Abstract
Background
Surgeons who perform laparotomy have a number of decisions to make regarding abdominal closure. Material and size of potential suture types varies widely. In addition, surgeons can choose to close the incision in anatomic layers or mass ('en masse'), as well as using either a continuous or interrupted suturing technique, of which there are different styles of each. There is ongoing debate as to which suturing techniques and suture materials are best for achieving definitive wound closure while minimising the risk of short‐ and long‐term complications.
Objectives
The objectives of this review were to identify the best available suture techniques and suture materials for closure of the fascia following laparotomy incisions, by assessing the following comparisons: absorbable versus non‐absorbable sutures; mass versus layered closure; continuous versus interrupted closure techniques; monofilament versus multifilament sutures; and slow absorbable versus fast absorbable sutures. Our objective was not to determine the single best combination of suture material and techniques, but to compare the individual components of abdominal closure.
Search methods
On 8 February 2017 we searched CENTRAL, MEDLINE, Embase, two trials registries, and Science Citation Index. There were no limitations based on language or date of publication. We searched the reference lists of all included studies to identify trials that our searches may have missed.
Selection criteria
We included randomised controlled trials (RCTs) that compared suture materials or closure techniques, or both, for fascial closure of laparotomy incisions. We excluded trials that compared only types of skin closures, peritoneal closures or use of retention sutures.
Data collection and analysis
We abstracted data and assessed the risk of bias for each trial. We calculated a summary risk ratio (RR) for the outcomes assessed in the review, all of which were dichotomous. We used random‐effects modelling, based on the heterogeneity seen throughout the studies and analyses. We completed subgroup analysis planned a priori for each outcome, excluding studies where interventions being compared differed by more than one component, making it impossible to determine which variable impacted on the outcome, or the possibility of a synergistic effect. We completed sensitivity analysis, excluding trials with at least one trait with high risk of bias. We assessed the quality of evidence using the GRADEpro guidelines.
Main results
Fifty‐five RCTs with a total of 19,174 participants met the inclusion criteria and were included in the meta‐analysis. Included studies were heterogeneous in the type of sutures used, methods of closure and patient population. Many of the included studies reported multiple comparisons.
For our primary outcome, the proportion of participants who developed incisional hernia at one year or more of follow‐up, we did not find evidence that suture absorption (absorbable versus non‐absorbable sutures, RR 1.07, 95% CI 0.86 to 1.32, moderate‐quality evidence; or slow versus fast absorbable sutures, RR 0.81, 95% CI 0.63 to 1.06, moderate‐quality evidence), closure method (mass versus layered, RR 1.92, 95% CI 0.58 to 6.35, very low‐quality evidence) or closure technique (continuous versus interrupted, RR 1.01, 95% CI 0.76 to 1.35, moderate‐quality evidence) resulted in a difference in the risk of incisional hernia. We did, however, find evidence to suggest that monofilament sutures reduced the risk of incisional hernia when compared with multifilament sutures (RR 0.76, 95% CI 0.59 to 0.98, I2 = 30%, moderate‐quality evidence).
For our secondary outcomes, we found that none of the interventions reduced the risk of wound infection, whether based on suture absorption (absorbable versus non‐absorbable sutures, RR 0.99, 95% CI 0.84 to 1.17, moderate‐quality evidence; or slow versus fast absorbable sutures, RR 1.16, 95% CI 0.85 to 1.57, moderate‐quality evidence), closure method (mass versus layered, RR 0.93, 95% CI 0.67 to 1.30, low‐quality evidence) or closure technique (continuous versus interrupted, RR 1.13, 95% CI 0.96 to 1.34, moderate‐quality evidence).
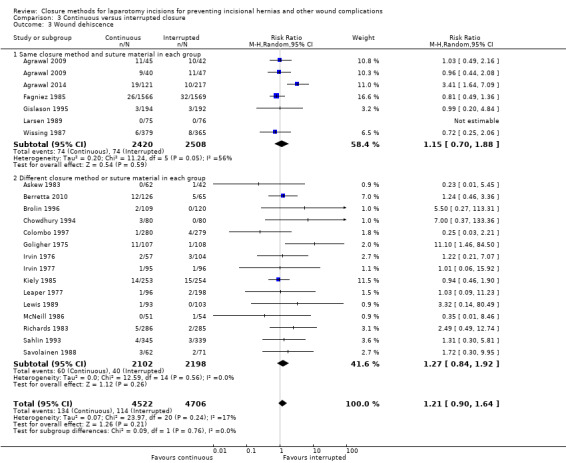
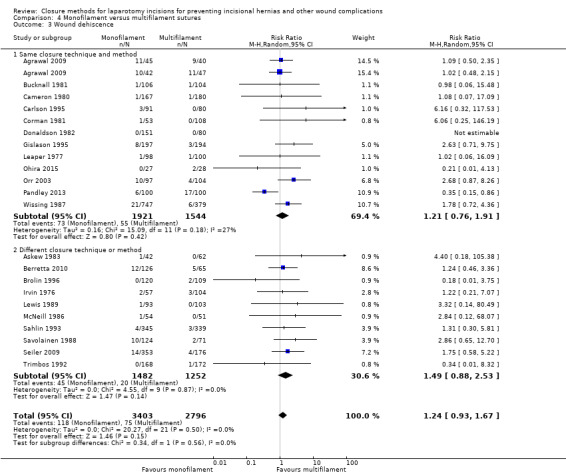
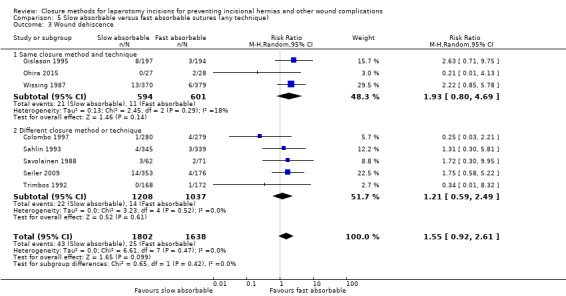
Similarily, none of the interventions reduced the risk of wound dehiscence whether based on suture absorption (absorbable versus non‐absorbable sutures, RR 0.78, 95% CI 0.55 to 1.10, moderate‐quality evidence; or slow versus fast absorbable sutures, RR 1.55, 95% CI 0.92 to 2.61, moderate‐quality evidence), closure method (mass versus layered, RR 0.69, 95% CI 0.31 to 1.52, moderate‐quality evidence) or closure technique (continuous versus interrupted, RR 1.21, 95% CI 0.90 to 1.64, moderate‐quality evidence).
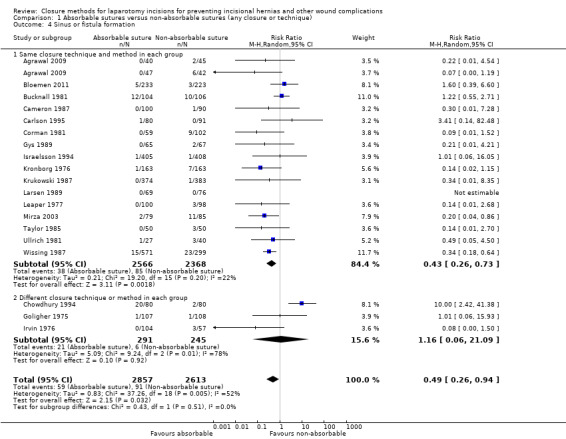
Absorbable sutures, compared with non‐absorbable sutures (RR 0.49, 95% CI 0.26 to 0.94, low‐quality evidence) reduced the risk of sinus or fistula tract formation. None of the other comparisons showed a difference (slow versus fast absorbable sutures, RR 0.88, 95% CI 0.05 to 16.05, very low‐quality evidence; mass versus layered, RR 0.49, 95% CI 0.15 to 1.62, low‐quality evidence; continuous versus interrupted, RR 1.51, 95% CI 0.64 to 3.61, very low‐quality evidence).
Authors' conclusions
Based on this moderate‐quality body of evidence, monofilament sutures may reduce the risk of incisional hernia. Absorbable sutures may also reduce the risk of sinus or fistula tract formation, but this finding is based on low‐quality evidence.
We had serious concerns about the design or reporting of several of the 55 included trials. The comparator arms in many trials differed by more than one component, making it impossible to attribute differences between groups to any one component. In addition, the patient population included in many of the studies was very heterogeneous. Trials included both emergency and elective cases, different types of disease pathology (e.g. colon surgery, hepatobiliary surgery, etc.) or different types of incisions (e.g. midline, paramedian, subcostal).
Consequently, larger, high‐quality trials to further address this clinical challenge are warranted. Future studies should ensure that proper randomisation and allocation techniques are performed, wound assessors are blinded, and that the duration of follow‐up is adequate. It is important that only one type of intervention is compared between groups. In addition, a homogeneous patient population would allow for a more accurate assessment of the interventions.
Plain language summary
What is the best way to close abdominal incisions following surgery?
What is the Issue?
Laparotomy, an incision through the abdominal wall to access the abdominal cavity, is performed for a variety of surgical procedures. Incisional hernia, infection, dehiscence (an opening of the wound or muscle layers) and chronic drainage from the wound, are potential complications of this procedure.
Why is it Important?
Incisional hernias affect up to 20% of people undergoing a laparotomy. Incisional hernias, as they enlarge over time, cause patient discomfort, which in turn, result in patients restricting their work and other physical activities. Cosmetic concerns may also arise.
We asked:
Does the type of suture material, or type of closure prevent these complications? We compared absorbable sutures (sutures that lose their tensile strength as they are dissolved by the patient's body) versus non‐absorbable (permanent) sutures; mass closure (closure of all anatomical layers of abdominal wall at once) versus layered closure (closing the anatomic layers individually); continuous closure (running suture) versus interrupted closure; monofilament sutures versus multifilament (braided) sutures; and slow absorbable sutures (those that maintain their tensile strength for more than 30 days) versus fast absorbable sutures (those that lose their tensile strength within 30 days).
We found:
A search of all relevant publications (up to date as of 8 February 2017) found a total of 55 studies with 19,174 participants to include in the review. The included studies differed greatly in the type of suture materials used, the closure technique and the type of underlying surgical procedures performed. We found that using monofilament sutures reduced the occurrence of incisional hernia. Absorbable sutures reduced the risk of chronic drainage from the wound (sinus or fistula formation).
This review included a notably large number of trials; however, we had concerns regarding their collective methodological design and scientific reporting.
This means:
Monofilament sutures can be considered for abdominal closure to reduce the risk of incisional hernia. Absorbable sutures can be considered to reduce the risk of chronic drainage from the wound.
Summary of findings
Summary of findings for the main comparison. Absorbable versus non‐absorbable sutures for laparotomy incisions.
| Absorbable versus non‐absorbable sutures for laparotomy incisions | |||||
| Patient or population: patients undergoing a laparotomy Setting: community and hospital‐based, outpatient and inpatient, worldwide Intervention: absorbable sutures for abdominal closure Comparison: non‐absorbable sutures for abdominal closure | |||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Quality of the evidence (GRADE) | |
| Risk with non‐absorbable sutures | Risk with absorbable sutures | ||||
| Incisional hernia follow‐up: 1 year | Study population | RR 1.07 (0.86 to 1.32) | 4720 (17 RCTs) | ⊕⊕⊕⊝ Moderate1 | |
| 107 per 1000 | 115 per 1000 (92 to 141) | ||||
| Wound infection at last follow‐up | Study population | RR 0.99 (0.84 to 1.17) | 8457 (29 RCTs) | ⊕⊕⊕⊝ Moderate1 | |
| 107 per 1000 | 105 per 1000 (89 to 125) | ||||
| Wound dehiscence at last follow‐up | Study population | RR 0.78 (0.55 to 1.10) | 9004 (34 RCTs) | ⊕⊕⊕⊝ Moderate1 | |
| 33 per 1000 | 26 per 1000 (18 to 36) | ||||
| Sinus or fistula formation at last follow‐up | Study population | RR 0.49 (0.26 to 0.94) | 5470 (19 RCTs) | ⊕⊕⊝⊝ Low1,2 | |
| 35 per 1000 | 17 per 1000 (9 to 33) | ||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RCT: randomised controlled trial; RR: risk ratio | |||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low quality: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect Very low quality: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect | |||||
1Downgraded one level for serious risk of bias (includes at least one study with overall high risk of bias). 2Downgraded one level for inconsistency (I2 = 52% ).
Summary of findings 2. Mass versus layered closure for laparotomy incisions.
| Mass versus layered closure for laparotomy incisions | |||||
| Patient or population: patients undergoing laparotomy incisions Setting: community and hospital‐based, outpatient and inpatient, worldwide Intervention: en masse for abdominal closure Comparison: layered closure for abdominal closure | |||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Quality of the evidence (GRADE) | |
| Risk with layered closure | Risk with mass closure | ||||
| Incisional hernia follow‐up: 1 year | Study population | RR 1.92 (0.58 to 6.35) | 1176 (5 RCTs) | ⊕⊝⊝⊝ Very low1,2,3 | |
| 27 per 1000 | 51 per 1000 (15 to 169) | ||||
| Wound infection at last follow‐up | Study population | RR 0.93 (0.67 to 1.30) | 2926 (11 RCTs) | ⊕⊕⊝⊝ Low1,4 | |
| 114 per 1000 | 106 per 1000 (76 to 148) | ||||
| Wound dehiscence at last follow‐up | Study population | RR 0.69 (0.31 to 1.52) | 2863 (11 RCTs) | ⊕⊕⊕⊝ Moderate1 | |
| 23 per 1000 | 16 per 1000 (7 to 35) | ||||
| Sinus or fistula formation at last follow‐up | Study population | RR 0.49 (0.15 to 1.62) | 1076 (6 RCTs) | ⊕⊕⊝⊝ Low1,2 | |
| 49 per 1000 | 24 per 1000 (7 to 79) | ||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RCT: randomised controlled trial; RR: risk ratio | |||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low quality: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect Very low quality: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect | |||||
1Downgraded one level for serious risk of bias (includes at least one study with overall high risk of bias). 2Downgraded one level for inconsistency (I2 = 61%). 3Downgraded one level for imprecision (overlapping no effect). 4Downgraded one level for inconsistency (I2 = 50%).
Summary of findings 3. Continuous versus interrupted closure for laparotomy incisions.
| Continuous versus interrupted closure for laparotomy incisions | |||||
| Patient or population: patients undergoing a laparotomy incision Setting: community and hospital‐based, outpatient and inpatient, worldwide Intervention: continuous closure Comparison: interrupted closure | |||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Quality of the evidence (GRADE) | |
| Risk with interrupted closure | Risk with continuous closure | ||||
| Incisional hernia follow‐up: 1 year | Study population | RR 1.01 (0.76 to 1.35) | 3854 (11 RCTs) | ⊕⊕⊕⊝ Moderate1 | |
| 95 per 1000 | 95 per 1000 (72 to 128) | ||||
| Wound infection at last follow‐up | Study population | RR 1.13 (0.96 to 1.34) | 10,039 (23 RCTs) | ⊕⊕⊕⊝ Moderate1 | |
| 86 per 1000 | 97 per 1000 (83 to 116) | ||||
| Wound dehiscence at last follow‐up | Study population | RR 1.21 (0.90 to 1.64) | 9228 (21 RCTs) | ⊕⊕⊕⊝ Moderate1 | |
| 24 per 1000 | 29 per 1000 (22 to 40) | ||||
| Sinus or fistula formation at last follow‐up | Study population | RR 1.51 (0.64 to 3.61) | 5082 (10 RCTs) | ⊕⊝⊝⊝ Very low1, 2,3 | |
| 24 per 1000 | 37 per 1000 (16 to 88) | ||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RCT: randomised controlled trial; RR: risk ratio | |||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low quality: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect Very low quality: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect | |||||
1Downgraded one level for serious risk of bias (includes at least one study with overall high risk of bias). 2Downgraded one level for inconsistency (I2 = 57%). 3Downgraded one level for imprecision (overlapping no effect).
Summary of findings 4. Monofilament versus multifilament sutures for laparotomy incisions.
| Monofilament versus multifilament sutures for laparotomy incisions | |||||
| Patient or population: patients undergoing a laparotomy incision Setting: community and hospital‐based, outpatient and inpatient, worldwide Intervention: monofilament Comparison: multifilament | |||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Quality of the evidence (GRADE) | |
| Risk with multifilament | Risk with monofilament | ||||
| Incisional hernia follow‐up: 1 year | Study population | RR 0.76 (0.59 to 0.98) | 4520 (16 RCTs) | ⊕⊕⊕⊝ Moderate1 | |
| 105 per 1000 | 80 per 1000 (62 to 103) | ||||
| Wound infection at last follow‐up | Study population | RR 1.08 (0.91 to 1.28) | 6557 (23 RCTs) | ⊕⊕⊕⊝ Moderate1 | |
| 105 per 1000 | 114 per 1000 (96 to 135) | ||||
| Wound dehiscence at last follow‐up | Study population | RR 1.24 (0.93 to 1.67) | 6199 (22 RCTs) | ⊕⊕⊕⊝ Moderate1 | |
| 27 per 1000 | 33 per 1000 (25 to 45) | ||||
| Sinus or fistula formation at last follow‐up | Study population | RR 1.91 (0.77 to 4.73) | 2285 (8 RCTs) | ⊕⊝⊝⊝ Very low1,2,3 | |
| 25 per 1000 | 48 per 1000 (19 to 118) | ||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RCT: randomised controlled trial; RR: risk ratio | |||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low quality: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect Very low quality: we have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | |||||
1Downgraded one level for serious risk of bias (includes at least one study with overall high risk of bias). 2Downgraded one level for inconsistency (I2 = 77%). 3Downgraded one level for imprecision (overlapping no effect).
Summary of findings 5. Fast absorbable versus slow absorbable sutures for laparotomy incision.
| Fast absorbable versus slow absorbable sutures for laparotomy incisions | |||||
| Patient or population: patients undergoing a laparotomy incision Setting: community and hospital‐based, outpatient and inpatient, worldwide Intervention: slow absorbable sutures Comparison: fast absorbable sutures | |||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Quality of the evidence (GRADE) | |
| Risk with fast absorbable sutures | Risk with slow absorbable sutures | ||||
| Incisional hernia follow‐up: 1 year | Study population | RR 0.81 (0.63 to 1.06) | 3643 (10 RCTs) | ⊕⊕⊕⊝ Moderate1 | |
| 113 per 1000 | 92 per 1000 (71 to 120) | ||||
| Wound infection at last follow‐up | Study population | RR 1.16 (0.85 to 1.57) | 4100 (11 RCTs) | ⊕⊕⊕⊝ Moderate1 | |
| 75 per 1000 | 87 per 1000 (64 to 118) | ||||
| Wound dehiscence at last follow‐up | Study population | RR 1.55 (0.92 to 2.61) | 3440 (8 RCTs) | ⊕⊕⊕⊝ Moderate1 | |
| 15 per 1000 | 24 per 1000 (14 to 40) | ||||
| Sinus or fistula formation at last follow‐up | Study population | RR 0.88 (0.05 to 16.05) | 911 (2 RCTs) | ⊕⊝⊝⊝ Very low1,2,3 | |
| 15 per 1000 | 13 per 1000 (1 to 243) | ||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RCT: randomised controlled trial; RR: risk ratio | |||||
| GRADE Working Group grades of evidence High quality: we are very confident that the true effect lies close to that of the estimate of the effect Moderate quality: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low quality: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect Very low quality: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect | |||||
1Downgraded one level for serious risk of bias (includes at least one study with overall high risk of bias). 2 Downgraded one level for inconsistency (I2 = 72%). 3Downgraded one level for imprecision (overlapping no effect).
Background
Description of the condition
Laparotomy is a surgical incision used to gain access to the organs of the abdominal cavity and is one of the most common surgical procedures performed globally. Sutures, most commonly, provide mechanical support for the closed wound during its initial healing. They approximate the wound edges and help to maintain wound closure until the healing process provides sufficient strength for the wound to withstand stress and strain. Surgeons have several choices for closing the abdominal fascia, but there is currently scant consensus as to the best suture material or closure method. For the majority of surgeons, the choice of a suture material in a given instance has mostly been directed by training exposure and local opinion, with many surgeons reluctant to attempt different techniques once their personal preferences have been established (Anthimidis 2013; Chalya 2015; Hodgson 2001; Tully 2002).
Incisional hernia is a frequent complication of laparotomy. It is a late manifestation of failure to secure fascial closure. The incidence following major abdominal surgery is reported to range from 2% to 20% across studies, depending on patient and wound factors (incidence may go up to 40% in those with wound infections) (Le Huu Nho 2012; Sanders 2012; Santora 1993). Incisional hernias, as they enlarge over time, cause the patient discomfort, which in turn, result in patients restricting their work and other physical activities. Cosmetic concerns may also arise. Overall, patient quality of life can be greatly affected. Complications of incisional hernias include pain, bowel obstruction, incarceration and strangulation and the risk of need for repeat surgery. In 2011, the number of incisional hernia repairs in the USA alone was estimated to be between 190,000 to 200,000, with approximately 1% to 2% annual growth in volume (Smith 2012). In addition, this volume reflects the economic impact of the condition given the surgical manpower and expensive mesh materials employed in hernia repairs (Rutkow 2003). Incisional hernia repair is also associated with hernia recurrence, ranging from 10% to 50%, and considerable morbidity and mortality. The rate of hernia recurrence is largely unchanged over time as surgeons continue to face increasing formidable patient factors such as older, more comorbid and more obese patients undergoing primary surgery (Anthony 2000; Hawn 2010; Helgstrand 2012; Langer 1985; Leber 1998; Mudge 1985; Stey 2015).
A large, prospective study (Itatsu 2014), in which patients were examined for hernia every 3 months following surgery, assessed the time from index surgery to the diagnosis of hernia. The study authors found that there was no time point in which the diagnosis of incisional hernia plateaued over the first two years following surgery. Approximately 5.2% of incisional hernias were diagnosed within the first 12 months, while 10.2% of hernias were diagnosed within the first 24 months. An additional study (Goodenough 2015) found that of those who developed an incisional hernia within 5 years of surgery, more than half were diagnosed within the first 12 months.
Several comorbid conditions have also been shown to be associated with the development of incisional hernia and these are listed in the right half of Table 6 (Bucknall 1982; Connelly 2015; Goodenough 2015; Lamont 1988; Sugerman 1996).
1. Factors associated with incisional hernia.
| In surgeon's control | Other factors |
Type of incision
|
Postoperative inflammatory response to sutures, which may be suture‐specific. For example, studies have shown that synthetic absorbable materials tend to induce lower levels of inflammation compared to catgut (Nilsson 1983; Postlethwait 1975) |
Incision technique
|
Associated co‐morbid conditions
|
| Preoperative surgical preparation of incision site and pre‐operative antibiotics |
Nature of wound
|
| Use of subcutaneous drains |
Neoadjuvant therapies
|
Suture material
|
|
Suture technique
|
Some studies have reported that the majority of incisional hernias occur within the first two years after surgery, suggesting that initial wound closure is an important factor in hernia prevention (Bucknall 1982; Lamont 1988). However, the limited follow‐up in these studies may have underestimated late occurrence of incisional hernia, as suggested by long‐term studies (Ellis 1983; George 1986; Mudge 1985; Pollock 1989; Spencer 2015).
The incidence of incisional hernia has been reported to vary with the type of incision, with a greater incidence reported with midline incisions compared to paramedian incisions (Brown 2005; Cox 1986; Guillou 1980; Kendall 1991). However, the midline incision remains the workhorse of open surgery due to its ideal properties in regards to optimal intraperitoneal access, exposure, speed and the simplicity of the incision and postoperative pain characteristics relative to the paramedian approach (Hughes 2009). One of the benefits of the modern uptake of laparoscopic surgery was thought to be a reduced rate of incisional hernias due to the use of smaller incisions. However, the modern evidence is variable in this regard and some studies demonstrate that laparoscopic surgery still results in notable rates of incisional hernia, in some cases, no different than when compared to the open approach (Benlice 2015; Ihedioha 2008; Llaguna 2010). In addition, many laparoscopic procedures (e.g. colectomy, splenectomy) require an incision to remove the specimen, and have an inherent hernia risk.
A number of factors influence the occurrence of postoperative wound infection and incisional hernia (Table 6). Some of these factors are considered to be under the control of the surgeon (such as the choice of incision), while others are only partly (e.g. the length of the incision or the duration of the operation), or not at all (e.g. most patient factors including diabetes and chronic lung disease) influenced by the surgeon. Risk factors for surgical wound infection should be considered additionally as incisional hernia risk factors, as infection disrupts wound healing, which in turn increases the risk of fascial dehiscence (Bucknall 1982). Fascial dehiscence that is not acutely diagnosed and repaired, or occurs in a delayed fashion, will ultimately become an incisional hernia.
This review explores how variations in the selection of closure techniques and suture materials in closing laparotomy (not laparoscopy) incisions affects the occurrence of post‐operative wound complications, such as development of incisional hernia and wound infection.
Description of the intervention
Fascial closure following laparotomy involves several key decisions. The first decision is whether to close the layers of the abdominal wall in separate anatomic layers (peritoneum, posterior fascia, anterior fascia, subcutaneous tissues) or 'en masse' (incorporating all layers of the fascia, with or without the peritoneum, into one suture line). We have considered layered closure to be closure of the peritoneum and linea alba separately in midline incisions. For non‐midline incisions, we defined layered closure as closure of the fascial layers (posterior fascia, anterior fascia) and peritoneum separately.
The second decision for surgeons is whether to close the fascia using an interrupted or a continuous method. We defined continuous closure as the use of a running suture on the fascia with knots only at either extreme of the wound, or the use of two running sutures with knots at the extremes of the wound, and tied together in the middle of the wound. We defined interrupted closure as the use of multiple knotted sutures to close the fascia. We did not distinguish between the types of interrupted closures (e.g. Smead Jones, simple, figure of eights). Interrupted closure has the advantage of ensuring closure, even if one of the suture knots breaks, but requires a longer closure time. Continuous closure is advantageous in that it disperses the tension more evenly and is more quickly completed. The disadvantage is that if the suture breaks, the entire incision may fall apart (dehisce).
The third decision is the type of suture material. Surgeons may choose from absorbable (i.e. sutures which will lose their tensile strength over time as the body breaks down the material) or non‐absorbable sutures (i.e. permanent). We further classified absorbable sutures into fast absorbable (those with loss of tensile strength within 30 days) and slow absorbable (loss of tensile strength greater than 30 days) in this review. A surgeon may also choose between monofilament or multifilament sutures.
How the intervention might work
Closing the abdominal wall allows for approximation of the cut edges from the laparotomy. Suturing the fascial layer closed protects the abdominal contents from critical dehydration, hypothermia, injury and infection, helps with pulmonary mechanics, and should reduce or eliminate the development of abdominal wall hernias postoperatively.
Why it is important to do this review
It is apparent that a multitude of factors play a role in the selection of an appropriate suture material in a given situation, including costs. The sequelae of a poorly closed wound can be considerable. Early wound failure (wound infection and dehiscence) can lead to a return to the operating room, and increased length and cost of stay. Late wound failures (incisional hernia, sinus and fistula formation) can lead to additional surgical procedures and can affect a patient's quality of life. Determining the optimal closure technique could help to reduce these issues. This review was concerned with suture materials and closure techniques in the closure of laparotomy incisions. Many randomised controlled trials have studied suture materials and closure techniques employed for fascial closure after laparotomy incisions. We have attempted to summarise the evidence and provide conclusive comments on the efficacy of different suture materials and closure techniques in prior meta‐analyses and reviews (Hodgson 2000; Rucinski 2001; Van't Riet 2002; Weiland 1998). However, each of the reviews was limited either by methodology, lack of comprehensive literature searching, restricted inclusion criteria, or a combination of these issues.
Objectives
The objectives of this review were to identify the best available suture techniques and suture materials for closure of the fascia following laparotomy incisions by assessing the following comparisons:
absorbable versus non‐absorbable sutures;
mass versus layered closure;
continuous versus interrupted closure techniques;
monofilament versus multifilament sutures; and
slow absorbable versus fast absorbable sutures.
Our objective was not to determine the single best combination of suture material and techniques, but to compare the individual components of abdominal closure.
Methods
Criteria for considering studies for this review
Types of studies
We included only randomised controlled trials (RCTs). Cluster‐randomised trials were also considered for inclusion. We did not restrict the inclusion of studies by duration of follow‐up (although we only included trials with a follow‐up of more than one year for the primary outcome, incisional hernia). We included studies regardless of how hernia was diagnosed (clinical, radiological or combination of both).
Types of participants
We included trials that compared the interventions of interest in adults and children. We included trials that performed abdominal incisions in all types of operations including, but not limited to, gastrointestinal surgery, obstetric procedures, emergency procedures including those for perforating or penetrating abdominal injuries, and surgical intervention for obesity. We included trials that enrolled participants undergoing laparotomy through any type of abdominal incision and with any septic status of the incision including clean, clean‐contaminated and septic or infected. We did not restrict inclusion based on the nutritional status or age of the participants. We excluded trials with participants undergoing laparoscopy and laparoscopic‐assisted operations.
Types of interventions
We included trials that compared any of the following interventions separately or in combination with each other for fascial closure following abdominal incisions.
Suture technique
Continuous suture
Interrupted suture
Mass closure either as a single mass layer or using the Smead‐Jones technique (internal mass closure) with or without inclusion of the peritoneal layer
Layered closure with or without inclusion of the peritoneal layer
Suture material
We classified the suture material as absorbable or non‐absorbable. Absorbable suture materials included, but were not limited to, surgical catgut, polyglactin, polyglycolic acid, polydioxanone and polyglyconate. We further classified absorbable sutures into fast absorbable (those with loss of tensile strength within 30 days) and slow absorbable (loss of tensile strength greater than 30 days). Non‐absorbable (i.e. permanent) suture materials included, and were not limited to, silk, polypropylene, stainless steel and nylon.
We also classified sutures as either monofilament or multifilament (i.e. braided). We did not exclude studies that compared monofilament versus multifilament sutures with different absorptive characteristics (e.g. we included studies that compared non‐absorbable monofilament sutures to absorbable multifilament sutures).
If multiple types of sutures were used, we categorised the trial based on what type of suture was used on the fascial layers (Table 7).
2. Sutures assessed.
| Suture material | Trade name(s) | Absorbability | Monofilament or multifilament |
| Catgut chromic | Catgut chromic | Fast absorbable | Monofilament |
| Polyamide (nylon) | Ethilon (monofilament), Nurolon (multifilament) | Non‐absorbable | Both |
| Polydioxanone | PDS | Slow absorbable | Monofilament |
| Polyester | Ethibond | Non‐absorbable | Multifilament |
| Polyglactin‐910 | Vicryl | Fast absorbable | Multifilament |
| Polyglycolic acid | PGA, Dexon | Fast absorbable | Available in both |
| Polyglyconate | Maxon | Slow absorbable | Monofilament |
| Polypropylene | Prolene, Premilene | Non‐absorbable | Monofilament |
| Silk | Silk | Non‐absorbable | Multifilament |
| Steel | Steel | Non‐absorbable | Monofilament |
We excluded trials that compared materials or techniques, or both, for the closure of the skin or peritoneum only. The use of retention sutures (defined as sutures that encompassed the entire abdominal wall (including the skin), placed in addition to the primary method of fascial closure) was also not compared in this review. We also excluded trials that only assessed stitch bites (small versus large) and not one of our other techniques.
Types of outcome measures
Primary outcomes
The primary outcome for the review was:
Proportion of participants who developed incisional hernia, as defined in the included studies, at one year or more of follow‐up.
Secondary outcomes
The secondary outcomes for the review were:
Wound infection, as defined and identified in the included studies.
Wound dehiscence (i.e. fascial breakdown in the postoperative period), as defined and identified in the included studies.
Wound sinus or fistula formation, as defined in included studies.
We focused on superficial surgical site infections, as these are most clinically relevant to the suture material and technique. If studies presented organ space, deep site and superficial site infections, we included only the superficial site infection in the outcome.
We did not incorporate the specific management of wound dehiscence into our review. We considered both dehiscence requiring reoperation and dehiscence managed non‐operatively for inclusion in our review.
Search methods for identification of studies
Electronic searches
On 8 February 2017 we searched the following electronic databases with no language or date of publication limitations:
Cochrane Central Register of Controlled Trials (CENTRAL; 2017, Issue 2) (Appendix 1);
MEDLINE (OVID) 1950 to 8 February 2017 (Appendix 2);
Embase (OVID) 1974 to 8 February 2017 (Appendix 3);
ClinicalTrials.gov, 8 February 2017 (Appendix 4); and
World Health Organization International Clinical Trials Registry Platform (ICTRP), 8 February 2017 (Appendix 5)
Searching other resources
We searched the reference lists of all included studies to identify RCTs that the electronic search may have failed to identify. We searched the Science Citation Index (8 February 2017) to identify additional trials that may have cited the included trials.
Data collection and analysis
Selection of studies
Review authors (SVP, DP, SS, SV, RN) independently assessed each title and abstract of all reports identified through the electronic and manual searches. We labelled each report as (a) definitely exclude, (b) unsure or (c) definitely include. We retrieved full texts for those classified as 'unsure' or 'definitely include'. Two review authors (from SVP, DP, SS, SV, RN) independently assessed these full‐text articles for inclusion. We included all eligible studies irrespective of whether measured outcome data were reported on in a usable way. We resolved differences through discussion.
Data extraction and management
Two of the review authors (from SSV, SVP, DP) independently extracted data for the study characteristics, and primary and secondary outcomes onto data collection forms developed for this purpose. We resolved discrepancies through discussion. We attempted to contact authors of studies with missing data or unclear methods. One review author (either SVP, SSV or DP) entered all data into Review Manager 5 (RevMan 5.3) (RevMan 2014) and a second review author (either SVP or DP) verified the data entered.
Assessment of risk of bias in included studies
Two review authors (from SVP, DP, SS, SV, RN) independently assessed the included studies for sources of systematic bias according to the guidelines in Chapter 8, sections 1 to 16, of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011a). We evaluated the studies for the following criteria: randomisation, allocation concealment (selection bias and performance bias), blinding of outcome assessors, rates of follow‐up and the use of an intention‐to‐treat analysis (attrition bias), selective reporting and other biases identified in the assessment process.
We assessed selective reporting for whether hernia outcomes were determined at a minimum of one year's follow‐up, and whether wound infection and dehiscence were reported in the perioperative period. We classified each bias as (a) low risk of bias, (b) high risk of bias or (c) unclear risk of bias, as described in the Cochrane 'Risk of bias' tool (Higgins 2011a, Appendix 6). We resolved differences between the two review authors by discussion. We judged trials as overall high risk of bias if we identified one or more domains as being at high risk of bias. We attempted to contact authors in studies that we judged to have 'unclear risk of bias' in any domain.
Measures of treatment effect
We measured all outcomes as dichotomous variables (i.e. occurring or not occurring) over the study period, and therefore measured the treatment effect using risk ratios (RR) with corresponding 95% confidence intervals (CI). We included postoperative outcomes (dehiscence and wound infection) if the trial measured these outcomes within the postoperative period, defined as within 30 days of surgery. We included sinus or fistula tract occurrence if identified at any point. We included incisional hernia if at least one year of follow‐up was completed for the study.
Unit of analysis issues
The unit of analysis in this review was the individual participant. We did not identify any cluster‐RCTs in the search, but should we do so in later updates, we will seek expert statistical advice to minimise potential unit‐of‐analysis issues.
Studies with more than two intervention groups
In studies with multiple comparison arms, we included pair‐wise data in all applicable meta‐analyses, as long as the groups were independent (i.e. did not share participants) and compared an intervention of interest. If two or more groups shared an intervention of interest and could be compared to a separate group (e.g. two groups using absorbable sutures, with a third using non‐absorbable sutures), we combined the two comparable groups for analysis. The exception was if an intervention differed by more than one component between groups. In this case, we included the groups differing by only one intervention in the meta‐analysis. For example, if there were three groups, group one using interrupted absorbable sutures, group two using continuous absorbable sutures and group three using non‐absorbable continuous sutures, we would compare group one to group two for analysis of continuous versus interrupted sutures, and group two to group three for analysis of absorbable versus non‐absorbable sutures.
Dealing with missing data
With regard to missing individuals from studies, we have based analyses on intention‐to‐treat analyses as far as permitted by published data for relevant outcome measures. For studies with dropout rates exceeding 10%, we performed best‐case/worst‐case sensitivity analyses for binary outcomes.
Assessment of heterogeneity
We assessed clinical and methodological heterogeneity using data collected to assess risk of bias and the table of Characteristics of included studies. We assessed statistical heterogeneity using the I2 statistic (Higgins 2003), categorizing heterogeneity into low (I2 less than 30%), moderate (I2 30% to 60%) or substantial (I2 more than 60%) as described in the Cochrane Handbook for Systematic Reviews of Interventions (Chapter 9.5 Deeks 2011). We anticipated that type of incision (midline, paramedian, subcostal), acuity of surgery (elective versus emergent) and wound contamination classification would be sources of heterogeneity.
We also considered studies that compared interventions differing by more than one component between groups to be a source of heterogeneity.
Assessment of reporting biases
We assessed reporting biases with the use of funnel plots. We created funnel plots for our primary outcome, incisional hernia, for each comparison where there were more than 10 included studies, as recommended in the Cochrane Handbook for Systematic Reviews of Interventions (Sterne 2011).
Data synthesis
We performed the meta‐analyses using RevMan 5 software provided by Cochrane (RevMan 2014). We calculated a summary RR for the dichotomous outcomes included in the review following guidelines in the Cochrane Handbook for Systematic Reviews of Interventions (Deeks 2011).
We analysed five comparisons for closure material and technique:
absorbable versus non‐absorbable materials;
continuous versus interrupted closure;
mass versus layered closure;
monofilament versus multifilament sutures; and
slow versus fast absorbable sutures.
If trials compared a combination of different materials and techniques (e.g. absorbable, continuous closure versus non‐absorbable, interrupted closure), we included the trial in all applicable analyses (i.e. absorbable versus non‐absorbable and continuous versus interrupted). For trials in which there were more than two comparator groups, we attempted to include outcome data for analysis in which only one component differed between groups (e.g. suture material or technique). If a third group differed by more than one component, we did not include it in the analysis.
We used random‐effects modelling exclusively throughout our analyses given the clinical heterogeneity of the included studies.
Subgroup analysis and investigation of heterogeneity
We undertook subgroup analyses for each outcome comparing the results for those trials that assessed interventions that differed only by the assessed comparison (e.g. absorbable sutures versus non‐absorbable sutures, both with continuous closure) to those that assessed interventions that differed by more than just this comparison (e.g. absorbable suture and continuous closure versus non‐absorbable sutures with interrupted closure).
We also conducted subgroup analysis to determine if the type of incision (the use of midline incision only ‐ there was insufficient data to assess paramedian incisions) affected the incidence of incisional hernia (this subgroup analysis only included comparisons where the intervention differed in a single component across groups).
We also planned a subgroup analysis to determine the effect of acuity of surgery (emergent versus elective) and wound classification on the association between our interventions and the primary outcome, but there were insufficient data to conduct these analyses.
Sensitivity analysis
We conducted sensitivity analyses to determine the impact of excluding studies with at least one domain identified as being at a high risk of bias. We also conducted best case/worst case sensitivity analysis as explained above for missing data.
'Summary of findings' tables
We evaluated the quality of evidence using the GRADE approach (Schünemann 2011) for each outcome. We presented the quality of evidence in 'Summary of Findings' tables for the following comparisons.
Absorbable versus non‐absorbable sutures for laparotomy incisions
Mass versus layered closure for laparotomy incisions
Continuous versus interrupted closure for laparotomy incisions
Monofilament versus multifilament sutures for laparotomy incisions
Fast absorbable versus slow absorbable sutures for laparotomy incisions
The GRADE system classifies the quality of evidence in one of four grades.
High quality: we are very confident that the true effect lies close to that of the estimate of the effect
Moderate quality: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different
Low quality: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect
Very low quality: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect.
The quality of evidence could be downgraded by one (serious concern) or two (very serious concern) for the following reasons: risk of bias, inconsistency (unexplained heterogeneity, inconsistency of results), indirectness (indirect population, intervention, control, outcomes), imprecision (wide confidence intervals, overlapping no effect), and publication bias.
Results
Description of studies
Results of the search
As seen in Figure 1, there were 2304 studies identified through the primary search. From these studies, we identified 85 for full‐text review, 55 of which were included in the quantitative analyses.
1.
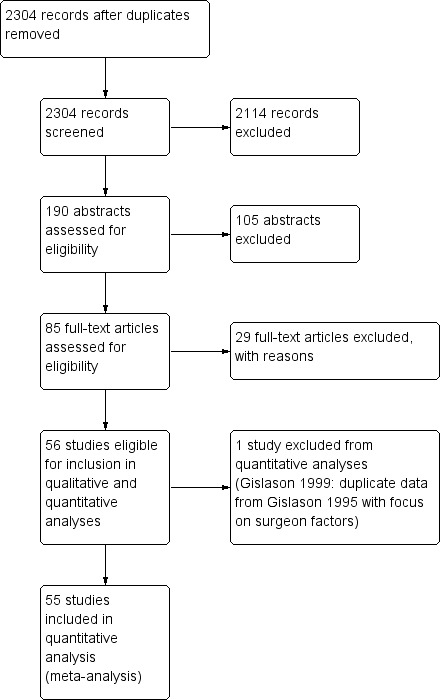
Study flow diagram
We furthermore identified six ongoing studies (NCT01965249; NCT00544583; ISRCTN25616490; NCT00514566; TCTR20150318001; NCT02145052), from searches in ClinicalTrials.gov and World Health Organization International Clinical Trials Registry Platform.
Included studies
We included a total of 55 studies with 19,174 participants in this review. Studies were published between 1975 and 2015. A summary of each study can be found in the Characteristics of included studies table. There was a large degree of heterogeneity in the types of comparisons performed within these studies, and they investigated a variety of absorbable sutures (including polyglactin‐910, polydioxanone, polyglycolic acid, polyglyconate and chromic catgut) and non‐absorbable sutures (nylon, polyester, polypropylene, silk, steel). There was a large amount of variability in the combination of suture material, closure technique (continuous versus interrupted) and closure method (mass versus layered). Commonly, we found that more than one component varied in the pair‐wise comparisons (i.e. absorbable, continuous, mass closure versus non‐absorbable, interrupted, layered closure).
In addition, 15 studies investigated more than two groups for comparison. Of these, only Agrawal 2009 was a factorial study with 4 interventional groups. For the purpose of our meta‐analyses, we included the individual group results in our analyses. Four studies included three or more groups, with only one component that differed between groups (Bresler 1995; Corman 1981; Donaldson 1982; Pollock 1979). Ten studies included three or more groups and had more than one component that differed between groups (Agrawal 2014; Berretta 2010; Gislason 1995; Goligher 1975; Irvin 1977; Larsen 1989; Leaper 1977; Savolainen 1988; Seiler 2009; Wissing 1987). The groups used for the outcome analyses are specified in the notes section of the Characteristics of included studies table.
There was a broad range of surgical indications for laparotomy (upper gastrointestinal, biliary tree, small bowel, colorectal, obesity surgery). Only one study looked only at emergency surgery patients (Agrawal 2009). In addition, the types of incision varied widely between studies (upper midline, lower midline, paramedian, subcostal, transverse) and even within studies. In total, 26 studies included participants undergoing only midline incisions (Agrawal 2009; Agrawal 2014; Berretta 2010; Bloemen 2011; Bresler 1995; Brolin 1996; Carlson 1995; Colombo 1997; Dan 2014; Deitel 1990; Efem 1980; Fagniez 1985; Israelsson 1994; Krukowski 1987; Lewis 1989; McNeill 1986; Ohira 2015; Orr 2003; Pandley 2013; Savolainen 1988; Seiler 2009; Siddique 2015; Taylor 1985; Trimbos 1992;Ullrich 1981Wissing 1987), while two studies included participants undergoing paramedian incisions alone (Donaldson 1982; Goligher 1975). The remaining studies included a combination of incisions, or did not specify the type of incisions used.
Follow‐up duration for the included studies included at least the perioperative period (allowing for assessment of wound infection and dehiscence). Follow‐up duration for the detection of incisional hernia varied greatly. We had to exclude several studies from the hernia analysis due to insufficient follow‐up duration (i.e. less than one year).
Excluded studies
After full‐text review, we excluded 29 studies for a variety of reasons. The reasons for exclusion can be found in the Characteristics of excluded studies table.
Risk of bias in included studies
We assessed only one trial as having a low risk of bias across all assessed categories (Bloemen 2011). Twenty‐six of the 55 trials had a high risk of bias in at least one category. The remainder had an unclear risk of bias. The large number of trials with an unclear risk of bias was due to poor reporting of their trial methods.
Allocation
The majority of the included trials suffered from poor reporting of their methods. Many trials did not specify the methods of randomisation and allocation concealment (Figure 2; Figure 3). Randomisation was adequate in 15 of 55 included studies, and allocation concealment was adequate in 16 of 55 studies. Of the 15 with adequate randomisation, nine studies had an unclear risk of bias for allocation concealment. Of the 16 studies with adequate allocation concealment, nine had either unclear or high risk of bias in randomisation.
2.
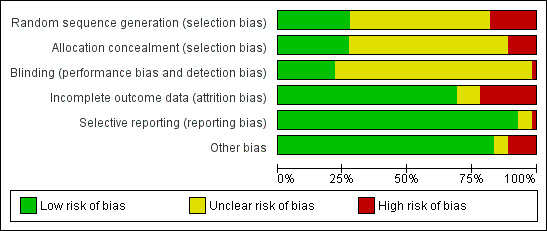
'Risk of bias' graph: review authors' judgements about each risk of bias item presented as percentages across all included studies
3.
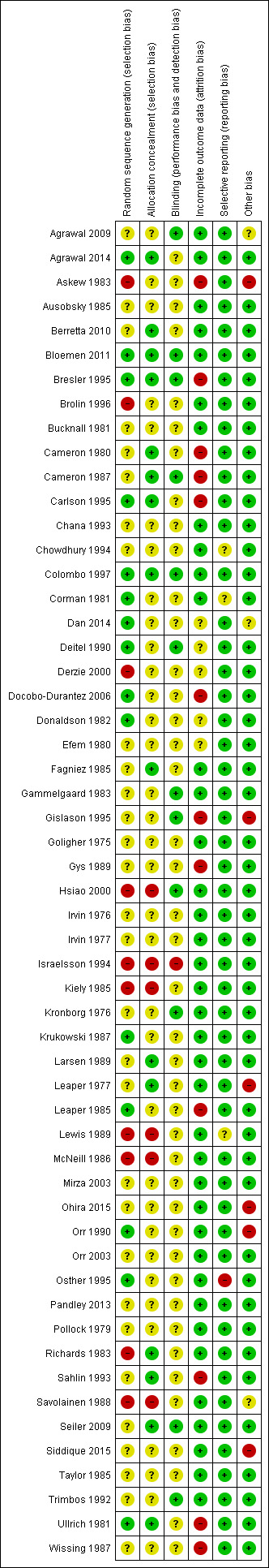
'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study
Blinding
Due to the nature of the intervention, blinding of the surgeon was not possible. The majority of studies did not explicitly discuss whether outcome assessors or participants were blinded to the intervention. Twelve of 55 studies reported avoiding detection bias by adequate outcome assessor blinding, while 43 studies were unclear about blinding or had high risk of bias of blinding (Figure 2; Figure 3).
Incomplete outcome data
Thirty‐seven of 55 studies had adequate follow‐up data, with few losses to follow‐up. Twelve studies were at high risk of bias due to high loss to follow‐up, without explanation as to the cause, or how this group differed from those who were followed up. The remainder of the studies did not adequately report the loss to follow‐up, so the potential for attrition bias is unclear (Figure 2; Figure 3).
Of the 55 included studies, only one did not report an intention‐to‐treat analysis (Leaper 1985).
Selective reporting
None of the included trials had a registered trial protocol. Of the included trials, three were judged to have unclear risk of selective repoting (Chowdhury 1994; Corman 1981; Lewis 1989) due to unclear length of follow up. In addition, one trial was felt to be high risk of selective reporting, as dehiscence was a prespecified outcome, but was not reported (Osther 1995). All other trials reported their outcomes and were judged to be at low risk of selective reporting (reporting bias) (Figure 2; Figure 3).
Other potential sources of bias
Six of the 55 studies were clearly at high risk of other sources of bias. The sources of bias included: early termination of a trial without an a priori stopping rule (Askew 1983), follow‐up through mailed surveys (Gislason 1995), surgeons refusing to randomise participants (Leaper 1977), participants not similar between groups (Ohira 2015), no available baseline characteristics (Orr 1990), or inappropriate exclusion criteria (Siddique 2015).
Effects of interventions
See: Table 1; Table 2; Table 3; Table 4; Table 5
1. Primary outcome: incisional hernia at one year or more of follow‐up
1.1 Absorbable versus non‐absorbable sutures
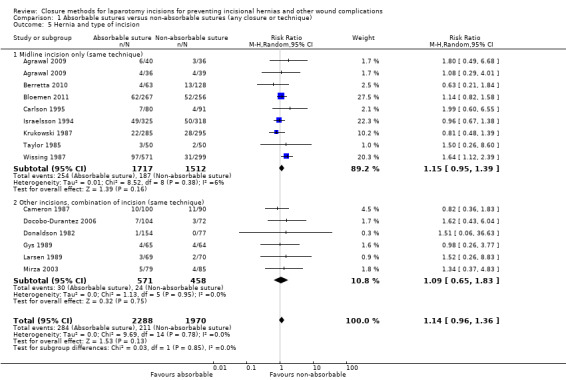
We included a total of 17 studies, with 4720 participants, in the analysis of absorbable versus non‐absorbable sutures for hernia formation. Overall, we found no evidence of a difference between absorbable and non‐absorbable suture material and the risk of hernia (risk ratio (RR) 1.07, 95% confidence interval (CI) 0.86 to 1.32, P = 0.53, I2 = 19%). A subgroup analysis, including only those studies that compared the same closure technique and method, found similar results (RR 1.13, 95% CI 0.95 to 1.34, P = 0.15, I2 = 0%). There was no evidence of a subgroup effect (P = 0.73) (Analysis 1.1; Figure 4). Of note, there were four comparison groups from the study by Agrawal 2009. As such, we included two comparisons from this study, the first compared interrupted closures between the two suture materials, while the second compared continuous closures between the two suture materials. We implemented a similar approach in other applicable analyses in which the study was included.
1.1. Analysis.
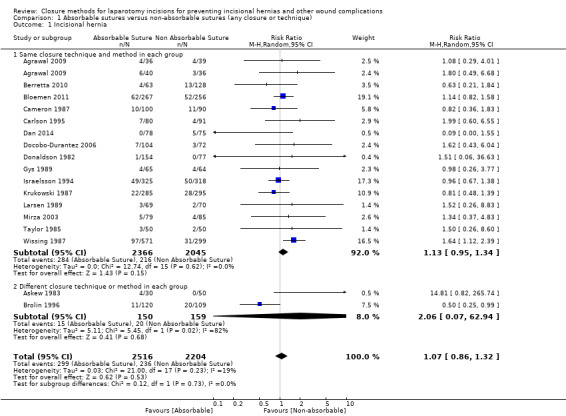
Comparison 1 Absorbable sutures versus non‐absorbable sutures (any closure or technique), Outcome 1 Incisional hernia.
4.
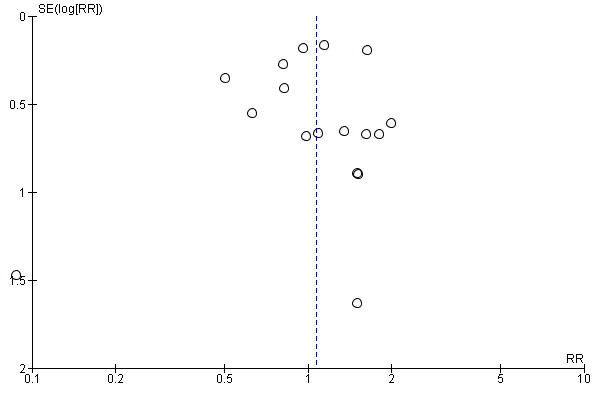
Funnel plot of comparison 1. Absorbable suture versus non‐absorbable sutures (any closure or technique), outcome 1.1: hernia
1.2 Mass versus layered closure
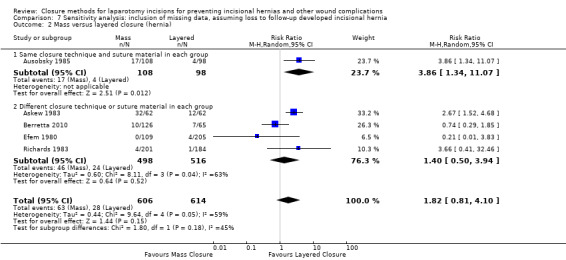
We included a total of five studies, with 1176 participants, in the analysis of mass versus layered closure for hernia formation. There was no evidence that mass versus layered closure resulted in an increased hernia risk (RR 1.92, 95% CI 0.58 to 6.35, P = 0.29, I2 = 61%). Only one study assessed mass versus layered closure, using the same type of suture and closure technique (Ausobsky 1985). This study found that mass closure resulted in increased hernia risk (RR 3.86, 95% CI 1.34 to 11.07, P = 0.01), although there was no evidence of a subgroup effect within this analysis (P = 0.31) (Analysis 2.1).
2.1. Analysis.
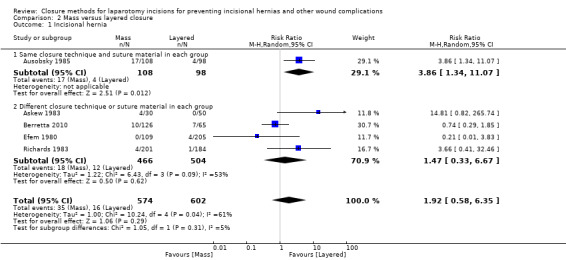
Comparison 2 Mass versus layered closure, Outcome 1 Incisional hernia.
1.3 Continuous versus interrupted closure
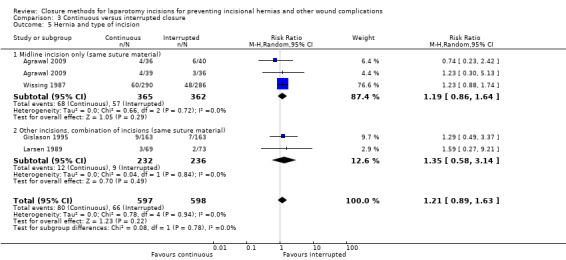
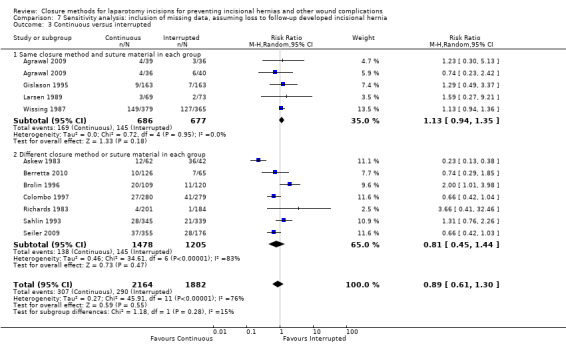
We included a total of 11 studies, with 3854 participants, in the analysis of continuous versus interrupted closure for hernia. The use of continuous or interrupted closure technique did not appear to affect the risk of hernia (RR 1.01, 95% CI 0.76 to 1.35, P = 0.94, I2 = 42%). A subgroup analysis, including only those studies that compared the same type of suture, found similar results, and the difference between subgroups was not significant (test of subgroup effect, P = 0.22) (Analysis 3.1). Of note, there were four comparison groups from the study by Agrawal 2009. Results were grouped accordingly (as described above).
3.1. Analysis.
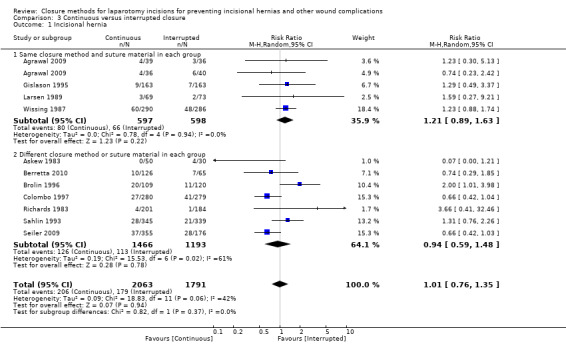
Comparison 3 Continuous versus interrupted closure, Outcome 1 Incisional hernia.
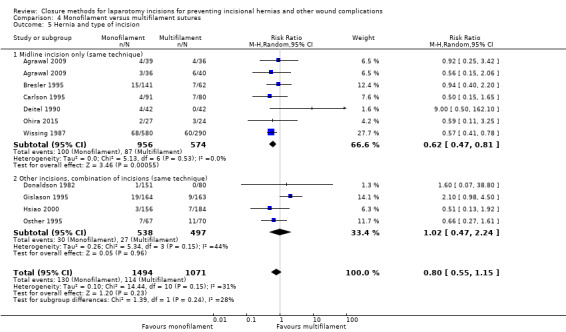
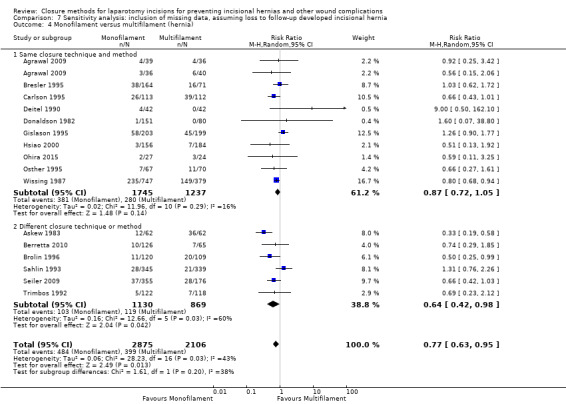
1.4 Monofilament versus multifilament sutures
We included a total of 16 studies, with 4520 participants, in the analysis of monofilament versus multifilament sutures for hernia. Of the 16 studies, nine compared groups with similar absorption of sutures (i.e. absorbable versus absorbable or non‐absorbable versus non‐absorbable) (Bresler 1995; Deitel 1990; Gislason 1995; Hsiao 2000; Ohira 2015; Osther 1995; Sahlin 1993; Seiler 2009; Trimbos 1992). Overall, there was evidence to suggest that monofilament sutures reduced the risk of hernia, relative to multifilament sutures (RR 0.76, 95% CI 0.59 to 0.98, P = 0.04, I2 = 30%). There was no evidence of a subgroup effect when we assessed trials with the same closure method and technique separately (test of subgroup differences P = 0.73) (Analysis 4.1).
4.1. Analysis.
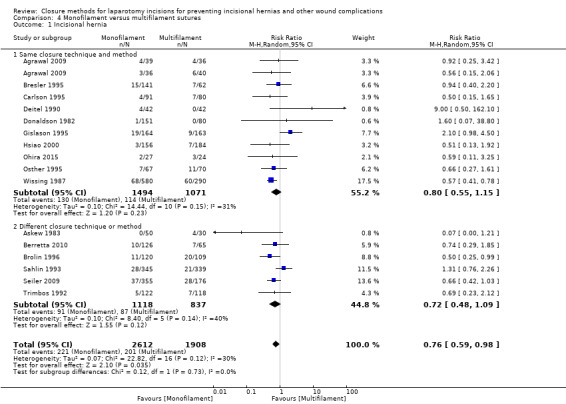
Comparison 4 Monofilament versus multifilament sutures, Outcome 1 Incisional hernia.
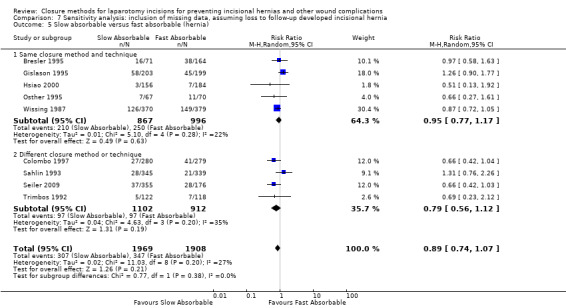
1.5 Slow absorbable versus fast absorbable sutures
We included a total of 10 studies, with 3643 participants, in the analysis of slow versus fast absorbable sutures for hernia formation. There was no evidence that the rate of absorption affected the risk of hernia (RR 0.81, 95% CI 0.63 to 1.06, P value = 0.12, I2 = 33%). We found no subgroup effect when comparing trials with the same closure methods to those with differing closure methods (test of subgroup effect P value = 0.78) (Analysis 5.1).
5.1. Analysis.
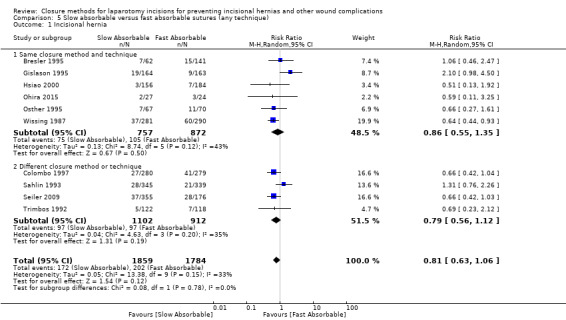
Comparison 5 Slow absorbable versus fast absorbable sutures (any technique), Outcome 1 Incisional hernia.
2. Secondary outcome: wound infection
2.1 Absorbable versus non‐absorbable sutures
We included a total of 29 studies, with 8457 participants, in the analysis of absorbable versus non‐absorbable sutures for wound infection. Overall, we found no evidence of a difference in the risk of wound infection between absorbable and non‐absorbable sutures (RR 0.99, 95% CI 0.84 to 1.17, P = 0.9, I2 = 35%). Subgroup analysis, including only those studies that compared the same closure technique and method, found similar results (test of subgroup effect P = 0.68) (Analysis 1.2).
1.2. Analysis.
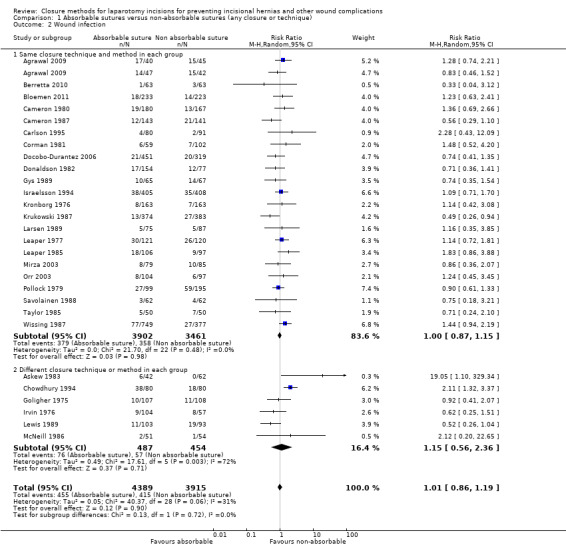
Comparison 1 Absorbable sutures versus non‐absorbable sutures (any closure or technique), Outcome 2 Wound infection.
2.2 Mass versus layered closure
We included a total of 11 studies, with 2926 participants, in the analysis of mass versus layered closure for wound infection. Overall, there was no evidence that mass versus layered closure resulted in a difference in wound infection (RR 0.93, 95% CI 0.67 to 1.30, P = 0.68, I2 = 50%). Only one study assessed mass versus layered closure, using the same type of suture and closure technique (Ausobsky 1985). There was no evidence of a subgroup effect within this analysis (P = 0.33) (Analysis 2.2).
2.2. Analysis.
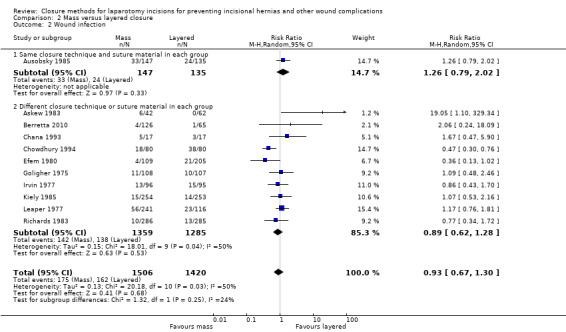
Comparison 2 Mass versus layered closure, Outcome 2 Wound infection.
2.3 Continuous versus interrupted closure
We included a total of 23 studies, with 10,039 participants, in the analysis of continuous versus interrupted closure for wound infection. There was no statistically significant evidence to suggest that interrupted sutures may result in a lower risk of wound infection (RR 1.13, 95% CI 0.96 to 1.34, P value = 0.15, I2 = 32%), We found similar results in the subgroup analysis of studies with the same closure methods and suture materials within each group (P value = 0.49) (Analysis 3.2).
3.2. Analysis.
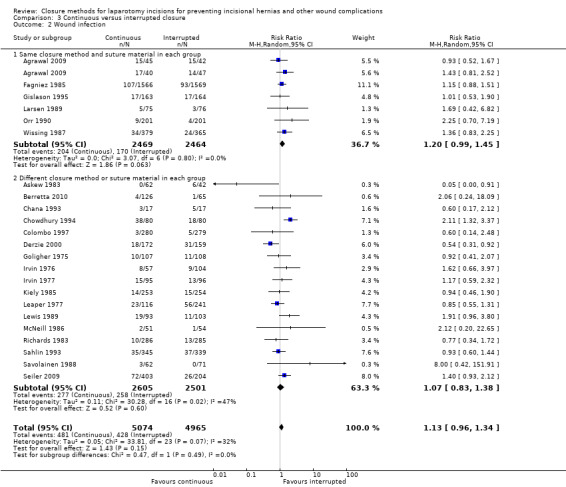
Comparison 3 Continuous versus interrupted closure, Outcome 2 Wound infection.
2.4 Monofilament versus multifilament sutures
We included a total of 23 studies, with 6557 participants, in the analysis of monofilament versus multifilament sutures for wound infection. Overall, there was no evidence of a difference in risk of wound infection between monofilament and multifilament suture materials (RR 1.08, 95% CI 0.91 to 1.28, P = 0.38, I2 = 21%). There was no evidence of a subgroup effect when we assessed trials with the same closure method and technique separately (test of subgroup differences P = 0.17) (Analysis 4.2).
4.2. Analysis.
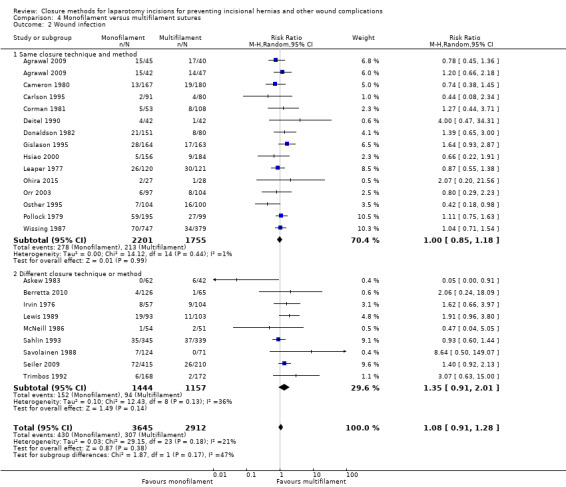
Comparison 4 Monofilament versus multifilament sutures, Outcome 2 Wound infection.
2.5 Slow absorbable versus fast absorbable sutures
We included a total of 11 studies, with 4100 participants, in the analysis of slow versus fast absorbable sutures for wound infection. There was no evidence that the rate of absorption affected the risk of wound infection (RR 1.16, 95% CI 0.85 to 1.57, P = 0.35, I2 = 36%). We found no subgroup effect when comparing trials with the same closure methods to those with differing closure methods (test of subgroup effect P value = 0.76) (Analysis 5.2).
5.2. Analysis.
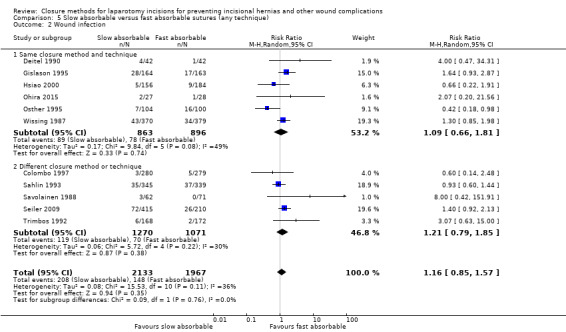
Comparison 5 Slow absorbable versus fast absorbable sutures (any technique), Outcome 2 Wound infection.
3. Secondary outcome: wound dehiscence
3.1 Absorbable versus non‐absorbable sutures
We included a total 34 studies, with 9004 participants, in the analysis of absorbable versus non‐absorbable sutures for dehiscence. Overall, we found no evidence of a difference in the risk of wound dehiscence between absorbable and non‐absorbable sutures (RR 0.78, 95% CI 0.55 to 1.10, P = 0.16, I2 = 32%). There was no evidence of a subgroup effect when comparing trials with the same closure methods to those with differing closure methods (P = 0.29) (Analysis 1.3).
1.3. Analysis.
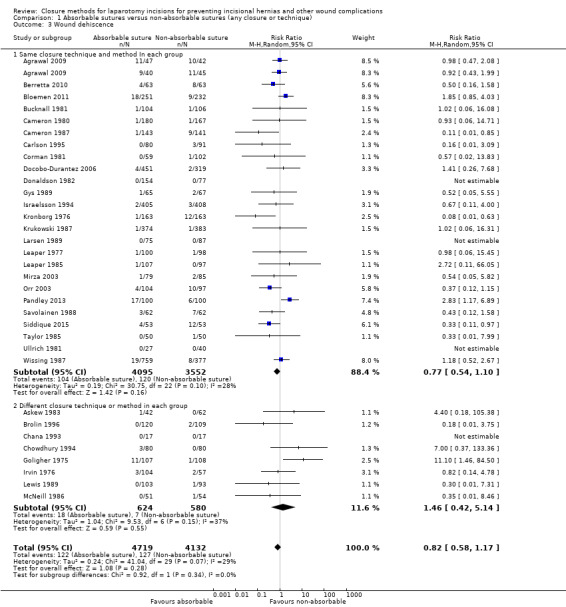
Comparison 1 Absorbable sutures versus non‐absorbable sutures (any closure or technique), Outcome 3 Wound dehiscence.
3.2 Mass versus layered closure
We included a total of 11 studies, with 2863 participants, in the analysis of mass versus layered closure for dehiscence. Overall, there was no conclusive evidence to suggest that layered closure may decrease wound dehiscence (RR 0.69, 95% CI 0.31 to 1.52, P = 0.35, I2 = 25%). Only one study assessed mass versus layered closure, using the same type of suture and closure technique (Ausobsky 1985). There was no evidence of a subgroup effect within this analysis (P = 0.75) (Analysis 2.3).
2.3. Analysis.
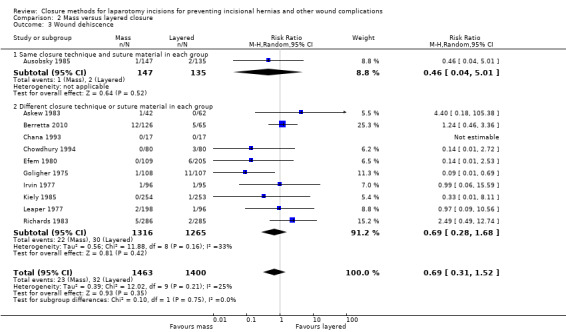
Comparison 2 Mass versus layered closure, Outcome 3 Wound dehiscence.
3.3 Continuous versus interrupted closure
We included a total of 21 studies, with 9228 participants, in the analysis of continuous versus interrupted closure for dehiscence. The use of continuous or interrupted closure technique did not affect the risk of dehiscence (RR 1.21, 95% CI 0.90 to 1.64, P = 0.21, I2 = 17%). There was no evidence of a subgroup effect, when analysing studies using a similar suture material and closure method (P = 0.76). (Analysis 3.3).
3.3. Analysis.
Comparison 3 Continuous versus interrupted closure, Outcome 3 Wound dehiscence.
3.4 Monofilament versus multifilament sutures
We included a total of 22 studies, with 6199 participants, in the analysis of monofilament versus multifilament sutures for dehiscence. Overall, there was no evidence that monofilament sutures increased the risk of dehiscence, compared to multifilament sutures (RR 1.24, 95% CI 0.93 to 1.67, P = 0.15, I2 = 0%). There was no evidence of a subgroup effect when we assessed trials with the same closure method and technique separately (test of subgroup differences P = 0.56) (Analysis 4.3).
4.3. Analysis.
Comparison 4 Monofilament versus multifilament sutures, Outcome 3 Wound dehiscence.
3.5 Slow absorbable versus fast absorbable sutures
We included a total of eight studies, with 3440 participants, in the analysis of slow versus fast absorbable sutures for dehiscence. There was no evidence to suggest that slow absorbable sutures may increase the risk of dehiscence (RR 1.55, 95% CI 0.92 to 2.61, P = 0.10, I2 = 0%). We found no subgroup effect when comparing trials with the same closure methods to those with differing closure methods (test of subgroup effect P value = 0.42) (Analysis 5.3).
5.3. Analysis.
Comparison 5 Slow absorbable versus fast absorbable sutures (any technique), Outcome 3 Wound dehiscence.
4. Secondary outcome: wound sinus or fistula formation
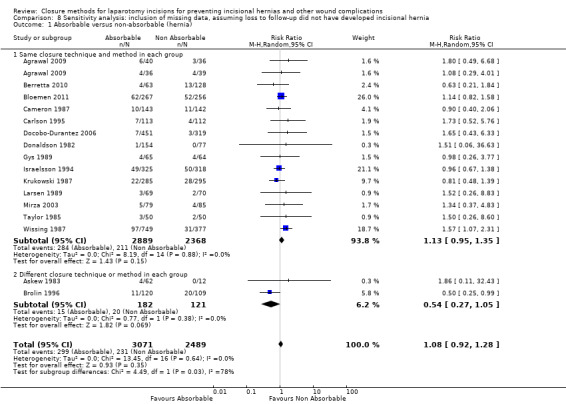
4.1 Absorbable versus non‐absorbable sutures
We included a total of 19 studies, with 5470 participants, in the analysis of absorbable versus non‐absorbable sutures for wound sinus or fistula formation. Overall, we found evidence that absorbable sutures decreased the risk of sinus or fistula tract formation (RR 0.49, 95% CI 0.26 to 0.94, P = 0.03, I2 = 52%). Subgroup analysis, including only those studies that compared the same closure technique and method, demonstrated similar results, with no evidence of a subgroup effect (P = 0.51) (Analysis 1.4).
1.4. Analysis.
Comparison 1 Absorbable sutures versus non‐absorbable sutures (any closure or technique), Outcome 4 Sinus or fistula formation.
4.2 Mass versus layered closure
We included a total of six studies, with 1076 participants, in the analysis of mass versus layered closure for sinus or fistula tract formation. Mass versus layered closure did not result in a difference in terms of fistula or sinus formation (RR 0.49, 95% CI 0.15 to 1.62, P = 0.24, I2 = 38%). Only one study assessed mass versus layered closure, using the same type of suture and closure technique (Ausobsky 1985). There was no evidence of a subgroup effect within this analysis (P = 0.55) (Analysis 2.4).
2.4. Analysis.
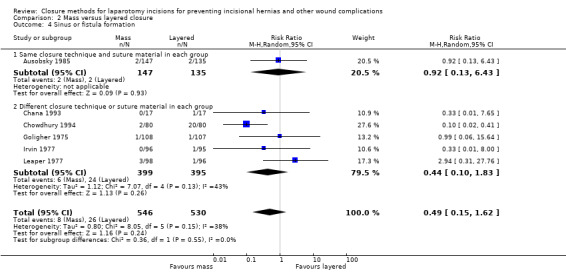
Comparison 2 Mass versus layered closure, Outcome 4 Sinus or fistula formation.
4.3 Continuous versus interrupted closure
We included a total of 10 studies, with 5082 participants, in the analysis of continuous versus interrupted closure for sinus or fistula formation. The use of continuous or interrupted closure technique did not appear to affect the risk of sinus or fistula tract formation (RR 1.51, 95% CI 0.64 to 3.61, P = 0.35, I2 = 57%). There was evidence of a subgroup effect (P = 0.005), although the analysis of studies with the same suture material and closure method found no evidence of a difference in sinus or fistula tract formation (RR 0.76, 95% CI 0.51 to 1.12, P = 0.17, I2 = 0%) (Analysis 3.4).
3.4. Analysis.
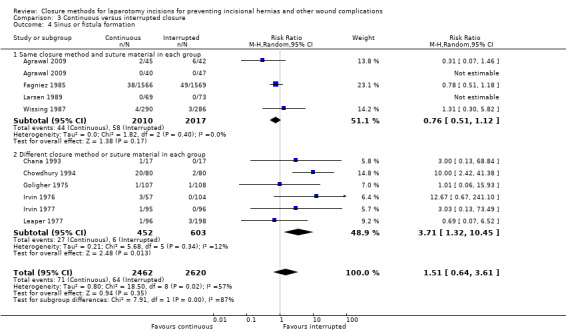
Comparison 3 Continuous versus interrupted closure, Outcome 4 Sinus or fistula formation.
4.5 Monofilament versus multifilament sutures
We included a total of eight studies, with 2285 participants, in the analysis of monofilament versus multifilament sutures for sinus or fistula tract formation. There was no evidence that the risk of sinus or fistula formation was increased with the use of monofilament versus multifilament suture materials (RR 1.91, 95% CI 0.77 to 4.73, P = 0.16, I2 = 51%). There was no evidence of a subgroup effect when we assessed trials with the same closure method and technique separately (P = 0.87) (Analysis 4.4).
4.4. Analysis.
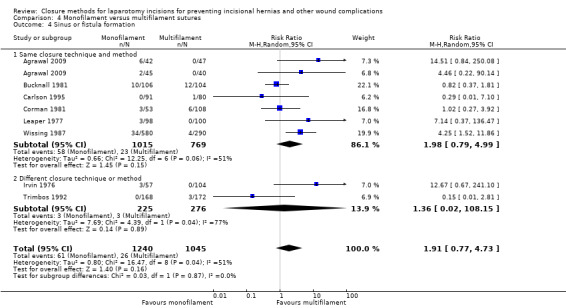
Comparison 4 Monofilament versus multifilament sutures, Outcome 4 Sinus or fistula formation.
4.6 Slow absorbable versus fast absorbable sutures
We included a total of two studies, with 911 participants, in the analysis of slow versus fast absorbable sutures for sinus or fistula formation. There was no evidence that the rate of absorption affected the risk of sinus or fistula formation (RR 0.88, 95% CI 0.05 to 16.05, P = 0.93, I2 = 72%). There was no significant evidence of a subgroup effect between the two studies (P = 0.07), (Analysis 5.4).
5.4. Analysis.
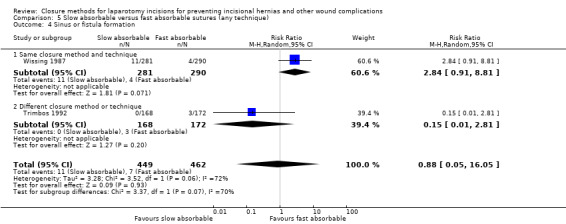
Comparison 5 Slow absorbable versus fast absorbable sutures (any technique), Outcome 4 Sinus or fistula formation.
5. Subgroup analyses
5.1 Effect of the type of incision
Of the included studies, 24 included participants who underwent a midline incision only (Agrawal 2009; Agrawal 2014; Berretta 2010; Bloemen 2011; Brolin 1996; Carlson 1995; Colombo 1997; Dan 2014; Deitel 1990; Efem 1980; Fagniez 1985; Israelsson 1994; Krukowski 1987; Lewis 1989; McNeill 1986; Ohira 2015; Orr 2003; Pandley 2013; Savolainen 1988; Seiler 2009; Siddique 2015; Taylor 1985; Trimbos 1992; Wissing 1987), and two included participants who underwent a paramedian incision only (Donaldson 1982; Goligher 1975). No other types of incisions were looked at in isolation by any of the included trials. Of the remaining studies, they either included a combination of the incision types, or did not specify the type of incision(s). Due to the small number of papers only studying paramedian incisions, we conducted a subgroup analysis for midline incisions only.
There were not enough studies reporting results for those having a midline incision within the fast absorbable versus slow absorbable comparison to complete the subgroup analysis for the outcomes in midline‐only incisions. A comparison of mass versus layered closure for midline‐only incisions seemed clinically implausible as all midline incisional closures should be mass by definition (with the exception of the peritoneum which was not of interest/excluded for the purposes of this review).
For trials that compared absorbable to non‐absorbable sutures, with the same closure methods and techniques between groups, we found no evidence of a difference between absorbable and non‐absorbable sutures in terms of hernia (RR 1.13, 95% CI 0.95 to 1.34, P = 0.15, I2 = 0%) and no subgroup effect with midline incisions compared with all other types of incision (P = 0.91) (Analysis 1.5). Similarly, we found no evidence of a difference between continuous and interrupted sutures in terms of hernia in those who had a midline incision (RR 1.19, 95% CI 0.86 to 1.64, P = 0.29, I2 = 0%) and no subgroup effect with midline incision compared to all other types of incision (P = 0.78) (Analysis 3.5).
1.5. Analysis.
Comparison 1 Absorbable sutures versus non‐absorbable sutures (any closure or technique), Outcome 5 Hernia and type of incision.
3.5. Analysis.
Comparison 3 Continuous versus interrupted closure, Outcome 5 Hernia and type of incision.
There was no evidence of a subgroup effect between participants with a midline incision versus other incisions, when comparing monofilament and multifilament sutures (P value = 0.24). However, when we analysed participants undergoing midline incision alone in isolation, monofilament sutures decreased the risk of incisional hernia, compared with multifilament closure (RR 0.62, 95% CI 0.47 to 0.81, P = 0.0005) (Analysis 4.5).
4.5. Analysis.
Comparison 4 Monofilament versus multifilament sutures, Outcome 5 Hernia and type of incision.
5.2 Effect of acuity of surgery
There was only one study that assessed emergent participants only (Agrawal 2009). As such, we were unable to perform a subgroup analysis to determine the effect of emergent versus elective participants on the association between the interventions and our primary outcome. Other studies that included both elective and emergent surgeries did not discriminate between these acuities when presenting their results.
5.3 Effect of wound contamination classification
Of the 55 studies, only 20 provided information for contamination classification distribution within each experimental group. The proportion of clean, clean‐contaminated, contaminated and dirty wounds varied greatly within these studies, and as such we could not perform any formal analysis to determine how this affected our analysis.
6. Sensitivity analysis
6.1 Excluding high risk of bias and multiple comparison studies
After excluding trials that had at least one category of 'high risk of bias' and trials that compared groups that differed by more than one component, we undertook a sensitivity analysis for our primary outcome, incisional hernia.
For the absorbable versus non‐absorbable analysis (Analysis 6.1), across nine qualifying studies with 2949 participants, there was no significant effect seen (RR 1.21, 95% CI 0.98 to 1.49, P = 0.07, I2 = 0%).
6.1. Analysis.
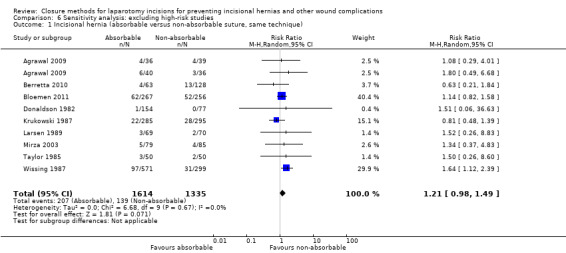
Comparison 6 Sensitivity analysis: excluding high‐risk studies, Outcome 1 Incisional hernia (absorbable versus non‐absorbable suture, same technique).
In the continuous versus interrupted analysis of three studies with 869 participants (Analysis 6.2), the sensitivity analysis was similar to the overall analysis, in showing no evidence of a difference in hernia, by technique (RR 1.20, 95% CI 0.87 to 1.64, P = 0.26, I2 = 0%).
6.2. Analysis.
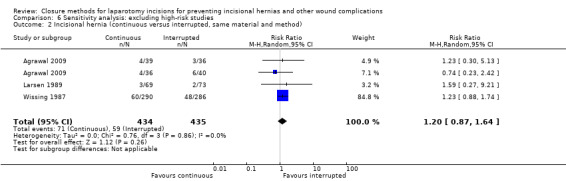
Comparison 6 Sensitivity analysis: excluding high‐risk studies, Outcome 2 Incisional hernia (continuous versus interrupted, same material and method).
For the analysis of monofilament versus multifilament sutures (Analysis 6.3), the sensitivity analysis of five studies with 1336 participants resulted in the same direction of effect (favouring monofilament sutures) (RR 0.65, 95% CI 0.42 to 1.01, P = 0.05, I2 = 9%).
6.3. Analysis.
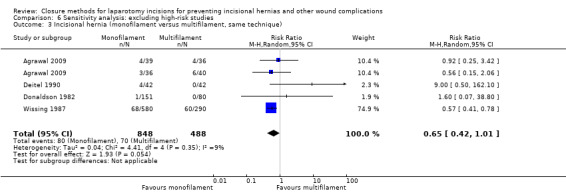
Comparison 6 Sensitivity analysis: excluding high‐risk studies, Outcome 3 Incisional hernia (monofilament versus multifilament, same technique).
We did not undertake a sensitivity analysis in the fast versus slow absorbable sutures comparison or in the mass versus layered analysis, as there was an insufficient number of trials with a low risk of bias to analyse (Table 8).
3. Findings from previous analyses for incisional hernia.
| Absorbable versus non‐absorbable | Mass versus layered | Continuous versus interrupted closure | Slow versus fast absorbable | |
| Hodgson 2000 | Favours non‐absorbable sutures (13 trials) | N/A | Favours continuous closure (6 trials) | N/A |
| Rucinski 2001 | Favours non‐absorbable sutures over braided absorbable (unclear number of trials) | N/A | N/A | N/A |
| Sajid 2011 | No difference (8 trials) | N/A | N/A | N/A |
| Van't Riet 2002 | No difference between slow absorbable and non‐absorbable sutures (5 trials) | N/A | No difference (7 trials) | Favours slow absorbable sutures (1 trial) |
| Weiland 1998 | Favours non‐absorbable sutures (7 studies) | Favours layered closure (9 studies) | Favours continuous closure (8 trials) | N/A |
6.2 Accounting for missing data in studies with high losses to follow‐up
Eight studies that had a high risk of bias due to incomplete outcome data (i.e. high losses to follow‐up) assessed hernia as an outcome (Askew 1983; Cameron 1987; Carlson 1995; Docobo‐Durantez 2006; Gislason 1995; Gys 1989; Sahlin 1993; Wissing 1987). Of these, two did not have group‐wise data available for inclusion in this sensitivity analysis (Gys 1989; Sahlin 1993). To account for missing data, we undertook two series of sensitivity analyses. The first (Analysis 7.1; Analysis 7.2; Analysis 7.3; Analysis 7.4; Analysis 7.5) assumed that all those lost to follow‐up all developed an incisional hernia. The second (Analysis 8.1; Analysis 8.2; Analysis 8.3; Analysis 8.4; Analysis 8.5) assumed all those lost to follow‐up did not develop an incisional hernia.
7.1. Analysis.
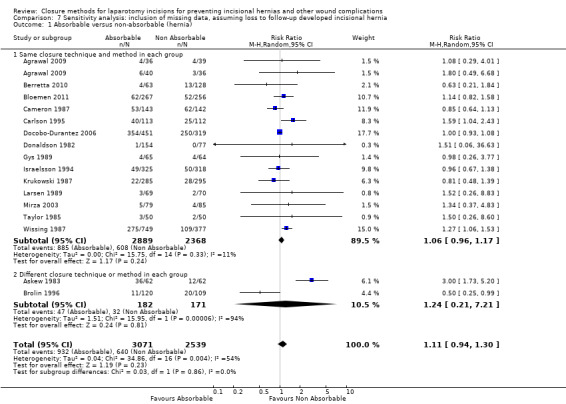
Comparison 7 Sensitivity analysis: inclusion of missing data, assuming loss to follow‐up developed incisional hernia, Outcome 1 Absorbable versus non‐absorbable (hernia).
7.2. Analysis.
Comparison 7 Sensitivity analysis: inclusion of missing data, assuming loss to follow‐up developed incisional hernia, Outcome 2 Mass versus layered closure (hernia).
7.3. Analysis.
Comparison 7 Sensitivity analysis: inclusion of missing data, assuming loss to follow‐up developed incisional hernia, Outcome 3 Continuous versus interrupted.
7.4. Analysis.
Comparison 7 Sensitivity analysis: inclusion of missing data, assuming loss to follow‐up developed incisional hernia, Outcome 4 Monofilament versus multifilament (hernia).
7.5. Analysis.
Comparison 7 Sensitivity analysis: inclusion of missing data, assuming loss to follow‐up developed incisional hernia, Outcome 5 Slow absorbable versus fast absorbable (hernia).
8.1. Analysis.
Comparison 8 Sensitivity analysis: inclusion of missing data, assuming loss to follow‐up did not have developed incisional hernia, Outcome 1 Absorbable versus non‐absorbable (hernia).
8.2. Analysis.
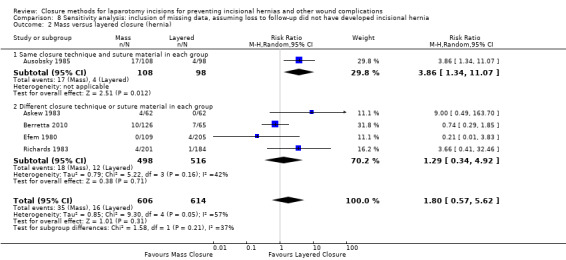
Comparison 8 Sensitivity analysis: inclusion of missing data, assuming loss to follow‐up did not have developed incisional hernia, Outcome 2 Mass versus layered closure (hernia).
8.3. Analysis.
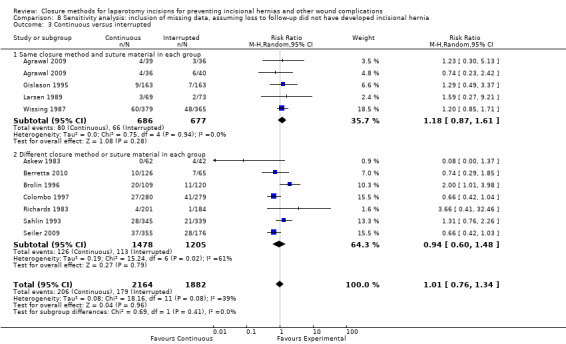
Comparison 8 Sensitivity analysis: inclusion of missing data, assuming loss to follow‐up did not have developed incisional hernia, Outcome 3 Continuous versus interrupted.
8.4. Analysis.
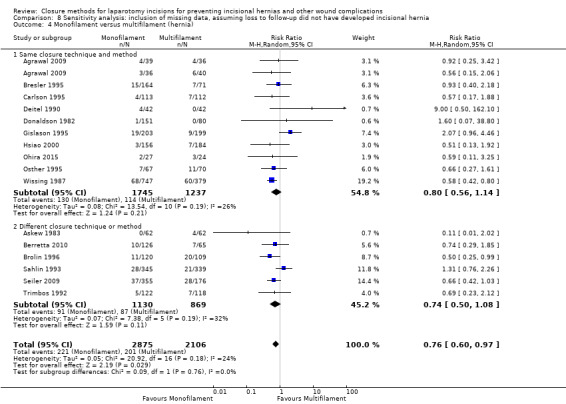
Comparison 8 Sensitivity analysis: inclusion of missing data, assuming loss to follow‐up did not have developed incisional hernia, Outcome 4 Monofilament versus multifilament (hernia).
8.5. Analysis.
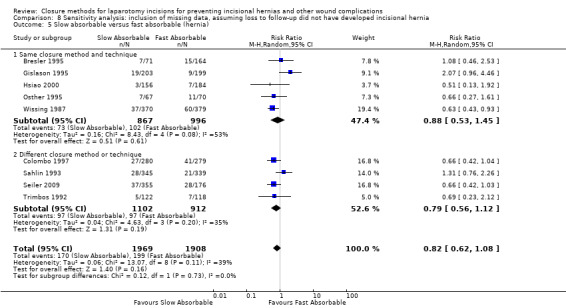
Comparison 8 Sensitivity analysis: inclusion of missing data, assuming loss to follow‐up did not have developed incisional hernia, Outcome 5 Slow absorbable versus fast absorbable (hernia).
In the first series of analyses where hernia was assumed in those lost to follow‐up, we found the following results: absorbable versus non‐absorbable sutures, no difference (RR 1.10, 95% CI 0.93 to 1.30, P = 0.28, I2 =54%); mass versus layered closure, no difference (RR 1.82, 95% CI 0.81 to 4.10, P = 0.15, I2 = 59%); continuous versus interrupted closure, no difference (RR 0.92, 95% CI 0.67 to 1.26, P = 0.58, I2 = 64% RR 0.89, 95% CI 0.61 to 1.30, P = 0.55, I2 = 76%); monofilament versus multifilament sutures, significantly less hernia in the monofilament population (RR 0.77, 95% CI 0.63 to 0.95, P = 0.01, I2 = 43%); and slow versus fast absorbable suture material, no difference (RR 0.89, 95% CI 0.74 to 1.07, P = 0.21, I2 = 27%).
In the second series of analyses where no hernia was assumed in those lost to follow‐up, we found the following results: absorbable versus non‐absorbable sutures, no difference (RR 1.07, 95% CI 0.91 to 1.27, P = 0.40, I2 = 0%); mass versus layered closure, no difference (RR 1.80, 95% CI 0.57 to 5.62, P = 0.31, I2 = 57%); continuous versus interrupted closure, no difference (RR 1.01, 95% CI 0.76 to 1.34, P = 0.96, I2 = 39%); monofilament versus multifilament sutures, significantly less hernia in the monofilament population (RR 0.76, 95% CI 0.60 to 0.97, P = 0.03, I2 = 24%); and slow versus fast absorbable suture material, no difference (RR 0.82, 95% CI 0.62 to 1.08, P = 0.16, I2 = 39%).
Furthermore four studies with high attrition bias are missing from the above list (Bresler 1995; Cameron 1980; Leaper 1985; Ullrich 1981). Data from Bresler 1995 is included in sensitivity analysis for monofilament versus multifilament and slow absorbable versus fast absorbable. Data from Cameron 1980 and Leaper 1985 was not included in hernia analysis due to inadequate duration of follow up, which is why the data are not included in the sensitivity analysis. Furthermore data from Ulrich 1981 did not assess hernia as an outcome.
7. Publication bias
We assessed publication bias for the incisional hernia outcome. We examined three analyses (absorbable versus non‐absorbable sutures, continuous versus interrupted closure, and monofilament versus multifilament sutures), each including at least 10 trials (Figure 4; Figure 5; Figure 6). In these funnel plots there appears to be adequate symmetry, suggesting no overt publication bias.
5.
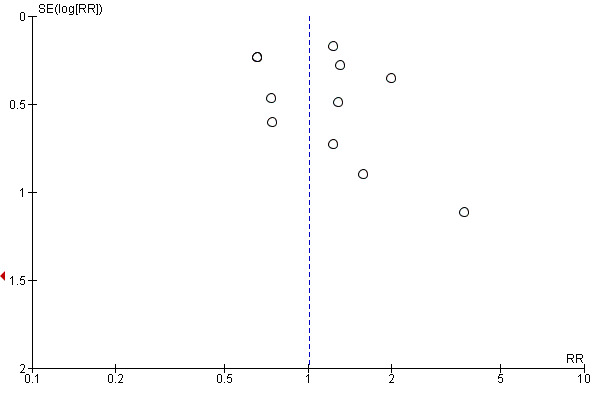
Funnel plot of comparison 3. Continuous versus interrupted closure, outcome 3.1: incisional hernia
6.
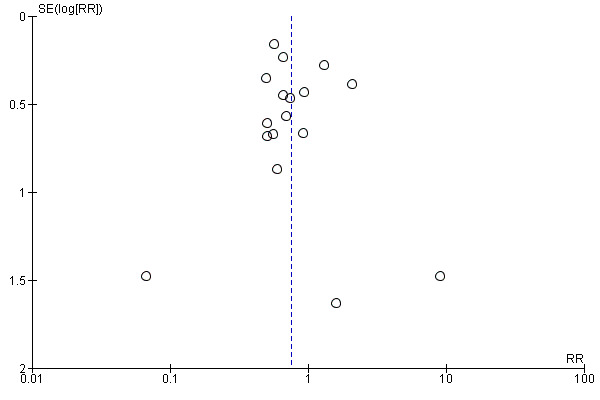
Funnel plot of comparison 4. Monofilament versus multifilament sutures, outcome 4.1: incisional hernia
Discussion
Summary of main results
This review included 55 studies that assessed the effects of suture materials, and closure techniques and methods on the development of incisional hernia, wound infection, wound dehiscence, or sinus or fistula tract formation. The combination of suture material (absorbable or non‐absorbable, monofilament or multifilament, fast or slow absorbable), suture technique (continuous or interrupted) and closure method (mass or layered) differed greatly between studies. As such, our focus was on determining the outcomes associated with each individual component.
Absorbable versus non‐absorbable sutures
Despite the hypothesis that non‐absorbable sutures would result in less incisional hernia formation, we did not find evidence of this effect when assessing and including all applicable trials. Even within the subgroup analysis, excluding those trials with differing technique and methods, there was no evidence that a treatment difference exists.
In terms of the other outcomes assessed, absorbable sutures decreased the risk of sinus or fistula tract formation (risk ratio (RR) 0.49, 95% confidence interval (CI) 0.26 to 0.94). There was high heterogeneity within this outcome (I2 = 52%). Heterogeneity was reduced when we assessed studies comparing groups with the same closure technique and methods as a subgroup (I2 = 22%). We did not find evidence that absorbable or non‐absorbable sutures reduced the risk of dehiscence or wound infection.
Mass versus layered closure
Few studies assessed the effect of mass versus layered closure on the risk of hernia formation. Overall, there was no evidence that mass or layered closure resulted in a higher risk of hernia. Only one study compared mass versus layered closures, using the same suture material and closure technique in each group (Ausobsky 1985). This study found that mass closure increased the risk of hernia, but it suffered from methodological deficiencies (unclear method of randomisation, unclear allocation concealment and unclear blinding of wound assessors). As such, the confidence we can have in this conclusion is low.
For the secondary outcomes, it appeared that mass or layered closure had no effect on wound infections, wound dehiscence or sinus or fistula tract formation. These outcomes suffered from the fact that only one study had a common suture material and closure technique between groups (Ausobsky 1985).
Continuous versus interrupted closure
We found no benefit of continuous or interrupted closure in terms of hernia risk. Subgroup analysis and sensitivity analysis did not show any evidence that one technique or another resulted in a decrease in the risk of hernia. None of the secondary outcomes (wound infection, dehiscence or sinus or fistula formation) was associated with continuous or interrupted closure. Neither wound dehiscence nor sinus or fistula tract formation seemed to be affected by the closure technique.
Monofilament versus multifilament sutures
The risk of hernia was reduced with monofilament sutures (RR 0.76, 95% CI 0.59 to 0.98). Despite the commonly held belief that multifilament sutures are associated with an increased risk of wound infection, we found no evidence of this within our analysis. The risk of dehiscence was not different between monofilament and multifilament sutures (RR 1.24, 95% CI 0.93 to 1.67). Sinus or fistula tract formation was not affected by monofilament or multifilament sutures (RR 1.91, 95% CI 0.77 to 4.73). This result had high heterogeneity (I2 = 51%), which was not resolved with subgroup analysis. This heterogeneity may have been persistent, as only one study defined the outcome adequately (Wissing 1987). In addition, there was variable duration of follow‐up to assess this outcome (from three months to two years).
Slow versus fast absorbable sutures
There did not appear to be a benefit for slow or fast absorbable sutures for hernia formation, wound infection or sinus formation. There was evidence to suggest a potential increase in dehiscence with slow absorbable sutures (RR 1.55, 95% CI 0.92 to 2.61). The finding that slow absorbable sutures may increase the risk of dehiscence is difficult to explain, as we expected that the longer duration of absorption would result in reinforcement of the wound edges for a longer period of time. One possible explanation for this may be the knot characteristics of polydioxanone versus Vicryl, etc. with the former, commonly‐used slow absorbable suture material having much poorer handling and knotting profiles than the latter, common absorbable suture agent.
Midline incision
We undertook subgroup analyses to determine whether incidence of the primary outcome (hernia) was affected by the type of incision; sufficient data were available only for midline incision. We found no evidence of a subgroup effect in the absorbable versus non‐absorbable sutures or continuous versus layered closure comparisons. For the monofilament versus multifilament comparison, we did find evidence of subgroup effect. The effect estimate favoured monofilament sutures in both the overall analysis as well as the midline incision subgroup.
Overall completeness and applicability of evidence
The primary objective of this review was to determine what a surgeon can do in terms of technique and material selection to prevent hernia, wound infection, wound dehiscence, and sinus or fistula formation following closure of a laparotomy incision. We assessed the surgeon‐controlled risk factors (the choice of closure material and techniques), which have been implicated in closure failure in previous reviews. It is important to remember that patient factors (e.g. diabetes) and surgical pathology (e.g perforated diverticulitis with fecal peritonitis) also affect the risk of surgical wound complications, but the surgeon has no control over these.
The most discussed technique that was not included in this review was the short‐stitch method described by Millbourn 2009 and others, as these trials had not been published at the time of acceptance of this study protocol. Although the early results appear promising, a limited number of trials are available for review.
The evidence presented in this review is applicable to any patient undergoing a laparotomy closure. We were able to identify over 19,000 participants from 55 studies for inclusion. This was a heterogeneous patient population and included patients undergoing emergency and elective procedures.
Quality of the evidence
Primary outcome, incisional hernia
We assessed the quality of evidence for each intervention using the methods described by Guyatt 2008. The quality of evidence can be found in Table 1; Table 2; Table 3; Table 4; and Table 5. For our primary outcome, incisional hernia, we found that there was moderate‐quality evidence for absorbable versus non‐absorbable sutures, continuous versus interrupted closure, monofilament versus multifilament sutures and slow versus fast absorbable sutures. We downgraded this outcome within these comparisons due to serious concerns regarding methodological quality and risk of bias. A rating of moderate quality (by definition) indicates that future research may have an important impact on our confidence in the estimate and may change the estimate (Guyatt 2008).
We graded the quality of evidence as very low for the mass versus layered closure outcomes. We downgraded this outcome for serious concerns about methodological quality, inconsistency and imprecision (few trials, with wide confidence intervals). A very low‐quality grade indicates that we are very uncertain about the estimate and that future research is definitely required to better the estimate (Guyatt 2008).
Secondary outcomes
Comparing absorbable to non‐absorbable sutures, we graded the quality of evidence for wound infections and dehiscence as moderate (downgraded for concerns about methodological quality), while we graded the quality of the evidence for sinus and fistula tract formation as low (downgraded for both poor methodological quality and inconsistency).
In the mass versus layered comparison, we graded the quality of the evidence for wound dehiscence as moderate (downgraded for concerns regarding risk of bias). We graded the quality of evidence for both sinus and fistula tract formation and wound infection as low (downgraded for methodological quality and inconsistency).
For the continuous versus interrupted outcomes, monofilament versus multifilament outcomes and slow versus fast absorbable sutures outcomes, we graded the quality of the evidence for wound infections and dehiscence as moderate (downgraded for concerns about methodological quality), while we graded the quality of the evidence for sinus or fistula tract formation as very low (downgraded for poor methodological quality, inconsistency and imprecision).
Potential biases in the review process
We minimised potential biases in the review process through duplication of study screening and data collection. We translated and included foreign language trials. We assessed all relevant studies and included them if they met our inclusion criteria. We included a transparent search strategy and full details of why we excluded studies from analysis. Additional sources of potential bias include the decision to base analyses on intention‐to‐treat analyses, or the decision to only include trials with a follow‐up of more than one year for the primary outcome, incisional hernia. Finally other potential sources of bias include the variability in the definition of individual studies of a hernia, wound infection and sinus.
Agreements and disagreements with other studies or reviews
There have been several previous meta‐analyses assessing at least one of our comparisons (Hodgson 2000; Rucinski 2001; Sajid 2011; Van't Riet 2002; Weiland 1998).
Hodgson 2000 identified 13 trials for inclusion, and compared the effect of non‐absorbable versus absorbable sutures and six trials comparing continuous versus interrupted sutures. They found a reduced odds of hernia with non‐absorbable sutures (odds ratio (OR) 0.68, 95% CI 0.52 to0.87), with no evidence of a difference in wound infection or dehiscence between groups. Sinus formation was higher in the non‐absorbable sutures groups (OR 2.18, 95% CI 1.48 to 3.22). Continuous closure was found to decrease the odds of hernia (OR 0.73, 95% CI 0.55 to 0.99), with no difference in the odds of wound infection or dehiscence.
Rucinski 2001 assessed non‐absorbable versus absorbable braided sutures or absorbable monofilament sutures (the number of trials is unclear). They found that the use of absorbable braided sutures increased the risk of hernia, compared with non‐absorbable sutures (RR 1.93, 95% CI 1.35 to 2.76), with no difference between monofilament absorbable and non‐absorbable sutures.
Sajid 2011 compared slow absorbable sutures (polydioxanone) to non‐absorbable sutures. Using eight trials, they found no difference in incisional hernia, wound infection, dehiscence or sinus formation.
Van't Riet 2002 compared continuous versus interrupted closure, as well fast absorbable versus slow absorbable, fast absorbable versus non‐absorbable and slow absorbable versus non‐absorbable sutures. They found non‐absorbable sutures and slow absorbable sutures decreased the risk of hernia formation (one study for each analysis). They found no difference in hernia formation in the slow absorbable versus non‐absorbable sutures comparison (five studies). Interrupted or continuous closure did not appear to affect incisional hernia risks. They did not find a difference in wound infections or wound dehiscence in any of the comparisons (slow versus fast absorbable, slow versus non‐absorbable, fast versus non‐absorbable, continuous versus interrupted closure).
Weiland 1998 compared continuous versus interrupted sutures, absorbable versus non‐absorbable sutures and mass versus layered closures. They found that continuous sutures decreased hernia (seven studies) and wound infection (eight studies). They also found that non‐absorbable sutures decreased hernia compared with absorbable sutures in continuous closures (seven studies) and interrupted closures (three studies). No difference was seen in wound infections. Dehiscence was less in the non‐absorbable groups versus the absorbable group for both continuous closures (seven studies) and interrupted closures (four studies). Layered closures were found to decrease hernia over mass closure (nine studies). This meta‐analysis included two non‐randomised controlled trials.
None of the reviews specifically addressed monofilament versus multifilament sutures. Of these reviews, only the one by van't Riet specified a required follow‐up duration for inclusion in analysis (Van't Riet 2002).
A summary of the findings from these meta‐analyses for incisional hernia can be found in Table 8. We found no evidence of a difference between absorbable and non‐absorbable sutures (16 trials), although the effect estimate favoured non‐absorbable sutures. We found no difference between mass and layered closures (five trials), which differs from the study by Weiland 1998. The previous study did not have clear criteria for follow‐up duration for hernia, and this likely explains the differences in our results. Our results showed no difference between continuous and interrupted sutures (11 trials), whereas two previous meta‐analyses did find a reduction in hernia (Hodgson 2000; Weiland 1998). However, our analysis incorporated more studies and previous analyses did not define a required follow‐up duration.
Authors' conclusions
Implications for practice.
We investigated the effect of suture material, method and technique for laparotomy closure on hernia occurrence and other important outcomes. Due to limitations in the quality of included studies, we cannot draw firm conclusions on suture material, closure method and technique. We do not have evidence to determine the best type of suture material (absorbable versus non‐absorbable; fast absorbable versus slow absorbable) or closure method (continuous versus interrupted, mass versus layered) to reduce hernia in patients undergoing a laparotomy. Monofilament sutures may reduce the risk of hernia in patients and can be considered (compared with multifilament sutures).
Implications for research.
This review has assessed many trials that have attempted to compare the effects of suture materials, methods or techniques on several important outcomes. The main limitation of this review was the study design and reporting limitations of many of the included trials. We felt that only a small proportion of trials did not have at least one category of 'high risk of bias'. This review has not definitively resolved the question of which materials and methods are best for wound outcomes. As such, surgeons should demand the performance of further, higher‐quality research on this topic.
The mass versus layered comparison was based on a small number of trials, with all but one comparing more than one intervention between groups. As such, there is a role for further work in this area.
With these factors in mind, further trials assessing laparotomy closure need to be more rigorously performed and reported. Adequate randomisation and allocation techniques, blinding of outcome assessors and adequate follow‐up for long‐term hernia outcomes are essential. In addition, it is important that future trials only compare one closure component between groups. Many of the included trials compared a combination of materials, methods or techniques, and thus it was difficult to determine the effect of each component on the outcomes. At the very least, trials seeking to assess multiple components should employ factorial designs.
Acknowledgements
We acknowledge Cochrane Colorectal Cancer Group and peer reviewers for their assistance with this review.
Appendices
Appendix 1. CENTRAL search strategy
#1 (sutur* near (continuous* or interrupt* or length))
#2 (closur* near (mass or layer*))
#3 (#1 OR #2)
#4 (sutur*)
#5 MeSH descriptor Sutures explode all trees
#6 (silk)
#7 MeSH descriptor Silk explode all trees
#8 (capromed dc)
#9 (stapling or staples)
#10 MeSH descriptor Surgical Staplers explode all trees
#11 (polydioxanone)
#12 MeSH descriptor Polydioxanone explode all trees
#13 (pds)
#14 (polypropylene*)
#15 MeSH descriptor Polypropylenes explode all trees
#16 (prolene*)
#17 MeSH descriptor Polyglactin 910 explode all trees
#18 (polyglactin 910)
#19 (ethilon)
#21 MeSH descriptor Nylons explode all trees
#22 (catgut)
#23 MeSH descriptor Catgut explode all trees
#24 (steel)
#25 MeSH descriptor Steel explode all trees
#26 (vicryl)
#27 (polyglycolic acid)
#28 MeSH descriptor Polyglycolic Acid explode all trees
#29 (maxon)
#30 (mersilene*)
#31 (#4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18 OR #19 OR #20 OR #21 OR #22 OR #23 OR #24 OR #25 OR #26 OR #27 OR #28 OR #29 OR #30)
#32 (#3 OR #31)
#33 (laparotomy)
#34 MeSH descriptor Laparotomy explode all trees
#35 (hysterectomy)
#36 MeSH descriptor Hysterectomy explode all trees
#37 (abdom* )
#38 MeSH descriptor Abdomen explode all trees
#39 (#37 OR #38)
#40 (injury)
#41 MeSH descriptor Abdominal Injuries explode all trees
#42 (wall)
#43 MeSH descriptor Abdominal Wall explode all trees
#44 (hernia)
#45 MeSH descriptor Hernia, Abdominal explode all trees
#46 (surger*)
#47 (closure*)
#48 (fascia*)
#49 MeSH descriptor Fascia explode all trees
#50 (wound)
#51 (#40 OR #41 OR #42 OR #43 OR #44 OR #45 OR #46 OR #47 OR #48 OR #49 OR #50)
#52 (#39 AND #51)
#53 (#33 OR #34 OR #35 OR #36 OR #37 OR #38 OR #52)
#54 (#32 AND #53)
#55 (rat* or rabbit* or rect* or anal* or laparoscop*):ti
#56 (#54 NOT #55)
Appendix 2. MEDLINE (Ovid) search strategy
1. (sutur* adj3 (continuous* or interrupt* or length)).mp.
2. (closur* adj3 (mass or layer*)).mp.
3. 1 or 2
4. (sutur* or silk or capromed or stapling or staples or polydioxanone* or pds or polypropylene* or prolene* or polyglactin 910 or polyglactin or ethilon or nylon* or catgut or steel or vicryl or polyglycolic acid or maxon or mersilene*).mp.
5. exp Sutures/
6. exp Silk/
7. exp Surgical Staplers/
8. exp Polydioxanone/
9. exp Polypropylenes/
10. exp Polyglactin 910/
11. exp Nylons/
12. exp Catgut/
13. exp Steel/
14. exp Polyglycolic Acid/
15. 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14
16. 3 or 15
17. (laparotom* or hysterectom*).mp.
18. exp Laparotomy/
19. exp Hysterectomy/
20. (abdom* adj3 (injury or wall or defect or hernia or surger* or closure* or fascia* or wound)).mp.
21. exp Abdomen/
22. exp Abdominal Injuries/
23. Abdominal Wall/
24. exp Hernia, Abdominal/
25. exp Fascia/
26. 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24 or 25
27. 16 and 26
28. randomized controlled trial.pt.
29. controlled clinical trial.pt.
30. randomized.ab.
31. placebo.ab.
32. clinical trials as topic.sh.
33. randomly.ab.
34. trial.ti.
35. 28 or 29 or 30 or 31 or 32 or 33 or 34
36. exp animals/ not humans.sh.
37. 35 not 36
38. 27 and 37
39. (rat* or rabbit* or rect* or anal* or laparoscop*).m_titl.
40. 38 not 39
Appendix 3. Embase (Ovid) search strategy
1. (sutur* adj3 (continuous* or interrupt* or length)).mp.
2. (closur* adj3 (mass or layer*)).mp.
3. 1 or 2
4. (sutur* or silk or capromed or stapling or staples or polydioxanone* or pds or polypropylene* or prolene* or polyglactin 910 or polyglactin or ethilon or nylon* or catgut or steel or vicryl or polyglycolic acid or maxon or mersilene*).mp.
5. exp suture/
6. exp SILK/
7. exp stapler/
8. exp POLYDIOXANONE/
9. exp polypropylene/
10. exp polyglactin/
11. exp nylon/
12. exp CATGUT/
13. exp STEEL/
14. exp polyglycolic acid/
15. 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14
16. 3 or 15
17. (laparotom* or hysterectom*).mp.
18. exp LAPAROTOMY/
19. exp HYSTERECTOMY/ or exp ABDOMINAL HYSTERECTOMY/
20. (abdom* adj3 (injury or wall or defect or hernia or surger* or closure* or fascia* or wound)).mp.
21. exp abdominal injury/su [Surgery]
22. exp abdominal wall/su [Surgery]
23. exp abdominal wall hernia/su [Surgery]
24. exp FASCIA/su [Surgery]
25. 17 or 18 or 19 or 20 or 21 or 22 or 23 or 24
26. 16 and 25
27. CROSSOVER PROCEDURE.sh.
28. DOUBLE‐BLIND PROCEDURE.sh.
29. SINGLE‐BLIND PROCEDURE.sh.
30. (crossover* or cross over*).ti,ab.
31. placebo*.ti,ab.
32. (doubl* adj blind*).ti,ab.
33. allocat*.ti,ab.
34. trial.ti.
35. RANDOMIZED CONTROLLED TRIAL.sh.
36. random*.ti,ab.
37. 27 or 28 or 29 or 30 or 31 or 32 or 33 or 34 or 35 or 36
38. (exp animal/ or exp invertebrate/ or animal.hw. or nonhuman/) not (exp human/ or human cell/ or (human or humans or man or men or wom?n).ti.)
39. 37 not 38
40. 26 and 39
41. (rat* or rabbit* or rect* or anal* or laparoscop*).m_titl.
42. 40 not 41
Appendix 4. ClinicalTrials.gov search strategy
Search Term: Suture OR Closure
Outcome = Hernia
Condition: Laparotomy
Appendix 5. WHO ICTRP
Laparotomy AND hernia AND closure
Laparotomy AND hernia AND suture
Appendix 6. Criteria for judging risk of bias in the Cochrane 'Risk of bias' assessment tool
|
Random sequence generation Selection bias (biased allocation to interventions) due to inadequate generation of a randomised sequence | |
| Criteria for a judgement of ‘low risk’ of bias | The investigators describe a random component in the sequence generation process such as:
aMinimisation may be implemented without a random element, and this is considered to be equivalent to being random. |
| Criteria for the judgement of ‘high risk’ of bias | The investigators describe a non‐random component in the sequence generation process. Usually, the description would involve some systematic, non‐random approach, for example:
Other non‐random approaches happen much less frequently than the systematic approaches mentioned above and tend to be obvious. They usually involve judgement or some method of non‐random categorisation of participants, for example:
|
| Criteria for the judgement of ‘unclear risk’ of bias | Insufficient information about the sequence generation process to permit judgement of ‘low risk’ or ‘high risk’ |
|
Allocation concealment Selection bias (biased allocation to interventions) due to inadequate concealment of allocations prior to assignment | |
| Criteria for a judgement of ‘low risk’ of bias | Participants and investigators enrolling participants could not foresee assignment because one of the following, or an equivalent method, was used to conceal allocation:
|
| Criteria for the judgement of ‘high risk’ of bias | Participants or investigators enrolling participants could possibly foresee assignments and thus introduce selection bias, such as allocation based on:
|
| Criteria for the judgement of ‘unclear risk’ of bias | Insufficient information to permit judgement of ‘low risk’ or ‘high risk’. This is usually the case if the method of concealment is not described or not described in sufficient detail to allow a definite judgement – for example if the use of assignment envelopes is described, but it remains unclear whether envelopes were sequentially numbered, opaque and sealed. |
|
Blinding of participants and personnel Performance bias due to knowledge of the allocated interventions by participants and personnel during the study | |
| Criteria for a judgement of ‘low risk’ of bias | Any one of the following:
|
| Criteria for the judgement of ‘high risk’ of bias | Any one of the following:
|
| Criteria for the judgement of ‘unclear risk’ of bias | Any one of the following:
|
|
Blinding of outcome assessment Detection bias due to knowledge of the allocated interventions by outcome assessors | |
| Criteria for a judgement of ‘low risk’ of bias | Any one of the following:
|
| Criteria for the judgement of ‘high risk’ of bias | Any one of the following:
|
| Criteria for the judgement of ‘unclear risk’ of bias | Any one of the following:
|
|
Incomplete outcome data Attrition bias due to amount, nature or handling of incomplete outcome data | |
| Criteria for a judgement of ‘low risk’ of bias | Any one of the following:
|
| Criteria for the judgement of ‘high risk’ of bias | Any one of the following:
|
| Criteria for the judgement of ‘unclear risk’ of bias | Any one of the following:
|
|
Selective reporting Reporting bias due to selective outcome reporting | |
| Criteria for a judgement of ‘low risk’ of bias | Any of the following:
|
| Criteria for the judgement of ‘high risk’ of bias | Any one of the following:
|
| Criteria for the judgement of ‘unclear risk’ of bias | Insufficient information to permit judgement of ‘low risk’ or ‘high risk’. It is likely that the majority of studies will fall into this category. |
|
Other bias Bias due to problems not covered elsewhere in the table | |
| Criteria for a judgement of ‘low risk’ of bias | The study appears to be free of other sources of bias. |
| Criteria for the judgement of ‘high risk’ of bias | There is at least one important risk of bias. For example, the study:
|
| Criteria for the judgement of ‘unclear risk’ of bias | There may be a risk of bias, but there is either:
|
Data and analyses
Comparison 1. Absorbable sutures versus non‐absorbable sutures (any closure or technique).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Incisional hernia | 17 | 4720 | Risk Ratio (M‐H, Random, 95% CI) | 1.07 [0.86, 1.32] |
| 1.1 Same closure technique and method in each group | 15 | 4411 | Risk Ratio (M‐H, Random, 95% CI) | 1.13 [0.95, 1.34] |
| 1.2 Different closure technique or method in each group | 2 | 309 | Risk Ratio (M‐H, Random, 95% CI) | 2.06 [0.07, 62.94] |
| 2 Wound infection | 28 | 8304 | Risk Ratio (M‐H, Random, 95% CI) | 1.01 [0.86, 1.19] |
| 2.1 Same closure technique and method in each group | 22 | 7363 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.87, 1.15] |
| 2.2 Different closure technique or method in each group | 6 | 941 | Risk Ratio (M‐H, Random, 95% CI) | 1.15 [0.56, 2.36] |
| 3 Wound dehiscence | 33 | 8851 | Risk Ratio (M‐H, Random, 95% CI) | 0.82 [0.58, 1.17] |
| 3.1 Same closure technique and method In each group | 25 | 7647 | Risk Ratio (M‐H, Random, 95% CI) | 0.77 [0.54, 1.10] |
| 3.2 Different closure technique or method in each group | 8 | 1204 | Risk Ratio (M‐H, Random, 95% CI) | 1.46 [0.42, 5.14] |
| 4 Sinus or fistula formation | 19 | 5470 | Risk Ratio (M‐H, Random, 95% CI) | 0.49 [0.26, 0.94] |
| 4.1 Same closure technique and method in each group | 16 | 4934 | Risk Ratio (M‐H, Random, 95% CI) | 0.43 [0.26, 0.73] |
| 4.2 Different closure technique or method in each group | 3 | 536 | Risk Ratio (M‐H, Random, 95% CI) | 1.16 [0.06, 21.09] |
| 5 Hernia and type of incision | 14 | 4258 | Risk Ratio (M‐H, Random, 95% CI) | 1.14 [0.96, 1.36] |
| 5.1 Midline incision only (same technique) | 8 | 3229 | Risk Ratio (M‐H, Random, 95% CI) | 1.15 [0.95, 1.39] |
| 5.2 Other incisions, combination of incision (same technique) | 6 | 1029 | Risk Ratio (M‐H, Random, 95% CI) | 1.09 [0.65, 1.83] |
Comparison 2. Mass versus layered closure.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Incisional hernia | 5 | 1176 | Risk Ratio (M‐H, Random, 95% CI) | 1.92 [0.58, 6.35] |
| 1.1 Same closure technique and suture material in each group | 1 | 206 | Risk Ratio (M‐H, Random, 95% CI) | 3.86 [1.34, 11.07] |
| 1.2 Different closure technique or suture material in each group | 4 | 970 | Risk Ratio (M‐H, Random, 95% CI) | 1.47 [0.33, 6.67] |
| 2 Wound infection | 11 | 2926 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.67, 1.30] |
| 2.1 Same closure technique and suture material in each group | 1 | 282 | Risk Ratio (M‐H, Random, 95% CI) | 1.26 [0.79, 2.02] |
| 2.2 Different closure technique or suture material in each group | 10 | 2644 | Risk Ratio (M‐H, Random, 95% CI) | 0.89 [0.62, 1.28] |
| 3 Wound dehiscence | 11 | 2863 | Risk Ratio (M‐H, Random, 95% CI) | 0.69 [0.31, 1.52] |
| 3.1 Same closure technique and suture material in each group | 1 | 282 | Risk Ratio (M‐H, Random, 95% CI) | 0.46 [0.04, 5.01] |
| 3.2 Different closure technique or suture material in each group | 10 | 2581 | Risk Ratio (M‐H, Random, 95% CI) | 0.69 [0.28, 1.68] |
| 4 Sinus or fistula formation | 6 | 1076 | Risk Ratio (M‐H, Random, 95% CI) | 0.49 [0.15, 1.62] |
| 4.1 Same closure technique and suture material in each group | 1 | 282 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.13, 6.43] |
| 4.2 Different closure technique or suture material in each group | 5 | 794 | Risk Ratio (M‐H, Random, 95% CI) | 0.44 [0.10, 1.83] |
Comparison 3. Continuous versus interrupted closure.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Incisional hernia | 11 | 3854 | Risk Ratio (M‐H, Random, 95% CI) | 1.01 [0.76, 1.35] |
| 1.1 Same closure method and suture material in each group | 4 | 1195 | Risk Ratio (M‐H, Random, 95% CI) | 1.21 [0.89, 1.63] |
| 1.2 Different closure method or suture material in each group | 7 | 2659 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.59, 1.48] |
| 2 Wound infection | 23 | 10039 | Risk Ratio (M‐H, Random, 95% CI) | 1.13 [0.96, 1.34] |
| 2.1 Same closure method and suture material in each group | 6 | 4933 | Risk Ratio (M‐H, Random, 95% CI) | 1.20 [0.99, 1.45] |
| 2.2 Different closure method or suture material in each group | 17 | 5106 | Risk Ratio (M‐H, Random, 95% CI) | 1.07 [0.83, 1.38] |
| 3 Wound dehiscence | 21 | 9228 | Risk Ratio (M‐H, Random, 95% CI) | 1.21 [0.90, 1.64] |
| 3.1 Same closure method and suture material in each group | 6 | 4928 | Risk Ratio (M‐H, Random, 95% CI) | 1.15 [0.70, 1.88] |
| 3.2 Different closure method or suture material in each group | 15 | 4300 | Risk Ratio (M‐H, Random, 95% CI) | 1.27 [0.84, 1.92] |
| 4 Sinus or fistula formation | 10 | 5082 | Risk Ratio (M‐H, Random, 95% CI) | 1.51 [0.64, 3.61] |
| 4.1 Same closure method and suture material in each group | 4 | 4027 | Risk Ratio (M‐H, Random, 95% CI) | 0.76 [0.51, 1.12] |
| 4.2 Different closure method or suture material in each group | 6 | 1055 | Risk Ratio (M‐H, Random, 95% CI) | 3.71 [1.32, 10.45] |
| 5 Hernia and type of incision | 4 | 1195 | Risk Ratio (M‐H, Random, 95% CI) | 1.21 [0.89, 1.63] |
| 5.1 Midline incision only (same suture material) | 2 | 727 | Risk Ratio (M‐H, Random, 95% CI) | 1.19 [0.86, 1.64] |
| 5.2 Other incisions, combination of incisions (same suture material) | 2 | 468 | Risk Ratio (M‐H, Random, 95% CI) | 1.35 [0.58, 3.14] |
Comparison 4. Monofilament versus multifilament sutures.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Incisional hernia | 16 | 4520 | Risk Ratio (M‐H, Random, 95% CI) | 0.76 [0.59, 0.98] |
| 1.1 Same closure technique and method | 10 | 2565 | Risk Ratio (M‐H, Random, 95% CI) | 0.80 [0.55, 1.15] |
| 1.2 Different closure technique or method | 6 | 1955 | Risk Ratio (M‐H, Random, 95% CI) | 0.72 [0.48, 1.09] |
| 2 Wound infection | 23 | 6557 | Risk Ratio (M‐H, Random, 95% CI) | 1.08 [0.91, 1.28] |
| 2.1 Same closure technique and method | 14 | 3956 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.85, 1.18] |
| 2.2 Different closure technique or method | 9 | 2601 | Risk Ratio (M‐H, Random, 95% CI) | 1.35 [0.91, 2.01] |
| 3 Wound dehiscence | 22 | 6199 | Risk Ratio (M‐H, Random, 95% CI) | 1.24 [0.93, 1.67] |
| 3.1 Same closure technique and method | 12 | 3465 | Risk Ratio (M‐H, Random, 95% CI) | 1.21 [0.76, 1.91] |
| 3.2 Different closure technique or method | 10 | 2734 | Risk Ratio (M‐H, Random, 95% CI) | 1.49 [0.88, 2.53] |
| 4 Sinus or fistula formation | 8 | 2285 | Risk Ratio (M‐H, Random, 95% CI) | 1.91 [0.77, 4.73] |
| 4.1 Same closure technique and method | 6 | 1784 | Risk Ratio (M‐H, Random, 95% CI) | 1.98 [0.79, 4.99] |
| 4.2 Different closure technique or method | 2 | 501 | Risk Ratio (M‐H, Random, 95% CI) | 1.36 [0.02, 108.15] |
| 5 Hernia and type of incision | 10 | 2565 | Risk Ratio (M‐H, Random, 95% CI) | 0.80 [0.55, 1.15] |
| 5.1 Midline incision only (same technique) | 6 | 1530 | Risk Ratio (M‐H, Random, 95% CI) | 0.62 [0.47, 0.81] |
| 5.2 Other incisions, combination of incisions (same technique) | 4 | 1035 | Risk Ratio (M‐H, Random, 95% CI) | 1.02 [0.47, 2.24] |
Comparison 5. Slow absorbable versus fast absorbable sutures (any technique).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Incisional hernia | 10 | 3643 | Risk Ratio (M‐H, Random, 95% CI) | 0.81 [0.63, 1.06] |
| 1.1 Same closure method and technique | 6 | 1629 | Risk Ratio (M‐H, Random, 95% CI) | 0.86 [0.55, 1.35] |
| 1.2 Different closure method or technique | 4 | 2014 | Risk Ratio (M‐H, Random, 95% CI) | 0.79 [0.56, 1.12] |
| 2 Wound infection | 11 | 4100 | Risk Ratio (M‐H, Random, 95% CI) | 1.16 [0.85, 1.57] |
| 2.1 Same closure method and technique | 6 | 1759 | Risk Ratio (M‐H, Random, 95% CI) | 1.09 [0.66, 1.81] |
| 2.2 Different closure method or technique | 5 | 2341 | Risk Ratio (M‐H, Random, 95% CI) | 1.21 [0.79, 1.85] |
| 3 Wound dehiscence | 8 | 3440 | Risk Ratio (M‐H, Random, 95% CI) | 1.55 [0.92, 2.61] |
| 3.1 Same closure method and technique | 3 | 1195 | Risk Ratio (M‐H, Random, 95% CI) | 1.93 [0.80, 4.69] |
| 3.2 Different closure method or technique | 5 | 2245 | Risk Ratio (M‐H, Random, 95% CI) | 1.21 [0.59, 2.49] |
| 4 Sinus or fistula formation | 2 | 911 | Risk Ratio (M‐H, Random, 95% CI) | 0.88 [0.05, 16.05] |
| 4.1 Same closure method and technique | 1 | 571 | Risk Ratio (M‐H, Random, 95% CI) | 2.84 [0.91, 8.81] |
| 4.2 Different closure method or technique | 1 | 340 | Risk Ratio (M‐H, Random, 95% CI) | 0.15 [0.01, 2.81] |
Comparison 6. Sensitivity analysis: excluding high‐risk studies.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Incisional hernia (absorbable versus non‐absorbable suture, same technique) | 9 | 2949 | Risk Ratio (M‐H, Random, 95% CI) | 1.21 [0.98, 1.49] |
| 2 Incisional hernia (continuous versus interrupted, same material and method) | 3 | 869 | Risk Ratio (M‐H, Random, 95% CI) | 1.20 [0.87, 1.64] |
| 3 Incisional hernia (monofilament versus multifilament, same technique) | 4 | 1336 | Risk Ratio (M‐H, Random, 95% CI) | 0.65 [0.42, 1.01] |
Comparison 7. Sensitivity analysis: inclusion of missing data, assuming loss to follow‐up developed incisional hernia.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Absorbable versus non‐absorbable (hernia) | 16 | 5610 | Risk Ratio (M‐H, Random, 95% CI) | 1.11 [0.94, 1.30] |
| 1.1 Same closure technique and method in each group | 14 | 5257 | Risk Ratio (M‐H, Random, 95% CI) | 1.06 [0.96, 1.17] |
| 1.2 Different closure technique or method in each group | 2 | 353 | Risk Ratio (M‐H, Random, 95% CI) | 1.24 [0.21, 7.21] |
| 2 Mass versus layered closure (hernia) | 5 | 1220 | Risk Ratio (M‐H, Random, 95% CI) | 1.82 [0.81, 4.10] |
| 2.1 Same closure technique and suture material in each group | 1 | 206 | Risk Ratio (M‐H, Random, 95% CI) | 3.86 [1.34, 11.07] |
| 2.2 Different closure technique or suture material in each group | 4 | 1014 | Risk Ratio (M‐H, Random, 95% CI) | 1.40 [0.50, 3.94] |
| 3 Continuous versus interrupted | 11 | 4046 | Risk Ratio (M‐H, Random, 95% CI) | 0.89 [0.61, 1.30] |
| 3.1 Same closure method and suture material in each group | 4 | 1363 | Risk Ratio (M‐H, Random, 95% CI) | 1.13 [0.94, 1.35] |
| 3.2 Different closure method or suture material in each group | 7 | 2683 | Risk Ratio (M‐H, Random, 95% CI) | 0.81 [0.45, 1.44] |
| 4 Monofilament versus multifilament (hernia) | 16 | 4981 | Risk Ratio (M‐H, Random, 95% CI) | 0.77 [0.63, 0.95] |
| 4.1 Same closure technique and method | 10 | 2982 | Risk Ratio (M‐H, Random, 95% CI) | 0.87 [0.72, 1.05] |
| 4.2 Different closure technique or method | 6 | 1999 | Risk Ratio (M‐H, Random, 95% CI) | 0.64 [0.42, 0.98] |
| 5 Slow absorbable versus fast absorbable (hernia) | 9 | 3877 | Risk Ratio (M‐H, Random, 95% CI) | 0.89 [0.74, 1.07] |
| 5.1 Same closure method and technique | 5 | 1863 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.77, 1.17] |
| 5.2 Different closure method or technique | 4 | 2014 | Risk Ratio (M‐H, Random, 95% CI) | 0.79 [0.56, 1.12] |
Comparison 8. Sensitivity analysis: inclusion of missing data, assuming loss to follow‐up did not have developed incisional hernia.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Absorbable versus non‐absorbable (hernia) | 16 | 5560 | Risk Ratio (M‐H, Random, 95% CI) | 1.08 [0.92, 1.28] |
| 1.1 Same closure technique and method in each group | 14 | 5257 | Risk Ratio (M‐H, Random, 95% CI) | 1.13 [0.95, 1.35] |
| 1.2 Different closure technique or method in each group | 2 | 303 | Risk Ratio (M‐H, Random, 95% CI) | 0.54 [0.27, 1.05] |
| 2 Mass versus layered closure (hernia) | 5 | 1220 | Risk Ratio (M‐H, Random, 95% CI) | 1.80 [0.57, 5.62] |
| 2.1 Same closure technique and suture material in each group | 1 | 206 | Risk Ratio (M‐H, Random, 95% CI) | 3.86 [1.34, 11.07] |
| 2.2 Different closure technique or suture material in each group | 4 | 1014 | Risk Ratio (M‐H, Random, 95% CI) | 1.29 [0.34, 4.92] |
| 3 Continuous versus interrupted | 11 | 4046 | Risk Ratio (M‐H, Random, 95% CI) | 1.01 [0.76, 1.34] |
| 3.1 Same closure method and suture material in each group | 4 | 1363 | Risk Ratio (M‐H, Random, 95% CI) | 1.18 [0.87, 1.61] |
| 3.2 Different closure method or suture material in each group | 7 | 2683 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.60, 1.48] |
| 4 Monofilament versus multifilament (hernia) | 16 | 4981 | Risk Ratio (M‐H, Random, 95% CI) | 0.76 [0.60, 0.97] |
| 4.1 Same closure technique and method | 10 | 2982 | Risk Ratio (M‐H, Random, 95% CI) | 0.80 [0.56, 1.14] |
| 4.2 Different closure technique or method | 6 | 1999 | Risk Ratio (M‐H, Random, 95% CI) | 0.74 [0.50, 1.08] |
| 5 Slow absorbable versus fast absorbable (hernia) | 9 | 3877 | Risk Ratio (M‐H, Random, 95% CI) | 0.82 [0.62, 1.08] |
| 5.1 Same closure method and technique | 5 | 1863 | Risk Ratio (M‐H, Random, 95% CI) | 0.88 [0.53, 1.45] |
| 5.2 Different closure method or technique | 4 | 2014 | Risk Ratio (M‐H, Random, 95% CI) | 0.79 [0.56, 1.12] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Agrawal 2009.
| Methods |
RCT Methods to control for contributory patient factors: none described |
|
| Participants |
Age: not described Gender: not described Types of incisions: all participants received a vertical midline incision Types of surgery: emergency surgery for peritonitis Contamination classification of included participants: not described Pre‐operative antibiotic use: all participants received ceftriaxone and metronidazole Prognostic patient factors: not described Inclusion criteria: all patients with peritonitis at a single centre Exclusion criteria: none described |
|
| Interventions |
Comparisons reported: Group 1: Suture: polygalactin‐910 (multifilament, fast absorbable) Suturing technique: continuous Closure method: mass Group 2: Suture: polygalactin‐910 (multifilament, fast absorbable) Suturing technique: interrupted Closure method: mass Group 3: Suture: polypropylene (monofilament, non‐absorbable) Suturing technique: continuous Closure method: mass Group 4: Suture: polypropylene (monofilament, non‐absorbable) Suturing technique: interrupted Closure method: mass Surgeon characteristics: "Trained surgeon with a minimum of three years of surgical residency" |
|
| Outcomes |
Incisional hernia: clinical exam, confirmed with ultrasound Follow‐up duration: 3 months and 4 years Wound infection: not defined Dehiscence: not defined Sinus or fistula: not defined |
|
| Notes | Hernia outcome data used from the 4‐year follow‐up period As this was a factorial design, the outcomes for each group were input separately against their comparison group |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Draw of lots" by nurse |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Outcome assessor blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants accounted for and analysed |
| Selective reporting (reporting bias) | Low risk | Hernia (at least 1 year); dehiscence and wound infection outcomes all reported |
| Other bias | Unclear risk | Exclusion criteria, postoperative care, etc. not described |
Agrawal 2014.
| Methods |
RCT Methods to control for contributory patient factors: none described |
|
| Participants |
Age: Group 1 (mean): 37 years Group 2 (mean): 36.5 years Group 3 (mean): 34.7 years Gender: Group 1 (%): 76.9% Female Group 2 (%): 81.0% Female Group 3 (%): 71.8% Female Types of incisions: all participants received a vertical midline incision Types of surgery: Group 1 (% emergent): 68.6% Group 2 (% emergent): 65.4% Group 3 (% emergent): 67.5% Contamination classification of included participants: Group 1 (% contaminated): 27.3% Group 2 (% contaminated): 25.5% Group 3 (% contaminated): 33.3% Prognostic patient factors: Average BMI: Group 1 22.5; Group 2 22.8; Group 3 21.6 Malignancy (%): Group 1 5%; Group 2 3.6%; Group 3 6% Inclusion criteria: elective or emergent gynaecology cases or emergency general surgery cases Exclusion criteria: patients with previous "Burst" Abdomen |
|
| Interventions |
Comparisons reported: Group 1: Suture: Prolene (monofilament, non‐absorbable) Suturing technique: continuous Closure method: mass Group 2: Sutures: Prolene (monofilament, non‐absorbable) Suturing technique: "X Technique" (interrupted) Closure method: mass Group 3: Sutures: Prolene (monofilament, non‐absorbable) Suturing technique: modified Smead Jones (interrupted) Closure method: mass Surgeon characteristics: not stated |
|
| Outcomes | Dehiscence: Intra‐abdominal components in the wound (30‐day follow‐up) | |
| Notes | Groups 2 & 3 combined into "Interrupted" closure for analysis | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Codes from randomization.com using permuted block design |
| Allocation concealment (selection bias) | Low risk | Sealed, opaque envelopes |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not specifically addressed |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No dropouts over study period |
| Selective reporting (reporting bias) | Low risk | There was no evidence of selective reporting |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Askew 1983.
| Methods |
RCT Methods to control for contributory patient factors: none described |
|
| Participants |
Age: Group 1 (mean): 54 years (male), 41 years (female) Group 2 (mean): 50 years (male), 47 years (female) Gender: Group 1: 52% female Group 2: 74% female Type of incision: Group 1: midline 19.4%, rectus split 56.5%, transverse 24.1%, other 0% Group 2: midline 26.2%, rectus split 61.9%, transverse 6.9%, other 5.0% Type of surgery: Group 1: biliary 67.7%, gastric 19.4%, liver/spleen/pancreas 12.9%; emergent 1.6% Group 2: biliary 61.9%, gastric 28.6%, liver/spleen/pancreas 9.5%; emergent 4.8% Contamination classification of included participants: not reported Pre‐operative antibiotic use: not reported Prognostic patient factors: Group 1: malignancy 12.0%, jaundice 8.1% Group 2: malignancy 2.4%, jaundice 2.4% Inclusion criteria: not clearly stated; consecutive participants undergoing upper abdominal laparotomy Exclusion criteria: none stated |
|
| Interventions |
Comparisons reported: Group 1: Suture: nylon (monofilament, non‐absorbable) Suturing technique: continuous Closure method: layered Group 2: Sutures: PGA (multifilament, fast absorbable) Suturing technique: Smead‐Jones (interrupted) Closure method: mass Surgeon characteristics: a single staff surgeon operated on all participants |
|
| Outcomes |
Incisional hernia: not defined Follow‐up duration: 12 months Dehiscence: not defined Wound infection: discharge of pus from the wound; at 6 months |
|
| Notes | ‐ | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | "Randomization was according to the date of operation, nylon closure on even dates and Dexon closure on odd dates." |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Only 60% followed up in clinic, while 21% followed up by telephone. No follow‐up available on 19% of participants |
| Selective reporting (reporting bias) | Low risk | Hernia (at least 1 year); dehiscence and wound infection outcomes all reported |
| Other bias | High risk | "The trial was designed to have at least 100 patients in each limb, but the trial was closed when analysis of the first 104 patients showed a significant difference in wound infection and incisional hernia between the two groups." No a priori stopping rules were described |
Ausobsky 1985.
| Methods |
RCT Methods to control for contributory patient factors: none described |
|
| Participants |
Age: not reported Gender: not reported Type of incision: Group 1: midline 60.5%, paramedian 10.2%, transverse/oblique 29.2% Group 2: midline 5.2%, paramedian 74.8%, transverse/oblique 20.0% Type of surgery: not reported Contamination classification of included participants: 37.4% in Group 1 and 28.9% in Group 2 classified as 'contaminated' (culture swabs collected before skin closure) Pre‐operative antibiotic use: cefuroxime or cephaloridine administered to all participants Prognostic patient factors: not reported Inclusion criteria: all emergency and elective major laparotomy procedures Exclusion criteria: grid‐iron incisions, Pfannenstiel incisions for exposure of bladder, incisions for exposure of kidneys and hernia repairs |
|
| Interventions |
Comparisons reported: Group 1: Suture: nylon suture (monofilament, non‐absorbable) Suturing technique: continuous Closure method: mass Group 2: Sutures: posterior rectus sheath with PGA (multifilament, fast absorbable), and anterior rectus sheath with nylon (monofilament, non‐absorbable) Suturing technique: continuous Closure method: layered Surgeon characteristics: no information provided |
|
| Outcomes |
Incisional hernia: visible bulge when coughing in standing position, together with a palpable sharp‐margined defect in the abdominal wall at the site of a scar Follow‐up duration: 1 to 4‐year follow‐up Wound infection: presence of pus in the wound Wound dehiscence: protrusion of abdominal viscera through the wound Suture sinus: no definition provided |
|
| Notes | Variable follow‐up duration; between 1 and 4 years | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Between January 1980 and May 1981, 282 consecutive patients who were admitted under the care of one consultant surgeon and who accepted elective or emergency major laparotomy were randomised to one or other of the closure regimens detailed below." |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | No information provided |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Participants who died within 6 months without developing an event were excluded from analysis |
| Selective reporting (reporting bias) | Low risk | Hernia (at least 1 year); dehiscence and wound infection outcomes all reported |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Berretta 2010.
| Methods |
RCT Methods to control for contributory patient factors: none described |
|
| Participants |
Age: Group 1 (mean): 59 years Group 2 (mean): 59 years Group 3 (mean): 56 years Gender: all participants were female Type of incision: all participants received a vertical midline incision Type of surgery: elective laparotomy for gynaecologic malignancy Contamination classification of included participants: not described Pre‐operative antibiotic use: all participants received ampicillin and sulbactam or clindamycin Prognostic patient factors: Group 1: diabetes 11%; obesity 32% Group 2: diabetes 13%; obesity 28% Group 3: diabetes 15%; obesity 32% Inclusion criteria: participants with ovarian, endometrial or cervical cancer and a life expectancy of > 1 year Exclusion criteria: pre‐existing ventral hernia, chemotherapy within 2 weeks of surgery, > 8 weeks of neoadjuvant radiation therapy, current immunosuppression, pre‐operative coagulopathy or collagen disorder |
|
| Interventions | Group 1:
Suture: polypropylene 1‐0 (monofilament, non‐absorbable)
Suturing technique: continuous
Closure method: mass closure
Group 2:
Suture: PDS 1‐0 (monofilament, slow absorbable)
Suturing technique: continuous
Closure method: mass Group 3: Sutures: polyester (multifilament, non‐absorbable) for fascia, polyglactin (absorbable) for peritoneum Suturing technique: interrupted Closure method: mass Surgeon characteristics: no information provided |
|
| Outcomes |
Incisional hernia: palpable defect in the fascia or a protrusion beyond the level of the fascia with the participant supine lifting both legs, and coughing or straining in an erect position; confirmed by ultrasound (in obese participants, ultrasound was performed routinely due to a lack of physical exam sensitivity) Follow‐up duration: 1 year Wound infection: defined as "dehiscence with secretion either of putrid or caliginous, smelly fluid or requiring antibiotic treatment or surgical intervention" Dehiscence: superficial (intact fascia), deep (complete disruption) |
|
| Notes | Groups 1 compared with Group 2 only for 'absorbable versus non‐absorbable' outcomes, as they had a common closure technique and method Groups 1 and 2 combined for 'continuous versus interrupted' outcomes Groups 1 and 2 combined for 'monofilament versus multifilament' outcomes |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Block randomisation by centre. Specific randomisation technique was not described |
| Allocation concealment (selection bias) | Low risk | Opaque envelopes |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not specified |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants included in analysis |
| Selective reporting (reporting bias) | Low risk | Hernia (at least 1 year); dehiscence and wound infection outcomes all reported |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Bloemen 2011.
| Methods |
RCT Methods to control for contributory patient factors: none described |
|
| Participants |
Age: Group 1 (mean): 63.1 years Group 2 (mean): 63.8 years Gender: Group 1: 40.6% female Group 2: 44.9% female Type of incision: all participants received midline incisions Type of surgery: Group 1: elective 80.1%; colorectal cancer 47.7%, aortic aneurysm 11.3%, benign colorectal 13.3%, gastric cancer 3.5%, cholelithiasis 5.5%, bowel perforation 3.9%, hiatal hernia 3.9%, appendicitis 2.0%, other 9.0% Group 2: elective 85.4%; colorectal cancer 53.2%, aortic aneurysm 10.9%, benign colorectal 12.3%, gastric cancer 4.9%, cholelithiasis 2.6%, bowel perforation 3.4%, hiatal hernia 2.6%, appendicitis 3.0%, other 7.1% Contamination classification of included participants: not described Pre‐operative antibiotic use: not described Prognostic patient factors: Group 1: DM 9.8%; mean BMI 25.6; steroids 6.3%; chronic pulmonary conditions 3.9% Group 2: DM 6.4%; mean BMI 25.8; steroids 7.9%; chronic pulmonary conditions 10.1% Inclusion criteria: elective or emergent laparotomy with midline incision Exclusion criteria: pregnancy, presence of an abdominal hernia, lack of informed consent, age < 18 years or life expectancy of < 1 year |
|
| Interventions | Group 1:
Suture: 1‐0 polypropylene (monofilament, non‐absorbable)
Suturing technique: continuous
Closure method: mass
Group 2:
Suture: 1‐0 PDS (monofilament, slowly absorbable)
Suturing technique: continuous
Closure method: mass Surgeon characteristics: consultant or resident surgeons |
|
| Outcomes |
Incisional hernia: defined as "any abdominal wall gap with or without a bulge in the area of a postoperative scar, perceptible or palpable by clinical examination or imaging" Follow‐up duration: up to 54 months Dehiscence: "Early post‐operative fascial dehiscence was distinguished from later incisional hernia, defined by a clinically palpable gap in the abdominal fascia with, or without wound dehiscence during the first 30 days after surgery..." Wound infection: not defined Sinus or fistula: not defined |
|
| Notes | Occurrence of incisional hernia at 1 year used in analysis | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomisation |
| Allocation concealment (selection bias) | Low risk | Sealed, opaque envelopes |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Outcome assessors blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants accounted for and included in analysis |
| Selective reporting (reporting bias) | Low risk | Hernia (at least 1 year); dehiscence and wound infection outcomes all reported |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Bresler 1995.
| Methods |
RCT Methods to control for contributory patient factors: none described |
|
| Participants |
Age: Group 1: < 40 years 3.6%; 40‐60 years 40.3%; > 60 years 29%** Group 2: < 40 years 25.7%; 40‐60 years 40.0%; > 60 years 34.2% Group 3: < 40 years 16.9%; 40 to 60 years 43.6%; > 60 years 39.4% Gender: Group 1: 61.2% female Group 2: 60% female Group 3: 67% female Type of incision: all participants received midline incisions Type of surgery: Cholecystectomy, digestive tract surgery, splenectomy, hiatal hernia repair, gastrectomy, hepato‐pancreatic (group‐wise data not given) Contamination classification of included participants: Group 1: clean 66.1%; clean‐contaminated 33.8% Group 2: clean 72.8%; clean‐contaminated 27.1% Group 3: clean 81.6%; clean‐contaminated 18.2% Pre‐operative antibiotic use: not described Prognostic patient factors: not described Inclusion criteria: laparotomy via midline incision Exclusion criteria: emergency surgery, presence of ascites, presence of carcinomatosis ** % do not add up to 100* |
|
| Interventions | Group 1:
Suture: polyglactin‐910 (multifilament, fast‐absorbable)
Suturing technique: continuous
Closure method: mass
Group 2:
Suture: PDS I (monofilament, slowly absorbable)
Suturing technique: continuous
Closure method: mass Group 2: Suture: PDS II (monofilament, slowly absorbable) Suturing technique: continuous Closure method: mass Surgeon characteristics: Group 1: attending surgeon 19.3%; assistant 59,6%; intern 20.9% Group 2: attending surgeon 25.7%; assistant 50%; intern 24.2% Group 3: attending surgeon 22.5%; assistant 56.3%; intern 21.1% |
|
| Outcomes |
Incisional hernia: not defined Follow‐up duration: 1 year |
|
| Notes | Group 1 and group 2 pooled as monofilament, slowly absorbable | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number table |
| Allocation concealment (selection bias) | Low risk | Allocation at time of closure by random number table |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Outcome assessor blinded |
| Incomplete outcome data (attrition bias) All outcomes | High risk | No outcome data on 15 participants in group 1, 8 participants group 2, 9 participants group 3 |
| Selective reporting (reporting bias) | Low risk | There was no evidence of selective reporting |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Brolin 1996.
| Methods |
RCT Methods to control for contributory patient factors: none described |
|
| Participants |
Age: Group 1 (mean): 39 years Group 2 (mean): 38 years Gender: Group 1: 81.6% female Group 2: 80.0% female Type of incision: all participants had midline incisions Type of surgery: all were elective bariatric procedures Group 1: vertical banded gastroplasty: 9.2%; Roux‐en‐Y gastric bypass 90.8% Group 2: vertical banded gastroplasty: 11.7%; Roux‐en‐Y gastric bypass 88.3% Contamination classification of included participants: no information provided Pre‐operative antibiotic use: all participants received either a cephalosporin or vancomycin Prognostic patient factors: all participants were morbidly obese Inclusion criteria: participants who had gastric‐restrictive bariatric procedures performed by one surgeon, for treatment of morbid obesity Exclusion criteria: no exclusion criteria were explicitly reported |
|
| Interventions |
Comparisons reported: Group 1: Suture: polyester (multifilament, non‐absorbable) Suturing technique: continuous Closure method: layered (polyester on fascia, other layers closed by same methods in both groups) Group 2: Suture: PDS (monofilament, slowly absorbable) Suturing technique: interrupted, 'figure‐of‐eight' Closure method: layered (PDS on fascia) Characteristics of surgeons: all procedures were performed by a chief resident |
|
| Outcomes |
Incisional hernia: participant‐reported symptoms of discomfort or lumps in their incision Follow‐up duration: mean follow‐up was 29.4 months, 65% followed for > 2 years Wound infection: not defined Wound dehiscence: acute dehiscence on the first postoperative day |
|
| Notes | Minimum follow‐up period not described; hernias at 1 year not specifically addressed | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | "Randomization was carried out in the operating room according to the last digit of the patient's hospital identification number. Patients with an even number (n = 109) had closure with [Polyester]; patients with an odd digit (n = 120) had closure using [Polydioxanone]." |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants accounted for and included in the analysis |
| Selective reporting (reporting bias) | Low risk | There was no evidence of selective reporting |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Bucknall 1981.
| Methods |
RCT Methods to control for contributory patient factors: none described |
|
| Participants |
Age: Group 1 (mean): 53.3 years Group 2 (mean): 50.5 years Gender: Group 1: 53.8% female Group 2: 61.5% female Type of incision: Group 1: midline 37.7%, paramedian 62.3% Group 2: midline 41.3%, paramedian 58.6% Type of surgery: Group 1: emergent 18.8%; "bowel surgery" 43.4%; malignancy 26.4% Group 2: emergent 17.3%; "bowel surgery" 39.4%; malignancy 20.2% Contamination classification of included participants: information not provided Pre‐operative antibiotic use: information not provided Prognostic patient factors: information not provided Inclusion criteria: all adult patients admitted to 1 hospital who underwent laparotomy through vertical incisions in the year 1979 Exclusion criteria: none described |
|
| Interventions |
Comparisons reported: Group 1 Suture: nylon (monofilament, non‐absorbable) Suturing technique: continuous Closure method: mass Group 2: Suture: PGA (multifilament, fast absorbable) Suturing technique: continuous Closure method: mass Surgeon characteristics: Group 1: consultant 32.1%; senior resident 44.3%; other resident 23.6% Group 2: consultant 26.0%; senior resident 49.0%; other resident 25.0% |
|
| Outcomes |
Incisional hernia: no definition provided Follow‐up duration: 8.3 months in nylon group, 8.5 months in PGA group Wound infection: no definition provided Wound dehiscence: "total wound disruption" Suture sinus or fistula: no definition provided |
|
| Notes | Hernia data not included in analysis due to inadequate follow‐up duration; other outcomes included | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "In 1979, all adult patients in the Professorial Surgical Unit at Westminster Hospital who underwent laparotomy through vertical incisions were randomised, by means of random number cards, into two groups." |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | No information provided |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | < 10% loss to follow‐up (4/110 in group 1, 2/106 in group 2) |
| Selective reporting (reporting bias) | Low risk | There was no evidence of selective reporting |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Cameron 1980.
| Methods |
RCT Methods to control for contributory patient factors: none described |
|
| Participants |
Age: not reported Gender: Group 1: 54.5% female Group 2: 51.1% female Type of incision: Group 1: midline 34.1%, paramedian 65.9% Group 2: midline 34.4%, paramedian 65.6% Type of surgery: Group 1: emergency 17.4% Group 2: emergency 22.2% Contamination classification of included participants: Group 1: contaminated 7.2% Group 2: contaminated 10.5% Pre‐operative antibiotic use: no information provided Prognostic patient factors: Group 1: corticosteroid use 1.8%, jaundice 1.2% Group 2: corticosteroid use 1.6%, jaundice 7.2% Inclusion criteria: age > 15 years, with vertical abdominal incisions Exclusion criteria: patients being re‐operated on via an incision made < 1 month previously |
|
| Interventions |
Comparisons reported: Group 1 Suture: polypropylene (monofilament, non‐absorbable) Suturing technique: interrupted ("figure‐of‐eight, near and far") Closure method: mass Group 2: Sutures: PGA (multifilament, fast absorbable) Suturing technique: interrupted ("figure‐of‐eight, near and far") Closure method: mass Surgeon characteristics: Group 1: consultant/senior resident 56.9%, registrar/senior health officer 43.1% Group 2: consultant/senior resident 56.7%, registrar/senior health officer 43.3% |
|
| Outcomes |
Incisional hernia: no definition provided Follow‐up duration: 6 months Wound infection: no definition provided Wound dehiscence: complete disruption |
|
| Notes | Hernia data not included in analysis due to inadequate follow‐up duration | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method to generate allocation sequence not described ("...randomly allocated...") |
| Allocation concealment (selection bias) | Low risk | "Patients were randomly allocated to a suture material by the opening of a sealed envelope during the procedure." |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | No information provided |
| Incomplete outcome data (attrition bias) All outcomes | High risk | High loss to follow‐up (33/167 in group 1, 49/180 in group 2) |
| Selective reporting (reporting bias) | Low risk | There was no evidence of selective reporting |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Cameron 1987.
| Methods |
RCT Methods to control for contributory patient factors: none described |
|
| Participants |
Age: Group 1 (mean): 60.2 years Group 2 (mean): 61.6 years Gender: Group 1: 56.0% female Group 2: 54.5% female Type of incision: Group 1: midline 66.7%; paramedian 33.3% Group 2: midline 56.0%; paramedian 44.0% Type of surgery: Group 1: emergent 19.6%; biliary 29.8%, gastric 17.7%, colon 29.1%, other 23.4% Group 2: emergent 19.9%; biliary 32.9%, gastric 23.1%, colon 21.0%, other 23.1% Contamination classification of included participants: Group 1: clean 77.3%, clean‐contaminated 9.2%, contaminated 13.5% Group 2: clean 79.7%, clean‐contaminated 6.3%, contaminated 14.0% Pre‐operative antibiotic use: "antibiotic prophylaxis was given according to the surgeon's usual routine" Prognostic patient factors: Group 1: obesity 26%, corticosteroid use 1.4%, jaundice 3.5% Group 2: obesity 24%, corticosteroid use 2.1%, jaundice 3.5% Inclusion criteria: patients undergoing laparotomy by vertical abdominal incision Exclusion criteria: patients who were being re‐operated on via the original incision were excluded |
|
| Interventions |
Comparisons reported: Group 1 Suture: polypropylene (monofilament, non‐absorbable) Suturing technique: interrupted, "figure‐of‐eight" Closure method: mass Group 2: Suture: PDS (monofilament, slowly absorbable) Suturing technique: interrupted, "figure‐of‐eight" Closure method: mass Surgeon characteristics: Group 1: senior resident 56.0%, junior resident 40.4% Group 2: senior resident 52.4%, junior resident 46.8% |
|
| Outcomes |
Incisional hernia: no definition provided Follow‐up duration: minimum 12 months (mean 14.7 months) Wound infection: "discharge of pus, up to one month of follow‐up" Wound dehiscence: "burst abdomen" Suture sinus or fistula: no definition provided |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Low risk | "At the end of the operation, the circulating nurse drew a sealed envelope and informed the surgeon of the suture to be used." |
| Blinding (performance bias and detection bias) All outcomes | Low risk | "This assessment was 'double‐blind', as neither the examiner nor the participant knew which suture had been used." |
| Incomplete outcome data (attrition bias) All outcomes | High risk | High loss to follow‐up (51/141 in group 1, 43/143 in group 2) |
| Selective reporting (reporting bias) | Low risk | Hernia (at least 1 year); dehiscence and wound infection outcomes all reported |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Carlson 1995.
| Methods |
RCT Methods to control for contributory patient factors: none described |
|
| Participants |
Age: not reported Gender: not reported Types of incisions: all incisions were in the vertical midline Type of surgery: Group 1: elective 75.8%; colon 26.4% Group 2: elective 76.2%; colon 18.7% Contamination classification of included participants: Group 1: clean 29.7%, clean‐contaminated 70.3% Group 2: clean 31.2%, clean‐contaminated 68.2% Pre‐operative antibiotic use: intravenous antibiotics were administered 30 min prior to surgery for clean‐contaminated wounds and oral antibiotics were given following lavage with PEG for participants undergoing colonic procedures, in both groups Prognostic patient factors: no information provided Inclusion criteria: patients undergoing laparotomy via a midline incision Exclusion criteria: life expectancy < 2 years, established peritonitis or pre‐existing ventral hernia |
|
| Interventions |
Comparisons reported: Group 1 Suture: nylon (monofilament, non‐absorbable) Suturing technique: continuous Closure method: mass Group 2: Suture: polyglyconate (multifilament, slowly absorbable) Suturing technique: continuous Closure method: mass Surgeon characteristics: all closures, in both groups, were performed by a senior or chief resident |
|
| Outcomes |
Incisional hernia definition: no definition provided Follow‐up duration: 2 years Wound infection: no definition provided Wound dehiscence: no definition provided Suture sinus or fistula: no definition provided |
|
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "...using a random number sequence..." |
| Allocation concealment (selection bias) | Low risk | "...using a random number sequence kept in serial sealed envelopes that were opened by the circulating nurse in the operating room." |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | "Follow‐up evaluation for the presence or absence of a ventral hernia was performed by the surgeon or an investigator through physical examination and communication with the patient's physician." |
| Incomplete outcome data (attrition bias) All outcomes | High risk | High loss to follow‐up (21/112 in group 1, 33/113 in group 2) |
| Selective reporting (reporting bias) | Low risk | Hernia (at least 1 year); dehiscence and wound infection outcomes all reported |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Chana 1993.
| Methods |
RCT Methods to control for contributory patient factors: none described |
|
| Participants |
Age: not reported Gender: not reported Type of incision: no group‐wise data were reported; overall: transverse 58.8%, vertical 20.6%, oblique 20.6% Type of surgery: emergent 55.9% (overall) Contamination classification of included participants: contaminated: 64.7% (overall) Pre‐operative antibiotic use: no information provided Prognostic patient factors: Group 1: malnutrition 53.0% Group 2: malnutrition 58.8% Inclusion criteria: infants and children < 12 years who underwent laparotomy Exclusion criteria: none explicitly mentioned |
|
| Interventions |
Comparisons reported: Group 1 Suture: polyglactin‐910 (multifilament, fast absorbable) Suturing technique: interrupted, 'figure‐of‐eight' Closure method: mass Group 2: Sutures: polyglactin‐910 (multifilament, fast absorbable) Suturing technique: continuous Closure method: layered Surgeon characteristics: no information provided |
|
| Outcomes |
Incisional hernia: no definition provided Follow‐up duration: unclear duration Wound infection: no definition provided Wound dehiscence: no definition provided Suture sinus or fistula: no definition provided |
|
| Notes | Incisions in group 1 included upper transverse and midline. Incisions in group 2 included transverse, subcostal and paramedian Hernia data excluded from analysis due to unclear follow‐up duration |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "...randomly allocated..." |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No losses to follow‐up were reported |
| Selective reporting (reporting bias) | Low risk | There was no evidence of selective reporting |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Chowdhury 1994.
| Methods |
RCT Methods to control for contributory patient factors: none described |
|
| Participants |
Age: Group 1 (range): 12‐78 years Group 2 (range): 10‐75 years Gender: Group 1: 35.0% female Group 2: 42.5% female Type of incision: Group 1: median 37.5%, paramedian 60.0%; transverse 2.5% Group 2: median 15.0%; paramedian 85.0%; transverse 0% Type of surgery: Group 1: emergent 42.5%; biliary 22.5%, gastric 27.5%, intestinal 27.5%, other 22.5% Group 2: emergent 20.0%; biliary 30.0%; gastric 32.5%, intestinal 15%, other 22.5% Contamination classification of included participants: no information provided Pre‐operative antibiotic use: no information provided Prognostic patient factors: Group 1: diabetes 5.0%, malignancy 15%, chronic pulmonary conditions 2.5%, anaemia 65%, malnutrition 30%, jaundice 20% Group 2: diabetes 2.5%, malignancy 15%, chronic pulmonary conditions 12.5%, anaemia 57.5%, malnutrition 20%, jaundice 12.5% Inclusion criteria: patients who had either a median, paramedian or transverse laparotomy incision Exclusion criteria: grid‐iron or Pfannenstiel incisions for kidney exposure and hernia operations |
|
| Interventions |
Comparisons reported: Group 1 Suture: nylon (monofilament, non‐absorbable) Suturing technique: interrupted, Smead‐Jones Closure method: mass Group 2: Sutures: chromic catgut (monofilament, fast absorbable) Suturing technique: continuous Closure method: layered (peritoneum and muscle/fascial layers closed separately) Surgeon characteristics: Group 1: consultant 30.0%, registrar 70.0% Group 2: consultant 52.5%, registrar 47.5% |
|
| Outcomes |
Incisional hernia: not reported Wound infection: discharge of pus from the wound Wound dehiscence: separation of all abdominal layers allowing visualisation or palpation of abdominal viscera Suture sinus or fistula: no definition provided |
|
| Notes | Follow‐up duration: 1‐15 months, no group‐wise data available. No specific follow‐up time described for primary analysis | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Out of these 160 patients, 80 patients were randomised to have the abdominal wall closed in mass closure and 80 in the layer closure." |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants included in analysis |
| Selective reporting (reporting bias) | Unclear risk | Unclear length of follow‐up for incisional hernia outcomes |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Colombo 1997.
| Methods |
RCT Methods to control for contributory patient factors: none described |
|
| Participants |
Age: Group 1 (mean): 51.1 years Group 2 (mean): 52.7 years Gender: all participants were female Type of incision: Group 1: lower midline 75%, complete midline 25% Group 2: lower midline 79%, complete midline 21% Type of surgery: Group 1: exploratory laparotomy 51.0%, exploratory laparotomy with bowel resection and anastomosis 13.3%, radical hysterectomy with pelvic lymphadenectomy 23.4%, total hysterectomy 10.1%, pelvic exenteration 2.3% Group 2: exploratory laparotomy 52.6%; exploratory laparotomy with bowel resection and anastomosis 11.1%; radical hysterectomy with pelvic lymphadenectomy 20.3%; total hysterectomy 15.0%; pelvic exenteration 1.0% Contamination classification of included participants: no information provided Pre‐operative antibiotic use: all participants in both groups received pre‐operative antibiotics: 1‐2 doses of intravenous cefazolin for procedures with no bowel resection and cefoxitin, gentamicin and metronidazole for procedures involving bowel resection Prognostic patient factors: all participants in both groups had malignancy Group 1: diabetes 2%, obesity (BMI ≥ 25 kg/m2) 30%, prior chemotherapy 38%, prior radiotherapy 5% Group 2: diabetes 3%, obesity (BMI ≥ 25 kg/m2) 32%, prior chemotherapy 32%, prior radiotherapy 6% Inclusion criteria: all women admitted for surgical treatment of gynaecological cancer using a vertical midline incision Exclusion criteria: none described |
|
| Interventions |
Comparisons reported: Group 1 Suture: polyglyconate (multifilament, slowly absorbable) Suturing technique: continuous Closure method: mass Group 2: Suture: PGA (multifilament, fast absorbable) Suturing technique: interrupted Closure method: mass Surgeon characteristics: "Most wounds were closed by house officers under the direct supervision of a senior staff gynaecologist..." |
|
| Outcomes |
Incisional hernia: any palpable defect in the fascia, even if an increase in intra‐abdominal pressure did not result in a swelling in the abdominal scar Follow‐up duration: 12, 24 and 36 months Wound infection: purulent discharge with or without a positive culture Wound dehiscence: no definition provided Suture sinus or fistula: no definition provided |
|
| Notes | Hernia data at 12 months used in analysis | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "...according to a table of computer‐generated random numbers..." |
| Allocation concealment (selection bias) | Low risk | "At the moment of abdominal‐wall suturing, a nurse assigned the patients to one of two closure techniques according to a table of computer‐generated random numbers and informed the surgeons of the type of closure to be used." |
| Blinding (performance bias and detection bias) All outcomes | Low risk | "Incisions were evaluated using careful palpation by physicians who were unaware of the type of suturing technique." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants included in analysis. Excluded participants discussed (met exclusion criteria) |
| Selective reporting (reporting bias) | Low risk | Hernia (at least 1 year); dehiscence and wound infection outcomes all reported |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Corman 1981.
| Methods |
RCT Methods to control for contributory patient factors: "Patients were further classified according to septic or contaminated status and whether or not steroids were required." |
|
| Participants |
Age: no information provided Gender: no information provided Type of incision: no information provided Type of surgery: overall: sigmoid colectomy 25%, right colectomy 20%, proctocolectomy 11%, low anterior resection 4%, Hartmann resection 3%, transverse colectomy 3%, other 11% Contamination classification of included participants: no information provided Pre‐operative antibiotic use: no information provided Prognostic patient factors: a total of 86 participants (53%) were operated for malignancy Sepsis: 8.9% in group 1, 9.4% in group 2 and 6.8% in group 3 Inclusion criteria: consecutive patients having a bowel operation employing a midline incision Exclusion criteria: none described |
|
| Interventions |
Comparisons reported: Group 1 Suture: nylon (multifilament, non‐absorbable) Suturing technique: interrupted, simple Closure method: mass Group 2: Suture: polypropylene (monofilament, non‐absorbable) Suturing technique: interrupted, simple Closure method: mass Group 3: Suture: polyglactin‐910 (multifilament, fast absorbable). Suturing technique: interrupted, simple Closure method: mass Surgeon characteristics: no clear information; "All procedures were performed by or under the direction of one of the three authors" |
|
| Outcomes |
Wound infection: no definition provided Follow‐up duration: mean follow‐up was 19 months overall; no group‐wise data available Incisional hernia: no definition provided Wound dehiscence: no definition provided Suture sinus or fistula: no definition provided |
|
| Notes | Hernia data excluded from analysis due to unclear follow‐up duration Groups 1 and 2 combined for analysis of absorbable versus non‐absorbable sutures Groups 1 and 3 combined for analysis of monofilament versus multifilament sutures |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "...the suture material to be used was randomly selected using a computer." |
| Allocation concealment (selection bias) | Unclear risk | "...the suture material to be used was randomly selected using a computer." |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | No information provided |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants analysed in the group they were assigned |
| Selective reporting (reporting bias) | Unclear risk | Unclear length of follow‐up for incisional hernia outcomes |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Dan 2014.
| Methods |
RCT Methods to control for contributory patient factors: unknown |
|
| Participants |
Age: groupwise data not available. Ages 30‐82 years Gender: groupwise data not available. Overall, Male = 59.5% Types of incisions: all midline Types of surgery: all elective surgery Contamination classification of included participants: not described Preoperative antibiotic use: not described Prognostic patient factors: not described Inclusion criteria: elective midline laparotomy Exclusion criteria: |
|
| Interventions |
Comparisons reported: Group 1: Sutures: polyglactin (multifilament, fast absorbable) Suture technique: interrupted Closure method: mass closure Group 2: Sutures: silk (multifilament, non‐absorbable) Suture technique: interrupted Closure method: mass closure |
|
| Outcomes |
Wound infection: not defined Dehiscence: not defined Sinus or fistula: "Suture rejection" |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomisation |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Loss to follow‐up and patient accountability not explicitly addressed |
| Selective reporting (reporting bias) | Low risk | There was no evidence of selective reporting |
| Other bias | Unclear risk | Follow‐up duration not described |
Deitel 1990.
| Methods |
RCT Methods to control for contributory patient factors: none described |
|
| Participants |
Age: Group 1 (mean): 34 years Group 2 (mean): 36 years Gender: Group 1: 36.6% female Group 2: 39.3% female Type of incision: all participants had an upper midline incision ending above the umbilicus Type of surgery: all participants underwent vertical banded gastroplasty Contamination classification of included participants: all wounds were classified as clean‐contaminated Pre‐operative antibiotic use: all participants received antibiotic prophylaxis with 2 g of cefazolin Prognostic patient factors: all participants were diagnosed with morbid obesity Inclusion criteria: consecutive participants who underwent vertical banded gastroplasty for morbid obesity Exclusion criteria: none described |
|
| Interventions |
Comparisons reported: Group 1 Suture: PGA (multifilament, fast absorbable) Suturing technique: continuous, reinforced with "a few" interrupted sutures Closure method: mass Group 2: Suture: polyglyconate (monofilament, slowly absorbable) Suturing technique: continuous sutures, reinforced with "a few" interrupted sutures Closure method: mass Surgeon characteristics: all procedures were performed by a senior resident under supervision |
|
| Outcomes |
Incisional hernia: no definition provided Follow‐up duration: no group‐wise data provided; all participants were followed up for > 2 years Wound infection: discharge of pus, associated with fever and increased leukocyte count Wound dehiscence: no definition provided |
|
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "The patients were allocated for closure with No.1 Dexon Plus or with No.1 Maxon by drawing a randomised card." |
| Allocation concealment (selection bias) | Unclear risk | Not clearly described |
| Blinding (performance bias and detection bias) All outcomes | Low risk | "All patients were followed up for more than 2 years by two surgeons who were blinded to the closure material used..." |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not clearly reported |
| Selective reporting (reporting bias) | Low risk | Hernia (at least 1 year); dehiscence and wound infection outcomes all reported |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Derzie 2000.
| Methods |
RCT Methods to control for contributory patient factors: none described |
|
| Participants |
Age: no information provided Gender: no information provided Types of incisions: no information provided Type of surgery: Group 1: Roux‐en‐Y gastric bypass 83.1%, vertical banded gastroplasty 2.3%, revision procedures 14.5%, additional cholecystectomy 14.0% Group 2: Roux‐en‐Y gastric bypass 84.3%, vertical banded gastroplasty 6.9%, revision procedures 8.8%, additional cholecystectomy 13.8% Contamination classification of included participants: no information provided Preoperative antibiotic use: all participants received either cefazolin or gentamicin and vancomycin (if allergic to penicillins) Prognostic patient factors: all participants were morbidly obese Inclusion criteria: none described Exclusion criteria: none described |
|
| Interventions |
Comparisons reported: Group 1: Sutures: nylon (in first 196 participants randomised), PDS (in the last 135 participants randomised) Suturing technique: continuous Closure method: mass Group 2: Sutures: nylon (in first 196 participants), PDS (in the last 135 participants) Suturing technique: interrupted, "figure‐of‐8" Closure method: mass Surgeon characteristics: no information provided |
|
| Outcomes |
Incisional hernia: not measured Wound infection: local or systemic inflammation and collection of purulent subcutaneous fluid from wound Deep wound complications: included deep surgical site infections and fascial dehiscence |
|
| Notes | Follow‐up duration: "All wounds were monitored for 30 postoperative days." Dehiscence (n = 2) were not separated from "wound complications". All "wound complications" analysed as wound infection | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | "All patients were randomised by odd or even medical record number at the time of fascial closure to either continuous or interrupted fascial closure." |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not clearly reported |
| Selective reporting (reporting bias) | Low risk | There was no evidence of selective reporting |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Docobo‐Durantez 2006.
| Methods |
RCT Methods to control for contributory patient factors: none described |
|
| Participants |
Age: Group 1: > 65 years 47.9% Group 2: > 65 years 49.2% Gender: Group 1: 47.2% female Group 2: 44.2% female Type of incision: overall, 78.1% were midline Type of surgery: Group 1: emergency 27.5% Group 2: emergency 28.2% Contamination classification of included participants: information not provided Pre‐operative antibiotic use: not described Prognostic patient factors: Group 1: malignancy 54.3%. obesity 17.1%, diabetes 18.4%, corticosteroids 4.4%, jaundice 4.2%, hypoproteinaemia 16.6%, renal failure 4.0%, ascites 1.3% Group 2: malignancy 52.7%, obesity 22.3%, diabetes 15.4%, corticosteroids 6.9%, jaundice 5.3%, hypoproteinaemia 13.8%, renal failure 5.0%, ascites 4.1% Inclusion criteria: laparotomies performed for gastrointestinal diseases and hepato‐biliopancreatic procedures (including transplant) in patients with at least 1 risk factor for wound complications: male, age > 65 years, pulmonary disease, haemodynamic instability, emergency surgery, hypoproteinaemia, clinical infection, obesity, renal failure, malignancy, ascites, steroids, hypertension, anaemia, jaundice or diabetes Exclusion criteria: hernia repair surgery, bariatric surgery, need for reinforcement sutures, uncommon incisions (including paramedian and McBurney incisions), life expectancy of < 1.5 years and deaths unrelated to wounds |
|
| Interventions |
Comparisons reported: Group 1 Suture: PDS (monofilament, slowly absorbable) Suturing technique: continuous Closure method: mass Group 2: Suture: nylon (monofilament, non‐absorbable) Suturing technique: continuous Closure method: mass Surgeon characteristics: information not provided |
|
| Outcomes |
Incisional hernia: no definition provided Follow‐up duration: 3, 6, 12 and 18 months Wound infection: "as per the Center for Disease Control (CDC) definition for surgical site infection" Dehiscence: no definition provided |
|
| Notes | Extremely high loss to follow‐up. Hernia data at 1 year used in analysis | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomisation tables created |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Only 104/451 in PDS group and 72/319 in nylon group followed up at 1 year |
| Selective reporting (reporting bias) | Low risk | Hernia (at least 1 year); dehiscence and wound infection outcomes all reported |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Donaldson 1982.
| Methods |
RCT Methods to control for contributory patient factors: none described |
|
| Participants |
Age: Group 1 (mean): 54.9 years Group 2 (mean): 53.4 years Group 3 (mean): 60.1 years Gender: Group 1: 55% female Group 2: 59% female Group 3: 53% female Type of incision: all participants underwent laparotomy through a lateral paramedian incision Group 1: upper abdominal 59%, mid‐abdominal 19%, lower abdominal 22% Group 2: upper abdominal 66%, mid‐abdominal 15%, lower abdominal 19% Group 3: upper abdominal 75%, mid‐abdominal 10%, lower abdominal 15% Type of surgery: Group 1: elective 68%; biliary 28%, pancreatic 1%, peptic ulcer 20%, colorectal cancer 15%, small bowel obstruction 3%, inflammatory bowel disease 9%, gastric cancer 5%, appendicitis 3%, other 13% Group 2: elective 72%; biliary 31%, pancreatic 0%, peptic ulcer 22%, colorectal cancer 14%, small bowel obstruction 3%, inflammatory bowel disease 5%, gastric cancer 5%, appendicitis 0%, other 15% Group 3: elective 75%; biliary 38%, pancreatic 1%, peptic ulcer 23%, colorectal cancer 13%, small bowel obstruction 5%, inflammatory bowel disease 4%, gastric cancer 9%, appendicitis 1%, other 3% Contamination classification of included participants: Group 1: clean 11%, clean‐contaminated 54%, contaminated 35% Group 2: clean 9%, clean‐contaminated 51%, contaminated 40% Group 3: clean 5%, clean‐contaminated 58%, contaminated 37% Preoperative antibiotic use: no prophylactic antibiotics were used Prognostic patient factors: Group 1: hypoalbuminaemia 33%, steroids 4%, diabetes 2.5%, uraemia 0%, jaundice 9%, respiratory disease 10% Group 2: hypoalbuminaemia 28%, steroids 0%, diabetes 0%, uraemia 3%, jaundice 8%, respiratory disease 9% Group 3: hypoalbuminaemia 34%, steroids 4%, diabetes 1%, uraemia 5%, jaundice 6%, respiratory disease 6% Inclusion criteria: all patients admitted between August 1978 and August 1979 for a laparotomy procedure under the care of the senior study author Exclusion criteria: patients with life‐threatening intra‐abdominal haemorrhage or who had a previous abdominal incision |
|
| Interventions |
Comparisons reported: Group 1 Suture: PGA (multifilament, fast absorbable) Suturing technique: continuous Closure method: layered Group 2: Sutures: chromic catgut (monofilament, fast absorbable) Suturing technique: continuous Closure method: layered Group 3: Sutures: polypropylene (monofilament, non‐absorbable) Suturing technique: continuous Closure method: layered Surgeon characteristics: no information provided |
|
| Outcomes |
Incisional hernia: no definition provided Follow‐up duration: "All wounds were further examined at 1, 3, 6, and 12 months after operation." Wound infection: wound discharge eliciting a positive bacterial culture Wound dehiscence: no definition provided Suture sinus: no definition provided |
|
| Notes | Groups 1 and 2 analysed together as "absorbable sutures" in the primary analysis Group 1 compared against Groups 2 and 3 (combined) in the monofilament versus multifilament analysis |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "However, closure of the anterior rectus sheath was randomly allocated (using a blind card system selected prior to the laparotomy)..." |
| Allocation concealment (selection bias) | Unclear risk | No clear description of the allocation procedure |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | None described |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Losses to follow‐up not clearly described |
| Selective reporting (reporting bias) | Low risk | Hernia (at least 1 year); dehiscence and wound infection outcomes all reported |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Efem 1980.
| Methods |
RCT Methods to control for contributory patient factors: none |
|
| Participants |
Age: not reported Gender: not reported Types of incisions: all participants underwent a vertical midline incision Types of surgery: Group 1: emergent 45% Group 2: emergent 45% Contamination classification of included participants: not reported Pre‐operative antibiotic use: not reported Prognostic patient factors: not reported Inclusion criteria: patients who underwent procedures through a vertical midline laparotomy Exclusion criteria: paramedian, transverse, oblique, gridiron, Pfannenstiel and Rutherford‐Morrison incisions were excluded |
|
| Interventions |
Comparisons reported: Group 1 Suture: nylon (monofilament, non‐absorbable) Suturing technique: interrupted, "Figure‐of‐8" Closure method: mass Group 2 Sutures: chromic catgut (monofilament, fast absorbable) and nylon (monofilament, non‐absorbable) Suturing technique: unclear Closure method: layered (#1 chromic for peritoneum, nylon for rectus sheath, 2‐0 chromic for fat) Surgeon characteristics: not reported |
|
| Outcomes |
Incisional hernia: no definition provided Follow‐up duration: 6‐18 months (80% for 8 months, 10% for 18 months) Wound infection: "Wound sepsis delaying discharge from hospital" Dehiscence: no definition provided Sinus or fistula: no definition provided |
|
| Notes | Hernia data excluded from analysis due to inadequate follow‐up duration at 1 year | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Unlcear how losses to follow‐up were accounted for |
| Selective reporting (reporting bias) | Low risk | There was no evidence of selective reporting |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Fagniez 1985.
| Methods |
RCT Methods to control for contributory patient factors: |
|
| Participants |
Age: Group 1 (mean): 54 years Group 2 (mean): 53 years Gender: Group 1: 55.0% female Group 2: 58.7% female Type of incision: Group 1: upper midline 55.1%; lower midline 32.7%; central midline 6.9%; complete midline 5.3% Group 2: upper midline 54.9%; lower midline 32.7%; central midline 6.8%; complete midline 5.6% Type of surgery: not reported Contamination classification of included participants: Group 1: clean 32.6%; clean‐contaminated 42.6%; contaminated 25.0% Group 2: clean 32.6%; clean‐contaminated 42.3%; contaminated 24.7% Pre‐operative antibiotic use: Group 1: 16.7% Group 2: 17.1% Prognostic patient factors: Group 1: obesity 11.9% Group 2: obesity 12.5% Inclusion criteria: all patients operated on who received a midline abdominal incision for any indication Exclusion criteria: patients operated on with incisions other than midline abdominal were excluded |
|
| Interventions |
Comparisons reported: Group 1: Sutures: PGA (multifilament, fast absorbable) Suture technique: interrupted Closure method: mass Group 2: Sutures: PGA (multifilament, fast absorbable) Suture technique: continuous Closure method: mass Surgeon characteristics: not reported |
|
| Outcomes |
Incisional hernia: not defined Follow‐up duration: unclear, but suggests 30 days Wound infection: "Wound abscess" Dehiscence: not defined Sinus or fistula: not defined |
|
| Notes | Hernia data excluded from analysis due to inadequate follow‐up duration | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Low risk | Sealed form opened by nurse at time of surgery |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants accounted for and analysed |
| Selective reporting (reporting bias) | Low risk | There was no evidence of selective reporting |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Gammelgaard 1983.
| Methods |
RCT Methods to control for contributory patient factors: none |
|
| Participants |
Age: Group 1 (median): 34 Group 2 (median): 38 Gender: Group 1: 63% female Group 2: 60% female Type of incision: Group 1: angular 13.9%, longitudinal 43.0%, transverse/oblique 43.0% Group 2: angular 10.1%, longitudinal 46.5%, transverse/oblique 40.9% Type of surgery: Group 1: emergency 29.0%; biliary 22.5%, gastric/duodenal 20.5%, intestinal 11.3%, appendectomy 24.5%, internal genitalia 21.2% Group 2: emergency 34.2%; biliary 20.1%, gastric/duodenal 19.5%, intestinal 10.1%, appendectomy 25.8%, internal genitalia 22.0% Contamination classification of included participants: not described Pre‐operative antibiotic use: not reported Prognostic patient factors: Group 1: obesity 34.4%, malignancy 15.2% Group 2: obesity 28.4%, malignancy 12.2% Inclusion criteria: consecutive abdominal incisions, either emergency or elective, for operations of the gastrointestinal tract or internal genital organs Exclusion criteria: hernioplasties, McBurney incisions, re‐operations within the follow‐up period, incisions in preparation for stoma operations, patients receiving steroids and non‐Danish patients |
|
| Interventions |
Comparisons reported: Group 1 Suture: polyglactin‐910 (multifilament, fast absorbable) Suturing technique: peritoneum ‐ continuous, fascia ‐ interrupted Closure method: layered Group 2: Sutures: PGA (multifilament, fast absorbable) Suturing technique: peritoneum ‐ continuous, fascia ‐ interrupted Closure method: layered Characteristics of surgeons: not reported |
|
| Outcomes |
Incisional hernia: no definition provided Follow‐up duration: 6 months Wound infection: defined as "wound abscess" Wound dehiscence: not defined Sinus or fistula tract: not defined |
|
| Notes | Hernia data excluded from analysis due to inadequate follow‐up duration | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Outcomes assessors blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants accounted for and analysed |
| Selective reporting (reporting bias) | Low risk | There was no evidence of selective reporting |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Gislason 1995.
| Methods |
RCT Methods to control for contributory patient factors: none |
|
| Participants |
Age: Group 1 (mean): 62 years Group 2 (mean): 60 years Group 3 (mean): 60 years Gender: Group 1: 1:1 (male:female) Group 2: 0.87:1 (male:female) Group 3: 1:1 (male:female) Type of incision: Group 1: midline 84%, transverse 16% Group 2: midline 83%, transverse 17% Group 3: midline 86%, transverse 14% Type of surgery: Group 1: emergency 36%; gastric/oesophageal 25.1%, hepato‐pancreaticobiliary 14.8%, small intestine 14.3%, colorectal 40.9%, other 4.9% Group 2: emergency 29%; gastric/oesophageal 19.1%, hepato‐pancreaticobiliary 19.1%, small intestine 15.6%, colorectal 42.7%, other 3.5% Group 3: emergency 32%; gastric/oesophageal 24.9%; hepato‐pancreaticobiliary 15.7%; small intestine 14.2%; colorectal 41.1%; other 4.1% Contamination classification of included participants: Group 1: clean 22%, clean‐contaminated/contaminated 66%, dirty 12% Group 2: clean 32%, clean‐contaminated/contaminated 59%, dirty 9% Group 3: clean 23%, clean‐contaminated/contaminated 66%, dirty 11% Pre‐operative antibiotic use: all received doxycycline or cefuroxime and metronidazole Prognostic patient factors: Group 1: mean weight 66 kg, malignancy 49.2% Group 2: mean weight 66 kg, malignancy 50.2% Group 3: mean weight 67 kg, malignancy 53.3% Inclusion criteria: "major GI surgery" (via laparotomy) Exclusion criteria: urological or gynaecological surgeries, "minor surgical procedures"; laparotomy within last 3 months |
|
| Interventions |
Comparisons reported: Group 1 Suture: polyglyconate (monofilament, slowly absorbable) Suturing technique: continuous Closure method: mass Group 2: Suture: polyglactin‐910 (multifilament, fast absorbable) Suturing technique: continuous Closure method: mass Group 3: Suture: polyglactin‐910 (multifilament, fast absorbable) Suturing technique: interrupted Closure method: mass Surgeon characteristics: not reported |
|
| Outcomes |
Incisional hernia: visible/palpable bulge with patient standing Follow‐up duration: 1 year Wound infection: inflammation of the wound with discharge, fever, increased leukocyte count or serum C‐reactive protein and a positive wound culture Wound dehiscence: ascites or abdominal viscera escaping from wound |
|
| Notes | Groups 2 compared with Group 3 in 'continuous versus interrupted' analysis Group 1 compared with Group 2 in 'monofilament versus multifilament' analysis Group 1 compared with Group 2 in 'slow versus fast absorbable' analysis |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Outcome assessors blinded |
| Incomplete outcome data (attrition bias) All outcomes | High risk | High rates of loss to follow‐up (39/203 in group 1, 36/199 in group 2) |
| Selective reporting (reporting bias) | Low risk | Hernia (at least 1 year); dehiscence and wound infection outcomes all reported |
| Other bias | High risk | Not all participants followed up within clinical setting. Some followed up by mailed survey only |
Goligher 1975.
| Methods |
RCT Methods to control for contributory patient factors: none |
|
| Participants |
Age: Group 1: < 60 years 66.4%, 60‐80 years 31.8%, > 80 years 1.9% Group 2: < 60 years 64.5%, 60‐80 years 33.6%, > 80 years 1.9% Group 3: < 60 years 61.8%, 60‐80 years 35.5%, > 80 years 2.7% Gender: Group 1: 45.8% female Group 2: 32.7% female Group 3: 46.3% female Type of incision: all paramedian incisions Type of surgery: all elective procedures Group 1: peptic ulcer disease 37.3%, colorectal cancer 18.7%, palliative 8.4%, inflammatory bowel disease 22.4%, other 13.1% Group 2: peptic ulcer disease 32.7%, colorectal cancer 23.3%, palliative 6.5%, inflammatory bowel disease 23.3%, other 14.0% Group 3: peptic ulcer disease 36.4%, colorectal cancer 17.2%, palliative 10.0%, inflammatory bowel disease 21.8%, other 14.5% Contamination classification of included participants: Group 1: contaminated 21.5% Group 2: contaminated 30.8% Group 3: contaminated 18.2% Pre‐operative antibiotic use: not described Prognostic patient factors: Group 1: obesity 30.8%, malignancy 27.1%, corticosteroids 8.4% Group 2: obesity 35.5%, malignancy 30.0%, corticosteroids 12.1% Group 3: obesity 40.0%, malignancy 27.3%, corticosteroids 10.0% Inclusion criteria: patients undergoing elective laparotomy through rectus‐displacing paramedian incisions Exclusion criteria: none described |
|
| Interventions |
Comparisons reported: Group 1 Suture: chromic catgut (monofilament, fast absorbable) Suturing technique: continuous, plus reinforcing interrupted sutures on the anterior rectus Closure method: layered Group 2: Sutures: chromic catgut (monofilament, fast absorbable) plus nylon retention sutures Suture technique: continuous, plus reinforcing interrupted nylon sutures on the anterior rectus Closure method: layered Group 3: Suture: stainless steel (monofilament, non‐absorbable) Suturing technique: interrupted, "figure‐of‐8" sutures Closure method: mass Surgeon characteristics: Group 1: consultant 30.0%, registrar 70.0% Group 2: consultant 30.8%, registrar 66.3%, unknown 2.8% Group 3: consultant 38.2%, registrar 60.0%, unknown 1.8% |
|
| Outcomes |
Incisional hernia: not defined Follow‐up duration: 6 months Wound infection: not defined Dehiscence: not defined Sinus or fistula: "Persistent wound infection and sinus formation" |
|
| Notes | Hernia data excluded, due to < 1 year's follow‐up Group 2 excluded from analysis (combined absorbable and non‐absorbable sutures) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Participants followed up for < 1 year for incisional hernia outcomes |
| Selective reporting (reporting bias) | Low risk | There was no evidence of selective reporting |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Gys 1989.
| Methods |
RCT Methods to control for contributory patient factors: none |
|
| Participants |
Age: Group 1 (mean): 64 years Group 2 (mean): 61 years Gender: Group 1: 48% female Group 2: 49% female Type of incision: Group 1: upper midline 30%, lower midline 39%, full midline 9%, subcostal 25%, other 7% Group 2: upper midline 30%, lower midline 34%, full midline 9%, subcostal 27%, other 0% Type of surgery: Group 1: emergency 24%; colorectal 34%, pancreaticobiliary 28%, oesophagogastric 22%, vascular 6%, other 10% Group 2: emergency 26%; colorectal 32%, pancreaticobiliary 34%, oesophagogastric 20%, vascular 3%, other 11% Contamination classification of included participants: Group 1: contaminated 9.0% Group 2: contaminated 4.6% Pre‐operative antibiotic use: not described Prognostic patient factors: Group 1: diabetes 9.0%, obesity 40.3%, malignancy 56.7%, respiratory failure 9.0%, jaundice 4.5% Group 2: diabetes 7.7%, obesity 30.8%, malignancy 44.6%, respiratory failure 9.2%, jaundice 7.7% Inclusion criteria: consecutive patients undergoing elective or emergency laparotomy Exclusion criteria: none described |
|
| Interventions |
Comparisons reported: Group 1 Suture: nylon (monofilament, non‐absorbable) Suturing technique: continuous Closure method: layered ('0' for peritoneum, '1' for musculo‐aponeurotic layer) Group 2: Suture: polyglyconate (monofilament, slowly absorbable) Suturing technique: continuous Closure method: layered ('0' for peritoneum, '1' for musculo‐aponeurotic layer) Surgeon characteristics: not described |
|
| Outcomes |
Incisional hernia: assessed by palpation with patient lying supine and with elevation of extended legs Follow‐up duration: 1 year Wound infection: postoperative purulent discharge with proven growth of a micro‐organism Dehiscence: "burst abdomen" Sinus or fistula: no definition provided |
|
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Of the total of 132 participants, 13 (9.8%) died within 1 year and 22 (17.0%) were lost to follow‐up |
| Selective reporting (reporting bias) | Low risk | Hernia (at least 1 year); dehiscence and wound infection outcomes all reported |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Hsiao 2000.
| Methods |
RCT Methods to control for contributory patient factors: none |
|
| Participants |
Age: Group 1 (mean): 60.9 years Group 2 (mean): 58.5 years Gender: Group 1: 44% female Group 2: 48% female Type of incision: Group 1: midline 50.5%, paramedian 4.3%, subcostal 26.1%, subcostal plus midline 4.9%, bilateral subcostal plus midline 14.1% Group 2: midline 45.5%, paramedian 5.1%, subcostal 26.3%, subcostal plus midline 5.1%, bilateral subcostal plus midline 17.9% Type of surgery: all surgeries were elective Group 1: upper GI 17.4%, hepato‐pancreaticobiliary 63.6%, lower GI 15.2%, vascular 3.3%, other 0.5% Group 2: upper GI 15.4%, hepato‐pancreaticobiliary 65.4%, lower GI 13.5%, vascular 1.2%, other 4.5% Contamination classification of included participants: not described Pre‐operative antibiotic use: all participants received cefmetazole and metronidazole Prognostic patient factors: Group 1: mean BMI 23.0, malignancy 58.1% Group 2: mean BMI 22.8, malignancy 54.4% Inclusion criteria: patients undergoing elective laparotomy Exclusion criteria: emergency laparotomies, history of laparotomy within 3 months, previous incisional hernia |
|
| Interventions |
Comparisons reported: Group 1 Suture: polyglactin‐910 (multifilament, fast absorbable) Suturing technique: continuous Closure method: mass Group 2: Suture: PDS (monofilament, slowly absorbable) Suturing technique: continuous Closure method: mass Surgeon characteristics: same surgeon for all procedures |
|
| Outcomes |
Incisional hernia: visible and palpable defect in the fascia or a protrusion in the wound when the participant was carefully examined in both horizontal and vertical positions Follow‐up duration: 24 months Wound infection: purulent discharge from the wound, confirmed by standard signs including fever and an elevated leukocyte count Dehiscence: no definition provided Sinus or fistula: no definition provided |
|
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Randomised based on last digit of hospital patient number |
| Allocation concealment (selection bias) | High risk | Randomised based on last digit of hospital patient number |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Outcome assessor blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants accounted for and analysed |
| Selective reporting (reporting bias) | Low risk | Hernia (at least 1 year); dehiscence and wound infection outcomes all reported |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Irvin 1976.
| Methods | RCT Methods to control for contributory patient factors: none | |
| Participants |
Age: Group 1 (mean): 51 years Group 2 (mean): 48 years Group 3 (mean): 50 years Gender: Group 1: 48.0% female Group 2: 38.5% female Group 3: 42.0% female Type of incision: Group 1: median 46.2%, paramedian 53.8% Group 2: median 48.0%, paramedian 52.0% Group 3: median 45.6%, paramedian 53.4% Type of surgery: all elective Group 1: biliary 36.5%, peptic ulcer 32.7%, intestinal 15.4%, other 15.4% Group 2: biliary 28.8%, peptic ulcer 42.3%, intestinal 15.4%, other 13.5% Group 3: biliary 28.1%, peptic ulcer 31.6%, intestinal 19.3%, other 21.0% Contamination classification of included participants: not specified Pre‐operative antibiotic use: not specified Prognostic patient factors: Group 1: obesity 38.5%, malignancy 9.6% Group 2: obesity 26.9%, malignancy 11.5% Group 3: obesity 26.3%, malignancy 14.0% Inclusion criteria: patients undergoing laparotomy through median or paramedian incisions Exclusion criteria: patients with prior median or paramedian scars |
|
| Interventions |
Comparisons reported: Group 1 Suture: PGA (multifilament, fast absorbable, absorbable) Suturing technique: continuous closure of peritoneum and posterior rectus sheath, interrupted closure of the anterior rectus sheath Closure method: layered Group 2: Suture: polyglactin XLG (multifilament, fast absorbable) Suturing technique: continuous closure of peritoneum and posterior rectus sheath, interrupted closure of the anterior rectus sheath Closure method: layered Group 3: Suture: polypropylene (monofilament, non‐absorbable) Suturing technique: continuous closure of peritoneum and both rectus sheaths Closure method: layered Surgeon characteristics: Group 1: consultant 67.3%, registrar 32.7% Group 2: consultant 53.9%, registrar 46.1% Group 3: consultant 52.6%, registrar 47.4% |
|
| Outcomes |
Incisional hernia: not defined Follow‐up duration: 6 months Wound infection: pus discharged from wound Dehiscence: not defined Sinus formation: not defined |
|
| Notes | Hernia data excluded from analysis due to inadequate follow‐up duration Groups 1 and 2 analysed together as 'absorbable sutures', as well as multifilament sutures |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Random allocation by drawing "trial cards" |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants discussed, with explanation of those not included in analysis |
| Selective reporting (reporting bias) | Low risk | There was no evidence of selective reporting |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Irvin 1977.
| Methods |
RCT Methods to control for contributory patient factors: "The method of randomisation took into account the type of surgery performed..." |
|
| Participants |
Age: unknown Gender: unknown Type of incision: Group 1: median 43.2%, paramedian 56.8% Group 2: median 40.6%, paramedian 59.4% Type of surgery: Group 1: emergent 16.8%, palliative 12.6%; biliary 27.4%, peptic ulcer 30.5%, intestinal 25.3%, other 16.8% Group 2: emergent 14.6%, palliative 10.4%; biliary 35.4%, peptic ulcer 25.0%, intestinal 20.8%, other 18.8% Contamination classification of included participants: 163 "clean" wounds, 28 "infected" wounds, not broken down by group Pre‐operative antibiotic use: not described Prognostic patient factors: not reported Inclusion criteria: patients going through exploratory laparotomy through median or paramedian incisions Exclusion criteria: not described |
|
| Interventions |
Comparisons reported: Group 1 Sutures: polypropylene (monofilament, non‐absorbable), polyester retention sutures Suturing technique: continuous (with interrupted retention sutures) Closure method: layered Group 2: Sutures: stainless steel (monofilament, non‐absorbable) Suturing technique: interrupted, 'figure‐of‐8' Closure method: mass Surgeon characteristics: Group 1: consultant 40.0%, registrar 60.0% Group 2: consultant 43.4%, registrar 56.6% |
|
| Outcomes |
Incisional hernia: palpable defect in abdominal fascia with straining Follow‐up duration: 6 months Wound dehiscence: no definition provided Wound infection: discharge of pus from wound |
|
| Notes | Hernia data excluded from analysis due to inadequate follow‐up duration | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "randomly allocated by drawing a trial card at the end of the abdominal procedure, and the method of randomisation took account of the type of surgery performed…" |
| Allocation concealment (selection bias) | Unclear risk | "randomly allocated by drawing a trial card at the end of the abdominal procedure, and the method of randomisation took account of the type of surgery performed…" |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants accounted for and dropouts adequately explained |
| Selective reporting (reporting bias) | Low risk | There was no evidence of selective reporting |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Israelsson 1994.
| Methods |
RCT Methods to control for contributory patient factors: not described |
|
| Participants |
Age: Group 1 (mean): 62 years Group 2 (mean): 62 years Gender: Group 1: 45.7% female Group 2: 48.0% female Type of incision: all incisions were midline Type of surgery: Group 1: emergency 30% Group 2: emergency 33% Contamination classification of included participants: Group 1: clean 34%, clean‐contaminated 55%, contaminated 11% Group 2: clean 34%, clean‐contaminated 56%, contaminated 10% Pre‐operative antibiotic use: not described Prognostic patient factors: not described Inclusion criteria: patients undergoing abdominal surgery through a midline incision Exclusion criteria: patients with an incisional hernia from previous abdominal surgery |
|
| Interventions |
Comparisons reported: Group 1: Suture: PDS (monofilament, slowly absorbable) Suturing technique: continuous Closure method: mass Group 2: Suture: nylon (monofilament, non‐absorbable) Suturing technique: continuous Closure method: mass Surgeon characteristics: group‐wise not described |
|
| Outcomes |
Incisional hernia: palpable defect in the fascia or a protrusion beyond the level of the fascia with the patient supine lifting both legs, and coughing or straining in an erect position Follow‐up duration: 12 months Wound infection: purulent discharge from the wound with or without generalised symptoms Dehiscence: no definition provided Sinus or fistula tract: no definition provided |
|
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Randomised based on alternating weeks |
| Allocation concealment (selection bias) | High risk | See above |
| Blinding (performance bias and detection bias) All outcomes | High risk | See above |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants accounted for and analysed |
| Selective reporting (reporting bias) | Low risk | Hernia (at least 1 year); dehiscence and wound infection outcomes all reported |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Kiely 1985.
| Methods | RCT | |
| Participants |
Age: infants and children Gender: Group 1: female 38.6% Group 2: female 36.4% Types of incisions Group 1: transverse 70%; vertical 30% Group 2: transverse 66.8%; vertical 33.2% Types of surgery: not specified Contamination Group 1: contaminated 38.2% Group 2: contaminated 37.1% Preoperative antibiotics: not described Inclusion criteria: all patients < 16 years undergoing laparotomy between 1980 and 1982 Exclusion criteria: none specified |
|
| Interventions |
Comparison reported: Group 1: Suture: PGA (fast absorbable, multifilament) Suture technique: interrupted Closure method: mass Group 2: Suture: PGA (fast absorbable, multifilament) Suture technique: continuous for each layer Closure method: layer |
|
| Outcomes |
Hernia: not defined Follow‐up duration: not defined Wound infection: not defined Dehiscence: not defined |
|
| Notes | Data excluded from hernia outcome, due to unclear follow‐up duration | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Alternate case allocation |
| Allocation concealment (selection bias) | High risk | Alternate case allocation |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants accounted for and analysed |
| Selective reporting (reporting bias) | Low risk | There was no evidence of selective reporting |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Kronborg 1976.
| Methods |
RCT Methods to control for contributory patient factors: none described |
|
| Participants |
Age: not described Gender: Group 1: female 59% Group 2: female 45% Types of incisions: Group 1: longitudinal 44%, transverse 45%, angular 11% Group 2: longitudinal 46.7%, transverse 41.1%, angular 12.2% Types of surgery: elective Group 1: colorectal 53.3%, gastric 28.8%, common bile duct 17.9% Group 2: colorectal 60.1%, gastric 27%, common bile duct 12.9% Contamination classification of included participants: not described Pre‐operative antibiotic use: not described Prognostic patient factors: Group 1: obesity 17.8% Group 2: obesity 16.0% Inclusion criteria: patients undergoing elective, major surgery of the GI tract Exclusion criteria: patients undergoing simple cholecystectomies, proximal gastric vagotomies, findings of inoperable cancers and with previous laparotomies |
|
| Interventions |
Comparisons reported: Group 1: Suture: PGA (multifilament, fast absorbable) for fascia Suturing technique: interrupted fascial closure; peritoneum closed with continuous catgut, subcutaneous tissues closed with interrupted catgut, skin closed with interrupted silk Closure method: layered Group 2: Suture: silk (multifilament, non‐absorbable) for fascia Suturing technique: interrupted fascial closure; peritoneum closed with continuous catgut, subcutaneous tissue closed with interrupted catgut, skin closed with interrupted silk Closure method: layered Surgeon characteristics: not described |
|
| Outcomes |
Incisional hernia: not defined Follow‐up duration: 3 months Wound infection: not defined Dehiscence: "wound rupture" with fascial dehiscence Sinus tract formation: "suture granuloma" |
|
| Notes | Incisional hernia data excluded due to inadequate follow‐up duration | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Blind paired sample principle" prior to fascial closure |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Outcome assessors blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants accounted for, analysed in group allocation |
| Selective reporting (reporting bias) | Low risk | There was no evidence of selective reporting |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Krukowski 1987.
| Methods |
RCT Methods to control for contributory patient factors: stratified by age (>/< 60 years), sex, emergent versus elective and degree of contamination |
|
| Participants |
Age: Group 1: 48.6% < 60 years Group 2: 49.1% < 60 years Gender: Group 1: 48.4% female Group 2: 46.2% female Type of incision: vertical midline incision for all participants Type of surgery: both emergent and elective Contamination classification of included participants: Group 1: clean 24.6%, clean‐contaminated 51.8%, contaminated 7.2%, dirty 16.3% Group 2: clean 26.6%, clean‐contaminated 49.6%, contaminated 8.0%, dirty 15.7% Pre‐operative antibiotic use: not described Prognostic patient factors: not described Inclusion criteria: patients undergoing laparotomy through a vertical midline incision Exclusion criteria: patients undergoing repair of an incisional hernia |
|
| Interventions |
Comparisons reported: Group 1: Suture: PDS (monofilament, slowly absorbable) Suturing technique: continuous Closure method: mass Group 2: Suture: polypropylene (monofilament, non‐absorbable) Suturing technique: continuous Closure method: mass Surgeon characteristics: all cases performed by 2 consultants |
|
| Outcomes |
Hernia: palpable gap without herniation or a diffuse bulge or obvious herniation Follow‐up duration: 12 months Wound infection: discharge of pus from the wound or growth of a pathogenic organism from serous or sanguineous discharge Dehiscence: evisceration Sinus or fistula: not defined |
|
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomisation tables |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Intention‐to‐treat, all participants accounted for |
| Selective reporting (reporting bias) | Low risk | Hernia (at least 1 year); dehiscence and wound infection outcomes all reported |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Larsen 1989.
| Methods |
RCT Methods to control for contributory patient factors: |
|
| Participants |
Age: Group 1 (median): 36 years Group 2 (median): 37 years Group 3 (median): 40 years Gender: Group 1: 84.0% female Group 2: 85.5% female Group 3: 86.8% female Type of incision: Group 1: transverse/oblique 76.0%, median/paramedian 24.0% Group 2: transverse/oblique 83.9%, median/paramedian 16.1% Group 3: transverse/oblique 71.1%, median/paramedian 28.9% Type of surgery: Group 1: emergent 28.0%, elective 72.0%; gastric 9.3%, biliary 30.7%, other non‐gynaecological 8.0%, caesarean section 28.0%, hysterectomy 17.3%, others 6.7% Group 2: emergent 29.9%, elective 70.1%; gastric 6.9%, biliary 28.7%, other non‐gynaecological 9.2%, caesarean 20.7%, hysterectomy 19.5%, others 15% Group 3: emergent 28.9%, elective 71.1%; gastric 9.2%, biliary 23.7%, non‐gynaecological 11.8%, caesarean 19.7%, hysterectomy 18.4%, others 17.1% Contamination classification of included participants: Preoperative antibiotic use: Prognostic patient factors: Inclusion criteria: patients undergoing clean and clean‐contaminated laparotomy Exclusion criteria: patients with ascites, appendectomy through an oblique muscle‐split incision, surgery through an old laparotomy scar, IDDM, thromboembolic prophylaxis with vitamin K‐antagonist |
|
| Interventions |
Comparisons reported: Group 1: Sutures: PGA (multifilament, fast absorbable) Suture technique: continuous Closure method: layered Group 2: Sutures: nylon (multifilament, non‐absorbable) Suture technique: continuous Closure method: layered Group 3: Sutures: PGA (multifilament, fast absorbable) Suture technique: interrupted Closure method: layered Characteristics of surgeons: not described |
|
| Outcomes |
Hernia: not defined Follow‐up duration: at 3 months then 14 to 52 months (median = 41 months) Wound infection: not defined Dehiscence: not defined Sinus/fistula: not defined |
|
| Notes | Hernia data from late follow‐up (median 41 months) Group 1 and 3 analysed together as 'absorbable' suture for absorbable versus non‐absorbable analysis, Group 1 and 2 analysed together as 'continuous' in the continuous versus interrupted analysis. Group 1 compared to Group 2 in subgroup analysis of absorbable versus non‐absorbable. Group 1 compared to group 3 in subgroup analysis of interrupted versus layered |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Type of randomisation not specified |
| Allocation concealment (selection bias) | Low risk | Sealed envelopes |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Intention‐to‐treat, all participants accounted for |
| Selective reporting (reporting bias) | Low risk | Reported on wound infections, dehiscence and had adequate follow‐up for hernia |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Leaper 1977.
| Methods |
RCT Methods to control for contributory patient factors: none |
|
| Participants |
Age: not stated Gender: Group 1 female 54.3% Group 2 female 53% Group 3 female 46.7% Types of incisions: Group 1 paramedian 11.2%, midline 56.9%, transverse 31.9% Group 2 paramedian 10.7%, midline 53.7%, transverse 35.5% Group 3 paramedian 10%, midline 54.1%, transverse 35.8% Types of surgery: Group 1 colorectal 26.7%, biliary 20.7%, gastric 28.4%, miscellaneous 24.1% Group 2 colorectal 26.4%, biliary 28.9%, gastric 22.3%, miscellaneous 22.3% Group 3 colorectal 27.5%, biliary 25.8%, gastric 34.2%, miscellaneous 12.5% Contamination classification of included participants: Preoperative antibiotic use: Prognostic patient factors: Malignancy: Group 1 25.8%, Group 2 34.7%, Group 3 36.7% COPD: Group 1 44%, Group 2 52%, Group 3 42% Hypoproteinaemia: Group 1 11%, Group 2 10%, Group 3 5% Inclusion criteria: major laparotomies Exclusion criteria: appendectomy through muscle‐splitting incision, lumbar sympathectomy, renal bladder and prostatic surgery, incisions through previous scars |
|
| Interventions |
Comparisons reported: Group 1: Sutures: nylon (monofilament, non‐absorbable) Suture technique: continuous Closure method: layered (peritoneum and posterior sheath closed with chromic catgut, anterior sheath by nylon) Group 2: Sutures: PGA (multifilament, fast absorbable) Suture technique: interrupted (Smead Jones) Closure method: mass closure Group 3: Sutures: steel (monofilament, non‐absorbable) Suture technique: interrupted (Smead Jones) Closure method: mass closure Characteristics of surgeons: Consultant: Group 1 25.8%, Group 2 28.9%, Group 3 30% |
|
| Outcomes |
Hernia: bulge noticeable by patient and assessor upon standing Follow‐up duration: 6 months Wound infection: primary sepsis is discharge of pus from a previously dry wound, secondary sepsis is acquisition of infection by a discharging wound. Major sepsis involves the deep layers of the wound and is accompanied by constitutional symptoms Dehiscence: separation of deep layers, heralded by discharge of ascites Sinus or fistula: not defined |
|
| Notes | Hernia data excluded from analysis due to inadequate follow‐up duration Group 2 compared with group 3 for 'absorbable versus non‐absorbable' and 'monofilament versus multifilament' as they share a common closure technique and method Group 2 and 3 analysed together as 'interrupted', 'mass' |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomisation was by "means of instructions in a sealed envelope" |
| Allocation concealment (selection bias) | Low risk | Sealed envelope |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants accounted for and analysed |
| Selective reporting (reporting bias) | Low risk | There was no evidence of selective reporting |
| Other bias | High risk | Surgeons refused randomisation in 17 cases |
Leaper 1985.
| Methods |
RCT Methods to control for contributory patient factors: |
|
| Participants |
Age (SD): Group 1 mean 57.4 years (1.8), Group 2 mean 57.9 years (1.7) Gender: Group 1 female 64%, Group 2 female 60% Types of incisions: Group 1: midline 77.3%, transverse 22.7% Group 2: midline 72%, transverse 28% Types of surgery: Group 1: oesophageal 14.4%, pancreaticobiliary 49.5%, small bowel 4.1%, colon 23.7%, unopened viscus 8.2% Group 2: oesophageal 17.7%, pancreaticobiliary 41.1%, small bowel 4.7%, colon 27.1%, unopened viscus 9.3% Contamination classification of included participants: Preoperative antibiotic use: single intravenous dose of third generation cephalosporin at induction for oesophago‐duodeno‐gastric, biliary and pancreatic operations; either the same or a combination with metronidazole at induction and at 6 and 12 h postoperatively for small bowel and colorectal operations Prognostic patient factors: Malignancy: Group 1 25.8%, Group 2 29% Jaundice: Group 1 25.8%, Group 2 16.3% Inclusion criteria: midline and transverse incisions Exclusion criteria: incisions through scar |
|
| Interventions |
Comparisons reported: Group 1: Sutures: nylon (monofilament, non‐absorbable) Suture technique: continuous Closure method: mass Group 2: Sutures: PDS (monofilament, slowly absorbable) Suture technique: continuous Closure method: mass Characteristics of surgeons: Group 1 consultants 33%, Group 2 consultants 37.4% |
|
| Outcomes |
Hernia: not defined Follow‐up duration: 6 months Wound infection: not defined Dehiscence: not defined |
|
| Notes | Hernia data excluded due to inadequate follow‐up duration | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated |
| Allocation concealment (selection bias) | Unclear risk | Not explicitly described |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not explicitly described |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Not an intention‐to‐treat analysis |
| Selective reporting (reporting bias) | Low risk | There was no evidence of selective reporting |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Lewis 1989.
| Methods |
RCT Methods to control for contributory patient factors: none |
|
| Participants |
Age: Group 1 mean 56.8 (17), Group 2 mean 55.8 (18) Gender: Group 1 female 57.3%, Group 2 female 48.4% Types of incisions: vertical laparotomy 100% Types of surgery: Group 1 biliary 46.6%, upper GI 22.3%, colorectal 29.1%, vascular 6.8%, miscellaneous 5.8% Group 1 biliary 37.6%, upper GI 40.8%, colorectal 25.8%, vascular 7.5%, miscellaneous 8.6% Contamination classification of included participants: Clean: Group 1 30%, Group 2 28% Clean‐contaminated: Group 1 51.5%, Group 2 54.8% Contaminated: Group 1 18.4%, Group 2 17.2% Preoperative antibiotic use: Group 1 65%, Group 2 68.8% Prognostic patient factors: Malignancy: Group 1 28.1%, Group 2 22.6% Corticosteroids: Group 1 5.8%, Group 2 4.3% Elevated bilirubin: Group 1 5.8%, Group 2 6.4% Inclusion criteria: vertical laparotomy > 10 cm Exclusion criteria: emergency procedures |
|
| Interventions |
Comparisons reported: Group 1: Sutures: PGA (multifilament, fast absorbable) Suture technique: interrupted (Smead Jones) Closure method: mass Group 2: Sutures: polypropylene (monofilament, non‐absorbable) Suture technique: continuous Closure method: mass Characteristics of surgeons: |
|
| Outcomes |
Hernia: defect with sharp fascial margins and presenting as a bulge when patient strained while standing Follow‐up duration: unknown Wound infection: pus from wound Dehiscence: evisceration |
|
| Notes | Hernia data excluded from analysis due to unclear follow‐up duration | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Randomised based on birth year (even versus odd) |
| Allocation concealment (selection bias) | High risk | Even versus odd birth year |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not explicitly described |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants accounted for, dropouts explained |
| Selective reporting (reporting bias) | Unclear risk | Follow‐up duration unclear, wound infection and dehiscence reported |
| Other bias | Low risk | The study appears to be free of other sources of bias |
McNeill 1986.
| Methods |
RCT Methods to control for contributory patient factors: none |
|
| Participants |
Age: Group 1 mean 35 (12), Group 2 mean 38 (11) Gender: Group 1 female 81.2%, Group 2 female 84.3% Types of incisions: vertical midline incision in all participants Types of surgery: Group 1: gastric bypass 33.3%, gastroplasty 66.7% Group 2: gastric bypass 27.5%, gastroplasty 72.5% Contamination classification of included participants: not described Preoperative antibiotic use: not described Prognostic patient factors: all participants undergoing surgery for morbid obesity Inclusion criteria: none clearly specified although patients were undergoing Roux‐en‐Y gastric bypass or gastroplasty for morbid obesity Exclusion criteria: none clearly specified |
|
| Interventions |
Comparisons reported: Group 1: Sutures: steel (monofilament, non‐absorbable) Suture technique: interrupted Smead Jones Closure method: mass Group 2: Sutures: PGA (multifilament, fast absorbable) Suture technique: continuous Closure method: mass Characteristics of surgeons: all closure by residents under supervision of consultant |
|
| Outcomes |
Hernia: not defined Follow‐up duration: 8‐35 months Wound infection: not defined Dehiscence: not defined |
|
| Notes | Hernia data excluded from analysis as not all participants followed up for at least 1 year | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Randomisation by hospital number – odd numbers to steel, even numbers to Dexon Plus |
| Allocation concealment (selection bias) | High risk | Randomisation by hospital number – odd numbers to steel, even numbers to Dexon Plus |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants accounted for; clear explanation of dropouts |
| Selective reporting (reporting bias) | Low risk | There was no evidence of selective reporting |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Mirza 2003.
| Methods |
RCT Methods to control for contributory patient factors: unknown |
|
| Participants |
Age: Group 1 (mean): 40.6 Group 2 (mean): 41.8 Gender: Group 1: female 45.6% Group 2: female 44.7% Types of incisions: Group 1: midline 51.9%, paramedian 13.9%, subcostal 27.8%, transverse 6.4% Group 1: midline 50.6%, paramedian 15.3%, subcostal 27.1%, transverse 7.0% Types of surgery: Emergency surgery: Group 1 23%; Group 2 33% Group 1: upper GI 8.9%; small bowel 34.2%; biliary tract 26.6%; large bowel 24.0%; solid organs 6.3% Group 2: upper GI 9.4%; small bowel 34.1%; biliary tract 27.1%; large bowel 23.5%; solid organs 5.9% Contamination classification of included participants: Group 1: clean 24.1%; clean‐contaminated 46.8%, contaminated 29.1% Group 2: clean 24.7%; clean‐contaminated 48.2%, contaminated 27.1% Preoperative antibiotic use: all participants received 3 doses of 2nd‐generation cephalosporin, participants with opening of bowel received metronidazole as well Prognostic patient factors: Group 1: malignancy 26.6%, diabetes 16.4%, jaundice 15.2%, obesity 7.6%, pulmonary disease 6.3%, steroids 5.1% Group 2: malignancy 25.9%, diabetes 17.6%, jaundice 15.3%, obesity 4.7%, pulmonary disease 5.9%, steroids 3.5% Inclusion criteria: elective and emergency patients Exclusion criteria: previous surgery through same incision within last 6 months, heavily contaminated operations |
|
| Interventions |
Comparisons reported: Group 1: Sutures: PDS (monofilament, slowly absorbable) Suture technique: continuous Closure method: mass closure of midline incision, layered closure of other incisions Group 2: Sutures: polypropylene (monofilament, non‐absorbable) Suture technique: continuous Closure method: mass closure of midline incision, layered closure of other incisions |
|
| Outcomes |
Hernia: visible swelling with positive cough impulse and palpable fascial defect Follow‐up duration: 12 months Wound infection: discharge of pus or growth of pathogenic microbes from wound discharge Dehiscence: operative closure of fascial wound necessitated Sinus or fistula: micro‐abscess or a chronic discharging sinus healed only after removal of suture |
|
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants accounted for and analysed |
| Selective reporting (reporting bias) | Low risk | Hernia follow‐up at least 1 year; wound infection and dehiscence reported |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Ohira 2015.
| Methods |
RCT Methods to control for contributory patient factors: unknown |
|
| Participants |
Age: not reported Gender: Group 1: female 7.1% Group 2: female 44.4% Types of incisions: all incisions were midline Types of surgery: all elective surgery Group 1: gastric 53.5%; colon 46.5% Group 2: gastric 55.6%; colon 44.4% Contamination classification of included participants: not reported Preoperative antibiotic use: not reported Prognostic patient factors: Group 1: diabetes 10.7%; average BMI 21.7 Group 2: diabetes 25.9%; average BMI 22.0 Inclusion criteria: gastric or colon cancer patients operated on with curative intent, aged 20‐80 years Exclusion criteria: non curative surgery, previous midline incision, laparoscopic surgery; immunosuppression (as defined by long‐term corticosteroid use, uncontrolled diabetes, or cirrhosis of the liver); and the surgeon’s judgment that the patient was unsuitable for the trial. |
|
| Interventions |
Comparisons reported: Group 1: Sutures: polyglactin (multifilament, fast absorbable) Suture technique: interrupted Closure method: mass closure Group 2: Sutures: PDS (monofilament, slowly absorbable) Suture technique: interrupted Closure method: mass closure |
|
| Outcomes |
Hernia: physical exam, CT scan every 6 months; follow‐up: up to 36 months (minimum 12 months) Wound Infection: not defined Dehiscence: not defined |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomisation sequence not clearly described |
| Allocation concealment (selection bias) | Unclear risk | Allocation concealment not clearly described |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Blinding of outcome assessors not clearly stated |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants accounted for |
| Selective reporting (reporting bias) | Low risk | There was no evidence of selective reporting |
| Other bias | High risk | Participants not similar at baseline (higher proportion of women in group 2, 2 vs 12); curative intent of surgery not determined until after randomisation |
Orr 1990.
| Methods | Methods to control for contributory patient factors: none | |
| Participants |
Age: not described Gender: not described Types of incisions: not described Types of surgery: not described Contamination classification of included participants: not described Preoperative antibiotic use: not described Prognostic patient factors: not described Inclusion criteria: patients included with risk criteria < 7 using prespecified criteria Exclusion criteria: none specifically described |
|
| Interventions |
Comparisons reported: Group 1: Sutures: polyglyconate (monofilament, slowly absorbable) Suture technique: continuous, non‐locking, 2 suture technique Closure method: mass Group 2: Sutures: polyglyconate (monofilament, slowly absorbable) Suture technique: interrupted, Smead Jones Closure method: mass Characteristics of surgeons: not described |
|
| Outcomes |
Hernia: no definition Follow‐up duration: 6 months Wound infection: no definition given |
|
| Notes | Hernia data excluded due to inadequate follow‐up duration | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants accounted for/dropouts described |
| Selective reporting (reporting bias) | Low risk | There was no evidence of selective reporting |
| Other bias | High risk | Baseline characteristics of groups not described |
Orr 2003.
| Methods |
RCT Methods to control for contributory patient factors: none |
|
| Participants |
Age: Group 1: mean 55.1 (SD 15.4) Group 2: mean 55.3 (SD 14.3) Gender: all female Types of incisions: Group 1: upper 19.2%, lower 33.7%, extended 47.1% Group 2: upper 21.6%, lower 30.9%, extended 47.4% Types of surgery: Group 1: gynaecological cancer 72%; GI cancer 3.8%; sarcoma 0.96%; lymphoma 0.96%; obesity 15.4%; GI disease 1.9%; pelvic mass 4.8% Group 2: gynaecological cancer 68%; GI cancer 5.1%; sarcoma 1%; lymphoma 0%; obesity 12.3%; GI disease 6.2%; pelvic mass 7.2% Contamination classification of included participants: All participants with clean or clean‐contaminated wounds. Group breakdown not given Preoperative antibiotic use: participants receive by protocol ≤ 3 doses of prophylactic antibiotics. Type of antibiotic and compliance not described Prognostic patient factors: Group 1: diabetes mellitus 15%, malignancy 22.9%, corticosteroids 9.5%, chronic pulmonary conditions 13.3% Group 2: diabetes mellitus 14%, malignancy 21.4%, corticosteroids 8.2%, chronic pulmonary conditions 12.2% Inclusion criteria: age ≥ 18 years, with at least one of: > 70 years of age; obesity; confirmed cancer; diabetes (requiring pharmacotherapy); COPD (FEV < 60% mL; resting PO2 < 70 mmHg, PCO2 > 45 mmHg); chronic steroid use (≥ 5 mg prednisone equivalent/day); altered nutritional status (albumin < 3.5 mg/dL or involuntary weight loss > 10% of body weight over the last 3 months); Ascites; chronic renal insufficiency (creatinine > 2.0 mg/dL); jaundice (total serum bilirubin > 2.5 mg/dL and clinical jaundice); prior radiation to surgical site; prior transverse incision that crosses the study vertical incision Exclusion criteria: not specifically described |
|
| Interventions |
Comparisons reported: Group 1: Sutures: 1 Poly (L‐lactide/glycolide) (multifilament, slowly absorbable); suture length: wound length > 4:1 Suture technique: continuous Closure method: mass closure Group 2: Sutures: polypropylene (monofilament, non‐absorbable); suture length: wound length > 4:1 Suture technique: continuous Closure method: mass closure Characteristics of surgeons: 9 institutions |
|
| Outcomes |
Hernia: no definition provided Follow‐up duration: 6 months Wound infection: no definition provided Dehiscence: no definition provided |
|
| Notes | Hernia data excluded due to inadequate follow‐up duration | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 203 participants enrolled, results of 201 participants presented |
| Selective reporting (reporting bias) | Low risk | There was no evidence of selective reporting |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Osther 1995.
| Methods |
RCT Methods to control for contributory patient factors: none |
|
| Participants |
Age: Group 1: median 75 Group 2: median 77 Gender: Group 1 female 53%; Group 2 56.7% Types of incisions: Group 1: median 9%; paramedian 59%; oblique 13%; transverse 19% Group 2: median 10.6%; paramedian 53.8%; oblique 11.5%; transverse 23.1% Types of surgery: not described Contamination classification of included participants: not described Preoperative antibiotic use: not described Prognostic patient factors: Group 1: malignancy 42% Group 2: malignancy 47.1% Inclusion criteria: undergoing laparotomy with ≥ 1 criteria for impaired wound healing including age > 70 years, COPD for at least 10 years, intra‐abdominal malignancy or diffuse peritonitis Exclusion criteria: appendectomy through an oblique muscle‐splitting incision, laparotomy through a previous scar |
|
| Interventions |
Comparisons reported: Group 1: Sutures: PGA (multifilament, fast absorbable) Suture technique: interrupted Closure method: mass Group 2: Sutures: polyglyconate (monofilament, slowly absorbable) Suture technique: interrupted Closure method: mass Characteristics of surgeons: not described |
|
| Outcomes |
Hernia: palpable protruding swelling and fascial defect Follow‐up duration: 10 days, 3 months and 12 months Wound infection: purulent discharge leading to surgical drainage Dehiscence: fascial disruption with operative closure necessary Sinus/fistula: no definition provided |
|
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random numbers using Geigy scientific tables |
| Allocation concealment (selection bias) | Unclear risk | Not explicitly described |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not explicitly described |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants accounted for. Loss to follow‐up described by group |
| Selective reporting (reporting bias) | High risk | Dehiscence not reported despite pre‐specified |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Pandley 2013.
| Methods |
RCT Methods to control for contributory patient factors: none |
|
| Participants |
Age: Group 1 (mean): 54 Group 2 (mean): 56 Gender: Group 1: female 26.0% Group 2: female 22.0% Types of incisions: all participants had a midline incision Types of surgery: Emergency surgery: Group 1 73.5%; Group 2 77.1% Group 1: bowel obstruction 15.1%, hemoperitoneum 9.4%; blunt trauma 10.4%; abdominal mass 9.4%; gut gangrene 1.9%; umbilical hernia 2.8% Group 2: bowel obstruction 17.1%, hemoperitoneum 11.4%; blunt trauma 8.6%; abdominal mass 13.3%; gut gangrene 2.9%; umbilical hernia 1.9% Contamination classification of included participants: not specifically reported. Reported "perforation" as Group 1 45.3%; Group 2 40.0% Preoperative antibiotic use: not described Prognostic patient factors: Group 1: BMI (mean) 28.4; diabetes 6.6%; smoker 24.5% Group 2: BMI (mean) 27.6; diabetes 8.6%; smoker 22.9% Inclusion criteria: all participants undergoing an elective or emergency midline laparotomy for various indications Exclusion criteria: pregnancy, presence of an abdominal hernia, lack of informed consent, age < 18 years, and previous laparotomy |
|
| Interventions |
Comparisons reported: Group 2: Sutures: polypropylene (monofilament, non‐absorbable) Suture technique: continuous Closure method: mass Group 2: Sutures: polyglactin‐910 (multifilament, fast absorbable) Suture technique: continuous Closure method: mass Characteristics of surgeons: not reported |
|
| Outcomes | Dehiscence: not defined | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not clearly described |
| Allocation concealment (selection bias) | Unclear risk | Not clearly described |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not clearly described |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants accounted for with no losses to follow‐up |
| Selective reporting (reporting bias) | Low risk | There was no evidence of selective reporting |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Pollock 1979.
| Methods |
RCT Methods to control for contributory patient factors: none |
|
| Participants |
Age: Group 1: 60.4% ≥ 60 Group 2: 61.6% ≥ 60 Group 3: 62.6% ≥ 60 Gender: Group 1: female 57.3% Group 2: female 58.6% Group 3: female 59.6% Types of incisions: Group 1: midline 56.3%; transverse 43.7% Group 1: midline 58.6%; transverse 41.4% Group 1: midline 55.6%; transverse 44.4% Types of surgery: Group 1: emergency 12.5% Group 2: emergency 21.2% Group 3: emergency 22.2% Contamination classification of included participants: not specified Preoperative antibiotic use: not specified Prognostic patient factors: Group 1: obesity 32.3%; jaundice 8.3% Group 2: obesity 41.4%; jaundice 6.1% Group 1: obesity 34.3%; jaundice 5.1% Inclusion criteria: consecutive patients undergoing emergency or elective major laparotomy Exclusion criteria: gridiron muscle‐splitting incision, Pfannenstiel for prostatectomy, lumbar and incisions through pre‐existing incisional hernias were excluded |
|
| Interventions |
Comparisons reported: Group 1: Sutures: steel (monofilament, non‐absorbable) Suture technique: continuous Closure method: mass Group 2: Sutures: PGA (multifilament, fast absorbable) Suture technique: continuous Closure method: mass Group 3: Sutures: nylon (monofilament, non‐absorbable) Suture technique: continuous Closure method: mass Characteristics of surgeons: consultant (50.8%) and registrar closures (49.2%) |
|
| Outcomes |
Hernia: visible bulge deep to the scar on straining, plus palpable defect in musculo‐aponeurosis Follow‐up duration: "Not less than 6 months" Wound infection: any discharge from wound within 1 month of surgery Sinus/fistula: no definition provided |
|
| Notes | Hernia data excluded from analysis due to inadequate follow‐up duration Group 1 and 3 analysed together as 'non‐absorbable' and 'monofilament' |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not specified |
| Allocation concealment (selection bias) | Unclear risk | Not specified |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not specified |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Participants accounted for; loss to follow‐up described by group |
| Selective reporting (reporting bias) | Low risk | There was no evidence of selective reporting |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Richards 1983.
| Methods |
RCT Methods to control for contributory patient factors: none |
|
| Participants |
Age: unknown Gender: unknown Types of incisions: Group 1: midline 85.3%; oblique 13.6%; paramedian 1.1% Group 2: midline 80.3%; oblique 17.5%; paramedian 2.1% Types of surgery: unknown Contamination classification of included participants: Group 1: clean 38.8%; clean‐contaminated 53.8%; contaminated 7.3% Group 2: clean 31.9%; clean‐contaminated 59.3%; contaminated 8.8% Preoperative antibiotic use: unknown Prognostic patient factors: not described Inclusion criteria: abdominal incision > 5 cm, excluding major trauma and heavily contaminated wounds |
|
| Interventions |
Comparisons reported: Group 1: Sutures: polypropylene (monofilament, non‐absorbable) Suture technique: continuous Closure method: mass Group 2: Sutures: PGA (multifilament, fast absorbable) for anterior sheath, polypropylene (monofilament, non‐absorbable) for posterior sheath Suture technique: interrupted Smead Jones for anterior, continuous for posterior/transverse/oblique Closure method: layered Characteristics of surgeons: unknown |
|
| Outcomes |
Hernia: no definition Follow‐up duration: 12 months Wound infection: no definition Dehiscence: no definition Sinus/fistula: no definition |
|
| Notes | Not included in absorbable versus non‐absorbable analysis as polypropylene was used on the fascia for both groups | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Method of closure determined by drawing a sealed card from 1 of 3 boxes |
| Allocation concealment (selection bias) | Low risk | Sealed card |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants accounted for and dropouts explained |
| Selective reporting (reporting bias) | Low risk | Hernia follow‐up at least 1 year; dehiscence and wound infection reported |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Sahlin 1993.
| Methods |
RCT Methods to control for contributory patient factors: none |
|
| Participants |
Age: Group 1 mean age 58 (SD 17); Group 2 mean age 58 (SD 17) Gender: Group 1 female 65.8%; Group 2 female 60.2% Types of incisions: Group 1: midline 42.9%; paramedian 11.3%; subcostal/transverse 44.9%; other 0.1% Group 2: midline 45.7%; paramedian 9.4%; subcostal/transverse 43.6%; other 0.1% Types of surgery: Group 1: upper GI 15.6%; HPB 41.4%; lower GI 35.6%; vascular 3.2%; other 4.1% Group 2: upper GI 17.4%; HPB 41.6%; lower GI 35.9%; vascular 3.2%; other 1.8% Contamination classification of included participants: unknown Preoperative antibiotic use: unknown Prognostic patient factors: malignancy: Group 1 18.8%, Group 2 17.7% Inclusion criteria: consecutive patients undergoing abdominal surgery |
|
| Interventions |
Comparisons reported: Group 1: Sutures: polyglyconate (monofilament, slowly absorbable) Suture technique: continuous Closure method: mass Group 2: Sutures: polyglactin (multifilament, fast absorbable) Suture technique: interrupted (Smead Jones) Closure method: mass Characteristics of surgeons: unknown |
|
| Outcomes |
Hernia: protrusion in the wound when patient lifted legs in supine position Follow‐up duration: 12 months Wound infection: no definition Dehiscence: no definition |
|
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Random sequence generation not described |
| Allocation concealment (selection bias) | Low risk | Sealed envelopes |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | High risk | All participants accounted for/dropouts explained. High loss to follow‐up: 308 of 988 participants lost to follow‐up (31%) |
| Selective reporting (reporting bias) | Low risk | Hernia follow‐up at least 1 year; wound infection and dehiscence reported |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Savolainen 1988.
| Methods |
RCT Methods to control for contributory patient factors: none |
|
| Participants |
Age: no information given Gender: no information given Types of incisions: upper midline incision only Types of surgery: no information Contamination classification of included participants: no information Preoperative antibiotic use: no information Prognostic patient factors: no information Inclusion criteria: all upper midline incisions within 1 year |
|
| Interventions |
Comparisons reported: Group 1: Sutures: PGA (multifilament, fast absorbable) Suture technique: interrupted, simple Closure method: mass Group 2: Sutures: polyglyconate (monofilament, slowly absorbable) Suture technique: continuous Closure method: mass Group 3: Sutures: polypropylene (monofilament, non‐absorbable) Suture technique: continuous Closure method: mass Characteristics of surgeons: not described |
|
| Outcomes |
Wound infection: no definition Dehiscence: no definition |
|
| Notes | Hernia not an outcome of this study Group 1 compared with Group 2 in 'interrupted versus continuous' analysis and 'slow versus fast absorbable' analysis, Group 2 compared with Group 3 in 'absorbable versus non‐absorbable' analysis |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Randomised according to birthday |
| Allocation concealment (selection bias) | High risk | Randomised according to birthday |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants accounted for/dropouts explained |
| Selective reporting (reporting bias) | Low risk | Dehiscence and wound infection reported |
| Other bias | Unclear risk | Duration of follow‐up not specified (in hospital only) |
Seiler 2009.
| Methods |
RCT Methods to control for contributory patient factors: none |
|
| Participants |
Age: Group 1 (mean): 65.5 Group 2 (mean): 63.8 Group 3 (mean): 64.7 Gender: Group 1: female 37.3% Group 2: female 39.7% Group 3: female 36.6% Types of incisions: all participants had a midline incision Types of surgery: all participants had elective surgery Group 1: colon 43%, rectum 25%, upper GI 15%, aortic aneurysm repair 4%, pancreas 7%, small bowel 1.5%, other 4.4% Group 2: colon 48%, rectum 23%, upper GI 10%, aortic aneurysm repair 3%, pancreas 6%, small bowel 1.5%, other 7.5% Group 3: colon 45%, rectum 24%, upper GI 15%, aortic aneurysm repair 3.4%, pancreas 10%, small bowel 1%, other 2.4% Contamination classification of included participants: not described Preoperative antibiotic use: not described Prognostic patient factors: Group 1: BMI (mean) 26.1 Group 2: BMI (mean) 25.6 Group 3: BMI (mean) 26.0 Inclusion criteria: elective primary midline laparotomy with an expected length of incision of at least 15 cm, informed consent, age ≥ 18 years and life expectancy > 1 year Exclusion criteria: patients requiring an emergency procedure, or undergoing current immunosuppressive therapy, or chemotherapy within 2 weeks or radiotherapy > 8 weeks before surgery; patients with coagulopathy or peritonitis or disorders that would preclude study participation (dementia, language problems) and patients participating in another trial |
|
| Interventions |
Comparisons reported: Group 1: Sutures: polyglactin‐910 (multifilament, fast absorbable) Suture technique: interrupted Closure method: mass Group 2: Sutures: PDS (monofilament, slowly absorbable) Suture technique: continuous Closure method: mass Group 3: Sutures: PDS ‐ MonoPlus (monofilament, slowly absorbable) Suture technique: continuous Closure method: mass Characteristics of surgeons: all performed by 1 surgeon |
|
| Outcomes |
Hernia: fascial dehiscence after completed superficial wound healing with or without a prolapse of abdominal organs, confirmed by abdominal ultrasound Follow‐up duration: 12 months Wound infection: redness, wound dehiscence with secretion either of putrid or caliginous smelly fluid or requiring antibiotic treatment or surgical intervention Dehiscence: missing continuity of abdominal fascia in combination with wound dehiscence with consecutive relapse operation |
|
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of randomisation not described |
| Allocation concealment (selection bias) | Low risk | Opaque, sealed envelopes |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Outcome assessors and participants blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants accounted for and analysed |
| Selective reporting (reporting bias) | Low risk | Hernia follow‐up at least 1 year; wound infection and dehiscence reported |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Siddique 2015.
| Methods |
RCT Methods to control for contributory patient factors: none |
|
| Participants |
Age: Group 1 (mean): 36 Group 2 (mean): 36 Gender: not reported Types of incisions: all participants had a midline incision Types of surgery: both elective and emergent (proportions not reported) Contamination classification of included participants: not described Preoperative antibiotic use: "all patients received antibiotics against gram negative and anaerobic organisms" Prognostic patient factors: not reported in detail Inclusion criteria: patients undergoing a midline laparotomy, age > 15, ASA 1 & 2 Exclusion criteria: patients who developed a wound infection |
|
| Interventions |
Comparisons reported: Group 1: Sutures: PDS (monofilament, slowly absorbable) Suture technique: continuous Closure method: mass Group 2: Sutures: polypropylene (monofilament, non‐absorbable) Suture technique: continuous Closure method: mass Characteristics of surgeons: not reported |
|
| Outcomes | Dehiscence: not defined, diagnosed within 7 days of surgery | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants accounted for, no losses to follow‐up |
| Selective reporting (reporting bias) | Low risk | There was no evidence of selective reporting |
| Other bias | High risk | Participants were excluded if they developed a wound infection |
Taylor 1985.
| Methods | RCT Methods to control for contributory patient factors: none | |
| Participants |
Age: Group 1 (mean): 45.9 years Group 2 (mean): 48.6 years Gender: Group 1: female 38% Group 2: female 36% Types of incisions: upper midline only Types of surgery: unknown Contamination classification of included participants: unknown Preoperative antibiotic use: at surgeon's discretion Prognostic patient factors: unknown Inclusion criteria: consecutive patients undergoing upper midline incision |
|
| Interventions |
Comparisons reported: Group 1: Sutures: PDS (monofilament, slowly absorbable) Suture technique: continuous Closure method: layered Group 2: Sutures: nylon (monofilament, non‐absorbable) Suture technique: continuous Closure method: layered Characteristics of surgeons: all performed by 1 surgeon |
|
| Outcomes |
Hernia: no definition Follow‐up duration: 12 months Wound infection: no definition Dehiscence: no definition Sinus or fistula: no definition |
|
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information |
| Allocation concealment (selection bias) | Unclear risk | No information |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | No information |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants accounted for/dropouts explained |
| Selective reporting (reporting bias) | Low risk | Hernia follow‐up at least 1 year; wound infection and dehiscence reported |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Trimbos 1992.
| Methods |
RCT Methods to control for contributory patient factors: none |
|
| Participants |
Age: Group 1 (mean): 50 Group 2 (mean): 51 Gender: all participants female Types of incisions: all participants with midline incision Types of surgery: not described Contamination classification of included participants: Group 1: clean 40%, clean‐contaminated 58%, contaminated 2% Group 2: clean 34%, clean‐contaminated 64%, contaminated 2% Preoperative antibiotic use: not described Prognostic patient factors: Group 1: diabetes 7%, obesity 50%, malignancy 45%, corticosteroids 5%, other immunosuppression 14%, chronic pulmonary conditions 5% Group 2: diabetes 6%, obesity 45%, malignancy 51%, corticosteroids 5%, other immunosuppression 14%, chronic pulmonary conditions 3% Inclusion criteria: women undergoing midline laparotomy Exclusion criteria: none specified |
|
| Interventions |
Comparisons reported: Group 1: Sutures: polyglyconate (monofilament, slowly absorbable) Suture technique: continuous Closure method: layered Group 2: Sutures: polyglactin‐910 (multifilament, fast absorbable) Suture technique: interrupted Closure method: layered Characteristics of surgeons: not described |
|
| Outcomes |
Hernia: swelling in the scar with increased intra‐abdominal pressure Follow‐up duration: 12 months Wound infection: purulent discharge from wound or wound fluid containing pathogenic microbes on culture Dehiscence: not defined Sinus or fistula: not defined |
|
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not explicitly described |
| Allocation concealment (selection bias) | Unclear risk | Not explicitly described |
| Blinding (performance bias and detection bias) All outcomes | Low risk | Outcome assessor blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants accounted for and analysed |
| Selective reporting (reporting bias) | Low risk | Hernia follow‐up at least 1 year; wound infection and dehiscence reported |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Ullrich 1981.
| Methods |
RCT Methods to control for contributory patient factors: none |
|
| Participants |
Age: not described Gender: 50.9% of participants were female Types of incisions: all participants with midline incision Types of surgery: not described, no exclusions Contamination classification of included participants: Group 1: clean 19%%, clean‐contaminated 56%%, contaminated 9%; dirty 16% Group 2: clean 17%%, clean‐contaminated 57%, contaminated 11%; dirty 15% Preoperative antibiotic use: not described Prognostic patient factors: not described Inclusion criteria: women undergoing midline laparotomy Exclusion criteria: none specified |
|
| Interventions |
Comparisons reported: Group 1: Sutures: PGA (multifilament, fast absorbable) Suture technique: continuous Closure method: layered Group 2: Sutures: polyester (multifilament, non‐absorbable) Suture technique: continuous Closure method: layered Characteristics of surgeons: not described |
|
| Outcomes |
Dehiscence: not defined Sinus or fistula: not defined |
|
| Notes | — | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random number table |
| Allocation concealment (selection bias) | Low risk | Opaque envelopes opened at start of case |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Not all participants accounted for (11/78, 14% lost to follow‐up) |
| Selective reporting (reporting bias) | Low risk | There was no evidence of selective reporting |
| Other bias | Low risk | The study appears to be free of other sources of bias |
Wissing 1987.
| Methods |
RCT Methods to control for contributory patient factors: none |
|
| Participants |
Age: Group 1: < 45 years 26.8%, 45‐59 years 26.0%, 60‐69 years 19.4%, > 70 27.9% Group 2: < 45 years 27.9%, 45‐59 years 22.4%, 60‐69 years 23.4%, > 70 26.3% Group 3: < 45 years 22.8%, 45‐59 years 23.9%, 60‐69 years 24.9%, > 70 28.4% Group 4: < 45 years 28.2%, 45‐59 years 26.9%, 60‐69 years 23.2%, > 70 21.7% Gender: Group 1 (female): 40.2% Group 2 (female): 43.3% Group 3 (female): 41.0% Group 4 (female): 42.6% Types of incisions: all incisions midline Types of surgery: Group 1: large intestine 21.8%, small intestine 4.5%, biliary tract 14.6%, stomach 19.7%, vascular 9.8%, other 29.5% Group 2: large intestine 22.3%, small intestine 5.5%, biliary tract 16.8%, stomach 12.1%, vascular 14.7%, other 28.6% Group 3: large intestine 19.7, small intestine 5.4, biliary tract 19.7, stomach 13.8, vascular 12.7%, other 28.6% Group 4: large intestine 19.6%, small intestine 5.0%, biliary tract 19.6%, stomach 15.6%, vascular 12.4%, other 27.8% Contamination classification of included participants: Group 1: clean 48.1%, clean‐contaminated 39.2%, contaminated 5.6%, dirty 7.1% Group 2: clean 47.5%, clean‐contaminated 39.4%, contaminated 7.8%, dirty 5.2% Group 3: clean 46.3%, clean‐contaminated 38.6%, contaminated 8.8%, dirty 6.4% Group 4: clean 49.3%, clean‐contaminated 36.7%, contaminated 7.9%, dirty 6.0% Preoperative antibiotic use: Group 1: 60.1% Group 2: 67.2% Group 3: 57.3% Group 4: 60.8% Prognostic patient factors: Group 1: diabetes 6.1%, obesity 28.3%, malignancy 35.4%, corticosteroids 2.9% Group 2: diabetes 6.8%, obesity 28.1%, malignancy 26.8%, corticosteroids 1.8% Group 3: diabetes 6.1%, obesity 30.4%, malignancy 26.1%, corticosteroids 1.3% Group 4: diabetes 5.8%, obesity 28.2%, malignancy 25.3%, corticosteroids 1.8% Inclusion criteria: all patients with midline laparotomy Exclusion criteria: those whose skin was not closed primarily and in whom abdominal cavity was irrigated with antimicrobial agents or local antibiotics used in the wound |
|
| Interventions |
Comparisons reported: Group 1: Sutures: polyglactin‐910 (multifilament, fast absorbable) Suture technique: interrupted Closure method: mass Group 2: Sutures: polyglactin‐910 (multifilament, fast absorbable) Suture technique: continuous Closure method: mass Group 3: Sutures: PDS (monofilament, slowly absorbable) Suture technique: continuous Closure method: mass Group 4: Sutures: nylon (monofilament, non‐absorbable) Suture technique: continuous Closure method: mass Characteristics of surgeons: not described |
|
| Outcomes |
Hernia: protruding swelling observed and fascial defect palpable in supine position with both legs lifted or when coughing Follow‐up duration: 12 months Wound infection: purulent discharge from wound spontaneously or after surgical drainage and isolation of pathogenic microbes Dehiscence: when new operative closure of fascia necessitated Sinus or fistula: sinus when a micro‐abscess or a chronic granulomatous inflammation resulted in a fistulous tract cured when the suture or knot was removed |
|
| Notes | Groups 2 and 3 combined in the 'absorbable versus non‐absorbable' analysis (same technique), Group 1 compared with Group 2 in 'continuous versus interrupted closure' analysis (same suture and method) Group 1 and 2 analysed as 'fast absorbable' Group 2 compared with Group 3 and 4 in 'monofilament versus multifilament' analysis Group 2 compared with Group 3 in 'fast versus slow absorbable' analysis |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Randomized by opening an envelope" |
| Allocation concealment (selection bias) | Unclear risk | "Randomized by opening an envelope" |
| Blinding (performance bias and detection bias) All outcomes | Unclear risk | Not described |
| Incomplete outcome data (attrition bias) All outcomes | High risk | All participants accounted for. Loss to follow‐up was 21%, but similar in each group |
| Selective reporting (reporting bias) | Low risk | Hernia follow‐up at least 1 year; wound infection and dehiscence reported |
| Other bias | Low risk | The study appears to be free of other sources of bias |
BMI: body mass index COPD: chronic obstructive pulmonary disease DM: diabetes mellitis FEV: forced expiratory volume GI: gastrointestinal PDS: polydioxanone PGA: polyglycolic acid RCT: randomised controlled trial SD: standard deviation
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Agarwal 2011 | Compared retention sutures versus no retention sutures. Primary outcome was dehiscence (not hernia) |
| Atul Kumar 2005 | Compared closure of uterine incision |
| Baracs 2011 | Compared PDS Plus versus PDS |
| Cengiz 2001 | Non‐human subjects |
| Deerenberg 2015 | Compared small bites to large bites. Did not compare suture material, or technique as we classified it |
| Ellis 1977 | Compared peritoneal versus non‐peritoneal closure |
| Gilbert 1987 | Compared peritoneal versus non‐peritoneal closure |
| Gislason 1999 | Duplicate of data from the Gislason 1995 article, with a focus on surgeon factors |
| Gorozpe‐Calvillo 1999 | Compared methods of skin closure |
| Harlaar 2011 | Suture length outside of the protocol |
| Hugh 1990 | Compared peritoneal versus non‐peritoneal closure |
| Hull 1991 | Compared peritoneal versus non‐peritoneal closure |
| Irion 1996 | Our primary and secondary outcomes were not assessed |
| Israelsson 1999 | Did not specify suture material |
| Johnson 1982 | Comment on Donaldson 1982 |
| Justinger 2013 | Compared the same suture material and technique in both arms. One arm contained antibiotic‐impregnated sutures |
| Khachatryan 2011 | Compared Vicryl with antimicrobial coating to Vicryl plain |
| Marwah 2005 | Compared "rectus sheath relaxation incision" versus no relaxation incision |
| Mattavelli 2011 | Compared Vicryl coated with antimicrobial coating to Vicryl plain |
| Mayer 1981 | Compared compression to normal closure (i.e. tightening suture to 5 kg of pressure versus not) |
| Millbourn 2009 | Suture length outside of the protocol |
| Millbourn 2011 | Suture length outside of the protocol |
| Nagele 1996 | Compared peritoneal versus non‐peritoneal closure |
| Niggebrugge 1999 | Compared 2 methods of closure with running PDS (continuous versus double double‐looped) |
| Pietrantoni 1991 | Compared peritoneal versus non‐peritoneal closure |
| Rasic 2011 | Compared antimicrobial suture to non‐coated suture |
| Rink 2000 | Compared the use of retention sutures to no retention sutures |
| Rosenberg 1975 | Compared the tension on retention sutures |
| Xiao‐dong 2009 | Compared 2 types of layered closures |
PDS: polydioxanone
Characteristics of ongoing studies [ordered by study ID]
ISRCTN25616490.
| Trial name or title | Hughes abdominal repair trial ‐ abdominal wall closure techniques to reduce incidence of incisional hernia |
| Methods | RCT |
| Participants | Midline laparotomy incision after colorectal surgery |
| Interventions | Hughes repair vs mass closure |
| Outcomes | Incisional hernia at 12 months |
| Starting date | January 2013 |
| Contact information | B Rees, HART@wales.nhs.uk |
| Notes |
NCT00514566.
| Trial name or title | PDS vs. polyamide for midline abdominal closure (PPMAC) |
| Methods | RCT |
| Participants | Patients with midline laparotomy |
| Interventions | Polyamide vs PDS |
| Outcomes | Wound complications |
| Starting date | October 2004 |
| Contact information | |
| Notes | Trial terminated early due to high wound dehiscence in the PDS group |
NCT00544583.
| Trial name or title | CONTINT Trial |
| Methods | RCT |
| Participants | Patients undergoing emergency midline laparotomy |
| Interventions | Continuous, absorbable monofilament closure vs interrupted, absorbable, multifilament closure |
| Outcomes | Incisional hernia at 12 months |
| Starting date | October 2007 |
| Contact information | NN Rahbari |
| Notes | No updates since January 2010 |
NCT01965249.
| Trial name or title | Effect of stitch technique on the occurence of incisional hernia after abdominal wall closure (ESTOIH) |
| Methods | RCT |
| Participants | Patients with median laparotomy |
| Interventions | Short stitch vs long stitch technique |
| Outcomes | Incisional hernia at 12 months |
| Starting date | February 2014 |
| Contact information | P. Baumann |
| Notes | Currently enrolling |
NCT02145052.
| Trial name or title | Optimal method of fascial closure in high risk patients undergoing laparotomy |
| Methods | RCT |
| Participants | High‐risk patients with a laparotomy |
| Interventions | Continuous vs interrupted closure |
| Outcomes | Dehiscence, wound infection, incisional hernia at 6, 12, 60 months |
| Starting date | 20 May 2014 |
| Contact information | MA Moya, Massachusetts General Hospital |
| Notes | Completed recruiting, no published results |
TCTR20150318001.
| Trial name or title | Randomized trial to compare dehiscence with continuous versus interrupted mass closure of transverse incisions in children with absorbable suture |
| Methods | RCT |
| Participants | Transverse incisions |
| Interventions | Continuous vs interrupted closures |
| Outcomes | Dehiscence |
| Starting date | Unknown |
| Contact information | Unknown |
| Notes |
PDS: polydioxanone RCT: randomised controlled trial
Differences between protocol and review
We analysed hernia outcomes at one year or later follow‐up. We did not include this outcome for trials that did not follow up participants for at least one year. If a trial had multiple follow‐up periods after one year, we only included the results at one year.
Due to the heterogeneous interventions used in the studies, we did not assess suture material and technique as a whole. Instead we compared sutures based on absorption (absorbable versus non‐absorbable and fast absorbable versus slow absorbable, any closure technique or method), closure technique (continuous versus interrupted, any suture material or method), closure method (mass versus layered, any suture material or technique) and filament (multifilament versus monofilament, any absorption, material, technique or method).
We did not explore further subgroup analyses (such as classification of wound contamination, type of surgery, etc.) due to the high variability between studies for these factors which make defining these factors for these potential analyses very difficult.
Updated the risk of bias methods to the most recent version of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011b).
Contributions of authors
Conceiving the review: RN Designing the review: RN, SSV, SS Co‐ordinating the review: SSV, SVP, DP Undertaking manual searches: SSV, SS Screening search results: SSV, SS, RN, SVP, DP Organising retrieval of papers: SSV, SVP Screening retrieved papers against inclusion criteria: SSV, SS, SVP, DP Appraising quality of papers: SSV, SS, RN, SVP, DP Abstracting data from papers: SSV, SS, RN, SVP, DP Writing to authors of papers for additional information: SSV, RN Providing additional data about papers: SSV, SS Obtaining and screening data on unpublished studies: RN, SSV Data management for the review: SSV, SVP, DP Entering data into Review Manager 5: SSV, SVP, DP Analysis of data: SSV, RN, SVP, DP Interpretation of data: SSV, RN, SS, SVP, DP Writing the review: RN, SSV, SS, SVP, DP Performing previous work that was the foundation of current study: RN Guarantor for the review: RN
Sources of support
Internal sources
None, Other.
External sources
None, Other.
Declarations of interest
SVP: none DP: none RN: none SSV: none SS: none
New
References
References to studies included in this review
Agrawal 2009 {published data only}
- Agrawal V, Sharma N, Joshi MK, Minocha VR. Role of suture material and technique of closure in wound outcome following laparotomy for peritonitis. Tropical Gastroenterology 2009;30(4):237‐40. [PubMed] [Google Scholar]
Agrawal 2014 {published data only}
- Agrawal CS, Tiwari P, Mishra S, Rao A, Hadke NS, Adhikari S, et al. Interrupted abdominal closure prevents burst: randomized controlled trial comparing interrupted‐X and conventional continuous closures in surgical and gynecological patients. Indian Journal of Surgery 2014;76(4):270‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Askew 1983 {published data only}
- Askew AR. A comparison of upper abdominal wound closure with monofilament nylon and polyglycolic acid. Australian & New Zealand Journal of Surgery 1983;53(4):353‐6. [DOI] [PubMed] [Google Scholar]
Ausobsky 1985 {published data only}
- Ausobsky JR, Evans M, Pollock AV. Does mass closure of midline laparotomies stand the test of time? A randomised controlled clinical trial. Annals of the Royal College of Surgeons of England 1985;67(3):159‐61. [PMC free article] [PubMed] [Google Scholar]
Berretta 2010 {published data only}
- Berretta R, Rolla M, Patrelli TS, Piantelli G, Merisio C, Melpignano M, et al. Randomised prospective study of abdominal wall closure in patients with gynaecological cancer. Australian and New Zealand Journal of Obstetrics and Gynecology 2010;50(4):391‐6. [DOI] [PubMed] [Google Scholar]
Bloemen 2011 {published data only}
- Bloemen A, Dooren P, Huizinga BF, Hoofwijk AGM. Randomized clinical trial comparing polypropylene or polydioxanone for midline abdominal wall closure. British Journal of Surgery 2011;98(5):633‐9. [DOI] [PubMed] [Google Scholar]
Bresler 1995 {published data only}
- Bresler L, Courbey PJ, Feldman L, Bilweiss J, Tortuyaux JM, Rauch P, et al. Results of a controlled trial comparing 3 slowly absorbable suture materials for the closure of supra‐umbilical midline laparotomies. Annales de Chirurgie 1995;49(6):544‐8. [PubMed] [Google Scholar]
Brolin 1996 {published data only}
- Brolin RE. Prospective, randomized evaluation of midline fascial closure in gastric bariatric operations. American Journal of Surgery 1996;172(4):328‐31. [DOI] [PubMed] [Google Scholar]
Bucknall 1981 {published data only}
- Bucknall TE, Ellis H. Abdominal wound closure‐‐a comparison of monofilament nylon and polyglycolic acid. Surgery 1981;89(6):672‐7. [PubMed] [Google Scholar]
Cameron 1980 {published data only}
- Cameron AEP, Gray RCF, Talbot RW, Wyatt AP. Abdominal wound closure: a trial of Prolene and Dexon. British Journal of Surgery 1980;67(7):487‐8. [DOI] [PubMed] [Google Scholar]
Cameron 1987 {published data only}
- Cameron AE, Parker CJ, Field ES, Gray RC, Wyatt AP. A randomised comparison of polydioxanone (PDS) and polypropylene (Prolene) for abdominal wound closure. Annals of the Royal College of Surgeons of England 1987;69(3):113‐5. [PMC free article] [PubMed] [Google Scholar]
Carlson 1995 {published data only}
- Carlson MA, Condon RE. Polyglyconate (Maxon registered trade mark) versus nylon suture in midline abdominal incision closure: a prospective randomized trial. American Surgeon 1995;61(11):980‐3. [PubMed] [Google Scholar]
Chana 1993 {published data only}
- Chana RS, Saxena VC, Agarwal A. A prospective study of closure techniques of abdominal incisions in infants and children. Journal of the Indian Medical Association 1993;91(3):59‐61. [PubMed] [Google Scholar]
Chowdhury 1994 {published data only}
- Chowdhury SK, Chowdhury SD. Mass closure versus layered closure of abdominal wound: a prospective clinical study. Journal of the Indian Medical Association 1994;92(7):229‐32. [PubMed] [Google Scholar]
Colombo 1997 {published data only}
- Colombo M, Maggioni A, Parma G, Scalambrino S, Milani R. A randomized comparison of continuous versus interrupted mass closure of midline incisions in patients with gynecologic cancer. Obstetrics and Gynecology 1997;89(5):684‐9. [DOI] [PubMed] [Google Scholar]
Corman 1981 {published data only}
- Corman ML, Veidenheimer MC, Coller JA. Controlled clinical trial of three suture materials for abdominal wall closure after bowel operations. American Journal of Surgery 1981;141(4):510‐3. [DOI] [PubMed] [Google Scholar]
Dan 2014 {published data only}
- Dan L, Jing Z, Yong‐Gang L, Hao Z, Kai‐Xuan C, Ke C, et al. Full fascia closure with interrupted absorbable suture and layered closure with interrupted silk suture in abdominal incision: comparison of curative effects and biocompatibility [可吸收缝线全筋膜与丝线间断缝合腹部切口:效果及生物相容性的比较]. Chinese Journal Of Tissue Engineering October 2014;43:6996‐7000. [Google Scholar]
Deitel 1990 {published data only}
- Deitel M, Alhindawi R, Yamen M, To TB, Burul CJ. Dexon Plus versus Maxon fascial closure in morbid obesity: a prospective randomized comparison. Canadian Journal of Surgery 1990;33(4):302‐4. [PubMed] [Google Scholar]
Derzie 2000 {published data only}
- Derzie AJ, Silvestri F, Liriano E, Benotti P. Wound closure technique and acute wound complications in gastric surgery for morbid obesity: a prospective randomized trial. Journal of the American College of Surgeons 2000;191(3):238‐43. [DOI] [PubMed] [Google Scholar]
Docobo‐Durantez 2006 {published and unpublished data}
- Docobo‐Durantez F, Sacristán‐Péreza C, Flor‐Civerab B, Lledó‐Matosesb S, Kreislercy E, Biondoc S. Randomized clinical study of polydioxanone and nylon sutures for laparotomy closure in high risk patients [Estudio clínico aleatorizado entre suturade polidioxanona y de naylon en el cierrede laparotomía en pacientes de riesgo]. Cirugía Española 2006;79(5):305‐9. [DOI] [PubMed] [Google Scholar]
Donaldson 1982 {published data only}
- Donaldson DR, Hall TJ, Zoltowski JA, Guillou PJ, Brennan TG. Does the type of suture material contribute to the strength of the lateral paramedian incision?. British Journal of Surgery 1982;69(3):163‐5. [DOI] [PubMed] [Google Scholar]
Efem 1980 {published data only}
- Efem SEE, Aja A. Layered versus mass closure of vertical midline laparotomy wounds in Negro Africans. Tropical Doctor 1988;18(2):67‐9. [DOI] [PubMed] [Google Scholar]
Fagniez 1985 {published data only}
- Fagniez PL, Hay JM, Lacaine, Thomsen C. Abdominal midline incision closure. A multicentric randomized prospective trial of 3,135 patients, comparing continuous vs interrupted polyglycolic acid sutures. Archives of Surgery 1985;120(12):1351‐3. [DOI] [PubMed] [Google Scholar]
Gammelgaard 1983 {published data only}
- Gammelgaard N, Jensen J. Wound complications after closure of abdominal incisions with Dexon or Vicryl. A randomized double‐blind study. Acta Chirurgica Scandinavica 1983;149(5):505‐8. [PubMed] [Google Scholar]
Gislason 1995 {published data only}
- Gislason H, Gronbech JE, Soreide O. Burst abdomen and incisional hernia after major gastrointestinal operations ‐ comparison of three closure techniques. Acta Chirurgica 1995;161(5):349‐54. [PubMed] [Google Scholar]
Goligher 1975 {published data only}
- Goligher JC, Irvin, TT, Johnston D, Dombal FT, Hill GL, Horrocks JC. A controlled clinical trial of three methods of closure of laparotomy wounds. British Journal of Surgery 1975;62(10):823‐9. [DOI] [PubMed] [Google Scholar]
Gys 1989 {published data only}
- Gys T, Hubens A. A prospective comparative clinical study between monofilament absorbable and non‐absorbable sutures for abdominal wall closure. Acta Chirurgica Belgica 1989;89(5):265‐70. [PubMed] [Google Scholar]
Hsiao 2000 {published data only}
- Hsiao WC, Young KC, Wang ST, Lin PW. Incisional hernia after laparotomy: prospective randomized comparison between early‐absorbable and late‐absorbable suture materials. World Journal of Surgery 2000;24(6):747‐52. [DOI] [PubMed] [Google Scholar]
Irvin 1976 {published data only}
- Irvin TT, Koffman CG, Duthie HL. Layer closure of laparotomy wounds with absorbable and non‐absorbable suture materials. British Journal of Surgery 1976;63(10):793‐6. [DOI] [PubMed] [Google Scholar]
Irvin 1977 {published data only}
- Irvin TT, Stoddard CJ, Greaney MG, Duthie HL. Abdominal wound healing: a prospective clinical study. British Medical Journal 1977;2(6083):351‐2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Israelsson 1994 {published data only}
- Israelsson LA, Jonsson T. Closure of midline laparotomy incisions with polydioxanone and nylon: the importance of suture technique. British Journal of Surgery 1994;81(11):1606‐8. [DOI] [PubMed] [Google Scholar]
Kiely 1985 {published data only}
- Kiely EM, Spitz L. Layered versus mass closure of abdominal wounds in infants and children. British Journal of Surgery 1985;72(9):739‐40. [DOI] [PubMed] [Google Scholar]
Kronborg 1976 {published data only}
- Kronborg O. Polyglycolic acid (Dexon) versus silk for fascial closure of abdominal incisions. Acta Chirurgica Scandinavica 1976;142(1):9‐12. [PubMed] [Google Scholar]
Krukowski 1987 {published data only}
- Krukowski ZH, Cusick EL, Engeset J, Matheson NA. Polydioxanone or polypropylene for closure of midline abdominal incisions: a prospective comparative clinical trial. British Journal of Surgery 1987;74(9):828‐30. [DOI] [PubMed] [Google Scholar]
Larsen 1989 {published data only}
- Larsen PN, Nielsen K, Mejdahl S, Larsen T, Moesgaard F, Shultz A. Closure of the abdominal fascia after clean and clean‐contaminated laparotomy. Acta Chirurgica Scandinavica 1989;155(9):461‐4. [PubMed] [Google Scholar]
Leaper 1977 {published data only}
- Leaper DJ, Pollock AV, Evans M. Abdominal wound closure: a trial of nylon, polyglycolic acid and steel sutures. British Journal of Surgery 1977;64(8):603‐6. [DOI] [PubMed] [Google Scholar]
Leaper 1985 {published data only}
- Leaper DJ, Allan A, May RE, Corfield AP, Kennedy RH. Abdominal wound closure: a controlled trial of polyamide (nylon) and polydioxanone suture (PDS). Annals of the Royal College of Surgeons of England 1985;67(5):273‐5. [PMC free article] [PubMed] [Google Scholar]
Lewis 1989 {published data only}
- Lewis RT, Wiegand FM. Natural history of vertical abdominal parietal closure: Prolene versus Dexon. Canadian Journal of Surgery 1989;32(3):196‐200. [PubMed] [Google Scholar]
McNeill 1986 {published data only}
- McNeil PM, Sugerman HJ. Continuous absorbable vs interrupted nonabsorbable fascial closure. A prospective, randomized comparison. Archives of Surgery 1986;121(7):821‐3. [DOI] [PubMed] [Google Scholar]
Mirza 2003 {published data only}
- Mirza SM, Hanif F, Khalid K, Ali AA, Chaudry A. Abdominal wound closure ‐ a prospective randomized trial of polypropylene and polydioxanone. Emirates Medical Journal 2003;21(1):45‐8. [Google Scholar]
Ohira 2015 {published data only}
- Ohira G, Kawahira H, Miyauchi H, Suzuki K, Nishimori T, Hanari N, et al. Synthetic polyglycomer short‐term absorbable sutures vs. polydioxanone long‐term absorbable sutures for preventing incisional hernia and wound dehiscence after abdominal wall closure: a comparative randomized study of patients treated for gastric or colon cancer. Surgery Today 2015;45(7):841‐5. [DOI] [PubMed] [Google Scholar]
Orr 1990 {published data only}
- Orr JW, Orr PF, Barrett JM, Ellington JR, Jennings RH, Paredes KB, et al. Continuous or interrupted fascial closure: a prospective evaluation of No. 1 Maxon suture in 402 gynecologic procedures. American Journal of Obstetrics and Gynecology 1990;163(5 pt 1):1485‐9. [DOI] [PubMed] [Google Scholar]
Orr 2003 {published data only}
- Orr JW, Montz FJ, Barter J, Schaitzberg SD, Delmore JE, Dodson MK, et al. Continuous abdominal fascial closure: a randomized controlled trial of poly (L‐lactide/glycolide). Gynecologic Oncology 2003;90(2):342‐7. [DOI] [PubMed] [Google Scholar]
Osther 1995 {published data only}
- Osther PJ, Gjøde P, Mortensen BB, Mortensen PB, Bartholin J, Gottrup F. Randomized comparison of polyglycolic acid and polyglyconate sutures for abdominal fascial closure after laparotomy in patients with suspected impaired wound healing. British Journal of Surgery 1995;82(8):1080‐2. [DOI] [PubMed] [Google Scholar]
Pandley 2013 {published data only}
- Pandey S, Singh M, Singh K, Sandhu S. A prospective randomized study comparing non‐absorbable polypropylene (Prolene®) and delayed absorbable polyglactin 910 (Vicryl®) suture material in mass closure of vertical laparotomy wounds. Indian Journal of Surgery 2013;75(4):306‐10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pollock 1979 {published data only}
- Pollock AV, Greenall MJ, Evans M. Single‐layer mass closure of major laparotomies by continuous suturing. Journal of the Royal Society of Medicine 1979;72(12):889‐93. [DOI] [PMC free article] [PubMed] [Google Scholar]
Richards 1983 {published data only}
- Richards PC, Balch CM, Aldrete JS. Abdominal wound closure. A randomized prospective study of 571 patients comparing continuous vs. interrupted suture techniques. Annals of Surgery 1983;197(2):238‐43. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sahlin 1993 {published data only}
- Sahlin S, Ahlberg J, Granstrom L, Ljungstrom KG. Monofilament versus multifilament absorbable sutures for abdominal closure. British Journal of Surgery 1993;80(3):322‐4. [DOI] [PubMed] [Google Scholar]
Savolainen 1988 {published data only}
- Savolainen H, Ristkari S, Mokka R. Early laparotomy wound dehiscence: a randomized comparison of three suture materials and two methods of fascial closure. Annales Chirurgiae et Gynaecologiae 1988;77(3):111‐3. [PubMed] [Google Scholar]
Seiler 2009 {published data only}
- Seiler CM, Bruckner T, Diener MK, Papyan A, Golcher H, Seidlmayer C, et al. Interrupted or continuous slowly absorbable sutures for closure of primary elective midline abdominal incisions: a multicenter randomized trial. Annals of Surgery 2009;249(4):576‐82. [DOI] [PubMed] [Google Scholar]
Siddique 2015 {published data only}
- Siddique A, Ahmed MA, Rehman Z. Polydioxanone vs. prolene closure for midline abdominal incisions: to compare postoperative wound dehiscence. Medical Forum Monthly 2015;26(6):40‐3. [Google Scholar]
Taylor 1985 {published data only}
- Taylor TV. The use of polydioxanone suture in midline incisions. Journal of the Royal College of Surgeons of Edinburgh 1985;30(3):191‐2. [PubMed] [Google Scholar]
Trimbos 1992 {published data only}
- Trimbos JB, Smit IB, Holm JP, Hermans J. A randomized clinical trial comparing two methods of fascia closure following midline laparotomy. Archives of Surgery 1992;127(10):1232‐4. [DOI] [PubMed] [Google Scholar]
Ullrich 1981 {published data only}
- Ullrich F, Henningsen B, Böttcher W. Fascial closure of median laparotomies with a synthetic, resorbable suture material (polyglycolic acid). Der Chirurg; Zeitschrift für alle Gebiete der operativen Medizen 1981;52(12):777‐9. [PubMed] [Google Scholar]
Wissing 1987 {published data only}
- Wissing J, Vroonhoven TJ, Schattenkerk ME, Veen HF, Ponsen RJ, Jeekel J. Fascia closure after midline laparotomy: results of a randomized trial. British Journal of Surgery 1987;74(8):738‐41. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Agarwal 2011 {published and unpublished data}
- Agarwal A, Hossain Z, Agarwal A, Das A, Chakraborty S, Mitra N, et al. Reinforced tension line suture closure after midline laparotomy in emergency surgery. Tropical Doctor 2011;41(4):193‐6. [DOI] [PubMed] [Google Scholar]
Atul Kumar 2005 {published data only}
- Atul Kumar S. Single versus double layer closure of low transverse uterine incision at cesarean section. Journal of Obstetrics and Gynecology of India 2005;55(3):231‐6. [Google Scholar]
Baracs 2011 {published and unpublished data}
- Baracs J, Huszar O, Sajjadi SG, Horvath OP. Surgical site infections after abdominal closure in colorectal surgery using triclosan‐coated absorbable suture (PDS Plus) vs. uncoated sutures (PDS II): a randomized multicenter study. Surgical Infections 2011;12(6):483‐9. [DOI] [PubMed] [Google Scholar]
Cengiz 2001 {published data only}
- Cengiz Y, Blomquist P, Israelsson LA. Small tissue bites and wound strength: an experimental study. Archives of Surgery 2001;136(3):272‐5. [DOI] [PubMed] [Google Scholar]
Deerenberg 2015 {published and unpublished data}
- Deerenberg EB, Harlaar JJ, Steyerberg EW, Lont HE, Doorn HC, Heisterkamp J, et al. Small bites versus large bites for closure of abdominal midline incisions (STITCH): a double blind, multicentre, randomised controlled trial. Lancet 2015;386(10000):1254‐60. [DOI] [PubMed] [Google Scholar]
Ellis 1977 {published data only}
- Ellis H, Heddle R. Does the peritoneum need to be closed at laparotomy?. British Journal of Surgery 1977;64(10):733‐6. [DOI] [PubMed] [Google Scholar]
Gilbert 1987 {published data only}
- Gilbert JM, Ellis H, Foweraker S. Peritoneal closure after lateral paramedian incision. British Journal of Surgery 1987;74(2):113‐5. [DOI] [PubMed] [Google Scholar]
Gislason 1999 {published data only}
- Gislason H, Soreide O, Viste A. Wound complications after major gastrointestinal operations. The surgeon as a risk factor. Digestive Surgery 1999;16(6):512‐4. [DOI] [PubMed] [Google Scholar]
Gorozpe‐Calvillo 1999 {published data only}
- Gorozpe‐Calvillo JI, Gonzalez‐Villamil J, Santoyo‐Hara S. Closure of skin with cyanoacrylate in cesarean section. Ginecologia y Obstetricia de Mexico 1999;67:491‐6. [PubMed] [Google Scholar]
Harlaar 2011 {published data only}
- Harlaar JJ, Deerenberg EB, Ramshorst GH, Lont HE, Borst EC, Schouten WR, et al. A multicenter randomized controlled trial evaluating the effect of small stitches on the incidence of incisional hernia in midline incisions. BMC Surgery 2011;11:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hugh 1990 {published data only}
- Hugh TB, Nankivell C, Meagher AP, Li B. Is closure of the peritoneal layer necessary in the repair of midline surgical abdominal wounds?. World Journal of Surgery 1990;14(2):231‐4. [DOI] [PubMed] [Google Scholar]
Hull 1991 {published and unpublished data}
- Hull DB, Varner MW. A randomized study of closure of the peritoneum at cesarean delivery. Obstetrics and Gynecology 1991;77(6):818‐21. [PubMed] [Google Scholar]
Irion 1996 {published and unpublished data}
- Irion O, Luzuy F, Beguin F. Nonclosure of the visceral and parietal peritoneum at caesarean section: a randomised controlled trial. British Journal of Obstetrics and Gynecology 1996;103(7):690‐4. [DOI] [PubMed] [Google Scholar]
Israelsson 1999 {published data only}
- Israelsson LA. Bias in clinical trials: the importance of suture technique. European Journal of Surgery 1999;165(1):3‐7. [DOI] [PubMed] [Google Scholar]
Johnson 1982 {published data only}
- Johnson CD, Bernhardt LW, Bentley PG. Incisional hernia after mass closure of abdominal incisions with Dexon and Prolene. British Journal of Surgery 1982;69:55‐7. [DOI] [PubMed] [Google Scholar]
Justinger 2013 {published and unpublished data}
- Justinger C, Slotta JE, Ningel S, Graber S, Kollmar O, Schilling MK. Surgical‐site infection after abdominal wall closure with triclosan‐impregnated polydioxanone sutures: results of a randomized clinical pathway facilitated trial (NCT00998907). Surgery 2013;154(3):589‐95. [DOI] [PubMed] [Google Scholar]
Khachatryan 2011 {published and unpublished data}
- Khachatryan N, Dibirov M, Omelyanovsky V, Chupalov M, Gasanova G. Prevention of postoperative infections in abdominal surgery using reabsorbable suture with antibacterial activity (Vicryl plus) versus reabsorbable standard sutures. 24th European Congress on Surgical Infections. 2011.
Marwah 2005 {published data only}
- Marwah S, Marwah N, Singh M, Kapoor A, Karwasra RK. Addition of rectus sheath relaxation incisions to emergency midline laparotomy for peritonitis to prevent fascial dehiscence. World Journal of Surgery 2005;29(2):235‐9. [DOI] [PubMed] [Google Scholar]
Mattavelli 2011 {published and unpublished data}
- Mattavelli I, Nespoli L, Alfieri S, Cantore F, Sebastian‐Douglas S, Cobianchi L, et al. Triclosan‐coated suture to reduce surgical site infection after colorectal surgery. 24th European Congress on Surgical Infections. 2011.
Mayer 1981 {published data only}
- Mayer AD, Ausobsky JR, Evans M, Pollock AV. Compression suture of the abdominal wall: a controlled trial in 302 major laparotomies. British Journal of Surgery 1981;68(9):634‐62. [DOI] [PubMed] [Google Scholar]
Millbourn 2009 {published data only}
- Millbourn D, Cengiz Y, Israelsson LA. Effect of stitch length on wound complications after closure of midline incisions: a randomized controlled trial. Archives of Surgery 2009;144(11):1056‐9. [DOI] [PubMed] [Google Scholar]
Millbourn 2011 {published data only}
- Millbourn D, Cengiz Y, Israelsson LA. Risk factors for wound complications in midline abdominal incisions related to the size of stitches. Hernia 2011;15(3):261‐6. [DOI] [PubMed] [Google Scholar]
Nagele 1996 {published data only}
- Nagele F, Karas H, Spitzer D, Staudach A, Karasegh S, Beck A, et al. Closure or nonclosure of the visceral peritoneum at cesarean delivery. American Journal of Obstetrics and Gynecology 1996;174(4):1366‐70. [DOI] [PubMed] [Google Scholar]
Niggebrugge 1999 {published data only}
- Niggebrugge AH, Trimbos JB, Hermans J, Steup WH, Velde CJ. Influence of abdominal‐wound closure technique on complications after surgery: a randomised study. Lancet 1999;353(9164):1563‐7. [DOI] [PubMed] [Google Scholar]
Pietrantoni 1991 {published data only}
- Pietrantoni M, Parsons MT, O'Brien WF, Collins E, Knuppel RA, Spellacy WN. Peritoneal closure or non‐closure at cesarean. Obstetrics & Gynecology 1991;77:293‐6. [DOI] [PubMed] [Google Scholar]
Rasic 2011 {published and unpublished data}
- Rasic Z, Schwarz D, Adam VN, Sever M, Lojo N, Rasic D, et al. Efficacy of antimicrobial triclosan‐coated polyglactin 910 (Vicryl Plus) suture for closure of the abdominal wall after colorectal surgery. Collegium Antropologicum 2011;35(2):439‐43. [PubMed] [Google Scholar]
Rink 2000 {published data only}
- Rink AD, Goldschmidt D, Dietrich J, Nagelschmidt M, Vestweber KH. Negative side‐effects of retention sutures for abdominal wound closure. A prospective randomised study. European Journal of Surgery 2000;166(12):932‐7. [DOI] [PubMed] [Google Scholar]
Rosenberg 1975 {published data only}
- Rosenberg IL, Brennan TG, Giles GR. How tight should tension sutures be tied? A controlled clinical trial. British Journal of Surgery 1975;62(12):950‐1. [DOI] [PubMed] [Google Scholar]
Xiao‐dong 2009 {published and unpublished data}
- Xiao‐dong W, Li J, Zhi F, Li L. Two‐layer suturing versus four‐layer suturing in abdominal median incision: a randomized controlled trial. Chinese Journal of Evidence‐Based Medicine 2009;9(2):199‐203. [Google Scholar]
References to ongoing studies
ISRCTN25616490 {unpublished data only}
- ISRCTN25616490. Hughes Abdominal Repair Trial (HART) ‐ abdominal wall closure techniques to reduce the incidence of incisional hernias: study protocol for a randomised controlled trial. www.isrctn.com/ISRCTN25616490 2016. [DOI] [PMC free article] [PubMed]
NCT00514566 {unpublished data only}
- NCT00514566. PDS vs. polyamide for midline abdominal closure PPMAC. clinicaltrials.gov/ct2/show/NCT00514566.
NCT00544583 {published and unpublished data}
- NCT00544583. Continuous versus interrupted abdominal wall closure after emergency midline laparotomy (CONTINT). clinicaltrials.gov/ct2/show/NCT00544583 2010. [DOI] [PMC free article] [PubMed]
NCT01965249 {unpublished data only}
- NCT01965249. Short stitch versus long stitch suture technique using monomax for abdominal wall closure after primary median laparotomy. A randomized controlled, double blinded, multicenter international trial. clinicaltrials.gov/ct2/show/NCT01965249.
NCT02145052 {unpublished data only}
- NCT02145052. Optimal method of fascial closure in high risk patients undergoing laparotomy: a prospective randomized trial. clinicaltrials.gov/ct2/show/NCT02145052.
TCTR20150318001 {unpublished data only}
- TCTR20150318001. Randomized trial to compare dehiscence with continuous versus interrupted mass closure of transverse incisions in children with absorbable suture (CLOSE). www.clinicaltrials.in.th/index.php?tp=regtrials&menu=trialsearch&smenu=fulltext&task=search&task2=view1&id=1335.
Additional references
Anthimidis 2013
- Anthimidis G, Gregoriou M, Stavrakis T, Vasiliadou K, Lyras I, Ioannidis K, et al. New‐fangled slowly‐absorbable versus non‐absorbable sutures for abdominal fascial closure. Have the goals towards an advantageous suture been met?. Surgical Science 2013;4(6):32282. [Google Scholar]
Anthony 2000
- Anthony T, Bergen PC, Kim LT. Factors affecting recurrence following incisional herniorrhaphy. World Journal of Surgery 2000;24:95‐101. [DOI] [PubMed] [Google Scholar]
Benlice 2015
- Benlice C, Stocchi L, Costedio M, Gorgun E, Hull T, Kessler H, et al. Laparoscopic IPAA is not associated with decreased rates of incisional hernia and small‐bowel obstruction when compared with open technique: long‐term follow‐up of a case‐matched study. Diseases of the Colon and Rectum 2015;58(3):314‐20. [DOI] [PubMed] [Google Scholar]
Brown 2005
- Brown SR, Tiernan J. Transverse verses midline incisions for abdominal surgery. Cochrane Database of Systematic Reviews 2005, Issue 4. [DOI: 10.1002/14651858.CD005199.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bucknall 1982
- Bucknall TE, Cox PJ, Ellis H. Burst abdomen and incisional hernia: a prospective study of 1129 major laparotomies. British Medical Journal (Clinical Research edition) 1984;284:931‐3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Chalya 2015
- Chayla PL, Massinde AN, Kihunrwa A, Mabula JB. Abdominal fascia closure following elective midline laparotomy: a surgical experience at a tertiary care hospital in Tanzania. BMC Research Notes 2015;8:281. [DOI] [PMC free article] [PubMed] [Google Scholar]
Connelly 2015
- Connelly TM, Tappouni R, Mathew P, Salgado J, Messaris E. Risk factors for the development of an incisional hernia after sigmoid resection for diverticulitis: an analysis of 33 patients, operative and disease‐associated factors. The American Surgeon May 2015;81(5):492‐7. [PubMed] [Google Scholar]
Cox 1986
- Cox PJ, Ausobsky JR, Ellis H, Pollock AV. Towards no incisional hernias: lateral paramedian versus midline incisions. Journal of the Royal Society of Medicine 1986;79:711‐3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Deeks 2011
- Deeks JJ, Higgins JPT, Altman DG (editors). Chapter 9: Analysing data and undertaking meta‐analyses. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Ellis 1983
- Ellis HG, George CD. Incisional hernias: when do they occur?. British Journal of Surgery 1983;70:290‐1. [DOI] [PubMed] [Google Scholar]
George 1986
- George CD, Ellis H. The results of incisional hernia repair: a twelve year review. Annals of the Royal College of Surgeons of England 1986;68:185‐7. [PMC free article] [PubMed] [Google Scholar]
Goodenough 2015
- Goodenough CJ, Ko TC, Kao LS, Nguyen MT, Holihan JL, Alawadi Z, et al. Development and validation of a risk stratification score for ventral incisional hernia after abdominal surgery: hernia expectation rates in intra‐abdominal surgery (the HERNIA Project). Journal of the American College of Surgeons 2015;220(4):405‐13. [DOI] [PMC free article] [PubMed] [Google Scholar]
Guillou 1980
- Guillou PJ, Hall TJ, Donaldson DR, Broughton AC, Brennan TG. Vertical abdominal incisions ‐ a choice?. British Journal of Surgery 1980;67:395‐9. [DOI] [PubMed] [Google Scholar]
Guyatt 2008
- Guyatt GH, Oxman AD, Kunz R, Vist GE, Falck‐Ytter Y, Schünemann HJ, GRADE Working Group. What is "quality of evidence" and why is it important to clinicians?. BMJ 2008;336(7651):995‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hawn 2010
- Hawn MT, Snyder CW, Graham LA, Gray SH, Finan KR, Vick CC. Long‐term follow‐up of technical outcomes for incisional hernia repair. Journal of the American College of Surgeons 2010;5:648‐55. [DOI] [PubMed] [Google Scholar]
Helgstrand 2012
- Helgstrand F, Rosenberg J, Kehlet H, Strandfelt P, Bisgaard T. Reoperation versus clinical recurrence rate after ventral hernia repair. Annals of Surgery December 2012;256(6):955‐8. [DOI] [PubMed] [Google Scholar]
Higgins 2003
- Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analyses. BMJ 2003;327:557‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011a
- Higgins JPT, Altman DG, Sterne JAC (editors). Chapter 8: Assessing risk of bias in included studies. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Higgins 2011b
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Hodgson 2000
- Hodgson NC, Malthaner RA, Ostbye T. The search for an ideal method of abdominal fascial closure: a meta‐analysis. Annals of Surgery 2000;231(3):436‐42. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hodgson 2001
- Hodgson NC, Malthaner RA, Ostbye T. Current practice of abdominal fascial closure: a survey of Ontario general surgeons. Canadian Journal of Surgery 2001;44(5):366‐70. [PMC free article] [PubMed] [Google Scholar]
Hughes 2009
- Hughes K, Selim NM. The lateral paramedian: revisiting a forgotten incision. The American Surgeon April 2009;75(4):321‐3. [PubMed] [Google Scholar]
Ihedioha 2008
- Ihedioha U, Mackay G, Leung E, Molloy RG, O'Dwyer PJ. Laparoscopic colorectal resection does not reduce incisional hernia rates when compared with open colorectal resection. Surgical Endoscopy March 2008;22(3):689‐92. [DOI] [PubMed] [Google Scholar]
Itatsu 2014
- Itatsu K, Yokoyama Y, Sugawara G, Kubota H, Tojima Y, Kurumiya Y, et al. Incidence of and risk factors for incisional hernia after abdominal surgery. British Journal of Surgery 2014;101(11):1439‐47. [DOI] [PubMed] [Google Scholar]
Kendall 1991
- Kendall WH, Brennan G, Guillou J. Suture length to wound length ratio and integrity of midline and lateral paramedian incisions. British Journal of Surgery 1991;78:705‐7. [DOI] [PubMed] [Google Scholar]
Lamont 1988
- Lamont PM, Ellis H. Incisional hernia in re‐opened abdominal incisions: an overlooked risk factor. British Journal of Surgery 1988;75:374‐6. [DOI] [PubMed] [Google Scholar]
Langer 1985
- Langer S, Christiansen J. Long term results after incisional hernia repair. Acta Chirurgica Scandinavica 1985;151:217‐9. [PubMed] [Google Scholar]
Le Huu Nho 2012
- Huu Nho R, Mege D, Ouaïssi M, Sielezneff I, Sastre B. Incidence and prevention of ventral incisional hernia. Journal of Visceral Surgery October 2012;149(5 (supplement)):e3‐14. [DOI] [PubMed] [Google Scholar]
Leber 1998
- Leber GE, Garb JL, Alexander AJ, Reed WP. Long‐term complications associated with prosthetic repair of incisional hernias. Archives of Surgery 1998;133:378‐82. [DOI] [PubMed] [Google Scholar]
Llaguna 2010
- Llaguna OH, Avgerinos DV, Lugo JZ, Matatov T, Abbadessa B, Martz JE, et al. Incidence and risk factors for the development of incisional hernia following elective laparoscopic versus opencolon resections. The American Journal of Surgery August 2010;200(2):265‐9. [DOI] [PubMed] [Google Scholar]
Mudge 1985
- Mudge M, Hughes LE. Incisional hernia: a 10 year prospective study of incidence and attitudes. British Journal of Surgery 1985;72:70‐1. [DOI] [PubMed] [Google Scholar]
Nilsson 1983
- Nilsson T. Abdominal wound repair: an experimental study of the wound healing mechanism in the rabbit. Danish Medical Bulletin 1983;30:394‐407. [PubMed] [Google Scholar]
Pollock 1989
- Pollock AV, Evans M. Early prediction of late incisional hernias. British Journal of Surgery 1989;76:953‐4. [DOI] [PubMed] [Google Scholar]
Postlethwait 1975
- Postlethwait RW, Willigan DA, Ulin AW. Human tissue reaction to sutures. Annals of Surgery 1975;181:144‐50. [DOI] [PMC free article] [PubMed] [Google Scholar]
RevMan 2014 [Computer program]
- Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager 5 (RevMan 5). Version 5.3. Copenhagen: Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Rucinski 2001
- Rucinski J, Margolis M, Panagopoulos G, Wise L. Closure of the abdominal midline fascia: meta‐analysis delineates the optimal technique. American Surgeon 2001;67(5):421‐6. [PubMed] [Google Scholar]
Rutkow 2003
- Rutkow IM. Demographic and socioeconomic aspects of hernia repair in the United States in 2003. Surgical Clinics of North America 2003;83:1045‐51. [DOI] [PubMed] [Google Scholar]
Sajid 2011
- Sajid MS, Parampalli U, Baig MK, McFall MR. A systematic review on the effectiveness of slowly‐absorbable versus non‐absorbable sutures for abdominal fascial closure following laparotomy. International Journal of Surgery 2011;9(8):615‐25. [DOI] [PubMed] [Google Scholar]
Sanders 2012
- Sanders DL, Kingsnorth AN. The modern management of incisional hernias. BMJ 2012;344:e2843. [DOI] [PubMed] [Google Scholar]
Santora 1993
- Santora TA, Roslyn JJ. Incisional hernia. Surgical Clinics of North America 1993;73:557‐70. [DOI] [PubMed] [Google Scholar]
Schünemann 2011
- Schünemann HJ, Oxman AD, Vist GE, Higgins JPT, Deeks JJ, Glasziou P, et al. on behalf of the Cochrane Applicability and Recommendations Methods Group. Chapter 12: Interpreting results and drawing conclusions. In: Higgins JPT, Green S (editors), Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Smith 2012
- Smith M. Surgeons face more complex hernias in more complex reimbursement world. General Surgery News January 2012;39(1):1. [Google Scholar]
Spencer 2015
- Spencer RJ, Hayes KD, Rose S, Zhao Q, Rathouz PJ, Rice LW, et al. Risk factors for early‐occurring and late‐occurring incisional hernias after primary laparotomy for ovarian cancer. Obstetrics and Gynecology February 2015;125(2):407‐13. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sterne 2011
- Sterne JAC, Egger M, Moher D (editors). Chapter 10: Addressing reporting biases. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Intervention. Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Stey 2015
- Stey AM, Russell MM, Sugar CA, Hall BL, Zingmond DS, Lawson EH, et al. Extending the value of the National Surgical Quality Improvement Program claims dataset to study long‐term outcomes: rate of repeat ventral hernia repair. Surgery 2015;157(6):1157‐65. [DOI] [PubMed] [Google Scholar]
Sugerman 1996
- Sugerman HJ, Kellum JM, Reines HD, DeMaria EJ, Newsome HH, Lowry JW. Greater risk of incisional hernia with morbidly obese than steroid‐dependent patients and low recurrence with prefascial polypropylene mesh. American Journal of Surgery 1996;171:80‐4. [DOI] [PubMed] [Google Scholar]
Tully 2002
- Tully L, Gates S, Brocklehurst P, McKenzie‐McHarg K, Ayers S. Surgical techniques used during caesarean section operations: results of a national survey of practice in the UK. European Journal of Obstetrics & Gynecology and Reproductive Biology 2002;102:120‐6. [DOI] [PubMed] [Google Scholar]
Van't Riet 2002
- Van't Riet M, Steyerberg EW, Nellensteyn J, Bonjer HJ, Jeekel J. Meta‐analysis of techniques for closure of midline abdominal incisions. British Journal of Surgery 2002;89(11):1350‐6. [DOI] [PubMed] [Google Scholar]
Weiland 1998
- Weiland DE, Bay RC, Sordi S. Choosing the best abdominal closure by meta‐analysis. American Journal of Surgery 1998;176(6):666‐70. [DOI] [PubMed] [Google Scholar]


