Key Points
Question
Is increased influenza activity associated with an increase in hospitalizations for heart failure and myocardial infarction?
Findings
In this community surveillance study of approximately 451 588 adults, a 5% absolute increase in influenza activity was associated with a 24% increase in heart failure hospitalizations rates within the same month but no significant increase in myocardial infarction hospitalizations.
Meaning
Increased levels of influenza activity are associated with increased hospitalizations for cardiovascular events, indicating that influenza activity should be addressed in efforts to prevent heart failure hospitalizations.
Abstract
Importance
Influenza is associated with an increased risk of cardiovascular events, but to our knowledge, few studies have explored the temporal association between influenza activity and hospitalizations, especially those caused by heart failure (HF).
Objective
To explore the temporal association between influenza activity and hospitalizations due to HF and myocardial infarction (MI). We hypothesized that increased influenza activity would be associated with an increase in hospitalizations for HF and MI among adults in the community.
Design, Setting, and Participants
As part of the community surveillance component of the Atherosclerosis Risk in Communities (ARIC) study, a population-based study with hospitalizations sampled from 4 US communities, data were collected from 451 588 adults aged 35 to 84 years residing in the ARIC communities from annual cross-sectional stratified random samples of hospitalizations during October 2010 to September 2014.
Exposures
Monthly influenza activity, defined as the percentage of patient visits to sentinel clinicians for influenza-like illness by state, as reported by the Centers for Disease Control and Prevention Surveillance Network.
Main Outcomes and Measures
The monthly frequency of MI hospitalizations (n = 3541) and HF hospitalizations (n = 4321), collected through community surveillance and adjudicated as part of the ARIC Study.
Results
Between October 2010 and September 2014, 2042 (47.3%) and 1599 (45.1%) of the sampled patients who were hospitalized for HF and MI, respectively, were women and 2391 (53.3%) and 2013 (57.4%) were white, respectively. A 5% monthly absolute increase in influenza activity was associated with a 24% increase in HF hospitalization rates, standardized to the total population in each community, within the same month after adjusting for region, season, race/ethnicity, sex, age, and number of MI/HF hospitalizations from the month before (incidence rate ratio, 1.24; 95% CI, 1.11-1.38; P < .001), while overall influenza activity was not significantly associated with MI hospitalizations (incidence rate ratio, 1.02; 95% CI, 0.90-1.17; P = .72). Influenza activity in the months before hospitalization was not associated with either outcome. Our model suggests that in a month with high influenza activity, approximately 19% of HF hospitalizations (95% CI, 10%-28%) could be attributable to influenza.
Conclusions and Relevance
Influenza activity was temporally associated with an increase in HF hospitalizations across 4 influenza seasons. These data suggest that influenza may contribute to the risk of HF hospitalization in the general population.
This community surveillance study uses data from communities in Maryland, Minnesota, Mississippi, and North Carolina to explore the association of monthly influenza-like illness activity with myocardial infarction and heart failure hospitalizations.
Introduction
In the United States, there are approximately 36 000 influenza-associated deaths during each influenza season and more than 200 000 influenza-associated excess hospitalizations.1 Influenza infection is known to be associated with an increased risk of cardiovascular (CV) events.2 Several studies have reported an increase in CV mortality and acute myocardial infarction (MI) during times when influenza was circulating. These findings are consistent across studies using various measures for MI, such as autopsy-confirmed MI deaths3 and International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) discharge diagnosis codes,4,5 and influenza activity at the population level through surveillance data2,3,4 and individual level with laboratory-confirmed infection.6 Two separate self-controlled case series studies found an increased risk for MI when preceded by acute respiratory infection, particularly in the week before the event.6,7 These results support a temporal association between influenza infections and acute CV events.
While several previous studies examining the association between influenza and CV disease have focused on mortality, fewer have explored the extent to which influenza contributes to CV hospitalizations specifically due to heart failure (HF). Patients with or at risk for HF are thought to be especially vulnerable to influenza-associated complications because of some degree of immunocompromise and have been shown to mount less vigorous responses to influenza vaccines.8 To our knowledge, the temporal association between influenza-like illness (ILI) and adjudicated hospitalizations for acute HF and MI has not been previously studied in a community population. We hypothesized that influenza activity would be associated with an increase in MI and HF hospitalizations among adults in a community population.
Methods
As part of the community surveillance component of the Atherosclerosis Risk in Communities (ARIC) study, data were collected from annual cross-sectional stratified random samples of hospitalizations of adults aged 35 to 84 years in 4 US communities from October 2010 to September 2014. The 4 communities were geographically diverse and included Jackson, Mississippi; some city suburbs of Minneapolis, Minnesota; and 2 rural communities: Forsyth County, North Carolina, and Washington County, Maryland. Based on the 2010 Census, 451 588 individuals between the ages of 35 to 84 years lived in the ARIC communities (eTable 1 in the Supplement).
Monthly ILI activity, the exposure of interest, was defined as the percentage of patient visits to sentinel clinicians for ILI in Mississippi, Minnesota, Maryland, and North Carolina as reported by the Centers for Disease Control and Prevention (CDC) US Outpatient Influenza-Like Illness Surveillance Network. Influenza-like illness was defined as a fever (temperature of 100°F [37.8°C] or higher), a cough and/or sore throat, and no known cause of symptoms. Influenza-like illness activity was defined at the month/region level and assumed constant across age/sex/race/ethnicity strata within a given month/site. The CDC also reports deaths due to pneumonia and influenza based on the National Center for Health Statistics Mortality Surveillance as well as cumulative influenza-associated hospitalization rates based on the surveillance of laboratory-confirmed influenza-associated hospitalizations.9 These measures of influenza or ILI were used to determine the severity of the influenza seasons and assess consistency across measures.
The number of hospitalizations for probable or definite MI and HF by month were adjudicated in the surveillance component of the ARIC Study. The methods of event ascertainment and classification have been described previously.10 A random sample of eligible hospitalizations were selected based on 3 criteria: (1) ICD-9-CM and ICD-10-CM discharge diagnosis codes for hospitalized MI (402, 410-414, 427, 428, 518.4, I11.x, I20.x, I21.x, I22.x, I24.x, I25.x, I46.x, I47.x, I48.x, I49.x, I50.x, J81.0, and R00.1), HF, or HF-associated conditions (398.91, 402.01, 402.11, 402.91, 404.01, 404.03, 404.11, 404.13, 404.91, 404.93, 415.0, 416.9, 425.4, 428.x, 518.4, and 786.0x) in any position; (2) age 35 to 84 years for MI and 55 years or older for HF at the time of hospital discharge; and (3) home address within the boundaries of the ARIC communities.10,11 The number of eligible hospitalizations that were abstracted was reduced by applying random sampling within strata defined by ICD diagnosis codes, age, sex, race/ethnicity, and communities of residence. The sampling fractions varied by strata and were defined to achieve similar standard errors for event rates across strata. We aggregated event counts by month, region, age, sex, and race/ethnicity. The range of dates were used as the study period because weekly ILI data by state were reported starting in 2010, and the adjudicated ARIC surveillance data were not available after 2014. This study was deemed exempt from review by the Brigham and Women’s institutional review board; none of the authors had direct access to information that could identify individuals and no informed consent was required.
We used a Poisson regression model to associate monthly influenza activity with hospitalizations for MI and HF. For these analyses, we combined new (incident) and recurrent hospitalized events. Models were adjusted for region, flu season, age, sex, race/ethnicity, and the number of hospitalizations from the month before to account for autocorrelation and included as an offset variable the log of the total population at risk living in the ARIC communities divided by the sampling fractions (eMethods in the Supplement). Given known seasonal differences in influenza virulence, we also stratified the models by season. For the analysis of HF hospitalizations, we also stratified the models to compare HF with preserved ejection fraction (left ventricular ejection fraction ≥50) vs HF with reduced ejection fraction (left ventricular ejection fraction <50) and incident vs recurrent hospitalizations. Additionally, we added interaction terms to assess if associations differed by age, sex, race/ethnicity, or region.
To account for the association of weather with influenza activity and CV outcomes, the monthly average temperature during the study period was also included in the analysis. The monthly average temperatures reported by the National Centers for Environmental Information National Oceanic and Atmospheric Administration was based on data collected at land-based weather stations within the study regions. Station details are provided in eTable 2 in the Supplement.
The number of MI and HF events were cross correlated with the percentage of patient visits for ILI from up to 6 months prior to assess the appropriate delay from exposure to outcome. To examine the temporal association between influenza and hospitalizations for HF or MI, we also evaluated separate models with the percentage of patient visits for ILI from a month prior as well as the subsequent month as the exposure variables. This was specifically to test for a lag in the association between influenza and hospitalizations for HF or MI or reverse causality. We used our final model to estimate the risk reduction associated with baseline ILI activity (ie, a month with 1% ILI) compared with elevated ILI activity (ie, a month with 6% ILI activity).
In a sensitivity analysis, we analyzed the correlation between ILI activity at the state level in North Carolina and at the county level in Forsyth County, North Carolina. County-level data were not available for the other ARIC communities. Influenza-like illness activity in Forsyth County was reported by the North Carolina Department of Health and Human Services/Department of Public Health Disease Event Tracking and Epidemiologic Collection Tool (NC DETECT), which is an advanced, statewide public health surveillance system that is funded by the North Carolina Division of Public Health and Public Health Emergency Preparedness Grant and managed through collaboration between the North Carolina Division of Public Health and the University of North Carolina at Chapel Hill Department of Emergency Medicine's Carolina Center for Health Informatics.
Analyses were performed using Stata, version 14 (StataCorp) and statistical significance was set at P < .05.
Results
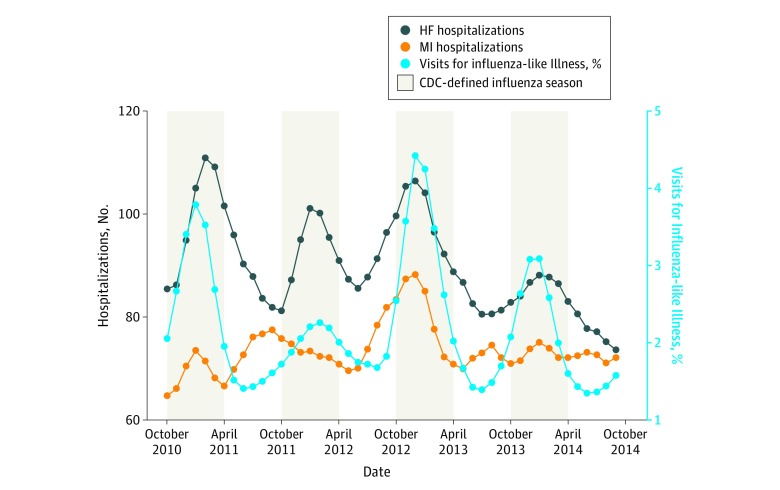
Influenza activity by season as reported by the CDC for the regions studied is shown in Table 1 and ILI activity over these regions by season is shown in Figure 1. Of the seasons studied, peak ILI activity was the highest in the 2012 to 2013 season and the lowest in the 2011 to 2012 season, with a peak of 10.1% vs 6.6% of visits to sentinel clinicians for ILI, respectively (Table 1). Concordant with ILI activity, the most pneumonia and influenza-associated deaths occurred during the 2012 to 2013 season (16 451 [27%]), and the lowest number occurred during the 2011 to 2012 season (14 449 [23%]).
Table 1. Influenza Activity by Season Reported by the US Centers for Disease Control and Prevention.
| Season | ILI Activity | Influenza-Associated Hospitalizations, Cumulative Rate per 100 000 Population | Pneumonia and Influenza Mortality, No. of Deaths | |
|---|---|---|---|---|
| Median (Range), % | Month of Peak ILI | |||
| 2010-2011 | 1.98 (0.38-8.51) | January | 20.5 | 15 581 |
| 2011-2012 | 2.10 (0.43-6.62) | March | 7.6 | 14 449 |
| 2012-2013 | 2.22 (0.11-10.13) | December | 50.4 | 16 451 |
| 2013-2014 | 1.78 (0.57-6.81) | January | 29.2 | 14 634 |
Abbreviation: ILI, influenza-like illness.
Figure 1. Average Influenza-like Illness Activity and Number of Hospitalizations Between October 2010 and September 2014.
This is based on moving averages that were calculated by taking the arithmetic mean of the observed values from each month with the values from the month before and after. CDC indicates Centers for Disease Control and Prevention; HF, heart failure; MI, myocardial infarction.
The demographics of the ARIC surveillance communities are shown in eTable 1 in the Supplement. Between October 2010 and September 2014, there were an unweighted total of 3541 MI hospitalizations and 4321 HF hospitalizations adjudicated within the ARIC communities (Tables 2 and 3). Weighted event counts by demographic strata are shown in eTables 3 and 4 in the Supplement.
Table 2. Average Influenza-like Illness Activity and Median Monthly Number of Heart Failure Hospitalizations by Season, Age, and Community.
| Season | Age, y | Forsyth County, North Carolina | Jackson, Mississippi | Minneapolis, Minnesota | Washington County, Maryland | ||||
|---|---|---|---|---|---|---|---|---|---|
| Average ILI, Mean (SD) | Event Count, Median (Range) | Average ILI, Mean (SD) | Event Count, Median (Range) | Average ILI, Mean (SD) | Event Count, Median (Range) | Average ILI, Mean (SD) | Event Count, Median (Range) | ||
| 2010-2011 | 55-74 | 1.20 (1.33) | 4.5 (1-13) | 3.70 (2.04) | 3.0 (0-9) | 1.19 (0.80) | 1.0 (0-5) | 1.79 (0.66) | 1.5 (0-6) |
| 75-85 | 3.5 (0-6) | 2.0 (0-5) | 0.5 (0-4) | 0.5 (0-4) | |||||
| 85+ | 2.0 (0-7) | 1.0 (0-4) | 0 (0-5) | 1.0 (0-5) | |||||
| 2011-2012 | 55-74 | 0.88 (0.24) | 4.5 (0-11) | 3.24 (0.71) | 4.0 (0-11) | 1.26 (0.53) | 0 (0-3) | 3.00 (1.71) | 1.0 (0-7) |
| 75-85 | 2.0 (0-8) | 2.0 (0-5) | 0.5 (0-3) | 0.5 (0-5) | |||||
| 85+ | 2.0 (0-6) | 1.0 (0-5) | 0 (0-6) | 0 (0-6) | |||||
| 2012-2013 | 55-74 | 1.50 (1.53) | 4.0 (0-8) | 4.17 (2.52) | 0 (0-14) | 1.24 (1.02) | 1.0 (0-3) | 1.97 (0.97) | 1.0 (0-8) |
| 75-85 | 2.0 (0-6) | 2.0 (0-5) | 0 (0-5) | 0.5 (0-6) | |||||
| 85+ | 2.0 (0-6) | 1.0 (0-5) | 1.0 (0-5) | 0 (0-5) | |||||
| 2013-2014 | 55-74 | 1.31 (0.63) | 4.0 (0-12) | 3.22 (1.70) | 3.0 (0-9) | 1.40 (0.69) | 1.0 (0-4) | 1.10 (0.47) | 1.0 (0-7) |
| 75-85 | 2.0 (0-6) | 1.0 (0-4) | 0 (0-5) | 0.5 (0-5) | |||||
| 85+ | 1.0 (0-4) | 1.0 (0-4) | 0 (0-5) | 0 (0-4) | |||||
Abbreviation: ILI, influenza-like illness.
Table 3. Average Influenza-like Illness Activity and Median Monthly Number of Myocardial Infarction Hospitalizations by Season, Age, and Community.
| Season | Age, y | Forsyth County, North Carolina | Jackson, Mississippi | Minneapolis, Minnesota | Washington County, Maryland | ||||
|---|---|---|---|---|---|---|---|---|---|
| Average ILI, Mean (SD) | Event Count, Median (Range) | Average ILI, Mean (SD) | Event Count, Median (Range) | Average ILI, Mean (SD) | Event Count, Median (Range) | Average ILI, Mean (SD) | Event Count, Median (Range) | ||
| 2010-2011 | 35-74 | 1.20 (1.33) | 5.0 (1-12) | 3.70 (2.04) | 3.0 (0-8) | 1.19 (0.80) | 2.0 (0-8) | 1.79 (0.66) | 1.5 (0-10) |
| 75-84 | 1.0 (0-5) | 0.0 (0-4) | 0 (0-3) | 1.0 (0-4) | |||||
| 2011-2012 | 35-74 | 0.88 (0.24) | 5.5 (1-11) | 3.24 (0.71) | 3.0 (0-9) | 1.26 (0.53) | 2.0 (0-6) | 3.00 (1.71) | 1.5 (0-11) |
| 75-84 | 2.0 (0-4) | 1.0 (0-4) | 0 (0-3) | 0 (0-3) | |||||
| 2012-2013 | 35-74 | 1.50 (1.53) | 5.0 (1-11) | 4.17 (2.52) | 3.0 (0-9) | 1.24 (1.02) | 2.0 (0-7) | 1.97 (0.97) | 2.0 (0-12) |
| 75-84 | 1.5 (0-9) | 1.0 (0-5) | 0 (0-4) | 1.0 (0-8) | |||||
| 2013-2014 | 35-74 | 1.31 (0.63) | 4.0 (0-13) | 3.22 (1.70) | 2.0 (0-7) | 1.40 (0.69) | 3.0 (0-7) | 1.10 (0.47) | 3.0 (0-7) |
| 75-84 | 1.5 (0-6) | 1.0 (0-4) | 0 (0-4) | 0 (0-3) | |||||
Abbreviation: ILI, influenza-like illness.
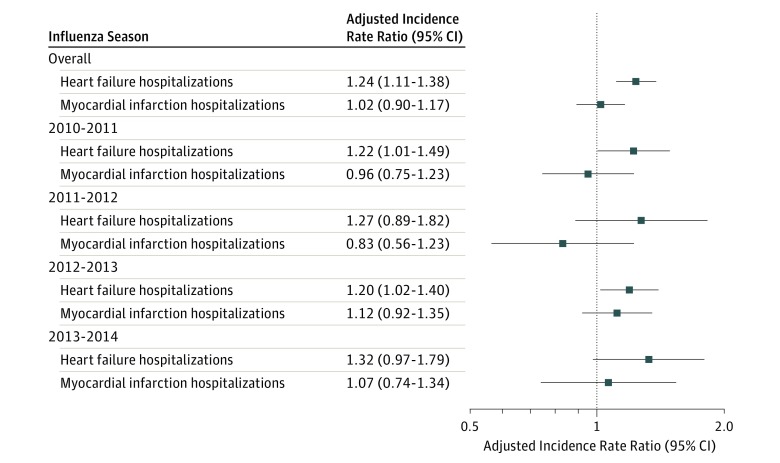
On average, a 5% increase in monthly ILI activity was associated with a 24% increase in HF hospitalization rates within the same month after multivariable adjustment (incidence rate ratio [IRR], 1.24; 95% CI, 1.11-1.38; P < .001) (Figure 2). Influenza-like illness activity was not significantly associated with MI hospitalizations (IRR, 1.02; 95% CI, 0.90-1.17; P = .72) when examined over the 4 seasons. During the 2 most severe influenza seasons (2010-2011 and 2012-2013), we observed a 22% and 20% temporally associated increased risk of HF (IRR, 1.22; 95% CI, 1.01-1.49; P = .04; and IRR, 1.20; 95% CI, 1.02-1.40; P = .02; respectively) and a positive but not significant association with MI in 2012 to 2013 (IRR, 1.12; 95% CI, 0.92-1.35; P = .25), suggesting that the influenza is associated with CV events especially during severe influenza seasons (Figure 2). Influenza-like illness activity in the months before hospitalization was not associated with either outcome. The estimated association between ILI activity and hospitalizations for HF and MI overall remained consistent after adjusting for monthly average temperatures (IRR, 1.17; 95% CI, 1.03-1.34 and IRR, 1.10; 95% CI, 0.94-1.28; respectively). The association between ILI activity and HF and MI hospitalizations was similar among men and women (IRR, 1.33; 95% CI, 1.16-1.54 vs IRR, 1.17; 95% CI, 0.99-1.36 and IRR, 1.13; 95% CI, 0.90-1.33 vs IRR, 0.96; 95% CI, 0.75-1.15; P value for interaction by sex = .45 and .24, respectively), among African American and white individuals (IRR, 1.31; 95% CI, 1.14-1.52 vs IRR, 1.25; 95% CI, 1.08-1.45 and IRR, 1.01; 95% CI, 0.96-1.38 and IRR, 1.38; 95% CI, 0.75-1.07; P value for interaction by race/ethnicity, .15 and .26, respectively), across age categories (IRR by age group for HF, 1.15; 95% CI, 1.00-1.33 among those aged 55-74 years vs 1.36; 95% CI, 1.13-1.65 among those aged 75-84 years vs 1.12; 95% CI, 0.88-1.41 among those 85 years or older; IRR by age group for MI, 1.02; 95% CI, 0.88-1.18 among those aged 35-74 years vs 1.03; 95% CI, 0.80-1.33 among those aged 75-84 years; P value for interaction by age, .09 and .72, respectively) and across region (IRR by region, 1.00; 95% CI, 0.70-1.41 and 0.86; 95% CI, 0.60-1.21 in Maryland vs 1.38; 95% CI, 0.83-2.00 and 0.71; 95% CI, 0.42-1.20 in Minnesota vs 1.22; 95% CI, 1.06-1.40 and 1.05; 95% CI, 0.87-1.26 in Mississippi vs 1.20; 95% CI, 0.96-1.48 and 1.14; 95% CI, 0.89-1.46 in North Carolina; P value for interaction, .41 and .25, respectively). The association between ILI activity and HF did not differ by ejection fraction (IRR, 1.31; 95% CI, 1.09-1.59 vs IRR, 1.24; 95% CI, 1.24-1.47; P value for interaction, .51; eTable 5 in the Supplement) or history of HF hospitalization (IRR, 1.05; 95% CI, 0.88-1.26 vs IRR, 1.21; 95% CI, 1.05-1.39; P value for interaction, .13; eTable 5 in the Supplement).
Figure 2. Association Between Monthly Influenza Activity and Hospitalizations for Heart Failure and Myocardial Infarction per 5% Increase in Influenza Activity by Season.
The Poisson models were adjusted for region, race, sex, age, season, and number of hospitalizations from the prior month to account for autocorrelation.
The corresponding risk reduction that was associated with reduced levels of ILI activity (IRR, 0.81; 95% CI, 0.72-0.90 per absolute 5% decrease in ILI) suggests that HF hospitalizations were 19% higher in months with elevated ILI activity (ie, a month with 6% ILI activity) when compared with a month with baseline ILI activity of 1%. No significant reduction in MI hospitalizations was associated with reduced levels of ILI activity (IRR, 0.98; 95% CI, 0.86 -1.11).
In a sensitivity analysis, we associated monthly ILI activity at the state level in North Carolina with county-level activity in Forsyth County, North Carolina. State-level and county-level activity were highly correlated (r = 0.92; P < .001). The estimated association between influenza and HF, as well as MI hospitalizations, remained unchanged when the analysis was performed using ILI activity data from Forsyth County, North Carolina, rather than state-level data (IRR, 1.25; 95% CI, 1.11-1.41 and IRR, 1.00; 95% CI, 0.86-1.15; respectively).
Discussion
In this study, we used surveillance data from 4 US communities to associate monthly ILI activity as reported by the CDC with MI and HF hospitalizations. Influenza-like illness activity was associated with an increase in HF hospitalizations within the same month. Myocardial infarction was positively but not significantly associated with ILI activity, with the highest point estimate during the most severe influenza season. These data suggest that influenza is temporally associated with the risk of CV hospitalization.
The exact mechanism by which influenza infection leads to an increased risk for acute CV events is not understood, but several mechanisms likely contribute. Influenza increases metabolic demand and, in the setting of hypoxemia, may exacerbate underlying cardiac conditions.12 Patients with HF have limited cardiac and respiratory reserves and are unlikely to tolerate infection-associated cardiac compromise. Infection-associated upregulated sympathetic nervous system activity may worsen HF, and infection concurrent with renal dysfunction may lead to volume overload. Proinflammatory cytokine level elevations during infection may precipitate plaque rupture and be associated with myocardial depression.13 Histologic findings from cardiac tissue samples from autopsies following deaths due to influenza have supported findings of acute myocarditis and myocyte necrosis.14
Our results are consistent with prior reports of increased admission rates for congestive HF during the influenza season15,16 and studies that have temporally associated acute CV events with influenza infection.6,7 In one study, investigators explored the effect of influenza on the risk of all-cause hospitalization among patients from 2 randomized, placebo-controlled trials among individuals with HF and found that the overall hospitalization rate was higher during the influenza season compared with noninfluenza seasons.15 However, another Canadian study that examined the association of CDC-reported influenza with HF hospital admissions did not detect significant associations between influenza and hospital admissions for HF among those older than 65 years.17 Investigators identified all hospital discharges in Ontario, Canada, with discharge diagnosis ICD-9 codes for HF between 1988 and 1993; there was no additional adjudication process to confirm the diagnosis. This study corroborates prior reports of an association between influenza and HF hospitalizations and elucidates the temporal association between these events.
Our results did not show an increased risk of MI following respiratory or influenza infection as previously reported.6,7 Two studies that examined the risk and timing of MI following acute infection found that MI risk was increased in the week after infection, but the association tapered over time.6,7 Therefore, it may not be possible to discern an association that occurs within a shorter time frame using event counts that were aggregated at the month level. The lack of a clear association in our analysis is likely a function of power and insufficient temporal resolution to detect the association between influenza infection and MI. In addition, the population sampled for MI in ARIC surveillance is younger than that sampled for HF hospitalizations and thus may be less likely to manifest the association.
Previous studies on the association between influenza and hospital morbidity have primarily focused on elderly populations.18 We found that hospitalizations for HF were associated with ILI activity in the broader study population, which included younger individuals, underscoring the vulnerability associated with HF regardless of age. The surveillance also covered urban, suburban, and rural communities, further generalizing these findings. Furthermore, we observed no heterogeneity by either sex or race/ethnicity.
We found an overall increased risk of HF associated with ILI activity throughout the 4 seasons studied. These data suggest that while hospitalizations for influenza and pneumonia, and deaths associated with these, are greatest during severe influenza seasons, acute CV events are also likely increased during periods of peak influenza activity. Of note, the A/H3N2 virus, which is associated with more severe morbidity and mortality, was the predominant strain that circulated during the 2012 to 2013 season. These data have implications for surveillance strategies aimed at identifying influenza as a cause of hospitalization in high-risk CV patients and vaccination strategies to mitigate this risk.
We were not able to directly assess the association between vaccination and influenza-associated CV risk at an individual level. Influenza vaccination is the most cost-effective way to attenuate the risk of influenza-associated cardiovascular events and has been shown in meta-analyses to reduce acute CV events.19 Currently, influenza vaccination is recommended by major guidelines in high-risk patients. The National Institutes of Health–supported INVESTED trial is testing whether a strategy using a high-dose formulation of the influenza vaccine, which may induce a more potent immune response, would reduce deaths or cardiopulmonary events more than the standard-dose vaccine.20
Limitations
Several limitations of this analysis should be noted. The individual influenza illness or vaccination status of those hospitalized for HF or MI was not known; therefore, we cannot make inferences at an individual patient level regarding influenza infection and subsequent CV events. Similarly, while we associated population-level ILI activity with events, it is possible that other infectious causes that might parallel influenza activity might have accounted for some of the association. It is also possible that another infectious cause accounted for the high MI/HF rates observed during the 2011 to 2012 season, which was reported as a low virulence year. Respiratory syncytial virus often cocirculates with influenza and may have been responsible for the high MI/HF rates that year.21 It is also possible that those admitted for severe flu with a prior history of HF may have been coded as having HF because prior knowledge of the disease. However, these hospitalizations were adjudicated and required specific criteria for classification as HF. While associating ILI at the state level with data with county-level surveillance data on HF and MI hospitalization sites could introduce bias into the results, our sensitivity analysis in North Carolina, where more granular information was available, suggested that influenza activity at the state level and county level are positively associated and assessing regional or state-level exposure did not modify our results. We were also unable to analyze the association between influenza severity and hospitalizations using other methods, such as the rate of influenza-associated hospitalizations. As shown in Table 1, the year with the lowest median ILI (2013-2014) had the second highest cumulative rate of influenza-associated hospitalizations. These observations may reflect that those infected with the circulating strain had a higher rate of hospitalizations but fewer individuals in the community-reported ILI. The inconsistency in influenza severity estimates across methods suggests that our results cannot be generalized to other measures of influenza activity. There were also relatively few events in each stratum that were stratified by age, race/ethnicity, and sex; therefore, there may be limited power to detect interaction effects. Finally, surveillance data are limited by sampling, which could result in inaccurate estimates of the total number of hospitalizations within the study communities; however, the risk of biased estimates based on surveillance data are minimized by a well-designed random sampling scheme to obtain a representative sample.
Conclusions
These data suggest that an increase in population levels of influenza activity is associated with an increase in hospitalizations for CV events, suggesting that addressing influenza activity may be valuable in efforts to prevent HF hospitalizations. Further studies are necessary to determine whether strategies to reduce influenza activity at the population level reduce the incidence of MI and HF hospitalizations.
eTable 1. Demographics of ARIC Surveillance Communities based on the 2010 U.S Census
eTable 2. Stations measuring monthly average temperatures
eTable 3. Median weighted monthly number of heart failure hospitalization by region and demographic strata
eTable 4. Median weighted monthly number of myocardial infarction hospitalization by region and demographic strata
eTable 5. Association between monthly influenza activity and hospitalizations for heart failure per 5% increase in influenza activity by age, region, ejection fraction and history of heart failure hospitalizations
eMethods
References
- 1.Thompson WW, Shay DK, Weintraub E, et al. . Influenza-associated hospitalizations in the United States. JAMA. 2004;292(11):1333-1340. doi: 10.1001/jama.292.11.1333 [DOI] [PubMed] [Google Scholar]
- 2.Kwok CS, Aslam S, Kontopantelis E, et al. . Influenza, influenza-like symptoms and their association with cardiovascular risks: a systematic review and meta-analysis of observational studies. Int J Clin Pract. 2015;69(9):928-937. doi: 10.1111/ijcp.12646 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Madjid M, Miller CC, Zarubaev VV, et al. . Influenza epidemics and acute respiratory disease activity are associated with a surge in autopsy-confirmed coronary heart disease death: results from 8 years of autopsies in 34,892 subjects. Eur Heart J. 2007;28(10):1205-1210. doi: 10.1093/eurheartj/ehm035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Warren-Gash C, Bhaskaran K, Hayward A, et al. . Circulating influenza virus, climatic factors, and acute myocardial infarction: a time series study in England and Wales and Hong Kong. J Infect Dis. 2011;203:1710-1718. doi: 10.1093/infdis/jir171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nguyen JL, Yang W, Ito K, Matte TD, Shaman J, Kinney PL; Journal of the American Medical Association . Seasonal influenza infections and cardiovascular disease mortality. JAMA Cardiol. 2016;1(3):274-281. doi: 10.1001/jamacardio.2016.0433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kwong JC, Schwartz KL, Campitelli MA, et al. . Acute myocardial infarction after laboratory-confirmed influenza infection. N Engl J Med. 2018;378(4):345-353. doi: 10.1056/NEJMoa1702090 [DOI] [PubMed] [Google Scholar]
- 7.Smeeth L, Thomas SL, Hall AJ, Hubbard R, Farrington P, Vallance P. Risk of myocardial infarction and stroke after acute infection or vaccination. N Engl J Med. 2004;351(25):2611-2618. doi: 10.1056/NEJMoa041747 [DOI] [PubMed] [Google Scholar]
- 8.Vardeny O, Sweitzer NK, Detry MA, Moran JM, Johnson MR, Hayney MS. Decreased immune responses to influenza vaccination in patients with heart failure. J Card Fail. 2009;15(4):368-373. doi: 10.1016/j.cardfail.2008.11.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brammer L, Budd A, Cox N. Seasonal and pandemic influenza surveillance considerations for constructing multicomponent systems. Influenza Other Respir Viruses. 2009;3(2):51-58. doi: 10.1111/j.1750-2659.2009.00077.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rosamond WD, Chang PP, Baggett C, et al. . Classification of heart failure in the atherosclerosis risk in communities (ARIC) study: a comparison of diagnostic criteria. Circ Heart Fail. 2012;5(2):152-159. doi: 10.1161/CIRCHEARTFAILURE.111.963199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.White AD, Folsom AR, Chambless LE, et al. . Community surveillance of coronary heart disease in the Atherosclerosis Risk in Communities (ARIC) study: methods and initial two years’ experience. J Clin Epidemiol. 1996;49(2):223-233. doi: 10.1016/0895-4356(95)00041-0 [DOI] [PubMed] [Google Scholar]
- 12.Corrales-Medina VF, Madjid M, Musher DM. Role of acute infection in triggering acute coronary syndromes. Lancet Infect Dis. 2010;10(2):83-92. doi: 10.1016/S1473-3099(09)70331-7 [DOI] [PubMed] [Google Scholar]
- 13.Takano T, Tajiri H, Kashiwagi Y, Kimura S, Kawashima H. Cytokine and chemokine response in children with the 2009 pandemic influenza A (H1N1) virus infection. Eur J Clin Microbiol Infect Dis. 2011;30(1):117-120. doi: 10.1007/s10096-010-1041-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fagnoul D, Pasquier P, Bodson L, Ortiz JA, Vincent JL, De Backer D. Myocardial dysfunction during H1N1 influenza infection. J Crit Care. 2013;28(4):321-327. doi: 10.1016/j.jcrc.2013.01.010 [DOI] [PubMed] [Google Scholar]
- 15.Upshur RE, Knight K, Goel V. Time-series analysis of the relation between influenza virus and hospital admissions of the elderly in Ontario, Canada, for pneumonia, chronic lung disease, and congestive heart failure. Am J Epidemiol. 1999;149(1):85-92. doi: 10.1093/oxfordjournals.aje.a009731 [DOI] [PubMed] [Google Scholar]
- 16.Araz OM, Bentley D, Muelleman RL. Using Google Flu Trends data in forecasting influenza-like-illness related ED visits in Omaha, Nebraska. Am J Emerg Med. 2014;32:1016-1023. doi: 10.1016/j.ajem.2014.05.052 [DOI] [PubMed] [Google Scholar]
- 17.Sandoval C, Walter SD, Krueger P, et al. . Risk of hospitalization during influenza season among a cohort of patients with congestive heart failure. Epidemiol Infect. 2007;135(4):574-582. doi: 10.1017/S095026880600714X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McBean AM, Babish JD, Warren JL. The impact and cost of influenza in the elderly. Arch Intern Med. 1993;153(18):2105-2111. doi: 10.1001/archinte.1993.00410180051005 [DOI] [PubMed] [Google Scholar]
- 19.Udell JA, Zawi R, Bhatt DL, et al. . Association between influenza vaccination and cardiovascular outcomes in high-risk patients: a meta-analysis. JAMA. 2013;310(16):1711-1720. doi: 10.1001/jama.2013.279206 [DOI] [PubMed] [Google Scholar]
- 20.Vardeny O, Udell JA, Joseph J, et al. . High-dose influenza vaccine to reduce clinical outcomes in high-risk cardiovascular patients: Rationale and design of the INVESTED trial. Am Heart J. 2018;202:97-103. doi: 10.1016/j.ahj.2018.05.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zambon MC, Stockton JD, Clewley JP, Fleming DM. Contribution of influenza and respiratory syncytial virus to community cases of influenza-like illness: an observational study. Lancet. 2001;358(9291):1410-1416. doi: 10.1016/S0140-6736(01)06528-X [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Demographics of ARIC Surveillance Communities based on the 2010 U.S Census
eTable 2. Stations measuring monthly average temperatures
eTable 3. Median weighted monthly number of heart failure hospitalization by region and demographic strata
eTable 4. Median weighted monthly number of myocardial infarction hospitalization by region and demographic strata
eTable 5. Association between monthly influenza activity and hospitalizations for heart failure per 5% increase in influenza activity by age, region, ejection fraction and history of heart failure hospitalizations
eMethods