Abstract
Background
Incidence of gestational diabetes mellitus (GDM) is increasing worldwide. Blood glucose monitoring plays a crucial part in maintaining glycaemic control in women with GDM and is generally recommended by healthcare professionals. There are several different methods for monitoring blood glucose which can be carried out in different settings (e.g. at home versus in hospital).
Objectives
The objective of this review is to compare the effects of different methods and settings for glucose monitoring for women with GDM on maternal and fetal, neonatal, child and adult outcomes, and use and costs of health care.
Search methods
We searched the Cochrane Pregnancy and Childbirth Group Trials Register (30 September 2016) and reference lists of retrieved studies.
Selection criteria
Randomised controlled trials (RCTs) or quasi‐randomised controlled trials (qRCTs) comparing different methods (such as timings and frequencies) or settings, or both, for blood glucose monitoring for women with GDM.
Data collection and analysis
Two authors independently assessed study eligibility, risk of bias, and extracted data. Data were checked for accuracy.
We assessed the quality of the evidence for the main comparisons using GRADE, for:
‐ primary outcomes for mothers: that is, hypertensive disorders of pregnancy; caesarean section; type 2 diabetes; and
‐ primary outcomes for children: that is, large‐for‐gestational age; perinatal mortality; death or serious morbidity composite; childhood/adulthood neurosensory disability;
‐ secondary outcomes for mothers: that is, induction of labour; perineal trauma; postnatal depression; postnatal weight retention or return to pre‐pregnancy weight; and
‐ secondary outcomes for children: that is, neonatal hypoglycaemia; childhood/adulthood adiposity; childhood/adulthood type 2 diabetes.
Main results
We included 11 RCTs (10 RCTs; one qRCT) that randomised 1272 women with GDM in upper‐middle or high‐income countries; we considered these to be at a moderate to high risk of bias. We assessed the RCTs under five comparisons. For outcomes assessed using GRADE, we downgraded for study design limitations, imprecision and inconsistency. Three trials received some support from commercial partners who provided glucose meters or financial support, or both.
Main comparisons
Telemedicine versus standard care for glucose monitoring (five RCTs): we observed no clear differences between the telemedicine and standard care groups for the mother, for:
‐ pre‐eclampsia or pregnancy‐induced hypertension (risk ratio (RR) 1.49, 95% confidence interval (CI) 0.69 to 3.20; 275 participants; four RCTs; very low quality evidence);
‐ caesarean section (average RR 1.05, 95% CI 0.72 to 1.53; 478 participants; 5 RCTs; very low quality evidence); and
‐ induction of labour (RR 1.06, 95% CI 0.63 to 1.77; 47 participants; 1 RCT; very low quality evidence);
or for the child, for:
‐ large‐for‐gestational age (RR 1.41, 95% CI 0.76 to 2.64; 228 participants; 3 RCTs; very low quality evidence);
‐ death or serious morbidity composite (RR 1.06, 95% CI 0.68 to 1.66; 57 participants; 1 RCT; very low quality evidence); and
‐ neonatal hypoglycaemia (RR 1.14, 95% CI 0.48 to 2.72; 198 participants; 3 RCTs; very low quality evidence).
There were no perinatal deaths in two RCTs (131 participants; very low quality evidence).
Self‐monitoring versus periodic glucose monitoring (two RCTs): we observed no clear differences between the self‐monitoring and periodic glucose monitoring groups for the mother, for:
‐ pre‐eclampsia (RR 0.17, 95% CI 0.01 to 3.49; 58 participants; 1 RCT; very low quality evidence); and
‐ caesarean section (average RR 1.18, 95% CI 0.61 to 2.27; 400 participants; 2 RCTs; low quality evidence);
or for the child, for:
‐ perinatal mortality (RR 1.54, 95% CI 0.21 to 11.24; 400 participants; 2 RCTs; very low quality evidence);
‐ large‐for‐gestational age (RR 0.82, 95% CI 0.50 to 1.37; 400 participants; 2 RCTs; low quality evidence); and
‐ neonatal hypoglycaemia (RR 0.64, 95% CI 0.39 to 1.06; 391 participants; 2 RCTs; low quality evidence).
Continuous glucose monitoring system (CGMS) versus self‐monitoring of glucose (two RCTs): we observed no clear differences between the CGMS and self‐monitoring groups for the mother, for:
‐ caesarean section (RR 0.91, 95% CI 0.68 to 1.20; 179 participants; 2 RCTs; very low quality evidence);
or for the child, for:
‐ large‐for‐gestational age (RR 0.67, 95% CI 0.43 to 1.05; 106 participants; 1 RCT; very low quality evidence) and
‐ neonatal hypoglycaemia (RR 0.79, 95% CI 0.35 to 1.78; 179 participants; 2 RCTs; very low quality evidence).
There were no perinatal deaths in the two RCTs (179 participants; very low quality evidence).
Other comparisons
Modem versus telephone transmission for glucose monitoring (one RCT): none of the review's primary outcomes were reported in this trial
Postprandial versus preprandial glucose monitoring (one RCT): we observed no clear differences between the postprandial and preprandial glucose monitoring groups for the mother, for:
‐ pre‐eclampsia (RR 1.00, 95% CI 0.15 to 6.68; 66 participants; 1 RCT);
‐ caesarean section (RR 0.62, 95% CI 0.29 to 1.29; 66 participants; 1 RCT); and
‐ perineal trauma (RR 0.38, 95% CI 0.11 to 1.29; 66 participants; 1 RCT);
or for the child, for:
‐ neonatal hypoglycaemia (RR 0.14, 95% CI 0.02 to 1.10; 66 participants; 1 RCT).
There were fewer large‐for‐gestational‐age infants born to mothers in the postprandial compared with the preprandial glucose monitoring group (RR 0.29, 95% CI 0.11 to 0.78; 66 participants; 1 RCT).
Authors' conclusions
Evidence from 11 RCTs assessing different methods or settings for glucose monitoring for GDM suggests no clear differences for the primary outcomes or other secondary outcomes assessed in this review.
However, current evidence is limited by the small number of RCTs for the comparisons assessed, small sample sizes, and the variable methodological quality of the RCTs. More evidence is needed to assess the effects of different methods and settings for glucose monitoring for GDM on outcomes for mothers and their children, including use and costs of health care. Future RCTs may consider collecting and reporting on the standard outcomes suggested in this review.
Plain language summary
Different methods and settings for glucose monitoring for women with gestational diabetes during pregnancy
What is the issue?
Gestational diabetes mellitus (GDM) is a glucose intolerance leading to high concentrations of glucose (sugar) in the blood (hyperglycaemia) that begins or is first recognised during pregnancy. Monitoring of blood glucose levels is an important way to maintain control of sugar concentrations in the blood. There are several different methods for monitoring blood glucose which can be carried out in different settings (e.g. at home or hospital), however it is not clear which is best for limiting health complications for women and their babies.
Why is this important?
Women with GDM are more likely to develop pre‐eclampsia (a dangerous condition characterised by high blood pressure) during pregnancy, and to have the birth induced, suffer trauma to the perineum during birth, or to give birth by caesarean section. Their babies are more likely to be large for their gestational age at birth, develop low blood sugar (hypoglycaemia), and suffer from complications leading to death. Both the women and their babies are more likely to develop long‐term health complications, including type 2 diabetes.
What evidence did we find?
We searched the medical literature in September 2016 and included 11 randomised controlled trials (RCTs) involving 1272 women with GDM and their babies. Three trials were supported by commercial partners.
We included five different comparisons:
1) telemedicine (transmission of glucose concentrations from home to healthcare professionals for review) versus standard care (face‐to‐face review in a clinic/hospital) (five RCTs);
2) self‐monitoring of glucose (at home) versus periodic monitoring of glucose (less frequently at face‐to‐face visits) (two RCTs);
3) use of a continuous glucose monitoring system (CCMS) versus less frequent self‐monitoring of glucose (two RCTs);
4) modem technology (transmitting glucose concentrations directly from glucose meters to healthcare professionals) versus telephone transmission of glucose concentrations (one RCT);
5) postprandial (after meal) versus preprandial (before meal) monitoring of glucose (one RCT).
Telemedicine versus standard care for glucose monitoring (five RCTs): there were no clear differences between women in the telemedicine and standard care groups for pre‐eclampsia or hypertension, caesarean section or induction of labour; or for their babies being born large‐for‐gestational age, developing a serious morbidity, or having hypoglycaemia. There were no deaths in the two RCTs that reported on deaths of babies.
Self‐monitoring versus periodic glucose monitoring (two RCTs): there were no clear differences between women in the self‐monitoring and periodic glucose monitoring groups for pre‐eclampsia or caesarean section; or for their babies dying, being born large‐for‐gestational age, or developing hypoglycaemia.
CGMS versus self‐monitoring of glucose (two RCTs): there was no clear difference between women in the CGMS and self‐monitoring groups for caesarean section; or for babies being born large‐for‐gestational age, or developing hypoglycaemia. There were no deaths of babies in the two RCTs.
Modem versus telephone transmission for glucose monitoring (one RCT): this RCT reported none of the outcomes we considered most important.
Postprandial versus preprandial glucose monitoring (one RCT): there were no clear differences between women in the postprandial and preprandial glucose monitoring groups for pre‐eclampsia, caesarean section or perineal trauma; or for babies developing hypoglycaemia. Babies born to women in the postprandial glucose monitoring group were less likely to be born large‐for‐gestational age than babies in the preprandial group.
The quality of the evidence for the above findings was low or very low. None of the 11 RCTs reported on postnatal depression, postnatal weight retention, return to pre‐pregnancy weight, or development of type 2 diabetes for the women; or disability, adiposity or development of type 2 diabetes for the babies as children or adults.
What does this mean?
Blood glucose monitoring is an important strategy for managing GDM, however it remains unclear what methods are best. Conclusive evidence from RCTs is not yet available to guide practice, although a range of methods has been investigated. Few RCTs have compared the same or similar interventions, RCTs have been small and have reported limited findings. Further large, well‐designed, RCTs are required to assess the effects of different methods and settings for blood glucose monitoring for women with GDM in order to improve outcomes for women and their babies in the short and long term.
Summary of findings
Background
Description of the condition
Gestational diabetes mellitus
Gestational diabetes mellitus (GDM) is defined as "carbohydrate intolerance of varying degrees of severity with onset or first recognition during pregnancy" (Metzger 1998). Therefore women with unrecognised pre‐existing type 1 or type 2 diabetes, whose first presentation of the disease is during pregnancy, are included in this definition (Hoffman 1998). Many physiological changes occur as a part of normal pregnancy. For example, maternal metabolic changes include the development of relative insulin resistance and reduced glucose sensitivity, particularly during the second trimester of pregnancy (Kuhl 1998); these physiological changes facilitate the transport of glucose across the placenta to stimulate adequate fetal growth and development (Setji 2005). Some women, however, are predisposed to an excessive maternal insulin resistance and are consequently at risk of hyperglycaemia (high blood glucose) and GDM during their pregnancy.
Diagnostic methods for GDM vary, and there are currently no uniformly accepted international diagnostic criteria. The World Health Organization has recommended a 75 g 2‐hour oral glucose tolerance test (OGTT) at 24 to 28 weeks' gestation (WHO 2013), and in some parts of the world, a 100 g 3‐hour OGTT is used. While universal screening has been encouraged, in some countries screening is only performed for 'high‐risk' women, due to the lack of identifiable risk factors in many women subsequently diagnosed with GDM. The effects of different methods of screening (Tieu 2014), and strategies for diagnosing GDM (Farrar 2015), are the topics of other Cochrane Reviews.
Epidemiology and risk factors
Due to the lack of consistent screening procedures and diagnostic criteria between (and within) countries, different populations of women are diagnosed with GDM in different parts of the world, and reported incidences vary greatly, and can be as high as 28% (Jiwani 2012). There is a general consensus however, that the incidence of GDM is increasing worldwide, in line with the increasing rates of both type 2 diabetes mellitus and maternal obesity (Dabelea 2005; Getahun 2008; Kim 2010; Lawrence 2008).
The HAPO (Hyperglycaemia and Adverse Pregnancy Outcomes) study explored the risks of adverse outcomes associated with different degrees of maternal hyperglycaemia (Coustan 2010; HAPO 2008). Following this, a task force from the International Association of Diabetes in Pregnancy Study Group (IADPSG) developed new consensus‐based criteria for GDM diagnosis using data from the study ‐ suggesting GDM diagnosis after a 75 g OGTT when any three of the following thresholds are met or exceeded: fasting plasma glucose: 5.1 mmol/L (92 mg/dL), 1‐hour plasma glucose: 10.0 mmol/L (180 mg/dL) or 2‐hour plasma glucose: 8.5 mmol/L (153 mg/dL) (IADPSG Consensus Panel 2010). Some studies published since these recommendations were made have revealed substantial increases in the numbers of women diagnosed with GDM when these criteria were applied (Benhalima 2013; Bodmer‐Roy 2012; Lapolla 2011; O'Sullivan 2011; Morikawa 2010). Accordingly, there is much debate surrounding the implications, including potential costs, risks and benefits of widespread use of these criteria.
In addition to obesity (a maternal body mass index of 30 kg/m² or higher), a range of risk factors for GDM have been identified, which include advanced maternal age, increased parity and certain ethnicities (ACOG 2013), with Indigenous Australian, Polynesian and South Asian (Indian) women being regarded as particularly high‐risk groups (Hoffman 1998). Women who have had GDM in a previous pregnancy are also at an increased risk of GDM in their subsequent pregnancies, as are women who have a family history of diabetes (ADA 2004).
Maternal and fetal complications
Hyperglycaemia has many end‐organ adverse effects and the diagnosis of GDM has implications for both mothers and their infants. The potential maternal complications of GDM include polyhydramnios (too much amniotic fluid) due to increased fetal urine production, pre‐eclampsia and caesarean birth (ACOG 2013). Maternal hyperglycaemia may cause accelerated fetal growth, and result in macrosomic (birthweight of at least 4000 g) or large‐for‐gestational‐age infants (Crowther 2005). While caesarean section is often the preferred mode of birth for a macrosomic infant, helping to avoid maternal perineal trauma and infant injury, this mode of birth may also be associated with increased maternal morbidity (Reece 2010).
There are well documented fetal and neonatal complications of GDM. Large‐for‐gestational‐age infants resulting from GDM can lead to shoulder dystocia (obstructed birth) and birth trauma such as nerve palsies and fractures (Crowther 2005; Dodd 2007; Landon 2009; Metzger 1998). Fetal hyperinsulinaemia (raised insulin levels) that occurs in response to maternal hyperglycaemia, may be associated with neonatal hypoglycaemia (HAPO 2008). Other potential complications for infants include neonatal respiratory distress syndrome, hyperbilirubinaemia (jaundice), polycythaemia (an excess of red blood cells) and hypocalcaemia (low blood calcium levels) (ADA 2004; Crowther 2005; Landon 2009; Metzger 1998).
As GDM is a result of physiological metabolic changes during pregnancy, maternal hyperglycaemia should resolve following birth, and does in the majority of cases. A repeat OGTT is recommended in the postpartum period, however, to confirm resolution of hyperglycaemia. Repeat testing is also recommended every one to two years in women with normalised glucose tolerance (ADA 2012; Hoffman 1998), as an obstetric history of GDM confers an increased risk of type 2 diabetes later in life for both mother and infant (Feig 2008; Kim 2002; O'Sullivan 1991; Pettitt 1985; Silverman 1998).
Description of the intervention
Different methods and settings for glucose monitoring for gestational diabetes mellitus
Treatment of GDM including lifestyle advice, monitoring of blood glucose, insulin therapy and oral hypoglycaemics, has been shown to significantly reduce the risk of maternal and perinatal complications (including perinatal mortality, shoulder dystocia, bone fracture, and nerve palsy) without increasing the risk of caesarean section (Crowther 2005; Landon 2009). Cochrane Reviews have assessed (or plan to assess) alternative management strategies for GDM (Alwan 2009), including lifestyle interventions (Brown 2017), insulin (Brown 2016), oral anti‐diabetic pharmacological therapies (Brown 2017b), exercise (Ceysens 2016), dietary supplementation with myo‐inositol (Brown 2016b), and different intensities of glycaemic control (Martis 2016).
Management of GDM relies on a multi‐disciplinary team approach to inform and educate the woman and to establish glycaemic control. Blood glucose monitoring is a crucial part in maintaining this control and is generally recommended by obstetric healthcare professionals (Gabbe 2004; NICE 2008). The decision to initiate active treatments for the management of GDM, including insulin therapy and oral hypoglycaemic agents, relies on the adequate monitoring of blood glucose. Consensus on the ideal methods (including frequency or timing) and settings for monitoring, however, has yet to be established.
Methods (including frequency and timing) of blood glucose monitoring
There is some evidence that more frequent blood glucose monitoring is associated with improved outcomes (Goldberg 1986: Langer 1994), although the optimal timing and frequency of testing is not known. Guidelines in different countries suggest monitoring three or four times daily (with both fasting and postprandial measurements recorded) (ACOG 2013; Nankervis 2013).
Debate continues about the best time to measure blood glucose concentrations, including whether postprandial monitoring, preprandial monitoring, or both should be conducted. Insulin peaks two to three hours after a meal, although this is likely to vary according to what is eaten and when. If carried out, it is not clear whether postprandial monitoring should take place one, or two, hours after meals (Weisz 2005). Similarly, if carried out, it is not clear when fasting or preprandial monitoring should be conducted (Ben‐Haroush 2004).
The benefits of continuous monitoring are also still in question; glucose monitoring systems can record concentrations at regular intervals over several days and this can give a full picture of changes throughout the day. There have been studies that suggested that such supplementary monitoring improves glycaemic control, which can have an impact on clinical outcomes (Murphy 2008; Yu 2014). As yet, there is insufficient evidence about the harms and benefits for women or babies for it to be generally recommended for GDM, although it may be a component of care for pregnant women with type 1 or 2 diabetes (ADA 2012). There is also a paucity of evidence about the optimal duration of continuous monitoring and the best time in pregnancy for it to be conducted, along with the cost‐effectiveness of such intensive monitoring (Voormolen 2013).
Settings for blood glucose monitoring
With the introduction of home reflectance monitors in the late 1970s, self‐monitoring of blood glucose became possible (Espersen 1985). Some early benefits of self‐monitoring for pregnant women with insulin‐dependent diabetes were observed, including declines in mean blood glucose concentrations and in the numbers of diabetes‐related hospitalisations (Espersen 1985). Self‐monitoring of blood glucose in the management of GDM has since become more widely practised (Gabbe 2004). Much debate, however, still exists surrounding its usefulness (Buchanan 2003; Jovanovic 2003), and particularly regarding the optimal timing and frequency of such self‐monitoring (Buchanan 2003; Gabbe 2004; Jovanovic 2003). Trials investigating treatments for GDM have generally used regular capillary blood glucose testing for monitoring, both in a hospital setting (with weekly testing) and home setting (with frequencies of testing ranging from seven times per day, to five days per week), with monthly glycated haemoglobin (HbA1c) concentrations also monitored in some trials (Alwan 2009).
More recent developments of digital technologies for self‐monitoring allow real‐time transfer of measurements to healthcare providers. Such devices mean that women are able to monitor their blood glucose from home; the results are relayed directly to healthcare providers, who in turn can offer advice or recommend changes in treatment without the women needing to attend a healthcare facility (Mackillop 2014). Electronic monitoring with direct transfer of results reduces the need for women to maintain diaries, and may reduce recording errors (Given 2013). As well as improving monitoring, such devices may enable timely intervention that could improve outcomes. Remote monitoring and feedback may also reduce the need for costly and inconvenient clinic visits, and many women are comfortable using smart‐phone and other interactive internet based technologies (Hirst 2015). However, some women may lack resources (such as internet access) or the confidence to use such devices, and may prefer monitoring to take place at regular clinic visits.
How the intervention might work
A consensus on the ideal method (including frequency and timing) and setting of monitoring is yet to be established. As the number of women affected by GDM increases there is an urgent need to identify the most cost‐effective means of monitoring blood glucose that achieves the best outcomes for women and their infants.
Glucose monitoring at both home and hospital, using a variety of methods, is currently part of the management of GDM, and trials investigating interventions for treating GDM have included testing in both locations (Alwan 2009). Home monitoring may be more likely to be well accepted or tolerated, and may allow more frequent and intensive monitoring. Barriers to home monitoring may include the reliance on women's adherence to the daily regimen, and their ability to use the self‐monitoring equipment appropriately. Glucose monitoring in the hospital setting may be less frequent (for example, weekly or fortnightly), but may encourage increased clinical contact and improved surveillance of measurements.
Non‐randomised studies have provided some support for home care in GDM and the more intensive self‐monitoring of blood glucose concentrations that it allows. In a non‐randomised study of 58 women with GDM, infants born to women who had undertaken home self‐monitoring were found to have lower rates of macrosomia than those born to women who had weekly in‐hospital 2‐hour postprandial capillary glucose monitoring (Goldberg 1986). The reduction of macrosomia was attributed, by the study authors, to the earlier detection of the need for insulin with home monitoring (Goldberg 1986). In a further prospective study of over 2000 women with GDM, intensive glucose self‐monitoring (seven times a day) using memory‐based reflectance meters was found to be associated with lower rates of macrosomia, caesarean birth, shoulder dystocia, stillbirth and neonatal intensive care unit days, when compared with conventional management (Langer 1994).
In addition to the potential health benefits of home care in the management of GDM, home glucose monitoring for women may prove to be more cost‐effective than hospital monitoring, which is an important public health consideration, given the increasing incidence of GDM.
Why it is important to do this review
GDM may be diagnosed through screening processes and potentially managed with adequate monitoring and appropriate initiation of active treatments, so it is vitally important that the most effective and safe monitoring strategies are identified. While blood glucose monitoring for women with GDM is commonly recommended, there is currently no consensus on whether self‐monitoring (which can be carried out at home) has benefits when compared with hospital glucose monitoring. With the increasing incidence of GDM, the optimal method and setting for blood glucose monitoring should be determined, with consideration of the public health and resource implications.
Objectives
The objective of this review is to compare the effects of different methods and settings for glucose monitoring for women with GDM on maternal and fetal, neonatal, child and adult outcomes, and use and costs of health care.
Methods
Criteria for considering studies for this review
Types of studies
We planned to include published, unpublished and ongoing randomised or quasi‐randomised controlled trials, however we only identified published trials for inclusion. We planned to include cluster‐randomised trials, however we did not identify any. Cross‐over trials are not eligible for inclusion in this review.
We classified trials that are currently available only as abstracts ‐ for which we could not obtain information about risk of bias and primary or secondary outcomes ‐ as 'awaiting classification'; we will reconsider these trials for inclusion once the full publications are available.
Types of participants
We included women diagnosed with GDM during their current pregnancy, as defined by individual trialists. We included women of any age, gestation and parity, but excluded women with previously diagnosed type 1 or type 2 diabetes.
Types of interventions
We included trials that compared different methods (including timings and frequencies) or settings, or both, for blood glucose monitoring.
This could include, for example, comparisons of ‘home’ (ambulatory or outpatient care) glucose monitoring with ‘hospital’ (acute care) glucose monitoring. ‘Home’ care could include studies where blood glucose self‐monitoring was performed predominately at home by the women (using a variety of methods, frequencies and timings). ‘Hospital’ care could include studies where blood glucose monitoring was performed predominately in the hospital (i.e. at antenatal hospital visits or as an inpatient) using a variety of methods, frequencies and timings. This could also include comparing different methods, frequencies or timings of glucose monitoring in the same setting (e.g. 'home').
Types of outcome measures
Primary outcomes
For the mother
Hypertensive disorders of pregnancy (including pre‐eclampsia, pregnancy‐induced hypertension, eclampsia)
Caesarean section
Development of type 2 diabetes
For the child
Perinatal mortality (stillbirth or neonatal mortality)
Large‐for‐gestational age
Death or serious morbidity composite
Neurosensory disability
Secondary outcomes
For the mother
Perinatal
Induction of labour
Perineal trauma
Placental abruption
Postpartum haemorrhage
Postpartum infection
Gestational weight gain
Adherence to the intervention
Behavioural changes associated with the intervention
Sense of well‐being and quality of life
Views of the intervention
Breastfeeding (e.g. at discharge, six weeks postpartum)
Use of additional pharmacotherapy
Maternal hypoglycaemia
Glycaemic control during or at end of treatment
Mortality
Long‐term
Postnatal depression
Postnatal weight retention or return to pre‐pregnancy weight
Body mass index (BMI)
GDM in a subsequent pregnancy
Type 1 diabetes
Impaired glucose tolerance
Cardiovascular health (e.g. blood pressure, hypertension, cardiovascular disease, metabolic syndrome)
For the child
Fetus/neonate
Stillbirth
Neonatal death
Gestational age at birth
Preterm birth (before 37 weeks' gestation; before 32 weeks' gestation)
Apgar score < 7 at five minutes
Macrosomia
Small‐for‐gestational age
Birthweight and z score
Head circumference and z score
Length and z score
Ponderal index
Adiposity
Shoulder dystocia
Nerve palsies
Bone fractures
Respiratory distress syndrome
Hypoglycaemia
Hyperbilirubinemia or jaundice
Hypocalcaemia
Polycythaemia
Child/adult
Weight and z score
Height and z score
Head circumference and z score
Adiposity (e.g. BMI, skinfold thickness, fat mass)
Cardiovascular health (e.g. blood pressure, hypertension, cardiovascular disease, metabolic syndrome)
Type 1 diabetes
Type 2 diabetes
Impaired glucose tolerance
Employment, education and social status or achievement
Use and costs of health services
Number of antenatal visits or admissions
Number of hospital or health professional visits (e.g. midwife, obstetrician, physician, dietician, diabetic nurse) (unscheduled and scheduled)
Admission to neonatal intensive care unit
Length of antenatal stay
Length of postnatal stay (mother)
Length of postnatal stay (baby)
Cost of maternal care
Cost of offspring care
Costs associated with the intervention
Costs to families associated with the management provided
(We used the standard outcome set agreed by consensus between review authors of Cochrane Pregnancy and Childbirth reviews for prevention and treatment of GDM and pre‐existing diabetes.)
Search methods for identification of studies
The following methods section of this review is based on a standard template used by Cochrane Pregnancy and Childbirth.
Electronic searches
We searched the Cochrane Pregnancy and Childbirth Trials Register by contacting their Information Specialist (30 September 2016).
The Register is a database containing over 21,000 reports of controlled trials in the field of pregnancy and childbirth. For full search methods used to populate the Pregnancy and Childbirth Group Trials Register including the detailed search strategies for CENTRAL, MEDLINE, Embase and CINAHL; the list of handsearched journals and conference proceedings, and the list of journals reviewed via the current awareness service, please follow this link to the editorial information about Cochrane Pregnancy and Childbirth in the Cochrane Library and select the ‘Specialized Register ’ section from the options on the left side of the screen.
Briefly, the Cochrane Pregnancy and Childbirth Trials Register is maintained by their Information Specialist and contains trials identified from:
monthly searches of the Cochrane Central Register of Controlled Trials (CENTRAL);
weekly searches of MEDLINE (Ovid);
weekly searches of Embase (Ovid);
monthly searches of CINAHL (EBSCO);
handsearches of 30 journals and the proceedings of major conferences;
weekly current awareness alerts for a further 44 journals plus monthly BioMed Central email alerts.
scoping searches of ClinicalTrials.gov and the WHO International Clinical Trials Registry Platform (ICTRP).
Search results are screened by two people from Cochrane Pregnancy and Childbirth, and the full text of all relevant trial reports identified through the searching activities described above is reviewed. Based on the intervention described, each trial report is assigned a number that corresponds to a specific Pregnancy and Childbirth review topic (or topics), and is then added to the Register. The Information Specialist searches the Register for each review using this topic number rather than keywords. This results in a more specific search set which has been fully accounted for in the relevant review sections (Included studies; Excluded studies; Studies awaiting classification; Ongoing studies).
Searching other resources
We searched reference lists of retrieved articles.
We did not apply any language or date restrictions.
Data collection and analysis
The following methods section of this review is based on a standard template used by Cochrane Pregnancy and Childbirth.
Selection of studies
Independently, two review authors assessed all the potential studies identified as a result of the search strategy for inclusion. We resolved any disagreement through discussion or, if required, we consulted the third review author.
Data extraction and management
At least two review authors extracted the data using the agreed form. We resolved discrepancies through discussion or, if required, we consulted the third review author. Data were entered into Review Manager 5 software (Review Manager 2014), and checked for accuracy.
When information regarding any of the above was unclear, we contacted authors of the original reports to provide further details.
Assessment of risk of bias in included studies
Two review authors independently assessed risk of bias for each study using the criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). Any disagreement was resolved by discussion or by involving a third assessor.
(1) Random sequence generation (checking for possible selection bias)
For each included study we described the method used to generate the allocation sequence in sufficient detail to allow an assessment of whether it should produce comparable groups.
We assessed the method as being at:
low risk of bias (any truly random process, e.g. random number table; computer random number generator);
high risk of bias (any non‐random process, e.g. odd or even date of birth; hospital or clinic record number);
unclear risk of bias.
(2) Allocation concealment (checking for possible selection bias)
For each included study we described the method used to conceal allocation to interventions prior to assignment and assessed whether intervention allocation could have been foreseen in advance of, or during recruitment, or changed after assignment.
We assessed the methods as being at:
low risk of bias (e.g. telephone or central randomisation; consecutively numbered sealed opaque envelopes);
high risk of bias (open random allocation; unsealed or non‐opaque envelopes, alternation; date of birth);
unclear risk of bias.
(3.1) Blinding of participants and personnel (checking for possible performance bias)
For each included study we described the methods used, if any, to blind study participants and personnel from knowledge of which intervention a participant received. We considered that studies were at low risk of bias if they were blinded, or if we judged that the lack of blinding unlikely to affect results. We assessed blinding separately for different outcomes or classes of outcomes.
We assessed the methods as being at:
low, high or unclear risk of bias for participants;
low, high or unclear risk of bias for personnel.
(3.2) Blinding of outcome assessment (checking for possible detection bias)
For each included study we described the methods used, if any, to blind outcome assessors from knowledge of which intervention a participant received. We assessed blinding separately for different outcomes or classes of outcomes.
We assessed methods used to blind outcome assessment as being at:
low, high or unclear risk of bias.
(4) Incomplete outcome data (checking for possible attrition bias due to the amount, nature and handling of incomplete outcome data)
For each included study, and for each outcome or class of outcomes, we described the completeness of data including attrition and exclusions from the analysis. We stated whether attrition and exclusions were reported and the numbers included in the analysis at each stage (compared with the total randomised participants), reasons for attrition or exclusion where reported, and whether missing data were balanced across groups or were related to outcomes. Where sufficient information was reported, or could be supplied by the study authors, we planned to re‐include missing data in the analyses which we undertook.
We assessed methods as being at:
low risk of bias (e.g. no missing outcome data; missing outcome data balanced across groups);
high risk of bias (e.g. numbers or reasons for missing data imbalanced across groups; ‘as treated’ analysis done with substantial departure of intervention received from that assigned at randomisation);
unclear risk of bias.
(5) Selective reporting (checking for reporting bias)
For each included study we described how we investigated the possibility of selective outcome reporting bias and what we found.
We assessed the methods as being at:
low risk of bias (where it was clear that all of the study’s prespecified outcomes and all expected outcomes of interest to the review were reported);
high risk of bias (where not all the study’s prespecified outcomes were reported; one or more reported primary outcomes were not prespecified; outcomes of interest were reported incompletely and so could not be used; study failed to include results of a key outcome that would have been expected to have been reported);
unclear risk of bias.
(6) Other bias (checking for bias due to problems not covered by (1) to (6) above)
For each included study we described any important concerns we had about other possible sources of bias.
(7) Overall risk of bias
We made explicit judgements about whether studies were at high risk of bias, according to the criteria given in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). With reference to (1) to (6) above, we assessed the likely magnitude and direction of the bias and whether we considered it was likely to have an impact on the findings. We explored the impact of the level of bias through undertaking sensitivity analyses ‐ seeSensitivity analysis.
Assessment of the quality of the evidence using the GRADE approach
We evaluated the quality of the evidence using the GRADE approach as outlined in the GRADE handbook for our three main comparisons.
Telemedicine versus standard care for glucose monitoring
Self‐monitoring versus periodic glucose monitoring
Continuous glucose monitoring system versus self‐monitoring of glucose
The GRADE approach uses five considerations (study limitations, consistency of effect, imprecision, indirectness and publication bias) to assess the quality of the body of evidence for specific outcomes. The evidence can be downgraded from 'high quality' by one level for serious (or by two levels for very serious) limitations, depending on assessments for risk of bias, indirectness of evidence, inconsistency, imprecision of effect estimates or publication bias. In this review we used the GRADE approach to assess the following outcomes, and reported them in 'Summary of findings' tables.
For the mother
Hypertensive disorders of pregnancy (including pre‐eclampsia, pregnancy‐induced hypertension, eclampsia)
Caesarean section
Development of type 2 diabetes
Induction of labour
Perineal trauma
Postnatal depression
Postnatal weight retention or return to pre‐pregnancy weight
For the child
Perinatal mortality (stillbirth or neonatal death)
Large‐for‐gestational age
Death or serious morbidity composite
Neurosensory disability
Hypoglycaemia
Adiposity (e.g. BMI, skinfold thickness, fat mass)
Type 2 diabetes
We used the GRADEpro Guideline Development Tool, GRADEpro 2014, to import data from Review Manager 5 in order to create ’Summary of findings’ tables (Review Manager 2014). A summary of the intervention effect and a measure of quality according to the GRADE approach is presented in the 'Summary of findings' tables for the outcomes listed above.
Measures of treatment effect
Dichotomous data
For dichotomous data, we presented results as summary risk ratios with 95% confidence intervals.
Continuous data
For continuous data, we used the mean difference. We planned to use the standardised mean difference to combine trials that measured the same outcome, but used different methods.
Unit of analysis issues
Cluster‐randomised trials
We did not identify any cluster‐randomised trials for inclusion in this review.
If cluster‐randomised trials are included in future updates of the review, we plan to include them in the analyses along with individually‐randomised trials. Their sample sizes will be adjusted using the methods described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011), using an estimate of the intra‐cluster correlation co‐efficient (ICC) derived from the trial (if possible), or from another source. If ICCs from other sources are used, we will report this and conduct sensitivity analyses to investigate the effect of variation in the ICC. If we identify both cluster‐randomised trials and individually‐randomised trials, we plan to synthesise the relevant information. We plan to consider it reasonable to combine the results from both, if there is little heterogeneity between the study designs, and the interaction between the effect of intervention and the choice of randomisation unit is considered to be unlikely. We plan to also acknowledge heterogeneity in the randomisation unit and perform a sensitivity analysis to investigate the effects of the randomisation units.
Cross‐over trials
We excluded trials with cross‐over designs.
Multi‐armed trials
If we had included multi‐armed trials, we planned to record and include all outcome data in the review as two‐arm comparisons. We planned to include the data for the different arms in independent two‐arm comparisons in separate meta‐analyses. In instances where we could not include the data in separate comparisons, we planned to combine them to create a single pair‐wise comparison (Higgins 2011). If the control group was shared by two or more study arms, we planned to divide it between relevant subgroup categories to avoid double‐counting the participants (for dichotomous data, we planned to divide the events and the total population, while for continuous data, we planned to assume the same mean and standard deviation (SD) but planned to divide the total population). We planned to describe the details in the 'Characteristics of included studies' tables.
Other unit of analysis issues
As infants from multiple pregnancies are not independent, we planned to use cluster‐trial methods in the analysis, where the data allowed, and where multiples made up a substantial proportion of the trial population, to account for non‐independence of variables (Gates 2004).
Dealing with missing data
For included studies, we noted levels of attrition. In future updates, if more eligible studies are included, we will explore the impact of including studies with high levels of missing data in the overall assessment of treatment effect by using sensitivity analyses.
For all outcomes, we carried out analyses, as far as possible, on an intention‐to‐treat basis, i.e. we attempted to include all participants randomised to each group in the analyses. The denominator for each outcome in each trial was the number randomised minus any participants whose outcomes were known to be missing.
Assessment of heterogeneity
We assessed statistical heterogeneity in each meta‐analysis using the Tau², I² and Chi² statistics. We regarded heterogeneity as substantial if an I² was greater than 30% and either the Tau² was greater than zero, or there was a low P value (less than 0.10) in the Chi² test for heterogeneity. If we identified substantial heterogeneity (above 30%), we planned to explore it using prespecified subgroup analyses.
Assessment of reporting biases
If there were 10 or more studies in the meta‐analysis, we planned to investigate reporting biases (such as publication bias) using funnel plots. We planned to assess funnel plot asymmetry visually. If asymmetry was suggested by a visual assessment, we planned to perform exploratory analyses to investigate it.
Data synthesis
We carried out statistical analysis using Review Manager 5 software (Review Manager 2014). We used fixed‐effect meta‐analysis for combining data where it was reasonable to assume that studies were estimating the same underlying treatment effect, that is, where studies examined the same intervention, and we judged the studies' populations and methods to be sufficiently similar.
Where there was clinical heterogeneity sufficient to expect that the underlying treatment effects differed between trials, or where substantial statistical heterogeneity was detected, we used random‐effects meta‐analysis to produce an overall summary, if an average treatment effect across trials was considered clinically meaningful. The random‐effects summary has been treated as the average range of possible treatment effects and we have discussed the clinical implications of treatment effects differing between trials. If the average treatment effect was not clinically meaningful, we planned not to combine trials. Where we used random‐effects analyses, the results have been presented as the average treatment effect with 95% confidence intervals, and the estimates of Tau² and I².
Subgroup analysis and investigation of heterogeneity
If we identified substantial heterogeneity, we planned to investigate it using subgroup analyses or sensitivity analyses. We planned to consider whether an overall summary is meaningful, and if it was, to use random‐effects analysis to produce it.
We planned to carry out the following subgroup analyses.
Timing of monitoring (i.e. postprandial versus preprandial)
Frequency of monitoring (i.e. multiple times per day versus daily)
Method of monitoring (i.e. use of glucose meter versus use of continuous glucose monitoring system)
Gestational age at randomisation, and at diagnosis (i.e. first trimester versus second trimester versus third trimester)
We planned to restrict subgroup analyses to the review's primary outcomes.
We planned to assess subgroup differences by interaction tests available within Review Manager 5 (Review Manager 2014). We planned to report the results of subgroup analyses quoting the Chi² statistic and P value, and the interaction test I² value.
Due to paucity of data in the review, however, we were not able to conduct planned subgroup analyses.
Sensitivity analysis
We planned to carry out a sensitivity analysis to explore the effects of trial quality assessed by omitting studies rated as 'high risk of bias' and 'unclear' when considering allocation concealment (selection bias) and incomplete outcome data (attrition bias). We planned to restrict this to the primary outcomes.
Due to paucity of data in the review, however, we were not able to conduct our planned sensitivity analyses.
Results
Description of studies
Results of the search
The search of the Cochrane Pregnancy and Childbirth Trials Register retrieved 39 reports, relating to 27 studies. We included 11 studies and excluded five.
Four studies are awaiting further classification (Ding 2012; Paramasivam 2014; Puricel 2014; Rigla 2015), and seven studies are ongoing (Evers 2016; Hanafusa 2015; Kim 2014; Mackillop 2016; Mendez‐Figueroa 2013; Rasekaba 2015a; Rudge 2013) (See Characteristics of studies awaiting classification; Characteristics of ongoing studies).
See Figure 1.
1.
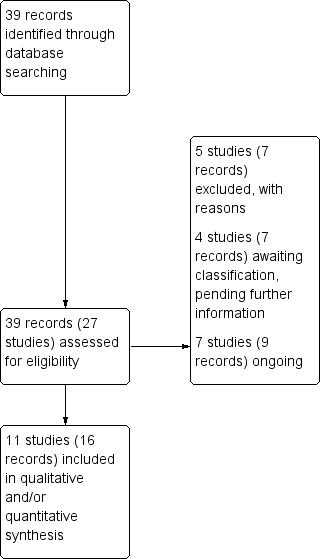
Study flow diagram
Included studies
We identified 11 trials that met the inclusion criteria for this review (Dalfra 2009; De Veciana 1995; Given 2015; Homko 2002; Homko 2007; Homko 2012; Kestila 2007; Kruger 2003; Perez‐Ferre 2010; Rey 1997; Wei 2016).
Design
One of the 11 included trials was a quasi‐randomised controlled trial (Dalfra 2009), and the other 10 were randomised controlled trials (De Veciana 1995; Given 2015; Homko 2002; Homko 2007; Homko 2012; Kestila 2007; Kruger 2003; Perez‐Ferre 2010; Rey 1997; Wei 2016).
Sample sizes
The 11 included trials randomised a total of 1272 pregnant women with GDM. Sample sizes ranged from 50 women in Given 2015, to 347 women in Rey 1997.
Settings and dates of trials
Five trials were conducted in the USA (De Veciana 1995; Homko 2002; Homko 2007; Homko 2012; Kruger 2003), and one trial was conducted in each of the following countries: Canada (Rey 1997), China (Wei 2016), Finland (Kestila 2007), Ireland (Given 2015), Italy (Dalfra 2009), and Spain (Perez‐Ferre 2010).
Trials ran between 1993 and 2013: Given 2015 took place between January 2012 and May 2013; Homko 2002 between March 1998 and November 1999; Homko 2007 between September 2004 and May 2006; Homko 2012 between September 2007 and November 2009; Perez‐Ferre 2010 between June and December 2007; Rey 1997 between June 1993 and May 1994; and Wei 2016 between September 2011 and December 2012. Four trials did not specify trial dates (Dalfra 2009; De Veciana 1995; Kestila 2007; Kruger 2003).
Participants
All 11 trials included women with gestational diabetes mellitus (GDM). One trial also included women with type 1 diabetes (Dalfra 2009), however, we have only included data related to the women with GDM in the review.
One trial (De Veciana 1995) diagnosed women with GDM according to the O'Sullivan and Mahan 1964 criteria (O'Sullivan 1964), four trials (Dalfra 2009; Homko 2007; Homko 2012; Perez‐Ferre 2010) used the Carpenter and Coustan 1982 criteria (Carpenter 1982), one trial (Given 2015) referenced the National Institute of Clinical Excellence: Diabetes in Pregnancy 2008 guidelines (NICE 2008) (however it did not specify the criteria used), and one trial (Wei 2016) reported that women were diagnosed according to criteria recommended by the American Diabetes Association 2011 (ADA 2012) and IADPSG 2010 (IADPSG Consensus Panel 2010). The Kestila 2007 trial used at least two abnormal values in a 2‐hour 75 g OGTT (fasting > 5.1 mmol/L, 1‐hour > 10 mmol/L, 2‐hour > 8.7 mmol/L). Rey 1997 (using plasma capillary blood) used a 1‐hour 50 g OGCT of ≥ 11.1 mmol/L, or between 8.9 and 11.0 mmol/L plus at least two abnormal values on a three‐hour 100 g OGTT. Abnormal values were dependent on gestation; before 26 weeks (fasting > 5.3 mmol/L, one‐hour > 10 mmol/L, two‐hour > 8.9 mmol/L; 3 hours > 7.8 mmol/L) or during and after 26 weeks (fasting > 5.6 mmol/L, one‐hour > 11.1 mmol/L; two‐hour > 9.2 mmol/L, three‐hour > 8.3 mmol/L). Two trials did not state diagnostic criteria used (Homko 2002; Kruger 2003).
After diagnosis of GDM, inclusion of women with varying gestational ages was reported: between 24 and 28 weeks' gestation (Given 2015; Wei 2016), within a week from diagnosis (mean of 28 weeks' gestation) (Dalfra 2009), before 28 weeks' gestation (Perez‐Ferre 2010), at or before 30 weeks' gestation (De Veciana 1995), at or before 33 weeks' gestation (Homko 2002; Homko 2007; Homko 2012), between 22 and 34 weeks' gestation (Kestila 2007), between 22 and 38 weeks' gestation (Rey 1997); Kruger 2003 did not specify gestational age.
Additional eligibility criteria varied across the trials, with Given 2015 also including women with impaired glucose tolerance (and referencing the National Institute of Clinical Excellence: Diabetes in Pregnancy 2008 guidelines (NICE 2008), however not specifying the criteria used); Homko 2002 required women to have a fasting glucose value of ≤ 5.3 mmol/L at the OGTT; and De Veciana 1995 included only women who required insulin (i.e. those with elevated fasting blood glucose values at the time of a 3‐hour OGTT or with weekly fasting and 1‐hour postprandial blood glucose values exceeding 5.8 mmol/L or 7.8 mmol/L respectively).
Six trials specified that only women with singleton pregnancies were included (De Veciana 1995; Kestila 2007; Wei 2016), or that women with multiple pregnancies were excluded (Homko 2007; Homko 2012; Rey 1997). Six trials detailed exclusion of women with a history of diabetes (type 1 or 2) (De Veciana 1995; Given 2015; Kruger 2003; Wei 2016) and/or prior glucose intolerance (Homko 2007; Homko 2012). Additional exclusion criteria reported included: pre‐existing hypertension, renal disease or autoimmune disorders (De Veciana 1995), receipt of oral steroid therapy (Given 2015), congential malformations, or current diet or insulin therapy (Rey 1997), and previous treatment for GDM, presence of infection, or other severe metabolic, endocrine, medical or psychological co‐morbidities (Wei 2016). Four trials did not specify exclusion criteria (Dalfra 2009; Homko 2002; Kestila 2007; Perez‐Ferre 2010).
Interventions and comparisons
We assessed the 11 included trials under five different comparisons.
Telemedicine versus standard care for glucose monitoring
Five trials compared the use of telemedicine versus standard care in glucose monitoring (Dalfra 2009; Given 2015; Homko 2007; Homko 2012; Perez‐Ferre 2010). Women in the telemedicine groups of these trials transmitted their blood glucose measurements weekly (Dalfra 2009; Given 2015; Homko 2012; Perez‐Ferre 2010), or at least three times per week (Homko 2007). The blood glucose measurements were sent to healthcare practitioners for review, using varying technologies, including: an interfacing device that converted values recorded by a blood glucose meter into audio tones which were sent via a normal telephone receiver to an Internet‐based server (Dalfra 2009); a cellular telephone (with an interfacing device) that converted values recorded by a blood glucose meter to messages sent via a short message service (SMS) to an Internet‐based application (Perez‐Ferre 2010); a telemedicine hub (with a small screen and three buttons to collect and transmit data) which sent stored values recorded by a blood glucose meter to a central server (Given 2015); and a computer using a web‐based disease management interactive healthcare delivery system composed of a secure Internet server and a database (Homko 2007; Homko 2012 (with the option of telephone communication (Homko 2012)). Following review of the information, women received feedback from the healthcare practitioners via telephone voice messages (Dalfra 2009), cellular telephone text messages (Rey 1997), telephone calls (Given 2015), or written messages on a web‐based system (Homko 2007; Homko 2012).
Regimens varied between trials: in the Perez‐Ferre 2010 trial, women in both groups were asked to self‐monitor their blood glucose six times daily during the first week, and then (if glycaemic control was achieved) three times daily or every other day. The Dalfra 2009, Homko 2007, and Homko 2012 trials requested self‐monitoring four times daily, while in Given 2015 it was required up to seven times a day. Medical examinations or specialist diabetes clinic visits occurred at least every two weeks in the Given 2015, Homko 2007 and Homko 2012 trials, and once a month in the Perez‐Ferre 2010 trial. In Dalfra 2009, women in the standard care group had visits every two weeks, while women in the telemedicine group had monthly visits.
Self‐monitoring versus periodic glucose monitoring
Two trials compared self‐monitoring of blood glucose with periodic (outpatient) monitoring (Homko 2002; Rey 1997). Women in the self‐monitoring groups were instructed to measure their blood glucose every day, alternating between three times daily (one hour after each meal) and four times daily (before each meal and at bed time) (Rey 1997); or four times daily (fasting and one hour after each meal) four times per week (Homko 2002). Women in the periodic monitoring groups had their blood glucose (fasting or one hour post breakfast, or both (Rey 1997), or fasting and one hour post meal (Homko 2002)) measured at each antenatal visit (Homko 2002) or at outpatient clinic visits every two weeks (Rey 1997).
Continuous glucose monitoring system versus self‐monitoring of glucose
Two trials compared the use of continuous glucose monitoring system (CGMS) with self‐monitoring of blood glucose, to determine subsequent management (i.e. need for anti‐diabetic drug therapy) within a week after initiating monitoring (Kestila 2007; Wei 2016). One of the trials assessed both early (24 to 28 weeks' gestation) and late (28 to 36 weeks' gestation) CGMS (Wei 2016). All women in both groups were taught to perform self‐monitoring of blood glucose, and were instructed to measure their blood glucose four times (Wei 2016), or five times (Kestila 2007), daily.
Modem versus telephone transmission for glucose monitoring
One trial compared the transmission of blood glucose data from a meter to an Endocrinology and Metabolism Clinic via a modem, with the transmission of data via telephone calls directly to clinic personnel (Kruger 2003). In both groups, women were instructed to measure their blood glucose five times daily (before breakfast, one hour after each meal (three meals), and before bed), and to report their concentrations daily for the first two weeks, and then weekly thereafter; the data were reviewed by clinic personnel who provided feedback and guidance to the women via the telephone (Kruger 2003).
Postprandial versus preprandial glucose monitoring
One trial compared daily monitoring of blood glucose before breakfast (fasting) and one hour after each meal (postprandial monitoring), with daily monitoring of fasting, before meal and bed time blood glucose (preprandial monitoring) (De Veciana 1995).
Funding and declarations of interest
Seven trials received funding support from non‐commercial organisations:
Given 2015: the Department for Employment and Learning for Northern Ireland and the Derry City Council, Ireland;
Homko 2002: the General Clinical Research Center Branch of the National Center for Research Resources, USA;
Homko 2007: the National Institute of Nursing Research, National Institutes of Health, USA;
Homko 2012: the National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health USA;
Kestila 2007 the Turku University Central Hospital Research Fund and the Foundation of Gynaecologists and Obstetricians, Finland;
Perez‐Ferre 2010: 'Fundacion para Estudios Metabolicos'; and
Wei 2016: the Social Development Project of JiangSu Province, China.
Three trials received some support from commercial partners: Homko 2002 was provided with glucose meters by LifeScan Inc; Kruger 2003 was provided with a grant, and glucose meters from Roche Diagnostics; and Rey 1997 was supported by Lilly Canada.
Two trials did not report any funding sources (Dalfra 2009; De Veciana 1995).
Given 2015 reported that one author had received research funding from Nova Biomedical (a manufacturer of glucose meters); and Homko 2012 reported that one author had stock ownership in, and another was a consultant for, Insight Telehealth Systems. Perez‐Ferre 2010 and Wei 2016 reported that the authors had no conflicts of interest. The other seven trials did not report on declarations of interest (Dalfra 2009; De Veciana 1995; Homko 2002; Homko 2007; Kestila 2007; Kruger 2003; Perez‐Ferre 2010).
For further details, see Characteristics of included studies.
Excluded studies
We excluded five studies (Bancroft 2000; Bartholomew 2015; Clarke 2005; Elnour 2008; Fung 1996). Two assessed treatment strategies for women with GDM (Bancroft 2000; Elnour 2008), two were cross‐over trials (Bartholomew 2015; Clarke 2005), and one included pregnant women (but not specifically women with GDM) (Fung 1996).
For further details, see Characteristics of excluded studies.
Risk of bias in included studies
Overall, we judged the trials to be at moderate to high risk of bias; lack of methodological detail led to 'unclear' risk of bias judgements across many of the domains (See Figure 2; Figure 3).
2.
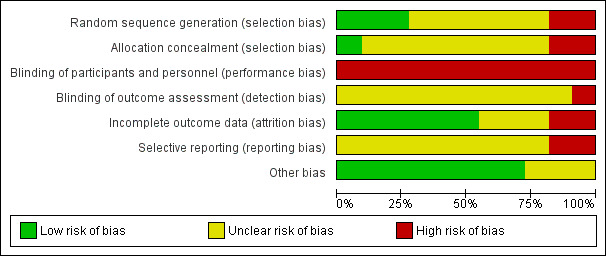
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies
3.
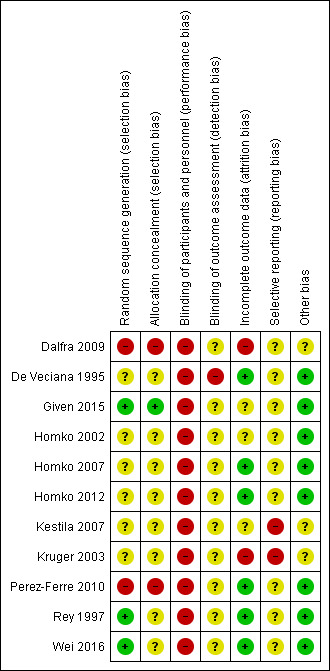
Risk of bias summary: review authors' judgements about each risk of bias item for each included study
Allocation
We judged one of the trials to be at low risk of selection bias, because it used an adequate method for sequence generation (random allocation software) and allocation concealment (an independent research secretary) (Given 2015). While two further trials detailed adequate methods for sequence generation (use of computer‐generated tables of random numbers), they did not detail methods for concealment of allocation, and thus we judged them to be at an unclear risk of selection bias (Rey 1997; Wei 2016).
Six of the trials did not provide sufficient detail regarding sequence generation or allocation concealment and therefore we judged them to be at an unclear risk of selection bias (De Veciana 1995; Homko 2002; Homko 2007; Homko 2012; Kestila 2007; Kruger 2003). The final two trials were judged to be at high risk of selection bias, with one trial using alternate allocation (Dalfra 2009), and another allocating a subgroup of women (those most likely to require treatment) to the intervention group (Perez‐Ferre 2010).
Blinding
We considered all of the 11 trials to be at a high risk of performance bias as, due to the nature of the interventions, it was not considered feasible for women or study personnel to be blinded (Dalfra 2009; De Veciana 1995; Given 2015; Homko 2002; Homko 2007; Homko 2012; Kestila 2007; Kruger 2003; Perez‐Ferre 2010; Rey 1997; Wei 2016).
Only one of the trials specifically detailed that it was unblinded, and this was also judged to be at high risk of detection bias (De Veciana 1995). In the other 10 trials, risk of detection bias was considered unclear, as no details were provided regarding whether outcome assessors could be blinded (Dalfra 2009; Given 2015; Homko 2002; Homko 2007; Homko 2012; Kestila 2007; Kruger 2003; Perez‐Ferre 2010; Rey 1997; Wei 2016).
Incomplete outcome data
We judged six of the trials to be at low risk of attrition bias, with either no missing outcome data (De Veciana 1995), or missing outcome data balanced in numbers across groups and/or similar reasons for missing data across groups (Homko 2007; Homko 2012; Perez‐Ferre 2010; Rey 1997; Wei 2016). We judged three trials to be at unclear risk of attrition bias, with insufficient reporting of attrition or exclusions to permit clear judgements (Given 2015; Homko 2002; Kestila 2007). We judged the other two trials to be at a high risk of attrition bias, with an imbalance in numbers or reasons for missing data across groups (Dalfra 2009), or a high proportion of missing outcome data (Kruger 2003).
Selective reporting
We judged nine of the trials to be at an unclear risk of reporting bias (Dalfra 2009; De Veciana 1995; Given 2015; Homko 2002; Homko 2007; Homko 2012; Perez‐Ferre 2010; Rey 1997; Wei 2016), as no trial protocols were available to help us assess whether the published reports included all prespecified outcomes. We judged the other two trials to be at a high risk of reporting bias, as they reported outcomes of interest incompletely (providing only narrative summaries in text; or P values), which meant they could not be entered in meta‐analyses (Kestila 2007; Kruger 2003), or did not present all of the prespecified outcomes (as per the 'Methods' section of the published report) (Kestila 2007).
Other potential sources of bias
In eight of the trials, there were no obvious sources of other bias (De Veciana 1995; Given 2015; Homko 2002; Homko 2007; Homko 2012; Perez‐Ferre 2010; Rey 1997; Wei 2016). We judged risk of other bias to be unclear in three of the trials, due to the lack of methodological detail provided (Dalfra 2009; Kestila 2007), or lack of information provided regarding the baseline characteristics of the women (Kruger 2003), or both.
Effects of interventions
See: Table 1; Table 2; Table 3; Table 4; Table 5; Table 6
Summary of findings for the main comparison. Telemedicine versus standard care for glucose monitoring for gestational diabetes during pregnancy (effect on mother).
| Telemedicine versus standard care for glucose monitoring for gestational diabetes during pregnancy (effect on mother) | ||||||
| Patient or population: women with gestational diabetes mellitus Setting: 2 RCTs in USA; 1 RCT each in Italy, Ireland and Spain set in clinics or hospitals Intervention: telemedicine Comparison: standard care | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Risk with standard care | Risk with telemedicine | |||||
| Hypertensive disorders of pregnancy including pre‐eclampsia, gestational hypertension and eclampsia | Study population | RR 1.49 (0.69 to 3.20) | 275 (4 RCTs) | ⊕⊝⊝⊝ VERY LOW1,2 | ||
| 58 per 1000 | 87 per 1000 (40 to 187) | |||||
| Caesarean section | Study population | RR 1.05 (0.72 to 1.53) | 478 (5 RCTs) | ⊕⊝⊝⊝ VERY LOW3,4,5 | ||
| 444 per 1000 | 467 per 1000 (320 to 680) | |||||
| Development of type 2 diabetes | Study population | not estimable | (0 RCTs) | ‐ | None of the included RCTs reported this outcome | |
| 0 per 1000 | 0 per 1000 (0 to 0) | |||||
| Induction of labour | Study population | RR 1.06 (0.63 to 1.77) | 47 (1 RCT) | ⊕⊝⊝⊝ VERY LOW 2,6 | ||
| 538 per 1000 | 571 per 1000 (339 to 953) | |||||
| Perineal trauma | Study population | Not estimable | (0 RCTs) | ‐ | None of the included RCTs reported this outcome | |
| 0 per 1000 | 0 per 1000 (0 to 0) | |||||
| Postnatal depression | Study population | Not estimable | (0 RCTs) | ‐ | None of the included RCTs reported this outcome | |
| 0 per 1000 | 0 per 1000 (0 to 0) | |||||
| Postnatal weight retention or return to pre‐pregnancy weight | Study population | Not estimable | (0 RCTs) | ‐ | None of the included RCTs reported this outcome | |
| 0 per 1000 | 0 per 1000 (0 to 0) | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RCT: randomised controlled trial; RR: risk ratio | ||||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: we are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low quality: our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low quality: we have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | ||||||
1Study limitations (downgraded 1 level): 4 RCTs with potentially serious or very serious design limitations 2Imprecision (downgraded 2 levels): wide confidence interval crossing the line of no effect, few events and small sample size(s) 3Study limitations (downgraded 2 levels): 5 RCTs with potentially serious or very serious design limitations (> 40% of weight from 2 RCTs with serious or very serious design limitations) 4Imprecision (downgraded 1 level): wide confidence interval crossing the line of no effect 5Inconsistency (downgraded 1 level): statistical heterogeneity (I² = 62%) 6Study limitations (downgraded 1 level): 1 RCT with potentially serious design limitations
Summary of findings 2. Telemedicine versus standard care for glucose monitoring in gestational diabetes during pregnancy (effect on child).
| Telemedicine versus standard care for glucose monitoring in gestational diabetes during pregnancy (effect on child) | ||||||
| Patient or population: women with gestational diabetes mellitus Setting: 2 RCTs in USA; 1 RCT each in Italy, Ireland, and Spain set in clinics or hospitals Intervention: telemedicine Comparison: standard care | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Risk with standard care | Risk with telemedicine | |||||
| Perinatal mortality (including stillbirth or neonatal death) | Study population | ‐ | 131 (2 RCTs) | ⊕⊝⊝⊝ VERY LOW1,2 | There were no perinatal deaths in 2 RCTs | |
| See comment | See comment | |||||
| Large‐for‐gestational age | Study population | RR 1.41 (0.76 to 2.64) | 228 (3 RCTs) | ⊕⊝⊝⊝ VERY LOW3,4 | ||
| 126 per 1000 | 178 per 1000 (96 to 333) | |||||
| Death or serious morbidity composite | Study population | RR 1.06 (0.68 to 1.66) | 57 (1 RCT) | ⊕⊝⊝⊝ VERY LOW4,5 | ||
| 560 per 1000 | 594 per 1000 (381 to 930) | |||||
| Neurosensory disability | Study population | Not estimable | (0 RCTS) | ‐ | None of the included RCTs reported this outcome | |
| 0 per 100 | 0 per 1000 (0 to 0) |
|||||
| Hypoglycaemia | Study population | RR 1.14 (0.48 to 2.72) | 198 (3 RCTs) | ⊕⊝⊝⊝ VERY LOW4,6 | ||
| 82 per 100 | 94 per 1000 (40 to 224) | |||||
| Adiposity (e.g. BMI, skinfold thickness, fat mass) | Study population | Not estimable | (0 RCTs) | ‐ | None of the included RCTs reported this outcome | |
| 0 per 1000 | 0 per 1000 (0 to 0) | |||||
| Type 2 diabetes | Study population | Not estimable | (0 RCTs) | ‐ | None of the included RCTs reported this outcome | |
| 0 per 1000 | 0 per 1000 (0 to 0) | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). BMI: body mass index;CI: confidence interval; RCT: randomised controlled trial; RR: risk ratio | ||||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: we are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low quality: our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low quality: we have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | ||||||
1Study limitations (downgraded 1 level): 2 RCTs with potentially serious design limitations 2Imprecision (downgraded 2 levels): no events and small sample size(s) 3Study limitations (downgraded 2 levels): 2 RCTs with potentially serious design limitations, and 1 RCT with serious or very serious design limitations (> 25% of weight) 4Imprecision (downgraded 2 levels): wide confidence interval crossing the line of no effect, (few events), small sample size(s) 5Study limitations (downgraded 1 level): 1 RCT with potentially serious design limitations 6Study limitations (downgraded 1 level): 2 RCTs with potentially serious design limitations, and 1 RCT with serious or very serious design limitations (< 7% of weight)
Summary of findings 3. Self‐monitoring versus periodic glucose monitoring for gestational diabetes during pregnancy (effect on mother).
| Self‐monitoring versus periodic glucose monitoring for gestational diabetes during pregnancy (effect on mother) | ||||||
|
Patient or population: women with gestational diabetes mellitus
Setting: 1 RCT in Canda, 1 RCT in USA set in clinics or hospitals Intervention: self‐monitoring of glucose Comparison: periodic glucose monitoring | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Risk with periodic glucose monitoring | Risk with self‐monitoring of glucose | |||||
| Hypertensive disorders of pregnancy: pre‐eclampsia | Study population | RR 0.17 (0.01 to 3.49) | 58 (1 RCT) | ⊕⊝⊝⊝ VERY LOW1,2 | ||
| 74 per 1000 | 13 per 1000 (1 to 259) | |||||
| Caesarean section | Study population | RR 1.18 (0.61 to 2.27) | 400 (2 RCTs) | ⊕⊕⊝⊝ LOW3,4,5 | ||
| 228 per 1000 | 270 per 1000 (139 to 519) | |||||
| Development of type 2 diabetes | Study population | Not estimable | (0 RCTs) | ‐ | Neither of the included RCTs reported this outcome | |
| 0 per 1000 | 0 per 1000 (0 to 0) | |||||
| Induction of labour | Study population | Not estimable | (0 RCTs) | ‐ | Neither of the RCTs reported this outcome | |
| 0 per 1000 | 0 per 1000 (0 to 0) | |||||
| Perineal trauma | Study population | Not estimable | (0 RCTs) | ‐ | Neither of the included RCTs reported this outcome | |
| 0 per 1000 | 0 per 1000 (0 to 0) | |||||
| Postnatal depression | Study population | Not estimable | (0 RCTs) | ‐ | Neither of the included RCTs reported this outcome | |
| 0 per 1000 | 0 per 1000 (0 to 0) | |||||
| Postnatal weight retention or return to pre‐pregnancy weight | Study population | Not estimable | (0 RCTs) | ‐ | Neither of the included RCTs reported this outcome | |
| 0 per 1000 | 0 per 1000 (0 to 0) | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RCT: randomised controlled trial; RR: risk ratio | ||||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: we are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low quality: our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low quality: we have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | ||||||
1Study limitations (downgraded 1 level): 1 RCT with potentially serious design limitations 2Imprecision (downgraded 2 levels): wide confidence interval crossing the line of no effect, few events and small sample size 3Study limitations (downgraded 1 level): 2 RCTs with potentially serious design limitations 4Imprecision (downgraded 1 level): wide confidence interval crossing the line of no effect 5Inconsistency: did not downgraded for statistical heterogeneity (I² = 49%)
Summary of findings 4. Self‐monitoring versus periodic for glucose monitoring for gestation diabetes during pregnancy (effect on child).
| Self‐monitoring versus periodic for glucose monitoring for gestation diabetes during pregnancy (effect on child) | ||||||
|
Patient or population: women with gestational diabetes mellitus
Setting: 1 RCT in Canda, 1 RCT in USA set in clinics or hospitals Intervention: self‐monitoring of glucose Comparison: periodic glucose monitoring | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Risk with periodic glucose monitoring | Risk with self‐monitoring of glucose | |||||
| Perinatal mortality (stillbirth or neonatal death) | Study population | RR 1.54 (0.21 to 11.24) | 400 (2 RCTs) | ⊕⊝⊝⊝ VERY LOW1,2 | ||
| 5 per 1000 | 8 per 1000 (1 to 57) | |||||
| Large‐for‐gestational age | Study population | RR 0.82 (0.50 to 1.37) | 400 (2 RCTs) | ⊕⊕⊝⊝ LOW1,3 | ||
| 142 per 1000 | 117 per 1000 (71 to 195) | |||||
| Death or serious morbidity composite | Study population | Not estimable | (0 RCTs) | ‐ | Neither of the included RCTs reported this outcome | |
| 0 per 1000 | 0 per 1000 (0 to 0) | |||||
| Neurosensory disability | Study population | Not estimable | (0 RCTs) | ‐ | Neither of the included RCTs reported this outcome | |
| 0 per 1000 | 0 per 1000 (0 to 0) | |||||
| Hypoglycaemia | Study population | RR 0.64 (0.39 to 1.06) | 391 (2 RCTs) | ⊕⊕⊝⊝ LOW1,3 | ||
| 173 per 1000 | 111 per 1000 (67 to 183) | |||||
| Adiposity (e.g. BMI, skinfold thickness, fat mass) | Study population | Not estimable | (0 RCTs) | ‐ | Neither of the included RCTs reported this outcome | |
| 0 per 1000 | 0 per 1000 (0 to 0) | |||||
| Type 2 diabetes | Study population | Not estimable | (0 RCTs) | ‐ | Neither of the included RCTs reported this outcome | |
| 0 per 1000 | 0 per 1000 (0 to 0) | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). BMI: body mass index;CI: confidence interval; RCT: randomised controlled trial; RR: risk ratio | ||||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: we are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low quality: our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low quality: we have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | ||||||
1Study limitations (downgraded 1 level): 2 RCTs with potentially serious design limitations 2Imprecision (downgraded 2 levels): wide confidence interval crossing the line of no effect and few events 3Imprecision (downgraded 1 level): wide confidence interval crossing the line of no effect
Summary of findings 5. Continuous glucose monitoring system versus self‐monitoring of glucose for gestational diabetes during pregnancy (effect on mother).
| Continuous glucose monitoring system versus self‐monitoring of glucose for gestational diabetes during pregnancy (effect on mother) | ||||||
|
Patient or population: women with gestational diabetes mellitus
Setting: 1 RCT in Finland, 1 RCT in China set in clinics or hospitals Intervention: continuous glucose monitoring system Comparison: self‐monitoring of glucose | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Risk with self‐monitoring of glucose | Risk with continuous glucose monitoring system | |||||
| Hypertensive disorders of pregnancy | Study population | Not estimable | (0 RCTs) | ‐ | Neither of the included RCTs reported this outcome | |
| 0 per 1000 | 0 per 1000 (0 to 0) | |||||
| Caesarean section | Study population | RR 0.91 (0.68 to 1.20) | 179 (2 RCTs) | ⊕⊕⊝⊝ VERY LOW1,2 | ||
| 500 per 1000 | 455 per 1000 (340 to 600) | |||||
| Development of type 2 diabetes | Study population | Not estimable | (0 RCTs) | ‐ | Neither of the included RCTs reported this outcome | |
| 0 per 1000 | 0 per 1000 (0 to 0) | |||||
| Induction of labour | Study population | Not estimable | (0 RCTs) | ‐ | Neither of the included RCTs reported this outcome | |
| 0 per 1000 | 0 per 1000 (0 to 0) | |||||
| Perineal trauma | Study population | Not estimable | (0 RCTs) | ‐ | Neither of the included RCTs reported this outcome | |
| 0 per 1000 | 0 per 1000 (0 to 0) | |||||
| Postnatal depression | Study population | Not estimable | (0 RCTs) | ‐ | Neither of the included RCTs reported this outcome | |
| 0 per 1000 | 0 per 1000 (0 to 0) | |||||
| Postnatal weight retention or return to pre‐pregnancy weight | Study population | Not estimable | (0 RCTs) | ‐ | Neither of the included RCTs reported this outcome | |
| 0 per 1000 | 0 per 1000 (0 to 0) | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RCT: randomised controlled trial; RR: risk ratio | ||||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: we are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low quality: our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low quality: we have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | ||||||
1Study limitations (downgraded 1 level): 2 RCTs with potentially serious design limitations 2Inconsistency (downgraded 1 level): wide confidence interval crossing the line of no effect and small sample sizes
Summary of findings 6. Continuous glucose monitoring system versus self‐monitoring of glucose for gestational diabetes during pregnancy (effect on child).
| Continuous glucose monitoring system versus self‐monitoring of glucose for gestational diabetes during pregnancy (effect on child) | ||||||
|
Patient or population: women with gestational diabetes mellitus
Setting: 1 RCT in Finland, 1 RCT in China set in clinics or hospitals Intervention: continuous glucose monitoring system Comparison: self‐monitoring of glucose | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Risk with self‐monitoring of glucose | Risk with continuous glucose monitoring system | |||||
| Perinatal mortality (stillbirth or neonatal death) | Study population | ‐ | 179 (2 RCTs) | ⊕⊕⊝⊝ VERY LOW1,2 | There were no perinatal deaths in the 2 RCTs | |
| See comment | See comment | |||||
| Large‐for‐gestational age | Study population | RR 0.67 (0.43 to 1.05) | 106 (1 RCT) | ⊕⊝⊝⊝ VERY LOW3,4 | ||
| 527 per 1000 | 353 per 1000 (227 to 554) | |||||
| Death or serious morbidity composite | Study population | Not estimable | (0 RCTs) | ‐ | Neither of the included RCTs reported this outcome | |
| 0 per 1000 | 0 per 1000 (0 to 0) | |||||
| Neurosensory disability | Study population | Not estimable | (0 RCTs) | ‐ | Neither of the included RCTs reported this outcome | |
| 0 per 1000 | 0 per 1000 (0 to 0) | |||||
| Hypoglycaemia | Study population | RR 0.79 (0.35 to 1.78) | 179 (2 RCTs) | ⊕⊝⊝⊝ VERY LOW1,5 | ||
| 130 per 1000 | 103 per 1000 (46 to 232) | |||||
| Adiposity (e.g. BMI, skinfold thickness, fat mass) | Study population | Not estimable | (0 RCTs) | ‐ | Neither of the included RCTs reported this outcome | |
| 0 per 1000 | 0 per 1000 (0 to 0) | |||||
| Type 2 diabetes | Study population | Not estimable | (0 RCTs) | ‐ | Neither of the included RCTs reported this outcome | |
| 0 per 1000 | 0 per 1000 (0 to 0) | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). BMI: body mass index; CI: confidence interval; RCT: randomised controlled trial; RR: risk ratio | ||||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: we are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low quality: our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low quality: we have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | ||||||
1Study limitations (downgraded 1 level): 2 RCTs with potentially serious design limitations 2Inconsistency (downgraded 2 levels): no events and small sample sizes 3Study limitations (downgraded 1 level): 1 RCT with potentially serious design limitations 4Inconsistency (downgraded 2 levels): wide confidence interval crossing the line of no effect and small sample size 5Inconsistency (downgraded 2 levels): wide confidence interval crossing the line of no effect, few events and small sample sizes
Telemedicine versus standard care for glucose monitoring
Five trials were included in this comparison (Dalfra 2009; Given 2015; Homko 2007; Homko 2012; Perez‐Ferre 2010).
Primary outcomes
For the mother
No clear differences between the telemedicine and standard care groups were observed for:
pre‐eclampsia or pregnancy‐induced hypertension (risk ratio (RR) 1.49, 95% confidence interval (CI) 0.69 to 3.20; 275 participants, 4 RCTs; very low quality evidence; Analysis 1.1); or
caesarean section (average RR 1.05, 95% CI 0.72 to 1.53; 478 participants, 5 RCTs; Tau² = 0.11; Chi² = 10.51; I² = 62%; very low quality evidence; Analysis 1.2).
1.1. Analysis.
Comparison 1 Telemedicine versus standard care for glucose monitoring, Outcome 1 Hypertensive disorders of pregnancy.
1.2. Analysis.
Comparison 1 Telemedicine versus standard care for glucose monitoring, Outcome 2 Caesarean section.
None of the trials reported on the development of type 2 diabetes.
For the child
There were no perinatal deaths in the two trials that reported on this outcome (131 participants, 2 RCTs; very low quality evidence; Analysis 1.3).
1.3. Analysis.
Comparison 1 Telemedicine versus standard care for glucose monitoring, Outcome 3 Perinatal mortality.
There were no clear differences between the telemedicine and standard care groups for:
large‐for‐gestational age (RR 1.41, 95% CI 0.76 to 2.64; 228 participants, 3 RCTs; very low quality evidence; Analysis 1.4); or
death or serious morbidity composite outcome (of neonatal intensive care unit admission, large‐for‐gestational age, respiratory outcomes (hyaline membrane disease, transient tachypnoea, need for respiratory support) hypoglycaemia, and hyperbilirubinaemia) (RR 1.06, 95% CI 0.68 to 1.66; 57 participants, 1 RCT; very low quality evidence; Analysis 1.5).
1.4. Analysis.
Comparison 1 Telemedicine versus standard care for glucose monitoring, Outcome 4 Large‐for‐gestational age.
1.5. Analysis.
Comparison 1 Telemedicine versus standard care for glucose monitoring, Outcome 5 Death or serious morbidity composite.
None of the trials reported on neurosensory disability.
Secondary outcomes
For the mother
No clear differences between the telemedicine and standard care groups were observed for:
operative vaginal birth (RR 0.50, 95% CI 0.11 to 2.30; 47 participants, 1 RCT; Analysis 1.6) ‐ this outcome was not prespecified;
induction of labour (RR 1.06, 95% CI 0.63 to 1.77; 47 participants, 1 RCT; very low quality evidence;Analysis 1.7);
placental abruption (RR 0.88, 95% CI 0.12 to 6.42; 154 participants, 2 RCTs; Analysis 1.8);
-
gestational weight gain (mean difference (MD) ‐0.47 kg, 95% CI ‐1.50 to 0.55; 300 participants, 2 RCTs; Analysis 1.9);
weight at 36 weeks (MD 5.50 kg, 95% CI ‐5.69 to 16.69; 44 participants, 1 RCT; Analysis 1.10);
adherence to the intervention (Analysis 1.11): appointments attended (MD 5.20, 95% CI ‐2.27 to 12.67; 47 participants, 1 RCT), average daily self‐monitoring of blood glucose frequency (as measured by meter memory (MD 0.50, 95% CI ‐0.42 to 1.42; 44 participants, 1 RCT) or diary (MD 0.10, 95% CI ‐0.66 to 0.86; 45 participants, 1 RCT), or frequency of monitoring as measured by number of data points (MD 21.10, 95% CI ‐9.33 to 51.53; 57 participants, 1 RCT), or number of data sets (MD 1.20, 95% CI ‐12.32 to 14.72; 74 participants, 1 RCT);
-
use of additional pharmacotherapy:
the use of oral anti‐diabetic agents (RR 0.85, 95% CI 0.50 to 1.42; 184 participants, 3 RCTs; Analysis 1.13);
the combined use of insulin and oral anti‐diabetic agents (RR 1.24, 95% CI 0.19 to 8.06; 47 participants, 1 RCT; Analysis 1.13);
-
maternal hypoglycaemia (no events; 203 participants, 1 RCT; Analysis 1.14);
self‐monitored glucose episodes < 3.9 mmol/L (MD ‐0.10%, 95% CI ‐1.64 to 1.44; 44 participants, 1 RCT; Analysis 1.15);
HbA1c less than 5.8% (RR 1.00, 95% CI 0.96 to 1.04; 97 participants, 1 RCT; Analysis 1.17);
HbA1c at 36 weeks (MD 0.20%, 95% CI ‐2.03 to 2.43; 30 participants, 1 RCT; Analysis 1.18);
self‐monitored blood glucose (MD 0.00 mmol/L, 95% CI ‐0.30 to 0.30; 44 participants, 1 RCT; Analysis 1.19);
fasting blood glucose (MD ‐0.50 mg/dL, 95% CI ‐5.38 to 4.38; 131 participants, 2 RCTs; Tau² = 5.54; Chi² = 1.80; I² = 44%; Analysis 1.20); and
2‐hour postprandial blood glucose (MD ‐0.21 mg/dL, 95% CI ‐5.09 to 4.67; 131 participants, 2 RCTs; Analysis 1.20).
1.6. Analysis.
Comparison 1 Telemedicine versus standard care for glucose monitoring, Outcome 6 Operative vaginal birth (not a prespecified outcome).
1.7. Analysis.
Comparison 1 Telemedicine versus standard care for glucose monitoring, Outcome 7 Induction of labour.
1.8. Analysis.
Comparison 1 Telemedicine versus standard care for glucose monitoring, Outcome 8 Placental abruption.
1.9. Analysis.
Comparison 1 Telemedicine versus standard care for glucose monitoring, Outcome 9 Gestational weight gain (kg).
1.10. Analysis.
Comparison 1 Telemedicine versus standard care for glucose monitoring, Outcome 10 Weight at 36 weeks (kg).
1.11. Analysis.
Comparison 1 Telemedicine versus standard care for glucose monitoring, Outcome 11 Adherence to the intervention.
1.13. Analysis.
Comparison 1 Telemedicine versus standard care for glucose monitoring, Outcome 13 Use of additional pharmacotherapy.
1.14. Analysis.
Comparison 1 Telemedicine versus standard care for glucose monitoring, Outcome 14 Maternal hypoglycaemia.
1.15. Analysis.
Comparison 1 Telemedicine versus standard care for glucose monitoring, Outcome 15 Maternal hypoglycaemia: self‐monitored blood glucose episodes hypoglycaemic (< 3.9 mmol/L) (%).
1.17. Analysis.
Comparison 1 Telemedicine versus standard care for glucose monitoring, Outcome 17 Glycaemic control: HbA1c < 5.8%.
1.18. Analysis.
Comparison 1 Telemedicine versus standard care for glucose monitoring, Outcome 18 Glycaemic control: HbA1c at 36 weeks (mmol/mol).
1.19. Analysis.
Comparison 1 Telemedicine versus standard care for glucose monitoring, Outcome 19 Glycaemic control: self‐monitored blood glucose (mmol/L).
1.20. Analysis.
Comparison 1 Telemedicine versus standard care for glucose monitoring, Outcome 20 Glycaemic control: fasting and 2‐hour post‐prandial blood glucose (mg/dL).
Women in the telemedicine group had an improved sense of well‐being and quality of life, as measured by the Diabetes Empowerment Scale (DES), compared with women in the standard care group:
for total score (MD 0.40, 95% CI 0.14 to 0.66; 57 participants, 1 RCT; Analysis 1.12), and
-
for subscale scores:
managing the psychosocial aspects of diabetes (MD 0.50, 95% CI 0.21 to 0.79; 57 participants, 1 RCT; Analysis 1.12),
assessing dissatisfaction and readiness to change (MD 0.40, 95% CI 0.14 to 0.66; 57 participants, 1 RCT; Analysis 1.12), and
setting and achieving diabetes goals (MD 0.30, 95% CI ‐0.04 to 0.64; 57 participants, 1 RCT; Analysis 1.12).
1.12. Analysis.
Comparison 1 Telemedicine versus standard care for glucose monitoring, Outcome 12 Sense of well‐being and quality of life: DES: Diabetes Empowerment Scale.
There was an approximate 50% relative increase in additional pharmacotherapy in the form of insulin use for women in the telemedicine group, compared with those in the standard care group (RR 1.52, 95% CI 1.18 to 1.96; 484 participants, 5 RCTs; Analysis 1.13), and improved glycaemic control with lower HbA1c levels were observed among women in the telemedicine group compared with those in the standard care group (MD ‐0.15%, 95% CI ‐0.26 to ‐0.04; 357 participants, 3 RCTs; Analysis 1.16).
1.16. Analysis.
Comparison 1 Telemedicine versus standard care for glucose monitoring, Outcome 16 Glycaemic control: HbA1c (%).
With regard to adherence, Dalfra 2009 reported that "Most of the women with diabetes sent their glycaemic profile weekly (76%), while 24% did so more frequently (2–4 times a week);" (this included women in the trial with type 1 diabetes). Homko 2007 noted that "Seven women (22%) in the intervention group never accessed the system," and that "Rates of appointment adherence were similar between the two groups (94% for women in the control group and 90% for women in the telemedicine group)". Homko 2012 reported that "Of the 36 women in the intervention group available for follow‐up until delivery, two women (6%) never used the system, and an additional five women (14%) used the system infrequently (< 10 transmissions)".
With regard to quality of life, although Dalfra 2009 also assessed women using the following questionnaires: CES‐D for depression, SF‐36 for health‐related quality of life, and Stress and Distress for the impact of diabetes, the trial authors did not report the data separately for the women in the trial with GDM.
With regard to the women's views of the intervention, Dalfra 2009 did not report this information separately for the women with GDM, while Perez‐Ferre 2010 reported in the Discussion: "When the Telemedicine system was offered, patients accepted the proposal in a positive way and showed their satisfaction at the end of the follow‐up. They highly appreciated the possibility to communicate with the healthcare team as required".
None of the trials reported on the other secondary outcomes for the mother (perineal trauma; postpartum haemorrhage; postpartum infection; behaviour changes associated with the intervention; breastfeeding; mortality).
For the mother in the longer term
None of the trials reported on any secondary outcomes for the mother in the longer term.
For the fetus/neonate
No clear differences between the telemedicine and standard care groups were observed for:
stillbirth (RR 0.41, 95% CI 0.02 to 9.55; 178 participants, 3 RCTs; Analysis 1.21);
neonatal death (no events; 131 participants, 2 RCTs; Analysis 1.22);
gestational age at birth (MD 0.10 weeks, 95% CI ‐0.18 to 0.37; 478 participants, 5 RCTs; Analysis 1.23);
preterm birth (RR 0.66, 95% CI 0.31 to 1.39; 275 participants, 4 RCTs; Analysis 1.24);
macrosomia (average RR 1.43, 95% CI 0.27 to 7.52; 249 participants, 2 RCTs; Tau² = 0.98; Chi² = 3.09; I² = 68%; Analysis 1.25);
small‐for‐gestational age (no events; 91 participants, 1 RCT; Analysis 1.26);
birthweight (MD 63.13 g, 95% CI ‐32.32 to 158.59; 477 participants, 5 RCTs; Analysis 1.27);
head circumference (MD 0.70 cm, 95% CI 0.02 to 1.38; 45 participants, 1 RCT; Analysis 1.28);
length (MD 0.20 cm, 95% CI ‐1.34 to 1.74; 42 participants, 1 RCT; Analysis 1.29);
shoulder dystocia (RR 0.33, 95% CI 0.01 to 7.83; 142 participants, 2 RCTs; Analysis 1.30);
respiratory distress syndrome (RR 0.63, 95% CI 0.26 to 1.49; 176 participants, 3 RCTs) (Analysis 1.31);
neonatal hypoglycaemia (RR 1.14, 95% CI 0.48 to 2.72; 198 participants, 3 RCTs; very low quality evidence; Analysis 1.32);
neonatal hyperbilirubinaemia or jaundice (RR 1.09, 95% CI 0.59 to 2.01; 176 participants, 3 RCTs; Analysis 1.33);
neonatal hypocalcaemia (no events; 97 participants, 1 RCT; Analysis 1.34); or
polycythaemia (no events; 97 participants, 1 RCT; Analysis 1.35).
1.21. Analysis.
Comparison 1 Telemedicine versus standard care for glucose monitoring, Outcome 21 Stillbirth.
1.22. Analysis.
Comparison 1 Telemedicine versus standard care for glucose monitoring, Outcome 22 Neonatal death.
1.23. Analysis.
Comparison 1 Telemedicine versus standard care for glucose monitoring, Outcome 23 Gestational age at birth (weeks).
1.24. Analysis.
Comparison 1 Telemedicine versus standard care for glucose monitoring, Outcome 24 Preterm birth < 37 weeks.
1.25. Analysis.
Comparison 1 Telemedicine versus standard care for glucose monitoring, Outcome 25 Macrosomia.
1.26. Analysis.
Comparison 1 Telemedicine versus standard care for glucose monitoring, Outcome 26 Small‐for‐gestational age.
1.27. Analysis.
Comparison 1 Telemedicine versus standard care for glucose monitoring, Outcome 27 Birthweight (g).
1.28. Analysis.
Comparison 1 Telemedicine versus standard care for glucose monitoring, Outcome 28 Head circumference (cm).
1.29. Analysis.
Comparison 1 Telemedicine versus standard care for glucose monitoring, Outcome 29 Length (cm).
1.30. Analysis.
Comparison 1 Telemedicine versus standard care for glucose monitoring, Outcome 30 Shoulder dystocia.
1.31. Analysis.
Comparison 1 Telemedicine versus standard care for glucose monitoring, Outcome 31 Respiratory distress syndrome.
1.32. Analysis.
Comparison 1 Telemedicine versus standard care for glucose monitoring, Outcome 32 Neonatal hypoglycaemia.
1.33. Analysis.
Comparison 1 Telemedicine versus standard care for glucose monitoring, Outcome 33 Hyperbilirubinaemia or jaundice.
1.34. Analysis.
Comparison 1 Telemedicine versus standard care for glucose monitoring, Outcome 34 Hypocalcaemia.
1.35. Analysis.
Comparison 1 Telemedicine versus standard care for glucose monitoring, Outcome 35 Polycythaemia.
None of the trials reported on the other secondary outcomes for the fetus/neonate (Apgar score < 7 at five minutes; ponderal index; adiposity; nerve palsies; bone fractures).
For the child and adult
None of the trials reported on any secondary outcomes for the child and adult.
Use and costs of health services
No clear differences between the telemedicine and standard care groups were observed for:
number of hospital or health professional visits: face‐to‐face visits (MD ‐0.36 visits, 95% CI ‐0.92 to 0.20; 97 participants, 1 RCT; Analysis 1.36); or neonatal intensive care unit admission (RR 1.05, 95% CI 0.62 to 1.79; 176 participants, 3 RCTs; Analysis 1.38).
There was a reduction in unscheduled face‐to‐face visits among women in the telemedicine group, compared with those in the standard care group (MD ‐0.62 visits, 95% CI ‐1.05 to ‐0.19; 97 participants, 1 RCT; Analysis 1.37).
With regard to the number of hospital or health professional visits, Dalfra 2009 reported that "Only 23% of the patients with gestational diabetes required extra medical examinations. The control group had a medical examination every two weeks, each visit taking about 30 minutes. In all, the control women with gestational diabetes visited the diabetes clinic 44% more often than the women followed up with telemedicine".
1.36. Analysis.
Comparison 1 Telemedicine versus standard care for glucose monitoring, Outcome 36 Number of hospital or health professional visits: face‐to‐face visits.
1.38. Analysis.
Comparison 1 Telemedicine versus standard care for glucose monitoring, Outcome 38 Neonatal intensive care unit admission.
1.37. Analysis.
Comparison 1 Telemedicine versus standard care for glucose monitoring, Outcome 37 Number of hospital or health professional visits: unscheduled face‐to‐face visits.
For length of postnatal stay (baby), Homko 2012 reported that the neonates from the intervention group (N = 4) admitted to the neonatal intensive care unit had a shorter length of stay than those from the control group (N = 7) "(5.5 days vs. 9.7 days), but none of these differences was statistically significant".
With regard to costs associated with the intervention, Perez‐Ferre 2010 reported that "In our study, the telemedicine system not only made attention more convenient for the patient, it was also less expensive for the health system in terms of use of health professionals’ time".
None of the trials reported on the other secondary outcomes for the use and costs of health services (number of antenatal visits or admissions; length of antenatal stay; length of postnatal stay (mother); cost of maternal care; cost of offspring care; costs to families associated with the management provided).
Non prespecified outcomes
Dalfra 2009 also reported on composite outcomes 'neonatal morbidity' and 'maternal morbidity' and observed no clear difference between the telemedicine and standard care groups for either outcome (RR 1.52, 95% CI 0.53 to 4.38; 203 participants, 1 RCT; Analysis 1.39); (RR 0.49, 95% CI 0.13 to 1.79; 203 participants, 1 RCT; Analysis 1.40).
1.39. Analysis.
Comparison 1 Telemedicine versus standard care for glucose monitoring, Outcome 39 'Neonatal morbidity' (neonatal complications: e.g. hypoglycaemia, hyperbilirubinaemia, respiratory distress syndrome, shoulder dystocia, malformations) (not a prespecified outcome).
1.40. Analysis.
Comparison 1 Telemedicine versus standard care for glucose monitoring, Outcome 40 'Maternal morbidity' (maternal complications: gestational hypertension, pre‐eclampsia, eclampsia, hypoglycaemic episodes) (not a prespecified outcome).
Self‐monitoring versus periodic glucose monitoring
Two trials were included in this comparison (Homko 2002; Rey 1997).
Primary outcomes
For the mother
We observed no clear differences between the self‐monitoring and periodic glucose monitoring groups for:
pre‐eclampsia (RR 0.17, 95% CI 0.01 to 3.49; 58 participants, 1 RCT; very low quality evidence; Analysis 2.1); or
caesarean section (average RR 1.18, 95% CI 0.61 to 2.27; 400 participants, 2 RCTs; Tau² = 0.12; Chi² = 1.95; I² = 49%; low quality evidence; Analysis 2.2).
2.1. Analysis.
Comparison 2 Self‐monitoring versus periodic glucose monitoring, Outcome 1 Hypertensive disorders of pregnancy: pre‐eclampsia.
2.2. Analysis.
Comparison 2 Self‐monitoring versus periodic glucose monitoring, Outcome 2 Caesarean section.
Neither of the trials reported on the development of type 2 diabetes.
For the child
No clear differences between the self‐monitoring and period glucose monitoring groups were observed for:
perinatal mortality (RR 1.54, 95% CI 0.21 to 11.24; 400 participants, 2 RCTs; very low quality evidence; Analysis 2.3); or
large‐for‐gestational age (RR 0.82, 95% CI 0.50 to 1.37; 400 participants, 2 RCTs; low quality evidence; Analysis 2.4).
2.3. Analysis.
Comparison 2 Self‐monitoring versus periodic glucose monitoring, Outcome 3 Perinatal mortality.
2.4. Analysis.
Comparison 2 Self‐monitoring versus periodic glucose monitoring, Outcome 4 Large‐for‐gestational age.
Neither of the trials reported on death or serious morbidity composite, or neurosensory disability.
Secondary outcomes
For the mother
No clear differences between the self‐monitoring and periodic glucose monitoring groups were observed for:
placental abruption (RR 2.63, 95% CI 0.11 to 61.88; 58 participants, 1 RCT; Analysis 2.5);
postpartum haemorrhage (RR 2.63, 95% CI 0.11 to 61.88; 58 participants, 1 RCT; Analysis 2.6);
gestational weight gain (MD ‐5.50 lb, 95% CI ‐13.57 to 2.57; 58 participants, 1 RCT; Analysis 2.8);
-
adherence to the intervention (less than 70% adherence to home blood glucose measurements or diabetes outpatient clinic appointments) (RR 0.74, 95% CI 0.32 to 1.71; 342 participants, 1 RCT; Analysis 2.9);
Dietary Compliance Questionnaire total compliance score (MD 1.50, 95% CI ‐0.47 to 3.47; 58 participants, 1 RCT)
mean compliance score (MD 0.00, 95% CI ‐0.40 to 0.40; 58 participants, 1 RCT; Analysis 2.10);
-
sense of wellbeing and quality of life:
Diabetes Empowerment Scale (DES) scores overall (MD 3.70, 95% CI ‐2.08 to 9.48; 47 participants, 1 RCT);
scores for setting goals (MD 0.65, 95% CI ‐1.10 to 2.40; 47 participants, 1 RCT); problem solving (MD 1.35, 95% CI ‐0.37 to 3.07; 47 participants, 1 RCT); motivating oneself (MD 0.63, 95% CI ‐0.89 to 2.15; 47 participants, 1 RCT); obtaining support (MD 0.94, 95% CI ‐0.09 to 1.97; 47 participants, 1 RCT); and making decisions (MD 0.01, 95% CI ‐1.39 to 1.41; 47 participants, 1 RCT; Analysis 2.11);
appraisal of Diabetes Scale delta scores (emotional adjustment) (MD 1.20, 95% CI ‐0.88 to 3.28; 47 participants, 1 RCT; Analysis 2.12);
use of additional pharmacotherapy: use of insulin (RR 1.31, 95% CI 0.69 to 2.48; 400 participants, 2 RCTs; Analysis 2.13);
-
Glycaemic control during or at end of treatment:
preprandial blood glucose (MD 0.06 mmol/L, 95% CI ‐0.08 to 0.19; 360 participants, 2 RCTs; Tau² = 0.01; Chi² = 3.12; I² = 36%; Analysis 2.14); or
postprandial blood glucose (MD ‐0.09 mmol/L, 95% CI ‐0.60 to 0.42; 395 participants, 2 RCTs; Tau² = 0.17; Chi² = 15.03; I² = 87%; Analysis 2.15).
2.5. Analysis.
Comparison 2 Self‐monitoring versus periodic glucose monitoring, Outcome 5 Placental abruption.
2.6. Analysis.
Comparison 2 Self‐monitoring versus periodic glucose monitoring, Outcome 6 Postpartum haemorrhage.
2.8. Analysis.
Comparison 2 Self‐monitoring versus periodic glucose monitoring, Outcome 8 Gestational weight gain (lb).
2.9. Analysis.
Comparison 2 Self‐monitoring versus periodic glucose monitoring, Outcome 9 Adherence to the intervention: < 70% adherence to home blood glucose measurements or diabetes outpatient clinic appointments.
2.10. Analysis.
Comparison 2 Self‐monitoring versus periodic glucose monitoring, Outcome 10 Adherence to the intervention: Dietary Compliance Questionnaire.
2.11. Analysis.
Comparison 2 Self‐monitoring versus periodic glucose monitoring, Outcome 11 Sense of well‐being and quality of life: Diabetes Empowerment Scale delta scores.
2.12. Analysis.
Comparison 2 Self‐monitoring versus periodic glucose monitoring, Outcome 12 Sense of well‐being and quality of life: emotional adjustment: Appraisal of Diabetes Scale delta scores.
2.13. Analysis.
Comparison 2 Self‐monitoring versus periodic glucose monitoring, Outcome 13 Use of additional pharmacotherapy: insulin.
2.14. Analysis.
Comparison 2 Self‐monitoring versus periodic glucose monitoring, Outcome 14 Glycaemic control: pre‐prandial blood glucose (mmol/L).
2.15. Analysis.
Comparison 2 Self‐monitoring versus periodic glucose monitoring, Outcome 15 Glycaemic control: 1‐hour post‐prandial blood glucose (mmol/L).
Weekly weight gain was, on average, 100 g less for women in the self‐monitoring group compared with those in the periodic glucose monitoring group (MD ‐0.10 kg/week, 95% CI ‐0.15 to ‐0.05; 342 participants, 1 RCT; (Analysis 2.7).
2.7. Analysis.
Comparison 2 Self‐monitoring versus periodic glucose monitoring, Outcome 7 Gestational weight gain (kg/week).
Neither trial reported on the other secondary outcomes for the mother (induction of labour; perineal trauma; postpartum infection; behavioural changes associated with the intervention; views of the intervention; breastfeeding; maternal hypoglycaemia; mortality).
For the mother in the longer term
Neither trial reported on any of the secondary outcomes for the mother in the longer term.
For the fetus/neonate
No clear differences between the self‐monitoring and periodic glucose monitoring groups were observed for:
stillbirth (RR 1.54, 95% CI 0.21 to 11.24; 400 participants, 2 RCTs; Analysis 2.16);
neonatal death (no events; 58 participants, 1 RCT; Analysis 2.17);
gestational age at birth (MD ‐0.03 weeks, 95% CI ‐0.32 to 0.27; 400 participants, 2 RCTs; Analysis 2.18);
macrosomia (RR 0.94, 95% CI 0.53 to 1.67; 342 participants, 1 RCT; Analysis 2.19);
small‐for‐gestational age (RR 1.19, 95% CI 0.53 to 2.67; 342 participants, 1 RCT; Analysis 2.20);
birthweight (MD ‐40.22 g, 95% CI ‐148.37 to 67.93; 400 participants, 2 RCTs; Analysis 2.21);
birthweight percentile (MD ‐0.67, 95% CI ‐6.75 to 5.42; 342 participants, 1 RCT; Analysis 2.22);
shoulder dystocia (RR 0.25, 95% CI 0.03 to 2.19; 342 participants, 1 RCT; Analysis 2.23);
hypoglycaemia (RR 0.64, 95% CI 0.39 to 1.06; 391 participants, 2 RCTs; low quality evidence; Analysis 2.24) or
hyperbilirubinaemia or jaundice (RR 0.63, 95% CI 0.39 to 1.04; 370 participants, 2 RCTs; Analysis 2.25).
2.16. Analysis.
Comparison 2 Self‐monitoring versus periodic glucose monitoring, Outcome 16 Stillbirth.
2.17. Analysis.
Comparison 2 Self‐monitoring versus periodic glucose monitoring, Outcome 17 Neonatal death.
2.18. Analysis.
Comparison 2 Self‐monitoring versus periodic glucose monitoring, Outcome 18 Gestational age at birth (weeks).
2.19. Analysis.
Comparison 2 Self‐monitoring versus periodic glucose monitoring, Outcome 19 Macrosomia.
2.20. Analysis.
Comparison 2 Self‐monitoring versus periodic glucose monitoring, Outcome 20 Small‐for‐gestational age.
2.21. Analysis.
Comparison 2 Self‐monitoring versus periodic glucose monitoring, Outcome 21 Birthweight (kg).
2.22. Analysis.
Comparison 2 Self‐monitoring versus periodic glucose monitoring, Outcome 22 Birthweight (percentile).
2.23. Analysis.
Comparison 2 Self‐monitoring versus periodic glucose monitoring, Outcome 23 Shoulder dystocia.
2.24. Analysis.
Comparison 2 Self‐monitoring versus periodic glucose monitoring, Outcome 24 Neonatal hypoglycaemia.
2.25. Analysis.
Comparison 2 Self‐monitoring versus periodic glucose monitoring, Outcome 25 Hyperbilirubinaemia or jaundice.
Neither trial reported on the other secondary outcomes for the fetus/neonate (preterm birth; Apgar score < 7 at five minutes; head circumference; length; ponderal index; adiposity; nerve palsies; bone fractures; respiratory distress syndrome; hypocalcaemia; polycythaemia).
For the child and adult
Neither trial reported on the other secondary outcomes for the child and adult.
Use and costs of health services
No clear differences between the self‐monitoring and periodic glucose monitoring groups were observed for number of antenatal visits with the diabetes team (MD 0.20, 95% CI ‐1.09 to 1.49; 58 participants, 1 RCT; Analysis 2.26); or neonatal intensive care unit admissions (RR 0.87, 95% CI 0.13 to 5.77; 58 participants, 1 RCT; Analysis 2.27).
2.26. Analysis.
Comparison 2 Self‐monitoring versus periodic glucose monitoring, Outcome 26 Number of antenatal visits or admissions: prenatal visits with the diabetes team.
2.27. Analysis.
Comparison 2 Self‐monitoring versus periodic glucose monitoring, Outcome 27 Neonatal intensive care unit admission.
With regard to costs associated with the intervention, Rey 1997 reported "the direct management costs (meter rental, equipment purchase, and clinic reagent strip) of the two follow‐ups in considering the transfer to home monitoring. On a weekly basis the expense was (US dollars): $10.80/woman on home monitoring, $0.50/woman with a breakfast result below 7.8 mmol/L on clinic follow up, and $6.80/woman with a breakfast result at or above 7.8 mmol/L on clinic follow up".
Neither trial reported on the other secondary outcomes related to the use and costs of health services (number of hospital or health professional visits; length of antenatal stay; length of postnatal stay (mother); length of postnatal stay (baby); cost of maternal care; cost of offspring care; costs to families associated with the management provided).
Non prespecified outcomes
No clear differences between the self‐monitoring and period glucose monitoring groups were observed for 'birth trauma' (RR 0.87, 95% CI 0.06 to 13.27; 58 participants, 1 RCT; Analysis 2.28); or 'respiratory complications' (RR 0.87, 95% CI 0.06 to 13.27; 58 participants, 1 RCT; Analysis 2.29).
2.28. Analysis.
Comparison 2 Self‐monitoring versus periodic glucose monitoring, Outcome 28 'Birth trauma' (not a prespecified outcome).
2.29. Analysis.
Comparison 2 Self‐monitoring versus periodic glucose monitoring, Outcome 29 'Respiratory complications' (not a prespecified outcome).
Continuous glucose monitoring system versus self‐monitoring of glucose
Two trials compared the use of continuous glucose monitoring system (CGMS) with self‐monitoring of glucose (Kestila 2007; Wei 2016).
Primary outcomes
For the mother
We observed no clear difference between the CGMS and self‐monitoring groups forcaesarean section (RR 0.91, 95% CI 0.68 to 1.20; 179 participants, 2 RCTs; very low quality evidence; Analysis 3.1). Kestila 2007 reported "There were no statistically significant differences between the two groups in … frequency of pre‐eclampsia, pregnancy‐induced hypertension".
3.1. Analysis.
Comparison 3 Continuous glucose monitoring system versus self‐monitoring of glucose, Outcome 1 Caesarean section.
Neither of the trials reported on the development of type 2 diabetes.
For the child
There were no perinatal deaths in the two trials (179 participants, very low quality evidence; Analysis 3.2).
3.2. Analysis.
Comparison 3 Continuous glucose monitoring system versus self‐monitoring of glucose, Outcome 2 Perinatal mortality.
We observed no clear difference between the CGMS and self‐monitoring groups for large‐for‐gestational age (RR 0.67, 95% CI 0.43 to 1.05; 106 participants, 1 RCT; very low quality evidence; Analysis 3.3).
3.3. Analysis.
Comparison 3 Continuous glucose monitoring system versus self‐monitoring of glucose, Outcome 3 Large‐for‐gestational age.
Neither of the trials reported on death or serious morbidity composite or neurosensory disability.
Secondary outcomes
For the mother
There was, on average, 1.26 kg less gestational weight gain among women in the CGMS group compared with those in the self‐monitoring group (MD ‐1.26 kg, 95% CI ‐2.28 to ‐0.24; 179 participants, 2 RCTs; Analysis 3.4). There was also an almost three‐fold increase in use of additional pharmacotherapy among women in the CGMS group compared with those in the self‐monitoring group (RR 2.86, 95% CI 1.47 to 5.56; 179 participants, 2 RCTs; Analysis 3.5).
3.4. Analysis.
Comparison 3 Continuous glucose monitoring system versus self‐monitoring of glucose, Outcome 4 Gestational weight gain (kg).
3.5. Analysis.
Comparison 3 Continuous glucose monitoring system versus self‐monitoring of glucose, Outcome 5 Use of additional pharmacotherapy.
We observed no clear difference between the CGMS and self‐monitoring groups for glycaemic control: HbA1c at 32 to 36 weeks (MD ‐0.10%, 95% CI ‐0.24 to 0.04; 106 participants, 1 RCT; Analysis 3.6).
3.6. Analysis.
Comparison 3 Continuous glucose monitoring system versus self‐monitoring of glucose, Outcome 6 Glycaemic control: HbA1c at 32 to 36 weeks (%).
With regard to perineal trauma, Kestila 2007 reported that "There were no statistically significant differences between the two groups in … maternal lacerations".
With regard to women's views of the intervention, Wei 2016 reported "The continuous glucose monitor was commonly well tolerated by the pregnant women in the CGMS group. No skin infections occurred at the sensor insertion site, but mild erythema, itchiness, and inflammation often occurred".
With regard to maternal hypoglycaemia, Wei 2016 reported that "The continuous glucose monitor was commonly well tolerated by the pregnant women in the CGMS group … An average of 568 ± 30 glucose measurements were recorded, and the reported hypoglycaemic episodes occurred primarily during early morning and early evening".
Neither trial reported on the other secondary outcomes for the mother (induction of labour, placental abruption, postpartum haemorrhage, postpartum infection, adherence to the intervention, behavioural changes associated with the intervention, sense of well‐being and quality of life, breastfeeding, or mortality).
For the mother in the longer term
Neither trial reported on any secondary outcomes for the mother in the longer term.
For the fetus/neonate
There were no stillbirths (Analysis 3.7) or neonatal deaths (Analysis 3.8) in either trial (179 participants).
3.7. Analysis.
Comparison 3 Continuous glucose monitoring system versus self‐monitoring of glucose, Outcome 7 Stillbirth.
3.8. Analysis.
Comparison 3 Continuous glucose monitoring system versus self‐monitoring of glucose, Outcome 8 Neonatal death.
No clear differences between the CGMS and self‐monitoring groups were observed for:
gestational age at birth (MD ‐0.17 weeks, 95% CI ‐0.52 to 0.19; 179 participants, 2 RCTs; Analysis 3.9);
preterm birth at less than 37 weeks' gestation (RR 1.03, 95% CI 0.15 to 6.91; 73 participants, 1 RCT; Analysis 3.10);
macrosomia (RR 0.85, 95% CI 0.35 to 2.05; 179 participants, 2 RCTs; Analysis 3.11);
small‐for‐gestational age (RR 1.08, 95% CI 0.16 to 7.37; 106 participants, 1 RCT; Analysis 3.12);
birthweight (MD ‐110.17 g, 95% CI ‐264.73 to 44.39; 179 participants, 2 RCTs; Analysis 3.13);
neonatal hypoglycaemia (RR 0.79, 95% CI 0.35 to 1.78; 179 participants, 2 RCTs; very low quality evidence; Analysis 3.14); or
hyperbilirubinaemia or jaundice (RR 1.03, 95% CI 0.28 to 3.80; 73 participants, 1 RCT; Analysis 3.15).
3.9. Analysis.
Comparison 3 Continuous glucose monitoring system versus self‐monitoring of glucose, Outcome 9 Gestational age at birth (weeks).
3.10. Analysis.
Comparison 3 Continuous glucose monitoring system versus self‐monitoring of glucose, Outcome 10 Preterm birth < 37 weeks.
3.11. Analysis.
Comparison 3 Continuous glucose monitoring system versus self‐monitoring of glucose, Outcome 11 Macrosomia.
3.12. Analysis.
Comparison 3 Continuous glucose monitoring system versus self‐monitoring of glucose, Outcome 12 Small‐for‐gestational age.
3.13. Analysis.
Comparison 3 Continuous glucose monitoring system versus self‐monitoring of glucose, Outcome 13 Birthweight (g).
3.14. Analysis.
Comparison 3 Continuous glucose monitoring system versus self‐monitoring of glucose, Outcome 14 Neonatal hypoglycaemia.
3.15. Analysis.
Comparison 3 Continuous glucose monitoring system versus self‐monitoring of glucose, Outcome 15 Hyperbilirubinaemia or jaundice.
Neither trial reported on the other secondary outcomes for the fetus/neonate (Apgar score < 7 at five minutes, macrosomia, head circumference, length, ponderal index, adiposity, shoulder dystocia, nerve palsies, bone fractures, respiratory distress syndrome, hypocalcaemia, polycythaemia).
For the child and adult
Neither trial reported on any secondary outcomes for the child and adult.
Use and costs of health services
No clear differences between the CGMS and self‐monitoring groups were observed for:
neonatal intensive care unit admission (RR 0.65, 95% CI 0.29 to 1.50; 73 participants, 1 RCT; Analysis 3.16); or
length of postnatal stay (baby; length of stay in neonatal intensive care) (MD ‐0.83 days, 95% CI ‐2.35 to 0.69; 18 participants, 1 RCT; Analysis 3.17).
3.16. Analysis.
Comparison 3 Continuous glucose monitoring system versus self‐monitoring of glucose, Outcome 16 Neonatal intensive care unit admission.
3.17. Analysis.
Comparison 3 Continuous glucose monitoring system versus self‐monitoring of glucose, Outcome 17 Length of postnatal stay (baby): length of stay in neonatal intensive care unit (days).
Neither trial reported on the other secondary outcomes for the use and costs of health services (number of antenatal visits or admissions; number of hospital or health professional visits; length of antenatal stay; length of postnatal stay (mother); cost of maternal care; cost of offspring care; costs associated with the intervention; costs to families associated with the management provided).
Modem versus telephone transmission for glucose monitoring
One trial was included in this comparison (Kruger 2003).
Primary outcomes
For the mother
Kruger 2003 did not report on any of our primary outcomes for the mother: hypertensive disorders of pregnancy, caesarean section, or development of type 2 diabetes.
For the child
Kruger 2003 did not report on any of our primary outcomes for the child: perinatal mortality, large‐for‐gestational age, death or serious morbidity composite, or neurosensory disability.
Secondary outcomes
For the mother
With regard to women's views of the intervention, no clear differences between the modem and telephone transmission groups were observed in response to the following statements:
'Overall, I am satisfied with how easy it is to use the Accu‐Check Complete, Acculink' (RR 1.11, 95% CI 0.90 to 1.38; 38 participants, 1 RCT);
'I feel comfortable using the Accu‐Chek Complete, Acculink' (RR 0.96, 95% CI 0.66 to 1.41; 38 participants, 1 RCT);
'Whenever I made a mistake using the Accu‐Chek Complete, Acculink, I could recover easily and quickly' (RR 0.92, 95% CI 0.67 to 1.25; 38 participants, 1 RCT);
'It was easy to learn to use the Accu‐Chek Complete, Acculink' (RR 1.05, 95% CI 0.82 to 1.34; 38 participants, 1 RCT); and
'The written material provided for the Accu‐Chek Complete was easy to understand' (RR 1.18, 95% CI 0.92 to 1.51; 38 participants, 1 RCT; Analysis 4.1).
4.1. Analysis.
Comparison 4 Modem versus telephone transmission for glucose monitoring, Outcome 1 Views of the intervention.
Kruger 2003 reported on the results of a survey of women's views, noting that "The results of this survey demonstrated that both groups of participants were very satisfied with the blood glucose meter. Participants in both groups stated they understood the written material provided by the meter’s manufacturer and felt confident in their blood glucose results. Participants in the modem group reported that they liked the convenience of transmitting their blood glucose results to the clinic by modem, that the modem saved them time, and that it resulted in more accurate data transmission".
Kruger 2003 did not report on any of the other secondary outcomes for the mother.
For the mother in the longer term
Kruger 2003 did not report on any of the secondary outcomes for the mother in the longer term.
For the fetus/neonate
Kruger 2003 reported that "No statistically significant differences between the modem group and control group were found for ... weeks of gestation (p = 0.24)."
Kruger 2003 did not report on any of the other secondary outcomes for the fetus/neonate.
For the child and adult
Kruger 2003 did not report on any secondary outcomes for the child and adult.
Use and costs of health services
Kruger 2003 did not report on any of the secondary outcomes related to the use and costs of health services.
Non‐prespecified outcomes
Kruger 2003 reported that there was "No statistically significant differences between the modem group and the control group were found for mean telephone consultation time (p = 0.71), length of clinic visit (p = 0.83)".
Postprandial versus preprandial glucose monitoring
One trial compared postprandial and preprandial glucose monitoring (De Veciana 1995).
Primary outcomes
For the mother
We observed no clear differences between the postprandial and preprandial glucose monitoring groups for:
pre‐eclampsia (RR 1.00, 95% CI 0.15 to 6.68; 66 participants, 1 RCT; Analysis 5.1); or
caesarean section (RR 0.62, 95% CI 0.29 to 1.29; 66 participants, 1 RCT; Analysis 5.2).
5.1. Analysis.
Comparison 5 Postprandial versus preprandial glucose monitoring, Outcome 1 Hypertensive disorders of pregnancy: pre‐eclampsia.
5.2. Analysis.
Comparison 5 Postprandial versus preprandial glucose monitoring, Outcome 2 Caesarean section.
De Veciana 1995 did not report on the development of type 2 diabetes.
For the child
There was an approximate 71% relative reduction in large‐for‐gestational‐age infants born to mothers in the postprandial compared with the preprandial glucose monitoring group (RR 0.29, 95% CI 0.11 to 0.78; 66 participants, 1 RCT; Analysis 5.3).
5.3. Analysis.
Comparison 5 Postprandial versus preprandial glucose monitoring, Outcome 3 Large‐for‐gestational age.
De Veciana 1995 did not report on: perinatal mortality, death or serious morbidity composite, or neurosensory disability.
Secondary outcomes
For the mother
We observed no clear differences between the postprandial and preprandial glucose monitoring groups for:
perineal trauma (RR 0.38, 95% CI 0.11 to 1.29; 66 participants, 1 RCT; Analysis 5.4);
gestational weight gain (MD ‐0.20 kg, 95% CI ‐2.81 to 2.41; 66 participants, 1 RCT; Analysis 5.5);
-
glycaemic control:
hospitalisation for glycaemic control (RR 1.33, 95% CI 0.32 to 5.50; 66 participants, 1 RCT; Analysis 5.9); or
success in glycaemic control (MD 2.00%, 95% CI ‐0.26 to 4.26; 66 participants, 1 RCT; Analysis 5.10).
5.4. Analysis.
Comparison 5 Postprandial versus preprandial glucose monitoring, Outcome 4 Perineal trauma.
5.5. Analysis.
Comparison 5 Postprandial versus preprandial glucose monitoring, Outcome 5 Gestational weight gain (kg).
5.9. Analysis.
Comparison 5 Postprandial versus preprandial glucose monitoring, Outcome 9 Glycaemic control: hospitalisation for glycaemic control.
5.10. Analysis.
Comparison 5 Postprandial versus preprandial glucose monitoring, Outcome 10 Glycaemic control: success in glycaemic control (%).
There was reduced compliance with the schedule (as a percentage) (adherence to the intervention) among women in the postprandial compared with the preprandial glucose monitoring group (MD ‐3.00%, 95% CI ‐3.99 to ‐2.01; 66 participants, 1 RCT; Analysis 5.6).
5.6. Analysis.
Comparison 5 Postprandial versus preprandial glucose monitoring, Outcome 6 Adherence to the intervention: compliance with schedule (%).
For use of additional pharmacotherapy, women in the postprandial glucose monitoring group used, on average, a 23.60 units/day higher insulin dose (MD 23.60 units/day, 95% CI 11.17 to 36.03; 66 participants, 1 RCT) and a 0.20 units/kg higher insulin dose during the last four weeks of pregnancy (MD 0.20 units/kg, 95% CI 0.12 to 0.28; 66 participants, 1 RCT; Analysis 5.7).
5.7. Analysis.
Comparison 5 Postprandial versus preprandial glucose monitoring, Outcome 7 Use of additional pharmacotherapy.
Women in the postprandial group also had, on average, a 2.4% greater glycaemic control with a reduction in HbA1c compared with women in the preprandial glucose monitoring group (MD ‐2.40%, 95% CI ‐3.33 to ‐1.47; 66 participants, 1 RCT; Analysis 5.8).
5.8. Analysis.
Comparison 5 Postprandial versus preprandial glucose monitoring, Outcome 8 Glycaemic control: change in HbA1c (%).
De Veciana 1995 did not report on the other secondary outcomes for the mother (induction of labour, placental abruption, postpartum haemorrhage, postpartum infection, behavioural changes associated with the intervention, sense of well‐being and quality of life, views of the intervention, breastfeeding (e.g. at discharge, six weeks postpartum), maternal hypoglycaemia, mortality).
For the mother in the longer term
De Veciana 1995 did not report on any secondary outcomes for the mother in the longer term.
For the fetus/neonate
We observed no clear differences between the postprandial and preprandial glucose monitoring groups for:
stillbirth (RR 0.33, 95% CI 0.01 to 7.90; 66 participants, 1 RCT; Analysis 5.11);
gestational age at birth (MD 0.30 weeks, 95% CI ‐1.08 to 1.68; 66 participants, 1 RCT; Analysis 5.12);
Apgar score < 7 at five minutes (RR 0.33, 95% CI 0.04 to 3.04; 66 participants, 1 RCT; Analysis 5.13);
small‐for‐gestational age (RR 3.00, 95% CI 0.13 to 71.07; 66 participants, 1 RCT; Analysis 5.15);
shoulder dystocia (RR 0.17, 95% CI 0.02 to 1.31; 66 participants, 1 RCT; Analysis 5.17);
nerve palsies (RR 0.50, 95% CI 0.05 to 5.25; 66 participants, 1 RCT; Analysis 5.18);
bone fractures (RR 1.00, 95% CI 0.07 to 15.33; 66 participants, 1 RCT; Analysis 5.19);
hypoglycaemia (RR 0.14, 95% CI 0.02 to 1.10; 66 participants, 1 RCT; Analysis 5.20); or
hyperbilirubinaemia or jaundice (RR 0.75, 95% CI 0.18 to 3.09; 66 participants, 1 RCT; Analysis 5.21).
5.11. Analysis.
Comparison 5 Postprandial versus preprandial glucose monitoring, Outcome 11 Stillbirth.
5.12. Analysis.
Comparison 5 Postprandial versus preprandial glucose monitoring, Outcome 12 Gestational age at birth (weeks).
5.13. Analysis.
Comparison 5 Postprandial versus preprandial glucose monitoring, Outcome 13 Apgar score < 7 at 5 minutes.
5.15. Analysis.
Comparison 5 Postprandial versus preprandial glucose monitoring, Outcome 15 Small‐for‐gestational age.
5.17. Analysis.
Comparison 5 Postprandial versus preprandial glucose monitoring, Outcome 17 Shoulder dystocia.
5.18. Analysis.
Comparison 5 Postprandial versus preprandial glucose monitoring, Outcome 18 Nerve palsies.
5.19. Analysis.
Comparison 5 Postprandial versus preprandial glucose monitoring, Outcome 19 Bone fractures.
5.20. Analysis.
Comparison 5 Postprandial versus preprandial glucose monitoring, Outcome 20 Neonatal hypoglycaemia.
5.21. Analysis.
Comparison 5 Postprandial versus preprandial glucose monitoring, Outcome 21 Hyperbilirubinaemia or jaundice.
There was an approximate 75% relative reduction in the risk of macrosomia for infants born to mothers in the postprandial compared with the preprandial glucose monitoring group (RR 0.25, 95% CI 0.08 to 0.81; 66 participants, 1 RCT; Analysis 5.14), and babies born to mothers in the postprandial monitoring group had, on average, 379 g lower birthweights than those born to mothers in the preprandial glucose monitoring group (MD ‐379.00 g, 95% CI ‐650.79 to ‐107.21; 66 participants, 1 RCT; Analysis 5.16).
5.14. Analysis.
Comparison 5 Postprandial versus preprandial glucose monitoring, Outcome 14 Macrosomia.
5.16. Analysis.
Comparison 5 Postprandial versus preprandial glucose monitoring, Outcome 16 Birthweight (g).
De Veciana 1995 did not report on the other secondary outcomes for the fetus/neonate (neonatal death, preterm birth, head circumference, length, ponderal index, adiposity, respiratory distress syndrome, hypocalcaemia, polycythaemia).
For the child and adult
De Veciana 1995 did not report on any secondary outcomes for the child and adult.
Use and costs of health services
De Veciana 1995 did not report on any secondary outcomes for the use and costs of health services.
Discussion
Summary of main results
We included 11 trials in the review (Dalfra 2009; De Veciana 1995; Given 2015; Homko 2002; Homko 2007; Homko 2012; Kestila 2007; Kruger 2003; Perez‐Ferre 2010; Rey 1997; Wei 2016); these randomised a total of 1272 pregnant women with GDM. We assessed the 11 trials under five comparisons.
Telemedicine versus standard care for glucose monitoring
Five trials investigated this comparison (Dalfra 2009; Given 2015; Homko 2007; Homko 2012; Perez‐Ferre 2010). For the primary outcomes of pre‐eclampsia or pregnancy‐induced hypertension, caesarean section, perinatal mortality (no events), large‐for‐gestational age, or a morbidity composite outcome there were no clear differences between the telemedicine and standard care groups (all very low quality evidence). Similarly, for the other important secondary outcomes of induction of labour or neonatal hypoglycaemia ‐ that we assessed using the GRADE approach ‐ we saw no clear differences between the telemedicine and standard care groups (both very low quality evidence). Very few other differences were observed between groups for secondary outcomes, except for an improved sense of well‐being and quality of life (one trial), increased insulin use (across five trials), lower HbA1c levels (across three trials), and fewer unscheduled face‐to‐face visits among women in the telemedicine group, compared with the standard care group (one trial).
Self‐monitoring versus periodic glucose monitoring
Two trials investigated this comparison (Homko 2002; Rey 1997). For the primary outcomes of pre‐eclampsia, caesarean section, perinatal mortality or large‐for‐gestational age, we observed no clear differences between the self‐monitoring and periodic glucose monitoring groups (all low or very low quality evidence). No clear difference was observed for another important secondary outcome, neonatal hypoglycaemia, assessed using the GRADE approach (low quality evidence). No other differences between groups were observed for secondary outcomes, except for a smaller weekly weight gain for women (one trial) in the self‐monitoring group compared with those in the periodic glucose monitoring group.
Continuous glucose monitoring system (CGMS) versus self‐monitoring of glucose
Two trials investigated this comparison (Kestila 2007; Wei 2016). For the primary outcomes of caesarean section, perinatal mortality (no events), or large‐for‐gestational age (all very low quality evidence) we observed no clear differences between the CGMS and self‐monitoring groups. We observed no clear difference for the important secondary outcome of neonatal hypoglycaemia (very low quality evidence), which we assessed using the GRADE approach. Very few other differences were observed between groups for secondary outcomes, except for less gestational weight gain (two trials), and increased use of additional pharmacotherapy (two trials) among women in the CGMS group compared with those in the self‐monitoring group.
Modem versus telephone transmission for glucose monitoring
One trial investigated this comparison (Kruger 2003). It reported none of our primary outcomes and we observed no clear difference between groups for the secondary outcomes reported.
Postprandial versus preprandial glucose monitoring
One trial investigated this comparison (De Veciana 1995). For the primary outcomes of pre‐eclampsia or caesarean section, we observed no clear differences between the post‐prandial and preprandial glucose monitoring groups, although a reduction in large‐for‐gestational‐age infants was observed for infants born to mothers in the post‐prandial monitoring group. Few other differences were observed between groups for the secondary outcomes, except for reduced compliance with the schedule, higher insulin dose across the last four weeks of pregnancy, greater change (reduction) in HbA1c levels, a reduced risk of macrosomia, and lower birthweights for mothers/infants in the post‐prandial glucose monitoring group.
Overall completeness and applicability of evidence
All of the 11 included trials, except Wei 2016, from China, were conducted in high‐income countries, with five from the USA, and one each from Canada, Finland, Ireland, Italy and Spain, which probably limits the generalisability of the findings. The trials used specific screening tests, diagnostic criteria, and subsequent management strategies for GDM, which may also limit applicability of their results for countries/settings that use different approaches, and with different practicality and feasibility considerations.
With regard to the important outcomes we selected for quality assessment using the GRADE approach: only five trials reported on hypertensive disorders of pregnancy, nine on caesarean section, one on induction of labour, six on perinatal mortality, six on large‐for‐gestational age, one on death or serious morbidity composite, and seven on neonatal hypoglycaemia. There were no data for the following outcomes for the mother: perineal trauma, type 2 diabetes, postnatal depression, and postnatal weight retention, or return to pre‐pregnancy weight, and no data for the child for: childhood/adulthood neurosensory disability, adiposity, or type 2 diabetes.
With regard to our secondary outcomes, none of the 11 trials reported on any longer‐term outcomes for the mother, or the infant, in childhood or adulthood.
Quality of the evidence
The risk of bias of the 11 included trials was mixed. Generally, the lack of methodological detail provided in the trial reports did not allow us to assess risk of bias across the trials, and led to many unclear 'Risk of bias' ratings across the various domains. We judged only one trial to be at a low risk of selection bias, and two at a high risk of selection bias. It was not possible to blind women or trial personnel (due to the nature of the interventions) in any of the trials; thus we considered all trials to be at a high risk of performance bias. It was not clear in the trials whether there were attempts to blind outcome assessors; therefore, we judged 10 trials to be at an unclear risk of detection bias. Due to lack of access to trial registrations and protocols, or limited reporting of important review outcomes, or both, we judged none of the trials to be at a low risk of reporting bias. Overall the risk of bias was moderate to high.
For outcomes assessed across the three main comparisons (telemedicine versus standard care; self‐monitoring versus periodic monitoring; CGMS versus self‐monitoring) using the GRADE approach, we determined the evidence to be low quality or very low quality. Evidence was predominately downgraded due to design limitations (risk of bias), and imprecision and inconsistencies (uncertain effect estimates, and at times, small sample sizes and low event rates).
Potential biases in the review process
We took steps to minimise bias in the review process. Data extraction was carried out by two researchers, independently, and all data were checked. The GRADE approach assessments were made by two people, independently, and discrepancies resolved by discussion.
Agreements and disagreements with other studies or reviews
This current review found no clear differences between the various methods or settings for glucose monitoring for women with GDM for our primary review outcomes, or the majority of our secondary review outcomes.
The Moy 2014 Cochrane Review also assessed different techniques of blood glucose monitoring during pregnancy, but specifically for women with pre‐existing diabetes (type 1 or 2 diabetes). Moy 2014 was able to include nine trials, with 506 women (the majority with type 1 diabetes), and included six comparisons, many of which were similar to those assessed in our review, namely:
self‐monitoring versus standard care;
self‐monitoring versus hospitalisation;
preprandial versus post‐prandial monitoring;
automated telemedicine monitoring versus conventional system;
CGMS versus intermittent monitoring;
constant CGMS versus intermittent CGMS.
The review found no clear differences between monitoring techniques for the primary or secondary outcomes assessed, and thus concluded that there was no clear evidence that any glucose monitoring technique was superior to any other technique, and that additional evidence from large well‐designed randomised trials was required to inform choices (Moy 2014).
We identified two further systematic reviews that specifically assessed the effects of telemedicine interventions for women with GDM (Rasekaba 2015b), or with diabetes in pregnancy (including GDM and pre‐existing type 1 or 2 diabetes) (Ming 2016). Rasekaba 2015b included three trials from our telemedicine versus standard care comparison (Homko 2007; Homko 2012; Perez‐Ferre 2010), but did not include Dalfra 2009 (as it was quasi‐randomised), or Given 2015 (as the search for the review was conducted in 2013). Ming 2016 included the same five trials that were included in our telemedicine versus standard care comparison, along with two additional trials in women with type 1 diabetes. In agreement with our review, Rasekaba 2015b showed no clear differences between groups for outcomes assessed, except for (as was observed in our review) positive findings of improved quality of life (measured with the Diabetes Empowerment Scale) (from Homko 2007), and reduced unscheduled face‐to‐face visits (from Perez‐Ferre 2010) with telemedicine. Rasekaba 2015b concluded that currently "Studies are limited and more trials that include cost evaluation are required". Ming 2016 also showed no clear differences between groups for clinical outcomes assessed for the mother and infant, though, in agreement with our review, did demonstrate an improvement in glycaemic control (as measured by HbA1c) with telemedicine. Ming 2016 thus concluded "There is currently insufficient evidence that telemedicine technology is superior to standard care for women with diabetes in pregnancy; however, there was no evidence of harm", which is in keeping with our review's findings.
Authors' conclusions
Implications for practice.
Evidence from 11 trials of different methods and settings for glucose monitoring for women with GDM, assessed under five different comparisons, suggests no clear differences between different methods/settings for primary review outcomes: hypertensive disorders of pregnancy (assessed by six trials under three comparisons), caesarean section (assessed by 10 trials under four comparisons), perinatal mortality (assessed by six trials under three comparisons), or a serious morbidity composite (assessed in one trial under one comparison). No clear difference was seen for large‐for‐gestational age (assessed by six trials under three comparisons), except for a possible reduction with post‐prandial compared with the preprandial glucose monitoring in one trial. None of the included trials reported on the other primary review outcomes: development of type 2 diabetes for the mother, and neurosensory disability for the child. Very few differences were seen for secondary review outcomes. For outcomes assessed using GRADE for our three main comparisons 1) telemedicine versus standard care for glucose monitoring; 2) self‐monitoring versus period glucose monitoring; 3) continuous glucose monitoring system (CGMS) versus self‐monitoring of glucose), the evidence was considered to be low to very‐low quality, with downgrading based on study limitations (risk of bias), imprecision, and inconsistency.
There is thus a limited and incomplete body of evidence from randomised trials assessing the effects of different methods and settings for glucose monitoring for women with GDM, which is insufficient to inform practice.
Implications for research.
The impact of different methods and settings for glucose monitoring for women with GDM on maternal (including hypertensive disorders of pregnancy; caesarean birth; and type 2 diabetes) and child (including large‐for‐gestational age; perinatal mortality; death or serious morbidity composite; and neurosensory disability) health outcomes is unclear. Large, high‐quality randomised controlled trials evaluating the effects of different methods or settings for glucose monitoring for women with GDM are required. Trials may consider collecting and reporting on the standard outcomes suggested in this review, including short‐term and long‐term maternal and child outcomes, and outcomes relating to the use and costs of health services. The data in the current review are further complicated by factors such as differing diagnostic criteria for GDM, and varied outcome descriptions and definitions; these are important issues for future trials to consider.
Acknowledgements
We acknowledge the support from the Cochrane Pregnancy and Childbirth editorial team in Liverpool, and the Australia and New Zealand Satellite of Cochrane Pregnancy and Childbirth (funded by the Australian National Health and Medical Research Council (NHMRC)).
We thank Madeleine Gill and Thuy‐My N Nguyen for their contribution to the protocol Gill 2014.
We thank Lambert Felix and Anna Cuthbert from Cochrane Pregnancy and Childbirth who provided support for this update, including assisting with producing the ’Summary of findings’ tables. Their contribution to this project was supported by the National Institute for Health Research (NIHR), via Cochrane programme grant funding to Cochrane Pregnancy and Childbirth. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, National Health Service or the Department of Health.
As part of the prepublication editorial process, this review has been commented on by three peer reviewers (an editor and two referees who are external to the editorial team), a member of Cochrane Pregnancy and Childbirth's international panel of consumers and the Group's Statistical Adviser.
This project was supported by the National Institute for Health Research, via Cochrane Infrastructure funding and Cochrane Programme Grant funding to Cochrane Pregnancy and Childbirth. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, NHS, or the Department of Health.
Data and analyses
Comparison 1. Telemedicine versus standard care for glucose monitoring.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Hypertensive disorders of pregnancy | 4 | 275 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.49 [0.69, 3.20] |
| 1.1 Pre‐eclampsia, pregnancy‐induced hypertension | 3 | 178 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.29 [0.58, 2.89] |
| 1.2 Pregnancy‐induced hypertension | 1 | 97 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.9 [0.24, 99.48] |
| 2 Caesarean section | 5 | 478 | Risk Ratio (M‐H, Random, 95% CI) | 1.05 [0.72, 1.53] |
| 3 Perinatal mortality | 2 | 131 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Large‐for‐gestational age | 3 | 228 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.41 [0.76, 2.64] |
| 5 Death or serious morbidity composite | 1 | 57 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.06 [0.68, 1.66] |
| 6 Operative vaginal birth (not a prespecified outcome) | 1 | 47 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.50 [0.11, 2.30] |
| 7 Induction of labour | 1 | 47 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.06 [0.63, 1.77] |
| 8 Placental abruption | 2 | 154 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.12, 6.42] |
| 9 Gestational weight gain (kg) | 2 | 300 | Mean Difference (IV, Fixed, 95% CI) | ‐0.47 [‐1.50, 0.55] |
| 10 Weight at 36 weeks (kg) | 1 | 44 | Mean Difference (IV, Fixed, 95% CI) | 5.5 [‐5.69, 16.69] |
| 11 Adherence to the intervention | 3 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 11.1 Appointments attended (%) | 1 | 47 | Mean Difference (IV, Fixed, 95% CI) | 5.20 [‐2.27, 12.67] |
| 11.2 Average daily self‐monitoring of blood glucose frequency: meter memory | 1 | 44 | Mean Difference (IV, Fixed, 95% CI) | 0.5 [‐0.42, 1.42] |
| 11.3 Average daily self‐monitoring of blood glucose frequency: diary | 1 | 45 | Mean Difference (IV, Fixed, 95% CI) | 0.10 [‐0.66, 0.86] |
| 11.4 Frequency of monitoring (number of data points) | 1 | 57 | Mean Difference (IV, Fixed, 95% CI) | 21.10 [‐9.33, 51.53] |
| 11.5 Frequency of monitoring (number of data sets) | 1 | 74 | Mean Difference (IV, Fixed, 95% CI) | 1.20 [‐12.32, 14.72] |
| 12 Sense of well‐being and quality of life: DES: Diabetes Empowerment Scale | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 12.1 Total | 1 | 57 | Mean Difference (IV, Fixed, 95% CI) | 0.40 [0.14, 0.66] |
| 12.2 Subscale 1: managing the psychosocial aspects of diabetes | 1 | 57 | Mean Difference (IV, Fixed, 95% CI) | 0.5 [0.21, 0.79] |
| 12.3 Subscale 2: assessing dissatisfaction and readiness to change | 1 | 57 | Mean Difference (IV, Fixed, 95% CI) | 0.40 [0.14, 0.66] |
| 12.4 Subscale 3: setting and achieving diabetes goals | 1 | 57 | Mean Difference (IV, Fixed, 95% CI) | 0.30 [‐0.04, 0.64] |
| 13 Use of additional pharmacotherapy | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 13.1 Insulin | 5 | 484 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.52 [1.18, 1.96] |
| 13.2 Oral agents | 3 | 184 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.85 [0.50, 1.42] |
| 13.3 Insulin and oral agents | 1 | 47 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.24 [0.19, 8.06] |
| 14 Maternal hypoglycaemia | 1 | 203 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 15 Maternal hypoglycaemia: self‐monitored blood glucose episodes hypoglycaemic (< 3.9 mmol/L) (%) | 1 | 44 | Mean Difference (IV, Fixed, 95% CI) | ‐0.10 [‐1.64, 1.44] |
| 16 Glycaemic control: HbA1c (%) | 3 | 357 | Mean Difference (IV, Fixed, 95% CI) | ‐0.15 [‐0.26, ‐0.04] |
| 17 Glycaemic control: HbA1c < 5.8% | 1 | 97 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.96, 1.04] |
| 18 Glycaemic control: HbA1c at 36 weeks (mmol/mol) | 1 | 30 | Mean Difference (IV, Fixed, 95% CI) | 0.20 [‐2.03, 2.43] |
| 19 Glycaemic control: self‐monitored blood glucose (mmol/L) | 1 | 44 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [‐0.30, 0.30] |
| 20 Glycaemic control: fasting and 2‐hour post‐prandial blood glucose (mg/dL) | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 20.1 Fasting blood glucose (mg/dL) | 2 | 131 | Mean Difference (IV, Random, 95% CI) | ‐0.50 [‐5.38, 4.38] |
| 20.2 2‐hour post‐prandial blood glucose (mg/dL) | 2 | 131 | Mean Difference (IV, Random, 95% CI) | ‐0.21 [‐5.09, 4.67] |
| 21 Stillbirth | 3 | 178 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.41 [0.02, 9.55] |
| 22 Neonatal death | 2 | 131 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 23 Gestational age at birth (weeks) | 5 | 478 | Mean Difference (IV, Fixed, 95% CI) | 0.10 [‐0.18, 0.37] |
| 24 Preterm birth < 37 weeks | 4 | 275 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.66 [0.31, 1.39] |
| 25 Macrosomia | 2 | 249 | Risk Ratio (M‐H, Random, 95% CI) | 1.43 [0.27, 7.52] |
| 26 Small‐for‐gestational age | 1 | 97 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 27 Birthweight (g) | 5 | 477 | Mean Difference (IV, Fixed, 95% CI) | 63.13 [‐32.32, 158.59] |
| 28 Head circumference (cm) | 1 | 45 | Mean Difference (IV, Fixed, 95% CI) | 0.70 [0.02, 1.38] |
| 29 Length (cm) | 1 | 42 | Mean Difference (IV, Fixed, 95% CI) | 0.20 [‐1.34, 1.74] |
| 30 Shoulder dystocia | 2 | 142 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.83] |
| 31 Respiratory distress syndrome | 3 | 176 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.63 [0.26, 1.49] |
| 32 Neonatal hypoglycaemia | 3 | 198 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.14 [0.48, 2.72] |
| 33 Hyperbilirubinaemia or jaundice | 3 | 176 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.09 [0.59, 2.01] |
| 34 Hypocalcaemia | 1 | 97 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 35 Polycythaemia | 1 | 97 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 36 Number of hospital or health professional visits: face‐to‐face visits | 1 | 97 | Mean Difference (IV, Fixed, 95% CI) | ‐0.36 [‐0.92, 0.20] |
| 37 Number of hospital or health professional visits: unscheduled face‐to‐face visits | 1 | 97 | Mean Difference (IV, Fixed, 95% CI) | ‐0.62 [‐1.05, ‐0.19] |
| 38 Neonatal intensive care unit admission | 3 | 176 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.05 [0.62, 1.79] |
| 39 'Neonatal morbidity' (neonatal complications: e.g. hypoglycaemia, hyperbilirubinaemia, respiratory distress syndrome, shoulder dystocia, malformations) (not a prespecified outcome) | 1 | 203 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.52 [0.53, 4.38] |
| 40 'Maternal morbidity' (maternal complications: gestational hypertension, pre‐eclampsia, eclampsia, hypoglycaemic episodes) (not a prespecified outcome) | 1 | 203 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.49 [0.13, 1.79] |
Comparison 2. Self‐monitoring versus periodic glucose monitoring.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Hypertensive disorders of pregnancy: pre‐eclampsia | 1 | 58 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.18 [0.01, 3.49] |
| 2 Caesarean section | 2 | 400 | Risk Ratio (M‐H, Random, 95% CI) | 1.18 [0.61, 2.27] |
| 3 Perinatal mortality | 2 | 400 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.54 [0.21, 11.24] |
| 4 Large‐for‐gestational age | 2 | 400 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.82 [0.50, 1.37] |
| 5 Placental abruption | 1 | 58 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.63 [0.11, 61.88] |
| 6 Postpartum haemorrhage | 1 | 58 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.63 [0.11, 61.88] |
| 7 Gestational weight gain (kg/week) | 1 | 342 | Mean Difference (IV, Fixed, 95% CI) | ‐0.1 [‐0.15, ‐0.05] |
| 7.1 1‐hour post‐breakfast glucose < 7.8 mmol/L | 1 | 227 | Mean Difference (IV, Fixed, 95% CI) | ‐0.10 [‐0.17, ‐0.03] |
| 7.2 1‐hour post‐breakfast glucose ≥ 7.8 mmol/L | 1 | 115 | Mean Difference (IV, Fixed, 95% CI) | ‐0.10 [‐0.17, ‐0.03] |
| 8 Gestational weight gain (lb) | 1 | 58 | Mean Difference (IV, Fixed, 95% CI) | ‐5.5 [‐13.57, 2.57] |
| 9 Adherence to the intervention: < 70% adherence to home blood glucose measurements or diabetes outpatient clinic appointments | 1 | 342 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.74 [0.32, 1.71] |
| 10 Adherence to the intervention: Dietary Compliance Questionnaire | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 10.1 Total compliance score | 1 | 58 | Mean Difference (IV, Fixed, 95% CI) | 1.5 [‐0.47, 3.47] |
| 10.2 Mean compliance score | 1 | 58 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [‐0.40, 0.40] |
| 11 Sense of well‐being and quality of life: Diabetes Empowerment Scale delta scores | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 11.1 Overall | 1 | 47 | Mean Difference (IV, Fixed, 95% CI) | 3.70 [‐2.08, 9.48] |
| 11.2 Setting goals | 1 | 47 | Mean Difference (IV, Fixed, 95% CI) | 0.65 [‐1.10, 2.40] |
| 11.3 Solving problems | 1 | 47 | Mean Difference (IV, Fixed, 95% CI) | 1.35 [‐0.37, 3.07] |
| 11.4 Motivating oneself | 1 | 47 | Mean Difference (IV, Fixed, 95% CI) | 0.63 [‐0.89, 2.15] |
| 11.5 Obtaining support | 1 | 47 | Mean Difference (IV, Fixed, 95% CI) | 0.94 [‐0.09, 1.97] |
| 11.6 Making decisions | 1 | 47 | Mean Difference (IV, Fixed, 95% CI) | 0.01 [‐1.39, 1.41] |
| 12 Sense of well‐being and quality of life: emotional adjustment: Appraisal of Diabetes Scale delta scores | 1 | 47 | Mean Difference (IV, Fixed, 95% CI) | 1.20 [‐0.88, 3.28] |
| 13 Use of additional pharmacotherapy: insulin | 2 | 400 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.31 [0.69, 2.48] |
| 14 Glycaemic control: pre‐prandial blood glucose (mmol/L) | 2 | 360 | Mean Difference (IV, Random, 95% CI) | 0.06 [‐0.08, 0.19] |
| 14.1 Breakfast glucose < 7.8 mmol/L | 1 | 192 | Mean Difference (IV, Random, 95% CI) | 0.10 [‐0.03, 0.23] |
| 14.2 Breakfast glucose ≥ 7.8 mmol/L | 1 | 110 | Mean Difference (IV, Random, 95% CI) | 0.10 [‐0.07, 0.27] |
| 14.3 All women | 1 | 58 | Mean Difference (IV, Random, 95% CI) | ‐0.21 [‐0.54, 0.12] |
| 15 Glycaemic control: 1‐hour post‐prandial blood glucose (mmol/L) | 2 | 395 | Mean Difference (IV, Random, 95% CI) | ‐0.09 [‐0.60, 0.42] |
| 15.1 1‐hour post‐breakfast glucose > 7.8 mmol/L | 1 | 222 | Mean Difference (IV, Random, 95% CI) | 0.0 [‐0.19, 0.19] |
| 15.2 1‐hour post‐breakfast glucose ≥ 7.8 mmol/L | 1 | 115 | Mean Difference (IV, Random, 95% CI) | ‐0.60 [‐0.90, ‐0.30] |
| 15.3 All women | 1 | 58 | Mean Difference (IV, Random, 95% CI) | 0.47 [‐0.12, 1.06] |
| 16 Stillbirth | 2 | 400 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.54 [0.21, 11.24] |
| 17 Neonatal death | 1 | 58 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 18 Gestational age at birth (weeks) | 2 | 400 | Mean Difference (IV, Fixed, 95% CI) | ‐0.03 [‐0.32, 0.27] |
| 18.1 1‐hour post‐breakfast glucose < 7.8 mmol/L | 1 | 227 | Mean Difference (IV, Fixed, 95% CI) | ‐0.20 [‐0.59, 0.19] |
| 18.2 1‐hour post‐breakfast glucose ≥ 7.8 mmol/L | 1 | 115 | Mean Difference (IV, Fixed, 95% CI) | 0.20 [‐0.31, 0.71] |
| 18.3 All neonates | 1 | 58 | Mean Difference (IV, Fixed, 95% CI) | 0.30 [‐0.78, 1.38] |
| 19 Macrosomia | 1 | 342 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.53, 1.67] |
| 20 Small‐for‐gestational age | 1 | 342 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.19 [0.53, 2.67] |
| 21 Birthweight (kg) | 2 | 400 | Mean Difference (IV, Fixed, 95% CI) | ‐40.22 [‐148.37, 67.93] |
| 21.1 1‐hour post‐breakfast glucose < 7.8 mmol/L | 1 | 227 | Mean Difference (IV, Fixed, 95% CI) | ‐10.0 [‐145.47, 125.47] |
| 21.2 1‐hour post‐breakfast glucose ≥ 7.8 mmol/L | 1 | 115 | Mean Difference (IV, Fixed, 95% CI) | ‐70.0 [‐283.34, 143.34] |
| 21.3 All neonates | 1 | 58 | Mean Difference (IV, Fixed, 95% CI) | ‐150.0 [‐482.61, 182.61] |
| 22 Birthweight (percentile) | 1 | 342 | Mean Difference (IV, Fixed, 95% CI) | ‐0.67 [‐6.75, 5.42] |
| 22.1 1‐hour post‐breakfast glucose < 7.8 mmol/L | 1 | 227 | Mean Difference (IV, Fixed, 95% CI) | 1.5 [‐5.71, 8.71] |
| 22.2 1‐hour post‐breakfast glucose ≥ 7.8 mmol/L | 1 | 115 | Mean Difference (IV, Fixed, 95% CI) | ‐6.00 [‐17.32, 5.32] |
| 23 Shoulder dystocia | 1 | 342 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.25 [0.03, 2.19] |
| 24 Neonatal hypoglycaemia | 2 | 391 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.64 [0.39, 1.06] |
| 25 Hyperbilirubinaemia or jaundice | 2 | 370 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.63 [0.39, 1.04] |
| 26 Number of antenatal visits or admissions: prenatal visits with the diabetes team | 1 | 58 | Mean Difference (IV, Fixed, 95% CI) | 0.20 [‐1.09, 1.49] |
| 27 Neonatal intensive care unit admission | 1 | 58 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.87 [0.13, 5.77] |
| 28 'Birth trauma' (not a prespecified outcome) | 1 | 58 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.87 [0.06, 13.27] |
| 29 'Respiratory complications' (not a prespecified outcome) | 1 | 58 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.87 [0.06, 13.27] |
Comparison 3. Continuous glucose monitoring system versus self‐monitoring of glucose.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Caesarean section | 2 | 179 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.68, 1.20] |
| 2 Perinatal mortality | 2 | 179 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 3 Large‐for‐gestational age | 1 | 106 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.43, 1.05] |
| 4 Gestational weight gain (kg) | 2 | 179 | Mean Difference (IV, Fixed, 95% CI) | ‐1.26 [‐2.28, ‐0.24] |
| 5 Use of additional pharmacotherapy | 2 | 179 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.86 [1.47, 5.56] |
| 6 Glycaemic control: HbA1c at 32 to 36 weeks (%) | 1 | 106 | Mean Difference (IV, Fixed, 95% CI) | ‐0.10 [‐0.24, 0.04] |
| 7 Stillbirth | 2 | 179 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 8 Neonatal death | 2 | 179 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 9 Gestational age at birth (weeks) | 2 | 179 | Mean Difference (IV, Fixed, 95% CI) | ‐0.17 [‐0.52, 0.19] |
| 10 Preterm birth < 37 weeks | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 11 Macrosomia | 2 | 179 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.85 [0.35, 2.05] |
| 12 Small‐for‐gestational age | 1 | 106 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.08 [0.16, 7.37] |
| 13 Birthweight (g) | 2 | 179 | Mean Difference (IV, Fixed, 95% CI) | ‐110.17 [‐264.73, 44.39] |
| 14 Neonatal hypoglycaemia | 2 | 179 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.79 [0.35, 1.78] |
| 15 Hyperbilirubinaemia or jaundice | 1 | 73 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.28, 3.80] |
| 16 Neonatal intensive care unit admission | 1 | 73 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.65 [0.29, 1.50] |
| 17 Length of postnatal stay (baby): length of stay in neonatal intensive care unit (days) | 1 | 18 | Mean Difference (IV, Fixed, 95% CI) | ‐0.83 [‐2.35, 0.69] |
Comparison 4. Modem versus telephone transmission for glucose monitoring.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Views of the intervention | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.1 Overall, I am satisfied with how easy it is to use Accu‐Chek Complete, Acculink | 1 | 38 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.11 [0.90, 1.38] |
| 1.2 I feel comfortable using the Accu‐Chek Complete, Acculink | 1 | 38 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.96 [0.66, 1.41] |
| 1.3 Whenever I made a mistake using the Accu‐Chek Complete, Acculink, I could recover easily and quickly | 1 | 38 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.92 [0.67, 1.25] |
| 1.4 It was easy to learn to use the Accu‐Chek Complete, Acculink | 1 | 38 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.05 [0.82, 1.34] |
| 1.5 The written material provided for the Accu‐Chek Complete was easy to understand | 1 | 38 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.18 [0.92, 1.51] |
Comparison 5. Postprandial versus preprandial glucose monitoring.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Hypertensive disorders of pregnancy: pre‐eclampsia | 1 | 66 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.15, 6.68] |
| 2 Caesarean section | 1 | 66 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.62 [0.29, 1.29] |
| 3 Large‐for‐gestational age | 1 | 66 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.29 [0.11, 0.78] |
| 4 Perineal trauma | 1 | 66 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.38 [0.11, 1.29] |
| 5 Gestational weight gain (kg) | 1 | 66 | Mean Difference (IV, Fixed, 95% CI) | ‐0.20 [‐2.81, 2.41] |
| 6 Adherence to the intervention: compliance with schedule (%) | 1 | 66 | Mean Difference (IV, Fixed, 95% CI) | ‐3.0 [‐3.99, ‐2.01] |
| 7 Use of additional pharmacotherapy | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 7.1 Insulin dose (during the last 4 weeks of pregnancy, including regular and intermediate acting) (units/day) | 1 | 66 | Mean Difference (IV, Fixed, 95% CI) | 23.60 [11.17, 36.03] |
| 7.2 Insulin dose (during the last 4 weeks of pregnancy, including regular and intermediate acting) (units/kg) | 1 | 66 | Mean Difference (IV, Fixed, 95% CI) | 0.20 [0.12, 0.28] |
| 8 Glycaemic control: change in HbA1c (%) | 1 | 66 | Mean Difference (IV, Fixed, 95% CI) | ‐2.4 [‐3.33, ‐1.47] |
| 9 Glycaemic control: hospitalisation for glycaemic control | 1 | 66 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.33 [0.32, 5.50] |
| 10 Glycaemic control: success in glycaemic control (%) | 1 | 66 | Mean Difference (IV, Fixed, 95% CI) | 2.0 [‐0.26, 4.26] |
| 11 Stillbirth | 1 | 66 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.01, 7.90] |
| 12 Gestational age at birth (weeks) | 1 | 66 | Mean Difference (IV, Fixed, 95% CI) | 0.30 [‐1.08, 1.68] |
| 13 Apgar score < 7 at 5 minutes | 1 | 66 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.33 [0.04, 3.04] |
| 14 Macrosomia | 1 | 66 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.25 [0.08, 0.81] |
| 15 Small‐for‐gestational age | 1 | 66 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.0 [0.13, 71.07] |
| 16 Birthweight (g) | 1 | 66 | Mean Difference (IV, Fixed, 95% CI) | ‐379.0 [‐650.79, ‐107.21] |
| 17 Shoulder dystocia | 1 | 66 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.17 [0.02, 1.31] |
| 18 Nerve palsies | 1 | 66 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.5 [0.05, 5.25] |
| 19 Bone fractures | 1 | 66 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.07, 15.33] |
| 20 Neonatal hypoglycaemia | 1 | 66 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.14 [0.02, 1.10] |
| 21 Hyperbilirubinaemia or jaundice | 1 | 66 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.75 [0.18, 3.09] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Dalfra 2009.
| Methods | Quasi‐randomised controlled trial | |
| Participants | 276 pregnant women enrolled – 240 had GDM and 36 had type 1 diabetes. Setting: 12 Italian diabetes clinics Inclusion criteria: 240 women with GDM were included within a week of diagnosis of GDM (Carpenter and Coustan 1982 criteria); mean of 28 weeks’ gestation. Exclusion criteria: not stated. |
|
| Interventions |
Telemedicine (n = unclear; 88 followed up) Women received standard care plus telemedicine. They were given training on the use of the equipment and were asked to submit their glycaemic data every week, and more often if necessary, and had a medical examination at the diabetes clinic once a month. Women were asked to report their glucose concentrations (as recorded by the glucometer) using an interfacing device that converted the values into audio tones which could be transmitted via a normal telephone receiver. Women dialled the Glucobeep server’s number and identified themselves by a code – the system received their glycaemic data; they could also record a voice message containing any details they deemed useful to help the physician interpret their glycaemic values. Physicians logged in to the server to download the women’s glucose values and any messages; they analysed the data and recorded prescriptions in a message on the server; women then called the server to hear the message containing any new prescriptions. Both women and physicians received a text message immediately when their messages were received by the other party. Standard care (n = not clear; 115 followed up) Women received standard care (see below for details). All women Women were given standard care according to the recommendations of the American Diabetes Association; women with GDM were placed on a diet and trained to monitor their blood glucose using a home monitor. Women were asked to measure their blood glucose 4 times per day. Insulin was provided when glucose exceeded 95 mg/dl (5.3 mmol/L) fasting, or 130 mg/dl (7.2 mmol/L) 1 hour after meals. Women had a medical examination every 2 weeks. All women could contact the physician whenever they wished. |
|
| Outcomes | Review outcomes reported: maternal morbidity (including gestational hypertension, pre‐eclampsia, eclampsia, hypoglycaemic episodes); caesarean section; use of additional pharmacotherapy (insulin therapy); glycaemic control (HbA1c in third trimester); maternal hypoglycaemia; gestational weight gain; adherence to intervention; quality of life; views of intervention; neonatal morbidity (including hypoglycaemic, hyperbilirubinaemia, respiratory distress syndrome, shoulder dystocia, malformations); macrosomia; gestational age at birth; birthweight; medical examinations and visits to diabetic clinic | |
| Notes |
Funding: not reported Declarations of interest: not reported Dates: not specified |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote: "Women were sequentially assigned to the two groups: one patient was followed up using the telemedicine approach, and the next using the conventional approach (usual care)." |
| Allocation concealment (selection bias) | High risk | As above |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not feasible to blind participants and personnel |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No detail provided; unclear how lack of blinding would have affected outcomes |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 270 pregnant women were enrolled (240 with GDM, 36 with type 1 diabetes); 203/240 women with GDM and 32/36 women with type 1 diabetes were analysed; the others were excluded as they did not complete the questionnaires at the end of the study. While the authors reported "The demographic, clinical and metabolic characteristics of the women excluded from the study were no different from those of the women who completed the study," there were unbalanced numbers of women with GDM included in the analysis (88 in intervention; 115 in control) indicating a higher rate of exclusion from the intervention group. |
| Selective reporting (reporting bias) | Unclear risk | No access to trial protocol to permit confident assessment of selective reporting. Some results (particularly surrounding adherence and views) reported incompletely in text. |
| Other bias | Unclear risk | Lack of methodological detail provided to determine risks of other bias. |
De Veciana 1995.
| Methods | Randomised controlled trial | |
| Participants | 66 women randomised Setting: University of California, Irvine and Long Beach Memorial Medical Centre, USA Inclusion criteria: women with GDM who required insulin at or before 30 weeks’ gestation, with a singleton fetus. Women with elevated fasting values at the time of a 3‐hour OGTT received insulin; for others, insulin therapy was initiated if weekly fasting and post‐prandial (1 hour after breakfast) values exceeded 105 mg/dL or 140 mg/dL, respectively. Women were screened for GDM at 24 to 28 weeks' gestation with a 50 g 1‐hour OGCT; if the value was ≥ 140 mg/dL (7.8 mmol/L) but < 190 mg/dL* (10.6 mmol/L) a 3‐hour OGTT was performed, with GDM diagnosed with any 2 of the following abnormal values: fasting > 105 mg/dL (5.9 mmol/L); 1‐hour > 190 mg/dL (10.6 mmol/L); 2‐hour > 165 mg/dL (9.2 mmol/L); or 3‐hour > 145 mg/dL (8.1 mmol/L). (O'Sullivan and Mahan 1964 criteria; O'Sullivan 1964). *Women with a value ≥ 190 mg/dL on the initial screening test were also diagnosed with GDM. Exclusion criteria: women with a history of diabetes before pregnancy, with pre‐existing hypertension, renal disease or autoimmune disorders |
|
| Interventions |
Postprandial monitoring plan (n = 33) Women were required to undertake daily monitoring of blood glucose concentrations before breakfast (fasting), and 1 hour after each meal for the duration of the pregnancy. preprandialmonitoring plan (n = 33) Women were required to undertake daily monitoring of fasting, preprandial and bedtime capillary blood glucose concentrations for the duration of the pregnancy. All women Women were evaluated weekly by the perinatal diabetes team (obstetrician, dietitian, nurse educator, counsellor) unless pregnancy complications (including poor glycaemic control, preterm labour or hypertension) made hospitalisation necessary. Women had a diet prescribed with 30 kcal to 35 kcal per kg of ideal body weight, divided into 3 meals and 1 to 3 snacks (with 40% to 45% of the energy provided by carbohydrates); calorie intake and food choices were adjusted at the weekly visits according to weight gain and blood glucose. All women received split‐dose therapy, with short‐ and intermediate‐acting human insulin, adjusted to achieve fasting blood glucose of 60 mg/dL to 90 mg/dL (3.3 mmol/L to 5 mmol/L) and preprandial values of 60 mg/dL to 105 mg/dL (3.3 mmol/L to 5.9 mmol/L) or post‐prandial values < 140 mg/dL. Women used memory‐based reflectance glucometers to measure their blood glucose; adjustments to insulin doses were made if any of the values were consistently higher than the target concentrations (with efforts made to normalise fasting glucose first). |
|
| Outcomes | Review outcomes reported: hypertensive disorders of pregnancy (pre‐eclampsia); caesarean section; perineal trauma (3rd or 4th degree lacerations); gestational weight gain; adherence to intervention (compliance with schedule); use of pharmacotherapy (insulin dose); glycaemic control (change in HbA1c; hospitalisation for glycaemic control; success in glycaemic control); large‐for‐gestational age; stillbirth; gestational age at birth; Apgar score < 7 at 5 minutes; macrosomia; small‐for‐gestational age; birthweight; shoulder dystocia; nerve palsy (Erb’s palsy); bone fracture; hypoglycaemia (requiring glucagon or dextrose infusion); hyperbilirubinaemia | |
| Notes |
Funding: not reported Declarations of interest: not reported Dates: not specified |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "permuted‐block randomization was used;" no further details provided. |
| Allocation concealment (selection bias) | Unclear risk | No further details provided. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not feasible to blind participants and personnel. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | As above; and described in Discussion as a "non‐blinded study". |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No losses to follow up or missing data. |
| Selective reporting (reporting bias) | Unclear risk | Reported all outcomes as per manuscript methods; however no access to trial protocol/registration to assess selective reporting further. |
| Other bias | Low risk | No other obvious risk of bias identified. |
Given 2015.
| Methods | Randomised controlled trial | |
| Participants | 50 women randomised. Setting: 2 specialist antenatal diabetes clinics in North Ireland and the Republic of Ireland from January 2012 and May 2013 Inclusion criteria: women with GDM or impaired glucose tolerance following an OGTT (usually at week 24 to 28 weeks); with the ability to use the telemedicine equipment following training, sufficient communication abilities to be fully involved, and willingness to use one of the approved blood glucose meters for the duration of the study (including women who had a previous diagnosis of GDM or impaired glucose tolerance). For GDM or impaired glucose tolerance diagnosis, the report referenced the National Institute of Clinical Excellence: Diabetes in Pregnancy 2008 guidelines. Exclusion criteria: prior diagnosis of type 1 or 2 diabetes; receipt of oral steroid therapy |
|
| Interventions |
Telemedicine (n = 24) Women received standard care plus telemedicine. Women were reviewed weekly using telemedicine (commercially available facilities from Northern Ireland). They were given a set of scales, a blood pressure monitor, blood glucose meter and telemedicine hub (with a small screen and 3 buttons to collect and transit data from the woman’s home). Once a week the hub would activate and remind the woman it was time for her telemedicine session; she would measure her weight and blood pressure and send 7‐day stored blood glucose values to the hub, and would answer 3 questions (Have you been taking your insulin? Have you had any hypoglycaemic episodes? Have you had any intercurrent illness?) using yes/no buttons; the information was transmitted to the central server where it could be accessed by the women’s healthcare practitioner. A website was available where women could review their data. 1 to 2 days after submission of the data, the healthcare practitioner reviewed the data; if there were any problems, the healthcare practitioner could contact the woman by telephone to discuss any changes needed, or arrange a visit. Standard care (n = 26) Women received standard care (see below for details). All women Standard care followed the National Institute for Health and Care Excellence (NICE) guidelines for the management of GDM or impaired glucose tolerance; women were asked to monitor their blood glucose 7 times per day (before and after each meal and before bed), and to attend a specialist diabetes clinic at least every 2 weeks, where weight and blood pressure were measured, urinalysis was performed and glycaemia was evaluated using self‐monitored blood glucose records and HbA1c. |
|
| Outcomes | Review outcomes reported: hypertensive disorders of pregnancy (pre‐eclampsia, pregnancy‐induced hypertension), caesarean section; induction of labour; use of additional pharmacotherapy (diabetes therapy at time of delivery); glycaemic control (HbA1c at 36 weeks; mean self‐monitored blood glucose); maternal hypoglycaemia; gestational weight gain (weight at 36 weeks); adherence (appointments attended; average daily self‐monitored blood glucose frequency (meter memory, diary)); average review length; stillbirth (intrauterine death); preterm birth; macrosomia; shoulder dystocia; respiratory distress syndrome (or transient tachypnoea of the newborn); hypoglycaemia (treated with dextrose); jaundice (no treatment needed; requiring phototherapy); malformations (diabetes‐related); neonatal intensive care unit admission; gestational age at birth; birthweight; head circumference; length | |
| Notes |
Funding: "This work constituted part of a PhD for J.E.G., which was funded by the Department for Employment and Learning for Northern Ireland. A small start‐up grant was provided for the study by Derry City Council. The telemedicine service was provided free of charge at one of the trial sites;" "There was no involvement of the funders of this research or the telemedicine service provider in study design, data collection, data analysis, and manuscript preparation or publication decisions." Declarations of interest: "M.J.O’K. has received research funding from Nova Biomedical (a manufacturer of glucose meters). J.E.G., B.P.B., F.D., and V.E.C. declare no competing financial interests exist." Dates: January 2012 and May 2013 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random allocation software was used to generate a stratified randomisation scheduled with blocks of 4‐6. |
| Allocation concealment (selection bias) | Low risk | An independent research secretary was used to allocate women to a group according to the schedule. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: "Because of the nature of the intervention it was not possible to blind participants or HCPs." |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No details provided; unclear how lack of blinding would have affected outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Of the 24 women allocated to the intervention group, 3 were excluded from analyses (2 did not have a landline and mobile network coverage to allow data transfer; 1 withdrew); none of the 26 women in the control group were excluded from analyses. Questionnaires completed by 19/24 women in the intervention group and 22/26 in the control group; unclear impact in already small sample. For a number of outcomes, data are taken from the supplementary tables which indicated missing data for some women/babies, for different outcomes (i.e. separate Ns are reported for each outcome). |
| Selective reporting (reporting bias) | Unclear risk | No access to trial protocol to confidently assess selective reporting. |
| Other bias | Low risk | Very few baseline characteristics reported, though no clear differences; no other obvious sources of bias identified. |
Homko 2002.
| Methods | Randomised controlled trial | |
| Participants | 61 women randomised Setting: The Diabetes‐in‐Pregnancy Program at Temple University Hospital, Philadelphia, USA and/or its satellite hospitals, from March 1998 to November 1999 Inclusion criteria: women with GDM ≤ 33 weeks' gestation and fasting blood glucose ≤ 95 mg/dL on OGTT. GDM criteria not defined. Exclusion criteria: none stated |
|
| Interventions |
Self‐monitoring (n = 31) Women were taught to perform self‐monitoring of blood glucose using a reflectance meter with memory (One Touch Profile) and asked to measure the blood glucose 4 times per day (fasting and 1 hour after meals), for a total of 4 times per week. Periodic monitoring (n = 30) Women had their blood glucose concentrations measured (fasting and 1 hour after a meal) at each prenatal visit, or more frequently if clinically indicated. All women The diabetes and obstetric management protocol was identical for both groups, except for glucose surveillance. Individualised teaching/counselling regarding GDM and its management was provided to all women by the diabetes educator. All women were treated to attain the same metabolic goals: fasting blood glucose < 95 mg/dL, and 1‐hour post‐prandial glucose < 120 mg/dL; women who failed to meet the targets at least 90% of the time, were started on insulin. |
|
| Outcomes | Review outcomes reported: pre‐eclampsia; caesarean section; perinatal mortality; large‐for‐gestational age; placental abruption; postpartum haemorrhage; gestational weight gain; adherence to the intervention (Dietary Compliance Questionnaire); sense of well‐being and quality of life (Diabetes Empowerment Scale; Appraisal of Diabetes Scale); use of additional pharmacotherapy; glycaemic control (preprandial and post‐prandial glucose); stillbirth; neonatal mortality; gestational age at birth; birthweight; hypoglycaemia; hyperbilirubinaemia; number of antenatal visits or admissions (visits with diabetes team); neonatal intensive care unit admission; 'birth trauma'; 'respiratory complications'. | |
| Notes |
Funding: "This work was supported by a grant from the General Clinical Research Center branch of the National Center for Research Resources, Grant No. 2M01‐RR‐349" and "We would also like to thank LifeScan Inc, who generously donated the glucose meters for this study." Declarations of interest: not reported Dates: March 1998 to November 1999 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "A randomized controlled trial was undertaken". |
| Allocation concealment (selection bias) | Unclear risk | As above; no further details provided. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not feasible to blind participants and personnel. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No detail provided; unclear how lack of blinding would have affected outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 3 women in the periodic monitoring group were lost to follow‐up and were removed, as no outcome data were available; for the Diabetes Empowerment Scale, results were reported for 28/31 (90%) and 19/27 (70%) women in the 2 groups, indicating fewer women in the control group completed the questionnaire, but no reasons were given. It appears that all 31 and 27 women completed the other questionnaires. |
| Selective reporting (reporting bias) | Unclear risk | Not possible to assess confidently; no access to trial protocol. Insulin therapy reported only in Abstract, and not in Results text of manuscript. |
| Other bias | Low risk | No other obvious sources of bias identified. |
Homko 2007.
| Methods | Randomised controlled trial | |
| Participants | 63 women randomised Setting: prenatal clinics at Temple University Hospital, Philadelphia, USA, or one of its satellites; from September 2004 to May 2006 Inclusion criteria: women with GDM (3‐hour OGTT using Carpenter and Coustan 1982 criteria), between 18 and 45 years, at 33 weeks' gestation or less Exclusion criteria: women with prior history of glucose intolerance, or with multiple gestations |
|
| Interventions |
Telemedicine (n = 34) Women were asked to transmit information via a diabetes health network at least 3 times per week to their healthcare provider. Women without access to the internet received a refurbished computer with free telephone‐based web access to be used during the study; they received a 1‐hour training session by graduate/undergraduate students on how to use a computer, how to access websites, how to set up an email address and receive/send emails. The intervention used 'ITSMyHealthfile', a web‐based disease management interactive healthcare delivery system, with a secure internet server and database which allowed women to send blood glucose and other health data directly to their care provider (blood glucose; fetal movement counts; insulin doses; episodes of hypoglycaemia; ask questions/messages), and receive information and advice from healthcare providers. It required a log‐on ID and password. Standard care (n = 29) Women were asked to record information in a log‐book, which was reviewed by the medical team at prenatal visits. All women All received standard care in the ‘diabetes‐in‐pregnancy program’: were seen for clinical evaluation every 2 weeks until 36 weeks, after which they were seen weekly. Care was provided by a team of maternal‐fetal medicine specialists, residents, diabetes educator, and nutritionists. All received individualised dietary counselling and diabetes education and were instructed in glucose self‐monitoring with portable reflectance meters – women were asked to monitor 4 times per day (before breakfast; 2 hours after meals), and were treated to maintain: fasting glucose ≤ 95 mg/dL, and 2‐hour ≤ 120 mg/dL; women who failed to meet the targets > 90% of the time were started on glyburide or insulin. Women were also asked to perform fetal movement counting 3 times per day and record insulin doses and episodes of hypoglycaemia. |
|
| Outcomes | Review outcomes reported: hypertensive disorders of pregnancy (pre‐eclampsia/gestational hypertension); caesarean section; placental abruption; use of additional pharmacotherapy (glyburide; insulin); glycaemic control (fasting blood sugar; blood glucose 2 hours post breakfast, lunch, dinner; mean; HbA1c at birth); adherence to intervention (frequency of monitoring; appointment adherence); sense of well‐being and quality of life (maternal feelings of diabetes self‐efficacy); large for gestational age; perinatal mortality; neonatal mortality or morbidity composite ('composite outcome'); stillbirth; neonatal mortality; preterm birth; respiratory distress syndrome/respiratory complications; hypoglycaemia; hyperbilirubinaemia/jaundice; neonatal intensive care unit admission; gestational age at birth; birthweight | |
| Notes |
Funding: "This study was supported by grant RO3 NR008776‐01 from the National Institute of Nursing Research, National Institutes of Health". Declarations of interest: not reported Dates: September 2004 to May 2006 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Women were randomized into one of two groups." |
| Allocation concealment (selection bias) | Unclear risk | As above; no further details provided. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not feasible to blind participants and personnel. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No detail provided; unclear how lack of blinding would have affected outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 29 women randomised to control group; 2 lost to follow‐up, 1 excluded (twin pregnancy), 1 did not meet criteria for GDM; therefore 25 included in analyses; 34 women randomised to intervention group, 2 formally withdrew; therefore 32 included in analyses. |
| Selective reporting (reporting bias) | Unclear risk | No access to trial protocol to enable confident assessment of selective reporting. |
| Other bias | Low risk | Comparable groups at baseline; no other obvious sources of bias apparent. |
Homko 2012.
| Methods | Randomised controlled trial | |
| Participants | 80 women randomised Setting: prenatal clinics at Temple University Hospital, Philadelphia, and Diabetes Education Program at Tallahassee Memorial Hospital, Tallahassee, USA; from September 2007 to November 2009 Inclusion criteria: women with GDM (on 3‐hour OGTT using the Carpenter and Coustan 1982 criteria), between 18 and 45 years, at 33 weeks' gestation or less Exclusion criteria: women with a prior history of glucose intolerance outside of pregnancy, or multiple gestations (twins, triplets) |
|
| Interventions |
Telemedicine (n = 40) Women were trained in the use of a computer and the internet, instructed on the details of the Internet program, and introduced to the website on a demonstration terminal at the clinic; automated telephone communication option and instructions were also offered for women with no Internet access. Women were provided with a password and log‐in name to gain access to the website, and an identification number to gain access to the telephone communication system. Women were prompted to input clinical data (blood glucose readings, changes in medications, episodes of hypoglycaemia) and identify the day or time. Women were provided with feedback, emotional support and reinforcement regarding self‐management with each transmission. Women received brief education message or suggestion each time they accessed the system. Women were asked to transmit information via phone/internet weekly to healthcare providers. The telemedicine system used was 'ITSMy Healthrecord', a web‐based, nurse‐co‐ordinated communication system, composed of a secure Internet server, a phone system and database, allowing data transfer (messages or clinical information) from patient to practice, and practice to patient in an asynchronous manner. Women dialled a toll‐free number or logged on through the internet using a unique log‐in and password – and could send messages or ask a question (45 seconds, or unlimited text input); nurses could then listen/review and respond (by typing a response that could be read or listened to); the system also provided reminders for women to record and transmit their data when required (3 phone call reminders, a day apart). Standard care (n = 40) Women were asked to record information in a logbook which was reviewed by the medical team at prenatal visits. All women Women were asked to monitor blood glucose daily (4 times per day: before breakfast and 2 hours after each meal). Women were treated to obtain metabolic goals: fasting glucose ≤ 95 mg/dL, 2‐hour: ≤ 120 mg/dL; women who did not meet these targets > 90% of the time were started on glyburide/insulin. Women were asked to perform fetal movement counting 3 times a day, and record insulin doses and episodes of hypoglycaemia. All women received standard care, and were seen for clinical evaluation every 2 weeks until 36 weeks, after which they were seen weekly (car provided by team: maternal‐fetal specialists, residents, diabetes educators, nutritionists); all women received individualised dietary counselling and diabetes education, and were instructed in glucose self‐monitoring. |
|
| Outcomes | Review outcomes reported: hypertensive disorders of pregnancy (pre‐eclampsia/gestational hypertension); caesarean section; use of additional pharmacotherapy (oral agents; insulin); glycaemic control (fasting blood sugar; blood glucose 2‐hour post breakfast, lunch, dinner; mean); adherence to intervention (frequency of monitoring); large‐for‐gestational age; perinatal mortality; stillbirth; neonatal mortality; preterm birth; respiratory distress syndrome/respiratory complications; hypoglycaemia; hyperbilirubinaemia/jaundice; neonatal intensive care unit admission; gestational age at birth; birthweight; length of stay in neonatal intensive care unit | |
| Notes |
Funding: "This study was supported by grant R21‐DK‐071694 from the National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health". Declarations of interest: "C.J.H., L.D., K.R., W.M., D.M., and J.G. have nothing to disclose. W.P.S. has stock ownership in Insight Telehealth Systems. A.A.B. is a consultant for Insight Telehealth Systems". Dates: September 2007 to November 2009 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Women were randomized into one of two groups." |
| Allocation concealment (selection bias) | Unclear risk | As above; no further details provided. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not feasible to blind participants and personnel. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No detail provided; unclear how lack of blinding would have affected outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 3/40 women in the intervention group and 2/40 in the control group were lost to follow‐up; 1 woman in the intervention group experienced a fetal loss at 19 weeks. |
| Selective reporting (reporting bias) | Unclear risk | No access to trial protocol to enable confident assessment of selective reporting. |
| Other bias | Low risk | Comparable groups at baseline; no other obvious sources of bias apparent. |
Kestila 2007.
| Methods | Randomised controlled trial | |
| Participants | 73 women randomised Setting: Finland Inclusion criteria: women with GDM, with singleton pregnancies. All women had a 2‐hour 75 g OGTT performed at 22 to 34 weeks' gestation as they belonged to a high‐risk group according to the evaluation system used in Finland (BMI > 25, > 40 years, previous child over 4500 g, glucosuria during pregnancy, weight gain during pregnancy > 20 kg, previous GDM or suspected fetal macrosomia). GDM was defined as having at least 2 abnormal high plasma glucose values out of 3 measurements in the 75 g OGTT (fasting > 5.1 mmol/L, 1‐hour > 10 mmol/L, 2‐hour > 8.7 mmol/L). Exclusion criteria: not reported |
|
| Interventions |
CGMS (n = 36) Women were taught how to use the CGMS equipment (and at least 4 daily plasma glucose calibration values were introduced to the apparatus); the mean duration of the registration period was 47.4 (2.5) hours. Women were asked not to take a shower during the monitoring period. Self‐monitoring (n = 37) All women All women came to the hospital for an interview and dietary counselling for low‐GI, low saturated fat eucaloric diet, and were taught how to measure plasma glucose, with an instruction to measure it 5 times per day (fasting plasma glucose, preprandial values and post‐prandial values 90 minutes after main meals), and asked to keep a dietary diary, and record exercise also. Treatment mode was determined within a week of starting monitoring; diet alone was considered insufficient if fasting plasma glucose was > 5.5 mmol/L twice, or was at least once > 5.5 mmol/L and post‐prandial value > 7.8 mmol/L or fasting plasma glucose ≤ 5.5 mmol/L but post‐prandial was at least twice > 7.8 mmol/L. Insulin was offered if at least 2 post‐prandial measurements were > 8.0 mmol/L; women with elevated fasting plasma glucose only were initially treated with metformin, and later combined with insulin if needed. |
|
| Outcomes | Review outcomes reported: hypertensive disorders of pregnancy (pre‐eclampsia, pregnancy‐induced hypertension); caesarean section; perineal trauma; use of additional pharmacotherapy (insulin; metformin); gestational weight gain (total); perinatal mortality; stillbirth; neonatal mortality; gestational age at birth; preterm birth; macrosomia; birthweight; hypoglycaemia; hyperbilirubinaemia (UV treated); neonatal intensive care unit admission; length of stay in neonatal intensive care unit. | |
| Notes |
Funding: "Turku University Central Hospital Research Fund, and The Foundation of Gynaecologists and Obstetricians in Finland supported this study". Declarations of interest: not reported Dates: not specified |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Patients were randomly allocated"; no further details provided. |
| Allocation concealment (selection bias) | Unclear risk | No details provided |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not feasible to blind participants and personnel. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No details provided; unclear how lack of blinding would have affected outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | It was not clear whether there were any women lost to follow‐up, or missing data for the outcomes reported, as this information was not provided. |
| Selective reporting (reporting bias) | High risk | Some results reported in text but not in tables, e.g. "There were no statistically significant differences between the two groups in… frequency of pre‐eclampsia, pregnancy‐induced hypertension, maternal lacerations… Apgar at… 10 min"; additional outcomes discussed in methods (e.g. shoulder dystocia, and PROM) not reported in results. Ns for hypoglycaemia and NICU admission unclear, as percentages indicate may not be 37 for control group. |
| Other bias | Unclear risk | Limited methodological details provided did not permit thorough assessment of other sources of bias. |
Kruger 2003.
| Methods | Randomised controlled trial | |
| Participants |
Setting: the Endocrinology and Metabolism Clinic of a large Midwestern health system; presumed to be in USA Inclusion criteria: pregnant women 18 years or older who sought treatment at the Endocrinology and Metabolism Clinic of a large Midwestern health system and were diagnosed with GDM. GDM diagnostic criteria not reported. Exclusion criteria: women who had been diagnosed with type 1 or 2 diabetes prior to pregnancy, or who were unwilling/unable to follow the protocol |
|
| Interventions |
Modem transmission (n = unclear; 72 across both groups; 18 analysed for satisfaction outcomes) Women transmitted blood glucose data to the clinic via the Acculink Modem; women were trained on how to use the modem to transmit blood glucose data from the meter to the clinic. Telephone transmission (n = 72 across both groups; 20 analysed for satisfaction outcomes) Women transmitted blood glucose data to the clinic via telephone calls directly to clinic personnel (research assistant/registered nurse). All women In both groups, women self‐tested blood glucose with an Accu‐Chek Complete meter. The duration of participation was from the first clinic visit to birth (thus length of participation was dependent on gestational age at GDM diagnosis; the mean duration was 6 weeks, with a range of 1 week to 22 weeks). At their first clinic visit, healthcare providers trained women about self‐monitoring of blood glucose, nutrition, and overall GDM management through educational literature and videos; if necessary, women received instruction on insulin administration; all women were asked to record the blood glucose results in a diary; all women were instructed to test and record their results 5 times daily, in accordance with standard care (before breakfast; 1 hour after each meal; before bed). Standard care involved reporting blood glucose values daily for the first 2 weeks after the first visit, then weekly thereafter; clinic personnel reviewed the blood glucose data received and provided feedback and guidance to the women via the telephone. Subsequent clinic visits were scheduled for 1 week after the first, and then every 2 weeks until 1 month before birth, then weekly until birth. |
|
| Outcomes | Review outcome reported: views of the intervention (percentages were provided and used to calculate group numbers); gestational age at birth | |
| Notes |
Funding: "Roche Diagnostics provided the authors with a grant as well as the blood glucose monitor supplies to do this study" Declarations of interest: not reported Dates: not specified |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "were randomized by block randomization into two groups". |
| Allocation concealment (selection bias) | Unclear risk | No further details provided |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not feasible to blind participants and personnel. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No details provided; unclear how lack of blinding would have affected outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Results reported incompletely (see below), therefore not possible to determine incomplete outcome data for some outcomes (mean telephone consultation time; length of clinic visit; weeks of gestation); participant satisfaction survey response rate was 52%. |
| Selective reporting (reporting bias) | High risk | No access to published trial protocol/trial registration; few outcomes reported (no clinical outcomes, except weeks of gestation) and focused on consultation time, and satisfaction only. A number of results reported as P values only. |
| Other bias | Unclear risk | No baseline characteristics were reported for the 2 groups (ethnicity and gestational age, and age across the population were reported). |
Perez‐Ferre 2010.
| Methods | Randomised controlled trial | |
| Participants | 100 women randomised Setting: the Unit of Gestational Diabetes of the Hospital Clinico Universitario San Carlos of Madrid, Spain from June to December 2007 Inclusion criteria: women with GDM (Carpenter‐Coustan criteria) before 28 weeks Exclusion criteria: not detailed |
|
| Interventions |
Telemedicine (n = 50) Women received a Glucometer (Accu‐Chek Compact Plus) with a cellular phone (which allowed the transmission of glucose values to the central database via a short message service SMS). Women were recommended to send their glucose values to the medical terminal once a week. An endocrinologist and diabetes nurse educator evaluated the data from a PC with Internet connection. Health professionals could then send text messages from their computer to the women, making recommendations for nutritional changes, or adjustments in insulin doses; women could send text messages with questions/answers. Standard care (n = 50) Women were followed according to standard protocol (face‐to‐face outpatient monitoring), and were given the opportunity to attend the outpatient clinic without prior appointment, and bring in their logbook when their glucose values were above the targets, of for any queries re: nutritional recommendations or insulin dose. All women Women were instructed by the nurse educator in nutritional habits and self‐monitoring of blood glucose and informed about the goals of glycaemic control: fasting blood glucose and preprandial blood glucose < 95 mg/dL; 1‐hour post‐prandial blood glucose < 120 mg/dL. At visit 1 (before 28 weeks' gestation), capillary blood glucose values were evaluated (6 measurements a day were recommended during the first week; if more than 4 of 5 fasting and pre‐meal glycaemic values were < 95 mg/dL in the first week, only 1‐hour post‐meal capillary blood glucose measurements were recommended daily or every other day until delivery). During the follow up, 4 face‐to‐face visits (once a month) were scheduled until birth; glucose values recorded by women in their log‐books were evaluated and episodes of mild/severe hypoglycaemia and insulin requirements registered. |
|
| Outcomes | Review outcomes reported: hypertensive disorders or pregnancy (pregnancy‐induced hypertension); caesarean section; placental abruption; use of additional pharmacotherapy (insulin treated); glycaemic control (HbA1c at visit 4 (39‐40 weeks); HbA1c < 5.8%); gestational weight gain; view of intervention; total contact hours per‐insulin treated woman; face‐to‐face visits; unscheduled visits; costs; large‐for‐gestational age; preterm birth; small‐for‐gestational age; shoulder dystocia; hypoglycaemia; hypocalcaemia; polycythaemia (poliglobulia); gestational age at birth; birthweight | |
| Notes |
Funding: "This work was supported by grants from Fundacion para Estudios Metabolicos". Declarations of interest: "The authors declare that they have no conflicts of interest" The 8 women most likely to require insulin after the evaluation of the first week were allocated to telemedicine group; and the other 92 were randomised to telemedicine or standard monitoring. Dates: June to December 2007 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote "were randomized;" see below |
| Allocation concealment (selection bias) | High risk | Not detailed; not achieved for 8 women most likely to require insulin who were allocated to telemedicine group. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not feasible to blind participants and personnel. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No detail provided; unclear how lack of blinding would have affected outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Of 100 women randomised, 97 (49 in the intervention group and 48 in the control group) completed the study. |
| Selective reporting (reporting bias) | Unclear risk | No access to trial protocol to enable confident assessment of selective reporting. Some data incompletely reported, e.g. "We did not detect differences in clinical and laboratory data during the follow up nor were differences in delivery and neonatal outcomes observed"; while the average total contact per insulin‐treated woman was reported, no variance was reported for this outcome; and the contact for all women was not clearly reported (only "There was a significant 62% reduction in outpatient clinic visits in women from the telemedicine group"). Methods detailed that loss of work days and the number of hospital admissions were regularly recorded, but no results were reported for these outcomes. |
| Other bias | Low risk | Comparable groups at baseline; no other obvious sources of bias apparent. |
Rey 1997.
| Methods | Randomised controlled trial | |
| Participants | 347 women randomised Setting: Sainte‐Justine Hospital, Montreal, Canada, from 1 June 1993 to 31 May 1994 Inclusion criteria: women with GDM (diagnosed according to institution criteria: 1‐hour 50 g glucose screen ≥ 11.1 mmol/L (200 mg/dL)); or glucose screen between 8.9 (160 mg/dL) and 11.0 mmol/L (198 mg/dL) with 2 or more abnormal values on a 3‐hour 100 g OGTT before 26 weeks (fasting: 5.3 mmol/L (95 mg/dL), 1‐hour: 10 mmol/L (180 mg/dL); 2‐hour: 8.9 mmol/L (160 mg/dL); 3‐hour: 7.8 mmol/L (140 mg/dL)); or during and after 26 weeks (fasting: 5.6 mmol/L (101 mg/dL), 1‐hour: 11.1 mmol/L (200 mg/dL); 2‐hour: 9.2 mmol/L (166 mg/dL); 3‐hour: 8.3 mmol/L (149 mg/dL)). Exclusion criteria: multiple pregnancy, fetus with congential malformation, current diet or insulin therapy, before 22 weeks or later than 38 weeks. Post‐randomisation exclusions: birth in another centre, birth within 2 weeks of randomisation, steroid therapy |
|
| Interventions |
Self‐monitoring (home) (n = 172; 112 with breakfast result < 7.8 mmol/L; 60 with breakfast result ≥ 7.8 mmol/L) Women took blood glucose measurements 3 times daily (1 hour after each meal) alternating with 4 times a day (before each meal and at bed time) using memory‐based reflectance meters, checked regularly. Periodic monitoring (outpatient follow‐up) (n = 170; 115 with breakfast result < 7.8 mmol/L; 55 with breakfast result ≥ 7.8 mmol/L) Women had outpatient clinic follow‐up, with capillary fasting and/or 1‐hour post‐breakfast glucose assessment by nurse educator every 2 weeks. Women were transferred to home monitoring as soon as 1 of their glucose assessments was higher than the goals. All women After an 8‐hour fast, women ingested standardised breakfast over 10 minutes, at 8am; 1 hour later, blood glucose was sampled: results were divided into those below and at or above 7.8 mmol/L (140 mg/dL). Target glucose concentrations were 5.3 mmol/L (95 mg/dL) fasting; 5.6 mmol/L (101 mg/dL) before dinner and supper and 7.8 mmol/L (140 mg/dL) 1‐hour post‐prandial. Women were started on insulin therapy when 25% or more of their home blood glucose concentrations during the previous 2 weeks were higher than the previously mentioned goals; insulin was adjusted to reach the same target goals. All women were prescribed a diet without refined carbohydrates, with 45% complex carbohydrate, 35% fat, 20% protein, divided into 3 meals and 4 snacks: 35 kcal/kg for non‐obese, 25 kcal/kg for obese women; all women were seen at 2‐week intervals. |
|
| Outcomes | Review outcomes reported: caesarean section; gestational weight gain; adherence (poor compliance); use of additional pharmacotherapy (insulin therapy); glycaemic control (preprandial glucose; post‐prandial glucose); perinatal mortality; large‐for‐gestational age; stillbirth; gestational age at birth; macrosomia; small‐for‐gestational age; birthweight; shoulder dystocia; hypoglycaemic; hyperbilirubinaemia; costs associated with the intervention | |
| Notes |
Funding: "This study was supported by a grant from Lilly Canada" Declarations of interest: not reported Dates: June 1993 to May 1994 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "women were randomized with stratification according to their ethnic origin (white and others) to either outpatient clinic follow‐up or self‐monitoring of blood glucose with a meter (home monitoring). A computer‐generated table of random numbers with permuted‐block randomization was used". |
| Allocation concealment (selection bias) | Unclear risk | No details provided |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not feasible to blind participants and personnel. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No detail provided; unclear how lack of blinding would have affected outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Of 347 women randomised, 5 were excluded (2 delivered preterm within 2 weeks of enrolment; 2 received long‐term high‐dose steroids for preterm labour; 1 delivered in another centre). Although 2.6% and 52.7% of women with a breakfast < 7.8 mmol/L and ≥ 7.8 mmol/L on clinic follow‐up were transferred to home monitoring respectively, "The data from the women included in the statistics were analysed according to their randomization". |
| Selective reporting (reporting bias) | Unclear risk | No access to trial protocol to enable confident assessment of selective reporting. |
| Other bias | Low risk | No other obvious sources of bias identified. |
Wei 2016.
| Methods | Randomised controlled trial | |
| Participants | 120 women randomised Setting: Department of Endocrinology, Zhongda Hospital, the Affiliated Hospital of Southeast University, China from September 2011 to December 2012 Inclusion criteria: women between 24 and 28 weeks' gestation with a singleton pregnancy, GDM, and written informed consent. All women underwent a 75 g OGTT at 24 to 28 weeks according to the criteria of the American Diabetes Association (ADA). Based on the 1‐step approached recommended by the World Health Organization, ADA and IADPSG, women were defined as having GDM if they had at least 1 abnormally high plasma glucose out of the 3 measurements: fasting > 92 mg/dL (5.1 mmol/L), 1‐hour > 180 mg/dL (10.0 mmol/L), or 2‐hour > 153 mg/dL (8.5 mmol/L). Exclusion criteria: diagnosis of diabetes mellitus, previous treatment for GDM, presence of infection, or other severe metabolic, endocrine, medical or psychological co‐morbidities |
|
| Interventions |
CGMS (n = 58*) There were 2 groups: CGMS early subgroup (n = 30): during gestational weeks 24 to 28; and CGMS late subgroup (n = 30): during gestational weeks 28 to 36. *There were 3 additional women who withdrew following allocation, it was unclear if they were allocated to the early or late subgroup. The CGMS group was monitoring using CGMS (Gold Medtronic MiniMed, Northbridge, CA, USA), with the sensor inserted into the upper outer buttock of the subjects. While women wore the sensor, glucose concentrations (bedtime, and 1 hour before the beginning of each meal) were also monitored using the Accu‐Chek meters and were input into the CGMS as calibration 4 times per day. Self‐monitoring (n = 62) All women Women were taught to perform self‐monitoring of blood glucose using Accu‐Chek Advantage meters (Roche Diagnostics, Manheim, Germany). Women were instructed to check their level 4 times per day (fasting, and 1 hour after the beginning of each meal) from the first visit at which they received the GDM diagnosis until birth (except during the period where the GGMS group used their device). Women underwent dietary counselling for a eucaloric diet with a low GI and low saturated fat levels (50% to 60% energy from carbohydrates; 25% to 30% from fat; 15% to 20% from protein; with energy intake distributed as equally as possible throughout the day, based on recommendations of the China Diabetic Association). Moderate intensity exercise was encouraged; 35 to 45 minute sessions, three times a week. A physiotherapist motivated the women to continue or start exercising, and provided written instructions, with walking, swimming and cycling recommended as types of exercise. Insulin treatment was administered under conditions of 2 fasting blood glucose values > 105 mg/dL (5.8 mmol/L), 2 1‐hour post‐prandial levels > 155 mg/dL (8.6 mmol/L), a 2‐hour post‐prandial level > 130 mg/dL (7.2 mmol/L), or a fasting blood glucose > 90 mg/dL (5.5 mmol/L) with at least 2 post‐prandial values > 141 mg/dL (7.5 mmol/L) according to ADA guidelines. Women received NPH insulin as an immediate acting insulin with an initial dose of 0.2 units/kg; if fasting levels were high, treatment was given before bed‐time; if post‐prandial levels were high, regular insulin or short acting insulin was given before meals. Follow‐up meetings were every 2 to 4 weeks until 28 weeks, fortnightly until 32 weeks, and weekly thereafter. |
|
| Outcomes | Review outcomes reported: caesarean section; use of additional pharmacotherapy (insulin use; dose); glycaemic control (HbA1c); hypoglycaemia; gestational weight gain (and excessive; inadequate; appropriate gain); views of intervention; large‐for‐gestational age; perineal mortality; stillbirth; neonatal death; preterm birth; macrosomia; small‐for‐gestational age; hypoglycaemia; gestational age at birth; birthweight | |
| Notes |
Funding: "This work was partially supported by the following foundation: the Social Development Project of JiangSu Province (No. SBE201170735, Wang SH)". Declarations of interest: "The authors declare no competing financial interests". Dates: September 2011 to December 2012 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "randomly allocated … by a computer generated random number table". |
| Allocation concealment (selection bias) | Unclear risk | No details provided |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not feasible to blind participants and personnel. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No detail provided; unclear how lack of blinding would have affected outcomes. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 120 women were randomised, and 106 were analysed; 58 were randomised to CGMS and 62 to self‐monitoring; overall 51/58 were analysed in the CGMS group and 55/62 in the self‐monitoring group. In the CGMS group, 2 withdrew, 1 had site discomfort, 3 were lost, and 1 discontinued; in the self‐monitoring group, 4 were lost, and 3 discontinued. |
| Selective reporting (reporting bias) | Unclear risk | No access to trial protocol to enable confident assessment of selective reporting. |
| Other bias | Low risk | No other obvious sources of bias identified. |
Abbreviations BMI: body‐mass index CGMS: continuous glucose monitoring system GDM: gestational diabetes mellitus GI: glycaemic index HbA1c: glycated haemoglobin
IADPSG: International Association of the Diabetes and Pregnancy Study Groups NICU: neonatal intensive care unit OGCT: oral glucose challenge test OGTT: oral glucose tolerance test PROM: preterm rupture of membranes
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Bancroft 2000 | This randomised trial is included in the Alwan 2009 Cochrane Review that assessed treatments for women with GDM. The monitored group were given standard dietary advice, glucose metabolism was monitored by capillary glucose series 5 days a week, HbA1c was measured monthly (insulin was introduced if 5 or more capillary measurements > 7.0 mmol/L in 1 week), serial ultrasound for growth and amniotic fluid, Doppler studies, CTG monitoring. The unmonitored group received dietary advice, and HbA1c monthly, but no capillary glucose measurements. |
| Bartholomew 2015 | This was a cross‐over randomised trial, in women with type 2 diabetes or GDM. The trial compared a traditional method of blood sugar reporting using telephone and voicemail and a novel method using cell phone/internet technology. |
| Clarke 2005 | This was a cross‐over randomised trial, in women with type 2 diabetes or GDM. The trial compared the use of Softsense and Optium (MediSense Products) meters. |
| Elnour 2008 | This randomised controlled trial assessed a structured pharmaceutical care service (including education and introduction of intensive self‐monitoring) for women with GDM. Women in the pharmaceutical care intervention group received care by a clinical pharmacist at baseline, and reinforced at monthly clinic visits, with education about GDM and its management (including advice on diet, exercise, blood glucose control, self‐monitoring of glucose, and adjustment of treatment if required; a printed educational booklet; and instructions for self‐monitoring of blood glucose). Control women received traditional care (which included monthly clinic visits and self‐monitoring of plasma glucose using diary cards, but did not include patient education or counselling by the clinical pharmacist, or liaison between the clinical pharmacist and the prescribing doctor). This trial is likely to be eligible for the Brown 2017 Cochrane Review. |
| Fung 1996 | Participants were pregnant women, not specifically women with GDM. All women received a 50 g 3‐hour and 75 g 2‐hour OGTT in a random order, 7 days apart between 28 and 32 weeks' gestation. Women were compared according to whether they received the 50 g test first or 75 g test first. |
Abbreviations CTG: cardiotocography GDM: gestational diabetes mellitus HbA1c: glycated haemoglobin OGTT: oral glucose tolerance test
Characteristics of studies awaiting assessment [ordered by study ID]
Ding 2012.
| Methods | Randomised controlled trial |
| Participants | 128 women with GDM |
| Interventions | Continuous glucose monitoring group (N = 68): women wore continuous glucose monitors for 72 hours. Control group (N = 60): women tested capillary blood glucose with a single spot blood glucose meter 7 times per day. |
| Outcomes | Abstract reported on hypoglycaemia and hyperglycaemia. |
| Notes | Published as an Abstract only; no contact details available for authors as at 19 September 2016. |
Paramasivam 2014.
| Methods | Randomised controlled trial |
| Participants | 50 women with insulin‐requiring GDM |
| Interventions | Continuous glucose monitoring group (N = 25): women underwent professional continuous glucose monitoring using the iPro2 Enlite 6‐day sensor at 28, 32 and 36 weeks' gestation. Control group (N = 25): no continuous glucose monitoring Women in both groups performed 7 point finger‐stick glucose profiles 3 times per week. |
| Outcomes | Abstract reported on HbA1c; hypoglycaemia, euglycaemia and hyperglycaemia; insulin dose; and birthweight. |
| Notes | Note: 2014 Abstract reported on 24 women; 2015 Abstract reported on 50 women (trial registration originally suggested 80 women were to be randomised, however this was updated to 50 women). Published as 2 Abstracts only; contacted trial author (sharmsp13@um.edu.my) re availability of full trial report on 19 September 2016. |
Puricel 2014.
| Methods | Randomised controlled trial |
| Participants | Women with GDM |
| Interventions | Telemedicine group (N = not reported): women were managed via the G‐DEMANDE PHS system. Standard protocol group (N = not reported): women were managed by regular clinic visits. |
| Outcomes | Abstract reported on acceptability (satisfaction; at ease with the technology), and blood glucose. |
| Notes | Published as an Abstract only; contacted trial author (serbanpuricel@icloud.com) re availability of full trial report on 19 September 2016. Received a response on 20 September 2016; as yet, the trial has not been published, or is not available as a full report. |
Rigla 2015.
| Methods | Randomised controlled trial |
| Participants | 69 women with GDM |
| Interventions | Active group (N = not reported): women used the computer‐based smart telemedicine system for automated support; and downloaded blood glucose data every 3 days. Control group (N = not reported): women attended usual weekly visits. |
| Outcomes | Abstract reported on blood glucose downloads; number of changes in diet automatically proposed; blood glucose and % blood glucose > 140 mg/dL; HbA1c; 'perinatal outcomes'; and face‐to‐face visits. |
| Notes | Published as an Abstract only; contacted trial author (mrigla@tauli.cat) re availability of full trial report on 19 September 2016. Received a response on 29 September 2016; as yet, the trial has not been published, or is not available as a full report. |
Abbreviations GDM: gestational diabetes mellitus HbA1c: glycated haemoglobin
Characteristics of ongoing studies [ordered by study ID]
Evers 2016.
| Trial name or title | GlucoMOMS trial |
| Methods | Randomised controlled trial |
| Participants | Pregnant women aged 18 and over with either diabetes mellitus type 1 or 2 on insulin therapy or with GDM requiring insulin therapy before 30 weeks of gestation. |
| Interventions | Intervention group: women will use continuous glucose monitoring for 5 to 7 days every 6 weeks; based on their profiles, they will receive dietary advice and insulin therapy adjustments if necessary. Control group: women will receive usual care. All women will determine their glycaemic control by self‐monitoring of blood glucose levels and HbA1c. |
| Outcomes | Primary outcome: macrosomia (birthweight > 90th centile) Secondary outcomes: maternal: pre‐eclampsia; caesarean section; hypoglycaemia; HbA1c levels; and glucose variability; neonatal: birthweight; preterm birth; perinatal death; birth trauma; hypoglycaemia; respiratory distress syndrome; bronchopulmonary dysplasia; intraventricular haemorrhage; necrotising enterocolitis; and sepsis |
| Starting date | Planned start date: 1 July 2011 |
| Contact information | Daphne N Voormolen: d.p.vanmunster‐2@umcutrecht.nl Department of Obstetrics and Gynaecology, University Medical Centre, Utrecht, The Netherlands |
| Notes | Recruitment target: 300 women 2016 Abstract reported that as of Septenber 2015, 300 pregnant women were included (N = 108 with GDM). |
Hanafusa 2015.
| Trial name or title | Evaluation of the efficacy of self monitoring blood glucose for GDM with 1 point abnormality |
| Methods | Randomised controlled trial |
| Participants |
|
| Interventions | Intervention group: self‐blood glucose monitoring |
| Outcomes | Outcomes: body weight; HbA1c; glycoalbumin plasma glucose; insrinogenic index; continuous glucose monitoring; neonatal complications; and complications of pregnancy |
| Starting date | Anticipated start date: 5 January 2016 |
| Contact information | Toshiaki Hanafusa: hanafusa@poh.osaka‐med.ac.jp Department of Internal Medicine, Osaka Medical College, Osaka, Japan |
| Notes | Recruitment target: 60 women |
Kim 2014.
| Trial name or title | Self‐blood glucose monitoring and real‐time continuous glucose monitoring in patients with GDM |
| Methods | Randomised controlled trial |
| Participants | Women with newly diagnosed GDM who meet 'two‐step' approach (Carpenter and Coustan criteria) at 24‐28 weeks' gestation. |
| Interventions | Intervention group: as per control group, plus real‐time continuous glucose monitoring Control group: women receive education every 1 to 2 weeks, about glucose controlling and diet, according to their self‐monitored glucose levels. |
| Outcomes | Primary outcome: composite maternal and neonatal outcome consisting of: pregnancy‐induced pre‐eclampsia; preterm birth; macrosomia/large‐for‐gestational age/small‐for‐gestational age; and obstetric trauma Secondary outcomes: caesarean birth; eclampsia, gestational hypertension; intrauterine fetal death; gestational age at birth; birthweight, birthweight percentile; neonatal hypoglycaemia; hyperbilirubinaemia; respiratory distress syndrome |
| Starting date | Anticipated date of first enrolment: 29 May 2015 |
| Contact information | Jae Hyeon KIm: jaehyeon@skku.edu Samsung Medical Center, Seoul, South Korea |
| Notes | Recruitment target: 178 women |
Mackillop 2016.
| Trial name or title | Trial of remote evaluation and treatment of GDM (TREAT‐GDM) |
| Methods | Randomised controlled trial |
| Participants | Women with abnormal glucose tolerance test in this pregnancy (as defined by IADPSG recommendations); not requiring pharmacological treatment at recruitment; started on oral hypoglycaemic therapy at recruitment; with a singleton pregnancy; able to travel to hospital independently |
| Interventions | Intervention group: women will receive the GDM‐health system and half the normal clinic visits. Control group: women will receive normal clinic care. |
| Outcomes | Primary outcome: mean blood glucose from recruitment to delivery calculated, with adjustments made for number of measurements, proportion of preprandial and post‐prandial readings and length of time in study Secondary outcomes: compliance; maternal and neonatal outcomes; glycaemic control using HbA1c and other blood glucose metrics; attitudes to care; resource use |
| Starting date | September 2013 |
| Contact information | Lucy Mackillop; lucy.mackillop@ouh.nhs.uk Nuffield Department of Obstetrics and Gynaecology, John Radcliffe Hospital, Oxford, UK |
| Notes | Recruitment target: 203 women |
Mendez‐Figueroa 2013.
| Trial name or title | Frequency of blood glucose monitoring in patients with GDM (GLIMPSE) |
| Methods | Randomised controlled trial |
| Participants | Women with GDM diagnosed using ACOG criteria; between 20‐32 weeks gestation; singleton pregnancies; not requiring medical therapy after the first weeks of blood glucose monitoring |
| Interventions | Intervention group: blood glucose monitoring every other day as per below Control group: blood glucose monitoring done every day (during a fasting state and 2 hours after breakfast, lunch and dinner) continued throughout gestation. |
| Outcomes | Primary outcome: neonatal weight Secondary outcome: macrosomia |
| Starting date | May 2013 |
| Contact information | Hector Mendez‐Figueroa: Hector.R.Mendezfigueroa@uth.tmc.edu The University of Texas Health Science Center, Houston, USA |
| Notes | Recruitment target: 286 women |
Rasekaba 2015a.
| Trial name or title | Telemedicine for insulin treated GDM (TeleGDM) |
| Methods | Randomised controlled trial |
| Participants | IADPSG criteria based clinical diagnosis of GDM confirmed by OGTT; 24 to 33 weeks' gestation, or earlier diagnosis if in high risk group; management of hyperglycaemia with insulin; smart phone/tablet with internet access and/or internet connected personal computer; not requiring an interpreter to navigate through the healthcare system |
| Interventions | Intervention group: telemedicine as an add‐on (adjunct) to usual care Control group: usual care |
| Outcomes | Primary outcome: patient service utilisation: assessed as a composite of scheduled face‐to‐face consultations, unscheduled face‐to‐face consultations, and telephone consultations. Secondary outcomes: glycaemic control; diabetes self efficacy; patient satisfaction; clinician satisfaction; service provision costs; technology capability and capacity; insulin adjustments; type of delivery (normal vaginal delivery, caesarean delivery or instrument deliveries); large‐for‐gestational age; macrosomia; and neonate admissions to special care nursery |
| Starting date | Anticipated date of first enrolment: 2 September 2014 |
| Contact information | Tshepo Rasekaba: tshepo.rasekaba@unimelb.edu.au School of Medicine,The University of Melbourne, Australia |
| Notes | Recruitment target: 100 women |
Rudge 2013.
| Trial name or title | Home versus hospital care in glucose monitoring of GDM and mild gestational hyperglycemia |
| Methods | Randomised controlled trial |
| Participants | Women with GDM, pre‐GDM or mild gestational hyperglycaemia |
| Interventions | Intervention group: home care, 'ambulatory care' or 'outpatient' care; blood glucose self‐monitoring by the women at home Control group: hospital care, 'acute care'; control of diabetes at hospitals by admission to hospital |
| Outcomes | Primary outcomes: maternal mortality and morbidity; perinatal mortality and morbidity Secondary outcomes: glucose control; maternal hospitalisation for any cause and prolonged hospitalisation; maternal prenatal and postnatal acute care visits; length of stay for delivery; postpartum repeated hospitalisation; biophysical profile tests; preterm birth; birthweight; infant repeated hospitalisation; infant acute care visits; costs |
| Starting date | May 2010 |
| Contact information | Marilza Rudge |
| Notes | Recruitment target: 80 women |
Abbreviations ACOG: American Congress of Obstetricians and Gynecologists GDM: gestational diabetes mellitus HbA1c: glycated haemoglobin IADPSG: International Association of the Diabetes and Pregnancy Study Groups OGTT: oral glucose tolerance test
Differences between protocol and review
There are a number of differences between the published protocol and this full review (Gill 2014).
Madeleine Gill and Thuy‐My N Nguyen left the review team and Therese Dowswell joined the review team.
We changed the title from protocol stage ('Home versus hospital glucose monitoring for gestational diabetes during pregnancy') to review stage ('Different methods and settings for glucose monitoring for gestational diabetes during pregnancy'), in line with the change in the scope of the review, which was expanded to incorporate another (now withdrawn) protocol ('Different techniques of blood glucose monitoring in women with gestational diabetes for improving maternal and infant health').
We revised the background and inclusion criteria in line with the expanded scope of the review.
We revised the outcomes, using the standard outcome set agreed by consensus between review authors of Cochrane Pregnancy and Childbirth reviews for prevention and treatment of GDM and pre‐existing diabetes. We also added a number of new outcomes that were not prespecified in the protocol, these are listed below.
Operative vaginal birth
Neonatal morbidity
Maternal morbidity
Birth trauma (neonatal)
Respiratory complications (neonatal)
For the outcome, 'use of additional pharmacotherapy' in the first comparison of telemedicine versus standard care for glucose monitoring, we split the analysis into insulin and others ‐ this was not a prespecified decision. We also reported scheduled and unscheduled hospital or health professional visits.
We updated the methods in line with those in the standard template used by Cochrane Pregnancy and Childbirth, specifically we included use of the GRADE approach to assess the quality of the body of evidence and the use of 'Summary of findings' tables.
Contributions of authors
Puvana Raman, Therese Dowswell and Emily Shepherd (née Bain) assessed studies for inclusion and extracted data. Puvana Raman, with guidance from Emily Shepherd, drafted the first version of the review and all authors made comments on subsequent drafts and contributed to the final version.
Madeleine Gill, Emily Shepherd and Thuy‐My Nguyen drafted the protocol, with Philippa Middleton and Caroline Crowther making comments and contributing to the final draft.
Sources of support
Internal sources
Australian Research Centre for Health of Women and Babies (ARCH), Robinson Research Institute, The University of Adelaide, Adelaide, Australia.
Healthy Mothers, Babies and Children, South Australian Health and Medical Research Institute (SAHMRI), Adelaide, Australia.
Liggins Institute, The University of Auckland, Auckland, New Zealand.
External sources
National Health and Medical Research Council, Australia.
-
National Institute for Health Research (NIHR), UK.
NIHR Cochrane Programme Grant Project: 13/89/05 – Pregnancy and childbirth systematic reviews to support clinical guidelines
Declarations of interest
Caroline Crowther ‐ none known.
Therese Dowswell is employed to on an NIHR Cochrane Programme Grant to work on a suite of Cochrane Reviews. In the last 36 months she has also been employed on a WHO project to work on other Cochrane Reviews. The funders have no influence on the content or conclusions of the reviews.
Philippa Middleton ‐ none known.
Puvaneswary Raman ‐ none known.
Emily Shepherd ‐ none known.
New
References
References to studies included in this review
Dalfra 2009 {published data only}
- Dalfra MG, Nicolucci A, Lapolla A, TISG. The effect of telemedicine on outcome and quality of life in pregnant women with diabetes. Journal of Telemedicine & Telecare 2009;15(5):238‐42. [DOI] [PubMed] [Google Scholar]
De Veciana 1995 {published data only}
- Veciana M, Major CA, Morgan MA, Asrat T, Toohey JS, Lien JM, et al. Postprandial vs preprandial blood glucose monitoring in women with gestational diabetes mellitus requiring insulin therapy. New England Journal of Medicine 1995;333:1237‐41. [DOI] [PubMed] [Google Scholar]
- Veciana M, Major CA, Morgan MA, Asrat T, Evans AT. Randomized trial comparing post‐prandial vs pre‐prandial glucose monitoring in class A2 gestational diabetics. American Journal of Obstetrics and Gynecology 1995;172:282. [Google Scholar]
Given 2015 {published data only}
- Given JE, Bunting BP, O'Kane MJ, Dunne F, Coates VE. Tele‐Mum: a feasibility study for a randomized controlled trial exploring the potential for telemedicine in the diabetes care of those with gestational diabetes. Diabetes Technology & Therapeutics 2015;17(12):880‐8. [DOI] [PubMed] [Google Scholar]
- Given JE, O'Kane M, Bunting BP, Dunne F, Moles K, King L, et al. Tele‐Mum: a feasibility study for a randomised controlled trial to explore the potential of using telemedicine for the diabetes care of those with gestational diabetes. Diabetic Medicine 2014;31(Suppl 1):146‐7. [Google Scholar]
- NCT01630759. Remote monitoring of diabetes in pregnancy: a feasibility study for a randomised controlled trial (Tele‐Mum). clinicaltrials.gov/ct2/show/NCT01630759 (first received 22 June 2012).
Homko 2002 {published data only}
- Homko CJ, Sivan E, Reece EA. The impact of self‐monitoring of blood glucose on self‐efficacy and pregnancy outcomes in women with diet‐controlled gestational diabetes. Diabetes Educator 2002;28(3):435‐43. [DOI] [PubMed] [Google Scholar]
Homko 2007 {published data only}
- Homko CJ, Santamore WP, Whiteman V, Bower M, Berger P, Geifman‐Holtzman O, et al. Use of an internet‐based telemedicine system to manage underserved women with gestational diabetes mellitus. Diabetes Technology & Therapeutics 2007;9(3):297‐306. [DOI] [PubMed] [Google Scholar]
Homko 2012 {published data only}
- Homko CJ, Deeb LC, Rohrbacher K, Mulla W, Mastrogiannis D, Gaughan J, et al. Impact of a telemedicine system with automated reminders on outcomes in women with gestational diabetes mellitus. Diabetes Technology and Therapeutics 2012;14(7):624‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kestila 2007 {published data only}
- Kestila KK, Ekblad UU, Ronnemaa T. Continuous glucose monitoring versus self‐monitoring of blood glucose in the treatment of gestational diabetes mellitus. Diabetes Research and Clinical Practice 2007;77(2):174‐9. [DOI] [PubMed] [Google Scholar]
Kruger 2003 {published data only}
- Kruger DF, White K, Galpern A, Mann K, Massirio A, McLellan M, et al. Effect of modem transmission of blood glucose data on telephone consultation time, clinic work flow, and patient satisfaction for patients with gestational diabetes mellitus. Journal of the American Academy of Nurse Practitioners 2003;15:371‐5. [DOI] [PubMed] [Google Scholar]
Perez‐Ferre 2010 {published data only}
- Perez‐Ferre N, Galindo M, Fernandez MD, Velasco V, Runkle I, Cruz MJ, et al. The outcomes of gestational diabetes mellitus after a telecare approach are not inferior to traditional outpatient clinic visits. International Journal of Endocrinology 2010;2010:386941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perez‐Ferre N, Galindo M, Fernandez MD, Velasco V, Cruz MJ, Martin P, et al. A telemedicine system based on Internet and short message service as a new approach in the follow‐up of patients with gestational diabetes. Diabetes Research and Clinical Practice 2010;87(2):e15‐e17. [DOI] [PubMed] [Google Scholar]
Rey 1997 {published data only}
- Rey E. Usefulness of a breakfast test in the management of women with gestational diabetes. Obstetrics & Gynecology 1997;89:981‐8. [DOI] [PubMed] [Google Scholar]
Wei 2016 {published data only}
- Wei Q, Sun Z, Yang Y, Yu H, Ding H, Wang S. Effect of a CGMS and SMBG on maternal and neonatal outcomes in gestational diabetes mellitus: a randomized controlled trial. Scientific Reports 2016;6:19920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wei Q, Wang S, Yang Y, Sun Z. Earlier management with continuous monitoring blood glucose decrease gestational weight gain in gestational diabetes mellitus: a randomised clinical trial. Diabetologia 2013; Vol. 56:S73.
References to studies excluded from this review
Bancroft 2000 {published data only}
- Bancroft K, Tuffnell DJ, Mason GC, Rogerson LJ, Mansfield M. A randomised controlled pilot study of the management of gestational impaired glucose tolerance. BJOG: an international journal of obstetrics and gynaecology 2000;107(8):959‐63. [DOI] [PubMed] [Google Scholar]
Bartholomew 2015 {published data only}
- Bartholomew LM, Soules K, Church K, Shaha S, Burlingame J, Graham G, et al. Managing diabetes in pregnancy using cell phone/internet technology. Clinical Diabetes 2015;33(4):169‐74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartholomew ML, Church K, Graham G, Burlingame J, Zalud I, Sauvage L, et al. Managing diabetes in pregnancy using cell phone/internet technology. American Journal of Obstetrics and Gynecology 2011;204(1 Suppl):S113‐4. [Google Scholar]
- NCT01907516. Managing diabetes in pregnancy using cell phone/internet technology. clinicaltrials.gov/ct2/show/NCT01907516. NCT01907516 (first received 22 July 2013).
Clarke 2005 {published data only}
- Clarke P, Coleman MA, Holt RI. Alternative site self blood glucose testing is preferred by women with gestational diabetes.. Diabetes Technology & Therapeutics 2005;7(4):604‐8. [DOI] [PubMed] [Google Scholar]
Elnour 2008 {published data only}
- Elnour AA, Mugammar IT, Jaber T, Revel T, McElnay JC. Pharmaceutical care of patients with gestational diabetes mellitus. Journal of Evaluation in Clinical Practice 2008;14(1):131‐40. [DOI] [PubMed] [Google Scholar]
Fung 1996 {published data only}
- Fung HY, Wong SP, Rogers M. The influence of glucose tolerance tests on subsequent carbohydrate metabolism in pregnancy. Acta Obstetricia et Gynecologica Scandinavica 1996;75(4):347‐51. [DOI] [PubMed] [Google Scholar]
References to studies awaiting assessment
Ding 2012 {published data only}
- Ding G, Liang P, Peng Y, Pang Y, Zheng Y. Evaluation of continuous glucose monitoring (CGM) on gestational diabetes mellitus in China. Diabetes 2012;61 Suppl 1:A588. [Google Scholar]
Paramasivam 2014 {published data only}
- NCT02204657. The effect of professional continuous glucose monitoring on diabetes management, hypoglycemia and glycemic control in insulin‐requiring gestational diabetes mellitus. clinicaltrials.gov/ct2/show/NCT02204657 (first recieved 28 July 2014).
- Paramasivam SS, Tan AT, Chan SP, Chinna K, Ratnasingam J, Ibrahim L, et al. The effect of professional continuous glucose monitoring on glycaemic control and hypoglycaemia in insulin‐requiring gestational diabetes mellitus. Diabetologia 2015;58(Suppl 1):S74‐5. [Google Scholar]
- Paramasivam SS, Tan AT, Chan SP, Tan PC, Omar SZ, Ratnasingam J, et al. The effect of professional continuous glucose monitoring on glycaemic control and hypoglycaemia in insulin‐requiring gestational diabetes mellitus. Diabetologia 2014; Vol. 57, issue 1 Suppl 1:S449.
Puricel 2014 {published data only}
- Puricel S, Bromuri S, Krampf J, Diolosa L, Puder J, Montreuil C, et al. Telemedical outpatient monitoring and management of gestational diabetes mellitus by the G‐demande system: a randomized controlled feasibility study (TELE‐GDM). Diabetes Technology & Therapeutics 2014;16:A120. [Google Scholar]
Rigla 2015 {published data only}
- NCT01850199. Intelligent and educational system for gestational diabetes management. clinicaltrials.gov/ct2/show/NCT01850199 (first received 3 May 2013).
- Rigla M, Garcia‐Saez G, Villaplana M, Caballero‐Ruiz E, Pons B, Mendez A, et al. Successful replacement of weekly face‐to‐face visits by unsupervised smart home telecare in diet‐treated gestational diabetes (GD). Diabetes 2015;64:A372. [Google Scholar]
References to ongoing studies
Evers 2016 {published data only}
- Evers I. Effectiveness of continuous glucose monitoring during diabetic pregnancy (GlucoMOMS trial); a randomised controlled trial. Diabetes Technology and Therapeutics 2016;18:A13‐A14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Voormolen DN, DeVries JH, Franx A, Mol BW, Evers IM. Effectiveness of continuous glucose monitoring during diabetic pregnancy (GlucoMOMS trial); a randomised controlled trial. BMC Pregnancy and Childbirth 2012;12:164. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hanafusa 2015 {published data only}
- UMIN0000172362015. Evaluation of the efficacy of self monitoring blood glucose for gestational diabetes mellitus with one point abnormality. upload.umin.ac.jp/cgi‐open‐bin/ctr_e/ctr_view.cgi?recptno=R000017870. UMIN000017236 (first received 22 April 2015).
Kim 2014 {published data only}
- Kim JH. Self‐blood glucose monitoring and real‐time continuous glucose monitoring in patients with gestational diabetes mellitus. Clinical Research Information Service ‐ Republic of Korea (cris.nih.go.kr/cris/en) (accessed 1 November 2015). KCT0001507 2014.
Mackillop 2016 {published data only}
- Mackillop LH, Bartlett K, Birks J, Farmer AJ, Gibson OJ, Kevat DA, et al. Trial protocol to compare the efficacy of a smartphone‐based blood glucose management system with standard clinic care in the gestational diabetic population. BMJ Open 2016;6(3):e009702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCT01916694. Trial of remote evaluation and treatment of gestational diabetes mellitus (TREAT‐GDM). clinicaltrials.gov/ct2/show/NCT01916694. NCT01916694 (first received 4 July 2013).
Mendez‐Figueroa 2013 {published data only}
- NCT01818557. Frequency of blood glucose monitoring in patients with gestational diabetes (GLIMPSE). clinicaltrials.gov/ct2/show/NCT01818557. NCT01818557 (first received 21 March 2013).
Rasekaba 2015a {published data only}
- ACTRN12614000934640. Effectiveness of telemedicine plus usual care for insulin treated women with gestational diabetes mellitus (TeleGDM): an exploratory pilot randomised controlled trial. anzctr.org.au/Trial/Registration/TrialReview.aspx?id=366740&isReview=true (first received 1 September 2014).
Rudge 2013 {published data only}
- NCT01441518. Home versus hospital care in glucose monitoring of gestational diabetes and mild gestational hyperglycemia. clinicaltrials.gov/ct2/show/NCT01441518 (first received 31 May 2011).
Additional references
ACOG 2013
- American College of Obstetricians and Gynecologists (ACOG). ACOG Practice Bulletin no. 137: Clinical Management Guidelines for Obstetrician‐Gynecologists. Gestational diabetes. Obstetrics and Gynecology 2013;122(2 Pt 1):406‐16. [Google Scholar]
ADA 2004
- American Diabetes Association (ADA). Gestational diabetes mellitus. Diabetes Care 2004;Suppl 1:S88‐S90. [DOI] [PubMed] [Google Scholar]
ADA 2012
- American Diabetes Association (ADA). Standards of medical care in diabetes ‐ 2012. Diabetes Care 2012;35(1):511‐63. [Google Scholar]
Alwan 2009
- Alwan N, Tuffnell DJ, West J. Treatments for gestational diabetes. Cochrane Database of Systematic Reviews 2009, Issue 3. [DOI: 10.1002/14651858.CD003395.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ben‐Haroush 2004
- Ben‐Haroush A, Yogev Y, Chen R, Rosenn B, Hod M, Langer O. The postprandial glucose profile in the diabetic pregnancy. American Journal of Obstetrics & Gynecology 2004;191(2):576‐81. [DOI] [PubMed] [Google Scholar]
Benhalima 2013
- Benhalima K, Hanssens M, Devlieger R, Verhaeghe J, Mathieu C. Analysis of pregnancy outcomes using the new IADPSG recommendation compared with the Carpenter and Coustan criteria in an area with a low prevalence of gestational diabetes. International Journal of Endocrinology 2013;2013:Article ID 248121. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bodmer‐Roy 2012
- Bodmer‐Roy S, Morin L, Cousineau J, Rey E. Pregnancy outcomes in women with and without gestational diabetes mellitus according to the International Association of the Diabetes and Pregnancy Study Groups criteria. Obstetrics and Gynecology 2012;120(4):746‐52. [DOI] [PubMed] [Google Scholar]
Brown 2016
- Brown J, Grzeskowiak L, Williamson K, Downie MR, Crowther CA. Insulin for the treatment of women with gestational diabetes. Cochrane Database of Systematic Reviews 2016, Issue 1. [DOI: 10.1002/14651858.CD012037] [DOI] [PMC free article] [PubMed] [Google Scholar]
Brown 2016b
- Brown J, Crawford TJ, Alsweiler J, Crowther CA. Dietary supplementation with myo‐inositol in women during pregnancy for treating gestational diabetes. Cochrane Database of Systematic Reviews 2016, Issue 9. [DOI: 10.1002/14651858.CD012048.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Brown 2017
- Brown J, Alwan NA, West J, Brown S, McKinlay CJ, Farrar D, et al. Lifestyle interventions for the treatment of women with gestational diabetes. Cochrane Database of Systematic Reviews 2017, Issue 5. [DOI: 10.1002/14651858.CD011970.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Brown 2017b
- Brown J, Martis R, Hughes B, Rowan J, Crowther CA. Oral anti‐diabetic pharmacological therapies for the treatment of women with gestational diabetes. Cochrane Database of Systematic Reviews 2017, Issue 1. [DOI: 10.1002/14651858.CD011967.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Buchanan 2003
- Buchanan TA, Kjos S. Counterpoint: glucose monitoring in gestational diabetes: lots of heat, not much light. Diabetes Care 2003;26:948‐9. [DOI] [PubMed] [Google Scholar]
Carpenter 1982
- Carpenter MW, Coustan DR. Criteria for screening tests for gestational diabetes. American Journal of Obstetrics and Gynecology 1982;144(7):768‐773. [DOI] [PubMed] [Google Scholar]
Ceysens 2016
- Ceysens G, Brown J, Boulvain M. Exercise for pregnant women with gestational diabetes for improving maternal and fetal outcomes. Cochrane Database of Systematic Reviews 2016, Issue 5. [DOI: 10.1002/14651858.CD012202] [DOI] [PMC free article] [PubMed] [Google Scholar]
Coustan 2010
- Coustan DR, Lowe LP, Metzger BE, Dyer AR, International Association of Diabetes and Pregnancy Study Groups. The hyperglycemia and adverse pregnancy outcome (HAPO) study: paving the way for new diagnostic criteria for gestational diabetes mellitus. American Journal of Obstetrics and Gynecology 2010;202(6):e1‐e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Crowther 2005
- Crowther C, Hiller J, Moss J, McPhee A, Jeffries W, Robinson J, et al. Effect of treatment of gestational diabetes mellitus on pregnancy outcomes. New England Journal of Medicine 2005;352:2477‐86. [DOI] [PubMed] [Google Scholar]
Dabelea 2005
- Dabelea D, Snell‐Bergeon JK, Hartsfield CL, Bischoff KJ, Hamman RF, McDuffie RS. Increasing prevalence of gestational diabetes mellitus (GDM) over time and by birth cohort: Kaiser Permanente of Colorado GDM screening program. Diabetes Care 2005;28(3):579‐84. [DOI] [PubMed] [Google Scholar]
Dodd 2007
- Dodd JM, Crowther CA, Antoniou G, Baghurst P, Robinson JS. Screening for gestational diabetes: the effect of varying blood glucose definitions in the prediction of adverse maternal and infant health outcomes. Australian and New Zealand Journal of Obstetrics and Gynaecology 2007;47(4):307‐12. [DOI] [PubMed] [Google Scholar]
Espersen 1985
- Espersen T, Klebe JG. Self‐monitoring of blood glucose in pregnant diabetics. Acta Obstetricia et Gynecologica Scandinavica 1985;64:11‐4. [DOI] [PubMed] [Google Scholar]
Farrar 2015
- Farrar D, Duley L, Medley N, Lawlor DA. Different strategies for diagnosing gestational diabetes to improve maternal and infant health. Cochrane Database of Systematic Reviews 2015, Issue 1. [DOI: 10.1002/14651858.CD007122.pub3] [DOI] [PubMed] [Google Scholar]
Feig 2008
- Feig DS, Zinman B, Wang X, Hux JE. Risk of development of diabetes mellitus after diagnosis of gestational diabetes. Canadian Medical Association Journal 2008;179(4):344. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gabbe 2004
- Gabbe SG, Gregory RP, Power ML, Williams SB, Schulkin J. Management of diabetes mellitus by obstetrician‐gynecologists. Obstetrics and Gynecology 2004;103(6):1229‐34. [DOI] [PubMed] [Google Scholar]
Gates 2004
- Gates S, Brocklehurst P. How should trials recruiting women with multiple pregnancies be analysed?. British Journal of Obstetrics and Gynaecology 2004;111:213‐9. [DOI] [PubMed] [Google Scholar]
Getahun 2008
- Getahun D, Nath C, Ananth CV, Chavez MR, Smulian JC. Gestational diabetes in the United States: temporal trends 1989 through 2004. American Journal of Obstetrics and Gynecology 2008;198:e1–e5. [DOI] [PubMed] [Google Scholar]
Given 2013
- Given JE, O'Kane MJ, Bunting BP, Coates VE. Comparing patient‐generated blood glucose diary records with meter memory in diabetes: a systematic review. Diabetic Medicine 2013;30(8):901‐13. [DOI] [PubMed] [Google Scholar]
Goldberg 1986
- Goldberg JD, Franklin B, Lasser D, Jornsay DL, Hausknecht RU, Ginsberg‐Fellner F, et al. Gestational diabetes: impact of home glucose monitoring on neonatal birthweight. American Journal of Obstetrics and Gynecology 1986;154:546‐60. [DOI] [PubMed] [Google Scholar]
GRADEpro 2014 [Computer program]
- McMaster University (developed by Evidence Prime). GRADEpro GDT. Hamilton (ON): McMaster University (developed by Evidence Prime), 2015.
HAPO 2008
- The HAPO Study Cooperative Research Group. Hyperglycemia and adverse pregnancy outcomes. New England Journal of Medicine 2008;358(19):1991‐2002. [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Hirst 2015
- Hirst JE, Mackillop L, Loerup L, Kevat DA, Bartlett K, Gibson O, et al. Acceptability and user satisfaction of a smartphone‐based, interactive blood glucose management system in women with gestational diabetes mellitus. Journal of Diabetes Science & Technology 2015;9(1):111‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hoffman 1998
- Hoffman L, Nolan C, Wilison J, Oats J, Simmons D. Gestational diabetes mellitus: management guidelines. Australasian Diabetes in Pregnancy Society. Medical Journal of Australia 1998;169(2):93‐7. [DOI] [PubMed] [Google Scholar]
IADPSG Consensus Panel 2010
- International Association of Diabetes and Pregnancy Study Groups Consensus Panel. International association of diabetes and pregnancy study groups recommendations on the diagnosis and classification of hyperglycemia in pregnancy. Diabetes Care 2010;33(2):676‐82. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jiwani 2012
- Jiwani A, Marseille E, Lohse N, Damm P, Hod M, Kahn JG. Gestational diabetes mellitus: results from a survey of country prevalence and practices. Journal of Maternal Fetal and Neonatal Medicine 2012;25(6):600‐10. [DOI] [PubMed] [Google Scholar]
Jovanovic 2003
- Jovanovic L. Point: yes, it is necessary to rely entirely on glycemic values for the insulin treatment of all gestational diabetes women review. Diabetes Care 2003;26:946‐7. [DOI] [PubMed] [Google Scholar]
Kim 2002
- Kim C, Newton KM, Knopp RH. Gestational diabetes and the incidence of type 2 diabetes: a systematic review. Diabetes Care 2002;25:1862‐8. [DOI] [PubMed] [Google Scholar]
Kim 2010
- Kim SY, England L, Wilson HG, Bish C, Satten GA, Dietz P. Percentage of gestational diabetes mellitus attributable to overweight and obesity. American Journal of Public Health 2010;100:1047‐52. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kuhl 1998
- Kuhl C. Etiology and pathogenesis of gestational diabetes. Diabetes Care 1998;21(Suppl 2):B19‐B26. [PubMed] [Google Scholar]
Landon 2009
- Landon MB, Spong CY, Thom E, Carpenter MW, Ramin SM, Casey B, et al. A multicenter, randomized trial of treatment for mild gestational diabetes. New England Journal of Medicine 2009;361:1339‐48. [DOI] [PMC free article] [PubMed] [Google Scholar]
Langer 1994
- Langer O, Rodriguez DA, Xenakis EM, McFarland MB, Berkus MD, Arrendondo F. Intensified versus conventional management of gestational diabetes. American Journal of Obstetrics and Gynecology 1994;170:1036‐47. [DOI] [PubMed] [Google Scholar]
Lapolla 2011
- Lapolla A, Dalfrà MG, Ragazzi E, Cata AP, Fedele D. New International Association of the Diabetes and Pregnancy Study Groups (IADPSG) recommendations for diagnosing gestational diabetes compared with former criteria: a retrospective study on pregnancy outcome. Diabetic Medicine 2011;28(9):1074‐7. [DOI] [PubMed] [Google Scholar]
Lawrence 2008
- Lawrence JM, Contreras R, Chen W, Sacks DA. Trends in the prevalence of preexisting diabetes and gestational diabetes mellitus among a racially/ethnically diverse population of pregnant women 1999–2005. Diabetes Care 2008;31:899‐904. [DOI] [PubMed] [Google Scholar]
Mackillop 2014
- Mackillop L, Loerup L, Bartlett K, Farmer A, Gibson OJ, Hirst JE, et al. Development of a real‐time smartphone solution for the management of women with or at high risk of gestational diabetes. Journal of Diabetes Science & Technology 2014;8(6):1105‐14. [DOI] [PMC free article] [PubMed] [Google Scholar]
Martis 2016
- Martis R, Brown J, Alsweiler J, Crawford TJ, Crowther CA. Different intensities of glycaemic control for women with gestational diabetes mellitus. Cochrane Database of Systematic Reviews 2016, Issue 4. [DOI: 10.1002/14651858.CD011624.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Metzger 1998
- Metzger BE, Coustan DR. Summary and recommendations of the fourth international workshop‐conference on gestational diabetes mellitus. Diabetes Care 1998;21(Suppl 2):B161‐B167. [PubMed] [Google Scholar]
Ming 2016
- Ming WK, Mackillop LH, Farmer AJ, Loerup L, Bartlett K, Levy JC, et al. Telemedicine technologies for diabetes in pregnancy: a systematic review and meta‐analysis. Journal of Medical Internet Research 2016;18(11):e290. [DOI] [PMC free article] [PubMed] [Google Scholar]
Morikawa 2010
- Morikawa M, Yamada T, Yamada T, Akaishi R, Nishida R, Cho K, et al. Change in the number of patients after the adoption of IADPSG criteria for hyperglycemia during pregnancy in Japanese women. Diabetes Research and Clinical Practice 2010;90(3):339‐42. [DOI] [PubMed] [Google Scholar]
Moy 2014
- Moy FM, Ray A, Buckley BS. Techniques of monitoring blood glucose during pregnancy for women with pre‐existing diabetes. Cochrane Database of Systematic Reviews 2014, Issue 4. [DOI: 10.1002/14651858.CD009613.pub2] [DOI] [PubMed] [Google Scholar]
Murphy 2008
- Murphy HR, Rayman G, Lewis K, Kelly S, Johal B, Duffield K, et al. Effectiveness of continuous glucose monitoring in pregnant women with diabetes: randomised clinical trial. BMJ 2008;337:a1680. [DOI] [PMC free article] [PubMed] [Google Scholar]
Nankervis 2013
- Nankervis A, Conn J. Gestational diabetes mellitus: negotiating the confusion. Australian Family Physician 2013;42(8):528‐31. [PubMed] [Google Scholar]
NICE 2008
- National Collaborating Centre for Women’s and Children’s Health, National Institute for Health and Clinical Excellence (NICE). Diabetes in Pregnancy: Management of Diabetes and its Complications from Pre‐conception to the Postnatal Period. NICE, 2008. [Google Scholar]
O'Sullivan 1964
- O'Sullivan JB, Mahan CM. Criteria for the oral glucose tolerance test in pregnancy. Diabetes 1964;13:278‐285. [PubMed] [Google Scholar]
O'Sullivan 1991
- O’Sullivan J. Diabetes mellitus after GDM. Diabetes 1991;29:131–5. [DOI] [PubMed] [Google Scholar]
O'Sullivan 2011
- O'Sullivan EP, Avalos G, O'Reilly M, Dennedy MC, Gaffney G, Dunne F, et al. Atlantic diabetes in pregnancy (DIP): the prevalence and outcomes of gestational diabetes mellitus using new diagnostic criteria. Diabetologia 2011;54(7):1670‐5. [DOI] [PubMed] [Google Scholar]
Pettitt 1985
- Pettitt DJ, Bennett PH, Knowler WC, Baird HR, Aleck KA. Gestational diabetes mellitus and impaired glucose tolerance during pregnancy: long‐term effects on obesity and glucose tolerance in the offspring. Diabetes 1985;34(Suppl 2):119‐22. [DOI] [PubMed] [Google Scholar]
Rasekaba 2015b
- Rasekaba TM, Furler J, Blackberry I, Tacey M, Gray K, Lim K. Telemedicine interventions for gestational diabetes mellitus: a systematic review and meta‐analysis. Diabetes Research and Clinical Practice 2015;110(1):1‐9. [DOI] [PubMed] [Google Scholar]
Reece 2010
- Reece EA. The fetal and maternal consequences of gestational diabetes mellitus. Journal of Maternal‐Fetal and Neonatal Medicine 2010;23(3):199‐203. [DOI] [PubMed] [Google Scholar]
Review Manager 2014 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager 5 (RevMan 5). Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Setji 2005
- Setji T, Brown A, Geinglos M. Gestational diabetes. Clincal Diabetes 2005;23:17‐24. [Google Scholar]
Silverman 1998
- Silverman BL, Rizzo TA, Nam H, Metzger BE. Long term effects of the intrauterine environment: the Northwestern University Diabetes in Pregnancy Center. Diabetes Care 1998;21(Suppl 2):B142‐B149. [PubMed] [Google Scholar]
Tieu 2014
- Tieu J, McPhee AJ, Crowther CA, Middleton P. Screening and subsequent management for gestational diabetes for improving maternal and infant health. Cochrane Database of Systematic Reviews 2014, Issue 2. [DOI: 10.1002/14651858.CD007222.pub3] [DOI] [PubMed] [Google Scholar]
Voormolen 2013
- Voormolen DN, DeVries JH, Evers IM, Mol BW, Franx A. The efficacy and effectiveness of continuous glucose monitoring during pregnancy: a systematic review. Obstetrical & Gynecological Survey 2013;68(11):753‐63. [DOI] [PubMed] [Google Scholar]
Weisz 2005
- Weisz B, Shrim A, Homko CJ, Schiff E, Epstein GS, Sivan E. One hour versus two hours postprandial glucose measurement in gestational diabetes: a prospective study. Journal of Perinatology 2005;25(4):241‐4. [DOI] [PubMed] [Google Scholar]
WHO 2013
- World Health Organization (WHO). Diagnostic Criteria and Classification of Hyperglycaemia First Detected in Pregnancy. Geneva: WHO, 2013. [PubMed] [Google Scholar]
Yu 2014
- Yu F, Lv L, Liang Z, Wang Y, Wen J, Lin X, et al. Continuous glucose monitoring effects on maternal glycemic control and pregnancy outcomes in patients with gestational diabetes mellitus: a prospective cohort study. Journal of Clinical Endocrinology & Metabolism 2014;99(12):4674‐82. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Gill 2014
- Gill MG, Nguyen TMN, Bain E, Crowther CA, Middleton P. Home versus hospital glucose monitoring for gestational diabetes during pregnancy. Cochrane Database of Systematic Reviews 2014, Issue 4. [DOI: 10.1002/14651858.CD011069] [DOI] [Google Scholar]


