Abstract
Objective: The goal of this research was to investigate the efficacy of perioperative manual acupuncture in the LV 3 and LI 4 points for lessening hemodynamic changes during endotracheal intubation in patients who were receiving anesthesia.
Materials and Methods: This double-blinded randomized controlled study enrolled patients who were undergoing endotracheal intubation, in 2015–2016, during general anesthesia in the general surgery department of the Imam Khomeini Hospital complex, in the Tehran University of Medical Sciences, Iran. The patients were randomly allocated into 2 groups with 30 patients in each group. In the treatment group, acupuncture needles were placed at LV 3 and LI 4, whereas, in the control group, the needles were placed 1 cm lateral to these points. Systolic blood pressure (SBP), diastolic blood pressure (DBP), mean arterial blood pressure (MAP), and heart rate (HR) before and after placing the acupuncture needles, after induction, immediately, 1 minute, and 3 minutes after intubation were measured and recorded prospectively.
Results: The patients had a mean age of 44.45 ± 12.72 years and included 35 (58.3%) males. Before acupuncture, demographic data, mean blood pressure (BP), and mean HR of the patients were not significantly different in the treatment and control groups. The mean SBP, DBP, MAP, and HR of all patients changed over time significantly (P < 0.001 for all). In the treatment group, mean SBP, DBP, and MAP changes immediately after the needles were placed were significantly less than those in the control group (P = 0.033, 0.024, and 0.024, respectively).
Conclusions: Although acupuncture could have a very–short-term effect that reduces BP during endotracheal intubation, hemodynamic changes might not be prevented during endotracheal intubation.
Keywords: acupuncture, intubation, hemodynamic indices
Introduction
Endotracheal intubation during general anesthesia can cause hemodynamic changes that can be life-threatening in elderly patients and those with cardiovascular diseases.1 During airway instrumentation, epipharyngeal and parapharyngeal areas can be stimulated leading to sympathoadrenal incitement and, consequently, significant rises in serum level of catecholamine, blood pressure (BP), and pulse. These rises can, in turn, lead to myocardial infarctions and arrhythmias in susceptible patients.2,3 The therapeutic effects of many drugs for attenuating the hemodynamic responses during laryngoscopy and prevention of significant increase in BP and workload of the heart during endotracheal intubation have been studied.4–6
Acupuncture as one of the basic pillars of complementary medicine is becoming more popular for managing various conditions, including hypertension, to avoid the adverse effects associated with pharmaceutical agents.7 It has been shown that acupuncture has a potential therapeutic effect for reducing BP in patients who have hypertension.8,9 The mechanisms of the antihypertensive action of acupuncture include reducing sympathomimetic substances such as norepinephrine and decreasing the activity of the renin angiotensin II system.10,11 In addition, it has been reported that perioperative acupuncture has both antihypotensive and antihypertensive effects, depending on different applied methods, and could stabilize hemodynamic changes during an operation by maintaining the balance of the sympathetic nervous system.12–15
In the present study, the current authors investigated the efficacy of perioperative manual acupuncture in the Liver 3 (LV 3) and Large Intestine 4 (LI 4) points for attenuating and preventing hemodynamic changes during endotracheal intubation in patients who were receiving general anesthesia in the general surgery department of the Imam Khomeini Hospital complex, at the Tehran University of Medical Sciences, Hamadan, Iran.
Materials and Methods
Patient Selections
In this double-blinded, randomized controlled study, patients who were undergoing general anesthesia with endotracheal intubation for surgery during 2015–2016 were enrolled. Inclusion criteria consisted of candidates for elective abdominal operations with physical status of classes 1 or 2 based on the American Society of Anesthesiologists physical status classification system.16 Patients with difficult intubation and repeated laryngoscopies; coagulation disorders; past or present histories of substance abuse; and/or alcoholism, pregnancy and neurologic disorders were excluded. Patients were randomly assigned into treatment and control groups according to a simple randomization method. A random number was assigned to each patient, using the random number table; patients who were assigned odd and even numbers were assigned to the treatment and control groups, respectively.
Study Protocol
First, the acupuncture points of LR 3 at the distal end of the first metatarsal space on the dorsum of the foot and LI 4 at the radial side of the middle of the second metacarpal bone of the hand were located using an acupuncture point–locator device (Acuhealth Pro 900, Australia). In the treatment group, the acupuncture needles were inserted at the proposed acupuncture points, whereas, in the control group, the acupuncture needles were placed 1 cm lateral to the proposed acupuncture points. Locating the points and placing the needles were performed by the same well-trained acupuncturist.
Just after placing the needles and taking measurements of the hemodynamic indices, midazolam (0.03 mg/kg) and fentanyl (0.002 mg/kg) were administered intravenously (i.v.) to each patient. Then, sodium thiopental (5 mg/kg) and atracurium (0.5 mg/kg) were administered i.v. for induction of general anesthesia. After 3 minutes, the patient was laryngoscoped and intubated by the same anesthesiologist.
Hemodynamic indices were measured using the same automated monitoring device before and after placing acupuncture needles; after induction; immediately; and 1, 3, and 5 minutes after intubation. The measurements included systolic BP (SBP), diastolic BP (DBP), mean arterial BP (MAP), and heart rate (HR). All measurements were recorded by the same anesthesia technician, who had no information about the patient's group.
Ethics
This study was performed only after approval of the ethical committee of the Tehran University of Medical Sciences. The entire procedure and its probable advantages and disadvantages were explained in detail to the patients prior to enrollment and signed informed consent was taken from each participant.
Statistical Analyses
Data analyses were performed using statistical software (SPSS for Windows, version 22.0, SPSS Inc., Chicago, IL). Qualitative and quantitative variables were evaluated with χ2 and Student's t-tests, respectively. Statistical significance was defined as P ≤ 0.05.
Results
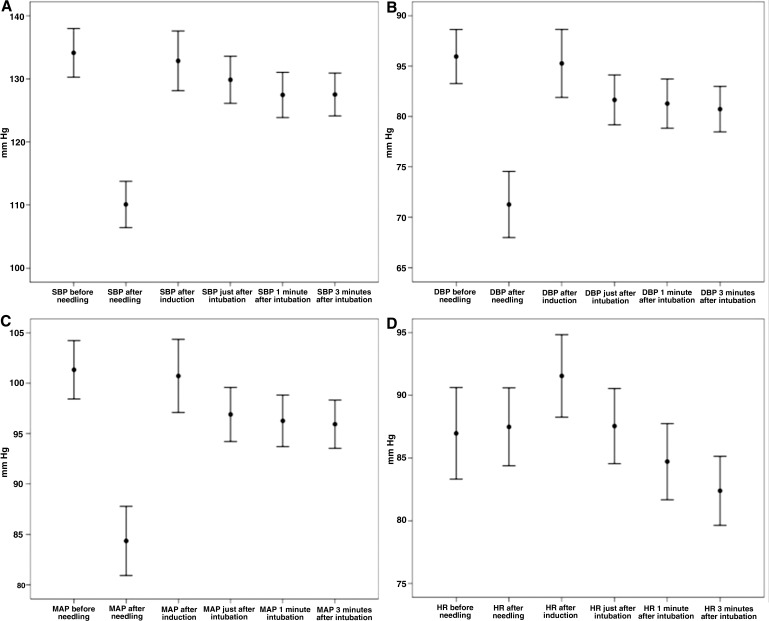
Sixty patients with a mean age of 44.45 ± 12.72 years (range: 17–63), including 35 (58.3%) males, were enrolled in the study. As shown in demographic data in Table 1, the mean BP and HR of the patients before placing the acupuncture needles were not significantly different in the treatment and control groups. Mean SBP, DBP, MAP, and HR of the patients changed significantly from the time before placing the acupuncture needles to 3 minutes after intubation (P < 0.001 for all). The trends of the means of SBP, DBP, MAP, and HR of the patients over time is shown in Figure 1.
Table 1.
Demographic Data of Patients and Mean BP and HR Before Acupuncture Needles Were Placed
| Characteristics | Treatment group (n = 30) | Control group (n = 30) | P-value |
|---|---|---|---|
| Gender, male | 21 (70%) | 14 (46.7%) | 0.058 |
| Age (years/old) | 41.7 ± 13.9 | 47.2 ± 10.9 | 0.094 |
| SBP (mm Hg) | 130.7 ± 15.5 | 137.5 ± 13.8 | 0.08 |
| DBP (mm Hg) | 85.3 ± 10.4 | 86.6 ± 10.5 | 0.65 |
| MAP (mm Hg) | 99.2 ± 11.7 | 103.5 ± 10.4 | 0.136 |
| HR (beats/minute) | 85.7 ± 18 | 88.2 ± 8.9 | 0.505 |
BP, blood pressure, HR, heart rate; SBP, systolic BP; DBP, diastolic BP; MAP, mean arterial BP.
FIG 1.
The trends of means of (A) systolic blood pressure (SBP), (B) diastolic blood pressure (DBP), (C) mean arterial blood pressure (MAP), and (D) heart rate (HR) of all studied patients over time.
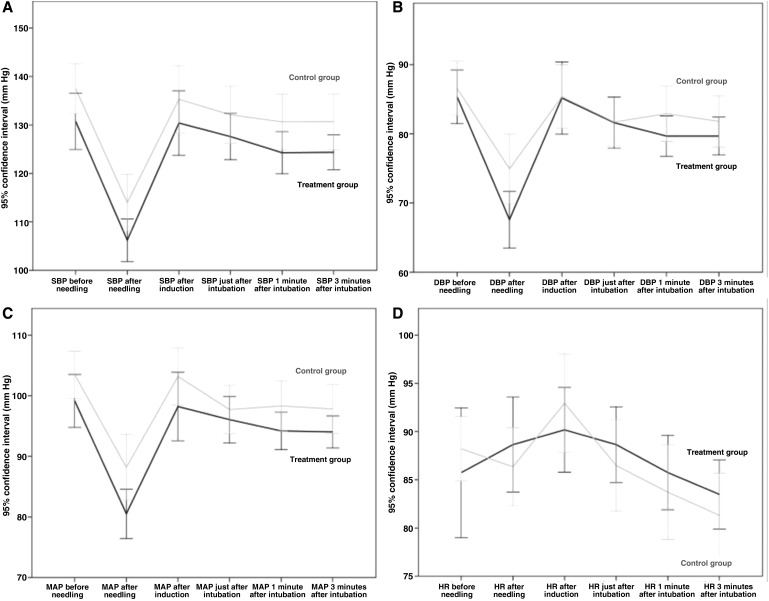
As shown in Table 2, the mean SBP, DBP, and MAP of the patients in the treatment group immediately after placing the needles were significantly less than those of the patients in the control group (P = 0.033, 0.024, and 0.024, respectively). However, subsequent measurements at other times were not significantly different across the 2 groups. Moreover, the mean HRs of the patients at all measurement timepoints were not significantly different between the 2 groups. The trends of the means of SBP, DBP, MAP, and HR over time in each group are depicted in Figure 2. The differences between the means of SBP, DBP, MAP, and HR before placing the needles and the next time sequences in each group are shown in Table 3.
Table 2.
Details for Mean of SBP, DBP, MAP and HR of Patients in Each Group
| Characteristics | Treatment group (n = 30) | Control group (n = 30) | P-value |
|---|---|---|---|
| SBP (mm Hg) | |||
| After needling | 106.2 ± 11.7 | 114 ± 15.6 | 0.033 |
| After induction | 130.4 ± 17.8 | 135.3 ± 18.8 | 0.304 |
| Just after intubation | 127.6 ± 12.8 | 132.1 ± 15.8 | 0.231 |
| 1 minute after intubation | 124.3 ± 11.7 | 130.6 ± 15.3 | 0.075 |
| 3 minutes after intubation | 124.4 ± 9.6 | 130.7 ± 15.4 | 0.063 |
| DBP (mm Hg) | |||
| After needling | 67.6 ± 10.9 | 74.9 ± 13.4 | 0.024 |
| After induction | 85.2 ± 14 | 85.4 ± 12.3 | 0.953 |
| Just after intubation | 81.6 ± 10 | 81.7 ± 9.4 | 0.968 |
| 1 minute after intubation | 79.7 ± 7.8 | 82.9 ± 10.7 | 0.187 |
| 3 minutes after intubation | 79.7 ± 7.3 | 81.8 ± 9.9 | 0.348 |
| MAP (mm/Hg) | |||
| After needling | 80.5 ± 10.9 | 88.2 ± 14.5 | 0.024 |
| After induction | 98.2 ± 15.1 | 103.2 ± 12.7 | 0.173 |
| Just after intubation | 96.1 ± 10.3 | 97.7 ± 10.6 | 0.539 |
| 1 minute after intubation | 94.2 ± 8.3 | 98.3 ± 11.1 | 0.107 |
| 3 minutes after intubation | 94.03 ± 7.1 | 97.8 ± 10.8 | 0.113 |
| HR (beats/minute) | |||
| After needling | 88.6 ± 13.2 | 86.3 ± 10.9 | 0.465 |
| After induction | 90.2 ± 11.8 | 92.9 ± 13.7 | 0.405 |
| Just after intubation | 88.6 ± 10.5 | 86.5 ± 12.7 | 0.475 |
| 1 minute after intubation | 85.7 ± 10.3 | 83.7 ± 13.1 | 0.507 |
| 3 minutes after intubation | 83.5 ± 9.5 | 81.3 ± 11.7 | 0.435 |
Bold represents significant results.
SBP, systolic blood pressure; DBP, diastolic blood pressure; MAP, mean arterial pressure; HR, heart rate.
FIG 2.
The trends of means of (A) systolic blood pressure (SBP), (B) diastolic blood pressure (DBP), (C) mean arterial blood pressure (MAP), and (D) heart rate (HR) over time in each group.
Table 3.
Differences Between Means of SBP, DBP, MAP and HR of Patients After Acupuncture Needle Placements, Induction, Intubation and 1 and 3 Minutes After Intubation in Each Group
| Characteristics | Treatment group (n = 30) | P-value | Control group (n = 30) | P-value |
|---|---|---|---|---|
| Systolic blood pressure (mm/Hg) | ||||
| After needling | 24.5 ± 2.0 | <0.001 | 23.5 ± 2.6 | <0.001 |
| After induction | 0.3 ± 2.7 | 0.904 | 2.2 ± 2.9 | 0.449 |
| Just after intubation | 3.1 ± 2.2 | 0.158 | 5.4 ± 2.1 | 0.015 |
| 1 minute after intubation | 6.5 ± 2 | 0.003 | 6.9 ± 2 | 0.002 |
| 3 minutes after intubation | 6.4 ± 2 | 0.004 | 6.8 ± 2.1 | 0.003 |
| DBP (mm Hg) | ||||
| After needling | 17.7 ± 1.8 | <0.001 | 11.6 ± 2.1 | <0.001 |
| After induction | 0.2 ± 2.4 | 0.945 | 1.2 ± 2.2 | 0.6 |
| Just after intubation | 3.7 ± 1.8 | 0.045 | 4.9 ± 1.6 | 00.005 |
| 1 minute after intubation | 5.7 ± 1.6 | 0.001 | 3.7 ± 1.5 | 0.02 |
| 3 minutes after intubation | 5.6 ± 1.7 | 0.002 | 4.8 ± 1.9 | 0.02 |
| MAP (mm Hg) | ||||
| After needling | 18.7 ± 2.0 | <0.001 | 15.3 ± 2.3 | <0.001 |
| After induction | 0.9 ± 2.5 | 0.71 | 0.3 ± 1.9 | 0.87 |
| Just after intubation | 3.1 ± 1.8 | 0.09 | 5.8 ± 1.5 | 0.001 |
| 1 minute after intubation | 5.0 ± 1.5 | 0.002 | 5.2 ± 1.5 | 0.002 |
| 3 minutes after intubation | 5.1 ± 1.7 | 0.005 | 5.7 ± 1.8 | 0.005 |
| HR (beats/minute) | ||||
| After needling | –2.9 ± 2.6 | 0.27 | 1.9 ± 2.0 | 0.36 |
| After induction | –4.4 ± 2.3 | 0.06 | −4.7 ± 2.7 | 0.09 |
| Just after intubation | –2.9 ± 2.3 | 0.23 | 1.7 ± 2.7 | 0.52 |
| 1 minute after intubation | 0 ± 2.3 | 1.0 | 4.5 ± 2.7 | 0.11 |
| 3 minutes after intubation | 2.3 ± 2.5 | 0.37 | 6.9 ± 2.5 | 0.01 |
Bold values denote statistical significance.
SBP, systolic blood pressure; DBP, diastolic blood pressure; MAP, mean arterial pressure; HR, heart rate.
Discussion
The current study showed that, immediately after placing the acupuncture needles at the proposed acupuncture points, SBP, DBP, and MAP were significantly reduced in the treatment group, compared to the control group. However, in the next time sequences these hemodynamic changes were not significantly different than those of the control group. Given that the demographics and hemodynamic indices of the patients before placing the acupuncture needles were comparable in both groups, the observed difference could suggest a very short-term effect of acupuncture for reducing BP during endotracheal intubation. However, in contrast, the HR of the patients in the treatment group was not significantly changed during acupuncture, compared to the control group. Similarly, in a study by Saleh, laser acupuncture at Pericardium (PC 6) and LV 3 in children who underwent surgery for strabismus resulted in decreased hemodynamic responses during endotracheal intubation; however, the response was not prevented.17 In that study, the MAP and HR were not significantly changed in poststimulation and postinduction times; however, these measures increased significantly after 1 and 2 minutes after intubation.17
Although, the role of cerebral and cerebellar regions in autonomic regulation has not yet been definitely identified, the central autonomic network (CAN) has been proposed as the controlling system of autonomic outflow in the cerebrum.4 Sympathetic and parasympathetic outflow of the brain and afferent–efferent integration of the autonomic nervous system (ANS) can be significantly influenced by the functionally connected networks of CAN.18 Sympathetic involvement was primarily seen in anterior, prefrontal, and right anterior and left posterior insular cortices. However, the bilateral dorsal anterior insula, hippocampal formation, and posterior cingulate and lateral temporal cortices were involved in parasympathetic regulation.4
Several reports have shown that brain functional connectivity in the regions of CAN might be modulated by using acupuncture in LV 3 and LI 4.19 In a study by Wu et al., a correlation between stimulating LV 3 and functional brain areas using resting-state functional magnetic resonance imaging (fMRI) was reported.20 The anterior cingulate gyrus, thalamus, and cerebellar posterior lobe—which are involved in sensation, pain, and emotion—were specifically altered during acupuncture at LV 3.20 Similarly, Zheng et al. showed that the medial, superior, and middle frontal gyri; inferior temporal and cingulate gyri; occipital lobe; inferior parietal lobule; insula; cuneus; precuneus; and cerebellar anterior lobe—most of which are associated with functional connectivity of emotion, vision, and autonomic function—were significantly altered after acupuncture in LV 3.21
In a study by Wang et al., several brain regions attributed to the limbic system—which were matched with known anatomical regions of pain and the CAN—were modulated during electroacupuncture of LI 4.22 Moreover, some studies suggested that acupuncture-induced pain modulation can be attributed to functional connectivity alterations in the cingulate gyrus, primary somatosensory cortex, prefrontal areas, and insula, which might play a major role in ANS regulation and cardiac control.15,23–25 Thus, functional connectivity alterations after acupuncture in LV 3 and LI 4 could be involved in the mechanism regulating HR variability and arterial BP.
Conclusions
The current study showed that, although acupuncture in LV 3 and LI 4 have have a very short-term effect for reducing the BP during endotracheal intubation, the hemodynamic changes might not be prevented during endotracheal intubation. More powered studies investigating dissimilar control groups and different acupuncture points are needed to elucidate the efficacy of acupuncture for reducing hemodynamic changes during endotracheal intubation.
Author Disclosure Statement
No competing financial conflicts exist.
References
- 1. Dix P, Howell S. Survey of cancellation rate of hypertensive patients undergoing anaesthesia and elective surgery. Br J Anaesth. 2001;86(6):789–793 [DOI] [PubMed] [Google Scholar]
- 2. Kayhan Z, Aldemir D, Mutlu H, Ögüs E. Which is responsible for the haemodynamic response due to laryngoscopy and endotracheal intubation—catecholamines, vasopressin or angiotensin? Eur J Anaesthesiol. 2005;22(10):780–785 [DOI] [PubMed] [Google Scholar]
- 3. Russell WJ, Morris RG, Frewin DB, Drew SE. Changes in plasma catecholamine concentrations during endotracheal intubation. Br J Anaesth. 1981;53(8):837–839 [DOI] [PubMed] [Google Scholar]
- 4. Beissner F, Meissner K, Bar KJ, Napadow V. The autonomic brain: An activation likelihood estimation meta-analysis for central processing of autonomic function. J Neurosci. 2013;33(25):10503–10511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Mendonca FT, de Queiroz LM, Guimaraes CC, Xavier AC. Effects of lidocaine and magnesium sulfate in attenuating hemodynamic response to tracheal intubation: Single-center, prospective, double-blind, randomized study. Braz J Anesthesiol. 2017;67(1):50–56 [DOI] [PubMed] [Google Scholar]
- 6. Nazir M, Salim B, Khan FA. Pharmacological agents for reducing the haemodynamic response to tracheal intubation in paediatric patients: A systematic review. Anaesth Intensive Care. 2016;44(6):681–691 [DOI] [PubMed] [Google Scholar]
- 7. Tindle HA, Davis RB, Phillips RS, Eisenberg DM. Trends in use of complementary and alternative medicine by US adults: 1997–2002. Alternat Ther Health Med. 2005;11(1):42–49 [PubMed] [Google Scholar]
- 8. Terenteva N, Chernykh O, Sanchez-Gonzalez MA, Wong A. Acupuncture therapy improves vascular hemodynamics and stiffness in middle-age hypertensive individuals. Complement Ther Clin Pract. 2018;30:14–18 [DOI] [PubMed] [Google Scholar]
- 9. Wang J, Xiong X, Liu W. Acupuncture for essential hypertension. Int J Cardiol. 2013;169(5):317–326 [DOI] [PubMed] [Google Scholar]
- 10. Chiu YJ, Chi A, Reid IA. Cardiovascular and endocrine effects of acupuncture in hypertensive patients. Clin Exp Hypertens. 1997;19(7):1047–1063 [DOI] [PubMed] [Google Scholar]
- 11. Zhou W, Longhurst JC. Neuroendocrine mechanisms of acupuncture in the treatment of hypertension. Evid Based Complement Alternat Med. 2012;2012:878673 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Lu Z, Dong H, Wang Q, Xiong L. Perioperative acupuncture modulation: More than anaesthesia. Br J Anaesth. 2015;115(2):183–193 [DOI] [PubMed] [Google Scholar]
- 13. Saghaei M, Ahmadi A, Rezvani M. Clinical trial of nitroglycerin-induced controlled hypotension with or without acupoint electrical stimulation in microscopic middle ear surgery under general anesthesia with halothane. Acta Anaesthesiol Taiwan. 2005;43(3):135–139 [PubMed] [Google Scholar]
- 14. Syuu Y, Matsubara H, Hosogi S, Suga H. Pressor effect of electroacupuncture on hemorrhagic hypotension. Am J Physiol Regul Integr Comp Physiol. 2003;285(6):R1446–R1452 [DOI] [PubMed] [Google Scholar]
- 15. Villarreal Santiago M, Tumilty S, Mącznik A, Mani R. Does acupuncture alter pain-related functional connectivity of the central nervous system? A systematic review. J Acupunct Meridian Stud. 2016;9(4):167–177 [DOI] [PubMed] [Google Scholar]
- 16. American Society of Anesthsiologists. Preoperative testing guidelines. http://www.choosingwisely.org/doctor-patient-lists/american-society-of-anesthesiologists/ Accessed April4, 2019
- 17. Saleh RH. Efficacy of laser acupuncture in attenuating hemodynamic response to orotracheal intubation and postoperative nausea and vomiting in children undergoing strabismus surgery. Egyptian J Anaesth. 2014;30(4):411–416 [Google Scholar]
- 18. Saper CB. The central autonomic nervous system: Conscious visceral perception and autonomic pattern generation. Annu Rev Neurosci. 2002;25:433–469 [DOI] [PubMed] [Google Scholar]
- 19. Sun R, Yang Y, Li Z, Li Y, Cheng S, Zeng F. Connectomics: A new direction in research to understand the mechanism of acupuncture. Evid Based Complement Alternat Med. 2014;2014:568429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Wu C, Qu S, Zhang J, et al. Correlation between the effects of acupuncture at Taichong (LR3) and functional brain areas: A resting-state functional magnetic resonance imaging study using true versus sham acupuncture. Evid Based Complement Alternat Med. 2014;2014:729091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Zheng Y, Wang Y, Lan Y, et al. Imaging of brain function based on the analysis of functional connectivity—imaging analysis of brain function by fMRI after acupuncture at LR3 in healthy individuals. Afr J Tradit Complement Altern Med. 2016;13(6):90–100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Wang W, Liu L, Zhi X, et al. Study on the regulatory effect of electro-acupuncture on Hegu point (LI4) in cerebral response with functional magnetic resonance imaging. Chin J Integr Med. 2007;13(1):10–16 [DOI] [PubMed] [Google Scholar]
- 23. Theysohn N, Choi KE, Gizewski ER, et al. Acupuncture-related modulation of pain-associated brain networks during electrical pain stimulation: A functional magnetic resonance imaging study. J Altern Complement Med. 2014;20(12):893–900 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Li K, Shan B, Xu J, et al. Changes in FMRI in the human brain related to different durations of manual acupuncture needling. J Altern Complement Med. 2006;12(7):615–623 [DOI] [PubMed] [Google Scholar]
- 25. Cechetto DF. Cortical control of the autonomic nervous system. Exp Physiol. 2014;99(2):326–231 [DOI] [PubMed] [Google Scholar]