Abstract
Adolescent idiopathic scoliosis (AIS) is the most common form of scoliosis, a 3-dimensional deviation in the axis of the spine. Etiology of AIS is unclear and the general belief is that AIS is multifactorial disorder possibly caused by different factors. It would be worthwhile to reveal new factors associated with AIS. The present study aimed to investigate association between sacroiliac joint (SIJ) dysfunction and AIS in young athletes.
This case–control study included 196 children athletes (basketball, football, volleyball, handball, ballet, and others), 82 males and 114 females aged 8 to 17, 98 of them with the diagnosis of AIS. The case group consisted of young athletes examined at a regular checkup by a sport physician and diagnosed with AIS. The control group consisted of athletes matched to the case group according to sex, age, sports, number of training years and number of training hours per week, but without AIS.
The scoliosis was diagnosed with Adams’ forward bend test and the scoliometer measurement. The SIJ dysfunction was determined using the palpation meter (PALM) measuring the sagittal pelvic position in standing position and in standing position with the hip flexion angle of 90°. The data were analyzed using Student t test, Mann–Whitney U test, contingency coefficients, and logistic regression.
The average difference in pelvic position in the sagittal plane (in standing position), with and without hip flexion 90° was found to be statistically different in the case and the control groups (t = 13.88, P = .00). There was a strong positive association between variables representing presence of AIS and SIJ dysfunction (determined by contingency coefficient C = 0.62, coefficient Phi = 0.79 and tetrachoric correlation coefficient 0.95).
The logistic regression indicated that the average difference in pelvic position in the sagittal plane (in standing position), with and without hip flexion 90° was significantly associated with the probability of scoliosis in young athletes (P = .00, Wald test).
There was a strong positive association between SIJ dysfunction and AIS in young athletes.
Keywords: adolescent idiopathic scoliosis, asymmetrical gait, palpation meter, sacroiliac joint dysfunction, sagittal pelvic position
1. Introduction
1.1. Background/rationale
Adolescent idiopathic scoliosis (AIS) is an abnormal curvature of the spine. The spine develops a side-to-side curvature, usually in an elongated “S” or “C” shape instead of growing straight, and the bones of the spine are also slightly twisted or rotated. AIS usually appears in late childhood or adolescence and it affects up to 3% of children aged 10 to 16.[1] Although clinical manifestations of scoliosis have been thoroughly investigated and well documented, the exact etiology of AIS is still unclear.[1–10] It would be worthwhile to reveal new factors associated with AIS.
The sacroiliac joint (SIJ) is the joint that links the iliac bone and the sacrum. SIJ transfers weight and forces between the upper body and the legs. There are several types of dysfunction in the SIJ which often cause lower back and leg pain.[11]
Dysfunction of the SIJ was noted in 54% of patients with AIS.[12]
1.2. Objectives
The aim of this study was to investigate relationship between SIJ dysfunction and AIS in the group of young athletes.
2. Materials and methods
The case-control study included 196 young athletes aged 8 to 17, 98 of them with the diagnosis of AIS - cases and 98 controls.
All children (cases and controls) were examined at a regular checkup by a sport physician in period of 15.September-15. December 2017 at Novi Sad Health Care Center, Sports Medicine Center.
The rationale for the choice of cases and controls: The case group consisted of young athletes diagnosed with AIS since the aim of the study was to reveal new factors associated with AIS.
Matching criteria: the control group was chosen from the group of young athletes without AIS. Controls were matched to the cases according to sex, age, sports, number of training years, and number of training hours per week. One control per case was chosen.
Matching of the cases and controls was done as follows. The case group consisted of all the children that were diagnosed with AIS during the checkup in the period of the study (taking into account also the power analysis). Control group consisted of children athletes matched to the case group according to sex, age, sports, and number of training hours but without AIS.
Inclusion criteria for the control group were that children chosen did not have any deviation of the spine.
Procedure for the choice of the control group was: a first child-athlete appearing at the checkup after a recorded athlete with AIS that had similar features (same sex, approximate age (± 1 year), similar type of sport, approximate number of training years (± 1 year), and same number of training hours per week) was chosen for the control group.
Variables chosen for the analysis were:
-
1.
Outcome variable: a binary variable representing presence or absence of AIS (which was taken to be 1 for the children from the case group and 0 for the children in the control group).
-
2.
Exposure variable: a continuous (independent variable), that was calculated as the difference (of measures) between 2 (standing) sagittal pelvic positions: with and without hip flexion of 90° (measured in degrees with PALM palpation meter) on the concave side of lumbothoracal curve of scoliosis, in the case group. This variable was calculated as the minimum (comparing both sides) of the differences between 2 positions in the control group.
-
3.
Predictor variable: a binary variable representing SIJ dysfunction, that was defined to be 1 if the difference in pelvic position in the sagittal plane (in standing position), with and without hip flexion 90° was less than 6 degrees. If the difference in pelvic position in the sagittal plane with and without hip flexion 90° was more than 6 degrees, then this variable was defined to be 0.
-
4.
Confounders (possible conditions that are connected to both, scoliosis and SIJ dysfunction, such as back pain, hip pain, leg length discrepancy) were eliminated since all participants were healthy children, athletes, without mentioned conditions. The past medical history was obtained to exclude non-idiopathic cause of scoliosis, so neuromuscular, congenital, syndromic and other disorders were ruled out taking into account the children's complete anamnesis.
-
5.
Concerning the potential effect modifier: sex, it was checked whether the effect exists equally in the male as well as in the female sub-group.
The scoliosis in all cases was determined with Adams’ forward bend test and scoliometer measurement.[7]
Pelvic position in the sagittal plane was assessed in standing position, with and without hip flexion 90° using PALM palpation meter (Performance Attainment Associates, St. Paul MN) on both sides.[13] A single experienced sports physician took all the measurements in all children.
The difference in degrees between 2 positions (with and without hip flexion 90°) was determined and the difference on the concave side of lumbothoracal curve of scoliosis was considered as the value of exposure variable, or the minimum difference (comparing both sides) if the scoliosis was not present.
In all types of scoliosis curves,[3] the side in which the concave part of the curve was lower was considered.
Efforts made to address potential sources of bias:
-
1.
Cases and controls were taken from the same population of children athletes.
-
2.
There was a risk of bias since the physician assessor of SIJ dysfunction was not blinded to the diagnosis of scoliosis. In order to prevent bias, all the measurements have been done 3 times and the average was applied.
The number of cases, children diagnosed with the AIS on the checkup at Novi Sad health care center, Sports medicine center, during the study period (3 months) determined the sample size (98 cases and 98 controls).
A continuous (independent variable), was calculated as the difference between 2 (standing) sagittal pelvic positions: with and without hip flexion of 90° (measured in degrees with PALM palpation meter) on the concave side of lumbothoracal curve of scoliosis, in case group and as the minimum (comparing both sides) difference between 2 positions in the control group. The SIJ dysfunction is characterized with the smaller (than usual) difference in 2 positions, and the significant difference between the case and the control group was obtained taking the minimum value in the case group. Even more significant difference would be obtained if the average value would be considered.
Statistical Analysis was performed using Dell Inc. (2016) Dell Statistica (data analysis software system), version 13. software.dell.com and IBM SPSS Statistics 20, Premium Faculty Pack.
Sample size calculation was done in the data analysis software system Statistica taking into account means of variables in the case and control groups, standard deviations, effects obtained, type I error rate alpha 0.0001, and power 0.9999. In order to achieve required rates of type I error and power, the sample size needed was 38 cases and 38 controls. The sample size of this study (98 cases and 98 controls) was well chosen to accomplish the required type I error rate and the power.
The data were analyzed using Student t tests for independent samples, Mann–Whitney U test, contingency coefficient, Phi coefficient, tetrachoric correlation coefficient, Somers’ D coefficients, and logistic regression.
Before statistical analyses, the assumption of normality of the data was checked by Shapiro–Wilk W test and Lilliefors test, P = .05. The data were tested for homogeneity of variances by Levene test, P = .05.
The first step to determine association between SIJ dysfunction and AIS was to show that the case group had in average significantly smaller difference in the pelvic position in the sagittal plane (since, as explained, smaller difference indicates SIJ dysfunction).
Association between AIS and SIJ dysfunction was determined by contingency coefficient, coefficient Phi and tetrachoric correlation coefficient and Somers’ D(X/Y).
A binary logistic regression was performed with the dependent variable representing presence or absence of AIS and the independent variable: the difference in sagittal pelvic positions.
The formula for the probability that a person with a value x of the variable representing the minimum difference in degrees in the sagittal pelvic position in standing position and in the standing position with hip flexion angle of 90° will have AIS was deduced by binary logistic regression (1).
The records with missing data were excluded from the study.
In regard to the sensitivity analyses (analysis of what the effect would be of varying the parameters of the model on the overall model fit), in this case, we had the only 1 predictor and instead of sensitivity analysis we confirmed the validity of the logistic model by the Omnibus test and Hosmer–Lemeshow test.
The study was approved by the Ethical committee of the Novi Sad health care center (no. 21/43-1, date 14.09.2017). The subjects provided their informed consent to participate in the study.
3. Results
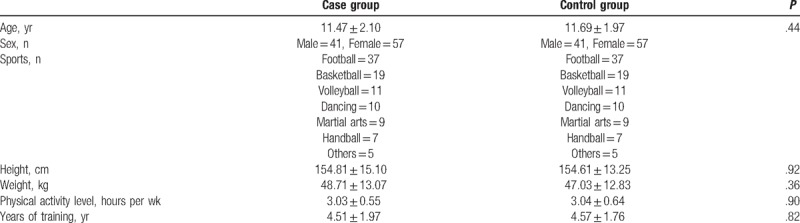
The case-control study included 196 children athletes, 82 males and 114 females aged 8 to 17 years (mean 11.58 ± 2.03), 98 of them with the diagnosis of AIS (41 males and 57 females)—cases and 98 controls (the same male-female ratio). All participants live in the urban area in Novi Sad and they participate in training of various sports (basketball, football, volleyball, handball, ballet, and others). Numbers of training hours per week were 2 to 4, median 3, in the case as well as in the control group. All children (cases and controls) were examined at a regular checkup by a sport physician at Novi Sad health care center, Sports medicine center and they were healthy children. Characteristics of all participants are presented in Table 1.
Table 1.
Characteristics of study participants.
-
1.
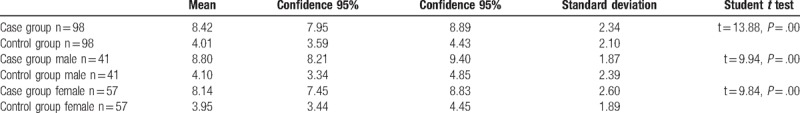
The average difference in pelvic position in the sagittal plane between measures with and without hip flexion 90° on the concave side of lumbothoracal curve of scoliosis in the case group was 4.01 ± 2.1 and in the control group the average of minimum differences was 8.42 ± 2.34.
The patients with AIS had around 4.4 degrees smaller difference in pelvic (95% confidence interval for difference (3.78,5.03)).
Using Student t-test for independent samples, the average difference in pelvic position in the sagittal plane (in standing position), with and without hip flexion 90° was found to be statistically different between the case and the control group (t = 13.88, P = .00) (Table 2). Although Levene test showed homoscedasticity and Student t test was correctly applied, this result was also confirmed by Mann–Whitney U test (Z = 9.45, P = .00).
It was demonstrated that this effect existed equally in male as well as in female sub-groups (Table 2).
The significant average differences were demonstrated for male and for female athletes separately (male cases compared to male controls and female cases compared to female controls) using Student t test for independent samples and Mann–Whitney U test. For male athletes there was a significant difference in the case and the control group that was demonstrated by Student t test (t = 9.94, P = .00) and confirmed by Mann–Whitney U test (Z = 6.63, P = .00) and similarly for female athletes: Student t test (t = 9.84, P = .00) and Mann–Whitney U test (Z = 6.92, P = .00).
-
2.
Contingency coefficient C = 0.62, coefficient Phi = 0.79 and tetrachoric correlation coefficient 0.95 indicated that there is a strong positive association between AIS and SIJ dysfunction. Somers’ D(X/Y) = 0.79 indicated that the variable representing presence of SIJ is a good predictor variable for the presence of AIS.
-
3.
The logistic regression indicated that the average difference in pelvic position in the sagittal plane (in standing position), with and without hip flexion 90° was significantly associated with the probability of scoliosis in young athletes (P = .00, Wald test).
Table 2.
Values of the average difference in pelvic position in the sagittal plane between measures with and without hip flexion 90° on the concave side of lumbothoracal curve of scoliosis (in degrees) in case and control group and in case and control group in males and females.
The Omnibus test (P = .00) confirmed that the final model was valid. The variance explained in the final model by Nagelkerke R2 was 60%. Hosmer–Lemeshow test indicated that the model fitted the data (P = .00). The model correctly predicted 87.7% of the cases with scoliosis (sensitivity 88.8 and specificity 86.6).
By logistic regression, coefficients −0.678 (with the variable) and the constant 4.224 were obtained, hence the probability that a person with a value x of the variable representing the minimum difference in degrees in the sagittal pelvic position in standing position and in the standing position with hip flexion angle of 90° would have AIS was given by formula (1).
4. Discussion
In our study, strong positive association between SIJ dysfunction and AIS was confirmed.
Statistical analysis demonstrated statistically significant difference in sagittal pelvic position in the case group compared with the control group. Significant differences between the male case and control groups as well as between the female case and control groups were also confirmed.
The variable representing the difference in pelvic position in the sagittal plane (in standing position), with and without hip flexion 90° was showed to be a good predictor for the presence of AIS.
In our study, the dysfunction of SIJ was considered in a particular way, reflected in walking and running. This special type of dysfunction considered in our study was witnessed by the smaller than normal difference in pelvic positions with and without hip flexion 90° (both in standing position).
It was defined differently and determined by different tests than the dysfunction considered in.[12] In paper [12] dysfunction of SIJ was also investigated in connection with scoliosis and the dysfunction was determined by assessment of SIJs using the following 4 tests: iliac spine test, Piedallu test in standing and sitting positions, Derbolowsky test and knee bending test in position lying on front. Dysfunction of SIJ on 1 side of the body was confirmed by a positive result in at least 3 of these tests. 54% out of 68 examined patients with AIS had this type of dysfunction of SIJ.[12]
In previous studies, it was indicated that the PALM palpation meter was a reliable tool for assessing sagittal pelvic position in standing, sitting and hip flexion (45° and 90°).[13–16]
Assessment of the pelvic position in 20 healthy participants was done[13] and it was concluded that the difference in pelvic position in healthy subjects in the sagittal plane (in standing position), with and without hip flexion 90° was in average around 9.5°. In the control group of children in our study, the average difference in pelvic position in children without scoliosis was 8.42 ± 2.34, which was compatible with previous findings.[13]
In a previous study, it was determined that the scoliosis was in correlation with muscle imbalance on both sides of the backbone and that it was possible to correct this imbalance with muscle strength training, and as a final result, to diminish scoliosis of the spine.[17]
Adolescents with AIS frequently experience back pain[18,19] and the lifetime prevalence of back pain was almost 60% in the group of children with scoliosis, which is almost double as in a group of children without scoliosis.[19] Back pain may also be connected with SIJ dysfunction.
Pelvic asymmetry and leg-length difference are also associated with scoliosis in 87% of the patients.[20] It was indicated[20] that acquired postural asymmetry of the SIJ may be cause of several pain-related symptoms and that the asymmetry characterized by leg-length difference and scoliosis may be reversible by a simple and safe treatment. Leg-length difference and scoliosis may be more often of reversible nature than previously considered. Acquired postural asymmetry of the SIJ may be a neglected cause of several neurologic and other pain-related symptoms that can be relieved by a simple and safe treatment.[20]
Another frequent phenomenon connected to AIS is sacral slanting, which is a compensatory mechanism for large lumbar curves. Moreover, a congenitally slanted upper sacrum may contribute to scoliosis in some cases.[21,22]
4.1. The mechanical explanation
SIJ motion during the normal gait cycle is well known.[11] First, at right heel strike right innominate rotates in a posterior direction and left innominate in an anterior direction. During this motion, the anterior surface of the sacrum is rotated to the left and the spine is straight and rotated to the left. Toward mid-stance, the right leg is straight and the innominate is rotated in an anterior direction, the sacrum is rotated right and side-bent left and the lumbar spine rotated left and side-bent right. At left heel strike, the opposite sequence happens and the cycle repeats.[11]
When walking and running, on the side of the leg that is raised, the iliac bone is rotated back comparing to the iliac bone of the leg that is on the ground.[11] Also, sacrum is bent towards the leg that is raised, and the lumbar spine is bent towards the leg that is on the ground and rotated towards the leg that is raised.
Theoretically, with the type of dysfunction of the SIJ that is described here, iliac bone is during walking and running steadily rotated forward to the side of dysfunction against the opposite side; lumbar segment of the spine is also constantly bent to the side of the lumbar dysfunction and rotated to the opposite side.
With the dysfunction, the lumbar segment of the spine does not change position from 1 side to the other during gait (as it is physiological), but it is constantly bent to 1 side only and this can be a cause of scoliosis.
This mechanical explanation is given according to the combined activities of right and left innominates, sacrum, and spine during walking.
Some studies showed that children with scoliosis demonstrated asymmetrical gait.[23–25] Our study suggests (as biomechanically explained) that a type of asymmetrical gait characteristic for the SIJ dysfunction might cause scoliosis.
In the control group there were a number of athletes, mostly girls, typically less than 10 years old with the type of dysfunction of the SIJ described in the paper, but without scoliosis. Hypothetically, if not corrected, the dysfunction of the SIJ might cause the scoliosis during the period of adolescent growth spurt.
A limitation of the study is that the diagnosis of scoliosis was not confirmed by X-rays (the reason is to avoid unnecessary X-rays on children in this study). Only clinical examinations (Adam's forward bend test and scoliometer) were used to determine scoliosis. According to [26] the forward bend test is a simple, reproducible and sensitive test for the detection of scoliosis. Further limitation is that the effect of training frequency, training age and sport type on development on scoliosis was not possible to be determined since those factors are made equal in the case and control groups. Finally, the generalization of results has been limited, since only young athletes were considered and not the population of children in general.
Strength of the study is that the cases and controls were members of a uniform group of healthy children athletes, which prevented the type of bias that might exist in choosing the control group.
Finally, although our findings may contribute to the present knowledge about the possible cause of AIS in young athletes, our study highlight the need to further investigate the correlations determined.
5. Conclusion
The present study demonstrated a strong positive association between SIJ dysfunction and AIS in young athletes. Further study toward non-athletic children with scoliosis in connection to SIJ dysfunction is needed. Further longitudinal studies are necessary to confirm the proposed mechanisms of association between AIS and SIJ dysfunction and possible causal relationship.
Acknowledgments
We are grateful to the reviewers whose valuable comments were very helpful in improving the manuscript.
Author contributions
Conceptualization: Zoran Sarcevic, Andreja Tepavcevic.
Data curation: Zoran Sarcevic.
Formal analysis: Zoran Sarcevic, Andreja Tepavcevic.
Funding acquisition: Zoran Sarcevic.
Investigation: Zoran Sarcevic, Andreja Tepavcevic.
Methodology: Zoran Sarcevic, Andreja Tepavcevic.
Project administration: Zoran Sarcevic, Andreja Tepavcevic.
Resources: Zoran Sarcevic, Andreja Tepavcevic.
Software: Andreja Tepavcevic.
Supervision: Zoran Sarcevic, Andreja Tepavcevic.
Validation: Zoran Sarcevic, Andreja Tepavcevic.
Visualization: Zoran Sarcevic, Andreja Tepavcevic.
Writing – Original Draft: Zoran Sarcevic, Andreja Tepavcevic.
Writing – Review & Editing: Zoran Sarcevic, Andreja Tepavcevic.
Zoran Sarcevic orcid: 0000-0001-8115-1430.
Andreja Tepavcevic orcid: 0000-0002-5716-604X.
Footnotes
Abbreviations: AIS = adolescent idiopathic scoliosis, SIJ = sacroiliac joint.
The study was approved by the Ethical committee of the Novi Sad Health Care Centre (no. 21/43-1). The subjects provided their informed consent to participate in the study.
The authors declare no conflicts of interest and do not have any financial disclosures.
The authors of this work have nothing to disclose.
References
- [1].de Seze M, Cugy E. Pathogenesis of idiopathic scoliosis: a review, pathogénies de la scoliose: une revue. Ann Phys Rehabil Med 2012;55:128–38. [DOI] [PubMed] [Google Scholar]
- [2].Altaf F, Gibson A, Dannawi Z, et al. Adolescent idiopathic scoliosis. BMJ 2013 2013;346:f2508. [DOI] [PubMed] [Google Scholar]
- [3].Wang WJ, Yeung HJ, Chu WCW, et al. Top theories for the etiopathogenesis of adolescent idiopathic scoliosis. J Pediatr Orthop 2011;31:S14–27. [DOI] [PubMed] [Google Scholar]
- [4].Shakil H, Iqbal ZA, Al-Ghadir AH. Scoliosis: review of types of curves, etiological theories and conservative treatment. J Back Musculoskelet Rehabil 2014;27:111–5. [DOI] [PubMed] [Google Scholar]
- [5].Hawasli AH, Hullar TE, Dorward IG. Idiopathic scoliosis and the vestibular system. Eur Spine J 2015;24:227–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Ahn UM, Ahn NU, Nallamshetty L, et al. The etiology of adolescent idiopathic scoliosis. Am J Orthop (Belle Mead NJ) 2001;31:387–95. [PubMed] [Google Scholar]
- [7].Hamad A, Ahmed EB, Tsirikos AI. Adolescent idiopathic scoliosis: a comprehensive approach to aetiology, diagnostic assessment and treatment. Orthop Trauma 2017;31:343–9. [Google Scholar]
- [8].Schlösser TPC, Colo D, Castelein RM. Etiology and pathogenesis of adolescent idiopathic scoliosis. Semin Spine Surg 2015;27:2–8. [Google Scholar]
- [9].Wren TAL, Ponrartana S, Poorghasamians E, et al. Biomechanical modeling of spine flexibility and its relationship to spinal range of motion and idiopathic scoliosis. Spine Deform 2017;5:225–30. [DOI] [PubMed] [Google Scholar]
- [10].Wajchenberg M, Astur N, Kanas M, et al. Adolescent idiopathic scoliosis: current concepts on neurological and muscular etiologies. Scoliosis Spinal Disord 2016;11:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Springer Science+Business Media, LLC 2010, Brolinson PG, Rogers M. Seidenberg PH, Bowen JD. Functional and Kinetic Chain Evaluation of the Hip and Pelvis. The Hip and Pelvis in Sports Medicine and Primary Care 2010;37–70. [Google Scholar]
- [12].Mortka K, Ostiak W, Kinel E, et al. Dysfunction of sacroiliac joint in patients with scoliosis and its connection with the setting of the pelvis. Issue Rehabil. Orthop Neurophysiol Sport Promot 2012;1:13–24. [Google Scholar]
- [13].Herrington L. Assessment of the degree of pelvic tilt within a normal asymptomatic population. Man Ther 2011;16:646–8. [DOI] [PubMed] [Google Scholar]
- [14].Azevedo DC, Santos H, Carneiro RL, et al. Reliability of sagittal pelvic position assessments in standing, sitting and during hip flexion using palpation meter. J Bodyw Mov Ther 2014;18:210–4. [DOI] [PubMed] [Google Scholar]
- [15].Hayes AM, Place HM, Hayden A, et al. The use of the PALM palpation meter for measuring pelvic tilt and its correlation with radiographic measures. Spine J 2016;16:S355–6. [Google Scholar]
- [16].Petrone MR, Guinn J, Reddin A, et al. Accuracy of the palpation meter (PALM) for measuring pelvic crest height difference and leg length discrepancy. J Orthop Sports Phys Ther 2003;33:319–25. [DOI] [PubMed] [Google Scholar]
- [17].Šarčević Z. Scoliosis: muscle imbalance and treatment. Br J Sports Med 2010;44:i16. [Google Scholar]
- [18].Théroux J, Stomski N, Hodgetts CJ, et al. Prevalence of low back pain in adolescents with idiopathic scoliosis: a systematic review. Chiropr Man Therap 2017;25:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Sato T, Hirano T, Ito T, et al. Back pain in adolescents with idiopathic scoliosis: epidemiological study for 43,630 pupils in Niigata City, Japan. Eur Spine J 2011;20:274–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Timgren J, Soinila S. Reversible pelvic asymmetry: an overlooked syndrome manifesting as scoliosis, apparent leg-length difference, and neurologic symptoms. J Manipulative Physiol Ther 2006 Sep 2006;29:561–5. [DOI] [PubMed] [Google Scholar]
- [21].Cho JH, Lee CS, Joo YS, et al. Association between sacral slanting and adjacent structures in patients with adolescent idiopathic scoliosis. Clin Orthop Surg 2017;9:57–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Lee CS, Ha JK, Kim DG, et al. The clinical importance of sacral slanting in patients with adolescent idiopathic scoliosis undergoing surgery. Spine J 2015;15:834–40. [DOI] [PubMed] [Google Scholar]
- [23].Yang JH, Suh SW, Sung PS, et al. Asymmetrical gait in adolescents with idiopathic scoliosis. Eur Spine J 2013;22:2407–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Haber CK, Sacco M. Scoliosis: lower limb asymmetries during the gait cycle. Arch Physiother 2015;5:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Nishida M, Nagura T, Fujita N, et al. Position of the major curve influences asymmetrical trunk kinematics during gait in adolescent idiopathic scoliosis. Gait Posture 2017;51:142–8. [DOI] [PubMed] [Google Scholar]
- [26].De Korvin G, Randriaminahiso T, Cugy E, et al. Detection of progressive idiopathic scoliosis during growth using back surface topography: A prospective study of 100 patients, Détection de l’évolution des scolioses idiopathiques en période de croissance par la topographie de surface du dos: étude prospective sur 100 patients. Ann Phys Rehabil Med 2014;57:629–39. [DOI] [PubMed] [Google Scholar]


