Abstract
Background
Preventive health care promotes health and prevents disease or injuries by addressing factors that lead to the onset of a disease, and by detecting latent conditions to reduce or halt their progression. Many risk factors for costly and disabling conditions (such as cardiovascular diseases, cancer, diabetes, and chronic respiratory diseases) can be prevented, yet healthcare systems do not make the best use of their available resources to support this process. Mobile phone messaging applications, such as Short Message Service (SMS) and Multimedia Message Service (MMS), could offer a convenient and cost‐effective way to support desirable health behaviours for preventive health care.
Objectives
To assess the effects of mobile phone messaging interventions as a mode of delivery for preventive health care, on health status and health behaviour outcomes.
Search methods
We searched: the Cochrane Central Register of Controlled Trials (CENTRAL, The Cochrane Library 2009, Issue 2), MEDLINE (OvidSP) (January 1993 to June 2009), EMBASE (OvidSP) (January 1993 to June 2009), PsycINFO (OvidSP) (January 1993 to June 2009), CINAHL (EbscoHOST) (January 1993 to June 2009), LILACS (January 1993 to June 2009) and African Health Anthology (January 1993 to June 2009).
We also reviewed grey literature (including trial registers) and reference lists of articles.
Selection criteria
We included randomised controlled trials (RCTs), quasi‐randomised controlled trials (QRCTs), controlled before‐after (CBA) studies, and interrupted time series (ITS) studies with at least three time points before and after the intervention. We included studies using SMS or MMS as a mode of delivery for any type of preventive health care. We only included studies in which it was possible to assess the effects of mobile phone messaging independent of other technologies or interventions.
Data collection and analysis
Two review authors independently assessed all studies against the inclusion criteria, with any disagreements resolved by a third review author. Study design features, characteristics of target populations, interventions and controls, and results data were extracted by two review authors and confirmed by a third author. Primary outcomes of interest were health status and health behaviour outcomes. We also considered patients’ and providers’ evaluation of the intervention, perceptions of safety, health service utilisation and costs, and potential harms or adverse effects. Because the included studies were heterogeneous in type of condition addressed, intervention characteristics and outcome measures, we did not consider that it was justified to conduct a meta‐analysis to derive an overall effect size for the main outcome categories; instead, we present findings narratively.
Main results
We included four randomised controlled trials involving 1933 participants.
For the primary outcome category of health, there was moderate quality evidence from one study that women who received prenatal support via mobile phone messages had significantly higher satisfaction than those who did not receive the messages, both in the antenatal period (mean difference (MD) 1.25, 95% confidence interval (CI) 0.78 to 1.72) and perinatal period (MD 1.19, 95% CI 0.37 to 2.01). Their confidence level was also higher (MD 1.12, 95% CI 0.51 to 1.73) and anxiety level was lower (MD ‐2.15, 95% CI ‐3.42 to ‐0.88) than in the control group in the antenatal period. In this study, no further differences were observed between groups in the perinatal period. There was low quality evidence that the mobile phone messaging intervention did not affect pregnancy outcomes (gestational age at birth, infant birth weight, preterm delivery and route of delivery).
For the primary outcome category of health behaviour, there was moderate quality evidence from one study that mobile phone message reminders to take vitamin C for preventive reasons resulted in higher adherence (risk ratio (RR) 1.41, 95% CI 1.14 to 1.74). There was high quality evidence from another study that participants receiving mobile phone messaging support had a significantly higher likelihood of quitting smoking than those in a control group at 6 weeks (RR 2.20, 95% CI 1.79 to 2.70) and at 12 weeks follow‐up (RR 1.55, 95% CI 1.30 to 1.84). At 26 weeks, there was only a significant difference between groups if, for participants with missing data, the last known value was carried forward. There was very low quality evidence from one study that mobile phone messaging interventions for self‐monitoring of healthy behaviours related to childhood weight control did not have a statistically significant effect on physical activity, consumption of sugar‐sweetened beverages or screen time.
For the secondary outcome of acceptability, there was very low quality evidence from one study that user evaluation of the intervention was similar between groups. There was moderate quality evidence from one study of no difference in adverse effects of the intervention, measured as rates of pain in the thumb or finger joints, and car crash rates.
None of the studies reported the secondary outcomes of health service utilisation or costs of the intervention.
Authors' conclusions
We found very limited evidence that in certain cases mobile phone messaging interventions may support preventive health care, to improve health status and health behaviour outcomes. However, because of the low number of participants in three of the included studies, combined with study limitations of risk of bias and lack of demonstrated causality, the evidence for these effects is of low to moderate quality. The evidence is of high quality only for interventions aimed at smoking cessation. Furthermore, there are significant information gaps regarding the long‐term effects, risks and limitations of, and user satisfaction with, such interventions.
Keywords: Female, Humans, Male, Pregnancy, Health Behavior, Multimedia, Text Messaging, Body Weight, Cell Phone, Health Status, Patient Satisfaction, Prenatal Care, Prenatal Care/methods, Primary Prevention, Primary Prevention/methods, Randomized Controlled Trials as Topic, Smoking Cessation
Plain language summary
Mobile phone messaging for preventive health care
Many costly and disabling conditions such as cardiovascular diseases, cancer or diabetes are linked by common preventable risk factors like tobacco use, unhealthy nutrition, physical inactivity and excessive alcohol use. However, prevention still plays a secondary role in many health systems as all too often, healthcare workers fail to seize interactions with patient as opportunities to inform them about health promotion and disease prevention strategies. This review examined whether mobile phone applications such as Short Message Service (SMS) and Multimedia Message Service (MMS) can support and enhance primary preventive health interventions.
There was moderate quality evidence from one study which showed that pregnant women who received supportive, informative text messages experienced higher satisfaction and confidence, and lower anxiety levels in the antenatal period than women who did not receive these. There was low quality evidence that there was no difference in pregnancy outcomes.
We found one trial that provided high quality evidence that regular support messages sent by text message can help people to quit smoking, at least in the short‐term. One study assessing whether mobile phone messaging promoted use of preventive medication reported moderate quality evidence of higher self‐reported adherence by people receiving the messages. A fourth study on healthy behaviours in children found very low quality evidence showing that the interventions had no effect.
There was very low quality evidence from one study that people's evaluation of the intervention was similar between groups. There was moderate quality evidence from one study of no difference in harms of the intervention, measured as rates of pain in the thumb or finger joints, and car crash rates. There were no studies reporting outcomes related to health service utilisation or costs.
Although we find that, overall, mobile phone messaging can be helpful for some aspects of preventive health care, much is not yet known about the long‐term effects or potential negative consequences.
Summary of findings
Summary of findings for the main comparison. Effect of mobile phone messaging interventions for preventive health care.
|
Patient or population: Various (pregnant women; daily smokers aged 16 and older; university students; children aged 5‐13) Settings: Various (antenatal clinics and postpartum wards in Thailand; outpatient settings in New Zealand, Canada and the USA) Intervention: Information and support for healthy behaviours delivered by mobile phone messaging Control: Usual care | |||
| Outcomes | Impact | No of Participants (studies) | Quality of the evidence (GRADE) |
| Health outcomes | |||
| Satisfaction, anxiety and confidence during pregnancy | Women who received mobile phone messages with information relating to abnormal symptoms during pregnancy showed significantly higher satisfaction scores in the antenatal and perinatal period. In the antenatal period their confidence level was also higher and their anxiety level lower, although in the perinatal period these differences were no longer statistically significant. | 61 (1 study) | ⊕⊕⊕⊝ moderate1 |
| Pregnancy outcomes | Mobile phone messages with information relating to abnormal symptoms during pregnancy had no statistically significant impacts on gestational age at birth, infant birth weight, frequency of preterm delivery or route of delivery. | 61 (1 study) | ⊕⊕⊝⊝ low1,2 |
| Health behaviour outcomes | |||
| Smoking cessation | Mobile phone messaging support for smoking cessation resulted in a significant increase of quit rates at 6 weeks (RR 2.20, 95% CI 1.79 to 2.70) and 12 weeks follow‐up (RR 1.55, 95% CI 1.30 to 1.84). The effect persisted at 26 weeks if last values were carried forward (RR 1.28, 95% CI 1.11 to 1.48). Continuous abstinence at 26 weeks, allowing three or fewer ‘lapses’ of two or fewer cigarettes per lapse, was also higher in the intervention group (RR 1.64, 95% CI 1.12 to 2.42), whereas there was no impact on continuous complete abstinence (RR 1.4, 95% CI 0.92 to 2.44). | 1705 (1 study) | ⊕⊕⊕⊕ high |
| Vitamin C adherence | Participants receiving mobile phone messaging reminders to take vitamin C tablets for preventive reasons showed significantly higher self‐reported adherence, and a marginal reduction in the number of missed tablets in the last 7 days compared to those who did not receive any reminders (MD ‐0.80, 95% CI ‐1.55 to ‐0.05). | 99 (1 study) | ⊕⊕⊕⊝ moderate1 |
| Healthy behaviour in children | Tracking of healthy behaviours in children using mobile phone messages did not result in any significant differences on their level of physical activity, consumption of sugar‐sweetened beverages or screen time, compared to tracking using a paper diary or no tracking at all. | 32 (1 study) | ⊕⊝⊝⊝ very low1,3 |
| User evaluation of the intervention | |||
| Acceptability | Children and their parents who used mobile phone messaging to track healthy behaviours in children reported no differences in acceptability of the intervention compared to groups using either paper diary reporting or no tracking. | 32 (1 study) | ⊕⊝⊝⊝ very low1,3 |
| Adverse effects of the intervention | |||
| Adverse effects | A mobile phone messaging intervention to support smoking cessation did not have any significant impact on the rates of pain in the thumb or finger joints (RR 1.08, 95% CI 0.74 to 1.59), or on car crash rates (RR 0.88, 95% CI 0.58 to 1.35) at 26 weeks of follow‐up. | 1705 (1 study) | ⊕⊕⊕⊝ moderate4 |
| Other outcomes | |||
| Health service utilisation | None of the included studies report on the impact of the intervention on health services utilisation | ||
| Cost | None of the included studies report on the cost or cost‐effectiveness of the intervention | ||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | |||
1 Low number of participants.
2 It is unlikely that the intervention would impact pregnancy outcomes such as gestational age, birth weight or duration of gestation. Although it is similarly unlikely that the intervention would directly impact emergency cesarean section rates, it is feasible that prenatal support would influence women's decision for mode of delivery.
3 Moderate risk of bias.
4 Very low number of adverse events reported in both groups.
Background
Mobile phone messaging is an important means of human communication globally. Mobile phone penetration is rapidly increasing, particularly in the Asia‐Pacific, with 90% of the global and 80% of rural population having access to a mobile network in 2010. The number of subscriptions in 2010 reached 5.3 billion, representing a 76.2% global penetration rate (ITU 2010). The penetration rates are 70% to 90% in high‐income countries, with a similar rate of increase across all socio‐economic groups (Atun 2006).
Most digital mobile phones provide Short Message Service (SMS), also known as text messaging, and Multimedia Message Service (MMS) for transmitting graphics, video clips and sound files. SMS, in particular, has developed into a powerful communication medium, particularly among young adults. The total number of text messages sent globally tripled between 2007 and 2010, from an estimated 1.8 trillion to 6.1 trillion, with about 200,000 messages sent every second (ITU 2010).These short messages, where up to 160 characters of text are sent from the Internet or from a mobile phone to one or several mobile phones, provide an important, inexpensive medium of communication. The terms text message, text, or txt are more commonly used in North America, the UK, Spain and the Philippines, while in many other countries the term SMS is used. In this review we will use the term ‘text messaging’ to refer to the use of SMS only, distinguishing it from the term ‘mobile phone messaging’, which encompasses both SMS and MMS. Increasingly, the latter term also refers to mobile email and ‘instant messaging’ delivered to the mobile phone.
Text messages, compared to other communication channels, have the advantage of instant transmission and low cost. There is also a smaller chance of being misplaced compared to print materials, and of being invasive to daily lives compared to phone calls (Kaplan 2006). Features such as ubiquity, mobility, direct and instantaneous access and direct communication offer the possibility of using mobile phones for health information transfer (Atun 2006). A literature review on the use of mobile phones in health care has demonstrated the wide application and potential of mobile phones to: increase access to health care; enhance efficiency of service delivery; improve diagnosis, treatment and rehabilitation; and support public health programmes (Atun 2006; Car 2008b). Mobile phone messaging has, for example, been used to provide appointment reminders (Bos 2005), to improve patient compliance with medications (Fairley 2003; Marquez Contreras 2004; Vilella 2004), to monitor chronic conditions (Ferrer‐Roca 2004; Kwon 2004; Ostojic 2005) and to provide psychological support (Bauer 2003). Mobile phones have also been used in managing communicable diseases (e.g. in contact tracing and partner notification for sexually transmitted illnesses (Newell 2001)) and in health promotion programmes (Obermayer 2004; Rodgers 2005). Furthermore, the use of mobile phones has been shown to improve service utilization among population groups such as teenagers and young adult males who do not typically use health services, by providing the opportunity to remotely access care providers for advice (Atun 2006b). However, for older adults, some of whom are less able or willing to use mobile phones, the effect on improved service utilization could be limited (Atun 2006b).
Challenges in using mobile phone applications in health care include incomplete coverage of mobile networks across regions, lack of standards, and possible information overload (Adler 2007).
This review is part of a series of four reviews which aim to determine the effects of mobile phone messaging in improving the processes of healthcare service delivery and service utilization:
Mobile phone messaging for preventive health care (this review);
Mobile phone messaging for communicating results of medical investigations (Gurol‐Urganci 2012);
Mobile phone messaging reminders for attendance at healthcare appointments (Car 2012);
Mobile phone messaging for facilitating self‐management of long‐term illnesses (de Jongh 2012)
Description of the condition
Many of the costly and disabling conditions (such as cardiovascular diseases, cancer and diabetes) facing health systems today are linked by shared risk factors like tobacco use, unhealthy nutrition, physical inactivity and excessive alcohol consumption, which can be addressed through preventive interventions (Goldstein 2004). Prevention measures in health systems can take various forms, and are generally divided into health promotion and disease prevention (Canadian 1994). Health promotion aims at encouraging people to adopt and maintain a healthful lifestyle. Disease prevention aims to prevent avoidable diseases or to identify diseases early, in order to minimise their impact.
Prevention measures targeted at specific illnesses (such as infectious diseases), risk factors (such as obesity), target groups (such as young people) and settings (such as schools) positively influence the health of populations. Effective strategies for the long‐term improvement of population health include primary, secondary and tertiary prevention interventions that are directed to the different stages of disease. Primary prevention increases a person’s ability to remain free of disease. The aim of secondary prevention is to identify asymptomatic individuals at an early stage of disease when early identification promises a significantly better response to treatment than after the disease has progressed. Tertiary prevention aims to minimize the disability caused by existing disease (McWhinney 1997). Prevention interventions such as counselling, screening, immunisation and chemoprophylaxis, when integrated into general clinical services, offer an efficient way of providing comprehensive care.
The ability of a health system to provide effective preventive health care is important not just from an ethical perspective but, equally, from an economic one. However, most health systems better respond to acute problems, urgent needs and pressing concerns of patients. Despite evidence of the effectiveness of preventive services, integration of preventive care guidelines into public health and clinical practice has been modest (Davis 1997; Wei 2005; Weingarten 1999). Barriers to the delivery of preventive health care include healthcare systems' traditional focus on a 'responsive' rather than a 'pro‐active' approach to individuals' and populations' health. Within the consultation context, factors such as lack of time, deficit of clinician expertise, logistic difficulties, lack of interest by patients, other urgent concerns, inadequate reimbursement, and patient concerns regarding the interventions, can play a role (Kottke 1993; Mirand 2002; Szilagyi 2005).
Inadequate delivery of preventive health care is well documented (Goldstein 1997; McGlynn 2003; Pollak 2002). With shortages of physicians in some countries (Bodenheimer 2006), and large and rapidly‐growing competing demands and guidelines, physicians will probably be able to do less rather than more preventive service during each visit (Pollak 2008). They may have to make choices about preventive services on a case by case basis, weighing patient characteristics, medical needs and time restraints against the need for intervention. Prioritising those patients needing preventive services may involve moving away from face‐to‐face patient care to various forms of patient education through telephone or electronic media (Atherton 2010; Yarnall 2003).
Patients are increasingly involved in managing their health care (Cline 2001), and providers are challenged to motivate, educate and help people adhere to healthy behaviours and medication regimens using new communication technologies (Demiris 2008). Advances in information technology have introduced new approaches to support healthcare delivery and patient education (Revere 2001). Understanding people's behaviour and identifying the factors underlying behavioural change help in the development and evaluation of effective health behaviour interventions (Bandura 1977; Glanz 1997; Prochaska 1997; Rhodes 1997).
Description of the intervention
Communication between patients and providers plays an important supportive role in preventive health care and can take a number of forms, such as face‐to‐face conversations, phone conversations or mobile phone messaging. In contrast to traditional sources of health information (such as print media), interactive health communication using mobile phone messaging offers the potential to combine the scalability of public health interventions (such as mass media campaigns) with individualized health care through the use of tailoring (Eng 1999; Robinson 1998). Relevant interventions support healthier lifestyles such as smoking cessation, increased physical activity, healthy nutrition, and weight control, or support health education or adherence to preventive medications.
How the intervention might work
Mobile phone messaging may help to address some preventive health challenges by enabling remote delivery of care, facilitating timely access to health advice and medications, prompting self‐monitoring and medication compliance, and educating patients (Demiris 2008). These interventions are particularly suitable for outpatient use, as patients can carry mobile phones with them easily. The price of mobile communication devices has dropped dramatically in the last decade; increasing functionality and decreasing cost provide opportunities for preventive interventions that were previously not feasible (Revere 2001). However, participants in preventive health behaviour interventions may not be motivated to initiate communication if they feel healthy.
Mobile phone messaging interventions can be used to enhance self‐efficacy (such as feedback on treatment success) (de Jongh 2012), to provide a form of social support (from peers and health professionals), or to establish social networks (support groups, peer‐to‐peer networks). By increasing self‐efficacy (Bandura 1977; Bandura 1982) and providing support mechanisms (Christakis 2004; Cobb 2002), these interventions may influence health behaviours and enhance preventive health care. Mobile phone messaging could affect health outcomes through individual tailoring, personalization and behavioural feedback. Tailoring refers to building an intervention, in part, on specific knowledge of actual characteristics of the individual receiving the intervention. Personalization involves designing the intervention to be delivered in a way that makes it specific for a given individual. Finally, behavioural feedback refers to providing consumers with messages regarding their status, well‐being, or progression through the intervention. These messages may come in many different forms. They can be motivational (such as "You did great today!") or purely data driven (such as "You completed 80 percent of your goal today").
Invitations and reminders may be an effective way to increase the uptake of preventive care activities such as adult immunisation (Vilella 2004) and cancer screening (Stone 2002). Electronic technology may facilitate communication with patients about preventive care based on clinical guidelines and strengthen the continuity of care between patient and clinician by improving access and supporting the coordination of healthcare activities from a single source (Balas 1997). Text messaging has been shown to facilitate adoption of healthier behaviours, such as smoking cessation (Rodgers 2005).
Our parallel review describes the use of text messaging in self‐management programmes for long‐term conditions, that are relevant for secondary and tertiary prevention (de Jongh 2012).
Acceptability and risks of the intervention
Possible risks of using mobile phone messaging include the risk of inaccurate data input (Norwell 2003); lack of understanding or misinterpretation of the information; and difficulties in reading for those with poor vision or problems with literacy. Furthermore, mobile phone messaging technology is intended to support or complement the process of care delivery rather than to substitute for it. A possible risk of a narrow focus on the technology is that providers may misinterpret it as an endpoint to their responsibilities within the care delivery process, believing that their work is completed once the message is sent. This may result in inadequate follow‐up of patients after the intervention. Additionally, text messaging cannot capture the verbal and non‐verbal cues that may also influence the interpretation of the message. Participants' perceptions of personal invasion and behavioural control may be affected by inappropriate SMS initiation methods and the intervention may have the opposite effect of that intended.
Having correct patient contact information and securely stored health records are essential to meet privacy, confidentiality and data protection requirements. Failures or delays in message delivery are rare but possible; however, harm is unlikely as senders are usually notified instantly in cases where there was a transmission problem. There may be additional monetary and time costs, as backup systems may be needed. Lastly, risks associated with mobile phone messaging in general may apply, such as an increased risk of car accidents as a result of messaging whilst driving.
Why it is important to do this review
Although there is some evidence on the use and effectiveness of mobile phone messaging in preventive health care, answers to questions regarding implementation of these technologies in routine care, such as the impact on patient health‐related outcomes or on processes of healthcare delivery, are unclear. We conducted this review to address these questions and propose directions for future research. This review complements available studies on the use of telephone consultations (Car 2003), email (Car 2004a; Car 2004b) and personal digital assistants (PDAs) (Baumgart 2005) in health care, as well as other Cochrane reviews by these authors on mobile phone messaging for a range of purposes (Car 2012; de Jongh 2012; Gurol‐Urganci 2012).
Objectives
To assess the effects of mobile phone messaging interventions as a mode of delivery for preventive health care on health status and health behaviour outcomes.
Methods
Criteria for considering studies for this review
Types of studies
We included randomised controlled trials (RCTs), quasi‐randomised controlled trials (QRCTs), controlled before and after studies (CBA) and interrupted time series (ITS) with at least three time points before and after the intervention.
We define QRCT as a controlled trial in which the participant allocation is not truly random, such as allocation by date of birth or the order in which participants are included in the study. We included QRCT, CBA and ITS designs because our initial literature searching suggested that only a small number of RCTs on mobile phone messaging interventions exist.
Types of participants
We included all study participants regardless of age, gender and ethnicity, as well as all types and stages of diseases. We included studies in all settings i.e. primary care settings (services of primary health care), outpatient settings (outpatient clinics), community settings (public health services, anywhere where a person can use a mobile phone) and hospital settings. We did not exclude studies according to the type of healthcare provider (e.g. nurse, doctor, allied staff).
Types of interventions
We included interventions using SMS or MMS as a mode of delivery for any type of preventive health care. The messaging needed to be between healthcare provider (either in person or automated) or a 'treatment buddy' (i.e. lay health worker or peer supporter) and participant, regardless of who sent the first message.
We excluded studies of mobile phone messaging to people other than those who were about to take part in preventive health care, or messaging between two healthcare providers. We also excluded studies in which mobile phone messaging was a part of a multifaceted intervention, as it would not be possible to separate the effects of messaging alone.
We aimed to make comparisons between mobile phone messaging and no intervention, as well as other modes of communication such as face‐to‐face, postal letters, calls to land line or mobile, email or via electronic health records; and if applicable, automated versus personal text messaging.
Types of outcome measures
A number of processes and outcomes may be affected by mobile phone messaging interventions that aim to facilitate communication between healthcare service users and healthcare providers.
Primary outcomes
As primary outcomes we included all outcomes related to health status or health behaviour, such as adoption of healthier lifestyles (e.g. smoking cessation, increased physical activity, weight control, nutrition and stress management), or improved quality of life.
Secondary outcomes
User (patient, carer or healthcare provider) evaluation of the intervention, including satisfaction, readiness to use, timeliness, availability and/or convenience;
Health service utilisation following the intervention;
Costs (direct and indirect) of the intervention;
User (patient, carer or healthcare provider) perceptions of safety;
Potential harms or adverse effects of the intervention, such as misreading or misinterpretation of data, transmission of inaccurate data, loss of verbal and non‐verbal communication cues, issues of privacy and disclosure, or failure or delay in the message delivery.
Search methods for identification of studies
We used a common search strategy for all four reviews (this review; Car 2012; de Jongh 2012; Gurol‐Urganci 2012) and allocated relevant studies to their respective reviews before assessing their risk of bias and extracting data. The search strategies for each database are given in Appendix 1 to Appendix 7.
Electronic searches
We restricted the searches to studies published since 1993 as the first commercial SMS message was sent in December 1992 (Wikipedia 2007). We included LILACS and the African Health Anthology because mobile phone messaging applications are increasingly used in low‐ and middle‐income regions. There were no language restrictions.
One review author (IGU) searched the following electronic databases on October 13, 2008 and updated the search on June 22, 2009:
The Cochrane Central Register of Controlled Trials (CENTRAL) (The Cochrane Library 2009, Issue 2)
MEDLINE (OvidSP) (January 1993 to June 22, 2009);
EMBASE (OvidSP) (January 1993 to June 22, 2009);
PsycINFO (OvidSP) (January 1993 to June 22, 2009);
CINAHL (EbscoHOST) (January 1993 to June 22, 2009);
LILACS (January 1993 to June 22, 2009);
African Health Anthology (January 1993 to June 22, 2009).
Searching other resources
For grey literature we searched:
Proceedings from AMIA Congresses;
WHO Clinical Trial Search Portal (www.who.int/trialsearch);
Current Controlled Trials (www.controlled‐trials.com);
Dissertation Abstracts International.
We searched the reference lists of included studies to identify additional studies. We contacted study authors for further information on their studies and to enquire whether they were aware of any other published or ongoing studies that would meet our inclusion criteria.
Data collection and analysis
Selection of studies
The selection of studies was done by IGU, TdJ and VVJ. IGU and TdJ independently assessed the relevance of all titles and abstracts identified from the electronic searches. We retrieved full text copies of all articles judged to be potentially relevant from the titles and abstracts. TdJ and VVJ independently assessed these articles for inclusion. IGU checked the final list of included and excluded studies, and any disagreements were resolved by discussion with VVJ, JC, and RA. Where the description of the intervention was not sufficiently detailed to allow the review authors to judge whether it met the inclusion criteria, we contacted the study authors for further details.
Data extraction and management
We extracted the following data from the included studies, using a modified version of the Cochrane Consumers and Communication Review Group’s data extraction template:
General information: title, authors, source, publication status, date published, language, review author information, date reviewed.
Study methods: aims of intervention, aim of study, study design, methods of participant recruitment, inclusion/exclusion criteria, informed consent and ethical approval, funding.
Risk of bias: data depended on the study design (see 'Assessment of risk of bias in included studies').
Participants: description, geographic location, setting, number, age, gender, ethnicity, socioeconomic status distribution. If relevant: principal health problem or diagnosis, stage of illness, treatment received.
Providers: description, geographic location, setting, age, gender.
Interventions: description including technical specifications on SMS and handset provider, duration of intervention, purpose of intervention, initiator of intervention, message content, details of control/usual or routine care, co‐interventions.
Outcomes: primary and secondary outcomes as specified above, methods of assessing outcomes, follow up for non‐respondents, timing of outcome assessment, adverse events.
Results: all reported measurements for the primary and secondary outcomes, including multiple timings for measurements, subgroup analyses or results in different measurement scales if applicable.
TdJ and VVJ independently extracted the above data onto a standard form. The forms were then assessed by one review author (IGU) who checked these data. Any discrepancies between the two data extraction sheets were discussed by two review authors (TdJ and VVJ), and resolved jointly with the two other review authors (IGU and JC). For missing data, we contacted the study authors to obtain the missing information.
Assessment of risk of bias in included studies
We assessed the risk of bias of included studies in accordance with the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011) which recommends the explicit reporting of sequence generation, allocation concealment, blinding of participants, providers and outcome assessors, incomplete outcome data, selective outcome reporting and other sources of bias for RCTs.
Had studies using other study designs been identified for inclusion in the review, we would have assessed these using a variation of the above tool.
Two review authors (TdJ, VVJ) independently assessed the risk of bias in the included studies, with any disagreements resolved by discussion and consensus of the team. We used a template to guide the assessment of risk of bias, and judged each domain as 'yes' (indicating a low risk of bias), 'no' (indicating a high risk of bias) or 'unclear' (indicating an uncertain risk of bias).
We present the results of the risk of bias assessment in tables, and provided a narrative discussion of risk of bias in individual domains.
Measures of treatment effect
We used risk ratios (RR) as effect measures for dichotomous outcomes and mean differences (MD) for continuous outcomes. RR and MDs have been derived from Manzel‐Haenszel and inverse variance methods respectively. We used a random‐effects model, where possible, to pool the results, and reported 95% confidence intervals with all measures of effect.
Unit of analysis issues
We noted the method of randomisation in each included trial, and considered additional issues regarding the assessment of risk of bias of cluster randomised trials as discussed in Chapter 16 of the Cochrane Handbook (Higgins 2011). In the case of repeated measurements, we defined several outcomes based on different periods of follow‐up and performed separate analyses for each outcome. In studies with more than two treatment groups, we made multiple pair‐wise comparisons between all possible pairs of intervention groups.
Dealing with missing data
We contacted the original investigators to request missing data. With incomplete outcome data (such as drop‐outs, loss to follow‐up and withdrawn study participants), we assessed and reported the risk of bias as high/unclear/low risk as guided by the Cochrane Handbook (Higgins 2011) and identified the numbers as well as the reasons for incomplete data. As the numbers and reasons for incomplete outcome data in included studies suggested that data were missing at random, we used only available data in the review and did not use imputation methods.
Assessment of reporting biases
We were unable to assess reporting bias statistically or using funnel plots, because the number of included studies was too small for a reliable analysis. We assessed selective outcome reporting using the Cochrane Risk of Bias assessment tool.
Data synthesis
Due to the heterogeneity in the interventions and outcomes reported in the included studies, it was not appropriate to combine the results of the studies statistically. We present a narrative overview of the findings, including tabular summaries of extracted data. We structured the reporting of the studies according to the intended purpose of the mobile phone message.
Subgroup analysis and investigation of heterogeneity
We were unable to conduct the planed subgroup analysis by participant age (0 to 18, 18 to 55, over 55) (MORI 2005), as planned, because of the small number of studies included and the absence of data for subgroups.
Sensitivity analysis
We did not conduct the planned sensitivity analyses due to the small number of studies included. We had aimed to determine the influence of the following factors on effect size:
excluding unpublished studies;
taking account of risk of bias of included studies, as specified above;
excluding any large studies to establish how they impact on the results;
excluding studies using the following filters: criteria used for clinical diagnosis and eligibility for intervention, language of publication, source of funding (industry versus other), country;
the length of the interval between delivery of the intervention and measurement of the effect.
Consumer participation
The draft review was circulated for peer review by consumers in The Cochrane Collaboration. The review received comments from two consumers through the Cochrane Consumers and Communication Review Group's standard editorial process. We also examined whether consumers were involved in the design and implementation of each included study.
Results
Description of studies
Results of the search
Our search across four reviews (this review; Car 2012; de Jongh 2012; Gurol‐Urganci 2012) identified 3937 citations. We excluded 3750 citations that, based on the abstract alone, showed insufficient relevance to the suite of reviews or did not meet the stated study design criteria. After review of the full text of the remaining 187 citations, a further 156 were subsequently rejected from this review for failing to meet the inclusion criteria. In the final selection stage, we excluded 27 of the remaining 31 citations (see Excluded studies below).
Included studies
We included four studies in this review (Cocosila 2009; Jareethum 2008; Rodgers 2005; Shapiro 2008) that cover the area of primary prevention. Two articles (Bramley 2005; Rodgers 2005) that used the same data set separately reported overall results (Rodgers 2005) and a sub‐analysis comparing results between Maori (the indigenous population of New Zealand) and non‐Maori (Bramley 2005). The latter sub‐analysis was not included in this review, and hence we list Bramley 2005 as an excluded study.
We present key characteristics of the included studies below and in the Characteristics of included studies table.
Methods
The included studies were all randomised controlled trials (RCTs) in which the unit of randomisation was the individual person. The studies' duration ranged from 1 month to 6 months: 1 month (Cocosila 2009), 8 weeks (Shapiro 2008), 6 months (Jareethum 2008; Rodgers 2005).
Three studies compared the effects of the text messaging intervention to existing practice (Cocosila 2009; Jareethum 2008; Rodgers 2005). Existing practice was no text messaging activity (Cocosila 2009), routine prenatal support (Jareethum 2008) and no restrictions on the use of other smoking cessation strategies by study participants (Rodgers 2005). One study compared the effect of a text messaging intervention to a second intervention consisting of monitoring of health behaviours through paper diaries, and to a control group with no monitoring (Shapiro 2008). Sample sizes ranged from 58 (Shapiro 2008) to 1705 participants (Rodgers 2005).
Participants
The studies were conducted in Canada (Cocosila 2009), Thailand (Jareethum 2008), New Zealand (Rodgers 2005), and the United States of America (Shapiro 2008). Use of SMS messaging was applied to four different clinical areas: adherence to preventive medication (Cocosila 2009), prenatal support (Jareethum 2008), smoking cessation (Rodgers 2005), and health behaviours (Shapiro 2008). Participants in three studies were people in the community (Cocosila 2009; Rodgers 2005; Shapiro 2008) and in one study healthy pregnant women attending an ambulatory antenatal clinic (Jareethum 2008). The target group for the intervention varied. Participants in one study were children aged 5 to 13 years and their parents (Shapiro 2008). Rodgers 2005 targeted current smokers aged over 16 years. The studies by Cocosila 2009 and Jareethum 2008 targeted participants aged over 18 years. Three studies included both men and women; the proportion of males included in the studies ranged from 38% to 45%. Jareethum 2008 included only women.
Participants in Rodgers 2005 came from all income levels: 26% from low, 42% from middle and 31% from higher income level. The intervention group in Jareethum 2008 had a higher proportion of pregnant women with a bachelor degree than the control group (P = 0.061). Other studies did not report the socio‐economic status of the participants. Ethnicity was reported in Rodgers 2005: the study included 21% Maori and 79% Non‐Maori participants. Details about race were presented only in the study by Shapiro 2008; the study included 60% white, 34% black, 1% Asian and 1% Hispanic/Latino participants.
Interventions
Purpose
The purpose of the SMS intervention varied across studies. One study used SMS to support antenatal care of healthy pregnant women (Jareethum 2008). In another study, current daily smokers interested in quitting within a month were sent regular, personalised text messages providing smoking cessation advice, support and distraction (Rodgers 2005). In addition, several other text message based services were provided for the intervention group: Quit buddies (participants with similar characteristics and quit days were put in touch with each other); TXT crave (participants could ‘pull’ text messages on demand by sending a text message to a short code number and they would receive a tip on how to get through the cravings); TXT polls (for example, messages sent to all participants on current topics, and the answers were sent back to all); and TXT quizzes (questions were sent out, followed by answers the next day).
Two studies involved two‐way communication between participants and an automated system. In Cocosila 2009 participants were sent SMS medication reminders, and, depending on their reply (i.e. acknowledgement or not), a reminding‐reinforcing or a reminding‐correcting message. Participants in Shapiro 2008 sent text messages to provide information on any of three targeted behaviours: pedometer usage, estimating beverage serving sizes, and estimating screen time (TV, video game, computers). For each SMS sent, they would receive an immediate, automated SMS feedback message.
Specifications
The mobile phone messaging interventions were delivered using different platforms. In Cocosila 2009 no information was provided other than that an automated delivery system was used. No technical details on the text messaging specifications were described in Jareethum 2008. In the study on smoking cessation an algorithm based on keyword matching was developed to match participant characteristics with a database of over 1000 text messages, so that an individualised programme was provided during a free month of text messaging (Rodgers 2005). In Shapiro 2008 for each SMS sent participants received an immediate, automated SMS feedback message from the program, which was hosted on a secure server.
Participants in Cocosila 2009 received compensation: in the control group 15 US dollars (USD) and those in the intervention group 30 USD (a higher amount covering additional activities and the SMS air‐time during the study). In Shapiro 2008 each family was given one phone to share for the duration of the study and they were instructed not to use the phone for anything except study‐related SMS. In three other studies participants used their own mobile phones.
Message content
In Cocosila 2009, participants in the intervention group were sent SMS medication reminders with fresh content from a virtual friend called ‘Tim’. Some messages included jokes and ended with a ‘smiley’. All texts were in a direct, non‐formal language. Three types of reminders were sent: basic (a medication reminder: after each such message participants were requested to reply with a one‐letter SMS after taking the vitamin, no later than the midnight of the same day), reinforcing (encouraging messages with fresh jokes, brief information) and correcting (those who did not acknowledge the basic reminders were sent brief information about the importance of taking the vitamin with no ‘smiley’). In Jareethum 2008 SMS messages were appropriate to the women’s gestational age, and contained information and warnings relating to abnormal symptoms that would require consultation with a doctor. The study on smoking cessation (Rodgers 2005) used personalised text messages providing smoking cessation advice, support, and distraction, by matching participant characteristics with a database of text messages . Participants’ nicknames were also incorporated into the text messages. In Shapiro 2008 hundreds of feedback messages were developed to avoid duplicate messages; algorithms were based on (1) how many goals were met and (2) enhancement or deterioration from the previous day (for example, “Wow, you met your step and screen time goals—Congratulations! What happened to beverages?”).
Timing and frequency
The timing and frequency with which messages were sent and received varied across studies. During the first two weeks of the one‐month Cocosila 2009 study, participants in the intervention group were sent one reminding‐basic message daily at random times within a two hour time interval and, depending on their reply (i.e. acknowledgement or not), a reminding‐reinforcing or a reminding‐correcting message every two days. In the last two weeks, participants received one reminding‐basic text message every other day, and either a reminding‐reinforcing or a reminding‐correcting message every three days. In Jareethum 2008 the study group received two text messages per week from 28 weeks of gestation until giving birth. SMS messages were sent on Mondays and Thursdays during the daytime to avoid making a disturbance.
In the study on smoking cessation (Rodgers 2005) five messages were sent per day for the week leading up to the quit day and for the following four weeks. Six weeks after randomisation, coinciding approximately with the end of the free text messaging month, the intervention became much less intensive, with the number of sent text messages reducing from five a day to three per week until the end of the 26‐week follow up.
Families in Shapiro 2008 began monitoring on day one of the program and sent two text messages per day (one for parent and one for child) for the full eight weeks of the study. For each text sent, they received an immediate, automated text feedback message, regardless of the time of day.
Outcomes
Cocosila 2009 reported on self‐reported adherence through missed tablets of preventive medicine (vitamin C) in the final week, increase in number of tablets taken per week and self‐reported increased adherence (SMS versus control) to taking the tablets. Jareethum 2008 reported on satisfaction levels, confidence scores, anxiety scores and pregnancy outcomes (e.g. gestational age at birth and fetal birth weight) in the antenatal and perinatal periods (SMS versus control). Rodgers 2005 on smoking cessation reported quit rates at 6 weeks, 12 weeks, and 26 weeks, and percentage abstaining from smoking at 26 weeks. Shapiro 2008 reported on treatment acceptability, attrition (SMS versus paper diaries versus control), adherence to self‐monitoring (percentage of total monitoring days: SMS versus paper diary) and preliminary efficacy of SMS in affecting behavior change in children. For determining the rate of attrition in this study, completers were defined as participants who completed the 8‐week post assessment and who attended at least two of three educational sessions.
Excluded studies
After review of the full text of 31 studies, we excluded 27 citations describing 21 individual studies from this review (see Characteristics of excluded studies for further details).
We excluded seven papers describing four studies relevant to secondary or tertiary prevention (Franklin 2006; Hanauer 2009; Marquez Contreras 2004; Ostojic 2005) as they are discussed in a separate review that examines the role of mobile phone messaging for facilitating self‐management of long term illnesses (de Jongh 2012). In 14 papers describing 11 studies, additional means of data transmission, such as digital subscriber line (DSL) Internet connection, wireless application protocol (WAP) or general packet radio service (GPRS), were used such that the independent effects of text messaging could not be separated from those of the overall intervention (i.e. they were multifaceted interventions), and three studies had no controls. At a later stage, we excluded two more studies (Chen 2008; Vilella 2004) that reported on mobile phone messaging reminders for facilitating the uptake of preventive activities. One of these (Chen 2008) is included in a separate review (Car 2012) that discusses the effects of mobile phone messaging reminders for attendance at healthcare appointments.
We excluded one paper (Bramley 2005) reporting a sub‐analysis of an included study (Rodgers 2005) comparing results between Maori (the indigenous population of New Zealand) and non‐Maori.
Ongoing studies
We identified eight studies potentially relevant to this review but for which no data were yet available. Of these, four studies were yet not recruiting participants at the time of this review (Balmford 2008; Bull 2008; Lim 2005; Kimball 2007); three were ongoing (Free 2007; Sutton 2009; Whittaker 2006); and one had already been completed but results had not yet been published (Sutton 2008). The studies by Balmford 2008, Free 2007, Sutton 2008, Sutton 2009 and Whittaker 2006 address smoking cessation; Bull 2008 and Lim 2005 sexual risk behaviour; and Kimball 2007 adherence to sunscreen use. We successfully contacted one study coordinator (Whittaker 2006) for additional information but the study was ongoing and we did not receive any preliminary findings. Studies will be assessed for inclusion in a subsequent update of this review.
Risk of bias in included studies
We summarise the risk of bias in included studies in Figure 1. The included studies were of varying methodological quality with some studies providing insufficient information to accurately assess the risk of bias.
1.
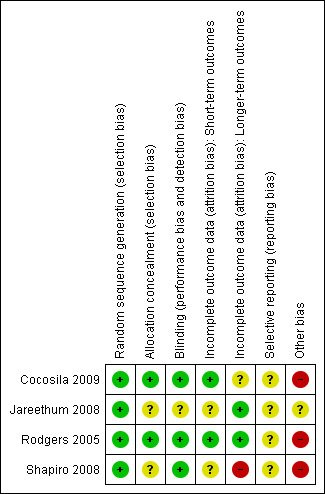
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
Adequate sequence generation
All four included studies reported the use of adequate sequence generation methods (computer generated random allocation sequences, central telephone randomisation or random number tables).
Allocation concealment
Allocation concealment was considered adequate in two studies (Cocosila 2009; Rodgers 2005). In Jareethum 2008 and Shapiro 2008 allocation concealment was unclear as the method of concealment was not described in sufficient detail.
Blinding
In none of the studies were participants blinded. We judged that the outcomes and outcome measurements were unlikely to have been influenced by lack of blinding. Only one study reported on blinding of personnel collecting and analysing the samples (Rodgers 2005). No mention is made in other studies of blinding of outcome assessors or researchers and this could have introduced a source of bias.
Incomplete outcome data
The number of study participants lost to follow‐up was relatively small compared to sample size in the study by Jareethum 2008. In Shapiro 2008 the sample size was too small to detect statistically significant differences between completers in the study groups. Also the percentage of participants who completed the study varied between groups (SMS 72% versus paper diaries 39% versus control 50%). In this study final analysis was performed on only those participants who had completed the study, which could influence generalisability of the findings (Shapiro 2008). The methods of analysing incomplete data collected varied across studies with analysis and reporting based on intention to treat analysis (ITT) in Cocosila 2009, and on only participants who completed the study (Shapiro 2008).
In the study on smoking cessation (Rodgers 2005) a number of sensitivity analyses were used to assess the potential effect of data missing from follow‐up, mis‐classified quit status, and adjustment for baseline prognostic variables. Assuming those participants lost to follow up as smokers is standard practice in cessation studies. However, sensitivity analyses were performed to evaluate the impact of other possibilities on the results in Rodgers 2005. The two main shortcomings of the study lay in the potential over‐reporting of quitting status and the comparatively large and differential loss to follow up. The results of salivary cotinine verification for those reporting to have quit at six weeks demonstrated over‐reporting of quit rates, with no clear evidence that this occurred at different rates in the intervention and control groups. These factors are unlikely to have biased the treatment effect estimates at six weeks, since at that time follow up was high and possible over‐reporting rates appeared similar in both groups. At 12 and 26 weeks there were more lost to follow‐up in the active group and so, assumptions of smoking status for those lost to follow‐up could have led to important differences to the treatment effect estimates. Researchers discussed the different scenarios modelled for treatment of missing data. Under all scenarios there remained a statistically significant increase in smoking cessation rates at six weeks, even under the most conservative assumptions. As well, there remained an increase in prevalence of non‐smoking in the active group compared to the control group at 12 weeks. However, the between‐group differences were less clear at 26 weeks.
Selective reporting
We were unable to review the original study protocols of the included studies, thus no fully informed inferences could be made about potential selective reporting, although the number of possible outcomes seemed restricted to those reported in the studies.
Other potential sources of bias
In the study on smoking cessation (Rodgers 2005) incentives for providing final follow‐up data differed between groups: one month of free text messaging was received by the control group on study completion whereas the intervention group had already received their month of free text messaging from their quit day and did not receive further incentives to complete the study. Consequently, follow‐up rates reduced to around 67% in the intervention group and to 78% in the control group by six months. The reported quit rates increased over time in the control group. One possible explanation is that some participants may have thought their free text month might depend on reporting quitting. Although differential use of incentives could have led to bias, this is expected to have led to an underestimation of effect rather than an overestimation.
In Cocosila 2009 the figures regarding vitamin C consumption increased for both groups at endpoint: by 246% for the intervention group and by 131% for the control group. However, the differences between groups were not significant. A possible cause of the non‐significant difference between the intervention and control group at endpoint may have been potential 'cross‐contamination' between intervention and control groups due to the way participants were selected for the study. In addition to the small sample size, Shapiro 2008 had several other limitations, including only English‐speaking families and intermittent difficulties with using SMS (e.g. phone companies merged, plans discontinued, changed coverage areas, which probably influenced generalisability. Furthermore, the questionnaire used to explore the preliminary efficacy of SMS in promoting behavioural change was not validated. There was also no validation of accuracy of reporting.
Effects of interventions
See: Table 1
All outcome measures reported in the included studies are presented in a single table (Table 1) as well as in Data and analyses. The primary outcomes have been grouped as health status outcomes and health behaviour outcomes. The secondary outcomes are grouped as participants' evaluation of the intervention, and adverse effects from the intervention. None of the included studies reported on the providers’ evaluation of the intervention, cost, or perceptions of the intervention's safety. Due to the heterogeneity across studies in areas of primary prevention, type of interventions, and outcome measures, it was not possible to quantify differences between groups or to calculate effect sizes across studies.
Health status outcomes
Satisfaction level of antenatal care and confidence and anxiety levels of healthy pregnant women
Jareethum 2008 compared healthy pregnant women's satisfaction levels with antenatal care between those who received text messages for prenatal support, and those who did not. The study also assessed the confidence and anxiety levels and pregnancy outcomes in the two groups. Satisfaction, anxiety and confidence were measured using a tested questionnaire involving a visual analogue scale from 1 to 10 points. Women who received prenatal support by text message were significantly more satisfied than those who did not receive the messages, both in the antenatal period (mean difference (MD) 1.25, 95% confidence interval (CI) 0.78 to 1.72) and perinatal period (MD 1.19, 95% CI 0.37 to 2.01). In the SMS group, women's confidence levels were higher (MD 1.12, 95% CI 0.51 to 1.73) and anxiety was lower (MD ‐2.15, 95% CI ‐3.42 to ‐0.88) (Analysis 1.1) than in the control group in the antenatal period. In the perinatal period there were no statistically significant differences for confidence and anxiety. Furthermore, no differences between the groups were found in pregnancy outcomes, including gestational age at birth, infant birth weight, preterm delivery and route of delivery (Analysis 1.2; Analysis 1.3; Table 1).
1.1. Analysis.
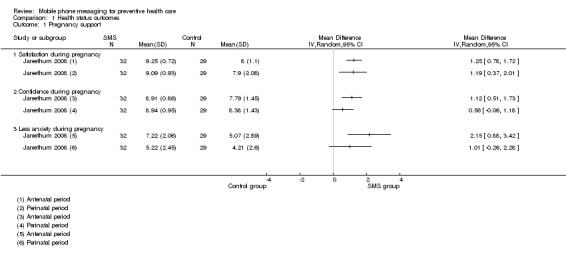
Comparison 1 Health status outcomes, Outcome 1 Pregnancy support.
1.2. Analysis.
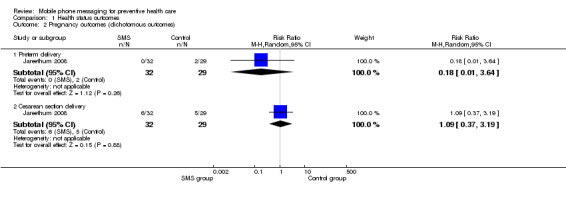
Comparison 1 Health status outcomes, Outcome 2 Pregnancy outcomes (dichotomous outcomes).
1.3. Analysis.

Comparison 1 Health status outcomes, Outcome 3 Pregnancy outcomes (continuous outcomes).
Health behaviour outcomes
Smoking cessation
Rodgers 2005 assessed the effects of a mobile phone text messaging smoking cessation programme (Analysis 2.1). More participants reported not smoking in the intervention group compared to the control group at 6 weeks (RR 2.20, 95% CI 1.79 to 2.70) and at 12 weeks follow‐up (RR 1.55, 95% CI 1.30 to 1.84) (Table 1).This treatment effect was consistent across subgroups defined by age, sex, income level, or geographic location. At 26 weeks there was no significant difference between groups, if missing values were assumed as smoking (RR 1.07, 95% CI 0.91 to 1.26). However, using last values carried forward, the difference between intervention and control groups persisted at 26 weeks (RR 1.28, 95% CI 1.11 to 1.48). Continuous abstinence rate (allowing three or fewer ‘lapses’ of two or fewer cigarettes per lapse) at 26 weeks was higher in the intervention group (RR 1.64, 95% CI 1.12 to 2.42), whereas there was no difference in the complete abstinence rate between groups (RR 1.5, 95% CI 0.92 to 2.44).
2.1. Analysis.
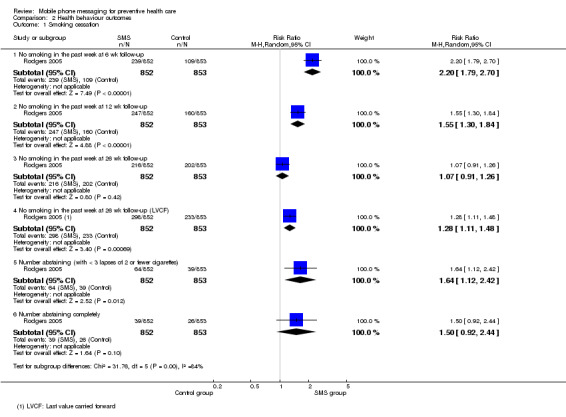
Comparison 2 Health behaviour outcomes, Outcome 1 Smoking cessation.
The authors attempted to verify smoking status in a random sample of self‐reported quitters at 6 weeks (n = 125, 35.9%). They used salivary cotinine as the biochemical measure and, although numbers were small, over‐reporting of quitting was evident in both intervention and control groups. Of those in the intervention group who were invited to provide a cotinine sample, 62.7% (n = 52) did not attend, and 57.1% (n = 24) of those invited in the control group did not attend. Of those who did provide a sample, 54.8% (n = 17) in the intervention group were verified as having quit, compared with 33.3% (n = 6) in the control group. Therefore the study demonstrates a higher degree of over‐reported quitting by those in the control group than those in the intervention group.
The evidence that mobile phone messaging interventions positively impact on smoking quit rates is considered to be of high quality (Table 1).
Self‐reported adherence to taking preventive medicine
Cocosila 2009 assessed the effectiveness of text messaging for improving adherence to taking preventive medicine (vitamin C) (Analysis 2.2). Both groups reported increased adherence at the end of the study, with a higher proportion of people in the intervention group reporting increased adherence (RR 1.41, 95% CI 1.14 to 1.74) and the average number of missed pills in the last 7 days was marginally lower in the intervention group (MD ‐0.80, 95% CI ‐1.55 to ‐0.05; Analysis 2.3). This evidence is of moderate quality and the finding may well be affected by further research in this area (Table 1).
2.2. Analysis.

Comparison 2 Health behaviour outcomes, Outcome 2 Vitamin C: increased adherence (dichotomous).
2.3. Analysis.
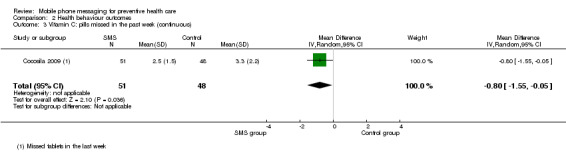
Comparison 2 Health behaviour outcomes, Outcome 3 Vitamin C: pills missed in the past week (continuous).
Monitoring of healthy behaviours
Shapiro 2008 examined acceptability, attrition, adherence, and preliminary efficacy of mobile phone text messaging for monitoring children's health behaviours. The outcomes relating to physical activity, consumption of sugar‐sweetened beverages or screen time did not differ between intervention and control groups, regardless of the method of assessment, using data from self‐monitoring versus self‐reported recall (Analysis 2.4).
2.4. Analysis.
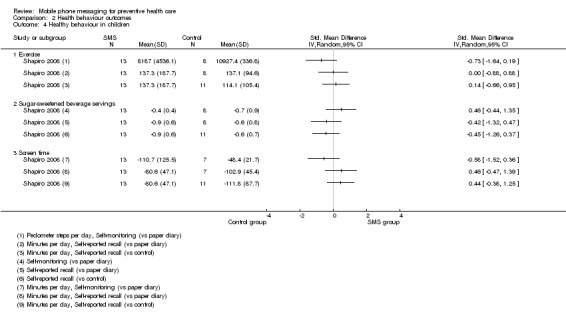
Comparison 2 Health behaviour outcomes, Outcome 4 Healthy behaviour in children.
Children in the SMS group had somewhat lower attrition n = 5 (28%) than those in the group using paper diary n = 11 (61%) and control group n = 11 (50%), and significantly greater adherence to self‐monitoring than the paper diary group (reported in the study as 43% versus 19%, P < 0.02). The quality of the evidence for phone messaging affecting health behaviours in children is, however, very low because of the very low number of participants enrolled and risk of bias in the study (Table 1). This means that further research is very likely to influence the observed effect size.
Participants’ evaluation of the intervention
The studies primarily focused on the effects of the interventions on health outcomes or health behaviours, with little or no discussion on participant satisfaction or acceptability of the intervention. The only study to explicitly address these issues was Shapiro 2008 in which authors measured acceptability using three questions each to the child and to the parent (Analysis 3.1). There were no differences in the individual or pooled scores for acceptability of SMS versus paper diary for children or parents.The only difference was in parental reports of likelihood of participating in such a study again, with parents in the non‐monitoring (C) group being more likely to participate than parents in the SMS group (MD ‐1.80, 95% CI ‐3.36 to ‐0.24).The small number of participants in this study, together with a moderate risk of bias in the included study, however, means that the quality of evidence for this measure is very low (Table 1).
3.1. Analysis.

Comparison 3 User evaluation of intervention, Outcome 1 Acceptability.
Adverse effects of the intervention
The adverse effects of text messaging were presented only in the study on smoking cessation (Rodgers 2005). During the 26 week study period the investigators were interested also in the rate of pain in the thumb or finger joints during texting, and car crash rates. There was no difference in the rate of pain in the thumb or finger joints during texting (RR 1.08, 95% CI 0.74 to 1.59), or in car crash rates (RR 0.88, 95% CI 0.58 to 1.35) (Analysis 4.1).The authors further note that a total of five crashes occurred during or after sending a text message whereas three occurred while smoking. The evidence for absence of adverse effects from the interventions is of moderate quality (Table 1).
4.1. Analysis.
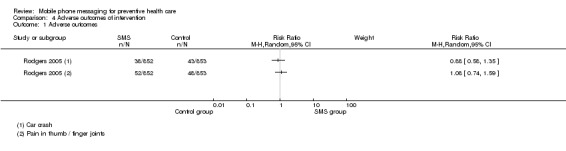
Comparison 4 Adverse outcomes of intervention, Outcome 1 Adverse outcomes.
Discussion
Summary of main results
This review brings together the evidence for delivering health interventions by text messaging that focus on preventive health care for healthy individuals. The results of our review show that using mobile phone messaging as a mode of delivery for preventive health care resulted in some improvements in the health status and health behaviours of the participants. One study focused on improving health status and three studies on promoting preventive health behaviour. However, participants' evaluation of the intervention and adverse effects were reported only in one study, which found no statistically significant results for participant evaluation, but also found no adverse effects of text messaging interventions. None of the included studies reported the cost of care, the providers’ evaluation of the intervention, or perceptions of safety of text messaging. All studies used tailored text messaging, and two of them involved two‐way communication between participants and an automated system (Cocosila 2009; Shapiro 2008).
The evidence on the effects of text messaging as a mode of delivery for preventive health care appears to be mixed. One study on satisfaction, confidence and anxiety levels of pregnant women who received SMS messages during their antenatal care demonstrated some potential to improve the health status of healthy pregnant women in the antenatal period. However, no difference was found in pregnancy outcomes (Jareethum 2008). The evidence on the effects of text messaging on smoking cessation comes from one large study (Rodgers 2005). This study reported significant short‐term beneficial effects on behaviour modification among the intervention group participants, but no significant effect was found for the long‐term. There were, however, significantly higher rates of continuous abstinence from smoking at 26 weeks among the intervention group participants.
We found very low quality evidence that text messaging had no effect on self‐monitoring healthy behaviours relevant to childhood weight control (specifically, increasing physical activity, and reducing sugary drink intake and screen time) (Shapiro 2008). However, the sample size was small, and no generalisations can be made until the intervention is rigorously evaluated in larger follow‐up studies that test the efficacy of the intervention.
We found moderate quality evidence that SMS medication reminders increased adherence to preventive medicines, in a small study (Cocosila 2009). Interestingly, this study used two‐way communication between participants and an automated system. Accordingly, it was possible to see if participants acknowledged their daily vitamin taking, and how late after the prescribed intake time this was done. As the research literature asks for more objective measures of adherence (Haynes 2008), this approach has the potential to become a suitable system for promptly reporting self‐reported adherence to medication.
Participants' evaluation of text messaging in supporting preventive healthcare measures was addressed in only one study (Shapiro 2008). In this small feasibility study no significant differences were found in most treatment acceptability measures across any of the groups; the only exception was that parents in the control group were more likely to participate again than those who received SMS messages. Evidently, the acceptability of text messaging in preventive healthcare is an area that requires further attention.
None of the included studies focused on direct and indirect costs associated with text messaging. It should, however, be recognised that such costs may depend on the nature of the intervention and the size and characteristics of the target group. Given the current global enthusiasm with which mHealth applications are being embraced, more attention to the cost implications seems warranted.
Overall completeness and applicability of evidence
We systematically collected and analysed the evidence to date on the effects of mobile phone messaging as a mode of delivery for preventive health care. However, when interpreting the results of this review, some of the limitations should be taken into consideration. Firstly, in considering studies for the review we have taken a narrow focus: including only those studies in which the intervention is exclusively delivered through text messaging, and communication is between provider and participant only. We excluded studies combining SMS with other forms of data transmission, such as email, Internet or General Packet Radio Service (GPRS), as it would be difficult to assess the independent effect of a text message within such complex interventions. However, this strategy restricted the body of evidence that we were able to examine. Our review thus contains only a small number of studies. Combined with the substantial heterogeneity in the selected studies, this means it is very difficult to assess to what extent the review's findings have more general relevance. Secondly, the fact that no data has been collected beyond a study period of 26 weeks means that it is difficult to predict the long‐term effects of text messaging in supporting the primary preventive measures directed to behavioral changes.
We included three studies from high income countries (Canada, New Zealand, USA) and one study from a lower‐middle income country (Thailand). Text messaging for preventive health care seemed promising in the area of smoking cessation and antenatal care. However, as our review contains only one study for each individual field of primary prevention, it is very difficult to assess to what extent our findings have more general relevance.
None of the studies evaluated potential loss or misinterpretation of the data, or considered issues of costs, security and confidentiality. Particularly in low‐income countries where mobile phones are frequently shared between family members, these are important issues that need to be taken into account.
Quality of the evidence
The included studies were of varying methodological quality; some studies provided insufficient information to accurately assess the risk of bias. On the whole, sequence generation for randomisation was considered adequate in all studies. Only two of the four studies provided information on allocation concealment. The lack of blinding of participants in all studies can be partly explained by the interactive nature of the SMS interventions, which does not permit the blinding of patients or their healthcare providers. There is, however, a potential for bias from the apparent lack of blinding of outcome assessors, as only one study reported on blinding of personnel collecting and analysing the samples. The individual studies examined a wide variety of outcomes, and the heterogeneity in these outcome measures makes it difficult to draw unambiguous conclusions on the effects of text messaging.
The study on smoking cessation attempted biochemical verification of self‐reported quit rates at 6 weeks and found greater over‐reporting of quitting in the control than the intervention group. Although the numbers involved were very small, it is possible that reliance on self‐report in this study could underestimate the effect of the intervention.
Some conclusions come from studies with small sample sizes, and the effects of these interventions need to be rigorously evaluated in larger follow up studies. While the study on adherence to preventive treatment is of moderate quality, the results have limited generalisability to improving treatment adherence for outpatients with more complex chronic disease regimens. It should also be taken into account that tools used to explore the preliminary efficacy of text messaging to promote behavioural change for children's weight control were not validated.
Because of the limited number of studies included in this review and the relatively small number of participants in some studies the effectiveness of using mobile phone messaging in supporting preventive health care cannot be assessed. However, despite these limitations this review provides a useful overview and has exposed important gaps in the current knowledge in this area which merit further research.
Potential biases in the review process
We believe that we have identified all the studies addressing the use of mobile phone messaging as a mode of delivery for preventive health care that met our study design criteria (RCT, QRCT, CBA, ITT) up to June 2009. We also successfully contacted four study coordinators to obtain additional information regarding ongoing studies and these will be assessed in a future update of the review. However, by excluding studies with possible confounding from other communication and/or data transmission methods, we may have introduced selection bias towards less successful interventions, as more complex interventions may be more effective at improving health and behavioural outcomes.
Agreements and disagreements with other studies or reviews
This review follows on two other reviews with a similar focus. Fjeldsoe 2009 reviewed the evidence for behaviour change interventions delivered by SMS, whereas Krishna 2009 more broadly looked at healthcare delivery via mobile phones in the management and prevention of disease. One study on smoking cessation (Rodgers 2005) in our review was also included in both of those reviews.
However, our review differs from these two reviews in several respects. First, Krishna 2009 focused on all possible fields of application for mobile phones in disease management and prevention, rather than on their utility as a mode of delivery for preventive health care alone. Their conclusions were thus based on an even more heterogeneous set of studies, complicating the process of deriving robust conclusions. Secondly, Krishna 2009 was not restricted to text messaging applications alone but also included interventions whereby mobile phones were used for regular phone calls or for data transmission by GPRS, e.g. to transmit data received from a wireless device, thus including a number of studies which we have excluded from our review to minimise possible confounding. Interestingly, Krishna 2009 is more positive overall regarding the effects of mobile phones on health outcomes, compliance with medication and self‐efficacy. A possible explanation could be that interventions employing a more extensive range of technologies in patient‐provider communication are better tailored to patients’ needs and preferences than those which rely exclusively on text messaging.
Fjeldsoe 2009's focus was somewhat closer to that of our review, as it looks specifically at behaviour change interventions, evaluating changes in both preventive health behaviour and those associated with the management of clinical conditions. The review, however, used less stringent selection criteria, and included studies without a control group. Furthermore, although text messaging had to be the main method of intervention delivery the review also considered studies in which other technologies were used as adjuncts. Despite the wider scope of the review and the inclusion of less rigorous studies, Fjeldsoe 2009's conclusions ‐ that text message based interventions can have some positive short‐term behavioural outcomes, but that further research into long‐term effects and acceptability is required ‐ are largely in line with those of our review.
Authors' conclusions
Implications for practice.
We identified four randomised controlled trials studying the effects of mobile phone messaging interventions as a mode of delivery for preventive health care. Despite the small number of studies and the small number of participants in three studies, results suggest that text messaging interventions have the potential to support health behavioural changes in the short‐term and they could add value to the provision of preventive health‐related information. There is no evidence that mobile phone messaging interventions have long‐term benefits for preventive health care. Furthermore, very little is known about costs, and possible risks and harms associated with the intervention. Before these issues are examined further, caution is advised about implementing these technologies on a large scale.
Implications for research.
The evidence is based on four randomised trials that tested text messaging for preventive health care for varied health behaviours. These studies used the individual person as the unit of randomisation. The number of participants in the included studies was low and most participants were young adults. The studies had a relatively short duration, with none exceeding 26 weeks. Causal pathways between interventions and outcomes were not clearly defined, especially in one study that also included financial compensation and where the effect of the SMS intervention and financial incentive could not be disaggregated. None of the studies included economic evaluations. These limitations, combined with the significant risk of bias, mean that the evidence on health effects is of low to moderate quality, and that long‐term effects or economic benefits cannot be demonstrated. It is also not possible to ascertain whether the effects can be sustained over a period of time. There is, therefore, a need for more robust studies into these issues.
Future studies should have larger sample sizes and include different age groups that may benefit from preventive health interventions. The studies should be for longer duration, preferably up to at least three years, to demonstrate whether such benefits can be sustained over time ‐ critically important as achieving sustained behaviour change is difficult. Studies which have a bundle of interventions, for example combining text messaging with professional support or financial incentives, should have appropriate designs to assess the effect of text messaging, both with and without such additional interventions.
Future studies should also compare effects in different contexts, for example in low and middle income countries with weaker health systems and significant shortages in the health workforce. In addition to demonstrating intermediate measures, such as uptake of interventions or sustained adherence to them, future studies should measure effects on health outcomes ‐ for example, reduced incidence and prevalence rates, or in the case of secondary prevention reduced disease progression, improved physiological measurements, reduced complication rates or lowered hospital admissions. In addition, future studies should explore acceptability of the interventions to users, as well as their economic costs and benefits.
Acknowledgements
We acknowledge the very helpful support of the Cochrane Consumers and Communication Review Group editorial base at different stages of this review.
Appendices
Appendix 1. MEDLINE (Ovid) search strategy
cellular phone/
text messag$.ab,ti.
texting.ab,ti.
short messag$.ab,ti.
sms.ab,ti.
(multimedia messag$ or multi‐media messag$).ab,ti.
mms.ab,ti.
((cellular phone$ or cell phone$ or mobile phone$) and (messag$ or text$)).ab,ti.
or/1‐8
randomized controlled trial.pt.
controlled clinical trial.pt.
randomized controlled trials.sh.
random allocation.sh.
double blind method.sh.
single blind method.sh.
or/10‐15
animals/ not (human/ and animals/)
16 not 17
clinical trial.pt.
exp clinical trials/
(clin$ adj25 trial$).ti,ab.
((singl$ or doubl$ or trebl$ or tripl$) adj25 (blind$ or mask$)).ti,ab.
placebos.sh.
placebo$.ti,ab.
random$.ti,ab.
research design.sh.
or/19‐26
27 not 17
18 or 28
exp evaluation studies/
follow up studies/
prospective studies/
(control$ or prospectiv$ or volunteer$).tw.
cross over studies/
comparative study/
or/30‐35
experiment$.tw.
(time adj series).tw.
(pre test or pretest or (posttest or post test)).tw.
(pre intervention or preintervention or (post intervention or postintervention)).tw.
(impact$ or intervention$ or chang$ or outcome$).tw.
effect$.tw.
or/37‐42
36 and 43
animals/ not (human/ and animals/
44 not 45
29 or 46
47 and 9
limit 48 to yr="1993 ‐ 2008"
Appendix 2. EMBASE (Ovid) search strategy
mobile phone/
wireless communication/
(cellular phone* or cellular telephon* or cell phone* or mobile phone* or mobile telephon* or wireless phone* or wireless telephon*).ti.
1 or 2 or 3
limit 4 to abstracts
(cellular phone* or cellular telephon* or cell phone* or mobile phone* or mobile telephon* or wireless phone* or wireless telephon*).tw.
(text* or messag* or multimedia or multi‐media or imag* or data or input* or sms or mms).tw.
(5 or 6) and 7
4 not 5
(text messag* or texting or texted).tw.
(short messag* or (sms not (somatostatin* or sphingomyelin*))).tw.
(multimedia messag* or multi‐media messag*).tw.
(mms and (multimedia or multi‐media)).tw.
or/8‐13
Randomized Controlled Trial/
random*.tw.
experiment*.tw.
time series.tw.
(pre test or pretest or post test or posttest).tw.
impact.tw.
intervention*.tw.
chang*.tw.
evaluat*.tw.
effect?.tw.
compar*.tw.
control*.tw.
or/15‐26
nonhuman/
27 not 28
14 and 29
limit 30 to yr="1993‐2009"
Appendix 3. PsycINFO (Ovid) search strategy
(cellular phone* or cellular telephon* or cell phone* or mobile phone* or mobile telephon* or wireless phone* or wireless telephon*).tw.
(text* or messag* or multimedia or multi‐media or imag* or data or input* or sms or mms).tw.
1 and 2
(text messag* or texting or texted).tw.
(short messag* or sms).tw.
(multimedia messag* or multi‐media messag*).tw.
(mms and (multimedia or multi‐media)).tw.
or/3‐7
random*.tw.
experiment*.tw.
trial.tw.
placebo.ab.
groups.ab.
((singl* or doubl* or trebl* or tripl*) and (blind* or mask*)).tw.
time series.tw.
time series/
(pre test or pretest or post test or posttest).tw.
(pre intervention or preintervention or post intervention or postintervention).tw.
(cross over or crossover).tw.
latin square.tw.
(prospective* or volunteer*).tw.
impact.tw.
intervention*.tw.
chang*.tw.
evaluat*.tw.
effect?.tw.
compar*.tw.
control*.tw.
treatment effectiveness evaluation/
mental health program evaluation/
exp experimental design/
or/9‐31
limit 32 to human
limit 33 to yr="1993‐2008"
(health* or medic* or telemedic* or patient* or illness* or therap* or psychiatr* or nurs* or remind* or consult*).tw.
("27" or "32" or "33" or "34").cc.
35 or 36
8 and 34
38 and 37
Appendix 4. CENTRAL search strategy
#1 "cellular phone":kw or "mobile phone":kw or ((text next messag*) or texting or texted or (short next messag*) or (sms not (somatostatin* or sphingomyelin*)) or (multimedia next messag*) or (multi‐media next messag*) or (mms and (multimedia or multi‐media)) or (cellular next phone*) or (cellular next telephon*) or (cell next phone*) or (mobile next phone*) or (mobile next telephon*) or (wireless next phone*) or (wireless next telephon*)):ti,ab in Clinical Trials
#2 human*:kw in Clinical Trials
#3 #1 and #2
Appendix 5. CINAHL (EBSCO) search strategy
| S15 | s14 |
| S14 | S10 or S13 |
| S13 | s11 and s12 |
| S12 | PT Research |
| S11 | S3 not S10 |
| S10 | s3 and s9 |
| S9 | S4 or S5 or S6 or S7 or S8 |
| S8 | pre test or pretest or post test or posttest or pre intervention or preintervention or post intervention or postintervention or time series |
| S7 | TI ((singl* or doubl* or trebl* or tripl*) and (blind* or mask*)) or AB ((singl* or doubl* or trebl* or tripl*) and (blind* or mask*)) |
| S6 | random* or trial or groups or placebo* or experiment* or control* or compar* or intervention* or chang* or evaluat* or impact* or effect? |
| S5 | PT Clinical Trial |
| S4 | MH Experimental Studies+ or MH Random Assignment or MH Comparative Studies or MH Comparative Studies or MH Crossover Design or MH Placebos or MH Quantitative Studies or MH Quasi‐Experimental Studies+ |
| S3 | S1 or S2 |
| S2 | cellular phone* or cellular telephon* or cell phone* or mobile phone* or mobile telephon* or wireless phone* or wireless telephon* or text messag* or texting or texted or short messag* or sms or multimedia messag* or multi‐media messag* or (mms and (phone* or telephon* or multimedia or multi‐media or messag*)) |
| S1 | MH Wireless Communications |
Appendix 6. African Health Anthology search strategy
1 ‐ Query 1:
| KEY WORDS/PHRASES |
RANDOM* OR TRIAL* OR CONTROL* OR PROSPECTIV* OR VOLUNTEER* OR EXPERIMENT* OR TIME SERIES OR PRE TEST OR PRETEST OR POST TEST OR POSTTEST OR PRE INTERVENTION OR PREINTERVENTION OR POST INTERVENTION OR POSTINTERVENTION OR IMPACT* OR INTERVENTION* OR CHANG* OR EFFECT* |
| TITLE | PLACEBO OR GROUPS |
| INDEX TERMS | RESEARCH DESIGN OR FOLLOW UP STUDIES OR PROSPECTIVE STUDIES OR CROSS OVER STUDIES OR DRUG THERAPY |
2 ‐ Query 2:
| KEY WORDS/PHRASES |
((TEXT* OR MESSAG* OR MULTIMEDIA OR MULTI‐MEDIA OR IMAG* OR DATA OR INPUT* OR SMS OR MMS) AND (CELLULAR PHONE* OR CELLULAR TELEPHON* OR CELL PHONE* OR MOBILE PHONE* OR MOBILE TELEPHON* OR WIRELESS PHONE* OR WIRELESS TELEPHON*)) OR TEXT MESSAG* OR TEXTING OR TEXTED OR SHORT MESSAG* OR (SMS NOT (SOMATOSTATIN* OR SPHINGOMYELIN*)) OR MULTIMEDIA MESSAG* OR MULTI‐MEDIA MESSAG* OR (MMS AND (MULTIMEDIA OR MULTI MEDIA)) |
| TITLE |
CELLULAR PHONE* OR CELLULAR TELEPHON* OR CELL PHONE* OR MOBILE PHONE* OR MOBILE TELEPHON* OR WIRELESS PHONE* OR WIRELESS TELEPHON* |
| INDEX TERMS | CELLULAR PHONE |
3 ‐ Query 1 and Query 2.
Appendix 7. Search Strategy for LILACS, trial portals and grey literature
cellular phone OR mobile phone OR cellular telephone* OR mobile telephone* OR text messag* OR
texting OR texted OR short messag* OR multimedia messag* OR sms OR mms
Data and analyses
Comparison 1. Health status outcomes.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pregnancy support | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.1 Satisfaction during pregnancy | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Confidence during pregnancy | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 Less anxiety during pregnancy | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Pregnancy outcomes (dichotomous outcomes) | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 2.1 Preterm delivery | 1 | 61 | Risk Ratio (M‐H, Random, 95% CI) | 0.18 [0.01, 3.64] |
| 2.2 Cesarean section delivery | 1 | 61 | Risk Ratio (M‐H, Random, 95% CI) | 1.09 [0.37, 3.19] |
| 3 Pregnancy outcomes (continuous outcomes) | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.1 Birth weight (gm) | 1 | 61 | Mean Difference (IV, Random, 95% CI) | ‐137.0 [‐412.87, 138.87] |
| 3.2 Gestational age in delivery (weeks) | 1 | 61 | Mean Difference (IV, Random, 95% CI) | 0.10 [‐0.45, 0.65] |
Comparison 2. Health behaviour outcomes.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Smoking cessation | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.1 No smoking in the past week at 6 wk follow‐up | 1 | 1705 | Risk Ratio (M‐H, Random, 95% CI) | 2.20 [1.79, 2.70] |
| 1.2 No smoking in the past week at 12 wk follow‐up | 1 | 1705 | Risk Ratio (M‐H, Random, 95% CI) | 1.55 [1.30, 1.84] |
| 1.3 No smoking in the past week at 26 wk follow‐up | 1 | 1705 | Risk Ratio (M‐H, Random, 95% CI) | 1.07 [0.91, 1.26] |
| 1.4 No smoking in the past week at 26 wk follow‐up (LVCF) | 1 | 1705 | Risk Ratio (M‐H, Random, 95% CI) | 1.28 [1.11, 1.48] |
| 1.5 Number abstaining (with < 3 lapses of 2 or fewer cigarettes) | 1 | 1705 | Risk Ratio (M‐H, Random, 95% CI) | 1.64 [1.12, 2.42] |
| 1.6 Number abstaining completely | 1 | 1705 | Risk Ratio (M‐H, Random, 95% CI) | 1.50 [0.92, 2.44] |
| 2 Vitamin C: increased adherence (dichotomous) | 1 | 99 | Risk Ratio (M‐H, Random, 95% CI) | 1.41 [1.14, 1.74] |
| 3 Vitamin C: pills missed in the past week (continuous) | 1 | 99 | Mean Difference (IV, Random, 95% CI) | ‐0.80 [‐1.55, ‐0.05] |
| 4 Healthy behaviour in children | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.1 Exercise | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.2 Sugar‐sweetened beverage servings | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4.3 Screen time | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
Comparison 3. User evaluation of intervention.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Acceptability | 1 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 Parent (SMS vs PD) | 1 | 63 | Mean Difference (IV, Random, 95% CI) | ‐0.00 [‐1.08, 1.08] |
| 1.2 Child (SMS vs PD) | 1 | 63 | Mean Difference (IV, Random, 95% CI) | 0.15 [‐0.32, 0.62] |
| 1.3 Parent (SMS vs C) | 1 | 72 | Mean Difference (IV, Random, 95% CI) | ‐0.45 [‐1.84, 0.94] |
| 1.4 Child (SMS vs C) | 1 | 72 | Mean Difference (IV, Random, 95% CI) | 0.46 [‐0.07, 1.00] |
Comparison 4. Adverse outcomes of intervention.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Adverse outcomes | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Cocosila 2009.
| Methods | Study design: RCT conducted over 1 month. | |
| Participants | Student population at an university in Canada; mean age 23.8 years; 54,9% female. Exclusion criteria: being allergic or intolerant to vitamin C; being pregnant or likely to become pregnant during the study if female. 102 randomised: 52 intervention SMS group, 50 control group. |
|
| Interventions | SMS group: Participants were sent SMS medication reminders to take vitamin C for preventive reasons, and depending on their reply (i.e. acknowledgement or not), a reminding‐reinforcing or a reminding‐correcting message by an automated system. They were sent at random times within a 2‐hr time interval one reminding‐basic message daily and, depending on their reply (i.e. acknowledgement or not), a reminding‐reinforcing or a reminding‐correcting message every 2 days. In the last 2 weeks participants received one reminding‐basic text message every other day, and either a reminding‐reinforcing or a reminding‐correcting message every 3 days. Control group: Participants received no SMS messages. |
|
| Outcomes | Self‐reported adherence: missed tablets of vitamin C in the final week, increase in number of tablets taken per week and self‐reported increased adherence. | |
| Notes | The study is derived from the thesis: User acceptance of wireless text messaging in telehealth: a case for adherence. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were randomly directed by a specialized Java script. |
| Allocation concealment (selection bias) | Low risk | Quote: “...Neither participants nor the investigators had any knowledge of the distribution process until it was fully completed.” |
| Blinding (performance bias and detection bias) Patient‐reported outcomes | Low risk | Blinding of participants not possible due to nature of intervention. Although researchers were not blinded and the authors do not discuss how this could have affected the results, it does not seem likely that the lack of blinding would have biased the analysis. |
| Incomplete outcome data (attrition bias) Short‐term outcomes | Low risk | 1 month: 1/52 missing from intervention group, 2/50 missing from control group. All randomised participants were included in ITT analysis. |
| Incomplete outcome data (attrition bias) Longer‐term outcomes | Unclear risk | NA, study last only 1 month |
| Selective reporting (reporting bias) | Unclear risk | The study protocol was not available but number of possible outcomes seems restricted to those reported so likely free of selective reporting. |
| Other bias | High risk | The intervention and control groups were comparable at baseline. A possible cause of the non‐significant difference between the intervention and control group at endpoint may have been affected by potential 'cross‐contamination' between intervention and control groups due to the way participants were selected for the study (i.e. included groups of friends and colleagues). |
Jareethum 2008.
| Methods | Study design: RCT conducted over 6 months. | |
| Participants | Healthy pregnant women at antenatal clinic and postpartum ward in Bangkok, Thailand; mean age 27.3 years. Education: none/primary school 21.3%, secondary school 57.4%, bachelors degree 21.3%. Parity: nulliparous 57.4%, multiparous 42.6%. 68 randomised: 34 intervention SMS group, 34 control group. |
|
| Interventions | SMS group: Participants received two SMS messages, via mobile phone, per week from the 28 weeks of gestation until delivery. The SMS messages were appropriate to the women’s gestational age and contained information and warnings relating to abnormal symptoms that, if the pregnant woman had, would require that they consult the doctor. Control group: routine antenatal and perinatal care. |
|
| Outcomes | Satisfaction level of women of antenatal and perinatal periods. Confidence scores from the antenatal and perinatal periods. Anxiety scores from the antenatal and perinatal periods. Pregnancy outcomes (i.e. gestational age at birth, fetal birth weight, route of delivery). |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Table of random numbers |
| Allocation concealment (selection bias) | Unclear risk | N/A |
| Blinding (performance bias and detection bias) Patient‐reported outcomes | Unclear risk | No information on blinding of researchers or providers provided, likely not done. Blinding of participants not possible due to nature of intervention |
| Incomplete outcome data (attrition bias) Short‐term outcomes | Unclear risk | N/A |
| Incomplete outcome data (attrition bias) Longer‐term outcomes | Low risk | 2/34 missing in the intervention group (2 women changed to deliver at another hospital); 5/34 missing in the control group 2 women changed to deliver at another hospital, 2 women were lost during the follow up and 1 woman had her pregnancy aborted before 28 weeks of gestation. Number of study participants lost to follow‐up is relatively small compared to sample size. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol was available but data presented match the outcome measures described in the section on methods so presumably free of selective reporting |
| Other bias | Unclear risk | There was no statistical difference between the groups at baseline, but the education level in study group was higher then in control group (P = 0.061). |
Rodgers 2005.
| Methods | Study design: RCT conducted over 26 weeks. | |
| Participants | Current daily smokers from community in New Zealand, interested in quitting within next month, with no restriction on the use of other smoking cessation strategies, current owners of mobile phone. Mean age 25 years, 58% female, from all income levels; English speaking. Ethnicity: Maori (21%) and non Maori. 1705 randomised: 852 intervention group, 853 control group; |
|
| Interventions | SMS group: A quit day was negotiated with each participant (within 30 days of randomisation) and five messages were sent per day for the week leading up to the quit day and the following four weeks. Six weeks after randomisation (end of the free text messaging month), the intervention became much less intensive (text messages reducing from five a day to three per week) until the end of the 26‐week follow up. Participants were sent regular, personalised text messages providing smoking cessation advice, support, and distraction. Also, several other text‐message based services were provided: participants could get in touch with each other; they could ‘pull’ text messages on demand; sent messages to all participants on current topics; and sent out questions, followed by answers the next day. Control group: Participants only received one text message every two weeks, thanking them for being in the study, providing study centre contact details, informing them that those who completed follow up would be rewarded with a free month of text messaging (whether they quit or not), and reminding them of the time until their free month at the end of follow up. |
|
| Outcomes | Primary outcome: Prevalence of current non‐smoking (that is, not smoking in the past week) 6 weeks after randomisation. Secondary outcomes: Biochemically‐verified abstinence rate at six weeks; Self‐reported current non‐smoking rate at 12 and 26 weeks; Continuous abstinence rate at 26 weeks. Adverse events: rates of car crash, rate of “text thumb” (ever having pain in the thumb or finger joints when texting during the six months). |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Central telephone randomisation. |
| Allocation concealment (selection bias) | Low risk | Sequence concealed until interventions were assigned. |
| Blinding (performance bias and detection bias) Patient‐reported outcomes | Low risk | Personal collecting and analysing the samples were unaware of treatment allocation. Participants were aware of which group they were allocated to (i.e. single blind). |
| Incomplete outcome data (attrition bias) Short‐term outcomes | Low risk | 6 weeks: 46/852 missing from intervention group; 35/853 missing from control group. A number of sensitivity analyses were performed to assess the potential impact of missing follow up data, mis‐classified quit status, and adjustment for baseline prognostic variables. |
| Incomplete outcome data (attrition bias) Longer‐term outcomes | Low risk | 12 weeks: 106/852 missing from intervention group; 65/853 missing from control group. 26 weeks: 261/852 missing from intervention group; 179/853 missing from control group. Researchers discussed the different scenarios modelled for treatment of missing data. |
| Selective reporting (reporting bias) | Unclear risk | The study protocol is not available. |
| Other bias | High risk | Study groups were comparable at baseline. Although differential use of incentives (control group received their month of free text messaging after the 26‐week follow‐up, the intervention group were not offered this incentive) could have led to introduction of bias, this is expected to have lead to an underestimation of effect rather than an overestimation. |
Shapiro 2008.
| Methods | Study design: RCT with 3 arms conducted over 8 weeks. | |
| Participants | Children (of any weight; no major metabolic problems associated with obesity) in the community with anticipated parent participation aged 5 to 13 in North Carolina, USA, English speaking. 58 children (families) randomised: 18 intervention SMS group, 18 intervention paper diaries (PD) group, 22 control group |
|
| Interventions | SMS group: Families began monitoring on day 1 of the program and provide information on the 3 targeted behaviours: pedometer usage, estimating beverage serving sizes, and estimating screen time (TV, video game, computers) They sent 2 SMS per day (one for parent and one for child) for the full 8 weeks of the study; for each SMS sent, they would each receive an immediate, automated SMS feedback message. Paper Diary (PD) group: Participants used self‐monitoring forms to record the 3 behaviours daily for both parent and child, turned in their forms at each of 3 weekly sessions, and received weekly verbal feedback. Families were instructed to complete the forms at the end of each day and not to back‐fill the forms. Control group: They participated in the 3 intervention sessions but were not expected to self‐monitor. All parents and children received a pedometer (AE 120 YAMAX digi‐walker for adults and Sportline 340 for children). Details of co‐interventions in all groups: All families participated in a total of 3 educational group sessions (90 minutes each) weekly, for 3 weeks. All groups were facilitated by the same psychologist.The only material that differed across groups was that presented in Session 1, which included training in either SMS or PD, or extended overview of the program for the control group. Session 1 provided instruction on the 3 targeted behaviours: pedometer usage, estimating beverage serving sizes, and estimating screen time (TV, video game, computers). Although no behavioral goals were discussed, those in the 2 monitoring conditions were instructed to monitor these 3 target behaviours before going to bed. Session 2 focused on increasing physical activity and decreasing screen time (behavioral goals for session 2 (for both the child and parent) were 5000 steps and under 60 minutes total screen time unrelated to school/work per day. Session 3 focused on the amount of sugar in sugar‐sweetened beverages (SSB). The session included demonstrations of the actual amount of sugar in various SSB and the health consequences of SSB. The goal for session 3 was zero SSB per day for both child and parent. |
|
| Outcomes | Treatment acceptability, attrition, adherence to self‐monitoring, preliminary efficacy (physical activity, screen time, sugar‐sweetened beverage consumption) (self‐monitoring data in SMS and PD groups and recall of targeted behaviours for all groups). | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer random number generator. |
| Allocation concealment (selection bias) | Unclear risk | The method of concealment is not described in sufficient detail to allow definitive judgment. |
| Blinding (performance bias and detection bias) Patient‐reported outcomes | Low risk | No blinding, but the outcome and the outcome measurement are not likely to be influenced by lack of blinding. |
| Incomplete outcome data (attrition bias) Short‐term outcomes | Unclear risk | N/A |
| Incomplete outcome data (attrition bias) Longer‐term outcomes | High risk | 8 weeks: Completers were defined as participants who completed the 8‐week post assessment and who attended at least 2 of the 3 educational sessions. The numbers of families who attended the weekly sessions were 39, 30, and 24 for the first, second, and third weeks, respectively. A total of 31 completed the study (SMS: 13/18, PD: 7/18, C: 11/22) and final analysis was performed on only those. Reasons for attrition differed across groups. |
| Selective reporting (reporting bias) | Unclear risk | The study protocol was not available but it is likely that the published reports include all expected outcomes. |
| Other bias | High risk | In addition to the small sample, the study has several limitations, including only English‐speaking families and intermittent difficulties with using SMS (e.g., phone companies merged, plans discontinued, coverage areas), which could influence generalizability.The questionnaire used to explore the preliminary efficacy of SMS was not validated. There was no validation of accurate reporting. |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Benhamou 2007 | RCT with multifaceted intervention, not possible to separate effects of SMS messaging alone. |
| Bramley 2005 | Uses same data set as Rodgers 2005, which is included. |
| Brendryen 2008 | RCT with multifaceted intervention, not possible to separate effects of SMS messaging alone. |
| Carrasco 2008 | RCT with multifaceted intervention, not possible to separate effects of SMS messaging alone. |
| Chen 2008 | RCT included in separate review on reminders (Car 2012). |
| Faridi 2008 | RCT with multifaceted intervention, not possible to separate effects of SMS messaging alone. |
| Ferrer‐Roca 2004 | Not an RCT, no control group. |
| Franklin 2006 | RCT included in separate review on self‐management (de Jongh 2012). |
| Hanauer 2009 | RCT included in separate review on self‐management (de Jongh 2012). |
| Hurling 2007 | RCT with multifaceted intervention, not possible to separate effects of SMS messaging alone. |
| Joo 2007 | Not an RCT, study with multifaceted intervention, not possible to separate effects of SMS messaging alone. |
| Kim 2007 | RCT with multifaceted intervention, not possible to separate effects of SMS messaging alone. |
| Kim 2008 | RCT with multifaceted intervention, not possible to separate effects of SMS messaging alone. |
| Marquez Contreras 2004 | Cluster RCT included in separate review on self‐management (de Jongh 2012). |
| Menon‐Johansson 2006 | Not an RCT, observational study (no control group). |
| Newton 2009 | RCT study with multifaceted intervention, not possible to separate effects of SMS messaging alone. |
| Obermayer 2004 | Not an RCT, no control group. |
| Ostojic 2005 | RCT included in separate review on self‐management (de Jongh 2012). |
| Patrick 2009 | RCT with multifaceted intervention, not possible to separate effects of SMS messaging alone. |
| Rami 2006 | RCT with multifaceted intervention, not possible to separate effects of SMS messaging alone. |
| Vilella 2004 | Cluster RCT on reminders for facilitating the uptake of preventive activities. Also not included in separate review on reminders (Car 2012) as the SMS reminder was used so that the patient would make an appointment, rather than attend a scheduled appointment. |
Characteristics of ongoing studies [ordered by study ID]
Balmford 2008.
| Trial name or title | Equit: A study of how smokers use electronic communication tools to help them quit smoking |
| Methods | RCT ‐ study duration 7 months |
| Participants | Current smoker, or quit within the last week older than 18 yrs. Not using any extensive interactive computer‐delivered or person‐delivered cessation program, no reported condition requiring referral to an in‐person service. Target sample size: 3600 |
| Interventions | QuitCoach Internet‐based interactive tailored advice designed to be used on multiple occasions; Quit onQ text messaging which sends a tailored program of 1‐8 messages daily for approximately 1 month; QuitCoach onQ integrated program consisting of daily messages plus use of the QuitCoach if more comprehensive assistance is desired |
| Outcomes | Primary outcome: 6‐month sustained abstinence from smoking, assessed by telephone interview. Secondary outcome: Point prevalence abstinence from smoking, assessed by telephone interview |
| Starting date | September 2008 |
| Contact information | Dr James Balmford, The Cancer Council Victoria, 1 Rathdowne St Carlton VIC 3053, Australia. James.Balmford@cancervic.org.au |
| Notes | Not yet recruiting |
Bull 2008.
| Trial name or title | Text Messaging for Abstinence and HIV Risk Prevention: The 411 on Safe Text |
| Methods | RCT (study duration 6 months) |
| Participants | 108 black urban males (aged 16 ‐20 yrs) in Philadelphia, Pennsylvania |
| Interventions | Experimental arm: Behavioral: HIV‐related text messaging Participants will receive up to 90 text messages related to abstinence, monogamy, and condom use over 3 months. Active Comparator: Behavioral: Nutrition‐related text messaging: Participants will receive up to 30 text messages about nutrition and healthy eating over 3 months |
| Outcomes | Primary Outcomes: Condom use (at baseline and Months 3 and 6), Abstinence (at baseline and Months 3 and 6), Monogamy(at baseline and Months 3 and 6); Secondary Outcomes: Attitudes, norms, self‐efficacy, and intentions to remain abstinent, remain monogamous, or use condoms (at baseline and Months 3 and 6) |
| Starting date | October 2008 |
| Contact information | University of Colorado at Denver and Health Sciences Center (Sheana Bull, PhD, MPH, Associate Professor) |
| Notes | Not yet recruiting |
Free 2007.
| Trial name or title | Stop smoking with mobile phones |
| Methods | RCT (study duration 6 months) |
| Participants | Individuals aged 16 yrs and over, currently smoking cigarettes daily and interested in quitting, owner of a mobile phone and familiar with text messaging capabilities, able to provide informed consent to participate in the study Target sample size: 5800 |
| Interventions | The intervention group will be encouraged to set a quit date within 14 days of randomisation. Five messages per day will be sent in the first five weeks after randomisation |
| Outcomes | Primary outcome (at 6 months): self reported abstinence verified by salivary cotinine testing using a cut‐off of 7 ng/ml of cotinine. Secondary outcomes: at 4 weeks: point prevalence of smoking; at 6 months: 28‐day continuous abstinence; involvement in any vehicle crashes |
| Starting date | March 2007 |
| Contact information | Dr Caroline Free Nutrition and Public Health Research Interventions Unit London School of Hygiene and Tropical Medicine Keppel Street London UK Caroline.Free@lshtm.ac.uk |
| Notes |
Kimball 2007.
| Trial name or title | Evaluation of Adherence to Topical Agents: Applying Communication Technology to Improve Sunscreen Use |
| Methods | RCT (study duration 6 weeks) |
| Participants | Individuals aged 18 yrs or older. Target sample size: 60 |
| Interventions | Use of text‐messages through cellular phones as reminders for subjects to use their sunscreen. Intervention group will receive the study sunscreen with the attached electronic monitor. In addition, they will receive daily text messages on their cellular phone to remind them to apply the sunscreen. The text message will also contain the daily weather information. This group will also be instructed to apply sunscreen once a day in the morning to the sun‐exposed areas of the body. If subjects are to have continuous sun exposure (for example, at a beach), they are to re‐apply the sunscreen every 3 hours. |
| Outcomes | Primary outcomes (at 6 weeks): number of days the subjects are adherent to using sunscreen, patient satisfaction with intervention. Secondary outcome (at 6 weeks): reasons for poor adherence. |
| Starting date | September 2007 |
| Contact information | Massachusetts General Hospital, Boston, MA 02114 ( Alexandra B. Kimball) |
| Notes | Not yet recruiting |
Lim 2005.
| Trial name or title | The impact of text and email messaging on the sexual risk behaviour of young men and women: a randomised controlled trial |
| Methods | RCT (study duration 12 months) |
| Participants | Victorian resident aged 16‐29 yrs. Target sample size: 340 |
| Interventions | Assigned to receive both SMS and email messages. SMS ‐ The intervention group will receive messages on their mobile phones at different times and on different days of the week. Message content and style will match the technology and age group. Email ‐ The intervention group will receive email messages such as: "If you have recently had unprotected sex with a new partner, you may be at risk of chlamydia infection and should consider being tested." SMS and email messages will also include contraception information, relevant web pages, and phone numbers for sexual health services |
| Outcomes | Primary outcome: Significantly increased self reported (and validated by contacting doctor) chlamydia testing during the intervention period in participants receiving the intervention. Secondary outcomes: significantly increased self reported condom use with casual or new partners during the intervention period in participants receiving the intervention, significantly increased rate of primary health care attendance for contraception advice on the part of female participants receiving the intervention |
| Starting date | January 2006 |
| Contact information | Megan Lim, Macfarlane Burnet Institute for Medical Research and Public Health Centre for Epidemiology and Population Health GPO Box 2284 Melbourne VIC 3001, Australia, lim@burnet.edu.au |
| Notes | Not yet recruiting |
Sutton 2008.
| Trial name or title | The MiQuit study: feasibility trial of a computer‐tailored smoking cessation intervention providing individualised written and mobile phone text message support to pregnant smokers |
| Methods | RCT (study duration 12 weeks) |
| Participants | Pregnant smokers aged at least 16 yrs, smoking at the time of booking for maternity care, owns or has the use of a mobile phone. Target sample size: 200 |
| Interventions | 2 arms: 1 arm ‐ Standard care and a generic smoking cessation self‐help leaflet. 2. Arm ‐ Standard care and an individually tailored smoking cessation self‐help leaflet plus 12 weeks of individualised mobile phone text message smoking cessation support |
| Outcomes | Primary outcomes (at 12 weeks): Self‐reported ratings of acceptability, usefulness and disengagement from the intervention.Secondary outcomes: Self‐reported and biochemically validated 7‐day point prevalence smoking rates, requested by text message at 4, 7 and 12 weeks; Self‐reported repeated 7‐day point prevalence rates across three time points, requested by text message at 4, 7 and 12 weeks; Infant birth weight, ascertained approximately 30 weeks after enrolment (depending upon number of weeks gestation at recruitment); Smoking status at delivery; Gestation at delivery |
| Starting date | November 2008 |
| Contact information | Prof Stephen Sutton, General Practice & Primary Care Research Unit Institute of Public Health University of Cambridge Forvie Site, Robinson Way, Cambridge, UK, srs34@medschl.cam.ac.uk |
| Notes | Completed but results not published yet |
Sutton 2009.
| Trial name or title | A randomised controlled trial to assess the feasibility, acceptability and effectiveness of tailored web‐ and text‐based facilitation of smoking cessation in primary care |
| Methods | RCT (study duration 6 months) |
| Participants |
Target sample size: 600. |
| Interventions | Participants will receive 'usual care' for smoking cessation, plus a printed patient‐tailored advice report generated by web‐based software, followed by a 90‐day program of patient‐tailored interactive SMS text messages |
| Outcomes | Primary outcomes: Self‐reported effectiveness, using a self report of being abstinent from smoking for at least 2 wks, at 8‐wk follow‐up from randomisation date, as assessed by postal questionnaire or telephone interview. Secondary outcomes: 1. Carbon monoxide (CO)‐verified self‐report of being abstinent from smoking for at least 2 wks, at 4‐wk follow‐up from quit date. 2. Self‐reported prolonged abstinence (at least 3 months) at 6‐month follow‐up from randomisation date. |
| Starting date | April 2009 |
| Contact information | Prof Stephen Sutton General Practice & Primary Care Research Unit Department of Public Health & Primary Care University of Cambridge, Institute of Public Health Forvie Site, Robinson Way, Cambridge, UK |
| Notes |
Whittaker 2006.
| Trial name or title | A RCT to determine if a multimedia mobile phone programme can help young people to stop smoking |
| Methods | RCT (study duration 6 months) |
| Participants | Resident in Auckland New Zealand, current smokers wanting to quit older than 16 yrs. Target sample size 1300 |
| Interventions | Intervention group: intensive multimedia smoking cessation programme delivered via mobile phone (such as daily video clips, SMS of quitting tips). Control group: less intensive (e.g. weekly) study‐related multimedia programme delivered via mobile phone |
| Outcomes | Primary outcome: Continuous abstinence at 6 months: Secondary outcomes: Point prevalence abstinence at 4 wks, 12 wks and 6 mths; Cost per quitter and satisfaction with programme at 6 mths |
| Starting date | November 2006 |
| Contact information | Robyn Whittaker, Clinical Trials Research Unit, University of Auckland Private Bag 92019 Auckland, New Zealand, r.whittaker@ctru.auckland.ac.nz |
| Notes |
RCT: Randomised Controlled Trial
mths: months
wks: weeks
wk: week
Differences between protocol and review
The protocol for this review was published in 2008 (Vodopivek‐Jamsek 2008).
Search strategy
We were not able to search the following databases we listed in the protocol:
Proceedings from the MEDNET Congresses: We could not access the proceedings.
TrialsCentralTM (www.trialscentral.org): The website for the data base was not functional at the time of review and did not allow for the search of clinical trials.
African Trials Register: The trials in the African Trials Register are collected with a search strategy using the Cochrane Controlled Trials Register and the African Health Anthology (AHA). As we searched both original sources, it was not necessary to access the African Trials Register separately.
Health Star: The database ceased to exist as of December 2000, with all peer‐reviewed journal articles transferred to PubMed.
Contributions of authors
Josip Car conceived the review together with Rifat Atun. He is the contact author for the reviews and coordinated all stages of the study, including the protocol stage. He advised on designing the search strategy, screening search results against inclusion criteria, and appraising quality of the papers. He assisted in interpreting the data and contributed to writing the review, providing clinical and consumer perspectives. He will also be responsible for future updates of this review.
Ipek Gurol‐Urganci developed the protocols. She has led the search process and assisted in screening the papers. She collected, analysed, interpreted the data and contributed to writing the review, providing methodological and policy perspectives.
Vlasta Vodopivec Jamek developed the protocols. She has been involved in data extraction and management. She led the screening and quality appraisal process and assisted in undertaking searches. She has collected, analysed and interpreted the data and contributed to writing the review, providing clinical and consumer perspectives.
Thyra de Jongh coordinated data extraction and management and was involved in the screening and quality appraisal process. She has collected, analysed and interpreted the data and contributed to writing the review, providing a methodological perspective.
Rifat Atun provided general direction for the studies and contributed to writing the review, and provided a policy perspective to the review findings.
Sources of support
Internal sources
-
eHealth Unit, Department of Primary Care and Social Medicine, Imperial College, UK.
salaries, office space
-
Centre for Health Management, Tanaka Business School, Imperial College, UK.
salaries, office space
-
Department of Family Medicine, Faculty of Medicine, University of Ljubljana, Slovenia.
salaries, office space
-
Imperial College London, UK.
salaries, office space
External sources
-
Ministry of Higher Education, Science and Technology, Slovenia.
grant funding
New
References
References to studies included in this review
Cocosila 2009 {published data only}
- Cocosila M, Archer N, Haynes RB, Yuan Y. Can wireless text messaging improve adherence to preventive activities? Results of a randomised controlled trial. International Journal of Medical Informatics 2009;78(4):230‐8. [DOI: 10.1016/j.ijmedinf.2008.07.011] [DOI] [PubMed] [Google Scholar]
Jareethum 2008 {published data only}
- Jareethum R, Titapant V, Tienthai C, Viboonchart S, Chuenwattana P, Chatchainoppakhun J. Satisfaction of healthy pregnant women receiving short message service via mobile phone for prenatal support: A randomized controlled trial. Journal of the Medical Association of Thailand 2008;91(4):458‐63. [PubMed] [Google Scholar]
Rodgers 2005 {published data only}
- Rodgers A, Corbett T, Bramley D, Riddell T, Wills M, Lin RB, et al. Do u smoke after txt? Results of a randomised trial of smoking cessation using mobile phone text messaging. Tobacco Control 2005;14(4):255‐61. [DOI: 10.1136/tc.2005.011577] [DOI] [PMC free article] [PubMed] [Google Scholar]
Shapiro 2008 {published data only}
- Shapiro JR, Bauer S, Hamer RM, Kordy H, Ward D, Bulik CM. Use of text messaging for monitoring sugar‐sweetened beverages, physical activity, and screen time in children: a pilot study. Journal of Nutrition Education and Behaviour 2008;40(6):385‐91. [DOI: 10.1016/j.jneb.2007.09.014] [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies excluded from this review
Benhamou 2007 {published data only}
- Benhamou PY, Melki V, Boizel R, Perreal F, Quesada JL, Bessieres‐Lacombe S, et al. One‐year efficacy and safety of Web‐based follow‐up using cellular phone in type 1 diabetic patients under insulin pump therapy: the PumpNet study. Diabetes/Metabolism Reviews 2007;33(3):220‐6. [DOI] [PubMed] [Google Scholar]
Bramley 2005 {published data only}
- Bramley D, Riddell T, Whittaker R, Corbett T, Lin R, Wills M, et al. Smoking cessation using mobile phone text messaging is as effective in Maori as non‐Maori. New Zealand Medical Journal 2005;118:1‐10. [PubMed] [Google Scholar]
Brendryen 2008 {published data only}
- Brendryen H, Drozd F, Kraft P. A digital smoking cessation program delivered through internet and cell phone without nicotine replacement (happy ending): randomized controlled trial. Journal of Medical Internet Research 2008;10(5):e51. [DOI] [PMC free article] [PubMed] [Google Scholar]
Carrasco 2008 {published data only}
- Carrasco MP, Salvador CH, Sagredo PG, Márquez‐Montes J, González de Mingo MA, Fragua JA, et al. Impact of patient‐general practitioner short‐messages‐based interaction on the control of hypertension in a follow‐up service for low‐to‐medium risk hypertensive patients: a randomized controlled trial. IEEE Transactions on Information Technology in Biomedicine 2008;12(6):780‐91. [DOI: 10.1109/TITB.2008.926429] [DOI] [PubMed] [Google Scholar]
Chen 2008 {published data only}
- Chen ZW, Fang LZ, Chen LY, Dai HL. Comparison of an SMS text messaging and phone reminder to improve attendance at a health promotion centre: a randomized controlled trial. Journal of Zhejiang University Science B 2008;9(1):34‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Faridi 2008 {published data only}
- Faridi Z, Liberti L, Shuval K, Northrup V, Ali A, Katz DL. Evaluating the impact of mobile telephone technology on type 2 diabetic patients' self‐management: the NICHE pilot study. Journal of Evaluation in Clinical Practice 2008;14(3):465‐9. [DOI] [PubMed] [Google Scholar]
Ferrer‐Roca 2004 {published data only}
- Ferrer‐Roca O, Cardenas A, Diaz‐Cardama A, Pulido P. Mobile phone text messaging in the management of diabetes. Journal of Telemedicine and Telecare 2004;10(5):282‐5. [DOI] [PubMed] [Google Scholar]
Franklin 2006 {published data only}
- Franklin V, Waller A, Pagliari C, Greene S. "Sweet Talk": text messaging support for intensive insulin therapy for young people with diabetes. Diabetes Technology & Therapeutics 2003;5(6):991‐6. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Franklin VL, Greene A, Waller A, Greene SA, Pagliari C. Patients' engagement with "Sweet Talk" ‐ a text messaging support system for young people with diabetes. Journal of Medical Internet Research 2008;10(2):e20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franklin VL, Waller A, Pagliari C, Greene SA. A randomized controlled trial of Sweet Talk, a text‐messaging system to support young people with diabetes. Diabetic Medicine 2006;23(12):1332‐8. [DOI] [PubMed] [Google Scholar]
- Waller A, Franklin V, Pagliari C, Greene S. Participatory design of a text message scheduling system to support young people with diabetes. Health Informatics Journal 2006 Dec;12(4):304‐18. [DOI] [PubMed] [Google Scholar]
Hanauer 2009 {published data only}
- Hanauer DA, Wentzell K, Laffel N, Laffel LM. Automated reminder diabetes system (CARDS): E‐mail and SMS cell phone text messaging reminders to support diabetes management. Diabetes Technology & Therapeutics 2009;11(2):99‐106. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hurling 2007 {published data only}
- Hurling R, Catt M, Boni MD, Fairley BW, Hurst T, Murray P, et al. Using internet and mobile phone technology to deliver an automated physical activity program: randomized controlled trial. Journal of Medical Internet Research 2007;9(2):e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Joo 2007 {published data only}
- Joo NS, Kim BT. Mobile phone short message service messaging for behaviour modification in a community‐based weight control programme in Korea. Journal of Telemedicine and Telecare 2007;13(8):416‐20. [PUBMED: 18078554] [DOI] [PubMed] [Google Scholar]
Kim 2007 {published data only}
- Kim H. A randomized controlled trial of a nurse short‐message service by cellular phone for people with diabetes. International Journal of Nursing Studies 2007;44(5):687‐92. [DOI] [PubMed] [Google Scholar]
- Kim HS, Jeong HS. A nurse short message service by cellular phone in type‐2 diabetic patients for six months. Journal of Clinical Nursing 2007;16(6):1082‐7. [DOI] [PubMed] [Google Scholar]
- Yoon KH, Kim HS. A short message service by cellular phone in type 2 diabetic patients for 12 months. Diabetes Research and Clinical Practice 2008;79(2):256‐61. [DOI] [PubMed] [Google Scholar]
Kim 2008 {published data only}
- Kim HS, Song MS. Technological intervention for obese patients with type 2 diabetes. Applied Nursing Research 2008;21(2):84‐9. [DOI] [PubMed] [Google Scholar]
- Kim SI, Kim HS. Effectiveness of mobile and internet intervention in patients with obese type 2 diabetes. International Journal of Medical Informatics 2008;77(6):399‐404. [PUBMED: 17881285 ] [DOI] [PubMed] [Google Scholar]
Marquez Contreras 2004 {published data only}
- Marquez Contreras E, Figuera von Wichmann M, Gil‐Guillen V, Ylla‐Catala A, Figueras M, Balana M, et al. Effectiveness of an intervention to provide information to patients with hypertension as short text messages and reminders sent to their mobile phone (HTA‐Alert). Atencion Primaria 2004;34(8):399‐405. [DOI] [PMC free article] [PubMed] [Google Scholar]
Menon‐Johansson 2006 {published data only}
- Menon‐Johansson AS, McNaught F, Mandalia S, Sullivan AK. Texting decreases the time to treatment for genital Chlamydia trachomatis infection. Sexually Transmitted Infections 2006;82(1):49‐51. [DOI] [PMC free article] [PubMed] [Google Scholar]
Newton 2009 {published data only}
- Newton KH, Wiltshire EJ, Elley CR. Pedometers and text messaging to increase physical activity: randomized controlled trial of adolescents with type 1 diabetes. Diabetes Care. 2009 May;32(5):813‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Obermayer 2004 {published data only}
- Obermayer JL, Riley WT, Jean‐Mary J. College smoking‐cessation using cell phone text messaging. Journal of American College Health 2004;53(2):71‐8. [DOI] [PubMed] [Google Scholar]
Ostojic 2005 {published data only}
- Ostojic V, Cvoriscec B, Ostojic SB, Reznikoff D, Stipic‐Markovic A, Tudjman Z. Improving asthma control through telemedicine: a study of short‐message service. Telemedicine Journal and e‐Health 2005;11(1):28‐35. [DOI] [PubMed] [Google Scholar]
Patrick 2009 {published data only}
- Patrick K, Raab F, Adams MA, Dillon L, Zabinski M, Rock CL, et al. A text message‐based intervention for weight loss: randomized controlled trial. Journal of Medical Internet Research 2009;11(1):e1. [PUBMED: 19141433] [DOI] [PMC free article] [PubMed] [Google Scholar]
Rami 2006 {published data only}
- Rami B, Popow C, Horn W, Waldhoer T, Schober E. Telemedical support to improve glycemic control in adolescents with type 1 diabetes mellitus. European Journal of Pediatrics 2006;165(10):701‐5. [DOI] [PubMed] [Google Scholar]
Vilella 2004 {published data only}
- Vilella A, Bayas JM, Diaz MT, Guinovart C, Diez C, Simo D, et al. The role of mobile phones in improving vaccination rates in travelers. Preventive Medicine 2004;38(4):503‐9. [DOI: 10.1016/j.ypmed.2003.12.005] [DOI] [PubMed] [Google Scholar]
References to ongoing studies
Balmford 2008 {unpublished data only}
- Equit: A study of how smokers use electronic communication tools to help them quit smoking. Ongoing study September 2008.
Bull 2008 {unpublished data only}
- Text Messaging for Abstinence and HIV Risk Prevention: The 411 on Safe Text. Ongoing study October 2008.
Free 2007 {unpublished data only}
- Stop smoking with mobile phones. Ongoing study March 2007.
Kimball 2007 {unpublished data only}
- Evaluation of Adherence to Topical Agents: Applying Communication Technology to Improve Sunscreen Use. Ongoing study September 2007.
Lim 2005 {unpublished data only}
- The impact of text and email messaging on the sexual risk behaviour of young men and women: a randomised controlled trial. Ongoing study January 2006.
Sutton 2008 {unpublished data only}
- The MiQuit study: feasibility trial of a computer‐tailored smoking cessation intervention providing individualised written and mobile phone text message support to pregnant smokers. Ongoing study November 2008.
Sutton 2009 {unpublished data only}
- A randomised controlled trial to assess the feasibility, acceptability and effectiveness of tailored web‐ and text‐based facilitation of smoking cessation in primary care. Ongoing study April 2009. [DOI] [PMC free article] [PubMed]
Whittaker 2006 {unpublished data only}
- A RCT to determine if a multimedia mobile phone programme can help young people to stop smoking. Ongoing study November 2006.
Additional references
Adler 2007
- Adler R. Health care unplugged: the evolving role of wireless technology. Chronic Health Care Foundation, 2007. [Google Scholar]
Atherton 2010
- Atherton H, Huckvale C, Car J. Communicating health promotion and disease prevention information to patients via email: a review. Journal of Telemedicine and Telecare 2010;16(4):172‐5. [PUBMED: 20511566] [DOI] [PubMed] [Google Scholar]
Atun 2006
- Atun RA, Sittampalam S. A review of the characteristics and benefits of SMS in delivering healthcare. The Role of Mobile Phones in Increasing Accessibility and Efficiency in Healthcare. Vodafone Group Plc, 2006:18‐28. [Google Scholar]
Atun 2006b
- Atun RA, Gurol‐Urganci I. Analysis of calls to NHS Direct. The Role of Mobile Phones in Increasing Accessibility and Efficiency in Healthcare. Vodafone Group Plc, 2006:12‐17. [Google Scholar]
Balas 1997
- Balas EA, Jaffrey F, Kuperman GJ, Boren SA, Brown GD, Pinciroli F, et al. Electronic communication with patients: evaluation of distance medicine technology. JAMA 1997;278(2):152‐9. [PubMed] [Google Scholar]
Bandura 1977
- Bandura A. Self‐efficacy: Toward a unifying theory of behaviour change. Psychological Review 1977;84:191‐215. [DOI] [PubMed] [Google Scholar]
Bandura 1982
- Bandura A. Self‐efficacy mechanism in human agency. American Psychologist 1982;37:122‐47. [Google Scholar]
Bauer 2003
- Bauer S, Percevic R, Okon E, Meermann R, Kordy H. Use of text messaging in the aftercare of patients with bulimia nervosa. European Eating Disorders Review 2003;11(3):279‐90. [Google Scholar]
Baumgart 2005
- Baumgart DC. Personal digital assistants in health care: experienced clinicians in the palm of your hand?. Lancet 2005;366(9492):1210‐22. [DOI] [PubMed] [Google Scholar]
Bodenheimer 2006
- Bodenheimer T. Primary care: will it survive?. New England Journal of Medicine 2006;355(9):861‐4. [DOI] [PubMed] [Google Scholar]
Bos 2005
- Bos A, Hoogstraten J, Prahl‐Andersen B. Failed appointments in an orthodontic clinic. American Journal of Orthodontics and Dentofacial Orthopedics 2005;127(3):355‐7. [DOI] [PubMed] [Google Scholar]
Canadian 1994
- Canadian Task Force on the Periodic Health Examination. The Canadian Guide to Clinical Preventive Health Care. Ottawa: Canadian Government Publishing, 1994. [Google Scholar]
Car 2003
- Car J, Sheikh A. Telephone consultations. BMJ 2003;326(7396):966‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Car 2004a
- Car J, Sheikh A. Email consultations in health care: 1‐scope and effectiveness. BMJ 2004;329(7463):435‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Car 2004b
- Car J, Sheikh A. Email consultations in health care: 2‐acceptability and safe application. BMJ 2004;329(7463):439‐42. [DOI] [PMC free article] [PubMed] [Google Scholar]
Car 2008b
- Car J, Ng C, Atun R, Card A. SMS text message healthcare appointment reminders in England. The Journal of Ambulatory Care Management 2008;31(3):216‐9. [DOI] [PubMed] [Google Scholar]
Car 2012
- Car J, Gurol‐Urganci I, Jongh T, Vodopivec‐Jamsek V, Atun R. Mobile phone messaging reminders for attendance at healthcare appointments. Cochrane Database of Systematic Reviews 2012, Issue 7. [DOI: 10.1002/14651858.CD007458.pub2] [DOI] [PubMed] [Google Scholar]
Christakis 2004
- Christakis NA. Social networks and collateral health effects. BMJ 2004;329:184‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cline 2001
- Cline RJ, Haynes KM. Consumer health information seeking on the Internet: the state of the art. Health Education Research 2001;16(6):671‐92. [DOI] [PubMed] [Google Scholar]
Cobb 2002
- Cobb S. Social support as a moderator of life stress. Psychosomatic Medicine 2002;38:300‐14. [DOI] [PubMed] [Google Scholar]
Davis 1997
- Davis DA, Taylor‐Vaisey A. Translating guidelines into practice: a systematic review of theoretic concepts, practical experience and research evidence in the adoption of clinical practice guidelines. Canadian Medical Association Journal 1997;157(4):408‐16. [MEDLINE: ] [PMC free article] [PubMed] [Google Scholar]
de Jongh 2012
- Jongh T, Gurol‐Urganci I, Vodopivec‐Jamsek V, Car J, Atun R. Mobile phone messaging telemedicine for facilitating self‐management of long‐term illnesses. Cochrane Database of Systematic Reviews 2012, Issue 12. [DOI: 10.1002/14651858.CD007459.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Demiris 2008
- Demiris G, Afrin LB, Speedie S, Courtney KL, Sondhi M, Vimarlund V, et al. Patient‐centered applications: use of information technology to promote disease management and wellness. A white paper by the AMIA knowledge in motion working group. Journal of the American Medical Informatics Association 2008;15(1):8‐13. [PUBMED: 17947617] [DOI] [PMC free article] [PubMed] [Google Scholar]
Eng 1999
- Eng TR, Gustafson DH, Henderson J, Jimison H, Patrick K. Introduction to evaluation of interactive health communication applications. Science Panel on Interactive Communication and Health. The American Journal of Preventive Medicine 1999;16(1):10‐5. [DOI] [PubMed] [Google Scholar]
Fairley 2003
- Fairley CK, Levy R, Rayner CR, Allardice K, Costello K, Thomas C, et al. Randomized trial of an adherence programme for clients with HIV. International Journal of STD & AIDS 2003;14(12):805‐9. [DOI] [PubMed] [Google Scholar]
Fjeldsoe 2009
- Fjeldsoe BS, Marshall AL, Miller YD. Behavior change interventions delivered by mobile telephone short‐message service. American Journal of Preventive Medicine 2009;36(2):165‐73. [PUBMED: 19135907] [DOI] [PubMed] [Google Scholar]
Glanz 1997
- Glanz K, Lewis FM, Rimer BK (eds). Health Behavior and Health Education: Theory, Research and Practice. 2nd Edition. San Francisco CA: Jossey‐Bass, 1997. [Google Scholar]
Goldstein 1997
- Goldstein MG, Niaura R, Willey‐Lessne C, DePue J, Eaton C, Rakowski W, et al. A population‐based survey of patients' perceptions of health care provider‐delivered smoking cessation interventions. Archives of Internal Medicine 1997;157(12):1313‐9. [DOI] [PubMed] [Google Scholar]
Goldstein 2004
- Goldstein M, Whitlock E, DePue J. Multiple behavioural risk factor interventions in primary care: summary of research evidence. American Journal of Preventive Medicine 2004;27(2):61‐79. [DOI] [PubMed] [Google Scholar]
Gurol‐Urganci 2012
- Gurol‐Urganci I, Jongh T, Vodopivec‐Jamsek V, Car J, Atun R. Mobile phone messaging for communicating results of medical investigations. Cochrane Database of Systematic Reviews 2012, Issue 6. [DOI: 10.1002/14651858.CD007456.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Haynes 2008
- Haynes RB, Ackloo E, Sahota N, McDonald HP, Yao X. Interventions for enhancing medication adherence. Cochrane Database of Systematic Reviews 2008, Issue 2. [DOI: 10.1002/14651858.CD000011.pub3] [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1 [updated March 2011]. The Cochrane Collaboration. Available from www.cochrane‐handbook.org, 2011. [Google Scholar]
ITU 2010
- International Telecommunications Union. The World in 2010: ICT Facts and Figures. http://www.itu.int/ITU‐D/ict/material/FactsFigures2010.pdf 2010.
Kaplan 2006
- Kaplan WA. Can the ubiquitous power of mobile phones be used to improve health outcomes in developing countries?. Global Health 2006;2:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kottke 1993
- Kottke TE, Brekke ML, Solberg LI. Making time for preventive services. Mayo Clinic Proceedings 1993;68(8):785‐91. [DOI] [PubMed] [Google Scholar]
Krishna 2009
- Krishna S, Boren SA, Balas EA. Healthcare via cell phones: a systematic review. Telemedicine Journal and e‐health 2009;15(3):231‐40. [DOI] [PubMed] [Google Scholar]
Kwon 2004
- Kwon HS, Cho JH, Kim HS, Lee JH, Song BR, Oh JA, at al. Development of web‐based diabetic patient management system using short message service (SMS). Diabetes Research and Clinical Practice 2004;66 Suppl 1:S133‐7. [DOI] [PubMed] [Google Scholar]
McGlynn 2003
- McGlynn EA, Asch SM, Adams J, Keesey J, Hicks J, DeCristofaro A, Kerr EA. The quality of health care delivered to adults in the United States. NEJM 2003 Jun 26;348(26):2635‐45. [PUBMED: 12826639] [DOI] [PubMed] [Google Scholar]
McWhinney 1997
- McWhinney I. The enhancement of health and the prevention of disease. In: McWhinney I editor(s). A Textbook of Family Medicine. 2nd Edition. New York: Oxford University Press, 1997:179‐227. [MEDLINE: ] [Google Scholar]
Mirand 2002
- Mirand AL, Beehler GP, Kuo CL, Mahoney MC. Explaining the de‐prioritization of primary prevention: physicians' perceptions of their role in the delivery of primary care. BMC Public Health 2003;3:15. [DOI: 10.1186/1471-2458-3-15] [DOI] [PMC free article] [PubMed] [Google Scholar]
MORI 2005
- Technology tracker. Technology Research at MORI. 2005. (http://www.mori.com/technology/techtracker.shtml).
Newell 2001
- Newell A. A mobile phone text message and Trichomonas vaginalis. Sexually Transmitted Infections 2001;77(3):225. [DOI] [PMC free article] [PubMed] [Google Scholar]
Norwell 2003
- Norwell N. Text messaging raises medicolegal issues. BMJ 2003;326(7399):1148. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pollak 2002
- Pollak KI, McBride CM, Scholes D, Grothaus LC, Civic D, Curry SJ. Women's reports of smoking cessation advice during reproductive health visits and subsequent smoking cessation. The American Journal of Managed Care 2002;8(10):837‐44. [PubMed] [Google Scholar]
Pollak 2008
- Pollak KI, Krause KM, Yarnall KS, Gradison M, Michener JL, Østbye T. Estimated time spent on preventive services by primary care physicians. BMC Health Services Research 2008;8:245. [DOI] [PMC free article] [PubMed] [Google Scholar]
Prochaska 1997
- Prochaska JO, Redding CA, Evers KE. The transtheoretical model and stages of change. In: Glanz K, Lewis FM, Rimer BK editor(s). Health Behaviour and Health Education: Theory, Research and Practice. 2nd Edition. San Francisco, CA: Jossey‐Bass, 1997:60‐84. [Google Scholar]
Revere 2001
- Revere D, Dunbar PJ. Review of computer‐generated outpatient health behavior interventions: clinical encounters "in absentia". Journal of the American Medical Informatics Association 2001;8(1):62‐79. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rhodes 1997
- Rhodes F, Fishbein M, Reis J. Using behavioral theory in computer‐based health promotion and appraisal. Health Education and Behavior 1997;24(1):20‐34. [DOI] [PubMed] [Google Scholar]
Robinson 1998
- Robinson TN, Patrick K, Eng TR, Gustafson D. An evidence‐based approach to interactive health communication: a challenge to medicine in the information age. Science Panel on Interactive Communication and Health. JAMA 1998;280(14):1264‐9. [DOI] [PubMed] [Google Scholar]
Stone 2002
- Stone EG, Morton SC, Hulscher ME, Maglione MA, Roth EA, Grimshaw JM, et al. Interventions that increase use of adult immunization and cancer screening services: a meta‐analysis. Annals of Internal Medicine 2002;136(9):641‐51. [DOI] [PubMed] [Google Scholar]
Szilagyi 2005
- Szilagyi PG, Shone LP, Barth R, Kouides RW, Long C, Humiston SG, et al. Physician practices and attitudes regarding adult immunizations. Preventive Medicine 2005;40(2):152‐61. [DOI] [PubMed] [Google Scholar]
Wei 2005
- Wei EK, Ryan CT, Dietrich AJ, Colditz GA. Improving colorectal cancer screening by targeting office systems in primary care practices: disseminating research results into clinical practice. Archives of Internal Medicine 2005;165(6):661‐6. [DOI] [PubMed] [Google Scholar]
Weingarten 1999
- Weingarten S. Using practice guideline compendiums to provide better preventive care. Annals of Internal Medicine 1999;130(5):454‐8. [DOI] [PubMed] [Google Scholar]
Wikipedia 2007
- Wikipedia. Short Message Service. http://en.wikipedia.org/wiki/short_message_service (accessed February 2007).
Yarnall 2003
- Yarnall KS, Pollak KI, Østbye T, Krause KM, Michener JL. Primary care: is there enough time for prevention?. American Journal of Public Health 2003;93(4):635‐41. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to other published versions of this review
Vodopivek‐Jamsek 2008
- Vodopivec‐Jamsek V, Jongh T, Gurol‐Urganci I, Atun R, Car J. Mobile phone messaging for preventive health care. Cochrane Database of Systematic Reviews 2008, Issue 4. [DOI: 10.1002/14651858.CD007457] [DOI] [PMC free article] [PubMed] [Google Scholar]


