Abstract
Objective
To understand contraceptive need and use among individuals with HIV/AIDS living in slums.
Methods
A sequential mixed-methods study was conducted in two slums in Nairobi, Kenya, from November 6th, 2009 to April 18th, 2010. Data were obtained by quantitative survey (n = 513), qualitative in-depth interviews (n = 41), and key informant interviews (n = 14).
Results
In all, 250 (55.5%) participants used contraceptives. Condoms were the most frequently reported modern method (n = 142; 60.4%), followed by injectables (n = 55; 23.4%) and dual methods (n = 38; 15.3%). Unmet need was reported by 151 (33.6%) individuals. Factors associated with contraceptive use were education, marital status, number of living children, discussion of contraception with a provider, and social support. Personal, conceptual, and structural barriers to contraceptive use were identified.
Conclusions
Individuals with HIV/AIDS wished to limit their fertility but experienced high unmet need for contraception. Multi-level interventions, including educational campaigns and integration of HIV and family planning services, are required to overcome barriers.
Keywords: Contraception, Family planning, HIV/AIDS, Kenya Slums, Unmet need
1. Introduction
More than two-thirds of the 35 million people diagnosed with HIV/AIDS worldwide live in Sub-Saharan Africa [1]. Of these affected individuals, in excess of 1.6 million are living in Kenya [1]. Urban prevalence rates of HIV/AIDS are almost twice as high as those reported in rural areas [2], and Kenyan urban slum residents have higher rates [3]. Estimates suggest that 72% of all urban residents in Sub-Saharan Africa live in slums [4]. Similarly, up to 70% of individuals living in the Kenyan capital of Nairobi are resident in slums or slum-like areas [5], making slum populations a substantial but poorly studied group.
The majority of individuals with HIV/AIDS in Sub-Saharan Africa are of reproductive age [6] and increased access to antiretroviral therapy has improved the prognosis of HIV. Approximately 50% of Kenyan adults living with HIV/AIDS are receiving antiretroviral therapy [1]. Internationally, there is also growing recognition of the fertility rights of people with HIV/AIDS [7].
Family planning plays a vital part in preventing transmission of HIV. Contraception is more cost-effective than prophylaxis with antiretroviral drugs for the prevention of mother-to-child transmission. The addition of family planning to programs designed to prevent such transmission in settings with a high prevalence of HIV could halve the number of infant infections compared to use of prevention of mother-to-child transmission strategies alone [8].
Little is currently known about the use of contraception or the contraceptive decision-making process among individuals with HIV/AIDS living in Sub-Saharan Africa in general and the Nairobi slums in particular. The contraceptive needs of this group are seldom met by health systems, which tend to focus on voluntary counseling and testing and services that provide antiretroviral therapy [9]. Research on family planning use among individuals with HIV/AIDS has predominantly focused on women, albeit with mixed findings. In some studies, knowledge of their HIV status increased contraceptive use among infected women [10], whereas no appreciable difference in contraceptive use was observed by HIV status in other studies [11]. Contraceptive use initially increases among women in response to learning their HIV status and receiving counseling but declines with time in settings with low contraceptive use and high fertility [12].
Many studies have examined determinants of contraceptive use in Sub-Saharan Africa [13,14]; however, few have assessed determinants of such behavior among individuals with HIV/AIDS. Uptake of contraception in this group might be affected by numerous issues. Factors that apply to the general population include level of education [15]; parity; marital status [13]; adverse effects and health concerns surrounding contraception [16]; cost of services and availability of stock [17]; discussion of family planning with a provider or spouse; and misconceptions [15]. Factors unique to individuals with HIV/AIDS include disclosure of HIV status to their partner [18], HIV-related stigma, and integration of family planning and voluntary counseling and testing services [12,15].
The aim of the present study was to investigate contraceptive use and its determinants among people with HIV/AIDS living in Nairobi slums.
2. Materials and methods
A sequential mixed-methods study [19] was conducted in two slums in Nairobi, Kenya, from November 6th 2009 to April 18th, 2010. The design involved a quantitative survey of individuals with HIV/AIDS (n = 513), followed by qualitative in-depth interviews among a subsample of the survey respondents (n = 41), which were in turn supplemented by key informant interviews (n = 14). The quantitative component described prevalence and correlates of contraceptive need and use, whereas the qualitative component focused on experiences of contraception and barriers to its use. The present study was approved by the institutional review boards of the Kenyan Medical Research Institute, Nairobi, and the London School of Economics, London, UK. All participants required the ability to give written informed consent.
The sample size for the quantitative survey was determined on the assumption that 50% of the cohort would desire to have a first child or additional children in the future, with a sampling error of 5% and a 95% confidence level [20]. Eligible respondents had been diagnosed with HIV/AIDS and were men aged older than 18 years or women aged 18–49 years. Individuals who were not registered members of the Nairobi Urban Health and Demographic Surveillance System were excluded from the present study, as were those deemed too weak or sick to be interviewed.
Respondents were recruited from the Nairobi Urban Health and Demographic Surveillance System slum sites of Korogocho and Viwandani. To ensure a representative survey sample, HIV sero-prevalence ratios by sex, marital status, ethnicity, age, and education level were used as quota guides to systematically select respondents, based on previous findings in these settings [3]. Eight experienced interviewers, who were supported by community health workers, approached individuals with HIV/AIDS to participate in the present study and recruitment continued until all quotas were filled. The recruitment process was iterative; regular meetings were held with interviewers and community health workers to evaluate and revise recruitment targets.
The quantitative survey respondents provided a sampling frame for the subsequent in-depth interviews, which were intentionally selected on the basis of participants’ responses. Individuals were typically selected for in-depth interview following classification as follows: (1) sexually abstinent during the past 12 months, no fertility desire, and not currently using contraceptives; (2) sexually active during the past 12 months, desire for future fertility, consistently using condoms, and currently using contraception; or (3) sexually active during the past 12 months, desire for future fertility, inconsistent or non-use of condoms, and not currently using any other form of contraception. Consequently, 45 individuals were identified to undergo in-depth interview; 41 interviews were conducted (three had moved and we were unable to trace them, one refused to be re-interviewed).
Data collected from the survey respondents was supplemented by the key informant interviews, which were intentionally designed to include a range of service providers (doctors, nurses, HIV counselors, and community health workers) for individuals with HIV/AIDS living in the Nairobi slums. Face-to-face interviews were conducted in a private setting of the respondent’s choice to ensure confidentiality.
The two outcome variables were contraceptive use and unmet need for contraception. Contraceptive use was defined as women or men who were using (or whose sexual partner was using) at least one method of contraception. These methods included both supply (modern) forms of contraception (i.e. female and male sterilization, oral contraceptives, intrauterine devices, injectable contraceptives, implants, and female and male condoms) and behavioral (traditional) forms of contraception (i.e. lactational amenorrhea, withdrawal, and terminal or periodic abstinence). Unmet need for contraception was defined on the basis of whether or not the respondent was sexually active and had reported that they did not want to have a first child (or further children) in the next 2 years or that they did not want to have any children (first or additional children), and that they were not using any method of contraception at the time of the interview.
The survey questionnaire collected information on socio-demographic, medical (e.g. duration since HIV diagnosis; use and duration of antiretroviral therapy), and behavioral (e.g. disclosure of HIV status to their sexual partners) factors. Detailed questions were used gather information from interviewees on current contraceptive use, sources of family planning methods, preferred contraceptive options for future use, and whether health providers had ever discussed family planning with them. Questions were also posed regarding stigma and psychological distress related to HIV; responses were assessed with item scales, averaged, and standardized into a composite score using the Cronbach α [21]. Household wealth quintiles were derived using factor analysis [22].
The in-depth interview items were open-ended and interviewers probed participants to elicit detailed responses. The interview guide included questions to explore the contexts of past and current contraceptive use, experiences of contraceptive use, and reasons for use or non-use. Key informant interviews focused on the sexual and reproductive health needs of individuals with HIV/AIDS and service provision challenges in slum settings.
Quantitative data were analyzed using Stata version 11 (Stata, College Station, TX, USA). Univariate, bivariate, and multivariate analyses assessed predictors of contraceptive use and unmet need. A multivariate logistic regression model with forward and backward selection, which used a P value of less than 0.05 as the entry criterion, was generated to calculate the odds ratios and 95% confidence intervals. Where appropriate, findings were compared with secondary data obtained from the general population of the Nairobi slums [23].
Qualitative data were managed and analyzed using Nvivo version 9 (QSR International, Melbourne, VIC, Australia). Interviews were first audio recorded in Kiswahili, then transcribed and translated into English. Interview transcripts were systematically reread to ensure familiarity with the content before the thematic analysis was conducted. A coding frame was developed to identify dominant themes and subthemes related to family planning experiences. Quantitative and qualitative data were both integrated in the present analysis and the interpretation of the findings.
3. Results
The socio-demographic characteristics of the 513 survey respondents are presented in Table 1. The proportion of men and women included in the present study reflected differential HIV infection rates among men (4.3%) and women (8.0%) in Kenya [24]. Just over half (54.8%) of the respondents were either married or co-habiting. Approximately two-thirds (65.3%) had attained primary level education and 28.3% had reached secondary level. The majority of the cohort comprised four ethnic groups (Kikuyu, Luo, Luyia, and Kamba). Approximately three-quarters (70.5%) of respondents were aged 30–49 years (mean, 38 years). The sample was almost evenly split with regards to antiretroviral therapy status; however, women were more likely to be receiving treatment and for a longer duration than men. This finding reflected women’s increased likelihood of early HIV testing, which is often related to prenatal testing. Almost three quarters (73.0%) of respondents had known their HIV status for less than 5.0 years (mean, 3.2 years).
Table 1.
Sociodemographic characteristics of the survey respondents.a
| Characteristic | Female respondents (n = 318) |
Male respondents (n = 195) |
Total cohort (n = 513) |
|---|---|---|---|
| Slum of residence | |||
| Korogocho | 155(48.7) | 105(53.9) | 260(50.7) |
| Viwandani | 163(51.3) | 90(46.1) | 253(49.3) |
| Ethnicity | |||
| Kikuyu | 105(33.0) | 51(26.2) | 156 (30.4) |
| Luo | 67(21.1) | 59(30.3) | 126(24.6) |
| Luyia | 66(20.8) | 38(19.5) | 104(20.3) |
| Kamba | 57(17.9) | 28(14.4) | 85(16.6) |
| Other | 23(7.2) | 19(9.7) | 42(8.2) |
| Education level | |||
| None | 23(7.2) | 10(5.1) | 33(6.4) |
| Primary | 230(72.3) | 105(53.9) | 333(65.3) |
| Secondary or higher | 65(20.4) | 80(41.3) | 145(28.3) |
| Marital status | |||
| Married or co-habiting | 134(42.1) | 147(75.4) | 281(54.8) |
| Divorced or separated | 67(21.1) | 24(12.3) | 91(17.7) |
| Widowed | 85(26.7) | 18(9.2) | 103(20.1) |
| Never married or co-habited | 32(10.1) | 6(3.1) | 38(7.4) |
| Age, y | |||
| 18–29 | 75(23.6) | 14(7.2) | 89(17.3) |
| 30–39 | 143(44.9) | 67(34.4) | 210(40.9) |
| 40–49 | 78(24.5) | 74(38.0) | 152(29.6) |
| ≥ 50 | 22(6.9) | 40(20.5) | 62(12.1) |
| HIV treatment status | |||
| Antiretroviral therapy | 184(57.9) | 84(43.1) | 268(52.2) |
| None | 134(42.1) | 111(56.9) | 245(48.0) |
| Duration of HIV, y | |||
| <1 | 60(18.9) | 55(28.2) | 115(22.4) |
| 1–2 | 90(28.3) | 64(32.8) | 154(30.0) |
| 3–4 | 63(19.8) | 42(21.5) | 105(20.5) |
| >4 | 105(33.2) | 34(17.4) | 139(27.1) |
Values given as number (percentage).
Family planning needs and use among survey respondents versus the general population of the Nairobi slums are summarized in Table 2. Secondary data for the Nairobi slums reported contraceptive use and need among currently married women [23]. Consequently, for the purposes of comparison, the present study reported the overall contraceptive use and need among all individuals with HIV/AIDS, as well as among married women. Two-thirds of the survey respondents wished to cease childbearing. In total, 73.7% of all women with HIV/AIDS and 66.9% of married women with HIV/AIDS living in Nairobi slums wanted to limit their fertility, compared to one-third of married women in the general slum population.
Table 2.
Fertility intentions, contraceptive use, and unmet need for contraception among the survey respondents.a
| Population |
||||||||
|---|---|---|---|---|---|---|---|---|
| Reproductive health indicator | Total cohort | Female respondents | Male respondents | Single female respondents | Single male respondents | Married male respondents | Married female respondents | Nairobi slums (married women only; b |
| Fertility intention | ||||||||
| Wants no more children | 306(66.2) | 199(73.7) | 107(55.7) | 118(79.2) | 22(45.8) | 85(59.0) | 81(66.9) | 33.2 |
| Wants children now or soon | 57(12.3) | 22(8.2) | 35(18.2) | 8(5.4) | 13 (27.1) | 22(15.2) | 14(11.6) | 13.2 |
| Wants children later (after 2 y) | 96(20.8) | 47(17.4) | 49(25.5) | 23(15.4) | 13(27.1) | 36(25.0) | 24(19.8) | 38.2 |
| Undecided | 3(0.7) | 2(0.7) | 1(0.5) | 0(0.0) | 0(0.0) | 1(0.7) | 1(0.8) | 8.0 |
| Contraceptive use | ||||||||
| None | 2000(44.4) | 123(46.8) | 77(41.2) | 89(60.5) | 37(77.1) | 40(28.8) | 34(29.3) | 37.2 |
| Traditionalc | 15(3.3) | 11(4.2) | 4(2.1) | 2(1.3) | 0(0.0) | 4(2.9) | 9(7.8) | 4.9 |
| Modernd | 235(52.2) | 129(49.1) | 106(56.7) | 56(38.2) | 11(23.9) | 95(78.1) | 73(62.9) | 58.0 |
| Total contraceptive use | 250(55.5) | 140(53.3) | 110(58.8) | 58(39.5) | 11(23.9) | 99(81.0) | 102(70.7) | 62.9 |
| Unmet need for contraception | ||||||||
| Limiting | 122(27.2) | 88(33.5) | 34(18.3) | 68(46.3) | 17(35.4) | 17(12.3) | 20(17.2) | 9.0 |
| Spacing | 29(6.5) | 16(6.1) | 13(7.0) | 11(7.5) | 4(8.3) | 9(6.5) | 6(4.3) | 13.0 |
| Total unmet need | 151(33.6) | 104(39.6) | 47(25.3) | 69(53.8) | 21(43.7) | 26(18.8) | 26(21.5) | 22.0 |
Source: PLWHA survey (2010) and Urban Reproductive Health Initiative (Tupange) (2010) [23].
Values given as number (percentage).
Derived from the general Nairobi slums population secondary data [23].
Traditional methods included periodic abstinence and withdrawal.
Modern methods included female and male sterilization; the contraceptive pill; intrauterine devices; injectable contraceptives; implants; condoms; and lactational amenorrhea.
Overall contraceptive use among the survey respondents was lower (55.5%) than that reported for the general Nairobi slum population (62.9%; Table 2). Nevertheless, women with HIV/AIDS who were married had the highest contraceptive use rate (70.7%), whereas single (i.e. never married or formerly married) women with HIV/AIDS had the lowest rate (23.9%). Overall, female survey respondents reported lower contraceptive use (53.3%) than male survey respondents (58.8%).
Unmet need for contraception among the present study cohort (33.6%) was higher than that reported for the general slum population (22.0%; Table 2). Reasons for unmet need varied. The rate of unmet need for limiting was 27.2% among the survey respondents and 9.0% among the general slum population. Women with HIV/AIDS who were not currently in a union reported the highest unmet need (53.8%), compared to 21.5% for those currently in a union.
Fertility desire, sexual activity, contraceptive use, and unmet need for contraception varied by background characteristics among the survey respondents (Table 3). Fertility desires and sexual activity were higher among men than women, although levels decreased with age. Sexual activity and fertility desires were higher among married people with HIV/AIDS than those who were formerly married. Contraceptive use was higher among married individuals with HIV/AIDS, and increased with age, education level, and household wealth. Unmet need was highest among the younger (18–29 years) and older (≥ 40 years) age groups. These findings highlighted unmet need for spacing among young respondents and unmet need for limiting among older women. Unmet need decreased with educational level and with increasing wealth.
Table 3.
Fertility desire, sexual activity, contraceptive use, and unmet need for contraception among the survey respondents).a
| Characteristic | Desired more children | Sexually active during the previous 12 mo | Currently using contraception | Unmet need for contraception |
|---|---|---|---|---|
| Age, y | ||||
| 18–29 | 41(47.8) | 70(78.7) | 42(53.2) | 28(35.4) |
| 30–39 | 71(36.4) | 155(75.7) | 110(57.0) | 58(30.1) |
| ≥40 | 45(24.7) | 149(69.6) | 98(55.1) | 65(36.7) |
| Marital status | ||||
| Married or co-habiting | 100(37.6) | 264(94.0) | 181(71.0) | 51(20.1) |
| Divorced or separated | 28(35.0) | 44(48.3) | 23(28.8) | 44(55.0) |
| Widowed | 15(17.9) | 50(48.5) | 38(45.8) | 36(43.4) |
| Never married or co-habited | 14(42.4) | 20(52.6) | 8(25.0) | 20(62.5) |
| Sex | ||||
| Female | 71(26.3) | 219 (68,9) | 140(53.2) | 104(39.5) |
| Male | 86(44.6) | 159(81.5) | 110(58.8) | 47(25.3) |
| Education level | ||||
| None | 8(38.10) | 20(60.6) | 6(31.6) | 9(47.4) |
| Primary | 95(31.5) | 250(74.6) | 165(56.3) | 100(34.3) |
| Secondary or higher | 54(38.6) | 108(74.5) | 79(57.3) | 42(30.4) |
| Wealth | ||||
| Poorest | 23(25.6) | 70(67.3) | 43(50.0) | 35(40.7) |
| Second | 32(33.3) | 76(74,5) | 53(56.4) | 30(31.0) |
| Third | 44(39.6) | 95(78.5) | 62(56.9) | 32(29.4) |
| Fourth | 26(35.1) | 59(70.2) | 33(46.5) | 33(46.5) |
| Richest | 32(34.8) | 79(76.5) | 59(65.6) | 21(23.6) |
Values given as number (percentage).
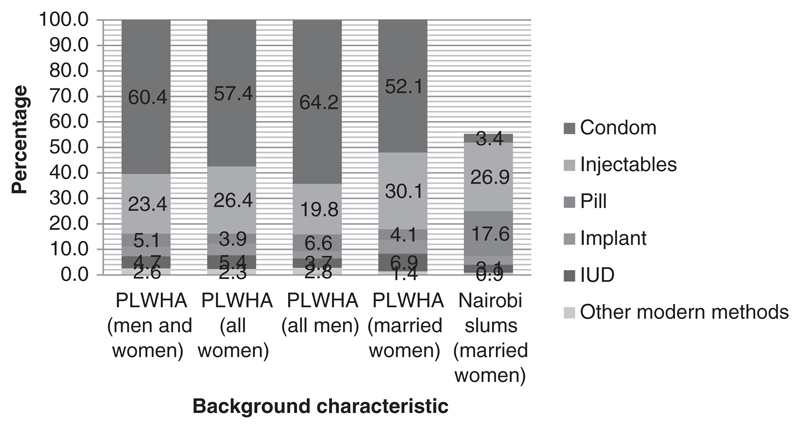
The two contraceptive methods most frequently used by individuals with HIV/AIDS were condoms and injectables (Fig. 1). This profile differed from that reported for the general slum population [23]. Men with HIV/AIDS reported higher condom use than women with HIV/AIDS; the rate of dual-method use (condom plus a supply method) was 15.3%.
Fig. 1.
Contraceptive methods supplied to survey respondents and the general Nairobi slum population [23]. Abbreviations: IUD, intrauterine device; PLWHA, people, living with HIV/AIDS.
The multivariate logistic regression analysis is shown in Table 4. Current contraceptive use was positively associated with formal education, being married, having more living children, ever having discussed family planning with a healthcare provider, and higher social support scale scores. The same factors were negatively associated with the likelihood of having unmet need for contraception.
Table 4.
Multivariate parsimonious model of predictors of contraceptive use and unmet need among sexually active individuals with HIV/AIDS living in the Nairobi slums (n = 450).a
| Characteristic | Contraceptive use | Unmet need for contraception | ||
|---|---|---|---|---|
| Adjusted OR (95% CI) |
P valueb | Adjusted OR (95% CI) |
P valueb | |
| Sex | ||||
| Female (reference) | 1.00 | 1.00 | ||
| Male | 1.01 (0.63–1.64) | 0.956 | 0.66 (0.41–1.07) | 0.091 |
| Education level | ||||
| None (reference) | 1.00 | 1.00 | ||
| Primary | 3.40 (1.16–9.93) | 0.026 | 0.51 (0.18–0.74) | 0.020 |
| Secondary or higher | 3.12 (1.04–9.40) | 0.043 | 0.53 (0.19–0.78) | 0.025 |
| Marital status | ||||
| Single (reference)c | 1.00 | 1.00 | ||
| Married or co-habiting | 5.25 (3.30–8.27) | <0.001 | 0.24 (0.16–0.38) | <0.001 |
| No. of living children | ||||
| 0 (reference) | 1.00 | 1.00 | ||
| 1–2 | 3.37 (1.08–10.52) | 0.036 | 2.35 (0.82–6.76) | 0.111 |
| 3–4 | 4.04 (1.30–12.57) | 0.016 | 2.28 (0.79–6.59) | 0.125 |
| ≥5 | 3.85 (1.20–12.31) | 0.023 | 3.12 (1.05–9.24) | 0.040 |
| Discussion with a health provider | ||||
| Never (reference) | 1.00 | 1.00 | ||
| Ever | 2.54 (1.60–4.04) | <0.001 | 0.65 (0.41–0.99) | 0.049 |
| Social support | 1.55 (1.08–2.24) | 0.017 | 0.76 (0.53–1.09) | 0.132 |
Abbreviations: CI, confidence interval; OR, odds ratio.
Logistic regression. The model was adjusted for age, ethnicity, duration of HIV infection, duration of antiretroviral therapy, disclosure of HIV status, stigma, and depression.
0.05.
Included all women who were divorced, separated, never married, and never cohabited.
The likelihood of using contraception increased more than three-fold for respondents with at least primary level education versus those with no formal schooling (OR 3.40; 95% CI 1.16-9.3; p = 0.026). The likelihood of having unmet need for contraception decreased with increasing level of education. Being in a union increased the likelihood of using contraception by a factor of 5.2 and reduced the likelihood of having unmet need by 76%.
The in-depth interviews conducted among 41 selected survey respondents indicated that individuals in partnerships might be more likely to discuss the issue of contraception and subsequently use family planning:
Interviewer: Have you discussed with your husband about family planning?
Respondent: Yes…we agreed with my husband that we first of all bring up the child that we already have. So I am using family [planning]. If the child is old enough we shall go for the check-up, because the issue of immunity is not only applicable to me as a woman. It also applies to my husband as well as his immunity level must be high enough. (Female aged 42 years; married with two children)
The likelihood of using contraception increased with parity, relative to those who were childless. However, respondents with five or more children had an increased likelihood of unmet need for family planning. Discussion of family planning with a health provider and high social support scores were associated with increased likelihood of contraceptive use (Table 4):
Interviewer: Why aren’t you using any method of family planning?
Respondent: I have not because whenever I go to the hospital they don’t tell me about family planning. They give me the drugs [antiretroviral therapy] I want and then ask me if I have a question for them, and I do not, then that is it. No one talks to me about family planning. (Female aged 41 years; married with four children)
Barriers to contraceptive use included fear of adverse effects, health concerns, previous negative experiences of using contraception, and spousal opposition. Some reasons were perceived to have been exacerbated by a positive HIV status:
Interviewer: You mentioned that you had problems with some methods of family planning?
Respondent: I used to use those pills but I would have extended blood flows during my periods. Now every month having periods three times for a person living with HIV/AIDS, you lose a lot of blood in the body and become very weak. So I stopped completely. (Female aged 41 years; married with four children)
Both men and women reported concerns about the ways in which contraception might interfere with sexual pleasure:
Interviewer: What are your concerns about family planning?
Respondent: Uuuh! Women who use [family planning] injections have nyege baridi (low libido)! They get wet. So if you have sex with her you don’t want to do it again with her. (Male aged 38 years; widower with four children)
Interviewer: Is there any problem you face with condom use?
Respondent: The problem is the man that I have sometimes says that the condom is not good. When having sex with condoms they [men] do not feel the sweetness of a woman. The condom prevents that warmth. (Female aged 34 years; never married, one child)
Specific concerns were voiced about concurrent antiretroviral therapy and contraceptive use:
Interviewer: Do you have any concerns about family planning methods?
Respondent: Some of them [family planning methods] are not compatible with antiretroviral therapy such as pills. Some of the pills can reduce the effectiveness of antiretroviral therapy. Antiretrovirals are also very strong…they “blow” family planning pills so people who use them can still conceive. (Female aged 25 years; widow with two children)
Concerns about contraindications between antiretroviral therapy and contraception were also articulated by healthcare workers during the key informant interviews (n = 14), revealing gaps in their knowledge:
Interviewer: Is there any problem with contraceptives and antiretroviral therapy use?
Respondent: For the general patients, I don’t see any contraindication unless the patient is in the terminal stage. (Clinical Officer)
Respondent: Some family planning methods are not safe when you are taking antiretroviral therapy drugs. Antiretrovirals make the pill to fail and somebody will become pregnant. (Clinical Officer)
Issues related to the supply chain made offering contraception difficult in the slums, especially for individuals with HIV/AIDS:
Respondent: Right now we don’t even have depo(depot medroxyprogesterone acetate) injection and they have to buy yet some of them cannot afford. (Nurse)
Respondent: Right now we don’t have injectables and intrauterine devices which are best for people living with HIV/AIDS. Bilateral tubal ligation in a private hospital is about 20,000 Kenyan shilling (US $213). We do it here freely but sometimes we cannot because we lack a few things. (Clinical Officer)
Infrastructure limitations reduced the potential effectiveness of HIV and contraceptive service integration in the slums:
Respondent: We are trying to integrate HIV and family planning services, but it has not picked up well because of the shortages we have with staff. So it has not gone the full integration as it were. One member of staff will have to attend to a very large number of clients. So the clients may not necessarily receive the proper service that they want. (Counselor)
Respondent: Integration is not possible here because of manpower constraints. If we have one person doing all that, counseling, giving drugs, providing family planning in one room, we would not be able to achieve much. So since we have family planning services for ordinary clients, then we just refer the HIV/AIDS clients to the same. (Clinical Officer)
4. Discussion
The present study documented contraceptive need and use among individuals with HIV/AIDS living in two Nairobi slums. The participants exhibited fertility desires geared toward limiting pregnancies: two in three wanted to stop having children versus just one in three individuals within the general slum population. Nonetheless, the majority of those surveyed relied on condoms or contraceptive methods with low effectiveness; the rate of dual method use among individuals with HIV/AIDS was only 15.3%.
Contraceptive use among individuals with HIV/AIDS enrolled in the present study was slightly lower than that reported for the general slum population. However, contraceptive use among married women with HIV/AIDS was higher than the general slum population. One in three individuals with HIV/AIDS had unmet need for contraception versus one in five individuals within the general slum population. The greatest unmet need was observed among those who were extremely poor, uneducated, and not in a union, suggesting inequities in access to family planning services. Unmet need among individuals with HIV/AIDS was greatest for limiting pregnancies, whereas in the general slum population the main unmet need was for spacing.
Other studies conducted among individuals with HIV/AIDS in sub-Saharan Africa settings also found that contraceptive use is associated with education, marital status, number of living children, and discussion of family planning with a provider [15]. The in-depth interviews and key informant interviews conducted in the present study revealed that the majority of individuals with HIV/AIDS faced barriers to contraceptive use, including fear of adverse effects, reduction in sexual pleasure, lack of discussion with providers and significant others, and little or no integration of services. Published evidence suggests that gaps in services for this population have continued because of the parallel provision of HIV and family planning services [26]. Barriers identified in the present study operated at individual, interpersonal, and structural levels, and so require multi-sector approaches and interventions.
Strengths of the present study included the fact that the sample was drawn from urban slums, an under-researched and growing population in Sub-Saharan Africa. Furthermore, the design took a mixed-methods approach and integrated quantitative and qualitative data to produce a holistic understanding of the reproductive lives of the target population.
Limitations of the present study included the cross-sectional nature, which precluded determination of causality; the use of self-reports, which were likely to be affected by social desirability bias; and the non-probabilistic sample, which limited the ability to generalize the findings.
In summary, integration of contraceptive and HIV services improves access and reduces stigma associated with their use [26]. The results of the present study emphasized the need to make contraceptive services an integral part of healthcare interventions for individuals with HIV/AIDS who are living in the Nairobi slums.
Acknowledgments
The present study was funded by the Wellcome Trust (078471/Z/05/A). A Fred H. Bixby Fellowship awarded to E.W. funded the time required to write the manuscript.
Footnotes
Conflict of interest
The authors have no conflicts of interest.
References
- [1].Joint United Nations Programme on HIV/AIDS. UNAIDS Report on the Global AIDS Epidemic 2012. [Accessed April 20,2015];2012 http://www.unaids.org/sites/default/files/media_asset/20121120_UNAIDS_Global_Report_2012_with_annexes_en_1.pdf.
- [2].Dyson T. HIV/AIDS and urbanization. Popul Dev Rev. 2003;29(3):427–42. [Google Scholar]
- [3].Madise NJ, Ziraba AK, Inungu J, Khamadi SA, Ezeh A, Zulu EM, et al. Are slum dwellers at heightened risk of HIV infection than other urban residents? Evidence from population-based HIV prevalence surveys in Kenya. Health Place. 2012;18(5):1144–52. doi: 10.1016/j.healthplace.2012.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].United Nations Human Settlements Programme. Slums of the World: The Face of Urban Poverty in the New Millennium? Nairobi: United Nations Human Settlements Programme; 2003. [Google Scholar]
- [5].Zulu EM, Beguy D, Ezeh AC, Bocquier P, Madise NJ, Cleland J, et al. Overview of migration, poverty and health dynamics in Nairobi City's slum settlements. J Urban Health. 2011;88(Suppl 2):S185–99. doi: 10.1007/s11524-011-9595-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].World Health Organization, Joint United Nations Programme on HIV/AIDS, United Nations International Children’s Emergency Fund. Towards Universal Access Scaling Up Priority HIV/AIDS Interventions in the Health Sector: Progress report 2008. [Accessed April 20, 2015];2008 http://www.who.int/hiv/pub/towards_universal_access_report_2008.pdf?ua=1.
- [7].Segurado AC, Paiva V. Rights of HIV positive people to sexual and reproductive health: parenthood. Reprod Health Matters. 2007;15(29 Suppl):27–45. doi: 10.1016/S0968-8080(07)29032-9. [DOI] [PubMed] [Google Scholar]
- [8].Halperin DT, Stover J, Reynolds HW. Benefits and costs of expanding access to family planning programs to women living with HIV. AIDS. 2009;23(Suppl 1):S123–30. doi: 10.1097/01.aids.0000363785.73450.5a. [DOI] [PubMed] [Google Scholar]
- [9].Lusti-Narasimhan M, Cottingham J, Berer M. Ensuring the sexual and reproductive health of people living with HIV: policies, programmes and health services. Reprod Health Matters. 2007;15(29 Suppl):1–3. [Google Scholar]
- [10].Elul B, Delvaux T, Munyana E, Lahuerta M, Horowitz D, Ndagije F, et al. Pregnancy desires, and contraceptive knowledge and use among prevention of mother-to-child transmission clients in Rwanda. AIDS. 2009;23(Suppl 1):S19–26. doi: 10.1097/01.aids.0000363774.91376.dc. [DOI] [PubMed] [Google Scholar]
- [11].Rutenberg N, Baek C. Field experiences integrating family planning into programs to prevent mother-to-child transmission of HIV. Stud Fam Plann. 2005;36(3):235–45. doi: 10.1111/j.1728-4465.2005.00064.x. [DOI] [PubMed] [Google Scholar]
- [12].Grabbe K, Stephenson R, Vwalika B, Ahmed Y, Vwalika C, Chomba E, et al. Knowledge, use, and concerns about contraceptive methods among serodiscordant couples in Rwanda and Zambia. J Womens Health (Larchmt) 2009;18(9):1449–56. doi: 10.1089/jwh.2008.1160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Magadi MA, Curtis SL. Trends and determinants of contraceptive method choice in Kenya. Stud Fam Plann. 2003;34(3):149–59. doi: 10.1111/j.1728-4465.2003.00149.x. [DOI] [PubMed] [Google Scholar]
- [14].Stephenson R, Baschieri A, Clements S, Hennink M, Madise N. Contextual influences on modern contraceptive use in Sub-Saharan Africa. Am J Public Health. 2007;97(7):1233–40. doi: 10.2105/AJPH.2005.071522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Nattabi B, Li J, Thompson S, Orach CG, Earnest J. Family planning among people living with HIV in post-conflict Northern Uganda: A mixed methods study. Confl Health. 2011;5:18. doi: 10.1186/1752-1505-5-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Laher F, Todd CS, Stibich MA, Phofa R, Behane X, Mohapi L, et al. A qualitative assessment of decisions affecting contraceptive utilization and fertility intentions among HIV-positive women in Soweto. S Afr AIDS Behav. 2009;13(Suppl 1):47–54. doi: 10.1007/s10461-009-9544-z. [DOI] [PubMed] [Google Scholar]
- [17].Bongaarts J, Sinding SW. A response to critics of family planning programs. Int Perspect Sex Reprod Health. 2009;35(1):39–44. doi: 10.1363/ifpp.35.039.09. [DOI] [PubMed] [Google Scholar]
- [18].Wanyenze RK, Tumwesigye NM, Kindyomunda R, Beyeza-Kashesya J, Atuyambe L, Kansiime A, et al. Uptake of family planning methods and unplanned pregnancies among HIV-infected individuals: a cross-sectional survey among clients at HIV clinics in Uganda. J Int AIDS Soc. 2011;14:35. doi: 10.1186/1758-2652-14-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Creswell JW, Plano Clark VL. Designing and Conducting Mixed Methods Research. Thousand Oaks: Sage; 2007. [Google Scholar]
- [20].Magnani R. Sampling guide. Arlington: MPACT Food Security and Nutrition Monitoring Project; 1997. http://pdf.usaid.gov/pdf_docs/pnacg172.pdf. [Google Scholar]
- [21].Gliem JA, Gliem RR. 2003 Midwest Research to Practice Conference in Adult, Continuing, and Community Education. Columbus: Ohio State University; 2003. Calculating, Interpreting and Reporting Cronbach's Alpha Reliability Coefficient for Likert-Type scales. [Google Scholar]
- [22].Filmer D, Pritchett LH. Estimating wealth effects without expenditure data–or tears: an application to educational enrollments in states of India. Demography. 2001;38(1):115–32. doi: 10.1353/dem.2001.0003. [DOI] [PubMed] [Google Scholar]
- [23].Kenya Urban Reproductive Health Initiative (Tupange) Kenya National Bureau of Statistics, Measurement, Learning & Evaluation Project for the Urban Reproductive Health Initiative. Kenya Urban Reproductive Health Initiative (Tupange) Report of the 2010 Baseline Household Survey. Published 2011; [Google Scholar]
- [24].Kenya National Bureau of Statistics, ICF Macro. [Accessed April 20,2015];Kenya Demographic and Health Survey 2008-09. 2010 http://dhsprogram.com/pubs/pdf/fr229/fr229.pdf.
- [26].Spaulding AB, Brickley DB, Kennedy C, Almers L, Packel L, Mirjahangir J, et al. Linking family planning with HIV/AIDS interventions: a systematic review of the evidence. AIDS. 2009;23(Suppl 1):S79–88. doi: 10.1097/01.aids.0000363780.42956.ff. [DOI] [PubMed] [Google Scholar]