Abstract
Obesity increases the risks of diabetes, hypertension, and cardiovascular diseases, ultimately contributing to mortality. Korean Society for the Study of Obesity (KSSO) was established to improve the management of obesity through research and education; to that end, the Committee of Clinical Practice Guidelines of KSSO reviews systemic evidence using expert panels to develop clinical guidelines. The clinical practice guidelines for obesity were revised in 2018 using National Health Insurance Service Health checkup data from 2006 to 2015. Following these guidelines, we added a category, class III obesity, which includes individuals with body mass index (BMI) ≥35 kg/m2. Agreeing with the International Federation for the Surgery of Obesity and Metabolic Disorders, Asian Pacific Chapter consensus, we determined that bariatric surgery is indicated for Korean patients with BMI ≥35 kg/m2 and for Korean patients with BMI ≥30 kg/m2 who have comorbidities. The new guidelines focus on guiding clinicians and patients to manage obesity more effectively. Our recommendations and treatment algorithms can serve as a guide for the evaluation, prevention, and management of overweight and obesity.
Keywords: Obesity, Clinical practice guidelines, Korea
INTRODUCTION
The prevalences of obesity and associated disease are rapidly increasing among Korean adults.1 Many health problems are associated with obesity and excessive fat.2 Obesity is associated with increased risks for type 2 diabetes mellitus (T2DM), hypertension (HTN), dyslipidemia, metabolic syndrome, coronary heart disease, other atherosclerotic diseases, and non-alcoholic fatty liver disease.2
Korean Society for the Study of Obesity (KSSO) was established to improve the management of obesity through research, education, and the development of clinical guidelines in 2000. The KSSO revised clinical practice guidelines for the prevention and treatment of obesity in 2003, 2009, 2012, 2014, and most recently in 2018. The most recent guidelines are based partly on an analysis of data from the Korean National Health Insurance Service Health Checkup database collected from 2006 to 2015. The data analyzed included a total of 84,690,131 Korean adults.1 The Committee of Clinical Practice Guidelines of KSSO reviewed systemic evidence for each topic using expert panels to produce the latest guidelines. The new revised guidelines summarize evidence-based recommendations and treatment guidelines, including the definition of obesity, behavioral therapy, and surgical therapy. In this article, we discuss the 2018 KSSO guidelines for the management of overweight and obesity in adults.
OBESITY PREVALENCE TRENDS BY SEX, AGE, AND THREE COMORBIDITIES, BASED ON THE PRESENCE OF ABDOMINAL OBESITY
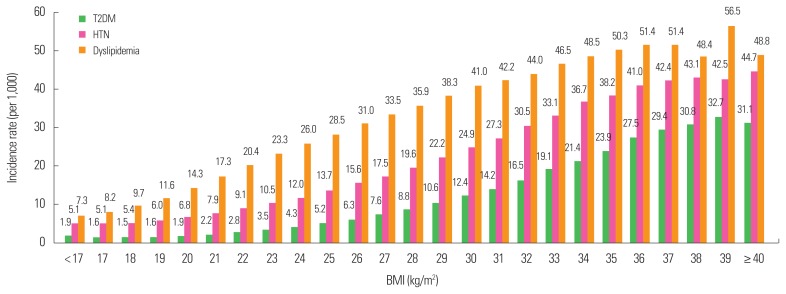
The prevalence of obesity steadily increased from 29.7% in 2009 to 32.4% in 2015, and that of abdominal obesity increased from 18.4% in 2009 to 20.8% in 2015.1 The prevalence of obesity combined with abdominal obesity increased steadily from 15.1% in 2009 to 17.7% in 2015.1 Abdominal obesity continuously increases from 20 to 80 years of age, but decreases after 80 years of age.1 The incidences of T2DM, HTN, and dyslipidemia increase gradually as body mass index (BMI) increases from the lowest level. The increases in the incidence rates of T2DM and HTN slowed down around BMI ≥35 kg/m2, while for dyslipidemia, the incidence rate slowed down at BMI ≥37 kg/m2 (Fig. 1).1
Figure 1.
Body mass index (BMI) and the incidence rates of type 2 diabetes mellitus (T2DM), hypertension (HTN), and dyslipidemia. Adapted from Seo MH, et al. J Obes Metab Syndr 2018;27:46–52.1
SOCIOECONOMIC COSTS OF OBESITY
According to the Korea National Health and Nutrition Examination Survey 2015 data, the estimated total cost of obesity in Korea was approximately $1.8 billion.3 These costs represent about 0.22% of the South Korean gross domestic product (GDP) and 3.7% of Korean national health care expenditures in 2005.3 Obesity was therefore a major health-related cause of socio-economic costs during this time period in Korea.3 Due to obesity, medical costs increased and labor productivity decreased, ultimately increasing the related socio-economic burden.3 The socioeconomic costs of obesity in Korea are still relatively low compared to developed Western countries. However, as the obese population of Korea rapidly increases in size, the socioeconomic costs associated with obesity are expected to increase.
DIAGNOSIS OF OBESITY
In clinical practice, body fat is measured using BMI.2 BMI is calculated as body weight (kg) divided by height squared (m2).4 BMI is easy to access, affordable to measure, and can conveniently be used to monitor weight changes.4 Adult obesity is defined as BMI ≥30 kg/m2 in Western populations, while overweight (also known as “pre-obese”) is defined as BMI between 25 and 29.9 kg/m2.5 Lower BMI cutoff points apply to other populations, including East Asians.6 East Asians generally have higher body fat percentages than non-Asians at the same BMI.7 Therefore, the cutoff values for defining overweight and obesity are lower for East Asians than for non-Asians according to the World Health Organization (WHO).8 Deurenberg et al.9 reported that at the same BMI, body fat percentages in Asians population were 3%–5% higher than in subjects of European descent, suggesting that the relationship between BMI and percentage body fat is different in Asians than in non-Asians.
Oh et al.10 conducted a cohort study of 773,915 Korean men and women between 30 and 59 years of age, with 8- to 10-year follow-up periods, and suggested that the number of individuals with BMI ≥25 kg/m2 is increasing rapidly and that these individuals are at significant risk for obesity-related disease. According to the 2017 Obesity Fact Sheet for Koreans based on National Health Insurance Service Health Checkup data collected from 2006 to 2015, the incidence rates of T2DM, HTN, and dyslipidemia increased steadily as BMI increased from 17 to 35 kg/m2. In this study, T2DM, HTN, and dyslipidemia increased significantly at BMI ≥25 kg/m2, which is also the diagnostic criterion for obesity defined by the KSSO. In addition, men with waist circumference (WC) ≥90 cm and women with WC ≥85 cm (i.e., abdominal obesity) were at high risk for T2DM, HTN, and dyslipidemia.1 These findings underscore the utility of current diagnostic criteria for identifying obesity outlined by the KSSO as well as their obesity treatment guidelines.1
By including the whole population of Korean citizens, for whom registering in the National Health Insurance Service Database (NHIS DB) is mandatory, Seo et al.1 were able to calculate the first and second cutoff points for increasing hazard ratios for any one of three comorbidities (T2DM, HTN, and dyslipidemia). The first and second cutoff BMI levels were 23 kg/m2 and 25 kg/m2, respectively. In addition, the incidences of T2DM, HTN, and dyslipidemia increased slowly as BMI increased, starting at the lowest level of BMI. In T2DM and HTN, the increase in incidence rates slowed at around BMI ≥35 kg/m2, while the incidence rate of dyslipidemia slowed at BMI ≥37 kg/m2.1 Higher BMIs are associated with higher metabolic and cardiovascular disease risks due to the accumulation of intra-abdominal fat.5
The classification of obesity into classes I, II, and III relies on adult BMI, in accordance with WHO guidelines for the Asia-Pacific region.8 Class I obesity is defined as BMI 25 kg/m2 to less than 30 kg/m2, class II obesity was defined as BMI 30 kg/m2 to less than 35 kg/m2, and class III obesity was newly defined in 2018 as greater than 35 kg/m2 (Table 1).
Table 1.
Risk of comorbidity according to obesity and abdominal obesity12
| Classification | Body mass index (kg/m2) | Risk of comorbidity according to abdominal obesity | |
|---|---|---|---|
| <90 cm (men), <85 cm (women) | ≥90 cm (men), ≥85 cm (women) | ||
| Underweight | <18.5 | Low | Average |
| Normal | 18.5–22.9 | Average | Increased |
| Pre-obese | 23–24.9 | Increased | Moderate |
| Obese class I | 25–29.9 | High | Severe |
| Obese class II | 30–34.9 | Moderate | Very severe |
| Obese class III | ≥35 | Severe | Very severe |
Pre-obese may be defined as overweight or at-risk weight, and obese class III may be defined as extreme obesity.
WC is highly associated with intraabdominal fat.5 WC is measured in the horizontal plane midway between the superior iliac crest and the lower margin of the last rib.6 According to the KSSO, abdominal obesity in Koreans is defined as WC ≥90 cm in men and ≥85 cm in women.11 The 2018 KSSO guidelines are summarized in Table 1.12 BMI cutoffs for the diagnosis of obesity in Korea are partly based on NHIS DB data.1
DETERMINING WEIGHT LOSS AND HEALTH GOALS
Maintaining a 3% to 5% weight loss can significantly reduce the risk of cardiovascular disease or diabetes. Therefore, we recommend a 5% to 10% weight loss within 6 months of diagnosis. In general, patients experiencing lifestyle modifications achieve maximum weight loss within 6 months of initiation. Their weight then becomes constant, and they typically regain weight over time. This increase in body weight also occurs during the use of medication although weight regain can be slowed with continued medication use.13 Patients undergoing bariatric surgery might be able to maintain weight for longer periods of time.14 Thus, patients should be advised to adhere to lifestyle (dietary and exercise) modifications for more than 1 year for successful maintenance of weight loss.11
TREATMENT OF OBESITY
Below, we discuss a three-part treatment strategy including lifestyle interventions, pharmacotherapy, and bariatric surgery according to the KSSO recommendations. Lifestyle interventions such as diet, physical activity, and behavior therapy are the first line of treatment for patients with obesity.5 Drug and surgical treatments are therapeutic options if you fail to get a first line of treatment with obesity.5
LIFESTYLE INTERVENTIONS
Cognitive behavior therapy can change patient beliefs and understanding about weight regulation.5 The KSSO behavior modification guidelines include dietary and exercise modifications.4 A meta-analysis by Peirson et al.15 including 68 studies of behavioral intervention therapy found that behavioral treatments led to greater weight loss of −3.02 kg (95% confidence interval [CI], −3.52 to −2.52 kg), greater reduction in WC of −2.78 cm (95% CI, −3.34 to −2.22 cm), and a greater reduction in BMI of −1.11 kg/m2 (95% CI, −1.39 to −0.84 kg/m2) compared to interventions without behavioral treatment. Therefore, behavior therapy is recommended to all participants who hope to lose weight.13 Weight loss requires the maintenance of a total energy deficit through caloric restriction and physical activity.13
Energy intake reductions of over 500 kcal/day can usually be achieved with a total daily intake of 1,200 to 1,500 kcal/day in female and 1,500 to 1,800 kcal/day in male.13 Various dietary approaches including low calorie diet, macronutrients modified diets and so on can be used to treat obesity based on individual characteristics. However, these approaches should be nutritionally adequate and create energy deficit.13
Physical activity is necessary for weight loss and weight maintenance. At the start, more than moderate physical activity is recommended. “Moderate” levels of physical activity include exercising between 30 minutes and 60 minutes five times per week. When including resistance exercises, it is recommended to engage in physical activity twice per week and in resistance training 8 to 10 times per week.11
Thus, the 2018 KSSO guidelines advise obese patients to pursue lifestyle changes such as food intake reductions and increased physical activity when attempting weight loss. It is recommended that behavior therapy be continued for at least 6 months to effectively lose weight and for at least 1 year to maintain weight loss.
Before treatment of obesity, the patient needs to be evaluated to determine whether they are ready to lose weight, and the treatment goals should be agreed upon between the physician and the patient according to the individual’s health condition. The primary goal of weight loss should be to reduce body weight by 5% to 10% within 6 months, but losses of only 3%–5% of body weight can improve cardiovascular risk factors.
To determine whether exercise is to be performed and to evaluate exercise capacity, the KSSO guidelines recommend that patients check their health before exercise. It is recommended that exercise regimens include recommendations regarding type, intensity, time, and frequency of exercise.
PHARMACOLOGIC INTERVENTIONS
The Asia-Pacific WHO recommendations suggest that the pharmacotherapy of obesity should be considered when BMI is ≥25 kg/m2, or ≥23 kg/m2 with associated comorbidities.8 The KSSO recommends that pharmacotherapy for obesity should be considered when intensive life style modifications fail to result in weight loss in obese patients with BMI ≥25 kg/m2. We recommend that pharmacotherapy be combined with diet, exercise, and behavior therapy, and that pharmacotherapy should be changed or discontinued if patient weight is not reduced by more than 5% within 3 months of initiating the drug. When choosing medications for weight control, clinicians should consider prescribing medications such as orlistat, lorcaserin, bupropion/naltrexone, and liraglutide 3 mg. Phentermine/topiramate cannot be prescribed because it is currently under review by Korea Ministry of Food and Drug Safety. In Korea, medical pharmacotherapy standards and administrative standards are different.
BARIATRIC SURGERY
Recent clinical studies suggest that bariatric surgery is a most effective treatment for morbidly obese patients and that it decreases the risks of obesity-related diseases and health-related costs.16 In 2013, the European Association for the Study of Obesity and the International Federation for the Surgery of Obesity and Metabolic Disorders-European Chapter jointly published a comprehensive review of surgical management for obesity, the Interdisciplinary European Guidelines on Metabolic and Bariatric Surgery.14,16 Kasama et al.14 reported that bariatric surgery was a good therapeutic choice in Western patients aged 18–60 years with BMI ≥40 kg/m2, or BMI ≥35 kg/m2 with obesity-related diseases who failed to maintain lifestyle modifications.
The risk of obesity-related disease is increased at relatively low BMIs in Asians.11 Therefore, according to the International Federation for the Surgery of Obesity and Metabolic Disorders, Asian Pacific Chapter Consensus statements 2011, bariatric surgery should be considered in Asian candidates when BMI is over 35 kg/m2.14 They also recommend that bariatric surgery be considered in Asian patients with diabetes and BMI ≥30 kg/m2 whose conditions are not controlled by drug therapy and lifestyle modifications.14 Surgical treatment may also be considered an alternative treatment for Asians with uncontrolled T2DM and BMI ≥27.5 kg/m2.14
Although there are differences according to type of bariatric surgery, many reports have shown that the remission rate for T2DM after surgery is about 45% to 90%.17,18 Hyperlipidemia is improved at rates of 70% or more and HTN is improved at rates of about 61%.17 The degree of weight loss after surgery depends on the surgical procedure performed.16 According to a meta-analysis, the mean average weight loss among bariatric surgery patients was 61.2% (95% CI, 58.1%–64.4%).17
According to the Committee of Korean Society for Metabolic and Bariatric Surgery, 1,687 bariatric procedures were performed at 29 institutions based on a nationwide survey.19 The most frequently performed surgery was adjustable gastric banding (71.8%), performed after sleeve gastrectomy (14.0%).19 The researchers emphasized that treatment outcomes significantly depended on, among other factors, patient compliance with long-term follow-up.16
The 2018 KSSO guidelines for the management of obesity include the following recommendations regarding bariatric surgery. First, surgical treatment should be considered if BMI ≥35 kg/m2 (obese class III) or if patients have BMI ≥30 kg/m2 (obese class II) with comorbidities, or if nonoperative treatment fails to result in weight loss. Second, surgical treatment is most effective for weight loss and maintenance of lost weight, and is effective in the management of obesity-associated diseases such as diabetes if conventional treatment fails. Third, in order to improve the efficacy and safety of bariatric treatment, consideration should be given to multidisciplinary approaches before and after surgery.
CONCLUSION
The prevalence of obesity and abdominal obesity are steadily increasing in Korea. KSSO has therefore tried to improve the management of obesity through continuing education initiatives and the development of clinical treatment guidelines. The most recent 2018 practice guidelines released by KSSO are designed to help patients and to distribute more information to physicians to help care for obese patients. Because obesity has multifactorial causes, appropriate care of obese patients requires coordinated multidisciplinary treatment teams. Future research is needed to gather more evidence and study clinical outcomes for the development of appropriate practice guidelines.
ACKNOWLEDGMENTS
This research was supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (HC16C2285).
Footnotes
CONFLICTS OF INTEREST
The authors declare no conflict of interest.
REFERENCES
- 1.Seo MH, Kim YH, Han K, Jung JH, Park YG, Lee SS, et al. Prevalence of obesity and incidence of obesity-related comorbidities in Koreans based on National Health Insurance Service Health Checkup Data 2006–2015. J Obes Metab Syndr. 2018;27:46–52. doi: 10.7570/jomes.2018.27.1.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Park JH, Yoon SJ, Lee H, Jo HS, Lee SI, Kim Y, et al. Burden of disease attributable to obesity and overweight in Korea. Int J Obes (Lond) 2006;30:1661–9. doi: 10.1038/sj.ijo.0803321. [DOI] [PubMed] [Google Scholar]
- 3.Kang JH, Jeong BG, Cho YG, Song HR, Kim KA. Socioeconomic costs of overweight and obesity in Korean adults. J Korean Med Sci. 2011;26:1533–40. doi: 10.3346/jkms.2011.26.12.1533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brauer P, Connor Gorber S, Shaw E, Singh H, Bell N, Shane AR, et al. Recommendations for prevention of weight gain and use of behavioural and pharmacologic interventions to manage overweight and obesity in adults in primary care. CMAJ. 2015;187:184–95. doi: 10.1503/cmaj.140887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yumuk V, Tsigos C, Fried M, Schindler K, Busetto L, Micic D, et al. European guidelines for obesity management in adults. Obes Facts. 2015;8:402–24. doi: 10.1159/000442721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organization. Obesity: preventing and managing the global epidemic. (World Health Organ Tech Rep Ser).Report of a WHO consultation. 2000;894:i–xii. [PubMed] [Google Scholar]
- 7.Jee SH, Sull JW, Park J, Lee SY, Ohrr H, Guallar E, et al. Body-mass index and mortality in Korean men and women. N Engl J Med. 2006;355:779–87. doi: 10.1056/NEJMoa054017. [DOI] [PubMed] [Google Scholar]
- 8.World Health Organization. The Asia-Pacific perspective: redefining obesity and its treatment. Sydney: Health Communications Australia; 2000. Regional Office for the Western Pacific. [Google Scholar]
- 9.Deurenberg P, Deurenberg-Yap M, Guricci S. Asians are different from Caucasians and from each other in their body mass index/body fat per cent relationship. Obes Rev. 2002;3:141–6. doi: 10.1046/j.1467-789X.2002.00065.x. [DOI] [PubMed] [Google Scholar]
- 10.Oh SW, Shin SA, Yun YH, Yoo T, Huh BY. Cut-off point of BMI and obesity-related comorbidities and mortality in middle-aged Koreans. Obes Res. 2004;12:2031–40. doi: 10.1038/oby.2004.254. [DOI] [PubMed] [Google Scholar]
- 11.Kim MK, Lee WY, Kang JH, Kang JH, Kim BT, Kim SM, et al. 2014 Clinical practice guidelines for overweight and obesity in Korea. Endocrinol Metab. 2014;29:405–9. doi: 10.3803/EnM.2014.29.4.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Korean Society for the Study of Obesity. Guideline for the management of obesity 2018. Seoul: Korean Society for the Study of Obesity; 2018. [Google Scholar]
- 13.Jensen MD, Ryan DH, Apovian CM, Ard JD, Comuzzie AG, Donato KA, et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. J Am Coll Cardiol. 2014;63(25 Pt B):2985–3023. doi: 10.1016/j.jacc.2013.11.004. [DOI] [PubMed] [Google Scholar]
- 14.Kasama K, Mui W, Lee WJ, Lakdawala M, Naitoh T, Seki Y, et al. IFSO-APC consensus statements 2011. Obes Surg. 2012;22:677–84. doi: 10.1007/s11695-012-0610-7. [DOI] [PubMed] [Google Scholar]
- 15.Peirson L, Douketis J, Ciliska D, Fitzpatrick-Lewis D, Ali MU, Raina P. Treatment for overweight and obesity in adult populations: a systematic review and meta-analysis. CMAJ Open. 2014;2:E306–17. doi: 10.9778/cmajo.20140012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fried M, Yumuk V, Oppert JM, Scopinaro N, Torres AJ, Weiner R, et al. Interdisciplinary European Guidelines on metabolic and bariatric surgery. Obes Facts. 2013;6:449–68. doi: 10.1159/000355480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Buchwald H, Avidor Y, Braunwald E, Jensen MD, Pories W, Fahrbach K, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292:1724–37. doi: 10.1001/jama.292.14.1724. [DOI] [PubMed] [Google Scholar]
- 18.Buchwald H, Estok R, Fahrbach K, Banel D, Jensen MD, Pories WJ, et al. Weight and type 2 diabetes after bariatric surgery: systematic review and meta-analysis. Am J Med. 2009;122:248–56.e5. doi: 10.1016/j.amjmed.2008.09.041. [DOI] [PubMed] [Google Scholar]
- 19.Ahn HS, Lee HJ, Kang SH, Kim GJ, Kim SS, Kim YJ, et al. 2013 Nationwide bariatric and metabolic surgery report in Korea. J Metab Bariatr Surg. 2014;3:38–43. [Google Scholar]