Abstract
Transformation of hematopoietic stem cells by the BCR-FGFR1 fusion kinase found in a variant of Stem Cell Leukemia/Lymphoma (SCLL) syndrome leads to development of B-lymphomas in syngeneic mice and humans. In this study, we show that the relatively rapid onset of this leukemia is potentially related to oncogenic domains within the BCR component. BCR recruited a guanidine nucleotide exchange factor (GEF) domain to the fusion kinase to facilitate activation of small GTPases such as RHOA. Deletion of this GEF domain increased leukemogenesis, enhanced cell survival and proliferation, and promoted stem cell expansion and lymph node metastasis. This suggests that, in an SCLL context, the presence of the endogenous GEF motif leads to reduced leukemogenesis. Indeed, loss of the GEF domain suppressed activation of RHOA and PTEN, leading to increased activation of AKT. Loss of the GEF domain enhanced cell proliferation and invasion potential, which was also observed in cells in which RHOA is knocked down, supported by the observation that overexpression of RHOA leads to reduced viability and invasion. In vivo, depletion of RHOA in SCLL cells significantly increased disease progression and shortened latency. Collectively, these data show that the BCR GEF domain affects phenotypes associated with progression of SCLL through suppression of RHOA signaling.
Keywords: RHOA, BCR-FGFR1, B-lymphoma, GEF domain
Introduction
The fibroblast growth factor receptor-1 (FGFR1) has important functions during normal embryonic development [1], but upregulation of its expression also plays a role in development of a variety of cancers [2]. The only disorder, however, where upregulation of FGFR1 expression leads consistently to the development of a specific disease, is in the stem cell leukemia/lymphoma syndrome (SCLL). This disorder typically presents as a chronic myeloproliferative disease accompanied by B-cell and T-cell lymphomas with rapid progression to AML [3]. The disease is characterized by chromosome rearrangements involving 8p11 breakpoints within the FGFR1 gene that combine with a wide variety of other chromosome sites leading to the generation of chimeric proteins. The consistent finding is that, as a result of these chromosome translocations, a chimeric FGFR1 kinase transcript is generated where the fusion partner provides a dimerization motif that leads to the ligand-independent, constitutive activation of the FGFR1 kinase [4–5]. Pharmacological suppression of FGFR1 function in these cells, both in vitro and in vivo, leads to suppression of the disease, demonstrating the importance of FGFR1 activation in the etiology of SCLL [6–8]. While activation of FGFR1 kinase is the consistent feature of the various chromosome translocations, it has become clear that the identity of the fusion partner gene may influence the phenotypic presentation of the disease [3].
The BCR-FGFR1 variant of SCLL is relatively rare, with only ~20 cases reported to date. It has been reported to occur with a higher median age compared with other SCLL variants and often presents with leukocytosis, neutrophilia and basophilia [9]. Clinically, it has often been described as similar to CML with lymphoid B-cells and myeloid cells, as well as blast cells at different levels of maturation [10]. Mouse models of BCR-FGFR1 SCLL have been generated where the phenotypes parallel those seen in the human disease with a pro-B-cell leukemia but with the caveat that syngeneic models do not develop AML [11–12], although AML develops in transduction and transplantation models using human CD34+ cells transplanted into immunocompromized mice [13]. In these mouse models, BCR-FGFR1 driven SCLL is the most aggressive of the chimeric kinases investigated.
While the BCR-FGFR1 rearrangement clearly activates the FGFR1 kinase domain through oligomerization, this is also the case for the other FGFR1 chimeric kinases. The more aggressive progression of BCR-FGFR1-driven disease, however, may be a result of the effects of unique domains within the BCR component of the chimeric protein. BCR, for example, contains a serine-threonine kinase (STK) domain which is retained in the fusion protein and potentially enhances specific signaling pathways through activation of specific targets. In addition, the retained 5’ portion of BCR contains a guanosine nucleotide exchange factor (GEF) domain which is responsible for activation of GTPases which often have important influences on cell growth and survival. To investigate the relative involvement of the BCR GEF subdomain for BCR-FGFR1 driven SCLL, we created deletion mutant isoforms of the chimeric protein and evaluated their relative contribution to SCLL development in a syngeneic, in vivo transduction and transplantation model. These studies demonstrated that, in fact, the GEF domain acts to suppress the potency of the BCR-FGFR1 kinase, since deletion constructs lead to an enhanced progression of SCLL in vivo with a shorter latency period. This promotion of leukemogenesis is related to reduced RHOA activation, PTEN activation and enhanced pAKT activation as a consequence.
Materials and Methods.
Transduction and transplantation in vivo.
All animal experiments were performed under an approved protocol from the Augusta University IACUC. Donor bone marrow cells from Balb/C mice were isolated and transduced with various constructs prepared in the MIG retroviral vector as described previously [14–15], then transplanted into sub-lethally irradiated, syngeneic hosts via tail vein injection. In this procedure, mice were pretreated i.p. with 5FU and BM cells collected 3 days later. Total harvested BM cells were then exposed to retroviral vectors in vitro and cultured for 2–3 days. 5 × 106 cells from the primary transduction were then transplanted into each of 5 mice in each cohort. Engraftment was monitored by weekly examination of the GFP population in peripheral blood. 1–2 × 106 BM cells (of which 80–90% are GFP+) from mice with the primary disease were transplanted into secondary recipients. Immunohistochemistry of formalin-fixed, paraffin-embedded tissues sections was carried out as described previously [14].
Molecular analyses.
BaF3 cells were obtained from ATCC and used within 4 passages following thawing. Transformation to IL3 independence confirmed the identity of these cells. SCLL cell lines were generated in-house and authenticated by the presence of the chimeric FGFR1 kinase. Cells were not routinely tested for mycoplasma. Western blot, DNA preparation/cloning, plasmid transfection and cell culture procedures are all standard and have been described extensively and in detail previously [16]. Flow cytometic analysis also followed standard procedures described elsewhere using antibodies B220-APC, IgM-PE, CD4-APC, CD8-PE/Cy7, Gr1-PE, Mac1-PerCP/Cy5.5, Sca1-PE/Cy7, c-Kit-APC from BD bioscience.
Invasion assays for adherent cells were performed as described previously [14, 17]. For primary bone marrow cells, CD19+ cells were flow sorted, layered (104 cells per well) on the upper surface of transwell chambers (in triplicate) and the number of cells that migrated through the matrix counted after 24 hours.
RHOA-GTP assays.
Quantitation of the GTP-bound form of the RHOA protein was performed using the RHOA Activation Assay kit (Cytoskeleton Inc, Denver, CO) according to the manufacturer’s instructions. Briefly, cell lysates were incubated at 4°C for 1 h with a GST fusion protein containing the RHO-binding domain of rhotekin (GST-RBD) immobilized on glutathione Sepharose beads. After washing the beads twice with lysis buffer and once with wash buffer provided by the manufacturer, bead-bound proteins were fractionated using 12% SDS-PAGE and immunoblotted with anti-RHOA antibodies. Total cell lysates were also blotted with anti-RHOA antibodies to assess the fractional ratios of rhotekin-bound RHOA proteins.
In vitro bone marrow transformation and differentiation analysis.
Transduced bone marrow cells were isolated using flow cytometry based on expression of GFP from the targeting vectors. Cells were then diluted to different concentrations in 24-well plates and cultured in RPMI media supplemented with 10% fetal bovine serum. After 3 weeks, individual wells were scored as positive if the cell numbers exceeded 1 × 106/ml. For detection and quantification of mouse hematopoietic progenitors in the bone marrow, colony formation assays using Methocult GMF M3434 and M3630 were performed according to the manufacturers’ instructions (Stem Cell, Vancouver, Canada).
The reverse phase protein array (RPPA) analysis.
The RPPA analysis was performed by the Functional Proteomics RPPA Core Facility of MD Anderson Cancer Center. https://www.mdanderson.org/research/research-resources/core-facilities/functional-proteomics-rppa-core.html
Results
Transformation in BaF3 cells in vitro.
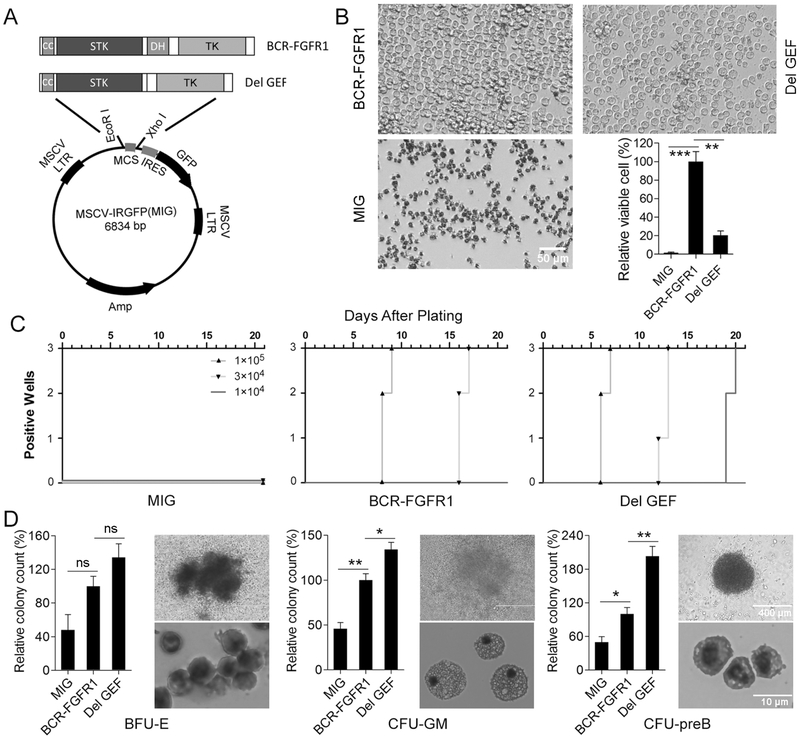
To investigate the role the BCR-FGFR1 GEF domain plays in leukemogenesis, we created deletion constructs in the MIG retroviral vector (Figure 1A) used for transduction and transplantation procedures [14–15]. The BaF3 cell system has been used extensively to determine the transforming ability of potential oncogenes. In this assay, the putative oncogene is expressed in these IL3-dependent pro-B cells, and transformation to IL3-independence over 24–72 hours indicates oncogenic activity. As shown in figure 1B, expression of the full length BCR-FGFR1 leads to significantly increased cell viability 3 days after withdrawal from IL3, compared to the empty vector control. In contrast, deletion of the GEF domain (ΔGEF) resulted in a less dramatic increase in viability, compared with the full-length chimeric kinase. It seems, therefore, that loss of GEF function reduces the oncogenicity of BCR-FGFR1 in this in vitro system.
Figure 1: Deletion of the GEF domain enhances proliferation and differentiation in vitro.
Schematic (A) showing the two derivative constructs of BCR-FGFR1 used in this study. When BaF/3 cells were transduced with the empty MIG vector (B) no viable cells were present after 72 hours following withdrawal of IL3. In contrast, cells transduced with BCR-FGFR1 show high levels of transformation to IL3-independence. In cells transduced with the GEF deletion construct, although showing significantly increased survival compared with the MIG transduced cells, the extent of IL3-independence was significantly lower than for the BCR-FGFR1 expressing cells. Using normal murine bone marrow cells transduced with the different constructs (C) plating efficiency was enhanced for the GEF deletion cells compared to the BCR-FGFR1. Analysis of B-lymphopoiesis and myelopoiesis (D) shows an increase in levels of primitive erythroid progenitors (BFU-E), granulocyte/macrophage differentiation (CFU-GM) and pre-B-lymphoid progenitor cells (CFU-preB) in cells expressing the GEF deletion. In each case, the colony counts are relative to the number of colonies seen for BCR-FGFR1 transduced cells. Colonies were first identified by the structure of the colony and then the staining characteristics of the individual cells in the colonies (shown on the right in each case in D). Using the Student’s t-test, n.s. = not significant, * p = <0.01, ** p = <0.001.
Deletion of the GEF domain enhances proliferation in primary bone marrow cells.
To study the impact in primary cells, bone marrow were transduced with retroviruses expressing BCR-FGFR/GFP and ΔGEF BCR-FGFR/GFP or GFP alone and sorted, GFP-positive cells were cultured in vitro. Each analysis was performed in triplicate, at three different seeding concentrations, as defined in Figure 1C. Wells were recorded as positive when they reached 1 × 106 cells/ml of culture medium. Cells transduced with the empty vector did not show evidence of growth or survival. In cells transduced with the BCR-FGFR1 construct, proliferation was detected only in the wells seeded at the two highest initial concentrations. Cells transduced with the GEF deletion construct, however, achieved 1 × 106 cells/ml more quickly than cells expressing BCR-FGFR1 and at the lowest seeding concentration over the 21-day observation period (Figure 1C). Thus, the GEF deletion leads to increased growth potential in cultured primary bone marrow cells.
To investigate the effect of the GEF on lymphopoiesis and myelopoeisis in bone marrow progenitor cells, we used colony-forming assays in custom methylcellulose medium that support growth of either primitive erythroid progenitors, granulocyte/macrophage progenitors or pre-B-lymphocytes (Figure 1D). 10,000 GFP+ sorted cells were plated into individual wells. Each experiment was performed in duplicate and on two separate occasions (n = 4). A significant increase in colony formation for all three cell types expressing the BCR-FGFR1 construct was observed, but this was further enhanced following expression of ΔGEF in the pro-B-progenitors (Figure 1D). The structure of the individual colonies in each case was consistent with that expected for the particular progenitor cell types, which was further confirmed following Hema 3 staining of individual dissociated cells from randomly selected colonies (Figure 1D).
Deletion of the GEF domain enhances in vivo progression of SCLL.
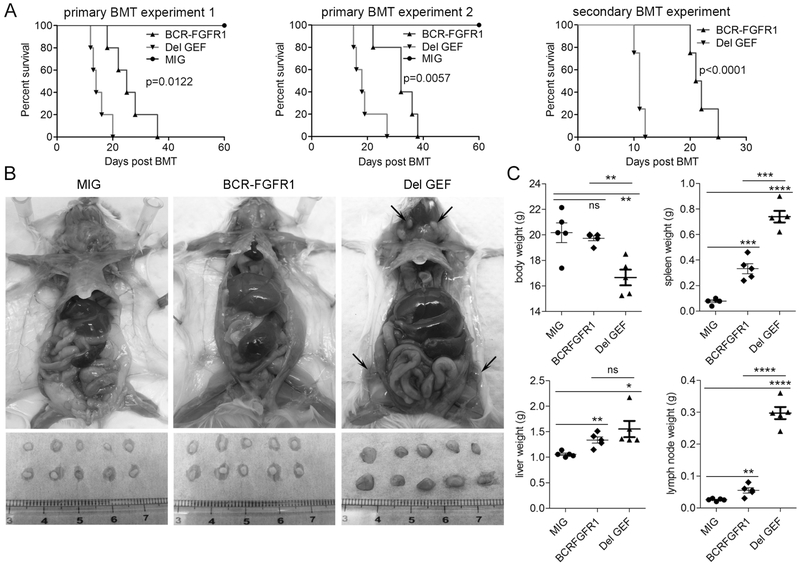
The transformation and transduction approach described previously [14–15], was used to investigate the effect of the GEF deletion on development of leukemia in vivo. In this approach bone marrow cells from donor BALB/c mice were infected ex vivo with the empty MIG vector, or with the two different BCR-FGFR1 constructs, and then introduced into the tail veins of recipient mice that had been pre-irradiated. Transduction efficiencies of the primary cells were assessed by flow analysis in each case, which demonstrated comparable levels of transformed (GFP+) cells between 10–15%. The survival time of the mice (n = 5) in two independent experiments was monitored to assess the relative aggressiveness of the transformed cells (Figure 2A). Mice injected with cells infected with the empty MIG vector did not develop disease over the observation period, as we have shown in previous studies [15], although systematic analysis of GFP+ cells in peripheral blood from these animals during the early stages showed successful engraftment (Supplementary Figure S1). In the mice infected with the construct lacking the GEF domain, disease developed within 12–27 days (median = 17 days), compared with the full-length kinase, which developed disease with a significantly longer latency period of 18–38 days (median = 28.9 days). It appears, therefore, that loss of the GEF domain enhances disease progression in vivo. Consistent with observations in this in vivo system, onset of disease in secondary transplants shows an even earlier onset of disease (10–12 days) in the GEF deletion cells compared to the full-length kinase (Figure 2A). Consistent with the dynamics of disease development in vivo, the mice transplanted with cells with the GEF deletion, had an overall lower body weight, increased spleen and liver size and a highly significant increase in overall size of lymph nodes (Figure 2B–C). Histological analysis of the GEF deletion tumors compared with BCR-FGFR1 and controls shows increased lymphocytes in the peripheral blood, increased hypercellularity in the bone marrow, greater disorganization in the spleen and increased infiltration in the liver (Supplementary Figure 2).
Figure 2: Deletion of the GEF domain enhances proliferation and differentiation in vivo.
Kaplan-Meier curves comparing survival of mice (N=5) transplanted with 5 × 106 total bone marrow cells transduced with either the BCR-FGFR1 full length chimeric kinase, the GEF deletion or the empty MIG vector from two different experiments shows significantly reduced survival in the mice receiving cells with the GEF deletion (A, left). On transplantation of ~2 × 106 bone marrow cells (80–90% GFP+) into secondary, irradiated hosts, the aggressive nature of the GEF deletion cells is confirmed (A, right). Autopsy of diseased mice from the three different constructs (B-C) shows enhanced spleen size and larger lymph nodes associated with the GEF deletion. Using Student’s t-test, n.s. = not significant, * p = <0.01, ** p = <0.001, *** p = <0.0001, **** p = <0.00001.
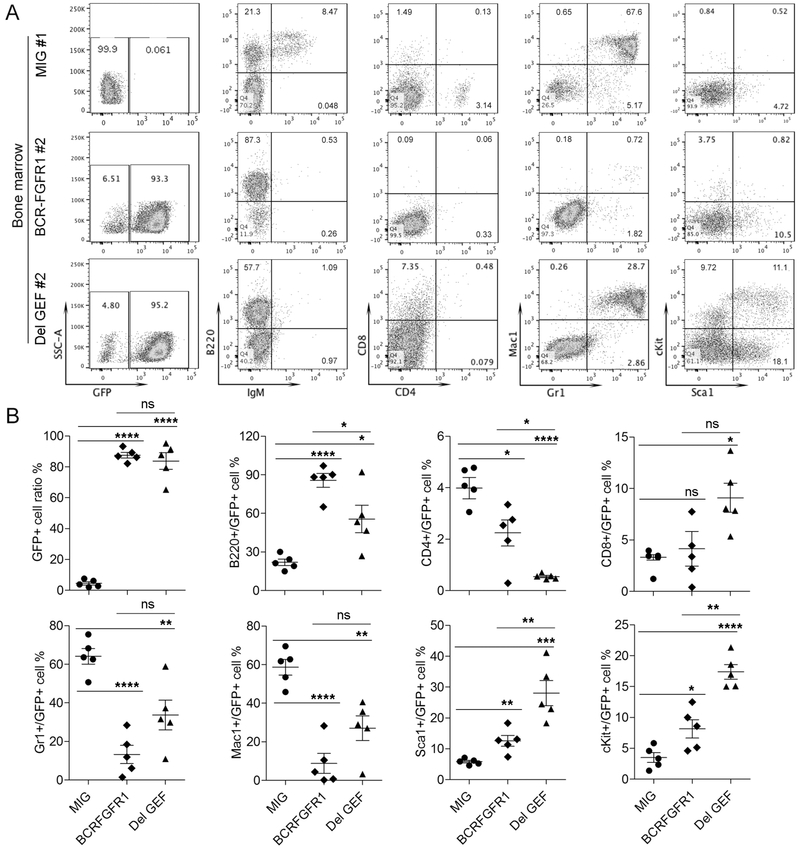
The disease that developed in the mice from the full length BCR-FGFR1 constructs, on autopsy, demonstrated the typical B220+, IgM-, CD4/CD8-, Mac1-Gr1- immunophenotype in the transformed cells isolated from the bone marrow (Figure 3A–B) as we have shown previously [12]. In the disease generated by the cells with the GEF deletion, a similar B220+, IgM-, CD4-CD8- immunophenotype was seen, but with significantly higher levels of Sca1+Kit+ cells, indicating a more stem cell-like phenotype (Figure 3A–B), as well as populations of Mac1+/Gr1+ myeloid cells, comparable with normal mice. The same profile was seen in the spleens of these animals (Supplementary Figure S3), with the possible reduction in the stem cell population (Sca1+, Kit1+). Notably, unlike the mice with BCR-FGFR1, which all displayed a B220+IgM- immunophenotype, the mice from GEF deletion displayed a gradual transition of disease from a myeloid disorder to B cell lymphoblastic leukemia, with an increase in the B220+IgM- population and decreased levels of Gr1+Mac1+ cells (Supplementary Figure S4).
Figure 3: Deletion of the GEF domain promotes pro-B-cell lymphomas with a stem cell immunophenotype.
At the time of autopsy of sick animals, representative flow cytometric analysis of GFP+ cells from the bone marrow (above) of mice transplanted with either full length BCR-FGFR1 chimeric kinase or GEF deletion construct are shown. GFP+ cells from mice transduced with cells using the empty vector (MIG) were performed after an arbitrary 60 days, a time when most experimental animals have succumbed to disease. In the BCR-FGFR1 transduced cells, the GFP+ population expresses B220 but is essentially negative for all other cell surface markers analyzed. In the mice transplanted with cells transduced with the GEF deletion, the GFP+ cells are similarly B220+, although at higher levels but now show a Mac1, GR1+ population of cells similar to the MIG control mice but uniquely show a population of cells expressing the Sca1 and Kit1+ stem cell markers. Comparison of the levels of the various cell surface markers for each of the five mice in each cohort is shown in (B). Using Student’s t-test, n.s. = not significant, * p = <0.01, ** p = <0.001, *** p = <0.0001, **** p = <0.00001.
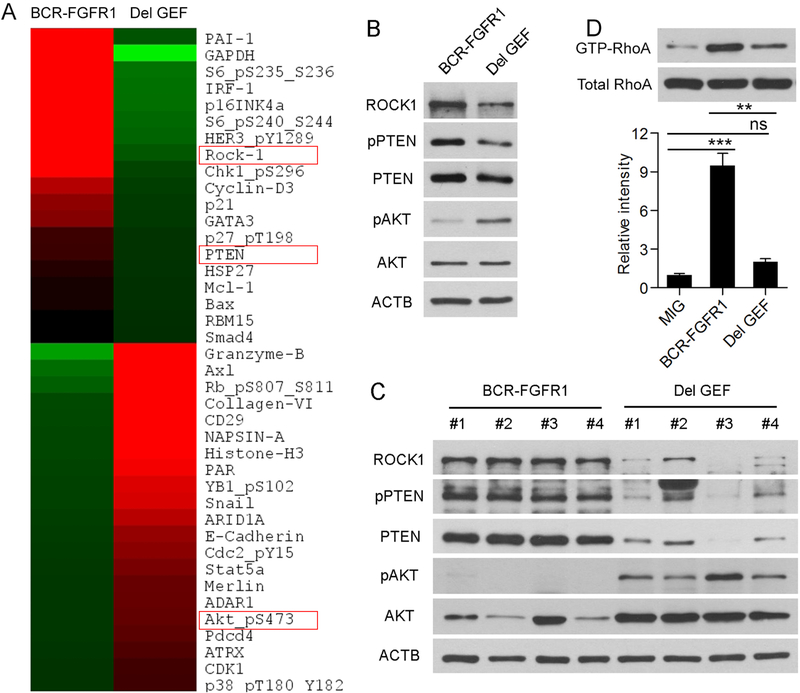
Deletion of the GEF domain suppresses RHOA/ROCK1/PTEN/Akt signaling.
To investigate differences in molecular signaling pathways in the cells expressing the different BCR-FGFR1 derivatives, we performed reverse phase protein array (RPPA) analysis comparing relative protein levels of well-characterized signal transduction proteins between BaF3 cells expressing either BCR-FGFR1 or the GEF deletion (Figure 4A). This assay analyzes expression levels of ~300 proteins using verified target- specific antibodies. In this analysis we observed 21 proteins were increased > 2-fold and 19 were decreased > 2-fold. Decreases in ROCK1 and PTEN levels, and an increase in activated AKT, were seen in the cells with the GEF deletion (Figure 4A, Supplementary Table 1). Downregulation of ROCK1 levels in the absence of the GEF domain was confirmed using western blotting compared with the BCR-FGFR1 transduced cells (Figure 4B). PTEN is one of the phosphorylation targets of ROCK1 [18] and, accordingly, the same proportional decrease for activated pPTEN was seen in the absence of the BCR GEF, but total PTEN protein levels were only slightly downregulated, confirming the RPPA data. Since PTEN suppresses activation of AKT, as expected, suppression of PTEN is accompanied by increased levels of activated AKT (Figure 4B). The same relationship between ROCK1, pPTEN and pAKT levels was seen in primary tumors from mice transplanted with bone marrow cells expressing either the full length BCR1-FGFR1 or the GEF deletion construct (Figure 4C). This increased dependence of pAKT for survival in the deletion GEF cells was confirmed using the GSK690693 AKT inhibitor (Supplementary Figure 5) where BCR-FGFR1 expressing cells were significantly less sensitive to the AKT inhibitor and showed reduced levels of apoptosis following treatment with the inhibitor compared with the deletion GEF expressing cells.
Figure 4: Deletion of the GEF domain suppresses ROCK1 signaling through PTEN and enhances AKT activation.
RPPA analysis (A) defined proteins that are downregulated (green) or upregulated (red) in BaF3 cells expressing the GEF deletion construct, including ROCK1, PTEN and pAKT (red boxes). These observations were confirmed using western blotting (B) showing reduced ROCK1 protein levels, slightly reduced total PTEN, significantly reduced activated PTEN (pPTEN) and proportionally increased levels of activated AKT (pAKT). Analysis of primary spleen cells from mice transplanted with the BCR-FGFR1 kinase show high levels of pPTEN and low levels of pAKT (C). In contrast spleen cells from the mice transplanted with cells expressing the GEF deletion show reduced levels of pPTEN and ROCK1 and increased levels of pAKT (C). Affinity immunoprecipitation of active RHOA demonstrates that BaF3 cells expressing the GEF deletion show reduced levels of active RHOA compared with the full length chimeric kinase (D). Relative intensity levels measured using ImageJ. Using Student’s t-test, n.s. = not significant, ** p = <0.001, *** p = <0.0001.
ROCK1 is a direct target of RHOA [19] and the GEF domain has been suggested as a GTPase-activating protein (GAP) for RHOA activation [20]. Since the BCR GEF domain is known to bind to RHOA, we investigated how loss of the BCR GEF influences RHOA activity, through analysis of the relative levels of the active and inactive forms of RHOA in BaF3 cells that have been transformed to IL3 independence through expression of either the wild type BCR-FGFR1 protein or the GEF deletion mutant. Using affinity precipitation assays (Figure 4D), expression of BCR-FGFR1 led to a large increase of activated RHOA protein levels compared with cells transduced with the empty MIG vector. In the absence of the BCR GEF domain, levels of active RHOA are highly significantly reduced, indicating a regulatory axis of RHOA/ROCK1/PTEN/pAkt in the BCR-FGFR1 driven SCLL.
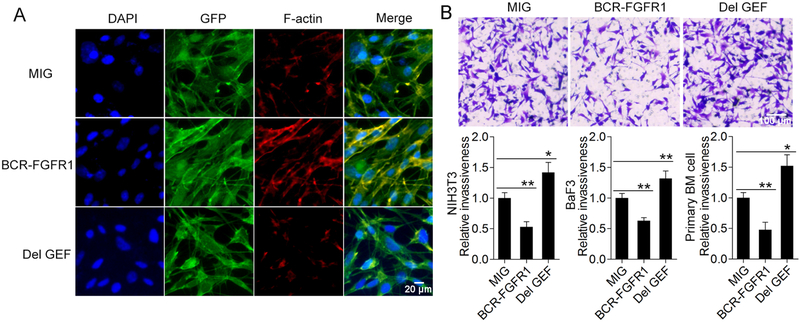
Deletion of GEF leads to actin cytoskeleton reorganization and increased cell migration
One of the primary consequences of RHOA activation of ROCK1 is the reorganization of the actin cytoskeleton [21] and to investigate how the BCR-FGFR1 or the GEF deletion affect this phenotype, we transduced NIH 3T3 cells which, because of their flat morphology in culture, allow changes to cytoskeleton organization to be readily ascertained. Using confocal microscopy, a dramatic increase in stress fibers was observed in cells transduced with BCR-FGFR1 compared with the empty vector, and no detectable change in stress fibers was seen in cells in which the GEF deletion was expressed compared with vector control (Figure 5A). To establish how this change in actin dynamics affects cell migration, we used transwell assays to measure invasion of the transduced NIH 3T3 cells (Figure 5B). Cells expressing the GEF deletion showed increased migration ability compared with cells transduced with the empty vector. Interestingly, cells transduced with the BCR-FGFR1 protein showed a reduced invasion potential compared with the empty vector control. The same effects were seen in BaF3 cells (Figure 5B) as well as in primary bone marrow cells from mice engrafted with the different constructs.
Figure 5: Deletion of the GEF domain leads to reduced stress fiber formation and enhances invasiveness.
Immunocytochemistry analysis of NIH3T3 cells transduced with the BCR-FGFR1 kinase show increased levels of stress fibers and focal adhesions compared with cells transduced with the empty vector (A). Stress fibers were not observed to the same extent in cells transduced with the GEF deletion construct. Transwell invasion assays for these transduced NIH3T3 cells (B), shows a reduced invasion potential in the cells expressing BCR-FGFR1 compared with the empty vector cells but invasion potential is significantly enhanced in the cells expressing the GEF deletion. Similarly, the GEF deletion induces significantly increased invasion in BaF3 cells as well as primary bone marrow cells from mice transplanted with cells expressing the GEF deletion. In each case the invasion measured was relative to that seen for cells transduced with the empty MIG vector. Using Student’s t-test, * p = <0.01, ** p = <0.001.
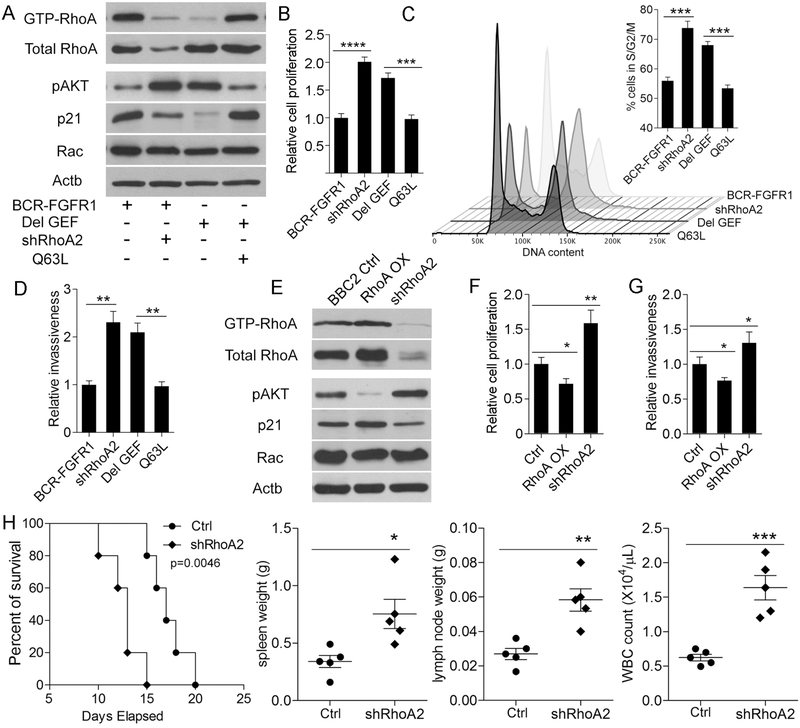
Knockdown of RHOA in BCR-FGFR1 expressing cells reproduces the phenotypes of GEF deletion.
To further investigate the role of RHOA in leukemogenesis, we downregulated RHOA in BaF3 cells expressing BCR1-FGFR1 using shRNAs. Two different shRNAs, (shRHOA1 and shRHOA2) gave varying degrees of knockdown, with shRHOA2 showing almost complete knockdown (Supplementary Figure S6). This shRNA was used exclusively in subsequent analyses. In these cells, suppression of RHOA expression led to reduced levels of the GTP-active form (Figure 6A), comparable with cells transduced with the GEF deletion construct, with proportional increases in pAKT. There were no changes in total RAC protein levels between the different cell lines. Analysis of cell viability in these cells showed that decreases in activated RHOA were associated with increased viability (Figure 6B), which is consistent with down regulation of p21 (Figure 6A, Supplementary Figure S6). Cell cycle analysis shows that this increase in viability correlated with increased levels of the population in the S/G2/M phase of the cell cycle (Figure 6C, Supplementary Figure S6). In transwell assays (Figure 6D), invasion potential was increased in cells in which RHOA function was suppressed either through shRNA treatment or deletion of the BCR GEF. To further investigate the role of RhoA in cell growth and invasion, we stably expressed a constitutively active (Q63L) RhoA gene in BaF3 cells expressing the ΔGEF construct. In these cells, the active RhoA levels increased comparable to those seen in the BCR-FGFR1 transformed cells (Figure 6A), pAKT was suppressed and p21 levels increased. Similarly, the Q63L mutant gene suppressed cell proliferation (Figure 6B), reduced the proportion of cells in S/G2/M (Figure 6C) and suppressed invasiveness (Figure 6D). Analysis of annexin V expression shows no significant changes in levels of apoptosis, whether RHOA was knocked down or the GEF domain deleted (Supplementary Figure S6). These cell viability and invasion data directly demonstrate that the BCR GEF domain serves as a negative regulator in disease progression, and suppression of RHOA activity in BCR-FGFR1 expressing cells leads to phenotypes similar to those seen in cells with the GEF domain deletion.
Figure 6: Knockdown of RHOA enhances cell viability, promotes progression through the cell cycle and enhances leukemogenesis.
BaF3 cells transduced with the GEF deletion construct show reduced levels of activated RHOA (A) and increased levels of pAKT. Knockdown of RHOA (shRHOA2) in cells expressing the full length fusion kinase demonstrated reduced levels of active RHOA and increased pAKT. Levels of Rac are unaffected but in both the GEF deletion and the shRHOA cells p21 is suppressed, which correlates with increased cell viability in these cells (B) compared with the BCR-FGFR1 control and an increase in cells in the S/G2/M phase of the cell cycle (C). In turn, suppression of RHOA in BaF3 cells leads to the same increase in invasion potential seen in the GEF deletion cells (D). In each of these analyses, expression of a constitutively active RhoA (Q63L) rescues the phenotypes to those seen in the BCR-FGFR1 expressing cells. Using SCLL BBC2 cells (E) overexpression (OX) of RHOA leads to suppression of pAKT and increased levels of p21, while shRNA knockdown of RHOA leads to increased pAKT levels and reduced levels of p21. Consistent with suppression of AKT activation and expression of p21, over expressing RHOA reduced cell viability compared with BCR-FGFR1 (F) and invasiveness (G) in BBC2 cells, while knockdown of RHOA led to increased cell viability and invasiveness. In vivo, mice transplanted with BBC2 cells in which RHOA was knocked down showed significantly poorer survival (H) and had increased spleen and lymph node sizes. White cell counts in the peripheral blood were also significantly increased. Using Student’s t-test, * p = <0.01, ** p = <0.001, *** p = <0.0001, **** p = <0.00001.
Knockdown of RHOA in SCLL cells leads to enhanced leukemogenesis.
During our previous development of the syngeneic mouse model for BCR-FGFR1-driven SCLL, we isolated the BBC2 cell line which showed a B220+/CD19+/CD24+/cKit+/CD43+/CD93+/IgM- immunophenotype, consistent with a pro-B cell origin [12]. To investigate the role of RHOA in these SCLL cells, we created BBC2 cells that either overexpressed RHOA or, through expression of shRNA, showed reduced levels of RHOA (Figure 6E). In these cells the inverse functional relationship between RHOA expression and pAKT and p21 levels was confirmed. Analysis of cell growth rates (Figure 6F) shows that knockdown of RHOA leads to increased cell viability compared with empty vector transduced cells and reduced cell viability when RHOA is overexpressed (Figure 6F). Similarly, overexpression of RHOA led to reduced invasion, and knockdown of RHOA led to increased invasion (Figure 6G). The observation in BBC2 SCLL cells further confirmed the direct function role of RHOA in progression of this disease.
To evaluate the effects of RHOA knockdown on development and progression of SCLL in vivo, we engrafted BBC2 cells, in which RHOA was knocked down, into subleathly irradiated Balb/C mice. As shown in figure 6H, disease in these mice developed more rapidly than for the parental BBC2 cells expressing the BCR-FGFR1 kinase. Spleen and lymph node sizes (Supplementary Figure S7) were significantly greater in the mice receiving the RHOA knockdown cells, and white blood cell counts were significantly increased (Supplementary Figure S7). Flow cytometry analysis of the cells in the bone marrow and spleen from the two different models confirmed a high ratio of GFP+ leukemia cell infiltration in both tissues with a significantly higher ratio in the peripheral blood and spleens from the RHOA knockdown mice (Supplementary Figure S7). This in vivo engraftment data, therefore, further confirmed the direct involvement of RHOA signaling in the BCR-FGFR1 driven SCLL.
Discussion.
The rapid onset of leukemia/lymphoma in mouse models of SCLL induced by BCR-FGFR1, compared with other variant chimeric kinases in this disease, suggested the possibility that components of the BCR gene retained in this oncogene contributes to its aggressiveness. Here we show that deletion of the plekstrin and double homology domain in BCR leads to increased viability, proliferation, invasiveness and tumor progression, suggesting that in the full length chimeric kinase it acts as a break on leukemogenesis. One of the ways in which this is achieved is through reduced RHOA activation. RHOA is a ubiquitously expressed protein that facilitates transmission of signaling cues from a variety of stimuli and is associated with actin cytoskeleton reorganization, cell proliferation, immune responses and many other functions [22–23]. Its transition between the active GTP-bound form and the inactive GDP-bound form has been described as a molecular switch that regulates these responses. These transitions are facilitated by interaction with proteins carrying a guanosine nucleotide exchange factor (GEF) such as the double-homology and plekstrin domain in BCR-FGFR1. This suggestion is supported by the observation that shRNA suppression of RHOA activation in the presence of BCR-FGFR1 expression, or as a result of deletion of the BCR-FGFR1 GEF domain, enhances cell proliferation, invasiveness and lymphomagenesis. These observations support a tumor suppressor role for RHOA activation during B-lymphoma development in SCLL. Further support for a tumor suppressor function for RHOA in leukemia came from mutation epidemiology studies in a variety of different leukemic subclasses which demonstrated a high incidence of mutational inactivation of RHOA. In angioimmunoblastic T cell lymphoma, for example, ~70% or cases analyzed carried a Gly17Val mutation which prevents GTP binding, thus inhibiting its function [24–25]. These mutations also led to attenuated stress fiber formation, increased cell proliferation and invasiveness of Jurkat T cells, consistent with phenotypes observed in SCLL cells. Similar observations were seen in peripheral T-cell leukemias [26] as well as adult T-cell leukemia/lymphoma caused by HTLV-1 [27]. It should be noted, however, that all reported cases of BCR-FGFR1 induced SCLL retain the GEF domain, and to date inactivating deletions within this domain have not been reported, although mutation analysis has not been routinely performed.
We have shown that deletion of the GEF domain in BCR-FGFR1 reduces transformation of BaF3 cells to IL3 independence, in a short term assay over 72 hours. In contrast, in already transformed SCLL cells deletion of the GEF domain increases cell proliferation in vitro and tumorigenicity in vivo. When transformed BaF3 cells are monitored over more extended periods, however, they also show increased proliferation, cell cycle progression and invasiveness. It appears, therefore, that while the GEF domain clearly acts consistently as a brake on aspects of tumor aggressiveness, it has an as yet undefined role in transformation of BaF3 cells to IL3 independence, possibly through regulation of genes promoting this phenotype.
SCLL driven by BCR-FGFR1 typically gives rise to B-lymphomas which is also the case in our in vivo models which show a pro-B-cell immunophenotype [12]. Loss of RHOA activation in this stem cell disorder leads to suppression of PTEN and activation of AKT, which provides one explanation for increased cell proliferation in these cells. It has been shown that inhibition of RHOA, through expression of a dominant negative mutant in normal hematopoietic stem/progenitor cells, enhances hematopoietic stem cell proliferation and engraftment into the stem cell niche [28]. These observations are consistent with our studies in SCLL cells where suppression of RHOA activation, either by deletion of the BCR GEF or shRNA knockdown of RHOA, leads to increased invasiveness and enhanced cell cycle progression. These observations suggest a common role for RHOA in normal stem cells and stem cell leukemias.
The development of BCR-FGFR1 SCLL shares similarities with the CML that develops due to expression of the BCR-ABL chimeric kinase in hematopoietic stem cells in murine models. In these studies, the BCR-ABL oncoprotein has two different isotypes, p210 and p190, that retain the ABL kinase domain but carry different contributions from the BCR gene. The p190 variant lacks the BCR-GEF domain and displayed a reduced ability to transform BaF3 cells [29], which is consistent with our observations in these cells in vitro. In vivo, however, mice transplanted with cells expressing the p190 variant showed a shorter latency period and more aggressive disease progression compared with the full-length p210 protein [30]. Mutation of the critical S506 amino acid within the GEF domain has the same disease phenotype as the p190 isotype. Thus, as in SCLL, the absence of the BCR GEF domain promotes more aggressive disease progression in vivo. Proteomics analyses have been used to investigate potential signaling pathways associated with the BCR GEF in BaF3 cells expressing either the p210 or p190 Bcr-Abl. In one study, activation of Lyn kinase and preferential interaction with the AP2 adaptor complex was seen in the p190 expressing cells. In p210 expressing cells, enrichment of the Sts1 phosphatase and stronger activation of the Stat5 and Erk1/2 were noted [31]. Another study, suggested that cells expressing p210 showed an increased engagement of membrane–associated molecules, while p190 showed preferential interaction with molecules associated with the cytoskeleton [32]. Here we show that the GEF domain activates the RHOA/ROCK1/PTEN/Akt signaling axis to regulate SCLL driven by the BCR-FGFR1. In this system RHOA activation is reduced in the absence of the BCR GEF domain leading to increased cell viability and progression through the cell cycle as well as increased invasion, consistent with the suggestion that loss of the GEF promotes interactions with proteins involved in cytoskeleton reorganization. Indeed, although beyond the scope of this study, many of the proteins found to be dysregulated using PRRA, influence cell migration/invasion, adhesion and proliferation. The increased cell invasiveness as a result of loss of RhoA activation in the GEF cells is consistent with a more aggressive disease, since the pathways involved are known to regulate leukemic cell mobilization from the bone marrow and intravasation into the blood and lymphatic systems. The higher levels of invasiveness seen in the bone marrow, spleen and liver of the mice transplanted with cells expressing the GEF deletion also support a role for the GEF in suppressing invasion through regulation of actin cytoskeleton dynamics.
Supplementary Material
Statement of significance;
RHOA activation is as a critical event in the progression of BCR-FGFR1 driven leukemogenesis in stem cell leukemia and lymphoma syndrome and is regulated by the BCR GEF domain.
Acknowledgements:
This study was supported by grant CA076167 from the National Institutes of Health. RPPA analysis was supported by grant CA16672 from the National Institutes of Health.
Grant support: This study was supported by grant CA076167 from the National Institutes of Health. RPPA analysis was supported by grant CA16672 from the National Institutes of Health.
Footnotes
Conflict of interests: The authors declare no conflicts of interest.
References
- 1.Ornitz DM, Itoh N. The Fibroblast Growth Factor signaling pathway. Wiley Interdiscip Rev Dev Biol 2015; 4:215–266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Turner N, Grose R. Fibroblast growth factor signalling: from development to cancer. Nat Rev Cancer 2010; 10:116–129. [DOI] [PubMed] [Google Scholar]
- 3.Jackson CC, Medeiros LJ, Miranda RN. 8p11 myeloproliferative syndrome: a review. Hum Pathol 2010; 41:461–476. [DOI] [PubMed] [Google Scholar]
- 4.Demiroglu A, Steer EJ, Heath C, Taylor K, Bentley M, Allen SL et al. The t(8;22) in chronic myeloid leukemia fuses BCR to FGFR1: transforming activity and specific inhibition of FGFR1 fusion proteins. Blood 2001; 98:3778–3783. [DOI] [PubMed] [Google Scholar]
- 5.Baumann H, Kunapuli P, Tracy E, Cowell JK. The oncogenic fusion protein-tyrosine kinase ZNF198/fibroblast growth factor receptor-1 has signaling function comparable with interleukin-6 cytokine receptors. J Biol Chem 2003; 278:16198–16208. [DOI] [PubMed] [Google Scholar]
- 6.Khodadoust MS, Luo B, Medeiros BC, Johnson RC, Ewait MD, Schalkwyk AS et al. Clinical activity of ponatinib in a patient with FGFR1-rearranged mixed-phenotype acute leukemia. Leukemia 2016;30: 947–950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ren M, Qin H, Ren R, Cowell JK. Ponatinib suppresses the development of myeloid and lymphoid malignancies associated with FGFR1 abnormalities. Leukemia 2013;27:32–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wu Q, Bhole A, Qin H, Karp J, Malek S, Cowell JK et al. SCLL. Targeting FGFR1 to suppress leukemogenesis in syndromic and de novo AML in murine models. Oncotarget 2016;7:49733–49742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Montenegro-Garreaud X, Miranda RN, Reynolds A, Tang G, Wang SA, Yabe M et al. Myeloproliferative neoplasms with t(8;22)(p11.2;q11.2)/BCR-FGFR1: a meta-analysis of 20 cases shows cytogenetic progression with B-lymphoid blast phase. Hum Pathol 2017;65:147–156. [DOI] [PubMed] [Google Scholar]
- 10.Murati A, Arnoulet C, Lafage-Pochitaloff M, et al. Dual lympho-myeloproliferative disorder in a patient with t(8;22) with BCR-FGFR1 gene fusion. Int J Oncol 2005;26:1485–1492. [PubMed] [Google Scholar]
- 11.Roumiantsev S, Krause DS, Neumann CA, Dimitri CA, Asiedu F, Cross NC et al. Distinct stem cell myeloproliferative/T lymphoma syndromes induced by ZNF198-FGFR1 and BCR-FGFR1 fusion genes from 8p11 translocations. Cancer Cell 2004;5:287–298. [DOI] [PubMed] [Google Scholar]
- 12.Ren M, Tidwell JA, Sharma S, Cowell JK. Acute progression of BCR-FGFR1 induced murine B-lympho/myeloproliferative disorder suggests involvement of lineages at the pro-B cell stage. PLoS One 2012; 7:e38265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cowell JK, Qin H, Chang CS, Kitamura E, Ren M. A model of BCR-FGFR1 driven human AML in immunocompromised mice. Br J Haematol 2016; 175:542–545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ren M, Li X, Cowell JK. Genetic fingerprinting of the development and progression of T-cell lymphoma in a murine model of atypical myeloproliferative disorder initiated by the ZNF198-fibroblast growth factor receptor-1 chimeric tyrosine kinase. Blood 2009;114:1576–1584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ren M, Cowell JK. Constitutive Notch pathway activation in murine ZMYM2-FGFR1-induced T-cell lymphomas associated with atypical myeloproliferative disease. Blood 2011;117:6837–6847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hu T, Chong Y, Qin H, Kitamura E, Chang CS, Silva J et al. The miR-17/92 cluster is involved in the molecular etiology of the SCLL syndrome driven by the BCR-FGFR1 chimeric kinase. Oncogene 2018; 37:1926–1938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sossey-Alaoui K, Ranalli TA, Li X, Cowell JK. WAVE3 promotes cell motility and invasion through the regulation of MMP-1, MMP-3 and MMP-9- expression. Exp Cell Res 2005;308:135–145. [DOI] [PubMed] [Google Scholar]
- 18.Li Z, Dong X, Wang Z, Liu W, Deng N, Ding Y et al. Regulation of PTEN by Rho small GTPases. Nat Cell Biol 2005;7:399–404. [DOI] [PubMed] [Google Scholar]
- 19.Julian L, Olson MF. Rho-associated coiled-coil containing kinases (ROCK): structure, regulation, and functions. Small GTPases 2014;5:e29846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dubash AD, Koetsier JL, Amargo EV, Najor NA, Harmon RM, Green KJ. (2013). The GEF Bcr activates RHOA/MAL signaling to promote keratinocyte differentiation via desmoglein-1. J Cell Biol 2013;202:653–666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Amano M, Nakayama M, Kaibuchi K. Rho-kinase/ROCK: A key regulator of the cytoskeleton and cell polarity. Cytoskeleton 2010;67:545–554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Thumkeo D, Watanabe S, Narumiya S. Physiological roles of Rho and Rho effectors in mammals. Eur J Cell Biol 2013; 92:303–315. [DOI] [PubMed] [Google Scholar]
- 23.Jaffe AB, Hall A. Rho GTPases: biochemistry and biology. Annu Rev Cell Dev Biol 2005;21:247–269. [DOI] [PubMed] [Google Scholar]
- 24.Yoo HY, Sung MK, Lee SH, Kim S, Lee H, Park S et al. A recurrent inactivating mutation in RHOA GTPase in angioimmunoblastic T cell lymphoma. Nat Genet 2014;46:371–375. [DOI] [PubMed] [Google Scholar]
- 25.Sakata-Yanagimoto M, Enami T, Yoshida K, Kim MY, Ambesi-Impiombato A, Perez-Garcia A et al. Somatic RHOA mutation in angioimmunoblastic T cell lymphoma. Nat Genet 2014;46:171–175. [DOI] [PubMed] [Google Scholar]
- 26.Palomero T, Couronné L, Khiabanian H, et al. Recurrent mutations in epigenetic regulators, RHOA and FYN kinase in peripheral T cell lymphomas. Nat Genet 2014;46:166–170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nagata Y, Kontani K, Enami T, Kataoka K, Ishii R, Totoki Y et al. Variegated RHOA mutations in adult T-cell leukemia/lymphoma. Blood 2016;127:596–604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ghiaur G, Lee A, Bailey J, Cancelas JA, Zheng Y, Williams DA. Inhibition of RHOA GTPase activity enhances hematopoietic stem and progenitor cell proliferation and engraftment. Blood 2006;108:2087–2094. [DOI] [PubMed] [Google Scholar]
- 29.Sahay S, Pannucci NL, Mahon GM, Rodriguez PL, Megjugorac NJ, Kostenko EV et al. The RhoGEF domain of p210 Bcr-Abl activates RHOA and is required for transformation. Oncogene 2008;27:2064–2071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tala I, Chen R, Hu T, Fitzpatrick ER, Williams DA, Whitehead IP. Contributions of the RhoGEF activity of p210 BCR/ABL to disease progression. Leukemia 2013;27:1080–1089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Reckel S, Hamelin R, Georgeon S, Armand F, Jolliet Q, Chiappe D et al. Differential signaling networks of Bcr-Abl p210 and p190 kinases in leukemia cells defined by functional proteomics. Leukemia 2017; 31:1502–1512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cutler JA, Tahir R, Sreenivasamurthy SK, Mitchell C, Renuse S, Nirujogi RS et al. Differential signaling through p190 and p210 BCR-ABL fusion proteins revealed by interactome and phosphoproteome analysis. Leukemia 2017;31:1513–1524. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.