ABSTRACT
Objectives: Impairment in upper cervical spine mobility is associated with cervicogenic headache severity and disability. Measures of such mobility include the flexion-rotation test (FRT), which requires full cervical flexion and may be influenced by lower cervical spine dysfunction. The C0-C2 axial rotation test also evaluates upper cervical mobility but normal values and reliability have not been reported. Our objective is to determine normal values, and intra-rater and inter-rater reliability of the C0-C2 axial rotation test.
Methods: Two therapists independently evaluated the FRT and C0-C2 axial rotation test with an iPhone compass application on 32 asymptomatic subjects with mean age 40.53 (SD 11.64) years on two occasions. Measurement procedures were standardized; and order of testing randomized.
Results: For the FRT and C0-C2 axial rotation test reliability was high (ICC > 0.88). For rater one, Mean range to the left during the FRT and C0-C2 axial rotation test was 45.0° (6.04) and 14.43° (2.94), respectively, while range to the right was 44.6° (6.57) and 15.44° (2.68). For the FRT and C0-C2 axial rotation test the standard error of measurement was at most 2°, while the minimum detectable change was at most 4°. A strong positive correlation exists between the FRT and C0-C2 axial rotation test (r = 0.84, P < 0.01).
Discussion: The range recorded during the C0-C2 axial rotation test and FRT have high levels of reliability when evaluated using an iPhone. The strong correlation between the FRT and C0-C2 axial rotation test indicate that both may be measuring similar constructs, but each test needs to be referenced to normal values.
KEYWORDS: Upper cervical spine rotation, flexion-rotation test, goniometer
Introduction
Determination of C0-C2 rotation mobility forms an integral part of examination of patients presenting with cervical spine disorders, but is particularly useful for the diagnosis of cervicogenic headache [1–4]. Indeed, impairment in C0-C2 rotation mobility is associated with cervicogenic headache severity and disability [4,5].
The flexion-rotation test (FRT) has found to be a valid and reliable measure of upper cervical mobility as it predominantly measures rotation between C1 and C2 vertebral levels [1,6]. A Delphi survey of international experts on physiotherapy management of headache suggested that the FRT was one of the most clinically useful tests in the assessment of patients with headache [7]. Support for this was provided by a review of screening tests for the diagnosis of cervicogenic headache, which found the FRT to have the highest level of diagnostic accuracy based on low risk of bias studies [8]. The FRT requires the subject to lay supine, with the cervical and upper thoracic spine in complete flexion to localize rotation to the C1-C2 motion segment. Range of motion (ROM) to the left and right are compared to normal values which is expected to be 44° to each side [1,2]. The presence of painful joints in the lower cervical spine pain reduces the available range on the FRT to 37.5° [9]. This indicates that lower cervical spine pain may influence to a small degree mobility recorded during the FRT when measured in supine, and hence may lead to a false positive FRT result.
Range of C0-C2 rotation mobility can also be evaluated with the C0-C2 axial rotation test. With the subject seated and neck placed in a neutral position, the therapist passively rotates the head to the left and right, isolating movement to segmental levels above C2 by stabilizing the second cervical vertebra with their index finger and thumb against the articular pillar and spinous process of C2 vertebra (Figure 1). This method does not require end-range flexion of the lower cervical spine and can, thus, be used to assess impairment of C0-C2 rotation mobility in the presence of lower cervical spine pain and dysfunction. Normal values for upper cervical rotation (C0-C2) combining left and right rotation ranges from 78° [6] to 88° [1,2]. However, during the C0-C2 axial rotation test, fixation of the C2 vertebra does not allow normal upper cervical movement to occur and MRI investigations of a variant of the C0-C2 axial rotation test in supine found a mean range of 22° combined rotation [10] which is much less range than recorded by the FRT. One explanation for this is that alar ligament tension is increased by fixation of the C2 vertebra [10], which limits full rotation movement at C0-C2. During clinical evaluation, normal mobility on this test is approximately 30° combined rotation to each side, although there are no studies to have reported normal values or that have evaluated the reliability of this test. While both tests measure rotation in the upper cervical spine, it is clear that the absolute value for each test will be different in an individual patient. However, if a patient were to present with impaired C0-C2 rotation mobility, then both tests should be able identify movement restriction at C0-C2 motion segment if referenced against a normal value for the test, yet no studies have investigated the correlation in range between tests.
Figure 1.

Hand Placement for stabilization of the C2 vertebra during the C0-C2 axial rotation test. During right rotation, the left side of the spinous process of C2 and the right laminar of C2 are fixed by the thumb and index finger respectively. Arrow indicates the direction of rotation. Circle indicates stabilization.
Reliability of measurement of C0-C2 rotation mobility during the FRT has been demonstrated with a number of devices including the cervical ROM device [11], as well as a more sophisticated ultrasound-based method [12]. Recently smartphones have been gaining popularity as a reliable measurement method used by physiotherapists in the assessment of musculoskeletal disorders to determine joint ROM [13–17]. Smartphones have the capability of measuring movement in all 3 planes using internal sensors and have been shown to have concurrent validity and accuracy [18,19]. Grondin et al. [20] reported that FRT range could be reliably measured by a physiotherapist using the compass application on an iPhone.
The purpose of the current study was to evaluate normal values for the C0-C2 axial rotation test and FRT when measured using the compass application on an iPhone 6. The primary objective was to assess intra-rater and inter-rater reliability of the measurement recorded during the C0-C2 axial rotation test. The secondary objective was to correlate range recorded for the FRT with that for the C0-C2 axial rotation test. Our hypothesis was the C0-C2 axial rotation test has good to excellent inter- and intra-rater reliability with a strong correlation between the 2 methods of measuring C0-C2 rotation mobility.
Methods
This was a repeated measures reliability study design investigating inter- and intra-rater reliability of the C0-C2 axial rotation test as measured with the compass application on an iPhone 6. Subjects were recruited in a manner of convenience from visitors, staff and students attending the Smt. Kashibai Navale Medical College and General Hospital and were naïve to the test and measurement method. Asymptomatic volunteers were included with an even distribution across genders and across eight age blocks (years 21–25; 26–30; 31–35; 36–40, etc.) between the ages of 21–60 years to provide variability in age. Hence, 2 males and 2 females for each age category were recruited before assessment of eligibility. Exclusion criteria were a significant history of neck pain, vertigo, headache or upper quadrant pain in the past 6 months, as well as recent upper quadrant surgery, fractures, infections, neurological disorders or malignancies. A total of 50 subjects were evaluated and 18 were excluded based on the exclusion criteria. Thus, a total 32 subjects (15 females) mean age 40.53 years (SD 11.64) were enrolled in this study. Additional demographic details of height, weight and BMI were also assessed (Table 1).
Table 1.
Descriptive statistics.
| Minimum | Maximum | Mean | Std. Deviation | |
|---|---|---|---|---|
| Age | 22.00 | 60.00 | 40.53 | 11.64 |
| Height (cm.) | 141.00 | 175.00 | 159.53 | 6.76 |
| Weight (kg.) | 40.00 | 80.00 | 61.78 | 10.57 |
| BMI | 17.60 | 32.10 | 24.24 | 3.77 |
Based on a Repeated Measures ANOVA, with a power of 0.8, effect size of 0.5, and alpha of 0.05, the required sample size was determined to be 25 subjects in each group. This number was increased to 32 to allow for 30% dropouts.
Subject’s demographic data including age, weight and height was recorded and the procedure was explained to the subject. An independent research assistant allocated consecutive subjects to each rater in random order, to avoid bias due to order effects
Two physiotherapists participated as the raters. Rater one had 15 years postgraduate experience while rater two was an inexperienced physiotherapist, an undergraduate intern, who had undergone extensive training for the measurement procedure and had been working on a clinical placement for two months. All the measurements were taken at the same time of day, in the same room without any interference from other electrical modalities to interfere with an iPhone.
An iPhone 6 (Apple Inc, Cupertino, CA, USA) was mounted on the apex of the subject’s head with elasticated Velcro straps (Figure 2). The in-built compass application was used to measure upper cervical rotation mobility. The compass application is designed to measure changes in angular orientation of an iPhone using internal sensors. The change in the angular rotation is expressed in degrees on an iPhone display. Range of rotation during the FRT in supine was determined by rater one according to previously published guidelines [1,3]. Following this, range was recorded for the C0-C2 axial rotation test in sitting while carefully maintaining a horizontal iPhone position. For this test, the second cervical vertebra is gently stabilized with the lateral side of the pad of the thumb placed on the contralateral side of the spinous process and the pad of the index finger placed on the articular pillar on the ipsilateral side of rotation (Figure 2). The subject’s trunk was stabilized by the therapist’s body leaning against the subject’s upper body. The subject’s head was passively rotated to the opposite side, the therapist was standing on until firm resistance prevented further movement. A research assistant silently recorded an iPhone compass application data ensuring the assessors were blind to all the measurements. The average of three readings was taken and recorded in degrees. After completing the measurements and following a 5-min rest period, the second rater who was blind to the measurements of first rater conducted the same test procedure in similar manner to the first rater.
Figure 2.

FRT (2 a) and C0-C2 axial rotation test (2 b) toward right side with an iPhone attachment.
To determine intra-rater reliability for each test, the same procedure was repeated by rater one the following day utilizing the same assessment process. Rater one did not have access to the data at any time ensuring blinding. Written informed consent was obtained from subjects who volunteered to participate in this study. Approval was granted by the ethical committee of Smt. Kashibai Navale College of Physiotherapy Narhe, Pune, India.
Statistical analysis
Statistical analysis was performed using SPSS V24.0 (SPSS Inc., 444 N. Michigan Avenue, Chicago, Illinois, 60,611). Alpha was set at 0.05 for each analysis. An independent samples t-test was calculated to determine differences in upper cervical rotation range between genders for range recorded during the FRT and C0-C2 axial rotation test. A single measure intra-class correlation coefficient (ICC2,1) and 95% confidence intervals (95% CI) were generated for range recorded during the FRT and the C0-C2 axial rotation test. These were used to compute the standard error of measurement (SEM) using the following formula to indicate the range of scores that can be expected upon re-testing in this population.
The minimum detectable change (MDC) at the 90% CI was calculated using the formula below to indicate the minimal change between two measurements required for the change to be considered a real change:
A Pearson’s correlation analysis was used to identify the relationships between range recorded on the FRT and the C0-C2 axial rotation test, and a simple linear regression analysis was calculated to predict range measured during the C0-C2 axial rotation test based on range recorded during the FRT.
Results
All data for ROM were normally distributed. Descriptive statistics for rater 1 and 2 are shown in Table 2. There was no significant difference in ROM between males and females for range recorded during the FRT (t (30) = 0.43, p = 0.67) or the C0-C2 axial rotation test (t (30) = −19.3, p = 0.06). Combined right and left range during the FRT and C0-C2 axial rotation test for rater one was recorded as 89.62 (SD 12.38) and 30.59 (SD 5.70), respectively. In all cases the end-point for ROM testing was firm resistance for the FRT and C0-C2 axial rotation test.
Table 2.
Mean values for rater one and two in degrees, ranges, and standard deviations for range recorded during the flexion rotation test (FRT) and C0-C2 axial rotation test.
| Mean range (SD) degrees | Mean range males (SD) degrees |
Mean range females (SD) degrees | |
|---|---|---|---|
| FRT R rater 1 | 44.6 (6.57) | 45.13 (7.20) | 44.12 (6.06) |
| FRT R rater 2 | 45.19 (5.25) | 45.50 (6.59) | 44.50 (5.60) |
| FRT L rater 1 | 45.0 (6.04) | 45.06 (4.85) | 45.0 (5.69) |
| FRT L rater 2 | 45.03 (5.2) | 45.06 (5.05) | 45.31 (6.61) |
| UCR R rater 1 | 15.44 (2.68) | 14.56 (2.73) | 16.13 (2.39) |
| UCR R rater 2 | 15.22 (2.79) | 15.0 (2.73) | 15.44 (2.93) |
| UCR L rater 1 | 14.43 (2.94) | 14.69 (2.65) | 16.19 (3.1) |
| UCR L rater 2 | 14.91 (2.29) | 14.37 (2.39) | 15.44 (2.14) |
FRT: Flexion rotation test, R: Right side, L: Left side
Intra-rater and inter-rater reliability coefficients for range record during the FRT and C0-C2 axial rotation test for rater one and two are shown in Table 3.
Table 3.
Summary of reliability analysis for range record during the flexion rotation test (FRT) and upper cervical rotation C0-C2 axial rotation test for rater one and two.
| ICC (2,1) | 95% CI |
SEM | MDC | ||
|---|---|---|---|---|---|
| Lower bound | Upper bound | ||||
| Inter rater FRT R | 0.93 | 0.85 | 0.97 | 1.74 | 4.05 |
| Intra rater FRT R | 0.90 | 0.80 | 0.95 | 2.08 | 4.85 |
| Inter rater FRT L | 0.92 | 0.84 | 0.96 | 1.71 | 3.98 |
| Intra rater FRT L | 0.91 | 0.82 | 0.95 | 1.81 | 4.23 |
| Inter rater UCR R | 0.92 | 0.84 | 0.96 | 0.76 | 1.77 |
| Intra rater UCR R | 0.91 | 0.82 | 0.96 | 0.84 | 1.95 |
| Inter rater UCR L | 0.89 | 0.78 | 0.94 | 0.97 | 2.27 |
| Intra rater UCR L | 0.88 | 0.77 | 0.94 | 1.02 | 2.38 |
FRT: Flexion rotation test, R: Right side, l: Left side, SEM: Smallest error in the measurement, MDC: Minimum detectable change
A bivariate Pearson’s correlation analysis was undertaken between range recorded on the FRT to each side and the range recorded during the C0-C2 axial rotation test. It was hypothesized that a positive relationship would exist between these variables for range recorded to the left and to the right side. Results of the correlation indicate that range to the left side recorded during the FRT was associated with range recorded during the C0-C2 axial rotation test (r = 0.84, p < 0.01). Similarly, range to the right side recorded during the FRT was associated with range recorded during the C0-C2 axial rotation test (r = 0.83, p < 0.01). The coefficient of determination was 71% for range to the left and 69% for range to the right. This indicates that 71 and 69% of range recorded during the C0-C2 axial rotation test is explained by range recorded on the FRT to the left and right, respectively.
A simple linear regression analysis on range to the left during the C0-C2 axial rotation test and the FRT identified a significant regression equation [F(1, 30) = 66.76, p < 0.000), with an R2 of 0.69]. Participants predicted range during the C0-C2 axial rotation test to the left is equal to (FRT-19.66)/1.71degrees when range recorded during the FRT to the left is measured in degrees. Participant’s left side range during the C0-C2 axial rotation test is increased 0.58° for each degree of range to the left on the FRT. Similarly, with respect to range to the right during the C0-C2 axial rotation test and the FRT, a simple linear regression analysis identified a significant regression equation [F(1, 30) = 70.49, p < 0.000), with an R2 of 0.70].
Participants predicted range to the right during the C0-C2 axial rotation test was equal to (FRT-12.88)/2.06 degrees when range recorded during the FRT to the right was measured in degrees. Participant’s right range during the C0-C2 axial rotation test was increased 0.48° for each degree of range to the right on the FRT. The representation of this analysis is shown in Figures 3 and 4.
Figure 3.
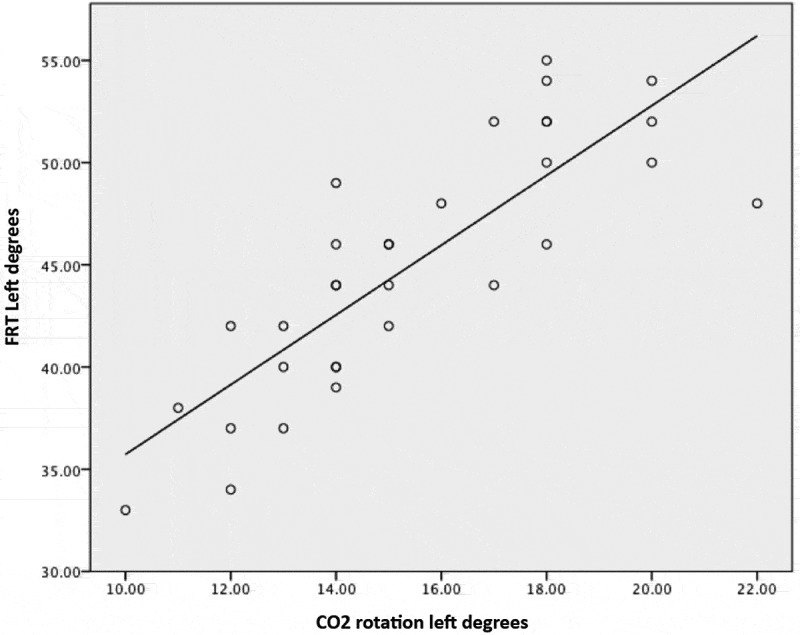
Simple linear regression analysis for range of rotation to the left during the flexion rotation test (FRT) and C0-C2 axial rotation test.
Figure 4.
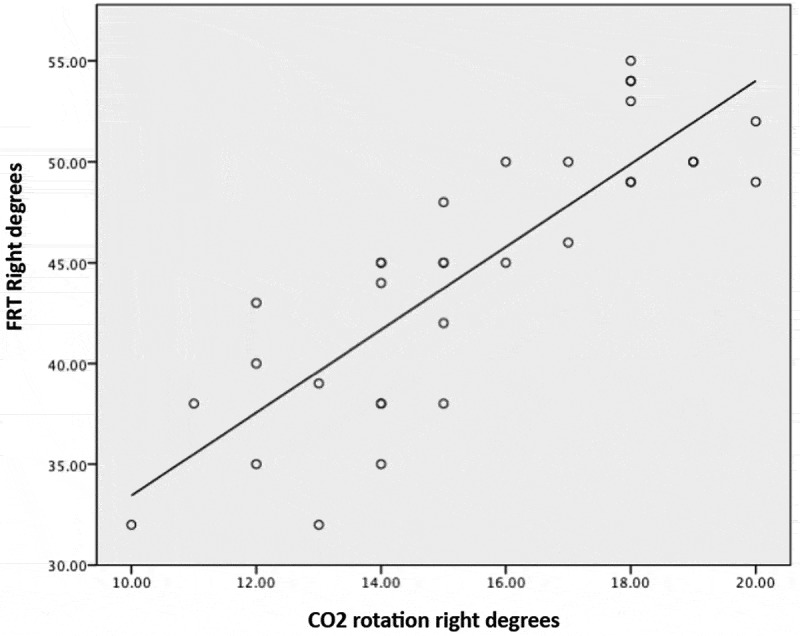
Simple linear regression analysis for range of rotation to the right during the flexion rotation test (FRT) and C0-C2 axial rotation test.
Discussion
This study is the first to examine the reliability of the C0-C2 axial rotation test using an iPhone compass application to measure C0-C2 rotation mobility. The FRT was used as a validated measure of upper cervical rotation and range compared between the two tests. The results indicate that mobility recorded during the FRT and C0-C2 axial rotation test can be reliably determined by the compass application on an iPhone.
Reliability is an important psychometric property that needs to be determined before an instrument can be considered valid [21]. Based on the results of this study intra- and inter-rater reliability can be considered as high [21] with all ICC values greater 0.88 for either test procedure (Table 3). These results are in accordance with a previous study assessing the reliability of the FRT using a modified cervical ROM device [ICC 0.93 (CI, 0.87–0.96)] [2] and using an iPhone [0.95 (CI, 0.88–0.98)] [20]. Interestingly inter-rater reliability was greater than intra-rater reliability, although the difference was very small. These results are contrary to most measurement studies assessing reliability.
A previous report of an iPhone used as a goniometer to measure cervical rotation has indicated poor reliability [16]. There are differences in the measurement methods described by Tousignant-Laflamme et al. [16] and the current study, which might explain the high levels of reliability found. First, both raters were well trained in the measurement procedure and had undergone vigorous training. Second, the readings were taken at consistent time in the same room without electromagnetic noise interfering with the magnetometer in the iPhone. Third, the end-point for range was firm resistance that was easy to identify by both raters. Fourth, the C2 spinous process is an easily palpable bony landmark, being the first bony prominence below the skull. Finally, we took the average of three measurements as a final reading. These factors may have enabled the high levels of reliability achieved.
Test measurement error is represented by the SEM and the MDC, which are presented in the similar units as that of original measurements. Variability among individuals does not affect values of the SEM and the MDC. In the current study, the SEM for the FRT was at most 2° and for the C0-C2 axial rotation test only 1°. Previous studies evaluating the FRT using a modified cervical ROM device also reported a similar small value for the SEM of 2–3° [4,22].
The MDC score provides an estimate of the difference in ROM required to identify a clinically meaningful change after an intervention [11]. The values for the MDC score indicate that to detect a true change in range determined by the FRT requires a difference of at least 4° and in the case of the C0-C2 axial rotation test a difference of at least 2°. A previous study by Hall et al. [23] reported a MDC of at least 5° when measured with a modified cervical ROM device. In the context of measurement error and statistically meaningful change, for both the FRT and C0-C2 axial rotation test, an iPhone compass application appears to be as effective as the modified cervical ROM device. The smaller measurement error in measuring upper cervical mobility with the C0-C2 axial rotation test and FRT using an iPhone justifies its use in clinical practice.
For example, patients with cervicogenic headache or temporomandibular dysfunction demonstrate significant C0-C2 rotation mobility deficit with range less than 25° determined by the FRT [3,4,24]. Lower SEM and MDC values for an iPhone application to determine ROM in both test methods used in this study provide confidence to identify this mobility deficit with ease.
For rater one, the FRT the mean range (SD) was found to be 44.06° (6.57) for right rotation and 45.0° (6.04) for left rotation. These values are similar to previous reports of range recorded for the FRT when measured using a modified cervical ROM device [3,25–27] and also when measured with more sophisticated measuring devices such as ultrasound-based measurement [12] or Fastrak [22]. For example, Hall et al. [2] reported mean values for the FRT for range to the right and left as 43° (SD 2.8°) and 44° (SD 3.1°), respectively. Having concordant values for the FRT provides a level of confidence in the study findings.
This is the first study to report on range of movement values for the C0-C2 axial rotation test. For rater one, mean values were 15.44° (2.68) for right rotation and 14.43° (2.94) for left rotation. Osmotherly et al. [10] was able to very accurately measure C0-C2 rotation range in normal subjects using high field strength MRI and reported a mean range of 11° with a SEM of 1°. These measurements were taken in supine position while stabilizing the C2 vertebrae in a different fashion to the one employed in the current study, which might explain the difference. Another explanation may be the different end-point, with firm resistance chosen in the current study, but not stated in the study by Osmotherly et al. [10]. Firm resistance as the end-point for range may be easy to define and achieve in clinical evaluation.
Another important finding from our study was the association between range recorded during the C0-C2 axial rotation test and that during the FRT, with a significant correlation between these two measurement procedures (p < 0.01) supported by Figures 3 and 4. Despite this correlation, there was almost a threefold difference in the magnitude of range between the two tests. Hence, it is important to clarify that the gross range recorded during the FRT and C0-C2 axial rotation test cannot be directly compared in the clinical setting. Rather, range must be interpreted as a proportion of normal values, for example, an impairment of 50% in range on one test should equate to an impairment of 50% on the other, but requires further investigation in symptomatic subjects to confirm this.
It has been reported that range recorded on the FRT is influenced by facet joint dysfunction in the lower cervical spine, perhaps as the test demands the complete flexion of lower cervical and upper thoracic spine, and a small part of the movement on the FRT occurs at levels other than C1-C2 vertebral segment. On some occasions it may not be possible to evaluate the FRT, for example, where there is an associated lower cervical spine disorder. Hence, the C0-C2 axial rotation test may be an alternative for the FRT.
There are some potential limitations to our study’s findings. The external validity of results are limited as we evaluated only healthy participants. Future studies should investigate the reliability of the C0-C2 axial rotation test and the correlation with range determined by the FRT in people with cervicogenic headache. In addition, criterion related validity of an iPhone should be determined with a gold standard test of cervical spine mobility such as MRI or x-ray.
Conclusion
This study is the first to evaluate the reliability of the C0-C2 axial rotation test using the compass application on an iPhone 6 and the first to have correlated mobility between the C0-C2 axial rotation test and the FRT. Measurements taken for both tests were found to have excellent intra- and inter-rater reliability in asymptomatic people, with a small SEM and MDC of at most 4°. Range recorded during the FRT correlated highly with range recorded on the C0-C2 axial rotation test.
Biography
Kiran Satpute is Under Graduate and Post Graduate teacher at Smt. Kashibai Navale College of Physiotherapy which is affiliated to Maharashtra Medical University Of Health Sciences Nashik, Maharashatra, India. Currently he is a PhD scholar at Sancheti College of Physiotherapy.
Disclosure statement
No potential conflict of interest was reported by the authors.
Supplemental Material
Supplemental data can be accessed here.
References
- [1].Hall T, Robinson K.. The flexion-rotation test and active cervical mobility–a comparative measurement study in cervicogenic headache. Man Ther. 2004;9:197–202. [DOI] [PubMed] [Google Scholar]
- [2].Hall TM, Robinson KW, Fujinawa O, et al. Intertester reliability and diagnostic validity of the cervical flexion-rotation test. J Manipulative Physiol Ther. 2008;31:293–300. [DOI] [PubMed] [Google Scholar]
- [3].Ogince M, Hall T, Robinson K, et al. Validity of the cervical flexion rotation test in C1-C2-related cervicogenic headache. Man Ther. 2007;12:256–262. [DOI] [PubMed] [Google Scholar]
- [4].Hall TM, Briffa K, Hopper D, et al. Comparative analysis and diagnostic accuracy of the cervical flexion-rotation test. J Headache Pain. 2010a;11:391–397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Ernst MJ, Crawford RJ, Schelldorfer S, et al. Extension and flexion in the upper cervical spine in neck pain patients. Man Ther. 2015;20:547–552. [DOI] [PubMed] [Google Scholar]
- [6].Takasaki H, Hall T, Oshiro S, et al. Normal kinematics of the upper cervical spine during the Flexion-Rotation Test in vivo measurements using magnetic resonance imaging. Man Ther. 2011;16(2):167–171. [DOI] [PubMed] [Google Scholar]
- [7].Luedtke K, Boissonnault W, Caspersen N, et al. International consensus on the most useful physical examination tests used by physiotherapists for patients with headache: a Delphi study. Man Ther. 2016;23:17–24. [DOI] [PubMed] [Google Scholar]
- [8].Rubio-Ochoa J, Benítez-Martínez J, Lluch E, et al. Physical examination tests for screening and diagnosis of cervicogenic headache: a systematic review. Man Ther. 2016;21:35–40. [DOI] [PubMed] [Google Scholar]
- [9].Hall T, Briffa K, Hopper D. The influence of lower cervical joint pain on range of motion and interpretation of the flexion–rotation test. J Man Manip Ther. 2010b;18:126–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Osmotherly PG, Rivett D, Rowe LJ. Toward understanding normal craniocervical rotation occurring during the rotation stress test for the alar ligaments. Phys Ther. 2013;93:986–992. [DOI] [PubMed] [Google Scholar]
- [11].Fletcher JP, Bandy WD. Intrarater reliability of CROM measurement of cervical spine active range of motion in persons with and without neck pain. J Orthop Sports Phys Ther. 2008;38:640–645. [DOI] [PubMed] [Google Scholar]
- [12].Schäfer A, Lüdtke K, Breuel F, et al. Validity of eyeball estimation for range of motion during the cervical flexion rotation test compared to an ultrasound-based movement analysis system. Physiother Theory Pract. 2018;34(8):622–628. [DOI] [PubMed] [Google Scholar]
- [13].Vohralik SL, Bowen AR, Burns J, et al. Reliability and validity of a Smartphone app to measure joint range. Am J Phys Med Rehabil. 2015;94(4):325–330. [DOI] [PubMed] [Google Scholar]
- [14].Mourcou Q, Fleury A, Diot B, et al. Mobile phonebased joint angle measurement for functional assessment and rehabilitation of proprioception. Biomed Res Int. 2015;2015:328142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Pourahmadi MR, Ebrahimi Takamjani I, Sarrafzadeh J, et al. Reliability and concurrent validity of a new iPhone® goniometric application for measuring active wrist range of motion: a cross-sectional study in asymptomatic subjects. J Anat. 2017;230(3):484–495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Tousignant- Laflamme Y, Boutin N, Dion AM, et al. Reliability and criterion validity of two applications of the iPhone to measure cervical range of motion in healthy participants. J Neuroeng Rehabil. 2013;10:69–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Guidetti L, Placentino U, Baldari C. Reliability and criterion validity of the smartphone inclinometer application to quantify cervical spine mobility. Clin Spine Surg. 2017;30(10):E1359–E1366. [DOI] [PubMed] [Google Scholar]
- [18].Jones A, Sealey R, Crowe M, et al. Concurrent validity and reliability of the simple goniometer iphone app compared with the universal goniometer. Physiother Theory Pract. 2014;30:512–516. [DOI] [PubMed] [Google Scholar]
- [19].Furness J, Schram B, Cox A, et al. Reliability and concurrent validity of the iPhone compass application to measure thoracic rotation range of motion (ROM) in healthy participants. Peer J. 2018;6:e4431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Grondin F, Hall T, von Piekartz H. Does altered mandibular position and dental occlusion influence upper cervical movement: a cross-sectional study in asymptomatic people. Musculoskelet Sci Pract. 2017;27:85–90. [DOI] [PubMed] [Google Scholar]
- [21].Portney LG, Watkins MP. Foundations of clinical research: applications to practice. 3rd ed. Upper Saddle River, NJ: Prentice Hall Health; 2015. [Google Scholar]
- [22].Amiri M, Jull G, Bullock-Saxton J. Measuring range of active cervical rotation in a position of full head flexion using the 3D Fastrak measurement system: an intra-tester reliability study. Man Ther. 2003;8:176–179. [DOI] [PubMed] [Google Scholar]
- [23].Hall T, Briffa K, Hopper D, et al. Long-term stability and minimal detectable change of the cervical flexion–rotation test. J Orthop Sports Phys Ther. 2010c;40:225–229. [DOI] [PubMed] [Google Scholar]
- [24].Grondin F, Hall T, Laurentjoye M, et al. Upper cervical range of motion is impaired in patients with temporomandibular disorders. Cranio. 2015;33(2):91–99. [DOI] [PubMed] [Google Scholar]
- [25].Hall T, Chan HT, Christensen L, et al. Efficacy of a C1-C2 self-sustained natural apophyseal glide (SNAG) in the management of cervicogenic headache. J Orthop Sports Phys Ther. 2007;37(3):100–107. [DOI] [PubMed] [Google Scholar]
- [26].Smith K, Hall T, Robinson K. The influence of age, gender, lifestyle factors and sub-clinical neck pain on the cervical flexion-rotation test and cervical range of motion. Man Ther. 2008;13:552–559. [DOI] [PubMed] [Google Scholar]
- [27].Bravo Petersen SM, Vardaxis VG. The flexion–rotation test performed actively and passively: a comparison of range of motion in patients with cervicogenic headache. J Man ManipTher. 2015;23:61–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


