Abstract
Rationale:
Traumatic neuroma is a reparative proliferative response of the nerve after trauma or surgery, which rarely occurs in the breast. However, it must be distinguished from tumor recurrence.
Patient concerns:
A 78-year-old woman underwent left-sided modified radical mastectomy for invasive carcinoma, 7 years before this case. Two painless nodules near the mastectomy scar were discovered in regular follow-up physical examination. A 62-year-old woman had received right-sided modified radical mastectomy for intraductal carcinoma, 4 years before this case. An asymptomatic nodule near the mastectomy scar was detected during follow-up ultrasound (US) examination.
Diagnosis:
The lesions in both patients were diagnosed as traumatic neuroma.
Interventions:
The first patient underwent excisional biopsy. The second patient underwent US guided core-needle aspiration, followed by conservative therapy.
Outcomes:
Neither patient complained of any discomfort, nor both exhibited normal physical and US findings during follow-up examinations.
Lessons:
Newly discovered nodules with the benign imaging features near the mastectomy site of a patient, especially with the tail sign, traumatic neuromas should be taken into consideration. Routine US examination is important for follow-up of breast cancer patients who have undergone mastectomy.
Keywords: imaging, mastectomy, traumatic neuroma
1. Introduction
Traumatic neuroma is a chronic reparative proliferative response of the nerve after trauma or surgery, which is composed of disorganized nerve fiber bundles with fibrous stroma, Schwann cells, perineural cells, axons, and endoneural fibroblasts; importantly, neuroma does not constitute tumor recurrence.[1] However, traumatic neuroma mimics tumor recurrence in mastectomy sites; thus far, it has been infrequently reported.[2–12] However, it is crucial to distinguish between neuroma and tumor recurrence to provide the appropriate patient prognosis.[13] Some reports have described a “tail sign” (focal thickening of adjacent nerve, similar to the dural tail sign) in ultrasound (US) images, which can be used to distinguish traumatic neuroma.[7,10] Nonetheless, it is difficult to identify this uncommon lesion based on its atypical appearance. Here, we report 2 cases of traumatic neuroma discovered during follow-up US examination near the mastectomy scar in 2 postmenopausal patients who had previously undergone mastectomy for breast cancer. Additionally, we reviewed the literature regarding the imaging features of traumatic neuroma in the breast. The West China Hospital of Sichuan University Research Ethics Committee approved this retrospective report and waived the requirement for written informed consent.
2. Case 1
A 71-year-old postmenopausal woman was diagnosed with invasive lobular and ductal carcinoma with a clinical stage of T2N0M0 in 2011. Left-sided modified radical mastectomy was subsequently performed. Additionally, anastrozole-based endocrine therapy was administered to the patient for 5 years. During routine follow-up, a lymph node—measuring 6 × 6 mm and exhibiting an abnormal structure—was discovered in the left supraclavicular area in 2015 (Fig. 1). US-guided fine-needle aspiration was performed as a conservative strategy. Lymph node reactive hyperplasia was confirmed by histology and the lymph node remained stable in follow-up US examinations. In 2018, 2 painless nodules near the mastectomy scar were discovered during regular follow-up physical examination. US examination revealed 2 oval, well-circumscribed, parallel subcutaneous nodules with homogenous hypoecho near the mastectomy scar in the upper-outer quadrant of the left breast (Fig. 1). The nodules were approximately 6 × 2 × 4 mm and 4 × 2 × 3 mm in size; neither exhibited any blood flow signals in color Doppler flow imaging (CDFI) or posterior acoustic features in routine US. Considering the high possibility of malignancy, excision biopsy of the nodule was performed. During the operation, 2 defined, regular nodules with intact capsule were detected near the mastectomy scar in the upper-outer quadrant of the left breast; these were movable and demonstrated no adhesion to the surrounding tissue. White homogeneous tissue was present on the cut surface. Histopathology showed disorganized proliferation of nerve fiber bundles, which is a typical characteristic of traumatic neuroma (Fig. 2). No abnormalities were found in 10 months of subsequent follow-up US examination.
Figure 1.
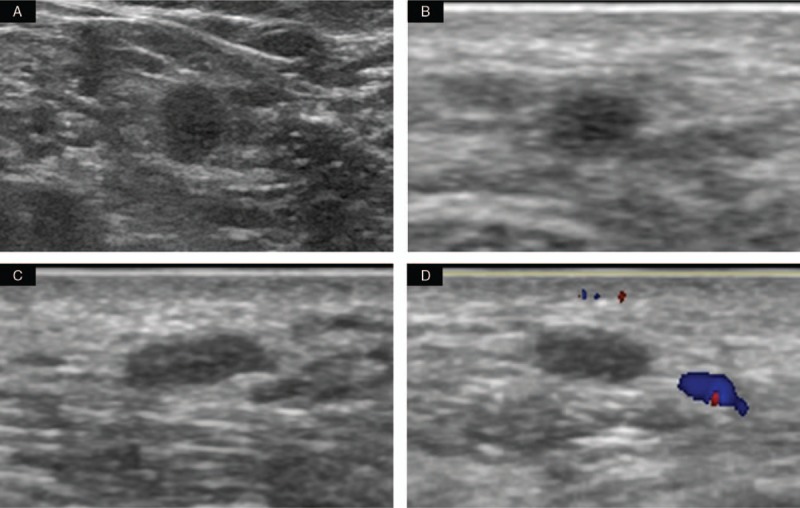
Ultrasound findings of a 78-year-old woman. (A) Grayscale sonogram of the left supraclavicular area demonstrated a lymph node with abnormal structure, which was approximately 6 × 6 mm in size. (B–D) Two oval, well-circumscribed, parallel nodules are shown in the upper-outer quadrant near the mastectomy scar. (B) Grayscale sonogram of the first nodule shows that it is approximately 4 × 2 × 3 mm in size. (C–D) Grayscale sonogram and color Doppler flow imaging of the second nodule show that it is approximately 6 × 2 × 4 mm in size.
Figure 2.
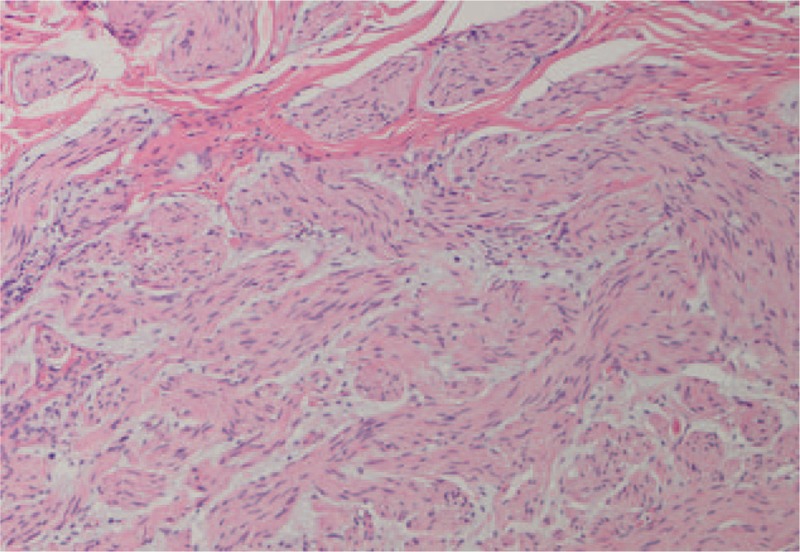
Histological examination shows disorganized proliferation of nerve fiber bundles (hematoxylin and eosin × 100).
3. Case 2
A 58-year-old postmenopausal woman was diagnosed with intraductal carcinoma (stage TisN0M0) in the right breast and underwent right-sided modified radical mastectomy in 2013. She subsequently received anastrozole-based endocrine therapy. Annual follow-up ultrasonography examination showed no abnormality in the operative site or axilla for 3 years. In 2017, a de novo nodule in the pectoral muscle layer near the mastectomy scar in the upper-outer quadrant of the right breast was revealed by US examination. The lesion was oval, well-circumscribed, homogenous hypoechoic, and measured 10 × 4 × 8 mm in size (Fig. 3). No blood flow signal was detected in CDFI and no posterior features were detected in routine US. The patient showed no symptoms and no abnormalities were observed in physical examination. In order to differentiate the lesion from recurrent tumor, US-guided core-needle aspiration was performed. Traumatic neuroma was confirmed by pathology (Fig. 4). The nodule was stable during 1 year of follow-up US examination.
Figure 3.
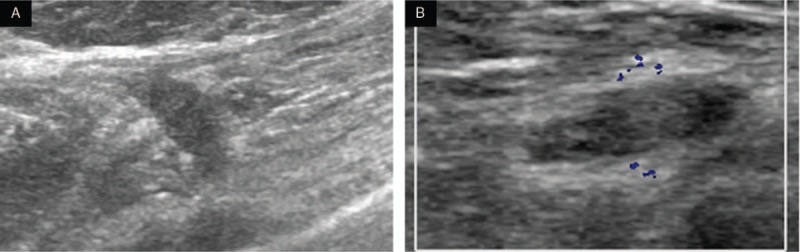
Ultrasound findings in a 62-year-old woman. (A) Baseline grayscale sonogram showed an oval, well-circumscribed mass of approximately 10 × 4 × 8 mm in size. (B) The mass was stable at the 1-year follow-up and demonstrated no blood flow in color Doppler flow imaging.
Figure 4.
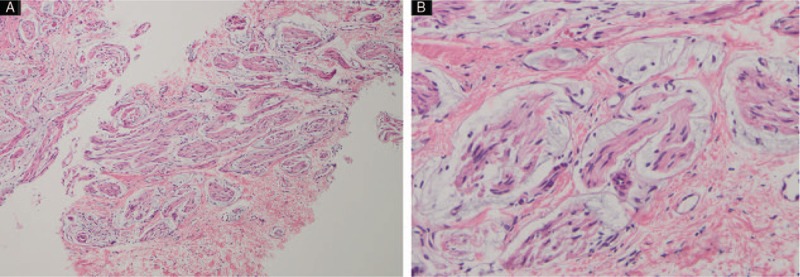
Histological findings in a 62-year-old woman. The mass consisted of disordered proliferative nerve fiber bundles with normal Schwann cells, perineural cells, axons, and endoneural fibroblasts surrounded by fibro-adipose tissues. (A) hematoxylin and eosin × 100, (B) hematoxylin and eosin × 200.
4. Discussion
Traumatic neuroma is the result of neural fiber regeneration and excessive disorganized proliferation after nerve injury, which frequently occurs in the lower extremities after surgical amputation, as well as after surgery in the head and neck.[1] We reviewed the English-language literature and found 11 publications regarding the imaging features of traumatic neuroma in the breast.[2–12]Table 1 summarizes the clinical findings and imaging features of these 11 reported cases, as well as our present report. Finally, 34 lesions in 26 patients were included for further analysis. Overall, the incidence of traumatic neuromas in breast is approximately 0.09%.[7] The age of the included patients ranged from 31 to 78 years. Neuromas occurred at 2 to 22 years after breast surgery, and were typically located in subcutaneous or pectoral muscle layer near the mastectomy scar. The size of the neuroma ranged from 0.2 to 1.6 cm. Patients were either asymptomatic or complained of pain, tenderness, or extreme pain during aspiration.[7,11] The mechanisms of neuroma-associated pain are not fully understood. Some research has indicated that increasing levels of nerve growth factor, alpha-smooth muscle actin, cannabinoid CB2 receptor, and unmyelinated fiber, as well as changes in peripheral and central sensitization, may be related to neuroma-associated pain.[14] In previous reports, patients typically underwent surgical excision or core needle biopsy. Therapy was generally considered unnecessary for patients who were asymptomatic. In contrast, patients with pain were administered conservative therapy, such as physical therapy, local injection of long-acting local anesthetics, steroid, or surgical excision.[14]
Table 1.
Review of clinical information and imaging features of traumatic breast neuromas published in the literature.
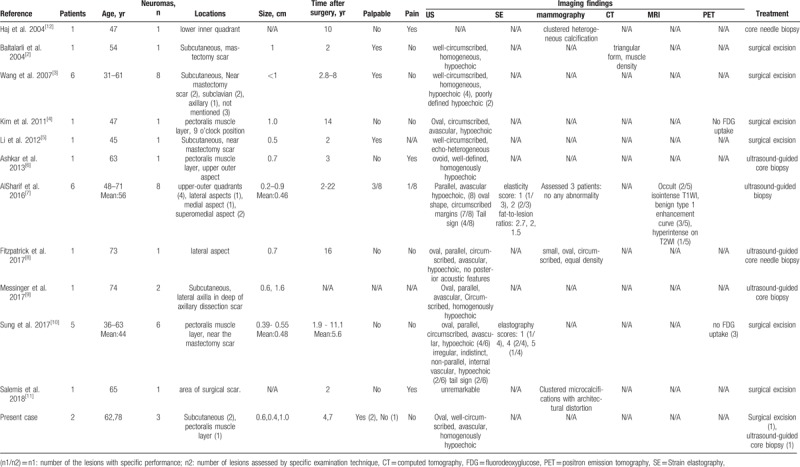
The majority of the reports described US findings of traumatic neuromas after breast surgery. In US, most lesions comprised oval, well-circumscribed, parallel, and avascular nodules that were homogenously hypoechoic,[4–10] which were consistent with our report. However, 4 lesions exhibited indistinct margin and irregular shape,[3,10] 2 lesions in 1 patient demonstrated inner vascularity,[10] and one 0.2-cm lesion was unremarkable in a surgical scar after breast-conserving surgery.[11] The tail sign was described in 2 reports with an incidence of 33.3% to 50%.[7,10] Nonetheless, this sign was absent in our cases. This might have been because the nerve was extremely thin and thus prevented detection, or the operator had not reached the appropriate section. Strain elastography was reported for the examination of 7 lesions in 2 papers.[7,10] All lesions in the first paper showed benign elasticity scores and benign fat-to-lesion ratios. In the second report, there were more lesions with low elasticity than with high elasticity. Traumatic neuromas were firm oval nodules in macroscopy,[1] which contradicted the findings of the first report. Notably, further confirmatory research is needed.
There have been a few reports of other imaging techniques for evaluation of traumatic neuromas after breast surgery. Six lesions were investigated by mammography.[7,8,11,12] However, 3 of these 6 nodules were not detected after breast-conserving surgery. Among the 3 remaining lesions, 1 demonstrated clustered heterogeneous calcification in the surgical site after nodule resection surgery; 1 showed clustered microcalcifications with architectural distortion after breast-conserving surgery; and the other comprised a small, oval, well-circumscribed, equal-density nodule in the mastectomy site. Baltalarli et al[2] reported 1 neuroma that presented as a triangular, muscle-dense nodule in computed tomography. AlSharif et al[7] investigated 5 lesions by magnetic resonance imaging (MRI); 2 of the 5 nodules were occult, while the remaining 3 were isointense foci on T1-weighted images with benign type 1 enhancement in time/signal intensity curves. Furthermore, 1 lesion was hyperintense on T2-weighted images. Finally, in positron emission tomography computed tomography, 3 neuromas showed no focal fluorodeoxyglucose uptake.[4,10]
The locoregional recurrence rate after mastectomy of breast cancer is approximately 5.3% to 8.95%.[15,16] The incidence of tumor recurrence is much higher than that of traumatic neuromas or other benign lesions. Therefore, a nodule discovered in a mastectomy site is suspected to be recurrent tumor. Early diagnosis of tumor recurrence, as well as appropriate and rapid therapy, is critical for optimal patient prognosis. Most recurrent cancers in mastectomy sites appear as hypoechoic lesions on US. [13] They are similar to some benign lesions, such as traumatic neuromas or granulomas. Additionally, some traumatic neuromas demonstrate indistinct margin and irregular shape with internal vascularity on US,[10] which resembles tumor recurrence. Therefore, misdiagnosis may occur based on US images. Some reports have described greater specificity on MRI, as most recurrent tumors demonstrated type 3 enhancement curves on MRI, whereas benign lesions always demonstrated type 1 enhancement curves.[17] These findings indicate that, when difficulties arise in differentiating recurrent tumor from traumatic neuroma on US, MRI examination may aid in distinguishing benign and malignant lesions. However, biopsy remains the most robust modality for definite diagnosis.
US, mammography, and MRI are the primary tools for use in follow-up of breast cancer patients after mastectomy. Some lesions in mastectomy sites may be enigmatic in mammography or MRI,[7] whereas nearly all lesions in mastectomy sites can be detected by US. US is an economic and widely available tool in most medical institutions. Additionally, US has few contraindications, whereas MRI should not be performed in patients with cardiac pacemakers or other metal implants. Breast US is important in early detection of abnormalities in breast cancer patients who have undergone mastectomy. In Salemis et al[11] report, a single lesion with diameter of 0.2 cm could not be detected in surgical sites by US after breast-conserving surgery, which maybe owing to the presence of operative scar and small nodule diameter. However, it could be identified as clustered microcalcifications with architectural distortion in mammography. Therefore, it is better to combine US with mammography or MRI for follow-up in breast cancer patients who have undergone breast-conserving surgery. According to previous reports, most traumatic neuromas appear as benign features. So, a nodule with benign features near the mastectomy site after breast cancer surgery, especially with the tail sign, is suggestive of traumatic neuroma.
Author contributions
Conceptualization: Yixuan Li, Zhang Zhang.
Data curation: Huan Zhang, Zhang Zhang.
Formal analysis: Yulan Peng.
Writing – original draft: Wenyi Chen.
Writing – review & editing: Wenyi Chen, Yulan Peng, Yixuan Li, Jiayan Huang.
Yulan Peng orcid: 0000-0003-3077-0746.
Footnotes
Abbreviations: CDFI = color Doppler flow imaging, MRI = magnetic resonance imaging, US = ultrasound.
This work was supported by National Natural Science Foundation of China (Project 81571694).
The authors report no conflicts of interest.
References
- [1].Foltan R, Klima K, Spackova J, et al. Mechanism of traumatic neuroma development. Med Hypotheses 2008;71:572–6. [DOI] [PubMed] [Google Scholar]
- [2].Baltalarli B, Demirkan N, Yagci B. Traumatic neuroma: unusual benign lesion occurring in the mastectomy scar. Clin Oncol (R Coll Radiol) 2004;16:503–4. [DOI] [PubMed] [Google Scholar]
- [3].Wang X, Cao X, Ning L. Traumatic neuromas after mastectomy. ANZ J Surg 2007;77:704–5. [DOI] [PubMed] [Google Scholar]
- [4].Kim EY, Kang DK, Kim TH, et al. Traumatic neuroma in a breast cancer patient after modified radical mastectomy: a case report. J Korean Soc Radiol 2011;64:518. [Google Scholar]
- [5].Li Q, Gao EL, Yang YL, et al. Traumatic neuroma in a patient with breast cancer after mastectomy: a case report and review of the literature. World J Surg Oncol 2012;10:35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Ashkar L, Omeroglu A, Halwani F, et al. Post-traumatic neuroma following breast surgery. Breast J 2013;19:671–2. [DOI] [PubMed] [Google Scholar]
- [7].AlSharif S, Ferre R, Omeroglu A, et al. Imaging features associated with posttraumatic breast neuromas. Am J Roentgenol 2016;206:660–5. [DOI] [PubMed] [Google Scholar]
- [8].Fitzpatrick KA, Borders MH, MacKerricher WS, et al. Traumatic neuroma of the breast after mastectomy. Appl Radiol 2017;46:26–8. [Google Scholar]
- [9].Messinger JD, Crawford SM. Traumatic neuroma in axillary dissection scar bed following mastectomy. Appl Radiol 2017;46:38–9. [Google Scholar]
- [10].Sung HS, Kim YS. Ultrasonographic features of traumatic neuromas in breast cancer patients after mastectomy. Ultrasonography 2017;36:33–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Salemis NS. Traumatic neuroma as a rare cause of intractable neuropathic breast pain following cancer surgery: Management and review of the literature. Intractable Rare Dis 2018;7:185–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Haj M, Bickel A, Cohen I. Osseous metaplasia of breast neuroma: diagnosis with stereotactic core biopsy. Breast J 2004;10:366–7. [DOI] [PubMed] [Google Scholar]
- [13].Kim SM, Park JM. Normal and abnormal US findings at the mastectomy site. Radiographics 2004;24:357–65. [DOI] [PubMed] [Google Scholar]
- [14].Lu CF, Sun X, Wang C, et al. Mechanisms and treatment of painful neuromas. Rev Neuroscience 2018;29:557–66. [DOI] [PubMed] [Google Scholar]
- [15].Lowery AJ, Kell MR, Glynn RW, et al. Locoregional recurrence after breast cancer surgery: a systematic review by receptor phenotype. Breast Cancer Res Treat 2012;133:831–41. [DOI] [PubMed] [Google Scholar]
- [16].Giuliano AE, Ballman K, McCall L, et al. Locoregional recurrence after sentinel lymph node dissection with or without axillary dissection in patients with sentinel lymph node metastases long-term follow-up from the American college of surgeons oncology group (alliance) ACOSOG Z0011 randomized trial. Ann Surg 2016;264:413–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Yilmaz MH, Esen G, Ayarcan Y, et al. The role of US and MR imaging in detecting local chest wall tumor recurrence after mastectomy. Diagn Interv Radiol 2007;13:13–8. [PubMed] [Google Scholar]


