Abstract
Background
Work‐related upper limb disorder (WRULD), repetitive strain injury (RSI), occupational overuse syndrome (OOS) and work‐related complaints of the arm, neck or shoulder (CANS) are the most frequently used umbrella terms for disorders that develop as a result of repetitive movements, awkward postures and impact of external forces such as those associated with operating vibrating tools. Work‐related CANS, which is the term we use in this review, severely hampers the working population.
Objectives
To assess the effects of conservative interventions for work‐related complaints of the arm, neck or shoulder (CANS) in adults on pain, function and work‐related outcomes.
Search methods
We searched the Cochrane Central Register of Controlled Trials (The Cochrane Library, 31 May 2013), MEDLINE (1950 to 31 May 2013), EMBASE (1988 to 31 May 2013), CINAHL (1982 to 31 May 2013), AMED (1985 to 31 May 2013), PsycINFO (1806 to 31 May 2013), the Physiotherapy Evidence Database (PEDro; inception to 31 May 2013) and the Occupational Therapy Systematic Evaluation of Evidence Database (OTseeker; inception to 31 May 2013). We did not apply any language restrictions.
Selection criteria
We included randomised controlled trials (RCTs) and quasi‐randomised controlled trials evaluating conservative interventions for work‐related complaints of the arm, neck or shoulder in adults. We excluded trials undertaken to test injections and surgery. We included studies that evaluated effects on pain, functional status or work ability.
Data collection and analysis
Two review authors independently selected trials for inclusion, extracted data and assessed risk of bias of the included studies. When studies were sufficiently similar, we performed statistical pooling of reported results.
Main results
We included 44 studies (62 publications) with 6,580 participants that evaluated 25 different interventions. We categorised these interventions according to their working mechanisms into exercises, ergonomics, behavioural and other interventions.
Overall, we judged 35 studies as having a high risk of bias mainly because of an unknown randomisation procedure, lack of a concealed allocation procedure, unblinded trial participants or lack of an intention‐to‐treat analysis.
We found very low‐quality evidence showing that exercises did not improve pain in comparison with no treatment (five studies, standardised mean difference (SMD) ‐0.52, 95% confidence interval (CI) ‐1.08 to 0.03), or minor intervention controls (three studies, SMD ‐0.25, 95% CI ‐0.87 to 0.37) or when provided as additional treatment (two studies, inconsistent results) at short‐term follow‐up or at long‐term follow‐up. Results were similar for recovery, disability and sick leave. Specific exercises led to increased pain at short‐term follow‐up when compared with general exercises (four studies, SMD 0.45, 95% CI 0.14 to 0.75)
We found very low‐quality evidence indicating that ergonomic interventions did not lead to a decrease in pain when compared with no intervention at short‐term follow‐up (three studies, SMD ‐0.07, 95% CI ‐0.36 to 0.22) but did decrease pain at long‐term follow‐up (four studies, SMD ‐0.76, 95% CI ‐1.35 to ‐0.16). There was no effect on disability but sick leave decreased in two studies (risk ratio (RR) 0.48, 95% CI 0.32 to 0.76). None of the ergonomic interventions was more beneficial for any outcome measures when compared with another treatment or with no treatment or with placebo.
Behavioural interventions had inconsistent effects on pain and disability, with some subgroups showing benefit and others showing no significant improvement when compared with no treatment, minor intervention controls or other behavioural interventions.
In the eight studies that evaluated various other interventions, there was no evidence of a clear beneficial effect of any of the interventions provided.
Authors' conclusions
We found very low‐quality evidence indicating that pain, recovery, disability and sick leave are similar after exercises when compared with no treatment, with minor intervention controls or with exercises provided as additional treatment to people with work‐related complaints of the arm, neck or shoulder. Low‐quality evidence also showed that ergonomic interventions did not decrease pain at short‐term follow‐up but did decrease pain at long‐term follow‐up. There was no evidence of an effect on other outcomes. For behavioural and other interventions, there was no evidence of a consistent effect on any of the outcomes.
Studies are needed that include more participants, that are clear about the diagnosis of work‐relatedness and that report findings according to current guidelines.
Keywords: Adult; Humans; Physical Therapy Modalities; Amitriptyline; Amitriptyline/therapeutic use; Analgesics, Non‐Narcotic; Analgesics, Non‐Narcotic/therapeutic use; Arm; Behavior Therapy; Behavior Therapy/methods; Cumulative Trauma Disorders; Cumulative Trauma Disorders/therapy; Ergonomics; Ergonomics/methods; Massage; Neck; Occupational Diseases; Occupational Diseases/therapy; Randomized Controlled Trials as Topic; Shoulder; Sick Leave; Sick Leave/statistics & numerical data
Plain language summary
Exercises, ergonomics and physical therapy for work‐related complaints of arm, neck or shoulder
Background
Work‐related complaints of the arm, neck or shoulder are also called repetitive strain injury or occupational overuse syndrome. They are a burden for individual workers, for their employers and for society at large because they impair functioning both in daily life and at work.
Studies included in the review
We included randomised controlled studies of all possible treatments such as exercises, ergonomic adjustments at the workplace, massage and manual therapy. These treatments aim to reduce pain and improve functioning, and they can be provided by general practitioners or physiotherapists. We excluded injections and surgical procedures that invade the body and require more special skills. We included studies only if the authors wrote that the people they studied had complaints that were work‐related. We searched electronic databases up until May 2013.
Findings
We found 44 studies that included 6,580 persons. Twenty‐one studies evaluated exercises, 13 evaluated ergonomic workplace adjustments and nine behavioural interventions. We combined the results of these studies per category. Eight other studies evaluated various other treatments.
We did not find a consistent effect of any treatment on pain, recovery, disability or sick leave. Ergonomic interventions reduced pain in the long term but not in the short term in several studies. We judged nine studies to be of high quality, but the results were very inconsistent. We found no reason for the variation in study results. Better studies are needed that are bigger, have a clearer diagnosis of work‐relatedness and comply with reporting guidelines.
Background
Description of the condition
Work‐related upper limb disorder (WRULD), repetitive strain injury (RSI), cumulative trauma disorder (CTD), occupational overuse syndrome (OOS) and work‐related complaints of the arm, neck or shoulder (CANS) are the most frequently used umbrella terms for disorders that develop as a result of repetitive movements, awkward postures and impact of external forces such as those associated with operating vibrating tools (Boocock 2009). Work‐related complaints can be divided into specific conditions with relatively clear diagnostic criteria and pathology, such as carpal tunnel syndrome, and non‐specific conditions, such as tension neck syndrome. These non‐specific conditions are primarily defined by the locations of complaints, and their pathophysiology is less clearly defined or is relatively unknown (Staal 2007).
In the USA, cumulative trauma disorders account for between 56% and 65% of all occupational injuries (Melhorn 1998; Pilligan 2000). Overall, the estimated prevalence of work‐related CANS is around 30% (Melhorn 1998), and several studies report a rapidly increasing incidence (Yassi 1997). Work‐related CANS severely hampers the working population in Western countries. Approximately one‐third of compensation costs in Australia and the USA are due to work‐related CANS (Shanahan 2006; Staal 2007). As a result, these complaints are responsible for a considerable number of lost working days. The Labour Force Survey shows that an estimated 3.8 million working days (full‐day equivalent) were lost in 2008‐2009 in the UK because of musculoskeletal disorders mainly affecting the upper limbs or neck, caused or made worse by work. On average, each affected person took an estimated 17.5 days off in that 12‐month period. This equates to an annual loss of 0.16 days per worker (HSE 2010).
The aetiology of CANS is considered to be multi‐factorial. In most people, no specific diagnosis can be made (Armstrong 1993). In addition, no pathological, neurological or radiological characteristics can be found to support the diagnosis of 'non‐specific' CANS (Staal 2007). Several personal and physical risk factors are found to be associated with CANS (Feleus 2007; Karels 2007; Roquelaure 2009), and increasing attention is being paid to its prevention and treatment (IJmker 2007; Shanahan 2006;Tulder 2007).
Description of the intervention
We defined conservative interventions as all interventions that are different from surgical interventions or injections. Types of conservative interventions that are prescribed or performed in the treatment of CANS include physiotherapy (exercises, mobilisation, electrotherapy and ultrasound), spinal manipulation, behavioural therapy and ergonomic measures or occupational therapy (e.g. working practices, splints). These interventions have in common that they are usually provided by general practitioners or physiotherapists, whereas the invasive interventions of surgery and injections require special skills and treatment facilities. Treatment may consist of a single intervention or of multiple interventions that may be provided by a member of a single discipline or members of several disciplines, as in multi‐disciplinary treatment, whereby a team involving members of different disciplines such as physiotherapists, occupational therapists and psychologists provides treatment. Ergonomic measures used in the treatment of CANS include specially designed office furniture, computer keyboards and computer mice.
How the intervention might work
Conservative interventions, such as physiotherapy and ergonomic adjustments, play a major role in the treatment of CANS (Staal 2007; Tulder 2007). The working mechanism at tissue level of most interventions is unclear. Below we describe hypothesised mechanisms. The principal aims of these treatments are to decrease pain levels and improve function through methods such as muscle relaxation and re‐education techniques, soft tissue mobilisation, cognitive interactions and workplace adjustments. Several exposures at the workplace are implied in the occupational origin of CANS, such as the use of too much force, too frequent (repetitive) movements and awkward positions. The aim of ergonomic and workplace adjustments is to influence these exposures by evaluating different sitting positions and making keyboard or mouse adjustments to prevent repetitive movements and awkward sitting postures. Physiotherapy interventions aim to (1) educate people about better sitting postures, (2) lower muscle intensity when working and (3) provide strengthening exercises to improve muscle condition and massage to relax muscles that are painful.
Why it is important to do this review
As shown above, work‐related CANS is a common disorder that has considerable impact on many individuals and society as a whole and frequently results in work loss. There is thus an imperative to find the best ways of treating people with CANS, especially so that they can return to work. Two previous Cochrane reviews on this topic found insufficient evidence to permit firm conclusions on the effectiveness of frequently applied treatment strategies (Karjalainen 2000; Verhagen 2006). However, several new studies have been published during the past few years. Therefore, there is a need to determine whether new evidence has an impact on previous results and to identify the most effective treatment strategy. Do conservative interventions have a significant impact on short‐term and long‐term outcomes? This new review, which replaces the two above‐mentioned reviews (Karjalainen 2000; Verhagen 2006), provides an update of the evidence on this topic.
Objectives
To assess the effects of conservative interventions for work‐related complaints of the arm, neck or shoulder (CANS) in adults on pain, function and work‐related outcomes.
Methods
Criteria for considering studies for this review
Types of studies
We considered for inclusion in this review all randomised controlled trials (RCTs) and quasi‐randomised controlled trials (using a method of allocating people to a treatment that is not strictly random, e.g. by date of birth or alternation). We also considered for inclusion cluster‐RCTs, wherein the unit of randomisation is a group of individuals, and cross‐over RCTs, in which participants, upon completion of one course of treatment, are switched to another.
Types of participants
We included studies that enrolled adults (18 years and older) suffering from work‐related complaints of the arm, neck or shoulder (CANS). We excluded studies in which participants had acute trauma, neoplasms or inflammatory or neurological diseases. We considered complaints to be work‐related when this was stated in the text, or when people were selected from a specific working population, such as an office, a factory or a laboratory.
Types of interventions
We considered all interventions that are not surgery or injections to be conservative interventions. We included all trials studying conservative interventions for the treatment of upper extremity work‐related disorders in adults. Conservative interventions include exercises, relaxation, biopsychosocial rehabilitation programmes, physical applications such as ultrasound, biofeedback (a method of treatment that uses monitors to provide feedback to patients on physiological information of which they are normally unaware), myofeedback (a form of biofeedback that specifically focuses on muscular activity) and workplace adjustments. These interventions can be applied within or outside the workplace, in specialised training centres or in fitness centres. Treatment providers can vary but may involve clinical professionals such as physiotherapists, occupational therapists and psychologists or fitness instructors.
We included single conservative interventions or combinations of conservative interventions versus no intervention (e.g. waiting list control) or a placebo control, or a different conservative intervention. The studied intervention could be the only treatment or an add‐on treatment. We excluded trials that tested injections and surgery.
We have set up separate comparisons for different categories of conservative interventions. We have grouped these primarily according to their working mechanisms as follows.
Exercises.
Ergonomic workplace adjustments.
Behavioural interventions.
Other interventions.
Types of outcome measures
We included studies that used the following primary outcome measures.
Primary outcomes
Functional status (e.g. Health Assessment Questionnaire (Fries 1982), Disabilities of the Arm, Shoulder and Hand Measurement Tool (DASH) (Hudak 1996)).
Pain (e.g. visual analogue scale (VAS) (Sriwatanakul 1983), West Haven‐Yale Multidimensional Pain Inventory (WHYMPI) (Kerns 1985), ordinal scale (Von Korff 2000)).
Ability to work (e.g. sickness absence (days off work), return to work, productivity loss at work, change of occupation).
Secondary outcomes
Global perceived effect (e.g. overall improvement) (Beurskens 1996).
Quality of life (e.g. Short Form 36 (SF‐36; Ware 1992), EQ‐5D (a generic measure of health status; Williams 1990), Sickness Impact Profile (de Bruin 1994)).
Healthcare consumption (e.g. physician consultations, physiotherapy, ergonomic adjustments, intake of analgesics).
Recurrence of injury, disorder or complaint.
Search methods for identification of studies
Electronic searches
For this updated version of our review, we searched the Cochrane Central Register of Controlled Trials (The Cochrane Library, 31 May 2013), MEDLINE (1950 to 31 May 2013), EMBASE (1988 to 31 May 2013), CINAHL (1982 to 31 May 2013), AMED (1985 to 31 May 2013), PsycINFO (1806 to 31 May 2013), PEDro (the Physiotherapy Evidence Database; inception to 31 May 2013) and OTseeker (the Occupational Therapy Systematic Evaluation of Evidence Database; inception to 31 May 2013). We did not apply any language restrictions.
In MEDLINE, we combined the subject‐specific strategy with the sensitivity‐ and precision‐maximising version of the Cochrane Highly Sensitive Search Strategy (Lefebvre 2009) for identifying randomised trials in MEDLINE and modified for use in other databases. Search strategies for the Cochrane Central Register of Controlled Trials, MEDLINE and EMBASE are shown in Appendix 1.
Searching other resources
We also searched reference lists of included articles and contacted experts in the field.
Data collection and analysis
Selection of studies
Three review authors (SMS, BWK and SMAB‐Z) independently selected trials by inspecting titles, keywords and abstracts to determine whether studies met the inclusion criteria regarding design, participants and interventions. Full publications of studies of any possible relevance were retrieved for final assessment. Next, the review authors independently performed a final selection of the trials to be included in the review using a standardised form. Disagreements were resolved by consensus and, if necessary, by fourth party adjudication (APV).
Data extraction and management
Two review authors (SMAB‐Z and APV) independently extracted data on trial methods, participants, settings, interventions, care providers, types of outcome measures, duration of follow‐up, loss to follow‐up and results using a standardised data extraction form from Verhagen 2006. Disagreements were resolved by consensus and, if necessary, by third party adjudication (HCWdV).
Assessment of risk of bias in included studies
Two review authors (BWK and SMS) independently assessed the risk of bias using a modified version of the assessment tool developed by The Cochrane Collaboration (Furlan 2009; Higgins 2011) (Table 1). This tool incorporates the Delphi list (Verhagen 1998), as used in previous versions of this review, and involves assessment of randomisation (sequence generation and allocation concealment), blinding (of participants, care providers and outcome assessors), completeness of outcome data, selection of outcomes reported and four other sources of bias. Disagreement was resolved by consensus or, if disagreement persisted, a third review author (APV) made the final decision.
1. Criteria for assessing risk of bias in randomised clinical trials.
| Item | Judgement |
| 1. Was the method of randomisation adequate? | Yes/No/Unsure |
| 2. Was the treatment allocation concealed? | Yes/No/Unsure |
| Was knowledge of the allocated interventions adequately prevented during the study? 3. Was the participant blinded to the intervention? 4. Was the care provider blinded to the intervention? 5. Was the outcome assessor blinded to the intervention? |
Yes/No/Unsure Yes/No/Unsure Yes/No/Unsure |
| Were incomplete outcome data adequately addressed? 6. Was the dropout rate described and acceptable? 7. Were all randomly assigned participants analysed in the group to which they were allocated? |
Yes/No/Unsure Yes/No/Unsure |
| 8. Are reports of the study free of suggestion of selective outcome reporting? | Yes/No/Unsure |
| Other sources of potential bias: 9. Were the groups similar at baseline regarding the most important prognostic indicators? 10. Were co‐interventions avoided or similar? 11. Was compliance acceptable in all groups? 12. Was the timing of the outcome assessment similar in all groups? |
Yes/No/Unsure Yes/No/Unsure Yes/No/Unsure Yes/No/Unsure |
Risk of bias was assessed using the 12 criteria above (Furlan 2009). The criteria for a judgement of 'Yes' are outlined in Appendix 2.
We derived the interobserver reliability of the risk of bias assessment by Kappa statistics. We considered Kappa values > 0.7 as showing good agreement, between 0.5 and 0.7 moderate agreement and < 0.5 poor agreement.
Measures of treatment effect
We presented the various outcome measures separately. For dichotomous data, we expressed results, if possible, as risk ratios (RRs) with corresponding 95% confidence intervals (95% CIs). For continuous data, we calculated mean differences or, when outcome measures were dissimilar, standardised mean differences (SMDs) with 95% confidence intervals (Lau 1997).
Unit of analysis issues
Most treatment was targeted to individuals. However, in some trials, treatment allocation was randomised by groups or clusters rather than individuals.
For cluster‐randomised trials that did not adjust for the cluster effect, we calculated the design effect based on the number of clusters and the number of participants and an assumed intraclass correlation (ICC) of 0.1 (Campbell 2001), as indicated in the Cochrane Handbook for Systematic Reviews of Interventions; Higgins 2011). We then used this design effect to adjust the number of participants included in the analysis.
When sufficient studies were available, we conducted a sensitivity analysis.
For cross‐over trials, we did not know what a suitable wash‐out period would be for the interventions of interest. Therefore, to avoid the carry‐over of the treatment from the first period, we restricted the analysis to the first period of the trial only. This was possible for two studies (Sjögren 2005; Ylinen 2007). One other study (Takala 1994) did not provide enough data for this analysis and we included this study as if it were a parallel group trial. We accept that this may have resulted in the underestimation of the treatment effect. The fourth cross‐over trial (Ferguson 1976) did not provide enough data to be included in the analysis.
Dealing with missing data
For dichotomous data, we performed an intention‐to‐treat analysis whereby all missing people were considered to have a bad outcome. However, for continuous data, when dropouts were identified, we used the actual number of participants contributing data at the relevant outcome assessment. Furthermore, we refrained from imputing values for standard deviations unless missing standard deviations could be derived from confidence intervals, standard errors or presented P values in the same study.
Assessment of heterogeneity
Clinicians on the review team assessed clinical heterogeneity on the basis of information on the study population (chronic vs. acute, specific vs non‐specific), interventions (exercises, massage, ergonomic interventions, etc.), control interventions (no treatment vs. active treatment), outcomes (pain, function, recovery and sick leave) and timing of follow‐up (short term: less than three months; long term: six months or longer). We assessed statistical heterogeneity between pooled trials using a combination of visual inspection of the graphs and consideration of the I2 statistic (Higgins 2011), as implemented in the forest plots in RevMan 5. We quantified the degree of heterogeneity using the I2 measure where an I2 value less than 40% indicates heterogeneity that is unimportant, 30% to 60% indicates a moderate degree of heterogeneity, values between 50% and 90% substantial heterogeneity and 75% to 100% considerable heterogeneity.
Assessment of reporting biases
We assessed publication bias by using a funnel plot.
Data synthesis
We used Review Manager (RevMan 2011) to analyse the data. We pooled studies that we judged to be similar with regard to participants, interventions, comparisons and outcomes.
We used the GRADE method as implemented in software GRADEpro (GRADEpro 2008) to evaluate the overall quality of evidence and the strength of recommendations (GRADE 2004).
The quality of the evidence for a specific outcome was based upon five domains and was downgraded by one level for each of the following factors if encountered.
Limitations in design (> 25% of participants came from studies with high risk of bias).
Inconsistency of results (significant statistical heterogeneity (I2 > 40%) or inconsistent findings among studies (≤ 75% of participants report findings in the same direction)).
Indirectness (i.e. generalisability of findings).
Imprecision (total number of participants < 300 for each outcome).
Other (e.g. publication bias, flawed design).
Two review authors (SMS, BWK) independently judged the quality of evidence for each outcome using these five factors. We considered single randomised studies (n < 300) to be inconsistent and imprecise and to provide "low quality evidence", which could be further downgraded to "very low quality evidence" if there were also limitations in design (i.e. high risk of bias), indirectness or other considerations. We rated the quality of the evidence as high, moderate, low or very low with the following implications.
High quality: Further research is very unlikely to change our confidence in the estimate of effect. Data are sufficient with narrow confidence intervals. No reporting biases are known or suspected; all domains were fulfilled.
Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate; one of the domains was not fulfilled.
Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change it; two of the domains were not fulfilled.
Very low quality: Great uncertainty surrounds the estimate; three of the domains were not fulfilled.
Subgroup analysis and investigation of heterogeneity
We performed subgroup analyses to evaluate the effects of specific work‐related CANS (e.g. a specific cause and diagnosis are established) versus non‐specific work‐related CANS, setting of treatment (work vs. outside work location), care provider (general practitioner, physiotherapist or occupational therapist), location of the complaint (neck/shoulder vs. arm) or duration of the complaint (chronic vs. (sub)acute).
Sensitivity analysis
We performed sensitivity analyses by pooling only results from studies that we considered to have a low risk of bias.
Results
Description of studies
Results of the search
We randomly allocated two out of four of the review authors (SMAB‐Z, SMS, BWK and APV) to perform the systematic search process independently. This resulted in 4,945 references after duplicates were removed. Based on title and abstract, we selected 275 references for full‐text retrieval. Of these, we finally selected 44 studies (62 publications) for inclusion in this review (Figure 1).
1.
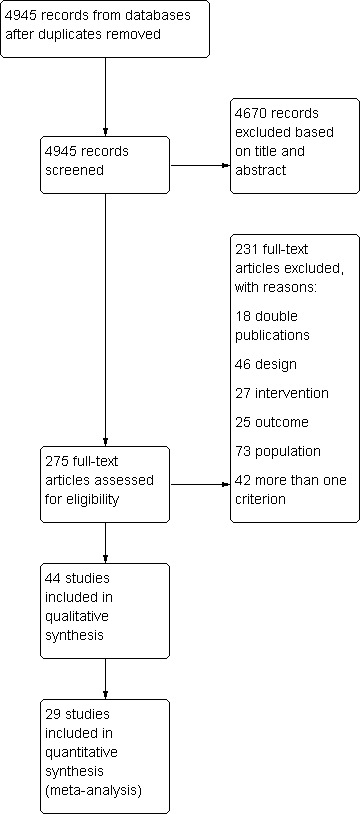
Study flow diagram.
Included studies
Study design
Of the 44 included studies, 35 studies randomly assigned participants individually to intervention or control groups. Two studies performed group randomisation (Heuvel 2003; Waling 2000), and three studies used cluster‐randomisation (Andersen 2008a; Andersen 2008b; Esmaeilzadeh 2012). Three studies used a cross‐over design (Ferguson 1976; Takala 1994; Ylinen 2007), and one study used a cross‐over design with cluster‐randomisation (Sjögren 2005). We adjusted the study outcome data for an assumed cluster effect for Heuvel 2003 and Andersen 2008b. We did not do so for Sjögren 2005 because this study used both a cluster‐randomised and a cross‐over design. For this study, we assumed that the too conservative estimate for the cross‐over design would balance the too narrow confidence intervals resulting from the cluster design. Equally, we did not adjust the data for Waling 2000 or Esmaeilzadeh 2012 because groups were clustered only on the basis of the most convenient timing for participants. We assumed that the cluster effect would be negligible here. Andersen 2008a did not provide data for meta‐analysis; therefore, we could not adjust study outcomes here. We excluded Ferguson 1976 from the analysis because these investigators did not present data from the first phase of the cross‐over trial.
Study size
One study (Abasolo 2005) was extremely large; researchers included 13 077 participants, of which 1,605 suffered from work‐related neck pain. In all other studies, the number of participants in each treatment group varied from nine to 187 (mean 108.4). In 19 of the other 43 studies, the smallest intervention group had fewer than 25 participants.
Setting
Of the 44 studies, 18 originated from the Scandinavian countries (eight from Finland alone); eight from the rest of Europe (of which five are from The Netherlands); 14 from the USA, Canada and Australia; ; two from China and two from Turkey.
Participants
In total, we included in this review data from 6,580 participants. Thirty‐three studies selected study populations such as industrial workers or hospital staff.
Thirty‐six studies included people with non‐specific neck and shoulder complaints or non‐specific upper extremity disorders. Three studies included people with work‐related carpal tunnel syndrome (Rempel 1999; Tittiranonda 1999; Werner 2005) and two rotator cuff tendinitis (Cheng 2007; Szcurko 2009), whereas shoulder impingement (Bang 2000), epicondylitis (Nourbakhsh 2008) and hand or wrist complaints (Stralka 1998) were included in one study each.
A total of 39 studies included people with chronic complaints varying in duration between three and 12 months. When people with 'prevalent complaints' were included, the mean duration of the complaints at baseline appeared to vary between three months and 11 years. Four studies involved people with recent (< six weeks) onset of complaints (Heuvel 2003; Ketola 2002; Moore 1996; Tittiranonda 1999).
Sixteen studies included only women, and one study included men only (Ferguson 1976); all other 27 studies included both men and women.
We evaluated the definition of 'work‐relatedness' in all studies. Most studies (n = 36) stated that work‐relatedness was due to including office or computer workers with musculoskeletal complaints or complaints caused by the work or by repetitive stress. Authors used statements such as "...reported a gradual onset of symptoms that were apparently work‐related", "...reported pain or complaints during work tasks", "...performed data processing tasks for 8 hours a day" or "...pain due to repetitive use or prolonged static postures".
Outcomes
Thirty‐nine studies used pain as an outcome measure, most often using a visual analogue scale (VAS) or a numerical rating scale (NRS). Eight studies used an index or composite score measure 'pain complaints', 12 studies used 'return to work' or 'sick leave' as an outcome measure and seven studies measured recovery, benefit or satisfaction. Other outcome measures included disability (by questionnaire) or strength (by dynamometer). We defined short‐term outcomes as outcomes measured within three months after randomisation, and long‐term outcomes as those measured more than three months after randomisation.
Interventions
The 44 included studies evaluated seven different types of interventions. Twenty‐five studies employed only two study arms, 14 studies had three and five studies used altogether four study arms. No studies compared a conservative treatment option versus other treatments such as oral medication, injection or surgery. Twenty‐nine studies included a control intervention such as placebo treatment (four studies: Goldman 2010; Nourbakhsh 2008Stralka 1998; Tittiranonda 1999), no treatment controls (13 studies: Dellve 2011; Esmaeilzadeh 2012; Heuvel 2003; Kamwendo 1991; Ketola 2002; Lundblad 1999; Ma 2011; Marangoni 2010; Rempel 2007; Sandsjö 2010; Sjögren 2005; Takala 1994; Viljanen 2003), a waiting list control group (four studies: Bru 1994; Moore 1996; Spence 1989; Spence 1995), a counselling or discussion control group (three studies: Andersen 2008a; Andersen 2008b; Waling 2000) or usual care controls (four studies: Abasolo 2005; Bernaards 2006; Martimo 2010; Meijer 2006).
One study did not evaluate a specific treatment but rather assessed treatment delivered by rheumatologist versus general practitioner (Abasolo 2005). All other interventions can be grouped as follows.
1. Exercises
Twenty‐one studies evaluated a form of exercise therapy including specific forms of exercises such as proprioceptive neuromuscular facilitation (PNF) (Ferguson 1976), Feldenkrais therapy (Lundblad 1999) or Mensendieck training (van Eijsden 2008). All 21 studies included participants with non‐specific neck and shoulder pain, except for one study, which included participants with rotator cuff tendinitis (Szcurko 2009).
Exercises were compared with a control group of no treatment or an intervention like counselling in 11 studies (Andersen 2008a; Andersen 2008b; Dellve 2011; Kamwendo 1991; Lundblad 1999; Ma 2011; Sjögren 2005; Takala 1994; Viljanen 2003; Waling 2000; Ylinen 2003), with other exercises in eight studies (Andersen 2008a; Andersen 2008b;Ferguson 1976; Hagberg 2000; Lundblad 1999; van Eijsden 2008; Waling 2000; Ylinen 2003), with behavioural therapy in three studies (Dellve 2011; Ma 2011; Viljanen 2003), with massage in two studies (Ferguson 1976; Levoska 1993) and with manual therapy (Ylinen 2007) and neuropathic care (Szcurko 2009) in one study each. Exercise was evaluated as an add‐on treatment to ergonomic instructions in two studies (Bernaards 2006; Omer 2003) and in addition to breaks during computer work in one study (Heuvel 2003). One study (Vasseljen 1995) compared physical therapy provided individually with group physical therapy, with both including exercises given at the workplace.
2. Ergonomics
Various ergonomic strategies were evaluated in 13 studies and can be regarded as two different strategies: work hardening strategies (Bernaards 2006; Cheng 2007; Ketola 2002; Lundblad 1999) and strategies related to workplace computer or keyboard use (Esmaeilzadeh 2012; Heuvel 2003; Kamwendo 1991; Marangoni 2010; Martimo 2010; Rempel 1999; Rempel 2007; Ripat 2006; Tittiranonda 1999). Three studies included participants with specific complaints such as rotator cuff tendinitis (Cheng 2007) or carpal tunnel syndrome (Rempel 1999; Tittiranonda 1999).
Eight studies compared ergonomic programmes versus a no treatment control group (Bernaards 2006; Esmaeilzadeh 2012; Heuvel 2003; Ketola 2002; Lundblad 1999; Marangoni 2010; Martimo 2010; Rempel 2007) and one versus placebo (Tittiranonda 1999). Five studies compared various ergonomic interventions versus each other (Ketola 2002; Marangoni 2010; Rempel 1999; Rempel 2007; Ripat 2006), and in two studies, ergonomic changes at the workplace were an add‐on treatment to exercises (Cheng 2007; Kamwendo 1991). One study compared both intensive ergonomic guidance and education in ergonomics (Ketola 2002) and an ergonomic programme versus an exercise group (Lundblad 1999).
3. Behavioural treatment
Nine studies evaluated a form of behavioural strategy, all in participants with non‐specific neck and shoulder pain (Bru 1994; Dellve 2011; Ma 2011; Moore 1996; Sandsjö 2010; Spence 1989; Spence 1995; Viljanen 2003; Voerman 2007). One other study evaluated a multi‐disciplinary treatment, including physical exercises and relaxation treatment, compared with usual care (Meijer 2006).
Four studies compared relaxation therapy, cognitive strategies or bio/myofeedback versus a waiting list control (Bru 1994; Moore 1996; Spence 1989; Spence 1995), two studies used a no‐treatment control group (Dellve 2011; Ma 2011) and another two studies compared with usual care (Sandsjö 2010; Viljanen 2003). One study evaluated a behavioural strategy as an add‐on treatment to ergonomic counselling (Voerman 2007).
4. Massage
Three studies evaluated massage as a part of the treatment compared with exercises in two studies (Ferguson 1976; Levoska 1993) and with additional treatment to spinal manipulative therapy in one study (Leboeuf 1987).
5. Electrical therapy
Two studies evaluated a splint. One study compared an energised splint versus placebo in participants with hand and wrist problems (Stralka 1998), and another study evaluated the use of a splint as add‐on treatment to video education in participants with carpal tunnel syndrome (Werner 2005). One study evaluated low‐frequency electrical stimulation versus placebo in participants with epicondylitis (Nourbakhsh 2008).
6. Manual therapy
Two studies evaluated a form of manual therapy (Bang 2000; Ylinen 2007). One study compared manual therapy versus exercises (Ylinen 2007), and another study evaluated manual therapy as an additional treatment to exercise in participants with shoulder impingement syndrome (Bang 2000).
7. Medication
One study compared amitriptyline, that is, pain medication, versus placebo in participants with non‐specific neck and shoulder pain (Goldman 2010).
Excluded studies
Most of the excluded studies did not differentiate between participants with a musculoskeletal disorder and those without. They included healthy workers, as well as workers with neck pain, without separate reporting of results. This means that both prevention and treatment were evaluated in the studies (Figure 1).
Risk of bias in included studies
Results of the risk of bias assessment are presented in the Characteristics of included studies table and in Figure 2.
2.
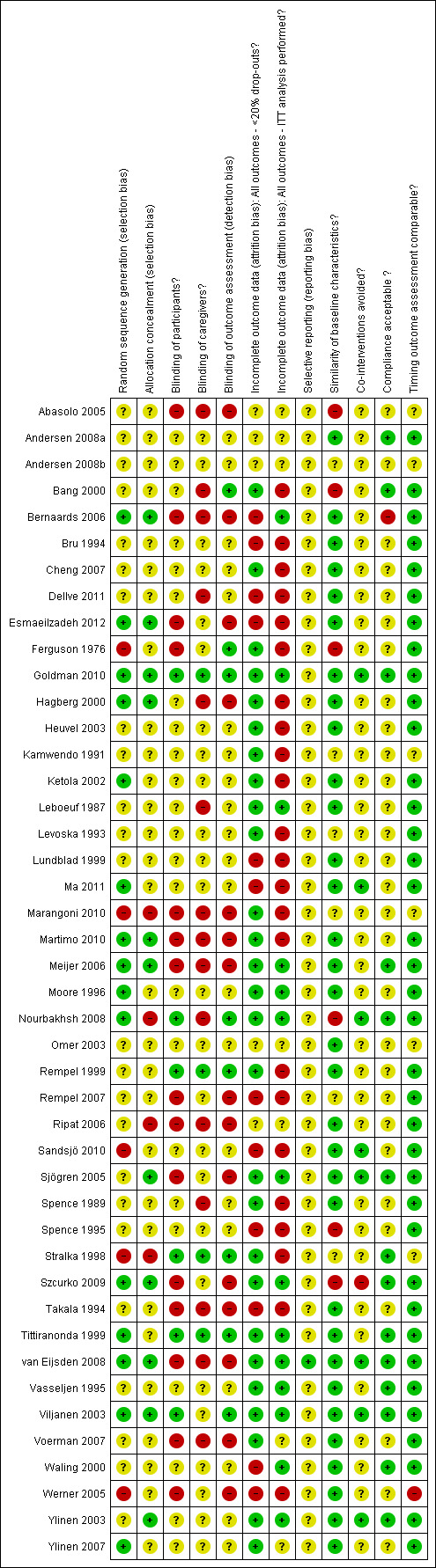
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Initially, there was agreement between both review authors of 83.5% (Kappa = 0.64), meaning a moderate level of agreement. The third review author made the final decision for 16 items.
Overall the amount of non‐information (i.e. items that scored unclear risk of bias) varied between 11.4% (dropout rate described) and 97.7% (selective outcome reporting). The items that scored high on risk of bias were intention‐to‐treat analysis (52.3%), dropout rate described and adequate (27.3%), non‐blinded participants (34.1%) and caregivers (34.1%) and outcome assessment (34.1%). See Figure 3.
3.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
Based on our criterion of low risk of bias, "an overall sum score 50 per cent or more of the maximum score", nine studies could be categorised as having low risk of bias (Meijer 2006; Nourbakhsh 2008; Rempel 1999; Stralka 1998; Szcurko 2009; Tittiranonda 1999; van Eijsden 2008; Viljanen 2003; Ylinen 2003). We consider these studies to have low risk of bias in our GRADE analysis, meaning that they do not downgrade the level of evidence because of the design.
Allocation
Twenty‐two studies provided no information on the randomisation procedure (Figure 2). We judged four studies to have an inadequate randomisation procedure (item 1) (Ferguson 1976; Marangoni 2010; Sandsjö 2010; Werner 2005).
We judged 11 studies to have described an adequate procedure for concealing allocation (item 2) (Bernaards 2006; Esmaeilzadeh 2012; Goldman 2010; Hagberg 2000; Meijer 2006; Sjögren 2005; Szcurko 2009; Tittiranonda 1999; van Eijsden 2008; Viljanen 2003; Ylinen 2003) and judged five studies to have done it inadequately (Marangoni 2010; Martimo 2010; Nourbakhsh 2008; Ripat 2006; Stralka 1998). The remaining 28 studies did not describe how or whether they concealed their randomisation procedure.
Blinding
Eight studies described blinding of outcome assessment (Bang 2000; Ferguson 1976; Goldman 2010; Nourbakhsh 2008; Rempel 1999; Stralka 1998; Tittiranonda 1999; Viljanen 2003), in six studies participants were blinded (Goldman 2010; Nourbakhsh 2008; Rempel 1999; Stralka 1998; Tittiranonda 1999; Viljanen 2003) and in four studies the care provider was blinded (Goldman 2010; Rempel 1999; Stralka 1998; Tittiranonda 1999).
Incomplete outcome data
We judged 23 (52.3%) of the included studies to have a high risk of bias, as they clearly did not perform an intention‐to‐treat (ITT) analysis. Only 14 (32.5%) of the included studies performed an ITT analysis or presented complete data. The dropout rate was described and acceptable, that is, was less than 20%, in 26 (59.1%) of the studies.
Selective reporting
We could retrieve a study protocol for only one study (van Eijsden 2008). Hence this was the only study that we scored as having a low risk of bias due to selective outcome presentation. We judged all remaining studies to have an unclear risk of bias due to selective reporting.
Other potential sources of bias
We assessed four other sources of bias: baseline imbalance, whether co‐interventions were avoided or similar, whether compliance was acceptable and whether timing was comparable. We judged 29 studies (65.9%) to have a low risk of bias as the result of no baseline imbalance, although in nine studies, baseline similarity was unclear.
Only five studies reported that co‐interventions were avoided or similar (Ma 2011; Nourbakhsh 2008; Sandsjö 2010; Viljanen 2003; Ylinen 2003), and two were considered to have a high risk of bias concerning co‐interventions (Andersen 2008b; Szcurko 2009). Seventeen studies reported acceptable compliance rates. Thirty‐seven studies reported comparable timing of outcome assessment. Only one study (Werner 2005) clearly reported that the 12‐month outcome assessment varied between seven and 15 months.
Effects of interventions
In total, 29 studies presented dichotomous data or point estimates and measures of variability for their primary outcomes. According to our judgement, studies overall had low power and high risk of bias. Therefore the quality of evidence varied between low and very low.
Pain
Exercise versus no treatment controls
Ten studies presented short‐term results on pain. Overall we found that exercise did not reduce pain when compared with no treatment or discussion controls, or when given as additional treatment (Analysis 1.1). Five studies (Dellve 2011; Ma 2011; Sjögren 2005; Takala 1994; Viljanen 2003) compared exercise versus no treatment and found no difference in pain (SMD ‐0.52, 95% CI ‐1.08 to 0.03). All studies concerned participants with chronic non‐specific complaints.
1.1. Analysis.
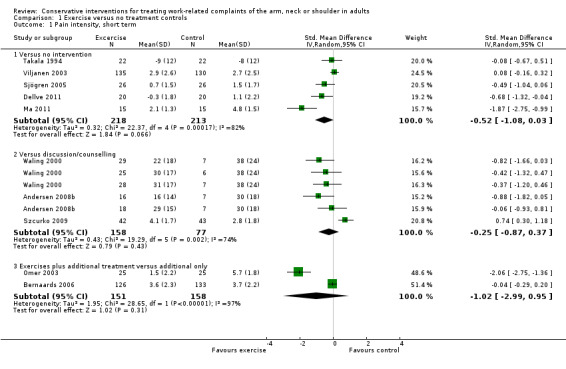
Comparison 1 Exercise versus no treatment controls, Outcome 1 Pain intensity, short term.
In a sensitivity analysis, we omitted all studies that we judged to have a high risk of bias (Dellve 2011; Ma 2011; Sjögren 2005; Takala 1994) and still found no differences between groups. According to four studies (Andersen 2008a; Andersen 2008b; Szcurko 2009; Waling 2000), exercise did not reduce pain any more than participating in a discussion group.
In a subgroup analysis of participants with specific complaints, one study (Szcurko 2009), which was the only study judged to have a low risk of bias, showed that participation in a discussion control group reduced pain more than exercise (mean difference (MD) 0.74, 95% CI 0.30 to 1.18). We found no differences in pain in the subgroup of chronic non‐specific complaints.
Two studies (Bernaards 2006; Omer 2003) compared exercise as an addition to work style education versus education alone and found conflicting results: One study (Omer 2003) reported significant benefit associated with additional exercises, and the other study (Bernaards 2006) found no differences.
Overall, this comparison suffered from major heterogeneity (I2 varied between 55% and 97%). This could be explained by clinical differences in the intervention or the population, although almost all participants had chronic non‐specific complaints, or by the fact that most studies in this comparison were judged to have a high risk of bias.
We conclude that for pain, very low‐quality evidence (downgraded by limitations of design, imprecision and inconsistency) that exercises lead to similar levels of pain as no treatment at both short‐term and long‐term follow‐up.
We also assessed publication bias for this comparison. The funnel plot (Figure 4) shows that small studies with negative effects are missing in the right lower quadrant, which indicates possible publication bias.
4.
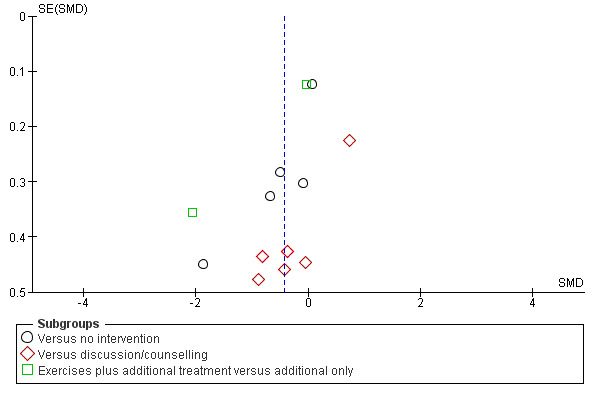
Funnel plot of comparison: 1 Exercise versus no treatment controls, outcome: 1.1 Pain intensity, short term.
Exercise versus active treatment controls
According to four studies (Andersen 2008b; van Eijsden 2008; Vasseljen 1995; Waling 2000), overall regular exercises reduce pain in the short term more than specific exercises (SMD 0.45, 95% CI 0.14 to 0.75) (Analysis 2.1). All four studies included participants with chronic non‐specific complaints.
2.1. Analysis.
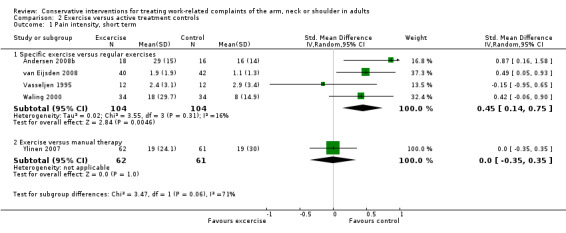
Comparison 2 Exercise versus active treatment controls, Outcome 1 Pain intensity, short term.
In a sensitivity analysis from which we omitted the studies we judged to have a high risk of bias (Andersen 2008b; Vasseljen 1995; Waling 2000), results showed that regular exercises reduce pain more than specific exercises. According to two studies (van Eijsden 2008; Ylinen 2003), both with a low risk of bias, regular exercise leads to less pain in the short term than specific exercises (MD 0.80, 95% CI 0.09 to 1.51) (van Eijsden 2008) but not in the long term (pooled SMD 0.10, 95% CI ‐0.18 to 0.38). One study (Ylinen 2007) compared exercises versus manual therapy and found no difference in short‐term pain (MD 0.00, 95% CI ‐9.63 to 9.63).
We conclude that for pain, low‐quality evidence (downgraded by limitations of design and imprecision) suggests a benefit of regular exercises over specific exercises at short‐term follow‐up only.
Ergonomic intervention versus no treatment controls
Five studies (Bernaards 2006; Cheng 2007; Ketola 2002; Martimo 2010; Tittiranonda 1999) compared ergonomic interventions versus placebo or no treatment or as an additional treatment for short‐term pain (Analysis 3.1). One study (Tittiranonda 1999) evaluated various keyboards versus placebo in participants with carpal tunnel syndrome (CTS) and found a reduction in pain with the placebo keyboard (SMD 0.53, 95% CI 0.01 to 1.04). Three studies (Bernaards 2006; Ketola 2002; Martimo 2010) compared ergonomic interventions versus no treatment in participants with non‐specific complaints and found no differences between the groups (SMD ‐0.07, 95% CI ‐0.36 to 0.22), although this analysis suffered from moderate heterogeneity (I2 = 49%). One study (Cheng 2007) compared ergonomic interventions on their own and when given in addition to exercises in participants with rotator cuff pain and found that the combination reduced pain more than ergonomic interventions on their own (SMD ‐0.60, 95% CI ‐1.01 to ‐0.18).
3.1. Analysis.
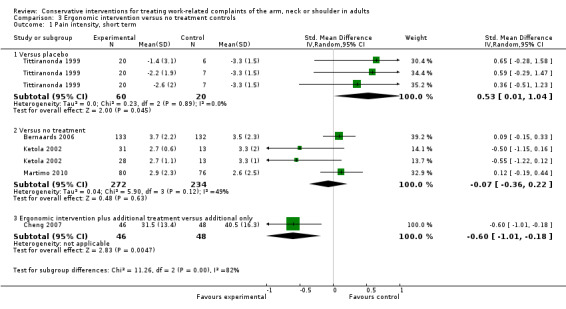
Comparison 3 Ergonomic intervention versus no treatment controls, Outcome 1 Pain intensity, short term.
Subgroup analysis of the study by Ketola 2002 involving subacute participants only showed pain to decrease more with ergonomic interventions than with no treatment (SMD ‐0.52, 95% CI ‐0.99 to ‐0.05), while the two studies with chronic complaints (Bernaards 2006; Martimo 2010) reported no difference (SMD 0.10, 95% CI ‐0.09 to 0.29).
Four studies (Bernaards 2006; Esmaeilzadeh 2012; Ketola 2002; Lundblad 1999) compared ergonomic interventions versus no treatment in reducing pain over the long term and found a significant difference in favour of the ergonomic intervention (SMD ‐0.76, 95% CI ‐1.35 to ‐0.16). However, this analysis (Analysis 3.2) exhibited large heterogeneity (I2 = 84%).
3.2. Analysis.
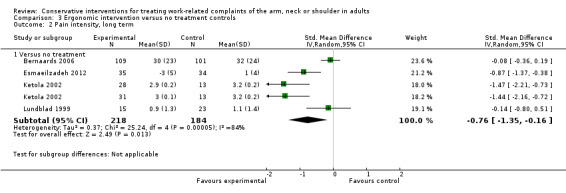
Comparison 3 Ergonomic intervention versus no treatment controls, Outcome 2 Pain intensity, long term.
We conclude that very low‐quality evidence (downgraded by limitations of design, imprecision and inconsistency) indicates that ergonomic interventions lead to similar results as no treatment in reducing pain in the short term. For the long term, very low‐quality evidence (downgraded by limitations of design, imprecision and inconsistency) shows a small benefit of ergonomic interventions when compared with no treatment.
In subgroups of subacute participants and in the subgroup of participants with specific complaints, we found a very low level of evidence (downgraded by limitations of design, imprecision and inconsistency) for ergonomic interventions reducing pain more than placebo, or when given as additional interventions to exercises.
Ergonomic intervention versus active treatment controls
One study (Rempel 1999) evaluated an experimental keyboard versus the standard one for reducing pain in the short term in participants with CTS. Another study (Tittiranonda 1999) evaluated three different keyboards versus placebo, also for reducing pain in the short term. One study (Ketola 2002) evaluated both short‐term and long‐term pain reduction with intensive versus standard ergonomic training in participants with recent non‐specific complaints, and another study evaluated reduction in pain over the long term due to ergonomic interventions versus regular exercises in participants with chronic non‐specific complaints (Lundblad 1999). Overall, we found no differences in pain between the groups in the short term (SMD 0.11, 95% CI ‐0.24 to 0.46) (Analysis 4.1) or over the long term (SMD ‐0.02, 95% CI ‐1.22 to 1.18) (Analysis 4.2).
4.1. Analysis.
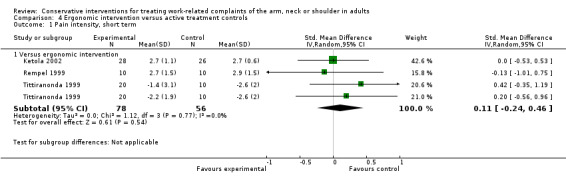
Comparison 4 Ergonomic intervention versus active treatment controls, Outcome 1 Pain intensity, short term.
4.2. Analysis.
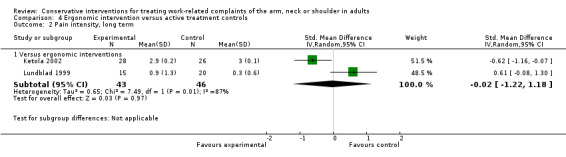
Comparison 4 Ergonomic intervention versus active treatment controls, Outcome 2 Pain intensity, long term.
We found very low‐quality evidence overall (downgraded by limitations of design, imprecision and inconsistency) showing that various ergonomic interventions lead to similar pain levels in the short term and over the long term.
Behavioural intervention versus no treatment controls
Four studies (Dellve 2011; Ma 2011; Sandsjö 2010; Viljanen 2003) evaluated a behavioural intervention versus no treatment and found no difference in pain (SMD ‐0.67, 95% CI ‐1.49 to 0.16) (Analysis 5.1; Analysis 5.2). Three studies (Moore 1996; Spence 1989; Spence 1995) compared a behavioural intervention versus a waiting list control group, all including participants with chronic non‐specific complaints, and found that the intervention reduced pain in the short term (SMD ‐0.74, 95% CI ‐1.32 to ‐0.15).
5.1. Analysis.
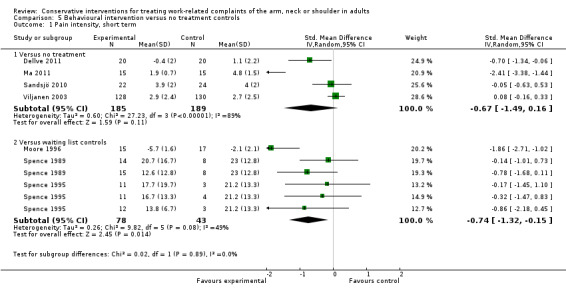
Comparison 5 Behavioural intervention versus no treatment controls, Outcome 1 Pain intensity, short term.
5.2. Analysis.
Comparison 5 Behavioural intervention versus no treatment controls, Outcome 2 Pain, short term.
In a sensitivity analysis we omitted the studies we judged to have a high or unclear risk of bias and only one remained (Viljanen 2003). This study reported no difference in pain intensity in the short term (SMD 0.08, 95% CI ‐0.16 to 0.33) or over the long term (SMD ‐0.04, 95% CI ‐0.28 to 0.20).
Meta‐analyses of behavioural interventions versus no treatment or a waiting list control suffered from moderate to large heterogeneity (I2 varied between 49% and 97%). We could not explain this by differences in participants, as all studies concerned participants with chronic non‐specific complaints. The only explanation left is low methodological rigour as we deemed that all but one of the studies (Viljanen 2003) to have a high risk of bias.
We conclude that very low‐quality evidence (downgraded by limitations of design, imprecision and inconsistency) indicates that behavioural intervention leads to similar pain levels at short term and over the long term as no treatment.
Behavioural intervention versus active treatment controls
Two studies (Spence 1989; Spence 1995) evaluated various behavioural interventions versus regular treatment and found no differences between the groups in terms of pain (SMD ‐0.23, 95% CI ‐0.73 to 0.27) (Analysis 6.1; Analysis 6.4). We judged all three studies to have a high risk of bias, and all included participants with chronic non‐specific complaints. Three studies (Dellve 2011; Ma 2011; Viljanen 2003) evaluated behavioural interventions versus exercises and found no differences in pain in the short term (SMD ‐0.02, 95% CI ‐0.24 to 0.19). Sensitivity analysis on the one study with low risk of bias (Viljanen 2003) also found no differences between groups in the short term (SMD 0.00, 95% CI ‐0.24 to 0.24) or over the long term (SMD 0.08, 95% CI ‐0.16 to 0.32).
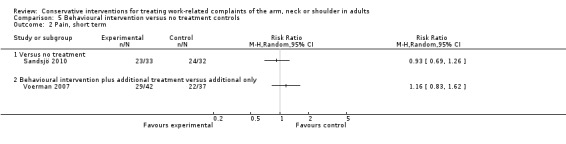
6.1. Analysis.
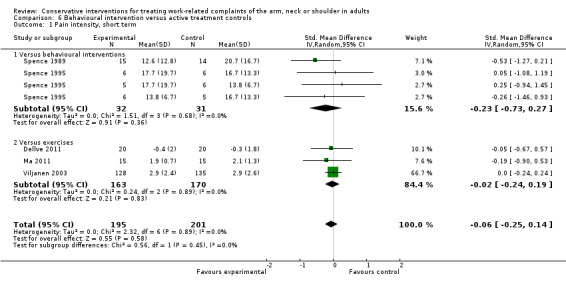
Comparison 6 Behavioural intervention versus active treatment controls, Outcome 1 Pain intensity, short term.
6.4. Analysis.
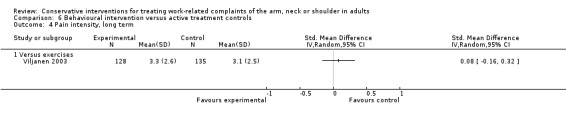
Comparison 6 Behavioural intervention versus active treatment controls, Outcome 4 Pain intensity, long term.
We conclude that very low‐quality evidence (downgraded by limitations of design, imprecision and inconsistency) indicates that various behavioural interventions lead to similar results in reducing pain in the short term and over the long term.
Disability
Exercise versus no treatment controls
Three studies (Ma 2011; Lundblad 1999; Viljanen 2003) evaluated exercise versus no treatment. When we pooled study results, we found no differences in disability between study groups at short‐term (SMD ‐0.77, 95% CI ‐2.50 to 0.97) or long‐term follow‐up (SMD 0.14, 95% CI ‐0.08 to 0.34; Analysis 1.3; Analysis 1.4; Analysis 1.5).
1.3. Analysis.
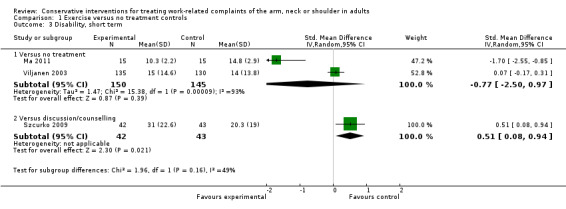
Comparison 1 Exercise versus no treatment controls, Outcome 3 Disability, short term.
1.4. Analysis.
Comparison 1 Exercise versus no treatment controls, Outcome 4 Disability, short term.
1.5. Analysis.
Comparison 1 Exercise versus no treatment controls, Outcome 5 Disability, long term.
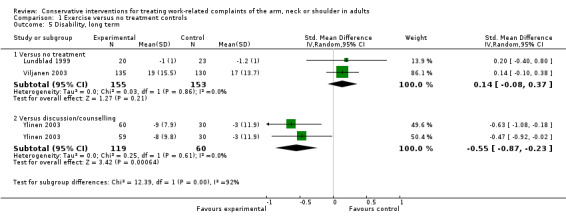
Exercise was compared with discussion in two studies (Szcurko 2009; Ylinen 2003). Szcurko 2009 found that discussion relieved disability better than exercise in the short term (SMD 0.51, 95% CI 0.08 to 0.94), whereas exercise produced better results in the long term in the study by Ylinen 2003 (SMD ‐0.55, 95% CI ‐0.87 to ‐0.23; Analysis 1.3; Analysis 1.5). Heterogeneity varied between 0 and 93%, and we could explain this by risk of bias or subgroups.
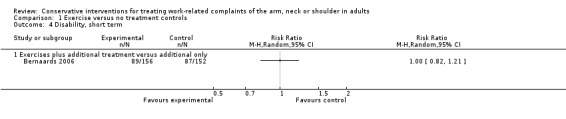
One study (Bernaards 2006), which we judged to have a high risk of bias, compared exercises only with exercises in addition to work style education. This study found no differences in disability (risk ratio (RR) 1.00, 95% CI 0.82 to 1.21; Analysis 1.4).
We conclude that very low‐quality evidence (downgraded by limitations of design, imprecision and inconsistency) indicates that exercises lead to similar levels of disability as no treatment both in the short term and over the long term.
Exercise versus active treatment controls
One study each compared the effects of different types of exercise (van Eijsden 2008) and exercise with manual therapy (Ylinen 2007) on disability in the short term. Neither study found a significant difference in disability in the short term: van Eijsden 2008—MD 2.00, 95% CI ‐2.18 to 6.18; Ylinen 2007—MD 1.00, 95% CI ‐2.20 to 4.20; Analysis 2.3.
2.3. Analysis.
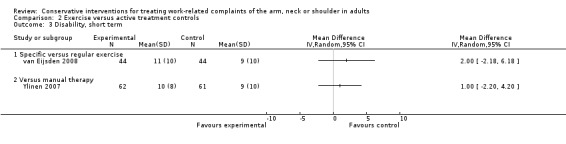
Comparison 2 Exercise versus active treatment controls, Outcome 3 Disability, short term.
Two studies compared the effects of different types of exercise (van Eijsden 2008; Ylinen 2003) on disability in the long term. No difference in disability was noted between exercises and other exercises in the long term in these two studies (SMD 0.11, 95% CI ‐0.17 to 0.38; Analysis 2.4).
2.4. Analysis.
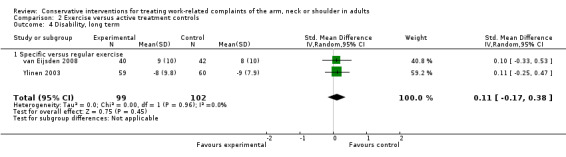
Comparison 2 Exercise versus active treatment controls, Outcome 4 Disability, long term.
We conclude that very low‐quality evidence (downgraded by limitations of design, imprecision and inconsistency) shows that exercises lead to similar levels of disability as other exercises or manual therapy both in the short term and over the long term.
Ergonomic intervention versus no treatment controls
One study (Tittiranonda 1999) evaluated various keyboards versus placebo in participants with carpal tunnel syndrome (CTS) and found that participants using the placebo keyboard felt less disabled (MD 0.93, 95% CI 0.28 to 1.57; Analysis 3.3).
3.3. Analysis.
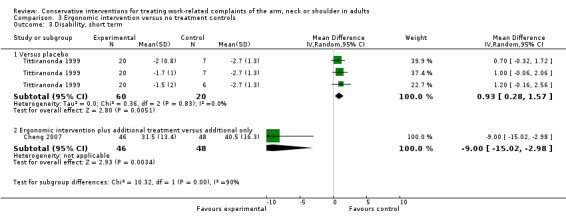
Comparison 3 Ergonomic intervention versus no treatment controls, Outcome 3 Disability, short term.
Three studies (Bernaards 2006; Esmaeilzadeh 2012; Lundblad 1999) evaluated ergonomic interventions in chronic non‐specific participants versus no treatment and found no differences in disability at long‐term follow‐up (RR 0.98, 95% CI 0.85 to 1.14; SMD ‐0.33, 95% CI ‐0.71 to 0.06; Analysis 3.4; Analysis 3.5).
3.4. Analysis.
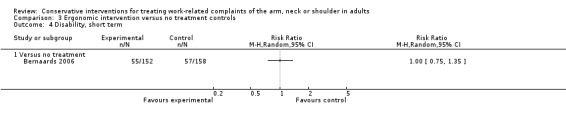
Comparison 3 Ergonomic intervention versus no treatment controls, Outcome 4 Disability, short term.
3.5. Analysis.
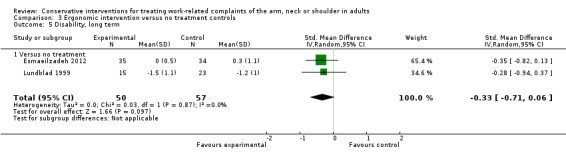
Comparison 3 Ergonomic intervention versus no treatment controls, Outcome 5 Disability, long term.
One study (Cheng 2007) found that ergonomic interventions and exercise decreased disability more than exercise alone in participants with rotator cuff pain (MD ‐9.00, 95% CI ‐15.02 to ‐2.98).
We conclude that very low‐quality evidence (downgraded by limitations of design, imprecision and inconsistency) shows that ergonomic interventions lead to similar levels of disability as no treatment both in the short term and over the long term.
Behavioural intervention versus no treatment controls
Two studies (Ma 2011; Viljanen 2003) compared behavioural interventions versus no treatment in reducing disability in the short term. Pooling their results led to such a large degree of heterogeneity (I2 = 96%) that meta‐analysis was not meaningful (Analysis 5.3). Another two studies (Spence 1989; Spence 1995) evaluated five different behavioural interventions versus a waiting list control group. When pooled together, the behavioural interventions appeared to decrease disability in the short term (SMD ‐0.58, 95% CI ‐1.05 to ‐0.12; Analysis 5.3).
5.3. Analysis.
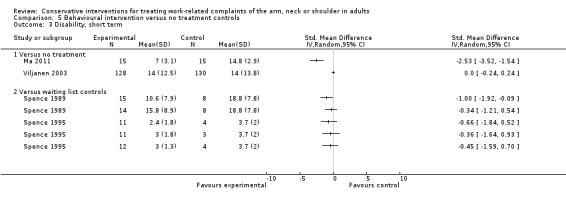
Comparison 5 Behavioural intervention versus no treatment controls, Outcome 3 Disability, short term.
We conclude that very low‐quality evidence (downgraded by limitations of design, imprecision and inconsistency) shows that in the short term behavioural interventions lead to similar levels of disability as no treatment. Furthermore, we conclude that very‐low quality evidence (downgraded by limitations of design, imprecision and inconsistency) suggests that behavioural interventions decrease disability in the short term more than being in a waiting list control group.
Behavioural intervention versus active treatment controls
Three studies (Ma 2011; Dellve 2011; Viljanen 2003) compared behavioural interventions and exercises in reducing disability or, conversely, in improving work ability in the short term. There was no difference between the groups in disability (SMD ‐0.57, 95% CI ‐1.66 to 0.52; Analysis 6.2) or in work ability (SMD ‐0.15, 95% CI ‐0.84 to 0.54; Analysis 6.3). One study (Viljanen 2003) also measured long‐term effects on disability and work ability and found no differences between behavioural interventions and exercises: disability—MD 0.00, 95% CI ‐3.65 to 3.65; Analysis 6.5; work ability—MD 0.20, 95% CI ‐0.09 to 0.49; Analysis 6.6.
6.2. Analysis.
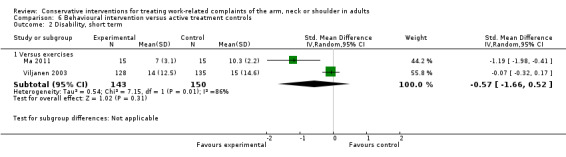
Comparison 6 Behavioural intervention versus active treatment controls, Outcome 2 Disability, short term.
6.3. Analysis.
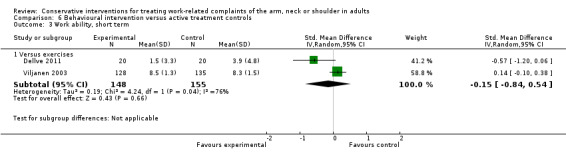
Comparison 6 Behavioural intervention versus active treatment controls, Outcome 3 Work ability, short term.
6.5. Analysis.
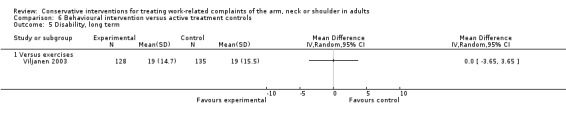
Comparison 6 Behavioural intervention versus active treatment controls, Outcome 5 Disability, long term.
6.6. Analysis.
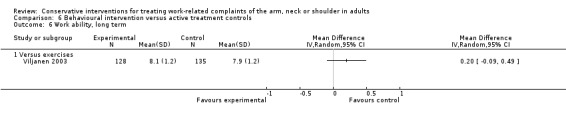
Comparison 6 Behavioural intervention versus active treatment controls, Outcome 6 Work ability, long term.
We conclude that very low‐quality evidence (downgraded by limitations of design, imprecision and inconsistency) shows that in the short term behavioural interventions lead to similar levels of disability as exercises.
Recovery
Exercise versus no treatment controls
Three studies, all with participants with chronic non‐specific complaints (Bernaards 2006; Heuvel 2003; Waling 2000), compared exercise with no treatment (Waling 2000) versus exercise additional to work style education (Bernaards 2006) and with computer breaks (Heuvel 2003) on short‐term recovery. We pooled the results of three different exercise interventions compared with no treatment in Waling 2000 and found that exercise improves recovery (RR 0.53, 95% CI 0.37 to 0.78; Analysis 1.6). In contrast, exercises conducted as additional treatment did not seem to improve recovery more than regular exercise in the two studies by Bernaards 2006 and Heuvel 2003 (RR 1.25, 95% CI 0.18 to 1.93; Analysis 1.7). We judged all three studies to have a high risk of bias. Ferguson 1976 did not find a significant effect on recovery, but the study could not be included in the meta‐analysis.
1.6. Analysis.
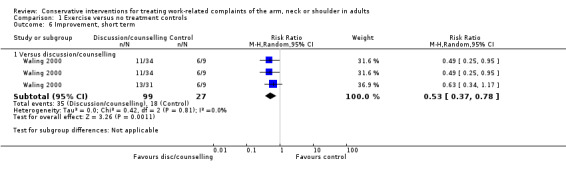
Comparison 1 Exercise versus no treatment controls, Outcome 6 Improvement, short term.
1.7. Analysis.
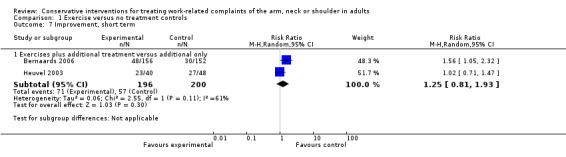
Comparison 1 Exercise versus no treatment controls, Outcome 7 Improvement, short term.
We conclude that very low‐quality evidence (downgraded by limitations of design, imprecision and inconsistency) suggests that in the short term exercises improve recovery more than no treatment, but there is no additional benefit on recovery if exercises are administered together with computer breaks or work style education.
Exercise versus active treatment controls
Three studies (van Eijsden 2008; Vasseljen 1995; Waling 2000) compared the effects of different types of exercise on recovery in the short term. One study (Levoska 1993) compared the recovery‐improving effects of exercise and massage, and another study (Ylinen 2007) compared exercise with manual therapy. There were no differences in effectiveness between different forms of exercise (RR 0.86, 95% CI 0.43 to 1.71; Analysis 2.5) or between exercises and massage (RR 0.78, 95% CI 0.55 to 1.11). Only manual therapy appeared to improve recovery more than exercises in one study (Ylinen 2007), which we judged to have a high risk of bias (RR 1.88, 95% CI 1.29 to 2.74; Analysis 2.5).
2.5. Analysis.
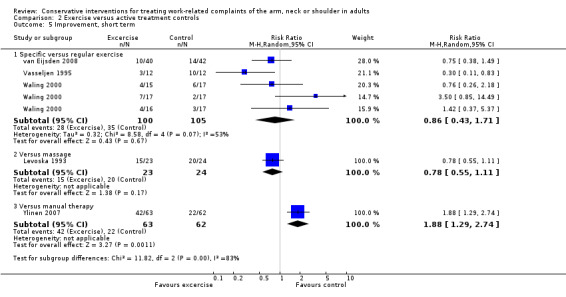
Comparison 2 Exercise versus active treatment controls, Outcome 5 Improvement, short term.
We conclude that very low‐quality evidence (downgraded by limitations of design, imprecision and inconsistency) shows no differences between different forms of exercise or between exercise and massage in recovery in the short term. Manual therapy may be more effective than exercise based on only one study with a high risk of bias.
Ergonomic intervention versus no treatment controls
One study (Tittiranonda 1999) compared the effects of different keyboards on recovery in the short term in participants with carpal tunnel syndrome (CTS). Recovery was better with participants who used a placebo keyboard (RR 1.89, 95% CI 0.85 to 4.21; Analysis 3.7). Another study (Bernaards 2006) compared an ergonomic intervention with no treatment in participants with chronic non‐specific complaints. Participants recovered better in the ergonomic intervention group when measured at short‐term (RR 0.88, 95% CI 0.78 to 0.99; Analysis 3.7) and at long‐term follow‐up (RR 0.90, 95% CI 0.81 to 1.00; Analysis 3.8).
3.7. Analysis.
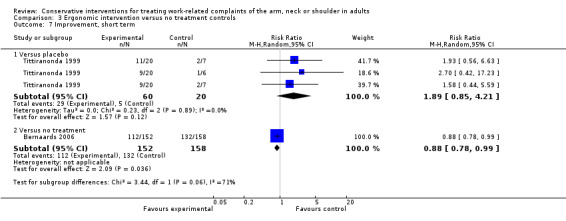
Comparison 3 Ergonomic intervention versus no treatment controls, Outcome 7 Improvement, short term.
3.8. Analysis.
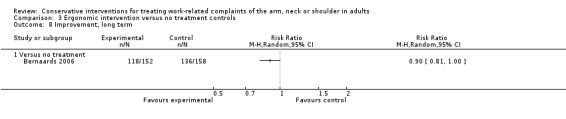
Comparison 3 Ergonomic intervention versus no treatment controls, Outcome 8 Improvement, long term.
We conclude that very low‐quality evidence (downgraded by limitations of design, imprecision and inconsistency) shows that both in the short term and over the long term ergonomic interventions improve recovery more than no treatment.
Sick leave
Exercise versus no treatment controls
Two studies (Lundblad 1999; Viljanen 2003) evaluated the effects of exercise versus no treatment on sick leave in the long term. We found no differences between groups (SMD ‐0.03, 95% CI ‐0.26 to 0.19; Analysis 1.8). We judged one of the two studies (Viljanen 2003) to have a low risk of bias.
1.8. Analysis.
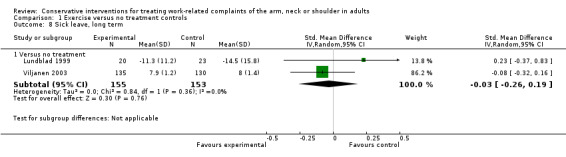
Comparison 1 Exercise versus no treatment controls, Outcome 8 Sick leave, long term.
We conclude that moderate‐quality evidence (downgraded by imprecision) shows no difference between exercise and no treatment on sick leave over the long term.
Ergonomic intervention versus no treatment controls
Two studies (Heuvel 2003; Martimo 2010) compared the effects of ergonomic interventions and no treatment on sick leave at short term and found no difference (RR 0.49, 95% CI 0.32 to 0.76; Analysis 3.9).
3.9. Analysis.
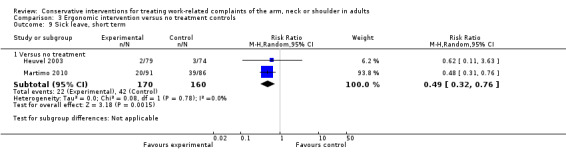
Comparison 3 Ergonomic intervention versus no treatment controls, Outcome 9 Sick leave, short term.
We conclude that low‐quality evidence (downgraded by limitations of design and imprecision) shows that in the short term ergonomic interventions lead to similar effects on sick leave as no treatment.
Behavioural intervention versus no treatment controls
Three studies (Dellve 2011; Sandsjö 2010; Viljanen 2003) compared the effects of behavioural interventions and no treatment on sick leave at short term. When we pooled the results of Dellve 2011 and Viljanen 2003, we found no differences (SMD 0.02, 95% CI ‐0.21 to 0.24; Analysis 5.5), nor did Sandsjö 2010 (RR 1.05, 95% CI 0.79 to 1.41; Analysis 5.6).
5.5. Analysis.
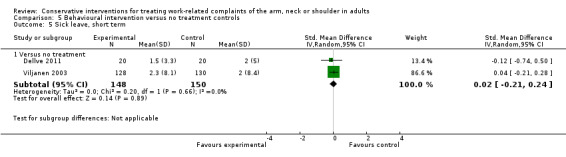
Comparison 5 Behavioural intervention versus no treatment controls, Outcome 5 Sick leave, short term.
5.6. Analysis.
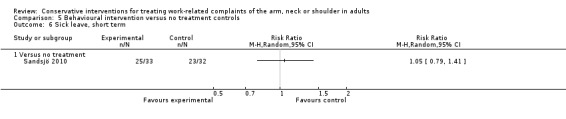
Comparison 5 Behavioural intervention versus no treatment controls, Outcome 6 Sick leave, short term.
We conclude that moderate‐quality evidence (downgraded by imprecision) shows that in the short term behavioural interventions lead to similar effects on sick leave as no treatment.
Nine of the remaining included studies (Abasolo 2005; Andersen 2008a; Bru 1994; Hagberg 2000; Kamwendo 1991; Marangoni 2010; Rempel 2007; Ripat 2006; Stralka 1998) did not provide data and therefore are not included in the comparisons above.
Other interventions
Behavioural interventions
One other study (Meijer 2006) evaluated a multi‐disciplinary treatment including physical exercises and relaxation treatment compared with usual care and found a statistically non‐significant benefit in favour of the multi‐disciplinary treatment (SMD ‐2.2, 95% CI ‐3.08 to 1.32) for pain at short term.
Massage
One study (Levoska 1993) compared the recovery‐improving effects of exercise and massage and found no differences in effectiveness between exercise and massage (RR 0.78, 95% CI 0.55 to 1.11; Analysis 2.5). Another study (Leboeuf 1987) evaluated manual therapy compared with manual therapy plus massage and found the combination reducing symptom severity more than manual therapy alone (RD 0.4, 95% CI 0.11 to 0.69).
Electrical therapy
One study evaluated the use of a splint as add‐on treatment to video education in participants with carpal tunnel syndrome (Werner 2005) and found no benefit of the additional splint for symptom severity score at short term (SMD ‐0,31, 95% CI ‐0.62 to 0). Another study evaluated low‐frequency electrical stimulation versus placebo in participants with epicondylitis (Nourbakhsh 2008) and found significant short‐term pain relief associated with the electrical stimulation (SMD ‐1.27, 95% CI ‐2,32 to ‐0.23).
Manual therapy
One study (Bang 2000) compared exercise versus exercise and manual therapy in participants with an impingement syndrome (shoulder pain). Investigators found significant pain reduction and disability reduction (SMD 0.8, 95% CI 0.2 to 1.4 for pain; SMD 0.8, 95% CI 0.2 to 11.3 for disability) for exercise plus manual therapy at short term. Another study (Ylinen 2007) compared exercise versus manual therapy and found no difference (SMD 0, 95% CI ‐0.35 to 0.35) in pain at short‐term follow‐up.
Medication
One study compared amitriptyline, that is, pain medication, versus placebo in participants with non‐specific neck and shoulder pain (Goldman 2010) and found no differences between the two groups in terms of pain at short‐term follow‐up (SMD 0.06, 95% CI ‐0.31 to 0.42).
Discussion
Summary of main results
In total, we included 44 studies and 6,580 participants in this review. The studies had an overall high risk of bias. We judged only nine studies to have a low risk of bias.
Overall we found no clear benefit of exercise over no treatment or discussion controls or as additional treatment for pain, disability or sick leave. In participants with chronic non‐specific complaints, regular exercises relieve pain more in the short‐term when compared with specific exercises. We found no differences in disability or recovery.
The placebo keyboard seems to be more effective than experimental keyboards in reducing pain and disability and improving recovery. Ergonomic interventions reduced pain at long term, but not at short term. Also, ergonomic interventions seem to reduce pain but not disability in subacute participants and in participants with rotator cuff syndrome, when compared with no treatment. None of the ergonomic interventions provided greater benefit compared with another, or compared with placebo, on any of the outcome measures.
Overall, behavioural interventions did not show benefit when compared with no treatment, waiting list controls or other behavioural interventions, except for short‐term pain when compared with waiting list controls.
Overall completeness and applicability of evidence
The aim of this review was to summarise existing evidence concerning the efficacy of frequently performed interventions in work‐related neck, arm or shoulder musculoskeletal disorders (CANS). We applied a broad search strategy aimed at finding all trials that included people suffering from work‐related CANS. No specific search strategy can be used to select participants with work‐related complaints, mostly because defining which disorders are work‐related appears to be rather difficult. Therefore, two independent review authors checked a large number of references.
Quality of the evidence
We considered only nine of the included studies to have low risk of bias. Most studies (n = 22) lacked information on the randomisation procedure and the analysis. Furthermore, blinding was difficult in these pragmatic studies.
Heterogeneity is another problem. We included several main groups of interventions, of which exercise was the largest. Each of these intervention groups consisted of a large variety of interventions and outcome measures. Although we were able to include 44 trials, it is disappointing that we could present so little evidence on the effects of interventions for CANS. In part, this is a result of the many different interventions available and the presentation of both short‐term and long‐term results, and it also reflects the overall high risk of bias. We found hardly any clinical heterogeneity in the study populations selected for inclusion in the original trials. Most studies included participants with chronic non‐specific neck or shoulder complaints. CANS is mostly divided into specific and non‐specific disorders, and the latter appear to constitute the larger group. This review contributes especially to the body of knowledge on non‐specific work‐related disorders.
Furthermore, 19 studies had small sample sizes (fewer than 25 participants in the smallest treatment arm). Although sample size does not contribute to the assessment of study risk of bias, it does show that most studies included in this review were underpowered to provide clear answers.
Potential biases in the review process
One of the possible biases of this review is selection bias. The most important difficulties include lack of a definition of work‐relatedness, the wide variety of interventions used to treat people with possible CANS and the overall poor methodological quality. There is no clear definition of the work‐relatedness of complaints. In the included trials, we noticed that defining the study population in this regard appeared to be difficult and subjective. Therefore, we might have missed studies that could have been included in this review.
The inconsistency in study results can also be due to our categorisation of studies into broad intervention categories. Even though we did our best to make the comparisons as homogeneous as possible, considerable variation is evident in intervention intensity and compliance. For example, Takala 1994 provided low‐intensity exercises and Szcurko 2009 high‐intensity training. However, a few studies (Ma 2011; Omer 2003) were clear outliers with exceptionally beneficial results that we could not explain by intervention intensity or compliance. The same argument holds for the category of ergonomic studies, which included a variety of interventions. Here too, we could find no proper explanation for the variable results. Heterogeneity could also have been the result of combining studies on all parts of the upper limb, neck and shoulder, but this did not explain the most pronounced differences in results.
Agreements and disagreements with other studies or reviews
The relevance of this systematic review in contributing to the body of knowledge concerning the efficacy of interventions in non‐specific work‐related CANS lies mainly in the fact that it points out a clear lack of evidence regarding the effectiveness of the interventions most often prescribed.
Although this version of the review includes 21 additional trials in comparison with the previous version (Verhagen 2006), the main conclusion of not finding clear evidence for the effectiveness of any treatment still holds. Some results of this updated review are slightly different compared with findings of the previous review. Our conclusion is in line with that of a large systematic review on the benefit of exercise for people with neck pain (Smidt 2005).
Authors' conclusions
Implications for practice.
This review concludes that low‐ to very low‐quality evidence indicates that exercise does not provide a clear benefit over no treatment or discussion controls or as additional treatment for pain, disability or sick leave for people with work‐related complaints of the arm, neck or shoulder. Specific exercises are less effective than regular ones. We also found low‐quality evidence suggesting that ergonomic interventions in the workplace and behavioural interventions lead to similar results to those obtained with no or alternative interventions.
Implications for research.
In this review, we evaluated a working population with a complaint. This complaint is not necessarily work‐related. We need an agreed upon definition of what can be considered a work‐related disorder. When consensus is reached, a clear participant population can be selected for future studies.
Future research should examine clear and well‐defined interventions and especially should compare the intervention versus a no treatment control group.
Larger and adequately powered trials are needed that will focus on appropriate allocation concealment; blinding, if possible, of participant and therapist, or keeping them naive; and adequate data presentation and analysis.
Acknowledgements
We thank Helen Handoll, Co‐ordinating Editor of the Bone, Joint and Muscle Trauma Review Group, and Jos Verbeek, Co‐ordinating Editor of the Cochrane Occupational Safety and Health Review Group, for their valuable comments and advice. We also thank Lesley Gillespie for her help with the search strategies, and Joanne Elliott, Lindsey Elstub and Amy Kavanagh for their help and comments about the protocol. We thank Jani Ruotsalainen, Managing Editor of the Cochrane Occupational Safety and Health Review Group, for his extensive comments on and editing of the review text. Finally, we thank Dolores Matthews for copy editing the text.
Appendices
Appendix 1. Search strategies
The Cochrane Central Register of Controlled Trials (Wiley InterScience interface)
#1 MeSH descriptor Cumulative Trauma Disorders explode all trees #2 MeSH descriptor Occupational Diseases, this term only #3 MeSH descriptor Hand‐Arm Vibration Syndrome, this term only #4 MeSH descriptor Occupational Health, this term only #5 ((occupational overuse or tension neck) NEXT syndrome):ti,ab #6 (cumulative trauma*):ti,ab #7 (work related):ti,ab #8 (repetit* NEXT (strain or stress or industr* or motion or movement or trauma)):ti,ab #9 (vibration NEXT (induced or related or syndrome*)):ti,ab #10 (#1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8 OR #9) #11 MeSH descriptor Neck Pain, this term only #12 MeSH descriptor Shoulder Pain, this term only #13 MeSH descriptor Hand Injuries explode all trees #14 MeSH descriptor Wrist Injuries, this term only #15 MeSH descriptor Musculoskeletal Diseases, this term only #16 (neck* or shoulder* or arm* or upper limb* or upper extremit* or elbow* or forearm* or wrist* or hand* or finger*):ti,ab #17 (carpal tunnel syndrome*):ti,ab #18 (#11 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17) #19 (#10 AND #18)
MEDLINE (Ovid interface)
1. exp Cumulative Trauma Disorders/ 2. Occupational Diseases/ or Hand‐Arm Vibration Syndrome/ 3. Occupational Health/ 4. ((occupational overuse or tension neck) adj syndrome).tw. 5. cumulative trauma$.tw. 6. work related.tw. 7. (repetit$ adj (strain or stress or industr$ or motion or movement or trauma)).tw. 8. (vibration adj (induced or related or syndrome$)).tw. 9. or/1‐8 10. Neck Pain/ or Shoulder Pain/ or exp Hand Injuries/ or Wrist Injuries/ 11. Musculoskeletal Diseases/ 12. (neck$1 or shoulder$1 or arm$1 or upper limb$1 or upper extremit$ or elbow$1 or forearm$1 or wrist$1 or hand$1 or finger$1).tw. 13. Carpal Tunnel Syndrome/ or carpal tunnel syndrome$.tw. 14. or/10‐13 15. and/9,14 16. Randomized Controlled Trial.pt. 17. Controlled Clinical Trial.pt. 18. randomized.ab. 19. placebo.ab. 20. Clinical Trials as Topic/ 21. randomly.ab. 22. trial.ti. 23. or/16‐22 24. exp animals/ not humans/ 25. 23 not 24 26. and/15,25
EMBASE (Elsevier)
('Cumulative Trauma Disorder'/exp OR ('Occupational Disease':de OR 'Hand Arm Vibration Syndrome':de) OR 'Occupational Health':de OR (('occupational overuse' OR 'tension neck') NEAR/1 syndrome*):ti,ab,de OR (cumulative NEAR/1 trauma*):ti,ab,de OR 'work related':ti,ab,de OR (repetitive NEAR/1 (strain* OR stress* OR industr* OR motion* OR movement* OR trauma*)):ti,ab,de OR (vibration NEAR/1 (induced OR related OR syndrome*)):ti,ab,de) AND ('Neck Pain':de OR 'Shoulder Pain':de OR 'Hand Injury':de OR 'Wrist Injury':de OR 'Musculoskeletal Disease':de OR neck:ti,ab,de OR shoulder:ti,ab,de OR arm:ti,ab,de OR 'upper limb':ti,ab,de OR (upper NEAR/1 extremit*):ti,ab,de OR elbow*:ti,ab,de OR forearm:ti,ab,de OR wrist:ti,ab,de OR hand:ti,ab,de OR finger:ti,ab,de OR thumb:ti,ab,de OR necks:ti,ab,de OR shoulders:ti,ab,de OR arms:ti,ab,de OR 'upper limbs':ti,ab,de OR elbow*s:ti,ab,de OR forearms:ti,ab,de OR wrists:ti,ab,de OR hands:ti,ab,de OR fingers:ti,ab,de OR thumbs:ti,ab,de OR ('carpal tunnel' NEAR/1 syndrome*):ti,ab,de) AND ('randomized controlled trial'/de OR 'controlled clinical trial'/de OR random*:ti,ab OR placebo:ti,ab OR 'clinical trial'/de OR trial:ti) NOT ('animal'/exp NOT 'human'/exp)
Appendix 2. Criteria for a judgement of 'Yes' for the sources of risk of bias (see Table 1)
1. Was the method of randomisation adequate?
A random (unpredictable) assignment sequence. Examples of adequate methods are coin toss (for studies with two groups), rolling of a dice (for studies with two or more groups), drawing of balls of different colours, drawing of ballots with the study group labels from a dark bag, computer‐generated random sequence, pre‐ordered sealed envelopes, sequentially ordered vials, telephone call to a central office and pre‐ordered list of treatment assignments.
Examples of inadequate methods include alternation, birth date, social insurance/security number, date on which they are invited to participate in the study and hospital registration number.
2. Was the treatment allocation concealed?
Assignment was generated by an independent person not responsible for determining the eligibility of patients. This person has no information about the persons included in the trial and has no influence on the assignment sequence or on the decision about eligibility of the patient.
Was knowledge of the allocated interventions adequately prevented during the study?
3. Was the participant blinded to the intervention?
This item should be scored 'Yes' if index and control groups were indistinguishable for the participants, or if the success of blinding was tested among the participants and it was successful.
4. Was the care provider blinded to the intervention?
This item should be scored 'Yes' if index and control groups were indistinguishable for the care providers, or if the success of blinding was tested among the care providers and it was successful.
5. Was the outcome assessor blinded to the intervention?
Adequacy of blinding should be assessed for the primary outcomes. This item should be scored 'Yes' if the success of blinding was tested among the outcome assessors and it was successful, or:
For participant‐reported outcomes for which the participant is the outcome assessor (e.g. pain, disability): The blinding procedure is adequate for outcome assessors if participant blinding is scored 'Yes'.
For outcome criteria assessed during scheduled visit and that suppose a contact between participants and outcome assessors (e.g. clinical examination): The blinding procedure is adequate if participants are blinded, and if the treatment or adverse effects of the treatment cannot be noticed during clinical examination.
For outcome criteria that do not suppose a contact with participants (e.g. radiography, magnetic resonance imaging): The blinding procedure is adequate if the treatment or adverse effects of the treatment cannot be noticed when the main outcome is assessed.
For outcome criteria that are clinical or therapeutic events that will be determined by the interaction between participants and care providers (e.g. co‐interventions, hospitalisation length, treatment failure), in which the care provider is the outcome assessor: The blinding procedure is adequate for outcome assessors if item 'E' is scored 'Yes'.
For outcome criteria that are assessed from data extracted from the medical forms: The blinding procedure is adequate if the treatment or adverse effects of the treatment cannot be noticed in the extracted data.
Were incomplete outcome data adequately addressed?
6. Was the dropout rate described and acceptable?
The number of participants included in the study but who did not complete the observation period or were not included in the analysis must be described and reasons given. If the percentage of withdrawals and dropouts does not exceed 20% for short‐term follow‐up and 30% for long‐term follow‐up and does not lead to substantial bias, a 'Yes' is scored. (N.B. These percentages are arbitrary, not supported by literature.)
7. Were all randomly assigned participants analysed in the group to which they were allocated?
All randomly assigned participants are reported/analysed in the group to which they were allocated by randomisation for the most important moments of effect measurement (minus missing values), irrespective of non‐compliance and co‐interventions.
8. Are reports of the study free of suggestion of selective outcome reporting?
To receive a ‘Yes’, the review author determines whether all results from all prespecified outcomes have been adequately reported in the published report of the trial. This information is obtained by comparing the protocol and the report or, in the absence of the protocol, by assessing that the published report includes enough information to make this judgement.
Other sources of potential bias
9. Were the groups similar at baseline regarding the most important prognostic indicators?
To receive a 'Yes', groups have to be similar at baseline regarding demographic factors, duration and severity of complaints, percentage of participants with neurological symptoms and value of main outcome measure(s).
10. Were co‐interventions avoided or similar?
This item should be scored 'Yes' if there were no co‐interventions, or if they were similar between index and control groups.
11. Was the compliance acceptable in all groups?
The review author determines whether compliance with the interventions is acceptable, based on reported intensity, duration, number and frequency of sessions for both the index intervention and control intervention(s). For example, physiotherapy treatment is usually administered over several sessions; therefore, it is necessary to assess how many sessions each participant attended. For single‐session interventions (e.g. surgery), this item is irrelevant.
12. Was the timing of the outcome assessment similar in all groups?
Timing of outcome assessment should be identical for all intervention groups and for all important outcome assessments.
Note: These instructions are adapted fromFurlan 2009and the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011).
Data and analyses
Comparison 1. Exercise versus no treatment controls.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pain intensity, short term | 10 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 Versus no intervention | 5 | 431 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.52 [‐1.08, 0.03] |
| 1.2 Versus discussion/counselling | 3 | 235 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.25 [‐0.87, 0.37] |
| 1.3 Exercises plus additional treatment versus additional only | 2 | 309 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.02 [‐2.99, 0.95] |
| 2 Pain intensity, long term | 4 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 Versus no treatment | 2 | 308 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.31 [‐0.96, 0.33] |
| 2.2 Versus discussion/counselling | 2 | 305 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.07 [‐0.68, 0.54] |
| 3 Disability, short term | 3 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.1 Versus no treatment | 2 | 295 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.77 [‐2.50, 0.97] |
| 3.2 Versus discussion/counselling | 1 | 85 | Std. Mean Difference (IV, Random, 95% CI) | 0.51 [0.08, 0.94] |
| 4 Disability, short term | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 4.1 Exercises plus additional treatment versus additional only | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Disability, long term | 3 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 5.1 Versus no treatment | 2 | 308 | Std. Mean Difference (IV, Random, 95% CI) | 0.14 [‐0.08, 0.37] |
| 5.2 Versus discussion/counselling | 1 | 179 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.55 [‐0.87, ‐0.23] |
| 6 Improvement, short term | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 6.1 Versus discussion/counselling | 1 | 126 | Risk Ratio (M‐H, Random, 95% CI) | 0.53 [0.37, 0.78] |
| 7 Improvement, short term | 2 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 7.1 Exercises plus additional treatment versus additional only | 2 | 396 | Risk Ratio (M‐H, Random, 95% CI) | 1.25 [0.81, 1.93] |
| 8 Sick leave, long term | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 8.1 Versus no treatment | 2 | 308 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.03 [‐0.26, 0.19] |
1.2. Analysis.
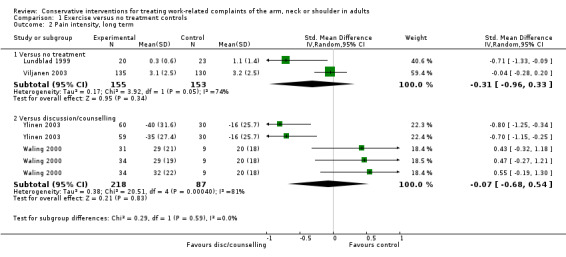
Comparison 1 Exercise versus no treatment controls, Outcome 2 Pain intensity, long term.
Comparison 2. Exercise versus active treatment controls.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pain intensity, short term | 5 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 Specific exercise versus regular exercises | 4 | 208 | Std. Mean Difference (IV, Random, 95% CI) | 0.45 [0.14, 0.75] |
| 1.2 Exercise versus manual therapy | 1 | 123 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [‐0.35, 0.35] |
| 2 Pain intensity, long term | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 Specific versus regular exercise | 2 | 201 | Std. Mean Difference (IV, Random, 95% CI) | 0.10 [‐0.18, 0.38] |
| 3 Disability, short term | 2 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 3.1 Specific versus regular exercise | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Versus manual therapy | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Disability, long term | 2 | 201 | Std. Mean Difference (IV, Random, 95% CI) | 0.11 [‐0.17, 0.38] |
| 4.1 Specific versus regular exercise | 2 | 201 | Std. Mean Difference (IV, Random, 95% CI) | 0.11 [‐0.17, 0.38] |
| 5 Improvement, short term | 5 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 5.1 Specific versus regular exercise | 3 | 205 | Risk Ratio (M‐H, Random, 95% CI) | 0.86 [0.43, 1.71] |
| 5.2 Versus massage | 1 | 47 | Risk Ratio (M‐H, Random, 95% CI) | 0.78 [0.55, 1.11] |
| 5.3 Versus manual therapy | 1 | 125 | Risk Ratio (M‐H, Random, 95% CI) | 1.88 [1.29, 2.74] |
2.2. Analysis.
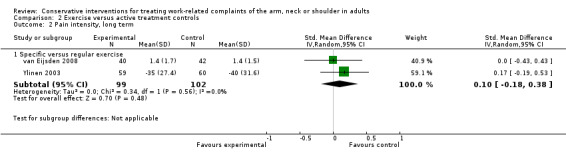
Comparison 2 Exercise versus active treatment controls, Outcome 2 Pain intensity, long term.
Comparison 3. Ergonomic intervention versus no treatment controls.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pain intensity, short term | 5 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 Versus placebo | 1 | 80 | Std. Mean Difference (IV, Random, 95% CI) | 0.53 [0.01, 1.04] |
| 1.2 Versus no treatment | 3 | 506 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.07 [‐0.36, 0.22] |
| 1.3 Ergonomic intervention plus additional treatment versus additional only | 1 | 94 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.60 [‐1.01, ‐0.18] |
| 2 Pain intensity, long term | 4 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 Versus no treatment | 4 | 402 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.76 [‐1.35, ‐0.16] |
| 3 Disability, short term | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.1 Versus placebo | 1 | 80 | Mean Difference (IV, Random, 95% CI) | 0.93 [0.28, 1.57] |
| 3.2 Ergonomic intervention plus additional treatment versus additional only | 1 | 94 | Mean Difference (IV, Random, 95% CI) | ‐9.0 [‐15.02, ‐2.98] |
| 4 Disability, short term | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 4.1 Versus no treatment | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Disability, long term | 2 | 107 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.33 [‐0.71, 0.06] |
| 5.1 Versus no treatment | 2 | 107 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.33 [‐0.71, 0.06] |
| 6 Disability, long term | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 6.1 Versus no treatment | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Improvement, short term | 2 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 7.1 Versus placebo | 1 | 80 | Risk Ratio (M‐H, Random, 95% CI) | 1.89 [0.85, 4.21] |
| 7.2 Versus no treatment | 1 | 310 | Risk Ratio (M‐H, Random, 95% CI) | 0.88 [0.78, 0.99] |
| 8 Improvement, long term | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 8.1 Versus no treatment | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 9 Sick leave, short term | 2 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 9.1 Versus no treatment | 2 | 330 | Risk Ratio (M‐H, Random, 95% CI) | 0.49 [0.32, 0.76] |
3.6. Analysis.
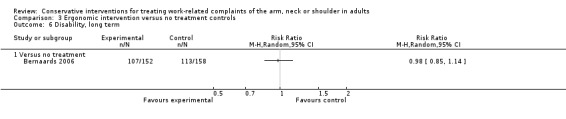
Comparison 3 Ergonomic intervention versus no treatment controls, Outcome 6 Disability, long term.
Comparison 4. Ergonomic intervention versus active treatment controls.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pain intensity, short term | 3 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 Versus ergonomic intervention | 3 | 134 | Std. Mean Difference (IV, Random, 95% CI) | 0.11 [‐0.24, 0.46] |
| 2 Pain intensity, long term | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 Versus ergonomic interventions | 2 | 89 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.02 [‐1.22, 1.18] |
Comparison 5. Behavioural intervention versus no treatment controls.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pain intensity, short term | 7 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 Versus no treatment | 4 | 374 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.67 [‐1.49, 0.16] |
| 1.2 Versus waiting list controls | 3 | 121 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.74 [‐1.32, ‐0.15] |
| 2 Pain, short term | 2 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2.1 Versus no treatment | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Behavioural intervention plus additional treatment versus additional only | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Disability, short term | 4 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 3.1 Versus no treatment | 2 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Versus waiting list controls | 2 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Disability, short term | 2 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 4.1 Versus no treatment | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 Behavioural intervention plus additional treatment versus additional only | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Sick leave, short term | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 5.1 Versus no treatment | 2 | 298 | Std. Mean Difference (IV, Random, 95% CI) | 0.02 [‐0.21, 0.24] |
| 6 Sick leave, short term | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 6.1 Versus no treatment | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Pain, long term | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 7.1 Versus no treatment | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8 Disability, long term | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 8.1 Versus no treatment | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
5.4. Analysis.
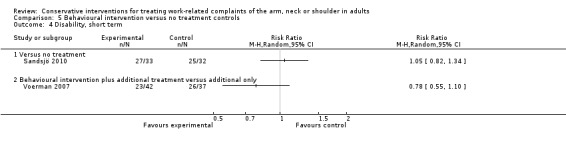
Comparison 5 Behavioural intervention versus no treatment controls, Outcome 4 Disability, short term.
5.7. Analysis.
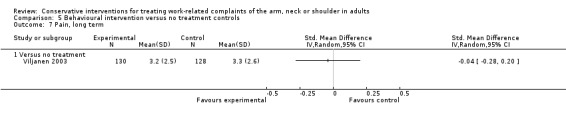
Comparison 5 Behavioural intervention versus no treatment controls, Outcome 7 Pain, long term.
5.8. Analysis.
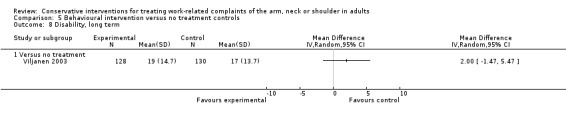
Comparison 5 Behavioural intervention versus no treatment controls, Outcome 8 Disability, long term.
Comparison 6. Behavioural intervention versus active treatment controls.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pain intensity, short term | 5 | 396 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.06 [‐0.25, 0.14] |
| 1.1 Versus behavioural interventions | 2 | 63 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.23 [‐0.73, 0.27] |
| 1.2 Versus exercises | 3 | 333 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.02 [‐0.24, 0.19] |
| 2 Disability, short term | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 Versus exercises | 2 | 293 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.57 [‐1.66, 0.52] |
| 3 Work ability, short term | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.1 Versus exercises | 2 | 303 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.15 [‐0.84, 0.54] |
| 4 Pain intensity, long term | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.1 Versus exercises | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Disability, long term | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5.1 Versus exercises | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Work ability, long term | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6.1 Versus exercises | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Abasolo 2005.
| Methods | RCT: method of randomisation unclear. Intervention: control ratios of 1:1 in district seven and 2:3 in districts four and nine | |
| Participants | All workers from three health districts who began sick leave with a diagnosis of an MSD during the study period (1998 to 2001) were included Sick leave episodes secondary to trauma, surgery or work accidents were excluded |
|
| Interventions |
Intervention: Rheumatologists acted as principal care providers in regular visits Interventions included education, pharmacological and non‐pharmacological treatments and timing of diagnostic tests in a stepwise manner. Participants were seen as often as necessary (n = 5,272) Control: Standard care was that provided by primary care physicians, with weekly administrative duties plus basic diagnostic and therapeutic procedures without prespecified protocols (n = 7,805) |
|
| Outcomes | Efficacy was defined as the difference between the intervention group and the control group in the number of days on sick leave per temporary work disability episode | |
| Notes | No separate data for CANS | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Unclear randomisation procedure |
| Allocation concealment (selection bias) | Unclear risk | Unclear whether allocation was concealed |
| Blinding of participants? | High risk | No participant blinding |
| Blinding of caregivers? | High risk | Caregivers not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Not told who compiled the outcome data |
| Incomplete outcome data (attrition bias) All outcomes ‐ <20% drop‐outs? | Unclear risk | Not clear from this paper how many dropouts: 62.8% attended the programme, but was this post randomisation? |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis performed? | Unclear risk | Unclear: "Data was analyzed on an intent to treat basis", but no numbers were given in the paper |
| Selective reporting (reporting bias) | Unclear risk | Unclear whether selective outcome was reported |
| Similarity of baseline characteristics? | High risk | Groups were not similar at baseline |
| Co‐interventions avoided? | Unclear risk | Unclear whether co‐interventions were avoided or were similar |
| Compliance acceptable ? | Unclear risk | Unclear compliance rate |
| Timing outcome assessment comparable? | Unclear risk | Not clear when outcome measure was calculated |
Andersen 2008a.
| Methods | RCT, cluster‐randomisation | |
| Participants | Forty‐eight employed women with chronic neck muscle pain (defined as a clinical diagnosis of trapezius myalgia). Recruited participants from seven workplaces characterised by monotonous jobs (e.g. computer‐intensive work) | |
| Interventions |
Specific strength training (SST): 10 weeks of specific strength training locally for the affected muscle; n = 18 General fitness training (GFT): leg bicycling with relaxed shoulders; n = 16 Control: health counselling without physical activity; n = 14 |
|
| Outcomes | Pain intensity (VAS). aerobic fitness (Astrand) | |
| Notes | Participants grouped as cases and controls post intervention. No analysis per intervention group | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Randomization at the cluster level .. in a balanced design..", but no specific details of method given |
| Allocation concealment (selection bias) | Unclear risk | Do not know who generated the assignment |
| Blinding of participants? | Unclear risk | Blinding was unlikely, but no info provided |
| Blinding of caregivers? | Unclear risk | Blinding was unlikely, but no info provided |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Blinding was unlikely, but no info provided |
| Incomplete outcome data (attrition bias) All outcomes ‐ <20% drop‐outs? | Unclear risk | Six dropouts in the REF group not adequately described |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis performed? | Unclear risk | Unclear whether ITT was used, but it looks like only 8/14 of the REF group were analysed |
| Selective reporting (reporting bias) | Unclear risk | Unclear |
| Similarity of baseline characteristics? | Low risk | Groups similar; see Table 1 and Table 2 |
| Co‐interventions avoided? | Unclear risk | Unclear whether cointerventions were addressed during the study |
| Compliance acceptable ? | Low risk | Duration similar in three groups, intensity similar in exercise groups and logbooks kept |
| Timing outcome assessment comparable? | Low risk | Figure 2: measures collected at each session and weekly in postintervention phase |
Andersen 2008b.
| Methods | RCT, cluster‐randomisation (n = 79 clusters) | |
| Participants | Office workers (n = 549) with neck/shoulder pain recruited from 12 geographically different units of a national Danish public administration authority | |
| Interventions |
Specific resistance training (SRT) for the neck/shoulder muscles. Training was performed three times a week, and each session lasted 20 minutes. Two of the three weekly sessions were supervised by experienced instructors; n = 180 All‐round physical exercise (APE) on a group level; n = 187 Reference intervention (REF) with counselling; n = 182 Interventions one hour per week for 12 months |
|
| Outcomes | Pain (NRS) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Participants randomly assigned at cluster level, but no details of method given |
| Allocation concealment (selection bias) | Unclear risk | Not told who allocated treatment |
| Blinding of participants? | Unclear risk | Blinding was unlikely, but no info provided |
| Blinding of caregivers? | Unclear risk | Blinding was unlikely, but no info provided |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Self‐reported participant outcomes, but we do not know whether participants were blinded |
| Incomplete outcome data (attrition bias) All outcomes ‐ <20% drop‐outs? | Unclear risk | No mention of dropouts |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis performed? | Unclear risk | Not clear from results how many participants were analysed after one year |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics? | Unclear risk | Baseline similarity unclear: only prevalence of pain symptoms reported |
| Co‐interventions avoided? | Unclear risk | No mention of avoiding co‐interventions during this time |
| Compliance acceptable ? | Unclear risk | Compliance not reported |
| Timing outcome assessment comparable? | Unclear risk | Timing unclear |
Bang 2000.
| Methods | RCT | |
| Participants | Fifty‐two participants diagnosed with shoulder impingement syndrome. Cumulative microtraumata during overuse and repetitive load are the theorised causes of primary impingement | |
| Interventions |
Manual therapy group: Standardised flexibility and strengthening programme under supervision of a physiotherapist and additional manual therapy directed at relevant movement limitations in the upper quarter; n = 28 Exercise group: Standardised flexibility and strengthening programme under supervision of a physiotherapist; n = 24 All treatments twice weekly for three weeks for a total of six visits |
|
| Outcomes | Pain response for functional activities (VAS), shoulder function (modified Oswestry: 0 to 45 (no limitations)), isometric strength (dynamometer) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Unclear randomisation procedure |
| Allocation concealment (selection bias) | Unclear risk | Unclear whether allocation was concealed |
| Blinding of participants? | Unclear risk | Unclear |
| Blinding of caregivers? | High risk | No blinding |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Testers were blinded to group assignment |
| Incomplete outcome data (attrition bias) All outcomes ‐ <20% drop‐outs? | Low risk | Less than 20% dropouts |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis performed? | High risk | No intention‐to‐treat analysis |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics? | High risk | Baseline not considered similar between groups |
| Co‐interventions avoided? | Unclear risk | Unclear whether co‐interventions were avoided |
| Compliance acceptable ? | Low risk | Compliance was acceptable |
| Timing outcome assessment comparable? | Low risk | Timing was acceptable |
Bernaards 2006.
| Methods | RCT; independent statistician prepared randomisation using computer‐generated random assignment. Block randomisation (blocks of three) |
|
| Participants | Computer workers (at least three days per week) with frequent or long‐term pain in neck and upper limb last two weeks | |
| Interventions |
Work style group (WS): focusing on behavioural change with regard to body posture, workplace adjustment, breaks and coping with high work demands; n = 152 Work style + physical activity group (WSPA): focusing on behavioural change with regard to body posture, workplace adjustment, breaks, coping with high work demands and additional physical activity; n = 156 Usual care group: These participants visited their occupational physician for neck and upper limb symptoms; they received usual care; n = 158 Interventions for the two intervention groups consisted of six interactive group meetings over a six‐month period. All group meetings took place at the workplace, during work time Intervention period of six month and measurements at baseline and after six and 12 months of follow‐up |
|
| Outcomes | Recovery (7‐point scale), pain intensity (11‐point NRS), disability (11‐point NRS) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Adequate randomisation procedure |
| Allocation concealment (selection bias) | Low risk | Prepared by an independent statistician, but researchers informed participants about their allocation |
| Blinding of participants? | High risk | Participant not blinded |
| Blinding of caregivers? | High risk | Caregivers not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participant not blinded for participant‐reported outcomes. Unblinded counsellors who also performed part of the follow‐up measurements |
| Incomplete outcome data (attrition bias) All outcomes ‐ <20% drop‐outs? | High risk | Figure 1: 32% dropout for long‐term follow‐up and differences in pain and activity levels may introduce bias |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis performed? | Low risk | ITT analysis was used |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics? | Low risk | Groups similar: see Table 1 and Table 3 |
| Co‐interventions avoided? | Unclear risk | Possibility of co‐interventions not addressed |
| Compliance acceptable ? | High risk | Table 2: differences in attendance at meetings between groups |
| Timing outcome assessment comparable? | Low risk | Timing comparable |
Bru 1994.
| Methods | RCT; no information on randomisation procedure | |
| Participants | Hospital staff with various degrees of musculoskeletal pain from neck, shoulders and/or low back; n = 119 | |
| Interventions |
I1: Relaxation training: relaxation exercise + autogenic training; n = 15 I2: Cognitive training: education, relationship, personality, work and complaints; n = 19 I3: Combination I1 + I2: n = 24 C: Waiting list controls: n = 53 10 sessions in ? weeks. Follow‐up: four months |
|
| Outcomes | Pain intensity (5‐point Likert), pain duration (4‐point Likert) | |
| Notes | No data available | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Unclear randomisation procedure |
| Allocation concealment (selection bias) | Unclear risk | Unclear whether allocation was concealed |
| Blinding of participants? | Unclear risk | Unclear |
| Blinding of caregivers? | Unclear risk | Unclear |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Unclear |
| Incomplete outcome data (attrition bias) All outcomes ‐ <20% drop‐outs? | High risk | 34% dropout |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis performed? | High risk | No intention‐to‐treat analysis |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics? | Low risk | Groups similar at baseline |
| Co‐interventions avoided? | Unclear risk | Unclear whether co‐interventions were avoided |
| Compliance acceptable ? | Unclear risk | Unclear compliance |
| Timing outcome assessment comparable? | Low risk | Timing comparable |
Cheng 2007.
| Methods | RCT; no information on randomisation procedure | |
| Participants | Workers recruited from workers' compensation insurance companies. Prevalent work‐related rotator cuff tendinitis; all sick listed > 90 days; n = 103 | |
| Interventions |
Clinical‐based work hardening (CWH): mobilisation, strength and endurance training; n = 52 I2: Workplace‐based work hardening (WWT): ergonomic education, stretching and strengthening exercises; n = 51 Training sessions three times per week for four weeks |
|
| Outcomes | Shoulder Pain and Disability Index (SPADI): functional capacity (FCE); return to work | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details of randomisation method given |
| Allocation concealment (selection bias) | Unclear risk | No details of who performed treatment allocation |
| Blinding of participants? | Unclear risk | We do not know whether participants were blinded |
| Blinding of caregivers? | Unclear risk | Unclear |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Self‐report outcome—we do not know whether patient was blinded |
| Incomplete outcome data (attrition bias) All outcomes ‐ <20% drop‐outs? | Low risk | 9/103 dropouts. < 20%. Reasons given |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis performed? | High risk | 94/103 analysed: no ITT analysis |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics? | Low risk | Groups similar: see Table 1 and Table 2 |
| Co‐interventions avoided? | Unclear risk | "Contaminating effect from collateral workplace based efforts was not investigated" |
| Compliance acceptable ? | Unclear risk | Three sessions a week but no record of attendance at sessions |
| Timing outcome assessment comparable? | Low risk | Timing comparable |
Dellve 2011.
| Methods | RCT | |
| Participants | Female human service organisation workers (35 to 60 years old) on long‐term (60 days) sick leave and with chronic neck pain. Reduction in degree of working should be at least 50%; n = 73 | |
| Interventions |
Myofeedback training: harness to muscle activity (EMG) from the upper trapezius muscles on the right and left sides; eight hours per week; n = 25; lost five Intensive strength training: two warm‐up movements, followed by four exercises for strengthening and coordinating upper extremities; five‐ to 10‐minute programme to be performed twice a day for six days/wk; n = 27; lost seven Control: n = 21 Intervention: one month; follow‐up: three months |
|
| Outcomes | Self‐reported (work ability, pain (VAS)) and laboratory‐observed data on health, pain, muscular activation and work ability | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomisation method is unclear |
| Allocation concealment (selection bias) | Unclear risk | Concealed randomisation is stated, but procedure is unclear |
| Blinding of participants? | Unclear risk | No mention of participant blinding |
| Blinding of caregivers? | High risk | One caregiver for all interventions, therefore not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Unclear blinding and outcome assessment |
| Incomplete outcome data (attrition bias) All outcomes ‐ <20% drop‐outs? | High risk | 23/73 lost, > 20% |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis performed? | High risk | No ITT analysis |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics? | Low risk | No differences |
| Co‐interventions avoided? | Unclear risk | Unclear |
| Compliance acceptable ? | Unclear risk | Unclear |
| Timing outcome assessment comparable? | Low risk | Timing comparable |
Esmaeilzadeh 2012.
| Methods | RCT; randomisation at department level, block randomisation | |
| Participants | Work‐related upper extremity musculoskeletal disorders (WUEMSDs) among computer workers | |
| Interventions |
Ergonomic intervention: to improve the computer user’s knowledge of office ergonomics, to teach workstation self‐assessment and to enable self‐adjustment and rearrangement of the office environment by comprehensive ergonomic training, ergonomic training brochure and workstation evaluation; n = 47; 12 dropouts; n = 35 Control group with no intervention/treatment; n = 47; 13 dropouts; n = 34 |
|
| Outcomes | Pain (VAS), duration of symptoms, Nordic musculoskeletal questionnaire, ergonomic questionnaire, medication use, sick leave | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | An independent blinded research assistant prepared the randomisation by using a computer‐generated random block sequence |
| Allocation concealment (selection bias) | Low risk | An independent blinded research assistant prepared the randomisation by using a computer‐generated random block sequence |
| Blinding of participants? | High risk | Investigators informed participants about their allocation directly after they completed their baseline assessment |
| Blinding of caregivers? | Unclear risk | No information |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participant was not blinded; therefore outcome assessment was not blinded |
| Incomplete outcome data (attrition bias) All outcomes ‐ <20% drop‐outs? | High risk | Dropouts (n = 25; > 20%) |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis performed? | High risk | Statistical analysis was performed with 69 (of 94) participants |
| Selective reporting (reporting bias) | Unclear risk | Unknown |
| Similarity of baseline characteristics? | Low risk | No significant difference was noted between the two groups at baseline assessment in terms of all outcome measures |
| Co‐interventions avoided? | Unclear risk | Unclear |
| Compliance acceptable ? | Unclear risk | Unclear |
| Timing outcome assessment comparable? | Low risk | Follow‐up at six months |
Ferguson 1976.
| Methods | RCT; allocated randomly in turn, cross‐over trial; observer blinded in part | |
| Participants | Prevalent neck/shoulder complaints (non‐specific); only men; n = 40. Full‐time operating telegraphists | |
| Interventions |
Group A: active exercise + ultrasound Group B: proprioceptive neuromuscular facilitation (PNF training) + ice Group C: massage Four‐week intervention, cross‐over after two, four months |
|
| Outcomes | Interview, observation of keyboard operation, self‐assessment, fear | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Allocation randomly in turn |
| Allocation concealment (selection bias) | Unclear risk | Unclear whether allocation is concealed |
| Blinding of participants? | High risk | Participants were not blinded |
| Blinding of caregivers? | Unclear risk | Unclear whether caregivers were blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Outcome assessment is regarded as blinded |
| Incomplete outcome data (attrition bias) All outcomes ‐ <20% drop‐outs? | Low risk | Varying dropout rates, all < 20% |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis performed? | High risk | No ITT analysis |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics? | High risk | Groups not similar at baseline |
| Co‐interventions avoided? | Unclear risk | Unclear whether co‐interventions were avoided |
| Compliance acceptable ? | Unclear risk | Unclear compliance rate |
| Timing outcome assessment comparable? | Low risk | Timing comparable |
Goldman 2010.
| Methods | RCT; randomisation by uninvolved assistant using envelopes; double‐blind, placebo‐controlled | |
| Participants | Adults with upper extremity pain due to repetitive use or prolonged static postures; n = 118 | |
| Interventions |
Amitriptyline (25 mg): n = 59 Placebo pill: n = 59 Treatment: six weeks, follow‐up at 10 weeks |
|
| Outcomes | Pain intensity (NRS), Levine Symptom Severity Scale (0 to 55), Upper Extremity Function Scale (8 to 88) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A permuted block randomisation with variable block sizes and assignments sealed in sequentially numbered opaque envelopes |
| Allocation concealment (selection bias) | Low risk | "Person performing randomization .. was at a separate site .. and had nothing to do with the study participants or collection of data" |
| Blinding of participants? | Low risk | Participant blinded |
| Blinding of caregivers? | Low risk | Caregivers blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | "Research assistants involved in data collection were also blinded to treatment assignment"; participant blinded for participant‐reported outcomes |
| Incomplete outcome data (attrition bias) All outcomes ‐ <20% drop‐outs? | Low risk | 51/59 amitriptyline and 55/59 placebo returned for post‐treatment assessment. < 20% dropouts |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis performed? | Low risk | Table 4: ITT analysis—imputed missing values |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics? | Low risk | "Well balanced on all variables (Table 1); no clinically significant differences" |
| Co‐interventions avoided? | Low risk | Placebo versus active pill but no mention of advising participants to refrain from co‐interventions |
| Compliance acceptable ? | Low risk | Adherence: "... figures at the end of treatment were 87% and 89% ..." |
| Timing outcome assessment comparable? | Low risk | Timing comparable |
Hagberg 2000.
| Methods | RCT; concealed randomisation, multi‐centre trial; n = 3 | |
| Participants | Woman industrial workers seeking medical attention for neck or shoulder pain. Chronic (three‐month) neck/shoulder complaints (non‐specific; n = 77). Industrial workers with gradual onset of symptoms during work | |
| Interventions |
Endurance training: isometric shoulder endurance training; n = 43 Strength training: isometric shoulder strength training; n = 34 Training once a week supervised by physiotherapist for 12 weeks. Follow‐up at 24 weeks |
|
| Outcomes | Pain (VAS), ROM, sick leave, strength (dynamometer), endurance (RPE) | |
| Notes | No data available | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Allocation by chance (dice) |
| Allocation concealment (selection bias) | Low risk | Principal investigator blinded for allocation |
| Blinding of participants? | Unclear risk | Unclear whether participant is blinded |
| Blinding of caregivers? | High risk | Not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Outcome assessment not blinded |
| Incomplete outcome data (attrition bias) All outcomes ‐ <20% drop‐outs? | Low risk | Eight dropouts, reasons given, < 20% |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis performed? | High risk | No ITT analysis |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics? | Low risk | Groups similar at baseline |
| Co‐interventions avoided? | Unclear risk | Unclear whether co‐interventions were avoided |
| Compliance acceptable ? | Unclear risk | Unclear compliance rate |
| Timing outcome assessment comparable? | Low risk | Timing comparable |
Heuvel 2003.
| Methods | RCT; cluster‐randomisation (n = 22 clusters). Randomisation by spreadsheet | |
| Participants | Participants were recruited from a large office organisation dealing with social security allowances. Neck, shoulder or arm pain > two weeks; non‐specific; n = 286. Workers from an office organisation who considered complaints work‐related | |
| Interventions |
Breaks: stimulated to take extra breaks of five minutes every 35 minutes; n = 97 Breaks + exercises: stimulated to perform exercises during the extra breaks (45 seconds) at the start of each break; n = 81 Control: no intervention; n = 90 Treatment during eight weeks |
|
| Outcomes | Perceived recovery (7‐point Likert), pain (11‐point NRS), sick leave (days) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Cluster‐randomisation, procedure unknown |
| Allocation concealment (selection bias) | Unclear risk | Unclear whether allocation was concealed |
| Blinding of participants? | Unclear risk | Unclear participant blinding |
| Blinding of caregivers? | Unclear risk | Unclear |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Unclear blinding outcome assessment |
| Incomplete outcome data (attrition bias) All outcomes ‐ <20% drop‐outs? | Low risk | Dropout rate < 20% |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis performed? | High risk | No ITT analysis |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics? | Low risk | Groups similar at baseline |
| Co‐interventions avoided? | Unclear risk | Unclear whether co‐interventions were avoided |
| Compliance acceptable ? | Unclear risk | Unclear compliance rate |
| Timing outcome assessment comparable? | Low risk | Timing comparable |
Kamwendo 1991.
| Methods | RCT | |
| Participants | Medical secretaries currently working. Chronic (> 12 months) neck/shoulder complaints (non‐specific); medical secretaries currently working (women); n = 79 | |
| Interventions |
Traditional neck school: Four‐hour traditional neck school conducted by a physiotherapist. Advice + exercises; n = 25 Traditional neck school + ergonomic changes: Four‐hour traditional neck school conducted by a physiotherapist and additional visit of the physiotherapist at the workplace; n = 28 Controls: not offered any intervention; n = 26 Two sessions/wk, four weeks. Follow‐up: six months |
|
| Outcomes | Pain (VAS), workload (VAS), fatigue (VAS), ROM (goniometer), sick leave, expectation | |
| Notes | No data available | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Unclear randomisation procedure |
| Allocation concealment (selection bias) | Unclear risk | Unclear whether allocation was concealed |
| Blinding of participants? | Unclear risk | Unclear blinding of participants |
| Blinding of caregivers? | Unclear risk | Unclear blinding of caregivers |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Unclear blinding of outcome assessment |
| Incomplete outcome data (attrition bias) All outcomes ‐ <20% drop‐outs? | Low risk | Dropout rate < 20% |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis performed? | High risk | No ITT analysis |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics? | Unclear risk | Unclear baseline similarity |
| Co‐interventions avoided? | Unclear risk | Unclear whether co‐interventions were avoided |
| Compliance acceptable ? | Unclear risk | Unclear compliance rate |
| Timing outcome assessment comparable? | Unclear risk | Timing comparable |
Ketola 2002.
| Methods | RCT; no info on randomisation procedure; ‘care‐giver’ blinded | |
| Participants | Employees working with video display units (VDUs). Neck/shoulder complaint > one month; non‐specific; n = 124. Employees who use the mouse currently | |
| Interventions |
Intensive ergonomics: two physiotherapists visited the worksite and changed worksite according to checklist; n = 39 Education ergonomics: workers attended a one‐hour training session in ergonomics; n = 35 Control group: one‐page leaflet; n = 35 Two‐ and 10‐month follow‐up |
|
| Outcomes | Discomfort (6‐point Likert), strain (6‐point Likert), pain (yes/no) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Using stratified random sampling—The three administrational units were used as a stratum. The success of the randomization was checked.." |
| Allocation concealment (selection bias) | Unclear risk | Unclear whether allocation was concealed |
| Blinding of participants? | Unclear risk | Participants unclear whether blinded |
| Blinding of caregivers? | Unclear risk | Unclear whether care provider blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Two blinded experts used to detect changes in workstations, but diary and questionnaires provided self‐reported outcomes; participants not fully blinded |
| Incomplete outcome data (attrition bias) All outcomes ‐ <20% drop‐outs? | Low risk | Seven dropouts: < 20% |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis performed? | High risk | No ITT analysis |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics? | Low risk | Groups similar at baseline |
| Co‐interventions avoided? | Unclear risk | Unclear whether co‐interventions were avoided |
| Compliance acceptable ? | Unclear risk | Unclear compliance rate |
| Timing outcome assessment comparable? | Low risk | Timing comparable |
Leboeuf 1987.
| Methods | RCT; no info on randomisation procedure. | |
| Participants | Thirty‐eight participants with repetitive strain injury of the upper limbs. Chronic (> three months) complaints of upper extremity (non‐specific; n = 38; 35 women). Symptoms were considered due to repetitive strain | |
| Interventions |
Spinal manipulative therapy + soft tissue therapy (massage): n = 21 Spinal manipulative therapy (SMT): n = 17 Five weeks, two sessions/wk. Follow‐up: at three and 12 months |
|
| Outcomes | Severity of symptoms, frequency of symptoms (Likert) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Unclear randomisation procedure |
| Allocation concealment (selection bias) | Unclear risk | Unclear whether allocation was concealed |
| Blinding of participants? | Unclear risk | Unclear blinding of participant |
| Blinding of caregivers? | High risk | No blinding |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Outcome assessment self‐reported, so blinding unclear |
| Incomplete outcome data (attrition bias) All outcomes ‐ <20% drop‐outs? | Low risk | No dropouts mentioned |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis performed? | Low risk | ITT analysis assumed |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics? | Low risk | Groups similar at baseline |
| Co‐interventions avoided? | Unclear risk | Unclear whether co‐interventions were avoided |
| Compliance acceptable ? | Unclear risk | Unclear compliance rate |
| Timing outcome assessment comparable? | Low risk | Timing comparable |
Levoska 1993.
| Methods | RCT, no info on randomisation procedure | |
| Participants | Prevalent neck/shoulder complaints (non‐specific); female office workers employed by a local bank or social insurance institution; n = 47 | |
| Interventions |
Active physiotherapy: stretching and dynamic muscle training exercise and daily home training exercise programme for 60 minutes; n = 23 Passive physiotherapy: massage, heat and exercises, each for 20 minutes; n = 24 Five weeks, three sessions/wk. Follow‐up three months |
|
| Outcomes | Pain, tender points, symptoms (Q), strength (dynamometer), endurance | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Unclear randomisation procedure |
| Allocation concealment (selection bias) | Unclear risk | Unclear whether allocation was concealed |
| Blinding of participants? | Unclear risk | Unclear |
| Blinding of caregivers? | Unclear risk | Unclear |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Unclear |
| Incomplete outcome data (attrition bias) All outcomes ‐ <20% drop‐outs? | Low risk | Three dropouts: < 20% |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis performed? | High risk | No ITT analysis |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics? | Unclear risk | Unclear baseline similarity |
| Co‐interventions avoided? | Unclear risk | Unclear whether co‐interventions were avoided |
| Compliance acceptable ? | Unclear risk | Unclear compliance rate |
| Timing outcome assessment comparable? | Low risk | Timing comparable |
Lundblad 1999.
| Methods | RCT; no info on randomisation procedure | |
| Participants | Prevalent neck/shoulder complaints (non‐specific); female employees currently working; n = 97 | |
| Interventions |
Physiotherapy: group‐based physiotherapy programme with an ergonomic programme and home exercises; n = 32; two sessions of 50 minutes/wk Feldenkrais: using sensory awareness with movements/exercises and home exercises; n = 33; one session of 50 minutes/wk Control group: no intervention; n = 32 Treatment duration of 16 weeks. Follow‐up of one year |
|
| Outcomes | Pain (VAS), function (?), complaints (?), ROM, sick leave (days) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Unclear randomisation procedure |
| Allocation concealment (selection bias) | Unclear risk | Unclear whether allocation was concealed |
| Blinding of participants? | Unclear risk | Unclear |
| Blinding of caregivers? | Unclear risk | Unclear |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Unclear |
| Incomplete outcome data (attrition bias) All outcomes ‐ <20% drop‐outs? | High risk | High dropout rate: 40% |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis performed? | High risk | No ITT analysis |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics? | Low risk | Groups similar at baseline |
| Co‐interventions avoided? | Unclear risk | Unclear whether co‐interventions were avoided |
| Compliance acceptable ? | Unclear risk | Unclear compliance rate |
| Timing outcome assessment comparable? | Low risk | Timing comparable |
Ma 2011.
| Methods | RCT; simple computer‐based randomisation | |
| Participants | Daily computer users with a history of computer‐related neck and shoulder discomfort; n = 72 | |
| Interventions |
Biofeedback: portable biofeedback, two hours daily for two weeks; n = 15 Exercise: standardised exercise programme with stretching and strengthening exercises using Thera‐band, 20 minutes four times a day; n = 15 Passive treatment: interferential therapy (20 minutes) and hotpacks 15 minutes two times per week; n = 15 Control: standard educational booklet; n = 15 Intervention period: six weeks, follow‐up at six months |
|
| Outcomes | Pain (VAS), disability (NDI) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Simple computer‐based randomisation |
| Allocation concealment (selection bias) | Unclear risk | Unclear |
| Blinding of participants? | Unclear risk | Unclear |
| Blinding of caregivers? | Unclear risk | Unclear |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Unclear |
| Incomplete outcome data (attrition bias) All outcomes ‐ <20% drop‐outs? | High risk | Dropout at follow‐up > 20% |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis performed? | High risk | No ITT |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics? | Low risk | Baseline similarity |
| Co‐interventions avoided? | Low risk | Co‐interventions avoided |
| Compliance acceptable ? | Unclear risk | Unclear compliance |
| Timing outcome assessment comparable? | Low risk | Timing comparable |
Marangoni 2010.
| Methods | RCT; randomisation by listing order | |
| Participants | Computer workers (88% female); n = 68 | |
| Interventions |
CAMP (computer‐assisted stretching programme): stretch via a computer programme; 10‐minute computer breaks/h; n = 22 FLIP (facsimile lessons with instructional pictures): stretching using a hard copy version of the stretches with pictures and written instructions (paper version of CASP); n = 23 Control: no intervention; n = 23 Both interventions stretched once every six minutes |
|
| Outcomes | Pain (VAS) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | "Alternating the interventions by assigning the CASP intervention to the first caller..." |
| Allocation concealment (selection bias) | High risk | Allocation done by using the list with date and time order from callers and emailers |
| Blinding of participants? | High risk | No blinding |
| Blinding of caregivers? | High risk | "The same physical therapist performed the intake and outtake evaluations" |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | "The same physical therapist performed the intake and outtake evaluations" |
| Incomplete outcome data (attrition bias) All outcomes ‐ <20% drop‐outs? | Low risk | Figure 7: < 20% dropout |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis performed? | High risk | No ITT |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics? | Unclear risk | No breakdown of group prognostic indicators given |
| Co‐interventions avoided? | Unclear risk | No details of any possible co‐interventions given |
| Compliance acceptable ? | Unclear risk | No details of compliance with the intervention given |
| Timing outcome assessment comparable? | Unclear risk | Intervention was 15 days, but author does not state when outcome assessment was completed |
Martimo 2010.
| Methods | RCT; randomisation using sealed envelopes in three blocks | |
| Participants | Workers with upper extremity disorders; n = 177 | |
| Interventions |
Ergonomic improvements at workplace: n = 91 Current best practice: n = 86 Follow‐up: eight and 12 weeks |
|
| Outcomes | Pain (VAS), sick leave, job strain (Job Content Questionnaire), production loss (yes/no) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Randomization using tables of random numbers in three blocks… Sealed envelopes were used" |
| Allocation concealment (selection bias) | Low risk | Assignment generated by the physician, who had information about persons included in the trial, as he/she had contacted each employee supervisor by phone |
| Blinding of participants? | High risk | Unblinded participants |
| Blinding of caregivers? | High risk | Unblinded caregiver |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | "Researcher conducting the interviews at 8 and 12 weeks follow up was not aware of the group assignment", but unblinded participant for participant‐reported outcome |
| Incomplete outcome data (attrition bias) All outcomes ‐ <20% drop‐outs? | Low risk | Dropout rate 12% to 13% |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis performed? | High risk | No ITT analysis |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics? | Low risk | Groups comparable at baseline |
| Co‐interventions avoided? | Unclear risk | Unclear whether co‐interventions were avoided |
| Compliance acceptable ? | Unclear risk | Unclear whether compliance was assessed |
| Timing outcome assessment comparable? | Low risk | Timing comparable |
Meijer 2006.
| Methods | RCT; cost‐effectiveness analysis. Concealed randomisation | |
| Participants | Bank employees, sick‐listed workers with non‐specific upper extremity musculoskeletal complaints. Prevalent non‐specific upper extremity musculoskeletal disorders; n = 38 | |
| Interventions |
I: Multidisciplinary treatment (Mt): outpatient training programme; physical and psychological sessions and relaxation exercises; n = 23 Sessions for two months, 13 full days, five return‐to‐work sessions and one feedback session C: Usual care (Uc): guidance by occupational physician or general practitioner; n = 15 Follow‐up one year (two, six and 12 months) |
|
| Outcomes | Pain (VAS), function (DASH), return‐to‐work, kinaesiophobia (TAMPA), costs | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Block randomisation computer‐generated random sequence table. Envelopes allocated on the basis of participants' consecutive registration numbers |
| Allocation concealment (selection bias) | Low risk | Opaque sealed envelopes kept by "researcher with no contact with therapists, physicians or patients" |
| Blinding of participants? | High risk | Participants were not blinded |
| Blinding of caregivers? | High risk | No blinding |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Does not mention who carried out objective outcome measures, but participants were unblinded for self‐reported outcome measures |
| Incomplete outcome data (attrition bias) All outcomes ‐ <20% drop‐outs? | Low risk | Figure 1: 4/38 dropouts (< 20%) |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis performed? | Low risk | Intention‐to‐treat analyses conducted |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics? | Low risk | Groups similar at baseline: see Table 2 |
| Co‐interventions avoided? | Unclear risk | Unclear whether co‐interventions were avoided |
| Compliance acceptable ? | Low risk | 18/21 of intervention group showed good compliance |
| Timing outcome assessment comparable? | Low risk | Timing comparable |
Moore 1996.
| Methods | RCT; no info on randomisation procedure | |
| Participants | Recent complaints upper extremity (non‐specific); n = 32 (28 women). Diagnosed as having upper extremity RSI, referred from occupational medicine department | |
| Interventions |
HVT (hypnotically induced vasodilatation treatment): relaxation training, biofeedback, hypnosis; n = 15; 45 minutes/wk, six weeks Waiting list controls: n = 17 |
|
| Outcomes | Comfort (VAS), temperature (hand) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Assigned by following a list of random numbers |
| Allocation concealment (selection bias) | Unclear risk | Unclear whether allocation was concealed |
| Blinding of participants? | Unclear risk | Unclear |
| Blinding of caregivers? | Unclear risk | Unclear |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Unclear whether outcome assessment was blinded |
| Incomplete outcome data (attrition bias) All outcomes ‐ <20% drop‐outs? | Low risk | No dropout mentioned |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis performed? | Low risk | ITT analysis assumed |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics? | Low risk | Groups similar at baseline |
| Co‐interventions avoided? | Unclear risk | Unclear whether co‐interventions were avoided |
| Compliance acceptable ? | Unclear risk | Unclear compliance |
| Timing outcome assessment comparable? | Low risk | Timing comparable |
Nourbakhsh 2008.
| Methods | RCT; randomisation by having participants draw a card out of a set of cards marked ‘Group A’ or ‘Group B’ | |
| Participants | Participants were involved in heavy or repetitive arm movements as part of their job or during recreational activities. Chronic lateral epicondylitis; n = 18 | |
| Interventions |
Low‐frequency electrical stimulation on trigger points; n = 10 Placebo: n = 8 Six sessions in two to three weeks; six months of follow‐up |
|
| Outcomes | Pain (NRS), functional status (Q) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Draw a card from a set of cards" |
| Allocation concealment (selection bias) | High risk | Treating therapist did the random assignment |
| Blinding of participants? | Low risk | Participant was blinded |
| Blinding of caregivers? | High risk | Therapists were not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Measuring therapists were blinded to participants' group assignment, and participant blinded for participant‐reported outcomes |
| Incomplete outcome data (attrition bias) All outcomes ‐ <20% drop‐outs? | Low risk | Two dropouts not described, but dropout rate does not exceed 20% |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis performed? | Low risk | Yes for post‐test measurement, not for six‐month follow‐up |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics? | High risk | Groups not similar in all outcome measures (e.g. grip strength); demographic features (e.g. age range, duration of symptoms) |
| Co‐interventions avoided? | Low risk | "Subjects did not receive any other form of treatment" |
| Compliance acceptable ? | Low risk | All participants received six treatment sessions over a two‐ to three‐week period |
| Timing outcome assessment comparable? | Low risk | Timing comparable |
Omer 2003.
| Methods | RCT; no info on randomisation procedure. | |
| Participants | Neck and upper extremity complaints (non‐specific); n = 50 (41 women). Computer operators > six hours a day | |
| Interventions |
Education + Exercises: education (one hour) + mobilisation, stretching, strengthening and relaxation exercises Education: education one hour Three sessions a week, eight weeks training |
|
| Outcomes | Pain (NRS, PDI), tiredness (TS), depression (BDI) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Unclear randomisation procedure |
| Allocation concealment (selection bias) | Unclear risk | Unclear whether allocation was concealed |
| Blinding of participants? | Unclear risk | Unclear participant blinding |
| Blinding of caregivers? | Unclear risk | Unclear |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Unclear whether outcome assessment was blinded |
| Incomplete outcome data (attrition bias) All outcomes ‐ <20% drop‐outs? | Unclear risk | Unclear number of dropouts |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis performed? | Unclear risk | Unclear whether ITT analysis was performed |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics? | Low risk | Groups similar at baseline |
| Co‐interventions avoided? | Unclear risk | Unclear whether co‐interventions were avoided |
| Compliance acceptable ? | Unclear risk | Unclear compliance |
| Timing outcome assessment comparable? | Unclear risk | Unclear whether timing was comparable |
Rempel 1999.
| Methods | RCT; no info on randomisation procedure. Matched pairs; participant and observer blinded | |
| Participants | Prevalent carpal tunnel syndrome (CTS) (specific); n = 24 (16 women). Full‐time laboratory personnel using a computer for > two hours a day, referred from an occupational medicine clinic for hand and wrist problems | |
| Interventions |
I: Keyboard A (Protouch): n = 12 C: Keyboard B (MacProPlus): control group with standard keyboard: n = 12 12 weeks, one hour of training |
|
| Outcomes | Pain (Likert), nerve conduction (electromyography), function and keyboard characteristics (Q) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Unclear randomisation procedure |
| Allocation concealment (selection bias) | Unclear risk | Unclear whether allocation was concealed |
| Blinding of participants? | Low risk | Participant was blinded |
| Blinding of caregivers? | Low risk | Caregiver was blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Participants self‐reported outcome, so outcome assessment was blinded |
| Incomplete outcome data (attrition bias) All outcomes ‐ <20% drop‐outs? | Low risk | Four dropouts < 20% |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis performed? | High risk | No ITT analysis |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics? | Low risk | Groups similar at baseline |
| Co‐interventions avoided? | Unclear risk | Unclear whether co‐interventions were avoided |
| Compliance acceptable ? | Unclear risk | Unclear compliance |
| Timing outcome assessment comparable? | Low risk | Timing was comparable |
Rempel 2007.
| Methods | RCT; no info on randomisation procedure | |
| Participants | Chronic neck and shoulder pain in sewing machine operators; n = 277. Performed sewing machine work for more than 20 hours per week | |
| Interventions |
Chair with flat seat: n = 72 Chair with curved seat: n = 100 Control: n = 105 Miscellaneous items provided to all participants were a footrest, a small table‐top storage box for items such as scissors, a side table, a task lamp and reading glasses Four months of follow‐up |
|
| Outcomes | Pain, job content (job content questionnaire) | |
| Notes | No data available | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details of randomisation method |
| Allocation concealment (selection bias) | Unclear risk | No details on treatment allocation |
| Blinding of participants? | High risk | Participant not blinded |
| Blinding of caregivers? | Unclear risk | Unclear whether caregiver was blinded |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participant‐reported outcomes and participant not blinded |
| Incomplete outcome data (attrition bias) All outcomes ‐ <20% drop‐outs? | High risk | 209/277 completed the study (25% dropout rate) |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis performed? | High risk | No ITT analysis |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics? | Unclear risk | Comparison of baseline outcome measures not given |
| Co‐interventions avoided? | Unclear risk | Unclear whether co‐interventions were avoided |
| Compliance acceptable ? | Unclear risk | Unclear compliance |
| Timing outcome assessment comparable? | Low risk | Timing was comparable |
Ripat 2006.
| Methods | RCT; no information on randomisation procedure | |
| Participants | Symptomatic workers employed by a single company recruited through public and/or electronic mail. Workers with two or more symptoms of work‐related upper extremity disorder (WRUED; n = 68) | |
| Interventions |
Modified keyboard (light touch): modified version of the same keyboard designed to reduce activation force, vibration and key travel; n = 43 Standard keyboard: commercially available ergonomic keyboard; n = 25 Keyboard use for 24 weeks |
|
| Outcomes | Symptom severity scale (SSS), functional status scale (FSS) | |
| Notes | No data available | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No details of method used |
| Allocation concealment (selection bias) | High risk | Some participants were placed in the adapted keyboard group as an "exception to the randomization process" |
| Blinding of participants? | High risk | Participants unblinded |
| Blinding of caregivers? | High risk | Caregivers not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Not told who did the outcome measures, but likely to be research assistant, who was not blinded. Also participants unblinded for participant‐reported outcomes |
| Incomplete outcome data (attrition bias) All outcomes ‐ <20% drop‐outs? | Unclear risk | Not told of any dropouts |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis performed? | Unclear risk | Unclear whether ITT analysis was performed |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics? | Low risk | Baseline comparable: see Table 2 |
| Co‐interventions avoided? | Unclear risk | Unclear whether co‐interventions were avoided |
| Compliance acceptable ? | Unclear risk | Unclear compliance |
| Timing outcome assessment comparable? | Low risk | Timing was comparable |
Sandsjö 2010.
| Methods | RCT; block randomisation (block size 2) | |
| Participants | Females; > 20‐hour computer work/wk with neck/shoulder pain; n = 65 | |
| Interventions |
Myofeedback teletreatment: four weeks of myofeedback‐based teletreatment. Participants had to use the myofeedback system for at least eight hours a week distributed over at least two days a week and during longer continuous (preferably two hours) sessions each day; n = 33 Control (usual care): not receive any intervention; n = 32 Follow‐up three months after intervention |
|
| Outcomes | Clinical improvement in pain (VAS > 13 mm), clinical improvement in disability (PDI > 7), clinical improvement in work ability (1 cm) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Block randomisation—one participant randomly assigned to intervention, one to control. Alternation method therefore inadequate |
| Allocation concealment (selection bias) | Unclear risk | No details given about treatment allocation method |
| Blinding of participants? | Unclear risk | Unclear blinding |
| Blinding of caregivers? | Unclear risk | Unclear blinding |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Self‐reported outcome measures, unclear blinding |
| Incomplete outcome data (attrition bias) All outcomes ‐ <20% drop‐outs? | High risk | Large dropout rate: four weeks 19/65 dropped out = 30%, three months 26/65 dropped out = 40% |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis performed? | High risk | No ITT |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics? | Low risk | Baseline comparable |
| Co‐interventions avoided? | Low risk | Co‐interventions: traced each participant's background activities via questionnaire |
| Compliance acceptable ? | Unclear risk | Unclear compliance |
| Timing outcome assessment comparable? | Low risk | Timing was comparable |
Sjögren 2005.
| Methods | RCT; cluster‐randomised, cross‐over trial; four clusters | |
| Participants | Office workers with headache, neck or shoulder pain; n = 53 | |
| Interventions |
I: Physical exercise: progressive light resistance training and guidance; n = 36 C: No intervention: n = 17 Treatment period: 15 weeks; cross‐over at 15 weeks |
|
| Outcomes | Pain (Borg CR10 Scale), strength | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Cluster‐randomisation, but method of randomisation not specified |
| Allocation concealment (selection bias) | Low risk | "Blind measurers allocated the workers into the two treatment sequences" |
| Blinding of participants? | High risk | Participants not blinded |
| Blinding of caregivers? | Unclear risk | Unclear |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Self‐reported outcomes used and participants not blinded |
| Incomplete outcome data (attrition bias) All outcomes ‐ <20% drop‐outs? | Low risk | Two participants lost to follow‐up: < 20% |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis performed? | Low risk | Figure 1: main analysis intention‐to‐treat, none excluded from analysis |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics? | Low risk | Baseline comparable: see Table 1 |
| Co‐interventions avoided? | Low risk | "Other physical activity performed outside the intervention was controlled by a structured interview" |
| Compliance acceptable ? | Low risk | Compliance: Participants maintained a weekly diary: 78% to 68% |
| Timing outcome assessment comparable? | Low risk | Timing was comparable |
Spence 1989.
| Methods | RCT; no info on randomisation procedure | |
| Participants | Chronic (> 10 months) occupational pain of the upper limbs (non‐specific); n = 45 (44 women). Upper extremity CTD and repetitive tasks in workplace | |
| Interventions |
ICBT: individual cognitive‐behavioural therapy: n = 15 GCBT: group cognitive‐behavioural therapy: n = 14 WCL: waiting list controls: n = 16 Nine weeks, nine sessions. Follow‐up: six months two years in intervention groups |
|
| Outcomes | Pain (McGill), function (SIP), return to work, satisfaction, fear (STAI), depression (BDI), coping (CSQ) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No info on randomisation procedure |
| Allocation concealment (selection bias) | Unclear risk | Unclear whether allocation was concealed |
| Blinding of participants? | Unclear risk | Unclear |
| Blinding of caregivers? | High risk | Care provider not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Unclear whether outcome assessment was blinded |
| Incomplete outcome data (attrition bias) All outcomes ‐ <20% drop‐outs? | Low risk | Seven dropouts: < 20% |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis performed? | High risk | No ITT analysis |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics? | Low risk | Baseline comparable |
| Co‐interventions avoided? | Unclear risk | Unclear whether co‐interventions were avoided |
| Compliance acceptable ? | Unclear risk | Unclear compliance |
| Timing outcome assessment comparable? | Low risk | Timing was comparable |
Spence 1995.
| Methods | RCT; no info on randomisation procedure | |
| Participants | Chronic (> 10 months) complaints, upper extremity (non‐specific) associated with repetitive tasks in the workplace; n = 48 (40 women) | |
| Interventions |
EMG biofeedback (EMG): auditory feedback on muscle tension levels + home‐based assignments; n = 12 EMG + relaxation (CO): combined treatment of EMG and ART; n = 12 Relaxation training (ART): consists of a range of relaxation techniques + home‐based assignments; n = 12 Waiting list controls (WCL): n = 12 Eight weeks. Follow‐up six months |
|
| Outcomes | Pain (Whimpy, Likert, PBQ), depression (BDI), ADL | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Unclear randomisation procedure |
| Allocation concealment (selection bias) | Unclear risk | Unclear whether allocation was concealed |
| Blinding of participants? | Unclear risk | Unclear |
| Blinding of caregivers? | Unclear risk | Unclear |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Unclear whether outcome assessment was blinded |
| Incomplete outcome data (attrition bias) All outcomes ‐ <20% drop‐outs? | High risk | Three dropouts at short term; eight at long term (> 20%) |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis performed? | High risk | No ITT analysis |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics? | High risk | Baseline groups were regarded as not comparable |
| Co‐interventions avoided? | Unclear risk | Unclear whether co‐interventions were avoided |
| Compliance acceptable ? | Unclear risk | Unclear compliance |
| Timing outcome assessment comparable? | Low risk | Timing was comparable |
Stralka 1998.
| Methods | RCT; even/odd numbers. Care provider and participant blinded | |
| Participants | Prevalent hand and wrist complaints (non‐specific); factory employees (data processing); n = 120 (84 women). Cumulative trauma disorders | |
| Interventions |
Energized splint: using a high‐voltage pulsed current in the wrist splint; n = 60 Placebo splint: n = 60 Seven weeks; 30 minutes of stimulation/20 sessions |
|
| Outcomes | Pain (VAS), ROM, strength (dynamometer), swelling (volume measurement) | |
| Notes | No data available | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Randomsiation was performed by odd and even number distribution |
| Allocation concealment (selection bias) | High risk | Allocation was probably concealed |
| Blinding of participants? | Low risk | Participant was blinded |
| Blinding of caregivers? | Low risk | Caregiver was blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Outcome assessment was blinded |
| Incomplete outcome data (attrition bias) All outcomes ‐ <20% drop‐outs? | Low risk | Dropouts: 21/141; < 20% |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis performed? | High risk | No ITT analysis |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics? | Unclear risk | Unclear baseline comparability |
| Co‐interventions avoided? | Unclear risk | Unclear whether co‐interventions were avoided |
| Compliance acceptable ? | Low risk | Compliance was monitored |
| Timing outcome assessment comparable? | Unclear risk | Timing was comparable |
Szcurko 2009.
| Methods | RCT; randomised using age‐ and sex‐matched central computer randomisation | |
| Participants | Postal workers with rotator cuff tendinitis; n = 89 | |
| Interventions |
PE: standardised physical exercises: range‐of‐motion exercises + placebo tablets; n = 42 NC: Naturopathic care: dietary counselling, acupuncture and Plogenzym; n = 43 12 weeks, one weekly session of 30 minutes |
|
| Outcomes | Pain (VAS), function (SPADI), quality of life (SF‐36) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Participants were randomized using age and sex matched computer randomization" |
| Allocation concealment (selection bias) | Low risk | "Allocation concealment using central randomization was preserved up to the point of treatment" |
| Blinding of participants? | High risk | Participant was not blinded |
| Blinding of caregivers? | Unclear risk | Unclear blinding |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | "Primary outcome is measured by patient and participant blinding is 'no'" |
| Incomplete outcome data (attrition bias) All outcomes ‐ <20% drop‐outs? | Low risk | Of 85 participants, 17 did not complete treatment (= 20%) |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis performed? | Low risk | Missing data at week 12 were replaced by values at week 8 for ITT analysis |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics? | High risk | No adequate baseline comparability: see Table 1 |
| Co‐interventions avoided? | High risk | Co‐interventions not similar between groups |
| Compliance acceptable ? | Low risk | Compliance for pills > 80%. Same number and duration of sessions for other groups |
| Timing outcome assessment comparable? | Low risk | Timing was comparable |
Takala 1994.
| Methods | RCT; matched, cross‐over, observer‐blinded | |
| Participants | Neck/shoulder complaints (> one month; non‐specific); female employees of security printing company; n = 44. All participants performed sedentary work and light repetitive tasks | |
| Interventions |
Exercise: group gymnastics, whole body exercises, 45 minutes once a week for 10 weeks; n = 22 C: Controls: n = 22 After four months, cross‐over |
|
| Outcomes | Pain (VAS), pressure pain (algometer) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Unclear randomisation procedure |
| Allocation concealment (selection bias) | Unclear risk | Unclear whether allocation was concealed |
| Blinding of participants? | High risk | Participant was not blinded |
| Blinding of caregivers? | High risk | Caregiver was not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Rater was blinded to treatment status (pain pressure); participant rated pain (VAS) and was not blinded |
| Incomplete outcome data (attrition bias) All outcomes ‐ <20% drop‐outs? | High risk | 14/44 dropouts: > 20% |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis performed? | High risk | No ITT analysis |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics? | Low risk | Baseline comparable |
| Co‐interventions avoided? | Unclear risk | Unclear whether co‐interventions were avoided |
| Compliance acceptable ? | Unclear risk | Compliance unclear |
| Timing outcome assessment comparable? | Low risk | Timing was comparable |
Tittiranonda 1999.
| Methods | RCT; placebo‐controlled, random permuted block method, observer blinded | |
| Participants | Carpal tunnel syndrome (CTS) or tendinitis wrist (complaints > one week; specific; n = 80; 46 women). Laboratory employees, computer users | |
| Interventions |
Kb1: Apple adjusted keyboard: n = 20 Kb2: Comfort keyboard system: n = 20 Kb3: Microsoft natural keyboard: n = 20 Placebo group: n = 20 |
|
| Outcomes | Pain (VAS), hand function (Q/VAS), physical examination, keyboard comfort (VAS) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random permuted block method |
| Allocation concealment (selection bias) | Unclear risk | Unclear randomisation concealment |
| Blinding of participants? | Low risk | Participant was blinded |
| Blinding of caregivers? | Low risk | Blinding |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Outcome assessment blinded because participants were blinded |
| Incomplete outcome data (attrition bias) All outcomes ‐ <20% drop‐outs? | Low risk | 14% dropouts mentioned |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis performed? | Low risk | ITT analysis performed |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics? | Low risk | Baseline comparable |
| Co‐interventions avoided? | Unclear risk | Unclear whether co‐interventions were avoided |
| Compliance acceptable ? | Low risk | Compliance was assessed and adequate |
| Timing outcome assessment comparable? | Low risk | Timing was comparable |
van Eijsden 2008.
| Methods | RCT; randomisation by independent research assistant; blocks of four were generated for each stratum (duration of complaints) using a computer‐generated random sequence table | |
| Participants | Visual display unit workers with early non‐specific work‐related upper limb disorders. Participants were recruited by advertisement in local newspapers; n = 88 | |
| Interventions |
Postural exercises: postural exercises according to the Mensendieck/Cesar approach; n = 44 Strength and fitness exercises: strength and fitness exercises delivered by four physiotherapists, who attended a course for work‐related upper limb disorders based on the latest evidence; n = 44 Intervention for 10 weeks; follow‐up at three, six and 12 months |
|
| Outcomes | Pain (VAS), disability (Disabilities of Arm, Shoulder and Hand Questionnaire), health‐related quality of life (Short Form‐36) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Blocks of four were generated for each stratum by means of a computer generated random sequence table" |
| Allocation concealment (selection bias) | Low risk | "Research assistant, who was not involved in the selection of participants, allocated participants to groups using a list of random numbers" |
| Blinding of participants? | High risk | No blinding of participants |
| Blinding of caregivers? | High risk | No blinding of caregivers |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | "All outcome measures were self report so they were not blind" |
| Incomplete outcome data (attrition bias) All outcomes ‐ <20% drop‐outs? | Low risk | "There were 6 drop outs" out of 88: < 20% |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis performed? | Low risk | Table 4: "analyses carried out according to the ITT principle" |
| Selective reporting (reporting bias) | Low risk | No selective reporting |
| Similarity of baseline characteristics? | Low risk | "Both groups were comparable at baseline for nearly all variables" |
| Co‐interventions avoided? | Low risk | No mention of co‐interventions, but also no mention of asking participants to avoid co‐interventions |
| Compliance acceptable ? | Low risk | "Compliance was 94% in the PE therapy group and 96% in the RP group" |
| Timing outcome assessment comparable? | Low risk | Timing comparable |
Vasseljen 1995.
| Methods | RCT | |
| Participants | Chronic (> six months) neck/shoulder complaints (non‐specific); female office workers; n = 24. Work‐related complaints | |
| Interventions |
IPT: individual physiotherapy: treated by local physiotherapist outside the workplace; massage, exercise, mobilisation, ergonomic adjustments; n = 12; 10 weeks, two sessions/ wk GPT: group physiotherapy: exercise at workplace by experienced physiotherapist; n = 12; six weeks, three sessions/wk Follow‐up: six months |
|
| Outcomes | Pain (VAS), trigger points (algometer), strength, muscle activity (EMG) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Unclear randomisation procedure |
| Allocation concealment (selection bias) | Unclear risk | Unclear whether allocation was concealed |
| Blinding of participants? | Unclear risk | Unclear participant blinding |
| Blinding of caregivers? | Unclear risk | Unclear |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Unclear whether outcome assessment was blinded |
| Incomplete outcome data (attrition bias) All outcomes ‐ <20% drop‐outs? | Low risk | No dropouts mentioned |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis performed? | Low risk | ITT analysis assumed |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics? | Low risk | Baseline comparable |
| Co‐interventions avoided? | Unclear risk | Unclear whether co‐interventions were avoided |
| Compliance acceptable ? | Low risk | Compliance with treatment regime was good |
| Timing outcome assessment comparable? | Low risk | Timing was comparable |
Viljanen 2003.
| Methods | RCT; concealed randomisation, random number table and numbered opaque envelopes, outcome assessor blinded | |
| Participants | Chronic (> three months) neck/shoulder complaints (non‐specific), female office workers; n = 393. Occupational complaints | |
| Interventions |
Dynamic muscle training: dynamic training using dumbbells, instructed by physiotherapist; n = 135 Relaxation training: various relaxation techniques, instructed by physiotherapist; n = 128 Control: ordinary activity; n = 130 Training for 12 weeks, three times/wk. Follow‐up three, six and 12 months |
|
| Outcomes | Neck pain (VAS), neck disability (Q), work ability (Likert), sick leave | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Using random number table |
| Allocation concealment (selection bias) | Low risk | Allocation was concealed using opaque sealed envelopes |
| Blinding of participants? | Low risk | Participants were blinded |
| Blinding of caregivers? | Unclear risk | Unclear |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Outcome was self‐reported, participants were blinded |
| Incomplete outcome data (attrition bias) All outcomes ‐ <20% drop‐outs? | Low risk | Dropout varies from 8% to 18% |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis performed? | Low risk | ITT analysis performed |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics? | Low risk | Baseline comparable |
| Co‐interventions avoided? | Low risk | Co‐interventions were avoided |
| Compliance acceptable ? | Low risk | Compliance was assessed |
| Timing outcome assessment comparable? | Low risk | Timing was comparable |
Voerman 2007.
| Methods | RCT; no info on randomisation procedure | |
| Participants | Female computer workers; age > 45. Prevalent non‐specific neck/shoulder complaints; n = 79 | |
| Interventions |
Mfb: Ergonomic counselling + Myofeedback: Cinderella‐based myofeedback on top of EC; four weeks for at least eight hours a week; n = 42 EC: Ergonomic counselling: diary, workplace investigation according to checklist, weekly visit by therapist; n = 37 Follow‐up three and six months |
|
| Outcomes | Pain intensity (VAS), pain disability (Pain Disability Index) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Block randomization was used to assign subjects.." Inadequate detail given to randomisation method |
| Allocation concealment (selection bias) | Unclear risk | Unclear whether allocation was concealed |
| Blinding of participants? | High risk | Participant was not blinded to intervention |
| Blinding of caregivers? | High risk | Caregivers were not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Participant was outcome assessor and was not blinded to intervention |
| Incomplete outcome data (attrition bias) All outcomes ‐ <20% drop‐outs? | Low risk | 14/79 (approximately 18%) dropouts |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis performed? | Unclear risk | Unclear whether dropouts were included in analysis |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics? | Low risk | Baseline comparable: see Table 1 and Table 2 |
| Co‐interventions avoided? | Unclear risk | Co‐interventions were not addressed |
| Compliance acceptable ? | Unclear risk | Compliance was partly assessed |
| Timing outcome assessment comparable? | Low risk | Timing was comparable |
Waling 2000.
| Methods | RCT; group randomisation; women choose a group (?) | |
| Participants | Chronic (> 12 months) neck/shoulder complaints (non‐specific); female employees; n = 126 (103). Work ‘contributed’ to the disorder | |
| Interventions |
I1: Coordination training: body awareness therapy; n = 31 (25) I2: Strength exercises: in a fitness centre with four different exercises; n = 34 (29) I3: Endurance training: arm cycling on an arm ergometer; n = 34 (28) C: Controls: discussion + stress management; n = 27 (21) Ten weeks, three sessions/wk |
|
| Outcomes | Pain (VAS), trigger points (algometer), function (Q), satisfaction (Q) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Unclear randomisation procedure |
| Allocation concealment (selection bias) | Unclear risk | Unclear whether allocation was concealed |
| Blinding of participants? | Unclear risk | Unclear |
| Blinding of caregivers? | Unclear risk | Unclear |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Unclear whether outcome assessment was blinded |
| Incomplete outcome data (attrition bias) All outcomes ‐ <20% drop‐outs? | High risk | 20/82 dropouts (> 20%) |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis performed? | Low risk | ITT analysis |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics? | Low risk | Baseline comparable |
| Co‐interventions avoided? | Unclear risk | Co‐interventions were not addressed |
| Compliance acceptable ? | Low risk | Compliance acceptable |
| Timing outcome assessment comparable? | Low risk | Timing was comparable |
Werner 2005.
| Methods | RCT; randomisation based on the last digit of Social Security number (odd or even) | |
| Participants | Active workers with carpal tunnel syndrome; n = 161 | |
| Interventions |
Splint and video education: Customised wrist splints, which were worn at night for six weeks + ergonomic education; n = 86 Video education: ergonomic education alone by viewing a 20‐minute video on CTS and ergonomic risk factors; n = 75 Follow‐up: three, six and 12 months |
|
| Outcomes | Pain (VAS), symptom severity scale | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Odd or even last digit Social Security number |
| Allocation concealment (selection bias) | Unclear risk | Unclear whether allocation was concealed |
| Blinding of participants? | High risk | Participant not blinded |
| Blinding of caregivers? | Unclear risk | Unclear |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Primary outcome was self‐reported symptom severity scale; participants were not blinded |
| Incomplete outcome data (attrition bias) All outcomes ‐ <20% drop‐outs? | High risk | Inadequate description of reasons for dropout. 112/161 dropouts = 30% |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis performed? | High risk | 49 of original 161 randomly assigned participants not included in final analysis. Figure 1: almost half of participants did not complete three‐ and six‐month questionnaires |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics? | Low risk | Baseline comparable: see Table 1 |
| Co‐interventions avoided? | Unclear risk | Not clear whether participants were monitored for co‐interventions or were asked to avoid |
| Compliance acceptable ? | Unclear risk | Unclear whether compliance was acceptable |
| Timing outcome assessment comparable? | High risk | Timing not comparable: 12 months of follow‐up; ranged from seven to 15 months |
Ylinen 2003.
| Methods | RCT; concealed randomisation: blinded block randomisation | |
| Participants | Chronic neck pain (> six months); female office workers recruited from occupational health care services; n = 180. Work‐related complaints | |
| Interventions |
Strength exercises: 12‐Day consecutive institutional rehabilitation period; used an elastic rubber band (Theraband) to train the neck flexor muscles in each session; n = 60 Endurance training: 12‐Day consecutive institutional rehabilitation period; exercised neck flexor muscles by lifting the head up from the supine position in three series of 20 repetitions; n = 60 Controls: home stretching exercises; n = 60 Both training groups also underwent a multi‐modal rehabilitation programme, which included relaxation training, aerobic training and behavioural support to reduce fear of pain and improve exercise motivation, as well as lectures and practical exercises in ergonomics Five sessions/wk, nine sessions in total, one‐month intervals during 12 months |
|
| Outcomes | Neck pain (VAS), disability (Q), depression, neck muscle strength, ROM | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Block randomization into 3 grps of 10 persons was performed blind… from each block 1 patient was randomized to 1 of the 2 training groups or to control group"; unclear procedure |
| Allocation concealment (selection bias) | Low risk | Block randomisation was performed blind |
| Blinding of participants? | Unclear risk | Unclear blinding |
| Blinding of caregivers? | Unclear risk | Unclear blinding |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Self‐reported outcome assessment; unclear blinding |
| Incomplete outcome data (attrition bias) All outcomes ‐ <20% drop‐outs? | Low risk | Only three of 180 did not complete programme (< 20%) |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis performed? | Low risk | ITT analysis performed |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics? | Low risk | Baseline similarity |
| Co‐interventions avoided? | Low risk | Groups given similar advice and other activities monitored by diaries |
| Compliance acceptable ? | Low risk | Training adherence 86%, 93% and 65% for three groups based on training diaries |
| Timing outcome assessment comparable? | Low risk | Timing comparable |
Ylinen 2007.
| Methods | RCT; examiner‐blinded randomised cross‐over trial | |
| Participants | Health services; female office workers with non‐specific neck pain; n = 125 | |
| Interventions |
Manual therapy, mobilisation and massage twice a week. No manipulation (i.e. high‐velocity thrusts with low amplitude were applied); n = 62 Stretching exercises, five times a week; n = 63 Treatment: four weeks; cross‐over after four weeks; follow‐up: 12 weeks |
|
| Outcomes | Benefit, pain (VAS), average and night time, disability (NSPD, NDI) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Tossing a coin |
| Allocation concealment (selection bias) | Unclear risk | Randomisation was performed by a person who had not seen the participants, but we do not know whether they had access to information about the participant |
| Blinding of participants? | Unclear risk | No information on blinding procedures |
| Blinding of caregivers? | Unclear risk | No information on blinding procedures |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information on blinding procedures |
| Incomplete outcome data (attrition bias) All outcomes ‐ <20% drop‐outs? | Low risk | Only two dropouts; therefore < 20%; they were not described |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis performed? | Unclear risk | Unable to tell from results what numbers were used in analysis |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics? | Low risk | Baseline comparable: see Table 1 |
| Co‐interventions avoided? | Unclear risk | Unclear whether co‐interventions were avoided |
| Compliance acceptable ? | Unclear risk | Unclear whether compliance was acceptable |
| Timing outcome assessment comparable? | Low risk | Timing was comparable |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Frost 2007 | No patients, mainly healthy people |
| Galinsky 2007 | No patients, only healthy people |
| Garg 2010 | No work‐relatedness |
| Huis in't Veld 2007 | Not an RCT |
| Michalsen 2009 | No work‐relatedness |
| Robertson 2013 | No patients, only healthy people |
| Shiri 2013 | No data separately on participants with upper extremity disorders |
| Spekle 2010 | Patients as well as healthy people were included; no subgroup analysis on participants |
| Tveito 2009 | No patients, only healthy people |
| von Thiele Schwarz 2008 | No patients, only healthy people |
| Zebis 2011 | No patients, only healthy people |
Characteristics of ongoing studies [ordered by study ID]
Sundstrup 2013.
| Trial name or title | Sundstrup 2013 |
| Methods | RCT |
| Participants | Slaughterhouse workers |
| Interventions | Strength training; participatory ergonomics |
| Outcomes | Pain; disability |
| Starting date | Unclear |
| Contact information | E Sundstrup |
| Notes | Protocol published in February 2013 |
Contributions of authors
APV, SMAB‐Z, AB, HCWdV and BWK are responsible for drafting the protocol. The search was performed by APV, SMS, HCWdV and BWK, and selection of the studies and data extraction by APV, SMS and SMAB‐Z. APV and AB are responsible for the analysis. All authors are responsible for the interpretation of results and for the final draft of the review.
Sources of support
Internal sources
-
Erasmus Medical Centre, University, Netherlands.
Salary and time to enable the review authors to perform the review
External sources
No sources of support supplied
Declarations of interest
None known.
New
References
References to studies included in this review
Abasolo 2005 {published data only}
- Abasolo L, Blanco M, Bachiller J, Candelas G, Collado P, Lajas C, et al. A health system program to reduce work disability related to musculoskeletal disorders. Annals of Internal Medicine 2005;143:404‐14. [DOI] [PubMed] [Google Scholar]
- Abasolo L, Carmona L, Hernandez‐Garcia C, Lajas C, Loza E, Blanco M, et al. Musculoskeletal work disability for clinicians: time course and effectiveness of specialized intervention program by diagnosis. Arthritis & Rheumatism 2007;57:335‐42. [DOI] [PubMed] [Google Scholar]
Andersen 2008a {published data only}
- Andersen LL, Andersen JL, Suetta C, Kjær M, Sjøgaard K, Sjøgaard G. Effect of contrasting physical exercise interventions on rapid force capacity of chronically painful muscles. Journal of Applied Physiology 2009;107:1413‐9. [DOI] [PubMed] [Google Scholar]
- Andersen LL, Kjær M, Sjøgaard K, Hansen L, Kryger AI, Sjøgaard G. Effect of two contrasting types of physical exercise on chronic neck muscle pain. Arthritis & Rheumatism 2008a;59:84‐91. [DOI] [PubMed] [Google Scholar]
Andersen 2008b {published data only}
- Andersen LL, Christensen KB, Holtermann A, Poulsen OM, Sjøgaard G, Pedersen MT, et al. Effect of physical exercise interventions on musculoskeletal pain in all body regions among office workers: a one year randomized controlled trial. Manual Therapy 2010;15:100‐4. [DOI] [PubMed] [Google Scholar]
- Andersen LL, Jørgensen MB, Blangsted AK, Pedersen MT, Hansen EA, Sjøgaard G. A randomized controlled intervention trial to relieve and prevent neck/shoulder pain. Medicine and Science in Sports and Exercise 2008b;40;983‐90:3‐9. [DOI] [PubMed] [Google Scholar]
- Blangsted AK, Sjøogaard K, Hansen EA, Hannerz H, Sjøgaard G. One‐year randomized controlled trial with different physical‐activity programs to reduce musculoskeletal symptoms in the neck and shoulders among office workers. Scandinavian Journal of Work, Environment and Health 2008;34:55–65. [DOI] [PubMed] [Google Scholar]
- Pedersen MT, Blangsted AK, Andersen LL, Jørgensen MB, Hansen EA, Sjøgaard G. The effect of work site physical activity intervention on physical capacity, health, and productivity: a 1‐year randomized controlled trial.. Journal of Occupational and Environmental Medicine 2009;51:759‐70. [DOI] [PubMed] [Google Scholar]
Bang 2000 {published data only}
- Bang MD, Deyle GD. Comparison of supervised exercise with and without manual physical therapy for patients with shoulder impingement syndrome. Journal of Orthopaedic and Sports Physical Therapy 2000;30:126‐37. [DOI] [PubMed] [Google Scholar]
Bernaards 2006 {published data only}
- Bernaards CM, Ariëns GAM, Hildebrandt VH. The (cost‐)effectiveness of a lifestyle physical activity intervention in addition to a work style intervention on the recovery from neck and upper limb symptoms in computer workers; study protocol. BMC Musculoskeletal Disorders 2006;7:80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernaards CM, Ariëns GAM, Knol DL, Hildebrandt VH. The effectiveness of a work style intervention and a life style physical activity intervention on the recovery from neck and upper limb symptoms in computer workers. Pain 2007;132:142‐53. [DOI] [PubMed] [Google Scholar]
- Bernaards CM, Ariëns GAM, Simons M, Knol DL, Hildebrandt VH. Improving work style behavior in computer workers with neck and upper limb symptoms. Journal of Occupational Rehabilitation 2008;18:87‐101. [DOI] [PubMed] [Google Scholar]
- Bernaards CM, Bosmans JE, Hildebrandt VH, Tulder MW, Heymans MW. The cost‐effectiveness of a lifestyle physical activity intervention in addition to a work style intervention on recovery from neck and upper limb symptoms and pain reduction in computer workers. Occupational and Environmental Medicine 2011;68:265‐72. [DOI] [PubMed] [Google Scholar]
Bru 1994 {published data only}
- Bru E, Mykletun RJ, Berge WT, Svebak S. Effects of different psychosocial interventions on neck, shoulder and low back pain in female hospital staff. Psychology and Health 1994;9:37:82. [DOI] [PubMed] [Google Scholar]
Cheng 2007 {published data only}
- Cheng ASK, Hung LK. Randomized controlled trial of workplace‐based rehabilitation for work‐related rotator cuff disorder. Journal of Occupational Rehabilitation 2007;17:487‐503. [DOI] [PubMed] [Google Scholar]
Dellve 2011 {published data only}
- Dellve L, Ahlström L, Jonsson A, Sandsjö L, Forsman M, Lindegård A, et al. Myofeedback training and intensive muscular strength training to decrease pain and improve work ability among female workers on long‐term sick leave with neck pain: a randomized controlled trial. International Archives of Occupational and Environmental Health 2011;84:335–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
Esmaeilzadeh 2012 {published data only}
- Esmaeilzadeh S, Ozcan E, Capan N. Effects of ergonomic intervention on work‐related upper extremity musculoskeletal disorders among computer workers: a randomized controlled trial. Internatinal Archives of Occupational and Environmental Health 2012;Dec 23:epub. [DOI] [PubMed] [Google Scholar]
Ferguson 1976 {published data only}
- Ferguson D, Duncan J. A trial of physiotherapy for symptoms in keyboard operating. Australian Journal of Physiotherapy 1976;22:61‐72. [DOI] [PubMed] [Google Scholar]
Goldman 2010 {published data only}
- Goldman RH, Stason WB, Park SK, Kim R, Mudgal S, Davis RB, et al. Low‐dose amitriptyline for treatment of persistent arm pain due to repetitive use. Pain 2010;149:117‐23. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hagberg 2000 {published data only}
- Hagberg M, Harms‐Ringdahl K, Nisell R, Hjelm EW. Rehabilitation of neck‐shoulder pain in woman industrial workers: a randomized trial comparing isometric shoulder endurance training with isometric shoulder strength training. Archives of Physical Medicine and Rehabilitation 2000;81:1051‐8. [DOI] [PubMed] [Google Scholar]
Heuvel 2003 {published data only}
- Heuvel SG van den, Looze MP, Hildebrandt VH, Thé KH. Effects of software programs stimulating regular breaks and exercises on work‐related neck and upper‐limb disorders. Scandinavian Journal of Work, Environmeant and Health 2003;29:106‐16. [DOI] [PubMed] [Google Scholar]
Kamwendo 1991 {published data only}
- Kamwendo K, Linton SJ. A controlled study of the effect of neck school in medical secretaries. Scandinavian Journal of Rehabilitation Medicine 1991;23:143‐52. [PubMed] [Google Scholar]
Ketola 2002 {published data only}
- Ketola R. Physical workload as a risk factor for symptoms in the neck and upper limbs: exposure assessment and ergonomic intervention. Journal of Sports Science and Medicine 2004;3:1‐46. [Google Scholar]
- Ketola R, Toivonen R, Häkkänen M, Luukkonen R, Takala EP, Viikari‐Juntura E. Effects of ergonomic intervention in work with video display units. Scandinavian Journal of Work, Environment and Health 2002;28:18‐24. [DOI] [PubMed] [Google Scholar]
Leboeuf 1987 {published data only}
- Leboeuf C, Grant BR, Maginnes GS. Chiropractic treatment of repetitive strain injuries: a preliminary prospective outcome study of SMT versus SMT combined with massage. Journal of Australian Chiropractors Association 1987;17:11‐4. [Google Scholar]
Levoska 1993 {published data only}
- Levoska A, Keinänen‐Kiukaanniemi S. A comparison of two treatment methods with a 1‐year follow‐up. Archives of Physical Medicine and Rehabilitation 1993;74:425‐30. [PubMed] [Google Scholar]
Lundblad 1999 {published data only}
- Lundblad I, Elert J, Gerdle B. Randomised controlled trial of physiotherapy and Feldenkrais interventions in female workers with neck‐shoulder complaints. Journal of Occupational Rehabilitation 1999;9:179‐94. [Google Scholar]
Ma 2011 {published data only}
- Ma C, Szeto GP, Yan T, Wu S, Lin C, Li L. Comparing Biofeedback With Active Exercise and Passive Treatment for the Management of Work‐Related Neck and Shoulder Pain: A Randomized Controlled Trial. Archives of Physical Medicine and Rehabilitation 2011;92:849‐58. [DOI] [PubMed] [Google Scholar]
Marangoni 2010 {published data only}
- Marangoni AH. Effects of intermittent stretching exercises at work on musculoskeletal pain associated with the use of a personal computer and the influence of media on outcome. Work 2010;36:27‐37. [DOI] [PubMed] [Google Scholar]
Martimo 2010 {published data only}
- Martimo KP, Shiri R, Miranda H, Ketola R, Varonen H, Viikari‐Juntura E. Effectiveness of an ergonomic intervention on the productivity of workers with upper extremity disorders; a randomized controlled trial. Scandinavian Journal of Work, Environment and Health 2010;36:25‐33. [DOI] [PubMed] [Google Scholar]
- Shiri R, Martimo KP, Miranda H, Ketola R, Kaila‐Kangas L, Liira H, et al. The effect of workplace intervention on pain and sickness absence caused by upper‐extremity musculoskeletal disorders. Scandinavian Journal of Work, Environment and Health 2011;37:120‐8. [DOI] [PubMed] [Google Scholar]
Meijer 2006 {published data only}
- Meijer EM, Sluiter JK, Heyma A, Sadiraj K, Frings‐Dresen MHW. Cost‐effectiveness of multidisciplinary treatment in sick‐listed patients with upper extremity musculoskeletal disorders: a randomized, controlled trial with one‐year follow‐up. International Archives of Occupational and Environmental Health 2006;79:654‐64. [DOI] [PubMed] [Google Scholar]
Moore 1996 {published data only}
- Moore LE, Wiesner SL. Hypnotically‐inducted vasodilation in the treatment of repetitive strain injuries. American Journal of Clinical Hypnosis 1996;39(2):97‐104. [DOI] [PubMed] [Google Scholar]
Nourbakhsh 2008 {published data only}
- Nourbakhsh MR, Fearon FJ. An alternative approach to treating epicondylitis; a randomised, placebo‐controlled, double‐blinded study. Clinical Rehabilitation 2008;22:601‐9. [DOI] [PubMed] [Google Scholar]
Omer 2003 {published data only}
- Omer SR, Ozcan E, Karan A, Ketenci A. Musculoskeletal system disorders in computer users: effectiveness of training and exercise programs. Journal of Back and Musculoskeletal Rehabilitation 2003/2004;17:9‐13. [Google Scholar]
Rempel 1999 {published data only}
- Rempel D, Tittiranonda P, Burastero S, Hudes M, So Y. Effect of keyboard keyswitch design on hand pain. Journal of Occupational and Environmental Medicine 1999;41:111‐9. [DOI] [PubMed] [Google Scholar]
Rempel 2007 {published data only}
- Rempel DM, Wang P‐C, Janowitz I, Harrison RJ, Yu F, Ritz BR. A randomized controlled trial evaluating the effects of a new task chair on shoulder and neck pain among sewing machine operators. Spine 2007;32:931‐8. [DOI] [PubMed] [Google Scholar]
- Wang PC, Harrison RJ, Yu F, Rempel DM, Ritz BR. Follow‐up of neck and shoulder pain among sewing machine operators: The Los Angeles garment study. American Journal of Industrial Medicine 2010;52:352‐60. [DOI] [PubMed] [Google Scholar]
Ripat 2006 {published data only}
- Ripat J, Scatliff T, Giesvrecht E, Quanbury A, Friesen M, Kelso S. The effect of alternate style keyboards on severity of symptoms and functional status of individuals with work related upper extremity disorders. Journal of Occupational Rehabilitation 2006;16:707‐18. [DOI] [PubMed] [Google Scholar]
Sandsjö 2010 {published data only}
- Sandsjö L, Larsman P, Huis in’t Veld R, Vollenbroek‐Hutten MMR. Clinical evaluation of a myofeedback‐based teletreatment service applied in the workplace: a randomized controlled trial. Journal of Telemedicine and Telecare 2010;16:329‐35. [DOI] [PubMed] [Google Scholar]
Sjögren 2005 {published data only}
- Sjögren T, Nissinen KJ, Järvenpää SK, Ojanen MT, Vanharanta H, Mälkiä EA. Effects of a workplace physical exercise intervention on the intensity of headache and neck and shoulder symptoms and upper extremity muscular strength of office workers: a cluster randomized controlled cross‐over trial. Pain 2005;116:119‐28. [DOI] [PubMed] [Google Scholar]
Spence 1989 {published data only}
- Spence SH. Cognitive‐behavior therapy in the management of chronic, occupational pain of the upper limbs. Behaviour Research and Therapy 1989;27:435‐46. [DOI] [PubMed] [Google Scholar]
- Spence SH. Cognitive‐behavior therapy in the treatment of chronic, occupational pain of the upper limbs: a 2 year follow‐up. Behaviour Research and Therapy 1991;29:503‐9. [DOI] [PubMed] [Google Scholar]
Spence 1995 {published data only}
- Spence SH, Sharpe L, Newton‐John T, Champion D. Effect of EMG Biofeedback compared to applied relaxation training with chronic, upper extremity cumulative trauma disorders. Pain 1995;63:199‐206. [DOI] [PubMed] [Google Scholar]
Stralka 1998 {published data only}
- Stralka SW, Jackson JA, Lewis AR. Treatment of hand and wrist pain. A randomized clinical trial of high voltage pulsed, direct current built into a wrist splint. American Association of Occupational Health Nurses Journal 1998;46:233‐6. [PubMed] [Google Scholar]
Szcurko 2009 {published data only}
- Szcurko O, Cooley K, Mills EJ, Zhou Q, Perri D, Seely D. Naturopathic treatment of rotator cuff tendinitis among Canadian postal workers: a randomized controlled trial. Arthritis & Rheumatism 2009;8:1037‐45. [DOI] [PubMed] [Google Scholar]
Takala 1994 {published data only}
- Takala EP, Viikari‐Juntura E, Tynkkynen EM. Does group gymnastics at the workplace help in neck pain? A controlled study. Scandinavian Journal of Rehabilitation Medicine 1994;26:17‐20. [PubMed] [Google Scholar]
Tittiranonda 1999 {published data only}
- Tittiranonda P, Rempel D, Armstrong T, Burastero S. Effect of four computer keyboards in computer users with upper extremity musculoskeletal disorders. American Journal of Industrial Medicine 1999;35:647‐61. [DOI] [PubMed] [Google Scholar]
van Eijsden 2008 {published data only}
- Eijsden MD, Gerhards SA, Bie RA, Severens JL. Cost‐effectiveness of postural exercise therapy versus physiotherapy in computer screen‐workers with early non‐specific work‐related upper limb disorders (WRULD); a randomized controlled trial. Trials 2009;10:103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eijsden MD, Staal BJ, Attekum A, Bie RA, Heuvel WJA. No difference between postural exercises and strength and fitness exercises for early, non‐specific, work‐related upper limb disorders in visual display unit workers: a randomised trial. Australian Journal of Physiotherapy 2008;54:95‐101. [DOI] [PubMed] [Google Scholar]
Vasseljen 1995 {published data only}
- Vasseljen O jr, Johansen BM, Westgaard RH. The effect of pain reduction on perceived tension and EMG‐recorded trapezius muscle activity in workers with shoulder and neck pain. Scandinavian Journal of Rehabilitation Medicine 1995;27:243‐52. [PubMed] [Google Scholar]
Viljanen 2003 {published data only}
- Viljanen M, Malmivaara A, Uitti J, Rinne M, Palmroos, Laippala P. Effectiveness of dynamic muscle training, relaxation training, or ordinary activity for chronic neck pain: randomized controlled trial. BMJ 2003;327:457. [DOI] [PMC free article] [PubMed] [Google Scholar]
Voerman 2007 {published data only}
- Voerman GE, Sandsjö L, Vollenbroek‐Hutten MMR, Larsman P, Kadefors R, Hermens HJ. Changes in cognitive‐behavioural factors and muscle activation patterns after interventions for work‐related neck‐shoulder complaints; relations with discomfort and disability. Journal of Occupational Rehabilitation 2007b;17:593‐609. [DOI] [PubMed] [Google Scholar]
- Voerman GE, Sandsjö L, Vollenbroek‐Hutten MMR, Larsman P, Kadefors R, Hermens HJ. Effects of ambulant myofeedback training and ergonomic counselling in female computer workers with work‐related neck‐shoulder complaints: A randomized controlled trial. Journal of Occupational Rehabilitation 2007a;17:137‐52. [DOI] [PMC free article] [PubMed] [Google Scholar]
Waling 2000 {published data only}
- Ahlgren C, Waling K, Kadi F, Djupsjöbacka M, Thornell LE, Sundelin G. Effects of physical performance and pain from three dynamic training programs for women with work‐related trapezius myalgia. Journal of Rehabilitation Medicine 2001;33:162‐9. [PubMed] [Google Scholar]
- Waling K, Järvholm B, Sundelin G. Effects of training on female trapezius myalgia; an intervention study with a 3‐year follow‐up period. Spine 2002;27:789‐96. [DOI] [PubMed] [Google Scholar]
- Waling K, Sundeling G, Ahlgren C, Järvholm B. Perceived pain before and after three exercise programs; a controlled clinical trial of women with work‐related trapezius myalgia. Pain 2000;85:201‐7. [DOI] [PubMed] [Google Scholar]
Werner 2005 {published data only}
- Werner RA, Franzblau A, Gell N. Randomized controlled trial of nocturnal splinting for active workers with symptoms of carpal tunnel syndrome. Archives of Physical Medicine and Rehabilitation 2005;86:1‐7. [DOI] [PubMed] [Google Scholar]
Ylinen 2003 {published data only}
- Nikander R, Mälkiä E, Parkkari J, Heinonen A, Starck H, Ylinen J. Dose‐response relationship of specific training to reduce chronic neck pain and disability. Medicine & Science in Sports & Exercise 2006;12:2068‐74. [DOI] [PubMed] [Google Scholar]
- Ylinen J, Takala EP, Nykänen M, Häkkinen A, Mälkiä E, Pohjolainen T, et al. Active neck muscle training in the treatment of chronic neck pain in woman; a randomised controlled trial. JAMA 2003;289:2509‐16. [DOI] [PubMed] [Google Scholar]
Ylinen 2007 {published data only}
- Ylinen J, Kautiainen H, Wiren K, Häkkinen A. Stretching exercises versus manual therapy in treatment of chronic neck pain: a randomized controlled cross‐over trial. Journal of Rehabilitation Medicine 2007;39:126‐32. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Frost 2007 {published data only}
- Frost P, Haahr JP, Andersen JH. Reduction of Pain‐Related Disability in Working Populations. A Randomized Intervention Study of the Effects of an Educational Booklet Addressing Psychosocial Risk Factors and Screening Workplaces for Physical Health Hazards. Spine 2007;32(18):1949–54. [DOI] [PubMed] [Google Scholar]
Galinsky 2007 {published data only}
- Galinsky T, Swanson N, Sauter S, Dunkin R, Hurrell J, Lawrence Schleifer L. Supplementary Breaks and Stretching Exercises for Data Entry Operators: A Follow‐Up Field Study. American Journal of Industrial Medicine 2007;50:519‐27. [DOI] [PubMed] [Google Scholar]
Garg 2010 {published data only}
- Garg R, Adamson GJ, Dawson PA, Shankwiler JA, Pink MM. A prospective randomized study comparing a forearm strap brace versus a wrist splint for the treatment of lateral epicondylitis. Journal of Shoulder and Elbow Surgery 2010;19:508‐12. [DOI] [PubMed] [Google Scholar]
Huis in't Veld 2007 {published data only}
- Huis in ’t Veld RMHA, Vollenbroek‐Hutten MMR, Groothuis‐Oudshoorn KCGM, Hermens HJ. The Role of the Fear‐avoidance Model in Female WorkersWith Neck‐shoulder Pain related to Computer Work. Clinical Journal of Pain 2007;23:28–34. [DOI] [PubMed] [Google Scholar]
Michalsen 2009 {published data only}
- Michalsen A, Bock S, Ludtke R, Rampp T, Baecker M, Bachmann J, Langhorst J, Musial F, Dobos GJ. Effects of Traditional Cupping Therapy in Patients With CarpalTunnel Syndrome: A Randomized Controlled Trial. The Journal of Pain 2009;10(6):601‐8. [DOI] [PubMed] [Google Scholar]
Robertson 2013 {published data only}
- Robertson MM, Ciriello VM, Garabet AM. Office ergonomics training and a sit‐stand workstation: effects on musculoskeletal and visual symptoms and performance of office workers. Applied Ergonomics 2013;44(1):73‐85. [DOI] [PubMed] [Google Scholar]
Shiri 2013 {published data only}
- Shiri R, Kausto J, Martimo KP, Kaila‐Kangas L, Takala EP, Viikari‐Juntura E. Health‐related effects of early part‐time sick leave due to musculoskeletal disorders: a randomized controlled trial. Scandinavian Journal of Work and Environmenatl Health 2013;39(1):37‐45. [DOI] [PubMed] [Google Scholar]
Spekle 2010 {published data only}
- Speklé EM, Hoozemans MJM, Blatter BM, Heinrich J, Beek AJ, Knol DL, Bongers PM, Dieën JH. Effectiveness of a questionnaire based intervention programme on the prevalence of arm, shoulder and neck symptoms, risk factors and sick leave in computer workers: A cluster randomised controlled trial in an occupational setting. BMC Musculoskeletal Disorders 2010;11:99. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tveito 2009 {published data only}
- Tveito TH, Eriksen HR. Integrated health programme: a workplace randomized controlled trial. Journal of Advanced Nursing 2009;65(1):110–9. [DOI] [PubMed] [Google Scholar]
von Thiele Schwarz 2008 {published data only}
- Thiele Schwarz U, Lindfors P, Lundberg U. Health‐related effects of worksite interventions involving physical exercise and reduced workhours. Scandinavian Journal of Work and Environmental Health 2008;34(3):179–88. [DOI] [PubMed] [Google Scholar]
Zebis 2011 {published data only}
- Zebis MK, Andersen LL, Pedersen MT, Mortensen P, Andersen CH, Pedersen MM, Boysen M, Roessler KK, Hannerz H, Mortensen OS, Sjøgaard G. Implementation of neck/shoulder exercises for pain relief among industrial workers:A randomized controlled trial. BMC Musculoskeletal Disorders 2011;12:205. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to ongoing studies
Sundstrup 2013 {published data only}
- Sundstrup E, Jakobsen MD, Andersen CH, Jay K, Persson R, Aagaard P, Andersen LL. Participatory ergonomic intervention versus strength training on chronic pain and work disability in slaughterhouse workers: study protocol for a single‐blind, randomized controlled trial. BMC Musculoskeletal Disorders 2013;Feb 21;14:67. [DOI] [PMC free article] [PubMed] [Google Scholar]
Additional references
Armstrong 1993
- Armstrong TJ, Buckle P, Fine LJ, Hagberg M, Jonsson B, Kilbom A, et al. A conceptual model for work‐related neck and upper‐limb musculoskeletal disorders. Scandinavian Journal of Work, Environment & Health 1993;19(2):73‐84. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Beurskens 1996
- Beurskens AJ, Vet HC, Koke AJ. Responsiveness of functional status in low back pain: a comparison of different instruments. Pain 1996;65(1):71‐6. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Boocock 2009
- Boocock MG, Collier JM, McNair PJ, Simmonds M, Larmer PJ, Armstrong B. A framework for the classification and diagnosis of work‐related upper extremity conditions: systematic review. Seminars in Arthritis & Rheumatism 2009;38(4):296‐311. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Campbell 2001
- Campbell MK, Mollison J, Grimshaw JM. Cluster trials in implementation research: estimation of intracluster correlation coefficients and sample size. Statistics in Medicine 2001;20(3):391‐9. [DOI] [PubMed] [Google Scholar]
de Bruin 1994
- Bruin AF, Diederiks JP, Witte LP, Stevens FC, Philipsen H. The development of a short generic version of the Sickness Impact Profile. Journal of Clinical Epidemiology 1994;47(4):407‐18. [DOI] [PubMed] [Google Scholar]
Feleus 2007
- Feleus A, Bierma‐Zeinstra SM, Miedema HS, Verhagen AP, Nauta AP, Burdorf A, et al. Prognostic indicators for non‐recovery of non‐traumatic complaints at arm, neck and shoulder in general practice ‐ 6 months follow‐up. Rheumatology 2007;46(1):169‐76. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Fries 1982
- Fries JF, Spitz PW, Young DY. The dimensions of health outcomes: the health assessment questionnaire, disability and pain scales. Journal of Rheumatology 1982;9(5):789‐93. [MEDLINE: ] [PubMed] [Google Scholar]
Furlan 2009
- Furlan AD, Pennick V, Bombardier C, Tulder M, from the Editorial Board of the Cochrane Back Review Group. 2009 updated method guidelines for systematic reviews in the Cochrane Back Review Group. Spine 2009;34(18):1929‐41. [DOI] [PubMed] [Google Scholar]
GRADE 2004
- Grade Working Group. Grading quality of evidence and strength of recommendations. BMJ 2004;328(7454):1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
GRADEpro 2008 [Computer program]
- Brozek J, Oxman A, Schünemann H. GRADEpro. Version 3.2 for Windows. GRADE working group, 2008.
Higgins 2011
- Higgins JPT, Altman DG (editors). Chapter 8: Assessing risk of bias in included studies. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. www.cochrane‐handbook.org.
HSE 2010
- Health and Safety Executive (HSE). Musculoskeletal disorders. http://www.hse.gov.uk/statistics/causdis/musculoskeletal/uln.htm (accessed 27 July 2010).
Hudak 1996
- Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand) [corrected]. The Upper Extremity Collaborative Group (UECG). American Journal of Industrial Medicine 1996;29(6):602‐8. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
IJmker 2007
- IJmker S, Huysmans MA, Blatter BM, Beek AJ, Mechelen W, Bongers PM. Should office workers spend fewer hours at their computer? A systematic review of the literature. Occupational & Environmental Medicine 2007;64(4):211‐22. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Karels 2007
- Karels CH, Bierma‐Zeinstra SM, Burdorf A, Verhagen AP, Nauta AP, Koes BW. Social and psychological factors influenced the course of arm, neck and shoulder complaints. Journal of Clinical Epidemiology 2007;60(8):839‐48. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Kerns 1985
- Kerns RD, Turk DC, Rudy TE. The West Haven‐Yale Multidimensional Pain Inventory (WHYMPI). Pain 1985;23(4):345–56. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Lau 1997
- Lau J, Ioannidis JP, Schmid CH. Quantitative synthesis in systematic reviews. Annals of Internal Medicine 1997;127(9):820‐6. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Lefebvre 2009
- Lefebvre C, Manheimer E, Glanville J. Chapter 6: Searching for studies In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. www.cochrane‐handbook.org.
Melhorn 1998
- Melhorn JM. Cumulative trauma disorders and repetitive strain injuries. The future. Clinical Orthopaedics & Related Research 1998;(351):107‐26. [MEDLINE: ] [PubMed] [Google Scholar]
Pilligan 2000
- Piligian G, Herbert R, Hearns M, Dropkin J, Landsbergis P, Cherniack M. Evaluation and management of chronic work‐related musculoskeletal disorders of the distal upper extremity. American Journal of Industrial Medicine 2000;37(1):75‐93. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
RevMan 2011 [Computer program]
- The Nordic Cochrane Centre. The Cochrane Collaboration. Review Manager (RevMan). Version 5.1. Copenhagen: The Nordic Cochrane Centre. The Cochrane Collaboration, 2011.
Roquelaure 2009
- Roquelaure Y, Ha C, Rouillon C, Fouquet N, Leclerc A, Descatha A, et al. Risk factors for upper‐extremity musculoskeletal disorders in the working population. Arthritis and Rheumatism 2009;61(10):1425‐34. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Shanahan 2006
- Shanahan EM, Jezukaitis P. Work related upper limb disorders. Australian Family Physician 2006;35(12):946‐50. [MEDLINE: ] [PubMed] [Google Scholar]
Smidt 2005
- Smidt N, Vet HC, Bouter LM, et al. Exercise Therapy Group. Effectiveness of exercise therapy: a best‐evidence summary of systematic reviews. Australian Journal of Physiotherapy 2005;51:71‐85. [DOI] [PubMed] [Google Scholar]
Sriwatanakul 1983
- Sriwatanakul K, Kelvie W, Lasagna L, Calimlim JF, Weis OF, Mehta G. Studies with different types of visual analog scales for measurement of pain. Clinical Pharmacology & Therapeutics 1983;34(2):234‐9. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Staal 2007
- Staal JB, Bie RA, Hendriks EJ. Aetiology and management of work‐related upper extremity disorders. Best Practice & Research Clinical Rheumatology 2007;21(1):123‐33. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Tulder 2007
- Tulder M, Malmivaara A, Koes B. Repetitive strain injury. Lancet 2007;369(9575):1815‐22. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Verhagen 1998
- Verhagen AP, Vet HCW, Bie RA, Kessels AGH, Boers M, Bouter LM, et al. The Delphi list: a criteria list for quality assessment of randomised clinical trials for conducting systematic reviews developed by Delphi consensus. Journal of Clinical Epidemiology 1998;51:1235‐41. [DOI] [PubMed] [Google Scholar]
Von Korff 2000
- Korff M, Jensen MP, Karoly P. Assessing global pain severity by self‐report in clinical and health services research. Spine 2000;25(24):3140‐51. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Ware 1992
- Ware JE Jr, Sherbourne CD. The MOS 36‐item short‐form health survey (SF‐36). I. Conceptual framework and item selection. Medical Care 1992;30(6):473‐83. [PubMed] [Google Scholar]
Williams 1990
- Williams A. EuroQol ‐ a new facility for the measurement of health‐related quality of life. The EuroQol Group. Health Policy 1990;16(3):199‐208. [EMBASE: 1991010271] [DOI] [PubMed] [Google Scholar]
Yassi 1997
- Yassi A. Repetitive strain injuries. Lancet 1997;349(9056):943‐7. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Karjalainen 2000
- Karjalainen KA, Malmivaara A, Tulder MW, Roine R, Jauhiainen M, Hurri H, et al. Biopsychosocial rehabilitation for upper limb repetitive strain injuries in working age adults. Cochrane Database of Systematic Reviews 2000, Issue 3. [DOI: 10.1002/14651858.CD002269] [DOI] [PubMed] [Google Scholar]
Verhagen 2006
- Verhagen AP, Karels C, Bierma‐Zeinstra SM, Burdorf L, Feleus A, Dahaghin S, et al. Ergonomic and physiotherapeutic interventions for treating work‐related complaints of the arm, neck or shoulder in adults. Cochrane Database of Systematic Reviews 2006, Issue 3. [DOI: 10.1002/14651858.CD003471.pub3] [DOI] [PubMed] [Google Scholar]
Verhagen 2007a
- Verhagen AP, Karels C, Bierma‐Zeinstra SM, Feleus A, Dahaghin S, Burdorf A, et al. Ergonomic and physiotherapeutic interventions for treating work‐related complaints of the arm, neck or shoulder in adults. A Cochrane systematic review. Europa Medicophysica 2007;43(3):391‐405. [MEDLINE: ] [PubMed] [Google Scholar]
Verhagen 2007b
- Verhagen AP, Karels C, Bierma‐Zeinstra SM, Feleus A, Dahaghin S, Burdorf A, et al. Exercise proves effective in a systematic review of work‐related complaints of the arm, neck, or shoulder. Journal of Clinical Epidemiology 2007;60(2):110‐7. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]


