Key Points
Question
Does juxtaposition of lethality trends for motor vehicle crashes and firearm injuries expose mechanism-specific injury severity trends?
Findings
In this repeated cross-sectional measures analysis of data on patients treated at level I or II trauma centers from 2003 to 2013, firearm assault and self-inflicted firearm injury were highly lethal in terms of case-fatality percentage and the percentage of out-of-hospital deaths. Annual trends significantly declined for motor vehicle crashes in all age groups but not for firearms in any intent or age group.
Meaning
Seen alongside trends in case-fatality percentage for motor vehicle crashes, it appears that injuries resulting from firearms may be worsening in severity.
Abstract
Importance
If changes over time in trauma care apply to both firearm injuries and motor vehicle crashes (MVCs) similarly, differences in mechanism-specific case-fatality trends may suggest changes over time in injury severity.
Objectives
To analyze national trends in case-fatality percentages at levels I and II trauma centers for injuries due to MVC, firearm assault, self-inflicted firearm injury, and unintentional firearm injury by age and to analyze trends in injury severity scores (ISSs) and the percentage of out-of-hospital deaths by mechanism.
Design, Setting, and Participants
From November 15, 2017, to July 4, 2018, repeated cross-sectional measures analysis of 1 335 044 patients treated at level I or II trauma centers from January 1, 2003, through December 31, 2013, was conducted using 2 data sources: the National Trauma Data Bank National Sample Program, with survey weights to estimate annual median ISS, total injuries and total deaths at levels I and II trauma centers, and the Centers for Disease Control and Prevention’s Wide-Ranging Online Data for Epidemiologic Research for percentages of out-of-hospital deaths.
Main Outcome Measures
The main outcome was annual case-fatality percentage (total died/total injured), calculated by mechanism across 3 age groups (15-34 years, 35-54 years, and ≥55 years) and 5 categories of ISS (1-15 [mild] 16-24, 25-40, 41-66, and 67-75 [severe]). Linear regression was performed to estimate annual trends in case-fatality percentage by mechanism, age group, and ISS. Annual trends in percentages of out-of-hospital deaths and median ISSs by mechanism were estimated. Sensitivity analyses included the Durbin-Watson statistic for autocorrelation and Prais-Winsten regression models.
Results
Among 1 335 044 patients treated at level I or II trauma centers, self-inflicted firearm injury had a case-fatality percentage of 42.8%, and assault with a firearm had a case-fatality percentage of 11.1%, the 2 highest of the injuries studied. The injury case-fatality percentage was lower each year for MVCs but did not change for any firearm intent overall or for any age group. Overall, median ISS increased annually for firearm suicide (0.31; 95% CI, 0.00-0.61). The annual percentage of out-of-hospital deaths was lower each year for MVCs (−0.24; 95% CI, −0.43 to −0.05) but not for any firearm intents. In sensitivity analyses, the annual percentage of out-of-hospital deaths for MVCs no longer showed a decline.
Conclusions and Relevance
Stagnant case-fatality percentages for firearm injuries juxtaposed to improvements for MVCs across age-groups and ISS categories suggests worsening severity of firearm injuries over the study period.
This repeated cross-sectional measures analysis of data from the National Trauma Data Bank National Sample Program compares trends in case-fatality percentages of motor vehicle crashes and firearm injuries in US levels I and II trauma centers across 10 years to assess whether firearm injuries are increasing in severity.
Introduction
Avoiding death from injury can be accomplished in 3 ways: prevent the fatal injury from happening, decrease the severity of injury, or provide coordinated, life-saving medical care immediately after the injury. The case-fatality percentage is a measure of injury lethality defined by the proportion of individuals who die from a particular injury.1 A higher case-fatality percentage suggests a more lethal injury given similar trauma care received.1 When the case-fatality percentage is high, primary prevention or decreasing the injury severity, as opposed to treatment of the injury, carries the greatest potential to minimize mortality. Motor vehicle crashes (MVCs) and injuries due to firearms are 2 of the top 3 causes of injury-related death for persons younger than 65 years.2 For firearms, severity and lethality of injury are related to the dimensions of the ammunition, the number and location of wounds, and the projectile velocity.3,4 Previous trends in increasing firearm lethality have been linked to changes over time in weapon and ammunition types.5,6 For MVCs, lethality may be associated with vehicle safety features, driver behavior, vehicle speed, and road features.7
There have been conflicting reports on trends in case-fatality percentages for firearm injuries in the United States. One analysis of data available publicly through the Centers for Disease Control and Prevention’s (CDC’s) web-based Injury Statistics Query and Reporting System concluded that firearm assault lethality declined from 2002 to 2011.8 Subsequent analyses did not find evidence of declining lethality after adjustment for reporting hospitals.9 Few studies have considered national trends in case-fatality percentages for firearms in the context of other injury mechanisms.10 Given a similar landscape of trauma care, juxtaposition of these trends can potentially unmask temporal changes that are not apparent when describing a single injury mechanism in isolation. Furthermore, earlier national investigations have not considered in-hospital and out-of-hospital deaths separately.
Our objective was to determine whether the trends in case-fatality percentage at levels I and II trauma centers for intent-specific firearm injuries and MVCs were similar in direction overall and across different age groups from 2003 to 2013. Given that trauma care at levels I and II trauma centers is considered the best care provided to injured patients nationally and that trends in care quality at these institutions are likely similar regardless of injury mechanism, we hypothesized that case-fatality trends would be similar in direction for all mechanisms.11 To test this hypothesis, we considered both in-hospital and out-of-hospital deaths. We sought to estimate case-fatality, as a measure of lethality, by age-group and injury mechanism (self-inflicted firearm injury, assault with a firearm, and unintentional firearm injury) and to assess whether trends in case-fatality percentage differed by age group and mechanism. Given that patients treated in trauma centers reflect only a subset of the burden of traumatic injury, we also sought to understand changes over time in the proportion of out-of-hospital deaths associated with these mechanisms. To test whether changes in case-fatality percentages were reflected in changes in measured injury severity, we assessed whether injury severity score (ISS) trends over time for specific mechanisms differed from zero and also calculated case-fatality trends by categories of ISS.
Methods
Data Sources
The National Trauma Data Bank (NTDB) National Sample Program (NSP) is a nationally representative sample from the NTDB consisting of 100 levels I and II trauma centers stratified by region and level of care.12 The purpose of the NSP was to provide a data structure and sampling scheme to compute reliable national estimates for levels I and II trauma centers.13 Sample hospitals are selected based on probability-proportional-to-size methodology considering counts of emergency department visits from American Hospital Association 2005 data.12 The sampling universe comes from the Trauma Information Exchange Program from 2003 consisting of 453 levels I and II trauma centers. The NSP is available annually for the years 2003 to 2013. The NSP is a subset of the larger NTDB and was discontinued after 2013. Although the full NTDB is available for the years 2014 through 2016, adding these years outside of the sampling and weighting methods used to design the NSP could introduce unpredictable bias. Furthermore, hospitals transitioned from using International Classification of Diseases, Ninth Revision to International Statistical Classification of Diseases and Related Health Problems, Tenth Revision during 2014 to 2016, adding additional uncertainty to comparisons in these years. Therefore, to reduce bias, years 2003 through 2013 were included in the analysis. From November 15, 2017, to July 4, 2018, we conducted repeated cross-sectional measures analysis of 1 335 044 patients treated at level I or II trauma centers from January 1, 2003, through December 31, 2013. Given that the systematic inclusion of children’s hospitals changed during the life of the NSP, we considered only patients 15 years or older. Because the data from both of our sources were deidentified, the study was exempt from institutional review board review per the Office of Human Research Protections guidelines.14
To account for the potential confounding effect of improvements in prehospital emergency medical services over the study period by which more severely injured patients reach the hospital before death, we investigated the percentage of out-of-hospital deaths among total deaths by mechanism. We obtained annual death counts by place of death from the CDC’s Wide-Ranging Online Data for Epidemiologic Research (WONDER) for firearm homicide, firearm suicide, unintentional firearm death, and death due to motor vehicle crash. The CDC’s WONDER sorts place of death into the following categories: medical facility–inpatient, medical facility–outpatient, or emergency department; medical facility–dead on arrival; decedent’s home, hospice facility, or nursing home/long-term care; other (such as street or public place); place of death unknown; and medical facility–status unknown. Deaths at the decedent’s home, medical facility–dead on arrival, and other were counted as out-of-hospital deaths.
Design, Measures, Exposure, and Control
We conducted an ecologic repeated cross-sectional analysis of age group–specific annual trends in case-fatality percentage by firearm intent (assault, unintentional, and suicide) and the annual age group–specific case-fatality percentage trends for occupant MVC. Our exposure was year. To calculate the case-fatality percentage, we first computed survey-weighted estimates for total counts of injured and deceased individuals among the 4 injury mechanisms/intents (occupant MVC, firearm assault, self-inflicted firearm injury, and unintentional firearm injury). We identified incidents according to e-codes. For occupant MVC, e-codes included 810.0 to 819.1. Firearm injury e-codes by intent included self-inflicted (955.0-955.4); assault (965.0-965.4, and 979.0); and unintentional (922.0-922.9). Case-fatality percentage was the survey-weighted total who died in trauma centers divided by the survey-weighted total estimated injured and treated individuals at trauma centers for each year, age group, and mechanism (MVC) or intent (firearm). We captured ISS as both annual survey-weighted means and medians by mechanism. We also estimated survey-weighted annual case-fatality percentages by categories of ISS (1-15 [mild], 16-24, 25-40, 41-66, and 67-75 [severe]). Percentages of out-of-hospital deaths were calculated by dividing out-of-hospital deaths by the total number of deaths by mechanism for that year.
Statistical Analysis
We generated total counts and 95% CIs using survey-weighted estimates according to the sampling scheme described by the NTDB/NSP user manual.12,13 Because our sample was limited to 11 years of data and included estimated totals, we generated 2-year rolling averages to smooth year-to-year variations. The limited number of time data points also restricted our ability to use time-series approaches that rely on greater numbers of observations.15 Even so, these approaches that correct for autocorrelation are most important when evaluating the association of a time-varying exposure (other than time itself) with an outcome. We performed linear regression using the ordinary least squares method, with year as the exposure and case-fatality percentage as a continuous outcome to estimate a coefficient and 95% CI for the annual change in case-fatality percentage. The null hypothesis for all models was that the annual case-fatality percentage did not change. Similarly, we performed linear regression, with year as the exposure and annual measures of ISS as the outcome. Last, we used linear regression with the ordinary least squares method to estimate trends in the percentage of out-of-hospital deaths by year. Statistical significance was set at 2-sided α = .05. All analyses were performed in Stata/SE, version 14.2 (StataCorp).
Sensitivity Analysis
To test the sensitivity of our results against the choices for our methodologic approaches, we conducted several additional analyses. For all ordinary least squares regression models, we calculated the Durbin-Watson statistic that tests for autocorrelation of outcome data.15 When this statistic is close to 2, the data are sufficiently independent. When the value is less than 2, a Prais-Winsten model with generalized least squares that corrects for autocorrelation may be more appropriate. For case-fatality percentage trends, we included Prais-Winsten regression models with and without 2-year moving averages.15 Finally, we calculated an out-of-hospital death group that did not include patients who were dead on arrival to account for possible changes in reporting criteria during the study period.
Results
From 2003 to 2013, the NSP included 1 667 395 observations weighted to an estimated 7 231 211 (95% CI, 6 236 718-8 225 704) incidents treated at level I or II trauma centers. For patients 15 years or older, we estimated a total of 1 335 044 (95% CI, 1 155 592-1 514 497) injured patients, of whom 87.0% were occupant MVCs (survey-weighted estimated total, 1 161 997), 10.0% were assaults with a firearm (survey-weighted estimated total, 133 289), 1.8% were self-inflicted firearm injury (survey-weighted estimated total, 24 376), and 1.2% were unintentional firearm injury (survey-weighted estimated total, 15 382) (Table 1). There were an estimated total 74 928 (95% CI, 63 651-86 205) in-hospital deaths, of which 49 294 (95% CI, 42 440-56 149) (65.8%; 95% CI, 62.0%-69.4%) were from occupant MVC, 14 718 (95% CI, 10 350-19 087) (19.7%; 95% CI, 16.1%-23.7%) from firearm homicide, 10 373 (95% CI, 8659-12 087) (13.8%; 95%CI, 12.3%-15.5%) from firearm suicide, and 541 (95% CI, 437-646) (0.7%; 95% CI, 0.6%-0.9%) from unintentional firearm injury (Table 1).
Table 1. Deaths, Injuries, and Trends in Case-Fatality Percentage by Mechanism of Injury Among Patients 15 Years or Older, 2003-2013a.
| Mechanism | Total No. | Overall Case-Fatality, % (95% CI) |
Annual Change in Case-Fatality, Percentage Point Change (95% CI) |
|
|---|---|---|---|---|
| Deaths (95% CI) | Injuries (95% CI) | |||
| Occupant motor vehicle crash | 49 294 (42 440 to 56 149) | 1 161 997 (1 014 640 to 1 309 353) | 4.3 (3.9 to 4.7) | −0.17 (−0.24 to −0.10)b |
| Firearm | ||||
| Assault | 14 718 (10 350 to 19 087) | 133 289 (94 792 to 171 787) | 11.1 (10.4 to 11.9) | −0.25 (−0.56 to 0.06) |
| Self-inflicted | 10 373 (8659 to 12 087) | 24 376 (20 293 to 28 459) | 42.8 (40.9 to 44.8) | −0.08 (−0.75 to 0.59) |
| Unintentional | 541 (437 to 646) | 15 382 (13 089 to 17 675) | 3.5 (3.1 to 4.1) | 0.14 (−0.17 to 0.45) |
All totals, proportions, and trends were generated using survey weighting rounded to the nearest whole number.
P < .05.
Overall, the case-fatality percentage among these 4 groups was 5.7% (95% CI, 5.3%-6.1%). The annual case-fatality percentages for each mechanism are presented in eTable 1 in the Supplement. The case-fatality percentage was highest for self-inflicted firearm injury (42.8%; 95% CI, 40.9%-44.8%) and lowest for unintentional firearm injury (3.5%; 95% CI, 3.1%-4.1%) (Table 1). Using 2-year rolling averages, the case-fatality percentage was lower each year for occupant MVC but did not significantly change for any of the firearm injuries regardless of intent (Table 1).
By total counts, the burden of total injuries and deaths was highest in the 15- to 34-year age group (eTable 2 in the Supplement). For total injuries, patients aged 35 to 54 years had the next highest number, but for fatalities, the group 55 years or older had the second highest number (eTable 2 in the Supplement). Although occupant MVC had the highest number of injuries and deaths in all 3 age groups, the case-fatality percentage from this mechanism was either the lowest or second lowest in all age groups. Self-inflicted firearm and assault with a firearm had the highest and second-highest case-fatality percentage in all 3 age groups, respectively (eTable 2 in the Supplement). Firearm homicide had the second-highest total death count in all age groups except the group 55 years or older, in which firearm suicide was the second highest (eTable 2 in the Supplement).
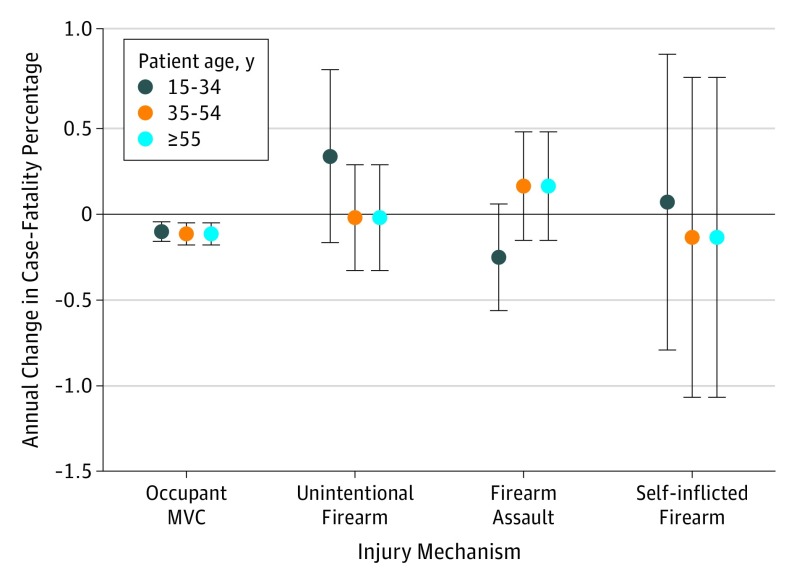
On average, the case-fatality percentage was lower each year in occupant MVCs for all groups (Table 2). By comparison, on average, none of the annual case-fatality percentages was significantly lower in any of the categories for firearm intent in any of the age groups (Figure). By mechanism, median ISS for self-inflicted firearm injury was 0.31 higher (95% CI, 0.00-0.61) each year (Table 3). By category of injury severity, the case-fatality percentage was lower each year for MVCs in all categories except ISS 25 to 40 (eTable 3 in the Supplement). For firearm assault and unintentional firearm injury, the data do not suggest annual changes in case-fatality percentages for any of the ISS categories. For self-inflicted firearm injury, on average, the case-fatality percentage was lower each year in the 2 lowest ISS categories (1-15 and 16-24) (eTable 3 in the Supplement).
Table 2. Annual Change in Case-Fatality Percentage by Age Group, 2003-2013.
| Mechanism | Age Group, Annual Percentage Point Change (95% CI) | ||
|---|---|---|---|
| 15-34 y | 35-54 y | ≥55 y | |
| Occupant motor vehicle crash | −0.13 (−0.19 to −0.08)a | −0.15 (−0.21 to −0.09)a | −0.36 (−0.55 to −0.17)a |
| Firearm | |||
| Assault | −0.28 (−0.58 to 0.02) | 0.12 (−0.19 to 0.42) | −1.06 (−2.16 to 0.05) |
| Self-inflicted | 0.03 (−0.80 to 0.86) | −0.17 (−1.06 to 0.72) | −0.05 (−1.33 to 1.22) |
| Unintentional | 0.28 (−0.20 to 0.77) | −0.06 (−0.35 to 0.24) | −0.17 (−0.63 to 0.29) |
P < .05.
Figure. Annual Change in Case-Fatality Percentage by Mechanism and Age Group.
MVC indicates motor vehicle crash. Error bars indicate 95% CI.
Table 3. Annual Trends in Injury Severity Score, NTDB NSP, 2003-2013.
| Mechanism/Intent | Mean (95% CI) ISS, OLS | Median (95% CI) ISS, OLS | Mean (95% CI) ISS, Prais-Winstena | Median (95% CI) ISS, Prais-Winstena |
|---|---|---|---|---|
| Occupant motor vehicle crash | 0.03 (−0.12 to 0.17) | 0.08 (−0.04 to 0.20) | 0.03 (−0.16 to 0.21) | NA |
| Firearm | ||||
| Homicide | −0.03 (−0.19 to 0.12) | −0.04 (−0.10 to 0.03) | −0.03 (−0.20 to 0.15) | NA |
| Suicide | 0.08 (−0.10 to 0.25) | 0.31 (0.00 to 0.61)b | NA | NA |
| Unintentional death | 0.05 (−0.04 to 0.15) | −0.08 (−0.35 to 0.18) | NA | −0.08 (−0.34 to 0.18) |
Abbreviations: ISS, injury severity score; NA, not applicable; NTDB NSP, National Trauma Data Bank National Sample Program; OLS, ordinary least squares method.
Prais-Winsten models were included if the Durbin-Watson statistic was less than 1.95.
P < .05.
For patients 15 years or older, 407 475 MVC deaths, 127 285 firearm homicide deaths, 202 191 firearm suicide deaths, and 6133 unintentional firearm injury deaths were captured from CDC’s WONDER from 2003 to 2013. Firearm suicides had the highest percentage of out-of-hospital deaths (86.5%) and MVC had the lowest (58.2%) (Table 4). The percentage of deaths occurring outside the hospital did not change across time for any of the firearm intents (Table 4). For occupant MVCs, on average, the percentage of out-of-hospital deaths was 0.24% lower each year (95% CI, −0.41 to −0.05).
Table 4. Annual Trends in Proportion of Out-of-Hospital Deaths in Patients 15 Years or Older, CDC’s WONDER, 2003-2013.
| Mechanism/Intent | No. of Out-of-Hospital Deaths | Total Deaths | Overall Out-of-Hospital Deaths. % | Annual Mean Percentage Point Change (95% CI) |
|---|---|---|---|---|
| Occupant motor vehicle crash | 237 113 | 407 475 | 58.2 | −0.24 (−0.43 to −0.05)a |
| Firearm | ||||
| Homicide | 75 877 | 127 285 | 59.6 | 0.13 (−0.15 to 0.42) |
| Suicide | 174 930 | 202 191 | 86.5 | 0.05 (−0.23 to 0.33) |
| Unintentional death | 3762 | 6133 | 61.3 | 0.64 (0.12 to 1.15)a |
Abbreviation: CDC’s WONDER, Centers for Disease Control and Prevention’s Wide-Ranging Online Data for Epidemiologic Research.
P < .05.
Results from the sensitivity analyses are included in eTables 4 and 5 in the Supplement. For out-of-hospital deaths, the declining trend for MVCs was no longer statistically significant using the Prais-Winsten regression model. All other results were similar to the main analysis.
Discussion
In the period from 2003 to 2013, these data suggest declining case-fatality percentages for patients 15 years or older injured in MVCs who were treated at levels I and II trauma centers, whereas the case-fatality percentages for all firearm intents remained unchanged. Although declining percentages of out-of-hospital deaths may have explained a portion of this finding by which more severely injured patients reach the hospital before death (potentially raising the in-hospital case-fatality percentage), our data suggest that these percentages have not changed during the study period or have decreased for MVCs only. This finding would create a bias toward no association or higher annual trends in the case-fatality percentage for MVCs. Decreasing percentages of out-of-hospital deaths may represent injuries becoming less fatal in the period immediately following injury. Our data do not suggest nonzero trends for ISS for any mechanism except self-inflicted firearm injury. Case-fatality percentages across nearly all ISS categories were decreasing for MVCs yet stayed flat for firearm assault and unintentional firearm injury. For self-inflicted firearm injury, lower annual case-fatality percentages for the least severe ISS categories in the context of a rising annual median ISS and a flat overall case-fatality percentage suggest that the overall proportion of patients in the lowest-severity ISS groups is decreasing over time.
Estimating trends in lethality of firearm injury is an area of active study. One report analyzed data from the CDC, combining annual counts of fatal and nonfatal firearm injury from 2002 to 2011 and concluded that firearm lethality was declining, evidenced by stagnant rates for firearm homicide with rising rates of nonfatal firearm assault.16 However, after correcting for facilities reporting to the sample, a separate analysis concluded that firearm lethality from assault has been constant from 2003 to 2012.9 There is active debate on the merits and limitations of both approaches.17
Our data do not provide evidence that the case-fatality percentage of firearm assault changed from 2003 to 2013 at levels I and II trauma centers, possibly suggesting that firearm lethality has been stagnant across this period. To place this stagnation in the context of the lower annual case-fatality percentage from MVCs may mean a relative worsening of firearm lethality assuming that trauma care improves in the same direction regardless of mechanism. Although our data do not suggest that ISS changed on average for assault with a firearm or unintentional firearm injury, there are data to suggest that this measure may be insufficiently sensitive to assess severity for penetrating injury.18,19 Data from the National Inpatient Sample from 1993 to 2014 suggest annual increases in the new ISS (NISS) for firearms.20 The NSP does not include the NISS. Given that the NISS may be more accurate in estimating mortality and complications in penetrating injuries, the trend reported using the NISS is not surprising, even when our analysis of the ISS showed no change.19 The data source, period, and analytic approach were also different from ours. Data from a level I trauma center in Denver, Colorado, reported an increasing firearm case-fatality percentage compared with other trauma mechanisms from 2000 to 2013.10
Our findings demonstrate that, for MVCs, the percentage of deaths occurring outside the hospital each year may be declining and the proportion of MVC occupants who die after being admitted to a level I or II trauma center is lower each year. This combination of findings suggests substantial achievements in reducing the severity of MVC injuries.
One possible explanation for the stagnant case-fatality percentage for firearm injuries amidst the improvements in trauma care suggested by trends in MVC case-fatality percentages is potentially associated with changes in the ballistic properties of firearms. Previous data analyses of linked hospital and police records suggest that changes in firearm properties over time also manifest in the aggregate on lethality.5,6 Developments in firearms technology that create more severe wounds through greater transfer of kinetic energy from projectiles to tissue or more tissue disruption from new bullet architecture may offset improvements in trauma care.21,22 There may also be an association between greater numbers of wounds that typically follow from firearms with rapid shooting capabilities and lethality.5 National data on the ballistic properties of civilian firearm injuries are not currently available for study.
Limitations
Facility requirements for reporting to the NTDB, and by extension the NSP, may change from year to year. Our results are limited to patients admitted to level I or II trauma centers, and these estimations are not designed to capture all injuries in the United States. Our analytic method imposed a linear association between time and the outcome measures, whereas that association may be nonlinear. Even so, uncovering quadratic, cubic, or other shapes of time associations with 11 data points may not be possible. Although our in-hospital analysis focused on levels I and II trauma centers, our analysis of out-of-hospital deaths included all deaths. Levels I and II trauma centers may exist within potentially more developed emergency medical systems with distinct trends for the proportion of out-of-hospital deaths. Results from our sensitivity analysis that remove the dead-on-arrival deaths from this analysis do not appreciably change the overall interpretation of these findings. When querying CDC WONDER, one is unable to limit the query to out-of-hospital deaths in areas served by levels I and II trauma centers.
Conclusions
We found stagnant case-fatality percentages for firearms alongside declining case-fatality percentages for occupant MVCs from 2003 to 2013. This may reflect a worsening of firearm injury severity over time. These findings are not likely explained by changes in the percentage of out-of-hospital deaths. Incorporating the study of firearm ballistics into longitudinal public health and trauma surgery research is necessary to better understand firearm lethality. Similar to the crash information collected in every fatal MVC, adding details on firearm type, ammunition used, shots fired, and number of wounds can provide a more complete picture of firearm injury severity over time and eventually lead to greater protections against death and disability due to firearm injuries.
eTable 1. Annual Case-Fatality Percentage (95% CI) by Mechanism, Ages 15 Years and Older
eTable 2. Survey Weighted Total Deaths, Injuries, and Case-Fatality by Mechanism and Age Group, 2003-2013, NTDB NSP
eTable 3. Annual Trends in Case-Fatality by Mechanism and ISS Category
eTable 4. Sensitivity Analysis, Durbin-Watson Statistic and Annual Change in Case Fatality Percentage Overall and by Age-Groups (2003-2013) Using Prais-Winsten Method
eTable 5. Sensitivity Analysis, Durbin-Watson Statistic and Annual Change in Percentage of Out-of-Hospital Deaths by Mechanism (2003-2013)
References
- 1.Principles of Epidemiology in Public Health Practice, Third Edition: An Introduction to Applied Epidemiology and Biostatistics: lesson 3: measures of risk. Centers for Disease Control and Prevention. https://www.cdc.gov/ophss/csels/dsepd/ss1978/lesson3/section3.html. Updated May 18, 2012. Accessed May 2, 2018.
- 2.10 Leading causes of injury deaths by age-group highlighting unintentional injury deaths, United States—2016. Centers for Diseases Control and Prevention. https://www.cdc.gov/injury/images/lc-charts/leading_causes_of_death_highlighting_unintentional_2016_1040w800h.gif. Published 2016. Accessed May 2, 2018.
- 3.Hargarten SW, Karlson TA, O’Brien M, Hancock J, Quebbeman E. Characteristics of firearms involved in fatalities. JAMA. 1996;275(1):42-45. doi: 10.1001/jama.1996.03530250046025 [DOI] [PubMed] [Google Scholar]
- 4.Fackler ML, Malinowski JA. The wound profile: a visual method for quantifying gunshot wound components. J Trauma. 1985;25(6):522-529. doi: 10.1097/00005373-198506000-00009 [DOI] [PubMed] [Google Scholar]
- 5.Wintemute GJ. The relationship between firearm design and firearm violence: handguns in the 1990s. JAMA. 1996;275(22):1749-1753. doi: 10.1001/jama.1996.03530460053031 [DOI] [PubMed] [Google Scholar]
- 6.Caruso RP, Jara DI, Swan KG. Gunshot wounds: bullet caliber is increasing. J Trauma. 1999;46(3):462-465. doi: 10.1097/00005373-199903000-00021 [DOI] [PubMed] [Google Scholar]
- 7.Bandi P, Silver D, Mijanovich T, Macinko J. Temporal trends in motor vehicle fatalities in the United States, 1968 to 2010—a joinpoint regression analysis. Inj Epidemiol. 2015;2(1):4. doi: 10.1186/s40621-015-0035-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jena AB, Sun EC, Prasad V. Does the declining lethality of gunshot injuries mask a rising epidemic of gun violence in the United States? J Gen Intern Med. 2014;29(7):1065-1069. doi: 10.1007/s11606-014-2779-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cook PJ, Rivera-Aguirre AE, Cerdá M, Wintemute G. Constant lethality of gunshot injuries from firearm assault: United States, 2003-2012. Am J Public Health. 2017;107(8):1324-1328. doi: 10.2105/AJPH.2017.303837 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sauaia A, Gonzalez E, Moore HB, Bol K, Moore EE. Fatality and severity of firearm injuries in a Denver trauma center, 2000-2013. JAMA. 2016;315(22):2465-2467. doi: 10.1001/jama.2016.5978 [DOI] [PubMed] [Google Scholar]
- 11.MacKenzie EJ, Rivara FP, Jurkovich GJ, et al. . A national evaluation of the effect of trauma-center care on mortality. N Engl J Med. 2006;354(4):366-378. doi: 10.1056/NEJMsa052049 [DOI] [PubMed] [Google Scholar]
- 12.National Sample Program Arrival Year 2012. Chicago, IL: American College of Surgeons; 2013. [Google Scholar]
- 13.Goble S, Neal M, Clark DE, et al. . Creating a nationally representative sample of patients from trauma centers. J Trauma. 2009;67(3):637-642. doi: 10.1097/TA.0b013e3181b84294 [DOI] [PubMed] [Google Scholar]
- 14.Office of Human Research Protections guidelines. https://www.hhs.gov/ohrp/. Accessed November 6, 2018.
- 15.Lagarde M. How to do (or not to do)…assessing the impact of a policy change with routine longitudinal data. Health Policy Plan. 2012;27(1):76-83. doi: 10.1093/heapol/czr004 [DOI] [PubMed] [Google Scholar]
- 16.Kalesan B, Adhikarla C, Pressley JC, et al. . The hidden epidemic of firearm injury: increasing firearm injury rates during 2001-2013. Am J Epidemiol. 2017;185(7):546-553. doi: 10.1093/aje/kww147 [DOI] [PubMed] [Google Scholar]
- 17.Kalesan B, Galea S, Fagan JA. Three authors reply. Am J Epidemiol. 2017;186(7):897-898. doi: 10.1093/aje/kwx280 [DOI] [PubMed] [Google Scholar]
- 18.Lawnick MM, Champion HR, Gennarelli T, et al. . Combat injury coding: a review and reconfiguration. J Trauma Acute Care Surg. 2013;75(4):573-581. doi: 10.1097/TA.0b013e3182a53bc6 [DOI] [PubMed] [Google Scholar]
- 19.Smith BP, Goldberg AJ, Gaughan JP, Seamon MJ. A comparison of injury severity score and new injury severity score after penetrating trauma: a prospective analysis. J Trauma Acute Care Surg. 2015;79(2):269-274. doi: 10.1097/TA.0000000000000753 [DOI] [PubMed] [Google Scholar]
- 20.Kalesan B, Zuo Y, Xuan Z, et al. . A multi-decade joinpoint analysis of firearm injury severity. Trauma Surg Acute Care Open. 2018;3(1):e000139. doi: 10.1136/tsaco-2017-000139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stefanopoulos PK, Pinialidis DE, Hadjigeorgiou GF, Filippakis KN. Wound ballistics 101: the mechanisms of soft tissue wounding by bullets. Eur J Trauma Emerg Surg. 2017;43(5):579-586. doi: 10.1007/s00068-015-0581-1 [DOI] [PubMed] [Google Scholar]
- 22.McGonigal MD, Cole J, Schwab CW, Kauder DR, Rotondo MF, Angood PB. Urban firearm deaths: a five-year perspective. J Trauma. 1993;35(4):532-536. doi: 10.1097/00005373-199310000-00006 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Annual Case-Fatality Percentage (95% CI) by Mechanism, Ages 15 Years and Older
eTable 2. Survey Weighted Total Deaths, Injuries, and Case-Fatality by Mechanism and Age Group, 2003-2013, NTDB NSP
eTable 3. Annual Trends in Case-Fatality by Mechanism and ISS Category
eTable 4. Sensitivity Analysis, Durbin-Watson Statistic and Annual Change in Case Fatality Percentage Overall and by Age-Groups (2003-2013) Using Prais-Winsten Method
eTable 5. Sensitivity Analysis, Durbin-Watson Statistic and Annual Change in Percentage of Out-of-Hospital Deaths by Mechanism (2003-2013)