Abstract
Background
For centuries, there has been controversy around whether being upright (sitting, birthing stools, chairs, squatting, kneeling) or lying down (lateral (Sim's) position, semi‐recumbent, lithotomy position, Trendelenburg's position) have advantages for women giving birth to their babies. This is an update of a review previously published in 2012, 2004 and 1999.
Objectives
To determine the possible benefits and risks of the use of different birth positions during the second stage of labour without epidural anaesthesia, on maternal, fetal, neonatal and caregiver outcomes.
Search methods
We searched Cochrane Pregnancy and Childbirth's Trials Register (30 November 2016) and reference lists of retrieved studies.
Selection criteria
Randomised, quasi‐randomised or cluster‐randomised controlled trials of any upright position assumed by pregnant women during the second stage of labour compared with supine or lithotomy positions. Secondary comparisons include comparison of different upright positions and the supine position. Trials in abstract form were included.
Data collection and analysis
Two review authors independently assessed trials for inclusion and assessed trial quality. At least two review authors extracted the data. Data were checked for accuracy. The quality of the evidence was assessed using the GRADE approach.
Main results
Results should be interpreted with caution because risk of bias of the included trials was variable. We included eleven new trials for this update; there are now 32 included studies, and one trial is ongoing. Thirty trials involving 9015 women contributed to the analysis. Comparisons include any upright position, birth or squat stool, birth cushion, and birth chair versus supine positions.
In all women studied (primigravid and multigravid), when compared with supine positions, the upright position was associated with a reduction in duration of second stage in the upright group (MD ‐6.16 minutes, 95% CI ‐9.74 to ‐2.59 minutes; 19 trials; 5811 women; P = 0.0007; random‐effects; I² = 91%; very low‐quality evidence); however, this result should be interpreted with caution due to large differences in size and direction of effect in individual studies. Upright positions were also associated with no clear difference in the rates of caesarean section (RR 1.22, 95% CI 0.81 to 1.81; 16 trials; 5439 women; low‐quality evidence), a reduction in assisted deliveries (RR 0.75, 95% CI 0.66 to 0.86; 21 trials; 6481 women; moderate‐quality evidence), a reduction in episiotomies (average RR 0.75, 95% CI 0.61 to 0.92; 17 trials; 6148 women; random‐effects; I² = 88%), a possible increase in second degree perineal tears (RR 1.20, 95% CI 1.00 to 1.44; 18 trials; 6715 women; I² = 43%; low‐quality evidence), no clear difference in the number of third or fourth degree perineal tears (RR 0.72, 95% CI 0.32 to 1.65; 6 trials; 1840 women; very low‐quality evidence), increased estimated blood loss greater than 500 mL (RR 1.48, 95% CI 1.10 to 1.98; 15 trials; 5615 women; I² = 33%; moderate‐quality evidence), fewer abnormal fetal heart rate patterns (RR 0.46, 95% CI 0.22 to 0.93; 2 trials; 617 women), no clear difference in the number of babies admitted to neonatal intensive care (RR 0.79, 95% CI 0.51 to 1.21; 4 trials; 2565 infants; low‐quality evidence). On sensitivity analysis excluding trials with high risk of bias, these findings were unchanged except that there was no longer a clear difference in duration of second stage of labour (MD ‐4.34, 95% CI ‐9.00 to 0.32; 21 trials; 2499 women; I² = 85%).
The main reasons for downgrading of GRADE assessment was that several studies had design limitations (inadequate randomisation and allocation concealment) with high heterogeneity and wide CIs.
Authors' conclusions
The findings of this review suggest several possible benefits for upright posture in women without epidural anaesthesia, such as a very small reduction in the duration of second stage of labour (mainly from the primigravid group), reduction in episiotomy rates and assisted deliveries. However, there is an increased risk blood loss greater than 500 mL and there may be an increased risk of second degree tears, though we cannot be certain of this. In view of the variable risk of bias of the trials reviewed, further trials using well‐designed protocols are needed to ascertain the true benefits and risks of various birth positions.
Plain language summary
Women’s position for giving birth without epidural anaesthesia
What is the issue?
Women often give birth in upright positions like kneeling, standing or squatting. Some women give birth on their backs in what are known as ‘supine’ positions ‐ including dorsal (the woman flat on her back), lateral (the woman lying on her side), semi‐recumbent (where the woman is angled partly upright) or lithotomy (where the woman’s legs are held up in stirrups). Birth position can be influenced by many different factors including setting, mother's choice, caregiver preference, or medical intervention. This Cochrane review assessed the possible benefits and risks to the mother and baby, by giving birth in upright positions compared with supine positions and also looked at some individual upright positions for benefits and harms.
Why is this important?
Giving birth in the supine position may have been adopted to make it more convenient for midwives and obstetricians to assist the labour and birth. However, many women report that giving birth on their backs feels painful, uncomfortable and difficult. It is suggested that women in upright positions give birth more easily because the pelvis is able to expand as the baby moves down; gravity may also be helpful and the baby may benefit because the weight of the uterus will not be pressing down on the mother’s major blood vessels which supply oxygen and nutrition to the baby.
We looked at the upright positions such as: sitting (on an obstetric chair or stool); kneeling (either on all fours or kneeling up) and squatting (unaided or using a birth cushion or a squatting bar). We compared these with supine positions such as: dorsal; lateral; semi‐recumbent and lithotomy. Our aim was to assess the effectiveness, benefits and possible disadvantages of the different positions for women without epidural, during the second stage of labour.
What evidence did we find?
We searched for evidence up to 30 November 2016. This review now includes data from 30 randomised controlled trials involving 9015 pregnant women who gave birth without epidural anaesthesia.
Overall, evidence was not of good quality. When women gave birth in an upright position, as compared with lying on their backs, the length of time they were pushing (second stage of labour) was reduced by around six minutes (19 trials, 5811 women; very low‐quality evidence). Fewer women had an assisted delivery, for example with forceps (21 trials, 6481 women; moderate‐quality evidence). The number of women having a caesarean section did not differ (16 trials, 5439 women; low‐quality evidence). Fewer women had an episiotomy (a surgical cut to the perineum to enlarge the opening for the baby to pass through) although there was a tendency for more women to have perineal tears (low‐quality evidence). There was no difference in number of women with serious perineal tears (6 trials, 1840 women; very low‐quality evidence) between those giving birth upright or supine. Women were more likely to have a blood loss of 500 mL or more (15 trials, 5615 women; moderate‐quality evidence) in the upright position but this may be associated with more accurate ways of measuring the blood loss. Fewer babies had problems with fast or irregular heart beats that indicate distress (2 trials, 617 women) when women gave birth in an upright position although the number of admissions to the neonatal unit was no different (4 trials, 2565 infants; low‐quality evidence).
What does this mean?
This review found that there could be benefits for women who choose to give birth in an upright position. The length of time they had to push may be reduced but the effect was very small and these women might lose more blood. The results should be interpreted with caution because of poorly conducted studies, variations between trials and in how the findings were analysed.
More research into the benefits and risks of different birthing positions would help us to say with greater certainty which birth position is best for most women and their babies. Overall, women should be encouraged to give birth in whatever position they find comfortable.
Summary of findings
Summary of findings for the main comparison. Any upright compared to supine position for the second stage of labour for women without epidural anaesthesia.
| Any upright compared to supine position for the second stage of labour for women without epidural anaesthesia | ||||||
| Patient or population: women in the second stage of labour without epidural anaesthesia Setting: hospital settings in Iran, India, Brazil, Mexico, Hong Kong, Ireland, UK, New Zealand, Finland, Thailand, France, and Sweden Intervention: any upright position Comparison: supine position | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Risk with supine position | Risk with Any upright | |||||
| Duration of second stage of labour | The mean duration of second stage of labour was 6.16 minutes shorter in the upright position (9.74 minutes shorter to 2.59 minutes shorter) | 5811 (19 RCTs) | ⊕⊝⊝⊝ VERY LOW 1 2 3 | Including multigravida and primigravida women | ||
| Mode of birth: assisted birth | Study population | RR 0.75 (0.66 to 0.86) | 6481 (21 RCTs) | ⊕⊕⊕⊝ MODERATE 1 | ||
| 128 per 1000 | 96 per 1000 (84 to 110) | |||||
| Mode of birth: caesarean section | Study population | RR 1.22 (0.81 to 1.81) | 5439 (16 RCTs) | ⊕⊕⊝⊝ LOW 4 5 | ||
| 14 per 1000 | 18 per 1000 (12 to 26) | |||||
| Trauma to the birth canal that required suturing: second degree perineal tears | Study population | average RR 1.20 (1.00 to 1.44) | 6715 (18 RCTs) | ⊕⊕⊝⊝ LOW 1 5 | ||
| 127 per 1000 | 153 per 1000 (127 to 184) | |||||
| Trauma to the birth canal that required suturing: third/fourth degree tears | Study population | RR 0.72 (0.32 to 1.65) | 1840 (6 RCTs) | ⊕⊝⊝⊝ VERY LOW 6 7 | ||
| 13 per 1000 | 9 per 1000 (4 to 21) | |||||
| Blood loss > 500 mL | Study population | average RR 1.48 (1.10 to 1.98) | 5615 (15 RCTs) | ⊕⊕⊕⊝ MODERATE 8 | ||
| 44 per 1000 | 65 per 1000 (49 to 88) | |||||
| Admission to neonatal intensive care unit | Study population | RR 0.79 (0.51 to 1.21) | 2565 (4 RCTs) | ⊕⊕⊝⊝ LOW 5 9 | ||
| 36 per 1000 | 28 per 1000 (18 to 43) | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio; OR: Odds ratio; | ||||||
| GRADE Working Group grades of evidence High quality: We are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low quality: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low quality: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | ||||||
1 Six studies have serious design limitations (inadequate randomisation and allocation concealment) though contribute less than 40% weight to analysis, all other studies have design limitations. (Downgraded 1 level).
2 High heterogeneity with variation in size and direction of effect. (Downgraded 2 levels).
3 Asymmetrical funnel plot. Small studies contributing data. (Downgraded 1 level).
4 Three studies have serious design limitations (inadequate randomisation and allocation concealment) though contribute less than 40% weight to analysis, all other studies have design limitations. (Downgraded 1 level).
5 Wide confidence intervals crossing the line of no effect. (Downgraded 1 level).
6 Three studies with serious design limitations contributing over 40% weight. (Downgraded 2 levels).
7 Wide confidence intervals crossing the line of no effect and few events. (Downgraded 2 levels).
8 Five studies have serious design limitations (inadequate randomisation and allocation concealment) though contribute less than 40% weight to analysis, all other studies have design limitations. (Downgraded 1 level).
9 All studies had design limitations. (Downgraded 1 level).
Background
Description of the condition
The position adopted naturally by women during birth has been described as early as 1882 (Engelmann 1882). Engelmann observed that women, not influenced by Western conventions, would try to avoid the dorsal position and would change position as and when they wished. Different upright positions could be achieved using posts, slung hammocks, furniture, holding on to ropes or knotted pieces of cloth, kneeling, crouching or squatting using bricks, stones, a pile of sand, or a birth stool (Balaskas 1992; Engelmann 1882; Jarcho 1934; Mead 1965; Simkin 2005). Today, most women in Western societies deliver in a dorsal, semi‐recumbent or lithotomy position. It is claimed that the dorsal position enables the midwife or obstetrician to monitor the fetus better and thus to ensure a safe birth, but it may be more convenient and give better control for the caregiver.
The position assumed by women during birth is influenced by several complex factors. 'Instinctive' behaviour is difficult to identify because behaviour is strongly influenced by cultural norms. For societies in which most births take place within a medical facility, cultural norms have over the years been moulded by the expectations and demands of medical attendants, as well as restrictions imposed by medical procedures such as fetal monitoring, intravenous therapy, anaesthesia including regional anaesthesia, medical examinations and medical procedures. During the second stage of labour, practices such as perineal support and assistance of the birth during 'spontaneous' birth have restricted options for positions assumed by women. Options for instrumental birth are also limited.
The influence of medical personnel and institutions over the positions adopted by women during labour and birth has been viewed as inconsiderate of women's comfort and need to experience birth as a positive event. In view of indirect evidence that a positive, supportive labour environment promotes a sense of competence and personal achievement experienced by women during childbirth, and their subsequent confidence as mothers and risk of postnatal depression (Wolman 1993), serious attention should be given to medical practices which may undermine or humiliate women during labour.
Description of the intervention
The supine or semi‐recumbent position for birth is widely used in contemporary obstetric practice. The parturient’s position changed from an upright positions to a semi‐recumbent position at the time of the introduction of the obstetric forceps by Hugh Chamberlen in 1670 (Atwood 1976). The main advantage cited is easy access of the caregiver to the woman's abdomen to monitor the fetal heart rate. Caregivers are comfortable with the dorsal position as it is the position in which they have usually been trained to conduct deliveries, including assisted vaginal deliveries, and is the conventional reference position for textbook descriptions of the mechanisms of vaginal birth.
The lithotomy position with the woman's legs fixed in stirrups is used in many institutions both for spontaneous and particularly for assisted vaginal deliveries (Dundes 1987). The use of stirrups may be combined with lateral pelvic tilting and a semi‐recumbent posture with the mother sitting up at about 45 degrees, to reduce aortocaval compression.
The lateral recumbent position is also used for both spontaneous and assisted deliveries, with the advantage of avoiding uterine compression of the aorta, the inferior vena cava, or both.
Kneeling positions may also be assumed by women in the second stage of labour. These may vary from upright kneeling to an 'all fours' position with the pelvis and shoulders at the same level.
A supported standing position was promoted by Odent in Pithiviers, France in the 1980s, but to our knowledge, has not been evaluated systematically.
The McRoberts' position with hyperflexed thighs was introduced to overcome shoulder dystocia. It has been shown to increase the expulsive force in the second stage of labour (Buhimschi 2001).
Birth in a birthing chair has been studied, but most of these studies have involved small sample sizes (Dunn 1978). There are conflicting data on the possible advantages and disadvantages of using a birthing chair for birth.
The deep squat is very similar to the habitual resting position of the chimpanzee and perhaps all of us might have squatted at some stage of our lives if our custom did not train us to adopt other postures (Hewes 1957). The squatting position is often termed the most natural position and is often used by women if left alone to choose their own position for birth (Kurokawa 1985; Romond 1985). However, the major disadvantage of the squatting position is that Western women may not have the appropriate muscular fitness and stamina to remain squatting for a considerable length of time, and that it may increase perineal trauma. This may be particularly true of Western women who no longer squat to defecate. In one study in Leeds, UK, only 16% of women allocated to squatting managed to do so, despite antenatal exercises (Gupta 1989). In many parts of Asia, Africa and Americas, people customarily work and rest in this posture. Consequently, the advent of a supported squatting position during giving birth, either using a birthing cushion or stool, seems attractive (Simkin 2005).
Observational studies have suggested that upright postures may reduce the risk of postpartum de novo urinary incontinence (Serati 2016) and enhances fathers' experience of having been positively and actively engaged in the birth process (Johansson 2015).
How the intervention might work
There is controversy around whether being upright or lying down has advantages for women delivering their babies. Several physiological advantages have been hypothesised and measured for non‐recumbent or upright labour: (i) the effects of gravity, (ii) lessened risk of aortocaval compression and improved acid‐base outcomes in the newborns (Ang 1969; Humphrey 1974; Scott 1963), (iii) stronger and more efficient uterine contractions (Caldeyro‐Barcia 1960; Méndez‐Bauer 1975), (iv) improved alignment of the fetus for passage through the pelvis ('drive angle') (Gold 1950), and (v) radiological evidence of larger antero‐posterior (Borell 1957b) and transverse (Russell 1969) pelvic outlet diameters, resulting in an increase in the total outlet area in the squatting (Gupta 1991; Lilford 1989; Russell 1982) and kneeling positions (Russell 1982).
We wanted to assess the maternal position in second stage of labour in women without epidural anaesthesia. There is a Cochrane Review in which epidural anaesthesia was assessed in the same population (Kemp 2013), but there is evidence that epidural anaesthesia can result in an increase in instrumental deliveries (Anim‐Somuah 2011). We therefore wanted to assess the effects of posture alone on birth outcomes.
Why it is important to do this review
Given the uncertainty regarding the optimal birth position, our aim was to evaluate the available evidence about the effectiveness, benefits and possible disadvantages for the use of different positions during the second stage of labour in women without epidural anaesthesia. A separate Cochrane Review has addressed women with epidural anaesthesia (Kemp 2013).
Objectives
To determine the possible benefits and risks of the use of different birth positions during the second stage of labour without epidural anaesthesia, on maternal, fetal, neonatal and caregiver outcomes.
Methods
Criteria for considering studies for this review
Types of studies
Any randomised controlled trial, including cluster‐randomised trials, that:
used random or quasi‐random allocation and appropriate follow‐up;
compared positions listed in the Review's types of interventions.
Cross‐over trials were not appropriate for the subject of this review and were not included. Trials in abstract form were included.
Types of participants
Pregnant women during the second stage of labour irrespective of choice of anaesthesia after randomisation.
Types of interventions
The main comparison was the use of any upright position during the second stage of labour compared with supine or lithotomy positions. Secondary comparisons included different upright positions and the supine position.
The various positions can be broadly categorised as being either neutral or upright (Atwood 1976). The neutral positions, in which a line connecting the centre of a woman's third and fifth vertebrae is more horizontal than vertical, which are generally used in modern Western obstetrics, are defined as supine positions:
lateral (Sim's) position;
dorsal (lying on back);
semi‐recumbent (trunk tilted forwards up to 30º to the horizontal);
lithotomy position; and
Trendelenburg's position (head lower than pelvis).
There are distinct upright positions (with gravity involved), namely:
sitting (obstetric chair/stool);
kneeling;
squatting (unaided or using squatting bars); and
squatting (aided with birth cushion).
Comparisons between any upright position during the second stage of labour compared with supine positions were eligible for inclusion.
Types of outcome measures
Primary outcomes
Maternal outcomes
Duration of second stage of labour
Secondary outcomes
Maternal outcomes
Pain.
Use of any analgesia or anaesthesia.
Mode of birth: assisted birth.
Mode of birth: caesarean section.
Trauma to the birth canal that required suturing: episiotomy.
Trauma to the birth canal that required suturing: second degree tear.
Trauma to the birth canal that required suturing: third or fourth degree tear.
Blood loss greater than 500 mL.
Need for blood transfusion (not pre‐specified).
Manual removal of placenta (not pre‐specified).
Shoulder dystocia (not pre‐specified).
Urinary or faecal incontinence.
Fetal outcomes
Abnormal fetal heart rate patterns needing intervention.
Neonatal outcomes
Admission to neonatal intensive care unit.
Perinatal death.
Search methods for identification of studies
The following methods section of this review is based on a standard template used by Cochrane Pregnancy and Childbirth.
Electronic searches
We searched Cochrane Pregnancy and Childbirth’s Trials Register by contacting their Information Specialist (30 November 2016).
The Register is a database containing over 22,000 reports of controlled trials in the field of pregnancy and childbirth. For full search methods used to populate Pregnancy and Childbirth’s Trials Register including the detailed search strategies for CENTRAL, MEDLINE, Embase and CINAHL; the list of handsearched journals and conference proceedings, and the list of journals reviewed via the current awareness service, please follow this link to the editorial information about the Cochrane Pregnancy and Childbirth in the Cochrane Library and select the ‘Specialized Register’ section from the options on the left side of the screen.
Briefly, Cochrane Pregnancy and Childbirth’s Trials Register is maintained by their Information Specialist and contains trials identified from:
monthly searches of the Cochrane Central Register of Controlled Trials (CENTRAL);
weekly searches of MEDLINE (Ovid);
weekly searches of Embase (Ovid);
monthly searches of CINAHL (EBSCO);
handsearches of 30 journals and the proceedings of major conferences;
weekly current awareness alerts for a further 44 journals plus monthly BioMed Central email alerts.
Search results were screened by two people and the full text of all relevant trial reports identified through the searching activities described above is reviewed. Based on the intervention described, each trial report is assigned a number that corresponds to a specific Pregnancy and Childbirth review topic (or topics), and is then added to the Register. The Information Specialist searches the Register for each review using this topic number rather than keywords. This results in a more specific search set which has been fully accounted for in the relevant review sections (Included studies; Excluded studies).
Searching other resources
We searched the reference lists of retrieved studies and contacted authors of published and unpublished trials for additional information when necessary.
We did not apply any language or date restrictions.
Data collection and analysis
For methods used in the previous version of this review, see Gupta 2012.
For this update, the following methods were used for assessing the 17 reports that were identified as a result of the updated search.
The following methods section of this review is based on a standard template used by Cochrane Pregnancy and Childbirth.
Selection of studies
Two review authors independently assessed for inclusion all the potential studies identified as a result of the search strategy. We resolved any disagreement through discussion or, if required, we consulted the third review author.
Data extraction and management
We designed a form to extract data. For eligible studies, two review authors extracted the data using the agreed form. We resolved discrepancies through discussion or, if required, we consulted the third review author. Data were entered into Review Manager software (RevMan 2014) and checked for accuracy.
When information regarding any of the above was unclear, we planned to contact authors of the original reports to provide further details.
Assessment of risk of bias in included studies
Two review authors independently assessed risk of bias for each study using the criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). Any disagreement was resolved by discussion or by involving a third assessor.
(1) Random sequence generation (checking for possible selection bias)
We described for each included study the method used to generate the allocation sequence in sufficient detail to enable assessment of whether it should produce comparable groups.
We assessed the method as:
low risk of bias (any truly random process, e.g. random number table; computer random number generator);
high risk of bias (any non‐random process, e.g. odd or even date of birth; hospital or clinic record number); or
unclear risk of bias.
(2) Allocation concealment (checking for possible selection bias)
We described for each included study the method used to conceal allocation to interventions prior to assignment and assessed whether intervention allocation could have been foreseen in advance of, or during recruitment, or changed after assignment.
We assessed the methods as:
low risk of bias (e.g. telephone or central randomisation; consecutively numbered sealed opaque envelopes);
high risk of bias (open random allocation; unsealed or non‐opaque envelopes, alternation; date of birth); or
unclear risk of bias.
(3.1) Blinding of participants and personnel (checking for possible performance bias)
We described for each included study the methods used, if any, to blind study participants and personnel from knowledge of which intervention a participant received. We considered that studies were at low risk of bias if they were blinded, or if we judged that the lack of blinding unlikely to affect results. We assessed blinding separately for different outcomes or classes of outcomes.
We assessed the methods as:
low, high or unclear risk of bias for participants; and
low, high or unclear risk of bias for personnel.
(3.2) Blinding of outcome assessment (checking for possible detection bias)
We described for each included study the methods used, if any, to blind outcome assessors from knowledge of which intervention a participant received. We assessed blinding separately for different outcomes or classes of outcomes.
We assessed methods used to blind outcome assessment as:
low, high or unclear risk of bias.
(4) Incomplete outcome data (checking for possible attrition bias due to the amount, nature and handling of incomplete outcome data)
We described for each included study, and for each outcome or class of outcomes, the completeness of data including attrition and exclusions from the analysis. We stated whether attrition and exclusions were reported and the numbers included in the analysis at each stage (compared with the total randomised participants), reasons for attrition or exclusion where reported, and whether missing data were balanced across groups or were related to outcomes. Where sufficient information was reported, or could be supplied by the trial authors, we planned to re‐include missing data in the analyses which we undertook.
We assessed methods as:
low risk of bias (e.g. no missing outcome data; missing outcome data balanced across groups);
high risk of bias (e.g. numbers or reasons for missing data imbalanced across groups; ‘as treated’ analysis done with substantial departure of intervention received from that assigned at randomisation); or
unclear risk of bias.
(5) Selective reporting (checking for reporting bias)
We described for each included study how we investigated the possibility of selective outcome reporting bias and what we found.
We assessed the methods as:
low risk of bias (where it is clear that all of the study’s pre‐specified outcomes and all expected outcomes of interest to the review have been reported);
high risk of bias (where not all the study’s pre‐specified outcomes have been reported; one or more reported primary outcomes were not pre‐specified; outcomes of interest are reported incompletely and so cannot be used; study fails to include results of a key outcome that would have been expected to have been reported); or
unclear risk of bias.
(6) Other bias (checking for bias due to problems not covered by (1) to (5) above)
We described for each included study any important concerns we had about other possible sources of bias.
(7) Overall risk of bias
We made explicit judgements about whether studies were at high risk of bias, according to the criteria given in the Handbook (Higgins 2011). With reference to (1) to (6) above, we planned to assess the likely magnitude and direction of the bias and whether we considered it is likely to impact on the findings. In future updates, we will explore the impact of the level of bias through undertaking sensitivity analyses ‐ seeSensitivity analysis.
Assessment of the quality of the evidence using the GRADE approach
For this update, the quality of the evidence was assessed using the GRADE approach as outlined in the GRADE handbook to assess the quality of the body of evidence relating to the following outcomes for the main comparison: any upright position versus supine position.
Duration of second stage of labour;
Mode of birth: assisted birth;
Mode of birth: caesarean section;
Trauma to the birth canal that required suturing: Second degree tear;
Trauma to the birth canal that required suturing: Third/fourth degree tear;
Blood loss greater than 500 mL; and
Admission to neonatal intensive care unit.
GRADEpro Guideline Development Tool was used to import data from Review Manager 5.3 (RevMan 2014) to create a ’Summary of findings’ table. A summary of the intervention effect and a measure of quality for each of the above outcomes were produced using the GRADE approach. The GRADE approach uses five considerations (study limitations, consistency of effect, imprecision, indirectness and publication bias) to assess the quality of the body of evidence for each outcome. The evidence can be downgraded from 'high quality' by one level for serious (or by two levels for very serious) limitations, depending on assessments for risk of bias, indirectness of evidence, serious inconsistency, imprecision of effect estimates or potential publication bias.
Measures of treatment effect
Dichotomous data
For dichotomous data, we presented results as summary risk ratio with 95% confidence intervals.
Continuous data
We used the mean difference if outcomes were measured in the same way between trials. In future updates, if appropriate, we will use the standardised mean difference to combine trials that measure the same outcome, but use different methods.
Unit of analysis issues
Cluster‐randomised trials
There were no cluster‐randomised trials included in this review. In future updates, cluster‐randomised trials will be included and analysed alongside individually randomised trials. We will adjust their sample sizes or standard errors using the methods described in the Handbook Section 16.3.4 or 16.3.6 using an estimate of the intracluster correlation co‐efficient (ICC) derived from the trial (if possible), from a similar trial or from a study of a similar population. If we use ICCs from other sources, we will report this and conduct sensitivity analyses to investigate the effect of variation in the ICC. If we identify both cluster‐randomised trials and individually‐randomised trials, we plan to synthesise the relevant information. We will consider it reasonable to combine the results from both if there is little heterogeneity between the study designs and the interaction between the effect of intervention and the choice of randomisation unit is considered to be unlikely.
Cross‐over trials
There were no cross‐over trials identified in this review. Cross‐over design trials are not appropriate for inclusion in this review, and will not be included in future updates.
Dealing with missing data
Levels of attrition were noted for included studies. In future updates, if more eligible studies are included, the impact of including studies with high levels of missing data in the overall assessment of treatment effect will be explored by using sensitivity analysis.
As far as possible analyses for all outcomes were conducted on an intention‐to‐treat basis, i.e. we attempted to include all participants randomised to each group in the analyses. The denominator for each outcome in each trial was the number randomised minus any participants whose outcomes were known to be missing.
Assessment of heterogeneity
We assessed statistical heterogeneity in each meta‐analysis using the Tau², I² and Chi² statistics. We regarded heterogeneity as substantial if I² was greater than 30% and either Tau² was greater than zero, or there was a low P value (less than 0.10) in the Chi² test for heterogeneity. If we identified substantial heterogeneity (above 30%), we planned to explore it by pre‐specified subgroup analysis. We considered whether an overall summary was meaningful, and if it was, we used random‐effects analysis to produce it.
Assessment of reporting biases
Where we included 10 or more studies in the meta‐analysis we investigated reporting biases (such as publication bias) using funnel plots. We assessed funnel plot asymmetry visually. If asymmetry was suggested by a visual assessment, we planned to perform exploratory analyses to investigate it.
Data synthesis
We carried out statistical analysis using the Review Manager software (RevMan 2014). We used fixed‐effect meta‐analysis for combining data where it was reasonable to assume that studies were estimating the same underlying treatment effect: i.e. where trials were examining the same intervention, and the trials’ populations and methods were judged sufficiently similar.
If there was clinical heterogeneity sufficient to expect that the underlying treatment effects differed between trials, or if substantial statistical heterogeneity was detected, we used random‐effects meta‐analysis to produce an overall summary if an average treatment effect across trials was considered clinically meaningful. The random‐effects summary will be treated as the average range of possible treatment effects and we will discuss the clinical implications of treatment effects differing between trials. If the average treatment effect is not clinically meaningful, we will not combine trials. If we used random‐effects analyses, the results were presented as the average treatment effect with 95% confidence intervals, and the estimates of Tau² and I².
Subgroup analysis and investigation of heterogeneity
If we identified substantial heterogeneity, we investigated it using subgroup analyses and sensitivity analyses. We considered whether an overall summary was meaningful, and if it was, we used random‐effects analysis to produce it.
We carried out the following subgroup analyses.
Parity (primigravidae versus multigravida women).
Subgroup analysis was restricted to the review's primary outcome where there was sufficient data to make subgroup analysis meaningful.
We assessed subgroup differences by interaction tests available within RevMan (RevMan 2014). We reported the results of subgroup analyses quoting the Chi² statistic and P value, and the interaction test I² value.
Sensitivity analysis
We carried out sensitivity analyses to explore the effect of trial quality assessed by concealment of allocation, high attrition rates, or both, with poor quality studies being excluded from the analyses in order to assess whether this makes any difference to the overall result. This sensitivity analysis was only carried out for the GRADE outcomes in the main comparison (upright versus supine), and the results are recorded under the relevant outcomes in comparison 1.
Results
Description of studies
This updated review now has 32 trials, with review outcome data for 30 studies (9015 women), 17 excluded studies, and one ongoing study.
Results of the search
From the November 2016 search, 18 new reports of 12 trials were identified. Nine new trials were added with outcome data for 1735 women to the review (Amiri 2012; Azhari 2013; Calvo Aguilar 2013; Phumdoung 2010; Phumdoung 2013; Sekhavat 2009; Schirmer 2011; Zaibunnisa 2015; Zhang 2016) and two trials excluded (Corton 2012; Thies‐Lagergren 2011). Two trials previously excluded due to none reporting of outcomes have been in included in this update (Liu 1986 and Schneider‐Affeld 1982). One trial previously included has now been excluded as it was found to compare two recumbent positions (Brément 2007). One trial is ongoing (Hofmeyr 2015). See Figure 1.
1.
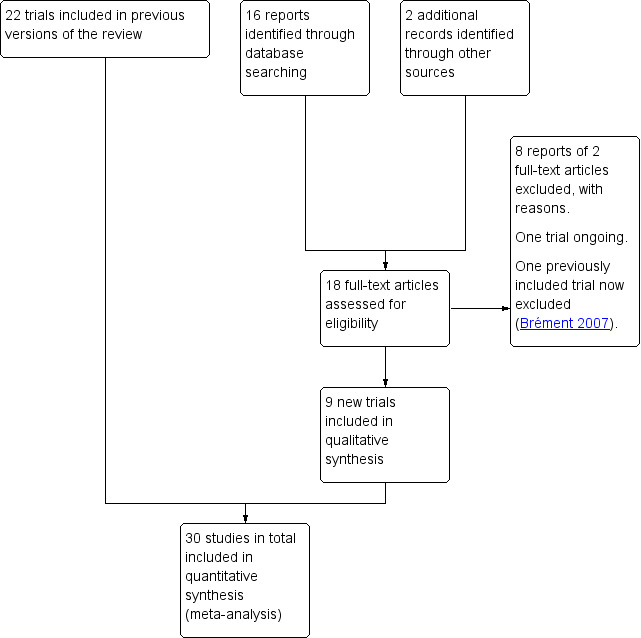
Study flow diagram.
Included studies
For more information, seeCharacteristics of included studies.
Methods
This review includes 32 randomised controlled trials, with outcome data from 30 trials.
Participants
Of trials contributing outcome data, fourteen studies reported on nulliparous women and five with multiparous women; 15 stated recruiting both parous and nulliparous women. Most trials included women at more than 36 weeks' gestation with no obstetric or medical complications. Exceptions were Crowley 1991, who included women at 34 weeks' gestation, and Hemminki 1986, who included women at 35 weeks' gestation.
Interventions and comparisons
All included studies reported on any upright position versus supine (Allahbadia 1992; Amiri 2012; Azhari 2013; Bhardwaj 1994; Bomfim‐Hyppólito 1998; Calvo Aguilar 2013; Chan 1963; Crowley 1991; De Jong 1997; Gardosi 1989a; Gardosi 1989b; Gupta 1989; Hemminki 1986; Hillan 1984; Jahanfar 2004; Liddell 1985; Liu 1986; Marttila 1983; Nasir 2007; Phumdoung 2010; Phumdoung 2013; Racinet 1999; Radkey 1991; Schneider‐Affeld 1982; Schirmer 2011; Sekhavat 2009; Stewart 1989; Suwanakam 1988; Turner 1986; Waldenström 1991; Zaibunnisa 2015; Zhang 2016).
We included 10 trials that compared women in supine position with those using a birthing or squat stool (Allahbadia 1992; De Jong 1997; Gardosi 1989a; Gardosi 1989b; Gupta 1989; Jahanfar 2004; Nasir 2007; Racinet 1999; Radkey 1991; Waldenström 1991). Three trials compared supine position with birth cushion (Bhardwaj 1994; Gardosi 1989a; Gardosi 1989b) and nine trials compared supine with birth chair (Bomfim‐Hyppólito 1998; Crowley 1991; Hemminki 1986; Hillan 1984; Liddell 1985; Marttila 1983; Stewart 1989; Suwanakam 1988; Turner 1986).
Settings
Most studies were conducted in hospital settings. Studies were distributed from various parts of the world. Out of 30 studies with outcome data, seven were from the UK, nine from Asian sub continent, five from EU, four from America and the remaining three from Middle east, one from Cape Town and one from New Zealand. The two studies without outcome data did not specify the setting.
Outcomes
Outcomes reported by most studies were maternal use of analgesia or anaesthesia, duration of second stage of labour, mode of birth, perineal tears or episiotomy, and blood loss greater than 500 mL. Incidence of urinary and faecal incontinence was not reported in any trial.
Funding
Funding sources were not specifically reported in the included studies.
Excluded studies
We excluded 17 trials because:
insufficient data were presented in abstract reports (4 trials: Ahmed 1985; Bonoan 1997; Caldeyro‐Barcia 1985; Hegab 2002);
not a randomised trial (Golay 1993);
multiple number of exclusions from the analysis (37%) (Chen 1987);
wrong population: women received an epidural prior to randomisation (2 trials: Downe 2004; Karraz 2003);
wrong intervention: intervention not continued into the active phase of labour (Golara 2002); comparing upright positions (3 trials: Altman 2007; Corton 2012; Ragnar 2006); comparing recumbent/supine positions (3 trials: Brément 2007; Humphrey 1973; Johnstone 1987); two trials investigated a birth seat with any other position (Thies‐Lagergren 2009; Thies‐Lagergren 2011); because other positions were not classified, comparison of upright position versus the birth seat was not possible. (See Characteristics of excluded studies).
Ongoing studies
The Gentle Assisted Pushing (GAP) trial is ongoing (Hofmeyr 2015; Characteristics of ongoing studies).
Risk of bias in included studies
Overall, risk of bias in the included trials was variable. Blinding of participants, personnel and outcome assessors was either not performed or unclear in all trials (Figure 2).
2.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
Random sequence generation was assessed at low risk of bias in eight trials, high risk in nine trials and unclear risk in 15 trials. Allocation concealment was classified as low risk in one trial, high risk in nine trials and unclear risk in 22 trials. Trials assessed as unclear risk of selection bias did not clearly describe randomisation or allocation methods. The nine trials that were at high risk of selection bias for randomisation and allocation issues (Bhardwaj 1994; Bomfim‐Hyppólito 1998; Chan 1963; Gardosi 1989a; Gardosi 1989b; Jahanfar 2004; Nasir 2007; Suwanakam 1988) were quasi‐randomised trials dependent on, for example, hospital admission, hospital number and height.
Blinding
Due to the nature of the intervention, it was not possible for women or carers to be blinded. Sekhavat 2009 did not provide adequate information to inform a judgement and was assessed as unclear risk of performance bias. In most studies it was unclear if an attempt was made to blind outcome assessors. Four studies reported that the attending midwife or research assistant, who were not blind to the allocation, assessed outcomes and were therefore assessed at high risk of detection bias (Gardosi 1989a; Gardosi 1989b; Phumdoung 2010; Stewart 1989).
Incomplete outcome data
Most trials reported complete outcome data (23 trials); while three trials were unclear risk of bias. Trials assessed at high risk of bias reported either post‐randomisation exclusions (Crowley 1991; Gupta 1989; Schirmer 2011; Turner 1986), missing data (Hemminki 1986; Racinet 1999; Zhang 2016), or both (Phumdoung 2013).
Selective reporting
Of the 32 included trials, nine (one at high risk of bias, eight at unclear risk) demonstrated selective reporting; 23 trials reported all data. Phumdoung 2013 was assessed as high risk of bias for this domain due to reporting data for several outcomes for all women rather than by position in second stage.
Other potential sources of bias
No other sources of bias were identified for any trials.
Effects of interventions
See: Table 1
We found that in many analyses, data were inconsistent with varying levels of heterogeneity. We analysed data as presented in the studies, and therefore advise cautious interpretation of results. Random‐effects meta‐analysis was conducted as an overall summary when considered appropriate.
Comparison 1: Any upright position compared with supine position
Primary outcome
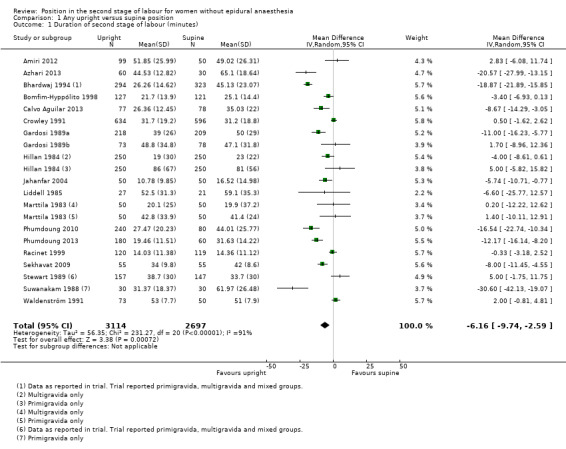
Duration of second stage
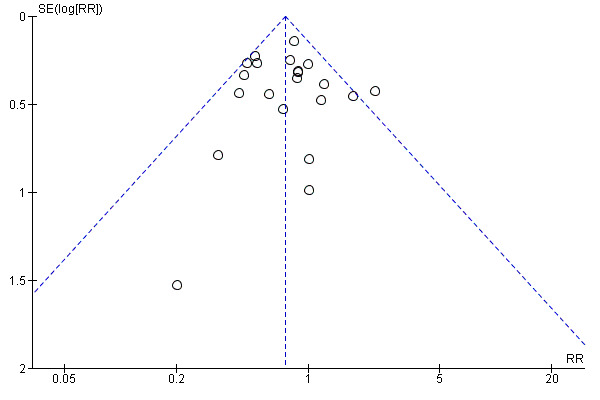
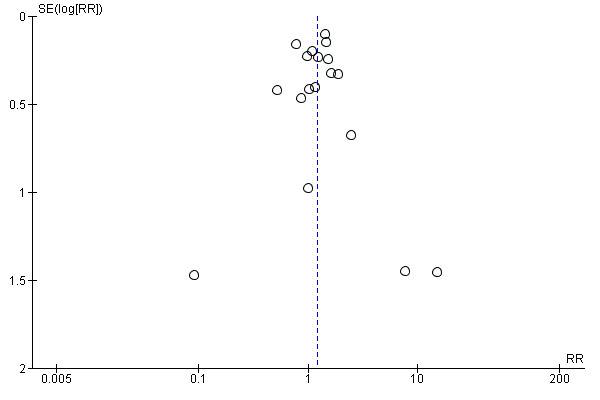
For all women allocated to upright positions the duration of the second stage of labour was reduced by a mean of 6.16 minutes (95% CI ‐9.74 to ‐2.59 minutes; 19 trials; 5811 women; P = 0.0007; random‐effects; I² = 91%; Tau² = 56.35; Analysis 1.1, Figure 3) (very low‐quality evidence). Because 19 trials contributed data to this analysis we plotted results on a funnel plot; visual examination suggested asymmetry with more pronounced treatment effects in some of the smaller studies; asymmetry may indicate publication bias and results should therefore be interpreted cautiously (Figure 3). We acknowledge extreme variability in mean duration, difference and standard deviations of the contributing data; therefore, we cannot be certain of these results. It is possible that the studies contributing data measured the duration of second stage from different time points.
1.1. Analysis.
Comparison 1 Any upright versus supine position, Outcome 1 Duration of second stage of labour (minutes).
3.
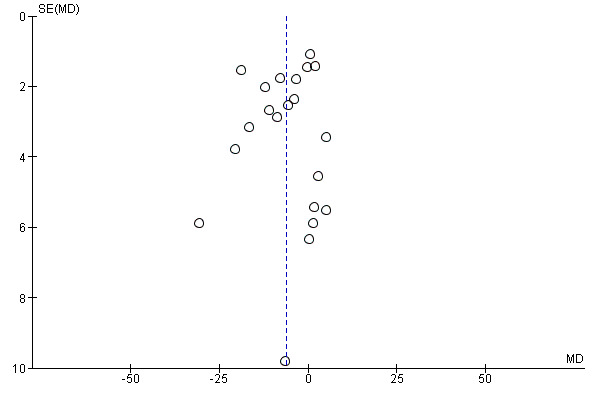
Funnel plot of comparison: 1 Any upright versus supine position, outcome: 1.1 Duration of second stage of labour (minutes).
For primigravid women only, duration of the second stage of labour was reduced by a mean of 7.8 minutes (95% CI ‐12.68 to ‐2.92 minutes; 14 trials; 3826 women; I² = 89%; Analysis 1.15). However, we found high levels of heterogeneity among trials. There was no evidence of subgroup differences among primiparous, multiparous, and mixed parity groups (test for subgroup differences: Chi² = 3.41, df = 2, P = 0.18, I² = 41.3%).
1.15. Analysis.
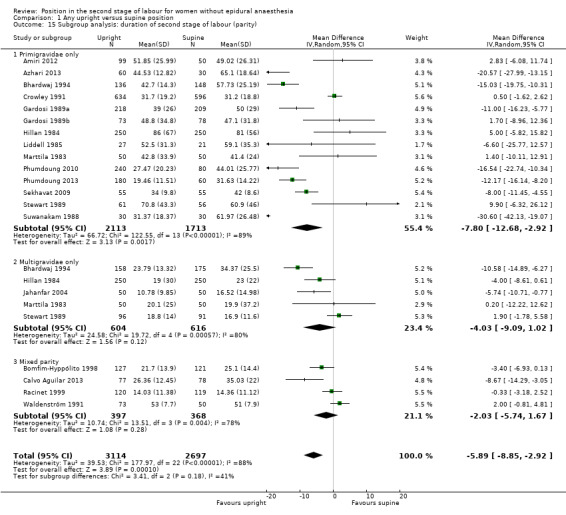
Comparison 1 Any upright versus supine position, Outcome 15 Subgroup analysis: duration of second stage of labour (parity).
We excluded nine trials (Bhardwaj 1994; Bomfim‐Hyppólito 1998; Crowley 1991; Gardosi 1989a; Gardosi 1989b; Jahanfar 2004; Phumdoung 2013; Racinet 1999; Suwanakam 1988) from this analysis as part of a sensitivity analysis based on trial quality (assessed by concealment of allocation, high attrition rates, or both). Excluding these trials resulted in a trend toward reduction of the second stage by a mean of 4.34 minutes (MD ‐4.34, 95% CI ‐9.00 to 0.32; 21 trials; 2499 women; I² = 85%; Analysis 5.1) for women in upright positions, although the CIs crossed the line of no effect and high level heterogeneity was present.
5.1. Analysis.
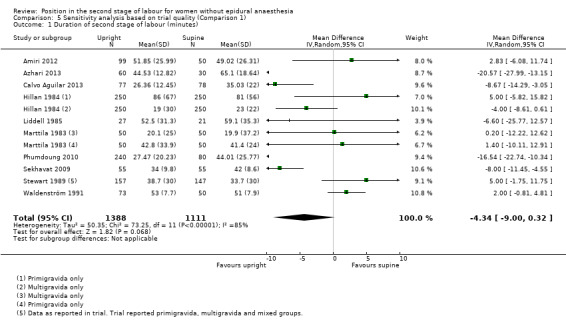
Comparison 5 Sensitivity analysis based on trial quality (Comparison 1), Outcome 1 Duration of second stage of labour (minutes).
Secondary outcomes
Pain
Four trials (Azhari 2013; Calvo Aguilar 2013; Phumdoung 2010; Phumdoung 2013) reported pain in the second stage of labour and postpartum (with higher scores indicating worse pain). Data from these studies contributed to subgroup reporting, such as distress, sensation, intensity in second stage, visual analogue scale scores (Analysis 1.2); however, data could not be pooled because studies used different ways to measure the same outcome. Overall, most trials (Azhari 2013; Phumdoung 2010; Phumdoung 2013) reported reduction in pain experienced by women in upright positions.
1.2. Analysis.
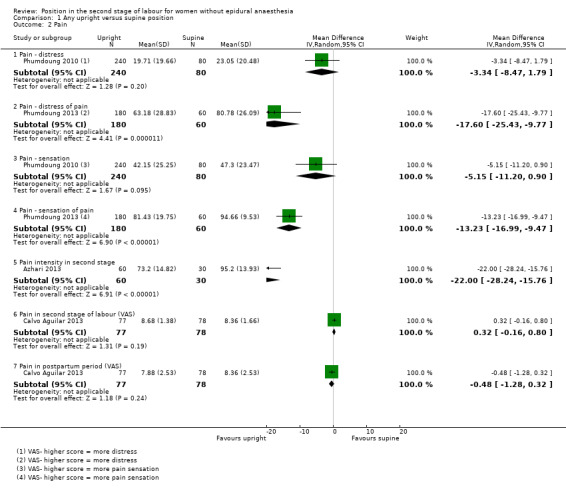
Comparison 1 Any upright versus supine position, Outcome 2 Pain.
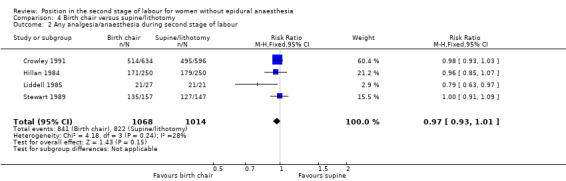
Use of any analgesia or anaesthesia
The upright position may lead to fewer women requiring analgesia or anaesthesia during the second stage of labour. However, the CIs crossed the line of no effect, so this result is not certain (RR 0.97, 95% CI 0.93 to 1.02; 7 trials; 3093 women; I² = 30%; Analysis 1.3). If there is an effect, it is likely to be very small.
1.3. Analysis.
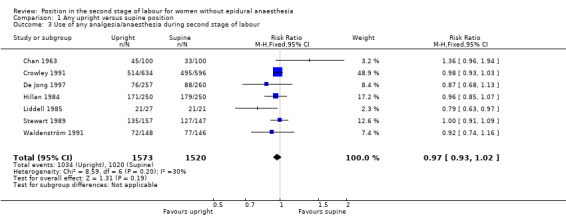
Comparison 1 Any upright versus supine position, Outcome 3 Use of any analgesia/anaesthesia during second stage of labour.
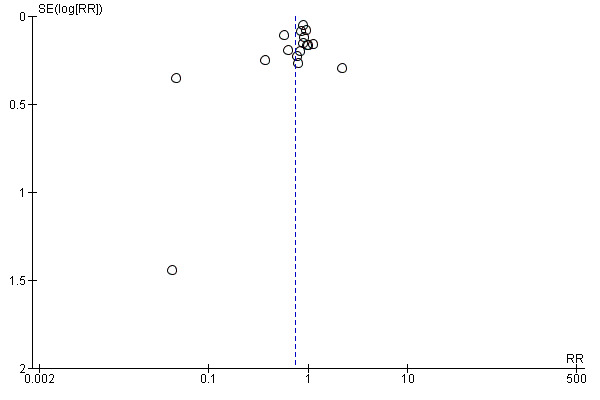
Mode of birth: assisted birth
There was a reduction in assisted deliveries (RR 0.75, 95% CI 0.66 to 0.860; 21 trials; 6481 women; Analysis 1.4, Figure 4) (moderate‐quality evidence). Because more than 10 trials contributed data to the analysis we constructed a funnel plot to look for any evidence of asymmetry which may suggest publication bias. Apart from one study there was no clear evidence of asymmetry from visual examination of the plot (Figure 4). A sensitivity analysis based on trial quality produced similar results for this outcome (RR 0.71, 95% CI 0.56 to 0.90; 21 trials; 2534 women; I² = 30%; Analysis 5.2).
1.4. Analysis.
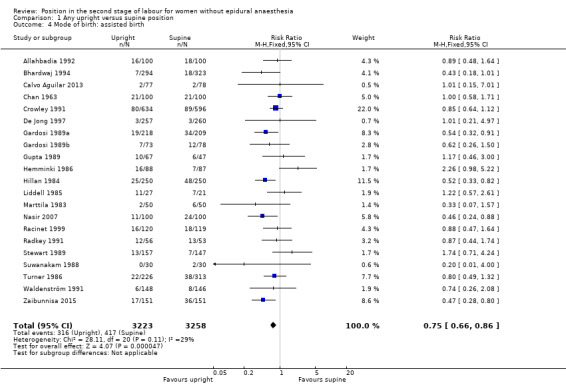
Comparison 1 Any upright versus supine position, Outcome 4 Mode of birth: assisted birth.
4.
Funnel plot of comparison: 1 Any upright versus supine position, outcome: 1.4 Mode of birth: assisted birth.
5.2. Analysis.
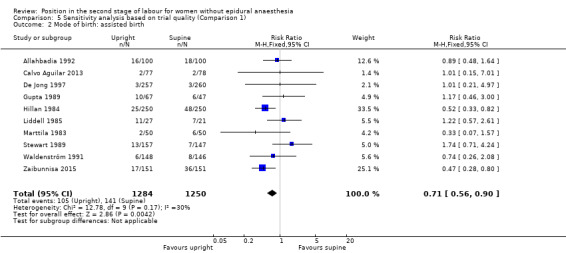
Comparison 5 Sensitivity analysis based on trial quality (Comparison 1), Outcome 2 Mode of birth: assisted birth.
Mode of birth: caesarean section
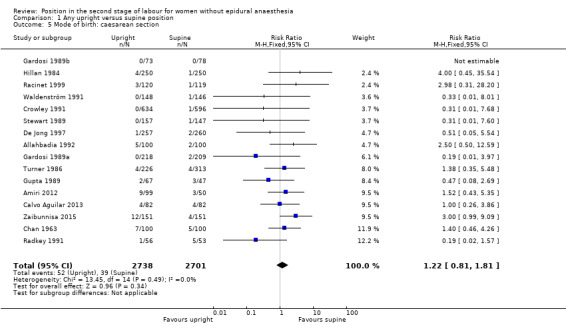
There was no clear difference in rates of caesarean section (RR 1.22, 95% CI 0.81 to 1.81; 16 trials; 5439 women; Analysis 1.5, Figure 5) (low‐quality evidence). There was no clear evidence of funnel plot asymmetry from visual examination.
1.5. Analysis.
Comparison 1 Any upright versus supine position, Outcome 5 Mode of birth: caesarean section.
5.
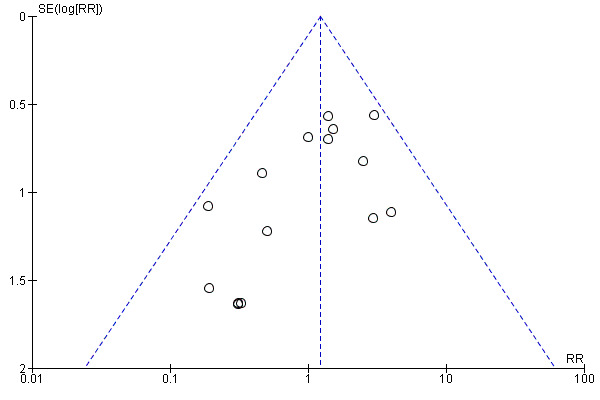
Funnel plot of comparison: 1 Any upright versus supine position, outcome: 1.5 Mode of birth: caesarean section.
Removing low quality trials from this analysis produced similar results for this outcome, with wide CIs crossing the line of no effect (RR 1.47, 95% CI 0.88 to 2.46; 16 trials; 2544 women; Analysis 5.3).
5.3. Analysis.
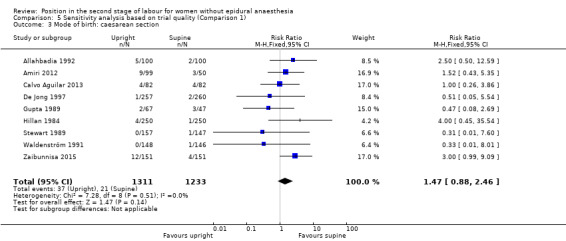
Comparison 5 Sensitivity analysis based on trial quality (Comparison 1), Outcome 3 Mode of birth: caesarean section.
Trauma to the birth canal that required suturing: episiotomy
Fewer episiotomies were performed for women randomised to upright position groups (average RR 0.75, 95% CI 0.61 to 0.92; 17 trials; 6148 women; random‐effects, I² = 88%; Tau² = 0.13; Analysis 1.6, Figure 6). There was some evidence of funnel plot asymmetry from visual examination, although it was difficult to assess if publication bias was present or not due to similar precision of many studies, and heterogeneity in the rates of outcomes between different trials. There was wide variation in episiotomy rates among the included studies, however, individual results from larger trials tended to favour reduction in episiotomy rates for upright positions. Episiotomy is heavily influenced by factors including policy, individual practice, and instrumental birth, therefore, results from this analysis should be interpreted with caution.
1.6. Analysis.
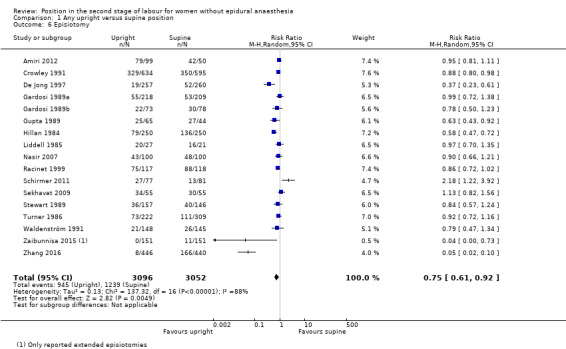
Comparison 1 Any upright versus supine position, Outcome 6 Episiotomy.
6.
Funnel plot of comparison: 1 Any upright versus supine position, outcome: 1.6 Episiotomy.
Trauma to the birth canal that required suturing: second degree perineal tear
Fewer episiotomies among women randomised to upright position groups was partly offset by a possible increase in second degree perineal tears, although the result touched the line of no effect (RR 1.20, 95% CI 1.00 to 1.44; 18 trials; 6715 women; random‐effects, I² = 43%; Tau² = 0.05; Analysis 1.7, Figure 7) (low‐quality evidence). There was no clear evidence of funnel plot asymmetry for this outcome from visual examination.
1.7. Analysis.
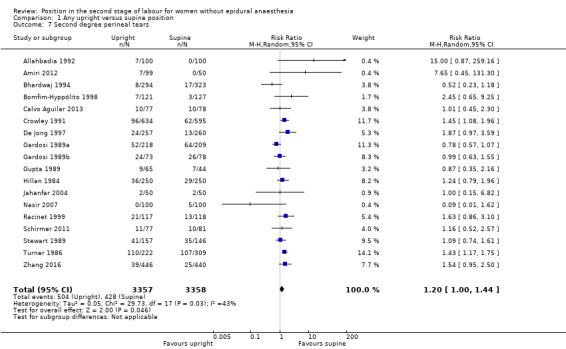
Comparison 1 Any upright versus supine position, Outcome 7 Second degree perineal tears.
7.
Funnel plot of comparison: 1 Any upright versus supine position, outcome: 1.7 Second degree perineal tears.
The sensitivity analysis based on trial quality produced similar results, but the CIs no longer crossed the line of no effect (RR 1.35, 95% CI 1.10 to 1.67; 9 trials; 2977 women; fixed‐effect; Analysis 5.4). Slightly more women in the upright position experienced second degree tear.
5.4. Analysis.
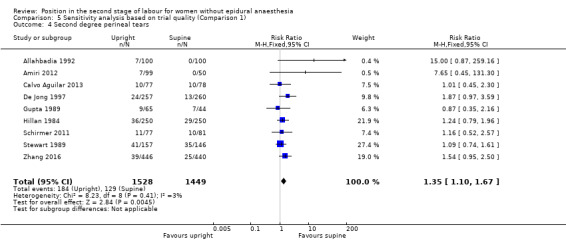
Comparison 5 Sensitivity analysis based on trial quality (Comparison 1), Outcome 4 Second degree perineal tears.
Trauma to the birth canal that required suturing: third or fourth degree tear
There was no clear difference in the number of third or fourth degree perineal tears between women in upright and supine positions (RR 0.72, 95% CI 0.32 to 1.65; 6 trials; 1840 women; Analysis 1.8) (very low‐quality evidence).
1.8. Analysis.
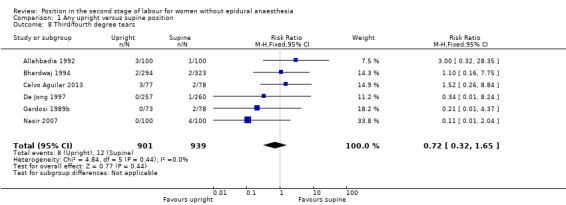
Comparison 1 Any upright versus supine position, Outcome 8 Third/fourth degree tears.
There was no clear difference among groups in the sensitivity analysis (RR 1.46, 95% CI 0.44 to 4.79; 6 trials; 872 women; Analysis 5.5).
5.5. Analysis.

Comparison 5 Sensitivity analysis based on trial quality (Comparison 1), Outcome 5 Third/fourth degree tears.
Blood loss greater than 500 mL
Estimated blood loss greater than 500 mL was more common in women allocated to the upright position (RR 1.48, 95% CI 1.10 to 1.98; 15 trials; 5615 women; random‐effects; I² = 33%; Tau² = 0.10; Analysis 1.9, Figure 8) (moderate‐quality evidence). There appeared to be funnel plot asymmetry which may suggest possible publication bias; some of the smaller studies appear to have larger effect sizes.
1.9. Analysis.
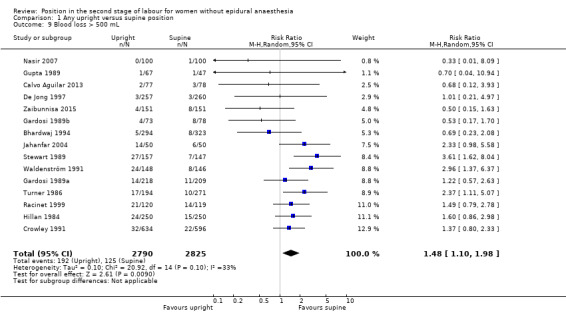
Comparison 1 Any upright versus supine position, Outcome 9 Blood loss > 500 mL.
8.
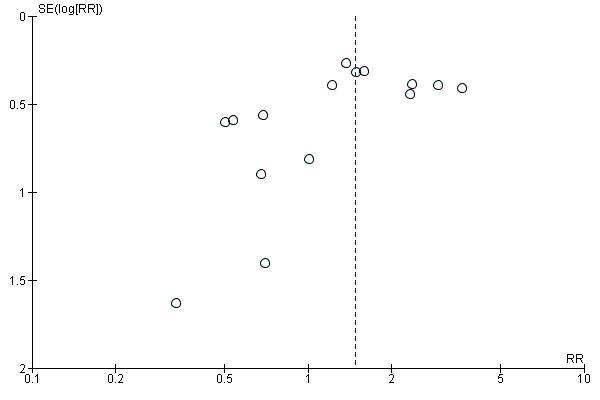
Funnel plot of comparison: 1 Any upright versus supine position, outcome: 1.9 Blood loss > 500 mL.
There was no clear difference in blood loss between groups when low quality trials were excluded from the analysis (RR 1.59, 95% CI 0.90 to 2.80; 15 trials; 2186 women; random‐effects; I² = 47%; Tau² = 0.24; Analysis 5.6).
5.6. Analysis.
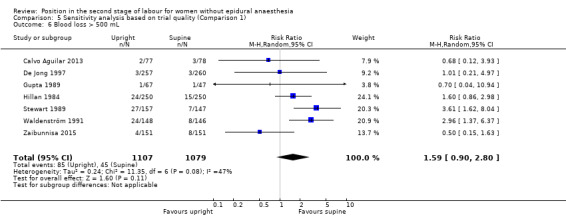
Comparison 5 Sensitivity analysis based on trial quality (Comparison 1), Outcome 6 Blood loss > 500 mL.
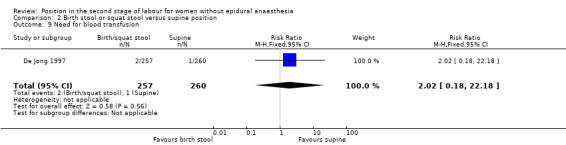
Need for blood transfusion (not pre‐specified)
There was no clear difference in numbers of blood transfusions for women in upright and supine positions (RR 1.66, 95% CI 0.70 to 3.94; 2 trials; 1747 women; Analysis 1.10).
1.10. Analysis.
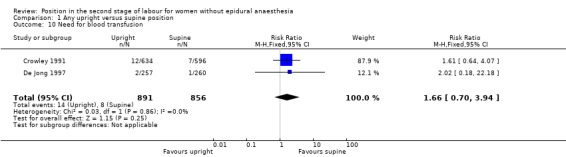
Comparison 1 Any upright versus supine position, Outcome 10 Need for blood transfusion.
Manual removal of placenta (not pre‐specified)
There was no clear difference in numbers of manual removals for women in upright and supine positions (RR 1.15, 95% CI 0.64 to 2.08; 5 trials; 2020 women; I² = 38%; Tau² = 0.60; Analysis 1.11).
1.11. Analysis.
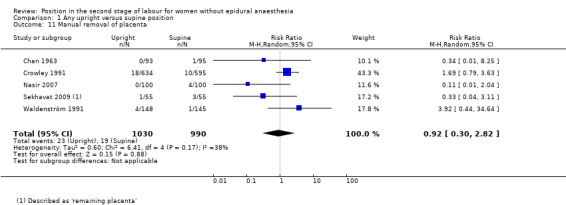
Comparison 1 Any upright versus supine position, Outcome 11 Manual removal of placenta.
Shoulder dystocia (not pre‐specified)
Shoulder dystocia was not reported in any of the included studies.
Urinary or faecal incontinence
The incidence of urinary or faecal incontinence was not reported in any of the included studies.
Abnormal fetal heart rate patterns needing intervention
Fewer abnormal fetal heart rate patterns were recorded for the upright position (RR 0.46, 95% CI 0.22 to 0.93; 2 trials; 617 women; Analysis 1.12).
1.12. Analysis.
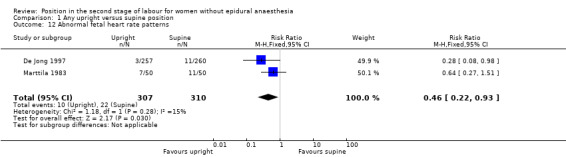
Comparison 1 Any upright versus supine position, Outcome 12 Abnormal fetal heart rate patterns.
Admission to neonatal intensive care unit
There was no clear difference in numbers of babies admitted to neonatal intensive care whose mothers gave birth in upright and supine positions (RR 0.79, 95% CI 0.51 to 1.21; 4 trials; 2565 infants; Analysis 1.13) (low‐quality evidence).
1.13. Analysis.
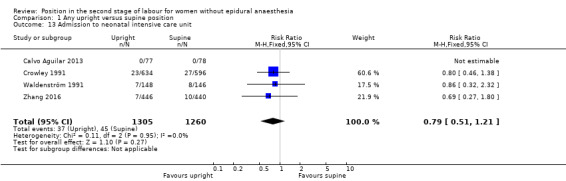
Comparison 1 Any upright versus supine position, Outcome 13 Admission to neonatal intensive care unit.
A similar result was found in the sensitivity analysis after excluding low quality studies (RR 0.86, 95% CI 0.32 to 2.32; 4 trials; 449 infants; Analysis 5.7).
5.7. Analysis.
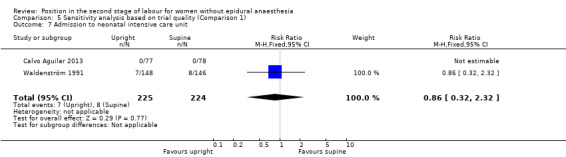
Comparison 5 Sensitivity analysis based on trial quality (Comparison 1), Outcome 7 Admission to neonatal intensive care unit.
Perinatal death
There was no clear difference in the perinatal mortality rate between women in upright and supine positions (RR 0.79, 95% CI 0.51 to 1.21; 4 trials; 982 infants; Analysis 1.14).
1.14. Analysis.
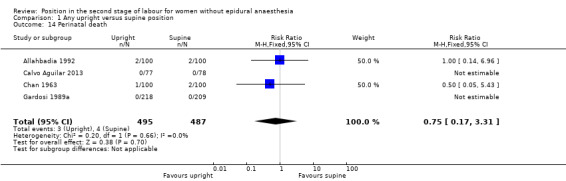
Comparison 1 Any upright versus supine position, Outcome 14 Perinatal death.
Comparison 2: Birth stool or squatting stool compared with supine position
Primary outcome
Duration of second stage labour
The effect of the use of a birth or squatting stool on the duration of second stage of labour showed no difference to the supine position in the four trials reporting this outcome (MD ‐0.57, 95% CI ‐3.83 to 2.68; 4 trials; 613 women; random‐effects, I² = 58%; Tau² = 5.81; Analysis 2.1).
2.1. Analysis.
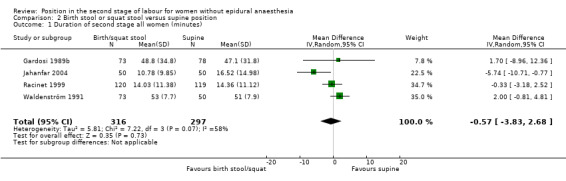
Comparison 2 Birth stool or squat stool versus supine position, Outcome 1 Duration of second stage all women (minutes).
Secondary outcomes
Pain
Pain was not reported in any of the included studies.
Use of any analgesia or anaesthesia
Fewer women in the birth stool group may have used analgesia or anaesthesia compared with women in supine position. However, the CIs crossed the line of no effect (RR 0.90, 95% CI 0.76 to 1.06; 2 trials; 811 women; Analysis 2.2).
2.2. Analysis.
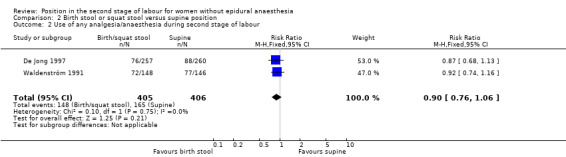
Comparison 2 Birth stool or squat stool versus supine position, Outcome 2 Use of any analgesia/anaesthesia during second stage of labour.
Mode of birth: assisted birth
Fewer women may require assisted births if they use a birth or squatting stool; the CIs just crossed the line of no effect (RR 0.77, 95% CI 0.58 to 1.01; 8 trials; 1824 women; Analysis 2.3).
2.3. Analysis.
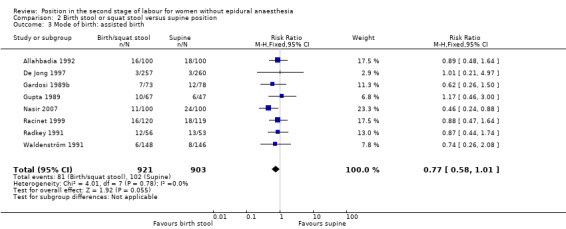
Comparison 2 Birth stool or squat stool versus supine position, Outcome 3 Mode of birth: assisted birth.
Mode of birth: caesarean section
There was no clear difference in the rates of caesarean section between women using a birth or squatting stool and in a supine position (RR 0.76, 95% CI 0.37 to 1.55; 8 trials; 1824 women; Analysis 2.4).
2.4. Analysis.
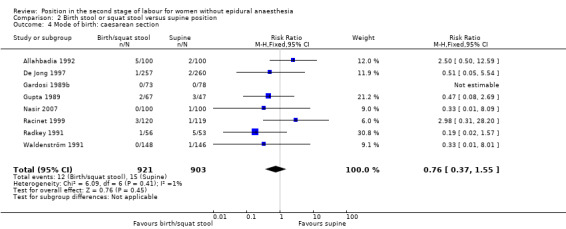
Comparison 2 Birth stool or squat stool versus supine position, Outcome 4 Mode of birth: caesarean section.
Trauma to the birth canal that required suturing: episiotomy
Fewer episiotomies were performed in the birthing stool or squatting position (RR 0.82, 95% CI 0.72 to 0.92; 7 trials; 1930 women; Analysis 2.5).
2.5. Analysis.
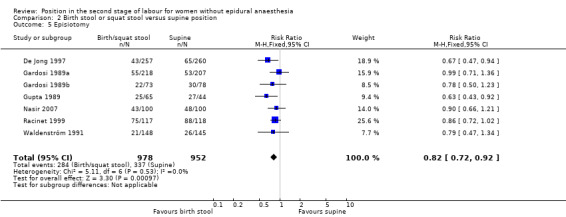
Comparison 2 Birth stool or squat stool versus supine position, Outcome 5 Episiotomy.
Trauma to the birth canal that required suturing: second degree perineal tear
There was no clear difference in the second degree perineal tear rate between women randomised to birthing or squatting stool versus supine position (average RR 1.34, 95% CI 0.79 to 2.27; 7 trials; 1505 women; random‐effects, I² = 51%; Tau² = 0.21; Analysis 2.6).
2.6. Analysis.
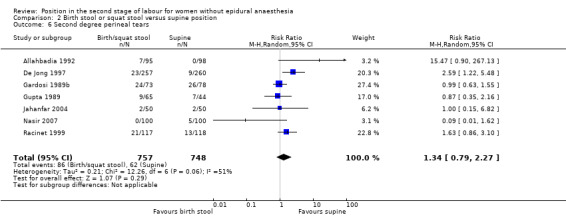
Comparison 2 Birth stool or squat stool versus supine position, Outcome 6 Second degree perineal tears.
Trauma to the birth canal that required suturing: third and fourth degree tear
There was no clear difference in the third and fourth degree tear rates (RR 0.49, 95% CI 0.16 to 1.48; 4 trials; 1061 women; Analysis 2.7) between women randomised to birthing or squatting stool versus supine position.
2.7. Analysis.
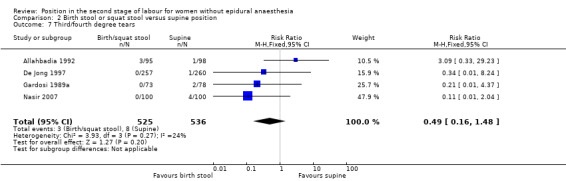
Comparison 2 Birth stool or squat stool versus supine position, Outcome 7 Third/fourth degree tears.
Blood loss greater than 500 mL
There was an increase in estimated blood loss greater than 500 mL in women who gave birth using birth or squat stools (RR 1.54, 95% CI 1.05 to 2.26; 7 trials; 1615 women; Analysis 2.8).
2.8. Analysis.
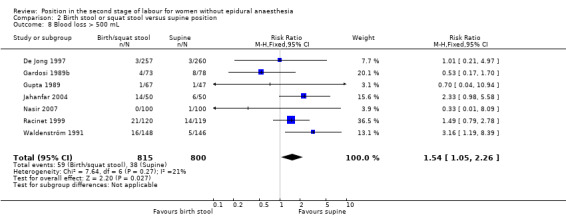
Comparison 2 Birth stool or squat stool versus supine position, Outcome 8 Blood loss > 500 mL.
Need for blood transfusion (not pre‐specified)
There was no difference in the need for blood transfusion between groups (RR 2.02, 95% CI 0.18 to 22.18; 1 trial; 517 women; Analysis 2.9).
2.9. Analysis.
Comparison 2 Birth stool or squat stool versus supine position, Outcome 9 Need for blood transfusion.
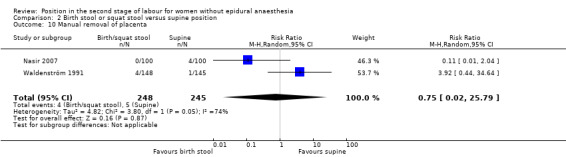
Manual removal of placenta (not pre‐specified)
There was no clear difference in the number of women who required manual removal of placenta (average RR 0.75, 95% CI 0.02 to 25.79; 2 trials; 493 women; I² = 74%; Tau² = 4.82; Analysis 2.10) between women randomised to birthing or squatting stool versus supine position.
2.10. Analysis.
Comparison 2 Birth stool or squat stool versus supine position, Outcome 10 Manual removal of placenta.
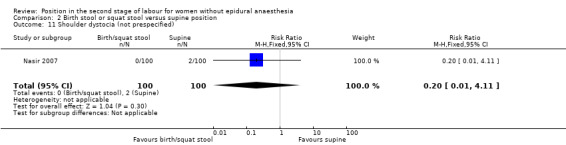
Shoulder dystocia (not pre‐specified)
There was no clear difference in numbers of shoulder dystocias between women randomised between birthing or squatting stool versus supine position (RR 0.20, 95% CI 0.01 to 4.11; 1 trial; 200 women; Analysis 2.11).
2.11. Analysis.
Comparison 2 Birth stool or squat stool versus supine position, Outcome 11 Shoulder dystocia (not prespecified).
Urinary or faecal incontinence
The incidence of urinary or faecal incontinence was not reported in any of the included studies.
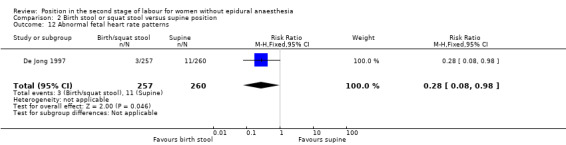
Abnormal fetal heart rate patterns
Fewer abnormal fetal heart rate patterns were detected in the birth or squatting stools group but this difference was border line and based on data from one trial (RR 0.28, 95% CI 0.08 to 0.98; 1 trial; 517 women; Analysis 2.12).
2.12. Analysis.
Comparison 2 Birth stool or squat stool versus supine position, Outcome 12 Abnormal fetal heart rate patterns.
Admission to neonatal intensive care unit
There was no clear difference in numbers of babies admitted to intensive care between birth stool or squatting stool compared with supine position (RR 0.86, 95% CI 0.32 to 2.30; 1 trial; 295 women; Analysis 2.13).
2.13. Analysis.
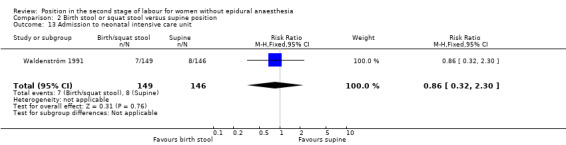
Comparison 2 Birth stool or squat stool versus supine position, Outcome 13 Admission to neonatal intensive care unit.
Perinatal death
There was no clear difference between birth stool or squatting stool and supine position groups in rates of perinatal mortality (RR 1.00, 95% CI 0.14 to 6.96; 1 trial; 200 women; Analysis 2.14).
2.14. Analysis.
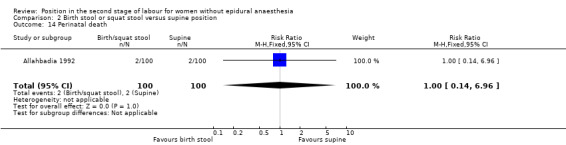
Comparison 2 Birth stool or squat stool versus supine position, Outcome 14 Perinatal death.
Comparison 3: Birth cushion compared with supine position
Primary outcome
Duration of second stage labour
Women allocated to using birth cushions had shorter second stages of labour. Trials were assessed as low quality and high levels of heterogeneity were present (average MD ‐10.64, 95% CI ‐20.15 to ‐1.12; 3 trials; 1193 women; random‐effects, I² = 89%; Tau² = 59.43; Analysis 3.1). Results between subgroups (primigravid and multigravid women) were very similar (Analysis 3.9).
3.1. Analysis.
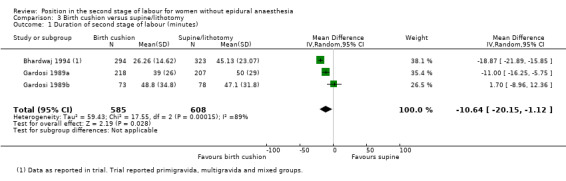
Comparison 3 Birth cushion versus supine/lithotomy, Outcome 1 Duration of second stage of labour (minutes).
3.9. Analysis.
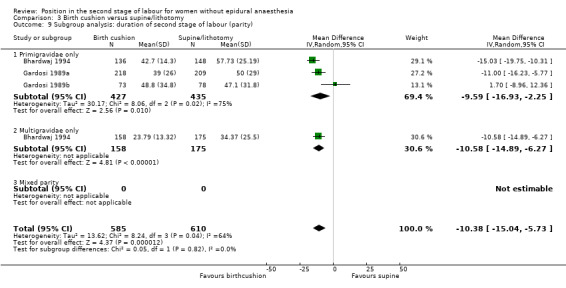
Comparison 3 Birth cushion versus supine/lithotomy, Outcome 9 Subgroup analysis: duration of second stage of labour (parity).
Secondary outcomes
Pain
Pain was not reported in any of the included studies.
Use of any analgesia or anaesthesia
Use of analgesia or anaesthesia was not reported in any of the included studies.
Mode of birth: assisted birth
There were fewer assisted deliveries among women using the birth cushion (RR 0.50, 95% CI 0.32 to 0.78; 2 trials; 1044 women; Analysis 3.2).
3.2. Analysis.
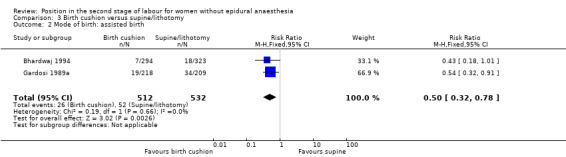
Comparison 3 Birth cushion versus supine/lithotomy, Outcome 2 Mode of birth: assisted birth.
Mode of birth: caesarean section
There was no clear difference in the rates of caesarean section between women using the birth cushion and those in supine position (RR 0.19, 95% CI 0.01 to 3.97; 1 trial; 427 women; Analysis 3.3).
3.3. Analysis.
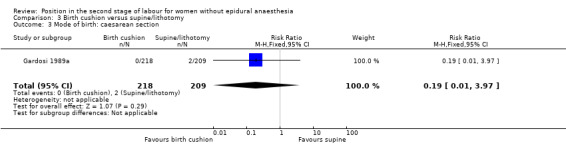
Comparison 3 Birth cushion versus supine/lithotomy, Outcome 3 Mode of birth: caesarean section.
Trauma to the birth canal that required suturing: episiotomy
A similar rate of episiotomies was observed in both birth cushion and supine position groups (RR 0.99, 95% CI 0.71 to 1.36; 1 trial; 425 women; Analysis 3.4).
3.4. Analysis.
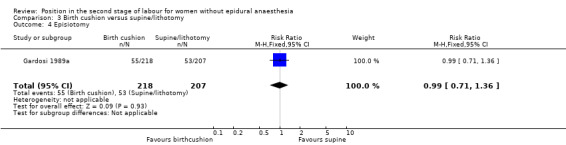
Comparison 3 Birth cushion versus supine/lithotomy, Outcome 4 Episiotomy.
Trauma to the birth canal that required suturing: second degree perineal tear
Fewer second degree perineal tears occurred in women using the birth cushion (RR 0.72, 95% CI 0.54 to 0.97; 2 trials; 1042 women; Analysis 3.5).
3.5. Analysis.
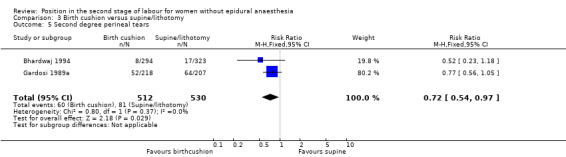
Comparison 3 Birth cushion versus supine/lithotomy, Outcome 5 Second degree perineal tears.
Trauma to the birth canal that required suturing: third and fourth degree tear
Similar rated of third and fourth degree tears were identified (RR 1.10, CI 0.16 to 7.75, 1 trial; 617 women; Analysis 3.6).
3.6. Analysis.
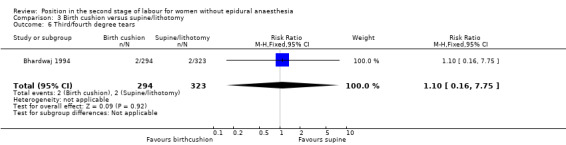
Comparison 3 Birth cushion versus supine/lithotomy, Outcome 6 Third/fourth degree tears.
Blood loss greater than 500 mL
The rate of estimated blood loss greater than 500 mL was not clearly different between groups (RR 1.00, 95% CI 0.54 to 1.88; 2 trials; 1044 women; Analysis 3.7).
3.7. Analysis.
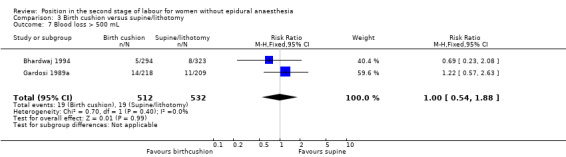
Comparison 3 Birth cushion versus supine/lithotomy, Outcome 7 Blood loss > 500 mL.
Need for blood transfusion (not pre‐specified)
Need for blood transfusion was not reported in any of the included studies.
Manual removal of placenta (not pre‐specified)
Manual removal of placenta was not reported in any of the included studies.
Shoulder dystocia (not pre‐specified)
Shoulder dystocia was not reported in any of the included studies.
Urinary or faecal incontinence
Urinary or faecal incontinence was not reported in any of the included studies.
Abnormal fetal heart rate patterns needing intervention
Abnormal fetal heart rate patters was not reported in any of the included studies.
Admission to neonatal intensive care unit
Admission to neonatal intensive care was not reported in any of the included studies.
Perinatal death
There were no perinatal deaths in one trial that involved 427 women reporting this outcome (Gardosi 1989a; Analysis 3.8).
3.8. Analysis.
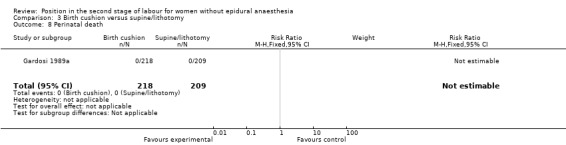
Comparison 3 Birth cushion versus supine/lithotomy, Outcome 8 Perinatal death.
Comparison 4: Birth chair compared with supine position
Primary outcome
Duration of second stage
There was no clear difference between women using birthing chairs or supine positions in duration of the second stage of labour (average MD ‐2.63, 95% CI ‐7.03 to 1.77; 9 trials; 3090 women; I² = 77%; Tau² = 26.93; Analysis 4.1). Subgroup analysis of primigravid, multigravid and mixed parity women revealed no clear differences and high heterogeneity within groups (Analysis 4.11).
4.1. Analysis.
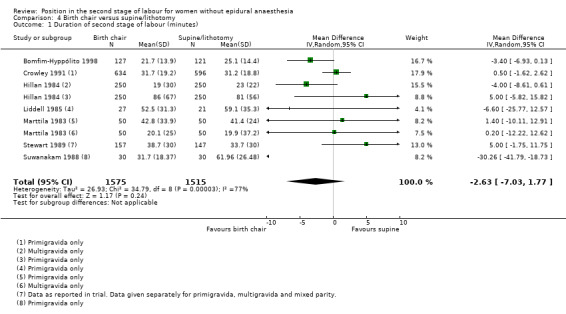
Comparison 4 Birth chair versus supine/lithotomy, Outcome 1 Duration of second stage of labour (minutes).
4.11. Analysis.
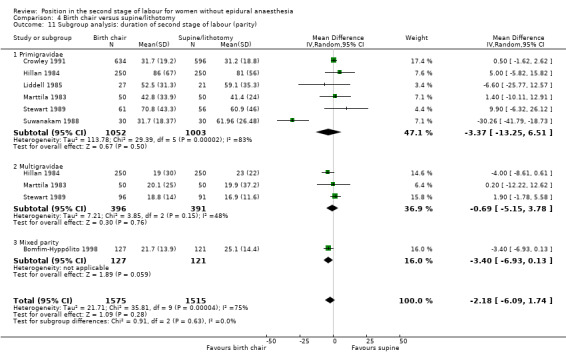
Comparison 4 Birth chair versus supine/lithotomy, Outcome 11 Subgroup analysis: duration of second stage of labour (parity).
Secondary outcomes
Pain
Pain was not reported in any of the included studies.
Use of any analgesia or anaesthesia
Similar numbers of women in the birth chair and supine position groups had any analgesia or anaesthesia during the second stage of labour (RR 0.97, 95% CI 0.93 to 1.01; 4 trials; 2082 women; I² = 28%; Analysis 4.2).
4.2. Analysis.
Comparison 4 Birth chair versus supine/lithotomy, Outcome 2 Any analgesia/anaesthesia during second stage of labour.
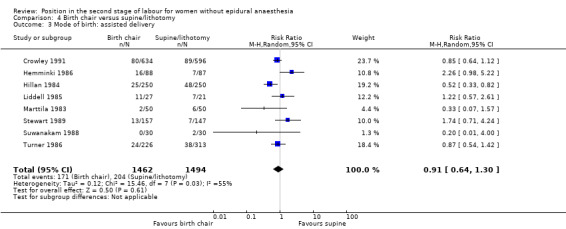
Mode of birth: assisted birth
No clear differences were demonstrated for assisted birth (average RR 0.91, 95% CI 0.64 to 1.30; 8 trials; 2956 women; I² = 55%; Tau² = 0.12; Analysis 4.3).
4.3. Analysis.
Comparison 4 Birth chair versus supine/lithotomy, Outcome 3 Mode of birth: assisted delivery.
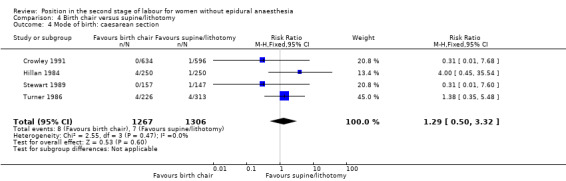
Mode of birth: caesarean section
There was no clear difference in rates of caesarean section between women using the birth chair and those in supine position (RR 1.29, 95% CI 0.50 to 3.32; 4 trials; 2573 women; Analysis 4.4).
4.4. Analysis.
Comparison 4 Birth chair versus supine/lithotomy, Outcome 4 Mode of birth: caesarean section.
Trauma to the birth canal that required suturing: episiotomy
Due to high levels of heterogeneity, we applied a random‐effects model to analyse rates of episiotomy. Rates were lower for women using the birth chair (average RR 0.82, 95% CI 0.68 to 0.99; 5 trials; 2620 women; random‐effects, I² = 71%; Tau² = 0.03; Analysis 4.5).
4.5. Analysis.
Comparison 4 Birth chair versus supine/lithotomy, Outcome 5 Episiotomy.
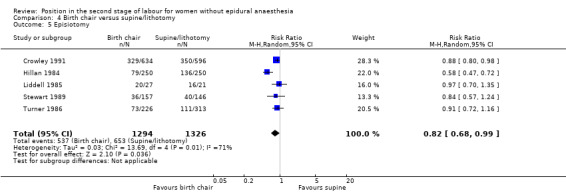
Trauma to the birth canal that required suturing: second degree perineal tears
Rates of second degree perineal tears were increased in the birth chair group (RR 1.37, 95% CI 1.18 to 1.59; 5 trials; 2819 women; Analysis 4.6).
4.6. Analysis.
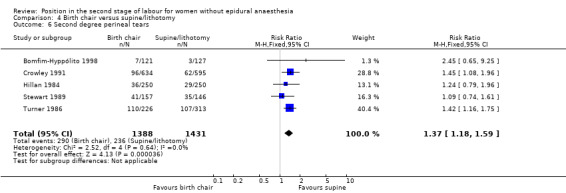
Comparison 4 Birth chair versus supine/lithotomy, Outcome 6 Second degree perineal tears.
Trauma to the birth canal that required suturing: third or fourth degree tear
Third or fourth degree tear was not reported in any of the included studies.
Blood loss greater than 500 mL
Estimated blood loss greater than 500 mL did not differ between groups (average RR 1.57, 95% CI 0.83 to 2.98; 4 trials; 2573 women; random‐effects, I² = 87%; Tau² = 0.35; Analysis 4.7).
4.7. Analysis.
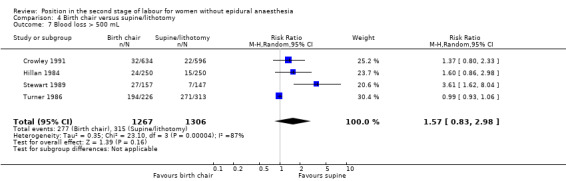
Comparison 4 Birth chair versus supine/lithotomy, Outcome 7 Blood loss > 500 mL.
Need for blood transfusion (not pre‐specified)
No clear difference was found between groups for women requiring blood transfusion (RR 1.61, 95% CI 0.64 to 4.07; 1 trial; 1230 women; Analysis 4.8).
4.8. Analysis.
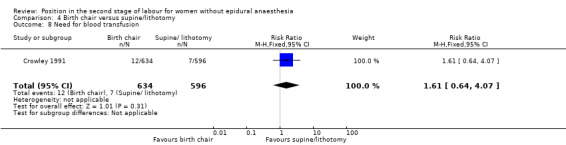
Comparison 4 Birth chair versus supine/lithotomy, Outcome 8 Need for blood transfusion.
Manual removal of placenta (not pre‐specified)
No clear difference was found between groups for women requiring manual removal of placenta (RR 1.69, 95% CI 0.79 to 3.63; 1 trial; 1229 women; Analysis 4.9).
4.9. Analysis.
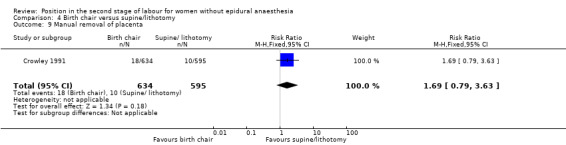
Comparison 4 Birth chair versus supine/lithotomy, Outcome 9 Manual removal of placenta.
Shoulder dystocia (not pre‐specified)
Shoulder dystocia was not reported in any of the included studies.
Urinary or faecal incontinence
Urinary or faecal incontinence was not reported in any of the included studies.
Abnormal fetal heart rate patterns needing intervention.
Abnormal fetal heart rate was not reported in any of the included studies.
Admission to neonatal intensive care unit
Similar numbers of babies were admitted to neonatal intensive care unit (RR 0.80, 95% CI 0.46 to 1.38; 1 trial; 1230 women; Analysis 4.10).
4.10. Analysis.
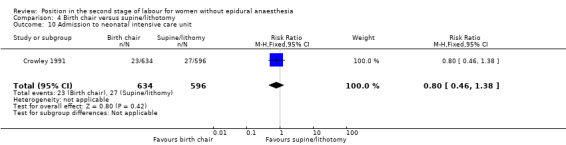
Comparison 4 Birth chair versus supine/lithotomy, Outcome 10 Admission to neonatal intensive care unit.
Perinatal death
Perinatal death was not reported in any of the included studies.
Funnel plots
We constructed and analysed funnel plots to investigate publication bias for six analyses (Analysis 1.1; Analysis 1.4; Analysis 1.5; Analysis 1.6; Analysis 1.7; Analysis 1.9). Funnel plots Figure 4 (Analysis 1.4) and Figure 5 (Analysis 1.5) showed no asymmetry. However, four plots were asymmetrical and suggest publication bias: Figure 3 (Analysis 1.1); Figure 6 (Analysis 1.6); Figure 7 (Analysis 1.7); and Figure 8 (Analysis 1.9).
Discussion
Summary of main results
Variability with risk of bias in trials, inconsistencies within trials, and heterogeneity of analyses, mean that results should be interpreted with caution. Furthermore, because blinding was not possible, negative or positive attitudes of caregivers to new techniques may have influenced the results. With upright postures, there was an overall reduction in duration of second stage of labour, largely contributed by the use of a birth cushion. No clear difference in duration of second stage was found with use of birth chair, birth stool or squatting stool. Fewer women had assisted delivery, for example using forceps, although using birth stools or birth chairs showed no effect. The number of women requiring caesarean section did not differ. Fewer women had episiotomies, those who did were mainly allocated to use of birthing stools or chairs, although there was a tendency for more women to have perineal tears in upright positions. There was no difference in numbers of women with serious perineal tears between those giving birth in upright or supine positions. Women were more likely to have blood losses of 500 mL or more in the upright position but this may be associated with more accurate ways of measuring blood loss. There was also a possibility of publication bias for blood loss (funnel plot asymmetry). Fewer babies had problems with fast or irregular heart rates that indicate distress in two trials (617 women) when women gave birth in an upright position although the number of admissions to the neonatal unit did not differ.
Overall completeness and applicability of evidence
The primary review outcome was reduction in duration of second stage labour, which has been demonstrated among women giving birth in the upright position. Most trials reported this outcome but the overall reduction in duration was small (less than 10 minutes) in the context of the whole duration of second stage labour. The largest reduction was achieved with the use of the birth cushion but these studies were conducted in the late 1980s. We are not aware if these cushions are commonly used in current obstetrics practice in other areas of the world; subsequent studies using these cushions have not been reported. The high heterogeneity for this outcome suggests that the included trials may have used different methods of measuring duration of second stage labour. It is also noteworthy that lack of blinding may have affected care provided for these women, for example rate of vaginal examinations and possible augmentation. Therefore, the overall applicability of the upright position to reduce the duration of second stage labour should be interpreted with caution.
There was no information in the included trials about compliance with allocation, and it is possible that in some trials women may have changed positions throughout second stage labour.
Most trials also reported on the review secondary outcome measures such as pain experienced (reduced), assisted deliveries (reduction), second degree tears (increased) and blood loss greater than 500 mL (increased) with the upright position. These measures can fit into the context of current practice, especially with regard to informing women of these risks during the counselling process.
Quality of the evidence
Overall, risk of bias in the included trials was variable. Blinding of participants, personnel and outcome assessors was either not performed or unclear in all trials (Figure 2).
Using GRADEpro software to assess evidence quality for selected important outcomes, we found moderate quality evidence for assisted birth (21 trials, 6481 women), and blood loss greater than 500 mL (15 trials, 5615 women). There were no outcomes graded as high quality; all other outcomes assessed were graded as either low (caesarean section; second degree perineal tears; admission to neonatal intensive care) or very low (duration of second stage of labour; third or fourth degree tears) quality (Table 1). The main reasons for downgrading GRADE assessment was that several studies had design limitations (inadequate randomisation and allocation concealment) with high heterogeneity and wide confidence intervals crossing the line of no effect.
Publication bias was assessed in funnel plots. Four analyses produced asymmetrical funnel plots (Figure 3 (Analysis 1.1); Figure 6 (Analysis 1.6); Figure 7 (Analysis 1.7); and Figure 8 (Analysis 1.9)) which could suggest that small studies had a large impact on the overall effect in the results and these analyses should be interpreted with caution.
Potential biases in the review process
The research question for this review was specific because another review of women with epidural anaesthesia had been undertaken (Kemp 2013). We attempted to identify all relevant studies and that all relevant data was obtained (non‐English papers were translated and data extracted), and the methods used for searching, study selection, data collection and analysis were completed as per robust Cochrane methodology. We acknowledge that we may have missed some relevant trials because we did not search trials registers such as ClinicalTrials.gov or the WHO International Clinical Trials Registry Platform ((ICTRP), but we will search these registers in the next update.
Agreements and disagreements with other studies or reviews
There was reasonable agreement between our findings and those of a similar Cochrane Review that assessed women in different positions who had epidural anaesthesia (Kemp 2013).
Authors' conclusions
Implications for practice.
The findings of this review suggest several possible benefits of upright posture for women without epidural anaesthesia, such as a small reduction in the duration of second stage of labour (mainly for primigravidae), reduction in episiotomy rates and assisted deliveries. However, there is an increased risk of blood loss greater than 500 mL, and there may be an increased risk of second degree tears, although this remains somewhat uncertain.
Implications for research.
In view of the variable quality of the trials reviewed, further studies using well‐designed protocols are needed. These should include a measure of the skill, confidence and attitudes of the midwives and obstetricians taking part in the trial. Attention must be paid to the way blood loss is measured, such as by haematocrit measurement before and after birth, and direct measurement of the blood loss.
What's new
| Date | Event | Description |
|---|---|---|
| 30 November 2016 | New search has been performed | Eleven new trials have been added to the review (Liu 1986; Schneider‐Affeld 1982; Amiri 2012; Azhari 2013; Calvo Aguilar 2013; Phumdoung 2010; Phumdoung 2013; Sekhavat 2009; Schirmer 2011; Zaibunnisa 2015; Zhang 2016) and two trials excluded (Corton 2012; Thies‐Lagergren 2011). One trial, Hofmeyr 2015, is ongoing. Two studies, previously excluded have been included in this update (Liu 1986; Schneider‐Affeld 1982), although they did not contribute any outcome data. One trial previously included has now been excluded as it was found to compare two recumbent positions(Brément 2007). There are now a total of 32 studies in the review, with 30 trials contributing data. |
| 30 November 2016 | New citation required but conclusions have not changed | Conclusions have not changed. |
History
Protocol first published: Issue 1, 2000 Review first published: Issue 1, 2000
| Date | Event | Description |
|---|---|---|
| 28 February 2012 | New citation required but conclusions have not changed | New co‐author helped prepare this update. The overall conclusions have not changed. |
| 28 February 2012 | New search has been performed | Four new studies, previously awaiting classification, have now been
incorporated into the review: three studies have been included (Bomfim‐Hyppólito 1998; Brement 2007a;
Nasir 2007) and one excluded (Ragnar 2006). Two studies (Humphrey 1973; Johnstone 1987) which were previously included have now been reclassified as excluded studies. New search conducted in February 2012 identified three studies: one has been included (Jahanfar 2004) and two excluded (Altman 2007; Thies‐Lagergren 2011). We also identified additional reports for Bhardwaj 1994; Jahanfar 2004 and Thies‐Lagergren 2011. This updated review is now comprised of 22 included studies and 16 excluded studies. |
| 12 June 2009 | Amended | Search updated. Three reports added to Studies awaiting classification (Brement 2007a; Nasir 2007; Ragnar 2006). |
| 12 May 2009 | Amended | Contact details updated. |
| 20 September 2008 | Amended | Converted to new review format. |
| 12 December 2005 | New search has been performed | New search conducted in September 2005 identified two new studies (Downe 2004; Karraz 2003), which were subsequently excluded. Suwanakam 1988, which was excluded in the previous version, has now been included. Bomfim‐Hyppolito1998a, which was previously excluded as large numbers of women were excluded from the analysis, is now in Characteristics of studies awaiting classification. The trial author has been contacted and has confirmed she will send the required data. These data will be analysed in the next update. Data from the report by Stewart 1983 has been superseded by data from another report for Hillan 1984. The methods section has been updated and sensitivity analysis performed based on excluding trials with clearly inadequate allocation concealment (rated C). The conclusions have not changed. |
| 11 November 2004 | Amended | The title of this Review has changed from 'Position for women during second stage of labour' to 'Position in the second stage of labour for women without epidural anaesthesia'' to differentiate its scope from the newly registered title 'Position in the second stage of labour for women with epidural anaesthesia'. |
| 12 November 2003 | New search has been performed | This update incorporates one new trial, Racinet 1999, and excludes several others. |
Acknowledgements
Cheryl Nikodem was involved in the preparation of the original review (Gupta 1999). We thank Rebecca Smyth for her contribution to the review update (Gupta 2004). We are grateful to Manjeet Shehmar for helping to update the 2012 review (Gupta 2012).
As part of the pre‐publication editorial process, this review has been commented on by two peers (an editor and referee who is external to the editorial team), a member of Cochrane Pregnancy and Childbirth's international panel of consumers and the Group's Statistical Adviser.
We thank Bita Mesgarpour for translating the following three trials Amiri 2012, Azhari 2013 and Sekhavat 2009.
The World Health Organization, Janesh Gupta, Akanksha Sood and G Justus Hofmeyr retain copyright and all other rights in their respective contributions to the manuscript of this Review as submitted for publication.
This project was supported by the National Institute for Health Research, via Cochrane Infrastructure funding to Cochrane Pregnancy and Childbirth. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, NHS or the Department of Health.
Data and analyses
Comparison 1. Any upright versus supine position.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Duration of second stage of labour (minutes) | 19 | 5811 | Mean Difference (IV, Random, 95% CI) | ‐6.16 [‐9.74, ‐2.59] |
| 2 Pain | 4 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 Pain ‐ distress | 1 | 320 | Mean Difference (IV, Random, 95% CI) | ‐3.34 [‐8.47, 1.79] |
| 2.2 Pain ‐ distress of pain | 1 | 240 | Mean Difference (IV, Random, 95% CI) | ‐17.6 [‐25.43, ‐9.77] |
| 2.3 Pain ‐ sensation | 1 | 320 | Mean Difference (IV, Random, 95% CI) | ‐5.15 [‐11.20, 0.90] |
| 2.4 Pain ‐ sensation of pain | 1 | 240 | Mean Difference (IV, Random, 95% CI) | ‐13.23 [‐16.99, ‐9.47] |
| 2.5 Pain intensity in second stage | 1 | 90 | Mean Difference (IV, Random, 95% CI) | ‐22.0 [‐28.24, ‐15.76] |
| 2.6 Pain in second stage of labour (VAS) | 1 | 155 | Mean Difference (IV, Random, 95% CI) | 0.32 [‐0.16, 0.80] |
| 2.7 Pain in postpartum period (VAS) | 1 | 155 | Mean Difference (IV, Random, 95% CI) | ‐0.48 [‐1.28, 0.32] |
| 3 Use of any analgesia/anaesthesia during second stage of labour | 7 | 3093 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.97 [0.93, 1.02] |
| 4 Mode of birth: assisted birth | 21 | 6481 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.75 [0.66, 0.86] |
| 5 Mode of birth: caesarean section | 16 | 5439 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.22 [0.81, 1.81] |
| 6 Episiotomy | 17 | 6148 | Risk Ratio (M‐H, Random, 95% CI) | 0.75 [0.61, 0.92] |
| 7 Second degree perineal tears | 18 | 6715 | Risk Ratio (M‐H, Random, 95% CI) | 1.20 [1.00, 1.44] |
| 8 Third/fourth degree tears | 6 | 1840 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.72 [0.32, 1.65] |
| 9 Blood loss > 500 mL | 15 | 5615 | Risk Ratio (M‐H, Random, 95% CI) | 1.48 [1.10, 1.98] |
| 10 Need for blood transfusion | 2 | 1747 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.66 [0.70, 3.94] |
| 11 Manual removal of placenta | 5 | 2020 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.30, 2.82] |
| 12 Abnormal fetal heart rate patterns | 2 | 617 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.46 [0.22, 0.93] |
| 13 Admission to neonatal intensive care unit | 4 | 2565 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.79 [0.51, 1.21] |
| 14 Perinatal death | 4 | 982 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.75 [0.17, 3.31] |
| 15 Subgroup analysis: duration of second stage of labour (parity) | 19 | 5811 | Mean Difference (IV, Random, 95% CI) | ‐5.89 [‐8.85, ‐2.92] |
| 15.1 Primigravidae only | 14 | 3826 | Mean Difference (IV, Random, 95% CI) | ‐7.80 [‐12.68, ‐2.92] |
| 15.2 Multigravidae only | 5 | 1220 | Mean Difference (IV, Random, 95% CI) | ‐4.03 [‐9.09, 1.02] |
| 15.3 Mixed parity | 4 | 765 | Mean Difference (IV, Random, 95% CI) | ‐2.03 [‐5.74, 1.67] |
Comparison 2. Birth stool or squat stool versus supine position.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Duration of second stage all women (minutes) | 4 | 613 | Mean Difference (IV, Random, 95% CI) | ‐0.57 [‐3.83, 2.68] |
| 2 Use of any analgesia/anaesthesia during second stage of labour | 2 | 811 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.76, 1.06] |
| 3 Mode of birth: assisted birth | 8 | 1824 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.77 [0.58, 1.01] |
| 4 Mode of birth: caesarean section | 8 | 1824 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.76 [0.37, 1.55] |
| 5 Episiotomy | 7 | 1930 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.82 [0.72, 0.92] |
| 6 Second degree perineal tears | 7 | 1505 | Risk Ratio (M‐H, Random, 95% CI) | 1.34 [0.79, 2.27] |
| 7 Third/fourth degree tears | 4 | 1061 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.49 [0.16, 1.48] |
| 8 Blood loss > 500 mL | 7 | 1615 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.54 [1.05, 2.26] |
| 9 Need for blood transfusion | 1 | 517 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.02 [0.18, 22.18] |
| 10 Manual removal of placenta | 2 | 493 | Risk Ratio (M‐H, Random, 95% CI) | 0.75 [0.02, 25.79] |
| 11 Shoulder dystocia (not prespecified) | 1 | 200 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.2 [0.01, 4.11] |
| 12 Abnormal fetal heart rate patterns | 1 | 517 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.28 [0.08, 0.98] |
| 13 Admission to neonatal intensive care unit | 1 | 295 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.86 [0.32, 2.30] |
| 14 Perinatal death | 1 | 200 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.14, 6.96] |
Comparison 3. Birth cushion versus supine/lithotomy.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Duration of second stage of labour (minutes) | 3 | 1193 | Mean Difference (IV, Random, 95% CI) | ‐10.64 [‐20.15, ‐1.12] |
| 2 Mode of birth: assisted birth | 2 | 1044 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.50 [0.32, 0.78] |
| 3 Mode of birth: caesarean section | 1 | 427 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.19 [0.01, 3.97] |
| 4 Episiotomy | 1 | 425 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.71, 1.36] |
| 5 Second degree perineal tears | 2 | 1042 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.72 [0.54, 0.97] |
| 6 Third/fourth degree tears | 1 | 617 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.10 [0.16, 7.75] |
| 7 Blood loss > 500 mL | 2 | 1044 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.54, 1.88] |
| 8 Perinatal death | 1 | 427 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 9 Subgroup analysis: duration of second stage of labour (parity) | 3 | 1195 | Mean Difference (IV, Random, 95% CI) | ‐10.38 [‐15.04, ‐5.73] |
| 9.1 Primigravidae only | 3 | 862 | Mean Difference (IV, Random, 95% CI) | ‐9.59 [‐16.93, ‐2.25] |
| 9.2 Multigravidae only | 1 | 333 | Mean Difference (IV, Random, 95% CI) | ‐10.58 [‐14.89, ‐6.27] |
| 9.3 Mixed parity | 0 | 0 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
Comparison 4. Birth chair versus supine/lithotomy.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Duration of second stage of labour (minutes) | 7 | 3090 | Mean Difference (IV, Random, 95% CI) | ‐2.63 [‐7.03, 1.77] |
| 2 Any analgesia/anaesthesia during second stage of labour | 4 | 2082 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.97 [0.93, 1.01] |
| 3 Mode of birth: assisted delivery | 8 | 2956 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.64, 1.30] |
| 4 Mode of birth: caesarean section | 4 | 2573 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.29 [0.50, 3.32] |
| 5 Episiotomy | 5 | 2620 | Risk Ratio (M‐H, Random, 95% CI) | 0.82 [0.68, 0.99] |
| 6 Second degree perineal tears | 5 | 2819 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.37 [1.18, 1.59] |
| 7 Blood loss > 500 mL | 4 | 2573 | Risk Ratio (M‐H, Random, 95% CI) | 1.57 [0.83, 2.98] |
| 8 Need for blood transfusion | 1 | 1230 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.61 [0.64, 4.07] |
| 9 Manual removal of placenta | 1 | 1229 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.69 [0.79, 3.63] |
| 10 Admission to neonatal intensive care unit | 1 | 1230 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.80 [0.46, 1.38] |
| 11 Subgroup analysis: duration of second stage of labour (parity) | 7 | 3090 | Mean Difference (IV, Random, 95% CI) | ‐2.18 [‐6.09, 1.74] |
| 11.1 Primigravidae | 6 | 2055 | Mean Difference (IV, Random, 95% CI) | ‐3.37 [‐13.25, 6.51] |
| 11.2 Multigravidae | 3 | 787 | Mean Difference (IV, Random, 95% CI) | ‐0.69 [‐5.15, 3.78] |
| 11.3 Mixed parity | 1 | 248 | Mean Difference (IV, Random, 95% CI) | ‐3.40 [‐6.93, 0.13] |
Comparison 5. Sensitivity analysis based on trial quality (Comparison 1).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Duration of second stage of labour (minutes) | 10 | 2499 | Mean Difference (IV, Random, 95% CI) | ‐4.34 [‐7.00, 0.32] |
| 2 Mode of birth: assisted birth | 10 | 2534 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.71 [0.56, 0.90] |
| 3 Mode of birth: caesarean section | 9 | 2544 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.47 [0.88, 2.46] |
| 4 Second degree perineal tears | 9 | 2977 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.35 [1.10, 1.67] |
| 5 Third/fourth degree tears | 3 | 872 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.46 [0.44, 4.79] |
| 6 Blood loss > 500 mL | 7 | 2186 | Risk Ratio (M‐H, Random, 95% CI) | 1.59 [0.90, 2.80] |
| 7 Admission to neonatal intensive care unit | 2 | 449 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.86 [0.32, 2.32] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Allahbadia 1992.
| Methods | Randomised controlled trial. Women were "randomly selected" irrespective of their age, parity, height, weight or baby's weight. | |
| Participants | 200 women at Lokmanya Tilak Municipal General Hospital, Bombay, India.
All women had full term (37 weeks completed) gestation; adequate pelvis; vertex presentation; no medical, surgical or obstetric complications. |
|
| Interventions | Study group: 100 women were kept ambulatory during the first stage of labour and were asked to squat on a birth cot during the second stage of labour. The last 20/42 primigravidae were subjected to prophylactic episiotomies. No support was given to the perineum at the time of birth. Control group: 100 women were kept in a supine position during the first and second stage of labour. All (46) primigravidae were subjected to prophylactic episiotomies. It is not stated whether support was given to the perineum at the time of birth. All women were in the supine position for the third stage of labour. |
|
| Outcomes |
|
|
| Notes | The randomisation method was unclear.
Not stated if support was
given to the perineum at the time of birth in the control group. Intervention group included first stage ambulation and squatting during second stage; control group were supine in first and second stage. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Women were "randomly selected" but there was no description of the randomisation method. |
| Allocation concealment (selection bias) | Unclear risk | Not described in the trial report. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and personnel aware of allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No missing data. |
| Selective reporting (reporting bias) | Low risk | All outcomes reported. |
| Other bias | Low risk | No other bias found. |
Amiri 2012.
| Methods | Randomised controlled trial. | |
| Participants | Taleghani Hospital in Arak, Iran. Primiparous and singleton women with gestational age of 37 to 42 weeks. Inclusion criteria: primiparous and singleton Iranian women, gestational age of 37 to 42 weeks, spontaneous labour, cephalic presentation, birthweight > 2500 g and < 4000 g. Exclusion criteria: prolonged rupture (> 12 hours), medical‐surgical disease in mother, fetal distress, accelerated or prolonged birth. |
|
| Interventions | Lithotomy position, N = 52 Control group 1: squatting position, N = 53. Control group 2: kneeling position, N = 55. |
|
| Outcomes | Times between full dilatation and effacement until the crowning stage, damage to the perineum, Apgar score. | |
| Notes | Outcomes only reported for 50 women (lithotomy), 49 women (squatting) and 55 women (kneeling). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Eligible women were randomised to three groups but there was no information regarding the generation of random sequence. |
| Allocation concealment (selection bias) | Unclear risk | No information provided. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and personnel aware of allocation/birth position. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All data entered. |
| Selective reporting (reporting bias) | Low risk | The study seems to adhere to the protocol IRCT201105113869N3. |
| Other bias | Low risk | None identified. |
Azhari 2013.
| Methods | Randomised controlled trial. | |
| Participants | Nulliparous women in Omolbanin Hospital, Mashhad (Iran), 2011 to 2012. Inclusion criteria: 42 weeks of pregnancy, single fetus, cephalic presentation, intact membranes, lack of infection of medical and midwifery, lack of fetal anomaly ultrasound proved by cervical dilation 3 to 5 cm. Exclusion criteria: women in the first stage or second stage of labour with fetal distress, fetal macrosomia and women, who because of his illness, were unable to get into certain positions. |
|
| Interventions | Intrvention ‐ kneeling, N = 30. Control group 1 ‐ sitting position, N = 30. Control group 2 ‐ supine position, N = 30. |
|
| Outcomes | Pain intensity before and after intervention. Duration of second stage of labour. |
|
| Notes | For the analysis, we combined kneeling and sitting into an “any upright” group. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | They were selected by convenience sampling method. |
| Allocation concealment (selection bias) | Unclear risk | No information provided. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and personnel aware of allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information provided. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All data entered. |
| Selective reporting (reporting bias) | Unclear risk | Protocol could not be located for comparison. |
| Other bias | Low risk | None identified. |
Bhardwaj 1994.
| Methods | Quasi‐randomised controlled trial. Women in labour were randomly allocated on admission in the labour ward to odd or even numbers, irrespective of their outpatient department number. Randomisation occurred before exclusion criteria were applied. Odd numbers = squatting and even numbers = lithotomy. | |
| Participants | 617 women, Latur, India.
All women had full‐term (> 36 weeks completed) gestation; vertex presentation. No medical, surgical or obstetric complications. Exclusion criteria: high‐risk pregnancies; previous caesarean sections; epilepsy; hypertension; jaundice in pregnancy; malaria; heart disease; diabetes; rhesus factor negative; post maturity (> 40 weeks); other than vertex presentation; antepartum haemorrhage; severe anaemia; cephalopelvic disproportion; premature labour; late registration in labour; those who refused to squat. |
|
| Interventions | 750 women were randomised before exclusion criteria were applied. These
included women who were randomised to squat, but who declined to do so. 617 women took part in the study.
All women were allowed to ambulate during the first stage of labour, although most preferred lying down. |
|
| Outcomes |
|
|
| Notes | Only abstract publication was available. Postpartum haemorrhage was not defined but assumed to be > 500 mL. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Inadequate ‐ odd numbers squatting, even numbers lithotomy. |
| Allocation concealment (selection bias) | High risk | Inadequate. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and personnel were aware of allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information provided. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data complete. |
| Selective reporting (reporting bias) | Low risk | All outcomes reported. |
| Other bias | Low risk | No other bias found. |
Bomfim‐Hyppólito 1998.
| Methods | Quasi‐randomised controlled trial. Women were divided into sitting versus lying positions during labour according to their height. If their height ended in an even figure, they were assigned to the sitting position, if in an odd number to the lying position. | |
| Participants | 248 women who delivered at the Maternidade Escola Assis Chateaubriand of
the Ceara Federal University. Included women with a singleton pregnancy at term with a vertex presentation. It excluded women who showed a preference for the other birthing position or who changed their minds during labour, those whose babies were less than 2500 g or heavier than 4000 g in weight and if the birth was any other than spontaneous vaginal. Also excluded seven patients who needed an episiotomy. |
|
| Interventions | 127 participants randomised to vertical (sitting) position during birth
defined as an inclination of the back support of the birth table at 60º with
support for the feet and legs bent at 90°. 121 participants randomised to horizontal (lying) position during birth on an ordinary birthing table. |
|
| Outcomes |
|
|
| Notes | Women who delivered in the vertical position were slightly but significantly younger than those who delivered in the horizontal position. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Dependent on height. If their height ended in an even figure, they were assigned to the sitting position, if in an odd number to the lying position. |
| Allocation concealment (selection bias) | High risk | Inadequate ‐ predetermined allocation according to height. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and personnel were aware of allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information provided. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No incomplete data. |
| Selective reporting (reporting bias) | Low risk | All outcomes reported. |
| Other bias | Low risk | No other bias found. |
Calvo Aguilar 2013.
| Methods | Randomised double blind study. Patients were assigned to the groups
randomly using Windows excel program. Sealed envelopes were used. Set in Mexico. |
|
| Participants | Normal pregnancy, irrespective of parity, gestation age > 36 weeks,
estimated fetal weight not > 3850 g, amniotic fluid volume > 4 cm,
cervical dilatation > 4 cm Patients who underwent caesarean section or were not placed in the corresponding position were excluded. |
|
| Interventions | 164 randomised. Study group, upright, N = 82 (outcomes for 77 reported; 4 had caesarean sections and 1 incomplete data). Control group, supine, N = 82 (outcomes for 78 reported; 4 had caesarean sections). |
|
| Outcomes | Blood loss, pain in the second stage of labour and immediate postpartum, duration of second stage of labour, perineal and vaginal tears, assisted birth, accomodation in position and perinatal outcome. | |
| Notes | Women were able to mobilise in first stage, with random assignment during
the second stage of labour. We used the author’s definition of duration of second stage, rather than adding their second stage plus time to expulsion (although it likely underestimated second stage compared to other trials). Initially 164 patients were recruited, and 5 from group 1 and 4 from group 2 were eliminated (likely post‐randomisation exclusion). Epidural status of enrolled women was not mentioned. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number tables were used. |
| Allocation concealment (selection bias) | Unclear risk | Sealed envelopes. No further information provided. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and personnel likely knew the allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information provided. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 9 women were excluded (post‐randomisation exclusion), however outcomes appear otherwise complete. |
| Selective reporting (reporting bias) | Low risk | All outcomes reported. |
| Other bias | Low risk | No other forms of bias were identified. |
Chan 1963.
| Methods | Quasi‐randomised controlled trial. Alternate primigravidae were assigned to 1 of 2 groups during the first stage of labour. Women in group A were kept in the erect position during first stage of labour; women in group B were kept in bed in the lateral or dorsal position during first stage of labour. During second stage, women in group A (study group) were propped up to 45º to 60º in the birth bed. Women in group B (control) delivered in the dorsal position. | |
| Participants | 200 women, Hong Kong.
Singleton and twin pregnancies were included (1 twin pregnancy in the study group), from 32 weeks' gestation. |
|
| Interventions | Study group: 100 women were kept ambulatory during the first stage of labour and were propped up to 45º to 60º in the bed during the second stage of labour. Control group: 100 women were kept in a supine or lateral position during the first of labour and in the dorsal position during the second stage of labour. |
|
| Outcomes | There were no statistically significant differences between groups
regarding maternal age, gestation or complications during labour.
|
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quasi‐randomisation "Alternate primigravidae, in whom elective caesarean section would not be done, were assigned at random to one of two groups, A and B". |
| Allocation concealment (selection bias) | High risk | Alternate participants. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and personnel were aware of allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information provided. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Complete data. |
| Selective reporting (reporting bias) | Low risk | All outcomes reported. |
| Other bias | Low risk | Nothing declared. |
Crowley 1991.
| Methods | Randomised controlled trial. Randomisation by numbered sealed opaque envelopes just before second stage of labour. | |
| Participants | 1250 women participated, at Coombe Lying‐in Hospital, Dublin between March
1984 and June 1985. There were 20 post randomisation withdrawals. 1230 women's results included.
Only nulliparae. All women had reached 34 weeks' completed gestation. Singleton pregnancies. Vertex presentation. Induced and augmented women were allowed to participate. No epidural anaesthesia. |
|
| Interventions | Study group: 634 women were allocated at the beginning of second stage to deliver in the "E‐Z birth chair" (413/634 did deliver in the chair). The height and angle of the chair were adjusted according to the preference of the midwife and the parturient. Control group: 596 women were allocated to deliver on the bed (576/596 did deliver on the bed). The women used any of the following positions: recumbent, semi‐recumbent, dorsal, or left lateral. | |
| Outcomes | There were no statistically significant differences between the groups for
meconium‐stained liquor, duration of first stage, birthweight and
gestational age.
|
|
| Notes | There were 20 post randomisation withdrawals of whom 7 had been allocated to the chair and 13 to the bed, and these women were not included in the analyses. Only 413/634 allocated to the chair, delivered in the chair and 576/596 allocated to the bed delivered in the bed. Analyses were done according to group allocation (intention‐to‐treat). The above short comings of the trial could have an effect on the results. A subgroup of women were interviewed (263 chair versus 289 bed). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Simple random allocation without balancing. |
| Allocation concealment (selection bias) | Unclear risk | Sealed opaque envelopes. No further information provided. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and personnel aware of allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information provided. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | There were 20 post‐randomisation withdrawals, and these were unbalanced between groups. |
| Selective reporting (reporting bias) | Low risk | All outcomes reported. |
| Other bias | Low risk | No other bias found. |
De Jong 1997.
| Methods | Randomised controlled trial. Randomisation was carried out in late first stage of labour by means of opaque sealed envelopes. | |
| Participants | 517 women, at St Monica’s Nursing Home, Cape Town, South Africa.
All women had full‐term (37 weeks completed) gestation. Singleton pregnancies. No contra‐indications for normal vaginal birth. Vertex presentation. No medical, surgical or obstetric complications. No epidural anaesthesia. |
|
| Interventions | Study group:
257 women were allocated to deliver in the upright
position. 249/257 did maintain the position during second stage. The women
used a 'step stool' covered with a foam mattress to deliver in a squatting
position. They were kept in this position for the third stage of labour. Control group: 260 women delivered in a supine position on a delivery bed. All women were encouraged to walk, sit or recline during the first stage of labour. |
|
| Outcomes | There were no statistically significant differences between groups for
maternal age, gravity, gestation, birthweight or Apgar scores.
|
|
| Notes | Correction on state of perineum and vulva data were incorporated in this review (De Jong 1999). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random sequencing. |
| Allocation concealment (selection bias) | Unclear risk | Opaque sealed envelopes. No further information provided. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and personnel aware of allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient not provided. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data complete. |
| Selective reporting (reporting bias) | Low risk | All outcomes reported. |
| Other bias | Low risk | No other bias found. |
Gardosi 1989a.
| Methods | Quasi‐randomised controlled trial. Randomisation was by adding the last digit of the women's hospital number to the date of admission. The groups were then allocated according to odd and even numbers. | |
| Participants | 427 primigravidae only, Milton Keynes, England.
All women had full‐term (37 weeks completed) gestation. Singleton pregnancies. No contraindications for normal vaginal birth. Vertex presentation. No medical, surgical or obstetric complications. Induced and spontaneous labours were included. No epidural anaesthesia. |
|
| Interventions | Study group:
218 women were allocated to the study group. Upright
second stage positions were defined as squatting using a birth cushion
(156/218), which was placed on the bed or floor. It was made of foam
plastic, and had a 'u' shape and side handles and enabled women to adopt a
modified squatting position during birth. Other upright positions used were
kneeling (15/218) and sitting (8/218). 39 women, who were allocated to
deliver in an upright position, used a semi‐recumbent or lateral position
during second stage. Control group: 209 women allocated to deliver in a conventional recumbent position, propped up to about 30 degrees from the horizontal, or on the side. 22 women spontaneously used an upright position, squatting (10/209), kneeling (6/209) or sitting (6/209) for birth. All women were free to walk about, sit up, or lie in the bed, during the first stage of labour. Episiotomy was not performed routinely. |
|
| Outcomes | There were no statistically significant differences between groups for
maternal age, gestation, birthweight and Apgar scores.
|
|
| Notes | Blood loss was estimated visually. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Addition of last digit of hospital number and the date of their admission and using quasi‐randomisation. |
| Allocation concealment (selection bias) | High risk | Allocated according to whether the sum of their last digit of hospital number and the date of admission was an even or odd number. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and personnel aware of allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Details of labour and its outcome were recorded by the midwife attending the birth. Therefore outcome assessor was not blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data complete. |
| Selective reporting (reporting bias) | Low risk | All outcomes reported. |
| Other bias | Low risk | No other bias found. |
Gardosi 1989b.
| Methods | Quasi‐randomised controlled trial. Randomisation was by adding the last digit of the woman's hospital number to the date of admission. The groups were then allocated according to odd and even numbers. | |
| Participants | 151 primigravidae only, Milton Keynes, England.
All women had full‐term (37 weeks completed) gestation. Maternal age between 16 years and 35 years. Singleton pregnancies. No contraindications for normal vaginal birth. Vertex presentation. No medical, surgical or obstetric complications. Induced and spontaneous labours were included. Had no epidural anaesthesia. |
|
| Interventions | Study group: 73 women were allocated to the study group. Upright second stage positions were defined as squatting, kneeling, sitting upright or standing. Control group: 78 women were allocated to deliver in a conventional recumbent position, propped up to about 30 degrees from the horizontal, or on the side. All women were free to walk about, sit up, or lie in the bed, during first stage of labour. Episiotomy was not done routinely. | |
| Outcomes | There were no statistically significant differences between groups for: maternal age, gestation, Apgar scores or birthweight.
|
|
| Notes | First‐stage positions were not controlled. Blood loss was estimated visually. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Addition of last digit of hospital number and the date of their admission and being a quasi‐randomised trial. |
| Allocation concealment (selection bias) | High risk | Allocated according to whether the sum of their last digit of hospital number and the date of admission was an even or odd number. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and personnel aware of allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Details of labour, outcome and the state of the newborn were recorded by the midwife managing the birth. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data complete. |
| Selective reporting (reporting bias) | Low risk | All outcomes reported. |
| Other bias | Low risk | No other bias found. |
Gupta 1989.
| Methods | Randomised controlled trial. Randomisation was by opaque sealed envelopes, determined by a random‐number generator. Randomisation took place at 30 weeks' gestation. | |
| Participants | 114 women, St. James’s University Hospital, Leeds, England.
No further details of participants available. Women had full‐term (37 weeks completed) gestation. Singleton pregnancies. Adequate pelvis. No contraindications for normal vaginal birth. Vertex presentation. No medical, surgical or obstetric complications. |
|
| Interventions | Study group: 67 women were allocated at 30 weeks of gestation to deliver in a squatting position. These women were asked to attend a special parent craft class, concentrating on special leg exercises. These women were given advice on the advantages of squatting during birth. Women were encouraged to adopt the squatting position when full cervical dilatation had been reached. Control group: 47 women were randomised to deliver in the conventional way. | |
| Outcomes |
|
|
| Notes | Additional data obtained from the author. Data in the published report not in useable format. Women were randomised at 30 weeks and received intensive advice on the benefits of the treatment. Data on duration of the second stage exclude the women who had caesarean sections or assisted deliveries. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number generator. |
| Allocation concealment (selection bias) | Low risk | Opaque sealed envelopes opened by a third party. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and personnel aware of allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information provided. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Not analysed according to intention‐to‐treat. |
| Selective reporting (reporting bias) | Low risk | All outcomes reported according to actual position of birth. |
| Other bias | Low risk | No additional sources of bias identified |
Hemminki 1986.
| Methods | Randomised controlled trial. Randomisation was by means of sealed envelopes in blocks of 10, stratified for gravidity. Women were randomised during the first stage of labour. | |
| Participants | 175 women, Kainuu Central Hospital, Kainuu, Finland.
All women had reached 35 weeks completed gestation. Singleton pregnancies. No contra‐indications for normal vaginal birth. Vertex presentation. No medical, surgical or obstetric complications. |
|
| Interventions | Study group: 88 women were randomised during the first stage of labour to use a birth chair. The mean cervical dilatation when transferred to the chair was 8.8 cm. The chair was made locally and was normally maintained with the back 60º to 70º from the horizontal. 12 women did not deliver in the chair. Control group: 87 women lay on their backs, propped up < 45º from the horizontal. | |
| Outcomes | There were no statistically significant differences between groups for
maternal age, gestation, gravidity, birthweight and Apgar scores.
|
|
| Notes | Data not in a usable format. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was in blocks of 10, stratified for gravidity. |
| Allocation concealment (selection bias) | Unclear risk | Sealed envelopes. No further information provided. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and personnel aware of allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information provided. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Missing data for mothers' preference in the next birth for both groups. In bed group, position in this birth missing for 16 women. These were not addressed. |
| Selective reporting (reporting bias) | Low risk | All outcomes reported. |
| Other bias | Low risk | No other bias found. |
Hillan 1984.
| Methods | Randomised controlled trial. | |
| Participants | 500 women, Glasgow, UK.
All women had singleton pregnancies, at 37 to 42 weeks' gestation, were of mixed parity (250 primigravidae, 250 multigravida), with a cephalic presentation, either in induced or spontaneous labour. |
|
| Interventions | Study group: 250 women were to be delivered in a 'Birth E‐Z' birthing chair. During birth the chair was maintained with the back 15º to 20º from the vertical. Control group: 250 women were to be delivered in a bed in the dorsal recumbent position, but could be propped up to a maximum of 20º from the horizontal. All women could remain ambulant throughout the first stage of labour. | |
| Outcomes | Duration of first stage of labour and active pushing, mode of birth, use of analgesia, blood loss, incidence of perineal damage. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation was in blocks of 10, separately for primiparae and multipara. |
| Allocation concealment (selection bias) | Unclear risk | Sealed envelopes. Allocation was by drawing a sealed envelope towards the end of the first stage of labour. No further information provided. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and personnel aware of allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Information was collected from the patient records, and by questionnaires to midwives and mothers. Does not indicate whether outcome assessors were blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data complete. |
| Selective reporting (reporting bias) | Low risk | All outcomes reported. |
| Other bias | Low risk | No other bias found. |
Jahanfar 2004.
| Methods | Quasi‐randomised controlled trial. Consecutive random sampling method according to the last digit on their registration number. Those with an odd number to the experimental group, even numbers to the control group. | |
| Participants | Multiparous women with singleton uncomplicated pregnancies gestation 38 to 42 weeks. Number in each group was 50. | |
| Interventions | Sitting position in a chair versus lithotomy. | |
| Outcomes | Length of second and third stage of labour, volume of blood loss during the third stage, first and fifth minutes Apgar scores. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Sequence generation by registration number. |
| Allocation concealment (selection bias) | High risk | Able to predict experimental/control group. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and personnel aware of allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information provided. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data complete. |
| Selective reporting (reporting bias) | Low risk | All outcomes reported. |
| Other bias | Low risk | No other bias found. |
Liddell 1985.
| Methods | Randomisation envelopes not opened until second stage of labour diagnosed. Motorised birthing chair used in study. | |
| Participants | 56 primigravid women, Auckland, New Zealand.
All women had 38 to 42 week singleton pregnancies. Both induced and spontaneous labours. |
|
| Interventions | 27 birthing chair; 21 supine. | |
| Outcomes | Epidural: no difference. Significantly less pethidine or no analgesia was used for women on the birthing chair. Duration of first and second stage: no difference. Mode of birth: no difference. Episiotomies, tears, birthweight, fetal distress in second stage, Apgar scores: no difference, but 2 women had extensive second degree tears in the chair. | |
| Notes | 5 women were excluded from analysis because of caesarean section. 3 assigned to use the birthing chair chose not to, and were excluded. 24 out of 27 using birthing chair would use it again in next pregnancy. It gave support to back and relief from back pain. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomly assigned sealed envelopes. Additional information not provided. |
| Allocation concealment (selection bias) | Unclear risk | Sealed envelopes. No further information provided. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and personnel aware of allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information provided. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data complete. |
| Selective reporting (reporting bias) | Low risk | All outcomes reported. |
| Other bias | Low risk | No other bias found. |
Liu 1986.
| Methods | Quasi‐randomized trial | |
| Participants | Setting not described 66 primigravidae women |
|
| Interventions | Group 1 – 30 degree upright with routine bearing down instructions during
second stage Group 2 – 30 degree upright without routine bearing down instructions during second stage Group 3 – zero‐degree recumbent position with bearing down instructions during second stage |
|
| Outcomes | The duration of labour is not reported separately for both groups, only the difference in mean time and p‐values. | |
| Notes | No data for review outcomes of interest could be extracted. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unable to blind participants/personnel to this intervention |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information provided |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information available to assess |
| Selective reporting (reporting bias) | Unclear risk | Insufficient information available to assess |
| Other bias | Low risk | No other sources of bias identified |
Marttila 1983.
| Methods | Randomised trial, although randomisation method unclear. Randomisation at full dilatation. | |
| Participants | 100 women, 60 primiparous and 40 multiparous, Helsinki, Finland. 97 spontaneous labours. 3 augmented labours. 38 to 42 weeks' gestation. Singleton pregnancies. | |
| Interventions | 50 supine position on bed (control). 50 'half‐sitting' (50º) in chair constructed from birth beds. First stage: supine in all except 8 ambulating women at 4 cm to 6 cm dilatation. Episiotomy in all except 2 multiparous women. No analgesia. | |
| Outcomes | Age, parity, gestational age, length of first stage, birthweight: no difference. Mode of birth: all delivered vaginally. Vacuum extraction rate was significantly higher in the supine position. No difference in duration of second stage. Late decelerations were more common in the supine position. | |
| Notes | 86% of women delivering in the supine position would choose this method again and 96% of those in the half‐sitting position. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method not described. |
| Allocation concealment (selection bias) | Unclear risk | Random but not described. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and personnel aware of allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information provided. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data complete. |
| Selective reporting (reporting bias) | Low risk | All outcomes reported. |
| Other bias | Low risk | No other bias found. |
Nasir 2007.
| Methods | Quasi‐randomised controlled trial. Random selection of patients then alternatively divided into squatting or supine position in second stage. | |
| Participants | 200 patients from Department of Obstetrics and Gynaecology, Jinnah
Postgraduate Medical Centre, Karachi. Gestation more than 37 weeks in active labour with cephalic presentation. Excluded patients with multiple gestation, malpresentation, previous scar, maternal fever and prenatal diagnosed fetal malformation. |
|
| Interventions | 100 in squatting position. 100 in control supine in lithotomy. |
|
| Outcomes |
|
|
| Notes | Outlet forceps for prolonged second stage due to inability to push. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Alternate group randomisation (quasi‐randomisation). |
| Allocation concealment (selection bias) | High risk | Able to predict next intervention group. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and personnel aware of allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information provided. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data complete. |
| Selective reporting (reporting bias) | Low risk | All outcomes reported. |
| Other bias | Low risk | No other bias found. |
Phumdoung 2010.
| Methods | 4‐arm randomised controlled trial. | |
| Participants | 320 primiparous women, labour unit of central hospital, Southern
Thailand. Inclusion criteria: primiparous; married; aged 18 years to 35 years; receiving antenatal care for at least the second trimester; 38 to 42 weeks' gestation; fetal heart rate (120 to 160 beats per minute); estimated fetal weight of 2500 tp 4000 g; without any prolonged latent or active phases; and, without any known personal or fetal health complications. |
|
| Interventions | Intervention group: Group 2 PSU locked‐upright position with knees‐to‐chest, N = 80. Group 3 PSU locked‐upright lithotomy position, N = 80. Group 4 upright lithotomy position, N = 80. (Subjects in Groups 2, 3 and 4 had the head of the birth table raised 45º to 60°) Control group: Group 1‐ lithotomy position, N = 80. |
|
| Outcomes | Duration of second stage of labour, pain (sensation and distress) and
comfort during second‐stage labour among primiparous women. Type of birth (vaginal or caesarean section); whether the woman received oxytocin or any type of analgesic drug; and, whether any complications were sustained by the woman during second‐stage labour. |
|
| Notes | In addition, participants in Groups 2 and 3 had their lumbar areas raised
30º to 40°, using a pillow. No information provided regarding use of epidural anaesthesia prior to enrolment. However, study reported that "subjects... reported moderate pain sensations, as well as mild distress from pain during second‐stage labor". 100% of women in the control group (lithotomy) received an episiotomy; episiotomy was not used in Groups 2, 3 and 4. Birth weight was not reported by group but authors reported it was similar across groups. 320 women had a normal birth, however use of instrumental vaginal birth was reported. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Participants were randomly allocated, method not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and personnel knew the allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Outcomes were assessed by research assistant, who was not blinded to allocation. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 326 primiparous women were recruited, however only 320 participated in the study, since 6 "failed to experience normal labor". While absolute numbers are not provided, it seems that all outcomes were reported for all women in each group. |
| Selective reporting (reporting bias) | Unclear risk | Use of oxytocin and anaesthesia, as well as "any complications" were
pre‐specified outcomes in methods section but not reported. However study
reports "No significant differences were found among the four groups
regarding demographic, obstetrical or infant data". A study protocol could not be located for comparison. |
| Other bias | Low risk | No additional biases identified. |
Phumdoung 2013.
| Methods | Randomised controlled trial. | |
| Participants | 240 primiparous women in a hospital in southern Thailand. Inclusion criteria: primiparous; aged 17 to 35 years; 37 to 42 weeks' gestation; vertex presentation; expected fetal weight 2500 g to 4000 g; able to read and write Thai. Exclusion criteria: pregnant women who had: anaemia; hypertension; asthma; an infection; a bleeding disorder; a history or presence of psychological problems; fetal distress; and, a prolapsed cord. |
|
| Interventions | 4 different types of beds/groups:
Group 1‐ PSU birthing bed without
a holding bar; N = 60. Group 2 ‐ PSU birthing bed with a holding bar; N = 60. Group 3 ‐ usual birthing bed with head elevated 45º to 60º; N = 60. Group 4 ‐ usual birthing bed with head elevated 15º; N = 60. |
|
| Outcomes |
|
|
| Notes | Total 334 women were recruited ‐ 240 included in final study ‐ rest of the
women had caesarean section/vacuum birth. For purposes of this review, Groups 1, 2 and 3 were combined (any upright position) and compared to Group 4 (supine). |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomisation done but method of sequence generation not described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and personnel knew the allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information provided. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | It appears there was considerable post‐randomisation exclusion of participants, 332 women were randomised. However, only 240 had outcome data reported (exclusions were 70 due to caesarean section and 22 due to vacuum birth). |
| Selective reporting (reporting bias) | High risk | Paper pre‐specified outcomes on the use of oxytocin and analgesic medication, episiotomy, and degree of perineal tear. However, these were not reported by group, only overall, hence unable to assess for any differences. |
| Other bias | Low risk | No other bias. |
Racinet 1999.
| Methods | Randomised method described as Zelen's design, envelopes, stratified for parity. | |
| Participants | 239 women, France.
Women at full cervical dilation able to assume squatting position of mixed parity. 120 study participants, gestation not stated in paper. |
|
| Interventions | Squatting versus lithotomy position for second stage bearing down. | |
| Outcomes | Duration of second stage, cord arterial pH, Apgar scores, method of birth, perineal trauma, blood loss and women's perspectives. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Drawn into lots and randomised by Zelen's design. |
| Allocation concealment (selection bias) | Unclear risk | Sealed envelopes. No further information provided. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and personnel knew the allocation. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information provided. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Missing data in maternal satisfaction rates ‐ response of 35 of 42 questionnaires. |
| Selective reporting (reporting bias) | Low risk | All outcomes reported. |
| Other bias | Low risk | No other bias found. |
Radkey 1991.
| Methods | Quasi‐randomised controlled trial. Randomisation method described as Zelen's design. Randomisation at time of admission, with consent of patient after randomisation. | |
| Participants | 197 primiparous women, gestation not stated in paper. Halifax, Nova Scotia. | |
| Interventions | Control group: managed 'normally' ‐ position of inclination < 45º. Study group: upright/squatting. | |
| Outcomes |
|
|
| Notes | Numbers in different groups do not match. Unsure as to the reasons for the disparity making analysis difficult. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Zelen's design was used. Method used to generate the random sequence was not described. |
| Allocation concealment (selection bias) | High risk | Quasi‐randomised trial, based on hospital admission |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and personnel were aware of position. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information provided. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not described. |
| Selective reporting (reporting bias) | Unclear risk | Not described. |
| Other bias | Low risk | No additional sources of bias were identified |
Schirmer 2011.
| Methods | Randomised trial to investigate the left lateral position and the upright half sitting position in the expulsive period of the parturition, in regard to perineal outcomes in nulliparous women. | |
| Participants | Hospital Geral de Itapecerica da Serra, São Paulo, Brazil. The sample size ‐ 158 nulliparous parturients, randomly divided into the experimental group or the control group. The inclusion criteria employed in the samples were: nulliparous women admitted at the first gestation period and parturition, single fetus, live birth, fetus well‐flexed in cephalic presentation, and absence of maternal and fetal disease. No exclusion criteria specified. |
|
| Interventions | Indicates allocation was blinded prior to randomisation during the
dilatation period ‐ "two identical and closed envelopes each containing the
indication of the left lateral position or the upright half‐sitting". 158 nulliparous parturients were allocated; experimental group (left lateral position), N = 81; control group (upright half‐sitting), N = 77. |
|
| Outcomes | Vulvar oedema – classified by the presence or absence of a lump or increase in volume in the vulva region, during parturition and postpartum. Perineal result – the effects of parturition on the perineum and obstetric interventions done classified as: entire perineum; first and second‐degree lacerations, episiotomy and position of perineal lacerations – categorised as: labial, paraurethral; vaginal, furcula and perineal body. | |
| Notes | 8 women withdrew; 6 had an obstetric indication for caesarean section, and 2 had dystocia. For these reasons, these women were replaced in the sample. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomly assigned sealed envelopes. Method of random sequence generation was not described. |
| Allocation concealment (selection bias) | Unclear risk | Sealed envelopes. No further information provided |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and personnel were aware of position. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information provided. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | During allocation, 8 women withdrew from participation; 6 of these women had an obstetric indication for caesarean section, and 2 had dystocia. These women were replaced in the sample. Not clear how these women were selected, or whether allocation was known before or after women withdrew |
| Selective reporting (reporting bias) | Unclear risk | All outcomes reported. Unable to locate protocol for comparison. |
| Other bias | Low risk | No additional sources of bias identified |
Schneider‐Affeld 1982.
| Methods | Randomised trial of 64 women | |
| Participants | women, not otherwise specified | |
| Interventions | vertical vs horizontal birth position (not otherwise specified). While the report indicates 29 and 35 women were randomized, it is not clear which arm they were randomized to | |
| Outcomes | Some data (including duration of labour) is reported separately for both
groups, however: ‐ data is ineligible ‐ a stratification is used (EP, AP) of unknown meaning / significance ‐ Mean of duration labour reported, but not standard deviation |
|
| Notes | No data for review outcomes of interest could be extracted | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind participants/personnel to this intervention |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information provided |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient data available to make an assessment |
| Selective reporting (reporting bias) | Unclear risk | Insufficient data available to make an assessment |
| Other bias | Low risk | No other sources of bias identified |
Sekhavat 2009.
| Methods | Parallel randomised controlled trial. Women individually randomised. | |
| Participants | 110 women, teaching hospital in Iran.
Inclusion criteria: first pregnancy, full‐term, singleton, the natural course of labour in the first stage, cephalic presentation with no contraindications to vaginal birth. Exclusion criteria: the first stage of labour with fetal distress, fixed fetal abnormalities by ultrasound, especially in the head, view posterior occipital stable, fetal macrosomia, women who were not able to get in a certain position due to their illness. |
|
| Interventions | 55 women adopted sitting position in the second stage. 55 women in lithotomy in the second stage. |
|
| Outcomes | Duration of second stage of labour, perinea trauma and the first 5 minutes Apgar. | |
| Notes | Translation and data extraction by Bita Mesgarpour. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | This clinical trial study was done on 110 term nulliparous women with normal conduct of labour in second stage, which divided randomly in sitting position, (N = 55) and lithotomy position (N = 55). |
| Allocation concealment (selection bias) | Unclear risk | No information provided. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information provided. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information provided. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All outcomes appear complete. Data reported for all women. |
| Selective reporting (reporting bias) | Unclear risk | Protocol of study was not available. |
| Other bias | Low risk | No evidence of other bias. |
Stewart 1989.
| Methods | Randomised controlled trial. Randomisation took place as late as possible in the first stage of labour. Randomisation was performed by opening sealed envelopes, and women were allocated to deliver in a newly‐designed birth chair or in an "edged'' dorsal position. | |
| Participants | 304 women, Sheffield, England. Participants recruited between May 1984 to
March 1986.
All women had full‐term (37 weeks completed) gestation. Singleton pregnancies. No contra‐indications for normal vaginal birth. Vertex presentation. No women who were augmented or who had epidural analgesia were included. |
|
| Interventions | All women were allowed to be ambulant during first stage of labour. Study group: 157 women were randomised to deliver in a special birth chair, kept at a recline of 15º to 20º from the upright. 22 women did not deliver in the chair but were analysed in the group. Control group: 147 women were randomised to deliver in a 'wedged' dorsal position. | |
| Outcomes | A sub‐sample of 92 women reported on comfort during birth. More women in
the chair group reported that they were comfortable all of the time (23/52
control versus 5/40 study) and 51/52 control and 35/40 study would prefer to
use the chair for their next birth.
Birthweight: no statistically significant differences. Neonatal condition. Apgar scores < 7 at 1 minute. No statistically significant difference. Cord blood gas: no statistically significant difference. |
|
| Notes | Method of blood loss not described. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomisation by Zelen's design. Method of generating the random sequence was not described. |
| Allocation concealment (selection bias) | Unclear risk | Sealed envelopes. No further information provided |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and personnel were aware of position. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | "Data regarding the labour, birth and condition of the infant were collected, but it was not possible to blind those collecting this information to the experimental group allocation." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Complete data. |
| Selective reporting (reporting bias) | Low risk | All outcomes reported. |
| Other bias | Low risk | No other biases identified. |
Suwanakam 1988.
| Methods | Quasi‐randomised controlled trial. Women were alternately divided into 2 groups as they came to the birth suite in spontaneous labour. | |
| Participants | 60 women, Sawan province, Thailand. 30 study participants and 30 control participants. All women were 'low risk' without any serious medical complication; primigravida; between 17 to 35 years whose heights were over 150 cm; their gestational ages were between 37 to 42 weeks. Throughout the first and second stage of labour, no intravenous fluid or any medications including oxytocin or analgesia. | |
| Interventions | Study group (sitting position): 30 women at the start of the second stage of labour were asked to sit on a specially designed delivery table with the head part raised 45º from the horizontal. Control group: 30 women were in the supine dorsal position. | |
| Outcomes | Characteristics of uterine contraction, duration of second stage of labour, type of birth, Apgar scores. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Alternate allocation. |
| Allocation concealment (selection bias) | High risk | Able to predict sequence. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and personnel were aware of position. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information provided. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data complete. |
| Selective reporting (reporting bias) | Low risk | All outcomes reported. |
| Other bias | Low risk | No other bias found. |
Turner 1986.
| Methods | Randomised controlled trial. Women were randomly allocated by the opening of a sealed envelope before the onset of second stage of labour. | |
| Participants | 636 women were randomised. 97 were excluded from analyses. London,
England.
All women had full‐term (37 weeks completed) gestation. Singleton pregnancies. Induced and spontaneous labours were included. Women who had epidural anaesthesia were included. |
|
| Interventions | Study group: 318 women were randomly allocated to deliver in a 'Birth E‐Z' chair. The birth was conducted with the chair tilted back to an angle of 40º. 92 women in the study group were excluded from the analyses as they did not deliver in the chair. Control group: 318 women were randomly allocated to deliver on the bed in the dorsal position, but were allowed to be propped up with a pillow. Five women were excluded from the analyses as they insisted on delivering in the chair. | |
| Outcomes |
|
|
| Notes | The authors excluded 92 women who were randomly allocated to use the chair, but delivered in the bed, from the analyses. Five women were excluded from the control group who insisted on using the chair for delivery. These exclusions could have affected the results and the data must be interpreted with care. 'Perineal tears' were included in review as second degree tears. It is not clear in the article if these include first degree tears. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Random opening of envelope. Method of randomisation not described. |
| Allocation concealment (selection bias) | Unclear risk | Sealed envelopes. No further information provided. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and personnel were aware of position. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information provided. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Data complete but there were post‐randomisation exclusions. |
| Selective reporting (reporting bias) | Low risk | All outcomes reported. |
| Other bias | Low risk | No other bias found. |
Waldenström 1991.
| Methods | At the end of first stage of labour, the midwife would open a sealed envelope containing 1 of 2 instructions: study group = encourage birth sitting on the birthing stool or control group = encourage birth in a conventional semirecumbent position. The women were unaware that they were taking part in a trial, and were only told about the trial 2 hours after birth. | |
| Participants | 294 women, Uppsala, Sweden.
Singleton and twin pregnancies were included of mixed parity; gestation not stated in paper. No contra‐indications to normal vaginal birth. Vertex and breech presentations were included. Fetal distress was an exclusion criterion. |
|
| Interventions | Study group: 148 women were encouraged to give birth on a Dutch‐designed birthing stool. The stool was moulded plastic in the shape of a horseshoe and 32 cm high. The women sat upright in a squatting position with their feet on the ground. 73/148 used the stool to give birth. Control group: 146 women were encouraged to give birth in a conventional semirecumbent position. 100/146 used the conventional position. Data were analysed according to group allocation. Other positions used to give birth were all fours, lateral recumbent and standing. | |
| Outcomes | Pain: women in the study group reported less pain on a 10‐point scale (6.9
study vs 7.6 control) and a similar proportion of women in both groups
experienced the birth position as not good (3% study versus 2% control).
More midwives reported the study working position as rather awkward (12.8% study versus 3% control). Fathers in the study group felt more supportive, involved and satisfied with their own contribution towards the second stage of labour than those in the control group. |
|
| Notes | Group allocations were not adhered to, which could have influenced the outcomes, although analyses were done according to intention‐to‐treat. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Unclear no description of how envelopes were selected. |
| Allocation concealment (selection bias) | Unclear risk | Sealed envelopes. No further information provided. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and personnel were aware of position. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information provided. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Complete data. |
| Selective reporting (reporting bias) | Low risk | All outcomes reported. |
| Other bias | Low risk | No other bias. |
Zaibunnisa 2015.
| Methods | Randomised controlled trial. | |
| Participants | Gynecology/Obstetrics Unit‐II, Sandeman Provincial Teaching Hospital,
Quetta, Pakistan. Participants recruited from 5 Oct 2011 to 05 April 2012. The inclusion criteria were ‐ all patients including booked/unbooked with term pregnancy of gestation > 37 and < 40 weeks, presenting in active labour and with only cephalic presentation. The exclusion criteria were malpresentation, multiple gestation, antepartum haemorrhage, previous surgery (caesarean, myomectomy), and antenatally diagnosed fetal anomalies. The patients were randomly divided into 2 groups, Group A (squatting position) and Group B (lithotomy position) for study purpose. |
|
| Interventions | Group 1‐ 151 patients ‐ lithotomy position. Group 2 ‐ 151 patient ‐ squatting position. |
|
| Outcomes | Perineal tears, periurethral tear, extended episiotomy, instrumental birth, caesarean section and primary postpartum haemorrhage. | |
| Notes | Method of randomisation not stated. For this review, "episiotomy extension" was interpreted to mean episiotomy, however we did not include periurethral tears as part of perineal tears. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Random, not otherwise described. |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and personnel were aware of position. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information provided. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data complete. |
| Selective reporting (reporting bias) | Unclear risk | All listed outcomes were reported, however we were unable to locate protocol for comparison. |
| Other bias | Low risk | No other bias found. |
Zhang 2016.
| Methods | Prospective, 2‐group randomised, controlled trial in 11 hospitals in China
(5 maternal and child health hospitals and 7 general hospitals). Data were
collected between May and December 2012. Equal numbers of 150 opaque and sealed envelopes containing randomisation assignments were randomly mixed, numbered, and placed in the office of the labour wards of each participating hospital. Each envelope also contained a data collection sheet. When a woman was admitted in active labour, the midwife asked whether the patient is willing to participate and if so, drew an envelope in strict numerical succession. |
|
| Participants | The study participants included women who gave birth at 11 hospitals in
China selected by convenience; these hospitals included 5 maternal and child
health hospitals and 7 general hospitals. Inclusion criteria:
Exclusion criteria: women with pregnancy complications, premature rupture of membranes, medical contraindications, physical limitations that do not allow the hands‐and‐knees position, and/or with fetus in the non‐cephalic presentation or breech position and/or of less than 37 or over 42 weeks of gestation. Women with epidural anaesthesia were also excluded. Both nulliparous and multiparous women were eligible. |
|
| Interventions | Study group, hands knees position, N = 446. Control group, supine position, N = 440. |
|
| Outcomes | Primary outcome ‐ episiotomy rate. Secondary outcomes
|
|
| Notes | Per protocol analysis used ‐ only women who completed protocol were
included in analysis. A group of women (18/700 in experimental and 12/700 in control) did complete the protocol, where outcome data were not available. Reason for this discrepancy was not reported. Authors reported that "episiotomy was regarded as second‐degree laceration", however this does not appear to be correct based on reported data. We have therefore used the data presented for second degree laceration and episiotomy rates. We have also taken neonatal asphyxia rates as those who needed neonatal intensive care. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Equal numbers of opaque and sealed envelopes containing randomisation assignments were randomly mixed, numbered, and placed in the office of the labor wards of each participating hospital." |
| Allocation concealment (selection bias) | Unclear risk | Randomisation using opaque sealed envelopes. No further information provided. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants and personnel were aware of position. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information provided, however does mention that all outcome data came from electronic case notes. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | It appears that a per‐protocol analysis was used, with no
intention‐to‐treat analysis conducted ‐ a total of 480 (254 in experimental
and 260 in control) randomised women "withdrew from the study because of
lack of willingness to follow the allocated intervention". Outcome data for
these women were not reported. In addition, a group of women (18/700 in experimental and 12/700 in control) did complete the protocol, but outcome data were not available. Reason for this was not reported. |
| Selective reporting (reporting bias) | Low risk | All outcomes reported. |
| Other bias | Low risk | No other bias found. |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Ahmed 1985 | Excluded because insufficient data presented in abstract. |
| Altman 2007 | This study compared 2 upright positions of kneeling and sitting. |
| Bonoan 1997 | Excluded because insufficient data presented in abstract. |
| Brément 2007 | This randomised trial compared 2 recumbent positions: Lateral versus dorsal. Both the rate of intact perineum and the blood loss were increased in the lateral recumbent group. |
| Caldeyro‐Barcia 1985 | Tried to contact trialists for details of their work. There was no contact made and therefore excluded from the analysis. |
| Chen 1987 | Excluded because of multiple (37%) exclusions from the analysis. |
| Corton 2012 | Excluded because comparison between delivery with stirrups and without stirrups. |
| Downe 2004 | Excluded because all women received an epidural. |
| Golara 2002 | Studied effect of ambulation versus recumbent position in only the passive phase of the second stage of labour, not during bearing down. |
| Golay 1993 | Cohort study. |
| Hegab 2002 | Insufficient data given in abstract. |
| Humphrey 1973 | Compared 2 supine positions, i.e. lateral versus supine positions. |
| Johnstone 1987 | Compared 2 supine positions, i.e. lateral versus supine positions. |
| Karraz 2003 | Excluded because all women received an epidural. |
| Ragnar 2006 | This randomised controlled trial compared 2 upright positions in labour: kneeling versus sitting. An analysis for this could not be made according to our methodology. |
| Thies‐Lagergren 2009 | This study (assessing feasibility of RCT) compared the birth seat (BirthRite seat) with ANY other position. As the other positions were not classified, comparison of upright versus the birth seat was not possible. |
| Thies‐Lagergren 2011 | This study compared the birth seat (BirthRite seat) with ANY other position. As the other positions were not classified, comparison of upright versus the birth seat was not possible. |
RCT: randomised controlled trial
Characteristics of ongoing studies [ordered by study ID]
Hofmeyr 2015.
| Trial name or title | The Gentle Assisted Pushing study (GAP). A multi‐centre randomised controlled trial of gentle assisted pushing in the upright posture (GAP) or upright posture alone compared with routine practice to reduce prolonged second stage of labour. |
| Methods | Randomised, controlled, unblinded, clinical trial with 3 parallel arms across 4 hospital sites in South Africa. |
| Participants | Inclusion
Exclusion
|
| Interventions | Intervention arm 1: Gentle Assisted Pushing. The woman will be assisted to
assume an upright kneeling or squatting posture on the bed. The trained
birth attendant will kneel behind her on the bed or stand behind her with
the woman positioned at right angles to the length of the bed and back close
to the side of the bed. The trained birth attendant will wrap her arms
around the woman passing below her axillae, and place both open palms,
overlapping, on the fundus of her uterus. Steady pressure in the long axis
of the uterus will be applied only during contractions. The duration of
pressure will be limited to 30 seconds with a minimum of 30 seconds rest
before the next pressure. Intervention arm 2: upright crouching or kneeling position for second stage. Control: recumbent/supine posture only. |
| Outcomes | The primary outcome is defined as mean time (minutes) from randomisation to
birth. Secondary outcomes include the following. Birth outcomes: ‐ No spontaneous birth within 15 minutes of randomisation ‐ Operative birth (vacuum, forceps or caesarean section) ‐ Episiotomy or 2nd/3rd degree tears Neonatal outcomes: ‐ Cord blood pH < 7.2 ‐ 5‐minute Apgar score < 7 ‐ Neonatal injury ‐ Neonatal encephalopathy ‐ Admission to neonatal high care nursery for ≥ 24 hours ‐ Neonatal death Mothers will also be asked to grade their discomfort experienced during the second stage of labour. All adverse events |
| Starting date | March 2015. |
| Contact information | Correspondence to vogeljo@who.int |
| Notes | Likely to finish June 2017. |
Differences between protocol and review
Outcomes were separated into Primary and Secondary outcomes, and the methods have been updated in accordance with the Cochrane Handbook (Higgins 2011).
Manual removal of placenta, shoulder dystocia, and need for blood transfusion were included in the review but were not listed as prespecified outcomes in our protocol.
The following outcomes were removed from the review for this update.
Uterine efficiency (contraction intensity, frequency).
Blood pressure.
Long‐term perineal pain/discomfort.
Dyspareunia.
Maternal experience of and satisfaction with second stage of labour.
Persistent occipito‐posterior position at birth.
Neonatal condition.
Contributions of authors
Janesh Gupta is guarantor for this review. Justus Hofmeyr updated an earlier version of the review, and reviewed the current update. Akanskha Sood assessed new papers, extracted data and assessed risk bias for the review and updated the review in light of new evidence. Joshua Vogel helped with analysis and review of the data.
Sources of support
Internal sources
(GJH) Effective Care Research Unit, University of the Witwatersrand, University of Fort Hare, Eastern Cape Department of Health, South Africa.
External sources
UNDP‐UNFPA‐UNICEF‐WHO‐World Bank Special Programme of Research, Development and Research Training in Human Reproduction (HRP), Department of Reproductive Health and Research (RHR), World Health Organization, Switzerland.
Declarations of interest
Janesh K Gupta: I am Editor‐in‐Chief for the European Journal of Obstetrics and Gynaecology (EJOG); I have received fees for consultancy from Femcare‐Nikodem Medicem and expert testimonies in relation to medicolegal reports; my institution has received money from Health Technology Assessment (HTA) grants; I have received royalties from core clinical cases undergraduate text books; and I am an author of a trial included in the systematic review (Gupta 1989) – trial assessment for inclusion, risk of bias, and data extraction were carried out by the other review authors (Justus Hofmeyr and Manjeet Shehmar (author in a previous version)), who were not directly involved in the study.
Akanksha Sood: None known.
G Justus Hofmeyr: GJH is conducting a study which may be considered for inclusion in this review (Hofmeyr 2015). He will not participate in decisions regarding the study.
Joshua P Vogel: JPV is conducting a study which may be considered for inclusion in this review (Hofmeyr 2015). He will not participate in decisions regarding the study.
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Allahbadia 1992 {published data only}
- Allahbadia GN, Vaidya PR. Squatting position for delivery. Journal of the Indian Medical Association 1993;90(1):13‐6. [PubMed] [Google Scholar]
- Allahbadia GN, Vaidya PR. Why deliver in the supine position?. Australian and New Zealand Journal of Obstetrics and Gynaecology 1992;32(2):104‐6. [DOI] [PubMed] [Google Scholar]
Amiri 2012 {published data only}
- Amiri L, Shirazi V, Rajabalipoor F. The effects of different positioning on the duration of the second stage of labor in primiparous women. Journal of Zanjan University of Medical Sciences and Health Services 2012;20(80):105‐14. [Google Scholar]
Azhari 2013 {published data only}
- Azhari S, Khalilian H, Tara F, Esmaeli H. Comparison the effect of sitting and kneeling positions during the second stage of labor on pain and duration of second stage of labor in nulliparous women. Iranian Journal of Obstetrics, Gynecology and Infertility 2013;15(38):7‐16. [Google Scholar]
Bhardwaj 1994 {published and unpublished data}
- Bhardwaj N. Randomised controlled trial on modified squatting position of birthing. International Journal of Gynecology & Obstetrics 1994;46:118. [Google Scholar]
- Bhardwaj N, Kukade JA, Patil S, Bhardwaj S. Randomised controlled trial on modified squatting position of delivery. Indian Journal of Maternal and Child Health 1995;6(2):33‐9. [PubMed] [Google Scholar]
Bomfim‐Hyppólito 1998 {published data only}
- Bomfim‐Hyppólito S. Influence of the position of the mother at delivery over some maternal and neonatal outcomes. International Journal of Gynecology & Obstetrics 1998;63(Suppl 1):S67‐73. [DOI] [PubMed] [Google Scholar]
- Bonfim‐Hyppólito S. A comparative study of normal delivery assistance on vertical and horizontal position. International Conference on Maternal and Neonatal Health; 1997 November 3‐5; Brazil. 1997.
Calvo Aguilar 2013 {published data only}
- Calvo Aguilar O, Flores Romero AL, Morales Garcia VE. Comparison of obstetric and perinatal results of childbirth vertical position vs. childbirth supine position. Ginecologia y Obstetricia de Mexico 2013;81(1):1‐10. [PubMed] [Google Scholar]
Chan 1963 {published data only}
- Chan DPC. Positions during labour. British Medical Journal 1963;1:100‐2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Crowley 1991 {published data only}
- Crowley P, Elbourne DR, Ashurst H, Garcia J, Murphy D, Duignan N. Delivery in an obstetric birth chair: a randomized controlled trial. British Journal of Obstetrics and Gynaecology 1991;98(7):667‐74. [DOI] [PubMed] [Google Scholar]
De Jong 1997 {published data only}
- Jong P. Randomised trial comparing the upright and supine positions for the second stage of labour. British Journal of Obstetrics and Gynaecology 1999;106(3):292. [DOI] [PubMed] [Google Scholar]
- Jong PR, Johanson R, Baxen P, Adrians VD, Westhuizen S, Jones P. St Monica's randomized controlled trial of upright vs dorsal position for the second stage of labour. 27th British Congress of Obstetrics and Gynaecology; 1995 July 4‐7; Dublin, Ireland. 1995:493.
- Jong PR, Johanson RB, Baxen P, Adrians VD, Westhuisen S, Jones PW. Randomised trial comparing the upright and supine positions for the second stage of labour. British Journal of Obstetrics and Gynaecology 1997;104(5):567‐71. [DOI] [PubMed] [Google Scholar]
- Eason E. Randomised trial comparing the upright and the supine positions for the second stage of labour. British Journal of Obstetrics and Gynaecology 1999;106(3):291‐2. [DOI] [PubMed] [Google Scholar]
Gardosi 1989a {published data only}
- Gardosi J. Cushion birth: the modern application of ancient principles. 4th European Congress of Allied Specialists in Maternal and Neonatal Care; 1989; Bruges, Belgium. 1989.
- Gardosi J. Randomised controlled trial of squatting in the second stage of labour. 9th Birth Conference; 1990; San Francisco, USA. 1990:74‐5. [DOI] [PubMed]
- Gardosi J. Squatting in the second stage of labour. 12th European Congress of Perinatal Medicine; 1990 Lyon, France. 1990:224.
- Gardosi J. The physiology of squatting during labour. American Journal of Obstetrics and Gynecology 1992;166:341. [Google Scholar]
- Gardosi J, Hutson N, Lynch CB. Randomised, controlled trial of squatting in the second stage of labour. Lancet 1989;2(8654):74‐7. [DOI] [PubMed] [Google Scholar]
- Gardosi J, Hutson N, Lynch CB. Squatting in the second stage of labour: a randomised controlled trial. 4th European Congress of Allied Specialists in Maternal and Neonatal Care; 1989; Bruges, Belgium. 1989.
- Gardosi J, Hutson N, Lynch CB. Squatting in the second stage of labour: a randomized controlled trial. British Journal of Obstetrics and Gynaecology 1989;96:1115. [DOI] [PubMed] [Google Scholar]
Gardosi 1989b {published data only}
- Gardosi J, Sylvester S, Lynch CB. Alternative positions in the second stage of labour: a randomized controlled trial. British Journal of Obstetrics and Gynaecology 1989;96(11):1290‐6. [DOI] [PubMed] [Google Scholar]
Gupta 1989 {published data only}
- Gupta JK, Brayshaw EM, Lilford RJ. An experiment of squatting birth. European Journal of Obstetrics, Gynecology, and Reproductive Biology 1989;30(3):217‐20. [DOI] [PubMed] [Google Scholar]
Hemminki 1986 {published data only}
- Hemminki E, Virkkunen A, Makela A, Hannikainen J, Pulkkis E, Moilanen K, et al. A trial of delivery in a birth chair. Journal of Obstetrics and Gynaecology 1986;6(3):162‐5. [Google Scholar]
Hillan 1984 {published data only}
- Hillan EM. The birthing chair trial. Research and the Midwife Conference; 1984; Manchester, UK. 1984:22‐37.
- Stewart P, Hillan E, Calder A. A randomised trial to evaluate the use of a birth chair for delivery. Lancet 1983;1(8337):1296‐8. [DOI] [PubMed] [Google Scholar]
- Stewart P, Hillan E, Calder AA. A study of the benefits of maternal ambulation during labour and the use of a birth chair for delivery. 8th European Congress of Perinatal Medicine; 1982 September 7‐10; Brussels, Belgum. 1982:113.
Jahanfar 2004 {published data only}
- Amini L, Jahanfar S, Jamshidi R, Kashanian M. The effect of sitting position during labour on 3rd stage duration and postpartum haemorrhage. Journal of Obstetrics and Gynaecology 2011;31(Suppl 1):33‐4. [Google Scholar]
- Amini L, Jahanfar S, Kashanian M, Rahiniha F, Jamshidi R. Sitting position: a right way to reduce labour pain with shortening duration of labor. Journal of Psychosomatic Obstetrics and Gynecology 2010;31(Suppl 1):104. [Google Scholar]
- Jahanfar S, Amini L, Jamshidi R. Third and fourth stages of labour: sitting position. British Journal of Midwifery 2004;12(7):437‐46. [Google Scholar]
Liddell 1985 {published data only}
- Liddell HS, Fisher PR. The birthing chair in the second stage of labour. Australian and New Zealand Journal of Obstetrics and Gynaecology 1985;25(1):65‐8. [DOI] [PubMed] [Google Scholar]
Liu 1986 {published data only}
- Liu YC. Effect of an upright position during childbirth. First Sigma Theta Tau, Alpha Tho Chapter National Research Conference. Living with change and choice in health; 1986; University of West Virginia, USA. 1986.
Marttila 1983 {published data only}
- Marttila M, Kajanoja P, Ylikorkala O. Maternal half‐sitting position in the second stage of labor. Journal of Perinatal Medicine 1983;11(6):286‐9. [DOI] [PubMed] [Google Scholar]
Nasir 2007 {published data only}
- Nasir A, Korejo R, Noorani KJ. Child birth in squatting position. Journal of the Pakistan Medical Association 2007;57(1):19‐22. [PubMed] [Google Scholar]
Phumdoung 2010 {published data only}
- Phumdoung S, Morkruengsai S, Tachapattarakul S, Lawantrakul J, Junsuwan P. Effect of the Prince of Songkla University locked‐upright position on the duration, pain and comfort of second‐stage labor in primiparous women. Pacific Rim International Journal of Nursing Research 2010;14(2):112‐21. [Google Scholar]
Phumdoung 2013 {published data only}
- Phumdoung S, Manasurakarn B, Rattanasombat K, Mahattanan S, Maneechot K, Chanudom B, et al. Effect of the Prince of Songkla University birthing bed on duration, pain, and comfort level during second‐stage labor in primiparous Thais. Pacific Rim International Journal of Nursing Research 2013;17(1):56‐68. [Google Scholar]
Racinet 1999 {published data only}
- Racinet C, Eymery P, Philibert L, Lucas C. Delivery in the squatting position. A randomized trial comparing the squatting position and the lithotomy position for the expulsion phrase [L'accouchement en position accroupie. Essai randomise comparant la position accroupie a la position classique en phase d' expulsion]. Journal de Gynecologie, Obstetrique et Biologie de la Reproduction 1999;28(3):263‐70. [PubMed] [Google Scholar]
Radkey 1991 {published data only}
- Radkey AL, Liston RM, Scott KE, Young C. Squatting: preventive medicine in childbirth?. Annual Meeting of the Society of Obstetricians and Gynaecologists of Canada; 1991;Toronto, Ontario, Canada. 1991:76.
Schirmer 2011 {published data only}
- Schirmer J, Fustinoni SM, Basile ALO. Perineal outcomes on the left lateral versus vertical semi sitting birth positions: a randomized study [Resultado perineal nas posições de parto lateral esquerda versus vertical semi‐sentada: estudorandomizado]. Acta Paulista de Enfermagem 2011;24(6):745‐50. [Google Scholar]
Schneider‐Affeld 1982 {published data only}
- Schneider‐Affeld F, Martin K. Delivery from a sitting position. Journal of Perinatal Medicine 1982;2(Suppl):70‐1. [Google Scholar]
Sekhavat 2009 {published data only}
- Sekhavat L, Dehghani‐Firuzabadi R, Karimzadah‐Mibodi M. Effect of maternal position on duration of second stage of labor and maternal and neonatal outcome in nulliparous women. Journal of Gorgan University of Medical Sciences 2009;11(2):33‐7. [Google Scholar]
Stewart 1989 {published data only}
- Stewart P, Spiby H. A randomized study of the sitting position for delivery using a newly designed obstetric chair. British Journal of Obstetrics and Gynaecology 1989;96(3):327‐33. [DOI] [PubMed] [Google Scholar]
Suwanakam 1988 {published data only}
- Suwanakam S, Linasmita V, Phuapradit W, Pongruengphant P. The effects of sitting position on second stage of labor. Journal of the Medical Association of Thailand 1988;71(Suppl 1):72‐5. [PubMed] [Google Scholar]
Turner 1986 {published data only}
- Turner MJ, Romney ML, Webb JB, Gordon H. The birthing chair: an obstetric hazard?. Journal of Obstetrics and Gynaecology 1986;6(4):232‐5. [Google Scholar]
Waldenström 1991 {published data only}
- Waldenström U, Gottval K. Randomized trial of birthing stool or conventional semi‐recumbent position for second‐stage labor. Jordemodern 1994;107(7‐8):261‐5. [PubMed] [Google Scholar]
- Waldenström U, Gottvall K. A randomised trial of the use of a birth stool in the second stage of labour. 22nd International Congress of Confederation of Midwives; 1991; Kobe, Japan. 1991:78.
- Waldenström U, Gottvall K. A randomized trial of birthing stool or conventional semirecumbent position for second‐stage labor. Birth 1991;18(1):5‐10. [DOI] [PubMed] [Google Scholar]
Zaibunnisa 2015 {published data only}
- Zaibunnisa, Ara F, Ara B, Kaker P, Aslam M. Child birth; comparison of complications between lithotomy position and squatting position during. Professional Medical Journal 2015;22(4):390‐4. [Google Scholar]
Zhang 2016 {published data only}
- Zhang HY, Shu R, Zhao NN, Lu YJ, Chen M, Li YX, et al. Comparing maternal and neonatal outcomes between hands‐and‐knees delivery position and supine position. International Journal of Nursing Sciences 2016;3(2):178‐84. [Google Scholar]
References to studies excluded from this review
Ahmed 1985 {published data only}
- Ahmed LT, Bouchetara K. The influence of maternal position on duration of labor. Archives of Gynecology 1985;237 Suppl:9. [Google Scholar]
Altman 2007 {published data only}
- Altman D, Ragnar I, Ekstrom A, Tyden T, Olsson SE. Anal sphincter lacerations and upright delivery postures ‐ a risk analysis from a randomized controlled trial. International Urogynecology Journal 2007;18(2):141‐6. [DOI] [PubMed] [Google Scholar]
Bonoan 1997 {published data only}
- Bonoan MJ, Otayza M, Garcia G. Acceptability of an indiginous birthing position using a filipino‐improvised birthing chair ‐ a third world tertiary care center prospective trial. Acta Obstetricia et Gynecologica Scandinavica 1997;76(167):45. [Google Scholar]
Brément 2007 {published data only}
- Brément S, Mossan S, Belery A, Racinet C. Delivery in lateral position. Randomized clinical trial comparing the maternal positions in lateral position and dorsal position for the second stage of labour [Accouchement en décubitus latéral. Essai clinique randomisé comparant les positions maternelles en décubitus latéral et en décubitus dorsal lors de la deuxième phase du travail]. Gynécologie Obstétrique & Fertilité 2007;35(7):637‐44. [DOI] [PubMed] [Google Scholar]
Caldeyro‐Barcia 1985 {published data only (unpublished sought but not used)}
- Caldeyro‐Barcia R, Alonso JG, Sugo M, Barron R, Dellepiane M. Fetal outcome of humanised labor. Personal communication 1985.
Chen 1987 {published data only}
- Chen SZ, Aisaka K, Mori H, Kigawa T. Effects of sitting position on uterine activity during labor. Obstetrics and Gynecology 1987;69(1):67‐73. [PubMed] [Google Scholar]
Corton 2012 {published data only}
- Corton MM, Lankford JC, Ames R, McIntire DD, Alexander JM, Leveno KJ. A randomized trial of birthing with and without stirrups. American Journal of Obstetrics and Gynaecology 2012;207(2):133.e1–133.e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Downe 2004 {published data only}
- Downe S, Gerrett D, Renfrew MJ. A prospective randomised trial on the effect of position in the passive second stage of labour on birth outcome in nulliparous women using epidural analgesia. Midwifery 2004;20(2):157‐68. [DOI] [PubMed] [Google Scholar]
Golara 2002 {published data only}
- Golara M, Plaat F Shennan AH. Upright versus recumbent position in the second stage of labour in women with combined spinal‐epidural analgesia. International Journal of Obstetric Anesthesia 2002;11(1):19‐22. [DOI] [PubMed] [Google Scholar]
- Plaat F, Golara M, Shennan A. Upright versus recumbent position with mobile extradurals in the early second stage of labour. British Journal of Anaesthesia 1996;76:102. [Google Scholar]
Golay 1993 {published data only}
- Golay J, Vedam S, Sorger L. The squatting position for the second stage of labor: effects on labor and on maternal and fetal well‐being. Birth 1993;20(2):73‐8. [DOI] [PubMed] [Google Scholar]
Hegab 2002 {published data only}
- Hegab H, Nagati A, Abd‐El Fatah H, Rizk A. Evaluation of the effect of four different maternal positions on the duration of the second stage in nulliparous women [abstract]. Journal of Obstetrics and Gynaecology Research 2002;28(1):64. [Google Scholar]
Humphrey 1973 {published data only}
- Humphrey M, Hounslow D, Morgan S, Wood C. The influence of maternal posture at birth on the fetus. Journal of Obstetrics and Gynaecology of the British Commonwealth 1973;80(12):1075‐80. [DOI] [PubMed] [Google Scholar]
- Humphrey MD, Chang A, Wood EC, Morgan S, Hounslow D. A decrease in fetal pH during the second stage of labour, when conducted in the dorsal position. Journal of Obstetrics and Gynaecology of the British Commonwealth 1974;81(8):600‐2. [DOI] [PubMed] [Google Scholar]
Johnstone 1987 {published data only}
- Johnstone FD, Aboelmagd MS, Harouny AK. Maternal posture in second stage and fetal acid base status. British Journal of Obstetrics and Gynaecology 1987;94(8):753‐7. [DOI] [PubMed] [Google Scholar]
Karraz 2003 {published data only}
- Karraz MA. Ambulatory epidural anesthesia and the duration of labor. International Journal of Gynaecology and Obstetrics 2003;80(2):117‐22. [DOI] [PubMed] [Google Scholar]
Ragnar 2006 {published data only}
- Ragnar I, Altman D, Tyden T, Olsson SE. Comparison of the maternal experience and duration of labour in two upright delivery positions ‐ a randomised controlled trial. BJOG: an international journal of obstetrics and gynaecology 2006;113(2):165‐70. [DOI] [PubMed] [Google Scholar]
Thies‐Lagergren 2009 {published data only}
- Thies‐Lagergren L, Kvist LJ. Assessing the feasibility of a randomised controlled trial of birth on a birthing seat. Evidence Based Midwifery 2009;7(4):122‐7. [Google Scholar]
Thies‐Lagergren 2011 {published data only}
- Thies‐Lagergren L, Hildingsson I, Christensson K, Kvist LJ. Who decides the position for birth? A follow‐up study of a randomised controlled trial. Women and Birth 2013;26(4):e99‐104. [DOI] [PubMed] [Google Scholar]
- Thies‐Lagergren L, Hildingsson I, Kvist L. Who decides the position for birth? ‐ a follow up study of a randomized controlled trial. International Confederation of Midwives 30th Triennial Congress. Midwives: Improving Women’s Health; 2014 June 1‐4; Prague, Czech Republic. 2014:P032. [DOI] [PubMed]
- Thies‐Lagergren L, Kvist LJ, Christensson K, Hildingsson I. Maternal outcomes in nulliparous women who gave vaginal birth on a birth seat or in any other position: results of a randomised controlled trial in Sweden. Journal of Paediatrics and Child Health 2011;47(Suppl 1):36‐7. [Google Scholar]
- Thies‐Lagergren L, Kvist LJ, Christensson K, Hildingsson I. Striving for scientific stringency: a re‐analysis of a randomised controlled trial considering first‐time mothers' obstetric outcomes in relation to birth position. BMC Pregnancy and Childbirth 2012;12:135. [DOI: 10.1186/1471-2393-12-135] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thies‐Lagergren L, Kvist LJ, Sandin‐Bojo AK, Christensson K, Hildingsson I. Augmentation of labour and fetal outcomes in relation to birth positions: A secondary analysis of an RCT evaluating birth seat births. Journal of Paediatrics and Child Health 2012;48(Suppl 1):101‐2. [DOI] [PubMed] [Google Scholar]
- Thies‐Lagergren L, Kvist LJ, Sandin‐Bojo AK, Christensson K, Hildingsson I. Labour augmentation and fetal outcomes in relation to birth positions: A secondary analysis of an RCT evaluating birth seat births. Midwifery 2013;29(4):344‐50. [DOI] [PubMed] [Google Scholar]
- Thies‐Lagregren L, Kvist LJ, Christensson K, Hildingsson I. No reduction in instrumental vaginal births and no increased risk for adverse perineal outcome in nulliparous women giving birth on a birth seat: results of a Swedish randomised controlled trial. BMC Pregnancy and Childbirth 2011;11:22. [DOI: 10.1186/1471-2393-11-22] [DOI] [PMC free article] [PubMed] [Google Scholar]
References to ongoing studies
Hofmeyr 2015 {published data only}
- Hofmeyr GJ, Singata M, Lawrie T, Vogel JP, Landoulsi S, Seuc AH, et al. A multicentre randomized controlled trial of gentle assisted pushing in the upright posture (GAP) or upright posture alone compared with routine practice to reduce prolonged second stage of labour (the Gentle Assisted Pushing study): study protocol. Reproductive Health. 2015;12(1):114. [DOI] [PMC free article] [PubMed] [Google Scholar]
Additional references
Ang 1969
- Ang CK, Tan TH, Walters WAW, Wood C. Postural influence on maternal capillary oxygen and carbon dioxide tension. British Medical Journal 1969;4(5677):201‐3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Anim‐Somuah 2011
- Anim‐Somuah M, Smyth RMD, Jones L. Epidural versus non‐epidural or no analgesia in labour. Cochrane Database of Systematic Reviews 2011, Issue 12. [DOI: 10.1002/14651858.CD000331.pub3] [DOI] [PubMed] [Google Scholar]
Atwood 1976
- Atwood RJ. Parturitional posture and related birth behaviour. Acta Obstetricia et Gynecologica Scandinavica. Supplement 1976;57:1‐25. [PubMed] [Google Scholar]
Balaskas 1992
- Balaskas J. Active Birth: The New Approach to Giving Birth Naturally. Boston: Harvard Common Press, 1992. [Google Scholar]
Borell 1957b
- Borell U, Fernström I. The movements at the sacro‐iliac joints and their importance to changes in the pelvic dimensions during parturition. Acta Obstetricia et Gynecologica Scandinavica 1957;36(1):42‐57. [DOI] [PubMed] [Google Scholar]
Buhimschi 2001
- Buhimschi CS, Buhimschi IA, Malinow A, Weiner CP. Use of McRoberts' position during delivery and increase in pushing efficiency. Lancet 2001;358(9280):470‐1. [DOI] [PubMed] [Google Scholar]
Caldeyro‐Barcia 1960
- Caldeyro‐Barcia R, Noriega‐Guerra L, Cibils LA, Alvarez H, Poseiro JJ, Pose SV, et al. Effect of position changes on the intensity and frequency of uterine contractions during labor. American Journal of Obstetrics and Gynecology 1960;80:284‐90. [Google Scholar]
Dundes 1987
- Dundes L. The evolution of maternal birthing position. American Journal of Public Health 1987;77(5):636–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dunn 1978
- Dunn PM. Posture in labour. Lancet 1978;i:496‐7. [PubMed] [Google Scholar]
Engelmann 1882
- Engelmann GJ. Labor Among Primitive Peoples. St. Louis: JH Chambers, 1882. [Google Scholar]
Gold 1950
- Gold EM. "Pelvic drive" in obstetrics: an X‐ray study of 100 cases. American Journal of Obstetrics and Gynecology 1950;59:890‐6. [Google Scholar]
Gupta 1991
- Gupta JK, Glanville JN, Johnson N, Lilford RJ, Dunham RJC, Watters JK. The effect of squatting on pelvic dimensions. European Journal of Obstetrics, Gynecology, and Reproductive Biology 1991;42(1):19‐22. [DOI] [PubMed] [Google Scholar]
Hewes 1957
- Hewes GW. The anthropology of posture. Scientific American 1957;196(2):123‐32. [Google Scholar]
Higgins 2011
- Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Humphrey 1974
- Humphrey MD, Chang A, Wood EC, Morgan S, Humslow D. The decrease in fetal pH during the second stage of labour when conducted in the dorsal position. Journal of Obstetrics and Gynaecology of the British Commonwealth 1974;81(8):600‐2. [DOI] [PubMed] [Google Scholar]
Jarcho 1934
- Jarcho J. Postures & Practices During Labor Among Primitive Peoples. New York: Paul Hoeber, 1934. [Google Scholar]
Johansson 2015
- Johansson M, Thies‐Lagergren L. Swedish fathers' experiences of childbirth in relation to maternal birth position: a mixed method study. Women Birth 2015;28(4):140‐7. [DOI] [PubMed] [Google Scholar]
Kemp 2013
- Kemp E, Kingswood CJ, Kibuka M, Thornton JG. Position in the second stage of labour for women with epidural anaesthesia. Cochrane Database of Systematic Reviews 2013, Issue 1. [DOI: 10.1002/14651858.CD008070.pub2] [DOI] [PubMed] [Google Scholar]
Kurokawa 1985
- Kurokawa J, Zilkoski MW. Adapting hospital obstetrics to birth in the squatting position. Birth 1985;12(2):87‐90. [DOI] [PubMed] [Google Scholar]
Lilford 1989
- Lilford RJ, Glanville JN, Gupta JK, Shrestha R, Johnson N. The action of squatting in the early postnatal period marginally increases pelvic dimensions. British Journal of Obstetrics and Gynaecology 1989;96(8):964‐6. [DOI] [PubMed] [Google Scholar]
Mead 1965
- Mead M, Newton N. Cultural patterning of perinatal behavior. In: Richardson A, Guttmacher A editor(s). Childbearing: Its Social and Psychological Aspects. Baltimore: Williams and Wilkins, 1965. [Google Scholar]
Méndez‐Bauer 1975
- Méndez‐Bauer C, Arroyo J, García Ramos C, Menéndez A, Lavilla M, Izquierdo F, et al. Effects of standing position on spontaneous uterine contractility and other aspects of labor. Journal of Perinatal Medicine 1975;3(2):89‐100. [DOI] [PubMed] [Google Scholar]
RevMan 2014 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Romond 1985
- Romond JL, Baker IT. Squatting in childbirth. A new look at an old tradition. Journal of Obstetric, Gynecologic, and Neonatal Nursing 1985;14(5):406‐11. [DOI] [PubMed] [Google Scholar]
Russell 1969
- Russell JGB. Moulding of the pelvic outlet. Journal of Obstetrics and Gynaecology of the British Commonwealth 1969;76(9):817‐20. [DOI] [PubMed] [Google Scholar]
Russell 1982
- Russell JGB. The rationale of primitive delivery positions. British Journal of Obstetrics and Gynaecology 1982;89(9):712‐5. [DOI] [PubMed] [Google Scholar]
Scott 1963
- Scott DB, Kerr MG. Inferior vena caval compression in late pregnancy. Journal of Obstetrics and Gynaecology of the British Commonwealth 1963;70:1044. [DOI] [PubMed] [Google Scholar]
Serati 2016
- Serati M, Dedda MC, Bogani G, Sorice P, Cromi A, Uccella S, et al. Position in the second stage of labour and de novo onset of post‐partum urinary incontinence. International Urogynecology Journal 2016;27(2):281‐6. [DOI] [PubMed] [Google Scholar]
Simkin 2005
- Simkin P, Ancheta R. The Labor Progress Handbook. Second Edition. Oxford: Blackwell Publishing, 2005. [Google Scholar]
Wolman 1993
- Wolman WL, Chambers B, Hofmeyr GJ, Nikodem VC. Post‐partum depression and companionship in the clinical birth environment: a randomised controlled study. American Journal of Obstetrics and Gynecology 1993;168(5):1388‐93. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Gupta 1999
- Gupta JK, Nikodem VC. Position for women during second stage of labour. Cochrane Database of Systematic Reviews 1999, Issue 3. [DOI: 10.1002/14651858.CD002006] [DOI] [PubMed] [Google Scholar]
Gupta 2004
- Gupta JK, Hofmeyr GJ, Smyth RMD. Position in the second stage of labour for women without epidural anaesthesia. Cochrane Database of Systematic Reviews 2004, Issue 1. [DOI: 10.1002/14651858.CD002006.pub2] [DOI] [PubMed] [Google Scholar]
Gupta 2012
- Gupta JK, Hofmeyr GJ, Shehmar M. Position in the second stage of labour for women without epidural anaesthesia. Cochrane Database of Systematic Reviews 2012, Issue 5. [DOI: 10.1002/14651858.CD002006.pub3] [DOI] [PubMed] [Google Scholar]
Nikodem 1995a
- Nikodem VC. Birthing chair vs recumbent position for 2nd stage of labour. [revised 03 October 1993] In: Enkin MW, Keirse MJNC, Renfrew MJ, Neilson JP, Crowther C (eds.) Pregnancy and Childbirth Module. In: The Cochrane Pregnancy and Childbirth Database [database on disk and CDROM]. The Cochrane Collaboration; Issue 2, Oxford: Update Software; 1995.
Nikodem 1995b
- Nikodem VC. Upright vs recumbent position during second stage of labour. [revised 06 May 1994] In: Enkin MW, Keirse MJNC, Renfrew MJ, Neilson JP, Crowther C (eds.) Pregnancy and Childbirth Module. In: The Cochrane Pregnancy and Childbirth Database [database on disk and CDROM]. The Cochrane Collaboration; Issue 2, Oxford: Update Software; 1995.


