Abstract
Genitourinary schistosomiasis is an acquired cause of urinary tract diseases, especially hematuria. Schistosoma haematobium can infect travelers after a single exposure. Bladder is the most frequent organ involved within the urinary tract, although upper tract can also be affected. Case report of 34-year-old woman with left upper urinary tract obstruction due to schistosomiasis is presented, as well as its diagnosis and minimally invasive surgical management through a laparoscopic ureteral reimplantation. After 1-year follow-up, she remains asymptomatic and without upper tract obstruction demonstrated by CT.
Introduction
Urinary tract obstruction remains a major clinical problem that can finally result in permanent renal damage or even end-stage renal disease (ESRD). Obstructive uropathy accounts for around 10% of all cases of renal failure. Schistosoma haematobium is an endemic parasite in Africa and Middle East that can affect travelers after a single exposure. It usually affects urinary system, especially the bladder, with hematuria as its main symptom and bladder squamous cell carcinoma as a severe complication.1 However, although less frequent, it can also result in upper tract involvement causing ureteral dilation, calcifications, strictures, squamous metaplasia and squamous cell carcinoma.2
Case report
A 34-year-old healthy Spanish female complained about hematuria after a work trip to Myanmar in 2014, where was diagnosed of bladder schistosomiasis caused by Schistosoma haematobium and received successful treatment with praziquantel 1200 mg/8 h. During first year follow-up she remained asymptomatic and with microbiological resolution of schistosomiasis. However, 2 years later a routine abdominal ultrasound revealed an unknown grade 3 left hydronephrosis with normal renal function (Cr 0.7 mg/dl), so was referred to our Department. Uro-CT confirmed left hydronephrosis due to a left distal ureteral stricture (Fig. 1), and isotope renogram (Tc-99 m) confirmed left obstructive uropathy without spontaneous urine elimination. Cystoscopy was normal and ureteroscopy showed an impassable distal ureteral stricture. Biopsy of distal ureter was performed and demonstrated fibrosis without parasite eggs in the bladder wall. Urine and blood serology were negative.
Fig. 1.
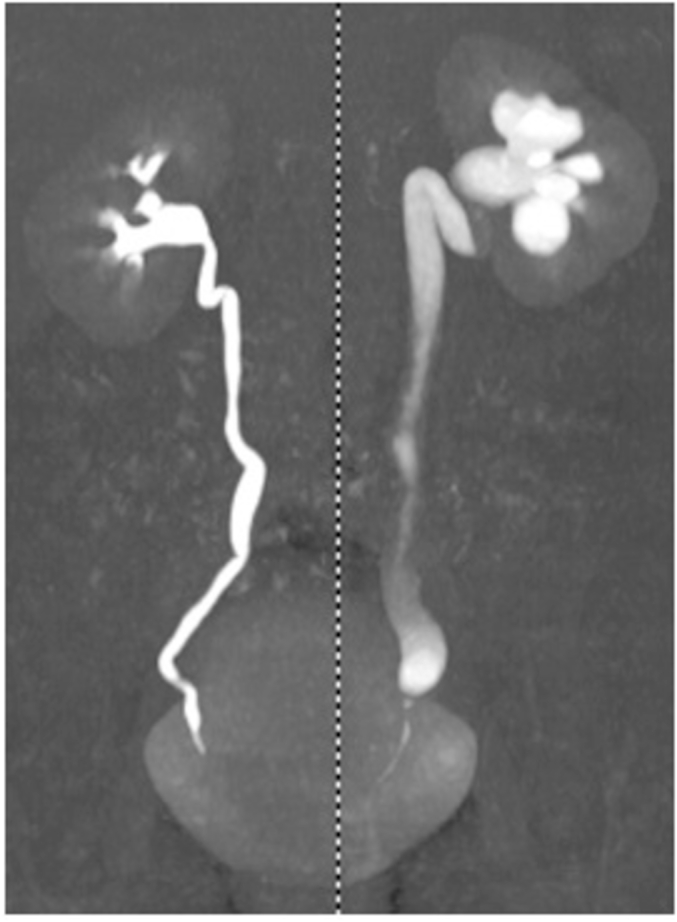
Left distal ureteral stenosis in Uro-TC.
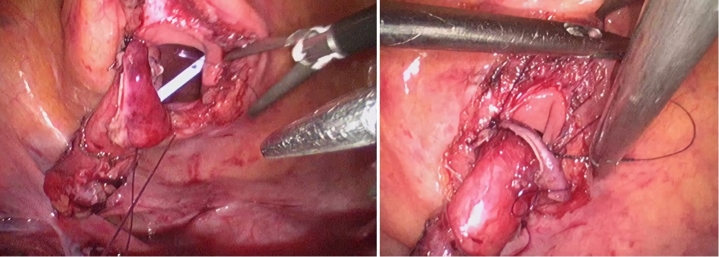
Laparoscopic extravesical ureteral reimplantation (ureteroneocystostomy) with 3 mm ports (Fig. 2) as well as distal ureter resection were performed, with uneventful postoperative course and discharged after 24 hours. Pathological assessment of the distal ureter specimen demonstrated inflammatory changes in ureteral wall secondary to granulomatous host response to schistosome eggs in the urinary tract.
Fig. 2.
Laparoscopic extravesical ureteral ureteroneocystostomy intraoperative images.
After 1-year follow-up, the patient remains asymptomatic, with normal caliber of ureteral reimplantation and without obstructive uropathy (Fig. 3).
Fig. 3.
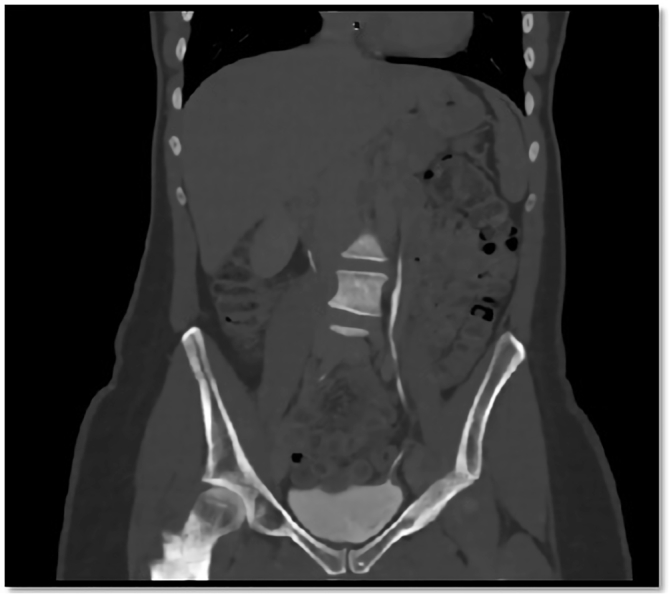
Postoperative Uro-CT 6-months after surgery. The patient presented a total resolution of left upper urinary tract obstruction, with proper contrast draining to bladder through the ureteroneocystostomy.
Discussion
According to the World Health Organization, schistosomiasis is one of the most widespread human parasitic infections, ranking second to malaria in terms of its effects on the socioeconomic status and health of populations living in tropical and subtropical regions. Schistosomiasis is a complex of parasitic infections that are caused by various trematodes of the genus Schistosoma, whose first hosts are aquatic or amphibious snail species that live in fresh water. Humans and other mammals may be infected through contact with water containing the parasites3.
Diagnosis of schistosomiasis is based in parasites detection through its eggs isolation or antibodies/serology demonstration in peripheral blood. Molecular testing of specific DNA sequences of the Schistosoma genome via PCR is a promising qualitative diagnostic assay as well. Once diagnosis has been made and successful treatment completed, image monitoring remains important to prevent ore early diagnose subsequent bladder malignancy.
There is no established protocol for image follow-up in patients with past history of schistosomiasis. Biannual ultrasound during first couple of years seems to be reasonable if the intention is to diagnose early ureteral involvement. If hematuria or low urinary tract symptoms are present during follow up, cystoscopy is mandatory to rule out bladder squamous cell carcinoma.
Only Schistosoma haematobium affects genitourinary system. This trematode worm is endemic throughout Africa, Madagascar, Mauritius, the southern shore of the Mediterranean, and the Middle East, including Turkey. Despite being endemic in these places tourist can been infected after a single exposure.1
Hematuria is the first symptom of genitourinary schistosomiasis related with the stage of egg deposition in the urinary tract, and appears 10–12 weeks after infection. In longstanding infections, a cellular reaction to dead ova produces calcification and fibrosis. Ureteral involvement in schistosomiasis has been reported up to 65% of the cases.4 The earliest change visible at urography is persistent filling of the distal ureteral segment of the ureter, followed by distal ureteral dilation (Fig. 1). Early-stage ureteral dilation results from ureteral dysfunction, is generally unilateral, and ranges from slight to severe. At a later stage, ureteral fibrosis resulting from tissue healing may lead to ureteral strictures. More than 80% of earliest ureteral strictures involve the intramural portion of the distal ureter (Fig. 1); second most common location is 2–5 cm above the orifice. The part of the ureter affected by fibrosis extends above and below the stenotic ureteral segment. As fibrosis progresses, the entire length of the ureter may be involved, with multiple strictures.3
Distal ureteral stenosis has been conventionally treated by open ureteral reimplantation. Several surgical techniques for ureteral reimplantation have been described; the most widely adopted are extravesical (Lich-Gregoir) or intravesical (Politano-Leadbetter). Regarding endourological approach, pneumatic dilation with or without stents are also possible.4 However, laparoscopic extravesical ureteral reimplantation was the earliest reported and most commonly used minimally invasive approach to treat distal ureteral strictures, reaching overall success rates similar to open surgery.5
Conclusion
Genitourinary schistosomiasis is an acquired cause of urinary tract diseases. Travelers can be infected by a single exposure. Ureteral involvement is not infrequent and distal intramural segment is the most commonly involved. Laparoscopic extravesical ureteral reimplantation is a feasible minimally invasive approach with comparable results to open surgery.
Declaration of interest
The authors declare no conflict of interest.
References
- 1.Cetron M.S., Chitsulo L., Sullivan J.J. Schistosomiasis in lake Malawi. Lancet. 1996;348:1274–1278. doi: 10.1016/S0140-6736(96)01511-5. [DOI] [PubMed] [Google Scholar]
- 2.Honeycutt J., Hammam O., Fu C.L., Hsieh M.H. Controversies and challenges in research on urogenital schistosomiasis-associated bladder cancer. Trends Parasitol. 2014;30:324–332. doi: 10.1016/j.pt.2014.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shebel H.M., Elsayes K.M., Abou El Atta H.M., Elguindy Y.M., El-Diasty T.A. Genitourinary schistosomiasis: life cycle and radiologic-pathologic findings. Radiographics. 2012;32(4):1031–1046. doi: 10.1148/rg.324115162. [DOI] [PubMed] [Google Scholar]
- 4.Taille A., Ravery V., Hoffmann P. Treatment of ureteral stenosis using high pressure dilatation catheters. Prog Urol. 1997 Jun;7(3):408–414. [PubMed] [Google Scholar]
- 5.Symons S., Kurien A., Desai M. Laparoscopic ureteral reimplantation: a single center experience and literature review. J Endourol. 2009;23:274. doi: 10.1089/end.2008.0266. [DOI] [PubMed] [Google Scholar]