Abstract
Background
Many preterm infants who survive go on to develop bronchopulmonary dysplasia, probably as the result of persistent inflammation in the lungs. Corticosteroids have powerful anti‐inflammatory effects and have been used to treat individuals with established bronchopulmonary dysplasia. However, it is unclear whether any beneficial effects outweigh the adverse effects of these drugs.
Objectives
To examine the relative benefits and adverse effects of late systemic postnatal corticosteroid treatment (> 7 days) for preterm infants with evolving or established bronchopulmonary dysplasia.
Search methods
For the 2017 update, we used the standard search strategy of Cochrane Neonatal to search the Cochrane Central Register of Controlled Trials (CENTRAL; 2017, Issue 1); MEDLINE via PubMed (January 2013 to 21 February 2017); Embase (January 2013 to 21 February 2017); and the Cumulative Index to Nursing and Allied Health Literature (CINAHL; January 2013 to 21 February 2017). We also searched clinical trials databases, conference proceedings, and reference lists of retrieved articles for randomised controlled trials and quasi‐randomised trials.
Selection criteria
We selected for inclusion in this review randomised controlled trials (RCTs) comparing systemic postnatal corticosteroid treatment versus placebo or nothing initiated more than seven days after birth for preterm infants with evolving or established bronchopulmonary dysplasia.
Data collection and analysis
We used the GRADE approach to assess the quality of evidence.
We extracted and analysed data regarding clinical outcomes including mortality, bronchopulmonary dysplasia, death or bronchopulmonary dysplasia, failure to extubate, complications during primary hospitalisation, and long‐term health outcomes.
Main results
Twenty‐one RCTs enrolling a total of 1424 participants were eligible for this review. All were RCTs, but methods used for random allocation were not always clear. Allocation concealment, blinding of the intervention, and blinding of outcome assessments most often were satisfactory. Late steroid treatment was associated with a reduction in neonatal mortality (at 28 days) but no reduction in mortality at 36 weeks, at discharge, or at latest reported age. Benefits of delayed steroid treatment included reductions in failure to extubate by 3, 7, or 28 days; bronchopulmonary dysplasia both at 28 days of life and at 36 weeks' postmenstrual age; need for late rescue treatment with dexamethasone; discharge on home oxygen; and death or bronchopulmonary dysplasia both at 28 days of life and at 36 weeks' postmenstrual age. Data revealed a trend towards increased risk of infection and gastrointestinal bleeding but no increase in risk of necrotising enterocolitis. Short‐term adverse affects included hyperglycaemia, glycosuria, and hypertension. Investigators reported an increase in severe retinopathy of prematurity but no significant increase in blindness. Trial results showed a trend towards reduction in severe intraventricular haemorrhage, but only five studies enrolling 247 infants reported this outcome. Trends towards an increase in cerebral palsy or abnormal neurological examination findings were partly offset by a trend in the opposite direction involving death before late follow‐up. The combined rate of death or cerebral palsy was not significantly different between steroid and control groups. Major neurosensory disability and the combined rate of death or major neurosensory disability were not significantly different between steroid and control groups. There were no substantial differences between groups for other outcomes in later childhood, including respiratory health or function, blood pressure, or growth, although there were fewer participants with a clinically important reduction in forced expired volume in one second (FEV1) on respiratory function testing in the dexamethasone group.
GRADE findings were high for all major outcomes considered, but review authors degraded the quality of evidence by one level because we found evidence of publication bias (bronchopulmonary dysplasia at 36 weeks).
Authors' conclusions
Benefits of late corticosteroid therapy may not outweigh actual or potential adverse effects. This review of postnatal systemic corticosteroid treatment for bronchopulmonary dysplasia initiated after seven days of age suggests that late therapy may reduce neonatal mortality without significantly increasing the risk of adverse long‐term neurodevelopmental outcomes. However, the methodological quality of studies determining long‐term outcomes is limited in some cases (some studies assessed surviving children only before school age, when some important neurological outcomes cannot be determined with certainty), and no studies were sufficiently powered to detect increased rates of important adverse long‐term neurosensory outcomes. Evidence showing both benefits and harms of treatment and limitations of available evidence suggests that it may be prudent to reserve the use of late corticosteroids for infants who cannot be weaned from mechanical ventilation, and to minimise both dose and duration for any course of treatment.
Plain language summary
Late (after seven days) systemic postnatal corticosteroids for preventing bronchopulmonary dysplasia in preterm infants
Review question: To determine the relative benefits and harms associated with treatment consisting of drugs that suppress inflammation, called corticosteroids, given after the first week after birth to prevent or treat lung injury, known as bronchopulmonary dysplasia (sometimes also called chronic lung disease), in babies born too early.
Background: Corticosteroids can reduce lung inflammation in newborns with bronchopulmonary dysplasia but may cause major adverse effects. Bronchopulmonary dysplasia is a major problem for newborn babies in neonatal intensive care units. It is associated with both a higher death rate and worse long‐term outcomes among survivors. Persistent inflammation of the lungs is the most likely cause of bronchopulmonary dysplasia. Corticosteroid drugs have strong anti‐inflammatory effects and so have been used to prevent or to treat bronchopulmonary dysplasia, particularly in babies who cannot be weaned from assisted ventilation.
Study characteristics: We reviewed all clinical trials in preterm babies that gave corticosteroids after the first week after birth and provided data on rates of bronchopulmonary dysplasia later in the newborn period.
Key results: This review of trials indicates that giving corticosteroids to infants at least seven days after birth produces short‐term benefits in reducing the need for assisted ventilation and the rate of bronchopulmonary dysplasia, perhaps also reducing death during the first 28 days of life. However, high doses in particular are associated with short‐term side effects such as bleeding from the stomach or bowel, higher blood pressure, and difficulty tolerating glucose. In contrast with early use of corticosteroids (in the first week of life), we found little evidence of long‐term complications and uncertainty regarding long‐term problems. It seems wise to limit late use of corticosteroids to babies who cannot be weaned from assisted ventilation, and to minimise the dose and duration of any course of treatment.
Quality of evidence: Overall the quality of evidence supporting our conclusions was high.
Summary of findings
Summary of findings for the main comparison. Systemic corticosteroids (dexamethasone or hydrocortisone) compared with control (placebo or nothing) for chronic lung disease in preterm infants.
| Systemic corticosteroids (dexamethasone or hydrocortisone) compared with control (placebo or nothing) for chronic lung disease in preterm infants | ||||||
| Patient or population: preterm infants with chronic lung disease Setting: neonatal intensive care units Intervention: systemic corticosteroids (dexamethasone or hydrocortisone) Comparison: control (placebo or nothing) | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | No. of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Risk with control (placebo or nothing) | Risk with systemic corticosteroids (dexamethasone or hydrocortisone) | |||||
| Mortality at 36 weeks | Study population | RR 0.82 (0.50 to 1.35) | 360 (7 RCTs) | ⊕⊕⊕⊕ HIGH | ||
| 162 per 1000 | 133 per 1000 (81 to 219) | |||||
| Mortality at latest reported age | Study population | RR 0.84 (0.66 to 1.07) | 1035 (19 RCTs) | ⊕⊕⊕⊕ HIGH | ||
| 206 per 1000 | 173 per 1000 (136 to 221) | |||||
| BPD at 36 weeks | Study population | RR 0.77 (0.67 to 0.88) | 580 (11 RCTs) | ⊕⊕⊕⊝ MODERATEa | ||
| 642 per 1000 | 494 per 1000 (430 to 565) | |||||
| Home on oxygen | Study population | RR 0.71 (0.54 to 0.94) | 611 (7 RCTs) | ⊕⊕⊕⊕ HIGH | ||
| 273 per 1000 | 194 per 1000 (147 to 256) | |||||
| Death or BPD at 36 weeks | Study population | RR 0.77 (0.70 to 0.86) | 580 (11 RCTs) | ⊕⊕⊕⊕ HIGH | ||
| 779 per 1000 | 600 per 1000 (545 to 670) | |||||
| Cerebral palsy ‐ at latest reported age | Study population | RR 1.16 (0.82 to 1.64) | 919 (16 RCTs) | ⊕⊕⊕⊕ HIGH | ||
| 114 per 1000 | 132 per 1000 (94 to 187) | |||||
| Death or cerebral palsy ‐ at latest reported age | Study population | RR 0.95 (0.78 to 1.15) | 919 (16 RCTs) | ⊕⊕⊕⊕ HIGH | ||
| 318 per 1000 | 302 per 1000 (248 to 366) | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; OR: odds ratio; RR: risk ratio. | ||||||
| GRADE Working Group grades of evidence. High quality: We are very confident that the true effect lies close to that of the estimate of the effect. Moderate quality: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low quality: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect. Very low quality: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect. | ||||||
aDowngraded one level because publication bias was suspected.
Background
Description of the condition
Surfactant therapy has improved outcomes for preterm infants with respiratory distress syndrome but has only modestly reduced risk of bronchopulmonary dysplasia (BPD) (Egberts 1997). More infants with BPD are being cared for in neonatal units, and management of their condition is both time‐consuming and costly. The term 'bronchopulmonary dysplasia' describes injury with maldevelopment of the lung that follows preterm birth and is a major problem in neonatal intensive care units. Persistent lung inflammation is the most likely underlying pathogenesis.
Description of the intervention
Postnatal corticosteroid treatment has been shown to have some acute effects on lung function in infants with established BPD, especially among those who are ventilator‐dependent (CDTG 1991; Mammel 1983). Corticosteroids may be given parenterally or enterally. Investigators have expressed concern that the benefits of steroids might not outweigh their adverse effects, which include hypertension, hyperglycaemia, intestinal perforation, and extreme catabolism (Anonymous 1991; Ng 1993). Animal studies have also raised concerns about adverse effects on the central nervous system of corticosteroids given perinatally to immature offspring (Flagel 2002; Gramsbergen 1998).
How the intervention might work
Corticosteroids might prevent or treat BPD through their potent anti‐inflammatory effects.
Why it is important to do this review
Multiple published systematic reviews have examined the use of systemic postnatal corticosteroids in infants with or at risk of BPD (Arias‐Camison 1999; Bhuta 1998; Doyle 2000; Doyle 2010a; Doyle 2010b; Doyle 2010c; Doyle 2014a; Doyle 2014b; Halliday 1997; Halliday 1999; Tarnow‐Mordi 1999). Other systematic reviews have addressed early versus late use of inhaled corticosteroids for preventing or treating BPD (Shah 2017 and Onland 2017a, respectively), as well as use of systemic versus inhaled steroids for preventing or treating BPD (Shah 2012a and Shah 2012b, respectively). Another review compared different systemic corticosteroid regimens (Onland 2017b).
Two existing Cochrane reviews have explored separately trials in which systemic postnatal corticosteroids were started within seven days of birth and more than seven days after birth (Doyle 2014a and Doyle 2014b, respectively). The present systematic review updates the review of systemic corticosteroids started more than seven days after birth.
Objectives
To examine the relative benefits and adverse effects of late systemic postnatal corticosteroid treatment (> 7 days) for preterm infants with evolving or established bronchopulmonary dysplasia.
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials (RCTs) of late postnatal corticosteroid treatment for preterm infants with evolving or established BPD that reported clinically important outcome variables.
Types of participants
Preterm infants with evolving or established BPD, defined as oxygen‐dependent, ventilator‐dependent, or both, with or without radiographic changes of BPD.
Types of interventions
Treatment with systemic corticosteroids (dexamethasone or hydrocortisone) versus control (placebo or nothing).
Types of outcome measures
Primary outcomes
Mortality
Bronchopulmonary dysplasia (including at 28 days of life, at 36 weeks' postmenstrual age, and at 36 weeks' postmenstrual age among survivors)
Death or BPD (at 28 days of life and at 36 weeks' postmenstrual age)
Long‐term outcomes (including blindness, deafness, cerebral palsy, and major neurosensory disability)
Secondary outcomes
Failure to extubate
Late rescue with corticosteroids
Need for home oxygen therapy
Complications during primary hospitalisation (including infection, hyperglycaemia, hypertension, pulmonary air leak, patent ductus arteriosus, severe intraventricular haemorrhage, periventricular leukomalacia, necrotising enterocolitis, gastrointestinal bleeding, intestinal perforation, and severe retinopathy of prematurity)
Later childhood outcomes, including respiratory function, blood pressure, and growth
Search methods for identification of studies
Electronic searches
We used the criteria and standard methods of Cochrane and Cochrane Neonatal (see the Cochrane Neonatal search strategy for specialized register).
For the 2017 update, we conducted a comprehensive search that included the Cochrane Central Register of Controlled Trials (CENTRAL; 2017, Issue 1) in the Cochrane Library; MEDLINE via PubMed (January 2013 to 21 February 2017); Embase (January 2013 to 21 February 2017); and the Cumulative Index to Nursing and Allied Health Literature (CINAHL) (January 2013 to 21 February 2017) using the following search terms: (adrenal cortex hormones OR dexamethasone OR betamethasone OR hydrocortisone OR steroid OR corticosteroid), plus database‐specific limiters for RCTs and neonates (see Appendix 1 for the full search strategy for each database). We did not apply language restrictions. We searched clinical trials registries for ongoing and recently completed trials (clinicaltrials.gov; the World Health Organization International Trials Registry and Platform (www.whoint/ictrp/search/en/); and the ISRCTN Registry).
See Appendix 2 for previous search strategies.
Searching other resources
We searched the reference lists of all identified publications for additional references not identified by the electronic literature search.
Data collection and analysis
We used the methods of the Cochrane Neonatal Group for data collection and analysis.
Selection of studies
We included all randomised and quasi‐randomised controlled trials that fulfilled the selection criteria presented in the previous section. Review authors independently reviewed results of the updated search and selected studies for inclusion. We resolved disagreements by discussion.
Data extraction and management
For each included trial, we sought information regarding methods of randomisation, blinding, and stratification, and whether the trial was single‐ or multi‐centred. Information on trial participants included birth weight, gestational age, and sex. We analysed information on the following clinical outcomes: mortality, BPD (including BPD at 28 days of life, BPD at 36 weeks' postmenstrual age, BPD at 36 weeks' postmenstrual age in survivors, late rescue with corticosteroids (among all infants and survivors), and need for home oxygen therapy), death or BPD (at 28 days and at 36 weeks' postmenstrual age), and long‐term outcomes (including blindness, deafness, cerebral palsy, and major neurosensory disability). Secondary outcomes included failure to extubate, complications during primary hospitalisation (including infection, hyperglycaemia, glycosuria, hypertension, echodensities on ultrasound scan of brain, necrotising enterocolitis, gastrointestinal bleeding, gastrointestinal perforation, and severe retinopathy of prematurity), and longer‐term outcomes of cognitive delay, respiratory health and function, blood pressure, and growth during childhood.
For each study, one review author entered final data into RevMan 5 (RevMan 2014); a second review author then checked the data for accuracy. We resolved discrepancies through discussion or through consultation with a third assessor.
We attempted to contact the authors of original reports to request further details when information regarding any of the above was unclear.
Assessment of risk of bias in included studies
Two review authors (LD, JC) independently assessed risk of bias (low, high, or unclear) of all included trials using the Cochrane ‘Risk of bias’ tool (Higgins 2011) for the following domains.
Sequence generation (selection bias).
Allocation concealment (selection bias).
Blinding of participants and personnel (performance bias).
Blinding of outcome assessment (detection bias).
Incomplete outcome data (attrition bias).
Selective reporting (reporting bias).
Any other bias.
We resolved disagreements by discussion or by consultation with a third assessor. See Appendix 3 for a more detailed description of risk of bias for each domain.
Measures of treatment effect
We used the standard methods of the Cochrane Neonatal Group to analyse data.
We performed statistical analyses using RevMan 5 (RevMan 2014). We analysed dichotomous data using risk ratio (RR), risk difference (RD), and the number needed to treat for an additional beneficial (NNTB) or harmful outcome (NNTH). We reported the 95% confidence interval (CI) for all estimates.
We analysed continuous data using mean difference (MD) or standardised mean difference (SMD) to combine trials that measured the same outcome using different methods.
Unit of analysis issues
For clinical outcomes such as episodes of sepsis, we analysed the data as proportions of neonates having one or more episodes.
Dealing with missing data
For included studies, we noted levels of attrition. When we had concern regarding the impact of including studies with high levels of missing data in the overall assessment of treatment effect, we planned to explore this concern using sensitivity analysis.
We performed all outcome analyses on an intention‐to‐treat basis (i.e. we included in the analyses all participants randomised to each group). The denominator for each outcome in each trial was the number randomised minus any participants whose outcomes were known to be missing.
Assessment of heterogeneity
We examined heterogeneity between trials by inspecting forest plots and quantifying the impact of heterogeneity using the I² statistic. If noted, we planned to explore possible causes of statistical heterogeneity using prespecified subgroup analysis (e.g. differences in study quality, participants, intervention regimens, or outcome assessments).
Assessment of reporting biases
We assessed possible publication bias and other biases by examining symmetry/asymmetry of funnel plots.
For included trials that were recently performed (and therefore prospectively registered), we used the websites www.clinicaltrials.gov and www.controlled‐trials.com to explore possible selective reporting of study outcomes by comparing primary and secondary outcomes for reports in which primary and secondary outcomes were proposed at trial registration. If we found such discrepancies, we planned to contact the primary investigators to request missing outcome data on outcomes prespecified at trial registration.
Data synthesis
Quality of evidence
We used the GRADE approach, as outlined in the GRADE Handbook (Schünemann 2013), to assess the quality of evidence for the following (clinically relevant) outcomes: mortality, BPD (including BPD at 28 days of life, BPD at 36 weeks' postmenstrual age, BPD at 36 weeks' postmenstrual age in survivors, late rescue with corticosteroids (among all infants and survivors), and need for home oxygen therapy), death or BPD (at 28 days of life and at 36 weeks' postmenstrual age), and long‐term outcomes (including blindness, deafness, cerebral palsy, and major neurosensory disability).
Two review authors independently assessed the quality of evidence for each of the outcomes above. We considered evidence from RCTs as high quality but downgraded the evidence one level for serious (or two levels for very serious) limitations based upon the following: design (risk of bias), consistency across studies, directness of evidence, precision of estimates, and presence of publication bias. We used the GRADEpro GDT Guideline Development Tool to create a ‘Summary of findings’ table to report the quality of the evidence.
The GRADE approach yields an assessment of the quality of a body of evidence and assignment to one of four grades.
High: We are very confident that the true effect lies close to that of the estimate of the effect.
Moderate: We are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different.
Low: Our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect.
Very low: We have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect.
When we judged meta‐analysis to be appropriate, we carried out the analysis using RevMan 5, supplied by Cochrane. We used the Mantel‐Haenszel method for estimates of typical risk ratio and risk difference. We analysed continuous measures using the inverse variance method, and computed mean differences or standardised mean differences.
We used the fixed‐effect model for all meta‐analyses.
Subgroup analysis and investigation of heterogeneity
We intended to include subgroup analyses by type of corticosteroid used (dexamethasone or hydrocortisone) if we identified a sufficient number of trials to make such subgroup analyses meaningful.
Sensitivity analysis
We planned to perform sensitivity analyses for situations where this might affect interpretation of significant results (e.g. when risk of bias was associated with the quality of some of included trials, when outcome data were missing). We thought no such analyses were necessary for this review.
Results
Description of studies
Results of the search
We identified no new RCTs through the literature search (Figure 1) but found a follow‐up report from an existing trial (Parikh 2016). For earlier reviews, we screened 521 potential references and 21 RCTs recruiting 1424 infants to determine eligibility for inclusion. These trials enrolled preterm infants who were oxygen‐ or ventilator‐dependent (or both) beyond seven days of age. Investigators typically used dexamethasone at an initial dose of 0.5 to 1.0 mg/kg/d, with initial duration of therapy ranging from three days to six weeks. In one study, the corticosteroid was solely hydrocortisone (Parikh 2013). Details are given below and in the Characteristics of included studies table.
1.
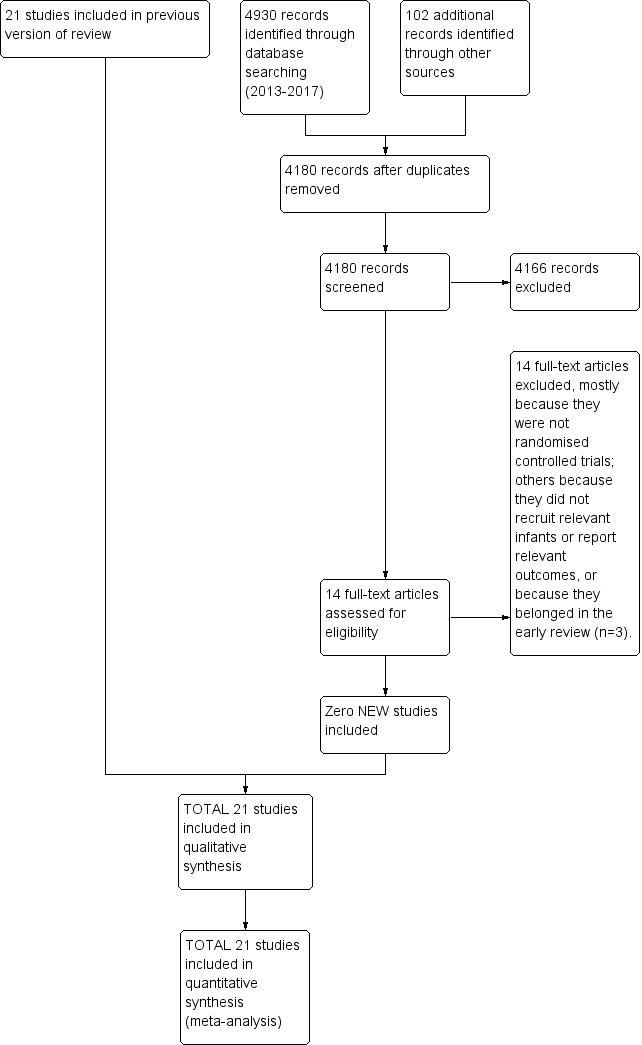
Study flow diagram: review update.
We discuss the excluded trials below and in the Characteristics of excluded studies table.
We identified two ongoing RCTs of hydrocortisone to prevent or treat BPD (NCT01353313; Onland 2011).
Included studies
Ariagno 1987 was updated with complete data provided by the investigators in September 2000. Investigators randomised 34 preterm infants of less than 1501 grams birth weight who were ventilator‐dependent and were not weaning from mechanical ventilation at three weeks of age to parenteral dexamethasone or placebo groups. Treated babies received one of two regimens: a 10‐day course of 1.0 mg/kg/d for four days and 0.5 mg/kg/d for six days, or a seven‐day course of 1.0 mg/kg/d for three days followed by 0.5 mg/kg/d for four days. Researchers calculated total respiratory system compliance from a pneumotachometer and made airway pressure measurements during mechanical inflation before and after seven days of treatment. Outcomes included mortality, duration of ventilation and oxygen therapy, and complications of prematurity and treatment.
Avery 1985 enrolled 16 infants with birth weight less than 1500 grams, a clinical and radiographic diagnosis of respiratory distress syndrome, inability to be weaned from the ventilator after two weeks, and radiological evidence of stage II or III BPD (Northway 1967). Researchers excluded babies if they had patent ductus arteriosus, congenital heart disease, sepsis, or pneumonia; had received intravenous lipids for at least 24 hours; and were over six weeks of age. To those randomised to receive dexamethasone, investigators gave 0.5 mg/kg/d intravenously in two divided doses for three days, followed by 0.3 mg/kg/d for a further three days, thereafter decreased by 10% of the current dose every three days until a dose of 0.1 mg/kg/d was reached. At that point, they gave the drug on alternate days for one week, then discontinued.
Brozanski 1995 was a prospective randomised double‐blind trial conducted to assess the efficacy and safety of pulse doses of dexamethasone for survival without supplemental oxygen given to very low birth weight infants at high risk of having BPD. Trial authors randomly assigned 78 infants with birth weight less than 1501 grams, who were ventilator‐dependent at seven days, to receive pulse doses of dexamethasone 0.5 mg/kg/d 12‐hourly or an equivalent volume of a saline placebo for three days at 10‐day intervals until they no longer required supplemental oxygen or assisted ventilation, or had reached 36 weeks' postmenstrual age. Trialists excluded from the study infants with complex congenital anomalies, pulmonary hypoplasia, or haemodynamic instability.
CDTG 1991 (Collaborative Dexamethasone Trial Group 1991) was a multi‐centre trial conducted at 31 centres in six countries over a period of two and a half years from August 1986 to January 1989. A total of 287 infants who were oxygen‐dependent and had been in a static or deteriorating condition over the preceding week were eligible for trial entry from around three weeks of age. Study authors excluded infants with major malformations and delayed trial entry to allow treatment of any intercurrent infection or heart failure. Infants did not require mechanical ventilation at the time of entry. Those allocated to the dexamethasone group received 0.6 mg/kg/d intravenously (or orally if there was no intravenous line) for one week. Trialists had the option to give a second tapering nine‐day course (0.6, 0.4, and 0.2 mg/kg/d for three days each) if, after initial improvement, relapse occurred. They gave an equivalent volume of saline placebo to control infants.
Investigators in Cummings 1989 randomised 36 preterm infants with birth weight less than 1251 grams and gestational age less than 31 weeks, who were dependent on oxygen (> 29%) and mechanical ventilation (rate > 14 per minute with no evidence of weaning during the previous 72 hours) at two weeks of age, to receive a 42‐day course of dexamethasone or an 18‐day course of dexamethasone or saline placebo. They did not include infants with symptomatic patent ductus arteriosus, renal failure, or sepsis. To infants in the 42‐day group, researchers administered dexamethasone at a dose of 0.5 mg/kg/d for three days and 0.3 mg/kg/d for the next three days. They then reduced the dose by 10% every three days until a dose of 0.1 mg/kg was reached on day 34. After three days at this dose, trialists gave the drug on alternate days for one week and then stopped. Infants in the 18‐day dexamethasone group received the same initial dose of 0.5 mg/kg/d for three days, but their dose was then decreased more rapidly by 50% every three days until a dose of 0.06 mg/kg was reached on day 10. After three days at this dose, study authors gave the drug on alternate days for one week and then stopped. For the remaining four treatment days, those infants received saline placebo. Infants in the control group received saline placebo for 42 days. Researchers combined the two treatment groups for the purposes of this meta‐analysis and provided additional data on some short‐term and long‐term outcomes for inclusion in this review.
Doyle 2006 enrolled from March 2000 to October 2002 a total of 70 infants of less than 1000 grams birth weight or born at less than 28 weeks' gestation, who were at least seven days of age and were ventilator‐dependent and considered eligible for postnatal corticosteroids. Exclusions were few and comprised only those with congenital anomalies likely to adversely affect long‐term neurological outcomes. Trialists worked at 11 collaborating centres within Australia, New Zealand, and Canada and performed stratification by centre. They randomly allocated infants to twice‐daily doses of a 10‐day tapering course of dexamethasone sodium phosphate (0.15 mg/kg/d for three days, 0.10 mg/kg/d for three days, 0.05 mg/kg/d for two days, 0.02 mg/kg/d for two days; for a total of 0.89 mg/kg over 10 days) (n = 35 infants) or to an equivalent volume of 0.9% saline placebo (n = 35 infants). A repeat course of the same blinded drug was a therapeutic option for attending physicians. The dexamethasone preparation did not contain bisulphite preservative. Researchers based the sample size calculation for the original trial on detecting improvement in survival free of major neurosensory disability from 50% to 60%, with a two‐sided type I error rate of 5% and 80% power, and required that a total of 814 infants be recruited. This study was stopped early at 70 infants, not only because less than 10% of the initial sample had been recruited after 2.5 years, making it unlikely that the total sample size of 814 would be achieved within a reasonable time, but also because the rate of recruitment had fallen, not increased, even though more centres had entered the study from the time of its inception.
Durand 1995 was a prospective randomised trial of 43 infants of birth weight 600 grams to 1500 grams and gestational age between 24 and 32 weeks who failed to be weaned from the ventilator at 7 to 14 days. Their oxygen requirement was > 29% and ventilator rate > 13 per minute. Investigators excluded infants with documented sepsis, evidence of systemic hypertension, congenital heart disease, renal failure, intraventricular haemorrhage (grade IV), and congenital anomalies. Infants in the treatment group received dexamethasone 0.5 mg/kg/d 12‐hourly intravenously for the first three days, 0.25 mg/kg/d for the next three days, and 0.10 mg/kg/d on the seventh day of treatment. Controls received no dexamethasone during the seven‐day study period. At the end of the week of the study, the attending clinician could start dexamethasone treatment for controls.
Harkavy 1989 randomised 21 preterm infants who were ventilator‐ and oxygen‐dependent at 30 days of age to receive dexamethasone or placebo. They gave dexamethasone 0.5 mg/kg/d in two or more doses either intravenously or by mouth, and gave an equivalent volume of saline to controls.
Kari 1993 was a randomised double‐blind placebo‐controlled trial that enrolled 41 infants with birth weight less than 1501 grams, gestational age greater than 23 weeks, dependence on mechanical ventilation at 10 days, and no signs of patent ductus arteriosus, sepsis, gastrointestinal bleeding, or major malformations. Infants in the dexamethasone group received 0.5 mg/kg/d intravenously in two doses for seven days, whereas the placebo group received normal saline.
In Kazzi 1990, 23 preterm infants with birth weight less than 1500 grams and radiological findings consistent with a diagnosis of BPD, who were ventilator‐dependent at three to four weeks of age, were eligible for study entry provided they needed more than 34% oxygen and had a ventilator rate greater than 14 per minute or peak inspiratory pressure > 17 cmH2O. Infants had to show lack of improvement in ventilator dependency during the preceding five days. Infants in the treatment group received dexamethasone 0.50 mg/kg/d for three days, given as a single daily dose by nasogastric tube. Trialists tapered this dose to 0.40 mg/kg/d for two days, then to 0.25 mg/kg/d for two days. Thereafter, infants received hydrocortisone administered in four divided doses every six hours, beginning with 8 mg/kg/d for two days and tapered by 50% of the dose every other day until 0.5 mg/kg/d was reached. After a total of 17 days (seven of dexamethasone and 10 of hydrocortisone), trialists discontinued treatment. Infants in the control group received equal volumes of saline.
In Kothadia 1999, researchers randomly allocated 118 preterm infants (birth weight < 1501 grams) between 15 and 25 days of age, who were ventilator‐dependent, to receive a 42‐day tapering course of dexamethasone or saline placebo. The dosage schedule was 0.25 mg/kg 12‐hourly for three days and 0.15 mg/kg 12‐hourly for three days, followed by a 10% reduction in dose every three days until a dose of 0.1 mg/kg had been received for three days, from which time they received 0.1 mg/kg every other day until 42 days after entry. Study authors provided additional data on some short‐term outcomes for inclusion in this review.
Kovacs 1998 was a double‐blind RCT conducted to assess the efficacy of a combination of prophylactic systemic dexamethasone and nebulised budesonide in reducing the incidence and severity of BPD in infants of less than 30 weeks' gestation and weighing less than 1501 grams who were ventilator‐dependent at the age of seven days. Thirty infants received dexamethasone 0.25 mg/kg twice daily for three days, followed by nebulised budesonide 500 µg twice daily for 18 days. Thirty control infants received systemic and inhaled saline. Study authors provided additional data on some short‐term and long‐term outcomes for inclusion in this review.
Noble‐Jamieson 1989 enrolled 18 infants over four weeks of age who required more than 30% oxygen. Congenital infection, gastric erosion, and necrotising enterocolitis were absolute contraindications to trial entry; investigators excluded one infant because of necrotising enterocolitis. Entry was postponed if an infant had a central venous catheter, active infection, untreated patent ductus arteriosus, glucose intolerance, or major segmental pulmonary collapse. Trial entry was postponed for 11 infants, mainly because of suspected sepsis. Researchers randomly allocated infants to receive either dexamethasone or saline. They gave dexamethasone orally or intravenously at a dose of 0.25 mg/kg twice daily for the first week, 0.125 mg/kg twice daily for the second week, and 0.10 mg/kg daily for the third week, and performed twice‐weekly cranial ultrasound scans on all infants and analysed them blindly after completion of the study.
Ohlsson 1992 enrolled 25 infants with birth weight less than 1501 grams after receiving parental informed consent, if the following criteria were met: postnatal age 21 to 35 days, inspired oxygen greater than 29%, chest radiograph consistent with BPD, and treatment with diuretics resulting in no signs of improvement in ventilator requirements during the previous 72 hours. Researchers excluded infants if they had a diagnosis of suspected or proven infection, significant congenital malformation, or clinical evidence of patent ductus arteriosus, necrotising enterocolitis, and gastrointestinal haemorrhage or perforation. The treatment group received dexamethasone 0.50 mg/kg 12‐hourly for three days, 0.25 mg/kg 12‐hourly for three days, 0.125 mg/kg 12‐hourly for three days, and 0.125 mg/kg daily for three days. Investigators gave dexamethasone intravenously at a standard volume of 1 mL. The Research Ethical Committee did not permit use of an intravenous placebo, so a physician not involved in subsequent care of the infant gave a sham injection of 1 mL of normal saline into the bed in the control group. Study authors provided additional data for some short‐term outcomes for inclusion in this review.
Papile 1998 was a double‐blind randomised controlled trial conducted to compare the benefits and hazards of initiating dexamethasone therapy at two weeks of age versus four weeks of age to 371 ventilator‐dependent very low birth weight (501 grams to 1500 grams) infants who had respiratory index scores (mean airway pressure (MAP) × fraction of inspired oxygen) ≥ 2.4 at two weeks of age. A total of 182 infants received dexamethasone for two weeks followed by placebo for two weeks, and 189 infants received placebo for two weeks followed by either dexamethasone (those with a respiratory index score ≥ 2.4 on treatment day 14) or additional placebo for two weeks. Trialists gave dexamethasone at a dose of 0.5 mg/kg/d intravenously or orally for five days, then tapered the dose. Only outcome data at 28 days were eligible for inclusion in this review (see below).
Parikh 2013 was a double‐blind RCT of hydrocortisone versus saline placebo given to 64 infants with birth weight ≤ 1000 grams who were ventilator‐dependent between 10 and 21 days of age, with the primary outcome of differences in brain tissue volumes on magnetic resonance imaging (MRI) at term‐equivalent age. Thirty‐one infants received a total of 17 mg/kg of hydrocortisone over seven days, and 33 infants received an identical volume of saline placebo. This trial included follow‐up at 18 to 22 months of age, corrected for prematurity.
Romagnoli 1997 was a randomised trial of 30 preterm infants who were ventilator‐ and oxygen‐dependent at 10 days and were at 90% risk of developing BPD based on the trial authors' own scoring system. Fifteen infants received dexamethasone 0.5 mg/kg/d for six days, 0.25 mg/kg/d for six days, and 0.125 mg/kg/d for three days (total dose 4.875 mg/kg). Control infants did not receive any steroid. Study authors provided additional data on some short‐term outcomes for inclusion in this review.
Scott 1997 was a double‐blind RCT of dexamethasone versus saline placebo given to 15 infants who were ventilator‐dependent between 11 and 14 days of age, with the primary outcome of cortisol response to adrenocorticotrophic hormone (ACTH). Ten infants received a total of 1.9 mg/kg of dexamethasone over five days, and five infants received an identical volume of saline placebo.
Vento 2004 was a randomised trial of 20 neonates with birth weight < 1251 grams and gestation < 33 weeks who were oxygen‐ and ventilator‐dependent on the 10th day of life. Infants received either dexamethasone 0.5 mg/kg/d for three days, 0.25 mg/kg/d for three days, and 0.125 mg/kg/d for one day or no steroid treatment.
In Vincer 1998, researchers randomly assigned 20 very low birth weight infants who were ventilator‐dependent at 28 days to receive either a six‐day course of intravenous dexamethasone 0.5 mg/kg/d for three days followed by 0.3 mg/kg/d for the final three days or an equal volume of saline placebo. This trial included a two‐year follow‐up. Study authors provided additional data on some short‐term outcomes for inclusion in this review.
Walther 2003 was a double‐blind randomised clinical trial involving preterm infants with birth weight > 599 grams, gestation of 24 to 32 weeks, and respiratory distress syndrome requiring mechanical ventilation with oxygen of > 29% between 7 and 14 days of life. Eligible infants received either dexamethasone 0.2 mg/kg/d for four days, 0.15 mg/kg/d for four days, and 0.25 mg/kg/d for two days (total dose 1.9 mg/kg over 14 days) or saline placebo.
Excluded studies
Doyle 2014a addressed the following studies on the use of postnatal corticosteroids commenced in the first week of life to prevent BPD in preterm infants: Anttila 2005; Baden 1972; Batton 2012; Biswas 2003; Bonsante 2007; Efird 2005; Garland 1999; Halac 1990; Kopelman 1999; Lin 1999; Mukhopadhyay 1998; Ng 2006; Peltoniemi 2005; Rastogi 1996; Romagnoli 1999; Sanders 1994; Shinwell 1996; Sinkin 2000; Soll 1999; Stark 2001; Subhedar 1997; Suske 1996; Tapia 1998; Vento 2004; Wang 1996; Watterberg 1999; Watterberg 2004; Yeh 1990; Yeh 1997. See Characteristics of excluded studies.
Risk of bias in included studies
Overall most studies had low risk of bias. All were RCTs, although the method of random allocation was not always clear. Allocation concealment applied to most studies. Blinding of investigators and others was achieved most often with use of placebo, usually saline solution. Follow‐up reporting for short‐term outcomes was most often complete but was more variable for long‐term outcomes beyond discharge and later into childhood.
Ariagno 1987 was a double‐blind trial in which the pharmacist performed randomisation. Trialists provided outcomes for all enrolled infants. Follow‐up consisted of the following: Investigators assessed surviving children at 12, 24, and 36 months of age, corrected for prematurity, in the High‐Risk Follow‐Up Clinic. Data included cerebral palsy and auditory status, but criteria were not defined. Personnel involved and blinding of assessors to treatment groups were unclear. The follow‐up rate of survivors was 96% (23/24) (Ariagno 2000).
Avery 1985 paired and compared treatment and control infants for success in weaning. Investigators stratified infants at entry by weight into three categories: less than 1000 grams, 1000 grams to 1250 grams, and 1251 grams to 1500 grams. Within each weight group, equal numbers of treatment cards and control cards were placed into envelopes for random selection. The first treated infant and the first control infant within a given weight category made the first pair, and researchers considered in the sequential analysis only infants who were paired for weaning success. If both infants in a pair were successful or had treatment failure, the result was a tie and trialists discarded the pair. If one infant weaned and the other did not, trialists scored the untied pair as favouring treatment or control. The study was stopped when significance was reached from weaning from the ventilator in the sequential analysis of untied pairs. At that time, 16 infants had been studied and 14 had been matched to form seven pairs. Study authors reported no follow‐up component.
In Brozanski 1995, researchers achieved randomisation by using a random numbers table and stratified infants according to sex and birth weight (< 1000 grams vs > 999 grams). They reported treatment allocation on cards inside sequentially numbered envelopes that were kept in the pharmacy where randomisation took place. Investigators enrolled 88 infants but provided outcome data, apart from survival without supplemental oxygen at 36 weeks' postmenstrual age, for only 78 infants. They withdrew 10 infants during the study because of pharmacy error (dexamethasone group two infants, placebo group one infant), parental choice (placebo group two infants), or attending physician request (dexamethasone group one infant, placebo group four infants). All five infants withdrawn from the study by the attending physician subsequently received an extended course of dexamethasone. Follow‐up consisted of the following (Hofkosh 1995): Unknown observer(s) blinded to treatment group allocation saw survivors at 12 months of age, corrected for prematurity. The follow‐up rate of survivors was 68% (44/65). Study authors did not specify criteria for the diagnosis of cerebral palsy. Psychological assessment included the Mental Developmental Index (MDI) of the Bayley Scales of Infant Development (BSID). Study authors provided no data on major disability.
CDTG 1991 assigned groups by telephone call to the Clinical Trial Service Unit in Oxford. Investigators stratified infants by clinical centre and by whether or not they were ventilator‐dependent. After completion of the trial, clinicians could give open steroids if this was clinically indicated because of life‐threatening deterioration. Researchers retained infants in the group to which they had been allocated for the purpose of analysis. They enrolled 287 infants in the trial; two were ineligible because of major malformations (Fallot's tetralogy, oesophageal atresia), leaving 285 infants included in the analysis. Follow‐up consisted of the following (Jones 1995): Researchrs provided data on survivors at 36 months of age, not corrected for prematurity. Primary sources of data, obtained in the UK and Ireland, were healthcare provider visitors, who provided data on major neurosensory diagnoses or other chronic problems, and general practitioners, who provided data on health and hospitalisations. Parents completed questionnaires, including the Minnesota Child Development Inventory (CDI). Parents, healthcare visitors, and general practitioners (GPs) were unaware of treatment group allocation. In some countries, investigators sought data from paediatricians only (< 10% cases). The follow‐up rate of survivors was 94% (209/223). Trialists did not specify criteria for the diagnosis of cerebral palsy or blindness, but they defined severe hearing loss (deafness) as hearing loss requiring either hearing aids or special schooling. Major disability comprised any types of non‐ambulant cerebral palsy at three years of age, < 50% of age level on the CDI, or predicted special schooling for sensory or other impairment. Further follow‐up at 13 to 17 years of age consisted of the following (Jones 2005a; Jones 2005b): Assessors who were blinded to treatment group allocation assessed surviving children from the 25 individual British and Irish study centres at 13 to 17 years of age. Families completed a questionnaire on functional status, diagnoses of potentially disabling conditions (visual or hearing impairment, learning disabilities, cerebral palsy, and epilepsy), and the child's schooling. Study authors asked GPs to complete a questionnaire to report known functional problems, diagnoses, and hospital admissions. The paediatrician responsible for each child's care made the diagnosis of cerebral palsy. One of three research nurses blinded to the children's original treatment allocation visited surviving children at home. They administered a non‐verbal reasoning test and the British Picture Vocabulary Scale and averaged these scores as a proxy for IQ. Investigators defined moderate disability as consisting of one or two of the following: IQ 2 to 3 standard deviations (SD) below the mean, ambulatory cerebral palsy, hearing deficits corrected with hearing aids, impaired vision, or a behaviour disorder with a major impact on schooling. They defined severe disability as any of the following: IQ > 3 SDs below the mean, wheelchair‐dependent cerebral palsy, uncorrectable hearing loss, blindness (perception of light only), or three moderate disabilities. Respiratory function included spirometry to measure forced expiratory volume in one second (FEV1), forced vital capacity (FVC), the FEV1/FVC ratio, and forced expired flow from 25% to 75% (FEF)25%‐75%, and study authors expressed results as standardised scores (z‐scores), as were growth measurements. They assessed other outcomes, but we did not include them in the review. These included data on types of schooling, teacher questionnaires on a child's ability, and the Strengths and Difficulties Questionnaire. The follow‐up rate of survivors at 13 to 17 years was 77% (150/195), as shown in data from five severely disabled children at three years of age who were not contacted as teenagers.
In Cummings 1989, investigators achieved randomisation by sequential assignment from a table of random numbers known only to a pharmacist who had no knowledge of the clinical status of infants. Study authors present outcome data for all 36 infants enrolled in the study. This trial included two experimental groups: one treated for 18 days, and another treated for 42 days, compared with a single control group. For these analyses, trialists combined treatment groups (n = 25) and compared data versus data derived from the control group (n = 11). Follow‐up consisted of the following: A paediatrician and an occupational therapist saw survivors at 15 months of age, corrected for prematurity. Observers were blinded to treatment group allocation. The follow‐up rate of survivors was 100% (23/23). Researchers specified criteria for the diagnosis of cerebral palsy but did not specify criteria for blindness or deafness. Psychological assessment included the MDI and the Psychomotor Developmental Index (PDI) of the BSID. Major disability comprised any of the following: cerebral palsy or MDI or PDI < 1 SD. Investigators later assessed survivors at four years of age and confirmed neurological status for all participants (Cummings 2002 (personal communication follow‐up of Cummings 1989)). Researchers provided further follow‐up at 15 years of age (Gross 2005). Assessors were blinded to treatment group allocation. Outcomes included growth (body size converted to z‐scores), general health, respiratory morbidity, and respiratory function testing. Trialists assessed cognition using the Wechsler Intelligence Scale for Children ‐ Third Edition (WISC‐III). Teachers completed data on class repetition, performance, and behaviour. Pulmonary function testing included spirometry to measure FEV1, FVC, and FEF25%‐75%, along with measurement of lung volumes (total lung capacity (TLC) and residual volume (RV)) by nitrogen washout; study authors expressed results as % predicted for age, height, and sex. Trial authors reported the numbers of surviving children with ongoing respiratory symptoms of wheezing or congestion and interpreted these as a diagnosis of asthma for meta‐analysis. They defined intact survival as a normal neurological examination, an IQ > 70, and receiving education in a normal classroom. For the meta‐analysis, investigators defined major neurological disability as any of an abnormal neurological examination (i.e. cerebral palsy), cognitive delay (IQ < 71), or not in a regular classroom (with or without additional help). They did not measure blood pressure.
Doyle 2006 was a double‐blind trial with randomisation performed centrally by non‐clinical staff independent of the chief investigators, with random variation in block sizes of two to eight for each centre. Trialists prepared and labelled syringes identically within the pharmacy department at the centre, concealing treatment allocation from study site investigators and the infant's caregivers. They discouraged but did not prohibit open‐label corticosteroids after randomisation; some infants may have received both a second course of their initially allocated study drug and open‐label corticosteroids. No one apart from the pharmacist at individual study sites had access to the treatment code. Trial authors reported short‐term outcomes for all enrolled infants. Follow‐up included the following (Doyle 2007 (follow‐up publication of Doyle 2006)): Paediatricians and psychologists who were blinded to treatment group allocation assessed surviving children at 24 months of age, corrected for prematurity, at individual study sites. They considered children to have a neurosensory impairment if they had cerebral palsy (criteria included abnormalities of tone and motor dysfunction), blindness (bilateral vision worse than 6/60), deafness requiring hearing aids or worse, or developmental delay (defined as a MDI on the BSID < 85 (< ‐1 SD) (Bayley 1993). Researchers graded severity of the neurosensory disability imposed by the impairment as follows: severe ‐ bilateral blindness, cerebral palsy with the child unlikely ever to walk, or MDI < 55 (< ‐3 SD); moderate ‐ deafness, cerebral palsy in children not walking at two years but expected to walk, or MDI from 55 to < 70 (‐3 SD to < ‐2 SD); mild ‐ cerebral palsy but walking at two years with only minimal limitation of movement or MDI 70 to < 85 (< ‐1 SD). They considered remaining children to have no neurosensory disability. Major neurosensory disability comprised moderate or severe disability. The follow‐up rate of survivors at two years was 98% (58/59).
In Durand 1995, investigators performed randomisation via blind drawing of random cards contained in sealed envelopes. Clinical personnel were not aware of the group assignment of any infant. Study authors present outcome data for 43 of the 44 enrolled infants. They excluded one infant in the control group from all analyses as the result of birth weight < 500 grams. Follow‐up consisted of the following (Durand 2012 (personal communication follow‐up of Durand 1995)): A developmental paediatrician, a paediatric neurologist, and other specialised personnel (including a psychologist) assessed surviving children at 12 months of age, corrected for prematurity. A paediatric ophthalmologist performed all eye examinations. All staff were blinded to treatment group allocation. Children were considered to have a neurosensory impairment if they had cerebral palsy (defined as non‐progressive motor impairment with abnormal muscle tone and decreased range of movements), blindness (bilateral vision worse than 6/60), deafness requiring hearing aids or worse, or developmental delay (defined as MDI < 70 on the BSID). The follow‐up rate of survivors at 12 months was 78% (29/37).
Harkavy 1989 achieved randomisation by using random numbers held in the pharmacy. Clinicians and investigators were unaware of treatment assignments. Study authors provided outcome data for 21 of the 22 enrolled infants. One infant died after consent but before random assignment to a treatment group. Follow‐up consisted of the following (Harkavy 2002 (personal communication follow‐up of Harkavy 1989)): A neonatologist and an occupational therapist saw survivors at ages ranging from 6 to 24 months, corrected for prematurity. Observers were blinded to treatment group allocation. The follow‐up rate of survivors was 32% (6/19). Trialists did not specify criteria for the diagnosis of cerebral palsy, blindness, or deafness. Psychological assessment included the MDI of the BSID. Study authors did not define major disability.
In Kari 1993, researchers performed randomisation in blocks of 10 for each participating hospital. Clinicians and investigators were unaware of treatment assignments. Study authors present outcomes for all 41 infants enrolled in the trial. The number of infants recruited was only 25% of the estimate required for the sample size. Therefore, the study was discontinued after 26 months. Follow‐up consisted of the following (Mieskonen 2003): Only one of four centres in this multi‐centre study provided follow‐up; this centre contributed 23 of the 41 participants to the original study. Three infants died before discharge (one dexamethasone; two placebo). No late deaths in childhood are known. Survivors were followed in the hospital's outpatient clinic. One child in the dexamethasone group had deafness requiring a hearing aid, seizures treated with anticonvulsants, and attention deficit hyperactivity disorder, and required assistance with schooling but did not have cerebral palsy at 7.8 years of age. This child would not co‐operate with the respiratory component of the study. Another child in the dexamethasone group had no confirmed cerebral palsy at 2.6 years of age and was not traced at school age but was said to be attending normal school. One child in the placebo group had multiple difficulties in speech and cognitive function at five years of age and was expected to require extra help at school but refused further follow‐up. Another child in the placebo group had minor difficulties in comprehension at five years of age but was lost to further follow‐up. In total, 16 children participated in the follow‐up study at seven to nine years of age. Trialists recorded neurological status at five years of age from hospital records, including assessments for cerebral palsy (abnormal muscle tone, increased tendon reflexes and positive Babinski sign, or persistent or exaggerated primitive reflexes, dyskinesia, or ataxia), visual or hearing deficits, and school maturity (details of testing not given). Severe disability comprised any of more than mild cerebral palsy, severe global delay (not defined), or sensory or other impairment requiring special schooling; moderate disability comprised any of mild cerebral palsy, severe deafness, moderate global delay (extra help needed at school, assessment of global retardation or language problems), or home oxygen beyond three years of age. For this meta‐analysis, we have extracted data for major neurological disability for those with more than mild cerebral palsy, blindness, or deafness, or needing extra help with schooling. One investigator blinded to neonatal details then assessed children at 7.8 to 9.2 years of age, including presumably treatment group allocation. Age was not corrected for prematurity. Study authors measured children for height and weight and performed lung function tests, electrocardiography (ECG), and echocardiography.
In Kazzi 1990, trialists achieved random assignment by drawing a pre‐coded card prepared from a table of random numbers. They stratified infants by birth weight into three groups: less than 1000 grams, 1000 grams to 1250 grams, and 1251 grams to 1500 grams. The pharmacist drew the card from the appropriate group, and neither investigators nor nursery staff were aware of the treatment group. Study authors provided outcome data for all 23 enrolled infants and reported no follow‐up component.
In Kothadia 1999, researchers randomised infants within six strata, defined in terms of birth weight (500 grams to 800 grams, 801 grams to 1100 grams, and 1101 grams to 1500 grams) and sex, with a block size of eight. They did not describe the exact method of randomisation. Control infants were given an equal volume of normal saline. Investigators assessed outcome data in a blinded fashion. Study authors initially described zero cross‐over in this trial, but review of data at age 19 years revealed that one child who was randomised to placebo received a 42‐day tapering course of placebo, then subsequently a 12‐day tapering course of dexamethasone. In addition, three of the children randomised to placebo received 24‐hour courses of dexamethasone for upper airway oedema. Follow‐up consisted of the following: A developmental paediatrician or one of two neonatologists and a physical therapist saw survivors at 12 months of age, corrected for prematurity, if any neurological abnormality was detected. Observers were blind to treatment group allocation. The follow‐up rate of survivors at 12 months of age was 98% (93/95). Trialists specified criteria for the diagnosis of cerebral palsy. Paediatric ophthalmologists diagnosed blindness. Study authors did not define deafness. Psychological assessment included the MDI of the BSID; investigators assessed the first 10 infants using the original Bayley Scales, and the remainder using BSID‐II. Major disability comprised any of cerebral palsy, blindness, or an MDI < ‐2 SD. Trialists assessed children again at 4 to 6 years of age and at 8 to 11 years of age (Nixon 2007; Washburn 2006). Parents, children, and follow‐up examiners were not aware of children's randomisation assignment. Investigators diagnosed cerebral palsy at 4 to 6 years if the child had a neuromotor abnormality detected on neurological examination by a nurse with specialised training in neurodevelopmental follow‐up, and if the parent reported that the child was receiving treatment for cerebral palsy. A parent was interviewed again at the 8‐ to 11‐year visit as to whether a diagnosis of cerebral palsy had ever been made. For intelligence and academic achievement, at the four‐ to six‐year visit, a child psychologist assessed the child using the Differential Abilities Scales (DAS), the Kaufman Survey of Early Academic and Language Skills (K‐SEALS), and the Vineland Adaptive Behavioral Scales (VABS). At the 8‐ to 11‐year visit, a child psychologist assessed the child using the Wechsler Individual Achievement Tests (WIAT), the Wechsler Intelligence Scale for Children ‐ Third Edition (WISC‐III), and the Vineland Adaptive Behavior Scale (VABS). Investigators defined a major neurodevelopmental impairment at 4 to 6 years and/or at 8 to 11 years as cerebral palsy, and at 4 to 6 years of age as mental retardation (IQ < 70 on either the DAS (n = 11 participants) or the WISC‐III (n = 71 participants) and a VABS composite score < 70) at last follow‐up. For five dexamethasone‐treated and eight placebo‐treated children who did not undergo intelligence testing at 4 to 6 years or at 8 to 11 years of age, they defined major neurodevelopmental impairment as blindness, cerebral palsy (at the most recent visit), or a Bayley MDI < 70 for adjusted age. Trialists assessed all survivors at least once at or beyond 1 year of age. The follow‐up rate at 4 to 11 years of age was 88% (84/95). Trialists collected respiratory data at 8 to 11 years of age using pulmonary function testing. They obtained forced expiratory flow rates and volumes (FVC, fFEV1, the FEV1/FVC ratio, and the FEF25%‐75%) expressed as % of predicted as appropriate and considered abnormal if below the fifth percentile. They determined TLC and RV from body plethysmography and expressed these as a ratio (RV/TLC), as well as pulmonary diffusing capacity (diffusing capacity of the lungs for carbon monoxide (DLCO)) via the single‐breath carbon monoxide technique. However, most children could not cope with plethysmography and the single‐breath diffusion manoeuvre, hence study authors did not analyse TLC, RV, and diffusing capacity data. Investigators also assessed asthma diagnosis and airway reactivity. They categorised children as having asthma if the parent or guardian reported that the child had asthma, had used medications for asthma treatment, or both. A subsample of children underwent maximal progressive exercise testing on a cycle ergometer as part of the larger study. Researchers repeated spirometry immediately and five minutes post exercise, as well as 20 minutes following three puffs of albuterol delivered with a spacer. They used a 15% decrease in FEV1 from pre‐exercise values as the criterion to define exercise‐induced bronchoconstriction and considered a 12% increase in FEV1 from pre‐exercise levels to be a positive bronchodilator response. The follow‐up rate at 8 to 11 years of age for respiratory data was 72% (68/95) but was 66% (63/95) for respiratory function testing.
Kovacs 1998 assigned eligible infants using a "blocked" randomisation procedure, and only the designated pharmacist who prepared all study medications was aware of group assignments. Researchers stratified infants before randomisation into two categories according to gestational age (22 to 26 weeks vs 27 to 29 weeks). Follow‐up consisted of the following (Kovacs 2002 (personal communication follow‐up of Kovacs 1998)): Study authors obtained data from the regular follow‐up clinic at ages up to 90 months in 70% (33/47) of survivors and did not specify personnel involved, blinding of assessors to treatment group, and criteria for various diagnoses, including cerebral palsy and major disability.
Noble‐Jamieson 1989 did not describe the method of randomisation. Medical and nursing staff were unaware of the drug given. Study authors provided outcome data for all 18 enrolled infants and reported no follow‐up component.
Ohlsson 1992 performed randomisation by using computer‐generated random numbers and wrote down allocation groups on cards enclosed in opaque envelopes and kept under lock in the pharmacy. Envelopes were available only to the pharmacist who drew the appropriate card and distributed the study drug. We have described under Description of studies the problem of administering placebo. Trialists discontinued treatment for suspected infection in one infant in each group and treatment for blood transfusion‐derived cytomegalovirus in one infant in the study group. They provided outcome data for all enrolled infants. Follow‐up consisted of the following (Ohlsson 1990 (additional publication of Ohlsson 1992)): Researchers saw survivors in the regular follow‐up clinic up to at least 18 months of age in 96% (23/24) of cases; the remaining survivor was developing normally when last seen at 12 months of age. Age was probably not corrected for prematurity. Study authors did not specify personnel involved and blinding of observers, nor did they specify criteria for the diagnoses of cerebral palsy and blindness. Psychological assessment included the MDI of the BSID.
In Papile 1998, random assignment took place at each centre's pharmacy via the urn method ‐ a procedure that promotes equal distribution of participants among treatment groups. To blind clinical staff to treatment group assignments, investigators prepared different volumes of placebo (saline) to match the various doses of dexamethasone. They reported no follow‐up component.
In Parikh 2013, an individual not involved in the study generated the randomisation sequence, but study authors did not specify the precise method. They described two strata ‐ one for birth weight (< 751 grams vs 751 to 1000 grams) and one for respiratory index score (2 to 4 vs > 4). Trialists limited access to the randomisation assignment to two study pharmacists, and maintained blinding by using an identical volume of saline placebo. Follow‐up consisted of the following (Parikh 2013): Certified examiners assessed survivors at 18 to 22 months of corrected age. Researchers blinded involved personnel to group allocation. Certified examiners diagnosed cerebral palsy and specified the criteria for diagnosis. Study authors defined bilateral deafness as bilateral hearing loss requiring amplification, and bilateral blindness as bilateral vision loss with only form or shadow vision or no useful vision. Psychological assessment included the Bayley Scales of Infant and Toddler Development ‐ Third Edition (Bayley III). Investigators defined any neurodevelopmental impairment as any of cerebral palsy, cognitive delay, language delay, blindness, or deafness.
Romagnoli 1997 achieved random allocation by opening numbered, sealed envelopes. Researchers did not give placebo to control infants. They reported outcome measures for all 30 infants included in the study. Follow‐up consisted of the following (Romagnoli 2002): One paediatrician and one neurologist saw survivors at 36 to 42 months of age, corrected for prematurity, with observers blinded to treatment group allocation. The follow‐up rate of survivors was 100% (30/30). The neurologist made the diagnosis of cerebral palsy, but study authors did not specify the criteria used and reported no specific criteria for blindness and deafness. Psychological assessment included the Stanford Binet Test ‐ 3rd Revision. Study authors provided no data on major disability.
Scott 1997 achieved randomisation using a random number table. Trialists maintained blinding by using an identical volume of saline placebo and reported no follow‐up component.
Vento 2004 did not state the method of randomisation. It is not clear whether clinicians caring for infants or those assessing outcomes were blinded to treatment group assignment. The control group did not receive a placebo. Follow‐up consisted of the following (Vento 2012 (personal communication follow‐up of Vento 2004)): A paediatric neurologist who was blinded to treatment group allocation assessed surviving children between one and four years of age, corrected for prematurity up to two years. They considered children to have a major neurosensory impairment if they had non‐ambulant cerebral palsy, blindness (bilateral vision worse than 6/60), deafness requiring hearing aids or worse, or severe cognitive delay (defined as an IQ < 55). The follow‐up rate of survivors at a mean age of 26 months was 100% (18/18).
Vincer 1998 achieved random allocation but did not describe in the abstract the method used. Trialists gave control infants equal volumes of saline placebo, which means that study authors concealed allocation. Follow‐up consisted of the following (Vincer 2002 (personal communication follow‐up of Vincer 1998): One of two neonatologists saw survivors at 24 months of age, corrected for prematurity. They referred children with a developmental abnormality to a neurologist. Observers were blind to treatment group allocation. The follow‐up rate of survivors was 100% (17/17). Study authors specified criteria for the diagnosis of cerebral palsy, but not for blindness or deafness. Psychological assessment included the MDI of the BSID. Major disability comprised any of moderate or severe cerebral palsy, bilateral blindness, deafness, or an MDI < 2 SD.
In Walther 2003, a staff pharmacist was in charge of randomisation and drug preparation. Investigators and clinical caregivers were unaware of treatment allocation. Infants in the control group received a saline placebo. Trialists used open‐label steroid therapy only if it became essential for management of ventilator dependency, ideally seven days after completion of therapy and at the discretion of the attending neonatologist. Follow‐up consisted of the following (Walther 2012 (personal communication follow‐up of Walther 2003): Trialists assessed surviving children at between one and four years of age but did not provide details about correction for prematurity and personnel involved; however, trial personnel were blinded to knowledge of treatment group allocation. They defined developmental delay as MDI < 70 on the BSID. The follow‐up rate of survivors was 78% (25/32).
Effects of interventions
See: Table 1
Results of meta‐analysis
Meta‐analysis of these 21 studies yielded the following results.
Mortality
Late steroid treatment was associated with reduced mortality at 28 days (typical risk ratio (RR) 0.49, 95% confidence interval (CI) 0.28 to 0.85; typical risk difference (RD) ‐0.06, 95% CI ‐0.10 to ‐0.01; 8 studies and 656 infants; Analysis 1.1) but had no significant effect on mortality before discharge (typical RR 0.86, 95% CI 0.66 to 1.13; typical RD ‐0.02, 95% CI ‐0.07 to 0.02; 19 studies and 1035 infants; Analysis 1.3) nor on mortality at the latest reported age (RR 0.84, 95% CI 0.66 to 1.07; RD ‐0.03, 95% CI ‐0.08 to 0.02; 19 studies and 1035 infants; Analysis 1.4). Review authors found no evidence of publication bias for mortality at the latest reported age upon examination of a funnel plot (Figure 2).
1.1. Analysis.
Comparison 1 Mortality, Outcome 1 Neonatal mortality before 28 days.
1.3. Analysis.
Comparison 1 Mortality, Outcome 3 Mortality to hospital discharge.
1.4. Analysis.
Comparison 1 Mortality, Outcome 4 Mortality at latest reported age.
2.
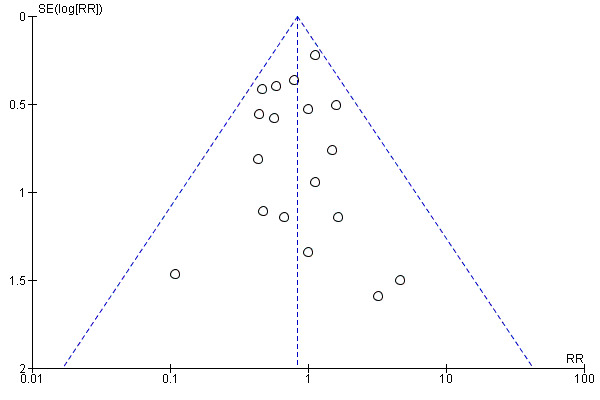
Funnel plot of comparison: 1 Mortality, outcome: 1.4 Mortality at latest reported age.
Bronchopulmonary dysplasia
The incidence of BPD was significantly decreased at 28 days of life (typical RR 0.87, 95% CI 0.81 to 0.94; typical RD ‐0.11, 95% CI ‐0.17 to ‐0.05; 6 studies and 623 infants; Analysis 2.1), at 36 weeks' postmenstrual age (typical RR 0.77, 95% CI 0.67 to 0.88; typical RD ‐0.15, 95% CI ‐0.22 to ‐0.07; 11 studies and 580 infants; Analysis 2.2), and at 36 weeks' postmenstrual age in survivors (typical RR 0.83, 95% CI 0.72 to 0.96; typical RD ‐0.13, 95% CI ‐0.22 to ‐0.03; 7 studies and 307 infants; Analysis 2.3). We noted some suggestion of publication bias upon examining a funnel plot for BPD at 36 weeks (Figure 3). Data show reduced need for late corticosteroids (typical RR 0.47, 95% CI 0.38 to 0.59; typical RD ‐0.17, 95% CI ‐0.22 to ‐0.12; 13 studies and 1096 infants; Analysis 2.4) and reduced need for home oxygen both overall (typical RR 0.71, 95% CI 0.54 to 0.94; typical RD ‐0.08, 95% CI ‐0.14 to ‐0.01; 7 studies and 611 infants; Analysis 2.5) and for survivors only (typical RR 0.69, 95% CI 0.51 to 0.94; typical RD ‐0.13, 95% CI ‐0.24 to ‐0.03; 6 studies and 277 infants; Analysis 2.6).
2.1. Analysis.
Comparison 2 Bronchopulmonary dysplasia (BPD), Outcome 1 BPD at 28 days.
2.2. Analysis.
Comparison 2 Bronchopulmonary dysplasia (BPD), Outcome 2 BPD at 36 weeks.
2.3. Analysis.
Comparison 2 Bronchopulmonary dysplasia (BPD), Outcome 3 BPD at 36 weeks in survivors.
3.
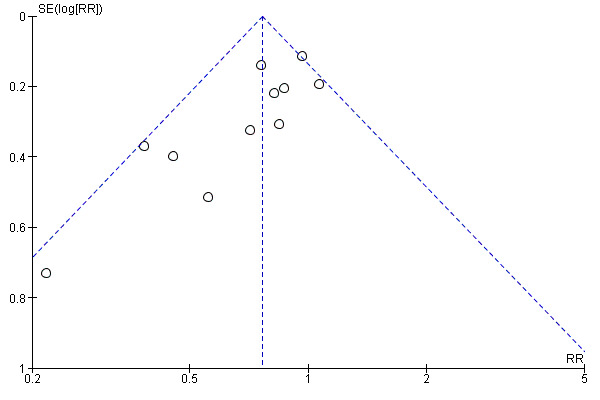
Funnel plot of comparison: 2 Bronchopulmonary dysplasia (BPD), outcome: 2.2 BPD at 36 weeks.
2.4. Analysis.
Comparison 2 Bronchopulmonary dysplasia (BPD), Outcome 4 Late rescue with corticosteroids.
2.5. Analysis.
Comparison 2 Bronchopulmonary dysplasia (BPD), Outcome 5 Home on oxygen.
2.6. Analysis.
Comparison 2 Bronchopulmonary dysplasia (BPD), Outcome 6 Survivors discharged home on oxygen.
Death or bronchopulmonary dysplasia
Mortality or BPD was decreased both at 28 days of life (typical RR 0.84, 95% CI 0.78 to 0.89; typical RD ‐0.15 to 95% CI ‐0.21 to ‐0.10; 5 studies and 563 infants; Analysis 3.1) and at 36 weeks' postmenstrual age (RR 0.77, 95% CI 0.70 to 0.86; RD ‐0.18, 95% CI ‐0.25 to ‐0.11; 11 studies and 580 infants; Analysis 3.2). We found some suggestion of publication bias upon examining a funnel plot for mortality or BPD at 36 weeks (Figure 4).
3.1. Analysis.
Comparison 3 Death or BPD, Outcome 1 Death or BPD at 28 days.
3.2. Analysis.
Comparison 3 Death or BPD, Outcome 2 Death or BPD at 36 weeks.
4.
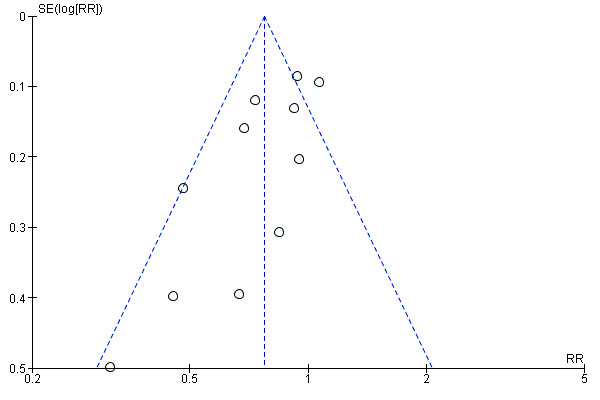
Funnel plot of comparison: 3 Death or BPD, outcome: 3.2 Death or BPD at 36 weeks.
Failure to extubate
Failure to extubate was significantly decreased at 3 days (typical RR 0.76, 95% CI 0.69 to 0.84; typical RD ‐0.22, 95% CI ‐0.29 to ‐0.10; 9 studies and 408 infants; Analysis 4.1), at 7 days (typical RR 0.65, 95% CI 0.59 to 0.72; typical RD ‐0.29, 95% CI ‐0.35 to ‐0.23; 15 studies and 761 infants; Analysis 4.2), and at 28 days (typical RR 0.57, 95% CI 0.37 to 0.89; typical RD ‐0.14, 95% CI ‐0.25 to ‐0.03; 3 studies and 236 infants; Analysis 4.4), but not at 14 days (typical RR 0.63, 95% CI 0.45 to 0.90; 4 studies and 124 infants; Analysis 4.3).
4.1. Analysis.
Comparison 4 Failure to extubate, Outcome 1 Failure to extubate by 3rd day.
4.2. Analysis.
Comparison 4 Failure to extubate, Outcome 2 Failure to extubate by 7th day.
4.4. Analysis.
Comparison 4 Failure to extubate, Outcome 4 Failure to extubate by 28th day.
4.3. Analysis.
Comparison 4 Failure to extubate, Outcome 3 Failure to extubate by 14th day.
Complications during primary hospitalisation
Metabolic complications
Data show increased risk of hyperglycaemia (typical RR 1.51, 95% CI 1.26 to 1.81; typical RD 0.10, 95% CI 0.06 to 0.15; 17 studies and 1291 infants; Analysis 5.2) and glycosuria (typical RR 8.03, 95% CI 2.43 to 26.5; typical RD 0.72, 95% CI 0.52 to 0.91; 2 studies and 48 infants; Analysis 5.3), as well as increased risk of hypertension (typical RR 2.12, 95% CI 1.45 to 3.10; typical RD 0.05, 95% CI 0.03 to 0.08; 14 studies and 1235 infants; Analysis 5.4).
5.2. Analysis.
Comparison 5 Complications during primary hospitalisation, Outcome 2 Hyperglycaemia.
5.3. Analysis.
Comparison 5 Complications during primary hospitalisation, Outcome 3 Glycosuria.
5.4. Analysis.
Comparison 5 Complications during primary hospitalisation, Outcome 4 Hypertension.
Gastrointestinal complications
No gastrointestinal complications were significantly increased: necrotising enterocolitis (typical RR 1.03, 95% CI 0.61 to 1.74; 9 studies and 1016 infants; Analysis 5.6), gastrointestinal bleeding (typical RR 1.38, 95% CI 0.99 to 1.93; 7 studies and 992 infants; Analysis 5.7), and gastrointestinal perforation (RR 1.60, 95% CI 0.28 to 9.31; 3 studies and 159 infants; Analysis 5.8).
5.6. Analysis.
Comparison 5 Complications during primary hospitalisation, Outcome 6 Necrotising enterocolitis (NEC).
5.7. Analysis.
Comparison 5 Complications during primary hospitalisation, Outcome 7 Gastrointestinal bleeding.
5.8. Analysis.
Comparison 5 Complications during primary hospitalisation, Outcome 8 Gastrointestinal perforation.
Other complications
Data show that infection rates were not significantly increased (typical RR 1.14, 95% CI 0.97 to 1.34; 18 studies and 1349 infants; Analysis 5.1). Hypertrophic cardiomyopathy was increased (typical RR 2.76, 95% CI 1.33 to 5.74; typical RD 0.13, 95% CI 0.05 to 0.20; 4 studies and 238 infants; Analysis 5.11), but reductions in pneumothorax (typical RR 0.89, 95% CI 0.53 to 1.49; 3 studies and 157 infants; Analysis 5.12) and in severe intraventricular haemorrhage (typical RR 0.44, 95% CI 0.19 to 1.02; 5 studies and 247 infants; Analysis 5.13) were not statistically significant. Severe retinopathy of prematurity was increased overall (typical RR 1.38, 95% CI 1.07 to 1.79; typical RD 0.09, 95% CI 0.02 to 0.16; 12 studies and 558 infants; Analysis 5.9) but not among survivors (typical RR 1.31, 95% CI 0.99 to 1.74; 9 studies and 416 infants; Analysis 5.10). The increase in retinopathy of prematurity did not translate into a significant increase in blindness, either overall (typical RR 0.78, 95% CI 0.35 to 1.73; 12 studies and 720 infants; Analysis 6.5) or in survivors assessed (typical RR 0.77, 95% CI 0.35 to 1.67; 12 studies and 502 infants; Analysis 6.6). One small study reported a non‐significant increase in new cranial echodensities (RR 7.00, 95% CI 0.41 to 118.7; 1 study and 18 infants) but provided no follow‐up of survivors (Analysis 5.5).
5.1. Analysis.
Comparison 5 Complications during primary hospitalisation, Outcome 1 Infection.
5.11. Analysis.
Comparison 5 Complications during primary hospitalisation, Outcome 11 Hypertrophic cardiomyopathy.
5.12. Analysis.
Comparison 5 Complications during primary hospitalisation, Outcome 12 Pneumothorax.
5.13. Analysis.
Comparison 5 Complications during primary hospitalisation, Outcome 13 Severe intraventricular haemorrhage (IVH).
5.9. Analysis.
Comparison 5 Complications during primary hospitalisation, Outcome 9 Severe retinopathy of prematurity (ROP).
5.10. Analysis.
Comparison 5 Complications during primary hospitalisation, Outcome 10 Severe ROP in survivors.
6.5. Analysis.
Comparison 6 Long‐term follow‐up, Outcome 5 Blindness.
6.6. Analysis.
Comparison 6 Long‐term follow‐up, Outcome 6 Blindness in survivors assessed.
5.5. Analysis.
Comparison 5 Complications during primary hospitalisation, Outcome 5 New cranial echodensities.
Follow‐up data
Rates of children with low cut‐off scores for the Mental Develomental Index on the Bayley Scales were not significantly reduced overall (typical RR 0.81, 95% CI 0.47 to 1.38; 7 and 333 infants; Analysis 6.1) nor among survivors assessed (typical RR 0.74, 95% CI 0.45 to 1.22; 7 studies and 232 infants; Analysis 6.2). Rates of children with low cut‐off scores for the Psychomotor Develomental Index on the Bayley Scales were not significantly reduced overall (typical RR 0.78, 95% CI 0.34 to 1.80; 1 study and 118 infants; Analysis 6.3) nor among survivors assessed (typical RR 0.67, 95% CI 0.30 to 1.50; 1 study and 90 infants; Analysis 6.4).
Blindness was not significantly reduced overall (typical RR 0.78, 95% CI 0.35 to 1.73; 13 studies and 784 infants; Analysis 6.5) nor among survivors assessed (typical RR 0.77, 95% CI 0.35 to 1.67; 13 studies and 539 infants; Analysis 6.6).
Deafness was not significantly reduced overall (typical RR 0.54, 95% CI 0.22 to 1.32; 8 studies and 565 infants; Analysis 6.7) nor among survivors assessed (typical RR 0.62, 95% CI 0.26 to 1.48; 8 studies and 362 infants; Analysis 6.8).
Cerebral palsy at the latest reported age was not significantly increased overall (typical RR 1.16, 95% CI 0.82 to 1.64; 16 studies and 919 infants; Analysis 6.9) nor among survivors assessed (typical RR 1.15, 95% CI 0.81 to 1.61; 16 studies and 628 infants; Analysis 6.12). Cerebral palsy was not significantly increased in studies limited to the first three years of life (typical RR 1.10, 95% CI 0.79 to 1.54; 15 studies and 940 infants; Analysis 6.9). The combined rate of either death or cerebral palsy at the latest reported age was not significantly decreased (typical RR 0.95, 95% CI 0.78 to 1.15; 16 studies and 919 infants; Analysis 6.11). The combined rate of death or cerebral palsy was little affected in studies limited to the first three years of life (typical RR 0.93, 95% CI 0.77 to 1.12; 15 studies and 940 infants; Analysis 6.11) and a funnel plot for the outcome death or cerebral palsy provided little evidence of publication bias (Figure 5).
6.1. Analysis.
Comparison 6 Long‐term follow‐up, Outcome 1 Bayley Mental Developmental Index (MDI) < ‐2 SD.
6.2. Analysis.
Comparison 6 Long‐term follow‐up, Outcome 2 Bayley MDI < ‐2 SD in survivors tested.
6.3. Analysis.
Comparison 6 Long‐term follow‐up, Outcome 3 Bayley Psychomotor Developmental Index (PDI) < ‐2 SD.
6.4. Analysis.
Comparison 6 Long‐term follow‐up, Outcome 4 Bayley PDI < ‐2 SD in survivors tested.
6.7. Analysis.
Comparison 6 Long‐term follow‐up, Outcome 7 Deafness.
6.8. Analysis.
Comparison 6 Long‐term follow‐up, Outcome 8 Deafness in survivors assessed.
6.9. Analysis.
Comparison 6 Long‐term follow‐up, Outcome 9 Cerebral palsy.
6.12. Analysis.
Comparison 6 Long‐term follow‐up, Outcome 12 Cerebral palsy in survivors assessed.
6.11. Analysis.
Comparison 6 Long‐term follow‐up, Outcome 11 Death or cerebral palsy.
5.
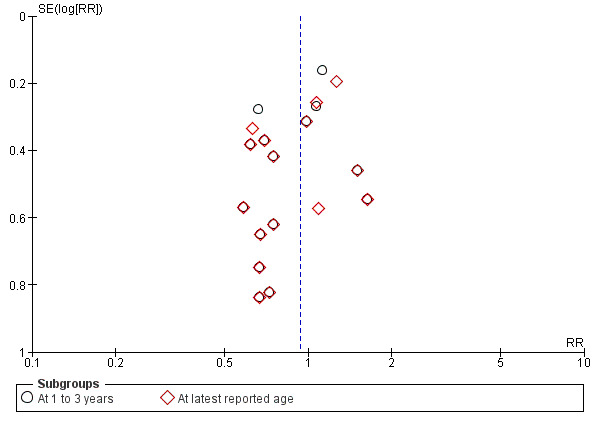
Funnel plot of comparison: 6 Long‐term follow‐up, outcome: 6.11 Death or cerebral palsy.
Major neurosensory disability was not significantly increased overall (typical RR 1.15, 95% CI 0.86 to 1.54; 9 studies and 719 infants; Analysis 6.13) nor among survivors assessed (typical RR 1.06, 95% CI 0.81 to 1.40; 9 studies and 517 infants; Analysis 6.16). The combined rate of death or major neurosensory disability was not significantly increased (typical RR 1.02, 95% CI 0.86 to 1.21; 9 studies and 719 infants; Analysis 6.15).
The rate of abnormal neurological examination overall was increased (typical RR 1.81, 95% CI 1.05 to 3.11; typical RD 0.13, 95% CI 0.02 to 0.24; 4 studies and 200 infants; Analysis 6.17), but the clinical importance of this finding is unclear in the absence of important increases in either cerebral palsy or major neurosensory disability. Rate of the combined outcome of death or abnormal neurological examination were not significantly different (typical RR 0.96, 95% CI 0.71 to 1.31; 4 studies and 200 infants; Analysis 6.19).
The only study reporting re‐hospitalisation rate over the first five years noted no significant difference (Analysis 6.21; Analysis 6.22). The same study with follow‐up of survivors to five years noted non‐significant increases in maternal reports of wheezing (RR 1.47, 95% CI 0.82 to 2.64; 1 study and 74 infants; Analysis 7.1), need for corrective lenses (RR 1.61, 95% CI 0.82 to 3.13; 1 study and 74 infants; Analysis 7.2), and need for physical therapy (RR 1.49, 95% CI 0.71 to 3.11; 1 study and 74 infants; Analysis 7.3), and a non‐significant decrease in the need for speech therapy (RR 0.46, 95% CI 0.21 to 1.02; 1 study and 74 infants; Analysis 7.4).
Data show no substantial differences between groups for other outcomes in later childhood, including IQ, respiratory health or function, blood pressure, or growth, with the exception of a significant reduction in rates of children with FEV1 < ‐2 SD (typical RR 0.58, 95% CI 0.36 to 0.94; 2 studies and 187 infants; Analysis 8.2).
6.13. Analysis.
Comparison 6 Long‐term follow‐up, Outcome 13 Major neurosensory disability (variable criteria ‐ see individual studies).
6.16. Analysis.
Comparison 6 Long‐term follow‐up, Outcome 16 Major neurosensory disability (variable criteria) in survivors assessed.
6.15. Analysis.
Comparison 6 Long‐term follow‐up, Outcome 15 Death or major neurosensory disability (variable criteria).
6.17. Analysis.
Comparison 6 Long‐term follow‐up, Outcome 17 Abnormal neurological exam (variable criteria ‐ see individual studies).
6.19. Analysis.
Comparison 6 Long‐term follow‐up, Outcome 19 Death or abnormal neurological exam (variable criteria).
6.21. Analysis.
Comparison 6 Long‐term follow‐up, Outcome 21 Rehospitalisation.
6.22. Analysis.
Comparison 6 Long‐term follow‐up, Outcome 22 Rehospitalisation in survivors seen at follow‐up.
7.1. Analysis.
Comparison 7 Later childhood outcomes, Outcome 1 Recurrent wheezing in survivors examined at 5 years.
7.2. Analysis.
Comparison 7 Later childhood outcomes, Outcome 2 Use of corrective lenses in survivors examined at 5 years.
7.3. Analysis.
Comparison 7 Later childhood outcomes, Outcome 3 Use of physical therapy in survivors examined at 5 years.
7.4. Analysis.
Comparison 7 Later childhood outcomes, Outcome 4 Use of speech therapy in survivors examined at 5 years.
8.2. Analysis.
Comparison 8 Respiratory outcomes in childhood ‐ after 5 years, Outcome 2 Forced expired volume in 1 second < ‐2 SD.
We found few outcomes with more than one study reporting results.
Results of individual trials
Ariagno 1987: Total respiratory system compliance improved in the dexamethasone group (P < 0.05). Time from initiation of treatment to first extubation was shorter for the dexamethasone group (6 vs 45 days; P = 0.0006), but time to final extubation was not significantly different (30 vs 48 days). Data show 10 deaths ‐ five in the dexamethasone group and five in the control group ‐ all occurring after the treatment period. Proportional weight gain was greater among control infants (P < 0.003) during treatment. Five dexamethasone‐treated infants had infection, as did two in the control group. Hyperglycaemia and hypertension were similar between groups. At follow‐up, trialists detected cerebral palsy in one child in the dexamethasone group at 36 months of age and in three controls at 12 months of age.
Avery 1985: Sequential analysis exceeded the criterion (P < 0.005) when seven consecutive untied pairs showed weaning with dexamethasone and failure to wean in control infants. Pulmonary compliance improved by 64% in the treated group and by 5% in the control group (P < 0.01). Results show no significant intergroup differences in mortality, length of hospital stay, sepsis, hypertension, hyperglycaemia, or electrolyte abnormalities.
Brozanski 1995: At 36 weeks' postmenstrual age, results show a significant increase in survival rates without oxygen supplementation (17/39 vs 7/39; P = 0.03) and a significant decrease in the incidence of BPD (46% vs 23%; P = 0.047) in the group that received pulse dexamethasone therapy. Supplemental oxygen requirements were also less throughout the study period in the dexamethasone group (P = 0.013). Mortality and durations of supplemental oxygen, ventilator support, and hospital stay did not differ significantly between groups. The need for insulin therapy for hyperglycaemia was increased in the dexamethasone group (P < 0.05). At follow‐up, data show no significant differences between groups in the rate of cerebral palsy among survivors assessed (20% vs 21%). The rate of death or survival among randomised children with cerebral palsy was lower in the dexamethasone group (23% vs 33%), but this difference was not statistically significant. The mean Mental Developmental Index (MDI) was 89.5 (SD 23.7) in the dexamethasone group and 80.8 (SD 26.0) in the control group ‐ a non‐significant difference.
CDTG 1991: Dexamethasone treatment significantly reduced the duration of assisted ventilation among infants who were ventilator‐dependent at entry (median days for survivors, 11 vs 17.5). Data show no statistically significant differences between total groups of survivors in time receiving supplemental oxygen and length of stay in hospital, although trends favoured the dexamethasone group. Twenty‐five infants in each group died before hospital discharge; most were ventilator‐dependent at trial entry. Open treatment with steroids was later given to 18% of the dexamethasone group and 43% of the placebo group (P < 0.001). We found little evidence of serious side effects and noted that infection rates in particular were similar in the two groups. At follow‐up, results show no clear differences between randomised groups in the original study for outcomes at three years. This conclusion held when data for cerebral palsy, blindness, and deafness were updated on the basis of results obtained at 13 to 17 years of age. Rates of intellectual impairment and moderate and severe disability at 13 to 17 years of age were similar in both groups, and data reveal no substantial differences in lung function or growth z‐scores, nor in proportions with high blood pressure.
Cummings 1989: Infants in the 42‐day dexamethasone group, but not those in the 18‐day group, were weaned from mechanical ventilation significantly faster than controls (medians 29, 73, and 84 days, respectively; P < 0.05) and from supplemental oxygen (medians 65, 190, and 136 days, respectively; P < 0.05). We noted no clinical complications of steroid administration. At follow‐up, combining both dexamethasone groups revealed no significant differences between dexamethasone‐treated and control children for rates of cerebral palsy, blindness, deafness, developmental delay, or major neurosensory disability among survivors, nor for death or survival with cerebral palsy or death or survival with major disability among those randomised. Neurological status was confirmed at four years of age for all children (Cummings 2002 (personal communication follow‐up of Cummings 1989)). Data show no significant differences in psychometric test scores at 15 months or 4 years of age. Between 4 and 15 years, one child in the 18‐day group had died, leaving 22 survivors, all of whom (100%) were assessed at 15 years of age. We found no significant differences between dexamethasone groups combined and the placebo group for any of the major neurological outcomes, nor for growth or respiratory function.
Doyle 2006: Substantially more infants were extubated successfully by 10 days in the dexamethasone group than in the control group (odds ratio (OR) 11.2, 95% confidence interval (CI) 3.2 to 39.0; P < 0.001). Twelve of 21 dexamethasone‐treated infants were reintubated after initial extubation compared with one of four placebo‐treated infants. Mortality was reduced but not significantly in the dexamethasone group (OR 0.52, 0.14 to 1.95; P = 0.33), and the same was true for BPD among survivors (OR 0.58, 0.08 to 3.32; P = 0.71). Combined rates of death or BPD (86% vs 91%; P = 0.45) and death or severe BPD (34% vs 46%; P = 0.33) were not different between groups. During the first 10 days, mean airway pressure (MAP), peak inspiratory pressure, and inspired oxygen concentration all decreased significantly in the dexamethasone group compared with the placebo group. Data show no differences between groups in rates of high blood glucose levels or high blood pressure. Open‐label use of corticosteroids, sepsis, necrotising enterocolitis, patent ductus arteriosus, and severe retinopathy of prematurity were similar for the two groups. No infant had gastrointestinal perforation or bleeding. One infant in the placebo group had cardiac hypertrophy, but none in the dexamethasone group. At follow‐up, rates of cerebral palsy, blindness, and deafness, of Bayley MDI or Psychomotor Developmental Index (PDI) < ‐1 SD, or of major neurological disability were similar in the two groups, as were combined rates of death or cerebral palsy, or death or major disability.
Durand 1995: Data show significant differences in compliance and tidal volume in the dexamethasone group compared with the control group (P < 0.001). Dexamethasone also significantly decreased inspired oxygen concentration and MAP (both P < 0.001) and facilitated successful weaning from mechanical ventilation. Bronchopulmonary dysplasia (supplemental oxygen at 36 weeks' postmenstrual age, chest radiograph changes) was significantly decreased in the dexamethasone group (2/21 vs 8/17; P < 0.01). Survival with BPD was also better in the dexamethasone group (19/23 vs 9/20; P < 0.02). Except for transient increases in blood pressure and plasma glucose, we found no evidence of adverse effects of treatment and no significant differences in rates of infection, intraventricular haemorrhage, and retinopathy of prematurity. Thirteen infants in the control group subsequently received dexamethasone.
Harkavy 1989: Dexamethasone treatment reduced age at extubation (39.4 days vs 57.2 days) compared with placebo. Average oxygen requirements for the steroid‐treated group were significantly lower during the first 10 days of treatment, but data show no significant differences between groups in age of weaning to room air (74.9 days vs 95.5 days), age at discharge (111 days vs 119 days), or number of deaths (1 (11%) vs 2 (17%)). Dexamethasone therapy was associated with a significantly increased incidence of hyperglycaemia (89% vs 8%; P = 0.01) but did not influence significantly the incidence of hypertension, intraventricular haemorrhage, infection, or retinopathy of prematurity. Steroid‐treated infants also had a significant delay in weight gain (P < 0.02) during the first three weeks of treatment. Among the small number of children followed up, cerebral palsy was diagnosed in one of three in the dexamethasone group and in two of three controls.
Kari 1993: At 28 days of life, pulmonary outcome was significantly better among girls treated with dexamethasone but not in all infants. Data show no significant differences between groups in long‐term outcomes, except for a shorter duration of supplemental oxygen among dexamethasone‐treated female infants. After one week of dexamethasone treatment, results show significant but short‐lived suppression of basal cortisol concentrations and of the adrenal response to ACTH. Investigators observe no serious side effects. At follow‐up, the only hospital providing follow‐up data reported no significant differences between dexamethasone and control children in rates of mortality, cerebral palsy, blindness, deafness, or major neurological disability, nor of death or survival with cerebral palsy or death or survival with major neurological disability among those randomised. At seven to nine years of age, data show some improvement in lung function among eight steroid‐treated children compared with seven controls, and no substantial differences in height or weight between steroid and placebo groups, but data were not reported in a form that would allow meta‐analysis. No children had hypertrophic cardiomyopathy.
Kazzi 1990: Infants who received dexamethasone required less oxygen on days eight and 17 (P < 0.005) and were more likely to be extubated eight days after therapy (8/12 vs 3/11; P < 0.05, P = 0.12 after Yates correction) compared with infants in the control group. Dexamethasone significantly shortened the duration of mechanical ventilation (median 4 vs 22 days; P < 0.05), but we found no evidence of effects on durations of oxygen therapy, hospitalisation, or home oxygen therapy, nor on the occurrence and severity of retinopathy of prematurity, rate of growth, or mortality.
Kothadia 1999: Infants treated with dexamethasone were on assisted ventilation and supplemental oxygen for fewer days after study entry (median days on ventilator: 5th and 95th centiles, 13 (1 to 64) vs 25 (6 to 104); days on oxygen: 59 (6 to 247) vs 100 (11 to 346)). Fewer infants in the dexamethasone group had failed to be extubated by the third day (82% vs 97%) or the seventh day (63% vs 90%). Data show no significant differences in rates of death, infection, or severe retinopathy of prematurity. At one‐year follow‐up, more surviving dexamethasone‐treated infants had cerebral palsy (24% vs 7%) and abnormal findings on neurological examination (42% vs 18%). However, deaths before one year were more frequent in the placebo group (26%) than in the dexamethasone group (12%); thus, rates of the combined outcome, death or cerebral palsy at one year, were not significantly different (dexamethasone 33% vs placebo 31%). An additional child in the placebo group was reported to have cerebral palsy at age four to six years. Risk of cerebral palsy was higher among surviving dexamethasone‐treated children at four to six years of age, although cognitive, functional, and medical outcomes were not significantly different between treated and non‐treated survivors. The combined outcome, death or cerebral palsy, was also similar at four‐ to six‐year follow‐up. Results show no substantial differences in rates of asthma, nor in blood pressure or growth. Fewer participants in the dexamethasone group had a low value for FEV1 at between 8 and 11 years (dexamethasone 40% vs placebo 68%).
Kovacs 1998: Mortality in hospital was not significantly different in the two groups (27% dexamethasone vs 17% controls). Steroid‐treated infants required less ventilatory support between 9 and 17 days of age, and less supplemental oxygen between 8 and 10 days of age. Fewer infants in the dexamethasone group had failed to be extubated by the seventh day (73% vs 93%). Infants in this group also had better pulmonary compliance at 10 days, but comparison with controls revealed that all improvements were not maintained over ensuing weeks. Incidences of BPD at 28 days of life and at 36 weeks' postmenstrual age among survivors were not significantly different between groups (80% vs 87% at 28 days of life; 45% vs 56% at 36 weeks' postmenstrual age). We found no evidence of steroid‐related adverse effects, other than transient glycosuria. At follow‐up, data show no significant differences between dexamethasone‐treated and control children in rates of cerebral palsy, blindness, deafness, developmental delay, or major neurosensory disability among survivors assessed, nor in death or survival with cerebral palsy or death or survival with major disability among those randomised.
Noble‐Jamieson 1989: Dexamethasone‐treated infants showed more rapid improvement in ventilation requirements during the first week of treatment, although the overall duration of oxygen therapy was similar in both groups. Cranial ultrasound examination revealed new periventricular abnormalities in three out of five dexamethasone‐treated infants with previous normal scans, compared with none of four placebo‐treated infants.
Ohlsson 1992: Dexamethasone facilitated weaning from assisted ventilation (P = 0.015). The incidence of infection was not significantly increased, although glycosuria (P = 0.0002) and systolic blood pressure (P = 0.003) were increased and heart rate (P = 0.0001) and weight gain (P = 0.0002) were decreased in the dexamethasone‐treated group. At follow‐up among survivors, cerebral palsy was diagnosed in one of 11 children in the dexamethasone group, and in three of 13 controls.
Papile 1998: As infants in the early group were given dexamethasone from 14 days, they can be considered as having been treated late by our definition (> 7 days of age). Upon examination of only 28‐day outcomes, babies in this study's late group can be considered as controls, as they did not receive dexamethasone until after 28 days. Mortality at 28 days was 7/182 in the early group (treated) compared with 16/189 in the late group (controls). Oxygen was required on day 28 in 141/182 versus 168/189, and the combination of 28‐day mortality or oxygen requirement was evident in 147/182 versus 184/189; the latter was significant (P < 0.001). It is not possible to use long‐term follow‐up data in this meta‐analysis, as all infants were eligible for dexamethasone after 28 days.
Parikh 2013: Data show no substantial differences in brain tissue volumes between groups. Low‐dose hydrocortisone had little effect on any other reported outcomes, including mortality, BPD, and acute complications. The follow‐up rate of survivors was 86% overall (37/43). Cerebral palsy was diagnosed in 15% (3/20) of survivors in the steroid group and in 6% (1/17) of those in the placebo group. Rates of cognitive and language delay, defined as < 80 on the Bayley III, were 21% versus 47% and 50% versus 59% in steroid and placebo groups, respectively. Rates of cognitive and language delay could not be pooled with others in the meta‐analysis that used earlier versions of the Bayley Scales, because tests and definitions were different. Rates of any neurodevelopmental impairment were similar between the two groups.
Romagnoli 1997: Treated infants showed an increase in dynamic respiratory compliance and a decreased incidence of BPD at 28 days of life and at 36 weeks' postmenstrual age. Fewer infants in the dexamethasone group had failed to be extubated by the seventh day (40% vs 87%). Dexamethasone‐treated infants had a lower weight gain during treatment and a significantly higher incidence of hypertrophic cardiomyopathy compared with controls. Data show no significant differences between groups regarding incidences of hypertension, sepsis, necrotising enterocolitis, or hyperglycaemia. At follow‐up, data show no significant differences between dexamethasone‐treated and control children for rates of cerebral palsy, blindness, deafness, or intellectual impairment among survivors assessed, nor for death or survival with cerebral palsy among those randomised.
Scott 1997: Cortisol responses to ACTH were lower in the dexamethasone group than in the placebo group. On day 28 of life, eight of 10 infants in the dexamethasone group no longer required assisted ventilation, compared with none of five infants in the placebo group (P = 0.04, as reported by trial authors).
Vento 2004: Six dexamethasone‐treated infants and five control infants were extubated within seven days. Data show no significant differences between groups regarding respiratory distress syndrome, patent ductus arteriosus, or severe intraventricular haemorrhage (grade 3 or 4), as well as lower absolute cell counts (P ≤ 0.05) and proportions of polymorphonuclear cells (P < 0.001) in tracheal aspirate fluid in the treated group on day seven. Treated infants also had an increase in dynamic pulmonary compliance, which was significant compared with the control group at seven days (P < 0.05). We noted no significant differences between groups regarding inspired oxygen concentration but found that infants in the dexamethasone group had significantly lower MAP on day seven (P < 0.05).
Vincer 1998: Two of 11 dexamethasone‐treated infants died before hospital discharge compared with one of nine control infants. The number of days when infants had apneic spells (14 vs 2; P = 0.005) was greater in the dexamethasone‐treated group. Fewer infants in the dexamethasone group had failed to be extubated by the third day (27% vs 100%) or the seventh day (27% vs 100%). Data show a trend towards more retinopathy of prematurity in the dexamethasone group (64% vs 22%; P = 0.064) but similarities in all other outcome variables between groups. At follow‐up among survivors, cerebral palsy was diagnosed in four of nine children in the dexamethasone group and in two of eight controls.
Walther 2003: MAP on the first day of life was higher in the control group than in the dexamethasone group (9.1 vs 7.5 cmH2O; P < 0.05). More infants in the dexamethasone group were successfully extubated within 7 to 14 days than in the placebo group (P < 0.05). Hyperglycaemia occurred more frequently in the dexamethasone group (P < 0.05), and infants in the control group more often received open‐label dexamethasone (P < 0.05). Incidences of hypertension, sepsis, necrotising enterocolitis, spontaneous gastrointestinal perforation, gastrointestinal bleeding, intraventricular haemorrhage, or periventricular leukomalacia were not significantly different between groups. Similarly, data show no significant differences in durations of ventilation or oxygen, BPD, or mortality or survival without BPD between groups. Two infants in the control group were discharged home while on oxygen.
Discussion
Among infants with bronchopulmonary dysplasia (BPD), corticosteroids improve respiratory compliance (Ariagno 1987; Avery 1985), while reducing the need for oxygen supplementation (Harkavy 1989; Kazzi 1990), but data show no evidence of effects on duration of hospitalisation. Steroids facilitate extubation in ventilator‐dependent infants from seven days up to 28 days after treatment. In this review, we found a significant reduction in neonatal mortality, with number needed to treat for additional beneficial outcomes of 17 (95% confidence interval (CI) 10 to 100). Mortality in hospital or at latest reported age was not significantly reduced. Whether corticosteroids given after the first week of life really improve survival among infants developing BPD remains to be confirmed.
Steroids have other significant effects. They can cause weight loss or poor weight gain (Ariagno 1987; Harkavy 1989; Ohlsson 1992). Although catchup growth after steroid therapy has been reported (Gibson 1993), worries about reduced brain growth have been noted in animal and human studies (Gramsbergen 1998 and Weichsel 1977; Papile 1998, respectively). Animal studies have also shown abnormal lung growth (Tschanz 1995). The finding of a borderline statistically significant increase in severe retinopathy of prematurity among survivors was not accompanied by significant increases in either blindness or the need for corrective lenses.
For this review, data on long‐term neurosensory follow‐up were available from 16 studies comprising 940 randomised infants, but these studies were of varying methodological quality. The significant increase in abnormal neurological examination among those randomised is of potential concern; however, this is tempered by data showing that cerebral palsy and major neurosensory disability, both overall and among survivors, were not significantly increased, and that abnormal neurological examination findings were reported in only four of the 15 follow‐up studies and in only 200 randomised participants. It should be noted, however, that some of the studies reporting cerebral palsy as an outcome did so early in childhood; before five years of age, the diagnosis of cerebral palsy is not certain in all cases (Stanley 1982). Moreover, only one study was designed primarily to test effects of postnatal steroids on adverse long‐term neurosensory outcomes (Doyle 2006), and all studies were underpowered to detect clinically important differences in long‐term neurosensory outcomes. Researchers performing animal studies have expressed concern about possible adverse effects of corticosteroids used at these doses during early postnatal life on neurodevelopment of very immature infants (Weichsel 1977). Clearly, more information on long‐term outcomes of infants is needed.
Clinicians must weigh the benefits of acute improvement in respiratory function and increased chances of extubation (with possible improved survival) against potential detrimental effects, both metabolic and neurological. Dexamethasone may be a harmful drug for the immature brain, and clinicians must consider limiting its use to situations in which it is essential to achieve weaning from the ventilator. Lower doses and shorter courses should be considered for these infants; the DART study (a randomised controlled trial of low‐dose, short‐course dexamethasone in ventilator‐dependent infants), which provided a total dose of only 0.89 mg/kg over 10 days, reported short‐term benefits of extubation and reduced respiratory support (Doyle 2006). We found limited data on effects of inhaled steroids among infants with BPD (Giffin 1994;La Force 1993; Shah 2017), but this potentially useful intervention should lead to fewer systemic side effects and warrants further study. Additional studies of low‐dose systemic corticosteroids for infants at high risk of developing BPD beyond the first week of life are warranted.
Quality of the evidence
Review authors assessed the quality of evidence for seven major outcomes: mortality at 36 weeks, mortality at latest reported age, BPD at 36 weeks, home on oxygen, death or BPD at 36 weeks, cerebral palsy at latest reported age, and death or cerebral palsy at latest reported age (Table 1). We assessed the quality of evidence for all outcomes as high, except BPD at 36 weeks, which we downgraded to moderate quality because we noted risk of publication bias in these studies.
Authors' conclusions
Implications for practice.
The condition of the ventilator‐dependent infant with bronchopulmonary dysplasia (BPD) after the age of seven days may be at least transiently improved by a course of dexamethasone. Such treatment facilitates extubation from the ventilator and reduces the rate of BPD and the need for a later course of steroids and for home oxygen therapy. Survival to 28 days is generally improved, but whether this is maintained overall remains to be confirmed. However, researchers have reported significant short‐term side effects, including hyperglycaemia and hypertension, and, more important, some evidence of long‐term side effects, including severe retinopathy of prematurity and abnormal neurological examination findings. The methodological quality of studies determining long‐term outcomes is limited in some cases; surviving children have been assessed predominantly before school age, and no study has been sufficiently powered to detect important adverse long‐term neurosensory outcomes. Given evidence of both benefits and harms of treatment, and limitations of the evidence at present, it appears prudent to reserve the use of late corticosteroids for infants who cannot be weaned from mechanical ventilation via an endotracheal tube after the first week of life, and to minimise the dose and duration of any course of treatment.
Implications for research.
Studies are needed to examine the lowest safe dose of corticosteroid. Two large ongoing placebo‐controlled trials of hydrocortisone in ventilator‐dependent infants beyond the first week of life may be able to establish the role of hydrocortisone, if any, in intubated infants. Both studies reported a follow‐up component during early childhood. Hydrocortisone at more physiological doses should be compared with dexamethasone at lower doses for ventilator‐dependent infants. Researchers might find it worthwhile to undertake studies with other steroid drugs, such as betamethasone or methylprednisolone. Review authors have noted a compelling need for long‐term follow‐up studies on all children who have been enrolled in randomised trials of postnatal corticosteroids. Investigators must examine both major and more subtle (e.g. cognitive and behavioural) adverse neurological outcomes, in addition to long‐term visual function. Effects of inhaled corticosteroids also require further study. New studies should be designed to assess overall risks and benefits of corticosteroids and should be sufficiently powered to detect important adverse long‐term neurosensory sequelae.
Despite increasing use of non‐invasive ventilation, infants become oxygen‐dependent and may develop BPD. Outcomes of systemic corticosteroids given to infants on long‐term non‐invasive ventilation remain to be investigated..
What's new
| Date | Event | Description |
|---|---|---|
| 10 July 2017 | New search has been performed | This review updates the existing review "Late (> 7 days) postnatal corticosteroids for chronic lung disease in preterm infants". We have added follow‐up data on early childhood from one study (Parikh 2016). The short‐term benefits and side effects of postnatal corticosteroids are confirmed. Data from long‐term neurodevelopmental follow‐up are now available for 16 studies; small, non‐significant increases in cerebral palsy or major neurosensory disability were offset by small, non‐significant reductions in mortality. Hence data show little effect of postnatal corticosteroids on the combined outcomes of death with either cerebral palsy or major neurosensory disability. |
| 10 July 2017 | New citation required but conclusions have not changed | Conclusions remain unchanged. |
History
Protocol first published: Issue 3, 1998 Review first published: Issue 3, 1998
| Date | Event | Description |
|---|---|---|
| 8 January 2014 | New citation required but conclusions have not changed | Added reference for ongoing randomised controlled trial of hydrocortisone in infants with postnatal age of 7 to 14 days |
| 6 September 2013 | New search has been performed | Updated searches 22 August 2013 |
| 7 August 2013 | New search has been performed | This review updates the existing review "Late (> 7 days) postnatal corticosteroids for chronic lung disease in preterm infants". The short‐term benefits and side effects of postnatal corticosteroids are confirmed. Data from long‐term neurodevelopmental follow‐up are now available for 15 studies; small, non‐significant increases in cerebral palsy or major neurosensory disability were offset by small, non‐significant reductions in mortality. Hence data show little effect of postnatal corticosteroids on the combined outcomes of death with either cerebral palsy or major neurosensory disability. |
| 7 October 2008 | Amended | This review combines and updates the existing reviews "Delayed (> 3 weeks) postnatal corticosteroids for chronic lung disease in preterm infants" and "Moderately early (7‐14 days) postnatal corticosteroids for preventing chronic lung disease in preterm infants", published in the Cochrane Library, Issue 3, 2003. The short‐term benefits and side effects of postnatal corticosteroids are confirmed. Data on long‐term neurodevelopmental follow‐up are now available for 12 studies; small, non‐significant increases in cerebral palsy or major neurosensory disability were offset by small, non‐significant reductions in mortality. Hence data show little effect of postnatal corticosteroids on the combined outcomes of death with either cerebral palsy or major neurosensory disability. |
| 7 October 2008 | New citation required but conclusions have not changed | Prepared substantive update |
| 1 April 2008 | Amended | Converted to new review format |
| 11 November 2002 | New search has been performed | This review updates the existing review "Delayed (> 3 weeks) postnatal corticosteroids for chronic lung disease in preterm infants", published in the Cochrane Library, Issue 2, 2001. We have included additional long‐term neurodevelopmental follow‐up data for Harkavy 1989 (unpublished data provided by investigators) and Ohlsson 1992 (data obtained from Masters of Science thesis). With the addition of these follow‐up data, the previously reported non‐significant trend associating delayed steroid treatment with increased risk of cerebral palsy is somewhat less marked. |
| 11 November 2002 | New citation required and conclusions have changed | Made substantive amendments |
Acknowledgements
Additional follow‐up data that had been provided to the authors of another systematic review (Onland 2017b) were made available to the authors of this systematic review.
Appendices
Appendix 1. Standard search methods
PubMed: ((infant, newborn[MeSH] OR newborn OR neonate OR neonatal OR premature OR low birth weight OR VLBW OR LBW or infan* or neonat*) AND (randomised controlled trial [pt] OR controlled clinical trial [pt] OR randomised [tiab] OR placebo [tiab] OR drug therapy [sh] OR randomly [tiab] OR trial [tiab] OR groups [tiab]) NOT (animals [mh] NOT humans [mh]))
Embase: (infant, newborn or newborn or neonate or neonatal or premature or very low birth weight or low birth weight or VLBW or LBW or Newborn or infan* or neonat*) AND (human not animal) AND (randomised controlled trial or controlled clinical trial or randomised or placebo or clinical trials as topic or randomly or trial or clinical trial)
CINAHL: (infant, newborn OR newborn OR neonate OR neonatal OR premature OR low birth weight OR VLBW OR LBW or Newborn or infan* or neonat*) AND (randomised controlled trial OR controlled clinical trial OR randomised OR placebo OR clinical trials as topic OR randomly OR trial OR PT clinical trial)
Cochrane Library: (infant or newborn or neonate or neonatal or premature or preterm or very low birth weight or low birth weight or VLBW or LBW)
Appendix 2. Previous search methods
For the previous version of this review, we sought randomised controlled trials of postnatal corticosteroid therapy by searching the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE (1966 through August 2013), Embase, CINAHL, Clinical Trials.gov, and Controlled‐trials; by handsearching paediatric and perinatal journals; and by examining previous review articles and information received from practising neonatologists. We searched MEDLINE using the terms adrenal cortex hormones or dexamethasone or betamethasone or hydrocortisone or steroids or corticosteroids and limits randomised controlled trials, human, all infant: birth to 23 months. When possible, we contacted authors of all studies to confirm details of reported follow‐up studies or to obtain information about long‐term follow‐up when none had been reported.
Appendix 3. Risk of bias tool
We used standard methods of Cochrane and Cochrane Neonatal to assess the methodological quality (to meet the validity criteria) of trials. For each trial, we sought information regarding the method of randomisation and blinding and reporting of all outcomes of all infants enrolled in the trial. We assessed each criterion as low, high, or unclear risk. Two review authors separately assessed each study. We resolved disagreements by discussion. We added this information to the Characteristics of included studies table. We evaluated the following issues and entered findings into the risk of bias table.
1. Sequence generation (checking for possible selection bias). Was the allocation sequence adequately generated?
For each included study, we categorised the method used to generate the allocation sequence as:
a. Low risk (any truly random process, e.g. random number table; computer random number generator);
b. High risk (any non‐random process, e.g. odd or even date of birth; hospital or clinic record number); or
c. Unclear risk.
2. Allocation concealment (checking for possible selection bias). Was allocation adequately concealed?
For each included study, we categorised the method used to conceal the allocation sequence as:
a. Low risk (e.g. telephone or central randomisation; consecutively numbered sealed opaque envelopes);
b. High risk (open random allocation; unsealed or non‐opaque envelopes, alternation; date of birth); or
c. Unclear risk.
3. Blinding of participants and personnel (checking for possible performance bias). Was knowledge of the allocated intervention adequately prevented during the study?
For each included study, we categorised the methods used to blind study participants and personnel from knowledge of which intervention a participant received. Blinding was assessed separately for different outcomes or classes of outcomes. We categorised methods as:
a. Low risk, high risk, or unclear risk for participants; or
b. Low risk, high risk, or unclear risk for personnel.
4. Blinding of outcome assessment (checking for possible detection bias). Was knowledge of the allocated intervention adequately prevented at the time of outcome assessment?
For each included study, we categorised the methods used to blind outcome assessment. Blinding was assessed separately for different outcomes or classes of outcomes. We categorised the methods as:
a. Low risk for outcome assessors;
b. High risk for outcome assessors; or
c. Unclear risk for outcome assessors.
5. Incomplete outcome data (checking for possible attrition bias through withdrawals, dropouts, protocol deviations). Were incomplete outcome data adequately addressed?
For each included study and for each outcome, we described completeness of data including attrition and exclusions from the analysis. We noted whether attrition and exclusions were reported, numbers included in the analysis at each stage (compared with total randomised participants), reasons for attrition or exclusion when reported, and whether missing data were balanced across groups or were related to outcomes. When sufficient information was reported or supplied by trial authors, we re‐included missing data in the analyses. We categorised the methods as:
a. Low risk (< 20% missing data);
b. High risk (≥ 20% missing data); or
c. Unclear risk.
6. Selective reporting bias. Are reports of the study free of the suggestion of selective outcome reporting?
For each included study, we described how we investigated the possibility of selective outcome reporting bias and what we found. We assessed the methods as:
a. Low risk (when it is clear that all of the study's prespecified outcomes and all expected outcomes of interest to the review have been reported);
b. High risk (when not all of the study's prespecified outcomes have been reported; one or more reported primary outcomes were not prespecified outcomes of interest and are reported incompletely and so cannot be used; study fails to include results of a key outcome that would have been expected to have been reported); or
c. Unclear risk.
7. Other sources of bias. Was the study apparently free of other problems that could put it at high risk of bias?
For each included study, we described any important concerns we had about other possible sources of bias (e.g. whether there was a potential source of bias related to the specific study design, whether the trial was stopped early because of some data‐dependent process). We assessed whether each study was free of other problems that could put it at risk of bias as:
a. Low risk;
b. High risk; or
c. Unclear risk.
If needed, we explored the impact of the level of bias by undertaking sensitivity analyses.
Data and analyses
Comparison 1. Mortality.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Neonatal mortality before 28 days | 8 | 656 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.49 [0.28, 0.85] |
| 2 Mortality at 36 weeks | 7 | 360 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.82 [0.50, 1.35] |
| 3 Mortality to hospital discharge | 19 | 1035 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.86 [0.66, 1.12] |
| 4 Mortality at latest reported age | 19 | 1035 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.84 [0.66, 1.07] |
1.2. Analysis.
Comparison 1 Mortality, Outcome 2 Mortality at 36 weeks.
Comparison 2. Bronchopulmonary dysplasia (BPD).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 BPD at 28 days | 6 | 623 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.87 [0.81, 0.94] |
| 2 BPD at 36 weeks | 11 | 580 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.77 [0.67, 0.88] |
| 3 BPD at 36 weeks in survivors | 7 | 307 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.83 [0.72, 0.96] |
| 4 Late rescue with corticosteroids | 13 | 1096 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.47 [0.38, 0.59] |
| 5 Home on oxygen | 7 | 611 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.71 [0.54, 0.94] |
| 6 Survivors discharged home on oxygen | 6 | 277 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.69 [0.51, 0.94] |
Comparison 3. Death or BPD.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Death or BPD at 28 days | 5 | 563 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.84 [0.78, 0.89] |
| 2 Death or BPD at 36 weeks | 11 | 580 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.77 [0.70, 0.86] |
Comparison 4. Failure to extubate.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Failure to extubate by 3rd day | 9 | 408 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.76 [0.69, 0.84] |
| 2 Failure to extubate by 7th day | 15 | 761 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.65 [0.59, 0.72] |
| 3 Failure to extubate by 14th day | 4 | 124 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.63 [0.45, 0.90] |
| 4 Failure to extubate by 28th day | 3 | 236 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.58 [0.37, 0.89] |
Comparison 5. Complications during primary hospitalisation.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Infection | 18 | 1349 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.14 [0.97, 1.34] |
| 2 Hyperglycaemia | 17 | 1291 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.51 [1.26, 1.81] |
| 3 Glycosuria | 2 | 48 | Risk Ratio (M‐H, Fixed, 95% CI) | 8.03 [2.43, 26.52] |
| 4 Hypertension | 15 | 1235 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.12 [1.45, 3.10] |
| 5 New cranial echodensities | 1 | 18 | Risk Ratio (M‐H, Fixed, 95% CI) | 7.0 [0.41, 118.69] |
| 6 Necrotising enterocolitis (NEC) | 9 | 1016 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.61, 1.74] |
| 7 Gastrointestinal bleeding | 7 | 992 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.38 [0.99, 1.93] |
| 8 Gastrointestinal perforation | 3 | 159 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.60 [0.28, 9.31] |
| 9 Severe retinopathy of prematurity (ROP) | 12 | 558 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.38 [1.07, 1.79] |
| 10 Severe ROP in survivors | 9 | 416 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.31 [0.99, 1.74] |
| 11 Hypertrophic cardiomyopathy | 4 | 238 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.76 [1.33, 5.74] |
| 12 Pneumothorax | 3 | 157 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.53, 1.49] |
| 13 Severe intraventricular haemorrhage (IVH) | 5 | 247 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.44 [0.19, 1.02] |
Comparison 6. Long‐term follow‐up.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Bayley Mental Developmental Index (MDI) < ‐2 SD | 7 | 333 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.81 [0.47, 1.38] |
| 2 Bayley MDI < ‐2 SD in survivors tested | 7 | 232 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.74 [0.45, 1.22] |
| 3 Bayley Psychomotor Developmental Index (PDI) < ‐2 SD | 1 | 118 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.78 [0.34, 1.80] |
| 4 Bayley PDI < ‐2 SD in survivors tested | 1 | 90 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.30, 1.50] |
| 5 Blindness | 13 | 784 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.78 [0.35, 1.73] |
| 6 Blindness in survivors assessed | 13 | 539 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.77 [0.35, 1.67] |
| 7 Deafness | 8 | 565 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.54 [0.22, 1.32] |
| 8 Deafness in survivors assessed | 8 | 362 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.62 [0.26, 1.48] |
| 9 Cerebral palsy | 16 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 9.1 At 1 to 3 years | 15 | 940 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.10 [0.79, 1.54] |
| 9.2 At latest reported age | 16 | 919 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.16 [0.82, 1.64] |
| 10 Death before follow‐up in trials assessing cerebral palsy | 16 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 10.1 At 1 to 3 years | 15 | 940 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.83 [0.65, 1.08] |
| 10.2 At latest reported age | 16 | 919 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.82 [0.63, 1.07] |
| 11 Death or cerebral palsy | 16 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 11.1 At 1 to 3 years | 15 | 940 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.93 [0.77, 1.12] |
| 11.2 At latest reported age | 16 | 919 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.78, 1.15] |
| 12 Cerebral palsy in survivors assessed | 16 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 12.1 At 1 to 3 years | 15 | 668 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.08 [0.77, 1.50] |
| 12.2 At latest reported age | 16 | 628 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.15 [0.81, 1.61] |
| 13 Major neurosensory disability (variable criteria ‐ see individual studies) | 9 | 719 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.15 [0.86, 1.54] |
| 14 Death before follow‐up in trials assessing major neurosensory disability (variable criteria) | 9 | 719 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.85 [0.64, 1.12] |
| 15 Death or major neurosensory disability (variable criteria) | 9 | 719 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.86, 1.21] |
| 16 Major neurosensory disability (variable criteria) in survivors assessed | 9 | 517 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.06 [0.81, 1.40] |
| 17 Abnormal neurological exam (variable criteria ‐ see individual studies) | 4 | 200 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.81 [1.05, 3.11] |
| 18 Death before follow‐up in trials assessing abnormal neurological exam (variable criteria) | 4 | 200 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.57 [0.33, 0.99] |
| 19 Death or abnormal neurological exam (variable criteria) | 4 | 200 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.96 [0.71, 1.31] |
| 20 Abnormal neurological exam (variable criteria) in survivors assessed | 4 | 145 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.62 [0.96, 2.73] |
| 21 Rehospitalisation | 1 | 118 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.15 [0.79, 1.66] |
| 22 Rehospitalisation in survivors seen at follow‐up | 1 | 92 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.72, 1.34] |
6.10. Analysis.
Comparison 6 Long‐term follow‐up, Outcome 10 Death before follow‐up in trials assessing cerebral palsy.
6.14. Analysis.
Comparison 6 Long‐term follow‐up, Outcome 14 Death before follow‐up in trials assessing major neurosensory disability (variable criteria).
6.18. Analysis.
Comparison 6 Long‐term follow‐up, Outcome 18 Death before follow‐up in trials assessing abnormal neurological exam (variable criteria).
6.20. Analysis.
Comparison 6 Long‐term follow‐up, Outcome 20 Abnormal neurological exam (variable criteria) in survivors assessed.
Comparison 7. Later childhood outcomes.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Recurrent wheezing in survivors examined at 5 years | 1 | 74 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.47 [0.82, 2.64] |
| 2 Use of corrective lenses in survivors examined at 5 years | 1 | 74 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.61 [0.82, 3.13] |
| 3 Use of physical therapy in survivors examined at 5 years | 1 | 74 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.49 [0.71, 3.11] |
| 4 Use of speech therapy in survivors examined at 5 years | 1 | 74 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.46 [0.21, 1.02] |
| 5 Intellectual impairment in survivors tested at 5 or more years | 3 | 254 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.04 [0.71, 1.52] |
| 6 IQ | 2 | 92 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.06 [‐0.37, 0.49] |
7.5. Analysis.
Comparison 7 Later childhood outcomes, Outcome 5 Intellectual impairment in survivors tested at 5 or more years.
7.6. Analysis.
Comparison 7 Later childhood outcomes, Outcome 6 IQ.
Comparison 8. Respiratory outcomes in childhood ‐ after 5 years.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Asthma in survivors assessed | 2 | 213 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.71 [0.44, 1.16] |
| 2 Forced expired volume in 1 second < ‐2 SD | 2 | 187 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.58 [0.36, 0.94] |
| 3 Forced expired volume in 1 second ‐ z‐score | 1 | 124 | Mean Difference (IV, Fixed, 95% CI) | 0.28 [‐0.14, 0.70] |
| 4 Forced expired volume in 1 second ‐ % predicted | 2 | 78 | Mean Difference (IV, Fixed, 95% CI) | 5.68 [‐1.69, 13.05] |
| 5 Forced vital capacity < ‐2 SD | 2 | 183 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.57 [0.24, 1.34] |
| 6 Forced vital capacity ‐ z‐score | 1 | 120 | Mean Difference (IV, Fixed, 95% CI) | 0.09 [‐0.31, 0.49] |
| 7 Forced vital capacity ‐ % predicted | 2 | 78 | Mean Difference (IV, Fixed, 95% CI) | 8.71 [2.38, 15.03] |
| 8 FEV1/FVC % | 1 | 63 | Mean Difference (IV, Fixed, 95% CI) | 1.0 [‐3.70, 5.70] |
| 9 FEV1/FVC < ‐2 SD | 1 | 63 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.44, 1.77] |
| 10 FEF25%‐75% ‐ % predicted | 1 | 63 | Mean Difference (IV, Fixed, 95% CI) | 7.0 [‐5.40, 19.40] |
| 11 Exercise‐induced bronchoconstriction | 1 | 56 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.87 [0.13, 5.73] |
| 12 Positive bronchodilator response | 1 | 55 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.17 [0.42, 3.23] |
8.1. Analysis.
Comparison 8 Respiratory outcomes in childhood ‐ after 5 years, Outcome 1 Asthma in survivors assessed.
8.3. Analysis.
Comparison 8 Respiratory outcomes in childhood ‐ after 5 years, Outcome 3 Forced expired volume in 1 second ‐ z‐score.
8.4. Analysis.
Comparison 8 Respiratory outcomes in childhood ‐ after 5 years, Outcome 4 Forced expired volume in 1 second ‐ % predicted.
8.5. Analysis.
Comparison 8 Respiratory outcomes in childhood ‐ after 5 years, Outcome 5 Forced vital capacity < ‐2 SD.
8.6. Analysis.
Comparison 8 Respiratory outcomes in childhood ‐ after 5 years, Outcome 6 Forced vital capacity ‐ z‐score.
8.7. Analysis.
Comparison 8 Respiratory outcomes in childhood ‐ after 5 years, Outcome 7 Forced vital capacity ‐ % predicted.
8.8. Analysis.
Comparison 8 Respiratory outcomes in childhood ‐ after 5 years, Outcome 8 FEV1/FVC %.
8.9. Analysis.
Comparison 8 Respiratory outcomes in childhood ‐ after 5 years, Outcome 9 FEV1/FVC < ‐2 SD.
8.10. Analysis.
Comparison 8 Respiratory outcomes in childhood ‐ after 5 years, Outcome 10 FEF25%‐75% ‐ % predicted.
8.11. Analysis.
Comparison 8 Respiratory outcomes in childhood ‐ after 5 years, Outcome 11 Exercise‐induced bronchoconstriction.
8.12. Analysis.
Comparison 8 Respiratory outcomes in childhood ‐ after 5 years, Outcome 12 Positive bronchodilator response.
Comparison 9. Growth in childhood.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Height ‐ z‐score | 2 | 208 | Mean Difference (IV, Fixed, 95% CI) | 0.14 [‐0.18, 0.46] |
| 2 Height < ‐2 SD | 2 | 207 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.81 [0.34, 1.94] |
| 3 Weight ‐ z‐score | 2 | 207 | Mean Difference (IV, Fixed, 95% CI) | 0.03 [‐0.35, 0.40] |
| 4 Weight < ‐2 SD | 1 | 68 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.53 [0.09, 2.95] |
| 5 Body mass index (BMI) ‐ z‐score | 2 | 205 | Mean Difference (IV, Fixed, 95% CI) | 0.02 [‐0.34, 0.38] |
| 6 BMI < ‐2 SD | 1 | 67 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.49 [0.13, 1.87] |
9.1. Analysis.
Comparison 9 Growth in childhood, Outcome 1 Height ‐ z‐score.
9.2. Analysis.
Comparison 9 Growth in childhood, Outcome 2 Height < ‐2 SD.
9.3. Analysis.
Comparison 9 Growth in childhood, Outcome 3 Weight ‐ z‐score.
9.4. Analysis.
Comparison 9 Growth in childhood, Outcome 4 Weight < ‐2 SD.
9.5. Analysis.
Comparison 9 Growth in childhood, Outcome 5 Body mass index (BMI) ‐ z‐score.
9.6. Analysis.
Comparison 9 Growth in childhood, Outcome 6 BMI < ‐2 SD.
Comparison 10. Blood pressure in childhood.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Systolic blood pressure > 95th centile | 2 | 207 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.84 [0.49, 1.45] |
| 2 Systolic blood pressure z‐score | 1 | 67 | Mean Difference (IV, Fixed, 95% CI) | 0.04 [‐0.43, 0.52] |
| 3 Diastolic blood pressure > 95th centile | 2 | 206 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.04 [0.23, 4.60] |
| 4 Diastolic blood pressure z‐score | 1 | 67 | Mean Difference (IV, Fixed, 95% CI) | 0.01 [‐0.32, 0.34] |
10.1. Analysis.
Comparison 10 Blood pressure in childhood, Outcome 1 Systolic blood pressure > 95th centile.
10.2. Analysis.
Comparison 10 Blood pressure in childhood, Outcome 2 Systolic blood pressure z‐score.
10.3. Analysis.
Comparison 10 Blood pressure in childhood, Outcome 3 Diastolic blood pressure > 95th centile.
10.4. Analysis.
Comparison 10 Blood pressure in childhood, Outcome 4 Diastolic blood pressure z‐score.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Ariagno 1987.
| Methods | Double‐blind randomised controlled trial | |
| Participants | 34 preterm infants < 1501 grams birth weight, ventilator‐dependent, no weaning from mechanical ventilation at 3 weeks. CXR changes | |
| Interventions | 2 regimens were used in this study: 10‐day or 7‐day. 10‐day: intravenous dexamethasone 1 mg/kg/d for 4 days followed by 0.5 mg/kg/d for 6 days; 7‐day: 1 mg/kg/d for 3 days followed by 0.5 mg/kg/d for 4 days. Of 17 dexamethasone‐treated infants, 4 received the 10‐day protocol, and 13 the 7‐day protocol. Saline placebos were used during respective treatment periods. | |
| Outcomes | Pulmonary function tests, failure to extubate, mortality, hyperglycaemia, hypertension, infection, GI bleeding, NEC, mortality, time to extubation, rates of weight gain and head growth, need for home oxygen, duration of oxygen, ROP, CP | |
| Notes | Results in the abstract were updated with complete data provided by investigators in September 2000. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random allocation by pharmacist |
| Allocation concealment (selection bias) | Low risk | Blinding of randomisation: yes Random allocation by pharmacist |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Blinding of intervention: yes |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Use of placebo |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Blinding of outcome assessment: yes |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Complete follow‐up: yes for outcomes measured within the first year; no for later outcomes |
| Selective reporting (reporting bias) | Unclear risk | Insufficent information |
Avery 1985.
| Methods | Randomised controlled trial | |
| Participants | 16 infants < 1501 grams birth weight, age 2 to 6 weeks, had respiratory distress syndrome but at entry radiological signs of BPD of stage 2 or 3 by Northway Classification Exclusion for PDA, congenital heart disease, pneumonia, IV lipids within 24 hours | |
| Interventions | Intravenous dexamethasone 0.5 mg/kg/d every 12 hours intravenously for 3 days, 0.3 mg/kg/d for 3 days decreased by 10% every 3 days Placebo not administered | |
| Outcomes | Pulmonary function tests, extubation within 3 days, mortality, sepsis, hypertension, hyperglycaemia, duration of hospital stay | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Random allocation by opening sealed envelopes. Stratification by birth weight and sequential analysis |
| Allocation concealment (selection bias) | Low risk | Random allocation by opening sealed envelopes. Stratification by birth weight and sequential analysis Blinding of randomisation: yes |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Blinding of intervention: uncertain |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Blinding of intervention: uncertain |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Blinding of outcome: uncertain |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Complete follow‐up: yes |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes reported |
Brozanski 1995.
| Methods | Double‐blind randomised controlled trial | |
| Participants | 78 infants < 1501 grams who were ventilator‐dependent at 7 days Exclusions: complex congenital anomalies, pulmonary hypoplasia, haemodynamic instability | |
| Interventions | Dexamethasone 0.25 mg/kg/d 12‐hourly for 2 days, repeated every 10 days until 36 weeks' PMA or until ventilator support or supplemental oxygen no longer needed. An occasional dose of study drug was administered as an intramuscular injection when intravenous access was not possible. Control infants were given an equivalent volume of saline intravenously twice daily for 3 days. | |
| Outcomes | Inspired oxygen concentration, duration of supplemental oxygen, survival without oxygen at 30 days and 34 weeks, CLD, GI bleeding, IVH, death, NEC, ROP (> stage II), hyperglycaemia, pulmonary air leak, sepsis, worsening IVH (grade > II) | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random allocation via sealed envelopes kept in the pharmacy. Stratification by sex and birth weight (< 1000 grams vs ≥ 1000 grams) |
| Allocation concealment (selection bias) | Low risk | Random allocation via sealed envelopes kept in the pharmacy. Stratification by sex and birth weight (< 1000 grams vs ≥ 1000 grams) Blinding of randomisation: yes |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Blinding of intervention: yes |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Blinding of intervention: yes |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Blinding of outcome: yes |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Complete follow‐up: no; results given for 78 out of 88 enrolled infants |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes reported |
CDTG 1991.
| Methods | Multi‐centre double‐blind randomised controlled trial | |
| Participants | 287 preterm infants from 3 weeks of age with oxygen dependency, with or without mechanical ventilation, whose condition was static or deteriorating over the preceding week Exclusion: major malformations | |
| Interventions | Dexamethasone 0.6 mg/kg/d for 1 week intravenously or orally, with an option to give a second tapering 9‐day course (0.6, 0.4, and 0.2 mg/kg/d for 3 days each) if, after initial improvement, relapse occurred. Matching saline placebo was given intravenously (or orally if no intravenous line) for 1 week. | |
| Outcomes | Durations of mechanical ventilation, death, sepsis, NEC, pneumothorax, blood pressure, plasma glucose, GI bleeding, O2, hospital stay Cerebral palsy and blindness in survivors as assessed by questionnaires from general practitioners, healthcare visitors, and parents | |
| Notes | Babies could be enrolled if breathing spontaneously. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random allocation via unmarked vials and telephone randomisation. Stratification by clinical centre and by whether or not babies were ventilator‐dependent |
| Allocation concealment (selection bias) | Low risk | Random allocation via unmarked vials and telephone randomisation. Stratification by clinical centre and by whether or not babies were ventilator‐dependent Blinding of randomisation: yes |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Blinding of intervention: yes |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Blinding of intervention: yes |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Blinding of outcome measurement: yes |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Survivors at 3 years were followed up. 14 infants died after discharge, and follow‐up information was available for 209 of the 212 infants (99% follow‐up). |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes reported |
Cummings 1989.
| Methods | Double‐blind randomised controlled trial | |
| Participants | 36 two‐week‐old infants < 1251 grams birth weight, < 31 weeks, needing mechanical ventilation and > 29% oxygen at entry Exclusions: PDA, renal failure, sepsis Infants in control group received a saline placebo. |
|
| Interventions | Dexamethasone 0.5 mg/kg/d for 3 days, 0.3 mg/kg/d for 3 days, then reduced by 10% every 3 days to 0.1 mg/kg/d for 3 days, then alternate days for 2 days or 0.5 mg/kg/d for 3 days, reduced by 50% every 3 days to 0.06 mg/kg/d for 3 days, then alternate days for 7 days | |
| Outcomes | Durations of intermittent positive‐pressure ventilation (IPPV), oxygen, and hospital stay; rates of pneumothorax, hyperglycaemia, sepsis, GI bleeding, transfusions, ROP, mortality; growth and development. | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomised allocation to 1 of 3 groups via a table of random numbers kept in the pharmacy |
| Allocation concealment (selection bias) | Low risk | Randomised allocation to 1 of 3 groups via a table of random numbers kept in the pharmacy Blinding of randomisation: yes |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Blinding of intervention: yes |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Blinding of intervention: yes |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Blinding of outcome measurement: yes |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Complete follow‐up: yes Blinding of outcome measurement: yes |
| Selective reporting (reporting bias) | Unclear risk | All prespecified outcomes reported |
Doyle 2006.
| Methods | Multi‐centre double‐blind randomised controlled trial | |
| Participants | 70 infants < 28 weeks' gestation or < 1000 grams birth weight, ventilator‐dependent after 7 days Exclusions: congenital neurological defects, chromosomal anomalies, other disorders likely to cause long‐term neurological deficits | |
| Interventions | A 10‐day tapering course of dexamethasone (0.15 mg/kg/d for 3 days, 0.10 mg/kg/d for 3 days, 0.05 mg/kg/d for 2 days, and 0.02 mg/kg/d for 2 days). Total dose of dexamethasone 0.89 mg/kg over 10 days Control infants were given equivalent volumes of normal saline placebo. A repeat course of the same blinded drug was allowed at the discretion of attending clinicians. | |
| Outcomes | Ventilator settings, oxygen requirements, hyperglycaemia, hypertension, growth, BPD (any oxygen at 36 weeks), severe BPD (> 30% oxygen at 36 weeks' PMA), mortality, infection, NEC, GI bleeding, PDA, ROP, cardiac hypertrophy, cranial ultrasound abnormalities Long‐term follow‐up at 2 years of age by staff blinded to treatment allocation for neurological impairments and disabilities, including cerebral palsy |
|
| Notes | Sample size estimate was 814, but study was stopped early because of slow recruitment. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random allocation was computer‐generated centrally, independent of investigators, except the statistician, and was stratified by centre, with randomly permuted blocks of 2 to 8 infants. |
| Allocation concealment (selection bias) | Low risk | Blinding of randomisation: yes |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Blinding of intervention: yes |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Blinding of intervention: yes |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Blinding of outcome measurement: yes |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Complete follow‐up: yes |
| Selective reporting (reporting bias) | Unclear risk | All prespecified outcomes reported |
Durand 1995.
| Methods | Randomised controlled trial | |
| Participants | 43 preterm babies 7 to 14 days old with birth weight 501 grams to 1500 grams, gestational age 24 to 32 weeks, needing mechanical ventilation with < 30% oxygen Exclusions: congenital heart disease, IVH (grade IV), multiple anomalies | |
| Interventions | Intravenous dexamethasone 0.5 mg/kg/d for 3 days, then 0.25 mg/kg/d for 3 days and 0.10 mg/kg for 1 day Control infants were not given a placebo. | |
| Outcomes | Pulmonary function tests, inspired oxygen concentration, ventilator settings, BPD (36 weeks' PMA), infection, ROP, IVH | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Blind drawing of random cards in sealed envelopes |
| Allocation concealment (selection bias) | Low risk | Yes |
| Blinding (performance bias and detection bias) All outcomes | High risk | Blinding of intervention: no |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding of intervention: no |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Blinding of outcome measurement: only for respiratory mechanics |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Complete follow‐up: almost (43 of 44 randomised) |
| Selective reporting (reporting bias) | Unclear risk | All prespecified outcomes reported |
Harkavy 1989.
| Methods | Double‐blind randomised controlled trial | |
| Participants | 21 preterm infants with ventilator and O2 dependency at 30 days | |
| Interventions | Dexamethasone 0.5 mg/kg/d every 12 hours for 2 weeks intravenously or orally Saline placebo given to controls | |
| Outcomes | Inspired oxygen concentration, duration of oxygen, mortality, hypertension, hyperglycaemia, infection, ROP | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random allocation in the pharmacy via cards of random numbers |
| Allocation concealment (selection bias) | Low risk | Allocation concealment: yes |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Blinding of intervention: yes |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Blinding of intervention: yes |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Blinding of outcome: yes |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Complete follow‐up: yes |
| Selective reporting (reporting bias) | Unclear risk | All prespecified outcomes reported |
Kari 1993.
| Methods | Multi‐centre double‐blind randomised controlled trial | |
| Participants | 41 preterm infants 10 days old, weighing < 1500 grams with gestational age > 23 weeks, and ventilator‐dependent Exclusions: PDA, sepsis, GI bleeding, major malformation |
|
| Interventions | Dexamethasone 0.5 mg/kg/d given intravenously 12‐hourly for 7 days Infants in the control group received normal saline as a placebo. | |
| Outcomes | BPD, duration of IPPV, hypertension, hyperglycaemia, sepsis, perforated colon, cryotherapy for ROP | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Random allocation: method not stated |
| Allocation concealment (selection bias) | Low risk | Allocation concealment: yes |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Blinding of intervention: yes |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Blinding of intervention: yes |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Blinding of outcome measurement: yes |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Complete follow‐up: yes |
| Selective reporting (reporting bias) | Unclear risk | All prespecified outcomes reported |
Kazzi 1990.
| Methods | Double‐blind randomised controlled trial | |
| Participants | 23 preterm infants, 3 to 4 weeks old, who weighed < 1501 grams at birth, with radiological findings of BPD and needing mechanical ventilation in > 34% oxygen; failure of medical treatment Exclusions: PDA, pneumonia, sepsis, hypertension | |
| Interventions | Dexamethasone 0.5 mg/kg/d for 3 days, 0.4 mg/kg/d for 2 days, 0.25 mg/kg/d for 2 days, given by nasogastric tube as a single daily dose, then hydrocortisone every 6 hours for 10 days Infants in the control group received equal volumes of saline. | |
| Outcomes | Inspired oxygen concentration, ventilator settings, extubation < 9 days, hyperglycaemia, sepsis, hypertension, ROP; durations of oxygen, mechanical ventilation, and hospital stay | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random allocation achieved by drawing a card prepared from random number tables in the pharmacy; stratification for birth weight (< 1000 grams, 1000 grams to 1250 grams, and 1251 grams to 1500 grams) |
| Allocation concealment (selection bias) | Low risk | Allocation concealment: yes |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Blinding of intervention: yes |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Blinding of intervention: yes |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Blinding of outcome: yes |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Complete follow‐up: yes |
| Selective reporting (reporting bias) | Unclear risk | All prespecified outcomes reported |
Kothadia 1999.
| Methods | Double‐blind randomised controlled trial | |
| Participants | 118 preterm infants, < 1501 grams, age 15 to 25 days, ventilator‐dependent over 30% oxygen; no PDA, major malformation, HIV, or hepatitis B virus infection | |
| Interventions | 42‐Day tapering course of dexamethasone or equal volume of normal saline. Dexamethasone 0.25 mg/kg 12‐hourly for 3 days, 0.15 mg/kg 12‐hourly for 3 days, then 10% reduction in dose every 3 days until dose of 0.1 mg/kg had been given for 3 days, from which time 0.1 mg/kg every other day until 42 days after entry | |
| Outcomes | Duration of ventilation, oxygen, hospital stay; death, oxygen at 36 weeks' PMA, ROP (stage 3), infection, hypertension, hyperglycaemia Follow‐up: Bayley MDI and PDI, cerebral palsy, abnormal neurological examination findings | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random allocation within 6 strata according to birth weight (500 grams to 800 grams, 801 grams to 1100 grams, and 1101 grams to 1500 grams) and sex. Method not stated |
| Allocation concealment (selection bias) | Low risk | Random allocation within 6 strata according to birth weight (500 grams to 800 grams, 801 grams to 1100 grams, and 1101 grams to 1500 grams) and sex. Method not stated Blinding of randomisation: yes |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Blinding of intervention: yes |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Blinding of intervention: yes |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Blinding of outcome: yes |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Complete follow‐up: yes for outcomes measured within first year; no for outcomes measured at 5 or more years |
| Selective reporting (reporting bias) | Unclear risk | All prespecified outcomes reported |
Kovacs 1998.
| Methods | Double‐blind randomised controlled trial | |
| Participants | 60 ventilator‐dependent infants of < 30 weeks' gestation and < 1501 grams birth weight | |
| Interventions | Dexamethasone given systemically at a dose of 0.25 mg/kg twice daily for 3 days followed by nebulised budesonide 500 µg twice daily for 18 days Control infants received systemic and inhaled saline placebos. | |
| Outcomes | Survival to discharge, ventilatory support between 9 and 17 days, supplemental oxygen between 8 and 10 days, pulmonary compliance at 10 days, elastase/albumin ratios in tracheal aspirates, need for rescue dexamethasone, time to extubation, duration of oxygen in survivors, BPD at 36 weeks' PMA in survivors, duration of hospital stay | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random allocation in pharmacy, with stratification by gestational age (22 to 26 weeks vs 27 to 29 weeks) |
| Allocation concealment (selection bias) | Low risk | Allocation concealment: yes |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Blinding of intervention: yes |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Blinding of intervention: yes |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Blinding of outcome measurement: yes |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Complete follow‐up: yes |
| Selective reporting (reporting bias) | Unclear risk | All prespecified outcomes reported |
Noble‐Jamieson 1989.
| Methods | Double‐blind randomised controlled trial | |
| Participants | 18 preterm infants over 4 weeks old and needing < 30% oxygen Exclusion for congenital anomalies, infection, gastric erosion, and NEC | |
| Interventions | Dexamethasone 0.5 mg/kg/d for 7 days orally or intravenously, 0.25 mg/kg/d for 7 days, 0.1 mg/kg/d for 7 days Saline placebo given to controls | |
| Outcomes | Inspired oxygen concentration, duration of oxygen, leucocytosis, cranial ultrasound scan | |
| Notes | Spontaneously breathing infants could be enrolled. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Random allocation: method not stated |
| Allocation concealment (selection bias) | Unclear risk | Blinding of randomisation: not clear |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Blinding of intervention: yes |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Blinding of intervention: yes |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Blinding of outcome measurement: yes |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Complete follow‐up: yes |
| Selective reporting (reporting bias) | Unclear risk | Primary outcome not clearly specified |
Ohlsson 1992.
| Methods | Double‐blind randomised controlled trial | |
| Participants | 25 preterm infants, 21 to 35 days old, weighing < 1501 grams birth weight, and needing mechanical ventilation > 29% O2. Chest radiograph consistent with BPD Exclusions: infection, congenital anomalies, PDA, NEC, GI bleeding or perforation | |
| Interventions | Dexamethasone 0.5 mg/kg twice daily for 3 days, followed by 0.25 mg/kg twice daily for 3 days and 0.125 mg/kg twice daily for 3 days intravenously Intravenous placebo was not permitted by Ethics Committee. Sham injection of saline was given into the bed in the control group by a physician not involved in respiratory care of the infant or in the study. A band aid was affixed to a possible site for intravenous infusion | |
| Outcomes | Extubation < 7 days, change in chest radiograph, blood pressure, full blood picture, perforation of stomach, severe ROP, death | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Random allocation in pharmacy via sealed envelopes |
| Allocation concealment (selection bias) | Low risk | Allocation concealment: yes |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Blinding of intervention: probably, because control group received a sham injection by staff not involved in the trial |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Blinding of intervention: probably |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Blinding of outcome: yes |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Complete follow‐up: yes |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes reported |
Papile 1998.
| Methods | Multi‐centre double‐blind randomised controlled trial | |
| Participants | 371 very low birth weight (501 grams to 1500 grams) infants who were ventilator‐dependent at 2 weeks of age and had respiratory index scores (MAP x FiO2) ≥ 2.4, which had been increasing or minimally decreasing over the previous 48 hours, or a score ≥ 4.0 even if there had been improvement in the preceding 48 hours Exclusions if received steroid treatment after birth, signs of sepsis as judged by treating physician, or major congenital anomaly of cardiovascular, pulmonary, or central nervous system | |
| Interventions | Dexamethasone 0.50 mg/kg/d intravenously or orally for 5 days, followed by 0.30 mg/kg/d for 3 days, then 0.14 mg/kg/d for 3 days, and finally 0.06 mg/kg/d for 3 days, making a total period of 2 weeks followed by placebo for 2 weeks Control group did not receive dexamethasone until after 4 weeks. From 2 to 4 weeks, they received a saline placebo. | |
| Outcomes | 28‐Day mortality, need for oxygen at 28 days, 28‐day mortality, oxygen at 28 days | |
| Notes | This was described as an early (2 weeks) vs late (4 weeks) dexamethasone study. Infants in the "early" group were considered to have received late steroid treatment according to our definition (> 7 days), whereas infants in the "late" group served as controls for 28‐day outcomes before dexamethasone treatment was started. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random allocation in each centre's pharmacy by the urn method to promote equal distribution of participants between treatment groups |
| Allocation concealment (selection bias) | Low risk | Allocation concealment: yes |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Blinding of intervention: yes |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Blinding of intervention: yes |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Blinding of outcome measurements: yes |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Complete follow‐up: yes |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes reported |
Parikh 2013.
| Methods | Double‐blind randomised controlled trial | |
| Participants | 64 infants with birth weight < 1001 grams, ventilator‐dependent between 10 and 21 days of age, with a respiratory index ≥ 2 with estimated 75% risk of developing CLD |
|
| Interventions | Hydrocortisone total of 17 mg/kg over 7 days (3 mg/kg/d for 4 days, 2 mg/kg/d for 2 days, and 1 mg/kg/d for 1 day). Identical volume saline placebo | |
| Outcomes | Main outcome was brain tissue volume on MRI at term‐equivalent age.
Other outcomes included mortality, BPD, and acute complications. Outcomes at 18 to 22 months of age, corrected for prematurity, were also reported. |
|
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Random allocation by an individual not involved in the study. Exact method of randomisation not described. Birth weight (≤ 750 grams vs 751 grams to 1000 grams) and respiratory index score (2 to 4 vs > 4) strata |
| Allocation concealment (selection bias) | Low risk | Allocation concealment: yes |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Blinding of intervention: yes |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Blinding of intervention: yes |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Blinding of outcome measurement: yes |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Complete follow‐up: yes |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes reported |
Romagnoli 1997.
| Methods | Randomised controlled trial | |
| Participants | 30 preterm infants, oxygen‐ and ventilator‐dependent on 10th day and at high risk of BPD by authors' own scoring system (90% risk) | |
| Interventions | Dexamethasone 0.50 mg/kg/d for 6 days, 0.25 mg/kg/d for 6 days, and 0.125 mg/kg/d for 3 days (total dose 4.75 mg/kg) from 10th day intravenously. Control group received no placebo. | |
| Outcomes | Failure to extubate at 28 days, BPD (28 days of life and 36 weeks' PMA), infection, hyperglycaemia, hypertension, PDA, severe IVH, NEC, received late steroids, severe ROP, left ventricular hypertrophy | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Random allocation via numbered sealed envelopes |
| Allocation concealment (selection bias) | Low risk | Alloocation concealment: yes |
| Blinding (performance bias and detection bias) All outcomes | High risk | Blinding of intervention: no |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding of intervention: no |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Blinding of outcome measurement: yes |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Complete follow‐up: yes |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes reported |
Scott 1997.
| Methods | Double‐blind randomised controlled trial | |
| Participants | 15 infants ventilator‐dependent between 11 and 14 days of age with FiO2 > 0.60 | |
| Interventions | Dexamethasone 0.5 mg/kg/d for 2 days, then 0.3 mg/kg/d for 3 days (total dose 1.9 mg/kg) Identical volume saline placebo | |
| Outcomes | Main outcomes was cortisol response to ACTH. Other outcomes included mortality and acute complications. | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random allocation via a random number table |
| Allocation concealment (selection bias) | Unclear risk | Allocation concealment: yes |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Blinding of intervention: yes |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Blinding of intervention: yes |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Blinding of outcome measurement: yes |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Complete follow‐up: yes |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes reported |
Vento 2004.
| Methods | Randomised controlled trial | |
| Participants | 20 infants < 1250 grams birth weight and < 33 weeks' gestational age who were oxygen‐dependent on 10th day of life Exclusions: not specified | |
| Interventions | Intravenous dexamethasone 0.50 mg/kg/d for 3 days, 0.25 mg/kg/d for 3 days, and 0.125 mg/kg/d for 1 day (total dose 2.375 mg/kg) Control group received no steroid treatment. | |
| Outcomes | Tracheal aspirate fluid cell counts, pulmonary mechanics, extubation during the study, PDA, IVH (> grade II) | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Random allocation: method not specified |
| Allocation concealment (selection bias) | Unclear risk | Allocation concealment: unclear |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Blinding of intervention: not clear |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Blinding of intervention: not clear |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Blinding of outcome measurements: yes |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Complete follow‐up: yes |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes reported |
Vincer 1998.
| Methods | Double‐blind randomised controlled trial | |
| Participants | 20 very low birth weight infants who were ventilator‐dependent at 28 days' postnatal age | |
| Interventions | 6‐Day course of intravenous dexamethasone 0.50 mg/kg/d for 3 days followed by 0.30 mg/kg/d for the final 3 days Equal volume of saline placebo | |
| Outcomes | Mortality, median number of days ventilated after treatment, days of apnoeic spells, length of hospital stay, weight and head circumference at 2 years, corrected MDI, retinopathy of prematurity, cerebral palsy in survivors, blindness in survivors | |
| Notes | Published as an abstract only | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Random assignment: method not stated |
| Allocation concealment (selection bias) | Low risk | Allocation concealment: yes |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Blinding of intervention: probably |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Blinding of intervention: probably |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Blinding of outcome measurements: yes |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Complete follow‐up: yes |
| Selective reporting (reporting bias) | Unclear risk | Outcomes not clearly specified |
Walther 2003.
| Methods | Double‐blind randomised controlled trial | |
| Participants | 36 infants of gestation 24 to 32 weeks and birth weight > 599 grams with respiratory distress syndrome requiring mechanical ventilation with > 29% oxygen or respiratory index (MAP x inspired oxygen) > 1.9 and ventilator rate > 16/min on days 7 to 14 after birth Exclusions: sepsis, congenital heart disease, hypertension, unstable clinical status (renal failure, grade IV IVH), multiple congenital anomalies | |
| Interventions | 14‐Day course of dexamethasone (0.20 mg/kg/d for 4 days, 0.15 mg/kg/d for 4 days, 0.10 mg/kg/d for 4 days, and 0.05 mg/kg/d for 2 days). Total dose of dexamethasone 1.9 mg/kg over 14 days Control infants received equivalent amounts of normal saline placebo | |
| Outcomes | Ventilator settings, MAP, inspired oxygen concentration, extubation within 7 to 14 days, hyperglycaemia, hypertension, serum cortisol, received late dexamethasone, BPD (oxygen at 36 weeks' PMA), survival without BPD | |
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random allocation by staff pharmacist, with investigators and clinicians unaware of treatment assignment |
| Allocation concealment (selection bias) | Low risk | Allocation concealment: yes |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Blinding of intervention: yes |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Blinding of intervention: yes |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Blinding of outcome measurements: yes |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Complete follow‐up: yes |
| Selective reporting (reporting bias) | Low risk | All prespecified outcomes reported |
BPD: bronchopulmonary dysplasia. CLD: chronic lung disease. CP: cerebral palsy. CXR: chest x‐ray. FiO2: fraction of inspired oxygen. GI: gastrointestinal. HIV: human immunodeficiency virus. IPPV: intermittent positive‐pressure ventilation. IVH: intraventricular haemorrhage. IV: intravenous. MAP: mean airway pressure. MDI: Mental Developmental Index. MRI: magnetic resonance imaging. NEC: necrotising enterocolitis. PDA: patent ductus arteriosus. PDI: Psychomotor Developmental Index. PMA: postmenstrual age. ROP: retinopathy of prematurity.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Anttila 2005 | Early neonatal dexamethasone treatment for prevention of bronchopulmonary dysplasia ‐ in "Early (< 8 days) systemic postnatal corticosteroids for preventing bronchopulmonary dysplasia in preterm infants" review (Doyle 2017) |
| Armstrong 2002 | Follow‐up study of 2 different dexamethasone regimens without an untreated control group |
| Ashton 1994 | No clinical outcomes assessed |
| Baden 1972 | Controlled trial of hydrocortisone therapy in infants with respiratory distress syndrome ‐ in "Early (< 8 days) systemic postnatal corticosteroids for preventing bronchopulmonary dysplasia in preterm infants" review (Doyle 2017) |
| Batton 2012 | Feasibility study of early blood pressure management in extremely preterm infants ‐ in "Early (< 8 days) systemic postnatal corticosteroids for preventing bronchopulmonary dysplasia in preterm infants" review (Doyle 2017) |
| Biswas 2003 | Pulmonary effects of triiodothyronine (T3) and hydrocortisone (HC) supplementation in preterm infants at less than 30 weeks' gestation ‐ in "Early (< 8 days) systemic postnatal corticosteroids for preventing bronchopulmonary dysplasia in preterm infants" review (Doyle 2017) |
| Bloomfield 1998 | 2 different courses of dexamethasone compared; no placebo control group |
| Bonsante 2007 | Randomised placebo‐controlled trial of early low‐dose hydrocortisone in very preterm infants ‐ in "Early (< 8 days) systemic postnatal corticosteroids for preventing bronchopulmonary dysplasia in preterm infants" review (Doyle 2017) |
| Couser 1992 | Dexamethasone given only to facilitate extubation; no long‐term data reported |
| Cranefield 2004 | 2 dexamethasone regimens compared without an untreated control group |
| Durand 2002 | 2 different courses of dexamethasone compared without a placebo control group |
| Efird 2005 | Randomised controlled trial of prophylactic hydrocortisone supplementation for prevention of hypotension in extremely low birth weight infants ‐ in "Early (< 8 days) systemic postnatal corticosteroids for preventing bronchopulmonary dysplasia in preterm infants" review (Doyle 2017) |
| Ferrara 1990 | Single dose of intravenous dexamethasone given before extubation; no long‐term outcome data reported |
| Garland 1999 | Randomised controlled trial of a 3‐day course of dexamethasone therapy to prevent bronchopulmonary dysplasia in ventilated neonates ‐ in "Early (< 8 days) systemic postnatal corticosteroids for preventing bronchopulmonary dysplasia in preterm infants" review (Doyle 2017) |
| Groneck 1993 | No clinical outcomes reported |
| Halac 1990 | Controlled trial of prenatal and postnatal corticosteroid therapy to prevent neonatal necrotising enterocolitis ‐ in "Early (< 8 days) systemic postnatal corticosteroids for preventing bronchopulmonary dysplasia in preterm infants" review (Doyle 2017) |
| Kopelman 1999 | Single very early dexamethasone dose improves respiratory and cardiovascular adaptation in preterm infants ‐ in "Early (< 8 days) systemic postnatal corticosteroids for preventing bronchopulmonary dysplasia in preterm infants" review (Doyle 2017) |
| Lin 1999 | Prevention of bronchopulmonary dysplasia in preterm infants by early postnatal dexamethasone therapy ‐ in "Early (< 8 days) systemic postnatal corticosteroids for preventing bronchopulmonary dysplasia in preterm infants" review (Doyle 2017) |
| Mammel 1983 | Randomised trial with a cross‐over design so that all infants were treated at some time with dexamethasone |
| Merz 1999 | Dexamethasone started at 7 or 14 days with no placebo control group |
| Mukhopadhyay 1998 | Role of early postnatal dexamethasone in respiratory distress syndrome ‐ in "Early (< 8 days) systemic postnatal corticosteroids for preventing bronchopulmonary dysplasia in preterm infants" review (Doyle 2017) |
| Ng 2006 | Double‐blind randomised controlled study of a stress dose of hydrocortisone for rescue treatment of refractory hypotension in preterm infants ‐ in "Early (< 8 days) systemic postnatal corticosteroids for preventing bronchopulmonary dysplasia in preterm infants" review (Doyle 2017) |
| Odd 2004 | 2 dexamethasone regimens compared without an untreated control group |
| Peltoniemi 2005 | Trial of early neonatal hydrocortisone administration for prevention of bronchopulmonary dysplasia in high‐risk infants ‐ in "Early (< 8 days) systemic postnatal corticosteroids for preventing bronchopulmonary dysplasia in preterm infants" review (Doyle 2017) |
| Rastogi 1996 | Randomised controlled trial of dexamethasone to prevent bronchopulmonary dysplasia in surfactant‐treated infants ‐ in "Early (< 8 days) systemic postnatal corticosteroids for preventing bronchopulmonary dysplasia in preterm infants" review (Doyle 2017) |
| Romagnoli 1999 | Controlled trial of early dexamethasone treatment for prevention of bronchopulmonary dysplasia in preterm infants ‐ in "Early (< 8 days) systemic postnatal corticosteroids for preventing bronchopulmonary dysplasia in preterm infants" review (Doyle 2017) |
| Sanders 1994 | 2 doses of early intravenous dexamethasone for prevention of bronchopulmonary dysplasia in babies with respiratory distress syndrome ‐ in "Early (< 8 days) systemic postnatal corticosteroids for preventing bronchopulmonary dysplasia in preterm infants" review |
| Shinwell 1996 | Early postnatal dexamethasone treatment to prevent bronchopulmonary dysplasia in infants with respiratory distress syndrome ‐ in "Early (< 8 days) systemic postnatal corticosteroids for preventing bronchopulmonary dysplasia in preterm infants" review (Doyle 2017) |
| Sinkin 2000 | Early dexamethasone ‐ attempting to prevent bronchopulmonary dysplasia ‐ in "Early (< 8 days) systemic postnatal corticosteroids for preventing bronchopulmonary dysplasia in preterm infants" review (Doyle 2017) |
| Soll 1999 | Early postnatal dexamethasone therapy for prevention of bronchopulmonary dysplasia ‐ in "Early (< 8 days) systemic postnatal corticosteroids for preventing bronchopulmonary dysplasia in preterm infants" review (Doyle 2017) |
| Stark 2001 | Randomised trial of early dexamethasone to prevent death or bronchopulmonary dysplasia in extremely low birth weight infants ‐ in "Early (< 8 days) systemic postnatal corticosteroids for preventing bronchopulmonary dysplasia in preterm infants" review (Doyle 2017) |
| Subhedar 1997 | Open randomised controlled trial of inhaled nitric oxide and early dexamethasone in high‐risk preterm infants ‐ in "Early (< 8 days) systemic postnatal corticosteroids for preventing bronchopulmonary dysplasia in preterm infants" review (Doyle 2017) |
| Suske 1996 | Effects of early postnatal dexamethasone therapy on ventilator dependency in surfactant‐substituted preterm infants ‐ in "Early (< 8 days) systemic postnatal corticosteroids for preventing bronchopulmonary dysplasia in preterm infants" review (Doyle 2017) |
| Tapia 1998 | Early dexamethasone administration for bronchopulmonary dysplasia in preterm infants with respiratory distress syndrome ‐ in "Early (< 8 days) systemic postnatal corticosteroids for preventing bronchopulmonary dysplasia in preterm infants" review (Doyle 2017) |
| Wang 1996 | Measurement of pulmonary status and surfactant protein levels during dexamethasone treatment for neonatal respiratory distress syndrome ‐ in "Early (< 8 days) systemic postnatal corticosteroids for preventing bronchopulmonary dysplasia in preterm infants" review (Doyle 2017) |
| Watterberg 2004 | Prophylaxis of early adrenal insufficiency to prevent bronchopulmonary dysplasia: a multi‐centre trial ‐ in "Early (< 8 days) systemic postnatal corticosteroids for preventing bronchopulmonary dysplasia in preterm infants" review (Doyle 2017) |
| Wilson 1988 | Reported only short‐term hormonal changes; no long‐term outcome data |
| Yeh 1990 | Early postnatal dexamethasone therapy in premature infants with severe respiratory distress syndrome: a double‐blind, controlled study ‐ in "Early (< 8 days) systemic postnatal corticosteroids for preventing bronchopulmonary dysplasia in preterm infants" review (Doyle 2017) |
| Yeh 1997 | Early postnatal dexamethasone therapy for prevention of bronchopulmonary dysplasia in preterm infants with respiratory distress syndrome: a multi‐centre clinical trial. ‐ in "Early (< 8 days) systemic postnatal corticosteroids for preventing bronchopulmonary dysplasia in preterm infants" review (Doyle 2017) |
| Yoder 1991 | No clinical outcomes assessed |
HC: hydrocortisone. T3: triiodothyronine.
Characteristics of ongoing studies [ordered by study ID]
NCT01353313.
| Trial name or title | A Randomised Controlled Trial of the Effect of Hydrocortisone on Survival Without Bronchopulmonary Dysplasia and on Neurodevelopmental Outcomes at 22 to 26 Months of Age in Intubated Infants < 30 Weeks' Gestation Age |
| Methods | Randomised controlled trial comparing hydrocortisone vs placebo |
| Participants | Infants < 30 weeks' gestational age intubated between 14 and 28 days after birth |
| Interventions | Hydrocortisone: 4 mg/kg/d q 6 hours x 2 days; then 2 mg/kg/d q 6 hours x 3 days; then 1 mg/kg/d q 12 hours x 3 days; then 0.5 mg/kg/d as a single dose x 2 days Equal volume saline placebo |
| Outcomes | Improvement in survival without physiologically defined moderate to severe BPD. Survival without moderate or severe neurodevelopmental impairment at 18 to 22 months' corrected age |
| Starting date | September 2011 |
| Contact information | Kristi Watterberg, New Mexico |
| Notes | https://clinicaltrials.gov/ct2/show/NCT01353313?term=watterberg+AND+hydrocortisone&rank=1 |
Onland 2011.
| Trial name or title | Systemic Hydrocortisone to Prevent Bronchopulmonary Dysplasia in Preterm Infants (the SToP‐BPD Study): A Multicenter Randomised Placebo Controlled Trial |
| Methods | SToP‐BPD trial is a randomised double‐blind placebo‐controlled multi‐centre study. This trial will determine the efficacy and safety of postnatal hydrocortisone administration at moderately early postnatal onset vs placebo for reduction of the combined outcome mortality and BPD at 36 weeks' postmenstrual age in ventilator‐dependent preterm infants. |
| Participants | 400 very low birth weight infants (gestational age < 30 weeks and/or birth weight < 1250 grams) who are ventilator‐dependent at a postnatal age of 7 to 14 days |
| Interventions | Hydrocortisone (cumulative dose 72.5 mg/kg) or placebo administered during a 22‐day tapering schedule |
| Outcomes | Primary outcome: combined outcome mortality or BPD at 36 weeks' postmenstrual age
Secondary outcomes: short‐term effects on the pulmonary condition, adverse effects during hospitalisation; long‐term neurodevelopmental sequelae assessed at 2 years' corrected gestational age Analysis will be performed on an intention‐to‐treat basis. |
| Starting date | — |
| Contact information | — |
| Notes | Trial registration number Netherlands Trial Register (NTR): NTR2768 This trial is funded by a Project Grant from the The Netherlands Organisation for Health Research and Development ZonMW Priority Medicines for Children, No. 11‐32010‐02. |
BPD: bronchopulmonary dysplasia.
Differences between protocol and review
We added methods, plans for Summary of findings tables, and GRADE recommendations, which were not included in the original protocol. For the 2017 update, we changed the title of the review to "Late (> 7 days) systemic postnatal corticosteroids for prevention of bronchopulmonary dysplasia in preterm infants".
Contributions of authors
Lex Doyle collated data on long‐term neurosensory outcomes; he assisted Henry Halliday and Richard Ehrenkranz in identifying all studies, synthesising data, and writing some of the earlier versions of this review. Richard Ehrenkranz assisted Henry Halliday in identifying all studies, synthesising data, and writing earlier versions of the review. Henry Halliday identified all studies, synthesised data, and wrote earlier versions of this review. Jeanie Cheong assisted Lex Doyle in identifying all studies through the most recent literature search, synthesising data, and writing the current version of this review.
Sources of support
Internal sources
Action Research Grant to study long‐term follow‐up, UK.
Action Research (UK) Grant to study effects of postnatal steroids, UK.
External sources
National Health and Medical Research Council, Australia.
Declarations of interest
Lex Doyle was Chief Investigator of the DART study, a randomised controlled trial of low‐dose, short‐course dexamethasone in ventilator‐dependent infants, funded by the National Health and Medical Research Council of Australia.
Henry Halliday (HLH) is a retired neonatologist. He is joint Editor‐in‐Chief of the journal Neonatology, and sits on many Data Monitoring and Trial Steering Committees for various neonatal/perinatal trials. He received support for co‐ordinating the OSECT study (2000), for which AstraZeneca (Sweden) supplied metered‐dose inhalers of budesonide and placebo. HLH also acts as a consultant for Chiesi Farmiceutici (Italy), a company that sells two neonatal drugs ‐ Curosurf (a surfactant to treat respiratory distress syndrome) and Peyona (a caffeine preparation to treat apnoea of prematurity).
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Ariagno 1987 {published data only}
- Ariagno RL. Personal communication. email 2000.
- Ariagno RL, Sweeney TE, Baldwin RB, Inguillo D, Martin D. Controlled trial of dexamethasone in preterm infants at risk for bronchopulmonary dysplasia: lung function, clinical course and outcome at three years. Unpublished manuscript supplied by authors 2000.
- Ariagno RL, Sweeney TJ, Baldwin RB, Inguillo D, Martin D. Dexamethasone effects on lung function and risks in 3 week old ventilatory dependent preterm infants. American Reviews of Respiratory Disease 1987;135:A125. [Google Scholar]
Avery 1985 {published data only}
- Avery GB, Fletcher AB, Caplan M, Brudno DS. Control trial of dexamethasone in respirator‐dependent infants with bronchopulmonary dysplasia. Pediatrics 1985;75(1):106‐11. [PUBMED: 3880879] [PubMed] [Google Scholar]
Brozanski 1995 {published data only}
- Brozanski BS, Jones JG, Gilmore CH, Balsan MJ, Vazquez RL, Israel BA, et al. Effect of pulse dexamethasone therapy on the incidence and severity of chronic lung disease in the very low birthweight infant. Journal of Pediatrics 1995;126(5 Pt 1):769‐76. [DOI: ] [DOI] [PubMed] [Google Scholar]
- Gilmour CH, Sentipal‐Walerius JM, Jones JG, Doyle JM, Brozanski BS, Balsan MJ, et al. Pulse dexamethasone does not impair growth and body composition of very low birth weight infants. Journal of the American College of Nutrition 1995;14(5):455‐62. [PUBMED: 8522724] [DOI] [PubMed] [Google Scholar]
- Hofkosh D, Brozanski BS, Edwards MD, Williams LA, Jones JG, Cheng KP. One year outcome of infants treated with pulse dexamethasone for prevention of BPD. Pediatric Research 1995;37(4):259A. [Google Scholar]
CDTG 1991 {published data only}
- Collaborative Dexamethasone Trial Group. Dexamethasone therapy in neonatal chronic lung disease: an international placebo‐controlled trial. Pediatrics 1991;88:421‐7. [PubMed] [Google Scholar]
- Jones R, Wincott E, Elbourne D, Grant A. Controlled trial of dexamethasone in neonatal chronic lung disease: a 3 year follow‐up. Pediatrics 1995;96(5 Pt 1):897‐906. [PUBMED: 7478833] [PubMed] [Google Scholar]
- Jones RA, Collaborative Dexamethasone Trial Follow‐up Group. Randomized, controlled trial of dexamethasone in neonatal chronic lung disease: 13‐ to 17‐year follow‐up study: I. Neurologic, psychological, and educational outcomes. Pediatrics 2005;116(2):370‐8. [DOI: 10.1542/peds.2004-1818; PUBMED: 16061591] [DOI] [PubMed] [Google Scholar]
- Jones RA, Collaborative Dexamethasone Trial Follow‐up Group. Randomized, controlled trial of dexamethasone in neonatal chronic lung disease: 13‐ to 17‐year follow‐up study: II. Respiratory status, growth, and blood pressure. Pediatrics 2005;116(2):379‐84. [DOI: 10.1542/peds.2004-1819; PUBMED: 16061592] [DOI] [PubMed] [Google Scholar]
Cummings 1989 {published data only}
- Cummings JJ. Personal communication. email 2002.
- Cummings JJ, D'Eugenio DB, Gross SJ. A controlled trial of dexamethasone in preterm infants at high risk for bronchopulmonary dysplasia. New England Journal of Medicine 1989;320(23):1505‐10. [DOI: 10.1056/NEJM198906083202301; PUBMED: 2657423] [DOI] [PubMed] [Google Scholar]
- Gross SJ, Anbar RD, Mettelman BB. Follow‐up at 15 years of preterm infants from a controlled trial of moderately early dexamethasone for the prevention of chronic lung disease. Pediatrics 2005;115(3):681‐7. [DOI: 10.1542/peds.2004-0956; PUBMED: 15741372] [DOI] [PubMed] [Google Scholar]
Doyle 2006 {published data only}
- Doyle LW, Davis PG, Morley CJ, McPhee A, Carlin JB, DART Study Investigators. Low‐dose dexamethasone facilitates extubation among chronically ventilator‐dependent infants: a multicenter international randomized controlled trial. Pediatrics 2006;117(1):75‐83. [DOI: 10.1542/peds.2004-2843; PUBMED: 16396863] [DOI] [PubMed] [Google Scholar]
- Doyle LW, Davis PG, Morley CJ, McPhee A, Carlin JB, DART Study Investigators. Outcome at 2 years of age of infants from the DART study: a multicenter, international, randomized, controlled trial of low‐dose dexamethasone. Pediatrics 2007;119(4):716‐21. [DOI: 10.1542/peds.2006-2806; PUBMED: 17403842] [DOI] [PubMed] [Google Scholar]
Durand 1995 {published data only}
- Durand M. Personal communication. email 2012.
- Durand M, Sardesi S, McEvoy C. Effect of early dexamethasone therapy on pulmonary mechanics and chronic lung disease in very low birth weight infants: a randomized controlled trial. Pediatrics 1995;95(4):584‐90. [PUBMED: 7700763] [PubMed] [Google Scholar]
Harkavy 1989 {published data only}
- Harkavy KL. Personal communication. email 2002.
- Harkavy KL, Scanlow JW, Chowdhry PK, Grylack LJ. Dexamethasone therapy for chronic lung disease in ventilator‐ and oxygen‐dependent infants. A controlled trial. Journal of Pediatrics 1989;115(6):979‐83. [PUBMED: 2685220] [DOI] [PubMed] [Google Scholar]
Kari 1993 {published data only}
- Kari MA, Heinonen KO, Ikonen RS, Koivisto M, Raivio KO. Dexamethasone treatment in preterm infants at risk for bronchopulmonary dysplasia. Archives of Disease of Childhood 1993;68(5 Spec No):566‐9. [PUBMED: 8323356] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kari MA, Raivio KO, Venge P, Hallman M. Dexamethasone treatment of infants at risk of chronic lung disease: surfactant components and inflammatory parameters in airway specimens. Pediatric Research 1994;36(3):387‐93. [DOI: 10.1203/00006450-199409000-00020; PUBMED: 7808837] [DOI] [PubMed] [Google Scholar]
- Mieskonen S, Eronen M, Malmberg LP, Turpeinen M, Kari MA, Hallman M. Controlled trial of dexamethasone in neonatal chronic lung disease: an 8‐year follow‐up of cardiopulmonary function and growth. Acta Paediatrica 2003;92(8):896‐904. [PUBMED: 12948063] [PubMed] [Google Scholar]
Kazzi 1990 {published data only}
- Kazzi NJ, Brans YW, Poland RL. Dexamethasone effects on the hospital course of infants with bronchopulmonary dysplasia who are dependent on artificial ventilation. Pediatrics 1990;86(5):722‐7. [PUBMED: 2235226] [PubMed] [Google Scholar]
Kothadia 1999 {published data only}
- Bensky AS, Kothadia JM, Covitz W. Cardiac effects of dexamethasone in very low birth weight infants. Pediatrics 1996;97(6 Pt 1):818‐21. [PUBMED: 8657520] [PubMed] [Google Scholar]
- Goldstein DJ, Waldrep EL, VanPelt JC, O'Shea TM. Developmental outcome at 5 years following dexamethasone use for very low birth weight infants. Pediatric Research 2000;47(4):310A. Abstract 1832. [Google Scholar]
- Kothadia JM, O'Shea TM, Roberts D, Auringer ST, Weaver RG, Dillard RG. Randomized placebo‐controlled trial of a 42‐day tapering course of dexamethasone to reduce the duration of ventilator dependency in very low birthweight infants. Pediatrics 1999;104(1 Pt 1):22‐7, Erratum in: Pediatrics 2004;114(6):1746. [PUBMED: 10390255] [DOI] [PubMed] [Google Scholar]
- Nixon PA, Washburn LK, Schechter MS, O'Shea TM. Follow‐up study of a randomized controlled trial of postnatal dexamethasone therapy in very low birth weight infants: effects on pulmonary outcomes at age 8 to 11 years. Journal of Pediatrics 2007;150(4):345‐50. [DOI: 10.1016/j.jpeds.2006.12.013; PUBMED: 17382108] [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Shea TM, Goldstein DJ, Jackson BG, Kothadia JM, Dillard RG. Randomized trial of a 42‐day tapering course of dexamethasone in very low birth weight infants: neurological, medical and functional outcome at 5 years of age. Pediatric Research 2000;47:319A. Abstract 1883. [Google Scholar]
- O'Shea TM, Kothadia JM, Klinepeter KL, Goldstein DJ, Jackson BG, Weaver RG 3rd, et al. Randomized placebo‐controlled trial of a 42‐day tapering course of dexamethasone to reduce the duration of ventilator dependency in very low birth weight infants: outcome of study participants at 1‐year adjusted age. Pediatrics 1999;104(1 Pt 1):15‐21. [PUBMED: 10390254] [DOI] [PubMed] [Google Scholar]
- Washburn LK, Nixon PA, O'Shea TM. Follow‐up of a randomized, placebo‐controlled trial of postnatal dexamethasone: blood pressure and anthropometric measurements at school age. Pediatrics 2006;118(4):1592‐9. [DOI: 10.1542/peds.2006-0973; PUBMED: 17015551] [DOI] [PubMed] [Google Scholar]
Kovacs 1998 {published data only}
- Kovacs L, Davis GM, Faucher D, Papageorgiou A. Efficacy of sequential early systemic and inhaled corticosteroid therapy in the prevention of chronic lung disease of prematurity. Acta Paediatrica 1998;87(7):792‐8. [PUBMED: 9722255] [DOI] [PubMed] [Google Scholar]
- Kovacs LB. Personal communication. email 2002.
Noble‐Jamieson 1989 {published data only}
- Noble‐Jamieson CM, Regev R, Silverman M. Dexamethasone in neonatal chronic lung disease: pulmonary effects and intracranial complications. European Journal of Pediatrics 1989;148(4):365‐7. [DOI: ] [DOI] [PubMed] [Google Scholar]
Ohlsson 1992 {published data only}
- Ohlsson A. A Randomized Controlled Trial of Dexamethasone Treatment in Very Low Birthweight Infants With Ventilator Dependent Chronic Lung Disease [Masters of Scence Thesis]. Hamilton (ON): McMaster University, 1990. [Google Scholar]
- Ohlsson A, Calvert SA, Hosking M, Shennan AT. Randomized controlled trial of dexamethasone treatment in very‐low‐birth‐weight infants with ventilator‐dependent chronic lung disease. Acta Paediatrica 1992;81(10):751‐6. [PUBMED: 1421877] [DOI] [PubMed] [Google Scholar]
Papile 1998 {published data only}
- Papile LA, Tyson JE, Stoll BJ, Wright LL, Donovan EF, Bauer CR, et al. A multicenter trial of two dexamethasone regimens in ventilator‐dependent premature infants. New England Journal of Medicine 1998;338(16):1112‐8. [DOI: 10.1056/NEJM199804163381604; PUBMED: 9545359] [DOI] [PubMed] [Google Scholar]
- Stoll BJ, Temprosa M, Tyson JE, Papile LA, Wright LL, Bauer CR, et al. Dexamethasone therapy increases infection in low birth weight infants. Pediatrics 1999;104(5):e63. [PUBMED: 10545589] [DOI] [PubMed] [Google Scholar]
Parikh 2013 {published data only}
- Parikh NA, Kennedy KA, Lasky RE, McDavid GE, Tyson JE. Pilot randomized trial of hydrocortisone in ventilator‐dependent extremely preterm infants: effects on regional brain volumes. Journal of Pediatrics 2013;162(4):685‐90. [DOI: 10.1016/j.jpeds.2012.09.054; PUBMED: 23140612] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parikh NA, Kennedy KA, Lasky RE, Tyson JE. Neurodevelopmental outcomes of extremely preterm infants randomized to stress dose hydrocortisone. PLoS One 2015;10(9):e0137051. [DOI: 10.1371/journal.pone.0137051; PUBMED: 26376074] [DOI] [PMC free article] [PubMed] [Google Scholar]
Romagnoli 1997 {published data only}
- Romagnoli C, Vento G, Zecca E, Papacci P, Carolis MP, Maggio L, et al. Dexamethasone for the prevention of chronic lung disease in preterm neonates: a prospective randomized study [II desametazone nella prevenzione della patologia polmonare cronica del neonato pretermine: studio prospettico randomizzato]. Rivista Italiana di Pediatria [Italian Journal of Pediatrics] 1997;24:283‐8. [Google Scholar]
- Romagnoli C, Zecca E, Luciano R, Torrioli G, Tortorolo G. A three year follow‐up of preterm infants after moderately early treatment with dexamethasone. Archives of Disease in Childhood. Fetal and Neonatal Edition 2002;87(1):F55‐8. [PUBMED: 12091294] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Romagnoli C, Zecca E, Vento G, Maggio L, Papacci P, Tortorolo G. Effect on growth of two different dexamethasone courses for preterm infants at risk of chronic lung disease. Pharmacology 1999;59(5):266‐74. [PUBMED: 10529659] [DOI] [PubMed] [Google Scholar]
Scott 1997 {published data only}
- Scott SM, Backstrom C, Bessman S. Effect of five days of dexamethasone therapy on ventilator dependence and adrenocorticotropic hormone‐stimulated cortisol concentrations. Journal of Perinatology 1997;17(1):24‐8. [PUBMED: 9069060] [PubMed] [Google Scholar]
Vento 2004 {published data only}
- Vento G. Personal communication. email 2012.
- Vento G, Matassa PG, Zecca E, Tortorolo L, Martelli M, Carolis MP, et al. Effect of dexamethasone on tracheobronchial aspirate fluid cytology and pulmonary mechanics in preterm infants. Pharmacology 2004;71(3):113‐9. [DOI: 10.1159/000077444; PUBMED: 15161992] [DOI] [PubMed] [Google Scholar]
Vincer 1998 {published data only}
- Vincer MJ. Personal communication. email 2002.
- Vincer MJ, Allen AC. Double blind randomized controlled trial of 6‐day pulse of dexamethasone for very low birth weight infants (VLBW < 1500 grams) who are ventilator dependent at 4 weeks of age. Pediatric Research 1998;43:201A. [Google Scholar]
Walther 2003 {published data only}
- Walther F. Personal communication. email 2012.
- Walther FJ, Findlay RD, Durand M. Adrenal suppression and extubation rate after moderately early low‐dose dexamethasone therapy in very preterm infants. Early Human Development 2003;74(1):37‐45. [PUBMED: 14512180] [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Anttila 2005 {published data only}
- Anttila E, Peltoniemi O, Haumont D, Herting E, ter Horst H, Heinonen K, et al. Early neonatal dexamethasone treatment for prevention of bronchopulmonary dysplasia. Randomised trial and meta‐analysis evaluating the duration of dexamethasone therapy. European Journal of Pediatrics 2005;164(8):472‐81. [DOI: 10.1007/s00431-005-1645-8; PUBMED: 15864643] [DOI] [PubMed] [Google Scholar]
Armstrong 2002 {published data only}
- Armstrong DL, Penrice J, Bloomfield FH, Knight DB, Dezoete JA, Harding JE. Follow up of a randomised trial of two different courses of dexamethasone for preterm babies at risk of chronic lung disease. Archives of Disease of Childhood. Fetal and Neonatal Edition 2002;86(2):F102‐7. [PUBMED: 11882552] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ashton 1994 {published data only}
- Ashton MR, Postle AD, Smith DE, Hall MA. Surfactant phosphatidylcholine composition during dexamethasone treatment in chronic lung disease. Archives of Disease of Childhood. Fetal and Neonatal Edition 1994;71(2):F114‐7. [PUBMED: 7979464] [DOI] [PMC free article] [PubMed] [Google Scholar]
Baden 1972 {published data only}
- Baden M, Bauer CR, Colle E, Klein G, Taeusch HW Jr, Stern L. A controlled trial of hydrocortisone therapy in infants with respiratory distress syndrome. Pediatrics 1972;50(4):526‐34. [PUBMED: 4561296] [PubMed] [Google Scholar]
- Fitzhardinge PM, Eisen A, Lejtenyi C, Metrakos K, Ramsay M. Sequelae of early steroid administration to the newborn infant. Pediatrics 1974;53(6):877‐83. [PUBMED: 4598934] [PubMed] [Google Scholar]
Batton 2012 {published data only}
- Batton BJ, Li L, Newman NS, Das A, Watterberg KL, Yoder BA, et al. Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network. Feasibility study of early blood pressure management in extremely preterm infants. Journal of Pediatrics 2012;161(1):65‐9.e1. [PUBMED: 22336574] [DOI] [PMC free article] [PubMed] [Google Scholar]
Biswas 2003 {published data only}
- Biswas S, Buffery J, Enoch H, Bland M, Markiewicz M, Walters D. Pulmonary effects of triiodothyronine (T3) and hydrocortisone (HC) supplementation in preterm infants less than 30 weeks' gestation: results of the THORN trial ‐ thyroid hormone replacement in neonates. Pediatric Research 2003;53(1):48‐56. [DOI: 10.1203/00006450-200301000-00011; PUBMED: 12508081] [DOI] [PubMed] [Google Scholar]
Bloomfield 1998 {published data only}
- Bloomfield FH, Knight DB, Harding JE. Side effects of 2 different dexamethasone courses for preterm infants at risk of chronic lung disease: a randomized trial. Journal of Pediatrics 1998;133(3):395‐400. [PUBMED: 9738724] [DOI] [PubMed] [Google Scholar]
Bonsante 2007 {published data only}
- Bonsante F, Latorre G, Iacobelli S, Forziati V, Laforgia N, Esposito L, et al. Early low‐dose hydrocortisone in very preterm infants: a randomized, placebo‐controlled trial. Neonatology 2007;91(4):217‐21. [DOI: 10.1159/000098168; PUBMED: 17568152] [DOI] [PubMed] [Google Scholar]
Couser 1992 {published data only}
- Couser RJ, Ferrara TB, Falde B, Johnson K, Schilling CG, Hoekstra RE. Effectiveness of dexamethasone in preventing extubation failure in preterm infants at increased risk for airway edema. Journal of Pediatrics 1992;121(4):591‐6. [PUBMED: 1403397] [DOI] [PubMed] [Google Scholar]
Cranefield 2004 {published data only}
- Cranefield DJ, Odd DE, Harding JE, Teele RL. High incidence of nephrocalcinosis in extremely preterm infants treated with dexamethasone. Pediatric Radiology 2004;34(2):1090‐7. [DOI: 10.1007/s00247-003-1090-7; PUBMED: 14624322] [DOI] [PubMed] [Google Scholar]
Durand 2002 {published data only}
- Durand M, Mendoza MW, Tantivit P, Kugelman A, McEvoy C. A randomized trial of moderately early low‐dose dexamethasone therapy in very low birth weight infants: dynamic pulmonary mechanics, oxygenation, and ventilation. Pediatrics 2002;109(2):262‐8. [PUBMED: 11826205] [DOI] [PubMed] [Google Scholar]
Efird 2005 {published data only}
- Efird MM, Heerens AT, Gordon PV, Bose CL, Young DA. A randomized‐controlled trial of prophylactic hydrocortisone supplementation for the prevention of hypotension in extremely low birth weight infants. Journal of Perinatology 2005;25(2):119‐24. [DOI: 10.1038/sj.jp.7211193; PUBMED: 15329742] [DOI] [PubMed] [Google Scholar]
Ferrara 1990 {published data only}
- Ferrara TB, Georgieff MK, Ebert TJ, Fisher JB. Routine use of dexamethasone for the prevention of post‐extubation respiratory distress. Journal of Perinatology 1989;9(3):287‐90. [PUBMED: 2809781] [PubMed] [Google Scholar]
Garland 1999 {published data only}
- Garland JS, Alex CP, Pauly TH, Whitehead VL, Brand J, Winston JF, et al. A three‐day course of dexamethasone therapy to prevent chronic lung disease in ventilated neonates: a randomized trial. Pediatrics 1999;104(1 Pt 1):91‐9. [PUBMED: 10390266] [DOI] [PubMed] [Google Scholar]
Groneck 1993 {published data only}
- Groneck P, Reuss D, Gotze‐Speer B, Speer CP. Effects of dexamethasone on chemotactic activity and inflammatory mediators in tracheobronchial aspirates of preterm infants at risk for chronic lung disease. Journal of Pediatrics 1993;122(6):938‐44. [8388949] [DOI] [PubMed] [Google Scholar]
Halac 1990 {published data only}
- Halac E, Halac J, Begue EF, Casanas JM, Indiveri DR, Petit JF, et al. Prenatal and postnatal corticosteroid therapy to prevent neonatal necrotizing enterocolitis: a controlled trial. Journal of Pediatrics 1990;117(1 Pt 1):132‐8. [PUBMED: 2196355] [DOI] [PubMed] [Google Scholar]
Kopelman 1999 {published data only}
- Kopelman AE, Moise AA, Holbert D, Hegemier SE. A single very early dexamethasone dose improves respiratory and cardiovascular adaptation in preterm infants. Journal of Pediatrics 1999;135(3):345‐50. [PUBMED: 10484801] [DOI] [PubMed] [Google Scholar]
Lin 1999 {published data only}
- Lin YJ, Yeh TF, Hsieh WS, Chi YC, Lin HC, Lin CH. Prevention of chronic lung disease in preterm infants by early postnatal dexamethasone therapy. Pediatric Pulmonology 1999;27(1):21‐6. [PUBMED: 10023787] [DOI] [PubMed] [Google Scholar]
Mammel 1983 {published data only}
- Mammel MC, Green TP, Johnson TR, Thompson TR. Controlled trial of dexamethasone therapy in infants with bronchopulmonary dysplasia. Lancet 1983;1(8338):1356‐8. [PUBMED: 6134136] [DOI] [PubMed] [Google Scholar]
Merz 1999 {published data only}
- Merz U, Peschgens T, Kusenbach G, Hörnchen H. Early versus late dexamethasone treatment in preterm infants at risk for chronic lung disease: a randomized pilot study. European Journal of Pediatrics 1999;158(4):318‐22. [PUBMED: 10206132] [DOI] [PubMed] [Google Scholar]
Mukhopadhyay 1998 {published data only}
- Mukhopadhyay K, Kumar P, Narang A. Role of early postnatal dexamethasone in respiratory distress syndrome. Indian Pediatrics 1998;35(2):117‐22. [PUBMED: 9707853] [PubMed] [Google Scholar]
Ng 2006 {published data only}
- Ng PC, Lee CH, Bnur FL, Chan IH, Lee AW, Wong E, et al. A double‐blind, randomized, controlled study of a "stress dose" of hydrocortisone for rescue treatment of refractory hypotension in preterm infants. Pediatrics 2006;117(2):367‐75. [DOI: 10.1542/peds.2005-0869; PUBMED: 16452355] [DOI] [PubMed] [Google Scholar]
Odd 2004 {published data only}
- Odd DE, Armstrong DL, Teele RL, Kuschel CA, Harding JE. A randomized trial of two dexamethasone regimens to reduce side‐effects in infants treated for chronic lung disease of prematurity. Journal of Paediatrics and Child Health 2004;40(5‐6):282‐9. [DOI: 10.1111/j.1440-1754.2004.00364.x; PUBMED: 15151582] [DOI] [PubMed] [Google Scholar]
Peltoniemi 2005 {published data only}
- Peltoniemi O, Kari MA, Heinonen K, Saarela T, Nikolajev K, Andersson S, et al. Pretreatment cortisol values may predict responses to hydrocortisone administration for the prevention of bronchopulmonary dysplasia in high‐risk infants. Journal of Pediatrics 2005;146(5):632‐7. [DOI: 10.1016/j.jpeds.2004.12.040; PUBMED: 15870666] [DOI] [PubMed] [Google Scholar]
- Peltoniemi OM, Lano A, Puosi R, Yliherva A, Bonsante F, Kari MA, et al. Neonatal Hydrocortisone Working Group. Trial of early neonatal hydrocortisone: two‐year follow‐up. Neonatology 2009;95(3):240‐7. [DOI: 10.1159/000164150; PUBMED: 18931525] [DOI] [PubMed] [Google Scholar]
Rastogi 1996 {published data only}
- Morales P, Rastogi A, Bez ML, Akintorin SM, Pyati S, Andes SM, et al. Effect of dexamethasone therapy on the neonatal ductus arteriosus. Pediatric Cardiology 1998;19(3):225‐9. [DOI: 10.1007/s002469900290; PUBMED: 9568218] [DOI] [PubMed] [Google Scholar]
- Rastogi A, Akintorin SM, Bez ML, Morales P, Pildes RS. A controlled trial of dexamethasone to prevent bronchopulmonary dysplasia in surfactant‐treated infants. Pediatrics 1996;98(2 Pt 1):204‐10. [PUBMED: 8692619] [PubMed] [Google Scholar]
Romagnoli 1999 {published data only}
- Romagnoli C, Zecca E, Luciano R, Torrioli G, Tortorolo G. Controlled trial of early dexamethasone treatment for the prevention of chronic lung disease in preterm infants: a 3‐year follow‐up. Pediatrics 2002;109(6):e85. [PUBMED: 12042579] [DOI] [PubMed] [Google Scholar]
- Romagnoli C, Zecca E, Vento G, Carolis MP, Papacci P, Tortorolo G. Early postnatal dexamethasone for the prevention of chronic lung disease in high‐risk preterm infants. Intensive Care Medicine 1999;25(7):717‐21. [PUBMED: 10470576] [DOI] [PubMed] [Google Scholar]
- Romagnoli C, Zecca E, Vento G, Maggio L, Papacci P, Tortorolo G. Effect on growth of two different dexamethasone courses for preterm infants at risk of chronic lung disease. Pharmacology 1999;59(5):266‐74. [DOI: ; PUBMED: 10529659] [DOI] [PubMed] [Google Scholar]
Sanders 1994 {published data only}
- Sanders RJ, Cox C, Phelps DL, Sinkin RA. Two doses of early intravenous dexamethasone for the prevention of bronchopulmonary dysplasia in babies with respiratory distress syndrome. Pediatric Research 1994;36(1 Pt 1):122‐8. [DOI: 10.1203/00006450-199407001-00022; PUBMED: 7936832] [DOI] [PubMed] [Google Scholar]
Shinwell 1996 {published data only}
- Shinwell ES. Early dexamethasone therapy is associated with increased incidence of cerebral palsy. Hot Topics '99 in Neonatology 1999:240‐54.
- Shinwell ES, Karplus M, Reich D, Weintraub Z, Blazer S, Bader D, et al. Early postnatal dexamethasone treatment and increased incidence of cerebral palsy. Archives of Disease in Childhood. Fetal and Neonatal Edition 2000;83(3):F177‐81. [PUBMED: 11040164] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shinwell ES, Karplus M, Zmora E, Reich D, Rothschild A, Blazer S, et al. Failure of early postnatal dexamethasone to prevent chronic lung disease in infants with respiratory distress syndrome. Archives of Disease in Childhood. Fetal and Neonatal Edition 1996;74(1):F33‐7. [PUBMED: 8653433] [DOI] [PMC free article] [PubMed] [Google Scholar]
Sinkin 2000 {published data only}
- D'Angio CT, Maniscalco WM, Ryan RM, Avissar NE, Basavegowda K, Sinkin RA. Vascular endothelial growth factor in pulmonary lavage fluid from premature infants: effects of age and postnatal dexamethasone. Biology of the Neonate 1999;76(5):266‐73. [PUBMED: 10516393] [DOI] [PubMed] [Google Scholar]
- Sinkin RA, Dweck HS, Horgan MJ, Gallaher KJ, Cox C, Maniscalco WM, et al. Early dexamethasone ‐ attempting to prevent chronic lung disease. Pediatrics 2000;105(3 Pt 1):542‐8. [PUBMED: 10699107] [DOI] [PubMed] [Google Scholar]
Soll 1999 {published data only}
- Soll RF, Vermont Oxford Network Steroid Study Group. Early postnatal dexamethasone therapy for the prevention of chronic lung disease. Pediatric Research 1999;45:226A. [DOI] [PubMed] [Google Scholar]
- Vermont Oxford Network Steroid Study Group. Early postnatal dexamethasone therapy for the prevention of chronic lung disease. Pediatrics 2001;108(3):741‐8. [PUBMED: 11533345] [DOI] [PubMed] [Google Scholar]
Stark 2001 {published data only}
- Stark AR, Carlo WA, Tyson JE, Papile LA, Wright LL, Shankaran S, et al. National Institute of Child Health and Human Development Neonatal Research Network. Adverse effects of early dexamethasone in extremely‐low‐birth‐weight infants. New England Journal of Medicine 2001;344(2):95‐101. [DOI: 10.1056/NEJM200101113440203; PUBMED: 11150359] [DOI] [PubMed] [Google Scholar]
- Stark AR, Carlo WA, Vohr BR, Papile LA, Saha S, Bauer CR, et al. Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network. Death or neurodevelopmental impairment at 18 to 22 months corrected age in a randomized trial of early dexamethasone to prevent death or chronic lung disease in extremely low birth weight infants. Journal of Pediatrics 2014; Vol. 164, issue 1:34‐39.e2. [DOI: 10.1016/j.jpeds.2013.07.027; PUBMED: 23992673] [DOI] [PMC free article] [PubMed]
Subhedar 1997 {published data only}
- Subhedar NV, Bennett AJ, Wardle SP, Shaw NJ. More trials on early treatment with corticosteroids are needed. BMJ (Clinical Research Ed.) 2000;320(7239):941. [PUBMED: 10742018] [PMC free article] [PubMed] [Google Scholar]
- Subhedar NV, Ryan SW, Shaw NJ. Open randomised controlled trial of inhaled nitric oxide and early dexamethasone in high risk preterm infants. Archives of Disease in Childhood. Fetal and Neonatal Edition 1997;77(3):F185‐90. [PUBMED: 9462187] [DOI] [PMC free article] [PubMed] [Google Scholar]
Suske 1996 {published data only}
- Suske G, Oestreich K, Varnholt V, Lasch P, Kachel W. Influence of early postnatal dexamethasone therapy on ventilator dependency in surfactant‐substituted preterm infants. Acta Paediatrica 1996;85(6):713‐8. [PUBMED: 8816210] [DOI] [PubMed] [Google Scholar]
Tapia 1998 {published data only}
- Tapia JL, Ramirez R, Cifuentes J, Fabres J, Hubner ME, Bancalari A, et al. The effect of early dexamethasone administration on bronchopulmonary dysplasia in preterm infants with respiratory distress syndrome. Journal of Pediatrics 1998;132(1):48‐52. [PUBMED: 9469999] [DOI] [PubMed] [Google Scholar]
Wang 1996 {published data only}
- Wang JY, Yeh TF, Lin YC, Miyamura K, Holmskov U, Reid KB. Measurement of pulmonary status and surfactant protein levels during dexamethasone treatment of neonatal respiratory distress syndrome. Thorax 1996;51(9):907‐13. [PUBMED: 8984701] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang JY, Yeh TF, Lin YJ, Chen WY, Lin CH. Early postnatal dexamethasone therapy may lessen lung inflammation in premature infants with respiratory distress syndrome on mechanical ventilation. Pediatrics 1997;23(3):193‐7. [PUBMED: 9094727] [DOI] [PubMed] [Google Scholar]
Watterberg 2004 {published data only}
- Watterberg KL, Gerdes JS, Cole CH, Aucott SW, Thilo EH, Mammel MC, et al. Prophylaxis of early adrenal insufficiency to prevent bronchopulmonary dysplasia: a multicenter trial. Pediatrics 2004;114(6):1649‐57. [DOI: 10.1542/peds.2004-1159; PUBMED: 15574629] [DOI] [PubMed] [Google Scholar]
- Watterberg KL, Shaffer ML, Mishefske MJ, Leach CL, Mammel MC, Couser RJ, et al. Growth and neurodevelopmental outcomes after early low‐dose hydrocortisone treatment in extremely low birth weight infants. Pediatrics 2007;120(1):40‐8. [DOI: 10.1542/peds.2006-3158; PUBMED: 17606560] [DOI] [PubMed] [Google Scholar]
Wilson 1988 {published data only}
- Wilson DM, Baldwin RB, Ariagno RL. A randomized, placebo‐controlled trial of effects of dexamethasone on hypothalamic‐pituitary‐adrenal axis in preterm infants. Journal of Pediatrics 1988;113(4):764‐8. [PUBMED: 3050006] [DOI] [PubMed] [Google Scholar]
Yeh 1990 {published data only}
- Yeh TF, Torre JA, Rastogi A, Anyebuno MA, Pildes RS. Early postnatal dexamethasone therapy in premature infants with severe respiratory distress syndrome: a double‐blind, controlled study. Journal of Pediatrics 1990;117(2 Pt 1):273‐82. [PUBMED: 2199642] [DOI] [PubMed] [Google Scholar]
Yeh 1997 {published data only}
- Lin YJ, Lin CH, Wu JM, Tsai WH, Yeh TF. The effects of early postnatal dexamethasone therapy on pulmonary outcome in premature infants with respiratory distress syndrome: a two‐year follow‐up study. Acta Paediatrica 2005;94(3):310‐6. [PUBMED: 16028649] [DOI] [PubMed] [Google Scholar]
- Lin YJ, Yeh TF, Lin HC, Wu JM, Lin CH, Yu CY. Effects of early postnatal dexamethasone therapy on calcium homeostasis and bone growth in preterm infants with respiratory distress syndrome. Acta Paediatrica 1998;87(10):1061‐5. [PUBMED: 9825973] [DOI] [PubMed] [Google Scholar]
- Peng CT, Lin HC, Lin YJ, Tsai CH, Yeh TF. Early dexamethasone therapy and blood cell count in preterm infants. Pediatrics 1999;104(3 Pt 1):476‐81. [PUBMED: 10469772] [DOI] [PubMed] [Google Scholar]
- Yeh TF, Lin IJ, Hsieh WS, Lin H, Lin C, Chen J, et al. Prevention of chronic lung disease (CLD) in premature RDS infants with early and prolonged dexamethasone (D) therapy ‐ a multicenter double‐blind controlled study. Pediatric Research 1994;35(4):262A. [Google Scholar]
- Yeh TF, Lin YJ, Hsieh WS, Lin HC, Lin CH, Chen JY, et al. Early postnatal dexamethasone therapy for the prevention of chronic lung disease in preterm infants with respiratory distress syndrome: a multicenter clinical trial. Pediatrics 1997;100(4):E3. [PUBMED: 9310536] [DOI] [PubMed] [Google Scholar]
- Yeh TF, Lin YJ, Huang CC, Chen YJ, Lin CH, Lin HC, et al. Early dexamethasone therapy in preterm infants: a follow‐up study. Pediatrics 1998;101(5):E7. [PUBMED: 9565440] [DOI] [PubMed] [Google Scholar]
- Yeh TF, Lin YJ, Lin HC, Huang CC, Hsieh WS, Lin CH, et al. Outcomes at school age after postnatal dexamethasone therapy for lung disease of prematurity. New England Journal of Medicine 2004;350(13):1304‐13. [DOI: 10.1056/NEJMoa032089; PUBMED: 15044641] [DOI] [PubMed] [Google Scholar]
Yoder 1991 {published data only}
- Yoder MC, Chua R, Tepper R. Effect of dexamethasone on pulmonary inflammation and pulmonary function in ventilator‐dependent infants with bronchopulmonary dysplasia. American Review of Respiratory Disease 1991;143(5 Pt 1):1044‐8. [DOI: 10.1164/ajrccm/143.5_Pt_1.1044; PUBMED: 2024813] [DOI] [PubMed] [Google Scholar]
References to ongoing studies
NCT01353313 {unpublished data only}
- NCT01353313. A randomized controlled trial of the effect of hydrocortisone on survival without bronchopulmonary dysplasia and on neurodevelopmental outcomes at 22 ‐ 26 months of age in intubated infants < 30 weeks' gestation age. clinicaltrials.gov/show/NCT01353313 (first received 20 April 2011).
Onland 2011 {unpublished data only}
- Onland W, Offringa M, Cools F, Jaegere AP, Rademaker K, Blom H, et al. Systemic hydrocortisone to prevent bronchopulmonary dysplasia in preterm infants (the SToP‐BPD study); a multicenter randomized placebo controlled trial. BMC Paediatrics 2011;11:102. [DOI: 10.1186/1471-2431-11-102; PUBMED: 22070744 ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Additional references
Anonymous 1991
- Anonymous. Dexamethasone for neonatal chronic lung disease. Lancet 1991;338(8773):982‐3. [PUBMED: 1681347] [PubMed] [Google Scholar]
Ariagno 2000
- Ariagno RL, Sweeney TE, Baldwin RB, Inguillo D, Martin D. Controlled trial of dexamethasone in preterm infants at risk for bronchopulmonary dysplasia: lung function, clinical course and outcome at three years. Unpublished manuscript supplied by authors 2000.
Arias‐Camison 1999
- Arias‐Camison JM, Lau J, Cole CH, Frantz ID 3rd. Meta‐analysis of dexamethasone therapy started in the first 15 days of life for prevention of chronic lung disease in premature infants. Pediatric Pulmonology 1999;28(3):167‐74. [PUBMED: 10495332] [DOI] [PubMed] [Google Scholar]
Bayley 1993
- Bayley N. Bayley Scales of Infant Development. 2nd Edition. San Antonio: The Psychological Corporation, 1993. [Google Scholar]
Bhuta 1998
- Bhuta T, Ohlsson A. Systematic review and meta‐analysis of early postnatal dexamethasone for prevention of chronic lung disease. Archives of Disease of Childhood. Fetal and Neonatal Edition 1998;79(1):F26‐3. [PUBMED: 9797621] [DOI] [PMC free article] [PubMed] [Google Scholar]
Doyle 2000
- Doyle LW, Davis PG. Postnatal corticosteroids in preterm infants: systematic review of effects on mortality and motor function. Journal of Paediatrics and Child Health 2000;36(2):101‐7. [PUBMED: 10760004] [DOI] [PubMed] [Google Scholar]
Doyle 2010a
- Doyle LW, Ehrenkranz RA, Halliday HL. Postnatal hydrocortisone for preventing or treating bronchopulmonary dysplasia in preterm infants: a systematic review. Neonatology 2010;98(2):111‐7. [DOI: 10.1159/000279992; PUBMED: 20150750] [DOI] [PubMed] [Google Scholar]
Doyle 2010b
- Doyle LW, Ehrenkranz RA, Halliday HL. Dexamethasone treatment in the first week of life for preventing bronchopulmonary dysplasia in preterm infants: a systematic review. Neonatology 2010;98(3):217‐24. [DOI: 10.1159/000286210; PUBMED: 20389126] [DOI] [PubMed] [Google Scholar]
Doyle 2010c
- Doyle LW, Ehrenkranz RA, Halliday HL. Dexamethasone treatment after the first week of life for bronchopulmonary dysplasia in preterm infants: a systematic review. Neonatology 2010;98(4):289‐96. [DOI: 10.1159/000286212; PUBMED: 20453523] [DOI] [PubMed] [Google Scholar]
Doyle 2014a
- Doyle LW, Ehrenkranz RE, Halliday HL. Early (< 8 days) postnatal corticosteroids for preventing chronic lung disease in preterm infants. Cochrane Database of Systematic Reviews 2014, Issue 5. [DOI: 10.1002/14651858.CD001146.pub4] [DOI] [PubMed] [Google Scholar]
Doyle 2017
- Doyle LW, Ehrenkranz RE, Halliday HL. Early (< 8 days) systemic postnatal corticosteroids for prevention of bronchopulmonary dysplasia in preterm infants. Cochrane Database of Systematic Reviews 2017, Issue 10. [DOI: 10.1002/14651858.CD001146.pub5] [DOI] [PMC free article] [PubMed] [Google Scholar]
Egberts 1997
- Egberts J, Brand R, Walti H, Bevilacqua G, Breart G, Gardini F. Mortality, severe respiratory distress syndrome and chronic lung disease of the newborn are reduced more after prophylactic than after therapeutic administration of the surfactant Curosurf. Pediatrics 1997;100(1):E4. [PUBMED: 9200378] [DOI] [PubMed] [Google Scholar]
Flagel 2002
- Flagel SB, Vazquez DM, Watson SJ Jr, Neal CR. Effects of tapering neonatal dexamethasone on rat growth, neurodevelopment, and stress response. American Journal of Regulatory Integrative Comparative Physiology 2002;282(1):R55‐66. [PUBMED: 11742823] [DOI] [PubMed] [Google Scholar]
Gibson 1993
- Gibson AT, Pearse RG, Wales JKH. Growth retardation after dexamethasone administration: assessment by knemometry. Archives of Disease of Childhood 1993;69(5 Spec No):505‐9. [PUBMED: 8285754] [DOI] [PMC free article] [PubMed] [Google Scholar]
Giffin 1994
- Giffin F, Greenough A. A pilot study assessing inhaled budesonide in chronically oxygen‐dependent infants. Acta Paediatrica 1994;83(6):669‐71. [PUBMED: 7919769] [DOI] [PubMed] [Google Scholar]
GRADEpro GDT [Computer program]
- GRADE Working Group, McMaster University. GRADEpro GDT. Version accessed 21 February 2017. Hamilton (ON): GRADE Working Group, McMaster University, 2014. Available from gradepro.org.
Gramsbergen 1998
- Gramsbergen A, Mulder EJH. The influence of betamethasone and dexamethasone on motor development in young rats. Pediatric Research 1998;44(1):105‐10. [DOI: 10.1203/00006450-199807000-00017; PUBMED: 9667379] [DOI] [PubMed] [Google Scholar]
Gross 2005
- Gross SJ, Anbar RD, Mettelman BB. Follow‐up at 15 years of preterm infants from a controlled trial of moderately early dexamethasone for the prevention of chronic lung disease. Pediatrics 2005;115(3):681‐7. [DOI: 10.1542/peds.2004-0956; PUBMED: 15741372] [DOI] [PubMed] [Google Scholar]
Halliday 1997
- Halliday HL. A review of postnatal corticosteroids for treatment and prevention of chronic lung disease in the preterm infant. Prenatal and Neonatal Medicine 1997;2:1‐12. [Google Scholar]
Halliday 1999
- Halliday HL. Clinical trials of postnatal corticosteroids: inhaled and systemic. Biology of the Neonate 1999;76(Suppl 1):29‐40. [DOI: ; PUBMED: 10393391] [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JP, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Hofkosh 1995
- Hofkosh D, Brozanski BS, Edwards MD, Williams LA, Jones JG, Cheng KP. One year outcome of infants treated with pulse dexamethasone for prevention of BPD. Pediatric Research 1995;37(4):259A. [Google Scholar]
Jones 1995
- Jones R, Wincott E, Elbourne D, Grant A. Controlled trial of dexamethasone in neonatal chronic lung disease: a 3 year follow‐up. Pediatrics 1995;96(5 Pt 1):897‐906. [PUBMED: 7478833] [PubMed] [Google Scholar]
Jones 2005a
- Jones RA, Collaborative Dexamethasone Trial Follow‐up Group. Randomized, controlled trial of dexamethasone in neonatal chronic lung disease: 13‐ to 17‐year follow‐up study: I. Neurologic, psychological, and educational outcomes. Pediatrics 2005;116(2):370‐8. [PUBMED: 16061591] [DOI] [PubMed] [Google Scholar]
Jones 2005b
- Jones RA, Collaborative Dexamethasone Trial Follow‐up Group. Randomized, controlled trial of dexamethasone in neonatal chronic lung disease: 13‐ to 17‐year follow‐up study: II. Respiratory status, growth, and blood pressure. Pediatrics 2005;116(2):379‐84. [PUBMED: 16061592] [DOI] [PubMed] [Google Scholar]
La Force 1993
- Force WR, Budno DS. Controlled trial of beclomethasone dipropionate by rehydration in oxygen‐ and ventilator‐dependent infants. Journal of Pediatrics 1993;122(2):285‐8. [PUBMED: 8429447] [DOI] [PubMed] [Google Scholar]
Mieskonen 2003
- Mieskonen S, Eronen M, Malmberg LP, Turpeinen M, Kari MA, Hallman M. Controlled trial of dexamethasone in neonatal chronic lung disease: an 8‐year follow‐up of cardiopulmonary function and growth. Acta Paediatrica 2003;92(8):896‐904. [PUBMED: 12948063] [PubMed] [Google Scholar]
Ng 1993
- Ng PC. The effectiveness and side effects of dexamethasone in preterm infants with bronchopulmonary dysplasia. Archives of Disease of Childhood 1993;68(3 Spec No):330‐6. [PUBMED: 8466274] [DOI] [PMC free article] [PubMed] [Google Scholar]
Nixon 2007
- Nixon PA, Washburn LK, Schechter MS, O'Shea TM. Follow‐up study of a randomized controlled trial of postnatal dexamethasone therapy in very low birth weight infants: effects on pulmonary outcomes at age 8 to 11 years. Journal of Pediatrics 2007;150(4):345‐50. [DOI: 10.1016/j.jpeds.2006.12.013; PUBMED: 17382108] [DOI] [PMC free article] [PubMed] [Google Scholar]
Northway 1967
- Northway WH Jr, Rosan RC, Porter DY. Pulmonary disease following respirator therapy of hyaline‐membrane disease. Bronchopulmonary dysplasia. New England Journal of Medicine 1967;276(7):357‐68. [DOI: 10.1056/NEJM196702162760701; PUBMED: 5334613] [DOI] [PubMed] [Google Scholar]
Onland 2017a
- Onland W, Offringa M, Kaam A. Late (≥ 7 days) inhalation corticosteroids to reduce bronchopulmonary dysplasia in preterm infants. Cochrane Database of Systematic Reviews 2017, Issue 8. [DOI: 10.1002/14651858.CD002311.pub4] [DOI] [PMC free article] [PubMed] [Google Scholar]
Onland 2017b
- Onland W, Jaegere AP, Offringa M, Kaam A. Systemic corticosteroid regimens for prevention of bronchopulmonary dysplasia in preterm infants. Cochrane Database of Systematic Reviews 2017, Issue 1. [DOI: 10.1002/14651858.CD010941.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Parikh 2016
- Parikh NA, Kennedy KA, Lasky RE, Tyson JE. Neurodevelopmental outcomes of extremely preterm infants randomized to stress dose hydrocortisone. PLoS One 2015;10(9):e0137051. [DOI: 10.1371/journal.pone.0137051; PUBMED: 26376074] [DOI] [PMC free article] [PubMed] [Google Scholar]
RevMan 2014 [Computer program]
- Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager 5 (RevMan 5). Version 5.3. Copenhagen: Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Romagnoli 2002
- Romagnoli C, Zecca E, Luciano R, Torrioli G, Tortorolo G. A three year follow‐up of preterm infants after moderately early treatment with dexamethasone. Archives of Disease of Childhood. Fetal and Neonatal Edition 2002;87(1):F55‐8. [PUBMED: 12091294] [DOI] [PMC free article] [PubMed] [Google Scholar]
Schünemann 2013
- Schünemann H, Brożek J, Guyatt G, Oxman A, editors. GRADE Working Group. GRADE Handbook for Grading Quality of Evidence and Strength of Recommendations. Available from https://gdt.gradepro.org/app/handbook/handbook.html. Updated October 2013.
Shah 2012a
- Shah SS, Ohlsson A, Halliday HL, Shah VS. Inhaled versus systemic corticosteroids for preventing chronic lung disease in ventilated very low birth weight preterm neonates. Cochrane Database of Systematic Reviews 2012, Issue 5. [DOI: 10.1002/14651858.CD002058.pub2] [DOI] [PubMed] [Google Scholar]
Shah 2012b
- Shah SS, Ohlsson A, Halliday HL, Shah VS. Inhaled versus systemic corticosteroids for the treatment of chronic lung disease in ventilated very low birth weight preterm infants. Cochrane Database of Systematic Reviews 2012, Issue 5. [DOI: 10.1002/14651858.CD002057.pub3] [DOI] [PubMed] [Google Scholar]
Shah 2017
- Shah VS, Ohlsson A, Halliday HL, Dunn MS. Early administration of inhaled corticosteroids for preventing chronic lung disease in very low birth weight preterm neonates. Cochrane Database of Systematic Reviews 2017, Issue 1. [DOI: 10.1002/14651858.CD001969.pub4] [DOI] [PMC free article] [PubMed] [Google Scholar]
Stanley 1982
- Stanley FJ. Using cerebral palsy data in the evaluation of neonatal intensive care: a warning. Developmental Medicine and Child Neurology 1982;24(1):93‐4. [PUBMED: 7106413] [DOI] [PubMed] [Google Scholar]
Tarnow‐Mordi 1999
- Tarnow‐Mordi W. Postnatal dexamethasone in preterm infants is potentially lifesaving, but follow up studies are urgently needed. BMJ 1999;319(7222):1385‐6. [PUBMED: 10574836] [DOI] [PMC free article] [PubMed] [Google Scholar]
Tschanz 1995
- Tschanz SA, Damke BM, Burri PH. Influence of postnatally administered glucocorticoids on rat lung growth. Biology of the Neonate 1995;68(4):229‐45. [PUBMED: 8580214] [DOI] [PubMed] [Google Scholar]
Washburn 2006
- Washburn LK, Nixon PA, O'Shea TM. Follow‐up of a randomized, placebo‐controlled trial of postnatal dexamethasone: blood pressure and anthropometric measurements at school age. Pediatrics 2006;118(4):1592‐9. [DOI: 10.1542/peds.2006-0973; PUBMED: 17015551] [DOI] [PubMed] [Google Scholar]
Watterberg 1999
- Watterberg KL, Gerdes JS, Gifford KL, Lin HM. Prophylaxis against early adrenal insufficiency to prevent chronic lung disease in premature infants. Pediatrics 1999;104(6):1258‐63. [PUBMED: 10585975] [DOI] [PubMed] [Google Scholar]
Weichsel 1977
- Weichsel ME. The therapeutic use of glucocorticoid hormones in the perinatal period: potential neurologic hazards. Annals of Neurology 1977;2(5):364‐6. [DOI: 10.1002/ana.410020503; PUBMED: 617574] [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Doyle 2014b
- Doyle LW, Ehrenkranz RE, Halliday HL. Late (> 7 days) postnatal corticosteroids for chronic lung disease in preterm infants. Cochrane Database of Systematic Reviews 2014, Issue 5. [DOI: 10.1002/14651858.CD001145.pub3] [DOI] [PubMed] [Google Scholar]
Halliday 1998
- Halliday HL. Postnatal corticosteroids in the preterm infants with chronic lung disease: Late treatment (> 3 weeks). Cochrane Database of Systematic Reviews 1998, Issue 3. [DOI: 10.1002/14651858.CD001145] [DOI] [Google Scholar]
Halliday 2000a
- Halliday HL, Ehrenkranz RA. Moderately early (7‐14 days) postnatal corticosteroids for preventing chronic lung disease in preterm infants. Cochrane Database of Systematic Reviews 2000, Issue 2. [DOI: 10.1002/14651858.CD001144] [DOI] [PubMed] [Google Scholar]
Halliday 2000b
- Halliday HL, Ehrenkranz RA. Delayed (> 3 weeks) postnatal corticosteroids for chronic lung disease in preterm infants. Cochrane Database of Systematic Reviews 2000, Issue 4. [DOI: 10.1002/14651858.CD001145] [DOI] [PubMed] [Google Scholar]
Halliday 2001a
- Halliday HL, Ehrenkranz RA. Delayed (> 3 weeks) postnatal corticosteroids for chronic lung disease in preterm infants. Cochrane Database of Systematic Reviews 2001, Issue 2. [DOI: 10.1002/14651858.CD001145] [DOI] [PubMed] [Google Scholar]
Halliday 2001b
- Halliday HL, Ehrenkranz RA. Moderately early (7‐14 days) postnatal corticosteroids for preventing chronic lung disease in preterm infants. Cochrane Database of Systematic Reviews 2001, Issue 1. [DOI: 10.1002/14651858.CD001144] [DOI] [PubMed] [Google Scholar]
Halliday 2003a
- Halliday HL, Ehrenkranz RA, Doyle LW. Moderately early (7‐14 days) postnatal corticosteroids for preventing chronic lung disease in preterm infants. Cochrane Database of Systematic Reviews 2003, Issue 1. [DOI: 10.1002/14651858.CD001144] [DOI] [PubMed] [Google Scholar]
Halliday 2003b
- Halliday HL, Ehrenkranz RA, Doyle LW. Delayed (> 3 weeks) postnatal corticosteroids for chronic lung disease in preterm infants. Cochrane Database of Systematic Reviews 2003, Issue 1. [DOI: 10.1002/14651858.CD001145] [DOI] [PubMed] [Google Scholar]
Halliday 2009
- Halliday HL, Ehrenkranz RA, Doyle LW. Late (> 7 days) postnatal corticosteroids for chronic lung disease in preterm infants. Cochrane Database of Systematic Reviews 2009, Issue 1. [DOI: 10.1002/14651858.CD001145.pub2] [DOI] [PubMed] [Google Scholar]


