Abstract
Background
Lay health workers (LHWs) are widely used to provide care for a broad range of health issues. Little is known, however, about the effectiveness of LHW interventions.
Objectives
To assess the effects of LHW interventions in primary and community health care on maternal and child health and the management of infectious diseases.
Search methods
For the current version of this review we searched The Cochrane Central Register of Controlled Trials (including citations uploaded from the EPOC and the CCRG registers) (The Cochrane Library 2009, Issue 1 Online) (searched 18 February 2009); MEDLINE, Ovid (1950 to February Week 1 2009) (searched 17 February 2009); MEDLINE In‐Process & Other Non‐Indexed Citations, Ovid (February 13 2009) (searched 17 February 2009); EMBASE, Ovid (1980 to 2009 Week 05) (searched 18 February 2009); AMED, Ovid (1985 to February 2009) (searched 19 February 2009); British Nursing Index and Archive, Ovid (1985 to February 2009) (searched 17 February 2009); CINAHL, Ebsco 1981 to present (searched 07 February 2010); POPLINE (searched 25 February 2009); WHOLIS (searched 16 April 2009); Science Citation Index and Social Sciences Citation Index (ISI Web of Science) (1975 to present) (searched 10 August 2006 and 10 February 2010). We also searched the reference lists of all included papers and relevant reviews, and contacted study authors and researchers in the field for additional papers.
Selection criteria
Randomised controlled trials of any intervention delivered by LHWs (paid or voluntary) in primary or community health care and intended to improve maternal or child health or the management of infectious diseases. A 'lay health worker' was defined as any health worker carrying out functions related to healthcare delivery, trained in some way in the context of the intervention, and having no formal professional or paraprofessional certificate or tertiary education degree. There were no restrictions on care recipients.
Data collection and analysis
Two review authors independently extracted data using a standard form and assessed risk of bias. Studies that compared broadly similar types of interventions were grouped together. Where feasible, the study results were combined and an overall estimate of effect obtained.
Main results
Eighty‐two studies met the inclusion criteria. These showed considerable diversity in the targeted health issue and the aims, content, and outcomes of interventions. The majority were conducted in high income countries (n = 55) but many of these focused on low income and minority populations. The diversity of included studies limited meta‐analysis to outcomes for four study groups. These analyses found evidence of moderate quality of the effectiveness of LHWs in promoting immunisation childhood uptake (RR 1.22, 95% CI 1.10 to 1.37; P = 0.0004); promoting initiation of breastfeeding (RR = 1.36, 95% CI 1.14 to 1.61; P < 0.00001), any breastfeeding (RR 1.24, 95% CI 1.10 to 1.39; P = 0.0004), and exclusive breastfeeding (RR 2.78, 95% CI 1.74 to 4.44; P <0.0001); and improving pulmonary TB cure rates (RR 1.22 (95% CI 1.13 to 1.31) P <0.0001), when compared to usual care. There was moderate quality evidence that LHW support had little or no effect on TB preventive treatment completion (RR 1.00, 95% CI 0.92 to 1.09; P = 0.99). There was also low quality evidence that LHWs may reduce child morbidity (RR 0.86, 95% CI 0.75 to 0.99; P = 0.03) and child (RR 0.75, 95% CI 0.55 to 1.03; P = 0.07) and neonatal (RR 0.76, 95% CI 0.57 to 1.02; P = 0.07) mortality, and increase the likelihood of seeking care for childhood illness (RR 1.33, 95% CI 0.86 to 2.05; P = 0.20). For other health issues, the evidence is insufficient to draw conclusions regarding effectiveness, or to enable the identification of specific LHW training or intervention strategies likely to be most effective.
Authors' conclusions
LHWs provide promising benefits in promoting immunisation uptake and breastfeeding, improving TB treatment outcomes, and reducing child morbidity and mortality when compared to usual care. For other health issues, evidence is insufficient to draw conclusions about the effects of LHWs.
Keywords: Child, Preschool; Humans; Infant, Newborn; Health Promotion; Breast Feeding; Child Abuse; Child Abuse/prevention & control; Child Health Services; Child Health Services/standards; Child Mortality; Community Health Workers; Community Health Workers/standards; Home Health Aides; Immunization; Infant, Low Birth Weight; Maternal Health Services; Maternal Health Services/standards; Parent‐Child Relations; Randomized Controlled Trials as Topic; Tuberculosis, Pulmonary; Tuberculosis, Pulmonary/prevention & control
Plain language summary
The effect of lay health workers on mother and child health and infectious diseases
A review of the effect of using lay health workers to improve mother and child health and to help people with infectious diseases was carried out by researchers in The Cochrane Collaboration. After searching for all relevant studies, they found 82 studies. Their findings are summarised below.
What is a lay health worker?
A lay health worker is a member of the community who has received some training to promote health or to carry out some healthcare services, but is not a healthcare professional. In the studies in this review, lay health workers carried out different tasks. These included giving help and advice about issues such as child health, child illnesses, and medicine taking. In some studies, lay health workers also treated people for particular health problems.
The studies took place in different settings. In many of the studies, lay health workers worked among people on low incomes in wealthy countries, or among people living in poor countries.
What the research says
The use of lay health workers, compared to usual healthcare services:
‐ probably leads to an increase in the number of women who start to breastfeed their child; who breastfeed their child at all; and who feed their child with breastmilk only;
‐ probably leads to an increase in the number of children who have their immunization schedule up to date;
‐ may lead to slightly fewer children who suffer from fever, diarrhoea and pneumonia;
‐ may lead to fewer deaths among children under five;
‐ may increase the number of parents who seek help for their sick child.
The use of lay health workers, compared to people helping themselves or going to a clinic:
‐ probably leads to an increase in the number of people with tuberculosis who are cured;
‐ probably makes little or no difference in the number of people who complete preventive treatment for tuberculosis.
Summary of findings
Summary of findings for the main comparison. LHWs to promote immunisation uptake in children compared to usual care.
| LHWs to promote immunisation uptake in children compared to usual care | ||||||
| Patient or population: patients with improving immunisation uptake among children < 2 years whose vaccination is not up to date Settings: USA(3), Ireland(1) Intervention: LHWs Comparison: usual care | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| usual care | LHWs | |||||
| Immunisation schedule up to date Interviews with mothers, record reviews Follow‐up: 6.5‐24 months | Low risk population1 | RR 1.22 (1.1 to 1.37) | 3568 (4 studies5) | ⊕⊕⊕⊝ moderate2,3,4 | ||
| 340 per 1000 | 415 per 1000 (374 to 466) | |||||
| High risk population1 | ||||||
| 560 per 1000 | 683 per 1000 (616 to 767) | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio; | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1 Selected the next to lowest and next to highest figures to represent the control risk. 2 In Barnes 1999, only 37.5% of eligible families consented to participate, 21.2% refused to particpate, 14.3% were living out of the country or in another state. A significantly greater percentage of non‐enrolled children were covered by Medicaid insurance than enrolled children (p=0.02). The quality of evidence was downgraded by 0.5 because of these design limitations (also see footnote 3). 3 In Johnson 1993 the outcomes were recorded by a family development nurse who knew the group assignment of the mother‐child pair. 4 There is wide variation in the estimates of the included studies from no effect to a 36% relative increase. The quality of evidence was downgraded by 0.5 because of these inconsistencies. 5 Barnes 1999, Johnson 1993, LeBaron 2004, Rodewald 1999
Summary of findings 2. LHW support compared to conventional support or care for breastfeeding.
| LHW support compared to conventional support or care for breastfeeding | ||||||
| Patient or population: patients with breastfeeding Settings: UK (5 studies); USA (4 studies); Bangladesh (3 studies); Brazil (2 studies); Canada; Phillipines; Mexico; India 1 Intervention: LHW support Comparison: usual care | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| usual care | LHW support | |||||
| Initiation of breastfeeding Self‐report Follow‐up: 0.3 ‐ 16 months2 | Low risk population3 | RR 1.36 (1.14 to 1.61) | 17159 (12 studies5) | ⊕⊕⊕⊝ moderate4 | ||
| 150 per 1000 | 204 per 1000 (171 to 242) | |||||
| Medium risk population3 | ||||||
| 540 per 1000 | 734 per 1000 (616 to 869) | |||||
| High risk population3 | ||||||
| 680 per 1000 | 925 per 1000 (775 to 1000) | |||||
| Any breastfeeding Self‐report Follow‐up: 0.3 ‐ 12 months6 | Low risk population7 | RR 1.24 (1.1 to 1.39) | 8104 (12 studies9) | ⊕⊕⊕⊝ moderate8 | ||
| 150 per 1000 | 186 per 1000 (165 to 208) | |||||
| Medium risk population7 | ||||||
| 320 per 1000 | 397 per 1000 (352 to 445) | |||||
| High risk population7 | ||||||
| 660 per 1000 | 818 per 1000 (726 to 917) | |||||
| Exclusive breastfeeding Self‐report Follow‐up: 3 ‐ 6 months10 | Low risk population11 | RR 2.78 (1.74 to 4.44) | 4334 (10 studies) | ⊕⊕⊕⊝ moderate12 | ||
| Medium risk population11 | ||||||
| 70 per 1000 | 195 per 1000 (122 to 311) | |||||
| High risk population11 | ||||||
| 250 per 1000 | 695 per 1000 (435 to 1000) | |||||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio; | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1 This list includes all studies that measured breastfeeding outcomes, regardless of whether these outcomes were included in a meta‐analysis. 2 Length of follow‐up is for the study as a whole, which generally included other outcomes. Length of follow‐up for 'Initiation of breastfeeding' not always specified, but is likely to have shorter. 3 Control group risks based on baseline risks found in the included studies, specifically the next to lowest, the median and the next to highest. 4 Large inconsistencies in results. Caulfield 1998, Haider 2000 and Kumar 2008 had much higher RRs for initiation of breastfeeding, possibly explained by differences in control group rates between these 3 studies and the remaining trials. 5 Study countries: USA (3); Canada (1); Mexico (1); Bangladesh (3); UK (3); India (1). 6 Length of follow‐up is for the study as a whole, which generally included other outcomes. 7 Control group risks based on baseline risks found in the included studies, specifically the next to lowest, the median and the next to highest. 8 Moderate inconsistencies in results. Agrasada 2005, Caulfield 1998 and Coutinho 2005 measured higher rates of any breastfeeding than the other included studies. 9 Study countries: USA (3); UK (3); Brazil (2); Canada (1); Mexico (1); Bangladesh (1); Phillipines (1). 10 Length of follow‐up is for the study as a whole, which generally included other outcomes. 11 'Low' control group risk was 0%. 12 No explanation was provided.
Summary of findings 3. LHWs compared to usual care for reducing mortality and morbidity in children <5 years.
| LHWs compared to usual care for reducing mortality and morbidity in children <5 years | ||||||
| Patient or population: patients with reducing mortality and morbidity in children <5 years Settings: Bangladesh (3 studies), Ethiopia, Tanzania, Nepal, Ghana, Thailand, Viet Nam, India, Burkina Faso Intervention: LHWs Comparison: usual care | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| usual care | LHWs | |||||
| Mortality among children less than 5 years Verbal autopsy Follow‐up: 1‐2 years | Study population1 | RR 0.75 (0.55 to 1.03) | 56378 (3 studies5) | ⊕⊕⊝⊝ low2,3,4 | ||
| 74 per 1000 | 56 per 1000 (41 to 76) | |||||
| Medium risk population1 | ||||||
| 50 per 1000 | 38 per 1000 (28 to 51) | |||||
| Morbidity e.g. fever, diarrhoea, ARI Verbal reports obtained during home visits, record reviews Follow‐up: 4‐33 months | Study population6 | RR 0.86 (0.75 to 0.99) | 17408 (7 studies9) | ⊕⊕⊝⊝ low7,8 | ||
| 398 per 1000 | 342 per 1000 (298 to 394) | |||||
| Low risk population6 | ||||||
| 300 per 1000 | 258 per 1000 (225 to 297) | |||||
| High risk population6 | ||||||
| 540 per 1000 | 464 per 1000 (405 to 535) | |||||
| Neonatal Mortality verbal autopsy Follow‐up: 12 ‐ 24 months | 45 per 1000 | 34 per 1000 (26 to 46) | RR 0.76 (0.57 to 1.02) | 29217 (4 studies12) | ⊕⊕⊝⊝ low10,11 | |
| Morbidity ‐ care seeking practice hospital record review Follow‐up: 12 ‐ 33 months | 131 per 1000 | 174 per 1000 (113 to 269) | RR 1.33 (0.86 to 2.05) | 11195 (3 studies15) | ⊕⊕⊝⊝ low13,14 | |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio; | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1 Median baseline control group risk among included studies. 2 In Pence 2005, only 2 clusters were randomised for this comparison and there were significant baseline imbalances. The quality of evidence was therefore downgraded for limitations in design. None of the 3 trials in this analysis adjusted adequately for clustering in the original report. After the design effect was taken into account, the CIs for the effect estimates were wider than reported in the original papers. 3 In Kidane 2000, cause of death from malaria was obtained from verbal autopsies during a period when measles and chronic wasting were also important health problems. Some of the deaths attributed to malaria may have been due to these other causes. In addition, authors verified only 1/3 of the deaths using a second assessor who was blinded. 4 The quality of evidence was downgraded for imprecision as the pooled estimate of effect included both no effect and appreciable benefit. The imprecision is related to the small number of clusters in Pence 2005 (2 clusters) and Kidane 2000 (24 clusters), giving a design effect of 267,7 and 12.4 for these two studies respectively. 5 Mtango 1986, Kidane 2000, Pence 2005. 6 Selected the next to lowest and next to highest control group risk. 7 For all studies it is not clear whether outcome assessors were blinded or not. The reliance on verbal reporting of outcomes may have introduced reporting bias. 8 There are moderate levels of heterogeneity across these studies (I2=69%, p=0.003) and the confidence intervals do not overlap for all of the studies. The reasons for this heterogeneity are not clear. 9 Chongsuvivatwong 1996, Sripaipan 2002, Manandhar 2004, Sloan 2008, Kumar 2008, Kouyate 2008, Bari 2006 10 There are high levels of heterogeneity across these studies (I2=78%, p=0.003) and the confidence intervals of the studies do not overlap. The effect sizes of the studies range from no effect to a 50% relative reduction. The reasons for this heterogeneity are not clear, but may relate to differences in the length of follow up across the studies (12‐24 months). 11 The quality of evidence was downgraded for imprecision as the pooled estimate of effect included both no effect and appreciable benefit. 12 Baqui 2008, Kumar 2008, Manandhar 2004, Sloan 2008. 13 There are high levels of heterogeneity across these studies (I2=77%, p=0.01) and the confidence intervals have minimal overlap. The reasons for this heterogeneity are not clear, but may relate to differences in the length of follow up across the studies (12‐33 months). 14 The 95% CI includes both no effect and appreciable benefit. 15 Bari 2006, Manandhar 2004, Sloan 2008.
Summary of findings 4. LHW support for tuberculosis (TB) treatment.
| LHW support for tuberculosis (TB) treatment | ||||||
| Patient or population: patients with tuberculosis (TB) treatment Settings: USA (4 studies); South Africa (2 studies); Tanzania (1 study); Iraq (1 study)1 Intervention: LHW support Comparison: without LHW support | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| without LHW support | LHW support | |||||
| Cure for smear positive TB patients (new and retreatment) Sputum smear test Follow‐up: 6 ‐ 8 months2 | 526 per 1000 | 642 per 1000 (594 to 689) | RR 1.22 (1.13 to 1.31) | 1203 (4 studies4) | ⊕⊕⊕⊝ moderate3 | |
| Completed preventive therapy with Isoniazid ‐ LHW supported self‐supervision or DOT compared with self‐supervision Follow‐up: mean 6 months5 | 766 per 1000 | 766 per 1000 (705 to 835) | RR 1.0 (0.92 to 1.09) | 595 (2 studies7) | ⊕⊕⊕⊝ moderate6 | |
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio; | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1 This includes all studies that measured tuberculosis treatment outcomes, regardless of whether these studies were included in all of the meta‐analyses presented below. Details of the settings for the studies included in each meta‐analysis are listed below. 2 Length of follow varied from 6 months (Clarke 2005, Lwilla 2003, Mohan 2003) to 8 months (Zwarenstein 2000 ‐ retreatment patients). 3 Risk of bias assessed as low for Clarke 2005 and Zwarenstein 2000. Risk of bias assessed as moderate for Lwilla 2003 (not clear how randomisation sequence generated; significant loss to follow up and these losses higher in intervention group) and Mohan 2003 (insufficient information on the sequence generation process and allocation concealment; rate of loss to follow‐up unclear; methods generally described poorly). 4 Settings: South Africa (2); Tanzania (1); Iraq (1). 5 Length of follow‐up for all studies = 6 months. 6 Risk of bias assessed as moderate for both studies: Chaisson 2001 (insufficient information provided on method of allocation concealment; incomplete outcome data not addressed ‐ reasons for loss to follow up not discussed); Morisky 2001 (insufficient information on the sequence generation process, method of concealment, blinding). 7 Settings: all conducted in the USA.
Background
Lay health workers (LHWs) perform diverse functions related to healthcare delivery. While LHWs are usually provided with job‐related training, they have no formal professional or paraprofessional tertiary education and can be involved in either paid or voluntary care. The term LHW is thus necessarily broad in scope and includes, for example, community health workers, village health workers, treatment supporters, and birth attendants.
The primary healthcare approach adopted by the World Health Organization (WHO) at Alma‐Ata promoted the initiation and rapid expansion of LHW programmes in low and middle income country (LMIC) settings in the 1970s, including a number of large national programmes (Walt 1990). However, the effectiveness and cost of such programmes came to be questioned in the following decade, particularly at a national level in the LMICs. Several evaluations were conducted and these indicated difficulties in the scaling up of LHW programmes, as a consequence of a range of factors. Important constraints included inadequate training and ongoing supervision; insecure funding for incentives, equipment and drugs; failure to integrate LHW initiatives with the formal health system; poor planning; and opposition from health professionals (Frankel 1992; Walt 1990). These constraints led to poor quality care and difficulties in retaining trained LHWs in many of the programmes. However, most of these evaluations were uncontrolled case studies that could not produce robust assessments of effectiveness.
The 1990s saw renewed interest in community or LHW programmes in LMICs. This was prompted by a number of factors including the growing AIDS epidemic; the resurgence of other infectious diseases; and the failure of the formal health system to provide adequate care for people with chronic illnesses (Hadley 2000; Maher 1999). The growing emphasis on decentralisation and partnership with community‐based organisations also contributed to this renewed interest. In high income country settings, a perceived need for mechanisms to deliver health care to minority communities and to support people with a wide range of health issues (Hesselink 2009; Witmer 1995) led to further growth in a wide range of LHW interventions.
More recently, the growing focus on the human resource crisis in health care in many LMICs has re‐energised debates regarding the roles that LHWs may play in extending services to 'hard to reach' groups and areas; and in substituting for health professionals for a range of tasks (Chopra 2008; WHO 2005; WHO 2006; WHO 2007). Task shifting is not a new concept, however it has been given particular prominence and urgency in the face of the demands placed on health systems in a number of settings by the increased need for treatment of HIV/AIDS (Hermann 2009; Lehmann 2009; Schneider 2008; Zachariah 2009). Within this context, it is thought that LHWs may be able to play an important role in helping to achieve the Millennium Development Goals for health, particularly for child survival and treatment of tuberculosis (TB) and HIV/AIDS (Chen 2004; Filippi 2006; Haines 2007; Lewin 2008). For example, LHWs may be one route to expanding the coverage of effective neonatal and child health interventions, such as exclusive breastfeeding and community‐based case management of pneumonia, which remains under 50% in many LMICs (Darmstadt 2005).
In contrast to earlier initiatives that tended to focus on generalist LHWs delivering a range of services within communities, more recent programmes have often been vertical in their approach. In these programmes LHWs deliver a single or a small number of focused interventions addressing a particular health issue, such as promotion of vaccination; or one aspect of treatment care, such as supporting treatment adherence for people with TB (Lehmann 2007; Schneider 2008). The growth of interest in LHW programmes, whether vertical or generalist, has, however, generally occurred in the absence of robust evidence on their effects. Given that these interventions may have adverse effects, for example if LHWs provide inappropriate care, in addition to having considerable direct and indirect costs, such evidence is needed to ensure LHWs do more good than harm.
In 2005, Lewin et al published a Cochrane systematic review examining the global evidence from randomised controlled trials (RCTs) (published up to 2001) on the effects of LHW interventions in primary and community health care (Lewin 2005). This review indicated promising benefits for LHW interventions in promoting immunization uptake; improving outcomes for selected infectious diseases; and for increasing the breastfeeding of infants in comparison with usual care. For other health issues, the review suggested that the outcomes were too diverse to allow statistical pooling. While a number of other reviews of LHW programmes have been published since, some have a focus that is wider than effectiveness (for example Lehmann 2007) while others examine the effects of LHWs for one area of intervention or health (for example Bhutta 2008).
This is an update of the 2005 systematic review, focusing on the effects of LHW interventions in improving maternal and child health (MCH) and managing infectious diseases. A second review, providing an update on the evidence of the effects of LHW interventions for chronic diseases, will be published later.
Objectives
To assess the effects of lay health worker interventions in primary and community health care on maternal and child health and the management of infectious diseases.
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials
Types of participants
Types of healthcare providers
Any lay health worker (paid or voluntary) including community health workers, village health workers, birth attendants, peer counsellors, nutrition workers, home visitors.
For the purposes of this review, we defined the term lay health worker as any health worker who:
performed functions related to healthcare delivery,
was trained in some way in the context of the intervention, but
had received no formal professional or paraprofessional certificate or tertiary education degree.
Exclusions
We excluded interventions in which a healthcare function was performed as an extension to a participant's profession (for example teachers providing health promotion in schools). We defined the term profession in this study as remunerated work for which formal tertiary education was required.
We did not consider formally trained nurse aides, medical assistants, physician assistants, paramedical workers in emergency and fire services, and other self‐defined health professionals or health paraprofessionals. We also excluded trainee health professionals and trainees of any of the cadres listed above.
We also made other exclusions. Some of these exclusions were not specified in the original protocol but were developed as issues emerged from papers considered for the original review and for this review update. They were interventions:
involving patient support groups only, as these interventions were seen as different to LHW interventions in that the lay people involved meet only to provide each other with informal support rather than to provide care or services to others, and also seldom receive training in the context of the intervention;
involving teachers delivering health promotion or related activities in schools. We reasoned that this large and important system of LHWs constitutes a unique group (teachers) and setting (schools) that, due to the scale and importance, would be better addressed in a separate systematic review;
involving peer health counselling programmes in schools, in which pupils teach other pupils about health issues as part of the school curriculum. Again, we reasoned that this type of intervention contains a unique group and setting that is better suited to a separate review;
in which the LHW was a family member trained to deliver care and provide support only to members of his or her own family (that is in which LHWs did not provide some sort of care or service to others, or were unavailable to other members of the community). These interventions were assessed as qualitatively different from other LHW interventions included in this review given that parents or spouses have an established close relationship with those receiving care which could affect the process and effects of the intervention.
All of these interventions targeted 'closed' groups of clients, that is clients who, for the purposes of the intervention, are not part of the general population.
We also excluded:
LHWs in non‐primary level institutions (e.g. referral hospitals);
RCTs of interventions to train self‐management tutors who were health professionals rather than lay persons. Furthermore, RCTs that compared lay self management with other forms of management (i.e. those that did not focus on the training of tutors etc.) were also excluded as these were concerned with the effects of empowering people to manage their own health issues rather than with the effects of interventions using LHWs. These studies are the subject of another Cochrane review (Foster 2007). RCTs of interventions to train self‐management tutors who were themselves lay persons were eligible for inclusion in this review;
'Head‐to‐head' comparisons of different LHW interventions. It was felt that these should be reviewed separately as they address the question of the relative effectiveness of different types of LHW interventions rather than the question of the effects of LHWs compared to other types of intervention;
Multi‐faceted interventions that included LHWs and professionals working together and did not include a comparison group that enabled us to separately assess the effects of the LHW intervention.
Types of recipients
There were no restrictions on the types of patients or recipients for whom data were extracted.
Types of interventions
Any intervention delivered by LHWs and intended to improve maternal or child health (MCH) or the management of infectious diseases. We included interventions if the description was adequate for us to establish that it was a LHW intervention. Where such detail was unclear, we contacted study authors, whenever possible, to establish whether the personnel described were LHWs.
For the purposes of this review, a MCH or infectious diseases intervention was defined as follows.
Child health: any interventions aimed at improving the health of children aged less than five years.
Maternal health: any interventions aimed at improving reproductive health, ensuring safe motherhood, or directed at women in their role as carers for children aged less than five years.
Infectious diseases: any interventions aimed at preventing, diagnosing, or treating communicable diseases such as tuberculosis, malaria, and diarrhoeal diseases.
We decided to include infectious diseases in this review (rather than in the sister review on chronic diseases) as many of these are highly relevant to MCH (for example diarrhoeal diseases, malaria). In addition, this review includes a number of comparisons that are of high interest to LMICs. LHW interventions to support adherence to TB and HIV treatment are also highly relevant to these settings.
Types of outcome measures
We included studies if they assessed any of the following primary and secondary outcomes.
Primary outcomes
Health behaviours, such as the type of care plan agreed, and adherence to care plans (medication, dietary advice etc.)
Healthcare outcomes as assessed by a variety of measures. These included mortality; physiological measures (e.g vitamin C levels); and participants' self reports of symptom resolution, quality of life, or patient self‐esteem
Harms or adverse effects
Secondary outcomes
Utilisation of services
Consultation processes, such as how healthcare providers interacted with healthcare users; or how often patients were managed correctly according to guidelines
Recipient satisfaction with care
Costs
Social development measures, such as the creation of support groups for the promotion of other community activities
We excluded studies which measured only recipients' knowledge, attitudes, or intentions. Such studies assessed, for example, knowledge of what constituted a 'healthy diet', or attitudes toward people with HIV/AIDS. These measures were not considered to be useful indicators of the effectiveness of LHW interventions.
Search methods for identification of studies
See: the Cochrane Effective Practice and Organisation of Care Group (EPOC) methods used in reviews.
For this update, we searched the following electronic databases for primary studies:
Cochrane Central Register of Controlled Trials (CENTRAL) which includes citations uploaded from the EPOC and Cochrane Consumers and Communication Group Trial Registers (The Cochrane Library 2009, Issue 1) (searched 18 February 2009);
MEDLINE, Ovid (1950 to February Week 1 2009, except August 2001 to December 2003 (see note below)) (searched 17 February 2009);
MEDLINE In‐Process & Other Non‐Indexed Citations, Ovid (February 13 2009) (searched 17 February 2009);
EMBASE, Ovid (1980 to 2009 Week 05, except August 2001 to December 2003 (see note below)) (searched 18 February 2009);
AMED, Ovid (1985 to February 2009) (searched 19 February 2009);
British Nursing Index and Archive, Ovid (1985 to February 2009) (searched 17 February 2009);
CINAHL, Ebsco (1982 to present) (searched 07 February 2010);
POPLINE (searched 25 February 2009);
WHOLIS (searched 16 April 2009).
Search strategies incorporated the methodological component of the EPOC search strategy combined with selected index terms and free text terms relating to LHWs (for example community health aides, home health aides, or voluntary workers). We translated the MEDLINE search strategy for use in the other databases using the appropriate controlled vocabulary, as applicable. We revised search strategies from the original review to reflect our improved knowledge, following the first version of this review, of terms used in the literature to describe LHW interventions. We tailored the search strategy to each database and performed a sensitivity analysis to ensure that most of the relevant studies retrieved during the first review were retrieved again. It should be noted that we did not search MEDLINE or EMBASE between August 2001 and 2004 as it was anticipated, during searches done in 2006, that all trials in these databases from that period would also appear in CENTRAL.
Full strategies for all databases are included in Appendix 1.
Other resources:
we searched the reference lists of all included papers and relevant reviews identified;
we contacted authors of relevant papers regarding any further published or unpublished work;
we searched the Science Citation Index and Social Sciences Citation Index (ISI Web of Science) from 1975 (searched 10 August 2006 for 55 studies and 10 February 2010 for 16 studies) for papers which cited the studies included in the review.
For this update, we did not search HealthStar as journal articles from this database are now indexed in MEDLINE. We did not search the Leeds Health Education Effectiveness Database as it seems to be comprised of journals that are indexed either in MEDLINE or EMBASE.
For the original review (Lewin 2005), we searched the following electronic databases:
MEDLINE (1966 to August 2001);
CENTRAL and specialised Cochrane Trial Registers (EPOC, Consumers and Communication Review Group) (to August 2001);
Science Citations (to August 2001);
EMBASE (1966 to August 2001);
CINAHL (1966 to August 2001);
Healthstar (1975 to 2000);
AMED (1966 to August 2001);
Leeds Health Education Effectiveness Database (www.hubley.co.uk).
Data collection and analysis
Selection of trials
Two review authors assessed independently the potential relevance of all titles and abstracts identified from the electronic searches. We retrieved full text copies of the articles identified as potentially relevant by either one or both review authors.
Assessment of the eligibility of interventions can vary between review authors. Therefore, each full paper was evaluated independently for inclusion by at least two review authors. When review authors disagreed, a discussion was held to obtain consensus. If no agreement was reached, a third review author was asked to make an independent assessment. Where appropriate, we contacted study authors for further information and clarification.
Reasons for the exclusion of studies at the data extraction stage are included in the table 'Characteristics of excluded studies'.
Assessment of risk of bias in included studies
We used the approach recommended by The Cochrane Collaboration for assessing risk of bias in studies included in Cochrane reviews (Higgins 2008).
Two review authors assessed independently the risk of bias of all included trials. We performed further analysis of the quality of evidence related to each of the key outcomes using the GRADE approach (Guyatt 2008; Higgins 2008). Using this approach, we rated the quality of the body of evidence for each key outcome as 'High', 'Moderate', 'Low', or 'Very Low'.
Data extraction and management
We extracted data from the included studies using a standard form. Two review authors independently extracted all outcome data. We then checked the data against each other and, if necessary, made reference to the original paper. Any outstanding discrepancies between the two data extraction sheets were discussed by the data extractors and resolved by consensus. We tried to contact study authors to obtain any missing information.
We extracted data relating to the following from all the included studies.
Participant (LHW and recipient) information. For LHWs this included terms used to describe the LHW, selection criteria, basic education, and tasks performed. For recipients, data included the health problems or treatments received, their age and demographic details, and their cultural background.
The healthcare setting (home, primary care facility, or other); the geographic setting (rural, formal urban, or informal urban settlement) and country.
The study design and its key features (e.g., whether the allocation to groups was at the level of individual healthcare provider or at the village or suburb level).
The intervention (specific training and ongoing monitoring and support (including duration, methods, who delivered the training etc.), and the healthcare tasks performed with recipients).
The number of LHWs who were approached, trained and followed up; the number of recipients enrolled at baseline; and the number and proportion followed up.
The outcomes assessed and timing of the outcome assessment.
The results (effects), organised into eight areas (healthcare behaviours, health status and wellbeing, harms or adverse effects, consultation processes, utilisation of services, recipient satisfaction with care, social development measures and costs).
Any recipient involvement in the selection, training, and management of the LHW interventions.
Data synthesis
We grouped together studies that compared broadly similar types of interventions (n = 76), as listed below. The remaining eight studies were extremely diverse and could not be usefully grouped. We considered grouping the studies by type of LHW. However, doing this would have resulted in groups of interventions that were very dissimilar in other ways (for example, peer counsellors to promote TB treatment taking and peer counsellors to support women at risk of abuse would have been included in one group), and for which it would not have been feasible, or useful from a policy perspective, to pool findings. We therefore grouped together studies according to the type of health issue that the LHWs addressed.
1. LHW interventions to promote immunisation uptake compared with usual care.
2. LHW interventions to reduce mortality and morbidity in children under five compared with usual care. Analysis was undertaken for the following outcomes:
2.1 mortality among children under five years,
2.2 neonatal mortality,
2.3 child morbidity,
2.4 care‐seeking behaviour.
3. LHW interventions to promote breastfeeding compared with usual care. Analysis was undertaken for the following outcomes:
3.1. initiation of breastfeeding,
3.2. any breastfeeding up to 12 months post partum,
3.3. exclusive breastfeeding up to six months post partum.
4. LHW interventions to provide support to mothers of sick children compared with usual care.
5. LHW interventions to prevent or reduce child abuse compared with usual care.
6. LHW interventions to promote parent‐child interaction or health promotion compared with usual care.
7. LHW interventions to support women with a high risk of low birthweight babies or other poor outcomes in pregnancy compared with usual care.
8. LHW interventions to improve TB treatment and prophylaxis outcomes compared with other forms of adherence support.
Where feasible, we combined the results of the included studies to obtain an overall estimate of effect. This was possible for the subgroups 1 to 3 and 8 listed above. Outcome comparisons for LHW interventions to promote the uptake of breastfeeding and immunization were expressed as adherence to beneficial health behaviour. Outcomes for the subgroups including LHW interventions to reduce morbidity and mortality in children were expressed as the number of events (mortality and morbidity). Only dichotomous outcomes were included in meta‐analysis owing to the methodological complications involved in combining and interpreting studies in which different continuous outcome measures have been used. Differences in baseline variables were rare and not considered influential. We re‐analysed data on an intention‐to‐treat basis, where possible: beneficial health behaviours were analysed on a worst case basis, that is persons lost to follow up were assumed to be non‐adherent to the beneficial health behaviours. In the same way, morbidity and mortality were analysed on a best case basis, that is persons lost to follow`up were assumed to be alive and not to have experienced any morbidity events.
In two studies, Baqui 2008 (outcome: initiated breastfeeding) and Kumar 2008 (outcomes: initiated breastfeeding and reported illness in children), the results were presented as cluster means. The number of events in each groups was estimated as (N*cluster mean/100).
We made adjustment for clustering for studies that used a cluster randomised design. Where no information on the intra‐cluster correlation coefficient (ICC) was reported in any of the cluster RCTs included in the analysis group, we assumed an ICC of 0.02 for this adjustment. This ICC is typical of primary and community care interventions (Campbell 2000). Where an ICC was reported among the studies in a group, this ICC was used for the adjustments to other studies. This was the case for the following analysis groups:
neonatal mortality, an ICC of 0.0012 was used from Kumar 2008;
breastfeeding, an ICC of 0.07 was used from MacArthur 2009.
We calculated log relative risks (RR) and standard errors (SE) of the log RR for both individual and cluster RCTs (unadjusted). We then adjusted the unadjusted SEs for cluster RCTs for the effect of clustering using the multiplicative factor square root of the design effect (= (1 + (mean cluster size‐1)*ICC)). We analysed the log RRs for individual RCTs and the adjusted log RRs for cluster RCTs together, using the generic inverse variance method in Review Manager 5. RRs were preferred to odds ratios because event rates were often high and, in these circumstances, odds ratios can be difficult to interpret (Altman 1998). Random‐effects model meta‐analysis was preferred because the studies were heterogeneous.
For the remaining groups of studies (LHW interventions to provide support for mothers of sick children; to prevent or reduce child abuse; to promote parent‐child interaction and health promotion; and to support women with a higher risk of low birthweight babies or other poor outcomes in pregnancy), the outcomes assessed and the settings in which the studies were conducted were very diverse. Consequently, we judged it inappropriate to combine the results of included studies quantitatively given that an overall estimate of effect would have little practical meaning. A descriptive review of these subgroups is presented in the results section below.
Subgroup analysis and investigation of heterogeneity
During the review process, we identified several factors that might explain heterogeneity. These included: characteristics of the participants and intervention setting (child immunisation uptake); risk of bias in included studies (child mortality); and characteristics of the intervention and comparator (cure for smear positive TB patients). These were undertaken as exploratory, hypothesis generating analyses since these factors were not identified a priori and a number of potential explanatory factors were considered.
Results
Description of studies
Results of the search
A total of 9705 titles and abstracts (excluding duplicates), written in English and other languages, was identified. We considered 526 full text papers for inclusion in this review, 89 of which met our inclusion criteria. When combined with the RCTs included in the last review (43 in total), a total of 132 trials were eligible for inclusion in this review update.
Given the very large number of studies eligible for inclusion in this review update, a decision was taken to split the updated review into two parts. This review includes all studies relevant to maternal and child health (MCH) and infectious diseases. A separate review (forthcoming) will include the following health issues: cancer screening; chronic diseases management including diabetes, mental illness and hypertension; and studies focusing on care of the elderly. This review, therefore, includes a total of 82 studies (including 21 from the original review) that are relevant to MCH and infectious diseases.
Setting
Of the 82 studies included in this review, 55 studies (67%) were conducted in six high income countries: Australia, Canada, Ireland, New Zealand, the UK, and the USA. Forty‐one of the 82 studies were conducted in the USA. Twelve studies (14.6%) were conducted in eight middle income countries (Brazil, China, India, Mexico, Philipines, Thailand, Turkey, and South Africa). Fifteen trials (18.3%) were from 10 low income countries (Bangladesh, Burkina Faso, Ethiopia, Ghana, Iraq, Jamaica, Nepal, Pakistan, Tanzania, and Vietnam). These assignments are based on the World Bank's classification of countries by gross national income per capita in 2008.
In 59 studies the intervention was delivered to patients based in their homes. Five interventions were based solely in a primary care facility (Chaisson 2001; Caulfield 1998; Merewood 2006; Olds 2002; Zaman 2008). A further eight studies involved a combination of home, primary care, and community‐based interventions. Four studies delivered the intervention mainly by telephone (Dennis 2002; Dennis 2009; Graffy 2004; Singer 1999), while one implemented the intervention through community meetings (Manandhar 2004). For five studies, other sites were used such as the workplace, churches, or homeless shelters.
Intervention characteristics
Objective of the interventions
The objectives of the interventions varied greatly and are discussed in more detail for each group of studies in the 'Effects of interventions' section below.
Mode of delivery
There was great variety in the mode of intervention delivery adopted in different studies. Some trials used very specific delivery techniques that were tailored to the individual recipient, while other intervention delivery approaches were far less specific. LHWs carried out home visits in many of the trials. In other trials, interventions were delivered through telephone calls and postcards; at community meetings; or during the recipient's visit to a healthcare centre. For more information, please see the description provided for each group of studies under 'Effects of interventions'.
Other characteristics
The involvement of recipients in the interventions was generally poorly described in the included studies. The most common form of involvement was the recruitment of people who had experienced a particular health condition to deliver the intervention to others who had the health condition. Few studies recorded that recipients or community members had been involved in the selection of LHWs. However, a number of trials recruited LHWs from participant communities, often to represent its demographic characteristics.
Participants
Lay health workers
Few studies documented the number of LHWs delivering care. Where this was reported, there were considerable differences in numbers. These ranged from two LHWs in Graham (1992) and Schuler (2000) to 150 LHWs in Chongsuvivatwong (1996).
It was difficult to group the studies in terms of either LHW selection or training because of a lack of information about these aspects in the trial reports. In some cases, individuals had been recruited for their familiarity with a target community or because of their experience of a particular health condition.
The level of education of the LHWs was often poorly reported but appears to have been very varied. Data on the duration of training received indicated a range of 0.4 to 146 days. The longest period (146 days) included six months of practical field training. The training approaches varied greatly between studies and were not described in the same level of detail in all of them. The terms used included: courses, classes, seminars, sessions, workshops, reading, discussion groups, meetings, role play, practical training, field work, video‐taped interviews, and in‐class practice.
Recipients
Different recipients were targeted in the different groups of studies. For more information, please go to the description provided for each subgroup under 'Effects of interventions'.
Outcomes
Most studies reported multiple effect measures and many did not specify a primary outcome. Relevant outcomes were extracted and were categorised for the analysis according to the results detailed below and in the 'Characteristics of included studies' tables.
Risk of bias in included studies
Assessments of the risk of bias for included studies are shown in the 'Characteristics of included studies' table and are summarised in Figure 1 and Figure 2. The risk of bias assessments were not used for deciding which studies should be included in the meta‐analyses. Rather, these assessments were used in interpreting the results and, particularly, in assessing the quality of evidence for specific effects of LHW interventions.
1.
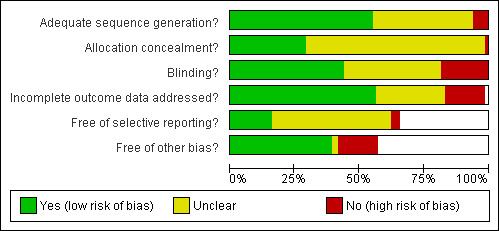
Methodological quality graph: review authors' judgements about each methodological quality item presented as percentages across all included studies.
2.
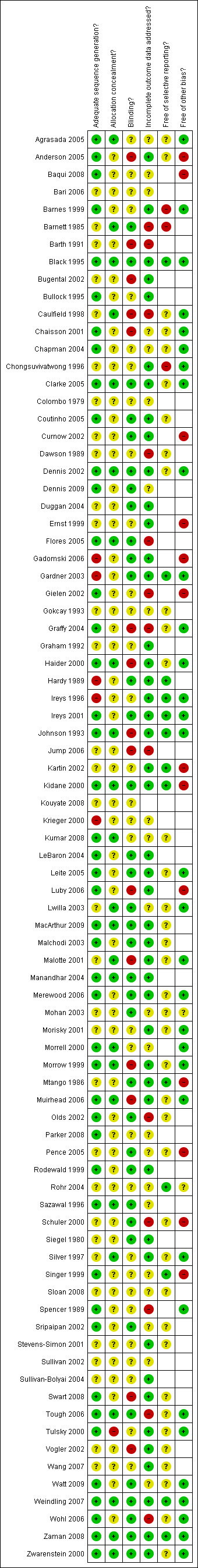
Methodological quality summary: review authors' judgements about each methodological quality item for each included study.
Effects of interventions
See: Table 1; Table 2; Table 3; Table 4
LHWs have been employed to deliver a wide range of interventions in many healthcare settings. Attempting to group studies by intervention type is therefore problematic; a more useful approach is to focus on the intended outcome or objective of each study. In this review, trials have been arranged into groups, each containing studies that used broadly similar methods to influence a single health care outcome or a group of closely related outcomes. Meta‐analysis was performed for four of the groups. In the majority of cases the analysis included the primary study outcome. Forest plots and GRADE tables for all meta‐analyses conducted are referenced below.
For the remaining groups, we considered the outcomes too diverse to be pooled usefully. The outcomes for studies not included in the meta‐analyses are reported briefly in the text and in Table 5 (for studies that could not be assigned to groups).
1. Outcomes for studies not assigned to any group or category.
| Study, and outcomes measured | Intervention data (number of participants) | Control data | Measure of effect (95% CI) | P value | Authors’ conclusion |
| Curnow 2002 | No intervention | Intervention group – clinical + Fibre Optic Transillumination (FOTI) | P value | Authors’ conclusions | |
| 24‐month DFS caries increments of first permanent molars: Clinical D1FS | 1.104 | 0.669 | 0.006 | Children in the intervention group had significantly less caries on their newly erupted permanent teeth when compared to the control group | |
| 24‐month DFS caries increments of first permanent molars: Clinical D3FS | 0.455 | 0.192 | 0.008 | ||
| 24‐month DFS caries increments of first permanent molars: Clinical + FOTI D1FS | 1.194 | 0.808 | 0.023 | ||
| 24‐month DFS caries increments of first permanent molars: Clinical + FOTI D3FS | 0.477 | 0.205 | 0.007 | ||
| Caries increment score 12 months after eruption of 1st permanent molars: clinical D1FS | 0.736 | 0.466 | 0.0316 | ||
| Caries increment score 12 months after eruption of 1st permanent molars: clinical D3FS | 0.264 | 0.105 | 0.0404 | ||
| Caries increment score 12 months after eruption of 1st permanent molars: clinical + FOTI D1FS | 0.788 | 0.524 | 0.0474 | ||
| Caries increment score 12 months after eruption of 1st permanent molars: clinical + FOTI D3FS | 0.28 | 0.111 | 0.0348 | ||
| Ernst 1999 | Hospital recruited clients (intervention) (N=28) | Hospital recruited controls (N=25) | Measure of effect (95% CI) | P value | Authors’ conclusion |
| Endpoint domain scores on 5 point Likert scale at 3 years : (1) Utilization of alcohol/drug treatment (Mean, SD) |
1 (4.9) | ‐0.6 (5.9) | Assessment of hospital recruited clients and controls after 3 years shows that clients scored significantly higher on the summary endpoint score of overall improvement in multiple domains. | ||
| (2) Abstinence from drug and alcohol (Mean, SD) | 3.9 (3.20) | 2.6 (4.2) | |||
| (3) Use of Family Planning (Mean, SD) | 2.3 (4.8) | 2.1 (4.70) | |||
| (4) Health and wellbeing of target child (Mean, SD) | 6.1 (2.3) | 4.1 (2.8) | |||
| (5) Appropriate connection with community services (Mean, SD) | 3.8 (4.7) | 1.9 (4.2) | |||
| (6) Multiple domains of the subjects' lives (Mean, SD) | 17.10 | 10.10 | t test ‐2.11 | 0,04 | |
| Flores 2005 | Case management (intervention) (N=139) | Control (N=136) | Measure of effect (95% CI) | P value | Authors’ conclusion |
| Proportion of children that obtained Health Insurance Coverage (primary outcome) | 96 | 57 | Adj. OR 7.78 [5.2 ‐11.64] | <0.0001 | Community based case managers were more effective in obtaining coverage for uninsured children than traditional Medicaid and SCHIP outreach and enrolment |
| Proportion continously insured (%) | 78 | 30 | <0.0001 | ||
| Proportion continously uninsured (%) | 4 | 43 | <0.0001 | ||
| Mean time (no.of days) to obtain insurance (SD) | 87.5 (68) | 134.8 (102.4) | <0.009 | ||
| Parents very satisfied with process of obtaining insurance (%) | 80 | 29 | <0.0001 | ||
| Mean parental satisfaction score for obtaining insurance (Likert scale 1‐5, SD) | 1.33 (0.77) | 2.4 (1.4) | <0.0001 | ||
| Gadomski 2006 | Intervention (N=416 farms) | Control (N=429 farms) | P value | Authors’ conclusions | |
| Mean Cumulative Injury density per 100 full time equivalents among children of all ages | 0.45 | 0.55 | 0.85 | Active dissemination of NAGCAT guidelines halved the incidence of NAGCAT preventable injuries among 7‐19 year olds on intervention farms in comparison to control farms. In 0 ‐ 19 years group, there was a sig increase in time span to occurence of a NAGCAT preventable injury in intervention compared to control group. | |
| Mean Cumulative incidence densities for strictly work related injuries all age groups | 0.34 | 0.44 | 0.31 | ||
| Injury incidence density/100 FTEs for children less than 7 years | 1.27 | 1.36 | 0.77 | ||
| Injury incidence density/100 FTEs for children 7 ‐ 16 years | 0.5 | 0.63 | 0.96 | ||
| North American Guidelines for Childrens Agricultural Tasks (NAGCAT) ‐ preventable injury incidence densities among 7 ‐19 year olds | 0.07 | 0.13 | 0.68 | ||
| All NAGCAT – related injury incidence densities among 7 – 19 year olds | 0.18 | 0.27 | 0.5 | ||
| Proportion reporting setting limits on amount of time child could perform work between breaks (%) | 25 | 16 | <0.01 | ||
| Proportion providing supervision to children while they were performing work (%) | 42 | 36 | 0.06 | ||
| Proportion preventing child from doing a particular job (%) | 61 | 61 | |||
| Proportion adding roll‐over protection structure during study period (%) | 3.5 | 2,9 | 0.89 | ||
| Proportion adding or repairing a power take off | 25 | 24 | 0.76 | ||
| Mean number of safety related changes made | 1.57 | 1.39 | 0.03 | ||
| Gielen 2002 | Enhanced intervention group | Standard intervention group | P value | Authors’ conclusions | |
| Proportion with hot water temperature ≤ 48.9 oC (N=115) | 47 | 47 | NS | There were no significant differences between the standard and enhanced intervention groups in the rates at which any of the safety practices were observed at home observation. | |
| Proportion with working smoke alarms (N=114) | 81 | 84 | NS | ||
| Proportion stairs protected by gate or door (N=96) | 27 | 23 | NS | ||
| Proportion poisons kept latched or locked up (N=121) | 10 | 12 | NS | ||
| Proportion homes with ipecac syrup (N=89) | 31 | 27 | NS | ||
| Parker 2008 | Intervention (N=23) | Control (N=30) | Intervention change (95% CI) | P value | Authors’ conclusion |
| Post‐intervention FEV1 intraday variability (Mean %, SD) | 14.4 (12.1) | 17.1 (13.7) | ‐1.3 [‐5.8, 3.0] | 0.559 | There was a significant beneficial effect on lung function in daily nadir FEV1 and daily nadir PF and reduced unscheduled health care utilization for asthma in the last 3 and 12 months. |
| Post‐intervention peak flow variability (Mean %, SD) | 8.7 (8.50) | 11.6 (9.7) | ‐2.1 [‐5.0, 0.8] | 0.153 | |
| Post‐intervention daily nadir FEV1 (% predicted, SD) | 83.1 (15.7) | 75.6 (18.5) | 10.0 [0.9, 19.1] | 0.032 | |
| Post‐intervention daily nadir peak flow (% predicted, SD) | 94.1(15) | 85.1(19,2) | 8.2 [1.1, 15.2] | 0.023 | |
| Proportion needed unscheduled medical care in last 12 months at post‐intervention | 59 (N=115) | 73 (n=112) | 0.40 [0.22, 0.74] | 0.004 | |
| Proportion needing unscheduled medical care in last 3 months at post‐intervention | 45 | 56 | 0.43 [0.23, 0.80] | 0.007 | |
| Proportion with any symptom more than 2 days per week, not on controller (corticosteriod) medication at post‐intervention | 42 | 46 | 0.56 [0.29, 1.06] | 0.073 | |
| Proportion with any symptom more than 2 days per week, not on any controller medication, at post‐intervention | 32 | 37 | 0.39 [0.20, 0.73] | 0.004 | |
| Swart 2008 | Intervention data (N=189) | Control data (N=188) | Mean difference (95% CI) | P value | Authors’ conclusion |
| Mean Total Injury Risk score (90) | 13.9 (0.53) | 14.2 (5.4) | ‐0.31 [‐1.8, 1.2] | 0.680 | Home visiting can effectively reduce home‐based child injury risks for burns related to unsafe practices. A non‐significant decline was noted for injuries related to electrical burns, paraffin burns and poison ingestion. |
| Mean risk score for burns, electrical (Total Risk score =20) | 1.1 (0.14) | 1.3 (0.14) | ‐0.19 [‐0.54, 0.16] | 0.294 | |
| Mean risk score for burns, paraffin (Total Risk score =20) | 3.2 (0.21) | 3.2 (0.21) | ‐0.03 [‐0.64, ‐0,57] | 0.911 | |
| Mean risk score for Burns, safety practices (Total Risk score =13) | 2.5 (0.12) | 2.9 (0.12) | ‐0.41 [‐0.76, ‐0.07] | 0.021 | |
| Mean risk score for Poison (Total Risk score =19) | 1.9 (0.20) | 2.4 (0.20) | ‐0.45 [‐1.01, 0.11] | 0.110 | |
| Mean risk score for Falls (Total Risk score =15) | 3.7 (0.24) | 3.6 (0.24) | 0.09 [‐0.60, 0.78] | 0.785 | |
| Zaman 2008 | LHW (N=52) | Usual care (N=53) | Measure of effect (95% CI) | P value | Authors’ conclusion |
| Communication skills: greets cordially (%) | 88.46 | 83.02 | OR 1.56 [0.29 – 8.32] | 0.597 | Nutrition counselling intervention resulted in (1) some improvements in LHW communication skills (2) more appropriate actions during consultations (3) improvements in child weight‐for‐age and weight‐for‐height at 180 days after the intervention, compared to usual care. |
| Communication skills: passes friendly remarks | 82.69 | 50.94 | OR 4.6 [1.32, 15.92] | 0.0160 | |
| Communication skills: pays attention to mothers | 90.38 | 84.91 | OR 1.67 [0.38, 7.34] | 0.498 | |
| Communication skills: encourages mothers to talk | 63.46 | 52.83 | OR 1.55 [0.48, 4.99] | 0.462 | |
| Communication skills: positive non‐verbal communication and body language | 94.23 | 90.57 | OR 1.7 [0.28, 10.51] | 0.563 | |
| Communication skills: asks about feeding and pays attention to reply | 50 | 24.53 | OR 3.07 [0.93] | 0.064 | |
| Communication skills: praises the mother about positive action | 36.54 | 7,55 | OR 7.5 [1.68, 29.5] | 0.008 | |
| Communication skills: recommends changes in inappropriate feeding practices | 32.69 | 3,77 | OR 12.38 [2.43, 63.25] | 0.003 | |
| Communication skills: explains why changes have to be done | 28.85 | 3,77 | OR 10.34 [2.05, 52.18] | 0.005 | |
| About feeding: asks if the child is breastfed | 50.03 | 27.27 | OR 3.15 [0.95, 10.43] | 0.060 | |
| About feeding: asks about other foods and drinks | 46.15 | 11,76 | OR 6.42 [1.37, 30.1] | 0.018 | |
| About feeding: asks size of portion | 27.45 | 5,66 | OR 6.18 [1.04, 36.6] | 0.045 | |
| About feeding: asks if changed feeding during illness | 15.56 | 9,09 | OR 2 [0.46, 8.73] | 0.353 | |
| Actions: weighs child | 57.69 | 47,17 | OR 1.52 [0.50 4,64] | 0.456 | |
| Actions: plots weight in growth chart | 36.54 | 7,95 | OR 7.05 [0.50, 4.64] | 0.034 | |
| Actions: checks current feeding against age recommended feeding | 38.46 | 5,66 | OR 10.4 [1.91, 56.8] | 0.007 | |
| Actions: checks if the mother has understood | 29.41 | 1,89 | OR 21.66 [2.6, 181.93] | 0.0046 | |
| Feeding practices: offered eggs 8 days ‐ 2 weeks | 47.68 (N=151) | 31. 95 (N=169) | OR 1.94 [1.04, 3.62] | 0.037 | |
| Feeding practices: offered chicken/beef/mutton 8 days ‐ 2 weeks | 49.67 | 31.95 | OR 2.1 [1.15, 3.83] | 0.016 | |
| Feeding practices: offered liver 8 days ‐ 2 weeks | 17.22 | 9.47 | OR 1.99 [0.89, 4.44] | 0.093 | |
| Feeding practices: added ghee/butter/oil 8 days ‐ 2 weeks | 30.46 | 24.85 | OR 1.32 [0.51, 3.42] | 0.562 | |
| Feeding practices: offered thick kitchuri 8 days ‐ 2 weeks | 61.59 | 44.97 | OR 1.96 [0.95, 4.05] | 0.068 | |
| Feeding practices: offered eggs at 180 days | 47.62 (N=126) | 26.72 (N=131) | OR 2.49 [1.03, 6.03] | 0.043 | |
| Feeding practices: offered chicken / beef / mutton at 180 days | 60.32 | 39.69 | OR 2.3 [0.996, 5.34] | 0.051 | |
| Feeding practices: offered liver at 180 days | 30.95 | 19.85 | OR 1.81 [0.79, 4.10] | 0.159 | |
| Feeding practices: added ghee/butter/oil at 180 days | 53.97 | 38.17 | OR 1.89 [0.75, 4.78] | 0.174 | |
| Feeding practices: offered thick kitchuri at 180 days | 65.87 | 44.27 | OR 2,43 [1.02, 5.76] | 0.044 | |
| Weight for age Z score ‐ 1st visit ‐ 2 weeks (Mean, SD) | ‐1.089 (1.23) | ‐1.439 (1.22) | 0.125 | ||
| Weight for age Z score ‐2nd visit ‐ 45 days (Mean, SD) | ‐1.319 (1.29) | ‐1.334 (1.19) | 0.950 | ||
| Weight for age Z score ‐ 3rd visit ‐ 180 days (Mean, SD) | ‐1.174(1.94) | ‐1.72 (1.27) | 0.012 | ||
| Height for age Z score ‐ 1st visit ‐ 2 weeks (Mean, SD) | ‐1.115 (1.36) | ‐1.407 (1.22) | 0.167 | ||
| Height for age Z score ‐2nd visit ‐ 45 days (Mean, SD) | ‐1.36 (1.29) | ‐1.575 (1.44) | 0.241 | ||
| Height for age Z score ‐ 3rd visit ‐ 180 days (Mean, SD) | ‐1.582 (1.58) | ‐1.705 (1.24) | 0.559 | ||
| Weight for height Z score ‐ 1st visit ‐ 2 weeks (Mean, SD) | ‐0.45 (1.01) | ‐0.559 (1.08) | 0.452 | ||
| Weight for height Z score ‐2nd visit ‐ 45 days (Mean, SD) | ‐0.536 (1.22) | ‐0.382 (1.08) | 0.447 | ||
| Weight for height Z score ‐ 3rd visit ‐ 180 days (Mean, SD) | ‐0.286 (1.22) | ‐0.794 (1.15) | 0.005 |
Detailed descriptions of the comparison groups for each study are available in the 'Characteristics of included studies' table.
LHW interventions to promote immunization uptake compared with usual care
Setting
Eight studies conducted in high and middle income countries were identified. One was conducted in China (Wang 2007), one in Ireland (Johnson 1993), one in Turkey (Gokcay 1993), and the remaining five in the USA (Barnes 1999; Colombo 1979; Krieger 2000; LeBaron 2004; Rodewald 1999). Apart from Wang 2007, conducted in a rural population, all other studies were implemented among urban communities.
Participants
Recipients: all studies were conducted among populations of low socioeconomic status. One study (Krieger 2000) was directed at an adult population (over 65 years of age). All other studies were directed at children of different age groups under five years.
LHWs: Krieger (2000) utilised peers selected from senior centres. In all other studies the LHWs were volunteers serving as outreach, village‐based workers or home visitors and recruited from the community. Information on educational background was available from three studies and indicated that the LHWs were college educated (LeBaron 2004; Rodewald 1999) or primary school graduates (Gokcay 1993). Only four studies provided specific information related to training: in Johnson (1993), LHWs were trained for four weeks on early childhood development principles, while Krieger (2000) reported training for only four hours. Both studies indicated that monitoring during implementation was provided. In Gockay (1993), LHWs were trained for three weeks on MCH, communication skills and on tasks to be undertaken during home visits. In Colombo 1979, coordinators were enrolled in a neighbouring college for education and training on communication skills, health care and education concepts over a six month period. Five studies indicated that monitoring or supervision was provided by a professional person but the methods used to monitor or evaluate delivery of the intervention were not specified.
Description of interventions
Immunization uptake was the primary goal in five of the studies. In four studies (Barnes 1999; Krieger 2000; LeBaron 2004; Rodewald 1999) LHWs were used to encourage individuals whose immunisation schedules were not up to date, or who had not received any vaccinations, to attend clinics to be vaccinated. This was done through postcards; phone calls or home visits, or both. In Wang (2007), LHWs delivered a birth dose of hepatitis B vaccine through a home visit to babies born in rural areas, using an out‐of‐cold chain delivery strategy. This intervention was compared to both hospital delivered vaccine and vaccine delivered using a prefilled injection device. In the remaining three studies (Colombo 1979; Gokcay 1993; Johnson 1993) immunization uptake was one of several goals tied to child health and development. Here, families were visited at home by the LHW and were given guidance and information about child health, including immunization, and were encouraged to get their children vaccinated at a clinic.
Results
Data from six studies on the outcome 'immunisation schedule up to date' were included in a meta‐analysis (Analysis 1.2; Figure 3; Table 1). This showed evidence of moderate quality that LHWs can increase the proportion of children with immunisation schedule up to date (RR 1.23, 95% CI 1.09 to 1.38; P = 0.0006), but the results were heterogeneous ( I2 = 70%, P = 0.005). In a post hoc analysis, we excluded Krieger (2000), a study focusing on adults, and Gokcay (1993), which had been implemented in a very different setting to the other studies (that is a middle rather than a high income country) (Analysis 1.3; Figure 4). The subsequent findings indicate that LHW‐based promotion strategies can increase immunisation uptake in children (RR 1.22, 95% CI 1.10 to 1.37; P = 0.0004). The control group risk was 47.4% (range 30% to 72%). However, the results were still heterogeneous (I2 = 58%, P = 0.07) suggesting that LHW interventions have variable effects. No compelling explanation for this heterogeneity was identified. In addition, there is only indirect data (from high income countries and one middle income country) regarding the effects of LHW interventions to promote immunization uptake in low income countries.
1.2. Analysis.

Comparison 1 LHW interventions to promote immunisation uptake in children under five compared with usual care, Outcome 2 Immunisation schedule up to date ‐ adjusted for clustering.
3.
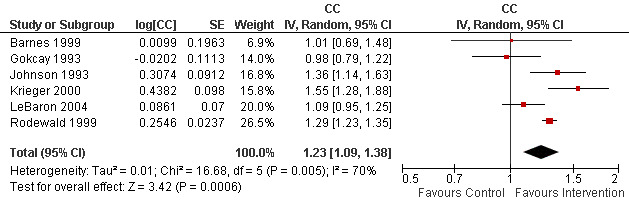
Forest plot of comparison: 1 LHW interventions to promote immunisation uptake in children under five compared with usual care, outcome: 1.5 Immunisation schedule up to date.
1.3. Analysis.

Comparison 1 LHW interventions to promote immunisation uptake in children under five compared with usual care, Outcome 3 Immunisation schedule up to date (excl. Gökcay and Krieger).
4.
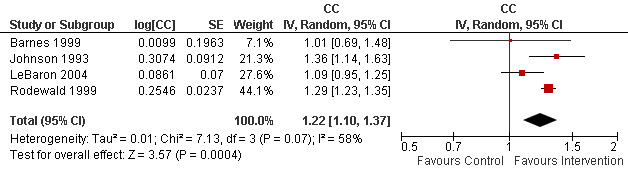
Forest plot of comparison: 1 LHW interventions to promote immunisation uptake in children under five compared with usual care, outcome: 1.8 Immunisation schedule up to date (excl. Gökcay and Krieger).
Two studies were not included in the meta‐analysis: Colombo 1979 did not provide sufficient data while Wang 2007 was different in intent to the other included studies (see above) and therefore measured different outcomes. Results from these two studies showed LHW interventions to have positive effects on immunization outcomes. In Colombo 1979, the subgroup for which outreach workers were specially trained to focus on preventive procedures for preschool children had markedly higher use rates for preventive care, such as immunization, when compared to the control group who received only routine care. In Wang 2007, coverage of the birth dose of hepatitis B vaccine increased in all three groups. There was a statistically significant (P < 0.05) difference between each of the groups in favour of the LHW interventions.
LHW interventions to reduce mortality and morbidity in children under five years compared with usual care
Setting
Fourteen studies conducted in 11 countries were identified. One study was implemented in the USA (Jump 2006) and all of the remaining studies were undertaken in LMICs: Bangladesh (Baqui 2008; Bari 2006; Sloan 2008), Burkina Faso (Kouyate 2008), Ethiopia (Kidane 2000), Ghana (Pence 2005), India (Kumar 2008; Sazawal 1996), Nepal (Manandhar 2004), Pakistan (Luby 2006), Tanzania (Mtango 1986), Thailand (Chongsuvivatwong 1996), and Vietnam (Sripaipan 2002). Aside from Jump 2006, all were community‐level interventions among rural or urban populations.
Participants
Recipients: these interventions targeted families of low socioeconomic status with children aged zero to five years. Jump 2003 was conducted among infants in an orphanage.
LHWs: these were nominated by village health committees or leaders in two studies (Manandhar 2004; Pence 2005) and by community members in two studies (Kidane 2000; Kouyate 2008). In Baqui 2008, LHWs were selected by a partner NGO while, in Sloan 2008, they were employees of the government’s nutrition programme. The LHWs in Jump 2006 were members of the staff of an orphanage. The education level of the LHWs was generally poorly described. In Kumar 2008, the LHWs had 12 years of education or more and, in Bari 2006, they had a minimum of 10th grade education. No information was provided on the educational background of the LHWs in the other included studies. Eight studies indicated that training was provided and this ranged from two days (Chongsuvivatwong 1996) to six weeks (Pence 2005). Supervision was performed by a village committee in two studies (Pence 2005; Sripaipan 2002); by the government trainers from the disease programme in two studies (malaria control in Kidane 2000; nutrition programme and partner NGO in Sloan 2008); by the regional programme supervisor in one study (Kumar 2008); or was not specified.
Description of interventions
The main purpose of these interventions was to promote health or essential newborn care and, in some cases, to manage or treat illness, including acute respiratory infections (ARI), malaria, diarrhoea, malnutrition, and other illnesses during the neonatal period. In five of the studies, the main LHW tasks included visiting homes to educate mothers about ARI or malaria; early recognition of symptoms; first line management of fever by tepid sponging; treatment with anti‐malarials or antibiotics; and referral of severe cases to health facilities (Chongsuvivatwong 1996; Kidane 2000; Kouyate 2008; Mtango 1986; Pence 2005). In the Pence study (2005), education about immunization, hygiene and other childhood illnesses was also given and the LHWs distributed multi‐vitamins, deworming tablets and vaccines in addition to anti‐malarials and antibiotics.
In five studies, LHW promoted birth preparedness and essential newborn care using various strategies. The LHW interventions were initiated in the antenatal period in two studies (Baqui 2008; Bari 2006), and included pregnancy surveillance, vitamin supplementation and promotion of birth preparedness. In the postnatal period, LHWs identifed and referred sick neonates after providing first line treatment. In Sloan 2008, the LHW promoted community‐based kangaroo care. In contrast, in Kumar 2008 the focus was on the identification of newborn stakeholders at community level and the promotion of behaviour change for improved survival of newborns. This was undertaken through folk songs and discussions at community level gatherings. In Manandhar (2004), the LHWs facilitated meetings where local perinatal health problems were identified and local strategies formulated to promote maternal and child health.
Four studies focused on the prevention or management of diarrhoeal diseases. In Luby (2006), LHWs arranged neighbourhood meetings and provided education concerning health problems associated with hand and water contamination. LHWs provided a broad range of interventions at household level for the prevention of diarrhoea, including: bleach; hand washing; a new disinfectant for drinking water; and a new disinfectant plus hand washing. The LHWs in Sazawal 1996 managed diarrhoea and prevented malnutrition by providing zinc preparations to children with diarrhoea. Growth monitoring, nutrition education, and referral to health facilities of those who were ill or failing to gain weight were the focus of activities in Sripaipan 2002. The LHWs also conducted rehabilitation programmes and made home visits to malnourished children. In the fourth study, the LHWs were trained to provided massage therapy as part of management of diarrhoea among children staying at an orphanage (Jump 2006).
Results
Data from seven studies were included in several meta‐analyses (Table 2). Findings are discussed below for the main outcomes measured by the included studies: mortality among children less than five years, neonatal mortality, child morbidity, and care‐seeking behaviour.
Outcome 1: mortality among children less than five years
This outcome was measured in three studies (Kidane 2000; Mtango 1986; Pence 2005). The results of the meta‐analysis for child mortality indicate that LHW interventions may reduce child mortality (RR 0.75, 95% CI 0.55 to 1.03; P = 0.07). However the evidence is of low quality (due to a wide confidence interval that includes no effect and due to a moderate risk of bias).There was no evidence of heterogeneity (I2 = 0%, P = 0.69) (Analysis 3.2; Figure 5) and the control group risk was 4.5% (range 4% to 5%). In a post hoc analysis, we excluded data from Pence (2005) from this analysis due to the measurement approach used in this study and its poor methodological quality. There was no major change in the final result (RR 0.75, 95% CI 0.54 to 1.03) (Analysis 3.3; Figure 6). In the excluded trial, the effect of LHW‐delivered care compared with health professional‐delivered care on child mortality was inconclusive (RR 0.89, 95% CI 0.25 to 3.33).
3.2. Analysis.

Comparison 3 LHW interventions to reduce mortality/morbidity in children under five compared with usual care, Outcome 2 Mortality among children < 5 years old.
5.
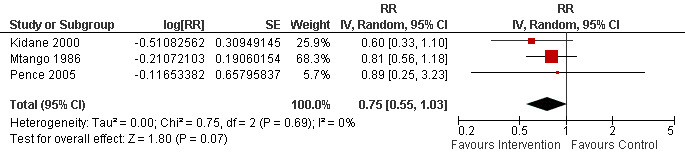
Forest plot of comparison: 3 LHW interventions to reduce mortality/morbidity in children under five compared with usual care, outcome: 3.2 Mortality among children < 5 years old.
3.3. Analysis.

Comparison 3 LHW interventions to reduce mortality/morbidity in children under five compared with usual care, Outcome 3 Mortality among children < 5 years old (Excl. Pence).
6.
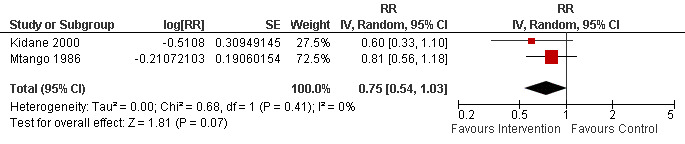
Forest plot of comparison: 3 LHW interventions to reduce mortality/morbidity in children under five compared with usual care, outcome: 3.3 Mortality among children < 5 years old (excluding Pence 2005).
Outcome 2: neonatal mortality
Four studies assessed this outcome and were included in a meta‐analysis (Baqui 2008; Kumar 2008; Manandhar 2004; Sloan 2008). The results of the meta‐analysis indicate that LHW interventions may reduce neonatal mortality (RR 0.76, 95% CI 0.57 to 1.02; P = 0.07). However the evidence is of low quality, due to a wide confidence interval that includes no effect and unexplained heterogeneity (I2 = 78%, P = 0.003) (Analysis 3.5; Figure 7).
3.5. Analysis.

Comparison 3 LHW interventions to reduce mortality/morbidity in children under five compared with usual care, Outcome 5 Neonatal mortality.
7.
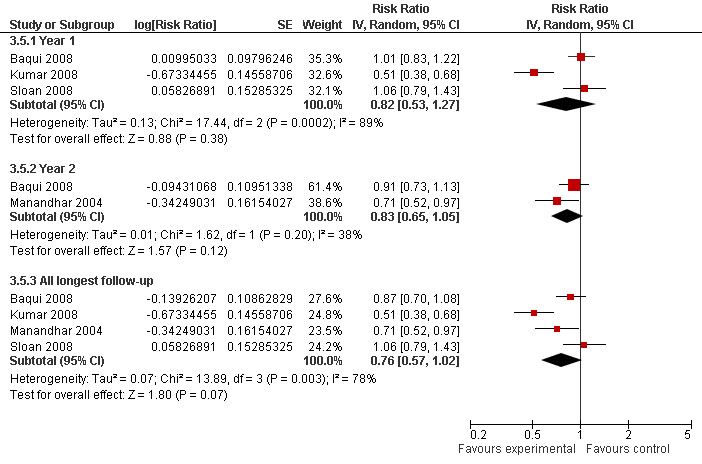
Forest plot of comparison: 3 LHW interventions to reduce mortality/morbidity in children under five compared with usual care, outcome: 3.5 Neonatal mortality.
Outcome 3: child morbidity
Seven studies measured morbidity from fever, acute respiratory infection (ARI) or diarrhoea among children under five years. When six of these studies were included in a meta‐analysis there was low quality evidence of reduced morbidity in favour of the LHW interventions compared with usual care (RR 0.86, 95% CI 0.75 to 0.99; P = 0.03). The results were heterogeneous (I2 = 69%, P = 0.003). However, all of the studies except for one (Sloan 2008: RR 1.11, 95% CI 0.98 to 1.26) found a moderate effect. The mean control group risk was 39.8% (range 25% to 55%) (Analysis 3.7; Figure 8). Luby (2006) presented insufficient raw data to allow its inclusion in this meta‐analysis but did document a lower prevalence of diarrhoea among children under five in the LHW arm.
3.7. Analysis.

Comparison 3 LHW interventions to reduce mortality/morbidity in children under five compared with usual care, Outcome 7 Morbidity; reported illness in children.
8.
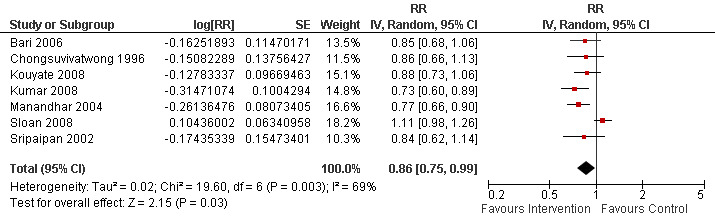
Forest plot of comparison: 3 LHW interventions to reduce mortality/morbidity in children under five compared with usual care, outcome: 3.7 Morbidity; reported illness in children.
Outcome 4: care‐seeking behaviour
Three studies measured this outcome and were included in a meta‐analysis (Analysis 3.9; Figure 9). The results suggest that LHWs may increase the likelihood of seeking care (RR 1.33, 95% CI 0.86 to 2.05). However the evidence is of low quality, due to a wide confidence interval that includes no effect and unexplained heterogeneity (I2 =77%, P = 0.01). The control group risk (that is the likelihood of seeking care) was 13.1% (range 4% to 26%).
3.9. Analysis.

Comparison 3 LHW interventions to reduce mortality/morbidity in children under five compared with usual care, Outcome 9 Morbidity; care‐seeking practice.
9.
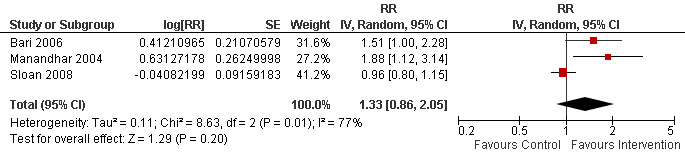
Forest plot of comparison: 3 LHW interventions to reduce mortality/morbidity in children under five compared with usual care, outcome: 3.9 Morbidity; care‐seeking practice.
LHW interventions to promote breastfeeding compared with usual care
Setting
Eighteen studies were identified of which 10 were conducted in high income countries (Anderson 2005; Caulfield 1998; Chapman 2004; Dennis 2002; Graffy 2004; MacArthur 2009; Merewood 2006; Morrell 2000; Muirhead 2006; Watt 2009); five in middle income countries (Agrasada 2005; Coutinho 2005; Kumar 2008; Leite 2005; Morrow 1999); and three in low income countries (Baqui 2008; Haider 2000; Sloan 2008). Most were implemented in urban settings apart from Baqui 2008, Kumar 2008 and Sloan 2008 which were conducted in rural areas; the setting for Agrasada 2005 was not clear.
Participants
Recipients: in five studies, the recipients were drawn from groups with higher socioeconomic status (Agrasada 2005; Dennis 2002; Graffy 2004; Morrell 2000; Muirhead 2006). Women in the other 13 studies were drawn from low income communities. The other characteristics of recipients, including parity, varied widely. Studies from LMICs focused mainly on younger mothers from low income settings.
LHWs: these were usually peers or volunteers selected from the community, although this was not clear in two studies (Coutinho 2005; Morrell 2000). In most studies, previous breastfeeding experience was a prerequisite. However, this was not the case in five studies (Baqui 2008; Coutinho 2005; Kumar 2008; Morrow 1999; and Sloan 2008) and was unclear in two studies (Morrell 2000; Watt 2009). The educational background of the LHWs was not reported consistently. Where reported (n = 7 studies), this typically included at least some secondary school education. Training of the LHWs varied in terms of intensity and content and was delivered by a range of different agencies and individuals. For example, in two studies training was by board‐certified lactation consultants (Anderson 2005; Chapman 2004); in one study by national childbirth accredited counsellors (Graffy 2004); and in three studies by specialists in lactation management (Agrasada 2005; Coutinho 2005; Morrow 1999). Duration of training varied from 2.5 hours of orientation (Dennis 2002) to approximately 280 hours in two studies (MacArthur 2009; Morrell 2000). Some studies included a substantial practice period for the LHWs. For instance, LHWs in the Morrow 1999 study practised for six months in a non‐study neighbourhood prior to the trial. While most programmes described some form of supervision of LHWs, the form of this varied.
Description of the interventions
Most studies (n = 14) intended to promote health or offer psychosocial support for breastfeeding through the provision of counselling, education and support to mothers. The interventions in the remaining studies (n = 4) had a range of objectives including (a) reducing neonatal and infant mortality through modifying high risk newborn care practices (Baqui 2008; Kumar 2008) and the use of community‐based kangaroo mother care (Sloan 2008); and (b) improving infant feeding practices more broadly (Watt 2009). All four of these studies also included breastfeeding outcomes.
Most of the interventions involved face to face contact with women in their homes to promote breastfeeding. However, in one study most of the contact was at primary care facilities (Caulfield 1998); two studies delivered support mainly by telephone (Dennis 2002; Graffy 2004); and several studies used a combination of all three of these approaches (for example Anderson 2005; Baqui 2008; MacArthur 2009). Discussions generally focused on ways to overcome potential obstacles to breastfeeding as well as on the importance and benefits of breastfeeding. In some studies, LHWs initiated contact before the third trimester of pregnancy (Anderson 2005; Caulfield 1998; Chapman 2004; MacArthur 2009; Morrow 1999; Sloan 2008) while in other studies contact was made only during the third trimester (Agrasada 2005; Coutinho 2005; Dennis 2002; Graffy 2004; Haider 2000; Leite 2005; Morrell 2000; Muirhead 2006). For two studies, LHW visits began only after birth (Merewood 2006; Watt 2009) while for the remaining studies community‐based programmes were ongoing (Baqui 2008; Kumar 2008).
Results
Data from 16 of the 18 breastfeeding studies were included in meta‐analyses (see below for list of studies; Table 3). Data from the remaining studies could not be included as these were not available in a form that allowed statistical pooling. Findings are presented below for the three main outcomes measured by the included studies: initiation of breastfeeding; any breastfeeding; and exclusive breastfeeding.
Outcome 1: initiation of breastfeeding
Twelve studies were included in this analysis (Anderson 2005; Baqui 2008; Caulfield 1998; Chapman 2004; Dennis 2002; Graffy 2004;Haider 2000; Kumar 2008; MacArthur 2009; Morrow 1999; Muirhead 2006; Sloan 2008). Breastfeeding promotion had a small impact on the initiation of breastfeeding, with studies showing an aggregate RR of 1.36 (95% CI 1.14 to 1.61). However, there was unexplained heterogeneity raising doubts about the suitability of a pooled estimate (I2 = 91%, P < 0.00001) (Analysis 2.4; Figure 10). The reasons for this heterogeneity will be explored a priori in the next update and include factors such as study setting (low, middle, or high income country); control group breastfeeding rates (for example < 30%; > 30%); and timing of the start of the intervention (in the first or second trimester of pregnancy, in the third trimester only).
2.4. Analysis.

Comparison 2 LHW interventions to promote breastfeeding compared with usual care, Outcome 4 Initiated Breastfeeding ‐ adjusted for clustering.
10.
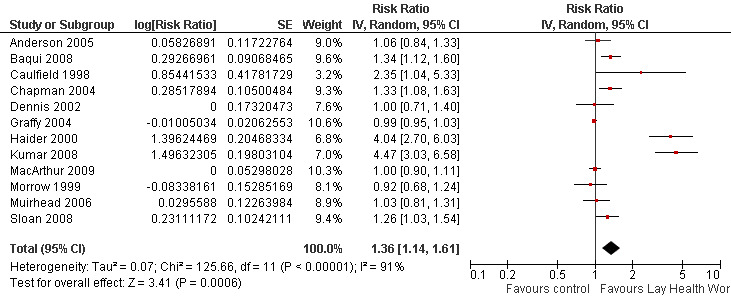
Forest plot of comparison: 2 LHW interventions to promote breastfeeding compared with usual care, outcome: 2.6 Initiated Breastfeeding ‐ adjusted for clustering.
Outcome 2: any breastfeeding up to 12 months post partum
Twelve studies were included in this analysis (Agrasada 2005; Anderson 2005; Caulfield 1998; Chapman 2004; Coutinho 2005; Dennis 2002; Graffy 2004; Leite 2005; Morrell 2000; Morrow 1999; Muirhead 2006; Sloan 2008). There was evidence, of moderate quality, that breastfeeding promotion had a small impact on any breastfeeding up to six months post partum (RR 1.24, 95% CI 1.10 to 1.39; P = 0.0004). However, the results were heterogeneous (I2 = 69%, P = 0.0002) (Analysis 2.5; Figure 11). The reasons for this heterogeneity are unclear and will be explored a priori in the next update. We will again consider factors such as study setting (low, middle, or high income country); control group breastfeeding rates; timing of the start of the intervention (in the first or second trimester of pregnancy, in the third trimester only); and time of outcome measurement.
2.5. Analysis.

Comparison 2 LHW interventions to promote breastfeeding compared with usual care, Outcome 5 Any Breastfeeding ‐ adjusted for clustering.
11.
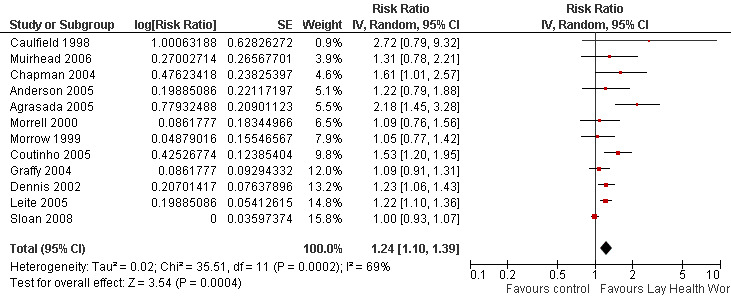
Forest plot of comparison: 2 LHW interventions to promote breastfeeding compared with usual care, outcome: 2.7 Any breastfeeding ‐ adjusted for clustering.
Outcome 3: exclusive breastfeeding up to six months postpartum
Ten studies were included in this analysis (Agrasada 2005; Anderson 2005; Coutinho 2005; Dennis 2002; Graffy 2004; Haider 2000; Leite 2005; Morrell 2000; Morrow 1999; Muirhead 2006). There was evidence, of moderate quality, that breastfeeding promotion by LHWs had a substantial impact on exclusive breastfeeding up to six months postpartum (RR 2.78, 95% CI 1.74 to 4.44; P < 0.0001). However, there was once again unexplained heterogeneity in these results (I2 = 87%, P < 0.00001) (Analysis 2.6; Figure 12). As for the other outcomes reported above, possible explanations for this heterogeneity will be explored a priori in the next update. We will again consider factors such as study setting (low, middle, or high income country); control group exclusive breastfeeding rates; timing of the start of the intervention; and time of outcome measurement.
2.6. Analysis.

Comparison 2 LHW interventions to promote breastfeeding compared with usual care, Outcome 6 Exclusive Breastfeeding ‐ adjusted for clustering.
12.
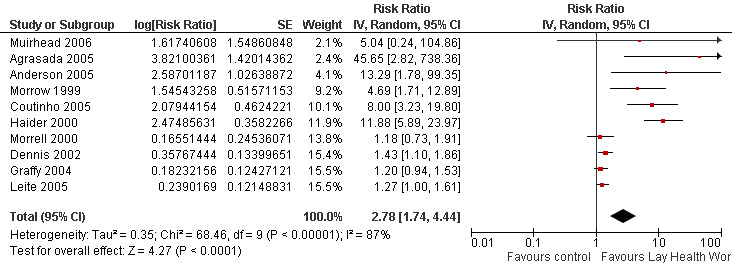
Forest plot of comparison: 2 LHW interventions to promote breastfeeding compared with usual care, outcome: 2.8 Exclusive breastfeeding ‐ adjusted for clustering.
LHW interventions to provide support to mothers of sick children compared with usual care
Setting
Eight studies were included in this group and all were conducted in urban settings within the the UK (Weindling 2007) or the United States of America (Black 1995; Ireys 1996; Ireys 2001; Silver 1997; Singer 1999; Sullivan‐Bolyai 2004; Vogler 2002).
Participants
Recipients: LHWs provided differing kinds of support to mothers of sick children. These included mothers of children with disabilities (Singer 1999; Weindling 2007); with juvenile rheumatoid arthritis (Ireys 1996); with chronic illnesses such as diabetes, asthma, and cystic fibrosis (Ireys 2001; Silver 1997; Sullivan‐Bolyai 2004); and children with non‐organic failure to thrive (Black 1995). Vogler 2002 was conducted among children with a high risk of developmental disabilities, for example children raised in foster care.
LHWs: these were largely volunteers who were parents or grandparents of children with the same or a similar chronic condition.Their education level was generally poorly described. Training received varied widely in intensity from 8 to 10 hours (Singer 1999) to 50 hours (Ireys 2001) and focused on enhancing skills, such as communication and other interpersonal skills, for providing psychosocial support. Where information on supervision was provided this varied from weekly meetings with professionals conducting the study in three studies, to fortnightly meetings in one study.
Description of interventions
The interventions intended to provide psycho‐social support and to promote health. Programmes were delivered both in the home and the community in three studies (Ireys 1996; Ireys 2001; Silver 1997). In contrast, four studies (Black 1995; Sullivan‐Bolyai 2004; Vogler 2002; Weindling 2007) provided only a home‐based intervention. In the Singer (1999) study, the intervention was delivered by telephone. The intensity of the interventions varied from four telephone calls over a two‐month period (Singer 1999) to weekly one‐hour home visits over six months (Weindling 2007). In addition, some studies included group events for the mother or parents (Ireys 1996; Ireys 2001; Silver 1997).
Results
These studies measured a wide range of maternal, parent and child health outcomes using different scales and it was not possible to combine these in a meta‐analysis. Five studies (Ireys 1996; Ireys 2001; Silver 1997; Sullivan‐Bolyai 2004; Weindling 2007) reported maternal health outcomes following interventions to provide support for mothers of sick children. Of these, two (Ireys 2001; Silver 1997) found maternal anxiety to be lower in the intervention group, but this was the only significant outcome of many reported. The same two studies also reported child mental health scores. Three scores (hostility; anxiety or depression; summary score of mental health) favoured the intervention group in one study (Ireys 2001). Other differences were not significant. Weindling 2007 reported only small effects on family needs and parental stress and no effect on the development of children with cerebral palsy. In Sullivan‐Bolyai 2004, parent‐mentored mothers had a significantly greater reduction in diabetes‐related concerns and perceived the impact of illness on the family as less negative over time.
Black (1995) reported a large number of child growth and development outcomes. No differences between the intervention and control groups were found for growth outcomes. However, outcomes measuring cognitive development, motor development, task engagement and negative affect showed significant differences in favour of the intervention group. Other differences in developmental measures were not significant. Singer (1999) reported four outcome measures: of these, scores for parental acceptance of family and disability and the extent to which primary needs were met favoured the intervention group. However, measures of empowerment showed no significant differences between intervention and control. Scores on the parental coping measure favoured the intervention, but only for parents who entered the study with low perceived coping skills.
Vogler 2002 reported outcomes measuring initiation and completion rates among children at risk for developmental delay. Children who received paraprofessional intensive case management had reduced time to completion of assessments or educational plans, and increased recommendation and initiation of needed services, compared to the group receiving basic case management.
Due to the heterogeneity of settings, interventions, and outcomes, it was not possible to draw robust, overall conclusions regarding the effects of LHWs providing support to mothers of sick children, compared with usual care. However, there were some suggestions of small benefits for child health and development.
LHW interventions to prevent or reduce child abuse compared with usual care
Setting
This group included eight studies (Barth 1991; Bugental 2002; Duggan 2004; Hardy 1989; Schuler 2000; Siegel 1980; Stevens‐Simon 2001; Sullivan 2002) conducted in the USA. Apart from Bugental 2002 in which the setting was not clear, all were delivered in urban settings.
Participants
Recipients: these were families at risk of child abuse and included mothers who were teenagers or those below 20 years (Barth 1991; Siegel 1980; Stevens‐Simon 2001); single mothers; those physically abused by their partners; mothers coping with situational crises; or mothers addicted to drugs and alcohol. Most of these families were of low socioeconomic status.
LHWs: only five studies provided some information on the background of the LHW. These were mainly mothers who were familiar with the community in which they worked and had a high school (n = 2), college level (n = 2), or undergraduate (n = 1) education. The training received was not well described. In Siegel 1980, training was for 60 days, including classroom teaching and field work, and focused on parent child interaction, child development, play and stimulation among others. In Barth 1991, training was over approximately 17 days and focused on the perinatal period, community resources, child abuse and reporting, as well as team building. The level of supervision provided varied from weekly meetings (n = 3), to twice weekly meetings for three hours for the first six months of the project in one study.
Description of interventions
All the interventions involved some form of home visitation to provide support to parents. In Barth (1991) and Steven‐Simons (2000), the interventions included both pre‐ and postnatal contact with LHWs whereas postnatal contact only was provided in Duggan 2004; Hardy 1989; Schuler 2000; and Siegel 1980. All attempted to assist parents in solving problems or dealing with stresses or crises and several also tried to improve access to or referral to local services (Duggan 2004; Siegel 1980; Stevens‐Simon 2001; Sullivan 2002).
Results
Most studies measured a wide range of healthcare behaviour, health status and social development outcomes and a meta‐analysis of these outcomes was therefore not useful. Three of the studies reported outcomes favouring the intervention group for measures of child abuse or neglect. Bugental (2002) showed a decrease in harsh parenting and in physical abuse in the cognitive appraisal group while Stevens‐Simon (2000) reported a decrease in the number of children removed due to child neglect in the intervention group compared with the control group. Hardy 1989 showed reduced child neglect, abuse, illnesses, hospitalisations, and improved compliance with well child care among the visited group, compared to the control group. The remaining studies showed no difference between the intervention and control groups for measures of child abuse. However, Duggan (2004) reported that, in families receiving a high dose of the intervention only, significant differences in favour of the intervention were measured for maternal problem alcohol use and physical abuse of women by partners. Stevens‐Simon (2000) also reported a significant increase in the use of a reliable form of hormonal contraception in the intervention group compared with control.
Given the range of outcomes measured and high loss to follow up in these studies, it is not possible to draw conclusions regarding the overall effectiveness of LHWs to reduce physical abuse among children.
LHW interventions to promote parent‐child interaction or health promotion compared with usual care
Setting
Five studies were included in this group. All were conducted in high income countries including Canada (Dennis 2009), Ireland (Johnson 1993), New Zealand (Bullock 1995), and the USA (Dawson 1989; Olds 2002). Apart from Dawson 1989, where the setting was not described clearly, all were among urban populations.
Participants
Recipients: these were mainly young (less than 20 years of age), single or first time mothers who were mainly of low socioeconomic status. In Dennis 2009, some mothers had a history of postpartum depression.
LHWs: these were mainly mothers who were selected from the community. In Dennis 2009, these mothers had a previous history of recovery from postpartum depression. The education level was poorly described. In Dawson 1989, the LHWs had a similar education level as the mothers (median of 12th grade), while in Dennis 2009 almost all the LHWs were educated beyond high school. Training varied from four hours (Dennis 2009) to 20 hours (Johnson 1993; Olds 2002) and included maternal and child health, child development and, in Dennis 2009, skills for telephone‐based support and referral to professional care. The LHWs were generally supervised but no details were provided on the intensity of this support.
Description of interventions
In all studies the intervention was intended to promote health, particularly child development, and to provide psychosocial support to low income mothers (Dawson 1989), first time mothers (Johnson 1993) or those with no previous live birth (Olds 2002), or single mothers with a partner who was not employed (Bullock 1995). In three of these studies the LHW interventions were delivered in the home while, in one study, care was delivered in primary health centres (Olds 2002), and in another by telephone (Dennis 2009). In three studies, participants were encouraged to also make use of local health and social service resources (Bullock 1995; Dawson 1989; Olds 2002). Olds (2002) also encouraged mothers to build social networks.
Results
The results of these studies were highly variable, with many of the studies reporting multiple outcome measures. Outcome data for these studies are available from the authors on request.
LHW interventions to support women with a high risk of low birthweight babies or other poor outcomes in pregnancy compared with usual care
Setting
Ten studies were included in this group. Eight of these were conducted in urban settings in high income countries including Australia (Barnett 1985), Canada (Tough 2006), New Zealand (Bullock 1995), the United Kingdom (Spencer 1989), and the USA (Black 1995; Graham 1992; Kartin 2002; Rohr 2004). Malchodi 2003 was conducted in the USA but in a rural setting while Gardner 2003 was conducted in Jamaica among an urban population.
Participants
Recipients: of the 10 studies, seven examined LHW support for pregnant women who were at risk of poor perinatal outcomes. Most women came from low income groups and were young, single mothers with low education levels. The included women were at high risk of giving birth to a low birthweight baby, as identified through a screening process (Gardner 2003; Graham 1992; Spencer 1989). In Rohr 2004, women had phenylketonuria and were pregnant or planning a pregnancy. Women at less than 20 weeks gestation and who were smoking more than one half a pack of cigarettes per day at baseline were the focus of the study by Bullock 1995. In Kartin 2002, the participating mothers used alcohol and drugs heavily during pregnancy. In the Barnett 1985 study, the included women were highly anxious primiparous mothers. Women whose babies were failing to thrive were included in Black 1995, while Tough 2006 included women who were healthy and of reasonable socioeconomic status and was intended to document the characteristics of women who opt out of prenatal care.
LHWs: these were mainly mothers who had good interpersonal skills or experienced mothers able to provide support to others. In Rohr 2004, these were mothers whose children had the same condition as the recipient, had similar adverse events to the recipients and functioned as a positive role model (Kartin 2002). In Malchodi 2003, they were non‐smoking women with similar social‐environmental and cultural qualities as the participants. Apart from Gradner 2003, where LHWs had at least four years of secondary education, no other studies provided information on the educational background of the LHW. Training was generally poorly described but tended to focus on aspects specific to the condition of interest (Black 1995; Bullock 1995; Graham 1992; Malchodi 2003; Rohr 2004). Training also focused on motivational counselling in Malchodi 2003 and on communication skills in two studies (Bullock 1995; Tough 2006). Limited information was available on the length of training provided and this ranged from one day in Malchodi 2003 to four days in Black 1995. Supervision was generally poorly described.
Description of interventions
All 10 studies involved the provision of psychosocial support to pregnant and postnatal women. In addition, LHWs provided help with daily tasks (Rohr 2004; Tough 2006) and with obtaining benefits, including housing (Spencer 1989). Graham 1992 provided health education and information on pregnancy health risks, antenatal care, and childbirth; while Spencer 1989 and Kartin 2002 promoted the appropriate use of health and social services. The study by Malchodi 2003 used non‐smoking women as LHWs to reinforce the anti‐smoking information and to support quitting efforts. In Black 1995, the LHWs identified family needs and then worked with mothers to develop an individualised plan of support. This was focused on interaction between mothers and their children so as to aid these children’s development.
Results
For both Graham 1992 and Spencer 1989, no differences were seen in the proportion of low birthweight babies born to high risk mothers in the LHW group, compared with control. In Graham, women in the intervention group showed a higher frequency of clinic attendance, and a dose response relationship with the number of LHW visits was noted. Spencer measured a large number of birth‐related outcomes, none of which showed significant differences between intervention and control. Similarly, Rohr 2004 measured a number of birth and maternal metabolic outcomes but did not demonstrate any statistically significant differences in these measures between intervention and control groups.
Malchodi 2003 found that, after controlling for baseline smoking rates, peer support by LHWs reduced the number of reported cigarettes smoked compared to usual care, especially among those that smoked 10 or more cigarettes per day. Bullock 1995 reported that women in the intervention group had decreased stress levels, higher self esteem, and reduced depressed mood in late pregnancy (34 weeks) when compared to the control group. The intervention did not, however, have an effect on smoking behaviour or drug use.
Barnett 1985 divided participants into high, moderate and low anxiety groups at baseline. For the high anxiety group, a significant difference in linear trend was found between the professional intervention and the control group for one measure of anxiety. No differences in linear trend were found between the LHW intervention and the control group for this measure. Direct comparisons of the professional and LHW groups were not reported for any of the groups (high, moderate, or low anxiety). Tough 2006 found no differences in the rates of completion of prenatal care by intervention arm.
Home visitation by lay advocates, the focus of the Kartin (2002) study, did not effectively influence the developmental abilities of children exposed to alcohol and drugs prenatally. However, Gardner 2003 documented a positive effect on problem solving and behaviour (cooperativeness and happiness) among low birthweight term babies whose mothers received LHW support, compared to low birthweight controls. Simiarly, lay home visitation in Black 1995 had a positive effect on infant cognitive and receptive language as well as on the home environment as compared to the control group.
Overall, these studies suggest that LHW interventions may not be useful in reducing the frequency of low birthweight babies in women at higher risk but may have an effect on children's development when implemented in the early postnatal period.
LHW interventions to improve tuberculosis (TB) treatment and prophylaxis outcomes compared with other forms of adherence support
Setting
Eight TB studies were included in this subgroup (Chaisson 2001; Clarke 2005; Lwilla 2003; Malotte 2001; Mohan 2003; Morisky 2001; Tulsky 2000; Zwarenstein 2000). One additional study (Wohl 2006) that evaluated LHW directly observed therapy (DOT) for anti‐retroviral treatment (ART) was included in this group because of its focus on adherence support and the close relations between TB and HIV in most settings. Four studies were conducted in low and middle income countries (Clarke 2005; Lwilla 2003; Mohan 2003; Zwarenstein 2000) and the remaining five studies in high income settings. All were conducted in urban settings apart from Clarke 2005 and Lwilla 2003 which were undertaken in rural areas.
Participants
Recipients: the recipients included adults with pulmonary TB (both clinically diagnosed and sputum or culture AFB positive TB patients) (Clarke 2005; Lwilla 2003; Mohan 2003; Zwarenstein 2000); adults and children receiving TB prophylaxis (Chaisson 2001; Malotte 2001; Morisky 2001; Tulsky 2000); and adults on ART (Wohl 2006). All but one of the studies were conducted in low income communities (this was unclear for Morisky 2001 although most participants were immigrants).
LHWs: in several studies, the LHWs were peers or people who had recently completed TB treatment (Chaisson 2001; Clarke 2005; Lwilla 2003; Morisky 2001; Tulsky 2000). In the remaining studies the LHWs were individuals from the local district (Mohan 2003; Zwarenstein 2000) or no information was provided (Malotte 2001; Wohl 2006). In both Clarke (2005) and Lwilla (2003), recipients participated in the selection of the LHWs. None of the studies provided information on the educational background of the LHWs. The training received was described in five studies (Chaisson 2001; Clarke 2005; Morisky 2001; Mohan 2003; Zwarenstein 2000). For example, in Clarke 2005 training consisted of 25 hours per week and focused on TB, primary health care, and community development principles. This training was conducted by a nurse and two LHW trainers. In Zwarenstein 2000, five mornings of interactive health promotion were delivered by a nurse who was also the project leader. Most studies also described specific supervision and monitoring of the LHWs, often by TB programme staff.
Description of the interventions
All interventions provided some form of adherence support to people with TB or HIV, although this was fairly varied and included LHW DOT, LHW support for self‐administration of treatment, LHW recall of patients who appeared to be non‐adherent to treatment and LHW support for clinic attendance.
In several studies, the LHWs supervised DOT for people on TB treatment or prophylaxis, or ART (Clarke 2005; Lwilla 2003; Malotte 2001; Tulsky 2000; Wohl 2006; Zwarenstein 2000) and this was generally compared to institution‐based therapy that would typically be supervised by a nurse, or to self‐supervision. Other tasks implemented by the LHWs included follow up of patients who had failed to adhere to treatment (for example Mohan 2003; Tulsky 2000); referral of patients with TB‐like symptoms (Clarke 2005); and, in the study by Lwilla (2003), the provision of drug refills. The intervention generally involved face to face contact with patients in their own homes, in the homes of LHWs, or in a community venue. Three studies from the USA also examined the additional effects on treatment adherence of an incentive (Malotte 2001; Morisky 2001; Tulsky 2000). These included an item agreed by parent and adolescent (Morisky 2001); USD 5 per treatment visit (Malotte 2001); and USD 5 per biweekly treatment visit (Tulsky 2000).
The outcomes measured focused mainly on healthcare behaviours (various measures of adherence to treatment or clinic appointment keeping) and health status (various measures of TB treatment including smear conversion, treatment success, and death). In addition, Wohl 2006 assessed a number of serological measures of HIV suppression, including viral load and CD4 count.
Results
Data from six of the eight TB studies were included in meta‐analyses. Findings are discussed below for the main outcomes measured by the included studies: smear positive TB patients (new and retreatment) cured; new smear positive TB patients cured; cure plus treatment completion (successful outcome) in all pulmonary TB patients; and completion of isoniazid preventive therapy at six months (Table 4).
Outcome 1: cure for smear positive TB patients (new and retreatment)
Data from four studies (Clarke 2005; Lwilla 2003; Mohan 2003; Zwarenstein 2000) were included in a meta‐analysis. This showed moderate quality evidence that LHWs have a small impact on cure rates for smear positive TB patients (new and retreatment) (RR 1.22, 95% CI 1.13 to 1.31). The control group risk range was 41% to 75%. The results were not heterogeneous (I2= 0%, P = 0.54) (Analysis 4.3; Figure 13). Because Clarke 2005 and Mohan 2003 assessed interventions and comparisons that could be considered different to those of the other two studies (Clarke compared LHW supported DOT to self‐supervision rather than to clinic‐based DOT, while Mohan examined LHW visits to find treatment defaulters compared to no visits), we repeated the analysis after removing these studies. This showed inconclusive evidence of the effects of LHWs on cure rates for smear positive TB patients (new and retreatment) (RR 1.16, 95% CI 0.93 to 1.46), with little heterogeneity (I2= 22%, P = 0.26) (Analysis 4.1; Figure 14).
4.3. Analysis.

Comparison 4 LHW interventions to improve TB treatment outcomes compared with other forms of adherence support, Outcome 3 Cure for smear positive TB patients (new and retreatment) ‐ adjusted for clustering.
13.
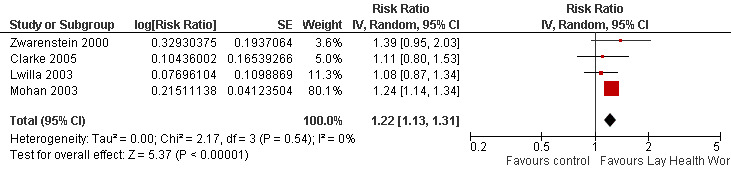
Forest plot of comparison: 4 LHW interventions to improve TB treatment outcomes compared with other forms of adherence support, outcome: 4.10 Cure for smear positive TB patients (new and retreatment) ‐ adjusted for clustering.
4.1. Analysis.

Comparison 4 LHW interventions to improve TB treatment outcomes compared with other forms of adherence support, Outcome 1 Cure for smear positive TB patients (new and retreatment) ‐ adjusted for clustering.
14.
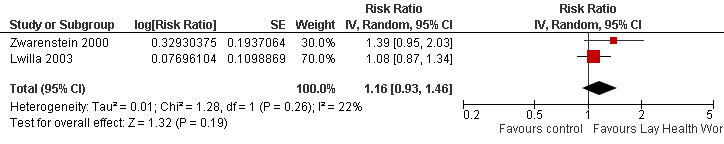
Forest plot of comparison: 4 LHW interventions to improve TB treatment outcomes compared with other forms of adherence support, outcome: 4.1 Cure for smear positive TB patients (new and retreatment), excluding Mohan 2003 and Clarke 2005 ‐ adjusted for clustering.
Outcome 2: cure for new smear positive TB patients
Two studies (Clarke 2005; Mohan 2003) reported cure rates for new smear positive TB patients. Because the interventions and comparisons assessed by these studies differed, a meta‐analysis was not conducted. Clarke 2005 compared LHW supported DOT in the community with self‐supervision of treatment in the community and found that the effects of LHW support were inconclusive (RR 1.11, 95% CI 0.8 to 1.53). Mohan 2003 compared LHW visits to locate TB treatment defaulters with no visits and found an effect on cure rates in favour of the LHW intervention (RR 1.24, 95% CI 1.14 to 1.34) (Analysis 4.4; Figure 15).
4.4. Analysis.

Comparison 4 LHW interventions to improve TB treatment outcomes compared with other forms of adherence support, Outcome 4 New smear positives cured ‐ adjusted for clustering.
15.
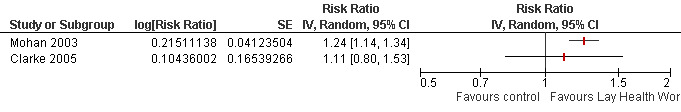
Forest plot of comparison: 4 LHW interventions to improve TB treatment outcomes compared with other forms of adherence support, outcome: 4.11 New smear positives cured ‐ adjusted for clustering.
Outcome 3: combined cure and treatment completion for all pulmonary TB patients
Three studies (Clarke 2005; Mohan 2003; Zwarenstein 2000) reported both cure and treatment completion rates for all pulmonary TB patients. Because the interventions and comparisons assessed by these studies differed, a meta‐analysis was not conducted. The interventions and comparisons for Clarke 2005 and Mogan 2003 are described above. Clarke 2005 found that the effects of LHW support were inconclusive (RR 1.08, 95% CI 0.92 to 1.27) while Mohan 2003 found an effect in favour of the LHW intervention (RR 1.23, 95% CI 1.13, 1.34). The Zwarenstein 2000 trial compared LHW supervision of DOT in the community with clinic‐based DOT and found inconclusive effects of LHW supervised DOT (RR 1.30, 95% CI 0.99 to 1.71) (Analysis 4.6; Figure 16).
4.6. Analysis.

Comparison 4 LHW interventions to improve TB treatment outcomes compared with other forms of adherence support, Outcome 6 Combined cure and treatment completion for all pulmonary TB patients ‐ adjusted for clustering.
16.
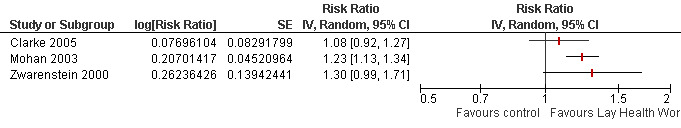
Forest plot of comparison: 4 LHW interventions to improve TB treatment outcomes compared with other forms of adherence support, outcome: 4.13 Combined cure and treatment completion for all pulmonary TB patients ‐ adjusted for clustering.
Outcome 4: completed preventive therapy with isoniazid
Four studies examined the effects of LHW support for completing preventive therapy with isoniazid. Because of heterogeneity of interventions and comparisons only two studies were included in a meta‐analysis (Chaisson 2001; Morisky 2001). These studies assessed LHW supported self‐supervision compared with self‐supervision without LHW support. There was evidence, of moderate quality, that this support had little or no effect on the completion of treatment (RR 1.00, 95% CI 0.92 to 1.09) (Analysis 4.7; Figure 17). The control group risk was 75% for Morisky 2001 and 79% for Chaisson 2001.
4.7. Analysis.

Comparison 4 LHW interventions to improve TB treatment outcomes compared with other forms of adherence support, Outcome 7 TB Preventive therapy with Isoniazid ‐ completed therapy.
17.
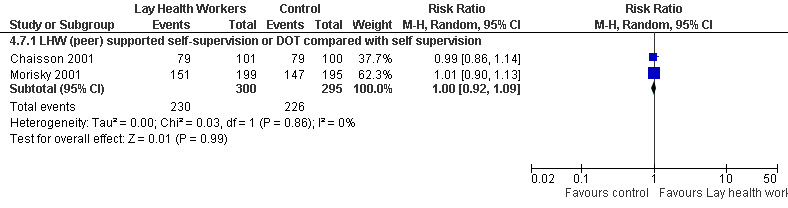
Forest plot of comparison: 4 LHW interventions to improve TB treatment outcomes compared with other forms of adherence support, outcome: 4.14 TB Preventive therapy with Isoniazid ‐ completed therapy.
Malotte 2001 compared LHW DOT plus incentive with clinic DOT plus incentive and reported inconclusive effects (RR 0.88, 95% CI 0.63 to 1.23). Tulsky 2000 compared the effects of LHW DOT with self‐supervision and found inconclusive effects on completion of isoniazid preventive therapy (RR 1.24, 95% CI 0.67 to 2.29).
Studies not assigned to any of the groups above
Owing to the range of interventions described and outcomes measured, eight studies could not be assigned to subgroups (Curnow 2002; Ernst 1999; Flores 2005; Gadomski 2006; Gielen 2002; Parker 2008; Swart 2008; Zaman 2008). In these studies, LHWs focused on the following health issues.
Curnow 2002: reducing dental caries in children.
Ernst 1999: improving health and social outcomes for substance using mothers and their children.
Flores 2005: providing information and support for the enrolment of uninsured Latino children in a state insurance programme.
Gadomski 2006: reducing childhood agricultural injuries on farms.
Gielen 2002: enhancing parents' home safety practices to reduce child injuries.
Parker 2008: improving childhood asthma through reducing household environmental triggers.
Swart 2008: improving home safety to reduce child injuries.
Zaman 2008: nutrition counselling to reduce growth faltering in children.
These studies are described in detail in the 'Characteristics of included studies' table and outcome data are reported in additional Table 5.
Discussion
Summary of main results
This review identified 82 RCTs evaluating the effects of LHW interventions for maternal and child health and the management of infectious diseases in primary and community health care. The diversity of included studies limited meta‐analysis to outcomes for four study groups. These analyses show evidence of moderate quality of the effectiveness of LHWs in promoting immunisation uptake in children; increasing breastfeeding; and improving TB cure rates, when compared to usual care. There was moderate quality evidence that LHW support had little or no effect on TB preventive treatment completion. There was also low quality evidence of the effectiveness of LHWs in reducing child morbidity; in reducing child and neonatal mortality; and in increasing the likelihood of seeking care for childhood illness. For other health issues, evidence is insufficient to draw conclusions regarding the effects of LHWs. There is also insufficient evidence to determine which LHW training or intervention strategies are likely to be most effective.
The addition of new studies has led to differences in the results compared with those presented in the original review, as follows.
Meta‐analysis findings now suggest that people with smear positive TB receiving LHW support are more likely to be cured than those receiving other forms of treatment delivery or support. However, LHW supported self‐supervision or DOT does not appear to be more effective than self‐supervision for completion of TB preventive therapy. In the original review, there were insufficient studies to conduct meta‐analyses for these outcomes.
Meta‐analysis has now been conducted separately on studies on child and neonatal mortality. The findings suggest that LHW interventions may be effective in reducing both child and neonatal mortality, although the quality of evidence is low. The original analysis suggested that LHWs were effective in reducing child mortality as well as mortality and morbidity combined. This difference is a result of changes in the way in which the studies have been analysed.
Meta‐analysis findings suggest that LHW interventions are effective in increasing the initiation of breastfeeding as well as any breastfeeding and exclusive breastfeeding. For the last outcome, the effect size is large. The original review did not separately examine outcomes for the initiation of breastfeeding, any breastfeeding, and exclusive breastfeeding. The new findings corroborate those of another Cochrane review focusing on the effectiveness of different forms of support for breastfeeding (Britton 2007).
Overall completeness and applicability of evidence
When extrapolating the meta‐analysis findings to large scale programmes, the following issues need to be considered. Firstly, LHWs in experimental studies may be more carefully selected; receive substantial training and support from highly motivated project leaders; and work with carefully selected recipient groups. Secondly, the review does not assess the sustainability of the effects of LHW interventions. Most trials have relatively short follow‐up periods and may involve higher levels of support and supervision than may be available in non‐experimental settings. These factors may be important to the long term success and sustainability of large routine LHW programmes (Berman 1987; Bosch‐Capblanch 2008; Hermann 2009; Walt 1989). Reviews including other study designs may be necessary to address the question of sustainability (for example Lehmann 2007). Thirdly, few studies described how LHW‐provided services linked with other health system components, such as referral systems. This might create difficulties or at least uncertainties for scaling up. As others have noted, the success of task shifting to LHWs, or the extension of services using LHWs, depends in part on the embedding of such programmes within broader health system strengthening initiatives (Darmstadt 2008; Lehmann 2009).
In the text below, we outline a number of other considerations regarding the applicability of the evidence presented in this review.
Because the number of studies in each analysis subgroup was small, and the interventions were often poorly described, it was not possible to:
explore differential effects across different socioeconomic settings;
examine the impact of different forms of LHW training and support, and different intensities of intervention, on outcomes;
examine the impact of different forms of LHW incentives and payment on programme outcomes (Bhattacharyya 2001; Glenton 2010);
explore the inter‐relationships between different elements of these complex interventions (Craig 2008; Shepperd 2009), which may include provision of information, support, and treatment by LHWs.
Information on these relationships would help those designing LHW programmes. Inadequate intervention descriptions also make difficult the development of a typology of LHW training interventions, which could be useful for grouping studies for analysis (Michie 2009).
Studies included in this review did not always compare LHW interventions with similar services delivered by professionals (substitution). Instead, many interventions involved LHWs being used as an extension of usual care, which was often described poorly and in some cases appeared to be no care. The studies comparing LHW programmes with similar services delivered by professionals (for example Black 1995; Lwilla 2003; Olds 2002; Pence 2005) presented mixed findings, with different outcomes favouring either professional or LHW interventions. It is possible therefore that replacing professionals with LHWs may, in some circumstances, do harm rather than good, and this should be considered more carefully in future studies. We would suggest that the available data allow no overall conclusions to be drawn regarding the effectiveness of LHWs in substituting for professional providers.
Few studies reported cost data. Examples of such reported information include the marginal costs per additional person immunized (Krieger 2000); the cost effectiveness of community postnatal support workers (Morrell 2000); and the costs of a programme to improve MCH (Olds 2002). LHWs could potentially reduce the costs of health care if substituted for professionals, through lower costs of training and remuneration. LHWs may also reduce costs for health services users by providing care at a level closer to their home or workplace. However, as others have noted, there is a conspicuous lack of data on the cost effectiveness of such interventions across different settings (Walker 2005). For example, a recent systematic review of the cost effectiveness of LHW interventions for vaccination promotion and delivery identified few relevant studies (Corluka 2009). In this review, we are unable to draw any conclusions regarding the cost of LHW interventions compared to similar interventions delivered by health professionals.
Most of the studies included in this review did not report on the possible harms or adverse effects of these interventions, either to individual patients or the health system. It is therefore difficult to draw conclusions regarding the trade‐off between benefits and harms (Oxman 2009). The key determinants for harms are likely to be the extent to which LHWs provide inappropriate care (or do not provide care where needed), make inappropriate referrals or otherwise use resources inappropriately. The benefits are also likely to vary according to the focus of the intervention, the setting in which it is implemented, and other services provided within the health system.
Few studies reported involving local people in the development of the interventions, the selection of LHWs, or the support of the LHW programmes and we, therefore, could not assess the impacts of such involvement on intervention effectiveness. Other systematic reviews of the participation of citizens in decision making for healthcare delivery have shown some benefits, but include few studies from LMIC settings (Crawford 2002; NICE 2008; Nilsen 2010).
A substantial proportion of the included studies (33%, n = 27) were conducted in LMICs or were directed at low income groups in high income countries. Based on the premise that low income groups across different countries share similar constraints in accessing health care, it may be concluded that these interventions could potentially be extrapolated to other settings, be effective in reaching low income groups, and contribute to reducing health inequalities. However, the degree to which the findings from studies in high income settings can be generalised to low income settings remains unclear and requires further empirical research. This is a particularly important consideration in the context of the two subgroups (LHWs providing support to mothers of sick children; and LHWs to prevent child abuse), where all of the studies were conducted in the United States. Given the high socioeconomic diversity within the USA, generalisation may well be possible, but using such location‐specific research findings as a basis for programmes in other settings should be undertaken with caution.
Factors that need to be considered in assessing whether the effects of LHW programmes, as outlined above, are likely to be transferable to other settings with different systems of health care delivery include (Lavis 2009) the following.
Whether the studies from which the evidence was drawn were conducted in similar settings to that in which the implementation decision is being taken.
Whether there are important differences in on‐the‐ground realities and constraints that might substantially alter the feasibility and acceptability of a LHW programme, compared to the sites in which the studies were done. For example, whether there is financial and political support for LHW programmes, including support (or resistance) from health professional organizations and service users. Also whether there are sufficient resources to provide ongoing clinical and managerial support for LHWs; to ensure the availability of supplies and equipment, such as drugs and vaccines; and to provide access to referral centres (for example for those at risk of child abuse, needing treatment for childhood illnesses, or requiring developmental assessment).
Whether there are important differences in health system arrangements that may mean that a LHW programme could not work in the same way as in the sites in which the studies were conducted. For example, if there are comparable mechanisms for employing and remunerating LHWs within the health system in the implementation setting.
Whether there are important differences in the baseline conditions between where the studies were done and the implementation setting. For example, if the incidence of TB is much lower than in the study settings, perhaps making it less cost effective to employ LHWs to support TB patients.
The availability of routine data on who might benefit from the intervention (for example children whose immunization is not up to date). These data are needed to target these programmes towards the areas of greatest need.
At present, detailed information on the trial settings and interventions is often not available in trial reports, making it difficult to assess the transferability of the results across different settings.
Quality of the evidence
The review includes 82 RCTs covering a wide range of interventions and settings. For studies included in the meta‐analyses the evidence was of low to moderate quality as assessed using GRADE.
Assessment of risk of bias in the studies included in the review suggests concerns regarding insufficient information on sequence generation and allocation concealment and regarding the failure to address adequately incomplete outcome data. A number of the studies were small and were probably underpowered. Where meta‐analysis was possible, the results were fairly consistent in showing improvements in favour of the LHW interventions, although for some interventions and outcomes there was important variation in the reported effects that could not be explained.
Some studies assessed large numbers of outcomes, increasing the probability of finding statistically significant differences for some outcomes by chance. Furthermore, the diversity of the psychometric and other outcome measures used made statistical pooling of outcome data difficult. An additional concern was the failure of a number of cluster randomised studies to adjust for clustering (resulting in misleadingly low P values and narrow CIs).
Potential biases in the review process
Firstly, LHW RCTs remain poorly indexed in electronic databases. For example, a very large number of terms are used in the literature to describe LHWs; we identified over 40 such terms in the course of this review. It is therefore possible that, despite the very extensive searches undertaken, some relevant RCTs were not identified. Most of the meta‐analyses included too few studies to allow for a meaningful assessment of assymetry that might potentially suggest publication bias. However, many of the included trials reported results that were statistically non‐significant and the studies were conducted by a wide range of investigators, so there are not specific reasons for suspecting a high risk of publication bias.
Secondly, there is no single widely accepted definition of this cadre of health workers (Lehmann 2007; Love 1997; Witmer 1995) and some readers may disagree with the inclusion decisions made. Furthermore, applying any definition to published studies is difficult as many studies do not describe adequately the training and background of the included health workers.
Thirdly, the meta‐analysis findings need to be interpreted with caution. The results were heterogenous for several analyses and the explanations for this remain unclear. This is in part because the small number of studies in some analyses does not allow us to meaningfully explore the reasons for the heterogeneity, examine differential effects across different socioeconomic settings, or other factors.
Authors' conclusions
Implications for practice.
There is moderate quality evidence of the effectiveness of LHWs in promoting immunisation uptake in children; increasing breastfeeding; and improving TB cure rates, when compared to usual care. There is also low quality evidence of the effectiveness of LHWs in reducing child morbidity; in reducing child and neonatal mortality; and in increasing the likelihood of seeking care for childhood illness. Health planners could consider including LHW interventions as components of health service strategies in these areas.
For other health issues, evidence is insufficient so far to draw conclusions regarding the effectiveness of LHW interventions. There is also insufficient evidence to determine which LHW training or intervention strategies are likely to be most effective. However, LHWs are most likely to be useful as a cadre of healthcare providers when they have an effective healthcare intervention that they are able to deliver appropriately. LHWs could also potentially reduce the direct and indirect costs of health care if substituted for professionals, through reduced training and remuneration costs and by providing care at a level closer to people’s homes. However, evidence for this is currently weak.
When LHWs are used either to substitute for professionals (task shifting) or to extend services for a range of purposes, such as the delivery of treatment support for people with HIV/AIDS (Farmer 2001; Hermann 2009; Loewenson 2004), policy makers, funders, and researchers should be aware of the need to rigorously evaluate these programmes given important uncertainties regarding their effects.
Implications for research.
The large number of trials, from a wide range of settings, of LHW programmes in maternal and child health and infectious diseases indicates the feasibility and value of rigorous evaluations and the potential for LHWs to have important benefits for a range of health issues. The implications for research are organised into key messages for trialists, systematic review authors, and other researchers.
Trialists
For health issues where LHW interventions demonstrate benefits, such as the support of breastfeeding women, research needs to shift to understanding which components of these often multi‐faceted interventions are most effective. Trials of head to head comparisons of LHW programmes may contribute to addressing this question.
Trials are also needed of the effectiveness of:
different approaches to the (initial and ongoing) training of LHWs and the delivery of services provided by LHWs, including mechanisms for supportive supervision;
LHWs as compared to professional healthcare providers in delivering interventions in the fields of health education, promotion, and the management of disease.
Greater attention needs to be paid to the quality of study designs, particularly where cluster randomisation is used. Also, investigators should specify a primary outcome; consider whether the measurement of large number of related outcomes is useful; describe more thoroughly the training and support strategies used, any co‐interventions and health care organisation and system issues; assess possible harms of the interventions; and report findings according to the relevant CONSORT guidelines.
Economic studies and process evaluations (Craig 2008; Lewin 2009; Oakley 2006) should also accompany trials to establish the cost effectiveness of different LHW interventions and to better understand the factors affecting their successful implementation.
Systematic review authors
Further systematic reviews, including of studies of effects, process evaluations, and economic evaluations, are needed on:
factors affecting the sustainability of LHW interventions when scaled up;
the effectiveness of different approaches to ensure programme sustainability, including the use of different kinds of incentives and payment systems for LHWs;
the cost effectiveness of LHW interventions for different health issues;
mechanisms for integrating LHW programmes into the formal health system;
the equity impacts of these programmes.
Other researchers
Given the wide range of health issues, recipients, settings, training strategies, and delivery mechanisms for LHW interventions, there is a need for the development of a coherent typology of LHW interventions that could help to guide research and practice in this field. Such a typology might allow LHW interventions to be conceptualised in terms of their lay component rather than in terms of the specific health issues on which they focus.
Further research is also needed on:
the effects of involving local people in the planning and support of LHW programmes;
the impacts of new technologies, such as mobile phones and uniject devices (simple, non‐reusable, prefilled injection devices) on the range of tasks that LHWs can undertake effectively.
What's new
| Date | Event | Description |
|---|---|---|
| 14 February 2010 | New search has been performed | This review is an update of the review "Lay health workers in primary and community health care" which was first published in Issue 1, 2005 of The Cochrane Library (Lewin 2005). The original review has been split into two reviews and the second review, focusing on lay health workers for chronic diseases, will be published during 2010. This review includes searches to February 2009. |
| 14 February 2010 | New citation required and conclusions have changed | The review includes new studies and the conclusions have been amended accordingly. The review also focuses only on maternal and child health and infectious diseases. |
History
Protocol first published: Issue 1, 2003 Review first published: Issue 1, 2005
| Date | Event | Description |
|---|---|---|
| 21 August 2008 | Amended | Converted to new review format. |
| 8 November 2004 | New citation required and conclusions have changed | Substantive amendment |
Notes
This review is an update of the review "Lay health workers in primary and community health care" which was first published in Issue 1, 2005 of The Cochrane Library (Lewin 2005). The original review has been split into two reviews and the second review, focusing on lay health workers interventions for chronic diseases, will be published during 2010.
An earlier version of this update was developed for a meeting hosted by the WHO: An International Dialogue on Evidence‐informed Action to Achieve Health Goals in Developing Countries. It can be assessed at: www.who.int/rpc/meetings/LHW_review.pdf (Lewin 2006).
Acknowledgements
Our thanks to the many study authors who gave us additional information regarding study designs and interventions.
Past and present staff at the editorial bases for the Cochrane Effective Practice and Organisation of Care and Consumers and Communication Review Groups also provided considerable assistance and support: Elizabeth Paulsen, Alain Mayhew, Kjetil Olsen, Hilda Bastian, Cynthia Fraser, Sophie Hill, Laura McAuley, Jessie McGowan, and Graham Mowatt. Nanna Kurtze assisted with the screening of titles and abstracts. Particular thanks to our contact editor, Andy Oxman, for his ongoing support and advice.
We would also like to acknowledge several authors of the original review who were not involved in this update: Judy Dick, Mary Patrick, and Philip Pond. Our thanks also to Craig Ramsay for statistical advice on the original review; and to Marina Clarke for assisting with inclusion assessments on the original review.
Administrative support was ably provided by Aud Ingeborg Urdahl at the Norwegian Knowledge Centre for the Health Services; Gloria Azalde at SINTEF Health Research; and Sylvia Louw at the Medical Research Council, South Africa.
We are also grateful for the comments of several consumer representatives; several anonymous peer‐reviewers; and many others who shared with us their insights into lay health worker programs.
Funding for this review was provided by the Research Council of Norway (179 355/S50). Funding for the original review was provided by: German Technical Development (GTZ) (95.2068.5‐001.00); WHO (M12/370/1); and the European Union funded AFDOT project (ICFP500A4PRO2). Additional funding for members of the review team was provided by the Medical Research Council of South Africa.
Appendices
Appendix 1. Search strategies
Please note that a database syntax guide appears at the end of this appendix.
CENTRAL
#1 MeSH descriptor Community Health Aides, this term only
#2 MeSH descriptor Allied Health Personnel, this term only
#3 MeSH descriptor Home Health Aides, this term only
#4 MeSH descriptor Voluntary Workers, this term only
#5 MeSH descriptor Home Nursing, this term only
#6 MeSH descriptor Peer Group, this term only
#7 MeSH descriptor Social Support, this term only
#8 (lay or voluntary or volunteer* or untrained or unlicensed or nonprofessional* or non next professional*) NEAR/5 (worker* or visitor* or attendant* or aide or aides or support* or person* or helper* or carer* or caregiver* or care next giver* or consultant* or assistant* or staff or visit* or midwife or midwives):ti OR (lay or voluntary or volunteer* or untrained or unlicensed or nonprofessional* or non next professional*) NEAR/5 (worker* or visitor* or attendant* or aide or aides or support* or person* or helper* or carer* or caregiver* or care next giver* or consultant* or assistant* or staff or visit* or midwife or midwives):ab OR lay next volunteer*:ti OR lay next volunteer*:ab
#9 (paraprofessional* or paramedic or paramedics or paramedical NEXT worker* or paramedical NEXT personnel or allied NEXT health NEXT personnel or allied NEXT health NEXT worker* or support NEXT worker* or home NEXT health NEXT aide*):ti OR (paraprofessional* or paramedic or paramedics or paramedical NEXT worker* or paramedical NEXT personnel or allied NEXT health NEXT personnel or allied NEXT health NEXT worker* or support NEXT worker* or home next health next aide*):ab
#10 (trained NEAR/3 (volunteer* or (health next worker*) or mother*)):ti OR (trained NEAR/3 (volunteer* or (health next worker*) or mother*)):ab
#11 (community or village*) NEAR/3 ((health next worker*) or (health next care next worker*) or (healthcare next worker*)):ti OR (community or village*) NEAR/3 ((health next worker*) or (health next care next worker*) or (healthcare next worker*)):ab
#12 (community NEAR/3 (volunteer* or aide or aides or support)):ti or (community NEAR/3 (volunteer* or aide or aides or support)):ab
#13 (birth or childbirth labor or labour) NEXT (attendant* or assistant*):ti OR (birth or childbirth or labor or labour) NEXT (attendant* or assistant*):ab
#14 (doula* or douladural*):ti OR (doula* or douladural*):ab
#15 (monitrice*):ti OR (monitrice*):ab
#16 (peer NEXT (volunteer* or counsel* or support or intervention*)):ti OR (peer NEXT (volunteer* or counsel* or support or intervention*)):ab
#17 outreach:ti OR outreach:ab
#18 (church next based) NEAR/3 (intervention* or program* or counsel*):ti OR (church next based) NEAR/3 (intervention* or program* or counsel*):ab
#19 (linkworker* or (link next worker*)):ti OR (linkworker* or (link next worker*)):ab
#20 (barefoot next doctor*):ti OR (barefoot next doctor*):ab
#21 (home NEXT (care or aide or aides or nursing or support or intervention* or treatment* or visit*)):ti OR (home NEXT (care or aide or aides or nursing or support or intervention* or treatment* or visit*)):ab
#22 (care or aide or aides or nursing or support or intervention* or treatment* or visit*) NEAR/3 (lay or volunteer* or voluntary):ti OR (care or aide or aides or nursing or support or intervention* or treatment* or visit*) NEAR/3 (lay or volunteer* or voluntary):ab
#23 (#21 AND #22)
#24 (#1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18 OR #19 OR #20 OR #23)
MEDLINE
1. Community Health Aides/
2. Home Health Aides/
3. Allied Health Personnel/
4. Voluntary Workers/
5. Home Nursing/
6. Peer Group/
7. Social Support/
8. ((lay or voluntary or volunteer? or untrained or unlicensed or nonprofessional? or non professional?) adj5 (worker? or visitor? or attendant? or aide or aides or support$ or person$ or helper? or carer? or caregiver? or care giver? or consultant? or assistant? or staff or visit$ or midwife or midwives)).tw.
9. lay volunteer?.tw.
10. (paraprofessional? or paramedic or paramedics or paramedical worker? or paramedical personnel or allied health personnel or allied health worker? or support worker? or home health aide?).tw.
11. (trained adj3 (volunteer? or health worker? or mother?)).tw.
12. ((community or village?) adj3 (health worker? or health care worker? or healthcare worker?)).tw.
13. (community adj3 (volunteer? or aide or aides or support)).tw.
14. ((birth or childbirth or labor or labour) adj (attendant? or assistant?)).tw.
15. (doula? or douladural?).tw.
16. monitrice?.tw.
17. (peer adj (volunteer? or counsel$ or support or intervention?)).tw.
18. (church based adj3 (intervention$ or program$ or counsel$)).tw.
19. (linkworker? or link worker?).tw.
20. barefoot doctor?.tw.
21. outreach.tw.
22. (home adj (care or aide or aides or nursing or support or intervention? or treatment? or visit$)).tw.
23. ((care or aide or aides or nursing or support or intervention? or treatment? or visit$) adj3 (lay or volunteer? or voluntary)).tw.
24. 22 and 23
25. or/1‐21,24
26. randomized controlled trial.pt.
27. controlled clinical trial.pt.
28. randomized.ab.
29. placebo.ab.
30. drug therapy.fs.
31. randomly.ab.
32. trial.ab.
33. groups.ab.
34. or/26‐33
35. humans.sh.
36. 34 and 35
37. editorial.pt.
38. comment.pt.
39. 37 or 38
40. 36 not 39
41. 25 and 40
MEDLINE In‐Process & Other Non‐Indexed Citations
1. ((lay or voluntary or volunteer? or untrained or unlicensed or nonprofessional? or non professional?) adj5 (worker? or visitor? or attendant? or aide or aides or support$ or person$ or helper? or carer? or caregiver? or care giver? or consultant? or assistant? or staff or visit$ or midwife or midwives)).tw.
2. lay volunteer?.tw.
3. (paraprofessional? or paramedic or paramedics or paramedical worker? or paramedical personnel or allied health personnel or allied health worker? or support worker? or home health aide?).tw.
4. (trained adj3 (volunteer? or health worker? or mother?)).tw.
5. ((community or village?) adj3 (health worker? or health care worker? or healthcare worker?)).tw.
6. (community adj3 (volunteer? or aide or aides or support)).tw.
7. ((birth or childbirth or labor or labour) adj (attendant? or assistant?)).tw.
8. (doula? or douladural?).tw.
9. monitrice?.tw.
10. (peer adj (volunteer? or counsel$ or support or intervention?)).tw.
11. (church based adj3 (intervention$ or program$ or counsel$)).tw.
12. (linkworker? or link worker?).tw.
13. barefoot doctor?.tw.
14. outreach.tw.
15. (home adj (care or aide or aides or nursing or support or intervention? or treatment? or visit$)).tw.
16. ((care or aide or aides or nursing or support or intervention? or treatment? or visit$) adj3 (lay or volunteer? or voluntary)).tw.
17. 15 and 16
18. or/1‐14,17
19. random$.tw.
20. ((clinical or control$) adj2 trial?).tw.
21. or/19‐20
22. 18 and 21
EMBASE
1. Voluntary Worker/
2. Paramedical Personnel/
3. Health Auxiliary/
4. Peer Group/
5. Health Visitor/
6. Doula/
7. ((lay or voluntary or volunteer? or untrained or unlicensed or nonprofessional? or non professional?) adj5 (worker? or visitor? or attendant? or aide or aides or support$ or person$ or helper? or carer? or caregiver? or care giver? or consultant? or assistant? or staff or visit$ or midwife or midwives)).tw.
8. lay volunteer?.tw.
9. (paraprofessional? or paramedic or paramedics or paramedical worker? or paramedical personnel or allied health personnel or allied health worker? or support worker? or home health aide?).tw.
10. (trained adj3 (volunteer? or health worker? or mother?)).tw.
11. ((community or village?) adj3 (health worker? or health care worker? or healthcare worker?)).tw.
12. (community adj3 (volunteer? or aide or aides or support)).tw.
13. ((birth or childbirth or labor or labour) adj (attendant? or assistant?)).tw.
14. (doula? or douladural?).tw.
15. monitrice?.tw.
16. (peer adj (volunteer? or counsel$ or support or intervention?)).tw.
17. (church based adj3 (intervention$ or program$ or counsel$)).tw.
18. (linkworker? or link worker?).tw.
19. barefoot doctor?.tw.
20. outreach.tw.
21. (home adj (care or aide or aides or nursing or support or intervention? or treatment? or visit$)).tw.
22. ((care or aide or aides or nursing or support or intervention? or treatment? or visit$) adj3 (lay or volunteer? or voluntary)).tw.
23. 21 and 22
24. or/1‐20,23
25. random$.tw. or clinical trial$.mp. or exp Health Care Quality/
26. Nonhuman/
27. 25 not 26
28. 24 and 27
AMED
1. Voluntary Workers/
2. Home Nursing/
3. Allied Health Personnel/
4. Caregivers/
5. Peer Group/
6. Social Support/
7. ((lay or voluntary or volunteer? or untrained or unlicensed or nonprofessional? or non professional?) adj5 (worker? or visitor? or attendant? or aide or aides or support$ or person$ or helper? or carer? or caregiver? or care giver? or consultant? or assistant? or staff or visit$ or midwife or midwives)).tw.
8. lay volunteer?.tw.
9. (paraprofessional? or paramedic or paramedics or paramedical worker? or paramedical personnel or allied health personnel or allied health worker? or support worker? or home health aide?).tw.
10. (trained adj3 (volunteer? or health worker? or mother?)).tw.
11. ((community or village?) adj3 (health worker? or health care worker? or healthcare worker?)).tw.
12. (community adj3 (volunteer? or aide or aides or support)).tw.
13. ((birth or childbirth or labor or labour) adj (attendant? or assistant?)).tw.
14. (doula? or douladural?).tw.
15. monitrice?.tw.
16. (peer adj (volunteer? or counsel$ or support or intervention?)).tw.
17. (church based adj3 (intervention$ or program$ or counsel$)).tw.
18. (linkworker? or link worker?).tw.
19. barefoot doctor?.tw.
20. outreach.tw.
21. (home adj (care or aide or aides or nursing or support or intervention? or treatment? or visit$)).tw.
22. ((care or aide or aides or nursing or support or intervention? or treatment? or visit$) adj3 (lay or volunteer? or voluntary)).tw.
23. 21 and 22
24. or/1‐20,23
25. Randomized controlled trials/
26. randomized controlled trial.pt.
27. Random Allocation/
28. Double Blind Method/
29. exp Clinical Trials/
30. clinical trial.pt.
31. (clinic$ adj trial$1).tw.
32. ((singl$ or doubl$ or treb$ or tripl$) adj (blind$3 or mask$3)).tw.
33. Placebos/
34. placebo$.tw.
35. Comparative Study/
36. random$.tw.
37. or/25‐36
38. 24 and 37
British Nursing Index and Archive
1. Voluntary Organisations/
2. Carers/
3. Health Care Assistants/
4. Health Visiting/
5. ((lay or voluntary or volunteer? or untrained or unlicensed or nonprofessional? or non professional?) adj5 (worker? or visitor? or attendant? or aide or aides or support$ or person$ or helper? or carer? or caregiver? or care giver? or consultant? or assistant? or staff or visit$ or midwife or midwives)).tw.
6. lay volunteer?.tw.
7. (paraprofessional? or paramedic or paramedics or paramedical worker? or paramedical personnel or allied health personnel or allied health worker? or support worker? or home health aide?).tw.
8. (trained adj3 (volunteer? or health worker? or mother?)).tw.
9. ((community or village?) adj3 (health worker? or health care worker? or healthcare worker?)).tw.
10. (community adj3 (volunteer? or aide or aides or support)).tw.
11. ((birth or childbirth or labor or labour) adj (attendant? or assistant?)).tw.
12. (doula? or douladural? or monitrice?).tw.
13. (peer adj (volunteer? or counsel$ or support or intervention?)).tw.
14. (church based adj3 (intervention$ or program$ or counsel$)).tw.
15. (linkworker? or link worker?).tw.
16. barefoot doctor?.tw.
17. outreach.tw.
18. (home adj (care or aide or aides or nursing or support or intervention? or treatment? or visit$)).tw.
19. ((care or aide or aides or nursing or support or intervention? or treatment? or visit$) adj3 (lay or volunteer? or voluntary)).tw.
20. 18 and 19
21. or/1‐17,20
22. random$.tw.
23. ((clinical or control$) adj2 trial?).tw.
24. 22 or 23
25. 21 and 24
CINAHL, Ovid (1982 to 2006 Week 31)
1. Volunteer Workers/
2. Health Personnel, Unlicensed/
3. Home Health Aides/
4. Allied Health Personnel/
5. Community Health Workers/
6. Home Nursing/
7. Lay Midwives/
8. Doulas/
9. Nursing Assistants/
10. Caregivers/
11. Peer Group/
12. Community Networks/
13. ((lay or voluntary or volunteer? or untrained or unlicensed or nonprofessional? or non professional?) adj5 (worker? or visitor? or attendant? or aid or aides or support$ or personnel or helper? or carer? or caregiver? or care giver? or consultant? or assistant? or staff or visit$ or midwife or midwives)).tw.
14. lay volunteer?.tw.
15. paraprofessional?.tw.
16. (paramedical adj (person$ or staff or aid or aides or assistant?)).tw.
17. (trained adj3 (volunteer? or lay person$ or health worker? or mother?)).tw.
18. ((community or primary or village?) adj3 (health worker? or health care worker? or healthcare worker?)).tw.
19. (community adj3 (volunteer? or aid or aides or support)).tw.
20. ((birth or childbirth or child birth or labor or labour) adj (attendant? or assistant?)).tw.
21. (doula? or douladural?).tw.
22. monitrice?.tw.
23. (peer adj (volunteer? or counsel$ or outreach or support)).tw.
24. "peer to peer".tw.
25. "mother to mother".tw.
26. "family to family".tw.
27. (church based adj3 (intervention$ or program$ or counsel$)).tw.
28. (linkworker? or link worker?).tw.
29. barefoot doctor?.tw.
30. (home adj (care or aid or aides or nursing or support or intervention? or treatment? or visit$)).tw.
31. ((care or aid or aides or nursing or support or intervention? or treatment? or visit$) adj3 (lay or volunteer? or voluntary)).tw.
32. 30 and 31
33. or/1‐29,32
34. exp Clinical trials/
35. clinical trial.pt.
36. (clinic$ adj trial$1).tw.
37. ((singl$ or doubl$ or trebl$ or tripl$) adj (blind$3 or mask$3)).tw.
38. Randomi?ed control$ trial$.tw.
39. Random assignment/
40. Random$ allocat$.tw.
41. Quantitative studies/
42. Allocat$ random$.tw.
43. exp clinical research/
44. evaluation research/
45. comparative studies/
46. or/34‐45
47. 33 and 46
CINAHL, Ebsco (2006 to present)
S42 S35 and S41
S41 S36 or S37 or S38 or S39 or S40
S40 EM 2010
S39 EM 2009
S38 EM 2008
S37 EM 2007
S36 EM 2006
S35 S33 and S34
S34 S29 or S30 or S31 or S32
S33 S1 or S2 or S3 or S4 or S5 or S6 or S7 or S8 or S9 or S10 or S11 or S12 or S13 or S14 or S15 or S16 or S17 or S18 or S19 or S20 or S21 or S22 or S23 or S24 or S25 or S26 or S27 or S28
S32 TI ( randomi* or randomly or "controlled trial" or "controlled clinical trial" or "controlled study" or "controlled design" ) or AB ( randomi* or randomly or "controlled trial" or "controlled clinical trial" or "controlled study" or "controlled design" )
S31 (MH "Random Assignment")
S30 (MH "Clinical Trials")
S29 PT clinical trial
S28 TI ( "home care" N3 volunteer* or "home aide" N3 volunteer* or "home aides" N3 volunteer* or "home nursing" N3 volunteer* or "home support" N3 volunteer* or "home intervention" N3 volunteer* or "home treatment" N3 volunteer* or "home visit" N3 volunteer* ) or AB ( "home care" N3 volunteer* or "home aide" N3 volunteer* or "home aides" N3 volunteer* or "home nursing" N3 volunteer* or "home support" N3 volunteer* or "home intervention" N3 volunteer* or "home treatment" N3 volunteer* or "home visit" N3 volunteer* )
S27 TI ( "home care" N3 voluntary or "home aide" N3 voluntary or "home aides" N3 voluntary or "home nursing" N3 voluntary or "home support" N3 voluntary or "home intervention" N3 voluntary or "home treatment" N3 voluntary or "home visit" N3 voluntary ) or AB ( "home care" N3 voluntary or "home aide" N3 voluntary or "home aides" N3 voluntary or "home nursing" N3 voluntary or "home support" N3 voluntary or "home intervention" N3 voluntary or "home treatment" N3 voluntary or "home visit" N3 voluntary )
S26 TI ( "home care" N3 lay or "home aide" N3 lay or "home aides" N3 lay or "home nursing" N3 lay or "home support" N3 lay or "home intervention" N3 lay or "home treatment" N3 lay or "home visit" N3 lay ) or AB ( "home care" N3 lay or "home aide" N3 lay or "home aides" N3 lay or "home nursing" N3 lay or "home support" N3 lay or "home intervention" N3 lay or "home treatment" N3 lay or "home visit" N3 lay )
S25 TI ( "church based" N3 intervention* or "church based" N3 program* or "church based" N3 counsel* or outreach ) or AB ( "church based" N3 intervention* or "church based" N3 program* or "church based" N3 counsel* or outreach )
S24 TI ( peer W1 volunteer* or peer W1 counsel* or peer W1 support or peer W1 intervention* ) or AB ( peer W1 volunteer* or peer W1 counsel* or peer W1 support or peer W1 intervention* )
S23 TI ( birth W1 attendant* or childbirth W1 attendant* or labor W1 attendant* or labour W1 attendant* or birth W1 assistant* or childbirth W1 assistant* or labor W1 assistant* or labour W1 assistant* or doula* or douladural* or monitrice* or linkworker* or link W1 worker* or barefoot W1 doctor* ) or AB ( birth W1 attendant* or childbirth W1 attendant* or labor W1 attendant* or labour W1 attendant* or birth W1 assistant* or childbirth W1 assistant* or labor W1 assistant* or labour W1 assistant* or doula* or douladural* or monitrice* or linkworker* or link W1 worker* or barefoot W1 doctor* )
S22 TI ( community N3 volunteer* or community N3 aide or community N3 aides or community N3 support ) or AB ( community N3 volunteer* or community N3 aide or community N3 aides or community N3 support )
S21 TI ( community N3 "health worker" or community N3 "health workers" or community N3 "health care worker" or community N3 "health care workers" or community N3 "healthcare worker" or community N3 "healthcare workers" or village* N3 "health worker" or village* N3 "health workers" or village* N3 "health care worker" or village* N3 "health care workers" or village* N3 "healthcare worker" or village* N3 "healthcare workers" ) or AB ( community N3 "health worker" or community N3 "health workers" or community N3 "health care worker" or community N3 "health care workers" or community N3 "healthcare worker" or community N3 "healthcare workers" or village* N3 "health worker" or village* N3 "health workers" or village* N3 "health care worker" or village* N3 "health care workers" or village* N3 "healthcare worker" or village* N3 "healthcare workers" )
S20 TI ( trained N3 volunteer* or trained N3 "health worker" or trained N3 "health workers" or trained N3 "health care worker" or trained N3 "health care workers" or trained N3 "healthcare worker" or trained N3 "healthcare workers" or trained N3 mother* ) or AB ( trained N3 volunteer* or trained N3 "health worker" or trained N3 "health workers" or trained N3 "health care worker" or trained N3 "health care workers" or trained N3 "healthcare worker" or trained N3 "healthcare workers" or trained N3 mother* )
S19 TI ( "lay volunteer" or "lay volunteers" or paraprofessional* or paramedic or paramedics or "paramedical worker" or "paramedical workers" or "paramedical personnel" or "allied health personnel" or "allied health worker" or "allied health workers" or "support worker" or "support workers" or "home health aide" or "home health aides" ) or AB ( "lay volunteer" or "lay volunteers" or paraprofessional* or paramedic or paramedics or "paramedical worker" or "paramedical workers" or "paramedical personnel" or "allied health personnel" or "allied health worker" or "allied health workers" or "support worker" or "support workers" or "home health aide" or "home health aides" )
S18 TI ( "non professional" N5 worker* or "non professional" N5 visitor* or "non professional" N5 attendant* or "non professional" N5 aide or "non professional" N5 aides or "non professional" N5 support* or "non professional" N5 personnel or "non professional" N5 helper* or "non professional" N5 carer* or "non professional" N5 caregiver* or "non professional" N5 "care giver" or "non professional" N5 "care givers" or "non professional" N5 consultant* or "non professional" N5 assistant* or "non professional" N5 staff or "non professional" N5 visit* or "non professional" N5 midwife or "non professional" N5 midwives ) or AB ( "non professional" N5 worker* or "non professional" N5 visitor* or "non professional" N5 attendant* or "non professional" N5 aide or "non professional" N5 aides or "non professional" N5 support* or "non professional" N5 personnel or "non professional" N5 helper* or "non professional" N5 carer* or "non professional" N5 caregiver* or "non professional" N5 "care giver" or "non professional" N5 "care givers" or "non professional" N5 consultant* or "non professional" N5 assistant* or "non professional" N5 staff or "non professional" N5 visit* or "non professional" N5 midwife or "non professional" N5 midwives )
S17 TI ( nonprofessional N5 worker* or nonprofessional N5 visitor* or nonprofessional N5 attendant* or nonprofessional N5 aide or nonprofessional N5 aides or nonprofessional N5 support* or nonprofessional N5 personnel or nonprofessional N5 helper* or nonprofessional N5 carer* or nonprofessional N5 caregiver* or nonprofessional N5 "care giver" or nonprofessional N5 "care givers" or nonprofessional N5 consultant* or nonprofessional N5 assistant* or nonprofessional N5 staff or nonprofessional N5 visit* or nonprofessional N5 midwife or nonprofessional N5 midwives ) or AB ( nonprofessional N5 worker* or nonprofessional N5 visitor* or nonprofessional N5 attendant* or nonprofessional N5 aide or nonprofessional N5 aides or nonprofessional N5 support* or nonprofessional N5 personnel or nonprofessional N5 helper* or nonprofessional N5 carer* or nonprofessional N5 caregiver* or nonprofessional N5 "care giver" or nonprofessional N5 "care givers" or nonprofessional N5 consultant* or nonprofessional N5 assistant* or nonprofessional N5 staff or nonprofessional N5 visit* or nonprofessional N5 midwife or nonprofessional N5 midwives )
S16 TI ( unlicensed N5 worker* or unlicensed N5 visitor* or unlicensed N5 attendant* or unlicensed N5 aide or unlicensed N5 aides or unlicensed N5 support* or unlicensed N5 personnel or unlicensed N5 helper* or unlicensed N5 carer* or unlicensed N5 caregiver* or unlicensed N5 "care giver" or unlicensed N5 "care givers" or unlicensed N5 consultant* or unlicensed N5 assistant* or unlicensed N5 staff or unlicensed N5 visit* or unlicensed N5 midwife or unlicensed N5 midwives ) or AB ( unlicensed N5 worker* or unlicensed N5 visitor* or unlicensed N5 attendant* or unlicensed N5 aide or unlicensed N5 aides or unlicensed N5 support* or unlicensed N5 personnel or unlicensed N5 helper* or unlicensed N5 carer* or unlicensed N5 caregiver* or unlicensed N5 "care giver" or unlicensed N5 "care givers" or unlicensed N5 consultant* or unlicensed N5 assistant* or unlicensed N5 staff or unlicensed N5 visit* or unlicensed N5 midwife or unlicensed N5 midwives )
S15 TI ( untrained N5 worker* or untrained N5 visitor* or untrained N5 attendant* or untrained N5 aide or untrained N5 aides or untrained N5 support* or untrained N5 personnel or untrained N5 helper* or untrained N5 carer* or untrained N5 caregiver* or untrained N5 "care giver" or untrained N5 "care givers" or untrained N5 consultant* or untrained N5 assistant* or untrained N5 staff or untrained N5 visit* or untrained N5 midwife or untrained N5 midwives ) or AB ( untrained N5 worker* or untrained N5 visitor* or untrained N5 attendant* or untrained N5 aide or untrained N5 aides or untrained N5 support* or untrained N5 personnel or untrained N5 helper* or untrained N5 carer* or untrained N5 caregiver* or untrained N5 "care giver" or untrained N5 "care givers" or untrained N5 consultant* or untrained N5 assistant* or untrained N5 staff or untrained N5 visit* or untrained N5 midwife or untrained N5 midwives )
S14 TI ( volunteer N5 worker* or volunteer N5 visitor* or volunteer N5 attendant* or volunteer N5 aide or volunteer N5 aides or volunteer N5 support* or volunteer N5 personnel or volunteer N5 helper* or volunteer N5 carer* or volunteer N5 caregiver* or volunteer N5 "care giver" or volunteer N5 "care givers" or volunteer N5 consultant* or volunteer N5 assistant* or volunteer N5 staff or volunteer N5 visit* or volunteer N5 midwife or volunteer N5 midwives ) or AB ( volunteer N5 worker* or volunteer N5 visitor* or volunteer N5 attendant* or volunteer N5 aide or volunteer N5 aides or volunteer N5 support* or volunteer N5 personnel or volunteer N5 helper* or volunteer N5 carer* or volunteer N5 caregiver* or volunteer N5 "care giver" or volunteer N5 "care givers" or volunteer N5 consultant* or volunteer N5 assistant* or volunteer N5 staff or volunteer N5 visit* or volunteer N5 midwife or volunteer N5 midwives )
S13 TI ( voluntary N5 worker* or voluntary N5 visitor* or voluntary N5 attendant* or voluntary N5 aide or voluntary N5 aides or voluntary N5 support* or voluntary N5 personnel or voluntary N5 helper* or voluntary N5 carer* or voluntary N5 caregiver* or voluntary N5 "care giver" or voluntary N5 "care givers" or voluntary N5 consultant* or voluntary N5 assistant* or voluntary N5 staff or voluntary N5 visit* or voluntary N5 midwife or voluntary N5 midwives ) or AB ( voluntary N5 worker* or voluntary N5 visitor* or voluntary N5 attendant* or voluntary N5 aide or voluntary N5 aides or voluntary N5 support* or voluntary N5 personnel or voluntary N5 helper* or voluntary N5 carer* or voluntary N5 caregiver* or voluntary N5 "care giver" or voluntary N5 "care givers" or voluntary N5 consultant* or voluntary N5 assistant* or voluntary N5 staff or voluntary N5 visit* or voluntary N5 midwife or voluntary N5 midwives )
S12 TI ( lay N5 worker* or lay N5 visitor* or lay N5 attendant* or lay N5 aide or lay N5 aides or lay N5 support* or lay N5 personnel or lay N5 helper* or lay N5 carer* or lay N5 caregiver* or lay N5 "care giver" or lay N5 "care givers" or lay N5 consultant* or lay N5 assistant* or lay N5 staff or lay N5 visit* or lay N5 midwife or lay N5 midwives ) or AB ( lay N5 worker* or lay N5 visitor* or lay N5 attendant* or lay N5 aide or lay N5 aides or lay N5 support* or lay N5 personnel or lay N5 helper* or lay N5 carer* or lay N5 caregiver* or lay N5 "care giver" or lay N5 "care givers" or lay N5 consultant* or lay N5 assistant* or lay N5 staff or lay N5 visit* or lay N5 midwife or lay N5 midwives )
S11 (MH "Peer Group")
S10 (MH "Doulas")
S9 (MH "Lay Midwifery")
S8 (MH "Lay Midwives")
S7 (MH "Health Personnel, Unlicensed")
S6 (MH "Nursing Assistants")
S5 (MH "Allied Health Personnel")
S4 (MH "Home Nursing")
S3 (MH "Home Health Aides")
S2 (MH "Community Health Workers")
S1 (MH "Volunteer Workers")
POPLINE
(17 individual Subject searches ‐ limited to the last 5 years)
1.
(lay w5 worker* / lay w5 visit* / lay w5 attendant* / lay w5 aide / lay w5 aides / lay w5 support* / lay w5 person* / lay w5 helper* / lay w5 carer* / lay w5 caregiver* / lay w5 giver* / lay w5 consultant* / lay w5 assistant* / lay w5 staff / lay w5 midwife / lay w5 midwives) & (random* / trial)
2.
(voluntary w5 worker* / voluntary w5 visit* / voluntary w5 attendant* / voluntary w5 aide / voluntary w5 aides / voluntary w5 support* / voluntary w5 person* / voluntary w5 helper* / voluntary w5 carer* / voluntary w5 caregiver* / voluntary w5 giver* / voluntary w5 consultant* / voluntary w5 assistant* / voluntary w5 staff / voluntary w5 midwife / voluntary w5 midwives) & (random* / trial)
3.
(volunteer* w5 worker* / volunteer* w5 visit* / volunteer* w5 attendant* / volunteer* w5 aide / volunteer* w5 aides / volunteer* w5 support* / volunteer* w5 person* / volunteer* w5 helper* / volunteer* w5 carer* / volunteer* w5 caregiver* / volunteer* w5 giver* / volunteer* w5 consultant* / volunteer* w5 assistant* / volunteer* w5 staff / volunteer* w5 midwife / volunteer* w5 midwives) & (random* / trial)
4.
(untrained w5 worker* / untrained w5 visit* / untrained w5 attendant* / untrained w5 aide / untrained w5 aides / untrained w5 support* / untrained w5 person* / untrained w5 helper* / untrained w5 carer* / untrained w5 caregiver* / untrained w5 giver* / untrained w5 consultant* / untrained w5 assistant* / untrained w5 staff / untrained w5 midwife / untrained w5 midwives) & (random* / trial)
5.
(unlicensed w5 worker* / unlicensed w5 visit* / unlicensed w5 attendant* / unlicensed w5 aide / unlicensed w5 aides / unlicensed w5 support* / unlicensed w5 person* / unlicensed w5 helper* / unlicensed w5 carer* / unlicensed w5 caregiver* / unlicensed w5 giver* / unlicensed w5 consultant* / unlicensed w5 assistant* / unlicensed w5 staff / unlicensed w5 midwife / unlicensed w5 midwives) & (random* / trial)
6.
(nonprofessional* w5 worker* / nonprofessional* w5 visit* / nonprofessional* w5 attendant* / nonprofessional* w5 aide / nonprofessional* w5 aides / nonprofessional* w5 support* / nonprofessional* w5 person* / nonprofessional* w5 helper* / nonprofessional* w5 carer* / nonprofessional* w5 caregiver* / nonprofessional* w5 giver* / nonprofessional* w5 consultant* / nonprofessional* w5 assistant* / nonprofessional* w5 staff / nonprofessional* w5 midwife / nonprofessional* w5 midwives) & (random* / trial)
7.
(non w1 professional*) & (worker* / visitor* / attendant* / aide / aides / support* / person* / helper* / carer* / caregiver* or care giver* / consultant* / assistant* / staff / visit* / midwife / midwives) & (random* / trial)
8.
(paraprofessional* / paramedical person* / paramedical staff / paramedical aide / paramedical aides / paramedical assistant* / support worker* / home health aide* / lay volunteer*) & (random* / trial)
9.
(trained w3 volunteer* / trained w3 lay / trained w3 worker* / trained w3 mother*) & (random* / trial)
10.
(community w3 worker* / village* w3 worker* / community w3 volunteer* / village w3 volunteer*) & (random* / trial)
11.
(community w3 aide / community w3 aides / community w3 support) & (random* / trial)
12.
(birth attendant* / childbirth attendant* / labor attendant* / labour attendant* / birth assistant* / childbirth assistant * / labor assistant * / labour assistant*) & (random* / trial)
13.
(doula* / douladural* / monitrice*) & (random* / trial)
14.
(peer volunteer* / peer counsel* / peer support / peer intervention*) & (random* / trial)
15.
(church w3 intervention* / church w3 counsel* / church w3 program*) & (random* / trial)
16.
(linkworker* / link worker* / barefoot doctor*) & (random* / trial)
17.
(home w3 care / home w3 aide / home w3 aides / home w3 nursing / home w3 support / home w3 intervention* / home w3 treatment* / home w3 visit*) & (random* / trial)
WHOLIS
(7 individual searches searched in words or phrase)
1. (lay or voluntary or volunteer? or untrained or unlicensed or nonprofessional? or (non adj professional?)) and (random$ or trial)
2. (paraprofessional? or paramedic or paramedics or (paramedical near3 worker?) or (paramedical near3 personnel)) and (random$ or trial)
3. ((allied near3 personnel) or (allied near3 worker?) or (support adj worker?)) and (random$ or trial)
4. (community or village?) and ((health$ near3 worker?) or volunteer? or aide or aides or support) and (random$ or trial)
5. (doula? or douladural? or monitrice? or peer or mother? or linkworker? or (link adj worker?) or (barefoot adj doctor?)) and (random$ or trial)
6. (outreach or home) and (random$ or trial)
7. ((trained near3 volunteer?) or (trained near3 worker?) or (trained near3 mother?))
Database Syntax Guide
| CENTRAL ‐ Cochrane Library Online | ||
| AND | AND operator | Includes both terms |
| OR | OR operator | Includes either both, the one or the other term |
| MeSH descriptor | Subject Heading | |
| :ti | Title word | |
| :ab | Abstract word | |
| * | Truncation | Adds non or more characters |
| NEAR/n | NEAR operator | Requires words are adjacent within n words regardless of word order |
| NEXT | NEXT operator | Requires words are adjacent to each other in the order typed in |
| Ovid databases | ||
| AND | AND operator | Includes both terms |
| OR | OR operator | Includes either both, the one or the other term |
| / | Subject Heading | |
| .ab. | Abstract word | |
| .tw. | Text Word | Word in title or abstract field |
| .fs. | Floating subheading | Subheading of any Subject Heading |
| .pt. | Publication type | |
| .sh. | Subject Heading | |
| .mp. | Will search in title, abstract and in Subject Heading field | |
| exp | Explode | Will include narrower terms to the Subject Heading being exploded |
| $ | Truncation/wild card | Adds non or more characters |
| $n | Truncation/wild card | Adds non to n characters |
| ? | Truncation/wild card | Adds non or one character |
| adj | Adjacency | Requires words are adjacent to each other in the order typed in |
| adjn | Adjacency | Requires words are adjacent within n words regardless of word order |
| ” ‐ ” | Double quotation mark | Exact phrase searching |
| POPLINE | ||
| Subject search | Will search in title, abstract and in keyword field | |
| & | AND operator | Includes both terms |
| / | OR operator | Includes either both, the one or the other term |
| Wn | WITHIN operator | Requires words are adjacent within n words regardless of word order |
| * | Truncation | Adds non or more characters |
| WHOLIS | ||
| AND | AND operator | Includes both terms |
| OR | OR operator | Includes either both, the one or the other term |
| $ | Truncation | Adds non or more characters |
| ? | Truncation | Adds non or one character |
| NEARn | NEAR operator | Requires words are adjacent within n words regardless of word order |
Data and analyses
Comparison 1. LHW interventions to promote immunisation uptake in children under five compared with usual care.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Immunisation schedule up to date ‐ unadjusted | 6 | 4546 | Risk Ratio (M‐H, Random, 95% CI) | 1.21 [1.07, 1.37] |
| 2 Immunisation schedule up to date ‐ adjusted for clustering | 6 | CC (Random, 95% CI) | 1.23 [1.09, 1.38] | |
| 3 Immunisation schedule up to date (excl. Gökcay and Krieger) | 4 | CC (Random, 95% CI) | 1.22 [1.10, 1.37] |
1.1. Analysis.

Comparison 1 LHW interventions to promote immunisation uptake in children under five compared with usual care, Outcome 1 Immunisation schedule up to date ‐ unadjusted.
Comparison 2. LHW interventions to promote breastfeeding compared with usual care.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Initiated Breastfeeding | 12 | 17159 | Risk Ratio (M‐H, Random, 95% CI) | 1.45 [1.14, 1.84] |
| 2 Any Breastfeeding | 12 | 8104 | Risk Ratio (M‐H, Random, 95% CI) | 1.28 [1.10, 1.48] |
| 3 Exclusive breastfeeding (6 weeks ‐ 6 months) | 10 | 4334 | Risk Ratio (M‐H, Random, 95% CI) | 3.17 [1.74, 5.75] |
| 4 Initiated Breastfeeding ‐ adjusted for clustering | 12 | Risk Ratio (Random, 95% CI) | 1.36 [1.14, 1.61] | |
| 5 Any Breastfeeding ‐ adjusted for clustering | 12 | Risk Ratio (Random, 95% CI) | 1.24 [1.10, 1.39] | |
| 6 Exclusive Breastfeeding ‐ adjusted for clustering | 10 | Risk Ratio (Random, 95% CI) | 2.78 [1.74, 4.44] |
2.1. Analysis.

Comparison 2 LHW interventions to promote breastfeeding compared with usual care, Outcome 1 Initiated Breastfeeding.
2.2. Analysis.

Comparison 2 LHW interventions to promote breastfeeding compared with usual care, Outcome 2 Any Breastfeeding.
2.3. Analysis.

Comparison 2 LHW interventions to promote breastfeeding compared with usual care, Outcome 3 Exclusive breastfeeding (6 weeks ‐ 6 months).
Comparison 3. LHW interventions to reduce mortality/morbidity in children under five compared with usual care.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Mortality among children < 5 years old ‐ unadjusted | 3 | 56378 | Risk Ratio (M‐H, Random, 95% CI) | 0.76 [0.61, 0.95] |
| 2 Mortality among children < 5 years old | 3 | RR (Random, 95% CI) | 0.75 [0.55, 1.03] | |
| 3 Mortality among children < 5 years old (Excl. Pence) | 2 | RR (Random, 95% CI) | 0.75 [0.54, 1.03] | |
| 4 Neonatal mortality ‐ unadjusted | 4 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 4.1 Year 1 | 3 | 24229 | Risk Ratio (M‐H, Random, 95% CI) | 0.82 [0.54, 1.26] |
| 4.2 Year 2 | 2 | 20954 | Risk Ratio (M‐H, Random, 95% CI) | 0.83 [0.65, 1.05] |
| 4.3 All longest follow‐up | 4 | 29217 | Risk Ratio (M‐H, Random, 95% CI) | 0.76 [0.57, 1.01] |
| 5 Neonatal mortality | 4 | Risk Ratio (Random, 95% CI) | Subtotals only | |
| 5.1 Year 1 | 3 | Risk Ratio (Random, 95% CI) | 0.82 [0.53, 1.27] | |
| 5.2 Year 2 | 2 | Risk Ratio (Random, 95% CI) | 0.83 [0.65, 1.05] | |
| 5.3 All longest follow‐up | 4 | Risk Ratio (Random, 95% CI) | 0.76 [0.57, 1.02] | |
| 6 Morbidity; reported illness in children ‐ unadjusted | 7 | 17408 | Risk Ratio (M‐H, Random, 95% CI) | 0.86 [0.74, 0.99] |
| 7 Morbidity; reported illness in children | 7 | RR (Random, 95% CI) | 0.86 [0.75, 0.99] | |
| 8 Morbidity; care‐seeking practice ‐ unadjusted | 3 | 11132 | Risk Ratio (M‐H, Random, 95% CI) | 1.38 [0.88, 2.15] |
| 9 Morbidity; care‐seeking practice | 3 | RR (Random, 95% CI) | 1.33 [0.86, 2.05] |
3.1. Analysis.

Comparison 3 LHW interventions to reduce mortality/morbidity in children under five compared with usual care, Outcome 1 Mortality among children < 5 years old ‐ unadjusted.
3.4. Analysis.

Comparison 3 LHW interventions to reduce mortality/morbidity in children under five compared with usual care, Outcome 4 Neonatal mortality ‐ unadjusted.
3.6. Analysis.

Comparison 3 LHW interventions to reduce mortality/morbidity in children under five compared with usual care, Outcome 6 Morbidity; reported illness in children ‐ unadjusted.
3.8. Analysis.

Comparison 3 LHW interventions to reduce mortality/morbidity in children under five compared with usual care, Outcome 8 Morbidity; care‐seeking practice ‐ unadjusted.
Comparison 4. LHW interventions to improve TB treatment outcomes compared with other forms of adherence support.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Cure for smear positive TB patients (new and retreatment) ‐ adjusted for clustering | 2 | Risk Ratio (Random, 95% CI) | 1.16 [0.93, 1.46] | |
| 2 Cure for smear positive TB patients (new and retreatment) | 4 | 1203 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.18 [1.09, 1.28] |
| 3 Cure for smear positive TB patients (new and retreatment) ‐ adjusted for clustering | 4 | Risk Ratio (Random, 95% CI) | 1.22 [1.13, 1.31] | |
| 4 New smear positives cured ‐ adjusted for clustering | 2 | Risk Ratio (Random, 95% CI) | Totals not selected | |
| 5 Combined cure and treatment completion for all pulmonary TB patients | 3 | 756 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.20 [1.12, 1.29] |
| 6 Combined cure and treatment completion for all pulmonary TB patients ‐ adjusted for clustering | 3 | Risk Ratio (Random, 95% CI) | Totals not selected | |
| 7 TB Preventive therapy with Isoniazid ‐ completed therapy | 2 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 7.1 LHW (peer) supported self‐supervision or DOT compared with self supervision | 2 | 595 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.92, 1.09] |
4.2. Analysis.

Comparison 4 LHW interventions to improve TB treatment outcomes compared with other forms of adherence support, Outcome 2 Cure for smear positive TB patients (new and retreatment).
4.5. Analysis.

Comparison 4 LHW interventions to improve TB treatment outcomes compared with other forms of adherence support, Outcome 5 Combined cure and treatment completion for all pulmonary TB patients.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Agrasada 2005.
| Methods | RCT. | |
| Participants | LHW: Village volunteers, selected after seminar attendance to undergo counselling training. 22‐50 years old. Similar formal education as mothers, willing to do home visits. All women who underwent breastfeeding (bf) training had previous positive personal bf experience. TRAINING: 40 hour interactive didactics, role playing and practical training by certified lactation counsellor. A maternal and child healthcare specialist used the same training approach for the childcare group. PARTICIPANTS: First time mothers, 18 years or older, intending to breastfeed, vaginally delivered a low birth baby with no health problems. The infants had to be born between 37 and 42 weeks gestation. TOTAL = 204; INTERVENTION 1 (breastfeeding counselling) = 68; INTERVENTION 2 (childcare counselling) = 67; CONTROL = 69. |
|
| Interventions | OBJECTIVE: To provide home‐based, postnatal peer counselling to improve breastfeeding exclusivity and duration. INTERVENTION 1: 8 visits: 3‐5 days, 7‐10 days, 21 days, 1.5 months, then monthly till 5.5 months. Mothers were informed of the benefits of exclusive breastfeeding up to 6 months and assisted in preventing and managing breastfeeding problems. 8 visits: 3‐5 days, 7‐10 days, 21 days, 1.5 months, then monthly till 5.5 months. A semi‐structured home visit guide was used. The counsellors were not paid a salary, but received local transport costs. INTERVENTION 2: Counsellors assisted mothers in infant care and attempted to increase mother‐infant interaction through activities such as infant massage and smile therapy. 8 visits: 3‐5 days, 7‐10 days, 21 days, 1.5 months, then monthly till 5.5 months. A semi‐structured home visit guide was used. The counsellors were not paid a salary, but received local transport costs. CONTROL: No counselling. MODE OF DELIVERY: Peer counsellor visits to mothers at home. RECIPIENT INVOLVEMENT IN SELECTION/TRAINING/MANAGEMENT: not described. GEOGRAPHICAL SETTING: urban formal, Phillipines HEALTHCARE SETTING: home. |
|
| Outcomes | HEALTHCARE BEHAVIOURS: Proportion of mothers still breast‐feeding at 6 months; Proportion of mothers still breastfeeding at 4 weeks; Proportion of mothers still breastfeeding at 8 weeks; Proportion of mothers still breastfeeding at 12 weeks; Exclusive breastfeeding in the last 7 days at 6 months; Exclusive breastfeeding from birth to 6 months. HEALTH STATUS AND WELLBEING: mean weight for age; rates of diarrhoea. LENGTH OF FOLLOW UP: 6 months. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | 'The allocation sequence, based on a table of random numbers...' (p1110). |
| Allocation concealment? | Low risk | '...the research assistant drew the topmost, opaque, sequentially numbered envelope from the pack' (p1110). |
| Blinding? All outcomes | Unclear risk | For breastfeeding outcomes, unclear whether outcome assessors blinded. '...a trained interviewer asked to carefully recall when and how the infact had been fed' (p1111). Participants and personnel not blinded. |
| Incomplete outcome data addressed? All outcomes | Unclear risk | Missing data balanced in numbers across intervention groups. Unclear whether similar reasons for missing data across groups. |
| Free of selective reporting? | Unclear risk | Insufficient information to make an assessment. |
| Free of other bias? | Low risk | |
Anderson 2005.
| Methods | RCT. | |
| Participants | LHW: Prior to the start of the study, 2 mothers from the greater Hartford area, who had successfully breastfed a child for no less than 6 months and who had the motivation to help other mothers breastfeed their infants, were hired. TRAINING: An international board certified lactation consultant trained these women over 2 weeks using the 40‐hour World Health Organization/United Nations Children's Fund Breastfeeding Counseling Training Course (WHO/UNICEF 1993) and the Hispanic Health Council Breastfeeding Training Manual (Damio 1995), while the exclusive breastfeeding component was handled by the study field coordinator. The training included theory (anatomy and physiology of the breast and management of breastfeeding), roleplays, and hands‐on practice with mother‐infant dyads, and communication skills, as well as observing the lactation consultant during routine ward rounds and home visits. The peer counselors were observed for 2 months by the lactation consultant, who assisted women with breastfeeding problems. PARTICIPANTS: Low income predominantly Latina community. 18 yrs or older, gestation age of 32 weeks or younger, healthy and abscence of any medical condition (diabetes, hypertension, HIV/AIDS or using illegal drugs) that were likely to impair breastfeeding. To qualify for participation, the woman should have been: (1) considering breastfeeding her newborn; (2) planning to deliver at Hartford Hospital; (3) willing to stay in the study area for at least 3 months after delivery; (4) living in a household earning 185% of the federal poverty level; (5) available to be contacted by telephone; and (6) willing to participate in the study. TOTAL = 182; INTERVENTION = 90; CONTROL = 92. |
|
| Interventions | OBJECTIVE: To provide community‐based peer counselling to improve exclusive breastfeeding among low‐income mothers. INTERVENTION: Women assigned to the peer counseling group were offered 3 prenatal home visits, 9 postpartum home visits, and daily in‐hospital visits during postpartum hospitalisation, from the assigned peer counselor (in addition to the routine breastfeeding support received by the control group). During the prenatal visits, the woman was provided with an opportunity to watch a breastfeeding video. The family was also encouraged to participate in the education, especially the person expected to support the woman after delivery. The mothers could contact the counsellors by phone if they had any urgent breastfeeding problems between visits. The assigned peer counselor also visited the mother‐infant pair at least once a day starting within 24 hours after delivery and continued for as long as the dyad remained hospitalised. CONTROL: Women assigned to the control group only received conventional breastfeeding education prenatally from the Women’s Ambulatory Health Services clinic staff. On delivery, they received hands‐on breastfeeding assistance and education from the maternity ward nursing staff. If any of these mothers experienced breastfeeding problems requiring assistance beyond that routinely provided by staff nurses, the hospital’s lactation consultant on duty was called to assist the patient. MODE OF DELIVERY: Counsellors contacted mother within a week of assignment to make an appointment for the first pre‐natal home visit. In addition to visits, telephone support was also available. RECIPIENT INVOLVEMENT IN SELECTION/TRAINING/MANAGEMENT: not described. GEOGRAPHICAL SETTING: urban formal, USA HEALTHCARE SETTING: home. |
|
| Outcomes | HEALTHCARE BEHAVIOURS: Mothers with exclusive breastfeeding at discharge; Incidence of exclusive breastfeeding 24 hours recall at 1 month; Incidence of exclusive breastfeeding 24 hours recall at 2 months; Incidence of exclusive breastfeeding 24 hours recall at 3 months; Incidence of exclusive breastfeeding, previous 1 week recall at 1 month; Incidence of exclusive breastfeeding, previous 1 week recall at 2 months; Incidence of exclusive breastfeeding, previous 1 week recall at 3 months; Incidence of exclusive breastfeeding, since birth recall at 1 month; Incidence of exclusive breastfeeding, since birth recall at 2 months; Incidence of exclusive breastfeeding, since birth recall at 3 months. HEALTH STATUS AND WELLBEING: Diarrhoea episodes in infant; return of menses, as assessed at 3 months post partum LENGTH OF FOLLOW UP: 3 months. |
|
| Notes | Incidence of exclusive breastfeeding 24 hours recall at 1 month. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | 'SPSS software for Windows was used to randomly assign subjects to study groups' (p837). |
| Allocation concealment? | Unclear risk | 'Participants were randomly assigned to either the intervention or control group by the study field co‐ordinator' (p837). No further information provided. |
| Blinding? All outcomes | High risk | 'it was not a double‐blind study and the interviewer (data collector) knew the study hypotheses' (p840). |
| Incomplete outcome data addressed? All outcomes | Low risk | Missing data balanced in numbers across intervention groups. 'the characteristics of dropouts was similar to those completing the follow‐up' (p840). |
| Free of selective reporting? | Unclear risk | Insufficient information to make an assessment. |
| Free of other bias? | High risk | |
Baqui 2008.
| Methods | RCT, Cluster randomised. | |
| Participants | LHW: Used female community health workers, community mobilisers and resource people (both male and female). Community health workers were recruited by an NGO partner, one for every 4 villages (about 4000 people), no information on the criteria for recruitment of all other LHWs. Community resource women were usually traditional birth attendants in their communities. TRAINING: Mention training only for community health worker ‐ 6 weeks training in tertiary hospital and households. Included skills development for behaviour change communication, provision of essential newborn care, clinical assessment and management of neonates. PARTICIPANTS: Mean age of mothers was about 27 years (SD6, Range 15‐49), mean years of school were 3 (SD3.5). Mean birth order was 3 (SD2.5), range 2‐13. INTERVENTIONS: Intervention 1 (Essential Newborn care) = 1632 pregnancies, Intervention 2 = 1179 pregnancies; Control= |
|
| Interventions | OBJECTIVE: Implemented a community‐based intervention package to reduce neonatal mortality. CONTROL: Usual health services provided by government, non‐governmental organisations and private providers. Government workers in all arms of study received refresher training. Study staff ensured antibiotic availability at all subdistrict hospitals. MODE OF DELIVERY: Community health worker ‐ identified pregnancies through routine surveillance, promoted birth and newborncare preparedness (2 ANC, 3 Postnatal home visits, provided supplements (iron and folate tablets), assessed all live neonates and classified any sickness to very severe disease, possible very severe disease with one sign or more than one sign. Provided referral for very severe disease or possible very severe disease.Gave first line treatment before referral (injected procaine penicillin and gentamicin), if family unable to go to hospital continued treatment for 10 days. Community mobilisers ‐ held group meetings for dissemination of birth and newborn care messages for both intervnetion arms.In the community care arm, visits were once every 4months (male mobilisers visited once every 10months), in home care arm once every 8 months. Community resource people identified pregnant women and encouraged them to attend community meetings, receive routine ANC and seek care for serious illness in mother and child. RECIPIENT INVOLVEMENT IN SELECTION/TRAINING/MANAGEMENT: Yes, in selection of LHWs. GEOGRAPHICAL SETTING: Bangladesh, Rural HEALTHCARE SETTING: Home. |
|
| Outcomes | HEALTHCARE UTILISATION: Newborn care birth preparedness. HEALTH STATUS AND WELLBEING: Neonatal mortality ratesall births and singleton, perinatal mortality rates. HEALTH BEHAVIOUR: Routine care during pregnancy, hygienic delivery and immediate newborn care, Thermocare including skin to skin care, umbilical cord and skin care, breastfeeding. CONSULTATION: Danger sign recognition and care seeking. UTILISATION: Care‐seeking providers used. LENGTH OF FOLLOW UP: 16 months. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Used computer generated pseudo‐random number sequence by an investigator who had no role in the study. |
| Allocation concealment? | Unclear risk | Not mentioned. |
| Blinding? All outcomes | Unclear risk | Not clear if the survey team that implemented the subsequent surveys was different from those delivering the intervention. |
| Incomplete outcome data addressed? All outcomes | Unclear risk | All clusters followed up to the end, length of study 30 months. |
| Free of other bias? | High risk | May be recall bias on some newborn care practices eg. use of clean instrument for cord cutting. |
Bari 2006.
| Methods | RCT. | |
| Participants | LHW: Were 36 community health workers (CHWs), each responsible for about 4000 people, all female, 20‐40 years old. Average age of CHWs was 27years, 79% were married, average schooling years was 11. TRAINING: One month initial training to equip them with a package of maternal and newborn care included 6 days of field practice. Trained through didactic sessions, videos and practice on sick and healthy newborn babies in Kumudini hosp. Materials used included visit record forms to record all CHW visits, standard algorithm adapted from IMCI Bangladesh. Issued referral slips to mthers of sick newborns, had birth and neonatal care preparedness cards with Identification numbers which they issued to mothers. Had referral tracking forms, free inpatient care at Kumudini hospital, a system of emergency transport and training of TBAs to promote referral of newborns with danger signs. Developed a manual for initial and refreasher training in 6 areas ‐ pregnancy registration and surveillance, management of neoborn at birth including resuscitation, continuing essential newborn care, routine neonatal assessment and illness classification, management of illness according to the Mirzapur CHW algorithm. PARTICIPANTS: 4508 women estimated to have their due date in the 9 months of study period. 72.5% of recently delivered attended at least one antenatal care visit, 87.6% had at least one Antenatal birth and neonatal care preparedness visit by CHW. INTERVENTIONS: Baseline survey: 2053 newborns, Survey at year 2: 523 newborns; Survey at year 2 and 9 months 520 newborns. CONTROL= Baseline survey: 2290 newborns, Survey at year 2: 550 newborns; Survey at year 2 and 9 months 548 newborns. |
|
| Interventions | OBJECTIVE: To promote care seeking for sick newborns through health education of families, identification and referral of sick newborns in the community and strengthening of neonatal care in the referral hospital. CONTROL: Not clear. MODE OF DELIVERY: Community health workers did bimonthly pregnancy surveillance and registration of married women of reproductive age, made home visits in third and eighth month of pregnancy for counselling on birth and neonatal preparedness. After delivery, home visits to promote evidence based domiciliary newborn care and identify and refer sick newborns and mothers on day 1(at birth), 3, 6, 9 days. For families refusing referral and babies with at least one danger sign of severe disease or 2 signs of possible severe disease, home treatment with antibiotics was given. RECIPIENT INVOLVEMENT IN SELECTION/TRAINING/MANAGEMENT: None. GEOGRAPHICAL SETTING: Bangladesh; Rural. HEALTHCARE SETTING: Home. |
|
| Outcomes | HEALTHCARE UTILISATION: Reported care seeking outside home, care seeking from qualified providers, care seeking from Kumudini hospital, Care seeking from unqualified providers. HEALTH STATUS AND WELLBEING: Number of newborns reported sick. LENGTH OF FOLLOW UP: 2 years, 9 months. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | No description of method used to randomly allocate clusters to interview or comparison. |
| Allocation concealment? | Unclear risk | Not mentioned. |
| Blinding? All outcomes | Unclear risk | Not clear who assessors were and if they were blinded or not. |
| Incomplete outcome data addressed? All outcomes | Unclear risk | Follow‐up rate not clear. |
Barnes 1999.
| Methods | RCT. | |
| Participants | LHW: Community volunteers, recruited from a volunteer organisation. No information provided on number of volunteers. Most of them were bilingual. Education level not clear. TRAINING: not described. Supervision was provided by the coordinator of the volunteer organisation. PATIENTS: children <2 years of age who enrolled in one of two ambulatory clinics and were not immunized. Predominantly Hispanic low income children, part of a highly mobile immigrant community from the Dominican Republic. TOTAL=434; INTERVENTION=218; CONTROL=216. | |
| Interventions | OBJECTIVE: to increase rate of immunization in children <2 years of age. INTERVENTION: immunization outreach, tracking and follow up. CONTROL: no intervention. MODE OF DELIVERY: LHWs contacted participants offering basic immunization education and referral, reminders of upcoming vaccinations and contact to ensure that vaccination was received. They also provided support/assistance to obtain immunization services eg clinic contact, escort for appointments. Control families were informed of child's immunization record and told to reschedule missed appointments. RECIPIENT INVOLVEMENT IN DESIGN/DEVELOPMENT/DELIVERY: not described. ORGANISATIONAL BASE OF THE INTERVENTION: not described. GEOGRAPHICAL SETTING: urban formal USA HEALTHCARE SETTING: Home. | |
| Outcomes | HEALTHCARE BEHAVIOURS: immunization status (up to date/due/late). FOLLOW UP TIME: minimum of 5 months follow up. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Used computer generated random numbers. |
| Allocation concealment? | Unclear risk | Not mentioned. |
| Blinding? All outcomes | Unclear risk | Not mentioned. It is not clear if the data collectors were different from the volunteers that administered the intervention. |
| Incomplete outcome data addressed? All outcomes | Low risk | Outcomes stated in the objectives are reflected in the data presented. |
| Free of selective reporting? | High risk | High attrition rates. Of the 434 children eligible for the intervention and randomisation, only 37.5% consented to participate. These are the data presented. |
| Free of other bias? | Low risk | |
Barnett 1985.
| Methods | RCT. | |
| Participants | LHW: Support mother was an experienced mother, who had volunteered to assist with the study and who met the requirements for a support figure. They would offer common sense advice, support, and practical help, but avoid proselytising any particular narrow model of mothering. TRAINING: Not specified. PARTICIPANTS: Highly anxious primiparous mothers, attending obstetric units on 3rd or 4th day postpartum. Mean age was 28 yrs. TOTAL= 3015; INTERVENTIONS: Tracking/Outreach‐prompting 732, Tracking/Outreach =715, Prompting only=801. CONTROL=767. |
|
| Interventions | OBJECTIVE: To assess the longitudinal adaptation of primiparous mothers that differed in levels of anxiety, to reduce anxiety in two subgroups of the highly anxious subjects. CONTROL: No intervention. MODE OF DELIVERY: Support mothers contacted participants by phone to offer advice and support. RECIPIENT INVOLVEMENT IN SELECTION/TRAINING/MANAGEMENT: no. GEOGRAPHICAL SETTING: Australia, Urban Formal. HEALTHCARE SETTING: Home. |
|
| Outcomes | HEALTH STATUS AND WELLBEING: Changes in anxiety state levels, Anxiety state over time. LENGTH OF FOLLOW UP: 1 year. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Participants were stratified by scores on Spielberger trait and state anxiety score before random allocation. |
| Allocation concealment? | Low risk | Used sealed envelopes. |
| Blinding? All outcomes | Low risk | Interviewer unaware of group allocation until interview was completed and group allocation discovered after interview so as to deliver intervention to high anxiety groups. |
| Incomplete outcome data addressed? All outcomes | High risk | Out of those originally screened and randomised, only 30% finally participated. |
| Free of selective reporting? | High risk | Results not presented by randomised group. |
Barth 1991.
| Methods | RCT. | |
| Participants | LHW: all parenting consultants were either mothers or had significant experience of bringing up infants and were recruited to represent ethnic and geographical communities in the service area. TRAINING: volunteers were trained for over 100 hours about the perinatal period, community resources, child abuse, and child abuse reporting and team building. They were also taught the basics of a task centered approach which focuses on the identification of goals for self improvement and child care, and enhances the client's ability to identify and complete tasks that forward goal attainment. Training organised by Child Parent Enrichment Project (CPEP), a community based, private, non‐profit agency. PATIENTS: mainly white women with a high school education and a mean age of 22.4 years. Most had one child already and 72% had a family income <$10,000 per year. The mean duration of pregnancy on recruitment was 5 months. TOTAL=65; INTERVENTION=29; CONTROL=36. | |
| Interventions | OBJECTIVE: to prevent abuse in children using a perinatal prevention program involving pre‐natal education and support; early/extended post partum contact; parent education; home visitation by professionals, paraprofessionals or volunteers. INTERVENTION: parenting consultants. CONTROL: no intervention. MODE OF DELIVERY: Services were provided for 6 months and home visits occurred approximately twice a month. Consultants saw approximately 10 families and worked for 20 hours per week. LHWs assisted mothers to identify goals for improved self and child care; enhanced the mothers ability to identify and complete tasks that forward goal attainment; tasks were recorded on sheets for clients and LHWs and accountability of task achievement; tasks included preparing a clean room for the infant to come home to, visiting the labor room prior delivery, etc. RECIPIENT INVOLVEMENT IN DESIGN/DEVELOPMENT/DELIVERY: not described. ORGANISATIONAL BASE OF THE INTERVENTION: CPEP. GEOGRAPHICAL SETTING: urban USA HEALTHCARE SETTING: home. | |
| Outcomes | HEALTH STATUS AND WELLBEING: psychological measures of parent and infant wellbeing. FOLLOW‐UP TIME: 6 months after birth of infant. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Not mentioned. |
| Allocation concealment? | Unclear risk | Not mentioned. |
| Blinding? All outcomes | High risk | Interviewers knew clients' assignment before interviewing them. |
| Incomplete outcome data addressed? All outcomes | High risk | 61% completed study. |
Black 1995.
| Methods | RCT. | |
| Participants | LHW: 3 lay home visitors were recruited. Each had experience with children, interpersonal skills and community knowledge. TRAINING: visitors received an 8 session training program featuring lectures, discussions on children's health/nutrition, infant/toddler development, activities to promote child's development, parent‐child interaction, behavior management, relationship building, family relationships, child/family advocacy, problem solving strategies, community resources and services. Training organised by university growth and nutrition clinic and community based agency. PATIENTS: children <25 months of age. Weight for age below the 5th percentile based on National Centre for Health statistics growth charts; gestational age of at least 36 weeks; birth weight appropriate for gestational age; no significant history of perinatal complications, no congenital disorders. Patients were recrutied from clinics serving low income families. TOTAL=130; INTERVENTION=64; CONTROL=66. | |
| Interventions | OBJECTIVE: to improve growth and development among children with non‐organic failure to thrive (NOFTT). INTERVENTION: home visits and clininc services.
CONTROL: clinic services.
MODE OF DELIVERY: The home visiting program involved a mean number of visits = 19.2 (SD = 11.5) lasting for approximately 1 hour at a time. Home visits using an individualised family service plan to assist the formation of a therapeutic alliance/support to the mother's familial, personal and environmental needs. The Hawaii Early Learning Program was used as curriculum and home visitors demonstrated developmentally appropriate activities to facilitate parent‐child interaction and supported recommendations from clinic nutritionist. RECIPIENT INVOLVEMENT IN DESIGN/DEVLOPMENT/DELIVERY: not described. ORGANISATIONAL BASE OF THE INTERVENTION: not described. GEOGRAPHICAL SETTING: urban USA HEALTHCARE SETTING: home. |
|
| Outcomes | HEALTH STATUS AND WELLBEING: growth, cognitive development, motor development, language development, parent‐child interaction, home environment. FOLLOW‐UP TIME: 12 months after intervention. | |
| Notes | Home visitors were supervised by a community health nurse and accompanied on some visits by an off‐duty police officer. Both intervention and control groups received nutrition information/support from the clinic. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Used random numbers table and stratfieid randomisation procedure with blocking variables by age, race and gender. |
| Allocation concealment? | Low risk | Allocation was done by community group who were different from the assessors (hospital team). |
| Blinding? All outcomes | Low risk | Assessors/data collectors were blinded. |
| Incomplete outcome data addressed? All outcomes | Low risk | Report on all outcomes stated in objectives, follow‐up rate 89%. |
| Free of selective reporting? | Low risk | |
| Free of other bias? | Low risk | |
Bugental 2002.
| Methods | RCT. | |
| Participants | LHW: Home visitors that served as facilitators, assisting parents in making a causal appraisal of the possible reasons for an identified care giving problem and in designing a strategic plan for the future. Conducted 20 home visits in one year. TRAINING: Were trained in home methods through the National Parents as Teachers program. Trained by Parents as Teachers Center in National City California. Two trainers: one Caucasian and one Latino. PARTICIPANTS: Families at moderate risk of child abuse, expecting the birth of a child or having recently given birth to a child. Some families (48%) did not include a husband or partner, 50% of mothers had been physically abused themselves. Average education of mothers was 7.8yrs (SD3.1) and average age was 25.5yrs (SD 6.1). TOTAL= 96 families; INTERVENTIONS: Unenhanced home visiting (modeled after the Healthy Start program)= 31‐34 families; Enhanced home visiting = 32‐35 families. CONTROL=22‐27 families. |
|
| Interventions | OBJECTIVE: To assess the incremental utility of cognitive retraining as a component within a program designed to prevent child maltreatment. CONTROL: Received no direct services but were provided information regarding existing services available in the community. MODE OF DELIVERY: Parents in the unenhanced home visitation condition received home visitation consistent with the Home visitation program (Duggan 2004) supplemented with information regarding existing community services. Families in the enhanced condition received information on exisiting community services, combined with methods used in the Healthy Start program and a brief attributionally based problem‐solving discussion at the start of each visit (causal appraisal followed by problem‐focused appraisal). Home visitors served as facilitators, assisting parents in making a causal appraisal of the possible reasons for an identified caregiving problem and in designing a strategic plan for the future. RECIPIENT INVOLVEMENT IN SELECTION/TRAINING/MANAGEMENT: none described. GEOGRAPHICAL SETTING: USA HEALTHCARE SETTING: Home. |
|
| Outcomes | HEALTH STATUS AND WELLBEING: Harsh parenting Mean score, Prevalence of physical abuse, Child health Score, Changes in maternal depression, anxiety, Adult control factor, Child control factor. LENGTH OF FOLLOW UP: 1 year. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Method used not described. |
| Allocation concealment? | Unclear risk | Not mentioned. |
| Blinding? All outcomes | High risk | Home visitors who delivered the intervention also recorded the outcomes. |
| Incomplete outcome data addressed? All outcomes | Low risk | Follow‐up rate 76%. |
Bullock 1995.
| Methods | RCT. | |
| Participants | LHW: 19 volunteers were recruited although the procedure is not described. TRAINING: initial training included information about the research program, research methods, communication techniques and general information about normal occurrences in antenatal/prenatal periods. It was followed by periodic meetings to give information/support to the volunteers. PATIENTS: antenatal women who were either single/in relationship where partner was unemployed (53% single; 18% married; 21% de facto married: 8% separated). Mean age = 24 years. TOTAL=131; INTERVENTION=65; CONTROL=66. | |
| Interventions | OBJECTIVE: to provide support for pregnant women. INTERVENTION: telephone support. CONTROL: no intervention. MODE OF DELIVERY: weekly telephone calls unto 12 weeks after birth of baby. 8 check‐off questions to be asked weekly. Referred women to health care provider if there was medical problem and encouraged women to seek assistance from community agencies. RECIPIENT INVOLVEMENT IN DESIGN/DEVELOPMENT/DELIVERY: not described. ORGANISATIONAL BASE OF THE INTERVENTION: not described. GEOGRAPHICAL SETTING: urban New Zealand HEALTHCARE SETTING: home. | |
| Outcomes | HEALTHCARE BEHAVIOURS: smoking, drinking, marijuana use, nutrition, utilisation of community resources. HEALTH STATUS AND WELLBEING: stress, social support from partner, social support from others, self esteem, anxiety. LENGTH OF FOLLOW UP: 34 weeks after gestation. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Used computer generated numbers in balanced blocks. |
| Allocation concealment? | Unclear risk | Not mentioned. |
| Blinding? All outcomes | Unclear risk | Not clear. |
| Incomplete outcome data addressed? All outcomes | Low risk | |
Caulfield 1998.
| Methods | Cluster RCT. | |
| Participants | LHW: peer counsellors were former women, infants and children (WIC) clinic clients who had successfully breastfed at least one child. TRAINING: all counsellors completed a 5‐week training programme adapted from a WIC Manual and administered by the study investigators and staff. PATIENTS: pregnant women who were before 24 weeks gestation and were WIC eligible, carrying single pregnancy, planning to keep the baby, remain in clinic's catchment area. Women were excluded if pregnancy was contra‐indicated. 64‐86% of women had <high school education; 82‐89% were single; 23‐37% <18 years of age; 40‐53% 18‐25 years; 20‐27% >25 years of age. TOTAL=548. | |
| Interventions | OBJECTIVE: to promote and support breastfeeding. INTERVENTION 1: peer counsellors. INTERVENTION 2: video education. INTERVENTION 3: peer counsellors and video education. CONTROL: no intervention. MODE OF DELIVERY: peer counsellors followed up those women interested in breastfeeding three or more times during pregnancy and then weekly to 16 weeks postpartum as long as they continued to breastfeed. One clinic in the study received a video based intervention as well. A random quality assurance visit was made to one clinic each week during the study. A checklist was completed to assess whether the intervention was being delivered as planned and any problems were rectified. RECIPIENT INVOLVEMENT IN DESIGN/DEVELOPMENT/DELIVERY: not described. ORGANISATIONAL BASE OF THE INTERVENTION: WIC clinics. GEOGRAPHICAL SETTING: urban USA HEALTHCARE SETTING: primary care facility (WIC clinics). | |
| Outcomes | HEALTHCARE BEHAVIOURS: initiated breastfeeding, still breastfeeding at 7‐10 days. LENGTH OF FOLLOW UP: 7‐10 days post partum. | |
| Notes | Three intervention arms: peer counsellors, video, both. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Insufficient information. |
| Allocation concealment? | Low risk | Cluster RCT ‐ 'The four clinics were randomly assigned to control and treatment groups.' (p16). |
| Blinding? All outcomes | High risk | No blinding or incomplete blinding. |
| Incomplete outcome data addressed? All outcomes | High risk | Very large loss to follow up, although few differences between women who could and could not be followed were noted (including no differences in intention to breastfeed). (p17). |
| Free of selective reporting? | Unclear risk | Insufficient information to make an assessment. |
| Free of other bias? | Low risk | |
Chaisson 2001.
| Methods | RCT. | |
| Participants | LHW: Peer counsellors were former injection drug users who had completed isoniazid preventive therapy.
TRAINING: Trained in counselling patients with tuberculosis and HIV regarding health promotion, prevention, treatment adherence and life‐coping strategies.
PARTICIPANTS: Were at least 18 years old (mean age 41yrs), used injection drugs and included people living with HIV. Three fourths were male patients, 20% were HIV positive. 40 ‐50% had less than high school education; most were unemployed (about 80%); and most were black (about 90%). TOTAL = 18 TB treatment units (522 patients); INTERVENTION = 9 units (221 patients); CONTROL = 9 units (301 patients). |
|
| Interventions | OBJECTIVE: To improve adherence to tuberculosis preventive therapy among injecting drug users. INTERVENTION 1: Patients in the self‐administered therapy group with peer support and counselling were given a months supply of tablets and instructions on dosage. They were asked to return to the TB clinic monthly for a refill and to see the nurse. In addition, peer counsellors met with patients twice weekly during the first month of TB treatment and thereafter once a month. Counsellors also appeared to run group meetings monthly which patients were asked to attend. Counsellors were supervised by a professional health educator. INTERVENTION 2: Patients in the directly observed preventive therapy group were assigned to an outreach nurse who met with them twice a week, administered medication and observed patients swallow this. This was done either at the clinic or a mutually convenient community location. CONTROL: The routine care group received monthly supply of isoniazid from a tuberculosis clinic nurse and were instructed to take 1 pill a day. Patient received initial counseling from a nurse, were encouraged to ask questions, and had monthly scheduled meetings at which they were asked about adherence and encouraged to continue medication. Had monthly visits to the TB clinic for clinical assessment and refills. MODE OF DELIVERY: treatment support delivered by peer counsellor in the community. RECIPIENT INVOLVEMENT IN SELECTION/TRAINING/MANAGEMENT: none. GEOGRAPHICAL SETTING: urban formal, USA HEALTHCARE SETTING: Home, community centres, primary health care TB clinic. |
|
| Outcomes | HEALTHCARE BEHAVIOURS: therapy completion as reported by the patient; proportion of doses taken as monitored by a nurse or patient self‐report; the presence of isoniazid metabolites in the urine during monthly screening; medication bottle opening as measured by electronic monitoring caps. | |
| Notes | Patients within each of the 3 trial arms were also randomly assigned to receive an immediate or deferred monthly USD10 stipend for maintaining adherence. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | 'Randomisation was performed by computer algorithm' (p611). |
| Allocation concealment? | Unclear risk | 'Patients were randomly assigned to 6 months of treatment according to one of three primary strategies and one of two financial incentives.' (p611). Comment: insufficient information provided on method of concealment. |
| Blinding? All outcomes | High risk | 'Blinding of the study was not possible' (p611). Comment: no blinding and some of the outcome measures are likely to be influenced by a lack of blinding. |
| Incomplete outcome data addressed? All outcomes | Unclear risk | Insufficient reporting to permit a judgement. Reasons for loss to follow up were not discussed. |
| Free of selective reporting? | Unclear risk | Insufficient information to make an assessment. |
| Free of other bias? | Low risk | |
Chapman 2004.
| Methods | RCT. | |
| Participants | LHW: Peer counsellors in this programme were community women who have (1) completed high school, (2) breastfed a child for a minimum of 6 months, and (3) been trained in breastfeeding management. They were recruited through job postings at the participating hospital and the Hispanic Health Council, through contact with clients who have successfully breastfed, and by word of mouth. Preference was given to candidates who were bilingual, were enthusiastic about breastfeeding, were flexible regarding scheduling, and had a mature, positive demeanour. At least one of the peer counsellors was bilingual and of Puerto Rican background. TRAINING: Peer counsellors receive 30 hours of classroom training from the program coordinator, using the combined curricula of the La Leche League International Peer Counseling Programme and the Hispanic Health Council's 'Breastfeeding: Heritage and Pride' peer counselling programme. They then spend 3 to 6 months working with experienced peer counselors, gradually progressing from observation to directly managing clients under supervision. Once competence is demonstrated, peer counsellors work independently with clients. Close contact with the program coordinator is maintained through biweekly case review meetings. Each month the staff members receive 1 hour of continuing education. PARTICIPANTS: Inclusion criteria specified that women must be (1) at least 18 years old, (2) considering breastfeeding their infant, (3) residents of the greater Hartford area, (4) available for telephone follow up, (5) low income (ie, WIC participant, food stamp recipient, or household income less than 180% of federal poverty level), 6) at no more than 26 weeks gestation, and 7) not yet enrolled in the peer counselling programme. Average age = 24.8 years; average education = 11.6 years; 12.8% had US residency; 23% were married; 15.9% and 22% were employed full time and part time respectively; 80% were Hispanic, 8.5% were African American, 3.6% were White and 7.9% were other; 26.5% spoke English at home. TOTAL = 165; INTERVENTION = 90; CONTROL = 75. |
|
| Interventions | OBJECTIVE: to provide peer support to increase breastfeeding in a low income, predominantly Latina population. INTERVENTION: Those in the intervention group received all of the services of the control group, plus prenatal, perinatal, and postnatal (minimum of 3) peer counsellor services. Peer counsellors carried out at least one prenatal home visit per client and, during these visits, reviewed benefits of breastfeeding, screened for inverted nipples, provided written material, discussed common breastfeeding myths, reviewed positioning and provided anticipatory guidance. A breastfeeding video was viewed, if possible. Additional prenatal visits were provided as needed. Postnatally, participants received at least daily visits. Hands‐on assistance was provided to demonstrate correct breastfeeding technique and participants were also provided with information on infant cues, expected breastfeeding frequency, signs of adequate breastfeeding and management of breastfeeding problems. Participants were also able to contact a peer counsellor by pager. CONTROL: routine breastfeeding education provided by the local hospital. This included prenatal education in response to questions and written materials; perinatal breastfeeding education, assistance and written materials; and postnatal access to a nurse telephone hotline. MODE OF DELIVERY: through visits at home and the hospital and via pager. RECIPIENT INVOLVEMENT IN DESIGN/DEVELOPMENT/DELIVERY: not described. GEOGRAPHICAL SETTING: urban formal, USA HEALTHCARE SETTING: home and hospital. | |
| Outcomes | HEALTHCARE BEHAVIOURS: breastfeeding status at birth and breastfeeding rates at 1,3 and 6 months post partum. LENGTH OF FOLLOW UP: 6 months post partum. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | 'Participants were randomized to either the control group or the intervention group by means of a computer software program' (p898). |
| Allocation concealment? | Unclear risk | 'Participants were randomized to either the control group or the intervention group by means of a computer software program' (p898). Not clear whether allocation was concealed. |
| Blinding? All outcomes | Unclear risk | Data collected through participant interviewer (p899). Unclear whether interviewer was blinded. Participants and personnel not blinded. |
| Incomplete outcome data addressed? All outcomes | Unclear risk | Significant loss to follow up by end of study (intervention = 36/113; control = 39/106), but balanced in numbers across intervention groups. Unclear whether similar reasons for missing data across groups. |
| Free of selective reporting? | Unclear risk | Insufficient information to make an assessment. |
| Free of other bias? | Low risk | |
Chongsuvivatwong 1996.
| Methods | Cluster RCT. | |
| Participants | LHW: there were approximately 10 volunteers for each of the 15 villages included in the study. TRAINING: health workers trained by paediatricians at regional hospital conducted 2 day training workshop for health volunteers from intervention villages. Training included a video program, lecture, demonstration and simulation, was conducted in Thai/local Malay dialect. The curriculum/media for training was modified from those developed by WHO PATIENTS: children <5 years of age. Mean age = 2.0 years in intervention group and 2.2 years in control control group. There were slightly more males than females. TOTAL=1313; INTERVENTION=664; CONTROL=649. | |
| Interventions | OBJECTIVE: to improve detection of serious acute respiratory infection (ARI). INTERVENTION: village health volunteers. CONTROL: no intervention. MODE OF DELIVERY: volunteers detected serious ARI, gave initial care by sponging and advised referral of cases to a health centre where antibiotics could be given and made a referral to hospital if necessary. RECIPIENT INVOLVEMENT IN DESIGN/DEVELOPMENT/DELIVERY OF INTEVENTION: not described. ORGANISATIONAL BASE OF THE INTERVENTION: not described. GEOGRAPHICAL SETTING: rural Thailand. HEALTHCARE SETTING: home. | |
| Outcomes | HEALTHCARE BEHAVIOUR: healthcare utilisation in past week. HEALTH STATUS AND WELLBEING: ARI event in the last week, severity of ARI attack. LENGTH OF FOLLOW UP: up to a maximum of 19 weeks. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Districts were randomly selected but not clear how this was done. |
| Allocation concealment? | Unclear risk | Not mentioned. |
| Blinding? All outcomes | Unclear risk | Not mentioned. |
| Incomplete outcome data addressed? All outcomes | Low risk | Data presented on outcomes stated in objectives. |
| Free of selective reporting? | High risk | Collected information on the outcomes 2 to 19 weeks after the intervention (training of village health workers) and average duration of observation in the intervention group was slightly longer. |
| Free of other bias? | Low risk | |
Clarke 2005.
| Methods | Cluster RCT. | |
| Participants | LHW: Suitable farm dwelling peers selected by adult co‐workers at the farm. Selection according to pre‐specified guidelines including role, function, characteristics. 84 LHWs were trained. TRAINING: Training focused on TB with PHC and community development principles. LHWs attended 5 one‐week training modules of 25 hours each. The content of the modules included: becoming a LHW, tuberculosis, AIDS, first aid and home based care. Small tasks as homework and these were reviewed at the next training session. The training conducted by a nurse and two LHW trainers. Monthly support visits were provided thereafter. PARTICIPANTS: People with TB who had been commenced on treatment. All were 15 years of age or more and permanent dwellers on farms. These farm workers are among the most disadvantaged groups in South Africa, have low levels of education and are dependent socially and economically on the farmers. TOTAL = 211 farms; INTERVENTION = 106 farms; CONTROL = 105 farms. |
|
| Interventions | OBJECTIVE: To improve treatment completion among farmworkers with TB.
INTERVENTION: For TB patients on directly observed therapy (DOT) by LHW, recorded treatment adherence. Monthly weighing and TB screening, referral of patients with symptoms suggestive of TB. LHW mentoring role in case of self‐supervision group. Addressed non‐adherence promptly. Also responsible for record keeping. CONTROL: Routine TB care. Patients are issued with sufficient drugs for 1–4 weeks, depending on the distance they live from the clinic nurse supervising treatment. Patients living further from the clinic receive larger supplies. Clinic nurses encourage TB patients to select a second person to supervise each dose taken. MODE OF DELIVERY: At patients' homes on farms. RECIPIENT INVOLVEMENT IN SELECTION/TRAINING/MANAGEMENT: LHWs selected by farm dwellers following local meetings on each farm. ORGANISATIONAL BASE OF THE INTERVENTION: not described. GEOGRAPHICAL SETTING: rural South Africa, farms. HEALTHCARE SETTING: home. |
|
| Outcomes | HEALTHCARE BEHAVIOURS: successful treatment completion in new smear positive pulmonary TB patients (primary outcome). OTHER: TB case finding. LENGTH OF FOLLOW UP: 1 year. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | 'Farms were allocated a number within the strata. All the numbers were randomly drawn from containers and allocated sequentially to the intervention or control group' (p675). |
| Allocation concealment? | Low risk | Cluster randomised. See above. |
| Blinding? All outcomes | Low risk | No blinding of personnel or outcome assessors, but the outcomes and the outcome measurement were not likely to be influenced by lack of blinding. |
| Incomplete outcome data addressed? All outcomes | Low risk | No missing outcome data. |
| Free of selective reporting? | Unclear risk | Insufficient information to make an assessment. |
| Free of other bias? | Low risk | |
Colombo 1979.
| Methods | RCT. | |
| Participants | LHW: 15 neighbourhood health coordinators, mostly women, 30 to 60 years of age and indigenous to the poverty community. Education level not clear. TRAINING: 6 month education and training program. Enrolled in courses at a local community college that taught communication skills, health care and health education concepts and related subjects. The in service program specifically addressed the importance of and rationale for the preventive services. Supervision not described. PARTICIPANTS: Federally‐financed poverty population. TOTAL=738 preschool children; INTERVENTION=569 children; CONTROL=169 children. |
|
| Interventions | OBJECTIVE: To determine if intervention by outreach workers trained in health education techniques could affect the use of preventive services by preschool children in poor families. CONTROL: Usual care. MODE OF DELIVERY: Recruited poor families to the project, taught family members the value of good health and health practices, motivated persons to utilise health services appropriate to their needs, assisted project members in participating effectively in the Kaiser‐Permanente medical care system, and directed families to community resources for other, non medical problems common to a poverty population. RECIPIENT INVOLVEMENT IN SELECTION/TRAINING/MANAGEMENT: No. GEOGRAPHICAL SETTING: Urban formal, USA HEALTHCARE SETTING: Home. |
|
| Outcomes | HEALTHCARE UTILISATION: Average number of primary procedures for preschool children among adult education group. Preventive use in the base year preceding the special coordinator intervention program. HEALTH STATUS AND WELLBEING: Primary preventive or early detection procedures and examinations for preschool children; Average number of primary procedures for preschool children among school age education group. LENGTH OF FOLLOW UP: 1 year. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | All families currently enrolled were 'randomly divided to three groups' but not told how they did this. |
| Allocation concealment? | Unclear risk | Not mentioned. |
| Blinding? All outcomes | Unclear risk | Not mentioned if those collecting data were blinded. |
| Incomplete outcome data addressed? All outcomes | Unclear risk | Not clear how many children completed the study. |
Coutinho 2005.
| Methods | RCT. | |
| Participants | LHW: Five women recruited to serve as home visitors. Secondary school education similar to that of community health agents in national programme. Personal breastfeeding experience not prerequisite. TRAINING:18 hour WHO/UNICEF Baby Friendly Hospitals training, 2 hour WHO/UNICEF Breastfeeding Counselling, which included training on how to listen, to learn from mothers, establishing a good relationship, building mothers confidence and how to offer support. Also received five days of “Helping mothers to breastfeed” (book). Included practice on how to discuss key topics with mothers using an illustrated book. PARTICIPANTS: Mothers of all 'healthy' singleton births at two hospitals during study period. 65% of mothers were 20 years or older, about 60% in each group had parity of two or more. Families had incomes below the poverty line of 0.5 minimum salaries per person per month (USD60 preintervention and USD40 at the time of the trial). Many living in environments with no indoor toilets (42%) and waste disposal (32%) preintervention. TOTAL = 375; INTERVENTION 1 = 175; INTERVENTION 2 = 175. |
|
| Interventions | OBJECTIVE: to provide support for exclusive breastfeeding.
INTERVENTION 1: Hospital, Maternity staff expected to support, guide and encourage all mothers to initiate and maintain exclusive breastfeeding throughout their hospital stay and at home for 6 months, to continue breastfeeding for at least 2 years. Used video, talk, discussions, advice. INTERVENTION 2: Hospital + home visitors, Home visitors expected to make 10 home visits until 6 months. Illustrated booklet given to mothers. Expected to encourage exclusive breastfeeding for 6 months and continued breastfeeding until at least 2 years, answer questions, discuss doubts, and use booklet as basis for discussion. Each visit had a mean duration of 30 minutes. MODE OF DELIVERY: See above. RECIPIENT INVOLVEMENT IN SELECTION/TRAINING/MANAGEMENT: not described. ORGANISATIONAL BASE OF THE INTERVENTION: not described. GEOGRAPHICAL SETTING: urban Brazil, formal housing. HEALTHCARE SETTING: home. |
|
| Outcomes | HEALTHCARE BEHAVIOURS: Rate of exclusive breastfeeding from birth to 6 months; proportion of infants breastfed at least partially from birth to 6 months; proportion of infants given foods other than breastmilk. LENGTH OF FOLLOW UP: 6 months. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | 'random numbers table' (p1095). |
| Allocation concealment? | Unclear risk | 'Concealment was achieved by drawing numbers from envelopes at the time of assignment' (p1095). |
| Blinding? All outcomes | Low risk | 'Data were collected...by four researchers who were not aware of group allocation and were unconnected with the delivery of the interventions' (p1096). |
| Incomplete outcome data addressed? All outcomes | Low risk | 'the mother‐infact pairs lost did not differ from those who remained for any of the variables studied' (p1096) Missing outcome data balanced in numbers across intervention groups. |
| Free of selective reporting? | Unclear risk | Insufficient information to make an assessment. |
Curnow 2002.
| Methods | RCT. | |
| Participants | LHW: Supervisors were local mothers who had some connection whether paid or voluntary with the school and were paid for the duration of 1hr per school day. TRAINING: All the supervisors were trained in cross‐infection control procedures and record keeping. PARTICIPANTS: Children in their first year of primary school, Mean age 5.3 years. The schools were located in relatively deprived areas with a history from school screening data, of above average numbers of children with caries experience at school entry. These children were designated to be high caries risk. TOTAL= 595 children; INTERVENTION:298 children CONTROL: 297 children. |
|
| Interventions | OBJECTIVE: To determine the reduction in 2 years caries increment that can be achieved by daily supervised tooth brushing on school days. CONTROL: No intervention. MODE OF DELIVERY: Supervised tooth brushing on school days. Were initially instructed to ensure that the toothbrush and toothpaste were in contact with the teeth, and moving around the mouth to ensure distribution of toothpaste to all quadrants. All trays were taken to the designated cleaning area and each tray and contents seperately cleaned by the supervisor. Supervised maintained a daily register of childrens attendance as a brushing record. RECIPIENT INVOLVEMENT IN SELECTION/TRAINING/MANAGEMENT: GEOGRAPHICAL SETTING: Urban formal, Scotland HEALTHCARE SETTING: Classroom. |
|
| Outcomes | HEALTH STATUS AND WELLBEING: Caries increment scores at 12 and 24 months. LENGTH OF FOLLOW UP: 2years. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | One class in each school was randomly allocated to intervention and the other being the within school control. not clear method used to allocate class. |
| Allocation concealment? | Unclear risk | Not mentioned. |
| Blinding? All outcomes | Low risk | Single calibrated examiner who examined children was blind to individual childrens group allocation. |
| Incomplete outcome data addressed? All outcomes | Low risk | Follow‐up rate 86%. |
| Free of other bias? | High risk | Within school control may have adapted tooth brushing as well. |
Dawson 1989.
| Methods | RCT. | |
| Participants | LHW: Home visitors were mothers who were carefully selected for warmth, empathy, and interest in helping people. The home visitors' educational level (median of 12th grade) was close to that of the women they visited, so that they could relate as peers rather than as authorities. TRAINING: 30 hours of training covering pregnancy, birth, infant care, safety, nutrition, child development, community resources and family life. PARTICIPANTS: Mothers that were expecting first or second child, were 20‐26weeks pregnant, were at least 16yrs. Mothers median education was 11th grade. 71% lived with baby's father, 19% with own parents. All had low incomes, median family income was $5500. 74% white, 25% Mexican‐American, 1 black. All English‐speaking. TOTAL=172 women; INTERVENTIONS: Intervention 1 (Routine services plus weekly home visits) = 42, Intervention 2 (routine services, weekly home visits plus group meetings) = 50; CONTROL= 53. |
|
| Interventions | OBJECTIVE: To enhance mother‐infant interaction. CONTROL: Received routine maternity and paediatric care including nutrition and social services, occasional visits by public health nurses and delivery at university hospital. MODE OF DELIVERY: Home visitors sought to develop trusting relationships with families, primarily mothers. Provided emotional support by listening to mothers, and showing understanding. Provided concrete help eg rides to clinics, babysitting provided information on pregnancy and infant care, enhanced mothers informal and formal social networks by helping mothers access community resources such as housing, food stamps, child care, etc. They responded to what mothers felt they needed to cope better, discussed and encouraged contraception, talked about infant feeding and listened to mother's description of child's minor illnesses. RECIPIENT INVOLVEMENT IN SELECTION/TRAINING/MANAGEMENT: no. GEOGRAPHICAL SETTING: USA HEALTHCARE SETTING: Home. |
|
| Outcomes | LENGTH OF FOLLOW UP: 14months. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Women were stratified by race and parity and assigned to race parity subgroups.The first woman entering each subgroup was assigned at random to control or one of two experimental groups. The next woman entering the subgroup was assigned at random to one of two other experimental conditions. |
| Allocation concealment? | Unclear risk | Not mentioned. |
| Blinding? All outcomes | Unclear risk | Not clear who data assessors were and if they were blinded or not. |
| Incomplete outcome data addressed? All outcomes | High risk | 35% of the sample was lost to attrition. Authors stated that subjects remained equivalent with regard to parity, ethnic group, maternal age and education and famil stress and that this did not impair comparability of groups. No further analysis provided. |
| Free of selective reporting? | Unclear risk | Insufficient information to make an assessment. |
Dennis 2002.
| Methods | RCT. | |
| Participants | LHW: 58 volunteer mothers, with minimum of 6 months previous breastfeeding experience and a positive breastfeeding attitude, were recruited into the participating community organisation specifically for the trial. 86.9% had post‐secondary education. TRAINING: mothers completed a 2.5 hour orientation session. The focus of the orientation session was to develop the peer volunteers' telephone support and referral skills; role playing and the verification of problem‐solving skills were important components of the session. PARTICIPANTS: mothers with singleton births at 37 weeks gestation or greater. All participants >16 years of age. Majority (75%) aged 25‐34 years; approximately 90% married; >60% had college or undergraduate university training; approximately 40% had an annual household income of 40,000‐79,999 Can$. TOTAL=258; INTERVENTION=132; CONTROL=126. | |
| Interventions | OBJECTIVE: to provide peer support to increase breastfeeding duration. INTERVENTION: peer support by volunteers. CONTROL: no intervention. MODE OF DELIVERY: volunteers contacted a new mother by telephone within 48 hours after hospital discharge and as frequently thereafter as the mother deemed necessary: 97% telephone interactions; 3% face‐to‐face meetings. The mean duration of contact: 53.1 days and 96% contacts made within the first week post partum. Volunteers provided peer support, defined as specific type of social support that incorporates informational, appraisal (feedback) and emotional assistance. RECIPIENT INVOLVEMENT IN DESIGN/DEVELOPMENT/DELIVERY: not described. ORGANISATIONAL BASE OF THE INTERVENTION: not described. GEOGRAPHICAL SETTING: urban Canada. HEALTHCARE SETTING: home. | |
| Outcomes | HEALTHCARE BEHAVIOURS: self reported breast feeding (exclusive, almost exclusive, high, partial, token, bottle feeding). LENGTH OF FOLLOW UP: 12 weeks post partum. | |
| Notes | A 43‐page handbook was distributed to all peer volunteers. The handbook outlined provisional services available for referral and was to be used as a reference guide. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | 'Randomization was achieved using consecutively numbered, sealed, opaque envelopes containing randomly generated numbers constructed by a biostatistician who was not involved in the recruitment process.' (p22). |
| Allocation concealment? | Low risk | 'Randomization was achieved using consecutively numbered, sealed, opaque envelopes containing randomly generated numbers constructed by a biostatistician who was not involved in the recruitment process.' (p22). |
| Blinding? All outcomes | Low risk | 'A research assistant blinded to group allocation telephoned all participants...to collect data...' (p22). |
| Incomplete outcome data addressed? All outcomes | Low risk | Only 2 participants lost to follow up (p24). |
| Free of selective reporting? | Unclear risk | Insufficient information to make an assessment. |
| Free of other bias? | Low risk | |
Dennis 2009.
| Methods | RCT. | |
| Participants | LHW: Peer support (mother to mother) or peer volunteers were recruited through distributed flyers, advertisements in local papers, word of mother. 204 women from community met criteria and were selected. Were volunteers from the community, able to speak and understand English, self reported history of and recovery from postnatal depression. Most were married 82%, 61% had more than one pregnancy, 41% were employed and 54% reported their ethnicity as non‐Canadian. 145 peer volunteers participated, each providing support to an average of 2 women (range 1‐7). 91% had further education beyond high school. TRAINING: Had a 4 hour training session, focus was to develop skills for effective telephone based support and make referrals to professionals as necessary. Had role playing as a part of the training. Used a 121 page training manual developed by the principal investigator. Training was implemented by a paid peer coordinator. PARTICIPANTS: Were new mothers, about 2 weeks or less post partum, 18 years and above, able to speak English, had a live birth and discharged from hospital. Most were 20‐34 years of age (78%), married or cohabiting (92%), undergraduate or university graduate level (50%). Most were primiparous (59%), had a vaginal delivery (63%) and had a history of depression (69%). Most had an annual household income ≥80,000$C (45% in intervention, 38% in control), about 30% had between 40 ‐79,999$C total household income. TOTAL=701women; INTERVENTIONS: Peer Support=349; Control=352. |
|
| Interventions | OBJECTIVE: To evaluate the effectiveness of telephone based peer support in the prevention of postnatal depression. CONTROL: Standard community post partum care which could include mothers proactively seeking services from public health nurses and other providers including various community resources including drop‐in centres. MODE OF DELIVERY: Peer volunteers initiated telephone contact 48‐72hrs after random allocation to provide support for postpartum depression. Were to make a minimum of 4 contacts and then interact as necessary. RECIPIENT INVOLVEMENT IN SELECTION/TRAINING/MANAGEMENT: no. GEOGRAPHICAL SETTING: Canada, Urban formal. HEALTHCARE SETTING: Other, telephone counselling. |
|
| Outcomes | HEALTH STATUS AND WELLBEING: Postnatal depression (Edinburgh postnatal depression scale EDS), Structured clinical interview for depression (SCID), Short version of the UCLA loneliness score, Hospital utilisation. LENGTH OF FOLLOW UP: 24 weeks. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Stratified by self‐reported history of depression then randomised using web‐based service(www.randomize.net). |
| Allocation concealment? | Unclear risk | Not mentioned. |
| Blinding? All outcomes | Low risk | Trial nurses blinded to group allocation collected data at 12 and 24 weeks post partum. Health providers of standard care were not aware of mothers group allocation. |
| Incomplete outcome data addressed? All outcomes | Unclear risk | Follow‐up rate >80%. |
Duggan 2004.
| Methods | RCT. | |
| Participants | LHW: Were home visitors whose aim, through long‐term, intensive home visiting of at‐risk families, was to (1) establish a trusting relationship with parents; (2) help parents address existing crises; (3) model problem‐solving skills; (4) help families access community resources. TRAINING: Not specified. PARTICIPANTS: Families at risk for child abuse and neglect, with children aged 3‐5 years. Over half of mothers were <20 years old, 33% were Native Hawaiian or Pacific Islander. 28% were Asian or Filipino. TOTAL=643 families; INTERVENTIONS: Home visiting=373 families; CONTROL=270 families. |
|
| Interventions | OBJECTIVE: To assess the impact of a home visitation program in reducing malleable parental risk factors for child abuse in families of newborns identified, through population‐based screening, as at risk of child abuse. CONTROL: No intervention. MODE OF DELIVERY: Home visits were guided by an individual family support plan (family goals and steps to achieve them). Supervisor and home visitor identify key issues by examining the family's stress checklist assessment and concerns. They decided what areas of concern were appropriate for the home visitor to address with the family in addition to goals nominated by the family. The home visitor and supervision referred to the goals at least every 2 months, the goals were updated by the visitor and family every 6 months. RECIPIENT INVOLVEMENT IN SELECTION/TRAINING/MANAGEMENT: no. GEOGRAPHICAL SETTING: USA HEALTHCARE SETTING: Home. |
|
| Outcomes | HEALTH STATUS AND WELLBEING: Maternal mental health ? Depressive symptoms, severe parenting stress, poor general mental health. Maternal substance abuse (illicit drug and problem alcohol use), Partner violence, psychological abuse, physical abuse. LENGTH OF FOLLOW UP: 3 years. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Offered all at risk study enrollment and random assigment. |
| Allocation concealment? | Unclear risk | Not mentioned. |
| Blinding? All outcomes | Low risk | Used trained research assistants blinded to randomisation status and not delivering intervention. |
| Incomplete outcome data addressed? All outcomes | Low risk | Follow‐up rate >80% over 3 year period. |
Ernst 1999.
| Methods | RCT. | |
| Participants | LHW: Advocates, paraprofessionals who had personal experience with many of the types of adverse life experiences as clients and acted as positive role models with an experienced and realistic perspective. TRAINING: Not specified. PARTICIPANTS: High risk alcohol and drug abusing mothers, mean age at enrolment was 27 years, mean number of years of education was 11, about 70% were single or separated/divorced. About 75% were multiparous mean number of children was 3. Mean IQ score was about 80. About 75% had one or both parents that abused alcohol, 65% sexually or physically abused as children. Almost 60% lived in a foster home at some time. About 85% were receiving public assistance, about half were transitional or homeless, 80% had ever been jailed. African American about 45%, 35% white, 15% native American. TOTAL=103 women; INTERVENTION: 65 women; CONTROL: 31 women.7 refused enrolment. |
|
| Interventions | OBJECTIVE: To examine the efficacy of a paraprofessional advocacy program for improving health and social outcomes of high risk substance abusing mothers and their children. CONTROL: no intervention but free to access services available in the community. MODE OF DELIVERY: Motivated clients to make changes, assisted them in identifying personal goals, ensured that clients followed up on referrals, offered guidance and a watchful eye. Linked women and their families with an array of existing community resources. RECIPIENTCONSUMER INVOLVEMENT IN SELECTION/TRAINING/MANAGEMENT: No. GEOGRAPHICAL SETTING: Urban formal, USA HEALTHCARE SETTING: Home. |
|
| Outcomes | HEALTHCARE UTILISATION: Family connection with services. HEALTH STATUS AND WELLBEING: Multiple domains of the subjects lives. BEHAVIOUR: indicators of alcohol/drug treatment, abstinence, use of family planning. LENGTH OF FOLLOW UP: 3 years. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Clients meeting eligibility criteria 'were assigned at random to client or control group (every third women assigned to control group) to obtain a two to one ratio of clients to control'. |
| Allocation concealment? | Unclear risk | Not mentioned. |
| Blinding? All outcomes | Unclear risk | Not clear if the data collectors for the client group were blind. Interviewers for the control group were 'blind in respect to subject status and source of recruitment'. |
| Incomplete outcome data addressed? All outcomes | Low risk | Follow‐up rates were 92% for clients and 86% for control. |
| Free of other bias? | High risk | Some self‐reported outcomes among high risk drug and alcohol users may not be reliable. |
Flores 2005.
| Methods | RCT. | |
| Participants | LHW: Case managers were bilingual Latina women of Dominican, Puerto Rican, Mexican and Columbian origin, between 22 and 36 years, all graduated from high school, some with college degree, 1 postgraduate training. None had experience working as case managers providing in insurance for children. Were recruited through job listings posted in employment offices of Boston colleges and universities. All graduated from high school, some with college degree, 1 postgraduate training. TRAINING: 1 day training on obstacles to obtaining insurance, following up on applications, coverage decisions made, disputing applications made, and the study protocol. Had 1 week training on Massachusetts health eligibility requirements, 4 hr session on insurance eligibility rules, 2hrs on Massachusetts managed care programs and rules, 1 day session on children’s medical security plan, 1 session on programs for impoverished families by and NGO providing care for these families. 1 week supervised case manager training in the community, monthly technical forums by the division of medical assistance. PARTICIPANTS: Uninsured Latino children and their families. Children aged 0‐18years, uninsured for at least 3 months or more. Parent speaking English or Spanish, parent identified child’s ethnicity as Latino. Mean age of children 9 years (SD 5) Mean age of parent 36.7(sd 9.1). At least half were legal residents, 40% undocumented, almost 80% with 1 parent fully employed. About 45% married, 20% single parents, about 30% high school graduate, 15% college graduate. Combined family income almost USD13,000 (range 0‐72,000 in intervention group, 0‐18,0000 control group. Almost 70% were in the 0‐100% federal poverty threshold, about 25% in the 101‐200% federal poverty threshold. Latino mostly from Columbia (40%), Dominican (18%) and Salvado(20%), others from Mexico and Guatemala. TOTAL=275 uninsured children and their families; INTERVENTION: 139 families; CONTROL: 136 families. |
|
| Interventions | OBJECTIVE: To evaluate whether case managers are more effective than traditional methods in insuring uninsured Latino children. CONTROL: Received standard of care and outreach efforts by the Massachusetts Health and Child Medical Security Plan. Efforts by the health department include mailings, press releases, door to door canvassing, radio, adverts, flyers, health fairs etc, mini grants to community organisations for outreach and assistance with applications, toll free telephone for applying for health benefits. MODE OF DELIVERY: Provide information on types of insurance available and application process; 2) information on eligibility requirements; 3) complete and submit insurance application on behalf of the family; 4) Expedite insurance coverage decisions including early contact with state agencies providing insurance (Division of medical assistance, division of public health responsible for Medicaid and children medical security plan respectively in Massachusetts; 5) act as family advocate or liaison with state agencies; 6) Rectify with the agencies situations where the child was deemed ineligible or insurance coverage inappropriately terminated. RECIPIENT INVOLVEMENT IN SELECTION/TRAINING/MANAGEMENT: No. GEOGRAPHICAL SETTING: Urban formal, USA HEALTHCARE SETTING: Community. |
|
| Outcomes | HEALTH STATUS AND WELLBEING: Health insurance obtained, Satisfaction with process of obtaining insurance. LENGTH OF FOLLOW UP: 2 years. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | "Subjects were allocated to the case management intervention group or the control group with a computer‐generated, stratified,randomization process. Randomization was stratified by community site, with separate allocation schedules prepared for participants from East Boston and Jamaica Plain. The randomization schedule was prepared with the RANUNI function of SAS software, version 8.2.28". |
| Allocation concealment? | Low risk | "Sequentially numbered, opaque, sealed envelopes were produced for each community site, to ensure adequate allocation concealment". |
| Blinding? All outcomes | Low risk | "Bilingual Latina research assistants who did not participate in any aspect of preparation of randomization schedules opened the envelopes in the presence of enrolled participants, to inform them of their group assignment". |
| Incomplete outcome data addressed? All outcomes | High risk | 72% in intervention and 62% in control group were followed up after 1 year. |
Gadomski 2006.
| Methods | RCT. | |
| Participants | LHW: Lay educators who had farming backgrounds. No further description provided. TRAINING: Not described. PARTICIPANTS: Farming community of central New York state. Had to have children resident or employed on farm. TOTAL=931 farms; INTERVENTION: 462 farms; CONTROL: 469 farms. |
|
| Interventions | OBJECTIVE: To assess whether active dissemination of North American Guidelines for Childrens Agricultural Tasks reduced childhood agricultural injuries. CONTROL: No intervention. MODE OF DELIVERY: Visit farms to review North American Guidelines for Childrens Agricultural Tasks to prevent injuries to children on farms. Tailored guidelines to each farm setting. Also provided booster interventions‐ post card, calender and fridge magnet. RECIPIENT INVOLVEMENT IN SELECTION/TRAINING/MANAGEMENT: not mentioned. GEOGRAPHICAL SETTING: Rural, USA HEALTHCARE SETTING: Farm. |
|
| Outcomes | HEALTH STATUS AND WELLBEING: Injury incidence, Injury density per full time equivalent. BEHAVIOUR: Proportion setting limits on amount of time child could perform work btw breaks, Providing supervision to children while they were performing work; Preventing child from doing a particular job; Adding role over protection structure during study period; Making safety related changes, Adding or repairing a power take off. LENGTH OF FOLLOW UP: 21 months. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | High risk | Told farms were '462 farms were allocated to intervention group and 469 allocated to control group' and later Mention simple random assignment of farms. |
| Allocation concealment? | Unclear risk | Not mentioned. |
| Blinding? All outcomes | Low risk | Surveillance telephone callers were unaware of the intervention status of the farms. |
| Incomplete outcome data addressed? All outcomes | Low risk | Follow‐up rates over 80%. |
| Free of other bias? | High risk | Data collected included reports of injuries among children working on farms and this information may be under reported. |
Gardner 2003.
| Methods | RCT. | |
| Participants | LHW: Community Health workers or paraprofessionals with at least 4 years of secondary education. TRAINING: Not specified. PARTICIPANTS: Mother‐baby pairs where Infants weighed <2500g at full term. Mothers were at 36 to 37 weeks gestational age at recruitment, education below 3 secondary level examination passes, mainly low income mothers. TOTAL= 140 LBW babies, 87 NBW babies; INTERVENTIONS: LBW‐T intervened=66; CONTROL= LBW‐T control=69, NBW babies=87. |
|
| Interventions | OBJECTIVE: To determine whether early psychosocial intervention with low birthweight term infants improved with cognition and behaviour and to compare (LBW‐T with normal birthweight infants. CONTROL: Weekly home visits, but without psychosocial intervention component. Had two control groups, one with LBW‐Term infants but did not receive the intervention and also compared to Normal birthweight babies. MODE OF DELIVERY: Visited up to 20 children weekly for the first 8 weeks of life. During home visits, were to ask about feeding and any illness in the infant. For intervention group, mothers were asked about the things they thought were important in the care of the infant and chatted about issues raised with emphasis on the importance of showing love to the infant. They were shown what to do to help their child develop well, for example, talking, singing and showing affection to the infant. RECIPIENT INVOLVEMENT IN SELECTION/TRAINING/MANAGEMENT: no. GEOGRAPHICAL SETTING: Jamaica, Urban Formal. HEALTHCARE SETTING: Home. |
|
| Outcomes | HEALTH STATUS AND WELLBEING: Intentional problem solving ability scores: Cover test, Support test; Behaviour ratings: Activity, Cooperation, General emotional tone, Vocalisation. LENGTH OF FOLLOW UP: 7 months. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | High risk | Used systematic random assignment. |
| Allocation concealment? | Unclear risk | Not mentioned. |
| Blinding? All outcomes | Low risk | Observers measuring outcome were unaware of infant group. |
| Incomplete outcome data addressed? All outcomes | Low risk | Attrition low, outcomes reported reflect those stated in objectives. |
| Free of selective reporting? | Low risk | |
| Free of other bias? | Low risk | |
Gielen 2002.
| Methods | RCT. | |
| Participants | LHW: Community health workers, no other details. TRAINING: Not described in detail, but mentions that they received specific training from investigators to conduct home visits. PARTICIPANTS: Participants were mostly infants mothers, mean age 24yrs, 13% were married, 12% had high school education and 23% were employed. Infants mean age was 3 months. Were generally low income families with 39% of households reporting household incomes <5000USD per year. 94% were African American. TOTAL=187 parents; INTERVENTION: 93 parents; CONTROL: 94 parents. |
|
| Interventions | OBJECTIVE: To enhance parents home safety practices through pediatric safety counselling. CONTROL: No intervention received. MODE OF DELIVERY: Assessed injury hazards for falls, burns and poisonings with the parent. Made recommendations about appropriate safety products and practices. Referred children to the childrens' safety center. RECIPIENT INVOLVEMENT IN SELECTION/TRAINING/MANAGEMENT: not mentioned. GEOGRAPHICAL SETTING: Urban formal, USA HEALTHCARE SETTING: Home. |
|
| Outcomes | BEHAVIOUR: Working smoke alarms, Hot water temperature record, Stairs protected by gate or door, Poisons kept latched or locked up, Homes with ipecac syrup. LENGTH OF FOLLOW UP: 1 year. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | The project director (EMM) used a table of random numbers to assign participating residents to the standard or enhanced intervenion group. |
| Allocation concealment? | Unclear risk | Not mentioned. |
| Blinding? All outcomes | Unclear risk | Not mentioned if the data collectors were blinded. Not clear if the two research assistants who listened to the audiotapes and coded mention of the 5 safety practices were blinded. |
| Incomplete outcome data addressed? All outcomes | High risk | Follow‐up rates were about 64% for intervention group and 66% for control group and this effect not fully explored at analysis. |
| Free of other bias? | High risk | Some of the data collected was on self‐reports of use of safety measures and visits to the child safety centre. |
Gokcay 1993.
| Methods | RCT. | |
| Participants | LHW: 3 lady home visitors from the same community, all primary school graduates. TRAINING: 3 week training session on MCH, communication skills, and tasks involved in home visits. Supervision not described. PARTICIPANTS: Children less than 5 yrs, Pregnant women and mothers. TOTAL=244 families; INTERVENTIONS: Followed up by lay health visitors=141 families. CONTROL: Followed up by midwives=103 families. |
|
| Interventions | OBJECTIVE: To compare the performance of midwives with that of lady visitors. CONTROL: Care by midwives. MODE OF DELIVERY: Identify those at risk, i.e. not attending any health institution and/or in health need. Invite those families to the clinic. Offer guidance on family planning, ANC, well child control, immunization and other mother, child health‐related problems. RECIPIENT INVOLVEMENT IN SELECTION/TRAINING/MANAGEMENT: No. GEOGRAPHICAL SETTING: Urban informal, Turkey (squatter area of Istanbul) HEALTHCARE SETTING: Home. |
|
| Outcomes | HEALTHCARE BEHAVIOURS: Use of family planning, Proportion of planned pregnancies, antenatal visits, deliveries attended by a healthcare provider. HEALTH STATUS AND WELLBEING: Infants fulfilling immunisation schedule, children under 5 years fully immunized, infants and children 1‐5 years receiving at least 1 health check up. LENGTH OF FOLLOW UP: 24 months. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Told each visitor was randomly assigned to each visiting unit. |
| Allocation concealment? | Unclear risk | Not mentioned. |
| Blinding? All outcomes | Unclear risk | Probably no blinding of data collectors as home visitor received mother at MCH centre on appointment day, data from home visits and clinic recorded on same card. |
| Incomplete outcome data addressed? All outcomes | Unclear risk | Attrition rate not clear but reported that 497 households not evaluated as moved away from project area. Lay visitors followed up 473 households initially, 713 for midwives. |
| Free of selective reporting? | Unclear risk | Insufficient data to make assessment. |
Graffy 2004.
| Methods | ||
| Participants | LHW: 28 accredited counsellors for the National Childbirth Trust. Had themselves breastfed, had undertaken training in counselling mothers. TRAINING: Training in counselling mothers, delivered by the National Childbirth Trust, UK. No further information provided. Their code of conduct emphasises a non‐directive approach and strengthening mothers' confidence in their own abilities. PARTICIPANTS: Any parity, considering breastfeeding, not having breastfed a previous child for more than 6 weeks. Most aged 20‐34 years; caucasian; and pregnant with their first child. Pregnant women approached at 28‐36 weeks gestation, delivered 36 weeks. About 70% having first child, 5% less than 20 years of age. Mainly in social classes II and III (UK). Living in mixed or deprived populations. About 20% in social class IV, V. White (UK) = 59%; White (other) = 10%; African or Caribbean = 15%; Indian = 8%; other = 7%. TOTAL = 720; INTERVENTION = 363; CONTROL = 357. |
|
| Interventions | OBJECTIVE: To improve the duration of, and satisfaction with, breastfeeding. INTERVENTION: Visited pregnant women once before birth to offer postnatal breastfeeding support by telephone or further home visits if requested. At the antenatal visits, women were given a contact card and 2 leaflets published by the National Childbirth Trust and the Health Education Authority. CONTROL: No counselling. MODE OF DELIVERY: Peer counsellor visits to mothers at home once before birth and provided further postnatal support by telephone. RECIPIENT INVOLVEMENT IN SELECTION/TRAINING/MANAGEMENT: not described. GEOGRAPHICAL SETTING: urban formal, United Kingdom HEALTHCARE SETTING: home and telephone. |
|
| Outcomes | RECIPIENT SATISFACTION WITH CARE: satisfaction with breastfeeding at 6 weeks; problems encountered in breastfeeding, at 6 weeks; whether the advice that they received was helpful, at 6 weeks. HEALTHCARE BEHAVIOURS: Prevalence of any breastfeeding at 6 weeks (primary outcome); Initiated breastfeeding at birth; Prevalence of any breastfeeding or bottle feeding at 4 months; Exclusive breastfeeding at 6 weeks; time to introduction of bottle feeds. LENGTH OF FOLLOW UP: 4 months. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | 'Randomisation was achieved using numbered, sealed envelopes prepared by the statistical advisor from random permuted blocks and held in the study office.' (p2). |
| Allocation concealment? | Unclear risk | 'Randomisation was achieved using numbered, sealed envelopes prepared by the statistical advisor from random permuted blocks and held in the study office.' (p2) Not clear if envelopes were opaque. |
| Blinding? All outcomes | High risk | Self‐assessment of outcomes using a questionnaire. |
| Incomplete outcome data addressed? All outcomes | High risk | Loss to follow up at 4 months = 11% overall (intervention = 26/357; control = 26/363), and this was similar across intervention and control groups. 'Women who had discontinued breastfeeding were significantly more likely to need a telephone reminder to return the questionnaire at six weeks' (p3). |
| Free of selective reporting? | Unclear risk | Insufficient data to make an assessment. |
| Free of other bias? | Low risk | |
Graham 1992.
| Methods | RCT. | |
| Participants | LHW: 2 home visitors were non‐professional Black women who demonstrated rapport with patients from clinic population and had children of their own. TRAINING: specific training was in childbirth education, community resources, and nutrition during pregnancy. The training included reading, discussion groups, weekly meetings, and attendance at hospital prenatal classes. PATIENTS: low income, Black inner city mothers at risk of low birthweight babies. Mean age was 24 years with 21% being between 14 and 20 years and 4% over the age of 35 years. Mothers lived within a 5 mile radius of the hospital. Only 'high risk' participants, initially identified by a medical/psychosocial screening questionnaire, were randomised; a low risk category formed another, non‐randomised control population. TOTAL=232; 4 HOME VISITS=87; SOME HOME VISITS=87; CONTROL=58. | |
| Interventions | OBJECTIVE: to reduce the incidence of low birthweight babies (<2500g) among high risk mothers. INTERVENTION: non‐professional home visitors. CONTROL: no intervention. MODE OF DELVIERY: 4 x 1 hour home visits at 2 to 4 week intervals. Intervention was family focused with goal of strengthening intrafamilial interpersonal support system. Home visitors provided psychosocial support, made efforts to reduce family stress, provided information on health risks during pregnancy (smoking, drinking cessation techniques), provided nutrition education/information for prenatal/childbirth and gave a small gift at each visit. RECIPIENT INVOLVEMENT IN DESIGN/DEVELOPMENT/DELIVERY: not described. ORGANISATIONAL BASE OF THE INTERVENTION: not described. GEOGRAPHICAL SETTING: urban USA HEALTHCARE SETTING: home. | |
| Outcomes | HEALTHCARE BEHAVIOURS: frequency of clinic attendance. HEALTH STATUS AND WELLBEING: proportion of low birthweight babies born to high risk mothers. LENGTH OF FOLLOW UP: not described. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Not mentioned. |
| Allocation concealment? | Unclear risk | Not mentioned. |
| Blinding? All outcomes | Unclear risk | Not mentioned. |
| Incomplete outcome data addressed? All outcomes | Low risk | Report on outcomes stated in objectives. |
Haider 2000.
| Methods | Cluster RCT. | |
| Participants | LHW: counsellors were local mothers with personal breastfeeding experience, at least 4 years schooling, a willingness to help other mothers and residence in the intervention areas. TRAINING: 40 hours (4 hours x 10 days) by demonstrators and role play using WHO/UNICEF breastfeeding counseling course and King's book (1992). 2 week pilot where volunteers practiced with pregnant mothers and mothers with newborns. Performance monitored at least 3 times during study by breast feeding supervisors. PATIENTS: pregnant women of lower‐middle and lower socioeconomic status, aged 16‐35 years, with 3 living children or less or parity 5. TOTAL=726; INTERVENTION=363; CONTROL=363. | |
| Interventions | OBJECTIVE: the promotion of exclusive breastfeeding among pregnant women. INTERVENTION: community‐based peer counsellors. CONTROL: no intervention. MODE OF DELIVERY: one counsellor responsible for 12‐25 mothers residing in the same zone. During 15 visits (20‐40 mins long) over 5 months counsellors explained the benefits of exclusive breastfeeding for 5 months. Prenatally, mothers were encouraged to eat more and avoid exhaustion. Mothers were also encouraged to hold babies within a few minutes of delivery, and initiate breast feeding within one hour of delivery. Prelacteal and postlacteal foods were discouraged. 15 homebased counselling visits were scheduled, with 2 visits in the first trimester, three in early post partum and the 2/52 until the infant was 5 months old. RECIPIENT INVOLVEMENT IN DESIGN/DEVELOPMENT/DELIVERY: not described. ORGANISATIONAL BASE OF THE INTERVENTION: WHO/UNICEF breastfeeding counselling course. GEOGRAPHICAL SETTING: informal urban Bangledesh HEALTHCARE SETTING: home. | |
| Outcomes | HEALTHCARE BEHAVIOURS: holding infants after delivery, breastfeeding initiation, exclusive breastfeeding, use of prelacteal foods, use of post lacteal foods. LENGTH OF FOLLOW UP: 5 months. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | 'random number tables were used ' (p1643). |
| Allocation concealment? | Low risk | Cluster randomised. |
| Blinding? All outcomes | High risk | 'inteviewers...were aware of which zones had peer counsellors and therefore of group assigment' (p1644). |
| Incomplete outcome data addressed? All outcomes | Low risk | Missing outcome data balanced in numbers across groups. 'There were no significant differences in the socioeconomic and demographic characteristics of the losses compared with those who completed 5 months' follow‐up.' (p1646). |
| Free of selective reporting? | Unclear risk | Insufficient information to make an assessment. |
| Free of other bias? | Low risk | |
Hardy 1989.
| Methods | RCT. | |
| Participants | LHW: The home visitor was a middle‐aged black college‐educated black woman who had previously lived in the community. TRAINING: Training was done but no details provided. The curriculum developed for home visitor use was based on experience in providing parenting education to adolescent and more mature mothers in this population. It included topics appropriate for the age of the infants visited. PARTICIPANTS: African American single parents, 18‐33 years(mean age of mothers was 22.6yrs). Majority (78%) were single parents, very poor and living in inner‐city ghettos. About 90% of children were eligible for Medicaid. TOTAL= 290 women; INTERVENTIONS: =143; CONTROL= 147. |
|
| Interventions | OBJECTIVE: To describe the results of an experimental program designed to provide inner‐city mothers with health and parenting education, as an extension of the services provided in the clinics of the children and youth program. CONTROL: No intervention. MODE OF DELIVERY: Provided parenting education to adolescents and more mature mothers in this population. Teaching was tailored to the age of the baby and to meet the individual needs and abilities of the parent. Provided information for adequate parenting and child care skills. Covered child's well and sick care, feeding, clothing, safety, development milestones, contact information for health providers, social worker for childs safety. She refered the family to a social worker or educator if there were any psychosocial issues. The first home visit was made when the child was 7 to 10 days old. Subsequent routine visits ocurred 2 to 3 weeks before the C&Y visits made at months 2, 4, 6, 9, 12, 15, 18, 21, and 24. Additional visits were made at the discretion of staff members. The home visitor was also available to the families by telephone. Routine visits lasted 40‐60 minutes. A calendar was developed and given to each parent at the first visit. It included information on child development, etc.The mothers were encouraged to list the date and time of their next clinic appoinment on the calendar. In addition to the calendar, childcare information was given to the families through the use of single‐issue pamphlets that had been developed in the adolescent‐parenting program, spesifically for use wih this disadvantages population. There were 36 booklets. RECIPIENT INVOLVEMENT IN ELECTION/TRAINING/MANAGEMENT: no. GEOGRAPHICAL SETTING: USA, Urban informal. HEALTHCARE SETTING: Home. |
|
| Outcomes | LENGTH OF FOLLOW UP: 23months. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | High risk | Infants whose medical record number ended in odd digits were enrolled in intervention group and those whose number ended in odd digits were enrolled as controls. |
| Allocation concealment? | Unclear risk | Not mentioned. |
| Blinding? All outcomes | Low risk | Visited children and controls not identified in medical records and the study was operated seperate from clinic services. |
| Incomplete outcome data addressed? All outcomes | Low risk | Follow‐up rates were 92% in intervention group and 90% in control group. |
| Free of selective reporting? | Low risk | |
Ireys 1996.
| Methods | RCT. | |
| Participants | LHW: 5 mothers (mentors) with children aged 18 to 24 who had juvenile rheumatoid arthritis (JRA) since childhood. TRAINING: the mentors participated in a 30 hour training programme. The programme focused on enhancing three types of social support: (1) informational support (2) affirmational support (3) emotional support. No information on methods used. PATIENTS: mothers who had been active patients of the pediatric rheumatology clinic at Johns Hopkins Hospital. 87.2% were married; 91.7% had at least high school education; 64.6% worked outside of home at least part‐time. Children with (JRA). Mean age = 7.7 years; 75% were female; 76% of the children had had JRA for 3 years or more. TOTAL=45; INTERVENTION=25; CONTROL=20. | |
| Interventions | OBJECTIVE: to provide social support for mothers with children who have juvenile rheumatoid arthritis (JRA). INTERVENTION: A‐PLUS mentors. CONTROL: no intervention. MODE OF DELIVERY: the mentors aimed to enhance social support (informational, affirmational and emotional) and overall mental health. Their protocol specified that they should (1) make telephone contacts of 5 minutes or more with each assigned mother every 2 weeks (2) meet individually with each mother every 6 weeks (3) hold occasional special events such as picnics. Weekly supervision was provided by the programme coordinators ‐ a psychologist and a social worker. Each mentor also met individually with the social worker once a month to review all assigned families. RECIPIENT INVOLVEMENT IN DESIGN/DEVELOPMENT/DELIVERY: social support provided by mothers with older children who had previously suffered from JRA. ORGANISATIONAL BASE OF THE INTERVENTION: A‐PLUS (Arthritis Parents: Learning, Understanding Sharing) mentors, a commnuity‐based scheme. GEOGRAPHICAL SETTING: urban USA HEALTHCARE SETTING: home and community. | |
| Outcomes | HEALTH STATUS AND WELLBEING: maternal mental health, perceived availability of social support. LENGTH OF FOLLOW UP: 15 months after intervention. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | High risk | Quote:' Randomly assigned to intervention and control group by putting names in a hat'. |
| Allocation concealment? | Unclear risk | Not mentioned. |
| Blinding? All outcomes | Unclear risk | Not mentioned but ascertainment bias possible with instruments with varying scales. |
| Incomplete outcome data addressed? All outcomes | Low risk | Reported on all outcomes stated in objectives. |
| Free of selective reporting? | Low risk | |
| Free of other bias? | Low risk | |
Ireys 2001.
| Methods | RCT. | |
| Participants | LHW: 39 'veteran mothers' or 'experienced' mothers with young adult children affected by chronic disease (diabetes, sickle cell anaemia, moderate to severe asthma and cystic fibrosis). The Network Mothers (NM) were recruited by asking directors and staff of speciality clinics to nominate suitable mothers whose affected child was 18 years or older. TRAINING: network mothers: 30 hour training program, focusing on enhancing skills in listening, reflecting and "story swapping". Role plays, videotaped interviews, and in‐class practice interviews were used. Successful graduates of the training were invited to participate in the programme and then underwent an additional 20 hours of training along with the child life specialists to reinforce the team aspects of the program and to review operational procedures. The network mothers and child life specialists met together weekly with a paediatrician and a social worker to ensure that the intervention was being delivered as planned. These meetings served to co‐ordinate efforts within and across teams, address ongoing problems, and review issues related to recent or upcoming contacts or special events. PATIENTS: Women with children aged 7 to 11 years with one of the following chronic illnesses: diabetes (40%), sickle cell anaemia (19%), cystic fibrosis (9%), moderate to severe asthma (32%). 29% were single mothers of whom 35% only had high school education or less. 70% of mothers had some form of employment. TOTAL=161; INTERVENTION=86; CONTROL=75. | |
| Interventions | OBJECTIVE: to provide social support for mothers of children suffering from chronic illness. INTERVENTION: social support from 'network mothers'. CONTROL: mothers were given a telephone number through which they could reach an experienced parent is they so wished. The experienced parent did not go through any training and did not initiate telephone calls. MODE OF DELIVERY: volunteer mothers performed the following tasks. 7 visits of 60 to 90 minutes to each assigned family, either alone or with the child life specialist; biweekly telephone contacts of at least 5 minutes to build and maintain support, follow up on issues previously discussed or plan future meetings; participation in 3 special events, such as bowling parties or small‐group lunches that would allow program parents to meet each other in a nonstressful venue. Through these interventions, the LHWs provided 3 types of support. 1) informational support, by linking families with existing health and community resources and by sharing information among mothers about child behaviour, parenting and coping. 2) affirmational support, by enhancing a mother's confidence in parenting and by reassuring her that her concerns and issues were appropriate. 3) emotional support, by being available to listen to a parent's concerns, demonstrating a continued interest in the mother's viewpoints and experiences, and effectively communicating an understanding of the mother's feelings and concerns. Each network mother had 1 to 7 assigned families and was paid hourly for all program‐related efforts. RECIPIENT INVOLVEMENT IN DESIGN/DEVELOPMENT/DELIVERY: social support provided by mothers with older children who had previously suffered from a chronic illness. ORGANISATIONAL BASE OF THE INTERVENTION: not described. GEOGRAPHICAL SETTING: urban U.S.A. HEALTHCARE SETTING: home and community. | |
| Outcomes | HEALTH STATUS AND WELLBEING: maternal physical health, maternal anxiety, maternal depression, stressful life events, child psychological adjustment, child depression, child report of general anxiety, child self esteem. CONSULTATION PROCESS: number of contact minutes. | |
| Notes | Child life specialists: this component was designed to enhance the mental health, adjustment and self esteem of children with selected conditions and was delivered by professionals. It was analysed separately. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Randomly assigned participants by using blocks of four cells. |
| Allocation concealment? | Unclear risk | Not mentioned. |
| Blinding? All outcomes | Low risk | Interviewers were blinded, questions pertaining to the group were left to the end. |
| Incomplete outcome data addressed? All outcomes | Low risk | Report on all outcomes stated in objectives, follow‐up rate about 84%. |
| Free of selective reporting? | Low risk | |
| Free of other bias? | Low risk | |
Johnson 1993.
| Methods | RCT. | |
| Participants | LHW: 90 community mothers living in disadvantaged areas who were identified by a local public nurse and interviewed by regional family development nurse to assess suitability. Education level not clear. Community leaders/self promoting individuals were generally excluded. TRAINING: Four weeks of training, during which the concepts of the programme are explained. Community mothers also meet, exchange ideas and explore ways of delivering the programme. Supervised by family nurse. PATIENTS: First time mothers with infant <1 year old. In the control group mean age=23.1 years and in the intervention group mean age=24.1 years. 56% were single; 17% (control) to 29% (intervention) employed; 12% social class I, II, IIINM; 88% social class IIIM,IV,V; 40% live in private housing; 60% live in local authority housing; 42% of fathers employed. TOTAL=262; INTERVENTION=141; CONTROL=121. | |
| Interventions | OBJECTIVE: to deliver a child development programme (early reading as a child, language development, cognitive development through play) to disadvantaged mothers. INTERVENTION: non‐professional community mothers. CONTROL: no intervention. MODE OF DELIVERY: one volunteer mother supports 5 to 15 first time parents with guidance on health/development. After training, each community mother works under the guidance of a family development nurse, who serves as a resource person, confidante, and monitor. RECIPIENT INVOLVEMENT IN DESIGN/DEVELOPMENT/DELIVERY: not described. ORGANISATIONAL BASE OF THE INTERVENTION: based upon the principles inherent in the Early Childhood Development Unit in the University of Bristol. GEOGRAPHICAL SETTING: urban Ireland. HEALTHCARE SETTING: home. | |
| Outcomes | HEALTHCARE BEHAVIOURS: immunisations, dietry nutrition intake, number of mothers who read to their children, the extent to which mothers use nursery rhyme and song with their children. HEALTH STATUS AND WELLBEING: mother's self esteem, relative risk of having an accident, mother's feeling in year since child was born, hospital admissions. LENGTH OF FOLLOW UP: one year. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Used table of random numbers. |
| Allocation concealment? | Low risk | Cards were sealed, put in marked envelopes and drawn in consecutive order. |
| Blinding? All outcomes | High risk | The family development nurse who told mothers the group they were assigned to also collected data and could lead to bias in reporting. |
| Incomplete outcome data addressed? All outcomes | Low risk | Outcomes stated in objectives are reported. |
| Free of selective reporting? | Low risk | |
| Free of other bias? | Low risk | |
Jump 2006.
| Methods | RCT. | |
| Participants | LHW: Volunteers who were members of staff at orphanages. TRAINING: Were trained in infant massage by PHD level certified instructor, but there is no indication how long training lasted. PARTICIPANTS: Were about 10month old infants, entered into orphanage at 2‐3months, most were females. TOTAL: 37 children; INTERVENTIONS: 17 children; CONTROL= 20 children. |
|
| Interventions | OBJECTIVE: To investigate whether therapeutic infant massage could reduce diarrhoeal episodes and decrease overall illnesses of infants. CONTROL: standard care at orphanage, no intervention. MODE OF DELIVERY: Supervised and took care of daily needs of infants in orphanage. As part of the intervention, they gave infants full body massage. RECIPIENT INVOLVEMENT IN SELECTION/TRAINING/MANAGEMENT: None. GEOGRAPHICAL SETTING: Urban Formal, Ecuador HEALTHCARE SETTING: Institution ‐ Orphanage. |
|
| Outcomes | HEALTH STATUS AND WELLBEING: Incidence rate of diarrhoea, Incidence rate of any illness. LENGTH OF FOLLOW UP: 53 days. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | After matching children by age, randomly assigned them to intervention or control groups. No details how this was done. |
| Allocation concealment? | Unclear risk | Not mentioned. |
| Blinding? All outcomes | High risk | Orphanage staff were not blinded, delivered the intervention as well as data on the outcome. |
| Incomplete outcome data addressed? All outcomes | High risk | 71% follow‐up rate. Followed children for only 53 days. |
Kartin 2002.
| Methods | RCT. | |
| Participants | LHW: Paraprofessional advocates that had personal experience with many of the same types of adverse life circumstances as their clients and functioned as positive role models with a realistic perspective. TRAINING: Not specified. PARTICIPANTS: Mothers who abuse alcohol and drugs heavily during pregnancy and effect on child development. Aim of intervention to assist mothers in obtaining alcohol/drug treatment and staying in recovery and to help families resolve the complex problems that arises within context of maternal substance abuse. TOTAL= 78; INTERVENTIONS: Intervention=53; CONTROL=25. |
|
| Interventions | OBJECTIVE: To describe the performance of children whose mothers abused alcohol and drugs heavily during pregnancy and to examine the effects of study group, prenatal binge alcohol exposure, and prematurity on developmental outcome. CONTROL: Had access to community social, health services but did not receive home visitation and advocacy intervention. MODE OF DELIVERY: Weekly home visits for first 6 wks, then twice monthly or more frequent depending on clients needs. Linked clients with appropriate service providers and transported them and their children to important appointments. Worked actively within the context of the clients' extended families. If child did not remain in mothers custody, advocates made every attempt to work with child's caregiver. Advocates linked clients with health care, parenting classes, and therapeutic childcare as available in the mothers' communities and substance abuse treatment programs. RECIPIENT INVOLVEMENT IN SELECTION/TRAINING/MANAGEMENT: no. GEOGRAPHICAL SETTING: USA, urban formal. HEALTHCARE SETTING: Home. |
|
| Outcomes | HEALTH STATUS AND WELLBEING: Growth at 3 years ? height, weight, head circumference, Mental Developmental Index, Psychomotor Developmental Index. LENGTH OF FOLLOW UP: 3 years. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Assigned at random to either hospital recruited group or control. |
| Allocation concealment? | Unclear risk | Not mentioned. |
| Blinding? All outcomes | Unclear risk | Not clear if primary investigator who assessed the children was aware of group assignment. |
| Incomplete outcome data addressed? All outcomes | Low risk | Reported on all stated in objectives. |
| Free of selective reporting? | Low risk | |
| Free of other bias? | High risk | Children referred from the community were assigned to the intervention group though baseline assessments are said to have been similar to the children in the hospital and control groups. |
Kidane 2000.
| Methods | Cluster RCT. | |
| Participants | LHW: mother coordinators chosen by neighborhood groups of 10‐44 households. TRAINING: 2 months of malaria specific training from Malaria Control Program (MCP) including how to teach neighborhood mothers to recognise symptoms of malaria in children <5 years; give appropriate course of treatment; recognise adverse drug reactions, share chloroquine appropriately. PATIENTS: children <5 years and their mothers. TOTAL=13,677 children in 24 tabias; INTERVENTION=6383 children in 12 tabias; CONTROL=7294 children in 12 tabias. | |
| Interventions | OBJECTIVE: to recognise malaria symptoms in children <5 years old, give appropriate course of treatment, recognise adverse drug reactions and share chloroquine appropriately. INTERVENTION: mother coordinators deliver malaria specific services as well as keep check on births/deaths and have information on where to refer sick children. CONTROL: coordinators but no malaria specific services. MODE OF DELIVERY: mother coordinators were supplied with drugs for distribution to all households and were responsible for monitoring/replenishing drugs (using pictorial treatment charts to calculate dosage by age). They refered children for further treatment if no improvement in 48 hours. RECIPIENT INVOLVEMENT IN DESIGN/DEVELOPMENT/DELIVERY: households within the villages selected their mother coordinators. ORGANISATIONAL BASE OF THE INTERVENTION: Malaria Control Program (MCP), organised by the department of health. GEOGRAPHICAL SETTING: rural Ethiopia. HEALTHCARE SETTING: home. | |
| Outcomes | HEALTH STATUS AND WELLBEING: mortality rate in children <5 years old, number of possible malaria deaths in children <5 years old. LENGTH OF FOLLOW UP: one year after intervention. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | One tabia of each of the 12 groups was selected by random number (not clear how this was generated, but was probably done). |
| Allocation concealment? | Low risk | Each tabia assigned a code before pairing and randmonising to intervention and control. |
| Blinding? All outcomes | Low risk | Blinding not possible, Mortality is outcome of interest. |
| Incomplete outcome data addressed? All outcomes | Low risk | Data on all clusters presented, attrition rate at individual level not reported. |
| Free of selective reporting? | Low risk | Outcome stated in objectives are reflected in results presented. |
| Free of other bias? | High risk | Used verbal autopsies to identify cause of death as malaria when illnesses such as measles and chronic wasting, were occuring. Authors addressed this by verifying 1/3 of the reported deaths plus using a second assessor who was masked. |
Kouyate 2008.
| Methods | RCT. | |
| Participants | LHW: Community members from intervention villages selected women group leaders. Inclusion criteria were permanent residence in sub‐village, age 30‐50years, honesty, respect by community. TRAINING: Were trained in peripheral health centres by health workers under supervision of the investigators. Were trained for two days on relevant aspects of malaria knowledge and management including referral criteria. Training included discussions as well as practical sessions using locally produced pictorial sensitisation material and role play, with one refresher course over the study period. Were supplied with a free, six month supply of prepacked choloroquine and paracetamol doses from the health district. Drugs were sold to the mothers at a small profit used as an incentive. PARTICIPANTS: Households with children below 5 years of age. Total of 1,083 children at baseline and 1006 children at follow up were included in the study. Median age in months was about 30 ‐ 35 months with a median age range of 4‐60. Were mostly from the Marka and Bobo ethnic groups, socioeconomic status was not clear. TOTAL=1083 children at baseline and 1006 at follow up. INTERVENTION: 542 at baseline survey, 496 at follow up. CONTROL: 496 at follow up and 510 at baseline. |
|
| Interventions | OBJECTIVE: To evaluate the feasibility and effectiveness of an intervention aimed at improving case management of malaria in under five children through primary caretakers in collaboration with local women groups and existing health centres. CONTROL: Usual care. MODE OF DELIVERY: Under the supervision of local health workers, women leaders trained an average of 15 mothers for half a day in their sub‐villages on correct malaria management. Had a stock of pre‐packaged treatment for malaria (chloroquine and paracetamol), provided early treatment for febrile children and directly supervised its consumption, visited sick child on day two and three. In case of danger signs at any point during treatment, women group leaders refered the child to the health centre. RECIPIENT INVOLVEMENT IN SELECTION/TRAINING/MANAGEMENT: In selection. GEOGRAPHICAL SETTING: Burkina Faso, Rural HEALTHCARE SETTING: Home. |
|
| Outcomes | HEALTH STATUS AND WELLBEING: Presence of fever, anemia, Falciparum malaria, splenic enlargement. Median weight (kg). LENGTH OF FOLLOW UP: 2 years. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Randomisation process for the clusters not clear. |
| Allocation concealment? | Unclear risk | Not mentioned. |
| Blinding? All outcomes | Unclear risk | Assessors were located at another site but it is not clear if the physician and laboratory assessors were blinded. |
Krieger 2000.
| Methods | RCT. | |
| Participants | LHW: peer to peer outreach volunteers were predominantly African‐American senior centre members. TRAINING: 4 hours training including role play sessions. PATIENTS: participants were aged >65 years and resident in targeted ZIP code areas. Ethnically diverse; most low income; most had no complete college. TOTAL=1246; INTERVENTION=622; CONTROL=624. | |
| Interventions | OBJECTIVE: to encourage immunization against influenza and pneumonia. INTERVENTION: Peer to peer outreach volunteers. CONTROL: no intervention. MODE OF DELIVERY: each volunteer contacted 20‐25 intervention group participants and used script to encourage immunisation of defaulters (receipt of immunization/address barriers to immunization); mailing of educational material. Intervention lasted for 6 weeks. If volunteer could not reach participant after 5 attempts then alternative contact person phoned. Volunteers were assisted by an on site project coordinator. RECIPIENT INVOLVEMENT IN DESIGN/DEVELOPMENT/DELIVERY: volunteers were predominantly senior citizens. ORGANISATIONAL BASE OF THE INTERVENTION: not described. GEOGRAPHICAL SETTING: urban USA HEALTHCARE SETTING: home. | |
| Outcomes | HEALTHCARE BEHAVIOURS: influenza and pneumococcal immunization. COST: cost and cost effectiveness. OTHER: change in knowledge, perceived barriers to immunization, appraisal of the intervention. LENGTH OF FOLLOW UP: three months after intervention. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | High risk | Used systematic allocation of participants to intervention or control. |
| Allocation concealment? | Unclear risk | Not mentioned. |
| Blinding? All outcomes | Unclear risk | Not mentioned. |
| Incomplete outcome data addressed? All outcomes | Unclear risk | Report on all outcomes stated in objectives. Self report of immunization among group over 65 years may not be reliable however this would affect both groups. |
Kumar 2008.
| Methods | Cluster RCT. | |
| Participants | LHW: Community‐based healthworkers or Saksham‐ Sahayak, were recruited from community, with 12 years of education or more, proficient communication and reasoning skills, commitment towards community work, and references of community stakeholders. Were compensated similar to community‐based workers in India (USD35‐40). Also used volunteers from within the community (Saksham Karta) who played a key part in program advocacy, trust‐building and social legitimisation of changes in behaviour. Mothers that received the intervention and displayed exemplary practices were promoted as role models to inspire other pregnant women in the community. TRAINING: Had a 7 day training, classroom and apprenticeship‐based field training on essential newborn care within the community, behaviour change management and trust building. PARTICIPANTS: Pregnant women from 18,989 households that were visited. Mean number of residents per household was about 5 (SD 0.3), Most were Hindu (Mean about 93, sd5.9). Mean number of literate women in reproductive age group 15 ‐ 49 years was about 38, sd 9.7, most were married (Mean 83, SD2.4). Routine antenatal seeking behaviour was low <10%, more than 90% deliveries were at home, less than 15% attended by a skilled attendant . Most had medium standard of living index as calculated by the National family Health survey method (Mean 56, SD2), roughly one third had lowest standard of living. Mostly form scheduled caste/tribe ‐ the lowest caste designation. TOTAL= 29 clusters (2511 women). INTERVENTIONS: Intervention 1 (Essential Newborn care) = 13 clusters (1600 pregnant women); Intervention 2 (Essential newborn care + thermospot) = 13 clusters (1149 pregnant women); Control = 13 clusters (1141 pregnant women). |
|
| Interventions | OBJECTIVE: To modify high risk newborn care practices with an emphasis on hypothermia within a community with high neonatal mortality rate so as to improve care practices and reduce mortality. CONTROL: Usual services of government and non‐governmental organisations in the area. MODE OF DELIVERY: 1. Engaged community stakeholders in meetings to seek approval, sensitise them of the importance of their role in newborn survival, encourage shared learning and create a supportive environment. 2. Held folk song group meetings once every month where folk songs incorporating behavioural change mechanisms were used. Also held monthly meetings with newborn stakeholders and community volunteers to discuss experiences, challenges and strategies. 3. Early identification of pregnant women, seeking their consent, enrolling them, and providing the intervention. This was achieved by 3‐monthly door to door household visits. RECIPIENT INVOLVEMENT IN SELECTION/TRAINING/MANAGEMENT: Yes, in selection of LHWs. GEOGRAPHICAL SETTING: India, Rural HEALTHCARE SETTING: Home. |
|
| Outcomes | HEALTHCARE UTILISATION: Newborn care, birth preparedness. HEALTH STATUS AND WELLBEING: Neonatal mortality rates, all births and singleton, perinatal mortality rates. HEALTH BEHAVIOUR: Routine care during pregnancy, hygienic delivery and immediate newborn care, Thermocare including skin to skin care, umbilical cord and skin care, breastfeeding. CONSULTATION: Danger sign recognition and care seeking. UTILISATION: Care‐seeking providers used. LENGTH OF FOLLOW UP: 16 months. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Used stratified randomised design, randomisation done centrally by computer using stata 7.0. |
| Allocation concealment? | Low risk | Allocation not masked because of visibile nature of intervention. Closely monitored boundaries to limit communication between teams. |
| Blinding? All outcomes | Unclear risk | Not clear if the data collectors were different from those delivering the intervention. |
| Incomplete outcome data addressed? All outcomes | Unclear risk | No clusters lost to follow up, length of study 16 months, not clear if all outcomes reported. |
| Free of selective reporting? | Unclear risk | Insufficient information to make an assessment. |
LeBaron 2004.
| Methods | RCT. | |
| Participants | LHW: 2 outreach workers, college educated. TRAINING: not described. Supervised by a person with a doctorate in community psychology and extensive experience in conducting inner city studies. PARTICIPANTS: Children born over 1 year (July 1995‐August 1996), 51% female. Median age at start of study = 9 months, range 1‐14months. 76% Black, 14% Hispanic, 7% White non‐Hispanic, 3% other. This was an inner city population with a high proportion of minorities (93% of study population) and who utilised publicly funded health services. TOTAL=3050; INTERVENTIONS: Combination: LHW outreach and autodialler= 764, LHW outreach=760, Autodialler=763. CONTROL=763. |
|
| Interventions | OBJECTIVE: To evaluate the impact of large‐scale, registry‐based reminder‐recall interventions on low immunization rates in an inner‐city population. CONTROL: Usual care, in certain instances involved non‐automated postcard recall system. MODE OF DELIVERY: Outreach: If a child missed a vaccination, the outreach worker attempted to contact the family by telephone or postcard (attempted to contact family within 7 days of child failing to receive dose by the due date, sent postcard 7 days later if no contact). If the child was not brought for vaccination in the next 30 days, the outreach worker conducted a home visit to determine what was needed to assist the family in obtaining immunization. Made monthly contact until contact was made. Autodialler: A week before dose was due computer connected to telephone delivered a reminder to the family, if no answer or line busy, call repeated every 30 to 60 min. If failed to establish contact, an automated postcard sent not later than 5 days before due date. If no vaccination recorded 6 days after due date computerised telephone message (or postcard if no telephone) sent to the family. If no vaccination registered, telephone message repeated on day 11, 17 and 23 days. If no contact, a computerised postcard was sent on day 28. All calls were made 5‐9pm, with Spanish and English language options. RECIPIENT INVOLVEMENT IN SELECTION/TRAINING/MANAGEMENT: No. GEOGRAPHICAL SETTING: urban formal, USA HEALTHCARE SETTING: Home. |
|
| Outcomes | HEALTHCARE BEHAVIOURS: Proportion of children with complete vaccination at 24 months of age, with 1 missed opportunity for vaccination, with missed opportunities as a reason for under vaccination. LENGTH OF FOLLOW UP: 24 months. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Used computer generated numbers. |
| Allocation concealment? | Unclear risk | Not mentioned. |
| Blinding? All outcomes | Low risk | Authors reported not having attempted blinding. This is unlikely to cause bias as vaccination status is not subjective. |
| Incomplete outcome data addressed? All outcomes | Low risk | Report on outcomes stated in objectives but not clear what happened to the 25% who were randomised but did not receive intervention ‐ check to see if intention‐to‐treat analysis was done? |
Leite 2005.
| Methods | RCT. | |
| Participants | LHW: The lay counsellors had personal experience in breastfeeding. They comprise a workgroup associated for more than 5 years with the Milk Bank at the university undertaking the research. Paid US$4 for every visit.
TRAINING: Besides periodic training and supervision, the LHWs also received a 20 hour theory‐practice course adapted from a course described in 'Breastfeeding counselling: a training course' (Rea 1999).
PARTICIPANTS: Mothers of low birthweight (less than 3000g) but otherwise healthy babies. Inhabitants of Ceara in low income areas of Brazil, lower socioeconomic classes. Average age of mothers = 23 years; 18% single. Average schooling = 6 years; 11% illiterate. TOTAL = 1003; INTERVENTION = 503; CONTROL = 500. |
|
| Interventions | OBJECTIVE: To provide home‐based peer counselling to increase breastfeeding rates for unfavourably low birthweight babies. INTERVENTION: Visits were focused on problem identification, observation & counselling. Activities included: (1) interviews with the mother: (2) observation of the home environment; (3) observation of all aspects involved with the breastfeeding, including technical ones, as well as the mother‐child relationship; (4) identification of the difficulties faced by the mother during breastfeeding and the type of counselling providing. CONTROL: no specific intervention. They were instructed in the maternity ward, by a study employee, to seek out their local health service facility in case of any health problems. MODE OF DELIVERY: Mothers received visits on days 5, 15, 30, 60, 90 and 120 after delivery. Visits lasted an average of 30‐40 minutes. Each visit began with two open questions to the mother: 'How are you feeling? How is your child's health?' The counsellor would then identify specific difficulties or problems related to the breastfeeding itself and conclude with the necessary counselling. RECIPIENT INVOLVEMENT IN SELECTION/TRAINING/MANAGEMENT: not described. GEOGRAPHICAL SETTING: urban formal, Brazil HEALTHCARE SETTING: home. |
|
| Outcomes | HEALTHCARE BEHAVIOURS: Proportion of babies at 4 months of age who: exclusively breastfed; predominantly breastfed; partially breastfed; and artificially fed. LENGTH OF FOLLOW UP: 4 months. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | 'Groups were formed...using a table of computer‐generated random numbers' (p742). |
| Allocation concealment? | Unclear risk | '...designated each mother to one of the study groups after opening a sealed envelope that contained the respective group code' (742). Not described whether envelopes were opaque. |
| Blinding? All outcomes | Low risk | 'The interviewers had not had any prior contact with the mothers and were also unaware as to the objectives of the research' (p743). |
| Incomplete outcome data addressed? All outcomes | Low risk | Missing outcome data balanced in numbers across intervention groups. 'No difference was found in the variables studied for the pairs that had dropped out' (p743). |
| Free of selective reporting? | Unclear risk | Insufficient information to make an assessment. |
| Free of other bias? | Low risk | |
Luby 2006.
| Methods | RCT. | |
| Participants | LHW: Field workers recruited from the study or nearby communities. TRAINING: Trained extensively in interviewing techniques, data recording, general approaches to community motivation and in specific techniques for promoting handwashing and drinking water treatment. PARTICIPANTS: Households with at least 1 child under 5 years of age. Average of approximately 9 persons per household. Communities that received at least 1 hr of running water twice weekly. Mean no. of persons per household was 8‐10 in each group, 1‐2 rooms per house, mean no. of children<5yrs approx 2. TOTAL= 47 neighbourhoods. INTERVENTION: 10 bleach neighbourhoods; 9 handwashing neighbourhoods; 9 flocculant‐disinfectant neighbourhoods, 10 flocculant‐disinfectant plus handwashing neighbourhoods. CONTROL= 9 neighbourhoods. |
|
| Interventions | OBJECTIVE: To evaluate the effectiveness of point of use water treatment with flocculent‐disinfectant on reducing diarrhoea and the additional benefit of handwashing. CONTROL: no intervention, got regular supply of childrens books, notebooks, pens and pencils but no products expected to affect diarrhoea. MODE OF DELIVERY: (1) Arranged neighbourhood meetings where health problems resulting from hand and water contamination were discussed and instructions given on how to use the intervention; (2) Visited each participating household at least twice weekly to encourage use of the interventions, answer questions and provide supplies; (3) Provided specific instructions and support regarding the use of the intervention allocated to their neighbourhood; (4) Collected health outcome data from intervention and control households. RECIPIENT INVOLVEMENT IN SELECTION/TRAINING/MANAGEMENT: not specified. GEOGRAPHICAL SETTING: Pakistan, Urban informal. HEALTHCARE SETTING: Home. |
|
| Outcomes | HEALTHCARE UTILISATION: uptake of antenatal and delivery services, home care practice at delivery and post partum and healthcare seeking. HEALTH STATUS AND WELLBEING: Prevalence of diarrhoea. LENGTH OF FOLLOW UP: up to 37 weeks. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Used computer generated random numbers. |
| Allocation concealment? | Unclear risk | Not mentioned. |
| Blinding? All outcomes | High risk | Personnel and participants were not blinded to intervention. |
| Incomplete outcome data addressed? All outcomes | Low risk | Follow‐up rates were >80%. Report on all outcomes stated in objectives. |
| Free of other bias? | High risk | Intervention households were given supplies free of cost and this could have biased their responses. |
Lwilla 2003.
| Methods | Cluster RCT. | |
| Participants | LHW: Called Community‐based DOT (CBDOT) observers and were volunteers who lived in same village as the patient.
TRAINING: Trained by the district TB‐Leprosy coordinator to supervise the patient's intake of TB treatment during the intensive treatment phase.
PARTICIPANTS: Most people in this district were subsistence farmers, with very low overall family income. Mean age was 35 years, about 38% females in each group. TOTAL = 18 TB treatment units (522 patients); INTERVENTION = 9 units (221 patients); CONTROL = 9 units (301 patients). |
|
| Interventions | OBJECTIVE: To provide community‐based DOT to people with TB. INTERVENTION: Daily observation of patient's intake of TB medications during intensive phase of TB treatment (first 2 months). Depending on the patient's condition, they occasionally collected drugs from health facility but this was usually done by patients. Monitoring was by TB health worker from the health facility and once monthly by the District TB‐Leprosy officer. After the intensive phase, patients visited the clinic monthly to collect medication and self‐supervised treatment. CONTROL: During the intensive phase, patients visited the health facility daily to be observed while taking their TB medication. Thereafter they visited monthly to collect medication and self‐supervised treatment. MODE OF DELIVERY: DOT delivered in communities. RECIPIENT INVOLVEMENT IN SELECTION/TRAINING/MANAGEMENT: LHWs interviewed and selected by village leaders. GEOGRAPHICAL SETTING: rural Tanzania HEALTHCARE SETTING: home. |
|
| Outcomes | HEALTH STATUS AND WELLBEING: Proportion of AFB‐postive pulmonary TB patients with AFB‐negative sputum after 2 months of treatment (primary outcome); number of patients cured at 7 months. LENGTH OF FOLLOW UP: 7 months. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | 'Each pair (of clinics) was given a unique number...and one treatment unit within each pair was randomly assigned to IBDOT or CBDOT' (p206). Comment: not clear how the randomisation sequence was generated. |
| Allocation concealment? | Low risk | Cluster RCT. |
| Blinding? All outcomes | Low risk | No blinding, but the outcome and the outcome measurement are not likely to be influenced by lack of blinding. |
| Incomplete outcome data addressed? All outcomes | Unclear risk | 'Overall losses to follow‐up 2 months after recruitment were similar the IBDOT (33 of 301) and the CBDOT (24 of 241) groups...At 7 months, the overall loss to follow‐up was higher in CBDOT compared with IBDOT and significant heterogeneity between the two groups persisted' (p207) Comment: reason for missing outcome data may be related to outcome. However, sensitivity analyses on the results suggested that they would not be altered by more complete follow up. |
| Free of selective reporting? | Unclear risk | Insufficient information to make an assessment. |
| Free of other bias? | Low risk | |
MacArthur 2009.
| Methods | RCT, Cluster randomised. | |
| Participants | LHW: Peer support workers (n=11), were peers of women in the clinic in which they worked, selected on basis of ethnicity and language, personal successful experience of breastfeeding of several months duration. TRAINING: Received daily training over 8 weeks, based on UNICEF baby friendly breastfeeding management course, addressed cultural beliefs and barriers of the local population. Were oriented into the environment of the community antenatal service where they worked for three months. PARTICIPANTS: Were pregnant women, about 60% between 21 ‐ 30 years old, 70% had vaginal delivery, 65.6% were multiparous. Most of the deliveries are in hospital (96%). Most common ethnic group were Pakistani (40%), African Caribbean (15%), and Bangladeshi(10%), ethnic British were 9.4%. 70% were in the lowest 10th for deprivation (Townsend score), 11% for 2nd and 4th to 10th scores. TOTAL= 2511 women; INTERVENTIONS: Peer Support =1140; Control=1371. |
|
| Interventions | OBJECTIVE: To assess the effectiveness of an antenatal service using community based breastfeeding peer support workers on initiation of breastfeeding. CONTROL: Standard antenatal care including usual information and advice from midwives on breast feeding but without input from the community support workers. MODE OF DELIVERY: Contacted pregnant women in antenatal clinic followed by a minimum of two other contacts, one at 24‐26 weeks and another at 36 weeks and at least 1 visit at home. Provided information and advice on breastfeeding benefits and support to women with particular cultural barriers and concerns. RECIPIENT INVOLVEMENT IN SELECTION/TRAINING/MANAGEMENT: no. GEOGRAPHICAL SETTING: UK, Urban formal. HEALTHCARE SETTING: Primary Health Care and Home. |
|
| Outcomes | HEALTH BEHAVIOUR: Rates of initiation of breastfeeding. LENGTH OF FOLLOW UP: 6 months. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Stratified by size of antenatal clinic and midwifery team, and used computer program to randomise. |
| Allocation concealment? | Low risk | Statistician was blinded to the identity of antenatal clinics. |
| Blinding? All outcomes | Low risk | Data obtained in anonymised format from hospital records. Not possible to blind those delivering and receiving intervention. |
| Incomplete outcome data addressed? All outcomes | Low risk | Report on outcomes as reflected in objectives, follow‐up rates >80%. |
| Free of selective reporting? | Unclear risk | Insufficient information to make an assessment. |
Malchodi 2003.
| Methods | RCT. | |
| Participants | LHW: Peer counsellors selected from an existing pool of non‐smoking, female, community outreach workers who possessed the same social environmental and cultural qualities of the participants. TRAINING: 2 standardised training sessions in smoking cessation from local expert. Role playing and didactic format for basic strategies for motivational counselling. Training by a 'local expert'. PARTICIPANTS: Pregnant and smoking women less than 20 wks gestation, 18yrs or older, median age was 25yrs. Smoked more than one half a pack per day at baseline. Most had less than high school education, were mainly low income and Hispanic. TOTAL=142; INTERVENTIONS: Peer counselling group=67; CONTROL=75. |
|
| Interventions | OBJECTIVE: To evaluate a peer counselling intervention for pregnant smokers. CONTROL: Usual care provided by the clinic staff physicians, residents, nurse practitioners and nurses. MODE OF DELIVERY: Encouraged pregnant women in the quit attempt, communicate caring and concern, encourage the woman to talk about the quitting process, and to reinforce basic information about smoking and successful quitting. Support and reinforcement of the stop smoking messages of the health care providers using a standardised prompt sheet. RECIPIENT INVOLVEMENT IN SELECTION/TRAINING/MANAGEMENT: no. GEOGRAPHICAL SETTING:USA, Rural. HEALTHCARE SETTING: Home and Primary Health Care Clinic. |
|
| Outcomes | HEALTH STATUS AND WELLBEING: Change in number of cigarettes per day, Quit rates, Carbon monoxide level at 36 weeks, Proportion of subjects abstinent at 36 weeks. LENGTH OF FOLLOW UP: 2 years. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Used computer generated numbers list. |
| Allocation concealment? | Unclear risk | Not mentioned. |
| Blinding? All outcomes | Low risk | Used obstetric care providers who were blind to group assignment. |
| Incomplete outcome data addressed? All outcomes | Low risk | Report on all outcomes stated in objectives. At the end of the study 43% of the peer counseling group and 36% of the usual care group were lost to follow up. The differences were adjusted for at analysis. |
| Free of selective reporting? | Unclear risk | insufficient information to make an assessment. |
Malotte 2001.
| Methods | RCT. | |
| Participants | LHW: Outreach worker who observed treatment taking among participants ‐ no further information provided. TRAINING: No information on training or monitoring of LHWs. PARTICIPANTS: Injection or crack cocaine users with positive tuberculin skin test. Predominantly male 82%, mean age 42 years (range 23 ‐ 69), 68% used crack cocaine, 13% injecting drug users and 14% used both in past 30 days. 42.3% had high school education and 23.9% more than high school education. Predminantly unemployed; 87.7% had no work and 41.7% had their own home/apartment. 70.6% of participants were African American males; 13.5% were white. TOTAL=163; INTERVENTION 1=53; INTERVENTION 2=55; INTERVENTION 3=55. | |
| Interventions | OBJECTIVE: To improve the adherence to drug users to treatment for TB prophylaxis. INTERVENTION 1: Twice weekly directly observed therapy (DOT) of TB prophylaxis treatment taking among drug users. The LHWs supplied TB drugs to the participants, and observed them swallowing the drugs at a location chosen by the participant. Each participant also received a US$5 incentive at each visit. INTERVENTION 2: Same as intervention 1, but with no incentive. INTERVENTION 3: DOT at a study community site and a monetary incentive. MODE OF DELIVERY: No further information available. RECIPIENT INVOLVEMENT IN DESIGN/DEVELOPMENT/DELIVERY: not described. GEOGRAPHICAL SETTING: urban informal, USA HEALTHCARE SETTING: a community location chosen by each participant. |
|
| Outcomes | HEALTHCARE BEHAVIOURS: percentage of medications taken on time; completion of the course of medication. LENGTH OF FOLLOW UP: minimum of 26 weeks. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | 'Study participants were randomly assigned to one of three treatment conditions within blocks of 18.' (p104). Comment: insufficient information about the sequence generation process. |
| Allocation concealment? | Low risk | 'Numbered, opaque, sealed envelopes containing the treatment condition assignment were used sequentially...Once a number was assigned, it was not reassigned...' (p104). |
| Blinding? All outcomes | High risk | 'Masking of treatment condition was not possible' (p104). Comment: No blinding and outcome may have been influenced by lack of blinding. |
| Incomplete outcome data addressed? All outcomes | Low risk | No missing outcome data. |
| Free of selective reporting? | Unclear risk | Insufficient information to make an assessment. |
| Free of other bias? | Low risk | |
Manandhar 2004.
| Methods | RCT. | |
| Participants | LHW: A local female facilitator that was literate, locally resident women. Was nominated by community leaders, through advertisements, or word of mouth after which potential candidates were interviewed. TRAINING: Not specified. PARTICIPANTS: Married women of reproductive age(15‐49). Most (70%) were between 20‐39 yrs old women,80% had never been to school. TOTAL= 42 clusters; INTERVENTIONS: 12 clusters(1133 median households, 14,884 participants); CONTROL=12 clusters(733 median households, 14,047 participants). |
|
| Interventions | OBJECTIVE: To assess if community‐based participatory intervention could significantly reduce neonatal mortality rates. CONTROL: Standard of care, but for ethical reasons health services in both intervention and control areas were strengthened by equipping PHC centres with resuscitaires, phototherapy units, warm cots, neonatal resuscitation equipment. Shortfalls in essential neonatal drugs were remedied, discussed strategies for resupply with local health‐service managers. Training in essential newborn care for all cadres of government health staff, female community health volunteers and traditional birth attendants was given. MODE OF DELIVERY: Local facilitators helped convene, activate and strengthen women's group meetings. Provided support through an action research cycle. This involved: discussing issues about childbirth and care behaviour with the community that allowed facilitator develop participatory learning skills and generate information on pregnancy, childbirth, beliefs and practices. Together with the women they then identified the key problems, developed strategies to overcome them. The women groups then implemented and assessed their strategies. RECIPIENT INVOLVEMENT IN SELECTION/TRAINING/MANAGEMENT: yes, in identification of facilitators, problem prioritisation and development of strategies. GEOGRAPHICAL SETTING: Nepal; Rural. HEALTHCARE SETTING: Rural Nepal, has district hospital (7852 people per hospital bed) with maternal child health services, health service has network of primary health care centres, health posts, subhealth posts, outreach clinics. |
|
| Outcomes | HEALTHCARE UTILISATION: uptake of antenatal and delivery services, home care practice at delivery and postpartum and healthcare seeking. HEALTH STATUS AND WELLBEING: Neonatal mortality rates, stillbirth rate, maternal death, infant morbidity. LENGTH OF FOLLOW UP: 2 years. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Used random numbers to select 12 clusters. Used coin toss to allocate one of each pair to intervention or control groups. |
| Allocation concealment? | Low risk | Concealed cluster allocation sequence in city before enrolment of the participants. |
| Blinding? All outcomes | Low risk | Blinding not possible because of nature of the intervention. |
| Incomplete outcome data addressed? All outcomes | Low risk | Data reflects the outcomes stated in objectives. All clusters selected received the allocated intervention, dropout rates about 5% in each group. |
Merewood 2006.
| Methods | RCT. | |
| Participants | LHW: women with breastfeeding experience drawn from local community. Used 2 US born African‐American women, 1 non US‐born Mexican woman, 1 white US‐born woman and 1 native white American woman. Two of the women were also employed at the hospital as lay childbirth assistants and two were former teenage mothers.
TRAINING: 5 day breastfeeding course operated by Centre for Breastfeeding [www.healthychildren.cc/index4.htm]. Were trained in hospital about NICU procedures, breastfeeding techniques and at regular, mandatory breastfeeding days for maternity staff throughout the course of their employment.
PARTICIPANTS: Eligible women had a healthy premature infant (26‐37 weeks gestation); spoke English or Spanish; were eligible to breastfeed according to current guidelines and chose to do so. 72.9% and 66% in intervention and control groups respectively were African American. About 505 in each group were on Medicaid. TOTAL=108; INTERVENTION=53; CONTROL=55. |
|
| Interventions | OBJECTIVE: Infant feeding counselling with emphasis on encouraging breastfeeding to mothers with preterm babies.
INTERVENTION: Emphasis was placed on face to face contact. One face to face meeting (at least 30 minutes) at hospital within 72 hours of birth. Thereafter weekly until 6 weeks. Met with mother whenever possible before discharge. Thereafter telephone contact unless mother chose to come to hospital. Peer counselors followed written guidelines for each contact to establish consistency of care. Counsellors had immediate daily access to a lactation consultant working on the unit and to project managers.The lactation consultants and the project managers presence helped to ensure peer counsellor consistency, accuracy of knowledge and reliability. CONTROL: Control group women received standard of care treatment, which in the baby friendly hospital included referral to the lactation consultant when needed, use of a pump in hospital, access to 3 breastfeeding classes per week and staff highly trained in lactation. MODE OF DELIVERY: Face to face contact initially and telephone contact thereafter. RECIPIENT INVOLVEMENT IN SELECTION/TRAINING/MANAGEMENT: not described. GEOGRAPHICAL SETTING: USA, urban formal. HEALTHCARE SETTING: home. |
|
| Outcomes | HEALTHCARE BEHAVIOURS: Any breastmilk at 12 weeks; mostly breastmilk at 12 weeks (more than 50% of feeds); only breastmilk at 12 weeks. LENGTH OF FOLLOW UP: 12 weeks. |
|
| Notes | Although this intervention was initiated in the hospital setting, it was decided to include it in the review as much of the intervention was delivered once the mothers and babies had been discharged home. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | 'Randomization was performed using SAS' (p682). |
| Allocation concealment? | Unclear risk | 'Numbered envelopes were prepared by the primary investigator...opened the sealed envelope' (p682). |
| Blinding? All outcomes | Low risk | 'Infant feeding status was assessed by a research assistant unaware of the mother's group assignment' (p682). |
| Incomplete outcome data addressed? All outcomes | Low risk | Missing outcome data balanced in numbers across intervention groups, with similar reasons for missing data across groups. |
| Free of selective reporting? | Unclear risk | Insufficient information to make an assessment. |
| Free of other bias? | Low risk | |
Mohan 2003.
| Methods | RCT. | |
| Participants | LHW: All were women from the same district where the study was conducted and were volunteers with no payment except an allowance for transport. The selection process was not well described. Volunteers selected from a local NGO, the Iraqi Women's Federation. TRAINING: LHWs were trained but the content was not specified. They received standardised instructions and were assessed in a pilot study before start of main study. Their work was monitored by the TB coordinator. PARTICIPANTS: New smear positive pulmonary TB patients who had never been treated previously and delayed coming to collect their drugs from the health centre 3 days after their scheduled appointment. Limited socio‐demographic information provided: participants were recruited from 15 randomly chosen health centres in Baghdad and appeared to be of low socioeconomic status. TOTAL=480; INTERVENTION=240; CONTROL=240. | |
| Interventions | OBJECTIVE: To improve the adherence to TB patients to their treatment. INTERVENTION: A patient who was recorded late for collection of drugs was visited by the volunteer and asked to return to the health centre. If patient refused to return to the centre, the LHW tried to convince them with the help of the family. Home visitors also carried out health education for the patient and his/her family. CONTROL: Received no home visits. MODE OF DELIVERY: LHW visited participants in their homes to encourage them to attend the health centre for TB treatment. RECIPIENT INVOLVEMENT IN DESIGN/DEVELOPMENT/DELIVERY: not described. GEOGRAPHICAL SETTING: urban formal, Iraq HEALTHCARE SETTING: home. | |
| Outcomes | HEALTH STATUS AND WELLBEING: Final TB treatment outcome ‐ treatment success, default, treatment failure or death. LENGTH OF FOLLOW UP: 6 months. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | 'Equal numbers of patients were randomly allocated to the control or intervention group after the first episode of delaying.' (p704) Comment: insufficient information about the sequence generation process provided. |
| Allocation concealment? | Unclear risk | 'Equal numbers of patients were randomly allocated to the control or intervention group after the first episode of delaying.' (p704) Comment: insufficient information about allocation concealment provided. |
| Blinding? All outcomes | Low risk | 'Blinding of the selection was impossible, as the intervention as known to patients...The evaluation was blind as the information about outcome was collected by a field worker who did not know which group the patients was assigned to.' (p704). |
| Incomplete outcome data addressed? All outcomes | Unclear risk | Rate of loss to follow up unclear. Probably 4/240 for intervention and 10/240. |
| Free of selective reporting? | Unclear risk | Insufficient information to make an assessment. |
| Free of other bias? | Unclear risk | Methods generally poorly described. |
Morisky 2001.
| Methods | RCT. | |
| Participants | LHW: The 'peer counsellors' were adolescents who had completed therapy for latent TB infection. TRAINING: LHWs were trained in their roles and responsibilities including need for strict confidentiality and followed a strict protocol. They were supervised by a site co‐ordinator at each clinic. No more information provided. PARTICIPANTS: Adolescents who required therapy for latent TB infection. Age of participants ranged from 11 to 19, mean age 15.2 (SD 1.9). Females were 51%. Approximately half were in middle school and half in high school. Predominantly Hispanic Americans 77.8%, followed by Asians 9.4% and African Americans 8.1%. TOTAL=794; INTERVENTION 1=199; INTERVENTION 2= 204; INTERVENTION 3= 196; CONTROL=195. | |
| Interventions | OBJECTIVE: To improve the adherence to treatment for latent TB infection among adolescents.
INTERVENTION 1: LHWs contacted all participants by telephone just after they were placed on treatment to, initially, establish rapport, explain the role of the peer counselor and stress the importance of clinic attendance and medication adherence. Later telephone contacts addressed issues identified by participants in their baseline interview and any problems that had arisen during treatment.
INTERVENTION 2: 'Parent‐participant contingency contract intervention' group: parents and adolescents, with the assistance of program staff, negotiated incentives to provided by the parent, according to a schedule, if the adolescent adhered to TB treatment. INTERVENTION 3: 'Combined intervention': received both peer counselling and parent‐participant contingency contract interventions. CONTROL: 'Usual care' group received all of the treatment and educational services customarily provided by the clinic, including health education from TB clinic staff and assessment of physical health. MODE OF DELIVERY: LHW support delivered by telephone. RECIPIENT INVOLVEMENT IN DESIGN/DEVELOPMENT/DELIVERY: not described. GEOGRAPHICAL SETTING: urban formal, USA HEALTHCARE SETTING: contacted by telephone at home. |
|
| Outcomes | HEALTHCARE BEHAVIOURS: Completion of TB treatment (Isoniazid); medication behaviour. LENGTH OF FOLLOW UP: 6 months. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | 'participants...were randomly assigned to one of four intervention groups' (p116). Comment: insufficient information about the sequence generation process. |
| Allocation concealment? | Unclear risk | 'participants...were randomly assigned to one of four intervention groups' (p116). Comment: insufficient information about the method of concealment. |
| Blinding? All outcomes | Unclear risk | Insufficient information. |
| Incomplete outcome data addressed? All outcomes | Low risk | Missing data imputed using appropriate methods. |
| Free of selective reporting? | Unclear risk | Insufficient information to make an assessment. |
| Free of other bias? | Low risk | |
Morrell 2000.
| Methods | RCT. | |
| Participants | LHW: not described. TRAINING: National vocational qualification (level 2) postnatal care award, endorsement units for domiciliary care award and competence in the care of young children through an 8 week training programme. PARTICIPANTS: women >17 years old who delivered live baby. Mean age was approximately 28 years. TOTAL=623; INTERVENTION=311; CONTROL=312. | |
| Interventions | OBJECTIVE: to provide practical and emotional postnatal support for mothers, including help in gaining confidence in caring for baby and reinforcement of midwifery advice on infant feeding. INTERVENTION: community postnatal support workers. CONTROL: no intervention. MODE OF DELIVERY: the intervention group were offered 10 visits from a support worker for up to 3 hours per day in the first 28 postnatal days. Most women received 6 visits and 15% received 10 visits. The length of visits ranged from 10‐375 minutes. Time was spent on: housework (38%); talking with the mother (23%); dealing with the baby (9%); dealing with other siblings (8%); bottle feeding (7%); talking about the baby (6%); discussing breastfeeding (3%). RECIPIENT INVOLVEMENT IN DESIGN/DEVELOPMENT/DELIVERY: not described. ORGANISATIONAL BASE OF THE INTERVENTION: not described. GEOGRAPHICAL SETTING: urban UK HEALTHCARE SETTING: home. | |
| Outcomes | RECIPIENT SATISFACTION WITH CARE: recipient satisfaction with midwife, health visitor and general practitioner. HEALTH STATUS AND WELLBEING: general health perception, depression, social support, breastfeeding rates. COST: NHS costs, use of social services, personal expenditure. LENGTH OF FOLLOW UP: 6 months after intervention. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | 'The allocation sequence was prepared in advance by using random digit tables.' (p594). |
| Allocation concealment? | Low risk | 'Individual women were randomly allocated to intervention or control group with sequentially numbered, sealed opaque envelopes' (p594). |
| Blinding? All outcomes | Unclear risk | 'Postal follow‐up questionnaires' (p593). No reporting of blinding of personnel or outcome assessors. |
| Incomplete outcome data addressed? All outcomes | Unclear risk | 'At six weeks 551 (88.4%) women returned with questionnaire...'. |
| Free of other bias? | Low risk | |
Morrow 1999.
| Methods | Cluster RCT. | |
| Participants | LHW: counsellors who previously worked for Instituto National de la Nutrician as field data collectors, lived in the study neighbourhood, were aged 25‐30 years, had a high‐school education and a commitment to breastfeeding, although did not necessarily have previous personal breastfeeding experience. TRAINING: peer counsellors were trained and supervised by staff of La Leche League of Mexico and the physician study coordinator, who was also trained in lactation management. The peer‐counsellor training consisted of 1 week of classes, 2 months in lactation clinics and with mother‐to‐mother support groups, and 1 day of observation and demonstration by visiting experts. Peer counsellors also practiced in a non‐study neighbourhood for 6 months before the trial and refined the content of messages and their problem solving skills. PATIENTS: all women residing in the periurban study area. Majority had primary or no schooling and were married. Few (7‐15%) were employed outside the home. 27% of mothers were primiparous and 31% gave birth by caesarian section. TOTAL=130; INTERVENTION 1=44; INTERVENTION 2=52; CONTROL=34. | |
| Interventions | OBJECTIVE: to promote breastfeeding among pregnant and lactating women. INTERVENTION 1: six home visits. INTERVENTION 2: three home visits. CONTROL: no home visits. MODE OF DELIVERY: Home visits to pregnant women focused on the benefits of exclusive breastfeeding; basic lactation anatomy and physiology; infant positioning; common myths; typical problems and solutions; and preparation for birth. Post partum visits focused on establishing a healthy breastfeeding pattern; addressing maternal concerns; and providing information and social support. RECIPIENT INVOLVEMENT IN DESIGN/DEVELOPMENT/DELIVERY: not described. ORGANISATIONAL BASE OF THE INTERVENTION: support provided by staff of La Leche League, Mexico. GEOGRAPHICAL SETTING: informal urban Mexico HEALTHCARE SETTING: home. | |
| Outcomes | RECIPIENT SATISFACTION WITH CARE: maternal satisfaction. HEALTHCARE BEHAVIOURS: exclusive breastfeeding in previous week at 2 weeks and 3 months, practice of exclusive breastfeeding at all five measurement times, duration of any breastfeeding, incidence of diarrhoea in children >3 months of age. LENGTH OF FOLLOW UP: up to 3 months post partum. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | '13 clusters were randomly allocated to each study group, stratified by subdivision. This randomisation schedule was generated by computer' (p1227). |
| Allocation concealment? | Low risk | Cluster randomised: '13 clusters were randomly allocated to each study group, stratified by subdivision. This randomisation schedule was generated by computer' (p1227). |
| Blinding? All outcomes | High risk | 'All data were collected...by two experienced staff other than peer counsellors. The study hypothesis could not be concealed from these staff, but they were trained to administer all questions in a standard manner, and they undertook an equal proportion of interviews in each study group' (p1227). |
| Incomplete outcome data addressed? All outcomes | Low risk | Missing outcome data balanced in numbers across groups. |
| Free of selective reporting? | Unclear risk | Protocol not available. |
| Free of other bias? | Low risk | |
Mtango 1986.
| Methods | Cluster RCT. | |
| Participants | LHW: village health workers. TRAINING: courses on acute respiratory infections (ARI). PATIENTS: 18% of children in villages in Bagamoya District were aged <5 years, predominantly Muslim and mainly of Bantu descent. The district's economic base is mainly agricultural, income per capita is among lowest in Tanzania. TOTAL=16,126 (YEAR 1); 19,014 (YEAR 2); INTERVENTION=8028 (YEAR 1); 9099 (YEAR 2); CONTROL=8098 (YEAR 1); 9915 (YEAR 2). | |
| Interventions | OBJECTIVE: to improve diagnosis, referral and treatment of ARI. INTERVENTION: village health workers (VHW). CONTROL: no intervention. MODE OF DELIVERY: utilisation of VHWs to include higher levels of primary care by visiting each household with child <5 years every 6‐8 weeks, giving health education to mothers about childhood symptoms/signs of ARI, treating pneumonia immediately with cotrimoxazole and referring severe cases to higher level of care. RECIPIENT INVOLVEMENT IN DESIGN/DEVELOPMENT/DELIVERY: not described. ORGANISATIONAL BASE OF THE INTERVENTION: not described. GEOGRAPHICAL SETTING: rural Tanzania HEALTHCARE SETTING: home. | |
| Outcomes | HEALTH STATUS AND WELLBEING: mortality rate for children <5 years of age. LENGTH OF FOLLOW UP: 2 years. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Randomly divided villages into two population groups, butnot clear how this was done. |
| Allocation concealment? | Unclear risk | Not mentioned. |
| Blinding? All outcomes | Low risk | Not possible for mortality data, but for morbidity data, village health workers who delivered the intervention also collected data. Later resorted to a yearly census as VHWs were not reporting all events. |
| Incomplete outcome data addressed? All outcomes | Low risk | Attrition rate at individual level not stated. At cluster level, the two clusters completed the study. |
| Free of selective reporting? | Low risk | Data presented reflects the outcomes stated in the objectives. |
| Free of other bias? | High risk | The only district that implemented this study was chosen because it was the field practice area for the university. This was a crossover trial, so the control group implemented the intervention in year 2. |
Muirhead 2006.
| Methods | RCT. | |
| Participants | LHW: 12 peer supporters ‐ experienced breastfeeding mothers known to the trial team ‐ were recruited and trained. Two written references were required and security vetting was carried out in all cases.
TRAINING: Designed by authors. Included two full days of training and four evening sessions, plus regular follow up sessions (in the form of case study discussions). The training covered: breastfeeding, transferable skills, health and safety and confidentiality, relationship with patient and professionals (see Box 1 of trial paper for further detail). The LHWs consulted supervisors as required. For the first 6 months, they attended a monthly supervision meeting of around 3 hrs duration with the supporters and trial team. From 6 months onwards, supervision continued by direct contact between the trial team and pairs of LHWs working with each mother.
PARTICIPANTS: Women of 28 weeks gestation from a general practice in Scotland. Mean age 27.8yrs (intervention group) and 28.5 years (control) and mostly caucasian. TOTAL = 225; INTERVENTION =112; CONTROL = 113. |
|
| Interventions | OBJECTIVE: To provide peer support for breastfeeding, so as to increase the initiation and duration of breastfeeding. INTERVENTION: Received normal breastfeeding support, as for control participants below. In addition, 2 peer supporters were assigned to each mother. Peer supporters visited participants at least once during antenatal period. Further antenatal support provided to women who requested it. Peer support was available to women in the intervention group if they were breastfeeding on return home after delivery and if the peer supporters were informed in time. Peer supporters therefore had little or no contact with women in hospital so that only midwives helped mothers in both groups to initiate feeding. CONTROL: normal breastfeeding support, i.e. a community midwife for the first 10 days, health visitor after 10 days, breastfeeding support groups and breastfeeding workshops. MODE OF DELIVERY: Mothers still breastfeeding on return home would be contacted by their peer supporter at least every 2 days or as often as required either by phone or a personal visit up until day 28. If mothers requested further support, this was provided until 16 weeks. RECIPIENT INVOLVEMENT IN SELECTION/TRAINING/MANAGEMENT: not described. GEOGRAPHICAL SETTING: urban formal, Scotland HEALTHCARE SETTING: home. |
|
| Outcomes | HEALTHCARE BEHAVIOURS: Proportion of women breastfeeding at birth (initiation of breastfeeding) and at 10 days, 6 weeks, 8 weeks and 16 weeks; median breastfeeding duration; exclusive breastfeeding at 6 and 8 weeks; no formula feeding by 16 weeks. LENGTH OF FOLLOW UP: 16 weeks. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | 'Allocation sequences...were generated at the start of the trial by computer' (p193). |
| Allocation concealment? | Low risk | 'allocation of each woman was done by post‐recruitment telephone call' (p193). |
| Blinding? All outcomes | High risk | 'There was no post‐allocation concealment' (p193) 'The 10‐day questionnaire was completed in the presence of the health visitor. The 8‐week and 16‐week questionnaires were completed in the presence of a GP or practice nurse' (p194). |
| Incomplete outcome data addressed? All outcomes | Low risk | Minimal missing outcome data (5/225 women). |
| Free of selective reporting? | Unclear risk | Insufficient data to make an assessment. |
| Free of other bias? | Low risk | |
Olds 2002.
| Methods | RCT. | |
| Participants | LHW: paraprofessional home visitors were required to have high school education but excluded if they had college preparation in the helping disciplines or a bachelor's degree in any discipline as well as strong people skills. Preference was given to those who had previously worked in human services agencies. TRAINING: one month intensive training. Volunteers then served 2 families in a pilot program to gain experience with the model and performed regular in service training to cover aspects of MCH/development. PATIENTS: low income women from from 21 antepartum clinics in the Denver metropolitan area, who had no previous live births and who qualified for Medicaid or had no private health insurance. Mean age=19.76 years; 84% of whom were unmarried; had a mean=11 years education; no previous live births; qualified for Medicaid/no private insurance. TOTAL=735; INTERVENTION 1=245; INTERVENTION 2=235; CONTROL=255. | |
| Interventions | OBJECTIVE: child and maternal health promotion to 1) improve maternal/fetal health during pregnancy; 2) improve health/development of child by helping parents provide more competent care; 3) enhance parent's personal development, planning future pregnancies, further education and find work. INTERVENTION 1: paraprofessional home visits. INTERVENTION 2: nurse home visits. CONTROL: no intervention. MODE OF DELIVERY: each visitor managed a case load of 25 families. There were 2 supervisors for 10 visitors. 3/10 visitors left the study and replacements were hired. Paraprofessionals completed approximately 6.3 home visits during pregnancy and 16 visits during infancy. By the end of the program 48% of the paraprofessional visited families had discontinued the program. RECIPIENT INVOLVEMENT IN DESIGN/DEVELOPMENT/DELIVERY: not described. ORGANISATIONAL BASE OF THE INTERVENTION: not described. GEOGRAPHICAL SETTING: urban USA HEALTHCARE SETTING: home. | |
| Outcomes | CONSULTATION PROCESS MEASURES: length of visit, family members participating, % time devoted to different progress areas, attempted visits not completed. UTILISATION OF LHW: program dropout, relationship continuity. RECIPIENT SATISFACTION WITH CARE: mother's rating of helping relationship. COST: cost of program or 2 or 5 years service per family. HEALTH CARE BEHAVIOURS: number/timing of subsequent pregnancies, mother‐infant interaction, use of psychoactive substances, use of nicotine, marijuana or cocaine, change in tobacco use. HEALTH STATUS AND WELLBEING: child emotional, mental and behavioural development, language development. LENGTH OF FOLLOW UP: up to 24 months. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Used computer program to randomise within strata from a model with 3 classification factors: race/ethnicity, gestational age at enrollment, geographic region of residence. |
| Allocation concealment? | Unclear risk | Not mentioned. |
| Blinding? All outcomes | Low risk | Assessors were blinded., home visitors records were used to collect some information. |
| Incomplete outcome data addressed? All outcomes | High risk | By the end of the intervention, 38% of the mothers in the nurse‐visited group and 48% in the paraprofessional visited group had dropped out of the study. Insufficent analysis of differences between those who completed the study and those who did not. |
| Free of selective reporting? | Unclear risk | Insufficient data for this assessment. |
Parker 2008.
| Methods | RCT. | |
| Participants | LHW: Community environmental specialists who made applications, were interviewed and hired by subcommittee of community and academic members of steering committee. Were all Detroit residents, two were bilingual (Spanish and English). Had a minimum of high school education. TRAINING: Intensive 4‐week training, had ongoing training activities throughout the year. Topics included clinical aspects of asthma, allergens and relation to asthma, environmental tobacco smoke, risks and strategies to reduce exposure, household chemicals, assessing the medical care system, provision of referrals, enrolment in medical care, and other social services, help with paying electricity bills. Were trained on strategies for behaviour change and integrated pest management. PARTICIPANTS: Children aged 7‐11years that were likely to have persistent asthma, attending elementary school in the area. Mean age of recruited children was about 9 years (SD 1.5), about 40% were females. Most of the caregivers were female (about 95%), about 40% were smokers. Almost 70% had a previous diagnosis of asthma, about 45% had moderate to severe asthma. Almost 40% had a positive skin test for dust mites, 30% for grasses. Almost 40% were from households where income was <$10,000. Almost 80% were of African‐American ethnicity, 10% Hispanic, 5% Caucasian. TOTAL= 328 children; INTERVENTION: 162 children CONTROL: 166 children. |
|
| Interventions | OBJECTIVE: To improve childrens asthma related health by reducing household environmental triggers for asthma. CONTROL: Received booklet on global initiative for Asthma that provides general basic information on asthma. MODE OF DELIVERY: Worked with families to make environmental changes in the home to reduce childs exposure to multiple common asthma triggers.At initial visit, provided general information on asthma and role of environmental triggers, assessed families major social services needs including if child had physician and health insurance. Made referrals to clinics, public health insurance programs and social service agents when appropriate.. At second visit, provided results from skin prick allergy test and bed room dust allegen concentrations, developed action plan with focus on priority list of environmental triggers identified. After this, subsequent visits covered strategies to reduce dust mites, environmental tobacco smoke, cockroaches, pet dander, rodents and mold. At each visit, reviewed the action plan, occssionally revisiting items initially considered lower priority. Visits planned every 6 weeks, scheduled additional visits as necessary. Worked with professional exterminators on homes with major infestations. RECIPIENT INVOLVEMENT IN SELECTION/TRAINING/MANAGEMENT: Yes, in selection of LHWs. GEOGRAPHICAL SETTING: Urban Formal, USA HEALTHCARE SETTING: Home . |
|
| Outcomes | HEALTHCARE UTILISATION: Unscheduled medical care. HEALTH STATUS AND WELLBEING: Measures of lung function (Daily nadir, FEV), any symptoms. BEHAVIOUR: Reports of vacuum cleaning dusting etc. LENGTH OF FOLLOW UP: 4 months. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Stratified by household, used random number generator method. |
| Allocation concealment? | Unclear risk | Not mentioned. |
| Blinding? All outcomes | Unclear risk | Not clear if assessors were blinded. Not clear if community environmental specialists collected some of this data. |
| Incomplete outcome data addressed? All outcomes | Unclear risk | About 69% participants completed the study. Used GEE models that take into account this missing data. |
Pence 2005.
| Methods | RCT. | |
| Participants | LHW: health volunteers (and also traditional village authorities). TRAINING: 6 weeks of initial training and quarterly refresher training sessions. PARTICIPANTS: Communities with high childhood mortality rates. Mean age of mothers was approximately 28 years and fathers was 38 years. Most parents were always resident in the household with the child. Children less than 5 yrs old. INTERVENTION: Community mobilisation (LHWs) = 8218; Ministry of Health = 8109; Combined= 18,350; CONTROL= 18,457. |
|
| Interventions | OBJECTIVE: To address the need for practical field trials of organisational strategies for community health service delivery. CONTROL: Received services according to standard Ministry of Health guidelines. MODE OF DELIVERY: (A) Community mobilisation arm (LHWs): (1) Visited households to discuss hygiene, child immunisationand other health issues and to make the community aware that they are available for basic treatment and referrals. (2) Provided the following treatments: paracetamol, chloroquine, aludrox, multivitamins. (3) Provided referrals to clinics and hospitals for more complicated services. (B) MOH mobilisation arm: All nurses in the area covered by this arm were reassigned from subdistrict clinics to villages and given door‐to‐door service delivery responsibilities. (1) Provided ambulatory care at their place of residence. (2) Visited all compounds in a 90 day cycle for health education, follow up and diagnosis. (3) Organised immunisation and outreach days. (4) Provided referral to clinics or hospital as appropriate. RECIPIENT INVOLVEMENT IN SELECTION/TRAINING/MANAGEMENT: village health committees appointed lay health workers GEOGRAPHICAL SETTING: Ghana, rural. HEALTHCARE SETTING: Home. |
|
| Outcomes | HEALTH STATUS AND WELLBEING: All‐cause childhood mortality rates. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Randomly assigned study region to four clusters but no details provided on how this was done. |
| Allocation concealment? | Unclear risk | Not mentioned. |
| Blinding? All outcomes | Low risk | Used field workers to collect the information, not clear if they were blinded or not. Used surveillance methods to record deaths, this was a cluster trial, bias probably low. |
| Incomplete outcome data addressed? All outcomes | Unclear risk | 4 clusters completed the trial, all outcomes reported. |
| Free of selective reporting? | Unclear risk | insufficient data to make assessment. |
| Free of other bias? | High risk | Results presented by the authors did not reflect the clustering. |
Rodewald 1999.
| Methods | RCT. | |
| Participants | LHW: Lay outreach workers (no information on number), recruited from neighbourhoods in which the study practices were located; had some college education. (1) Set up an immunization tracking system for their site and determined the immunization status of each participating child; (2) Used postcards and telephone calls to recall under immunized children to the primary care providers offices; (3) conducted a home visit where parents did not respond to the above. TRAINING: Not described. Backup support from a hospital social work department when assistance with unexpected situations was required. PARTICIPANTS: Children born over 1 year(March 1993‐Feb 1994), Approximately 50% male; mean age at enrolment = 8.5 months; one‐third African‐American, 15% White, 10% Hispanic, 40% unknown. Approximately two‐thirds received Medicaid. 13% were uninsured for immunizations and 25% were insured for immunizations. TOTAL= 3015; INTERVENTIONS: Tracking/Outreach‐prompting 732, Tracking/Outreach =715, Prompting only=801; CONTROL=767. |
|
| Interventions | OBJECTIVE: To compare and measure the effects and cost effectiveness of two interventions designed to raise immunization rates. CONTROL: Standard of care, no intervention. MODE OF DELIVERY: Tracking/Outreach:(1) Lay Outreach workers set up an immunisation tracking system(tickler file) for their site and determined the immunization status of each participating child; (2) Used postcards and telephone calls to recall under immunized children to the primary care providers offices; (3) conducted a home visit where parents did not respond to the above. Prompting: Programme to reduce missed opportunities for immunization in primary care offices. This involved: (a) discussions with practice site physicians on missed immunization opportunities; (b) encouraging practices to agree to immunize children who were no up‐to‐date at any visit to the practice; (c) marking the charts of children in the prompting group; (d) assessment by a nurse of the immunization status of children assigned to this group on presentation and the placement of a 'missed opportunity card' on the chart as a prompt, where necessary; (e) bimonthly provider feedback on provider‐specific missed opportunity rates. CONSUMER INVOLVEMENT IN SELECTION/TRAINING/MANAGEMENT: no. GEOGRAPHICAL SETTING: urban formal, USA HEALTHCARE SETTING: Home. |
|
| Outcomes | HEALTHCARE UTILISATION: Mean number of preventive visits, primary care visits , anaemia screenings, lead exposure screenings, appointments kept, missed immunisation opportunities. HEALTH STATUS AND WELLBEING: Proportion of children with up to date vaccination, Mean days of delay in vaccination. LENGTH OF FOLLOW UP: 18 months. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Randomly allocated using a computer program. |
| Allocation concealment? | Unclear risk | Not mentioned. |
| Blinding? All outcomes | Low risk | Data collection group was separate from those delivering intervention. Chart reviewers were blinded to study allocation. |
| Incomplete outcome data addressed? All outcomes | Low risk | Follow‐up rate >80%, report on all outcomes stated in objectives. |
Rohr 2004.
| Methods | RCT. | |
| Participants | LHW: Resource mothers were a self‐selected group of women who have children with phenylketonuria (PKU), age 6 months to 35 years. TRAINING: During the first 2 years of the study, 2‐day training sessions were held for the 30 resource mothers and 8 coordinators. Included information on PKU, maternal PKU, nutrition, pregnancy, psychosocial issues and home visitation. Coordinators also received training in supervision of resource mothers and data collection methods. PARTICIPANTS: Women (pregnant or planning pregnancy) with phenylketonuria. Mean age 29 years (SD 5), 48% in intervention and 65% in control were on diet before pregnancy. TOTAL= 50; INTERVENTIONS: Resource mothers group=27; CONTROL=23. |
|
| Interventions | OBJECTIVE: To provide social support and enhance positive attitudes in women with PKU who were pregnant or planning pregnancy. CONTROL: Were also treated according to the maternal PKU protocol. MODE OF DELIVERY: A resource mother is trained to visit the homes of the women with PKU to offer support and technical assistance in adhering to medical recommendations. She might help with cooking, meal planning, ordering low‐protein food and supervising blood drawing, simply listening and offering emotional support. They offer social support to pregnant women and women who are planning to conceive who have been recommended to follow a phenylalanine (phe)restricted diet. These were treated according to the maternal PKU protocol. The resource mother contacted the woman with PKU within one week if she was pregnant or in 2 weeks if she was planning a pregnancy. A maximum of 20 visits including a post partum visit were made by the Resource mother, with more frequent intervention in early pregnancy. RECIPIENT INVOLVEMENT IN SELECTION/TRAINING/MANAGEMENT: no. GEOGRAPHICAL SETTING: USA, Urban formal. HEALTHCARE SETTING: Home. |
|
| Outcomes | HEALTH STATUS AND WELLBEING: Weeks gestation after which blood phe remained <360 micromol/L, % under metabolic control by 10 wks gestation, Birthweight z‐score, Birth length z‐score, Birth head circumference z‐score. LENGTH OF FOLLOW UP: 3 years. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Told randomly assigned participants to control or treatment groups. |
| Allocation concealment? | Unclear risk | Not mentioned. |
| Blinding? All outcomes | Unclear risk | Not mentioned. |
| Incomplete outcome data addressed? All outcomes | Unclear risk | Attrition rates low, data reported reflects outcomes stated in objectives. |
| Free of selective reporting? | Low risk | |
| Free of other bias? | Unclear risk | Contamination in the control group could have led to healthier eating habits. |
Sazawal 1996.
| Methods | RCT. | |
| Participants | LHW: Field assistant. TRAINING: Not clear. PARTICIPANTS: Children aged 6‐35 months with at least 4 episodes of unformed stools in previous 24 hours, diarrhoea duration of <7 days attending diarrhoea clinic were enrolled. Mean age was about 16 months (+‐8 months), about 38% children were 6‐11months, 40% 12‐23 months. About 76% were breast fed with or without other foods. Almost 7% were wasted, about 40% stunted, 13% both wasted and stunted. About 67% had 3 doses of DPT vaccine and 65% had diarrhoea in the last 2 months. Family size was about 5 members +‐2 with about 35% with 1 child in the family. The water supply was from hand pump for 40% of the families. Low socioeconomic status, in this population 94% women and 50% men are illiterate. Income was about 16000 (+‐12000) rupees per year. TOTAL: 579 children INTERVENTIONS: 286 children CONTROL= 293 children. |
|
| Interventions | OBJECTIVE: To investigate the effect of zinc supplementation on incidence of persistent diarrhoea and dysentery. CONTROL: Received vitamin supplements ‐ Vitamin A, thiamin, riboflavin, vitamin B6, cholecalciferol, vit. E, and niacin but no zinc. MODE OF DELIVERY: Field assistants visited family every day and fed zinc preparation to child. If child not home, or Sundays/holidays, measured daily dose of the liquid and left it in separate vials for mother to feed. CONSUMER INVOLVEMENT IN SELECTION/TRAINING/MANAGEMENT: None. GEOGRAPHICAL SETTING: Urban Formal, India HEALTHCARE SETTING: Home. |
|
| Outcomes | HEALTH STATUS AND WELLBEING: Effect of zinc supplementation on incidence of persistent diarrhoea and dysentery. LENGTH OF FOLLOW UP: 4 months after last diarrhoea episode. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Random allocation after stratification by nutrition and breastfeeding status using permuted blocks of fixed length of 10. |
| Allocation concealment? | Low risk | Used sealed envelope opened at enrollment. Envelop contained assigned group and code assignment of supplement. |
| Blinding? All outcomes | Low risk | Assessors were differnt from those delivering the intervention. Control group received vitamin supplementation (placebo) but probably less frequent follow up. |
| Incomplete outcome data addressed? All outcomes | Unclear risk | Follow‐up rates >80%, followed up for 4 months after a diarrhoea episode. |
Schuler 2000.
| Methods | RCT. | |
| Participants | LHW: lay visitors were two middle aged African‐American women who had previous experience of making home visits and were familiar with the community where the mothers lived. TRAINING: trained to pursue HELP at Home (Hawaii Early Learning Profile, 1991). PATIENTS: women with mean age=27 years. 97.7‐100% unemployed; 91.7‐96.4% single. TOTAL=171; INTERVENTION=84; CONTROL=87. | |
| Interventions | OBJECTIVE: to increase maternal empowerment and infant development. INTERVENTION: home visitors. CONTROL: no intervention. MODE OF DELIVERY: home visitors delivered a developmentally orientated intervention based on program used by IHDP, providing information on drug use/treatment to increase maternal empowerment and infant development. Home visitors modelled behavior/activity on a sheet. Weekly visits in the first 6 months (mean=8.9) of mean length=30.1 min. RECIPIENT INVOLVEMENT IN DESIGN/DEVELOPMENT/DELIVERY: not described. ORGANISATIONAL BASE OF THE INTERVENTION: not described. GEOGRAPHICAL SETTING: urban USA HEALTHCARE SETTING: home. | |
| Outcomes | HEALTHCARE BEHAVIOURS: cocaine/heroin, marijuana, alcohol use. HEALTH STATUS AND WELLBEING: mother infant interaction (maternal responsiveness and infant warmth). LENGTH OF FOLLOW UP: 6 months post‐intervention. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Used random assignment, not clear how this was done. |
| Allocation concealment? | Unclear risk | Not mentioned. |
| Blinding? All outcomes | Low risk | Used trained coders who were not aware of group assignment. |
| Incomplete outcome data addressed? All outcomes | High risk | Follow up rate was approximately 64%. Insufficient exploration of differences between those lost of follow up and those that completed the study. |
| Free of selective reporting? | Unclear risk | Insufficient information to make an assessment. |
| Free of other bias? | High risk | Lay workers visited the control group to minimise loss to follow up. |
Siegel 1980.
| Methods | RCT. | |
| Participants | LHW: paraprofessional infant care workers. TRAINING: 200 hours of preservice training including 3 months of multi‐method classroom learning experiences and field work during last month of training . Began with orientation to research project then covered mother‐infant attachment, child care/development, importance of play/stimulation, special needs of mothers/infants, use of community resources, skills in relating to mothers. Continuous supervision provided by project field director who had a degree in child development. Public health nurses participated in training and served as continuing resources to infant care workers, the relationship was facilitated by the health department. PATIENTS: women in third trimester of pregnancy who received care at public prenatal clinic. TOTAL=202; INTERVENTION 1=47; INTERVENTION 2=50; INTERVENTION 3=53; CONTROL=52. | |
| Interventions | OBJECTIVE: to promote mother's involvement with children and support mothers coping with situational stresses. INTERVENTION 1: home visits and extended contact in hospital. INTERVENTION 2: extended contact in hospital only. INTERVENTION 3: home visits only. CONTROL: normal hospital care (approximately 2 ½ hours of routine contact per day). MODE OF DELIVERY: infant care workers first visited mothers in hospital then made 9 visits during first 3 months of infant's life. Hospital contact consisted of at least 45 mins during first three hours after delivery and then at least 5 additional hours each day during hospital stay. During first 6 months of intervention workers met as a group with field director for three hours twice a week (once a week after 6 months). RECIPIENT INVOLVEMENT IN DESIGN/DEVELOPMENT/DELIVERY: not described. ORGANISATIONAL BASE OF THE INTERVENTION: not described. GEOGRAPHICAL SETTING: urban formal, USA HEALTHCARE SETTING: home. | |
| Outcomes | HEALTHCARE BEHAVIOURS: acceptance, interaction/stimulation, consolling, infant positive/negative behaviour. HEALTH STATUS AND WELLBEING: reports of child abuse and neglect. OTHER: health care utilization by infants. LENGTH OF FOLLOW UP: up to 12 months. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Participants were randomly assigned but no mention of method used. |
| Allocation concealment? | Unclear risk | Not mentioned. |
| Blinding? All outcomes | Low risk | Data collectors had no information on group assignment. |
| Incomplete outcome data addressed? All outcomes | Low risk | Analysed data including all 47 subjects that lacked data and without them, producing the same results. |
Silver 1997.
| Methods | RCT. | |
| Participants | LHW: 3 lay counsellors were recruited through advertisements in neighbourhood newspapers. They were all women who had raised children with ongoing health conditions. Further selection of counsellors occurred, but no information provided on how this occurred. TRAINING: 40 hour training programme focusing on listening, reflection and communication skills and on the issues that mothers of children with ongoing conditions experience. A second intensive training programme covered home visiting, coordinating schedules and how to describe the programme to participants. 10 women received 40 hour training program. 6 proceeded to further training and 3 women accepted jobs as lay interveners. PATIENTS: mothers and children with a variety of ongoing health conditions. Mothers had an average age of approximately 34 years; one‐third were high school graduates, one‐third had attended some college and 20% had less than high school education; approximately 40% of mothers were employed; just under half of families were on welfare. Children had an average age of approximately 7 years; on average had been diagnosed for 5 years; both parents were present in fewer than half of households. TOTAL=265; INTERVENTION=183; CONTROL=182. | |
| Interventions | OBJECTIVE: to provide social support and increased access to relevant information, services and knowledgeable advisors for mothers of children with ongoing health conditions. INTERVENTION: support and information from lay counsellors. CONTROL: no intervention. MODE OF DELIVERY: through face to face home meetings and biweekly telephone calls and group activities the project attempted to 1. Link mothers with community support/resources; 2. Share information about child health/behavior; 3. Enhance maternal confidence in parenting; 4. Provide source of emotional support; 5. Help identify support among mothers' naturally occurring network of friends/family. Lay intervenors worked approximately 21 hours per week and were supervised by a clinical psychologist and a social worker. RECIPIENT INVOLVEMENT IN DESIGN/DEVELOPMENT/DELIVERY: social support provided by mothers with older children who had previously suffered from on going health conditions. ORGANISATIONAL BASE OF THE INTERVENTION: not described. GEOGRAPHICAL SETTING: urban USA HEALTHCARE SETTING: home and community. | |
| Outcomes | UTILIZATION OF LHW: program participation. HEALTH STATUS AND WELLBEING: children's illness related functional impairment, stressful life events. OTHER: maternal capacity to provide care. LENGTH OF FOLLOW UP: 12 months after intervention. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Quote: 'Had preestablished random procedure'. Comment: probably done but not clear. |
| Allocation concealment? | Low risk | Person randomising was unaware of baseline response and had no role in the intervention. |
| Blinding? All outcomes | Unclear risk | Trained research assistants collected data, was not clear if they were blinded. |
| Incomplete outcome data addressed? All outcomes | Low risk | Follow up was for 12 months, rate was 77%. |
| Free of selective reporting? | Unclear risk | Report on all outcomes stated in objectives, but no protocol not available. |
| Free of other bias? | Low risk | |
Singer 1999.
| Methods | RCT. | |
| Participants | LHW: Parents or foster parents or grandparents of children with a disability or chronic health problem who volunteered to assist families. Parents who have children with disabilities, matched with parents who are experiencing similar problems to what they experienced. TRAINING: Received an average of 8‐10 hours of group instruction on communication skills, information about services, advocacy and support for families. PARTICIPANTS: Were parents or foster parents, grandparents of children with a disability or chronic health condition. Mean age of children was 6.9(SD 4.69) in intervention and 7.7(SD7.8) in waiting list group. Almost half in each group had moderate disability. Over 60% of parents were married, 25% with high school education, slightly over 30% with some college education. TOTAL=128; INTERVENTIONS: Intervention =56; Control=72. |
|
| Interventions | OBJECTIVE: To evaluate the efficacy of the parent to parent mentoring program in five states. CONTROL: Received parent to parent support after end of trial. MODE OF DELIVERY: Made four calls to the help‐seeking parents over two months. Parent to parent programs provide mothers with emotional support, practical information about caring for a child with disability, and information about obtaining services. RECIPIENT INVOLVEMENT IN SELECTION/TRAINING/MANAGEMENT: no. GEOGRAPHICAL SETTING: USA; urban formal. HEALTHCARE SETTING: Telephone support. |
|
| Outcomes | HEALTH STATUS AND WELLBEING: Cognitive adaptation at pre and post‐test, Coping, Progress on meeting need. LENGTH OF FOLLOW UP: 2 months. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Used a toss of a coin. |
| Allocation concealment? | Unclear risk | Not mentioned. |
| Blinding? All outcomes | Unclear risk | Not mentioned. |
| Incomplete outcome data addressed? All outcomes | Unclear risk | Not clear. |
| Free of selective reporting? | Low risk | |
| Free of other bias? | High risk | Used self‐reported outcomes, response bias is possible. 74% provided complete information. |
Sloan 2008.
| Methods | RCT. | |
| Participants | LHW: Community nutrition workers from the government's nutrition program. TRAINING: Were trained by a physician to teach community‐based kangaroo care of neonates. PARTICIPANTS: Eligible women were 12‐50 age group. Mean age was 23 years SD5.91. Mean gravidity was 2 SD1.96, almost 30% were nulliparous. Close to 9% had parity ≥5, with households of about 6 people. About 60% had children <5years of age, 18% had a past neonatal loss. About 85% had home births, about 13% had institutional delivery, close to 35% had skilled birth attendant. Mean distance to capitol city was 11km SD7. Close to 70% ever attended school, about 40% were illiterate. About 84% were housewives. Close to 7% received some wages. About 6% had husbands who were professionals, a little over 20% were agricultural workers, close to 70% had other widely varying occupations. TOTAL= 42 clusters; INTERVENTIONS: 21 clusters(2121 live births); CONTROL = 21 clusters(2044 live births). |
|
| Interventions | OBJECTIVE: To test whether community‐based kangaroo mother care reduces the overall neonatal mortality rate by 27.5%, infant mortality by 25% and low birthweight neonatal mortality by 30%. CONTROL: Seemed like community workers did measure birthweights for the control group but no other intervention. MODE OF DELIVERY: Taught community‐based kangaroo method of care to expectant mothers and their families. Obtained birthweights using the Salter scales weighing to the nearest 100gm within 72 hours of birth. Community‐based kangaroo care is promoted for all infants, regardless of birthweight, requiring no clinical judgement. Teaches that skin to skin care is provided as long as infant accepts it. RECIPIENT INVOLVEMENT IN SELECTION/TRAINING/MANAGEMENT: not described. GEOGRAPHICAL SETTING: Bangladesh; Rural. HEALTHCARE SETTING: Home. |
|
| Outcomes | HEALTH STATUS AND WELLBEING: Neonatal and infant mortality, Morbidity and Growth, Maternal outcomes. BEHAVIOUR: Community‐Based kangaroo care behaviours such as skin to skin care, breastfeeding, bathing after birth, clinic/hospital visits for well care check up or perceived illness. LENGTH OF FOLLOW UP: 1 year. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Stratified by union population size, distance to capital before randomly allocating half to intervention and control. Randmonly selected 1 village per union, according to population size. Not clear how achieved this. |
| Allocation concealment? | Unclear risk | Not mentioned. |
| Blinding? All outcomes | Unclear risk | Not mentioned if data collectors were blinded. |
| Incomplete outcome data addressed? All outcomes | Unclear risk | Over 80% follow up rate, study lasted 1 year. |
| Free of selective reporting? | Unclear risk | Insufficient information to make an assessment. |
Spencer 1989.
| Methods | RCT. | |
| Participants | LHW: Family workers were women, selected for the posts on the basis of personality and general experiences, they had no formal qualifications in the health or social services. TRAINING: Not specified. PARTICIPANTS: Pregnant women at above average risk of giving birth to a low weight baby, Mean age 23years. Inter‐pregnancy interval less or equal to 6months and parity 3 or more. TOTAL= 1288; INTERVENTIONS: =655; CONTROL=633. |
|
| Interventions | OBJECTIVE: To provide additional support to pregnant women at above average risk of giving birth to low birthweight babies. CONTROL: No intervention. MODE OF DELIVERY: Tasks varied according to individual situations. These ranged from providing help with obtaining state benefits, with housing, shopping, and other domestic work and child care, to promoting appropriate use of health and social services and community facilities. RECIPIENT INVOLVEMENT IN SELECTION/TRAINING/MANAGEMENT: no. GEOGRAPHICAL SETTING: UK, Urban informal. HEALTHCARE SETTING: Home. |
|
| Outcomes | HEALTH STATUS AND WELLBEING: Mean birthweight, Length of gestation, Proportion of preterm births, miscarriages, stillbirths. LENGTH OF FOLLOW UP: 2 years. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Used random table of numbers. |
| Allocation concealment? | Unclear risk | Not mentioned. |
| Blinding? All outcomes | Unclear risk | Not mentioned. |
| Incomplete outcome data addressed? All outcomes | High risk | Only 41% of the women in the intervention group received it. Those who received the intervention were also more likely to have had a previous low birthweight. |
| Free of other bias? | Low risk | |
Sripaipan 2002.
| Methods | RCT. | |
| Participants | LHW: Health volunteers. TRAINING: Trainers were trained by NGO(Save the Childrens Fund) and, in turn, trained health volunteers. PARTICIPANTS: Children less than 3 years of age and their mothers (5 to 25 months old children). Average age of mothers = 26 years. Approximately half had not completed secondary school.53% males, 56% lived in high/midland. 33% of the eligible children were malnourished. About half of the mothers and fathers were educated to junior high school or higher. TOTAL= 238 children; INTERVENTION: 119 children; CONTROL=119 children. |
|
| Interventions | OBJECTIVE: To assess if community‐based participatory intervention could significantly reduce neonatal mortality rates. CONTROL: no intervention. MODE OF DELIVERY: (1) Undertook growth monitoring and promotion sessions 2 monthly for children less than 3 years; (2) provided growth counselling, reinforced good child caring behaviour and referred ill children or those who failed to gain weight; (3) conducted the 'positive deviance inquiry' with other staff; (4) conducted monthly nutrition education and rehabilitation programme sessions with mothers of malnourished children, including the teaching of hygiene, child development and the prepartion of cheap but nutritious foods. RECIPIENT INVOLVEMENT IN SELECTION/TRAINING/MANAGEMENT: not clear. GEOGRAPHICAL SETTING: Vietnam, Rural. HEALTHCARE SETTING: Home, community. |
|
| Outcomes | HEALTHCARE UTILISATION: uptake of antenatal and delivery services, home care practice at delivery and postpartum and healthcare seeking. HEALTH STATUS AND WELLBEING: Caregiver report of at least one day of diarrhoea or respiratory illness in the 14 days preceding the interview, Weight‐for‐age Z score, Height‐for‐age Z score, Weight‐for‐height Z score. Breastfeeding frequency. LENGTH OF FOLLOW UP: up to 1 year. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Randomly assigned by coin toss. |
| Allocation concealment? | Unclear risk | Not mentioned. |
| Blinding? All outcomes | Low risk | Authors say blinding of subjects or data collectors was not feasible. |
| Incomplete outcome data addressed? All outcomes | Unclear risk | Attrition rates not clear. Report on all outcomes stated in objectives. |
| Free of selective reporting? | Unclear risk | Probably not as since reports of cough, running nose or sore throat may be reported differentially. |
Stevens‐Simon 2001.
| Methods | RCT. | |
| Participants | LHW: Only one home visitor used. Was a middle‐aged college educated, Hispanic woman who also served as a paraprofessional health educator in the CAMP prenatal clinic. Drew on her experiences as a mother. TRAINING: Not specified. PARTICIPANTS: Teenage mothers (13‐19years) at risk of abusing or neglecting their children, were poor (94% on Medicaid), predominantly unmarried and primiparous mothers who scored 25 or higher on the family stress checklist. TOTAL= 145 families; INTERVENTIONS: Home visiting=58 families; CONTROL=87 families. |
|
| Interventions | OBJECTIVE: To determine if adding an intensive home visitation component to a comprehensive adolescent‐oriented maternity program prevents child abuse and neglect. CONTROL: No intervention. MODE OF DELIVERY: In the prenatal period, met with parents individually and in groups and introduced concepts and information she planned to cover in detail after the delivery. During home visits: Assess individual and environmental strengths and weaknesses, and identify attitudes and behaviours that antedate child abuse and neglect. Help the teenagers develop a sense of competency and self‐efficacy by identifying and performing small achievable objectives. Present didactic material about age‐appropriate ways of enhancing child development and disciplining children, well and sick child care, and peaceful, adaptive techniques for managing stress. Help the teenagers appreciate and manage individual differences in infant temperament. Enhance informal support from family and friends. Coordinate referrals to social service agencies and educational and vocational training programmes. Monitor and promote appropriate utilization of medical services. RECIPIENT INVOLVEMENT IN SELECTION/TRAINING/MANAGEMENT: no. GEOGRAPHICAL SETTING: USA HEALTHCARE SETTING: Home and primary health care |
|
| Outcomes | HEALTHCARE UTILISATION: Immunization, Healthcare utilisation (no. of CAMP clinic, emergency dept visits, hospitalisations). HEALTH STATUS AND WELLBEING: Any maltreatment, Abuse (physical, sexual, emotional), Neglect (failure to provide basic shelter, supervision, medical care or support, Abandonment(the mother left the home, putting a friend or relative in charge of the child's care), Child's mental and motor development, Teenager's next pregnancy, Use of hormonal contraception, Qualities of home environment and parental care, Post partum school return. LENGTH OF FOLLOW UP: 2 years. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | No mention of the process used to randomise participants. |
| Allocation concealment? | Unclear risk | Not mentioned. |
| Blinding? All outcomes | Unclear risk | Mention blinding of trained assistants that collected information on child development but not clear if others that collected data on other variables were blinded. |
| Incomplete outcome data addressed? All outcomes | Low risk | High attrition rate in intervention arm. By study end only 53.4% of study participants were visited. Student t test for selective loss of participants showed no significant differences between those who were lost and those who were not. |
| Free of selective reporting? | Unclear risk | Insufficient evidence to make an assessment. |
Sullivan 2002.
| Methods | RCT. | |
| Participants | LHW: Used advocates/paraprofessionals that were female undergraduates. TRAINING: Not specified. PARTICIPANTS: Women that had experienced some type of physical violence from an intimate partner or ex‐partner in the previous 4 months. Mean income 1,200 USD/month. Women with at least one child between 7 and 11 years living with them, planning to remain in area for 8 months, at least one of those children interested in participating. Participants exiting a domestic violence shelter program, or obtained services from a community‐based family service organisation or a State Social Department. TOTAL= 643 families; INTERVENTIONS: Home visiting=373 families; CONTROL=270 families. |
|
| Interventions | OBJECTIVE: To examine the effectiveness of a community‐based support and advocacy intervention for battered women and their children. CONTROL: No intervention, were also paid for participation. MODE OF DELIVERY: Spent 5.16hrs per week meeting face to face with children and 2.66 with the mothers. They were responsible for assessment, facilitated access to community resources (legal, housing, child care), monitoring, secondary implementation. They made sure that everything was set up in 16weeks when the advocates stopped their actions. RECIPIENTCONSUMER INVOLVEMENT IN SELECTION/TRAINING/MANAGEMENT: no. GEOGRAPHICAL SETTING: USA HEALTHCARE SETTING: Home |
|
| Outcomes | HEALTH STATUS AND WELLBEING: Child wellbeing (Self competence, assailant abuse witnessed, assailant abuse of child), Maternal wellbeing (depression, self esteem, quality of life, social support, assailant abuse). LENGTH OF FOLLOW UP: 8 months. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Randomly allocated to intervention and control, not clear how. |
| Allocation concealment? | Unclear risk | Not mentioned. |
| Blinding? All outcomes | Unclear risk | Not mentioned. |
| Incomplete outcome data addressed? All outcomes | Unclear risk | Follow‐up rates over 80%, but for relatively short time. |
Sullivan‐Bolyai 2004.
| Methods | RCT. | |
| Participants | LHW: Parent mentor that was selected by the principal investigator and diabetes team among mothers of diabetic children in the involved clinics. Mothers who were judged to be knowledgeable in management of type 1 diabetes, child development issues and identifying community resources were identified. TRAINING: Were knowledgeable in management of diabetes type 1, child development, community resources, managing their own children?s diabetes, team work, role models. They were trained in the Irey's curriculum. PARTICIPANTS: Mothers with diabetic children, were mostly women in their 30s; mothers of 2 to 3 children; at least one with diabetes type 1. TOTAL=1288; INTERVENTIONS: 655; Control=633. |
|
| Interventions | OBJECTIVE: To examine the feasibility of a post diagnosis parent mentoring intervention with mothers of young children (1‐10 years old) newly diagnosed with type 1 diabetes. CONTROL: Transitional follow‐up care (negotiated home visits and phone calls). MODE OF DELIVERY: Support to mothers over 6 months of intervention. Provided practical support and information, emotional support, "tricks of the trade". RECIPIENTCONSUMER INVOLVEMENT IN SELECTION/TRAINING/MANAGEMENT: no. GEOGRAPHICAL SETTING: USA; urban informal. HEALTHCARE SETTING: Home. |
|
| Outcomes | HEALTHCARE UTILISATION: Emergency room or acute‐care visits, Calls to diabetes team. HEALTH STATUS AND WELLBEING: Parental concern, Maternal confidence, Impact on family, Home care resources, Haemoglobin A1C levels. LENGTH OF FOLLOW UP: 6 months. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Participants were randomly assigned but no details provided. |
| Allocation concealment? | Unclear risk | Not mentioned. |
| Blinding? All outcomes | Unclear risk | No mention of who the assessors were and if they were blinded. |
| Incomplete outcome data addressed? All outcomes | Low risk | Follow‐up rates almost 100%. |
Swart 2008.
| Methods | Cluster RCT. | |
| Participants | LHW: Home visitors who were community residents. Some had worked with injury prevention work, acted as volunteers for a local safety promotion team. TRAINING: Received training by research team on unintentional injury prevention methods. Had a manual for home visitors training. Had two site coordinators who met daily with the home visiting teams for debriefing and supervision. PARTICIPANTS: Visited 410 households out of 731 who were mainly from a low income community. Average age of caregivers was 34 years. Most respondents (about 80%) were the mother or father. Mean number of people per household, about 5 (SD 2.1), mean number of years staying in that house was 7 (SD3.7), No. Of children les than 10years was 1.7 (SD1). Almost 20% of the time, child left in care of person <16 years. About 32%caretakers had primary school level education. Out of a maximum score of 37, the mean positive safety attitude was 248 SD3.8). TOTAL = 52 housing blocks (410 households); INTERVENTION: 26 blocks (208 households); CONTROL: 26 blocks (202 households). |
|
| Interventions | OBJECTIVE: To investigate the effectiveness of a paraprofessional visitation program to improve home safety and prevent injuries among children living in low income settings. CONTROL: Did not receive any visits. MODE OF DELIVERY: Made home visits for child development and prevention of burns, poisoning and falls. At each visit, provided caregivers with information on safety practices, completed an injury hazard checklist with the caregiver, discussed possible changes to reduce risks for child injuries. Gave caregivers safety devices e.g. child proof locks, paraffin container safety caps and demonstrated their use. RECIPIENT INVOLVEMENT IN SELECTION/TRAINING/MANAGEMENT: No. GEOGRAPHICAL SETTING: Urban informal, South Africa HEALTH CARE SETTING: Home. |
|
| Outcomes | BEHAVIOUR: Prescence of household hazards for burns, poisoning and falls. LENGTH OF FOLLOW UP: 5 months. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Eligible blocks were randomly allocated to intervention and control groups. |
| Allocation concealment? | Unclear risk | Not mentioned. |
| Blinding? All outcomes | High risk | Not clear if data collectors were different from home visitors. Were unlikely to have been blinded at post intervention. Authors state that " they might have been alerted to intervention houses". |
| Incomplete outcome data addressed? All outcomes | Low risk | Complete reports on all outcomes stated in objectives. Follow‐up data were available for 92% of the households. |
| Free of selective reporting? | Unclear risk | Insufficient information to make an assessment. |
Tough 2006.
| Methods | RCT | |
| Participants | LHW: Home visitors were multi‐lingual and trained to provide culturally appropriate care. Number of LHWs not specified. TRAINING: The intervention was based on 3 existing programme models: 'Invest in kids', 'Wisconsin' and 'Within our reach'. Training addressed the role of home visitors, the philosophy of home visiting, conduct in the harm, injury prevention, safety, diversity, communication skills and substance use. PARTICIPANTS: Community‐based population of pregnant women. Age of women 29.2 years; 76% currently married; 98% had a current partner; 75% caucasian; 61% previously pregnant. Education: 9% of women had less than high school education; 18% had high school education; 73% had college, university or trade education. Employment: 67% of women worked full or part‐time. Earnings: 25% of women earned less than $40,000 per year; 42% earned $40,000 ‐ $80,000; 33% earned more than $80,000. 66% owned their own home. 6% used a good bank within the 12 months before their pregnancy. TOTAL: 1737 women. INTERVENTION 1 (Nurse + home visitor (LHW)): 577; INTERVENTION 2 (Nurse only): 578. CONTROL: 860. |
|
| Interventions | OBJECTIVE: To improve the use of prenatal resources among women at low medical risk, including those experiencing challenges such as poverty, language barriers etc. INTERVENTION 1: Nurse + home visitor: In addition to the nurse intervention (see below), the home visitors provided non‐medical, peer‐like practical support in women's homes. This focused on social support, practical assistance, supporting optimal prenatal health and connecting the client/family with community resources. INTERVENTION 2: Nurse intervention: women met with nurses at the maternity practice and received support around their goals and needs. The nurses received additional training to deliver this intervention, including in person‐centred approaches. CONTROL: Usual care provided by family physicians and nurses in maternity practices. MODE OF DELIVERY: The LHWs worked with the nurses to reduce service duplication and best address priority goal areas for each woman. The frequency and duration of home visits were determined jointly by the participating women and the LHW or nurse. It was anticipated that LHWs would make 4‐6 visits to each woman. RECIPIENT INVOLVEMENT IN SELECTION/TRAINING/MANAGEMENT: Recipients were not involved in the selection, training or management of the LHWs. GEOGRAPHICAL SETTING: Canada, urban formal. HEALTHCARE SETTING: home. |
|
| Outcomes | CONSULTATION PROCESS: Informational support discussed by healthcare provider with participant, including on smoking, alcohol, street drugs, prenatal classes, diet, parenting classes, preterm labour, breastfeeding, post partum depression, stress, vaginal infections, physical abuse, emotional abuse, seat belt use, car seat use, sleep position for infants, smoke alarms, diabetes, weight gain, folic acid. UTILISATION OF LHWs: Use of a range of available resources including prenatal classes, parenting classes, breastfeeding support, written resource guide, nutrition counselling, resource libraries, food banks, counselling services for personal concerns. HEALTHCARE BEHAVIOURS: Alcohol use (1st trimester, mid‐pregnancy, 3rd trimester); smoking (1st trimester, mid‐pregnancy, after deliver). LENGTH OF FOLLOW UP: 8 weeks post‐delivery. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | 'The clinics were located in two quadrants of the city. Within each clinic, a random list of assignment to a study group was generated using 10 blocked sequences of 90 records. Randomization was undertaken by an off‐site research associate using a pregenerated randomised table developed using the Microsoft Access program. The names of participants randomised to an intervention group (nurse or nurse + home visitor) were forwarded to the nurse who made the initial contact.' (p186). Comment: used a computer random number generator. |
| Allocation concealment? | Low risk | 'The names of participants randomised to an intervention group (nurse or nurse + home visitor) were forwarded to the nurse who made the initial contact.' (p186). Comment: central allocation. |
| Blinding? All outcomes | Low risk | 'Women received no instructions about discussing their allocation with their physician because purposefully withholding this information would not reflect program goals in ‘‘real life.’’ (p186).
'Interviewers were not involved with the intervention.' (p187). Comment: No blinding, but outcome reporting by participants unlikely to have been influenced by knowledge of allocation. |
| Incomplete outcome data addressed? All outcomes | High risk | 'Of those who agreed to participate, 78 percent (1,352/1,737) completed all three questionnaires (Fig. 1). Noncompletion rates did not differ by study group, but women who did not complete the study tended to be younger, non‐Caucasian, and less educated than those who completed the study.' (p188). Comment: Missing outcome data balanced in numbers across intervention groups, but reasons for missing data across groups varied, with a higher proportion of women in the nurse + LHW group refusing the intervention. |
| Free of selective reporting? | Unclear risk | Comment: insufficient information available. |
| Free of other bias? | Low risk | |
Tulsky 2000.
| Methods | RCT. | |
| Participants | LHW: The peer health advisors were referred to the programme by social workers. They were homeless, or recently homeless, people who were reliable in coming to meetings, had a caring and responsible attitude, and an ability to assimilate basic medical information about TB. Peers were employed by University of California for 12 hours a week at USD8.98 per hour, plus beepers and bus passes. 8 advisors hired. TRAINING: Not clear ‐ basic information about TB appears to have been given by the study clinicians. PARTICIPANTS: Homeless or 'marginally housed' people exposed to TB. Median age was 37 yrs, 86% were male, 13% were currently married, 32% with less than high school education, 31% were veterans. On night before screening, 58% had stayed in shelter, 21% in low cost residential housing. Median time since last employement was 14 months, 78% had used a free meal program in the past. 36% had lifetime history of injecting drug use, 64% used crack cocaine, 56% had history of alchoholism. TOTAL: 118. INTERVENTION 1 (monetary incentive + lay person): 43. INTERVENTION 2 (peer heatlh advisor (LHW)): 37. CONTROL: 38. |
|
| Interventions | OBJECTIVE: To provide support to improve adherence to TB prophylaxis. INTERVENTION 1: Participants received isoniazid with DOT by a research assistant twice a week at a site near the TB clinic and received USD5 each time. Problems were referred to a physician or the TB clinic. If a dose was missed, attempts to contact the participant were made through letters or telephone calls. The research assistants were lay persons trained by the study physicians. They were encouraged to be friendly and respectful to the participants but were explicitly discouraged from giving special assistance or medical referrals. INTERVENTION 2: Each participant was introduced to a peer health advisor who was responsible for directly observed therapy of 900 mg of Isoniazide twice weekly for 6 months. Where Isoniazid was not dispensed immediately, the advisor visited the participant twice a week for a review of TB symptoms. The advisor also checked for drug side effects before administering each dose and referred these on to the clinic. Also, the advisor accompanied participants to the clinic for monthly refill appointment and searched for the participants if they missed an appointment. CONTROL: TB clinic staff instructed patients who were prescribed isoniazid in daily self‐administered dosing. Participants were given 1 month's supply of pills and scheduled for monthly drop‐in appointments at the clinic for symptom review and pill refills. Adherence to appointments was monitored by reviewing TB clinic charts. If participants failed to return, the clinic followed a standard protocol including 3 letters or 3 telephone calls before closing the chart to further treatment. Participants were assumed to be adherent if they collected their pills monthly. MODE OF DELIVERY: See above. RECIPIENT INVOLVEMENT IN SELECTION/TRAINING/MANAGEMENT: None. GEOGRAPHICAL SETTING: urban formal, USA HEALTHCARE SETTING: home (for LHWs), community site and TB clinic. |
|
| Outcomes | HEALTHCARE BEHAVIOURS: Completion of 6 months of TB prevention treatment (isoniazid); Months of isoniazid dispensed; Probablility of receiving at least 3 months of isoniazid. LENGTH OF FOLLOW UP: 6 months. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | 'A block randomization method was used in which one third of consenting subjects were assigned to each arm at each screening. To carry out the randomization, subjects made a blinded selection of labeled coins taken from a bag.' (p698). |
| Allocation concealment? | High risk | 'A block randomization method was used in which one third of consenting subjects were assigned to each arm at each screening. To carry out the randomization, subjects made a blinded selection of labeled coins taken from a bag.' (p698). Comment: participants or investigators could possibly forsee assignments and thus introduce selection bias. |
| Blinding? All outcomes | Unclear risk | Participants and personnel not blinded. Not clear whether outcome assessors blinded. It is possible that the outcome measure was influenced by a lack of blinding. |
| Incomplete outcome data addressed? All outcomes | Low risk | No missing outcome data. |
| Free of selective reporting? | Unclear risk | Insufficient information to make an assessment. |
| Free of other bias? | Low risk | |
Vogler 2002.
| Methods | RCT. | |
| Participants | LHW: Paraprofessionals who were fluent in Spanish. No other details provided. TRAINING: Over 3 months had lectures on community resources for spcial needs children, common medical, developmental and behavioural issues experienced by these children, information on how to use the data entry forms, arrange transport for the families, access medical records and other practical topics. Met weekly with the project manager, an early childhood educator and therapy consultant to monitor progress and receive input. Lectures were by community agencies, e.g. Denver Public Schools child Fund, developmental specialists and representatives from relevant Denver health departments. PARTICIPANTS: Children at high risk of development disability due to difficult family situation, e.g. foster care. Children were less than 6 years of age including those from foster homes, with single‐parent fathers. Median age was 2 yrs, about 65% were 0‐2 yrs, 60% male. Median age of mothers was about 26 years with median of 10yrs education. About 45% were single parents, and 45% married.About 40% received aid to families with dependant children and about 60% were Hispanic, 20% were African American. TOTAL: 159 children. INTERVENTION : 88 children. CONTROL: 71 children. |
|
| Interventions | OBJECTIVE:To efficiently place qualified preschool children into appropriate programs by dealing with real or perceived family and system barriers. CONTROL: Received basic case management by study nurse, visited home, referred child to specific therapies or assessment sites. Visited again 1 to 2 months later. Both groups got services from family support groups, family specific binders containing medical and early intervention information, access to toy‐lending library. MODE OF DELIVERY: Visited families and helped them choose suitable early intervention programs, arranged family therapy appointments, served as translators and informally monitored early intervention activity attendance. RECIPIENT INVOLVEMENT IN SELECTION/TRAINING/MANAGEMENT: None. GEOGRAPHICAL SETTING: USA HEALTHCARE SETTING: home. |
|
| Outcomes | HEALTHCARE BEHAVIOURS: Compliance rates. UTILISATION: Early intervention programmes and speciality therapies recommended, initiated and completed. LENGTH OF FOLLOW UP: 1 year. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Participants were randomised but the process is not described. |
| Allocation concealment? | Unclear risk | Not mentioned. |
| Blinding? All outcomes | High risk | Not told if data collectors were blinded. However the "Prinicipal investigator performed a detailed source review including attendance logs, chart notes" etc. |
| Incomplete outcome data addressed? All outcomes | Low risk | All outcomes stated in objectives were reported. Follow‐up rate was 79% (85% among Intensive case management arm and 72% among those receiving basic case management). |
| Free of selective reporting? | Unclear risk | Insufficient data to make assessment. |
Wang 2007.
| Methods | Cluster RCT. | |
| Participants | LHW: Village‐based health workers (no information on number). Education level not clear. TRAINING: Not described. Supervision not described. PARTICIPANTS: 6988 infants that were born during the study period. At baseline 42.4% were born at home, in follow‐up survey 38.5% were born at home. TOTAL= 1202 infants; Group 1/Control (ampoule inside the cold chain) = 401; Group 2 (ampoule outside the cold chain) = 391 infants; Group 3 (HB‐uniject outside the cold chain) = 410 infants. |
|
| Interventions | OBJECTIVE: To prevent perinatal transmission of hepatitis B virus by delivering hepatitis B vaccine within 24 hours after birth. CONTROL: got hepatitis B vaccine from the hospital. There was additional awareness raising about the importance of vaccination. MODE OF DELIVERY: Delivered hepatitis B vaccine to infants in their homes. RECIPIENT INVOLVEMENT IN ELECTION/TRAINING/MANAGEMENT: GEOGRAPHICAL SETTING: Rural, China HEALTHCARE SETTING: Home |
|
| Outcomes | HEALTH STATUS AND WELLBEING: Proportion of children who received the birth dose of hepatitis B vaccine within 24 hours of birth. LENGTH OF FOLLOW UP: 1 year. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Told counties were randomised, no details on how this was done. |
| Allocation concealment? | Unclear risk | Not mentioned. |
| Blinding? All outcomes | Unclear risk | Not mentioned if assessors were blinded or not or if they were different from those delivering the intervention. |
| Incomplete outcome data addressed? All outcomes | Low risk | Report on all outcomes stated in objectives. All clusters completed the study. |
| Free of selective reporting? | Unclear risk | Insufficient information to make assessment. |
Watt 2009.
| Methods | RCT. | |
| Participants | LHW: Were a group of local mothers.
TRAINING: 12 session programme held over 4 weeks.
PARTICIPANTS: 62% were first time mothers, 50% described as being from ethnic minority group. Mean age of mothers at birth of first child was 30 years, infants' mean age was 10 weeks. Mothers were relatively disadvantaged with 28% as lone parents, 57% living in social housing, 33% receiving income support/jobseekers allowance. 50% were from minority groups, 50% were white. TOTAL = 312; INTERVENTION =157; CONTROL = 155. |
|
| Interventions | OBJECTIVE: To support mothers to improve infant feeding practices. INTERVENTION: Based on a social support theoretical model and consisted of the offer of practical and non‐judgemental support and advice on infant feeding, in particular complementary feeding. A holistic approach to infant nutrition was taken with the intention of empowering women to follow infant feeding guidance. LHWs offered practical support, offered a listening ear to mothers concerns and worries about infant feeding. CONTROL: Standard professional support from health visitors and GPs. MODE OF DELIVERY: Made monthly home visits from when the baby was 3 months until their first birthday.. RECIPIENT INVOLVEMENT IN SELECTION/TRAINING/MANAGEMENT: not described. GEOGRAPHICAL SETTING: urban formal, England HEALTHCARE SETTING: home. |
|
| Outcomes | HEALTHCARE BEHAVIOURS: infant feeding habits; infant fruit and vegetable consumption; mother's consumption of fruit and vegetables. HEALTH STATUS AND WELLBEING: Vitamin C from fruit at 12 months (primary outcome); selected macro‐ and micro‐nutrients; supine length and weight. LENGTH OF FOLLOW UP: 18 months. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | 'A random allocation schedule was prepared in advance using random digit computer tables' (p157). |
| Allocation concealment? | Unclear risk | '...women were allocated a sequential identification number and simple randomisation was used to allocate them to either interventio nor control group. The study administrator was responsible for the randomisation process' (p157). Comment: method not described in sufficient detail. |
| Blinding? All outcomes | Low risk | 'those responsible for recruiting and assessing outcomes were all masked to group assignment' (p157). |
| Incomplete outcome data addressed? All outcomes | Unclear risk | Proportion followed up: intervention = 66%; control = 70%. Unclear whether similar reasons for missing data across groups. |
| Free of selective reporting? | Unclear risk | Insufficient data to make an assessment. |
| Free of other bias? | Low risk | |
Weindling 2007.
| Methods | RCT. | |
| Participants | LHW: Family support workers were parents of children with cerebral palsy. No other details provided. TRAINING: Had 12 weekly sessions each 3 hours long. Had talks and practical exercises focussing on family and child needs, interpersonal and counselling skills. PARTICIPANTS: Children with cerebal palsy. Mean age of children was 19.8 months, almost 9 months after diagnosis made. 39% of children had hemiplegia, 40% had tetraplegia, 21% were diplegic. Most were boys (61%). Gestational period was shorter and birthweight lower than normal. There were more multiple births. Mean motor and cognitive quotients fell 1 SD from norm of 100. Mean stress scores and number of cases above threshold on the Parenting Stress Index (PSI) and General Health Questionaire (measures anxiety, depression and social isolation) were higher than normally found in the normal population. On the family situation, most children were living with both parents (78%), primary caretaker was the mother (88%). TOTAL = 88 families; CONTROL = 29; Physiotherapy assistant group = 28; Family support worker group = 31. |
|
| Interventions | INTERVENTION: Provided support for daily needs to family with child with spastic cerebral palsy. OBJECTIVE: (1) To evaluate the effect of increasing the frequency of neurodevelopmental therapy (NDT). (2) To examine the belief that the effect of physical therapy on the child is not just through physical support but also through supporting the family. (3) To examine the cost effectiveness of the intervention against a broader evaluation of service costs. (4) To provide information about the way in which families with children with cerebral palsy functioned, the amount of services received and the factors that determined this. CONTROL: Received physiotherapy and support in the routine manner provided in their clinic. There was no attempt to standardise style of physiotherapy given. All provided NDT in a similar way. MODE OF DELIVERY: Made weekly home visits that lasted 1 hour over 6 months. Discussed family needs and how best could help family. Ethos for equal partnership with joint decision making about family needs and how they could be met. RECIPIENT INVOLVEMENT IN SELECTION/TRAINING/MANAGEMENT: No. GEOGRAPHICAL SETTING: Urban formal, UK HEALTHCARE SETTING: Home. |
|
| Outcomes | HEALTH STATUS AND WELLBEING: Child outcomes: Gross motor function measure; Vineland daily living and Griffiths raw scores. Family outcomes: PSI parent domain and family needs. LENGTH OF FOLLOW UP: 2 years. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Used minimisation techniques, randomised stratified children by maternal education, pattern of spasticity and geographical area where treatment was based. |
| Allocation concealment? | Low risk | Central allocation by independent statistician in remote site. |
| Blinding? All outcomes | Low risk | Assessments done by senior paediatrician physiotherapist blinded to group allocation. Had independent assessor check the home environment. |
| Incomplete outcome data addressed? All outcomes | Low risk | Loss to follow up low, at analysis take into account the differential withdrawal of families with high mean family needs score. |
| Free of selective reporting? | Low risk | |
| Free of other bias? | Low risk | |
Wohl 2006.
| Methods | RCT. | |
| Participants | LHW: Bilingual community workers. Their educational background was not described. TRAINING: The training and monitoring of the LHWs was not specified. PATIENTS: HIV treatment naive and treatment experienced persons for who no more than 1 prior regimen had failed. Most were men (75%), aged 30yrs and more (82%) and were non‐white, self identified as heterosexual (56%). 62% were borne outside the US and 57% were monolingual Spanish speakers. 64% were Latino, 24% African American. Self‐reported mode of exposure to HIV was commonly sex with men (included men having sex with men who also reported injection drug use, 29% heterosexual contact). 46% were treatment naive, and 54% treatment experienced. Most were unemployed (73%), and reported annual incomes of <US$10,000. TOTAL=250; INTERVENTION 1=82; INTERVENTION 2=84; CONTROL=84. |
|
| Interventions | OBJECTIVE: To improve adherence to anti‐retroviral treatment (ART). INTERVENTION 1: Daily direct observation of ART treatment taking in the home. INTERVENTION 2: Self‐administration of ART with weekly meetings with a trained case manager for 6 months. These meetings aimed to overcome barriers to ART adherence while also engaging in traditional case management activities, including health care referrals, housing support, drug abuse treatment, legal services and nutritional support. CONTROL: 'Standard of care', study clinic offered adherence counselling as part of primary care services, meetings with a case manager every 3‐4 months and access to community‐based social support services, including adherence support by community pharmacies and others. During the course of the study, weekly adherence clinics were established by staff uninvolved in the study at the 2 larger clinics at which patients in the control arm could receive one to one adherence counselling from providers. MODE OF DELIVERY: Delivered daily evening, weekend and holiday doses for self administration and observed participants take their medication. Addressed adherence problems immediately where possible and referred participants to the clinic when necessary. RECIPIENT INVOLVEMENT IN DESIGN/DEVELOPMENT/DELIVERY: Not specified. GEOGRAPHICAL SETTING: urban formal, USA HEALTHCARE SETTING: home. |
|
| Outcomes | HEALTHCARE BEHAVIOURS: proportion of patients who reported missing no doses of ART; A: completed 6 months of follow up. HEALTH STATUS AND WELLBEING: Proportion of patients with viral load <400copies/ml (primary outcome); 6 month HIV‐1 RNA Level ≤400 copies/Ml; 6 month HIV‐1 RNA Level ≤400 copies/ml; change in CD4 count; development of a new or recurrent opportunistic infection. LENGTH OF TREATMENT: 6 months. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | 'computer generated random‐number assignment' (p1620). |
| Allocation concealment? | Unclear risk | 'treatment assignment was concealed from study staff in sealed envelopes' (p1620). Comment: insufficient information on methods of concealment. |
| Blinding? All outcomes | Low risk | Participants and personnel not blinded. Primary outcomes not likely to be influenced by lack of blinding. For behavioural outcomes, patients were interviewed by staff not involved in the intervention, but unclear if these staff were blinded. |
| Incomplete outcome data addressed? All outcomes | High risk | 'more patients in the DAART arm (18%) exiting the study early, compared with those in the SOC arm (4%)', ' the differences between pateints in the DAART and SOC arms lost to follow‐up was statistically significant' (p1621). Comment: Reason for missing data likely to be related to true outcome. |
| Free of selective reporting? | Unclear risk | Insufficient information to make an assessment. |
| Free of other bias? | Low risk | |
Zaman 2008.
| Methods | RCT. | |
| Participants | LHW: Lady health visitors. TRAINING: Trained in nutrition counselling for five half days and included updating infant feeding knowledge and practice sessions for development of counselling and communication skills. Used the 'Counsel the mother training module' of the WHO/UNICEF IMCI training course, Had a local adaptation of the Pakistani's IMCI 'feeding counselling card'. PARTICIPANTS: Prevention of malnutrition among sick children ‐ about 25% were aged 6‐9 months, almost 40% were 9‐12 months, a little less than 40% were 12+ months. Close to 40% of mothers had no schooling, 10% had 1‐5 years of school, about 35% had 6 ‐ 12 years of school. TOTAL= 375 mother child pairs; INTERVENTION:189 Mother child pairs; CONTROL: 186 mother child pairs. |
|
| Interventions | OBJECTIVE: To determine the efficacy of training health workers in nutrition counselling in enhancing their communication skills and performance, improving feeding practices, and reducing growth faltering in the children aged 6‐24 months. CONTROL: No intervention. MODE OF DELIVERY: Lady health visitor provided counselling to mothers bringing sick children to the health unit. She highlighted recommended foods and frequency of feeding. She discussed these with mother and provided a 'feeding counselling card' as a reminder to the mother. RECIPIENT INVOLVEMENT IN SELECTION/TRAINING/MANAGEMENT: No. GEOGRAPHICAL SETTING: Rural, Pakistan HEALTHCARE SETTING: Primary Health Clinic. |
|
| Outcomes | HEALTH STATUS AND WELLBEING: Weight for age Z score, height for age Z score, Weight for height Z score. BEHAVIOUR: communication skills, feeding practices reported. LENGTH OF FOLLOW UP: 180 days. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | 'One member of each of 20 pairs was allocated to the intervention group and the other to the control group randomly by flipping a coin' (p211). |
| Allocation concealment? | Low risk | Comment: Cluster RCT with clinics as unit of randomisation. |
| Blinding? All outcomes | Low risk | 'blind evaluation...Due to the characteristics of the study, it was not possible to carry a double‐blind trial' (p220). Comment: health providers and patients were not blinded. Outcome assessors were blinded. |
| Incomplete outcome data addressed? All outcomes | Low risk | 'Four centres were dropped from the study after the initial allocation as either intervention (n=2) or controls groups (n=2) because their use was so low that it would not be operationally feasible to reach the target number of 10 mother/child pairs recruited within six months after training.' (p212). Comment: loss to follow up of participants was similar across the intervention and control groups at each outcome assessment. |
| Free of selective reporting? | Low risk | Comment: no evidence of selective outcome reporting found. |
| Free of other bias? | Low risk | |
Zwarenstein 2000.
| Methods | RCT. | |
| Participants | LHW: many of the lay health workers (LHW) were previous TB patients, or had experienced TB in their family. TRAINING: 5 mornings of interactive health promotion education. The rationale was that the process of training the LHW volunteers would increase knowledge of the disease in the community. PATIENTS: pulmonary tuberculosis patients of whom 49% <35 years of age; 58% male; 69% single; 89% living in formal housing; 11% employed; 22% had >11 years of schooling. TOTAL=156; INTERVENTION 1=54; INTERVENTION 2=44; CONTROL=58. | |
| Interventions | OBJECTIVE: to improve tuberculosis (TB) treatment outcomes for pulmonary TB. INTERVENTION 1: observation of TB treatment taking by lay health workers. INTERVENTION 2: self‐observed TB treatment taking. CONTROL: nurse observed TB treatment taking at a clinic MODE OF DELIVERY: LHW supervised the daily dose of anti‐tuberculosis medication. The TB patient came to the LHW's house each day, and the LHW administered the medication from the supplies that they held. They then monitored this on a compliance record. If the patient missed a day's treatment, the LHW visited the patient's home. If the LHW could not solve the problem, a staff member of the managing non‐government organisation (NGO) visited the patient. RECIPIENT INVOLVEMENT IN DESIGN/DEVELOPMENT/DELIVERY: many LHWs were previous TB patients or family members of TB patients. ORGANISATIONAL BASE OF THE INTERVENTION: SANTA, a TB NGO. GEOGRAPHICAL SETTING: urban South Africa HEALTHCARE SETTING: home. | |
| Outcomes | HEALTH STATUS AND WELLBEING: successful TB treatment completion (patients cured and patients completely cured), successful treatment in new patients, successful treatment in recurrent patients, successful treatment in female patients, successful treatment in male patients. LENGTH OF TREATMENT: 6 months. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | 'The randomisation sequence was generated by computer algorithm.' (p551). |
| Allocation concealment? | Low risk | '...the nurse drew an envelope from the top of a box of consecutively numbered opaque sealed envelopes, recording the allocation in the trial book for that clinic' (p551). |
| Blinding? All outcomes | Low risk | Participants not blinded, personnel not blinded. Not clear if outcome assessors blinded but outcome assessment was not likely to be influenced by the lack of blinding. |
| Incomplete outcome data addressed? All outcomes | Low risk | No missing outcome data. |
| Free of selective reporting? | Unclear risk | Insufficient information to make an assessment. |
| Free of other bias? | Low risk | |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Akram 1997 | Not a RCT |
| Anderson 1998 | Not a RCT |
| Andresen 1992 | Review article |
| Arlotti 1998 | Not a RCT |
| Armstrong 1999 | Not a RCT |
| Bailey 1996 | Not an RCT, not a LHW. This study compared 2 ways of training LHW |
| Bang 1993 | Controlled field study |
| Bang 1994 | Field trial |
| Bang 1999 | Not a RCT |
| Barlow 2006 | This study compared 2 LHW interventions |
| Berry 1991 | Not a RCT |
| Bhandari 2003 | Complex intervention involving both LHW and professionals |
| Bhandari 2008 | Multifaceted intervention and effects of LHWs alone cannot be assessed |
| Bhattacharya 1988 | Quasi randomisation, ? systematic. Not LHW intervention. Training for mothers and family members |
| Bhutta 2008 | LHW in both arms of the trial |
| Boone 2007 | LHW in both arms of the trial |
| Brennan 1991 | RCT but not a LHW |
| Brown 2007 | An intervention to promote the uptake of LHWs and a range of other interventions but not LHW delivering intervention |
| Brugha 1996 | Complex intervention involving both professionals and LHW |
| Bullough 1989 | Both groups have LHW involvement |
| Chen 1999 | RCT but not LHW |
| Christopher 1990 | Not a RCT |
| Cox 1998 | Not a LHW study |
| Das 2008 | Not RCT |
| Davies‐Adetugbo 1997 | Controlled before and after |
| Delacollette 1996 | Not a RCT |
| DiCenso 1997 | Not LHW study |
| Dick 1997 | Not a RCT |
| Doherty 2006 | Family members delivering care to other family members only ‐ excluded by our definition of LHW |
| Drummond 2008 | Quasi‐randomised study |
| Durand 1992 | Not a RCT |
| Durlak 1981 | NOT a RCT |
| Gill 2007 | Quasi‐randomised study |
| Goodburn 2000 | Not a RCT |
| Graham 2002 | School‐based, teacher led intervention |
| Gray 1980 | Professional staff who administer the intervention |
| Greenwood 1989 | Not LHW study |
| Gupta 1992 | Not a LHW study |
| Haider 1997 | Not a RCT |
| Hampson 1980 | RCT, not a LHW project |
| Heikens 1993 | RCT but not LHW. Both groups provided with care |
| Heins 1987 | Not a RCT |
| Hill 2000 | Not a RCT |
| Hodnett 1989 | Not LHWs but midwives in training to become professional |
| Hofmeyr 1991 | Referral facility, unlikely primary health care |
| Jepson 1999 | RCT but not a LHW |
| Jessop 1991 | Not LHW study |
| Johnstone 2000 | RCT but not an LHW |
| Jokhio 2005 | Complex intervention including traditional birth attendants and health professionals |
| Kaag 1996 | Not LHW study |
| Kamolratanakul 1999 | Within intervention arm allocation to LHW or professional supervision was not random |
| Kennell 1991 | Quasi‐experimental design |
| Kent 1997 | Not a RCT |
| Kitzman 2000 | Not LHW study |
| Langer 1998 | Not LHW |
| Larson 1980 | Not RCT, visits by undergraduate students |
| Lasater 1996 | Not LHW study |
| Lefeber 1997 | Not a RCT |
| Lindsay 1993 | Not a RCT |
| Madi 1999 | Female relative ‐ excluded from our definition |
| May 1986 | Not a RCT |
| Mbonye 2007 | Not a RCT |
| McFarlane 1997 | Not a RCT |
| McInnes 2000 | This study is a CCT not a RCT |
| Menendez 1994a | Study measuring effectivness |
| Menendez 1994b | Not LHW study |
| Mercier 1992 | Not a RCT or a LHW project |
| Moongtui 2000 | Not LHW study |
| Neittaanmaki 1980 | Not a RCT |
| Newell 2006 | LHW in more than one arm |
| Niccols 2008 | Not LHW study |
| Nikodem 2001 | Institutionalised care |
| Pbert 2006 | Complex intervention that includes both professional and LHW |
| Robinson 1988 | RCT but both groups have LHWs. Family caregivers intervention is training to LHW |
| Rubenstein 1978 | Not a RCT |
| Saylor 1983 | Not a RCT |
| Scarano 1987 | Not a RCT |
| Schafer 1998 | Controlled before and after |
| Sciacca 1995 | Knowledge attitude practice study |
| Shamir 2007 | School‐based intervention trial |
| Shargie 2006 | Complex intervention |
| Shaughnessy 1996 | Not a RCT |
| Shaw 1999 | Not a RCT |
| Smith 2000a | Not a RCT |
| Sosa 1980 | Hospital‐based and not primary health care |
| Spiby 1999 | Not a RCT |
| Strawczynski 1973 | Not a LHW project |
| Terefe 1993 | RCT but both groups have LHW involvement. The intervention was husband involvement |
| Tessaro 1997 | Not a LHW study |
| Thouw 1992 | Not a RCT |
| Townsend 1976 | Not LHW |
| Tuckman 1994 | Not a RCT |
| Uphold 2000 | Not a LHW project or a RCT |
| Victora 1994 | Not LHW study |
| Walker 2004 | Nursing aides ‐ not LHW |
| Walley 2001 | Family members, not considered LHW |
| Walraven 1995 | Not LHW study |
| Walton 1993 | RCT but not LHW |
| Weiler 1993 | Not an RCT or LHW study |
| Wolf 1985 | Intervention used Visiting Nurse Association |
Differences between protocol and review
1) In the original review protocol, we aimed to address the following comparisons:
LHW interventions compared to no intervention;
LHW interventions involving activities not now undertaken by health professionals and delegated to LHWs compared to no intervention;
LHW interventions involving activities not now performed adequately by health professionals and delegated to LHWs compared to no intervention;
LHW interventions involving activities now performed by health professionals but delegated to LHWs to reduce resource consumption compared to the same activities performed by health professionals;
The effectiveness of the lay health worker intervention related to intensity of training.
As the data included in published studies did not allow these comparisons to be addressed meaningfully, we have not included them in this review update.
2) Exclusions: where necessary, we have tailored the exclusion criteria for the review based on new configurations of interventions identified during this update. In particular, we have now excluded interventions in which the LHW was a family member trained to deliver care and provide support only to members of his or her own family (that is in which LHWs did not provide some sort of care or service to others or were unavailable to other members of the community). See above for further explanation (Types of participants).
Contributions of authors
The protocol for the original review was written by SL, MZ, and Judy Dick, with contributions from GA and BvW. This review update was led by SL and SMB. MJ developed and ran the searches. SL, SMB, CG, KD, XBC, BvW, GA, MZ, and IBS assessed studies for inclusion. SL, SMB, CG, XBC, BvW, and IBS participated in data extraction and contributed to data analysis. JOJ, SL, and SMB undertook the meta‐analysis with assistance from the other authors. SMB and SL drafted the review, drawing on contributions from a number of the review authors, and all authors commented on this.
Sources of support
Internal sources
Medical Research Council, South Africa.
Norwegian Knowledge Centre for the Health Services, Norway.
-
SINTEF Health Research, Not specified.
For review update
External sources
-
Research Council of Norway, Norway.
For review update
-
World Health Organisation, Switzerland.
For original review only
-
German Technical Co‐operation (GTZ), Germany.
For original review only
Declarations of interest
JOJ, MZ, SL, and SMB are editors for the Cochrane Effective Practice and Organisation of Care Review Group. SL and CG are editors for the Cochrane Consumers and Communication Review Group. MJ is a trial search coordinator for the Cochrane Effective Practice and Organisation of Care Review Group. MZ was the principal investigator on one of the included trials (Zwarenstein 2000).
New search for studies and content updated (conclusions changed)
References
References to studies included in this review
Agrasada 2005 {published data only}
- Agrasada GV, Gustafsson J, Kylberg E, Ewald U. Postnatal peer counselling on exclusive breastfeeding of low‐birthweight infants: a randomized, controlled trial. Acta Paediatrica 2005;94(0803‐5253 (Print), 8):1109‐15. [DOI] [PubMed] [Google Scholar]
Anderson 2005 {published data only}
- Anderson AK, Damio G, Young S, Chapman DJ, Perez‐Escamilla R. A randomized trial assessing the efficacy of peer counseling on exclusive breastfeeding in a predominantly Latina low‐income community. Archives of Pediatrics & Adolescent Medicine 2005;159(1072‐4710 (Print), 9):836‐41. [DOI] [PubMed] [Google Scholar]
Baqui 2008 {published data only}
- Baqui AH, Arifeen S, Darmstadt GL, Ahmed S, Williams EK, Seraji HR, et al. Effect of community‐based newborn‐care intervention package implemented through two service‐delivery strategies in Sylhet district, Bangladesh: a cluster‐randomised controlled trial. Lancet 2008;371(9628):1936‐44. [DOI] [PubMed] [Google Scholar]
Bari 2006 {published data only}
- Bari S, Mannan I, Rahman MA, Darmstadt GL, Serajil MH, Baqui AH, et al. Trends in use of referral hospital services for care of sick newborns in a community‐based intervention in Tangail District, Bangladesh. Journal of Health, Population, and Nutrition 2006;24(4):519‐29. [PMC free article] [PubMed] [Google Scholar]
Barnes 1999 {published data only}
- Barnes K, Friedman SM, Brickner Namerow P, Honig J. Impact of community volunteers on immunization rates of children younger than 2 years. Archives of Pediatrics & Adolescent Medicine 1999;153(5):518‐24. [DOI] [PubMed] [Google Scholar]
Barnett 1985 {published data only}
- Barnett B, Parker G. Professional and non‐professional intervention for highly anxious primiparous mothers. British Journal of Psychiatry 1985;146(0007‐1250 (Print)):287‐93. [DOI] [PubMed] [Google Scholar]
Barth 1991 {published data only}
- Barth RP. An experimental evaluation of in‐home child abuse prevention services. Child Abuse & Neglect 1991;15(4):363‐75. [DOI] [PubMed] [Google Scholar]
- Barth RP, Hacking S, Ash JR. Preventing child abuse: an experimental evaluation of the child parent enrichment project. Journal of Primary Prevention 1988;8(4):201‐17. [DOI] [PubMed] [Google Scholar]
Black 1995 {published data only}
- Black MM, Dubowitz H, Hutcheson J, Berenson‐Howard J, Starr RH Jr. A randomized clinical trial of home intervention for children with failure to thrive. Pediatrics 1995;95(6):807‐14. [PubMed] [Google Scholar]
- Hutcheson JJ, Black MM, Talley M, Dubowitz H, Howard JB, Starr RH Jr, et al. Risk status and home intervention among children with failure‐to‐thrive: follow‐up at age 4. Journal of Pediatric Psychology 1997;22(5):651‐68. [DOI] [PubMed] [Google Scholar]
Bugental 2002 {published data only}
- Bugental DB, Ellerson PC, Lin EK, Rainey B, Kokotovic A, O'Hara N. A cognitive approach to child abuse prevention. Journal of Family Psychology 2002;16(0893‐3200 (Print), 3):243‐58. [DOI] [PubMed] [Google Scholar]
Bullock 1995 {published data only}
- Bullock LF, Wells JE, Duff GB, Hornblow AR. Telephone support for pregnant women: outcome in late pregnancy. New Zealand Medical Journal 1995;108(1012):476‐8. [PubMed] [Google Scholar]
Caulfield 1998 {published data only}
- Caulfield LE, Gross SM, Bentley ME, Bronner Y, Kessler L, Jensen J, et al. WIC‐based interventions to promote breastfeeding among African‐American women in Baltimore: effects on breastfeeding initiation and continuation. Journal of Human Lactation 1998;14(1):15‐22. [DOI] [PubMed] [Google Scholar]
Chaisson 2001 {published data only}
- Chaisson RE, Barnes GL, Hackman J, Watkinson L, Kimbrough L, Metha S, et al. A randomized, controlled trial of interventions to improve adherence to isoniazid therapy to prevent tuberculosis in injection drug users. American Journal of Medicine 2001;110(0002‐9343 (Print), 8):610‐5. [DOI] [PubMed] [Google Scholar]
Chapman 2004 {published data only}
- Chapman DJ, Damio G, Young S, Perez‐Escamilla R. Effectiveness of breastfeeding peer counseling in a low‐income, predominantly Latina population: a randomized controlled trial. Archives of Pediatrics & Adolescent Medicine 2004;158(1072‐4710 (Print), 9):897‐902. [DOI] [PubMed] [Google Scholar]
Chongsuvivatwong 1996 {published data only}
- Chongsuvivatwong V, Mo‐Suwan L, Tayakkanonta K, Vitsupakorn K, McNeil R. Impacts of training of village health volunteers in reduction of morbidity from acute respiratory infections in childhood in southern Thailand. Southeast Asian Journal of Tropical Medicine and Public Health 1996;27(2):333‐8. [PubMed] [Google Scholar]
Clarke 2005 {published data only}
- Clarke M, Dick J, Zwarenstein M, Lombard CJ, Diwan VK. Lay health worker intervention with choice of DOT superior to standard TB care for farm dwellers in South Africa: a cluster randomised control trial. International Journal of Tuberculosis and Lung Disease 2005;9(1027‐3719 (Print), 6):673‐9. [PubMed] [Google Scholar]
Colombo 1979 {published data only}
- Colombo TJ, Freeborn DK, Mullooly JP, Burnham VR. The effect of outreach workers' educational efforts on disadvantaged preschool children's use of preventive services. American Journal of Public Health 1979;69(0090‐0036 (Print), 5):465‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Coutinho 2005 {published data only}
- Coutinho SB, Lira PI, Carvalho Lima M, Ashworth A. Comparison of the effect of two systems for the promotion of exclusive breastfeeding. Lancet 2005;366(1474‐547X (Electronic), 9491):1094‐100. [DOI] [PubMed] [Google Scholar]
Curnow 2002 {published data only}
- Curnow MM, Pine CM, Burnside G, Nicholson JA, Chesters RK, Huntington E. A randomised controlled trial of the efficacy of supervised toothbrushing in high‐caries‐risk children. Caries Research 2002;36(0008‐6568 (Print), 4):294‐300. [DOI] [PubMed] [Google Scholar]
Dawson 1989 {published data only}
- Dawson P, Doorninck WJ, Robinson JL. Effects of home‐based, informal social support on child health. Journal of Developmental and Behavioral Pediatrics 1989;10(0196‐206X (Print), 2):63‐7. [PubMed] [Google Scholar]
Dennis 2002 {published data only}
- Dennis CL. Breastfeeding peer support: maternal and volunteer perceptions from a randomized controlled trial. Birth 2002;29(3):169‐76. [DOI] [PubMed] [Google Scholar]
- Dennis CL, Hodnett E, Gallop R, Chalmers B. The effect of peer support upon breast‐feeding duration among primiparous women: a randomized controlled trial. CMAJ 2002;166(1):21‐8. [PMC free article] [PubMed] [Google Scholar]
Dennis 2009 {published data only}
- Dennis CL, Hodnett E, Kenton L, Weston J, Zupancic J, Stewart DE, et al. Effect of peer support on prevention of postnatal depression among high risk women: multisite randomised controlled trial. BMJ 2009;338:a3064. [DOI] [PMC free article] [PubMed] [Google Scholar]
Duggan 2004 {published data only}
- Duggan A, Fuddy L, Burrell L, Higman SM, McFarlane E, Windham A, et al. Randomized trial of a statewide home visiting program to prevent child abuse: impact in reducing parental risk factors. Child Abuse and Neglect 2004;28(0145‐2134 (Print), 6):623‐43. [DOI] [PubMed] [Google Scholar]
Ernst 1999 {published data only}
- Ernst CC, Grant TM, Streissguth AP, Sampson PD. Intervention with high‐risk alcohol and drug‐abusing mothers: II. Three‐year findings from the Seattle model of paraprofessional advocacy. Journal of Community Psychology 1999;27(1):19‐38. [Google Scholar]
Flores 2005 {published data only}
- Flores G, Abreu M, Chaisson CE, Meyers A, Sachdeva RC, Fernandez H, et al. A randomized, controlled trial of the effectiveness of community‐based case management in insuring uninsured Latino children. Pediatrics 2005;116(6):1433‐41. [DOI] [PubMed] [Google Scholar]
Gadomski 2006 {published data only}
- Gadomski A, Ackerman S, Burdick P, Jenkins P. Efficacy of the North American guidelines for children's agricultural tasks in reducing childhood agricultural injuries. American Journal of Public Health 2006;96(0090‐0036 (Print), 4):722‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gardner 2003 {published data only}
- Gardner JM, Walker SP, Powell CA, Grantham‐McGregor S. A randomized controlled trial of a home‐visiting intervention on cognition and behavior in term low birth weight infants. Jornal de Pediatria 2003;143(0022‐3476 (Print), 5):634‐9. [DOI] [PubMed] [Google Scholar]
Gielen 2002 {published data only}
- Gielen AC, McDonald EM, Wilson ME, Hwang WT, Serwint JR, Andrews JS, et al. Effects of improved access to safety counseling, products, and home visits on parents' safety practices: results of a randomized trial. Archives of Pediatrics and Adolescent Medicine 2002;156(1072‐4710 (Print), 1):33‐40. [DOI] [PubMed] [Google Scholar]
Gokcay 1993 {published data only}
- Gökçay G, Bulut A, Neyzi O. Paraprofessional women as health care facilitators in mother and child health. Tropical Doctor 1993;23(2):79‐81. [DOI] [PubMed] [Google Scholar]
Graffy 2004 {published data only}
- Graffy J, Taylor J, Williams A, Eldridge S. Randomised controlled trial of support from volunteer counsellors for mothers considering breast feeding. BMJ 2004;328(7430):26. [DOI] [PMC free article] [PubMed] [Google Scholar]
Graham 1992 {published data only}
- Graham AV, Frank SH, Zyzanski SJ, Kitson GC, Reeb KG. A clinical trial to reduce the rate of low birth weight in an inner‐city black population. Family Medicine 1992;24(6):439‐46. [PubMed] [Google Scholar]
Haider 2000 {published data only}
- Haider R, Ashworth A, Kabir I, Huttly SR. Effect of community‐based peer counsellors on exclusive breastfeeding practices in Dhaka, Bangladesh: a randomised controlled trial [see commments]. Lancet 2000;356(9242):1643‐7. [DOI] [PubMed] [Google Scholar]
Hardy 1989 {published data only}
- Hardy JB, Streett R. Family support and parenting education in the home: an effective extension of clinic‐based preventive health care services for poor children. Jornal de Pediatria 1989;115(0022‐3476 (Print), 6):927‐31. [DOI] [PubMed] [Google Scholar]
Ireys 1996 {published data only}
- Chernoff RG, Ireys HT, DeVet KA, Kim YJ. A randomized, controlled trial of a community‐based support program for families of children with chronic illness: pediatric outcomes. Archives of Pediatrics & Adolescent Medicine 2002;156(6):533‐9. [DOI] [PubMed] [Google Scholar]
- Ireys HT, Sills EM, Kolodner KB, Walsh BB. A social support intervention for parents of children with juvenile rheumatoid arthritis: results of a randomized trial. Journal of Pediatric Psychology 1996;21(5):633‐41. [DOI] [PubMed] [Google Scholar]
Ireys 2001 {published data only}
- Ireys HT, Chernoff R, DeVet KA, Kim Y. Maternal outcomes of a randomized controlled trial of a community‐based support program for families of children with chronic illnesses. Archives of Pediatrics & Adolescent Medicine 2001;155(7):771‐6. [DOI] [PubMed] [Google Scholar]
Johnson 1993 {published data only}
- Johnson Z, Howell F, Molloy B. Community mothers' programme: randomised controlled trial of non‐professional intervention in parenting. BMJ 1993;306(6890):1449‐52. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jump 2006 {published data only}
- Jump VK, Fargo JD, Akers JF. Impact of massage therapy on health outcomes among orphaned infants in Ecuador: results of a randomized clinical trial. Family and Community Health 2006;29(4):314‐9. [DOI] [PubMed] [Google Scholar]
Kartin 2002 {published data only}
- Kartin D, Grant TM, Streissguth AP, Sampson PD, Ernst CC. Three‐year developmental outcomes in children with prenatal alcohol and drug exposure. Pediatric Physical Therapy 2002;14(0898‐5669 (Print), 3):145‐53. [DOI] [PubMed] [Google Scholar]
Kidane 2000 {published data only}
- Kidane G, Morrow RH. Teaching mothers to provide home treatment of malaria in Tigray, Ethiopia: a randomised trial. Lancet 2000;356(9229):550‐5. [DOI] [PubMed] [Google Scholar]
Kouyate 2008 {published data only}
- Kouyate B, Some F, Jahn A, Coulibaly B, Eriksen J, Sauerborn R, et al. Process and effects of a community intervention on malaria in rural Burkina Faso: randomized controlled trial. Malaria Journal 2008;7:50. [DOI] [PMC free article] [PubMed] [Google Scholar]
Krieger 2000 {published data only}
- Krieger JW, Castorina JS, Walls ML, Weaver MR, Ciske S. Increasing influenza and pneumococcal immunization rates: a randomized controlled study of a senior center‐based intervention. American Journal of Preventive Medicine 2000;18(2):123‐31. [DOI] [PubMed] [Google Scholar]
Kumar 2008 {published data only}
- Kumar V, Mohanty S, Kumar A, Misra RP, Santosham M, Awasthi S, et al. Effect of community‐based behaviour change management on neonatal mortality in Shivgarh, Uttar Pradesh, India: a cluster‐randomised controlled trial. Lancet 2008;372(9644):1151‐62. [DOI] [PubMed] [Google Scholar]
LeBaron 2004 {published data only}
- LeBaron CW, Starnes DM, Rask KJ. The impact of reminder‐recall interventions on low vaccination coverage in an inner‐city population. Archives of Pediatrics & Adolescent Medicine 2004;158(1072‐4710 (Print), 3):255‐61. [DOI] [PubMed] [Google Scholar]
Leite 2005 {published data only}
- Leite AJ, Puccini RF, Atalah AN, Alves Da Cunha AL, Machado MT. Effectiveness of home‐based peer counselling to promote breastfeeding in the northeast of Brazil: a randomized clinical trial. Acta Paediatrica 2005;94(0803‐5253 (Print), 6):741‐6. [DOI] [PubMed] [Google Scholar]
Luby 2006 {published data only}
- Luby SP, Agboatwalla M, Painter J, Altaf A, Billhimer W, Keswick B, et al. Combining drinking water treatment and hand washing for diarrhoea prevention, a cluster randomised controlled trial. Tropical Medicine and International Health 2006;11(1360‐2276 (Print), 4):479‐89. [DOI] [PubMed] [Google Scholar]
Lwilla 2003 {published data only}
- Lwilla F, Schellenberg D, Masanja H, Acosta C, Galindo C, Aponte J, et al. Evaluation of efficacy of community‐based vs. institutional‐based direct observed short‐course treatment for the control of tuberculosis in Kilombero district, Tanzania. Tropical Medicine and International Health 2003;8(1360‐2276 (Print), 3):204‐10. [DOI] [PubMed] [Google Scholar]
MacArthur 2009 {published data only}
- MacArthur C, Jolly K, Ingram L, Freemantle N, Dennis CL, Hamburger R, et al. Antenatal peer support workers and initiation of breast feeding: cluster randomised controlled trial. BMJ 2009;338:b131. [DOI] [PMC free article] [PubMed] [Google Scholar]
Malchodi 2003 {published data only}
- Malchodi CS, Oncken C, Dornelas EA, Caramanica L, Gregonis E, Curry SL. The effects of peer counseling on smoking cessation and reduction. Obstetrics and Gynecology 2003;101(0029‐7844 (Print), 3):504‐10. [DOI] [PubMed] [Google Scholar]
Malotte 2001 {published data only}
- Malotte CK, Hollingshead JR, Larro M. Incentives vs outreach workers for latent tuberculosis treatment in drug users. American Journal of Preventive Medicine 2001;20(0749‐3797 (Print), 2):103‐7. [DOI] [PubMed] [Google Scholar]
Manandhar 2004 {published data only}
- Manandhar DS, Osrin D, Shrestha BP, Mesko N, Morrison J, Tumbahangphe KM, et al. Effect of a participatory intervention with women's groups on birth outcomes in Nepal: cluster‐randomised controlled trial. Lancet 2004;364(1474‐547X (Electronic), 9438):970‐9. [DOI] [PubMed] [Google Scholar]
Merewood 2006 {published data only}
- Merewood A, Chamberlain LB, Cook JT, Philipp BL, Malone K, Bauchner H. The effect of peer counselors on breastfeeding rates in the neonatal intensive care unit: results of a randomized controlled trial. Archives of Pediatrics & Adolescent Medicine 2006;160(1072‐4710 (Print), 7):681‐5. [DOI] [PubMed] [Google Scholar]
Mohan 2003 {published data only}
- Mohan A, Nassir H, Niazi A. Does routine home visiting improve the return rate and outcome of DOTS patients who delay treatment?. Eastern Mediterranean Health Journal 2003;9(1020‐3397 (Print), 4):702‐8. [PubMed] [Google Scholar]
Morisky 2001 {published data only}
- Morisky DE, Malotte CK, Ebin V, Davidson P, Cabrera D, Trout PT, et al. Behavioral interventions for the control of tuberculosis among adolescents. Public Health Reports 2001;116(0033‐3549 (Print), 6):568‐74. [DOI] [PMC free article] [PubMed] [Google Scholar]
Morrell 2000 {published data only}
- Morrell CJ, Spiby H, Stewart P, Walters S, Morgan A. Costs and effectiveness of community postnatal support workers: randomised controlled trial. BMJ 2000;321(7261):593‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Morrow 1999 {published data only}
- Morrow AL, Guerrero ML, Shults J, Calva JJ, Lutter C, Bravo J, et al. Efficacy of home‐based peer counselling to promote exclusive breastfeeding: a randomised controlled trial. Lancet 1999;353(9160):1226‐31. [DOI] [PubMed] [Google Scholar]
Mtango 1986 {published data only}
- Mtango FD, Neuvians D. Acute respiratory infections in children under five years. Control project in Bagamoyo District, Tanzania. Transactions of the Royal Society of Tropical Medicine and Hygiene 1986;80(6):851‐8. [DOI] [PubMed] [Google Scholar]
Muirhead 2006 {published data only}
- Muirhead PE, Butcher G, Rankin J, Munley A. The effect of a programme of organised and supervised peer support on the initiation and duration of breastfeeding: a randomised trial. British Journal of General Practice 2006;56(0960‐1643 (Print), 524):191‐7. [PMC free article] [PubMed] [Google Scholar]
Olds 2002 {published data only}
- Korfmacher J, O'Brien R, Hiatt S, Olds D. Differences in program implementation between nurses and paraprofessionals providing home visits during pregnancy and infancy: a randomized trial. American Journal of Public Health 1999;89(12):1847‐51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olds DL, Robinson J, O'Brien R, Luckey DW, Pettitt LM, Henderson CR Jr, et al. Home visiting by paraprofessionals and by nurses: a randomized, controlled trial. Pediatrics 2002;110(3):486‐96. [DOI] [PubMed] [Google Scholar]
Parker 2008 {published data only}
- Parker EA, Israel BA, Robins TG, Mentz G, Xihong Lin, Brakefield‐Caldwell W, et al. Evaluation of Community Action Against Asthma: a community health worker intervention to improve children's asthma‐related health by reducing household environmental triggers for asthma. Health Education and Behavior 2008;35(3):376‐95. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pence 2005 {published data only}
- Pence BW, Nyarko P, Phillips JF, Debpuur C. The effects of community nurses and health volunteers on child mortality: The Navrongo Community Health Family Planning Project. Population Council 2005;200:1‐27. [DOI] [PubMed] [Google Scholar]
Rodewald 1999 {published data only}
- Rodewald LE, Szilagyi PG, Humiston SG, Barth R, Kraus R, Raubertas RF. A randomized study of tracking with outreach and provider prompting to improve immunization coverage and primary care. Pediatrics 1999;103(1098‐4275 (Electronic), 1):31‐8. [DOI] [PubMed] [Google Scholar]
Rohr 2004 {published data only}
- Rohr F, Munier A, Sullivan D, Bailey I, Gennaccaro M, Levy H, et al. The Resource Mothers Study of Maternal Phenylketonuria: preliminary findings. Journal of Inherited Metabolic Disease 2004;27(0141‐8955 (Print), 2):145‐55. [DOI] [PubMed] [Google Scholar]
Sazawal 1996 {published data only}
- Sazawal S, Black RE, Bhan MK, Jalla S, Bhandari N, Sinha A, et al. Zinc supplementation reduces the incidence of persistent diarrhea and dysentery among low socioeconomic children in India. Journal of Nutrition 1996;126(2):443‐50. [DOI] [PubMed] [Google Scholar]
Schuler 2000 {published data only}
- Schuler ME, Nair P, Black MM, Kettinger L. Mother‐infant interaction: effects of a home intervention and ongoing maternal drug use. Journal of Clinical Child Psychology 2000;29(3):424‐31. [DOI] [PMC free article] [PubMed] [Google Scholar]
Siegel 1980 {published data only}
- Siegel E, Bauman KE, Schaefer ES, Saunders MM, Ingram DD. Hospital and home support during infancy: impact on maternal attachment, child abuse and neglect, and health care utilization. Pediatrics 1980;66(2):183‐90. [PubMed] [Google Scholar]
Silver 1997 {published data only}
- Silver E, Ireys HT, Bauman LJ, Stein RE. Psychological outcomes of a support intervention in mothers of children with ongoing health conditions. The parent‐to‐parent network. Journal of Community Psychology 1997;25(3):249‐64. [Google Scholar]
Singer 1999 {published data only}
- Singer GHS, Marquis J, Powers LK, Blanchard L, Divenere N, Santelli B, et al. A multi‐site evaluation of parent to parent programs for parents of children with disabilities. Journal of Early Intervention 1999;22(3):217‐29. [Google Scholar]
Sloan 2008 {published data only}
- Sloan NL, Ahmed S, Mitra SN, Choudhury N, Chowdhury M, Rob U, et al. Community‐based kangaroo mother care to prevent neonatal and infant mortality: a randomized, controlled cluster trial. Pediatrics 2008;121(5):e1047‐59. [DOI] [PubMed] [Google Scholar]
Spencer 1989 {published data only}
- Spencer B, Thomas H, Morris J. A randomized controlled trial of the provision of a social support service during pregnancy: the South Manchester Family Worker Project. BJOG 1989;96(0306‐5456 (Print), 3):281‐8. [DOI] [PubMed] [Google Scholar]
Sripaipan 2002 {published data only}
- Sripaipan T, Schroeder DG, Marsh DR, Pachon H, Dearden KA, Ha TT, et al. Effect of an integrated nutrition program on child morbidity due to respiratory infection and diarrhea in northern Viet Nam. Food and Nutrition Bulletin 2002;23 Suppl(0379‐5721 (Print), 4):70‐7. [PubMed] [Google Scholar]
Stevens‐Simon 2001 {published data only}
- Stevens‐Simon C, Nelligan D, Kelly L. Adolescents at risk for mistreating their children. Part II: A home‐ and clinic‐based prevention program. Child Abuse and Neglect 2001;25(0145‐2134 (Print), 6):753‐69. [DOI] [PubMed] [Google Scholar]
Sullivan 2002 {published data only}
- Sullivan CM, Byebee DI, Allen NE. Findings from a community‐based program for battered women and their children. Journal of Interpersonal Violence 2002;17(9):915‐36. [Google Scholar]
Sullivan‐Bolyai 2004 {published data only}
- Sullivan‐Bolyai S, Grey M, Deatrick J, Gruppuso P, Giraitis P, Tamborlane W. Helping other mothers effectively work at raising young children with type 1 diabetes. The Diabetes Educator 2004;30(0145‐7217 (Print), 3):476‐84. [DOI] [PubMed] [Google Scholar]
Swart 2008 {published data only}
- Swart L, Niekerk A, Seedat M, Jordaan E. Paraprofessional home visitation program to prevent childhood unintentional injuries in low‐income communities: a cluster randomized controlled trial. Injury Prevention 2008;14(3):164‐9. [DOI] [PubMed] [Google Scholar]
Tough 2006 {published data only}
- Tough SC, Johnston DW, Siever JE, Jorgenson G, Slocombe L, Lane C, et al. Does supplementary prenatal nursing and home visitation support improve resource use in a universal health care system? A Randomized Controlled Trial in Canada. Birth 2006;33(3):183‐94. [DOI] [PubMed] [Google Scholar]
Tulsky 2000 {published data only}
- Pilote L, Tulsky JP, Zolopa AR, Hahn JA, Schecter GF, Moss AR. Tuberculosis prophylaxis in the homeless. A trial to improve adherence to referral. Archives of Internal Medicine 1996;156(2):161‐5. [PubMed] [Google Scholar]
- Tulsky JP, Pilote L, Hahn JA, Zolopa AJ, Burke M, Chesney M, et al. Adherence to isoniazid prophylaxis in the homeless: a randomized controlled trial. Archives of Internal Medicine 2000;160(0003‐9926 (Print), 5):697‐702. [DOI] [PubMed] [Google Scholar]
Vogler 2002 {published data only}
- Vogler SD, Davidson AJ, Crane LA, Steiner JF, Brown JM. Can paraprofessional home visitation enhance early intervention service delivery?. Journal of Developmental and Behavioral Pediatrics 2002;23(0196‐206X (Print), 4):208‐16. [DOI] [PubMed] [Google Scholar]
Wang 2007 {published data only}
- Wang L, Li J, Chen H, Li F, Armstrong GL, Nelson C, et al. Hepatitis B vaccination of newborn infants in rural China: evaluation of a village‐based, out‐of‐cold‐chain delivery strategy. Bulletin of the World Health Organization 2007;85(9):688‐94. [DOI] [PMC free article] [PubMed] [Google Scholar]
Watt 2009 {published data only}
- Watt RG, Tull KI, Hardy R, Wiggins M, Kelly Y, Molloy B, et al. Effectiveness of a social support intervention on infant feeding practices: randomised controlled trial. Journal of Epidemiology and Community Health 2009;63(2):156‐62. [DOI] [PubMed] [Google Scholar]
Weindling 2007 {published data only}
- Weindling AM, Cunningham CC, Glenn SM, Edwards RT, Reeves DJ. Additional therapy for young children with spastic cerebral palsy: a randomised controlled trial. Health Technology Assessment 2007;11(16):iii‐x, 1. [DOI] [PubMed] [Google Scholar]
Wohl 2006 {published data only}
- Wohl AR, Garland WH, Valencia R, Squires K, Witt MD, Kovacs A, et al. A randomized trial of directly administered antiretroviral therapy and adherence case management intervention. Clinical Infectious Diseases 2006;42(1537‐6591 (Electronic), 11):1619‐27. [DOI] [PubMed] [Google Scholar]
Zaman 2008 {published data only}
- Zaman S, Ashraf RN, Martines J. Training in complementary feeding counselling of healthcare workers and its influence on maternal behaviours and child growth: A cluster randomized controlled trial in Lahore, Pakistan. Journal of Health, Population, and Nutrition 2008;26(2):210‐22. [PMC free article] [PubMed] [Google Scholar]
Zwarenstein 2000 {published data only}
- Zwarenstein M, Schoeman JH, Vundule C, Lombard CJ, Tatley M. A randomised controlled trial of lay health workers as direct observers for treatment of tuberculosis. The International Journal of Tuberculosis and Lung Disease 2000;4(6):550‐4. [PubMed] [Google Scholar]
References to studies excluded from this review
Akram 1997 {published data only}
- Akram DS, Agboatwalla M, Shamshad S. Effect of intervention on promotion of exclusive breast feeding. JPMA. The Journal of the Pakistan Medical Association 1997;47(2):46‐8. [PubMed] [Google Scholar]
Anderson 1998 {published data only}
- Anderson SE, Brewer B, Stein M. Closing the distance. Nursing Management 1998;29(11):44‐8. [PubMed] [Google Scholar]
Andresen 1992 {published data only}
- Andresen PA, Telleen SL. The relationship between social support and maternal behaviors and attitudes: a meta‐analytic review. American Journal of Community Psychology 1992;20(6):753‐74. [PubMed] [Google Scholar]
Arlotti 1998 {published data only}
- Arlotti JP, Cottrell BH, Lee SH, Curtin JJ. Breastfeeding among low‐income women with and without peer support. Journal of Community Health Nursing 1998;15(3):163‐78. [DOI] [PubMed] [Google Scholar]
Armstrong 1999 {published data only}
- Armstrong KL, Fraser JA, Dadds MR, Morris J. A randomized, controlled trial of nurse home visiting to vulnerable families with newborns. Journal of Paediatrics and Child Health 1999;35(3):237‐44. [DOI] [PubMed] [Google Scholar]
Bailey 1996 {published data only}
- Bailey JE, Coombs DW. Effectiveness of an Indonesian model for rapid training of Guatemalan health workers in diarrhea case management. Journal of Community Health 1996;21(4):269‐76. [DOI] [PubMed] [Google Scholar]
Bang 1993 {published data only}
- Bang AT, Bang RA, Morankar VP, Sontakke PG, Solanki JM. Pneumonia in neonates: can it be managed in the community?. Archives of Disease in Childhood 1993;68(5 Spec No):550‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bang 1994 {published data only}
- Bang AT, Bang RA, Sontakke PG. Management of childhood pneumonia by traditional birth attendants. The SEARCH Team. Bulletin of the World Health Organization 1994;72(6):897‐905. [PMC free article] [PubMed] [Google Scholar]
Bang 1999 {published data only}
- Bang AT, Bang RA, Baitule SB, Reddy MH, Deshmukh MD. Effect of home‐based neonatal care and management of sepsis on neonatal mortality: field trial in rural India. Lancet 1999;345(9194):1955‐61. [DOI] [PubMed] [Google Scholar]
Barlow 2006 {published data only}
- Barlow J, Powell L, Gilchrist M. The influence of the training and support programme on the self‐efficacy and psychological well‐being of parents of children with disabilities: a controlled trial. Complementary Therapies in Clinical Practice 2006;12:(1):55‐63. [DOI] [PubMed] [Google Scholar]
Berry 1991 {published data only}
- Berry GL, Zarit SH, Rabatin VX. Caregiver activity on respite and nonrespite days: a comparison of two service approaches. The Gerontologist 1991;31(6):830‐5. [DOI] [PubMed] [Google Scholar]
Bhandari 2003 {published data only}
- Bhandari N, Bahl R, Mazumdar S, Martines J, Black RE, Bhan MK. Effect of community‐based promotion of exclusive breastfeeding on diarrhoeal illness and growth: a cluster randomised controlled trial. Lancet 2003;361(0140‐6736 (Print), 9367):1418‐23. [DOI] [PubMed] [Google Scholar]
Bhandari 2008 {published data only}
- Bhandari Nita, Mazumder Sarmila, Taneja Sunita, Dube Brinda, Agarwal RC, Mahalanabis Dilip, et al. Effectiveness of zinc supplementation plus oral rehydration salts compared with oral rehydration salts alone as a treatment for acute diarrhea in a primary care setting: a cluster randomized trial. Pediatrics 2008;121(5):e1279‐85. [DOI] [PubMed] [Google Scholar]
Bhattacharya 1988 {published data only}
- Bhattacharya R, Kaur P, Reddy DC. Impact of education in the knowledge and practices of rural mothers and key family members on diarrhoea and its treatment at home. Journal of Diarrhoeal Diseases Research 1988;6(1):15‐20. [PubMed] [Google Scholar]
Bhutta 2008 {published data only}
- Bhutta ZA, Memon ZA, Soofi S, Salat MS, Cousens S, Martines J. Implementing community‐based perinatal care: results from a pilot study in rural Pakistan. Bulletin of the World Health Organization 2008;86(6):452‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Boone 2007 {published data only}
- Boone Peter, Mann Vera, Eble Alexander, Mendiratta Tarana, Mukherjee Rohini, Figueiredo Ryan, et al. Community health and medical provision: impact on neonates (the CHAMPION trial). BMC Pediatrics 2007;7:26. [DOI] [PMC free article] [PubMed] [Google Scholar]
Brennan 1991 {published data only}
- Brennan PF, Moore SM, Smyth KA. ComputerLink: electronic support for the home caregiver. ANS. Advances in Nursing Science 1991;13(4):14‐27. [DOI] [PubMed] [Google Scholar]
Brown 2007 {published data only}
- Brown H, Hofmeyr GJ, Nikodem VC, Smith H, Garner P. Promoting childbirth companions in South Africa: a randomised pilot study. BMC Medicine 2007;5:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Brugha 1996 {published data only}
- Brugha RF, Kevany JP. Maximizing immunization coverage through home visits: a controlled trial in an urban area of Ghana. Bulletin of the World Health Organization 1996;74(0042‐9686 (Print), 5):517‐24. [PMC free article] [PubMed] [Google Scholar]
Bullough 1989 {published data only}
- Bullough CH, Msuku RS, Karonde L. Early suckling and postpartum haemorrhage: controlled trial in deliveries by traditional birth attendants. Lancet 1989;2(8662):522‐5. [DOI] [PubMed] [Google Scholar]
Chen 1999 {published data only}
- Chen M. The effectiveness of health promotion counseling to family caregivers. Public Health Nursing (Boston, Mass.) 1999;16(2):125‐32. [DOI] [PubMed] [Google Scholar]
Christopher 1990 {published data only}
- Christopher FS, Roosa MW. An evaluation of an adolescent pregnancy prevention programme: is 'just say no' enough?. Family Relations 1990;39(1):68‐72. [Google Scholar]
Cox 1998 {published data only}
- Cox GB, Walker RD, Freng SA, Short BA, Meijer L, Gilchrist L. Outcome of a controlled trial of the effectiveness of intensive case management for chronic public inebriates. Journal of Studies on Alcohol 1998;59(5):523‐32. [DOI] [PubMed] [Google Scholar]
Das 2008 {published data only}
- Das Lalit K, Jambulingam Purushothaman, Sadanandane Candasamy. Impact of community‐based presumptive chloroquine treatment of fever cases on malaria morbidity and mortality in a tribal area in Orissa State, India. Malaria Journal 2008;7:75. [DOI] [PMC free article] [PubMed] [Google Scholar]
Davies‐Adetugbo 1997 {published data only}
- Davies‐Adetugbo AA, Adebawa HA. The Ife South Breastfeeding Project: training community health extension workers to promote and manage breastfeeding in rural communities. Bulletin of the World Health Organization 1997;75(4):323‐32. [PMC free article] [PubMed] [Google Scholar]
Delacollette 1996 {published data only}
- Delacollette C, Stuyft P, Molima K. Using community health workers for malaria control: experience in Zaire. Bulletin of the World Health Organization 1996;74(4):423‐30. [PMC free article] [PubMed] [Google Scholar]
DiCenso 1997 {published data only}
- Mitchell‐DiCenso A, Thomas BH, Devlin MC, Goldsmith CH, Willan A, Singer J, et al. Evaluation of an educational program to prevent adolescent pregnancy. Health Education & Behavior 1997;24(3):300‐12. [DOI] [PubMed] [Google Scholar]
Dick 1997 {published data only}
- Dick J, Clarke M, Tibbs J, Schoeman H. Combating tuberculosis‐‐lessons learnt from a rural community project in the Klein Drakenstein area of the Western Cape. South African Medical Journal 1997;87 Suppl(8):1042‐7. [PubMed] [Google Scholar]
Doherty 2006 {published data only}
- Doherty William J, Erickson Martha Farrell, LaRossa Ralph. An intervention to increase father involvement and skills with infants during the transition to parenthood. Journal of Family Psychology 2006;20(3):438‐47. [DOI] [PubMed] [Google Scholar]
Drummond 2008 {published data only}
- Drummond JE, Letourneau N, Neufeld SM, Stewart M, Weir A. Effectiveness of teaching an early parenting approach within a community‐based support service for adolescent mothers. Research in Nursing & Health 2008;31(1):12‐22. [DOI] [PubMed] [Google Scholar]
Durand 1992 {published data only}
- Duran AM. The safety of home birth: the farm study. American Journal of Public Health 1992;82(3):450‐3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Durlak 1981 {published data only}
- Durlak JA. Evaluating comparative studies of paraprofessional and professional helpers: a reply to Nietzel and Fisher. Psychological Bulletin 1981;89(3):566‐9. [PubMed] [Google Scholar]
Gill 2007 {published data only}
- Gill SL, Reifsnider E, Lucke JF. Effects of support on the initiation and duration of breastfeeding. Western Journal of Nursing Research 2007;29(6):708‐23. [DOI] [PubMed] [Google Scholar]
Goodburn 2000 {published data only}
- Goodburn EA, Chowdhury M, Gazi R, Marshall T, Graham W. Training traditional birth attendants in clean delivery does not prevent postpartum infection. Health Policy and Planning 2000;15(4):394‐9. [DOI] [PubMed] [Google Scholar]
Graham 2002 {published data only}
- Graham A, Moore L, Sharp D, Diamond I. Improving teenagers' knowledge of emergency contraception: cluster randomised controlled trial of a teacher led intervention. BMJ 2002;324(7347):1179. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gray 1980 {published data only}
- Gray SW, Ruttle K. The family‐oriented home visiting program: a longitudinal study. Genetic Psychology Monographs 1980;102(2):299‐316. [PubMed] [Google Scholar]
Greenwood 1989 {published data only}
- Greenwood BM, Greenwood AM, Snow RW, Byass P, Bennett S, Hatib‐N'Jie AB. The effects of malaria chemoprophylaxis given by traditional birth attendants on the course and outcome of pregnancy. Transactions of the Royal Society of Tropical Medicine and Hygiene 1989;83(5):589‐94. [DOI] [PubMed] [Google Scholar]
Gupta 1992 {published data only}
- Gupta PC, Mehta FS, Pindborg JJ, Bhonsle RB, Murti PR, Daftary DK, et al. Primary prevention trial of oral cancer in india: a 10‐year follow‐up study. Journal of Oral Pathology & Medicine 1992;21(10):433‐9. [DOI] [PubMed] [Google Scholar]
Haider 1997 {published data only}
- Haider R, Kabir I, Hamadani JD, Habte D. Reasons for failure of breast‐feeding counselling: mothers' perspectives in Bangladesh. Bulletin of the World Health Organization 1997;75(3):191‐6. [PMC free article] [PubMed] [Google Scholar]
Hampson 1980 {published data only}
- Hampson RB, Tavormina JB. Relative effectiveness of behavioral and reflective group training with foster mothers. Journal of Consulting and Clinical Psychology 1980;48(2):294‐5. [DOI] [PubMed] [Google Scholar]
Heikens 1993 {published data only}
- Heikens GT, Schofield WN, Dawson S. The Kingston Project. II. The effects of high energy supplement and metronidazole on malnourished children rehabilitated in the community: anthropometry. European Journal of Clinical Nutrition 1993;47(3):160‐73. [PubMed] [Google Scholar]
Heins 1987 {published data only}
- Heins HC Jr, Nance NW, Ferguson JE. Social support in improving perinatal outcome: the Resource Mothers Program. Obstetrics and Gynecology 1987;70(2):263‐6. [PubMed] [Google Scholar]
Hill 2000 {published data only}
- Hill AG, MacLeod WB, Joof D, Gomez P, Walraven G. Decline of mortality in children in rural Gambia: the influence of village‐level primary health care. Tropical Medicine & International Health 2000;5(2):107‐18. [DOI] [PubMed] [Google Scholar]
Hodnett 1989 {published data only}
- Hodnett ED, Osborn RW. A randomized trial of the effects of monitrice support during labor: mothers' views two to four weeks postpartum. Birth 1989;16(4):177‐84. [DOI] [PubMed] [Google Scholar]
- Hodnett ED, Osborn RW. Effects of continuous intrapartum professional support on childbirth outcomes. Research in Nursing & Health 1989;12(5):289‐97. [DOI] [PubMed] [Google Scholar]
Hofmeyr 1991 {published data only}
- Hofmeyr GJ, Nikodem VC, Wolman WL, Chalmers BE, Kramer T. Companionship to modify the clinical birth environment: effects on progress and perceptions of labour, and breastfeeding. Br.J.Obstet.Gynaecol. 1991;98(0306‐5456 (Print), 8):756‐64. [DOI] [PubMed] [Google Scholar]
Jepson 1999 {published data only}
- J Jepson C, McCorkle R, Adler D, Nuamah I, Lusk E. Effects of home care on caregivers' psychosocial status. Image‐‐The Journal of Nursing Scholarship 1999;31(2):115‐20. [DOI] [PubMed] [Google Scholar]
Jessop 1991 {published data only}
- Jessop DJ, Stein RE. Who benefits from a pediatric home care program?. Pediatrics 1991;88(3):497‐505. [PubMed] [Google Scholar]
Johnstone 2000 {published data only}
- Johnston B, Wheeler L, Deuser J, Sousa KH. Outcomes of the Kaiser Permanente Tele‐Home Health Research Project. Archives of Family.Medicine 2000;9(1):40‐5. [DOI] [PubMed] [Google Scholar]
Jokhio 2005 {published data only}
- Jokhio AH, Winter HR, Cheng KK. An intervention involving traditional birth attendants and perinatal and maternal mortality in Pakistan. New England Journal of Medicine 2005;352(1533‐4406 (Electronic), 20):2091‐9. [DOI] [PubMed] [Google Scholar]
Kaag 1996 {published data only}
- Kaag ME, Wijkel D, Jong D. Primary health care replacing hospital care‐‐the effect on quality of care. International Journal for Quality in Health Care 1996;8(4):367‐73. [DOI] [PubMed] [Google Scholar]
Kamolratanakul 1999 {published data only}
- Kamolratanakul P, Sawert H, Lertmaharit S, Kasetjaroen Y, Akksilp S, Tulaporn C, et al. Randomized controlled trial of directly observed treatment (DOT) for patients with pulmonary tuberculosis in Thailand. Transactions of the Royal Society of Tropical Medicine and Hygiene 1999;93(5):552‐7. [DOI] [PubMed] [Google Scholar]
Kennell 1991 {published data only}
- Kennell J, Klaus M, McGrath S, Robertson S, Hinkley C. Continuous emotional support during labor in a US hospital. A randomized controlled trial. JAMA 1991;265(0098‐7484 (Print), 17):2197‐201. [PubMed] [Google Scholar]
Kent 1997 {published data only}
- Kent RM, Chandler BJ. A comparison of community care services provided for younger and elderly disabled people. Clinical Rehabilitation 1997;11:265‐70. [Google Scholar]
Kitzman 2000 {published data only}
- Kitzman H, Olds DL, Sidora K, Henderson CR Jr, Hanks C, Cole R, et al. Enduring effects of nurse home visitation on maternal life course: a 3‐year follow‐up of a randomized trial. JAMA 2000;283(15):1983‐9. [DOI] [PubMed] [Google Scholar]
Langer 1998 {published data only}
- Langer A, Campero L, Garcia C, Reynoso S. Effects of psychosocial support during labour and childbirth on breastfeeding, medical interventions, and mothers' wellbeing in a Mexican public hospital: a randomised clinical trial. British Journal of Obstetrics and Gynaecology 1998;105(0306‐5456 (Print), 10):1056‐63. [DOI] [PubMed] [Google Scholar]
Larson 1980 {published data only}
- Larson CP. Efficacy of prenatal and postpartum home visits on child health and development. Pediatrics 1980;66(2):191‐7. [PubMed] [Google Scholar]
Lasater 1996 {published data only}
- Lasater M. The effect of a nurse‐managed CHF clinic on patient readmission and length of stay. Home Healthcare Nurse 1996;14(5):351‐6. [DOI] [PubMed] [Google Scholar]
Lefeber 1997 {published data only}
- Lefèber Y, Voorhoever H. Practices and beliefs of traditional birth attendants: lessons for obstetrics in the north?. Tropical Medicine & International Health 1997;2(12):1175‐9. [DOI] [PubMed] [Google Scholar]
Lindsay 1993 {published data only}
- Lindsay SW, Alonso PL, Armstrong Schellenberg JR, Hemingway J, Thomas PJ, Shenton FC, et al. A malaria control trial using insecticide‐treated bed nets and targeted chemoprophylaxis in a rural area of The Gambia, west Africa. 3. Entomological characteristics of the study area. Transactions of the Royal Society of Tropical Medicine and Hygiene 1993;87 Suppl 2:19‐23. [DOI] [PubMed] [Google Scholar]
Madi 1999 {published data only}
- Madi BC, Sandall J, Bennett R, MacLeod C. Effects of female relative support in labor: a randomized controlled trial. Birth 1999;26(0730‐7659 (Print), 1):4‐8. [DOI] [PubMed] [Google Scholar]
May 1986 {published data only}
- May D, McKeganey N, Flood M. Extra hands or extra problems?. Nursing Times 1986;82(36):35‐8. [PubMed] [Google Scholar]
Mbonye 2007 {published data only}
- Mbonye Anthony K, Bygbjerg IC, Magnussen Pascal. A community‐based delivery system of intermittent preventive treatment of malaria in pregnancy and its effect on use of essential maternity care at health units in Uganda. Transactions of the Royal Society of Tropical Medicine and Hygiene 2007;101(11):1088‐95. [DOI] [PubMed] [Google Scholar]
McFarlane 1997 {published data only}
- McFarlane J, Wiist W. Preventing abuse to pregnant women: implementation of a "mentor mother" advocacy model. Journal of Community Health Nursing 1997;14(4):237‐49. [DOI] [PubMed] [Google Scholar]
McInnes 2000 {published data only}
- McInnes RJ, Love JG, Stone DH. Evaluation of a community‐based intervention to increase breastfeeding prevalance. Journal of Public Health Medicine 2000;22(2):138‐45. [DOI] [PubMed] [Google Scholar]
Menendez 1994a {published data only}
- Menendez C, Todd J, Alonso PL, Francis N, Lulat S, Ceesay S, et al. The effects of iron supplementation during pregnancy, given by traditional birth attendants, on the prevalence of anaemia and malaria. Transactions of the Royal Society of Tropical Medicine and Hygiene 1994;88(5):590‐3. [DOI] [PubMed] [Google Scholar]
Menendez 1994b {published data only}
- Menendez C, Todd J, Alonso PL, Lulat S, Francis N, Greenwood BM. Malaria chemoprophylaxis, infection of the placenta and birth weight in Gambian primigravidae. Journal of Tropical Medicine and Hygiene 1994;97(4):244‐8. [PubMed] [Google Scholar]
Mercier 1992 {published data only}
- Mercier C, Tempier R, Renaud C. Community services and quality of life: a study of the impact in a remote region [Services communautaires et qualiité de la vie: une étude d'Impact en région éloignée]. Canadian Journal of Psychiatry 1992;37(8):553‐63. [DOI] [PubMed] [Google Scholar]
Moongtui 2000 {published data only}
- Moongtui W, Gauthier DK, Turner JG. Using peer feedback to improve handwashing and glove usage among Thai health care workers. American Journal of Infection Control 2000;28(5):365‐9. [DOI] [PubMed] [Google Scholar]
Neittaanmaki 1980 {published data only}
- Neittaanmäki L, Koskela K, Puska P, McAlister AL. The role of lay workers in community health education: experiences of the North Karelia project. Scandinavian Journal of Social Medicine 1980;8(1):1‐7. [DOI] [PubMed] [Google Scholar]
Newell 2006 {published data only}
- Newell JN, Baral SC, Pande SB, Bam DS, Malla P. Family‐member DOTS and community DOTS for tuberculosis control in Nepal: cluster‐randomised controlled trial. Lancet 2006;367(1474‐547X (Electronic), 9514):903‐9. [DOI] [PubMed] [Google Scholar]
Niccols 2008 {published data only}
- Niccols A. 'Right from the Start': randomized trial comparing an attachment group intervention to supportive home visiting. Journal of Child Psychology and Psychiatry, and Allied Disciplines 2008;49(7):754‐64. [DOI] [PubMed] [Google Scholar]
Nikodem 2001 {published data only}
- Nikodem VC, Nolte AG, Wolman W, Gülmezoglu AM, Hofmeyr GJ. Companionship by a lay labour supporter to modify the clinical birth environment: long‐term effects on mother and child. Curationis 2001;21(1):8‐12. [DOI] [PubMed] [Google Scholar]
Pbert 2006 {published data only}
- Pbert L, Fletcher KE, Flint AJ, Young MH, Druker S, DiFranza J. Smoking prevention and cessation intervention delivery by pediatric providers, as assessed with patient exit interviews. Pediatrics 2006;118(3):e810‐24. [DOI] [PubMed] [Google Scholar]
Robinson 1988 {published data only}
- Robinson KM. A social skills training program for adult caregivers. ANS. Advances in Nursing Science 1988;10(2):59‐72. [DOI] [PubMed] [Google Scholar]
Rubenstein 1978 {published data only}
- Rubenstein JS, Armentrout JA, Levin S, Herald D. The parent‐therapist program: alternate care for emotionally disturbed children. The American Journal of Orthopsychiatry 1978;48(4):654‐62. [DOI] [PubMed] [Google Scholar]
Saylor 1983 {published data only}
- Saylor DE. Orientation programs prepare volunteers for patient contact. Hospital Progress 1983;64(5):53, 66. [PubMed] [Google Scholar]
Scarano 1987 {published data only}
- Scarano S. Victim volunteers mobilize to minister. Emergency 1987;19(3):47‐9. [PubMed] [Google Scholar]
Schafer 1998 {published data only}
- Schafer E, Vogel MK, Viegas S, Hausafus C. Volunteer peer counselors increase breastfeeding duration among rural low‐income women. Birth 1998;25(2):101‐6. [DOI] [PubMed] [Google Scholar]
Sciacca 1995 {published data only}
- Sciacca JP, Dube DA, Phipps BL, Ratliff MI. A breast feeding education and promotion program: effects on knowledge, attitudes, and support for breast feeding. Journal of Community Health 1995;20(0094‐5145 (Print), 6):473‐90. [DOI] [PubMed] [Google Scholar]
Shamir 2007 {published data only}
- Shamir A, Lazerovitz T. Peer mediation intervention for scaffolding self‐regulated learning among children with learning disabilities. European Journal of Special Needs Education 2007;22(3):255‐73. [Google Scholar]
Shargie 2006 {published data only}
- Shargie EB, Morkve O, Lindtjorn B. Tuberculosis case‐finding through a village outreach programme in a rural setting in southern Ethiopia: community randomized trial. Bulletin of the World Health Organization 2006;84(0042‐9686 (Print), 2):112‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Shaughnessy 1996 {published data only}
- Shaughnessy PW, Schlenker RE, Crisler KS, Arnold AG, Powell MC, Beaudry JM. Home care: moving forward with continuous quality improvement. Journal of Aging & Social Policy 1996;7(3‐4):149‐67. [DOI] [PubMed] [Google Scholar]
Shaw 1999 {published data only}
- Shaw E, Kaczorowski J. The effect of a peer counseling program on breastfeeding initiation and longevity in a low‐income rural population. Journal of Human Lactation 1999;15(1):19‐25. [DOI] [PubMed] [Google Scholar]
Smith 2000a {published data only}
- Smith JB, Coleman NA, Fortney JA, Johnson JD, Blumhagen DW, Grey TW. The impact of traditional birth attendant training on delivery complications in Ghana. Health Policy and Planning 2000;15(3):326‐31. [DOI] [PubMed] [Google Scholar]
Sosa 1980 {published data only}
- Sosa R, Kennell J, Klaus M, Robertson S, Urrutia J. The effect of a supportive companion on perinatal problems, length of labor, and mother‐infant interaction. New England Journal of Medicine 1980;303(0028‐4793 (Print), 11):597‐600. [DOI] [PubMed] [Google Scholar]
Spiby 1999 {published data only}
- Spiby H, Crowther S. Dutch materninty aides: a transferable model. RCM Midwives Journal 1999;2(3):20‐1. [Google Scholar]
Strawczynski 1973 {published data only}
- Strawczynski H, Stachewitsch A, Morgenstern G, Shaw ME. Delivery of care to hemophilic children: home care versus hospitalization. Pediatrics 1973;51(6):986‐91. [PubMed] [Google Scholar]
Terefe 1993 {published data only}
- Terefe A, Larson CP. Modern contraception use in Ethiopia: does involving husbands make a difference?. American Journal of Public Health 1993;83(11):1567‐71. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tessaro 1997 {published data only}
- Tessaro I, Campbell M, O'Meara C, Herrick H, Buescher P, Meyer R, et al. State health department and university evaluation of North Carolina's Maternal Outreach Worker Program. American Journal of Preventive Medicine 1997;13 Suppl(6):38‐44. [PubMed] [Google Scholar]
Thouw 1992 {published data only}
- Thouw J. Delegation of obstetric care in Indonesia. International Journal of Gynecology and Obstetrics 1992;38 Suppl:45‐7. [DOI] [PubMed] [Google Scholar]
Townsend 1976 {published data only}
- Townsend PW, Flanagan JJ. Experimental preadmission program to encourgage home care for severely and profoundly retarded children. American Journal of Mental Deficiency 1976;80(5):562‐9. [PubMed] [Google Scholar]
Tuckman 1994 {published data only}
- Tuckman HP, Chang CF. The healthcare volunteer. Hospital Topics 1994;72(2):23‐7. [DOI] [PubMed] [Google Scholar]
Uphold 2000 {published data only}
- Uphold CR, Lenz ER, Soeken KL. Social support transactions between professional and nonprofessional women and their mothers. Research in Nursing & Health 2000;23(6):447‐60. [DOI] [PubMed] [Google Scholar]
Victora 1994 {published data only}
- Victora CG, Langer A, Barros F, Belizan J, Farnot U, Villar J. The Latin American Multicenter Trial on psychosocial support during pregnancy: methodology and baseline comparability. Latin American Network for Perinatal and Reproductive Research (LANPER). Controlled Clinical Trials 1994;15(5):379‐94. [DOI] [PubMed] [Google Scholar]
Walker 2004 {published data only}
- Walker SP, Chang SM, Powell CA, Grantham‐McGregor SM. Psychosocial intervention improves the development of term low‐birth‐weight infants. Journal of Nutrition 2004;134(6):1417‐23. [DOI] [PubMed] [Google Scholar]
Walley 2001 {published data only}
- Walley JD, Khan MA, Newell JN, Khan MH. Effectiveness of the direct observation component of DOTS for tuberculosis: a randomised controlled trial in Pakistan. Lancet 2001;357(9257):664‐9. [DOI] [PubMed] [Google Scholar]
Walraven 1995 {published data only}
- Walraven GE, Mkanje RJ, Roosmalen J, Dongen PW, Dolmans WM. Perinatal mortality in home births in rural Tanzania. European Journal of Obstetrics, Gynecology, and Reproductive Biology 1995;58(2):131‐4. [DOI] [PubMed] [Google Scholar]
Walton 1993 {published data only}
- Walton E, Fraser MW, Lewis RE, Pecora PJ, Walton WK. In‐home family‐focused reunification: an experimental study. Child Welfare 1993;72(5):473‐87. [PubMed] [Google Scholar]
Weiler 1993 {published data only}
- Weiler K. Volunteer family members assisting with care. Journal of Gerontological Nursing 1993;19(7):43. [DOI] [PubMed] [Google Scholar]
Wolf 1985 {published data only}
- Wolf RS, Halas KT, Green LB, McNiff ML. A model for the integration of community‐based health and social services. Home Health Care Services Quarterly 1985‐1986;6(4):41‐57. [DOI] [PubMed] [Google Scholar]
References to studies awaiting assessment
Andersson 2009 {published data only}
- Andersson N, Cockcroft A, Ansari NM, Omer K, Baloch M, Ho Foster A, Shea B, Wells GA, Soberanis JL. Evidence‐based discussion increases childhood vaccination uptake: a randomised cluster controlled trial of knowledge translation in Pakistan. BMC International Health and Human Rights 2009;14(9):Suppl 1:S8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Aracena 2009 {published data only}
- Aracena M, Krause M, Perez C, Mendez MJ, Salvatierra L, Soto M, et al. A cost‐effectiveness evaluation of a home visit program for adolescent mothers. Journal of Health Psychology 2009;14(7):878‐87. [DOI] [PubMed] [Google Scholar]
Barnes 2009 {published data only}
- Barnes J, Senior R, MacPherson K. The utility of volunteer home‐visiting support to prevent maternal depression in the first year of life. Child: care, health and development 2009;35(6):807‐16. [DOI] [PubMed] [Google Scholar]
Flores 2009 {published data only}
- Flores G, Bridon C, Torres S, Perez R, Walter T, Brotanek J, et al. Improving asthma outcomes in minority children: a randomized, controlled trial of parent mentors. Pediatrics 2009;124(6):1522‐32. [DOI] [PubMed] [Google Scholar]
Helgadottir 2007 {published data only}
- Helgadottir HL. Education for parents to manage children's pain at home after tonsillectomy. Thesis / dissertation. University of Nebraska Medical Center 2007.
Mausezahl 2009 {published data only}
- Mausezahl D, Christen A, Pacheco GD, Tellez FA, Iriarte M, Zapata ME, et al. Solar drinking water disinfection (SODIS) to reduce childhood diarrhoea in rural Bolivia: a cluster‐randomized, controlled trial. PLoS Medicine 2009;6(8):e1000125. [DOI] [PMC free article] [PubMed] [Google Scholar]
Nield 2008 {published data only}
- Nield LS. Improving Cultural Competence in the Pediatric Clinic. Pediatric.Annals 2008;37:830‐5. [DOI] [PubMed] [Google Scholar]
Odendaal 2009 {published data only}
- Odendaal W, Niekerk A, Jordaan E, Seedat M. The impact of a home visitation programme on household hazards associated with unintentional childhood injuries: a randomised controlled trial. Accident; analysis and prevention 2009;41(1):183‐90. [DOI] [PubMed] [Google Scholar]
Rahman 2009 {published data only}
- Rahman A, Iqbal Z, Roberts C, Husain N. Cluster randomized trial of a parent‐based intervention to support early development of children in a low‐income country. Child: care, health and development 2009;35(1):56‐62. [DOI] [PubMed] [Google Scholar]
Simon 2009 {published data only}
- Simon GE. CBT improves maternal perinatal depression in rural Pakistan. Evidence Based Mental Health 2009;12(2):45. [DOI] [PubMed] [Google Scholar]
Stockdale 2008 {published data only}
- Stockdale J, Sinclair M, Kernohan WG, Keller JM, Dunwoody L, Cunningham JB. Feasibility study to test DESIGNER BREASTFEEDING: a randomised controlled trial. Evidence Based Midwifery 2008;6:76‐82. [Google Scholar]
Taylor 2009 {published data only}
- Taylor VM, Hislop TG, Tu SP, Teh C, Acorda E, Yip MP, et al. Evaluation of a hepatitis B lay health worker intervention for Chinese Americans and Canadians. Journal of Community Health 2009;34(3):165‐72. [DOI] [PMC free article] [PubMed] [Google Scholar]
Additional references
Altman 1998
- Altman DG, Deeks JJ, Sackett DL. Odds ratios should be avoided when events are common. BMJ 1998;317(7168):1318. [DOI] [PMC free article] [PubMed] [Google Scholar]
Berman 1987
- Berman PA, Gwatkin DR, Burger SE. Community‐based health workers: head start or false start towards health for all?. Social Science & Medicine 1987;25(5):443‐59. [DOI] [PubMed] [Google Scholar]
Bhattacharyya 2001
- Bhattacharyya K, Winch P, Ban K, Thien M. Community health worker incentives and disincentives: How they affect motivation, retention, and sustainability. Community health worker incentives and disincentives: How they affect motivation, retention, and sustainability. Arlington, Virginia: BASICS II, 2001. [Google Scholar]
Bhutta 2008
- Bhutta ZA, Ali S, Cousens S, Ali TM, Haider BA, Rizvi A, et al. Alma‐Ata: Rebirth and Revision 6 Interventions to address maternal, newborn, and child survival: what difference can integrated primary health care strategies make?. Lancet 2008;372(9642):972‐89. [DOI] [PubMed] [Google Scholar]
Bosch‐Capblanch 2008
- Bosch‐Capblanch X, Garner P. Primary health care supervision in developing countries. Tropical Medicine & International Health 2008;13:369‐83. [DOI] [PubMed] [Google Scholar]
Britton 2007
- Britton C, McCormick FM, Renfrew MJ, Wade A, King SE. Support for breastfeeding mothers. Cochrane Database of Systematic Reviews 2007, Issue 1. [DOI] [PubMed] [Google Scholar]
Campbell 2000
- Campbell MK, Grimshaw JM, Steen IN. Sample size calculations for cluster randomised controlled trials. Journal of Health Services Research & Policy 2000;5:12‐6. [DOI] [PubMed] [Google Scholar]
Chen 2004
- Chen L, Evans T, Anand S, Boufford JI, Brown H, Chowdhury, M, et al. Human resources for health: overcoming the crisis. Lancet 2004;364(9449):1984‐90. [DOI] [PubMed] [Google Scholar]
Chopra 2008
- Chopra M, Munro S, Lavis JN, Vist G, Bennett S. Effects of policy options for human resources for health: an analysis of systematic reviews. Lancet 2008;371:668‐74. [DOI] [PubMed] [Google Scholar]
Corluka 2009
- Corluka A, Walker DG, Lewin S, Glenton C, Scheel IB. Are vaccination programmes delivered by lay health workers cost‐effective? A systematic review. Human Resources for Health 2009; Vol. 7:81. [DOI] [PMC free article] [PubMed]
Craig 2008
- Craig P, Dieppe P, Macintyre S, Michie S, NazarethI, Petticrew M. Medical Research Council Guidance. Developing and evaluating complex interventions: the new Medical Research Council guidance. British Medical Journal 2008;337:a1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
Crawford 2002
- Crawford MJ, Rutter D, Manley C, Weaver T, Bhui K, Fulop N, et al. Systematic review of involving patients in the planning and development of health care. British Medical Journal 2002;325(7375):1263. [DOI] [PMC free article] [PubMed] [Google Scholar]
Damio 1995
- Damio G, Hill N, Lebron E. Breastfeeding: Heritage and Pride. Hartford, Conn: Hispanic Health Council, 1995. [Google Scholar]
Darmstadt 2005
- Darmstadt GL, Bhutta ZA, Cousens S, Adam T, Walker N, Bernis L, et al. Evidence‐based, cost‐effective interventions: how many newborn babies can we save?. Lancet 2005;365(9463):977‐88. [DOI] [PubMed] [Google Scholar]
Darmstadt 2008
- Darmstadt GL, Walker N, Lawn JE, Bhutta ZA, Haws RA, Cousens S. Saving newborn lives in Asia and Africa: cost and impact of phased scale‐up of interventions within the continuum of care. Health Policy and Planning 2008;23(2):101‐17. [DOI] [PubMed] [Google Scholar]
Farmer 2001
- Farmer P, Léandre F, Mukherjee J, Gupta R, Tarter L, Kim JY. Community‐based treatment of advanced HIV disease: introducing DOT‐HAART (directly observed therapy with highly active antiretroviral therapy). Bulletin of the World Health Organization 2001;79(12):1145‐51. [PMC free article] [PubMed] [Google Scholar]
Filippi 2006
- Filippi V, Ronsmans C, Campbell OM, Graham WJ, Mills A, Borghi J, et al. Maternal health in poor countries: the broader context and a call for action. Lancet 2006;368(9546):1535‐41. [DOI] [PubMed] [Google Scholar]
Foster 2007
- Foster G, Taylor SJC, Eldridge S, Ramsay J, Griffiths CJ. Self‐management education programmes by lay leaders for people with chronic conditions. Cochrane Database of Systematic Reviews 2007;4:Art. No.: CD005108. [DOI: 10.1002/14651858.CD005108.pub2] [DOI] [PubMed] [Google Scholar]
Frankel 1992
- Frankel S. The community health worker: effective programmes for developing countries. Oxford: Oxford University Press, 1992. [Google Scholar]
Glenton 2010
- Glenton C, Scheel IB, Pradhan S, Lewin S, Hodgins S, Shrestha V. The Female Community Health Volunteer Programme in Nepal: decision makers' perceptions of volunteerism, payment and other incentives. Social Science and Medicine 2010;In press. [DOI] [PubMed] [Google Scholar]
Guyatt 2008
- Guyatt GH, Oxman AD, Kunz R, Vist GE, Falck‐Ytter Y, Schunemann HJ, et al. What is 'quality of evidence' and why is it important to clinicians?. BMJ 2008;336:995‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hadley 2000
- Hadley M, Maher D. Community involvement in tuberculosis control: lessons from other health care programmes. International Journal of Tuberculosis and Lung Disease 2000;4(5):401‐8. [PubMed] [Google Scholar]
Haines 2007
- Haines A, Sanders D, Lehmann U, Rowe AK, Lawn JE, Jan S, et al. Achieving child survival goals: potential contribution of community health workers. Lancet 2007;369(9579):2121‐31. [DOI] [PubMed] [Google Scholar]
Hermann 2009
- Hermann K, Damme W, Pariyo GW, Schouten E, Assefa Y, Cirera A, et al. Community health workers for ART in sub‐Saharan Africa: learning from experience ‐ capitalizing on new opportunities. Human Resources for Health 2009;7:31. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hesselink 2009
- Hesselink AE, Verhoeff AP, Stronks K. Ethnic health care advisors: a good strategy to improve the access to health care and social welfare services for ethnic minorities?. Journal of Community Health 2009;34(5):419‐29. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2008
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.2 [updated September 2009]. Available from www.cochrane‐handbook.org.: The Cochrane Collaboration, 2008. [Google Scholar]
Lavis 2009
- Lavis JN, Oxman AD, Souza NM, Lewin S, Gruen RL, Fretheim A. SUPPORT Tools for evidence‐informed health Policymaking (STP): 9. Assessing the applicability of the findings of a systematic review. Health Research Policy and Systems 2009;7 Suppl 1:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lehmann 2007
- Lehmann U, Sanders D. Community health workers: What do we know about them? The state of the evidence on programmes, activities, costs and impact on health outcomes of using community health workers. Community health workers: What do we know about them? The state of the evidence on programmes, activities, costs and impact on health outcomes of using community health workers. Geneva: Evidence and Information for Policy, Department of Human Resources for Health, World Health Organization, 2007. [Google Scholar]
Lehmann 2009
- Lehmann U, Damme W, Barten F, Sanders D. Task shifting: the answer to the human resources crisis in Africa?. Human Resources for Health 2009;7:49. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lewin 2008
- Lewin S, Lavis JN, Oxman AD, Bastías G, Chopra M, Ciapponi A, et al. Supporting the delivery of cost‐effective interventions in primary health‐care systems in low‐income and middle‐income countries: an overview of systematic reviews. Lancet 2008;372(9642):928‐39. [DOI] [PubMed] [Google Scholar]
Lewin 2009
- Lewin S, Glenton C, Oxman A. Use of qualitative methods alongside randomised controlled trials of complex healthcare interventions: methodological study. BMJ 2009;339:b3496. [DOI] [PMC free article] [PubMed] [Google Scholar]
Loewenson 2004
- Loewenson R, McCoy D. Access to antiretroviral treatment in Africa. new resources and sustainable health systems are needed. BMJ 2004;328:241‐2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Love 1997
- Love MB, Gardner K, Legion V. Community Health Workers: who are they and what do they do?. Health Education & Behavior 1997;24(4):510‐22. [DOI] [PubMed] [Google Scholar]
Maher 1999
- Maher D, Gondrie PCFM, Raviglione M. Community contribution to tuberculosis care in countries with high tuberculosis prevalence: past, present and future. The International Journal of Tuberculosis and Lung Disease 1999;3(9):762‐8. [PubMed] [Google Scholar]
Michie 2009
- Michie S, Fixsen D, Grimshaw JM, Eccles MP. Specifying and reporting complex behaviour change interventions: the need for a scientific method. Implementation Science 2009;4:40. [DOI] [PMC free article] [PubMed] [Google Scholar]
NICE 2008
- NICE. Community engagement to improve health. London: National Institute for Health and Clinical Excellence, 2008. [Google Scholar]
Nilsen 2010
- Nilsen ES, Myrhaug HT, Johansen M, Oliver S, Oxman AD. Methods of consumer involvement in developing healthcare policy and research, clinical practice guidelines and patient information material. Cochrane Database of Systematic Reviews 2010, Issue 3. [DOI: 10.1002/14651858.CD004563.pub2.] [DOI] [PMC free article] [PubMed] [Google Scholar]
Oakley 2006
- Oakley A, Strange V, Bonell C, Allen E, Stephenson J. RIPPLE Study Team. Process evaluation in randomised controlled trials of complex interventions. BMJ 2006;332:413‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Oxman 2009
- Oxman AD, Lavis JN, Fretheim A, Lewin S. SUPPORT Tools for evidence‐informed health Policymaking (STP): 16. Using research evidence in balancing the pros and cons of policies. Health Research Policy and Systems 2009;7 Suppl 1:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rea 1999
- Rea MF, Venancio SI, Martines JC, Savage F. Counselling on breastfeeding: assessing knowledge and skills. Bulletin of the World Health Organization 1999;77(6):492‐8. [PMC free article] [PubMed] [Google Scholar]
Schneider 2008
- Schneider H, Hlophe H, Rensburg D. Community health workers and the response to HIV/AIDS in South Africa: tensions and prospects. Health Policy and Planning 2008;23:179‐87. [DOI] [PubMed] [Google Scholar]
Shepperd 2009
- Shepperd S, Lewin S, Strauss S, Clarke M, Eccles MP, et al. Can we systematically review studies that evaluate complex interventions?. PLoS Medicine 2009;6(8):e1000086. [DOI] [PMC free article] [PubMed] [Google Scholar]
Walker 2005
- Walker DG, Jan S. How do we determine whether community health workers are costeffective? Some core methodological issues. Journal of Community Health 2005;30(3):221‐9. [DOI] [PubMed] [Google Scholar]
Walt 1989
- Walt G, Perera M, Heggenhougen K. Are large‐scale volunteer community health worker programmes feasible? The case of Sri Lanka. Social Science & Medicine 1989;29(5):599‐608. [DOI] [PubMed] [Google Scholar]
Walt 1990
- Walt G. Community health workers in national programmes: just another pair of hands?. Community health workers in national programmes: just another pair of hands?. Open University Press, 1990. [Google Scholar]
WHO 2005
- WHO. Report of the WHO Task Force on Health Systems Research. 2005; Vol. Available at:http://www.who.int/rpc/summit/en/Task_Force_on_Health_Systems_Research.pdf.
WHO 2006
- WHO. The World Health Report 2006: working together for health. Geneva: World Health Organization, 2006. [Google Scholar]
WHO 2007
- WHO. Task shifting: rational redistribution of tasks among health workforce teams. Geneva: World Health Organization, 2007. [Google Scholar]
WHO/UNICEF 1993
- World Health Organization/United Nations Children’s Fund. Breastfeeding Counselling:A Training Course. Breastfeeding Counselling:A Training Course. Geneva, Switzerland: World Health Organization and United Nations Children’s Fund, 1993. [Google Scholar]
Witmer 1995
- Witmer A, Seifer SD, Finocchio L, Leslie J, O'Neil EH. Community health workers: integral members of the health care work force. American Journal of Public Health 1995;85(8 Pt 1):1055‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Zachariah 2009
- Zachariah R, Ford N, Philips M, Lynch S, Massaquoi M, Janssens V, et al. Task shifting in HIV/AIDS: opportunities, challenges and proposed actions for sub‐Saharan Africa. Transactions of the Royal Society of Tropical Medicine and Hygiene 2009;103:549‐58. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Lewin 2005
- Lewin S, Dick J, Pond P, Zwarenstein M, Aja GN, Wyk BE, Bosch‐Capblanch X, Patrick M. Lay health workers in primary and community health care. Cochrane Database of Systematic Reviews 2005, Issue Issue 1. [DOI: 10.1002/14651858.CD004015.pub2.] [DOI] [PubMed] [Google Scholar]
Lewin 2006
- Lewin SA, Babigumira SM, Bosch‐Capblanch X, Aja G, Wyk B, Glenton C, Scheel I, Zwarenstein M, Daniels K. Lay health workers in primary and community health care: A systematic review of trials. A policy brief prepared for the International Dialogue on Evidence‐Informed Action to Achieve Health Goals in Developing Countries (IDEAHealth). Available from: http://www.who.int/rpc/meetings/LHW_review.pdf December 2006.


