Abstract
The aim of the current study was to establish animal scar models in a simple and rapid manner by comparing three methods. Wounds were created on the buttocks of Sprague Dawley rats. For Group 1, the initial wound was created by surgical incision. For Groups 2 and 3, a 1470-nm laser was employed to generate dermal burns as the initial wound. The wounds in Groups 1 and 3 were then sutured for three days. After the wound healing, Group 2 generated the largest collagen proportion with abundant collagen type I and significant increases in α-SMA and TGF-β1. The proposed method can be an efficient way to develop rat scar models in a simple manner for evaluating scar treatment.
1. Introduction
Of the 100 million people suffering from scarring in the developed world annually, 55 million of them were the result of elective operations while 25 million were due to operations after trauma (or traumatic injuries) [1]. The scar forms during a normal wound healing process, which is naturally accompanied by trauma, injury, and burn [2]. The process is classified into three main phases based on morphological changes: inflammation, proliferation, and remodeling or maturation [3]. Immediately after injury, platelets in the blood clot release a variety of cytokines and growth factors, which further recruit macrophages and fibroblasts [4]. In the proliferation phase, re-epithelialization proceeds, the new blood vessels are formed, and fibroplasia occurs [5]. In addition, granulation tissue is developed during the process, and fibroblasts are activated in the granulation tissue. As well, the activated fibroblasts acquire α-SMA expression and become myofibroblasts, which play a primary role in the contraction and maturation of the granulation tissue [6]. The final remodeling process takes place several months after the injury. During the remodeling, the dermis reacts to injury by the production of collagen and protein matrix [5,7]. As the granulation tissue is remodeled and matured, the process of scar formation occurs at the final stage. Although collagen degradation happens during the scarring process, the synthesis is stimulated to a higher degree, and the total amount of collagen continues to increase as a result of the body’s homeostatic response. However, excessive neocollagenesis leads to abnormal scars such as hypertrophic scar and keloid scar. In the remodeling phase, wounds are transformed into natural matrix components. Collagen type III, which is produced in the early stage of wound healing, is replaced by type I over time. In this process, the maturation of scarring is progressive, pale, and flat. The texture of the surface is often different from that of the surrounding skin [8,9]. During the wound healing, the activated cytokines such as TGF-β1 regulate myofibroblast differentiation. Normally, the myofibroblasts disappear from the granulation tissue by apoptosis. However, if these cells persist in the granulation tissue, they contribute to scar formation [10]. Thus, the scar shows the increases in α-SMA and TGF-β1 expressions as the key markers of the skin scar that are involved in myofibroblasts [11].
Scars often lead to cosmetic and functional troubles. Furthermore, patients with extensive burns feel uncomfortable with mobility because the scars affect physical movements due to their contraction and stiffness. Some scars also accompany itching and pain, and the quality of life may decrease due to psychosocial problems caused by cosmetic disfigurement [12,13]. Thus, a number of studies on the scar treatment have been conducted to resolve the unmet clinical needs. For the studies, both in vitro and in vivo may help identify the underlying mechanisms of scar formation and may develop and validate various types of therapies [14]. The in vitro testing can be used to explain the cellular responses to the new scar treatment and to establish safety dose ranges for human use. However, preclinical animal models are still needed to ensure efficacy and safety of the new treatment prior to clinical applications [15]. A variety of the animal models have been established in diverse species such as a rodent, leporine, and porcine [16–25]. Mice models have widely been used to investigate wound healing and hypertrophic scar by using mechanical loads and splinting after the skin is cut out [16,19,24]. Rat models have been established for assessment of scarring by cutting buttocks skin and inducing burns with hot water on the dorsal skin [20,21]. The rodent models have the advantage of being economical and easy to handle although they may be different from human wounds due to rapid wound contractions [25]. Compared with the rats, the mice have thinner skin thickness, and the overall range of the sites that can create wounds is smaller, which makes it difficult to assess the mechanism of the scar treatments [24]. Rabbit models have been applied mainly for the study of developing hypertrophic scars by using a biopsy punch in the ears [20,23]. Porcine models have been used to study deep dermal burn caused by scalding and chronic ischemic wound responses [17,18,22]. However, both the rabbits and the pigs are difficult to handle due to their large size. It should be noted that the time to create a scar in the animal models ranged from 25 days to 24 weeks [16–20,22–24]. Furthermore, the long-term animal testing can cause significant stress to the animals.
Previously, various methods (physical, chemical, and thermal wounds) were compared to create scarring in mice models [26]. The previous study reported that despite the second largest scar size, application of 1470 nm laser light showed a relatively consistent and simple method to induce scar formation due to light absorption by the skin. Some surgical wounds involved rapid wound healing with no or minimal scarring [26]. The laser-induced wounds yielded a consistent initial wound size with a two-fold smaller standard deviation in comparison with the surgical incision with a biopsy punch, indicating a more reliable and predictable wound model. In turn, a short optical penetration led to heat generation and accumulation confined within the epidermis and the dermis, contributing to precise control of thermal injury. However, the mice model had very thin dermis, which made it difficult to develop thick scarring tissue caused by injury such as deep thermal burns. Dermal tissue thicker than mouse tissue can result in the evident changes in the scarring tissue. Thus, animal models with relatively thicker skin are still needed to validate the feasible light application in terms of mature scar formation. Therefore, the purpose of the current study was to establish in vivo mature scar models (using rats) in a rapid and simple manner in light of investigating the scars induced by various methods.
2. Materials and methods
2.1 Animal preparation
The current study used a total of nine male Sprague Dawley rats (age = 7 weeks, weight = 200 ~250 g, and three animals per group). Before the experiments, all the rats were anesthetized by applying intraperitoneal injection with zoletil and rompun in a 3:1 mixture solution (i.e., 0.4 cc per rat). Then, both buttocks of each rat were shaved with a clipper, and a waxing cream (Nair sensitive hair removal cream, Nair, Australia) was applied to the shaved areas to completely remove the hair. Since a single wound was created on each shaved buttock, each animal had two wounds for testing (i.e., the total number of wounds = 18). No antibiotics were administered to the animals during the wound healing to exclude any effect of the antibiotics on scar formation. No wound infection was seen during healing. The animal experiments were approved by Institutional Animal Care and Use Committee at Pukyong National University (2017-44).
2.2 Wound creation
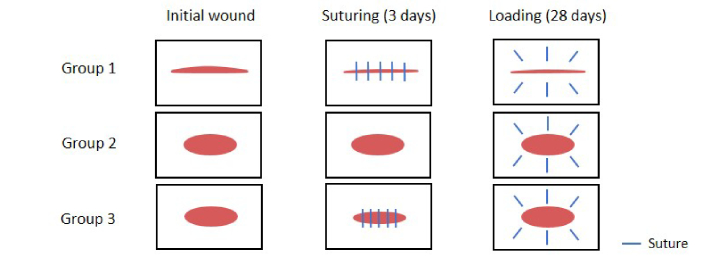
Physical wounds were created by using three different methods to simply and rapidly develop mature scar formation in a rodent model (Fig. 1). For Group 1, the initial wound (1.5 cm long and 0.5 mm wide) was created on the buttock skin by surgical incision. For Groups 2 and 3, a 1470-nm wavelength laser (FC-W-1470, CNI Optoelectronics Tech. Co., China) was used to generate the initial circular wound (1 cm diameter) on the skin. The preliminary studies tested mice and rats at various conditions (power and irradiation time) and identified that the conditions of 5 W and 30 s were appropriate for inducing thermal wounds without any carbonization and resulted in thermally-induced scars after four weeks. Before irradiation, a 600-μm multimode fiber was vertically positioned 25 mm above the skin surface. The beam spot size was 0.3 cm2, and the corresponding irradiance was 16.7 W/cm2. Based upon the preliminary skin tests, the optical fiber transmitted laser power of 5 W for 30 s to create 1~2 mm thick coagulation in the epidermis and dermis of the rat skin. Thin injury (shallower than 1~2 mm) led to the complete healing (scar-free), while a thicker injury deeper than 2 mm caused animal death. No visible carbonization (black discoloration) was observed in the wounded area (Fig. 2). Upon creation, the wounds in two groups (Groups 1 and 3) were closed by using 6-0 nylon suture for three days to evaluate the effect of suturing on wound development. The wound in Group 2 had no suture closure for three days (Fig. 2). It should be noted that Day 0 represents the day when the suturing period is finished (i.e., three days after initial wound generation). After three days, the sutures in Groups 1 and 3 were removed. All groups were loaded in radially outward suturing for 28 days to maximize mature scar formation based on the previous studies (Fig. 1 [16,24]). Although the previous studies applied dynamic loading for six months, the current study selected 28 days for the testing to identify whether mature scar could be achieved in a relatively shorter period. The radial suture was applied 1 cm from the wound edge on six different areas (0.5 cm apart) to circumscribe the entire wounded area (Fig. 1). Each wounded area was photographed weekly to observe variations in the wound size. Image J (National Institute of Health, Bethesda, MD, USA) was used to estimate the wound size from the acquired images by using boundary detection and area estimation. The initial wound size was measured to be 66.2 ± 4.3 mm2, and each condition was repeated six times.
Fig. 1.
Experimental conditions for wound generation in SD rats: Group 1 (incision and suture), Group 2 (burn), and Group 3 (burn and suture)
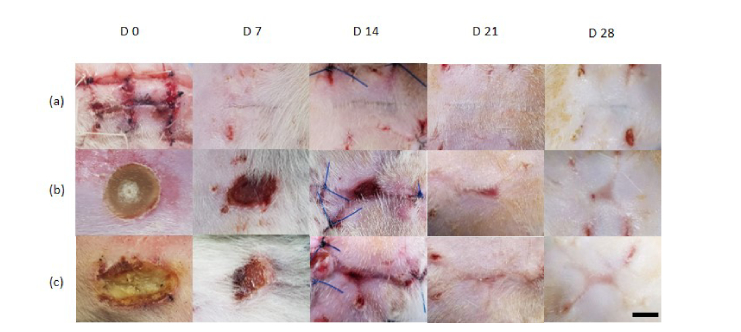
Fig. 2.
Top-view images of wound on days 0, 7, 14, 21, and 28 after injury: (a) Group 1 (incision and suture), (b) Group 2 (burn), and (c) Group 3 (burn and suture). Scale bar = 5 mm
2.3 Histology
Each group of rats was euthanized on Day 28, and scar tissues were harvested to estimate histological variations. The tissue sections were initially embedded in 10% formalin during 48 h for fixation. To prepare histology slides, the paraffin blocks were made and sectioned by 6 μm thickness. Then, all the sections were stained in Masson’s trichrome (MT; American MasterTech, California, USA) and Picrosirius red (PR; Abcam, Cambridge, United Kingdom). The MT staining was used to observe the extent of collagen generation in each group. To estimate collagen expression in MT staining images, dermal regions of interest were initially selected and fixed to quantify the collagenous areas by using MATLAB. Based on the RGB value, the blue color was chosen from each fixed image to detect the boundary of the collagen sites (blue), and the proportion of the color in the fixed area was computed. Five random fields were measured in each image, and all values were averaged. The use of 10% formalin could have shrunk the tissue during fixation because of its cross-linking process and could eventually have underestimated the area measurements. However, the aim of the quantification was to compare scar groups induced by various methods relatively. As all the tissues underwent the formalin fixation for the same period of time, we assumed that the volumetric contraction would not be critical for the relative comparison. The PR staining visualized the collagen and muscle in the tissue sections. Then, an optical microscope (DM 500, Leica, Germany) with a polarization filter (Leica Microsystem™ KIT POLARISATION, Leica, Germany) was used to distinguish collagen types I and III. Collagen type I (thick fibers) exhibits red-orange birefringence while collagen type III (thin fibers) accompanies green birefringence under the polarized microscopy. To quantify red and green color intensities, Image J was used to initially change the background color of the image to black. Then, the gray value was set to 0 to prevent intensity detection of other colors in the background, and a histogram function was used to measure the red and green color intensity.
2.4 Immunohistochemistry
To perform immunohistochemical analysis, the wounded tissues were harvested from the rat buttocks on Day 28 and were fixed in 4-% paraformaldehyde for 12 hr. Paraffin sections of 6 μm thickness were prepared for immunohistochemical staining. The tissue sections with paraffin embedding were washed after deparaffinization and rehydration. Endogenous peroxidase was inactivated by covering tissue with 3% hydrogen peroxide, and each slide was washed. Each slide was incubated at room temperature for 90 minutes with the primary antibodies. The primary antibodies included anti-alpha smooth muscle actin (α-SMA) antibody (ab7817) and TGF-β1 monoclonal antibody (MA5-16949). For the antigen retrieval step, the tissues were placed in citrate buffer (pH 6.0) and incubated at 120 °C for 10 minutes by using a cooker. The cell density (cells/mm2) was counted in five random sites of the dermis to confirm the positive cell staining of α-SMA and TGF-β1.
2.5 Statistical analysis
All data were represented as mean ± one standard deviation. For nonparametric statistical analysis, the Mann-Whitney U test using Bonferroni correction was performed for each group when there was a significant difference (p < 0.05) between groups after the Kruskal-Wallis test.
3. Results
3.1 Macroscopic observations
To identify physical changes in the wound over time, top-view images of each wound area were captured every week. The sutures were temporarily removed for the photographs (except Day 14). Figure 2 shows the photographs acquired from all the groups at various times (Day 0 ~28). Day 0 represents the time when 3-day suturing was finished (Fig. 2). Regardless of group, the overall wound size was reduced with healing time, and cicatrization (line shape) was confirmed at Day 28. Group 1 showed a straight line (middle) at Day 0, and the wound size was estimated to be 14.8 ± 2.6 mm2. Interestingly, the wound in Group 1 was nearly healed during the suturing period as the wound was almost closed [Fig. 2(a)]. A straight scar formed seven days after the wound was loaded, and both the size and the shape were constantly maintained until Day 28 (wound size = 2.1 ± 0.3 mm2). Group 2 (no sutures) demonstrated that the shape of the initial wound was preserved in a round shape with an area of 83.6 ± 9.1 mm2 [Fig. 2(b)]. At Day 7, the scab on the skin surface was removed, and the margin of the wound was torn. Furthermore, the depressed wound was severely damaged, and the granulation tissue was visible. After the wound loading (i.e., outward suturing in Fig. 1), the scar was slightly stretched out along the direction of the applied tension, and the corresponding area was estimated to be 11.1 ± 1.8 mm2 at Day 28. Unlike Group 2, the wound in Group 3 festered from suturing at Day 0 (wound size = 78.8 ± 23.3 mm2), but after seven days, the shape and size of the wound were comparable to those from Group 2. At Day 28, Group 3 showed a scar area of 12.5 ± 2.8 mm2. The wound sizes from Groups 2 and 3 were up to six-fold larger than those in Group 1.
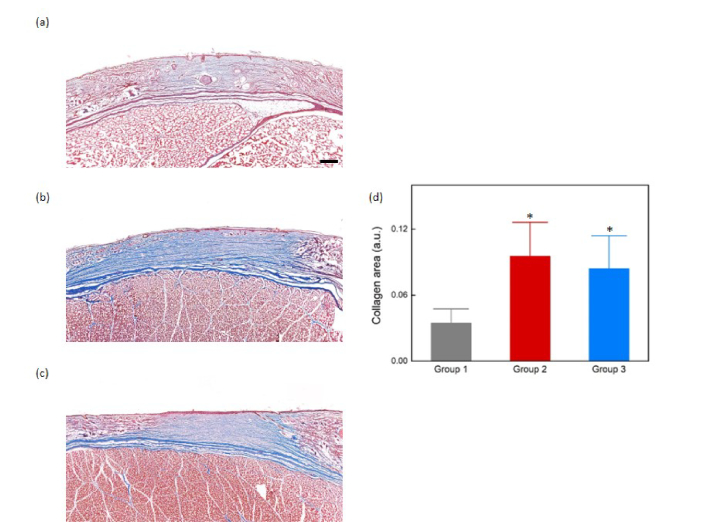
3.2 Histological analysis
To quantify the collagen area of each group, Masson's trichrome staining was performed at Day 28 (Fig. 3). The collagen fibers were stained blue to visualize collagen expressions and to quantify the proportion of collagen in the tissue. In comparison with Group 1, both Groups 2 and 3 showed a larger collagen proportion, represented by thick and dense blue layers below the epidermis [Figs. 3(a-c)]. For quantitative evaluations of the collagen generated in the dermis, Fig. 3(d) shows the proportion of collagen generation measured from the captured images for the three groups.Both Groups 2 and 3 yielded significantly larger collagen fibers than Group 1 (e.g., collagen proportions for Groups 1 and 2 = 0.034 ± 0.013 and 0.095 ± 0.031 in arbitrary unit, respectively; p < 0.001). At Day 28, the overall scar thickness for all the groups was estimated to be 1.1 ± 0.2 mm.
Fig. 3.
Masson’s trichrome staining of normal skin and wounded regions: (a) Group 1 (incision and suture), (b) Group 2 (burn), and (c) Group 3 (burn and suture) and graph of collagen area: (d). Scale bar = 500 μm. (*p < 0.001 vs. Group 1)
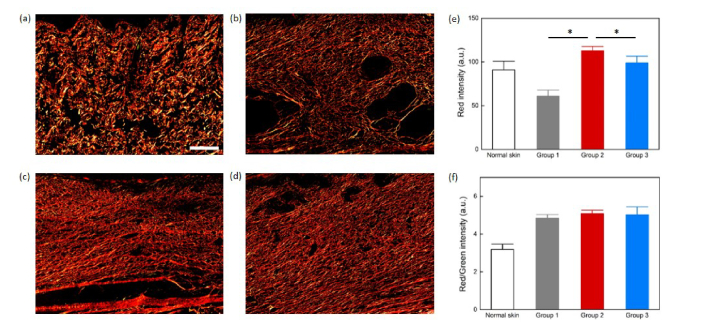
Figure 4 presents the formation of collagen types I and III in each group by using the PR staining along with polarization microscopy. Because of the PR staining, collagen type I (thick fiber) shows red-orange birefringence while collagen type III (thin fiber) shows green birefringence Normal skin showed randomly distributed thick collagen fibers: collagen type I was widely spread out, and more collagen type III was observed, compared with the other groups [Fig. 4(a)]. When collagen is regenerated, fibroblasts produce collagen type III (i.e., baby collagen), which is replaced by type I over time [8]. During the wound healing time, the basket weave pattern (normal collagen) changes to one directional pattern (scar tissue collagen). To develop a mature scar model in a rapid manner, the formation of collagen type I is a critical factor for evaluating the scar models. Group 1 yielded lower collagen type I with a more organized lattice-like structure of the collagen fibers [Fig. 4(b)]. In Group 2, the amount of collagen type I (strong red intensity) was larger than those from the other groups, and the collagen fibers were oriented in one direction [Fig. 4(c)]. Furthermore, Group 3 showed one direction collagen fiber arrangements and higher red intensity than Group 1 [Fig. 4(d)]. For quantitative evaluations, the intensity of red birefringence was measured and compared in Fig. 4(e). Group 2 had about 85% higher red intensity (vs. Group 1), and 14% higher intensity (vs. Group 3) than the other groups (Group 2 = 112.8 ± 4.8 vs. Group 1 = 60.9 ± 7.1 and Group 3 = 98.9 ± 7.7 in arbitrary unit; p < 0.05). In Fig. 4(f), Group 2 had no significance in red / green intensity compared to Group 1 and Group 3 (Group 1 = 4.9 ± 0.2, Group 2 = 5.1 ± 0.2 and Group 3 = 5.0 ± 0.4 in arbitrary unit; p = 0.11 by Kruskal-Wallis test).
Fig. 4.
Picrosirius red with polarization microscope. (a) normal skin, (b) Group 1 (incision and suture), (c) Group 2 (burn), (d) Group 3 (burn and suture), (e) red intensity graph, and (f) red/green intensity graph. Scale bar = 200 μm. (*p < 0.05).
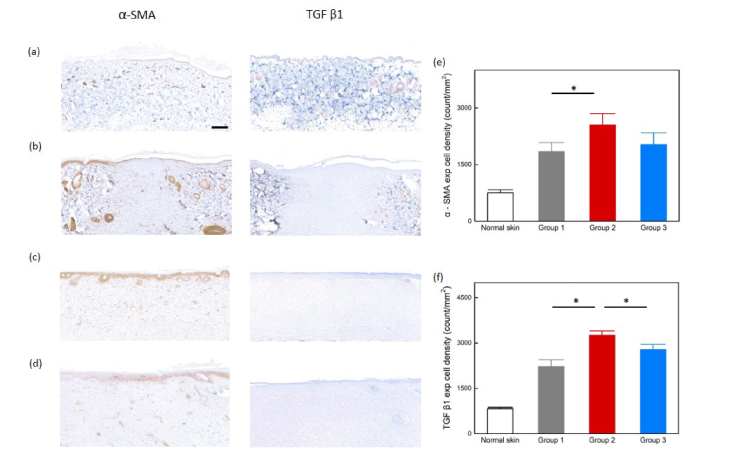
3.3 Immunohistochemistry
Both α-SMA and TGF-β1 are important markers in forming scars. Immuno-histochemical analysis was performed to observe the positively stained cells to evaluate fibrotic effects in each group. Overall, the scar tissue was more excessively stained than the normal skin, and the scar areas for all groups showed a dense population of cells (Fig. 5). The α-SMA was used to identify myofibroblasts in the dermal region, and the positively stained cells showed a spindle shape. Compared with the scar tissue groups, normal skin yielded a lower cell density (754.1 ± 80.5). However, Group 2 showed a significant increase in the cell density [2552.5 ± 300.7 for Group 2 vs. 1839.3 ± 248.5 for Group 1; p < 0.05; Fig. 5(e)]. An increase in TGF-β1 often leads to overproduction of collagen by fibroblasts, which cause excessive scarring [11]. The cell density was lower in normal skin, compared to the other groups (826.2 ± 45.0). However, the TGF-β1 positive cells, such as fibroblasts, significantly increased in Group 2 [3254.1 ± 145.8 for Group 2 vs. 2221.6 ± 223.7 Group 1 and 2778.7 ± 177.0 for Group 3; p < 0.05; Fig. 5(f)]. Groups 1 and 3 were not significantly different in antibodies [α-SMA: 1839.3 ± 248.5 for Group 1 vs. 2026.2 ± 315 for Group 3; p = 0.525 and TGF-β1: 2221.6 ± 223.7 for Group 1 vs. 2778.7 ± 177.0 for Group 3; p = 0.084; Fig. 5(f)]. These results indicate that the wound loaded after laser irradiation without suturing (Group 2) yielded the most scar reaction from significant increases in α-SMA and TGF-β1.
Fig. 5.
Immunohistochemistry: (a) normal skin, (b) Group 1 (incision and suture), (c) Group 2 (burn), (d) Group 3 (burn and suture), (e) α-SMA expressing graph, and (f) TGF β1 expressing graph. Scale bar = 200 μm. (*p < 0.05).
4. Discussion
Scars remain major problems for patients who have undergone surgery or burns and accompany cosmetic and functional troubles. The current study aimed to develop animal scar models in a relatively simple and rapid manner. According to the results, Groups 2 and 3 produced larger wound areas and more collagen expression than Group 1 (Figs. 2 and 3). As the ultimate goal of our study was to apply the proposed model for scar treatment evaluations, a large wound area would be more beneficial in assessing various treatments. Furthermore, the collagen-type analysis with PR staining showed that the intensity of the collagen type I was highest in Group 2, implicating the most mature collagen distribution (Fig. 4). According to immunohistochemistry, the expressed cell density (both α-SMA and TGF-β1) was higher in all three groups, compared to normal tissue, but Group 2 showed the most positive cells, such as myofibroblasts and fibroblasts (Fig. 5). Therefore, the laser-induced wound with no suturing could be a simple and reliable model to develop mature scars in a short period, compared with other wound models.
A number of scarring and treatment studies have been conducted in animal models [16,20,25,27]. However, development of the animal scar models is often complicated and time-consuming. Rodent models are inexpensive and easy to handle, making them widely used in scar research. A variety of wounds and scars using mice and rats have been made in different ways to evaluate scar treatments [16,20,25,27]. Scalded rat models were most commonly used in the study of burns, and dorsum, and ventral regions were scaled and exposed to various temperatures of hot water (60~106 °C) to create burns [25]. Although the scald burn models using mice were also established with a temperature of 54~100 °C [25], the rat models have an advantage because the overall total body surface area is larger than that of mouse models [25]. The scalding method has been used for various burn studies [25]. However, hot water is difficult to maintain uniformly high temperature and can often be dangerous to investigators. In addition, because of complex procedures and difficulty controlling the wound area, the scalding method can hardly predict the degree of thermal injury to the skin. On the other hand, the laser-induced model involves a relatively easy procedure of applying light for 30 s. Both a short optical penetration and constant heat flux can determine the extent of thermal coagulation in the skin in a reliable manner. Table 1 shows a summary of comparison between the scalding and the laser-induced rat models. However, for in-depth comprehension of different thermal responses, numerical modeling on temperature elevation should be developed and compared between the laser-induced and the hot water models. For instance, a constant heat flux case (laser-induced model) can be evaluated with a constant surface temperature case (hot water model) in terms of thermal penetration depth and transient thermal behavior of the rat dermal tissue. In addition, the degree of thermal injury as a function of time should be computed to predict spatial distribution of scar formation and to understand any correlation between the thermal injury and the scar development.
Table 1. Comparison of scalding and laser-induced rat models.
| Model | Method | Advantage | Disadvantage |
|---|---|---|---|
| Scalding model | Direct application of hot water to skin | · Most common type of burns | · Difficult to maintain uniform high temperature and to predict wound |
| · Constant surface temperature | · Dangerous to investigators | ||
| · Standardized model | · Complex procedures | ||
|
| |||
| Laser-induced model | Irradiation of 1470 nm light on skin | · Constant heat flux | · Laser system required |
| · Easy to control thermal injury | · Difficult to develop large wound area | ||
| · Simple procedure | · May cause carbonization | ||
Another model was a rat, split-thickness, skin graft model that transplants clinical skin [27]. Dorsum graft and inguinal graft were divided and were observed for 28 days after the transplantation. In the grafting study, histology and immunohistochemistry using Ki67 and CD68 were analyzed. Overall, the collagen distribution in Masson’s trichrome staining was different from normal skin after 28 days, but the collagen deposition significantly increased in the inguinal graft model, which was similar to the findings from the current study (Fig. 4). For the graft model, a thick epidermis was obtained and prepared in a short period of time (Day 28), but the procedure was complicated since it required a donation of clinical skin. Rat skin models were also used for therapeutic studies to treat wounds and to minimize scarring. Both sides of the buttocks were cut into a circle (2 cm in diameter) and observed for 145 days to compare the scar size of untreated and treated skin after wound healing [20]. Masson’s trichrome staining was performed for evaluating histopathological changes. By 45 days post-healing, collagen fibers were arranged in parallel, in comparison with nine days after wounding tissue (loosely arranged) as shown in Fig. 4. Lastly, mechanical loading models using mice were established to emulate human hypertrophic scars [16]. Two-2 cm, linear, full-thickness incisions were made on the back of the mice, followed by suturing left for four days and tensioning with biomechanical loading devices for two weeks. After the two-week loading, the model was observed for 24 weeks and showed the most similar hypertrophic scars to those of humans. As shown in Fig. 1, the rat model in the current study had sutures for three days after wounding and loaded for four weeks to emulate the previous mechanical loading models. Instead of the mechanical loading device, the current study applied the outward suturing for four weeks. The suturing was difficult to maintain in position because of frequent animal resistance and the inability to provide sufficient tension to the wounded area to raise scars eventually. Although the models failed to develop human-like, raised, hypertrophic scars, the proposed method was able to create mature scars in a relatively shorter time (31 days in total).
A previous study reported a comparison of mouse scar models by using various methods (physical, chemical, and thermal wounds) [26]. A biopsy punch was used to partially remove back skin, chemical burns were conducted by NaOH, and thermal wounds were generated by using a 1470-nm laser system on dorsal mouse skin. Among the three methods, the use of the chemical method yielded the largest scar size and increased the thickness of the epidermis and dermis. From large variations in the initial wound area, the chemical method was quite difficult to control and to predict the degree of injury. In contrast, the current study focused on the development of a constant and simple method to create animal scar models. The deviation of the initial wound size from the previous chemical burn was 39.7%, whereas the deviation of the initial wound size in the current study significantly decreased to 9.9%. Unlike chemical wounding, laser wounding with loading provided an almost constant initial wound size because of the controlled irradiation conditions (area and fluence rate) and eventually increased collagen areas after four weeks (Figs. 2 and 3).Tthis study used a 1470-nm laser because of its short optical penetration depth (0.2 mm) and strong water absorption (major chromophore) [28]. Furthermore, more controlled chemical models will be developed by combining a photoablative or physical method to achieve a consistent chemical approach. For instance, a biopsy punch or Er:YAG laser ablation will be applied to precisely remove a well-defined cross-section of the epidermis, and then the open wound will be treated with a fixed amount of NaOH.
Variations in collagen types during wound healing and scarring have widely been researched [2,29–31]. Collagen type III, which increases as the wound proliferates, is typically replaced by collagen type I over time. Figure 4 shows that collagen type I was the most abundant in Group 2 and collagen type I/III ratio showed no significance from other scar groups. Many studies have examined the collagen type of hypertrophic scars. However, the studies of the deposition of collagen types I and III during scar formation were rather contradictory [2,30,31]. In some studies, collagen type III was relatively increased in the hypertrophic scars [30,31], but in other studies, the ratio of collagen type I/III (6:1) was similar between the hypertrophic scars (abnormal scars) and the normal scars [2]. According to Fig. 4, a large deposition of collagen type I in Group 2 was seen in a mature scar. However, since hypertrophic scars also mature over time [32], the scars from the current model still need to be defined in detail. Therefore, further investigations of collagen types at Day 0, 7, 14, and 21 are required to validate changes in the collagen types during the scar formation. Analyzing the red to green intensity ratio immediately or shortly after laser injury will also be performed to confirm the current collagen analysis.
Collagen type III increases at the proliferative stage, compared to collagen type I during wound healing. In the scar maturation stage, the collagen type I/III ratio can decrease to a normal level [2], and the reduced collagen type III can remain in the scar area. In the experiment, Group 1 yielded a lower collagen type I intensity than normal skin, and Group 2 verified that the collagen type I/III ratio was similar to those of other scar groups, as shown in the red to green intensity (from PR staining with polarization filter) graph [Fig. 4(f)]. As wound maturation is prolonged, the collagen content no longer increases, and the process of remodeling continues for up to two years. The alignment of the collagen fibers tends to have a more organized, lattice-like structure [33]. An old mature scar can re-establish a collagen I/III ratio similar to that of normal skin [33]. The scar from Group 1 matured for a longer time while the surgically-induced wound underwent the healing process first (i.e., faster recovery) in comparison with the other groups. As a result, Group 1 had a lattice-like structure and lower collagen type I intensity than Groups 2 and 3 [Fig. 4(b)]. Despite a higher collagen I/III ratio and more cell expressions, the current study found that the collagen I level of Group 1 was somewhat lower than that of normal skin. Thus, further studies need to validate the current findings by confirming the reliability of collagen I quantification with PR staining and the relevance of the wound healing period. Additionally, the color and intensity of the birefringence appeared from differences in thickness and packing of the collagen fibers. The thin and poorly packed fibers were green polarized while the thick and tightly packed fibers showed a red-polarized color [34]. Thus, analysis of the packing of the collagen fibers in the scar tissues is needed to supplement the results of the red intensity in Group 2. To further differentiate the scars among the groups, the arrangement of collagen type I (red) to collagen type III (green) will be taken as a metric of measurements. The ratio of the area of the unidirectional fiber over the area of the haphazardly-oriented fiber will also be estimated to clearly define the scar in the tissue [35].
The current study compared the scar deposition of each group in terms of α-SMA and TGF-β1 after scar formation (Fig. 5). As the prolonged inflammatory response increases fibrosis [11], both CD68 (stain macrophages) and mast cells can be used to assess the fibrosis, particularly during the inflammation phase [27]. Ki67 can be used as a proliferation marker to identify any variations in hypertrophic scars [17]. Accordingly, immunohistochemistry with various antibodies will be performed to evaluate the current scar model at different time points (i.e., Day 0, 7, 14, 21, and 28) and to elucidate the mechanism of scar formation in a quantitative manner. MT is a nonspecific, collagen stain and is usually used only to demonstrate overall collagen distribution and not the level of collagen because its staining could differ from donor to donor. Thus to differentiate mature collagen from neocollagen, a monoclonal antibody such as procollagen I will be used for more accurate quantitative comparison [36]. For the sake of impartial comparison, various thermal applications including laser, radiofrequency, and microwave also need to be evaluated for thermal scar formation in terms of the degree of thermal injury, scar dimension, and reproducibility. In this study, injuries in both Groups 1 and 3 were closed by suture for 3 days after incision and laser-induced wound, respectively, before they were loaded for 28 days. Accordingly, immunohistochemistry appeared to suggest that the biomarkers indicating overproduction of collagen by fibroblasts, α-SMA and TGF-β1, were not statistically significantly different. In order to ascertain the benefit of the laser-induced scar in Group 2, a nonsutured surgical incision followed by loading will be conducted for direct comparison. Various studies of scar treatment have been carried out in animal models, and the proposed model, which causes the rapid development of scarring, can be an efficient tool to evaluate scar treatment modalities, such as CO2 laser resurfacing and anti-scar drug [37–39].
5. Conclusion
Animal scar models with three different methods were comparatively investigated to develop mature scars in a simple and rapid manner. The proposed laser application can be an efficient method to create mature animal scar models in a simple and rapid manner for scar treatment research. The loaded-laser burn without sutures created the dense scar models rapidly because of the large proportion of collagen and increased expressions of α-SMA and TGF-β1. Further immunohistochemistry with various antibodies will be conducted to explian the underlying mechanism of scar formation.
Acknowledgment
We would like to thank Dr. Kathy Wiemers for her professional editing and valuable advice.
Funding
Technology Development Program (S2436204) funded by the Ministry of SMEs and Startups (MSS, Korea).
Disclosures
The authors declare that there are no conflicts of interest related to this article.
References
- 1.Sund B., Arrow A. K., “New developments in wound care,” Clin. Rep. 45, 379 (2000). [Google Scholar]
- 2.Xue M., Jackson C. J., “Extracellular matrix reorganization during wound healing and its impact on abnormal scarring,” Adv. Wound Care (New Rochelle) 4(3), 119–136 (2015). 10.1089/wound.2013.0485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Singer A. J., Clark R. A., “Cutaneous wound healing,” N. Engl. J. Med. 341(10), 738–746 (1999). 10.1056/NEJM199909023411006 [DOI] [PubMed] [Google Scholar]
- 4.S. Ghatak, V. C. Hascall, R. M. Rodriguez, R. R. Markwald, and S. Misra, “Inflammation, Wound Healing, and Fibrosis,” Wound Healing: Stem Cells Repair and Restorations, Basic and Clinical Aspects, 195 (2017).
- 5.Kirsner R. S., Eaglstein W. H., “The wound healing process,” Dermatol. Clin. 11(4), 629–640 (1993). 10.1016/S0733-8635(18)30216-X [DOI] [PubMed] [Google Scholar]
- 6.Darby I. A., Laverdet B., Bonté F., Desmoulière A., “Fibroblasts and myofibroblasts in wound healing,” Clin. Cosmet. Investig. Dermatol. 7, 301–311 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Velnar T., Bailey T., Smrkolj V., “The wound healing process: an overview of the cellular and molecular mechanisms,” J. Int. Med. Res. 37(5), 1528–1542 (2009). 10.1177/147323000903700531 [DOI] [PubMed] [Google Scholar]
- 8.Mutsaers S. E., Bishop J. E., McGrouther G., Laurent G. J., “Mechanisms of tissue repair: from wound healing to fibrosis,” Int. J. Biochem. Cell Biol. 29(1), 5–17 (1997). 10.1016/S1357-2725(96)00115-X [DOI] [PubMed] [Google Scholar]
- 9.Bayat A., McGrouther D. A., “Clinical management of skin scarring,” Skinmed 4(3), 165–173 (2005). 10.1111/j.1540-9740.2005.02507.x [DOI] [PubMed] [Google Scholar]
- 10.Sarrazy V., Billet F., Micallef L., Coulomb B., Desmoulière A., “Mechanisms of pathological scarring: role of myofibroblasts and current developments,” Wound Repair Regen. 19(Suppl 1), s10–s15 (2011). 10.1111/j.1524-475X.2011.00708.x [DOI] [PubMed] [Google Scholar]
- 11.Wang J., Ding J., Jiao H., Honardoust D., Momtazi M., Shankowsky H. A., Tredget E. E., “Human hypertrophic scar-like nude mouse model: characterization of the molecular and cellular biology of the scar process,” Wound Repair Regen. 19(2), 274–285 (2011). 10.1111/j.1524-475X.2011.00672.x [DOI] [PubMed] [Google Scholar]
- 12.Van Loey N. E., Bremer M., Faber A. W., Middelkoop E., Nieuwenhuis M. K., Group R., “Itching following burns: epidemiology and predictors,” Br. J. Dermatol. 158(1), 95–100 (2008). [DOI] [PubMed] [Google Scholar]
- 13.Bock O., Schmid-Ott G., Malewski P., Mrowietz U., “Quality of life of patients with keloid and hypertrophic scarring,” Arch. Dermatol. Res. 297(10), 433–438 (2006). 10.1007/s00403-006-0651-7 [DOI] [PubMed] [Google Scholar]
- 14.Ramos M. L. C., Gragnani A., Ferreira L. M., “Is there an ideal animal model to study hypertrophic scarring?” J. Burn Care Res. 29(2), 363–368 (2008). 10.1097/BCR.0b013e3181667557 [DOI] [PubMed] [Google Scholar]
- 15.Hillmer M. P., MacLeod S. M., “Experimental keloid scar models: a review of methodological issues,” J. Cutan. Med. Surg. 6(4), 354–359 (2002). 10.1177/120347540200600408 [DOI] [PubMed] [Google Scholar]
- 16.Aarabi S., Bhatt K. A., Shi Y., Paterno J., Chang E. I., Loh S. A., Holmes J. W., Longaker M. T., Yee H., Gurtner G. C., “Mechanical load initiates hypertrophic scar formation through decreased cellular apoptosis,” FASEB J. 21(12), 3250–3261 (2007). 10.1096/fj.07-8218com [DOI] [PubMed] [Google Scholar]
- 17.Cuttle L., Kempf M., Phillips G. E., Mill J., Hayes M. T., Fraser J. F., Wang X.-Q., Kimble R. M., “A porcine deep dermal partial thickness burn model with hypertrophic scarring,” Burns 32(7), 806–820 (2006). 10.1016/j.burns.2006.02.023 [DOI] [PubMed] [Google Scholar]
- 18.DeBruler D. M., Blackstone B. N., McFarland K. L., Baumann M. E., Supp D. M., Bailey J. K., Powell H. M., “Effect of skin graft thickness on scar development in a porcine burn model,” Burns 44(4), 917–930 (2018). 10.1016/j.burns.2017.11.011 [DOI] [PubMed] [Google Scholar]
- 19.Galiano R. D., Michaels J., 5th, Dobryansky M., Levine J. P., Gurtner G. C., “Quantitative and reproducible murine model of excisional wound healing,” Wound Repair Regen. 12(4), 485–492 (2004). 10.1111/j.1067-1927.2004.12404.x [DOI] [PubMed] [Google Scholar]
- 20.Li P., Liu P., Xiong R. P., Chen X. Y., Zhao Y., Lu W. P., Liu X., Ning Y. L., Yang N., Zhou Y. G., “Ski, a modulator of wound healing and scar formation in the rat skin and rabbit ear,” J. Pathol. 223(5), 659–671 (2011). 10.1002/path.2831 [DOI] [PubMed] [Google Scholar]
- 21.Mitsunaga Junior J. K., Gragnani A., Ramos M. L. C., Ferreira L. M., “Rat an experimental model for burns: a systematic review,” Acta Cir. Bras. 27(6), 417–423 (2012). 10.1590/S0102-86502012000600010 [DOI] [PubMed] [Google Scholar]
- 22.Roy S., Biswas S., Khanna S., Gordillo G., Bergdall V., Green J., Marsh C. B., Gould L. J., Sen C. K., “Characterization of a preclinical model of chronic ischemic wound,” Physiol. Genomics 37(3), 211–224 (2009). 10.1152/physiolgenomics.90362.2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Saulis A. S., Mogford J. H., Mustoe T. A., Tredget E. E., Anzarut A., “Effect of Mederma on hypertrophic scarring in the rabbit ear model,” Plast. Reconstr. Surg. 110(1), 177–183, discussion 184–186 (2002). 10.1097/00006534-200207000-00029 [DOI] [PubMed] [Google Scholar]
- 24.Wong V. W., Sorkin M., Glotzbach J. P., Longaker M. T., Gurtner G. C., “Surgical approaches to create murine models of human wound healing,” J. Biomed. Biotechnol. 2011, 969618 (2011). 10.1155/2011/969618 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Abdullahi A., Amini-Nik S., Jeschke M. G., “Animal models in burn research,” Cell. Mol. Life Sci. 71(17), 3241–3255 (2014). 10.1007/s00018-014-1612-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kim M., Kim H., Kang H. W., “Comparative evaluations of hypertrophic scar formation in in vivo models,” Lasers Surg. Med. 50(6), 661–668 (2018). 10.1002/lsm.22783 [DOI] [PubMed] [Google Scholar]
- 27.Zhai Q., Zhou F., Ibrahim M. M., Zhao J., Liu X., Wu J., Chen L., Qi S., “An immune-competent rat split thickness skin graft model: useful tools to develop new therapies to improve skin graft survival,” Am. J. Transl. Res. 10(6), 1600–1610 (2018). [PMC free article] [PubMed] [Google Scholar]
- 28.Poluektova A. A., Malskat W. S., van Gemert M. J., Vuylsteke M. E., Bruijninckx C. M., Neumann H. A., van der Geld C. W., “Some controversies in endovenous laser ablation of varicose veins addressed by optical-thermal mathematical modeling,” Lasers Med. Sci. 29(2), 441–452 (2014). 10.1007/s10103-013-1450-y [DOI] [PubMed] [Google Scholar]
- 29.Hayakawa T., Hashimoto Y., Myokei Y., Aoyama H., Izawa Y., “Changes in type of collagen during the development of human post-burn hypertrophic scars,” Clin. Chim. Acta 93(1), 119–125 (1979). 10.1016/0009-8981(79)90252-3 [DOI] [PubMed] [Google Scholar]
- 30.Arno A. I., Gauglitz G. G., Barret J. P., Jeschke M. G., “Up-to-date approach to manage keloids and hypertrophic scars: a useful guide,” Burns 40(7), 1255–1266 (2014). 10.1016/j.burns.2014.02.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Oliveira G. V., Hawkins H. K., Chinkes D., Burke A., Tavares A. L. P., Ramos-e-Silva M., Albrecht T. B., Kitten G. T., Herndon D. N., “Hypertrophic versus non hypertrophic scars compared by immunohistochemistry and laser confocal microscopy: type I and III collagens,” Int. Wound J. 6(6), 445–452 (2009). 10.1111/j.1742-481X.2009.00638.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ogawa R., “Mechanobiology of scarring,” Wound Repair Regen. 19(Suppl 1), s2–s9 (2011). 10.1111/j.1524-475X.2011.00707.x [DOI] [PubMed] [Google Scholar]
- 33.C. Theoret, “Physiology of wound healing,” Equine wound management, 1–13 (2016). 10.1002/9781118999219.ch1 [DOI]
- 34.Velidandla S., Gaikwad P., Ealla K. K. R., Bhorgonde K. D., Hunsingi P., Kumar A., “Histochemical analysis of polarizing colors of collagen using Picrosirius Red staining in oral submucous fibrosis,” J. Int. Oral Health 6(1), 33–38 (2014). [PMC free article] [PubMed] [Google Scholar]
- 35.Smitha B., Donoghue M., “Clinical and histopathological evaluation of collagen fiber orientation in patients with oral submucous fibrosis,” J. Oral Maxillofac. Pathol. 15(2), 154–160 (2011). 10.4103/0973-029X.84481 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Riaz Y., Cook H. T., Wangoo A., Glenville B., Shaw R. J., “Type 1 procollagen as a marker of severity of scarring after sternotomy: effects of topical corticosteroids,” J. Clin. Pathol. 47(10), 892–899 (1994). 10.1136/jcp.47.10.892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Grbavac R. A. O., Veeck E. B., Bernard J.-P., Ramalho L. M. P., Pinheiro A. L. B., “Effects of laser therapy in CO2 laser wounds in rats,” Photomed. Laser Surg. 24(3), 389–396 (2006). 10.1089/pho.2006.24.389 [DOI] [PubMed] [Google Scholar]
- 38.Chen X., Peng L.-H., Li N., Li Q.-M., Li P., Fung K.-P., Leung P.-C., Gao J.-Q., “The healing and anti-scar effects of astragaloside IV on the wound repair in vitro and in vivo,” J. Ethnopharmacol. 139(3), 721–727 (2012). 10.1016/j.jep.2011.11.035 [DOI] [PubMed] [Google Scholar]
- 39.Boucard N., Viton C., Agay D., Mari E., Roger T., Chancerelle Y., Domard A., “The use of physical hydrogels of chitosan for skin regeneration following third-degree burns,” Biomaterials 28(24), 3478–3488 (2007). 10.1016/j.biomaterials.2007.04.021 [DOI] [PubMed] [Google Scholar]