Abstract
Rationale:
Bile duct injury (BDI), a major complication of cholecystectomy, usually needs hepaticojejunostomy or primary repair over T-tube in severe cases. There were few cases about retained fragments of T-tube. Whereas, intact T-tube retained in common bile duct (CBD) for years after BDI was very rare.
Patient Concerns:
A 55-year-old female complaining of a retained T-tube in the right upper quadrant for 10 years with bilious exudation for 3 months.
Diagnosis:
Based on the medical history of reoperation after the initial laparoscopic cholecystectomy (LC), the retained T-tube, the bilious exudation, and the feature of image modalities, she was diagnosed with retained biliary T-tube, biliary leak, hepatolithiasis, and BDI.
Interventions:
After nonsurgical management at local hospitals, the patient had her indwelling T-tube removal during laparotomy in our center finally. During this procedure, bile duct exploration, hilar bile ducts reconstruction, and primary Roux-en-Y hepaticojejunostomy were performed.
Outcomes:
Unfortunately, bile leakage occurred postoperatively. After drainage of the peritoneal bilious fluid, the patient recovered gradually without further complication.
Lessons:
T-tube in CBD could act as nidus for stone formation after long-time placement. As a result of gradual stone formation on T-tube, severe hepatic ducts dilatation may occur without the presence of jaundice. Timely follow-up and proper surgical intervention should be suggested for patients with T-tube placement or iatrogenic BDI to avoid further impacts.
Keywords: bile duct injury, cholecystectomy, long-time placement, T-tube
1. Introduction
Cholecystectomy is one of the most common intra-abdominal procedure performed on most general surgical services.[1,2] Despite the change from open cholecystectomy to laparoscopic cholecystectomy (LC), the enhancement of technique, the multiple modalities of preoperative assessment, bile duct injury (BDI) continues to be a major concern of this procedure.[2–4] Iatrogenic BDI is a severe complication that may have a great impact on the patient's mental and physical quality of life.[5] The definitive therapy for BDI depends on the type of lesion and the timing of its recognition. In cases of complex BDI like common BDI with leakage, hepaticojejunostomy, or primary repair over T-tube through open approach are considered the standard of care.[6,7]
We present here a rare case of iatrogenic BDI with a retained T-tube in common bile duct (CBD) for 10 years. The aim of our case is to show the relevant impacts to the patient, including the physiological and pathological changes after such long-time period T-tube placement from different aspects like laboratory test, image modalities, and surgical findings. Meanwhile, we also try to present a proper procedure for this condition.
2. Case report
A 55-year-old female was referred to our hospital with chief complaint of a retained T-tube for 10 years and discomfort in the right upper quadrant of abdomen with bilious exudation along the outwall of T-tube for 3 months, without complaints of jaundice, vomiting or fever. The patient had suffered from loss of appetite, diarrhea and weight loss. At the time of admission, the patient was on no regular medication and had no medical history concerning hepatic or biliary disease except for LC in 2008 at a periphery hospital due to cholecystitis. However, reoperation was conducted and a T-tube was placed several days after that LC for postoperative jaundice and increase in liver function tests. Since then, the patient had lived with an indwelling T-tube for 10 years. She had sought for medical help at several local clinics during this episode. Unfortunately, nonsurgical management did not resolve her major concern.
On physical examination, the patient was in chronic distress with remarkable emaciation (37 kg). She was afebrile (37.1°C), normotensive (104/68 mmHg), and without signs of jaundice. Abdominal examination revealed a retained T-tube in the right upper quadrant with massive bile-like fluid leaking along the out wall of it. Mild tenderness was observed in the upper abdomen. Serological analysis and biochemical investigation showed anemia (red blood cell count 3.54∗1012 /L, reference range: 3.8–5.1∗1012 /L; hemoglobin 104 g/L, reference range: 115–150 g/L); slightly elevated direct bilirubin (10.2 μmol/L, reference range: <8.8 μmol/L); decreased albumin (33.7 g/L, reference range: 40–55 g/L); elevated carcinoembryonic antigen (10.8 ng/ml, reference range: <3.4 ng/mL). Inflammatory factors including leukocyte count, erythrocyte sedimentation rate, and C-reactive protein were normal.
Ten years after the last operation, cholangiography through the T-tube was performed for the initial evaluation of the disease, which showed significant intrahepatic ducts dilation (19 mm–21 mm) with small amount of contrast medium in distal intestinal lumen, without obvious presentation of the CBD (Fig. 1A). Owing to her history of BDI and undefinable reasons behind such long-time placement, removing the T-tube directly was not possible. Thus, to further evaluate the anatomy of hepatic hilum and exclude the presence of tumor formation, magnetic resonance cholangiopancreatography (MRCP) and magnetic resonance imaging (MRI) were performed. MRCP further confirmed the significantly dilated intrahepatic ducts without the presentation of primary hepatic ducts convergence (Fig. 1B, white arrow). Besides, multiple intrahepatic stones in the right and left hepatic ducts were demonstrated on the axial and coronal MRI images, respectively (Fig. 2 A and B, black and white arrows). Three-dimensional MRI images revealed the exact location of T-tube with circled high signal around it, which indicated chronic inflammation (Fig. 3). Unexpectedly, remarkable gastric dilatation was showed on the coronal section (Fig. 3, white arrows). All the above evidences support the diagnoses of retained biliary T-tube, biliary leak, hepatolithiasis, and BDI.
Figure 1.
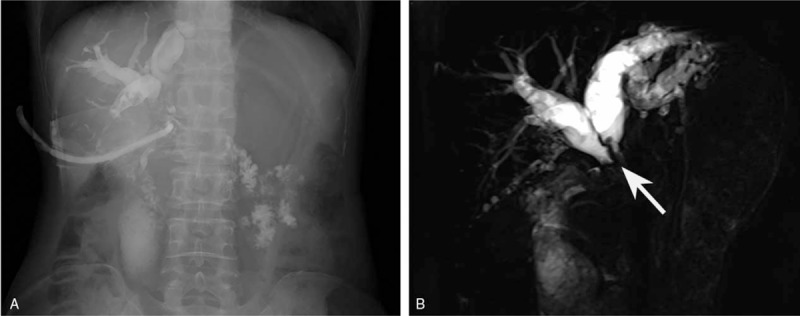
Cholangiogram and MRCP for the patient. (A) Cholangiogram showed significant intrahepatic ducts dilation (19 mm - 21 mm) with bits of contrast medium in the distal intestinal lumen, but without obvious presentation of the CBD. (B) MRCP further confirmed the significantly dilated intrahepatic ducts without the presentation of primary hepatic ducts convergence (white arrow). CBD = common bile duct, MRCP = magnetic resonance cholangiopancreatography.
Figure 2.
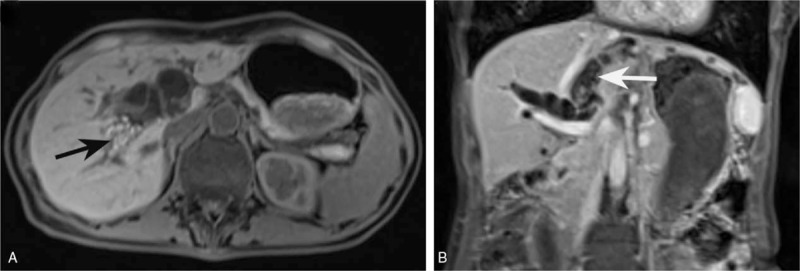
Axial and coronal MRI images demonstrated multiple intrahepatic stones both in the right (A, black arrow) and left (B, white arrow) hepatic ducts. MRI = magnetic resonance imaging.
Figure 3.
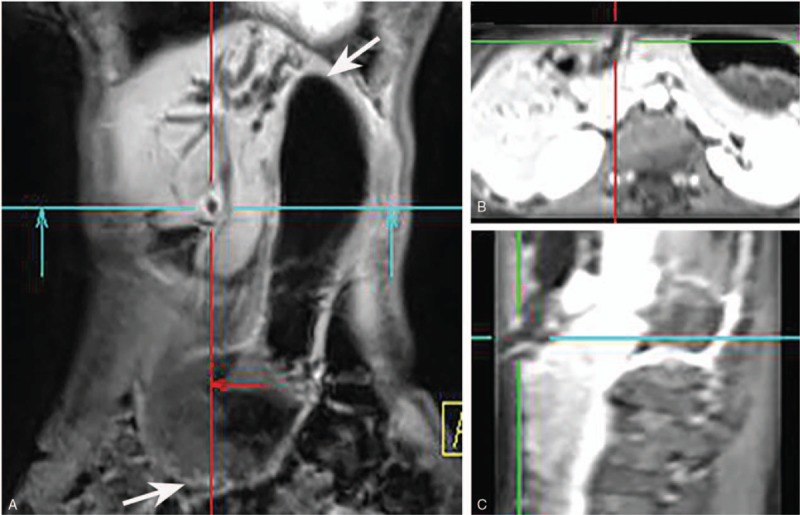
Three-dimensional MRI images revealed the exact location of T-tube with circled high signal around it, indicating chronic inflammation. Remarkable gastric dilatation was also showed on the coronal section (white arrows). MRI = magnetic resonance imaging.
Choledochoscope was not considered initially because the frangibility of the aging T-tube. Furthermore, the patient could not suffer the indwelling T-tube and leaking bilious fluid which had been affecting her health and life quality severely. Because of these reasons, an open surgical decision was taken. After a right subcostal incision, we found a T-tube with coral-like appearance and stone-like adhesions (Fig. 4A) in hilar common hepatic duct. The CBD below the T-tube site could not be recognized clearly for severe adhesions. Afterward, intraoperative choledochoscope exploration was made to remove as many gallstones as possible (Fig. 4B). Subsequently, hilar hepatic ducts reconstruction and Roux-en-Y hepaticojejunostomy were performed. Fortunately, the intraoperative frozen pathological examination of the suspicious margin of bile duct showed sterile chronic inflammatory lesion without presence of malignancy. By performing this procedure, we attempted to bring the patient back to a normal life without T-tube. Although biliary leakage occurred on the 6th postoperative day, unfortunately, the patient recovered gradually after drainage of peritoneal bilious fluid collections and was discharged 19 days postoperatively. The patient showed no further complications at a 1-month follow-up.
Figure 4.
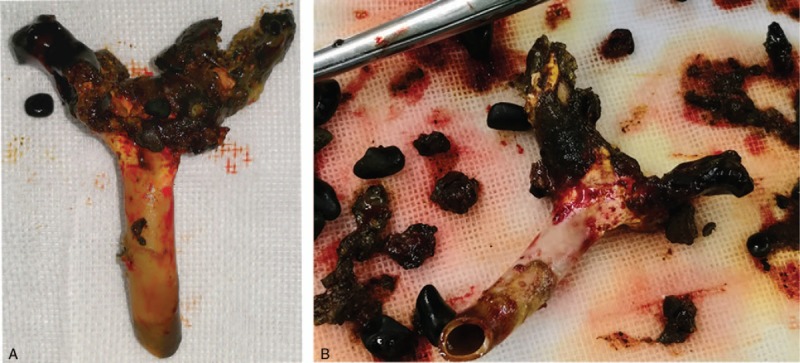
Coral-like T-tube (A) and multiple stones (B) taken out during operation.
The Ethics Committee of West China Hospital of Sichuan University, Chengdu, China, waived the need to obtain informed consent.
3. Discussion
T-tubes are suggested to be removed within 1 month after bile duct exploration.[8] And long-term placement is usually unintentional for various reasons, such as poor compliance, lack of health care insurance, patient migration, loss of communication, and so on.[8] To the best of our knowledge, there were only few cases about long-time retained T-tubes or fragments after cholecystectomy.[9–12] But none of them had reported an intact retained T-tube that last for over 10 years, nor the pathological and physiological changes caused by such long-time placement. We report here a rare case with an intact retained T-tube which was placed in CBD for over 10 years. In the present case, we speculated that extremely poor compliance after the iatrogenic BDI during LC might be the main reason for this 10-year endurance. In fact, the patient might not search for medical help without the presence of bile leakage.
Foreign bodies, like T-tube, in CBD for a prolonged period promote bacterial proliferation and release of the enzyme beta-glucuronidase, which results in the precipitation of calcium bilirubinate. Calcium bilirubinate then aggregates into stones by an anionic glycoprotein. Finally, foreign bodies in CBD could act as nidus for stone formation.[13] Besides, foreign bodies in CBD alter the local host defense and response mechanism as a consequence of which there is increase susceptibility to infection and eventually fibrosis occurs.[14] In the present case, we found a coral-like T-tube with stone-like adhesions, and the T-tube became fragile after such a long-time placement. Thus, to confirm the clearance of foreign matters in the CBD, we used choledochoscope to eliminate the possible T-tube fragments and extract the intrahepatic gallstones. Although we could not speculate the time of the initial stone formation on the T-tube, we could demonstrate that the absence of bile leakage could last for 10 years after the initial placement of T-tube in CBD. Actually, this is another learning point of this case.
Meanwhile, there were some specific pathological changes after such long-time placement of the T-tube. One specific change needs to be mentioned was that the patient had extremely dilated hepatic ducts, but without significant elevated bilirubin. And this could be explained by the gradual formation of the stones on the wall of T-tube. Another specific change was gastric dilatation. This was probably because the recurrent chronic inflammation and subsequent abdominal adhesions around the T-tube, which led to gastric output obstruction. As long placement of foreign bodies may lead to malignancies,[15,16] biopsy of the suspicious tissue of the surgical area was conducted. Fortunately, there was no presence of malignancy in the present case. On the other hand, the 10-year retained T-tube had changed the patient's personality and physical status, besides the pathological changes. She was in depression and suffered from insomnia for the inconvenience of the retained T-tube. As an adult, the patient weight only 37 kg at the time of admission with slight anemia. Thus, she was not competent for a proper job. And financial strain of her family was another reason for such long duration.
As the rarity of similar condition, the standard procedure could not be found for the present patient. Reconstructive hepaticojejunostomy is recommended for major BDI during cholecystectomy.[17] Whereas, considering the poor quality of the remaining bile and hepatic ducts, what procedure should be performed for a BDI with a retained T-tube for more than 10 years remains inconclusive. Hoffman et al reported a case with a T-tube fragment that had remained in the CBD for more than 9 years after surgery.[10] They use a Dormia basket to remove the fragment and bilirubin-containing calculus in the CBD during endoscopic retrograde cholangiopancreatography (ERCP). However, an intact T-tube could not be removed like that. In the present case, T-tube removal and reconstructive hepaticojejunostomy were performed during laparotomy. Despite the presence of temporary bile leakage in the present patient, our case report emphasis the importance of timely follow-up and early surgical intervention of such BDI cases.
4. Conclusion
Iatrogenic BDI is a severe complication which could impact the patient's mental and physical quality of life, especially in the present case. T-tube in CBD could act as nidus for stone formation after long-time placement. As a result of gradual stone formation on T-tube, severe hepatic ducts dilatation may occur without the presence of jaundice. Gastric obstruction and dilation may also occur for the severe abdominal adhesions caused by long-time placement of T-tube. The last but not the least, timely follow-up must be highlighted for patients with placement of T-tubes in CBDs to avoid ridiculous and incredible events.
Author contributions
Conceptualization: Li Wang.
Data curation: Yi Zhang.
Investigation: Li Wang, Yi Zhang.
Project administration: Ping Dong.
Software: Li Wang, Ping Dong.
Supervision: Xubao Liu, Bole Tian.
Writing – original draft: Li Wang.
Writing – review & editing: Xubao Liu, Bole Tian.
Footnotes
Abbreviations: BDI = bile duct injury, CBD = common bile duct, LC = laparoscopic cholecystectomy, MRCP = magnetic resonance cholangiopancreatography, MRI = magnetic resonance imaging.
The authors declare that there is no conflict of interests.
References
- [1].Giulianotti PC, Quadri P, Durgam S, et al. Reconstruction/repair of iatrogenic biliary injuries: is the robot offering a new option? Short clinical report. Ann Surg 2018;267:e7–9. [DOI] [PubMed] [Google Scholar]
- [2].Schmidt SC, Langrehr JM, Hintze RE, et al. Long-term results and risk factors influencing outcome of major bile duct injuries following cholecystectomy. Br J Surg 2005;92:76–82. [DOI] [PubMed] [Google Scholar]
- [3].Parmeggiani D, Cimmino G, Cerbone D, et al. Biliary tract injuries during laparoscopic cholecystectomy: three case reports and literature review. G Chir 2010;31:16–9. [PubMed] [Google Scholar]
- [4].Bordley Jt, White TT. Causes for 340 reoperations on the extrahepatic bile ducts. Ann Surg 1979;189:442–6. [PMC free article] [PubMed] [Google Scholar]
- [5].Boerma D, Rauws EA, Keulemans YC, et al. Impaired quality of life 5 years after bile duct injury during laparoscopic cholecystectomy: a prospective analysis. Ann Surg 2001;234:750–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Pitt HA, Sherman S, Johnson MS, et al. Improved outcomes of bile duct injuries in the 21st century. Ann Surg 2013;258:490–9. [DOI] [PubMed] [Google Scholar]
- [7].Karvonen J, Gullichsen R, Laine S, et al. Bile duct injuries during laparoscopic cholecystectomy: primary and long-term results from a single institution. Surg Endosc 2007;21:1069–73. [DOI] [PubMed] [Google Scholar]
- [8].Tang SJ, Armstrong L, Lara LF, et al. De novo stent-stone complex after long-term biliary stent placement: pathogenesis, diagnosis, and endotherapy. Gastrointest Endosc 2007;66:193–200. [DOI] [PubMed] [Google Scholar]
- [9].Haq A, Morris J, Goddard C, et al. Delayed cholangitis resulting from a retained T-tube fragment encased within a stone: a rare complication. Surg Endosc 2002;16:714. [DOI] [PubMed] [Google Scholar]
- [10].Hoffman A, Kiesslich R, Galle PR, et al. A 9-year retained T-tube fragment encased within a stone as a rare cause of jaundice. Z Gastroenterol 2008;46:700–3. [DOI] [PubMed] [Google Scholar]
- [11].Muhammad SR, Gatehouse D. Removal of a retained T-tube from the common bile duct. J Pak Med Assoc 1997;47:194–5. [PubMed] [Google Scholar]
- [12].Tekant Y, Goh P, Isaac J. Endoscopic removal of a retained T tube. Gastrointest Endosc 1993;39:108–9. [DOI] [PubMed] [Google Scholar]
- [13].Upwanshi MH, Shaikh ST, Ghetla SR, et al. De novo choledocholithiasis in retained common bile duct stent. J Clin Diagn Res 2015;9:PD17–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Yu JL, Andersson R, Wang LQ, et al. Experimental foreign-body infection in the biliary tract in rats. Scand J Gastroenterol 1995;30:478–83. [DOI] [PubMed] [Google Scholar]
- [15].Bayar S, Saxena R, Salem RR. Foreign body reaction to a metal clip causing a benign bile duct stricture 16 years after open cholecystectomy: report of a case. Surg Today 2000;30:534–6. [DOI] [PubMed] [Google Scholar]
- [16].Shaltz AT, Leath CA., 3rd Wiedenhoefer JF, Sundborg MJ. Reaction to a surgical implant foreign body masquerading as recurrent uterine sarcoma. Obstet Gynecol 2011;117:450–2. [DOI] [PubMed] [Google Scholar]
- [17].Holte K, Bardram L, Wettergren A, et al. Reconstruction of major bile duct injuries after laparoscopic cholecystectomy. Dan Med Bull 2010;57:A4135. [PubMed] [Google Scholar]


