Abstract
Background
Approaches, tools, and technologies for atrial fibrillation (AF) ablation have evolved significantly since its inception. We sought to characterize secular trends in AF ablation success rates.
Methods
We performed a systematic review and meta-analysis of AF ablation from January 1, 1990, to August 1, 2016, searching PubMed, Scopus, and Cochrane databases. Major exclusion criteria were insufficient outcome reporting and ablation strategies that were not prespecified and uniform. We stratified treatment arms by AF type (paroxysmal AF; nonparoxysmal AF) and analyzed single-procedure outcomes. Multivariate meta-regressions analyzed effects of study, patient, and procedure characteristics on success rate trends. Registered in PROSPERO (CRD42016036549).
Results
A total of 180 trials and observational studies with 28,118 patients met inclusion. For paroxysmal AF ablation studies, unadjusted success rate summary estimates ranged from 73.1% in 2003 to 77.1% in 2016, increasing by 0.9%/year (95% CI 0.4%−1.4%; P = .001; I2 = 90%). After controlling for study design and patient demographics, rate of improvement in success rate summary estimate increased (1.6%/year; 95% CI 0.9%−2.2%; P = .001; I2 = 87%). For nonparoxysmal AF ablation studies, unadjusted success rate summary estimates ranged from 70.0% in 2010 to 64.3% in 2016 (1.1%/year; 95% CI −1.3% to 3.5%; P = .37; I2 = 85%), with no improvement in multivariate analyses.
Conclusions
Despite substantial research investment and health care expenditure, improvements in AF ablation success rates have been incremental. Meaningful improvements may require major paradigm or technology changes, and evaluation of clinical outcomes such as mortality and quality of life may prove to be important going forward.
Since the initial proof of concept of ablation of pulmonary vein triggers as a means to prevent initiation of atrial fibrillation (AF),1 catheter ablation for AF has undergone substantial evolution in procedural approaches (pulmonary vein isolation,2 linear and other ablation strategies,3 rotor mapping,4 fibrosis-guided ablation5), tools (cryoablation,6 laser balloon,7 contact force catheters8), and technologies (3-dimensional electroanatomic mapping9). However, changes in procedural efficacy and effectiveness have been difficult to quantify because of substantial variation in evaluated ablation strategies, study designs, and enrolled populations. Attempts at evidence synthesis have been limited and primarily restricted to specific ablation strategies; prior meta-analyses have not adequately accounted for all plausible contributors to high study heterogeneity.10–12
Therefore, we sought to perform a contemporary systematic review and meta-analysis of trials and observational studies of catheter ablation for AF spanning the totality of the published evidence base. We also evaluated secular trends in success rates and explored features associated with high study heterogeneity.
Methods
The Systematic Review and Meta-analysis of Ablation Strategy Heterogeneity in AF (SMASH-AF) study is a comprehensive cohort of trials and observational studies investigating catheter ablation for AF from January 1, 1990, to August 1, 2016. The full project protocol was registered with PROSPERO prior to data analysis.13 Methods for cohort creation have been previously described in detail.14
Data sources and searches
We identified relevant articles in PubMed, Scopus, and Cochrane databases using a sensitive search strategy (Supplementary Table I), developed in collaboration with Lane Medical Library (Stanford University), designed to capture both contemporary studies and all studies included in prior AF ablation systematic reviews.10,15 Search terms were selected to capture the full spectrum of AF ablation approaches, tools, and technologies.
Study selection
Studies were screened for SMASH-AF cohort inclusion if they reported outcomes of interest, which were defined as any one or more of the following: (1) AF ablation success rate, (2) safety profile, (3) quality of life postablation, or (4) procedure cost. Major exclusion criteria included (1) no treatment or outcomes of interest; (2) insufficient reporting of patient demographics, ablation strategy, or outcomes of interest; (3) ablation strategies that were not prespecified and uniform across the treatment arm; and (4) small study size (ie, <40 patients in a treatment arm). Full exclusion criteria are available in Supplementary Tables II and III. We screened studies for exclusion criteria in 2 steps: (1) review of title and abstract performed by 1 project member (G. L.) and (2) review of full text performed by 3 project members (G. L., A. C., F. Y.) with 2-reviewer agreement required for final inclusion or exclusion. All exclusion conflicts were settled by a single project member (A. P.).
Data extraction and quality assessment
We identified necessary data assumptions and simplifications (Supplementary Table IV) and performed data abstraction form optimization through a trial abstraction of 20 random articles. Data abstraction was performed by 3 project members (G. L., A. C., F. Y.) with abstracted data categories available in Supplementary Table V. Ablation protocol exclusion criteria (Supplementary Table II, criteria 5–11) were used to assess quality, bias, and reproducibility of included studies. All aspects of SMASH-AF followed the Standards for Systematic Reviews established by the Institute of Medicine,16 which have been adopted in the Methodology Standards of the Patient-Centered Outcomes Research Institute.17 Reporting of results is in accordance with both Institute of Medicine and Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines.16,18
Data synthesis and analysis
For the secular trends in AF ablation success rate analysis, from the previously described SMASH-AF cohort, we excluded treatment arms (1) published in a year with <2 total treatment arms; (2) that did not report a single-procedure success rate; and (3) that were not exclusively comprised of paroxysmal (PAF) or nonparoxysmal (NPAF) patients. We abstracted success rate as reported single-procedure arrhythmia-free survival. If multiple recurrence definitions were reported, the highest priority definition was included in the analysis based on the following priority order: (1) atrial tachyarrhythmia without antiarrhythmic agents; (2) AF without antiarrhythmic agents; (3) atrial tachyarrhythmia with antiarrhythmic agents; and (4) AF with antiarrhythmic agents. To account for variable definitions of success, we abstracted (1) arrhythmia duration threshold that qualified as a recurrence; (2) whether recurrence arrhythmia was defined as atrial fibrillation only or any atrial tachyarrhythmia; and (3) whether antiarrhythmic drugs were prohibited postablation. We also determined studies’ percentage of follow up with rhythm monitoring based on reported postablation screening protocol.
For the primary analysis, we determined success rate summary estimates for all included PAF and NPAF studies by year of publication and determined secular trends. We also performed the following sensitivity analyses for PAF studies: (1) randomized study type, any lesion sets, and any energy type; (2) any study type, pulmonary vein isolation (PVI) lesion set only, and any energy type; and (3) any study type, PVI lesion set only, and radiofrequency (RF) energy type only. Because of limited numbers of studies in PAF subgroups, success rate summary estimates in subgroup analyses were determined for nonoverlapping adjacent year groups (ie, 2003 and 2004, 2005 and 2006, etc). Sensitivity analyses were not performed for the NPAF cohort because of the limited number of included studies.
We used multivariate meta-regressions to evaluate the effect of covariates on success rate secular trends. Covariates included (1) study design (study type [randomized, prospective, retrospective, case control], recurrence definitions [AF or atrial tachyarrhythmia, recurrence duration threshold], follow-up protocol [duration of follow-up, percentage of mean follow-up with rhythm monitoring], antiarrhythmic drug prohibition, study size), (2) patient demographics (age, percent female), and (3) procedure characteristics (ablation energy type, catheter [balloon, contact force, irrigated], and lesions sets). Study design and procedure characteristic covariates were selected a priori based on plausible modifiers of success rate, whereas patient demographic covariates were selected based on uniform reporting.
For PAF studies, we also determined secular trends from 2003 to 2008 and 2009 to 2016 and compared the following study variables by these time periods: (1) follow-up protocol (duration of follow-up, percentage of mean follow-up with rhythm monitoring), (2) definition of success (recurrence duration threshold, recurrence arrhythmia definition, antiarrhythmic drug prohibition postablation), and (3) patient demographics (age, percent female, hypertension prevalence). Publications before and after 2008 were compared because unadjusted yearly success rate summary estimates in the full cohort of included PAF studies reached a nadir in this year. Hypertension prevalence was selected as a surrogate for comorbidity burden because it was the most frequently reported comorbidity. Time period analyses were not performed for the NPAF cohort because no included NPAF studies were published before 2010.
Meta-analyses used DerSimonian and Laird methodology with random effects. Statistical heterogeneity was assessed using the I2 statistic. The t test or Mann-Whitney U test was used to compare time period group variables of interest depending on variable normality and variance. Evidence Partner DistillerSR (Ottawa, Canada) was used for (1) reference management; (2) creation, distribution, and completion of screening and data collection forms; (3) recording exclusion rationale; and (4) storage of abstracted data. All analyses were performed using STATA, version 12.1 (College Station, TX). The work was supported by a seed grant from the Meta-Research Center at Stanford (METRICS), Stanford University (Stanford, CA). The authors are solely responsible for the design and conduct of this study, all study analyses, the drafting and editing of the paper, and its final contents.
Results
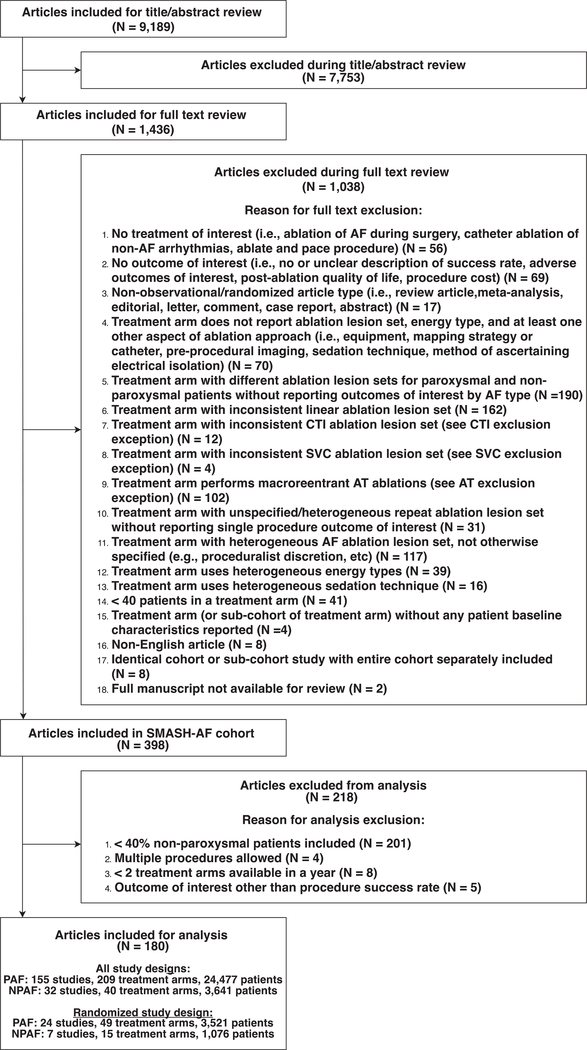
The analysis cohort included 180 studies with 28,118 patients (PAF: 155 studies, 209 treatment arms, 24,477 patients; NPAF: 32 studies, 40 treatment arms, 3,641 patients), of which 31 studies were randomized (PAF: 24 studies, 49 treatment arms, 3,521 patients; NPAF 7 studies, 15 treatment arms, 1,076 patients) (Figure 1). The PAF analysis cohort did not include studies prior to 2003 or from 2007. The NPAF analysis cohort did not include studies prior to 2010. For PAF studies (age: 58.1 years; sex: 30.4% female), reported success rates ranged from 29.2% to 94.0% with a summary estimate of 70.6% (95% CI 68.9%−72.4%; I2 = 90.3%) over a weighted mean follow-up of 21 months (range: 5–77 months). For NPAF studies (age: 60.1 years; sex: 26.9% female), reported success rates ranged from 34.0% to 83.3% with a summary estimate of 57.9% (95% CI 53.7%−62.0%; I2 = 85.7%) over a weighted mean follow-up of 22 months (range: 3–60 months).
Figure 1.
Flow diagram.Inclusion and exclusion criteria used to select analysis cohort. AT, atrial tachycardia; CTI, cavotricuspid isthmus; SVC, superior vena cava. N = study number.
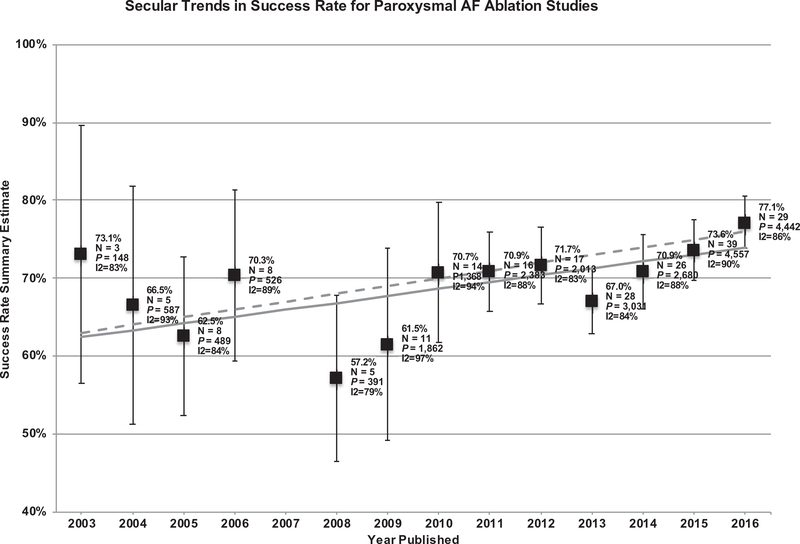
PAF ablation
For PAF studies, unadjusted success rate summary estimates ranged from 73.1% in 2003 to 77.1% in 2016 with a nadir in 2008 (57.5%) (Figure 2). From 2003 to 2016, unadjusted success rate summary estimates increased by 0.9% per year (95% CI 0.4%−1.4%; P = .001; I2 = 90%). Unadjusted success rate summary estimates did not significantly change from 2003 to 2008 and increased by 1.4% per year (95% CI 0.6%−2.2%; P = .001; I2 = 90%) from 2009 to 2016. After adjusting for study design and patient demographics, rate of improvement in success rate summary estimate from 2003 to 2016 increased (1.6% per year; 95% CI 0.9%−2.2%; P = .001; I2 = 87%) as compared to the unadjusted rate. Additional adjustment for procedure characteristics partially accounted for improvement in success rate per year (Table I).
Figure 2.
Secular trends in success rate for PAF ablation studies. Studies of PAF ablation (155 studies, 24,477 patients), with unadjusted summary estimates reported by year. Unadjusted analysis (solid line): (0.9%/year; 95% CI 0.4%−1.4%; P = .001; I2 = 90%). Adjusting for 12-month follow-up duration (dashed line): (1.0%/year; 95% CI 0.5%−1.5%; P < .001; I2 = 90%). N = treatment arms, P = patients.
Table I.
Secular trends in success rate for PAF ablation studies
| Meta-regression model |
2003–2016 |
2003–2008 |
2009–2016 |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| All studies* | %/y† | 95% CI | P value | I2 | %/y† | 95% CI | P value | I2 | %/y† | 95% CI | P value | I2 |
| Univariate (year) | 0.9% | 0.4%–1.4% | .001 | 90% | −2.1% | −5.8% to 1.5% | .24 | 88% | 1.4% | 0.6%–2.2% | .001 | 90% |
| Follow-up duration covariate | 1.0% | 0.5%–1.5% | <.001 | 90% | −1.5% | −5.3% to 2.3% | .44 | 88% | 1.3% | 0.5%–2.1% | .001 | 90% |
| Study design covariates‡ | 1.4% | 0.8%–2.0% | <.001 | 89% | 1.8% | −4.7% to 8.2% | .57 | 83% | 1.9% | 1.0%–2.8% | <.001 | 89% |
| Study design and patient demographics covariates§ | 1.6% | 0.9%–2.2% | <.001 | 88% | 1.5% | −6.0% to 8.9% | .68 | 85% | 2.2% | 1.3%–3.2% | <.001 | 89% |
| All covariates|| | 1.4% | 0.6%–2.2% | .001 | 87% | Insufficient observations | 1.8% | 0.7%–2.9% | .002 | 88% | |||
| RCT only# |
||||||||||||
| Univariate (year) | −0.4% | −1.4% to 0.7% | .48 | 86% | 1.4% | −10.2% to 13.0% | .78 | 83% | 0.6% | −1.6% to 2.8% | .57 | 87% |
| Follow-up duration covariate | −0.3% | −1.4% to 0.8% | .57 | 86% | 3.8% | −11.4% to 18.9% | .55 | 84% | 0.6% | −1.6% to 2.8% | .59 | 87% |
| Study design covariates‡ | −0.6% | −2.2% to 1.0% | .46 | 86% | Insufficient observations | 0.3% | −2.5% to 3.1% | .81 | 87% | |||
| Study design and patient demographics covariates§ | −1.6% | −3.5% to 0.3% | .10 | 85% | Insufficient observations | −0.6% | −3.9% to 2.8% | .73 | 86% | |||
| All covariates|| | −2.0% | −3.8% to −0.2% | .03 | 82% | Insufficient observations | −3.3% | −6.9% to 3.0% | .07 | 83% | |||
| PVI only** |
||||||||||||
| Univariate (year) | 1.4% | 0.7%–2.1% | <.001 | 88% | −0.3% | −5.5 to 4.9% | .89 | 83% | 2.3% | 1.3%–3.3% | <.001 | 88% |
| Follow-up duration covariate | 1.6% | 1.0%–2.3% | <.001 | 86% | 1.0% | −4.7 to 6.7% | .71 | 82% | 2.4% | 1.4%–3.3% | <.001 | 86% |
| Study design covariates‡ | 2.1% | 1.4%–2.9% | <.001 | 87% | Insufficient observations | 3.0% | 1.9%–4.0% | <.001 | 87% | |||
| Study design and patient demographics covariates§ | 2.3% | 1.5%–3.1% | <.001 | 86% | Insufficient observations | 3.2% | 2.2%–4.2% | <.001 | 85% | |||
| All covariates|| | 1.8% | 0.9%–2.6% | <.001 | 85% | Insufficient observations | 2.4% | 1.3%–3.6% | <.001 | 85% | |||
| PVI and RF only†† |
||||||||||||
| Univariate (year) | 1.0% | 0.2%–1.8% | .01 | 88% | 1.5% | −3.9 to 6.9% | .55 | 76% | 1.9% | 0.7%–3.1% | .002 | 88% |
| Follow-up duration covariate | 1.2% | 0.4%–1.9% | .002 | 87% | 3.3% | −2.3 to 8.9% | .22 | 72% | 1.9% | 0.8%–3.0% | .001 | 87% |
| Study design covariates‡ | 1.6% | 0.7%–2.5% | .001 | 87% | Insufficient observations | 2.4% | 1.1%–3.6% | <.001 | 88% | |||
| Study design and patient demographics covariates§ | 1.7% | 0.7%–2.7% | .001 | 87% | Insufficient observations | 2.6% | 1.3%–3.9% | <.001 | 87% | |||
| All covariates|| | 1.6% | 0.6%–2.6% | .003 | 87% | Insufficient observations | 2.2% | 0.8%–3.6% | .002 | 87% | |||
n = treatment arms.
All studies: n = 209 (2003–2016), n = 29 (2003–2008), n = 180 (2009–2016).
Percent increase per year.
Study design covariates (study type [randomized, prospective, retrospective, case control], recurrence definitions [AF or atrial tachyarrhythmia, arrhythmia duration definition], follow-up protocol [duration of follow-up and rhythm monitoring percentage], antiarrhythmic drug prohibition, study size).
Patient demographic covariates (age, percent female) and study design covariates.
Procedure characteristic covariates (ablation energy, equipment, and lesion set) and study design and patient demographic covariates.
RCT only: n = 49 (2003–2016), n = 8 (2003–2008), n = 41 (2009–2016).
PVI only: n = 148 (2003–2016), n = 12 (2003–2008), n = 136 (2003–2016).
PVI and RF only: n = 110 (2003–2016), n = 11 (2003–2008), n = 99 (2009–2016).
Unadjusted success rates for randomized PAF studies (49 treatment arms, 24 studies, 3,521 patients) did not change significantly during any analyzed time period, with no increase in success rates per year after controlling for study design and patient demographic covariates (Table I, Supplementary Figure 1). PVI-only studies (148 treatment arms, 115 studies, 16,500 patients) and PVI- and RF-only studies (110 treatment arms, 87 studies, 12,479 patients) had similar improvements in success rate over time as compared to all studies, with greater absolute increases in success rate per year (Table I, Supplementary Figures 2 and 3).
When comparing PAF studies published from 2003 to 2008 to those published from 2009 to 2016, earlier studies generally had less rigorous study methodology and included patients who were slightly younger and less diverse (by sex) and were substantially less comorbid (by hypertensive prevalence) (Table II).
Table II.
Study design and patient demographics of PAF studies* by time period
| 2003–2008 | 2009–2016 | Difference | 95% CI | P value | |
|---|---|---|---|---|---|
| Follow-up duration (months) | 12.7 | 18.1 | 5.4 | 1.0–9.8 | .016 |
| Rhythm monitoring percentage†,‡ | 1.1% | 1.8% | 0.6% | −0.2% to 1.4% | .13 |
| Recurrence threshold definition: 30 s | 24.1% | 76.7% | 52.5% | 35.7%–69.3% | <.0001 |
| Recurrence arrhythmia definition: AF or AFL/AT | 51.7% | 15.6% | −36.2% | −51.4% to −20.9% | <.0001 |
| Postablation AAD prohibited | 82.8% | 78.9% | −3.9% | −19.9% to 12.1% | .63 |
| Randomized study design | 27.6% | 22.8% | −4.8% | −21.6% to 12.0% | .57 |
| Patients per treatment arm | 74 | 124 | 50 | 10–90 | .014 |
| Age (years) | 55.8 | 58.5 | 2.6 | 1.2–4.1 | <.001 |
| Sex (percent female) | 26.3% | 30.8% | 4.4% | 0.9%–8.0% | .015 |
| Hypertension prevalence§ | 29.3% | 44.2% | 15.0% | 4.2%–25.7% | .007 |
AFL, atrial flutter; AT, atrial tachycardia; AAD, antiarrhythmic drugs.
All studies.
Percent of mean follow-up duration that was screened with rhythm monitoring.
Excluded studies that used continuous rhythm monitoring during follow-up (ie, implantable loop recorders).
Reported in 83% of treatment arms.
NPAF ablation
For NPAF studies, unadjusted success rate summary estimates ranged from 70.0% in 2010 to 64.3% in 2016 (Figure 3). From 2010 to 2016, unadjusted success rate summary estimates were unchanged (1.1% per year; 95% CI −1.3% to 3.5%; P = .37; I2 = 85%). There was no increase in success rate summary estimate per year after adjustment for follow-up duration, all study design covariates, and patient demographics (Table III).
Figure 3.
Secular trends in success rate for NPAF ablation studies. Studies of NPAF ablation (32 studies, 3,641 patients), with unadjusted summary estimates reported by year. Unadjusted analysis (solid line): (1.1%/year; 95% CI −1.3% to 3.5%; P = .37; I2 = 85%) (solid line). Adjusting for 12-month follow-up duration (dashed line): (1.4%/year; 95% CI −1.0% to 3.7%; P = .25; I2 = 84%). N = treatment arm, P = patients.
Table III.
Secular trends in success rate for NPAF ablation studies
| Meta-regression model |
2010–2016 |
|||
|---|---|---|---|---|
| All studies (N = 40) | %/y* | 95% CI | P value | I2 |
| Univariate (y) | 1.1% | −1.3% to 3.5% | .37 | 85% |
| Follow-up duration covariate | 1.4% | −1.0% to 3.7% | .25 | 84% |
| Study design covariates† | −0.3% | −3.1% to 3.1% | .99 | 80% |
| Study design and patient demographics covariates‡ | −1.0% | −3.8% to 3.2% | .86 | 80% |
| All covariates§ | Insufficient observations | |||
Percent increase per year.
Study design covariates (study type [randomized, prospective, retrospective, case control], recurrence definitions [AF or atrial tachyarrhythmia, arrhythmia duration definition], follow-up protocol [duration of follow-up and rhythm monitoring percentage], antiarrhythmic drug prohibition, and study size).
Patient demographic covariates (age, percent female) and study design covariates.
Procedure characteristics covariates (ablation energy, equipment, and lesion set) and study design and patient demographic covariates.
Discussion
We found that, despite substantial research investment and health care expenditure, success rates of trials and observational studies of PAF ablation improved only incrementally, whereas no improvements in NPAF ablation success rates were detected. These data indicate that maturation of approaches, tools, and technology to perform catheter ablation of AF have not resulted in marked improvements in success rate, arguing that major paradigm or technology changes may be necessary to achieve a highly efficacious procedure to restore and maintain sinus rhythm.
In 1998, the reported success rate of PAF ablation was 62%.1 Over the subsequent 20 years, there has been substantial evolution in procedural approaches, tools, and technologies. Despite these advances, a prior review of the literature that included studies published before 2008 did not detect improvements in AF ablation efficacy over time,10 similar to our findings during this time period. However, real-world data from Denmark have been used to show reductions in AF-related clinical encounters after AF ablation from 2005 to 2014, suggesting secular improvements in AF ablation effectiveness.19 In a contemporary and rigorous review of the literature, we did not detect any improvements in NPAF ablation efficacy over time. Importantly though, incremental gains in PAF procedural success appear to have occurred, with important caveats and implications.
With multiple stakeholders committed to improving quality of research reporting18,22 and study methodology23 and AF ablation guideline statements outlining optimal trial design and reporting in 200724 and 2012,25 it is plausible that AF ablation study quality may have improved, resulting in underestimation of success rate improvements. In support of this hypothesis, we found that PAF ablation studies performed from 2009 to 2016, as compared to 2003 to 2008, had mean durations of follow-up that were longer, were more likely to use a 30-second recurrence threshold as recommended by consensus statements, included more patients, and trended toward higher percentages of mean follow-up with rhythm monitoring. For unclear reasons, specifying that any atrial tachyarrhythmia will be counted as a recurrence (as compared to AF only) has become less common. Importantly though, after controlling for study design, there were larger improvements in PAF ablation success rates over time.
Proof of concept and early utilization of novel procedures are performed in carefully selected patients, who are often not representative of the full denominator of patients with a disease state. Over time, intentional selection bias of early studies can be balanced if procedure efficacy and safety are investigated in more diverse populations. PAF ablation studies performed from 2009 to 2016, compared to 2003 to 2008, included older patients, more women, and patients with higher prevalence of comorbidities. Although we accounted for age and sex in our regressions, reporting of comorbidities was highly variable across included studies, preventing adjustment for variables known to effect procedure outcome. Considering that hypertension prevalence increased over time, suggesting sicker patients are undergoing ablation, our adjusted estimates may underestimate procedural gains.
Notably, when analyses were restricted to PAF studies that only performed PVI, larger success rate improvements per year were found as compared to all included studies. Possible explanations for this finding include (1) a more accurate estimate of secular trends in procedural success due to lower heterogeneity between studies that used similar ablation strategies, (2) reductions in postablation atypical flutter which has been associated with some non-PVI lesion sets, or (3) chance. However, this finding suggests meaningful improvement in procedural approaches, tools, or technologies to achieve PVI.
In general, advances in procedural approaches, tools, and technologies would be expected to account for improvements in success rate over time. However, there was residual improvement over time after adjusting for procedure covariates. This observation requires further exploration and could be due to a number of factors, including our methods not accounting for all procedural variables that affect creation of durable lesions, including mapping techniques and operator or study site experience.
Importantly, interpretation of our findings must be done in the context of no improvements over time (or trends toward an improvement) detected in PAF success rates from randomized trials and reported success rates from all PAF studies published in 2016 only reaching 77.1%, with several recent multicenter randomized trials for PAF ablation showing single-procedure success rates less than 66%.20,21 These findings argue that major paradigm or technology changes may be necessary to achieve a highly efficacious procedure to restore and maintain sinus rhythm. Importantly though, large residual heterogeneity despite inclusion of studies deemed high quality based on rigorous exclusion criteria which prioritized reproducibility and methods that accounted for numerous study design variables argues that further improvements in study quality and lesion set reproducibility are also needed to accurately evaluate procedural advances.
Looking beyond time to first recurrence, recent studies have focused on clinical end points, demonstrating improvements in mortality and health care utilization with reductions in AF burden achieved through ablation in certain populations.26,27 There could be substantial gains in these end points that are independent of time to first recurrence. Continuous assessment of AF burden to clinical end points may also help to reframe optimal choice of primary and secondary outcomes for future AF trials and observational studies.28
There are several notable limitations, including large heterogeneity in summary estimates by year and residual heterogeneity in meta-regressions despite stratification by AF type and accounting for numerous study design covariates and patient age and sex. Unfortunately, highly variable reporting of patient baseline characteristics and comorbidities, duration of AF and prior treatments, and operator experience prevented controlling for these important characteristics in meta-regressions, contributing to residual heterogeneity and possibly underestimation of procedural gains. As with all systematic reviews and meta-analyses, small study effects may bias results.
Despite substantial evolution of approaches, tools, and technologies and widespread diffusion of AF ablation, improvements over time in PAF ablation have only been incremental, whereas no improvements for NPAF ablation were detected. Meaningful improvements in procedure efficacy may not occur without major paradigm or technology changes, and evaluation of clinical outcomes such as mortality and quality of life may prove to be important going forward.
Supplementary Material
Acknowledgements
Christopher Stave, MLS (Lane Medical Library, Stanford University School of Medicine, USA), consulted on search strategy development. Ewoud Schuit, MSc, PhD (Julius Centre for Health Sciences and Primary Care, University Medical Centre Utrecht, Utrecht, Netherlands), consulted on statistical methodology. The work was supported by a seed grant from the Meta-Research Center at Stanford (METRICS), Stanford University (Stanford, USA).
Footnotes
Disclosures
A. C. Perino: none. G. C. Leef: none. A. Cluckey: none. F. N. Yunus: none. M. Askari: none. P. A. Heidenreich: none. S. M. Narayan: research grant, significant: National Institutes of Health (HL13359). Ownership interest, significant: Topera. Consulting, modest: Abbott. Consulting, minor: Uptodate, American College of Cardiology. P. J. Wang: research grant, modest: Medtronic, Inc, Siemens, Cardiofocus, ARCA. Other research support, modest: Medtronic, Inc, St Jude Medical, Boston Scientific Corp, Biosense Webster. Honoraria, modest: Janssen Pharmaceuticals, St Jude Medical, Medtronic, Inc, Amgen, Johnson & Johnson. Ownership interest, modest: Vytronus. Consultant/advisory board, modest: Janssen Pharmaceuticals, St Jude Medical, Medtronic, Inc, Amgen. M. Turakhia: research grant, significant: Janssen Pharmaceuticals, Medtronic Inc, AstraZeneca, Veterans Health Administration, Cardiva Medical Inc. Other research support, Modest: AliveCor Inc, Amazon, Zipline Medical Inc, iBeat Inc, iRhythm Technologies Inc. Honoraria, significant: Abbott. Honoraria, modest: Medtronic Inc, Boehringer Ingelheim, Precision Health Economics, iBeat Inc, Akebia, Cardiva Medical Inc, Medscape/theheart.org.
Appendix. Supplementary methods and data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ahj.2018.10.006.
References
- 1.Haissaguerre M, Jais P, Shah DC, et al. Spontaneous initiation of atrial fibrillation by ectopic beats originating in the pulmonary veins. N Engl J Med 1998;339(10):659–66, 10.1056/NEJM199809033391003. [DOI] [PubMed] [Google Scholar]
- 2.Pappone C, Rosanio S, Oreto G, et al. Circumferential radiofrequency ablation of pulmonary vein ostia: a new anatomic approach for curing atrial fibrillation. Circulation 2000;102(21):2619–28. [DOI] [PubMed] [Google Scholar]
- 3.Ernst S, Ouyang F, Lober F, et al. Catheter-induced linear lesions in the left atrium in patients with atrial fibrillation: an electroanatomic study. J Am Coll Cardiol 2003;42(7):1271–82. [DOI] [PubMed] [Google Scholar]
- 4.Narayan SM, Krummen DE, Shivkumar K, et al. Treatment of atrial fibrillation by the ablation of localized sources: CONFIRM (Conventional Ablation for Atrial Fibrillation With or Without Focal Impulse and Rotor Modulation) trial. J Am Coll Cardiol 2012;60(7): 628–36, 10.1016/j.jacc.2012.05.022 [Epub 2012 Jul 18]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Marrouche NF, Wilber D, Hindricks G, et al. Association of atrial tissue fibrosis identified by delayed enhancement MRI and atrial fibrillation catheter ablation: the DECAAF study. JAMA 2014;311(5): 498–506, 10.1001/jama.2014.3. [DOI] [PubMed] [Google Scholar]
- 6.Packer DL, Kowal RC, Wheelan KR, et al. Cryoballoon ablation of pulmonary veins for paroxysmal atrial fibrillation: first results of the North American Arctic Front (STOP AF) pivotal trial. J Am Coll Cardiol 2013;61(16):1713–23, 10.1016/j.jacc.2012.11.064. [DOI] [PubMed] [Google Scholar]
- 7.Reddy VY, Neuzil P, Themistoclakis S, et al. Visually-guided balloon catheter ablation of atrial fibrillation: experimental feasibility and first-in-human multicenter clinical outcome. Circulation 2009;120(1): 12–20, 10.1161/CIRCULATIONAHA.108.840587. [Epub 2009 Jun 22]. [DOI] [PubMed] [Google Scholar]
- 8.Natale A, Reddy VY, Monir G, et al. Paroxysmal AF catheter ablation with a contact force sensing catheter: results of the prospective, multicenter SMART-AF trial. J Am Coll Cardiol 2014;64(7):647–56, 10.1016/j.jacc.2014.04.072. [DOI] [PubMed] [Google Scholar]
- 9.Martinek M, Nesser HJ, Aichinger J, et al. Impact of integration of multislice computed tomography imaging into three-dimensional electroanatomic mapping on clinical outcomes, safety, and efficacy using radiofrequency ablation for atrial fibrillation. Pacing Clin Electrophysiol 2007;30(10):1215–23, 10.1111/j.1540-8159.2007.00843.x. [DOI] [PubMed] [Google Scholar]
- 10.Calkins H, Reynolds MR, Spector P, et al. Treatment of atrial fibrillation with antiarrhythmic drugs or radiofrequency ablation: two systematic literature reviews and meta-analyses. Circ Arrhythm Electrophysiol 2009;2(4): 349–61, 10.1161/CIRCEP.108.824789. [published Online First: 2009/10/08]. [DOI] [PubMed] [Google Scholar]
- 11.Ganesan AN, Shipp NJ, Brooks AG, et al. Long-term outcomes of catheter ablation of atrial fibrillation: a systematic review and meta-analysis. J Am Heart Assoc 2013;2(2), e004549, 10.1161/JAHA.112.004549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wynn GJ, Das M, Bonnett LJ, et al. Efficacy of catheter ablation for persistent atrial fibrillation: a systematic review and meta-analysis of evidence from randomized and nonrandomized controlled trials. Circ Arrhythm Electrophysiol 2014;7(5):841–52, 10.1161/CIRCEP.114.001759. [Epub 2014 Aug 16]. [DOI] [PubMed] [Google Scholar]
- 13.Turakhia M, Perino AC. National Institute for Health Research. Systematic review and meta-analysis of ablation strategy heterogeneity in atrial fibrillation. PROSPERO: International prospective register of systematic reviews; 2016. Available at:, http://www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42016036549. Accessed October 9, 2017.
- 14.Leef GC, Perino AC, Cluckey A, et al. Geographic and racial representation and reported success rates of studies of catheter ablation for atrial fibrillation: Findings from the SMASH-AF meta-analysis study cohort. J Cardiovasc Electrophysiol 2018, 10.1111/jce.13439. [published Online First: 2018/0½5]. [DOI] [PubMed] [Google Scholar]
- 15.Perino AC, Hoang DD, Holmes TH, et al. Association between success rate and citation count of studies of radiofrequency catheter ablation for atrial fibrillation: possible evidence of citation bias. Circ Cardiovasc Qual Outcomes 2014;7(5):687–92, 10.1161/CIRCOUTCOMES.114.000912. [DOI] [PubMed] [Google Scholar]
- 16.Institute of Medicine (U.S.), Committee on Standards for Systematic Reviews of Comparative Effectiveness Research, Eden J Finding what works in health care: standards for systematic reviews. Washington, D.C.: National Academies Press; 2011 [PubMed] [Google Scholar]
- 17.The PCORI methodology report. Patient Centered Outcomes Research Institute. Available at, http://www.pcori.org/sites/default/files/PCORI-Methodology-Standards.pdf 2013. Accessed December , 2016.
- 18.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 2009;151(4):264–9. [W64]. [DOI] [PubMed] [Google Scholar]
- 19.Pallisgaard JL, Gislason GH, Hansen J, et al. Temporal trends in atrial fibrillation recurrence rates after ablation between 2005 and 2014: a nationwide Danish cohort study. Eur Heart J 2018;39(6):442–9, 10.1093/eurheartj/ehx466. [published Online First: 2017/10/12]. [DOI] [PubMed] [Google Scholar]
- 20.Reddy VY, Dukkipati SR, Neuzil P, et al. Randomized, controlled trial of the safety and effectiveness of a contact force-sensing irrigated catheter for ablation of paroxysmal atrial fibrillation: results of the TactiCath Contact Force Ablation Catheter Study for Atrial Fibrillation (TOCCAS-TAR) study. Circulation 2015;132(10):907–15, 10.1161/CIRCULATIONAHA.114.014092. [Epub 2015 Aug 26]. [DOI] [PubMed] [Google Scholar]
- 21.Kuck KH, Brugada J, Furnkranz A, et al. Cryoballoon or radiofrequency ablation for paroxysmal atrial fibrillation. N Engl J Med 2016;374(23):2235–45, 10.1056/NEJMoa1602014. [DOI] [PubMed] [Google Scholar]
- 22.Schulz KF, Altman DG, Moher D, et al. CONSORT 2010 statement: updated guidelines for reporting parallel group randomized trials. Ann Intern Med 2010;152(11):726–32, 10.7326/0003-4819-152-11-201006010-00232. [DOI] [PubMed] [Google Scholar]
- 23.Zarin DA, Tse T, Williams RJ, et al. The ClinicalTrials.gov results database—update and key issues. N Engl J Med 2011;364(9): 852–60, 10.1056/NEJMsa1012065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Calkins H, Brugada J, Packer DL, et al. HRS/EHRA/ECAS expert consensus statement on catheter and surgical ablation of atrial fibrillation: recommendations for personnel, policy, procedures and follow-up. A report of the Heart Rhythm Society (HRS) Task Force on Catheter and Surgical Ablation of Atrial Fibrillation developed in partnership with the European Heart Rhythm Association (EHRA) and the European Cardiac Arrhythmia Society (ECAS); in collaboration with the American College of Cardiology (ACC), American Heart Association (AHA), and the Society of Thoracic Surgeons (STS). Endorsed and approved by the governing bodies of the American College of Cardiology, the American Heart Association, the European Cardiac Arrhythmia Society, the European Heart Rhythm Association, the Society of Thoracic Surgeons, and the Heart Rhythm Society. Europace 2007;9(6):335–79, 10.1093/europace/eum120. [DOI] [PubMed] [Google Scholar]
- 25.Calkins H, Kuck KH, Cappato R, et al. 2012 HRS/EHRA/ECAS expert consensus statement on catheter and surgical ablation of atrial fibrillation: recommendations for patient selection, procedural techniques, patient management and follow-up, definitions, endpoints, and research trial design: a report of the Heart Rhythm Society (HRS) Task Force on Catheter and Surgical Ablation of Atrial Fibrillation. Developed in partnership with the European Heart Rhythm Association(EHRA),a registered branch of the European Society of Cardiology (ESC) and the European Cardiac Arrhythmia Society (ECAS); and in collaboration with the American College of Cardiology (ACC), American Heart Association (AHA), the Asia Pacific Heart Rhythm Society (APHRS), and the Society of Thoracic Surgeons (STS). Endorsed by the governing bodies of the American College of Cardiology Foundation, the American Heart Association, the European Cardiac Arrhythmia Society, the European Heart Rhythm Association, the Society of Thoracic Surgeons, the Asia Pacific Heart Rhythm Society, and the Heart Rhythm Society. Heart Rhythm 2012;9(4):632–96 e21, 10.1016/j.hrthm.2011.12.016. [DOI] [PubMed] [Google Scholar]
- 26.Marrouche NF, Brachmann J, Andresen D, et al. Catheter ablation for atrial fibrillation with heart failure. N Engl J Med 2018;378(5):417–27, 10.1056/NEJMoa1707855. [DOI] [PubMed] [Google Scholar]
- 27.Catheter Ablation vs Anti-arrhythmic Drug Therapy for Atrial Fibrillation Trial (CABANA). NCT00911508. U.S. National Library of Medicine: ClinicalTrials.gov. Available at, https://clinicaltrials.gov/ct2/show/NCT00911508 2017. Accessed October 9, 2017.
- 28.Chen LY, Chung MK, Allen LA, et al. Atrial fibrillation burden: moving beyond atrial fibrillation as a binary entity: a scientific statement from the American Heart Association. Circulation 2018;137(20):e623–44, 10.1161/CIR.0000000000000568. [published Online First: 2018/04/18]. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.