Abstract
Background:
Return to sport (RTS) after meniscectomy is an important metric for young, active patients. However, the impact of the duration from surgery to RTS on clinical outcomes is not fully understood and is not reflected in outcome scores.
Purpose:
To establish when patients RTS after meniscectomy and to determine predictive measures for the ability to return to their preinjury activity.
Study Design:
Case-control study; Level of evidence, 3.
Methods:
All patients undergoing meniscectomy between 2016 and 2017 from a single institution were assessed for inclusion. RTS, type of activity, and level of function upon returning were obtained. The minimal clinically important difference (MCID), substantial clinical benefit, and patient acceptable symptom state (PASS) were calculated for the Knee injury and Osteoarthritis Outcome Score (KOOS) and International Knee Documentation Committee (IKDC) questionnaire using anchor-based and distribution-based approaches. Preoperative knee-specific and generic quality-of-life scores were analyzed to determine their predictive power of RTS. A multivariate logistical analysis was also performed to determine which demographic variables corresponded to RTS.
Results:
Overall, 94 patients (mean age, 51.0 ± 11.1 years) who underwent meniscectomy participated in sports within 6 months of surgery. Of these patients, 76.6% returned to sport without permanent restrictions at a mean of 8.6 ± 6.9 weeks postoperatively. RTS rates for low-, medium-, and high-intensity activities were 75.0%, 70.0%, and 82.5%, respectively. RTS was associated with achieving the PASS for the KOOS–Physical Function short form (PS), KOOS-Pain, and KOOS-Sports (P = .004, P = .007, and P = .006, respectively) but not for the IKDC questionnaire (P = .3). Achieving the MCID was associated with RTS for the KOOS-Sports, KOOS-Pain, and IKDC questionnaire (P < .001, P = .03, and P = .001, respectively). There was no preoperative or intraoperative variable that was predictive of RTS. Preoperative KOOS-PS scores ≥37.8 (area under the curve = 76.3%) and KOOS-Pain scores ≥51.4 (area under the curve = 72.5%) were predictive of RTS.
Conclusion:
Approximately 77% of patients returned to sport after meniscectomy at a mean of 2 months postoperatively. The level of activity intensity did not significantly alter the rate of RTS. Higher preoperative scores on the KOOS-PS and KOOS-Pain were predictive of RTS. Identifying these factors allows physicians to counsel patients on expected outcomes after meniscectomy.
Keywords: meniscectomy, minimal clinically important difference, substantial clinical benefit, patient acceptable symptom state, return to sport
The meniscus is a semicircular fibrocartilaginous structure that functions to provide lubrication, proprioception, knee stability, load distribution, and shock absorption.1,29 Once the meniscus is disrupted, the risk of joint degeneration, pain, and morbidity increases. Meniscal tears affect 60 to 70 people per 100,000 person-years, and approximately one-third of injuries are related to sport activity.5 In patients who are active and wish to return to sport (RTS), partial meniscectomy may provide the quickest path to RTS, despite the long-term risk of developing osteoarthritis.17 However, the effect on clinical outcomes of the duration from surgery to RTS is not fully understood and is not reflected in outcome scores.
RTS is often reported as an outcome measure because it is an important goal for patients2; the RTS rate has ranged from 50% to 98% after meniscectomy.21,28,34 Because of the variable rates of RTS, it is unknown whether RTS has a positive, negative, or neutral effect on patient-reported outcome measures (PROMs). Thus, its effect on clinically meaningful knee-specific and generic quality-of-life outcomes after meniscectomy should be evaluated. After anterior cruciate ligament (ACL) reconstruction, patients report that they wish to participate in sports without knee difficulties above all other occupational or family activities.7 This suggests that participation in sports is a priority for many patients. Within orthopaedic surgery, preoperative functional outcomes have been shown to be important predictors of postoperative outcomes after hip arthroplasty,3 shoulder arthroplasty,37 femoroacetabular impingement,25 and ACL reconstruction.24 However, the use of PROMs to predict the likelihood of RTS after meniscectomy has yet to be elucidated. Identifying threshold values of functional outcome scores that are predictive of RTS can assist with patient education to promote realistic expectations.
Outcome reporting is highly variable because it is dependent on subjective PROMs, such as the Knee injury and Osteoarthritis Outcome Score (KOOS) and International Knee Documentation Committee (IKDC) questionnaire.19,35 Statistically significant differences in PROMs are commonly reported; however, this may not equate to clinically meaningful improvements. Additionally, PROMs may exhibit a ceiling effect in which they may be unable to detect further functional improvements.12,30 Therefore, an emphasis should be placed on clinically significant improvements.27,35 The minimal clinically important difference (MCID), substantial clinical benefit (SCB), and patient acceptable symptom state (PASS) have been developed as measurement tools to determine clinically meaningful differences in PROMs.23–26 Additionally, the 12-Item Short Form Health Survey, a general health–related questionnaire, has been used to assess patients’ mental and physical quality of life.26 When implemented together, both disease-specific and general health surveys provide a holistic assessment of a patient’s well-being in response to an intervention.24 PROMs are used to track the clinical progress of patients after meniscectomy; however, no study has established whether these outcome measures have any relation to RTS.
The purpose of this investigation was to identify a timeline of RTS after isolated meniscectomy with respect to various levels of activity intensity and to determine if outcome measures were predictive of RTS. We hypothesized that knee-specific PROMs have threshold values that are predictive of RTS after meniscectomy.
Methods
Demographics
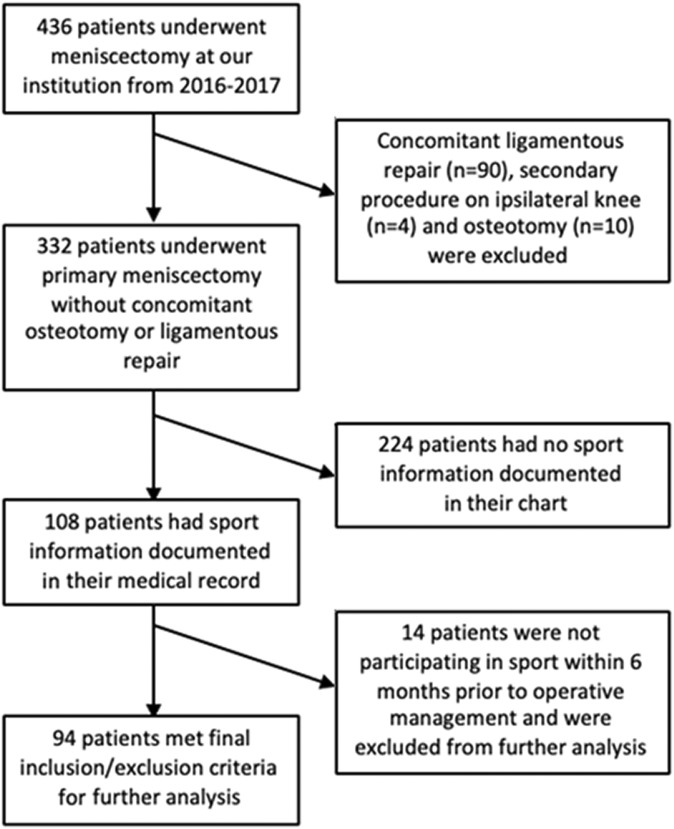
From 2016 to 2017, a total of 436 patients aged ≥18 years at the time of surgery underwent meniscectomy by 1 of 3 fellowship-trained sports physicians (B.J.C., B.F., and N.N.V.) at our institution. Patients undergoing a secondary procedure on the ipsilateral knee (n = 4), concomitant ligamentous repair (n = 90), or concomitant osteotomy (n = 10) were excluded from this investigation. Thus, there were 332 patients who underwent meniscectomy with or without concomitant chondroplasty or plica excision over the course of the study period. Patients who underwent concomitant chondroplasty were included in this investigation.4 Of this patient cohort, a total of 108 patients had documented preoperative sport information in their medical record. In comparison with patients who did not have RTS information available (n = 224), there was a statistical difference with regard to age and workers’ compensation status (P < .001 and P = .02, respectively) (Table 1). Baseline KOOS–Physical Function short form (KOOS-PS) scores were significantly different between both groups (P = .03); however, baseline IKDC, KOOS-Symptoms, KOOS–Joint Replacement, KOOS-Pain, KOOS–Activities of Daily Living, KOOS-Sports, and KOOS–Quality of Life scores were not significantly different (P > .05). The mean age of patients with sport data within their record was 51.0 ± 11.1 years (range, 18-68 years), with 80.6% of patients being older than 40 years at the time of surgery.
TABLE 1.
Baseline Characteristics of Patients With Return-to-Sport Informationa
| Sport Data Provided (n = 108) | Sport Data Not Provided (n = 224) | P Value | |
|---|---|---|---|
| Age, y | 51.0 ± 11.1 | 43.2 ± 14.6 | <.001 |
| Sex, male:female, n (% male) | 65:43 (60.2) | 123:101 (54.9) | .4 |
| Body mass index, kg/m2 | 30.3 ± 6.6 | 29.0 ± 6.3 | .1 |
| Smoker, n (%) | 15 (13.9) | 30 (13.4) | .9 |
| History of diabetes, n (%) | 2 (1.9) | 3 (1.3) | .1 |
| History of thyroid problems, n (%) | 7 (6.5) | 13 (5.8) | .06 |
| Symptom duration, mo | 9.4 ± 10.7 | 12.2 ± 25.0 | .3 |
| Workers’ compensation, n (%) | 9 (8.3) | 40 (17.9) | .02 |
| Outcome scores | |||
| IKDC | 43.0 ± 15.5 | 45.6 ± 19.7 | .2 |
| KOOS–Joint Replacement | 55.9 ± 12.4 | 59.0 ± 14.1 | .1 |
| KOOS–Physical Function short form | 43.0 ± 12.7 | 38.4 ± 9.9 | .03 |
| KOOS-Symptoms | 55.2 ± 17.0 | 59.1 ± 19.4 | .1 |
| KOOS-Pain | 55.0 ± 15.1 | 56.0 ± 18.7 | .6 |
| KOOS–Activities of Daily Living | 63.0 ± 17.9 | 65.2 ± 22.0 | .4 |
| KOOS-Sports | 33.8 ± 21.5 | 32.2 ± 24.8 | .6 |
| KOOS–Quality of Life | 28.8 ± 19.1 | 25.6 ± 18.4 | .1 |
aData are reported as mean ± SD unless otherwise indicated. Bolded P values indicate a statistically significant difference between groups. IKDC, International Knee Documentation Committee; KOOS, Knee injury and Osteoarthritis Outcome Score.
To assess RTS after meniscectomy, the patient group with documented preoperative sport information was further filtered. Patients were included if they were aged ≥18 years at the time of surgery, were participating in a sport within 6 months before operative management, and had completed PROMs at the time of surgery as well as at 6 months postoperatively. Patients were excluded if they were younger than 18 years at the time of surgery, were not participating in a sport within 6 months before surgery, and did not complete PROMs at the time of surgery or at 6 months postoperatively. Patients were also excluded if RTS information was not obtainable, they underwent a secondary procedure on the ipsilateral knee, or they underwent concomitant ligamentous repair or osteotomy. After inclusion and exclusion criteria, 94 patients were included for a further analysis (Figure 1).
Figure 1.
Flow chart of final cohort for analysis of predictive factors and rate of return to sport.
Data Collection
Preoperative PROMs were completed on the day of surgery. Questionnaires were completed in a time-sensitive manner at the 6-month postoperative time point to prevent the heterogeneity of patient outcomes being recorded before or after this time point. All PROM scores were collected and retrieved electronically using a data collection service (Outcomes Based Electronic Research Database; Universal Research Solutions). Patients were contacted via email every 5 days for 1 month, and the survey expired after this interval.
Medical records were then reviewed for duration of symptoms, surgical history, and complications or imposed restrictions in the postoperative period. Preoperative and postoperative sports as well as the duration to RTS were recorded. Patient-reported activities were stratified into low-, medium-, and high-intensity lower extremity demands (Table 2).8,9 If patients participated in multiple sports, they were categorized based on the highest demand activity. The duration of symptoms and time to return to previous activity were measured in weeks. Baseline characteristics, such as PROM scores, age, sex, body mass index (BMI), comorbidities, smoking status, workers’ compensation status, and tear patterns, were also collected for a regression analysis.
TABLE 2.
Categorization of Sports by Activity Intensity
| Intensity | Sports |
|---|---|
| Low | Golf, swimming, bowling, nature sports, fitness sports, yoga |
| Medium | Rowing, cycling, cross-country skiing, downhill skiing, softball, baseball |
| High | Running, basketball, football, tennis, volleyball, soccer |
Patient-Reported Outcome Measures
Patients completed knee-specific PROMs, including the IKDC questionnaire and KOOS. Patients also completed general health questionnaires, including the mental and physical components of the Veterans RAND 12-Item Health Survey (VR-12), as well as the Veterans RAND 6-Dimension. Clinical improvement was assessed through patients’ ability to achieve the MCID, SCB, or PASS on PROMs. These were calculated using distribution-based and anchor-based methods.25,37 The MCID, SCB, and PASS were calculated with the entire cohort of patients who underwent meniscectomy with or without concomitant chondral debridement, chondroplasty, or plica excision (n = 332). An area under the receiver operating characteristic (ROC) curve (AUC) analysis was performed to determine the threshold values to achieve the MCID, SCB, and PASS for each PROM. AUC values >70% were considered acceptable, and AUC values >80% were considered excellent.24 Threshold values for the MCID, SCB, and PASS were determined using the Youden index, which maximizes the sensitivity and specificity in a given relationship (Table 3). Calculated MCID, SCB, and PASS values were then correlated with the ability to RTS.
TABLE 3.
Calculated MCID, SCB, and PASS Thresholds After Meniscectomya
| MCID | SCB | PASS | |
|---|---|---|---|
| IKDC | 10.4 | 25.3 | 57.9 |
| KOOS-Symptoms | 10.4 | 7.1 | 71.4 |
| KOOS-Pain | 9.7 | 22.2 | 76.4 |
| KOOS–Activities of Daily Living | 10.5 | 16.9 | 89.0 |
| KOOS-Sport | 14.7 | 27.5 | 55.6 |
| KOOS–Quality of Life | 13.2 | 34.4 | 46.9 |
| KOOS–Joint Replacement | 10.9 | 13.2 | 68.3 |
| KOOS–Physical Function short form | –8.5 | –11.3 | 26.2 |
aIKDC, International Knee Documentation Committee; KOOS, Knee injury and Osteoarthritis Outcome Score; MCID, minimal clinically important difference; PASS, patient acceptable symptom state; SCB, substantial clinical benefit.
Statistical Analysis
Statistical analyses were performed using RStudio software version 1.0.143. The rate of RTS was analyzed for the overall population and then for each level of activity intensity. A Pearson chi-square analysis was performed to assess the differences in the rate of RTS based on the level of activity intensity. All demographic and intraoperative variables were included in a multivariate logistical regression model. From the regression analysis, an odds ratio (OR) was calculated for each variable. A nonparametric ROC curve was created for each preoperative PROM score to determine the future ability of a patient to RTS. An AUC analysis was subsequently performed to determine if this association was predictive of RTS. The chi-square test was used to determine if there was a correlation between returning to sport at full capacity and achieving the MCID, SCB, and PASS. A final analysis of each statistical test was considered significant at P < .05.
Results
Operative Data
Operative data were collected and assessed for their ability to affect RTS at full capacity. Chondroplasty was performed in 12 of 94 patients (12.8%). Medial meniscal tears were present in 65 patients (69.1%), lateral tears were present in 16 patients (17.0%), and 13 patients (13.8%) had medial and lateral tears. Sixty-one patients (64.9%) suffered a traumatic meniscal tear, while 33 (35.1%) suffered degenerative tears. There were 88 patients with documented tear patterns, as presented in Table 4. No patient returned to the operating room after the index procedure at the time of final follow-up. However, 19 patients (20.2%) received an intra-articular steroid injection after operative management by the time of final follow-up.
TABLE 4.
Tear Patterns
| Pattern | n (%) |
|---|---|
| Complex | 27 (28.7) |
| Flap | 12 (12.8) |
| Oblique | 12 (12.8) |
| Transverse | 12 (12.8) |
| Degenerative | 8 (8.5) |
| Horizontal | 6 (6.4) |
| Vertical | 4 (4.3) |
| Root | 3 (3.2) |
| Bucket handle | 2 (2.1) |
| Discoid | 2 (2.1) |
RTS Outcomes
After meniscectomy, 72 patients (76.6%) returned to their previous level of sport at a mean time of 8.6 ± 6.9 weeks (Table 5). However, only 57 of those who returned to sport (79.2%) reported that they were at the same or better level of performance upon returning. There was also no statistical difference between the rate of RTS and the level of activity intensity (P = .5). Patients who participated in low-intensity activities returned to sport sooner than patients who participated in high-intensity activities; however, this was not statistically significant (P = .2).
TABLE 5.
RTS Rate and Time After Meniscectomya
| Participation in Sports, n | Rate of RTS, % | Weeks to RTS, Mean ± SD | ||
|---|---|---|---|---|
| Before Meniscectomy | After Meniscectomy | |||
| Low | 20 | 15 | 75.0 | 6.1 ± 4.3 |
| Medium | 20 | 14 | 70.0 | 8.2 ± 4.9 |
| High | 40 | 33 | 82.5 | 10.1 ± 8.2 |
| Totalb | 94 | 72 | 76.6 | 8.6 ± 6.9 |
aRTS, return to sport.
bTotal patients is greater than the sum of patients with activity intensity status, as there were several patients in whom activity intensity status was not provided.
Furthermore, IKDC, KOOS, VR-6D, and VR-12 physical component scores significantly increased by 6 months postoperatively (P < .001). However, the VR-12 mental component score did not improve significantly by final follow-up (P = .1).
Achieving the PASS for the KOOS-PS, KOOS-Pain, and KOOS-Sports was correlated with RTS (P = .004, P = .007, and P = .006, respectively). However, achieving the PASS for the IKDC questionnaire was not associated with the ability to RTS (P = .3). Last, achieving the MCID for the KOOS-Sports, KOOS-Pain, and IKDC questionnaire was predictive of RTS (P < .001, P = .03, and P = .001, respectively). The relationship of achieving the MCID, SCB, and PASS to RTS stratified by level of activity intensity is provided in Table 6.
TABLE 6.
Relationship Between Achieving the MCID, SCB, and PASS for Outcome Measures and Return to Sport by Activity Intensitya
| P Value | ||||
|---|---|---|---|---|
| Low Intensity | Medium Intensity | High Intensity | Overall | |
| IKDC | ||||
| Achieving MCID | .6 | .4 | <.001 | .001 |
| Achieving SCB | .4 | .6 | .3 | .2 |
| Achieving PASS | .04 | .3 | .3 | .3 |
| KOOS–Physical Function short form | ||||
| Achieving MCID | .2 | .4 | .02 | .1 |
| Achieving SCB | .4 | .4 | .1 | .2 |
| Achieving PASS | .1 | .02 | .1 | .004 |
| KOOS-Pain | ||||
| Achieving MCID | .1 | .6 | .1 | .03 |
| Achieving SCB | .1 | .9 | .1 | .03 |
| Achieving PASS | .04 | .4 | .1 | .007 |
| KOOS-Sports | ||||
| Achieving MCID | .01 | .05 | .03 | <.001 |
| Achieving SCB | .3 | .5 | .6 | .2 |
| Achieving PASS | .1 | .1 | .1 | .006 |
aBolded P values indicate a statistical significance. IKDC, International Knee Documentation Committee; KOOS, Knee injury and Osteoarthritis Outcome Score; MCID, minimal clinically important difference; PASS, patient acceptable symptom state; SCB, substantial clinical benefit.
A multivariate analysis of patient demographics and operative findings revealed that increased BMI was associated with a decreased rate of RTS (OR, 0.8; P = .001) and that lateral meniscal tears were associated with a decreased rate of return to previous sport activity (OR, 0.1; P = .02). Workers’ compensation status, concomitant chondroplasty, and oblique, discoid, or flap tear patterns were not predictive of RTS (P > .05).
Predictive Metrics of RTS
A score of ≥37.8 on the KOOS-PS had a specificity of 94.4% and a sensitivity of 47.3% in predicting RTS (AUC = 76.3%). Within the low-intensity and medium-intensity subgroups, scores of ≥39.5 and ≥52.8 on the KOOS-PS were predictive of RTS (AUC = 86.5% and 88.2%, respectively). There was no threshold value that was predictive of RTS in the high-intensity subgroup. Additional threshold preoperative values on PROMs and their predictive value toward RTS are provided in Table 7.
TABLE 7.
Predictive Values of Preoperative Outcome Scores Toward Return to Sporta
| Threshold | Specificity, % | Sensitivity, % | AUC, % | |
|---|---|---|---|---|
| Low intensity | ||||
| IKDC | 32.4 | 57.1 | 95.7 | 72.0 |
| KOOS-PS | 39.5 | 100.0 | 58.8 | 86.5 |
| KOOS-Pain | 48.6 | 71.4 | 82.6 | 74.5 |
| KOOS-Sports | 15.0 | 57.1 | 100.0 | 66.8 |
| VR-12 MC | 59.5 | 71.4 | 73.9 | 65.2 |
| VR-12 PC | 43.6 | 42.9 | 78.3 | 47.8 |
| Medium intensity | ||||
| IKDC | 29.3 | 66.7 | 95.0 | 83.3 |
| KOOS-PS | 52.8 | 83.3 | 91.7 | 88.2 |
| KOOS-Pain | 44.4 | 100.0 | 85.0 | 94.2 |
| KOOS-Sports | 39.9 | 83.3 | 75.0 | 83.8 |
| VR-12 MC | 55.7 | 66.7 | 61.1 | 53.7 |
| VR-12 PC | 36.8 | 83.3 | 77.8 | 82.4 |
| High intensity | ||||
| IKDC | 38.3 | 50.0 | 82.5 | 59.8 |
| KOOS-PS | 41.1 | 71.4 | 59.3 | 63.2 |
| KOOS-Pain | 51.4 | 62.5 | 70.0 | 57.7 |
| KOOS-Sports | 32.5 | 75.0 | 55.0 | 59.2 |
| VR-12 MC | 66.1 | 100.0 | 20.0 | 53.9 |
| VR-12 PC | 38.9 | 50.0 | 71.4 | 57.5 |
| Overall | ||||
| IKDC | 31.4 | 52.4 | 92.6 | 69.8 |
| KOOS-PS | 37.8 | 94.4 | 47.3 | 76.3 |
| KOOS-Pain | 51.4 | 81.0 | 66.7 | 72.5 |
| KOOS-Sports | 12.5 | 42.9 | 87.5 | 64.9 |
| VR-12 MC | 60.2 | 66.7 | 53.9 | 56.6 |
| VR-12 PC | 38.9 | 57.1 | 72.4 | 54.3 |
aBolded rows indicate values that meet the minimum AUC that is considered acceptable (70%). AUC, area under the curve; IKDC, International Knee Documentation Committee; KOOS, Knee injury and Osteoarthritis Outcome Score; MC, mental component; PC, physical component; PS, Physical Function short form; VR-12, Veterans RAND 12-Item Health Survey.
Discussion
In this investigation, we found that 76.6% of patients returned to their previous sport at a mean of 8.6 ± 6.9 weeks after isolated meniscectomy. As the level of activity intensity increased, the proportion of patients who returned to sport increased and the duration to RTS increased; however, these findings were not statistically significant. RTS was correlated with a patient’s ability to achieve the PASS and MCID on several knee-specific outcome measures. With regard to achieving the SCB, the only outcome measure that correlated with RTS was KOOS-Pain.
RTS is a commonly reported outcome metric after orthopaedic procedures, as it serves as an identifiable milestone for patients. Currently, there is a dearth of evidence to suggest that collected outcome scores are predictive of RTS. In this investigation, achieving the MCID on the IKDC questionnaire as well as the KOOS-Sports and KOOS-Pain was correlated with RTS. This finding is in contrast to that of Nwachukwu et al,24 who found that achieving the MCID on the IKDC questionnaire was not correlated with RTS after ACL reconstruction. In ACL reconstruction, minimal improvements may result in reduced pain or improved ability to perform activities of daily living; however, these improvements may be insufficient to allow for RTS. For isolated meniscal injuries, pain and discomfort may be the primary deterrents for patients to participate in sport. By removing the pain generator, patients are able to demonstrate sufficient improvement, as reflected by achieving the MCID, to RTS. Furthermore, achieving the SCB on the IKDC questionnaire, KOOS-Sports, and KOOS-PS was not correlated with a patient’s ability to RTS. Patients who are higher functioning at the time of surgery may be unable to achieve an improvement in PROM scores that exceeds the SCB, but achieving the MCID is more attainable. However, patients with worse symptoms have a lower baseline level of function, which may be preventative of RTS. Therefore, the amount of improvement that is necessary to achieve the SCB may be unattainable. Regardless of the level of preoperative function, pain reduction may be the most important factor that dictates RTS, as minimal to significant improvements in pain were found to be correlated with RTS.
Although the MCID and SCB establish clinically relevant changes in PROMs, these changes may not reflect a patient’s overall state of health or satisfaction.39 The PASS is a robust measure of a patient’s overall satisfaction and adaptation to his or her current symptom state.39 Patient outcomes after meniscectomy are variable13,15,20,32; however, in this investigation, we demonstrated that RTS is correlated with achieving a satisfactory state. This finding suggests that RTS plays an important factor in achieving an acceptable symptom state after isolated meniscectomy. By identifying a timeline as well as predictors of RTS, physicians can manage patient expectations.
Patients with meniscal injuries often present with varying degrees of pain and symptoms. Thus, the degree of preoperative pain and functional impairment may be predictive of RTS. This finding demonstrates that patients with higher levels of impairment or painful symptoms are less likely to RTS. Psychosocial and sociodemographic factors have previously been shown to be determinants of pain levels in patients with knee osteoarthritis undergoing meniscectomy.6 Additionally, patients with more severe osteoarthritis undergoing meniscectomy are at an increased risk of interventional failure and need to undergo subsequent total knee arthroplasty.38 Patients who have significant baseline functional impairment or pain levels, as defined by their preoperative PROM scores, can be counseled that meniscectomy may only be a temporary solution that may optimize their daily function and quality of life; however, it may not allow them to RTS.
More than 50% of patients included in this investigation were older than 50 years at the time of surgery. Previous investigations have demonstrated that there is no difference in PROM scores in middle-aged patients undergoing arthroscopic partial meniscectomy versus sham surgery or physical therapy.10,11,13,16,33 Although there is no difference in functional outcomes between patients in this age group, it is possible that PROMs impose a ceiling effect in which additional improvement may not be detected. Therefore, arthroscopic partial meniscectomy may provide sufficient pain relief to allow patients to return to work or sport earlier than conservative management. The results of this investigation demonstrate that RTS is an important component in patient satisfaction. Because satisfaction influences clinical outcomes,36 it may be more efficacious to perform meniscectomy in active patients regardless of age instead of conservative management to improve function, activity levels, and quality of life.
Previous investigations have identified complex tears,28 concomitant cartilaginous lesions,28 age >30 years,14 level of competition,14 and lateral meniscectomy21 as negative predictors of RTS after isolated meniscectomy. In this investigation, we identified that elevated BMI as well as lateral meniscal tears decreased the likelihood of RTS. Lateral meniscectomy has been shown to have worse clinical and radiological outcomes than medial meniscectomy.31 Because of the convexity of the femoral condyle and tibial plateau as well as the majority of rotational movement occurring in the lateral aspect of the tibiofemoral joint, the lateral meniscus is more susceptible to injuries.18,22 The lateral meniscus supports approximately 70% of load transmission at the tibiofemoral joint2; patients undergoing lateral meniscectomy have shown lower rates of RTS and a higher rate of complications in comparison with patients who undergo medial meniscectomy.14,21 As a result, Aune et al2 demonstrated that speed-position players in the National Football League were less likely to RTS after lateral meniscectomy than non–speed-position players. This may be because of the differences in athletic requirements by these positions to perform frequent directional changes and tackling, which place significant stress on the lateral meniscus.2 Identifying surgical and demographic variables that are predictive of decreased rates of RTS is important for appropriate patient consultation and education regarding postoperative expectations.
While the data for this investigation were collected prospectively, this study was conducted in a retrospective manner, which has intrinsic limitations such as an inability to control baseline characteristics or variations in patient management across different physicians. It should be noted that the mean age of patients included in this investigation was 51.0 years; thus, the results of this investigation may lack external validity and may only be applicable to middle-aged patients. It is possible that the rate of RTS would be higher in a younger patient population that is more motivated to return to their previous activity. Younger patients could also demonstrate a lower rate and longer duration to RTS, as this population may participate in higher intensity activity. There was no information available regarding the degree of osteoarthritis, which may contribute to a patient’s ability to RTS. Furthermore, there were statistical differences in the age, proportion with workers’ compensation status, and several baseline PROM scores of patients with sport data recorded in their chart and those without that information, which may limit the external validity of this investigation.
This study would benefit from a longer duration of follow-up to capture patients’ ability to maintain their level of function, as their ability to perform sport-related activities may be influenced by additional factors such as lifestyle changes, personal matters, or other socioeconomic considerations. These variables may directly affect a patient’s capacity to participate in sport activities or may prevent a patient’s capability to participate in rehabilitation after meniscectomy. A longer follow-up would also be beneficial, as meniscectomy has been shown to provide no improvement in outcomes in patients older than 50 years by 2-year follow-up.16
Patients were categorized based on the level of lower extremity activity intensity.8,9 Pivoting sports, such as golf, are classified as low-intensity sports; however, these sports may place additional force on the meniscus, which may affect the ability of a patient to RTS. Patients with isolated medial or lateral defects as well as those with defects in both compartments were included in a single analysis. It is possible that the rate and duration to RTS may vary based on the location of the abnormality. Additionally, a larger patient population and longer follow-up would be beneficial to evaluate clinical symptoms after RTS, as pain and effusion have been reported in patients who RTS after meniscectomy. The results of this investigation are subject to nonresponse bias, as approximately two-thirds of patients did not have documented information pertaining to RTS. Because physicians at our institution typically evaluate this population of patients up to 3 months postoperatively, RTS may not have been documented by the time of final follow-up.
Conclusion
Approximately 77% of patients returned to sport after meniscectomy at a mean of 2 months postoperatively. The level of activity intensity did not significantly alter the rate of RTS. Higher preoperative scores on the KOOS-PS and KOOS-Pain were predictive of RTS. Identifying these factors allows physicians to counsel patients on expected outcomes after meniscectomy.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: B.J.C. has received research support from Aesculap/B. Braun, Arthrex, Geistlich, National Institutes of Health, Sanofi-Aventis, and Zimmer Biomet; has received educational support from Arthrex; has received consulting fees from Anika Therapeutics, Arthrex, Bioventus, Flexion, Geistlich, Genzyme, Pacira Pharmaceuticals, Smith & Nephew, Vericel, and Zimmer Biomet; has received speaking fees from Arthrex, Carticept Medical, and LifeNet Health; has received hospitality payments from DePuy and GE Healthcare; receives royalties from Arthrex, DJ Orthopedics, Elsevier, Encore Medical, and Operative Techniques in Sports Medicine; and has stock/stock options in Aqua Boom, Biometrix, GiteliScope, Ossio, and Regentis. B.F. has received research support from Arthrex and Stryker; has received educational/fellowship support from Medwest, Smith & Nephew, and Ossur; has received consulting fees from Sonoma Orthopedics and Stryker; has received honoraria from Arthrosurface; receives royalties from Elsevier; and has stock/stock options in Jace Medical. N.N.V. has received research support from Arthrex, Arthrosurface, DJ Orthopedics, Ossur, Athletico, ConMed Linvatec, Miomed, and Mitek; has received educational support from Medwest; has received consulting fees from Arthrex, Medacta, Minivasive, Orthospace, and Smith & Nephew; has received speaking fees from Pacira Pharmaceuticals; receives royalties from Arthroscopy, Smith & Nephew, and Vindico Medical Education–Orthopedics Hyperguide; and has stock/stock options in CyMedica, Minivasive, and Omeros. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the Rush University Medical Center Institutional Review Board.
References
- 1. Andrews S, Shrive N, Ronsky J. The shocking truth about meniscus. J Biomech. 2011;44(16):2737–2740. [DOI] [PubMed] [Google Scholar]
- 2. Aune KT, Andrews JR, Dugas JR, Cain EL., Jr Return to play after partial lateral meniscectomy in National Football League athletes. Am J Sports Med. 2014;42(8):1865–1872. [DOI] [PubMed] [Google Scholar]
- 3. Berliner JL, Brodke DJ, Chan V, SooHoo NF, Bozic KJ. John Charnley Award: preoperative patient-reported outcome measures predict clinically meaningful improvement in function after THA. Clin Orthop Relat Res. 2016;474(2):321–329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bisson LJ, Kluczynski MA, Wind WM, et al. Patient outcomes after observation versus debridement of unstable chondral lesions during partial meniscectomy: the Chondral Lesions And Meniscus Procedures (ChAMP) randomized controlled trial. J Bone Joint Surg Am. 2017;99(13):1078–1085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Brelin AM, Rue JP. Return to play following meniscus surgery. Clin Sports Med. 2016;35(4):669–678. [DOI] [PubMed] [Google Scholar]
- 6. Eberly L, Richter D, Comerci G, et al. Psychosocial and demographic factors influencing pain scores of patients with knee osteoarthritis. PLoS One. 2018;13(4):e0195075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Filbay SR, Ackerman IN, Russell TG, Crossley KM. Return to sport matters: longer-term quality of life after ACL reconstruction in people with knee difficulties. Scand J Med Sci Sports. 2017;27(5):514–524. [DOI] [PubMed] [Google Scholar]
- 8. Garcia GH, Mahony GT, Fabricant PD, et al. Sports- and work-related outcomes after shoulder hemiarthroplasty. Am J Sports Med. 2016;44(2):490–496. [DOI] [PubMed] [Google Scholar]
- 9. Garcia GH, Taylor SA, DePalma BJ, et al. Patient activity levels after reverse total shoulder arthroplasty: what are patients doing? Am J Sports Med. 2015;43(11):2816–2821. [DOI] [PubMed] [Google Scholar]
- 10. Hare KB, Lohmander LS, Christensen R, Roos EM. Arthroscopic partial meniscectomy in middle-aged patients with mild or no knee osteoarthritis: a protocol for a double-blind, randomized sham-controlled multi-centre trial. BMC Musculoskelet Disord. 2013;14:71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Herrlin SV, Wange PO, Lapidus G, Hallander M, Werner S, Weidenhielm L. Is arthroscopic surgery beneficial in treating non-traumatic, degenerative medial meniscal tears? A five year follow-up. Knee Surg Sports Traumatol Arthrosc. 2013;21(2):358–364. [DOI] [PubMed] [Google Scholar]
- 12. Hsu JE, Nacke E, Park MJ, Sennett BJ, Huffman GR. The Disabilities of the Arm, Shoulder, and Hand questionnaire in intercollegiate athletes: validity limited by ceiling effect. J Shoulder Elbow Surg. 2010;19(3):349–354. [DOI] [PubMed] [Google Scholar]
- 13. Katz JN, Brophy RH, Chaisson CE, et al. Surgery versus physical therapy for a meniscal tear and osteoarthritis. N Engl J Med. 2013;368(18):1675–1684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kim SG, Nagao M, Kamata K, Maeda K, Nozawa M. Return to sport after arthroscopic meniscectomy on stable knees. BMC Sports Sci Med Rehabil. 2013;5(1):23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kirkley A, Birmingham TB, Litchfield RB, et al. A randomized trial of arthroscopic surgery for osteoarthritis of the knee. N Engl J Med. 2008;359(11):1097–1107. [DOI] [PubMed] [Google Scholar]
- 16. Kise NJ, Risberg MA, Stensrud S, Ranstam J, Engebretsen L, Roos EM. Exercise therapy versus arthroscopic partial meniscectomy for degenerative meniscal tear in middle aged patients: randomised controlled trial with two year follow-up. Br J Sports Med. 2016;50(23):1473–1480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Longo UG, Ciuffreda M, Candela V, et al. Knee osteoarthritis after arthroscopic partial meniscectomy: prevalence and progression of radiographic changes after 5 to 12 years compared with contralateral knee [published online May 3, 2018]. J Knee Surg. doi:10.1055/s-0038-1646926 [DOI] [PubMed] [Google Scholar]
- 18. McDermott I. Meniscal tears, repairs and replacement: their relevance to osteoarthritis of the knee. Br J Sports Med. 2011;45(4):292–297. [DOI] [PubMed] [Google Scholar]
- 19. Monk P, Garfjeld Roberts P, Palmer AJ, et al. The urgent need for evidence in arthroscopic meniscal surgery. Am J Sports Med. 2017;45(4):965–973. [DOI] [PubMed] [Google Scholar]
- 20. Moseley JB, O’Malley K, Petersen NJ, et al. A controlled trial of arthroscopic surgery for osteoarthritis of the knee. N Engl J Med. 2002;347(2):81–88. [DOI] [PubMed] [Google Scholar]
- 21. Nawabi DH, Cro S, Hamid IP, Williams A. Return to play after lateral meniscectomy compared with medial meniscectomy in elite professional soccer players. Am J Sports Med. 2014;42(9):2193–2198. [DOI] [PubMed] [Google Scholar]
- 22. Nepple JJ, Dunn WR, Wright RW. Meniscal repair outcomes at greater than five years: a systematic literature review and meta-analysis. J Bone Joint Surg Am. 2012;94(24):2222–2227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Nwachukwu BU, Chang B, Fields K, et al. Defining the “substantial clinical benefit” after arthroscopic treatment of femoroacetabular impingement. Am J Sports Med. 2017;45(6):1297–1303. [DOI] [PubMed] [Google Scholar]
- 24. Nwachukwu BU, Chang B, Voleti PB, et al. Preoperative Short Form Health Survey score is predictive of return to play and minimal clinically important difference at a minimum 2-year follow-up after anterior cruciate ligament reconstruction. Am J Sports Med. 2017;45(12):2784–2790. [DOI] [PubMed] [Google Scholar]
- 25. Nwachukwu BU, Fields K, Chang B, Nawabi DH, Kelly BT, Ranawat AS. Preoperative outcome scores are predictive of achieving the minimal clinically important difference after arthroscopic treatment of femoroacetabular impingement. Am J Sports Med. 2017;45(3):612–619. [DOI] [PubMed] [Google Scholar]
- 26. Nwachukwu BU, Hamid KS, Bozic KJ. Measuring value in orthopaedic surgery. JBJS Rev. 2013;1(1):01874474–201311000-00003. [DOI] [PubMed] [Google Scholar]
- 27. Nwachukwu BU, Runyon RS, Kahlenberg CA, Gausden EB, Schairer WW, Allen AA. How are we measuring clinically important outcome for operative treatments in sports medicine? Phys Sportsmed. 2017;45(2):159–164. [DOI] [PubMed] [Google Scholar]
- 28. Osti L, Liu SH, Raskin A, Merlo F, Bocchi L. Partial lateral meniscectomy in athletes. Arthroscopy. 1994;10(4):424–430. [DOI] [PubMed] [Google Scholar]
- 29. Petrigliano FA, Musahl V, Suero EM, Citak M, Pearle AD. Effect of meniscal loss on knee stability after single-bundle anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2011;19 (suppl 1):S86–S93. [DOI] [PubMed] [Google Scholar]
- 30. Ra HJ, Kim HS, Choi JY, Ha JK, Kim JY, Kim JG. Comparison of the ceiling effect in the Lysholm score and the IKDC subjective score for assessing functional outcome after ACL reconstruction. Knee. 2014;21(5):906–910. [DOI] [PubMed] [Google Scholar]
- 31. Salata MJ, Gibbs AE, Sekiya JK. A systematic review of clinical outcomes in patients undergoing meniscectomy. Am J Sports Med. 2010;38(9):1907–1916. [DOI] [PubMed] [Google Scholar]
- 32. Sihvonen R, Paavola M, Malmivaara A, et al. Arthroscopic partial meniscectomy versus placebo surgery for a degenerative meniscus tear: a 2-year follow-up of the randomised controlled trial. Ann Rheum Dis. 2018;77(2):188–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Sihvonen R, Paavola M, Malmivaara A, et al. Arthroscopic partial meniscectomy versus sham surgery for a degenerative meniscal tear. N Engl J Med. 2013;369(26):2515–2524. [DOI] [PubMed] [Google Scholar]
- 34. Stein T, Mehling AP, Welsch F, von Eisenhart-Rothe R, Jager A. Long-term outcome after arthroscopic meniscal repair versus arthroscopic partial meniscectomy for traumatic meniscal tears. Am J Sports Med. 2010;38(8):1542–1548. [DOI] [PubMed] [Google Scholar]
- 35. Thorlund JB, Englund M, Christensen R, et al. Patient reported outcomes in patients undergoing arthroscopic partial meniscectomy for traumatic or degenerative meniscal tears: comparative prospective cohort study. BMJ. 2017;356:J356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Tirico LEP, McCauley JC, Pulido PA, Demange MK, Bugbee WD. Is patient satisfaction associated with clinical outcomes after osteochondral allograft transplantation in the knee? Am J Sports Med. 2019;47(1):82–87. [DOI] [PubMed] [Google Scholar]
- 37. Werner BC, Chang B, Nguyen JT, Dines DM, Gulotta LV. What change in American Shoulder and Elbow Surgeons score represents a clinically important change after shoulder arthroplasty? Clin Orthop Relat Res. 2016;474(12):2672–2681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Winter AR, Collins JE, Katz JN. The likelihood of total knee arthroplasty following arthroscopic surgery for osteoarthritis: a systematic review. BMC Musculoskelet Disord. 2017;18(1):408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Wright AA, Hensley CP, Gilbertson J, Leland JM, 3rd, Jackson S. Defining patient acceptable symptom state thresholds for commonly used patient reported outcomes measures in general orthopedic practice. Man Ther. 2015;20(6):814–819. [DOI] [PubMed] [Google Scholar]