Abstract
Cardiovascular and metabolic diseases (CVMD) are the leading causes of death worldwide, underscoring the urgent necessity to develop new pharmacotherapies. Berberine (BBR) is an eminent component of traditional Chinese and Ayurvedic medicine for more than 2000 years. Recently, BBR has attracted much interest for its pharmacological actions in treating and/or managing CVMD. Recent discoveries of basic, translational and clinical studies have identified many novel molecular targets of BBR (such as AMPK, SIRT1, LDLR, PCSK9, and PTP1B) and provided novel evidences supporting the promising therapeutic potential of BBR to combat CVMD. Thus, this review provides a timely overview of the pharmacological properties and therapeutic application of BBR in CVMD, and underlines recent pharmacological advances which validate BBR as a promising lead drug against CVMD.
Keywords: berberine, cardiovascular diseases, metabolic diseases, targets, therapeutics
Introduction
Cardiovascular diseases (including atherosclerosis, myocardial infarction, hypertension, cardiac hypertrophy and heart failure), and metabolic diseases (including diabesity, obesity, and non-alcoholic fatty liver disease), are the leading causes of death worldwide 1-8. These diseases are caused by the combined effects of multiple pathological factors, and their pathogenesis has not been fully clarified yet 1-8. Although the prevention and treatment of cardiovascular diseases and metabolic diseases (CVMD) have made great progress in the past 20 years, the morbidity and mortality arising from CVMD are still very high 1-8. Western medicine is still the mainstream therapy of CVMD 9-12. For example, hypoglycemic agents, statins, anticoagulants, beta receptor blockers, nitrates, and anti-thrombotic drugs are widely used in patients with CVMD 9-11, 13, 14. Despite widespread evidences showing that these drugs are effective in a treatment of CVMD, potentially serious adverse consequences remain key challenges 9-14. Therefore, there is an urgent need to identify alternative and complementary therapies to better manage CVMD. Berberine (BBR) is widely used in Asian countries (mainly in China) due to its good clinical and safety profile 15-17. With the advances of pharmacological research, BBR is considered to be one of the most promising natural product-derived drug for the treatment of CVMD (Figure 1). To this end, we provide a timely and insightful overview of the therapeutic potential and molecular targets of BBR in treating CVMD.
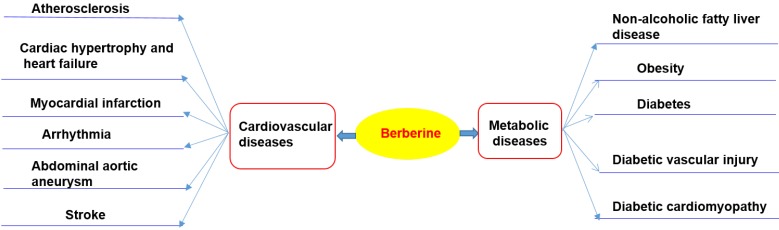
Figure 1.
Therapeutic potential of BBR in cardiometabolic diseases. Current researches support that BBR may play a therapeutic role in the treatment of cardiovascular disease (including atherosclerosis, heart failure, myocardial infarction, arrhythmia, abdominal aortic aneurysm, stroke) and metabolic diseases (including nonalcoholic fatty liver, obesity, diabetes and its cardiovascular complications).
BBR - basic characteristics and history of use
BBR is the principal bioactive ingredient of Rhizoma coptidis (also named 'Huang Lian' in Chinese), a common traditional Chinese medicinal herb used for the therapy of inflammatory disorders and diabetes mellitus (DM) 18, 19. The earliest record of the use of Rhizoma coptidis as a medication is dated in A.D. 200 in the book of 'Shen Nong Ben Cao Jing' 18, 19. For the first time, the anti-diabetic effect of Rhizoma coptidis was recorded in the book Note of Elite Physicians in about 1500 years ago by Hongjing Tao 20.
BBR (C20H18NO4) is a quaternary ammonium salt derived from isoquinoline alkaloid, with a molar weight of 336.36 g/mol 21, 22. BBR is a yellow powder that is odorless and has characteristic alkaloid bitterness 21. It is sparingly soluble in water, slightly soluble in ethanol or methanol; however, the salt form is relatively water-soluble 21, 22. BBR can be easily obtained from medicinal plants or through total synthesis 23, 24.
Bioavailability and metabolism of BBR
Chloride or sulfate of BBR are commonly used for clinical purposes 15, 17. Nevertheless, pharmacokinetic data in rodents and humans have revealed poor absorption from the gut and rapid metabolism in the body that caused its low oral bioavailability 21. For example, BBR is converted to ionic form under physiological conditions and self-aggregates at low pH values 25-27. Self-aggregation of BBR reduces its solubility in the gastrointestinal tract and its ability to permeate the gut wall 26, 27. P-glycoprotein (P-gp) is located in the epithelial cell membrane and can efflux many drugs (including BBR), thereby limiting their oral bioavailability 26. P-gp inhibitors, including D-tocopheryl polyethylene glycol 1000 succinate, are common adjuvants to increase the oral bioavailability of BBR 25. In addition, penetration enhancers and lipid particle delivery systems can also increase the bioavailability of BBR 27. BBR is metabolized by oxidative demethylation and glucuronidation to berberrubine, thalifendine, demethyleneberberine and jatrorrhizine and their corresponding glucuronides in the liver 21, 28 (Figure 2). CYP2D6 is the major cytochrome P450 (CYPs) for BBR metabolism, followed by CYP1A2, 3A4, 2E1 and CYP2C19. Finally, BBR metabolites are excreted through bile, feces, and urine 21, 28.
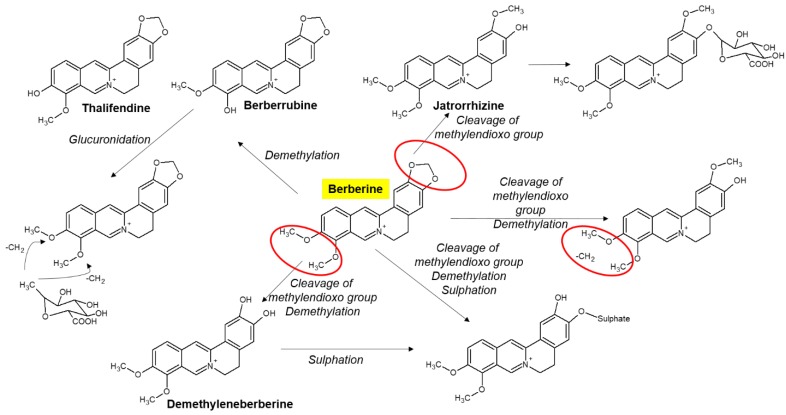
Figure 2.
Selected metabolites of BBR in human. BBR is metabolized in the body by metabolic pathways (such as demethylation, glucuronidation etc) to thalifendin, berberrubine, jatrorrhizin, demethyleneberberin.
Although plasma concentration of BBR is low, the tissue concentrations of BBR and its metabolites are high 29. BBR and its metabolites are widely distributed in the liver, kidney, muscle, lung, brain, heart, pancreas and adipose tissue 29-31. BBR can also penetrate the blood-brain barrier 32. Specifically, the rapid clearance of BBR from plasma as compared to the hippocampus indicates that BBR may have an important effect on hippocampal neurons 31. Moreover, infusion of BBR (2 μg/h, 28d) by bilateral hypothalamic paraventricular nucleus (PVN) through an osmotic minipump can reduce hypertension and sympathoexcitation in two-kidney, one-clip (2K1C) renovascular hypertensive rats by ROS/ERK1/2 (extracellular-signal regulated kinase 1/2)/ inducible nitric oxide (iNOS) pathway 33.
Emerging studies have shown that BBR is almost safe at conventional doses, with a relatively low incidence of adverse reactions, such as gastrointestinal discomfort, and transient increases in plasma bilirubin levels 27, 34. Although the safety of BBR is relatively high, it should be taken carefully to avoid adverse reactions in specific cases. For example, BBR replaces bilirubin in binding to albumin (in nearly 10 times greater effect compared to phenylbutazone), so any BBR containing herbs should be avoided in jaundice in pregnant women and infants 35. BBR interacts with macrolides and it may lead to potentially dangerous arrhythmias 36. BBR in combination with statins increases cardiotoxicity by inhibiting CYP3A4 and human ether-a-go-go related genes (hERG) potassium channels 37. On the other hand, BBR can prevent toxic reactions in different tissues caused by antitumor drugs such as cisplatin 38, cyclophosphamide 39, doxorubicin 40 and bleomycin 41 as well as side effects of analgesics (e.g. acetaminophen 42).
BBR in the treatment of cardiovascular diseases
Atherosclerosis
Atherosclerosis is mainly a lipid metabolic disorder which underlies multiple cardio- and cerebro-vascular diseases 43-46. Atherosclerosis commences with endothelial dysfunction, followed by neointima formation, lipid accumulation, foam cell formation, and plaque rupture 43, 44, 46-48. BBR exerts protective effects against atherosclerosis by modulating various pro-atherogenic cellular events (Figure 3).
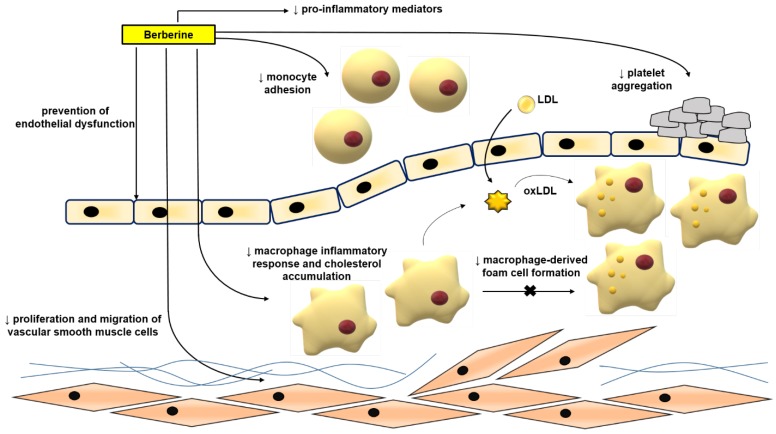
Figure 3.
Anti-atherosclerotic effects of BBR. The role of BBR in inhibiting atherosclerosis includes improving endothelial dysfunction; inhibiting smooth muscle cell proliferation and migration; reducing monocyte adhesion, macrophage inflammation and cholesterol aggregation, foam cell formation, and platelet aggregation. Abbreviations: low density lipoprotein (LDL); oxidized LDL (oxLDL).
Mechanism of BBR in protecting against atherosclerosis in vitro
Normalizing endothelial function
Endothelial dysfunction and its related complications are typically specified by reduced local bioavailability of nitric oxide (NO) and excessive oxidative stress; the increased NADH/NADPH and xanthine-oxidase activity are important factors for oxidative stress in endothelial cells 49-51. Enhanced adhesion of leukocytes to the endothelium plays an initiating role in inflammation 3, 7, 52, 53. Studies have proven the ameliorative effects of BBR in endothelial dysfunction via regulating reactive oxygen species (ROS)/NO balance 49, 52, 54. BBR treatment is capable to reduce oxidized low density lipoprotein (oxLDL)-stimulated production of ROS in human umbilical vein endothelial cells (HUVECs) 54. BBR could inhibit oxLDL‑stimulated monocyte adhesion to HUVECs via the mechanism associated with the suppression of vascular cell adhesion molecule-1 (VCAM‑1) and intercellular adhesion molecule-1 (ICAM‑1) 52. BBR has been shown to reduce the tumor necrosis factor α (TNFα)‑stimulated expression of the pro-inflammatory monocyte chemotactic protein-1 (MCP-1) and ICAM‑1 in human amniotic epithelial cells (HAECs) and to suppress the activation of nuclear factor kappa B (NF‑κB) in HAECs involving AMP protein kinase (AMPK)‑dependent pathway 55. The exposure of HUVECs to oxLDL or TNFα significantly increased the expression of lectin-like oxidized low density lipoprotein receptor-1 (LOX-1) and the production of intracellular ROS 56-58. Treatment with BBR reduced ERK1/2 signaling pathway, the expression of nicotinamide adenine dinucleotide phosphate-oxidase 2 (NOX2) and the expression of VCAM-1 and ICAM-1 56. BBR protected against palmitate-induced endothelial dysfunction via increasing NO level, and endothelial nitric oxide synthase (eNOS) expression and down-regulating the expression of NOX4 in HUVECs 59. BBR also contributed to the inhibition of the vascular inflammation via preventing angiotensin II (Ang II)-induced adhesion of monocytes to endothelial cells and reduced ROS and MCP-1 expression in HUVECs 60. Berberrubine, the active metabolite of BBR, has recently been shown to decrease xanthine oxidase activity and reduce TNFα-induced ICAM-1 expression in HUVECs 61.
BBR also dose-dependently inhibited the proliferation of HUVECs induced by oxLDL; its anti-proliferative and anti-inflammatory properties are exerted through decreasing the expression of NF-кB, LOX-1, proliferating cell nuclear antigen (PCNA) and inhibiting the phosphorylation of the phosphoinositide 3-kinase (PI3K)/Akt, ERK1/2, p38 mitogen activated protein kinases (MAPKs) signaling pathways 62. In HUVECs, BBR treatment showed protective effects also against oxLDL-induced endothelial injury and apoptosis through cytochrome c-mediated caspase activation pathway 54.
Inhibiting migration and proliferation of vascular smooth muscle cells (VSMCs)
The enhancement of VSMCs proliferation and migration is an important factor for causing of neointimal hyperplasia and luminal stenosis after vascular injury 63. Components of extracellular matrix, cytokines, shear stress, ROS, and other factors can significantly reduce the expression of markers of the differentiation of VSMCs, increase VSMCs proliferation and migration, and also a capacity for the synthesis of the extracellular matrix and promotion of neointimal formation 64. BBR had a beneficial effect on vascular remodeling 65, 66. BBR inhibited fetal bovine serum-induced proliferation of VSMCs by up-regulation of peroxisome proliferator-activated receptor α (PPARα) expression and NO concentration 67. BBR inhibited the migration of human aortic VSMCs by down-regulating matrix metalloproteinase (MMP)-2 and MMP-9, as well as urokinase-type plasminogen activator (u-PA) 68. Similarly, BBR attenuated Chlamydia pneumoniae infection-induced VSMCs migration by inhibiting PI3K and down-regulating the expression of MMP-3 and MMP-9 69.
In addition to its effect on the extracellular matrix, BBR reduced platelet-derived growth factor (PDGF)-induced proliferation of VSMCs by activating AMPK/p53/p21 signaling, while simultaneously inactivating Ras/Rac1/Cyclin D/Cdks, and attenuated PDGF-induced migration by inhibiting Rac1 and Cdc42 70. BBR limited the proliferation and migration of lysophosphatidylcholine (lysoPC)-stimulated VSMCs by decreasing ROS level and subsequent activation of the ERK1/2 pathway 71. BBR also significantly decreased the proliferation and migration of VSMCs stimulated by Ang II and heparin binding epidermal growth factor (HB-EGF) by inhibiting the activation of Akt pathway 65. In norepinephrine (NE)-induced pulmonary arterial VSMC proliferation and migration models, BBR can reverse the effect of NE by increasing protein phosphatase 2A (PP2A) signaling, suggesting that BBR may have a therapeutic effect in pulmonary hypertension 72. Furthermore, BBR induced the cell cycle arrest of A7r5 cells by disrupting the combination of p27, p21 and Skp2, inhibited the proliferation of A7r5 induced by PDGF-BB and enhanced the anti-proliferative effect of adrenal steroid dehydroepiandrosterone sulfate on A7r5 73. BBR blocked the cell cycle progression of VSMCs at G(1) phase by down-regulating the expression of cyclin D1, without affecting G(2)/M phase 74.
Inhibiting of macrophage-derived foam cell formation, inflammation, and inflammasome activation
The uptake of oxLDL into macrophages is mediated by diverse scavenger receptors (SRs), such as scavenger receptor A (SR-A)I/II, scavenger receptor class B type I (SR-BI), LOX-1, and the cluster of differentiation 36 (CD36)75. When oxLDL is endocytosed into macrophages, they develop into foam cells that form the core of atherosclerotic lesion 76, 77. BBR reduced oxLDL uptake by inhibiting CD36 and LOX-1, and promoted cholesterol efflux by suppressing the expression of adipocyte enhancer-binding protein 1 (AEBP1) in macrophages 78. BBR also inhibited the effect of oxLDL on macrophage-derived foam cell formation by inhibiting LOX-1, while up-regulating SR-BI expression 79. Moreover, it has been reported that BBR minimized the accumulation of lipids in human macrophages exposed to hypercholesterolemic serum by reducing the process of micropinocytosis and also decreased the secretion of MCP-1 80. Furthermore, BBR eliminated foam cells by enhancing liver X receptor α (LXRα) and ATP-binding membrane cassette transport protein A1 (ABCA1)-stimulated cholesterol efflux 81. The combination of atorvastatin and BBR suppressed the foam cells formation more effectively than atorvastatin alone 82. BBR suppressed the formation of foam cells from THP-1-derived macrophages by increasing the expression of AMPK and silent information regulator 1 (SIRT1), by decreasing the expression of PPARγ, and reducing the uptake of oxLDL 82. In addition, BBR combined with atorvastatin diminished the levels of serum triglyceride (TG), TC, and low-density lipoprotein cholesterol (LDL-C) and inflammation and oxidative stress markers 83. BBR combined with atorvastatin down-regulated the expression of LOX-1 through endothelin 1 receptor (ET-1R) in monocytes/macrophages 83, and in macrophages-derived foam cells, BBR-mediated sonodynamic therapy enhanced cholesterol efflux by promoting the production of ROS, and enhanced autophagy through the PI3K/Akt/mammalian target of rapamycin (mTOR) signaling pathway 84. However, it was shown that BBR induced the foam cell formation and promoted atherosclerosis by inducing the expression of SR-A in macrophages and increasing the uptake of modified low-density lipoprotein (LDL) 85. Although the vast majority of above mentioned studies show that BBR can suppress foam cell formation and the progression of atherosclerosis, this conclusion is still controversial.
BBR also exerted anti-inflammatory effects in macrophages stimulated with oxLDL. BBR down-regulated lipopolysaccharide (LPS)-induced IL-1β, IL-6, iNOS, MCP-1, cyclooxygenase (COX)-2 and MMP-9 expression, and p-MAPKs (including p38, c-Jun N-terminal kinase (JNK), and ERK) by activating AMPK 86. BBR reduced the production of inflammatory markers and induced autophagy in oxLDL-exposed J774A.1 cells 87. The mechanism of effect was associated with the activation of AMPK/mTOR signaling pathway 87. Furthermore, BBR inhibited the activation of the Nod-like receptor family pyrin domain containing-3 (NLRP3) inflammasome: BBR exposure reduced ROS-dependent activation of NLRP3 inflammasome in macrophages and inhibited the expression and release of IL-1β by inhibition of NF-κB 88. BBR can also reduce NLRP3 inflammatory expression in PMA-stimulated macrophages by inhibiting Toll-like receptor 4 (TLR4)/ myeloid differentiation factor 88 (MyD88)/NF-κB signaling pathway 89. BBR decreased sodium uric acid crystal induced inflammasome activation by suppressing the expression of NLRP3 and IL-1β 90. In addition, in adipose tissue-derived macrophages, BBR suppressed NLRP3 inflammasome activation and IL-1β production stimulated by saturated fatty acid (palmitate), by activating AMPK-dependent autophagy 91. BBR also inhibited the activation of the NLRP3 inflammasome pathway, and then improved liver injury in mice by inhibiting the purinoreceptor P2X7 92. TNFα and LPS stimulated the expression of miR-23a in RAW 264.7 macrophages, resulting in TLR4/TNF receptor-associated factor 2 (TRAF2)-mediated activation of apoptosis-signaling kinase 1 (ASK1) and phosphorylation of p38, which mediate inflammatory reaction 93. BBR treatment inhibited LPS and TNFα-induced inflammatory responses by up-regulating miR-23a, ameliorating TLR4, TRAF2, TNFα, IL-6 and IL-23 gene expression, and inhibiting TLR4/TRAF2-mediated ASK1/p38 phosphorylation 93. After percutaneous coronary intervention, macrophage activation plays an essential role in neovascular atherosclerosis and in-stent restenosis 94. Galectin-3, which was mainly expressed on macrophages, is an important mediator of inflammation. BBR down-regulated oxLDL-induced macrophage activation by down-regulating Galectin-3 via NF-κB and AMPK signaling pathways 94.
Inhibiting platelet activation
BBR has been shown to effectively prevent thrombus formation in arteries 95, and assisted thrombolysis induced by the plasminogen activators urokinase and streptokinase 96. The anti-platelet aggregation effects of BBR have been demonstrated in platelets isolated from healthy subjects, patients with platelet hyperaggregability, and also patients with atherosclerotic cerebral infarction 95. Chu et al. well reviewed the effect of BBR on platelets in 1996 97. BBR in vitro could inhibit platelet aggregation stimulated by adenosine diphosphate (ADP), collagen, adrenaline, arachidonic acid (AA), and calcium ionophore A23187 97. It also had inhibitory effect on clot retraction induced by ADP 98. BBR inhibited platelet activation by modulating the effect on cAMP level in platelets, antagonistic activity against Ca2+, partial and competitive binding with α2-adrenoreceptors on platelet membrane, affecting AA metabolism and ADP release from platelets 97.
BBR chloride decreased plasmatic levels of thromboxane B2 and P-selectin in mice with dextran sulphate sodium-stimulated colitis 99. BBR chloride also inhibited platelet activation via down-regulation of P-selectin expression and inhibiting fibrinogen binding to platelet GP IIb/IIIa integrin receptor on the surface of platelets 100. Shah et al. 101 reported that BBR inhibited collagen-induced platelet aggregation without affecting the platelet responses to the other platelet agonists including platelet-activating factor (PAF), AA and adrenaline. Its anti-platelet activity has been suggested to be exerted via suppressing with the collagen-induced adhesion process without any effect on cAMP, or A23187-induced platelet aggregation 101. While in one animal study investigating the effect of BBR on GPVI (glycoprotein receptor for collagen, expressed in platelets) BBR could not statistically inhibit the expression of GPVI 102, another study has proven the protective effects of BBR in combination with ligustrazine (alkylpyrazine from Ligusticum chuanxiong) in a rat model of coronary microembolization 103. In this study, ADP-induced platelet activation, von Willebrand factor, ET-1, and levels of TNFα, IL-1β, and ICAM-1 in serum and heart tissues were decreased by BBR/ligustrazine combination 103. Tissue factor (TF) is closely related to coagulation; its expression by vascular cells surrounding blood vessels is stimulated by pro-inflammatory substances such as LPS or TNFα 104. In this regard, BBR attenuated LPS-stimulated TF protein expression by suppressing NF-κB, Akt and MAPK signaling pathways in THP-1 cells 105. However, another study revealed that BBR could increase TNFα-stimulated TF expression in HAECs, and could decrease the expression of TF pathway inhibitor in HAECs and in arteries of apolipoprotein E-deficient mice (ApoE-/-) mice, what might promote thrombosis 104. BBR therefore might act bidirectionally on TF expression in different cell types 105.
Anti-atherosclerotic effects of BBR in vivo
Diverse investigations have reported the therapeutic potential of BBR to inhibit atherosclerosis in mouse models of atherosclerosis. For example, BBR treatment (150 mg/kg/d, p.o., 12wk) obviously reduced the atherosclerotic plaque area and displayed suppression of inflammatory and oxidative markers 106. Specifically, BBR diminished the serum levels of IL-1β and TNFα, and decreased the expression of ICAM-1, iNOS, and IL-6 in the aorta. Furthermore, the treatment with BBR reduced the translocation of NF-κB to the nucleus 106. In homocysteine thiolactone (HTL)-fed ApoE-/- mice, BBR (1.0 g/kg/d, p.o., 8wk) increased atherosclerotic plaque stability in the carotid artery and normalized the redox state. These protective effects on vascular function might be ascribed to an activation of PPARγ, which leads to a down-regulation of oxidative stress 107. BBR also abrogated the HTL-induced oxidative stress in HUVECs by activating PPARγ 107.
Visfatin is a pro-inflammatory adipokine, which is expressed in visceral fat and induces endothelial dysfunction by promoting the production of inflammatory and adhesion molecules 108. Oral administration of BBR (5 mg/kg/d, p.o., 12wk) in ApoE-/- mice lowered the serum expression of visfatin and inflammatory cytokines (TNFα and IL-6), as well as it reduced the distribution of visfatin in the atherosclerotic plaques 108. BBR pretreatment also reversed the visfatin-induced increase of IL-6 and TNFα in HUVECs 108. The amelioration of visfatin-induced endothelial dysfunction was associated with the inhibition of MAPK signaling pathway (p38 and JNK) 108. Moreover, BBR suppressed the increase of p-p38 MAPK, p-JNK and Bcl2- associated X protein (Bax) in visfatin-induced endothelial dysfunction in HUVECs 108. Furthermore, it was suggested that the protective effects of BBR (in drinking water (0.5 g/L), 14wk) in ApoE-/- mice can be related to the modulation of gut microbiota, specifically an up-regulation in Akkermansia spp. abundance which has been known to regulate inflammation, metabolic endotoxemia, and gut barrier integrity 109. A recent study showed that BBR (50 mg/kg, p.o., twice weekly, 12wk) inhibition of HFD-induced atherosclerosis in ApoE-/- mice is associated with changes in gut microbiota composition, such as BBR treatment altering an occurrence of Firmicutes and Verrucomicrobia 110.
Increased circulating endothelial microparticles in the peripheral circulation show the state of endothelial damage and endothelial cell activation, apoptosis and injury 111. BBR treatment (1.2 g/d, p.o.) in healthy humans led to a decrease in serum malondialdehyde and circulating CD31+/CD4- microparticles (as markers of endothelial injury) and the improvement of flow-mediated vasodilation. BBR contributed to an improvement of endothelial function via up-regulating eNOS expression and down-regulating NOX4 expression, and ROS production in HUVECs 112-114.
The MyD88 dependent TLR4 signaling pathway plays a critical role in hypertension-induce endothelial damage. TLR4 activation could activate NF-κB, leading to endothelial cell injury via an increased production of inflammatory enzymes and mediators (including COX-2, IL-1, and IL-6) 115. An increased level of TNFα initiates apoptosis and endothelial cell turnover, resulting in the formation of atherosclerotic plaques 115. BBR treatment inhibited the apoptosis, decreased the expression of NF-κB as well as the levels of TNFα and IL-6 in aortic endothelial cells isolated from spontaneously hypertensive rats (SHR) by decreasing the expression of TLR4 and MyD88 116. Endothelium-dependent contractions (EDCs) are also involved in endothelial dysfunction, and EDCs are caused by contracting factors such as endothelial COX-produced prostanoids or augmented level of ROS 117. EDCs of the carotid arteries of SHR were reduced by BBR administration 118. This effect has been reported to be caused by triggering of activated AMPK, inhibition of endoplasmic reticulum (ER) stress, reduction of ROS and expression of COX-2 118. BBR (5, 10 mg/kg, i.p.) has also been reported to inhibit NF-κB activity and decrease VCAM-1 production in lung of LPS-stimulated rats 119.
Cardiac hypertrophy and heart failure
Cardiac remodeling is associated with progressive cardiac hypertrophy, fibrosis, and the eventual occurrence of heart failure (HF) 120-123. Interventions in cardiac remodeling are important strategies for the treatment of HF 124. The effect of BBR on HF is shown in Figure 4.
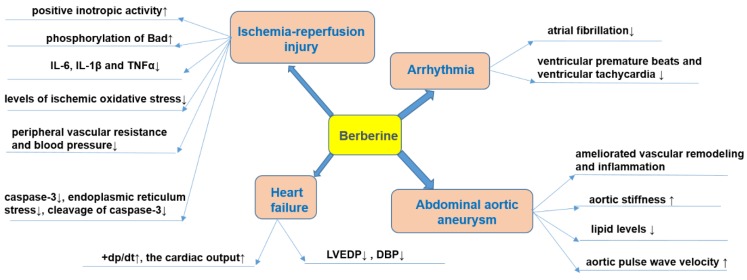
Figure 4.
Effects of BBR on heart failure, arrhythmia, myocardial ischemia and abdominal aortic aneurysm. Specifically, BBR prevents ischemia/reperfusion injury via its positive inotropic activity, increased phosphorylation of Bad, decreased production of pro-inflammatory mediators (IL-6, IL-1β, and TNFα), reducing oxidative stress, blood-pressure lowering, anti-apoptotic effects and protective effects against endoplasmic reticulum stress. BBR prevents heart failure by increasing cardiac output, and decreasing LVEDP and DBP. BBR prevents arrhythmia by reducing ventricular premature beats and tachycardia. BBR prevents abdominal aortic aneurysm by reducing vascular remodeling and pressure, reducing aortic stiffness, modulating lipid level, and increase aortic pulse wave velocity. ↑indicates increase or activation, and ↓indicates decrease or suppression. Abbreviations: Bad, Bcl-2-associated death promoter; diastolic blood pressure (DBP), interleukin-1β (IL-1β), interleukin-6 (IL-6), left ventricular end-diastolic pressure (LVEDP) , peak rate of rise of left ventricular pressure (+dp/dt), tumor necrosis factor α (TNFα).
In animal models, BBR can reduce the degree of HF. For example, in ischemic left ventricular heart failure dogs, intravenous injection of BBR (1 mg/kg, within 3 min) and then repeated infusion (0.2 mg/kg/min, 30 min) for 10 consecutive days, increased the cardiac output and peak rate of rise of left ventricular pressure (+dp/dt) while left ventricular end-diastolic pressure (LVEDP), diastolic blood pressure (DBP), and systemic vascular resistance were decreased125. The total saponins of Panax ginseng (20 mg/kg/d) combined with BBR (20 mg/kg/d), and captopril were administered for 12 consecutive days to rats in a model of HF induced by injecting of high dose of isoproterenol (s.c.), and a similar anti-HF effect was observed in both groups 126. BBR (63 mg/kg/d, p.o., 4wk) further proved to be a potential drug for improving HF symptoms by inhibiting the Ca2+ overload in cardiomyocytes 127.
Pathological cardiac hypertrophy is a critical intermediate step toward HF and other cardiac diseases 128. BBR (10 mg/kg/d, p.o., 8wk) prevented the development of left ventricular hypertrophy in rats caused by pressure overload; +dp/dt increased, while the weight of the whole heart and left ventricle decreased, and the increase of left ventricular myocardial cell size was significantly reduced 129, 130. Mechanistic studies have shown that BBR can up-regulate F-Box protein 32 (FBXO32), an E3 ubiquitin ligase, and down-regulated mTOR, ERK1/2, as well as p38 phosphorylation, which enhances autophagy and thus inhibits cardiac hypertrophy 128, 131. Cardiac fibrosis is an important pathological change in the development of HF, arrhythmia and cardiac arrest 132. BBR can restrict cardiac fibrosis by up-regulating the expression of relaxin in vitro 133. BBR administration (5, 10 mg/kg/d, p.o., 4wk) also obviously reduced cardiac fibrosis in two-kidney, two-clip (2K2C) rats via increased levels of NO and cAMP in left ventricular tissue134.
Abdominal aortic aneurysm
Abdominal aortic aneurysm is characterized by dilatation of the abdominal aorta with an etiology not completely understood 135. The presence of aneurysm leads to the weakening of the aortic wall, followed by a progressive dilatation and potential risk of aortic rupture 136. To date, only very limited studies investigating the effects of BBR against abdominal aortic aneurysm were published. One of the potential causes of formation of aneurysms is the increase in the ratio of collagen to elastin 137. It has been evidenced that BBR significantly reduced collagen synthesis in cardiac fibroblasts subjected to Ang II 138. The activation of MMPs is also a mechanism that participates in the etiology of aneurysms since it weakens the aortic media 139. In this sense, it was reported that BBR obviously decreased the activity and expression of MMP-9 as well as the expression of extracellular MMP inducer (EMMPRIN) in stimulated macrophages 140. In addition, BBR treatment ameliorated vascular remodeling in a rat model of metabolic syndrome by reducing the aortic levels of MMP-2 141.
It is well established that the formation of abdominal aortic aneurysm is related to abnormal wall stiffness 142. A clinical study investigated the effects of the two months consumption of 200 mg red yeast rice (RYR), 500 mg BBR and 10 mg policosanols in 70 hypercholesterolemic patients 143. The intervention significantly improved aortic stiffness by reducing lipid levels and increasing aortic pulse wave velocity 143. Furthermore, in aged mice, it has been evidenced that BBR induced the relaxation of VSMCs with decreasing of blood pressure and also reduced vascular stiffness via suppression of the activity of Ca2+ channel transient receptor potential vanilloid 4 (TRPV4) 144. The effect of BBR on abdominal aortic aneurysm was summarized in Figure 4.
Ischemia-reperfusion injury
Ischemic heart disease (ISHD) is primarily caused by coronary atherosclerosis and its complications 145, 146. Myocardial infarction is the most severe ISHD with high mortality 145. Reperfusion is beneficial for ischemia, but it can also cause severe cardiac damage 145. Thus, studying the underlying mechanisms of myocardial ischemia-reperfusion (I/R), contributes to the treatment of I/R injury in myocardial tissue 145, 146. The effect of BBR on myocardial ischemia was shown in Figure 4.
Experiments on isolated cardiomyocytes in hypoxia-reoxygenation model showed that pretreatment with BBR resulted in reduction in lactate dehydrogenase (LDH) and malondialdehyde (MDA) release, which are biomarkers of the extent of I/R injury 147. BBR inhibited I/R injury by the following mechanisms: i) direct and/or indirect antioxidant activity 148; ii) post-ischemic anti-inflammatory activity 149; iii) vasodilation of coronary arteries 150; iv) anti‑apoptotic activity on cardiomyocytes 151; v) suppressing an activation of autophagy during I/R152; vi) promoting angiogenesis in heart after I/R injury153.
Antioxidant activity of BBR
BBR showed direct antioxidant activity in several cell-free systems, such as DPPH radical scavenging assay 154, 155. Moreover, antioxidant activity was observed in cultured cells subject to oxidative stress 148, 156. BBR inhibited oxidative stress by increasing super oxide dismutase (SOD), uncoupling protein 2 (UCP2) and decreasing NOX expression, via SIRT1/FoxO (forkhead box O) or AMPK signaling pathways 157.
Anti-inflammatory effects of BBR
BBR is anti-inflammatory active by decreasing the secretion of an array of pro-inflammatory cytokines/mediators (IL-6, IL-1β, and TNFα) in myocardial tissue and serum by suppressing PI3K/Akt signaling pathway 157-159. BBR in cardiomyocytes in the mouse model of I/R injury inhibited inflammatory responses through the suppression of NF-κB signaling pathway 149. Another study showed that BBR can also activate SIRT1 signaling, and thus further reduce myocardial inflammatory response 160.
Hypotensive effects of BBR
BBR has hypotensive effects by functioning as a vasodilator in isolated blood vessels 161, 162. Vasodilation of coronary arteries and thus coronary flow is of key importance during the I/R injury of the heart 163. In this context, BBR enhanced coronary blood flow in isolated guinea pig hearts with ventricular fibrillation 150. Moreover, BBR can stimulate cardiac contractility (positive inotropic activity) by increasing intracellular calcium levels in addition to lowering peripheral vascular resistance and blood pressure 127. Several mechanisms are proposed for vasodilation and/or hypotensive effect of BBR: i) the antagonism on α1-adrenoreceptors on VSMCs 164, 165; ii) the enhancement of the hypotensive effect of acetylcholine (ACh) on nervus vagus, and thus the inhibition of carotid sinus pressor reflex 166; iii) the endothelium-dependent release of NO 167, 168; iv) via angiotensin-converting enzyme (ACE) inhibition of the NO-cGMP axis 169; v) the direct activation of K+ channels in arterial VSMCs leading to hyperpolarization, thereby the inhibition of calcium influx leading to smooth muscle relaxation 168, 170; vi) the inhibition of L- and T-type voltage-gated Ca2+ currents in ventricular myocytes 171.
Anti-apoptotic effects of BBR
One of the main mechanisms of BBR in protecting against I/R injury is the inhibition of apoptosis of cardiomyocytes. For example, in a mouse model of myocardial I/R, BBR inhibited the activation of caspase-3, caspase-9 and apoptotic protease-activating factor 1 (Apaf-1) in cardiomyocytes, while increased the expression of Bcl-2-like protein 1 and p53 149. In the rat hearts subjected to I/R injury, BBR treatment decreased AMPK and Bcl-2-like protein 1 in the myocardial risk areas, while increased AMPK in the non-ischemia areas compared to the control hearts 172. In neonatal rat cardiomyocytes, BBR decreased hypoxia-reoxygenation-stimulated cardiomyocytes apoptosis, increased Bcl-2/Bax ratio, activated PI3K-Akt, AMPK and eNOS phosphorylation, while decreased caspase-3 expression 173, 174. Recent studies on hypoxia-reoxygenation injury on H9C2 rat cardiac myoblasts proposed that BBR prevents apoptosis by modulating Notch1/Hes1-PTEN (phosphatase and tensin homolog)/Akt signaling pathway 175, as well as Smad7 (Mothers against decapentaplegic homolog 7) activation 151. BBR-mediated activation of Smad7 pathway resulted in the suppression of caspase-3 expression and activity. Indeed, the Smad7 knockdown confirmed this hypothesis 151. Importantly, BBR also activated the Janus kinase 2 (JAK2)/ signal transducer and activator of transcription 3 (STAT3) pathway, and thus decreased the endoplasmic reticulum (ER) stress 176.
Effect of BBR on autophagy and angiogenesis
Inhibition of activation of autophagy is an additional mechanism underlying the protective effects of BBR 152. Incubation of the cells with BBR or treatment with BBR increased survival of cells, decreased the infarct zone in mice hearts, and suppressed autophagy, which was confirmed by the decreased expression levels of autophagy-related proteins such as SIRT1, BNIP3, and Beclin-1 152. BBR can also be useful after I/R injury, since BBR can promote angiogenesis of the small vascular beds in coronary arteries 153. Post-ischemic application of BBR for 14 days reduced the infract zone, improved the heart function, as well as up-regulated miR-29b expression, and enhanced cell proliferation and migration in endothelial cells from left anterior descending (LAD) coronary artery 153.
Importantly, similar protective activities of BBR against I/R injury were observed also in non‑cardiac tissues 177. In neuronal cells during ischemia, BBR reduced p53 and cyclin D1, enhanced phosphorylation of Bad and decreased cleavage of caspase-3, thereby inducing cell cycle arrest and inhibiting apoptosis 177. During the reperfusion phase, BBR protected from cerebral ischemia injury via activating the PI3K/Akt signaling pathway 177. A pretreatment with BBR significantly preserved cells in response to a strong oxidant (CoCl2) 178. BBR injections were given prior to I/R surgery in rats and led to increased survival of neurons due to anti‑apoptotic effects mediated by PI3K/Akt signaling pathway 179. Moreover, in a mouse model of cerebral ischemia, BBR decreased the neuronal apoptosis via activating PI3K/Akt signaling pathway 180.
Protective activity was not only BBR-specific but it can be related to the other members of structural class of isoquinoline alkaloids, as both coptisine 181 and palmatine 182 showed similar protective effects against I/R injury on hearts of rats.
Furthermore, administration of BBR (100 mg/ kg/d, p.o., 14d) in rats prior to I/R injury (a surgical occlusion of LAD coronary artery) resulted in a reduced size of infarction and protection from arrhythmias 172. BBR prevented the occurrence and duration of isolated premature beats, ventricular fibrillation and ventricular tachycardia 172. In another model of acute myocardial infarction (induction by isoproterenol injection), BBR (30, 60 mg/kg/d, p.o., 14d) decreased the ST elevation stimulated by acute myocardial ischemia, and also down-regulated serum levels of ischemic biomarkers muscle/brain (MB) isoenzyme of creatine kinase (CK-MB), IL-6, TNFα and LDH 183. Moreover, ex vivo experiments evaluating I/R on isolated hearts showed that hearts pre-treated with BBR before ischemia had improved preservation of left ventricular developed pressure and LVEDP when compared to the non-treated group 172. Importantly, BBR had no influence on these parameters per se (on hearts without I/R injury) 172. In addition, a solid dispersion of BBR and sodium citrate (HGSD) improved BBR bioavailability and membrane permeability, and HGSD treatment (12.5, 25, 50 mg/kg/d, p.o., 7d) protected the rat heart from I/R injury by attenuating NF-κB and JNK signaling pathways 184.
Stroke
Similar to myocardial infarction, stroke also results from vascular or microvascular diseases which cause an interruption of cerebral blood supply and consequently brain dysfunction 185. To date, the reperfusion is the merely approved treatment for acute ischemic stroke 186. Consistently, thrombolytic/anti-platelet agents and surgery are the only available options 187. However, due to the fact that multiple mechanisms are involved in stroke progression, the therapeutic effect of current regimens is limited and agents that possess multiple pharmacologic actions have attracted much attention. Inflammation, apoptosis, and oxidation are three major mechanisms for the pathogenic proceeding of stroke 188.
In addition to the routine treatment, the administration of BBR 300 mg (t.i.d., p.o.) significantly reduced serum levels of macrophage migration inhibitory factor (MIF) and IL-6 in patients with acute cerebral ischemic stroke and to a certain extent decreased the carotid atherosclerosis and neurological deficit 189.
The right carotid artery of rats was ligated (ischemic injury) and BBR solution (0.2‒2 mg/kg) was intraperitoneally injected. After 30 min, the rats were subjected to hypoxic conditions by breathing in air with 10% oxygen and 90% nitrogen (a model of hypoxic damage). BBR dose-dependently reduced cerebral ischemia-hypoxic injury 190. BBR (0.2, 0.5, 1 or 2 mg/kg, i.p. or 0.2, 0.02, 0.002 mg/kg, i.v.) inhibited ischemia-induced apoptosis via enhancing the PI3K/Akt signaling pathway and exerted its neuroprotective effects in vivo and in vitro 179, 191. Additional mechanisms of BBR in preventing ischemic brain damage include reducing intracellular ROS levels and subsequently inhibiting of the mitochondrial apoptotic pathway 192. Moreover, BBR (10, 40 mg/kg) can reduce the ischemic brain injury in rats by promoting the activation of Akt/GSK3β (glycogen synthase kinase 3β) signaling pathway and claudin-5, while down-regulating the NF-κB expression 32. A similar study showed that BBR (25, 50 mg/kg/d, p.o., 14d) pretreatment dose-dependently reduced infarct size, neurological deficits, and cerebral edema in model of cortical tissue ischemia performed by transient middle cerebral artery occlusion 193. Its mechanism may depend on its anti-inflammatory effects, including an inhibition of nuclear translocation of high-mobility group box1 (HMGB1) and NF-κB, as well as TLR4 expression 193. In addition, BBR can promote angiogenesis in rats suffering from cerebral ischemia-reperfusion injury, which may be related to increased expression of hypoxia-inducible factor 1α (HIF-1α) and its downstream gene-vascular endothelial growth factor (VEGF) 194.
BBR can protect neurons during focal cerebral ischemia by up-regulating anti-inflammatory cytokines and down-regulating pro-inflammatory cytokines 195. The combination of BBR and other drugs has been tested to improve cerebral ischemia. For example, rats were reperfused after bilateral common carotid occlusion to induce a transient global cerebral ischemia model. Co-administration of BBR (5, 10, 20 mg/kg/d, 19d) and verapamil (2mg/kg/d, 19d) enhanced brain uptake of BBR and improved brain functions in rats 196. Berberis koreana extract (containing 7.39±0.78 mg/g of BBR) significantly ameliorated nerve injury induced by ischemic stroke in gerbils, by inhibiting COX-2 expression and PGE2 production 197. The main components of Huang-Lian-Jie-Du-Decoction (HLJDD) are BBR, baicalin and jasminoidin, which are commonly used in traditional Chinese medicine to treat ischemic stroke 198. HLJDD administration ameliorated ischemic stroke in rats by improving abnormal metabolism and regulating oxidative stress, neuronal autophagy, and inflammatory responses 198. A study evaluating the Yi-qi-jie-du formula (YJ) with the main constituents ginsenosides (G), BBR and jasminoidin (J) (in a ratio 3 (G): 2 (BBR): 0.5 (J)) showed the improvement of state in the focal cerebral ischemia in rats 199.
Arrhythmia
The anti-arrhythmic effect of BBR was firstly reported by Huang et al. in 1989 200. The authors induced ischemic ventricular arrhythmias in canines through occluding the LAD coronary artery and showed that BBR can prevent total ventricular premature beats and ventricular tachycardia 200. Recently, BBR (2 mg/kg, i.v.) hindered ACh-induced atrial fibrillation in rabbits via extension of action potential (AP) and effective refractory period in atrial myocytes 201. In addition, BBR (at a concentration of 300 mmol/L) prevented stretch-induced arrhythmia in isolated myocardial infracted hearts of Wistar rats 202.
Early studies proposed that BBR has class III anti-arrhythmic effects (by blocking K+ channel) 203. However, further studies revealed that BBR targets several types of channels such as the cardiac slow (IKs) and rapid (IKr) delayed rectifier K+ channels, ATP-sensitive K+ channel (KATP), inwardly-rectifying K+ channel (IKl), L-type Ca2+ (ICa) 166 and human hyperpolarization-activated cyclic nucleotide-gated 4 (hHCN4) channels 204. BBR (10, 20 mg/kg, p.o.) suppressed expression of IKr channel in rat ventricular tissues 205. Moreover, BBR inhibited the expression of hERG channel in hERG-transfected HEK293 cells 205. HERG channel encoded by hERG is an important subunit of Ikr channel 206. It crucially contributes to cardiac repolarization and its defect leads to long QT syndrome with manifestations such as delayed repolarization and prolonged QT interval 206. BBR (27.1 mg/kg, p.o..) induced extension of the AP duration and the QT interval in guinea pigs 207. BBR caused mature hERG reduction through inducing defect in channel trafficking, which led to an immature hERG response (unfolded protein response), and defective hERG underwent degradation in lysosomes and proteasomes 207. Fexofenadine and resveratrol, as two drugs preventing hERG trafficking defect, can reverse BBR-induced prolongation of AP duration 208. BBR can also block hERG channel directly via interacting with residues V625, Y652, and F656, respectively, in the central cavity of the channel 209. The effect of BBR on arrhythmia was summarized in Figure 4.
BBR in treating metabolic diseases
BBR in diabetes mellitus and its cardiovascular complications
Diabetes mellitus (DM) is linked to chronic hyperglycemia and abnormal metabolism of carbohydrates, lipids, and lipoproteins, which are caused by an inadequate production of insulin and/or insulin action 210, 211. DM is increasingly being recognized as a significant cause of mortality and morbidity, and profoundly contributes to the global health burden and death toll 210, 211. Based on the latest disease statistical report (The International Diabetes Federation, https://www.idf.org/): approximately 425 million people were diabetics in 2017 and this number is anticipated to increase to 629 million by 2045. There are two categories of DM: Type 1 diabetes (T1DM) and Type 2 diabetes (T2DM) 212. T1DM is characterized by the absolute deficiency of insulin secretion, while T2DM, the most common one, has features of insulin resistance (IR) and an insufficient compensatory insulin secretory response 212. Therapeutic effects of BBR on diabetes mellitus and its cardiovascular complications were summarized in Figure 5.
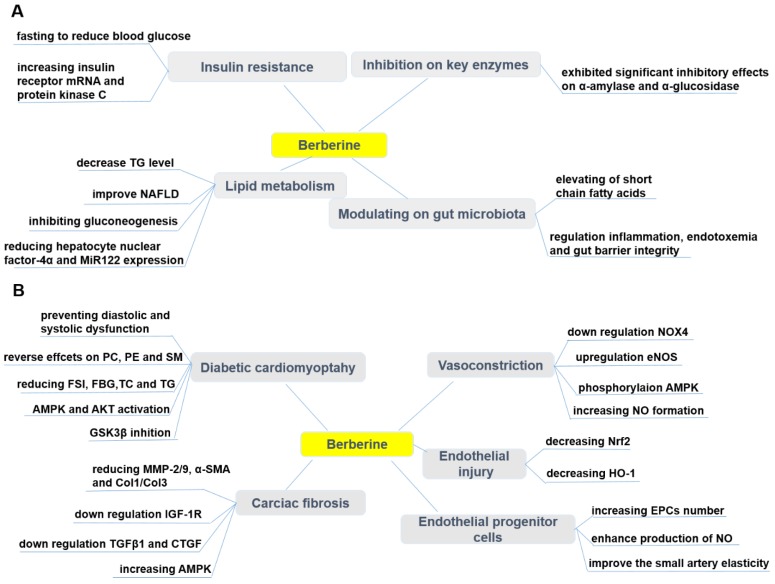
Figure 5.
Pharmacological effects of berberine in treating diabetes (A) and its cardiovascular complications (B). BBR exerts protective effects in diabetes by ameliorating insulin resistance, modulating lipid metabolism and gut microbiota, inhibiting α-amylase and α-glucosidase activity. BBR also prevents cardiovascular complications associated with diabetes, such as diabetic cardiomyopathy, cardiac fibrosis, endothelial injury, endothelial progenitor cell dysfunction, and vasoconstriction. ↑indicates increase or activation, and ↓indicates decrease or suppression. Abbreviations: AMP protein kinase (AMPK), α-smooth muscle actin (α-SMA), cholesterol (TC), collagen (Col), connective tissue growth factor (CTGF), dinucleotide phosphate-oxidase (NOX), endothelial nitric oxide synthase (eNOS), endothelial progenitor cells (EPCs), fasting blood glucose (FBG), fasting serum insulin (FSI), glycogen synthase kinase 3β (GSK3β), heme oxygenase-1 (HO-1), insulin-like growth factor-1 receptor (IGF-1R), matrix metalloproteinase (MMP), non-alcoholic fatty liver disease (NAFLD), nitric oxide (NO), nuclear factor erythroid 2-related factor 2 (Nrf2), phosphatidylcholine (PC), phosphatidylethanolamine (PE), protein kinase B (Akt), sphingolipid (SM), triglyceride (TG), transforming growth factor β1 (TGFβ1).
Effects of BBR on T1DM and T2DM
Physiologically, blood glucose level is regulated by the liver (gluconeogenesis and glycogenolysis) and glucose utilization by the peripheral tissues. An increase in the hepatic glucose production due to an inadequate insulin secretion/action is the major cause of hyperglycemia in DM patients 210, 211. DM can lead to many complications such as hyperlipidemia, hypertension, atherosclerosis, hyperinsulinemia, retinopathy, nephropathy and peripheral neuropathy 213, 214. Approved oral hyperglycemic drugs such as derivatives of sulfonylurea, metformin, and thiazolidinediones are reported to induce some side effects 9-11. In addition to the adverse effects, the conventional medicines are expensive and not always satisfactory in maintaining normal level of blood glucose 215. Many herbal medicines with potential of anti-diabetic effect have been widely used for treating DM in various traditional systems of medicine worldwide since the immemorial time 216. Nowadays, the market for natural anti-diabetic drugs is booming as they are preferred for their effectiveness, lower occurrence of side effects and relative low costs 216.
Recently, a plethora of investigations has shown that BBR is a promising hypoglycemic, and anti-hyperlipidemic compound by modulating various signaling pathways 217-221. It diminished body mass in DM patients 217-219. The exact mechanism of action underlying the hypoglycemic effect of BBR is not fully elucidated. In vitro and in vivo studies have highlighted that BBR contributed to its therapeutic activities via variety of mechanisms and signaling pathways, including improving IR, activating AMPK, modulating gut microbiota, reducing gluconeogenesis in liver and enhancing glycolysis in peripheral tissues 217, 222-224. Although many studies have shown that BBR is an AMPK activator 30, 225, 226, in HepG2 and C2C12 cells BBR promoted glucose metabolism by stimulating glycolysis, and this effect may be independent of AMPK activity 227. A recent study has shown that BBR (150 mg/kg/d, p.o., 7d) promoted glucose uptake and restrict gluconeogenesis in rats by inhibiting SIRT3 and promoting ubiquitination of phosphoenol pyruvate carboxykinase 1 (PEPCK1) 228. The entry of pyruvate into the mitochondria via the mitochondrial pyruvate carrier (MPC) is a central step in hepatic gluconeogenesis 229. BBR limited the gluconeogenesis of mitochondrial pyruvate by inhibiting the deacetylation of MPC1 by SIRT3 229. This can be a therapeutic strategy to prevent excessive hepatic glucose production 229. The hypoglycemic effect of BBR was also partially mediated by an anti-inflammatory and antioxidative mechanism 157, 230, 231. It is challenging to justify the clinical efficacy of BBR due to its low oral bioavailability, although it is clinically active, and it exerted therapeutic effects through different mechanisms 232, 233.
Effects of BBR on insulin resistance (IR)
BBR has been shown to ameliorate IR, which is the main metabolic abnormality culminating not only to T2DM, but also to metabolic syndrome 234. It can be defined as a state in which normal or increased insulin level produces an attenuated biological response 235. Several researchers have reported that BBR is effective in mitigating the IR through different pathways. Kong et al. 236 have investigated the molecular mechanism of BBR against IR and BBR was found to reduce the fasting blood glucose (FBG) and fasting serum insulin (FSI), increase insulin receptor (InsR) mRNA and insulin sensitivity as well as protein kinase C (PKC) activity both in vitro and in T2DM rats. Mahmoud et al. 237 have demonstrated that treating rats, with IR syndrome, with 50 mg/kg/day of BBR for 2 weeks was effective against IR syndrome by improving IR, lipid profile, antioxidant enzymes, pro-inflammatory cytokines, and IFN-γ. Liu et al. 238, 239 have also revealed the effectiveness of BBR against IR. Increased branched-chain amino acids (BCAAs) are involved in obesity and IR as Yue et al. 240 have reported that BBR (200 mg/kg/d, p.o., 10wk) can improve IR in HFD-fed mice and diabetic patients by altering the intestinal microbiota of BCAAs biosynthesis and BCAAs catabolism in liver and adipose tissue.
Effects of BBR on lipid metabolism
BBR is well-known to improve glucose and lipid metabolic disorders. BBR was an approved component of nutraceuticals for treatment of hyperlipidemia in many countries 241. Kong et al. 23 have described BBR as “a new lipid-lowering drug” after they observed the efficacy of BBR in lowering lipid level in vitro and in vivo, which was comparable to that of statins. Zhao et al. 242 have reported that BBR (150 mg/kg/d, p.o., 16wk) improved NAFLD, a critical hepatic manifestation of metabolic syndrome, by inhibiting gluconeogenesis and regulating lipid metabolism. BBR (40, 60 mg/kg/d, p.o., 4wk) regulated hepatic gluconeogenesis and lipid metabolism in T2DM mice via reducing the expression of hepatocyte nuclear factor-4α and miR122 243. The main metabolite of BBR in vivo, berberrubine (M3), showed the most potential hypolipidemic effect by up-regulating LDLR expression in HepG2 cells 244. Nine berberrubine analogs modified at the C9 position were tested for their lipid-lowering activity. The results showed that berberrubine and hydroxypropyl-berberine can regulate the expression of liver LDLR and PCSK9 through ERK signaling pathway. Hydroxypropyl-berberine showing a greater effect, which may indicate it as a candidate drug for anti-hyperlipidemia 244.
Effect of BBR on modulating gut microbiota
Human gut microbiota plays a vital role in mediating obesity-related metabolic dysfunction, including T2DM 245. For example, Fei et al. 246 have revealed that an endotoxin-producing Enterobacter cloacae B29, obtained from the gut of obese subjects, induced IR and obesity in germ-free mice. Another study has shown that endotoxin produced by the pathogen in the gut, such as Escherichia coli, caused obesity and IR when it was subcutaneously administered into mice 247. As BBR has been known for treating intestinal infection-related diarrhea, Han et al. 248 hypothesized that gut microbiota regulation can be one of the anti-diabetic mechanisms of BBR. Recently, Zhu et al. 109 have reported that BBR (in drinking water (0.5 g/L), 14wk) treatment significantly reduced atherosclerosis in HFD treated mice by up-regulating the population of Akkermansia spp. which was confirmed to regulate inflammation, endotoxemia and gut barrier integrity. The study carried by Zhang et al. 233 showed that BBR (100 mg/kg/d, p.o., 18wk) modulated gut microbiota, and it is particularly important that the observed elevating of short chain fatty acids (SCFAs) levels in the intestine, may contribute to its therapeutic effect against DM, obesity and other metabolic diseases.
BBR as inhibitors of α-amylase and α-glucosidase
Inhibition of key carbohydrate hydrolyzing enzymes, in clinic relevant α-amylase and α-glucosidase, has been acknowledged as one of the most effective approaches for managing of DM and delaying postprandial hyperglycemia 249, 250. Enzymes α-amylase and α-glucosidase are present in the small intestine and its brush border and are responsible for hydrolytic breakdown of complex oligosaccharides and disaccharides into glucose and further monosaccharides suitable for absorption 249, 250. Inhibition of these enzymes delayed carbohydrate digestion, resulting in a down-regulation in the rate of intestinal glucose absorption and subsequent reduction of the post-prandial glucose levels 249, 250. Interestingly, BBR has been found to exhibit significant inhibitory potency against both α-amylase and α-glucosidase 223, 249, 251, 252.
Effect of BBR on DM-induced cardiovascular disease and complications
Chronic exposure to hyperglycemic conditions (accompanying DM), can cause damages to various tissues, as well as induces vascular injury and cardiomyopathy 253, 254. High glucose level plays an important role for endothelial injury. BBR (100 mg/kg/d, p.o., 8wk) ameliorated impaired endothelium-dependent vasorelaxation of aorta in T2DM rats by down-regulating NOX4 expression and up-regulating eNOS expression 255. Normal vascular tone is sustained by various dilatory and constrictory agents where NO is the major vasodilator. A main feature of endothelial dysfunction is impaired endothelium-dependent relaxation 256. An effect of BBR on vascular tone has been reported in different studies 168, 169, 257. BBR caused vasorelaxation in isolated rat aorta cells via phosphorylation of AMPK and eNOS 257. BBR has been evidenced to exert its protective effects on vascular endothelium via increasing NO formation 168, 169. In addition, it has been shown that BBR (50, 100, 200 mg/kg/d, p.o., 4wk) might contribute to the protection against endothelial injuries in retinal tissue of DM rats via decreasing the expressions of nuclear factor erythroid 2-related factor 2 (Nrf2) and heme oxygenase-1 (HO-1) 258. Both the endothelium and the underlying VSMCs could be affected by BBR to induce relaxation 168. BBR, as a sensitizer of the insulin signal in HUVECs, also improved insulin-mediated vasodilatation in diabetic rats involving PI3K/Akt and AMPK activation via the up-regulation of the InsR 259. The vasodilator effect of BBR (200 mg/kg/d, p.o., 4wk) also improved ACh-induced mesenteric artery vasodilation in diabetic rats 259. There are findings indicating that the decrease in UCP2 expression and mitochondrial ROS accumulation are related to vascular damage 260. UCP2 has been found to reduce high glucose-induced apoptosis in HUVECs by increasing Bcl-2 while decreasing caspase-3 and cytochrome c 261. Concurrently, BBR promoted the mitochondrial biogenesis and enhance UCP2 mRNA and protein expression in cultured HUVECs 262. BBR exerted this pharmacological effect through AMPK-dependent manner, which led to reduction in oxidative stress and vascular inflammation 262. Increased atherothrombotic events due to platelet activation and apoptosis are the leading cause of high mortality and morbidity during DM 263. Platelet hyperresponsiveness and apoptosis during DM are ROS accumulation caused by activation of aldose reductase (AR) and NOX. BBR protects platelets by suppressing AR and NOX activity in high glucose treated platelets 263.
Endothelial progenitor cells (EPCs) play a significant role in endothelial function 264. The reduced number and impaired function of circulating EPCs are markers of vascular diseases, and contribute to impaired arterial elasticity and endothelial dysfunction, particularly in cardiovascular diseases 264. BBR (1.2 g/d, p.o., 30d) has been confirmed to increase the number of circulating EPCs 265, 266, enhanced the production of NO265 and improved the small artery elasticity 266 in healthy volunteers. However, in one randomized trial there were no changes in circulating EPCs in individuals with dyslipidemia after treatment with a nutraceutical formulation containing BBR 267. Oppositely, another trial concluded the improvement of endothelial function after treatment by combination of BBR, RYR and policosanols, through increasing the endothelial-dependent flow-mediated dilation (FMD) in patients with hypercholesterolemia 268.
Diabetic cardiomyopathy (DCM) is considered to be a clinical pathology independent of concomitant vascular diseases and can be primarily caused by disturbances in the energy substrate 269. In the high-sucrose and HFD/streptozotocin (STZ)-induced rat DCM model, BBR (10, 30 mg/kg/d, p.o., 16wk) significantly prevented diastolic and systolic dysfunction, and cardiac hypertrophy 269. Phosphatidylcholine (PC), phosphatidylethanolamine (PE) and sphingolipid (SM) are potential biomarkers of DCM, and the protective effect of BBR on DCM can be through reversal of PC, PE and SM metabolic disturbances 269. BBR treatment (100 mg/kg/d, p.o., 16wk) of diabetic rats can partially improve cardiac function and significantly reduce FSI, FBG, total TC and TG levels. The underlying mechanism can be that BBR activated cardiac AMPK and Akt in diabetic rats and inhibited GSK3β activity 270. Similarly, in the palmitate-induced H9C2 cell hypertrophy model, BBR up-regulated alpha-myosin heavy chain (α-MHC) expression, down-regulated beta-myosin heavy chain (β-MHC) expression and thus inhibited H9C2 cell hypertrophy 270. Moreover, BBR also enhanced AMPK and Akt activation in H9C2 cells and inhibited GSK3β activity 270, 271. Diabetic hearts are more sensitive to I/R injury, and BBR treatment protected the heart of diabetic rats from I/R damage 272. This protective effect of BBR was achieved by activating AMPK and Akt activity, while inhibiting GSK3β activity in non-ischemic regions of the diabetic rat hearts 272.
Diabetic cardiac fibrosis causes ventricular stiffness and leads to diastolic dysfunction 273. In a diabetic rat model, BBR treatment (100 mg/kg/d, p.o., 4wk) improved cardiac fibrosis and dysfunction by down-regulating insulin-like growth factor-1 receptor (IGF-1R) expression in cardiac fibroblasts, specifically by reducing expression of MMP-2/9, α-smooth muscle actin (α-SMA) and type 1 collagen (Col1) in diabetic hearts. BBR also exerted a similar effect in cardiac fibroblasts exposed to high levels of glucose 273. Furthermore, BBR (50, 100, 150 mg/kg/d, p.o., 12wk) reduced cardiac fibrosis in DM rats by down-regulating the expression of transforming growth factor β1 (TGFβ1) and connective tissue growth factor (CTGF), reducing the expression of Col1 and Col3 274. In addition, BBR treatment promoted glucose depletion and glucose uptake as well as improved IR in H9C2 cells, at least partially by increasing AMPK activity 222. Further, BBR (100 mg/kg/day, p.o., 7d) ameliorated arrhythmias induced by ischemia (LAD ligature) in diabetic rats 275. Researchers have shown that BBR reversed the down-regulation of the transient outward K+ current (Ito) and ICa 275. In a similar study, BBR (60 mg/kg/day, p.o., 14d) led to the restoration of diminished inwardly rectifying potassium channel Kir2.1 to nearly normal levels 276. The effect of BBR on Kir2.1, the main subunit of IK1, was associated with recovering of resting membrane potential and alleviating of ischemia-induced arrhythmias in diabetic rats 276.
In conclusion, BBR is a promising candidate for therapy of T2DM and metabolic syndrome. However, further investigations of the mechanisms of BBR are required for its appropriate application in clinical settings.
Obesity
Obesity is a complex metabolic disease occurring in both developed and developing countries 277. Obesity contributes to the development of several other health problems, such as cardiovascular diseases, DM, cancer, chronic obstructive pulmonary disease, and depression 277. Etiology of obesity is multi-factorial and is associated with the energy input exceeding energy output 278. Most commonly, it is induced by excessive food intake, imbalanced nutrition, physical inactivity, and genetic predisposeitions. Other causes of obesity include endocrine dysfunction, mental illnesses, or iatrogenic etiologies 278.
BBR reduced food intake in the mice fed with HFD, and decreased their weight gain 279. Such an effect led to the question as to how BBR affects the appetite. BBR can improve lipid dysregulation by controlling both peripheral and central AMPK activity 280. Although BBR cannot cross the cerebrovascular barrier, studies have shown that an application of BBR intraperitoneally caused a 47% up-regulation in serotonin levels in the brain 281. The expression of glucagon-like peptide 1 receptor (GLP-1R), orexin A and neuropeptide Y in brain of tested animals were found to be up-regulated 282. Together with changes observed in hypothalamus, this can be a factor causing the decrease of body weight, enhanced lipolysis, and decrease of IR in obese experimental animals and even humans.
It is clear, that anti-obesity effects of BBR are associated with its anti-diabetic activity 283. Many studies identified BBR as an activator of AMPK, which is, besides other effects, responsible for triggering of the glucose uptake and fatty acid oxidation in skeletal muscles, and regulation of insulin secretion by pancreatic β-secretory cells 30, 225, 226. Effects of BBR on an increase of glucagon-like peptide-1 (GLP-1) via enhancing GLP-1 secretion and GLP-1 biosynthesis in enteroendocrine L-cells and some neurons were also observed, and BBR stimulated GLP-1 secretion can trigger the feeling of satiety and decrease the food intake 284. Mitochondrial stress responses (e.g., mitochondrial swelling and membrane rupture) and GLP-1 expression were decreased in the colon of diet-induced obese mice 285. Administration of BBR (100 mg/kg/d, p.o., 8wk) up-regulated GLP-1 expression in mice and prevented mitochondrial stress response 285. All these pharmacological effects of BBR can translate to improved outcomes in DM and obesity.
Several studies have shown altered intestinal architecture as a result of a shift in gut microbiota composition to the phyla Bacteroidetes and Firmicutes 286. The pivotal barrier-protecting function conferred by BBR was mediated by elevated levels of SCFAs 233. Gene profiling analysis showed that BBR can regulate gut microbiota diversity. In the group of BBR-treated rats (100 mg/kg/d, p.o., 18wk), the shift to bacteria producing SCFAs was shown to be significant 233. On the other hand, fasting-induced adipose factor (FIAF), which inhibits circulating lipoprotein lipase (LPL), is a regulator as a putative mediator of microbial modulation of energy storage, and fat mobilization 287. BBR (200 mg/kg/d, p.o., 6wk) up-regulated FIAF expression in adipose tissues and intestinal and also changed the abundance of fecal Bacteroidetes and Firmicutes in total bacteria in the gut of mice fed with HFD 288. Additionally, Chae et al.289 showed modulation of growth of gut microbiota, especially Lactobacillus and Bifidobacterium by BBR.
Non-alcoholic fatty liver disease (NAFLD)
NAFLD is manifested as an accumulation of TG in liver 290. NAFLD is closely related to the obesity and related metabolic risk factors (T2DM and dyslipidemia). Untreated NAFLD can progress to non-alcoholic steatohepatitis (NASH), characterized by persistent hepatocyte inflammation and injury with or without fibrosis. NASH can progress to cirrhosis and liver cancer 291, 292.
According to the main characteristics of NAFLD, the first therapeutic option is the restoration of dysregulated lipid metabolism, which leads to the fat reduction and weight loss 290. BBR (5 mg/kg/d, p.o., 3wk) improved fatty liver in obese mice by regulating neural signaling from the central nervous system and peripheral AMPK signaling 293. Sterol regulatory element binding protein 1c (SREBP1c) can be regulated by AMPK via direct phosphorylation 294. AMPK activation suppresses SREBP-1c activity and lowers hepatic and plasma levels of TG and TC 294. BBR acted as a potent inhibitor of SREBP-1c, possibly through AMPK pathway 295, 296. BBR (100 mg/kg) can down-regulate SREBP-1c and ameliorate lipid profile in rats 297. The combination of BBR (50 mg/kg/d, p.o., 8wk) and curcumin (50 mg/kg/d, p.o., 8wk) is more effective than lovastatin (100 mg/kg/d, p.o., 8wk) 298. BBR can reverse the disorder of lipid metabolism in 3T3-L1 cells induced by olanzapine, a second-generation antipsychotic drug, by inhibiting SREBP and activating AMPKα 299. Overexpression of SREBP-1c leads to the down-regulation of insulin receptor substrate 2 (IRS-2) mRNA levels which is closely linked to the hepatic IR 300. BBR reduced liver TC levels by down-regulation of sterol carrier protein 2 expression and inhibiting COX-2 induced prostaglandin production301. The improvement of IR by increasing IRS-2 mRNA expression is one of the possible mechanisms in the treatment of NAFLD with BBR 302.
Another transcription factor carbohydrate-responsive element binding protein (ChREBP) also participated in the modulation of lipogenic genes (e.g. L-PK) as it has been demonstrated in the liver of carbohydrate-fed rats 303. BBR (380 mg/kg/d, p.o., 5wk) was able to suppress the expression of ChREBP and ameliorated fatty acid synthesis in the liver 304. BBR has been reported as a potential PPARα activator in diabetic hamsters 305, although this finding is inconsistent with the results of the study conducted previously 306, where BBR did not influence the expression of PPARα, but directly up-regulated the expression of microsomal triglyceride transfer protein (MTTP) through reduction of methylation of MTTP promoter. MTTP regulated the assembly and secretion of ApoB-containing lipoproteins (including LDL and VLDL) 306. Similarly, BBR (200 mg/kg/d, p.o., 16wk) can ameliorate the symptoms of NAFLD in rats by increasing the expression of LXRα/FAS 307, UCP2 308 and MTTP 306 in hepatocytes. In addition, BBR (50mg/kg/d, p.o., 8wk) inhibited HFD-induced down-regulation of carnitine-palmitoyltransferase 1A (CPT 1A) and PPARα expression in fish 309. BBR obviously reduced TC and LDL-C in hyperlipidemic rats while up-regulated high-density lipoprotein-cholesterol (HDL-C) and CPT 1A expression 310. BBR (5 mg/kg/d, p.o., 4wk) maintained the energy balance and reduced hepatic steatosis in mice by enhancing autophagy and activating fibroblast growth factor 21 (FGF21), and this effect was dependent on SIRT1 311, which is the inductor of the expression of PPARα. The depletion of SIRT1 attenuated PPARα signaling and fatty acid β-oxidation, and it can lead to the development of ER stress, hepatic inflammation, and hepatic steatosis 312. Thus, BBR may be effective in reversing steatohepatitis and fibrosis similarly as fibrates and other PPARα agonists in mice, although there was no significant improvement in histological findings in human subjects 313. C‑C motif ligand 19 (CCL19) was highly expressed in patients with NAFLD 314. In a model of HFD-induced rat NAFLD, metformin and BBR improved NAFLD by activating AMPK signaling, and metformin and BBR significantly reduced high expression of CCL19 in NAFLD rats. It is postulated that inhibition of CCL19 may be an effective treatment for NAFLD 314.
Oxidative stress, lipid peroxidation, and inflammatory cytokines lead to the development of hepatic steatosis that can progress to devastating NASH, potentially leading to fibrosis and cirrhosis 315. An increased inflammatory response (e.g. TNFα, IL-6 up-regulation) has been observed in patients with NAFLD 316. TNFα is recognized as a critical factor in NAFLD and related liver diseases and an inhibition of pro-inflammatory cytokines production could be an important strategy to treat NAFLD 316. BBR obviously reduced the p-JNK1 in mouse primary hepatocytes, whereas the level of p-AMPK was not significantly changed. These results showed, that the inhibition of inflammation by BBR could have AMPK-independent mechanisms 317, although Jeong et al. 86 have reported that BBR (5 mg/kg/d, i.p., 3wk) down-regulated the production of pro-inflammatory cytokines (IL-6, IL-1β and TNFα) in adipose tissue of obese db/db mice through AMPK activation. Additional mechanisms of attenuation of hepatic steatosis can be the modulation of gut microbiota 318. HFD could cause the overgrowth of Gram negative bacteria in the intestine and subsequently the alternation of composition of intestinal microbiota, which leads to the increase of the intestinal permeability and inflammation 319. BBR (150 mg/kg/d, p.o., 4 wk) could decrease the level of Faecalibacterium prausnitzii in rats 320 as well as the number of Firmicutes and Bacteroidetes in the feces of mice fed a HFD 288.
Taken together, BBR represents a very promising therapeutic drug in various metabolic diseases via its pleiotropic effects, including the regulation of lipid and glucose metabolism, oxidative stress, and inflammatory response. Since most studies are performed in pre-clinical animal models, more randomized large-scale clinical trials are needed to evaluate the metabolic effects of BBR in human patients.
Molecular targets of BBR
BBR modulates multiple cellular events involved in cardiometabolic diseases by modulating multiple disease-relevant targets (Figure 6). The major molecular targets involved in the cardioprotective and metabolic effects are AMPK, PPAR, LDL receptor (LDLR), hepatocyte nuclear factor 1α (HNF1α), IκB kinase β (IKKβ), silent information regulator (SIRT1), and gut microbiota. In this section, a detailed account on the molecular targets of BBR in various CVMD will be summarized.
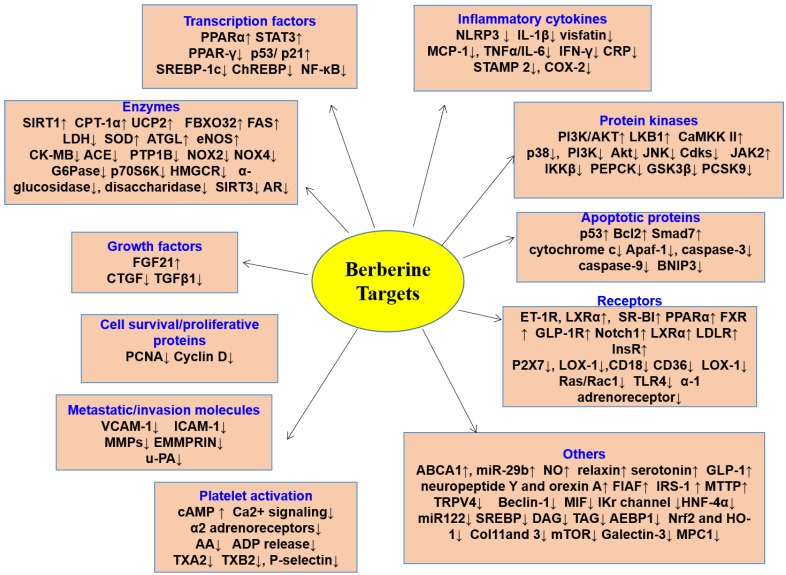
Figure 6.
Molecular targets of BBR. BBR exerts its pharmacological effects by regulating the expression of genes/proteins responsible for transcription factors, enzymes, growth factors, cell survival/proliferative proteins, metastatic/invasion molecules, platelet activation, inflammatory cytokines, protein kinases, apoptotic proteins, receptors, and the others. By targeting these molecules, BBR prevents the development of multiple cardiovascular and metabolic diseases. ↑indicates increase or activation, and ↓indicates decrease or suppression. Abbreviations: arachidonic acid (AA), ATP-binding membrane cassette transport protein A1 (ABCA1), angiotensin-converting enzyme (ACE), adenosine diphosphate (ADP), adipocyte enhancer-binding protein 1 (AEBP1), apoptotic protease-activating factor 1 (Apaf-1), adipose triglyceride lipase (ATGL), aldose reductase (AR), calmodulin-dependent kinase II (CaMKK II), C‑C motif ligand 19 (CCL19), the cluster of differentiation 18 (CD18), the cluster of differentiation 36 (CD36), carbohydrate responsive element binding protein (ChREBP), MB isoenzyme of creatine kinase (CK-MB), type 1 collagen (Col1), C-reactive protein (CPR), connective tissue growth factor (CTGF), 1,2-diacyl-sn-glycerol (DAG), endoplasmic reticulum (ER), extracellular MMP inducer (EMMPRIN), endothelin 1 receptor(ET-1R), fatty acid synthase (FAS), fibroblast growth factor 21 (FGF21), fasting-induced adipose factor (FIAF), farnesoid X receptor (FXR), glucose-6-phosphatase (G6Pase), glucagon-like peptide 1 receptor (GLP-1R), 3-hydroxy-3-methylglutaryl-CoA reductase (HMGCR), hepatocyte nuclear factor-4α (HNF-4α), intercellular adhesion molecule-1 (ICAM-1), IκB kinase β (IKKβ), interleukin-1β (IL-1β), interleukin-6 (IL-6), insulin receptor (InsR), insulin receptor substrate 2 (IRS-2), N-terminal kinase (JNK), lactate dehydrogenase (LDH), LDL receptor (LDLR), lectin-like oxidized low density lipoprotein receptor-1 (LOX-1), monocyte chemotactic protein-1 (MCP-1), migration inhibitory factor (MIF), matrix metalloproteinases (MMPs), mitochondrial pyruvate carrier (MPC), microsomal triglyceride transfer protein (MTTP), nuclear factor-kappaB (NF-κB), Nod-like receptor family pyrin domain containing3 (NLRP3), nitric oxide (NO), nicotinamide adenine dinucleotide phosphate oxidase 2 (NOX2), nicotinamide adenine dinucleotide phosphate oxidase 4 (NOX4), nuclear factor erythroid-2-related factor-2 (Nrf2), protein S6 kinase (p70S6K), proprotein convertase subtilisin/kexin type 9 (PCSK9), ribosomal proliferating cell nuclear antigen (PCNA), P-glycoprotein (P-gp), phosphoenol pyruvate carboxykinase (PEPCK), phosphatidylinositol 3 kinase (PI3K), peroxisome proliferator-activated receptor α (PPARα), peroxisome proliferator-activated receptor γ (PPARγ), protein tyrosine phosphatase1B (PTP1B), activate silent information regulator 1 (SIRT1), super oxide dismutase (SOD), scavenger receptor class B type I (SR-BI), sterol regulatory element binding protein (SREBP), 1,2,3-triacyl-sn-glycerol (TAG), tissue growth factor-β1(TGFβ1), Toll-like receptor 4 (TLR4), tumor necrosis factor α (TNFα), TNF receptor-associated factor 2 (TRAF2), transient receptor potential vanilloid 4 (TRPV4), uncoupling protein 2 (UCP2), urokinase-type plasminogen activator (u-PA), vascular cell adhesion molecule-1 (VCAM-1).
Increased ratio of AMP/ATP promotes the activation of AMPK, which is a decisive regulator of energy metabolism and is responsible for controlling several features of cellular resistance 321, 322. BBR was found to decrease ROS production by either up-regulation of SOD expression 323, 324 or negative regulation of NOXs, probably through AMPK activation 30, 225. Pharmacological actions of BBR are similar to that of metformin, which acts through regulation of different effectors in lipid and energy metabolism, such as PKC, AMPK, and MAPK 236, 325. The enhancement of adipose triglyceride lipase (ATGL) expression, which was mediated by AMPK, was mainly considered to be responsible for the long term body weight losing effect of BBR and this effect is also attributed to the enhancement of basal lipolysis of TG present in the adipocytes which is directly correlated with dyslipidemia and obesity 326. However, the proliferation of preadipocytes was inhibited by BBR, via C/EBPα and PPARγ pathways 327, 328. One of the risk factor of CVD, LDL-C, was also lowered by BBR and this effect was via increasing LDLR expression, which also upsurges the LDLR-mediated liver clearance and BBR-caused stabilization of LDLR mRNA was regulated through the ERK signaling pathway revealed the mechanism behind cholesterol lowering effect of BBR 23, 329. The modulation of LDLR takes place at a post translational level where BBR degraded and ubiquitinized HNF1α 330-332. Moreover, the up-regulation of LDLR expression is dependent on the ERK activation 23.
The up-regulation of AMP level and consequent activation of AMPK by BBR was also related to the inhibition of mitochondrial respiratory complex 1 which represents a prominent target for the compounds which improve entire body insulin sensitivity 333. BBR blocked complex 1 and led to the enhancement of lactate release and glucose consumption. This process is independent of AMPK activation 331, 334. Modulation of glycolipid metabolism by BBR occurred through enhancing PPARα/δ expression and down-regulated PPARγ expression in liver 335. Lipid and glucose SOD homeostasis is also regulated by AMPK 336. Zhao et al. 337 have demonstrated that in normal and Mac-CM-damaged adipocytes, nandinine, a BBR derivative, and BBR attenuated IR via the reduction of inflammation mediated by an effect on AMPK and also by targeting IKKβ. Apparent suppression of pro-inflammatory responses by AMPK activation in macrophages by BBR has also been reported 86, 337 Thus, the authors recommend the use of BBR and nandinine as dietary supplement in obesity.
The principal lipid-lowering mechanism of BBR was hepatic LDLR stabilization, which was mediated via intensification of the signal regulated kinase dependent pathway, along with the enhanced LDLR promoter transcriptional activity responsible for its cardioprotective effect against I/R injury 272. A recent study has reported that BBR was beneficial for the maintenance of energy supply to diabetic hearts during I/R injury 272. BBR inhibited Col1 and Col2 synthesis, promoted IL-10 secretion both in Ang II stimulated heart fibroblasts and suppressed TGFβ1 secretion 138. The same study also revealed that AMPK phosphorylation was increased by BBR 138. After Ang II stimulation in cardiac fibroblasts, protein S6 kinase (p70S6K) and mTOR phosphorylation was down-regulated by BBR. Moreover, myofibroblasts transformation could also be inhibited by BBR via decreasing the α-SMA expression 138. BBR also exhibited inhibitory effects on protein tyrosine phosphatase 1B (PTP1B) which functions as a mediator of insulin signaling and catalyzes protein dephosphorylation by interacting InsR, and showed insulin mimicking effects in myocytes and adipocytes which suggested that BBR is a representative of a different class of anti-hyperglycemic agent 338.
Apart from the effect on AMPK, an effect of BBR on human health was plausible due to the stimulation of the SIRT1, which is also responsible for the potential effects against consequences of oxidative stress 339. A recent study has shown that BBR (5 mg/kg/day, i.p., 3 wk) attenuated oxidative stress in diabetic mice via miR-106b/SIRT1 signaling pathway340. BBR also affected the islet function and thus was beneficial in plummeting cardiovascular risk factors in DM 340. Another study has revealed that BBR has the potential not only to suppress formation of foam cells, but also the ability to adjust lipid accumulation 82. This effect was mediated through activation of AMPK-SIRT1-PPARγ pathway 82. Additionally, the same study has shown that the foam cell inhibitory effect was increased when both BBR and atorvastatin were used in combination rather than atorvastatin alone 82. Another study performed in doxorubicin treated H9C2 cardiomyoblasts showed that pre-treatment with BBR up-regulated the protein levels of SIRT1 and SIRT3 in the presence of doxorubicin 341. BBR also repressed the activation of caspase-3 and caspase-9 induced by doxorubicin. In doxorubicin- treated H9C2 cardiomyoblasts, BBR showed an autophagy modulating effect and increased mitochondrial biogenesis markers and hence BBR can be used as a modulator in decreasing doxorubicin induced cardiotoxicity 341. The SIRT1/ER stress pathway represents a vital mechanism for the neuroprotective effects of BBR in diabetic encephalopathy 342. BBR has been found to up-regulate SIRT1 protein expression and down-regulate the expression of proteins associated with ER stress, such as protein disulfide isomerase (PDI), inositol-requiring enzyme (IRE)1α, eukaryotic translation initiation factor 2 (eIF2), C/EBP homologous protein (CHOP) and PKR-like endoplasmic reticulum kinase (PERK) 342.
The regulation of gut microbiota is another important target of BBR in hyperglycemia, hyperlipidemia, IR, DM, and atherosclerosis 109, 233, 343-346. Gut microbiota converted BBR to an absorbable form of dihydroberberine, which can be further oxidized to BBR after intestinal absorption 347. The increase of gut Akkermansia may contribute to atheroprotective and metabolic protective effects of BBR 109. BBR increases the amount of gut microbiota that produces SCFAs, contributing to the beneficial effects on the host 343. Similar conclusions have appeared from several studies 233, 344-346. Supplementation of BBR in broiler diet promoted intestinal colonization of healthy microbiota at high stocking densities 348. By normalizing gut microbiota, BBR alleviated NASH and its predisposing factors in mice 349. BBR also regulated energy metabolism as it could reduce lipids by regulating the turnover of bile acids, and subsequent ileal FXR signaling pathway 350. Therefore, BBR acts through numerous signaling pathways which clearly suggests that it does not act via a ubiquitous mechanism and it acts through distinct mechanisms to combat cardiovascular and metabolic diseases.
Clinical trials of BBR in cardiometabolic diseases
Several clinical trials have been performed to study the effects of BBR in the therapy of cardiometabolic diseases and/or conditions related to them. These ongoing or completed clinical trials are summarized in Supplementary Table 1 (in supplemental material) 23, 112, 325, 351-364. Trials testing the effects of BBR-based nutraceuticals combination were excluded, because the observed effects are not specifically attributable to BBR, but, probably, to the synergistic effects of all bioactive components. Generally, BBR is tested in dosage ranged from 0.5 to 2.0 g/d as well as treatment period ranged from 4 to 24 weeks. In these trials, BBR has been demonstrated to improve blood lipid profile 23, 112, 325, 351-360, glucose level 112, 325, 351, 357-361, blood pressure 112, 357, 360, IR 358, 360, endothelial function 112, body weight 357, 362, and systemic inflammation 356.
Selected clinical trials have been carried out on subjects with hypercholesterolemia 23, 112, 352, 353, 355, T2DM 325, 354, 360, 361, 363, obesity 362, congestive heart failure (CHF) 364, acute coronary syndrome (ACS) 356, metabolic syndrome 357, NAFLD 351, 359, and polycystic ovary syndrome (PCOS) 358. Only one study was conducted on healthy subjects 112. Particularly, 25 subjects were randomized into two groups: 1.2 g/d BBR treatment group and a control group without any treatment. After 4 weeks of treatment, TC, LDL-C, fasting blood glucose (FBG) and blood pressure were obviously decreased. In addition, improved endothelial function, and a reduction of levels of CD31+/CD42- microparticles were observed 112.
Clinical trial of metabolic diseases
The effect of BBR in patients with T2DM
In patients with T2DM, BBR ameliorated glucose metabolism and improved insulin sensitivity 361. A pilot study was conducted in diabetic patients to investigate the efficacy of BBR. 36 diabetic patients were randomized into two groups: BBR or metformin (both 1.5 g/d, 12wk) 361. After the treatment, in both groups, a statistically significant down-regulation in levels of glycosylated HbA1c (p<0.01), FPG and postprandial blood glucose (PBG) (p<0.01) were observed, suggesting that BBR exerted a hypoglycemic effect comparable to that of metformin. Further, BBR significantly reduced the levels of TG and TC 361. Zhang et al. 325 have compared the effects of BBR (1.0 g/d) and metformin (1.5 g/d) or rosiglitazone (4.0 g/d) for 8 weeks in patients with T2DM. After the treatment period, BBR lowered the level of FPG and HbA1c. The effects of BBR were comparable to that of metformin and rosiglitazone. To evaluate the potential effects and mechanism of BBR in IR, the expression levels of InsR were assessed on peripheral blood lymphocytes (PBL) isolated from subjects before and after BBR treatment 325. A significant up-regulation of InsR-expressing PBL was observed (p<0.01), suggesting that BBR can be effective in treating IR by up-regulation of InsR expression 325.
The effect of BBR in patients with T2DM and dyslipidemia
Zhang et al. 360 conducted a randomized, placebo-controlled, double-blinded study on 106 subjects with T2DM and dyslipidemia. After 12 weeks of treatment with BBR (1.0 g/d), a obvious improvement was observed in levels of FBG, post-load blood glucose (P-LBG), HbA1c, TG, TC, and LDL-C and insulin-sensitivity 360. In addition, BBR also reduced systolic (SBP, p = 0.001) and DBP 360. Similarly, Gu et al. 363 have shown that BBR (1.0 g/d, 12wk) improved lipid profile and insulin sensitivity. In addition, BBR treatment reduced serum concentration of 13 free fatty acids (FFAs), suggesting that BBR was effective in the T2DM-related pathological conditions reducing the level of FFAs 363.
The effect of BBR in patients with dyslipidemia
Kong et al. 23 have reported that BBR (1.0 g/d, 12wk) in a clinical study reduced the lipids (TC, TG and LDL-C) and increased LDLR expression. The proprotein convertase subtilisin/kexin type 9 (PCSK9) negatively regulates LDLR and has become a potential target for hypercholesterolemia 330, 365, and it was shown, that BBR can significantly improve dyslipidemia and LPS-induced inflammatory response in mice by down-regulation of the expression of PCSK9 in the liver and then up-regulating LDLR expression 365. The specific mechanism by which BBR inhibited PCSK9 expression may be through a decrease in HNF1α expression 366 and attenuation of HNF1α and SREBP2 transcription of PCSK9 332. This increased LDLR mRNA is independent on HMGCR activity, suggesting that BBR is able to lower lipid level by a mechanism different from statins 23. A follow-up study evaluated the hypolipidemic effects of BBR (1.0 g/d) and simvastatin (0.2 g/d) alone or in combination for 8 weeks, in subjects with hypercholesterolemia 355. In the combination therapy, the serum levels of LDL-C, TC and TG were obviously reduced after the treatment. Interestingly, BBR monotherapy was more effective that simvastatin in reducing LDL-C, TC and TG 355.
Clinical trial of cardiovascular diseases
BBR also exerted beneficial effects in patients with CVD 356, 364. In 12 patients with refractory CHF, an infusion (0.02 or 0.2 mg/kg/min, 30 min) of high doses of BBR could reduce systemic vascular resistance and enhanced cardiac index, while in the lower dosed group only reduced the patients' heart rate 367. Reaching the plasma concentration of BBR in patients with CHF greater than 0.11 mg/L, significantly reduced the frequency and complexity of ventricular premature beats (VPBs) while left ventricular ejection fraction (LVEF) was increased 368. 79 patients with CHF received BBR 1.2 to 2.0 g/day and routine anti-HF treatment for 8 consecutive weeks. BBR significantly increased exercise capacity and the dyspnea-fatigue index, while decreased frequency and complexity of VPBs 364. Meng et al. 356 have evaluated the effects of BBR in 130 patients with ACS. Subjects were randomized into a treatment group (BBR 0.9 g/d as add-on therapy for 4 weeks) and a control group (only standard therapy). After treatment period, BBR reduced TC and LDL-C levels as well as markers of inflammation (including hypersensitive CRP, IL-6, MMP-9, VCAM-1, ICAM-1and MCP-1), suggesting that BBR is effective in the global management of CVD 356. A recent clinical study evaluated the effect of an oral nutraceutical combination comprised of RYR and BBR on subclinical inflammation, lipid profile, PCSK9, and arterial stiffness in antiretroviral therapy treated HIV-infected patients 369. The results of this study showed positive effect and reported that the nutraceutical combination substantially reduced PCSK9 and plasma cholesterol levels and improved arterial stiffness 369.
New development of BBR derivatives in treating cardiometabolic diseases
Many derivatives of BBR were synthesized with an aim to improve its relatively low bioavailability and to decrease the dosage necessary to trigger the desired therapeutic effects. The main positions of the BBR skeleton are depicted in Figure 7. Especially positions 7, 8, 9, 12 and 13 were targets of BBR modifications 370. It has been observed that alkylation and acylation of BBR on the ring D can change bioavailability 370. As example, pseudoberberine (10,11-dimethoxyderivative) IMB-Y53 in vivo increased the glucose lowering properties, probably due to diminished affinity to P-gp 371. BBR has relatively low oral bioavailability due to extensive P-gp mediated drug efflux in gastrointestinal tract 372. To address this issue, IMB‑Y53 was prepared with the increased gastrointestinal uptake and thus further anti-diabetic effects 371. The potential of IMB-Y53 in CVMD remains to be investigated in future.
Figure 7.
Derivatives of BBR in treating cardiovascular and metabolic diseases. Currently, there are several derivatives being developed based on BBR structural skeleton. These derivatives, such as dihydroberberine, 6-protoberberine, Raisanberine, IMB-Y53, and berberine-baicaline hybrids etc have therapeutic potential in treating cardiovascular and metabolic diseases.
Similarly, dihydroberberine and its analog 8,8-dimethyldihydroberberine were synthesized and tested. Dihydroberberine and 8,8-dimethyldihydroberberine were more potent than BBR and appeared to have similar pharmacodynamic effects in treatment of type 2 diabetes at lower doses 373 . A study by Turner et al. 333 indicated that 560 mg/kg of BBR in a model of rats fed HFD had similar effects compared to 100 mg/kg of dihydroberberine in slowing the adiposity, tissue TG accumulation and IR. It represents a novel therapeutic agent for the therapy of T2DM 333. Furthermore, BBR metabolites were studied, their activity was explored, and they were also used for synthesis of derivatives with more pronounced activity. As examples, we can mention derivatives of 12-aminomethyl berberrubine (e.g. 12-(N-methyl-piperazine-4-methyl)-berberrubine), which were synthetized as potential anti-diabetic substances, and tested on 3T3-L1 adipocytes and L6 myotubes to evaluate their effects on the insulin-resistant reversal activity and glucose transportation. Their effect was comparable to rosiglitazone 374. Further in vitro assay analyzed effect of berberrubine derivatives (e.g. [2-oxo-2-[2-[(2,3,4-trihydroxyphenyl)methylene]hydrazinyl]ethoxy]-9-berberrubine) on the α-glucosidase, showing their ability to inhibit this enzyme and to be a potential anti-diabetic drug 370.
BBR is an isoquinoline alkaloid that, and due to its quaternary ammonium ion, can form compounds with other molecules with negative charge, such as BBR-baicalin, BBR-wogonoside, and BBR-glycyrrhizin 375. These complexes have been shown to possess improved bioavailability due to increased lipophilicity in comparison to parent drug BBR 375. A good example of such as complex compound is berberrubine-magnolol, which was synthesized as anti-diabetic compound. When assayed, this derivative showed low toxicity, and improved absorption, metabolism time, and even greater effect on decreasing glycemia 376.
6-Protoberberine showed hypotensive activity, namely it decreased SBP and heart rate by a central sympatholytic effect 377. Tetrahydroprotoberberine is a competitive antagonist at α1-adrenoceptors in rat aorta, and showed no endothelium-dependent vasorelaxatory activity 378. Some protoberberine complexes, e.g. tetrahydroprotoberberine-aporphine dimer, were described in nature 379. Novel tetrahydroprotoberberine derivatives are recently being developed as selective inhibitors of dopamine D1 receptor 380.
Raisanberine (p-chlorobenzyltetrahydroberberine chloride), named also CPU 86017, is a novel cardioprotective drug for the therapy of pulmonary arterial hypertension (PAH), HF and arrhythmia 381-384. In a rat model of PAH, CPU 86017 reduced ET-1 in lung tissues, reversed an increase of iNOS mRNA level 381. CPU 86017 also improved heart function and hemodynamic parameters in rats subject to development of artificial myocardial infarction 382. The main mechanism of protective effects of CPU 86017 were attributed to the inhibitory effects on calcium influx, and stabilized expression of PLB, FKBP12.6, and SERCA2a 382.
Analysis of pharmacological activity in LPS-stimulated RAW264.7 macrophages and acute inflammation mouse models indicate that BBR and its natural derivatives have anti-inflammatory effects, with the order of oxyberberine (OBB) > BBR> reduced derivatives (two hydroquinone, DHBB) 385. The mechanisms of BBR and its derivatives involve the inhibition of the NF-κB signaling pathway 385. Further elucidation of the mechanism and therapeutic potential of BBR derivatives in cardiometabolic diseases are warranted.
Concluding remarks and future perspectives
Emerging studies over the past decade have convincingly shown that BBR has diverse therapeutic effects on various cardiometabolic diseases, including cardiac hypertrophy, HF, atherosclerosis, stroke, DM, and NAFLD. The efficacy of BBR for treating multiple diseases is mediated by its multi-target pharmacological profile, including amelioration of AMPK, PTP1B, SIRT1, PCSK9, LDLR, PPAR, NF-κB, and modulation of gut microbiota.
The safety of BBR may be based on the poor oral absorption. High doses of BBR can inhibit certain types of CYPs, such as CYP3A11 and CYP3A25 386, 387 and repeated oral administration of BBR (0.3 g three times daily) can reduce the activity of CYP2D6, CYP2C9 and CYP3A4 in healthy subjects 388. This may affect the metabolism of other drugs and could cause some herb-drug interactions; however, this should be further studied and supported by clinical investigations.
As mentioned, the low bioavailability of BBR due its poor oral absorption and extensive metabolism are main obstacles for practical application of BBR. Modern oral dosage forms offer a number of benefits including reduced frequency of dosing, better therapeutic control, and fewer side effects. Advances in polymer materials, particle engineering and nanotechnology could solve some of the problems described for BBR. Different types of nanocarriers (polymers, magnetic mesoporous silica, lipids, graphene, gold and silver nanoparticles) encapsulating BBR can also overcome its deficiencies 389. In addition. BBR has been recently recommended by several groups of experts as an effective lipid-lowering nutraceutical both in low-risk patients and in statin-intolerant ones 390, 391.
Plants with content of BBR are commonly part of preparations used in Traditional Chinese Medicine and other traditional medicinal systems. Besides of this alkaloid, they contain other related compounds and derivatives of BBR. Preparations of TCM are commonly complex and also contain other, structurally unrelated plant secondary metabolites. This inspired research on combinations of BBR and other substances. As example, the oligomeric proanthocyanidins (OPCs) are the main anti-diabetic components in Cinnamon water extracts 392. The combination of OPCs and BBR can significantly improve the pharmacokinetics of BBR in diabetic mice (by inhibiting the expression of P-gp in Caco-2 intestinal cells and thereby reducing the efflux of BBR) and hypoglycemic efficacy 392. The combination of BBR and resveratrol has an enhanced hypolipidemic effect in mice fed with HFD 393. Mechanistic studies have shown that the combination of BBR and resveratrol significantly increased the expression of LDLR in HepG2 cells to approximately one-fold compared to the two drugs alone 393.
Collectively, BBR represents a promising naturally-occurring lead compound for treating CVMD. Further structural modification of BBR may improve the oral bioavailability, efficacy, and reduces potential toxicity of BBR. However, study outcomes of BBR mixture with other nutraceuticals or compounds have to be analyzed carefully since not pure BBR was used for these studies. Furthermore, well-designed, large-scale, high-quality, and multi-center clinical trials are required to assess the safety, toxicology profile, clinical utility of BBR (as compared to traditional treatment regimens) on CVMD in human patients.
Acknowledgments
The work was supported by National Nature Science Foundation of China (81603339, 81602344) and Natural Science Foundation of Anhui Province (1708085QH175). S. X. is a recipient of Career Development Award from American Heart Association (18CDA34110359). L. Z. was supported by Slovenian Research Agency ARRS (J3-8209). A. S. was supported by the Institute of Health Carlos III (Project CIBEROBN CB12/03/30038).
Supplementary Material
Supplementary table 1.
References
- 1.Chandirasegaran G, Elanchezhiyan C, Ghosh K. Effects of Berberine chloride on the liver of streptozotocin-induced diabetes in albino Wistar rats. Biomed Pharmacother. 2018;99:227–36. doi: 10.1016/j.biopha.2018.01.007. [DOI] [PubMed] [Google Scholar]
- 2.Xu S, Xu Y, Yin M, Zhang S, Liu P, Koroleva M. et al. Flow-dependent epigenetic regulation of IGFBP5 expression by H3K27me3 contributes to endothelial anti-inflammatory effects. Theranostics. 2018;8:3007–21. doi: 10.7150/thno.21966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Xu S, Bai P, Little PJ, Liu P. Poly(ADP-ribose) polymerase 1 (PARP1) in atherosclerosis: from molecular mechanisms to therapeutic implications. Med Res Rev. 2014;34:644–75. doi: 10.1002/med.21300. [DOI] [PubMed] [Google Scholar]
- 4.Benjamin EJ, Virani SS, Callaway CW, Chamberlain AM, Chang AR, Cheng S. et al. Heart Disease and Stroke Statistics-2018 Update: A Report From the American Heart Association. Circulation. 2018;137:e67–e492. doi: 10.1161/CIR.0000000000000558. [DOI] [PubMed] [Google Scholar]
- 5.Timmis A, Townsend N, Gale C, Grobbee R, Maniadakis N, Flather M. et al. European Society of Cardiology: Cardiovascular Disease Statistics 2017. Eur Heart J. 2018;39:508–79. doi: 10.1093/eurheartj/ehx628. [DOI] [PubMed] [Google Scholar]
- 6.Xu S, Pelisek J, Jin ZG. Atherosclerosis Is an Epigenetic Disease. Trends Endocrinol Metab; 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fang J, Little PJ, Xu S. Atheroprotective Effects and Molecular Targets of Tanshinones Derived From Herbal Medicine Danshen. Med Res Rev. 2018;38:201–28. doi: 10.1002/med.21438. [DOI] [PubMed] [Google Scholar]
- 8.Saklayen MG. The Global Epidemic of the Metabolic Syndrome. Curr Hypertens Rep. 2018;20:12. doi: 10.1007/s11906-018-0812-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bodmer M, Meier C, Krähenbühl S, Jick SS, Meier CR. Metformin, sulfonylureas, or other antidiabetes drugs and the risk of lactic acidosis or hypoglycemia: a nested case-control analysis. Diabetes care. 2008;31:2086–91. doi: 10.2337/dc08-1171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pillai GKG, Bharate SS, Awasthi A, Verma R, Mishra G, Singh AT. et al. Antidiabetic potential of polyherbal formulation DB14201: Preclinical development, safety and efficacy studies. J Ethnopharmacol. 2017;197:218–30. doi: 10.1016/j.jep.2016.07.062. [DOI] [PubMed] [Google Scholar]
- 11.Stafford JM, Elasy T. Treatment update: thiazolidinediones in combination with metformin for the treatment of type 2 diabetes. Vasc Health Risk Manag. 2007;3:503. [PMC free article] [PubMed] [Google Scholar]
- 12.Zhao M, Klipstein-Grobusch K, Wang X, Reitsma JB, Zhao D, Grobbee DE. et al. Prevalence of cardiovascular medication on secondary prevention after myocardial infarction in China between 1995-2015: A systematic review and meta-analysis. PLoS One. 2017;12:e0175947. doi: 10.1371/journal.pone.0175947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Squizzato A, Bellesini M, Takeda A, Middeldorp S, Donadini MP. Clopidogrel plus aspirin versus aspirin alone for preventing cardiovascular events. Cochrane Database Syst Rev. 2017;12:CD005158. doi: 10.1002/14651858.CD005158.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Blessberger H, Kammler J, Domanovits H, Schlager O, Wildner B, Azar D. et al. Perioperative beta-blockers for preventing surgery-related mortality and morbidity. Cochrane Database Syst Rev. 2018;3:CD004476. doi: 10.1002/14651858.CD004476.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jin Y, Khadka DB, Cho WJ. Pharmacological effects of berberine and its derivatives: a patent update. Expert Opin Ther Pat. 2016;26:229–43. doi: 10.1517/13543776.2016.1118060. [DOI] [PubMed] [Google Scholar]
- 16.Ju J, Li J, Lin Q, Xu H. Efficacy and safety of berberine for dyslipidaemias: A systematic review and meta-analysis of randomized clinical trials. Phytomedicine. 2018;50:25–34. doi: 10.1016/j.phymed.2018.09.212. [DOI] [PubMed] [Google Scholar]
- 17.Lin X, Zhang N. Berberine: Pathways to protect neurons. Phytother Res. 2018;32:1501–10. doi: 10.1002/ptr.6107. [DOI] [PubMed] [Google Scholar]
- 18.Pang B, Yu X-T, Zhou Q, Zhao T-Y, Wang H, Gu C-J. et al. Effect of Rhizoma coptidis (Huang Lian) on treating diabetes mellitus. Evid Based Complement Alternat Med. 2015;2015:921416. doi: 10.1155/2015/921416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tan H-L, Chan K-G, Pusparajah P, Duangjai A, Saokaew S, Mehmood Khan T. et al. Rhizoma coptidis: a potential cardiovascular protective agent. Front Pharmacol. 2016;7:362. doi: 10.3389/fphar.2016.00362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhang Q, Xiao X, Li M, Li W, Yu M, Zhang H. et al. Berberine moderates glucose metabolism through the GnRH-GLP-1 and MAPK pathways in the intestine. BMC Complement Altern Med. 2014;14:188. doi: 10.1186/1472-6882-14-188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wang K, Feng X, Chai L, Cao S, Qiu F. The metabolism of berberine and its contribution to the pharmacological effects. Drug Metab Rev. 2017;49:139–57. doi: 10.1080/03602532.2017.1306544. [DOI] [PubMed] [Google Scholar]
- 22.Battu SK, Repka MA, Maddineni S, Chittiboyina AG, Avery MA, Majumdar S. Physicochemical characterization of berberine chloride: a perspective in the development of a solution dosage form for oral delivery. AAPS PharmSciTech. 2010;11:1466–75. doi: 10.1208/s12249-010-9520-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kong W, Wei J, Abidi P, Lin M, Inaba S, Li C. et al. Berberine is a novel cholesterol-lowering drug working through a unique mechanism distinct from statins. Nat Med. 2004;10:1344–51. doi: 10.1038/nm1135. [DOI] [PubMed] [Google Scholar]
- 24.Huang ZJ, Zeng Y, Lan P, Sun PH, Chen WM. Advances in structural modifications and biological activities of berberine: an active compound in traditional Chinese medicine. Mini Rev Med Chem. 2011;11:1122–9. doi: 10.2174/138955711797655362. [DOI] [PubMed] [Google Scholar]
- 25.Chen W, Miao YQ, Fan DJ, Yang SS, Lin X, Meng LK. et al. Bioavailability study of berberine and the enhancing effects of TPGS on intestinal absorption in rats. AAPS PharmSciTech. 2011;12:705–11. doi: 10.1208/s12249-011-9632-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pan GY, Wang GJ, Liu XD, Fawcett JP, Xie YY. The involvement of P-glycoprotein in berberine absorption. Pharmacol Toxicol. 2002;91:193–7. doi: 10.1034/j.1600-0773.2002.t01-1-910403.x. [DOI] [PubMed] [Google Scholar]
- 27.Liu CS, Zheng YR, Zhang YF, Long XY. Research progress on berberine with a special focus on its oral bioavailability. Fitoterapia. 2016;109:274–82. doi: 10.1016/j.fitote.2016.02.001. [DOI] [PubMed] [Google Scholar]
- 28.Guo Y, Li F, Ma X, Cheng X, Zhou H, Klaassen CD. CYP2D plays a major role in berberine metabolism in liver of mice and humans. Xenobiotica. 2011;41:996–1005. doi: 10.3109/00498254.2011.597456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tan XS, Ma JY, Feng R, Ma C, Chen WJ, Sun YP. et al. Tissue distribution of berberine and its metabolites after oral administration in rats. PLoS One. 2013;8:e77969. doi: 10.1371/journal.pone.0077969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kumar A, Ekavali, Chopra K, Mukherjee M, Pottabathini R, Dhull DK. Current knowledge and pharmacological profile of berberine: An update. Eur J Pharmacol. 2015;761:288–97. doi: 10.1016/j.ejphar.2015.05.068. [DOI] [PubMed] [Google Scholar]
- 31.Wang X, Wang R, Xing D, Su H, Ma C, Ding Y. et al. Kinetic difference of berberine between hippocampus and plasma in rat after intravenous administration of Coptidis rhizoma extract. Life Sci. 2005;77:3058–67. doi: 10.1016/j.lfs.2005.02.033. [DOI] [PubMed] [Google Scholar]
- 32.Zhang X, Zhang X, Wang C, Li Y, Dong L, Cui L. et al. Neuroprotection of early and short-time applying berberine in the acute phase of cerebral ischemia: up-regulated pAkt, pGSK and pCREB, down-regulated NF-kappaB expression, ameliorated BBB permeability. Brain Res. 2012;1459:61–70. doi: 10.1016/j.brainres.2012.03.065. [DOI] [PubMed] [Google Scholar]
- 33.Tian H, Kang YM, Gao HL, Shi XL, Fu LY, Li Y. et al. Chronic infusion of berberine into the hypothalamic paraventricular nucleus attenuates hypertension and sympathoexcitation via the ROS/Erk1/2/iNOS pathway. Phytomedicine. 2019;52:216–24. doi: 10.1016/j.phymed.2018.09.206. [DOI] [PubMed] [Google Scholar]
- 34.Imenshahidi M, Hosseinzadeh H. Berberis Vulgaris and Berberine: An Update Review. Phytother Res. 2016;30:1745–64. doi: 10.1002/ptr.5693. [DOI] [PubMed] [Google Scholar]
- 35.Chan E. Displacement of bilirubin from albumin by berberine. Biol Neonate. 1993;63:201–8. doi: 10.1159/000243932. [DOI] [PubMed] [Google Scholar]
- 36.Zhi D, Feng PF, Sun JL, Guo F, Zhang R, Zhao X. et al. The enhancement of cardiac toxicity by concomitant administration of Berberine and macrolides. Eur J Pharm Sci. 2015;76:149–55. doi: 10.1016/j.ejps.2015.05.009. [DOI] [PubMed] [Google Scholar]
- 37.Feng P, Zhao L, Guo F, Zhang B, Fang L, Zhan G. et al. The enhancement of cardiotoxicity that results from inhibiton of CYP 3A4 activity and hERG channel by berberine in combination with statins. Chem Biol Interact. 2018;293:115–23. doi: 10.1016/j.cbi.2018.07.022. [DOI] [PubMed] [Google Scholar]
- 38.Domitrovic R, Cvijanovic O, Pernjak-Pugel E, Skoda M, Mikelic L, Crncevic-Orlic Z. Berberine exerts nephroprotective effect against cisplatin-induced kidney damage through inhibition of oxidative/nitrosative stress, inflammation, autophagy and apoptosis. Food Chem Toxicol. 2013;62:397–406. doi: 10.1016/j.fct.2013.09.003. [DOI] [PubMed] [Google Scholar]
- 39.Germoush MO, Mahmoud AM. Berberine mitigates cyclophosphamide-induced hepatotoxicity by modulating antioxidant status and inflammatory cytokines. J Cancer Res Clin Oncol. 2014;140:1103–9. doi: 10.1007/s00432-014-1665-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hao G, Yu Y, Gu B, Xing Y, Xue M. Protective effects of berberine against doxorubicin-induced cardiotoxicity in rats by inhibiting metabolism of doxorubicin. Xenobiotica. 2015;45:1024–9. doi: 10.3109/00498254.2015.1034223. [DOI] [PubMed] [Google Scholar]
- 41.Chitra P, Saiprasad G, Manikandan R, Sudhandiran G. Berberine attenuates bleomycin induced pulmonary toxicity and fibrosis via suppressing NF-kappaB dependant TGF-beta activation: a biphasic experimental study. Toxicol Lett. 2013;219:178–93. doi: 10.1016/j.toxlet.2013.03.009. [DOI] [PubMed] [Google Scholar]
- 42.Janbaz KH, Gilani AH. Studies on preventive and curative effects of berberine on chemical-induced hepatotoxicity in rodents. Fitoterapia. 2000;71:25–33. doi: 10.1016/s0367-326x(99)00098-2. [DOI] [PubMed] [Google Scholar]
- 43.Geovanini GR, Libby P. Atherosclerosis and inflammation: overview and updates. Clin Sci (Lond) 2018;132:1243–52. doi: 10.1042/CS20180306. [DOI] [PubMed] [Google Scholar]
- 44.Bentzon JF, Otsuka F, Virmani R, Falk E. Mechanisms of plaque formation and rupture. Circ Res. 2014;114:1852–66. doi: 10.1161/CIRCRESAHA.114.302721. [DOI] [PubMed] [Google Scholar]
- 45.Nowak WN, Deng J, Ruan XZ, Xu Q. Reactive Oxygen Species Generation and Atherosclerosis. Arterioscler Thromb Vasc Biol. 2017;37:e41–e52. doi: 10.1161/ATVBAHA.117.309228. [DOI] [PubMed] [Google Scholar]
- 46.Libby P, Ridker PM, Hansson GK. Progress and challenges in translating the biology of atherosclerosis. Nature. 2011;473:317–25. doi: 10.1038/nature10146. [DOI] [PubMed] [Google Scholar]
- 47.Escarcega RO, Lipinski MJ, Garcia-Carrasco M, Mendoza-Pinto C, Galvez-Romero JL, Cervera R. Inflammation and atherosclerosis: Cardiovascular evaluation in patients with autoimmune diseases. Autoimmun Rev. 2018;17:703–8. doi: 10.1016/j.autrev.2018.01.021. [DOI] [PubMed] [Google Scholar]
- 48.Raggi P, Genest J, Giles JT, Rayner KJ, Dwivedi G, Beanlands RS. et al. Role of inflammation in the pathogenesis of atherosclerosis and therapeutic interventions. Atherosclerosis. 2018;276:98–108. doi: 10.1016/j.atherosclerosis.2018.07.014. [DOI] [PubMed] [Google Scholar]
- 49.Halcox JPJ. Chapter 66 - Endothelial Dysfunction A2 - Robertson, David. In: Biaggioni I, Burnstock G, Low PA, Paton JFR, editors. Primer on the Autonomic Nervous System (Third Edition) San Diego: Academic Press; 2012. p. 319-24. [Google Scholar]
- 50.Xu S, Kamato D, Little PJ, Nakagawa S, Pelisek J, Jin ZG. Targeting epigenetics and non-coding RNAs in atherosclerosis: from mechanisms to therapeutics. Pharmacol Ther. 2018 doi: 10.1016/j.pharmthera.2018.11.003. doi: 10.1016/j.pharmthera.2018.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Nafisa A, Gray SG, Cao Y, Wang T, Xu S, Wattoo FH. et al. Endothelial function and dysfunction: Impact of metformin. Pharmacol Ther. 2018;192:150–62. doi: 10.1016/j.pharmthera.2018.07.007. [DOI] [PubMed] [Google Scholar]
- 52.Huang Z, Cai X, Li S, Zhou H, Chu M, Shan P. et al. Berberine-attenuated monocyte adhesion to endothelial cells induced by oxidized low-density lipoprotein via inhibition of adhesion molecule expression. Mol Med Rep. 2013;7:461–5. doi: 10.3892/mmr.2012.1236. [DOI] [PubMed] [Google Scholar]
- 53.Xu S, Pelisek J, Jin ZG. Atherosclerosis Is an Epigenetic Disease. Trends Endocrinol Metab. 2018;29:739–42. doi: 10.1016/j.tem.2018.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hsieh YS, Kuo WH, Lin TW, Chang HR, Lin TH, Chen PN. et al. Protective effects of berberine against low-density lipoprotein (LDL) oxidation and oxidized LDL-induced cytotoxicity on endothelial cells. J Agric Food Chem. 2007;55:10437–45. doi: 10.1021/jf071868c. [DOI] [PubMed] [Google Scholar]
- 55.Liu SJ, Yin CX, Ding MC, Wang YZ, Wang H. Berberine inhibits tumor necrosis factor-alpha-induced expression of inflammatory molecules and activation of nuclear factor-kappaB via the activation of AMPK in vascular endothelial cells. Mol Med Rep. 2015;12:5580–6. doi: 10.3892/mmr.2015.4061. [DOI] [PubMed] [Google Scholar]
- 56.Caliceti C, Rizzo P, Ferrari R, Fortini F, Aquila G, Leoncini E. et al. Novel role of the nutraceutical bioactive compound berberine in lectin-like OxLDL receptor 1-mediated endothelial dysfunction in comparison to lovastatin. Nutr Metab Cardiovasc Dis. 2017;27:552–63. doi: 10.1016/j.numecd.2017.04.002. [DOI] [PubMed] [Google Scholar]
- 57.Xu S, Ogura S, Chen J, Little PJ, Moss J, Liu P. LOX-1 in atherosclerosis: biological functions and pharmacological modifiers. Cell Mol Life Sci. 2013;70:2859–72. doi: 10.1007/s00018-012-1194-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Tian K, Ogura S, Little PJ, Xu SW, Sawamura T. Targeting LOX-1 in atherosclerosis and vasculopathy: current knowledge and future perspectives. Ann N Y Acad Sci. 2018 doi: 10.1111/nyas.13984. doi: 10.1111/nyas.13984. [DOI] [PubMed] [Google Scholar]
- 59.Zhang M, Wang C-M, Li J, Meng Z-J, Wei S-N, Li J. et al. Berberine protects against palmitate-induced endothelial dysfunction: involvements of upregulation of AMPK and eNOS and downregulation of NOX4. Mediators Inflamm. 2013;2013:260464. doi: 10.1155/2013/260464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ko YJ, Lee J-S, Park BC, Shin HM, Kim J-A. Inhibitory effects of Zoagumhwan water extract and berberine on angiotensin II-induced monocyte chemoattractant protein (MCP)-1 expression and monocyte adhesion to endothelial cells. Vascul Pharmacol. 2007;47:189–96. doi: 10.1016/j.vph.2007.06.004. [DOI] [PubMed] [Google Scholar]
- 61.Porru E, Franco P, Calabria D, Spinozzi S, Roberti M, Caliceti C. et al. Combined analytical approaches to define biodistribution and biological activity of semi-synthetic berberrubine, the active metabolite of natural berberine. Anal Bioanal Chem. 2018;410:3533–45. doi: 10.1007/s00216-018-0884-2. [DOI] [PubMed] [Google Scholar]
- 62.Xu RX, Sun XC, Ma CY, Yao YH, Li XL, Guo YL. et al. Impacts of berberine on oxidized LDL-induced proliferation of human umbilical vein endothelial cells. Am J Transl Res. 2017;9:4375–89. [PMC free article] [PubMed] [Google Scholar]
- 63.Alexander MR, Owens GK. Epigenetic control of smooth muscle cell differentiation and phenotypic switching in vascular development and disease. Annu Rev Physiol. 2012;74:13–40. doi: 10.1146/annurev-physiol-012110-142315. [DOI] [PubMed] [Google Scholar]
- 64.Hayashi K, Takahashi M, Nishida W, Yoshida K, Ohkawa Y, Kitabatake A. et al. Phenotypic modulation of vascular smooth muscle cells induced by unsaturated lysophosphatidic acids. Circ Res. 2001;89:251–8. doi: 10.1161/hh1501.094265. [DOI] [PubMed] [Google Scholar]
- 65.Lee S, Lim HJ, Park HY, Lee KS, Park JH, Jang Y. Berberine inhibits rat vascular smooth muscle cell proliferation and migration in vitro and improves neointima formation after balloon injury in vivo. Berberine improves neointima formation in a rat model. Atherosclerosis. 2006;186:29–37. doi: 10.1016/j.atherosclerosis.2005.06.048. [DOI] [PubMed] [Google Scholar]
- 66.Liang KW, Ting CT, Yin SC, Chen YT, Lin SJ, Liao JK. et al. Berberine suppresses MEK/ERK-dependent Egr-1 signaling pathway and inhibits vascular smooth muscle cell regrowth after in vitro mechanical injury. Biochem Pharmacol. 2006;71:806–17. doi: 10.1016/j.bcp.2005.12.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Qiu H, Wu Y, Wang Q, Liu C, Xue L, Wang H. et al. Effect of berberine on PPARalpha-NO signalling pathway in vascular smooth muscle cell proliferation induced by angiotensin IV. Pharm Biol. 2017;55:227–32. doi: 10.1080/13880209.2016.1257642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Liu SJ, Yin CX, Ding MC, Xia SY, Shen QM, Wu JD. Berberine suppresses in vitro migration of human aortic smooth muscle cells through the inhibitions of MMP-2/9, u-PA, AP-1, and NF-kappaB. BMB Rep. 2014;47:388–92. doi: 10.5483/BMBRep.2014.47.7.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Ma L, Zhang L, Wang B, Wei J, Liu J, Zhang L. Berberine inhibits Chlamydia pneumoniae infection-induced vascular smooth muscle cell migration through downregulating MMP3 and MMP9 via PI3K. Eur J Pharmacol. 2015;755:102–9. doi: 10.1016/j.ejphar.2015.02.039. [DOI] [PubMed] [Google Scholar]
- 70.Liang KW, Yin SC, Ting CT, Lin SJ, Hsueh CM, Chen CY. et al. Berberine inhibits platelet-derived growth factor-induced growth and migration partly through an AMPK-dependent pathway in vascular smooth muscle cells. Eur J Pharmacol. 2008;590:343–54. doi: 10.1016/j.ejphar.2008.06.034. [DOI] [PubMed] [Google Scholar]
- 71.Cho BJ, Im EK, Kwon JH, Lee KH, Shin HJ, Oh J. et al. Berberine inhibits the production of lysophosphatidylcholine-induced reactive oxygen species and the ERK1/2 pathway in vascular smooth muscle cells. Mol Cells. 2005;20:429–34. [PubMed] [Google Scholar]
- 72.Luo J, Gu Y, Liu P, Jiang X, Yu W, Ye P. et al. Berberine attenuates pulmonary arterial hypertension via protein phosphatase 2A signaling pathway both in vivo and in vitro. J Cell Physiol. 2018;233:9750–62. doi: 10.1002/jcp.26940. [DOI] [PubMed] [Google Scholar]
- 73.Liu J, Xiu J, Cao J, Gao Q, Ma D, Fu L. Berberine cooperates with adrenal androgen dehydroepiandrosterone sulfate to attenuate PDGF-induced proliferation of vascular smooth muscle cell A7r5 through Skp2 signaling pathway. Mol Cell Biochem. 2011;355:127–34. doi: 10.1007/s11010-011-0846-x. [DOI] [PubMed] [Google Scholar]
- 74.Tanabe H, Suzuki H, Mizukami H, Inoue M. Double blockade of cell cycle progression by coptisine in vascular smooth muscle cells. Biochem Pharmacol. 2005;70:1176–84. doi: 10.1016/j.bcp.2005.07.010. [DOI] [PubMed] [Google Scholar]
- 75.Levitan I, Volkov S, Subbaiah PV. Oxidized LDL: diversity, patterns of recognition, and pathophysiology. Antioxid Redox Signal. 2010;13:39–75. doi: 10.1089/ars.2009.2733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Moore KJ, Sheedy FJ, Fisher EA. Macrophages in atherosclerosis: a dynamic balance. Nat Rev Immunol. 2013;13:709–21. doi: 10.1038/nri3520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Xu S, Huang Y, Xie Y, Lan T, Le K, Chen J. et al. Evaluation of foam cell formation in cultured macrophages: an improved method with Oil Red O staining and DiI-oxLDL uptake. Cytotechnology. 2010;62:473–81. doi: 10.1007/s10616-010-9290-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Huang Z, Dong F, Li S, Chu M, Zhou H, Lu Z. et al. Berberine-induced inhibition of adipocyte enhancer-binding protein 1 attenuates oxidized low-density lipoprotein accumulation and foam cell formation in phorbol 12-myristate 13-acetate-induced macrophages. Eur J Pharmacol. 2012;690:164–9. doi: 10.1016/j.ejphar.2012.07.009. [DOI] [PubMed] [Google Scholar]
- 79.Guan S, Wang B, Li W, Guan J, Fang X. Effects of berberine on expression of LOX-1 and SR-BI in human macrophage-derived foam cells induced by ox-LDL. Am J Chin Med. 2010;38:1161–9. doi: 10.1142/S0192415X10008548. [DOI] [PubMed] [Google Scholar]
- 80.Zimetti F, Adorni MP, Ronda N, Gatti R, Bernini F, Favari E. The natural compound berberine positively affects macrophage functions involved in atherogenesis. Nutr Metab Cardiovasc Dis. 2015;25:195–201. doi: 10.1016/j.numecd.2014.08.004. [DOI] [PubMed] [Google Scholar]
- 81.Liang H, Wang Y. Berberine alleviates hepatic lipid accumulation by increasing ABCA1 through the protein kinase C delta pathway. Biochem Biophys Res Commun. 2018;498:473–80. doi: 10.1016/j.bbrc.2018.03.003. [DOI] [PubMed] [Google Scholar]
- 82.Chi L, Peng L, Pan N, Hu X, Zhang Y. The anti-atherogenic effects of berberine on foam cell formation are mediated through the upregulation of sirtuin 1. Int J Mol Med. 2014;34:1087–93. doi: 10.3892/ijmm.2014.1868. [DOI] [PubMed] [Google Scholar]
- 83.Chi L, Peng L, Hu X, Pan N, Zhang Y. Berberine combined with atorvastatin downregulates LOX1 expression through the ET1 receptor in monocyte/macrophages. Int J Mol Med. 2014;34:283–90. doi: 10.3892/ijmm.2014.1748. [DOI] [PubMed] [Google Scholar]
- 84.Kou JY, Li Y, Zhong ZY, Jiang YQ, Li XS, Han XB. et al. Berberine-sonodynamic therapy induces autophagy and lipid unloading in macrophage. Cell Death Dis. 2017;8:e2558. doi: 10.1038/cddis.2016.354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Li K, Yao W, Zheng X, Liao K. Berberine promotes the development of atherosclerosis and foam cell formation by inducing scavenger receptor A expression in macrophage. Cell Res. 2009;19:1006–17. doi: 10.1038/cr.2009.76. [DOI] [PubMed] [Google Scholar]
- 86.Jeong HW, Hsu KC, Lee JW, Ham M, Huh JY, Shin HJ. et al. Berberine suppresses proinflammatory responses through AMPK activation in macrophages. Am J Physiol Endocrinol Metab. 2009;296:E955–64. doi: 10.1152/ajpendo.90599.2008. [DOI] [PubMed] [Google Scholar]
- 87.Fan X, Wang J, Hou J, Lin C, Bensoussan A, Chang D. et al. Berberine alleviates ox-LDL induced inflammatory factors by up-regulation of autophagy via AMPK/mTOR signaling pathway. J Transl Med. 2015;13:92. doi: 10.1186/s12967-015-0450-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Jiang Y, Huang K, Lin X, Chen Q, Lin S, Feng X. et al. Berberine Attenuates NLRP3 Inflammasome Activation in Macrophages to Reduce the Secretion of Interleukin-1beta. Ann Clin Lab Sci. 2017;47:720–8. [PubMed] [Google Scholar]
- 89.Huang Z, Ye B, Han J, Kong F, Shan P, Lu Z. et al. NACHT, LRR and PYD domains-containing protein 3 inflammasome is activated and inhibited by berberine via toll-like receptor 4/myeloid differentiation primary response gene 88/nuclear factor-kappaB pathway, in phorbol 12-myristate 13-acetate-induced macrophages. Mol Med Rep. 2018;17:2673–80. doi: 10.3892/mmr.2017.8189. [DOI] [PubMed] [Google Scholar]
- 90.Liu YF, Wen CY, Chen Z, Wang Y, Huang Y, Tu SH. Effects of Berberine on NLRP3 and IL-1beta Expressions in Monocytic THP-1 Cells with Monosodium Urate Crystals-Induced Inflammation. Biomed Res Int. 2016;2016:2503703. doi: 10.1155/2016/2503703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Zhou H, Feng L, Xu F, Sun Y, Ma Y, Zhang X. et al. Berberine inhibits palmitate-induced NLRP3 inflammasome activation by triggering autophagy in macrophages: A new mechanism linking berberine to insulin resistance improvement. Biomed Pharmacother. 2017;89:864–74. doi: 10.1016/j.biopha.2017.03.003. [DOI] [PubMed] [Google Scholar]
- 92.Vivoli E, Cappon A, Milani S, Piombanti B, Provenzano A, Novo E. et al. NLRP3 inflammasome as a target of berberine in experimental murine liver injury: interference with P2X7 signalling. Clin Sci (Lond) 2016;130:1793–806. doi: 10.1042/CS20160400. [DOI] [PubMed] [Google Scholar]
- 93.Sujitha S, Dinesh P, Rasool M. Berberine modulates ASK1 signaling mediated through TLR4/TRAF2 via upregulation of miR-23a. Toxicol Appl Pharmacol. 2018;359:34–46. doi: 10.1016/j.taap.2018.09.017. [DOI] [PubMed] [Google Scholar]
- 94.Pei C, Zhang Y, Wang P, Zhang B, Fang L, Liu B. et al. Berberine alleviates oxidized low-density lipoprotein-induced macrophage activation by downregulating galectin-3 via the NF-kappaB and AMPK signaling pathways. Phytother Res. 2019;33:294–308. doi: 10.1002/ptr.6217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Huang CG, Chu ZL, Wei SJ, Jiang H, Jiao BH. Effect of berberine on arachidonic acid metabolism in rabbit platelets and endothelial cells. Thromb Res. 2002;106:223–7. doi: 10.1016/s0049-3848(02)00133-0. [DOI] [PubMed] [Google Scholar]
- 96.Zhao L CZ. The assisting effect of berberine on urokinase- and streptokinase-induced thrombolysis. Chin Pharmacol Bull. 1998;14:359–61. [Google Scholar]
- 97.Chu Z-L, Huang C-G, Xu Z-P. Antiplatelet effects and mechanisms of berberine. Chinese Journal of Integrated Traditional and Western Medicine. 1996;2:75–7. [Google Scholar]
- 98.Chu Z-L, Huang C-G, Lai F-S. The anti-platelet-rich-plasma-clot-retraction effect of berberine and its mechanism. Chin Pharmacol Bull. 1994;10:114–6. [Google Scholar]
- 99.Gui-xian J, Bang-mao W, Wei-li F. The effects of berberine chloride on platelet activation of mice with dextransulphate sodium-induced colitis [J] Journal of Tianjin Medical University. 2004;2:008. [Google Scholar]
- 100.Allijn IE, Vaessen SF, Quarles van Ufford LC, Beukelman KJ, de Winther MP, Storm G. et al. Head-to-Head Comparison of Anti-Inflammatory Performance of Known Natural Products In Vitro. PLoS One. 2016;11:e0155325. doi: 10.1371/journal.pone.0155325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Shah BH, Nawaz Z, Saeed SA, Gilani AHJPR. Agonist-dependent differential effects of berberine in human platelet aggregation. 2010; 12: S60-S2.
- 102.LU L, ZHANG H-q, CHEN G-r, WU J-b, CHEN Z-l, ZHOU X-y. et al. Effects of Berberine on the Expression of GPVI on Platelets of Diabetes Rats [J] Herald of Medicine. 2007;11:012. [Google Scholar]
- 103.Zhang Y, Ma XJ, Guo CY, Wang MM, Kou N, Qu H. et al. Pretreatment with a combination of ligustrazine and berberine improves cardiac function in rats with coronary microembolization. Acta Pharmacol Sin. 2016;37:463–72. doi: 10.1038/aps.2015.147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Holy EW, Akhmedov A, Lüscher TF, Tanner FC. Berberine, a natural lipid-lowering drug, exerts prothrombotic effects on vascular cells. J Mol Cell Cardiol. 2009;46:234–40. doi: 10.1016/j.yjmcc.2008.10.011. [DOI] [PubMed] [Google Scholar]
- 105.Gao M-y, Chen L, Yang L, Yu X, Kou J-p, Yu B-y. Berberine inhibits LPS-induced TF procoagulant activity and expression through NF-κB/p65, Akt and MAPK pathway in THP-1 cells. Pharmacol Rep. 2014;66:480–4. doi: 10.1016/j.pharep.2013.12.004. [DOI] [PubMed] [Google Scholar]
- 106.Feng M, Zou Z, Zhou X, Hu Y, Ma H, Xiao Y. et al. Comparative effect of berberine and its derivative 8-cetylberberine on attenuating atherosclerosis in ApoE(-/-) mice. Int Immunopharmacol. 2017;43:195–202. doi: 10.1016/j.intimp.2016.12.001. [DOI] [PubMed] [Google Scholar]
- 107.Li H, He C, Wang J, Li X, Yang Z, Sun X. et al. Berberine activates peroxisome proliferator-activated receptor gamma to increase atherosclerotic plaque stability in Apoe(-/-) mice with hyperhomocysteinemia. J Diabetes Investig. 2016;7:824–32. doi: 10.1111/jdi.12516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Wan Q, Liu Z, Yang Y, Cui X. Suppressive effects of berberine on atherosclerosis via downregulating visfatin expression and attenuating visfatin-induced endothelial dysfunction. Int J Mol Med. 2018;41:1939–48. doi: 10.3892/ijmm.2018.3440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Zhu L, Zhang D, Zhu H, Zhu J, Weng S, Dong L. et al. Berberine treatment increases Akkermansia in the gut and improves high-fat diet-induced atherosclerosis in Apoe(-/-) mice. Atherosclerosis. 2018;268:117–26. doi: 10.1016/j.atherosclerosis.2017.11.023. [DOI] [PubMed] [Google Scholar]
- 110.Shi Y, Hu J, Geng J, Hu T, Wang B, Yan W. et al. Berberine treatment reduces atherosclerosis by mediating gut microbiota in apoE-/- mice. Biomed Pharmacother. 2018;107:1556–63. doi: 10.1016/j.biopha.2018.08.148. [DOI] [PubMed] [Google Scholar]
- 111.Van Ierssel SH, Hoymans VY, Van Craenenbroeck EM, Van Tendeloo VF, Vrints CJ, Jorens PG. et al. Endothelial microparticles (EMP) for the assessment of endothelial function: an in vitro and in vivo study on possible interference of plasma lipids. PLoS One. 2012;7:e31496. doi: 10.1371/journal.pone.0031496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Wang JM, Yang Z, Xu MG, Chen L, Wang Y, Su C. et al. Berberine-induced decline in circulating CD31+/CD42- microparticles is associated with improvement of endothelial function in humans. Eur J Pharmacol. 2009;614:77–83. doi: 10.1016/j.ejphar.2009.04.037. [DOI] [PubMed] [Google Scholar]
- 113.Chen S. Inhibition of endothelial microparticles-mediated oxidative stress by berberine and its relation with endothelial function in humans. Heart. 2011;97:A90–A1. [Google Scholar]
- 114.Cheng F, Wang Y, Li J, Su C, Wu F, Xia W-H. et al. Berberine improves endothelial function by reducing endothelial microparticles-mediated oxidative stress in humans. Int J Cardiol. 2013;167:936–42. doi: 10.1016/j.ijcard.2012.03.090. [DOI] [PubMed] [Google Scholar]
- 115.Csiszar A, Wang M, Lakatta EG, Ungvari Z. Inflammation and endothelial dysfunction during aging: role of NF-κB. J Appl Physiol. 2008;105:1333–41. doi: 10.1152/japplphysiol.90470.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Wang Y, Ding Y. Berberine protects vascular endothelial cells in hypertensive rats. Int J Clin Exp. 2015;8:14896–905. [PMC free article] [PubMed] [Google Scholar]
- 117.Versari D, Daghini E, Virdis A, Ghiadoni L, Taddei S. Endothelium-dependent contractions and endothelial dysfunction in human hypertension. Br J Pharmacol. 2009;157:527–36. doi: 10.1111/j.1476-5381.2009.00240.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Liu L, Liu J, Huang Z, Yu X, Zhang X, Dou D. et al. Berberine improves endothelial function by inhibiting endoplasmic reticulum stress in the carotid arteries of spontaneously hypertensive rats. Biochem Biophys Res Commun. 2015;458:796–801. doi: 10.1016/j.bbrc.2015.02.028. [DOI] [PubMed] [Google Scholar]
- 119.Wu Y, Chuang S, Hong W, Lai Y, Chang G, Pang JS. Berberine reduces leukocyte adhesion to LPS-stimulated endothelial cells and VCAM-1 expression both in vivo and in vitro. Int J Immunopathol Pharmacol. 2012;25:741–50. doi: 10.1177/039463201202500320. [DOI] [PubMed] [Google Scholar]
- 120.Pfeffer MA, Braunwald E. Ventricular remodeling after myocardial infarction. Experimental observations and clinical implications. Circulation. 1990;81:1161–72. doi: 10.1161/01.cir.81.4.1161. [DOI] [PubMed] [Google Scholar]
- 121.Rizzello V, Poldermans D, Biagini E, Schinkel AF, Boersma E, Boccanelli A. et al. Prognosis of patients with ischaemic cardiomyopathy after coronary revascularisation: relation to viability and improvement in left ventricular ejection fraction. Heart. 2009;95:1273–7. doi: 10.1136/hrt.2008.163972. [DOI] [PubMed] [Google Scholar]
- 122.Le K, Li R, Xu S, Wu X, Huang H, Bao Y. et al. PPARalpha activation inhibits endothelin-1-induced cardiomyocyte hypertrophy by prevention of NFATc4 binding to GATA-4. Arch Biochem Biophys. 2012;518:71–8. doi: 10.1016/j.abb.2011.11.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Zou J, Le K, Xu S, Chen J, Liu Z, Chao X. et al. Fenofibrate ameliorates cardiac hypertrophy by activation of peroxisome proliferator-activated receptor-alpha partly via preventing p65-NFkappaB binding to NFATc4. Mol Cell Endocrinol. 2013;370:103–12. doi: 10.1016/j.mce.2013.03.006. [DOI] [PubMed] [Google Scholar]
- 124.Konstam MA, Kramer DG, Patel AR, Maron MS, Udelson JE. Left ventricular remodeling in heart failure: current concepts in clinical significance and assessment. JACC Cardiovasc Imaging. 2011;4:98–108. doi: 10.1016/j.jcmg.2010.10.008. [DOI] [PubMed] [Google Scholar]
- 125.Huang WM, Yan H, Jin JM, Yu C, Zhang H. Beneficial effects of berberine on hemodynamics during acute ischemic left ventricular failure in dogs. Chin Med J (Engl) 1992;105:1014–9. [PubMed] [Google Scholar]
- 126.Li Y, Chen X, Liu H, Luo F, Li G. [Effects of ginseng total saponins with berberine on plasma brain natriuretic peptide and Ca2+ concentration in experimental rats with chronic congestive heart failure] Zhongguo Zhong Yao Za Zhi. 2009;34:324–7. [PubMed] [Google Scholar]
- 127.Zhang XD, Ren HM, Liu L. [Effects of different dose berberine on hemodynamic parameters and [Ca2+]i of cardiac myocytes of diastolic heart failure rat model] Zhongguo Zhong Yao Za Zhi. 2008;33:818–21. [PubMed] [Google Scholar]
- 128.Tsui H, Zi M, Wang S, Chowdhury SK, Prehar S, Liang Q. et al. Smad3 Couples Pak1 With the Antihypertrophic Pathway Through the E3 Ubiquitin Ligase, Fbxo32. Hypertension. 2015;66:1176–83. doi: 10.1161/HYPERTENSIONAHA.115.06068. [DOI] [PubMed] [Google Scholar]
- 129.Hong Y, Hui SC, Chan TY, Hou JY. Effect of berberine on regression of pressure-overload induced cardiac hypertrophy in rats. Am J Chin Med. 2002;30:589–99. doi: 10.1142/S0192415X02000612. [DOI] [PubMed] [Google Scholar]
- 130.Hong Y, Hui SS, Chan BT, Hou J. Effect of berberine on catecholamine levels in rats with experimental cardiac hypertrophy. Life Sci. 2003;72:2499–507. doi: 10.1016/s0024-3205(03)00144-9. [DOI] [PubMed] [Google Scholar]
- 131.Li MH, Zhang YJ, Yu YH, Yang SH, Iqbal J, Mi QY. et al. Berberine improves pressure overload-induced cardiac hypertrophy and dysfunction through enhanced autophagy. Eur J Pharmacol. 2014;728:67–76. doi: 10.1016/j.ejphar.2014.01.061. [DOI] [PubMed] [Google Scholar]
- 132.Daskalopoulos EP, Dufeys C, Bertrand L, Beauloye C, Horman S. AMPK in cardiac fibrosis and repair: Actions beyond metabolic regulation. J Mol Cell Cardiol. 2016;91:188–200. doi: 10.1016/j.yjmcc.2016.01.001. [DOI] [PubMed] [Google Scholar]
- 133.Gu HP, Lin S, Xu M, Yu HY, Du XJ, Zhang YY. et al. Up-regulating relaxin expression by G-quadruplex interactive ligand to achieve antifibrotic action. Endocrinology. 2012;153:3692–700. doi: 10.1210/en.2012-1114. [DOI] [PubMed] [Google Scholar]
- 134.Zhao HP, Hong Y, Xie JD, Xie XR, Wang J, Fan JB. [Effect of berberine on left ventricular remodeling in renovascular hypertensive rats] Yao Xue Xue Bao. 2007;42:336–41. [PubMed] [Google Scholar]
- 135.Ailawadi G, Eliason JL, Upchurch GR Jr. Current concepts in the pathogenesis of abdominal aortic aneurysm. J Vasc Surg. 2003;38:584–8. doi: 10.1016/s0741-5214(03)00324-0. [DOI] [PubMed] [Google Scholar]
- 136.Calero A, Illig KA. Overview of aortic aneurysm management in the endovascular era. Semin Vasc Surg. 2016;29:3–17. doi: 10.1053/j.semvascsurg.2016.07.003. [DOI] [PubMed] [Google Scholar]
- 137.Wills A, Thompson MM, Crowther M, Sayers RD, Bell PR. Pathogenesis of abdominal aortic aneurysms-cellular and biochemical mechanisms. Eur J Vasc Endovasc Surg. 1996;12:391–400. doi: 10.1016/s1078-5884(96)80002-5. [DOI] [PubMed] [Google Scholar]
- 138.Ai F, Chen M, Yu B, Yang Y, Xu G, Gui F. et al. Berberine regulates proliferation, collagen synthesis and cytokine secretion of cardiac fibroblasts via AMPK-mTOR-p70S6K signaling pathway. Int J Clin Exp Pathol. 2015;8:12509–16. [PMC free article] [PubMed] [Google Scholar]
- 139.van Vlijmen-van Keulen CJ, Pals G, Rauwerda JA. Familial abdominal aortic aneurysm: a systematic review of a genetic background. Eur J Vasc Endovasc Surg. 2002;24:105–16. doi: 10.1053/ejvs.2002.1692. [DOI] [PubMed] [Google Scholar]
- 140.Huang Z, Wang L, Meng S, Wang Y, Chen T, Wang C. Berberine reduces both MMP-9 and EMMPRIN expression through prevention of p38 pathway activation in PMA-induced macrophages. Int J Cardiol. 2011;146:153–8. doi: 10.1016/j.ijcard.2009.06.023. [DOI] [PubMed] [Google Scholar]
- 141.Li XX, Li CB, Xiao J, Gao HQ, Wang HW, Zhang XY. et al. Berberine Attenuates Vascular Remodeling and Inflammation in a Rat Model of Metabolic Syndrome. Biol Pharm Bull. 2015;38:862–8. doi: 10.1248/bpb.b14-00828. [DOI] [PubMed] [Google Scholar]
- 142.Raaz U, Zollner AM, Schellinger IN, Toh R, Nakagami F, Brandt M. et al. Segmental aortic stiffening contributes to experimental abdominal aortic aneurysm development. Circulation. 2015;131:1783–95. doi: 10.1161/CIRCULATIONAHA.114.012377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Pirro M, Lupattelli G, Del Giorno R, Schillaci G, Berisha S, Mannarino MR. et al. Nutraceutical combination (red yeast rice, berberine and policosanols) improves aortic stiffness in low-moderate risk hypercholesterolemic patients. PharmaNutrition. 2013;1:73–7. [Google Scholar]
- 144.Wang J, Guo T, Peng QS, Yue SW, Wang SX. Berberine via suppression of transient receptor potential vanilloid 4 channel improves vascular stiffness in mice. J Cell Mol Med. 2015;19:2607–16. doi: 10.1111/jcmm.12645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Heusch G. Molecular basis of cardioprotection: signal transduction in ischemic pre-, post-, and remote conditioning. Circ Res. 2015;116:674–99. doi: 10.1161/CIRCRESAHA.116.305348. [DOI] [PubMed] [Google Scholar]
- 146.Heusch G. Cardioprotection Is Alive But Remains Enigmatic: The Nitric Oxide-Protein Kinases-Mitochondria Signaling Axis. Circulation. 2017;136:2356–8. doi: 10.1161/CIRCULATIONAHA.117.031978. [DOI] [PubMed] [Google Scholar]
- 147.Zheng L, Zhou Z, Tao D, Lan T. [Protective effect of berberine on cardiac myocyte injured by ischemia-reperfusion] Sichuan Da Xue Xue Bao Yi Xue Ban. 2003;34:452–4. [PubMed] [Google Scholar]
- 148.Tan Y, Tang Q, Hu BR, Xiang JZ. Antioxidant properties of berberine on cultured rabbit corpus cavernosum smooth muscle cells injured by hydrogen peroxide. Acta Pharmacol Sin. 2007;28:1914–8. doi: 10.1111/j.1745-7254.2007.00705.x. [DOI] [PubMed] [Google Scholar]
- 149.Wang L, Ma H, Xue Y, Shi H, Ma T, Cui X. Berberine inhibits the ischemia-reperfusion injury induced inflammatory response and apoptosis of myocardial cells through the phosphoinositide 3-kinase/RAC-alpha serine/threonine-protein kinase and nuclear factor-kappaB signaling pathways. Exp Ther Med. 2018;15:1225–32. doi: 10.3892/etm.2017.5575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Huang W. [The role and mechanism of berberine on coronary arteries] Zhonghua Xin Xue Guan Bing Za Zhi. 1990;18:231–4. 54-5. [PubMed] [Google Scholar]
- 151.Yao W, Wang X, Xiao K. Protective effect of berberine against cardiac ischemia/reperfusion injury by inhibiting apoptosis through the activation of Smad7. Mol Cell Probes. 2018;38:38–44. doi: 10.1016/j.mcp.2017.12.002. [DOI] [PubMed] [Google Scholar]
- 152.Huang Z, Han Z, Ye B, Dai Z, Shan P, Lu Z. et al. Berberine alleviates cardiac ischemia/reperfusion injury by inhibiting excessive autophagy in cardiomyocytes. Eur J Pharmacol. 2015;762:1–10. doi: 10.1016/j.ejphar.2015.05.028. [DOI] [PubMed] [Google Scholar]
- 153.Zhu ML, Yin YL, Ping S, Yu HY, Wan GR, Jian X. et al. Berberine promotes ischemia-induced angiogenesis in mice heart via upregulation of microRNA-29b. Clin Exp Hypertens. 2017;39:672–9. doi: 10.1080/10641963.2017.1313853. [DOI] [PubMed] [Google Scholar]
- 154.Pongkittiphan V, Chavasiri W, Supabphol R. Antioxidant Effect of Berberine and its Phenolic Derivatives Against Human Fibrosarcoma Cells. Asian Pac J Cancer Prev. 2015;16:5371–6. doi: 10.7314/apjcp.2015.16.13.5371. [DOI] [PubMed] [Google Scholar]
- 155.Shirwaikar A, Shirwaikar A, Rajendran K, Punitha IS. In vitro antioxidant studies on the benzyl tetra isoquinoline alkaloid berberine. Biol Pharm Bull. 2006;29:1906–10. doi: 10.1248/bpb.29.1906. [DOI] [PubMed] [Google Scholar]
- 156.Chatuphonprasert W, Lao-Ong T, Jarukamjorn K. Improvement of superoxide dismutase and catalase in streptozotocin-nicotinamide-induced type 2-diabetes in mice by berberine and glibenclamide. Pharm Biol. 2013;52:419–27. doi: 10.3109/13880209.2013.839714. [DOI] [PubMed] [Google Scholar]
- 157.Li Z, Geng YN, Jiang JD, Kong WJ. Antioxidant and anti-inflammatory activities of berberine in the treatment of diabetes mellitus. Evid Based Complement Alternat Med. 2014;2014:289264. doi: 10.1155/2014/289264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Shang W, Liu J, Yu X, Zhao J. [Effects of berberine on serum levels of inflammatory factors and inflammatory signaling pathway in obese mice induced by high fat diet] Zhongguo Zhong Yao Za Zhi. 2010;35:1474–7. [PubMed] [Google Scholar]
- 159.Qin-Wei Z, Yong-Guang LI. Berberine attenuates myocardial ischemia reperfusion injury by suppressing the activation of PI3K/AKT signaling. Exp Ther Med. 2016;11:978–84. doi: 10.3892/etm.2016.3018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Yu L, Li Q, Yu B, Yang Y, Jin Z, Duan W. et al. Berberine Attenuates Myocardial Ischemia/Reperfusion Injury by Reducing Oxidative Stress and Inflammation Response: Role of Silent Information Regulator 1. Oxid Med Cell Longev. 2016;2016:1689602. doi: 10.1155/2016/1689602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Chun YT, Yip TT, Lau KL, Kong YC, Sankawa U. A biochemical study on the hypotensive effect of berberine in rats. Gen Pharmacol. 1979;10:177–82. doi: 10.1016/0306-3623(79)90085-5. [DOI] [PubMed] [Google Scholar]
- 162.Fatehi-Hassanabad Z, Jafarzadeh M, Tarhini A, Fatehi M. The antihypertensive and vasodilator effects of aqueous extract from Berberis vulgaris fruit on hypertensive rats. Phytother Res. 2005;19:222–5. doi: 10.1002/ptr.1661. [DOI] [PubMed] [Google Scholar]
- 163.Heusch G. Myocardial Ischemia: Lack of Coronary Blood Flow or Myocardial Oxygen Supply/Demand Imbalance? Circ Res. 2016;119:194–6. doi: 10.1161/CIRCRESAHA.116.308925. [DOI] [PubMed] [Google Scholar]
- 164.Cheng B, Luo LY, Fang DC, Jiang MX. Cardiovascular aspects of pharmacology of berberine: I. Alpha-adrenoceptor blocking action of berberine in isolated rat anococcygeus muscle and rabbit aortic strip. J Tongji Med Univ. 1987;7:239–41. doi: 10.1007/BF02888450. [DOI] [PubMed] [Google Scholar]
- 165.Olmez E, Ilhan M. Evaluation of the alpha-adrenoceptor antagonistic action of berberine in isolated organs. Arzneimittelforschung. 1992;42:1095–7. [PubMed] [Google Scholar]
- 166.Lau CW, Yao XQ, Chen ZY, Ko WH, Huang Y. Cardiovascular actions of berberine. Cardiovasc Drug Rev. 2001;19:234–44. doi: 10.1111/j.1527-3466.2001.tb00068.x. [DOI] [PubMed] [Google Scholar]
- 167.Wong KK. Mechanism of the aortic relaxation induced by low concentrations of berberine. Planta Med. 1998;64:756–7. doi: 10.1055/s-2006-957575. [DOI] [PubMed] [Google Scholar]
- 168.Ko W-H, Yao X-Q, Lau C-W, Law W-I, Chen Z-Y, Kwok W. et al. Vasorelaxant and antiproliferative effects of berberine. Eur J Pharmacol. 2000;399:187–96. doi: 10.1016/s0014-2999(00)00339-3. [DOI] [PubMed] [Google Scholar]
- 169.Kang DG, Sohn EJ, Kwon EK, Han JH, Oh H, Lee HS. Effects of berberine on angiotensin-converting enzyme and NO/cGMP system in vessels. Vascul Pharmacol. 2002;39:281–6. doi: 10.1016/s1537-1891(03)00005-3. [DOI] [PubMed] [Google Scholar]
- 170.Chiou WF, Chen J, Chen CF. Relaxation of corpus cavernosum and raised intracavernous pressure by berberine in rabbit. Br J Pharmacol. 1998;125:1677–84. doi: 10.1038/sj.bjp.0702249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Xu SZ, Zhang Y, Ren JY, Zhou ZN. Effects of berberine of L- and T-type calcium channels in guinea pig ventricular myocytes. Zhongguo Yao Li Xue Bao. 1997;18:515–8. [PubMed] [Google Scholar]
- 172.Chang W, Zhang M, Li J, Meng Z, Xiao D, Wei S. et al. Berberine attenuates ischemia-reperfusion injury via regulation of adenosine-5'-monophosphate kinase activity in both non-ischemic and ischemic areas of the rat heart. Cardiovasc Drugs Ther. 2012;26:467–78. doi: 10.1007/s10557-012-6422-0. [DOI] [PubMed] [Google Scholar]
- 173.Chen K, Li G, Geng F, Zhang Z, Li J, Yang M. et al. Berberine reduces ischemia/reperfusion-induced myocardial apoptosis via activating AMPK and PI3K-Akt signaling in diabetic rats. Apoptosis. 2014;19:946–57. doi: 10.1007/s10495-014-0977-0. [DOI] [PubMed] [Google Scholar]
- 174.Wang Y, Liu J, Ma A, Chen Y. Cardioprotective effect of berberine against myocardial ischemia/reperfusion injury via attenuating mitochondrial dysfunction and apoptosis. Int J Clin Exp Med. 2015;8:14513–9. [PMC free article] [PubMed] [Google Scholar]
- 175.Yu L, Li F, Zhao G, Yang Y, Jin Z, Zhai M. et al. Protective effect of berberine against myocardial ischemia reperfusion injury: role of Notch1/Hes1-PTEN/Akt signaling. Apoptosis. 2015;20:796–810. doi: 10.1007/s10495-015-1122-4. [DOI] [PubMed] [Google Scholar]
- 176.Zhao GL, Yu LM, Gao WL, Duan WX, Jiang B, Liu XD. et al. Berberine protects rat heart from ischemia/reperfusion injury via activating JAK2/STAT3 signaling and attenuating endoplasmic reticulum stress. Acta Pharmacol Sin. 2016;37:354–67. doi: 10.1038/aps.2015.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Chai YS, Hu J, Lei F, Wang YG, Yuan ZY, Lu X. et al. Effect of berberine on cell cycle arrest and cell survival during cerebral ischemia and reperfusion and correlations with p53/cyclin D1 and PI3K/Akt. Eur J Pharmacol. 2013;708:44–55. doi: 10.1016/j.ejphar.2013.02.041. [DOI] [PubMed] [Google Scholar]
- 178.Zhang Q, Qian Z, Pan L, Li H, Zhu H. Hypoxia-inducible factor 1 mediates the anti-apoptosis of berberine in neurons during hypoxia/ischemia. Acta Physiol Hung. 2012;99:311–23. doi: 10.1556/APhysiol.99.2012.3.8. [DOI] [PubMed] [Google Scholar]
- 179.Hu J, Chai Y, Wang Y, Kheir MM, Li H, Yuan Z. et al. PI3K p55gamma promoter activity enhancement is involved in the anti-apoptotic effect of berberine against cerebral ischemia-reperfusion. Eur J Pharmacol. 2012;674:132–42. doi: 10.1016/j.ejphar.2011.11.014. [DOI] [PubMed] [Google Scholar]
- 180.Yang J, Yan H, Li S, Zhang M. Berberine Ameliorates MCAO Induced Cerebral Ischemia/Reperfusion Injury via Activation of the BDNF-TrkB-PI3K/Akt Signaling Pathway. Neurochem Res. 2018;43:702–10. doi: 10.1007/s11064-018-2472-4. [DOI] [PubMed] [Google Scholar]
- 181.Gong LL, Fang LH, Wang SB, Sun JL, Qin HL, Li XX. et al. Coptisine exert cardioprotective effect through anti-oxidative and inhibition of RhoA/Rho kinase pathway on isoproterenol-induced myocardial infarction in rats. Atherosclerosis. 2012;222:50–8. doi: 10.1016/j.atherosclerosis.2012.01.046. [DOI] [PubMed] [Google Scholar]
- 182.Kim YM, Ha YM, Jin YC, Shi LY, Lee YS, Kim HJ. et al. Palmatine from Coptidis rhizoma reduces ischemia-reperfusion-mediated acute myocardial injury in the rat. Food Chem Toxicol. 2009;47:2097–102. doi: 10.1016/j.fct.2009.05.031. [DOI] [PubMed] [Google Scholar]
- 183.Zhang T, Yang S, Du J. Protective Effects of Berberine on Isoproterenol-Induced Acute Myocardial Ischemia in Rats through Regulating HMGB1-TLR4 Axis. Evid Based Complement Alternat Med. 2014;2014:849783. doi: 10.1155/2014/849783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Yu Y, Zhang M, Hu Y, Zhao Y, Teng F, Lv X. et al. Increased Bioavailable Berberine Protects Against Myocardial Ischemia Reperfusion Injury Through Attenuation of NFkappaB and JNK Signaling Pathways. Int Heart J. 2018;59:1378–88. doi: 10.1536/ihj.17-458. [DOI] [PubMed] [Google Scholar]
- 185.Kalani A, Kamat PK, Kalani K, Tyagi N. Epigenetic impact of curcumin on stroke prevention. Metab Brain Dis. 2015;30:427–35. doi: 10.1007/s11011-014-9537-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Li W, Suwanwela NC, Patumraj S. Curcumin prevents reperfusion injury following ischemic stroke in rats via inhibition of NFkappaB, ICAM-1, MMP-9 and caspase-3 expression. Mol Med Rep. 2017;16:4710–20. doi: 10.3892/mmr.2017.7205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Adams HP Jr, del Zoppo G, Alberts MJ, Bhatt DL, Brass L, Furlan A. et al. Guidelines for the early management of adults with ischemic stroke: a guideline from the American Heart Association/American Stroke Association Stroke Council, Clinical Cardiology Council, Cardiovascular Radiology and Intervention Council, and the Atherosclerotic Peripheral Vascular Disease and Quality of Care Outcomes in Research Interdisciplinary Working Groups: The American Academy of Neurology affirms the value of this guideline as an educational tool for neurologists. Circulation. 2007;115:e478–534. doi: 10.1161/CIRCULATIONAHA.107.181486. [DOI] [PubMed] [Google Scholar]
- 188.Li W, Suwanwela NC, Patumraj S. Curcumin by down-regulating NF-kB and elevating Nrf2, reduces brain edema and neurological dysfunction after cerebral I/R. Microvasc Res. 2016;106:117–27. doi: 10.1016/j.mvr.2015.12.008. [DOI] [PubMed] [Google Scholar]
- 189.Li Y, Wang P, Chai MJ, Yang F, Li HS, Zhao J. et al. [Effects of berberine on serum inflammatory factors and carotid atherosclerotic plaques in patients with acute cerebral ischemic stroke] Zhongguo Zhong Yao Za Zhi. 2016;41:4066–71. doi: 10.4268/cjcmm20162128. [DOI] [PubMed] [Google Scholar]
- 190.Benaissa F, Mohseni-Rad H, Rahimi-Moghaddam P, Mahmoudian M. Berberine reduces the hypoxic-ischemic insult in rat pup brain. Acta Physiol Hung. 2009;96:213–20. doi: 10.1556/APhysiol.96.2009.2.6. [DOI] [PubMed] [Google Scholar]
- 191.Kim M, Shin MS, Lee JM, Cho HS, Kim CJ, Kim YJ. et al. Inhibitory Effects of Isoquinoline Alkaloid Berberine on Ischemia-Induced Apoptosis via Activation of Phosphoinositide 3-Kinase/Protein Kinase B Signaling Pathway. Int Neurourol J. 2014;18:115–25. doi: 10.5213/inj.2014.18.3.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Zhou XQ, Zeng XN, Kong H, Sun XL. Neuroprotective effects of berberine on stroke models in vitro and in vivo. Neurosci Lett. 2008;447:31–6. doi: 10.1016/j.neulet.2008.09.064. [DOI] [PubMed] [Google Scholar]
- 193.Zhu JR, Lu HD, Guo C, Fang WR, Zhao HD, Zhou JS. et al. Berberine attenuates ischemia-reperfusion injury through inhibiting HMGB1 release and NF-kappaB nuclear translocation. Acta Pharmacol Sin. 2018;39:1706–15. doi: 10.1038/s41401-018-0160-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Liu H, Ren X, Ma C. Effect of Berberine on Angiogenesis and HIF-1α / VEGF Signal Transduction Pathway in Rats with Cerebral Ischemia - Reperfusion Injury. J Coll Physicians Surg Pak. 2018;28:753–7. [PubMed] [Google Scholar]
- 195.Maleki SN, Aboutaleb N, Souri F. Berberine confers neuroprotection in coping with focal cerebral ischemia by targeting inflammatory cytokines. J Chem Neuroanat. 2018;87:54–9. doi: 10.1016/j.jchemneu.2017.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Singh DP, Chopra K. Verapamil augments the neuroprotectant action of berberine in rat model of transient global cerebral ischemia. Eur J Pharmacol. 2013;720:98–106. doi: 10.1016/j.ejphar.2013.10.043. [DOI] [PubMed] [Google Scholar]
- 197.Yoo KY, Hwang IK, Kim JD, Kang IJ, Park J, Yi JS. et al. Antiinflammatory effect of the ethanol extract of Berberis koreana in a gerbil model of cerebral ischemia/reperfusion. Phytother Res. 2008;22:1527–32. doi: 10.1002/ptr.2527. [DOI] [PubMed] [Google Scholar]
- 198.Zhang Q, Fu X, Wang J, Yang M, Kong L. Treatment Effects of Ischemic Stroke by Berberine, Baicalin, and Jasminoidin from Huang-Lian-Jie-Du-Decoction (HLJDD) Explored by an Integrated Metabolomics Approach. Oxid Med Cell Longev. 2017;2017:9848594. doi: 10.1155/2017/9848594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Li S, Wu C, Chen J, Lu P, Chen C, Fu M. et al. An effective solution to discover synergistic drugs for anti-cerebral ischemia from traditional Chinese medicinal formulae. PLoS One. 2013;8:e78902. doi: 10.1371/journal.pone.0078902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Huang W, Wu Z, Gan Y. Effects of berberine on ischemic ventricular arrhythmia. Zhonghua Xin Xue Guan Bing Za Zhi. 1989;17:300–1. 19. [PubMed] [Google Scholar]
- 201.Zhou Z-W, Zheng H-C, Zhao L-F, Li W, Hou J-W, Yu Y. et al. Effect of berberine on acetylcholine-induced atrial fibrillation in rabbit. Am J Transl Res. 2015;7:1450–7. [PMC free article] [PubMed] [Google Scholar]
- 202.Jun-xian C, Lu F, Yu-hui D, Yan-li D, Jun-xian C. THE EFFECT OF BERBERINE ON ARRHYTHMIA CAUSED BY STRETCH OF ISOLATED MYOCARDIAL INFARCTED HEARTS IN RATS. Heart. 2012;98:E84. [Google Scholar]
- 203.Neto FR. Electropharmacological effects of berberine on canine cardiac Purkinje fibres and ventricular muscle and atrial muscle of the rabbit. Br J Pharmacol. 1993;108:534–7. doi: 10.1111/j.1476-5381.1993.tb12836.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Chen H, Chen Y, Tang Y, Yang J, Wang D, Yu T. et al. Berberine attenuates spontaneous action potentials in sinoatrial node cells and the currents of human HCN4 channels expressed in Xenopus laevis oocytes. Mol Med Rep. 2014;10:1576–82. doi: 10.3892/mmr.2014.2377. [DOI] [PubMed] [Google Scholar]
- 205.Wei T, Liang Z, Jin Y, Zhang L. [Effect of berberine, liensinine and neferine on HERG channel expression] Zhongguo Zhong yao za zhi. 2013;38:239–44. [PubMed] [Google Scholar]
- 206.Sanguinetti MC, Tristani-Firouzi M. hERG potassium channels and cardiac arrhythmia. Nature. 2006;440:463. doi: 10.1038/nature04710. [DOI] [PubMed] [Google Scholar]
- 207.Zhang K, Zhi D, Huang T, Gong Y, Yan M, Liu C. et al. Berberine Induces hERG Channel Deficiency through Trafficking Inhibition. Cell Physiol Biochem. 2014;34:691–702. doi: 10.1159/000363034. [DOI] [PubMed] [Google Scholar]
- 208.Yan M, Zhang K, Shi Y, Feng L, Lv L, Li B. Mechanism and pharmacological rescue of berberine-induced hERG channel deficiency. Drug Des Devel Ther. 2015;9:5737–47. doi: 10.2147/DDDT.S91561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Rodriguez-Menchaca A, Ferrer-Villada T, Lara J, Fernandez D, Navarro-Polanco RA, Sanchez-Chapula JA. Block of hERG Channels by Berberine: Mechanisms of Voltage- and State-Dependence Probed With Site-Directed Mutant Channels. J Cardiovasc Pharmacol. 2006;47:21–9. doi: 10.1097/01.fjc.0000191564.52242.00. [DOI] [PubMed] [Google Scholar]
- 210.Llorent-Martínez EJ, Zengin G, Lobine D, Molina-García L, Mollica A, Mahomoodally MF. Phytochemical characterization, in vitro and in silico approaches for three Hypericum species. New J Chem. 2018;42:5204–14. [Google Scholar]
- 211.American Diabetets Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2009;32(Suppl 1):S62–7. doi: 10.2337/dc09-S062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Association AD. Diagnosis and classification of diabetes mellitus. Diabetes care. 2010;33:S62. doi: 10.2337/dc10-S062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Horr S, Nissen S. Managing hypertension in type 2 diabetes mellitus. Best Pract Res Clin Endocrinol Metab. 2016;30:445–54. doi: 10.1016/j.beem.2016.06.001. [DOI] [PubMed] [Google Scholar]
- 214.Li J-w, Yuan K, Shang S-c, Guo Y. A safer hypoglycemic agent for type 2 diabetes—Berberine organic acid salt. J Funct Foods. 2017;38:399–408. [Google Scholar]
- 215.Raman B, Krishna N, Rao N, Saradhi P, Rao B. Plants with antidiabetic activities and their medicinal values. Int Res J Pharm. 2012;3:11–5. [Google Scholar]
- 216.Grover JK, Yadav S, Vats V. Medicinal plants of India with anti-diabetic potential. J Ethnopharmacol. 2002;81:81–100. doi: 10.1016/s0378-8741(02)00059-4. [DOI] [PubMed] [Google Scholar]
- 217.Chang W, Chen L, Hatch GM. Berberine as a therapy for type 2 diabetes and its complications: From mechanism of action to clinical studies. Biochem Cell Biol. 2014;93:479–86. doi: 10.1139/bcb-2014-0107. [DOI] [PubMed] [Google Scholar]
- 218.Dong H, Zhao Y, Zhao L, Lu F. The effects of berberine on blood lipids: a systemic review and meta-analysis of randomized controlled trials. Planta Medica. 2013;79:437–46. doi: 10.1055/s-0032-1328321. [DOI] [PubMed] [Google Scholar]
- 219.Gong J, Hu M, Huang Z, Fang K, Wang D, Chen Q. et al. Berberine attenuates intestinal mucosal barrier dysfunction in type 2 diabetic rats. Front Pharmacol. 2017;8:42. doi: 10.3389/fphar.2017.00042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Lan T, Shen X, Liu P, Liu W, Xu S, Xie X. et al. Berberine ameliorates renal injury in diabetic C57BL/6 mice: Involvement of suppression of SphK-S1P signaling pathway. Arch Biochem Biophys. 2010;502:112–20. doi: 10.1016/j.abb.2010.07.012. [DOI] [PubMed] [Google Scholar]
- 221.Jiang Q, Liu P, Wu X, Liu W, Shen X, Lan T. et al. Berberine attenuates lipopolysaccharide-induced extracelluar matrix accumulation and inflammation in rat mesangial cells: involvement of NF-kappaB signaling pathway. Mol Cell Endocrinol. 2011;331:34–40. doi: 10.1016/j.mce.2010.07.023. [DOI] [PubMed] [Google Scholar]
- 222.Chang W, Zhang M, Li J, Meng Z, Wei S, Du H. et al. Berberine improves insulin resistance in cardiomyocytes via activation of 5'-adenosine monophosphate-activated protein kinase. Metabolism. 2013;62:1159–67. doi: 10.1016/j.metabol.2013.02.007. [DOI] [PubMed] [Google Scholar]
- 223.Pan G, Wang G, Sun J, Huang Z, Zhao X, Gu Y. et al. Inhibitory action of berberine on glucose absorption. Yao xue xue bao. 2003;38:911–4. [PubMed] [Google Scholar]
- 224.Vuddanda PR, Chakraborty S, Singh S. Berberine: a potential phytochemical with multispectrum therapeutic activities. Expert Opin Investig Drugs. 2010;19:1297–307. doi: 10.1517/13543784.2010.517745. [DOI] [PubMed] [Google Scholar]
- 225.Eid AA, Ford BM, Block K, Kasinath BS, Gorin Y, Ghosh-Choudhury G. et al. AMP-activated protein kinase (AMPK) negatively regulates Nox4-dependent activation of p53 and epithelial cell apoptosis in diabetes. J Biol Chem. 2010;285:37503–12. doi: 10.1074/jbc.M110.136796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Zhao L, Sun L, Nie H, Wang X, Guan G. Berberine improves kidney function in diabetic mice via AMPK activation. PLoS ONE. 2014;9:e113398. doi: 10.1371/journal.pone.0113398. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 227.Xiao Y, Xu M, Alimujiang M, Bao Y, Wei L, Yin J. Bidirectional regulation of adenosine 5'-monophosphate-activated protein kinase activity by berberine and metformin in response to changes in ambient glucose concentration. J Cell Biochem. 2018;119:9910–20. doi: 10.1002/jcb.27312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Zhang B, Pan Y, Xu L, Tang D, Dorfman RG, Zhou Q. et al. Berberine promotes glucose uptake and inhibits gluconeogenesis by inhibiting deacetylase SIRT3. Endocrine. 2018;62:576–87. doi: 10.1007/s12020-018-1689-y. [DOI] [PubMed] [Google Scholar]
- 229.Li A, Liu Q, Li Q, Liu B, Yang Y, Zhang N. Berberine Reduces Pyruvate-driven Hepatic Glucose Production by Limiting Mitochondrial Import of Pyruvate through Mitochondrial Pyruvate Carrier 1. EBioMedicine. 2018;34:243–55. doi: 10.1016/j.ebiom.2018.07.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Xie W, Du L. Diabetes is an inflammatory disease: evidence from traditional Chinese medicines. Diabetes Obes Metab. 2011;13:289–301. doi: 10.1111/j.1463-1326.2010.01336.x. [DOI] [PubMed] [Google Scholar]
- 231.Ma X, Chen Z, Wang L, Wang G, Wang Z, Dong X. et al. The Pathogenesis of Diabetes Mellitus by Oxidative Stress and Inflammation: Its Inhibition by Berberine. Front Pharmacol. 2018;9:782. doi: 10.3389/fphar.2018.00782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Hua W, Ding L, Chen Y, Gong B, He J, Xu G. Determination of berberine in human plasma by liquid chromatography-electrospray ionization-mass spectrometry. J Pharm Biomed Anal. 2007;44:931–7. doi: 10.1016/j.jpba.2007.03.022. [DOI] [PubMed] [Google Scholar]
- 233.Zhang X, Zhao Y, Zhang M, Pang X, Xu J, Kang C. et al. Structural changes of gut microbiota during berberine-mediated prevention of obesity and insulin resistance in high-fat diet-fed rats. PLoS One. 2012;7:e42529. doi: 10.1371/journal.pone.0042529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Roberts CK, Hevener AL, Barnard RJ. Metabolic syndrome and insulin resistance: underlying causes and modification by exercise training. Compr Physiol. 2013;3:1–58. doi: 10.1002/cphy.c110062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Cefalu WT. Insulin resistance: cellular and clinical concepts. Exp Biol Med. 2001;226:13–26. doi: 10.1177/153537020122600103. [DOI] [PubMed] [Google Scholar]
- 236.Kong WJ, Zhang H, Song DQ, Xue R, Zhao W, Wei J. et al. Berberine reduces insulin resistance through protein kinase C-dependent up-regulation of insulin receptor expression. Metabolism. 2009;58:109–19. doi: 10.1016/j.metabol.2008.08.013. [DOI] [PubMed] [Google Scholar]
- 237.Mahmoud MA, Ghareeb DA, Sahyoun HA, Elshehawy AA, Elsayed MM. In Vivo Interrelationship between Insulin Resistance and Interferon Gamma Production: Protective and Therapeutic Effect of Berberine. Evid Based Complement Alternat Med. 2016;2016:2039897. doi: 10.1155/2016/2039897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Liu LZ, Cheung SC, Lan LL, Ho SK, Xu HX, Chan JC. et al. Berberine modulates insulin signaling transduction in insulin-resistant cells. Mol Cell Endocrinol. 2010;317:148–53. doi: 10.1016/j.mce.2009.12.027. [DOI] [PubMed] [Google Scholar]
- 239.Liu D, Zhang Y, Liu Y, Hou L, Li S, Tian H. et al. Berberine Modulates Gut Microbiota and Reduces Insulin Resistance via the TLR4 Signaling Pathway. Exp Clin Endocrinol Diabetes. 2018;126:513–20. doi: 10.1055/s-0043-125066. [DOI] [PubMed] [Google Scholar]
- 240.Yue SJ, Liu J, Wang AT, Meng XT, Yang ZR, Peng C. et al. Berberine alleviates insulin resistance by reducing peripheral branched-chain amino acids. Am J Physiol Endocrinol Metab. 2019;316:E73–E85. doi: 10.1152/ajpendo.00256.2018. [DOI] [PubMed] [Google Scholar]
- 241.Affuso F, Mercurio V, Fazio V, Fazio S. Cardiovascular and metabolic effects of Berberine. World J Cardiol. 2010;2:71. doi: 10.4330/wjc.v2.i4.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Zhao L, Cang Z, Sun H, Nie X, Wang N, Lu Y. Berberine improves glucogenesis and lipid metabolism in nonalcoholic fatty liver disease. BMC Endocr Disord. 2017;17:13. doi: 10.1186/s12902-017-0165-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Wei S, Zhang M, Yu Y, Lan X, Yao F, Yan X. et al. Berberine Attenuates Development of the Hepatic Gluconeogenesis and Lipid Metabolism Disorder in Type 2 Diabetic Mice and in Palmitate-Incubated HepG2 Cells through Suppression of the HNF-4alpha miR122 Pathway. PLoS One. 2016;11:e0152097. doi: 10.1371/journal.pone.0152097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Cao S, Xu P, Yan J, Liu H, Liu L, Cheng L, Berberrubine and its analog, hydroxypropyl-berberrubine, regulate LDLR and PCSK9 expression via the ERK signal pathway to exert cholesterol-lowering effects in human hepatoma HepG2 cells. J Cell Biochem; 2018. [DOI] [PubMed] [Google Scholar]
- 245.Han JL, Lin HL. Intestinal microbiota and type 2 diabetes: from mechanism insights to therapeutic perspective. World J Gastroenterol. 2014;20:17737–45. doi: 10.3748/wjg.v20.i47.17737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Fei N, Zhao L. An opportunistic pathogen isolated from the gut of an obese human causes obesity in germfree mice. The ISME journal. 2013;7:880. doi: 10.1038/ismej.2012.153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Cani PD, Amar J, Iglesias MA, Poggi M, Knauf C, Bastelica D. et al. Metabolic endotoxemia initiates obesity and insulin resistance. Diabetes. 2007;56:1761–72. doi: 10.2337/db06-1491. [DOI] [PubMed] [Google Scholar]
- 248.Han J, Lin H, Huang W. Modulating gut microbiota as an anti-diabetic mechanism of berberine. Med Sci Monit. 2011;17:RA164. doi: 10.12659/MSM.881842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.Jhong CH, Riyaphan J, Lin SH, Chia YC, Weng CF. Screening alpha-glucosidase and alpha-amylase inhibitors from natural compounds by molecular docking in silico. Biofactors. 2015;41:242–51. doi: 10.1002/biof.1219. [DOI] [PubMed] [Google Scholar]
- 250.Sales PM, Souza PM, Simeoni LA, Magalhães PO, Silveira D. α-Amylase inhibitors: a review of raw material and isolated compounds from plant source. J Pharm Pharm Sci. 2012;15:141–83. doi: 10.18433/j35s3k. [DOI] [PubMed] [Google Scholar]
- 251.El-Wahab AEA, Ghareeb DA, Sarhan EE, Abu-Serie MM, El Demellawy MA. In vitro biological assessment of berberis vulgaris and its active constituent, berberine: antioxidants, anti-acetylcholinesterase, anti-diabetic and anticancer effects. BMC Complement Altern Med. 2013;13:218. doi: 10.1186/1472-6882-13-218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Xiao-Ping Y, Chun-Qing S, Ping Y, Ren-Gang M. α-Glucosidase and α-amylase inhibitory activity of common constituents from traditional Chinese medicine used for diabetes mellitus. Chinese Journal of Natural Medicines. 2010;8:349–52. [Google Scholar]
- 253.Retnakaran R, Zinman B. Type 1 diabetes, hyperglycaemia, and the heart. Lancet. 2008;371:1790–9. doi: 10.1016/S0140-6736(08)60767-9. [DOI] [PubMed] [Google Scholar]
- 254.Rao Kondapally Seshasai S, Kaptoge S, Thompson A, Di Angelantonio E, Gao P, Sarwar N. et al. Diabetes mellitus, fasting glucose, and risk of cause-specific death. N Engl J Med. 2011;364:829–41. doi: 10.1056/NEJMoa1008862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Wang C, Li J, Lv X, Zhang M, Song Y, Chen L. et al. Ameliorative effect of berberine on endothelial dysfunction in diabetic rats induced by high-fat diet and streptozotocin. Eur J Pharmacol. 2009;620:131–7. doi: 10.1016/j.ejphar.2009.07.027. [DOI] [PubMed] [Google Scholar]
- 256.Wong SL, Wong WT, Tian XY, Lau CW, Huang Y. Chapter 3 - Prostaglandins in Action: Indispensable Roles of Cyclooxygenase-1 and -2 in Endothelium-Dependent Contractions. Adv Pharmacol. 2010;60:61–83. doi: 10.1016/B978-0-12-385061-4.00003-9. [DOI] [PubMed] [Google Scholar]
- 257.Wang Y, Huang Y, Lam KS, Li Y, Wong WT, Ye H. et al. Berberine prevents hyperglycemia-induced endothelial injury and enhances vasodilatation via adenosine monophosphate-activated protein kinase and endothelial nitric oxide synthase. Cardiovasc Res. 2009;82:484–92. doi: 10.1093/cvr/cvp078. [DOI] [PubMed] [Google Scholar]
- 258.Tao K, Chen J, Wang L. Effects of berberine on the expressions of NRF2 and HO-1 in endothelial cells of diabetic rat. Biomedical Research. 2017;28:3860–64. [Google Scholar]
- 259.Geng FH, Li GH, Zhang X, Zhang P, Dong MQ, Zhao ZJ. et al. Berberine improves mesenteric artery insulin sensitivity through up-regulating insulin receptor-mediated signalling in diabetic rats. Br J Pharmacol. 2016;173:1569–79. doi: 10.1111/bph.13466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Pierelli G, Stanzione R, Forte M, Migliarino S, Perelli M, Volpe M. et al. Uncoupling Protein 2: A Key Player and a Potential Therapeutic Target in Vascular Diseases. Oxid Med Cell Longev. 2017;2017:7348372. doi: 10.1155/2017/7348372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.He Y, Wang N, Shen Y, Zheng Z, Xu X. Inhibition of high glucose-induced apoptosis by uncoupling protein 2 in human umbilical vein endothelial cells. Int J Mol Med. 2014;33:1275–81. doi: 10.3892/ijmm.2014.1676. [DOI] [PubMed] [Google Scholar]
- 262.Wang Q, Zhang M, Liang B, Shirwany N, Zhu Y, Zou M-H. Activation of AMP-activated protein kinase is required for berberine-induced reduction of atherosclerosis in mice: the role of uncoupling protein 2. PLoS One. 2011;6:e25436. doi: 10.1371/journal.pone.0025436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.Paul M, Hemshekhar M, Kemparaju K, Girish KS. Berberine mitigates high glucose-potentiated platelet aggregation and apoptosis by modulating aldose reductase and NADPH oxidase activity. Free Radic Biol Med. 2018;130:196–205. doi: 10.1016/j.freeradbiomed.2018.10.453. [DOI] [PubMed] [Google Scholar]
- 264.Sen S, McDonald SP, Coates PT, Bonder CS. Endothelial progenitor cells: novel biomarker and promising cell therapy for cardiovascular disease. Clin Sci (Lond) 2011;120:263–83. doi: 10.1042/CS20100429. [DOI] [PubMed] [Google Scholar]
- 265.Xu MG, Wang JM, Chen L, Wang Y, Yang Z, Tao J. Berberine-induced upregulation of circulating endothelial progenitor cells is related to nitric oxide production in healthy subjects. Cardiology. 2009;112:279–86. doi: 10.1159/000157336. [DOI] [PubMed] [Google Scholar]
- 266.Xu MG, Wang JM, Chen L, Wang Y, Yang Z, Tao J. Berberine-induced mobilization of circulating endothelial progenitor cells improves human small artery elasticity. J Hum Hypertens. 2008;22:389–93. doi: 10.1038/sj.jhh.1002311. [DOI] [PubMed] [Google Scholar]
- 267.Spigoni V, Aldigeri R, Antonini M, Micheli MM, Fantuzzi F, Fratter A. et al. Effects of a New Nutraceutical Formulation (Berberine, Red Yeast Rice and Chitosan) on Non-HDL Cholesterol Levels in Individuals with Dyslipidemia: Results from a Randomized, Double Blind, Placebo-Controlled Study. Int J Mol Sci. 2017;18:1498. doi: 10.3390/ijms18071498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.Affuso F, Ruvolo A, Micillo F, Sacca L, Fazio S. Effects of a nutraceutical combination (berberine, red yeast rice and policosanols) on lipid levels and endothelial function randomized, double-blind, placebo-controlled study. Nutr Metab Cardiovasc Dis. 2010;20:656–61. doi: 10.1016/j.numecd.2009.05.017. [DOI] [PubMed] [Google Scholar]
- 269.Dong S, Zhang S, Chen Z, Zhang R, Tian L, Cheng L. et al. Berberine Could Ameliorate Cardiac Dysfunction via Interfering Myocardial Lipidomic Profiles in the Rat Model of Diabetic Cardiomyopathy. Front Physiol. 2018;9:1042. doi: 10.3389/fphys.2018.01042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270.Chang W, Zhang M, Meng Z, Yu Y, Yao F, Hatch GM. et al. Berberine treatment prevents cardiac dysfunction and remodeling through activation of 5'-adenosine monophosphate-activated protein kinase in type 2 diabetic rats and in palmitate-induced hypertrophic H9c2 cells. Eur J Pharmacol. 2015;769:55–63. doi: 10.1016/j.ejphar.2015.10.043. [DOI] [PubMed] [Google Scholar]
- 271.Hang W, He B, Chen J, Xia L, Wen B, Liang T. et al. Berberine Ameliorates High Glucose-Induced Cardiomyocyte Injury via AMPK Signaling Activation to Stimulate Mitochondrial Biogenesis and Restore Autophagic Flux. Front Pharmacol. 2018;9:1121. doi: 10.3389/fphar.2018.01121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 272.Chang W, Li K, Guan F, Yao F, Yu Y, Zhang M. et al. Berberine Pretreatment Confers Cardioprotection Against Ischemia-Reperfusion Injury in a Rat Model of Type 2 Diabetes. J Cardiovasc Pharmacol Ther. 2016;21:486–94. doi: 10.1177/1074248415627873. [DOI] [PubMed] [Google Scholar]
- 273.Li G, Xing W, Zhang M, Geng FH, Yang H, Zhang H. et al. Anti-fibrotic cardioprotection of berberine via down-regulating myocardial IGF-1 receptor-regulated MMP-2/9 expression in diabetic rats. Am J Physiol Heart Circ Physiol. 2018;315:H802–h13. doi: 10.1152/ajpheart.00093.2018. [DOI] [PubMed] [Google Scholar]
- 274.Lu K, Shen Y, He J, Liu G, Song W. [Berberine inhibits cardiac fibrosis of diabetic rats] Xi Bao Yu Fen Zi Mian Yi Xue Za Zhi. 2016;32:1352–5. [PubMed] [Google Scholar]
- 275.Wang LH, Li XL, Li Q, Fu Y, Yu HJ, Sun YQ. et al. Berberine alleviates ischemic arrhythmias via recovering depressed I(to) and I(Ca) currents in diabetic rats. Phytomedicine. 2012;19:206–10. doi: 10.1016/j.phymed.2011.11.002. [DOI] [PubMed] [Google Scholar]
- 276.Wang L-h, Yu C-h, Fu Y, Li Q, Sun Y-q. Berberine elicits anti-arrhythmic effects via IK1/Kir2.1 in the rat type 2 diabetic myocardial infarction model. Phytother Res. 2011;25:33–7. doi: 10.1002/ptr.3097. [DOI] [PubMed] [Google Scholar]
- 277.Jung UJ, Choi MS. Obesity and its metabolic complications: the role of adipokines and the relationship between obesity, inflammation, insulin resistance, dyslipidemia and nonalcoholic fatty liver disease. Int J Mol Sci. 2014;15:6184–223. doi: 10.3390/ijms15046184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 278.Wang FF, Wu Y, Zhu YH, Ding T, Batterham RL, Qu F. et al. Pharmacologic therapy to induce weight loss in women who have obesity/overweight with polycystic ovary syndrome: a systematic review and network meta-analysis. Obes Rev. 2018;19:1424–45. doi: 10.1111/obr.12720. [DOI] [PubMed] [Google Scholar]
- 279.Hu Y, Davies GE. Berberine inhibits adipogenesis in high-fat diet-induced obesity mice. Fitoterapia. 2010;81:358–66. doi: 10.1016/j.fitote.2009.10.010. [DOI] [PubMed] [Google Scholar]
- 280.Ma X, Egawa T, Kimura H, Karaike K, Masuda S, Iwanaka N. et al. Berberine-induced activation of 5'-adenosine monophosphate-activated protein kinase and glucose transport in rat skeletal muscles. Metabolism. 2010;59:1619–27. doi: 10.1016/j.metabol.2010.03.009. [DOI] [PubMed] [Google Scholar]
- 281.Kulkarni SK, Dhir A. On the mechanism of antidepressant-like action of berberine chloride. Eur J Pharmacol. 2008;589:163–72. doi: 10.1016/j.ejphar.2008.05.043. [DOI] [PubMed] [Google Scholar]
- 282.Sun H, Wang N, Cang Z, Zhu C, Zhao L, Nie X. et al. Modulation of Microbiota-Gut-Brain Axis by Berberine Resulting in Improved Metabolic Status in High-Fat Diet-Fed Rats. Obes Facts. 2016;9:365–78. doi: 10.1159/000449507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 283.Yin J, Ye J, Jia W. Effects and mechanisms of berberine in diabetes treatment. Acta Pharmaceutica Sinica B. 2012;2:327–34. [Google Scholar]
- 284.Yu Y, Liu L, Wang X, Liu X, Liu X, Xie L. et al. Modulation of glucagon-like peptide-1 release by berberine: in vivo and in vitro studies. Biochem Pharmacol. 2010;79:1000–6. doi: 10.1016/j.bcp.2009.11.017. [DOI] [PubMed] [Google Scholar]
- 285.Sun Y, Jin C, Zhang X, Jia W, Le J, Ye J. Restoration of GLP-1 secretion by Berberine is associated with protection of colon enterocytes from mitochondrial overheating in diet-induced obese mice. Nutr Diabetes. 2018;8:53. doi: 10.1038/s41387-018-0061-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 286.Sommer F, Adam N, Johansson ME, Xia L, Hansson GC, Backhed F. Altered mucus glycosylation in core 1 O-glycan-deficient mice affects microbiota composition and intestinal architecture. PLoS One. 2014;9:e85254. doi: 10.1371/journal.pone.0085254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 287.Backhed F, Manchester JK, Semenkovich CF, Gordon JI. Mechanisms underlying the resistance to diet-induced obesity in germ-free mice. Proc Natl Acad Sci U S A. 2007;104:979–84. doi: 10.1073/pnas.0605374104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 288.Xie W, Gu D, Li J, Cui K, Zhang Y. Effects and action mechanisms of berberine and Rhizoma coptidis on gut microbes and obesity in high-fat diet-fed C57BL/6J mice. PLoS One. 2011;6:e24520. doi: 10.1371/journal.pone.0024520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 289.Chae SH, Jeong IH, Choi DH, Oh JW, Ahn YJ. Growth-inhibiting effects of Coptis japonica root-derived isoquinoline alkaloids on human intestinal bacteria. J Agric Food Chem. 1999;47:934–8. doi: 10.1021/jf980991o. [DOI] [PubMed] [Google Scholar]
- 290.Chalasani N, Younossi Z, Lavine JE, Diehl AM, Brunt EM, Cusi K. et al. The diagnosis and management of non-alcoholic fatty liver disease: practice Guideline by the American Association for the Study of Liver Diseases, American College of Gastroenterology, and the American Gastroenterological Association. Hepatology. 2012;55:2005–23. doi: 10.1002/hep.25762. [DOI] [PubMed] [Google Scholar]
- 291.Michelotti GA, Machado MV, Diehl AM. NAFLD, NASH and liver cancer. Nat Rev Gastroenterol Hepatol. 2013;10:656–65. doi: 10.1038/nrgastro.2013.183. [DOI] [PubMed] [Google Scholar]
- 292.Cohen JC, Horton JD, Hobbs HH. Human fatty liver disease: old questions and new insights. Science. 2011;332:1519–23. doi: 10.1126/science.1204265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 293.Kim WS, Lee YS, Cha SH, Jeong HW, Choe SS, Lee MR. et al. Berberine improves lipid dysregulation in obesity by controlling central and peripheral AMPK activity. Am J Physiol Endocrinol Metab. 2009;296:E812–9. doi: 10.1152/ajpendo.90710.2008. [DOI] [PubMed] [Google Scholar]
- 294.Li Y, Xu S, Mihaylova MM, Zheng B, Hou X, Jiang B. et al. AMPK phosphorylates and inhibits SREBP activity to attenuate hepatic steatosis and atherosclerosis in diet-induced insulin-resistant mice. Cell Metab. 2011;13:376–88. doi: 10.1016/j.cmet.2011.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 295.Yuebin G, Yan Z, Rui L, Wei C, Yang L, Guoxun C. Berberine regulated Gck, G6pc, Pck1 and Srebp-1c expression and activated AMP-activated protein kinase in primary rat hepatocytes. Int J Biol Sci. 2011;7:673–84. doi: 10.7150/ijbs.7.673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 296.Jang J, Jung Y, Seo S, Kim SM, Shim Y, Cho S. et al. Berberine activates AMPK to suppress proteolytic processing, nuclear translocation and target DNA binding of SREBP-1c in 3T3-L1 adipocytes. Mol Med Rep. 2017;15:4139–47. doi: 10.3892/mmr.2017.6513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 297.Lee YS, Kim WS, Kim KH, Yoon MJ, Cho HJ, Shen Y. et al. Berberine, a natural plant product, activates AMP-activated protein kinase with beneficial metabolic effects in diabetic and insulin-resistant states. Diabetes. 2006;55:2256–64. doi: 10.2337/db06-0006. [DOI] [PubMed] [Google Scholar]
- 298.Feng WW, Kuang SY, Tu C, Ma ZJ, Pang JY, Wang YH. et al. Natural products berberine and curcumin exhibited better ameliorative effects on rats with non-alcohol fatty liver disease than lovastatin. Biomed Pharmacother. 2018;99:325–33. doi: 10.1016/j.biopha.2018.01.071. [DOI] [PubMed] [Google Scholar]
- 299.Li Y, Zhao X, Feng X, Liu X, Deng C, Hu CH. Berberine Alleviates Olanzapine-Induced Adipogenesis via the AMPKalpha-SREBP Pathway in 3T3-L1 Cells. Int J Mol Sci. 2016;17:1865. doi: 10.3390/ijms17111865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 300.Ide T, Shimano H, Yahagi N, Matsuzaka T, Nakakuki M, Yamamoto T. et al. SREBPs suppress IRS-2-mediated insulin signalling in the liver. Nat Cell Biol. 2004;6:351–7. doi: 10.1038/ncb1111. [DOI] [PubMed] [Google Scholar]
- 301.Sun H, Liu Q, Hu H, Jiang Y, Shao W, Wang Q. et al. Berberine ameliorates blockade of autophagic flux in the liver by regulating cholesterol metabolism and inhibiting COX2-prostaglandin synthesis. Cell Death Dis. 2018;9:824. doi: 10.1038/s41419-018-0890-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 302.Xing LJ, Zhang L, Liu T, Hua YQ, Zheng PY, Ji G. Berberine reducing insulin resistance by up-regulating IRS-2 mRNA expression in nonalcoholic fatty liver disease (NAFLD) rat liver. Eur J Pharmacol. 2011;668:467–71. doi: 10.1016/j.ejphar.2011.07.036. [DOI] [PubMed] [Google Scholar]
- 303.Uyeda K, Repa JJ. Carbohydrate response element binding protein, ChREBP, a transcription factor coupling hepatic glucose utilization and lipid synthesis. Cell Metab. 2006;4:107–10. doi: 10.1016/j.cmet.2006.06.008. [DOI] [PubMed] [Google Scholar]
- 304.Xia X, Yan J, Shen Y, Tang K, Yin J, Zhang Y. et al. Berberine improves glucose metabolism in diabetic rats by inhibition of hepatic gluconeogenesis. PLoS One. 2011;6:e16556. doi: 10.1371/journal.pone.0016556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 305.Liu X, Li G, Zhu H, Huang L, Liu Y, Ma C. et al. Beneficial effect of berberine on hepatic insulin resistance in diabetic hamsters possibly involves in SREBPs, LXRalpha and PPARalpha transcriptional programs. Endocr J. 2010;57:881–93. doi: 10.1507/endocrj.k10e-043. [DOI] [PubMed] [Google Scholar]
- 306.Chang X, Yan H, Fei J, Jiang M, Zhu H, Lu D. et al. Berberine reduces methylation of the MTTP promoter and alleviates fatty liver induced by a high-fat diet in rats. J Lipid Res. 2010;51:2504–15. doi: 10.1194/jlr.M001958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 307.Han L, Yang QH, Zhang YP, Yan HZ, Zhu XF, Gong XW. et al. [Intervention of berberine on lipid deposition in liver cells of non-alcoholic fatty liver disease rats induced by high fat diet] Zhongguo Zhong Xi Yi Jie He Za Zhi. 2015;35:314–9. [PubMed] [Google Scholar]
- 308.Yang QH, Hu SP, Zhang YP, Xie WN, Li N, Ji GY. et al. Effect of berberine on expressions of uncoupling protein-2 mRNA and protein in hepatic tissue of non-alcoholic fatty liver disease in rats. Chin J Integr Med. 2011;17:205–11. doi: 10.1007/s11655-011-0668-4. [DOI] [PubMed] [Google Scholar]
- 309.Lu KL, Zhang DD, Wang LN, Xu WN, Liu WB. Molecular characterization of carnitine palmitoyltransferase IA in Megalobrama amblycephala and effects on its expression of feeding status and dietary lipid and berberine. Comp Biochem Physiol B Biochem Mol Biol. 2016;191:20–5. doi: 10.1016/j.cbpb.2015.08.010. [DOI] [PubMed] [Google Scholar]
- 310.Wang H, Shi L, Yin H, Zhou Q. [Study on effect of berberine on modulating lipid and CPT I A gene expression] Zhongguo Zhong Yao Za Zhi. 2011;36:2715–8. [PubMed] [Google Scholar]
- 311.Sun Y, Xia M, Yan H, Han Y, Zhang F, Hu Z. et al. Berberine attenuates hepatic steatosis and enhances energy expenditure in mice by inducing autophagy and fibroblast growth factor 21. Br J Pharmacol. 2018;175:374–87. doi: 10.1111/bph.14079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 312.Purushotham A, Schug TT, Xu Q, Surapureddi S, Guo X, Li X. Hepatocyte-specific deletion of SIRT1 alters fatty acid metabolism and results in hepatic steatosis and inflammation. Cell Metab. 2009;9:327–38. doi: 10.1016/j.cmet.2009.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 313.Liss KH, Finck BN. PPARs and nonalcoholic fatty liver disease. Biochimie. 2017;136:65–74. doi: 10.1016/j.biochi.2016.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 314.Zhao J, Wang Y, Wu X, Tong P, Yue Y, Gao S. et al. Inhibition of CCL19 benefits nonalcoholic fatty liver disease by inhibiting TLR4/NFkappaBp65 signaling. Mol Med Rep. 2018;18:4635–42. doi: 10.3892/mmr.2018.9490. [DOI] [PubMed] [Google Scholar]
- 315.Lim JS, Mietus-Snyder M, Valente A, Schwarz JM, Lustig RH. The role of fructose in the pathogenesis of NAFLD and the metabolic syndrome. Nat Rev Gastroenterol Hepatol. 2010;7:251–64. doi: 10.1038/nrgastro.2010.41. [DOI] [PubMed] [Google Scholar]
- 316.Tilg H, Moschen AR. Insulin resistance, inflammation, and non-alcoholic fatty liver disease. Trends Endocrinol Metab. 2008;19:371–9. doi: 10.1016/j.tem.2008.08.005. [DOI] [PubMed] [Google Scholar]
- 317.Guo T, Woo SL, Guo X, Li H, Zheng J, Botchlett R. et al. Berberine Ameliorates Hepatic Steatosis and Suppresses Liver and Adipose Tissue Inflammation in Mice with Diet-induced Obesity. Sci Rep. 2016;6:22612. doi: 10.1038/srep22612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 318.Feng W, Wang H, Zhang P, Gao C, Tao J, Ge Z. et al. Modulation of gut microbiota contributes to curcumin-mediated attenuation of hepatic steatosis in rats. Biochim Biophys Acta Gen Subj. 2017;1861:1801. doi: 10.1016/j.bbagen.2017.03.017. [DOI] [PubMed] [Google Scholar]
- 319.Bischoff SC, Barbara G, Buurman W, Ockhuizen T, Schulzke JD, Serino M. et al. Intestinal permeability - a new target for disease prevention and therapy. Bmc Gastroenterology. 2014;14:189. doi: 10.1186/s12876-014-0189-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 320.Li D, Zheng J, Hu Y, Hou H, Hao S, Liu N. et al. Amelioration of Intestinal Barrier Dysfunction by Berberine in the Treatment of Nonalcoholic Fatty Liver Disease in Rats. Pharmacogn Mag. 2017;13:677–82. doi: 10.4103/pm.pm_584_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 321.Abel ED, O'Shea KM, Ramasamy R. Insulin resistance: metabolic mechanisms and consequences in the heart. Arterioscler Thromb Vasc Biol. 2012;32:2068–76. doi: 10.1161/ATVBAHA.111.241984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 322.Salminen A, Kaarniranta K. AMP-activated protein kinase (AMPK) controls the aging process via an integrated signaling network. Ageing Res Rev. 2012;11:230–41. doi: 10.1016/j.arr.2011.12.005. [DOI] [PubMed] [Google Scholar]
- 323.Xie Z, Zhang J, Wu J, Viollet B, Zou MH. Upregulation of mitochondrial uncoupling protein-2 by the AMP-activated protein kinase in endothelial cells attenuates oxidative stress in diabetes. Diabetes. 2008;57:3222–30. doi: 10.2337/db08-0610. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 324.Kukidome D, Nishikawa T, Sonoda K, Imoto K, Fujisawa K, Yano M. et al. Activation of AMP-activated protein kinase reduces hyperglycemia-induced mitochondrial reactive oxygen species production and promotes mitochondrial biogenesis in human umbilical vein endothelial cells. Diabetes. 2006;55:120–7. [PubMed] [Google Scholar]
- 325.Zhang H, Wei J, Xue R, Wu JD, Zhao W, Wang ZZ. et al. Berberine lowers blood glucose in type 2 diabetes mellitus patients through increasing insulin receptor expression. Metabolism. 2010;59:285–92. doi: 10.1016/j.metabol.2009.07.029. [DOI] [PubMed] [Google Scholar]
- 326.Jiang D, Wang D, Zhuang X, Wang Z, Ni Y, Chen S. et al. Berberine increases adipose triglyceride lipase in 3T3-L1 adipocytes through the AMPK pathway. Lipids Health Dis. 2016;15:214. doi: 10.1186/s12944-016-0383-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 327.Evans R, Barish G, Wang Y. PPARs and the complex journey to obesity. Nat Med. 2004;10:355–61. doi: 10.1038/nm1025. [DOI] [PubMed] [Google Scholar]
- 328.Huang C, Zhang Y, Gong Z, Sheng X, Li Z, Zhang W. et al. Berberine inhibits 3T3-L1 adipocyte differentiation through the PPARgamma pathway. Biochem Biophys Res Commun. 2006;348:571–8. doi: 10.1016/j.bbrc.2006.07.095. [DOI] [PubMed] [Google Scholar]
- 329.Abidi P, Zhou Y, Jiang J, Liu J. Extracellular signal-regulated kinase-dependent stabilization of hepatic low-density lipoprotein receptor mRNA by herbal medicine berberine. Arterioscler Thromb Vasc Biol. 2005;25:2170–6. doi: 10.1161/01.ATV.0000181761.16341.2b. [DOI] [PubMed] [Google Scholar]
- 330.Cameron J, Ranheim T, Kulseth MA, Leren TP, Berge KE. Berberine decreases PCSK9 expression in HepG2 cells. Atherosclerosis. 2008;201:266–73. doi: 10.1016/j.atherosclerosis.2008.02.004. [DOI] [PubMed] [Google Scholar]
- 331.Wang H, Zhu C, Ying Y, Luo L, Huang D, Luo Z. Metformin and berberine, two versatile drugs in treatment of common metabolic diseases. Oncotarget. 2018;9:10135–46. doi: 10.18632/oncotarget.20807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 332.Li H, Dong B, Park SW, Lee HS, Chen W, Liu J. Hepatocyte nuclear factor 1alpha plays a critical role in PCSK9 gene transcription and regulation by the natural hypocholesterolemic compound berberine. J Biol Chem. 2009;284:28885–95. doi: 10.1074/jbc.M109.052407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 333.Turner N, Li JY, Gosby A, To SW, Cheng Z, Miyoshi H. et al. Berberine and its more biologically available derivative, dihydroberberine, inhibit mitochondrial respiratory complex I: a mechanism for the action of berberine to activate AMP-activated protein kinase and improve insulin action. Diabetes. 2008;57:1414–8. doi: 10.2337/db07-1552. [DOI] [PubMed] [Google Scholar]
- 334.Xu M, Xiao Y, Yin J, Hou W, Yu X, Shen L. et al. Berberine promotes glucose consumption independently of AMP-activated protein kinase activation. PLoS ONE. 2014;9:e103702. doi: 10.1371/journal.pone.0103702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 335.Xu Z, Feng W, Shen Q, Yu N, Yu K, Wang S. et al. Rhizoma Coptidis and Berberine as a Natural Drug to Combat Aging and Aging-Related Diseases via Anti-Oxidation and AMPK Activation. Aging Dis. 2017;8:760–77. doi: 10.14336/AD.2016.0620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 336.Towler M, Hardie D. AMP-activated protein kinase in metabolic control and insulin signaling. Circ Res. 2007;100:328–41. doi: 10.1161/01.RES.0000256090.42690.05. [DOI] [PubMed] [Google Scholar]
- 337.Zhao W, Ge H, Liu K, Chen X, Zhang J, Liu B. Nandinine, a Derivative of Berberine, Inhibits Inflammation and Reduces Insulin Resistance in Adipocytes via Regulation of AMP-Kinase Activity. Planta Med. 2017;83:203–9. doi: 10.1055/s-0042-110576. [DOI] [PubMed] [Google Scholar]
- 338.Chen C, Zhang Y, Huang C. Berberine inhibits PTP1B activity and mimics insulin action. Biochem Biophys Res Commun. 2010;397:543–7. doi: 10.1016/j.bbrc.2010.05.153. [DOI] [PubMed] [Google Scholar]
- 339.Fusi J, Bianchi S, Daniele S, Pellegrini S, Martini C, Galetta F. et al. An in vitro comparative study of the antioxidant activity and SIRT1 modulation of natural compounds. Biomed Pharmacother. 2018;101:805. doi: 10.1016/j.biopha.2018.03.006. [DOI] [PubMed] [Google Scholar]
- 340.Chen DL, Yang KY. Berberine Alleviates Oxidative Stress in Islets of Diabetic Mice by Inhibiting miR-106b Expression and Up-Regulating SIRT1. J Cell Biochem. 2017;118:4349–57. doi: 10.1002/jcb.26089. [DOI] [PubMed] [Google Scholar]
- 341.Coelho AR, Martins TR, Couto R, Deus C, Pereira CV, Simoes RF. et al. Berberine-induced cardioprotection and Sirt3 modulation in doxorubicin-treated H9c2 cardiomyoblasts. Biochim Biophys Acta Mol Basis Dis. 2017;1863:2904–23. doi: 10.1016/j.bbadis.2017.07.030. [DOI] [PubMed] [Google Scholar]
- 342.Li HY, Wang XC, Xu YM, Luo NC, Luo S, Hao XY. et al. Berberine Improves Diabetic Encephalopathy Through the SIRT1/ER Stress Pathway in db/db Mice. Rejuvenation Res. 2018;21:200–9. doi: 10.1089/rej.2017.1972. [DOI] [PubMed] [Google Scholar]
- 343.Zhang X, Zhao Y, Xu J, Xue Z, Zhang M, Pang X. et al. Modulation of gut microbiota by berberine and metformin during the treatment of high-fat diet-induced obesity in rats. Sci Rep. 2015;5:14405. doi: 10.1038/srep14405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 344.Qin C, Zhang H, Zhao L, Zeng M, Huang W, Fu G. et al. Microbiota transplantation reveals beneficial impact of berberine on hepatotoxicity by improving gut homeostasis. Sci China Life Sci. 2018;61:1537–44. doi: 10.1007/s11427-017-9202-0. [DOI] [PubMed] [Google Scholar]
- 345.Wang Y, Shou JW, Li XY, Zhao ZX, Fu J, He CY. et al. Berberine-induced bioactive metabolites of the gut microbiota improve energy metabolism. Metabolism. 2017;70:72–84. doi: 10.1016/j.metabol.2017.02.003. [DOI] [PubMed] [Google Scholar]
- 346.Li M, Shu X, Xu H, Zhang C, Yang L, Zhang L. et al. Integrative analysis of metabolome and gut microbiota in diet-induced hyperlipidemic rats treated with berberine compounds. J Transl Med. 2016;14:237. doi: 10.1186/s12967-016-0987-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 347.Feng R, Shou JW, Zhao ZX, He CY, Ma C, Huang M. et al. Transforming berberine into its intestine-absorbable form by the gut microbiota. Sci Rep. 2015;5:12155. doi: 10.1038/srep12155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 348.Zhang HY, Piao XS, Zhang Q, Li P, Yi JQ, Liu JD. et al. The effects of Forsythia suspensa extract and berberine on growth performance, immunity, antioxidant activities, and intestinal microbiota in broilers under high stocking density. Poult Sci. 2013;92:1981–8. doi: 10.3382/ps.2013-03081. [DOI] [PubMed] [Google Scholar]
- 349.Cao Y, Pan Q, Cai W, Shen F, Chen GY, Xu LM. et al. Modulation of Gut Microbiota by Berberine Improves Steatohepatitis in High-Fat Diet-Fed BALB/C Mice. Arch Iran Med. 2016;19:197–203. [PubMed] [Google Scholar]
- 350.Sun R, Yang N, Kong B, Cao B, Feng D, Yu X. et al. Orally Administered Berberine Modulates Hepatic Lipid Metabolism by Altering Microbial Bile Acid Metabolism and the Intestinal FXR Signaling Pathway. Mol Pharmacol. 2017;91:110–22. doi: 10.1124/mol.116.106617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 351.Chang X, Wang Z, Zhang J, Yan H, Bian H, Xia M. et al. Lipid profiling of the therapeutic effects of berberine in patients with nonalcoholic fatty liver disease. J Transl Med. 2016;14:266. doi: 10.1186/s12967-016-0982-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 352.Cicero AF, Rovati LC, Setnikar I. Eulipidemic effects of berberine administered alone or in combination with other natural cholesterol-lowering agents. A single-blind clinical investigation. Arzneimittelforschung. 2007;57:26–30. doi: 10.1055/s-0031-1296582. [DOI] [PubMed] [Google Scholar]
- 353.Derosa G, D'Angelo A, Bonaventura A, Bianchi L, Romano D, Maffioli P. Effects of berberine on lipid profile in subjects with low cardiovascular risk. Expert Opin Biol Ther. 2013;13:475–82. doi: 10.1517/14712598.2013.776037. [DOI] [PubMed] [Google Scholar]
- 354.Di Pierro F, Putignano P, Villanova N, Montesi L, Moscatiello S, Marchesini G. Preliminary study about the possible glycemic clinical advantage in using a fixed combination of Berberis aristata and Silybum marianum standardized extracts versus only Berberis aristata in patients with type 2 diabetes. Clin Pharmacol. 2013;5:167–74. doi: 10.2147/CPAA.S54308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 355.Kong WJ, Wei J, Zuo ZY, Wang YM, Song DQ, You XF. et al. Combination of simvastatin with berberine improves the lipid-lowering efficacy. Metabolism. 2008;57:1029–37. doi: 10.1016/j.metabol.2008.01.037. [DOI] [PubMed] [Google Scholar]
- 356.Meng S, Wang LS, Huang ZQ, Zhou Q, Sun YG, Cao JT. et al. Berberine ameliorates inflammation in patients with acute coronary syndrome following percutaneous coronary intervention. Clin Exp Pharmacol Physiol. 2012;39:406–11. doi: 10.1111/j.1440-1681.2012.05670.x. [DOI] [PubMed] [Google Scholar]
- 357.Perez-Rubio KG, Gonzalez-Ortiz M, Martinez-Abundis E, Robles-Cervantes JA, Espinel-Bermudez MC. Effect of berberine administration on metabolic syndrome, insulin sensitivity, and insulin secretion. Metab Syndr Relat Disord. 2013;11:366–9. doi: 10.1089/met.2012.0183. [DOI] [PubMed] [Google Scholar]
- 358.Wei W, Zhao H, Wang A, Sui M, Liang K, Deng H. et al. A clinical study on the short-term effect of berberine in comparison to metformin on the metabolic characteristics of women with polycystic ovary syndrome. Eur J Endocrinol. 2012;166:99–105. doi: 10.1530/EJE-11-0616. [DOI] [PubMed] [Google Scholar]
- 359.Yan HM, Xia MF, Wang Y, Chang XX, Yao XZ, Rao SX. et al. Efficacy of Berberine in Patients with Non-Alcoholic Fatty Liver Disease. PLoS One. 2015;10:e0134172. doi: 10.1371/journal.pone.0134172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 360.Zhang Y, Li X, Zou D, Liu W, Yang J, Zhu N. et al. Treatment of type 2 diabetes and dyslipidemia with the natural plant alkaloid berberine. J Clin Endocrinol Metab. 2008;93:2559–65. doi: 10.1210/jc.2007-2404. [DOI] [PubMed] [Google Scholar]
- 361.Yin J, Xing H, Ye J. Efficacy of berberine in patients with type 2 diabetes mellitus. Metabolism. 2008;57:712–7. doi: 10.1016/j.metabol.2008.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 362.Hu Y, Ehli EA, Kittelsrud J, Ronan PJ, Munger K, Downey T. et al. Lipid-lowering effect of berberine in human subjects and rats. Phytomedicine. 2012;19:861–7. doi: 10.1016/j.phymed.2012.05.009. [DOI] [PubMed] [Google Scholar]
- 363.Gu Y, Zhang Y, Shi X, Li X, Hong J, Chen J. et al. Effect of traditional Chinese medicine berberine on type 2 diabetes based on comprehensive metabonomics. Talanta. 2010;81:766–72. doi: 10.1016/j.talanta.2010.01.015. [DOI] [PubMed] [Google Scholar]
- 364.Zeng XH, Zeng XJ, Li YY. Efficacy and safety of berberine for congestive heart failure secondary to ischemic or idiopathic dilated cardiomyopathy. Am J Cardiol. 2003;92:173–6. doi: 10.1016/s0002-9149(03)00533-2. [DOI] [PubMed] [Google Scholar]
- 365.Xiao HB, Sun ZL, Zhang HB, Zhang DS. Berberine inhibits dyslipidemia in C57BL/6 mice with lipopolysaccharide induced inflammation. Pharmacol Rep. 2012;64:889–95. doi: 10.1016/s1734-1140(12)70883-6. [DOI] [PubMed] [Google Scholar]
- 366.Dong B, Li H, Singh AB, Cao A, Liu J. Inhibition of PCSK9 transcription by berberine involves down-regulation of hepatic HNF1alpha protein expression through the ubiquitin-proteasome degradation pathway. J Biol Chem. 2015;290:4047–58. doi: 10.1074/jbc.M114.597229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 367.Marin-Neto JA, Maciel BC, Secches AL, Gallo Junior L. Cardiovascular effects of berberine in patients with severe congestive heart failure. Clin Cardiol. 1988;11:253–60. doi: 10.1002/clc.4960110411. [DOI] [PubMed] [Google Scholar]
- 368.Zeng X, Zeng X. Relationship between the clinical effects of berberine on severe congestive heart failure and its concentration in plasma studied by HPLC. Biomed Chromatogr. 1999;13:442–4. doi: 10.1002/(SICI)1099-0801(199911)13:7<442::AID-BMC908>3.0.CO;2-A. [DOI] [PubMed] [Google Scholar]
- 369.Pirro M, Francisci D, Bianconi V, Schiaroli E, Mannarino MR, Barsotti F. et al. NUtraceutical TReatment for hYpercholesterolemia in HIV-infected patients: The NU-TRY(HIV) randomized cross-over trial. Atherosclerosis. 2018;280:51–7. doi: 10.1016/j.atherosclerosis.2018.11.026. [DOI] [PubMed] [Google Scholar]
- 370.Xiao D, Liu Z, Zhang S, Zhou M, He F, Zou M. et al. Berberine Derivatives with Different Pharmacological Activities via Structural Modifications. Mini Rev Med Chem. 2018;18:1424–41. doi: 10.2174/1389557517666170321103139. [DOI] [PubMed] [Google Scholar]
- 371.Shan YQ, Ren G, Wang YX, Pang J, Zhao ZY, Yao J. et al. Berberine analogue IMB-Y53 improves glucose-lowering efficacy by averting cellular efflux especially P-glycoprotein efflux. Metabolism. 2013;62:446–56. doi: 10.1016/j.metabol.2012.09.009. [DOI] [PubMed] [Google Scholar]
- 372.Maeng HJ, Yoo HJ, Kim IW, Song IS, Chung SJ, Shim CK. P-glycoprotein-mediated transport of berberine across Caco-2 cell monolayers. J Pharm Sci. 2002;91:2614–21. doi: 10.1002/jps.10268. [DOI] [PubMed] [Google Scholar]
- 373.Cheng Z, Chen AF, Wu F, Sheng L, Zhang HK, Gu M. et al. 8,8-Dimethyldihydroberberine with improved bioavailability and oral efficacy on obese and diabetic mouse models. Bioorg Med Chem. 2010;18:5915–24. doi: 10.1016/j.bmc.2010.06.085. [DOI] [PubMed] [Google Scholar]
- 374.Li R, Wu J, He Y, Hai L, Wu Y. Synthesis and in vitro evaluation of 12-(substituted aminomethyl) berberrubine derivatives as anti-diabetics. Bioorg Med Chem Lett. 2014;24:1762–5. doi: 10.1016/j.bmcl.2014.02.032. [DOI] [PubMed] [Google Scholar]
- 375.Wang JR, Tanaka T, Zhang H, Kouno I, Jiang ZH. Formation and conformation of baicalin-berberine and wogonoside-berberine complexes. Chem Pharm Bull (Tokyo) 2012;60:706–11. doi: 10.1248/cpb.60.706. [DOI] [PubMed] [Google Scholar]
- 376.Yan L, Xiao Y, Rong X, Ying G, Qiu Z, Zhang Z. et al. Design, synthesis and biological evaluation of a hybrid compound berberine and magnolol for improvement of glucose and lipid metabolism. RSC Adv. 2016;6:81924–31. [Google Scholar]
- 377.Liu JC, Chan P, Chen YJ, Tomlinson B, Hong SH, Cheng JT. The antihypertensive effect of the berberine derivative 6-protoberberine in spontaneously hypertensive rats. Pharmacology. 1999;59:283–9. doi: 10.1159/000028331. [DOI] [PubMed] [Google Scholar]
- 378.Ko FN, Chang YL, Chen CM, Teng CM. (+/-)-Govadine and (+/-)-THP, two tetrahydroprotoberberine alkaloids, as selective alpha 1-adrenoceptor antagonists in vascular smooth muscle cells. J Pharm Pharmacol. 1996;48:629–34. doi: 10.1111/j.2042-7158.1996.tb05986.x. [DOI] [PubMed] [Google Scholar]
- 379.Al-Howiriny TA, Zemaitis MA, Gao CY, Hadden CE, Martin GE, Lin FT. et al. Thalibealine, a novel tetrahydroprotoberberine-aporphine dimeric alkaloid from Thalictrum wangii. J Nat Prod. 2001;64:819–22. doi: 10.1021/np010095y. [DOI] [PubMed] [Google Scholar]
- 380.Qian W, Lu W, Sun H, Li Z, Zhu L, Zhao R. et al. Design, synthesis, and pharmacological evaluation of novel tetrahydroprotoberberine derivatives: selective inhibitors of dopamine D(1) receptor. Bioorg Med Chem. 2012;20:4862–71. doi: 10.1016/j.bmc.2012.05.057. [DOI] [PubMed] [Google Scholar]
- 381.Zhang TT, Cui B, Dai DZ, Su W. CPU 86017, p-chlorobenzyltetrahydroberberine chloride, attenuates monocrotaline- induced pulmonary hypertension by suppressing endothelin pathway. Acta Pharmacol Sin. 2005;26:1309–16. doi: 10.1111/j.1745-7254.2005.00214.x. [DOI] [PubMed] [Google Scholar]
- 382.Qi MY, Feng Y, Dai DZ, Li N, Cheng YS, Dai Y. CPU86017, a berberine derivative, attenuates cardiac failure through normalizing calcium leakage and downregulated phospholamban and exerting antioxidant activity. Acta Pharmacol Sin. 2010;31:165–74. doi: 10.1038/aps.2009.180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 383.Gao J, Tang YQ, Dai DZ, Cheng YS, Zhang GL, Zhang C. et al. Raisanberine protected pulmonary arterial rings and cardiac myocytes of rats against hypoxia injury by suppressing NADPH oxidase and calcium influx. Acta Pharmacol Sin. 2012;33:625–34. doi: 10.1038/aps.2012.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 384.Zhang GL, Dai DZ, Zhang C, Dai Y. Apocynin and raisanberine alleviate intermittent hypoxia induced abnormal StAR and 3beta-HSD and low testosterone by suppressing endoplasmic reticulum stress and activated p66Shc in rat testes. Reprod Toxicol. 2013;36:60–70. doi: 10.1016/j.reprotox.2012.12.002. [DOI] [PubMed] [Google Scholar]
- 385.Li CL, Tan LH, Wang YF, Luo CD, Chen HB, Lu Q. et al. Comparison of anti-inflammatory effects of berberine, and its natural oxidative and reduced derivatives from Rhizoma Coptidis in vitro and in vivo. Phytomedicine. 2019;52:272–83. doi: 10.1016/j.phymed.2018.09.228. [DOI] [PubMed] [Google Scholar]
- 386.Hermann R, von Richter O. Clinical evidence of herbal drugs as perpetrators of pharmacokinetic drug interactions. Planta Med. 2012;78:1458–77. doi: 10.1055/s-0032-1315117. [DOI] [PubMed] [Google Scholar]
- 387.Guo Y, Pope C, Cheng X, Zhou H, Klaassen CD. Dose-response of berberine on hepatic cytochromes P450 mRNA expression and activities in mice. J Ethnopharmacol. 2011;138:111–8. doi: 10.1016/j.jep.2011.08.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 388.Guo Y, Chen Y, Tan ZR, Klaassen CD, Zhou HH. Repeated administration of berberine inhibits cytochromes P450 in humans. Eur J Clin Pharmacol. 2012;68:213–7. doi: 10.1007/s00228-011-1108-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 389.Mirhadi E, Rezaee M, Malaekeh-Nikouei B. Nano strategies for berberine delivery, a natural alkaloid of Berberis. Biomed Pharmacother. 2018;104:465–73. doi: 10.1016/j.biopha.2018.05.067. [DOI] [PubMed] [Google Scholar]
- 390.Banach M, Patti AM, Giglio RV, Cicero AFG, Atanasov AG, Bajraktari G. et al. The Role of Nutraceuticals in Statin Intolerant Patients. J Am Coll Cardiol. 2018;72:96–118. doi: 10.1016/j.jacc.2018.04.040. [DOI] [PubMed] [Google Scholar]
- 391.Patti AM, Al-Rasadi K, Giglio RV, Nikolic D, Mannina C, Castellino G. et al. Natural approaches in metabolic syndrome management. Arch Med Sci. 2018;14:422–41. doi: 10.5114/aoms.2017.68717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 392.Zhang H, Wang X, Wang T, Chen K, Wang H, Jia Q, Enhancement of Berberine Hypoglycemic Activity by Oligomeric Proanthocyanidins. Molecules; 2018. p. 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 393.Zhu X, Yang J, Zhu W, Yin X, Yang B, Wei Y, Combination of Berberine with Resveratrol Improves the Lipid-Lowering Efficacy. Int J Mol Sci; 2018. p. 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary table 1.