Abstract
Background
This is one of three Cochrane reviews examining the role of the telephone in HIV/AIDS services. Telephone interventions, delivered either by landline or mobile phone, may be useful in the management of people living with HIV (PLHIV) in many situations. Telephone delivered interventions have the potential to reduce costs, save time and facilitate more support for PLHIV.
Objectives
To assess the effectiveness of voice landline and mobile telephone delivered interventions for reducing morbidity and mortality in people with HIV infection.
Search methods
We searched The Cochrane Central Register of Controlled Trials, MEDLINE, PubMed Central, EMBASE, PsycINFO, ISI Web of Science, Cumulative Index to Nursing & Allied Health, World Health Organisation’s The Global Health Library and Current Controlled Trials from 1980 to June 2011. We searched the following grey literature sources: Dissertation Abstracts International, Centre for Agriculture Bioscience International Direct Global Health database, The System for Information on Grey Literature Europe, The Healthcare Management Information Consortium database, Google Scholar, Conference on Retroviruses and Opportunistic Infections, International AIDS Society, AIDS Educational Global Information System and reference lists of articles.
Selection criteria
Randomised controlled trials (RCTs), quasi‐randomised controlled trials, controlled before and after studies, and interrupted time series studies comparing the effectiveness of telephone delivered interventions for reducing morbidity and mortality in persons with HIV infection versus in‐person interventions or usual care, regardless of demographic characteristics and in all settings. Both mobile and landline telephone interventions were included, but mobile phone messaging interventions were excluded.
Data collection and analysis
Two reviewers independently searched, screened, assessed study quality and extracted data. Primary outcomes were change in behaviour, healthcare uptake or clinical outcomes. Secondary outcomes were appropriateness of the mode of communication, and whether underlying factors for change were altered. Meta‐analyses, each of three studies, were performed for medication adherence and depressive symptoms. A narrative synthesis is presented for all other outcomes due to study heterogeneity.
Main results
Out of 14 717 citations, 11 RCTs met the inclusion criteria (1381 participants).
Six studies addressed outcomes relating to medication adherence, and there was some evidence from two studies that telephone interventions can improve adherence. A meta‐analysis of three studies for which there was sufficient data showed no significant benefit (SMD 0.49, 95% CI ‐1.12 to 2.11). There was some evidence from a study of young substance abusing HIV positive persons of the efficacy of telephone interventions for reducing risky sexual behaviour, while a trial of older persons found no benefit. Three RCTs addressed virologic outcomes, and there is very little evidence that telephone interventions improved virologic outcomes. Five RCTs addressed outcomes relating to depressive and psychiatric symptoms, and showed some evidence that telephone interventions can be of benefit. Three of these studies which focussed on depressive symptoms were combined in a meta‐analysis, which showed no significant benefit (SMD 0.02, 95% CI ‐0.18 to 0.21 95% CI).
Authors' conclusions
Telephone voice interventions may have a role in improving medication adherence, reducing risky sexual behaviour, and reducing depressive and psychiatric symptoms, but current evidence is sparse, and further research is needed.
Keywords: Humans, Telephone, Age Factors, Cell Phone, Depression, Depression/therapy, HIV Infections, HIV Infections/psychology, HIV Infections/therapy, HIV Infections/virology, Medication Adherence, Mental Disorders, Mental Disorders/therapy, Morbidity, Randomized Controlled Trials as Topic, Unsafe Sex, Unsafe Sex/prevention & control
The use of the telephone to improve the health of people with HIV infection
More than 34 million people were living with HIV in 2010, and more than 2.7 million new infections occurred in that year. Improvements in drug treatments for HIV mean that the life expectancy of people living with HIV/AIDS (PLHIV) is now almost the same as that of non‐infected people. However, the disease is still incurable, and patients require support to cope with their chronic illness and need for lifelong medication. Interventions often require people to go for face to face consultations, but barriers to healthcare, such as lack of money, transportation problems and the stigma sometimes associated with attending a clinic for HIV treatment, can prevent people from receiving the care they need. Using the telephone to deliver care to PLHIV may overcome some of these barriers, and ultimately improve health. It may also reduce costs, save time, and reduce effort. This could allow for a greater frequency of contact with patients, and the opportunity to reach more people in need of care. Mobile phones are widely used in both developed and developing countries, making them a feasible method to deliver health interventions for PLHIV.
The aim of this review was to assess the effectiveness of using the telephone to deliver interventions to improve the health of PLHIV compared to standard care. A comprehensive search of various scientific databases and other resources found 11 relevant studies. All of the studies were performed in the United States, and so the results may not apply to other countries, particularly developing countries. Some studies were aimed at any HIV positive person in the area in which the study was carried out, and others focused on specific groups of people, such as young substance using PLHIV, or older PLHIV. There were a lot of differences in the types of telephone interventions used in each study. There was some evidence that telephone interventions can improve medication adherence, reduce risky sexual behaviour, and reduce symptoms of depression in PLHIV. However, there were also a number of studies that suggested that telephone interventions were no more effective than usual care alone. We need more studies conducted in different settings to assess the effectiveness of telephone interventions for improving the health of PLHIV.
Summary of findings
Summary of findings for the main comparison.
Effects of the interventions aimed at improving medication adherence for reducing morbidity and mortality in people with HIV infection
| Effects of the interventions aimed at improving medication adherence for reducing morbidity and mortality in people with HIV infection | ||||||
| Patient or population: People living with HIV infection Settings: All Intervention: Voice landline and mobile telephone delivered interventions to improve medication adherence | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Effects of the interventions aimed at improving medication adherence | |||||
| ART adherence | The mean art adherence in the intervention groups was 0.49 higher (1.12 lower to 2.11 higher) | 191 (3 studies) | ⊕⊕⊝⊝ low1,2 | |||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1 Results of the studies are inconsistent. 2 All of the included studies had fewer than 400 participants.
Summary of findings 2.
Effects of the interventions aimed at improving depressive symptoms for reducing morbidity and mortality in people with HIV infection
| Effects of the interventions aimed at improving depressive symptoms for reducing morbidity and mortality in people with HIV infection | ||||||
| Patient or population: People living with HIV infection Settings: All Intervention: Voice landline and mobile telephone delivered interventions to improve depressive symptoms | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | Effects of the interventions aimed at improving depressive and psychiatric symptoms | |||||
| Depressive symptoms Beck Depression Inventory Score | The mean depressive symptoms in the intervention groups was 0.02 higher (0.18 lower to 0.21 higher) | 447 (3 studies) | ⊕⊕⊝⊝ low1,2,3 | |||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1 All three studies have an unclear risk of bias due to missing information. 2 Studies have wide confidence intervals.
3 All the included studies had fewer than 400 participants.
Background
This review is one of three Cochrane reviews that examine the role of the telephone in the delivery of HIV/AIDS services. The other two reviews are entitled: ‘Telephone‐delivered interventions for preventing HIV infection in HIV‐negative persons’ (Van Velthoven 2012b) and ‘Telephone communication of HIV testing results for improving knowledge of HIV infection status’ (Tudor Car 2012). The titles emerged from a preliminary systematic overview of the literature (Van Velthoven 2012a). While the preliminary systematic review focussed on PLHIV, people recently being tested for HIV, and people at risk for HIV, it was felt that the population of interest was too broadly defined as those three groups are not necessarily the same groups of people. Therefore, we decided to produce three reviews with distinct populations by which we aimed to make results more cohesive and valuable. These reviews will provide a comprehensive synthesis of the evidence of the use of voice telephone interventions in HIV/AIDS services. Studies using mobile phone text messaging were excluded, as another Cochrane review is focusing on messaging for long‐term diseases management (de Jongh 2008), and a Cochrane review of mobile phone text messaging for promoting adherence to anti‐retroviral therapy in patients with HIV infection has been published (Horvath 2012).
Description of the condition
HIV/AIDS contributes significantly to the global burden of disease. In 2010, 34 million people were living with HIV (WHO 2011), and this number is expected to increase significantly over the next few decades as the AIDS epidemic continues (The aids2031 Consortium 2011).
Improvements in antiretroviral therapy (ART) have greatly increased the life expectancy of people living with HIV/AIDS (PLHIV). Life expectancy of treatment naive asymptomatic PLHIV now approaches that of non‐infected people (Van Sighem 2010). However, without a cure available, patients have to continually manage their illness, which includes the use of lifelong medication (Volberding 2010).
Adherence to ART is important, with high adherence (90‐95%) being essential for stability of viral suppression (Paterson 2000). Low adherence is related to treatment failure and can also cause drug resistance (Knobel 2001). However, many patients fail to adhere to their prescribed medication. Evidence from the United States shows that at least 10% of PLHIV reported missing one or more pills on any given day, and 30‐50% of patients reported missing pills in the past two to four weeks (Reynolds 2004). Medication side effects, complicated medication regimes and psychological factors can result in poor adherence (Singh 1999). Many studies have evaluated interventions to improve adherence to long‐term medication in those with chronic illnesses such as hypertension, rheumatoid arthritis and diabetes mellitus. However, effective interventions appear to be complex and even the most effective interventions do not appear to provide great increases in adherence (Haynes 2008).
While mortality from directly AIDS‐related causes is decreasing, deaths indirectly related to AIDS such as cancer, pulmonary disease and cardiovascular disease are increasing (Palella 2006). One of the side effects of prolonged ART use is an increase in cardiovascular disease risk factors such as cholesterol, lipodystrophy and insulin resistance (Mondy 2007).
PLHIV often experience discrimination, stigma and psychological distress in addition to their infection (Bravo 2010). A study reported that almost 40% of HIV positive persons living in rural areas in the United States had experienced suicidal thoughts in the past week (Heckman 2002). Psychological symptoms are linked to lower quality of life in PLHIV (Cleary 1993). The most common psychiatric co‐morbidity of HIV/AIDS is depression (Bing 2001). A meta‐analysis concluded that the frequency of a major depressive disorder was around two times higher in PLHIV compared with HIV negative participants (Ciesla 2001). However, there are many barriers to PLHIV receiving treatment for depression and psychiatric distress, including health beliefs, stigma, lack of time and transportation problems (Tobias 2007).
HIV/AIDS is also a huge burden to healthcare systems. The number of PLHIV receiving ART in low and middle‐income countries rapidly increased from only 400,000 in 2003 (WHO 2009), to 7.4 million in 2011, with a further seven million people eligible for treatment but unable to access it (WHO 2011). Healthcare systems must continue to provide acute care for people with advanced AIDS, chronic services to the increasing number of PLHIV who are maintained on ART, and preventative interventions for at risk populations (Ullrich 2011). Therefore, low cost, effective interventions are needed (Atun 2011).
Description of the intervention
Telephones are widely used both in daily life and in health care. As far back as the 1970s clinicians described the telephone as “having become as much a part of standard medical equipment as the stethoscope” (Car 2003). Telephone contacts are frequently used to extend, or substitute for traditional face to face contacts with healthcare workers (Wasson 1992; Car 2004). Clinicians have reported that they value the convenience and flexibility afforded by the telephone, as it can facilitate regular follow up and sometimes obviate the need for home visits (Car 2003). Patients have reported that they value the increased choice in the way they can receive healthcare, quicker access to care and greater convenience (Car 2004). Studies showed that patients were satisfied with using the telephone for consultation (Bunn 2005) and want to be given the opportunity to consult with their doctors by telephone (Hallam 1993).
Mobile phones have become ubiquitous with an estimated six billion users at the end of 2011 (ITU‐D 2011). Mobile phones can have advantages over landline telephones, as people often carry their mobile phone with them at all times. However, using mobile phones can pose problems, including limited privacy in certain situations, depletion of battery during a call and running out of prepaid credit (depending on who is paying). Mobile phone messaging is very popular and shows promise as a simple and cost‐effective mode of healthcare communication for HIV/AIDS services (Van Velthoven 2012c). However, the use of mobile phone messaging in HIV care may be limited by illiteracy and the short space available in a message. Mobile phone calling can overcome some of these barriers. Toll‐free numbers offer a solution for the potential costs of calling that many people living in low and middle‐income countries may not be able to afford.
Telephone consultation, either by landline or mobile phone, may be useful in the management of PLHIV in many situations. A study evaluating two HIV/AIDS clinics described three patient cases of successful telephone consultations from triage nurses to PLHIV. The patient’s complaints and symptoms were addressed and instructions by the nurse were given to deal with them (Morrison 1998).
How the intervention might work
The telephone can be used to deliver simple interventions, such as giving test results or reminding patients of appointments. It may also be used to deliver more complex interventions, such as behavioural or mental health therapy. Complex interventions can use theoretical models, such as the self‐efficacy model for HIV prevention (Fishbein 2000), the self‐regulation theory for improving medication adherence (Reynolds 2003), or the cognitive behavioural theory for depression. This may enhance knowledge, understanding and self‐efficacy and thereby change emotions and behaviour. This could encourage people to adopt healthier behaviours (e.g. reduce risky sexual behaviour, improve medication adherence, facilitate smoking cessation) or improve the uptake of healthcare (e.g. increase the proportion of healthcare appointments attended), which ultimately could improve health outcomes and survival rates.
Using telephones for consultation compared to face to face delivery of care may reduce costs, save time, reduce effort, and facilitate more support. Telephone consultations may reduce waiting times, travel time and expenses (Lattimer 1998; Mohr 2010). Telephone consultations can also be shorter than face to face consultations, which may facilitate doctors to consult with more patients within a given time (Bunn 2005). More consultations in less time could improve communication, by meeting the need for regular medical review and addressing issues of compliance and perceived lack of support for PLHIV. This is important for long‐term disease management, where the quality of physician‐patient communication can make a considerable difference to patient health outcomes (Stewart 1995).
Improving access to healthcare is a major priority for both patients and healthcare providers (McKinstry 2006). Using telephones for healthcare is especially valuable for people living in rural areas and those whose health or social circumstances make visits to healthcare providers difficult (Foster 1999; Lattimer 1998). The burden of HIV/AIDS is highest in resource‐limited settings, where there is poor infrastructure and transport. People living in these settings often face additional barriers, including limited financial means for travelling, fear of stigma and partner violence. Using telephones could overcome some of these barriers, improve access to care and strengthen communication (Lester 2006). The use of telephone interventions may also help to overcome barriers experienced by PLHIV relating to confidentiality. Individuals who fear stigma can avoid an in‐person interaction and in some cases be given the opportunity to use a pseudonym. While providing telephone care may increase access to care, it may reduce self‐screening for the client, who may only need to make a simple phone call instead of travelling to a provider. For behavioural interventions, this could influence the motivation of the patient to put effort into their treatment regime (Roffman 2007).
The effective and safe use of telephone support in healthcare depends on qualified healthcare workers delivering the intervention to avoid adverse events from occurring, such as increased out‐of hours contact and accident and emergency attendance (Bunn 2005). Health workers may be concerned about providing telephone based care and the potential risk of missing a serious condition (Hull 2002).
Why it is important to do this review
There is a large gap between theory and the empirically proven effects of eHealth applications such as telephone interventions (Black 2011). The evidence for the feasibility and effectiveness of telephone interventions in the management of PLHIV is inconclusive (Bunn 2005; Van Velthoven 2012a). Little is known about the content of telephone consultations used for different purposes (e.g. acute triage, disease management, and follow up consultations) or the quality of the advice given by telephone in comparison with face to face consulting (Car 2004). Safe and effective telephone consultations require good training of healthcare personnel (Car 2004). The key approaches for clinicians have to be defined and the skills required of them for efficient practice also need to be ascertained. Considering the potential that telephone consultation can offer to improve HIV/AIDS care, it is important to assess the effectiveness. This review intends to summarise data on how the telephone can be used for PLHIV, and will inform current and new initiatives to focus on the best interventions. We aim contribute to an evidence base for the effective and safe use of this intervention.
Objectives
Primary Objective
To assess the effectiveness of voice landline and mobile telephone delivered interventions for improving health of PLHIV.
Secondary Objective
To assess the user evaluation, costs and adverse events associated with telephone delivered interventions for PLHIV.
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials (RCTs), quasi‐randomised controlled trials (qRCTs), controlled before and after studies (CBAs) with at least two intervention and two control groups, and interrupted time series (ITS) studies with at least three time points before and after the intervention. We considered qRCTs and CBAs, because our preliminary search showed that there was a limited number of RCTs. The other study types can provide additional evidence. Including ITS studies is valuable in assessing the ongoing qualities of a new technology requiring an introduction period. We also planned to evaluate any relevant trials with economic evaluations.
Types of participants
PLHIV who receive telephone delivered consultations regardless of any demographic characteristic (e.g. age, gender, education, marital status, employment status, or income) in all settings (e.g. community settings, primary care settings, outpatient settings and hospital settings).
Types of interventions
We considered studies using a telephone for delivering the intervention. The comparison group was face to face consultation, usual care (e.g. recommended standard care for medication adherence) or other ways of delivering brief interventions for PLHIV. Outcome measures for patients who received telephone delivered interventions were compared with the outcomes of patients assigned to the usual care or control group. We only included studies where telephone delivered intervention happened between the health care provider and the PLHIV.
Studies using mobile phones for calling were included. Studies using mobile phone messaging (SMS, MMS) were excluded, as another Cochrane review is focusing on messaging for long‐term diseases management (de Jongh 2008). We excluded studies focused on smoking cessation as this is covered by two other Cochrane reviews (Stead 2006; Whittaker 2009). Studies which use telephones only as a part of their intervention were excluded when the telephone component could not be separately evaluated. Studies in which a telephone voice intervention was used in combination with mobile phone text messaging were excluded when the telephone component could not be evaluated separately. Studies using automated calls were also excluded (including those for a reminder). Studies which focused on any telephone delivered intervention for PLHIV, not only restricted to an intervention specific to the care of HIV, were excluded when the effectiveness of the telephone intervention specific to the HIV care of PLHIV could not be separately evaluated.
Types of outcome measures
We included studies which report on at least one of the following primary or secondary outcomes.
Primary outcomes
To evaluate the effectiveness of telephone delivered interventions we were interested in whether they can change behaviour, healthcare uptake and ultimately change clinical outcomes.
1. Behaviour outcomes (e.g. adherence to treatment (e.g. pill counts, electronic monitoring, medications diaries, patient self‐report, provider report, clinic and pharmacy records), reported health‐enhancing behaviours, disease coping, reported risky behaviour)
2. Healthcare uptake related outcomes (e.g. proportion of healthcare appointments attended)
3. Clinical outcomes (e.g. immunologic and virologic outcomes (clinic and pharmacy records reports of viral load, reports of immunology CD4+ cells), depressive symptoms and psychiatric symptoms, quality of life, HIV/AIDS related mortality (directly and indirectly related causes).
Secondary outcomes
To evaluate whether a telephone intervention is an appropriate mode of communication we were also interested in the following outcomes:
1. Patient evaluation outcomes (e.g. acceptability of service, patient‐reported communication with provider, ease and timeliness with which patients were able to obtain and maintain needed services, barriers to services, health service utilization)
2. Provider evaluation outcomes (e.g. readiness to use, timeliness and/or convenience, satisfaction)
3. Economic outcomes (e.g. cost‐effectiveness, cost‐benefit, resources used)
4. Adverse outcomes regarding the communication mode (e.g. lower quality of telephone consultations, increased out‐of hours contact for the provider, breach of confidentiality, misinterpretation of information)
For the working mechanism of effectiveness we were also interested in whether underlying factors for change such as knowledge and support from relatives were improved.
5. Proximal outcomes (e.g. knowledge, understanding, self‐efficacy)
6. Social outcomes (e.g. perceived support from family and friends, loneliness)
Search methods for identification of studies
We used terms specific to the telephone and HIV/AIDS to create a general search for all three reviews. We consulted a librarian and Cochrane HIV/AIDS Review Group's Trial Search Coordinator when developing the search strategy. Articles in all languages but with an English abstract, regardless of publication year were included. We included both peer‐reviewed studies and grey literature. Two reviewers independently performed the searches. The detailed search strategies for all databases searched are presented in the appendices (Appendix 1; Appendix 2; Appendix 3; Appendix 4; Appendix 5; Appendix 6; Appendix 7; Appendix 8; Appendix 9; Appendix 10; Appendix 11; Appendix 12; Appendix 13; Appendix 14; Appendix 15; Appendix 16; Appendix 17.)
Electronic searches
The Cochrane Central Register of Controlled Trials (CENTRAL, The Cochrane Library)
MEDLINE (Ovid); 1980 ‐ June 2011.
PubMed Central (PMC)
EMBASE (Ovid); 1980 ‐ June 2011.
PsycINFO (Ovid); 1980 ‐ June 2011.
ISI Web of Science which includes: Social Sciences Citation Index (SSCI), Conference Proceedings Citation Index‐ Science (CPCI‐S), Science Citation Index Expanded (SCI‐EXPANDED), Arts & Humanities Citation Index (A&HCI)
Cumulative Index to Nursing & Allied Health (CINAHL); 1981‐ June 2011.
WHOs The Global Health Library (Regional indexes)
Searching other resources
We searched online trial registers for ongoing and recently completed studies (Current Controlled Trials: www.controlled‐trials.com). This database contains the following registers:
‐ Action Medical Research United Kingdom (UK) ‐ subset from ISRCTN Register
‐ Medical Research Council UK ‐ subset from ISRCTN Register
‐ NIH ClinicalTrials.gov Register (International) ‐ subset of randomised trial records
‐ NIHR Health Technology Assessment Programme (HTA) UK ‐ subset from ISRCTN Register
‐ The Wellcome Trust UK ‐ subset from ISRCTN Register
‐ UK trials ‐ subset from ISRCTN Register, UK trials only.
Reference lists
We searched reference lists of studies being included in the review, relevant systematic reviews and key articles in this area (as described or referred to by experts in the field).
Grey literature
We also searched Dissertation Abstracts International and Centre for Agricultural Bioscience International Direct Global Health, the System for Information on Grey Literature and The Healthcare Management Information Consortium database . A preliminary Google Scholar search showed a large number of hits, so we scanned the first 500 results.
Conference proceedings
We searched the following conference databases:
‐ Conference on Retroviruses and Opportunistic Infections (CROI)
‐ International AIDS Society (IAS)
‐ AIDS Education Global Information System (AEGIS)
Data collection and analysis
Selection of studies
Search results were merged across databases using Endnote X4, and duplicates removed. Two groups of two authors (SG and MvV, SG and LTC) independently examined titles and abstracts according to pre‐specified inclusion criteria to determine study eligibility. Studies for which eligibility was uncertain on the basis of the title and abstract alone were examined with the full text. Study authors were contacted if the information contained in the abstract or full text was not sufficient to make a judgement. Three authors discussed which studies should finally be included (SG, MvV and LTC).
Data extraction and management
The full texts of the included studies were retrieved, and data extracted independently by three groups of two authors (SG and MvV, SG and LTC, MvV and LTC) using a standardised data extraction sheet. Disagreements were resolved by discussion. Data extracted included:
Study citation
Methods: study aims, design, duration, recruitment method and setting, inclusion and exclusion criteria, control or comparison group, incentives for participation and duration of follow‐up
Participants: demographic characteristics, diagnostic criteria, location of study centre(s), intervention setting, power calculation details, number recruited/excluded/declined and number randomised/withdrawn/lost to follow‐up with reasons
Intervention: intervention content, intervention target, frequency of delivery, duration of intervention, who delivered the intervention, number of providers, training for patients and providers, initiator of the intervention, adherence, exposure, quality of delivery, participant responsiveness, mode of delivery, behaviour change theory used, implementation fidelity, program differentiation and security arrangements
Outcomes: outcomes collected, outcomes reported, outcome definition, method of assessing outcome, time points for assessment, measurements involved and adverse effects.
Results: quantitative data was collected for all relevant outcomes. Qualitative data was collected on health economics, adverse effects, acceptability to patients and providers, patient knowledge and understanding and social outcomes.
Key conclusions of the study were recorded.
Risk of bias data was collected in order to perform risk of bias assessment, as outlined below.
Assessment of risk of bias in included studies
Three groups of two authors (SG and MvV, SG and LTC, MvV and LTC) independently assessed each trial and performed assessment of risk of bias. Disagreements were be resolved by consensus.
Bias in RCTs was assessed as described by The Cochrane Handbook (Higgins 2009) and EPOC group (EPOC 2002) for six domains:
1. Sequence generation; whether the study used a mechanism that ensured that the same sorts of participants were allocated to the intervention and control groups.
2. Allocation sequence concealment; whether the study made sure that those who admitted participants to the intervention and control groups did not know in which intervention the participants were randomised, before the intervention started.
3. Blinding; whether personnel and people assessing outcomes were being kept unaware of the allocation of the intervention after inclusion of participants (blinding of participants obviously is not feasible in this context).
4. Incomplete outcome data; whether the study addressed attrition, reasons for attrition and how this was handled during analysis.
5. Selective outcome reporting; whether all pre‐specified outcomes, described in the methods or the outcomes one would expect, were reported in the results.
6. Other potential biases; relevant for this review were comparability of intervention and control group characteristics at baseline, imbalance of outcome measures at baseline and protection against contamination.
Assessment of heterogeneity
Qualitative examination revealed a fairly high degree of clinical heterogeneity between the included studies in terms of: intervention characteristics; type of provider of the intervention; characteristics of participants; and context of study population and outcomes. Three studies assessing the effect of telephone delivered interventions for improving medication adherence were deemed sufficiently homogenous, and sufficient data was available, for meta‐analysis to be performed. Three studies of the effect of telephone delivered interventions to reduce depressive symptoms, as measured using the Beck Depression Inventory, were also deemed sufficiently homogenous for meta‐analysis. For all other outcomes, a narrative synthesis of findings is presented, with effect sizes calculated for outcomes where there was sufficient data. Where possible, an assessment is made on the quality, size of the effect observed and statistical significance of the studies.
Where meta‐analysis was performed, statistical heterogeneity was examined for using the I2 statistic (Higgins 2011). This statistic gives the percentage of the variability in effect estimates that can be attributed to heterogeneity rather than chance. A value of greater than 50% is considered substantial heterogeneity.Values of I2 >50% were not found, indicating that there was not substantial statistical heterogeneity.
Data synthesis
We have systematically described the included studies according to design, setting, participants, control, and outcomes. When available, we have also aimed to provide additional information such as intervention integrity (e.g. adherence, exposure, quality of delivery, participant responsiveness etc). We have grouped the included studies according to intervention type. We have presented each included study in a "Characteristics of included studies" Table and provided a risk of bias assessment and quality assessment of included studies. The excluded studies are presented in "Excluded studies" with reasons for exclusion. We have presented the effects of interventions according to the groups listed under "Types of outcome measures".
We present a summary of treatment effect by type of intervention. Analysis was performed using Review Manager. Continuous outcomes were calculated as mean difference and weighted mean difference with 95% CI. Where appropriate, data were pooled using a fixed‐effects model with standardised mean differences (SMDs) for continuous outcomes. Results for the different outcomes were analysed separately. Missing data (e.g. studies, outcomes, summary data and individuals) was sought from original investigators. The GRADE approach was used to evaluate the aggregate quality of the evidence (Higgins 2011) for the primary outcomes.
Results
Description of studies
We describe the studies in the Characteristics of included studies and Characteristics of excluded studies Tables.
Results of the search
The joint search strategy for the three Cochrane reviews on the use of telephone delivered interventions for HIV yielded 14 717 citations. We found ten relevant studies focused on the use of telephone delivered interventions for reducing morbidity and mortality in people with HIV infection (Collier 2005; Heckman 2007; Kalichman 2011; Lovejoy 2011; Lucy 1994; Ransom 2008; Reynolds 2008; Rotheram‐Borus 2004; Stein 2007; Watakasol 2010) and one relevant conference proceeding (Cox 2006). We found no relevant on‐going trials.
We present the search process in the form of a flow diagram in Figure 1.
Figure 1.
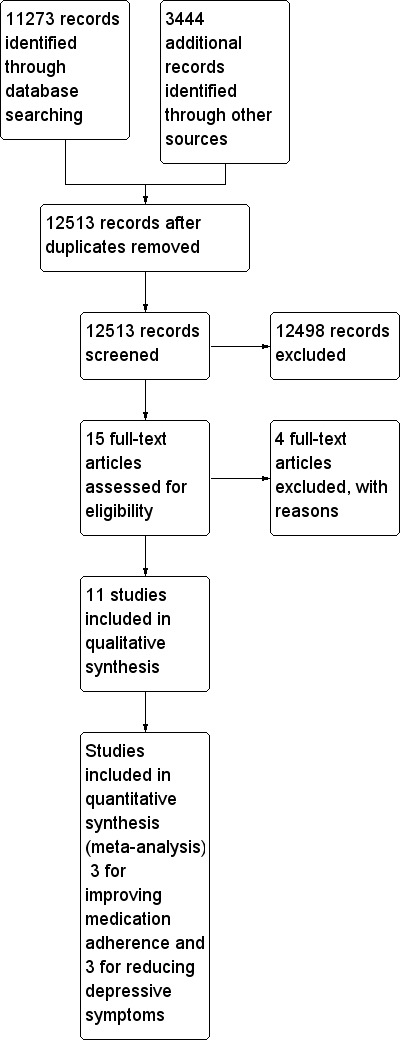
Study flow diagram.
Included studies
Design
We identified 11 eligible studies, all of which were RCTs.
Sample sizes
Studies varied in size. The largest (Heckman 2007) was a multicentre trial with 299 participants. The second largest study had 282 participants from 30 different study sites in three countries (United States, Italy and Puerto Rico) (Collier 2005). The number of participants in the other included multicentre trials were 175 (Rotheram‐Borus 2004), 109 (Reynolds 2008), 100 (Lovejoy 2011), 79 (Ransom 2008) and 42 (Watakasol 2010). Of the four single centre trials included, the largest had 177 participants (Stein 2007), the second 61 participants (Cox 2006), the third 40 participants (Kalichman 2011) and the smallest just 17 participants (Lucy 1994).
Setting
All studies were based in the United States, although one of the studies also had sites in Italy and Puerto Rico (Collier 2005). Three of the included studies focused on PLHIV living in rural areas (Heckman 2007; Ransom 2008; Watakasol 2010). Heckman 2007 defined rural as residence in a community with a population of 50,000 or less that was at least 20 miles from a city with 100,000 or more residents; Ransom 2008 defined rural as residence in a community with a population of 50,000 or less; and Watakasol 2010 defined rural as living in a county that met the United States Department of Agricultures definition of rural.
Participants
All participants in the included studies were HIV positive. Three studies included only participants living in rural areas (Heckman 2007; Ransom 2008; Watakasol 2010), and two studies included only participants with comorbid depression (Ransom 2008; Stein 2007). One study included only late middle‐age and older adults (Lovejoy 2011), and another only young substance users who engaged in risky sexual behaviour (Rotheram‐Borus 2004). Two studies included only participants initiating antiretroviral therapy (Collier 2005; Reynolds 2008), one of which included only those with advanced HIV infection (Collier 2005). The majority of participants were men in all the included studies, and one study included only men (Lucy 1994). One study enrolled patients with their self‐identified care giver, if they had one (Stein 2007). Further details on the characteristics of participants in the included studies can be found in the Characteristics of included studies tables.
Interventions
Five studies involved telephone interventions focused on improving adherence to antiretroviral medication. The intervention used by Reynolds 2008 involved structured proactive telephone calls based on self‐regulation theory.The intervention was delivered by registered nurse specialists from a central site over 16 weeks and 24‐hour support was also available via a toll free number. The intervention was designed not only to provide information about the antiretroviral regimen, but also to assist patients in recognising, self‐managing and effectively solving problems that commonly affect adherence over time. Kalichman 2011 also used an intervention based on self‐regulation theory. Participants received four unannounced telephone calls over an eight week period, in which a pill count was performed, followed by self‐regulation counselling to try to improve medication adherence. Collier 2005 gave participants in the intervention group up to 16 scripted telephone calls over 96 weeks delivered by study site staff members, mostly nurses. The calls focused on medication taking behaviour, barriers to adherence and development of strategies to increase adherence. The intervention was delivered by a masters level social worker with experience working in AIDS services. Cox 2006 was the only study to use an intervention delivered by a pharmacist. Calls were made at day four, two weeks, and then monthly for six months. The intervention involved correcting ART medication dose or frequency, suggesting methods to minimise adverse effects, arranging clinic appointments for adverse effects, assistance with medication supply and advice on medication storage requirements.Watakasol 2010 used a single session telephone administered motivational interviewing (MI) adherence improvement intervention. The intervention lasted 60 minutes and was delivered by a psychologist.
One study involved a telephone intervention focused on reducing risky sexual behaviour (Lovejoy 2011), and also used MI. The study had two intervention groups, one in which participants received one session of MI, and one in which participants received four sessions of MI. With the exception of treatment dose, the interventions were designed to be identical. The intervention was delivered by masters level psychology students. Participants sexual relationship dynamics and their readiness to always engage in condom protected sex were explored. For those in the pre‐contemplation and contemplation stages of change, providers tried to move the participant towards readiness to change. For those who felt ready to engage in condom protected sex on all occasions, providers addressed participant confidence to carry out their intentions, barriers to carrying out their intentions, and ways to overcome these barriers.
Four studies involved telephone interventions focused on reducing depressive and psychiatric symptoms. Heckman 2007 had two telephone delivered group interventions; a telephone‐delivered coping improvement intervention and a telephone‐delivered information support group. Both interventions involved eight 90 minute sessions, delivered once weekly over eight weeks. Both had six to eight participants per group, and used teleconference technology to conduct the sessions. Separate intervention groups were conducted for men who had sex with men, heterosexual men and women. The coping improvement intervention groups were co‐facilitated by two masters or PhD level clinicians, who used cognitive behavioural principles to identify stressors and their severity and develop and optimise coping skills. The information support groups were co‐facilitated by two nurse practitioners and/or social workers, who provided information and directed discussion on assigned topics (e.g. HIV symptoms management, exercise and nutrition) for the first hour of the session, and then facilitated discussion of topics generated by group members for the remaining 30 minutes. This was the only study to use a group telephone intervention. Lucy 1994 used weekly structured telephone calls lasting 20‐45 minutes, primarily aimed at providing psychosocial support but also at health monitoring, HIV education and early referrals to appropriate services, given over a 16 week period. Ransom 2008 used six 50 minutes sessions of telephone‐delivered interpersonal psychotherapy provided by a psychologist. This intervention aimed to treat depressive symptoms by improving interpersonal relations. Stein 2007 gave 12 psychoeducational telephone calls delivered by a social worker, a clinical psychologist, or a nurse, over a six month period to both HIV positive participants and their identified informal care giver. The telephone intervention was structured to provide education, and encourage problem appraisal and resolution through referral.
One study's intervention (Rotheram‐Borus 2004) addressed improving antiretroviral medication adherence, reducing risky sexual behaviour and reducing emotional distress. This was a three module intervention, with one module targeting each of the aforementioned areas. Each of the three modules was six sessions long, and each session lasted two hours. Module one aimed to improve adherence to ART; module two aimed to decrease unprotected sexual acts and substance use by identifying situations in which the participant was more likely to partake in risky behaviour and suggesting how they might modify their behaviour; and module three was aimed at reducing emotional distress by anticipating situations in which negative feelings may arise (such as anxiety or anger) and suggesting techniques to control these emotions, such as relaxation, self‐instruction and meditation. This intervention was initially planned as a group intervention, but slower than anticipated recruitment, difficulties agreeing mutually suitable times for the group sessions, and poor adherence to the intervention resulted in changing it to a one‐to‐one intervention.
Intervention integrity was only mentioned in one study (Lovejoy 2011) where therapist providing motivational interviewing were evaluated for intervention fidelity using the using the Motivational Interviewing Treatment Integrity (MITI) code. All therapists were at least proficient and often competent in the majority of the domains evaluated by the MITI code, suggesting that intervention fidelity in the study was retained.
All the included studies compared a telephone intervention to a control group with no active intervention. One study compared a telephone intervention to an in‐person intervention group, and to a control group with no active intervention (Rotheram‐Borus 2004). One study compared two different telephone interventions to a control group with no active intervention (Heckman 2007). One study compared the same telephone intervention, given once or given four times, to a control group with no active intervention (Lovejoy 2011).
Outcomes
Six of the studies addressed outcomes relating to medication adherence (Collier 2005; Cox 2006; Kalichman 2011; Reynolds 2008; Rotheram‐Borus 2004; Watakasol 2010). Three studies addressed outcomes relating to immunologic and/or virologic improvements (Collier 2005; Cox 2006; Ransom 2008). Two studies addressed outcomes relating to risky sexual behaviour (Lovejoy 2011; Rotheram‐Borus 2004). Five studies addressed outcomes relating to depressive and/or psychiatric symptoms (Heckman 2007; Lucy 1994; Ransom 2008; Rotheram‐Borus 2004; Stein 2007). Two of these studies included only PLHIV who had comorbid depression (Ransom 2008; Stein 2007).
Excluded studies
We excluded four studies at the full text screening stage (Konkle‐Parker 2010; Puccio 2006; Uzma 2011; Wang 2010). Three (Konkle‐Parker 2010; Uzma 2011; Wang 2010) were excluded because they assessed the efficacy of interventions with both a telephone and a face‐to‐face component, and the telephone component could not be separately evaluated. One (Puccio 2006) study was excluded due to ineligible study design.
Risk of bias in included studies
Two of the included studies (Kalichman 2011 and Lovejoy 2011) were at low risk of bias. The remaining studies (Collier 2005; Cox 2006; Heckman 2007; Lucy 1994; Ransom 2008; Reynolds 2008; Rotheram‐Borus 2004; Stein 2007; Watakasol 2010) had an unclear risk of bias due to lack of available detail about their methodology. See Figure 2 (Risk of bias graph) and Figure 3 (Risk of bias summary) for summaries of the risk of bias assessment of included studies. See Characteristics of included studies for explanation of the risk of bias assessment for each study. The criteria for assessing risk of bias are described in the Methods section.
Figure 2.
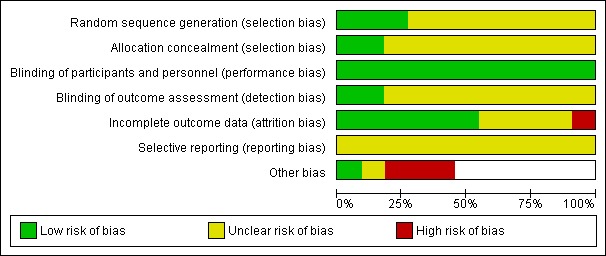
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
Figure 3.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
Risk of selection bias was low in three studies (Kalichman 2011; Lovejoy 2011; Watakasol 2010) and unclear in the remaining studies, as it was not mentioned.
Blinding
We believe that blinding of participants was unlikely to be feasible in all the included studies, due to the type of interventions being used. However, we do not think that this will have affected the results, and so we judged all the included studies to be at low risk of performance bias.
Risk of detection bias was low in Kalichman 2011 and Lovejoy 2011 as both stated that blinding of outcome assessment was performed. None of the other included studies mentioned the risk of detection bias, and so was judged to be unclear.
Incomplete outcome data
Ransom 2008 was deemed at high risk of bias, as a greater number of participants (n=10) discontinued from the intervention group than the control group (n=3). Collier 2005, Heckman 2007, Kalichman 2011, Lovejoy 2011, Reynolds 2008 and Watakasol 2010 were thought to be at low risk of attrition bias, and Cox 2006, Lucy 1994, Rotheram‐Borus 2004 and Stein 2007 were unclear.
Selective reporting
Reporting bias was unclear for all the included studies, as none of the study protocols were available to us.
Other potential sources of bias
Collier 2005 was thought to be at high risk of bias for contamination. Lucy 1994 and Rotheram‐Borus 2004 were both thought to be at high risk of bias from baseline differences between the intervention and control groups.
Effects of interventions
We will describe the effects of the interventions by type of outcome.
Primary outcomes
Behaviour outcomes
Improving medication adherence
Six included studies reported on outcomes related to medication adherence (Collier 2005; Cox 2006; Kalichman 2011; Reynolds 2008; Rotheram‐Borus 2004; Watakasol 2010).
Three of the studies (Cox 2006; Watakasol 2010; Rotheram‐Borus 2004 ) found no evidence that the telephone interventions used improved medication adherence. Cox 2006 found no significant difference in the proportion of participants who were adherent to their medication between the intervention and control groups (P=0.08). Watakasol 2010 found no significant differences in dose adherence or schedule adherence between the intervention and control groups. Repeated‐measures multivariate analysis of variance revealed ‘no statistically significant ‘Condition x Time’ interaction' (P=0.81) on the combined set of outcome variables. Univariate analysis revealed that the percentage schedule adherence increased over time in both the intervention and the control groups (P=0.01). There were no significant differences between groups in readiness to change, intrinsic motivation or adherence self‐efficacy. Adherence self‐efficacy improved over time in both groups. The authors suggest that the improvements in both groups in schedule adherence and adherence self‐efficacy may be due to the use of medication diaries to collect adherence data. It is important to note that this study was performed on a rural population, and was a single session telephone intervention. Rotheram‐Borus 2004 states that ‘The proportion of ART use and adherence to ART medication were similar among intervention conditions over time.’
Results of two studies suggested that the telephone interventions used did improve adherence to medication (Kalichman 2011; Reynolds 2008). Kalichman 2011 found that adherence in the self‐regulation counselling telephone intervention group showed significant improvements in all outcomes compared to the control group. Adherence in the telephone intervention group improved from 87.4% (SD 17.7) at baseline to 94.1% (SD 9.8) at four month follow up (P<0.01). Adherence in the control group decreased from 91.0% (SD 9.7) to 87.8% (SD 17.2) at four month follow up. There was also a significant improvement in the intervention group in self‐efficacy (P <0.05) and use of adherence behavioural strategies (P <0.05). Reynolds 2008 found that mean self‐reported adherence was consistently higher in the intervention group than in the control group at each time point for assessment (99.7% versus 97.3%, P=0.032).
One study (Collier 2005) suggested that the telephone intervention used could improve medication adherence. There was no evidence of a difference in self‐reported adherence between intervention and control groups (odds ration [OR]=0.86 [95% confidence interval {CI}, 0.57‐1.29]; P=0.46). However, participants in the intervention group who received a higher proportion of telephone calls had a lower likelihood of low adherence (OR=0.46 [95% CI, 0.23‐0.90]; P=0.02). This suggests that telephone calls may be a useful tool in improving adherence, but that the intensity of the intervention may need to be greater than that used in this study, or that it is only beneficial to particular patient populations.
A meta‐analysis of the three studies for which there was sufficient data (Kalichman 2011; Reynolds 2008; Watakasol 2010) showed no significant difference between telephone delivered intervention and control (SMD 0.49, 95% CI ‐1.12,2.11) (Analysis 1.1, Figure 4). The quality of evidence for this outcome was deemed to be low (Table 1).
Analysis 1.1.
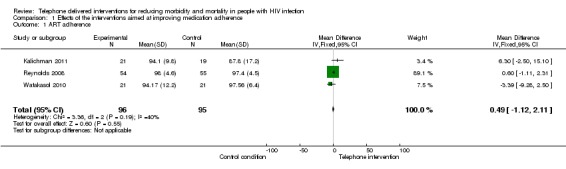
Comparison 1 Effects of the interventions aimed at improving medication adherence, Outcome 1 ART adherence.
Figure 4.

Forest plot of comparison: 1 Effects of the interventions for improving medication adherence, outcome: 1.1 ART adherence.
There is some weak evidence that telephone interventions may be able to improve medication adherence in PLHIV. It is not clear what type of intervention, if any, is most effective, the frequency of intervention delivery required to improve adherence, or the target population(s) that are most likely to benefit.
Reducing risky sexual behaviour
Two studies reported on outcomes relating to risky sexual behaviour (Lovejoy 2011; Rotheram‐Borus 2004). Both studies measured the proportion of protected sexual acts.
One study of young drug users living with HIV (age 16‐29, had used illicit drugs at least five times in the last three months) (Rotheram‐Borus 2004) had a telephone intervention group, an in‐person intervention group, and a control group. No significant difference was found in the proportion of protected sexual acts between the telephone intervention group and the control group over time. Those in the in‐person group had a significantly higher proportion of protected sexual acts compared to participants in the telephone group (P<0.01). No significant differences were found between any groups for number of sexual partners, disclosure of serostatus to partners, or any drug use related outcomes.
A second study of late middle‐aged and older adults (age 45‐66) (Lovejoy 2011) had a one session telephone intervention group, a four session telephone intervention group, and a control group. There was no significant difference in the mean number of condom protected acts between the control group and the one session intervention group at three months (OR=0.81 [0.47‐1.41]) or six months (OR=0.61 [0.35‐1.09]). The control group had approximately three times as many unprotected sexual acts as the four session intervention group at three months (OR=3.24, 95% CI [1.79‐5.85]) and six months (OR=2.70 [1.45‐5.00]). There was no difference in the proportion of participants who were in an action stage for always using protection during anal and/or vaginal intercourse between the one session intervention group and the control group at three months (OR=2.69 [0.88‐8.27]) or six months (OR=1.87 [0.66‐5.30]). Participants in the four session intervention group were three times as likely to be in the action stage for always using protection at three months (OR=3.15 [1.02–9.72]), but this relationship was no longer significant at six months (OR=2.23 [0.78–6.40]).
Effect sizes were not estimable due to missing data. There is some evidence that telephone interventions may be able to reduce risky sexual behaviour in a middle‐aged and older adult population.
Healthcare uptake related outcomes
Healthcare uptake related outcomes (e.g. proportion of healthcare appointments attended, proportion of patients receiving test results) were not measured in any of the included studies.
Clinical outcomes
The clinical outcomes reported in the included studies can be divided into immunologic or virologic related outcomes, and psychiatric or depressive symptom related outcomes.
Immunologic and virologic outcomes
Three of the included studies addressed immunologic and/or virologic outcomes (Collier 2005; Cox 2006; Reynolds 2008). The telephone interventions had no statistically significant effects on time to virologic failure in Collier 2005 and Reynolds 2008. Only one of four immunologic and virologic measures used by Cox 2006 showed a statistically significant effect of the telephone intervention.
In one trial (Collier 2005) 37% (n=52) of participants in the usual care group had virologic failure, compared to 32% (n=45) in the intervention group. There was no statistically significant difference in time to virologic failure between the two groups (P=0.32).
In a second trial (Reynolds 2008) a Kaplan‐Meier survival curve for the intervention group remained above the control group from weeks 20 to 64, suggesting a lower risk of regimen failure. However, being in the intervention group was not a statistically significant predictor of virologic failure (P=0.21, 95% CI: 0.38 to 1.23)
In a third trial (Cox 2006) the following were measured: change in CD4 lymphocyte count; log change in HIV RNA copies/mL; proportion of participants with HIV RNA <50 copies/mL at the end of follow up; and percentage of patients with HIV RNA >50 copies/mL over time. A significant difference was found only in the percentage of participants with <50 HIV RNA copies at the end of follow up (P=0.03). Average CD4 count for the intervention group was 67 cells/mm3, and 47 cells/mm3 in the control group (P=0.35). Log HIV RNA was ‐3.3 copies/mL in the control group, and ‐3.4 copies/mL in the intervention group (P=0.93).
Effect sizes were not estimable due to missing data. There was little evidence that telephone interventions used in these studies had any affect on immunologic and virologic outcomes.
Depressive and psychiatric symptoms
Six studies reported outcomes related to depressive and/or psychiatric symptoms (Lucy 1994; Ransom 2008; Heckman 2007; Stein 2007; Rotheram‐Borus 2004; Watakasol 2010).
Three studies reporting depressive symptoms using the Beck Depression Inventory (BDI) (Heckman 2007; Ransom 2008; Stein 2007) were deemed to be sufficiently heterogeneous to be combined into a meta‐analysis, which showed no significant difference between telephone delivered intervention and control (SMD 0.2, 95% CI 0.18 to 0.21, Analysis 2.1, Figure 5).The quality of this evidence was judged to be low (Table 2). Heckman 2007 had two telephone intervention groups. One was an eight session Information Support Group Intervention, and the other was an eight session Coping Improvement Group Intervention. These were compared to a control group, which received usual care. Participants in the Information Support telephone intervention group reported receiving significantly more support from friends than participants in the control group at four month follow‐up (P<0.04) and eight month follow up (P<0.05) and fewer barriers to care (P<0.05). Ransom 2008 assessed depressive symptoms, psychiatric symptoms, social support and loneliness using the BDI, the Outcomes Quesionnaire (OQ), the University of California Los Angeles (UCLA) Loneliness Scale and the Provision of Social Relations Scale (PSRS) respectively. Participants in the teletherapy group reported significant reductions in BDI scores from pre intervention (28.7, SD 11.2) to postintervention (23.5, SD 12.5) (mean change score=5.2). ANOVA of BDI scores found a significant time x condition interaction (P <0.05). Those in the teletherapy group had greater decreases in Outcomes Questionnaire score from pre‐intervention (87.0, SD 24.0) to postintervention (78.5, SD 31.1) (mean change score=1.5) and ANOVA conducted using total scores on the Outcomes Questionnaire found a significant time x condition interaction (P<0.05). The only information provided for results of the University of California Los Angeles Loneliness scale and Provision of Social Relations Scale was: 'No hypothesized condition × time interactions were found for the UCLA Loneliness Scale or the PSRS.' Stein 2007 assessed change in depressive symptoms; change in depression severity category; percentage of participants with a 50% or greater decrease in depressive symptoms; and whether the patient went into remission for their depression or not. All of these were measured using the BDI. Results showed that at 6 months there was no significant difference between groups for depression outcomes, and the study authors concluded that the psycho‐educational telephone support intervention did not reduce depressive symptoms for HIV patients more than an assessment only control condition.
Analysis 2.1.

Comparison 2 Effects of the interventions aimed at improving depressive and psychiatric symptoms, Outcome 1 Depressive symptoms (BDI score).
Figure 5.

Forest plot of comparison: 2 Effects of the interventions aimed at improving depressive and psychiatric symptoms, outcome: 2.1 Depressive symptoms (BDI score).
Rotheram‐Borus 2004 focussed on a young substance abusing population who participated in risky sexual behaviour, and used a different tool for measuring depressive/psychiatric symptoms, the Brief Symptom Inventory (BSI), which assesses global severity of mental health symptoms. At 15 months, log emotional distress was 0.8 in the telephone group, 0.9 in the in‐person group, and 0.9 in the control group. The study authors stated that ‘Logs of the overall score for emotional distress on the BSI were similar between intervention conditions over time.’ Effect size was not estimable due to missing data. Lucy 1994 measured reduction in psychiatric distress using the General Severity Index of the BSI. Change in General Severity Index was ‐5.83 (SD 4.97) in the intervention group and 0.93 (SD 5.82) in the control group (P<0.05), meaning there was a significant decline in psychological distress in the intervention group as compared to the control group. However, there was no significant difference in total GSI score between groups at the end of the study period (SMD ‐6.53, 95% CI 11.71 to ‐1.35, (Analysis 2.2).
Analysis 2.2.

Comparison 2 Effects of the interventions aimed at improving depressive and psychiatric symptoms, Outcome 2 Psychiatric distress (General Severity Index of the Brief Symptom Index).
A further study (Watakasol 2010) assessed depression using the BDI. However, they measured it only as an adherence related variable, to use when conducting explanatory analysis. Their intervention was aimed at improving adherence, not depressive symptoms, so they did not expect or observe any change in depressive symptoms. As the intervention did not aim to reduce depressive symptoms it was not included in the meta‐analysis.
There is some weak evidence of low quality for the use of voice landline and mobile telephone delivered interventions for reducing depressive and psychiatric symptoms in PLHIV.
Secondary outcomes
Very few studies addressed our secondary outcomes. Patient and provider evaluation outcomes, proximal outcomes and social outcomes were not addressed in any of the included studies. Economic outcomes were briefly mentioned in Kalichman 2011, which stated that the resources used for the telephone intervention mirror those typically available in routine clinical services, but no further analysis of cost‐effectiveness was performed. Rotheram‐Borus 2004 was the only study to give details of the costings. The study authors stated ‘The total cost of the in‐person intervention for the three modules was $3500 per participant (approximately $1167 per module), which was higher than the cost of the $2692 per participant for the telephone intervention (approximately $897 per module). The excess cost of travelling time and expenses for in‐person sessions accounted for this difference. Personnel counted for most of the total costs: 65% for in‐person sessions and 60% for telephone sessions. Overhead costs averaged 25% and material and instrumental costs averaged 12% of total costs across intervention conditions.' Adverse outcomes were very briefly mentioned by Lovejoy 2011, which states ‘No adverse outcomes were reported during the clinical trial’. They were not mentioned in any of the other included studies.
Discussion
Summary of main results
The aim of this systematic review was to assess the effectiveness of telephone delivered interventions for reducing morbidity and mortality in people with HIV infection. This is one of three Cochrane reviews examining the role of the telephone in HIV/AIDS services. Eleven eligible studies were identified and included in this review.
Evidence for whether telephone interventions can reduce risky sexual behaviour in people living with HIV is limited, with only two included studies with outcomes related to risky sexual behaviour. The studies had very different participant populations (late middle‐age and older PLHIV Lovejoy 2011 versus young substance using PLWA Rotheram‐Borus 2004). In the first study (Lovejoy 2011), a significant reduction in outcomes related to risky sexual behaviour was seen only in the group receiving a four‐session intervention. There was no difference in outcomes between those receiving a one session intervention, and those in the control group. The second study (Rotheram‐Borus 2004) found no significant differences in outcomes relating to risky sexual behaviour between those receiving an 18‐session telephone intervention, and those in the control group. Differences in the results of the study may be related to the very different study populations.
There was some evidence that telephone interventions can improve medication adherence. Six studies reported on outcomes related to adherence. Three of the studies (Cox 2006; Watakasol 2010; Rotheram‐Borus 2004) reported no significant difference between participants in the telephone intervention group and those in the control group. Two studies (Kalichman 2011; Reynolds 2008) found a significant difference between the telephone intervention group and the control group for adherence related outcomes. One study (Collier 2005) was inconclusive, with some suggestion that the telephone intervention used could improve medication adherence. There was no evidence of a difference in self‐reported adherence between intervention and control groups, but participants in the intervention group who received a higher proportion of telephone calls had a lower likelihood of low adherence, suggesting that telephone calls may be a useful tool in improving adherence. Only three of the six included studies had sufficient data to include in a meta‐analysis (Kalichman 2011; Reynolds 2008; Watakasol 2010) and this showed that the telephone interventions had no significant effect on ART adherence at the end of the studies follow‐up periods.
There was very little evidence that telephone interventions can improve immunologic and virologic outcomes. Three of the included studies addressed immunologic and/or virologic outcomes (Collier 2005; Cox 2006; Reynolds 2008). The telephone interventions had no statistically significant effects on time to virologic failure in Collier 2005 and Reynolds 2008. Only one of four immunologic and virologic measures used by Cox 2006 showed a statistically significant effect of the telephone intervention.
There was some evidence that telephone interventions can reduce depressive and/or psychiatric symptoms. Six studies reported outcomes related to depressive and/or psychiatric symptoms (Lucy 1994; Ransom 2008; Heckman 2007; Stein 2007; Rotheram‐Borus 2004; Watakasol 2010). Two of the studies (Rotheram‐Borus 2004 and Stein 2007) found no evidence that a telephone intervention can reduce depressive and/or psychiatric symptoms in PLWA. Three studies (Heckman 2007; Lucy 1994; Ransom 2008) found evidence that telephone interventions can reduce psychiatric symptoms in PLHIV. A further study (Watakasol 2010) assessed depression using the BDI, but only as an adherence related variable to use when conducting explanatory analysis, and there was no expectation or observation of an improvement in depressive symptoms, as the intervention used was not targeted at reducing depressive symptoms. A meta‐analysis of three studies (Heckman 2007; Ransom 2008; Stein 2007) found no significant effect of the telephone intervention compared to the control group at the end of the studies follow‐up periods.
None of the eligible studies provided any information about healthcare uptake related outcomes, patient or providers acceptability of telephone delivered interventions, proximal outcomes or social outcomes. Information on cost‐effectiveness and adverse events was sparse.
Whilst the interventions were very heterogeneous, there were some important commonalities that may suggest features that demonstrate or lack effectiveness. The characteristics of the included participants appears to be potentially important to the efficacy of an intervention. The two studies focusing on risky sexual behaviour (Lovejoy 2011 and Rotheram‐Borus 2004) had conflicting results but included very different populations. Lovejoy 2011 included middle aged and older adults, while Rotheram‐Borus 2004 included young substance users who display risky sexual behaviour. In the studies focusing on depressive and psychiatric symptoms (Heckman 2007; Lucy 1994; Ransom 2008; Rotheram‐Borus 2004; Stein 2007), those in which there was no significant difference between the intervention and control groups focused on specific populations. As previously mentioned, Rotheram‐Borus 2004 included young substance users who display risky sexual behaviour, while Stein 2007 included only those living in rural areas. Intervention intensity also appears to be important. Lovejoy 2011 found a significant reduction in risky sexual behaviour in participants randomised to a 4 session intervention compared to control, but no significant difference between those randomised to a 1 session intervention and control. The single session intervention used by Watakasol 2010 also appeared ineffective. Collier 2005 found no evidence of a difference in self‐reported adherence between intervention and control, but found that participants in the intervention group who received a higher proportion of telephone calls had a lower likelihood of low adherence. This perhaps suggests that greater intensity of intervention is beneficial, or that only a particular population benefited from the intervention.However, with such a small number of included studies, and heterogeneity of interventions, participants and outcomes, identifying components of interventions that demonstrated or lacked effectiveness is challenging.
Overall completeness and applicability of evidence
We performed a thorough search of an extensive range of databases and considered as eligible all experimental study designs accepted by The Cochrane Collaboration. We found only 11 eligible studies. The heterogeneity of studies in terms of study population, interventions, and outcomes is fairly high, resulting in low comparability.
All the eligible studies were performed in the United States, with one study (Collier 2005) also having study sites in Italy and Puerto Rico. The applicability of these results to other settings, particularly in low and middle‐income countries with a high burden of HIV infection is unclear. None of the eligible studies provided any information about healthcare uptake related outcomes, patients' or providers' acceptability of telephone delivered interventions, proximal outcomes or social outcomes. Information on cost‐effectiveness and adverse events was extremely limited.
Rapidly rising mobile phone use in developed and developing countries (ITU‐D 2011) at least theoretically provides a great opportunity for improvement of health and healthcare in resource‐limited settings (Lester 2006). Technology has the potential to be highly beneficial in reducing morbidity and mortality in PLHIV, given the high prevalence and poor treatment outcomes of HIV infection in developing countries. However, the existing evidence offers insufficient information on the efficacy of telephone interventions for reducing morbidity and mortality in people with HIV infection, either in developed or developing countries.
Quality of the evidence
The overall quality of evidence included in this systematic review is relatively poor. Two of the included studies (Kalichman 2011 and Lovejoy 2011) were at low risk of bias. The remaining studies (Collier 2005; Cox 2006; Heckman 2007; Lucy 1994; Ransom 2008; Reynolds 2008; Rotheram‐Borus 2004; Stein 2007; Watakasol 2010), however, had an unclear risk of bias due to lack of available detail about their methodology.
Potential biases in the review process
This review has a number of strengths. We rigorously followed The Cochrane Collaboration methodology, performed a comprehensive search and included all Cochrane accepted experimental study designs. We believe it is unlikely that we missed any relevant study.
Nine out of 11 included studies were at unclear risk of bias (Collier 2005; Cox 2006; Heckman 2007; Lucy 1994; Ransom 2008; Reynolds 2008; Rotheram‐Borus 2004; Stein 2007; Watakasol 2010) due to lack of available detail about the methodology even after we had contacted the authors. It is possible that if we had sufficient information to properly evaluate the risk of bias in these studies that it may have been high.
The heterogeneity of the included studies in terms of participants, interventions and outcomes meant we were unable to pool the studies in a meta‐analysis for all outcomes. Our narrative synthesis uses the study as the unit of analysis, which may introduce reporting bias. All the included studies were conducted in the United States (although Collier 2005 also had sites in Puerto Rico and Italy), perhaps limiting generalisability.
Agreements and disagreements with other studies or reviews
The studies included in this review suggest that voice telephone interventions may reduce morbidity and mortality in PLHIV in the USA by improving medication adherence, reducing risky sexual behaviour, and reducing the burden of depressive and psychiatric symptoms. However, the evidence is inconsistent and sparse. The evidence for the use of mobile phone text messaging for improving adherence to ART in developing countries is more conclusive. A Cochrane review evaluating the use of mobile phone text messaging for promoting adherence to ART in PLHIV (Horvath 2012) included two studies, both of which were RCTs. Meta‐analysis of both trials found that weekly text messaging was associated with a lower risk of non‐adherence (RR 0.78, 95% CI 0.68 to 0.89). One trial found that weekly text messaging was associated with non‐occurrence of virologic failure at 12 months (RR 0.83, 95% CI 0.69 to 0.99). A systematic review of the evidence for the effectiveness of interventions to increase ART adherence in PLHIV in sub‐Saharan Africa suggested that a variety of interventions, including mobile phone text messaging, can effectively increase adherence (Barnighausen 2011).
There is also high quality evidence for the use of telephone‐administered psychotherapy for patients with depression, a common comorbidity in PLHIV. A meta‐analysis of patients with depression, some of whom were PLHIV and some of whom had other health problems or depression alone, showed a significant reduction in depressive symptoms for patients enrolled in telephone‐administered psychotherapy as compared to control conditions (d=0.26, 95% CI = 0.14‐0.39, P<0.0001) (Mohr 2008). Attrition rates were also considerably lower in participants receiving telephone interventions.
There is also evidence suggesting that interactive voice response systems may be effective. Tucker 2012 assessed the efficacy of using an interactive voice response system for PLHIV to self‐monitor HIV risk behaviours daily. Results showed that this intervention was able to assess and reduce risky behaviour in rural PLHIV. A study of PLHIV who use non‐injection drugs by Aharonovich 2012 aimed to extend brief motivational interviewing (MI) delivered in person by using a HealthCall intervention in addition. Participants were randomised to receive either MI alone, or MI plus HealthCall. Those who received HealthCall were asked to call a specified number daily for 30 days, where they answered a short set of pre‐recorded questions about their drug use on the previous day. The information collected was used to provide personalised feedback about their drug use. Results suggested that HealthCall was a feasible and acceptable method of extending patient involvement in a brief intervention.
Authors' conclusions
The included studies show inconsistent evidence for all types of outcomes. There is some evidence that voice telephone interventions can reduce morbidity and mortality in people with HIV infection in the United States, by improving medication adherence, reducing risky sexual behaviour, and reducing the burden of psychiatric symptoms. However, current evidence is scarce. We cannot currently recommend the use of voice telephone interventions of reducing morbidity and mortality in people with HIV infection in practice.
There is a lack of evidence for the effectiveness of voice telephone use for reducing morbidity and mortality in people with HIV infection. All of the included studies were performed in the United States, although one study also had sites in Italy and Puerto Rico This review did not look at mobile phone text messaging, for which good evidence of efficacy in improving ART adherence in Kenya was found in another Cochrane review (Horvath 2012). Further research is needed into the potential efficacy of voice telephone interventions for reducing morbidity and mortality in people with HIV infection in both developed and developing settings. None of the studies included in our review evaluated patients or providers satisfaction with the intervention, and there was very limited assessment of economic outcomes or adverse effects. Some of the included studies suggest that telephone interventions may have a role in reducing risky sexual behaviour, improving medication adherence, and reducing depressive and psychiatric symptoms. Further high quality research is needed to identify what types of intervention are effective, the frequency of delivery required for efficacy, and the patient populations in which the intervention is effective.
Acknowledgements
We are grateful to Prescilla Sawmynaden and Tapio Paljarvi for providing comments on the protocol of this review. We are very grateful to Joy Oliver from the Cochrane HIV/AIDS group for helping us develop the search strategy. We are also very grateful to Tara Horvath and the rest of the Cochrane HIV/AIDS group for their support and guidance.
Appendices
Appendix 1. MEDLINE search strategy
| Number | Search terms |
| #1 | phone* |
| #2 | telephon* |
| #3 | telefon* |
| #4 | telephone intervention |
| #5 | call |
| #6 | calls |
| #7 | calling |
| #8 | telemedicine |
| #9 | teleconsult* |
| #10 | telecounsel* |
| #11 | Telephone[MeSH] |
| #12 | Hotlines[MeSH] |
| #13 | Cellular phone[MeSH] |
| #14 | Cellular phone |
| #15 | Mobile phone |
| #16 | Cell phone |
| #17 | #1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14 OR #15 OR #16 |
| #18 | HIV Infections[MeSH] |
| #19 | HIV[MeSH] |
| #20 | hiv[tw] |
| #21 | hiv‐1*[tw] |
| #22 | hiv‐2*[tw] |
| #23 | hiv1[tw] |
| #24 | hiv2[tw] |
| #25 | hiv infect*[tw] |
| #26 | human immunodeficiency virus[tw] |
| #27 | human immunedeficiency virus[tw] |
| #28 | human immune‐deficiency virus[tw] |
| #29 | ((human immun*) AND(deficiency virus[tw])) |
| #30 | “Acquired Immunodeficiency Syndrome”[MeSH] |
| #31 | acquired immunodeficiency syndrome[tw] |
| #32 | acquired immunedeficiency syndrome[tw] |
| #33 | acquired immuno‐deficiency syndrome[tw] |
| #34 | acquired immune‐deficiency syndrome[tw] |
| #35 | ((acquired immun*) AND (deficiency syndrome[tw])) |
| #36 | #18 OR #19 OR #20 OR #21 OR #22 OR #23 OR #24 OR #25 OR #26 OR #27 OR #28 OR #29 OR #30 OR #31 OR #32 OR #33 OR #34 OR #35 |
| #37 | # 17 AND # 36 |
Appendix 2. Pubmed Central (PMC) search strategy
Choose Advanced search from the list of terms above the search box
On Advance search interface, enter the following search string into the search box:
(TELEPHONE OR PHONE[Body ‐ Key Terms]) AND HIV OR AIDS[Body ‐ Key Terms]
Click on limits from the list of terms above the search box and enter
01/01/1980‐13/06/2011 into dates
Appendix 3. EMBASE search strategy
| No. | Query |
| #9 | #1 AND #7 AND [humans]/lim AND [embase]/lim AND [1980‐2011]/py |
| #8 | #1 AND #7 |
| #7 | #2 OR #3 OR #6 |
| #6 | 'telemedicine'/syn OR teleconsult* OR 'remote consulting' OR 'remote consultation'/syn OR 'remote consultations' OR telecounsel* |
| #3 | telephon* OR phone* OR telefon* OR hotline* |
| #2 | 'telephone'/syn OR 'mobile phone'/syn |
| #1 | 'human immunodeficiency virus infection'/exp OR 'human immunodeficiency virus infection'/de OR 'human immunodeficiency virus infection' OR 'human immunodeficiency virus'/exp OR 'human immunodeficiency virus'/de OR 'human immunodeficiency virus' OR hiv:ti OR hiv:ab OR 'hiv‐1':ti OR 'hiv‐1':ab OR 'hiv‐2':ti OR 'hiv‐2':ab OR 'human immunodeficiency virus':ti OR 'human immunodeficiency virus':ab OR 'human immuno‐deficiency virus':ti OR 'human immuno‐deficiency virus':ab OR 'human immunedeficiency virus':ti OR 'human immunedeficiency virus':ab OR 'human immune‐deficiency virus':ti OR 'human immune‐deficiency virus':ab OR 'acquired immune‐deficiency syndrome':ti OR 'acquired immune‐deficiency syndrome':ab OR 'acquired immunedeficiency syndrome':ti OR 'acquired immunedeficiency syndrome':ab OR 'acquired immunodeficiency syndrome':ti OR 'acquired immunodeficiency syndrome':ab OR 'acquired immuno‐deficiency syndrome':ti OR 'acquired immuno‐deficiency syndrome':ab |
Appendix 4. PsycINFO search strategy
| Number | Search terms |
| 1 | phone*.af. |
| 2 | Telephon*.af. |
| 3 | telefon*.af. |
| 4 | telephone intervention.af. |
| 5 | call.af. |
| 6 | calls.af. |
| 7 | calling.af. |
| 8 | teleconsult*.af. |
| 9 | telecounsel*.af. |
| 10 | Hotline.af. |
| 11 | Telephone Hotlines.af. |
| 12 | Hotline, Telephone.af. |
| 13 | Telephone Hotline.af. |
| 14 | Phone, Cellular.af. |
| 15 | Cellular Telephone.af. |
| 16 | Cellular Telephones.af. |
| 17 | Cell Phone.af. |
| 18 | Phone, Cell.af. |
| 19 | Phones, Cell.af. |
| 20 | Mobile Phone.af. |
| 21 | Phone, Mobile.af. |
| 22 | Phones, Mobile.af. |
| 23 | Car Phone.af. |
| 24 | Car Phones.af. |
| 25 | exp Telephone Systems / |
| 26 | exp Cellular Phones / |
| 27 | exp Hot Line Services/ |
| 28 | exp telemedicine / |
| 29 | 1 OR 2 OR 3 OR 4 OR 5 OR 6 OR 7 OR 8 OR 9 OR 10 OR 11 OR 12 OR 13 OR 14 OR 15 OR 16 OR 17 OR 18 OR 19 OR 20 OR 21 OR 22 OR 23 OR 24 OR 25 OR 26 OR 27 OR 28 |
| 30 | exp hiv/ |
| 31 | exp hiv testing/ |
| 32 | hiv.ti. OR hiv.ab. |
| 33 | hiv‐1.ti. OR hiv‐1.ab. |
| 34 | hiv‐2.ti. OR hiv‐2.ab. |
| 35 | human immunodeficiency virus.ti. OR human immuno deficiency.ab. |
| 36 | human immuno‐deficiency virus.ti. OR human immuno‐deficiency virus.ab. |
| 37 | human immunedeficiency virus.ti. OR human immune deficiency virus.ab. |
| 38 | human immune‐deficiency virus.ti. OR human immune‐deficiency virus.ab. |
| 39 | acquired immune‐deficiency syndrome.ti. OR acquired immune‐deficiency syndrome.ab. |
| 40 | acquired immunodeficiency syndrome.ti. OR acquired immunodeficiency syndrome.ab. |
| 41 | acquired immuno‐deficiency syndrome.ti. OR acquired immuno‐deficiency syndrome.ab. |
| 42 | exp aids/ |
| 43 | 30 OR 31 OR 32 OR 33 OR 34 OR 35 OR 36 OR 37 OR 38 OR 39 OR 40 OR 41 OR 42 |
| 44 | 29 AND 43 |
Appendix 5. ISI Web of Science search strategy
| Number | Search terms |
| 1 | TS=phone* |
| 2 | TS=Telephon* |
| 3 | TS=telefon* |
| 4 | TS=telephone intervention |
| 5 | TS=call |
| 6 | TS=calls |
| 7 | TS=calling |
| 8 | TS=telecounsel* |
| 9 | TS=Hotline |
| 10 | TS=Telephone Hotlin* |
| 11 | TS=Cellular Phon* |
| 12 | TS=Cellular Telephon* |
| 13 | TS=Cell Phon* |
| 14 | TS=Portable Cellular Phon* |
| 15 | TS=Mobile Phon* |
| 16 | TS=Car Phon* |
| 17 | TS=telemedicine |
| 18 | TS=teleconsult* |
| 19 | TS=teletherapy |
| 20 | TS=telehealth |
| 21 | 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20 |
| 22 | TS=AIDS |
| 23 | TS=HIV |
| 24 | TS=HIV‐1* |
| 25 | TS=HIV‐2* |
| 26 | TS=HIV1 |
| 27 | TS=HIV2 |
| 28 | TS=HIV INFECT* |
| 29 | TS=HUMAN IMMUNODEFICIENCY VIRUS |
| 30 | TS=HUMAN IMMUNEDEFICIENCY VIRUS |
| 31 | TS=HUMAN IMMUNO DEFICIENCY VIRUS |
| 32 | TS=HUMAN IMMUNE‐DEFICIENCY VIRUS |
| 33 | (TS=HUMAN IMMUN*) AND (TS=DEFICIENCY VIRUS) |
| 34 | TS=ACQUIRED IMMUNODEFICIENCY SYNDROME |
| 35 | TS=ACQUIRED IMMUNEDEFICIENCY SYNDROME |
| 36 | TS=ACQUIRED IMMUNO‐DEFICIENCY SYNDROME |
| 37 | TS=ACQUIRED IMMUNE‐DEFICIENCY SYNDROME |
| 38 | (TS=ACQUIRED IMMUN*) AND (TS=DEFICIENCY SYNDROME) |
| 39 | TS=VIRAL SEXUALLY TRANSMITTED DISEASES |
| 40 | 22 or 23 or 24 or 25 or 26 or 27 or 28 or 29 or 30 or 31 or 32 or 33 or 34 or 35 or 36 or 37 or 38 or 39 |
| 41 | 21 and 40 |
Appendix 6. CINAHL search strategy
| Number | Search terms |
| 1 | phone* |
| 2 | Telephon* |
| 3 | telefon* |
| 4 | telephone intervention |
| 5 | call |
| 6 | calls |
| 7 | calling |
| 8 | telecounsel* |
| 9 | Hotline |
| 10 | Telephone Hotlines |
| 11 | Hotline, Telephone |
| 12 | Hotlines, Telephone |
| 13 | Telephone Hotline |
| 14 | Cellular Phones |
| 15 | Phone, Cellular |
| 16 | Cellular Telephone |
| 17 | Cellular Telephones |
| 18 | Telephones, Cellular |
| 19 | Cell Phone |
| 20 | Cell Phones |
| 21 | Phone, Cell |
| 22 | Phones, Cell |
| 23 | Portable Cellular Phone |
| 24 | Portable Cellular Phones |
| 25 | Cellular Phone, Portable |
| 26 | Cellular Phones, Portable |
| 27 | Portable Cellular Phones |
| 28 | Cellular Phone, Transportable |
| 29 | Cellular Phones, Transportable |
| 30 | Mobile Phone |
| 31 | Mobile Phones |
| 32 | Phone, Mobile |
| 33 | Phones, Mobile |
| 34 | Car Phone |
| 35 | Car Phones |
| 36 | Phone, Car |
| 37 | Phones, Car |
| 38 | Phones, Cellular |
| 39 | Telephone, Cellular |
| 40 | telemedicine |
| 41 | teleconsult* |
| 42 | teletherapy |
| 43 | telehealth |
| 44 | 1 OR 2 OR 3 OR 4 OR 5 OR 6 OR 7 OR 8 OR 9 OR 10 OR 11 OR 12 OR 13 OR 14 OR 15 OR 16 OR 17 OR 18 OR 19 OR 20 OR 21 OR 22 OR 23 OR 24 OR 25 OR 26 OR 27 OR 28 OR 29 OR 30 OR 31 OR 32 OR 33 OR 34 OR 35 OR 36 OR 37 OR 38 OR 39 OR 40 OR 41 OR 42 OR 43 |
| 45 | AIDS |
| 46 | HIV |
| 47 | HIV‐1* |
| 48 | HIV‐2* |
| 49 | HIV1 |
| 50 | HIV2 |
| 51 | (HIV INFECT*) |
| 52 | (HUMAN IMMUNODEFICIENCY VIRUS) |
| 53 | (HUMAN IMMUNEDEFICIENCY VIRUS) |
| 54 | (HUMAN IMMUNO‐DEFICIENCY VIRUS) |
| 55 | (HUMAN IMMUNE‐DEFICIENCY VIRUS) |
| 56 | ((HUMAN IMMUN*) AND (DEFICIENCY VIRUS) ) |
| 57 | (ACQUIRED IMMUNODEFICIENCY SYNDROME) |
| 58 | (ACQUIRED IMMUNEDEFICIENCY SYNDROME) |
| 59 | (ACQUIRED IMMUNO‐DEFICIENCY SYNDROME) |
| 60 | (ACQUIRED IMMUNE‐DEFICIENCY SYNDROME) |
| 61 | ((ACQUIRED IMMUN*) AND (DEFICIENCY SYNDROME)) |
| 62 | (VIRAL SEXUALLY TRANSMITTED DISEASES) |
| 63 | 45 OR 46 OR 47 OR 48 OR 49 OR 50 OR 51 OR 52 OR 53 OR 54 OR 55 OR 56 OR 57 OR 58 OR 59 OR 60 OR 61 OR 62 |
| 64 | 44 AND 63 |
Appendix 7. WHOs The Global Health Library search strategy
Search for: Title in Regional indexes with the following terms:
(phone* or telephon* or telefon* or telephone intervention or call or calls or calling or telemedicine or teleconsult* OR telecounsel* or "Telephone" OR "Telephone Hotlines" OR "Telephone, Cellular") AND ( hiv or hiv‐1* or hiv‐2* or hiv‐1 or hiv‐2 or (human immunodeficiency virus) or (human immunedeficiency virus) or (human immune‐deficiency virus) or ((human immun*) AND (deficiency virus)) or (acquired immunodeficiency syndrome) or (acquired immunedeficiency syndrome) or (acquired immuno‐deficiency syndrome) or (acquired immune‐deficiency syndrome) or ((acquired immun*) AND (deficiency syndrome)) or hiv infect* or aids or "HIV" OR "AIDS" OR "HIV Infections")
Appendix 8. CENTRAL search strategy
| ID | Search |
| #1 | MeSH descriptor HIV Infections explode all trees |
| #2 | MeSH descriptor HIV explode all trees |
| #3 | hiv OR hiv‐1* OR hiv‐2* OR hiv1 OR hiv2 OR HIV INFECT* OR HUMAN IMMUNODEFICIENCY VIRUS OR HUMAN IMMUNEDEFICIENCY VIRUS OR HUMAN IMMUNE‐DEFICIENCY VIRUS OR HUMAN IMMUNO‐DEFICIENCY VIRUS OR HUMAN IMMUN* DEFICIENCY VIRUS OR ACQUIRED IMMUNODEFICIENCY SYNDROME OR ACQUIRED IMMUNEDEFICIENCY SYNDROME OR ACQUIRED IMMUNO‐DEFICIENCY SYNDROME OR ACQUIRED IMMUNE‐DEFICIENCY SYNDROME OR ACQUIRED IMMUN* DEFICIENCY SYNDROME |
| #4 | MeSH descriptor Lymphoma, AIDS‐Related, this term only |
| #5 | MeSH descriptor Sexually Transmitted Diseases, Viral, this term only |
| #6 | (#1 OR #2 OR #3 OR #4 OR #5) |
| #7 | MeSH descriptor Telephone explode all trees |
| #8 | MeSH descriptor Hotlines, this term only |
| #9 | MeSH descriptor Telemedicine explode tree 2 |
| #10 | MeSH descriptor Health Education, this term only |
| #11 | phone*:ti,ab,kw OR telephon*:ti,ab,kw OR telefon*:ti,ab,kw OR telemedicine:ti,ab,kw OR mobile health*:ti,ab,kw OR teleconsult*:ti,ab,kw OR remote consultation*:ti,ab,kw OR hotline*:ti,ab,kw OR telecounsel*:ti,ab,kw OR health communication:ti,ab,kw |
| #12 | (#7 OR #8 OR #9 OR #10 OR #11) |
| #13 | (#6 AND #12) |
| #14 | (#6 AND #12), from 1980 to 2011 |
Appendix 9. DAI search strategy
cabs(phone* or telephon* or telefon* or "telephone intervention" or call or calls or calling or telecounsel* or Hotline or "Mobile Phon*" or telemedicine or teleconsult* or teletherapy or telehealth) AND cabs((HIV OR "AIDS" OR "HIV infect*" OR "human immunodeficiency virus" OR "acquired immunodeficiency syndrome"))
LIMIT FOR: SINCE 1980
Appendix 10. CABI search strategy
| Number | Search terms |
| 1 | phone* |
| 2 | Telephon* |
| 3 | telefon* |
| 4 | telephone intervention |
| 5 | call |
| 6 | calls |
| 7 | calling |
| 8 | telecounsel* |
| 9 | Hotline |
| 10 | Telephone Hotlines |
| 11 | Hotline, Telephone |
| 12 | Hotlines, Telephone |
| 13 | Telephone Hotline |
| 14 | Cellular Phones |
| 15 | Phone, Cellular |
| 16 | Cellular Telephone |
| 17 | Cellular Telephones |
| 18 | Telephones, Cellular |
| 19 | Cell Phone |
| 20 | Cell Phones |
| 21 | Phone, Cell |
| 22 | Phones, Cell |
| 23 | Portable Cellular Phone |
| 24 | Portable Cellular Phones |
| 25 | Cellular Phone, Portable |
| 26 | Cellular Phones, Portable |
| 27 | Portable Cellular Phones |
| 28 | Cellular Phone, Transportable |
| 29 | Cellular Phones, Transportable |
| 30 | Mobile Phone |
| 31 | Mobile Phones |
| 32 | Phone, Mobile |
| 33 | Phones, Mobile |
| 34 | Car Phone |
| 35 | Car Phones |
| 36 | Phone, Car |
| 37 | Phones, Car |
| 38 | Phones, Cellular |
| 39 | Telephone, Cellular |
| 40 | telemedicine |
| 41 | teleconsult* |
| 42 | teletherapy |
| 43 | telehealth |
| 44 | 1 OR 2 OR 3 OR 4 OR 5 OR 6 OR 7 OR 8 OR 9 OR 10 OR 11 OR 12 OR 13 OR 14 OR 15 OR 16 OR 17 OR 18 OR 19 OR 20 OR 21 OR 22 OR 23 OR 24 OR 25 OR 26 OR 27 OR 28 OR 29 OR 30 OR 31 OR 32 OR 33 OR 34 OR 35 OR 36 OR 37 OR 38 OR 39 OR 40 OR 41 OR 42 OR 43 |
| 45 | AIDS |
| 46 | (HIV INFECTIONS) |
| 47 | HIV |
| 48 | HIV‐1* |
| 49 | HIV‐2* |
| 50 | HIV1 |
| 51 | HIV2 |
| 52 | (HIV INFECT*) |
| 53 | (HUMAN IMMUNODEFICIENCY VIRUS) |
| 54 | (HUMAN IMMUNEDEFICIENCY VIRUS) |
| 55 | (HUMAN IMMUNO‐DEFICIENCY VIRUS) |
| 56 | (HUMAN IMMUNE‐DEFICIENCY VIRUS) |
| 57 | ((HUMAN IMMUN*) AND (DEFICIENCY VIRUS) ) |
| 58 | (ACQUIRED IMMUNODEFICIENCY SYNDROME) |
| 59 | (ACQUIRED IMMUNEDEFICIENCY SYNDROME) |
| 60 | (ACQUIRED IMMUNO‐DEFICIENCY SYNDROME) |
| 61 | (ACQUIRED IMMUNE‐DEFICIENCY SYNDROME) |
| 62 | ((ACQUIRED IMMUN*) AND (DEFICIENCY SYNDROME)) |
| 63 | (VIRAL SEXUALLY TRANSMITTED DISEASES) |
| 64 | 45 OR 46 OR 47 OR 48 OR 49 OR 50 OR 51 OR 52 OR 53 OR 54 OR 55 OR 56 OR 57 OR 58 OR 59 OR 60 OR 61 OR 62 OR 63 |
| 65 | 44 AND 64 |
Appendix 11. OpenSIGLE search strategy
Simple search required:
((telephon*) AND (hiv OR aids))
Appendix 12. HMIC search strategy
| Number | Search terms |
| 1 | phone*.af. |
| 2 | Telephon*.af. |
| 3 | telefon*.af. |
| 4 | telephone intervention.af. |
| 5 | call.af. |
| 6 | calls.af. |
| 7 | calling.af. |
| 8 | Hotline.af. |
| 9 | Telephone Hotlines.af. |
| 10 | Telephone Hotline.af. |
| 11 | Cellular Phones.af. |
| 12 | Cellular Telephone.af. |
| 13 | Cellular Telephones.af. |
| 14 | Cell Phones.af. |
| 15 | Mobile Phones.af. |
| 16 | Phones, Mobile.af. |
| 17 | exp telephone/ |
| 18 | exp telemedicine/ |
| 19 | exp teletherapy / |
| 20 | 1 OR 2 OR 3 OR 4 OR 5 OR 6 OR 7 OR 8 OR 9 OR 10 OR 11 OR 12 OR 13 OR 14 OR 15 OR 16 OR 17 OR 18 OR 19 |
| 21 | exp human immunodeficiency virus/ |
| 22 | hiv.ti. OR hiv.ab. |
| 23 | hiv‐1.ti. OR hiv‐1.ab. |
| 24 | hiv‐2.ti. OR hiv‐2.ab. |
| 25 | human immunodeficiency virus.ti. OR human immuno deficiency.ab. |
| 26 | human immuno‐deficiency virus.ti. OR human immuno‐deficiency virus.ab. |
| 27 | human immune‐deficiency virus.ti. OR human immune‐deficiency virus.ab. |
| 28 | acquired immune‐deficiency syndrome.ti. OR acquired immune‐deficiency syndrome.ab. |
| 29 | acquired immunedeficiency syndrome.ti. OR acquired immunedeficiency syndrome.ab. |
| 30 | acquired immunodeficiency syndrome.ti. OR acquired immunodeficiency syndrome.ab. |
| 31 | acquired immuno‐deficiency syndrome.ti. OR acquired immuno‐deficiency syndrome.ab. |
| 32 | exp acquired immune deficiency syndrome/ |
| 33 | 21 OR 22 OR 23 OR 24 OR 25 OR 26 OR 27 OR 28 OR 29 OR 30 OR 31 OR 32 |
| 34 | 20 AND 33 |
Appendix 13. Google Scholar search strategy
((telephon*) AND (hiv OR aids))
Appendix 14. Conference on Retroviruses and Opportunistic Infections (CROI)
Source: http://www.retroconference.org/AbstractSearch/default.aspx
Search strategy: telephone HIV AIDS
Match on all words entered
Include Prior 14 Conferences (1997 ‐ 2011)
Appendix 15. International AIDS Society (IAS)
Source: http://www.iasociety.org/Default.aspx?pageId=7
Search strategy: telephone phone
Search conference IAS 2009
Search conference AIDS 2010
Appendix 16. AEGIS search strategy
telephon* OR phone* OR hotline* OR telecounsel* OR telemedicine OR teleconsult*
Appendix 17. Current Controlled Trials search strategy
hiv AND (telephone OR phone OR hotline OR text message OR messaging OR telemedicine OR telecounseling)
Data and analyses
Comparison 1.
Effects of the interventions aimed at improving medication adherence
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 ART adherence | 3 | 191 | Mean Difference (IV, Fixed, 95% CI) | 0.49 [‐1.12, 2.11] |
Comparison 2.
Effects of the interventions aimed at improving depressive and psychiatric symptoms
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Depressive symptoms (BDI score) | 3 | 447 | Mean Difference (IV, Fixed, 95% CI) | 0.02 [‐0.18, 0.21] |
| 2 Psychiatric distress (General Severity Index of the Brief Symptom Index) | 1 | 17 | Mean Difference (IV, Fixed, 95% CI) | ‐6.53 [‐11.71, ‐1.35] |
| 3 Psychiatric distress (Outcomes questionnaire score) | 1 | 79 | Mean Difference (IV, Fixed, 95% CI) | 1.80 [‐10.98, 14.58] |
| 4 Psychological distress (Total SCL‐90‐R score) | 1 | 191 | Mean Difference (IV, Fixed, 95% CI) | ‐0.10 [‐0.11, ‐0.09] |
| 5 Life stressor burden (HIV‐related life‐stressor burden scale) | 1 | 191 | Mean Difference (IV, Fixed, 95% CI) | ‐0.01 [‐0.02, 0.00] |
| 6 Support from family (PSRS) | 1 | 191 | Mean Difference (IV, Fixed, 95% CI) | 0.16 [0.14, 0.18] |
| 7 Support from friends (PSRS) | 1 | 191 | Mean Difference (IV, Fixed, 95% CI) | 0.22 [0.20, 0.24] |
| 8 Barriers to care (BACS) | 1 | 191 | Mean Difference (IV, Fixed, 95% CI) | ‐0.06 [‐0.08, ‐0.04] |
| 9 Coping self‐efficacy (Coping self‐efficacy scale) | 1 | 191 | Mean Difference (IV, Fixed, 95% CI) | 0.38 [0.34, 0.42] |
| 10 Social well‐being (Social/family well‐being subscale of the FAHI) | 1 | 191 | Mean Difference (IV, Fixed, 95% CI) | 0.02 [‐0.00, 0.04] |
| 11 Emotional well‐being (Emotional well‐being subscale of the FAHI) | 1 | 191 | Mean Difference (IV, Fixed, 95% CI) | 0.05 [0.03, 0.07] |
Analysis 2.3.

Comparison 2 Effects of the interventions aimed at improving depressive and psychiatric symptoms, Outcome 3 Psychiatric distress (Outcomes questionnaire score).
Analysis 2.4.
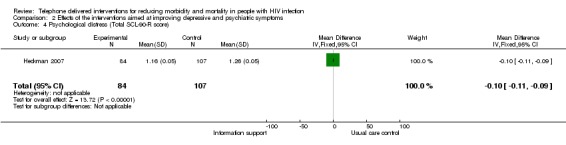
Comparison 2 Effects of the interventions aimed at improving depressive and psychiatric symptoms, Outcome 4 Psychological distress (Total SCL‐90‐R score).
Analysis 2.5.
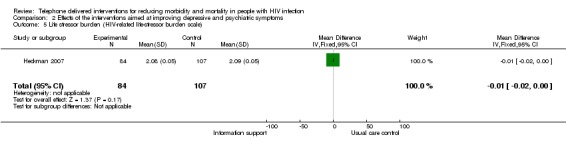
Comparison 2 Effects of the interventions aimed at improving depressive and psychiatric symptoms, Outcome 5 Life stressor burden (HIV‐related life‐stressor burden scale).
Analysis 2.6.
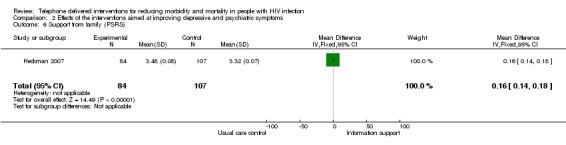
Comparison 2 Effects of the interventions aimed at improving depressive and psychiatric symptoms, Outcome 6 Support from family (PSRS).
Analysis 2.7.
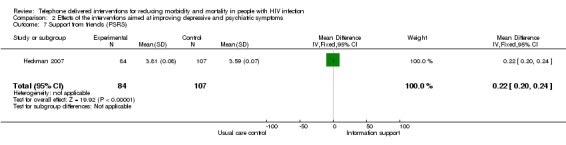
Comparison 2 Effects of the interventions aimed at improving depressive and psychiatric symptoms, Outcome 7 Support from friends (PSRS).
Analysis 2.8.
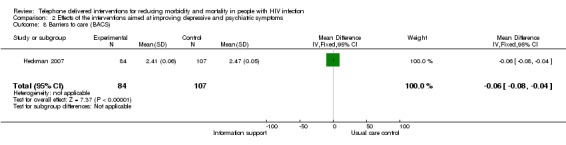
Comparison 2 Effects of the interventions aimed at improving depressive and psychiatric symptoms, Outcome 8 Barriers to care (BACS).
Analysis 2.9.
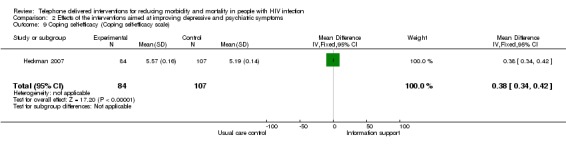
Comparison 2 Effects of the interventions aimed at improving depressive and psychiatric symptoms, Outcome 9 Coping self‐efficacy (Coping self‐efficacy scale).
Analysis 2.10.
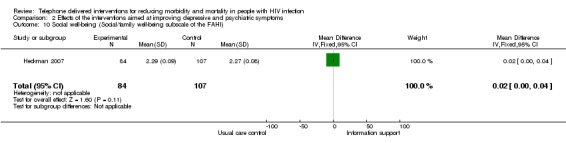
Comparison 2 Effects of the interventions aimed at improving depressive and psychiatric symptoms, Outcome 10 Social well‐being (Social/family well‐being subscale of the FAHI).
Analysis 2.11.

Comparison 2 Effects of the interventions aimed at improving depressive and psychiatric symptoms, Outcome 11 Emotional well‐being (Emotional well‐being subscale of the FAHI).
History
| Date | Event | Description |
|---|---|---|
| 31 July 2012 | Amended | final revisions |
Differences between protocol and review
There are a number of differences between the protocol and this review. These are mostly due to the fact that we only found RCTs, and due to the heterogeneity of the included studies.
1. Assessment of risk of bias in included studies: our searches found only eligible studies of RCT design. If we had found eligible studies of other designs, other tools would have been used to assess risk of bias (EPOC 1998; EPOC 2009) as stated in the protocol.
2. Data analysis: Our searches found only eligible studies of randomised controlled trial design. If we had found eligible studies of other study designs that met our inclusion criteria, we would have reported each study design separately. If any eligible ITS studies had been found, we would have reported mean differences in before and after values. If we had found eligible studies of more than one study design we would have presented a summary of the treatment effect by study design. Instead, we present only a summary of treatment effect by type of intervention. We planned to calculate dichotomous data as relative risk (95% CIs), but all data in the included studies was continuous. If heterogeneity had been detected and it had still been appropriate to combine the trials, we would have used a random‐effects model.
3. Data synthesis: We would have separately analysed the results of different study types.
4. Assessment of heterogeneity: If substantial statistical heterogeneity had been identified by an I2 statistic value of >50% subgroup analysis and sensitivity analysis (Higgins 2011) would have been performed to further explore this, and data would not have been combined in a meta‐analysis. A random‐effect model would have been used in sensitivity analysis.
5. Sensitivity analyses to evaluate the effect on effect size of the following factors would have been considered: lower quality studies, studies with higher/lower risk of bias (as specified above), studies of low statistical power, unpublished studies, studies in languages other than English, research undertaken in various countries, source of funding (industry versus other) and different statistical models (fixed‐ and random‐effects models).
6. Subgroup analysis: We would have considered subgroup analyses based on demographic outcomes such as race/ethnicity/nationality, age, gender and HIV risk factors.
7. Reporting bias: We would have used funnel plots to examine the potential existence of reporting biases (small study bias). We would have performed a test for funnel plot asymmetry to examine whether the association between estimated intervention effects and a measure of study size is greater than might be expected to occur by chance, and to add further consideration to the visual inspection of the funnel plot.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | Randomised controlled trial conducted over a 96 week period. | |
| Participants | Participants (n=282) with advanced HIV infection (CD4 count less than or equal to 200 cells/mm3 or >80,000 HIV RNA copies/mL of plasma at screening) who were initiating antiretroviral therapy (no previous use of lamivudine, nonnucleoside reverse transcriptase inhibitors, or protease inhibitors) were enrolled in this adherence substudy of a treatment trial. Participants were recruited from 30 sites in the United States of America, Puerto Rico and Italy, 48% identified as white, 32% black and 15% Hispanic and 19% of participants were women. There were no significant baseline differences between the intervention and control groups. | |
| Interventions | Participants were randomised to a usual support measures group (n=140) or a telephone intervention group (n=142). Participants in the usual care support group received their study site's usual adherence support measures. These may have included 35 minutes of in‐person counselling, written material or informal telephone calls. Those in the telephone intervention group received their site's usual support measures plus up to 16 scripted telephone calls from study site members (mostly nurses) over the 96 week study period. Calls focused on each subject's medication taking behaviour and barriers to adherence, and developed individual strategies to increase adherence. Social support and assistance with medical side effects were also provided. | |
| Outcomes | Outcomes were virologic failure and self‐reported adherence. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No mention of sequence generation in the study. |
| Allocation concealment (selection bias) | Unclear risk | No mention of allocation concealment in the study. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Blinding of participants and personnel was unlikely to be feasible in this study, but we do not think this will have affected the results. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No mention of blinding to outcome assessment in the study. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Of the 282 enrollees, 239 (85%) completed the trial, 35 (12%) discontinued prematurely, six (2%) died, and two (1%) discontinued for other reasons. The reasons for not completing the trial were similar between groups. |
| Selective reporting (reporting bias) | Unclear risk | Protocol of the study was unavailable. |
| Other bias | High risk | We judged the risk of contamination to be high. The same study site staff members were counselling participants in both groups. Subjects who were anticipated to have problems with adherence at all study sites received counselling. It is possible that the approach used for the usual support measures group may have been influenced by the additional support measures used for the calls group if the study site staff members inadvertently used counselling strategies they learned from the standardised script. According to a study site survey, 67% of study sites reported that they provided written materials to study participants as part of their usual adherence support measures. In addition, 41% of study sites reported making at least one telephone call to selected participants (who were judged by study site staff members as being at high risk for low adherence) as part of their usual support measures; telephone calls were made to a minority of participants, the number of telephone calls per subject was limited, and the content was not standardized. |
| Methods | A randomised controlled trial of 12 months duration. | |
| Participants | HIV positive persons (n=61) in the United States of America. In the intervention group 70.5% were black, 23.5% white, 3% Hispanic, and 3% mixed Hispanic and African American. In the control group 81% were black and 19% white. 50% of the intervention group, and 46% of the control group, were female. | |
| Interventions | Participants were randomised to an intervention group (n=34) or a control group (n=27). The control group received monthly visits until their viral load was <50, including physician visit, CD4, VL and pharmacist adherence review. The intervention group received the control group intervention plus telephone calls from a pharmacist at day four, two weeks, then monthly for six months. | |
| Outcomes | Outcomes were: adherence; change in CD4 lymphocyte count; and virologic response. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details of random sequence generation in the study. |
| Allocation concealment (selection bias) | Unclear risk | No mention of allocation concealment in the study. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Blinding of participants and personnel was unlikely to be feasible in this study, but we do not think this will have affected the results. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No mention of blinding to outcome analysis. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | In the intervention group, one participant withdrew and five were lost to follow up. In the control group, one participant withdrew and seven were lost to follow up. Reasons for these were not mentioned in the study. |
| Selective reporting (reporting bias) | Unclear risk | Protocol was unavailable to us. |
| Methods | A randomised controlled trial. | |
| Participants | Rural (defined as residence in a community of 50,000 persons or fewer that was at least 20 miles from a city of 100,000 or more) persons (n=299) with a self‐reported diagnosis of HIV in the United States. The majority (75%) of participants were white. 30% were women. No inclusion or exclusion criteria related to psychological functioning were employed. Study quote: 'There were no differences between the treatment conditions at pre‐intervention with the exception of education. Post‐hoc comparisons revealed that Information Support Group Intervention participants completed fewer years of education than Coping Improvement Group Intervention participants.' |
|
| Interventions | Participants were assigned to a telephone‐delivered eight session information support group (n=84), a telephone‐delivered eight session coping improvement intervention group (n=108), or a usual care control group (n=107). Both intervention conditions had separate groups for men who had sex with men (MSM), heterosexual men and women. There were six to eight participants per group, and the interventions were conducted using teleconference technology. The control group received no active intervention, but were able to access services provided by their AIDS service organisation. |
|
| Outcomes | Outcomes were: BDI score; Symptom Checklist 90‐Revisied score; HIV‐Related Life‐Stressor Burden Scale score; Provision of Social Relations Scale score; The Barriers to Care Scale score; Functional Assessment of HIV Infection Inventory score; Coping Self‐Efficacy Scale score; and demographic characteristics. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information on random sequence generation in the study. |
| Allocation concealment (selection bias) | Unclear risk | No mention of allocation concealment in the study. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Blinding of participants and personnel was unlikely to be feasible in this study, but we do not think this will have affected the results. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No mention of blinding of outcome assessment. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 73% (n=78) of the usual care condition, 68% (n=57) of the Information Support Group condition, and 82% (n=88) of the Coping Improvement Group condition completed eight month follow‐up assessment. |
| Selective reporting (reporting bias) | Unclear risk | Protocol was unavailable to us. |
| Methods | A randomised controlled trial. | |
| Participants | Participants were 26 men and 14 women recruited from infectious diseases clinics in Atlanta, Georgia, receiving and less than 95% adherent to anti‐retroviral therapy. The majority (92.5%) were black, with the remainder (7.5%) being white. 35% of participants were women. Study quote: 'Initial comparisons between conditions on all baseline characteristics and adherence did not indicate any significant differences between conditions, indicating that the randomisation scheme achieved balanced conditions.' |
|
| Interventions | Participants were randomised to telephone‐delivered behavioural self‐regulation counselling (n=21) or a usual care control group (n=19). Study quote: 'Those in the telephone intervention group received a single office session followed by four biweekly cell phone counselling sessions that were grounded in behavioural self‐management model of medication adherence using data from phone‐based unannounced pill counts to provide feedback‐guided adherence strategies. The control condition received usual care and matched office and cell phone/pill count contacts.' |
|
| Outcomes | Outcomes were: ART adherence; medication adherence self‐efficacy; adherence behavioural strategies; process measures. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Study quote: 'Allocation was accomplished by using a computer generated simple randomization scheme. Randomization was not breached throughout the trial.' |
| Allocation concealment (selection bias) | Low risk | Study quote: 'Recruitment, screening, and office‐based assessment staff remained blinded to condition throughout the study.' |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Blinding of participants and personnel was unlikely to be feasible in this study, but we do not think this will have affected the results. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Study quote: 'office‐based assessment staff remained blinded to condition throughout the study and the adherence counsellor never conducted outcome assessments.' |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | One control group participant was lost to follow up. |
| Selective reporting (reporting bias) | Unclear risk | Protocol was unavailable to us. |
| Other bias | Low risk | |
| Methods | Randomised controlled trial conducted between December 2009 and March 2010. | |
| Participants | Self‐reported HIV‐positive people (n=100) over 45 years of age (mean age 54) who participated in risky sexual behaviour (had engaged in one or more occasions of unprotected anal or vaginal intercourse in the past 3 months). Participants were recruited from five metropolitan areas: New York City, Atlanta, Philadelphia, Cincinnati and Columbus The majority were black (87%), and the remainder white (13%). 46% were female. Participants did not differ on any baseline demographic or clinical variables across the three study conditions. | |
| Interventions | Participants were randomised to four sessions of telephone delivered motivational interviewing (n= 38), one session of telephone delivered motivational interviewing (n=39) or a control group (n=23) in which they received no motivational interviewing sessions. Participants in the four session MI group received four sessions of MI, in which a therapist aimed to explore the participants’ relationship dynamics, increase readiness to engage in condom‐protected sex, discuss and overcome barriers to condom use and improve clients’ confidence to engage in condom‐protected sex. Exactly what was included depended on the patients’ readiness to change. Participants in the one‐session MI group received the same intervention as the four session group, with the exception of treatment dose (one session as opposed to four sessions). Participants in the control group did not receive any active intervention, but were encouraged to seek support from their local AIDS service organisations, HIV‐related and other support groups, information websites, and any other resources available to them. No formal referrals to these services were made. |
|
| Outcomes | Outcomes were: the number of self‐reported non‐condom protected anal and vaginal sex acts in the last three months; and readiness to engage in condom protected behaviours (assessed by asking participants to endorse one of five statements which most represented their willingness to change). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Study quote: 'Prior to initiating the study, off‐site personnel utilized a random numbers table and weighted simple random assignment to generate the allocation sequence, yielding a 2 (1‐session MI): 2 (4‐session MI): 1 (control) ratio.' |
| Allocation concealment (selection bias) | Low risk | Study quote: 'Immediately following the baseline interview, participants were assigned to one of three parallel study conditions using concealment of allocation procedures. Sealed, consecutively numbered, opaque envelopes prepared by off‐site personnel contained the randomly allocation conditions.' |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Study quote: 'All research personnel were blind to participant condition prior to, and during, the baseline interview.' Blinding of participants was unlikely to be feasible in this study, but we do not think this will have affected the results. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Study quote: 'Interviewers were blind to participant condition when conducting all interviews.' |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Two participants in the four session MI group, three participants in the one session MI group, and zero participants in the control group did not complete six month follow‐up. Reasons were: unable to locate (n=2); dropped out of study (n=1); deceased (n=1); and too sick (n=1). |
| Selective reporting (reporting bias) | Unclear risk | Protocol was unavailable to us. |
| Methods | Randomised controlled trial of 16 weeks duration. | |
| Participants | English‐speaking men (n=17) aged 25‐68 and in the early stages of HIV. They were well educated (college=5, graduate school=12), largely employed (full time=10, part time=2, unemployed=3, student=1, retired=1). 71% were white, 18% African American and 12% Latino. There were significant differences in sexual orientation between the intervention and the control group. In the intervention group one participant was bisexual and eight homosexual. In the control group, three participants were heterosexual and five were homosexual. | |
| Interventions | Participants were randomised to a telephone intervention group (n=9) or a control group (n=8). Those in the intervention group received weekly structured telephone calls for 16 weeks. These incorporated psychosocial support; ongoing monitoring of health, stress, mood and interpersonal satisfaction; information and education regarding HIV infection and AIDS; and early referral to other services where appropriate.The control group was a wait‐list no intervention control group. | |
| Outcomes | Outcome was psychiatric distress, measured using the General Severity Index of the BSI. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details about random sequence generation. |
| Allocation concealment (selection bias) | Unclear risk | No mention of allocation concealment in the study. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Blinding of participants and personnel was unlikely to be feasible in this study, but we do not think this will have affected the results. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No mention of blinding of outcome assessment in the study. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No mention of incomplete outcome data in the study. |
| Selective reporting (reporting bias) | Unclear risk | Protocol was not available to us. |
| Other bias | High risk | High risk of bias for baseline differences. There were significant differences in sexual orientation between the intervention and the control group. In the intervention group one participant was bisexual and eight homosexual. In the control group, three participants were heterosexual and five were homosexual. |
| Methods | A pilot randomised controlled trial carried out between February 2006 and March 2007. | |
| Participants | Self‐reported HIV (n=79) positive persons living an urban area (definition) and with depression (met diagnostic criteria for a depression‐spectrum disorder according to a telephone‐administered mood module of the Primary Care Evaluation of Mental Disorders). The majority of participants were white (77%), followed by African American (10%), Latino (9%), Hispanic (3%) and Native American (1%). Just 16% of participants were women. There were no significant baseline differences between the intervention and control groups. | |
| Interventions | Participants were randomly allocated to an intervention group (n=41) or a usual care control group (n=38). The intervention group received a six‐session, telephone‐delivered interpersonal psychotherapy intervention plus usual care. Those in the usual care control group received no active therapeutic intervention, but had access to services provided by their AIDS service organisation (for example support groups). | |
| Outcomes | Outcomes were BDI‐II score; Outcomes Questionnaire score; Provision of Social Relations Scale score; and the University of California Los Angeles Lonliness Scale score. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Study quote: 'randomly assigned'. No further detail. |
| Allocation concealment (selection bias) | Unclear risk | No mention of allocation concealment in the study. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Blinding of participants and personnel was unlikely to be feasible in this study, but we do not think this will have affected the results. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No mention of blinding of outcome assessment in the study. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Study quote: 'Participants in the teletherapy group were marginally more likely to discontinue study involvement (n=10) than those in the control group (n=3), although this association was not significant.' Study quote: 'Participants with missing postintervention data (n=13) were retained for final outcome analyses by using a last‐observation‐carried‐forward approach.' |
| Selective reporting (reporting bias) | Unclear risk | The only information provided on the University of California Los Angeles (UCLA) Lonliness Scale and Provision of Social Relations Scale (PSRS) results is: 'No hypothesized condition x time interactions were found for the UCLA Loneliness Scale or the PSRS.' |
| Methods | A randomised controlled trial carried out over 64 weeks. An adherence substudy of a large multicentre treatment trial evaluating different strategies for initiating antiretroviral therapy in HIV‐infected individuals. | |
| Participants | Anti‐retroviral therapy naive participants (n=109) in five sites in the United States of America. 51% of participants were white and 43% black. 15% of participants were women. 73% had comorbid depression. There were no significant differences in demographics between the two groups. | |
| Interventions | Participants were randomised to an intervention group (n=54) and a control group (n=55). Those in the intervention group received standard clinic‐based patient education plus structured proactive telephone calls provided by a trained registered nurse specialist and access to a 24‐hour toll free helpline. Those in the control group received standard clinic‐based patient education. | |
| Outcomes | Outcomes were self‐reported adherence and time to virologic failure. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Study states that participants 'were randomized', but no further detail is given. |
| Allocation concealment (selection bias) | Unclear risk | No mention of allocation concealment in the study. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Blinding of participants and personnel was unlikely to be feasible in this study, but we do not think this will have affected the results. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No mention of blinding of outcome assessment. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Fourteen participants in the intervention group and 20 in the control group were lost to follow up, due to dropping out of parent study or reaching the endpoint of the parent study. |
| Selective reporting (reporting bias) | Unclear risk | The study protocol was unavailable to us. |
| Methods | A randomised controlled trial | |
| Participants | Drug using (must have used illicit drugs at least 5 times in the last 3 months) young people (n=175) (aged 16‐29) with HIV infection. 42% were Latino, 26% black, 23% white and 8% of unspecified ethnicity. 22% were women. The in‐person intervention condition had a higher proportion of protected acts across all sexual partners, among HIV‐positive sexual partners, and among HIV‐negative sexual partners compared with the delayed‐intervention condition (P <0.05). The telephone intervention condition had a higher proportion of protected acts across all sexual partners and among HIV‐negative sexual partners compared with the delayed‐intervention condition (P <0.05). The telephone intervention condition also had a higher proportion of protected acts across all sexual partners and among HIV‐negative sexual partners compared with in‐person intervention condition (P <0.05). | |
| Interventions | Participants were randomised into a telephone intervention group (n=59), an in‐person intervention group (n=61), or a delayed intervention control group (n=55). The intervention consisted of 18 one‐on‐one interventions divided up in to three modules, and delivered via telephone or in‐person. Each module lasted six sessions and focused on a different target behaviour: improving physical health, reducing sexual and substance use acts, and improving mental health. | |
| Outcomes | Outcomes were: sexual risk acts; substance abuse; medication adherence; health behaviours; self‐report health status; mental health outcome; and cost analysis. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details of sequence generation in the study. |
| Allocation concealment (selection bias) | Unclear risk | No mention of allocation concealment in the study. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Blinding of participants and personnel was unlikely to be feasible in this study, but we do not think this will have affected the results. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No mention of blinding to outcome assessment. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Study quote: 'Fewer young people completed all 18 sessions (35%): 41% of those receiving individual sessions and 29% of those receiving the telephone interventions.' No further information given. |
| Selective reporting (reporting bias) | Unclear risk | Protocol unavailable, but unlikely given the number of outcomes. |
| Other bias | High risk | High risk of bias for baseline differences between the two intervention groups and the control group. The in‐person intervention condition had a higher proportion of protected acts across all sexual partners, among HIV‐positive sexual partners, and among HIV‐negative sexual partners compared with the delayed‐intervention condition (P<0.05). The telephone intervention condition had a higher proportion of protected acts across all sexual partners and among HIV‐negative sexual partners compared with the delayed‐intervention condition (P< 0.05). The telephone intervention condition also had a higher proportion of protected acts across all sexual partners and among HIV‐negative sexual partners compared with in‐person intervention condition (P<0.05). |
| Methods | A randomised controlled trial carried out over a six month period. | |
| Participants | HIV positive persons (n=177) with depression (defined as a BDI score of 10 or more), co‐enrolled with their self‐identified primary informal care giver (if they were able to identify one) in the United States of America. 41% of participants were Caucasian. 44% were female. Participants had an average BDI score of 22.7. Study quote: 'Participants randomized to treatment had significantly lower CD4 counts at baseline and reported significantly poorer mean physical function scores on SF‐36. Treatment groups did not differ significantly with respect to any other variables. Baseline depression was not correlated significantly with baseline CD4 counts or months since diagnosis.' |
|
| Interventions | Participants were randomised to a telephone‐contact intervention group (n=89) and a control group (n=88). Those in the intervention group received 12 structured psychoeducational telephone calls over six months, which provided education and encouraged problem‐appraisal and resolution‐through‐referral, with the aim of reducing problems related to mood in HIV positive patients. Those in the control group received assessment only. | |
| Outcomes | Outcome measures were: change in depressive symptoms over time (six months, measured using BDI); whether the patient goes in to remission for depression or not (measured using BDI); change in severity of depressive symptoms category; use of psychiatric medications during follow‐up period; mental and physical function subscales of SF‐36. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Study quote: 'Patients were randomly assigned to either an assessment only group or to a phone intervention group'. No further detail provided. |
| Allocation concealment (selection bias) | Unclear risk | No mention of allocation concealment in the study. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Blinding of participants and personnel was unlikely to be feasible in this study, but we do not think this will have affected the results. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No mention of blinding to outcome assessment in the study. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Ten participants in the intervention group, and seven participants in the control group were lost to follow up. Reasons for this were not given. |
| Selective reporting (reporting bias) | Unclear risk | Protocol of the study was unavailable. |
| Methods | A pilot randomised controlled trial conducted between December 2009 and May 2010. | |
| Participants | Rural persons (n=42) living with HIV in the United States of America. The majority (81%) were white, 7.1% were black and 4.9% were 'other' ethnicity. 40% of participants were female. | |
| Interventions | Participants were randomised to a telephone‐administered motivational interviewing adherence improvement intervention (n=21) and a self‐monitoring comparison condition control group (n=21). Those in the intervention group received a one‐session telephone‐administered 60 minute structured scripted adherence improvement intervention. Those in the control group received no active intervention, but were asked to complete medication diaries over a five‐week period, which was equal to the number of weeks that intervention participants completed medication diaries. | |
| Outcomes | Outcomes were: dose adherence; schedule adherence; readiness to change; intrinsic motivation; self‐efficacy; depression; and reasons for non‐adherence. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Study quote: 'Block randomization with a 1:1 allocation using a random block size of two was used to ensure equal numbers within both conditions. Specifically, every time two participants returned their pre‐intervention questionnaires; a researcher drew a card from an envelope. The envelope contained two cards; one was labelled 'Intervention group' and the other one was labelled 'Control group'. |
| Allocation concealment (selection bias) | Unclear risk | It does not mention whether the envelopes used were sealed and opaque. Assignment envelopes may have been used without appropriate safeguards. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Blinding of participants and personnel was unlikely to be feasible in this study, but we do not think this will have affected the results. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No mention of blinding of outcome assessment in the study. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Study quote: 'All participants completed the pre‐intervention questionnaire and the 2‐week medication diary. However, two intervention (9.5%) and two control group participants (9.5%) did not return 3‐week medication diaries. One intervention group (4.7%) and one control group participant (4.7%) did not return the post‐intervention questionnaires. Contact was lost with these participants and the reasons for their termination in the study remain unknown.' |
| Selective reporting (reporting bias) | Unclear risk | Protocol was unavailable to us. |
| Other bias | Unclear risk | There may be risk of bias due to significant baseline differences between the intervention and the control group. Study quote: 'There were significant differences between conditions at baseline on number of years on ART medications, number of different ART medications, and number of total ART pills prescribed. On average, intervention participants (15.3 years) were on ART medications for a longer period of time compared to controls (11.1 years). Compared to control group participants (2.1), intervention group participants (3.1) were prescribed a greater number of different ART medications and a greater number of total ART pills (intervention group= 5.4, control group=3.2).' However, we feel that this may have been inevitable given the small sample size. |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Konkle‐Parker 2010 | This RCT pilot trial assessed the efficacy of an intervention with both a face‐to‐face and a telephone component to improve medication adherence in PLHIV. We excluded the study because the use of the telephone was only a part of the intervention and could not be separately evaluated. |
| Puccio 2006 | This pilot study assessed the use of cell phone reminder calls for improving adherence to ART in young PLHIV. We excluded the study because of was not of an eligible study design. |
| Uzma 2011 | This RCT assessed the efficacy of an intervention combining both telephone calls and face‐to‐face sessions for improving ART adherence in PLHIV. We excluded the study because the use of the telephone was only a part of the intervention and could not be separately evaluated. |
| Wang 2010 | This study assessed the efficacy of a nurse delivered intervention combining home visits and telephone calls designed to improve medication adherence and quality of life. We excluded the study because the use of the telephone was only a part of the intervention and could not be separately evaluated. |
Contributions of authors
JC conceived the idea for the review. MvV wrote the protocol. SG, MvV and LTC performed searches, screened citations and extracted data. SG wrote the review. MvV, LTC and JC provided comments on the review.
Sources of support
Internal sources
-
Global eHealth Unit, Department of Primary Care and Public Health, Imperial College London, UK, UK.
salaries, office space, etc
External sources
The Department of Primary Care and Public Health at Imperial College London is grateful for support from the NIHR Collaboration for Leadership in Applied Health Research & Care (CLAHRC) scheme, the NIHR Biomedical Research Centre scheme, and the Imperial Centrefor Patient Safety and Service Quality., UK.
Declarations of interest
None to declare.
New
References
References to studies included in this review
- Collier AC, Rubaudo H, Mukherjee L, Feinbery J, Fischl MA, Chesney M, et al. A randomized study of serial telephone call support to increase adherence and thereby improve virologic outcome in persons initiating antiretroviral therapy. The Journal of Infectious Diseases 2005;192(8):1398‐406. [DOI] [PubMed] [Google Scholar]
- Cox HL, Johnson JW, Williamson JC, Russell GB, Wilkin AM. Clinician‐initiated telephone follow‐up improves virologic outcomes in an HIV outpatient clinic. AIDS 2006. XCI International AIDS Conference: Abstract no. TUPR0144. [Google Scholar]
- Heckman TG, Carlson B. A randomized clinical trial of two telephone‐delivered, mental health interventions for HIV infected persons in rural areas of the United States. AIDS and Behaviour 2007 Jan;11(1):5‐14. [DOI] [PubMed] [Google Scholar]
- Kalichman SC, Kalichman MO, Cherry C, Swetzes C, Amaral CM, White D, et al. Brief behavioural self‐regulation counselling for HIV treatment adherence delivered by cell phone: an initial test of concept trial. AIDS Patient Care and STDs 2011;25(5):303‐10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovejoy TI, Heckman TG, Suhr JA, Anderson T, Heckman BD, France CR. Telephone‐administered motivational interviewing reduces risky sexual behaviour in HIV‐positive late middle‐age and older adults: a pilot randomized controlled trial. AIDS and Behaviour 2011;15(8):1623‐34. [DOI] [PubMed] [Google Scholar]
- Lucy JR. The effects of TELECARE on psychosocial symptoms in HIV‐seropositive individuals. Thesis (PhD), Fuller Theological Seminary1994.
- Ransom D, Heckman TG, Anderson T, Garske J, Holyrod K, Basta T. Telephone‐delivered, interpersonal psychotherapy for HIV‐infected rural persons with depression: a pilot trial. Psychiatric Services 2008;59(8):871‐7. [DOI] [PubMed] [Google Scholar]
- Reynolds NR, Testa MA, Su M, Chesney MA, Neidig JF, Frank I, et al. Telephone support to improve antiretroviral medications adherence: a multisite randomized controlled trial. Journal of Acquired Immune Deficiency Syndromes 2008;47(1):62‐8. [DOI] [PubMed] [Google Scholar]
- Rotheram‐Borus MJ, Swendeman D, Comulada WS, Weiss RE, Lee M, Lightfoot M. Prevention for substance‐using HIV‐positive young people: telephone and in‐person delivery. Journal of Acquired Immune Deficiency Syndromes 2004;37 (suppl 2):S68‐S77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein MD, Herman DS, Bishop D, Anderson BJ, Trisvan E, Lopez R, et al. A telephone‐based intervention for depression in HIV patients: negative results from a randomized clinical trial. AIDS and Behaviour 2007;11(1):15‐23. [DOI] [PubMed] [Google Scholar]
- Watakasol R. Telephone administered intervention to improve medication adherence in HIV‐infected rural persons: a pilot randomized clinical trial. Thesis (PhD), Ohio University2010.
References to studies excluded from this review
- Konkle‐Parker DJ, Erlen JA, Dubbert PM. Lessons learned from an HIV adherence pilot study in the Deep South. Patientient Education and Counseling 2010;78(1):91‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puccio JA, Belzer M, Olson J, Martinez M, Salata C, Tucker D, et al. The use of cell phone reminder calls for assisting HIV‐infected adolescents and young adults to adhere to highly active antiretroviral therapy: a pilot study. AIDS Patient Care and STDs 2006;20(6):438‐44. [DOI] [PubMed] [Google Scholar]
- Uzma, Emmanuel F, Ather U, Zaman S. Efficacy of interventions for improving antiretroviral therapy adherence in HIV/AIDS cases at PIMS, Islamabad. Journal of the International Association of Physicians in AIDS Care 2011;10(6):373‐83. [DOI] [PubMed] [Google Scholar]
- Wang H, Zhou J, Huang L, Li X, Fennie KP, Williams AB. Effects of nurse‐delivered home visits combined with telephone calls on medication adherence and quality of life in HIV‐infected heroin users in Hunan of China. Journal of Clinical Nursng 2010;19(3‐4):380‐8. [DOI] [PubMed] [Google Scholar]
Additional references
- Aharonovich E, Greenstein E, O'Leary A, Johnston B, Seol SG, Hasin DS. HealthCall: technology‐based extension of motivational interviewing to reduce non‐injection drug use in HIV primary care patients ‐ a pilot study. AIDS Care 2012;24(12):1461‐9.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atun R, Bataringaya J. Building a durable response to HIV/AIDS: implications for health systems. Journal of Acquired Immune Deficiency Syndromes 2011;57 Suppl 2:S91‐5. [DOI] [PubMed] [Google Scholar]
- Barnighausen T, Chaiyachati K, Chimbindi N, Peoples A, Haberer J, Newell ML. Interventions to increase antiretroviral adherence in sub‐Saharan Africa: a systematic review of evaluation studies. The Lancet Infectious Diseases 2011;11(12):942‐51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bing E G, Burnam A, Longshore D, Fleishman J A, Sherbourne C D, London A S, et al. Psychiatric disorders and drug use among human immunodeficiency virus‐infected adults in the United States. Archives of General Psychiatry 2001;58:721‐8. [DOI] [PubMed] [Google Scholar]
- Black AD, Car, J, Pagliari C, Anandan C, Cresswell K, Bokun T, et al. The impact of eHealth on the quality and safety of health care: a systematic overview. PloS Medicine 2011;8(1):e1000387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bravo P, Edwards A, Rollnick S, Elwyn G. Tough decisions faced by people living with HIV: a literature review of psychosocial problems. Aids Reviews 2010;12:76‐88. [PubMed] [Google Scholar]
- Bunn F, Byrne G, Kendall S. Telephone consultation and triage: effects on health care use and patient satisfaction. Cochrane Database of Systematic Reviews 2004;3:CD004180. [DOI] [PubMed] [Google Scholar]
- Car J, Sheikh A. Telephone consultations. British Medical Journal 2003;326:966‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Car J, Freeman GK, Partridge MR, Sheikh A. Improving quality and safety of telephone based delivery of care: teaching telephone consultation skills. Quality & Safety in Health Care 2004;13:2‐3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ciesla JA, Roberts JE. Meta‐analysis of the relationship between HIV infection and risk for depressive disorders. American Journal of Psychiatry 2001;158:725‐30. [DOI] [PubMed] [Google Scholar]
- Cleary PD, Fowler FJ, Weissman J, Massagli MP, Wilson I, Seage GR, et al. Health‐related quality of life in persons with acquired immune deficiency syndrome. Medical Care 1993;31:569‐80. [DOI] [PubMed] [Google Scholar]
- Jongh T, Gurol‐Urganci I, Vodopivec‐Jamsek V, Car J, Atun R. Mobile phone messaging telemedicine for facilitating self management of long‐term illnesses (Protocol). Cochrane Database of Systematic Review. Chichester, UK: John Wiley & Sons, Ltd, 2008; Vol. 4:CD007459.
- Thomson Reuters. Endnote. Version 4. Thomson Reuters, 2009.
- Cochrane Effective Practice and Organisation of Care group. Draft EPOC methods paper: including interrupted time series (ITS) designs in a EPOC review. http://epoc.cochrane.org/sites/epoc.cochrane.org/files/uploads/inttime.pdf1998.
- Cochrane Effective Practice and Organisation of Care group. Cochrane effective practice and organisation of care review group: data collection checklist. http://epoc.cochrane.org/sites/epoc.cochrane.org/files/uploads/datacollectionchecklist.pdf2002.
- Cochrane Effective Practice and Organisation of Care group. Risk of Bias. http://epoc.cochrane.org/epoc‐resources‐review‐authors2009.
- Fishbein M. The role of theory in HIV prevention. Aids Care‐Psychological and Socio‐Medical Aspects of Aids/Hiv 2000;12:273‐8. [DOI] [PubMed] [Google Scholar]
- Foster J, Jessopp L, Dale J. Concerns and confidence of general practitioners in providing telephone consultations. British Journal of General Practice 1999;49:111‐3. [PMC free article] [PubMed] [Google Scholar]
- Hallam L. Access to general practice and general practitioners by telephone ‐ the patients view. British Journal of General Practice 1993;43:331‐5. [PMC free article] [PubMed] [Google Scholar]
- Haynes RB, Ackloo E, Sahota N, McDonald H P, Yao X. Interventions for enhancing medication adherence. Cochrane Database of Systematic Reviews 2008;2:CD00011. [DOI] [PubMed] [Google Scholar]
- Heckman TG, Heckman BD, Kochman A, Sikkema KJ, Suhr J, Goodkin K. Psychological symptoms among persons 50 years of age and older living with HIV disease. Aging & Mental Health 2002;6:121‐8. [DOI] [PubMed] [Google Scholar]
- Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.2 [updated September 2009]. The Cochrane Collaboration 2009. [Google Scholar]
- Higgins J, Green S. Cochrane Handbook for Systematic Reivews of Interventions. Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org2011.
- Horvath T, Azman H, Kennedy GE, Rutherford GW. Mobile phone text messaging for promoting adherence to antiretroviral therapy in patients with HIV infection. Cochrane Library of Systematic Reviews 2012;3:CD009756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hull S, Hagdrup N, Hart B, Griffiths C, Hennessy E. Boosting uptake of influenza immunisation: a randomised controlled trial of telephone appointing in general practice. British Journal of General Practice 2002;52:712‐6. [PMC free article] [PubMed] [Google Scholar]
- ITU‐D. The world in 2011 facts and figures. Available from http://www.itu.int/ITU‐D/ict/ 2011.
- Knobel H, Guelar A, Carmona A, Espona M, Gonzalez A, Lopez‐Colomes JL, et al. Virologic outcome and predictors of virologic failure of highly active antiretroviral therapy containing protease inhibitors. AIDS Patient Care and STDs 2001;15:193‐9. [DOI] [PubMed] [Google Scholar]
- Lattimer V, George S, Thompson F, Thomas E, Mullee M, Turnbull J, et al. Safety and effectiveness of nurse telephone consultation in out of hours primary care: randomised controlled trial. British Medical Journal 1998;317:1054‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lester RT, Gelmon L, Plummer FA. Cell phones: tightening the communication gap in resource‐limited antiretroviral programmes?. Aids 2006;20:2242‐4. [DOI] [PubMed] [Google Scholar]
- McKinstry B, Sheikh A. Unresolved questions in telephone consulting. Journal of the Royal Society of Medicine 2006;99:2‐3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohr DC, Vella L, Hart S, Heckman T, Simon G. The effect of telephone‐administered psychotherapy on symptoms of depression and attrition: a meta‐analysis. Clinical Psychology Science and Practice 2008;15:243‐53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohr DC, Siddique J, Ho J, Duffecy J, Jin L, Fokuo JK. Interest in behavioral and psychological treatments delivered face‐to‐face, by telephone, and by internet. Annals of Behavioural Medicine 2010;40(1):89‐98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mondy K, Tebas P. Cardiovascular risks of antiretroviral therapies. Annual Review of Medicine 2007;58:141‐55. [DOI] [PubMed] [Google Scholar]
- Morrison RE, Black D. Telephone medical care of patients with HIV/AIDS. AIDS Patient Care and STDs 1998;12:131‐4. [DOI] [PubMed] [Google Scholar]
- Palella FJ, Baker RK, Moorman AC, Chmiel JS, Wood KC, Brooks JT, et al. Mortality in the highly active antiretroviral therapy era ‐ Changing causes of death and disease in the HIV outpatient study. Journal of Acquired Immune Deficiency Syndromes 2006;43:27‐34. [DOI] [PubMed] [Google Scholar]
- Paterson DL, Swindells S, Mohr J, Brester M, Vergis EN, Squier C, et al. Adherence to protease inhibitor therapy and outcomes in patients with HIV infection. Annals of Internal Medicine 2000;133:21‐30. [DOI] [PubMed] [Google Scholar]
- Reynolds NR. The problem of antiretroviral adherence: a self‐regulatory model for intervention. Aids Care‐Psychological and Socio‐Medical Aspects of Aids/Hiv 2003;15:117‐24. [DOI] [PubMed] [Google Scholar]
- Reynolds NR. Adherence to antiretroviral therapies: state of the science. Current HIV Research 2004;2:207‐14. [DOI] [PubMed] [Google Scholar]
- Roffman R. Telephone‐delivered interventions for people living with HIV/AIDS: Guest editorial. Aids and Behavior 2007;11:3‐4. [DOI] [PubMed] [Google Scholar]
- Singh N, Berman SM, Swindells S, Justis JC, Mohr JA, Squier C, et al. Adherence of human immunodeficiency virus‐infected patients to antiretroviral therapy. Clinical Infectious Diseases 1999;29:824‐30. [DOI] [PubMed] [Google Scholar]
- Stead LF, Perera R, Lancaster T. Telephone counselling for smoking cessation. Cochrane Database of Systematic Reviews 2006;3:CD002850. [DOI] [PubMed] [Google Scholar]
- Stewart MA. Effective physician‐patient communication and health outcomes ‐ a review. Canadian Medical Association Journal 1995;152:1423‐33. [PMC free article] [PubMed] [Google Scholar]
- The aids2031 Consortium. AIDS: Taking a long‐term view. FT Press2011.
- Tobias CR, Cunningham W, Cabral HD, Cunningham CO, Eldred L, Naar‐King S, et al. Living with HIV but without medical care: barriers to engagement. AIDS Patient Care and STDs 2007;21:426‐34. [DOI] [PubMed] [Google Scholar]
- Tucker JA, Blum ER, Xie L, Roth DL, Simpson CA. Interactive voice response self‐monitoring to assess risk behaviours in rural substance users living with HIV/AIDS. AIDS and Behaviour 2012;16(2):432‐40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tudor Car L, Gentry S, Velthoven MH, Car J. Telephone communication of HIV testing results for improving knowledge of HIV infection status. Cochrane Database of Systematic Reviews. 2013;1:CD009192. [DOI] [PubMed] [Google Scholar]
- Ullrich A, Ott JJ, Vitoria M, Martin‐Moreno JM, Atun R. Long‐term care of AIDS and non‐communicable diseases. Lancet 2011;377(9766):639‐40. [DOI] [PubMed] [Google Scholar]
- Sighem AI, Gras LA, Reiss P, Brinkman K, Wolf F. Life expectancy of recently diagnosed asymptomatic HIV‐infected patients approaches that of uninfected individuals. AIDS (London, England) 2010;24(10):1527‐35. [PUBMED: 20467289] [DOI] [PubMed] [Google Scholar]
- Velthoven MH, Tudor Car L, Car J, Atun R. Telephone consultation for improving health of people living with or at risk of HIV: a systematic review. PLoS One 2012;7(5):e36105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Velthoven MH, Tudor Car L, Gentry S, Car J. Telephone‐delivered interventions for preventing HIV infection in HIV‐negative persons. Cochrane Database of Systematic Reviews. 2013. [DOI] [PubMed] [Google Scholar]
- Van Velthoven, M. H, Brusamento, S, Majeed, A, et al. Scope and effectiveness of mobile phone messaging for HIV/AIDS care: A systematic review. Psychol Health Med 2012 Jul 12 [Epub ahead of print]. [DOI] [PubMed]
- Volberding PA, Deeks SG. Antiretroviral therapy and management of HIV infection. The Lancet 2010;376:49‐62. [DOI] [PubMed] [Google Scholar]
- Wasson J, Gaudette C, Whaley F, Sauvigne A, Baribeau P, Welch H G. Telephone care as a substitute for routine clinic follow‐up. The Journal of the American Medical Association 1992;267:1788‐93. [PubMed] [Google Scholar]
- Whittaker R, Borland R, Bullen C, Lin RB, McRobbie H, Rodgers A. Mobile phone‐based interventions for smoking cessation. Cochrane Database of Systematic Reviews 2009;4:CD006611. [DOI] [PubMed] [Google Scholar]
- WHO. Towards universal access: scaling up priority HIV/AIDS interventions in the health sector : progress report 2009. http://www.who.int/hiv/pub/tuapr_2009_en.pdf 2009. [Google Scholar]
- WHO. Global HIV/AIDS response: epidemic update and health sector progress towards universal access: progress report 2011. Publications of the WHO are available on the WHO website (www.who.int)2011.


