ABSTRACT
Background: Abnormalities in serum potassium levels have been associated with variable mortality risk among hospitalized patients with heart failure (HF). We aim to use a large database study to further characterize risk of mortality, demographic factors, and associated comorbidities among heart failure inpatients.
Methods: Our sample population was from the US National Inpatient Sample database from the year 2009–2011. The inclusion criteria used to identify patients was those with a diagnosis of heart failure as per ICD-9 classification. Other demographic factors considered in data collection included income, and cardiac risk factors. Taking these factors into consideration, a univariate association of potassium level and mortality was performed, as well as multivariable logistic regression controlling for demographic factors and associated conditions.
Results: Of the 2,660,609 patients who were discharged with a diagnosis of heart failure during this time period, patients with hypokalemia during hospitalization had increased mortality risk (OR: 1.96, 95% CI: 1.91–2.01) when compared with those with hyperkalemia who had decreased inpatient mortality risk OR: 0.94,95% CI: 0.91–0.96) versus those not coded for potassium abnormalities. This finding was significant even regardless of the etiology of the hypokalemia while the hyperkalemic patients were noted to have no difference or a decreased risk in all subtypes and groups.
Conclusion: Unlike heart failure patients with hyperkalemia, those with hypokalemia are at an increased inpatient mortality risk. Whether our mortality findings translate to longer-term outpatient settings where significantly less monitoring is possible is a matter for further study.
KEYWORDS: Heart failure, hypokalemia, hyperkalemia, mortality, National Inpatient Sample
1. Introduction
According to the American Heart Association, approximately 6.5 million adults in the USA (US) are living with heart failure (HF) [1]. In 2014, 68,626 had heart failure listed as the underlying cause of death [1].
Among heart failure patients, studies have shown that hypokalemia, in comparison to normokalemia, has been associated with increased risk of mortality, with hazard ratios ranging from 1.2 to 2.3 [2–5]. Decrease in potassium levels by >15% or >0.7 mmol/l, even within normal range among patients admitted with acute decompensated heart failure was associated with increased 180-day all-cause mortality [6]. Hypokalemia in patients with heart failure has been postulated to be caused by the use of non-potassium sparing diuretics and activation of neurohormones [3,5,7]. Low serum potassium is known to increase the transmembrane resting potential of myocardial cells, resulting in hyperpolarization and increased excitability. Increased excitability leads to a higher risk of ventricular arrhythmia [4,5,8], which is the most common cause of sudden cardiac death in heart failure patients [9]. This may be especially relevant in heart failure patients with structural heart disease such as myocardial infarction and valvular heart disease, where effects of potassium are currently unknown [2,4,5,10]. On the other hand, hyperkalemia has been associated with both increased and decreased mortality risk in various outpatient studies [5,11–14]). Studies have reported no association between lower ranges of hyperkalemia (K 5.0–6.0 mEq/l) and death [5], an association between hyperkalemia and fewer deaths [11] and association between hyperkalemia and higher rates of death and hospitalization [12–14]. Patients with heart failure, particularly those on angiotensin-converting enzyme (ACE) inhibitors, angiotensin-receptor blockers (ARBs) and aldosterone receptor antagonists are susceptible to develop hyperkalemia [15]. Therefore it is critical to understand whether these evidence-based medications can have their doses safely increased without concerns for provoking additional mortality risk.
In order to better characterize some of the discrepancies in observed effects and establish relationship between in-hospital mortality among heart failure patients and serum potassium levels, we studied a large US inpatient database (National Inpatient Sample) to ascertain relationships between diagnosed potassium disorders and inpatient mortality.
2. Methods
2.1. Study population
We utilized the National Inpatient Sample (NIS) database from years 2009–2011. NIS is the largest all–payer inpatient care database in the US and contains discharge level information of 7 to 8 million hospital stays. This is a 20% stratified clustered sample from all US hospitals. It is federally sponsored by Agency for Healthcare Research and Quality [16].
We selected non-pregnant adult patients (≥18 years) admitted with a diagnosis of heart failure in US hospitals from 2009 to 2011. Patients with heart failure were selected based on Clinical Classification Software code 108, which represents all patients with parent ICD-9 (International Classification of disease-9) code 428. CCS codes are supplied by HCUP to facilitate researchers into selecting patients with one or few disease conditions grouped together into a clinically meaningful category (HCUP CCS). We additionally included ICD-9 codes 402.01, 402.11, 402.91, 404.01, 404.03, 404.11, 404.13, 404.91 and 404.93 to include heart failure patients not included under CCS code 108. We categorized patients with heart failure into systolic, diastolic, combined and unspecified based on their coded ICD-9 classification. Analyses were based on 3 different groups of potassium levels: hypokalemia, normokalemia (defined as not coded for either hypokalemia or hyperkalemia) and hyperkalemia. The ICD-9 codes 267.7 and 276.8 were used to classify hyperkalemia and hypokalemia respectively. ICD-9 coding does not specify any particular potassium levels for these diagnoses. Patients coded for both hyperkalemia and hypokalemia were excluded from further analysis. The HCUP-NIS database also contains data for baseline characteristics such as age, gender, race, expected primary payer, location of hospital and mean household income for patient’s ZIP code (HCUP-US NIS). The primary outcome for this study group was in-hospital mortality.
3. Statistical analysis
STATA version 13.0 (College Station, TX) was used for analysis of this survey sample data. Categorical data were expressed as proportion or percentage with Chi-square testing used to compare proportions. Continuous variables were reported as means with standard errors. Mortality associations between potassium categories were initially compared by univariate analysis, then were also included in multivariable logistic regression analyses. Multivariable analyses were controlled for age, sex, race, smoking, obesity, dyslipidemia, diabetes, hypertension, chronic kidney disease and Charlson comorbidity index (a predictor of 10-year mortality for patients with multiple comorbidities). Two tailed p-value of p < 0.05 was assumed to have statistical significance.
4. Results
The total number of discharge records in the NIS database (sample) from 2009 to 2011 was 23,634,793. The weighted count in the universe of the database (US population) was N = 117,033,987. Details of the selection process is depicted in Figure 1. Our final study population was based on 549,044 inpatient hospital discharge records.
Figure 1.
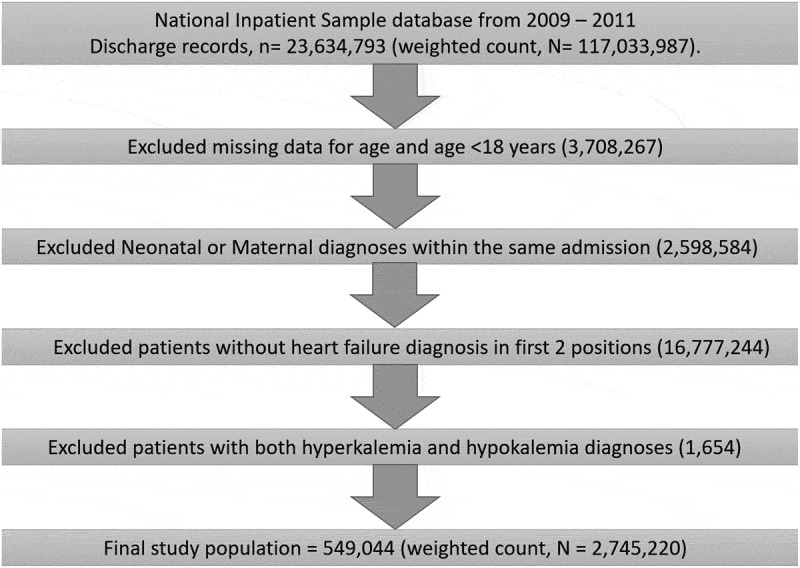
Selection process for the discharge records used in final analysis.
The baseline characteristics of HF patients are presented in Table 1. Hypokalemic heart failure patients were slightly younger (72.3 vs. 73.6 years, p < 0.001), less likely to be Caucasian (61.5 vs. 67.3, p < 0.001), more likely to be admitted to an urban hospital (86.8 vs. 83.2%, p < 0.001), and were more likely to have obesity, hypertension and diabetes when compared to normokalemic heart failure patients. Chronic renal failure was much more likely to be present in hypokalemic patients (69.1% vs 38.8%, p < 0.001). Hyperkalemic heart failure patients were slightly younger (73.2 vs. 73.6 years, p < 0.001), slightly more likely to be Caucasian (68.4% vs. 67.3%), and more likely to have comorbidities of obesity, smoking and hypertension but less likely to have chronic kidney disease (36.6% vs. 38.9%, p < 0.001) as compared to those normokalemic heart failure patients. We found that higher number of heart failure inpatients, regardless of potassium levels, were of lower income than of higher income.
Table 1.
Baseline characteristics of HF patients with different categories of potassium levels.
| Baseline characteristics | HF with normokalemia | HF with hyperkalemia | HF with hypokalemia | p-value |
|---|---|---|---|---|
| Age | 73.67 (SE:0.15) | 73.21 (SE:0.18) | 72.39 (SE:0.18) | <0.0001 |
| Female | 51.13 | 55.39 | 52.40 | <0.0001 |
| Race | ||||
| Caucasian | 67.37 | 68.45 | 61.58 | <0.0001 |
| Black | 20.40 | 21.78 | 22.02 | |
| Hispanic | 7.61 | 5.81 | 10.77 | |
| Asian or Pacific Islander | 1.65 | 1.43 | 2.44 | |
| Native American | 0.58 | 0.56 | 0.56 | |
| Expected primary payer | ||||
| Medicare | 76.02 | 74.69 | 78.20 | <0.0001 |
| Medicaid | 7.78 | 7.63 | 8.83 | |
| Primary insurance | 11.16 | 12.03 | 9.45 | |
| Self-pay | 3.11 | 3.83 | 2.12 | |
| No charge | 0.29 | 0.34 | 0.22 | |
| Location of hospital | ||||
| Rural | 16.73 | 16.90 | 13.12 | <0.0001 |
| Urban | 83.27 | 83.10 | 86.88 | |
| Mean household income for patient’s Zip code | ||||
| 0–25th percentile | 33.24 | 32.87 | 33.00 | <0.0001 |
| 26th–50th percentile | 26.42 | 26.04 | 24.99 | |
| 51st–75th percentile | 22.71 | 23.38 | 23.50 | |
| 76th–100th percentile | 17.64 | 17.70 | 18.51 | |
| Mean Charlson comorbidity index | 3.16 | 3.06 | 3.99 | <0.0001 |
| Risk factors | ||||
| Obesity | 14.20 | 14.96 | 15.10 | <0.0001 |
| Smoking | 21.31 | 22.41 | 21.10 | 0.0001 |
| Hypertension | 75.69 | 77.32 | 81.15 | <0.0001 |
| Dyslipidemia | 39.36 | 39.68 | 37.90 | 0.0006 |
| Diabetes mellitus | 43.62 | 39.35 | 53.36 | <0.0001 |
| Chronic kidney disease | 38.86 | 36.64 | 69.12 | <0.0001 |
Univariate analysis comparing potassium diagnosis and inpatient death showed a lower odds of inpatient mortality among HF patients coded for a diagnosis of hyperkalemia as compared to normokalemia (OR = 0.73, 95% CI: 0.69–0.78) and a higher odds of mortality among those coded for a diagnosis of hypokalemia as compared to normokalemia (OR = 2.27, 95% CI: 2.15–2.40). (Table 2) The reported length of stay was significantly increased in patients with codes for hypokalemia and was decreased for hyperkalemia. Patients with heart failure without a potassium diagnosis code, as compared to hyperkalemia and hypokalemia, stayed in the hospital for a mean of 4.55, 5.36 and 5.93 days respectively. Multivariable analysis using inpatient death as the dependent variable and controlling for age, sex, race, smoking, obesity, dyslipidemia, diabetes, hypertension, chronic kidney disease and Charlson comorbidity index showed similar significant results as with univariate analysis, with a lower odds of death in those with hyperkalemia (OR: 0.77, 95% CI: 0.72–0.83) as compared to those without a potassium diagnosis. Similarly, hypokalemia was associated with a higher odds of death in multivariate analysis when above factors were controlled than those without a potassium diagnosis. (OR: 2.37, 95% CI: 2.24–2.52). (Table 2)
Table 2.
Univariate and multivariable analyses with logistic regression of mortality, length of stay (LOS) and cost among HF patients in relation to normokalemia.
| Characteristics | Unadjusted Odds Ratio OR (95% CI), p-value |
Adjusted* Odds Ratio OR (95% CI), p-value |
|---|---|---|
| Mortality | ||
| Hyperkalemia | 0.73 (0.69–0.78), p < 0.001 | 0.77 (0.72–0.83), p < 0.001 |
| Hypokalemia | 2.27 (2.15–2.40), p < 0.001 | 2.37 (2.24–2.52), p < 0.001 |
| LOS | ||
| Hyperkalemia | 0.81 (0.74–0.88), p < 0.001 | 0.88(0.81–0.94), p < 0.001 |
| Hypokalemia | 1.37 (1.30–1.45), p < 0.001 | 1.16 (1.09–1.24), p < 0.001 |
| Cost | ||
| Hyperkalemia | 1270.81 (1083.19–1458.44), p < 0.001 | 1428.22 (1229.40–1627.04), p < 0.001 |
| Hypokalemia | 3070.33 (2855.78–3284.89), p < 0.001 | 2511.57 (2307.19–2715.95), p < 0.001 |
*Adjusted for age, sex, race, smoking, obesity, dyslipidemia, diabetes, hypertension, Charlson comorbidity index.
The rate of inpatient mortality of patients with heart failure without a diagnosis of abnormal potassium, with hyperkalemia and with hypokalemia were 2.85, 2.11 and 6.24 percent respectively (Table 3). Inpatient mortality among different subcategories of HF, namely systolic heart failure, diastolic heart failure and combined systolic and diastolic heart failure followed similar trends as the composite HF group (Table 3). Multivariable analysis of mortality in subtypes of HF and possible etiologies of HF (acute coronary syndrome, ischemic heart disease, valvular heart disease, cardiomyopathy, atrial fibrillation) are presented in Supplementary Table 1. The subtypes and etiologies follow the same pattern of mortality among different serum potassium categories as was seen with HF and its subtypes. All associations were statistically significant except for hyperkalemic patients with combined systolic and diastolic, valvular heart disease, hypertensive heart disease and cardiomyopathy in comparison to normokalemia.
Table 3.
Classification of mortality in HF and based on etiology and subtypes of HF with different categories of potassium levels.
| Subtypes and etiologies | Normokalemia (%) | Hyperkalemia (%) | Hypokalemia (%) | p-value |
|---|---|---|---|---|
| HF | 2.85 | 2.11 | 6.24 | <0.0001 |
| SHF | 2.50 | 1.94 | 6.58 | <0.0001 |
| DHF | 2.12 | 1.79 | 4.75 | <0.0001 |
| SDHF | 2.58 | 2.19 | 5.42 | <0.0001 |
| IHD | 2.67 | 2.21 | 5.35 | <0.0001 |
| VHD | 2.87 | 2.01 | 7.16 | <0.0001 |
| HHD | 0.82 | 0.75 | 5.75 | 0.06 |
| CM | 2.08 | 1.40 | 4.88 | <0.0001 |
| AF | 3.88 | 2.72 | 9.92 | <0.0001 |
(HF: heart failure; SHF: systolic heart failure; DHF: diastolic heart failure; SDHF: systolic and diastolic heart failure; UHF: unspecified heart failure; ACS: acute coronary syndrome; IHD: ischemic heart disease; VHD: valvular heart disease; HHD: hypertensive heart disease; CM: cardiomyopathy; AF: atrial fibrillation)
5. Discussion
In this US database study, we found increased inpatient mortality in HF patients diagnosed with hypokalemia when compared to those without abnormal potassium diagnosis, which is in line with prior outpatient studies [2–5,12]. Our study found a higher overall calculated risk of mortality in comparison to other studies except Hoss et al., where their odds ratio was comparable to ours [2–5,12]. Our findings of increased mortality risk were similar regardless of the subtype or etiology of HF (OR: 2.16–5.94).
The risk for developing hyperkalemia increases with advancing age, male gender, renal failure and diabetes, all of which are themselves independently associated with chronic kidney disease [13,15,17]. Paradoxically, our cohort identified significantly more CKD in the hypokalemic HF patients than the normokalemic or hyperkalemic groups. It is possible that hypokalemia is a marker for patients who have more decompensated heart failure and/or higher diuretic doses, a theory postulated by Bowling et al. to explain the higher rates of death and rehospitalization in their cohort of HF patients with hypokalemia [4]. We found that hyperkalemia was associated with an overall small but decreased odds of mortality among HF patients without abnormal potassium. Although some heart failure etiologies and subtypes did not demonstrate a significant association between hyperkalemia and decreased mortality, none showed a significant increase in mortality. This finding is in line with previous studies which showed either no difference of a decrease in mortality associated with hyperkalemia [5,18]. This finding is particularly important because of the increase in inpatient mortality seen following the publication of the RALES trial, in which hyperkalemia related hospitalizations and mortality both increased [14], a finding that made physicians more concerned about the use of evidence based medicines that may be associated with hyperkalemia alone or in combination.
6. Limitations
The database that we utilized uses ICD-9 codes to categorize potassium disorders. No ICD-9 definitions specify what levels of potassium constitute hypo- or hyperkalemia. It was not possible to know whether potassium abnormalities were one-time or sustained. Potassium abnormalities that occurred only once should be less likely to result in mortality. Furthermore, it is possible that hypokalemia may be a confounding variable for patients who needed more aggressive diuresis due to more significant volume overload; if this is the case, hypokalemia may be a marker for disease severity but not an independent risk factor on its own. We were not able to subcategorize high serum potassium into multiple groups as was done by Hoss et al. and Ahmed et al. and calculate mortality risk in high-normal serum potassium (serum K 5.0–5.5 mEq/l) due to the aforementioned limitations in the ICD-9 diagnoses [5,18]. This limitation would be present using ICD-10 coding as well. It is possible that hospitals with greater resources may have had coding personnel, allowing them to identify hyperkalemia in their heart failure patients more often, which would raise the question of whether other unmeasured confounders such as patient or hospital resources may explain differences in mortality seen in our study. However, those same coding resources would also have identified hypokalemia, and the hypokalemic cohort fared significantly worse than those patients without potassium diagnoses. Furthermore, surrogate analysis of patient ZIP codes did not suggest that the cohorts had very different financial resources. Although ICD −9 does distinguish between acute and chronic heart failure, we chose to select all heart failure diagnoses in the first two diagnosis positions in order to most broadly capture all heart failure patients for whom it was believed heart failure was one of their top two admission diagnoses. Despite this, it is possible that some of the patients included in the study may have had chronic but not acute decompensated failure.
7. Conclusion
Hypokalemia is associated with an increased odds of mortality among patients with HF, regardless of the etiology or type of heart failure. Conversely, hyperkalemia, is associated with a similar or lower odds of mortality. Whether our mortality findings translate to longer-term outpatient settings where significantly less monitoring is possible is a matter for further study, but our current work supports the use of aggressive goal-directed therapy and establishment of normal potassium levels in the inpatient setting.
Disclosure statement
2017 Heart Failure Society of America Annual Meeting Travel Grant Award
Supplementary material
Supplemental data for this article can be accessed here.
References
- [1].Benjamin EJ, Blaha MJ, Chiuve SE, et al. Heart disease and stroke statistics-2017 update: a report from the American Heart Association. Circulation. 2017January DOI: 10.1161/CIR.0000000000000485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Alper AB, Campbell RC, Anker SD, et al. A propensity-matched study of low serum potassium and mortality in older adults with chronic heart failure. Int J Cardiol. 2009;137(1):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Ahmed A, Zannad F, Love TE, et al. A propensity matched study of the association of low serum potassium levels and mortality in chronic heart failure. Eur Heart J. 2007;28(11):1334–1343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Bowling CB, Pitt B, Ahmed MI, et al. Hypokalemia and outcomes in patients with chronic heart failure and chronic kidney disease: findings from propensity-matched studies. Circ Heart Fail. 2010;3(2):253–260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Hoss S, Elizur Y, Luria D, et al. Serum potassium levels and outcome in patients with chronic heart failure. Am J Cardiol. 2016;118(12):1868–1874. [DOI] [PubMed] [Google Scholar]
- [6].Salah K, Pinto YM, Eurlings LW, et al. Serum potassium decline during hospitalization for acute decompensated heart failure is a predictor of 6-month mortality, independent of N-terminal pro-B-type natriuretic peptide levels: an individual patient data analysis. Am Heart J. 2015;170(3):531–542.e1. [DOI] [PubMed] [Google Scholar]
- [7].Gotsman I, Zwas D, Lotan C, et al. Heart failure and preserved left ventricular function: long term clinical outcome. PloS One. 2012;7(7):e41022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Macdonald JE, Struthers AD.. What is the optimal serum potassium level in cardiovascular patients? J Am Coll Cardiol. 2004;43(2):155–161. [DOI] [PubMed] [Google Scholar]
- [9].Cleland JG, Dargie HJ, Ford I.. Mortality in heart failure: clinical variables of prognostic value. Br Heart J. 1987;58(6):572–582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Cooper HA, Dries DL, Davis CE, et al. Diuretics and risk of arrhythmic death in patients with left ventricular dysfunction. Circulation. 1999;100(12):1311–1315. [DOI] [PubMed] [Google Scholar]
- [11].Pitt B, Zannad F, Remme WJ, et al. The effect of spironolactone on morbidity and mortality in patients with severe heart failure. Randomized aldactone evaluation study investigators. N Engl J Med. 1999;341(10):709–717. [DOI] [PubMed] [Google Scholar]
- [12].Collins AJ, Pitt B, Reaven N, et al. Association of serum potassium with all-cause mortality in patients with and without heart failure, chronic kidney disease, and/or diabetes. Am J Nephrol. 2017;46(3):213–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Desai AS, Swedberg K, McMurray JJV, et al. Incidence and predictors of hyperkalemia in patients with heart failure: an analysis of the CHARM program. J Am Coll Cardiol. 2007;50(20):1959–1966. [DOI] [PubMed] [Google Scholar]
- [14].Juurlink DN, Mamdani MM, Lee DS, et al. Rates of hyperkalemia after publication of the randomized aldactone evaluation study. N Engl J Med. 2004;351(6):543–551. [DOI] [PubMed] [Google Scholar]
- [15].Tromp J, Ter Maaten JM, Damman K, et al. Serum potassium levels and outcome in acute heart failure (data from the PROTECT and COACH trials). Am J Cardiol. 2017;119(2):290–296. [DOI] [PubMed] [Google Scholar]
- [16].HCUP HCUP-US NIS overview. [cited2017April6]. Available from: https://www.hcup-us.ahrq.gov/nisoverview.jsp
- [17].López-Vilella R, Morillas-Climent H, Plaza-López D, et al. Hyperkalemia in heart failure patients: current challenges and future prospects. Research Reports in Clinical Cardiology. 2016February9 [cited 2017 April9]. Available from: https://www.dovepress.com/hyperkalemia-in-heart-failure-patients-current-challenges-and-future-p-peer-reviewed-fulltext-article-RRCC
- [18].Ahmed MI, Ekundayo OJ, Mujib M, et al. Mild hyperkalemia and outcomes in chronic heart failure: a propensity matched study. Int J Cardiol. 2010;144(3):383–388. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


