Key Points
Question
What are the patterns of hospitalizations, treatments, and outcomes for older patients with acute myocardial infarction (AMI) over a recent 20-year period in the United States?
Findings
In this cohort study of data from more than 4.3 million Medicare fee-for-service beneficiaries aged 65 years and older discharged with AMI, declines were found in AMI hospitalizations (914 to 566 per 100 000 beneficiary-years), 30-day mortality (20.0% to 12.4%), and 30-day all-cause readmissions (21.0% to 15.3%). There were increases in the 2014 Consumer Price Index–adjusted median Medicare inpatient payment per AMI discharge ($9282 to $11 031) and 30-day inpatient catheterization (44.2% to 59.9%).
Meaning
The last 2 decades were marked by large changes in the number of people hospitalized with AMI—and marked improvements in the short- and long-term outcomes along with increases in cost per hospitalization and number of procedures.
This cohort study reports patterns of hospitalizations, treatments, and outcomes for US Medicare fee-for-service beneficiaries aged 65 years or older with acute myocardial infarction from 1995 to 2014.
Abstract
Importance
Medicare and other organizations have focused on improving quality of care for patients with acute myocardial infarction (AMI) over the last 2 decades. However, there is no comprehensive perspective on the evolution of outcomes for AMI during that period, and it is unknown whether temporal changes varied by patient subgroup, hospital, or county.
Objective
To provide a comprehensive evaluation of national trends in inpatient outcomes and costs of AMI during this period.
Design, Setting, and Participants
This cohort study included analysis of data from a sample of 4 367 485 Medicare fee-for-service beneficiaries aged 65 years or older from January 1, 1995, through December 31, 2014, across 5680 hospitals in the United States. Analyses were conducted from January 15 to June 5, 2018.
Main Outcomes and Measures
Thirty-day all-cause mortality at the patient, hospital, and county levels. Additional outcomes included 30-day all-cause readmissions; 1-year recurrent AMI; in-hospital mortality; length of hospital stay; 2014 Consumer Price Index–adjusted median Medicare inpatient payment per AMI discharge; and rates of catheterization, percutaneous coronary intervention, and coronary artery bypass graft surgery.
Results
The cohort included 4 367 485 Medicare fee-for-service patients aged 65 years or older hospitalized for AMI during the study period. Between 1995 and 2014, the mean (SD) age of patients increased from 76.9 (7.2) to 78.2 (8.7) years, the percentage of female patients declined from 49.5% to 46.1%, the percentage of white patients declined from 91.0% to 86.2%, and the percentage of black patients increased from 5.9% to 8.0%. There were declines in AMI hospitalizations (914 to 566 per 100 000 beneficiary-years); 30-day mortality (20.0% to 12.4%; difference, 7.6 percentage points; 95% CI, 7.3-7.8 percentage points); 30-day all-cause readmissions (21.0% to 15.3%; difference, 5.7 percentage points; 95% CI, 5.4-6.0 percentage points); and 1-year recurrent AMI (7.1% to 5.1%; difference, 2.0 percentage points; 95% CI, 1.8-2.2 percentage points). There were increases in the 2014 Consumer Price Index–adjusted median (interquartile range) Medicare inpatient payment per AMI discharge ($9282 [$6969-$12 173] to $11 031 [$8099-$16 861]); 30-day inpatient catheterization (44.2% to 59.9%; difference, 15.7 percentage points; 95% CI, 15.4-16.0 percentage points); and inpatient percutaneous coronary intervention (18.8% to 43.3%; difference, 24.5 percentage points; 95% CI, 24.2-24.7 percentage points). Coronary artery bypass graft surgery rates decreased from 14.4% to 10.2% (difference, 4.2 percentage points; 95% CI, 3.9-4.3 percentage points). There was heterogeneity by hospital and county in the mortality changes over time.
Conclusions and Relevance
This study shows marked improvements in short-term mortality and readmissions, with an increase in in-hospital procedures and payments, for the increasingly smaller number of Medicare beneficiaries with AMI.
Introduction
Acute myocardial infarction (AMI) is undergoing a transition. For the last 2 decades, Medicare has focused on improving quality of care for patients with AMI, starting with the Cooperative Cardiovascular Project.1 Studies2,3,4,5,6,7,8,9,10,11 have reported improvements in quality and reductions in AMI hospitalizations and risk of short-term mortality during various periods within this time span. However, there is no comprehensive perspective on the evolution of outcomes for AMI across the last 2 decades, including cost, length of stay, treatments, and rehospitalizations. It is also unknown whether changes over time varied by patient subgroup, hospital, or county.
Accordingly, we sought to provide a comprehensive view of treatments and outcomes for patients with AMI over a recent 20-year period in the United States. We used Medicare fee-for-service data to characterize changes in 30-day mortality at the patient, hospital, and county levels and examined trends in the rates of 30-day all-cause readmissions and 1-year recurrent AMI. Finally, we assessed the changes in 3 common in-hospital AMI-specific surgical procedures (catheterization, percutaneous coronary intervention [PCI], and coronary artery bypass graft [CABG]) within 30 days from the date of an AMI index admission.
Methods
Study Population
This was a cohort study. The Yale University institutional review board reviewed the study protocol and granted a waiver of informed consent for the use of this deidentified database. We used Medicare enrollment data from the Centers for Medicare & Medicaid Services (CMS) to identify individuals in the Medicare population aged 65 years or older enrolled in the fee-for-service program for at least 1 month between January 1995 and December 2014. We then linked the fee-for-service population data to the Medicare inpatient claims data to identify patients discharged from an acute-care nonfederal hospital from January 1, 1995, through December 31, 2014, with a principal discharge diagnosis of AMI as determined using International Classification of Diseases, Ninth Revision, Clinical Modification diagnostic codes 410.xx (with the exception of 410.x2). The linked data include patient demographic characteristics, principal and secondary diagnosis codes, and procedure codes. If a patient had more than 1 AMI hospitalization during the entire study period, we selected the first AMI hospitalization, the index admission, and excluded subsequent hospitalizations (n = 548 546). To ensure that patients did not have an AMI in 1995, we also excluded patients who were hospitalized with an AMI in 1994. The study followed the guidelines for cohort studies described in the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline for observational studies.12
Patient, Hospital, and County Characteristics
Patient demographic information included age, sex, race (white, black, or other), and dual eligibility status for Medicaid and Medicare. We identified clinical comorbidities that represent additional coexisting illnesses with the method used by CMS to profile hospital 30-day mortality measures for AMI.13,14 We determined comorbidities for the index hospitalization from secondary diagnosis codes as well as the principal and secondary diagnosis codes from all hospitalizations for up to 12 months before the index hospitalization. Because the maximum number of diagnosis codes in Medicare data increased from 10 to 25 in 2011,15 we restricted the 2011 to 2014 data to the first 10 diagnosis codes to align with the 1995 to 2010 data. Hospital characteristics included hospital structure, patient population, and in-hospital care information. Information about hospital structure was obtained from the 2013 American Hospital Association Surveys, including ownership status, geographic location (urban vs rural), teaching status, Medicare and Medicaid volume, nurse-to-patient ratio, safety-net hospital status (yes vs no), and hospital capacity to provide CABG surgery. Information about in-hospital care included rates of AMI transfer in and transfer out, rates of in-hospital PCI and CABG procedures, and discharge disposition (rates of discharge to home for self-care, to home with home health care, and to skilled nursing home facilities). Information about the patient population and in-hospital care was drawn from CMS inpatient all-cause claims data.
County characteristics included Consumer Price Index–adjusted median income, proportion of people aged 65 years or older, people below the national poverty level (eTable in the Supplement), and a binary variable to indicate whether a county belongs to a health priority area as defined in one of our previous studies.16 The priority area has had a persistently high all-cause mortality over time.
Outcomes
Our primary outcome was 30-day all-cause mortality, defined as death within 30 days from the date of admission for an index AMI hospitalization, regardless of cause. We evaluated mortality at the individual patient level, the hospital level, and the county level. Additional outcomes included (1) 30-day all-cause readmissions, defined as an unplanned rehospitalization within 30 days from the index AMI discharge among individuals who survived to discharge; (2) 1-year recurrent AMI, defined as a recurrent AMI hospitalization within 1 year from the index AMI discharge; (3) in-hospital mortality, defined as all-cause death during the index AMI hospitalization; and (4) length of hospital stay. Additionally, we examined the change in AMI hospitalizations per 100 000 beneficiary-years by using the total number of AMI hospitalizations for each year divided by the corresponding number of beneficiary-years of fee-for-service enrollments, based on the total months that people were in fee-for-service. We also assessed the Consumer Price Index–adjusted Medicare payment for an index AMI hospitalization, referring to the year 2014. For each year, we also measured the rates of individuals who received catheterization, PCI, and CABG, defined as a patient who underwent a targeted procedure in an acute-care hospital within 30 days of an index AMI admission among admitted patients with AMI in each year.
Statistical Analysis
We conducted analyses at the patient, hospital, and county levels. At the patient level, we assessed changes in patient characteristics over the study period via a logistic regression to model each individual characteristic as a function of a year parameterized as a count, ranging from 0 to 19, corresponding to years 1995 to 2014. To assess the changes in individual patients’ risk of 30-day deaths over time, we used the 2014 data (the end of the study period data) to fit a mixed model with hospital random effects and a logit link function to model mortality as a function of patient age, sex, and comorbidities. Using the estimated parameters, we calculated an expected probability of 30-day death for each patient hospitalized in 1995 to 2013. We then calculated a standardized mortality ratio as the observed 30-day deaths divided by the expected deaths for each year of 1995 to 2013. For a given year, a ratio greater than 1.0 indicates that the risk of death for such a patient is expected to be lower if that patient were hospitalized in 2014. We conducted a nonparametric bootstrapping with replacement to construct a 95% confidence interval for this standardized mortality ratio. To assess potential inequalities in the changes in patients’ risk of death, we compared the standardized mortality ratios across age, sex, race, and dual-eligible subgroups.
At the hospital level, we assessed hospital performance by calculating a 30-day risk-standardized mortality rate for each hospital and each year based on the CMS method for profiling hospitals.13,14,17,18 To assess hospital characteristics associated with mortality declines, we fitted a mixed model with the state as random effects and an identity link function to model the absolute difference in risk-standardized mortality between 1995 and 2014 as a function of hospital characteristics, adjusting for hospitals’ baseline risk-standardized mortality rate.
At the county level, to ensure that each county had an adequate number of patients with AMI, we divided the 20-year period into 5 intervals, each combining 4 sequential years of data (1995-1998, 1999-2002, 2003-2006, 2007-2010, and 2011-2014). We calculated the risk-standardized 30-day mortality rate for each county and each subperiod by extending the CMS method to the county level, adjusted for patient characteristics (age, sex, race [white, black, Hispanic, all others], dual eligibility, and comorbidities). We then mapped counties using a gradient from red, yellow, and green (increase in red, on average in yellow, and decrease in green). To assess county characteristics associated with the decline in mortality, we fitted a mixed model with state as random effects and an identity link function to model the absolute difference in risk-standardized mortality between 1995 to 1998 and 2011 to 2014 as a function of county characteristics. To facilitate data presentation, we report patient characteristics and outcomes by the five 4-year intervals defined in the county-level analysis.
Analyses were conducted between January 15 and June 5, 2018, using SAS statistical software, version 9.4, 64-bit Windows version (SAS Institute, Inc). As of 2019, the data were 5 years old. All statistical tests were 2-tailed, at a significance level of .05.
Results
Study Population and Patient Characteristics
There were 4 367 485 unique Medicare fee-for-service patients aged 65 years or older hospitalized for AMI across 5680 unique hospitals during the 20-year period. Between 1995 and 2014, the mean (SD) age of patients with AMI increased from 76.9 (7.2) to 78.2 (8.7) years, an absolute difference of 2.7 years; the proportion of female patients declined from 49.5% to 46.1%; the percentage of white patients declined from 91.0% to 86.2%; and the percentage of black patients increased from 5.9% to 8.0% (all P values for trends <.001).
The rate of hospitalization for an initial AMI declined over the period from 914 to 566 per 100 000 beneficiary-years, a relative 38.1% reduction (eFigure 1 in the Supplement). Most comorbidities increased during the study period, but the proportions of patients with cerebrovascular disease, stroke, anterior AMI location, inferior lateral AMI, unstable angina, and valvular heart disease declined (eFigure 2 in the Supplement; Table).
Table. Patient Characteristics.
| Characteristic | 1995-1998 (n = 1 012 897) | 1999-2002 (n = 999 009) | 2003-2006 (n = 919 981) | 2007-2010 (n = 742 812) | 2011-2014 (n = 692 786) | Aggregated (N = 4 367 485) |
|---|---|---|---|---|---|---|
| Demographic characteristics and comorbidities, No. (%) | ||||||
| Age, mean (SD), y | 77.3 (7.3) | 78.4 (7.8) | 78.6 (8.1) | 78.6 (8.5) | 78.1 (8.6) | 78.2 (8.0) |
| Female | 505 015 (49.9) | 505 786 (50.6) | 461 401 (50.2) | 366 863 (49.4) | 326 029 (47.1) | 2 165 094 (49.6) |
| White | 914 985 (90.3) | 889 941 (89.1) | 809 239 (88.0) | 650 931 (87.6) | 599 774 (86.6) | 3 864 870 (88.5) |
| Black | 61 039 (6.0) | 68 416 (6.8) | 67 842 (7.4) | 56 564 (7.6) | 55 536 (8.0) | 309 397 (7.1) |
| Other race | 31 440 (3.1) | 40 652 (4.1) | 42 900 (4.7) | 35 317 (4.8) | 37 476 (5.4) | 193 218 (4.4) |
| Heart failure | 134 488 (13.3) | 144 952 (14.5) | 136 957 (14.9) | 106 029 (14.3) | 92 039 (13.3) | 614 465 (14.1) |
| Myocardial infarction | 46 391 (4.6) | 49 164 (4.9) | 45 062 (4.9) | 36 292 (4.9) | 33 072 (4.8) | 209 981 (4.8) |
| Unstable angina | 56 939 (5.6) | 49 009 (4.9) | 33 820 (3.7) | 21 471 (2.9) | 17 680 (2.6) | 178 919 (4.1) |
| Chronic atherosclerosis | 680 245 (67.2) | 655 429 (65.6) | 630 149 (68.5) | 519 313 (69.9) | 496 177 (71.6) | 2 981 313 (68.3) |
| Cardiorespiratory disease | 21 737 (2.1) | 25 313 (2.5) | 27 667 (3.0) | 34 521 (4.6) | 36 762 (5.3) | 146 000 (3.3) |
| Hypertension | 485 258 (47.9) | 537 800 (53.8) | 532 660 (57.9) | 477 564 (64.3) | 468 670 (67.7) | 2 501 952 (57.3) |
| Stroke | 20 517 (2.0) | 20 595 (2.1) | 17 841 (1.9) | 13 913 (1.9) | 12 405 (1.8) | 85 271 (2.0) |
| Cerebrovascular disease | 40 588 (4.0) | 52 259 (5.2) | 42 135 (4.6) | 30 768 (4.1) | 27 183 (3.9) | 192 933 (4.4) |
| Renal failure | 31 353 (3.1) | 45 552 (4.6) | 64 392 (7.0) | 87 220 (11.7) | 92 187 (13.3) | 320 704 (7.3) |
| Chronic obstructive pulmonary disease | 204 168 (20.2) | 227 051 (22.7) | 223 856 (24.3) | 158 333 (21.3) | 138 327 (20.0) | 951 735 (21.8) |
| Pneumonia | 91 977 (9.1) | 126 982 (12.7) | 131 896 (14.3) | 114 628 (15.4) | 101 380 (14.6) | 566 863 (13.0) |
| Protein calorie malnutrition | 9810 (1.0) | 24 282 (2.4) | 27 512 (3.0) | 33 123 (4.5) | 36 604 (5.3) | 131 331 (3.0) |
| Dementia | 50 051 (4.9) | 92 066 (9.2) | 95 134 (10.3) | 81 219 (10.9) | 47 194 (6.8) | 365 664 (8.4) |
| Functional disability | 18 090 (1.8) | 25 823 (2.6) | 21 925 (2.4) | 18 419 (2.5) | 17 522 (2.5) | 101 779 (2.3) |
| Peripheral vascular disease | 52 800 (5.2) | 61 473 (6.2) | 60 671 (6.6) | 49 220 (6.6) | 41 585 (6.0) | 265 749 (6.1) |
| Metastatic cancer | 23 717 (2.3) | 62 611 (6.3) | 60 943 (6.6) | 50 061 (6.7) | 44 158 (6.4) | 241 490 (5.5) |
| Trauma in past year | 41 581 (4.1) | 51 883 (5.2) | 56 273 (6.1) | 45 483 (6.1) | 37 689 (5.4) | 232 909 (5.3) |
| Major psychiatric disorder | 12 524 (1.2) | 18 274 (1.8) | 16 481 (1.8) | 14 918 (2.0) | 15 113 (2.2) | 77 310 (1.8) |
| Liver disease | 4222 (0.4) | 5673 (0.6) | 6337 (0.7) | 5102 (0.7) | 5751 (0.8) | 27 085 (0.6) |
| Depression | 22 740 (2.2) | 44 332 (4.4) | 48 799 (5.3) | 40 341 (5.4) | 41 069 (5.9) | 197 281 (4.5) |
| Diabetes | 334 688 (33.0) | 293 433 (29.4) | 277 281 (30.1) | 225 956 (30.4) | 229 613 (33.1) | 1 360 971 (31.2) |
| Outcomes, % (95% CI) | ||||||
| 30-d mortality | 19.1 (19.1-19.2) | 19.2 (19.2-19.3) | 17.1 (17.1-17.2) | 15.2 (15.1-15.3) | 13.4 (13.3-13.5) | 17.2 (17.1-17.2) |
| In-hospital mortality | 14.3 (14.2-14.4) | 14.1 (14.0-14.1) | 11.5 (11.5-11.6) | 9.2 (9.15-9.28) | 7.7 (7.63-7.76) | 11.7 (11.7-11.8) |
| 30-d readmission | 21.3 (21.2-21.4) | 21.8 (21.7-21.9) | 21.4 (21.3-21.5) | 20.2 (20.1-20.3) | 17.4 (17.3-17.5) | 20.4 (20.3-20.4) |
| Discharge to home | 44.5 (44.4-44.6) | 46.1 (46.0-46.2) | 45.1 (45.0-45.2) | 46.9 (46.8-47.0) | 50.2 (50.1-50.3) | 46.3 (46.3-46.3) |
| Discharge to home with home health service | 9.1 (9.06-9.17) | 9.6 (9.51-9.62) | 12.1 (12.1-12.2) | 13.2 (13.2-13.3) | 13.2 (13.1-13.3) | 11.2 (11.2-11.2) |
| Discharge to skilled nursing home | 10.5 (10.4-10.5) | 14.0 (13.9-14.1) | 15.9 (15.8-16.0) | 16.6 (16.6-16.7) | 15.4 (15.3-15.5) | 11.8 (11.8-11.9) |
| Discharge to hospice | 0 (0.01-0.01) | 0.3 (0.30-0.32) | 1.7 (1.64-1.69) | 2.7 (2.71-2.78) | 3.0 (2.96-3.04) | 1.4 (1.35-1.38) |
| Transferred to another acute-care hospital | 19.0 (18.9-19.1) | 11.7 (11.6-11.7) | 8.8 (8.70-8.82) | 6.6 (6.57-6.68) | 5.6 (5.59-5.70) | 10.9 (10.9-11.0) |
| Length of stay, mean (SD), d | 6.5 (6.0) | 6.5 (6.7) | 6.2 (6.5) | 5.7 (5.9) | 5.1 (5.2) | 6.1 (6.2) |
Changes in Risk of Mortality at the Patient Level
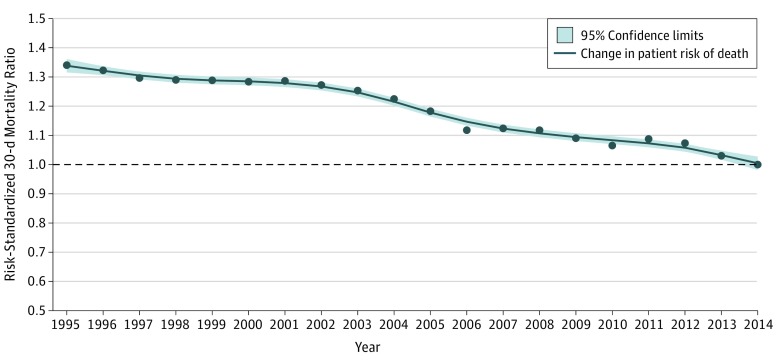
Patient risk of 30-day mortality declined significantly over the 20-year period. The observed 30-day mortality declined from 20.0% in 1995 to 12.4% in 2014 (difference, 7.6 percentage points; 95% CI, 7.3-7.8 percentage points). This reduction in observed mortality was found across age, sex, race, and dual-eligibility subgroups (eFigure 3 in the Supplement); the gap in mortality decreased between the dual-eligible and non–dual-eligible subgroups (24.1% vs 19.4%; difference, 4.7 percentage points; 95% CI, 4.3-5.2 percentage points in 1995 and 14.0% vs 12.1%; difference, 1.9 percentage points; 95% CI, 1.4-2.3 percentage points in 2014) and between the female and male subgroups (21.8% vs 18.2%; difference, 3.6 percentage points; 95% CI, 3.4-4.0 percentage points in 1995 and 13.4% vs 11.6%; difference, 1.8 percentage points; 95% CI, 1.4-2.1 percentage points in 2014) (P < .001 for interactions). There were no differences in mortality by the race subgroups. Between 1995 and 2014, mortality declined from 13.4% to 7.5% (difference, 5.9 percentage points; 95% CI, 5.6-6.2 percentage points) for patients aged 65 to 74 years, 21.7% to 11.7% (difference, 10.0 percentage points; 95% CI, 9.6-10.4 percentage points) for patients aged 75 to 84 years, and 32.2% to 22.0% (difference, 10.2 percentage points; 95% CI, 9.7-10.9 percentage points) for patients aged 85 years or older. An interaction effect (P < .001) between year and age was observed. For a patient hospitalized in 1995, with demographic characteristics and comorbidities unchanged, the adjusted risk of 30-day mortality would be 34% (95% CI, 31.0%-37.2%) lower if the hospitalization occurred in 2014 (Figure 1). This reduction in the adjusted risk of mortality between 1995 and 2014 was lower in patients aged 85 years or older (24%; 95% CI, 20.1%-28.0%), men (25.8%; 95% CI, 21.4%-28.6%), nonwhite and nonblack patients (27.3%; 95% CI, 23.4%-30.5%), and non–dual-eligible patients (32.4%; 95% CI, 29.3%-35.6%) than the national average (eFigure 4 in the Supplement).
Figure 1. Change in Adjusted Risk of 30-Day Acute Myocardial Infarction Mortality at the Patient Level Between 1995 and 2014.
Points indicate year-specific risk-standardized 30-day mortality ratios. The line was smoothed using the locally estimated scatterplot smoothing (LOESS) method (local regression).
Changes in Risk of Mortality at the Hospital Level
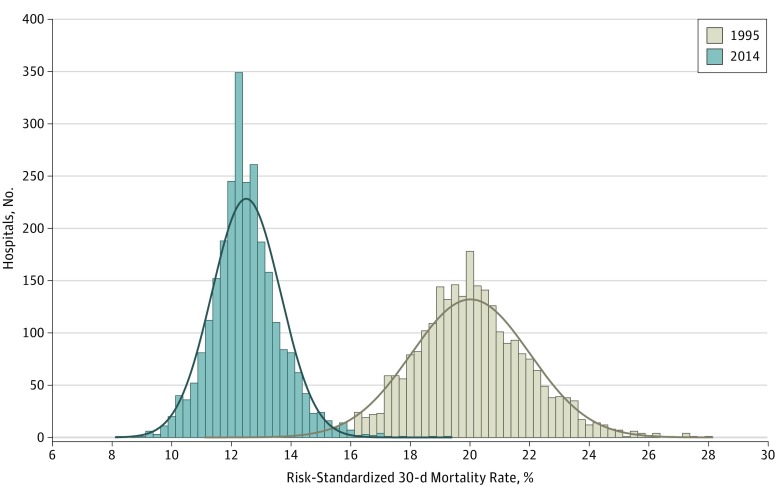
Between 1995 and 2014, the number of unique hospitals that treated at least 1 patient with AMI each year declined from 4989 to 3056; the median (interquartile range) hospital AMI volume remained unchanged from 31 (11-71) to 31 (8-79). The mean (SD) risk-standardized mortality rate, at the individual hospital level, declined from 20.0% (1.7%) in 1995 to 12.5% (1.1%) in 2014 (difference, 7.5 percentage points; 95% CI, 7.4-7.6 percentage points) (Figure 2). The distributions of risk-standardized mortality are shown in eFigure 5 in the Supplement. Overall, the annual national decline was 2.2%.
Figure 2. Change in Hospital-Specific Risk-Standardized 30-Day Acute Myocardial Infarction Mortality Rates Between 1995 and 2014.
The size of each bar reflects the number of hospitals that filled in a particular interval of risk-standardized mortality rate as well as the distributions (ranges) of rates in 1995 and 2014. The curves represent distribution of the data. Mean (SD) risk-standardized 30-day mortality rates were 20.0% (2.0%) and 12.5% (1.2%) for 1995 and 2014, respectively (n = 2635 hospitals). Restricted to hospitals that had at least 1 case in both 1995 and 2014.
There were 2635 hospitals represented in both 1995 and 2014. Among these, the absolute change in mortality between 1995 and 2014 ranged from a decrease of 15.4 percentage points to an increase of 2.5 percentage points, with 4 hospitals having increased mortality (increases ranging from 0.7-2.5 percentage points). A reduction in between-hospital heterogeneity in mortality was also observed: the hospital-specific mortality ranged from 11.3% to 28.0% (difference, 16.7 percentage points) in 1995 and ranged from 8.3% to 19.4% (difference, 11.1 percentage points) in 2014. Hospital characteristics were not associated with the decline in risk-standardized 30-day mortality (eFigure 6 in the Supplement).
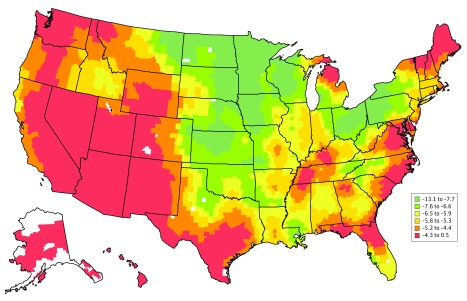
Changes in Risk of Mortality at the County Level
From 1995 to 1998 and 2011 to 2014, the county-specific mean (SD) 30-day risk-standardized mortality rate, adjusted for patient characteristics (age, sex, race [white, black, Hispanic, and all others], dual-eligible status, and comorbidities), declined from 19.2% (1.3%) to 13.4% (0.6%). Across counties, the absolute decline in percentage points ranged from 0.1 to 13.1, with 2 counties having increases (0.2 and 0.5 percentage points) (Figure 3). A reduction in between-county heterogeneity in mortality was also observed: the county-specific mortality ranged from 15.4% to 23.1% in 1995 to 1998 and from 12.2% to 13.9% in 2011 to 2014 (eFigure 7 in the Supplement).
Figure 3. Difference in County-Specific 30-Day Risk-Standardized Acute Myocardial Infarction Mortality Rates Between 1995 to 1998 and 2011 to 2014.
The difference was calculated as the percentage point between the 2011 to 2014 combined rate minus the 1995 to 1998 combined rate. Counties are shaded according to the difference in percentage points of the risk-standardized acute myocardial infarction mortality rates (percentage). Counties with negative values had mortality rates that were lower in 2011 to 2014 than in 1995 to 1998. Counties with the largest decline between 2011 to 2014 and 1995 to 1998 are shaded green, while those with the smallest decline or even increase in mortality between 2011 to 2014 and 1995 to 1998 are shaded red. Counties are shaded white if there were missing or insufficient data that precluded the calculation of mortality rates.
Overall, counties with a high rate of individuals enrolled in a Medicare Advantage plan, a high proportion of rural areas, and a high rate of residents who lived in the county for at least 1 year were more likely to have declines in mortality, but counties with high proportions of Medicare beneficiaries not enrolled in the Medicare Part B plan, unemployed residents, and a high risk of potential life lost were less likely to show declines in mortality (eFigure 8 in the Supplement). Counties in the health priority areas were less likely to have a decline in mortality (point estimate = −0.41; 95% CI, −0.60 to −0.23 points).
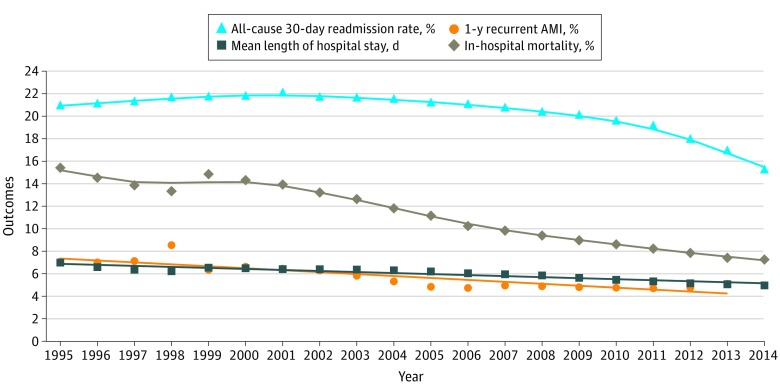
Changes in Readmissions, In-Hospital Mortality, Length of Stay, and Medicare Payment
Between 1995 and 2014 (2013 for 1-year recurrent AMI), the rates of 30-day all-cause readmissions, 1-year recurrent AMI, and in-hospital mortality declined from 21.0% to 15.3% (difference, 5.7 percentage points; 95% CI, 5.4-6.0 percentage points), 7.1% to 5.1% (difference, 2.0 percentage points; 95% CI, 1.8-2.2 percentage points), and 15.4% to 7.3% (difference, 8.1 percentage points; 95% CI, 7.9-8.3 percentage points), respectively (Figure 4). The median (interquartile range) length of stay declined from 6.0 (3.0-8.0) days in 1995 to 3.0 (2.0-6.0) days in 2014. Between 1995 and 2014, the 2014 Consumer Price Index–adjusted median (interquartile range) Medicare inpatient payment per AMI discharge increased from $9282 ($6969-$12 173) to $11 031 ($8099-$16 861). Although the association between 30-day risk-standardized mortality and Medicare inpatient payment was negative over the study period (eFigure 9 in the Supplement), the effect size was small and it declined slightly over time. In 1995, a $10 000 increase in the payment was associated with an 0.5–percentage point decrease in 30-day risk-standardized mortality; in 2014, the same dollar amount was associated with a decrease of 0.3 percentage points.
Figure 4. Changes in 30-Day All-Cause Readmissions, 1-Year Recurrent Acute Myocardial Infarction (AMI), In-Hospital Mortality, and Length of Stay .
Symbols denote observed values and lines represent changes over time. Lines were smoothed using the locally estimated scatterplot smoothing (LOESS) method (local regression). Triangles indicate 30-day all-cause readmissions; circles, 1-year recurrent AMI; diamonds, in-hospital mortality; and squares, length of stay.
Changes in Inpatient Procedures
Between 1995 and 2014, the rate of 30-day inpatient catheterization increased from 44.2% to 59.9% (difference, 15.7 percentage points; 95% CI, 15.4-16.0 percentage points), the rate of inpatient PCI increased from 18.8% to 43.3% (difference, 24.5 percentage points; 95% CI, 24.2-24.7 percentage points), and the rate of CABG decreased from 14.4% to 10.2% (difference, 4.2 percentage points; 95% CI, 3.9-4.3 percentage points) (eFigure 10 in the Supplement). All 3 procedure rates were correlated at the hospital level. The weighted Pearson correlation coefficients were 0.68 (PCI and CABG), 0.91 (PCI and catheterization), and 0.75 (CABG and catheterization). An increase of 1% in the PCI rate was associated with a decrease in mortality of 0.72 percentage points (95% CI, −0.80 to −0.64 percentage points), but the decrease in CABG rate was not associated with changes in mortality rate. Although we measured these procedures within a 30-day period from the index AMI hospitalization, the majority (96.0% of catheterizations, 96.3% of PCI, and 83.0% of CABG) were performed at the index hospitalization.
Discussion
From 1995 through 2014, the Medicare fee-for-service population experienced a remarkable and progressive improvement in the hospitalization rates for AMI and the 30-day mortality rate after AMI. In addition, the 2.7-year increase in the average age of patients suggests progress in delaying the onset of AMI. Mortality after AMI is at a historic low of 12%, a reduction of 34% since 1995, accounting for changes in patient characteristics. The improvements were consistent across demographic groups defined by age, sex, race, and eligibility for Medicaid. Almost all hospitals improved over this period, although there was some heterogeneity in the improvement over time, and almost every county experienced improvement, although the size of the change varied. The in-hospital mortality, length of stay, 30-day all-cause rehospitalization, and 1-year recurrent AMI rates also declined, while payments and rates of revascularization increased. The decline in in-hospital mortality was unlikely to have been affected by the decline in length of stay, given the decline in 30-day mortality.
This work extends the prior literature in several ways. Previous studies2,3,4,7,8,10,11,19 have reported some of these improvements, but not as comprehensively, or over a 20-year period or across the entire United States. As such, this work reveals novel insights about what has been achieved in reducing and mitigating AMI among Medicare beneficiaries. Moreover, even as payments per hospitalization have increased, outcomes improved and total cost declined because the number of hospitalizations was greatly reduced.
There are several potential explanations for our findings, including changes in the treatment of AMI over this period. By the beginning of the period, it was established that aspirin, β-blockers, and rapid reperfusion therapy could improve outcomes for patients with AMI and that statins and risk factor control could reduce risk. However, it became apparent that the translation of the evidence into practice was incomplete. In the early 1990s, the Health Care Financing Administration (now CMS) launched an improvement initiative focused specifically on AMI. Many patients who were ideal for particular clinical strategies were not receiving them.20,21,22,23 Moreover, PCI was emerging as a superior method of reperfusion but was used infrequently, in part because of its availability. Over the years, the use of evidence-based strategies improved dramatically. The speed of reperfusion therapy for ST-segment elevation AMI also improved, as did the use of PCI in general.3,24 All of this occurred as a result of concerted efforts by CMS, the American College of Cardiology, the American Heart Association, and other national organizations, along with local hospitals and clinicians, to improve population risk and acute care. Lifestyle changes likely also contributed to the change in the rates of AMI.25
We identified some county characteristics that were associated with changes over time. Perhaps most disconcerting is that the areas of the country with persistently highest mortality rates, which we previously termed health priority areas, also had slower-than-average decline in AMI mortality.16 These areas may particularly benefit from future improvement activities.
Limitations
The study has several limitations. We examined data about individuals in the Medicare fee-for-service population, and the findings may not reflect the changes in the Medicare Advantage population. Moreover, the growing Medicare Advantage population may have implications for trend analyses, but we have risk adjusted the outcomes data. Also, the hospitalization rate has been dropping over time, and there is no indication that the fee-for-service population is getting healthier over time.26 Because this is a Medicare population, we cannot be sure about how our results may reflect the experience of younger populations. The lack of laboratory data in our study precluded our ability to include troponin levels in the risk adjustments. The lack of clinical information in claims data precluded our ability to assess the changes in process of care over time, such as door-to-balloon time and the use of medications, which could explain the changes in outcomes. Nevertheless, other studies9,27 have shown remarkable improvement in AMI process measures over this period. Additionally, our assessments of comorbidities are dependent on codes and may not accurately reflect the condition of the patients, but the improvements were also present in unadjusted analyses. There may be some concerns that the higher sensitivity of biomarkers used to diagnose AMI may have contributed to the trend. Changing definitions of AMI do make comparisons difficult and likely led to shifting of patients among the categories of acute coronary syndromes. However, this improvement in mortality occurred in a period of a marked reduction in the number of hospitalizations.28 Moreover, the changes in mortality were gradual over time and did not show an abrupt change with the introduction of troponins—or level off after a period of adoption. Also, a systematic review of the validity of administrative codes did not find evidence of a secular trend in code sensitivity, although the evidence is limited.29 Finally, we also restricted this study to a period in which International Classification of Diseases, Ninth Revision, Clinical Modification codes were used so as not to introduce a new coding system into the assessment of the trends. Also, the effect of the expansion of codes during this period on risk determination is unclear, but this seems unlikely to affect the overall findings of this study.
Conclusions
This study charts the course of AMI among Medicare fee-for-service beneficiaries over a recent 20-year period. Hospitalization rates for AMI declined 38%, and there were improvements in 30-day mortality, readmissions, length of stay, and 1-year recurrent AMI, with only a modest increase in payments. Revascularization rates increased markedly. Thirty-day adjusted mortality, which declined 34%, touched almost every county and hospital in the country. Nevertheless, there was heterogeneity in the performance over time with some hospital and county characteristics associated with the change. Overall, however, we describe 2 decades of marked improvements in outcomes for AMI among the increasingly smaller number of people in the United States who experience it, representing a transition in the impact of this condition.
eTable. County-Specific Characteristics
eFigure 1. Change in Number of Initial AMI Hospitalizations per 100,000 Beneficiary-Years, 1995-2014
eFigure 2. Annual Relative Changes in Patient Characteristics
eFigure 3. Trend in Observed Mortality by Year and Sub-population
eFigure 4. Changes in Patient Risk of 30-Day Mortality Between 2014 and 1995 by Sub-population
eFigure 5. Nationwide Change in Hospital-Specific 30-Day Risk-Standardized Mortality Rate by Selected Years
eFigure 6. Hospital Characteristics Associated With Change in Difference in Hospital-Specific Risk-Standardized 30-Day Mortality Rates Between 1995 and 2014
eFigure 7. Change in County-Specific Risk-Standardized 30-Day Mortality in 1995-1998 (Top Panel) and in 2011-2014 (Bottom Panel)
eFigure 8. County-Specific Characteristics Associated With Difference in County-Specific Risk-Standardized 30-Day Mortality Between 1995-1998 and 2011-2014
eFigure 9. Association Between Medicare Inpatient Payment and 30-Day Risk-Standardized Mortality at the Hospital Level
eFigure 10. Annual Changes in the 30-Day Rates of Three Common AMI-Specific Procedures (Catheterization, CABG, and PCI)
References
- 1.Ellerbeck EF, Jencks SF, Radford MJ, et al. . Quality of care for Medicare patients with acute myocardial infarction: a four-state pilot study from the Cooperative Cardiovascular Project. JAMA. 1995;273(19):-. doi: 10.1001/jama.1995.03520430045037 [DOI] [PubMed] [Google Scholar]
- 2.Chen HY, Gore JM, Lapane KL, et al. . A 35-year perspective (1975 to 2009) into the long-term prognosis and hospital management of patients discharged from the hospital after a first acute myocardial infarction. Am J Cardiol. 2015;116(1):24-29. doi: 10.1016/j.amjcard.2015.03.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chen HY, Tisminetzky M, Lapane KL, et al. . Decade-long trends in 30-day rehospitalization rates after acute myocardial infarction. J Am Heart Assoc. 2015;4(11):e002291. doi: 10.1161/JAHA.115.002291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gerber Y, Weston SA, Jiang R, Roger VL. The changing epidemiology of myocardial infarction in Olmsted County, Minnesota, 1995-2012. Am J Med. 2015;128(2):144-151. doi: 10.1016/j.amjmed.2014.09.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Krumholz HM, Normand SL, Wang Y. Trends in hospitalizations and outcomes for acute cardiovascular disease and stroke, 1999-2011. Circulation. 2014;130(12):966-975. doi: 10.1161/CIRCULATIONAHA.113.007787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Krumholz HM, Wang Y, Chen J, et al. . Reduction in acute myocardial infarction mortality in the United States: risk-standardized mortality rates from 1995-2006. JAMA. 2009;302(7):767-773. doi: 10.1001/jama.2009.1178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McGovern PG, Pankow JS, Shahar E, et al. ; The Minnesota Heart Survey Investigators . Recent trends in acute coronary heart disease—mortality, morbidity, medical care, and risk factors. N Engl J Med. 1996;334(14):884-890. doi: 10.1056/NEJM199604043341403 [DOI] [PubMed] [Google Scholar]
- 8.Newman JD, Shimbo D, Baggett C, et al. ; ARIC Study Investigators . Trends in myocardial infarction rates and case fatality by anatomical location in four United States communities, 1987 to 2008 (from the Atherosclerosis Risk in Communities Study). Am J Cardiol. 2013;112(11):1714-1719. doi: 10.1016/j.amjcard.2013.07.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nuti SV, Wang Y, Masoudi FA, et al. . Improvements in the distribution of hospital performance for the care of patients with acute myocardial infarction, heart failure, and pneumonia, 2006-2011. Med Care. 2015;53(6):485-491. doi: 10.1097/MLR.0000000000000358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.O’Brien EC, Rose KM, Suchindran CM, et al. . Temporal trends in medical therapies for ST- and non-ST elevation myocardial infarction (from the Atherosclerosis Risk in Communities [ARIC] Surveillance Study). Am J Cardiol. 2013;111(3):305-311. doi: 10.1016/j.amjcard.2012.09.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rosamond WD, Chambless LE, Heiss G, et al. . Twenty-two-year trends in incidence of myocardial infarction, coronary heart disease mortality, and case fatality in 4 US communities, 1987-2008. Circulation. 2012;125(15):1848-1857. doi: 10.1161/CIRCULATIONAHA.111.047480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP; STROBE Initiative . The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. PLoS Med. 2007;4(10):e296. doi: 10.1371/journal.pmed.0040296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Krumholz HM, Wang Y, Mattera JA, et al. . An administrative claims model suitable for profiling hospital performance based on 30-day mortality rates among patients with an acute myocardial infarction. Circulation. 2006;113(13):1683-1692. doi: 10.1161/CIRCULATIONAHA.105.611186 [DOI] [PubMed] [Google Scholar]
- 14.Normand S-LT, Wang Y, Krumholz HM. Assessing surrogacy of data sources for institutional comparisons. Health Serv Outcomes Res Methodol. 2007;7:79-96. doi: 10.1007/s10742-006-0018-8 [DOI] [Google Scholar]
- 15.Centers for Medicare & Medicaid Services 5010 implementation—processing additional International Classification of Diseases, 9th Revision—Clinical Modification (ICD-9-CM) diagnosis and procedure codes in pricer, grouper, and the Medicare code editor (MCE). https://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/downloads/ R2028CP.pdf. Published August 13, 2010. Accessed January 30, 2019.
- 16.Krumholz HM, Normand ST, Wang Y. Geographical health priority areas for older Americans. Health Aff (Millwood). 2018;37(1):104-110. doi: 10.1377/hlthaff.2017.0744 [DOI] [PubMed] [Google Scholar]
- 17.Bratzler DW, Normand SL, Wang Y, et al. . An administrative claims model for profiling hospital 30-day mortality rates for pneumonia patients. PLoS One. 2011;6(4):e17401. doi: 10.1371/journal.pone.0017401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Krumholz HM, Wang Y, Mattera JA, et al. . An administrative claims model suitable for profiling hospital performance based on 30-day mortality rates among patients with heart failure. Circulation. 2006;113(13):1693-1701. doi: 10.1161/CIRCULATIONAHA.105.611194 [DOI] [PubMed] [Google Scholar]
- 19.Rosamond WD, Chambless LE, Folsom AR, et al. . Trends in the incidence of myocardial infarction and in mortality due to coronary heart disease, 1987 to 1994. N Engl J Med. 1998;339(13):861-867. doi: 10.1056/NEJM199809243391301 [DOI] [PubMed] [Google Scholar]
- 20.Krumholz HM, Murillo JE, Chen J, et al. . Thrombolytic therapy for eligible elderly patients with acute myocardial infarction. JAMA. 1997;277(21):1683-1688. doi: 10.1001/jama.1997.03540450039032 [DOI] [PubMed] [Google Scholar]
- 21.Krumholz HM, Radford MJ, Ellerbeck EF, et al. . Aspirin for secondary prevention after acute myocardial infarction in the elderly: prescribed use and outcomes. Ann Intern Med. 1996;124(3):292-298. doi: 10.7326/0003-4819-124-3-199602010-00002 [DOI] [PubMed] [Google Scholar]
- 22.Krumholz HM, Radford MJ, Ellerbeck EF, et al. . Aspirin in the treatment of acute myocardial infarction in elderly Medicare beneficiaries: patterns of use and outcomes. Circulation. 1995;92(10):2841-2847. doi: 10.1161/01.CIR.92.10.2841 [DOI] [PubMed] [Google Scholar]
- 23.Krumholz HM, Radford MJ, Wang Y, Chen J, Heiat A, Marciniak TA. National use and effectiveness of beta-blockers for the treatment of elderly patients after acute myocardial infarction: National Cooperative Cardiovascular Project. JAMA. 1998;280(7):623-629. doi: 10.1001/jama.280.7.623 [DOI] [PubMed] [Google Scholar]
- 24.Nallamothu BK, Normand SL, Wang Y, et al. . Relation between door-to-balloon times and mortality after primary percutaneous coronary intervention over time: a retrospective study. Lancet. 2015;385(9973):1114-1122. doi: 10.1016/S0140-6736(14)61932-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ornish D, Brown SE, Scherwitz LW, et al. . Can lifestyle changes reverse coronary heart disease? the Lifestyle Heart Trial. Lancet. 1990;336(8708):129-133. doi: 10.1016/0140-6736(90)91656-U [DOI] [PubMed] [Google Scholar]
- 26.Miller EA, Decker SL, Parker JD. Characteristics of Medicare Advantage and fee-for-service beneficiaries upon enrollment in Medicare at age 65. J Ambul Care Manage. 2016;39(3):231-241. doi: 10.1097/JAC.0000000000000107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Makam RC, Erskine N, McManus DD, et al. . Decade-long trends (2001 to 2011) in the use of evidence-based medical therapies at the time of hospital discharge for patients surviving acute myocardial infarction. Am J Cardiol. 2016;118(12):1792-1797. doi: 10.1016/j.amjcard.2016.08.065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dalen JE, Alpert JS, Goldberg RJ, Weinstein RS. The epidemic of the 20th century: coronary heart disease. Am J Med. 2014;127(9):807-812. doi: 10.1016/j.amjmed.2014.04.015 [DOI] [PubMed] [Google Scholar]
- 29.McCormick N, Lacaille D, Bhole V, Avina-Zubieta JA. Validity of myocardial infarction diagnoses in administrative databases: a systematic review. PLoS One. 2014;9(3):e92286. doi: 10.1371/journal.pone.0092286 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable. County-Specific Characteristics
eFigure 1. Change in Number of Initial AMI Hospitalizations per 100,000 Beneficiary-Years, 1995-2014
eFigure 2. Annual Relative Changes in Patient Characteristics
eFigure 3. Trend in Observed Mortality by Year and Sub-population
eFigure 4. Changes in Patient Risk of 30-Day Mortality Between 2014 and 1995 by Sub-population
eFigure 5. Nationwide Change in Hospital-Specific 30-Day Risk-Standardized Mortality Rate by Selected Years
eFigure 6. Hospital Characteristics Associated With Change in Difference in Hospital-Specific Risk-Standardized 30-Day Mortality Rates Between 1995 and 2014
eFigure 7. Change in County-Specific Risk-Standardized 30-Day Mortality in 1995-1998 (Top Panel) and in 2011-2014 (Bottom Panel)
eFigure 8. County-Specific Characteristics Associated With Difference in County-Specific Risk-Standardized 30-Day Mortality Between 1995-1998 and 2011-2014
eFigure 9. Association Between Medicare Inpatient Payment and 30-Day Risk-Standardized Mortality at the Hospital Level
eFigure 10. Annual Changes in the 30-Day Rates of Three Common AMI-Specific Procedures (Catheterization, CABG, and PCI)