherosclerosis-related markers (Aoi et al., 2016). Due to the observed association of NC with cardiovascular risk factors (lipid profile, insulin resistance, metabolic syndrome, and hypertension) in many studies (Ben-Noun & Laor, 2003, 2006; Liang et al., 2013; G. Yang et al., 2010), NC might be related to CHD. However, the results of clinical studies on the association of NC with CHD remained controversial. In a cross-sectional study, NC was found to be a better predictor of the risk of CHD compared to other anthropometric indices (Arjmand et al., 2015). However, the results from ELSA-Brazil study had shown that NC was not associated with coronary atherosclerosis (Baena et al., 2016).
A variety of study designs were used for this meta-analysis, with various study population (i.e., age, sex) and uncontrolled confounding factors (past history, cardiovascular risk factors). These variations may affect the heterogeneity and the results. In some studies related to NC and obesity, it was shown that NC in males was higher than that in females, so the cutoff of NC for evaluating obesity was sex-specific (G. Yang et al., 2010). However in the eight studies used in our meta-analysis, only one study assessed the sex-specific relationship between NC and CHD (Baena et al., 2016). To assess whether the difference in nation would affect the results, subgroup analyses were conducted stratified by nations. In each nation strata, no association was found between NC and CHD.
In studies used for the meta-analysis, CHD was diagnosed by using coronary angiography in four studies (Arjmand et al., 2015; Chagas et al., 2011; Liao et al., 2015; Zen et al., 2012), by using computed tomography scanner in two studies (Baena et al., 2016; Pokharel et al., 2014), and by history of past myocardial infarction, acute coronary syndrome, and cardiac death in two studies (Dai et al., 2016; G. Yang et al., 2016). In the subgroup analysis, the eight studies were stratified into three subgroups according to the criteria for diagnosing CHD. In the subgroup of coronary angiography, NC was also found to be associated with the prevalence of CHD with low heterogeneity. However, in the other subgroups, where computed tomography or past history were used to diagnose CHD, no association between NC and CHD was found. In the subgroup of computed tomography or past history, there were only two studies included in each subgroup, which may interfere with the results of the meta-analysis. In clinical practice, when people were suspected for CHD, coronary angiography will be recommended in most cases. When needed, a 64-detector computed tomography scanner is also used to evaluate the coronary atherosclerosis. Coronary angiography is recognized as the gold standard for diagnosing CHD. Based on the results of the subgroup of coronary angiography, there is statistically significant evidence that NC is associated with CHD. Furthermore, large-scale studies are needed to confirm this relationship. Whether NC can predict CHD also need prospective studies. In a Chinese cohort study, it was found that NC was related to the incident of CHD events (Dai et al., 2016). However, in the Framingham study, though NC was related to the cardiovascular risk factor, NC was not related to the incidence of cardiovascular events (Preis et al., 2010).
Due to the nature of observational studies used in the meta-analysis, the inherent biases cannot be controlled as in the randomized controlled studies, and some confounding effects are inevitable in observational studies. In addition, the study design and subject selection for each analysis are not coherent. For example, a cross-sectional study is more likely performed in a particular area with a high incidence, and is less likely in an area with a rare incidence. Therefore, the results could have bias and are difficul in generalizing the population of interest (Jung & Lee, 2009; Stroup et al., 2000).
Additional potential limitations to this meta-analysis include: (1) The limited number of studies included in the meta-analysis could affect the association between NC and CHD, for example, no statistical significant association exist between NC and CHD when the number of studies decreased to three; (2) Different diagnose criteria for CHD was used in these eight studies in the meta-analysis; (3) Participants in some studies were patients with high risk for CHD, for example, G. Yang et al. (2016) investigated the association between NC and CHD in type 2 diabetes, and Arjmand et al. (2015) investigated people with stable angina. (4) There were studies investigating the association of NC with cardiovascular risk factors in different populations, however, only several studies investigated the association of NC with CHD. The studies included in this meta-analysis were performed in Asia and America. The association of NC with CHD risk factors was also studied in Asian/Pacific Islanders (Aoi et al., 2016; Dixon & O’Brien, 2002; Lindarto et al., 2016). However, no studies evaluating the relationship between NC and CHD in Asian/Pacific Islanders were found. Further studies in this population are needed to confirm this association in Asian/Pacific Islanders. The reason for the increasing obesity in different population may be different. However, there were common risk factors for obesity in Chinese and Asian/Pacific Islands. Modern dietary pattern was reported to be positively associated with obesity in China (Xu, Hall, Byles, & Shi, 2015). Increased intake of fats and sugars was found to be one of the main reasons for obesity in the Pacific Islanders (Snowdon & Thow, 2013). Obesity is now a global public health problem. Nutrition education is a very important preventive strategy for both Chinese and Asian/Pacific Islanders. Studies on NC, an anthropometric indicator for obesity, and obesity related disease, such as CHD, would be helpful in future prevention and treatment of obesity in Asian/Pacific Islanders.
Our results indicate that NC may be associated with CHD, especially when coronary angiography was taken to diagnose CHD. Given the high incidence of CHD, further large-scale and prospective studies may be worthwhile to confirm this relationship between NC and CHD.
Acknowledgements
We would like to thank the anonymous reviewers for their insightful comments and suggestions that helped to improve our manuscript.
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest concerning the research, authorship, or publication of this article.
Funding
This study is supported by Capital’s Funds for Health Improvement and Research [2016-2-2054], and the Beijing Municipal Training Foundation for Highly-qualified and Technological Talents of Health System [2014-3-013]. Dr. Li’s, Dr. Zand’s, Mr. Fogg’s, and Dr. Dye’s time is supported by the University of Rochester’s Clinical and Translational Science Award (CTSA) number UL1 TR000042 and UL1 TR002001 from the National Center for Advancing Translational Sciences of the National Institutes of Health. Dr. Zand is also supported by the National Institute of Allergy and Infectious Diseases and the National Institute of Immunology, grant numbers AI098112 and AI069351. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References
- Aoi S., Miyake T., Iida T., Ikeda H., Ishizaki F., Chikamura C., ... Miyaguchi H. (2016). Association of changes in neck circumference with cardiometabolic risk in postmenopausal healthy women. Journal of Atherosclerosis and Thrombosis, 23(6), 728–736. 10.5551/jat.31963 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arjmand G., Shidfar F., Nojoomi M. M., & Amirfarhangi A. (2015). Anthropometric indices and their relationship with coronary artery diseases. Health Scope, 4(3). 10.17795/jhealthscope-25120 [DOI] [Google Scholar]
- Baena C. P., Lotufo P. A., Santos I. S., Goulart A. C., Bittencourt M. S., Duncan B. B., ... Bensenor I. M. (2016). Neck circumference is associated with carotid intimal-media thickness but not with coronary artery calcium: Results from The ELSA-Brasil. Nutrition, Metabolism & Cardiovascular Diseases, 26(3), 216–222. 10.1016/j.numecd.2016.01.004 [DOI] [PubMed] [Google Scholar]
- Ben-Noun L., & Laor A. (2003). Relationship of neck circumference to cardiovascular risk factors. Obesity Research, 11(2), 226–231. 10.1038/oby.2003.35 [DOI] [PubMed] [Google Scholar]
- Ben-Noun L. L., & Laor A. (2006). Relationship between changes in neck circumference and cardiovascular risk factors. Experimental & Clinical Cardiology, 11(1), 14–20. [PMC free article] [PubMed] [Google Scholar]
- Buchmueller T. C., & Johar M. (2015). Obesity and health expenditures: Evidence from Australia. Economics & Human Biology, 17, 42–58. 10.1016/j.ehb.2015.01.001 [DOI] [PubMed] [Google Scholar]
- Chagas P., Caramori P., Barcellos C., Galdino T. P., Gomes I., & Schwanke C. H. (2011). Association of different anthropometric measures and indices with coronary atherosclerotic burden. Arquivos Brasileiros de Cardiologia, 97(5), 397–401. 10.1590/S0066-782X2011005000093 [DOI] [PubMed] [Google Scholar]
- Czernichow S., Kengne A. P., Stamatakis E., Hamer M., & Batty G. D. (2011). Body mass index, waist circumference and waist-hip ratio: Which is the better discriminator of cardiovascular disease mortality risk?: Evidence from an individual-participant meta-analysis of 82 864 participants from nine cohort studies. Obesity Review, 12(9), 680–687. 10.1111/j.1467-789X.2011.00879.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dai Y., Wan X., Li X., & Jin E. (2016). Neck circumference and future cardiovascular events in a high-risk population—A prospective cohort study. Lipids in Health and Disease, 15 32 10.1186/s12944-016-0218-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dixon J. B., & O’Brien P. E. (2002). Neck circumference a good predictor of raised insulin and free androgen index in obese premenopausal women: Changes with weight loss. Clinical Endocrinology, 57(6), 769–778. 10.1046/j.1365-2265.2002.01665.x [DOI] [PubMed] [Google Scholar]
- Finucane M. M., Stevens G. A., Cowan M. J., Danaei G., Lin J. K., Paciorek C. J., ... Global Burden of Metabolic Risk Factors of Chronic Diseases Collaborating Group. (2011). National, regional, and global trends in body-mass index since 1980: Systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9.1 million participants. Lancet, 377(9765), 557–567. 10.1016/S0140-6736(10)62037-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flegal K. M., Carroll M. D., Kit B. K., & Ogden C. L. (2012). Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. JAMA, 307(5), 491–497. 10.1001/jama.2012.39 [DOI] [PubMed] [Google Scholar]
- Higgins J. P., & Thompson S. G. (2002). Quantifying heterogeneity in a meta-analysis. Statistics in Medicine, 21(11), 1539–1558. 10.1002/sim.1186 [DOI] [PubMed] [Google Scholar]
- Higgins J. P., Thompson S. G., Deeks J. J., & Altman D. G. (2003). Measuring inconsistency in meta-analyses. BMJ, 327(7414), 557–560. 10.1136/bmj.327.7414.557327/7414/557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jung D., & Lee S. M. (2009). BMI and breast cancer in Korean women: A meta-analysis. Asian Nursing Research (Korean Society of Nursing Science), 3(1), 31–40. 10.1016/S1976-1317(09)60014-1 [DOI] [PubMed] [Google Scholar]
- Kissebah A. H., Vydelingum N., Murray R., Evans D. J., Hartz A. J., Kalkhoff R. K., & Adams P. W. (1982). Relation of body fat distribution to metabolic complications of obesity. The Journal of Clinical Endocrinology & Metabolism, 54(2), 254–260. 10.1210/jcem-54-2-254 [DOI] [PubMed] [Google Scholar]
- Kumar N. V., Ismail M. H., Mahesha P., Girish M., & Tripathy M. (2014). Neck circumference and cardio-metabolic syndrome. Journal of Clinical and Diagnostic Research, 8(7), MC23–MC25. 10.7860/JCDR/2014/8455.4641 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laakso M., Matilainen V., & Keinanen-Kiukaanniemi S. (2002). Association of neck circumference with insulin resistance-related factors. International Journal of Obesity and Related Metabolic Disorders, 26(6), 873–875. 10.1038/sj.ijo.0802002 [DOI] [PubMed] [Google Scholar]
- Liang J., Teng F., Li Y., Liu X., Zou C., Wang Y., ... Qi L. (2013). Neck circumference and insulin resistance in Chinese adults: The Cardiometabolic Risk in Chinese (CRC) Study. Diabetes Care, 36(9), e145–e146. 10.2337/dc13-1114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang J., Wang Y., Li H., Liu X., Qiu Q., & Qi L. (2014). Neck circumference and early stage atherosclerosis: The Cardiometabolic Risk in Chinese (CRC) study. Cardiovascular Diabetology, 13 32 10.1186/s12933-014-0107-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liao H. Z., Liu Z. Y., Wang C. H., Zhang B. Q. (2015). Correlation analysis between lipid profile and neck circumference in patients with coronary heart disease. Henan Medical Journal, 26(24), 3623–3626. [Google Scholar]
- Lindarto D., Shierly , & Syafril S. (2016). Neck circumference in overweight/obese subjects who visited the Binjai Supermall in Indonesia. Open Access Macedonian Journal of Medical Sciences, 4(3), 319–323. 10.3889/oamjms.2016.072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mongraw-Chaffin M. L., Peters S. A., Huxley R. R., & Woodward M. (2015). The sex-specific association between BMI and coronary heart disease: A systematic review and meta-analysis of 95 cohorts with 1.2 million participants. The Lancet Diabetes & Endocrinology, 3(6), 437–449. 10.1016/S2213-8587(15)00086-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mozaffarian D., Benjamin E. J., Go A. S., Arnett D. K., Blaha M. J., Cushman M., ... Turner M. B. (2016). Heart Disease and Stroke Statistics—2016 update: A report from the American Heart Association. Circulation, 133(4), e38–e360. 10.1161/CIR.0000000000000350 [DOI] [PubMed] [Google Scholar]
- National Center for Cardiovascular Disease, China. (2012). Report on cardiovascular disease in China (2012).
- Okihiro M., & Harrigan R. (2005). An overview of obesity and diabetes in the diverse populations of the Pacific. Ethnicity & Disease, 15(4 Suppl 5), S5-71–S5-80. [PubMed] [Google Scholar]
- Onat A., Hergenc G., Yuksel H., Can G., Ayhan E., Kaya Z., & Dursunoglu D. (2009). Neck circumference as a measure of central obesity: Associations with metabolic syndrome and obstructive sleep apnea syndrome beyond waist circumference. Clinical Nutrition, 28(1), 46–51. 10.1016/j.clnu.2008.10.006 [DOI] [PubMed] [Google Scholar]
- Panapasa S. V., McNally J. W., Heeringa S. G., & Williams D. R. (2015). Impacts of long-term obesity on the health status of Samoan and Tongan men in the United States: Results from the Pacific Islander Health Study. Ethnicity & Disease, 25(3), 279–286. 10.18865/ed.25.3.279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pokharel Y., Macedo F. Y., Nambi V., Martin S. S., Nasir K., Wong N. D., ... Virani S. S. (2014). Neck circumference is not associated with subclinical atherosclerosis in retired National Football League players. Clinical Cardiology, 37(7), 402–407. 10.1002/clc.22270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preis S. R., Massaro J. M., Hoffmann U., D’Agostino Sr. R. B., Levy D., Robins S. J., ... Fox C. S. (2010). Neck circumference as a novel measure of cardiometabolic risk: The Framingham Heart Study. Journal of Clinical Endocrinology and Metabolism, 95(8), 3701–3710. 10.1210/jc.2009-1779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sjostrom C. D., Hakangard A. C., Lissner L., & Sjostrom L. (1995). Body compartment and subcutaneous adipose tissue distribution—Risk factor patterns in obese subjects. Obesity Research, 3(1), 9–22. 10.1002/j.1550-8528.1995.tb00116.x [DOI] [PubMed] [Google Scholar]
- Snowdon W., & Thow A. M. (2013). Trade policy and obesity prevention: Challenges and innovation in the Pacific Islands. Obesity Review, 14(Suppl 2), 150–158. 10.1111/obr.12090 [DOI] [PubMed] [Google Scholar]
- Stroup D. F., Berlin J. A., Morton S. C., Olkin I., Williamson G. D., Rennie D., ... Thacker S. B. (2000). Meta-analysis of observational studies in epidemiology: A proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA, 283(15), 2008–2012. 10.1001/jama.283.15.2008 [DOI] [PubMed] [Google Scholar]
- Viechtbauer W. (2010). Conducting meta-analyses in R with the metafor package. Journal of Statistical Software, 36(3), 1–48. 10.18637/jss.v036.i03 [DOI] [Google Scholar]
- Wormser D., Kaptoge S., Di Angelantonio E., Wood A. M., Pennells L., Thompson A., ... Danesh J. (2011). Separate and combined associations of body-mass index and abdominal adiposity with cardiovascular disease: Collaborative analysis of 58 prospective studies. Lancet, 377(9771), 1085–1095. 10.1016/S0140-6736(11)60105-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu X., Hall J., Byles J., & Shi Z. (2015). Dietary pattern is associated with obesity in older people in China: Data from China Health and Nutrition Survey (CHNS). Nutrients, 7(9), 8170–8188. 10.3390/nu7095386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang G. R., Yuan S. Y., Fu H. J., Wan G., Zhu L. X., Bu X. L., ... Li Y. (2010). Neck circumference positively related with central obesity, overweight, and metabolic syndrome in Chinese subjects with type 2 diabetes: Beijing Community Diabetes Study 4. Diabetes Care, 33(11), 2465–2467. 10.2337/dc10-0798 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang G. R., Yuan S., Fu H. J., Wan G., Zhu L. X., Yuan M. X., et al. (2016). Neck circumference in identifying cardiovascular disease and dyslipidemia in Chinese type 2 diabetes—Beijing Community Diabetes Study (BCDS-15). Chinese Journal of General Practitioners, 15(1), 19–24. https://dio.org/ 10.3760/cma.j.issn.1671-7368.2016.01.008 [Google Scholar]
- Yang L., Samarasinghe Y. P., Kane P., Amiel S. A., & Aylwin S. J. (2010). Visceral adiposity is closely correlated with neck circumference and represents a significant indicator of insulin resistance in WHO grade III obesity. Clinical Endocrinology, 73(2), 197–200. 10.1111/j.1365-2265.2009.03772.x [DOI] [PubMed] [Google Scholar]
- Zen V., Fuchs F. D., Wainstein M. V., Goncalves S. C., Biavatti K., Riedner C. E., ... Fuchs S. C. (2012). Neck circumference and central obesity are independent predictors of coronary artery disease in patients undergoing coronary angiography. American Journal of Cardiovascular Disease, 2(4), 323–330. [PMC free article] [PubMed] [Google Scholar]
- Zhou J. Y., Ge H., Zhu M. F., Wang L. J., Chen L., Tan Y. Z., ... Zhu H. L. (2013). Neck circumference as an independent predictive contributor to cardio-metabolic syndrome. Cardiovascular Diabetology, 12 32 10.1186/1475-2840-12-76 [DOI] [PMC free article] [PubMed] [Google Scholar]


