Abstract
Background
Contraception provides significant benefits for women's and children's health, yet an estimated 225 million women had an unmet need for modern contraceptive methods in 2014. Interventions delivered by mobile phone have been demonstrated to be effective in other health areas, but their effects on use of contraception have not been established.
Objectives
To assess the effects of mobile phone‐based interventions for improving contraception use.
Search methods
We searched for randomised controlled trials (RCTs) of client‐provider interventions delivered by mobile phone to improve contraception use compared with standard care or another intervention. We searched the electronic databases Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE, EMBASE, Global Health, PsycINFO, POPLINE, Africa‐Wide Information and Latin American Caribbean Health Sciences Literature (LILACS) from January 1993 to October 2014, as well as clinical trials registries, online mHealth resources and abstracts from key conferences.
Selection criteria
Randomised controlled trials of mobile phone‐based interventions to improve any form of contraception use amongst users or potential users of contraception. Outcome measures included uptake of contraception, measures of adherence, pregnancy and abortion.
Data collection and analysis
Two review authors independently screened titles and abstracts of studies retrieved using the search strategy and extracted data from the included studies. We calculated the Mantel‐Haenszel risk ratio (RR) for dichotomous outcomes and the mean difference (MD) for continuous outcomes, together with 95% confidence intervals (CIs). Differences in interventions and outcome measures did not permit us to undertake meta‐analysis.
Main results
Five RCTs met our inclusion criteria. Three trials aimed to improve adherence to a specific method of contraception amongst existing or new contraception users by comparing automated text message interventions versus standard care. Two trials aimed to improve both uptake and adherence, not limited to one method, in both users and non‐users of contraception. No trials were at low risk of bias in all areas assessed.
One trial in the USA reported improved self reported oral contraceptive (OC) continuation at six months from an intervention comprising a range of uni‐directional and interactive text messages (RR 1.19, 95% CI 1.05 to 1.35). One trial in Cambodia reported increased self reported use of effective contraception at four months post abortion from an intervention comprising automated interactive voice messages and phone counsellor support (RR 1.39, 95% CI 1.17 to 1.66).
One feasibility trial in the USA reported a lower mean number of days between scheduled and completed attendance for the first but not subsequent Depo‐Provera appointments using clinic records from an intervention comprising reminders and healthy self management text messages (mean difference (MD) ‐8.60 days, 95% CI ‐16.74 to ‐0.46). Simple text message OC reminders had no effect on missed pills as assessed by electronic medication monitoring in a small trial in the USA (MD 0.5 missed pills, 95% CI ‐1.08 to 2.08). No effect on self reported contraception use was noted amongst isotretinoin users from an intervention that provided health information via two uni‐directional text messages and mail (RR 1.26, 95% CI 0.84 to 1.89). One trial assessed potential adverse effects of the intervention and reported no evidence of road traffic accidents or domestic abuse.
Authors' conclusions
Our review provides limited evidence that interventions delivered by mobile phone can improve contraception use. Whilst evidence suggests that a series of interactive voice messages and counsellor support can improve post‐abortion contraception, and that a mixture of uni‐directional and interactive daily educational text messages can improve OC adherence, the cost‐effectiveness and long‐term effects of these interventions remain unknown. Further high‐quality trials are required to robustly establish the effects of interventions delivered by mobile phone to improve contraception use.
Plain language summary
Interventions delivered by mobile phone to support client use of family planning/contraception
Contraception ‐ methods or devices used to prevent pregnancy – has significant benefits for women's and children's health. Despite these benefits, an estimated 225 million women in developing countries were not using a modern contraceptive method in 2014 despite wanting to avoid pregnancy. Expansion of mobile phone use in recent years has led to increased interest in healthcare delivery via mobile phone and the potential to deliver support wherever the person is located, whenever it is needed, and to reach populations with restricted access to services. Mobile phone‐based interventions have been demonstrated to be effective in other health areas, but not yet in the field of contraception.
In 2014, we undertook computer searches for randomised trials evaluating mobile phone‐based interventions to increase contraception use. We found five trials. Three trials used text messaging to support women in continuing to use a specific method of contraception. Two trials aimed to improve both uptake and continued use of contraception ‐ one with voice and one with text messaging. Our review provides limited evidence that interventions delivered by mobile phone improve contraception use. One trial in the USA reported that women were more likely to continue to take the contraceptive pill from an intervention comprising a range of educational text messages. One trial in Cambodia reported increased use of contraception at four months post abortion from an intervention comprising voice messages and phone counsellor support. Another trial in the USA reported improved attendance for the first but not subsequent contraceptive injection appointments from an intervention comprising reminders and healthy self management text messages. Simple text message contraceptive pill reminders did not reduce missed pills in a small trial in the USA. No difference in contraception use was reported amongst users of isotretinoin (a drug used for acne) from an intervention that provided health information via text messages and mail.
In conclusion, evidence indicates that a series of voice messages and counsellor support can improve contraception amongst women seeking abortion services not wanting to get pregnant again at the current time, and data suggest that daily educational text messages can improve continued use of the contraceptive pill. However, the cost value and long‐term effectiveness of these interventions remain unknown. More good quality trials are needed to establish the effectiveness of interventions delivered by mobile phone to increase contraception use.
Summary of findings
for the main comparison.
| Intervention delivered by mobile phone compared with standard care to improve contraception use | ||||
|
Patient or population: female users or non‐users of contraception Settings: Various: USA, Cambodia, Israel Intervention: text messaging, voice messaging, telephone counselling Comparison: standard care (clinic‐based counselling), no additional mobile phone‐based support | ||||
| Outcomes | Relative effect (95% CI) | Number of participants (studies) | Quality of the evidence (GRADE) | Intervention |
| OC use (continuation) at 6 months |
RR 1.19 (1.05 to 1.35) |
683 (Castano 2012) | ⊕⊕⊝⊝ Low | Intervention comprised a range of different daily educational text messages for 180 days |
| Effective contraception use at 4 months |
RR 1.39 (1.17 to 1.66) |
431 (Smith 2014) | ⊕⊕⊕⊕ High | Intervention comprised a series of six voice messages ± counsellor delivered support |
| Mean number of missed pills (cycle 1) |
Mean difference
0.5 missed pills (‐1.08 to 2.08) |
73 (Hou 2010) | ⊕⊕⊕⊝ Moderate | Intervention comprised daily contraceptive pill reminder text message for 3 months |
| Contraceptive use during treatment with Isotretinoin at 3 months |
RR 1.26 (0.84 to 1.89) |
108 (Tsur 2008) | ⊕⊝⊝⊝ Very low | Intervention comprised 2 text messages together with information via mail |
| Mean number of days between scheduled appointment and completed visit for Depo‐Provera: first visit |
Mean difference ‐8.60 days (‐16.74 to ‐0.46) |
87 (Trent 2013) | ⊕⊕⊕⊝ Moderate | Intervention comprised daily text message appointment reminders 72 hours before appointment and healthy self management messages |
| GRADE Working Group grades of evidence. High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||
Background
Rapid expansion in the use of mobile phones in recent years has had a dramatic impact on interpersonal communication. Within the health domain, phone calls, text messages and smartphone applications offer new means of communication between service providers and clients. This review focuses on interventions delivered by mobile phone to improve contraception use.
Description of the condition
Contraception ‐ methods or devices used to prevent pregnancy – provides significant benefits for women's and children's health. Use of contraception prevents unintended pregnancies, reduces abortions and maternal deaths and can improve perinatal outcomes and child survival by widening the interval between successive pregnancies (Cleland 2012). Contraception also confers substantial social and economic benefits such as improved educational and employment opportunities for women, leading to increasing family savings and economic growth (Singh 2009).
Despite these benefits, the unmet need for contraception is significant. Unmet need can be defined as women not using a modern contraceptive method despite wanting to wait two or more years to give birth, or wanting no more children (Darroch 2013). The total number of women with unmet need was estimated to be 225 million in 2014 (Singh 2014). Women report not using contraception for many reasons. The most common reasons for non‐use are concerns about health and side effects of methods (Ali 2010; Bradley 2009; Westoff 2012). Other important barriers include lack of access to supplies and services, as well as factors outside the health system such as women's lack of education or empowerment (Singh 2014).
If the unmet need for modern methods of contraception were met amongst women in developing countries, the number of unintended pregnancies would be reduced by 52 million per year. This reduction in unintended pregnancies would avert an estimated 24 million abortions (of which around half would be unsafe), 70,000 maternal deaths and 500,000 newborn deaths (Singh 2014).
Description of the intervention
The past decade has seen rapid expansion in the delivery of healthcare interventions via mobile phone (Mechael 2010). Interventions delivered by mobile phone have been designed to improve health outcomes for individuals needing acute and chronic disease management and to facilitate health promotion. These interventions may be designed to improve medication adherence, encourage appointment attendance or promote behaviour change (Free 2013a; Free 2013b; Whittaker 2009). Interventions delivered by mobile phone have also provided a novel means of delivering patient test results (Bastawrous 2012).
Interventions can utilise different functions of mobile phones such as text messages, voice messages, videos and applications; may involve one‐direction or two‐way (interactive) communication (Free 2010; Kallander 2013); and can employ single functions or combined functions of mobile phones such as interactive text message‐based support or voice messaging combined with telephone counselling. Interventions delivered by mobile phone to improve contraception use could be provided as an adjunct or alternative to face‐to‐face services and, for non‐users of contraception, could aim to increase uptake of contraception. Interventions for existing contraceptive users could aim to improve adherence to contraception, reduce discontinuation of contraceptives or encourage switching rather than stopping contraceptives if the individual experiences side effects.
How the intervention might work
Interventions delivered by mobile phone offer potential advantages over face‐to‐face or landline phone healthcare delivery, as support can be delivered wherever the person is located, and whenever it is needed (Rodgers 2005). Such interventions can facilitate confidential access to healthcare information amongst younger populations, who are regular mobile phone users (UNICEF 2011; Whittaker 2009; Williamson 2013). Furthermore, these interventions have the potential to reach rural populations, for whom geographical distances can restrict access to services (Car 2012).
Intervention content could include information, pill or appointment reminders and/or content designed to increase or maintain motivation to use contraception. Behaviour change techniques used in face‐to‐face interventions can be modified for delivery by mobile phone (Free 2013a). Interventions could utilise a range of behaviour change techniques, such as encouraging women to make a clear plan about when, where and how they will use contraception (goal setting) (Abraham 2008). Multi‐faceted interventions that address a wide range of barriers to contraception use could be more effective than those targeting single barriers to use. Existing adherence research suggests that multi‐faceted interventions can be effective but uni‐faceted interventions provide at best modest benefits (Haynes 2008). Similarly, no evidence indicates that medication reminders delivered by mobile phone have benefits (pooled risk ratio 1.00, 95% confidence interval 0.77 to 1.30) (Free 2013a), whilst trials of more complex interventions to improve adherence to antiretroviral medication report benefits (Free 2013a; Lester 2010).
Several potential risks are associated with using mobile phones to improve contraception use. Road traffic accidents are the only adverse health effect of cell phone use for which evidence is available (CDC 2015; National Safety Council 2015; Rothman 2000). However, in the often sensitive context of contraception, the potential for physical or psychological adverse effects could arise as a result if other people access intervention content when mobile phones are shared. Further risk relates to the opportunity cost of investing substantial resources in developing a technologically focused intervention with most likely a moderate impact, instead of investing in alternative approaches. Additional challenges related to implementation of interventions delivered by mobile phone include limited literacy of target populations, incomplete network coverage, phone number switching and risk of incomplete data input and inaccurate data acted upon (Bullen 2013; Upadhyay 2009).
Why it is important to do this review
Interventions delivered by mobile phone have been demonstrated to be effective in other areas such as smoking cessation (Free 2011; Horvath 2012; Whittaker 2009). When interventions delivered by mobile phone have been shown to be effective, they have also been shown to be highly cost‐effective (Guerriero 2013). However, evidence related to interventions delivered by mobile phone for contraception is more limited.
In recent years, interest in interventions delivered by mobile phone has been growing, as reflected in a number of mobile phone‐based contraception initiatives that have been launched, and in some cases scaled up, such as Mobile Technology for Improved Family Planning (MOTIF), mAssist, Mobile for Reproductive Health (m4RH), CycleTel and Mobile Alliance for Maternal Action (MAMA) (Constant 2010; CycleTel 2011; L'engle 2013; MAMA 2013; Smith 2013). Although these initiatives seem promising, each uses different intervention and evaluation approaches, and the effect of interventions delivered by mobile phone on contraception has not been reliably established. Therefore a review of interventions delivered by mobile phone for contraception is timely.
Objectives
To assess the effects of mobile phone‐based interventions for improving contraception use.
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials (RCTs).
Types of participants
Eligible participants were men or women of reproductive age who were users or potential users of contraceptive methods. We included studies in all settings (e.g. primary care settings, outpatient settings, community settings, hospital settings). We did not exclude studies according to the types of healthcare providers who participated (e.g. doctor, nurse, allied staff).
Types of interventions
We included studies that examined any type of client‐provider intervention delivered by mobile phone designed to improve use of contraception compared with standard delivery of care or another intervention. We included interventions directed at both users and non‐users of contraception. Eligible interventions included those designed to do the following.
Improve uptake of contraception (including post‐abortion and post‐partum contraception).
Promote specific methods of contraception.
Improve adherence to contraception (e.g. interventions to support individuals experiencing side effects, reduce discontinuation, ensure safe method switching or send pill or appointment reminders).
We included interventions aimed at mobile phone users delivered by mobile phone that included some degree of automation, for example, text message, voice message and applications. We excluded trials in which mobile phones were used for two‐way voice communication (as a phone) alone, in keeping with previous reviews of mobile phone‐based interventions (Horvath 2012; Whittaker 2009). Web‐based interventions often can be accessed on mobile phones, as well as through other platforms, but in practice can be difficult to access via mobile phone unless they are adapted for mobile phone use. We excluded web‐based interventions unless study authors stated that they had been intended or adapted for mobile phone users. We excluded trials that focused only on preventing sexually transmitted disease rather than providing contraception.
Types of outcome measures
Primary outcomes
Uptake of contraception (including post‐abortion and post‐partum contraception).
Uptake of a specific method of contraception (e.g. a long‐acting method).
Adherence to contraceptive method (e.g. number of missed pills, attendance for repeat injection).
Safe method switching (e.g. from one effective method to another with no gap).
Discontinuation of contraception.
Pregnancy or abortion (objectively measured or self reported).
Secondary outcomes
Road traffic accidents ‐ the only adverse health effect of cell phone use for which evidence is available (Rothman 2000).
Any physical or psychological effect reported.
We included studies that assessed any form of contraceptive use and trials assessing a range of outcome measures related to contraceptive use, including uptake of contraception, selection of a specific method, use of measures of adherence (including discontinuation and safe switching), pregnancy or abortion.
We considered sustained and point prevalence measures as well as subjective (self reported) and objective (e.g. biochemically verified, electronic medication monitors used, clinical examination performed) assessment of contraception use.
Contraceptive methods can be classified in different ways. Contraception can be classed as modern (e.g. condom, oral contraceptive pills, injectables, intrauterine device, implant, emergency contraception) or traditional (e.g. rhythm or periodic abstinence, withdrawal) (Westoff 2012; WHO 2013). Furthermore, distinctions can be made between hormonal and non‐hormonal methods, and between short‐acting and long‐acting or permanent methods. The World Health Organization (WHO) classifies methods according to effectiveness on the basis of estimated rates of unintended pregnancy per 100 women per year (WHO 2011). For this review, we define effective modern methods as those associated with < 10% 12‐month pregnancy rates; commonly used methods include oral contraceptive, injectable, implant, intrauterine device and permanent methods.
Search methods for identification of studies
Electronic searches
We searched the following electronic databases between 6 and 9 October 2014.
Cochrane Central Register of Controlled Trials (CENTRAL).
MEDLINE using Ovid.
EMBASE using Ovid.
Global Health using Ovid.
PsycINFO using Ovid.
Population Information Online (POPLINE).
Africa‐Wide Information.
Latin American Caribbean Health Sciences Literature (LILACS).
We included Africa‐Wide Information and LILACS, given the proliferation of mobile phone‐based initiatives in low‐ and middle‐income regions. We searched for recent clinical trials separately via the WHO International Clinical Trials Registry Platform (www.who.int/trialsearch) and Current Controlled Trials (www.controlled‐trials.com), which included clinicaltrials.gov.
We searched for studies published in all languages from January 1993 until the present (i.e. the date of the search), as the first text message was sent in December 1992 (Kellon 2012). We presented in Appendix 1 the electronic database search strategies that we used.
Searching other resources
We wrote to the contact investigators of included studies to request additional information about studies when required, as well as information about trials not discovered in our search. To identify completed or ongoing studies that had not been identified in the electronic searches, we reviewed abstracts from the mHealth summit, Women Deliver and the International Conference on Family Planning. We also reviewed online repositories of mHealth interventions including Health Unbound, Royal Tropical Institute, mHealthinfo, K4Health and mHealth Evidence.
Data collection and analysis
Selection of studies
We exported search results into a software programme for bibliographic citation management and excluded duplicate references. Two review authors independently screened titles and abstracts of studies retrieved using the search strategy. We retrieved full articles for further assessment if the information given suggested that the study (1) included participants who were users or potential users of contraception, (2) compared use of an intervention delivered by mobile phone versus routine standard of care or another intervention or (3) assessed one or more relevant outcome measures.
If we had any doubt regarding these criteria from the information provided in the title and abstract, we retrieved the full article for clarification. Two review authors retrieved the full text of potentially eligible studies and independently assessed them for eligibility, with disagreements resolved through discussion with a third review author.
Data extraction and management
Two review authors independently extracted the following data from the included studies using a standardised data extraction form.
General information: title, study authors, complete citation, publication status, date published, language, review author information, date reviewed, sponsoring, setting.
Study characteristics: study design, aim of study, duration, participant recruitment, sampling, inclusion and exclusion criteria including numbers screened and eligible, randomisation, allocation concealment, method of allocation concealment, blinding, informed consent, power analysis.
Risk of bias (see Assessment of risk of bias in included studies).
Participants: description, geographical location, setting, number, age, ethnicity, socioeconomic status distribution.
Providers: description, geographical location, setting.
Intervention: description, aim of intervention, any behaviour change intervention (according to the study authors' description and our assessment according to an established typology of behaviour change techniques (Abraham 2008)), duration, frequency and 'dose', control or placebo intervention, technical specifications including device and mobile phone functions used (e.g. text message, voice message), message content, co‐interventions.
Outcomes: outcomes as specified above, other outcomes assessed, length of follow‐up, methods used to assess outcomes, completeness of outcome data, follow‐up for non‐respondents, adverse events.
Results: outcomes and times of assessment, intention‐to‐treat analysis (when all randomly assigned participants are included, irrespective of what happened subsequently (Newell 1992)).
Review authors discussed disagreements and resolved them through discussion with a third review author as necessary.
Assessment of risk of bias in included studies
Review authors assessed studies for risk of bias in accordance with the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011) across the following domains: random sequence generation, allocation concealment, blinding of outcome assessment, incomplete outcome data, selective outcome reporting and other potential biases. Two review authors independently assessed risk of bias, discussed disagreements and resolved them through discussion with a third review author as necessary. We used a standardised form to guide assessment of risk of bias, and judged each domain as having 'high', 'low' or 'unclear' risk. We presented all included studies by study type and risk of bias level. As required, we contacted study authors to ask for additional information. We presented the results of the risk of bias assessment in tables in the Characteristics of included studies section, and as a systematic narrative description.
Measures of treatment effect
We used risk ratios (RRs) as measures of treatment effect for dichotomous outcomes, and mean differences (MDs) for continuous outcomes. We reported 95% confidence intervals (CIs) with all measures of effect.
Unit of analysis issues
We planned to take into account unit of analysis issues resulting from cluster RCTs, repeated measurements and studies with more than one treatment group and, if appropriate, to analyse data in accordance with recommendations of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). However, we did not identify any unit of analysis issues.
Dealing with missing data
We planned to assess missing data on individuals as guided by the Cochrane Handbook for Systematic Reviews of Interventions. We would ignore missing data if they were assumed to be missing at random. If feasible, we planned to contact study authors to ask for missing data when it was assumed that they were not missing at random, for example, if some randomly assigned participants were excluded from analyses. If feasible, we planned to use statistical techniques, as appropriate to each study, to impute missing data to enable an available case or intention‐to‐treat analysis (Higgins 2011). For missing summary data, if feasible, we planned to approximate the correct analyses to impute missing summary statistics (e.g. standard deviations), in accordance with the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011).
Assessment of heterogeneity
We did not undertake a meta‐analysis, as the studies identified were so different in terms of both interventions and outcome measures.
Assessment of reporting biases
We did not assess reporting biases statistically, as the studies identified were so different in terms of both interventions and outcome measures.
Data synthesis
We conducted statistical analysis according to the guidelines provided in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We presented a narrative overview of the findings, together with tabular summaries of extracted data.
Differences in study populations, interventions, comparators and outcomes precluded us from pooling data across studies to estimate summary effect sizes. We used the Mantel‐Haenszel risk ratio fixed‐effect model for dichotomous data and mean differences (MDs) for continuous data. When meta‐analysis was not possible, we presented summary and descriptive statistics.
We summarised the quality of evidence provided by studies using the GRADE (Grades of Recommendation, Assessment, Development and Evaluation) approach while considering factors that decrease the quality level of a body of evidence (Higgins 2011). Randomised controlled trials were considered of high quality and were downgraded by one level (serious) or two levels (very serious) for each of the following reasons.
Limitations in design and implementation (e.g. lack of blinding, large losses to follow‐up).
Indirectness of evidence (e.g. trials that meet eligibility criteria but address a restricted version of the main review question in terms of population, intervention, comparator or outcomes).
Unexplained heterogeneity or inconsistency of results (e.g. when heterogeneity exists and affects interpretation of results, but study authors fail to identify a plausible explanation).
Imprecision of results (e.g. when studies include few participants and thus have wide confidence intervals).
High probability of publication bias (e.g. if investigators failed to report studies or outcomes on the basis of results).
Subgroup analysis and investigation of heterogeneity
We planned to perform subgroup analyses if one of the primary outcome parameters demonstrated statistically significant differences (at P value < 0.01) between treatment groups. These would have included meta‐analyses on studies amongst specific populations, specifically, younger versus older women; high‐income versus low‐income settings; and post delivery versus post abortion versus general clinic attendees. However, we did not identify studies appropriate for this subgroup analysis. We did not identify studies promoting traditional contraceptive methods; therefore we did not undertake the planned subgroup analysis including only modern methods, or methods considered effective or very effective by the WHO (WHO 2011).
Sensitivity analysis
We did not identify a sufficient number of studies to perform the following sensitivity analyses.
Repeating the analysis while excluding unpublished studies to investigate potential publication bias resulting from publication or non‐publication of research findings, depending on the nature and direction of the results (Higgins 2011).
Repeating the analysis while taking account of risk of bias of included studies, as specified above.
Results
Description of studies
Results of the search
We conducted searches during October 2014 and produced 759 records after removing duplicates. We discarded 683 records after review of titles and abstracts. We assessed 76 full‐text articles for eligibility. See Figure 1 for the study flowchart. We identified four ongoing studies (see Characteristics of ongoing studies below).
1.
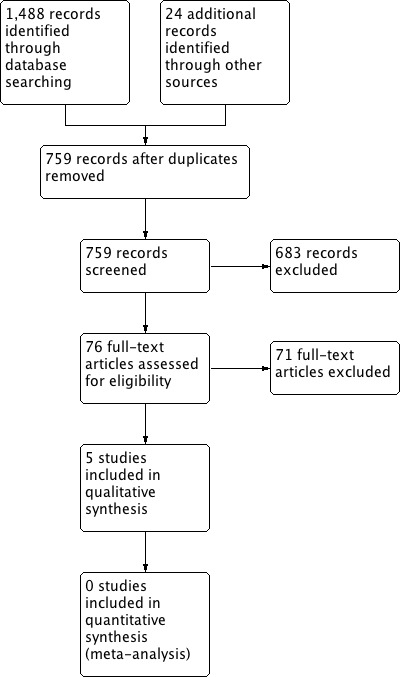
Study flow diagram.
Included studies
We identified five randomised controlled trials that fulfilled the inclusion criteria (Castano 2012; Hou 2010; Smith 2014; Trent 2013; Tsur 2008). Three trials were conducted in the USA (Castano 2012; Hou 2010; Trent 2013), one in Israel (Tsur 2008) and one in Cambodia (Smith 2014). One was multi‐site (Smith 2014), and four were single‐site (Castano 2012; Hou 2010; Trent 2013; Tsur 2008). Three trials recruited participants from urban clinics (Castano 2012; Hou 2010; Trent 2013), one trial from clinics serving both urban and rural populations (Smith 2014) and one trial from individuals who phoned an advice line (Tsur 2008). All trials included only female participants. Two trials focused on youth populations (Castano 2012; Trent 2013), and three included younger and older women of reproductive age (Hou 2010; Smith 2014; Tsur 2008). Two trials recruited new users of OC (Castano 2012; Hou 2010), one recruited existing injectable users (Trent 2013) and two recruited both users and non‐users of contraception (Smith 2014; Tsur 2008).
Interventions
Three trials aimed to improve adherence to a specific method of contraception by existing or new contraception users, comparing automated text message interventions versus standard care. Castano 2012 in the USA randomly assigned 962 new OC users 13 to 25 years of age ‐ 480 to mobile phone text messaging and 482 to standard care. The intervention aimed to improve OC continuation and comprised a range of daily uni‐directional and interactive educational text messages (e.g. “The pill improves anaemia”) for 180 days, in addition to standard care (face‐to‐face counselling and written educational handout). Hou 2010 in the USA randomly assigned 82 new OC users between 18 and 31 years of age ‐ 41 to mobile phone text messaging and 41 to standard care. The intervention aimed to improve OC adherence and comprised a daily text message, “Please remember to take your birth control pill”, sent at a designated time over the three‐month study period. Trent 2013 in the USA randomly assigned 100 current Depo‐Provera users between 13 and 21 years of age to mobile phone text messaging or standard care. The intervention aimed to improve follow‐up Depo‐Provera clinic attendance and comprised a welcome message, daily text appointment reminders starting 72 hours before the clinic visit and healthy self management messages sent over the course of the three‐month enrolment period.
Two trials aimed to improve both uptake and adherence, not limited to one method, in both users and non‐users of contraception. Smith 2014 in Cambodia randomly assigned 500 women > 18 years of age seeking abortion services who reported not wanting to get pregnant again at the current time: 249 to a semi automated intervention delivered by mobile phone and 251 to standard care. The intervention aimed to increase uptake and adherence to effective contraception (OC, injectable, implant, intrauterine device (IUD) and permanent methods) and comprised six interactive voice messages, counsellor‐delivered phone support according to the response to messages and additional reminder messages for OC or injectable users. Tsur 2008 in Israel randomly assigned 108 women of reproductive age (16 to 45 years of age) using isotretinoin (an acne treatment that is contraindicated in pregnancy): 50 to mobile phone text messaging and 58 to standard care. The intervention was automated and comprised two text messages (at one month and two months) together with information sent via mail, in addition to standard care (information given once during a phone interview).
One of the five trials provided limited details of the intervention (Tsur 2008). No trials reported using a particular behavioural theory to underpin the intervention. Smith 2014 reported a conceptual framework for the intervention in the study protocol (Smith 2013). The maximum number of behaviour change techniques according to our assessment using Abrahams and Michie's typology (Abraham 2008) for any intervention was six, and the median was three. The most commonly used behaviour change techniques were the following: provide information about behaviour‐health link (four interventions), provide information on consequences (three interventions) and provide instruction (three interventions) and prompt practice (three interventions). Behavioural change techniques identified by our assessment are found in Table 2.
1. Behaviour techniques used in interventions.
| Behaviour change technique | Studies |
| 1. Provide information about behaviour‐health link | Castano 2012 (e.g. "The pill improves anaemia"); Smith 2014 (e.g. information about amenorrhoea); Trent 2013 (healthy self management messages); Tsur 2008 (informed about importance of contraceptive use) |
| 2. Provide information on consequences | Castano 2012 ("The pill is very effective at preventing pregnancy"); Smith 2014 (e.g. "contraceptive methods are an effective and safe way to prevent unintended pregnancy"); Tsur 2008 (informed about teratogenic risk) |
| 3. Provide information about others' approval | |
| 4. Prompt intention formation | |
| 5. Prompt barrier identification | Smith 2014 (If client received a phone call, counsellors provided reassurance regarding side effects as per conceptual framework reported in the study protocol) |
| 6. Provide general encouragement | Castano 2012 (e.g. "Welcome to our study and thank u 4 participating") |
| 7. Set graded tasks | |
| 8. Provide instruction | Castano 2012 (e.g. "Tell every doctor u see that u r taking the pill"; Hou 2010 (if "Please remember to take your birth control pill" is considered 'telling a person how to perform a behaviour'); Smith 2014 (e.g. "press 1 if you would like me to call you back to discuss contraception") |
| 9. Model or demonstrate the behaviour | |
| 10. Provide specific goal setting | |
| 11. Prompt review of behavioural goals | |
| 12. Prompt self monitoring of behaviour | Hou 2010 (women kept a diary of their daily pill taking; the intervention may have prompted this behaviour) |
| 13. Provide feedback on performance | |
| 14. Provide contingent rewards | |
| 15. Teach or use prompts or cues | |
| 16. Agree on behavioural contract | |
| 17. Prompt practice | Hou 2010 ("Please remember to take your birth control pill"); Smith 2014 (participants who chose to receive the OC or injectable could receive additional reminders appropriate to their method); Trent 2013 (daily text appointment reminders 72 hours before the clinical visit) |
| 18. Use follow‐up prompts | |
| 19. Provide opportunities for social comparison | |
| 20. Plan social support or social change | Smith 2014 (If client received a phone call and requested, the counsellor would also discuss contraception with the husband or partner) |
| 21. Prompt identification as a role model | |
| 22. Prompt self‐talk | |
| 23. Relapse prevention | |
| 24. Stress management | |
| 25. Motivational interviewing | |
| 26. Time management |
Outcomes
Primary outcomes were reported as follows: Three trials reported on adherence. Castano 2012 defined OC continuation as the participant taking a pill within the previous seven days, assessed at six months. Hou 2010 reported missed pills per cycle as measured by electronic monitoring device (EMD) over a three‐month period. Trent 2013 reported days between next scheduled appointment and attendance for Depo‐Provera injection over three cycles (nine months) (NCT01641380). Two trials reported contraception use. Smith 2014 assessed self reported use of effective contraception, as assessed at four months (12 month follow‐up is also planned). Effective methods were considered as those with less than 10% failure rates as commonly used: OC, injectable, IUD, implant. Tsur 2008 assessed self reported contraceptive use (methods not defined) at three months.
Secondary outcomes were as follows: adherence (OC use at last sexual intercourse, interruptions in OC use greater than seven days, no missed pills during the past month) (Castano 2012), on‐time appointment for Depo‐Provera (Trent 2013), discontinuation of effective contraception (Smith 2014), long‐acting contraception use (Smith 2014), contraception use over the follow‐up period > 80% (Smith 2014), condom use for at least 50% of coital activity during the study (Hou 2010), use of two contraceptives (Tsur 2008), sexually active and not using contraception (Tsur 2008), emergency contraception use (Hou 2010), pregnancy (Hou 2010; Smith 2014), repeat abortion (Smith 2014), unintended outcomes (road traffic accident, domestic abuse) (Smith 2014) and measures of satisfaction with the intervention (Castano 2012; Hou 2010).
Excluded studies
We excluded three studies when mobile phones were used for two‐way voice communication (as a phone) alone (Berenson 2012; Katz 2011; Kirby 2010); two studies when the intervention was web‐based or tablet‐based and did not appear to have been adapted for mobile phone users (Bannink 2014; Sridhar 2013); three studies that did not have relevant outcome measures (Bracken 2014; Constant 2014; Hall 2013); five studies in which the intervention focused on preventing sexually transmitted disease rather than on providing contraception (Gold 2011; Juzang 2011; Kaoaiem 2012; Lim 2012; Suffoletto 2013) and four studies that were not randomised controlled trials (L'Engle 2013; Mackenzie 2009; O'Sullivan 2008; Walakira 2013). We provided details in Characteristics of excluded studies.
Risk of bias in included studies
We summarised risk of bias in Figure 2 and Figure 3. For Trent 2013, the conference abstract provided insufficient information for full assessment of risk of bias, but we were able to obtain additional data from the study investigator.
2.
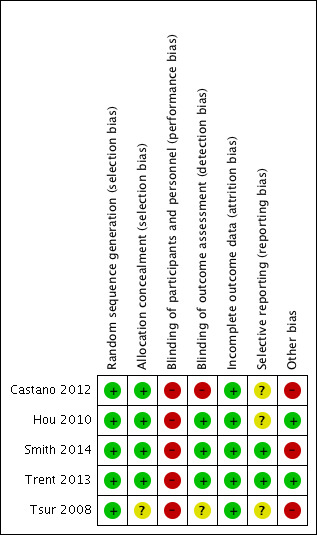
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
3.
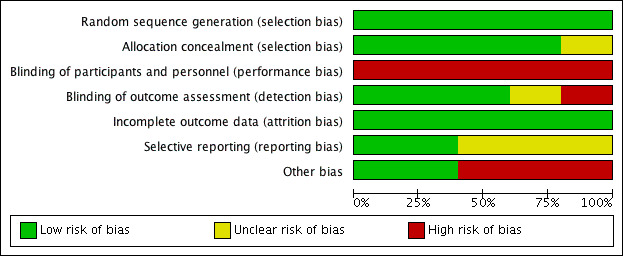
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
Allocation
All five studies specified random sequence generation methods. Four studies used computer‐generated sequences (Hou 2010; Smith 2014; Trent 2013; Tsur 2008), and one study used a random number table (Castano 2012). Four studies specified adequate allocation concealment methods (Castano 2012; Hou 2010; Smith 2014; Trent 2013), and in the remaining study these methods were unclear (Tsur 2008).
Blinding
As a result of the nature of the interventions, it was not possible to blind participants to intervention allocation; therefore the outcome could have been influenced by lack of blinding, resulting in performance bias. Hou 2010 reported that 68% of participants in the control group used a reminding system outside of the study protocol (e.g. alarm clock, mobile phone alarm) compared with 36% in the intervention group (P value = 0.003). This could have occurred in response to participation in the trial or frequent use of reminding systems in general.
Three studies reported outcome assessment as blinded (Hou 2010; Smith 2014; Trent 2013), but this was not stated in two studies (Castano 2012; Tsur 2008). In Castano 2012 and Hou 2010, participants were asked questions regarding their satisfaction with the intervention.
Incomplete outcome data
One trial reported loss to follow‐up of 20% or more (Castano 2012): 28% in the intervention group and 30% in the control group.
Selective reporting
One trial (Smith 2014) prespecified primary and secondary outcomes in its study protocol (Smith 2013). Three trials provided information on outcomes on a clinical trials registry (Castano 2012; Hou 2010; Trent 2013). For one trial, we were unable to locate a study protocol or a clinical trials registry record (Tsur 2008).
Other potential sources of bias
Two trials used objective measures for the primary outcome (Hou 2010; Trent 2013). Hou 2010 assessed mean pills missed per cycle using an electronic medication monitor, in addition to a self report patient diary. The overall rate of missed pills was 4.7 ± 3.2 per cycle according to the electronic monitoring device, and 1.2 ± 1.5 per cycle according to the patient diary (P value < 0.001). Trent 2013 assessed attendance for Depo‐Provera appointments using clinic records.
Three studies used self report measures for the primary outcome (Castano 2012; Smith 2014; Tsur 2008). Castano 2012 defined adherence as participants reporting that they took OC within the previous seven days. Smith 2014 defined self reported contraception use according to one of these methods: Participants currently had an implant or an IUD inserted; participants had received an injection within the previous three months; participants or husbands or partners had undergone a sterilisation or vasectomy procedure; or participants reported that they had taken OC within 24 hours of the interview or according to instructions. In addition, Smith 2014 attempted to conduct objective measurements amongst 50 participants to validate self report measures. Tsur 2008 did not report how contraceptive use was assessed.
Effects of interventions
See: Table 1
Primary outcomes
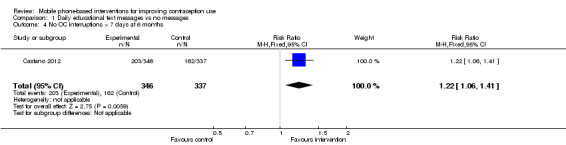
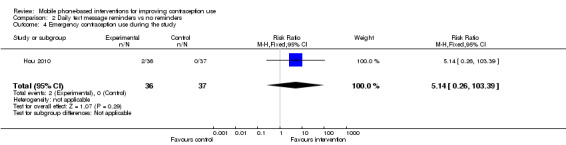
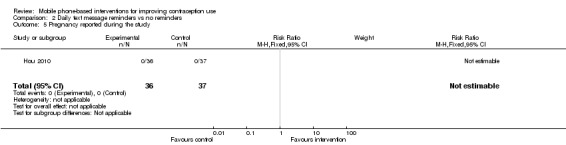
Three trials assessed adherence to a specific method of contraception. In Castano 2012, participants receiving daily educational text messages were more likely to report OC continuation at six months (RR 1.19, 95% CI 1.05 to 1.35) (Analysis 1.1). In Hou 2010, no significant difference was noted in the mean number of missed pills per contraceptive pill cycle using the electronic monitoring device between the text message group and the control group during cycle one (MD 0.5 missed pills, 95% CI ‐1.08 to 2.08) (Analysis 2.1), cycle two or cycle three (MD 0.80 missed pills; 95% CI ‐1.22 to 2.82) (Analysis 2.2).
1.1. Analysis.
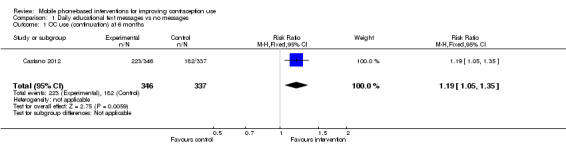
Comparison 1 Daily educational text messages vs no messages, Outcome 1 OC use (continuation) at 6 months.
2.1. Analysis.
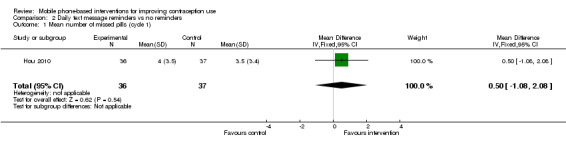
Comparison 2 Daily text message reminders vs no reminders, Outcome 1 Mean number of missed pills (cycle 1).
2.2. Analysis.
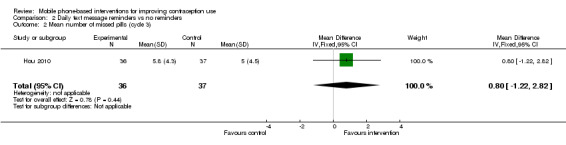
Comparison 2 Daily text message reminders vs no reminders, Outcome 2 Mean number of missed pills (cycle 3).
Trent 2013 reported that the group receiving text message reminders and healthy self management messages had a lower mean number of days between scheduled appointment and actual attendance for Depo‐Provera injection for visit one (MD ‐8.60 days, 95% CI ‐16.74 to ‐0.46) (Analysis 3.1) but not for visit two or three (Analysis 3.2) (data obtained from study investigator).
3.1. Analysis.
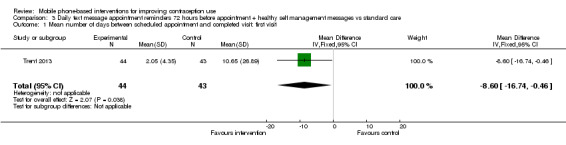
Comparison 3 Daily text message appointment reminders 72 hours before appointment + healthy self management messages vs standard care, Outcome 1 Mean number of days between scheduled appointment and completed visit: first visit.
3.2. Analysis.
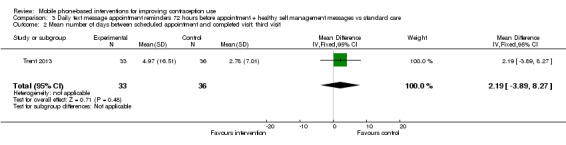
Comparison 3 Daily text message appointment reminders 72 hours before appointment + healthy self management messages vs standard care, Outcome 2 Mean number of days between scheduled appointment and completed visit: third visit.
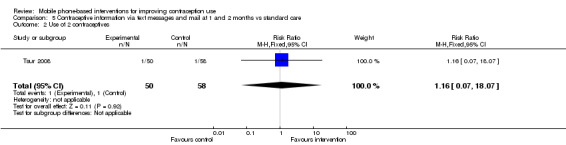
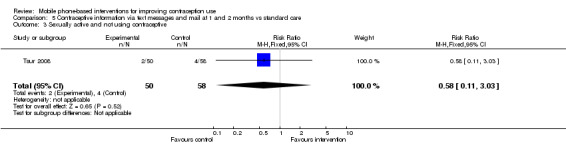
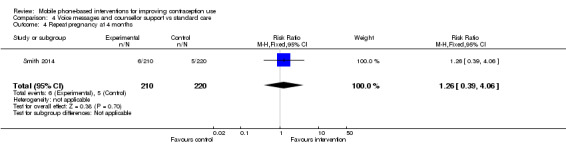
Two trials assessed uptake and adherence to more than one method of contraception. In Smith 2014, participants receiving voice messages and counsellor support were more likely to report using effective contraception at four months post abortion (RR 1.39, 95% CI 1.17 to 1.66) (Analysis 4.1). In Tsur 2008, no significant difference in contraceptive use was observed between participants receiving text messages together with information received via mail and the control group (RR 1.26, 95% CI 0.84 to 1.89) (Analysis 5.1).
4.1. Analysis.
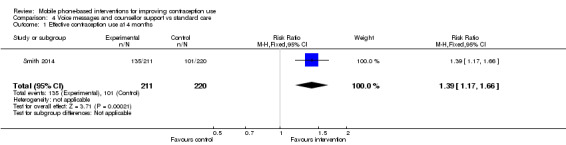
Comparison 4 Voice messages and counsellor support vs standard care, Outcome 1 Effective contraception use at 4 months.
5.1. Analysis.
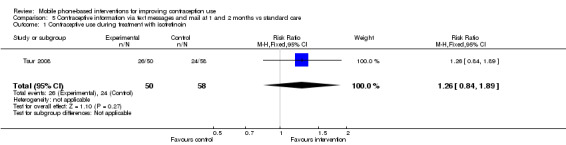
Comparison 5 Contraceptive information via text messages and mail at 1 and 2 months vs standard care, Outcome 1 Contraceptive use during treatment with isotretinoin.
Secondary outcomes
Four trials assessed measures of adherence. In Castano 2012, participants receiving the intervention were more likely to report no OC interruptions longer than seven days at six months (RR 1.22, 95% CI 1.06 to 1.41) (Analysis 1.4), more likely to report that they had missed no pills in the previous month (RR 1.44, 95% CI 1.16 to 1.79) (Analysis 1.5) and more likely to report OC use at last sexual intercourse (RR 1.15, 95% CI 1.03 to 1.28) (Analysis 1.6). In Hou 2010, participants receiving the intervention were more likely to report condom use for at least 50% of coital activity during the study (RR 1.94, 95% CI 1.00 to 3.78) (Analysis 2.3). In Smith 2014, participants receiving the intervention were more likely to use contraception over the four‐month post‐abortion period (> 80%, RR 1.35, 95% CI 1.10 to 1.67) (Analysis 4.3) and less likely to discontinue effective contraception if they had started a method during the first four weeks post abortion (hazard ratio 0.45, 95% CI 0.20 to 1.01). For Trent 2013, the abstract reported no overall differences among those who received injections within the optimal Depo‐Provera window due to additional clinical nursing outreach that resulted from missed visits per the existing clinical protocol for standard care.
1.4. Analysis.
Comparison 1 Daily educational text messages vs no messages, Outcome 4 No OC interruptions > 7 days at 6 months.
1.5. Analysis.
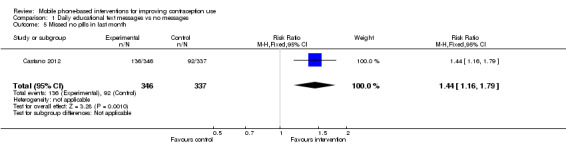
Comparison 1 Daily educational text messages vs no messages, Outcome 5 Missed no pills in last month.
1.6. Analysis.
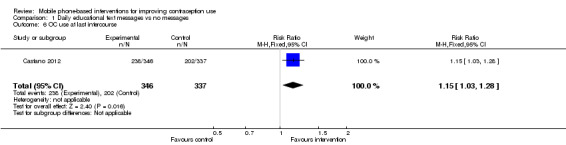
Comparison 1 Daily educational text messages vs no messages, Outcome 6 OC use at last intercourse.
2.3. Analysis.
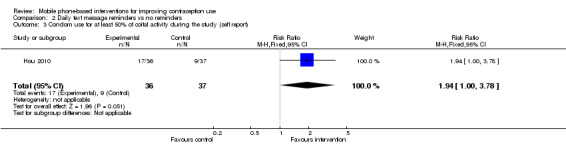
Comparison 2 Daily text message reminders vs no reminders, Outcome 3 Condom use for at least 50% of coital activity during the study (self report).
4.3. Analysis.
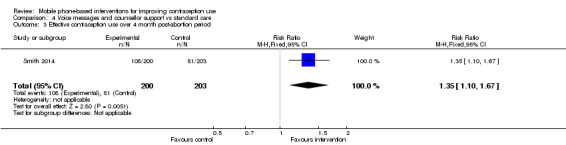
Comparison 4 Voice messages and counsellor support vs standard care, Outcome 3 Effective contraception use over 4 month post‐abortion period.
Three trials assessed use of additional contraceptive methods. In Smith 2014, participants receiving the intervention were more likely to be using long‐acting contraception (IUD or implant) at four months (RR 3.35, 95% CI 2.07 to 5.40) (Analysis 4.2). In Hou 2010, no difference was noted between intervention and control groups regarding emergency contraception use, but few events were reported (Analysis 2.4). In Tsur 2008, no difference was observed between intervention and control groups regarding using two contraceptives or being sexually active and not using contraception at three months, but few events were reported (Analysis 5.2; Analysis 5.3).
4.2. Analysis.
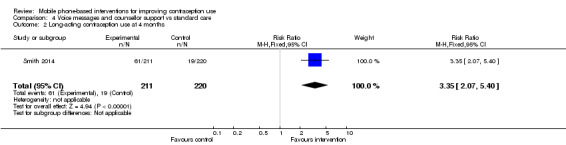
Comparison 4 Voice messages and counsellor support vs standard care, Outcome 2 Long‐acting contraception use at 4 months.
2.4. Analysis.
Comparison 2 Daily text message reminders vs no reminders, Outcome 4 Emergency contraception use during the study.
5.2. Analysis.
Comparison 5 Contraceptive information via text messages and mail at 1 and 2 months vs standard care, Outcome 2 Use of 2 contraceptives.
5.3. Analysis.
Comparison 5 Contraceptive information via text messages and mail at 1 and 2 months vs standard care, Outcome 3 Sexually active and not using contraceptive.
Two trials assessed pregnancy, and one trial assessed repeat abortion. In Hou 2010, no pregnancies were reported during the trial period. In Smith 2014, no difference was noted between intervention and control groups in repeat pregnancy or abortion at four months, but few events were reported (Analysis 4.4; Analysis 4.5).
4.4. Analysis.
Comparison 4 Voice messages and counsellor support vs standard care, Outcome 4 Repeat pregnancy at 4 months.
4.5. Analysis.
Comparison 4 Voice messages and counsellor support vs standard care, Outcome 5 Repeat abortion at 4 months.
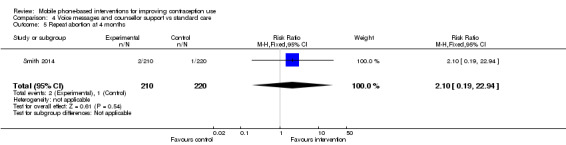
One trial assessed potential unintended outcomes. In Smith 2014, no road traffic accidents or domestic abuse was reported (Analysis 4.6; Analysis 4.7).
4.6. Analysis.
Comparison 4 Voice messages and counsellor support vs standard care, Outcome 6 Road traffic accident.
4.7. Analysis.
Comparison 4 Voice messages and counsellor support vs standard care, Outcome 7 Domestic abuse.
Exploratory analyses
Castano 2012 undertook an exploratory analysis to assess whether the effect of the intervention on the primary outcome differed if follow‐up occurred whilst the participant was still receiving the intervention. Participants receiving the intervention were more likely to report OC continuation if follow‐up took place whilst the intervention was ongoing (RR 1.41, 95% CI 1.13 to 1.74) (Analysis 1.2),and no evidence of effect was found if follow‐up was provided after the intervention ended (RR 1.11, 95% CI 0.95 to 1.29) (Analysis 1.3).
1.2. Analysis.
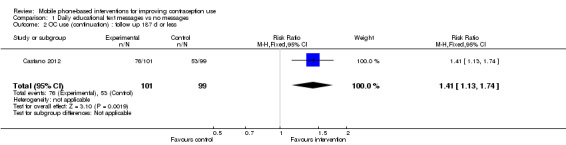
Comparison 1 Daily educational text messages vs no messages, Outcome 2 OC use (continuation) : follow up 187 d or less.
1.3. Analysis.
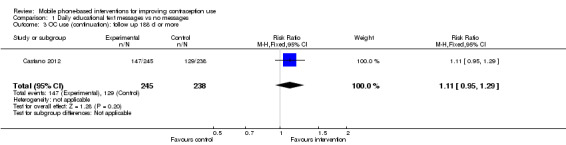
Comparison 1 Daily educational text messages vs no messages, Outcome 3 OC use (continuation): follow up 188 d or more.
Discussion
Summary of main results
Our review provides limited evidence that interventions delivered by mobile phone improve contraception use. We identified five trials ‐ three assessing adherence to a specific method of contraception and two assessing both uptake and adherence to more than one method. Most trials were conducted in high‐income countries. Differences in interventions and outcomes measures did not permit us to undertake meta‐analysis.
Two trials reported increased self reported contraception use. One trial in the USA reported improved OC continuation from an intervention comprising a range of uni‐directional and interactive text messages amongst participants who were still receiving the intervention (Castano 2012). One trial in Cambodia reported increased use of effective contraception at four months post abortion from an intervention comprising automated interactive voice messages and phone counsellor support (Smith 2014).
One feasibility trial in the USA reported a lower mean number of days between scheduled and completed attendance for the first but not subsequent Depo‐Provera appointments using clinic records from an intervention comprising reminders and healthy self management text messages (Trent 2013). Simple text messages as OC reminders had no effect on missed pills assessed by electronic medication monitor in a small trial in the USA (Hou 2010). No effect on self reported contraception use was observed amongst isotretinoin users from an intervention that provided health information via two uni‐directional text messages and mail (Tsur 2008). Only one trial assessed potential adverse effects of the intervention and reported no evidence of road traffic accidents or domestic abuse (Smith 2014).
Overall completeness and applicability of evidence
As predicted on the basis of previous reviews of mobile phone‐based interventions (Horvath 2012; Whittaker 2009), we identified insufficient high‐quality studies to address the objectives of the review, and thus its external validity. Evidence is insufficient to recommend a particular mode or frequency of communication. We cannot draw conclusions on the effectiveness of interventions delivered by mobile phone among younger or older populations, in high‐ or low‐income settings or among different outcomes, whether they involve uptake of or adherence with contraception. However, we identified several ongoing studies that may be included in future updates of this review.
At present, interventions delivered by mobile phone to increase contraception use are not standard practice for contraceptive service delivery organisations. Our review findings suggest that additional mobile phone‐based interventions to increase contraception use could be used in two contexts. First, daily educational text message reminders can improve self reported OC adherence in young females at the time they are receiving the intervention. Second, interactive voice messages and counsellor support can increase self reported use of effective contraception at four months post abortion. However, the follow caveats should be considered. First, information on the cost‐effectiveness of these interventions is lacking at the present time. None of the included studies presented data on intervention costs, although we may have identified articles if we had explicitly searched for cost‐effectiveness analyses. Second, the duration of follow‐up in all of the included trials ranged between three months and 12 months, and the long‐term effect of these interventions is unclear. Third, it is likely that these interventions would require adaptation for different settings, and it is not clear what behaviour change techniques, or combinations of, are effective. Lack of theory in the interventions was a limitation of all included studies. We used Abraham and Michie's typology of behaviour change techniques to code intervention content according to the intervention description provided in the papers or in protocols, which varied in the level of detail provided. Three trials provided details of specific message content (Castano 2012; Hou 2010; Smith 2014). Coding of the intervention content could have been more complete and accurate if additional detail on messages and other intervention content had been provided. The effective interventions used four (Castano 2012) or five (Smith 2014) behaviour change techniques, whilst the interventions that were not reported to be effective used two (Trent 2013; Tsur 2008) or three (Hou 2010) behaviour change techniques (Table 2). An inadequate number of studies assessed associations between use of particular behaviour change techniques and effectiveness of interventions.
Our review excluded studies in which mobile phones were used for two‐way voice communication alone. However, some of the excluded studies were recent and utilised mobile phones; therefore future reviews should consider inclusion of such studies. Our review did not include studies that aimed to increase contraceptive knowledge alone. Interventions that increase knowledge of contraception may lead to increased uptake and adherence, and future reviews should consider inclusion of such studies.
Quality of the evidence
We summarised the quality of evidence in Table 3 using the GRADE approach. We downgraded two trials because of limitations in design and implementation; lack of or insufficient information on blinding (Castano 2012; Tsur 2008); or large losses to follow‐up (Castano 2012). We downgraded one trial for indirectness of evidence, as it addressed a restricted version of the main review question by including only participants using a medication for acne, which could affect the generalisability of this study to other populations (Tsur 2008). We downgraded three trials with small sample sizes for imprecision of results (Hou 2010; Trent 2013; Tsur 2008). Overall, evidence was of high quality for one trial, moderate for two trials, low for one trial and very low for one trial.
2. Results by quality of evidence.
| Study | Limitations in design and implementation | Indirectness of evidence | Unexplained heterogeneity or inconsistency of results | Imprecision of results | High probability of publication bias | Quality of evidence | Evidence of effect |
| Castano 2012 | ‐2 | Low | Yes | ||||
| Hou 2010 | ‐1 | Moderate | No | ||||
| Smith 2014 | High | Yes | |||||
| Trent 2013 | ‐1 | Moderate | Yes | ||||
| Tsur 2008 | ‐1 | ‐1 | ‐1 | Very low | No |
Randomised controlled trials were considered of high quality, then were downgraded by one level (serious) or two levels (very serious) for each of the following: limitations in design and implementation (e.g. lack of blinding, large losses to follow‐up), indirectness of evidence, unexplained heterogeneity or inconsistency of results, imprecision of results, high probability of publication bias.
No trials were at low risk of bias in all areas assessed. Performance bias may have arisen from altered behaviour of participants based on allocation to the intervention or control group. Detection bias may have arisen as the result of lack of outcome assessment blinding, which was not apparent in all of the trials. Furthermore, bias may have arisen from use of self report measures of contraception. Although the standard in contraceptive research, self report measures have been shown to overestimate contraceptive use and underestimate abortion (Stuart 2009). Hou 2010 reported increased poorer OC adherence as measured by electronic medication monitoring compared with the patient diary. However, it should be considered that no gold standard measure of OC use is available, and objective assessment is challenging, as biological measures such as hormonal assays do not indicate consistent use (Hall 2010). To date, electronic medication monitors have been costly, and the appearance of the devices themselves could interfere with the intervention.
Participants randomly assigned to the intervention may have shared intervention content with participants recruited from the same centre, resulting in contamination across study groups and weakening of overall effect. None of the included trials reported on this. Three trials, all of which found no effect, included small sample sizes, which increased the possibility of Type II error (Hou 2010; Trent 2013; Tsur 2008).
Agreements and disagreements with other studies or reviews
To our knowledge, this is the first systematic review of mobile phone‐based interventions to improve contraception use. Our observation that interventions found to increase contraception use were multi‐faceted and more intensive is consistent with evidence on strategies to improve adherence and acceptability of hormonal methods of contraception (Halpern 2013). The finding that simple text message reminders had no effect is consistent with existing mHealth evidence from systematic reviews and trials that simple text message reminders have at best small effects (pooled RR 1.0, 95% CI 0.77 to 1.30), as well as findings of face‐to‐face adherence research (Free 2013a; Haynes 2008; Shet 2014).
Complex interventions delivered by mobile phone have been shown to be effective in other conditions, including human immunodeficiency virus (HIV) medication adherence and smoking cessation (Free 2011; Free 2013a; Horvath 2012; Lester 2010; Pop‐Eleches 2011). Interventions for different conditions should be compared with caution, as it is likely that factors influencing contraception use will be different from those influencing adherence to antiretroviral therapy or smoking cessation. However, mobile phone‐based interventions for HIV medication adherence are similar to those for contraception in the respect that they include populations for which confidentiality and privacy are of particular importance, and they can involve similar behaviours (i.e. taking a tablet). A Cochrane review of mobile phone text messaging for promoting adherence to antiretroviral therapy reported good evidence that text message support can improve adherence to treatment compared with standard care (Horvath 2012). However, since that time, Shet 2014 has reported no effect on virologic failure at two years when medication reminders were delivered by mobile. Thus, evidence for mobile phone‐based interventions for HIV adherence to date, as for contraception, is mixed and is likely to be dependent on intervention content, as well as the mechanism of delivery (mobile phone). Shared learning between researchers in different fields may occur over time.
Authors' conclusions
Implications for practice.
At the present time, evidence is insufficient to support widespread implementation of mobile phone‐based interventions to increase contraception use. Whilst evidence indicates that a series of interactive voice messages and counsellor support can improve post‐abortion contraception, and that a mixture of uni‐directional and interactive daily educational text messages may improve OC adherence, the cost‐effectiveness and long‐term effects of these interventions remain unknown.
Interventions delivered by mobile phone should be considered as part of the wider health service delivery. Future mobile phone‐based interventions should consider the context and needs of the population, for example, literacy, phone use, use of other services and what behaviour change techniques delivered by mobile phone are likely to be effective.
Implications for research.
Further high‐quality trials are required to robustly establish the effects of interventions delivered by mobile phone to increase contraception use. Larger trials could be powered for pregnancy and abortion outcomes. Trials should be complemented by process evaluations to enhance understanding of the mechanism that explains why a certain intervention works or does not work. The cost‐effectiveness of effective interventions should be established. To build the evidence base regarding which interventions and intervention components are effective, future interventions should be described in detail together with conceptual frameworks and use of theory, as appropriate. This would enable assessment of behaviour change techniques and replication or modification of interventions elsewhere. In areas where interventions have yielded inconclusive evidence, such as fully automated text message interventions for OC adherence, future research should focus on improving interventions before considering future evaluation by randomised controlled trials. Interventions that aim to improve adherence to a single method should consider additional facilitation of safe method switching, given that side effects and health concerns leading to discontinuation are common.
Consideration should be given to choice of outcome measures, whether measures of uptake or adherence. Use of consistent outcome measures would allow pooling of results and meta‐analysis in future reviews. Trials should aim to objectively assess contraception use, if feasible. If self report measures are used, outcome assessment should be blinded and questions carefully considered to reduce the likelihood of courtesy bias. For long‐acting contraception, objective measures of use such as clinical examination to assess IUD position are likely to be more robust but may be costly and less acceptable to patients, resulting in increased attrition. If appropriate, data on contraception use such as injectable methods could be obtained from clinical records. To assess oral contraceptive use, electronic medication monitors that have the same appearance as contraceptive pill blister packs should be considered.
Acknowledgements
We would like to thank Mousumi Rahman for her input on earlier drafts of the protocol, Jane Falconer for assistance with the search strategy and the Cochrane Fertility Regulation Group editors.
Appendices
Appendix 1. Search strategies
MEDLINE via Ovid (date of search: 6 October 2014)
(phone adj3 call*).mp. OR ((cell* or mobile or smart or google or nexus or iphone) adj3 (phone* or telephone*)).mp. OR smartphone*.mp. OR smart‐phone*.mp. OR (blackberr* not extract).mp. OR (black‐berr* not extract).mp. OR ((mobile adj3 health) not (van* or unit*)).mp. OR mhealth.mp OR m‐health.mp OR e‐health*.mp. OR ehealth*.mp. OR (electronic adj health).mp. OR (mobile adj3 technol*).mp. OR ((mobile or smartphone or smart‐phone or phone or software) adj3 app*).mp. OR MMS.mp. OR multimedia messaging service.mp OR SMS.mp. OR short messag* service.mp OR (text* adj messag*).mp. OR text‐messa*.mp. OR voice messag*.mp. OR interactive voice response.mp OR IVR.mp. OR Telemedicine/ OR cellular phone/ or text messaging/
AND
(contracept* or (family adj planning) or (Birth adj control)).mp. OR condom.mp. OR (OC adj pill).mp. OR (depot medroxyprogest* or NET‐EN or NET EN or Mesigyna or Cyclofem).mp. OR (intrauterine system or intra‐uterine system or IUS or intrauterine device or intra‐uterine device or IUD).mp. OR (vasectomy or sterilisation or sterilization or (tubal adj ligation)).mp. OR ((vaginal adj ring) or cycletel or cycle‐tel or abstain or abstinen* or lactational amenorr*).mp OR (pregnan* or abortion).mp OR exp Contraception/ OR exp Contraceptive Devices/ OR exp Pregnancy, Unplanned/ OR exp Pregnancy, Unwanted/ OR exp Abortion, Induced/ OR (NORPLANT or implanon or Femplant).mp.
Limit to yr="1993‐Current" and clinical trial, all
Global Health via Ovid (date of search: 6 October 2014)
(phone adj3 call*).mp. OR ((cell* or mobile or smart or google or nexus or iphone) adj3 (phone* or telephone*)).mp. OR smartphone*.mp. OR smart‐phone*.mp. OR (blackberr* not extract).mp OR (black‐berr* not extract).mp OR ((mobile adj3 health) not (van* or unit*)).mp. OR mhealth.mp OR m‐health.mp. OR e‐health*.mp. OR ehealth*.mp OR (electronic adj health).mp OR (mobile adj3 technol*).mp OR ((mobile or smartphone or smart‐phone or phone or software) adj3 app*).mp. OR MMS.mp OR multimedia messaging service.mp OR SMS.mp. OR short messag* service.mp OR (text* adj messag*).mp. OR text‐messa*.mp. OR voice messag*.mp. OR interactive voice response.mp OR IVR.mp OR Telemedicine/ OR cellular phone/ or text messaging/ OR exp mobile telephones/
AND
(contracept* or (family adj planning) or (Birth adj control)).mp. OR condom.mp OR (OC adj pill).mp. OR (depot medroxyprogest* or NET‐EN or NET EN or Mesigyna or Cyclofem).mp. OR (intrauterine system or intra‐uterine system or IUS or intrauterine device or intra‐uterine device or IUD).mp. OR (vasectomy or sterilisation or sterilization or (tubal adj ligation)).mp. OR ((vaginal adj ring) or cycletel or cycle‐tel or abstain or abstinen* or lactational amenorr*).mp OR (pregnan* or abortion).mp OR exp Contraception/ OR exp Contraceptive Devices/ OR exp Pregnancy, Unplanned/ OR exp Pregnancy, Unwanted/ OR exp Abortion, Induced/ OR (NORPLANT or implanon or Femplant).mp. OR induced abortion/
Limit to yr="1993‐Current"
PsycINFO via Ovid (date of search: 6 October 2014) (phone adj3 call*).mp. OR ((cell* or mobile or smart or google or nexus or iphone) adj3 (phone* or telephone*)).mp. OR smartphone*.mp OR smart‐phone*.mp. OR (blackberr* not extract).mp OR (black‐berr* not extract).mp OR ((mobile adj3 health) not (van* or unit*)).mp OR mhealth.mp. OR m‐health.mp. OR e‐health*.mp. OR ehealth*.mp OR (electronic adj health). OR (mobile adj3 technol*).mp OR ((mobile or smartphone or smart‐phone or phone or software) adj3 app*).mp. OR MMS.mp. OR multimedia messaging OR SMS.mp. OR short messag* service.mp OR (text* adj messag*).mp OR text‐messa*.mp OR voice messag*.mp OR interactive voice response.mp OR IVR.mp OR Telemedicine/ OR cellular phone/ or text messaging/
AND
(contracept* or (family adj planning) or (Birth adj control)).mp OR condom.mp. OR (OC adj pill).mp OR (depot medroxyprogest* or NET‐EN or NET EN or Mesigyna or Cyclofem).mp OR (intrauterine system or intra‐uterine system or IUS or intrauterine device or intra‐uterine device or IUD).mp. OR (vasectomy or sterilisation or sterilization or (tubal adj ligation)).mp OR ((vaginal adj ring) or cycletel or cycle‐tel or abstain or abstinen* or lactational amenorr*).mp OR (pregnan* or abortion).mp OR exp Contraception/ OR exp Contraceptive Devices/ OR exp Pregnancy, Unplanned/ OR exp Pregnancy, Unwanted/ OR exp Abortion, Induced/ OR (NORPLANT or implanon or Femplant).mp.
Limit to yr="1993‐Current" and clinical trial, all
EMBASE via Ovid (date of search: 6 October 2014) (phone adj3 call*).mp OR ((cell* or mobile or smart or google or nexus or iphone) adj3 (phone* or telephone*)).mp. OR smartphone*.mp. OR smart‐phone*.mp OR (blackberr* not extract).mp OR (black‐berr* not extract).mp OR ((mobile adj3 health) not (van* or unit*)).mp. OR mhealth.mp OR m‐health.mp. OR e‐health*.mp. OR ehealth*.mp. OR (electronic adj health).mp OR (mobile adj3 technol*).mp. OR ((mobile or smartphone or smart‐phone or phone or software) adj3 app*).mp OR MMS.mp. OR multimedia messaging service.mp OR SMS.mp OR short messag* service.mp. OR (text* adj messag*).mp OR text‐messa*.mp. OR voice messag*.mp OR interactive voice response.mp. OR IVR.mp. OR Telemedicine/ OR cellular phone/ or text messaging/
AND
(contracept* or (family adj planning) or (Birth adj control)).mp. OR condom.mp. OR (OC adj pill).mp. OR (depot medroxyprogest* or NET‐EN or NET EN or Mesigyna or Cyclofem).mp. OR (intrauterine system or intra‐uterine system or IUS or intrauterine device or intra‐uterine device or IUD).mp. OR (vasectomy or sterilisation or sterilization or (tubal adj ligation)).mp. OR ((vaginal adj ring) or cycletel or cycle‐tel or abstain or abstinen* or lactational amenorr*).mp. OR (pregnan* or abortion).mp. OR exp Contraception/ OR exp Contraceptive Devices/ OR exp Pregnancy, Unplanned/ OR exp Pregnancy, Unwanted/ OR exp Abortion, Induced/ OR (NORPLANT or implanon or Femplant).mp.
Limit to yr="1993‐Current", clinical trial, all and (clinical trial or randomized controlled trial or controlled clinical trial or multicenter study or phase 1 clinical trial or phase 2 clinical trial or phase 3 clinical trial or phase 4 clinical trial)
Cochrane Central register of Controlled trials (CENTRAL) (date of search: 6 October 2014)
(((phone NEAR3 call*) OR ((cell* or mobile or smart or google or nexus or iphone) NEAR3 (phone* or telephone*)) OR (smartphone*) OR (smart‐phone*) OR (blackberr* NOT extract) OR (black‐berr* NOT extract)) OR ((mobile NEAR3 (health NOT (van* or unit*))) OR (mhealth) OR (m‐health) OR (e‐health*) OR (ehealth*) OR (electronic health) OR (mobile NEAR3 technol*)) OR ((mobile or smartphone or smart‐phone or phone or software) NEAR3 (app*)) OR ((MMS) OR (multimedia messaging service) OR (SMS) OR (short messag* service) OR (text* messag*) OR (text‐messa*) OR (voice messag*) OR (interactive voice response) OR (IVR))) OR exp Telemedicine OR exp Cellular Phone
AND
(((contracept*) OR (family planning) OR (Birth control)) OR (condom) OR ((OC pill)) OR ((depot medroxyprogest*) OR (NET‐EN) OR (NET EN) OR (Mesigyna) OR (Cyclofem)) OR ((NORPLANT) OR (implanon) OR (Femplant)) OR ((intrauterine system) OR (intra‐uterine system) OR (IUS) OR (intrauterine device) OR (intra‐uterine device) OR (IUD)) OR ((vasectomy) OR (sterilisation) OR (sterilization) OR (tubal ligation)) OR ((vaginal ring) OR (cycletel) OR (cycle‐tel) or (abstain) OR (abstinen*) OR (lactational amenorr*)) OR ((pregnan*) OR (abortion))) OR exp Contraception OR exp Contraceptive Devices OR exp Pregnancy, Unplanned OR exp Pregnancy, Unwanted OR exp Abortion, Induced
Limit to 1993‐2014
POPLINE (date of search: 6 October 2014)
Family Planning OR Pregnancy Unplanned OR Pregnancy Unwanted AND Cellular Phone OR Mobile Devices OR Text Messaging (1993‐2014)
Africa‐Wide Information (date of search: 6 October 2014)
((phone n3 call*) OR ((cell* or mobile or smart or google or nexus or iphone) n3 (phone* or telephone*)) OR (smartphone*) OR (smart‐phone*) OR (blackberr* NOT extract) OR (black‐berr* NOT extract)) OR ((mobile n3 (health NOT (van* or unit*))) OR (mhealth) OR (m‐health) OR (e‐health*) OR (ehealth*) OR (electronic health) OR (mobile n3 technol*)) OR ((mobile or smartphone or smart‐phone or phone or software) n3 (app*)) OR ((MMS) OR (multimedia messaging service) OR (SMS) OR (short messag* service) OR (text* messag*) OR (text‐messa*) OR (voice messag*) OR (interactive voice response) OR (IVR))
AND
((contracept*) OR (family planning) OR (Birth control)) OR (condom) OR ((OC pill)) OR ((depot medroxyprogest*) OR (NET‐EN) OR (NET EN) OR (Mesigyna) OR (Cyclofem)) OR ((NORPLANT) OR (implanon) OR (Femplant)) OR ((intrauterine system) OR (intra‐uterine system) OR (IUS) OR (intrauterine device) OR (intra‐uterine device) OR (IUD)) OR ((vasectomy) OR (sterilisation) OR (sterilization) OR (tubal ligation)) OR ((vaginal ring) OR (cycletel) OR (cycle‐tel) or (abstain) OR (abstinen*) OR (lactational amenorr*)) OR ((pregnan*) OR (abortion))
LILACS (date of search: 6 October 2014)
(contracept$ OR family planning OR condom$ OR pregnan$ OR abortion$) AND (phone$ OR text messag$ OR mobil$ health)
WHO international trials registry (date of search: 9 October 2014)
Condition (family planning) intervention (mHealth): (family planning OR contracept* OR pregnanc* OR abortion* OR condom*) AND (phone OR text messag* OR cellular phon* OR mobile phon* OR mobile devic* OR mobile technol* Current controlled trials
(family planning OR contracept* OR unplanned pregnanc* OR unintended pregnanc* OR induced abortion* OR condom*) AND (phone OR text messag* OR cellular phon* OR mobile phon* OR mobile devic* OR mobile technol*)
Data and analyses
Comparison 1. Daily educational text messages vs no messages.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 OC use (continuation) at 6 months | 1 | 683 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.19 [1.05, 1.35] |
| 2 OC use (continuation) : follow up 187 d or less | 1 | 200 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.41 [1.13, 1.74] |
| 3 OC use (continuation): follow up 188 d or more | 1 | 483 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.11 [0.95, 1.29] |
| 4 No OC interruptions > 7 days at 6 months | 1 | 683 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.22 [1.06, 1.41] |
| 5 Missed no pills in last month | 1 | 683 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.44 [1.16, 1.79] |
| 6 OC use at last intercourse | 1 | 683 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.15 [1.03, 1.28] |
Comparison 2. Daily text message reminders vs no reminders.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Mean number of missed pills (cycle 1) | 1 | 73 | Mean Difference (IV, Fixed, 95% CI) | 0.5 [‐1.08, 2.08] |
| 2 Mean number of missed pills (cycle 3) | 1 | 73 | Mean Difference (IV, Fixed, 95% CI) | 0.80 [‐1.22, 2.82] |
| 3 Condom use for at least 50% of coital activity during the study (self report) | 1 | 73 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.94 [1.00, 3.78] |
| 4 Emergency contraception use during the study | 1 | 73 | Risk Ratio (M‐H, Fixed, 95% CI) | 5.14 [0.26, 103.39] |
| 5 Pregnancy reported during the study | 1 | 73 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
2.5. Analysis.
Comparison 2 Daily text message reminders vs no reminders, Outcome 5 Pregnancy reported during the study.
Comparison 3. Daily text message appointment reminders 72 hours before appointment + healthy self management messages vs standard care.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Mean number of days between scheduled appointment and completed visit: first visit | 1 | 87 | Mean Difference (IV, Fixed, 95% CI) | ‐8.60 [‐16.74, ‐0.46] |
| 2 Mean number of days between scheduled appointment and completed visit: third visit | 1 | 69 | Mean Difference (IV, Fixed, 95% CI) | 2.19 [‐3.89, 8.27] |
Comparison 4. Voice messages and counsellor support vs standard care.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Effective contraception use at 4 months | 1 | 431 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.39 [1.17, 1.66] |
| 2 Long‐acting contraception use at 4 months | 1 | 431 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.35 [2.07, 5.40] |
| 3 Effective contraception use over 4 month post‐abortion period | 1 | 403 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.35 [1.10, 1.67] |
| 4 Repeat pregnancy at 4 months | 1 | 430 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.26 [0.39, 4.06] |
| 5 Repeat abortion at 4 months | 1 | 430 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.10 [0.19, 22.94] |
| 6 Road traffic accident | 1 | 430 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Domestic abuse | 1 | 430 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
Comparison 5. Contraceptive information via text messages and mail at 1 and 2 months vs standard care.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Contraceptive use during treatment with isotretinoin | 1 | 108 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.26 [0.84, 1.89] |
| 2 Use of 2 contraceptives | 1 | 108 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.16 [0.07, 18.07] |
| 3 Sexually active and not using contraceptive | 1 | 108 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.58 [0.11, 3.03] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Castano 2012.
| Methods | Individual randomised controlled trial. Estimated 6‐month continuation rate in the control group of 40% and that a sample size of 960 would be required to detect a 10% change in OC continuation, with 80% power at a 0.05 level of significance, anticipating 15% loss to follow‐up | |
| Participants | 962 sexually active females 13 to 25 years of age electing to use OC at a Planned Parenthood family planning health centre in downtown Brooklyn, New York, USA | |
| Interventions | Control group: routine care including contraceptive counselling by staff and an educational information handout detailing use, effectiveness, benefits and risks Intervention group: routine care plus automated mobile phone‐based intervention comprising 180 daily text messages aiming to improve OC continuation. This included an introductory message, 3 reminders of how to change contact information or message time, 47 individual educational messages, repeated up to 4 times, which incorporated 6 domains of OC knowledge (risks, benefits, side effects, use, effectiveness and mechanisms of action), 12 two‐way messages for quality control and a final message. Intervention duration was 180 days |
|
| Outcomes | Primary outcome: self reported OC continuation (participant had taken OC within previous 7 days). Secondary outcomes: missed pills, interruptions in OC use > 7 days, use of OC at last sexual intercourse. All outcomes assessed by phone 6 months after enrolment | |
| Behaviour change techniques | As defined by study authors: The educational messages incorporated 6 domains of OC knowledge: risks, benefits, side effects, use, effectiveness and mechanisms of action According to Abraham and Michie's typology: 4 behaviour change techniques used (see Table 2) |
|
| Notes | Loss to follow‐up: 28% in the intervention group and 30% in the control group | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number table used to generate the sequence |
| Allocation concealment (selection bias) | Low risk | Sequentially numbered, opaque, sealed envelopes used |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding possible; outcome may have been influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Outcome assessors not blinded, as participants were asked about satisfaction with the intervention |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Main reason for incomplete data unlikely to be related to outcome |
| Selective reporting (reporting bias) | Unclear risk | Primary outcome of contraceptive continuation stated in the clinicaltrials.gov entry but insufficient detail on prespecified measurements |
| Other bias | High risk | Possibility of detection (social desirability or recall) bias with self report measures of contraception use |
Hou 2010.
| Methods | Individual randomised controlled trial. Estimated an average of 2.6 missed pills per cycle in the control group, and that a sample size of 68 would be required to detect a 1.6 pill improvement with standard deviation of 2 pills, with 90% power at a 0.05 level of significance, anticipating 15% loss to follow‐up | |
| Participants | 103 women enrolled to the study and 82 randomly assigned after a 1 month run‐in period. 82 sexually active females electing to start using OC, seeking care at Planned Parenthood League of Massachusetts, USA. Mean age of 22 years (range 18 to 31) | |
| Interventions | Control group: routine care according to standard clinic protocol (not stated) during 1 month run‐in period. Women in the control group did not receive text message reminders Study authors reported a high rate of reminder system use in the control group, particularly electronic systems such as cell phone alarms that mimicked the study intervention Intervention group: routine care according to standard clinic protocol (not stated) during 1 month run‐in period plus an automated daily text message aiming to improve OC adherence, “Please remember to take your birth control pill,” sent at a designated time chosen by the participant over the 3 month study period | |
| Outcomes | Number of missed pills per cycle (assessed over 3 months) assessed with electronic monitoring device and patient diary | |
| Behaviour change techniques | As defined by study authors: not described According to Abraham and Michie's typology: 3 behaviour change techniques used (see Table 2) |
|
| Notes | Loss to follow‐up: 12% intervention and 10% control | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomisation |
| Allocation concealment (selection bias) | Low risk | Sequentially numbered, opaque, sealed envelopes |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding possible; outcome may have been influenced by lack of blinding. Increased use of reminders in the control group suggests that allocation to intervention or control group may have altered behaviour |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Investigator blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Reason for missing data (mechanical and technological issues) unlikely to be related to true outcome |
| Selective reporting (reporting bias) | Unclear risk | Primary and secondary outcomes stated in the clinicaltrials.gov entry, but insufficient detail on prespecified measurements and subgroup analyses |
| Other bias | Low risk | Study appears to be free of other sources of bias (electronic medication monitor used to assess outcome) |
Smith 2014.
| Methods | Individual randomised controlled trial. Estimated that use of effective contraception at 4 months would be 35% in the control group, and a sample size of 500 would be required to detect a 13% improvement in contraceptive use, with 90% power at a 0·05 level of significance | |
| Participants | 500 participants; females 18 years of age or older, with a mobile phone primarily for their own use, reporting not wanting to be pregnant, willing to receive automated voice messages related to contraception, attending for induced abortion at 4 Marie Stopes International clinics in Cambodia | |
| Interventions | Control group: routine care, which included post‐abortion family planning counselling at the clinic in accordance with national guidelines, the offer of a clinic follow‐up appointment, the clinic phone number and the Hotline number operated by counsellors at MSI Cambodia Intervention group: routine care plus a mobile phone‐based intervention aiming to improve uptake and adherence comprising 6 automated, interactive voice messages, counsellor delivered phone support according to response to messages and additional reminder messages for OC or injectable users | |
| Outcomes | Primary outcome: self reported effective contraception use at 4 months post abortion. Secondary outcomes: use of long‐acting contraception (intrauterine device, implant, permanent method), repeat pregnancy, abortion, contraceptive use over the 4 month post‐abortion period > 80%, road traffic accident and domestic abuse. All outcomes assessed by phone at 4 months (12 month follow‐up is planned) | |
| Behaviour change techniques | As defined by study authors: Phone calls aimed to support contraceptive use by addressing participants' capability to use contraception by providing individualised information on a range of contraceptive methods, opportunity to use contraception (e.g. informing participants where they could access specific methods near to their residence) and motivation by re‐enforcing the benefits of contraception use According to Abraham and Michie's typology: 5 behaviour change techniques used (see Table 2) |
|
| Notes | Loss to follow‐up: 15% in the intervention group and 12% in the control group | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐based randomisation programme used |
| Allocation concealment (selection bias) | Low risk | Web‐based allocation performed after enrolment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding possible; outcome may have been influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Researchers who undertook data collection and analysis were masked to treatment allocation |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Missing outcome data balanced in numbers across intervention groups. Reasons for missing data unlikely to be related to true outcome |
| Selective reporting (reporting bias) | Low risk | Study’s prespecified (primary and secondary) outcomes have been reported as prespecified in the published study protocol |
| Other bias | High risk | Possibility of detection (social desirability or recall) bias with self report measures of contraception use |
Trent 2013.
| Methods | Pilot individual randomised controlled trial (primarily a feasibility and acceptability trial) | |
| Participants | 100 female adolescents (13 to 21 years of age) recruited from an urban academic practice in a high teen and unplanned pregnancy prevalence community in the USA, currently using Depo‐Provera, with a cell phone with text messaging capability for personal use. Most participants were African American and resided in low income, single parent, mother‐headed households | |
| Interventions | Control group: clinic protocol for standard care, which included participant‐initiated support and clinical nursing outreach for missed appointments Intervention group: routine care plus automated intervention aimed to improve follow‐up Depo‐Provera clinic attendance and comprised a welcome message, daily text appointment reminders starting 72 hours before the clinic visit with the option to cease messages by responding (yes or no) with their plans to attend the visit. Intervention adolescents also received prescheduled health messages over the course of the 3 month enrolment period regarding condom use for STI prevention, healthy weight management, encouragement to call the nurse for problems and an STI screening reminder. All message signatures indicated that they were from the nurse case manager to build relationships with the clinical team |
|
| Outcomes | Primary outcome: days between next scheduled appointment and attendance for Depo‐Provera injection over 3 cycles (9 months). Secondary outcome: on‐time appointment for Depo‐Provera injection over 3 cycles (9 months) | |
| Behaviour change techniques | As defined by study authors: not described According to Abraham and Michie's typology: 2 behaviour change techniques used (see Table 2) |
|
| Notes | Information from abstract and additional communication with investigator. Full text not yet published Loss to follow‐up: 12% in the intervention group and 14% in the control group |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation by permitted block design (according to investigator's communication) |
| Allocation concealment (selection bias) | Low risk | Allocation sealed in envelope for nurse until informed consent to participate (according to investigator's communication) |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding possible; outcome may have been influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | PI blinded to allocation (according to investigators' communication) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Missing outcome data balanced in numbers across intervention groups. Reasons for missing data unlikely to be related to true outcome |
| Selective reporting (reporting bias) | Low risk | Primary outcome prespecified in the clinicaltrials.gov record |
| Other bias | Low risk | Study appears to be free of other sources of bias |
Tsur 2008.
| Methods | Individual randomised controlled trial. Estimated that use of contraception would be 50% in the control group, and a sample size of 100 would be required to detect 30% improvement in contraceptive use, with 80% power at a 0·05 level of significance | |
| Participants | 108 females of reproductive age (16 to 45 years of age), some users and some not users of contraception, using or planning to use isotretinoin (a drug for acne), who phoned the Drug Consultation Centre at Assaf Harofeh Medical Center in Israel seeking advice regarding isotretinoin | |
| Interventions | Control group: Routine care comprised information on Isotretinoin including contraceptive use only during the initial interview. Intervention group: automated intervention aimed to increase contraception use and comprised routine care plus additional information about teratogenic risk and the importance of contraceptive use in mailed written form and by text messages sent to cellular phones 1 month and 2 months after the initial call | |
| Outcomes | Primary outcome: contraceptive use in women taking isotretinoin (methods of contraception not stated). Secondary outcomes: use of 2 contraceptives, sexual activity, contraceptive use amongst sexually active participants. All outcomes assessed by phone call at 3 months | |
| Behaviour change techniques | As defined by study authors: not described According to Abraham and Michie's typology: 2 behaviour change techniques used (see Table 2) |
|
| Notes | 5 participants (5%) lost to follow‐up at 3 months and not included in the final analysis. Differential loss to follow‐up between intervention and control groups not stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random numbers kept in sealed envelopes |
| Allocation concealment (selection bias) | Unclear risk | Method of allocation concealment not described in adequate detail. Sealed envelopes used, but unclear whether they were sequentially numbered and opaque |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding possible; outcome may have been influenced by lack of blinding |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Insufficient information on whether outcome assessors were aware of allocation |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Missing outcome data balanced in numbers across intervention groups |
| Selective reporting (reporting bias) | Unclear risk | Study protocol not available. The primary outcome is reported using measurements that were not prespecified in the Methods section of the paper |
| Other bias | High risk | Possibility of detection (social desirability) bias with self report measures of contraception use |
OC: oral contraceptive
STI: sexually transmitted infection
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Bannink 2014 | Web‐based intervention that does not appear to have been intended or adapted for mobile phone users |
| Berenson 2012 | Phone call only intervention |
| Bracken 2014 | No relevant contraception outcome measure |
| Constant 2014 | Post‐abortion family planning not the main focus of the intervention and not reported |
| Gold 2011 | Focus on preventing sexually transmitted disease rather than on providing contraception |
| Hall 2013 | Additional analysis of Castano 2012 but no relevant outcome measure (reported contraceptive knowledge) |
| Juzang 2011 | Focus on preventing sexually transmitted disease rather than on providing contraception |
| Kaoaiem 2012 | Focus on preventing sexually transmitted disease rather than on providing contraception, 'quasi‐experimental' design |
| Katz 2011 | Phone call only intervention |
| Kirby 2010 | Phone call only intervention |
| L'Engle 2013 | Not a randomised controlled trial |
| Lim 2012 | Focus on preventing sexually transmitted disease rather than on providing contraception |
| Mackenzie 2009 | Not a randomised controlled trial |
| O'Sullivan 2008 | Not a randomised controlled trial |
| Sridhar 2013 | Tablet‐based application for contraceptive counselling not adapted for mobile phone users |
| Suffoletto 2013 | Focus on preventing sexually transmitted disease rather than on providing contraception |
| Walakira 2013 | Not a randomised controlled trial (longitudinal comparison study) |
Characteristics of ongoing studies [ordered by study ID]
Johnson 2014.
| Trial name or title | Randomised Controlled Trial Evaluation of m4RH |
| Methods | Randomised controlled trial |
| Participants | Users or potential users of contraception who registered for m4RH with a text message |
| Interventions | m4RH text messaging intervention |
| Outcomes | Contraceptive knowledge and use |
| Starting date | 2014 |
| Contact information | Pamela Riley: Pamela_riley@abtassoc.com |
| Notes |
NCT01401816.
| Trial name or title | Advanced Provision of Emergency Contraception: Utilising Technology to Increase Prescription Fill Rates |
| Methods | Pilot randomised controlled trial (n = 60) of a text messaging intervention |
| Participants | Sexually active female adolescents 13 to 21 years of age who have been provided with a prescription for emergency contraception |
| Interventions | Follow‐up text message on the phone to remind them to fill the prescription |
| Outcomes | Primary outcome: prescription fill rates. Secondary outcomes: sexual activity, contraception use, risk of pregnancy, knowledge of emergency contraception |
| Starting date | July 2011 |
| Contact information | tracey.a.wilkinson@gmail.com |
| Notes |
NCT01545609.
| Trial name or title | A Text Message Support System for Effective Continuation of a Birth Control Method in Female Adolescents: 'BC 2U': NCT01545609 |
| Methods | Randomised controlled trial (n = 220) |
| Participants | Inner city, minority adolescent females (15 to 19 years of age), English speaking, owner of a working cell phone, wanting to start a birth control method and not on a method for the preceding 3 months, no contraindications to initiating a birth control method |
| Interventions | Intervention: tailored text messages about their method of contraception |
| Outcomes | Primary outcome: continuation of a birth control method at 4 months. Secondary outcomes: change in birth control method used, pregnancy |
| Starting date | March 2012 |
| Contact information | jf2815@cumc.columbia.edu |
| Notes | Expect publication in 2015 |
NCT02093884.
| Trial name or title | A Pilot Study Using Text Messaging to Communicate With Adolescent Females in the Pediatric Emergency Department T2 |
| Methods | Pilot randomised controlled trial (n = 100) using text messaging vs standard care to increase contraceptive use |
| Participants | Adolescent females at high risk of pregnancy in the emergency department who are potential users of contraception (high risk of pregnancy is defined as sexually active in the past 3 months and did not use effective contraception at last intercourse and is not on it now) |
| Interventions | Intervention: 3 months of 31 random text messages developed from qualitative interviews. Standard care: paper wallet card advertising family planning clinic |
| Outcomes | Primary outcome: initiation of highly effective contraception. Secondary outcomes: follow‐up, condom use, contraception counselling |
| Starting date | 2014 |
| Contact information | Lauren S Chernick: lc2243@cumc.columbia.edu |
| Notes | Expect publication in 2015 |
Differences between protocol and review
In the protocol, we stated that we would assess risk of bias across the following domains: random sequence generation, allocation concealment, blinding of outcome assessment, incomplete outcome data, selective outcome reporting and other potential biases. In the review, we assessed risk of bias across the following domains in accordance with the latest version of the Cochrane Handbook for Systematic Reviews of Interventions: random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting and other sources of bias.
Contributions of authors
Chris Smith and Caroline Free conceived of the review. Chris Smith oversaw the search and selection process, including the construction and implementation of search and quality appraisal strategies. He contacted authors of papers to ask for additional information from selected papers. Chris Smith and Colin Sumpter screened and selected studies and undertook data extraction. Judy Gold commented on selection of studies. Judy Gold and Caroline Free commented on risk of bias and assessment of behaviour change techniques. All of the review authors reviewed and commented on the review.
Sources of support
Internal sources
No sources of support supplied
External sources
CS is supported by a Medical Research Council (MRC) Population Scientist Fellowship, UK.
Declarations of interest
None known.
New
References
References to studies included in this review
Castano 2012 {published data only}
- Castano P, Bynum J, Andres R, Lara M, Westhoff C. Effect of daily text messages on oral contraceptive continuation: a randomised controlled trial. Obstetrics & Gynecology 2012;119(1):14‐20. [DOI: 10.1097/AOG.0b013e31823d4167] [DOI] [PubMed] [Google Scholar]
Hou 2010 {published data only}
- Hou M, Hurwitz S, Kavanagh E, Fortin J, Goldberg A. Using daily text‐message reminders to improve adherence with oral contraceptives: a randomized controlled trial. Obstetrics and Gynecology 2010;116(3):633‐40. [DOI: 10.1097/AOG.0b013e3181eb6b0f] [DOI] [PubMed] [Google Scholar]
Smith 2014 {unpublished data only}
- Smith C, Ngo T, Gold J, Vannak U, Ly S, Free C. MObile Technology for Improved Family Planning (MOTIF): a single blind randomised trial of a mobile phone‐based intervention to support post‐abortion family planning. Under review. [DOI] [PMC free article] [PubMed]
Trent 2013 {published and unpublished data}
- Trent M, Tomaszewski K. Family planning appointment attendance among urban youth: results from the depotext trial. Journal of Adolescent Health 2013;52(2):S88. [DOI: ] [Google Scholar]
Tsur 2008 {published data only}
- Tsur L, Kozer E, Berkovitch M. The effect of drug consultation center guidance on contraceptive use among women using isotretinoin: a randomized, controlled study. Journal of Women's Health 2008;17(4):579‐84. [DOI: 10.1089/jwh.2007.0623] [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Bannink 2014 {published data only}
- Bannink R, Broeren S, Joosten‐van Zwanenburg E, As E, Looij‐Jansen P, Raat H. Effectiveness of a web‐based tailored intervention (E‐health4Uth) and consultation to promote adolescents' health: randomized controlled trial. Journal of Medical Internet Research 2014;16(5):e143. [DOI: 10.2196/jmir.3163] [DOI] [PMC free article] [PubMed] [Google Scholar]
Berenson 2012 {published data only}
- Berenson A, Rahman M. A randomized controlled study of two educational interventions on adherence with oral contraceptives and condoms. Contraception 2012;86(6):716‐24. [DOI: 10.1016/j.contraception.2012.06.007] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bracken 2014 {published data only}
- Bracken H, Lohr P, Taylor J, Morroni C, Winikoff B. RU OK? The acceptability and feasibility of remote technologies for follow‐up after early medical abortion. Contraception 2014;90(1):29‐35. [DOI: 10.1016/j.contraception.2014.03.016] [DOI] [PubMed] [Google Scholar]
Constant 2014 {published data only (unpublished sought but not used)}
- Constant D, Tolly K, Harries J, Myer L. Mobile phone messages to provide support to women during the home phase of medical abortion in South Africa: a randomised controlled trial. Contraception 2014;90(3):226‐33. [DOI: 10.1016/j.contraception.2014.04.009] [DOI] [PubMed] [Google Scholar]
Gold 2011 {published data only}
- Gold J, Aitken C, Dixon H, Lim M, Gouillou M, Spelman T, et al. A randomised controlled trial using mobile advertising to promote safer sex and sun safety to young people. Health Education Research 2011;26(5):782‐94. [DOI: 10.1093/her/cyr020] [DOI] [PubMed] [Google Scholar]
Hall 2013 {published data only}
- Hall K, Westhoff C, Castano P. The impact of an educational text message intervention on young urban women's knowledge of oral contraception. Contraception 2013;87(4):449‐54. [DOI: 10.1016/j.contraception.2012.09.004] [DOI] [PMC free article] [PubMed] [Google Scholar]
Juzang 2011 {published data only}
- Juzang I, Fortune T, Black S, Wright E, Bull S. A pilot programme using mobile phones for HIV prevention. Journal of Telemedicine and Telecare 2011;17(3):150‐3. [DOI: 10.1258/jtt.2010.091107] [DOI] [PubMed] [Google Scholar]
Kaoaiem 2012 {published data only}
- Kaoaiem H. The effect of squad leader mentors through short message services for mobile phones in promoting safe sex among first (central) army area conscripts of Thailand. Journal of the Medical Association of Thailand 2012;95(2):249‐56. [PUBMED: 22435256] [PubMed] [Google Scholar]
Katz 2011 {published data only}
- Katz K, Rodan M, Milligan R, Tan S, Courtney L, Gantz M, et al. Efficacy of a randomized cell phone‐based counseling intervention in postponing subsequent pregnancy among teen mothers. Maternal and Child Health Journal 2011;15:S42‐S53. [DOI: 10.1007/s10995-011-0860-3] [DOI] [PubMed] [Google Scholar]
Kirby 2010 {published data only}
- Kirby D, Raine T, Yuen C, Sokoloff A, Potter S. Impact of an intervention to improve contraceptive use through follow‐up phone calls to female adolescent clinic patients. Perspectives on Sexual and Reproductive Health 2010;42(1):251‐7. [DOI: 10.1363/4225110.] [DOI] [PMC free article] [PubMed] [Google Scholar]
L'Engle 2013 {published data only}
- L'Engle K, Vahdat H, Ndakidemi E, Lasway C, Zan T. Evaluating feasibility, reach and potential impact of a text message family planning information service in Tanzania. Contraception 2013;87(2):251‐6. [DOI: 10.1016/j.contraception.2012.07.009] [DOI] [PubMed] [Google Scholar]
Lim 2012 {published data only}
- Lim M, Hocking J, Aitken C, Fairley C, Jordan L, Lewis J, et al. Impact of text and email messaging on the sexual health of young people: a randomised controlled trial. Journal of Epidemiology and Community Health 2012;66(1):69‐74. [DOI: 10.1136/jech.2009.100396] [DOI] [PubMed] [Google Scholar]
Mackenzie 2009 {published data only}
- Mackenzie H. A text messaging trial in family planning clinics. Studies in Health Technology and Informatics 2009;146:154‐9. [PUBMED: 19592826] [PubMed] [Google Scholar]
O'Sullivan 2008 {published data only}
- O'Sullivan G. The Saathiya trusted partner program in India: meeting young couples' reproductive health needs. Social Marketing Quarterly 2008;14(3):109‐20. [DOI: 10.1080/15245000802261324] [DOI] [Google Scholar]
Sridhar 2013 {published data only}
- Sridhar A, Chen A, Glik D. Plan a birth control: randomized controlled trial of a mobile health application. Abstracts / Contraception 2013;88:463. [DOI: 10.1016/j.contraception.2013.05.125] [DOI] [Google Scholar]
Suffoletto 2013 {published data only}
- Suffoletto B, Akers A, McGinnis K, Calabria J, Wiesenfeld H, Clark D. A sex risk reduction text‐message program for young adult females discharged from the emergency department. Journal of Adolescent Health 2013;53(3):387‐93. [DOI: 10.1016/j.jadohealth.2013.04.006] [DOI] [PubMed] [Google Scholar]
Walakira 2013 {published data only}
- Walakira B, Lubaale Y, Balidawa F, Nalule S, Githinji F. Can mobile phone text messaging increase uptake of family planning services in Uganda?. Measure Evaluation 2013. [http://www.cpc.unc.edu/measure/publications/wp‐13‐135]
References to ongoing studies
Johnson 2014 {unpublished data only}
- Johnson D, Riley P, Juras R, Choi S, L'Engle K, Okello F. m4RH impact evaluation. Presentation at the Global mHealth forum: http://www.mhealthsummit.org/globalmhealthforum. Washington DC, 2014.
NCT01401816 {published data only}
- NCT01401816. Advanced provision of emergency contraception: utilizing technology to increase prescription fill rates. clinicaltrials.gov/show/NCT01401816 (accessed 9 October 2014).
NCT01545609 {published data only}
- NCT01545609. A trial assessing the effectiveness of text messages in improving continuation of birth control (BC 2U). clinicaltrials.gov/ct2/show/NCT01545609 (accessed 22 Jan 2015).
NCT02093884 {published data only}
- NCT02093884. A pilot study using text messaging to communicate with adolescent females in the pediatric emergency department (T2I). clinicaltrials.gov/ct2/show/NCT02093884 (accessed 9 October 2014).
Additional references
Abraham 2008
- Abraham C, Michie S. A taxonomy of behavior change techniques used in interventions. Health Psychology 2008;27(3):379‐87. [DOI] [PubMed] [Google Scholar]
Ali 2010
- Ali M, Cleland J. Contraceptive switching after method‐related discontinuation: levels and differentials. Studies in Family Planning 2010;41(2):129‐33. [DOI] [PubMed] [Google Scholar]
Bastawrous 2012
- Bastawrous A, Cheeseman R, Kumar A. iPhones for eye surgeons. Eye 2012;26(3):343‐54. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bradley 2009
- Bradley S, Schwandt H, Khan S. Levels, trends, and reasons for contraceptive discontinuation. DHS Analytical studies 20: Measure DHS; 2009 Sept. Publication ID: AS20.
Bullen 2013
- Bullen P. Operational challenges in the Cambodian mHealth revolution. Journal of Mobile Technology in Medicine 2013;2(2):20‐3. [Google Scholar]
Car 2012
- Car J, Gurol‐Urganci I, Jongh T, Vodopivec‐Jamsek V, Atun R. Mobile phone messaging reminders for attendance at healthcare appointments. Cochrane Database of Systematic Reviews 2012, Issue 7. [DOI: 10.1002/14651858.CD007458.pub2] [DOI] [PubMed] [Google Scholar]
CDC 2015
- Centers for Disease Control and Prevention (CDC). Injury Prevention & Control: Motor Vehicle Safety. http://www.cdc.gov/motorvehiclesafety/distracted_driving/ (accessed 5 May 2015).
Cleland 2012
- Cleland J, Conde‐Agudelo A, Peterson H, Ross J, Tsui A. Contraception and health. Lancet 2012;380(9837):149‐56. [DOI] [PubMed] [Google Scholar]
Constant 2010
- Constant D, Tolley K. M‐assist: mobile in medical abortion. www.cell‐life.org/projects/m‐assist/ (accessed 19 December 2013).
CycleTel 2011
- CycleTel: The first family planning method via mobile phone. www.cycletel.org (accessed December 2013).
Darroch 2013
- Darroch J, Singh S. Trends in contraceptive need and use in developing countries in 2003, 2008, and 2012: an analysis of national surveys. Lancet 2013;381(9879):1756‐62. [DOI: 10.1016/S0140-6736(13)60597-8] [DOI] [PubMed] [Google Scholar]
Free 2010
- Free C, Phillips G, Felix L, Galli L, Patel V, Edwards P. The effectiveness of M‐health technologies for improving health and health services: a systematic review protocol. BMC Research Notes 2010;3(1):250. [http://biomedcentral.com/1756‐0500/3/250] [DOI] [PMC free article] [PubMed] [Google Scholar]
Free 2011
- Free C, Knight R, Robertson S, Whittaker R, Edwards P, Zhou W. Smoking cessation support delivered via mobile phone text messaging (txt2stop): a single‐blind, randomised trial. Lancet 2011;378(9785):49‐55. [DOI] [PMC free article] [PubMed] [Google Scholar]
Free 2013a
- Free C, Phillips G, Galli L, Watson L, Felix L, Edwards P, et al. The effectiveness of mobile‐health technology‐based health behaviour change or disease management interventions for health care consumers: a systematic review. PLoS Medicine 2013;10(1):e1001362. [DOI] [PMC free article] [PubMed] [Google Scholar]
Free 2013b
- Free C, Phillips G, Watson L, Galli L, Felix L, Edwards P, et al. The effectiveness of mobile‐health technologies to improve health care service delivery processes: a systematic review and meta‐analysis. Plos Medicine 2013;10(1):e1001363. [DOI] [PMC free article] [PubMed] [Google Scholar]
Guerriero 2013
- Guerriero C, Cairns J, Roberts I, Rodgers A, Whittaker R, Free C. The cost‐effectiveness of smoking cessation support delivered by mobile phone text messaging: txt2stop. The European Journal of Health Economics 2013;14(5):789‐97. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hall 2010
- Hall K, White K, Reame N, Westhoff C. Studying the use of oral contraception: a review of measurement approaches. Journal of Women's Health 2010;19(12):2203‐9. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Halpern 2013
- Halpern V, Lopez L, Grimes D, Stockton L, Gallo M. Strategies to improve adherence and acceptability of hormonal methods of contraception (Review). Cochrane Database of Systematic Reviews 2013, Issue 10. [DOI: 10.1002/14651858.CD004317.pub4] [DOI] [PubMed] [Google Scholar]
Haynes 2008
- Haynes R, Ackloo E, Sahota N, McDonald H, Yao X. Interventions for enhancing medication adherence (Review). Cochrane Database of Systematic Reviews 2008, Issue 2. [DOI: 10.1002/14651858.CD000011.pub3] [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. www.cochrane‐handbook.org. Version 5.1.0 [updated March 2011]. The Cochrane Collaboration.
Horvath 2012
- Horvath T, Azman H, Kennedy GE, Rutherford GW. Mobile phone text messaging for promoting adherence to antiretroviral therapy in patients with HIV infection. Cochrane Database of Systematic Reviews 2012, Issue 4. [DOI: 10.1002/14651858.CD009756] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kallander 2013
- Kallander K, Tibenderana J, Akpogheneta O, Strachan D, Hill Z, Asbroek A, et al. Mobile health (mHealth) approaches and lessons for increased performance and retention of community health workers in low‐ and middle‐income countries: a review. Journal of Medical Internet Research 2013;15(1):e17. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kellon 2012
- Kellon L. Texting SMS pioneer Matti Makkonen 20 years on. www.bbc.co.uk/news/technology‐20555620 (accessed 19 December 2013).
L'engle 2013
- L'Engle K, Vahdat H, Ndakidemi E, Lasway C, Zan T. Evaluating feasibility, reach and potential impact of a text message family planning information service in Tanzania. Contraception 2013;87(2):251‐6. [DOI] [PubMed] [Google Scholar]
Lester 2010
- Lester R, Ritvo P, Mills E, Kariri A, Karanja S, Chung M, et al. Effects of a mobile phone short message service on antiretroviral treatment adherence in Kenya (WelTel Kenya1): a randomised trial. Lancet 2010;376(9755):1838‐45. [DOI] [PubMed] [Google Scholar]
MAMA 2013
- MAMA: Mobile Alliance for Maternal Action. The power of health in every mama's hand. http://mobilemamaalliance.org (accessed 19 December 2013).
Mechael 2010
- Mechael P, Batavia H, Kaonga N, Searle S, Kwan A, Goldberger A, et al. Barriers and gaps affecting mHealth in low and middle income countries: policy white paper. Centre for Global Health and Economic Development, Earth Institute, Columbia University, May 2010.
National Safety Council 2015
- National Safety Council. The problem of cell phone distracted driving. http://www.nsc.org/learn/NSC‐Initiatives/Pages/distracted‐driving‐problem‐of‐cell‐phone‐distracted‐driving.aspx (accessed on 5 May 2015).
NCT01641380
- NCT01641380. Meaningful use of technology to improve health care delivery (DepoText). clinicaltrials.gov/ct2/show/NCT01641380 (accessed 9 October 2014).
Newell 1992
- Newell D. Intention‐to‐treat analysis: implications for quantitative and qualitative research. International Journal of Epidemiology 1992;21(5):837‐41. [DOI] [PubMed] [Google Scholar]
Pop‐Eleches 2011
- Pop‐Eleches C, Thirumurthy H, Habyarimana JP, Zivin JG, Goldstein MP, Walque D, et al. Mobile phone technologies improve adherence to antiretroviral treatment in a resource‐limited setting: a randomised controlled trial of text message reminders. AIDS 2011;25(6):825‐34. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rodgers 2005
- Rodgers A, Corbett T, Bramley D, Riddell T, Wills M, Lin R, et al. Do u smoke after txt? Results of a randomised trial of smoking cessation using mobile phone text messaging. Tobacco Control 2005;14(4):255‐61. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rothman 2000
- Rothman K. Epidemiological evidence on health risks of cellular telephones. Lancet 2000;356(9244):1837‐40. [DOI] [PubMed] [Google Scholar]
Shet 2014
- Shet A, Costa A, Kumarasamy N, Rodrigues R, Rewari B, Ashorn P, et al. Effect of mobile telephone reminders on treatment outcome in HIV: evidence from a randomised controlled trial in India. British Medical Journal 2014;347:1‐11. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Singh 2009
- Singh S, Darroch J, Ashford L, Vlassoff M. Adding It Up: The Costs and Benefits of Investing in Family Planning and Maternal and Newborn Health. New York: Guttmacher Institute and UNFPA, 2009.
Singh 2014
- Singh S, Darroch JE, Ashford LS. Adding It Up: Costs and Benefits of Investing in Sexual and Reproductive Health 2014. New York: Guttmacher Institute, 2014. [http://www. guttmacher.org/pubs/AIU‐2012‐estimates.pdf]
Smith 2013
- Smith C, Uk V, Ly S, Ngo T, Gold G, Khut K, et al. MObile technology for improved family planning services (MOTIF): study protocol for a randomised control trial. Trials 2013; Vol. 14, issue 427:1‐9. [DOI] [PMC free article] [PubMed]
Stuart 2009
- Stuart G, Grimes D. Social desirability bias in family planning studies: a neglected problem. Contraception 2009;80:108‐12. [DOI: 10.1016/j.contraception.2009.02.009] [DOI] [PubMed] [Google Scholar]
UNICEF 2011
- United Nations Children's Fund (UNICEF). Adolescence: an age of opportunity. http://www.unicef.org/sowc2011/pdfs/SOWC‐2011‐Main‐Report_EN_02092011.pdf (accessed 11 May 2015).
Upadhyay 2009
- Upadhyay N, Kokalj Kokot M, Kokalj Kokot M, Car J, Svab I. Mobile phone messaging ‐ a telemedicine for people with diabetes mellitus. Cochrane Database of Systematic Reviews 2009, Issue 1. [DOI: 10.1002/14651858.CD006393] [DOI] [Google Scholar]
Westoff 2012
- Westoff CF. Unmet need for modern contraceptive methods. DHS Analytical Studies 28: Office of Population Research, Princeton University; 2012 Sept. Publication ID: AS28.
Whittaker 2009
- Whittaker R, Borland R, Bullen C, Lin RB, McRobbie H, Rodgers A. Mobile phone‐based interventions for smoking cessation. Cochrane Database of Systematic Reviews 2009, Issue 4. [DOI: 10.1002/14651858.CD006611.pub2] [DOI] [PubMed] [Google Scholar]
WHO 2011
- World Health Organization Department of Reproductive Health and Research (WHO/RHR) and Johns Hopkins Bloomberg School of Public Health/Center for Communication Programs (CCP), Knowledge for Health Project. Family Planning: A Global Handbook for Providers [2011 update]. Baltimore and Geneva: CCP and WHO, 2011. [Google Scholar]
WHO 2013
- World Health Organization. Family Planning. http://www.who.int/mediacentre/factsheets/fs351/en/ (accessed 10 June 2014).
Williamson 2013
- Williamson J. SMS 4 SRH: Using mobile phones to reduce barriers to youth access to sexual and reproductive health services and information. Marie Stopes International, 2013. http://www.msi‐us.org/sites/www.msi‐us.org/files/SMS 4 SRH %282013 11 13%29.pdf.


